User login
Patient Navigators for Serious Illnesses Can Now Bill Under New Medicare Codes
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.
In a move that acknowledges the gauntlet the US health system poses for people facing serious and fatal illnesses, Medicare will pay for a new class of workers to help patients manage treatments for conditions like cancer and heart failure.
The 2024 Medicare physician fee schedule includes new billing codes, including G0023, to pay for 60 minutes a month of care coordination by certified or trained auxiliary personnel working under the direction of a clinician.
A diagnosis of cancer or another serious illness takes a toll beyond the physical effects of the disease. Patients often scramble to make adjustments in family and work schedules to manage treatment, said Samyukta Mullangi, MD, MBA, medical director of oncology at Thyme Care, a Nashville, Tennessee–based firm that provides navigation and coordination services to oncology practices and insurers.
“It just really does create a bit of a pressure cooker for patients,” Dr. Mullangi told this news organization.
Medicare has for many years paid for medical professionals to help patients cope with the complexities of disease, such as chronic care management (CCM) provided by physicians, nurses, and physician assistants.
The new principal illness navigation (PIN) payments are intended to pay for work that to date typically has been done by people without medical degrees, including those involved in peer support networks and community health programs. The US Centers for Medicare and Medicaid Services(CMS) expects these navigators will undergo training and work under the supervision of clinicians.
The new navigators may coordinate care transitions between medical settings, follow up with patients after emergency department (ED) visits, or communicate with skilled nursing facilities regarding the psychosocial needs and functional deficits of a patient, among other functions.
CMS expects the new navigators may:
- Conduct assessments to understand a patient’s life story, strengths, needs, goals, preferences, and desired outcomes, including understanding cultural and linguistic factors.
- Provide support to accomplish the clinician’s treatment plan.
- Coordinate the receipt of needed services from healthcare facilities, home- and community-based service providers, and caregivers.
Peers as Navigators
The new navigators can be former patients who have undergone similar treatments for serious diseases, CMS said. This approach sets the new program apart from other care management services Medicare already covers, program officials wrote in the 2024 physician fee schedule.
“For some conditions, patients are best able to engage with the healthcare system and access care if they have assistance from a single, dedicated individual who has ‘lived experience,’ ” according to the rule.
The agency has taken a broad initial approach in defining what kinds of illnesses a patient may have to qualify for services. Patients must have a serious condition that is expected to last at least 3 months, such as cancer, heart failure, or substance use disorder.
But those without a definitive diagnosis may also qualify to receive navigator services.
In the rule, CMS cited a case in which a CT scan identified a suspicious mass in a patient’s colon. A clinician might decide this person would benefit from navigation services due to the potential risks for an undiagnosed illness.
“Regardless of the definitive diagnosis of the mass, presence of a colonic mass for that patient may be a serious high-risk condition that could, for example, cause obstruction and lead the patient to present to the emergency department, as well as be potentially indicative of an underlying life-threatening illness such as colon cancer,” CMS wrote in the rule.
Navigators often start their work when cancer patients are screened and guide them through initial diagnosis, potential surgery, radiation, or chemotherapy, said Sharon Gentry, MSN, RN, a former nurse navigator who is now the editor in chief of the Journal of the Academy of Oncology Nurse & Patient Navigators.
The navigators are meant to be a trusted and continual presence for patients, who otherwise might be left to start anew in finding help at each phase of care.
The navigators “see the whole picture. They see the whole journey the patient takes, from pre-diagnosis all the way through diagnosis care out through survival,” Ms. Gentry said.
Gaining a special Medicare payment for these kinds of services will elevate this work, she said.
Many newer drugs can target specific mechanisms and proteins of cancer. Often, oncology treatment involves testing to find out if mutations are allowing the cancer cells to evade a patient’s immune system.
Checking these biomarkers takes time, however. Patients sometimes become frustrated because they are anxious to begin treatment. Patients may receive inaccurate information from friends or family who went through treatment previously. Navigators can provide knowledge on the current state of care for a patient’s disease, helping them better manage anxieties.
“You have to explain to them that things have changed since the guy you drink coffee with was diagnosed with cancer, and there may be a drug that could target that,” Ms. Gentry said.
Potential Challenges
Initial uptake of the new PIN codes may be slow going, however, as clinicians and health systems may already use well-established codes. These include CCM and principal care management services, which may pay higher rates, Mullangi said.
“There might be sensitivity around not wanting to cannibalize existing programs with a new program,” Dr. Mullangi said.
In addition, many patients will have a copay for the services of principal illness navigators, Dr. Mullangi said.
While many patients have additional insurance that would cover the service, not all do. People with traditional Medicare coverage can sometimes pay 20% of the cost of some medical services.
“I think that may give patients pause, particularly if they’re already feeling the financial burden of a cancer treatment journey,” Dr. Mullangi said.
Pay rates for PIN services involve calculations of regional price differences, which are posted publicly by CMS, and potential added fees for services provided by hospital-affiliated organizations.
Consider payments for code G0023, covering 60 minutes of principal navigation services provided in a single month.
A set reimbursement for patients cared for in independent medical practices exists, with variation for local costs. Medicare’s non-facility price for G0023 would be $102.41 in some parts of Silicon Valley in California, including San Jose. In Arkansas, where costs are lower, reimbursement would be $73.14 for this same service.
Patients who get services covered by code G0023 in independent medical practices would have monthly copays of about $15-$20, depending on where they live.
The tab for patients tends to be higher for these same services if delivered through a medical practice owned by a hospital, as this would trigger the addition of facility fees to the payments made to cover the services. Facility fees are difficult for the public to ascertain before getting a treatment or service.
Dr. Mullangi and Ms. Gentry reported no relevant financial disclosures outside of their employers.
A version of this article first appeared on Medscape.com.

VA Choice Bill Defeated in the House
A U.S. House of Representatives appropriation to fund the Veterans Choice Program surprisingly went down to defeat on Monday. The VA Choice Program is set to run out of money in September, and VA officials have been calling for Congress to provide additional funding for the program. Republican leaders, hoping to expedite the bill’s passage and thinking that it was not controversial, submitted the bill in a process that required the votes of two-thirds of the representatives. The 219-186 vote fell well short of the necessary two-thirds, and voting fell largely along party lines.
Many veterans service organizations (VSOs) were critical of the bill and called on the House to make substantial changes to it. Seven VSOs signed a joint statement calling for the bill’s defeat. “As organizations who represent and support the interests of America’s 21 million veterans, and in fulfillment of our mandate to ensure that the men and women who served are able to receive the health care and benefits they need and deserve, we are calling on Members of Congress to defeat the House vote on unacceptable choice funding legislation (S. 114, with amendments),” the statement read.
AMVETS, Disabled American Veterans , Military Officers Association of America, Military Order of the Purple Heart, Veterans of Foreign Wars, Vietnam Veterans of America, and Wounded Warrior Project all signed on to the statement. The chief complaint was that the legislation “includes funding only for the ‘choice’ program which provides additional community care options, but makes no investment in VA and uses ‘savings’ from other veterans benefits or services to ‘pay’ for the ‘choice’ program.”
The bill would have allocated $2 billion for the Veterans Choice Program, taken funding for veteran housing loan fees, and would reduce the pensions for some veterans living in nursing facilities that also could be paid for under the Medicaid program.
The fate of the bill and funding for the Veterans Choice Program remains unclear. Senate and House veterans committees seem to be far apart on how to fund the program and for efforts to make more substantive changes to the program. Although House Republicans eventually may be able to pass a bill without Democrats, in the Senate, they will need the support of at least a handful of Democrats to move the bill to the President’s desk.
A U.S. House of Representatives appropriation to fund the Veterans Choice Program surprisingly went down to defeat on Monday. The VA Choice Program is set to run out of money in September, and VA officials have been calling for Congress to provide additional funding for the program. Republican leaders, hoping to expedite the bill’s passage and thinking that it was not controversial, submitted the bill in a process that required the votes of two-thirds of the representatives. The 219-186 vote fell well short of the necessary two-thirds, and voting fell largely along party lines.
Many veterans service organizations (VSOs) were critical of the bill and called on the House to make substantial changes to it. Seven VSOs signed a joint statement calling for the bill’s defeat. “As organizations who represent and support the interests of America’s 21 million veterans, and in fulfillment of our mandate to ensure that the men and women who served are able to receive the health care and benefits they need and deserve, we are calling on Members of Congress to defeat the House vote on unacceptable choice funding legislation (S. 114, with amendments),” the statement read.
AMVETS, Disabled American Veterans , Military Officers Association of America, Military Order of the Purple Heart, Veterans of Foreign Wars, Vietnam Veterans of America, and Wounded Warrior Project all signed on to the statement. The chief complaint was that the legislation “includes funding only for the ‘choice’ program which provides additional community care options, but makes no investment in VA and uses ‘savings’ from other veterans benefits or services to ‘pay’ for the ‘choice’ program.”
The bill would have allocated $2 billion for the Veterans Choice Program, taken funding for veteran housing loan fees, and would reduce the pensions for some veterans living in nursing facilities that also could be paid for under the Medicaid program.
The fate of the bill and funding for the Veterans Choice Program remains unclear. Senate and House veterans committees seem to be far apart on how to fund the program and for efforts to make more substantive changes to the program. Although House Republicans eventually may be able to pass a bill without Democrats, in the Senate, they will need the support of at least a handful of Democrats to move the bill to the President’s desk.
A U.S. House of Representatives appropriation to fund the Veterans Choice Program surprisingly went down to defeat on Monday. The VA Choice Program is set to run out of money in September, and VA officials have been calling for Congress to provide additional funding for the program. Republican leaders, hoping to expedite the bill’s passage and thinking that it was not controversial, submitted the bill in a process that required the votes of two-thirds of the representatives. The 219-186 vote fell well short of the necessary two-thirds, and voting fell largely along party lines.
Many veterans service organizations (VSOs) were critical of the bill and called on the House to make substantial changes to it. Seven VSOs signed a joint statement calling for the bill’s defeat. “As organizations who represent and support the interests of America’s 21 million veterans, and in fulfillment of our mandate to ensure that the men and women who served are able to receive the health care and benefits they need and deserve, we are calling on Members of Congress to defeat the House vote on unacceptable choice funding legislation (S. 114, with amendments),” the statement read.
AMVETS, Disabled American Veterans , Military Officers Association of America, Military Order of the Purple Heart, Veterans of Foreign Wars, Vietnam Veterans of America, and Wounded Warrior Project all signed on to the statement. The chief complaint was that the legislation “includes funding only for the ‘choice’ program which provides additional community care options, but makes no investment in VA and uses ‘savings’ from other veterans benefits or services to ‘pay’ for the ‘choice’ program.”
The bill would have allocated $2 billion for the Veterans Choice Program, taken funding for veteran housing loan fees, and would reduce the pensions for some veterans living in nursing facilities that also could be paid for under the Medicaid program.
The fate of the bill and funding for the Veterans Choice Program remains unclear. Senate and House veterans committees seem to be far apart on how to fund the program and for efforts to make more substantive changes to the program. Although House Republicans eventually may be able to pass a bill without Democrats, in the Senate, they will need the support of at least a handful of Democrats to move the bill to the President’s desk.
How to explain physician compounding to legislators
In Ohio, new limits on drug compounding in physicians’ offices went into effect in April and have become a real hindrance to care for dermatology patients. The State of Ohio Board of Pharmacy has defined compounding as combining two or more prescription drugs and has required that physicians who perform this “compounding” must obtain a “Terminal Distributor of Dangerous Drugs” license. Ohio is the “test state,” and these rules, unless vigorously opposed, will be coming to your state.
[polldaddy:9779752]
The rules state that “compounded” drugs used within 6 hours of preparation must be prepared in a designated clean medication area with proper hand hygiene and the use of powder-free gloves. “Compounded” drugs that are used more than 6 hours after preparation, require a designated clean room with access limited to authorized personnel, environmental control devices such as a laminar flow hood, and additional equipment and training of personnel to maintain an aseptic environment. A separate license is required for each office location.
The state pharmacy boards are eager to restrict physicians – as well as dentists and veterinarians – and to collect annual licensing fees. Additionally, according to an article from the Ohio State Medical Association, noncompliant physicians can be fined by the pharmacy board.
