User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Feds May End Hospital System’s Noncompete Contract for Part-Time Docs
Mount Sinai Health System in New York City is forcing part-time physicians to sign employment contracts that violate their labor rights, according to a June 2024 complaint by the National Labor Relations Board (NLRB).
The complaint stems from no-poaching and confidentiality clauses in the agreements required as a condition of employment, NLRB officials alleged.
according to a copy of the terms included in NLRB’s June 18 complaint.
By requiring the agreements, NLRB officials claimed, Mount Sinai is “interfering with, restraining, and coercing employees” in violation of the National Labor Relations Act. The health system’s “unfair labor practices” affects commerce as outlined under the law, according to the NLRB. The Act bans employers from burdening or obstructing commerce or the free flow of commerce.
Mount Sinai did not respond to requests for comment.
The NLRB’s complaint follows a landmark decision by the Federal Trade Commission (FTC) to ban noncompete agreements nationwide. In April 2024, the FTC voted to prohibit noncompetes indefinitely in an effort to protect workers.
“Noncompete clauses keep wages low, suppress new ideas, and rob the American economy of dynamism, including from the more than 8500 new startups that would be created a year once noncompetes are banned,” FTC Chair Lina M. Khan said in a statement. “The FTC’s final rule to ban noncompetes will ensure Americans have the freedom to pursue a new job, start a new business, or bring a new idea to market.”
Business groups and agencies have since sued to challenge against the ban, including the Chamber of Commerce. The Chamber and other business groups argue that noncompete agreements are important for companies to protect trade secrets, shield recruiting investments, and hide confidential information. The lawsuits are ongoing.
A Physician Blows the Whistle
An anonymous physician first alerted the NLRB to the contract language in November 2023. The doctor was required the sign the hospital system’s agreement for part-time physicians. The complaint does not say if the employee is still employed by the hospital system.
To remedy the unfair labor practices alleged, the NLRB seeks an order requiring the health system to rescind the contract language, stop any actions against current or former employees to enforce the provisions, and make whole any employees who suffered financial losses related to the contract terms.
The allegation against Mount Sinai is among a rising number of grievances filed with the NLRB that claim unfair labor practices. During the first 6 months of fiscal year 2024, unfair labor practice charges filed across the NLRB’s field offices increased 7% — from 9612 in 2023 to 10,278 in 2024, according to a news release.
NLRB, meanwhile has been cracking down on anticompetitive labor practices and confidentiality provisions that prevent employees from speaking out.
In a February 2023 decision for instance, NLRB ruled that an employer violates the National Labor Relations Act by offering severance agreements to workers that include restrictive confidentiality and nondisparagement terms. In 2022, the NLRB and the Federal Trade Commission forged a partnership to more widely combat unfair, anticompetitive, and deceptive business practices.
“Noncompete provisions reasonably tend to chill employees in the exercise of Section 7 rights when the provisions could reasonably be construed by employees to deny them the ability to quit or change jobs by cutting off their access to other employment opportunities that they are qualified for,” NLRB General Counsel Jennifer Abruzzo said in a 2023 release.
Ms. Abruzzo stressed in a memo that NLR Act is committed to an interagency approach to restrictions on the exercise of employee rights, “including limits to workers’ job mobility, information sharing, and referrals to other agencies.”
Mount Sinai Health System must respond to the NLRB’s complaint by July 16, and an administrative law judge is scheduled to hear the case on September 24.
A version of this article first appeared on Medscape.com.
Mount Sinai Health System in New York City is forcing part-time physicians to sign employment contracts that violate their labor rights, according to a June 2024 complaint by the National Labor Relations Board (NLRB).
The complaint stems from no-poaching and confidentiality clauses in the agreements required as a condition of employment, NLRB officials alleged.
according to a copy of the terms included in NLRB’s June 18 complaint.
By requiring the agreements, NLRB officials claimed, Mount Sinai is “interfering with, restraining, and coercing employees” in violation of the National Labor Relations Act. The health system’s “unfair labor practices” affects commerce as outlined under the law, according to the NLRB. The Act bans employers from burdening or obstructing commerce or the free flow of commerce.
Mount Sinai did not respond to requests for comment.
The NLRB’s complaint follows a landmark decision by the Federal Trade Commission (FTC) to ban noncompete agreements nationwide. In April 2024, the FTC voted to prohibit noncompetes indefinitely in an effort to protect workers.
“Noncompete clauses keep wages low, suppress new ideas, and rob the American economy of dynamism, including from the more than 8500 new startups that would be created a year once noncompetes are banned,” FTC Chair Lina M. Khan said in a statement. “The FTC’s final rule to ban noncompetes will ensure Americans have the freedom to pursue a new job, start a new business, or bring a new idea to market.”
Business groups and agencies have since sued to challenge against the ban, including the Chamber of Commerce. The Chamber and other business groups argue that noncompete agreements are important for companies to protect trade secrets, shield recruiting investments, and hide confidential information. The lawsuits are ongoing.
A Physician Blows the Whistle
An anonymous physician first alerted the NLRB to the contract language in November 2023. The doctor was required the sign the hospital system’s agreement for part-time physicians. The complaint does not say if the employee is still employed by the hospital system.
To remedy the unfair labor practices alleged, the NLRB seeks an order requiring the health system to rescind the contract language, stop any actions against current or former employees to enforce the provisions, and make whole any employees who suffered financial losses related to the contract terms.
The allegation against Mount Sinai is among a rising number of grievances filed with the NLRB that claim unfair labor practices. During the first 6 months of fiscal year 2024, unfair labor practice charges filed across the NLRB’s field offices increased 7% — from 9612 in 2023 to 10,278 in 2024, according to a news release.
NLRB, meanwhile has been cracking down on anticompetitive labor practices and confidentiality provisions that prevent employees from speaking out.
In a February 2023 decision for instance, NLRB ruled that an employer violates the National Labor Relations Act by offering severance agreements to workers that include restrictive confidentiality and nondisparagement terms. In 2022, the NLRB and the Federal Trade Commission forged a partnership to more widely combat unfair, anticompetitive, and deceptive business practices.
“Noncompete provisions reasonably tend to chill employees in the exercise of Section 7 rights when the provisions could reasonably be construed by employees to deny them the ability to quit or change jobs by cutting off their access to other employment opportunities that they are qualified for,” NLRB General Counsel Jennifer Abruzzo said in a 2023 release.
Ms. Abruzzo stressed in a memo that NLR Act is committed to an interagency approach to restrictions on the exercise of employee rights, “including limits to workers’ job mobility, information sharing, and referrals to other agencies.”
Mount Sinai Health System must respond to the NLRB’s complaint by July 16, and an administrative law judge is scheduled to hear the case on September 24.
A version of this article first appeared on Medscape.com.
Mount Sinai Health System in New York City is forcing part-time physicians to sign employment contracts that violate their labor rights, according to a June 2024 complaint by the National Labor Relations Board (NLRB).
The complaint stems from no-poaching and confidentiality clauses in the agreements required as a condition of employment, NLRB officials alleged.
according to a copy of the terms included in NLRB’s June 18 complaint.
By requiring the agreements, NLRB officials claimed, Mount Sinai is “interfering with, restraining, and coercing employees” in violation of the National Labor Relations Act. The health system’s “unfair labor practices” affects commerce as outlined under the law, according to the NLRB. The Act bans employers from burdening or obstructing commerce or the free flow of commerce.
Mount Sinai did not respond to requests for comment.
The NLRB’s complaint follows a landmark decision by the Federal Trade Commission (FTC) to ban noncompete agreements nationwide. In April 2024, the FTC voted to prohibit noncompetes indefinitely in an effort to protect workers.
“Noncompete clauses keep wages low, suppress new ideas, and rob the American economy of dynamism, including from the more than 8500 new startups that would be created a year once noncompetes are banned,” FTC Chair Lina M. Khan said in a statement. “The FTC’s final rule to ban noncompetes will ensure Americans have the freedom to pursue a new job, start a new business, or bring a new idea to market.”
Business groups and agencies have since sued to challenge against the ban, including the Chamber of Commerce. The Chamber and other business groups argue that noncompete agreements are important for companies to protect trade secrets, shield recruiting investments, and hide confidential information. The lawsuits are ongoing.
A Physician Blows the Whistle
An anonymous physician first alerted the NLRB to the contract language in November 2023. The doctor was required the sign the hospital system’s agreement for part-time physicians. The complaint does not say if the employee is still employed by the hospital system.
To remedy the unfair labor practices alleged, the NLRB seeks an order requiring the health system to rescind the contract language, stop any actions against current or former employees to enforce the provisions, and make whole any employees who suffered financial losses related to the contract terms.
The allegation against Mount Sinai is among a rising number of grievances filed with the NLRB that claim unfair labor practices. During the first 6 months of fiscal year 2024, unfair labor practice charges filed across the NLRB’s field offices increased 7% — from 9612 in 2023 to 10,278 in 2024, according to a news release.
NLRB, meanwhile has been cracking down on anticompetitive labor practices and confidentiality provisions that prevent employees from speaking out.
In a February 2023 decision for instance, NLRB ruled that an employer violates the National Labor Relations Act by offering severance agreements to workers that include restrictive confidentiality and nondisparagement terms. In 2022, the NLRB and the Federal Trade Commission forged a partnership to more widely combat unfair, anticompetitive, and deceptive business practices.
“Noncompete provisions reasonably tend to chill employees in the exercise of Section 7 rights when the provisions could reasonably be construed by employees to deny them the ability to quit or change jobs by cutting off their access to other employment opportunities that they are qualified for,” NLRB General Counsel Jennifer Abruzzo said in a 2023 release.
Ms. Abruzzo stressed in a memo that NLR Act is committed to an interagency approach to restrictions on the exercise of employee rights, “including limits to workers’ job mobility, information sharing, and referrals to other agencies.”
Mount Sinai Health System must respond to the NLRB’s complaint by July 16, and an administrative law judge is scheduled to hear the case on September 24.
A version of this article first appeared on Medscape.com.
Stroke Recurrence Risk Doubles in Patients With AF Who Stop Anticoagulation Therapy
, a new Danish nationwide cohort study finds.
Among 8,119 patients aged 50 years and older (54.1% male, mean age 78.4), 4.3% had a recurrent stroke within 1 year following discharge for the initial stroke, reported David Gaist, PhD, of Odense University Hospital, Odense, Denmark, and colleagues in JAMA Neurology.
An adjusted analysis found that those who stopped therapy were more than twice as likely to experience another stroke over a mean 2.9 years (13.4% vs 6.8%, adjusted odds ratio [aOR] = 2.13; 95% confidence interval [CI], 1.57-2.89).
The findings highlight the preventive power of OAC therapy, Dr. Gaist said in an interview, and point to the importance of counseling patients about the benefits of the drugs. “Clinicians can provide balanced information on the pros and cons of discontinuing oral anticoagulants as well as lay out plans on when to restart the medication,” he said.
The researchers launched the study “to provide data on how often recurrent ischemic strokes occur in a large, unselected cohort of patients with atrial fibrillation who had a stroke and started or restarted oral anticoagulants, a situation mirroring what we see in our everyday lives as clinicians,” Dr. Gaist said. “We also wanted to see if patients with breakthrough strokes had particular characteristics compared with patients who did not have a recurrent stroke. Finally, we wanted to quantify a very simple cause of breakthrough stroke by answering the following question: How many of these patients had stopped taking their oral anticoagulant?”
A Large, Unselected Patient Cohort
Dr. Gaist and colleagues tracked 8,119 patients with ischemic stroke and atrial fibrillation who started or restarted OAC therapy within 30 days following their discharge between 2014 and 2021. Patients either had atrial fibrillation before their stroke or developed it afterward.
Eighty-one percent of patients had hypertension, 19.7% had diabetes, and 27.3% had ischemic heart disease; 35.3% had never smoked and smoking information was missing for 15.9%. Race/ethnicity information was not provided.
Patients were followed for an average of 2.9 years until 2022, and all were alive at least 30 days after discharge. During that time, 663 patients had a recurrent ischemic stroke (4.3%), of whom 80.4% were on OAC therapy. The percentage who had stroke at 2 years rose to 6.5%.
While the researchers thought the number of strokes was high, Dr. Gaist said, this isn’t a sign that the drugs aren’t working. “Oral anticoagulant use in secondary prevention in atrial fibrillation is guideline-supported as it has been proven to reduce the risk of stroke by roughly two thirds.”
Of study participants at baseline, 37.9% took oral anticoagulants, 23.5% took direct oral anticoagulants (DOACs; dabigatran, rivaroxaban, apixaban, and edoxaban), and 15.1% took vitamin K antagonists. In a nested case-control analysis of 663 cases (58.7% men, mean age 80.1) matched to 2,652 controls, at admission for ischemic stroke, 80.4% were on OAC therapy, and 8%-11% of patients stopped OAC therapy after their strokes, the researchers reported.
Patients who stopped OAC therapy had more severe strokes than those who didn’t at 7 days (median recurrent ischemic stroke Scandinavian Stroke Scale [SSS] score = 40.0 vs 46.0, respectively; aOR = 2.10; 95% CI, 1.31-3.36). Those who stopped OAC therapy also had higher mortality rates at 7 days (11.2% vs 3.9%, respectively) and 30 days (28.1% vs 10.9%, respectively).
It’s not clear why some patients discontinued OAC therapy. “We looked for evidence of serious bleeding or surgical procedures around the time of anticoagulant discontinuation but found this only to be the case in roughly 10% of these patients,” Dr. Gaist said.
He added that the study probably “underestimates the issue of anticoagulant discontinuation, particularly for DOACs, where a shorter half-life compared with warfarin means that even a short drug-break of a few days puts the patient at increased risk of stroke.”
The authors noted study limitations, including the lack of data on actual medication usage, alcohol usage, stroke etiology, lesion location, and socioeconomic status. And, they wrote, the study population is mostly of European origin.
No Surprises
Steven R. Messe, MD, professor of neurology at the Hospital of the University of Pennsylvania, Philadelphia, who didn’t take part in the study but is familiar with its findings, said in an interview that the study is a “well-done analysis.”
The findings are not surprising, he said. “The overall risk of stroke recurrence was 4.3% at 1 year while the mortality rate was higher at 15.4%. Given that the median CHA2DS2-VASc score was 4 and the average age was 79, the stroke recurrence rate and mortality rate are in line with prior studies.”
In regard to the power of OAC therapy to prevent recurrent strokes, Dr. Messe noted that patients may not be adhering to prescribed regimens. Also, “while DOACs are clearly safer that vitamin K–dependent anticoagulants, the medications are generally not dose adjusted. It is possible that adjusting the dose based on measured anti-Xa levels to insure therapeutic anticoagulant effects may reduce the stroke risk further.”
He added that “most of these patients with prior stroke and atrial fibrillation are vasculopathic and at risk of additional strokes due to other mechanisms such as small vessel or large vessel disease.”
In the big picture, the study “confirms again that anticoagulation should be prescribed to all patients with atrial fibrillation and prior stroke, unless there is a strong bleeding risk contraindication,” Dr. Messe said. These patients are clearly at high risk of stroke recurrence and mortality, and all risk factors should be aggressively managed.”
Researchers are exploring other options, he said. “For example, there are studies of factor XI inhibitors that could be added to a DOAC for additional reductions in ischemic stroke. In addition, in patients undergoing cardiac surgery, the randomized trial LAOS III demonstrated that surgical left atrial occlusion in addition to anticoagulation may provide additional stroke prevention.”
Dr. Gaist disclosed personal fees from Pfizer and Bristol Myers Squibb, and grants from Bayer. Several other authors reported various relationships with industry. Dr. Messe has no disclosures.
, a new Danish nationwide cohort study finds.
Among 8,119 patients aged 50 years and older (54.1% male, mean age 78.4), 4.3% had a recurrent stroke within 1 year following discharge for the initial stroke, reported David Gaist, PhD, of Odense University Hospital, Odense, Denmark, and colleagues in JAMA Neurology.
An adjusted analysis found that those who stopped therapy were more than twice as likely to experience another stroke over a mean 2.9 years (13.4% vs 6.8%, adjusted odds ratio [aOR] = 2.13; 95% confidence interval [CI], 1.57-2.89).
The findings highlight the preventive power of OAC therapy, Dr. Gaist said in an interview, and point to the importance of counseling patients about the benefits of the drugs. “Clinicians can provide balanced information on the pros and cons of discontinuing oral anticoagulants as well as lay out plans on when to restart the medication,” he said.
The researchers launched the study “to provide data on how often recurrent ischemic strokes occur in a large, unselected cohort of patients with atrial fibrillation who had a stroke and started or restarted oral anticoagulants, a situation mirroring what we see in our everyday lives as clinicians,” Dr. Gaist said. “We also wanted to see if patients with breakthrough strokes had particular characteristics compared with patients who did not have a recurrent stroke. Finally, we wanted to quantify a very simple cause of breakthrough stroke by answering the following question: How many of these patients had stopped taking their oral anticoagulant?”
A Large, Unselected Patient Cohort
Dr. Gaist and colleagues tracked 8,119 patients with ischemic stroke and atrial fibrillation who started or restarted OAC therapy within 30 days following their discharge between 2014 and 2021. Patients either had atrial fibrillation before their stroke or developed it afterward.
Eighty-one percent of patients had hypertension, 19.7% had diabetes, and 27.3% had ischemic heart disease; 35.3% had never smoked and smoking information was missing for 15.9%. Race/ethnicity information was not provided.
Patients were followed for an average of 2.9 years until 2022, and all were alive at least 30 days after discharge. During that time, 663 patients had a recurrent ischemic stroke (4.3%), of whom 80.4% were on OAC therapy. The percentage who had stroke at 2 years rose to 6.5%.
While the researchers thought the number of strokes was high, Dr. Gaist said, this isn’t a sign that the drugs aren’t working. “Oral anticoagulant use in secondary prevention in atrial fibrillation is guideline-supported as it has been proven to reduce the risk of stroke by roughly two thirds.”
Of study participants at baseline, 37.9% took oral anticoagulants, 23.5% took direct oral anticoagulants (DOACs; dabigatran, rivaroxaban, apixaban, and edoxaban), and 15.1% took vitamin K antagonists. In a nested case-control analysis of 663 cases (58.7% men, mean age 80.1) matched to 2,652 controls, at admission for ischemic stroke, 80.4% were on OAC therapy, and 8%-11% of patients stopped OAC therapy after their strokes, the researchers reported.
