User login
MMR/MSI Testing for CRC Climbs, But Variations Persist
TOPLINE:
with testing rates differing by cancer stage, individual hospital, patient sex, race, and insurance status.
METHODOLOGY:
- In 2017, the National Comprehensive Cancer Network (NCCN) recommended universal testing for MMR and MSI among patients with CRC, but studies suggest that testing may still be underused.
- To assess trends and factors associated with MMR/MSI testing in the United States, researchers evaluated 834,797 patients diagnosed with stage I-IV CRC between 2012 and 2021 across 1366 Commission on Cancer–accredited hospitals in the National Cancer Database.
- The variability in MMR/MSI testing was assessed in relation to both patient and hospital-level factors.
- Overall, 70.7% patients had colon cancer, 7.3% had rectosigmoid cancer, and 22.0% had rectal cancer. The median patient age was 66 years; just over half (53%) were men, 81.8% were White, and 11.9% were Black.
TAKEAWAY:
- Overall, 43.9% patients underwent MMR/MSI testing, but testing rates increased more than threefold between 2012 and 2021 — from 22.7% to 71.5%. Still, testing rates varied depending on a range of factors.
- About 22% variability in MMR/MSI testing was attributed to hospital-level variations, with the best vs worst performing hospitals reporting testing rates of 90% vs 2%. This hospital-level variation may be caused by testing protocol differences at individual institutions, the authors said.
- The likelihood of undergoing MMR/MSI testing was lower in patients with stage IV vs stage I disease (adjusted odds ratio [aOR], 0.78) but higher in those with stage II (aOR, 1.53) and III (aOR, 1.40) disease.
- The likelihood of undergoing MMR/MSI testing was slightly lower for men than for women (aOR, 0.98) and for Black patients than for White patients (aOR, 0.97). Having a lower household income, public or no insurance (vs private insurance), or living a longer distance (more than 5 miles) from the treatment facility was also associated with lower odds of testing.
IN PRACTICE:
“This cohort study indicated that MMR/MSI testing increased markedly, suggesting increased NCCN guideline adherence,” the authors said. However, variations still exist by cancer stage, hospital, and patient factors. Implementing “widespread institution-level reflexive testing for every initial diagnostic biopsy” can improve testing rates and reduce disparities, the authors suggested.
SOURCE:
This study, led by Totadri Dhimal, MD, University of Rochester Medical Center in New York, was published online in JAMA Oncology.
LIMITATIONS:
The study lacked clinical granularity, and potential coding inaccuracies and incomplete data could have affected the interpretation and generalizability of the findings.
DISCLOSURES:
No funding information was provided for the study. One author reported receiving author royalties from UpToDate outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
with testing rates differing by cancer stage, individual hospital, patient sex, race, and insurance status.
METHODOLOGY:
- In 2017, the National Comprehensive Cancer Network (NCCN) recommended universal testing for MMR and MSI among patients with CRC, but studies suggest that testing may still be underused.
- To assess trends and factors associated with MMR/MSI testing in the United States, researchers evaluated 834,797 patients diagnosed with stage I-IV CRC between 2012 and 2021 across 1366 Commission on Cancer–accredited hospitals in the National Cancer Database.
- The variability in MMR/MSI testing was assessed in relation to both patient and hospital-level factors.
- Overall, 70.7% patients had colon cancer, 7.3% had rectosigmoid cancer, and 22.0% had rectal cancer. The median patient age was 66 years; just over half (53%) were men, 81.8% were White, and 11.9% were Black.
TAKEAWAY:
- Overall, 43.9% patients underwent MMR/MSI testing, but testing rates increased more than threefold between 2012 and 2021 — from 22.7% to 71.5%. Still, testing rates varied depending on a range of factors.
- About 22% variability in MMR/MSI testing was attributed to hospital-level variations, with the best vs worst performing hospitals reporting testing rates of 90% vs 2%. This hospital-level variation may be caused by testing protocol differences at individual institutions, the authors said.
- The likelihood of undergoing MMR/MSI testing was lower in patients with stage IV vs stage I disease (adjusted odds ratio [aOR], 0.78) but higher in those with stage II (aOR, 1.53) and III (aOR, 1.40) disease.
- The likelihood of undergoing MMR/MSI testing was slightly lower for men than for women (aOR, 0.98) and for Black patients than for White patients (aOR, 0.97). Having a lower household income, public or no insurance (vs private insurance), or living a longer distance (more than 5 miles) from the treatment facility was also associated with lower odds of testing.
IN PRACTICE:
“This cohort study indicated that MMR/MSI testing increased markedly, suggesting increased NCCN guideline adherence,” the authors said. However, variations still exist by cancer stage, hospital, and patient factors. Implementing “widespread institution-level reflexive testing for every initial diagnostic biopsy” can improve testing rates and reduce disparities, the authors suggested.
SOURCE:
This study, led by Totadri Dhimal, MD, University of Rochester Medical Center in New York, was published online in JAMA Oncology.
LIMITATIONS:
The study lacked clinical granularity, and potential coding inaccuracies and incomplete data could have affected the interpretation and generalizability of the findings.
DISCLOSURES:
No funding information was provided for the study. One author reported receiving author royalties from UpToDate outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
with testing rates differing by cancer stage, individual hospital, patient sex, race, and insurance status.
METHODOLOGY:
- In 2017, the National Comprehensive Cancer Network (NCCN) recommended universal testing for MMR and MSI among patients with CRC, but studies suggest that testing may still be underused.
- To assess trends and factors associated with MMR/MSI testing in the United States, researchers evaluated 834,797 patients diagnosed with stage I-IV CRC between 2012 and 2021 across 1366 Commission on Cancer–accredited hospitals in the National Cancer Database.
- The variability in MMR/MSI testing was assessed in relation to both patient and hospital-level factors.
- Overall, 70.7% patients had colon cancer, 7.3% had rectosigmoid cancer, and 22.0% had rectal cancer. The median patient age was 66 years; just over half (53%) were men, 81.8% were White, and 11.9% were Black.
TAKEAWAY:
- Overall, 43.9% patients underwent MMR/MSI testing, but testing rates increased more than threefold between 2012 and 2021 — from 22.7% to 71.5%. Still, testing rates varied depending on a range of factors.
- About 22% variability in MMR/MSI testing was attributed to hospital-level variations, with the best vs worst performing hospitals reporting testing rates of 90% vs 2%. This hospital-level variation may be caused by testing protocol differences at individual institutions, the authors said.
- The likelihood of undergoing MMR/MSI testing was lower in patients with stage IV vs stage I disease (adjusted odds ratio [aOR], 0.78) but higher in those with stage II (aOR, 1.53) and III (aOR, 1.40) disease.
- The likelihood of undergoing MMR/MSI testing was slightly lower for men than for women (aOR, 0.98) and for Black patients than for White patients (aOR, 0.97). Having a lower household income, public or no insurance (vs private insurance), or living a longer distance (more than 5 miles) from the treatment facility was also associated with lower odds of testing.
IN PRACTICE:
“This cohort study indicated that MMR/MSI testing increased markedly, suggesting increased NCCN guideline adherence,” the authors said. However, variations still exist by cancer stage, hospital, and patient factors. Implementing “widespread institution-level reflexive testing for every initial diagnostic biopsy” can improve testing rates and reduce disparities, the authors suggested.
SOURCE:
This study, led by Totadri Dhimal, MD, University of Rochester Medical Center in New York, was published online in JAMA Oncology.
LIMITATIONS:
The study lacked clinical granularity, and potential coding inaccuracies and incomplete data could have affected the interpretation and generalizability of the findings.
DISCLOSURES:
No funding information was provided for the study. One author reported receiving author royalties from UpToDate outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
New Treatment Effective for Male Postpartum Depression
A psychosocial intervention designed to improve depressive symptoms and promote good parenting skills can be an effective way of treating male postpartum depression, according to new research.
In a study conducted in Pakistan, about 70% fathers with postpartum depression who received the intervention showed complete remission of their depressive symptoms and experienced enhanced relationships with their children and domestic partners.
Called Learning Through Play Plus Dads (LTP + Dads), the intervention, which can be delivered by community health workers, could improve paternal mental health and child development not only in Pakistan but also in other populations, the authors stated.
The results of the study were published on October 2, 2024, in JAMA Psychiatry.
Stigmatized and Understudied
“Pakistan is a patriarchal society with strict gender roles, and male mental health, particularly postpartum depression in new fathers, is stigmatized and understudied,” lead investigator Ishrat Husain, MD, a senior scientist at the Centre for Addiction and Mental Health and associate professor of psychiatry at the University of Toronto in Ontario, Canada, said in an interview.
“Historically, and rightly so, the focus has always been on the mother, but men also experience significant emotional challenges as they adapt to being a parent. Fathers are also in need of support,” said Husain.
Male postpartum depression is prevalent in all populations. Globally, about 10% fathers have postpartum depression. But in societies like Pakistan, rates of male postpartum depression have been reported to be as high as 23.5%.
The study included 357 fathers aged 18 years or older (mean age, 31.44 years) with a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnosis of major depressive episode and a child younger than 30 months.
They were randomly assigned either to receive treatment as usual (n = 186) or to participate in the LTP + Dads program (n = 171). LTP + Dads is a parenting and mental health initiative adapted from a similar program for Pakistani mothers. It combines parenting skills training, play therapy, and cognitive behavioral therapy. In this study, the initiative was delivered by community health workers in 12 group sessions over 4 months. Sessions took place weekly for the first 2 months and biweekly thereafter.
The researchers assessed changes in the 17-item Hamilton Depression Rating Scale (HDRS-17) score at 4 months and at 6 months. They also looked at anxiety symptoms; parenting stress; intimate partner violence; functioning; quality of life; and child social, emotional, and physical health outcomes.
Improved Child Development
There were significantly greater reductions in HDRS-17 scores in the LTP + Dads group than in the treatment as usual group at 4 months (group difference ratio [GDR], 0.66; P < .001) and at 6 months (GDR, 0.67; P < .001).
Similar results were seen for anxiety (GDR, 0.62; P < .001), parenting stress (GDR, −12.5; P < .001), intimate partner violence (GDR, 0.89; P = .05), disability (GDR, 0.77; P = .03), and health-related quality of life (GDR, 12.7; P < .001) at 4 months. The differences in depression and parenting stress were sustained at 6 months.
In addition, children of fathers who received the parenting intervention showed significantly greater improvements in social-emotional development scores (mean difference, −20.8; P < .001) at 6 months than children of those who received the treatment as usual.
“We believe that this program could also be successful in other countries, including Canada,” said Husain. “Canada is multicultural, and similar patterns of male postpartum depression probably exist here. We know that cultural and social pressures create barriers to seeking mental health support for men. Stigma and cultural beliefs often prevent new fathers from seeking the help they need. Programs like LTP + Dads can help men transition to their new role as fathers by giving them support to process their emotions,” he said.
Husain added that the program will be expanded throughout Pakistan to include about 4000 fathers and their partners.
‘Remarkable’ Success Rate
“Postpartum depression in men is still something that people are trying to understand,” John Ogrodniczuk, MD, professor of psychiatry and director of the psychotherapy program at The University of British Columbia, Vancouver, Canada, said in an interview. He did not participate in the study.
“Obviously, men aren’t going through the same endocrine changes that women are, but nonetheless, a lot of men do actually struggle with it,” said Ogrodniczuk, who is also the founder of HeadsUpGuys, a mental health resource for men.
“Understandably, most of the literature is around postpartum depression in women, not so much around men. The positive results seen here are interesting, especially in a country that is patriarchal and where there is not a lot of uptake of mental health interventions and services by men,” he said.
“The success rate of this psychosocial intervention is remarkable, so I am excited to see that the researchers have secured funding to expand the study and validate their results with a larger group of participants,” Simon B. Sherry, PhD, professor of psychology and neuroscience at Dalhousie University, Halifax, Nova Scotia, Canada, said in an interview.
“I am also encouraged by the inclusion of play-based activities in addition to cognitive behavioral therapy. Perhaps more than any other role we hold through life, the role of parent comes with copious societal and personal expectations, plus with all that pressure, transitioning into that role is hard for everyone, but especially for those with postpartum depression. Supporting parents and improving their mental well-being goes a long way toward raising mentally healthy kids,” said Sherry, who was not part of the study.
The study was funded by a grant from Grand Challenges Canada, an Academic Scholars Award from the Department of Psychiatry at the University of Toronto, and a Tier 2 Canada Research Chair from the Canadian Institutes of Health Research. Husain reported receiving grants from COMPASS Pathfinder, stock options from Mindset Pharma, and personal fees from Wake Network, outside the submitted work. He previously served as a trustee for the Pakistan Institute of Living and Learning. Ogrodniczuk and Sherry reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A psychosocial intervention designed to improve depressive symptoms and promote good parenting skills can be an effective way of treating male postpartum depression, according to new research.
In a study conducted in Pakistan, about 70% fathers with postpartum depression who received the intervention showed complete remission of their depressive symptoms and experienced enhanced relationships with their children and domestic partners.
Called Learning Through Play Plus Dads (LTP + Dads), the intervention, which can be delivered by community health workers, could improve paternal mental health and child development not only in Pakistan but also in other populations, the authors stated.
The results of the study were published on October 2, 2024, in JAMA Psychiatry.
Stigmatized and Understudied
“Pakistan is a patriarchal society with strict gender roles, and male mental health, particularly postpartum depression in new fathers, is stigmatized and understudied,” lead investigator Ishrat Husain, MD, a senior scientist at the Centre for Addiction and Mental Health and associate professor of psychiatry at the University of Toronto in Ontario, Canada, said in an interview.