We are talking big money, power, and dreams of clinical relevancy (and billable activities) here.
What can dermatologists do to prevent this regulatory overreach? I encourage you to plan a visit to your state representative, where you can demonstrate how these restrictions affect you and your patients – an exercise that should be both fun and compelling. All you need to illustrate your case is a simple kit that includes a syringe (but no needles in the statehouse!), a bottle of lidocaine with epinephrine, a bottle of 8.4% bicarbonate, alcohol pads, and gloves.
First, explain to your audience that there is a skin cancer epidemic with more than 5.4 million new cases a year and that, over the past 20 years, the incidence of skin cancer has doubled and is projected to double again over the next 20 years. Further, explain that dermatologists treat more than 70% of these cases in the office setting, under local anesthesia, at a huge cost savings to the public and government (it costs an average of 12 times as much to remove these cancers in the outpatient department at the hospital). Remember, states foot most of the bill for Medicaid and Medicare gap indigent coverage.
Take the bottle of lidocaine with epinephrine and open the syringe pack (Staffers love this demonstration; everyone is fascinated with shots.). Put on your gloves, wipe the top of the lidocaine bottle with an alcohol swab, and explain that this medicine is the anesthetic preferred for skin cancer surgery. Explain how it not only numbs the skin, but also causes vasoconstriction, so that the cancer can be easily and safely removed in the office.
Then explain that, in order for the epinephrine to be stable, the solution has to be very acidic (a pH of 4.2, in fact). Explain that this makes it burn like hell unless you add 0.1 cc per cc of 8.4% bicarbonate, in which case the perceived pain on a 10-point scale will drop from 8 to 2. Then pick up the bottle of bicarbonate and explain that you will no longer be able to mix these two components anymore without a “Terminal Distributor of Dangerous Drugs” license because your state pharmacy board considers this compounding. Your representative is likely to give you looks of astonishment, disbelief, and then a dawning realization of the absurdity of the situation.
Follow-up questions may include “Why can’t you buy buffered lidocaine with epinephrine from the compounding pharmacy?” Easy answer: because each patient needs an individual prescription, and you may not know in advance which patient will need it, and how much the patient will need, and it becomes unstable once it has been buffered. It also will cost the patient $45 per 5-cc syringe, and it will be degraded by the time the patient returns from the compounding pharmacy. Explain further that it costs you only 84 cents to make a 5-cc syringe of buffered lidocaine; that some patients may need as many as 10 syringes; and that these costs are all included in the surgery (free!) if the physician draws it up in the office.
A simple summary is – less pain, less cost – and no history of infections or complications.
It is an eye-opener when you demonstrate how ridiculous the compounding rules being imposed are for physicians and patients. I’ve used this demonstration at the state and federal legislative level, and more recently, at the Food and Drug Administration.
If you get the chance, when a state legislator is in your office, become an advocate for your patients and fellow physicians. Make sure physician offices are excluded from these definitions of com
This column was updated June 22, 2017.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@frontlinemedcom.com.
In Ohio, new limits on drug compounding in physicians’ offices went into effect in April and have become a real hindrance to care for dermatology patients. The State of Ohio Board of Pharmacy has defined compounding as combining two or more prescription drugs and has required that physicians who perform this “compounding” must obtain a “Terminal Distributor of Dangerous Drugs” license. Ohio is the “test state,” and these rules, unless vigorously opposed, will be coming to your state.
[polldaddy:9779752]
The rules state that “compounded” drugs used within 6 hours of preparation must be prepared in a designated clean medication area with proper hand hygiene and the use of powder-free gloves. “Compounded” drugs that are used more than 6 hours after preparation, require a designated clean room with access limited to authorized personnel, environmental control devices such as a laminar flow hood, and additional equipment and training of personnel to maintain an aseptic environment. A separate license is required for each office location.
The state pharmacy boards are eager to restrict physicians – as well as dentists and veterinarians – and to collect annual licensing fees. Additionally, according to an article from the Ohio State Medical Association, noncompliant physicians can be fined by the pharmacy board.
We are talking big money, power, and dreams of clinical relevancy (and billable activities) here.
What can dermatologists do to prevent this regulatory overreach? I encourage you to plan a visit to your state representative, where you can demonstrate how these restrictions affect you and your patients – an exercise that should be both fun and compelling. All you need to illustrate your case is a simple kit that includes a syringe (but no needles in the statehouse!), a bottle of lidocaine with epinephrine, a bottle of 8.4% bicarbonate, alcohol pads, and gloves.
First, explain to your audience that there is a skin cancer epidemic with more than 5.4 million new cases a year and that, over the past 20 years, the incidence of skin cancer has doubled and is projected to double again over the next 20 years. Further, explain that dermatologists treat more than 70% of these cases in the office setting, under local anesthesia, at a huge cost savings to the public and government (it costs an average of 12 times as much to remove these cancers in the outpatient department at the hospital). Remember, states foot most of the bill for Medicaid and Medicare gap indigent coverage.
Take the bottle of lidocaine with epinephrine and open the syringe pack (Staffers love this demonstration; everyone is fascinated with shots.). Put on your gloves, wipe the top of the lidocaine bottle with an alcohol swab, and explain that this medicine is the anesthetic preferred for skin cancer surgery. Explain how it not only numbs the skin, but also causes vasoconstriction, so that the cancer can be easily and safely removed in the office.
Then explain that, in order for the epinephrine to be stable, the solution has to be very acidic (a pH of 4.2, in fact). Explain that this makes it burn like hell unless you add 0.1 cc per cc of 8.4% bicarbonate, in which case the perceived pain on a 10-point scale will drop from 8 to 2. Then pick up the bottle of bicarbonate and explain that you will no longer be able to mix these two components anymore without a “Terminal Distributor of Dangerous Drugs” license because your state pharmacy board considers this compounding. Your representative is likely to give you looks of astonishment, disbelief, and then a dawning realization of the absurdity of the situation.
Follow-up questions may include “Why can’t you buy buffered lidocaine with epinephrine from the compounding pharmacy?” Easy answer: because each patient needs an individual prescription, and you may not know in advance which patient will need it, and how much the patient will need, and it becomes unstable once it has been buffered. It also will cost the patient $45 per 5-cc syringe, and it will be degraded by the time the patient returns from the compounding pharmacy. Explain further that it costs you only 84 cents to make a 5-cc syringe of buffered lidocaine; that some patients may need as many as 10 syringes; and that these costs are all included in the surgery (free!) if the physician draws it up in the office.
A simple summary is – less pain, less cost – and no history of infections or complications.
It is an eye-opener when you demonstrate how ridiculous the compounding rules being imposed are for physicians and patients. I’ve used this demonstration at the state and federal legislative level, and more recently, at the Food and Drug Administration.
If you get the chance, when a state legislator is in your office, become an advocate for your patients and fellow physicians. Make sure physician offices are excluded from these definitions of com
This column was updated June 22, 2017.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@frontlinemedcom.com.
In Ohio, new limits on drug compounding in physicians’ offices went into effect in April and have become a real hindrance to care for dermatology patients. The State of Ohio Board of Pharmacy has defined compounding as combining two or more prescription drugs and has required that physicians who perform this “compounding” must obtain a “Terminal Distributor of Dangerous Drugs” license. Ohio is the “test state,” and these rules, unless vigorously opposed, will be coming to your state.
[polldaddy:9779752]
The rules state that “compounded” drugs used within 6 hours of preparation must be prepared in a designated clean medication area with proper hand hygiene and the use of powder-free gloves. “Compounded” drugs that are used more than 6 hours after preparation, require a designated clean room with access limited to authorized personnel, environmental control devices such as a laminar flow hood, and additional equipment and training of personnel to maintain an aseptic environment. A separate license is required for each office location.
The state pharmacy boards are eager to restrict physicians – as well as dentists and veterinarians – and to collect annual licensing fees. Additionally, according to an article from the Ohio State Medical Association, noncompliant physicians can be fined by the pharmacy board.
We are talking big money, power, and dreams of clinical relevancy (and billable activities) here.
What can dermatologists do to prevent this regulatory overreach? I encourage you to plan a visit to your state representative, where you can demonstrate how these restrictions affect you and your patients – an exercise that should be both fun and compelling. All you need to illustrate your case is a simple kit that includes a syringe (but no needles in the statehouse!), a bottle of lidocaine with epinephrine, a bottle of 8.4% bicarbonate, alcohol pads, and gloves.
First, explain to your audience that there is a skin cancer epidemic with more than 5.4 million new cases a year and that, over the past 20 years, the incidence of skin cancer has doubled and is projected to double again over the next 20 years. Further, explain that dermatologists treat more than 70% of these cases in the office setting, under local anesthesia, at a huge cost savings to the public and government (it costs an average of 12 times as much to remove these cancers in the outpatient department at the hospital). Remember, states foot most of the bill for Medicaid and Medicare gap indigent coverage.
Take the bottle of lidocaine with epinephrine and open the syringe pack (Staffers love this demonstration; everyone is fascinated with shots.). Put on your gloves, wipe the top of the lidocaine bottle with an alcohol swab, and explain that this medicine is the anesthetic preferred for skin cancer surgery. Explain how it not only numbs the skin, but also causes vasoconstriction, so that the cancer can be easily and safely removed in the office.
Then explain that, in order for the epinephrine to be stable, the solution has to be very acidic (a pH of 4.2, in fact). Explain that this makes it burn like hell unless you add 0.1 cc per cc of 8.4% bicarbonate, in which case the perceived pain on a 10-point scale will drop from 8 to 2. Then pick up the bottle of bicarbonate and explain that you will no longer be able to mix these two components anymore without a “Terminal Distributor of Dangerous Drugs” license because your state pharmacy board considers this compounding. Your representative is likely to give you looks of astonishment, disbelief, and then a dawning realization of the absurdity of the situation.
Follow-up questions may include “Why can’t you buy buffered lidocaine with epinephrine from the compounding pharmacy?” Easy answer: because each patient needs an individual prescription, and you may not know in advance which patient will need it, and how much the patient will need, and it becomes unstable once it has been buffered. It also will cost the patient $45 per 5-cc syringe, and it will be degraded by the time the patient returns from the compounding pharmacy. Explain further that it costs you only 84 cents to make a 5-cc syringe of buffered lidocaine; that some patients may need as many as 10 syringes; and that these costs are all included in the surgery (free!) if the physician draws it up in the office.
A simple summary is – less pain, less cost – and no history of infections or complications.
It is an eye-opener when you demonstrate how ridiculous the compounding rules being imposed are for physicians and patients. I’ve used this demonstration at the state and federal legislative level, and more recently, at the Food and Drug Administration.
If you get the chance, when a state legislator is in your office, become an advocate for your patients and fellow physicians. Make sure physician offices are excluded from these definitions of com
This column was updated June 22, 2017.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at dermnews@frontlinemedcom.com.
Special Report II: Tackling Burnout
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Last month, we introduced the epidemic of burnout and the adverse consequences for both our vascular surgery patients and ourselves. Today we will outline a framework for addressing these issues. The foundation of this framework is informed by the social and neurosciences.
From the perspective of the social scientist: Christina Maslach, the originator of the widely used Maslach Burnout Inventory, theorized that burnout arises from a chronic mismatch between people and their work setting in some or all of the following domains: Workload (too much, wrong kind); control (lack of autonomy, or insufficient control over resources); reward (insufficient financial or social rewards commensurate with achievements); community (loss of positive connection with others); fairness (lack of perceived fairness, inequity of work, pay, or promotion); and values (conflict of personal and organizational values). The reality of practicing medicine in today’s business milieu – of achieving service efficiencies by meeting performance targets – brings many of these mismatches into sharp focus.
From the perspective of the neuroscientist: Recent advances, including functional MRI, have demonstrated that the human brain is hard wired for compassion. Compassion is the deep feeling that arises when confronted with another’s suffering, coupled with a strong desire to alleviate that suffering. There are at least two neural pathways: one activated during empathy, having us experience another’s pain; and the other activated during compassion, resulting in our sense of reward. Thus, burnout is thought to occur when you know what your patient needs but you are unable to deliver it. Compassionate medical care is purposeful work, which promotes a sense of reward and mitigates burnout.
