User login
Ready for post-acute care?
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”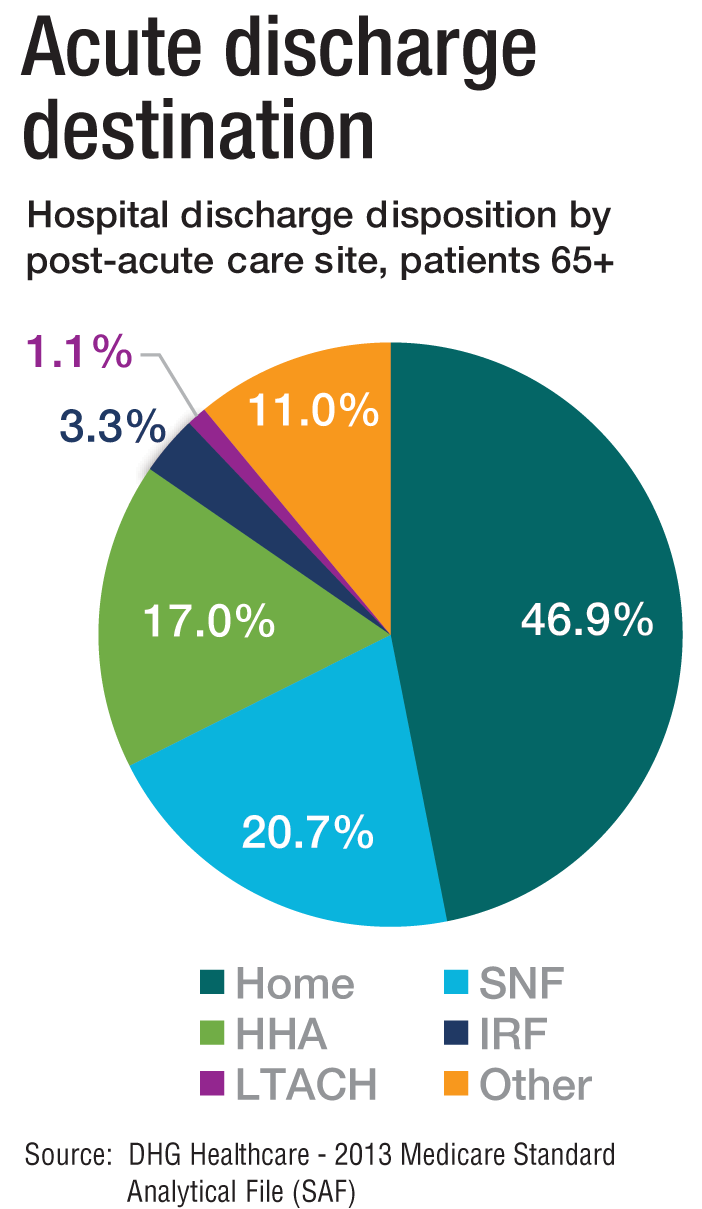
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”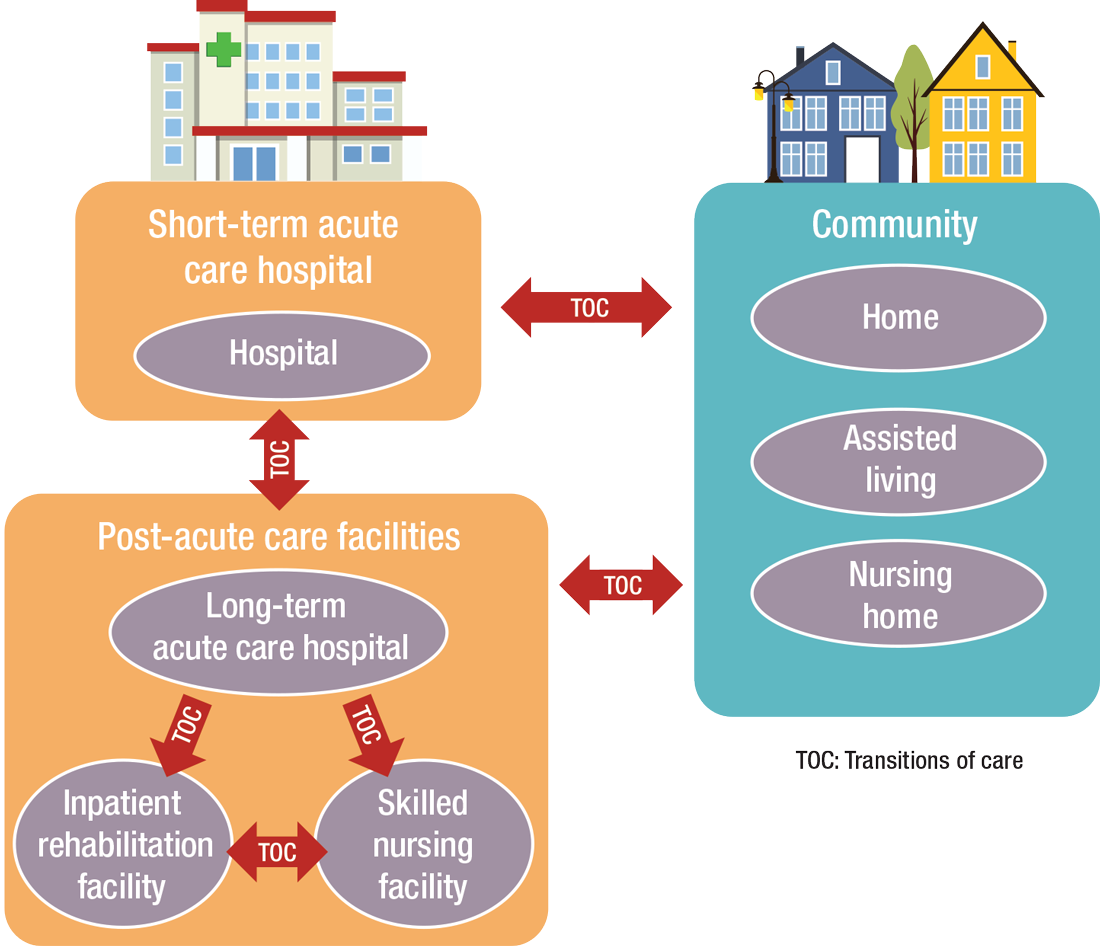
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”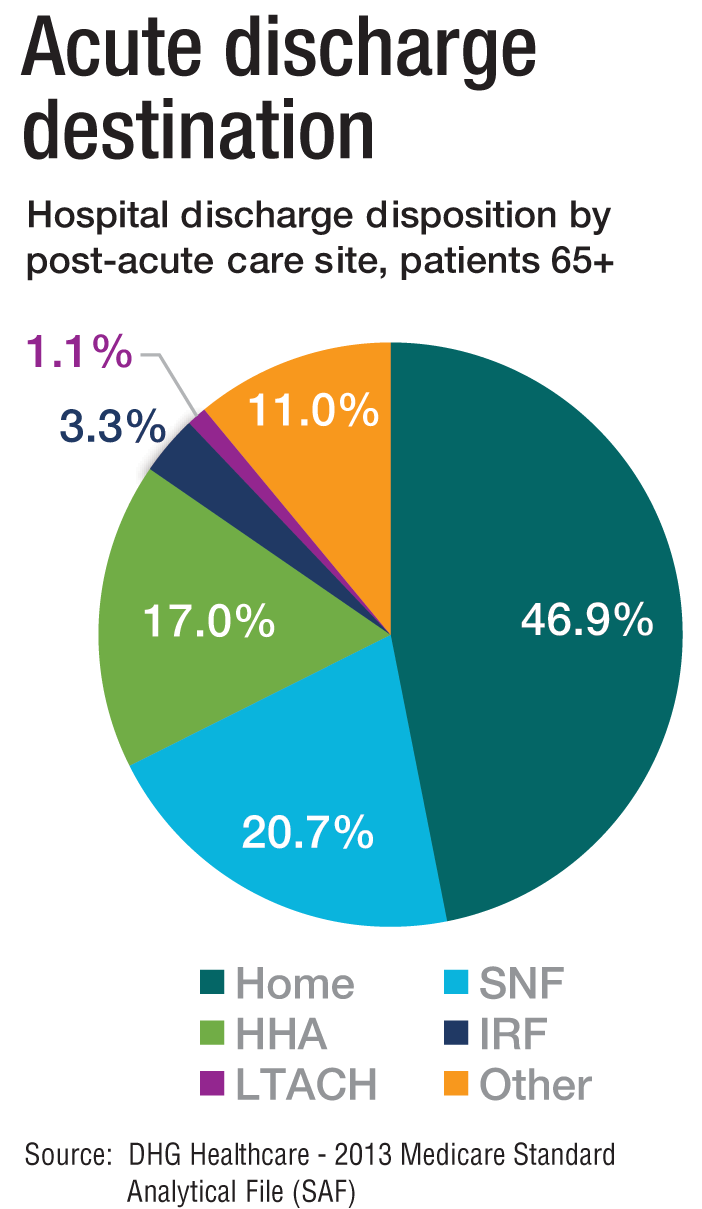
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”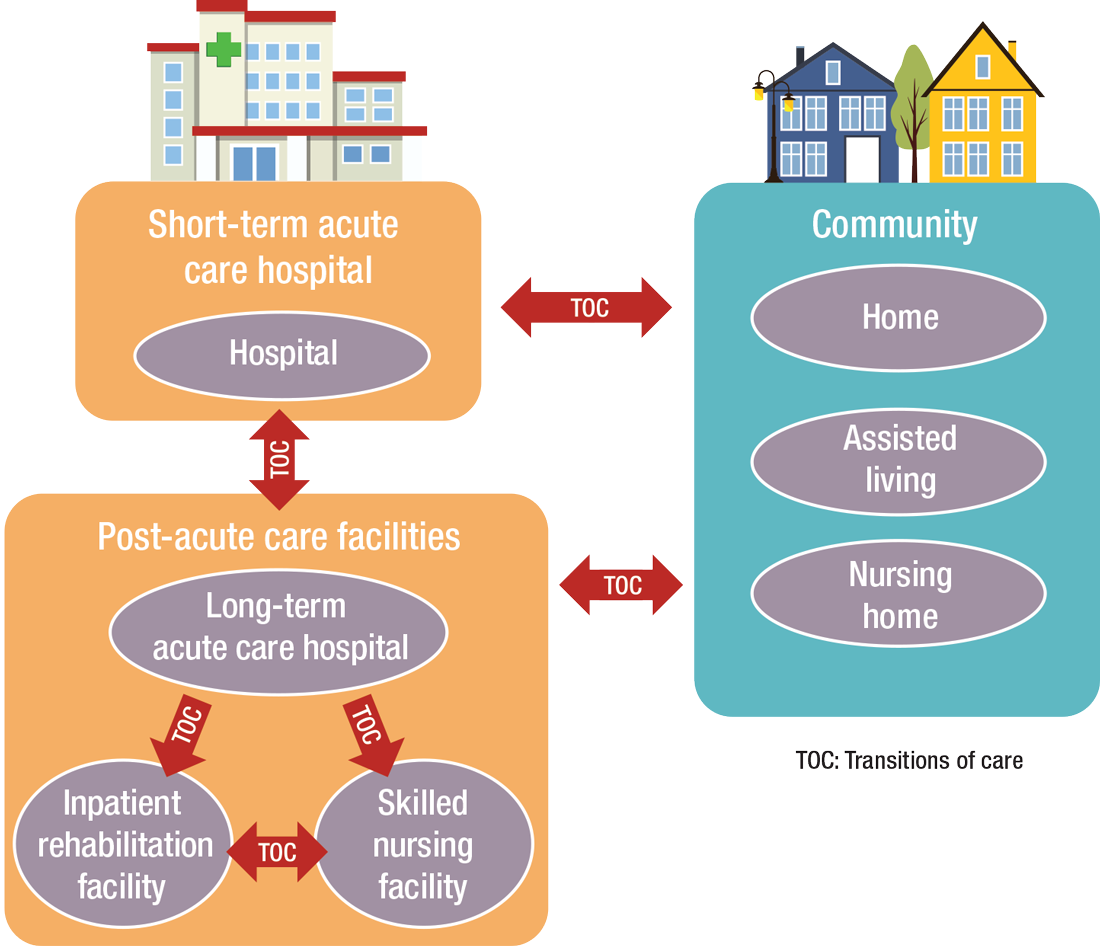
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
The definition of “hospitalist,” according to the SHM website, is a clinician “dedicated to delivering comprehensive medical care to hospitalized patients.” For years, the hospital setting was the specialties’ identifier. But as hospitalists’ scope has expanded, and post-acute care (PAC) in the United States has grown, more hospitalists are extending their roles into this space.
PAC today is more than the traditional nursing home, according to Manoj K. Mathew, MD, SFHM, national medical director of Agilon Health in Los Angeles.
Many of those expanded settings Dr. Mathew describes emerged as a result of the Affordable Care Act. Since its enactment in 2010, the ACA has heightened providers’ focus on the “Triple Aim” of improving the patient experience (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of healthcare.1 Vishal Kuchaculla, MD, New England regional post-acute medical director of Knoxville,Tenn.-based TeamHealth, says new service lines also developed as Medicare clamped down on long-term inpatient hospital stays by giving financial impetus to discharge patients as soon as possible.
“Over the last few years, there’s been a major shift from fee-for-service to risk-based payment models,” Dr. Kuchaculla says. “The government’s financial incentives are driving outcomes to improve performance initiatives.”
“Today, LTACHs can be used as substitutes for short-term acute care,” says Sean R. Muldoon, MD, MPH, FCCP, chief medical officer of Kindred Healthcare in Louisville, Ky., and former chair of SHM’s Post-Acute Care Committee. “This means that a patient can be directly admitted from their home to an LTACH. In fact, many hospice and home-care patients are referred from physicians’ offices without a preceding hospitalization.”

Hospitalists can fill a need

More hospitalists are working in PACs for a number of reasons. Dr. Mathew says PAC facilities and services have “typically lacked the clinical structure and processes to obtain the results that patients and payors expect.
“These deficits needed to be quickly remedied as patients discharged from hospitals have increased acuity and higher disease burdens,” he adds. “Hospitalists were the natural choice to fill roles requiring their expertise and experience.”
Dr. Muldoon considers the expanded scope of practice into PACs an additional layer to hospital medicine’s value proposition to the healthcare system.
“As experts in the management of inpatient populations, it’s natural for hospitalists to expand to other facilities with inpatient-like populations,” he says, noting SNFs are the most popular choice, with IRFs and LTACHs also being common places to work. Few hospitalists work in home care or hospice.
PAC settings are designed to help patients who are transitioning from an inpatient setting back to their home or other setting.
“Many patients go home after a SNF stay, while others will move to a nursing home or other longer-term care setting for the first time,” says Tiffany Radcliff, PhD, a health economist in the department of health policy and management at Texas A&M University School of Public Health in College Station. “With this in mind, hospitalists working in PAC have the opportunity to address each patient’s ongoing care needs and prepare them for their next setting. Hospitalists can manage medication or other care regimen changes that resulted from an inpatient stay, reinforce discharge instructions to the patient and their caregivers, and identify any other issues with continuing care that need to be addressed before discharge to the next care setting.”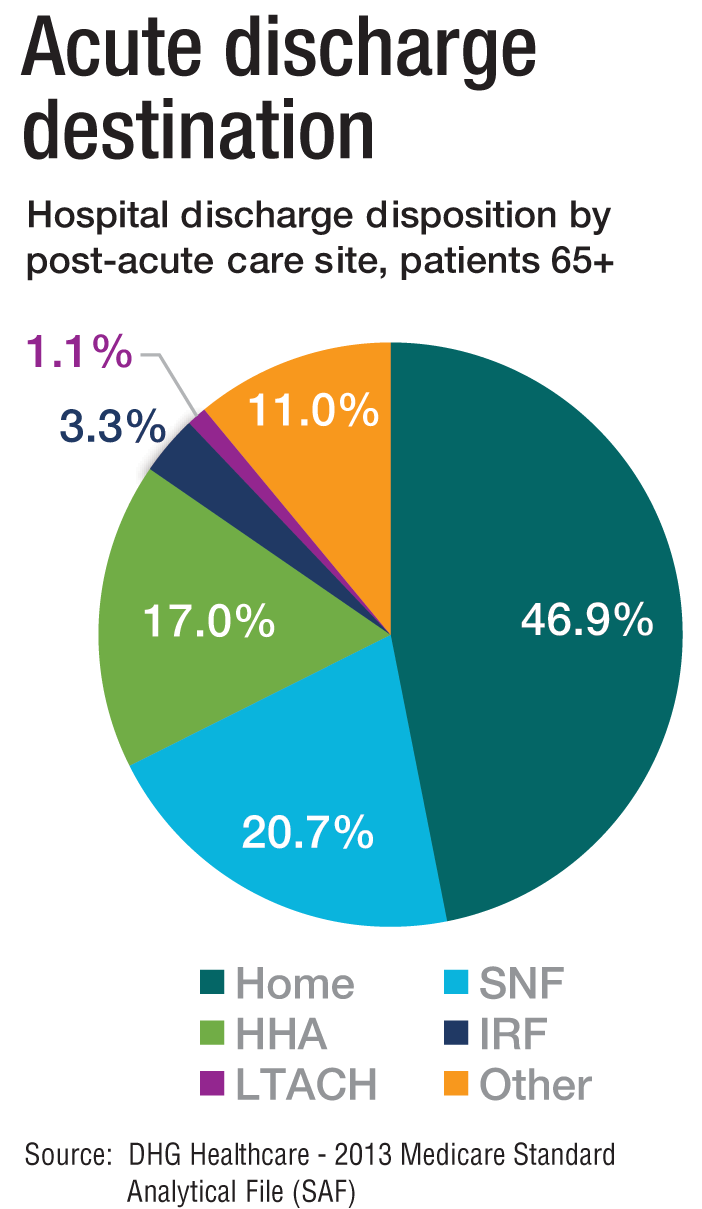
Transitioning Care
Even if a hospitalist is not employed at a PAC, it’s important that they know something about them.
“As patients are moved downstream earlier, hospitalists are being asked to help make a judgment regarding when and where an inpatient is transitioned,” Dr. Muldoon says. As organizations move toward becoming fully risk capable, it is necessary to develop referral networks of high-quality PAC providers to achieve the best clinical outcomes, reduce readmissions, and lower costs.2“Therefore, hospitalists should have a working knowledge of the different sites of service as well as some opinion on the suitability of available options in their community,” Dr. Muldoon says. “The hospitalist can also help to educate the hospitalized patient on what to expect at a PAC.”
