User login
About Half of Canadian Physicians Report High Burnout Levels
About Half of Canadian Physicians Report High Burnout Levels
Nearly half of physicians in Canada report high levels of burnout, according to preliminary data from the 2025 National Physician Health Survey (NPHS). The new data show that 46% of physicians report high levels of burnout, down from 2021 (53%) but significantly above the level of 2017 (30%), when the first survey was conducted. The full NPHS 2025 Foundational Report will be released later this year.
Other significant findings include the following:
- 74% of physicians reported experiencing bullying, harassment, microaggressions, or discrimination, a slight but meaningful reduction form 78% in 2021.
- 64% of physicians reported spending significant time on electronic medical records outside regular hours.
- 46% of physicians said that their mental health is worse than it was before the start of the pandemic, down 14% from 2021.
- 60% reported being satisfied or very satisfied with work-life balance, an improvement from 49% in 2021, though slightly below 2017 (62%).
- 37% of physicians plan to reduce their clinical hours in the next 2 years.
Margot Burnell, MD, president of the Canadian Medical Association (CMA), told Medscape Medical News that she was "disappointed" with the results.
"I hoped that the burnout numbers would decrease more than they have," she said. "Physicians are still under extreme stress in trying to provide the care for patients that they wish to give."
Reductions in Hours
The most distressing finding is that > one-third of physicians (37%) plan to reduce their hours within 24 hours -- at a time of growing physician shortages -- said Burnell.
"The one positive (finding) that stands out is that physicians are taking care of their own health and wellness and report that it's helping," she said. About 65% of physicians reported having accessed at least 1 wellness support in the past 5 years, up 11% since 2021.
The NPHS includes responses from about 3300 practicing physicians, medical residents, and fellows who were surveyed from March 14 to April 15.
Among the CMA's top priorities is to reduce the administrative burden because that tops the list of what physicians say would help them with burnout, said Burnell.
"The other area is to provide and encourage team-based care," she continued. "That provides some relief for physicians." It also is important to promote the approaches that seem to be helping, such as wellness support and artificial intelligence (AI), she said. In this survey, 59% of respondents who used AI said that it decreased their time spent on administrative tasks.
Burnout by Specialty
Future analyses will examine burnout by specialty, Burnell said. Burnout is particularly high among emergency physicians, regardless of province, according to previous work by Kerstin de Wit, MD, emergency physician and research director for the Department of Emergency Medicine at Queen's University in Kingston, Ontario, and colleagues.
The NPHS findings are not surprising, she told Medscape Medical News. "We resurveyed all our emergency physicians in January and found similar results, in that the levels of burnout were marginally less than they were in 2022 but still significantly higher than they were in 2020. Still, a majority of (emergency department) physicians qualify as having high burnout levels."
The Pandemic's Role
A telling finding of her team's research is that emergency physician burnout levels are now higher than they were in December 2020, the first year of the COVID pandemic, said De Wit. "I don't think you can say burnout is because of COVID. It's because of the problems in the medical system."
Among those problems in hospitals are a shortage of beds, physicians, and nurses and inadequate numbers of physicians in outpatient clinics "so patients are waiting for years" for conditions to be treated, she added.
"We don't have the resources that we need to maintain the standards that we had even 10, 15 years ago. The whole system is collapsing. Government underfunding is huge. Routinely, our emergency department is 100% full of ward patients, so we don't have a room with a door or a curtain to see patients in. All the emergency patients are seen in corridors or the waiting room in full view of everyone else. We have people with serious medical conditions who are dying in waiting rooms because we can't get them in."
The issues are complex, but the overarching problem is chronic underfunding that results in physicians "feeling overworked and powerless to help patients," said De Wit.
Burnell and de Wit reported having no relevant financial relationships.
Marcia Frellick is an independent health care journalist and a regular contributor to Medscape Medical News.
A version of this article first appeared on Medscape.com.
Nearly half of physicians in Canada report high levels of burnout, according to preliminary data from the 2025 National Physician Health Survey (NPHS). The new data show that 46% of physicians report high levels of burnout, down from 2021 (53%) but significantly above the level of 2017 (30%), when the first survey was conducted. The full NPHS 2025 Foundational Report will be released later this year.
Other significant findings include the following:
- 74% of physicians reported experiencing bullying, harassment, microaggressions, or discrimination, a slight but meaningful reduction form 78% in 2021.
- 64% of physicians reported spending significant time on electronic medical records outside regular hours.
- 46% of physicians said that their mental health is worse than it was before the start of the pandemic, down 14% from 2021.
- 60% reported being satisfied or very satisfied with work-life balance, an improvement from 49% in 2021, though slightly below 2017 (62%).
- 37% of physicians plan to reduce their clinical hours in the next 2 years.
Margot Burnell, MD, president of the Canadian Medical Association (CMA), told Medscape Medical News that she was "disappointed" with the results.
"I hoped that the burnout numbers would decrease more than they have," she said. "Physicians are still under extreme stress in trying to provide the care for patients that they wish to give."
Reductions in Hours
The most distressing finding is that > one-third of physicians (37%) plan to reduce their hours within 24 hours -- at a time of growing physician shortages -- said Burnell.
"The one positive (finding) that stands out is that physicians are taking care of their own health and wellness and report that it's helping," she said. About 65% of physicians reported having accessed at least 1 wellness support in the past 5 years, up 11% since 2021.
The NPHS includes responses from about 3300 practicing physicians, medical residents, and fellows who were surveyed from March 14 to April 15.
Among the CMA's top priorities is to reduce the administrative burden because that tops the list of what physicians say would help them with burnout, said Burnell.
"The other area is to provide and encourage team-based care," she continued. "That provides some relief for physicians." It also is important to promote the approaches that seem to be helping, such as wellness support and artificial intelligence (AI), she said. In this survey, 59% of respondents who used AI said that it decreased their time spent on administrative tasks.
Burnout by Specialty
Future analyses will examine burnout by specialty, Burnell said. Burnout is particularly high among emergency physicians, regardless of province, according to previous work by Kerstin de Wit, MD, emergency physician and research director for the Department of Emergency Medicine at Queen's University in Kingston, Ontario, and colleagues.
The NPHS findings are not surprising, she told Medscape Medical News. "We resurveyed all our emergency physicians in January and found similar results, in that the levels of burnout were marginally less than they were in 2022 but still significantly higher than they were in 2020. Still, a majority of (emergency department) physicians qualify as having high burnout levels."
The Pandemic's Role
A telling finding of her team's research is that emergency physician burnout levels are now higher than they were in December 2020, the first year of the COVID pandemic, said De Wit. "I don't think you can say burnout is because of COVID. It's because of the problems in the medical system."
Among those problems in hospitals are a shortage of beds, physicians, and nurses and inadequate numbers of physicians in outpatient clinics "so patients are waiting for years" for conditions to be treated, she added.
"We don't have the resources that we need to maintain the standards that we had even 10, 15 years ago. The whole system is collapsing. Government underfunding is huge. Routinely, our emergency department is 100% full of ward patients, so we don't have a room with a door or a curtain to see patients in. All the emergency patients are seen in corridors or the waiting room in full view of everyone else. We have people with serious medical conditions who are dying in waiting rooms because we can't get them in."
The issues are complex, but the overarching problem is chronic underfunding that results in physicians "feeling overworked and powerless to help patients," said De Wit.
Burnell and de Wit reported having no relevant financial relationships.
Marcia Frellick is an independent health care journalist and a regular contributor to Medscape Medical News.
A version of this article first appeared on Medscape.com.
Nearly half of physicians in Canada report high levels of burnout, according to preliminary data from the 2025 National Physician Health Survey (NPHS). The new data show that 46% of physicians report high levels of burnout, down from 2021 (53%) but significantly above the level of 2017 (30%), when the first survey was conducted. The full NPHS 2025 Foundational Report will be released later this year.
Other significant findings include the following:
- 74% of physicians reported experiencing bullying, harassment, microaggressions, or discrimination, a slight but meaningful reduction form 78% in 2021.
- 64% of physicians reported spending significant time on electronic medical records outside regular hours.
- 46% of physicians said that their mental health is worse than it was before the start of the pandemic, down 14% from 2021.
- 60% reported being satisfied or very satisfied with work-life balance, an improvement from 49% in 2021, though slightly below 2017 (62%).
- 37% of physicians plan to reduce their clinical hours in the next 2 years.
Margot Burnell, MD, president of the Canadian Medical Association (CMA), told Medscape Medical News that she was "disappointed" with the results.
"I hoped that the burnout numbers would decrease more than they have," she said. "Physicians are still under extreme stress in trying to provide the care for patients that they wish to give."
Reductions in Hours
The most distressing finding is that > one-third of physicians (37%) plan to reduce their hours within 24 hours -- at a time of growing physician shortages -- said Burnell.
"The one positive (finding) that stands out is that physicians are taking care of their own health and wellness and report that it's helping," she said. About 65% of physicians reported having accessed at least 1 wellness support in the past 5 years, up 11% since 2021.
The NPHS includes responses from about 3300 practicing physicians, medical residents, and fellows who were surveyed from March 14 to April 15.
Among the CMA's top priorities is to reduce the administrative burden because that tops the list of what physicians say would help them with burnout, said Burnell.
"The other area is to provide and encourage team-based care," she continued. "That provides some relief for physicians." It also is important to promote the approaches that seem to be helping, such as wellness support and artificial intelligence (AI), she said. In this survey, 59% of respondents who used AI said that it decreased their time spent on administrative tasks.
Burnout by Specialty
Future analyses will examine burnout by specialty, Burnell said. Burnout is particularly high among emergency physicians, regardless of province, according to previous work by Kerstin de Wit, MD, emergency physician and research director for the Department of Emergency Medicine at Queen's University in Kingston, Ontario, and colleagues.
The NPHS findings are not surprising, she told Medscape Medical News. "We resurveyed all our emergency physicians in January and found similar results, in that the levels of burnout were marginally less than they were in 2022 but still significantly higher than they were in 2020. Still, a majority of (emergency department) physicians qualify as having high burnout levels."
The Pandemic's Role
A telling finding of her team's research is that emergency physician burnout levels are now higher than they were in December 2020, the first year of the COVID pandemic, said De Wit. "I don't think you can say burnout is because of COVID. It's because of the problems in the medical system."
Among those problems in hospitals are a shortage of beds, physicians, and nurses and inadequate numbers of physicians in outpatient clinics "so patients are waiting for years" for conditions to be treated, she added.
"We don't have the resources that we need to maintain the standards that we had even 10, 15 years ago. The whole system is collapsing. Government underfunding is huge. Routinely, our emergency department is 100% full of ward patients, so we don't have a room with a door or a curtain to see patients in. All the emergency patients are seen in corridors or the waiting room in full view of everyone else. We have people with serious medical conditions who are dying in waiting rooms because we can't get them in."
The issues are complex, but the overarching problem is chronic underfunding that results in physicians "feeling overworked and powerless to help patients," said De Wit.
Burnell and de Wit reported having no relevant financial relationships.
Marcia Frellick is an independent health care journalist and a regular contributor to Medscape Medical News.
A version of this article first appeared on Medscape.com.
About Half of Canadian Physicians Report High Burnout Levels
About Half of Canadian Physicians Report High Burnout Levels
Helicobacter pylori May Shift Gastric Cancer Earlier
Helicobacter pylori May Shift Gastric Cancer Earlier
ORLANDO, Fl — , new data suggested.
H pylori infection is a leading risk factor for gastric carcinoma, accounting for as many as 90% of cases. As the new data show, failure to screen routinely for the bacteria could be leading to younger people developing easily preventable forms of gastric cancer, experts said.
“The most concerning and the most interesting finding for us was we found higher prevalence” of gastric cancer linked to H pylori in the younger group, Neel Patel, MD, MPH, with the Department of Pathology at Staten Island University Hospital in Staten Island, New York, told GI & Hepatology News.
“This does not mean most patients are young. Rather, it means H pylori increases the likelihood of gastric cancer appearing earlier in life compared with non-H pylori cases.”
For the study, Patel and his colleagues, who presented their findings at the annual meeting of the College of American Pathologists (CAP) 2025, used 2016-2020 data from the Nationwide Inpatient Sample, which included records for adults with primary diagnoses of gastric cancer. They looked at outcomes of those whose cancer was associated with H pylori compared with the non-H pylori group.
Among 91,670 adult hospitalizations, 1830 (2%) had gastric cancer linked to H pylori (2016-2020). Patel said the low percentage resulted from focusing solely on diagnostic codes for primary diagnoses of gastric cancer and excluding secondary diagnoses.
These cancers were twice as prevalent in patients aged 18-49 years (3.97%) as in those older than 65 years (1.65%).
Septicemia Odds Higher in H pylori Group
Patients in the H pylori group also had a higher burden of comorbidities such as anemia, chronic blood loss, and metastatic cancer, according to the data. The researcher found these patients also had significantly higher odds of septicemia (odds ratio, 1.62; 95% CI, 1.17-2.24; P = .003) and spent an average of 8 days in the hospital — two more than those with cancers not associated with the infection.
Dipti M. Karamchandani, MD, a professor of pathology at the University of Texas Southwestern Medical Center in Dallas, who was not part of the study, said the longer hospital stays and greater risk for septicemia may be related to increased comorbidities among people who get H pylori infection in general. The infection often is caused by unsanitary conditions, and the groups infected may also be more likely to experience malnutrition, anemia, or lower body reserves, for example, she said.
“Also, H pylori often causes gastric ulcers, even before causing cancer, and those patients may be prone to chronic blood loss,” Karamchandani said. “These are all reasons that these patients may be more prone to longer hospital stay.”
US Guidelines Lacking
H pylori infection is a strong predictor of gastric cancer, but it often goes undetected. “Sometimes we ignore the symptoms,” Patel said.
“There are no standard guidelines for screening for H pylori,” he added. “We need to stop the transition from H pylori to gastric cancer.”
“This abstract highlights an important issue: Gastric cancer is rising among younger adults in the US, particularly in noncardia gastric cancer, which is most often associated with Helicobacter pylori infection,” said Chul S. Hyun, MD, PhD, MPH, director of the Gastric Cancer Prevention and Screening Program at Yale School of Medicine in New Haven, Connecticut.
Hyun said the 2% of patients in the study diagnosed with gastric cancer associated with H pylori likely reflected undercoding and “incomplete capture” in the database and noted that subgroup comparisons “become difficult to interpret reliably.” By extension, the findings also underscore, “We are not adequately capturing H pylori in routine US coding and claims.”
“What we do know is that H pylori is the central, modifiable driver of risk, and that prevention efforts should focus on high prevalence populations — including Asian, Hispanic, and immigrant communities — where systematic H pylori screening remains a major unmet need,” said Hyun, who was not involved in the new research.
Currently no US society guideline recommends systematic screening, Hyun said. “Other high-incidence countries, such as Japan and Korea, already incorporate H pylori and gastroscopy screening into national policy,” he said. “For these reasons, guidelines urgently need to evolve to recommend targeted H pylori screening in high prevalence groups.”
Patel, Karamchandani, and Hyun reported having no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
ORLANDO, Fl — , new data suggested.
H pylori infection is a leading risk factor for gastric carcinoma, accounting for as many as 90% of cases. As the new data show, failure to screen routinely for the bacteria could be leading to younger people developing easily preventable forms of gastric cancer, experts said.
“The most concerning and the most interesting finding for us was we found higher prevalence” of gastric cancer linked to H pylori in the younger group, Neel Patel, MD, MPH, with the Department of Pathology at Staten Island University Hospital in Staten Island, New York, told GI & Hepatology News.
“This does not mean most patients are young. Rather, it means H pylori increases the likelihood of gastric cancer appearing earlier in life compared with non-H pylori cases.”
For the study, Patel and his colleagues, who presented their findings at the annual meeting of the College of American Pathologists (CAP) 2025, used 2016-2020 data from the Nationwide Inpatient Sample, which included records for adults with primary diagnoses of gastric cancer. They looked at outcomes of those whose cancer was associated with H pylori compared with the non-H pylori group.
Among 91,670 adult hospitalizations, 1830 (2%) had gastric cancer linked to H pylori (2016-2020). Patel said the low percentage resulted from focusing solely on diagnostic codes for primary diagnoses of gastric cancer and excluding secondary diagnoses.
These cancers were twice as prevalent in patients aged 18-49 years (3.97%) as in those older than 65 years (1.65%).
Septicemia Odds Higher in H pylori Group
Patients in the H pylori group also had a higher burden of comorbidities such as anemia, chronic blood loss, and metastatic cancer, according to the data. The researcher found these patients also had significantly higher odds of septicemia (odds ratio, 1.62; 95% CI, 1.17-2.24; P = .003) and spent an average of 8 days in the hospital — two more than those with cancers not associated with the infection.
Dipti M. Karamchandani, MD, a professor of pathology at the University of Texas Southwestern Medical Center in Dallas, who was not part of the study, said the longer hospital stays and greater risk for septicemia may be related to increased comorbidities among people who get H pylori infection in general. The infection often is caused by unsanitary conditions, and the groups infected may also be more likely to experience malnutrition, anemia, or lower body reserves, for example, she said.
“Also, H pylori often causes gastric ulcers, even before causing cancer, and those patients may be prone to chronic blood loss,” Karamchandani said. “These are all reasons that these patients may be more prone to longer hospital stay.”
US Guidelines Lacking
H pylori infection is a strong predictor of gastric cancer, but it often goes undetected. “Sometimes we ignore the symptoms,” Patel said.