Because burnout affects all caregivers (anyone who touches the patient), a successful program addressing workforce well-being must be comprehensive and organization wide, similar to successful patient safety, CPI [continuous process improvement] and LEAN [Six Sigma] initiatives.
There are no shortcuts. Creating a culture of compassionate, collaborative care requires an understanding of the interrelationships between the individual provider, the unit or team, and organizational leadership.
1) The individual provider: There is evidence to support the use of programs that build personal resilience. A recently published meta-analysis by West and colleagues concluded that while no specific physician burnout intervention has been shown to be better than other types of interventions, mindfulness, stress management, and small-group discussions can be effective approaches to reducing burnout scores. Strategies to build individual resilience, such as mindfulness and meditation, are easy to teach but place the burden for success on the individual. No amount of resilience can withstand an unsupportive or toxic workplace environment, so both individual and organizational strategies in combination are necessary.
2) The unit or team: Scheduling time for open and honest discussion of social and emotional issues that arise in caring for patients helps nourish caregiver to caregiver compassion. The Schwartz Center for Compassionate Healthcare is a national nonprofit leading the movement to bring compassion to every patient-caregiver interaction. More than 425 health care organization are Schwartz Center members and conduct Schwartz Rounds™ to bring doctors, nurses, and other caregivers together to discuss the human side of health care. (www.theschwartzcenter.org). Team member to team member support is essential for navigating the stressors of practice. With having lunch in front of your computer being the norm, and the disappearance of traditional spaces for colleagues to connect (for example, nurses’ lounge, physician dining rooms), the opportunity for caregivers to have a safe place to escape, a place to have their own humanity reaffirmed, a place to offer support to their peers, has been eliminated.
3) Organizational Leadership: Making compassion a core value, articulating it, and establishing metrics whereby it can be measured, is a good start. The barriers to a culture of compassion are related to our systems of care. There are burgeoning administrative and documentation tasks to be performed, and productivity expectations that turn our clinics and hospitals into assembly lines. No, we cannot expect the EMR [electronic medical records] to be eliminated, but workforce well-being cannot be sustainable in the context of inadequate resources. A culture of compassionate collaborative care requires programs and policies that are implemented by the organization itself. Examples of organization-wide initiatives that support workforce well-being and provider engagement include: screening for caregiver burnout, establishing policies for managing adverse events with an eye toward the second victim, and most importantly, supporting systems that preserve work control autonomy of physicians and nurses in clinical settings. The business sector has long recognized that workplace stress is a function of how demanding a person’s job is and how much control that person has over his or her responsibilities. The business community has also recognized that the experience of the worker (provider) drives the experience of the customer (patient). In a study of hospital compassionate practices and HCAHPS [the Hospital Consumer Assessment of Healthcare Providers and Systems], McClelland and Vogus reported that how well a hospital compassionately supports it employees and rewards compassionate acts is significantly and positively is associated with that hospital’s ratings and likelihood of patients recommending it.
How does the Society of Vascular Surgery, or any professional medical/nursing society for that matter, fit into this model?
We propose that the SVS find ways to empower their members to be agents for culture change within their own health care organizations. How might this be done:
- Teach organizational leadership skills, starting with the SVS Board of Directors, the presidential line, and the chairs of committees. Offer leadership courses at the Annual Meeting.
- Develop a community of caregivers committed to creating a compassionate collaborative culture. The SVS is a founding member of the Schwartz Center Healthcare Society Leadership Council, and you, as members of the SVS benefit from reduced registration at the Annual Compassion in Action Healthcare Conference, June 24-27, 2017 in Boston. (http://compassioninactionconference.org) This conference is designed to be highly experiential, using a hands-on “how to do it” model.
- The SVS should make improving the overall wellness of its members a specific goal and find specific metrics to monitor our progress towards this goal. Members can be provided with the tools to identify, monitor, and measure burnout and compassion. Each committee and council of the SVS can reexamine their objectives through the lens of reducing burnout and improving the wellness of vascular surgeons.
- Provide members with evidence-based programs that build personal resilience. This will not be a successful initiative unless our surgeons recognize and acknowledge the symptoms of burnout, and are willing to admit vulnerability. Without doing so, it is difficult to reach out for help.