If a patient is inappropriately prepared for the PAC setting, it could lead to incomplete management of their condition, which ultimately could lead to readmission.
“When hospitalists know how care is provided in a PAC setting, they are better able to ensure a smoother transition of care between settings,” says Tochi Iroku-Malize, MD, MPH, MBA, FAAFP, SFHM, chair of family medicine at Northwell Health in Long Island, N.Y. “This will ultimately prevent unnecessary readmissions.”
Further, the quality metrics that hospitals and thereby hospitalists are judged by no longer end at the hospital’s exit.
“The ownership of acute-care outcomes requires extending the accountability to outside of the institution’s four walls,” Dr. Mathew says. “The inpatient team needs to place great importance on the transition of care and the subsequent quality of that care when the patient is discharged.”
Robert W. Harrington Jr., MD, SFHM, chief medical officer of Plano, Texas–based Reliant Post-Acute Care Solutions and former SHM president, says the health system landscapes are pushing HM beyond the hospitals’ walls.
How PAC settings differ from hospitals
Practicing in PAC has some important nuances that hospitalists from short-term acute care need to get accustomed to, Dr. Muldoon says. Primarily, the diagnostic capabilities are much more limited, as is the presence of high-level staffing. Further, patients are less resilient to medication changes and interventions, so changes need to be done gradually.
“Hospitalists who try to practice acute-care medicine in a PAC setting may become frustrated by the length of time it takes to do a work-up, get a consultation, and respond to a patient’s change of condition,” Dr. Muldoon says. “Nonetheless, hospitalists can overcome this once recognizing this mind shift.”
According to Dr. Harrington, another challenge hospitalists may face is the inability of the hospital’s and PAC facility’s IT platforms to exchange electronic information.
“The major vendors on both sides need to figure out an interoperability strategy,” he says. “Currently, it often takes 1-3 days to receive a new patient’s discharge summary. The summary may consist of a stack of paper that takes significant time to sort through and requires the PAC facility to perform duplicate data entry. It’s a very highly inefficient process that opens up the doors to mistakes and errors of omission and commission that can result in bad patient outcomes.”
Arif Nazir, MD, CMD, FACP, AGSF, chief medical officer of Signature HealthCARE and president of SHC Medical Partners, both in Louisville, Ky., cites additional reasons the lack of seamless communication between a hospital and PAC facility is problematic. “I see physicians order laboratory tests and investigations that were already done in the hospital because they didn’t know they were already performed or never received the results,” he says. “Similarly, I see patients continue to take medications prescribed in the hospital long term even though they were only supposed to take them short term. I’ve also seen patients come to a PAC setting from a hospital without any formal understanding of their rehabilitative period and expectations for recovery.”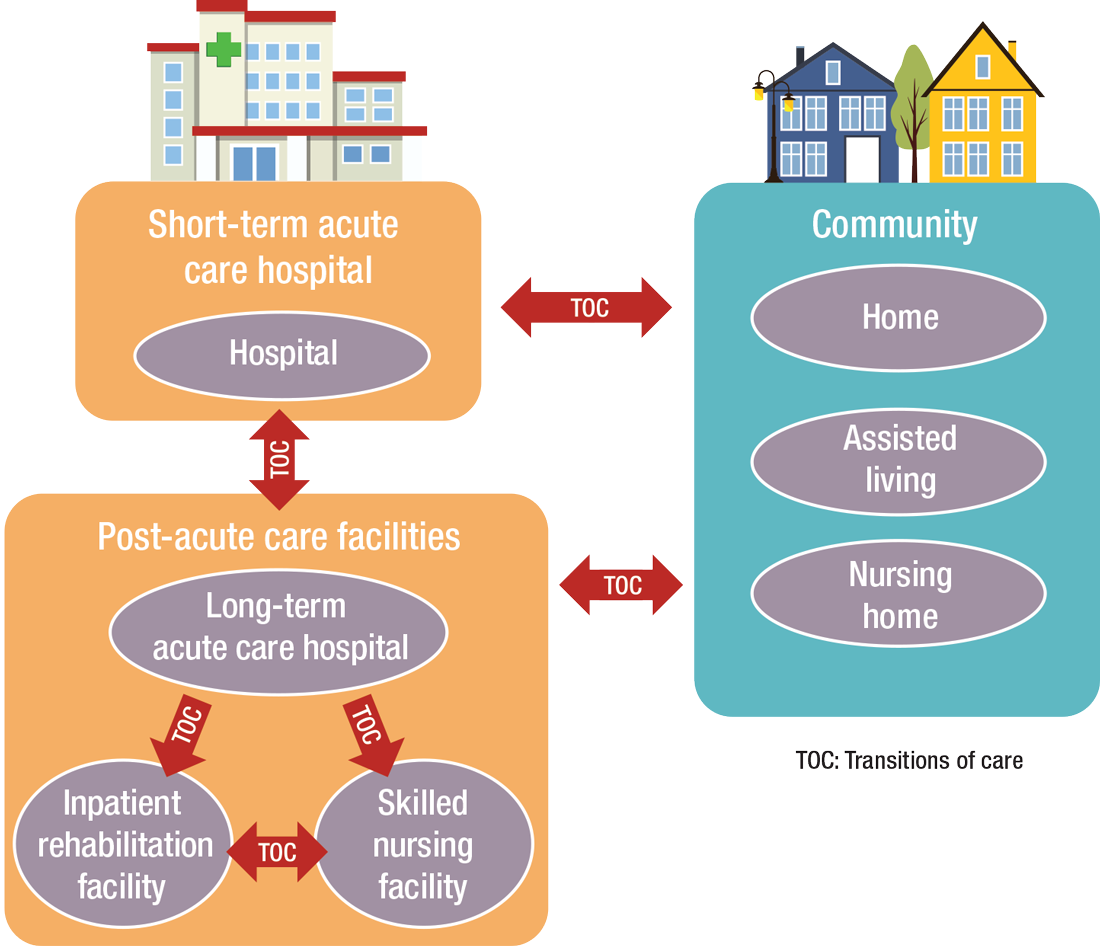
What’s ahead?
Looking to the future, Surafel Tsega, MD, clinical instructor at Mount Sinai Hospital in New York, says he thinks there will be a move toward greater collaboration among inpatient and PAC facilities, particularly in the discharge process, given that hospitals have an added incentive to ensure safe transitions because reimbursement from the Centers for Medicare & Medicaid Services is tied to readmissions and there are penalties for readmission. This involves more comprehensive planning regarding “warm handoffs” (e.g., real-time discussions with PAC providers about a patient’s hospital course and plan of care upon discharge), transferring of information, and so forth.
And while it can still be challenging to identify high-risk patients or determine the intensity and duration of their care, Dr. Mathew says risk-stratification tools and care pathways are continually being refined to maximize value with the limited resources available. In addition, with an increased emphasis on employing a team approach to care, there will be better integration of non-medical services to address the social determinants of health, which play significant roles in overall health and healing.
“Working with community-based organizations for this purpose will be a valuable tool for any of the population health–based initiatives,” he says.
Dr. Muldoon says he believes healthcare reform will increasingly view an inpatient admission as something to be avoided.
“If hospitalization can’t be avoided, then it should be shortened as much as possible,” he says. “This will shift inpatient care into LTACHs, SNFs, and IRFs. Hospitalists would be wise to follow patients into those settings as traditional inpatient census is reduced. This will take a few years, so hospitalists should start now in preparing for that downstream transition of individuals who were previously inpatients.”
The cost of care, and other PAC facts and figures
The amount of money that Medicare spends on post-acute care (PAC) has been increasing. In 2012, 12.6% of Medicare beneficiaries used some form of PAC, costing $62 billion.2 That amounts to the Centers for Medicare & Medicaid Services spending close to 25% of Medicare beneficiary expenses on PAC, a 133% increase from 2001 to 2012. Among the different types, $30.4 billion was spent on skilled nursing facilities (SNFs), $18.6 billion on home health, and $13.1 billion on long-term acute care (LTAC) and acute-care rehabilitation.2
It’s also been reported that after short-term acute-care hospitalization, about one in five Medicare beneficiaries requires continued specialized treatment in one of the three typical Medicare PAC settings: inpatient rehabilitation facilities (IRFs), LTAC hospitals, and SNFs.3
What’s more, hospital readmission nearly doubles the cost of an episode, so the financial implications for organizations operating in risk-bearing arrangements are significant. In 2013, 2,213 hospitals were charged $280 million in readmission penalties.2
References
1. The role of post-acute care in new care delivery models. American Hospital Association website. Available at: http://www.aha.org/research/reports/tw/15dec-tw-postacute.pdf. Accessed Nov. 7, 2016.
2. Post-acute care integration: Today and in the future. DHG Healthcare website. Available at: http://www2.dhgllp.com/res_pubs/HCG-Post-Acute-Care-Integration.pdf. Accessed Nov. 7, 2016.
3. Overview: Post-acute care transitions toolkit. Society for Hospital Medicine website. Available at: http://www.hospitalmedicine.org/Web/Quality___Innovation/Implementation_Toolkit/pact/Overview_PACT.aspx?hkey=dea3da3c-8620-46db-a00f-89f07f021958. Accessed Nov. 10, 2016.
Does morning discharge really improve hospital throughput?
‘Perennial debate’ likely to be reignited
A recent study published in the Journal of Hospital Medicine examined patient discharges from hospitals in Ontario, Canada, to determine if morning discharges were associated with positive outcomes. Some hospitalist programs have embraced discharge before noon (DBN) initiatives like those studied in the article.1 Unfortunately, the researchers concluded that the Canadian DBNs did not positively impact hospital length of stay, readmissions, or mortality rates.
DBN has been a quality improvement target for hospitals hoping to improve throughput and free up scarce beds, while promoting patient safety by encouraging discharge as soon as patients are ready to leave. Yet other researchers have questioned its actual impact on quality metrics. One author called DBN’s purported impact an “urban legend,”2 while a JHM editorial accompanying the Ontario study noted, “Hospitals are delicate organisms; a singular focus on one metric will undoubtedly impact others.”3
Might DBN be an artificial target that doesn’t actually enhance throughput, but leads instead to unintended consequences, such as patients being held over for an additional night in the hospital, rather than being discharged when they are ready to go on the afternoon before, in order to boost DBN rates? A perennial debate in hospital medicine is likely to be reignited by the new findings.
‘No significant overall association’
Quality improvement initiatives targeting morning discharges have included stakeholder meetings, incentives programs, discharge-centered breakfast programs, and creation of deadlines for discharge orders, the new study’s authors noted. Although these initiatives have gained support, critics have suggested that their supporting evidence is not robust.
The Canadian researchers retrospectively reviewed all patient admissions to general internal medicine services (GIMs) – largely similar to hospital medicine services in the United States – at seven hospitals in Toronto and Mississauga over a 7-year period ending Oct. 31, 2017, counting all of these patients who were discharged alive between 8 a.m. and noon. DBN averaged 19% of total live discharges across the diverse hospitals, with their diverse discharge practices.
But they found no significant overall association between morning discharge and hospital or emergency department length of stay. “Our findings suggest that increasing the number of morning discharges alone is unlikely to substantially improve patient throughput in GIM, but further research is needed to determine the effectiveness of specific interventions,” they concluded.
“We used a very narrow lens, looking specifically at throughput for the hospitals and emergency departments and whether DBN makes it more efficient,” said corresponding author Amol Verma, MD, MPhil, FRCPC, clinician-scientist at St. Michael’s Hospital, University of Toronto, in a recent interview. “What we found was that, on days when more patients are discharged in the morning, patients do not flow more quickly through the hospital. That suggests that increasing morning discharges is unlikely to make a difference.”
What does DBN really mean?
The semantics of DBN deserve further exploration. Is DBN about the actual hour of discharge, or the time when the hospitalist signs a discharge order – which may be well before the patient actually gets a wheelchair ride down to the hospital’s front doors? And if DBN is an organized program promoting morning discharges, how is it incentivized or otherwise rewarded?
Other factors, such as arrival of medications from the pharmacy or results from clinical tests, access to an ambulance if needed, transport to the front door, and bed cleaning will impact how quickly a doctor’s discharge orders get acted upon – and how quickly the newly emptied bed is available for the next occupant.
The clinician’s views on discharge practices may diverge from hospital administrator or health system perspectives, with its imperatives for efficient throughput in order to bring in more patients, Dr. Verma said. The hospitalist is also concerned about whether the patient feels ready to go home. “We can all agree that patients should leave the hospital as soon as they are medically able to do so,” he said. Longer hospital stays are associated with increased rates of hospital-acquired infections and other iatrogenic complications.
But there is not agreement on the components of a safe discharge – or on the other dimensions of effective patient flow and transitions of care. How do we optimize treatments initiated in the hospital? Does the patient need one more CAT scan? And what about the concerns of patient-centered care? Does the patient have a caregiver able to help them when they get home? There is a lot of uncertainty, Dr. Verma said. “These kinds of decisions have to get made many times every day by hospitalists,” he noted.
“We find ourselves trying to mirror the ebbs and flows of the emergency department with what’s happening in the hospital,” said Venkat Gundareddy, MBBS, MPH, associate director of the division of hospital medicine at Johns Hopkins Medicine in Baltimore. “The majority of hospital discharges happen during business hours, but the emergency department doesn’t stop admitting overnight, thus creating a throughput challenge.” Discharges are also based on clinical outcomes and on patients transferring to other facilities that prefer patients to arrive earlier in the day.
“Hospitalists may not fully appreciate these dynamics, because we’re siloed on our units,” Dr. Gundareddy said. “There is a subset of patients who would fit the bill for early discharge, but other patients come into the hospital with greater complexities, and a need for more coordination. Their discharges are harder to predict, although it gets clearer as their care progresses.”
The hospitals included in the Ontario study are at 90% -100% capacity, so their flexibility is constrained and throughput is a critical issue, Dr. Verma said. “But if you start with the target of more efficient throughput, there is no logical or practical reason to assume that discharge before noon would help. If we believe someone is ready for discharge based on physiologic changes, their response to treatment, and the conclusion of medical investigations, none of these conform to the clock. It’s equally likely the patient achieves them in the afternoon or evening.”
Other views on morning discharge
An alternative perspective comes from New York University’s Langone Medical Center, which has published positive results, including earlier subsequent arrivals to the inpatient unit from the emergency department, from increasing its hospital’s DBN rate.4
The hospital has continued to encourage morning discharges, which have consistently run 35%-40% or more of total discharges on two acute inpatient units at Langone’s Tisch Hospital. A previous study described the multidisciplinary intervention that resulted in a statistically significant increase in DBN – from 11% to 38% in the first 13 months – while significantly reducing high-frequency admission peaks.5
“We’ve been doing DBN for a number of years,” said Benjamin Wertheimer, MD, a hospitalist at Langone Medical Center and one of the studies’ authors. It is an achievable – and sustainable – goal. “Many hospitals around the country have problems with the flow of patients. Many hospitals are full – even before accounting for the COVID pandemic.” There is good evidence that, for a patient who no longer requires hospitalization, getting them out as early as possible, with a safe plan for their discharge, is a good thing, he said. “We see DBN as an important operational metric.”
If the necessary work is done correctly on the afternoon before the discharge, then a DBN approach can push communication, coordination, and advance planning, Dr Wertheimer said. Otherwise, essential discharge tasks may lag until the last minute. “We try to put the pieces in place the day before through a better planned process. But it should never be that DBN takes precedence over when the patient is safely ready to go,” he said.
“Our true measure of success would be how well we are preparing, communicating, putting safe plans into place,” he added. “DBN does not in and of itself answer all the safety and quality concerns. We set priorities around specific quality targets. DBN is just one of our operational and safety measures.”
The DBN intervention at Langone started with a multidisciplinary kickoff event in which all team members received education on its importance, a clear description of roles in the DBN process, and a corresponding checklist of daily responsibilities. The checklist was utilized at newly implemented afternoon interdisciplinary rounds, scripted to identify next-day DBNs, and make sure everything is in place for them, he explained.
“We provide daily feedback to floor staff on the DBN percentage, celebrate success, and offer real-time opportunities for case review,” Dr. Wertheimer said. “We have been careful about how we message this goal. Quality and safety come first, and we want to be prepared for discharge in advance of when the patient is ready.”
A boost for discharges
Mark Williams, MD, MHM, recently appointed chief of hospital medicine at Washington University School of Medicine in St. Louis, and a principal investigator for Project BOOST (Better Outcomes by Optimizing Safe Transitions), SHM’s quality improvement mentoring initiative aimed at helping hospitals improve care transitions, said that debates about DBN have gone on for a long time in hospital medicine.
“Around 2002, consultants told the CEO of a community hospital affiliated with Emory Healthcare that if our hospitalists could discharge patients before noon it would improve throughput,” he recalled. The consultants came from the hospitality industry, where DBN is easier to achieve.
But in hospital medicine, he said, “We use the whole day of the discharge in delivering care. I said to the CEO, ‘I can get you 100% discharge before noon – I’ll just hold the patients overnight,’” he explained. “In our initial experience, we pushed DBN up to about 10% -15%, and it opened up a few beds, which rapidly filled.”
Project BOOST encouraged the goal of getting patients ready to go out as soon as they were clinically ready, but did not advocate specifically for DBN, Dr. Williams said. “The problem is that hospital throughput starts to gum up when occupancy goes over 80% or 90%, and many academic medical centers regularly reach occupancy rates greater than 100%, particularly in the afternoon.” The deluge of patients includes transfers from other hospitals, postsurgical patients, and admissions from the emergency department.
“Boarding in the ED is a real issue,” he said. “Right now, it’s a crisis of overoccupancy, and the problem is that the pipeline is pouring patients into the system faster than they can be discharged.”
Dr. Williams believes there needs to be bigger thinking about these issues. Could hospitals, health systems, and hospitalists practice more preventive medicine so that some of these patients don’t need to come to the hospital? “Can you better address high blood pressure to prevent strokes and make sure patients with heart disease risk factors are enrolled in exercise and nutrition programs? What about access to healthy foods and the other social determinants of health? What if we provided adequate, consistent housing and transportation to medical visits?” he wondered.
Hospital at home programs may also offer some relief, he said. “If suddenly there weren’t so many emergency room visits by patients who need to get admitted, we’d have enough beds in the hospital.”
A more holistic view
John Nelson, MD, MHM, hospital medicine pioneer and management consultant, has been studying hospital throughput and policies to improve it for a long time. His 2010 column in The Hospitalist, “The Earlier the Better,” said attaching a financial incentive for hospitalists to discharge patients by a preset hour has produced mixed results.6 But Dr. Nelson offered some easy steps hospitalists can take to maximize earlier discharges, including to write “probable discharge tomorrow” as an order in the patient’s medical record.
