User login
Making sense of LAMA discharges
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
Converge 2021 session
LAMA’s DRAMA: Left AMA – Documentation and Rules of AMA
Presenter
Venkatrao Medarametla, MD, SFHM
Session summary
Most hospitalists equate LAMA (left against medical advice) patients with noncompliance and stop at that. During the recent SHM Converge conference session on LAMA, Dr. Venkatrao Medarametla, medical director for hospital medicine at Baystate Medical Center, Springfield, Mass., delved into the etiology and pathophysiology of LAMA discharges.
According to Dr. Medarametla, LAMA accounts for 1.4% of all discharges amounting to more than 500,000 discharges per year nationwide. LAMA discharges are at high risk for readmissions (20%-40% higher), have longer length of stay on readmission, higher morbidity and mortality (10% higher), and result in higher costs of care (56% higher).
The reasons for LAMA discharges could be broadly divided into patient and provider factors. Patient factors include refusal to wait for administrative delays, extenuating domestic and social concerns, conflicts with care providers, disagreement with providers’ judgment of health status, mistrust of the health system, substance dependence with inadequate treatment for withdrawal, patient’s perception of respect, stereotyping or stigma, and even ambiance and diet at the hospital.
Provider factors include conflict with the patient, concerns of legal and ethical responsibilities, formally distancing from nonstandard plan, and deflecting blame for worse outcomes.
Faced with a LAMA discharge, the important role of a hospitalist is to assess capacity. Help may be sought from other specialists such as psychiatrists and geriatricians. Some of the best practices also include a clear discussion of risks of outpatient treatment, exploration of safe alternative care plans, patient-centered care, shared decision-making (e.g., needle exchange), and harm reduction.
Dr. Medarametla advised hospitalists not to rely on the AMA forms the patients are asked to sign for liability protection. The forms may not stand up to legal scrutiny. Excellent documentation regarding the details of discussions with the patient, and determination of capacity encompassing the patients’ understanding, reasoning, and insight should be made. Hospitalists can also assess the barriers and mitigate them. Appropriate outpatient and alternative treatment plans should be explored. Postdischarge care and follow ups also should be facilitated.
According to Dr. Medarametla, another myth about AMA discharge is that insurance will not pay for it. About 57% of a survey sample of attendings and residents believed the same, and 66% heard other providers telling patients that insurance would not cover the AMA discharges. In a multicentric study of 526 patients, payment was refused only in 4.1% of AMA cases, mostly for administrative reasons.
Another prevalent myth is that patients who leave AMA will lose their right to follow up. Prescriptions also could be given to LAMA patients provided hospitalists adhere to detailed and relevant documentation. Overall, the session was very interesting and informative.
Key takeaways
- There are patient and provider factors leading to LAMA.
- Patients signing an AMA form does not provide legal protection for providers, but a stream-lined discharge process and a detailed documentation are likely to.
- There is no evidence that insurance companies will not pay for LAMA discharges.
- LAMA patients could be given prescriptions and follow up as long as they are well documented.
References
Schaefer G et al. Financial responsibility of hospitalized patients who left against medical advice: Medical urban legend? J Gen Intern Med. 2012 Jul;27(7):825-30. doi: 10.1007/s11606-012-1984-x.
Wigder H et al. Insurance companies refusing payment for patients who leave the emergency department against medical advice is a myth. Ann Emerg Med. 2010 Apr;55(4):393. doi: 10.1016/j.annemergmed.2009.11.024.
Dr. Kumar is a hospitalist in Port Huron, Mich. He is a member of the editorial advisory board for the Hospitalist.
FROM SHM CONVERGE 2021
Hospital at Home: Delivering hospital-level care without the hospital
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
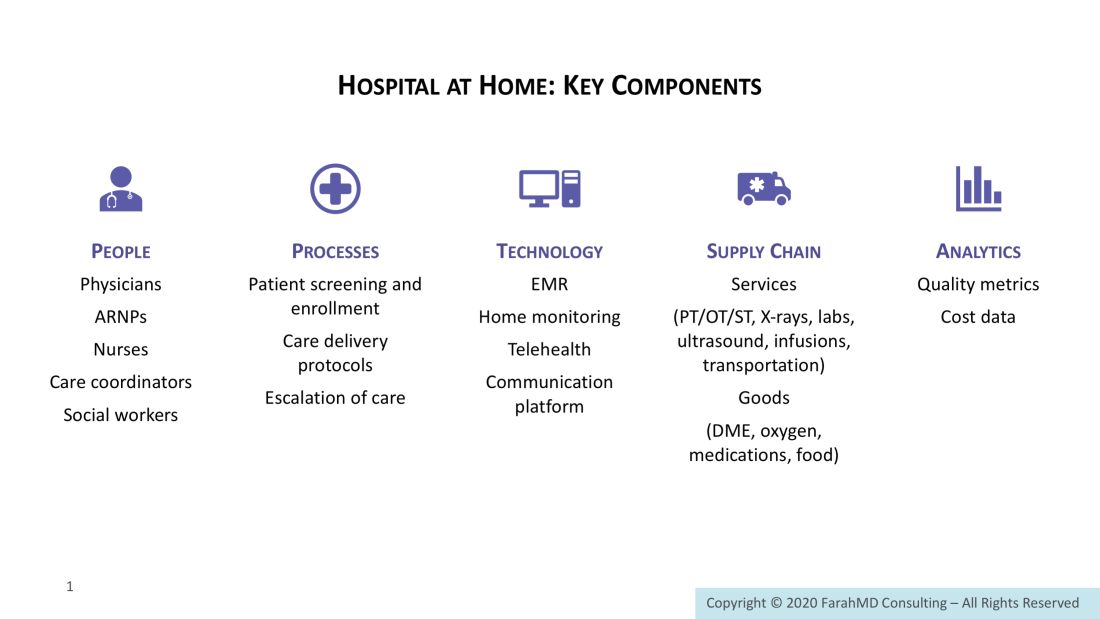
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
How to implement a new model of care
How to implement a new model of care
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
The United States spends one-third of the nation’s health dollars on hospital care, amounting to $1.2 trillion in 2018.1 U.S. hospital beds are prevalent2, and expensive to build and operate, with most hospital services costs related to buildings, equipment, salaried labor, and overhead.3
Despite their mission to heal, hospitals can be harmful, especially for frail and elderly patients. A study completed by the Office of the Inspector General (OIG) found that 13.5% of hospitalized Medicare patients experienced an adverse event that resulted in a prolonged hospital stay, permanent harm, a life-sustaining intervention or death.4 In addition, there is growing concern about acquired post-hospitalization syndrome caused by the physiological stress that patients experience in the hospital, leaving them vulnerable to clinical adverse events such as falls and infections.5
In the mid-1990s, driven by a goal to “avoid the harm of inpatient care and honor the wishes of older adults who refused to go to the hospital”, Dr. Bruce Leff, director of the Center for Transformative Geriatric Research and professor of medicine at Johns Hopkins University in Baltimore, and his team set out to develop and test Hospital at Home (HaH) – an innovative model for delivering hospital-level care to selected patients in the safety of their homes.
More than 20 years later, despite extensive evidence supporting HaH safety and efficacy, and its successful rollout in other countries, the model has not been widely adopted in the U.S. However, the COVID-19 pandemic amplified interest in HaH by creating an urgent need for flexible hospital bed capacity and heightening concerns about hospital care safety, especially for vulnerable adults.
In this article, we will introduce HaH history and efficacy, and then discuss what it takes to successfully implement HaH.
Hospital at Home: History, efficacy, and early adoption
The earliest HaH study, a 17-patient pilot conducted by Dr. Leff’s team from 1996 to 1998, proved that HaH was feasible, safe, highly satisfactory and cost-effective for selected acutely ill older patients with community-acquired pneumonia, chronic heart failure, chronic obstructive pulmonary disease or cellulitis.6 In 2000 to 2002, a National Demonstration and Evaluation Study of 455 patients across three sites determined that patients treated in Hospital at Home had statistically significant shorter length of stay (3.2 vs 4.9 days), lower cost ($5,081 vs. $7,480) and complications.7 Equipped with evidence, Dr. Leff and his team focused on HaH dissemination and implementation across several health care systems.8
Presbyterian Healthcare Services in Albuquerque, N.M., was one of the earliest adopters of HaH and launched the program in 2008. The integrated system serves one-third of New Mexicans and includes nine hospitals, more than 100 clinics and the state’s largest health plan. According to Nancy Guinn, MD, a medical director of Presbyterian Healthcare at Home, “Innovation is key to survive in a lean environment like New Mexico, which has the lowest percentage of residents with insurance from their employer and a high rate of government payers.”
Presbyterian selected nine diagnoses for HaH focus: congestive heart failure, chronic obstructive pulmonary disease, community-acquired pneumonia, cellulitis, deep venous thrombosis, pulmonary embolism, complicated urinary tract infection or urosepsis, nausea and vomiting, and dehydration. The HaH care, including physician services, is reimbursed via a partial DRG (diagnosis-related group) payment that was negotiated internally between the health system and Presbyterian Health Plan.
The results demonstrated that, compared to hospitalized patients with similar conditions, patients in HaH had a lower rate of falls (0% vs. .8%), lower mortality (.93% vs. 3.4%), higher satisfaction (mean score 90.7 vs. 83.9) and 19% lower cost.9 According to Dr. Guinn, more recent results showed even larger cost savings of 42%.10 After starting the HaH model, Presbyterian has launched other programs that work closely with HaH to provide a seamless experience for patients. That includes the Complete Care Program, which offers home-based primary, urgent, and acute care to members covered through Presbyterian Health Plan and has a daily census of 600-700 patients.
Another important milestone came in 2014 when Icahn School of Medicine at Mount Sinai in New York was awarded $9.6 million by the Center for Medicare and Medicaid Innovation (CMMI) to test the HaH model during acute illness and for 30 days after admission. A case study of 507 patients enrolled in the program in 2014 through 2017 revealed that HaH patients had statistically significant shorter length of stay (3.2 days vs. 5.5 days), and lower rates of all-cause 30-day hospital readmissions (8.6% vs. 15.6%), 30-day ED revisits (5.8% vs. 11.7%), and SNF admissions (1.7% vs. 10.4%), and were also more likely to rate their hospital care highly (68.8% vs. 45.3%).11
In 2017, using data from their CMMI study, Mount Sinai submitted an application to the Physician-Focused Payment Model Technical Advisory Committee (PTAC) to implement Hospital at Home as an alternative payment model that bundles the acute episode with 30 days of post‐acute transitional care. The PTAC unanimously approved the proposal and submitted their recommendations to the Secretary of Health and Human Services (HHS) to implement HaH as an alternative payment model that included two parts:
1. A bundled payment equal to a percentage of the prospective DRG (diagnosis-related group) payment that would have been paid to a hospital.
2. A performance-based payment (shared savings/losses) based on (a) total spending during the acute care phase and 30 days afterward relative to a target price, and (b) performance on quality measures.12
In June 2018, the HHS secretary announced that he was not approving the proposal as written, citing, among other things, concerns about proposed payment methodology and patient safety.13
Hospital at Home: Present state
Despite additional evidence of HaH’s impact on lowering cost, decreasing 30-day readmissions, improving patient satisfaction and functional outcomes without an adverse effect on mortality,14, 15 the model has not been widely adopted, largely due to lack of fee-for-service reimbursement from the public payers (Medicare and Medicaid) and complex logistics to implement it.
However, the COVID-19 pandemic created an urgent need for flexible hospital bed capacity and amplified concerns about hospital care safety for vulnerable populations. In response, the Centers for Medicare and Medicaid Services (CMS) introduced its Hospitals without Walls initiative that allowed hospitals to provide services in other health care facilities and sites that are not part of the existing hospital.16 On November 25, 2020, CMS announced expansion of the Hospital without Walls initiatives to include a Hospital Care at Home program that allows eligible hospitals to treat eligible patients at home.17
With significant evidence supporting HaH’s safety and efficacy, and long overdue support from CMS, it’s now a matter of how to successfully implement it. Let’s explore what it takes to select and enroll patients, deliver acute care at home, and ensure a smooth post-acute transition within the HaH model.
Successfully implementing Hospital at Home
HaH implementation requires five key components – people, processes, technology, supply chain, and analytics – to select and enroll patients, deliver acute care at home, and ensure a smooth postacute transition. Let’s discuss each of them in more detail below.
Selecting and enrolling patients
Patients eligible for HaH are identified based on their insurance, as well as clinical and social criteria. Despite a lack of public payer support, several commercial payers embraced the model for selected patients who consented to receive acute hospital care at home. The patients must meet criteria for an inpatient admission, be medically stable and have a low level of diagnostic uncertainty. Advances in home monitoring technology expanded clinical criteria to include acutely ill patients with multiple comorbidities, including cancer. It is important that patients reside in a safe home environment and live within a reasonable distance from the hospital.
CareMore Health, an integrated health care delivery system serving more than 180,000 Medicare Advantage and Medicaid patients across nine states and Washington D.C., launched Hospital at Home in December 2018, and rapidly scaled from a few referrals to averaging more than 20 new patients per week.
Sashidaran Moodley, MD, medical director at CareMore Health and Aspire Health, in Cerritos, Calif., shared a valuable lesson regarding launching the program: “Do not presume that if you build it, they will come. This is a new model of care that requires physicians to change their behavior and health systems to modify their traditional admission work flows. Program designers should not limit their thinking around sourcing patients just from the emergency department.”