- Redesign postgraduate resident and fellowship education. Standardizing clinical care may reduce variation and promote efficiency. However, when processes such as time-limited appointment scheduling, EMR templates, and protocols that drive physician-patient interactions are embedded in Resident and Fellowship education, the result may well be inflexibility in practice, reduced face time with patients, and interactions that lack compassion; all leading to burnout. Graduate Medical Education leaders must develop programs that support the learner’s ability to connect with patients and families, cultivate and role-model skills and behaviors that strengthen compassionate interactions, and strive to develop clinical practice models that increase Resident and Fellow work control autonomy.
The SVS should work proactively to optimize workload, fairness, and reward on a larger scale for its members as it relates to the EMR, reimbursement, and systems coverage. While we may be relatively small in size, as leaders, we are perfectly poised to address these larger, global issues. Perhaps working within the current system (i.e., PAC and APM task force) and considering innovative solutions at a national leadership scale, the SVS can direct real change!
Changing culture is not easy, nor quick, nor does it have an easy-to-follow blueprint. The first step is recognizing the need. The second is taking a leadership role. The third is thinking deeply about implementation.
*The authors extend their thanks and appreciation for the guidance, resources and support of Michael Goldberg, MD, scholar in residence, Schwartz Center for Compassionate Care, Boston and clinical professor of orthopedics at Seattle Children’s Hospital.
REFERENCES
1. J Managerial Psychol. (2007) 22:309-28
2. Annu Rev Neurosci. (2012) 35:1-23
3. Medicine. (2016) 44:583-5
4. J Health Organization Manag. (2015) 29:973-87
5. De Zulueta P Developing compassionate leadership in health care: an integrative review. J Healthcare Leadership. (2016) 8:1-10
6. Dolan ED, Morh D, Lempa M et al. Using a single item to measure burnout in primary care staff: A psychometry evaluation. J Gen Intern Med. (2015) 30:582-7
7. Karasek RA Job demands, job decision latitude, and mental strain: implications for job design. Administrative Sciences Quarterly (1979) 24: 285-308
8. Lee VS, Miller T, Daniels C, et al. Creating the exceptional patient experience in one academic health system. Acad Med. (2016) 91:338-44
9. Linzer M, Levine R, Meltzer D, et al. 10 bold steps to prevent burnout in general internal medicine. J Gen Intern Med. (2013) 29:18-20
10. Lown BA, Manning CF The Schwartz Center Rounds: Evaluation of an interdisciplinary approach to enhancing patient-centered communication, teamwork, and provider support. Acad Med. (2010) 85:1073-81
11. Lown BA, Muncer SJ, Chadwick R Can compassionate healthcare be measured? The Schwartz Center Compassionate Care Scale. Patient Education and Counseling (2015) 98:1005-10
12. Lown BA, McIntosh S, Gaines ME, et. al. Integrating compassionate collaborative care (“the Triple C”) into health professional education to advance the triple aim of health care. Acad Med (2016) 91:1-7
13. Lown BA A social neuroscience-informed model for teaching and practicing compassion in health care. Medical Education (2016) 50: 332-342
14. Maslach C, Schaufeli WG, Leiter MP Job burnout. Annu Rev Psychol (2001) 52:397-422
15. McClelland LE, Vogus TJ Compassion practices and HCAHPS: Does rewarding and supporting workplace compassion influence patient perceptions? HSR: Health Serv Res. (2014) 49:1670-83
16. Shanafelt TD, Noseworthy JH Executive leadership and physician well-being: Nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. (2016) 6:1-18
17. Shanafelt TD, Dyrbye LN, West CP Addressing physician burnout: the way forward. JAMA (2017) 317:901-2
18. Singer T, Klimecki OM Empathy and compassion Curr Biol. (2014) 24: R875-8
19. West CP, Dyrbye LN, Satele DV et. al. Concurrent validity of single-item measures of emotional exhaustion and depersonalization in burnout assessment. J Gen Intern Med. (2012) 27:1445-52
20. West CP, Dyrbye LN, Erwin PJ, et al. Interventions to address and reduce physician burnout: a systematic review and meta-analysis. Lancet. (2016) 388:2272-81
21. Wuest TK, Goldberg MJ, Kelly JD Clinical faceoff: Physician burnout-Fact, fantasy, or the fourth component of the triple aim? Clin Orthop Relat Res. (2016) doi: 10.1007/5-11999-016-5193-5
Ready for post-acute care?
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”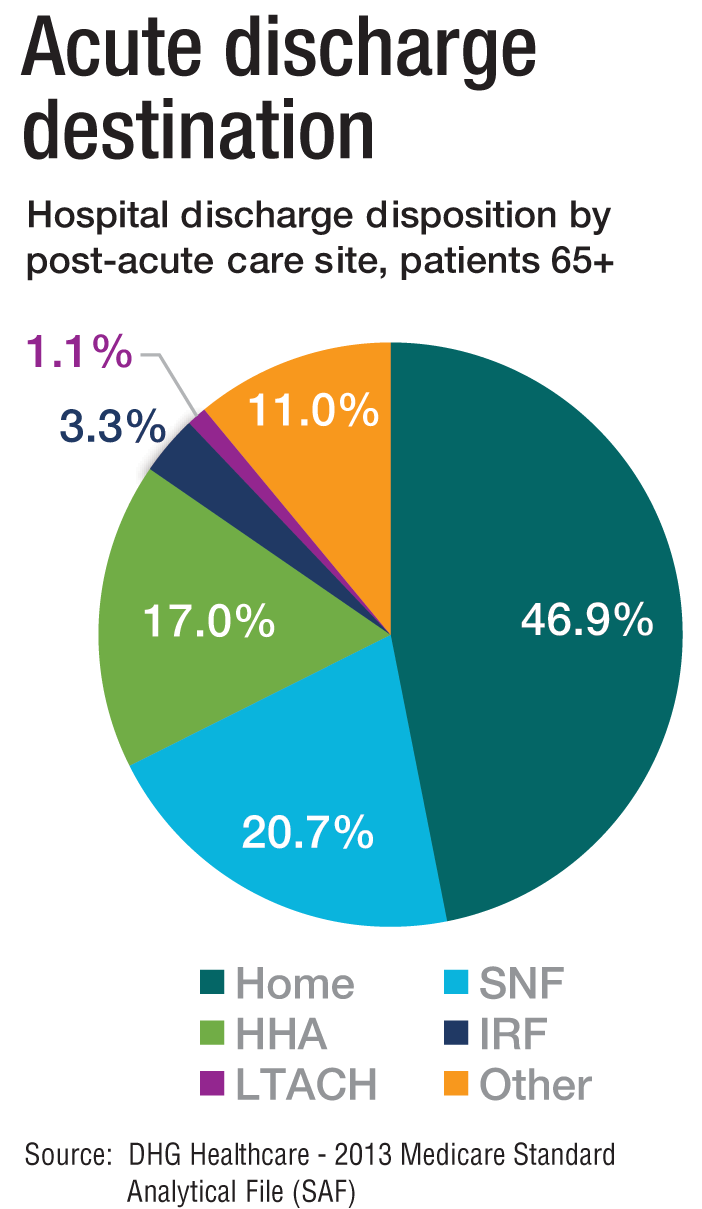
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”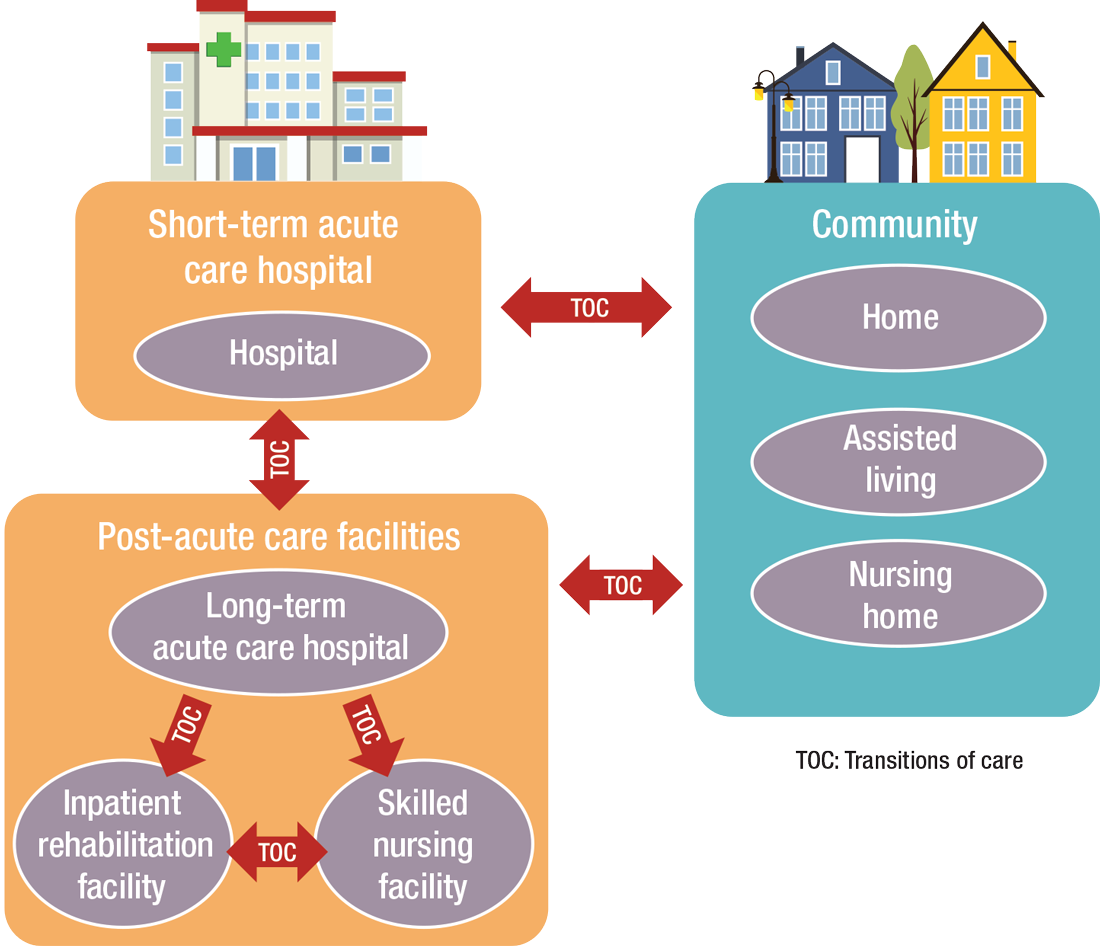
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”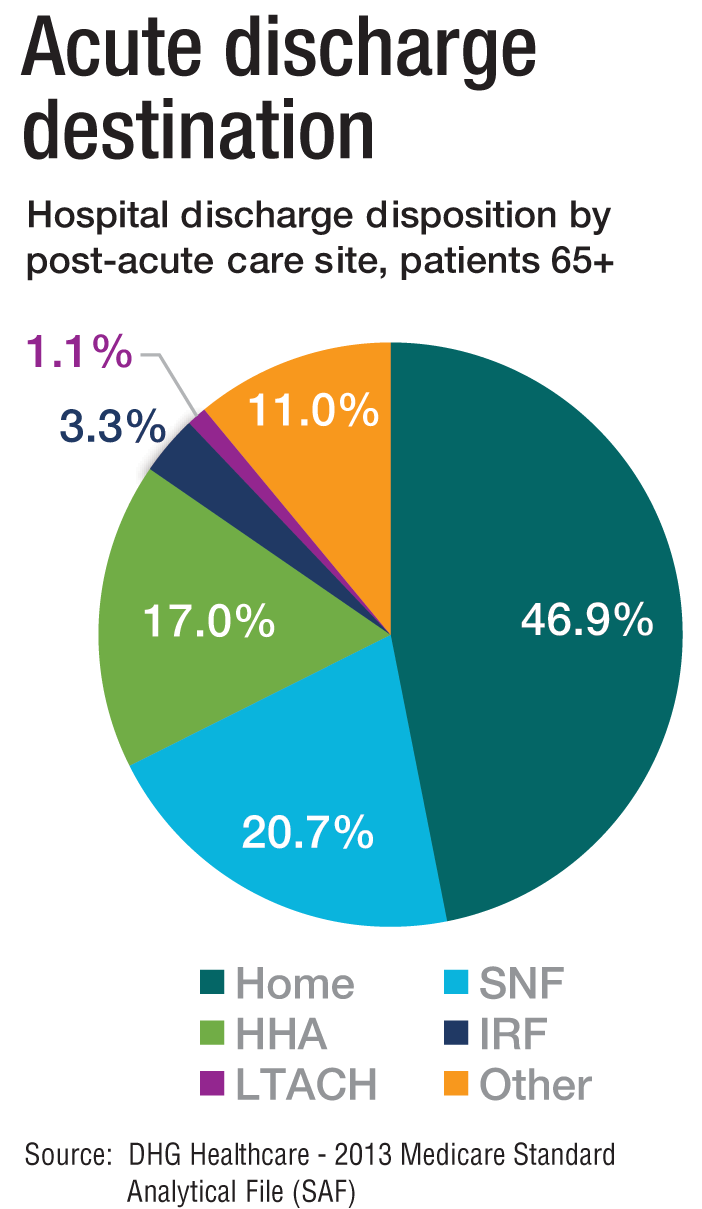
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”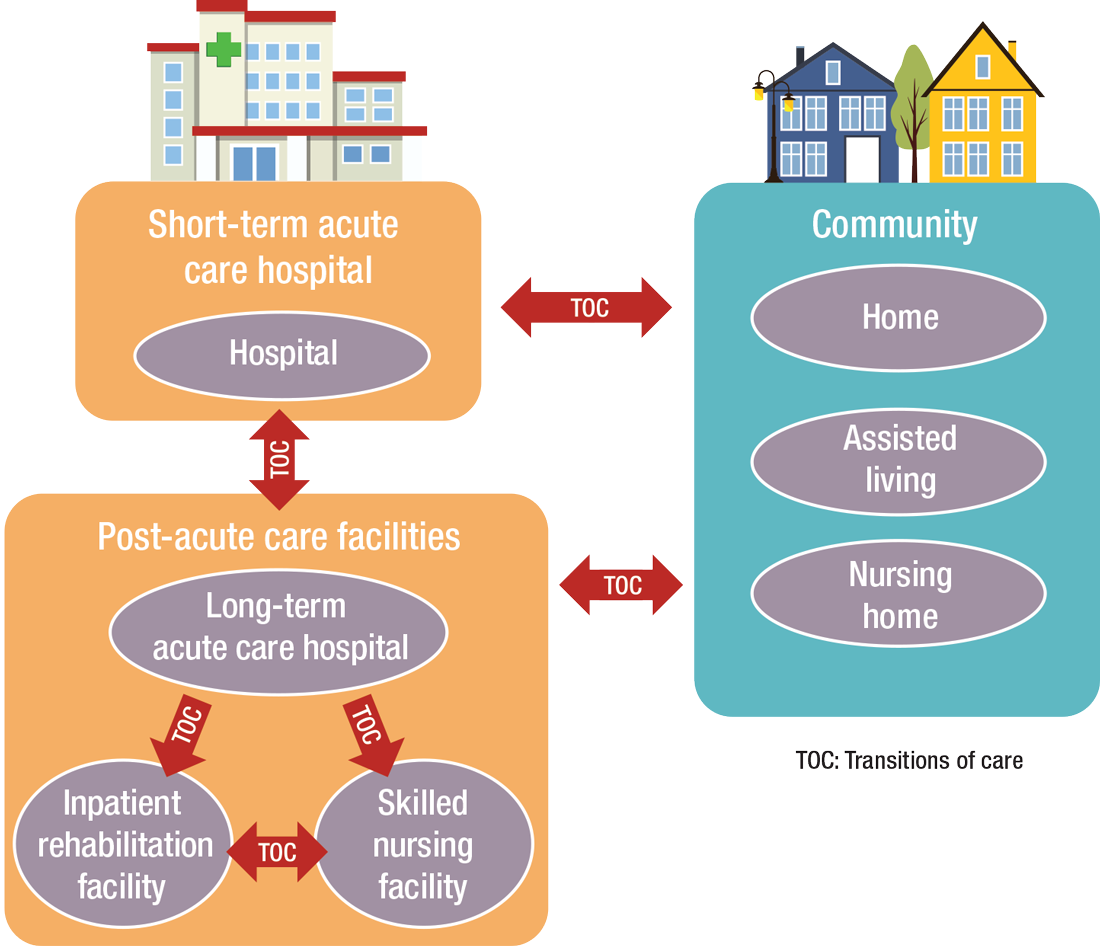
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”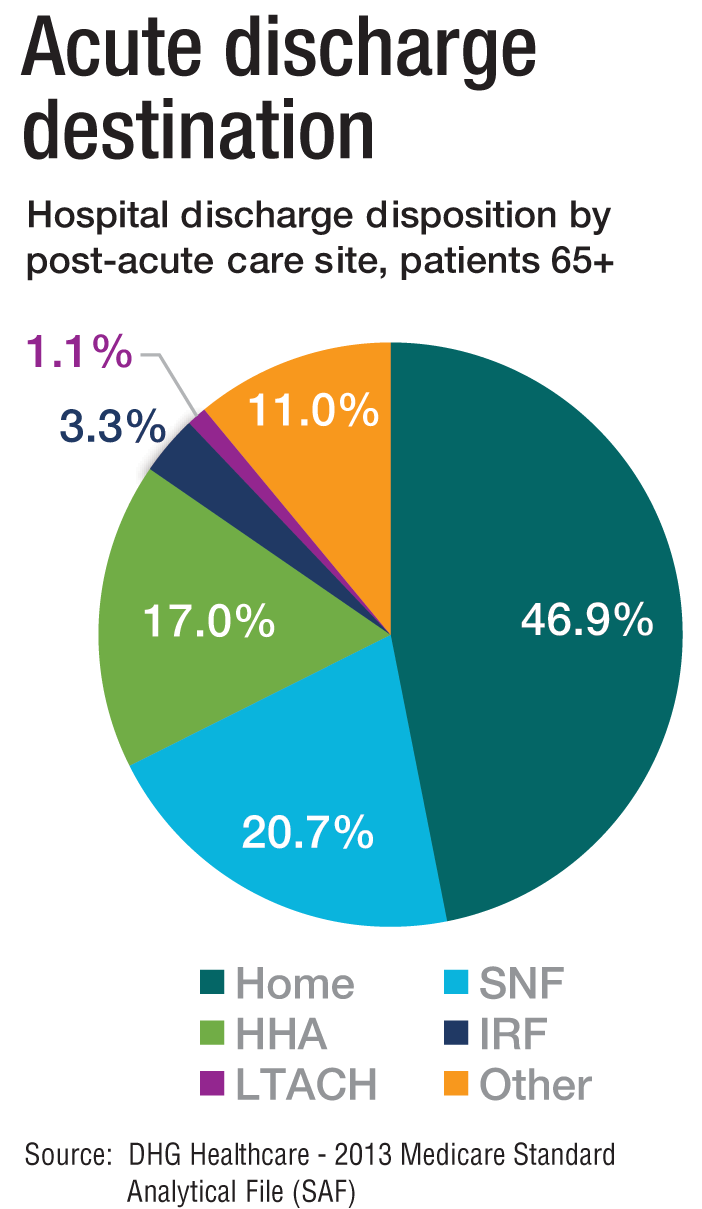
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”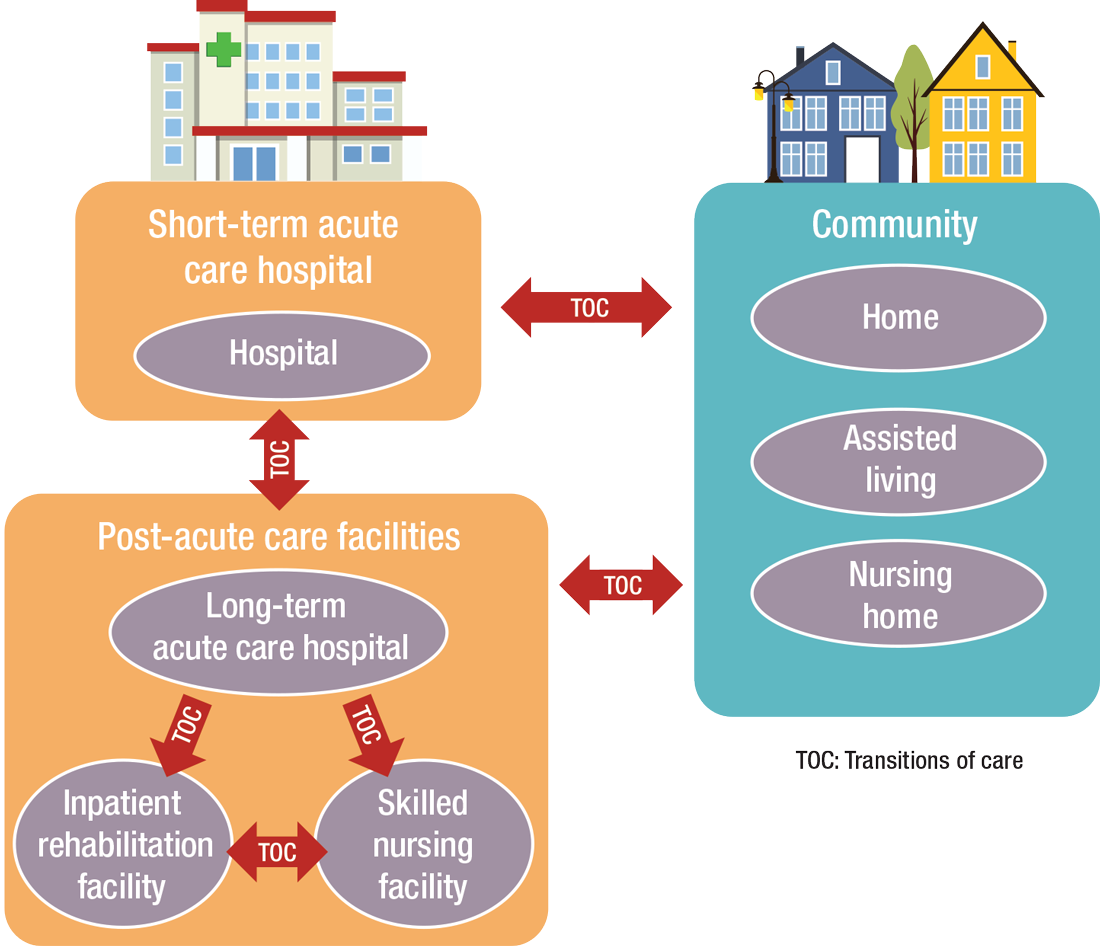
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
High-Deductible Plans May Be Linked to Worse Cancer Survival
High-Deductible Plans May Be Linked to Worse Cancer Survival
TOPLINE:
A new analysis found that high-deductible health plans were associated with worse overall survival and cancer-specific survival among cancer survivors. High-deductible plans, however, were not associated with worse overall survival among adults without a history of cancer.