The afternoon before a planned discharge, the hospitalist could talk to a patient’s family members about the discharge plan and order any outstanding tests to be done that evening to be ready for morning rounds – which he suggested should start by 7:00 a.m. The hospitalist could dictate the discharge summary the afternoon before. Even if a discharge can’t proceed as planned, the time isn’t necessarily wasted.
In a recent interview, Dr. Nelson noted that the movement to reduce average length of stay in the hospital has complicated the discharge picture by reducing a hospital’s flexibility. But he added that it’s still worth tracking and collecting data on discharge times, and to keep the conversation going. “Just don’t lose sight of the real goal, which is not DBN but optimal length-of-stay management,” he said.
Dr. Gundareddy said that, as his group has dealt with these issues, some steps have emerged to help manage discharges and throughput. “We didn’t have case management and social work services over the weekend, but when we added that support, it changed how our Mondays went.”
He encourages hospitalists to focus on the actual processes that create bottlenecks preventing throughput. “A good example of effective restructuring is lab testing. It’s amazing to think that you could have lab test results available for 7:00 a.m. rounds. There are areas that deserve more attention and more research regarding DBN. What is the impact of discharge before noon programs on the patients who aren’t being planned for discharge that day? Do they get neglected? I feel that happens sometimes.”
The COVID pandemic has further complicated these questions, Dr. Gundareddy said. “Early on in the pandemic, we were unsure how things were going with discharges, since all of the focus was on the COVID crisis. A lot of outpatient and surgical services came to a standstill, and there weren’t enough of the right kinds of beds for COVID patients. It was hard to align staff appropriately with the new clinical goals and to train them during the crisis.” Now, patients who delayed care during the pandemic are turning up at the hospital with greater acuity.
As with all incentives, DBN can have unintended consequences – especially if you monetize the practice, Dr. Verma said. “Most hospitalists are already working so hard – making so many decisions every day. These incentives could push decisions that aren’t in anybody’s best interests.”
Various groups have created comprehensive packages of protocols for improving transitions of care, he said. Organized programs to maximize efficiency of transitions and patient flow, including Project BOOST and Project RED (Re-Engineered Discharge) at Boston University Medical Center, are important sources of tools and resources. “But we should stop flogging hospitalists to discharge patients before noon,” Dr. Verma said, “Discharge is more complex than that. Instead, we should work to improve discharges in more holistic ways.”
References
1. Kirubarajan A et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021 Jun;16(6):333-8. doi: 10.12788/jhm.3605.
2. Shine D. Discharge before noon: An urban legend. Am J Med. 2015 May;128(5):445-6. doi:10.1016/j.amjmed.2014.12.011.
3. Zorian A et al. Discharge by noon: Toward a better understanding of benefits and costs. J Hosp Med. 2021 Jun;16(6):384. doi: 10.12788/jhm.3613.
4. Wertheimer B et al. Discharge before noon: Effect on throughput and sustainability. J Hosp Med. 2015 Oct;10(10):664-9. doi: 10.1002/jhm.2412.
5. Wertheimer B et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014 Apr;9(4):210-4. doi: 10.1002/jhm.2154.
6. Nelson J. The earlier, the better. The Hospitalist. 2010 May.
‘Perennial debate’ likely to be reignited
‘Perennial debate’ likely to be reignited
A recent study published in the Journal of Hospital Medicine examined patient discharges from hospitals in Ontario, Canada, to determine if morning discharges were associated with positive outcomes. Some hospitalist programs have embraced discharge before noon (DBN) initiatives like those studied in the article.1 Unfortunately, the researchers concluded that the Canadian DBNs did not positively impact hospital length of stay, readmissions, or mortality rates.
DBN has been a quality improvement target for hospitals hoping to improve throughput and free up scarce beds, while promoting patient safety by encouraging discharge as soon as patients are ready to leave. Yet other researchers have questioned its actual impact on quality metrics. One author called DBN’s purported impact an “urban legend,”2 while a JHM editorial accompanying the Ontario study noted, “Hospitals are delicate organisms; a singular focus on one metric will undoubtedly impact others.”3
Might DBN be an artificial target that doesn’t actually enhance throughput, but leads instead to unintended consequences, such as patients being held over for an additional night in the hospital, rather than being discharged when they are ready to go on the afternoon before, in order to boost DBN rates? A perennial debate in hospital medicine is likely to be reignited by the new findings.
‘No significant overall association’
Quality improvement initiatives targeting morning discharges have included stakeholder meetings, incentives programs, discharge-centered breakfast programs, and creation of deadlines for discharge orders, the new study’s authors noted. Although these initiatives have gained support, critics have suggested that their supporting evidence is not robust.
The Canadian researchers retrospectively reviewed all patient admissions to general internal medicine services (GIMs) – largely similar to hospital medicine services in the United States – at seven hospitals in Toronto and Mississauga over a 7-year period ending Oct. 31, 2017, counting all of these patients who were discharged alive between 8 a.m. and noon. DBN averaged 19% of total live discharges across the diverse hospitals, with their diverse discharge practices.
But they found no significant overall association between morning discharge and hospital or emergency department length of stay. “Our findings suggest that increasing the number of morning discharges alone is unlikely to substantially improve patient throughput in GIM, but further research is needed to determine the effectiveness of specific interventions,” they concluded.
“We used a very narrow lens, looking specifically at throughput for the hospitals and emergency departments and whether DBN makes it more efficient,” said corresponding author Amol Verma, MD, MPhil, FRCPC, clinician-scientist at St. Michael’s Hospital, University of Toronto, in a recent interview. “What we found was that, on days when more patients are discharged in the morning, patients do not flow more quickly through the hospital. That suggests that increasing morning discharges is unlikely to make a difference.”
What does DBN really mean?
The semantics of DBN deserve further exploration. Is DBN about the actual hour of discharge, or the time when the hospitalist signs a discharge order – which may be well before the patient actually gets a wheelchair ride down to the hospital’s front doors? And if DBN is an organized program promoting morning discharges, how is it incentivized or otherwise rewarded?
Other factors, such as arrival of medications from the pharmacy or results from clinical tests, access to an ambulance if needed, transport to the front door, and bed cleaning will impact how quickly a doctor’s discharge orders get acted upon – and how quickly the newly emptied bed is available for the next occupant.
The clinician’s views on discharge practices may diverge from hospital administrator or health system perspectives, with its imperatives for efficient throughput in order to bring in more patients, Dr. Verma said. The hospitalist is also concerned about whether the patient feels ready to go home. “We can all agree that patients should leave the hospital as soon as they are medically able to do so,” he said. Longer hospital stays are associated with increased rates of hospital-acquired infections and other iatrogenic complications.
But there is not agreement on the components of a safe discharge – or on the other dimensions of effective patient flow and transitions of care. How do we optimize treatments initiated in the hospital? Does the patient need one more CAT scan? And what about the concerns of patient-centered care? Does the patient have a caregiver able to help them when they get home? There is a lot of uncertainty, Dr. Verma said. “These kinds of decisions have to get made many times every day by hospitalists,” he noted.
“We find ourselves trying to mirror the ebbs and flows of the emergency department with what’s happening in the hospital,” said Venkat Gundareddy, MBBS, MPH, associate director of the division of hospital medicine at Johns Hopkins Medicine in Baltimore. “The majority of hospital discharges happen during business hours, but the emergency department doesn’t stop admitting overnight, thus creating a throughput challenge.” Discharges are also based on clinical outcomes and on patients transferring to other facilities that prefer patients to arrive earlier in the day.
“Hospitalists may not fully appreciate these dynamics, because we’re siloed on our units,” Dr. Gundareddy said. “There is a subset of patients who would fit the bill for early discharge, but other patients come into the hospital with greater complexities, and a need for more coordination. Their discharges are harder to predict, although it gets clearer as their care progresses.”
The hospitals included in the Ontario study are at 90% -100% capacity, so their flexibility is constrained and throughput is a critical issue, Dr. Verma said. “But if you start with the target of more efficient throughput, there is no logical or practical reason to assume that discharge before noon would help. If we believe someone is ready for discharge based on physiologic changes, their response to treatment, and the conclusion of medical investigations, none of these conform to the clock. It’s equally likely the patient achieves them in the afternoon or evening.”
Other views on morning discharge
An alternative perspective comes from New York University’s Langone Medical Center, which has published positive results, including earlier subsequent arrivals to the inpatient unit from the emergency department, from increasing its hospital’s DBN rate.4
The hospital has continued to encourage morning discharges, which have consistently run 35%-40% or more of total discharges on two acute inpatient units at Langone’s Tisch Hospital. A previous study described the multidisciplinary intervention that resulted in a statistically significant increase in DBN – from 11% to 38% in the first 13 months – while significantly reducing high-frequency admission peaks.5
“We’ve been doing DBN for a number of years,” said Benjamin Wertheimer, MD, a hospitalist at Langone Medical Center and one of the studies’ authors. It is an achievable – and sustainable – goal. “Many hospitals around the country have problems with the flow of patients. Many hospitals are full – even before accounting for the COVID pandemic.” There is good evidence that, for a patient who no longer requires hospitalization, getting them out as early as possible, with a safe plan for their discharge, is a good thing, he said. “We see DBN as an important operational metric.”
If the necessary work is done correctly on the afternoon before the discharge, then a DBN approach can push communication, coordination, and advance planning, Dr Wertheimer said. Otherwise, essential discharge tasks may lag until the last minute. “We try to put the pieces in place the day before through a better planned process. But it should never be that DBN takes precedence over when the patient is safely ready to go,” he said.
“Our true measure of success would be how well we are preparing, communicating, putting safe plans into place,” he added. “DBN does not in and of itself answer all the safety and quality concerns. We set priorities around specific quality targets. DBN is just one of our operational and safety measures.”
The DBN intervention at Langone started with a multidisciplinary kickoff event in which all team members received education on its importance, a clear description of roles in the DBN process, and a corresponding checklist of daily responsibilities. The checklist was utilized at newly implemented afternoon interdisciplinary rounds, scripted to identify next-day DBNs, and make sure everything is in place for them, he explained.
“We provide daily feedback to floor staff on the DBN percentage, celebrate success, and offer real-time opportunities for case review,” Dr. Wertheimer said. “We have been careful about how we message this goal. Quality and safety come first, and we want to be prepared for discharge in advance of when the patient is ready.”
A boost for discharges
Mark Williams, MD, MHM, recently appointed chief of hospital medicine at Washington University School of Medicine in St. Louis, and a principal investigator for Project BOOST (Better Outcomes by Optimizing Safe Transitions), SHM’s quality improvement mentoring initiative aimed at helping hospitals improve care transitions, said that debates about DBN have gone on for a long time in hospital medicine.
“Around 2002, consultants told the CEO of a community hospital affiliated with Emory Healthcare that if our hospitalists could discharge patients before noon it would improve throughput,” he recalled. The consultants came from the hospitality industry, where DBN is easier to achieve.
But in hospital medicine, he said, “We use the whole day of the discharge in delivering care. I said to the CEO, ‘I can get you 100% discharge before noon – I’ll just hold the patients overnight,’” he explained. “In our initial experience, we pushed DBN up to about 10% -15%, and it opened up a few beds, which rapidly filled.”
Project BOOST encouraged the goal of getting patients ready to go out as soon as they were clinically ready, but did not advocate specifically for DBN, Dr. Williams said. “The problem is that hospital throughput starts to gum up when occupancy goes over 80% or 90%, and many academic medical centers regularly reach occupancy rates greater than 100%, particularly in the afternoon.” The deluge of patients includes transfers from other hospitals, postsurgical patients, and admissions from the emergency department.
“Boarding in the ED is a real issue,” he said. “Right now, it’s a crisis of overoccupancy, and the problem is that the pipeline is pouring patients into the system faster than they can be discharged.”
Dr. Williams believes there needs to be bigger thinking about these issues. Could hospitals, health systems, and hospitalists practice more preventive medicine so that some of these patients don’t need to come to the hospital? “Can you better address high blood pressure to prevent strokes and make sure patients with heart disease risk factors are enrolled in exercise and nutrition programs? What about access to healthy foods and the other social determinants of health? What if we provided adequate, consistent housing and transportation to medical visits?” he wondered.
Hospital at home programs may also offer some relief, he said. “If suddenly there weren’t so many emergency room visits by patients who need to get admitted, we’d have enough beds in the hospital.”
A more holistic view
John Nelson, MD, MHM, hospital medicine pioneer and management consultant, has been studying hospital throughput and policies to improve it for a long time. His 2010 column in The Hospitalist, “The Earlier the Better,” said attaching a financial incentive for hospitalists to discharge patients by a preset hour has produced mixed results.6 But Dr. Nelson offered some easy steps hospitalists can take to maximize earlier discharges, including to write “probable discharge tomorrow” as an order in the patient’s medical record.
The afternoon before a planned discharge, the hospitalist could talk to a patient’s family members about the discharge plan and order any outstanding tests to be done that evening to be ready for morning rounds – which he suggested should start by 7:00 a.m. The hospitalist could dictate the discharge summary the afternoon before. Even if a discharge can’t proceed as planned, the time isn’t necessarily wasted.
In a recent interview, Dr. Nelson noted that the movement to reduce average length of stay in the hospital has complicated the discharge picture by reducing a hospital’s flexibility. But he added that it’s still worth tracking and collecting data on discharge times, and to keep the conversation going. “Just don’t lose sight of the real goal, which is not DBN but optimal length-of-stay management,” he said.
Dr. Gundareddy said that, as his group has dealt with these issues, some steps have emerged to help manage discharges and throughput. “We didn’t have case management and social work services over the weekend, but when we added that support, it changed how our Mondays went.”
He encourages hospitalists to focus on the actual processes that create bottlenecks preventing throughput. “A good example of effective restructuring is lab testing. It’s amazing to think that you could have lab test results available for 7:00 a.m. rounds. There are areas that deserve more attention and more research regarding DBN. What is the impact of discharge before noon programs on the patients who aren’t being planned for discharge that day? Do they get neglected? I feel that happens sometimes.”
The COVID pandemic has further complicated these questions, Dr. Gundareddy said. “Early on in the pandemic, we were unsure how things were going with discharges, since all of the focus was on the COVID crisis. A lot of outpatient and surgical services came to a standstill, and there weren’t enough of the right kinds of beds for COVID patients. It was hard to align staff appropriately with the new clinical goals and to train them during the crisis.” Now, patients who delayed care during the pandemic are turning up at the hospital with greater acuity.
As with all incentives, DBN can have unintended consequences – especially if you monetize the practice, Dr. Verma said. “Most hospitalists are already working so hard – making so many decisions every day. These incentives could push decisions that aren’t in anybody’s best interests.”
Various groups have created comprehensive packages of protocols for improving transitions of care, he said. Organized programs to maximize efficiency of transitions and patient flow, including Project BOOST and Project RED (Re-Engineered Discharge) at Boston University Medical Center, are important sources of tools and resources. “But we should stop flogging hospitalists to discharge patients before noon,” Dr. Verma said, “Discharge is more complex than that. Instead, we should work to improve discharges in more holistic ways.”
References
1. Kirubarajan A et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021 Jun;16(6):333-8. doi: 10.12788/jhm.3605.
2. Shine D. Discharge before noon: An urban legend. Am J Med. 2015 May;128(5):445-6. doi:10.1016/j.amjmed.2014.12.011.
3. Zorian A et al. Discharge by noon: Toward a better understanding of benefits and costs. J Hosp Med. 2021 Jun;16(6):384. doi: 10.12788/jhm.3613.
4. Wertheimer B et al. Discharge before noon: Effect on throughput and sustainability. J Hosp Med. 2015 Oct;10(10):664-9. doi: 10.1002/jhm.2412.
5. Wertheimer B et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014 Apr;9(4):210-4. doi: 10.1002/jhm.2154.
6. Nelson J. The earlier, the better. The Hospitalist. 2010 May.
A recent study published in the Journal of Hospital Medicine examined patient discharges from hospitals in Ontario, Canada, to determine if morning discharges were associated with positive outcomes. Some hospitalist programs have embraced discharge before noon (DBN) initiatives like those studied in the article.1 Unfortunately, the researchers concluded that the Canadian DBNs did not positively impact hospital length of stay, readmissions, or mortality rates.
DBN has been a quality improvement target for hospitals hoping to improve throughput and free up scarce beds, while promoting patient safety by encouraging discharge as soon as patients are ready to leave. Yet other researchers have questioned its actual impact on quality metrics. One author called DBN’s purported impact an “urban legend,”2 while a JHM editorial accompanying the Ontario study noted, “Hospitals are delicate organisms; a singular focus on one metric will undoubtedly impact others.”3
Might DBN be an artificial target that doesn’t actually enhance throughput, but leads instead to unintended consequences, such as patients being held over for an additional night in the hospital, rather than being discharged when they are ready to go on the afternoon before, in order to boost DBN rates? A perennial debate in hospital medicine is likely to be reignited by the new findings.
‘No significant overall association’
Quality improvement initiatives targeting morning discharges have included stakeholder meetings, incentives programs, discharge-centered breakfast programs, and creation of deadlines for discharge orders, the new study’s authors noted. Although these initiatives have gained support, critics have suggested that their supporting evidence is not robust.
The Canadian researchers retrospectively reviewed all patient admissions to general internal medicine services (GIMs) – largely similar to hospital medicine services in the United States – at seven hospitals in Toronto and Mississauga over a 7-year period ending Oct. 31, 2017, counting all of these patients who were discharged alive between 8 a.m. and noon. DBN averaged 19% of total live discharges across the diverse hospitals, with their diverse discharge practices.
But they found no significant overall association between morning discharge and hospital or emergency department length of stay. “Our findings suggest that increasing the number of morning discharges alone is unlikely to substantially improve patient throughput in GIM, but further research is needed to determine the effectiveness of specific interventions,” they concluded.
“We used a very narrow lens, looking specifically at throughput for the hospitals and emergency departments and whether DBN makes it more efficient,” said corresponding author Amol Verma, MD, MPhil, FRCPC, clinician-scientist at St. Michael’s Hospital, University of Toronto, in a recent interview. “What we found was that, on days when more patients are discharged in the morning, patients do not flow more quickly through the hospital. That suggests that increasing morning discharges is unlikely to make a difference.”
What does DBN really mean?
The semantics of DBN deserve further exploration. Is DBN about the actual hour of discharge, or the time when the hospitalist signs a discharge order – which may be well before the patient actually gets a wheelchair ride down to the hospital’s front doors? And if DBN is an organized program promoting morning discharges, how is it incentivized or otherwise rewarded?