Dr. Moodley recommends moving upstream and bring awareness to the program to drive additional referrals from primary care providers, case managers, and remote patient monitoring programs (for example, heart failure).
Linda DeCherrie, MD, clinical director of Mount Sinai at Home, based in New York, says that “educating and involving hospitalists is key.” At Mount Sinai, patients eligible for HaH are initially evaluated by hospitalists in the ED who write initial orders and then transfer care to HaH hospitalists.
HaH also can enroll eligible patients who still require hospital-level care to complete the last few days of acute hospitalization at home. Early discharge programs have been implemented at CareMore, Presbyterian Healthcare Services in Albuquerque, N.M., and Mount Sinai. At Mount Sinai, a program called Completing Hospitalization at Home initially started with non-COVID patients and expanded to include COVID-19 early discharges, helping to free up much-needed hospital beds.
Delivering acute care at home
HaH requires a well-coordinated multidisciplinary team. Patient care is directed by a team of physicians and nurse practitioners who provide daily in-person or virtual visits. To enable provider work flow, an ambulatory version of electronic medical records (for example, Epic) must be customized to include specialized order sets that mimic inpatient orders and diagnoses-specific care delivery protocols. HaH physicians and nurse practitioners are available 24/7 to address acute patient issues.
In addition, patients receive at least daily visits from registered nurses (RNs) who carry out orders, administer medications, draw labs, and provide clinical assessment and patient education. Some organizations employ HaH nurses, while others contract with home health agencies.
Typically, patients are provided with a tablet to enable telehealth visits, as well as a blood pressure monitor, thermometer, pulse oximeter, and, if needed, scale and glucometer, that allow on-demand or continuous remote monitoring. Recent technology advances in home monitoring enhanced HaH’s capability to care for complex, high-acuity patients, and increased the potential volume of patients that can be safely treated at home.
Providence St. Joseph Health, a not-for-profit health care system operating 51 hospitals and 1,085 clinics across seven states, launched their HaH program earlier this year. Per Danielsson, MD, executive medical director for hospital medicine at Swedish Medical Center in Seattle, describes it as a “high-touch, high-tech program anchored by hospitalists.” The Providence HaH team utilizes a wearable medical device for patients that enables at-home continuous monitoring of vital signs such as temperature, blood pressure, heart rate, respirations, and pulse oximetry. Single-lead EKG monitoring is available for selected patients. Individual patient data is transmitted to a central command center, where a team of nurses and physicians remotely monitor HaH patients. According to Todd Czartoski, MD, chief medical technology officer at Providence, “Hospital at Home improves quality and access, and can substitute for 20%-30% of hospital admissions.”
In addition to patient monitoring and 24/7 provider access, some HaH programs partner with community paramedics for emergency responses. At Mount Sinai, HaH providers can trigger paramedic response, if needed. Paramedics can set up a video link with a doctor and, under the direction of a physician, will provide treatment at home or transport patients to the hospital.
HaH would be impossible without a partnership with local ancillary service providers that can promptly deliver services and goods to patient homes. Raphael Rakowski, CEO of Medically Home, a Boston-based company that partners with health care providers to build virtual hospitals at home, calls it an “acute rapid response supply chain.” The services, both clinical and nonclinical, consist of infusions; x-rays; bedside ultrasound; laboratory; transportation; and skilled physical, occupational, and speech therapy. If patients require services that are not available at home (for example, a CT scan), patients can be transported to and from a diagnostic center. Medical and nonmedical goods include medications, oxygen, durable medical equipment, and even meals.
Delivery of hospital-level services at home requires a seamless coordination between clinical teams and suppliers that relies on nursing care coordinators and supporting nonclinical staff, and is enabled by a secure text messaging platform to communicate within the care team, with suppliers, and with other providers (for example, primary care providers and specialists).
Ensuring smooth postacute transition
Thirty days after hospital discharge is the most critical period, especially for elderly patients. According to one study, 19% of patients experienced adverse events within 3 weeks after hospital discharge.18 Adverse drug events were the most common postdischarge complication, followed by procedural complications and hospital-acquired infections. Furthermore, 30-day all-cause hospital readmissions is a common occurrence. Per the Healthcare Cost and Utilization Project database, 17.1% of Medicare and 13.9% of all-payers patients were readmitted to the hospital within 30 days in 2016.19
It is not surprising that some organizations offer ongoing home care during the postacute period. At Mount Sinai, patients discharged from HaH continue to have access to the HaH team around the clock for 30 days to address emergencies and health concerns. Recovery Care Coordinators and social workers monitor patient health status, develop a follow-up plan, coordinate care, and answer questions. Medically Home provides 24/7 care to HaH patients for the entire duration of the acute care episode (34 days) to ensure maximum access to care and no gaps in care and communication. At Presbyterian, most HaH patients are transitioned into a Home Health episode of care to ensure continued high-quality care.
In addition to people, processes, technology, and the supply chain, HaH implementation requires capabilities to collect and analyze quality and cost data to measure program efficacy and, in some arrangements with payers, to reconcile clams data to determine shared savings or losses.
Partnering with third parties
Considering the resources and capabilities required for HaH program development and implementation, it is not surprising that health care providers are choosing to partner with third parties. For example, Mount Sinai partnered with Contessa Health, a Nashville, Tenn.–based company that offers hospitals a turn-key Home Recovery Care program, to assist with supply chain contracting and management, and claims data reconciliation.
Medically Home has partnered with seven health care systems, including the Mayo Clinic, Tufts Medical Center in Boston, and Adventist Health in southern California, to create virtual beds, and is expected to launch the program with 15 health care systems by the end of 2020.
Medically Home offers the following services to its partners to enable care for high-acuity patients at home:
- Assistance with hiring and training of clinical staff.
- Proprietary EMR-integrated orders, notes, and clinical protocols.
- Technology for patient monitoring by the 24/7 central command center; tablets that provide health status updates and daily schedules, and enable televisits; a video platform for video communication; and secure texting.
- Selection, contracting and monitoring the performance of supply chain vendors.
- Analytics.
The future of Hospital at Home
There is no question that HaH can offer a safe, high-quality, and lower-cost alternative to hospitalizations for select patients, which is aligned with the Centers for Medicare and Medicaid Services’ triple aim of better care for individuals, better health for populations, and lower cost.20
The future of HaH depends on development of a common payment model that will be adopted beyond the pandemic by government and commercial payers. Current payment models vary and include capitated agreements, discounted diagnosis-related group payments for the acute episode, and discounted DRG payments plus shared losses or savings.
The COVID-19 pandemic has created, arguably, the biggest crisis that U.S. health care has ever experienced, and it is far from over. Short term, Hospital at Home offers a solution to create flexible hospital bed capacity and deliver safe hospital-level care for vulnerable populations. Long term, it may be the solution that helps achieve better care for individuals, better health for populations and lower health care costs.
Dr. Farah is a hospitalist, physician advisor, and Lean Six Sigma Black Belt. She is a performance improvement consultant based in Corvallis, Ore., and a member of the Hospitalist’s editorial advisory board.
References
1. Source: www.cms.gov/files/document/nations-health-dollar-where-it-came-where-it-went.pdf
2. Source: www.aha.org/statistics/fast-facts-us-hospitals
3. Roberts RR, et al. Distribution of variable vs fixed costs of hospital care. JAMA. 1999 Feb;281(7):644-9.
4. Levinson DR; US Department of Health and Human Services; HHS; Office of the Inspector General; OIG.
5. Krumholz HM. Post-Hospital Syndrome – An Acquired, Transient Condition of Generalized Risk. N Engl J Med. 2013 Jan;368:100-102.
6. Leff B, et al. Home hospital program: a pilot study. J Am Geriatr Soc. 1999 Jun;47(6):697-702.
7. Leff B, et al. Hospital at home: Feasibility and outcomes of a program to provide hospital-level care at home for acutely ill older patients. Ann Intern Med. 2005 Dec;143(11):798-808.
8. Source: www.johnshopkinssolutions.com/solution/hospital-at-home/
9. Cryer L, et al. Costs for ‘Hospital at Home’ Patients Were 19 Percent Lower, with Equal or Better Outcomes Compared to Similar Inpatients. Health Affairs. 2012 Jun;31(6):1237–43.
10. Personal communication with Presbyterian Health Services. May 20, 2020.
11. Federman A, et al. Association of a bundled hospital-at-home and 30-day postacute transitional care program with clinical outcomes and patient experiences. JAMA Intern Med. 2018 Aug;178(8):1033–40.
12. Source: aspe.hhs.gov/system/files/pdf/255906/MtSinaiHAHReportSecretary.pdf
13. Source: aspe.hhs.gov/system/files/pdf/255906/Secretarial_Responses_June_13_2018.508.pdf
14. Shepperd S, et al. Admission avoidance hospital at home. Cochrane Database Syst Rev. 2016;9(9):CD007491. DOI:10.1002/14651858.CD007491.pub2.
15. Levine DM, et al. Hospital-level care at home for acutely ill adults: a randomized controlled trial. Ann Intern Med. 2020 Jan;172(2);77-85.
16. Source: www.cms.gov/files/document/covid-hospitals.pdf
17. Centers for Medicare & Medicaid Services. CMS Announces Comprehensive Strategy to Enhance Hospital Capacity Amid COVID-19 Surge. 2020 Nov 20.
18. Forster AJ et al. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003 Mar;138(3):161-7. doi: 10.7326/0003-4819-138-3-200302040-00007.
19. Bailey MK et al. Characteristics of 30-Day All-Cause Hospital Readmissions, 2010-2016. Statistical Brief 248. Agency for Healthcare Research and Quality. 2019 Feb 12. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb248-Hospital-Readmissions-2010-2016.jsp.
20. Centers for Medicare & Medicaid Services. What are the value-based programs? 2020 Jan 6. https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/Value-Based-Programs.
Survey offers a snapshot of nationwide COVID-19 discharge practices
Discharge practices for COVID-19 patients vary widely at the nation’s academic medical centers, but there are some areas of strong concordance, especially related to procedures for isolation and mitigating transmission of COVID-19.
In addition, most sites use some form of clinical criteria to determine discharge readiness, S. Ryan Greysen, MD, MHS, SFHM, said on May 5 at SHM Converge, the annual conference of the Society of Hospital Medicine.
Those rank among the key findings from of a survey of 22 academic medical centers conducted by the Hospital Medicine Re-engineering Network (HOMERuN), which was launched in 2011 as a way to advance hospital medicine through rigorous research to improve the care of hospitalized patients.
“When COVID came and changed all of our lives, HOMERuN was well positioned to examine the state of practices in member hospitals, and we set out some key principles,” Dr. Greysen said. “First, we wanted to respect the challenges and needs of sites during this extraordinary time. We wanted to support speed and flexibility from our study design to get results to the front lines as quickly as possible. Therefore, we used lightweight research methods such as cross-sectional surveys, periodic evaluations, and we use the data to support operational needs. We have developed linkages to more granular datasets such as electronic health records, but our focus to date has been mostly on the frontline experience of hospitalists and gathering consensus around clinical practice, especially in the early stages of the pandemic.”
In March and April of 2020, Dr. Greysen and colleagues collected and analyzed any discharge protocols, policies, or other documents from 22 academic medical centers. From this they created a follow-up survey containing 21 different domains that was administered to the same institutions in May and June of 2020. “It’s not meant to be a completely comprehensive list, but these 21 domains were the themes we saw coming out of these discharge practice documents,” explained Dr. Greysen, chief of hospital medicine at the University of Pennsylvania, Philadelphia, which is one of the participating sites.
Next, the researchers used a concordance table to help them keep track of which institution responded in which way for which domain, and they bundled the discharge criteria into five higher order domains: procedures for isolation and mitigating transmission; clinical criteria for discharge; nonclinical/nonisolation issues; discharge to settings other than home, and postdischarge instructions, monitoring, and follow-up.
In the procedures for isolation and mitigating transmission domain, Dr. Greysen reported that the use of isolation guidelines was the area of greatest consensus in the study, with 19 of 22 sites (86%) citing the Centers for Disease Control and Prevention and 7 (32%) also citing state department of health guidance. “Specifically, most sites included the ability to socially isolate at home (until no longer necessary per CDC guidance) as part of the criteria,” he said. Most sites (73%) required use of personal protective equipment (PPE) in transportation from the hospital and 73% gave masks and other PPE for use at home.
Session copresenter Maralyssa A. Bann, MD, a hospitalist at the University of Washington/Harborview Medical Center, Seattle, another participating site, pointed out that the institutions surveyed look to the CDC as being “the single source of truth on discharge practices,” specifically material for health care workers related to discharging COVID-19 patients. “Notable specific recent updates include the recommendation that meeting criteria for discontinuation of Transmission-Based Precautions is not a prerequisite for discharge from a health care facility,” Dr. Bann said. “Also, as of August 2020, use of symptom-based strategy for discontinuation of isolation precautions instead of repeat testing is recommended for most patients. This is a rapidly evolving area.”
Practices in the clinical criteria for discharge domain varied by site. Slightly more than one-quarter of sites (27%) gave little or no guidance by using terms like “use clinical judgment,” while 14% gave very specific detailed algorithms. “Most sites fell in between and gave some parameters, usually along the lines of symptom improvement, temperature, and oxygen requirement, but the criteria were variable,” Dr. Greysen said. “For example, in terms of temperature, many sites said that patients should be afebrile for a specific length of time, 24-72 hours, while other sites simply said afebrile at discharge.” Meanwhile, the following criteria for discharge were addressed by relatively few sites: lab criteria (36%), age (36%), high-risk comorbidities (32%), or ID consultation (18%).