“Historically, and rightly so, the focus has always been on the mother, but men also experience significant emotional challenges as they adapt to being a parent. Fathers are also in need of support,” said Husain.
Male postpartum depression is prevalent in all populations. Globally, about 10% fathers have postpartum depression. But in societies like Pakistan, rates of male postpartum depression have been reported to be as high as 23.5%.
The study included 357 fathers aged 18 years or older (mean age, 31.44 years) with a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnosis of major depressive episode and a child younger than 30 months.
They were randomly assigned either to receive treatment as usual (n = 186) or to participate in the LTP + Dads program (n = 171). LTP + Dads is a parenting and mental health initiative adapted from a similar program for Pakistani mothers. It combines parenting skills training, play therapy, and cognitive behavioral therapy. In this study, the initiative was delivered by community health workers in 12 group sessions over 4 months. Sessions took place weekly for the first 2 months and biweekly thereafter.
The researchers assessed changes in the 17-item Hamilton Depression Rating Scale (HDRS-17) score at 4 months and at 6 months. They also looked at anxiety symptoms; parenting stress; intimate partner violence; functioning; quality of life; and child social, emotional, and physical health outcomes.
Improved Child Development
There were significantly greater reductions in HDRS-17 scores in the LTP + Dads group than in the treatment as usual group at 4 months (group difference ratio [GDR], 0.66; P < .001) and at 6 months (GDR, 0.67; P < .001).
Similar results were seen for anxiety (GDR, 0.62; P < .001), parenting stress (GDR, −12.5; P < .001), intimate partner violence (GDR, 0.89; P = .05), disability (GDR, 0.77; P = .03), and health-related quality of life (GDR, 12.7; P < .001) at 4 months. The differences in depression and parenting stress were sustained at 6 months.
In addition, children of fathers who received the parenting intervention showed significantly greater improvements in social-emotional development scores (mean difference, −20.8; P < .001) at 6 months than children of those who received the treatment as usual.
“We believe that this program could also be successful in other countries, including Canada,” said Husain. “Canada is multicultural, and similar patterns of male postpartum depression probably exist here. We know that cultural and social pressures create barriers to seeking mental health support for men. Stigma and cultural beliefs often prevent new fathers from seeking the help they need. Programs like LTP + Dads can help men transition to their new role as fathers by giving them support to process their emotions,” he said.
Husain added that the program will be expanded throughout Pakistan to include about 4000 fathers and their partners.
‘Remarkable’ Success Rate
“Postpartum depression in men is still something that people are trying to understand,” John Ogrodniczuk, MD, professor of psychiatry and director of the psychotherapy program at The University of British Columbia, Vancouver, Canada, said in an interview. He did not participate in the study.
“Obviously, men aren’t going through the same endocrine changes that women are, but nonetheless, a lot of men do actually struggle with it,” said Ogrodniczuk, who is also the founder of HeadsUpGuys, a mental health resource for men.
“Understandably, most of the literature is around postpartum depression in women, not so much around men. The positive results seen here are interesting, especially in a country that is patriarchal and where there is not a lot of uptake of mental health interventions and services by men,” he said.
“The success rate of this psychosocial intervention is remarkable, so I am excited to see that the researchers have secured funding to expand the study and validate their results with a larger group of participants,” Simon B. Sherry, PhD, professor of psychology and neuroscience at Dalhousie University, Halifax, Nova Scotia, Canada, said in an interview.
“I am also encouraged by the inclusion of play-based activities in addition to cognitive behavioral therapy. Perhaps more than any other role we hold through life, the role of parent comes with copious societal and personal expectations, plus with all that pressure, transitioning into that role is hard for everyone, but especially for those with postpartum depression. Supporting parents and improving their mental well-being goes a long way toward raising mentally healthy kids,” said Sherry, who was not part of the study.
The study was funded by a grant from Grand Challenges Canada, an Academic Scholars Award from the Department of Psychiatry at the University of Toronto, and a Tier 2 Canada Research Chair from the Canadian Institutes of Health Research. Husain reported receiving grants from COMPASS Pathfinder, stock options from Mindset Pharma, and personal fees from Wake Network, outside the submitted work. He previously served as a trustee for the Pakistan Institute of Living and Learning. Ogrodniczuk and Sherry reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A psychosocial intervention designed to improve depressive symptoms and promote good parenting skills can be an effective way of treating male postpartum depression, according to new research.
In a study conducted in Pakistan, about 70% fathers with postpartum depression who received the intervention showed complete remission of their depressive symptoms and experienced enhanced relationships with their children and domestic partners.
Called Learning Through Play Plus Dads (LTP + Dads), the intervention, which can be delivered by community health workers, could improve paternal mental health and child development not only in Pakistan but also in other populations, the authors stated.
The results of the study were published on October 2, 2024, in JAMA Psychiatry.
Stigmatized and Understudied
“Pakistan is a patriarchal society with strict gender roles, and male mental health, particularly postpartum depression in new fathers, is stigmatized and understudied,” lead investigator Ishrat Husain, MD, a senior scientist at the Centre for Addiction and Mental Health and associate professor of psychiatry at the University of Toronto in Ontario, Canada, said in an interview.
“Historically, and rightly so, the focus has always been on the mother, but men also experience significant emotional challenges as they adapt to being a parent. Fathers are also in need of support,” said Husain.
Male postpartum depression is prevalent in all populations. Globally, about 10% fathers have postpartum depression. But in societies like Pakistan, rates of male postpartum depression have been reported to be as high as 23.5%.
The study included 357 fathers aged 18 years or older (mean age, 31.44 years) with a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, diagnosis of major depressive episode and a child younger than 30 months.
They were randomly assigned either to receive treatment as usual (n = 186) or to participate in the LTP + Dads program (n = 171). LTP + Dads is a parenting and mental health initiative adapted from a similar program for Pakistani mothers. It combines parenting skills training, play therapy, and cognitive behavioral therapy. In this study, the initiative was delivered by community health workers in 12 group sessions over 4 months. Sessions took place weekly for the first 2 months and biweekly thereafter.
The researchers assessed changes in the 17-item Hamilton Depression Rating Scale (HDRS-17) score at 4 months and at 6 months. They also looked at anxiety symptoms; parenting stress; intimate partner violence; functioning; quality of life; and child social, emotional, and physical health outcomes.
Improved Child Development
There were significantly greater reductions in HDRS-17 scores in the LTP + Dads group than in the treatment as usual group at 4 months (group difference ratio [GDR], 0.66; P < .001) and at 6 months (GDR, 0.67; P < .001).
Similar results were seen for anxiety (GDR, 0.62; P < .001), parenting stress (GDR, −12.5; P < .001), intimate partner violence (GDR, 0.89; P = .05), disability (GDR, 0.77; P = .03), and health-related quality of life (GDR, 12.7; P < .001) at 4 months. The differences in depression and parenting stress were sustained at 6 months.
In addition, children of fathers who received the parenting intervention showed significantly greater improvements in social-emotional development scores (mean difference, −20.8; P < .001) at 6 months than children of those who received the treatment as usual.
“We believe that this program could also be successful in other countries, including Canada,” said Husain. “Canada is multicultural, and similar patterns of male postpartum depression probably exist here. We know that cultural and social pressures create barriers to seeking mental health support for men. Stigma and cultural beliefs often prevent new fathers from seeking the help they need. Programs like LTP + Dads can help men transition to their new role as fathers by giving them support to process their emotions,” he said.
Husain added that the program will be expanded throughout Pakistan to include about 4000 fathers and their partners.
‘Remarkable’ Success Rate
“Postpartum depression in men is still something that people are trying to understand,” John Ogrodniczuk, MD, professor of psychiatry and director of the psychotherapy program at The University of British Columbia, Vancouver, Canada, said in an interview. He did not participate in the study.
“Obviously, men aren’t going through the same endocrine changes that women are, but nonetheless, a lot of men do actually struggle with it,” said Ogrodniczuk, who is also the founder of HeadsUpGuys, a mental health resource for men.
“Understandably, most of the literature is around postpartum depression in women, not so much around men. The positive results seen here are interesting, especially in a country that is patriarchal and where there is not a lot of uptake of mental health interventions and services by men,” he said.
“The success rate of this psychosocial intervention is remarkable, so I am excited to see that the researchers have secured funding to expand the study and validate their results with a larger group of participants,” Simon B. Sherry, PhD, professor of psychology and neuroscience at Dalhousie University, Halifax, Nova Scotia, Canada, said in an interview.
“I am also encouraged by the inclusion of play-based activities in addition to cognitive behavioral therapy. Perhaps more than any other role we hold through life, the role of parent comes with copious societal and personal expectations, plus with all that pressure, transitioning into that role is hard for everyone, but especially for those with postpartum depression. Supporting parents and improving their mental well-being goes a long way toward raising mentally healthy kids,” said Sherry, who was not part of the study.
The study was funded by a grant from Grand Challenges Canada, an Academic Scholars Award from the Department of Psychiatry at the University of Toronto, and a Tier 2 Canada Research Chair from the Canadian Institutes of Health Research. Husain reported receiving grants from COMPASS Pathfinder, stock options from Mindset Pharma, and personal fees from Wake Network, outside the submitted work. He previously served as a trustee for the Pakistan Institute of Living and Learning. Ogrodniczuk and Sherry reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Room for Improvement in Screening for Sexually Transmitted Diseases
Syphilis. It is often called the “great imitator.” It is speculated that this infection led to King George III of England going mad and likely contributing to his death. In the modern era, the discovery of penicillin in 1928 was instrumental in treating this once-deadly infection. Over the ensuing decades, rates of syphilis continued to decline. However, according to the Centers for Disease Control and Prevention, from 2018-2022 reported cases of syphilis in the United States have increased by 79% and continue to increase each year. Men who have sex with men (MSM) accounted for 41.4% of infections nationwide during this time period. This extraordinary rise highlights the need for better screening in our patients.
I currently live and practice in Texas, so I will use it as a case example. In 2013, Texas reported 1,471 cases of primary or secondary syphilis. By 2022, this number had risen to 4,655, a 216% increase. CDC data shows that Texas cases among men increased from 1,917 in 2019 to 3,324 in 2022, with MSM accounting for 1,341 (40%) of those infections. Adolescents and young adults aged 15-24 accounted for the second-highest number of new infections. Interestingly, rates of syphilis in men began to rise in Texas starting in 2013, the first full year that Truvada (emtricitabine and tenofovir disoproxil fumarate) was available for HIV pre-exposure prophylaxis (PrEP). While no definitive study has proven that the availability of PrEP caused an increase in condomless sexual intercourse, the number of high school students in Texas who did not use a condom at their last intercourse increased from 47.1% in 2013 to 50% in 2021.
The data above highlights the need to increase screening, especially in primary care and emergency room settings. According to the 2021 Youth Risk Behavior Survey, 94.8% of high school students surveyed that they were not tested for STIs in the 12 months prior to the survey. This compares with 91.4% in the 2019 survey. When STI testing is done, many adolescents often choose to forgo blood testing for HIV and syphilis and decide only to do urine NAATs testing for Neisseria gonorrhoeae and Chlamydia trachomatis. Therefore, those physicians and other healthcare providers who take care of adolescents and young adults must work to improve screening for ALL STIs. According to the American Academy of Pediatrics Bright Futures Periodicity Guidelines, pediatricians should screen for HIV in all patients at least once starting at age 15 and then thereafter based on risk assessment. Adding syphilis screening at the same time as the above HIV screening is an easy way to improve testing and treatment for this potentially deadly condition. If access to phlebotomy is not available, there are rapid HIV and syphilis tests that can be done in physicians’ offices. To perform these risk assessments, pediatricians must spend time alone with their adolescent and young patients at nearly every visit to discuss behaviors. Pediatricians should also be aware to consider syphilis on their differential for patients with unexplained rashes, sores in the mouth, or flu-like symptoms if that young person is sexually active.
Compounding the issue of increasing cases of syphilis is a national shortage of intramuscular penicillin G benzathine, the preferred treatment, which began in April 2023 only recently began to improve as of August 2024. Oral doxycycline can be used as a backup for some patients. Still, IM penicillin G is the only recommended treatment available for pregnant patients or those with advanced disease. The increasing number of cases, as well as the medication shortages, remind all of us that
Dr. M. Brett Cooper, is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
Syphilis. It is often called the “great imitator.” It is speculated that this infection led to King George III of England going mad and likely contributing to his death. In the modern era, the discovery of penicillin in 1928 was instrumental in treating this once-deadly infection. Over the ensuing decades, rates of syphilis continued to decline. However, according to the Centers for Disease Control and Prevention, from 2018-2022 reported cases of syphilis in the United States have increased by 79% and continue to increase each year. Men who have sex with men (MSM) accounted for 41.4% of infections nationwide during this time period. This extraordinary rise highlights the need for better screening in our patients.
I currently live and practice in Texas, so I will use it as a case example. In 2013, Texas reported 1,471 cases of primary or secondary syphilis. By 2022, this number had risen to 4,655, a 216% increase. CDC data shows that Texas cases among men increased from 1,917 in 2019 to 3,324 in 2022, with MSM accounting for 1,341 (40%) of those infections. Adolescents and young adults aged 15-24 accounted for the second-highest number of new infections. Interestingly, rates of syphilis in men began to rise in Texas starting in 2013, the first full year that Truvada (emtricitabine and tenofovir disoproxil fumarate) was available for HIV pre-exposure prophylaxis (PrEP). While no definitive study has proven that the availability of PrEP caused an increase in condomless sexual intercourse, the number of high school students in Texas who did not use a condom at their last intercourse increased from 47.1% in 2013 to 50% in 2021.