“There are no standard guidelines for screening for H pylori,” he added. “We need to stop the transition from H pylori to gastric cancer.”
“This abstract highlights an important issue: Gastric cancer is rising among younger adults in the US, particularly in noncardia gastric cancer, which is most often associated with Helicobacter pylori infection,” said Chul S. Hyun, MD, PhD, MPH, director of the Gastric Cancer Prevention and Screening Program at Yale School of Medicine in New Haven, Connecticut.
Hyun said the 2% of patients in the study diagnosed with gastric cancer associated with H pylori likely reflected undercoding and “incomplete capture” in the database and noted that subgroup comparisons “become difficult to interpret reliably.” By extension, the findings also underscore, “We are not adequately capturing H pylori in routine US coding and claims.”
“What we do know is that H pylori is the central, modifiable driver of risk, and that prevention efforts should focus on high prevalence populations — including Asian, Hispanic, and immigrant communities — where systematic H pylori screening remains a major unmet need,” said Hyun, who was not involved in the new research.
Currently no US society guideline recommends systematic screening, Hyun said. “Other high-incidence countries, such as Japan and Korea, already incorporate H pylori and gastroscopy screening into national policy,” he said. “For these reasons, guidelines urgently need to evolve to recommend targeted H pylori screening in high prevalence groups.”
Patel, Karamchandani, and Hyun reported having no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
ORLANDO, Fl — , new data suggested.
H pylori infection is a leading risk factor for gastric carcinoma, accounting for as many as 90% of cases. As the new data show, failure to screen routinely for the bacteria could be leading to younger people developing easily preventable forms of gastric cancer, experts said.
“The most concerning and the most interesting finding for us was we found higher prevalence” of gastric cancer linked to H pylori in the younger group, Neel Patel, MD, MPH, with the Department of Pathology at Staten Island University Hospital in Staten Island, New York, told GI & Hepatology News.
“This does not mean most patients are young. Rather, it means H pylori increases the likelihood of gastric cancer appearing earlier in life compared with non-H pylori cases.”
For the study, Patel and his colleagues, who presented their findings at the annual meeting of the College of American Pathologists (CAP) 2025, used 2016-2020 data from the Nationwide Inpatient Sample, which included records for adults with primary diagnoses of gastric cancer. They looked at outcomes of those whose cancer was associated with H pylori compared with the non-H pylori group.
Among 91,670 adult hospitalizations, 1830 (2%) had gastric cancer linked to H pylori (2016-2020). Patel said the low percentage resulted from focusing solely on diagnostic codes for primary diagnoses of gastric cancer and excluding secondary diagnoses.
These cancers were twice as prevalent in patients aged 18-49 years (3.97%) as in those older than 65 years (1.65%).
Septicemia Odds Higher in H pylori Group
Patients in the H pylori group also had a higher burden of comorbidities such as anemia, chronic blood loss, and metastatic cancer, according to the data. The researcher found these patients also had significantly higher odds of septicemia (odds ratio, 1.62; 95% CI, 1.17-2.24; P = .003) and spent an average of 8 days in the hospital — two more than those with cancers not associated with the infection.
Dipti M. Karamchandani, MD, a professor of pathology at the University of Texas Southwestern Medical Center in Dallas, who was not part of the study, said the longer hospital stays and greater risk for septicemia may be related to increased comorbidities among people who get H pylori infection in general. The infection often is caused by unsanitary conditions, and the groups infected may also be more likely to experience malnutrition, anemia, or lower body reserves, for example, she said.
“Also, H pylori often causes gastric ulcers, even before causing cancer, and those patients may be prone to chronic blood loss,” Karamchandani said. “These are all reasons that these patients may be more prone to longer hospital stay.”
US Guidelines Lacking
H pylori infection is a strong predictor of gastric cancer, but it often goes undetected. “Sometimes we ignore the symptoms,” Patel said.
“There are no standard guidelines for screening for H pylori,” he added. “We need to stop the transition from H pylori to gastric cancer.”
“This abstract highlights an important issue: Gastric cancer is rising among younger adults in the US, particularly in noncardia gastric cancer, which is most often associated with Helicobacter pylori infection,” said Chul S. Hyun, MD, PhD, MPH, director of the Gastric Cancer Prevention and Screening Program at Yale School of Medicine in New Haven, Connecticut.
Hyun said the 2% of patients in the study diagnosed with gastric cancer associated with H pylori likely reflected undercoding and “incomplete capture” in the database and noted that subgroup comparisons “become difficult to interpret reliably.” By extension, the findings also underscore, “We are not adequately capturing H pylori in routine US coding and claims.”
“What we do know is that H pylori is the central, modifiable driver of risk, and that prevention efforts should focus on high prevalence populations — including Asian, Hispanic, and immigrant communities — where systematic H pylori screening remains a major unmet need,” said Hyun, who was not involved in the new research.
Currently no US society guideline recommends systematic screening, Hyun said. “Other high-incidence countries, such as Japan and Korea, already incorporate H pylori and gastroscopy screening into national policy,” he said. “For these reasons, guidelines urgently need to evolve to recommend targeted H pylori screening in high prevalence groups.”
Patel, Karamchandani, and Hyun reported having no relevant financial conflicts of interest.
A version of this article appeared on Medscape.com.
Helicobacter pylori May Shift Gastric Cancer Earlier
Helicobacter pylori May Shift Gastric Cancer Earlier
Ostomy Innovation Grabs ‘Shark Tank’ Win
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
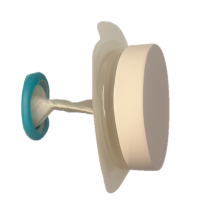
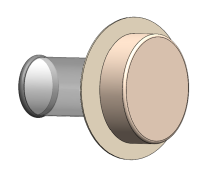
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
The “Shark Tank” winning innovation at the American Gastroenterological Association (AGA) Tech Summit in Chicago this April has “life-altering” potential for ostomy patients, according to one of the judges, and eliminates the need for constant pouch wear.
The innovation is called Twistomy and it is designed to replace current ostomy-pouch systems that can cause leaks, odor, skin irritation, embarrassment, and social and emotional distress. The AGA Committee for GI Innovation and Technology (CGIT) organizes the annual Tech Summit.
Twistomy’s winning design includes a flexible ring and sleeve, which are inserted into the stoma and secured on the outside with a set of rings that make up the housing unit attached to a standard wafer. The housing unit twists the sleeve closed, allowing the user to control fecal output. For evacuation, the user attaches a pouch, untwists the sleeve, evacuates cleanly and effectively, and then discards the pouch.
Twistomy cofounders Devon Horton, BS, senior bioengineer, and Lily Williams, BS, biomedical researcher and engineer, both work for the department of surgery at University of Colorado, Denver.
Horton said in an interview that when he was approached with the idea to create a better ostomy solution for a senior-year capstone project he was intrigued because the traditional ostomy system “has not changed in more than 70 years. It was crazy that no one had done anything to change that.”
The Twistomy team also won the Grand Prize this spring at the Emerging Medical Innovation Valuation Competition at the Design of Medical Devices Conference held at the University of Minnesota, Minneapolis.
Witnessing the Struggle as a CNA
Horton also works as a certified nursing assistant at an inpatient unit at University of Colorado Hospital and the ostomy patients he sees there every shift help drive his passion to find a better solution.
He hears the emotional stories of people who manage their ostomy daily.
“Many express feelings of depression and anxiety, feeling isolated with their severe inability to go out and do things because of the fear of the noise the stoma makes, or the crinkling of the plastic bag in a yoga class,” he said. “We want to help them regain that control of quality of life.”
They also hope to cut down on the ostomy management time. “Initial user testing [for Twistomy] was less than 75 seconds to insert and assemble,” he said. “I did an interview with a patient yesterday who said they probably spend an hour a day managing their ostomy,” including cleaning and replacing.
Horton and Williams have a patent on the device and currently use three-dimensional printing for the prototypes.
Williams said they are now conducting consumer discovery studies through the National Science Foundation and are interviewing 30 stakeholders — “anyone who has a relationship with an ostomy,” whether a colorectal surgeon, a gastrointestinal nurse, ostomy patients, or insurers.
Those interviews will help in refining the device so they can start consulting with manufacturers and work toward approval as a Class II medical device from the US Food and Drug Administration (FDA), Williams said.
Saving Healthcare Costs
Another potential benefit for Twistomy is its ability to cut healthcare costs, Horton said. Traditional ostomies are prone to leakage, which can lead to peristomal skin complications.
He pointed to a National Institutes of Health analysis that found that on average peristomal skin complications caused upwards of $80,000 more per ostomy patient in increased healthcare costs over a 3-month period than for those without the complications.
“With Twistomy, we are reducing leakage most likely to zero,” Horton said. “We set out to say if we could reduce [infections] by half or a little less than half, we can cut out those tens of thousands of dollars that insurance companies and payers are spending.”
Permanent and Temporary Ostomy Markets
He pointed out that not all ostomies are permanent ostomies, adding that the reversal rate “is about 65%.” Often those reversal surgeries cannot take place until peristomal skin complications have been healed.
“We’re not only hoping to market to the permanent stoma patients, but the patients with temporary stomas as well,” he said.
The team estimates it will need $4 million–$6 million in funding for manufacturing and consultation costs as well as costs involved in seeking FDA approval.
Horton and Williams project the housing unit cost will be $399 based on known out-of-pocket expenses for patients with ostomy care products and the unit would be replaced annually. Disposable elements would be an additional cost.
Assuming insurance acceptance of the product, he said, “With about an 80/20 insurance coverage, typical for many patients, it would be about $100 in out-of-pocket expenses per month to use our device, which is around the lower end of what a lot of patients are spending out of pocket.”
One of the Tech Summit judges, Somaya Albhaisi, MD, a gastroenterology/hepatology fellow at University of Southern California, Los Angeles, said in an interview that the Shark Tank results were unanimous among the five judges and Twistomy also took the fan favorite vote.
She said the teams were judged on quality of pitch, potential clinical impact, and feasibility of business plan. Teams got 5-7 minutes to pitch and answered questions afterward.
“Deep Understanding” of Patient Need
“They combined smart engineering with deep understanding of patient need, which is restoring control, dignity, and quality of life for ostomy users while also reducing healthcare costs. It is rare to see a solution this scalable and impactful. It was a deeply empathetic solution overall.” She noted that nearly 1 million people in the United States currently use an ostomy.
Ostomy users’ quality of life is compromised, and they often have mental health challenges, Albhaisi said. This innovation appears to offer easy use, more dignity and control.
The other four Shark Tank finalists were:
- AI Lumen, which developed a retroview camera system, which attaches to the colonoscope and enhances imaging to detect hidden polyps that may evade conventional endoscopes.
- Amplified Sciences, which developed an ultrasensitive diagnostic platform that detects biomarker activities in minute volumes of fluid from pancreatic cystic lesions, helping to stratify patients into low risk or potential malignancy, reducing unneeded surgeries, costs, and comorbidities.
- KITE Endoscopic Innovations, which designed the Dynaflex TruCut needle to offer a simpler endoscopic ultrasound (EUS)–guided biopsy procedure with fewer needle passes, deeper insights into tumor pathology, and more tissue for geonomic analysis.
- MicroSteer, which designed a device to facilitate semiautomated endoscopic submucosal dissection (ESD) by decoupling the dissecting knife from the endoscope, enhancing safety and effectiveness during the procedure.
The Twistomy Team “Surprised Everyone”
The competitors’ scores were “very close,” one of the judges, Kevin Berliner, said in an interview. “The Twistomy team surprised everyone — the judges and the crowd — with their succinct, informative, and impactful pitch. That presentation disparity was the tiebreaker for me,” said Berliner, who works for Medtronic, a sponsor of the competition, in Chicago.
He said Horton and Williams were the youngest presenters and had the earliest stage pitch they judged, but they “outpresented other competitors in clarity, simplification, and storytelling.”
Also impressive was their description of their “commercially viable path to success” and their plan for the challenges ahead, he said.
Those challenges to get Twistomy to market center “on the ongoing changing climate we have with research funds lately,” Horton said. “We’re giving it an estimate of 3-5 years.”
Horton, Williams, Albhaisi, and Berliner reported no relevant financial relationships.
Most Kids With COVID-Linked MIS-C Recover by 6 Months
Children who were severely ill with multisystem inflammatory syndrome in children (MIS-C) related to COVID-19 infection appear to show excellent cardiovascular and noncardiovascular outcomes by 6 months, according to data published in JAMA Pediatrics.
MIS-C is a life-threatening complication of COVID-19 infection and data on outcomes are limited, wrote the authors, led by Dongngan T. Truong, MD, MSSI, with Children’s Healthcare of Atlanta Cardiology, Emory University School of Medicine in Atlanta, Georgia. These 6-month results are from the Long-Term Outcomes After the Multisystem Inflammatory Syndrome in Children (MUSIC) study, sponsored by the National Heart, Lung, and Blood Institute.
Researchers found in this cohort study of 1204 participants that by 6 months after hospital discharge, 99% had normalization of left ventricular systolic function, and 92.3% had normalized coronary artery dimensions. More than 95% reported being more than 90% back to baseline health.
Patient-Reported Outcomes Measurement Information Systems (PROMIS) Global Health scores were at least equivalent to prepandemic population normative values. PROMIS Global Health parent/guardian proxy median T scores for fatigue, global health, and pain interference improved significantly from 2 weeks to 6 months: fatigue, 56.1 vs 48.9; global health, 48.8 vs 51.3; pain interference, 53.0 vs 43.3 (P < .001).
The most common symptoms reported at 2 weeks were fatigue (15.9%) and low stamina/energy (9.2%); both decreased to 3.4% and 3.3%, respectively, by 6 months. The most common cardiovascular symptom at 2 weeks was palpitations (1.5%), which decreased to 0.6%.
Chest Pain Increased Over Time
Reports of chest pain, however, reportedly increased over time, with 1.3% reporting chest pain at rest at 2 weeks and 2.2% at 6 months. Although gastrointestinal symptoms were common during the acute MIS-C, only 5.3% of respondents reported those symptoms at 2 weeks.
Children in the cohort had a median age of 9 years, and 60% were men. They self-identified with the following races and ethnicities: American Indian or Alaska Native (0.1%), Asian (3.3%), Black (27.0%), Hawaiian Native or Other Pacific Islander (0.2%), Hispanic or Latino (26.9%), multiracial (2.7%), White (31.2%), other (1.0%), and unknown or refused to specify (7.6%). Authors wrote that the cohort was followed-up to 2 years after illness onset and long-term results are not yet known.
Time to Exhale
David J. Goldberg, MD, with the Cardiac Center, Children’s Hospital of Philadelphia, Pennsylvania, and colleagues, wrote in an accompanying editorial that “the decreased frequency of the disease along (with) the reassuring reports on midterm outcomes can allow the pediatric community a moment of collective exhale.”
The editorialists note that of those who initially presented with myocardial dysfunction, all but one patient evaluated had a normal ejection fraction at follow-up. Energy, sleep, appetite, cognition, and mood also normalized by midterm.
“The results of the MUSIC study add to the emerging midterm outcomes data suggesting a near-complete cardiovascular recovery in the overwhelming majority of patients who develop MIS-C,” Goldberg and colleagues wrote. “Despite initial concerns, driven by the severity of acute presentation at diagnosis and longer-term questions that remain (for example, does coronary microvascular dysfunction persist even after normalization of coronary artery z score?), these data suggest an encouraging outlook for the long-term health of affected children.”
The Centers for Disease Control and Prevention and other agencies have reported a declining overall incidence of MIS-C and highlighted the protective value of vaccination.
The editorialists add, however, that while the drop in MIS-C cases is encouraging, cases are still reported, especially amid high viral activity periods, “and nearly half of affected children continue to require intensive care in the acute phase of illness.”
Truong reported grants from the National Institutes of Health and serving as coprincipal investigator for Pfizer for research on COVID-19 vaccine-associated myocarditis funded by Pfizer and occurring through the framework of the National Heart, Lung, and Blood Institute’s Pediatric Heart Network outside the submitted work. One coauthor reported grants from Pfizer and Boston Scientific outside the submitted work. One coauthor reported receiving grants from Additional Ventures Foundation outside the submitted work. One coauthor reported receiving consultant fees from Amryt Pharma, Chiesi, Esperion, and Ultragenyx outside the submitted work. A coauthor reported receiving consultant fees from Larimar Therapeutics for mitochondrial therapies outside the submitted work. One coauthor reported being an employee of Takeda Pharmaceuticals since July 2023. One editorialist reported grants from Childhood Arthritis and Rheumatology Research Alliance and the Arthritis Foundation, Academy Health, and the Gordon and Betty Moore Foundation during the conduct of the study.
A version of this article first appeared on Medscape.com.
Children who were severely ill with multisystem inflammatory syndrome in children (MIS-C) related to COVID-19 infection appear to show excellent cardiovascular and noncardiovascular outcomes by 6 months, according to data published in JAMA Pediatrics.
MIS-C is a life-threatening complication of COVID-19 infection and data on outcomes are limited, wrote the authors, led by Dongngan T. Truong, MD, MSSI, with Children’s Healthcare of Atlanta Cardiology, Emory University School of Medicine in Atlanta, Georgia. These 6-month results are from the Long-Term Outcomes After the Multisystem Inflammatory Syndrome in Children (MUSIC) study, sponsored by the National Heart, Lung, and Blood Institute.
Researchers found in this cohort study of 1204 participants that by 6 months after hospital discharge, 99% had normalization of left ventricular systolic function, and 92.3% had normalized coronary artery dimensions. More than 95% reported being more than 90% back to baseline health.