In the nonclinical/nonisolation domain, 73% of sites assessed for level of support available, though this was variably defined. Slightly more than half (55%) specifically assessed activities of daily living or the presence of a caregiver to assist, while 18% reported addressing durable medical equipment such as beds and toilets and access to food or medication supplies in ways that were specific for COVID-19 patients.
In the discharge to settings other than home domain, 77% of sites addressed discharge to skilled nursing facilities, inpatient rehabilitation, or long-term care, although specific requirements were often set by the accepting facilities. In addition, 65% of sites gave specific guidance for patients experiencing unstable housing/homelessness, usually recommending a respite facility or similar, and 59% addressed congregate/shared living spaces such as assisted living facilities. “Often the strictest criteria [two negative COVID tests] were applied to discharge to these types of settings,” he said.
In the postdischarge instructions, monitoring, and follow-up domain, 73% of sites reported providing home monitoring and/or virtual follow-up care. Programs ranged from daily texting via SMS or patient portals, RN phone calls, home pulse oximeters, and/or thermometers. In addition, 55% of sites had created COVID-specific brochures, discharge instructions, and other materials to standardize content such as use of PPE, travel restrictions, social distancing, signs and symptoms to watch out for, and what to do if worsening clinically.
Dr. Bann predicted future trends on the heels of the HOMERuN survey, including the development of more evidence and consensus related to discharge criteria. “Clarity is needed specifically around hypoxemia at rest/on ambulation, as well as more flexible criteria for oxygen supplementation,” she said. “We also think there will be a considerable amount of growth in posthospitalization monitoring and support, in particular home-based and virtual/remote monitoring.”
HOMERuN is supported by the Gordon and Betty Moore Foundation, the AAMC, the Patient-Centered Outcomes Research Institute, the Clinical Data Research Networks, the Patient-Powered Research Networks, and Agency for Healthcare Research and Quality. Dr. Greysen and Dr. Bann reported having no financial disclosures.
Discharge practices for COVID-19 patients vary widely at the nation’s academic medical centers, but there are some areas of strong concordance, especially related to procedures for isolation and mitigating transmission of COVID-19.
In addition, most sites use some form of clinical criteria to determine discharge readiness, S. Ryan Greysen, MD, MHS, SFHM, said on May 5 at SHM Converge, the annual conference of the Society of Hospital Medicine.
Those rank among the key findings from of a survey of 22 academic medical centers conducted by the Hospital Medicine Re-engineering Network (HOMERuN), which was launched in 2011 as a way to advance hospital medicine through rigorous research to improve the care of hospitalized patients.
“When COVID came and changed all of our lives, HOMERuN was well positioned to examine the state of practices in member hospitals, and we set out some key principles,” Dr. Greysen said. “First, we wanted to respect the challenges and needs of sites during this extraordinary time. We wanted to support speed and flexibility from our study design to get results to the front lines as quickly as possible. Therefore, we used lightweight research methods such as cross-sectional surveys, periodic evaluations, and we use the data to support operational needs. We have developed linkages to more granular datasets such as electronic health records, but our focus to date has been mostly on the frontline experience of hospitalists and gathering consensus around clinical practice, especially in the early stages of the pandemic.”
In March and April of 2020, Dr. Greysen and colleagues collected and analyzed any discharge protocols, policies, or other documents from 22 academic medical centers. From this they created a follow-up survey containing 21 different domains that was administered to the same institutions in May and June of 2020. “It’s not meant to be a completely comprehensive list, but these 21 domains were the themes we saw coming out of these discharge practice documents,” explained Dr. Greysen, chief of hospital medicine at the University of Pennsylvania, Philadelphia, which is one of the participating sites.
Next, the researchers used a concordance table to help them keep track of which institution responded in which way for which domain, and they bundled the discharge criteria into five higher order domains: procedures for isolation and mitigating transmission; clinical criteria for discharge; nonclinical/nonisolation issues; discharge to settings other than home, and postdischarge instructions, monitoring, and follow-up.
In the procedures for isolation and mitigating transmission domain, Dr. Greysen reported that the use of isolation guidelines was the area of greatest consensus in the study, with 19 of 22 sites (86%) citing the Centers for Disease Control and Prevention and 7 (32%) also citing state department of health guidance. “Specifically, most sites included the ability to socially isolate at home (until no longer necessary per CDC guidance) as part of the criteria,” he said. Most sites (73%) required use of personal protective equipment (PPE) in transportation from the hospital and 73% gave masks and other PPE for use at home.
Session copresenter Maralyssa A. Bann, MD, a hospitalist at the University of Washington/Harborview Medical Center, Seattle, another participating site, pointed out that the institutions surveyed look to the CDC as being “the single source of truth on discharge practices,” specifically material for health care workers related to discharging COVID-19 patients. “Notable specific recent updates include the recommendation that meeting criteria for discontinuation of Transmission-Based Precautions is not a prerequisite for discharge from a health care facility,” Dr. Bann said. “Also, as of August 2020, use of symptom-based strategy for discontinuation of isolation precautions instead of repeat testing is recommended for most patients. This is a rapidly evolving area.”
Practices in the clinical criteria for discharge domain varied by site. Slightly more than one-quarter of sites (27%) gave little or no guidance by using terms like “use clinical judgment,” while 14% gave very specific detailed algorithms. “Most sites fell in between and gave some parameters, usually along the lines of symptom improvement, temperature, and oxygen requirement, but the criteria were variable,” Dr. Greysen said. “For example, in terms of temperature, many sites said that patients should be afebrile for a specific length of time, 24-72 hours, while other sites simply said afebrile at discharge.” Meanwhile, the following criteria for discharge were addressed by relatively few sites: lab criteria (36%), age (36%), high-risk comorbidities (32%), or ID consultation (18%).
In the nonclinical/nonisolation domain, 73% of sites assessed for level of support available, though this was variably defined. Slightly more than half (55%) specifically assessed activities of daily living or the presence of a caregiver to assist, while 18% reported addressing durable medical equipment such as beds and toilets and access to food or medication supplies in ways that were specific for COVID-19 patients.
In the discharge to settings other than home domain, 77% of sites addressed discharge to skilled nursing facilities, inpatient rehabilitation, or long-term care, although specific requirements were often set by the accepting facilities. In addition, 65% of sites gave specific guidance for patients experiencing unstable housing/homelessness, usually recommending a respite facility or similar, and 59% addressed congregate/shared living spaces such as assisted living facilities. “Often the strictest criteria [two negative COVID tests] were applied to discharge to these types of settings,” he said.
In the postdischarge instructions, monitoring, and follow-up domain, 73% of sites reported providing home monitoring and/or virtual follow-up care. Programs ranged from daily texting via SMS or patient portals, RN phone calls, home pulse oximeters, and/or thermometers. In addition, 55% of sites had created COVID-specific brochures, discharge instructions, and other materials to standardize content such as use of PPE, travel restrictions, social distancing, signs and symptoms to watch out for, and what to do if worsening clinically.
Dr. Bann predicted future trends on the heels of the HOMERuN survey, including the development of more evidence and consensus related to discharge criteria. “Clarity is needed specifically around hypoxemia at rest/on ambulation, as well as more flexible criteria for oxygen supplementation,” she said. “We also think there will be a considerable amount of growth in posthospitalization monitoring and support, in particular home-based and virtual/remote monitoring.”
HOMERuN is supported by the Gordon and Betty Moore Foundation, the AAMC, the Patient-Centered Outcomes Research Institute, the Clinical Data Research Networks, the Patient-Powered Research Networks, and Agency for Healthcare Research and Quality. Dr. Greysen and Dr. Bann reported having no financial disclosures.
Discharge practices for COVID-19 patients vary widely at the nation’s academic medical centers, but there are some areas of strong concordance, especially related to procedures for isolation and mitigating transmission of COVID-19.
In addition, most sites use some form of clinical criteria to determine discharge readiness, S. Ryan Greysen, MD, MHS, SFHM, said on May 5 at SHM Converge, the annual conference of the Society of Hospital Medicine.
Those rank among the key findings from of a survey of 22 academic medical centers conducted by the Hospital Medicine Re-engineering Network (HOMERuN), which was launched in 2011 as a way to advance hospital medicine through rigorous research to improve the care of hospitalized patients.
“When COVID came and changed all of our lives, HOMERuN was well positioned to examine the state of practices in member hospitals, and we set out some key principles,” Dr. Greysen said. “First, we wanted to respect the challenges and needs of sites during this extraordinary time. We wanted to support speed and flexibility from our study design to get results to the front lines as quickly as possible. Therefore, we used lightweight research methods such as cross-sectional surveys, periodic evaluations, and we use the data to support operational needs. We have developed linkages to more granular datasets such as electronic health records, but our focus to date has been mostly on the frontline experience of hospitalists and gathering consensus around clinical practice, especially in the early stages of the pandemic.”
In March and April of 2020, Dr. Greysen and colleagues collected and analyzed any discharge protocols, policies, or other documents from 22 academic medical centers. From this they created a follow-up survey containing 21 different domains that was administered to the same institutions in May and June of 2020. “It’s not meant to be a completely comprehensive list, but these 21 domains were the themes we saw coming out of these discharge practice documents,” explained Dr. Greysen, chief of hospital medicine at the University of Pennsylvania, Philadelphia, which is one of the participating sites.
Next, the researchers used a concordance table to help them keep track of which institution responded in which way for which domain, and they bundled the discharge criteria into five higher order domains: procedures for isolation and mitigating transmission; clinical criteria for discharge; nonclinical/nonisolation issues; discharge to settings other than home, and postdischarge instructions, monitoring, and follow-up.
In the procedures for isolation and mitigating transmission domain, Dr. Greysen reported that the use of isolation guidelines was the area of greatest consensus in the study, with 19 of 22 sites (86%) citing the Centers for Disease Control and Prevention and 7 (32%) also citing state department of health guidance. “Specifically, most sites included the ability to socially isolate at home (until no longer necessary per CDC guidance) as part of the criteria,” he said. Most sites (73%) required use of personal protective equipment (PPE) in transportation from the hospital and 73% gave masks and other PPE for use at home.
Session copresenter Maralyssa A. Bann, MD, a hospitalist at the University of Washington/Harborview Medical Center, Seattle, another participating site, pointed out that the institutions surveyed look to the CDC as being “the single source of truth on discharge practices,” specifically material for health care workers related to discharging COVID-19 patients. “Notable specific recent updates include the recommendation that meeting criteria for discontinuation of Transmission-Based Precautions is not a prerequisite for discharge from a health care facility,” Dr. Bann said. “Also, as of August 2020, use of symptom-based strategy for discontinuation of isolation precautions instead of repeat testing is recommended for most patients. This is a rapidly evolving area.”
Practices in the clinical criteria for discharge domain varied by site. Slightly more than one-quarter of sites (27%) gave little or no guidance by using terms like “use clinical judgment,” while 14% gave very specific detailed algorithms. “Most sites fell in between and gave some parameters, usually along the lines of symptom improvement, temperature, and oxygen requirement, but the criteria were variable,” Dr. Greysen said. “For example, in terms of temperature, many sites said that patients should be afebrile for a specific length of time, 24-72 hours, while other sites simply said afebrile at discharge.” Meanwhile, the following criteria for discharge were addressed by relatively few sites: lab criteria (36%), age (36%), high-risk comorbidities (32%), or ID consultation (18%).
In the nonclinical/nonisolation domain, 73% of sites assessed for level of support available, though this was variably defined. Slightly more than half (55%) specifically assessed activities of daily living or the presence of a caregiver to assist, while 18% reported addressing durable medical equipment such as beds and toilets and access to food or medication supplies in ways that were specific for COVID-19 patients.
In the discharge to settings other than home domain, 77% of sites addressed discharge to skilled nursing facilities, inpatient rehabilitation, or long-term care, although specific requirements were often set by the accepting facilities. In addition, 65% of sites gave specific guidance for patients experiencing unstable housing/homelessness, usually recommending a respite facility or similar, and 59% addressed congregate/shared living spaces such as assisted living facilities. “Often the strictest criteria [two negative COVID tests] were applied to discharge to these types of settings,” he said.
In the postdischarge instructions, monitoring, and follow-up domain, 73% of sites reported providing home monitoring and/or virtual follow-up care. Programs ranged from daily texting via SMS or patient portals, RN phone calls, home pulse oximeters, and/or thermometers. In addition, 55% of sites had created COVID-specific brochures, discharge instructions, and other materials to standardize content such as use of PPE, travel restrictions, social distancing, signs and symptoms to watch out for, and what to do if worsening clinically.
Dr. Bann predicted future trends on the heels of the HOMERuN survey, including the development of more evidence and consensus related to discharge criteria. “Clarity is needed specifically around hypoxemia at rest/on ambulation, as well as more flexible criteria for oxygen supplementation,” she said. “We also think there will be a considerable amount of growth in posthospitalization monitoring and support, in particular home-based and virtual/remote monitoring.”
HOMERuN is supported by the Gordon and Betty Moore Foundation, the AAMC, the Patient-Centered Outcomes Research Institute, the Clinical Data Research Networks, the Patient-Powered Research Networks, and Agency for Healthcare Research and Quality. Dr. Greysen and Dr. Bann reported having no financial disclosures.
FROM SHM CONVERGE 2021
In-hospital mobility impairment in older MI patients predicts postdischarge functional decline
Background: The ability to independently perform daily activities is highly valued by patients, yet it is commonly impaired in older adults after hospitalization for MI. Risk of functional decline in this population is not well understood, but may relate to reduced mobility while hospitalized.