The data above highlights the need to increase screening, especially in primary care and emergency room settings. According to the 2021 Youth Risk Behavior Survey, 94.8% of high school students surveyed that they were not tested for STIs in the 12 months prior to the survey. This compares with 91.4% in the 2019 survey. When STI testing is done, many adolescents often choose to forgo blood testing for HIV and syphilis and decide only to do urine NAATs testing for Neisseria gonorrhoeae and Chlamydia trachomatis. Therefore, those physicians and other healthcare providers who take care of adolescents and young adults must work to improve screening for ALL STIs. According to the American Academy of Pediatrics Bright Futures Periodicity Guidelines, pediatricians should screen for HIV in all patients at least once starting at age 15 and then thereafter based on risk assessment. Adding syphilis screening at the same time as the above HIV screening is an easy way to improve testing and treatment for this potentially deadly condition. If access to phlebotomy is not available, there are rapid HIV and syphilis tests that can be done in physicians’ offices. To perform these risk assessments, pediatricians must spend time alone with their adolescent and young patients at nearly every visit to discuss behaviors. Pediatricians should also be aware to consider syphilis on their differential for patients with unexplained rashes, sores in the mouth, or flu-like symptoms if that young person is sexually active.
Compounding the issue of increasing cases of syphilis is a national shortage of intramuscular penicillin G benzathine, the preferred treatment, which began in April 2023 only recently began to improve as of August 2024. Oral doxycycline can be used as a backup for some patients. Still, IM penicillin G is the only recommended treatment available for pregnant patients or those with advanced disease. The increasing number of cases, as well as the medication shortages, remind all of us that
Dr. M. Brett Cooper, is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
Syphilis. It is often called the “great imitator.” It is speculated that this infection led to King George III of England going mad and likely contributing to his death. In the modern era, the discovery of penicillin in 1928 was instrumental in treating this once-deadly infection. Over the ensuing decades, rates of syphilis continued to decline. However, according to the Centers for Disease Control and Prevention, from 2018-2022 reported cases of syphilis in the United States have increased by 79% and continue to increase each year. Men who have sex with men (MSM) accounted for 41.4% of infections nationwide during this time period. This extraordinary rise highlights the need for better screening in our patients.
I currently live and practice in Texas, so I will use it as a case example. In 2013, Texas reported 1,471 cases of primary or secondary syphilis. By 2022, this number had risen to 4,655, a 216% increase. CDC data shows that Texas cases among men increased from 1,917 in 2019 to 3,324 in 2022, with MSM accounting for 1,341 (40%) of those infections. Adolescents and young adults aged 15-24 accounted for the second-highest number of new infections. Interestingly, rates of syphilis in men began to rise in Texas starting in 2013, the first full year that Truvada (emtricitabine and tenofovir disoproxil fumarate) was available for HIV pre-exposure prophylaxis (PrEP). While no definitive study has proven that the availability of PrEP caused an increase in condomless sexual intercourse, the number of high school students in Texas who did not use a condom at their last intercourse increased from 47.1% in 2013 to 50% in 2021.
The data above highlights the need to increase screening, especially in primary care and emergency room settings. According to the 2021 Youth Risk Behavior Survey, 94.8% of high school students surveyed that they were not tested for STIs in the 12 months prior to the survey. This compares with 91.4% in the 2019 survey. When STI testing is done, many adolescents often choose to forgo blood testing for HIV and syphilis and decide only to do urine NAATs testing for Neisseria gonorrhoeae and Chlamydia trachomatis. Therefore, those physicians and other healthcare providers who take care of adolescents and young adults must work to improve screening for ALL STIs. According to the American Academy of Pediatrics Bright Futures Periodicity Guidelines, pediatricians should screen for HIV in all patients at least once starting at age 15 and then thereafter based on risk assessment. Adding syphilis screening at the same time as the above HIV screening is an easy way to improve testing and treatment for this potentially deadly condition. If access to phlebotomy is not available, there are rapid HIV and syphilis tests that can be done in physicians’ offices. To perform these risk assessments, pediatricians must spend time alone with their adolescent and young patients at nearly every visit to discuss behaviors. Pediatricians should also be aware to consider syphilis on their differential for patients with unexplained rashes, sores in the mouth, or flu-like symptoms if that young person is sexually active.
Compounding the issue of increasing cases of syphilis is a national shortage of intramuscular penicillin G benzathine, the preferred treatment, which began in April 2023 only recently began to improve as of August 2024. Oral doxycycline can be used as a backup for some patients. Still, IM penicillin G is the only recommended treatment available for pregnant patients or those with advanced disease. The increasing number of cases, as well as the medication shortages, remind all of us that
Dr. M. Brett Cooper, is an assistant professor of pediatrics at University of Texas Southwestern, Dallas, and an adolescent medicine specialist at Children’s Medical Center Dallas.
GI Docs Will Need to Forge a ‘Human-Computer Cooperative’
Several artificial intelligence (AI) technologies are emerging that will change the management of gastrointestinal (GI) diseases sooner rather than later. One of the leading researchers working toward that AI-driven future is Ryan W. Stidham, MD, MS, AGAF, associate professor of gastroenterology and computational medicine and bioinformatics at the University of Michigan, Ann Arbor.
Stidham’s work focuses on leveraging AI to develop automated systems that better quantify disease activity and aid gastroenterologists in their decision-making. He also serves as a meber of AGA's AI Task Force. what the technology may do to improve physician efficiency, and why gastroenterologists shouldn’t be worried about being replaced by machines any time soon.
How did you first become involved in studying AI applications for GI conditions?
My medical training coincided with the emergence of electronic health records (EHRs) making enormous amounts of data, ranging from laboratory results to diagnostic codes and billing records, readily accessible.
I quickly contracted data analytics fever, but a major problem became apparent: EHRs and medical claims data alone only weakly describe a patient. Researchers in the field were excited to use machine learning for personalizing treatment decisions for GI conditions, including inflammatory bowel disease (IBD). But no matter how large the dataset, the EHRs lacked the most rudimentary descriptions: What was the patient’s IBD phenotype? Where exactly was the disease located?
I could see machine learning had the potential to learn and reproduce expert decision-making. Unfortunately, we were fueling this machine-learning rocket ship with crude data unlikely to take us very far. Gastroenterologists rely on data in progress notes, emails, interpretations of colonoscopies, and radiologists’ and pathologists’ reviews of imaging to make treatment decisions, but that information is not well organized in any dataset.
I wanted to use AI to retrieve that key information in text, images, and video that we use every day for IBD care, automatically interpreting the data like a seasoned gastroenterologist. Generating higher-quality data describing patients could take our AI models from interesting research to useful and reliable tools in clinical care.
How did your early research go about trying to solve that problem?
My GI career began amid the IBD field shifting from relying on symptoms alone to objective biomarkers for IBD assessment, particularly focusing on standardized scoring of endoscopic mucosal inflammation. However, these scores were challenged with interobserver variability, prompting the need for centralized reading. More importantly, these scores are qualitative and do not capture all the visual findings an experienced physician appreciates when assessing severity, phenotype, and therapeutic effect. As a result, even experts could disagree on the degree of endoscopic severity, and patients with obvious differences in the appearance of mucosa could have the same endoscopic score.
I asked myself: Are we really using these measures to make treatment decisions and determine the effectiveness of investigational therapies? I thought we could do better and aimed to improve endoscopic IBD assessments using then-emerging digital image analysis techniques.
Convolutional neural network (CNN) modeling was just becoming feasible as computing performance increased. CNNs are well suited for complex medical image interpretation, using an associated “label,” such as the presence or grade of disease, to decipher the complex set of image feature patterns characterizing an expert’s determination of disease severity.
How did you convert the promise of CNN into tangible results?
The plan was simple: Collect endoscopic images from patients with IBD, find some experts to grade IBD severity on the images, and train a CNN model using the images and expert labels.
In 2016, developing a CNN wasn’t easy. There was no database of endoscopic images or simple methods for image labeling. The CNN needed tens of thousands of images. How were we to collect enough images with a broad range of IBD severity? I also reached some technical limits and needed help solving computational challenges.
Designing our first IBD endoscopic CNN took years of reading, coursework, additional training, and a new host of collaborators.
Failure was frequent, and my colleagues and I spent a lot of nights and weekends looking at thousands of individual endoscopic images. But we eventually had a working model for grading endoscopic severity, and its performance exceeded our expectations.
To our surprise, the CNN model grading of ulcerative colitis severity almost perfectly matched the opinion of IBD experts. We introduced the proof of concept that AI could automate complex disease measurement for IBD.
What took us 3 years in 2016 would take about 3 weeks today.
You have said that AI could help reduce the substantial administrative burdens in medicine today. What might an AI-assisted future look like for time-strapped gastroenterologists?
We will be spending more time on complex decision-making and developing treatment plans, with less time needed to hunt for information in the chart and administrative tasks.
The practical applications of AI will chip away at tedious mechanical tasks, soon to be done by machines, reclaiming time for gastroenterologists.
For example, automated documentation is almost usable, and audio recordings in the clinic could be leveraged to generate office notes.
Computer vision analysis of endoscopic video is generating draft procedural notes and letters to patients in a shared language, as well as recommending surveillance intervals based on the findings.
Text processing is already being used to automate billing and manage health maintenance like vaccinations, laboratory screening, and therapeutic drug monitoring.
Unfortunately, I don’t think that AI will immediately help with burnout. These near-term AI administrative assistant advantages, however, will help us manage the increasing patient load, address physician shortages, and potentially improve access to care in underserved areas.
Were there any surprises in your work?
I must admit, I was certain AI would put us gastroenterologists to shame. Over time, I have reversed that view.
AI really struggles to understand the holistic patient context when interpreting disease and predicting what to do for an individual patient. Humans anticipate gaps in data and customize the weighting of information when making decisions for individuals. An experienced gastroenterologist can incorporate risks, harms, and costs in ways AI is several generations from achieving.
With certainty, AI will outperform gastroenterologists for tedious and repetitive tasks, and we should gladly expect AI to assume those responsibilities. However, many unknowns remain in the daily management of GI conditions. We will continue to rely on the clinical experience, creativity, and improvisation of gastroenterologists for years to come.
Has there been a turning-point moment when it felt like this technology moved from being more theoretical to something with real-world clinical applications?
Last spring, I saw a lecture by Peter Lee, who is president of Microsoft Research and a leader in developing AI-powered applications in medicine and scientific research, demonstrating how a large language model (LLM) could “understand” medical text and generate responses to questions. My jaw dropped.
We watched an LLM answer American Board of Internal Medicine questions with perfect explanations and rationale. He demonstrated how an audio recording of a clinic visit could be used to automatically generate a SOAP (subjective, objective assessment and plan) note. It was better than anything I would have drafted. He also showed how the LLM could directly ingest EHR data, without any modification, and provide a great diagnosis and treatment plan. Finally, LLM chatbots could carry on an interactive conversation with a patient that would be difficult to distinguish from a human physician.
The inevitability of AI-powered transformations in gastroenterology care became apparent.
Documentation, billing, and administrative work will be handled by AI. AI will collect and organize information for me. Chart reviews and even telephone/email checkups on patients will be a thing of the past. AI chatbots will be able to discuss an individual patient’s condition and test results. Our GI-AI assistants will proactively collect information from patients after hospitalization or react to a change in labs.
AI will soon be an amazing diagnostician and will know more than me. So do we need to polish our resumes for new careers? No, but we will need to adapt to changes, which I believe on the whole will be better for gastroenterologists and patients.
What does adaptation look like for gastroenterologists over the next handful of years?
Like any other tool, gastroenterologists will be figuring out how to use AI prediction models, chatbots, and imaging analytics. Value, ease of use, and information-gain will drive which AI tools are ultimately adopted.
Memory, information recall, calculations, and repetitive tasks where gastroenterologists occasionally error or find tiresome will become the job of machines. We will still be the magicians, now aided by machines, applying our human strengths of contextual awareness, judgment, and creativity to find customized solutions for more patients.
That, I think, is the future that we are reliably moving toward over the next decade — a human-computer cooperative throughout gastroenterology (including IBD) and, frankly, all of medicine.
A version of this article appeared on Medscape.com.
Several artificial intelligence (AI) technologies are emerging that will change the management of gastrointestinal (GI) diseases sooner rather than later. One of the leading researchers working toward that AI-driven future is Ryan W. Stidham, MD, MS, AGAF, associate professor of gastroenterology and computational medicine and bioinformatics at the University of Michigan, Ann Arbor.
Stidham’s work focuses on leveraging AI to develop automated systems that better quantify disease activity and aid gastroenterologists in their decision-making. He also serves as a meber of AGA's AI Task Force. what the technology may do to improve physician efficiency, and why gastroenterologists shouldn’t be worried about being replaced by machines any time soon.
How did you first become involved in studying AI applications for GI conditions?
My medical training coincided with the emergence of electronic health records (EHRs) making enormous amounts of data, ranging from laboratory results to diagnostic codes and billing records, readily accessible.
I quickly contracted data analytics fever, but a major problem became apparent: EHRs and medical claims data alone only weakly describe a patient. Researchers in the field were excited to use machine learning for personalizing treatment decisions for GI conditions, including inflammatory bowel disease (IBD). But no matter how large the dataset, the EHRs lacked the most rudimentary descriptions: What was the patient’s IBD phenotype? Where exactly was the disease located?