METHODOLOGY:
- Previous studies have linked high-deductible health plans with decreased or delayed health utilization among cancer survivors and higher out-of-pocket costs. However, it’s not clear whether these plans influence cancer outcomes.
- In a cross-sectional study, researchers analyzed data from 147,254 respondents (aged 18 to 84 years) in the National Health Interview Survey from 2011 to 2018 and identified individuals with high-deductible plans — 2331 cancer survivors and 37,473 people without a history of cancer.
- The researchers acquired linked mortality files from the National Death Index, which included data on mortality events through the end of 2019.
- High-deductible health plans were identified through survey responses and defined as plans with yearly deductibles of at least $1200-$1350 for individuals or at least $2400-$2700 for families.
- The primary endpoints included overall survival and cancer-specific survival. Researchers adjusted for insurance status, marital status, sex, comorbidities, education, household income, geographic region, cancer site, and time since diagnosis.
TAKEAWAY:
- Among cancer survivors, having a high-deductible health plan was associated with worse overall survival (hazard ratio [HR], 1.46) and cancer-specific survival (HR, 1.34). However, sensitivity analyses incorporating time since diagnosis slightly attenuated the cancer-specific survival association (HR, 1.20; 95% CI, 0.92-1.55).
- Among adults without a history of cancer, having a high-deductible health plan was not associated with significantly worse overall survival (HR, 1.08; 95% CI, 0.96-1.21).
- General concerns over finances, worry about medical bills, cost-related delays, or forgone care, as well as cost-related underuse of medications were significant mediators of the associations between high-deductible health plan status and mortality outcomes among cancer survivors.
- High-deductible health plan status was also associated with worse cancer-specific survival among cancer survivors with incomes at least 400% of the federal poverty level (HR, 1.65; P for interaction = .03).
IN PRACTICE:
“These data suggest that insurance coverage that financially discourages medical care may financially discourage necessary care and ultimately worsen cancer outcomes,” the study authors wrote. “This danger appears to be unique to cancer survivors, as [high-deductible health plans] were not associated with survival among adults without a cancer history.”
SOURCE:
The study, led by Justin M. Barnes, MD, MS, Department of Radiation Oncology, Mayo Clinic in Rochester, Minnesota, was published online on January 29 in JAMA Network Open.
LIMITATIONS:
High-deductible health plan status was self-reported and may have been inaccurate for some individuals, with more than half of consumers being unsure about their annual deductible amount. The study lacked specific plan details and exact deductible amounts, and high-deductible health plan status was based on a single time point during survey participation. Additionally, researchers lacked information about cancer stage, cancer-directed therapies, recurrences, or complications, and cancer mortality could be from cancers diagnosed after survey participation.
DISCLOSURES:
Meera Ragavan, MD, MPH, disclosed receiving personal fees from Trial Library and AstraZeneca and grants from Merck, outside the submitted work. Other authors reported receiving personal fees from Costs of Care during the study. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
A new analysis found that high-deductible health plans were associated with worse overall survival and cancer-specific survival among cancer survivors. High-deductible plans, however, were not associated with worse overall survival among adults without a history of cancer.
METHODOLOGY:
- Previous studies have linked high-deductible health plans with decreased or delayed health utilization among cancer survivors and higher out-of-pocket costs. However, it’s not clear whether these plans influence cancer outcomes.
- In a cross-sectional study, researchers analyzed data from 147,254 respondents (aged 18 to 84 years) in the National Health Interview Survey from 2011 to 2018 and identified individuals with high-deductible plans — 2331 cancer survivors and 37,473 people without a history of cancer.
- The researchers acquired linked mortality files from the National Death Index, which included data on mortality events through the end of 2019.
- High-deductible health plans were identified through survey responses and defined as plans with yearly deductibles of at least $1200-$1350 for individuals or at least $2400-$2700 for families.
- The primary endpoints included overall survival and cancer-specific survival. Researchers adjusted for insurance status, marital status, sex, comorbidities, education, household income, geographic region, cancer site, and time since diagnosis.
TAKEAWAY:
- Among cancer survivors, having a high-deductible health plan was associated with worse overall survival (hazard ratio [HR], 1.46) and cancer-specific survival (HR, 1.34). However, sensitivity analyses incorporating time since diagnosis slightly attenuated the cancer-specific survival association (HR, 1.20; 95% CI, 0.92-1.55).
- Among adults without a history of cancer, having a high-deductible health plan was not associated with significantly worse overall survival (HR, 1.08; 95% CI, 0.96-1.21).
- General concerns over finances, worry about medical bills, cost-related delays, or forgone care, as well as cost-related underuse of medications were significant mediators of the associations between high-deductible health plan status and mortality outcomes among cancer survivors.
- High-deductible health plan status was also associated with worse cancer-specific survival among cancer survivors with incomes at least 400% of the federal poverty level (HR, 1.65; P for interaction = .03).
IN PRACTICE:
“These data suggest that insurance coverage that financially discourages medical care may financially discourage necessary care and ultimately worsen cancer outcomes,” the study authors wrote. “This danger appears to be unique to cancer survivors, as [high-deductible health plans] were not associated with survival among adults without a cancer history.”
SOURCE:
The study, led by Justin M. Barnes, MD, MS, Department of Radiation Oncology, Mayo Clinic in Rochester, Minnesota, was published online on January 29 in JAMA Network Open.
LIMITATIONS:
High-deductible health plan status was self-reported and may have been inaccurate for some individuals, with more than half of consumers being unsure about their annual deductible amount. The study lacked specific plan details and exact deductible amounts, and high-deductible health plan status was based on a single time point during survey participation. Additionally, researchers lacked information about cancer stage, cancer-directed therapies, recurrences, or complications, and cancer mortality could be from cancers diagnosed after survey participation.
DISCLOSURES:
Meera Ragavan, MD, MPH, disclosed receiving personal fees from Trial Library and AstraZeneca and grants from Merck, outside the submitted work. Other authors reported receiving personal fees from Costs of Care during the study. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
TOPLINE:
A new analysis found that high-deductible health plans were associated with worse overall survival and cancer-specific survival among cancer survivors. High-deductible plans, however, were not associated with worse overall survival among adults without a history of cancer.
METHODOLOGY:
- Previous studies have linked high-deductible health plans with decreased or delayed health utilization among cancer survivors and higher out-of-pocket costs. However, it’s not clear whether these plans influence cancer outcomes.
- In a cross-sectional study, researchers analyzed data from 147,254 respondents (aged 18 to 84 years) in the National Health Interview Survey from 2011 to 2018 and identified individuals with high-deductible plans — 2331 cancer survivors and 37,473 people without a history of cancer.
- The researchers acquired linked mortality files from the National Death Index, which included data on mortality events through the end of 2019.
- High-deductible health plans were identified through survey responses and defined as plans with yearly deductibles of at least $1200-$1350 for individuals or at least $2400-$2700 for families.
- The primary endpoints included overall survival and cancer-specific survival. Researchers adjusted for insurance status, marital status, sex, comorbidities, education, household income, geographic region, cancer site, and time since diagnosis.
TAKEAWAY:
- Among cancer survivors, having a high-deductible health plan was associated with worse overall survival (hazard ratio [HR], 1.46) and cancer-specific survival (HR, 1.34). However, sensitivity analyses incorporating time since diagnosis slightly attenuated the cancer-specific survival association (HR, 1.20; 95% CI, 0.92-1.55).
- Among adults without a history of cancer, having a high-deductible health plan was not associated with significantly worse overall survival (HR, 1.08; 95% CI, 0.96-1.21).
- General concerns over finances, worry about medical bills, cost-related delays, or forgone care, as well as cost-related underuse of medications were significant mediators of the associations between high-deductible health plan status and mortality outcomes among cancer survivors.
- High-deductible health plan status was also associated with worse cancer-specific survival among cancer survivors with incomes at least 400% of the federal poverty level (HR, 1.65; P for interaction = .03).
IN PRACTICE:
“These data suggest that insurance coverage that financially discourages medical care may financially discourage necessary care and ultimately worsen cancer outcomes,” the study authors wrote. “This danger appears to be unique to cancer survivors, as [high-deductible health plans] were not associated with survival among adults without a cancer history.”
SOURCE:
The study, led by Justin M. Barnes, MD, MS, Department of Radiation Oncology, Mayo Clinic in Rochester, Minnesota, was published online on January 29 in JAMA Network Open.
LIMITATIONS:
High-deductible health plan status was self-reported and may have been inaccurate for some individuals, with more than half of consumers being unsure about their annual deductible amount. The study lacked specific plan details and exact deductible amounts, and high-deductible health plan status was based on a single time point during survey participation. Additionally, researchers lacked information about cancer stage, cancer-directed therapies, recurrences, or complications, and cancer mortality could be from cancers diagnosed after survey participation.
DISCLOSURES:
Meera Ragavan, MD, MPH, disclosed receiving personal fees from Trial Library and AstraZeneca and grants from Merck, outside the submitted work. Other authors reported receiving personal fees from Costs of Care during the study. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article first appeared on Medscape.com.
High-Deductible Plans May Be Linked to Worse Cancer Survival
High-Deductible Plans May Be Linked to Worse Cancer Survival
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
It's hardly news that the United States is experiencing a mental health crisis -- the CDC says as much. But experts in the field say that the current administration has severely compounded the problem by eliminating agency funding and national programs, slashing research grants and data resources, and creating new barriers to behavioral health care.
Philanthropic foundations aim to do what they can to address the shortfall. The numbers, however, just don't add up.