Study design: Prospective cohort.
Setting: A total of 94 academic and community hospitals in the United States.
Synopsis: More than 3,000 adults aged 75 years and older who were hospitalized for acute myocardial infarction were enrolled in the prospective cohort SILVER-AMI; 2,587 patients within this cohort were evaluated for in-hospital mobility with the Timed “Up and Go” test. At 6-month follow-up, loss of independent performance of activities of daily living (ADL) and of the ability to walk 0.25 miles were both associated in a dose-dependent manner with in-hospital mobility. Severe in-hospital mobility impairment was associated with ADL decline with an adjusted odds ratio of 5.45 (95% confidence interval, 3.29-9.01).
While in-hospital mobility is predictive of future functional decline in this population, this observational study cannot establish whether attempts to improve mobility in hospitalized patients will prevent future functional decline.
Bottom line: Lower performance on the Timed “Up and Go” test of mobility among older patients hospitalized for MI is associated with functional decline 6 months after hospitalization.
Citation: Hajduk AM et al. Association between mobility measured during hospitalization and functional outcomes in older adults with acute myocardial infarction in the SILVER-AMI study. JAMA Intern Med. 2019 Oct 7. doi: 10.1001/jamainternmed.2019.4114.
Dr. Gerstenberger is a hospitalist and clinical assistant professor of medicine at the University of Utah, Salt Lake City.
Background: The ability to independently perform daily activities is highly valued by patients, yet it is commonly impaired in older adults after hospitalization for MI. Risk of functional decline in this population is not well understood, but may relate to reduced mobility while hospitalized.
Study design: Prospective cohort.
Setting: A total of 94 academic and community hospitals in the United States.
Synopsis: More than 3,000 adults aged 75 years and older who were hospitalized for acute myocardial infarction were enrolled in the prospective cohort SILVER-AMI; 2,587 patients within this cohort were evaluated for in-hospital mobility with the Timed “Up and Go” test. At 6-month follow-up, loss of independent performance of activities of daily living (ADL) and of the ability to walk 0.25 miles were both associated in a dose-dependent manner with in-hospital mobility. Severe in-hospital mobility impairment was associated with ADL decline with an adjusted odds ratio of 5.45 (95% confidence interval, 3.29-9.01).
While in-hospital mobility is predictive of future functional decline in this population, this observational study cannot establish whether attempts to improve mobility in hospitalized patients will prevent future functional decline.
Bottom line: Lower performance on the Timed “Up and Go” test of mobility among older patients hospitalized for MI is associated with functional decline 6 months after hospitalization.
Citation: Hajduk AM et al. Association between mobility measured during hospitalization and functional outcomes in older adults with acute myocardial infarction in the SILVER-AMI study. JAMA Intern Med. 2019 Oct 7. doi: 10.1001/jamainternmed.2019.4114.
Dr. Gerstenberger is a hospitalist and clinical assistant professor of medicine at the University of Utah, Salt Lake City.
Background: The ability to independently perform daily activities is highly valued by patients, yet it is commonly impaired in older adults after hospitalization for MI. Risk of functional decline in this population is not well understood, but may relate to reduced mobility while hospitalized.
Study design: Prospective cohort.
Setting: A total of 94 academic and community hospitals in the United States.
Synopsis: More than 3,000 adults aged 75 years and older who were hospitalized for acute myocardial infarction were enrolled in the prospective cohort SILVER-AMI; 2,587 patients within this cohort were evaluated for in-hospital mobility with the Timed “Up and Go” test. At 6-month follow-up, loss of independent performance of activities of daily living (ADL) and of the ability to walk 0.25 miles were both associated in a dose-dependent manner with in-hospital mobility. Severe in-hospital mobility impairment was associated with ADL decline with an adjusted odds ratio of 5.45 (95% confidence interval, 3.29-9.01).
While in-hospital mobility is predictive of future functional decline in this population, this observational study cannot establish whether attempts to improve mobility in hospitalized patients will prevent future functional decline.
Bottom line: Lower performance on the Timed “Up and Go” test of mobility among older patients hospitalized for MI is associated with functional decline 6 months after hospitalization.
Citation: Hajduk AM et al. Association between mobility measured during hospitalization and functional outcomes in older adults with acute myocardial infarction in the SILVER-AMI study. JAMA Intern Med. 2019 Oct 7. doi: 10.1001/jamainternmed.2019.4114.
Dr. Gerstenberger is a hospitalist and clinical assistant professor of medicine at the University of Utah, Salt Lake City.
Higher 10-day mortality of lower-acuity patients during times of increased ED crowding
Background: Studies have assessed mortality effect from ED crowding on high-acuity patients, but limited evidence exists for how this affects lower-acuity patients who are discharged home.
Study design: Retrospective cohort study.
Setting: Emergency department, Karolinska University Hospital, Solna, Sweden.
Synopsis: During 2009-2016, 705,813 encounters seen in the ED, triaged to lower-acuity levels 3-5 and discharged without further hospitalization needs were identified. A total of 623 patients died within 10 days of the initial ED visit (0.09%). The study evaluated the association of 10-day mortality with mean ED length of stay and ED-occupancy ratio.
The study demonstrated an increased 10-day mortality for mean ED length of stay of 8 hours or more vs. less than 2 hours (adjusted odds ratio, 5.86; 95% CI, 2.15-15.94). It also found an increased mortality rate for occupancy ratio quartiles with an aOR for quartiles 2, 3, and 4 vs. quartile 1 of 1.48 (95% CI, 1.14-1.92), 1.63 (95% CI, 1.24-2.14), and 1.53 (95% CI, 1.15-2.03), respectively.
While this suggests increased 10-day mortality in this patient population, additional studies should be conducted to determine if this risk is caused by ED crowding and length of stay or by current limitations in triage scoring.
Bottom line: There is an increased 10-day mortality rate for lower-acuity triaged patients who were discharged from the ED without hospitalization experiencing increased ED length of stay and during times of ED crowding.
Citation: Berg L et al. Associations between crowding and 10-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019 Sep;74(3):345-56.
Dr. Merando is a hospitalist and assistant professor of internal medicine at St. Louis University School of Medicine.
Background: Studies have assessed mortality effect from ED crowding on high-acuity patients, but limited evidence exists for how this affects lower-acuity patients who are discharged home.
Study design: Retrospective cohort study.
Setting: Emergency department, Karolinska University Hospital, Solna, Sweden.
Synopsis: During 2009-2016, 705,813 encounters seen in the ED, triaged to lower-acuity levels 3-5 and discharged without further hospitalization needs were identified. A total of 623 patients died within 10 days of the initial ED visit (0.09%). The study evaluated the association of 10-day mortality with mean ED length of stay and ED-occupancy ratio.
The study demonstrated an increased 10-day mortality for mean ED length of stay of 8 hours or more vs. less than 2 hours (adjusted odds ratio, 5.86; 95% CI, 2.15-15.94). It also found an increased mortality rate for occupancy ratio quartiles with an aOR for quartiles 2, 3, and 4 vs. quartile 1 of 1.48 (95% CI, 1.14-1.92), 1.63 (95% CI, 1.24-2.14), and 1.53 (95% CI, 1.15-2.03), respectively.
While this suggests increased 10-day mortality in this patient population, additional studies should be conducted to determine if this risk is caused by ED crowding and length of stay or by current limitations in triage scoring.
Bottom line: There is an increased 10-day mortality rate for lower-acuity triaged patients who were discharged from the ED without hospitalization experiencing increased ED length of stay and during times of ED crowding.
Citation: Berg L et al. Associations between crowding and 10-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019 Sep;74(3):345-56.
Dr. Merando is a hospitalist and assistant professor of internal medicine at St. Louis University School of Medicine.
Background: Studies have assessed mortality effect from ED crowding on high-acuity patients, but limited evidence exists for how this affects lower-acuity patients who are discharged home.
Study design: Retrospective cohort study.
Setting: Emergency department, Karolinska University Hospital, Solna, Sweden.
Synopsis: During 2009-2016, 705,813 encounters seen in the ED, triaged to lower-acuity levels 3-5 and discharged without further hospitalization needs were identified. A total of 623 patients died within 10 days of the initial ED visit (0.09%). The study evaluated the association of 10-day mortality with mean ED length of stay and ED-occupancy ratio.
The study demonstrated an increased 10-day mortality for mean ED length of stay of 8 hours or more vs. less than 2 hours (adjusted odds ratio, 5.86; 95% CI, 2.15-15.94). It also found an increased mortality rate for occupancy ratio quartiles with an aOR for quartiles 2, 3, and 4 vs. quartile 1 of 1.48 (95% CI, 1.14-1.92), 1.63 (95% CI, 1.24-2.14), and 1.53 (95% CI, 1.15-2.03), respectively.
While this suggests increased 10-day mortality in this patient population, additional studies should be conducted to determine if this risk is caused by ED crowding and length of stay or by current limitations in triage scoring.
Bottom line: There is an increased 10-day mortality rate for lower-acuity triaged patients who were discharged from the ED without hospitalization experiencing increased ED length of stay and during times of ED crowding.
Citation: Berg L et al. Associations between crowding and 10-day mortality among patients allocated lower triage acuity levels without need of acute hospital care on departure from the emergency department. Ann Emerg Med. 2019 Sep;74(3):345-56.
Dr. Merando is a hospitalist and assistant professor of internal medicine at St. Louis University School of Medicine.
CMS launches hospital-at-home program to free up hospital capacity
As an increasing number of health systems implement “hospital-at-home” (HaH) programs to increase their traditional hospital capacity, the Centers for Medicare & Medicaid Services has given the movement a boost by changing its regulations to allow acute care to be provided in a patient’s home under certain conditions.
The CMS announced Nov. 25 that it was launching its Acute Hospital Care at Home program “to increase the capacity of the American health care system” during the COVID-19 pandemic.
At the same time, the agency announced it was giving more flexibility to ambulatory surgery centers (ASCs) to provide hospital-level care.
The CMS said its new HaH program is an expansion of the Hospitals Without Walls initiative that was unveiled last March. Hospitals Without Walls is a set of “temporary new rules” that provide flexibility for hospitals to provide acute care outside of inpatient settings. Under those rules, hospitals are able to transfer patients to outside facilities, such as ASCs, inpatient rehabilitation hospitals, hotels, and dormitories, while still receiving Medicare hospital payments.
Under CMS’ new Acute Hospital Care at Home, which is not described as temporary, patients can be transferred from emergency departments or inpatient wards to hospital-level care at home. The CMS said the HaH program is designed for people with conditions such as the acute phases of asthma, heart failure, pneumonia, and chronic obstructive pulmonary disease. Altogether, the agency said, more than 60 acute conditions can be treated safely at home.
However, the agency didn’t say that facilities can’t admit COVID-19 patients to the hospital at home. Rami Karjian, MBA, cofounder and CEO of Medically Home, a firm that supplies health systems with technical services and software for HaH programs, said in an interview that several Medically Home clients plan to treat both COVID-19 and non-COVID-19 patients at home when they begin to participate in the CMS program in the near future.
The CMS said it consulted extensively with academic and private industry leaders in building its HaH program. Before rolling out the initiative, the agency noted, it conducted successful pilot programs in leading hospitals and health systems. The results of some of these pilots have been reported in academic journals.
Participating hospitals will be required to have specified screening protocols in place before beginning acute care at home, the CMS announced. An in-person physician evaluation will be required before starting care at home. A nurse will evaluate each patient once daily in person or remotely, and either nurses or paramedics will visit the patient in person twice a day.
In contrast, Medicare regulations require nursing staff to be available around the clock in traditional hospitals. So the CMS has to grant waivers to hospitals for HaH programs.
While not going into detail on the telemonitoring capabilities that will be required in the acute hospital care at home, the release said, “Today’s announcement builds upon the critical work by CMS to expand telehealth coverage to keep beneficiaries safe and prevent the spread of COVID-19.”
More flexibility for ASCs
The agency is also giving ASCs the flexibility to provide 24-hour nursing services only when one or more patients are receiving care on site. This flexibility will be available to any of the 5,700 ASCs that wish to participate, and will be immediately effective for the 85 ASCs currently participating in the Hospital Without Walls initiative, the CMS said.
The new ASC regulations, the CMS said, are aimed at allowing communities “to maintain surgical capacity and other life-saving non-COVID-19 [care], like cancer surgeries.” Patients who need such procedures will be able to receive them in ASCs without being exposed to known COVID-19 cases.
Similarly, the CMS said patients and families not diagnosed with COVID-19 may prefer to receive acute care at home if local hospitals are full of COVID-19 patients. In addition, the CMS said it anticipates patients may value the ability to be treated at home without the visitation restrictions of hospitals.
Early HaH participants
Six health systems with extensive experience in providing acute hospital care at home have been approved for the new HaH waivers from Medicare rules. They include Brigham and Women’s Hospital (Massachusetts); Huntsman Cancer Institute (Utah); Massachusetts General Hospital (Massachusetts); Mount Sinai Health System (New York City); Presbyterian Healthcare Services (New Mexico); and UnityPoint Health (Iowa).
The CMS said that it’s in discussions with other health care systems and expects new applications to be submitted soon.
To support these efforts, the CMS has launched an online portal to streamline the waiver request process. The agency said it will closely monitor the program to safeguard beneficiaries and will require participating hospitals to report quality and safety data on a regular basis.