Patients who stopped OAC therapy had more severe strokes than those who didn’t at 7 days (median recurrent ischemic stroke Scandinavian Stroke Scale [SSS] score = 40.0 vs 46.0, respectively; aOR = 2.10; 95% CI, 1.31-3.36). Those who stopped OAC therapy also had higher mortality rates at 7 days (11.2% vs 3.9%, respectively) and 30 days (28.1% vs 10.9%, respectively).
It’s not clear why some patients discontinued OAC therapy. “We looked for evidence of serious bleeding or surgical procedures around the time of anticoagulant discontinuation but found this only to be the case in roughly 10% of these patients,” Dr. Gaist said.
He added that the study probably “underestimates the issue of anticoagulant discontinuation, particularly for DOACs, where a shorter half-life compared with warfarin means that even a short drug-break of a few days puts the patient at increased risk of stroke.”
The authors noted study limitations, including the lack of data on actual medication usage, alcohol usage, stroke etiology, lesion location, and socioeconomic status. And, they wrote, the study population is mostly of European origin.
No Surprises
Steven R. Messe, MD, professor of neurology at the Hospital of the University of Pennsylvania, Philadelphia, who didn’t take part in the study but is familiar with its findings, said in an interview that the study is a “well-done analysis.”
The findings are not surprising, he said. “The overall risk of stroke recurrence was 4.3% at 1 year while the mortality rate was higher at 15.4%. Given that the median CHA2DS2-VASc score was 4 and the average age was 79, the stroke recurrence rate and mortality rate are in line with prior studies.”
In regard to the power of OAC therapy to prevent recurrent strokes, Dr. Messe noted that patients may not be adhering to prescribed regimens. Also, “while DOACs are clearly safer that vitamin K–dependent anticoagulants, the medications are generally not dose adjusted. It is possible that adjusting the dose based on measured anti-Xa levels to insure therapeutic anticoagulant effects may reduce the stroke risk further.”
He added that “most of these patients with prior stroke and atrial fibrillation are vasculopathic and at risk of additional strokes due to other mechanisms such as small vessel or large vessel disease.”
In the big picture, the study “confirms again that anticoagulation should be prescribed to all patients with atrial fibrillation and prior stroke, unless there is a strong bleeding risk contraindication,” Dr. Messe said. These patients are clearly at high risk of stroke recurrence and mortality, and all risk factors should be aggressively managed.”
Researchers are exploring other options, he said. “For example, there are studies of factor XI inhibitors that could be added to a DOAC for additional reductions in ischemic stroke. In addition, in patients undergoing cardiac surgery, the randomized trial LAOS III demonstrated that surgical left atrial occlusion in addition to anticoagulation may provide additional stroke prevention.”
Dr. Gaist disclosed personal fees from Pfizer and Bristol Myers Squibb, and grants from Bayer. Several other authors reported various relationships with industry. Dr. Messe has no disclosures.
, a new Danish nationwide cohort study finds.
Among 8,119 patients aged 50 years and older (54.1% male, mean age 78.4), 4.3% had a recurrent stroke within 1 year following discharge for the initial stroke, reported David Gaist, PhD, of Odense University Hospital, Odense, Denmark, and colleagues in JAMA Neurology.
An adjusted analysis found that those who stopped therapy were more than twice as likely to experience another stroke over a mean 2.9 years (13.4% vs 6.8%, adjusted odds ratio [aOR] = 2.13; 95% confidence interval [CI], 1.57-2.89).
The findings highlight the preventive power of OAC therapy, Dr. Gaist said in an interview, and point to the importance of counseling patients about the benefits of the drugs. “Clinicians can provide balanced information on the pros and cons of discontinuing oral anticoagulants as well as lay out plans on when to restart the medication,” he said.
The researchers launched the study “to provide data on how often recurrent ischemic strokes occur in a large, unselected cohort of patients with atrial fibrillation who had a stroke and started or restarted oral anticoagulants, a situation mirroring what we see in our everyday lives as clinicians,” Dr. Gaist said. “We also wanted to see if patients with breakthrough strokes had particular characteristics compared with patients who did not have a recurrent stroke. Finally, we wanted to quantify a very simple cause of breakthrough stroke by answering the following question: How many of these patients had stopped taking their oral anticoagulant?”
A Large, Unselected Patient Cohort
Dr. Gaist and colleagues tracked 8,119 patients with ischemic stroke and atrial fibrillation who started or restarted OAC therapy within 30 days following their discharge between 2014 and 2021. Patients either had atrial fibrillation before their stroke or developed it afterward.
Eighty-one percent of patients had hypertension, 19.7% had diabetes, and 27.3% had ischemic heart disease; 35.3% had never smoked and smoking information was missing for 15.9%. Race/ethnicity information was not provided.
Patients were followed for an average of 2.9 years until 2022, and all were alive at least 30 days after discharge. During that time, 663 patients had a recurrent ischemic stroke (4.3%), of whom 80.4% were on OAC therapy. The percentage who had stroke at 2 years rose to 6.5%.
While the researchers thought the number of strokes was high, Dr. Gaist said, this isn’t a sign that the drugs aren’t working. “Oral anticoagulant use in secondary prevention in atrial fibrillation is guideline-supported as it has been proven to reduce the risk of stroke by roughly two thirds.”
Of study participants at baseline, 37.9% took oral anticoagulants, 23.5% took direct oral anticoagulants (DOACs; dabigatran, rivaroxaban, apixaban, and edoxaban), and 15.1% took vitamin K antagonists. In a nested case-control analysis of 663 cases (58.7% men, mean age 80.1) matched to 2,652 controls, at admission for ischemic stroke, 80.4% were on OAC therapy, and 8%-11% of patients stopped OAC therapy after their strokes, the researchers reported.
Patients who stopped OAC therapy had more severe strokes than those who didn’t at 7 days (median recurrent ischemic stroke Scandinavian Stroke Scale [SSS] score = 40.0 vs 46.0, respectively; aOR = 2.10; 95% CI, 1.31-3.36). Those who stopped OAC therapy also had higher mortality rates at 7 days (11.2% vs 3.9%, respectively) and 30 days (28.1% vs 10.9%, respectively).
It’s not clear why some patients discontinued OAC therapy. “We looked for evidence of serious bleeding or surgical procedures around the time of anticoagulant discontinuation but found this only to be the case in roughly 10% of these patients,” Dr. Gaist said.
He added that the study probably “underestimates the issue of anticoagulant discontinuation, particularly for DOACs, where a shorter half-life compared with warfarin means that even a short drug-break of a few days puts the patient at increased risk of stroke.”
The authors noted study limitations, including the lack of data on actual medication usage, alcohol usage, stroke etiology, lesion location, and socioeconomic status. And, they wrote, the study population is mostly of European origin.
No Surprises
Steven R. Messe, MD, professor of neurology at the Hospital of the University of Pennsylvania, Philadelphia, who didn’t take part in the study but is familiar with its findings, said in an interview that the study is a “well-done analysis.”
The findings are not surprising, he said. “The overall risk of stroke recurrence was 4.3% at 1 year while the mortality rate was higher at 15.4%. Given that the median CHA2DS2-VASc score was 4 and the average age was 79, the stroke recurrence rate and mortality rate are in line with prior studies.”
In regard to the power of OAC therapy to prevent recurrent strokes, Dr. Messe noted that patients may not be adhering to prescribed regimens. Also, “while DOACs are clearly safer that vitamin K–dependent anticoagulants, the medications are generally not dose adjusted. It is possible that adjusting the dose based on measured anti-Xa levels to insure therapeutic anticoagulant effects may reduce the stroke risk further.”
He added that “most of these patients with prior stroke and atrial fibrillation are vasculopathic and at risk of additional strokes due to other mechanisms such as small vessel or large vessel disease.”
In the big picture, the study “confirms again that anticoagulation should be prescribed to all patients with atrial fibrillation and prior stroke, unless there is a strong bleeding risk contraindication,” Dr. Messe said. These patients are clearly at high risk of stroke recurrence and mortality, and all risk factors should be aggressively managed.”
Researchers are exploring other options, he said. “For example, there are studies of factor XI inhibitors that could be added to a DOAC for additional reductions in ischemic stroke. In addition, in patients undergoing cardiac surgery, the randomized trial LAOS III demonstrated that surgical left atrial occlusion in addition to anticoagulation may provide additional stroke prevention.”
Dr. Gaist disclosed personal fees from Pfizer and Bristol Myers Squibb, and grants from Bayer. Several other authors reported various relationships with industry. Dr. Messe has no disclosures.
FROM JAMA NEUROLOGY
Does An Elevated Lp(a) Call for Low-dose Aspirin?
Should a patient with high lipoprotein (a), or Lp(a), be started on low-dose aspirin?
This is the conundrum facing many physicians and patients, but even getting to that point will require more availability and coverage of tests and a greater appreciation of the risk associated with Lp(a), said cardiologists.
Lp(a): The Silent Risk
On Lp(a) Awareness Day, C. Michael Gibson, MD, MA, CEO of the Baim Institute for Clinical Research, Boston, Massachusetts, and PERFUSE took the opportunity to talk about his experiences with testing on X.
The professor of medicine at Harvard Medical School, also in Boston, said he was surprised to find that he had a very high calcium score, despite a low-density lipoprotein (LDL) cholesterol level of just 70 mg/dL. Eventually, he found out that he had a “very, very high Lp(a),” which was particularly concerning because his grandfather died of a heart attack at 45 years of age.
But how much risk does that represent?
A 2022 consensus statement from the European Atherosclerosis Society (EAS) highlighted that epidemiologic and genetic studies “strongly support a causal and continuous association between Lp(a) concentration and cardiovascular outcomes,” even at very low LDL cholesterol levels.
This is because Lp(a) has proinflammatory and proatherosclerotic properties, and high levels are associated with both micro- and macrocalcification of the aortic valve. Findings from a US registry study also suggest the threshold related to increased cardiovascular risk may differ for primary and secondary prevention populations (J Am Coll Cardiol. 2024 Mar 5;83[9]:873-886).
Lp(a) is, however, genetically determined, and there are no drugs available that directly lower levels, although some are on the horizon. In the meantime, the experts behind the consensus statement recommend that all adults be tested at least once in their lifetime.
Testing Cost and Availability
This recommendation has been translated into guidelines in “many, many” countries, said lead author Florian Kronenberg, MD, MAE, Institute of Genetic Epidemiology, Medical University of Innsbruck, Innsbruck, Austria, but “we are far away from reaching that goal.”
“We’ve got a real problem,” added Stephen Nicholls, MD, PhD, director of the Victorian Heart Institute and a professor of cardiology at Monash University, Melbourne, Australia, as there is “not a country in the world where there’s good access to Lp(a) testing.”
Dr. Kronenberg said that the consensus statement “created a kind of momentum” toward universal testing.
Ulrich Laufs, MD, PhD, professor and chair, Department of Cardiology, University Hospital Leipzig, Leipzig, Germany, agreed, saying that, overall, Lp(a) testing has “increased dramatically,” albeit from “extremely low levels.”
Dr. Kronenberg believes that “we have to be really patient.” He cited a lack of knowledge among physicians as one of the biggest barriers to greater uptake of testing.
“There is still no appreciation of the role of Lp(a),” agreed Alberico L. Catapano, MD, PhD, director of Cardiovascular Research and of the Lipoproteins and Atherosclerosis Laboratory of IRCCS Multimedica, Milan, Italy, and past president of the EAS.
“That’s why it’s not mentioned” to patients, he said. “What is really needed is to inform physician colleagues that Lp(a) is not only a risk factor but is the cause” of atherosclerotic cardiovascular disease (ASCVD).
Dr. Kronenberg said that the pressure for testing can often come from the patient themselves.
Physicians then question why the patient wants to be tested when there are no medications to treat it, he added. “We really tried very hard when we did the consensus paper to say that we should perform the test and give people advice on what to do.”
Dr. Catapano believes that another major obstacle is the cost of the test, which remains high “because very few people do it,” and there is some debate over which test to use.
Taken together, these issues have meant that “payers are really struggling with the idea of funding Lp(a),” said Dr. Nicholls, adding that “there seems to be this fixation on: ‘Well, if you can’t lower Lp(a), why measure it?’ ”
Rather than blame the payers, he says there is a need to educate about the science behind testing and underline that Lp(a) is an “important risk enhancer” for cardiovascular disease.
“Because if we’re going to make people pay out of pocket, then you’re creating a massive equity issue in that only those who can afford the test have it.”
High Lp(a) Now What?
But once the test has been performed, there then comes the question as to what to do about the result.
“Before we get anywhere near an agent that effectively lowers Lp(a) and get it into the clinic, there are lots of things that we can do today,” said Dr. Nicholls.
If someone has an intermediate or high background cardiovascular risk and they have got a high Lp(a) level, they “should be treated more intensively, as we know that high Lp(a) patients do better if their LDL cholesterol and their blood pressure is lower.”
For Dr. Catapano, this means having the “same mindset as you do with [a patient with] high blood pressure, high LDL cholesterol, and so on, because it’s exactly the same thing: It’s interacting with your other risk factors to increase your overall risk.”
Dr. Gibson agreed. Through a range of measures, including weight loss and statin therapy, he was able to reduce his overall cardiovascular risk, and his LDL cholesterol level dropped to just 20 mg/dL.
A Role for Aspirin?
It gained added momentum when Pablo Corral, MD, a lipidologist and a professor in the School of Medicine, Pharmacology Department, FASTA University, Mar del Plata, Buenos Aires, Argentina, highlighted the issue on X.
He pointed to a recent study, which showed that regular aspirin use was associated with a significantly lower rate of ASCVD mortality in adults without clinical ASCVD but who had elevated Lp(a).
Dr. Nicholls said that, when you “peel away the layers” of the current evidence, there is some suggestion that Lp(a)may be prothrombotic. “So in theory, perhaps aspirin might be maybe more intuitively useful there.”
He noted that the ASPREE primary prevention study found that low-dose aspirin in older adults resulted in a significantly higher risk for major hemorrhage over placebo and did not significantly reduce the risk for cardiovascular disease.
But an analysis he and his colleagues did suggest that aspirin may indeed benefit older individuals if they have elevated Lp(a) genotypes.
An Individual Decision
For Dr. Kronenberg and Dr. Laufs, there is currently a lack of appropriate data to make a recommendation either way, particularly for primary prevention.
They warned that the risk for thrombosis in patients with mildly elevated Lp(a) cannot be discounted, and in most cases either “the existing risk of bleeding exceeds the beneficial effects [of aspirin], or it’s not indicated,” said Dr. Laufs.
“When we make a recommendation, we should have evidence-based data,” Dr. Kronenberg said, but, at the moment, people “somehow put their finger in the air and see” which way the wind is blowing.
Dr. Catapano urged patients to talk to their physician, as even low-dose aspirin is “very potent” at inhibiting platelets.
Dr. Gibson agreed, saying that he is in two minds, as the potential benefit has to be weighed against the bleeding risk.
He personally takes low-dose aspirin because “I know I have a low bleeding risk,” but it is a decision “that has to be taken individually between a patient and their physician.”
Dr. Gibson, Dr. Kronenberg, Dr. Nicholls, and Dr. Catapano all reported conflicts of interest with numerous pharmaceutical companies and organizations.
A version of this article first appeared on Medscape.com.
Should a patient with high lipoprotein (a), or Lp(a), be started on low-dose aspirin?
This is the conundrum facing many physicians and patients, but even getting to that point will require more availability and coverage of tests and a greater appreciation of the risk associated with Lp(a), said cardiologists.
Lp(a): The Silent Risk
On Lp(a) Awareness Day, C. Michael Gibson, MD, MA, CEO of the Baim Institute for Clinical Research, Boston, Massachusetts, and PERFUSE took the opportunity to talk about his experiences with testing on X.
The professor of medicine at Harvard Medical School, also in Boston, said he was surprised to find that he had a very high calcium score, despite a low-density lipoprotein (LDL) cholesterol level of just 70 mg/dL. Eventually, he found out that he had a “very, very high Lp(a),” which was particularly concerning because his grandfather died of a heart attack at 45 years of age.
But how much risk does that represent?
A 2022 consensus statement from the European Atherosclerosis Society (EAS) highlighted that epidemiologic and genetic studies “strongly support a causal and continuous association between Lp(a) concentration and cardiovascular outcomes,” even at very low LDL cholesterol levels.
This is because Lp(a) has proinflammatory and proatherosclerotic properties, and high levels are associated with both micro- and macrocalcification of the aortic valve. Findings from a US registry study also suggest the threshold related to increased cardiovascular risk may differ for primary and secondary prevention populations (J Am Coll Cardiol. 2024 Mar 5;83[9]:873-886).
Lp(a) is, however, genetically determined, and there are no drugs available that directly lower levels, although some are on the horizon. In the meantime, the experts behind the consensus statement recommend that all adults be tested at least once in their lifetime.
Testing Cost and Availability
This recommendation has been translated into guidelines in “many, many” countries, said lead author Florian Kronenberg, MD, MAE, Institute of Genetic Epidemiology, Medical University of Innsbruck, Innsbruck, Austria, but “we are far away from reaching that goal.”
“We’ve got a real problem,” added Stephen Nicholls, MD, PhD, director of the Victorian Heart Institute and a professor of cardiology at Monash University, Melbourne, Australia, as there is “not a country in the world where there’s good access to Lp(a) testing.”
Dr. Kronenberg said that the consensus statement “created a kind of momentum” toward universal testing.
Ulrich Laufs, MD, PhD, professor and chair, Department of Cardiology, University Hospital Leipzig, Leipzig, Germany, agreed, saying that, overall, Lp(a) testing has “increased dramatically,” albeit from “extremely low levels.”
Dr. Kronenberg believes that “we have to be really patient.” He cited a lack of knowledge among physicians as one of the biggest barriers to greater uptake of testing.
“There is still no appreciation of the role of Lp(a),” agreed Alberico L. Catapano, MD, PhD, director of Cardiovascular Research and of the Lipoproteins and Atherosclerosis Laboratory of IRCCS Multimedica, Milan, Italy, and past president of the EAS.
“That’s why it’s not mentioned” to patients, he said. “What is really needed is to inform physician colleagues that Lp(a) is not only a risk factor but is the cause” of atherosclerotic cardiovascular disease (ASCVD).
Dr. Kronenberg said that the pressure for testing can often come from the patient themselves.
Physicians then question why the patient wants to be tested when there are no medications to treat it, he added. “We really tried very hard when we did the consensus paper to say that we should perform the test and give people advice on what to do.”