"Some big foundations and philanthropies have said they're going to increase what they give out in the next 4 years, but they'll never be able to fill the gap," said Morgan F. McDonald, MD, national director of population health at the Milbank Memorial Fund in New York City, which works with states on health policy. "Even if every one of them were to spend down their endowments, they still couldn't."
Given the financial limitations, some foundations are taking a different tack. While looking for ways to join forces with fellow nonprofits, they are providing emergency grants to bridge funding in the short term to keep research from grinding to a halt.
Budget Cuts Reach Far and Wide
Mental health research certainly didn't escape the extensive grant cancellations at the National Institutes of Health and the National Science Foundation.
"It's already affecting our ability to stay on the cutting edge of research, best practices, and treatment approaches," said Zainab Okolo, EdD, senior vice president of policy, advocacy, and government relations at The Jed Foundation in New York City, which focuses on the emotional health of teens and young adults.
The upheaval is evident in an array of government agencies. The Health Resources and Services Administration, which last year awarded $12 billion in grants to community health centers and addiction treatment services, has seen > one-fourth of its staff eliminated. The Substance Abuse and Mental Health Services Administration has lost more than a third of its staff as federal cuts took a $1 billion bite out of its operating budget. The Education Department has halted $1 billion in grants used to hire mental health workers in school districts nationwide.
"We're very, very concerned about cuts to behavioral health systems," said Alonzo Plough, PhD, chief science officer at the Robert Wood Johnson Foundation in Princeton, New Jersey. "Doctors and nurses working in safety-net clinics are seeing tremendous reductions."
All in all, the new tax and spending law means $1 trillion in cuts to health care programs including Medicaid -- the nation's largest payer for mental health services -- Medicare, and Affordable Care Act insurance. An estimated 10 million Americans are expected to lose their health coverage as a result.
"When accessibility to care goes down, there's a chance that more people will die by suicide," said Jill Harkavy-Friedman, PhD, senior vice president of research at the American Foundation for Suicide Prevention. "But it also means people will come into care later in the course of their difficulties. Health professionals will be dealing with worse problems."
Foundations Take Emergency Measures
Even if private dollars can't replace what's been lost, philanthropic and medical foundations are stepping up.
We're seeing a lot of foundations and funders that are shifting their funding," said Alyson Niemann, CEO of Mindful Philanthropy, an organization that works with > 1000 private funders to marshal resources for mental health. This year, in response to federal cuts, "many increased funding to health and well-being, doubling or even tripling it," Niemann noted.
"They're making a great deal of effort to respond with emergency funds, really getting in the trenches and being good partners to their grantees," she said. "We've seen them asking deliberate questions, thinking about where their funding can have the most impact."
The American Psychological Foundation (APF), a longtime supporter of research and innovation, is addressing the current crisis with 2 initiatives, Michelle Quist Ryder, PhD, the organization's CEO, explained in an email. The first is APF Director Action, which funds innovative interventions at the community level. The second, Direct Action Crisis Funding Grants, will help continue research that is at risk of stalling because of budget cuts.
"Studies that are 'paused' or lose funding often cannot simply pick back up where they left off. Having to halt progress on a project can invalidate the work already completed," Ryder wrote. "These Direct Action Crisis Grants help bridge funding gaps and keep research viable."
At the same time, collaboration between foundations is becoming more widespread as they seek to maximize their impact. Philanthropic organizations are sharing ideas and best practices as well as pooling fundings.
"The goal of philanthropy is to help people," Harkavy-Friedman said. "There's strength in numbers and more dollars in numbers."
Some See Hope in Raised Voices
Despite the emergency scrambling, many of those in the trenches remain surprisingly optimistic. Some point out that the current turmoil has put a helpful spotlight on behavioral health care. Practitioners, meanwhile, have an essential role to play.
"There's a reason that things were the way they were: People advocated for many years to get where we've gotten," Harkavy-Friedman said, citing veterans' mental health care, the national violent death reporting system, and 988 as examples. "We have to raise our voices louder -- professionals in particular, because they know the impact a person in the general public many not fully grasp."
As a growing numbers of health professionals call attention to the damage wrought by deep cuts in the federal budget, foundation executives see an opportunity.
"In the mental health field, there's a deficit in the narrative, where there's a lot of focus on crisis. What we're hoping to do is shift the narrative toward 'How do we flourish together?'" Niemann said. "Sometimes deficits are where the most incredible innovations appear."
Debbie Koenig is a health writer whose work has been published by WebMD, The New York Times, and The Washington Post.
A version of this article first appeared on Medscape.com.
It's hardly news that the United States is experiencing a mental health crisis -- the CDC says as much. But experts in the field say that the current administration has severely compounded the problem by eliminating agency funding and national programs, slashing research grants and data resources, and creating new barriers to behavioral health care.
Philanthropic foundations aim to do what they can to address the shortfall. The numbers, however, just don't add up.
"Some big foundations and philanthropies have said they're going to increase what they give out in the next 4 years, but they'll never be able to fill the gap," said Morgan F. McDonald, MD, national director of population health at the Milbank Memorial Fund in New York City, which works with states on health policy. "Even if every one of them were to spend down their endowments, they still couldn't."
Given the financial limitations, some foundations are taking a different tack. While looking for ways to join forces with fellow nonprofits, they are providing emergency grants to bridge funding in the short term to keep research from grinding to a halt.
Budget Cuts Reach Far and Wide
Mental health research certainly didn't escape the extensive grant cancellations at the National Institutes of Health and the National Science Foundation.
"It's already affecting our ability to stay on the cutting edge of research, best practices, and treatment approaches," said Zainab Okolo, EdD, senior vice president of policy, advocacy, and government relations at The Jed Foundation in New York City, which focuses on the emotional health of teens and young adults.
The upheaval is evident in an array of government agencies. The Health Resources and Services Administration, which last year awarded $12 billion in grants to community health centers and addiction treatment services, has seen > one-fourth of its staff eliminated. The Substance Abuse and Mental Health Services Administration has lost more than a third of its staff as federal cuts took a $1 billion bite out of its operating budget. The Education Department has halted $1 billion in grants used to hire mental health workers in school districts nationwide.
"We're very, very concerned about cuts to behavioral health systems," said Alonzo Plough, PhD, chief science officer at the Robert Wood Johnson Foundation in Princeton, New Jersey. "Doctors and nurses working in safety-net clinics are seeing tremendous reductions."
All in all, the new tax and spending law means $1 trillion in cuts to health care programs including Medicaid -- the nation's largest payer for mental health services -- Medicare, and Affordable Care Act insurance. An estimated 10 million Americans are expected to lose their health coverage as a result.
"When accessibility to care goes down, there's a chance that more people will die by suicide," said Jill Harkavy-Friedman, PhD, senior vice president of research at the American Foundation for Suicide Prevention. "But it also means people will come into care later in the course of their difficulties. Health professionals will be dealing with worse problems."
Foundations Take Emergency Measures
Even if private dollars can't replace what's been lost, philanthropic and medical foundations are stepping up.
We're seeing a lot of foundations and funders that are shifting their funding," said Alyson Niemann, CEO of Mindful Philanthropy, an organization that works with > 1000 private funders to marshal resources for mental health. This year, in response to federal cuts, "many increased funding to health and well-being, doubling or even tripling it," Niemann noted.
"They're making a great deal of effort to respond with emergency funds, really getting in the trenches and being good partners to their grantees," she said. "We've seen them asking deliberate questions, thinking about where their funding can have the most impact."
The American Psychological Foundation (APF), a longtime supporter of research and innovation, is addressing the current crisis with 2 initiatives, Michelle Quist Ryder, PhD, the organization's CEO, explained in an email. The first is APF Director Action, which funds innovative interventions at the community level. The second, Direct Action Crisis Funding Grants, will help continue research that is at risk of stalling because of budget cuts.
"Studies that are 'paused' or lose funding often cannot simply pick back up where they left off. Having to halt progress on a project can invalidate the work already completed," Ryder wrote. "These Direct Action Crisis Grants help bridge funding gaps and keep research viable."
At the same time, collaboration between foundations is becoming more widespread as they seek to maximize their impact. Philanthropic organizations are sharing ideas and best practices as well as pooling fundings.
"The goal of philanthropy is to help people," Harkavy-Friedman said. "There's strength in numbers and more dollars in numbers."
Some See Hope in Raised Voices
Despite the emergency scrambling, many of those in the trenches remain surprisingly optimistic. Some point out that the current turmoil has put a helpful spotlight on behavioral health care. Practitioners, meanwhile, have an essential role to play.
"There's a reason that things were the way they were: People advocated for many years to get where we've gotten," Harkavy-Friedman said, citing veterans' mental health care, the national violent death reporting system, and 988 as examples. "We have to raise our voices louder -- professionals in particular, because they know the impact a person in the general public many not fully grasp."
As a growing numbers of health professionals call attention to the damage wrought by deep cuts in the federal budget, foundation executives see an opportunity.
"In the mental health field, there's a deficit in the narrative, where there's a lot of focus on crisis. What we're hoping to do is shift the narrative toward 'How do we flourish together?'" Niemann said. "Sometimes deficits are where the most incredible innovations appear."
Debbie Koenig is a health writer whose work has been published by WebMD, The New York Times, and The Washington Post.
A version of this article first appeared on Medscape.com.
It's hardly news that the United States is experiencing a mental health crisis -- the CDC says as much. But experts in the field say that the current administration has severely compounded the problem by eliminating agency funding and national programs, slashing research grants and data resources, and creating new barriers to behavioral health care.
Philanthropic foundations aim to do what they can to address the shortfall. The numbers, however, just don't add up.
"Some big foundations and philanthropies have said they're going to increase what they give out in the next 4 years, but they'll never be able to fill the gap," said Morgan F. McDonald, MD, national director of population health at the Milbank Memorial Fund in New York City, which works with states on health policy. "Even if every one of them were to spend down their endowments, they still couldn't."
Given the financial limitations, some foundations are taking a different tack. While looking for ways to join forces with fellow nonprofits, they are providing emergency grants to bridge funding in the short term to keep research from grinding to a halt.
Budget Cuts Reach Far and Wide
Mental health research certainly didn't escape the extensive grant cancellations at the National Institutes of Health and the National Science Foundation.
"It's already affecting our ability to stay on the cutting edge of research, best practices, and treatment approaches," said Zainab Okolo, EdD, senior vice president of policy, advocacy, and government relations at The Jed Foundation in New York City, which focuses on the emotional health of teens and young adults.
The upheaval is evident in an array of government agencies. The Health Resources and Services Administration, which last year awarded $12 billion in grants to community health centers and addiction treatment services, has seen > one-fourth of its staff eliminated. The Substance Abuse and Mental Health Services Administration has lost more than a third of its staff as federal cuts took a $1 billion bite out of its operating budget. The Education Department has halted $1 billion in grants used to hire mental health workers in school districts nationwide.
"We're very, very concerned about cuts to behavioral health systems," said Alonzo Plough, PhD, chief science officer at the Robert Wood Johnson Foundation in Princeton, New Jersey. "Doctors and nurses working in safety-net clinics are seeing tremendous reductions."
All in all, the new tax and spending law means $1 trillion in cuts to health care programs including Medicaid -- the nation's largest payer for mental health services -- Medicare, and Affordable Care Act insurance. An estimated 10 million Americans are expected to lose their health coverage as a result.
"When accessibility to care goes down, there's a chance that more people will die by suicide," said Jill Harkavy-Friedman, PhD, senior vice president of research at the American Foundation for Suicide Prevention. "But it also means people will come into care later in the course of their difficulties. Health professionals will be dealing with worse problems."
Foundations Take Emergency Measures
Even if private dollars can't replace what's been lost, philanthropic and medical foundations are stepping up.
We're seeing a lot of foundations and funders that are shifting their funding," said Alyson Niemann, CEO of Mindful Philanthropy, an organization that works with > 1000 private funders to marshal resources for mental health. This year, in response to federal cuts, "many increased funding to health and well-being, doubling or even tripling it," Niemann noted.
"They're making a great deal of effort to respond with emergency funds, really getting in the trenches and being good partners to their grantees," she said. "We've seen them asking deliberate questions, thinking about where their funding can have the most impact."