Support from hospitals
The first health systems participating in the CMS HaH appear to be supportive of the program, with some hospital leaders submitting comments to the CMS about their view of the initiative.
“The CMS has taken an extraordinary step today, facilitating the rapid expansion of Hospitalization at Home, an innovative care model with proven results,” said Kenneth L. Davis, MD, president and CEO of the Mount Sinai Health System in New York City. “This important and timely move will enable hospitals across the country to use effective tools to safely care for patients during this pandemic.”
David Levine, MD, assistant professor of medicine and medical director of strategy and innovation for Brigham Health Home Hospital in Boston, was similarly laudatory: “Our research at Brigham Health Home has shown that we can deliver hospital-level care in our patients’ homes with lower readmission rates, more physical mobility, and a positive patient experience,” he said. “During these challenging times, a focus on the home is critical. We are so encouraged that CMS is taking this important step, which will allow hospitals across the country to increase their capacity while delivering the care all patients deserve.”
Scaling up quickly
If other hospitals and health systems recognize the value of HaH, how long might it take them to develop and implement these programs in the midst of a pandemic?
Atrium Health, a large health system in the Southeast, ramped up a hospital-at-home initiative last spring for its 10 hospitals in the Charlotte, N.C., area, in just 2 weeks. However, it had been working on the project for some time before the pandemic struck. Focusing mostly on COVID-19 patients, the initiative reduced the COVID-19 patient load by 20%-25% in Atrium’s hospitals.
Medically Home, the HaH infrastructure company, said in a news release that it “enables health systems to establish new hospital-at-home services in as little as 30 days.” Medically Home has partnered in this venture with Huron Consulting Group, which has about 200 HaH-trained consultants, and Cardinal Health, a large global medical supplies distributor.
Mr. Karjian said in an interview that he expects private insurers to follow CMS’ example, as they often do. “We think this decision will cause not only CMS but private insurers to cover hospital at home after the pandemic, if it becomes the standard of care, because patients have better outcomes when treated at home,” he said.
Asked for his view on why the CMS specified that patients could be admitted to an HaH only from emergency departments or inpatient settings, Mr. Karjian said that the CMS wants to make sure that patients have access to brick-and-mortar hospital care if that’s what they need. Also, he noted, this model is new to most hospitals, so the CMS wants to make sure it starts “with all the safety guardrails” in place.
Overall, Mr. Karjian said, “This is an exciting development for patients across the country. What CMS has done is terrific in terms of letting patients get the care they want, where they want it, and get the benefit of better outcomes while the nation is going through this capacity crunch for hospital beds.”
A version of this article originally appeared on Medscape.com.
As an increasing number of health systems implement “hospital-at-home” (HaH) programs to increase their traditional hospital capacity, the Centers for Medicare & Medicaid Services has given the movement a boost by changing its regulations to allow acute care to be provided in a patient’s home under certain conditions.
The CMS announced Nov. 25 that it was launching its Acute Hospital Care at Home program “to increase the capacity of the American health care system” during the COVID-19 pandemic.
At the same time, the agency announced it was giving more flexibility to ambulatory surgery centers (ASCs) to provide hospital-level care.
The CMS said its new HaH program is an expansion of the Hospitals Without Walls initiative that was unveiled last March. Hospitals Without Walls is a set of “temporary new rules” that provide flexibility for hospitals to provide acute care outside of inpatient settings. Under those rules, hospitals are able to transfer patients to outside facilities, such as ASCs, inpatient rehabilitation hospitals, hotels, and dormitories, while still receiving Medicare hospital payments.
Under CMS’ new Acute Hospital Care at Home, which is not described as temporary, patients can be transferred from emergency departments or inpatient wards to hospital-level care at home. The CMS said the HaH program is designed for people with conditions such as the acute phases of asthma, heart failure, pneumonia, and chronic obstructive pulmonary disease. Altogether, the agency said, more than 60 acute conditions can be treated safely at home.
However, the agency didn’t say that facilities can’t admit COVID-19 patients to the hospital at home. Rami Karjian, MBA, cofounder and CEO of Medically Home, a firm that supplies health systems with technical services and software for HaH programs, said in an interview that several Medically Home clients plan to treat both COVID-19 and non-COVID-19 patients at home when they begin to participate in the CMS program in the near future.
The CMS said it consulted extensively with academic and private industry leaders in building its HaH program. Before rolling out the initiative, the agency noted, it conducted successful pilot programs in leading hospitals and health systems. The results of some of these pilots have been reported in academic journals.
Participating hospitals will be required to have specified screening protocols in place before beginning acute care at home, the CMS announced. An in-person physician evaluation will be required before starting care at home. A nurse will evaluate each patient once daily in person or remotely, and either nurses or paramedics will visit the patient in person twice a day.
In contrast, Medicare regulations require nursing staff to be available around the clock in traditional hospitals. So the CMS has to grant waivers to hospitals for HaH programs.
While not going into detail on the telemonitoring capabilities that will be required in the acute hospital care at home, the release said, “Today’s announcement builds upon the critical work by CMS to expand telehealth coverage to keep beneficiaries safe and prevent the spread of COVID-19.”
More flexibility for ASCs
The agency is also giving ASCs the flexibility to provide 24-hour nursing services only when one or more patients are receiving care on site. This flexibility will be available to any of the 5,700 ASCs that wish to participate, and will be immediately effective for the 85 ASCs currently participating in the Hospital Without Walls initiative, the CMS said.
The new ASC regulations, the CMS said, are aimed at allowing communities “to maintain surgical capacity and other life-saving non-COVID-19 [care], like cancer surgeries.” Patients who need such procedures will be able to receive them in ASCs without being exposed to known COVID-19 cases.
Similarly, the CMS said patients and families not diagnosed with COVID-19 may prefer to receive acute care at home if local hospitals are full of COVID-19 patients. In addition, the CMS said it anticipates patients may value the ability to be treated at home without the visitation restrictions of hospitals.
Early HaH participants
Six health systems with extensive experience in providing acute hospital care at home have been approved for the new HaH waivers from Medicare rules. They include Brigham and Women’s Hospital (Massachusetts); Huntsman Cancer Institute (Utah); Massachusetts General Hospital (Massachusetts); Mount Sinai Health System (New York City); Presbyterian Healthcare Services (New Mexico); and UnityPoint Health (Iowa).
The CMS said that it’s in discussions with other health care systems and expects new applications to be submitted soon.
To support these efforts, the CMS has launched an online portal to streamline the waiver request process. The agency said it will closely monitor the program to safeguard beneficiaries and will require participating hospitals to report quality and safety data on a regular basis.
Support from hospitals
The first health systems participating in the CMS HaH appear to be supportive of the program, with some hospital leaders submitting comments to the CMS about their view of the initiative.
“The CMS has taken an extraordinary step today, facilitating the rapid expansion of Hospitalization at Home, an innovative care model with proven results,” said Kenneth L. Davis, MD, president and CEO of the Mount Sinai Health System in New York City. “This important and timely move will enable hospitals across the country to use effective tools to safely care for patients during this pandemic.”
David Levine, MD, assistant professor of medicine and medical director of strategy and innovation for Brigham Health Home Hospital in Boston, was similarly laudatory: “Our research at Brigham Health Home has shown that we can deliver hospital-level care in our patients’ homes with lower readmission rates, more physical mobility, and a positive patient experience,” he said. “During these challenging times, a focus on the home is critical. We are so encouraged that CMS is taking this important step, which will allow hospitals across the country to increase their capacity while delivering the care all patients deserve.”
Scaling up quickly
If other hospitals and health systems recognize the value of HaH, how long might it take them to develop and implement these programs in the midst of a pandemic?
Atrium Health, a large health system in the Southeast, ramped up a hospital-at-home initiative last spring for its 10 hospitals in the Charlotte, N.C., area, in just 2 weeks. However, it had been working on the project for some time before the pandemic struck. Focusing mostly on COVID-19 patients, the initiative reduced the COVID-19 patient load by 20%-25% in Atrium’s hospitals.
Medically Home, the HaH infrastructure company, said in a news release that it “enables health systems to establish new hospital-at-home services in as little as 30 days.” Medically Home has partnered in this venture with Huron Consulting Group, which has about 200 HaH-trained consultants, and Cardinal Health, a large global medical supplies distributor.
Mr. Karjian said in an interview that he expects private insurers to follow CMS’ example, as they often do. “We think this decision will cause not only CMS but private insurers to cover hospital at home after the pandemic, if it becomes the standard of care, because patients have better outcomes when treated at home,” he said.
Asked for his view on why the CMS specified that patients could be admitted to an HaH only from emergency departments or inpatient settings, Mr. Karjian said that the CMS wants to make sure that patients have access to brick-and-mortar hospital care if that’s what they need. Also, he noted, this model is new to most hospitals, so the CMS wants to make sure it starts “with all the safety guardrails” in place.
Overall, Mr. Karjian said, “This is an exciting development for patients across the country. What CMS has done is terrific in terms of letting patients get the care they want, where they want it, and get the benefit of better outcomes while the nation is going through this capacity crunch for hospital beds.”
A version of this article originally appeared on Medscape.com.
As an increasing number of health systems implement “hospital-at-home” (HaH) programs to increase their traditional hospital capacity, the Centers for Medicare & Medicaid Services has given the movement a boost by changing its regulations to allow acute care to be provided in a patient’s home under certain conditions.
The CMS announced Nov. 25 that it was launching its Acute Hospital Care at Home program “to increase the capacity of the American health care system” during the COVID-19 pandemic.
At the same time, the agency announced it was giving more flexibility to ambulatory surgery centers (ASCs) to provide hospital-level care.
The CMS said its new HaH program is an expansion of the Hospitals Without Walls initiative that was unveiled last March. Hospitals Without Walls is a set of “temporary new rules” that provide flexibility for hospitals to provide acute care outside of inpatient settings. Under those rules, hospitals are able to transfer patients to outside facilities, such as ASCs, inpatient rehabilitation hospitals, hotels, and dormitories, while still receiving Medicare hospital payments.
Under CMS’ new Acute Hospital Care at Home, which is not described as temporary, patients can be transferred from emergency departments or inpatient wards to hospital-level care at home. The CMS said the HaH program is designed for people with conditions such as the acute phases of asthma, heart failure, pneumonia, and chronic obstructive pulmonary disease. Altogether, the agency said, more than 60 acute conditions can be treated safely at home.
However, the agency didn’t say that facilities can’t admit COVID-19 patients to the hospital at home. Rami Karjian, MBA, cofounder and CEO of Medically Home, a firm that supplies health systems with technical services and software for HaH programs, said in an interview that several Medically Home clients plan to treat both COVID-19 and non-COVID-19 patients at home when they begin to participate in the CMS program in the near future.
The CMS said it consulted extensively with academic and private industry leaders in building its HaH program. Before rolling out the initiative, the agency noted, it conducted successful pilot programs in leading hospitals and health systems. The results of some of these pilots have been reported in academic journals.
Participating hospitals will be required to have specified screening protocols in place before beginning acute care at home, the CMS announced. An in-person physician evaluation will be required before starting care at home. A nurse will evaluate each patient once daily in person or remotely, and either nurses or paramedics will visit the patient in person twice a day.
In contrast, Medicare regulations require nursing staff to be available around the clock in traditional hospitals. So the CMS has to grant waivers to hospitals for HaH programs.
While not going into detail on the telemonitoring capabilities that will be required in the acute hospital care at home, the release said, “Today’s announcement builds upon the critical work by CMS to expand telehealth coverage to keep beneficiaries safe and prevent the spread of COVID-19.”
More flexibility for ASCs
The agency is also giving ASCs the flexibility to provide 24-hour nursing services only when one or more patients are receiving care on site. This flexibility will be available to any of the 5,700 ASCs that wish to participate, and will be immediately effective for the 85 ASCs currently participating in the Hospital Without Walls initiative, the CMS said.
The new ASC regulations, the CMS said, are aimed at allowing communities “to maintain surgical capacity and other life-saving non-COVID-19 [care], like cancer surgeries.” Patients who need such procedures will be able to receive them in ASCs without being exposed to known COVID-19 cases.
Similarly, the CMS said patients and families not diagnosed with COVID-19 may prefer to receive acute care at home if local hospitals are full of COVID-19 patients. In addition, the CMS said it anticipates patients may value the ability to be treated at home without the visitation restrictions of hospitals.
Early HaH participants
Six health systems with extensive experience in providing acute hospital care at home have been approved for the new HaH waivers from Medicare rules. They include Brigham and Women’s Hospital (Massachusetts); Huntsman Cancer Institute (Utah); Massachusetts General Hospital (Massachusetts); Mount Sinai Health System (New York City); Presbyterian Healthcare Services (New Mexico); and UnityPoint Health (Iowa).
The CMS said that it’s in discussions with other health care systems and expects new applications to be submitted soon.
To support these efforts, the CMS has launched an online portal to streamline the waiver request process. The agency said it will closely monitor the program to safeguard beneficiaries and will require participating hospitals to report quality and safety data on a regular basis.
Support from hospitals
The first health systems participating in the CMS HaH appear to be supportive of the program, with some hospital leaders submitting comments to the CMS about their view of the initiative.
“The CMS has taken an extraordinary step today, facilitating the rapid expansion of Hospitalization at Home, an innovative care model with proven results,” said Kenneth L. Davis, MD, president and CEO of the Mount Sinai Health System in New York City. “This important and timely move will enable hospitals across the country to use effective tools to safely care for patients during this pandemic.”
David Levine, MD, assistant professor of medicine and medical director of strategy and innovation for Brigham Health Home Hospital in Boston, was similarly laudatory: “Our research at Brigham Health Home has shown that we can deliver hospital-level care in our patients’ homes with lower readmission rates, more physical mobility, and a positive patient experience,” he said. “During these challenging times, a focus on the home is critical. We are so encouraged that CMS is taking this important step, which will allow hospitals across the country to increase their capacity while delivering the care all patients deserve.”
Scaling up quickly
If other hospitals and health systems recognize the value of HaH, how long might it take them to develop and implement these programs in the midst of a pandemic?
Atrium Health, a large health system in the Southeast, ramped up a hospital-at-home initiative last spring for its 10 hospitals in the Charlotte, N.C., area, in just 2 weeks. However, it had been working on the project for some time before the pandemic struck. Focusing mostly on COVID-19 patients, the initiative reduced the COVID-19 patient load by 20%-25% in Atrium’s hospitals.
Medically Home, the HaH infrastructure company, said in a news release that it “enables health systems to establish new hospital-at-home services in as little as 30 days.” Medically Home has partnered in this venture with Huron Consulting Group, which has about 200 HaH-trained consultants, and Cardinal Health, a large global medical supplies distributor.
Mr. Karjian said in an interview that he expects private insurers to follow CMS’ example, as they often do. “We think this decision will cause not only CMS but private insurers to cover hospital at home after the pandemic, if it becomes the standard of care, because patients have better outcomes when treated at home,” he said.
Asked for his view on why the CMS specified that patients could be admitted to an HaH only from emergency departments or inpatient settings, Mr. Karjian said that the CMS wants to make sure that patients have access to brick-and-mortar hospital care if that’s what they need. Also, he noted, this model is new to most hospitals, so the CMS wants to make sure it starts “with all the safety guardrails” in place.
Overall, Mr. Karjian said, “This is an exciting development for patients across the country. What CMS has done is terrific in terms of letting patients get the care they want, where they want it, and get the benefit of better outcomes while the nation is going through this capacity crunch for hospital beds.”
A version of this article originally appeared on Medscape.com.
Adverse events occur in LTC residents transitioning from hospital to nursing home
Background: Adverse events in the immediate posthospitalization period are a serious threat to patients 65 years and older who are residents of long-term care facilities. Changes during hospitalization – such as fasting for procedures, immobility, change in surroundings, disruption of sleep, and medication adjustments – can lead to adverse events such as falls, pressure ulcers, adverse drug reactions, and health care–acquired infections. However, the frequency and preventability of these adverse events has not been measured.
Study design: Prospective cohort study.
Setting: Nursing homes in the New England states.
Synopsis: This study sampled 762 hospital discharges for 555 long-term care residents of 32 nursing homes who were discharged from the hospital back to their same long-term care facility and followed for 45 days. A trained nurse reviewed records using a trigger tool developed by the Institute for Healthcare Improvement. Each trigger linked to a possible harm was reviewed by two physicians. Adverse events were categorized into health care–acquired infections and events related to resident care, medications, and procedures. The severity and preventability of each event was assessed.
Of the 555 residents, 65.5% were female and the mean age was 82.2. There were 379 adverse events identified; 52% involved pressure ulcers, skin tears, and falls with injury, which were deemed preventable. Healthcare-acquired infections totaled 28.5% and adverse drug events were 16.5%. Close to half of the events were serious, life threatening, or fatal. The study was limited by subjectivity in classifying the adverse events.
Hospitalists should ensure proper coordination and handoff when transitioning patients back to their nursing home.
Bottom line: Adverse events occur in 4 of 10 discharges from the hospital to long-term care facilities, and most events are preventable.
Citation: Kapoor A et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019 Jul 22;179(9):1254-61.
Dr. Ali is assistant professor of internal medicine and section chief of hospital medicine at St. Louis University School of Medicine.
Background: Adverse events in the immediate posthospitalization period are a serious threat to patients 65 years and older who are residents of long-term care facilities. Changes during hospitalization – such as fasting for procedures, immobility, change in surroundings, disruption of sleep, and medication adjustments – can lead to adverse events such as falls, pressure ulcers, adverse drug reactions, and health care–acquired infections. However, the frequency and preventability of these adverse events has not been measured.
Study design: Prospective cohort study.
Setting: Nursing homes in the New England states.
Synopsis: This study sampled 762 hospital discharges for 555 long-term care residents of 32 nursing homes who were discharged from the hospital back to their same long-term care facility and followed for 45 days. A trained nurse reviewed records using a trigger tool developed by the Institute for Healthcare Improvement. Each trigger linked to a possible harm was reviewed by two physicians. Adverse events were categorized into health care–acquired infections and events related to resident care, medications, and procedures. The severity and preventability of each event was assessed.
Of the 555 residents, 65.5% were female and the mean age was 82.2. There were 379 adverse events identified; 52% involved pressure ulcers, skin tears, and falls with injury, which were deemed preventable. Healthcare-acquired infections totaled 28.5% and adverse drug events were 16.5%. Close to half of the events were serious, life threatening, or fatal. The study was limited by subjectivity in classifying the adverse events.
Hospitalists should ensure proper coordination and handoff when transitioning patients back to their nursing home.
Bottom line: Adverse events occur in 4 of 10 discharges from the hospital to long-term care facilities, and most events are preventable.
Citation: Kapoor A et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019 Jul 22;179(9):1254-61.
Dr. Ali is assistant professor of internal medicine and section chief of hospital medicine at St. Louis University School of Medicine.
Background: Adverse events in the immediate posthospitalization period are a serious threat to patients 65 years and older who are residents of long-term care facilities. Changes during hospitalization – such as fasting for procedures, immobility, change in surroundings, disruption of sleep, and medication adjustments – can lead to adverse events such as falls, pressure ulcers, adverse drug reactions, and health care–acquired infections. However, the frequency and preventability of these adverse events has not been measured.
Study design: Prospective cohort study.
Setting: Nursing homes in the New England states.
Synopsis: This study sampled 762 hospital discharges for 555 long-term care residents of 32 nursing homes who were discharged from the hospital back to their same long-term care facility and followed for 45 days. A trained nurse reviewed records using a trigger tool developed by the Institute for Healthcare Improvement. Each trigger linked to a possible harm was reviewed by two physicians. Adverse events were categorized into health care–acquired infections and events related to resident care, medications, and procedures. The severity and preventability of each event was assessed.
Of the 555 residents, 65.5% were female and the mean age was 82.2. There were 379 adverse events identified; 52% involved pressure ulcers, skin tears, and falls with injury, which were deemed preventable. Healthcare-acquired infections totaled 28.5% and adverse drug events were 16.5%. Close to half of the events were serious, life threatening, or fatal. The study was limited by subjectivity in classifying the adverse events.
Hospitalists should ensure proper coordination and handoff when transitioning patients back to their nursing home.
Bottom line: Adverse events occur in 4 of 10 discharges from the hospital to long-term care facilities, and most events are preventable.
Citation: Kapoor A et al. Adverse events in long-term care residents transitioning from hospital back to nursing home. JAMA Intern Med. 2019 Jul 22;179(9):1254-61.
Dr. Ali is assistant professor of internal medicine and section chief of hospital medicine at St. Louis University School of Medicine.
‘Hospital at home’ increases COVID capacity in large study
A “hospital at home” (HaH) program at Atrium Health, a large integrated delivery system in the Southeast, expanded its hospital capacity during the early phase of the COVID-19 pandemic by providing hospital-level acute care to COVID-19 patients at home, according to a new study in Annals of Internal Medicine.
“Virtual hospital programs have the potential to provide health systems with additional inpatient capacity during the COVID-19 pandemic and beyond,” wrote Kranthi Sitammagari, MD, from the Atrium Health Hospitalist Group, Monroe, N.C., and colleagues.
Whereas most previous HaH programs have relied on visiting nurses and physicians, the new study uses telemedicine to connect with patients. Advocate Health Care researchers published the only other study using the telemedicine-powered model in 2015.
The new Atrium Health study evaluated 1,477 patients who received care in the HaH program between March 23 and May 7 of this year after having been diagnosed with COVID-19. The program provided home monitoring and hospital-level care in a home-based virtual observation unit (VOU) and a virtual acute care unit (VACU).
Patients were tested for the virus in Atrium emergency departments, primary care clinics, urgent care centers, and external testing sites. Those who tested positive were invited to be cared for either in the VOU, if they had mild to moderate symptoms, or in the VACU, if they were sick enough to be admitted to the hospital.
Patients hop onboard
Nearly all COVID-positive patients tested in these sites agreed to be admitted to the hospital at home, coauthor Stephanie Murphy, DO, medical director of the Atrium Health HaH program, said in an interview.
Patients with moderate symptoms were glad to be monitored at home, she said. When they got to the point where the nurse supervising their care felt they needed escalation to acute care, they were asked whether they wanted to continue to be cared for at home. Most opted to stay home rather than be admitted to the hospital, where their loved ones couldn’t visit them.
Low-acuity patients in the VOU received daily telemonitoring by a nurse to identify disease progression and escalate care as needed. For those who required more care and were admitted to the VACU, a team of paramedics and registered nurses (RNs; mobile clinicians) visited the patient’s home within 24 hours, setting up a hospital bed, other necessary medical equipment, videoconferencing gear, and a remote-monitoring kit that included a blood pressure cuff, a pulse oximeter, and a thermometer.
Dedicated hospitalists and nurses managed patients with 24/7 coverage and monitoring, bringing in other specialties as needed for virtual consults. Mobile clinician and virtual provider visits continued daily until a patient’s condition improved to the point where they could be deescalated back to the VOU. After that, patients received mobile app-driven symptom monitoring and telephone follow-up with a nurse until they got better.
Few patients go to hospital
Overall, patients had a median length of stay of 11 days in the VOU or the VACU or both. The vast majority, 1,293 patients (88%), received care in the VOU only. In that cohort, just 40 patients (3%) required hospitalization in an Atrium facility. Sixteen of those patients spent time in an ICU, seven required ventilator support, and two died in the hospital.
A total of 184 patients (12%) were admitted to the VACU. Twenty-one (11%) required intravenous fluids, 16 (9%) received antibiotics, 40 (22%) required inhaler or nebulizer treatments, 41 (22%) used supplemental oxygen, and 24 (13%) were admitted to a conventional hospital. Of the latter patients, 10 were admitted to an ICU, one required a ventilator, and none died in the hospital.
Dr. Sitammagari, a hospitalist and comedical director for quality at Atrium Health, told this news organization that, overall, the outcomes for patients in the system’s HaH were comparable to those seen in the literature among other COVID-19 cohorts.
Augmenting hospital capacity
The authors note that treating the 160 VACU patients within the HaH saved hospital beds for other patients. The HaH maintained a consistent census of between 20 and 30 patients for the first 6 weeks as COVID-19 cases spread.
Since last spring, Dr. Murphy said, the Atrium HaH’s daily census has grown to between 30 and 45 patients. “We could absorb 50 patients if our hospitals required it.”
How much capacity does that add to Atrium Health? While there are 50 hospitals in the health system, the HaH was set up mainly to care for COVID-19 patients who would otherwise have been admitted to the 10 acute-care hospitals in the Charlotte, N.C., area. In the 4 weeks ending Nov. 16, these facilities carried an average daily census of around 160 COVID-19 patients, Dr. Murphy noted. “During that time, the Atrium Health HaH has carried, on average, about 20%-25% of that census.”
If the pandemic were to overwhelm area hospitals, she added, “the structure would support flexing up our staffing and supplies to expand to crisis capacity,” which could be up to 200 patients a day.
For the nurses who make most of the phone calls to patients, patients average about 12 to 15 per RN, Dr. Murphy said, and there’s one mobile clinician for every six to nine patients. That’s pretty consistent with the staffing on med-surg floors in hospitals, she said.
The physicians in the program include hospitalists dedicated to telemedicine and some doctors who can’t work in the regular hospital because they’re immunocompromised. The physicians round virtually, covering 12-17 HaH patients per day, according to Dr. Murphy.
Prior planning paid off
Unlike some other health care systems that have launched HaH programs with the aid of outside vendors, Atrium Health developed its own HaH and brought it online just 2 weeks after deciding to launch the program. Atrium was able to do this, Dr. Sitammagari explained, because before the pandemic its hospitalist program was already developing an HaH model to improve the care of high-risk patients after hospital discharge to prevent readmission.
While Atrium’s electronic health record system wasn’t designed for hospital at home, its health information technology department and clinicians collaborated in rewriting some of the workflows and order sets in the EHR. For example, they set up a nursing questionnaire to administer after VACU admission, and they created another form for automatic admission to the HaH after a patient tested positive for COVID-19. Atrium staff also modified a patient-doctor communications app to help clinicians monitor HaH patients, Dr. Murphy noted.
Other hospital systems have gotten up to speed on HaH pretty quickly by using platforms supplied by outside vendors. Adventist Health in Los Angeles, for example, started admitting patients to its hospital at home just a month after approaching a vendor called Medically Home.
COVID vs. non-COVID patients
Atrium’s decision to focus its HaH effort on COVID-19 patients is unusual among the small but growing number of health systems that have adopted the HaH model to increase their capacity. (Atrium is now transferring some hospitalized patients with other conditions to its HaH, but is still focusing mainly on COVID-19 in its HaH program.)
Bruce Leff, MD, a professor of health policy and management at Johns Hopkins Bloomberg School of Public Health, Baltimore, a leading expert on the HaH model, agrees that it can increase hospital capacity significantly.
Dr. Leff praised the Atrium Health study. “It proves that within an integrated delivery system you can quickly deploy and implement a virtual hospital in the specific-use case of COVID, and help patients and help the system at scale,” he said. “They took a bunch of people into the virtual observation unit and thereby kept people from overwhelming their [emergency department] and treated those people safely at home.”
Dr. Leff had no problem with Atrium’s focus on patients with COVID-19 rather than other conditions. “My guess is that they have the ability to take what they developed and apply it to other conditions. Once you have the ability to do acute care at home, you can do a lot at home.”
The biggest barrier to the spread of hospital at home remains the lack of insurer coverage. Dr. Murphy said that health plans are covering virtual physician consultations with patients in the HaH, as well as some other bits and pieces, but not the entire episode of acute care.
Dr. Leff believes that this will start changing soon. COVID-19 has altered the attitudes of physicians and hospitals toward telehealth, he noted, “and it has moved policy makers and payers to start thinking about the new models – home-based care in general and hospital at home in particular. For the first time in 25 years, payers are starting to get interested.”
Most of the authors are employees of Atrium Health. In addition, one coauthor reports being the cofounder of a digital health company, iEnroll, and receiving grants from The Heineman Foundation. Dr. Leff is an advisor to Medically Home, which provides support to hospital at home programs.
A version of this article originally appeared on Medscape.com.
A “hospital at home” (HaH) program at Atrium Health, a large integrated delivery system in the Southeast, expanded its hospital capacity during the early phase of the COVID-19 pandemic by providing hospital-level acute care to COVID-19 patients at home, according to a new study in Annals of Internal Medicine.
“Virtual hospital programs have the potential to provide health systems with additional inpatient capacity during the COVID-19 pandemic and beyond,” wrote Kranthi Sitammagari, MD, from the Atrium Health Hospitalist Group, Monroe, N.C., and colleagues.
Whereas most previous HaH programs have relied on visiting nurses and physicians, the new study uses telemedicine to connect with patients. Advocate Health Care researchers published the only other study using the telemedicine-powered model in 2015.
The new Atrium Health study evaluated 1,477 patients who received care in the HaH program between March 23 and May 7 of this year after having been diagnosed with COVID-19. The program provided home monitoring and hospital-level care in a home-based virtual observation unit (VOU) and a virtual acute care unit (VACU).
Patients were tested for the virus in Atrium emergency departments, primary care clinics, urgent care centers, and external testing sites. Those who tested positive were invited to be cared for either in the VOU, if they had mild to moderate symptoms, or in the VACU, if they were sick enough to be admitted to the hospital.
Patients hop onboard
Nearly all COVID-positive patients tested in these sites agreed to be admitted to the hospital at home, coauthor Stephanie Murphy, DO, medical director of the Atrium Health HaH program, said in an interview.
Patients with moderate symptoms were glad to be monitored at home, she said. When they got to the point where the nurse supervising their care felt they needed escalation to acute care, they were asked whether they wanted to continue to be cared for at home. Most opted to stay home rather than be admitted to the hospital, where their loved ones couldn’t visit them.
Low-acuity patients in the VOU received daily telemonitoring by a nurse to identify disease progression and escalate care as needed. For those who required more care and were admitted to the VACU, a team of paramedics and registered nurses (RNs; mobile clinicians) visited the patient’s home within 24 hours, setting up a hospital bed, other necessary medical equipment, videoconferencing gear, and a remote-monitoring kit that included a blood pressure cuff, a pulse oximeter, and a thermometer.
Dedicated hospitalists and nurses managed patients with 24/7 coverage and monitoring, bringing in other specialties as needed for virtual consults. Mobile clinician and virtual provider visits continued daily until a patient’s condition improved to the point where they could be deescalated back to the VOU. After that, patients received mobile app-driven symptom monitoring and telephone follow-up with a nurse until they got better.
Few patients go to hospital
Overall, patients had a median length of stay of 11 days in the VOU or the VACU or both. The vast majority, 1,293 patients (88%), received care in the VOU only. In that cohort, just 40 patients (3%) required hospitalization in an Atrium facility. Sixteen of those patients spent time in an ICU, seven required ventilator support, and two died in the hospital.
A total of 184 patients (12%) were admitted to the VACU. Twenty-one (11%) required intravenous fluids, 16 (9%) received antibiotics, 40 (22%) required inhaler or nebulizer treatments, 41 (22%) used supplemental oxygen, and 24 (13%) were admitted to a conventional hospital. Of the latter patients, 10 were admitted to an ICU, one required a ventilator, and none died in the hospital.
Dr. Sitammagari, a hospitalist and comedical director for quality at Atrium Health, told this news organization that, overall, the outcomes for patients in the system’s HaH were comparable to those seen in the literature among other COVID-19 cohorts.
Augmenting hospital capacity
The authors note that treating the 160 VACU patients within the HaH saved hospital beds for other patients. The HaH maintained a consistent census of between 20 and 30 patients for the first 6 weeks as COVID-19 cases spread.
Since last spring, Dr. Murphy said, the Atrium HaH’s daily census has grown to between 30 and 45 patients. “We could absorb 50 patients if our hospitals required it.”
How much capacity does that add to Atrium Health? While there are 50 hospitals in the health system, the HaH was set up mainly to care for COVID-19 patients who would otherwise have been admitted to the 10 acute-care hospitals in the Charlotte, N.C., area. In the 4 weeks ending Nov. 16, these facilities carried an average daily census of around 160 COVID-19 patients, Dr. Murphy noted. “During that time, the Atrium Health HaH has carried, on average, about 20%-25% of that census.”
If the pandemic were to overwhelm area hospitals, she added, “the structure would support flexing up our staffing and supplies to expand to crisis capacity,” which could be up to 200 patients a day.
For the nurses who make most of the phone calls to patients, patients average about 12 to 15 per RN, Dr. Murphy said, and there’s one mobile clinician for every six to nine patients. That’s pretty consistent with the staffing on med-surg floors in hospitals, she said.
The physicians in the program include hospitalists dedicated to telemedicine and some doctors who can’t work in the regular hospital because they’re immunocompromised. The physicians round virtually, covering 12-17 HaH patients per day, according to Dr. Murphy.
Prior planning paid off
Unlike some other health care systems that have launched HaH programs with the aid of outside vendors, Atrium Health developed its own HaH and brought it online just 2 weeks after deciding to launch the program. Atrium was able to do this, Dr. Sitammagari explained, because before the pandemic its hospitalist program was already developing an HaH model to improve the care of high-risk patients after hospital discharge to prevent readmission.
While Atrium’s electronic health record system wasn’t designed for hospital at home, its health information technology department and clinicians collaborated in rewriting some of the workflows and order sets in the EHR. For example, they set up a nursing questionnaire to administer after VACU admission, and they created another form for automatic admission to the HaH after a patient tested positive for COVID-19. Atrium staff also modified a patient-doctor communications app to help clinicians monitor HaH patients, Dr. Murphy noted.
Other hospital systems have gotten up to speed on HaH pretty quickly by using platforms supplied by outside vendors. Adventist Health in Los Angeles, for example, started admitting patients to its hospital at home just a month after approaching a vendor called Medically Home.
COVID vs. non-COVID patients
Atrium’s decision to focus its HaH effort on COVID-19 patients is unusual among the small but growing number of health systems that have adopted the HaH model to increase their capacity. (Atrium is now transferring some hospitalized patients with other conditions to its HaH, but is still focusing mainly on COVID-19 in its HaH program.)
Bruce Leff, MD, a professor of health policy and management at Johns Hopkins Bloomberg School of Public Health, Baltimore, a leading expert on the HaH model, agrees that it can increase hospital capacity significantly.
Dr. Leff praised the Atrium Health study. “It proves that within an integrated delivery system you can quickly deploy and implement a virtual hospital in the specific-use case of COVID, and help patients and help the system at scale,” he said. “They took a bunch of people into the virtual observation unit and thereby kept people from overwhelming their [emergency department] and treated those people safely at home.”
Dr. Leff had no problem with Atrium’s focus on patients with COVID-19 rather than other conditions. “My guess is that they have the ability to take what they developed and apply it to other conditions. Once you have the ability to do acute care at home, you can do a lot at home.”
The biggest barrier to the spread of hospital at home remains the lack of insurer coverage. Dr. Murphy said that health plans are covering virtual physician consultations with patients in the HaH, as well as some other bits and pieces, but not the entire episode of acute care.
Dr. Leff believes that this will start changing soon. COVID-19 has altered the attitudes of physicians and hospitals toward telehealth, he noted, “and it has moved policy makers and payers to start thinking about the new models – home-based care in general and hospital at home in particular. For the first time in 25 years, payers are starting to get interested.”
Most of the authors are employees of Atrium Health. In addition, one coauthor reports being the cofounder of a digital health company, iEnroll, and receiving grants from The Heineman Foundation. Dr. Leff is an advisor to Medically Home, which provides support to hospital at home programs.
A version of this article originally appeared on Medscape.com.
A “hospital at home” (HaH) program at Atrium Health, a large integrated delivery system in the Southeast, expanded its hospital capacity during the early phase of the COVID-19 pandemic by providing hospital-level acute care to COVID-19 patients at home, according to a new study in Annals of Internal Medicine.
“Virtual hospital programs have the potential to provide health systems with additional inpatient capacity during the COVID-19 pandemic and beyond,” wrote Kranthi Sitammagari, MD, from the Atrium Health Hospitalist Group, Monroe, N.C., and colleagues.
Whereas most previous HaH programs have relied on visiting nurses and physicians, the new study uses telemedicine to connect with patients. Advocate Health Care researchers published the only other study using the telemedicine-powered model in 2015.
The new Atrium Health study evaluated 1,477 patients who received care in the HaH program between March 23 and May 7 of this year after having been diagnosed with COVID-19. The program provided home monitoring and hospital-level care in a home-based virtual observation unit (VOU) and a virtual acute care unit (VACU).
Patients were tested for the virus in Atrium emergency departments, primary care clinics, urgent care centers, and external testing sites. Those who tested positive were invited to be cared for either in the VOU, if they had mild to moderate symptoms, or in the VACU, if they were sick enough to be admitted to the hospital.
Patients hop onboard
Nearly all COVID-positive patients tested in these sites agreed to be admitted to the hospital at home, coauthor Stephanie Murphy, DO, medical director of the Atrium Health HaH program, said in an interview.
Patients with moderate symptoms were glad to be monitored at home, she said. When they got to the point where the nurse supervising their care felt they needed escalation to acute care, they were asked whether they wanted to continue to be cared for at home. Most opted to stay home rather than be admitted to the hospital, where their loved ones couldn’t visit them.
Low-acuity patients in the VOU received daily telemonitoring by a nurse to identify disease progression and escalate care as needed. For those who required more care and were admitted to the VACU, a team of paramedics and registered nurses (RNs; mobile clinicians) visited the patient’s home within 24 hours, setting up a hospital bed, other necessary medical equipment, videoconferencing gear, and a remote-monitoring kit that included a blood pressure cuff, a pulse oximeter, and a thermometer.
Dedicated hospitalists and nurses managed patients with 24/7 coverage and monitoring, bringing in other specialties as needed for virtual consults. Mobile clinician and virtual provider visits continued daily until a patient’s condition improved to the point where they could be deescalated back to the VOU. After that, patients received mobile app-driven symptom monitoring and telephone follow-up with a nurse until they got better.
Few patients go to hospital
Overall, patients had a median length of stay of 11 days in the VOU or the VACU or both. The vast majority, 1,293 patients (88%), received care in the VOU only. In that cohort, just 40 patients (3%) required hospitalization in an Atrium facility. Sixteen of those patients spent time in an ICU, seven required ventilator support, and two died in the hospital.
A total of 184 patients (12%) were admitted to the VACU. Twenty-one (11%) required intravenous fluids, 16 (9%) received antibiotics, 40 (22%) required inhaler or nebulizer treatments, 41 (22%) used supplemental oxygen, and 24 (13%) were admitted to a conventional hospital. Of the latter patients, 10 were admitted to an ICU, one required a ventilator, and none died in the hospital.
Dr. Sitammagari, a hospitalist and comedical director for quality at Atrium Health, told this news organization that, overall, the outcomes for patients in the system’s HaH were comparable to those seen in the literature among other COVID-19 cohorts.
Augmenting hospital capacity
The authors note that treating the 160 VACU patients within the HaH saved hospital beds for other patients. The HaH maintained a consistent census of between 20 and 30 patients for the first 6 weeks as COVID-19 cases spread.
Since last spring, Dr. Murphy said, the Atrium HaH’s daily census has grown to between 30 and 45 patients. “We could absorb 50 patients if our hospitals required it.”
How much capacity does that add to Atrium Health? While there are 50 hospitals in the health system, the HaH was set up mainly to care for COVID-19 patients who would otherwise have been admitted to the 10 acute-care hospitals in the Charlotte, N.C., area. In the 4 weeks ending Nov. 16, these facilities carried an average daily census of around 160 COVID-19 patients, Dr. Murphy noted. “During that time, the Atrium Health HaH has carried, on average, about 20%-25% of that census.”
If the pandemic were to overwhelm area hospitals, she added, “the structure would support flexing up our staffing and supplies to expand to crisis capacity,” which could be up to 200 patients a day.
For the nurses who make most of the phone calls to patients, patients average about 12 to 15 per RN, Dr. Murphy said, and there’s one mobile clinician for every six to nine patients. That’s pretty consistent with the staffing on med-surg floors in hospitals, she said.
The physicians in the program include hospitalists dedicated to telemedicine and some doctors who can’t work in the regular hospital because they’re immunocompromised. The physicians round virtually, covering 12-17 HaH patients per day, according to Dr. Murphy.
Prior planning paid off
Unlike some other health care systems that have launched HaH programs with the aid of outside vendors, Atrium Health developed its own HaH and brought it online just 2 weeks after deciding to launch the program. Atrium was able to do this, Dr. Sitammagari explained, because before the pandemic its hospitalist program was already developing an HaH model to improve the care of high-risk patients after hospital discharge to prevent readmission.
While Atrium’s electronic health record system wasn’t designed for hospital at home, its health information technology department and clinicians collaborated in rewriting some of the workflows and order sets in the EHR. For example, they set up a nursing questionnaire to administer after VACU admission, and they created another form for automatic admission to the HaH after a patient tested positive for COVID-19. Atrium staff also modified a patient-doctor communications app to help clinicians monitor HaH patients, Dr. Murphy noted.
Other hospital systems have gotten up to speed on HaH pretty quickly by using platforms supplied by outside vendors. Adventist Health in Los Angeles, for example, started admitting patients to its hospital at home just a month after approaching a vendor called Medically Home.
COVID vs. non-COVID patients
Atrium’s decision to focus its HaH effort on COVID-19 patients is unusual among the small but growing number of health systems that have adopted the HaH model to increase their capacity. (Atrium is now transferring some hospitalized patients with other conditions to its HaH, but is still focusing mainly on COVID-19 in its HaH program.)
Bruce Leff, MD, a professor of health policy and management at Johns Hopkins Bloomberg School of Public Health, Baltimore, a leading expert on the HaH model, agrees that it can increase hospital capacity significantly.
Dr. Leff praised the Atrium Health study. “It proves that within an integrated delivery system you can quickly deploy and implement a virtual hospital in the specific-use case of COVID, and help patients and help the system at scale,” he said. “They took a bunch of people into the virtual observation unit and thereby kept people from overwhelming their [emergency department] and treated those people safely at home.”
Dr. Leff had no problem with Atrium’s focus on patients with COVID-19 rather than other conditions. “My guess is that they have the ability to take what they developed and apply it to other conditions. Once you have the ability to do acute care at home, you can do a lot at home.”
The biggest barrier to the spread of hospital at home remains the lack of insurer coverage. Dr. Murphy said that health plans are covering virtual physician consultations with patients in the HaH, as well as some other bits and pieces, but not the entire episode of acute care.
Dr. Leff believes that this will start changing soon. COVID-19 has altered the attitudes of physicians and hospitals toward telehealth, he noted, “and it has moved policy makers and payers to start thinking about the new models – home-based care in general and hospital at home in particular. For the first time in 25 years, payers are starting to get interested.”
Most of the authors are employees of Atrium Health. In addition, one coauthor reports being the cofounder of a digital health company, iEnroll, and receiving grants from The Heineman Foundation. Dr. Leff is an advisor to Medically Home, which provides support to hospital at home programs.
A version of this article originally appeared on Medscape.com.
Predicting patient risk of medication-related harm
A new tool is the first of its kind
“An increasing number of older adults are using multiple medicines, and it is important that the benefits are outweighing the risks,” said Nikesh Parekh, MBBS, MPH, lead author of a recent study of a new predictive tool. The study was done in the context of the World Health Organization campaign to halve the incidence of medication-related harm (MRH) by 2022 – reducing MRH following hospital discharge was identified as a priority area.
This works allows clinicians to calculate the risk of a patient suffering MRH post-discharge requiring health care, said Dr. Parekh, a research fellow at Brighton and Sussex Medical School in Great Britain. “This enables practitioners and policy makers to target interventions to reduce MRH at those with highest risk. This should support the delivery of cost-effective care. The knowledge of individual risk can also prompt clinicians to reconsider any high-risk medicines that they intend on prescribing at discharge.”
This is the first prediction tool to calculate individual patient risk of serious MRH post-discharge, he added.The high readmission rate for older adults is often an avoidable pressure for hospitalists, particularly where MRH is the underlying cause. “The prediction tool has the potential to significantly reduce this burden for hospitalists/patients by identifying those individuals at high risk upon discharge and ensuring that monitoring and additional support is provided to them in the community with their medications,” Dr. Parekh said.
This electronic tool could be integrated into the electronic discharge summaries so that the information can be shared with primary care clinicians in a straightforward way. “The risk score should be calculated automatically by a self-population of the tool’s fields from information that exists on the patient within the electronic discharge system.”The tool now needs to be externally validated through testing in new settings to assess its validity and reliability in new populations. “If the tool is found to be usable by hospitalists and demonstrates reasonable predictive accuracy, then it should be implemented widely to reduce the incidence of MRH,” Dr. Parekh said.
Reference
1. Parekh N, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. Published Online First 2019 Sept 16. doi: 10.1136/bmjqs-2019-009587.
A new tool is the first of its kind
A new tool is the first of its kind
“An increasing number of older adults are using multiple medicines, and it is important that the benefits are outweighing the risks,” said Nikesh Parekh, MBBS, MPH, lead author of a recent study of a new predictive tool. The study was done in the context of the World Health Organization campaign to halve the incidence of medication-related harm (MRH) by 2022 – reducing MRH following hospital discharge was identified as a priority area.
This works allows clinicians to calculate the risk of a patient suffering MRH post-discharge requiring health care, said Dr. Parekh, a research fellow at Brighton and Sussex Medical School in Great Britain. “This enables practitioners and policy makers to target interventions to reduce MRH at those with highest risk. This should support the delivery of cost-effective care. The knowledge of individual risk can also prompt clinicians to reconsider any high-risk medicines that they intend on prescribing at discharge.”
This is the first prediction tool to calculate individual patient risk of serious MRH post-discharge, he added.The high readmission rate for older adults is often an avoidable pressure for hospitalists, particularly where MRH is the underlying cause. “The prediction tool has the potential to significantly reduce this burden for hospitalists/patients by identifying those individuals at high risk upon discharge and ensuring that monitoring and additional support is provided to them in the community with their medications,” Dr. Parekh said.
This electronic tool could be integrated into the electronic discharge summaries so that the information can be shared with primary care clinicians in a straightforward way. “The risk score should be calculated automatically by a self-population of the tool’s fields from information that exists on the patient within the electronic discharge system.”The tool now needs to be externally validated through testing in new settings to assess its validity and reliability in new populations. “If the tool is found to be usable by hospitalists and demonstrates reasonable predictive accuracy, then it should be implemented widely to reduce the incidence of MRH,” Dr. Parekh said.
Reference
1. Parekh N, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. Published Online First 2019 Sept 16. doi: 10.1136/bmjqs-2019-009587.
“An increasing number of older adults are using multiple medicines, and it is important that the benefits are outweighing the risks,” said Nikesh Parekh, MBBS, MPH, lead author of a recent study of a new predictive tool. The study was done in the context of the World Health Organization campaign to halve the incidence of medication-related harm (MRH) by 2022 – reducing MRH following hospital discharge was identified as a priority area.
This works allows clinicians to calculate the risk of a patient suffering MRH post-discharge requiring health care, said Dr. Parekh, a research fellow at Brighton and Sussex Medical School in Great Britain. “This enables practitioners and policy makers to target interventions to reduce MRH at those with highest risk. This should support the delivery of cost-effective care. The knowledge of individual risk can also prompt clinicians to reconsider any high-risk medicines that they intend on prescribing at discharge.”
This is the first prediction tool to calculate individual patient risk of serious MRH post-discharge, he added.The high readmission rate for older adults is often an avoidable pressure for hospitalists, particularly where MRH is the underlying cause. “The prediction tool has the potential to significantly reduce this burden for hospitalists/patients by identifying those individuals at high risk upon discharge and ensuring that monitoring and additional support is provided to them in the community with their medications,” Dr. Parekh said.
This electronic tool could be integrated into the electronic discharge summaries so that the information can be shared with primary care clinicians in a straightforward way. “The risk score should be calculated automatically by a self-population of the tool’s fields from information that exists on the patient within the electronic discharge system.”The tool now needs to be externally validated through testing in new settings to assess its validity and reliability in new populations. “If the tool is found to be usable by hospitalists and demonstrates reasonable predictive accuracy, then it should be implemented widely to reduce the incidence of MRH,” Dr. Parekh said.
Reference
1. Parekh N, et al. Medication-related harm in older adults following hospital discharge: development and validation of a prediction tool. BMJ Qual Saf. Published Online First 2019 Sept 16. doi: 10.1136/bmjqs-2019-009587.
AMA discharge linked to increased readmissions, discontinuity of care
Background: AMA discharges are common (1%-2% of all U.S. discharges) and disproportionately affect vulnerable patient populations, specifically those of lower socioeconomic status and the uninsured. Previous studies have been insufficiently powered to assess the effects of AMA discharge on 30-day readmission rates at a national level.
Study design: Retrospective cohort.
Setting: Community and teaching hospitals in 22 states.
Synopsis: With use of the 2014 Nationwide Readmissions Database of 23,110,641 index hospitalizations of patients 18 years or older, this study found that AMA discharge occurred with 1.3% of admissions. AMA discharge was associated with greater than twice the odds of 30-day readmission, compared with routine discharge. Of patients discharged AMA, 20.2% had an unplanned readmission within 30 days, compared with 10.1% of patients discharged routinely (OR, 2.25; 95% CI, 2.20-2.30; P less than .001).
Patients who were discharged AMA had almost 20 times the odds of undergoing repeat AMA discharge at readmission (OR, 18.41; 95% CI, 17.46-19.41; P less than .001) and twice the odds of presenting to a different hospital (OR, 2.35; 95% CI, 2.22-2.49; P less than .001). The study did not capture readmissions in a different state than that of the index hospital and was limited to the 22 states participating in the 2014 Readmissions Database.
Bottom line: Discharge AMA is associated with significantly higher odds of 30-day readmission, subsequent AMA discharge and presentation to another hospital, compared with routine discharge.
Citation: Kumar N. Burden of 30-day readmissions associated with discharge against medical advice among inpatients in the United States. Am J Med. 2019 Jun;132(6):708-17.
Dr. Webber is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: AMA discharges are common (1%-2% of all U.S. discharges) and disproportionately affect vulnerable patient populations, specifically those of lower socioeconomic status and the uninsured. Previous studies have been insufficiently powered to assess the effects of AMA discharge on 30-day readmission rates at a national level.
Study design: Retrospective cohort.
Setting: Community and teaching hospitals in 22 states.
Synopsis: With use of the 2014 Nationwide Readmissions Database of 23,110,641 index hospitalizations of patients 18 years or older, this study found that AMA discharge occurred with 1.3% of admissions. AMA discharge was associated with greater than twice the odds of 30-day readmission, compared with routine discharge. Of patients discharged AMA, 20.2% had an unplanned readmission within 30 days, compared with 10.1% of patients discharged routinely (OR, 2.25; 95% CI, 2.20-2.30; P less than .001).
Patients who were discharged AMA had almost 20 times the odds of undergoing repeat AMA discharge at readmission (OR, 18.41; 95% CI, 17.46-19.41; P less than .001) and twice the odds of presenting to a different hospital (OR, 2.35; 95% CI, 2.22-2.49; P less than .001). The study did not capture readmissions in a different state than that of the index hospital and was limited to the 22 states participating in the 2014 Readmissions Database.
Bottom line: Discharge AMA is associated with significantly higher odds of 30-day readmission, subsequent AMA discharge and presentation to another hospital, compared with routine discharge.
Citation: Kumar N. Burden of 30-day readmissions associated with discharge against medical advice among inpatients in the United States. Am J Med. 2019 Jun;132(6):708-17.
Dr. Webber is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.
Background: AMA discharges are common (1%-2% of all U.S. discharges) and disproportionately affect vulnerable patient populations, specifically those of lower socioeconomic status and the uninsured. Previous studies have been insufficiently powered to assess the effects of AMA discharge on 30-day readmission rates at a national level.
Study design: Retrospective cohort.
Setting: Community and teaching hospitals in 22 states.
Synopsis: With use of the 2014 Nationwide Readmissions Database of 23,110,641 index hospitalizations of patients 18 years or older, this study found that AMA discharge occurred with 1.3% of admissions. AMA discharge was associated with greater than twice the odds of 30-day readmission, compared with routine discharge. Of patients discharged AMA, 20.2% had an unplanned readmission within 30 days, compared with 10.1% of patients discharged routinely (OR, 2.25; 95% CI, 2.20-2.30; P less than .001).
Patients who were discharged AMA had almost 20 times the odds of undergoing repeat AMA discharge at readmission (OR, 18.41; 95% CI, 17.46-19.41; P less than .001) and twice the odds of presenting to a different hospital (OR, 2.35; 95% CI, 2.22-2.49; P less than .001). The study did not capture readmissions in a different state than that of the index hospital and was limited to the 22 states participating in the 2014 Readmissions Database.
Bottom line: Discharge AMA is associated with significantly higher odds of 30-day readmission, subsequent AMA discharge and presentation to another hospital, compared with routine discharge.
Citation: Kumar N. Burden of 30-day readmissions associated with discharge against medical advice among inpatients in the United States. Am J Med. 2019 Jun;132(6):708-17.
Dr. Webber is a hospitalist at Vanderbilt University Medical Center, Nashville, Tenn.