User login
How to give a talk
I have to give a talk. Get this – the topic is how to give a good talk. Very meta.
I’ve given a hundred or so presentations in my career, including a couple of TEDx talks. With each one, I try to get a little better. Effective speaking is always simple but never easy. Let me share with you a few things I’ve learned.
Even if you don’t want to become a TEDMED phenom, you should know a few fundamentals. Giving good talks enhances your reputation and can jump-start your practice or career. For any talk, you must master three things: preparation, content, and delivery.
Just as we choose movies with actors we like, people choose speakers they want to see. Who you are matters. If you are introduced by an emcee, then be sure he or she bills you as a star. However, don’t try to be someone you aren’t – If I gave a talk on robotic prostate surgery, I’d be sure to lose no matter how witty I was. That’s why writing your own intro can sometimes be your best option.
Next up: content. It’s the king of speaking as well as marketing. Although you can pick up points for style, if you want to be remembered, you have to deliver something worth remembering. This starts with your preparation. Resist the temptation to focus exclusively on your slides. As in writing, it is best to brainstorm what you want to cover, then outline your ideas, then fill in content with slides.
Most presentations require visuals; however, there are times when you can do without. Go for it! Nothing is more freeing or more intimate than you one-on-one with your audience. If you must have slides, then follow the one-idea one-slide rule. Slides crammed with information actually detract from your presentation. Here’s a tip: Write only what you can fit with a marker on a Post-it pad. Then, laying out the Post-its, you can rearrange slides getting a feel for the flow or argument of the talk.
Did you ever wonder why headlines like, “Why I never use this suture” and “How I cut my EMR documentation time in half” work so well? They tap into a core human instinct: curiosity. Your opening should introduce some sense of wonder. What is she going to share? Really, how does he do that? Starting with a problem and taking them to a solution is also a great game plan that will often yield success.
When it comes to slides, be clean and concise. Taking a cue from wildly popular TED talks, use images and art instead of words. Use sentence fragments, not sentences, and limit content to the width of the slide (no easy feat). Sometimes you need the slide to prompt your talking point. Put only the data or fact you need and leave the rest at the bottom in your notes section.
Humor is almost always a good idea and more difficult to execute than most realize. Cartoons with captions don’t work. I know that’s hard for many of you to hear, but it’s true. Delete them from your decks. Go ahead, I’ll wait.
Instead, try finding something relevant to the audience that only they will find funny. Inside jokes not only have a higher chance of success, but will also help you bond with your audience. A joke about ICD10 as it relates to neurology is better than the funniest Calvin and Hobbes strip. Self-deprecating humor is always appreciated. I’m not among the gifted who can come up with a great one-liner on the spot. It’s OK to plan it ahead.
Once you’ve got your talk built, it’s time to run it. This is hard, as it requires planning to have your content done in time to rehearse. Find the discipline to do it. The first time you run it, you’ll likely realize that 1/3 of the content needs to be cut. Cut it. Indeed, plan to run 10% less than the time allotted. Leave your audience wanting for more rather than wishing for less.
As I’ve learned, your talking points and slides will always be most appreciated in your own head. Keeping to time shows your respect for your audience and makes you appear polished.
The day of, get to the venue well ahead of time and check the sound, lights, and temperature. All of your preparation will be for naught if they can’t hear you, see your slides, or feel their fingers due to the frigid AC.
One of the reasons I love giving talks is because they are live. You and your audience are intimately engaged, and like any conversation, you’ll sense how it’s going. Are they looking at you or at their phones? Do they seem bored? Do they laugh easily, even when you weren’t expecting them to? Observe what is happening and adjust your performance accordingly. Are you losing them? Pause. Let them catch up. Are you putting them to sleep? Pick up the pace. Try that bit of humor now.
Your delivery is critical to your success. If you’re on the dais and behind the podium of a large audience, then be big, Greek theatre big, which means bigger facial expressions and bigger arm and hand gestures. Vary the tone and pace of your voice. Speed it up to build excitement. Slow down and lower your pitch for gravity and authority. Pause for 3-4 seconds to create suspense and drama.