Patient-Reported Outcomes Measurement Information Systems (PROMIS) Global Health scores were at least equivalent to prepandemic population normative values. PROMIS Global Health parent/guardian proxy median T scores for fatigue, global health, and pain interference improved significantly from 2 weeks to 6 months: fatigue, 56.1 vs 48.9; global health, 48.8 vs 51.3; pain interference, 53.0 vs 43.3 (P < .001).
The most common symptoms reported at 2 weeks were fatigue (15.9%) and low stamina/energy (9.2%); both decreased to 3.4% and 3.3%, respectively, by 6 months. The most common cardiovascular symptom at 2 weeks was palpitations (1.5%), which decreased to 0.6%.
Chest Pain Increased Over Time
Reports of chest pain, however, reportedly increased over time, with 1.3% reporting chest pain at rest at 2 weeks and 2.2% at 6 months. Although gastrointestinal symptoms were common during the acute MIS-C, only 5.3% of respondents reported those symptoms at 2 weeks.
Children in the cohort had a median age of 9 years, and 60% were men. They self-identified with the following races and ethnicities: American Indian or Alaska Native (0.1%), Asian (3.3%), Black (27.0%), Hawaiian Native or Other Pacific Islander (0.2%), Hispanic or Latino (26.9%), multiracial (2.7%), White (31.2%), other (1.0%), and unknown or refused to specify (7.6%). Authors wrote that the cohort was followed-up to 2 years after illness onset and long-term results are not yet known.
Time to Exhale
David J. Goldberg, MD, with the Cardiac Center, Children’s Hospital of Philadelphia, Pennsylvania, and colleagues, wrote in an accompanying editorial that “the decreased frequency of the disease along (with) the reassuring reports on midterm outcomes can allow the pediatric community a moment of collective exhale.”
The editorialists note that of those who initially presented with myocardial dysfunction, all but one patient evaluated had a normal ejection fraction at follow-up. Energy, sleep, appetite, cognition, and mood also normalized by midterm.
“The results of the MUSIC study add to the emerging midterm outcomes data suggesting a near-complete cardiovascular recovery in the overwhelming majority of patients who develop MIS-C,” Goldberg and colleagues wrote. “Despite initial concerns, driven by the severity of acute presentation at diagnosis and longer-term questions that remain (for example, does coronary microvascular dysfunction persist even after normalization of coronary artery z score?), these data suggest an encouraging outlook for the long-term health of affected children.”
The Centers for Disease Control and Prevention and other agencies have reported a declining overall incidence of MIS-C and highlighted the protective value of vaccination.
The editorialists add, however, that while the drop in MIS-C cases is encouraging, cases are still reported, especially amid high viral activity periods, “and nearly half of affected children continue to require intensive care in the acute phase of illness.”
Truong reported grants from the National Institutes of Health and serving as coprincipal investigator for Pfizer for research on COVID-19 vaccine-associated myocarditis funded by Pfizer and occurring through the framework of the National Heart, Lung, and Blood Institute’s Pediatric Heart Network outside the submitted work. One coauthor reported grants from Pfizer and Boston Scientific outside the submitted work. One coauthor reported receiving grants from Additional Ventures Foundation outside the submitted work. One coauthor reported receiving consultant fees from Amryt Pharma, Chiesi, Esperion, and Ultragenyx outside the submitted work. A coauthor reported receiving consultant fees from Larimar Therapeutics for mitochondrial therapies outside the submitted work. One coauthor reported being an employee of Takeda Pharmaceuticals since July 2023. One editorialist reported grants from Childhood Arthritis and Rheumatology Research Alliance and the Arthritis Foundation, Academy Health, and the Gordon and Betty Moore Foundation during the conduct of the study.
A version of this article first appeared on Medscape.com.
Children who were severely ill with multisystem inflammatory syndrome in children (MIS-C) related to COVID-19 infection appear to show excellent cardiovascular and noncardiovascular outcomes by 6 months, according to data published in JAMA Pediatrics.
MIS-C is a life-threatening complication of COVID-19 infection and data on outcomes are limited, wrote the authors, led by Dongngan T. Truong, MD, MSSI, with Children’s Healthcare of Atlanta Cardiology, Emory University School of Medicine in Atlanta, Georgia. These 6-month results are from the Long-Term Outcomes After the Multisystem Inflammatory Syndrome in Children (MUSIC) study, sponsored by the National Heart, Lung, and Blood Institute.
Researchers found in this cohort study of 1204 participants that by 6 months after hospital discharge, 99% had normalization of left ventricular systolic function, and 92.3% had normalized coronary artery dimensions. More than 95% reported being more than 90% back to baseline health.
Patient-Reported Outcomes Measurement Information Systems (PROMIS) Global Health scores were at least equivalent to prepandemic population normative values. PROMIS Global Health parent/guardian proxy median T scores for fatigue, global health, and pain interference improved significantly from 2 weeks to 6 months: fatigue, 56.1 vs 48.9; global health, 48.8 vs 51.3; pain interference, 53.0 vs 43.3 (P < .001).
The most common symptoms reported at 2 weeks were fatigue (15.9%) and low stamina/energy (9.2%); both decreased to 3.4% and 3.3%, respectively, by 6 months. The most common cardiovascular symptom at 2 weeks was palpitations (1.5%), which decreased to 0.6%.
Chest Pain Increased Over Time
Reports of chest pain, however, reportedly increased over time, with 1.3% reporting chest pain at rest at 2 weeks and 2.2% at 6 months. Although gastrointestinal symptoms were common during the acute MIS-C, only 5.3% of respondents reported those symptoms at 2 weeks.
Children in the cohort had a median age of 9 years, and 60% were men. They self-identified with the following races and ethnicities: American Indian or Alaska Native (0.1%), Asian (3.3%), Black (27.0%), Hawaiian Native or Other Pacific Islander (0.2%), Hispanic or Latino (26.9%), multiracial (2.7%), White (31.2%), other (1.0%), and unknown or refused to specify (7.6%). Authors wrote that the cohort was followed-up to 2 years after illness onset and long-term results are not yet known.
Time to Exhale
David J. Goldberg, MD, with the Cardiac Center, Children’s Hospital of Philadelphia, Pennsylvania, and colleagues, wrote in an accompanying editorial that “the decreased frequency of the disease along (with) the reassuring reports on midterm outcomes can allow the pediatric community a moment of collective exhale.”
The editorialists note that of those who initially presented with myocardial dysfunction, all but one patient evaluated had a normal ejection fraction at follow-up. Energy, sleep, appetite, cognition, and mood also normalized by midterm.
“The results of the MUSIC study add to the emerging midterm outcomes data suggesting a near-complete cardiovascular recovery in the overwhelming majority of patients who develop MIS-C,” Goldberg and colleagues wrote. “Despite initial concerns, driven by the severity of acute presentation at diagnosis and longer-term questions that remain (for example, does coronary microvascular dysfunction persist even after normalization of coronary artery z score?), these data suggest an encouraging outlook for the long-term health of affected children.”
The Centers for Disease Control and Prevention and other agencies have reported a declining overall incidence of MIS-C and highlighted the protective value of vaccination.
The editorialists add, however, that while the drop in MIS-C cases is encouraging, cases are still reported, especially amid high viral activity periods, “and nearly half of affected children continue to require intensive care in the acute phase of illness.”
Truong reported grants from the National Institutes of Health and serving as coprincipal investigator for Pfizer for research on COVID-19 vaccine-associated myocarditis funded by Pfizer and occurring through the framework of the National Heart, Lung, and Blood Institute’s Pediatric Heart Network outside the submitted work. One coauthor reported grants from Pfizer and Boston Scientific outside the submitted work. One coauthor reported receiving grants from Additional Ventures Foundation outside the submitted work. One coauthor reported receiving consultant fees from Amryt Pharma, Chiesi, Esperion, and Ultragenyx outside the submitted work. A coauthor reported receiving consultant fees from Larimar Therapeutics for mitochondrial therapies outside the submitted work. One coauthor reported being an employee of Takeda Pharmaceuticals since July 2023. One editorialist reported grants from Childhood Arthritis and Rheumatology Research Alliance and the Arthritis Foundation, Academy Health, and the Gordon and Betty Moore Foundation during the conduct of the study.
A version of this article first appeared on Medscape.com.
FROM JAMA PEDIATRICS
High Radon Levels Linked to Gestational Diabetes
New data link higher county-level radon exposure to gestational diabetes (GD) in women who haven’t previously given birth, emphasizing the need to consider environmental risks in maternal and fetal healthcare.
Yijia Zhang, PhD, with the Department of Obstetrics and Gynecology, Vagelos College of Physicians and Surgeons at Columbia University Irving Medical Center in New York, and colleagues found in a study of 9107 nulliparous pregnant women that those living in US counties with higher radon levels (2 picocuries [pCi]/L) had higher odds of developing GD than those in counties with lower (< 1 pCi/L) radon levels (odds ratio [OR], 1.37; 95% CI, 1.02-1.84.) The researchers used three radon categories, and the middle level was 1 to < 2 pCi/L.
Findings were published online on January 10 in JAMA Network Open. The researchers used data from The Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a multicenter, prospective cohort study that examines factors associated with pregnancy-related outcomes.
“To our knowledge, this is the first study to examine the association between radon exposure and the risk of GD,” the authors wrote.
GD Affects 10% of Pregnancies
GD affects about 10% of pregnancies every year in the United States, according to the Centers for Disease Control and Prevention, and can affect women and offspring long term as it raises mothers’ risk of type 2 diabetes and cardiovascular disease and raises the risk for childhood obesity. Radon exposure’s link with lung cancer risk has been well established, but its link to other health risks is uncertain, the authors note.
The authors said their findings are hypothesis-generating and said, “It is vital to conduct studies that incorporate individual-level indoor radon exposure data,” to get closer to understanding the underlying mechanisms.
Individual-Level Exposure Measures Needed
They note that the average radon level in a county might not reflect an individual’s exposure and individual-level residential factors involved with radon exposure, such as household mitigation, and whether a dwelling has a basement, for instance, “are crucial for enhancing the precision of exposure assessment.”
In an invited commentary, Alberto Ruano-Ravina, PhD, and Lucía Martín-Gisbert, MSc, both with the Department of Preventive Medicine and Public Health at the University of Santiago de Compostela in Galicia, Spain, also urged that individual-level studies be conducted to further investigate radon’s link to health risks, noting that “[r]adon is possibly the most prevalent indoor carcinogen to which human beings are exposed.”
“There is no reason for not having these studies once we have some evidence of an association from ecological studies,” they wrote. They point out that reliable radon assessments are easy and inexpensive.
“The potential association of radon exposure with gestational diabetes or any other disease should be better analyzed using exclusively radon-prone areas. An observance of a dose-response effect may be indicative of a causal relationship, and it could be easily evidenced in radon-prone areas should such a relationship exist,” the commenters wrote.
Such areas have low, medium, high, and extremely high concentration levels, the commenters wrote. Zhang’s team, they point out, had to use only three exposure levels because the number of residents in high-exposure areas (exceeding 3 pCi/L) was too small.
“It is time now to move forward and really understand the full implications of radon exposure for health,” they concluded.
One coauthor reported serving on the board of directors for Merck for Mothers and as a board member for March for Moms outside the submitted work. One coauthor reported grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health (NIH) during the conduct of the study. Four coauthors reported grants from the NIH during the conduct of the study. One coauthor reported grants from the NIH during the conduct of the study and being a cofounder of Naima Health and receiving personal fees from Organon outside the submitted work. Both commenters reported no relevant financial disclosures.
A version of this article appeared on Medscape.com.
New data link higher county-level radon exposure to gestational diabetes (GD) in women who haven’t previously given birth, emphasizing the need to consider environmental risks in maternal and fetal healthcare.
Yijia Zhang, PhD, with the Department of Obstetrics and Gynecology, Vagelos College of Physicians and Surgeons at Columbia University Irving Medical Center in New York, and colleagues found in a study of 9107 nulliparous pregnant women that those living in US counties with higher radon levels (2 picocuries [pCi]/L) had higher odds of developing GD than those in counties with lower (< 1 pCi/L) radon levels (odds ratio [OR], 1.37; 95% CI, 1.02-1.84.) The researchers used three radon categories, and the middle level was 1 to < 2 pCi/L.
Findings were published online on January 10 in JAMA Network Open. The researchers used data from The Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a multicenter, prospective cohort study that examines factors associated with pregnancy-related outcomes.
“To our knowledge, this is the first study to examine the association between radon exposure and the risk of GD,” the authors wrote.
GD Affects 10% of Pregnancies
GD affects about 10% of pregnancies every year in the United States, according to the Centers for Disease Control and Prevention, and can affect women and offspring long term as it raises mothers’ risk of type 2 diabetes and cardiovascular disease and raises the risk for childhood obesity. Radon exposure’s link with lung cancer risk has been well established, but its link to other health risks is uncertain, the authors note.
The authors said their findings are hypothesis-generating and said, “It is vital to conduct studies that incorporate individual-level indoor radon exposure data,” to get closer to understanding the underlying mechanisms.
Individual-Level Exposure Measures Needed
They note that the average radon level in a county might not reflect an individual’s exposure and individual-level residential factors involved with radon exposure, such as household mitigation, and whether a dwelling has a basement, for instance, “are crucial for enhancing the precision of exposure assessment.”
In an invited commentary, Alberto Ruano-Ravina, PhD, and Lucía Martín-Gisbert, MSc, both with the Department of Preventive Medicine and Public Health at the University of Santiago de Compostela in Galicia, Spain, also urged that individual-level studies be conducted to further investigate radon’s link to health risks, noting that “[r]adon is possibly the most prevalent indoor carcinogen to which human beings are exposed.”
“There is no reason for not having these studies once we have some evidence of an association from ecological studies,” they wrote. They point out that reliable radon assessments are easy and inexpensive.
“The potential association of radon exposure with gestational diabetes or any other disease should be better analyzed using exclusively radon-prone areas. An observance of a dose-response effect may be indicative of a causal relationship, and it could be easily evidenced in radon-prone areas should such a relationship exist,” the commenters wrote.
Such areas have low, medium, high, and extremely high concentration levels, the commenters wrote. Zhang’s team, they point out, had to use only three exposure levels because the number of residents in high-exposure areas (exceeding 3 pCi/L) was too small.
“It is time now to move forward and really understand the full implications of radon exposure for health,” they concluded.
One coauthor reported serving on the board of directors for Merck for Mothers and as a board member for March for Moms outside the submitted work. One coauthor reported grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health (NIH) during the conduct of the study. Four coauthors reported grants from the NIH during the conduct of the study. One coauthor reported grants from the NIH during the conduct of the study and being a cofounder of Naima Health and receiving personal fees from Organon outside the submitted work. Both commenters reported no relevant financial disclosures.
A version of this article appeared on Medscape.com.
New data link higher county-level radon exposure to gestational diabetes (GD) in women who haven’t previously given birth, emphasizing the need to consider environmental risks in maternal and fetal healthcare.
Yijia Zhang, PhD, with the Department of Obstetrics and Gynecology, Vagelos College of Physicians and Surgeons at Columbia University Irving Medical Center in New York, and colleagues found in a study of 9107 nulliparous pregnant women that those living in US counties with higher radon levels (2 picocuries [pCi]/L) had higher odds of developing GD than those in counties with lower (< 1 pCi/L) radon levels (odds ratio [OR], 1.37; 95% CI, 1.02-1.84.) The researchers used three radon categories, and the middle level was 1 to < 2 pCi/L.
Findings were published online on January 10 in JAMA Network Open. The researchers used data from The Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-to-Be (nuMoM2b), a multicenter, prospective cohort study that examines factors associated with pregnancy-related outcomes.
“To our knowledge, this is the first study to examine the association between radon exposure and the risk of GD,” the authors wrote.
GD Affects 10% of Pregnancies
GD affects about 10% of pregnancies every year in the United States, according to the Centers for Disease Control and Prevention, and can affect women and offspring long term as it raises mothers’ risk of type 2 diabetes and cardiovascular disease and raises the risk for childhood obesity. Radon exposure’s link with lung cancer risk has been well established, but its link to other health risks is uncertain, the authors note.
The authors said their findings are hypothesis-generating and said, “It is vital to conduct studies that incorporate individual-level indoor radon exposure data,” to get closer to understanding the underlying mechanisms.
Individual-Level Exposure Measures Needed
They note that the average radon level in a county might not reflect an individual’s exposure and individual-level residential factors involved with radon exposure, such as household mitigation, and whether a dwelling has a basement, for instance, “are crucial for enhancing the precision of exposure assessment.”
In an invited commentary, Alberto Ruano-Ravina, PhD, and Lucía Martín-Gisbert, MSc, both with the Department of Preventive Medicine and Public Health at the University of Santiago de Compostela in Galicia, Spain, also urged that individual-level studies be conducted to further investigate radon’s link to health risks, noting that “[r]adon is possibly the most prevalent indoor carcinogen to which human beings are exposed.”
“There is no reason for not having these studies once we have some evidence of an association from ecological studies,” they wrote. They point out that reliable radon assessments are easy and inexpensive.
“The potential association of radon exposure with gestational diabetes or any other disease should be better analyzed using exclusively radon-prone areas. An observance of a dose-response effect may be indicative of a causal relationship, and it could be easily evidenced in radon-prone areas should such a relationship exist,” the commenters wrote.