Dr. Catapano believes that another major obstacle is the cost of the test, which remains high “because very few people do it,” and there is some debate over which test to use.
Taken together, these issues have meant that “payers are really struggling with the idea of funding Lp(a),” said Dr. Nicholls, adding that “there seems to be this fixation on: ‘Well, if you can’t lower Lp(a), why measure it?’ ”
Rather than blame the payers, he says there is a need to educate about the science behind testing and underline that Lp(a) is an “important risk enhancer” for cardiovascular disease.
“Because if we’re going to make people pay out of pocket, then you’re creating a massive equity issue in that only those who can afford the test have it.”
High Lp(a) Now What?
But once the test has been performed, there then comes the question as to what to do about the result.
“Before we get anywhere near an agent that effectively lowers Lp(a) and get it into the clinic, there are lots of things that we can do today,” said Dr. Nicholls.
If someone has an intermediate or high background cardiovascular risk and they have got a high Lp(a) level, they “should be treated more intensively, as we know that high Lp(a) patients do better if their LDL cholesterol and their blood pressure is lower.”
For Dr. Catapano, this means having the “same mindset as you do with [a patient with] high blood pressure, high LDL cholesterol, and so on, because it’s exactly the same thing: It’s interacting with your other risk factors to increase your overall risk.”
Dr. Gibson agreed. Through a range of measures, including weight loss and statin therapy, he was able to reduce his overall cardiovascular risk, and his LDL cholesterol level dropped to just 20 mg/dL.
A Role for Aspirin?
It gained added momentum when Pablo Corral, MD, a lipidologist and a professor in the School of Medicine, Pharmacology Department, FASTA University, Mar del Plata, Buenos Aires, Argentina, highlighted the issue on X.
He pointed to a recent study, which showed that regular aspirin use was associated with a significantly lower rate of ASCVD mortality in adults without clinical ASCVD but who had elevated Lp(a).
Dr. Nicholls said that, when you “peel away the layers” of the current evidence, there is some suggestion that Lp(a)may be prothrombotic. “So in theory, perhaps aspirin might be maybe more intuitively useful there.”
He noted that the ASPREE primary prevention study found that low-dose aspirin in older adults resulted in a significantly higher risk for major hemorrhage over placebo and did not significantly reduce the risk for cardiovascular disease.
But an analysis he and his colleagues did suggest that aspirin may indeed benefit older individuals if they have elevated Lp(a) genotypes.
An Individual Decision
For Dr. Kronenberg and Dr. Laufs, there is currently a lack of appropriate data to make a recommendation either way, particularly for primary prevention.
They warned that the risk for thrombosis in patients with mildly elevated Lp(a) cannot be discounted, and in most cases either “the existing risk of bleeding exceeds the beneficial effects [of aspirin], or it’s not indicated,” said Dr. Laufs.
“When we make a recommendation, we should have evidence-based data,” Dr. Kronenberg said, but, at the moment, people “somehow put their finger in the air and see” which way the wind is blowing.
Dr. Catapano urged patients to talk to their physician, as even low-dose aspirin is “very potent” at inhibiting platelets.
Dr. Gibson agreed, saying that he is in two minds, as the potential benefit has to be weighed against the bleeding risk.
He personally takes low-dose aspirin because “I know I have a low bleeding risk,” but it is a decision “that has to be taken individually between a patient and their physician.”
Dr. Gibson, Dr. Kronenberg, Dr. Nicholls, and Dr. Catapano all reported conflicts of interest with numerous pharmaceutical companies and organizations.
A version of this article first appeared on Medscape.com.
Should a patient with high lipoprotein (a), or Lp(a), be started on low-dose aspirin?
This is the conundrum facing many physicians and patients, but even getting to that point will require more availability and coverage of tests and a greater appreciation of the risk associated with Lp(a), said cardiologists.
Lp(a): The Silent Risk
On Lp(a) Awareness Day, C. Michael Gibson, MD, MA, CEO of the Baim Institute for Clinical Research, Boston, Massachusetts, and PERFUSE took the opportunity to talk about his experiences with testing on X.
The professor of medicine at Harvard Medical School, also in Boston, said he was surprised to find that he had a very high calcium score, despite a low-density lipoprotein (LDL) cholesterol level of just 70 mg/dL. Eventually, he found out that he had a “very, very high Lp(a),” which was particularly concerning because his grandfather died of a heart attack at 45 years of age.
But how much risk does that represent?
A 2022 consensus statement from the European Atherosclerosis Society (EAS) highlighted that epidemiologic and genetic studies “strongly support a causal and continuous association between Lp(a) concentration and cardiovascular outcomes,” even at very low LDL cholesterol levels.
This is because Lp(a) has proinflammatory and proatherosclerotic properties, and high levels are associated with both micro- and macrocalcification of the aortic valve. Findings from a US registry study also suggest the threshold related to increased cardiovascular risk may differ for primary and secondary prevention populations (J Am Coll Cardiol. 2024 Mar 5;83[9]:873-886).
Lp(a) is, however, genetically determined, and there are no drugs available that directly lower levels, although some are on the horizon. In the meantime, the experts behind the consensus statement recommend that all adults be tested at least once in their lifetime.
Testing Cost and Availability
This recommendation has been translated into guidelines in “many, many” countries, said lead author Florian Kronenberg, MD, MAE, Institute of Genetic Epidemiology, Medical University of Innsbruck, Innsbruck, Austria, but “we are far away from reaching that goal.”
“We’ve got a real problem,” added Stephen Nicholls, MD, PhD, director of the Victorian Heart Institute and a professor of cardiology at Monash University, Melbourne, Australia, as there is “not a country in the world where there’s good access to Lp(a) testing.”
Dr. Kronenberg said that the consensus statement “created a kind of momentum” toward universal testing.
Ulrich Laufs, MD, PhD, professor and chair, Department of Cardiology, University Hospital Leipzig, Leipzig, Germany, agreed, saying that, overall, Lp(a) testing has “increased dramatically,” albeit from “extremely low levels.”
Dr. Kronenberg believes that “we have to be really patient.” He cited a lack of knowledge among physicians as one of the biggest barriers to greater uptake of testing.
“There is still no appreciation of the role of Lp(a),” agreed Alberico L. Catapano, MD, PhD, director of Cardiovascular Research and of the Lipoproteins and Atherosclerosis Laboratory of IRCCS Multimedica, Milan, Italy, and past president of the EAS.
“That’s why it’s not mentioned” to patients, he said. “What is really needed is to inform physician colleagues that Lp(a) is not only a risk factor but is the cause” of atherosclerotic cardiovascular disease (ASCVD).
Dr. Kronenberg said that the pressure for testing can often come from the patient themselves.
Physicians then question why the patient wants to be tested when there are no medications to treat it, he added. “We really tried very hard when we did the consensus paper to say that we should perform the test and give people advice on what to do.”
Dr. Catapano believes that another major obstacle is the cost of the test, which remains high “because very few people do it,” and there is some debate over which test to use.
Taken together, these issues have meant that “payers are really struggling with the idea of funding Lp(a),” said Dr. Nicholls, adding that “there seems to be this fixation on: ‘Well, if you can’t lower Lp(a), why measure it?’ ”
Rather than blame the payers, he says there is a need to educate about the science behind testing and underline that Lp(a) is an “important risk enhancer” for cardiovascular disease.
“Because if we’re going to make people pay out of pocket, then you’re creating a massive equity issue in that only those who can afford the test have it.”
High Lp(a) Now What?
But once the test has been performed, there then comes the question as to what to do about the result.
“Before we get anywhere near an agent that effectively lowers Lp(a) and get it into the clinic, there are lots of things that we can do today,” said Dr. Nicholls.
If someone has an intermediate or high background cardiovascular risk and they have got a high Lp(a) level, they “should be treated more intensively, as we know that high Lp(a) patients do better if their LDL cholesterol and their blood pressure is lower.”
For Dr. Catapano, this means having the “same mindset as you do with [a patient with] high blood pressure, high LDL cholesterol, and so on, because it’s exactly the same thing: It’s interacting with your other risk factors to increase your overall risk.”
Dr. Gibson agreed. Through a range of measures, including weight loss and statin therapy, he was able to reduce his overall cardiovascular risk, and his LDL cholesterol level dropped to just 20 mg/dL.
A Role for Aspirin?
It gained added momentum when Pablo Corral, MD, a lipidologist and a professor in the School of Medicine, Pharmacology Department, FASTA University, Mar del Plata, Buenos Aires, Argentina, highlighted the issue on X.
He pointed to a recent study, which showed that regular aspirin use was associated with a significantly lower rate of ASCVD mortality in adults without clinical ASCVD but who had elevated Lp(a).
Dr. Nicholls said that, when you “peel away the layers” of the current evidence, there is some suggestion that Lp(a)may be prothrombotic. “So in theory, perhaps aspirin might be maybe more intuitively useful there.”
He noted that the ASPREE primary prevention study found that low-dose aspirin in older adults resulted in a significantly higher risk for major hemorrhage over placebo and did not significantly reduce the risk for cardiovascular disease.
But an analysis he and his colleagues did suggest that aspirin may indeed benefit older individuals if they have elevated Lp(a) genotypes.
An Individual Decision
For Dr. Kronenberg and Dr. Laufs, there is currently a lack of appropriate data to make a recommendation either way, particularly for primary prevention.
They warned that the risk for thrombosis in patients with mildly elevated Lp(a) cannot be discounted, and in most cases either “the existing risk of bleeding exceeds the beneficial effects [of aspirin], or it’s not indicated,” said Dr. Laufs.
“When we make a recommendation, we should have evidence-based data,” Dr. Kronenberg said, but, at the moment, people “somehow put their finger in the air and see” which way the wind is blowing.
Dr. Catapano urged patients to talk to their physician, as even low-dose aspirin is “very potent” at inhibiting platelets.
Dr. Gibson agreed, saying that he is in two minds, as the potential benefit has to be weighed against the bleeding risk.
He personally takes low-dose aspirin because “I know I have a low bleeding risk,” but it is a decision “that has to be taken individually between a patient and their physician.”
Dr. Gibson, Dr. Kronenberg, Dr. Nicholls, and Dr. Catapano all reported conflicts of interest with numerous pharmaceutical companies and organizations.
A version of this article first appeared on Medscape.com.
Facial Temperature Can Reveal Age and Disease
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
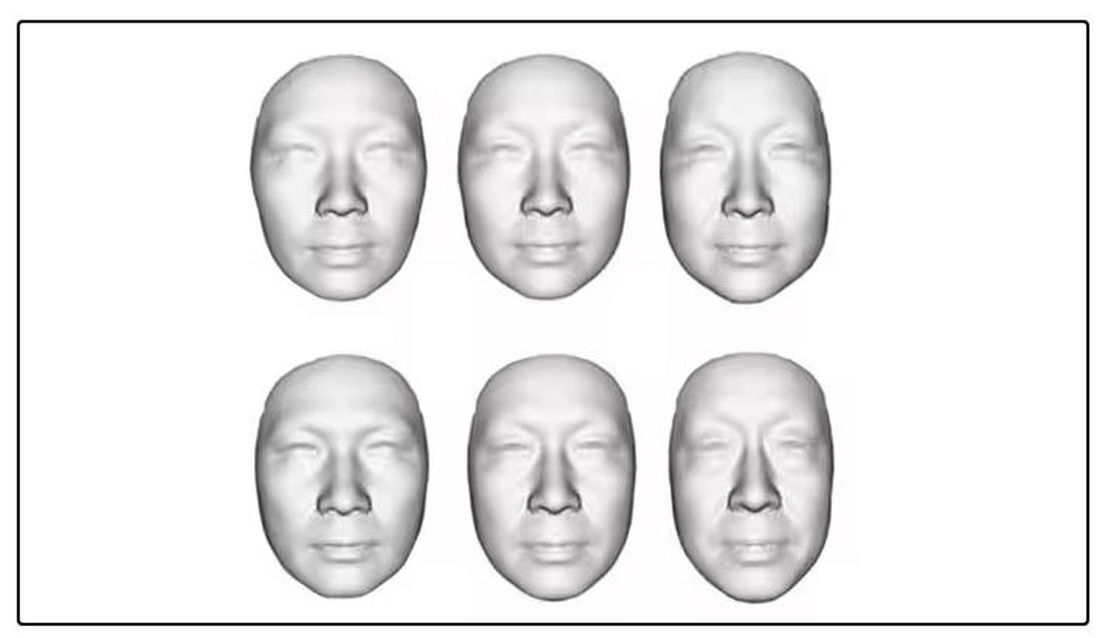
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those.
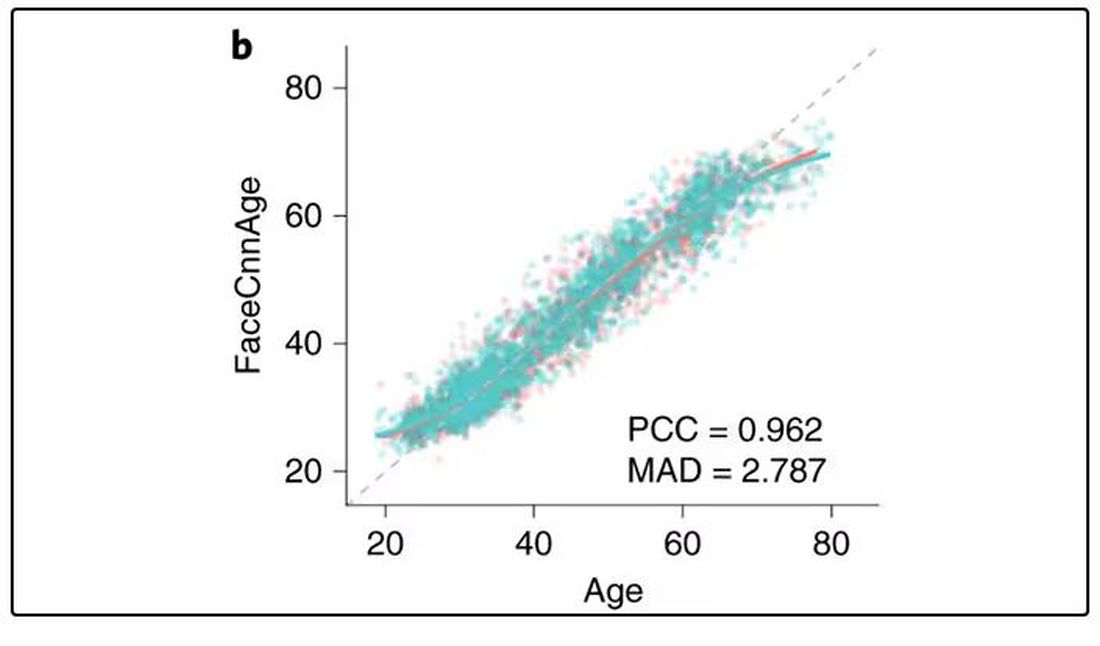
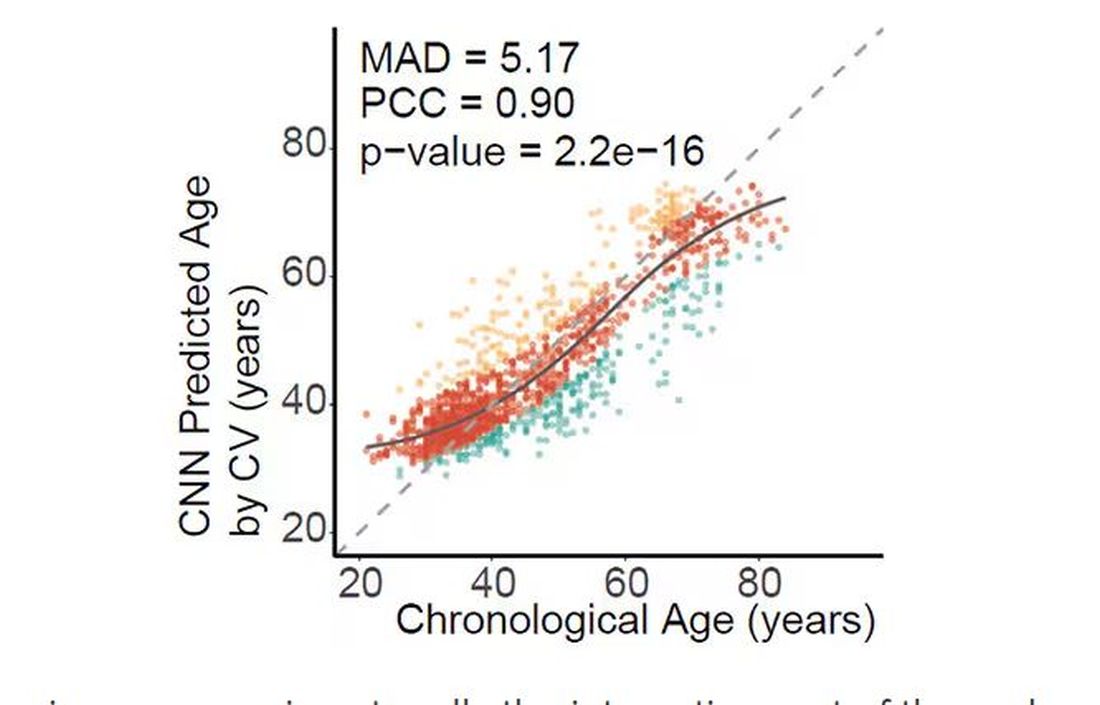
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally.