Leave time for discussion when possible. Invite the audience to engage by asking, What do you think? Finally, on the plane ride home, or even as you walk back from the auditorium to your clinic, think about your presentation: What worked? What fell flat? What roused the audience? How can you deliver it better next time?
Even if it didn’t go well, remember, there’s always next week. It’s on to Cincinnati.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@frontlinemedcom.com.
I have to give a talk. Get this – the topic is how to give a good talk. Very meta.
I’ve given a hundred or so presentations in my career, including a couple of TEDx talks. With each one, I try to get a little better. Effective speaking is always simple but never easy. Let me share with you a few things I’ve learned.
Even if you don’t want to become a TEDMED phenom, you should know a few fundamentals. Giving good talks enhances your reputation and can jump-start your practice or career. For any talk, you must master three things: preparation, content, and delivery.
Just as we choose movies with actors we like, people choose speakers they want to see. Who you are matters. If you are introduced by an emcee, then be sure he or she bills you as a star. However, don’t try to be someone you aren’t – If I gave a talk on robotic prostate surgery, I’d be sure to lose no matter how witty I was. That’s why writing your own intro can sometimes be your best option.
Next up: content. It’s the king of speaking as well as marketing. Although you can pick up points for style, if you want to be remembered, you have to deliver something worth remembering. This starts with your preparation. Resist the temptation to focus exclusively on your slides. As in writing, it is best to brainstorm what you want to cover, then outline your ideas, then fill in content with slides.
Most presentations require visuals; however, there are times when you can do without. Go for it! Nothing is more freeing or more intimate than you one-on-one with your audience. If you must have slides, then follow the one-idea one-slide rule. Slides crammed with information actually detract from your presentation. Here’s a tip: Write only what you can fit with a marker on a Post-it pad. Then, laying out the Post-its, you can rearrange slides getting a feel for the flow or argument of the talk.
Did you ever wonder why headlines like, “Why I never use this suture” and “How I cut my EMR documentation time in half” work so well? They tap into a core human instinct: curiosity. Your opening should introduce some sense of wonder. What is she going to share? Really, how does he do that? Starting with a problem and taking them to a solution is also a great game plan that will often yield success.
When it comes to slides, be clean and concise. Taking a cue from wildly popular TED talks, use images and art instead of words. Use sentence fragments, not sentences, and limit content to the width of the slide (no easy feat). Sometimes you need the slide to prompt your talking point. Put only the data or fact you need and leave the rest at the bottom in your notes section.
Humor is almost always a good idea and more difficult to execute than most realize. Cartoons with captions don’t work. I know that’s hard for many of you to hear, but it’s true. Delete them from your decks. Go ahead, I’ll wait.
Instead, try finding something relevant to the audience that only they will find funny. Inside jokes not only have a higher chance of success, but will also help you bond with your audience. A joke about ICD10 as it relates to neurology is better than the funniest Calvin and Hobbes strip. Self-deprecating humor is always appreciated. I’m not among the gifted who can come up with a great one-liner on the spot. It’s OK to plan it ahead.
Once you’ve got your talk built, it’s time to run it. This is hard, as it requires planning to have your content done in time to rehearse. Find the discipline to do it. The first time you run it, you’ll likely realize that 1/3 of the content needs to be cut. Cut it. Indeed, plan to run 10% less than the time allotted. Leave your audience wanting for more rather than wishing for less.
As I’ve learned, your talking points and slides will always be most appreciated in your own head. Keeping to time shows your respect for your audience and makes you appear polished.
The day of, get to the venue well ahead of time and check the sound, lights, and temperature. All of your preparation will be for naught if they can’t hear you, see your slides, or feel their fingers due to the frigid AC.
One of the reasons I love giving talks is because they are live. You and your audience are intimately engaged, and like any conversation, you’ll sense how it’s going. Are they looking at you or at their phones? Do they seem bored? Do they laugh easily, even when you weren’t expecting them to? Observe what is happening and adjust your performance accordingly. Are you losing them? Pause. Let them catch up. Are you putting them to sleep? Pick up the pace. Try that bit of humor now.