I could see machine learning had the potential to learn and reproduce expert decision-making. Unfortunately, we were fueling this machine-learning rocket ship with crude data unlikely to take us very far. Gastroenterologists rely on data in progress notes, emails, interpretations of colonoscopies, and radiologists’ and pathologists’ reviews of imaging to make treatment decisions, but that information is not well organized in any dataset.
I wanted to use AI to retrieve that key information in text, images, and video that we use every day for IBD care, automatically interpreting the data like a seasoned gastroenterologist. Generating higher-quality data describing patients could take our AI models from interesting research to useful and reliable tools in clinical care.
How did your early research go about trying to solve that problem?
My GI career began amid the IBD field shifting from relying on symptoms alone to objective biomarkers for IBD assessment, particularly focusing on standardized scoring of endoscopic mucosal inflammation. However, these scores were challenged with interobserver variability, prompting the need for centralized reading. More importantly, these scores are qualitative and do not capture all the visual findings an experienced physician appreciates when assessing severity, phenotype, and therapeutic effect. As a result, even experts could disagree on the degree of endoscopic severity, and patients with obvious differences in the appearance of mucosa could have the same endoscopic score.
I asked myself: Are we really using these measures to make treatment decisions and determine the effectiveness of investigational therapies? I thought we could do better and aimed to improve endoscopic IBD assessments using then-emerging digital image analysis techniques.
Convolutional neural network (CNN) modeling was just becoming feasible as computing performance increased. CNNs are well suited for complex medical image interpretation, using an associated “label,” such as the presence or grade of disease, to decipher the complex set of image feature patterns characterizing an expert’s determination of disease severity.
How did you convert the promise of CNN into tangible results?
The plan was simple: Collect endoscopic images from patients with IBD, find some experts to grade IBD severity on the images, and train a CNN model using the images and expert labels.
In 2016, developing a CNN wasn’t easy. There was no database of endoscopic images or simple methods for image labeling. The CNN needed tens of thousands of images. How were we to collect enough images with a broad range of IBD severity? I also reached some technical limits and needed help solving computational challenges.
Designing our first IBD endoscopic CNN took years of reading, coursework, additional training, and a new host of collaborators.
Failure was frequent, and my colleagues and I spent a lot of nights and weekends looking at thousands of individual endoscopic images. But we eventually had a working model for grading endoscopic severity, and its performance exceeded our expectations.
To our surprise, the CNN model grading of ulcerative colitis severity almost perfectly matched the opinion of IBD experts. We introduced the proof of concept that AI could automate complex disease measurement for IBD.
What took us 3 years in 2016 would take about 3 weeks today.
You have said that AI could help reduce the substantial administrative burdens in medicine today. What might an AI-assisted future look like for time-strapped gastroenterologists?
We will be spending more time on complex decision-making and developing treatment plans, with less time needed to hunt for information in the chart and administrative tasks.
The practical applications of AI will chip away at tedious mechanical tasks, soon to be done by machines, reclaiming time for gastroenterologists.
For example, automated documentation is almost usable, and audio recordings in the clinic could be leveraged to generate office notes.
Computer vision analysis of endoscopic video is generating draft procedural notes and letters to patients in a shared language, as well as recommending surveillance intervals based on the findings.
Text processing is already being used to automate billing and manage health maintenance like vaccinations, laboratory screening, and therapeutic drug monitoring.
Unfortunately, I don’t think that AI will immediately help with burnout. These near-term AI administrative assistant advantages, however, will help us manage the increasing patient load, address physician shortages, and potentially improve access to care in underserved areas.
Were there any surprises in your work?
I must admit, I was certain AI would put us gastroenterologists to shame. Over time, I have reversed that view.
AI really struggles to understand the holistic patient context when interpreting disease and predicting what to do for an individual patient. Humans anticipate gaps in data and customize the weighting of information when making decisions for individuals. An experienced gastroenterologist can incorporate risks, harms, and costs in ways AI is several generations from achieving.
With certainty, AI will outperform gastroenterologists for tedious and repetitive tasks, and we should gladly expect AI to assume those responsibilities. However, many unknowns remain in the daily management of GI conditions. We will continue to rely on the clinical experience, creativity, and improvisation of gastroenterologists for years to come.
Has there been a turning-point moment when it felt like this technology moved from being more theoretical to something with real-world clinical applications?
Last spring, I saw a lecture by Peter Lee, who is president of Microsoft Research and a leader in developing AI-powered applications in medicine and scientific research, demonstrating how a large language model (LLM) could “understand” medical text and generate responses to questions. My jaw dropped.
We watched an LLM answer American Board of Internal Medicine questions with perfect explanations and rationale. He demonstrated how an audio recording of a clinic visit could be used to automatically generate a SOAP (subjective, objective assessment and plan) note. It was better than anything I would have drafted. He also showed how the LLM could directly ingest EHR data, without any modification, and provide a great diagnosis and treatment plan. Finally, LLM chatbots could carry on an interactive conversation with a patient that would be difficult to distinguish from a human physician.
The inevitability of AI-powered transformations in gastroenterology care became apparent.
Documentation, billing, and administrative work will be handled by AI. AI will collect and organize information for me. Chart reviews and even telephone/email checkups on patients will be a thing of the past. AI chatbots will be able to discuss an individual patient’s condition and test results. Our GI-AI assistants will proactively collect information from patients after hospitalization or react to a change in labs.
AI will soon be an amazing diagnostician and will know more than me. So do we need to polish our resumes for new careers? No, but we will need to adapt to changes, which I believe on the whole will be better for gastroenterologists and patients.
What does adaptation look like for gastroenterologists over the next handful of years?
Like any other tool, gastroenterologists will be figuring out how to use AI prediction models, chatbots, and imaging analytics. Value, ease of use, and information-gain will drive which AI tools are ultimately adopted.
Memory, information recall, calculations, and repetitive tasks where gastroenterologists occasionally error or find tiresome will become the job of machines. We will still be the magicians, now aided by machines, applying our human strengths of contextual awareness, judgment, and creativity to find customized solutions for more patients.
That, I think, is the future that we are reliably moving toward over the next decade — a human-computer cooperative throughout gastroenterology (including IBD) and, frankly, all of medicine.
A version of this article appeared on Medscape.com.
Several artificial intelligence (AI) technologies are emerging that will change the management of gastrointestinal (GI) diseases sooner rather than later. One of the leading researchers working toward that AI-driven future is Ryan W. Stidham, MD, MS, AGAF, associate professor of gastroenterology and computational medicine and bioinformatics at the University of Michigan, Ann Arbor.
Stidham’s work focuses on leveraging AI to develop automated systems that better quantify disease activity and aid gastroenterologists in their decision-making. He also serves as a meber of AGA's AI Task Force. what the technology may do to improve physician efficiency, and why gastroenterologists shouldn’t be worried about being replaced by machines any time soon.
How did you first become involved in studying AI applications for GI conditions?
My medical training coincided with the emergence of electronic health records (EHRs) making enormous amounts of data, ranging from laboratory results to diagnostic codes and billing records, readily accessible.
I quickly contracted data analytics fever, but a major problem became apparent: EHRs and medical claims data alone only weakly describe a patient. Researchers in the field were excited to use machine learning for personalizing treatment decisions for GI conditions, including inflammatory bowel disease (IBD). But no matter how large the dataset, the EHRs lacked the most rudimentary descriptions: What was the patient’s IBD phenotype? Where exactly was the disease located?
I could see machine learning had the potential to learn and reproduce expert decision-making. Unfortunately, we were fueling this machine-learning rocket ship with crude data unlikely to take us very far. Gastroenterologists rely on data in progress notes, emails, interpretations of colonoscopies, and radiologists’ and pathologists’ reviews of imaging to make treatment decisions, but that information is not well organized in any dataset.
I wanted to use AI to retrieve that key information in text, images, and video that we use every day for IBD care, automatically interpreting the data like a seasoned gastroenterologist. Generating higher-quality data describing patients could take our AI models from interesting research to useful and reliable tools in clinical care.
How did your early research go about trying to solve that problem?
My GI career began amid the IBD field shifting from relying on symptoms alone to objective biomarkers for IBD assessment, particularly focusing on standardized scoring of endoscopic mucosal inflammation. However, these scores were challenged with interobserver variability, prompting the need for centralized reading. More importantly, these scores are qualitative and do not capture all the visual findings an experienced physician appreciates when assessing severity, phenotype, and therapeutic effect. As a result, even experts could disagree on the degree of endoscopic severity, and patients with obvious differences in the appearance of mucosa could have the same endoscopic score.
I asked myself: Are we really using these measures to make treatment decisions and determine the effectiveness of investigational therapies? I thought we could do better and aimed to improve endoscopic IBD assessments using then-emerging digital image analysis techniques.
Convolutional neural network (CNN) modeling was just becoming feasible as computing performance increased. CNNs are well suited for complex medical image interpretation, using an associated “label,” such as the presence or grade of disease, to decipher the complex set of image feature patterns characterizing an expert’s determination of disease severity.
How did you convert the promise of CNN into tangible results?
The plan was simple: Collect endoscopic images from patients with IBD, find some experts to grade IBD severity on the images, and train a CNN model using the images and expert labels.
In 2016, developing a CNN wasn’t easy. There was no database of endoscopic images or simple methods for image labeling. The CNN needed tens of thousands of images. How were we to collect enough images with a broad range of IBD severity? I also reached some technical limits and needed help solving computational challenges.
Designing our first IBD endoscopic CNN took years of reading, coursework, additional training, and a new host of collaborators.
Failure was frequent, and my colleagues and I spent a lot of nights and weekends looking at thousands of individual endoscopic images. But we eventually had a working model for grading endoscopic severity, and its performance exceeded our expectations.
To our surprise, the CNN model grading of ulcerative colitis severity almost perfectly matched the opinion of IBD experts. We introduced the proof of concept that AI could automate complex disease measurement for IBD.
What took us 3 years in 2016 would take about 3 weeks today.
You have said that AI could help reduce the substantial administrative burdens in medicine today. What might an AI-assisted future look like for time-strapped gastroenterologists?
We will be spending more time on complex decision-making and developing treatment plans, with less time needed to hunt for information in the chart and administrative tasks.
The practical applications of AI will chip away at tedious mechanical tasks, soon to be done by machines, reclaiming time for gastroenterologists.
For example, automated documentation is almost usable, and audio recordings in the clinic could be leveraged to generate office notes.
Computer vision analysis of endoscopic video is generating draft procedural notes and letters to patients in a shared language, as well as recommending surveillance intervals based on the findings.
Text processing is already being used to automate billing and manage health maintenance like vaccinations, laboratory screening, and therapeutic drug monitoring.
Unfortunately, I don’t think that AI will immediately help with burnout. These near-term AI administrative assistant advantages, however, will help us manage the increasing patient load, address physician shortages, and potentially improve access to care in underserved areas.
Were there any surprises in your work?
I must admit, I was certain AI would put us gastroenterologists to shame. Over time, I have reversed that view.
AI really struggles to understand the holistic patient context when interpreting disease and predicting what to do for an individual patient. Humans anticipate gaps in data and customize the weighting of information when making decisions for individuals. An experienced gastroenterologist can incorporate risks, harms, and costs in ways AI is several generations from achieving.
With certainty, AI will outperform gastroenterologists for tedious and repetitive tasks, and we should gladly expect AI to assume those responsibilities. However, many unknowns remain in the daily management of GI conditions. We will continue to rely on the clinical experience, creativity, and improvisation of gastroenterologists for years to come.
Has there been a turning-point moment when it felt like this technology moved from being more theoretical to something with real-world clinical applications?
Last spring, I saw a lecture by Peter Lee, who is president of Microsoft Research and a leader in developing AI-powered applications in medicine and scientific research, demonstrating how a large language model (LLM) could “understand” medical text and generate responses to questions. My jaw dropped.
We watched an LLM answer American Board of Internal Medicine questions with perfect explanations and rationale. He demonstrated how an audio recording of a clinic visit could be used to automatically generate a SOAP (subjective, objective assessment and plan) note. It was better than anything I would have drafted. He also showed how the LLM could directly ingest EHR data, without any modification, and provide a great diagnosis and treatment plan. Finally, LLM chatbots could carry on an interactive conversation with a patient that would be difficult to distinguish from a human physician.
The inevitability of AI-powered transformations in gastroenterology care became apparent.
Documentation, billing, and administrative work will be handled by AI. AI will collect and organize information for me. Chart reviews and even telephone/email checkups on patients will be a thing of the past. AI chatbots will be able to discuss an individual patient’s condition and test results. Our GI-AI assistants will proactively collect information from patients after hospitalization or react to a change in labs.
AI will soon be an amazing diagnostician and will know more than me. So do we need to polish our resumes for new careers? No, but we will need to adapt to changes, which I believe on the whole will be better for gastroenterologists and patients.
What does adaptation look like for gastroenterologists over the next handful of years?
Like any other tool, gastroenterologists will be figuring out how to use AI prediction models, chatbots, and imaging analytics. Value, ease of use, and information-gain will drive which AI tools are ultimately adopted.
Memory, information recall, calculations, and repetitive tasks where gastroenterologists occasionally error or find tiresome will become the job of machines. We will still be the magicians, now aided by machines, applying our human strengths of contextual awareness, judgment, and creativity to find customized solutions for more patients.