The American Psychological Foundation (APF), a longtime supporter of research and innovation, is addressing the current crisis with 2 initiatives, Michelle Quist Ryder, PhD, the organization's CEO, explained in an email. The first is APF Director Action, which funds innovative interventions at the community level. The second, Direct Action Crisis Funding Grants, will help continue research that is at risk of stalling because of budget cuts.
"Studies that are 'paused' or lose funding often cannot simply pick back up where they left off. Having to halt progress on a project can invalidate the work already completed," Ryder wrote. "These Direct Action Crisis Grants help bridge funding gaps and keep research viable."
At the same time, collaboration between foundations is becoming more widespread as they seek to maximize their impact. Philanthropic organizations are sharing ideas and best practices as well as pooling fundings.
"The goal of philanthropy is to help people," Harkavy-Friedman said. "There's strength in numbers and more dollars in numbers."
Some See Hope in Raised Voices
Despite the emergency scrambling, many of those in the trenches remain surprisingly optimistic. Some point out that the current turmoil has put a helpful spotlight on behavioral health care. Practitioners, meanwhile, have an essential role to play.
"There's a reason that things were the way they were: People advocated for many years to get where we've gotten," Harkavy-Friedman said, citing veterans' mental health care, the national violent death reporting system, and 988 as examples. "We have to raise our voices louder -- professionals in particular, because they know the impact a person in the general public many not fully grasp."
As a growing numbers of health professionals call attention to the damage wrought by deep cuts in the federal budget, foundation executives see an opportunity.
"In the mental health field, there's a deficit in the narrative, where there's a lot of focus on crisis. What we're hoping to do is shift the narrative toward 'How do we flourish together?'" Niemann said. "Sometimes deficits are where the most incredible innovations appear."
Debbie Koenig is a health writer whose work has been published by WebMD, The New York Times, and The Washington Post.
A version of this article first appeared on Medscape.com.
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
As Federal Cuts Deepen Mental Health Crisis, Philanthropy Scrambles to Fill the Gap
VA Exempts Clinical Staff From OPM Deferred Resignation Program
The US Department of Veterans Affairs (VA) announced on Feb. 7, 2025, that 116 Veterans Health Administration job classifications will not be eligible for the deferred resignation plan emailed by the Office of Personnel Management (OPM). The exemptions include Title 38 and Hybrid Title 38 positions, including doctors, nurses, and most medical staff.
The original OPM email offer had a Feb. 6, 2025, deadline for accepting the offer and a resignation date of no later than Sept. 30, 2025. However, the offer has been put on hold following a limited temporary restraining order from a Federal District Court in Massachusetts. Judge George O’Toole enjoined the OPM from “taking any further action to implement the so-called Fork Directive.” Arguments on the program’s legal merits began at a separate hearing on Monday.
The 116 roles exempted include physicians, nurses, pharmacists and pharmacy technicians, therapists, data scientists, dieticians, health and medical instrument technicians, among other roles.
OPM also included Voluntary Early Retirement Authority (VERA) in the deferred resignation offer. In a Feb. 6 email, the VA’s Office of the Chief Human Capital Officer (OCHCO) said: “The Department of Veterans Affairs established a list of occupations that are excluded from participating in DRP and VERA. If your occupation is on this list, you are not eligible to participate in the DRP.”
The US Department of Veterans Affairs (VA) announced on Feb. 7, 2025, that 116 Veterans Health Administration job classifications will not be eligible for the deferred resignation plan emailed by the Office of Personnel Management (OPM). The exemptions include Title 38 and Hybrid Title 38 positions, including doctors, nurses, and most medical staff.
The original OPM email offer had a Feb. 6, 2025, deadline for accepting the offer and a resignation date of no later than Sept. 30, 2025. However, the offer has been put on hold following a limited temporary restraining order from a Federal District Court in Massachusetts. Judge George O’Toole enjoined the OPM from “taking any further action to implement the so-called Fork Directive.” Arguments on the program’s legal merits began at a separate hearing on Monday.
The 116 roles exempted include physicians, nurses, pharmacists and pharmacy technicians, therapists, data scientists, dieticians, health and medical instrument technicians, among other roles.
OPM also included Voluntary Early Retirement Authority (VERA) in the deferred resignation offer. In a Feb. 6 email, the VA’s Office of the Chief Human Capital Officer (OCHCO) said: “The Department of Veterans Affairs established a list of occupations that are excluded from participating in DRP and VERA. If your occupation is on this list, you are not eligible to participate in the DRP.”
The US Department of Veterans Affairs (VA) announced on Feb. 7, 2025, that 116 Veterans Health Administration job classifications will not be eligible for the deferred resignation plan emailed by the Office of Personnel Management (OPM). The exemptions include Title 38 and Hybrid Title 38 positions, including doctors, nurses, and most medical staff.
The original OPM email offer had a Feb. 6, 2025, deadline for accepting the offer and a resignation date of no later than Sept. 30, 2025. However, the offer has been put on hold following a limited temporary restraining order from a Federal District Court in Massachusetts. Judge George O’Toole enjoined the OPM from “taking any further action to implement the so-called Fork Directive.” Arguments on the program’s legal merits began at a separate hearing on Monday.
The 116 roles exempted include physicians, nurses, pharmacists and pharmacy technicians, therapists, data scientists, dieticians, health and medical instrument technicians, among other roles.
OPM also included Voluntary Early Retirement Authority (VERA) in the deferred resignation offer. In a Feb. 6 email, the VA’s Office of the Chief Human Capital Officer (OCHCO) said: “The Department of Veterans Affairs established a list of occupations that are excluded from participating in DRP and VERA. If your occupation is on this list, you are not eligible to participate in the DRP.”
Impact of Return to Office on VA Telehealth Remains Unclear
Nearly 96,000 US Department of Veterans Affairs (VA) employees—about 20% of the workforce—will be required to return to in-office work by the end of February. The announcement follows a Jan. 20 presidential memorandum, which states agency heads must “take all necessary steps to terminate remote work arrangements and require employees to return to work in-person at their respective duty stations on a full-time basis.” According to a Jan. 28 email sent from the Office of Personnel Management but without a signature, federal employees who refuse will be offered “dignified, fair departure from the federal government utilizing a deferred resignation program.”
The revised VA work policy states “eligible employees must work full-time at their respective duty stations (agency worksites) unless excused due to a disability, qualifying medical condition or other compelling reason.” All nonbargaining unit employees and supervisors who are within 50 miles of their office have until Feb. 24 to return. The VA stated that further guidance is coming for those who live > 50 miles from a facility.
“VA’s policy allows exceptions for arrangements approved for employees as a reasonable accommodation due to a disability or a qualifying medical condition. Exceptions may also be allowed for military spouses with permanent change of station orders,” according to a VA press release.
“This is a commonsense step toward treating all VA employees equally,” acting VA Secretary Todd Hunter said. “Most VA clinical staff don’t have the luxury of working remotely, and we believe the performance, collaboration and productivity of the department will improve if all VA employees are held to the same standard.”
The impact on Veterans Health Administration operations remains difficult to determine. The order appears to include personnel providing telehealth care from remote locations, including those at the Clinical Resource Hub (CRH) program. CRH uses a hub and spoke model for limited time primary care and mental health care staffing to cover local clinician vacancies. CRH clinicians have provided > 500,000 veterans with care, averaging > 25,000 encounters in the program’s first year. Started during fiscal year 2020 amid the COVID-19 pandemic, CRH employed 636 clinicians, but more recent data are not available. The VA provided > 28 million telehealth sessions to veterans across all of its telehealth modalities in 2023. Details on how many CRH clinicians and other telehealth practitioners work remotely are also not available.
On Feb. 3, the Office of Personnel Management issued a memo to federal agency heads arguing that any collective bargaining agreements that include teleworking may “conflict with management rights” and therefore may be “unlawful and cannot be enforced.”
The American Federation of Government Employees (AFGE), which represents 800,000 federal employees, disputed the memo. “Federal employees should know that approved union contracts are enforceable by law, and the President does not have the authority to make unilateral changes to those agreements,” AFGE President Everett Kelley said. “AFGE members will not be intimidated. If our contracts are violated, we will aggressively defend them.”
The VA must decide where to put the more than 47,000 workers who may be coming back. According to the Government Accountability Office, “Federal agencies have long struggled to determine how much office space they needed to fulfill their missions efficiently.” The VA has reduced its office space by > 290,000 ft2 over the last few years in the National Capital Region alone.
In his confirmation hearing last month, VA Secretary nominee Doug Collins told lawmakers that, if confirmed, he would “encourage employees to come back to work,” but he also said he would ensure the department was following the White House’s remote work limits. “We’re going to make sure that we get people in there,” he said, “because at the end of the day, it’s about veterans.”
Nearly 96,000 US Department of Veterans Affairs (VA) employees—about 20% of the workforce—will be required to return to in-office work by the end of February. The announcement follows a Jan. 20 presidential memorandum, which states agency heads must “take all necessary steps to terminate remote work arrangements and require employees to return to work in-person at their respective duty stations on a full-time basis.” According to a Jan. 28 email sent from the Office of Personnel Management but without a signature, federal employees who refuse will be offered “dignified, fair departure from the federal government utilizing a deferred resignation program.”
The revised VA work policy states “eligible employees must work full-time at their respective duty stations (agency worksites) unless excused due to a disability, qualifying medical condition or other compelling reason.” All nonbargaining unit employees and supervisors who are within 50 miles of their office have until Feb. 24 to return. The VA stated that further guidance is coming for those who live > 50 miles from a facility.
“VA’s policy allows exceptions for arrangements approved for employees as a reasonable accommodation due to a disability or a qualifying medical condition. Exceptions may also be allowed for military spouses with permanent change of station orders,” according to a VA press release.
“This is a commonsense step toward treating all VA employees equally,” acting VA Secretary Todd Hunter said. “Most VA clinical staff don’t have the luxury of working remotely, and we believe the performance, collaboration and productivity of the department will improve if all VA employees are held to the same standard.”
The impact on Veterans Health Administration operations remains difficult to determine. The order appears to include personnel providing telehealth care from remote locations, including those at the Clinical Resource Hub (CRH) program. CRH uses a hub and spoke model for limited time primary care and mental health care staffing to cover local clinician vacancies. CRH clinicians have provided > 500,000 veterans with care, averaging > 25,000 encounters in the program’s first year. Started during fiscal year 2020 amid the COVID-19 pandemic, CRH employed 636 clinicians, but more recent data are not available. The VA provided > 28 million telehealth sessions to veterans across all of its telehealth modalities in 2023. Details on how many CRH clinicians and other telehealth practitioners work remotely are also not available.
On Feb. 3, the Office of Personnel Management issued a memo to federal agency heads arguing that any collective bargaining agreements that include teleworking may “conflict with management rights” and therefore may be “unlawful and cannot be enforced.”
The American Federation of Government Employees (AFGE), which represents 800,000 federal employees, disputed the memo. “Federal employees should know that approved union contracts are enforceable by law, and the President does not have the authority to make unilateral changes to those agreements,” AFGE President Everett Kelley said. “AFGE members will not be intimidated. If our contracts are violated, we will aggressively defend them.”
The VA must decide where to put the more than 47,000 workers who may be coming back. According to the Government Accountability Office, “Federal agencies have long struggled to determine how much office space they needed to fulfill their missions efficiently.” The VA has reduced its office space by > 290,000 ft2 over the last few years in the National Capital Region alone.
In his confirmation hearing last month, VA Secretary nominee Doug Collins told lawmakers that, if confirmed, he would “encourage employees to come back to work,” but he also said he would ensure the department was following the White House’s remote work limits. “We’re going to make sure that we get people in there,” he said, “because at the end of the day, it’s about veterans.”
Nearly 96,000 US Department of Veterans Affairs (VA) employees—about 20% of the workforce—will be required to return to in-office work by the end of February. The announcement follows a Jan. 20 presidential memorandum, which states agency heads must “take all necessary steps to terminate remote work arrangements and require employees to return to work in-person at their respective duty stations on a full-time basis.” According to a Jan. 28 email sent from the Office of Personnel Management but without a signature, federal employees who refuse will be offered “dignified, fair departure from the federal government utilizing a deferred resignation program.”