Such areas have low, medium, high, and extremely high concentration levels, the commenters wrote. Zhang’s team, they point out, had to use only three exposure levels because the number of residents in high-exposure areas (exceeding 3 pCi/L) was too small.
“It is time now to move forward and really understand the full implications of radon exposure for health,” they concluded.
One coauthor reported serving on the board of directors for Merck for Mothers and as a board member for March for Moms outside the submitted work. One coauthor reported grants from the National Heart, Lung, and Blood Institute and the National Institutes of Health (NIH) during the conduct of the study. Four coauthors reported grants from the NIH during the conduct of the study. One coauthor reported grants from the NIH during the conduct of the study and being a cofounder of Naima Health and receiving personal fees from Organon outside the submitted work. Both commenters reported no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Meta-Analysis Finding of a Fluoride-IQ Link Controversial
Results published from a systematic review and meta-analysis find an inverse association and a dose-response link between fluoride exposure and children’s IQ scores.
Kyla W. Taylor, PhD, with the Division of Translational Toxicology at the National Institutes of Health, Morrisville, North Carolina, led the multicountry study published online in JAMA Pediatrics.
Two accompanying editorials offer two very different perspectives on how to interpret the researchers’ conclusions.
Study Results
The authors noted that, of the 74 studies included in the review (64 cross-sectional and 10 cohort studies), most (45) were conducted in China. Other countries included were Canada (3), Denmark (1), India (12), Iran (4), Mexico (4), New Zealand (1), Pakistan (2), Spain (1), and Taiwan (1). “Fifty-two studies were rated high risk of bias, and 22 were rated low risk of bias,” the authors stated.
Researchers found that 64 of the 74 studies reported inverse associations between fluoride exposure measures and children’s IQ scores. Their analysis of 59 studies with group-level measures of fluoride in drinking water, dental fluorosis, or other measures of fluoride exposure showed an inverse relationship between fluoride exposure and IQ (pooled standardized mean difference [SMD], −0.45; 95% CI, −0.57 to −0.33; P < .001). Of those 59 studies, encompassing 20,932 children, 47 had high risk for bias and 12 had low risk for bias.
In 31 studies that reported fluoride measurements in drinking water, a dose-response relationship was found between exposed and reference groups (SMD, –0.15; 95% CI, –0.20 to –0.11; P < .001). That relationship remained inverse when exposed groups were limited to less than 4 mg fluoride/L and less than 2 mg/L. However, the association was not seen at less than 1.5 mg/L.
In 20 studies reporting fluoride measured in urine, there was an inverse dose-response association (SMD, –0.15; 95% CI, –0.23 to –0.07; P < .001). Those inverse relationships held at levels less than 4 mg/L, less than 2 mg/L, and less than 1.5 mg/L fluoride in urine.
For perspective, in the United States, the US Public Health Service in 2015 lowered the recommended concentration of fluoride in drinking water from a range of 0.7-1.2 mg/L to 0.7 mg/L to reduce the risk for dental fluorosis while keeping its protective effect against dental caries.
When Taylor’s team analyzed 13 studies with individual-level measures, they found an IQ score decrease of 1.63 points (95% CI, –2.33 to –0.93; P < .001) per 1-mg/L increase in urinary fluoride. Among studies with a low risk for bias, they observed an IQ score decrease of 1.14 points (95% CI, –1.68 to –0.61; P < .001). The inverse relationship remained when stratified by factors including risk for bias, sex, age, country, outcome assessment type, exposure timing (prenatal or postnatal), and exposure matrix (urinary fluoride, intake and water fluoride), the authors wrote.
The authors conclude both that inverse relationships and a dose-response association between fluoride measured in urine and drinking water and children’s IQs were found across the literature examined but also that “there were limited data and uncertainty in the dose-response association between fluoride exposure and children’s IQ when fluoride exposure was estimated by drinking water alone at concentrations less than 1.5 mg/L.”
The authors point out that, “To our knowledge, no studies of fluoride exposure and children’s IQ have been performed in the United States and no nationally representative urinary fluoride levels are available, hindering application of these findings to the US population.”
Editorial: Time to Reassess Systemic Fluoride
Bruce P. Lanphear, MD, MPH, with Simon Fraser University, Vancouver, British Columbia, Canada, is the lead author on an editorial that suggests these data point to the need to reassess systemic fluoride exposure.
“Their study is the largest and includes the most rigorous series of meta-analyses of fluoride ever conducted,” Lanphear and colleagues wrote. “It is time for health organizations and regulatory bodies to reassess the risks and benefits of fluoride, particularly for pregnant women and infants.”
Lanphear’s team says distinguishing between water fluoride and urinary fluoride levels is important in these results “because regulatory and public health agencies must consider total fluoride intake when assessing risks.”
Taylor and colleagues’ finding that there was no statistically significant association between water fluoride les than 1.5 mg/L and children’s IQ scores in the dose-response meta-analysis doesn’t mean fluoride is not a potential risk for lower IQ scores in fluoridated communities, they wrote. “Water fluoride concentration does not capture the amount of water ingested or other sources of ingested fluoride. In contrast, urinary fluoride is a biological measure of total fluoride exposure, including the dynamic interface between bone fluoride stores and blood fluoride.”
Editorial: Be Cautious About the Conclusions
Steven M. Levy, DDS, MPH, cites “major areas of concern” in the meta-analysis in his editorial.
He points to the large majority of studies in the meta-analysis that were at “high risk of bias” (47 high risk vs 12 that were low risk). He also cited information from a further look at the low-risk-of-bias studies included in the supplement.
“The studies with lower risk of bias showed a negligible effect (standardized mean difference [SMD], −0.19; 95% CI, −0.35 to −0.04) with very high heterogeneity (I2 = 87%), and a majority of publications (8 of 12) did not show a negative association between fluoride and childhood IQ,” Levy wrote.
“Taylor et al do not adequately justify selection or omission of studies or explain or justify the calculated individual effect sizes presented in the main analysis. Also, readers are not told which studies with lower risk of bias are included in the subanalyses for water fluoride levels less than 1.5 mg/L, less than 2.0 mg/L, and less than 4.0 mg/L; therefore, readers cannot independently consider important differences across these studies.”
Levy also states that the magnitudes of the possible IQ differences are unfairly inflated. For the United Staes and most of the world, he points out, the recommended community water fluoridation level is 0.7 mg/L. Therefore, the difference between a community with low fluoride levels (about 0.2 mg/L) and one with optimal levels is about 0.5 mg/L.
“However, Taylor and colleagues use a difference of 1.0 mg/L in their calculations, artificially doubling the estimated impact on IQ,” Levy wrote.
The meta-analysis should not affect public policy on adding fluoride to community water systems “and the widespread use of fluoride for caries prevention should continue,” Levy concluded.
Concerns About Quality of Studies Included
Charlotte Lewis, MD, MPH, associate professor of pediatrics at the University of Washington School of Medicine and part of Seattle Children’s Multidisciplinary Infant Nutrition and Feeding Team, Seattle, who was not involved in the meta-analysis or editorials, said that systemic fluoridation should not change based on these results, citing what she said are problems with methodology.
“There are many concerns about the quality of studies included in this meta-analysis,” Lewis said. “Although the authors claim to have separated out low-bias studies, it is important to note that many of these same studies have substantial methodological flaws.”
She said studies deemed low-bias and included in the meta-analysis “relied on multiple examiners for cognitive testing without consideration for inter-rater variation or reliability measures.” She added that “a number of the studies failed to account for maternal IQ scores, breastfeeding, lead exposure, or other factors that could affect cognitive development, further contributing to biased conclusions.”
Importantly, she said, many of the studies, including one by Rivka Green and colleagues published in JAMA Pediatrics, relied on maternal spot urinary fluoride to assess fetal exposure to fluoride. “This is not a valid way to assess fetal exposure to fluoride and including such studies in this meta-analysis has led to inappropriate conclusions because they are based on studies using a flawed exposure measure.”
She pointed to recent longitudinal, population-based studies, including one by Jayant V Kumar and colleagues that have found no adverse impact on IQ, or other cognitive tests, of drinking water with low levels of fluoride present, comparable to US community water fluoridation standards.
“Relative to the small convenience-sample, cross-sectional studies included in this meta-analysis, longitudinal, population-based studies are considered significantly more reliable for establishing cause and effect,” she said.
Fluoride Levels Different Globally
Lewis said in some parts of the world fluoride is present in the environment in much higher levels than in fluoridated water in the United States.
“There are known adverse health effects of high fluoride ingestion in these endemic regions found primarily in China, India, and Iran. This points to the importance of dose response. What is beneficial at low levels can be toxic at high levels and that appears to be the case, not surprisingly, for fluoride as well. However, at 0.7 ppm, the level of fluoride in community water fluoridation, we experience fluoride’s beneficial effects when we regularly drink optimally fluoridated water.”
“Water fluoridation is an important public health approach available and beneficial to all, even those unable to afford or access dental care,” she said. “Water fluoridation diminishes oral health disparities, and its removal threatens to worsen disparities and increased suffering from dental disease. I remain confident in the benefits and safety of community water fluoridation.”
Taylor and colleagues reported no relevant financial relationships. Lanphear reported grants from the National Institute of Environmental Health Sciences and the Canadian Institute for Health Research and having served as a nonretained and unpaid expert witness in a federal fluoride suit against the US EPA. Levy reported past grants from the National Institute of Dental and Craniofacial Research related to fluoride, dental caries, dental fluorosis, and bone development. He reported small grant funding from the Centers for Disease Control and Prevention related to fluoride, dental caries, and fluorosis. He consults for the Centers for Disease Control and Prevention and the National Institute of Dental and Craniofacial Research and serves on the National Fluoride Advisory Committee for the American Dental Association.
A version of this article appeared on Medscape.com.
Results published from a systematic review and meta-analysis find an inverse association and a dose-response link between fluoride exposure and children’s IQ scores.
Kyla W. Taylor, PhD, with the Division of Translational Toxicology at the National Institutes of Health, Morrisville, North Carolina, led the multicountry study published online in JAMA Pediatrics.
Two accompanying editorials offer two very different perspectives on how to interpret the researchers’ conclusions.
Study Results
The authors noted that, of the 74 studies included in the review (64 cross-sectional and 10 cohort studies), most (45) were conducted in China. Other countries included were Canada (3), Denmark (1), India (12), Iran (4), Mexico (4), New Zealand (1), Pakistan (2), Spain (1), and Taiwan (1). “Fifty-two studies were rated high risk of bias, and 22 were rated low risk of bias,” the authors stated.
Researchers found that 64 of the 74 studies reported inverse associations between fluoride exposure measures and children’s IQ scores. Their analysis of 59 studies with group-level measures of fluoride in drinking water, dental fluorosis, or other measures of fluoride exposure showed an inverse relationship between fluoride exposure and IQ (pooled standardized mean difference [SMD], −0.45; 95% CI, −0.57 to −0.33; P < .001). Of those 59 studies, encompassing 20,932 children, 47 had high risk for bias and 12 had low risk for bias.
In 31 studies that reported fluoride measurements in drinking water, a dose-response relationship was found between exposed and reference groups (SMD, –0.15; 95% CI, –0.20 to –0.11; P < .001). That relationship remained inverse when exposed groups were limited to less than 4 mg fluoride/L and less than 2 mg/L. However, the association was not seen at less than 1.5 mg/L.
In 20 studies reporting fluoride measured in urine, there was an inverse dose-response association (SMD, –0.15; 95% CI, –0.23 to –0.07; P < .001). Those inverse relationships held at levels less than 4 mg/L, less than 2 mg/L, and less than 1.5 mg/L fluoride in urine.
For perspective, in the United States, the US Public Health Service in 2015 lowered the recommended concentration of fluoride in drinking water from a range of 0.7-1.2 mg/L to 0.7 mg/L to reduce the risk for dental fluorosis while keeping its protective effect against dental caries.
When Taylor’s team analyzed 13 studies with individual-level measures, they found an IQ score decrease of 1.63 points (95% CI, –2.33 to –0.93; P < .001) per 1-mg/L increase in urinary fluoride. Among studies with a low risk for bias, they observed an IQ score decrease of 1.14 points (95% CI, –1.68 to –0.61; P < .001). The inverse relationship remained when stratified by factors including risk for bias, sex, age, country, outcome assessment type, exposure timing (prenatal or postnatal), and exposure matrix (urinary fluoride, intake and water fluoride), the authors wrote.
The authors conclude both that inverse relationships and a dose-response association between fluoride measured in urine and drinking water and children’s IQs were found across the literature examined but also that “there were limited data and uncertainty in the dose-response association between fluoride exposure and children’s IQ when fluoride exposure was estimated by drinking water alone at concentrations less than 1.5 mg/L.”
The authors point out that, “To our knowledge, no studies of fluoride exposure and children’s IQ have been performed in the United States and no nationally representative urinary fluoride levels are available, hindering application of these findings to the US population.”
Editorial: Time to Reassess Systemic Fluoride
Bruce P. Lanphear, MD, MPH, with Simon Fraser University, Vancouver, British Columbia, Canada, is the lead author on an editorial that suggests these data point to the need to reassess systemic fluoride exposure.
“Their study is the largest and includes the most rigorous series of meta-analyses of fluoride ever conducted,” Lanphear and colleagues wrote. “It is time for health organizations and regulatory bodies to reassess the risks and benefits of fluoride, particularly for pregnant women and infants.”
Lanphear’s team says distinguishing between water fluoride and urinary fluoride levels is important in these results “because regulatory and public health agencies must consider total fluoride intake when assessing risks.”
Taylor and colleagues’ finding that there was no statistically significant association between water fluoride les than 1.5 mg/L and children’s IQ scores in the dose-response meta-analysis doesn’t mean fluoride is not a potential risk for lower IQ scores in fluoridated communities, they wrote. “Water fluoride concentration does not capture the amount of water ingested or other sources of ingested fluoride. In contrast, urinary fluoride is a biological measure of total fluoride exposure, including the dynamic interface between bone fluoride stores and blood fluoride.”
Editorial: Be Cautious About the Conclusions
Steven M. Levy, DDS, MPH, cites “major areas of concern” in the meta-analysis in his editorial.
He points to the large majority of studies in the meta-analysis that were at “high risk of bias” (47 high risk vs 12 that were low risk). He also cited information from a further look at the low-risk-of-bias studies included in the supplement.
“The studies with lower risk of bias showed a negligible effect (standardized mean difference [SMD], −0.19; 95% CI, −0.35 to −0.04) with very high heterogeneity (I2 = 87%), and a majority of publications (8 of 12) did not show a negative association between fluoride and childhood IQ,” Levy wrote.
“Taylor et al do not adequately justify selection or omission of studies or explain or justify the calculated individual effect sizes presented in the main analysis. Also, readers are not told which studies with lower risk of bias are included in the subanalyses for water fluoride levels less than 1.5 mg/L, less than 2.0 mg/L, and less than 4.0 mg/L; therefore, readers cannot independently consider important differences across these studies.”
Levy also states that the magnitudes of the possible IQ differences are unfairly inflated. For the United Staes and most of the world, he points out, the recommended community water fluoridation level is 0.7 mg/L. Therefore, the difference between a community with low fluoride levels (about 0.2 mg/L) and one with optimal levels is about 0.5 mg/L.
“However, Taylor and colleagues use a difference of 1.0 mg/L in their calculations, artificially doubling the estimated impact on IQ,” Levy wrote.
The meta-analysis should not affect public policy on adding fluoride to community water systems “and the widespread use of fluoride for caries prevention should continue,” Levy concluded.
Concerns About Quality of Studies Included
Charlotte Lewis, MD, MPH, associate professor of pediatrics at the University of Washington School of Medicine and part of Seattle Children’s Multidisciplinary Infant Nutrition and Feeding Team, Seattle, who was not involved in the meta-analysis or editorials, said that systemic fluoridation should not change based on these results, citing what she said are problems with methodology.
“There are many concerns about the quality of studies included in this meta-analysis,” Lewis said. “Although the authors claim to have separated out low-bias studies, it is important to note that many of these same studies have substantial methodological flaws.”
She said studies deemed low-bias and included in the meta-analysis “relied on multiple examiners for cognitive testing without consideration for inter-rater variation or reliability measures.” She added that “a number of the studies failed to account for maternal IQ scores, breastfeeding, lead exposure, or other factors that could affect cognitive development, further contributing to biased conclusions.”
Importantly, she said, many of the studies, including one by Rivka Green and colleagues published in JAMA Pediatrics, relied on maternal spot urinary fluoride to assess fetal exposure to fluoride. “This is not a valid way to assess fetal exposure to fluoride and including such studies in this meta-analysis has led to inappropriate conclusions because they are based on studies using a flawed exposure measure.”
She pointed to recent longitudinal, population-based studies, including one by Jayant V Kumar and colleagues that have found no adverse impact on IQ, or other cognitive tests, of drinking water with low levels of fluoride present, comparable to US community water fluoridation standards.
“Relative to the small convenience-sample, cross-sectional studies included in this meta-analysis, longitudinal, population-based studies are considered significantly more reliable for establishing cause and effect,” she said.
Fluoride Levels Different Globally
Lewis said in some parts of the world fluoride is present in the environment in much higher levels than in fluoridated water in the United States.
“There are known adverse health effects of high fluoride ingestion in these endemic regions found primarily in China, India, and Iran. This points to the importance of dose response. What is beneficial at low levels can be toxic at high levels and that appears to be the case, not surprisingly, for fluoride as well. However, at 0.7 ppm, the level of fluoride in community water fluoridation, we experience fluoride’s beneficial effects when we regularly drink optimally fluoridated water.”