That, I think, is the future that we are reliably moving toward over the next decade — a human-computer cooperative throughout gastroenterology (including IBD) and, frankly, all of medicine.
A version of this article appeared on Medscape.com.
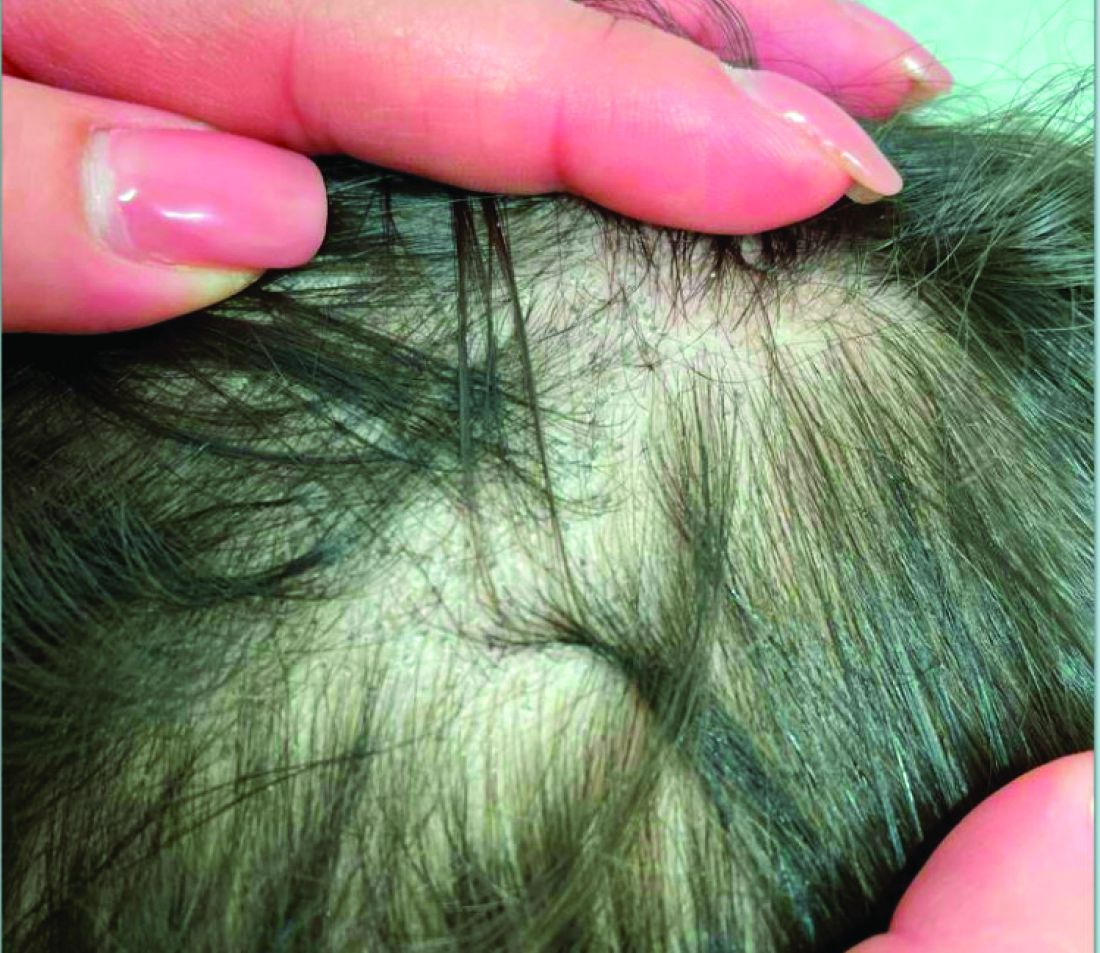
A 7-Year-Old Boy Presents With Dark Spots on His Scalp and Areas of Poor Hair Growth
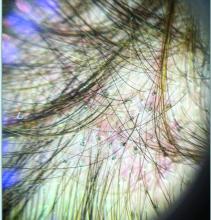
Given the trichoscopic findings, scrapings from the scaly areas were taken and revealed hyphae, confirming the diagnosis of tinea capitis. A fungal culture identified Trichophyton tonsurans as the causative organism.
Tinea capitis is the most common dermatophyte infection in children. Risk factors include participation in close-contact sports like wrestling or jiu-jitsu, attendance at daycare for younger children, African American hair care practices, pet ownership (particularly cats and rodents), and living in overcrowded conditions.
Diagnosis of tinea capitis requires a thorough clinical history to identify potential risk factors. On physical examination, patchy hair loss with associated scaling should raise suspicion for tinea capitis. Inflammatory signs, such as pustules and swelling, may suggest the presence of a kerion, further supporting the diagnosis. Although some practitioners use Wood’s lamp to help with diagnosis, its utility is limited. It detects fluorescence in Microsporum species (exothrix infections) but not in Trichophyton species (endothrix infections).
Trichoscopy can be a valuable tool when inflammation is minimal, and only hair loss and scaling are observed. Trichoscopic findings suggestive of tinea capitis include comma hairs, corkscrew hairs (as seen in this patient), Morse code-like hairs, zigzag hairs, bent hairs, block hairs, and i-hairs. Other common, though not characteristic, findings include broken hairs, black dots, perifollicular scaling, and diffuse scaling.
KOH (potassium hydroxide) analysis is another useful method for detecting fungal elements, though it does not identify the specific fungus and may not be available in all clinical settings. Mycologic culture remains the gold standard for diagnosing tinea capitis, though results can take 3-4 weeks. Newer diagnostic techniques, such as PCR analysis and MALDI-TOF/MS, offer more rapid identification of the causative organism.
The differential diagnosis includes:
- Seborrheic dermatitis, which presents with greasy, yellowish scales and itching, with trichoscopy showing twisted, coiled hairs and yellowish scaling.
- Psoriasis, which can mimic tinea capitis but presents with well-demarcated red plaques and silvery-white scales. Trichoscopy shows red dots and uniform scaling.
- Alopecia areata, which causes patchy hair loss without inflammation or scaling, with trichoscopic findings of exclamation mark hairs, black dots, and yellow dots.
- Trichotillomania, a hair-pulling disorder, which results in irregular patches of hair loss. Trichoscopy shows broken hairs of varying lengths, V-sign hairs, and flame-shaped residues at follicular openings.
Treatment of tinea capitis requires systemic antifungals and topical agents to prevent fungal spore spread. Several treatment guidelines are available from different institutions. Griseofulvin (FDA-approved for patients > 2 years of age) has been widely used, particularly for Microsporum canis infections. However, due to limited availability in many countries, terbinafine (FDA-approved for patients > 4 years of age) is now commonly used as first-line therapy, especially for Trichophyton species. Treatment typically lasts 4-6 weeks, and post-treatment cultures may be recommended to confirm mycologic cure.
Concerns about drug resistance have emerged, particularly for terbinafine-resistant dermatophytes linked to mutations in the squalene epoxidase enzyme. Resistance may be driven by limited antifungal availability and poor adherence to prolonged treatment regimens. While fluconazole and itraconazole are used off-label, growing evidence supports their effectiveness, although one large trial showed suboptimal cure rates with fluconazole.
Though systemic antifungals are generally safe, hepatotoxicity remains a concern, especially in patients with hepatic conditions or other comorbidities. Lab monitoring is advised for patients on prolonged or multiple therapies, or for those with coexisting conditions. The decision to conduct lab monitoring should be discussed with parents, balancing the very low risk of hepatotoxicity in healthy children against their comfort level.
An alternative to systemic therapy is photodynamic therapy (PDT), which has been reported as successful in treating tinea capitis infections, particularly in cases of T. mentagrophytes and M. canis. However, large-scale trials are needed to confirm PDT’s efficacy and safety.
In conclusion, children presenting with hair loss, scaling, and associated dark spots on the scalp should be evaluated for fungal infection. While trichoscopy can aid in diagnosis, fungal culture remains the gold standard for confirmation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Rudnicka L et al. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013 Oct;31(4):695-708, x. doi: 10.1016/j.det.2013.06.007.
Gupta AK et al. An update on tinea capitis in children. Pediatr Dermatol. 2024 Aug 7. doi: 10.1111/pde.15708.
Anna Waskiel-Burnat et al. Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020 Feb;10(1):43-52. doi: 10.1007/s13555-019-00350-1.
Given the trichoscopic findings, scrapings from the scaly areas were taken and revealed hyphae, confirming the diagnosis of tinea capitis. A fungal culture identified Trichophyton tonsurans as the causative organism.
Tinea capitis is the most common dermatophyte infection in children. Risk factors include participation in close-contact sports like wrestling or jiu-jitsu, attendance at daycare for younger children, African American hair care practices, pet ownership (particularly cats and rodents), and living in overcrowded conditions.
Diagnosis of tinea capitis requires a thorough clinical history to identify potential risk factors. On physical examination, patchy hair loss with associated scaling should raise suspicion for tinea capitis. Inflammatory signs, such as pustules and swelling, may suggest the presence of a kerion, further supporting the diagnosis. Although some practitioners use Wood’s lamp to help with diagnosis, its utility is limited. It detects fluorescence in Microsporum species (exothrix infections) but not in Trichophyton species (endothrix infections).
Trichoscopy can be a valuable tool when inflammation is minimal, and only hair loss and scaling are observed. Trichoscopic findings suggestive of tinea capitis include comma hairs, corkscrew hairs (as seen in this patient), Morse code-like hairs, zigzag hairs, bent hairs, block hairs, and i-hairs. Other common, though not characteristic, findings include broken hairs, black dots, perifollicular scaling, and diffuse scaling.
KOH (potassium hydroxide) analysis is another useful method for detecting fungal elements, though it does not identify the specific fungus and may not be available in all clinical settings. Mycologic culture remains the gold standard for diagnosing tinea capitis, though results can take 3-4 weeks. Newer diagnostic techniques, such as PCR analysis and MALDI-TOF/MS, offer more rapid identification of the causative organism.
The differential diagnosis includes:
- Seborrheic dermatitis, which presents with greasy, yellowish scales and itching, with trichoscopy showing twisted, coiled hairs and yellowish scaling.
- Psoriasis, which can mimic tinea capitis but presents with well-demarcated red plaques and silvery-white scales. Trichoscopy shows red dots and uniform scaling.
- Alopecia areata, which causes patchy hair loss without inflammation or scaling, with trichoscopic findings of exclamation mark hairs, black dots, and yellow dots.
- Trichotillomania, a hair-pulling disorder, which results in irregular patches of hair loss. Trichoscopy shows broken hairs of varying lengths, V-sign hairs, and flame-shaped residues at follicular openings.
Treatment of tinea capitis requires systemic antifungals and topical agents to prevent fungal spore spread. Several treatment guidelines are available from different institutions. Griseofulvin (FDA-approved for patients > 2 years of age) has been widely used, particularly for Microsporum canis infections. However, due to limited availability in many countries, terbinafine (FDA-approved for patients > 4 years of age) is now commonly used as first-line therapy, especially for Trichophyton species. Treatment typically lasts 4-6 weeks, and post-treatment cultures may be recommended to confirm mycologic cure.
Concerns about drug resistance have emerged, particularly for terbinafine-resistant dermatophytes linked to mutations in the squalene epoxidase enzyme. Resistance may be driven by limited antifungal availability and poor adherence to prolonged treatment regimens. While fluconazole and itraconazole are used off-label, growing evidence supports their effectiveness, although one large trial showed suboptimal cure rates with fluconazole.
Though systemic antifungals are generally safe, hepatotoxicity remains a concern, especially in patients with hepatic conditions or other comorbidities. Lab monitoring is advised for patients on prolonged or multiple therapies, or for those with coexisting conditions. The decision to conduct lab monitoring should be discussed with parents, balancing the very low risk of hepatotoxicity in healthy children against their comfort level.
An alternative to systemic therapy is photodynamic therapy (PDT), which has been reported as successful in treating tinea capitis infections, particularly in cases of T. mentagrophytes and M. canis. However, large-scale trials are needed to confirm PDT’s efficacy and safety.
In conclusion, children presenting with hair loss, scaling, and associated dark spots on the scalp should be evaluated for fungal infection. While trichoscopy can aid in diagnosis, fungal culture remains the gold standard for confirmation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Rudnicka L et al. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013 Oct;31(4):695-708, x. doi: 10.1016/j.det.2013.06.007.
Gupta AK et al. An update on tinea capitis in children. Pediatr Dermatol. 2024 Aug 7. doi: 10.1111/pde.15708.
Anna Waskiel-Burnat et al. Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020 Feb;10(1):43-52. doi: 10.1007/s13555-019-00350-1.
Given the trichoscopic findings, scrapings from the scaly areas were taken and revealed hyphae, confirming the diagnosis of tinea capitis. A fungal culture identified Trichophyton tonsurans as the causative organism.
Tinea capitis is the most common dermatophyte infection in children. Risk factors include participation in close-contact sports like wrestling or jiu-jitsu, attendance at daycare for younger children, African American hair care practices, pet ownership (particularly cats and rodents), and living in overcrowded conditions.
Diagnosis of tinea capitis requires a thorough clinical history to identify potential risk factors. On physical examination, patchy hair loss with associated scaling should raise suspicion for tinea capitis. Inflammatory signs, such as pustules and swelling, may suggest the presence of a kerion, further supporting the diagnosis. Although some practitioners use Wood’s lamp to help with diagnosis, its utility is limited. It detects fluorescence in Microsporum species (exothrix infections) but not in Trichophyton species (endothrix infections).