The revised VA work policy states “eligible employees must work full-time at their respective duty stations (agency worksites) unless excused due to a disability, qualifying medical condition or other compelling reason.” All nonbargaining unit employees and supervisors who are within 50 miles of their office have until Feb. 24 to return. The VA stated that further guidance is coming for those who live > 50 miles from a facility.
“VA’s policy allows exceptions for arrangements approved for employees as a reasonable accommodation due to a disability or a qualifying medical condition. Exceptions may also be allowed for military spouses with permanent change of station orders,” according to a VA press release.
“This is a commonsense step toward treating all VA employees equally,” acting VA Secretary Todd Hunter said. “Most VA clinical staff don’t have the luxury of working remotely, and we believe the performance, collaboration and productivity of the department will improve if all VA employees are held to the same standard.”
The impact on Veterans Health Administration operations remains difficult to determine. The order appears to include personnel providing telehealth care from remote locations, including those at the Clinical Resource Hub (CRH) program. CRH uses a hub and spoke model for limited time primary care and mental health care staffing to cover local clinician vacancies. CRH clinicians have provided > 500,000 veterans with care, averaging > 25,000 encounters in the program’s first year. Started during fiscal year 2020 amid the COVID-19 pandemic, CRH employed 636 clinicians, but more recent data are not available. The VA provided > 28 million telehealth sessions to veterans across all of its telehealth modalities in 2023. Details on how many CRH clinicians and other telehealth practitioners work remotely are also not available.
On Feb. 3, the Office of Personnel Management issued a memo to federal agency heads arguing that any collective bargaining agreements that include teleworking may “conflict with management rights” and therefore may be “unlawful and cannot be enforced.”
The American Federation of Government Employees (AFGE), which represents 800,000 federal employees, disputed the memo. “Federal employees should know that approved union contracts are enforceable by law, and the President does not have the authority to make unilateral changes to those agreements,” AFGE President Everett Kelley said. “AFGE members will not be intimidated. If our contracts are violated, we will aggressively defend them.”
The VA must decide where to put the more than 47,000 workers who may be coming back. According to the Government Accountability Office, “Federal agencies have long struggled to determine how much office space they needed to fulfill their missions efficiently.” The VA has reduced its office space by > 290,000 ft2 over the last few years in the National Capital Region alone.
In his confirmation hearing last month, VA Secretary nominee Doug Collins told lawmakers that, if confirmed, he would “encourage employees to come back to work,” but he also said he would ensure the department was following the White House’s remote work limits. “We’re going to make sure that we get people in there,” he said, “because at the end of the day, it’s about veterans.”
How Long Does It Take to See a Neurologist?
a cross-sectional analysis of Medicare data showed.
Wait times were not affected by the number of available neurologists. However, those with multiple sclerosis (MS), epilepsy, Parkinson’s disease, dementia, and sleep disorders had the longest wait times.
“In general, early referral to specialists has been shown to improve outcomes and increase patient satisfaction,” study author Chun Chieh Lin, PhD, MBA, of Ohio State University, Columbus, said in a press release. “Our findings underscore the need to develop new strategies to help people with neurological conditions see neurologists faster.”
The findings were published online in Neurology.
No National Benchmark for Wait Times
For this study, researchers analyzed a large sample of fee-for-service Medicare data from 2018 to 2019. Researchers identified patients with a year or less between their last referring physician visit and a new neurologist visit.
Exclusion criteria included enrollment in health maintenance organization plans without continuous enrollment in Medicare Part A and Part B for 2 years before the index neurologist visit, missing patient data, no physician referral at all, or referral by a different neurologist.
In addition to assessing wait times, investigators examined the availability of neurologists who provided medical services to Medicare beneficiaries in the 2018 dataset across 306 hospital referral regions in the United States, based on zip codes.
Results showed that 163,313 patients (average age, 74 years; 58% women; 85% White) were referred by 84,975 physicians to 10,250 neurologists across the United States.
Overall, the average wait time from physician referral to index neurologist visit was 34 days (range, 1-365 days), with longer wait times for White patients, women, and those aged 65-69 years. Overall, 18% waited longer than 90 days for an appointment.
The most common conditions diagnosed at the index neurologist visit were chronic pain/abnormality of gait (13%), sleep disorders (11%), and peripheral neuropathy (10%).
Using a linear mixed-effects statistical model, investigators found that patients with back pain waited an average of 30 days to see a neurologist, with longer waits for other conditions. Those with MS had an average wait that was 29 days longer, patients with epilepsy waited an average of 10 days longer, and those with Parkinson’s disease waited 9 days longer (P < .0001).
The number of available neurologists (range, 10-50 neurologists per 100,000 Medicare patients) did not affect wait times. However, there were differences in wait times across states because of different policies or regulations regarding healthcare access, with wait times ranging from a median high of 49 days in Idaho to a low of 24 days in Wyoming.
Notably, when patients saw a neurologist outside of their physician’s referral area, wait times were longer by an average of 11 days.
More than 40% of patients with new neurology referrals had prior office-based visits for the same neurologic diagnosis. For these patients, the median time between diagnosis and index neurologist visit was 342 days (range, 66-753 days).
Female patients in this category waited slightly longer (median, 353 days) than male patients (median, 328 days), and Black and Hispanic patients had longer median waits than White patients (389.5 days and 397 days respectively, vs 337 days; P = .0003).
“It is important to note that there is no national benchmark for determining appropriate wait times for specialist care, making it difficult to standardize expectations for timely access to specialists,” the authors noted.
The investigators suggested that a direct communication channel between primary care physicians and neurologists such as an eConsult service may hasten access to neurology consultation without the need for a formal appointment. Telemedicine in rural areas could also shorten wait times, they added.
Study limitations included the inability to determine if patients followed through with their index neurology visits or whether the last visit with the physician was the time of referral, as this could not be determined through the claims data.
This study was funded by the American Academy of Neurology. Lin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a cross-sectional analysis of Medicare data showed.
Wait times were not affected by the number of available neurologists. However, those with multiple sclerosis (MS), epilepsy, Parkinson’s disease, dementia, and sleep disorders had the longest wait times.
“In general, early referral to specialists has been shown to improve outcomes and increase patient satisfaction,” study author Chun Chieh Lin, PhD, MBA, of Ohio State University, Columbus, said in a press release. “Our findings underscore the need to develop new strategies to help people with neurological conditions see neurologists faster.”
The findings were published online in Neurology.
No National Benchmark for Wait Times
For this study, researchers analyzed a large sample of fee-for-service Medicare data from 2018 to 2019. Researchers identified patients with a year or less between their last referring physician visit and a new neurologist visit.
Exclusion criteria included enrollment in health maintenance organization plans without continuous enrollment in Medicare Part A and Part B for 2 years before the index neurologist visit, missing patient data, no physician referral at all, or referral by a different neurologist.
In addition to assessing wait times, investigators examined the availability of neurologists who provided medical services to Medicare beneficiaries in the 2018 dataset across 306 hospital referral regions in the United States, based on zip codes.
Results showed that 163,313 patients (average age, 74 years; 58% women; 85% White) were referred by 84,975 physicians to 10,250 neurologists across the United States.
Overall, the average wait time from physician referral to index neurologist visit was 34 days (range, 1-365 days), with longer wait times for White patients, women, and those aged 65-69 years. Overall, 18% waited longer than 90 days for an appointment.
The most common conditions diagnosed at the index neurologist visit were chronic pain/abnormality of gait (13%), sleep disorders (11%), and peripheral neuropathy (10%).
Using a linear mixed-effects statistical model, investigators found that patients with back pain waited an average of 30 days to see a neurologist, with longer waits for other conditions. Those with MS had an average wait that was 29 days longer, patients with epilepsy waited an average of 10 days longer, and those with Parkinson’s disease waited 9 days longer (P < .0001).
The number of available neurologists (range, 10-50 neurologists per 100,000 Medicare patients) did not affect wait times. However, there were differences in wait times across states because of different policies or regulations regarding healthcare access, with wait times ranging from a median high of 49 days in Idaho to a low of 24 days in Wyoming.
Notably, when patients saw a neurologist outside of their physician’s referral area, wait times were longer by an average of 11 days.
More than 40% of patients with new neurology referrals had prior office-based visits for the same neurologic diagnosis. For these patients, the median time between diagnosis and index neurologist visit was 342 days (range, 66-753 days).
Female patients in this category waited slightly longer (median, 353 days) than male patients (median, 328 days), and Black and Hispanic patients had longer median waits than White patients (389.5 days and 397 days respectively, vs 337 days; P = .0003).
“It is important to note that there is no national benchmark for determining appropriate wait times for specialist care, making it difficult to standardize expectations for timely access to specialists,” the authors noted.
The investigators suggested that a direct communication channel between primary care physicians and neurologists such as an eConsult service may hasten access to neurology consultation without the need for a formal appointment. Telemedicine in rural areas could also shorten wait times, they added.
Study limitations included the inability to determine if patients followed through with their index neurology visits or whether the last visit with the physician was the time of referral, as this could not be determined through the claims data.
This study was funded by the American Academy of Neurology. Lin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
a cross-sectional analysis of Medicare data showed.
Wait times were not affected by the number of available neurologists. However, those with multiple sclerosis (MS), epilepsy, Parkinson’s disease, dementia, and sleep disorders had the longest wait times.
“In general, early referral to specialists has been shown to improve outcomes and increase patient satisfaction,” study author Chun Chieh Lin, PhD, MBA, of Ohio State University, Columbus, said in a press release. “Our findings underscore the need to develop new strategies to help people with neurological conditions see neurologists faster.”
The findings were published online in Neurology.
No National Benchmark for Wait Times
For this study, researchers analyzed a large sample of fee-for-service Medicare data from 2018 to 2019. Researchers identified patients with a year or less between their last referring physician visit and a new neurologist visit.
Exclusion criteria included enrollment in health maintenance organization plans without continuous enrollment in Medicare Part A and Part B for 2 years before the index neurologist visit, missing patient data, no physician referral at all, or referral by a different neurologist.
In addition to assessing wait times, investigators examined the availability of neurologists who provided medical services to Medicare beneficiaries in the 2018 dataset across 306 hospital referral regions in the United States, based on zip codes.
Results showed that 163,313 patients (average age, 74 years; 58% women; 85% White) were referred by 84,975 physicians to 10,250 neurologists across the United States.
Overall, the average wait time from physician referral to index neurologist visit was 34 days (range, 1-365 days), with longer wait times for White patients, women, and those aged 65-69 years. Overall, 18% waited longer than 90 days for an appointment.
The most common conditions diagnosed at the index neurologist visit were chronic pain/abnormality of gait (13%), sleep disorders (11%), and peripheral neuropathy (10%).
Using a linear mixed-effects statistical model, investigators found that patients with back pain waited an average of 30 days to see a neurologist, with longer waits for other conditions. Those with MS had an average wait that was 29 days longer, patients with epilepsy waited an average of 10 days longer, and those with Parkinson’s disease waited 9 days longer (P < .0001).
The number of available neurologists (range, 10-50 neurologists per 100,000 Medicare patients) did not affect wait times. However, there were differences in wait times across states because of different policies or regulations regarding healthcare access, with wait times ranging from a median high of 49 days in Idaho to a low of 24 days in Wyoming.
Notably, when patients saw a neurologist outside of their physician’s referral area, wait times were longer by an average of 11 days.
More than 40% of patients with new neurology referrals had prior office-based visits for the same neurologic diagnosis. For these patients, the median time between diagnosis and index neurologist visit was 342 days (range, 66-753 days).
Female patients in this category waited slightly longer (median, 353 days) than male patients (median, 328 days), and Black and Hispanic patients had longer median waits than White patients (389.5 days and 397 days respectively, vs 337 days; P = .0003).
“It is important to note that there is no national benchmark for determining appropriate wait times for specialist care, making it difficult to standardize expectations for timely access to specialists,” the authors noted.
The investigators suggested that a direct communication channel between primary care physicians and neurologists such as an eConsult service may hasten access to neurology consultation without the need for a formal appointment. Telemedicine in rural areas could also shorten wait times, they added.
Study limitations included the inability to determine if patients followed through with their index neurology visits or whether the last visit with the physician was the time of referral, as this could not be determined through the claims data.
This study was funded by the American Academy of Neurology. Lin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY