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
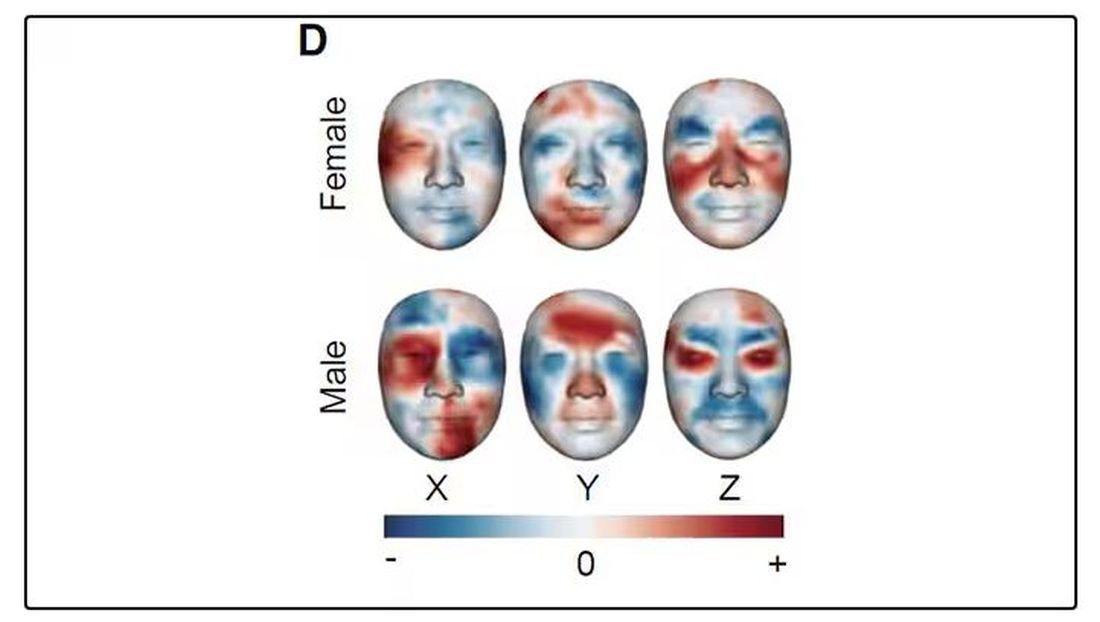
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.
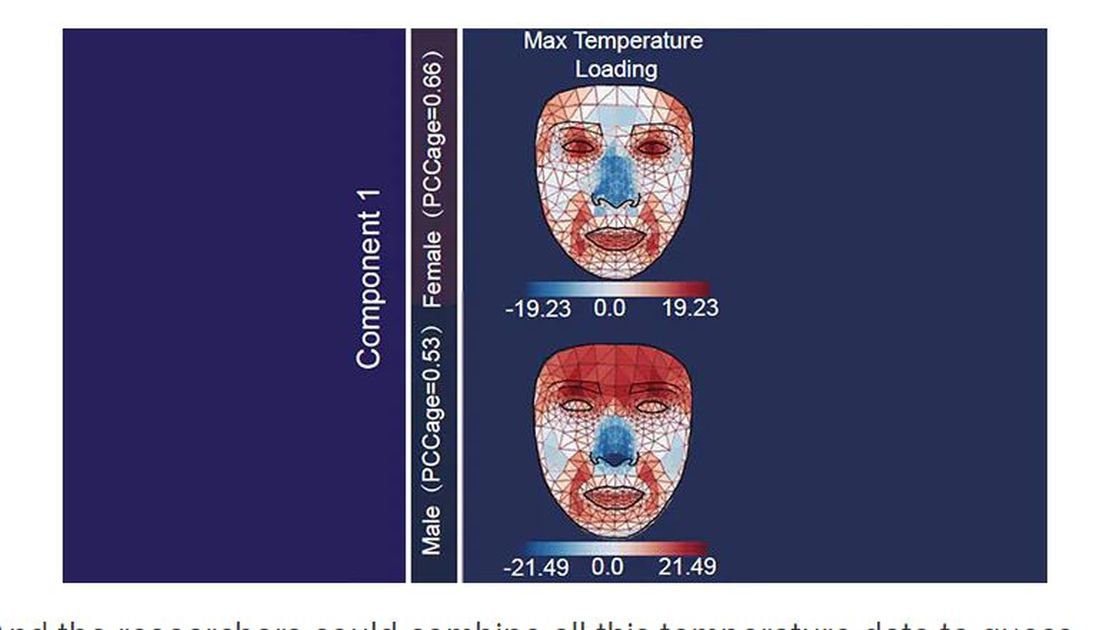
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
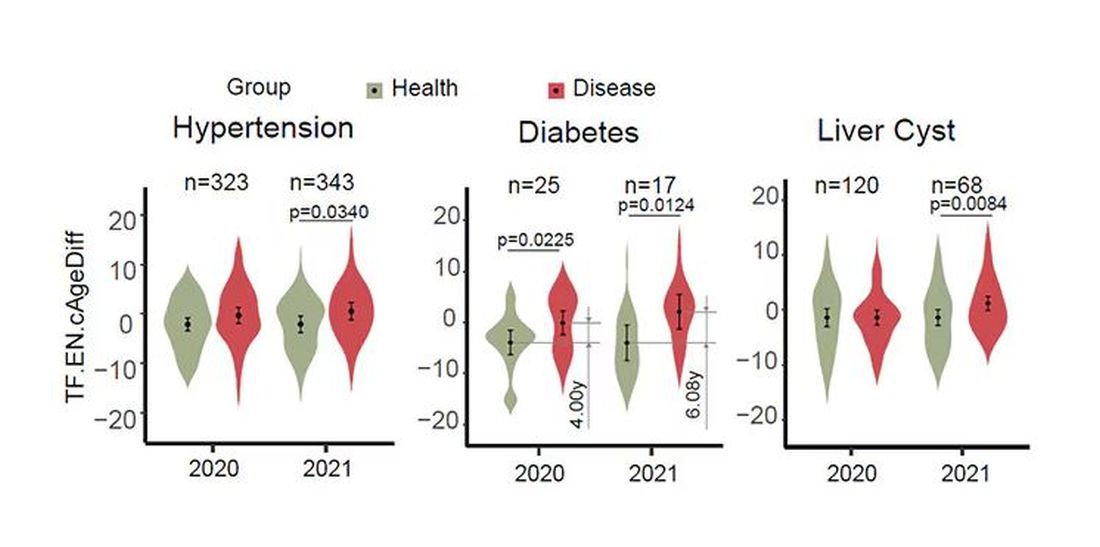
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.
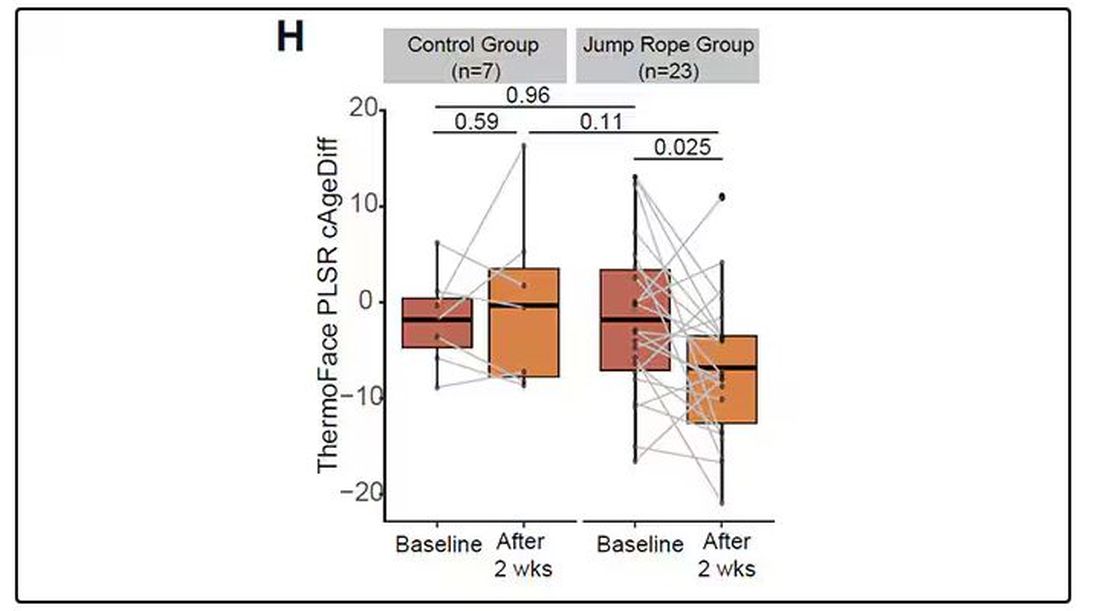
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those.
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally.
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
My oldest daughter is at sleepaway camp for a couple of weeks, and the camp has a photographer who goes around all day taking pictures of the kids, which get uploaded to a private Facebook group. In the past, I would go online every day (or, okay, several times a day) and scroll through all those pictures looking for one that features my kid.
I don’t have to do that anymore. This year, I simply uploaded a picture of my daughter to an app and artificial intelligence (AI) takes care of the rest, recognizing her face amidst the sea of smiling children, and flagging just those photos for me to peruse. It’s amazing, really. And a bit scary.
The fact that facial recognition has penetrated the summer camp market should tell you that the tech is truly ubiquitous. But today we’re going to think a bit more about what AI can do with a picture of your face, because the power of facial recognition is not just skin deep.
What’s got me hot and bothered about facial images is this paper, appearing in Cell Metabolism, which adds a new layer to the standard facial-analysis playbook: facial temperature.
To understand this paper, you need to understand a whole field of research that is developing various different “clocks” for age.
It turns out that age really is just a number. Our cells, our proteins, our biochemistry can be analyzed to give different numbers. These “clocks,” as distinct from the calendar we usually use to measure our age, might have more predictive power than the number itself.
There are numerous molecular clocks, such as telomere length, that not only correlate with calendar age but are superior to calendar age in predicting age-related complications. Testing telomere length typically requires a blood sample — and remains costly. But we can use other sources to estimate age; how about a photo?
I mean, we do this all the time when we meet someone new or, as a physician, when we meet a new patient. I have often written that a patient “appears younger than their stated age,” and we’ve all had the experience of hearing how old someone is and being shocked. I mean, have you seen Sharon Stone recently? She’s 66 years old. Okay — to be fair, there might be some outside help there. But you get the point.
Back to the Cell Metabolism paper. Researchers report on multiple algorithms to obtain an “age” from a picture of an individual’s face.
The first algorithm is pretty straightforward. Researchers collected 2811 images, all of Han Chinese individuals ranging in age from 20 to 90 years, and reconstructed a 3D facial map from those.
They then trained a convolutional neural network to predict the individuals’ ages from the pictures. It was quite accurate, as you can see here.
In the AI age, this may not seem that impressive. A brief search online turned up dozens of apps that promised to guess my age from a photo.
I sent this rather unflattering picture of myself to ChatGPT which, after initially demurring and saying it was not designed to guess ages, pegged me at somewhere between 35 and 45, which I am taking as a major victory.
But the Cell Metabolism paper goes deeper. Literally.
And this is where things start to get interesting. Because sure, the visible part of your face can change depending on makeup, expression, plastic surgery, and the like. But the temperature? That’s harder to fake.
It turns out that the temperature distribution in your face changes as you get older. There is a cooling of the nose and the cheeks, for example.
And the researchers could combine all this temperature data to guess someone’s calendar age fairly accurately, though notably not as accurately as the model that just looks at the pictures.
But guessing your age is not really the interesting part of thermal imaging of the face. It’s guessing — or, rather, predicting — the state of your metabolism. All these study participants had extensive metabolic testing performed, as well as detailed analysis of their lifestyle behaviors. And facial images could be used to predict those factors.
For example, the 3D reconstruction of the faces could predict who ate seafood (they tend to look younger than their actual age) compared with who ate poultry and meat (they tend to look older). The thermal imaging could predict who got more sleep (they look younger from a temperature perspective) and who ate more yogurt (also younger-appearing, temperature-wise). Facial temperature patterns could identify those with higher BMI, higher blood pressure, higher fasting glucose.
The researchers used the difference between actual and predicted age as a metric to measure illness as well. You can see here how, on average, individuals with hypertension, diabetes, and even liver cysts are “older,” at least by face temperature.
It may even be possible to use facial temperature as biofeedback. In a small study, the researchers measured the difference between facial temperature age and real age before and after 2 weeks of jump-roping. It turns out that 2 weeks of jump-roping can make you look about 5 years younger, at least as judged by a thermal camera. Or like the Predator.
Okay, this is all very cool, but I’m not saying we’ll all be doing facial temperature tests in the near future. No; what this study highlights for me is how much information about ourselves is available to those who know how to decode it. Maybe those data come from the wrinkles in our faces, or the angles of our smiles, or the speed with which we type, or the temperature of our elbows. The data have always been there, actually, but we’ve never had the tools powerful enough to analyze them until now.
When I was a kid, I was obsessed with Star Trek — I know, you’re shocked — and, of course, the famous tricorder, a scanner that could tell everything about someone’s state of health in 5 seconds from 3 feet away. That’s how I thought medicine really would be in the future. Once I got to medical school, I was disabused of that notion. But the age of data, the age of AI, may mean the tricorder age is not actually that far away.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Time Warp: Fax Machines Still Common in Oncology Practice. Why?
One minute, he’s working on sequencing a tumor genome. The next, he’s sifting through pages of disorganized data from a device that has been around for decades: the fax machine.
“If two doctors’ offices aren’t on the same electronic medical record, one of the main ways to transfer records is still by fax,” said Dr. Lewis, director of gastrointestinal oncology at Intermountain Healthcare in Murray, Utah. “I can go from cutting-edge innovation to relying on, at best, 1980s information technology. It just boggles my mind.”
Dr. Lewis, who has posted about his frustration with fax machines, is far from alone. Oncologists are among the many specialists across the country at the mercy of telecopiers.
According to a 2021 report by the Office of the National Coordinator for Health Information Technology, fax and mail continue to be the most common methods for hospitals and health systems to exchange care record summaries. In 2019, nearly 8 in 10 hospitals used mail or fax to send and receive health information, the report found.
Fax machines are still commonplace across the healthcare spectrum, said Robert Havasy, MS, senior director for informatics strategy at the Healthcare Information and Management Systems Society (HIMSS). Inertia, cost, and more pressing priorities for hospitals and medical institutions contribute to the technology sticking around, he explained.
“Post-COVID, my guess is we’re still at over 50% of healthcare practices using fax for some reason, on a daily basis,” Mr. Havasy said in an interview. “A lot of hospitals just don’t have the time, the money, or the staff to fix that problem because there’s always something a little higher up the priority chain they need to focus on.”
If, for instance, “you’re going to do a process redesign to reduce hospital total acquired infections, your fax machine replacement might be 10th or 12th on the list. It just never gets up to 1 or 2 because it’s ‘not that much of a problem,’ ” he added.
Or is it?
Administrators may not view fax machines as a top concern, but clinicians who deal with the machines daily see it differently.
“What worries me is we’re taking records out of an electronic storehouse [and] converting them to a paper medium,” Dr. Lewis said. “And then we are scanning into another electronic storehouse. The more steps, the more can be lost.”
And when information is lost, patient care can be compromised.
Slower Workflows, Care Concerns
Although there are no published data on fax machine use in oncology specifically, this outdated technology does come into play in a variety of ways along the cancer care continuum.
Radiation oncologist David R. Penberthy, MD, said patients often seek his cancer center’s expertise for second opinions, and that requires collecting patient records from many different practices.
“Ideally, it would come electronically, but sometimes it does come by fax,” said Dr. Penberthy, program director of radiation oncology at the University of Virginia School of Medicine in Charlottesville. “The quality of the fax is not always the best. Sometimes it’s literally a fax of a fax. You’re reading something that’s very difficult to read.”
Orders for new tests are also typically sent and received via fax temporarily while IT teams work to integrate them into the electronic health record (EHR), Dr. Penberthy said.
Insurers and third-party laboratories often send test results back by fax as well.
“Even if I haven’t actually sent my patient out of our institution, this crucial result may only be entered back into the record as a scanned document from a fax, which is not great because it can get lost in the other results that are reported electronically,” Dr. Lewis said. The risk here is that an ordering physician won’t see these results, which can lead to delayed or overlooked care for patients, he explained.
“To me, it’s like a blind spot,” Dr. Lewis said. “Every time we use a fax, I see it actually as an opportunity for oversight and missed opportunity to collect data.”
Dr. Penberthy said faxing can slow things down at his practice, particularly if he faxes a document to another office but receives no confirmation and has to track down what happened.
As for cybersecurity, data that are in transit during faxing are generally considered secure and compliant with the Health Insurance Portability and Accountability Act (HIPAA), said Mr. Havasy of HIMSS. However, the Privacy Rule also requires that data remain secure while at rest, which isn’t always possible, he added.
“That’s where faxes fall down, because generally fax machines are in public, if you will, or open areas in a hospital,” he said. “They just sit on a desk. I don’t know that the next nurse who comes up and looks through that stack was the nurse who was treating the patient.”
Important decisions or results can also be missed when sent by fax, creating headaches for physicians and care problems for patients.
Dr. Lewis recently experienced an insurance-related fax mishap over Memorial Day weekend. He believed his patient had access to the antinausea medication he had prescribed. When Dr. Lewis happened to check the fax machine over the weekend, he found a coverage denial for the medication from the insurer but, at that point, had no recourse to appeal because it was a long holiday weekend.
“Had the denial been sent by an electronic means that was quicker and more readily available, it would have been possible to appeal before the holiday weekend,” he said.
Hematologist Aaron Goodman, MD, encountered a similar problem after an insurer denied coverage of an expensive cancer drug for a patient and faxed over its reason for the denial. Dr. Goodman was not directly notified that the information arrived and didn’t learn about the denial for a week, he said.
“There’s no ‘ding’ in my inbox if something is faxed over and scanned,” said Dr. Goodman, associate professor of medicine at UC San Diego Health. “Once I realized it was denied, I was able to rectify it, but it wasted a week of a patient not getting a drug that I felt would be beneficial for them.”
Broader Health Policy Impacts
The use of outdated technology, such as fax machines, also creates ripple effects that burden the health system, health policy experts say.
Duplicate testing and unnecessary care are top impacts, said Julia Adler-Milstein, PhD, professor of medicine and chief of the division of clinical informatics and digital transformation at the University of California, San Francisco.
Studies show that 20%-30% of the $65 billion spent annually on lab tests is used on unnecessary duplicate tests, and another estimated $30 billion is spent each year on unnecessary duplicate medical imaging. These duplicate tests may be mitigated if hospitals adopt certified EHR technology, research shows.
Still, without EHR interoperability between institutions, new providers may be unaware that tests or past labs for patients exist, leading to repeat tests, said Dr. Adler-Milstein, who researches health IT policy with a focus on EHRs. Patients can sometimes fill in the gaps, but not always.
“Fax machines only help close information gaps if the clinician is aware of where to seek out the information and there is someone at the other organization to locate and transmit the information in a timely manner,” Dr. Adler-Milstein said.
Old technology and poor interoperability also greatly affect data collection for disease surveillance and monitoring, said Janet Hamilton, MPH, executive director for the Council of State and Territorial Epidemiologists. This issue was keenly demonstrated during the pandemic, Ms. Hamilton said.