Other factors, such as arrival of medications from the pharmacy or results from clinical tests, access to an ambulance if needed, transport to the front door, and bed cleaning will impact how quickly a doctor’s discharge orders get acted upon – and how quickly the newly emptied bed is available for the next occupant.
The clinician’s views on discharge practices may diverge from hospital administrator or health system perspectives, with its imperatives for efficient throughput in order to bring in more patients, Dr. Verma said. The hospitalist is also concerned about whether the patient feels ready to go home. “We can all agree that patients should leave the hospital as soon as they are medically able to do so,” he said. Longer hospital stays are associated with increased rates of hospital-acquired infections and other iatrogenic complications.
But there is not agreement on the components of a safe discharge – or on the other dimensions of effective patient flow and transitions of care. How do we optimize treatments initiated in the hospital? Does the patient need one more CAT scan? And what about the concerns of patient-centered care? Does the patient have a caregiver able to help them when they get home? There is a lot of uncertainty, Dr. Verma said. “These kinds of decisions have to get made many times every day by hospitalists,” he noted.
“We find ourselves trying to mirror the ebbs and flows of the emergency department with what’s happening in the hospital,” said Venkat Gundareddy, MBBS, MPH, associate director of the division of hospital medicine at Johns Hopkins Medicine in Baltimore. “The majority of hospital discharges happen during business hours, but the emergency department doesn’t stop admitting overnight, thus creating a throughput challenge.” Discharges are also based on clinical outcomes and on patients transferring to other facilities that prefer patients to arrive earlier in the day.
“Hospitalists may not fully appreciate these dynamics, because we’re siloed on our units,” Dr. Gundareddy said. “There is a subset of patients who would fit the bill for early discharge, but other patients come into the hospital with greater complexities, and a need for more coordination. Their discharges are harder to predict, although it gets clearer as their care progresses.”
The hospitals included in the Ontario study are at 90% -100% capacity, so their flexibility is constrained and throughput is a critical issue, Dr. Verma said. “But if you start with the target of more efficient throughput, there is no logical or practical reason to assume that discharge before noon would help. If we believe someone is ready for discharge based on physiologic changes, their response to treatment, and the conclusion of medical investigations, none of these conform to the clock. It’s equally likely the patient achieves them in the afternoon or evening.”
Other views on morning discharge
An alternative perspective comes from New York University’s Langone Medical Center, which has published positive results, including earlier subsequent arrivals to the inpatient unit from the emergency department, from increasing its hospital’s DBN rate.4
The hospital has continued to encourage morning discharges, which have consistently run 35%-40% or more of total discharges on two acute inpatient units at Langone’s Tisch Hospital. A previous study described the multidisciplinary intervention that resulted in a statistically significant increase in DBN – from 11% to 38% in the first 13 months – while significantly reducing high-frequency admission peaks.5
“We’ve been doing DBN for a number of years,” said Benjamin Wertheimer, MD, a hospitalist at Langone Medical Center and one of the studies’ authors. It is an achievable – and sustainable – goal. “Many hospitals around the country have problems with the flow of patients. Many hospitals are full – even before accounting for the COVID pandemic.” There is good evidence that, for a patient who no longer requires hospitalization, getting them out as early as possible, with a safe plan for their discharge, is a good thing, he said. “We see DBN as an important operational metric.”
If the necessary work is done correctly on the afternoon before the discharge, then a DBN approach can push communication, coordination, and advance planning, Dr Wertheimer said. Otherwise, essential discharge tasks may lag until the last minute. “We try to put the pieces in place the day before through a better planned process. But it should never be that DBN takes precedence over when the patient is safely ready to go,” he said.
“Our true measure of success would be how well we are preparing, communicating, putting safe plans into place,” he added. “DBN does not in and of itself answer all the safety and quality concerns. We set priorities around specific quality targets. DBN is just one of our operational and safety measures.”
The DBN intervention at Langone started with a multidisciplinary kickoff event in which all team members received education on its importance, a clear description of roles in the DBN process, and a corresponding checklist of daily responsibilities. The checklist was utilized at newly implemented afternoon interdisciplinary rounds, scripted to identify next-day DBNs, and make sure everything is in place for them, he explained.
“We provide daily feedback to floor staff on the DBN percentage, celebrate success, and offer real-time opportunities for case review,” Dr. Wertheimer said. “We have been careful about how we message this goal. Quality and safety come first, and we want to be prepared for discharge in advance of when the patient is ready.”
A boost for discharges
Mark Williams, MD, MHM, recently appointed chief of hospital medicine at Washington University School of Medicine in St. Louis, and a principal investigator for Project BOOST (Better Outcomes by Optimizing Safe Transitions), SHM’s quality improvement mentoring initiative aimed at helping hospitals improve care transitions, said that debates about DBN have gone on for a long time in hospital medicine.
“Around 2002, consultants told the CEO of a community hospital affiliated with Emory Healthcare that if our hospitalists could discharge patients before noon it would improve throughput,” he recalled. The consultants came from the hospitality industry, where DBN is easier to achieve.
But in hospital medicine, he said, “We use the whole day of the discharge in delivering care. I said to the CEO, ‘I can get you 100% discharge before noon – I’ll just hold the patients overnight,’” he explained. “In our initial experience, we pushed DBN up to about 10% -15%, and it opened up a few beds, which rapidly filled.”
Project BOOST encouraged the goal of getting patients ready to go out as soon as they were clinically ready, but did not advocate specifically for DBN, Dr. Williams said. “The problem is that hospital throughput starts to gum up when occupancy goes over 80% or 90%, and many academic medical centers regularly reach occupancy rates greater than 100%, particularly in the afternoon.” The deluge of patients includes transfers from other hospitals, postsurgical patients, and admissions from the emergency department.
“Boarding in the ED is a real issue,” he said. “Right now, it’s a crisis of overoccupancy, and the problem is that the pipeline is pouring patients into the system faster than they can be discharged.”
Dr. Williams believes there needs to be bigger thinking about these issues. Could hospitals, health systems, and hospitalists practice more preventive medicine so that some of these patients don’t need to come to the hospital? “Can you better address high blood pressure to prevent strokes and make sure patients with heart disease risk factors are enrolled in exercise and nutrition programs? What about access to healthy foods and the other social determinants of health? What if we provided adequate, consistent housing and transportation to medical visits?” he wondered.
Hospital at home programs may also offer some relief, he said. “If suddenly there weren’t so many emergency room visits by patients who need to get admitted, we’d have enough beds in the hospital.”
A more holistic view
John Nelson, MD, MHM, hospital medicine pioneer and management consultant, has been studying hospital throughput and policies to improve it for a long time. His 2010 column in The Hospitalist, “The Earlier the Better,” said attaching a financial incentive for hospitalists to discharge patients by a preset hour has produced mixed results.6 But Dr. Nelson offered some easy steps hospitalists can take to maximize earlier discharges, including to write “probable discharge tomorrow” as an order in the patient’s medical record.
The afternoon before a planned discharge, the hospitalist could talk to a patient’s family members about the discharge plan and order any outstanding tests to be done that evening to be ready for morning rounds – which he suggested should start by 7:00 a.m. The hospitalist could dictate the discharge summary the afternoon before. Even if a discharge can’t proceed as planned, the time isn’t necessarily wasted.
In a recent interview, Dr. Nelson noted that the movement to reduce average length of stay in the hospital has complicated the discharge picture by reducing a hospital’s flexibility. But he added that it’s still worth tracking and collecting data on discharge times, and to keep the conversation going. “Just don’t lose sight of the real goal, which is not DBN but optimal length-of-stay management,” he said.
Dr. Gundareddy said that, as his group has dealt with these issues, some steps have emerged to help manage discharges and throughput. “We didn’t have case management and social work services over the weekend, but when we added that support, it changed how our Mondays went.”
He encourages hospitalists to focus on the actual processes that create bottlenecks preventing throughput. “A good example of effective restructuring is lab testing. It’s amazing to think that you could have lab test results available for 7:00 a.m. rounds. There are areas that deserve more attention and more research regarding DBN. What is the impact of discharge before noon programs on the patients who aren’t being planned for discharge that day? Do they get neglected? I feel that happens sometimes.”
The COVID pandemic has further complicated these questions, Dr. Gundareddy said. “Early on in the pandemic, we were unsure how things were going with discharges, since all of the focus was on the COVID crisis. A lot of outpatient and surgical services came to a standstill, and there weren’t enough of the right kinds of beds for COVID patients. It was hard to align staff appropriately with the new clinical goals and to train them during the crisis.” Now, patients who delayed care during the pandemic are turning up at the hospital with greater acuity.
As with all incentives, DBN can have unintended consequences – especially if you monetize the practice, Dr. Verma said. “Most hospitalists are already working so hard – making so many decisions every day. These incentives could push decisions that aren’t in anybody’s best interests.”
Various groups have created comprehensive packages of protocols for improving transitions of care, he said. Organized programs to maximize efficiency of transitions and patient flow, including Project BOOST and Project RED (Re-Engineered Discharge) at Boston University Medical Center, are important sources of tools and resources. “But we should stop flogging hospitalists to discharge patients before noon,” Dr. Verma said, “Discharge is more complex than that. Instead, we should work to improve discharges in more holistic ways.”
References
1. Kirubarajan A et al. Morning discharges and patient length of stay in inpatient general internal medicine. J Hosp Med. 2021 Jun;16(6):333-8. doi: 10.12788/jhm.3605.
2. Shine D. Discharge before noon: An urban legend. Am J Med. 2015 May;128(5):445-6. doi:10.1016/j.amjmed.2014.12.011.
3. Zorian A et al. Discharge by noon: Toward a better understanding of benefits and costs. J Hosp Med. 2021 Jun;16(6):384. doi: 10.12788/jhm.3613.
4. Wertheimer B et al. Discharge before noon: Effect on throughput and sustainability. J Hosp Med. 2015 Oct;10(10):664-9. doi: 10.1002/jhm.2412.
5. Wertheimer B et al. Discharge before noon: an achievable hospital goal. J Hosp Med. 2014 Apr;9(4):210-4. doi: 10.1002/jhm.2154.
6. Nelson J. The earlier, the better. The Hospitalist. 2010 May.
Hospitalists helped plan COVID-19 field hospitals
‘It’s a great thing to be overprepared’
At the height of the COVID-19 pandemic’s terrifying first wave in the spring of 2020, dozens of hospitals in high-incidence areas either planned or opened temporary, emergency field hospitals to cover anticipated demand for beds beyond the capacity of local permanent hospitals.
Chastened by images of overwhelmed health care systems in Northern Italy and other hard-hit areas,1 the planners used available modeling tools and estimates for projecting maximum potential need in worst-case scenarios. Some of these temporary hospitals never opened. Others opened in convention centers, parking garages, or parking lot tents, and ended up being used to a lesser degree than the worst-case scenarios.
But those who participated in the planning – including, in many cases, hospitalists – believe they created alternate care site manuals that could be quickly revived in the event of future COVID surges or other, similar crises. Better to plan for too much, they say, than not plan for enough.
Field hospitals or alternate care sites are defined in a recent journal article in Prehospital Disaster Medicine as “locations that can be converted to provide either inpatient and/or outpatient health services when existing facilities are compromised by a hazard impact or the volume of patients exceeds available capacity and/or capabilities.”2
The lead author of that report, Sue Anne Bell, PhD, FNP-BC, a disaster expert and assistant professor of nursing at the University of Michigan (UM), was one of five members of the leadership team for planning UM’s field hospital. They used an organizational unit structure based on the U.S. military’s staffing structure, with their work organized around six units of planning: personnel and labor, security, clinical operations, logistics and supply, planning and training, and communications. This team planned a 519-bed step-down care facility, the Michigan Medicine Field Hospital, for a 73,000-foot indoor track and performance facility at the university, three miles from UM’s main hospital. The aim was to provide safe care in a resource-limited environment.
“We were prepared, but the need never materialized as the peak of COVID cases started to subside,” Dr. Bell said. The team was ready to open within days using a “T-Minus” framework of days remaining on an official countdown clock. But when the need and deadlines kept getting pushed back, that gave them more time to develop clearer procedures.
Two Michigan Medicine hospitalists, Christopher Smith, MD, and David Paje, MD, MPH, both professors at UM’s medical school, were intimately involved in the process. “I was the medical director for the respiratory care unit that was opened for COVID patients, so I was pulled in to assist in the field hospital planning,” said Dr. Smith.
Dr. Paje was director of the short-stay unit and had been a medical officer in the U.S. Army, with training in how to set up military field hospitals. He credits that background as helpful for UM’s COVID field hospital planning, along with his experience in hospital medicine operations.
“We expected that these patients would need the expertise of hospitalists, who had quickly become familiar with the peculiarities of the new disease. That played a role in the decisions we made. Hospitalists were at the front lines of COVID care and had unique clinical insights about managing those with severe disease,” Dr. Paje added.
“When we started, the projections were dire. You don’t want to believe something like that is going to happen. When COVID started to cool off, it was more of a relief to us than anything else,” Dr. Smith said. “Still, it was a very worthwhile exercise. At the end of the day, we put together a comprehensive guide, which is ready for the next crisis.”
Baltimore builds a convention center hospital
A COVID-19 field hospital was planned and executed at an exhibit hall in the Baltimore Convention Center, starting in March 2020 under the leadership of Johns Hopkins Bayview hospitalist Eric Howell, MD, MHM, who eventually handed over responsibilities as chief medical officer when he assumed the position of CEO for the Society of Hospital Medicine in July of that year.
Hopkins collaborated with the University of Maryland health system and state leaders, including the Secretary of Health, to open a 252-bed temporary facility, which at its peak carried a census of 48 patients, with no on-site mortality or cardiac arrests, before it was closed in June 2021 – ready to reopen if necessary. It also served as Baltimore’s major site for polymerase chain reaction COVID-19 testing, vaccinations, and monoclonal antibody infusions, along with medical research.
“My belief at the time we started was that my entire 20-year career as a hospitalist had prepared me for the challenge of opening a COVID field hospital,” Dr. Howell said. “I had learned how to build clinical programs. The difference was that instead of months and years to build a program, we only had a few weeks.”
His first request was to bring on an associate medical director for the field hospital, Melinda E. Kantsiper, MD, a hospitalist and director of clinical operations in the Division of Hospital Medicine at Johns Hopkins Bayview. She became the field hospital’s CMO when Dr. Howell moved to SHM. “As hospitalists, we are trained to care for the patient in front of us while at the same time creating systems that can adjust to rapidly changing circumstances,” Dr. Kantsiper said. “We did what was asked and set up a field hospital that cared for a total of 1,500 COVID patients.”
Hospitalists have the tools that are needed for this work, and shouldn’t be reluctant to contribute to field hospital planning, she said. “This was a real eye-opener for me. Eric explained to me that hospitalists really practice acute care medicine, which doesn’t have to be within the four walls of a hospital.”
The Baltimore field hospital has been a fantastic experience, Dr. Kantsiper added. “But it’s not a building designed for health care delivery.” For the right group of providers, the experience of working in a temporary facility such as this can be positive and exhilarating. “But we need to make sure we take care of our staff. It takes a toll. How we keep them safe – physically and emotionally – has to be top of mind,” she said.
The leaders at Hopkins Medicine and their collaborators truly engaged with the field hospital’s mission, Dr. Howell added.
“They gave us a lot of autonomy and helped us break down barriers. They gave us the political capital to say proper PPE was absolutely essential. As hard and devastating as the pandemic has been, one take-away is that we showed that we can be more flexible and elastic in response to actual needs than we used to think.”
Range of challenges
Among the questions that need to be answered by a field hospital’s planners, the first is ‘where to put it?’ The answer is, hopefully, someplace not too far away, large enough, with ready access to supplies and intake. The next question is ‘who is the patient?’ Clinicians must determine who goes to the field hospital versus who stays at the standing hospital. How sick should these patients be? And when do they need to go back to the permanent hospital? Can staff be trained to recognize when patients in the field hospital are starting to decompensate? The EPIC Deterioration Index3 is a proprietary prediction model that was used by more than a hundred hospitals during the pandemic.
The hospitalist team may develop specific inclusion and exclusion criteria – for example, don’t admit patients who are receiving oxygen therapy above a certain threshold or who are hemodynamically unstable. These criteria should reflect the capacity of the field hospital and the needs of the permanent hospital. At Michigan, as at other field hospital sites, the goal was to offer a step-down or postacute setting for patients with COVID-19 who were too sick to return home but didn’t need acute or ICU-level care, thereby freeing up beds at the permanent hospital for patients who were sicker.
Other questions: What is the process for admissions and discharges? How will patients be transported? What kind of staffing is needed, and what levels of care will be provided? What about rehabilitation services, or palliative care? What about patients with substance abuse or psychiatric comorbidities?
“Are we going to do paper charting? How will that work out for long-term documentation and billing?” Dr. Bell said. A clear reporting structure and communication pathways are essential. Among the other operational processes to address, outlined in Dr. Bell’s article, are orientation and training, PPE donning and doffing procedures, the code or rapid response team, patient and staff food and nutrition, infection control protocols, pharmacy services, access to radiology, rounding procedures, staff support, and the morgue.
One other issue that shouldn’t be overlooked is health equity in the field hospital. “Providing safe and equitable care should be the focus. Thinking who goes to the field hospital should be done within a health equity framework,” Dr. Bell said.4 She also wonders if field hospital planners are sharing their experience with colleagues across the country and developing more collaborative relationships with other hospitals in their communities.
“Field hospitals can be different things,” Dr. Bell said. “The important take-home is it doesn’t have to be in a tent or a parking garage, which can be suboptimal.” In many cases, it may be better to focus on finding unused space within the hospital – whether a lobby, staff lounge, or unoccupied unit – closer to personnel, supplies, pharmacy, and the like. “I think the pandemic showed us how unprepared we were as a health care system, and how much more we need to do in preparation for future crises.”
Limits to the temporary hospital
In New York City, which had the country’s worst COVID-19 outbreak during the first surge in the spring of 2020, a 1,000-bed field hospital was opened at the Jacob Javits Center in March 2020 and closed that June. “I was in the field hospital early, in March and April, when our hospitals were temporarily overrun,” said hospitalist Mona Krouss, MD, FACP, CPPS, NYC Health + Hospitals’ director of patient safety. “My role was to figure out how to get patients on our medical floors into these field hospitals, with responsibility for helping to revise admission criteria,” she said.
“No one knew how horrible it would become. This was so unanticipated, so difficult to operationalize. What they were able to create was amazing, but there were just too many barriers to have it work smoothly,” Dr. Krouss said.
“The military stepped in, and they helped us so much. We wouldn’t have been able to survive without their help.” But there is only so much a field hospital can do to provide acute medical care. Later, military medical teams shifted to roles in temporary units inside the permanent hospitals. “They came to the hospital wanting to be deployed,” she said.
“We could only send patients [to the field hospital] who were fairly stable, and choosing the right ones was difficult.” Dr. Krouss said. In the end, not a lot of COVID-19 patients from NYC Health + Hospitals ended up going to the Javits Center, in part because the paperwork and logistics of getting someone in was a barrier, Dr. Krouss said. A process was established for referring doctors to call a phone number and speak with a New York City Department of Health employee to go through the criteria for admission to the field hospital.
“That could take up to 30 minutes before getting approval. Then you had to go through the same process all over again for sign-out to another physician, and then register the patient with a special bar code. Then you had to arrange ambulance transfer. Doctors didn’t want to go through all of that – everybody was too busy,” she explained. Hospitalists have since worked on streamlining the criteria. “Now we have a good process for the future. We made it more seamless,” she noted.
Susan Lee, DO, MBA, hospitalist and chief medical officer for Renown Regional Medical Center in Reno, Nev., helped to plan an alternate care site in anticipation of up to a thousand COVID patients in her community – far beyond the scope of the existing hospitals. Hospitalists were involved the entire time in planning, design of the unit, design of staffing models, care protocols, and the like, working through an evidence-based medical committee and a COVID-19 provider task force for the Renown Health System.
“Because of a history of fires and earthquakes in this region, we had an emergency planning infrastructure in place. We put the field hospital on the first and second floors of a parking garage, with built-in negative pressure capacity. We also built space for staff break rooms and desk space. It took 10 days to build the hospital, thanks to some very talented people in management and facility design,” Dr. Lee said.
Then, the hospital was locked up and sat empty for 7 months, until the surge in December 2020, when Reno was hit by a bigger wave – this time exceeding the hospitals’ capacity. Through mid-January of 2021, clinicians cared for approximately 240 COVID-19 patients, up to 47 at a time, in the field hospital. A third wave in the autumn of 2021 plateaued at a level lower than the previous fall, so the field hospital is not currently needed.
Replicating hospital work flows
“We ensured that everybody who needed to be within the walls of the permanent hospitals was able to stay there,” said Dr. Lee’s colleague, hospitalist Adnan (Eddy) Akbar, MD. “The postacute system we ordinarily rely on was no longer accepting patients. Other hospitals in the area were able to manage within their capacity because Renown’s field hospital could admit excess patients. We tried to replicate in the field hospital, as much as possible, the work flows and systems of our main hospital.”
When the field hospital finally opened, Dr. Akbar said, “we had a good feeling. We were ready. If something more catastrophic had come down, we were ready to care for more patients. In the field hospital you have to keep monitoring your work flow – almost on a daily basis. But we felt privileged to be working for a system where you knew you can go and care for everyone who needed care.”
One upside of the field hospital experience for participating clinicians, Dr. Lee added, is the opportunity to practice creatively. “The downside is it’s extremely expensive, and has consequences for the mental health of staff. Like so many of these things, it wore on people over time – such as all the time spent donning and doffing protective equipment. And recently the patients have become a lot less gracious.”
Amy Baughman, MD, a hospitalist at Massachusetts General Hospital in Boston, was co-medical director of the postacute care section of a 1,000-bed field hospital, Boston Hope Medical Center, opened in April 2020 at the Boston Convention and Exhibition Center. The other half of the facility was dedicated to undomiciled COVID-19 patients who had no place else to go. Peak census was around 100 patients, housed on four units, each with a clinical team led by a physician.
Dr. Baughman’s field hospital experience has taught her the importance of “staying within your domain of expertise. Physicians are attracted to difficult problems and want to do everything themselves. Next time I won’t be the one installing hand sanitizer dispensers.” A big part of running a field hospital is logistics, she said, and physicians are trained clinicians, not necessarily logistics engineers.
“So it’s important to partner with logistics experts. A huge part of our success in building a facility in 9 days of almost continuous construction was the involvement of the National Guard,” she said. An incident command system was led by an experienced military general incident commander, with two clinical codirectors. The army also sent in full teams of health professionals.
The facility admitted a lot fewer patients than the worst-case projections before it closed in June 2020. “But at the end of the day, we provided a lot of excellent care,” Dr. Baughman said. “This was about preparing for a disaster. It was all hands on deck, and the hands were health professionals. We spent a lot of money for the patients we took care of, but we had no choice, based on what we believed could happen. At that time, so many nursing facilities and homeless shelters were closed to us. It was impossible to predict what utilization would be.”
Subsequent experience has taught that a lot of even seriously ill COVID-19 patients can be managed safely at home, for example, using accelerated home oxygen monitoring with telelinked pulse oximeters. But in the beginning, Dr. Baughman said, “it was a new situation for us. We had seen what happened in Europe and China. It’s a great thing to be overprepared.”
References
1. Horowitz J. Italy’s health care system groans under coronavirus – a warning to the world. New York Times. 2020 Mar 12.
2. Bell SA et al. T-Minus 10 days: The role of an academic medical institution in field hospital planning. Prehosp Disaster Med. 2021 Feb 18:1-6. doi: 10.1017/S1049023X21000224.
3. Singh K et al. Evaluating a widely implemented proprietary deterioration index model among hospitalized patients with COVID-19. Ann Am Thorac Soc. 2021 Jul;18(7):1129-37. doi: 10.1513/AnnalsATS.202006-698OC.
4. Bell SA et al. Alternate care sites during COVID-19 pandemic: Policy implications for pandemic surge planning. Disaster Med Public Health Prep. 2021 Jul 23;1-3. doi: 10.1017/dmp.2021.241.
‘It’s a great thing to be overprepared’
‘It’s a great thing to be overprepared’
At the height of the COVID-19 pandemic’s terrifying first wave in the spring of 2020, dozens of hospitals in high-incidence areas either planned or opened temporary, emergency field hospitals to cover anticipated demand for beds beyond the capacity of local permanent hospitals.
Chastened by images of overwhelmed health care systems in Northern Italy and other hard-hit areas,1 the planners used available modeling tools and estimates for projecting maximum potential need in worst-case scenarios. Some of these temporary hospitals never opened. Others opened in convention centers, parking garages, or parking lot tents, and ended up being used to a lesser degree than the worst-case scenarios.
But those who participated in the planning – including, in many cases, hospitalists – believe they created alternate care site manuals that could be quickly revived in the event of future COVID surges or other, similar crises. Better to plan for too much, they say, than not plan for enough.
Field hospitals or alternate care sites are defined in a recent journal article in Prehospital Disaster Medicine as “locations that can be converted to provide either inpatient and/or outpatient health services when existing facilities are compromised by a hazard impact or the volume of patients exceeds available capacity and/or capabilities.”2
The lead author of that report, Sue Anne Bell, PhD, FNP-BC, a disaster expert and assistant professor of nursing at the University of Michigan (UM), was one of five members of the leadership team for planning UM’s field hospital. They used an organizational unit structure based on the U.S. military’s staffing structure, with their work organized around six units of planning: personnel and labor, security, clinical operations, logistics and supply, planning and training, and communications. This team planned a 519-bed step-down care facility, the Michigan Medicine Field Hospital, for a 73,000-foot indoor track and performance facility at the university, three miles from UM’s main hospital. The aim was to provide safe care in a resource-limited environment.
“We were prepared, but the need never materialized as the peak of COVID cases started to subside,” Dr. Bell said. The team was ready to open within days using a “T-Minus” framework of days remaining on an official countdown clock. But when the need and deadlines kept getting pushed back, that gave them more time to develop clearer procedures.
Two Michigan Medicine hospitalists, Christopher Smith, MD, and David Paje, MD, MPH, both professors at UM’s medical school, were intimately involved in the process. “I was the medical director for the respiratory care unit that was opened for COVID patients, so I was pulled in to assist in the field hospital planning,” said Dr. Smith.
Dr. Paje was director of the short-stay unit and had been a medical officer in the U.S. Army, with training in how to set up military field hospitals. He credits that background as helpful for UM’s COVID field hospital planning, along with his experience in hospital medicine operations.
“We expected that these patients would need the expertise of hospitalists, who had quickly become familiar with the peculiarities of the new disease. That played a role in the decisions we made. Hospitalists were at the front lines of COVID care and had unique clinical insights about managing those with severe disease,” Dr. Paje added.
“When we started, the projections were dire. You don’t want to believe something like that is going to happen. When COVID started to cool off, it was more of a relief to us than anything else,” Dr. Smith said. “Still, it was a very worthwhile exercise. At the end of the day, we put together a comprehensive guide, which is ready for the next crisis.”
Baltimore builds a convention center hospital
A COVID-19 field hospital was planned and executed at an exhibit hall in the Baltimore Convention Center, starting in March 2020 under the leadership of Johns Hopkins Bayview hospitalist Eric Howell, MD, MHM, who eventually handed over responsibilities as chief medical officer when he assumed the position of CEO for the Society of Hospital Medicine in July of that year.
Hopkins collaborated with the University of Maryland health system and state leaders, including the Secretary of Health, to open a 252-bed temporary facility, which at its peak carried a census of 48 patients, with no on-site mortality or cardiac arrests, before it was closed in June 2021 – ready to reopen if necessary. It also served as Baltimore’s major site for polymerase chain reaction COVID-19 testing, vaccinations, and monoclonal antibody infusions, along with medical research.
“My belief at the time we started was that my entire 20-year career as a hospitalist had prepared me for the challenge of opening a COVID field hospital,” Dr. Howell said. “I had learned how to build clinical programs. The difference was that instead of months and years to build a program, we only had a few weeks.”
His first request was to bring on an associate medical director for the field hospital, Melinda E. Kantsiper, MD, a hospitalist and director of clinical operations in the Division of Hospital Medicine at Johns Hopkins Bayview. She became the field hospital’s CMO when Dr. Howell moved to SHM. “As hospitalists, we are trained to care for the patient in front of us while at the same time creating systems that can adjust to rapidly changing circumstances,” Dr. Kantsiper said. “We did what was asked and set up a field hospital that cared for a total of 1,500 COVID patients.”
Hospitalists have the tools that are needed for this work, and shouldn’t be reluctant to contribute to field hospital planning, she said. “This was a real eye-opener for me. Eric explained to me that hospitalists really practice acute care medicine, which doesn’t have to be within the four walls of a hospital.”
The Baltimore field hospital has been a fantastic experience, Dr. Kantsiper added. “But it’s not a building designed for health care delivery.” For the right group of providers, the experience of working in a temporary facility such as this can be positive and exhilarating. “But we need to make sure we take care of our staff. It takes a toll. How we keep them safe – physically and emotionally – has to be top of mind,” she said.
The leaders at Hopkins Medicine and their collaborators truly engaged with the field hospital’s mission, Dr. Howell added.
“They gave us a lot of autonomy and helped us break down barriers. They gave us the political capital to say proper PPE was absolutely essential. As hard and devastating as the pandemic has been, one take-away is that we showed that we can be more flexible and elastic in response to actual needs than we used to think.”
Range of challenges
Among the questions that need to be answered by a field hospital’s planners, the first is ‘where to put it?’ The answer is, hopefully, someplace not too far away, large enough, with ready access to supplies and intake. The next question is ‘who is the patient?’ Clinicians must determine who goes to the field hospital versus who stays at the standing hospital. How sick should these patients be? And when do they need to go back to the permanent hospital? Can staff be trained to recognize when patients in the field hospital are starting to decompensate? The EPIC Deterioration Index3 is a proprietary prediction model that was used by more than a hundred hospitals during the pandemic.
The hospitalist team may develop specific inclusion and exclusion criteria – for example, don’t admit patients who are receiving oxygen therapy above a certain threshold or who are hemodynamically unstable. These criteria should reflect the capacity of the field hospital and the needs of the permanent hospital. At Michigan, as at other field hospital sites, the goal was to offer a step-down or postacute setting for patients with COVID-19 who were too sick to return home but didn’t need acute or ICU-level care, thereby freeing up beds at the permanent hospital for patients who were sicker.
Other questions: What is the process for admissions and discharges? How will patients be transported? What kind of staffing is needed, and what levels of care will be provided? What about rehabilitation services, or palliative care? What about patients with substance abuse or psychiatric comorbidities?
“Are we going to do paper charting? How will that work out for long-term documentation and billing?” Dr. Bell said. A clear reporting structure and communication pathways are essential. Among the other operational processes to address, outlined in Dr. Bell’s article, are orientation and training, PPE donning and doffing procedures, the code or rapid response team, patient and staff food and nutrition, infection control protocols, pharmacy services, access to radiology, rounding procedures, staff support, and the morgue.
One other issue that shouldn’t be overlooked is health equity in the field hospital. “Providing safe and equitable care should be the focus. Thinking who goes to the field hospital should be done within a health equity framework,” Dr. Bell said.4 She also wonders if field hospital planners are sharing their experience with colleagues across the country and developing more collaborative relationships with other hospitals in their communities.
“Field hospitals can be different things,” Dr. Bell said. “The important take-home is it doesn’t have to be in a tent or a parking garage, which can be suboptimal.” In many cases, it may be better to focus on finding unused space within the hospital – whether a lobby, staff lounge, or unoccupied unit – closer to personnel, supplies, pharmacy, and the like. “I think the pandemic showed us how unprepared we were as a health care system, and how much more we need to do in preparation for future crises.”
Limits to the temporary hospital
In New York City, which had the country’s worst COVID-19 outbreak during the first surge in the spring of 2020, a 1,000-bed field hospital was opened at the Jacob Javits Center in March 2020 and closed that June. “I was in the field hospital early, in March and April, when our hospitals were temporarily overrun,” said hospitalist Mona Krouss, MD, FACP, CPPS, NYC Health + Hospitals’ director of patient safety. “My role was to figure out how to get patients on our medical floors into these field hospitals, with responsibility for helping to revise admission criteria,” she said.
“No one knew how horrible it would become. This was so unanticipated, so difficult to operationalize. What they were able to create was amazing, but there were just too many barriers to have it work smoothly,” Dr. Krouss said.
“The military stepped in, and they helped us so much. We wouldn’t have been able to survive without their help.” But there is only so much a field hospital can do to provide acute medical care. Later, military medical teams shifted to roles in temporary units inside the permanent hospitals. “They came to the hospital wanting to be deployed,” she said.
“We could only send patients [to the field hospital] who were fairly stable, and choosing the right ones was difficult.” Dr. Krouss said. In the end, not a lot of COVID-19 patients from NYC Health + Hospitals ended up going to the Javits Center, in part because the paperwork and logistics of getting someone in was a barrier, Dr. Krouss said. A process was established for referring doctors to call a phone number and speak with a New York City Department of Health employee to go through the criteria for admission to the field hospital.
“That could take up to 30 minutes before getting approval. Then you had to go through the same process all over again for sign-out to another physician, and then register the patient with a special bar code. Then you had to arrange ambulance transfer. Doctors didn’t want to go through all of that – everybody was too busy,” she explained. Hospitalists have since worked on streamlining the criteria. “Now we have a good process for the future. We made it more seamless,” she noted.
Susan Lee, DO, MBA, hospitalist and chief medical officer for Renown Regional Medical Center in Reno, Nev., helped to plan an alternate care site in anticipation of up to a thousand COVID patients in her community – far beyond the scope of the existing hospitals. Hospitalists were involved the entire time in planning, design of the unit, design of staffing models, care protocols, and the like, working through an evidence-based medical committee and a COVID-19 provider task force for the Renown Health System.
“Because of a history of fires and earthquakes in this region, we had an emergency planning infrastructure in place. We put the field hospital on the first and second floors of a parking garage, with built-in negative pressure capacity. We also built space for staff break rooms and desk space. It took 10 days to build the hospital, thanks to some very talented people in management and facility design,” Dr. Lee said.
Then, the hospital was locked up and sat empty for 7 months, until the surge in December 2020, when Reno was hit by a bigger wave – this time exceeding the hospitals’ capacity. Through mid-January of 2021, clinicians cared for approximately 240 COVID-19 patients, up to 47 at a time, in the field hospital. A third wave in the autumn of 2021 plateaued at a level lower than the previous fall, so the field hospital is not currently needed.
Replicating hospital work flows
“We ensured that everybody who needed to be within the walls of the permanent hospitals was able to stay there,” said Dr. Lee’s colleague, hospitalist Adnan (Eddy) Akbar, MD. “The postacute system we ordinarily rely on was no longer accepting patients. Other hospitals in the area were able to manage within their capacity because Renown’s field hospital could admit excess patients. We tried to replicate in the field hospital, as much as possible, the work flows and systems of our main hospital.”
When the field hospital finally opened, Dr. Akbar said, “we had a good feeling. We were ready. If something more catastrophic had come down, we were ready to care for more patients. In the field hospital you have to keep monitoring your work flow – almost on a daily basis. But we felt privileged to be working for a system where you knew you can go and care for everyone who needed care.”
One upside of the field hospital experience for participating clinicians, Dr. Lee added, is the opportunity to practice creatively. “The downside is it’s extremely expensive, and has consequences for the mental health of staff. Like so many of these things, it wore on people over time – such as all the time spent donning and doffing protective equipment. And recently the patients have become a lot less gracious.”
Amy Baughman, MD, a hospitalist at Massachusetts General Hospital in Boston, was co-medical director of the postacute care section of a 1,000-bed field hospital, Boston Hope Medical Center, opened in April 2020 at the Boston Convention and Exhibition Center. The other half of the facility was dedicated to undomiciled COVID-19 patients who had no place else to go. Peak census was around 100 patients, housed on four units, each with a clinical team led by a physician.
Dr. Baughman’s field hospital experience has taught her the importance of “staying within your domain of expertise. Physicians are attracted to difficult problems and want to do everything themselves. Next time I won’t be the one installing hand sanitizer dispensers.” A big part of running a field hospital is logistics, she said, and physicians are trained clinicians, not necessarily logistics engineers.
“So it’s important to partner with logistics experts. A huge part of our success in building a facility in 9 days of almost continuous construction was the involvement of the National Guard,” she said. An incident command system was led by an experienced military general incident commander, with two clinical codirectors. The army also sent in full teams of health professionals.
The facility admitted a lot fewer patients than the worst-case projections before it closed in June 2020. “But at the end of the day, we provided a lot of excellent care,” Dr. Baughman said. “This was about preparing for a disaster. It was all hands on deck, and the hands were health professionals. We spent a lot of money for the patients we took care of, but we had no choice, based on what we believed could happen. At that time, so many nursing facilities and homeless shelters were closed to us. It was impossible to predict what utilization would be.”
Subsequent experience has taught that a lot of even seriously ill COVID-19 patients can be managed safely at home, for example, using accelerated home oxygen monitoring with telelinked pulse oximeters. But in the beginning, Dr. Baughman said, “it was a new situation for us. We had seen what happened in Europe and China. It’s a great thing to be overprepared.”