Trichoscopy can be a valuable tool when inflammation is minimal, and only hair loss and scaling are observed. Trichoscopic findings suggestive of tinea capitis include comma hairs, corkscrew hairs (as seen in this patient), Morse code-like hairs, zigzag hairs, bent hairs, block hairs, and i-hairs. Other common, though not characteristic, findings include broken hairs, black dots, perifollicular scaling, and diffuse scaling.
KOH (potassium hydroxide) analysis is another useful method for detecting fungal elements, though it does not identify the specific fungus and may not be available in all clinical settings. Mycologic culture remains the gold standard for diagnosing tinea capitis, though results can take 3-4 weeks. Newer diagnostic techniques, such as PCR analysis and MALDI-TOF/MS, offer more rapid identification of the causative organism.
The differential diagnosis includes:
- Seborrheic dermatitis, which presents with greasy, yellowish scales and itching, with trichoscopy showing twisted, coiled hairs and yellowish scaling.
- Psoriasis, which can mimic tinea capitis but presents with well-demarcated red plaques and silvery-white scales. Trichoscopy shows red dots and uniform scaling.
- Alopecia areata, which causes patchy hair loss without inflammation or scaling, with trichoscopic findings of exclamation mark hairs, black dots, and yellow dots.
- Trichotillomania, a hair-pulling disorder, which results in irregular patches of hair loss. Trichoscopy shows broken hairs of varying lengths, V-sign hairs, and flame-shaped residues at follicular openings.
Treatment of tinea capitis requires systemic antifungals and topical agents to prevent fungal spore spread. Several treatment guidelines are available from different institutions. Griseofulvin (FDA-approved for patients > 2 years of age) has been widely used, particularly for Microsporum canis infections. However, due to limited availability in many countries, terbinafine (FDA-approved for patients > 4 years of age) is now commonly used as first-line therapy, especially for Trichophyton species. Treatment typically lasts 4-6 weeks, and post-treatment cultures may be recommended to confirm mycologic cure.
Concerns about drug resistance have emerged, particularly for terbinafine-resistant dermatophytes linked to mutations in the squalene epoxidase enzyme. Resistance may be driven by limited antifungal availability and poor adherence to prolonged treatment regimens. While fluconazole and itraconazole are used off-label, growing evidence supports their effectiveness, although one large trial showed suboptimal cure rates with fluconazole.
Though systemic antifungals are generally safe, hepatotoxicity remains a concern, especially in patients with hepatic conditions or other comorbidities. Lab monitoring is advised for patients on prolonged or multiple therapies, or for those with coexisting conditions. The decision to conduct lab monitoring should be discussed with parents, balancing the very low risk of hepatotoxicity in healthy children against their comfort level.
An alternative to systemic therapy is photodynamic therapy (PDT), which has been reported as successful in treating tinea capitis infections, particularly in cases of T. mentagrophytes and M. canis. However, large-scale trials are needed to confirm PDT’s efficacy and safety.
In conclusion, children presenting with hair loss, scaling, and associated dark spots on the scalp should be evaluated for fungal infection. While trichoscopy can aid in diagnosis, fungal culture remains the gold standard for confirmation.
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego.
References
Rudnicka L et al. Hair shafts in trichoscopy: clues for diagnosis of hair and scalp diseases. Dermatol Clin. 2013 Oct;31(4):695-708, x. doi: 10.1016/j.det.2013.06.007.
Gupta AK et al. An update on tinea capitis in children. Pediatr Dermatol. 2024 Aug 7. doi: 10.1111/pde.15708.
Anna Waskiel-Burnat et al. Trichoscopy of tinea capitis: A systematic review. Dermatol Ther (Heidelb). 2020 Feb;10(1):43-52. doi: 10.1007/s13555-019-00350-1.
Swollen elbow and knee joints
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 24-year-old woman presents for swollen and painful elbow and knee joints. The patient is 5 ft 7 in tall and weighs 235 lb (BMI 36.8). The patient says she has been overweight since her preteen years and has never been involved in sports or exercise activities. She has gained a significant amount of weight in the past 2 years since beginning work in an insurance office. She has lived at home with her parents since graduating from college.
Her elbows are tender to the touch; further examination reveals tender joints at her wrists, knees, and hips as well. Extremities are thick because of obesity.
Medical history includes diagnosis of type 2 diabetes (T2D) at age 22. In the office, her blood pressure is elevated (150/85 mm Hg), heart rate is 110 beats/min, and respiratory rate is 18 breaths/min. Lab results indicate A1c = 8.5%, low-density lipoprotein cholesterol = 145 mg/dL, and estimated glomerular filtration rate = 90 mL/min/1.73 m2; all other results are within normal range. Her only current medication is metformin 1000 mg daily.
In-office radiography reveals no obvious bone or joint damage.
Pulsed Dye Laser a “Go-To Device” Option for Acne Treatment When Access to 1726-nm Lasers Is Limited
CARLSBAD, CALIF. — Lasers and energy-based treatments alone or in combination with medical therapy may improve outcomes for patients with moderate to severe acne, according to Arielle Kauvar, MD.
At the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium, Kauvar, director of New York Laser & Skin Care, New York City, highlighted several reasons why using lasers for acne is beneficial. “First, we know that topical therapy alone is often ineffective, and antibiotic treatment does not address the cause of acne and can alter the skin and gut microbiome,” she said. “Isotretinoin is highly effective, but there’s an increasing reluctance to use it. Lasers and energy devices are effective in treating acne and may also treat the post-inflammatory hyperpigmentation and scarring associated with it.”
The pathogenesis of acne is multifactorial, she continued, including a disruption of sebaceous gland activity, with overproduction and alteration of sebum and abnormal follicular keratinization. Acne also causes an imbalance of the skin microbiome, local inflammation, and activation of both innate and adaptive immunity.
“Many studies point to the fact that inflammation and immune system activation may actually be the primary event” of acne formation, said Kauvar, who is also a clinical professor of dermatology at New York University, New York City. “This persistent immune activation is also associated with scarring,” she noted. “So, are we off the mark in terms of trying to kill sebaceous glands? Should we be concentrating on anti-inflammatory approaches?”
AviClear became the first 1726-nm laser cleared by the US Food and Drug Administration (FDA) for the treatment of mild to severe acne vulgaris in 2022, followed a few months later with the FDA clearance of another 1726-nm laser, the Accure Acne Laser System in November 2022. These lasers cause selective photothermolysis of sebaceous glands, but according to Kauvar, “access to these devices is somewhat limited at this time.”
What is available includes her go-to device, the pulsed dye laser (PDL), which has been widely studied and shown in a systematic review and meta-analysis of studies to be effective for acne. The PDL “targets dermal blood vessels facilitating inflammation, upregulates TGF-beta, and inhibits CD4+ T cell-mediated inflammation,” she said. “It can also treat PIH [post-inflammatory hyperpigmentation] and may be helpful in scar prevention.”
In an abstract presented at The American Society for Laser Medicine and Surgery (ASLMS) 2024 annual meeting, Kauvar and colleagues conducted a real-world study of PDL therapy in 15 adult women with recalcitrant acne who were maintained on their medical treatment regimen. Their mean age was 27 years, and they had skin types II-IV; they underwent four monthly PDL treatments with follow-up at 1 and 3 months. At each visit, the researchers took digital photographs and counted inflammatory acne lesions, non-inflammatory acne lesions, and post-inflammatory pigment alteration (PIPA) lesions.
The main outcomes of interest were the investigator global assessment (IGA) scores at the 1- and 3-month follow-up visits. Kauvar and colleagues observed a significant improvement in IGA scores at the 1- and 3-month follow-up visits (P < .05), with an average decrease of 1.8 and 1.6 points in the acne severity scale, respectively, from a baseline score of 3.4. By the 3-month follow-up visits, counts of inflammatory and non-inflammatory lesions decreased significantly (P < .05), and 61% of study participants showed a decrease in the PIPA count. No adverse events occurred.
Kauvar disclosed that she has conducted research for Candela, Lumenis, and Sofwave, and is an adviser to Acclaro.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIF. — Lasers and energy-based treatments alone or in combination with medical therapy may improve outcomes for patients with moderate to severe acne, according to Arielle Kauvar, MD.
At the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium, Kauvar, director of New York Laser & Skin Care, New York City, highlighted several reasons why using lasers for acne is beneficial. “First, we know that topical therapy alone is often ineffective, and antibiotic treatment does not address the cause of acne and can alter the skin and gut microbiome,” she said. “Isotretinoin is highly effective, but there’s an increasing reluctance to use it. Lasers and energy devices are effective in treating acne and may also treat the post-inflammatory hyperpigmentation and scarring associated with it.”
The pathogenesis of acne is multifactorial, she continued, including a disruption of sebaceous gland activity, with overproduction and alteration of sebum and abnormal follicular keratinization. Acne also causes an imbalance of the skin microbiome, local inflammation, and activation of both innate and adaptive immunity.
“Many studies point to the fact that inflammation and immune system activation may actually be the primary event” of acne formation, said Kauvar, who is also a clinical professor of dermatology at New York University, New York City. “This persistent immune activation is also associated with scarring,” she noted. “So, are we off the mark in terms of trying to kill sebaceous glands? Should we be concentrating on anti-inflammatory approaches?”
AviClear became the first 1726-nm laser cleared by the US Food and Drug Administration (FDA) for the treatment of mild to severe acne vulgaris in 2022, followed a few months later with the FDA clearance of another 1726-nm laser, the Accure Acne Laser System in November 2022. These lasers cause selective photothermolysis of sebaceous glands, but according to Kauvar, “access to these devices is somewhat limited at this time.”
What is available includes her go-to device, the pulsed dye laser (PDL), which has been widely studied and shown in a systematic review and meta-analysis of studies to be effective for acne. The PDL “targets dermal blood vessels facilitating inflammation, upregulates TGF-beta, and inhibits CD4+ T cell-mediated inflammation,” she said. “It can also treat PIH [post-inflammatory hyperpigmentation] and may be helpful in scar prevention.”
In an abstract presented at The American Society for Laser Medicine and Surgery (ASLMS) 2024 annual meeting, Kauvar and colleagues conducted a real-world study of PDL therapy in 15 adult women with recalcitrant acne who were maintained on their medical treatment regimen. Their mean age was 27 years, and they had skin types II-IV; they underwent four monthly PDL treatments with follow-up at 1 and 3 months. At each visit, the researchers took digital photographs and counted inflammatory acne lesions, non-inflammatory acne lesions, and post-inflammatory pigment alteration (PIPA) lesions.
The main outcomes of interest were the investigator global assessment (IGA) scores at the 1- and 3-month follow-up visits. Kauvar and colleagues observed a significant improvement in IGA scores at the 1- and 3-month follow-up visits (P < .05), with an average decrease of 1.8 and 1.6 points in the acne severity scale, respectively, from a baseline score of 3.4. By the 3-month follow-up visits, counts of inflammatory and non-inflammatory lesions decreased significantly (P < .05), and 61% of study participants showed a decrease in the PIPA count. No adverse events occurred.
Kauvar disclosed that she has conducted research for Candela, Lumenis, and Sofwave, and is an adviser to Acclaro.
A version of this article first appeared on Medscape.com.
CARLSBAD, CALIF. — Lasers and energy-based treatments alone or in combination with medical therapy may improve outcomes for patients with moderate to severe acne, according to Arielle Kauvar, MD.
At the Controversies and Conversations in Laser and Cosmetic Surgery annual symposium, Kauvar, director of New York Laser & Skin Care, New York City, highlighted several reasons why using lasers for acne is beneficial. “First, we know that topical therapy alone is often ineffective, and antibiotic treatment does not address the cause of acne and can alter the skin and gut microbiome,” she said. “Isotretinoin is highly effective, but there’s an increasing reluctance to use it. Lasers and energy devices are effective in treating acne and may also treat the post-inflammatory hyperpigmentation and scarring associated with it.”
The pathogenesis of acne is multifactorial, she continued, including a disruption of sebaceous gland activity, with overproduction and alteration of sebum and abnormal follicular keratinization. Acne also causes an imbalance of the skin microbiome, local inflammation, and activation of both innate and adaptive immunity.
“Many studies point to the fact that inflammation and immune system activation may actually be the primary event” of acne formation, said Kauvar, who is also a clinical professor of dermatology at New York University, New York City. “This persistent immune activation is also associated with scarring,” she noted. “So, are we off the mark in terms of trying to kill sebaceous glands? Should we be concentrating on anti-inflammatory approaches?”
AviClear became the first 1726-nm laser cleared by the US Food and Drug Administration (FDA) for the treatment of mild to severe acne vulgaris in 2022, followed a few months later with the FDA clearance of another 1726-nm laser, the Accure Acne Laser System in November 2022. These lasers cause selective photothermolysis of sebaceous glands, but according to Kauvar, “access to these devices is somewhat limited at this time.”
What is available includes her go-to device, the pulsed dye laser (PDL), which has been widely studied and shown in a systematic review and meta-analysis of studies to be effective for acne. The PDL “targets dermal blood vessels facilitating inflammation, upregulates TGF-beta, and inhibits CD4+ T cell-mediated inflammation,” she said. “It can also treat PIH [post-inflammatory hyperpigmentation] and may be helpful in scar prevention.”
In an abstract presented at The American Society for Laser Medicine and Surgery (ASLMS) 2024 annual meeting, Kauvar and colleagues conducted a real-world study of PDL therapy in 15 adult women with recalcitrant acne who were maintained on their medical treatment regimen. Their mean age was 27 years, and they had skin types II-IV; they underwent four monthly PDL treatments with follow-up at 1 and 3 months. At each visit, the researchers took digital photographs and counted inflammatory acne lesions, non-inflammatory acne lesions, and post-inflammatory pigment alteration (PIPA) lesions.
The main outcomes of interest were the investigator global assessment (IGA) scores at the 1- and 3-month follow-up visits. Kauvar and colleagues observed a significant improvement in IGA scores at the 1- and 3-month follow-up visits (P < .05), with an average decrease of 1.8 and 1.6 points in the acne severity scale, respectively, from a baseline score of 3.4. By the 3-month follow-up visits, counts of inflammatory and non-inflammatory lesions decreased significantly (P < .05), and 61% of study participants showed a decrease in the PIPA count. No adverse events occurred.
Kauvar disclosed that she has conducted research for Candela, Lumenis, and Sofwave, and is an adviser to Acclaro.
A version of this article first appeared on Medscape.com.
What Are the Best Tools for Early Childhood Developmental Concerns?
Early recognition of neurodevelopmental concerns and timely access to services have been shown to result in better outcomes for young children. But not all instruments are of equal value, and new research has sought to identify the most useful among them.
For their research, published online in Developmental Medicine & Child Neurology, Andrea Burgess, PhD, of the University of Queensland in Brisbane, Australia, and her colleagues looked at two decades’ worth of systematic reviews of screening, assessment, and diagnostic tools used in children younger than 6 years.
Eighty-six clinical reviews and six practice guidelines, all published between 2000 and 2023, were included in the scoping review, which covered nearly 250 different multi-domain and domain- and disorder-specific tools.
The diagnostic instruments were those used to diagnose the most common early childhood disorders, including intellectual disability, global developmental delay, communication disorders, autism spectrum disorder, attention-deficit/hyperactivity disorder, cerebral palsy, movement disorders, and fetal alcohol spectrum disorder. Burgess and her colleagues sought to determine which tools had the strongest evidence behind them, noting that comparisons were inherently limited by differences in the tested populations, cutoff values, and other factors.
Burgess and her colleagues identified 67 instruments — about a third of those analyzed in the study — “with good discriminative or predictive validity for the screening and assessment of developmental concerns or disability.” Recommended tools were classified by tool type and by patient age groups.
The reason a tool might not be recommended, Burgess said in an email, was for lack of psychometric testing or published evidence, or because the tool was very narrow in scope (eg, covering only a single aspect of a domain), had a small time window for use, or was too new to have been captured in published systematic reviews.
Top Recommendations
Among multi-domain assessment tools, the Bayley Scales of Infant and Toddler Development, the Battelle Developmental Inventory, and the Mullen Scales of Early Learning all emerged as highly recommended. The top diagnostic screening tool for autism was the revised version of Social Attention and Communication Surveillance. For cerebral palsy, the top-rated diagnostic assessment tools were Prechtl’s Qualitative Assessment of General Movements and the Hammersmith Infant Neurological Examination.
Ratifying findings by other groups, the researchers determined the Ages & Stages Questionnaires, Third Edition (ASQ-3) to be the best overall multi-domain screening instrument for early childhood development, thanks to its simplicity and ease of use by a wide range of practitioner types. Burgess and her colleagues noted, however, that the ASQ-3 “will not identify all children with developmental concerns and may incorrectly identify others,” and that it may be more accurate in children 2 years or older.
Patient Care Setting and Cultural, Socioeconomic Factors Are Key
This news organization spoke to two clinicians working with these and similar tools in the United States. Both said that the care setting can also influence the utility of tools, with cultural and socioeconomic factors playing important roles.
Liz Schwandt, PsyD, an early intervention specialist in Los Angeles, said in an interview that children living in high-risk communities in the United States have a larger burden of developmental delays. But for many families in these communities, accessing care can be complex, which is why well-designed, efficient screening tools like ASQ-3 are especially valuable in practice.
“The reality is you have 10 minutes with a lot of families, and if it’s an emergency, you need to know,” she said. “The ASQ-3 has a very broad age range for this type of instrument and can be used by different practitioner types. The reason it’s successful lies in its parent-centric approach and inherent ease of use. It’s quick, and you can score it using pencil and paper while chatting with the parent, and you can use it for multiple siblings in the space of one appointment.”
With very young children, in whom neurodevelopmental concerns often overlap domains, Schwandt said it can be more important to flag a potential problem early and initiate a nonspecific developmental intervention than wait for results from more precise assessments using more specialized tools. These often require multiple, multi-hour appointments, which can be difficult to attain in lower-resource settings in the United States and can delay care, she said.
Liza Mackintosh, MD, a pediatrician at a federally funded healthcare center in Los Angeles that serves mostly publicly insured families, called validated first-line screening tools “incredibly important.” While rates of developmental screenings in pediatric clinics are increasing, there is still room for improvement, she said.
Mackintosh’s institution does not currently use the ASQ-3 but a different screening tool, called the Survey of Well-Being of Young Children (SWYC), that is embedded into the electronic health record. (The SWYC was not among the tools highlighted in Burgess and colleagues’ review.) Like the ASQ-3, it is short and efficient, she said, and it is used in all children in the recommended age ranges.
“Our visits are on average only 20 minutes,” Mackintosh said. “There’s not enough time for an in-depth developmental assessment. We will flag things such as a speech delay, gross motor delay, or fine motor delay” and refer to early intervention centers for more in-depth developmental assessments as needed, she said.
“The biggest job of pediatricians working in communities that are under-resourced is advocating for those early intervention services,” Mackintosh added. “We really see our job as doing the recommended screening, putting that together with what we’re seeing clinically and on history, and then advocating for the right next step or early intervention. Because sometimes the diagnosis is — I don’t want to say irrelevant, but your treatment plan is still going to be the same. So while I don’t have a formal diagnosis yet, the child definitely needs therapies and we’re still going to get those therapies.”
Burgess and her colleagues stressed in their paper the importance of selecting tools that are culturally appropriate for Indigenous communities in Australia, noting that “inappropriate tools may lead to over- or under-recognition of children with developmental concerns.”
Schwandt and Mackintosh said that the same applies in US settings.
“We’ve done a good job translating screening tools into Chinese, Spanish, Vietnamese, and Russian,” Schwandt said. “But some of them assume a way of taking care of children that is not always shared across cultures. The expectations of how children should play and interact with adults can be very different, and there needs to be an understanding of that. Just putting something in Vietnamese doesn’t mean that there are obvious analogues to understanding what the questionnaire is asking.”
Mackintosh concurred. “A lot of times our patients will not do well on screening, even though they’re fine, because they don’t have the exposure to that activity that’s being asked about. So — is the child scribbling with crayons? Is she climbing up a ladder at a playground? In order to be able to do that, you need to have an environment that you are doing it in. The screeners have to really be appropriate for what the child is exposed to. And sometimes our patients just don’t have that exposure.”
Burgess and colleagues’ study was funded by the Australian government and the Merchant Charitable Foundation. The authors disclosed no financial conflicts of interest. Schwandt and Mackintosh disclosed no conflicts of interest related to their comments.
A version of this article appeared on Medscape.com.
Early recognition of neurodevelopmental concerns and timely access to services have been shown to result in better outcomes for young children. But not all instruments are of equal value, and new research has sought to identify the most useful among them.
For their research, published online in Developmental Medicine & Child Neurology, Andrea Burgess, PhD, of the University of Queensland in Brisbane, Australia, and her colleagues looked at two decades’ worth of systematic reviews of screening, assessment, and diagnostic tools used in children younger than 6 years.
Eighty-six clinical reviews and six practice guidelines, all published between 2000 and 2023, were included in the scoping review, which covered nearly 250 different multi-domain and domain- and disorder-specific tools.
The diagnostic instruments were those used to diagnose the most common early childhood disorders, including intellectual disability, global developmental delay, communication disorders, autism spectrum disorder, attention-deficit/hyperactivity disorder, cerebral palsy, movement disorders, and fetal alcohol spectrum disorder. Burgess and her colleagues sought to determine which tools had the strongest evidence behind them, noting that comparisons were inherently limited by differences in the tested populations, cutoff values, and other factors.
Burgess and her colleagues identified 67 instruments — about a third of those analyzed in the study — “with good discriminative or predictive validity for the screening and assessment of developmental concerns or disability.” Recommended tools were classified by tool type and by patient age groups.
The reason a tool might not be recommended, Burgess said in an email, was for lack of psychometric testing or published evidence, or because the tool was very narrow in scope (eg, covering only a single aspect of a domain), had a small time window for use, or was too new to have been captured in published systematic reviews.
Top Recommendations
Among multi-domain assessment tools, the Bayley Scales of Infant and Toddler Development, the Battelle Developmental Inventory, and the Mullen Scales of Early Learning all emerged as highly recommended. The top diagnostic screening tool for autism was the revised version of Social Attention and Communication Surveillance. For cerebral palsy, the top-rated diagnostic assessment tools were Prechtl’s Qualitative Assessment of General Movements and the Hammersmith Infant Neurological Examination.
Ratifying findings by other groups, the researchers determined the Ages & Stages Questionnaires, Third Edition (ASQ-3) to be the best overall multi-domain screening instrument for early childhood development, thanks to its simplicity and ease of use by a wide range of practitioner types. Burgess and her colleagues noted, however, that the ASQ-3 “will not identify all children with developmental concerns and may incorrectly identify others,” and that it may be more accurate in children 2 years or older.
Patient Care Setting and Cultural, Socioeconomic Factors Are Key
This news organization spoke to two clinicians working with these and similar tools in the United States. Both said that the care setting can also influence the utility of tools, with cultural and socioeconomic factors playing important roles.
Liz Schwandt, PsyD, an early intervention specialist in Los Angeles, said in an interview that children living in high-risk communities in the United States have a larger burden of developmental delays. But for many families in these communities, accessing care can be complex, which is why well-designed, efficient screening tools like ASQ-3 are especially valuable in practice.
“The reality is you have 10 minutes with a lot of families, and if it’s an emergency, you need to know,” she said. “The ASQ-3 has a very broad age range for this type of instrument and can be used by different practitioner types. The reason it’s successful lies in its parent-centric approach and inherent ease of use. It’s quick, and you can score it using pencil and paper while chatting with the parent, and you can use it for multiple siblings in the space of one appointment.”
With very young children, in whom neurodevelopmental concerns often overlap domains, Schwandt said it can be more important to flag a potential problem early and initiate a nonspecific developmental intervention than wait for results from more precise assessments using more specialized tools. These often require multiple, multi-hour appointments, which can be difficult to attain in lower-resource settings in the United States and can delay care, she said.
Liza Mackintosh, MD, a pediatrician at a federally funded healthcare center in Los Angeles that serves mostly publicly insured families, called validated first-line screening tools “incredibly important.” While rates of developmental screenings in pediatric clinics are increasing, there is still room for improvement, she said.
Mackintosh’s institution does not currently use the ASQ-3 but a different screening tool, called the Survey of Well-Being of Young Children (SWYC), that is embedded into the electronic health record. (The SWYC was not among the tools highlighted in Burgess and colleagues’ review.) Like the ASQ-3, it is short and efficient, she said, and it is used in all children in the recommended age ranges.
“Our visits are on average only 20 minutes,” Mackintosh said. “There’s not enough time for an in-depth developmental assessment. We will flag things such as a speech delay, gross motor delay, or fine motor delay” and refer to early intervention centers for more in-depth developmental assessments as needed, she said.
“The biggest job of pediatricians working in communities that are under-resourced is advocating for those early intervention services,” Mackintosh added. “We really see our job as doing the recommended screening, putting that together with what we’re seeing clinically and on history, and then advocating for the right next step or early intervention. Because sometimes the diagnosis is — I don’t want to say irrelevant, but your treatment plan is still going to be the same. So while I don’t have a formal diagnosis yet, the child definitely needs therapies and we’re still going to get those therapies.”
Burgess and her colleagues stressed in their paper the importance of selecting tools that are culturally appropriate for Indigenous communities in Australia, noting that “inappropriate tools may lead to over- or under-recognition of children with developmental concerns.”
Schwandt and Mackintosh said that the same applies in US settings.
“We’ve done a good job translating screening tools into Chinese, Spanish, Vietnamese, and Russian,” Schwandt said. “But some of them assume a way of taking care of children that is not always shared across cultures. The expectations of how children should play and interact with adults can be very different, and there needs to be an understanding of that. Just putting something in Vietnamese doesn’t mean that there are obvious analogues to understanding what the questionnaire is asking.”
Mackintosh concurred. “A lot of times our patients will not do well on screening, even though they’re fine, because they don’t have the exposure to that activity that’s being asked about. So — is the child scribbling with crayons? Is she climbing up a ladder at a playground? In order to be able to do that, you need to have an environment that you are doing it in. The screeners have to really be appropriate for what the child is exposed to. And sometimes our patients just don’t have that exposure.”
Burgess and colleagues’ study was funded by the Australian government and the Merchant Charitable Foundation. The authors disclosed no financial conflicts of interest. Schwandt and Mackintosh disclosed no conflicts of interest related to their comments.
A version of this article appeared on Medscape.com.
Early recognition of neurodevelopmental concerns and timely access to services have been shown to result in better outcomes for young children. But not all instruments are of equal value, and new research has sought to identify the most useful among them.
For their research, published online in Developmental Medicine & Child Neurology, Andrea Burgess, PhD, of the University of Queensland in Brisbane, Australia, and her colleagues looked at two decades’ worth of systematic reviews of screening, assessment, and diagnostic tools used in children younger than 6 years.
Eighty-six clinical reviews and six practice guidelines, all published between 2000 and 2023, were included in the scoping review, which covered nearly 250 different multi-domain and domain- and disorder-specific tools.
The diagnostic instruments were those used to diagnose the most common early childhood disorders, including intellectual disability, global developmental delay, communication disorders, autism spectrum disorder, attention-deficit/hyperactivity disorder, cerebral palsy, movement disorders, and fetal alcohol spectrum disorder. Burgess and her colleagues sought to determine which tools had the strongest evidence behind them, noting that comparisons were inherently limited by differences in the tested populations, cutoff values, and other factors.
Burgess and her colleagues identified 67 instruments — about a third of those analyzed in the study — “with good discriminative or predictive validity for the screening and assessment of developmental concerns or disability.” Recommended tools were classified by tool type and by patient age groups.
The reason a tool might not be recommended, Burgess said in an email, was for lack of psychometric testing or published evidence, or because the tool was very narrow in scope (eg, covering only a single aspect of a domain), had a small time window for use, or was too new to have been captured in published systematic reviews.
Top Recommendations
Among multi-domain assessment tools, the Bayley Scales of Infant and Toddler Development, the Battelle Developmental Inventory, and the Mullen Scales of Early Learning all emerged as highly recommended. The top diagnostic screening tool for autism was the revised version of Social Attention and Communication Surveillance. For cerebral palsy, the top-rated diagnostic assessment tools were Prechtl’s Qualitative Assessment of General Movements and the Hammersmith Infant Neurological Examination.
Ratifying findings by other groups, the researchers determined the Ages & Stages Questionnaires, Third Edition (ASQ-3) to be the best overall multi-domain screening instrument for early childhood development, thanks to its simplicity and ease of use by a wide range of practitioner types. Burgess and her colleagues noted, however, that the ASQ-3 “will not identify all children with developmental concerns and may incorrectly identify others,” and that it may be more accurate in children 2 years or older.
Patient Care Setting and Cultural, Socioeconomic Factors Are Key
This news organization spoke to two clinicians working with these and similar tools in the United States. Both said that the care setting can also influence the utility of tools, with cultural and socioeconomic factors playing important roles.
Liz Schwandt, PsyD, an early intervention specialist in Los Angeles, said in an interview that children living in high-risk communities in the United States have a larger burden of developmental delays. But for many families in these communities, accessing care can be complex, which is why well-designed, efficient screening tools like ASQ-3 are especially valuable in practice.
“The reality is you have 10 minutes with a lot of families, and if it’s an emergency, you need to know,” she said. “The ASQ-3 has a very broad age range for this type of instrument and can be used by different practitioner types. The reason it’s successful lies in its parent-centric approach and inherent ease of use. It’s quick, and you can score it using pencil and paper while chatting with the parent, and you can use it for multiple siblings in the space of one appointment.”
With very young children, in whom neurodevelopmental concerns often overlap domains, Schwandt said it can be more important to flag a potential problem early and initiate a nonspecific developmental intervention than wait for results from more precise assessments using more specialized tools. These often require multiple, multi-hour appointments, which can be difficult to attain in lower-resource settings in the United States and can delay care, she said.
Liza Mackintosh, MD, a pediatrician at a federally funded healthcare center in Los Angeles that serves mostly publicly insured families, called validated first-line screening tools “incredibly important.” While rates of developmental screenings in pediatric clinics are increasing, there is still room for improvement, she said.
Mackintosh’s institution does not currently use the ASQ-3 but a different screening tool, called the Survey of Well-Being of Young Children (SWYC), that is embedded into the electronic health record. (The SWYC was not among the tools highlighted in Burgess and colleagues’ review.) Like the ASQ-3, it is short and efficient, she said, and it is used in all children in the recommended age ranges.
“Our visits are on average only 20 minutes,” Mackintosh said. “There’s not enough time for an in-depth developmental assessment. We will flag things such as a speech delay, gross motor delay, or fine motor delay” and refer to early intervention centers for more in-depth developmental assessments as needed, she said.
“The biggest job of pediatricians working in communities that are under-resourced is advocating for those early intervention services,” Mackintosh added. “We really see our job as doing the recommended screening, putting that together with what we’re seeing clinically and on history, and then advocating for the right next step or early intervention. Because sometimes the diagnosis is — I don’t want to say irrelevant, but your treatment plan is still going to be the same. So while I don’t have a formal diagnosis yet, the child definitely needs therapies and we’re still going to get those therapies.”
Burgess and her colleagues stressed in their paper the importance of selecting tools that are culturally appropriate for Indigenous communities in Australia, noting that “inappropriate tools may lead to over- or under-recognition of children with developmental concerns.”
Schwandt and Mackintosh said that the same applies in US settings.
“We’ve done a good job translating screening tools into Chinese, Spanish, Vietnamese, and Russian,” Schwandt said. “But some of them assume a way of taking care of children that is not always shared across cultures. The expectations of how children should play and interact with adults can be very different, and there needs to be an understanding of that. Just putting something in Vietnamese doesn’t mean that there are obvious analogues to understanding what the questionnaire is asking.”
Mackintosh concurred. “A lot of times our patients will not do well on screening, even though they’re fine, because they don’t have the exposure to that activity that’s being asked about. So — is the child scribbling with crayons? Is she climbing up a ladder at a playground? In order to be able to do that, you need to have an environment that you are doing it in. The screeners have to really be appropriate for what the child is exposed to. And sometimes our patients just don’t have that exposure.”
Burgess and colleagues’ study was funded by the Australian government and the Merchant Charitable Foundation. The authors disclosed no financial conflicts of interest. Schwandt and Mackintosh disclosed no conflicts of interest related to their comments.
A version of this article appeared on Medscape.com.
A Hard Look at Toxic Workplace Culture in Medicine
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.
While Kellie Lease Stecher, MD, was working as an ob.gyn. in Minneapolis, Minnesota, a patient confided in her a sexual assault allegation about one of Stecher’s male colleagues. Stecher shared the allegation with her supervisor, who told Stecher not to file a report and chose not to address the issue with the patient. Stecher weighed how to do the right thing: Should she speak up? What were the ethical and legal implications of speaking up vs staying silent?
After seeking advice from her mentors, Stecher felt it was her moral and legal duty to report the allegation to the Minnesota Medical Board. Once she did, her supervisor chastised her repeatedly for reporting the allegation. Stecher soon found herself in a hostile work environment where she was regularly singled out and silenced by her supervisor and colleagues.
“I got to a point where I felt like I couldn’t say anything at any meetings without somehow being targeted after the meeting. There was an individual who was even allowed to fat-shame me with no consequences,” Stecher said. “[Being bullied at work is] a struggle because you have no voice, you have no opportunities, and there’s someone who is intentionally making your life uncomfortable.”
Stecher’s experience is not unusual. Mistreatment is a common issue among healthcare workers, ranging from rudeness to bullying and harassment and permeating every level and specialty of the medical profession. A 2019 research review estimated that 26.3% of healthcare workers had experienced bullying and found bullying in healthcare to be associated with mental health problems such as burnout and depression, physical health problems such as insomnia and headaches, and physicians taking more sick leave.
The Medscape Physician Workplace Culture Report 2024 found similarly bleak results:
- 38% said workplace culture is declining.
- 70% don’t see a big commitment from employers for positive culture.
- 48% said staff isn’t committed to positive culture.
The irony, of course, is that most physicians enter the field to care for people. As individuals go from medical school to residency and on with the rest of their careers, they often experience a rude awakening.
It’s Everywhere
Noticing the prevalence of workplace bullying in the medical field, endocrinologist Farah Khan, MD, at UW Medicine in Seattle, Washington, decided to conduct a survey on the issue.
Khan collected 122 responses from colleagues, friends, and acquaintances in the field. When asked if they had ever been bullied in medicine, 68% of respondents said yes. But here’s the fascinating part: She tried to pinpoint one particular area or source of toxicity in the progression of a physician’s career — and couldn’t because it existed at all levels.
More than one third of respondents said their worst bullying experiences occurred in residency, while 30% said mistreatment was worst in medical school, and 24% indicated their worst experience had occurred once they became an attending.
The litany of experiences included being belittled, excluded, yelled at, criticized, shamed, unfairly blamed, threatened, sexually harassed, subjected to bigotry and slurs, and humiliated.
“What surprised me the most was how widespread this problem is and the many different layers of healthcare it permeates through, from operating room staff to medical students to hospital HR to residents and attendings,” Khan said of her findings.
Who Cares for the Caregivers?
When hematologist Mikkael Sekeres, MD, was in medical school, he seriously considered a career as a surgeon. Following success in his surgical rotations, he scrubbed in with a cardiothoracic surgeon who was well known for both his status as a surgeon and his fiery temper. Sekeres witnessed the surgeon yelling at whoever was nearby: Medical students, fellows, residents, operating room nurses.
“At the end of that experience, any passing thoughts I had of going into cardiothoracic surgery were gone,” Sekeres said. “Some of the people I met in surgery were truly wonderful. Some were unhappy people.”
He has clear ideas why. Mental health struggles that are all too common among physicians can be caused or exacerbated by mistreatment and can also lead a physician to mistreat others.
“People bully when they themselves are hurting,” Sekeres said. “It begs the question, why are people hurting? What’s driving them to be bullies? I think part of the reason is that they’re working really hard and they’re tired, and nobody’s caring for them. It’s hard to care for others when you feel as if you’re hurting more than they are.”
Gail Gazelle, MD, experienced something like this. In her case, the pressure to please and to be a perfect professional and mother affected how she interacted with those around her. While working as a hospice medical director and an academician and clinician at Harvard Medical School, Boston, Massachusetts, she found herself feeling exhausted and burnt out but simultaneously guilty for not doing enough at work or at home.
Guess what happened? She became irritable, lashing out at her son and not putting her best foot forward with coworkers or patients.
After trying traditional therapy and self-help through books and podcasts, Gazelle found her solution in life coaching. “I realized just how harsh I was being on myself and found ways to reverse that pattern,” she said. “I learned ways of regulating myself emotionally that I definitely didn’t learn in my training.”
Today, Gazelle works as a life coach herself, guiding physicians through common challenges of the profession — particularly bullying, which she sees often. She remembers one client, an oncologist, who was being targeted by a nurse practitioner she was training. The nurse practitioner began talking back to the oncologist, as well as gossiping and bad-mouthing her to the nurses in the practice. The nurses then began excluding the oncologist from their cafeteria table at lunchtime, which felt blatant in such a small practice.
A core component of Gazelle’s coaching strategy was helping the client reclaim her self-esteem by focusing on her strengths. She instructed the client to write down what went well that day each night rather than lying in bed ruminating. Such self-care strategies can not only help bullied physicians but also prevent some of the challenges that might cause a physician to bully or lash out at another in the first place.
Such strategies, along with the recent influx of wellness programs available in healthcare facilities, can help physicians cope with the mental health impacts of bullying and the job in general. But even life coaches like Gazelle acknowledge that they are often band-aids on the system’s deeper wounds. Bullying in healthcare is not an individual issue; at its core, it’s an institutional one.
Negative Hierarchies in Healthcare
When Stecher’s contract expired, she was fired by the supervisor who had been bullying her. Stecher has since filed a lawsuit, claiming sexual discrimination, defamation, and wrongful termination.
The medical field has a long history of hierarchy, and while this rigidity has softened over time, negative hierarchical dynamics are often perpetuated by leaders. Phenomena like cronyism and cliques and behaviors like petty gossip, lunchroom exclusion (which in the worst cases can mimic high school dynamics), and targeting can be at play in the healthcare workplace.
The classic examples, Stecher said, can usually be spotted: “If you threaten the status quo or offer different ideas, you are seen as a threat. Cronyism ... strict hierarchies ... people who elevate individuals in their social arena into leadership positions. Physicians don’t get the leadership training that they really need; they are often just dumped into roles with no previous experience because they’re someone’s golfing buddy.”
The question is how to get workplace culture momentum moving in a positive direction. When Gazelle’s clients are hesitant to voice concerns, she emphasizes doing so can and should benefit leadership, as well as patients and the wider healthcare system.
“The win-win is that you have a healthy culture of respect and dignity and civility rather than the opposite,” she said. “The leader will actually have more staff retention, which everybody’s concerned about, given the shortage of healthcare workers.”
And that’s a key incentive that may not be discussed as much: Talent drain from toxicity. The Medscape Workplace Culture Report asked about culture as it applies to physicians looking to join up. Notably, 93% of doctors say culture is important when mulling a job offer, 70% said culture is equal to money, and 18% ranked it as more important than money, and 46% say a positive atmosphere is the top priority.
Ultimately, it comes down to who is willing to step in and stand up. Respondents to Khan’s survey counted anonymous reporting systems, more supportive administration teams, and zero-tolerance policies as potential remedies. Gazelle, Sekeres, and Stecher all emphasize the need for zero-tolerance policies for bullying and mistreatment.
“We can’t afford to have things going on like this that just destroy the fabric of the healthcare endeavor,” Gazelle said. “They come out sideways eventually. They come out in terms of poor patient care because there are greater errors. There’s a lack of respect for patients. There’s anger and irritability and so much spillover. We have to have zero-tolerance policies from the top down.”
A version of this article appeared on Medscape.com.