“It was tragic, quite honestly,” she said. “There was such an immense amount of data that needed to be moved quickly, and that’s when computers are at their best.”
But, she said, “we didn’t have the level of systems in place to do it well.”
Specifically, the lack of electronic case reporting in place during the pandemic — where diagnoses are documented in the record and then immediately sent to the public health system — led to reports that were delayed, not made, or had missing or incomplete information, such as patients’ race and ethnicity or other health conditions, Ms. Hamilton said.
Incomplete or missing data hampered the ability of public health officials and researchers to understand how the virus might affect different patients.
“If you had a chronic condition like cancer, you were less likely to have a positive outcome with COVID,” Ms. Hamilton said. “But because electronic case reporting was not in place, we didn’t get some of those additional pieces of information. We didn’t have people’s underlying oncology status to then say, ‘Here are individuals with these types of characteristics, and these are the things that happen if they also have a cancer.’”
Slow, but Steady, Improvements
Efforts at the state and federal levels have targeted improved health information exchange, but progress takes time, Dr. Adler-Milstein said.
Most states have some form of health information exchange, such as statewide exchanges, regional health information organizations, or clinical data registries. Maryland is often held up as a notable example for its health information exchange, Dr. Adler-Milstein noted.
According to Maryland law, all hospitals under the jurisdiction of the Maryland Health Care Commission are required to electronically connect to the state-designated health information exchange. In 2012, Maryland became the first state to connect all its 46 acute care hospitals in the sharing of real-time data.
The Health Information Technology for Economic and Clinical Health (HITECH) Act provided federal-enhanced Medicaid matching funds to states through 2021 to support efforts to advance electronic exchange. Nearly all states used these funds, and most have identified other sources to sustain the efforts, according to a recent US Government Accountability Office (GAO) report. However, GAO found that small and rural providers are less likely to have the financial and technological resources to participate in or maintain electronic exchange capabilities.
Nationally, several recent initiatives have targeted health data interoperability, including for cancer care. The Centers for Disease Control and Prevention’s Data Modernization Initiative is a multiyear, multi–billion-dollar effort to improve data sharing across the federal and state public health landscape.
Meanwhile, in March 2024, the Biden-Harris administration launched United States Core Data for Interoperability Plus Cancer. The program will define a recommended minimum set of cancer-related data to be included in a patient’s EHR to enhance data exchange for research and clinical care.
EHR vendors are also key to improving the landscape, said Dr. Adler-Milstein. Vendors such as Epic have developed strong sharing capabilities for transmitting health information from site to site, but of course, that only helps if providers have Epic, she said.
“That’s where these national frameworks should help, because we don’t want it to break down by what EHR vendor you have,” she said. “It’s a patchwork. You can go to some places and hear success stories because they have Epic or a state health information exchange, but it’s very heterogeneous. In some places, they have nothing and are using a fax machine.”
Mr. Havasy believes fax machines will ultimately go extinct, particularly as a younger, more digitally savvy generation enters the healthcare workforce. He also foresees that the growing use of artificial intelligence will help eradicate the outdated technology.
But, Ms. Hamilton noted, “unless we have consistent, ongoing, sustained funding, it is very hard to move off [an older] technology that can work. That’s one of the biggest barriers.”
“Public health is about protecting the lives of every single person everywhere,” Ms. Hamilton said, “but when we don’t have the data that comes into the system, we can’t achieve our mission.”
A version of this article appeared on Medscape.com.
One minute, he’s working on sequencing a tumor genome. The next, he’s sifting through pages of disorganized data from a device that has been around for decades: the fax machine.
“If two doctors’ offices aren’t on the same electronic medical record, one of the main ways to transfer records is still by fax,” said Dr. Lewis, director of gastrointestinal oncology at Intermountain Healthcare in Murray, Utah. “I can go from cutting-edge innovation to relying on, at best, 1980s information technology. It just boggles my mind.”
Dr. Lewis, who has posted about his frustration with fax machines, is far from alone. Oncologists are among the many specialists across the country at the mercy of telecopiers.
According to a 2021 report by the Office of the National Coordinator for Health Information Technology, fax and mail continue to be the most common methods for hospitals and health systems to exchange care record summaries. In 2019, nearly 8 in 10 hospitals used mail or fax to send and receive health information, the report found.
Fax machines are still commonplace across the healthcare spectrum, said Robert Havasy, MS, senior director for informatics strategy at the Healthcare Information and Management Systems Society (HIMSS). Inertia, cost, and more pressing priorities for hospitals and medical institutions contribute to the technology sticking around, he explained.
“Post-COVID, my guess is we’re still at over 50% of healthcare practices using fax for some reason, on a daily basis,” Mr. Havasy said in an interview. “A lot of hospitals just don’t have the time, the money, or the staff to fix that problem because there’s always something a little higher up the priority chain they need to focus on.”
If, for instance, “you’re going to do a process redesign to reduce hospital total acquired infections, your fax machine replacement might be 10th or 12th on the list. It just never gets up to 1 or 2 because it’s ‘not that much of a problem,’ ” he added.
Or is it?
Administrators may not view fax machines as a top concern, but clinicians who deal with the machines daily see it differently.
“What worries me is we’re taking records out of an electronic storehouse [and] converting them to a paper medium,” Dr. Lewis said. “And then we are scanning into another electronic storehouse. The more steps, the more can be lost.”
And when information is lost, patient care can be compromised.
Slower Workflows, Care Concerns
Although there are no published data on fax machine use in oncology specifically, this outdated technology does come into play in a variety of ways along the cancer care continuum.
Radiation oncologist David R. Penberthy, MD, said patients often seek his cancer center’s expertise for second opinions, and that requires collecting patient records from many different practices.
“Ideally, it would come electronically, but sometimes it does come by fax,” said Dr. Penberthy, program director of radiation oncology at the University of Virginia School of Medicine in Charlottesville. “The quality of the fax is not always the best. Sometimes it’s literally a fax of a fax. You’re reading something that’s very difficult to read.”
Orders for new tests are also typically sent and received via fax temporarily while IT teams work to integrate them into the electronic health record (EHR), Dr. Penberthy said.
Insurers and third-party laboratories often send test results back by fax as well.
“Even if I haven’t actually sent my patient out of our institution, this crucial result may only be entered back into the record as a scanned document from a fax, which is not great because it can get lost in the other results that are reported electronically,” Dr. Lewis said. The risk here is that an ordering physician won’t see these results, which can lead to delayed or overlooked care for patients, he explained.
“To me, it’s like a blind spot,” Dr. Lewis said. “Every time we use a fax, I see it actually as an opportunity for oversight and missed opportunity to collect data.”
Dr. Penberthy said faxing can slow things down at his practice, particularly if he faxes a document to another office but receives no confirmation and has to track down what happened.
As for cybersecurity, data that are in transit during faxing are generally considered secure and compliant with the Health Insurance Portability and Accountability Act (HIPAA), said Mr. Havasy of HIMSS. However, the Privacy Rule also requires that data remain secure while at rest, which isn’t always possible, he added.
“That’s where faxes fall down, because generally fax machines are in public, if you will, or open areas in a hospital,” he said. “They just sit on a desk. I don’t know that the next nurse who comes up and looks through that stack was the nurse who was treating the patient.”
Important decisions or results can also be missed when sent by fax, creating headaches for physicians and care problems for patients.
Dr. Lewis recently experienced an insurance-related fax mishap over Memorial Day weekend. He believed his patient had access to the antinausea medication he had prescribed. When Dr. Lewis happened to check the fax machine over the weekend, he found a coverage denial for the medication from the insurer but, at that point, had no recourse to appeal because it was a long holiday weekend.
“Had the denial been sent by an electronic means that was quicker and more readily available, it would have been possible to appeal before the holiday weekend,” he said.
Hematologist Aaron Goodman, MD, encountered a similar problem after an insurer denied coverage of an expensive cancer drug for a patient and faxed over its reason for the denial. Dr. Goodman was not directly notified that the information arrived and didn’t learn about the denial for a week, he said.
“There’s no ‘ding’ in my inbox if something is faxed over and scanned,” said Dr. Goodman, associate professor of medicine at UC San Diego Health. “Once I realized it was denied, I was able to rectify it, but it wasted a week of a patient not getting a drug that I felt would be beneficial for them.”
Broader Health Policy Impacts
The use of outdated technology, such as fax machines, also creates ripple effects that burden the health system, health policy experts say.
Duplicate testing and unnecessary care are top impacts, said Julia Adler-Milstein, PhD, professor of medicine and chief of the division of clinical informatics and digital transformation at the University of California, San Francisco.
Studies show that 20%-30% of the $65 billion spent annually on lab tests is used on unnecessary duplicate tests, and another estimated $30 billion is spent each year on unnecessary duplicate medical imaging. These duplicate tests may be mitigated if hospitals adopt certified EHR technology, research shows.
Still, without EHR interoperability between institutions, new providers may be unaware that tests or past labs for patients exist, leading to repeat tests, said Dr. Adler-Milstein, who researches health IT policy with a focus on EHRs. Patients can sometimes fill in the gaps, but not always.
“Fax machines only help close information gaps if the clinician is aware of where to seek out the information and there is someone at the other organization to locate and transmit the information in a timely manner,” Dr. Adler-Milstein said.
Old technology and poor interoperability also greatly affect data collection for disease surveillance and monitoring, said Janet Hamilton, MPH, executive director for the Council of State and Territorial Epidemiologists. This issue was keenly demonstrated during the pandemic, Ms. Hamilton said.
“It was tragic, quite honestly,” she said. “There was such an immense amount of data that needed to be moved quickly, and that’s when computers are at their best.”
But, she said, “we didn’t have the level of systems in place to do it well.”
Specifically, the lack of electronic case reporting in place during the pandemic — where diagnoses are documented in the record and then immediately sent to the public health system — led to reports that were delayed, not made, or had missing or incomplete information, such as patients’ race and ethnicity or other health conditions, Ms. Hamilton said.
Incomplete or missing data hampered the ability of public health officials and researchers to understand how the virus might affect different patients.
“If you had a chronic condition like cancer, you were less likely to have a positive outcome with COVID,” Ms. Hamilton said. “But because electronic case reporting was not in place, we didn’t get some of those additional pieces of information. We didn’t have people’s underlying oncology status to then say, ‘Here are individuals with these types of characteristics, and these are the things that happen if they also have a cancer.’”
Slow, but Steady, Improvements
Efforts at the state and federal levels have targeted improved health information exchange, but progress takes time, Dr. Adler-Milstein said.
Most states have some form of health information exchange, such as statewide exchanges, regional health information organizations, or clinical data registries. Maryland is often held up as a notable example for its health information exchange, Dr. Adler-Milstein noted.
According to Maryland law, all hospitals under the jurisdiction of the Maryland Health Care Commission are required to electronically connect to the state-designated health information exchange. In 2012, Maryland became the first state to connect all its 46 acute care hospitals in the sharing of real-time data.
The Health Information Technology for Economic and Clinical Health (HITECH) Act provided federal-enhanced Medicaid matching funds to states through 2021 to support efforts to advance electronic exchange. Nearly all states used these funds, and most have identified other sources to sustain the efforts, according to a recent US Government Accountability Office (GAO) report. However, GAO found that small and rural providers are less likely to have the financial and technological resources to participate in or maintain electronic exchange capabilities.
Nationally, several recent initiatives have targeted health data interoperability, including for cancer care. The Centers for Disease Control and Prevention’s Data Modernization Initiative is a multiyear, multi–billion-dollar effort to improve data sharing across the federal and state public health landscape.
Meanwhile, in March 2024, the Biden-Harris administration launched United States Core Data for Interoperability Plus Cancer. The program will define a recommended minimum set of cancer-related data to be included in a patient’s EHR to enhance data exchange for research and clinical care.
EHR vendors are also key to improving the landscape, said Dr. Adler-Milstein. Vendors such as Epic have developed strong sharing capabilities for transmitting health information from site to site, but of course, that only helps if providers have Epic, she said.
“That’s where these national frameworks should help, because we don’t want it to break down by what EHR vendor you have,” she said. “It’s a patchwork. You can go to some places and hear success stories because they have Epic or a state health information exchange, but it’s very heterogeneous. In some places, they have nothing and are using a fax machine.”
Mr. Havasy believes fax machines will ultimately go extinct, particularly as a younger, more digitally savvy generation enters the healthcare workforce. He also foresees that the growing use of artificial intelligence will help eradicate the outdated technology.
But, Ms. Hamilton noted, “unless we have consistent, ongoing, sustained funding, it is very hard to move off [an older] technology that can work. That’s one of the biggest barriers.”
“Public health is about protecting the lives of every single person everywhere,” Ms. Hamilton said, “but when we don’t have the data that comes into the system, we can’t achieve our mission.”
A version of this article appeared on Medscape.com.
One minute, he’s working on sequencing a tumor genome. The next, he’s sifting through pages of disorganized data from a device that has been around for decades: the fax machine.
“If two doctors’ offices aren’t on the same electronic medical record, one of the main ways to transfer records is still by fax,” said Dr. Lewis, director of gastrointestinal oncology at Intermountain Healthcare in Murray, Utah. “I can go from cutting-edge innovation to relying on, at best, 1980s information technology. It just boggles my mind.”
Dr. Lewis, who has posted about his frustration with fax machines, is far from alone. Oncologists are among the many specialists across the country at the mercy of telecopiers.
According to a 2021 report by the Office of the National Coordinator for Health Information Technology, fax and mail continue to be the most common methods for hospitals and health systems to exchange care record summaries. In 2019, nearly 8 in 10 hospitals used mail or fax to send and receive health information, the report found.
Fax machines are still commonplace across the healthcare spectrum, said Robert Havasy, MS, senior director for informatics strategy at the Healthcare Information and Management Systems Society (HIMSS). Inertia, cost, and more pressing priorities for hospitals and medical institutions contribute to the technology sticking around, he explained.
“Post-COVID, my guess is we’re still at over 50% of healthcare practices using fax for some reason, on a daily basis,” Mr. Havasy said in an interview. “A lot of hospitals just don’t have the time, the money, or the staff to fix that problem because there’s always something a little higher up the priority chain they need to focus on.”
If, for instance, “you’re going to do a process redesign to reduce hospital total acquired infections, your fax machine replacement might be 10th or 12th on the list. It just never gets up to 1 or 2 because it’s ‘not that much of a problem,’ ” he added.
Or is it?
Administrators may not view fax machines as a top concern, but clinicians who deal with the machines daily see it differently.
“What worries me is we’re taking records out of an electronic storehouse [and] converting them to a paper medium,” Dr. Lewis said. “And then we are scanning into another electronic storehouse. The more steps, the more can be lost.”
And when information is lost, patient care can be compromised.
Slower Workflows, Care Concerns
Although there are no published data on fax machine use in oncology specifically, this outdated technology does come into play in a variety of ways along the cancer care continuum.
Radiation oncologist David R. Penberthy, MD, said patients often seek his cancer center’s expertise for second opinions, and that requires collecting patient records from many different practices.
“Ideally, it would come electronically, but sometimes it does come by fax,” said Dr. Penberthy, program director of radiation oncology at the University of Virginia School of Medicine in Charlottesville. “The quality of the fax is not always the best. Sometimes it’s literally a fax of a fax. You’re reading something that’s very difficult to read.”
Orders for new tests are also typically sent and received via fax temporarily while IT teams work to integrate them into the electronic health record (EHR), Dr. Penberthy said.
Insurers and third-party laboratories often send test results back by fax as well.
“Even if I haven’t actually sent my patient out of our institution, this crucial result may only be entered back into the record as a scanned document from a fax, which is not great because it can get lost in the other results that are reported electronically,” Dr. Lewis said. The risk here is that an ordering physician won’t see these results, which can lead to delayed or overlooked care for patients, he explained.
“To me, it’s like a blind spot,” Dr. Lewis said. “Every time we use a fax, I see it actually as an opportunity for oversight and missed opportunity to collect data.”
Dr. Penberthy said faxing can slow things down at his practice, particularly if he faxes a document to another office but receives no confirmation and has to track down what happened.
As for cybersecurity, data that are in transit during faxing are generally considered secure and compliant with the Health Insurance Portability and Accountability Act (HIPAA), said Mr. Havasy of HIMSS. However, the Privacy Rule also requires that data remain secure while at rest, which isn’t always possible, he added.
“That’s where faxes fall down, because generally fax machines are in public, if you will, or open areas in a hospital,” he said. “They just sit on a desk. I don’t know that the next nurse who comes up and looks through that stack was the nurse who was treating the patient.”
Important decisions or results can also be missed when sent by fax, creating headaches for physicians and care problems for patients.
Dr. Lewis recently experienced an insurance-related fax mishap over Memorial Day weekend. He believed his patient had access to the antinausea medication he had prescribed. When Dr. Lewis happened to check the fax machine over the weekend, he found a coverage denial for the medication from the insurer but, at that point, had no recourse to appeal because it was a long holiday weekend.
“Had the denial been sent by an electronic means that was quicker and more readily available, it would have been possible to appeal before the holiday weekend,” he said.
Hematologist Aaron Goodman, MD, encountered a similar problem after an insurer denied coverage of an expensive cancer drug for a patient and faxed over its reason for the denial. Dr. Goodman was not directly notified that the information arrived and didn’t learn about the denial for a week, he said.
“There’s no ‘ding’ in my inbox if something is faxed over and scanned,” said Dr. Goodman, associate professor of medicine at UC San Diego Health. “Once I realized it was denied, I was able to rectify it, but it wasted a week of a patient not getting a drug that I felt would be beneficial for them.”
Broader Health Policy Impacts
The use of outdated technology, such as fax machines, also creates ripple effects that burden the health system, health policy experts say.
Duplicate testing and unnecessary care are top impacts, said Julia Adler-Milstein, PhD, professor of medicine and chief of the division of clinical informatics and digital transformation at the University of California, San Francisco.
Studies show that 20%-30% of the $65 billion spent annually on lab tests is used on unnecessary duplicate tests, and another estimated $30 billion is spent each year on unnecessary duplicate medical imaging. These duplicate tests may be mitigated if hospitals adopt certified EHR technology, research shows.
Still, without EHR interoperability between institutions, new providers may be unaware that tests or past labs for patients exist, leading to repeat tests, said Dr. Adler-Milstein, who researches health IT policy with a focus on EHRs. Patients can sometimes fill in the gaps, but not always.
“Fax machines only help close information gaps if the clinician is aware of where to seek out the information and there is someone at the other organization to locate and transmit the information in a timely manner,” Dr. Adler-Milstein said.
Old technology and poor interoperability also greatly affect data collection for disease surveillance and monitoring, said Janet Hamilton, MPH, executive director for the Council of State and Territorial Epidemiologists. This issue was keenly demonstrated during the pandemic, Ms. Hamilton said.
“It was tragic, quite honestly,” she said. “There was such an immense amount of data that needed to be moved quickly, and that’s when computers are at their best.”
But, she said, “we didn’t have the level of systems in place to do it well.”
Specifically, the lack of electronic case reporting in place during the pandemic — where diagnoses are documented in the record and then immediately sent to the public health system — led to reports that were delayed, not made, or had missing or incomplete information, such as patients’ race and ethnicity or other health conditions, Ms. Hamilton said.
Incomplete or missing data hampered the ability of public health officials and researchers to understand how the virus might affect different patients.
“If you had a chronic condition like cancer, you were less likely to have a positive outcome with COVID,” Ms. Hamilton said. “But because electronic case reporting was not in place, we didn’t get some of those additional pieces of information. We didn’t have people’s underlying oncology status to then say, ‘Here are individuals with these types of characteristics, and these are the things that happen if they also have a cancer.’”
Slow, but Steady, Improvements
Efforts at the state and federal levels have targeted improved health information exchange, but progress takes time, Dr. Adler-Milstein said.
Most states have some form of health information exchange, such as statewide exchanges, regional health information organizations, or clinical data registries. Maryland is often held up as a notable example for its health information exchange, Dr. Adler-Milstein noted.
According to Maryland law, all hospitals under the jurisdiction of the Maryland Health Care Commission are required to electronically connect to the state-designated health information exchange. In 2012, Maryland became the first state to connect all its 46 acute care hospitals in the sharing of real-time data.
The Health Information Technology for Economic and Clinical Health (HITECH) Act provided federal-enhanced Medicaid matching funds to states through 2021 to support efforts to advance electronic exchange. Nearly all states used these funds, and most have identified other sources to sustain the efforts, according to a recent US Government Accountability Office (GAO) report. However, GAO found that small and rural providers are less likely to have the financial and technological resources to participate in or maintain electronic exchange capabilities.
Nationally, several recent initiatives have targeted health data interoperability, including for cancer care. The Centers for Disease Control and Prevention’s Data Modernization Initiative is a multiyear, multi–billion-dollar effort to improve data sharing across the federal and state public health landscape.
Meanwhile, in March 2024, the Biden-Harris administration launched United States Core Data for Interoperability Plus Cancer. The program will define a recommended minimum set of cancer-related data to be included in a patient’s EHR to enhance data exchange for research and clinical care.
EHR vendors are also key to improving the landscape, said Dr. Adler-Milstein. Vendors such as Epic have developed strong sharing capabilities for transmitting health information from site to site, but of course, that only helps if providers have Epic, she said.
“That’s where these national frameworks should help, because we don’t want it to break down by what EHR vendor you have,” she said. “It’s a patchwork. You can go to some places and hear success stories because they have Epic or a state health information exchange, but it’s very heterogeneous. In some places, they have nothing and are using a fax machine.”
Mr. Havasy believes fax machines will ultimately go extinct, particularly as a younger, more digitally savvy generation enters the healthcare workforce. He also foresees that the growing use of artificial intelligence will help eradicate the outdated technology.
But, Ms. Hamilton noted, “unless we have consistent, ongoing, sustained funding, it is very hard to move off [an older] technology that can work. That’s one of the biggest barriers.”
“Public health is about protecting the lives of every single person everywhere,” Ms. Hamilton said, “but when we don’t have the data that comes into the system, we can’t achieve our mission.”
A version of this article appeared on Medscape.com.
Trading TV Time for Physical Activity Boosts Healthy Aging
TOPLINE:
, but substituting it with any physical activity — or even sleeping, in case of women with inadequate sleep — may lead to better overall health.
METHODOLOGY:
- Previous studies have shown that replacing sedentary behavior with physical activity may improve mortality outcomes, but whether this increased lifespan is accompanied by better overall health remains an unanswered question.
- To understand the impact of sedentary behavior and physical activity on healthy aging, researchers analyzed data from the prospective cohort Nurses’ Health Study.
- They included 45,176 women aged > 50 years in 1992 (mean age, 59.2 years) who were free of major chronic diseases and were followed up for 20 years.
- In 1992, validated questionnaires were used to record exposure to sedentary behavior, different levels of physical activity, and sleep. The time spent watching television was the primary exposure in the sedentary behavior category.
- The main outcome was healthy aging, defined as survival to ≥ 70 years of age and maintenance of four domains of health — being free of 11 main chronic diseases and having no impairment of subjective memory, physical function, or mental health.
TAKEAWAY:
- At 20 years of follow-up, 8.6% of the women achieved healthy aging, while 41.4% had none of the 11 chronic diseases, 16.1% had no physical function impairment, 44.1% had no mental health limitation, and 51.9% reported no memory impairment.
- For each increase of 2 hours per day spent sitting and watching television, the odds of healthy aging dropped by 12% (95% confidence interval [CI], 7%-17%).
- Conversely, every additional 2 hours per day of low-level physical activity at work upped the odds of healthy aging by 6% (95% CI, 3%-9%); furthermore, each extra hour per day of standardized moderate to vigorous physical activity (normal pace walking or the equivalent) was associated with 14% higher odds (95% CI, 11%-16%) of healthy aging.
- In a theoretical modeling analysis, individuals could increase their odds of healthy aging by replacing 1 hour of television time per day with low levels of physical activity at home and work or with moderate to vigorous levels of physical activity — or even sleeping, for those who slept for ≤ 7 hours.
IN PRACTICE:
“These findings expand on the literature reporting that replacing sedentary behavior with light or moderate to vigorous physical activity is associated with decreased mortality by suggesting that this increased lifespan might be accompanied by better overall health,” the authors wrote.
SOURCE:
Hongying Shi, PhD, Department of Epidemiology and Health Statistics, School of Public Health, Wenzhou Medical University, Wenzhou, China, led this study, which was published online in JAMA Network Open.
LIMITATIONS:
The measures of different behaviors were self-reported and may, therefore, be less accurate than objective measurement methods. Measurement error may have attenuated the effect of low levels of physical activity. The single exposure assessment at baseline may not reflect the long-term pattern of these activities.
DISCLOSURES:
The lead author was supported by the National Social Science Foundation Project of China and the Zhejiang Provincial Philosophy and Social Sciences Planning Project. A co-author and the Nurses’ Health Study were supported by the US National Institutes of Health. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, but substituting it with any physical activity — or even sleeping, in case of women with inadequate sleep — may lead to better overall health.
METHODOLOGY:
- Previous studies have shown that replacing sedentary behavior with physical activity may improve mortality outcomes, but whether this increased lifespan is accompanied by better overall health remains an unanswered question.
- To understand the impact of sedentary behavior and physical activity on healthy aging, researchers analyzed data from the prospective cohort Nurses’ Health Study.
- They included 45,176 women aged > 50 years in 1992 (mean age, 59.2 years) who were free of major chronic diseases and were followed up for 20 years.
- In 1992, validated questionnaires were used to record exposure to sedentary behavior, different levels of physical activity, and sleep. The time spent watching television was the primary exposure in the sedentary behavior category.
- The main outcome was healthy aging, defined as survival to ≥ 70 years of age and maintenance of four domains of health — being free of 11 main chronic diseases and having no impairment of subjective memory, physical function, or mental health.
TAKEAWAY:
- At 20 years of follow-up, 8.6% of the women achieved healthy aging, while 41.4% had none of the 11 chronic diseases, 16.1% had no physical function impairment, 44.1% had no mental health limitation, and 51.9% reported no memory impairment.
- For each increase of 2 hours per day spent sitting and watching television, the odds of healthy aging dropped by 12% (95% confidence interval [CI], 7%-17%).
- Conversely, every additional 2 hours per day of low-level physical activity at work upped the odds of healthy aging by 6% (95% CI, 3%-9%); furthermore, each extra hour per day of standardized moderate to vigorous physical activity (normal pace walking or the equivalent) was associated with 14% higher odds (95% CI, 11%-16%) of healthy aging.
- In a theoretical modeling analysis, individuals could increase their odds of healthy aging by replacing 1 hour of television time per day with low levels of physical activity at home and work or with moderate to vigorous levels of physical activity — or even sleeping, for those who slept for ≤ 7 hours.
IN PRACTICE:
“These findings expand on the literature reporting that replacing sedentary behavior with light or moderate to vigorous physical activity is associated with decreased mortality by suggesting that this increased lifespan might be accompanied by better overall health,” the authors wrote.
SOURCE:
Hongying Shi, PhD, Department of Epidemiology and Health Statistics, School of Public Health, Wenzhou Medical University, Wenzhou, China, led this study, which was published online in JAMA Network Open.
LIMITATIONS:
The measures of different behaviors were self-reported and may, therefore, be less accurate than objective measurement methods. Measurement error may have attenuated the effect of low levels of physical activity. The single exposure assessment at baseline may not reflect the long-term pattern of these activities.
DISCLOSURES:
The lead author was supported by the National Social Science Foundation Project of China and the Zhejiang Provincial Philosophy and Social Sciences Planning Project. A co-author and the Nurses’ Health Study were supported by the US National Institutes of Health. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
TOPLINE:
, but substituting it with any physical activity — or even sleeping, in case of women with inadequate sleep — may lead to better overall health.
METHODOLOGY:
- Previous studies have shown that replacing sedentary behavior with physical activity may improve mortality outcomes, but whether this increased lifespan is accompanied by better overall health remains an unanswered question.
- To understand the impact of sedentary behavior and physical activity on healthy aging, researchers analyzed data from the prospective cohort Nurses’ Health Study.
- They included 45,176 women aged > 50 years in 1992 (mean age, 59.2 years) who were free of major chronic diseases and were followed up for 20 years.
- In 1992, validated questionnaires were used to record exposure to sedentary behavior, different levels of physical activity, and sleep. The time spent watching television was the primary exposure in the sedentary behavior category.
- The main outcome was healthy aging, defined as survival to ≥ 70 years of age and maintenance of four domains of health — being free of 11 main chronic diseases and having no impairment of subjective memory, physical function, or mental health.
TAKEAWAY:
- At 20 years of follow-up, 8.6% of the women achieved healthy aging, while 41.4% had none of the 11 chronic diseases, 16.1% had no physical function impairment, 44.1% had no mental health limitation, and 51.9% reported no memory impairment.
- For each increase of 2 hours per day spent sitting and watching television, the odds of healthy aging dropped by 12% (95% confidence interval [CI], 7%-17%).
- Conversely, every additional 2 hours per day of low-level physical activity at work upped the odds of healthy aging by 6% (95% CI, 3%-9%); furthermore, each extra hour per day of standardized moderate to vigorous physical activity (normal pace walking or the equivalent) was associated with 14% higher odds (95% CI, 11%-16%) of healthy aging.
- In a theoretical modeling analysis, individuals could increase their odds of healthy aging by replacing 1 hour of television time per day with low levels of physical activity at home and work or with moderate to vigorous levels of physical activity — or even sleeping, for those who slept for ≤ 7 hours.
IN PRACTICE:
“These findings expand on the literature reporting that replacing sedentary behavior with light or moderate to vigorous physical activity is associated with decreased mortality by suggesting that this increased lifespan might be accompanied by better overall health,” the authors wrote.
SOURCE:
Hongying Shi, PhD, Department of Epidemiology and Health Statistics, School of Public Health, Wenzhou Medical University, Wenzhou, China, led this study, which was published online in JAMA Network Open.
LIMITATIONS:
The measures of different behaviors were self-reported and may, therefore, be less accurate than objective measurement methods. Measurement error may have attenuated the effect of low levels of physical activity. The single exposure assessment at baseline may not reflect the long-term pattern of these activities.
DISCLOSURES:
The lead author was supported by the National Social Science Foundation Project of China and the Zhejiang Provincial Philosophy and Social Sciences Planning Project. A co-author and the Nurses’ Health Study were supported by the US National Institutes of Health. The authors declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
Does Semaglutide Reduce Inflammation?
LYON, FRANCE — The anti-obesity drug semaglutide is associated with significant reductions in the inflammatory marker high-sensitivity C-reactive protein (CRP), even in patients who do not lose substantial amounts of weight with the drug, according to data from the SELECT clinical trial.
The research, presented at the European Atherosclerosis Society 2024, involved over 17,600 patients with overweight or obesity and had established cardiovascular disease but not diabetes.
“Weight loss was associated with greater high-sensitivity CRP reduction in both treatment groups,” said study presenter Jorge Plutzky, MD, director of Preventive Cardiology at Brigham and Women’s Hospital, Boston, but “with increased high-sensitivity CRP reductions in those receiving semaglutide.”
The drug also “significantly reduced high-sensitivity CRP early,” he said, “prior to major weight loss and in those who did not lose significant amounts of weight.” The reductions reached approximately 12% at 4 weeks and around 20% at 8 weeks, when the weight loss “was still quite modest,” at 2% and 3% of body weight, respectively. Even among patients who achieved weight loss of less than 2% body weight, semaglutide was associated with a reduction in high-sensitivity CRP levels.
In the SELECT trial, semaglutide also resulted in a consistent reduction of around 20% vs placebo in major adverse cardiovascular events such as cardiovascular mortality, nonfatal myocardial infarction, or nonfatal stroke.
But Naveed Sattar, MD, PhD, professor of cardiometabolic medicine at the University of Glasgow, Scotland, said in an interview that body weight “is probably the major driver” of CRP levels in the population, accounting for between 20% and 30% of the variation.
Dr. Sattar, who was not involved in the study, said that because drugs like semaglutide lower weight but also have anti-inflammatory effects, the question becomes: “Could the anti-inflammatory effects be part of the mechanisms by which these drugs affect the risk of major adverse cardiovascular events?”
Reducing Cardiovascular Events
The current analysis, however, cannot answer the question, he said. “All it tells us is about associations.”
“What we do know is semaglutide, predominantly by lowering weight, is lowering CRP levels and equally, we know that when you lose weight, you improve blood pressure, you improve lipids, and you reduce the risk of diabetes,” he said.
Dr. Sattar also took issue with the researchers’ conclusion that the high-sensitivity CRP reductions seen in SELECT occurred prior to major weight loss because the “pattern of CRP reduction and weight reduction is almost identical.”
Dr. Sattar also pointed out in a recent editorial that the drug appears to have a direct effect on blood vessels and the heart, which may lead to improvements in systemic inflammation. Consequently, he said, any assertion that semaglutide is genuinely anti-inflammatory is, at this stage, “speculation.”
Dr. Plutzky said that “systemic, chronic inflammation is implicated as a potential mechanism and therapeutic target in atherosclerosis and major adverse cardiovascular events, as well as obesity,” and high-sensitivity CRP levels are an “established biomarker of inflammation and have been shown to predict cardiovascular risk.”
However, the relationship between high-sensitivity CRP, responses to glucagon-like peptide 1 receptor agonists like semaglutide, and cardiovascular outcomes in obesity “remains incompletely understood,” said Dr. Plutzky.
A version of this article appeared on Medscape.com.
LYON, FRANCE — The anti-obesity drug semaglutide is associated with significant reductions in the inflammatory marker high-sensitivity C-reactive protein (CRP), even in patients who do not lose substantial amounts of weight with the drug, according to data from the SELECT clinical trial.
The research, presented at the European Atherosclerosis Society 2024, involved over 17,600 patients with overweight or obesity and had established cardiovascular disease but not diabetes.
“Weight loss was associated with greater high-sensitivity CRP reduction in both treatment groups,” said study presenter Jorge Plutzky, MD, director of Preventive Cardiology at Brigham and Women’s Hospital, Boston, but “with increased high-sensitivity CRP reductions in those receiving semaglutide.”
The drug also “significantly reduced high-sensitivity CRP early,” he said, “prior to major weight loss and in those who did not lose significant amounts of weight.” The reductions reached approximately 12% at 4 weeks and around 20% at 8 weeks, when the weight loss “was still quite modest,” at 2% and 3% of body weight, respectively. Even among patients who achieved weight loss of less than 2% body weight, semaglutide was associated with a reduction in high-sensitivity CRP levels.
In the SELECT trial, semaglutide also resulted in a consistent reduction of around 20% vs placebo in major adverse cardiovascular events such as cardiovascular mortality, nonfatal myocardial infarction, or nonfatal stroke.
But Naveed Sattar, MD, PhD, professor of cardiometabolic medicine at the University of Glasgow, Scotland, said in an interview that body weight “is probably the major driver” of CRP levels in the population, accounting for between 20% and 30% of the variation.
Dr. Sattar, who was not involved in the study, said that because drugs like semaglutide lower weight but also have anti-inflammatory effects, the question becomes: “Could the anti-inflammatory effects be part of the mechanisms by which these drugs affect the risk of major adverse cardiovascular events?”
Reducing Cardiovascular Events
The current analysis, however, cannot answer the question, he said. “All it tells us is about associations.”
“What we do know is semaglutide, predominantly by lowering weight, is lowering CRP levels and equally, we know that when you lose weight, you improve blood pressure, you improve lipids, and you reduce the risk of diabetes,” he said.
Dr. Sattar also took issue with the researchers’ conclusion that the high-sensitivity CRP reductions seen in SELECT occurred prior to major weight loss because the “pattern of CRP reduction and weight reduction is almost identical.”
Dr. Sattar also pointed out in a recent editorial that the drug appears to have a direct effect on blood vessels and the heart, which may lead to improvements in systemic inflammation. Consequently, he said, any assertion that semaglutide is genuinely anti-inflammatory is, at this stage, “speculation.”
Dr. Plutzky said that “systemic, chronic inflammation is implicated as a potential mechanism and therapeutic target in atherosclerosis and major adverse cardiovascular events, as well as obesity,” and high-sensitivity CRP levels are an “established biomarker of inflammation and have been shown to predict cardiovascular risk.”
However, the relationship between high-sensitivity CRP, responses to glucagon-like peptide 1 receptor agonists like semaglutide, and cardiovascular outcomes in obesity “remains incompletely understood,” said Dr. Plutzky.
A version of this article appeared on Medscape.com.
LYON, FRANCE — The anti-obesity drug semaglutide is associated with significant reductions in the inflammatory marker high-sensitivity C-reactive protein (CRP), even in patients who do not lose substantial amounts of weight with the drug, according to data from the SELECT clinical trial.
The research, presented at the European Atherosclerosis Society 2024, involved over 17,600 patients with overweight or obesity and had established cardiovascular disease but not diabetes.
“Weight loss was associated with greater high-sensitivity CRP reduction in both treatment groups,” said study presenter Jorge Plutzky, MD, director of Preventive Cardiology at Brigham and Women’s Hospital, Boston, but “with increased high-sensitivity CRP reductions in those receiving semaglutide.”
The drug also “significantly reduced high-sensitivity CRP early,” he said, “prior to major weight loss and in those who did not lose significant amounts of weight.” The reductions reached approximately 12% at 4 weeks and around 20% at 8 weeks, when the weight loss “was still quite modest,” at 2% and 3% of body weight, respectively. Even among patients who achieved weight loss of less than 2% body weight, semaglutide was associated with a reduction in high-sensitivity CRP levels.
In the SELECT trial, semaglutide also resulted in a consistent reduction of around 20% vs placebo in major adverse cardiovascular events such as cardiovascular mortality, nonfatal myocardial infarction, or nonfatal stroke.
But Naveed Sattar, MD, PhD, professor of cardiometabolic medicine at the University of Glasgow, Scotland, said in an interview that body weight “is probably the major driver” of CRP levels in the population, accounting for between 20% and 30% of the variation.
Dr. Sattar, who was not involved in the study, said that because drugs like semaglutide lower weight but also have anti-inflammatory effects, the question becomes: “Could the anti-inflammatory effects be part of the mechanisms by which these drugs affect the risk of major adverse cardiovascular events?”
Reducing Cardiovascular Events
The current analysis, however, cannot answer the question, he said. “All it tells us is about associations.”
“What we do know is semaglutide, predominantly by lowering weight, is lowering CRP levels and equally, we know that when you lose weight, you improve blood pressure, you improve lipids, and you reduce the risk of diabetes,” he said.
Dr. Sattar also took issue with the researchers’ conclusion that the high-sensitivity CRP reductions seen in SELECT occurred prior to major weight loss because the “pattern of CRP reduction and weight reduction is almost identical.”
Dr. Sattar also pointed out in a recent editorial that the drug appears to have a direct effect on blood vessels and the heart, which may lead to improvements in systemic inflammation. Consequently, he said, any assertion that semaglutide is genuinely anti-inflammatory is, at this stage, “speculation.”
Dr. Plutzky said that “systemic, chronic inflammation is implicated as a potential mechanism and therapeutic target in atherosclerosis and major adverse cardiovascular events, as well as obesity,” and high-sensitivity CRP levels are an “established biomarker of inflammation and have been shown to predict cardiovascular risk.”
However, the relationship between high-sensitivity CRP, responses to glucagon-like peptide 1 receptor agonists like semaglutide, and cardiovascular outcomes in obesity “remains incompletely understood,” said Dr. Plutzky.
A version of this article appeared on Medscape.com.
Cardiovascular Health Becoming a Major Risk Factor for Dementia
That’s according to researchers from University College London (UCL) in the United Kingdom who analyzed 27 papers about dementia that had data collected over more than 70 years. They calculated what share of dementia cases were due to different risk factors. Their findings were recently published in the Lancet Public Health.
Top risk factors for dementia over the years have been hypertension, obesity, diabetes, education, and smoking, according to a news release on the findings. But the prevalence of risk factors has changed over the decades.
Researchers said smoking and education have become less important risk factors because of “population-level interventions,” such as stop-smoking campaigns and compulsory public education. On the other hand, obesity and diabetes rates have increased and become bigger risk factors.
Hypertension remains the greatest risk factor, even though doctors and public health groups are putting more emphasis on managing the condition, the study said.
“Cardiovascular risk factors may have contributed more to dementia risk over time, so these deserve more targeted action for future dementia prevention efforts,” said Naaheed Mukadam, PhD, an associate professor at UCL and the lead author of the study.
Eliminating modifiable risk factors could theoretically prevent 40% of dementia cases, the release said.
The CDC says that an estimated 5.8 million people in the United States have Alzheimer’s disease and related dementias, including 5.6 million people ages 65 and older and about 200,000 under age 65. The UCL release said an estimated 944,000 in the U.K. have dementia.
A version of this article first appeared on WebMD.com.
That’s according to researchers from University College London (UCL) in the United Kingdom who analyzed 27 papers about dementia that had data collected over more than 70 years. They calculated what share of dementia cases were due to different risk factors. Their findings were recently published in the Lancet Public Health.
Top risk factors for dementia over the years have been hypertension, obesity, diabetes, education, and smoking, according to a news release on the findings. But the prevalence of risk factors has changed over the decades.
Researchers said smoking and education have become less important risk factors because of “population-level interventions,” such as stop-smoking campaigns and compulsory public education. On the other hand, obesity and diabetes rates have increased and become bigger risk factors.
Hypertension remains the greatest risk factor, even though doctors and public health groups are putting more emphasis on managing the condition, the study said.
“Cardiovascular risk factors may have contributed more to dementia risk over time, so these deserve more targeted action for future dementia prevention efforts,” said Naaheed Mukadam, PhD, an associate professor at UCL and the lead author of the study.
Eliminating modifiable risk factors could theoretically prevent 40% of dementia cases, the release said.
The CDC says that an estimated 5.8 million people in the United States have Alzheimer’s disease and related dementias, including 5.6 million people ages 65 and older and about 200,000 under age 65. The UCL release said an estimated 944,000 in the U.K. have dementia.
A version of this article first appeared on WebMD.com.
That’s according to researchers from University College London (UCL) in the United Kingdom who analyzed 27 papers about dementia that had data collected over more than 70 years. They calculated what share of dementia cases were due to different risk factors. Their findings were recently published in the Lancet Public Health.
Top risk factors for dementia over the years have been hypertension, obesity, diabetes, education, and smoking, according to a news release on the findings. But the prevalence of risk factors has changed over the decades.
Researchers said smoking and education have become less important risk factors because of “population-level interventions,” such as stop-smoking campaigns and compulsory public education. On the other hand, obesity and diabetes rates have increased and become bigger risk factors.
Hypertension remains the greatest risk factor, even though doctors and public health groups are putting more emphasis on managing the condition, the study said.
“Cardiovascular risk factors may have contributed more to dementia risk over time, so these deserve more targeted action for future dementia prevention efforts,” said Naaheed Mukadam, PhD, an associate professor at UCL and the lead author of the study.
Eliminating modifiable risk factors could theoretically prevent 40% of dementia cases, the release said.
The CDC says that an estimated 5.8 million people in the United States have Alzheimer’s disease and related dementias, including 5.6 million people ages 65 and older and about 200,000 under age 65. The UCL release said an estimated 944,000 in the U.K. have dementia.
A version of this article first appeared on WebMD.com.
FROM THE LANCET PUBLIC HEALTH
Similar Outcomes With Labetalol, Nifedipine for Chronic Hypertension in Pregnancy
Treatment for chronic hypertension in pregnancy with labetalol showed no significant differences in maternal or neonatal outcomes, compared with treatment with nifedipine, new research indicates.
The open-label, multicenter, randomized CHAP (Chronic Hypertension in Pregnancy) trial showed that treating mild chronic hypertension was better than delaying treatment until severe hypertension developed, but still unclear was whether, or to what extent, the choice of first-line treatment affected outcomes.
Researchers, led by Ayodeji A. Sanusi, MD, MPH, with the Division of Maternal and Fetal Medicine at the University of Alabama at Birmingham, conducted a secondary analysis of CHAP to compare the primary treatments. Mild chronic hypertension in the study was defined as blood pressure of 140-159/90-104 mmHg before 20 weeks of gestation.
Three Comparisons
Three comparisons were performed in 2292 participants based on medications prescribed at enrollment: 720 (31.4%) received labetalol; 417 (18.2%) initially received nifedipine; and 1155 (50.4%) had standard care. Labetalol was compared with standard care; nifedipine was compared with standard care; and labetalol was compared with nifedipine.
The primary outcome was occurrence of superimposed preeclampsia with severe features; preterm birth before 35 weeks of gestation; placental abruption; or fetal or neonatal death. The key secondary outcome was a small-for-gestational age neonate. Researchers also compared adverse effects between groups.
Among the results were the following:
- The primary outcome occurred in 30.1% in the labetalol group; 31.2% in the nifedipine group; and 37% in the standard care group.
- Risk of the primary outcome was lower among those receiving treatment. For labetalol vs standard care, the adjusted relative risk (RR) was 0.82; 95% confidence interval (CI), 0.72-0.94. For nifedipine vs standard care, the adjusted RR was 0.84; 95% CI, 0.71-0.99. There was no significant difference in risk when labetalol was compared with nifedipine (adjusted RR, 0.98; 95% CI, 0.82-1.18).
- There were no significant differences in numbers of small-for-gestational age neonates or serious adverse events between those who received labetalol and those using nifedipine.
Any adverse events were significantly more common with nifedipine, compared with labetalol (35.7% vs 28.3%, P = .009), and with nifedipine, compared with standard care (35.7% vs 26.3%, P = .0003). Adverse event rates were not significantly higher with labetalol when compared with standard care (28.3% vs 26.3%, P = .34). The most frequently reported adverse events were headache, medication intolerance, dizziness, nausea, dyspepsia, neonatal jaundice, and vomiting.
“Thus, labetalol compared with nifedipine appeared to have fewer adverse events and to be better tolerated,” the authors write. They note that labetalol, a third-generation mixed alpha- and beta-adrenergic antagonist, is contraindicated for those who have obstructive pulmonary disease and nifedipine, a dihydropyridine calcium channel blocker, is contraindicated in people with tachycardia.
The authors write that their results align with other studies that have not found differences between labetalol and nifedipine. “[O]ur findings support the use of either labetalol or nifedipine as initial first-line agents for the management of mild chronic hypertension in pregnancy to reduce the risk of adverse maternal and other perinatal outcomes with no increased risk of fetal harm,” the authors write.
Dr. Sanusi reports no relevant financial relationships. Full coauthor disclosures are available with the full text of the paper.
Treatment for chronic hypertension in pregnancy with labetalol showed no significant differences in maternal or neonatal outcomes, compared with treatment with nifedipine, new research indicates.
The open-label, multicenter, randomized CHAP (Chronic Hypertension in Pregnancy) trial showed that treating mild chronic hypertension was better than delaying treatment until severe hypertension developed, but still unclear was whether, or to what extent, the choice of first-line treatment affected outcomes.
Researchers, led by Ayodeji A. Sanusi, MD, MPH, with the Division of Maternal and Fetal Medicine at the University of Alabama at Birmingham, conducted a secondary analysis of CHAP to compare the primary treatments. Mild chronic hypertension in the study was defined as blood pressure of 140-159/90-104 mmHg before 20 weeks of gestation.
Three Comparisons
Three comparisons were performed in 2292 participants based on medications prescribed at enrollment: 720 (31.4%) received labetalol; 417 (18.2%) initially received nifedipine; and 1155 (50.4%) had standard care. Labetalol was compared with standard care; nifedipine was compared with standard care; and labetalol was compared with nifedipine.
The primary outcome was occurrence of superimposed preeclampsia with severe features; preterm birth before 35 weeks of gestation; placental abruption; or fetal or neonatal death. The key secondary outcome was a small-for-gestational age neonate. Researchers also compared adverse effects between groups.
Among the results were the following:
- The primary outcome occurred in 30.1% in the labetalol group; 31.2% in the nifedipine group; and 37% in the standard care group.
- Risk of the primary outcome was lower among those receiving treatment. For labetalol vs standard care, the adjusted relative risk (RR) was 0.82; 95% confidence interval (CI), 0.72-0.94. For nifedipine vs standard care, the adjusted RR was 0.84; 95% CI, 0.71-0.99. There was no significant difference in risk when labetalol was compared with nifedipine (adjusted RR, 0.98; 95% CI, 0.82-1.18).
- There were no significant differences in numbers of small-for-gestational age neonates or serious adverse events between those who received labetalol and those using nifedipine.
Any adverse events were significantly more common with nifedipine, compared with labetalol (35.7% vs 28.3%, P = .009), and with nifedipine, compared with standard care (35.7% vs 26.3%, P = .0003). Adverse event rates were not significantly higher with labetalol when compared with standard care (28.3% vs 26.3%, P = .34). The most frequently reported adverse events were headache, medication intolerance, dizziness, nausea, dyspepsia, neonatal jaundice, and vomiting.
“Thus, labetalol compared with nifedipine appeared to have fewer adverse events and to be better tolerated,” the authors write. They note that labetalol, a third-generation mixed alpha- and beta-adrenergic antagonist, is contraindicated for those who have obstructive pulmonary disease and nifedipine, a dihydropyridine calcium channel blocker, is contraindicated in people with tachycardia.
The authors write that their results align with other studies that have not found differences between labetalol and nifedipine. “[O]ur findings support the use of either labetalol or nifedipine as initial first-line agents for the management of mild chronic hypertension in pregnancy to reduce the risk of adverse maternal and other perinatal outcomes with no increased risk of fetal harm,” the authors write.
Dr. Sanusi reports no relevant financial relationships. Full coauthor disclosures are available with the full text of the paper.
Treatment for chronic hypertension in pregnancy with labetalol showed no significant differences in maternal or neonatal outcomes, compared with treatment with nifedipine, new research indicates.
The open-label, multicenter, randomized CHAP (Chronic Hypertension in Pregnancy) trial showed that treating mild chronic hypertension was better than delaying treatment until severe hypertension developed, but still unclear was whether, or to what extent, the choice of first-line treatment affected outcomes.
Researchers, led by Ayodeji A. Sanusi, MD, MPH, with the Division of Maternal and Fetal Medicine at the University of Alabama at Birmingham, conducted a secondary analysis of CHAP to compare the primary treatments. Mild chronic hypertension in the study was defined as blood pressure of 140-159/90-104 mmHg before 20 weeks of gestation.
Three Comparisons
Three comparisons were performed in 2292 participants based on medications prescribed at enrollment: 720 (31.4%) received labetalol; 417 (18.2%) initially received nifedipine; and 1155 (50.4%) had standard care. Labetalol was compared with standard care; nifedipine was compared with standard care; and labetalol was compared with nifedipine.
The primary outcome was occurrence of superimposed preeclampsia with severe features; preterm birth before 35 weeks of gestation; placental abruption; or fetal or neonatal death. The key secondary outcome was a small-for-gestational age neonate. Researchers also compared adverse effects between groups.
Among the results were the following:
- The primary outcome occurred in 30.1% in the labetalol group; 31.2% in the nifedipine group; and 37% in the standard care group.
- Risk of the primary outcome was lower among those receiving treatment. For labetalol vs standard care, the adjusted relative risk (RR) was 0.82; 95% confidence interval (CI), 0.72-0.94. For nifedipine vs standard care, the adjusted RR was 0.84; 95% CI, 0.71-0.99. There was no significant difference in risk when labetalol was compared with nifedipine (adjusted RR, 0.98; 95% CI, 0.82-1.18).
- There were no significant differences in numbers of small-for-gestational age neonates or serious adverse events between those who received labetalol and those using nifedipine.
Any adverse events were significantly more common with nifedipine, compared with labetalol (35.7% vs 28.3%, P = .009), and with nifedipine, compared with standard care (35.7% vs 26.3%, P = .0003). Adverse event rates were not significantly higher with labetalol when compared with standard care (28.3% vs 26.3%, P = .34). The most frequently reported adverse events were headache, medication intolerance, dizziness, nausea, dyspepsia, neonatal jaundice, and vomiting.
“Thus, labetalol compared with nifedipine appeared to have fewer adverse events and to be better tolerated,” the authors write. They note that labetalol, a third-generation mixed alpha- and beta-adrenergic antagonist, is contraindicated for those who have obstructive pulmonary disease and nifedipine, a dihydropyridine calcium channel blocker, is contraindicated in people with tachycardia.
The authors write that their results align with other studies that have not found differences between labetalol and nifedipine. “[O]ur findings support the use of either labetalol or nifedipine as initial first-line agents for the management of mild chronic hypertension in pregnancy to reduce the risk of adverse maternal and other perinatal outcomes with no increased risk of fetal harm,” the authors write.
Dr. Sanusi reports no relevant financial relationships. Full coauthor disclosures are available with the full text of the paper.
FROM OBSTETRICS & GYNECOLOGY
Scope of Practice Concerns Lead to Hospital’s Temp Ban on CRNAs
Two hospitals in California in recent months have been cited by state inspectors for allowing certified registered nurse anesthetists (CRNAs) to practice beyond their scope, leading to one hospital temporarily stopping use of CRNAs in surgeries.
In one case, a CRNA changed a physician’s order from general anesthesia to spinal anesthesia for a patient who later became unresponsive and had to be transferred to another hospital, according to The Modesto Bee.
The unusual situation highlights the ongoing, often contentious debate about the proper role of CRNAs in surgery amid widely varying state scope of practice laws.
Elizabeth Bamgbose, CRNA, past president of the California Association of Nurse Anesthetists (CANA), said that the absence of CRNAs at Doctors Medical Center (DMC) in Modesto, California, had led to the cancellation of hundreds of procedures. It was an unnecessary step, she said.
“It’s unfortunate that a single surveyor has taken it upon themselves to reinterpret state regulations and redefine a practice that was efficient and safe,” said Ms. Bamgbose, a member of the CANA practice committee.
In late May, the California Department of Public Health (CDPH) issued an “immediate jeopardy” warning about DMC of Modesto. The state agency, like its counterparts in other states, acts on behalf of the Centers for Medicare and Medicaid Services (CMS) in surveying healthcare facilities. CMS defines immediate jeopardy as “a situation in which entity noncompliance has placed the health and safety of recipients in its care at risk for serious injury, serious harm, serious impairment, or death.”
The administrative warning comes with fines and requires the facility to submit an action plan to remediate the situation. The state determines through a follow-up survey whether the plan is sufficient for the facility to avoid being dropped from participation in Medicare and Medicaid.
Before the immediate jeopardy action was taken against DMC, the state had issued three previous such warnings in 2024, according to the CDPH enforcement actions dashboard.
CRNA Claims to Be in Charge
Stanislaus Surgical Hospital in Modesto, California, was the first facility to attract CDPH attention. It reportedly was cited in August 2023 and January 2024 surveys for a number of violations of the CMS conditions of participation, including allowing nurse anesthetists to practice beyond their scope.
According to The Modesto Bee, CDPH issued an “immediate jeopardy” order for Stanislaus in January.
The paper reported that state regulators took issue with a CRNA claiming to be the lead manager of the hospital’s anesthesia group, referring to herself as the “chief CRNA.”
Jennifer Banek, MSN, CRNA, a member of the American Association of Nurse Anesthesiology board, declined comment on the Stanislaus hospital but said that “it would not be unusual for a nurse anesthetist to serve as a leader, especially (for a) rural or underserved population.”
In April, CMS informed Stanislaus it was being terminated from Medicare, but several Congressional representatives from the Modesto area asked CMS to reconsider. The agency eventually reversed the sanction, The Modesto Bee reported.
CDPH subsequently cited DMC for CRNA scope of practice issues. A department spokesman said that CDPH teams went to DMC “to investigate practices that may not be compliant with state and federal requirements.” The agency declined to comment further until its investigations were complete.
CDPH is monitoring DMC to ensure the hospital complies with state requirements and will return for an unannounced follow-up survey “so it can provide safe, high-quality care to patients that need it,” the spokesperson said.
Although DMC would not confirm it on the record, the immediate jeopardy order led to the removal of all CRNAs, according to Ms. Banek, Ms. Bamgbose, and The Modesto Bee.
The hospital said in a statement that it is working with CDPH to address its concerns and will await a follow-up survey. “Our hospital will continue to fully participate in the Medicare and Medicaid programs during this process.”
Scope of Practice Confusion?
But that does not supersede state laws or hospital bylaws governing practice, said American Society of Anesthesiologists (ASA) president Ronald Harter, MD.
Five states — Alaska, Delaware, Montana, New Hampshire, and Oregon — have laws that allow nurse anesthetists to practice without physician oversight or involvement, said Dr. Harter, professor of anesthesiology at The Ohio State University Wexner Medical Center in Columbus, Ohio.
“There’s a lot of various opinions on what exactly constitutes scope of practice of a nurse anesthetist,” Dr. Harter said. “The vast majority of them work under the direction of an anesthesiologist, and in those settings, it’s typically very clear to everybody who performs what tasks within the care team,” he said.
It’s less common for nurse anesthetists to work totally independent of physician oversight, he said.
Ms. Bamgbose, however, said there is no California statute requiring physician supervision of CRNAs.
The ASA maintains that CRNAs should always be under the supervision of a physician, which can be an anesthesiologist, obstetrician, gastroenterologist, surgeon, or other physician conducting a procedure. An anesthesiologist does not necessarily have to be physically on site, but in those circumstances, the physician conducting the procedure would be, said Dr. Harter.
Nurse anesthetists are “excellent advanced practice nurses,” Dr. Harter said. “But they haven’t been to medical school; they haven’t conducted a residency in anesthesiology. [They] don’t have the medical knowledge and skills that are required to manage the medical problems that patients either bring to the OR with them or that can arise during the time that they’re under anesthesia.”
Filling a Gap
Nurse anesthetists see things differently.
CRNAs, by virtue of their certification, can “practice to the full extent and to the full scope, which is complete service of anesthesia,” said Ms. Bamgbose. “You can practice independently of anyone, any type of supervision,” she said.
She acknowledges that “the bylaws of any institution will govern the scope at which any healthcare professional can practice at that institution.”
Most nurse anesthetists see themselves as independent practitioners.
Seventy-five percent of CRNAs who responded to a 2023 Medscape Medical News survey said they practice independently. But even Ms. Banek said that often, the meaning of “independent” is in the eye of the beholder. “It could mean different things to various providers, especially depending on the state that they are residing in,” she said.
Ms. Banek and Ms. Bamgbose said that CRNAs can help fill a gap in anesthesiology services in underserved areas.
The Bureau of Labor Statistics estimates there are currently 32,530 anesthesiologists in the United States, with California employing the largest number, at about 5300. The Association of American Medical Colleges estimated the number at 42,263 in 2022. But the federal Health Resources and Services Administration projects a shortage of 6300 anesthesiologists over the next 15 years.
Some 61,000 CRNAs are currently practicing, with 2400 graduating each year. They are required to be board-certified and are recredentialed every 4 years. By 2025, all will be required to have a doctoral degree. Most have already achieved that status, said Ms. Banek.
“Nurse anesthetists provide care predominantly to rural and underserved areas,” she said, adding, “In many rural hospitals across the country and in all three branches of the military, CRNAs practice autonomously.”
There are 3000 CRNAs in California, said Ms. Bamgbose. Nurse anesthetists are the only anesthesiology professionals in four of 58 California counties, she said.
Ms. Banek said she had heard that some 200 cases were canceled in 1 week at DMC due to the lack of CRNAs. Having physician supervision, which she called redundant, “is really creating a barrier to care,” she said.
“We have countless state and national studies that show the safety and efficacy of our practice,” said Ms. Bamgbose. “To interrupt that care ... is incredibly disruptive to the system.”
A version of this article first appeared on Medscape.com.
Two hospitals in California in recent months have been cited by state inspectors for allowing certified registered nurse anesthetists (CRNAs) to practice beyond their scope, leading to one hospital temporarily stopping use of CRNAs in surgeries.
In one case, a CRNA changed a physician’s order from general anesthesia to spinal anesthesia for a patient who later became unresponsive and had to be transferred to another hospital, according to The Modesto Bee.
The unusual situation highlights the ongoing, often contentious debate about the proper role of CRNAs in surgery amid widely varying state scope of practice laws.
Elizabeth Bamgbose, CRNA, past president of the California Association of Nurse Anesthetists (CANA), said that the absence of CRNAs at Doctors Medical Center (DMC) in Modesto, California, had led to the cancellation of hundreds of procedures. It was an unnecessary step, she said.
“It’s unfortunate that a single surveyor has taken it upon themselves to reinterpret state regulations and redefine a practice that was efficient and safe,” said Ms. Bamgbose, a member of the CANA practice committee.
In late May, the California Department of Public Health (CDPH) issued an “immediate jeopardy” warning about DMC of Modesto. The state agency, like its counterparts in other states, acts on behalf of the Centers for Medicare and Medicaid Services (CMS) in surveying healthcare facilities. CMS defines immediate jeopardy as “a situation in which entity noncompliance has placed the health and safety of recipients in its care at risk for serious injury, serious harm, serious impairment, or death.”
The administrative warning comes with fines and requires the facility to submit an action plan to remediate the situation. The state determines through a follow-up survey whether the plan is sufficient for the facility to avoid being dropped from participation in Medicare and Medicaid.
Before the immediate jeopardy action was taken against DMC, the state had issued three previous such warnings in 2024, according to the CDPH enforcement actions dashboard.
CRNA Claims to Be in Charge
Stanislaus Surgical Hospital in Modesto, California, was the first facility to attract CDPH attention. It reportedly was cited in August 2023 and January 2024 surveys for a number of violations of the CMS conditions of participation, including allowing nurse anesthetists to practice beyond their scope.
According to The Modesto Bee, CDPH issued an “immediate jeopardy” order for Stanislaus in January.
The paper reported that state regulators took issue with a CRNA claiming to be the lead manager of the hospital’s anesthesia group, referring to herself as the “chief CRNA.”
Jennifer Banek, MSN, CRNA, a member of the American Association of Nurse Anesthesiology board, declined comment on the Stanislaus hospital but said that “it would not be unusual for a nurse anesthetist to serve as a leader, especially (for a) rural or underserved population.”
In April, CMS informed Stanislaus it was being terminated from Medicare, but several Congressional representatives from the Modesto area asked CMS to reconsider. The agency eventually reversed the sanction, The Modesto Bee reported.
CDPH subsequently cited DMC for CRNA scope of practice issues. A department spokesman said that CDPH teams went to DMC “to investigate practices that may not be compliant with state and federal requirements.” The agency declined to comment further until its investigations were complete.
CDPH is monitoring DMC to ensure the hospital complies with state requirements and will return for an unannounced follow-up survey “so it can provide safe, high-quality care to patients that need it,” the spokesperson said.
Although DMC would not confirm it on the record, the immediate jeopardy order led to the removal of all CRNAs, according to Ms. Banek, Ms. Bamgbose, and The Modesto Bee.
The hospital said in a statement that it is working with CDPH to address its concerns and will await a follow-up survey. “Our hospital will continue to fully participate in the Medicare and Medicaid programs during this process.”
Scope of Practice Confusion?
But that does not supersede state laws or hospital bylaws governing practice, said American Society of Anesthesiologists (ASA) president Ronald Harter, MD.
Five states — Alaska, Delaware, Montana, New Hampshire, and Oregon — have laws that allow nurse anesthetists to practice without physician oversight or involvement, said Dr. Harter, professor of anesthesiology at The Ohio State University Wexner Medical Center in Columbus, Ohio.
“There’s a lot of various opinions on what exactly constitutes scope of practice of a nurse anesthetist,” Dr. Harter said. “The vast majority of them work under the direction of an anesthesiologist, and in those settings, it’s typically very clear to everybody who performs what tasks within the care team,” he said.
It’s less common for nurse anesthetists to work totally independent of physician oversight, he said.
Ms. Bamgbose, however, said there is no California statute requiring physician supervision of CRNAs.
The ASA maintains that CRNAs should always be under the supervision of a physician, which can be an anesthesiologist, obstetrician, gastroenterologist, surgeon, or other physician conducting a procedure. An anesthesiologist does not necessarily have to be physically on site, but in those circumstances, the physician conducting the procedure would be, said Dr. Harter.
Nurse anesthetists are “excellent advanced practice nurses,” Dr. Harter said. “But they haven’t been to medical school; they haven’t conducted a residency in anesthesiology. [They] don’t have the medical knowledge and skills that are required to manage the medical problems that patients either bring to the OR with them or that can arise during the time that they’re under anesthesia.”
Filling a Gap
Nurse anesthetists see things differently.
CRNAs, by virtue of their certification, can “practice to the full extent and to the full scope, which is complete service of anesthesia,” said Ms. Bamgbose. “You can practice independently of anyone, any type of supervision,” she said.
She acknowledges that “the bylaws of any institution will govern the scope at which any healthcare professional can practice at that institution.”
Most nurse anesthetists see themselves as independent practitioners.
Seventy-five percent of CRNAs who responded to a 2023 Medscape Medical News survey said they practice independently. But even Ms. Banek said that often, the meaning of “independent” is in the eye of the beholder. “It could mean different things to various providers, especially depending on the state that they are residing in,” she said.
Ms. Banek and Ms. Bamgbose said that CRNAs can help fill a gap in anesthesiology services in underserved areas.
The Bureau of Labor Statistics estimates there are currently 32,530 anesthesiologists in the United States, with California employing the largest number, at about 5300. The Association of American Medical Colleges estimated the number at 42,263 in 2022. But the federal Health Resources and Services Administration projects a shortage of 6300 anesthesiologists over the next 15 years.
Some 61,000 CRNAs are currently practicing, with 2400 graduating each year. They are required to be board-certified and are recredentialed every 4 years. By 2025, all will be required to have a doctoral degree. Most have already achieved that status, said Ms. Banek.
“Nurse anesthetists provide care predominantly to rural and underserved areas,” she said, adding, “In many rural hospitals across the country and in all three branches of the military, CRNAs practice autonomously.”
There are 3000 CRNAs in California, said Ms. Bamgbose. Nurse anesthetists are the only anesthesiology professionals in four of 58 California counties, she said.
Ms. Banek said she had heard that some 200 cases were canceled in 1 week at DMC due to the lack of CRNAs. Having physician supervision, which she called redundant, “is really creating a barrier to care,” she said.
“We have countless state and national studies that show the safety and efficacy of our practice,” said Ms. Bamgbose. “To interrupt that care ... is incredibly disruptive to the system.”
A version of this article first appeared on Medscape.com.
Two hospitals in California in recent months have been cited by state inspectors for allowing certified registered nurse anesthetists (CRNAs) to practice beyond their scope, leading to one hospital temporarily stopping use of CRNAs in surgeries.
In one case, a CRNA changed a physician’s order from general anesthesia to spinal anesthesia for a patient who later became unresponsive and had to be transferred to another hospital, according to The Modesto Bee.
The unusual situation highlights the ongoing, often contentious debate about the proper role of CRNAs in surgery amid widely varying state scope of practice laws.
Elizabeth Bamgbose, CRNA, past president of the California Association of Nurse Anesthetists (CANA), said that the absence of CRNAs at Doctors Medical Center (DMC) in Modesto, California, had led to the cancellation of hundreds of procedures. It was an unnecessary step, she said.
“It’s unfortunate that a single surveyor has taken it upon themselves to reinterpret state regulations and redefine a practice that was efficient and safe,” said Ms. Bamgbose, a member of the CANA practice committee.
In late May, the California Department of Public Health (CDPH) issued an “immediate jeopardy” warning about DMC of Modesto. The state agency, like its counterparts in other states, acts on behalf of the Centers for Medicare and Medicaid Services (CMS) in surveying healthcare facilities. CMS defines immediate jeopardy as “a situation in which entity noncompliance has placed the health and safety of recipients in its care at risk for serious injury, serious harm, serious impairment, or death.”
The administrative warning comes with fines and requires the facility to submit an action plan to remediate the situation. The state determines through a follow-up survey whether the plan is sufficient for the facility to avoid being dropped from participation in Medicare and Medicaid.
Before the immediate jeopardy action was taken against DMC, the state had issued three previous such warnings in 2024, according to the CDPH enforcement actions dashboard.
CRNA Claims to Be in Charge
Stanislaus Surgical Hospital in Modesto, California, was the first facility to attract CDPH attention. It reportedly was cited in August 2023 and January 2024 surveys for a number of violations of the CMS conditions of participation, including allowing nurse anesthetists to practice beyond their scope.
According to The Modesto Bee, CDPH issued an “immediate jeopardy” order for Stanislaus in January.
The paper reported that state regulators took issue with a CRNA claiming to be the lead manager of the hospital’s anesthesia group, referring to herself as the “chief CRNA.”
Jennifer Banek, MSN, CRNA, a member of the American Association of Nurse Anesthesiology board, declined comment on the Stanislaus hospital but said that “it would not be unusual for a nurse anesthetist to serve as a leader, especially (for a) rural or underserved population.”
In April, CMS informed Stanislaus it was being terminated from Medicare, but several Congressional representatives from the Modesto area asked CMS to reconsider. The agency eventually reversed the sanction, The Modesto Bee reported.
CDPH subsequently cited DMC for CRNA scope of practice issues. A department spokesman said that CDPH teams went to DMC “to investigate practices that may not be compliant with state and federal requirements.” The agency declined to comment further until its investigations were complete.
CDPH is monitoring DMC to ensure the hospital complies with state requirements and will return for an unannounced follow-up survey “so it can provide safe, high-quality care to patients that need it,” the spokesperson said.
Although DMC would not confirm it on the record, the immediate jeopardy order led to the removal of all CRNAs, according to Ms. Banek, Ms. Bamgbose, and The Modesto Bee.
The hospital said in a statement that it is working with CDPH to address its concerns and will await a follow-up survey. “Our hospital will continue to fully participate in the Medicare and Medicaid programs during this process.”
Scope of Practice Confusion?
But that does not supersede state laws or hospital bylaws governing practice, said American Society of Anesthesiologists (ASA) president Ronald Harter, MD.
Five states — Alaska, Delaware, Montana, New Hampshire, and Oregon — have laws that allow nurse anesthetists to practice without physician oversight or involvement, said Dr. Harter, professor of anesthesiology at The Ohio State University Wexner Medical Center in Columbus, Ohio.
“There’s a lot of various opinions on what exactly constitutes scope of practice of a nurse anesthetist,” Dr. Harter said. “The vast majority of them work under the direction of an anesthesiologist, and in those settings, it’s typically very clear to everybody who performs what tasks within the care team,” he said.
It’s less common for nurse anesthetists to work totally independent of physician oversight, he said.
Ms. Bamgbose, however, said there is no California statute requiring physician supervision of CRNAs.
The ASA maintains that CRNAs should always be under the supervision of a physician, which can be an anesthesiologist, obstetrician, gastroenterologist, surgeon, or other physician conducting a procedure. An anesthesiologist does not necessarily have to be physically on site, but in those circumstances, the physician conducting the procedure would be, said Dr. Harter.
Nurse anesthetists are “excellent advanced practice nurses,” Dr. Harter said. “But they haven’t been to medical school; they haven’t conducted a residency in anesthesiology. [They] don’t have the medical knowledge and skills that are required to manage the medical problems that patients either bring to the OR with them or that can arise during the time that they’re under anesthesia.”
Filling a Gap
Nurse anesthetists see things differently.
CRNAs, by virtue of their certification, can “practice to the full extent and to the full scope, which is complete service of anesthesia,” said Ms. Bamgbose. “You can practice independently of anyone, any type of supervision,” she said.
She acknowledges that “the bylaws of any institution will govern the scope at which any healthcare professional can practice at that institution.”
Most nurse anesthetists see themselves as independent practitioners.
Seventy-five percent of CRNAs who responded to a 2023 Medscape Medical News survey said they practice independently. But even Ms. Banek said that often, the meaning of “independent” is in the eye of the beholder. “It could mean different things to various providers, especially depending on the state that they are residing in,” she said.
Ms. Banek and Ms. Bamgbose said that CRNAs can help fill a gap in anesthesiology services in underserved areas.
The Bureau of Labor Statistics estimates there are currently 32,530 anesthesiologists in the United States, with California employing the largest number, at about 5300. The Association of American Medical Colleges estimated the number at 42,263 in 2022. But the federal Health Resources and Services Administration projects a shortage of 6300 anesthesiologists over the next 15 years.
Some 61,000 CRNAs are currently practicing, with 2400 graduating each year. They are required to be board-certified and are recredentialed every 4 years. By 2025, all will be required to have a doctoral degree. Most have already achieved that status, said Ms. Banek.
“Nurse anesthetists provide care predominantly to rural and underserved areas,” she said, adding, “In many rural hospitals across the country and in all three branches of the military, CRNAs practice autonomously.”
There are 3000 CRNAs in California, said Ms. Bamgbose. Nurse anesthetists are the only anesthesiology professionals in four of 58 California counties, she said.
Ms. Banek said she had heard that some 200 cases were canceled in 1 week at DMC due to the lack of CRNAs. Having physician supervision, which she called redundant, “is really creating a barrier to care,” she said.
“We have countless state and national studies that show the safety and efficacy of our practice,” said Ms. Bamgbose. “To interrupt that care ... is incredibly disruptive to the system.”
A version of this article first appeared on Medscape.com.