References
1. Horowitz J. Italy’s health care system groans under coronavirus – a warning to the world. New York Times. 2020 Mar 12.
2. Bell SA et al. T-Minus 10 days: The role of an academic medical institution in field hospital planning. Prehosp Disaster Med. 2021 Feb 18:1-6. doi: 10.1017/S1049023X21000224.
3. Singh K et al. Evaluating a widely implemented proprietary deterioration index model among hospitalized patients with COVID-19. Ann Am Thorac Soc. 2021 Jul;18(7):1129-37. doi: 10.1513/AnnalsATS.202006-698OC.
4. Bell SA et al. Alternate care sites during COVID-19 pandemic: Policy implications for pandemic surge planning. Disaster Med Public Health Prep. 2021 Jul 23;1-3. doi: 10.1017/dmp.2021.241.
At the height of the COVID-19 pandemic’s terrifying first wave in the spring of 2020, dozens of hospitals in high-incidence areas either planned or opened temporary, emergency field hospitals to cover anticipated demand for beds beyond the capacity of local permanent hospitals.
Chastened by images of overwhelmed health care systems in Northern Italy and other hard-hit areas,1 the planners used available modeling tools and estimates for projecting maximum potential need in worst-case scenarios. Some of these temporary hospitals never opened. Others opened in convention centers, parking garages, or parking lot tents, and ended up being used to a lesser degree than the worst-case scenarios.
But those who participated in the planning – including, in many cases, hospitalists – believe they created alternate care site manuals that could be quickly revived in the event of future COVID surges or other, similar crises. Better to plan for too much, they say, than not plan for enough.
Field hospitals or alternate care sites are defined in a recent journal article in Prehospital Disaster Medicine as “locations that can be converted to provide either inpatient and/or outpatient health services when existing facilities are compromised by a hazard impact or the volume of patients exceeds available capacity and/or capabilities.”2
The lead author of that report, Sue Anne Bell, PhD, FNP-BC, a disaster expert and assistant professor of nursing at the University of Michigan (UM), was one of five members of the leadership team for planning UM’s field hospital. They used an organizational unit structure based on the U.S. military’s staffing structure, with their work organized around six units of planning: personnel and labor, security, clinical operations, logistics and supply, planning and training, and communications. This team planned a 519-bed step-down care facility, the Michigan Medicine Field Hospital, for a 73,000-foot indoor track and performance facility at the university, three miles from UM’s main hospital. The aim was to provide safe care in a resource-limited environment.
“We were prepared, but the need never materialized as the peak of COVID cases started to subside,” Dr. Bell said. The team was ready to open within days using a “T-Minus” framework of days remaining on an official countdown clock. But when the need and deadlines kept getting pushed back, that gave them more time to develop clearer procedures.
Two Michigan Medicine hospitalists, Christopher Smith, MD, and David Paje, MD, MPH, both professors at UM’s medical school, were intimately involved in the process. “I was the medical director for the respiratory care unit that was opened for COVID patients, so I was pulled in to assist in the field hospital planning,” said Dr. Smith.
Dr. Paje was director of the short-stay unit and had been a medical officer in the U.S. Army, with training in how to set up military field hospitals. He credits that background as helpful for UM’s COVID field hospital planning, along with his experience in hospital medicine operations.
“We expected that these patients would need the expertise of hospitalists, who had quickly become familiar with the peculiarities of the new disease. That played a role in the decisions we made. Hospitalists were at the front lines of COVID care and had unique clinical insights about managing those with severe disease,” Dr. Paje added.
“When we started, the projections were dire. You don’t want to believe something like that is going to happen. When COVID started to cool off, it was more of a relief to us than anything else,” Dr. Smith said. “Still, it was a very worthwhile exercise. At the end of the day, we put together a comprehensive guide, which is ready for the next crisis.”
Baltimore builds a convention center hospital
A COVID-19 field hospital was planned and executed at an exhibit hall in the Baltimore Convention Center, starting in March 2020 under the leadership of Johns Hopkins Bayview hospitalist Eric Howell, MD, MHM, who eventually handed over responsibilities as chief medical officer when he assumed the position of CEO for the Society of Hospital Medicine in July of that year.
Hopkins collaborated with the University of Maryland health system and state leaders, including the Secretary of Health, to open a 252-bed temporary facility, which at its peak carried a census of 48 patients, with no on-site mortality or cardiac arrests, before it was closed in June 2021 – ready to reopen if necessary. It also served as Baltimore’s major site for polymerase chain reaction COVID-19 testing, vaccinations, and monoclonal antibody infusions, along with medical research.
“My belief at the time we started was that my entire 20-year career as a hospitalist had prepared me for the challenge of opening a COVID field hospital,” Dr. Howell said. “I had learned how to build clinical programs. The difference was that instead of months and years to build a program, we only had a few weeks.”
His first request was to bring on an associate medical director for the field hospital, Melinda E. Kantsiper, MD, a hospitalist and director of clinical operations in the Division of Hospital Medicine at Johns Hopkins Bayview. She became the field hospital’s CMO when Dr. Howell moved to SHM. “As hospitalists, we are trained to care for the patient in front of us while at the same time creating systems that can adjust to rapidly changing circumstances,” Dr. Kantsiper said. “We did what was asked and set up a field hospital that cared for a total of 1,500 COVID patients.”
Hospitalists have the tools that are needed for this work, and shouldn’t be reluctant to contribute to field hospital planning, she said. “This was a real eye-opener for me. Eric explained to me that hospitalists really practice acute care medicine, which doesn’t have to be within the four walls of a hospital.”
The Baltimore field hospital has been a fantastic experience, Dr. Kantsiper added. “But it’s not a building designed for health care delivery.” For the right group of providers, the experience of working in a temporary facility such as this can be positive and exhilarating. “But we need to make sure we take care of our staff. It takes a toll. How we keep them safe – physically and emotionally – has to be top of mind,” she said.
The leaders at Hopkins Medicine and their collaborators truly engaged with the field hospital’s mission, Dr. Howell added.
“They gave us a lot of autonomy and helped us break down barriers. They gave us the political capital to say proper PPE was absolutely essential. As hard and devastating as the pandemic has been, one take-away is that we showed that we can be more flexible and elastic in response to actual needs than we used to think.”
Range of challenges
Among the questions that need to be answered by a field hospital’s planners, the first is ‘where to put it?’ The answer is, hopefully, someplace not too far away, large enough, with ready access to supplies and intake. The next question is ‘who is the patient?’ Clinicians must determine who goes to the field hospital versus who stays at the standing hospital. How sick should these patients be? And when do they need to go back to the permanent hospital? Can staff be trained to recognize when patients in the field hospital are starting to decompensate? The EPIC Deterioration Index3 is a proprietary prediction model that was used by more than a hundred hospitals during the pandemic.
The hospitalist team may develop specific inclusion and exclusion criteria – for example, don’t admit patients who are receiving oxygen therapy above a certain threshold or who are hemodynamically unstable. These criteria should reflect the capacity of the field hospital and the needs of the permanent hospital. At Michigan, as at other field hospital sites, the goal was to offer a step-down or postacute setting for patients with COVID-19 who were too sick to return home but didn’t need acute or ICU-level care, thereby freeing up beds at the permanent hospital for patients who were sicker.
Other questions: What is the process for admissions and discharges? How will patients be transported? What kind of staffing is needed, and what levels of care will be provided? What about rehabilitation services, or palliative care? What about patients with substance abuse or psychiatric comorbidities?
“Are we going to do paper charting? How will that work out for long-term documentation and billing?” Dr. Bell said. A clear reporting structure and communication pathways are essential. Among the other operational processes to address, outlined in Dr. Bell’s article, are orientation and training, PPE donning and doffing procedures, the code or rapid response team, patient and staff food and nutrition, infection control protocols, pharmacy services, access to radiology, rounding procedures, staff support, and the morgue.
One other issue that shouldn’t be overlooked is health equity in the field hospital. “Providing safe and equitable care should be the focus. Thinking who goes to the field hospital should be done within a health equity framework,” Dr. Bell said.4 She also wonders if field hospital planners are sharing their experience with colleagues across the country and developing more collaborative relationships with other hospitals in their communities.
“Field hospitals can be different things,” Dr. Bell said. “The important take-home is it doesn’t have to be in a tent or a parking garage, which can be suboptimal.” In many cases, it may be better to focus on finding unused space within the hospital – whether a lobby, staff lounge, or unoccupied unit – closer to personnel, supplies, pharmacy, and the like. “I think the pandemic showed us how unprepared we were as a health care system, and how much more we need to do in preparation for future crises.”
Limits to the temporary hospital
In New York City, which had the country’s worst COVID-19 outbreak during the first surge in the spring of 2020, a 1,000-bed field hospital was opened at the Jacob Javits Center in March 2020 and closed that June. “I was in the field hospital early, in March and April, when our hospitals were temporarily overrun,” said hospitalist Mona Krouss, MD, FACP, CPPS, NYC Health + Hospitals’ director of patient safety. “My role was to figure out how to get patients on our medical floors into these field hospitals, with responsibility for helping to revise admission criteria,” she said.
“No one knew how horrible it would become. This was so unanticipated, so difficult to operationalize. What they were able to create was amazing, but there were just too many barriers to have it work smoothly,” Dr. Krouss said.
“The military stepped in, and they helped us so much. We wouldn’t have been able to survive without their help.” But there is only so much a field hospital can do to provide acute medical care. Later, military medical teams shifted to roles in temporary units inside the permanent hospitals. “They came to the hospital wanting to be deployed,” she said.
“We could only send patients [to the field hospital] who were fairly stable, and choosing the right ones was difficult.” Dr. Krouss said. In the end, not a lot of COVID-19 patients from NYC Health + Hospitals ended up going to the Javits Center, in part because the paperwork and logistics of getting someone in was a barrier, Dr. Krouss said. A process was established for referring doctors to call a phone number and speak with a New York City Department of Health employee to go through the criteria for admission to the field hospital.
“That could take up to 30 minutes before getting approval. Then you had to go through the same process all over again for sign-out to another physician, and then register the patient with a special bar code. Then you had to arrange ambulance transfer. Doctors didn’t want to go through all of that – everybody was too busy,” she explained. Hospitalists have since worked on streamlining the criteria. “Now we have a good process for the future. We made it more seamless,” she noted.
Susan Lee, DO, MBA, hospitalist and chief medical officer for Renown Regional Medical Center in Reno, Nev., helped to plan an alternate care site in anticipation of up to a thousand COVID patients in her community – far beyond the scope of the existing hospitals. Hospitalists were involved the entire time in planning, design of the unit, design of staffing models, care protocols, and the like, working through an evidence-based medical committee and a COVID-19 provider task force for the Renown Health System.
“Because of a history of fires and earthquakes in this region, we had an emergency planning infrastructure in place. We put the field hospital on the first and second floors of a parking garage, with built-in negative pressure capacity. We also built space for staff break rooms and desk space. It took 10 days to build the hospital, thanks to some very talented people in management and facility design,” Dr. Lee said.
Then, the hospital was locked up and sat empty for 7 months, until the surge in December 2020, when Reno was hit by a bigger wave – this time exceeding the hospitals’ capacity. Through mid-January of 2021, clinicians cared for approximately 240 COVID-19 patients, up to 47 at a time, in the field hospital. A third wave in the autumn of 2021 plateaued at a level lower than the previous fall, so the field hospital is not currently needed.
Replicating hospital work flows
“We ensured that everybody who needed to be within the walls of the permanent hospitals was able to stay there,” said Dr. Lee’s colleague, hospitalist Adnan (Eddy) Akbar, MD. “The postacute system we ordinarily rely on was no longer accepting patients. Other hospitals in the area were able to manage within their capacity because Renown’s field hospital could admit excess patients. We tried to replicate in the field hospital, as much as possible, the work flows and systems of our main hospital.”
When the field hospital finally opened, Dr. Akbar said, “we had a good feeling. We were ready. If something more catastrophic had come down, we were ready to care for more patients. In the field hospital you have to keep monitoring your work flow – almost on a daily basis. But we felt privileged to be working for a system where you knew you can go and care for everyone who needed care.”
One upside of the field hospital experience for participating clinicians, Dr. Lee added, is the opportunity to practice creatively. “The downside is it’s extremely expensive, and has consequences for the mental health of staff. Like so many of these things, it wore on people over time – such as all the time spent donning and doffing protective equipment. And recently the patients have become a lot less gracious.”
Amy Baughman, MD, a hospitalist at Massachusetts General Hospital in Boston, was co-medical director of the postacute care section of a 1,000-bed field hospital, Boston Hope Medical Center, opened in April 2020 at the Boston Convention and Exhibition Center. The other half of the facility was dedicated to undomiciled COVID-19 patients who had no place else to go. Peak census was around 100 patients, housed on four units, each with a clinical team led by a physician.
Dr. Baughman’s field hospital experience has taught her the importance of “staying within your domain of expertise. Physicians are attracted to difficult problems and want to do everything themselves. Next time I won’t be the one installing hand sanitizer dispensers.” A big part of running a field hospital is logistics, she said, and physicians are trained clinicians, not necessarily logistics engineers.
“So it’s important to partner with logistics experts. A huge part of our success in building a facility in 9 days of almost continuous construction was the involvement of the National Guard,” she said. An incident command system was led by an experienced military general incident commander, with two clinical codirectors. The army also sent in full teams of health professionals.
The facility admitted a lot fewer patients than the worst-case projections before it closed in June 2020. “But at the end of the day, we provided a lot of excellent care,” Dr. Baughman said. “This was about preparing for a disaster. It was all hands on deck, and the hands were health professionals. We spent a lot of money for the patients we took care of, but we had no choice, based on what we believed could happen. At that time, so many nursing facilities and homeless shelters were closed to us. It was impossible to predict what utilization would be.”
Subsequent experience has taught that a lot of even seriously ill COVID-19 patients can be managed safely at home, for example, using accelerated home oxygen monitoring with telelinked pulse oximeters. But in the beginning, Dr. Baughman said, “it was a new situation for us. We had seen what happened in Europe and China. It’s a great thing to be overprepared.”
References
1. Horowitz J. Italy’s health care system groans under coronavirus – a warning to the world. New York Times. 2020 Mar 12.
2. Bell SA et al. T-Minus 10 days: The role of an academic medical institution in field hospital planning. Prehosp Disaster Med. 2021 Feb 18:1-6. doi: 10.1017/S1049023X21000224.
3. Singh K et al. Evaluating a widely implemented proprietary deterioration index model among hospitalized patients with COVID-19. Ann Am Thorac Soc. 2021 Jul;18(7):1129-37. doi: 10.1513/AnnalsATS.202006-698OC.
4. Bell SA et al. Alternate care sites during COVID-19 pandemic: Policy implications for pandemic surge planning. Disaster Med Public Health Prep. 2021 Jul 23;1-3. doi: 10.1017/dmp.2021.241.
New prescription for loop diuretic improves 30-day heart failure outcomes
Background: In patients with heart failure, loop diuretics are used to manage symptoms. However, the effect of loop diuretics on morbidity and mortality is not well studied.
Study design: Retrospective matched cohort study.
Setting: OPTIMIZE-HF registry.
Synopsis: Using the data from the OPTIMIZE-HF registry to develop a matched cohort of 2,191 pairs of patients, researchers showed that patients hospitalized for heart failure who were not previously taking any diuretic had significantly better 30-day clinical outcomes if they were discharged on a loop diuretic. Specifically, a loop diuretic on discharge resulted in a lower 30-day all-cause mortality (hazard ratio, 0.73; 95% CI, 0.57-0.94; P = .016) and a lower risk of 30-day heart failure readmission (HR, 0.79; 95% CI, 0.63-0.99; P = .037), compared with patients not discharged on a loop diuretic.
Neither of these associations was statistically significant during a 60-day follow-up, and the authors acknowledge that significant 30-day associations may be sensitive to an unmeasured confounder.
Bottom line: Starting an outpatient loop diuretic on discharge for patients hospitalized for heart failure improves 30-day all-cause mortality and lowers the risk of 30-day heart failure readmission.
Citation: Faselis C et al. Loop diuretic prescription and 30-day outcomes in older patients with heart failure. J Am Coll Cardiol. 2020;76:669-79.
Dr. Wallenhorst is a hospitalist and palliative medicine physician at the Lexington (Ky) VA Health Care System.
Background: In patients with heart failure, loop diuretics are used to manage symptoms. However, the effect of loop diuretics on morbidity and mortality is not well studied.
Study design: Retrospective matched cohort study.
Setting: OPTIMIZE-HF registry.
Synopsis: Using the data from the OPTIMIZE-HF registry to develop a matched cohort of 2,191 pairs of patients, researchers showed that patients hospitalized for heart failure who were not previously taking any diuretic had significantly better 30-day clinical outcomes if they were discharged on a loop diuretic. Specifically, a loop diuretic on discharge resulted in a lower 30-day all-cause mortality (hazard ratio, 0.73; 95% CI, 0.57-0.94; P = .016) and a lower risk of 30-day heart failure readmission (HR, 0.79; 95% CI, 0.63-0.99; P = .037), compared with patients not discharged on a loop diuretic.
Neither of these associations was statistically significant during a 60-day follow-up, and the authors acknowledge that significant 30-day associations may be sensitive to an unmeasured confounder.
Bottom line: Starting an outpatient loop diuretic on discharge for patients hospitalized for heart failure improves 30-day all-cause mortality and lowers the risk of 30-day heart failure readmission.
Citation: Faselis C et al. Loop diuretic prescription and 30-day outcomes in older patients with heart failure. J Am Coll Cardiol. 2020;76:669-79.
Dr. Wallenhorst is a hospitalist and palliative medicine physician at the Lexington (Ky) VA Health Care System.
Background: In patients with heart failure, loop diuretics are used to manage symptoms. However, the effect of loop diuretics on morbidity and mortality is not well studied.
Study design: Retrospective matched cohort study.
Setting: OPTIMIZE-HF registry.
Synopsis: Using the data from the OPTIMIZE-HF registry to develop a matched cohort of 2,191 pairs of patients, researchers showed that patients hospitalized for heart failure who were not previously taking any diuretic had significantly better 30-day clinical outcomes if they were discharged on a loop diuretic. Specifically, a loop diuretic on discharge resulted in a lower 30-day all-cause mortality (hazard ratio, 0.73; 95% CI, 0.57-0.94; P = .016) and a lower risk of 30-day heart failure readmission (HR, 0.79; 95% CI, 0.63-0.99; P = .037), compared with patients not discharged on a loop diuretic.
Neither of these associations was statistically significant during a 60-day follow-up, and the authors acknowledge that significant 30-day associations may be sensitive to an unmeasured confounder.
Bottom line: Starting an outpatient loop diuretic on discharge for patients hospitalized for heart failure improves 30-day all-cause mortality and lowers the risk of 30-day heart failure readmission.
Citation: Faselis C et al. Loop diuretic prescription and 30-day outcomes in older patients with heart failure. J Am Coll Cardiol. 2020;76:669-79.
Dr. Wallenhorst is a hospitalist and palliative medicine physician at the Lexington (Ky) VA Health Care System.
Symptoms persist in patients after acute COVID-19
Background: A large proportion of Italian patients with COVID-19 presented with symptoms, most commonly cough, fever, dyspnea, myalgias, anosmia, and gastrointestinal symptoms. Information is lacking on persistent symptoms after recovery.
Study design: Retrospective observational study.
Setting: Hospital system in Rome.
Synopsis: A postacute outpatient service for individuals discharged after recovery from COVID-19 was established. All patients who met World Health Organization criteria for discontinuation of quarantine (no fever for 3 consecutive days, improved symptoms, and two negative SARS-CoV-2 tests 24 hours apart) were offered a comprehensive medical assessment. Patients were asked to retrospectively recount the presence or absence of symptoms during the acute phase of COVID-19 and whether each symptom persisted at the time of the visit.
From April 21 to May 29, 2020, 179 patients were potentially eligible; 143 ultimately were included. During hospitalization, 72.7% of participants had evidence of interstitial pneumonia. Patients were assessed a mean of 60.3 days after onset of the first COVID-19 symptom. Only 18 (12.6%) were completely free of any COVID-19–related symptoms, 32% had one or two symptoms, and 55% had three or more. Worsened quality of life was observed among 44.1% of patients.
Bottom line: 87.4% of patients who had recovered from COVID-19 reported persistence of at least one symptom, particularly fatigue and dyspnea.
Citation: Carfi A et al. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603-5.
Dr. Walker is a hospitalist at the Lexington (Ky.) VA Health Care System.
Background: A large proportion of Italian patients with COVID-19 presented with symptoms, most commonly cough, fever, dyspnea, myalgias, anosmia, and gastrointestinal symptoms. Information is lacking on persistent symptoms after recovery.
Study design: Retrospective observational study.
Setting: Hospital system in Rome.
Synopsis: A postacute outpatient service for individuals discharged after recovery from COVID-19 was established. All patients who met World Health Organization criteria for discontinuation of quarantine (no fever for 3 consecutive days, improved symptoms, and two negative SARS-CoV-2 tests 24 hours apart) were offered a comprehensive medical assessment. Patients were asked to retrospectively recount the presence or absence of symptoms during the acute phase of COVID-19 and whether each symptom persisted at the time of the visit.
From April 21 to May 29, 2020, 179 patients were potentially eligible; 143 ultimately were included. During hospitalization, 72.7% of participants had evidence of interstitial pneumonia. Patients were assessed a mean of 60.3 days after onset of the first COVID-19 symptom. Only 18 (12.6%) were completely free of any COVID-19–related symptoms, 32% had one or two symptoms, and 55% had three or more. Worsened quality of life was observed among 44.1% of patients.
Bottom line: 87.4% of patients who had recovered from COVID-19 reported persistence of at least one symptom, particularly fatigue and dyspnea.
Citation: Carfi A et al. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603-5.
Dr. Walker is a hospitalist at the Lexington (Ky.) VA Health Care System.
Background: A large proportion of Italian patients with COVID-19 presented with symptoms, most commonly cough, fever, dyspnea, myalgias, anosmia, and gastrointestinal symptoms. Information is lacking on persistent symptoms after recovery.
Study design: Retrospective observational study.
Setting: Hospital system in Rome.
Synopsis: A postacute outpatient service for individuals discharged after recovery from COVID-19 was established. All patients who met World Health Organization criteria for discontinuation of quarantine (no fever for 3 consecutive days, improved symptoms, and two negative SARS-CoV-2 tests 24 hours apart) were offered a comprehensive medical assessment. Patients were asked to retrospectively recount the presence or absence of symptoms during the acute phase of COVID-19 and whether each symptom persisted at the time of the visit.
From April 21 to May 29, 2020, 179 patients were potentially eligible; 143 ultimately were included. During hospitalization, 72.7% of participants had evidence of interstitial pneumonia. Patients were assessed a mean of 60.3 days after onset of the first COVID-19 symptom. Only 18 (12.6%) were completely free of any COVID-19–related symptoms, 32% had one or two symptoms, and 55% had three or more. Worsened quality of life was observed among 44.1% of patients.
Bottom line: 87.4% of patients who had recovered from COVID-19 reported persistence of at least one symptom, particularly fatigue and dyspnea.
Citation: Carfi A et al. Persistent symptoms in patients after acute COVID-19. JAMA. 2020;324(6):603-5.
Dr. Walker is a hospitalist at the Lexington (Ky.) VA Health Care System.
Hotspotting does not reduce readmissions
Background: In the United States, 5% of the population use half of the annual spending for health care services and 1% account for approximately a quarter of annual spending, considered “superutilizers” of U.S. health care services. The Camden Coalition of Healthcare Providers (the Coalition) developed a model using hospital admission data to identify superutilizers, termed “hotspotting,” which has gained national recognition. Unlike other similar programs, this model targets a more diverse population with higher utilization than other programs that have been studied.
Study design: Randomized, controlled trial.
Setting: Two hospitals in Camden, N.J., from June 2, 2014, to March 31, 2018.
Synopsis: Eight-hundred superutilizers (at least one hospital admission at any of the four Camden-area hospital systems in the past 6 months, greater than one chronic medical condition, more than one high-risk traits/conditions) were randomly assigned to the intervention group or usual care. Once enrolled in the hospital, a multidisciplinary team began working with the patient in the intervention group on discharge. Team members conducted home visits, scheduled/took patients to appointments, managed medications, monitored and coached patients in disease-specific self-care, and assisted with applying for social and other assistive programs.
The readmission rate within 180 days after hospital discharge (primary outcome) between groups was not significant, with 62.3% readmitted in the intervention group and 61.7% in the control group. There was also no effect on the defined secondary outcomes (number of readmissions, proportion of patients with more than two readmissions, hospital days, charges, payments received, mortality).
The trial was not powered to detect smaller reductions in readmissions or to analyze effects within specific subgroups.
Bottom line: The addition of the Coalition’s program to patients with very high use of health care services did not decrease hospital readmission rate when compared to usual care.
Citation: Finkelstein A et al. Health care hotspotting – a randomized, controlled trial. N Engl J Med. 2020;382:152-62.
Dr. Trammell-Velasquez is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: In the United States, 5% of the population use half of the annual spending for health care services and 1% account for approximately a quarter of annual spending, considered “superutilizers” of U.S. health care services. The Camden Coalition of Healthcare Providers (the Coalition) developed a model using hospital admission data to identify superutilizers, termed “hotspotting,” which has gained national recognition. Unlike other similar programs, this model targets a more diverse population with higher utilization than other programs that have been studied.
Study design: Randomized, controlled trial.
Setting: Two hospitals in Camden, N.J., from June 2, 2014, to March 31, 2018.
Synopsis: Eight-hundred superutilizers (at least one hospital admission at any of the four Camden-area hospital systems in the past 6 months, greater than one chronic medical condition, more than one high-risk traits/conditions) were randomly assigned to the intervention group or usual care. Once enrolled in the hospital, a multidisciplinary team began working with the patient in the intervention group on discharge. Team members conducted home visits, scheduled/took patients to appointments, managed medications, monitored and coached patients in disease-specific self-care, and assisted with applying for social and other assistive programs.
The readmission rate within 180 days after hospital discharge (primary outcome) between groups was not significant, with 62.3% readmitted in the intervention group and 61.7% in the control group. There was also no effect on the defined secondary outcomes (number of readmissions, proportion of patients with more than two readmissions, hospital days, charges, payments received, mortality).
The trial was not powered to detect smaller reductions in readmissions or to analyze effects within specific subgroups.
Bottom line: The addition of the Coalition’s program to patients with very high use of health care services did not decrease hospital readmission rate when compared to usual care.
Citation: Finkelstein A et al. Health care hotspotting – a randomized, controlled trial. N Engl J Med. 2020;382:152-62.
Dr. Trammell-Velasquez is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: In the United States, 5% of the population use half of the annual spending for health care services and 1% account for approximately a quarter of annual spending, considered “superutilizers” of U.S. health care services. The Camden Coalition of Healthcare Providers (the Coalition) developed a model using hospital admission data to identify superutilizers, termed “hotspotting,” which has gained national recognition. Unlike other similar programs, this model targets a more diverse population with higher utilization than other programs that have been studied.
Study design: Randomized, controlled trial.
Setting: Two hospitals in Camden, N.J., from June 2, 2014, to March 31, 2018.
Synopsis: Eight-hundred superutilizers (at least one hospital admission at any of the four Camden-area hospital systems in the past 6 months, greater than one chronic medical condition, more than one high-risk traits/conditions) were randomly assigned to the intervention group or usual care. Once enrolled in the hospital, a multidisciplinary team began working with the patient in the intervention group on discharge. Team members conducted home visits, scheduled/took patients to appointments, managed medications, monitored and coached patients in disease-specific self-care, and assisted with applying for social and other assistive programs.
The readmission rate within 180 days after hospital discharge (primary outcome) between groups was not significant, with 62.3% readmitted in the intervention group and 61.7% in the control group. There was also no effect on the defined secondary outcomes (number of readmissions, proportion of patients with more than two readmissions, hospital days, charges, payments received, mortality).
The trial was not powered to detect smaller reductions in readmissions or to analyze effects within specific subgroups.
Bottom line: The addition of the Coalition’s program to patients with very high use of health care services did not decrease hospital readmission rate when compared to usual care.
Citation: Finkelstein A et al. Health care hotspotting – a randomized, controlled trial. N Engl J Med. 2020;382:152-62.
Dr. Trammell-Velasquez is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Post–acute kidney injury proteinuria predicts subsequent kidney disease progression
Background: Recent studies have shown that the level of proteinuria increases after AKI. It is not yet shown if this increases risk of kidney disease progression.
Study design: Prospective matched cohort study.
Setting: North American hospitals.
Synopsis: A total of 769 hospitalized adults with AKI were matched with those without based on clinical center and preadmission chronic kidney disease (CKD) status. Study authors found that albumin/creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) 3 months after hospitalization were highly associated with kidney disease progression, with a hazard ratio of 1.53 for each doubling (95% confidence interval, 1.43-1.64).
Episodes of AKI were also associated with progression, but this is severely attenuated once adjusted for ACR, eGFR, and traditional CKD risk factors. This suggests more routine quantification of proteinuria after AKI for better risk stratification.
Bottom line: Posthospitalization ACR predicts progression of kidney disease.
Citation: Hsu CY et al. Post–acute kidney injury proteinuria and subsequent kidney disease progression. JAMA Intern Med. 2020 Jan 27. doi: 10.1001/jamainternmed.2019.6390.
Dr. Ho is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Recent studies have shown that the level of proteinuria increases after AKI. It is not yet shown if this increases risk of kidney disease progression.
Study design: Prospective matched cohort study.
Setting: North American hospitals.
Synopsis: A total of 769 hospitalized adults with AKI were matched with those without based on clinical center and preadmission chronic kidney disease (CKD) status. Study authors found that albumin/creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) 3 months after hospitalization were highly associated with kidney disease progression, with a hazard ratio of 1.53 for each doubling (95% confidence interval, 1.43-1.64).
Episodes of AKI were also associated with progression, but this is severely attenuated once adjusted for ACR, eGFR, and traditional CKD risk factors. This suggests more routine quantification of proteinuria after AKI for better risk stratification.
Bottom line: Posthospitalization ACR predicts progression of kidney disease.
Citation: Hsu CY et al. Post–acute kidney injury proteinuria and subsequent kidney disease progression. JAMA Intern Med. 2020 Jan 27. doi: 10.1001/jamainternmed.2019.6390.
Dr. Ho is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Background: Recent studies have shown that the level of proteinuria increases after AKI. It is not yet shown if this increases risk of kidney disease progression.
Study design: Prospective matched cohort study.
Setting: North American hospitals.
Synopsis: A total of 769 hospitalized adults with AKI were matched with those without based on clinical center and preadmission chronic kidney disease (CKD) status. Study authors found that albumin/creatinine ratio (ACR) and estimated glomerular filtration rate (eGFR) 3 months after hospitalization were highly associated with kidney disease progression, with a hazard ratio of 1.53 for each doubling (95% confidence interval, 1.43-1.64).
Episodes of AKI were also associated with progression, but this is severely attenuated once adjusted for ACR, eGFR, and traditional CKD risk factors. This suggests more routine quantification of proteinuria after AKI for better risk stratification.
Bottom line: Posthospitalization ACR predicts progression of kidney disease.
Citation: Hsu CY et al. Post–acute kidney injury proteinuria and subsequent kidney disease progression. JAMA Intern Med. 2020 Jan 27. doi: 10.1001/jamainternmed.2019.6390.
Dr. Ho is a hospitalist and associate professor of medicine at University of Texas Health, San Antonio.
Hospital-level care at home for acutely ill adults may be as safe as inpatient care
Background: Providing hospital-level care at home for select patients has proven to reduce health care cost, usage, and readmission rates, while maintaining quality and safety in other developed countries but few studies exist in the United States.
Study design: Randomized, controlled, unblinded, parallel-design trial.
Setting: Home hospital care versus inpatient care at two Boston academic hospitals, during June 2017–January 2018.
Synopsis: The study enrolled 91 adult patients from the emergency department who were deemed appropriate for non-ICU admission for treatment of prespecified diagnoses (i.e., COPD exacerbation, heart failure exacerbation, etc.). Participants were randomized to usual inpatient care or home hospital care. All home hospital patients received daily internist visits, twice-daily nursing visits, home access to additional services (physical/occupational therapy, social work, etc.), oxygen, IV medications, labs, radiology, and continuous monitoring. The authors found that home hospital care resulted in a lower total cost (P < .001), lower use of imaging and labs, and lower 30-day readmission rate, without appreciable differences in quality or safety between the two groups. Given that the study was performed at only two academic hospitals, it is unclear if these findings can be generalized to other health systems.
Bottom line: For the care of select illnesses, hospital-level care at home may be cheaper, may be just as safe, and reduced readmission rates when compared with inpatient care.
Citation: Levine D et al. Hospital-level care at home for acutely ill adults. Ann Intern Med. 2020;172:77-85.
Dr. Persaud is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Background: Providing hospital-level care at home for select patients has proven to reduce health care cost, usage, and readmission rates, while maintaining quality and safety in other developed countries but few studies exist in the United States.
Study design: Randomized, controlled, unblinded, parallel-design trial.
Setting: Home hospital care versus inpatient care at two Boston academic hospitals, during June 2017–January 2018.
Synopsis: The study enrolled 91 adult patients from the emergency department who were deemed appropriate for non-ICU admission for treatment of prespecified diagnoses (i.e., COPD exacerbation, heart failure exacerbation, etc.). Participants were randomized to usual inpatient care or home hospital care. All home hospital patients received daily internist visits, twice-daily nursing visits, home access to additional services (physical/occupational therapy, social work, etc.), oxygen, IV medications, labs, radiology, and continuous monitoring. The authors found that home hospital care resulted in a lower total cost (P < .001), lower use of imaging and labs, and lower 30-day readmission rate, without appreciable differences in quality or safety between the two groups. Given that the study was performed at only two academic hospitals, it is unclear if these findings can be generalized to other health systems.
Bottom line: For the care of select illnesses, hospital-level care at home may be cheaper, may be just as safe, and reduced readmission rates when compared with inpatient care.
Citation: Levine D et al. Hospital-level care at home for acutely ill adults. Ann Intern Med. 2020;172:77-85.
Dr. Persaud is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Background: Providing hospital-level care at home for select patients has proven to reduce health care cost, usage, and readmission rates, while maintaining quality and safety in other developed countries but few studies exist in the United States.
Study design: Randomized, controlled, unblinded, parallel-design trial.
Setting: Home hospital care versus inpatient care at two Boston academic hospitals, during June 2017–January 2018.
Synopsis: The study enrolled 91 adult patients from the emergency department who were deemed appropriate for non-ICU admission for treatment of prespecified diagnoses (i.e., COPD exacerbation, heart failure exacerbation, etc.). Participants were randomized to usual inpatient care or home hospital care. All home hospital patients received daily internist visits, twice-daily nursing visits, home access to additional services (physical/occupational therapy, social work, etc.), oxygen, IV medications, labs, radiology, and continuous monitoring. The authors found that home hospital care resulted in a lower total cost (P < .001), lower use of imaging and labs, and lower 30-day readmission rate, without appreciable differences in quality or safety between the two groups. Given that the study was performed at only two academic hospitals, it is unclear if these findings can be generalized to other health systems.
Bottom line: For the care of select illnesses, hospital-level care at home may be cheaper, may be just as safe, and reduced readmission rates when compared with inpatient care.
Citation: Levine D et al. Hospital-level care at home for acutely ill adults. Ann Intern Med. 2020;172:77-85.
Dr. Persaud is a hospitalist, Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Hospitalists play key role in advance care planning
Advance care planning (ACP) is a process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences for future medical care, according to Meredith A. MacMartin, MD, director of inpatient palliative care at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
ACP “is really about planning for care in advance,” and in many ways, the inpatient setting is uniquely suited to this process, Dr. MacMartin said in a presentation at SHM Converge 2021, the annual conference of the Society of Hospital Medicine. “The key part is the advance part. You want conversations to happen before the care is actually needed,” she said.
Dr. MacMartin emphasized the importance of distinguishing between ACP and advance directives (ADs). ACP is a process, whereas ADs are documentation, “ideally of the content of advance care planning discussions,” she explained. ACP involves discussion about what is important to the patients, their goals, what information is helpful for them, and whether their current care is aligned with their goals, Dr. MacMartin said. ADs might involve a designated power of attorney for health care, a living will, and, in some states, specific clinician-signed orders regarding resuscitation or transport to hospital.
ACP is “more than whether a patient wants CPR [cardiopulmonary resuscitation] or not,” said Dr. MacMartin. ACP matters because it helps ensure that the care a patient receives aligns with the patient’s wishes and values, she said. ACP increases the likelihood that patients will die in their preferred locations, it allows them to discuss their wishes and prepare for decline, and it relieves family members of the burden of decision making, she said. From a hospital perspective, data show that use of an ACP can decrease intensive care unit (ICU) utilization and overall health care costs. “Often, when people are given the opportunity to express their wishes, they get less unnecessary care,” Dr. MacMartin noted.