“Water fluoridation is an important public health approach available and beneficial to all, even those unable to afford or access dental care,” she said. “Water fluoridation diminishes oral health disparities, and its removal threatens to worsen disparities and increased suffering from dental disease. I remain confident in the benefits and safety of community water fluoridation.”
Taylor and colleagues reported no relevant financial relationships. Lanphear reported grants from the National Institute of Environmental Health Sciences and the Canadian Institute for Health Research and having served as a nonretained and unpaid expert witness in a federal fluoride suit against the US EPA. Levy reported past grants from the National Institute of Dental and Craniofacial Research related to fluoride, dental caries, dental fluorosis, and bone development. He reported small grant funding from the Centers for Disease Control and Prevention related to fluoride, dental caries, and fluorosis. He consults for the Centers for Disease Control and Prevention and the National Institute of Dental and Craniofacial Research and serves on the National Fluoride Advisory Committee for the American Dental Association.
A version of this article appeared on Medscape.com.
Results published from a systematic review and meta-analysis find an inverse association and a dose-response link between fluoride exposure and children’s IQ scores.
Kyla W. Taylor, PhD, with the Division of Translational Toxicology at the National Institutes of Health, Morrisville, North Carolina, led the multicountry study published online in JAMA Pediatrics.
Two accompanying editorials offer two very different perspectives on how to interpret the researchers’ conclusions.
Study Results
The authors noted that, of the 74 studies included in the review (64 cross-sectional and 10 cohort studies), most (45) were conducted in China. Other countries included were Canada (3), Denmark (1), India (12), Iran (4), Mexico (4), New Zealand (1), Pakistan (2), Spain (1), and Taiwan (1). “Fifty-two studies were rated high risk of bias, and 22 were rated low risk of bias,” the authors stated.
Researchers found that 64 of the 74 studies reported inverse associations between fluoride exposure measures and children’s IQ scores. Their analysis of 59 studies with group-level measures of fluoride in drinking water, dental fluorosis, or other measures of fluoride exposure showed an inverse relationship between fluoride exposure and IQ (pooled standardized mean difference [SMD], −0.45; 95% CI, −0.57 to −0.33; P < .001). Of those 59 studies, encompassing 20,932 children, 47 had high risk for bias and 12 had low risk for bias.
In 31 studies that reported fluoride measurements in drinking water, a dose-response relationship was found between exposed and reference groups (SMD, –0.15; 95% CI, –0.20 to –0.11; P < .001). That relationship remained inverse when exposed groups were limited to less than 4 mg fluoride/L and less than 2 mg/L. However, the association was not seen at less than 1.5 mg/L.
In 20 studies reporting fluoride measured in urine, there was an inverse dose-response association (SMD, –0.15; 95% CI, –0.23 to –0.07; P < .001). Those inverse relationships held at levels less than 4 mg/L, less than 2 mg/L, and less than 1.5 mg/L fluoride in urine.
For perspective, in the United States, the US Public Health Service in 2015 lowered the recommended concentration of fluoride in drinking water from a range of 0.7-1.2 mg/L to 0.7 mg/L to reduce the risk for dental fluorosis while keeping its protective effect against dental caries.
When Taylor’s team analyzed 13 studies with individual-level measures, they found an IQ score decrease of 1.63 points (95% CI, –2.33 to –0.93; P < .001) per 1-mg/L increase in urinary fluoride. Among studies with a low risk for bias, they observed an IQ score decrease of 1.14 points (95% CI, –1.68 to –0.61; P < .001). The inverse relationship remained when stratified by factors including risk for bias, sex, age, country, outcome assessment type, exposure timing (prenatal or postnatal), and exposure matrix (urinary fluoride, intake and water fluoride), the authors wrote.
The authors conclude both that inverse relationships and a dose-response association between fluoride measured in urine and drinking water and children’s IQs were found across the literature examined but also that “there were limited data and uncertainty in the dose-response association between fluoride exposure and children’s IQ when fluoride exposure was estimated by drinking water alone at concentrations less than 1.5 mg/L.”
The authors point out that, “To our knowledge, no studies of fluoride exposure and children’s IQ have been performed in the United States and no nationally representative urinary fluoride levels are available, hindering application of these findings to the US population.”
Editorial: Time to Reassess Systemic Fluoride
Bruce P. Lanphear, MD, MPH, with Simon Fraser University, Vancouver, British Columbia, Canada, is the lead author on an editorial that suggests these data point to the need to reassess systemic fluoride exposure.
“Their study is the largest and includes the most rigorous series of meta-analyses of fluoride ever conducted,” Lanphear and colleagues wrote. “It is time for health organizations and regulatory bodies to reassess the risks and benefits of fluoride, particularly for pregnant women and infants.”
Lanphear’s team says distinguishing between water fluoride and urinary fluoride levels is important in these results “because regulatory and public health agencies must consider total fluoride intake when assessing risks.”
Taylor and colleagues’ finding that there was no statistically significant association between water fluoride les than 1.5 mg/L and children’s IQ scores in the dose-response meta-analysis doesn’t mean fluoride is not a potential risk for lower IQ scores in fluoridated communities, they wrote. “Water fluoride concentration does not capture the amount of water ingested or other sources of ingested fluoride. In contrast, urinary fluoride is a biological measure of total fluoride exposure, including the dynamic interface between bone fluoride stores and blood fluoride.”
Editorial: Be Cautious About the Conclusions
Steven M. Levy, DDS, MPH, cites “major areas of concern” in the meta-analysis in his editorial.
He points to the large majority of studies in the meta-analysis that were at “high risk of bias” (47 high risk vs 12 that were low risk). He also cited information from a further look at the low-risk-of-bias studies included in the supplement.
“The studies with lower risk of bias showed a negligible effect (standardized mean difference [SMD], −0.19; 95% CI, −0.35 to −0.04) with very high heterogeneity (I2 = 87%), and a majority of publications (8 of 12) did not show a negative association between fluoride and childhood IQ,” Levy wrote.
“Taylor et al do not adequately justify selection or omission of studies or explain or justify the calculated individual effect sizes presented in the main analysis. Also, readers are not told which studies with lower risk of bias are included in the subanalyses for water fluoride levels less than 1.5 mg/L, less than 2.0 mg/L, and less than 4.0 mg/L; therefore, readers cannot independently consider important differences across these studies.”
Levy also states that the magnitudes of the possible IQ differences are unfairly inflated. For the United Staes and most of the world, he points out, the recommended community water fluoridation level is 0.7 mg/L. Therefore, the difference between a community with low fluoride levels (about 0.2 mg/L) and one with optimal levels is about 0.5 mg/L.
“However, Taylor and colleagues use a difference of 1.0 mg/L in their calculations, artificially doubling the estimated impact on IQ,” Levy wrote.
The meta-analysis should not affect public policy on adding fluoride to community water systems “and the widespread use of fluoride for caries prevention should continue,” Levy concluded.
Concerns About Quality of Studies Included
Charlotte Lewis, MD, MPH, associate professor of pediatrics at the University of Washington School of Medicine and part of Seattle Children’s Multidisciplinary Infant Nutrition and Feeding Team, Seattle, who was not involved in the meta-analysis or editorials, said that systemic fluoridation should not change based on these results, citing what she said are problems with methodology.
“There are many concerns about the quality of studies included in this meta-analysis,” Lewis said. “Although the authors claim to have separated out low-bias studies, it is important to note that many of these same studies have substantial methodological flaws.”
She said studies deemed low-bias and included in the meta-analysis “relied on multiple examiners for cognitive testing without consideration for inter-rater variation or reliability measures.” She added that “a number of the studies failed to account for maternal IQ scores, breastfeeding, lead exposure, or other factors that could affect cognitive development, further contributing to biased conclusions.”
Importantly, she said, many of the studies, including one by Rivka Green and colleagues published in JAMA Pediatrics, relied on maternal spot urinary fluoride to assess fetal exposure to fluoride. “This is not a valid way to assess fetal exposure to fluoride and including such studies in this meta-analysis has led to inappropriate conclusions because they are based on studies using a flawed exposure measure.”
She pointed to recent longitudinal, population-based studies, including one by Jayant V Kumar and colleagues that have found no adverse impact on IQ, or other cognitive tests, of drinking water with low levels of fluoride present, comparable to US community water fluoridation standards.
“Relative to the small convenience-sample, cross-sectional studies included in this meta-analysis, longitudinal, population-based studies are considered significantly more reliable for establishing cause and effect,” she said.
Fluoride Levels Different Globally
Lewis said in some parts of the world fluoride is present in the environment in much higher levels than in fluoridated water in the United States.
“There are known adverse health effects of high fluoride ingestion in these endemic regions found primarily in China, India, and Iran. This points to the importance of dose response. What is beneficial at low levels can be toxic at high levels and that appears to be the case, not surprisingly, for fluoride as well. However, at 0.7 ppm, the level of fluoride in community water fluoridation, we experience fluoride’s beneficial effects when we regularly drink optimally fluoridated water.”
“Water fluoridation is an important public health approach available and beneficial to all, even those unable to afford or access dental care,” she said. “Water fluoridation diminishes oral health disparities, and its removal threatens to worsen disparities and increased suffering from dental disease. I remain confident in the benefits and safety of community water fluoridation.”
Taylor and colleagues reported no relevant financial relationships. Lanphear reported grants from the National Institute of Environmental Health Sciences and the Canadian Institute for Health Research and having served as a nonretained and unpaid expert witness in a federal fluoride suit against the US EPA. Levy reported past grants from the National Institute of Dental and Craniofacial Research related to fluoride, dental caries, dental fluorosis, and bone development. He reported small grant funding from the Centers for Disease Control and Prevention related to fluoride, dental caries, and fluorosis. He consults for the Centers for Disease Control and Prevention and the National Institute of Dental and Craniofacial Research and serves on the National Fluoride Advisory Committee for the American Dental Association.
A version of this article appeared on Medscape.com.
FROM JAMA PEDIATRICS
Why Aren’t More Primary Care Physicians Prescribing Contraceptives?
In 2024, the Guttmacher Institute reported that eight states enacted or proposed limits on contraceptive access. Currently, more than 19 million women aged 13-44 years in the United States live in “contraceptive deserts” or places that lack access to a full range of birth control methods. About 1.2 million of those women live in counties that don’t have a single health center that has complete birth control services.
Providing contraceptive care in primary care settings has long been deemed a best practice by the Centers for Disease Control and Prevention (CDC). But the percentage of primary care physicians (PCPs) prescribing contraception or offering contraceptive procedures is strikingly low.
Only Half of Family Physicians (FPs) Prescribe Contraceptives
Research by Candice Chen, MD, MPH, and colleagues found that while 73.1% of obstetrician-gynecologists (OB/GYNs) and 72.6% of nurse-midwives prescribed the pill, patch, or vaginal ring; only 51% of FPs, 32.4% of pediatricians, and 19.8% of internal medicine physicians did so. And while 92.8% of OB/GYNs provided intrauterine device (IUD) services, only 16.4% of FPs, 2.6% of internists, and 0.6% of pediatricians did so.
One reason primary care is positioned so well to fill contraception gaps is found in the sheer numbers of PCPs. Chen and colleagues found that while the percentage of FPs prescribing contraception was much smaller (51.4%) than the percentage of OB/GYN prescribers (72.6%), the numbers translate to 72,725 FPs prescribing contraceptives, which is nearly double the number of OB/GYNs prescribing them (36,887).
Access to contraception services took a big hit with the COVID-19 pandemic as did access to healthcare in general. And the 2022 Supreme Court ruling that struck down Roe V. Wade has shaken up the landscape for reproductive services with potential consequences for contraceptive access.
Why Aren’t More PCPs Offering Contraceptive Services?
Reasons for the relatively low numbers of PCPs prescribing contraceptives include lack of training in residency, health systems’ financial choices, insurance barriers, and expectation by some physicians and many patients that birth control belongs in the OB/GYN sector. Access, patient awareness that PCPs can provide the care, expectations, and options vary by states and regions.
Angeline Ti, MD, an FP who teaches in a residency program at Wellstar Douglasville Medical Center in Douglasville, Georgia, told this news organization that the awareness issue might be the easiest change for PCPs as many patients aren’t aware you can get contraceptive services in primary care.
Things PCPs ‘Could Do Tomorrow’
Those physicians who want to add those services might want to start with universal screening, Ti said — having conversations with patients about contraceptive needs and letting them know they don’t have to get those prescriptions from an OB/GYN. The conversations could center on laying out the options and counseling on risks and benefits of various options and providing referrals, if that is the best option. “There are definitely things that you could do tomorrow,” she said.
PCPs should be familiar with the CDC’s Contraceptive Guidance for Health Care Providers and the federal Office of Population Affairs’ Quality Family Planning Recommendations for providers, which offer practice-level information, Ti said.
PCPs should not feel they need to be able to provide same-day contraceptive care to get started. Having nurses and medical assistants and practice managers on board who are passionate about adding the services can also help bring about change with a team approach, she said.
Even when the provider is enthusiastic about providing the care and is trained to do so, however, insurance barriers may exist, Ti acknowledged. For example, at her clinic a common IUD insertion requires prior authorization.
Including Other Providers
Julia Strasser, DrPH, MPH, a member of the core faculty at the Fitzhugh Mullan Institute for Health Workforce Equity in Washington, DC, told this news organization that including other clinicians could help expand contraceptive services in primary care. Her research showed that the proportion of the contraception workforce that is made up of advanced practice clinicians and nurse practitioners is increasing, whereas the proportion that includes physicians is either static or declining.
A paper by her team found that although OB/GYNs and nurse-midwives were more likely to prescribe the pill, patch, or ring, the largest numbers of contraception prescribers were FPs (72,725) and advanced practice nurses (70,115).
“We also know that pharmacists can safely prescribe contraception, and some states have authorized this practice, but uptake is low and policies vary by state,” she said. “Some health systems have pharmacists embedded in their practice — for example in federally qualified health centers and others.”
It’s important, she said, not to frame the gaps in contraceptive care as a failure on the part of individual clinicians but rather as: “How can we change some of the system-level factors that have gotten us to this point?”
Yalda Jabbarpour, MD, an FP and director of the Robert Graham Center of the American Academy of Family Physicians, said sometimes it’s the health center’s cost analysis that stands in the way. She gave an example from her own health system.
“The health system doesn’t want to pay for us to have the IUDs stored in our offices and provide that procedure because they feel it’s more cost effective if the OB/GYNs do it.” IUD insertions take more appointment time than the standard appointment, which also goes into the cost analysis. “Even though you’re trained to do it, you can’t necessarily do it when you get to the real world,” Jabbarpour said.
She said the thinking is that while OB/GYNs focus on women, FPs cover all ages and family members, so having the equipment and the storage space is best left to the OB/GYNs. She said that thinking may be short sighted.
“We have good data that the highest number of office visits in the United States actually happen in the family physician’s office,” she said. Not providing the services injects a barrier into the system as women are being referred for a simple procedure to a physician they’ve never seen. “That’s not very patient centered,” Jabbarpour noted.
In systems that refer contraceptive procedures to OB/GYNs, doctors also can’t practice skills they learned in residency and then may not feel comfortable performing the procedures when they enter a health system that offers the procedures in primary care.
Number of FPs Prescribing Long-Acting Contraception Growing
Jabbarpour said there has been some improvement in that area in terms of long-acting reversible contraception.
She pointed to a study of recertifying FPs that found that the percent of FPs who offer either IUDs or implants increased from 23.9% in 2018 to 30% in 2022. The share of FPs providing implant insertion increased from 12.9% to 20.8%; those providing IUDs also increased from 22.9% to 25.5% from 2018 to 2022.
FPs also have the advantage of being more widely distributed in rural and remote areas than OB/GYNs, she noted. “They are in almost every county in the United States.”
Jabbarpour said the education must start with health system leaders. If they deem it important to offer these services in primary care, then residency programs will see that their residents must be appropriately trained to provide it.
“Right now, it’s not an expectation of many of the employers that primary care physicians should do this,” she said.
Ti said that expectation should change. The value proposition for all PCPs and health systems, she said, is this: “Most of contraceptive care is well within the scope of primary care providers. This is care that we can do, and it’s care that we should be doing. So why aren’t we doing it?”
Ti, Strasser, and Jabbarpour reported no relevant financial disclosures.
A version of this article appeared on Medscape.com.
In 2024, the Guttmacher Institute reported that eight states enacted or proposed limits on contraceptive access. Currently, more than 19 million women aged 13-44 years in the United States live in “contraceptive deserts” or places that lack access to a full range of birth control methods. About 1.2 million of those women live in counties that don’t have a single health center that has complete birth control services.
Providing contraceptive care in primary care settings has long been deemed a best practice by the Centers for Disease Control and Prevention (CDC). But the percentage of primary care physicians (PCPs) prescribing contraception or offering contraceptive procedures is strikingly low.
Only Half of Family Physicians (FPs) Prescribe Contraceptives
Research by Candice Chen, MD, MPH, and colleagues found that while 73.1% of obstetrician-gynecologists (OB/GYNs) and 72.6% of nurse-midwives prescribed the pill, patch, or vaginal ring; only 51% of FPs, 32.4% of pediatricians, and 19.8% of internal medicine physicians did so. And while 92.8% of OB/GYNs provided intrauterine device (IUD) services, only 16.4% of FPs, 2.6% of internists, and 0.6% of pediatricians did so.
One reason primary care is positioned so well to fill contraception gaps is found in the sheer numbers of PCPs. Chen and colleagues found that while the percentage of FPs prescribing contraception was much smaller (51.4%) than the percentage of OB/GYN prescribers (72.6%), the numbers translate to 72,725 FPs prescribing contraceptives, which is nearly double the number of OB/GYNs prescribing them (36,887).
Access to contraception services took a big hit with the COVID-19 pandemic as did access to healthcare in general. And the 2022 Supreme Court ruling that struck down Roe V. Wade has shaken up the landscape for reproductive services with potential consequences for contraceptive access.
Why Aren’t More PCPs Offering Contraceptive Services?
Reasons for the relatively low numbers of PCPs prescribing contraceptives include lack of training in residency, health systems’ financial choices, insurance barriers, and expectation by some physicians and many patients that birth control belongs in the OB/GYN sector. Access, patient awareness that PCPs can provide the care, expectations, and options vary by states and regions.
Angeline Ti, MD, an FP who teaches in a residency program at Wellstar Douglasville Medical Center in Douglasville, Georgia, told this news organization that the awareness issue might be the easiest change for PCPs as many patients aren’t aware you can get contraceptive services in primary care.
Things PCPs ‘Could Do Tomorrow’
Those physicians who want to add those services might want to start with universal screening, Ti said — having conversations with patients about contraceptive needs and letting them know they don’t have to get those prescriptions from an OB/GYN. The conversations could center on laying out the options and counseling on risks and benefits of various options and providing referrals, if that is the best option. “There are definitely things that you could do tomorrow,” she said.
PCPs should be familiar with the CDC’s Contraceptive Guidance for Health Care Providers and the federal Office of Population Affairs’ Quality Family Planning Recommendations for providers, which offer practice-level information, Ti said.
PCPs should not feel they need to be able to provide same-day contraceptive care to get started. Having nurses and medical assistants and practice managers on board who are passionate about adding the services can also help bring about change with a team approach, she said.
Even when the provider is enthusiastic about providing the care and is trained to do so, however, insurance barriers may exist, Ti acknowledged. For example, at her clinic a common IUD insertion requires prior authorization.
Including Other Providers
Julia Strasser, DrPH, MPH, a member of the core faculty at the Fitzhugh Mullan Institute for Health Workforce Equity in Washington, DC, told this news organization that including other clinicians could help expand contraceptive services in primary care. Her research showed that the proportion of the contraception workforce that is made up of advanced practice clinicians and nurse practitioners is increasing, whereas the proportion that includes physicians is either static or declining.
A paper by her team found that although OB/GYNs and nurse-midwives were more likely to prescribe the pill, patch, or ring, the largest numbers of contraception prescribers were FPs (72,725) and advanced practice nurses (70,115).
“We also know that pharmacists can safely prescribe contraception, and some states have authorized this practice, but uptake is low and policies vary by state,” she said. “Some health systems have pharmacists embedded in their practice — for example in federally qualified health centers and others.”
It’s important, she said, not to frame the gaps in contraceptive care as a failure on the part of individual clinicians but rather as: “How can we change some of the system-level factors that have gotten us to this point?”
Yalda Jabbarpour, MD, an FP and director of the Robert Graham Center of the American Academy of Family Physicians, said sometimes it’s the health center’s cost analysis that stands in the way. She gave an example from her own health system.
“The health system doesn’t want to pay for us to have the IUDs stored in our offices and provide that procedure because they feel it’s more cost effective if the OB/GYNs do it.” IUD insertions take more appointment time than the standard appointment, which also goes into the cost analysis. “Even though you’re trained to do it, you can’t necessarily do it when you get to the real world,” Jabbarpour said.
She said the thinking is that while OB/GYNs focus on women, FPs cover all ages and family members, so having the equipment and the storage space is best left to the OB/GYNs. She said that thinking may be short sighted.
“We have good data that the highest number of office visits in the United States actually happen in the family physician’s office,” she said. Not providing the services injects a barrier into the system as women are being referred for a simple procedure to a physician they’ve never seen. “That’s not very patient centered,” Jabbarpour noted.
In systems that refer contraceptive procedures to OB/GYNs, doctors also can’t practice skills they learned in residency and then may not feel comfortable performing the procedures when they enter a health system that offers the procedures in primary care.
Number of FPs Prescribing Long-Acting Contraception Growing
Jabbarpour said there has been some improvement in that area in terms of long-acting reversible contraception.
She pointed to a study of recertifying FPs that found that the percent of FPs who offer either IUDs or implants increased from 23.9% in 2018 to 30% in 2022. The share of FPs providing implant insertion increased from 12.9% to 20.8%; those providing IUDs also increased from 22.9% to 25.5% from 2018 to 2022.
FPs also have the advantage of being more widely distributed in rural and remote areas than OB/GYNs, she noted. “They are in almost every county in the United States.”
Jabbarpour said the education must start with health system leaders. If they deem it important to offer these services in primary care, then residency programs will see that their residents must be appropriately trained to provide it.
“Right now, it’s not an expectation of many of the employers that primary care physicians should do this,” she said.
Ti said that expectation should change. The value proposition for all PCPs and health systems, she said, is this: “Most of contraceptive care is well within the scope of primary care providers. This is care that we can do, and it’s care that we should be doing. So why aren’t we doing it?”
Ti, Strasser, and Jabbarpour reported no relevant financial disclosures.
A version of this article appeared on Medscape.com.
In 2024, the Guttmacher Institute reported that eight states enacted or proposed limits on contraceptive access. Currently, more than 19 million women aged 13-44 years in the United States live in “contraceptive deserts” or places that lack access to a full range of birth control methods. About 1.2 million of those women live in counties that don’t have a single health center that has complete birth control services.
Providing contraceptive care in primary care settings has long been deemed a best practice by the Centers for Disease Control and Prevention (CDC). But the percentage of primary care physicians (PCPs) prescribing contraception or offering contraceptive procedures is strikingly low.
Only Half of Family Physicians (FPs) Prescribe Contraceptives
Research by Candice Chen, MD, MPH, and colleagues found that while 73.1% of obstetrician-gynecologists (OB/GYNs) and 72.6% of nurse-midwives prescribed the pill, patch, or vaginal ring; only 51% of FPs, 32.4% of pediatricians, and 19.8% of internal medicine physicians did so. And while 92.8% of OB/GYNs provided intrauterine device (IUD) services, only 16.4% of FPs, 2.6% of internists, and 0.6% of pediatricians did so.
One reason primary care is positioned so well to fill contraception gaps is found in the sheer numbers of PCPs. Chen and colleagues found that while the percentage of FPs prescribing contraception was much smaller (51.4%) than the percentage of OB/GYN prescribers (72.6%), the numbers translate to 72,725 FPs prescribing contraceptives, which is nearly double the number of OB/GYNs prescribing them (36,887).
Access to contraception services took a big hit with the COVID-19 pandemic as did access to healthcare in general. And the 2022 Supreme Court ruling that struck down Roe V. Wade has shaken up the landscape for reproductive services with potential consequences for contraceptive access.
Why Aren’t More PCPs Offering Contraceptive Services?
Reasons for the relatively low numbers of PCPs prescribing contraceptives include lack of training in residency, health systems’ financial choices, insurance barriers, and expectation by some physicians and many patients that birth control belongs in the OB/GYN sector. Access, patient awareness that PCPs can provide the care, expectations, and options vary by states and regions.
Angeline Ti, MD, an FP who teaches in a residency program at Wellstar Douglasville Medical Center in Douglasville, Georgia, told this news organization that the awareness issue might be the easiest change for PCPs as many patients aren’t aware you can get contraceptive services in primary care.
Things PCPs ‘Could Do Tomorrow’
Those physicians who want to add those services might want to start with universal screening, Ti said — having conversations with patients about contraceptive needs and letting them know they don’t have to get those prescriptions from an OB/GYN. The conversations could center on laying out the options and counseling on risks and benefits of various options and providing referrals, if that is the best option. “There are definitely things that you could do tomorrow,” she said.
PCPs should be familiar with the CDC’s Contraceptive Guidance for Health Care Providers and the federal Office of Population Affairs’ Quality Family Planning Recommendations for providers, which offer practice-level information, Ti said.
PCPs should not feel they need to be able to provide same-day contraceptive care to get started. Having nurses and medical assistants and practice managers on board who are passionate about adding the services can also help bring about change with a team approach, she said.
Even when the provider is enthusiastic about providing the care and is trained to do so, however, insurance barriers may exist, Ti acknowledged. For example, at her clinic a common IUD insertion requires prior authorization.
Including Other Providers
Julia Strasser, DrPH, MPH, a member of the core faculty at the Fitzhugh Mullan Institute for Health Workforce Equity in Washington, DC, told this news organization that including other clinicians could help expand contraceptive services in primary care. Her research showed that the proportion of the contraception workforce that is made up of advanced practice clinicians and nurse practitioners is increasing, whereas the proportion that includes physicians is either static or declining.
A paper by her team found that although OB/GYNs and nurse-midwives were more likely to prescribe the pill, patch, or ring, the largest numbers of contraception prescribers were FPs (72,725) and advanced practice nurses (70,115).
“We also know that pharmacists can safely prescribe contraception, and some states have authorized this practice, but uptake is low and policies vary by state,” she said. “Some health systems have pharmacists embedded in their practice — for example in federally qualified health centers and others.”
It’s important, she said, not to frame the gaps in contraceptive care as a failure on the part of individual clinicians but rather as: “How can we change some of the system-level factors that have gotten us to this point?”
Yalda Jabbarpour, MD, an FP and director of the Robert Graham Center of the American Academy of Family Physicians, said sometimes it’s the health center’s cost analysis that stands in the way. She gave an example from her own health system.
“The health system doesn’t want to pay for us to have the IUDs stored in our offices and provide that procedure because they feel it’s more cost effective if the OB/GYNs do it.” IUD insertions take more appointment time than the standard appointment, which also goes into the cost analysis. “Even though you’re trained to do it, you can’t necessarily do it when you get to the real world,” Jabbarpour said.
She said the thinking is that while OB/GYNs focus on women, FPs cover all ages and family members, so having the equipment and the storage space is best left to the OB/GYNs. She said that thinking may be short sighted.
“We have good data that the highest number of office visits in the United States actually happen in the family physician’s office,” she said. Not providing the services injects a barrier into the system as women are being referred for a simple procedure to a physician they’ve never seen. “That’s not very patient centered,” Jabbarpour noted.
In systems that refer contraceptive procedures to OB/GYNs, doctors also can’t practice skills they learned in residency and then may not feel comfortable performing the procedures when they enter a health system that offers the procedures in primary care.
Number of FPs Prescribing Long-Acting Contraception Growing
Jabbarpour said there has been some improvement in that area in terms of long-acting reversible contraception.
She pointed to a study of recertifying FPs that found that the percent of FPs who offer either IUDs or implants increased from 23.9% in 2018 to 30% in 2022. The share of FPs providing implant insertion increased from 12.9% to 20.8%; those providing IUDs also increased from 22.9% to 25.5% from 2018 to 2022.
FPs also have the advantage of being more widely distributed in rural and remote areas than OB/GYNs, she noted. “They are in almost every county in the United States.”
Jabbarpour said the education must start with health system leaders. If they deem it important to offer these services in primary care, then residency programs will see that their residents must be appropriately trained to provide it.
“Right now, it’s not an expectation of many of the employers that primary care physicians should do this,” she said.
Ti said that expectation should change. The value proposition for all PCPs and health systems, she said, is this: “Most of contraceptive care is well within the scope of primary care providers. This is care that we can do, and it’s care that we should be doing. So why aren’t we doing it?”
Ti, Strasser, and Jabbarpour reported no relevant financial disclosures.
A version of this article appeared on Medscape.com.
‘New Hope’ for Alcohol Use Disorder Treatment
Evidence is mounting that new therapies already used to treat gut diseases, type 2 diabetes, and obesity may help people with alcohol use disorder (AUD).
Glucagon-like peptide 1 (GLP-1) receptor agonists, first used to treat diabetes and now widely used for weight loss, and fecal microbiota transplants (FMTs), used to treat diseases such as recurrent Clostridioides difficile infection, are advancing in clinical trials as potential options for treating AUD.
AUD Affects 28.9 Million People in the United States
In 2023, 28.9 million people aged 12 years or older in the United States had AUD (10.2% of the people in this age group). The Food and Drug Administration (FDA) has approved three medical therapies: Acamprosate, naltrexone, and disulfiram to help keep people with the disorder from returning to heavy drinking. Acamprosate’s mechanism of action is not clear, but it is thought to modulate and normalize alcohol-related changes in brain activity, thereby reducing withdrawal symptoms. Naltrexone blocks opioid receptors to reduce alcohol cravings. Disulfiram causes a toxic physical reaction when mixed with alcohol.
Some with AUD also benefit from behavioral therapies and support groups such as Alcoholics Anonymous. But for others, nothing has worked, and that’s part of the reason Lorenzo Leggio, MD, PhD, a scientist in the field of alcohol addiction with the National Institutes of Health (NIH), told this news organization that this is the “most exciting moment” for AUD treatment in his more than 2 decades of research in this area.
GLP-1 Agonists Showing Consistent Results
GLP-1 receptor agonists work by modulating the brain’s reward pathways, including the areas that regulate cravings and motivation.
“By dampening the reward signals associated with alcohol consumption, GLP-1 agonists may reduce cravings and heavy drinking episodes,” Fares Qeadan, PhD, MS, associate professor of biostatistics in the Department of Public Health Sciences at Loyola University Chicago in Illinois, told this news organization.
“The unique aspect of GLP-1 agonists is their ability to target both metabolic and reward systems in the brain,” he said. While naltrexone or acamprosate blocks the effects of alcohol or reduces withdrawal symptoms, “GLP-1 agonists approach addiction through a broader mechanism, potentially addressing underlying factors that contribute to cravings and compulsive behaviors,” he said.
As part of a study published in October in Addiction, Qeadan’s team found that people with AUD who were prescribed GLP-1 agonists had a 50% lower rate of severe intoxication than those who were not prescribed those medications.
“While this is observational and not yet definitive, it highlights the potential of these drugs to complement existing treatments for AUD,” he said.
Another study, a nationwide cohort study published in JAMA Psychiatry, found that using the GLP-1 receptor agonists semaglutide and liraglutide was linked to a lower risk for AUD-related hospitalizations than traditional AUD medications.
A systematic review, published last month in eClinical Medicine, concluded that, though there is little high-quality evidence demonstrating the effect of GLP-1 receptor agonists on alcohol use, “subgroup analysis from two [randomized, controlled trials] and supporting data from four observational studies suggest that GLP-1 [receptor agonists] may reduce alcohol consumption and improve outcomes in some individuals.”
Studying individual differences in response may have implications for personalized medicine, Qeadan said, as treatments could be tailored to those most likely to benefit, such as people with both metabolic dysfunction and AUD.
“These medications may offer hope for patients who struggle with addiction and have not responded to traditional therapies,” Qeadan said.
Exploring FMT as AUD Treatment
FMT is also a new research focus for treating AUD. Jasmohan Bajaj, MD, a gastroenterologist and liver specialist at Virginia Commonwealth University Medical Center, Richmond, is leading the Intestinal Microbiota Transplant in Alcohol-Associated Liver Disease (IMPACT) trial.
AUD has been linked with gut microbial alterations that worsen with cirrhosis. Research has shown that alcohol consumption changes the diversity of bacteria and can lead to bacterial overgrowth and progression of alcohol-associated liver disease.
FMT has been effective in rebalancing gut bacteria by transferring healthy stool from screened donors into patients who have developed an overgrowth of harmful bacteria. In the IMPACT trial, participants, who have not previously received traditional treatment for AUD or for whom treatment has not worked, are randomized either to the oral treatment capsule, which contains freeze-dried stool from a donor with healthy gut bacteria, or placebo.
The trial, sponsored by the NIH, is halfway through its target enrollment of 80.
In a previous smaller, placebo-controlled, phase 1 study, also led by Bajaj and published in Hepatology, 9 of the 10 volunteers who had severe AUD and cirrhosis experienced fewer alcohol cravings and had lower consumption after 15 days. Only three of the placebo participants saw similar improvements. Those who received the microbiota transplant also had fewer AUD-related events over 6 months.
Bajaj said that, if trials show FMT is safe and effective, he envisions the treatment as one tool in a multidisciplinary, integrated clinic that would include a hepatologist and mental health clinicians.
One benefit of the FMT treatment approach is it is given once or twice only, rather than administered regularly.
Current Treatments Work, But More are Needed
Leggio, who is clinical director of the National Institute on Drug Abuse Intramural Research Program, said: “We know that alcohol use disorder, and addiction in general, is a brain disease. We also know that the brain does not work in isolation. The brain is constantly interacting with the rest of the body, including with the gut.”
Leggio said it’s important to note that the three FDA-approved medications do work for alcohol addiction. He said they work as well as selective serotonin reuptake inhibitors for depression and beta-blockers for chronic heart failure.
But there are only three, and they don’t work for everyone, he noted. Those are among the reasons developing new treatments is important. New treatments could be used as an alternative or in combination with already approved treatments.
FMT is in “the very early stages” of trials testing its use for AUD, Leggio noted, adding that the studies by Bajaj’s team are among the very few addressing gut dysbiosis in AUD, and all have involved small numbers of patients. “It’s promising. It’s intriguing. It’s exciting. But we are just at the beginning.”
Results Consistent Across Species, Labs
GLP-1 agonists are further along in trials but still not ready for prescribing for AUD, Leggio said. The positive results have been consistent across species, different labs, and different research teams around the world.
Researchers have also explored through electronic health record emulation trials whether people already taking GLP-1 agonists for diabetes or obesity drink less alcohol compared with matched cohorts not taking GLP-1s. “They consistently show that the people who are on GLP-1s drink less,” he said.
“[Emulation trials] don’t replace the need for randomized controlled trials, Leggio noted. Leggio’s team is currently working on a randomized, placebo-controlled, double-blinded trial studying GLP-1s in relation to AUD.
New Directions 20-Year Highlight
This whole line of research represents “new hope” and has many implications, Leggio said. “I have been in this business for 20-plus years, and I think this is themost exciting moment when we have a very promising target in GLP-1s.”
Regardless of efficacy, he said, the focus on GLP-1 agonists and FMT for AUD has people talking more about addiction and the brain-body connection rather than assuming AUD is a result of poor choices and “bad behavior.”
The momentum of new treatments could also lead to patients and physicians having conversations about existing treatments.
“Hopefully, this momentum will help us destigmatize addiction, and by destigmatizing addiction, there will be an uptick in use of currently approved medications,” Leggio said.
Qeadan, Bajaj, and Leggio reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Evidence is mounting that new therapies already used to treat gut diseases, type 2 diabetes, and obesity may help people with alcohol use disorder (AUD).
Glucagon-like peptide 1 (GLP-1) receptor agonists, first used to treat diabetes and now widely used for weight loss, and fecal microbiota transplants (FMTs), used to treat diseases such as recurrent Clostridioides difficile infection, are advancing in clinical trials as potential options for treating AUD.
AUD Affects 28.9 Million People in the United States
In 2023, 28.9 million people aged 12 years or older in the United States had AUD (10.2% of the people in this age group). The Food and Drug Administration (FDA) has approved three medical therapies: Acamprosate, naltrexone, and disulfiram to help keep people with the disorder from returning to heavy drinking. Acamprosate’s mechanism of action is not clear, but it is thought to modulate and normalize alcohol-related changes in brain activity, thereby reducing withdrawal symptoms. Naltrexone blocks opioid receptors to reduce alcohol cravings. Disulfiram causes a toxic physical reaction when mixed with alcohol.
Some with AUD also benefit from behavioral therapies and support groups such as Alcoholics Anonymous. But for others, nothing has worked, and that’s part of the reason Lorenzo Leggio, MD, PhD, a scientist in the field of alcohol addiction with the National Institutes of Health (NIH), told this news organization that this is the “most exciting moment” for AUD treatment in his more than 2 decades of research in this area.
GLP-1 Agonists Showing Consistent Results
GLP-1 receptor agonists work by modulating the brain’s reward pathways, including the areas that regulate cravings and motivation.
“By dampening the reward signals associated with alcohol consumption, GLP-1 agonists may reduce cravings and heavy drinking episodes,” Fares Qeadan, PhD, MS, associate professor of biostatistics in the Department of Public Health Sciences at Loyola University Chicago in Illinois, told this news organization.
“The unique aspect of GLP-1 agonists is their ability to target both metabolic and reward systems in the brain,” he said. While naltrexone or acamprosate blocks the effects of alcohol or reduces withdrawal symptoms, “GLP-1 agonists approach addiction through a broader mechanism, potentially addressing underlying factors that contribute to cravings and compulsive behaviors,” he said.
As part of a study published in October in Addiction, Qeadan’s team found that people with AUD who were prescribed GLP-1 agonists had a 50% lower rate of severe intoxication than those who were not prescribed those medications.
“While this is observational and not yet definitive, it highlights the potential of these drugs to complement existing treatments for AUD,” he said.
Another study, a nationwide cohort study published in JAMA Psychiatry, found that using the GLP-1 receptor agonists semaglutide and liraglutide was linked to a lower risk for AUD-related hospitalizations than traditional AUD medications.
A systematic review, published last month in eClinical Medicine, concluded that, though there is little high-quality evidence demonstrating the effect of GLP-1 receptor agonists on alcohol use, “subgroup analysis from two [randomized, controlled trials] and supporting data from four observational studies suggest that GLP-1 [receptor agonists] may reduce alcohol consumption and improve outcomes in some individuals.”
Studying individual differences in response may have implications for personalized medicine, Qeadan said, as treatments could be tailored to those most likely to benefit, such as people with both metabolic dysfunction and AUD.
“These medications may offer hope for patients who struggle with addiction and have not responded to traditional therapies,” Qeadan said.
Exploring FMT as AUD Treatment
FMT is also a new research focus for treating AUD. Jasmohan Bajaj, MD, a gastroenterologist and liver specialist at Virginia Commonwealth University Medical Center, Richmond, is leading the Intestinal Microbiota Transplant in Alcohol-Associated Liver Disease (IMPACT) trial.
AUD has been linked with gut microbial alterations that worsen with cirrhosis. Research has shown that alcohol consumption changes the diversity of bacteria and can lead to bacterial overgrowth and progression of alcohol-associated liver disease.
FMT has been effective in rebalancing gut bacteria by transferring healthy stool from screened donors into patients who have developed an overgrowth of harmful bacteria. In the IMPACT trial, participants, who have not previously received traditional treatment for AUD or for whom treatment has not worked, are randomized either to the oral treatment capsule, which contains freeze-dried stool from a donor with healthy gut bacteria, or placebo.
The trial, sponsored by the NIH, is halfway through its target enrollment of 80.
In a previous smaller, placebo-controlled, phase 1 study, also led by Bajaj and published in Hepatology, 9 of the 10 volunteers who had severe AUD and cirrhosis experienced fewer alcohol cravings and had lower consumption after 15 days. Only three of the placebo participants saw similar improvements. Those who received the microbiota transplant also had fewer AUD-related events over 6 months.
Bajaj said that, if trials show FMT is safe and effective, he envisions the treatment as one tool in a multidisciplinary, integrated clinic that would include a hepatologist and mental health clinicians.
One benefit of the FMT treatment approach is it is given once or twice only, rather than administered regularly.
Current Treatments Work, But More are Needed
Leggio, who is clinical director of the National Institute on Drug Abuse Intramural Research Program, said: “We know that alcohol use disorder, and addiction in general, is a brain disease. We also know that the brain does not work in isolation. The brain is constantly interacting with the rest of the body, including with the gut.”
Leggio said it’s important to note that the three FDA-approved medications do work for alcohol addiction. He said they work as well as selective serotonin reuptake inhibitors for depression and beta-blockers for chronic heart failure.
But there are only three, and they don’t work for everyone, he noted. Those are among the reasons developing new treatments is important. New treatments could be used as an alternative or in combination with already approved treatments.
FMT is in “the very early stages” of trials testing its use for AUD, Leggio noted, adding that the studies by Bajaj’s team are among the very few addressing gut dysbiosis in AUD, and all have involved small numbers of patients. “It’s promising. It’s intriguing. It’s exciting. But we are just at the beginning.”
Results Consistent Across Species, Labs
GLP-1 agonists are further along in trials but still not ready for prescribing for AUD, Leggio said. The positive results have been consistent across species, different labs, and different research teams around the world.
Researchers have also explored through electronic health record emulation trials whether people already taking GLP-1 agonists for diabetes or obesity drink less alcohol compared with matched cohorts not taking GLP-1s. “They consistently show that the people who are on GLP-1s drink less,” he said.
“[Emulation trials] don’t replace the need for randomized controlled trials, Leggio noted. Leggio’s team is currently working on a randomized, placebo-controlled, double-blinded trial studying GLP-1s in relation to AUD.
New Directions 20-Year Highlight
This whole line of research represents “new hope” and has many implications, Leggio said. “I have been in this business for 20-plus years, and I think this is themost exciting moment when we have a very promising target in GLP-1s.”
Regardless of efficacy, he said, the focus on GLP-1 agonists and FMT for AUD has people talking more about addiction and the brain-body connection rather than assuming AUD is a result of poor choices and “bad behavior.”
The momentum of new treatments could also lead to patients and physicians having conversations about existing treatments.
“Hopefully, this momentum will help us destigmatize addiction, and by destigmatizing addiction, there will be an uptick in use of currently approved medications,” Leggio said.
Qeadan, Bajaj, and Leggio reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Evidence is mounting that new therapies already used to treat gut diseases, type 2 diabetes, and obesity may help people with alcohol use disorder (AUD).
Glucagon-like peptide 1 (GLP-1) receptor agonists, first used to treat diabetes and now widely used for weight loss, and fecal microbiota transplants (FMTs), used to treat diseases such as recurrent Clostridioides difficile infection, are advancing in clinical trials as potential options for treating AUD.
AUD Affects 28.9 Million People in the United States
In 2023, 28.9 million people aged 12 years or older in the United States had AUD (10.2% of the people in this age group). The Food and Drug Administration (FDA) has approved three medical therapies: Acamprosate, naltrexone, and disulfiram to help keep people with the disorder from returning to heavy drinking. Acamprosate’s mechanism of action is not clear, but it is thought to modulate and normalize alcohol-related changes in brain activity, thereby reducing withdrawal symptoms. Naltrexone blocks opioid receptors to reduce alcohol cravings. Disulfiram causes a toxic physical reaction when mixed with alcohol.
Some with AUD also benefit from behavioral therapies and support groups such as Alcoholics Anonymous. But for others, nothing has worked, and that’s part of the reason Lorenzo Leggio, MD, PhD, a scientist in the field of alcohol addiction with the National Institutes of Health (NIH), told this news organization that this is the “most exciting moment” for AUD treatment in his more than 2 decades of research in this area.
GLP-1 Agonists Showing Consistent Results
GLP-1 receptor agonists work by modulating the brain’s reward pathways, including the areas that regulate cravings and motivation.
“By dampening the reward signals associated with alcohol consumption, GLP-1 agonists may reduce cravings and heavy drinking episodes,” Fares Qeadan, PhD, MS, associate professor of biostatistics in the Department of Public Health Sciences at Loyola University Chicago in Illinois, told this news organization.
“The unique aspect of GLP-1 agonists is their ability to target both metabolic and reward systems in the brain,” he said. While naltrexone or acamprosate blocks the effects of alcohol or reduces withdrawal symptoms, “GLP-1 agonists approach addiction through a broader mechanism, potentially addressing underlying factors that contribute to cravings and compulsive behaviors,” he said.
As part of a study published in October in Addiction, Qeadan’s team found that people with AUD who were prescribed GLP-1 agonists had a 50% lower rate of severe intoxication than those who were not prescribed those medications.
“While this is observational and not yet definitive, it highlights the potential of these drugs to complement existing treatments for AUD,” he said.
Another study, a nationwide cohort study published in JAMA Psychiatry, found that using the GLP-1 receptor agonists semaglutide and liraglutide was linked to a lower risk for AUD-related hospitalizations than traditional AUD medications.
A systematic review, published last month in eClinical Medicine, concluded that, though there is little high-quality evidence demonstrating the effect of GLP-1 receptor agonists on alcohol use, “subgroup analysis from two [randomized, controlled trials] and supporting data from four observational studies suggest that GLP-1 [receptor agonists] may reduce alcohol consumption and improve outcomes in some individuals.”
Studying individual differences in response may have implications for personalized medicine, Qeadan said, as treatments could be tailored to those most likely to benefit, such as people with both metabolic dysfunction and AUD.
“These medications may offer hope for patients who struggle with addiction and have not responded to traditional therapies,” Qeadan said.
Exploring FMT as AUD Treatment
FMT is also a new research focus for treating AUD. Jasmohan Bajaj, MD, a gastroenterologist and liver specialist at Virginia Commonwealth University Medical Center, Richmond, is leading the Intestinal Microbiota Transplant in Alcohol-Associated Liver Disease (IMPACT) trial.
AUD has been linked with gut microbial alterations that worsen with cirrhosis. Research has shown that alcohol consumption changes the diversity of bacteria and can lead to bacterial overgrowth and progression of alcohol-associated liver disease.
FMT has been effective in rebalancing gut bacteria by transferring healthy stool from screened donors into patients who have developed an overgrowth of harmful bacteria. In the IMPACT trial, participants, who have not previously received traditional treatment for AUD or for whom treatment has not worked, are randomized either to the oral treatment capsule, which contains freeze-dried stool from a donor with healthy gut bacteria, or placebo.
The trial, sponsored by the NIH, is halfway through its target enrollment of 80.
In a previous smaller, placebo-controlled, phase 1 study, also led by Bajaj and published in Hepatology, 9 of the 10 volunteers who had severe AUD and cirrhosis experienced fewer alcohol cravings and had lower consumption after 15 days. Only three of the placebo participants saw similar improvements. Those who received the microbiota transplant also had fewer AUD-related events over 6 months.
Bajaj said that, if trials show FMT is safe and effective, he envisions the treatment as one tool in a multidisciplinary, integrated clinic that would include a hepatologist and mental health clinicians.
One benefit of the FMT treatment approach is it is given once or twice only, rather than administered regularly.
Current Treatments Work, But More are Needed
Leggio, who is clinical director of the National Institute on Drug Abuse Intramural Research Program, said: “We know that alcohol use disorder, and addiction in general, is a brain disease. We also know that the brain does not work in isolation. The brain is constantly interacting with the rest of the body, including with the gut.”
Leggio said it’s important to note that the three FDA-approved medications do work for alcohol addiction. He said they work as well as selective serotonin reuptake inhibitors for depression and beta-blockers for chronic heart failure.
But there are only three, and they don’t work for everyone, he noted. Those are among the reasons developing new treatments is important. New treatments could be used as an alternative or in combination with already approved treatments.
FMT is in “the very early stages” of trials testing its use for AUD, Leggio noted, adding that the studies by Bajaj’s team are among the very few addressing gut dysbiosis in AUD, and all have involved small numbers of patients. “It’s promising. It’s intriguing. It’s exciting. But we are just at the beginning.”
Results Consistent Across Species, Labs
GLP-1 agonists are further along in trials but still not ready for prescribing for AUD, Leggio said. The positive results have been consistent across species, different labs, and different research teams around the world.
Researchers have also explored through electronic health record emulation trials whether people already taking GLP-1 agonists for diabetes or obesity drink less alcohol compared with matched cohorts not taking GLP-1s. “They consistently show that the people who are on GLP-1s drink less,” he said.
“[Emulation trials] don’t replace the need for randomized controlled trials, Leggio noted. Leggio’s team is currently working on a randomized, placebo-controlled, double-blinded trial studying GLP-1s in relation to AUD.
New Directions 20-Year Highlight
This whole line of research represents “new hope” and has many implications, Leggio said. “I have been in this business for 20-plus years, and I think this is themost exciting moment when we have a very promising target in GLP-1s.”
Regardless of efficacy, he said, the focus on GLP-1 agonists and FMT for AUD has people talking more about addiction and the brain-body connection rather than assuming AUD is a result of poor choices and “bad behavior.”
The momentum of new treatments could also lead to patients and physicians having conversations about existing treatments.
“Hopefully, this momentum will help us destigmatize addiction, and by destigmatizing addiction, there will be an uptick in use of currently approved medications,” Leggio said.
Qeadan, Bajaj, and Leggio reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New Investigation Casts Doubt on Landmark Ticagrelor Trial
New questions about the landmark trial that launched the antiplatelet drug ticagrelor worldwide are being raised after an investigation uncovered more information about how the PLATO study was conducted.
Peter Doshi, PhD, senior editor at The BMJ, obtained primary records for the trial and unpublished data through a Freedom of Information Act request, and has detailed inconsistencies and omissions in data reporting from the 2009 trial originally published in The New England Journal of Medicine (NEJM). The new investigation into the Platelet Inhibition and Patient Outcomes (PLATO) trial is published in The BMJ.
The findings come as generic versions of ticagrelor (Brilinta) are expected to become available soon in the United States. Ticagrelor is the only P2Y12 inhibitor still under patent, and in 2022, the United States spent more than $750 million on it, according to the report.
PLATO, sponsored by ticagrelor manufacturer AstraZeneca, included more than 18,000 patients in 43 countries. Investigators reported that ticagrelor reduced deaths from vascular causes, heart attack, or stroke compared with clopidogrel (Plavix). However, in a subgroup analysis, among US patients, there were more deaths in the ticagrelor group, and AstraZeneca failed its first bid for approval from the US Food and Drug Administration (FDA).
Failed First Bid for FDA Approval
AstraZeneca resubmitted its application, which was met with objections by some FDA staff members, including medical officer Thomas Marciniak, who called the resubmission “the worst in my experience regarding completeness of the submissions and the sponsor responding completely and accurately to requests,” Doshi reports.
Despite the objections, the FDA in 2011 approved ticagrelor for acute coronary syndrome, kicking off intense controversy over the trial, as several other studies have failed to replicate PLATO’s positive results.
Doubts have grown about its apparent advantage over cheaper, off-patent P2Y12 inhibitors such as clopidogrel and prasugrel.
“Critics said it was noteworthy that ticagrelor failed in the US,” Doshi writes, “the only high enrolling country where sites were not monitored by the sponsor itself.” Doshi’s report points out that critics of the trial “highlight that AstraZeneca itself carried out the data monitoring for PLATO except for sites that were monitored by third party contract research organizations. In the four countries exclusively monitored by non-sponsor personnel—Georgia, Israel, Russia, and the US—ticagrelor fared worse.”
Victor Serebruany, MD, from Johns Hopkins University, said he was initially impressed by the trial results but became skeptical after noticing inconsistencies and anomalies in the data. He filed a complaint with the US District Court in the District of Columbia, suggesting that the cardiovascular events in the study “may have been manipulated.”
US Department of Justice Investigation
The US Department of Justice (DOJ) opened an investigation in 2013 and closed it in 2014 with no further action. Serebruany continues to publish critiques of the trial 15 years later but told The BMJ he has little hope that the questions will be resolved unless the DOJ re-engages with an investigation.
Doshi also points out discrepancies in the data reported. In the 2009 paper, published as an intent-to-treat analysis, investigators said there were 905 total deaths from any cause among all randomized patients. “An internal company report states, however, that 983 patients had died at this point. While 33 deaths occurred after the follow-up period, the NEJM tally still leaves out 45 deaths ‘discovered after withdrawal of consent,’” he reports.
The NEJM responded to Doshi that while it didn’t dispute the error in the number of deaths, it was uncertain about publishing a correction, citing new — not yet published — guidelines from the International Committee of Medical Journal Editors. NEJM Editor-in-Chief Eric Rubin told The BMJ that “for older manuscripts, correction is not necessarily appropriate unless there would be an effect on clinical practice.”
Doshi’s investigation includes an interview with Eric Bates, MD, professor of internal medicine at the University of Michigan in Ann Arbor, and a co-author of the US guidelines that recommend ticagrelor, who said he was “increasingly disturbed by how trial after trial came out as being not dramatically positive in any way.” Bates is now calling for a review of ticagrelor’s recommendation in guidelines, according to the report.
AstraZeneca declined to be interviewed for the BMJ investigation, according to Doshi, and a spokesperson from the company told the journal by email that they have “nothing to add,” directing editors to its 2014 public statement after the DOJ’s investigation into PLATO. The BMJ said PLATO trial co-chairs Robert A. Harrington, MD, and Lars Wallentin, MD, did not respond to The BMJ’s requests for comment.
Will the Guidelines Be Changed Now?
“I know and have worked with Drs Wallentin and Harrington,” Bates told Medscape Medical News, “and find them to be honest, intelligent clinical scientists with the highest ethical standards who manage conflicts of interest as well as can be done in the clinical research arena, where industry support is required to develop new knowledge,” he said.
“If there is a concern that AstraZeneca was manipulating the dataset and FDA submission, that is an important issue,” Bates said. “The US paradox and the failure of any other antiplatelet trial to find a comparative mortality advantage are two unexplained issues with PLATO that provide good fodder for conspiracy theories. I agree with the NEJM that this trial is 15 years old and may not be worth readjudicating in the current treatment era.”
Other calls for revisiting guidelines have come after disappointing postlicensure studies have repeatedly demonstrated that ticagrelor has “similar efficacy to clopidogrel but with increased bleeding and [dyspnea],” Doshi reports.
“My concern is the marketing spin by AstraZeneca and the promotion of ticagrelor by six to eight ‘thought leaders’ consistently funded by AstraZeneca over the past 10 years,” said Bates. “They have flooded the literature with supportive subset and post hoc analyses, review articles, and ‘meta-analyses’ flawed by selection and intellectual bias, and public interviews that consistently discount the findings of the many subsequent randomized controlled trials that have not supported the superiority of ticagrelor over clopidogrel or prasugrel.”
A version of this article first appeared on Medscape.com.
New questions about the landmark trial that launched the antiplatelet drug ticagrelor worldwide are being raised after an investigation uncovered more information about how the PLATO study was conducted.
Peter Doshi, PhD, senior editor at The BMJ, obtained primary records for the trial and unpublished data through a Freedom of Information Act request, and has detailed inconsistencies and omissions in data reporting from the 2009 trial originally published in The New England Journal of Medicine (NEJM). The new investigation into the Platelet Inhibition and Patient Outcomes (PLATO) trial is published in The BMJ.
The findings come as generic versions of ticagrelor (Brilinta) are expected to become available soon in the United States. Ticagrelor is the only P2Y12 inhibitor still under patent, and in 2022, the United States spent more than $750 million on it, according to the report.
PLATO, sponsored by ticagrelor manufacturer AstraZeneca, included more than 18,000 patients in 43 countries. Investigators reported that ticagrelor reduced deaths from vascular causes, heart attack, or stroke compared with clopidogrel (Plavix). However, in a subgroup analysis, among US patients, there were more deaths in the ticagrelor group, and AstraZeneca failed its first bid for approval from the US Food and Drug Administration (FDA).
Failed First Bid for FDA Approval
AstraZeneca resubmitted its application, which was met with objections by some FDA staff members, including medical officer Thomas Marciniak, who called the resubmission “the worst in my experience regarding completeness of the submissions and the sponsor responding completely and accurately to requests,” Doshi reports.
Despite the objections, the FDA in 2011 approved ticagrelor for acute coronary syndrome, kicking off intense controversy over the trial, as several other studies have failed to replicate PLATO’s positive results.
Doubts have grown about its apparent advantage over cheaper, off-patent P2Y12 inhibitors such as clopidogrel and prasugrel.
“Critics said it was noteworthy that ticagrelor failed in the US,” Doshi writes, “the only high enrolling country where sites were not monitored by the sponsor itself.” Doshi’s report points out that critics of the trial “highlight that AstraZeneca itself carried out the data monitoring for PLATO except for sites that were monitored by third party contract research organizations. In the four countries exclusively monitored by non-sponsor personnel—Georgia, Israel, Russia, and the US—ticagrelor fared worse.”
Victor Serebruany, MD, from Johns Hopkins University, said he was initially impressed by the trial results but became skeptical after noticing inconsistencies and anomalies in the data. He filed a complaint with the US District Court in the District of Columbia, suggesting that the cardiovascular events in the study “may have been manipulated.”
US Department of Justice Investigation
The US Department of Justice (DOJ) opened an investigation in 2013 and closed it in 2014 with no further action. Serebruany continues to publish critiques of the trial 15 years later but told The BMJ he has little hope that the questions will be resolved unless the DOJ re-engages with an investigation.
Doshi also points out discrepancies in the data reported. In the 2009 paper, published as an intent-to-treat analysis, investigators said there were 905 total deaths from any cause among all randomized patients. “An internal company report states, however, that 983 patients had died at this point. While 33 deaths occurred after the follow-up period, the NEJM tally still leaves out 45 deaths ‘discovered after withdrawal of consent,’” he reports.
The NEJM responded to Doshi that while it didn’t dispute the error in the number of deaths, it was uncertain about publishing a correction, citing new — not yet published — guidelines from the International Committee of Medical Journal Editors. NEJM Editor-in-Chief Eric Rubin told The BMJ that “for older manuscripts, correction is not necessarily appropriate unless there would be an effect on clinical practice.”
Doshi’s investigation includes an interview with Eric Bates, MD, professor of internal medicine at the University of Michigan in Ann Arbor, and a co-author of the US guidelines that recommend ticagrelor, who said he was “increasingly disturbed by how trial after trial came out as being not dramatically positive in any way.” Bates is now calling for a review of ticagrelor’s recommendation in guidelines, according to the report.
AstraZeneca declined to be interviewed for the BMJ investigation, according to Doshi, and a spokesperson from the company told the journal by email that they have “nothing to add,” directing editors to its 2014 public statement after the DOJ’s investigation into PLATO. The BMJ said PLATO trial co-chairs Robert A. Harrington, MD, and Lars Wallentin, MD, did not respond to The BMJ’s requests for comment.
Will the Guidelines Be Changed Now?
“I know and have worked with Drs Wallentin and Harrington,” Bates told Medscape Medical News, “and find them to be honest, intelligent clinical scientists with the highest ethical standards who manage conflicts of interest as well as can be done in the clinical research arena, where industry support is required to develop new knowledge,” he said.
“If there is a concern that AstraZeneca was manipulating the dataset and FDA submission, that is an important issue,” Bates said. “The US paradox and the failure of any other antiplatelet trial to find a comparative mortality advantage are two unexplained issues with PLATO that provide good fodder for conspiracy theories. I agree with the NEJM that this trial is 15 years old and may not be worth readjudicating in the current treatment era.”
Other calls for revisiting guidelines have come after disappointing postlicensure studies have repeatedly demonstrated that ticagrelor has “similar efficacy to clopidogrel but with increased bleeding and [dyspnea],” Doshi reports.
“My concern is the marketing spin by AstraZeneca and the promotion of ticagrelor by six to eight ‘thought leaders’ consistently funded by AstraZeneca over the past 10 years,” said Bates. “They have flooded the literature with supportive subset and post hoc analyses, review articles, and ‘meta-analyses’ flawed by selection and intellectual bias, and public interviews that consistently discount the findings of the many subsequent randomized controlled trials that have not supported the superiority of ticagrelor over clopidogrel or prasugrel.”
A version of this article first appeared on Medscape.com.
New questions about the landmark trial that launched the antiplatelet drug ticagrelor worldwide are being raised after an investigation uncovered more information about how the PLATO study was conducted.
Peter Doshi, PhD, senior editor at The BMJ, obtained primary records for the trial and unpublished data through a Freedom of Information Act request, and has detailed inconsistencies and omissions in data reporting from the 2009 trial originally published in The New England Journal of Medicine (NEJM). The new investigation into the Platelet Inhibition and Patient Outcomes (PLATO) trial is published in The BMJ.
The findings come as generic versions of ticagrelor (Brilinta) are expected to become available soon in the United States. Ticagrelor is the only P2Y12 inhibitor still under patent, and in 2022, the United States spent more than $750 million on it, according to the report.
PLATO, sponsored by ticagrelor manufacturer AstraZeneca, included more than 18,000 patients in 43 countries. Investigators reported that ticagrelor reduced deaths from vascular causes, heart attack, or stroke compared with clopidogrel (Plavix). However, in a subgroup analysis, among US patients, there were more deaths in the ticagrelor group, and AstraZeneca failed its first bid for approval from the US Food and Drug Administration (FDA).
Failed First Bid for FDA Approval
AstraZeneca resubmitted its application, which was met with objections by some FDA staff members, including medical officer Thomas Marciniak, who called the resubmission “the worst in my experience regarding completeness of the submissions and the sponsor responding completely and accurately to requests,” Doshi reports.
Despite the objections, the FDA in 2011 approved ticagrelor for acute coronary syndrome, kicking off intense controversy over the trial, as several other studies have failed to replicate PLATO’s positive results.
Doubts have grown about its apparent advantage over cheaper, off-patent P2Y12 inhibitors such as clopidogrel and prasugrel.
“Critics said it was noteworthy that ticagrelor failed in the US,” Doshi writes, “the only high enrolling country where sites were not monitored by the sponsor itself.” Doshi’s report points out that critics of the trial “highlight that AstraZeneca itself carried out the data monitoring for PLATO except for sites that were monitored by third party contract research organizations. In the four countries exclusively monitored by non-sponsor personnel—Georgia, Israel, Russia, and the US—ticagrelor fared worse.”
Victor Serebruany, MD, from Johns Hopkins University, said he was initially impressed by the trial results but became skeptical after noticing inconsistencies and anomalies in the data. He filed a complaint with the US District Court in the District of Columbia, suggesting that the cardiovascular events in the study “may have been manipulated.”
US Department of Justice Investigation
The US Department of Justice (DOJ) opened an investigation in 2013 and closed it in 2014 with no further action. Serebruany continues to publish critiques of the trial 15 years later but told The BMJ he has little hope that the questions will be resolved unless the DOJ re-engages with an investigation.
Doshi also points out discrepancies in the data reported. In the 2009 paper, published as an intent-to-treat analysis, investigators said there were 905 total deaths from any cause among all randomized patients. “An internal company report states, however, that 983 patients had died at this point. While 33 deaths occurred after the follow-up period, the NEJM tally still leaves out 45 deaths ‘discovered after withdrawal of consent,’” he reports.
The NEJM responded to Doshi that while it didn’t dispute the error in the number of deaths, it was uncertain about publishing a correction, citing new — not yet published — guidelines from the International Committee of Medical Journal Editors. NEJM Editor-in-Chief Eric Rubin told The BMJ that “for older manuscripts, correction is not necessarily appropriate unless there would be an effect on clinical practice.”
Doshi’s investigation includes an interview with Eric Bates, MD, professor of internal medicine at the University of Michigan in Ann Arbor, and a co-author of the US guidelines that recommend ticagrelor, who said he was “increasingly disturbed by how trial after trial came out as being not dramatically positive in any way.” Bates is now calling for a review of ticagrelor’s recommendation in guidelines, according to the report.
AstraZeneca declined to be interviewed for the BMJ investigation, according to Doshi, and a spokesperson from the company told the journal by email that they have “nothing to add,” directing editors to its 2014 public statement after the DOJ’s investigation into PLATO. The BMJ said PLATO trial co-chairs Robert A. Harrington, MD, and Lars Wallentin, MD, did not respond to The BMJ’s requests for comment.
Will the Guidelines Be Changed Now?
“I know and have worked with Drs Wallentin and Harrington,” Bates told Medscape Medical News, “and find them to be honest, intelligent clinical scientists with the highest ethical standards who manage conflicts of interest as well as can be done in the clinical research arena, where industry support is required to develop new knowledge,” he said.
“If there is a concern that AstraZeneca was manipulating the dataset and FDA submission, that is an important issue,” Bates said. “The US paradox and the failure of any other antiplatelet trial to find a comparative mortality advantage are two unexplained issues with PLATO that provide good fodder for conspiracy theories. I agree with the NEJM that this trial is 15 years old and may not be worth readjudicating in the current treatment era.”
Other calls for revisiting guidelines have come after disappointing postlicensure studies have repeatedly demonstrated that ticagrelor has “similar efficacy to clopidogrel but with increased bleeding and [dyspnea],” Doshi reports.
“My concern is the marketing spin by AstraZeneca and the promotion of ticagrelor by six to eight ‘thought leaders’ consistently funded by AstraZeneca over the past 10 years,” said Bates. “They have flooded the literature with supportive subset and post hoc analyses, review articles, and ‘meta-analyses’ flawed by selection and intellectual bias, and public interviews that consistently discount the findings of the many subsequent randomized controlled trials that have not supported the superiority of ticagrelor over clopidogrel or prasugrel.”
A version of this article first appeared on Medscape.com.
FROM THE BMJ
Key Updates in Resuscitation Procedure After Drowning
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
New recommendations on rescuing adults and children who have drowned include an important update for healthcare professionals, trained rescuers, and untrained lay rescuers.
The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have issued recommendations that highlight delivering rescue breaths as well as calling 911 and performing chest compressions in cardiopulmonary resuscitation (CPR) as first steps when a person pulled from the water is in cardiac arrest.
This is the first collaboration between the two organizations on resuscitation after drowning. The recommendations were published simultaneously in Circulation and Pediatrics.
Included in the recommendations are two key principles:
- Anyone pulled from the water who has no signs of normal breathing or consciousness should be presumed to be in cardiac arrest.
- Rescuers should immediately start CPR that includes rescue breathing in addition to chest compressions. Multiple large studies show more people with cardiac arrest from noncardiac causes such as drowning survive when CPR includes rescue breaths, compared with hands-only CPR (calling 911 and pushing hard and fast in the center of the chest).
If someone is untrained, unwilling, or unable to give breaths, they can perform chest compressions until help arrives, the recommendations advise.
Reasoning Behind the Update
The authors, led by writing group cochair Tracy E. McCallin, MD, associate professor in the division of pediatric emergency medicine at Rainbow Babies and Children’s Hospital in Cleveland , Ohio, explained that drowning generally advances from initial respiratory arrest from submersion-related hypoxia to cardiac arrest, and therefore it can be difficult to distinguish respiratory arrest from cardiac arrest because pulses are difficult to accurately palpate within the recommended 10-second window.
“Therefore, resuscitation from cardiac arrest due to this specific circumstance must focus on restoring breathing as much as it does circulation,” the authors wrote.
Resuscitation after drowning may begin in the water with rescue breathing when safely provided by trained rescuers and should continue with chest compressions, once the drowned person and the rescuer are on land or in a boat, the report authors wrote.
“The focused update on drowning contains the most up-to-date, evidence-based recommendations on how to resuscitate someone who has drowned,” McCallin states in a press release.
In addition to the new guidance on rescue breaths, the update includes new topics that the AHA has not previously addressed with treatment recommendations, such as oxygen administration after drowning; automated external defibrillator use in cardiac arrest after drowning and public-access defibrillation programs.
Pediatricians Can Help Spread the Word
Alexandra Stern, MD, assistant professor in the Department of Pediatrics at University of Florida, Gainesville, who was not part of the update, said pediatricians can help disseminate this new information.
“Water safety is a topic frequently discussed as a pediatrician, with focus often being on primary prevention of drowning,” she said. “We stress the importance of the multiple layers of protection against drowning, such as touch supervision (staying within arm’s length); secure fencing, access to appropriate life jackets, and teaching our children to swim. Learning CPR is a large part of these measures and continuing these discussions with our patients and families is important.”
She added that updating the recommended procedures will likely require changes to all forms of education and community outreach regarding drowning from basic life support classes to more advanced lifeguard training. She noted that the update provides practical guidance not just for trained rescuers and healthcare professionals, but also for family members.
The paper notes that drowning is the third leading cause of death from unintentional injury globally, accounting for 7% of all injury-related deaths. In the United States, drowning is the leading cause of death in children aged 1-4 years and the second leading cause of death from unintentional injury in children aged 5-14 years.
The update is based on systematic reviews from 2021 to 2023 performed by the International Liaison Committee on Resuscitation related to the resuscitation of drowning.
The authors and Stern reported no relevant financial relationships.
A version of this article appeared on Medscape.com.
From Pediatrics