Although ACP often takes place in an outpatient setting, hospitalists are in a unique position to conduct some ACP conversations with their patients, Dr. MacMartin said. “Hospitalists are available” and are physically present at least once a day, so there is a pragmatic advantage. Also, some data suggest that patients may feel more comfortable having ACP conversations with a hospitalist than with a primary care provider with whom they have a long-standing relationship, Dr. MacMartin added.
Another important advantage of ACP in the hospital setting is that, “as hospitalists, you are the expert on inpatient illness; you know what sick looks like, and you have a unique perspective on prognostication that may be harder to recreate in the outpatient setting,” Dr. MacMartin said.
Barriers to ACP include patient identification, logistics, attitudes
Settings in which ACP is appropriate include those in which a patient is undergoing “sentinel hospitalization,” meaning that the patient is at a transition point in the disease course. Examples are a patient newly diagnosed with metastatic solid cancer, a patient with progressive chronic kidney disease who is considering hemodialysis, or a patient who receives treatment in the ICU for longer than 7 days, Dr. MacMartin said.
Guidelines for identifying patients who might benefit from ACP include the use of the “surprise question” (“would you be surprised if this patient dies in the next year?”) as well as functional status assessments using tools such as the Australia-modified Karnofsky Performance Status or the Eastern Cooperative Oncology Group score, said Dr. MacMartin. Some studies suggest that any hospitalized patient older than 65 years should have an ACP discussion, she added.
Time pressure remains a significant barrier to ACP conversations. Some strategies to overcome this problem include enlisting help from other specialists, particularly social workers, Dr. MacMartin said. Social workers report a higher comfort level for talking to patients about death than any other medical specialty; “this is something they want to be doing,” she said. Also, the possibility of reimbursement may act as a buffer to create more time to have ACP conversations with patients, she noted.
Addressing clinicians’ discomfort with ACP conversations can be “a tougher nut to crack,” Dr. MacMartin acknowledged. Clinicians report that they don’t want to cause their patients distress, and some report that having conversations about end-of-life care is distressing for them as well. Some of these barriers can be overcome with skills training, including use of a prepared guideline or framework to help increase the comfort level for both clinicians and patients, said Dr. MacMartin.
A look ahead: Training strategies and COVID-19 impact
“For hospitalists interested in developing their ACP skills, I highly recommend two resources,” Dr. MacMartin said in an interview. “The Serious Illness Conversation Guide, from Ariadne Labs, is an excellent tool for any clinician to guide discussion about a patient’s goals and values,” she said.
“For clinicians wanting to build or improve their communication, including advance care planning discussions but also topics like responding to patient’s emotions, VitalTalk training offers a deeper dive into core communications skills,” she added.
“If your hospital has a palliative care team, they may also have more local resources available to you. To learn more about billing for ACP discussions, I recommend starting with your institutional billing and coding group, as these practices vary some between practices, and they will be able to provide the best guidance for clinicians. These are new codes that aren’t yet being very widely used so it’s a chance to innovate,” Dr. MacMartin noted.
“The hospital setting is an opportunity for patients to reflect on their health, both present and in the future, with a physician who has expertise in acute illness and prognostication and who is available for discussion on a daily basis during the hospitalization,” Dr. MacMartin emphasized.
As for whether the COVID-19 pandemic has affected ACP in the inpatient setting, the data are limited, but more information is forthcoming, Dr. MacMartin said. “In my personal experience and in talking to colleagues elsewhere, the pandemic has highlighted the need for ACP in some ways, as we have tried to ensure that people who wouldn’t want things like intensive care are identified early,” she said. “I hope that some of the workflows developed to identify patients who should get ACP in the hospital stay in practice and are strengthened over time,” she added.
Dr. MacMartin has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Advance care planning (ACP) is a process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences for future medical care, according to Meredith A. MacMartin, MD, director of inpatient palliative care at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
ACP “is really about planning for care in advance,” and in many ways, the inpatient setting is uniquely suited to this process, Dr. MacMartin said in a presentation at SHM Converge 2021, the annual conference of the Society of Hospital Medicine. “The key part is the advance part. You want conversations to happen before the care is actually needed,” she said.
Dr. MacMartin emphasized the importance of distinguishing between ACP and advance directives (ADs). ACP is a process, whereas ADs are documentation, “ideally of the content of advance care planning discussions,” she explained. ACP involves discussion about what is important to the patients, their goals, what information is helpful for them, and whether their current care is aligned with their goals, Dr. MacMartin said. ADs might involve a designated power of attorney for health care, a living will, and, in some states, specific clinician-signed orders regarding resuscitation or transport to hospital.
ACP is “more than whether a patient wants CPR [cardiopulmonary resuscitation] or not,” said Dr. MacMartin. ACP matters because it helps ensure that the care a patient receives aligns with the patient’s wishes and values, she said. ACP increases the likelihood that patients will die in their preferred locations, it allows them to discuss their wishes and prepare for decline, and it relieves family members of the burden of decision making, she said. From a hospital perspective, data show that use of an ACP can decrease intensive care unit (ICU) utilization and overall health care costs. “Often, when people are given the opportunity to express their wishes, they get less unnecessary care,” Dr. MacMartin noted.
Although ACP often takes place in an outpatient setting, hospitalists are in a unique position to conduct some ACP conversations with their patients, Dr. MacMartin said. “Hospitalists are available” and are physically present at least once a day, so there is a pragmatic advantage. Also, some data suggest that patients may feel more comfortable having ACP conversations with a hospitalist than with a primary care provider with whom they have a long-standing relationship, Dr. MacMartin added.
Another important advantage of ACP in the hospital setting is that, “as hospitalists, you are the expert on inpatient illness; you know what sick looks like, and you have a unique perspective on prognostication that may be harder to recreate in the outpatient setting,” Dr. MacMartin said.
Barriers to ACP include patient identification, logistics, attitudes
Settings in which ACP is appropriate include those in which a patient is undergoing “sentinel hospitalization,” meaning that the patient is at a transition point in the disease course. Examples are a patient newly diagnosed with metastatic solid cancer, a patient with progressive chronic kidney disease who is considering hemodialysis, or a patient who receives treatment in the ICU for longer than 7 days, Dr. MacMartin said.
Guidelines for identifying patients who might benefit from ACP include the use of the “surprise question” (“would you be surprised if this patient dies in the next year?”) as well as functional status assessments using tools such as the Australia-modified Karnofsky Performance Status or the Eastern Cooperative Oncology Group score, said Dr. MacMartin. Some studies suggest that any hospitalized patient older than 65 years should have an ACP discussion, she added.
Time pressure remains a significant barrier to ACP conversations. Some strategies to overcome this problem include enlisting help from other specialists, particularly social workers, Dr. MacMartin said. Social workers report a higher comfort level for talking to patients about death than any other medical specialty; “this is something they want to be doing,” she said. Also, the possibility of reimbursement may act as a buffer to create more time to have ACP conversations with patients, she noted.
Addressing clinicians’ discomfort with ACP conversations can be “a tougher nut to crack,” Dr. MacMartin acknowledged. Clinicians report that they don’t want to cause their patients distress, and some report that having conversations about end-of-life care is distressing for them as well. Some of these barriers can be overcome with skills training, including use of a prepared guideline or framework to help increase the comfort level for both clinicians and patients, said Dr. MacMartin.
A look ahead: Training strategies and COVID-19 impact
“For hospitalists interested in developing their ACP skills, I highly recommend two resources,” Dr. MacMartin said in an interview. “The Serious Illness Conversation Guide, from Ariadne Labs, is an excellent tool for any clinician to guide discussion about a patient’s goals and values,” she said.
“For clinicians wanting to build or improve their communication, including advance care planning discussions but also topics like responding to patient’s emotions, VitalTalk training offers a deeper dive into core communications skills,” she added.
“If your hospital has a palliative care team, they may also have more local resources available to you. To learn more about billing for ACP discussions, I recommend starting with your institutional billing and coding group, as these practices vary some between practices, and they will be able to provide the best guidance for clinicians. These are new codes that aren’t yet being very widely used so it’s a chance to innovate,” Dr. MacMartin noted.
“The hospital setting is an opportunity for patients to reflect on their health, both present and in the future, with a physician who has expertise in acute illness and prognostication and who is available for discussion on a daily basis during the hospitalization,” Dr. MacMartin emphasized.
As for whether the COVID-19 pandemic has affected ACP in the inpatient setting, the data are limited, but more information is forthcoming, Dr. MacMartin said. “In my personal experience and in talking to colleagues elsewhere, the pandemic has highlighted the need for ACP in some ways, as we have tried to ensure that people who wouldn’t want things like intensive care are identified early,” she said. “I hope that some of the workflows developed to identify patients who should get ACP in the hospital stay in practice and are strengthened over time,” she added.
Dr. MacMartin has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Advance care planning (ACP) is a process that supports adults at any age or stage of health in understanding and sharing their personal values, life goals, and preferences for future medical care, according to Meredith A. MacMartin, MD, director of inpatient palliative care at the Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
ACP “is really about planning for care in advance,” and in many ways, the inpatient setting is uniquely suited to this process, Dr. MacMartin said in a presentation at SHM Converge 2021, the annual conference of the Society of Hospital Medicine. “The key part is the advance part. You want conversations to happen before the care is actually needed,” she said.
Dr. MacMartin emphasized the importance of distinguishing between ACP and advance directives (ADs). ACP is a process, whereas ADs are documentation, “ideally of the content of advance care planning discussions,” she explained. ACP involves discussion about what is important to the patients, their goals, what information is helpful for them, and whether their current care is aligned with their goals, Dr. MacMartin said. ADs might involve a designated power of attorney for health care, a living will, and, in some states, specific clinician-signed orders regarding resuscitation or transport to hospital.
ACP is “more than whether a patient wants CPR [cardiopulmonary resuscitation] or not,” said Dr. MacMartin. ACP matters because it helps ensure that the care a patient receives aligns with the patient’s wishes and values, she said. ACP increases the likelihood that patients will die in their preferred locations, it allows them to discuss their wishes and prepare for decline, and it relieves family members of the burden of decision making, she said. From a hospital perspective, data show that use of an ACP can decrease intensive care unit (ICU) utilization and overall health care costs. “Often, when people are given the opportunity to express their wishes, they get less unnecessary care,” Dr. MacMartin noted.
Although ACP often takes place in an outpatient setting, hospitalists are in a unique position to conduct some ACP conversations with their patients, Dr. MacMartin said. “Hospitalists are available” and are physically present at least once a day, so there is a pragmatic advantage. Also, some data suggest that patients may feel more comfortable having ACP conversations with a hospitalist than with a primary care provider with whom they have a long-standing relationship, Dr. MacMartin added.
Another important advantage of ACP in the hospital setting is that, “as hospitalists, you are the expert on inpatient illness; you know what sick looks like, and you have a unique perspective on prognostication that may be harder to recreate in the outpatient setting,” Dr. MacMartin said.
Barriers to ACP include patient identification, logistics, attitudes
Settings in which ACP is appropriate include those in which a patient is undergoing “sentinel hospitalization,” meaning that the patient is at a transition point in the disease course. Examples are a patient newly diagnosed with metastatic solid cancer, a patient with progressive chronic kidney disease who is considering hemodialysis, or a patient who receives treatment in the ICU for longer than 7 days, Dr. MacMartin said.
Guidelines for identifying patients who might benefit from ACP include the use of the “surprise question” (“would you be surprised if this patient dies in the next year?”) as well as functional status assessments using tools such as the Australia-modified Karnofsky Performance Status or the Eastern Cooperative Oncology Group score, said Dr. MacMartin. Some studies suggest that any hospitalized patient older than 65 years should have an ACP discussion, she added.
Time pressure remains a significant barrier to ACP conversations. Some strategies to overcome this problem include enlisting help from other specialists, particularly social workers, Dr. MacMartin said. Social workers report a higher comfort level for talking to patients about death than any other medical specialty; “this is something they want to be doing,” she said. Also, the possibility of reimbursement may act as a buffer to create more time to have ACP conversations with patients, she noted.
Addressing clinicians’ discomfort with ACP conversations can be “a tougher nut to crack,” Dr. MacMartin acknowledged. Clinicians report that they don’t want to cause their patients distress, and some report that having conversations about end-of-life care is distressing for them as well. Some of these barriers can be overcome with skills training, including use of a prepared guideline or framework to help increase the comfort level for both clinicians and patients, said Dr. MacMartin.
A look ahead: Training strategies and COVID-19 impact
“For hospitalists interested in developing their ACP skills, I highly recommend two resources,” Dr. MacMartin said in an interview. “The Serious Illness Conversation Guide, from Ariadne Labs, is an excellent tool for any clinician to guide discussion about a patient’s goals and values,” she said.
“For clinicians wanting to build or improve their communication, including advance care planning discussions but also topics like responding to patient’s emotions, VitalTalk training offers a deeper dive into core communications skills,” she added.
“If your hospital has a palliative care team, they may also have more local resources available to you. To learn more about billing for ACP discussions, I recommend starting with your institutional billing and coding group, as these practices vary some between practices, and they will be able to provide the best guidance for clinicians. These are new codes that aren’t yet being very widely used so it’s a chance to innovate,” Dr. MacMartin noted.
“The hospital setting is an opportunity for patients to reflect on their health, both present and in the future, with a physician who has expertise in acute illness and prognostication and who is available for discussion on a daily basis during the hospitalization,” Dr. MacMartin emphasized.
As for whether the COVID-19 pandemic has affected ACP in the inpatient setting, the data are limited, but more information is forthcoming, Dr. MacMartin said. “In my personal experience and in talking to colleagues elsewhere, the pandemic has highlighted the need for ACP in some ways, as we have tried to ensure that people who wouldn’t want things like intensive care are identified early,” she said. “I hope that some of the workflows developed to identify patients who should get ACP in the hospital stay in practice and are strengthened over time,” she added.
Dr. MacMartin has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM SHM CONVERGE 2021
Hospital admissions of nursing home patients declined after ACA quality initiatives
Background: Following the ACA’s implementation, several measures were introduced to reduce unnecessary admissions of long-term nursing home residents to hospitals. These measures included an initiative to enhance a nursing home’s on-site capability to handle target populations; the accountable care organization payment model; and the Hospital Readmissions Reduction Program.
Study design: Cross-sectional study using the claims-based nationwide Minimum Data Set during 2011-2016.
Setting: Federally licensed nursing homes in the United States.
Synopsis: The authors examined the number of transfers between federally funded nursing homes and the hospital settings (EDs, observation, or inpatient hospitalizations) for greater than 460,000 long term–stay patients with advanced dementia, advanced heart failure, and/or advanced chronic obstructive pulmonary disease (COPD). A risk-adjusted model showed that, during 2011-2016, there were significant decreases in transfers rates for potentially avoidable conditions, measured as the mean number of transfers per person-year alive, for patients with advanced dementia (2.4 vs. 1.6), heart failure (8.5 vs. 6.7), and COPD (7.8 vs 5.5). Most of this decrease was linked to reductions in acute hospitalizations. Notably, hospice enrollment remained low throughout this time period, despite a high 1-year mortality.
Bottom line: During the 2011-2016 period, transfer rates for patients with advanced dementia, heart failure, and/or COPD from nursing homes to the hospital setting decreased.
Citation: McCarthy EP et al. Hospital transfer rates among U.S. nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2019 Dec 30. doi: 10.1001/jamainternmed.2019.6130.
Dr. Cool is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Background: Following the ACA’s implementation, several measures were introduced to reduce unnecessary admissions of long-term nursing home residents to hospitals. These measures included an initiative to enhance a nursing home’s on-site capability to handle target populations; the accountable care organization payment model; and the Hospital Readmissions Reduction Program.
Study design: Cross-sectional study using the claims-based nationwide Minimum Data Set during 2011-2016.
Setting: Federally licensed nursing homes in the United States.
Synopsis: The authors examined the number of transfers between federally funded nursing homes and the hospital settings (EDs, observation, or inpatient hospitalizations) for greater than 460,000 long term–stay patients with advanced dementia, advanced heart failure, and/or advanced chronic obstructive pulmonary disease (COPD). A risk-adjusted model showed that, during 2011-2016, there were significant decreases in transfers rates for potentially avoidable conditions, measured as the mean number of transfers per person-year alive, for patients with advanced dementia (2.4 vs. 1.6), heart failure (8.5 vs. 6.7), and COPD (7.8 vs 5.5). Most of this decrease was linked to reductions in acute hospitalizations. Notably, hospice enrollment remained low throughout this time period, despite a high 1-year mortality.
Bottom line: During the 2011-2016 period, transfer rates for patients with advanced dementia, heart failure, and/or COPD from nursing homes to the hospital setting decreased.
Citation: McCarthy EP et al. Hospital transfer rates among U.S. nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2019 Dec 30. doi: 10.1001/jamainternmed.2019.6130.
Dr. Cool is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.
Background: Following the ACA’s implementation, several measures were introduced to reduce unnecessary admissions of long-term nursing home residents to hospitals. These measures included an initiative to enhance a nursing home’s on-site capability to handle target populations; the accountable care organization payment model; and the Hospital Readmissions Reduction Program.
Study design: Cross-sectional study using the claims-based nationwide Minimum Data Set during 2011-2016.
Setting: Federally licensed nursing homes in the United States.
Synopsis: The authors examined the number of transfers between federally funded nursing homes and the hospital settings (EDs, observation, or inpatient hospitalizations) for greater than 460,000 long term–stay patients with advanced dementia, advanced heart failure, and/or advanced chronic obstructive pulmonary disease (COPD). A risk-adjusted model showed that, during 2011-2016, there were significant decreases in transfers rates for potentially avoidable conditions, measured as the mean number of transfers per person-year alive, for patients with advanced dementia (2.4 vs. 1.6), heart failure (8.5 vs. 6.7), and COPD (7.8 vs 5.5). Most of this decrease was linked to reductions in acute hospitalizations. Notably, hospice enrollment remained low throughout this time period, despite a high 1-year mortality.
Bottom line: During the 2011-2016 period, transfer rates for patients with advanced dementia, heart failure, and/or COPD from nursing homes to the hospital setting decreased.
Citation: McCarthy EP et al. Hospital transfer rates among U.S. nursing home residents with advanced illness before and after initiatives to reduce hospitalizations. JAMA Intern Med. 2019 Dec 30. doi: 10.1001/jamainternmed.2019.6130.
Dr. Cool is a hospitalist at Beth Israel Deaconess Medical Center, and instructor in medicine, Harvard Medical School, both in Boston.






