Your delivery is critical to your success. If you’re on the dais and behind the podium of a large audience, then be big, Greek theatre big, which means bigger facial expressions and bigger arm and hand gestures. Vary the tone and pace of your voice. Speed it up to build excitement. Slow down and lower your pitch for gravity and authority. Pause for 3-4 seconds to create suspense and drama.
Leave time for discussion when possible. Invite the audience to engage by asking, What do you think? Finally, on the plane ride home, or even as you walk back from the auditorium to your clinic, think about your presentation: What worked? What fell flat? What roused the audience? How can you deliver it better next time?
Even if it didn’t go well, remember, there’s always next week. It’s on to Cincinnati.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@frontlinemedcom.com.
I have to give a talk. Get this – the topic is how to give a good talk. Very meta.
I’ve given a hundred or so presentations in my career, including a couple of TEDx talks. With each one, I try to get a little better. Effective speaking is always simple but never easy. Let me share with you a few things I’ve learned.
Even if you don’t want to become a TEDMED phenom, you should know a few fundamentals. Giving good talks enhances your reputation and can jump-start your practice or career. For any talk, you must master three things: preparation, content, and delivery.
Just as we choose movies with actors we like, people choose speakers they want to see. Who you are matters. If you are introduced by an emcee, then be sure he or she bills you as a star. However, don’t try to be someone you aren’t – If I gave a talk on robotic prostate surgery, I’d be sure to lose no matter how witty I was. That’s why writing your own intro can sometimes be your best option.
Next up: content. It’s the king of speaking as well as marketing. Although you can pick up points for style, if you want to be remembered, you have to deliver something worth remembering. This starts with your preparation. Resist the temptation to focus exclusively on your slides. As in writing, it is best to brainstorm what you want to cover, then outline your ideas, then fill in content with slides.
Most presentations require visuals; however, there are times when you can do without. Go for it! Nothing is more freeing or more intimate than you one-on-one with your audience. If you must have slides, then follow the one-idea one-slide rule. Slides crammed with information actually detract from your presentation. Here’s a tip: Write only what you can fit with a marker on a Post-it pad. Then, laying out the Post-its, you can rearrange slides getting a feel for the flow or argument of the talk.
Did you ever wonder why headlines like, “Why I never use this suture” and “How I cut my EMR documentation time in half” work so well? They tap into a core human instinct: curiosity. Your opening should introduce some sense of wonder. What is she going to share? Really, how does he do that? Starting with a problem and taking them to a solution is also a great game plan that will often yield success.
When it comes to slides, be clean and concise. Taking a cue from wildly popular TED talks, use images and art instead of words. Use sentence fragments, not sentences, and limit content to the width of the slide (no easy feat). Sometimes you need the slide to prompt your talking point. Put only the data or fact you need and leave the rest at the bottom in your notes section.
Humor is almost always a good idea and more difficult to execute than most realize. Cartoons with captions don’t work. I know that’s hard for many of you to hear, but it’s true. Delete them from your decks. Go ahead, I’ll wait.
Instead, try finding something relevant to the audience that only they will find funny. Inside jokes not only have a higher chance of success, but will also help you bond with your audience. A joke about ICD10 as it relates to neurology is better than the funniest Calvin and Hobbes strip. Self-deprecating humor is always appreciated. I’m not among the gifted who can come up with a great one-liner on the spot. It’s OK to plan it ahead.
Once you’ve got your talk built, it’s time to run it. This is hard, as it requires planning to have your content done in time to rehearse. Find the discipline to do it. The first time you run it, you’ll likely realize that 1/3 of the content needs to be cut. Cut it. Indeed, plan to run 10% less than the time allotted. Leave your audience wanting for more rather than wishing for less.
As I’ve learned, your talking points and slides will always be most appreciated in your own head. Keeping to time shows your respect for your audience and makes you appear polished.
The day of, get to the venue well ahead of time and check the sound, lights, and temperature. All of your preparation will be for naught if they can’t hear you, see your slides, or feel their fingers due to the frigid AC.
One of the reasons I love giving talks is because they are live. You and your audience are intimately engaged, and like any conversation, you’ll sense how it’s going. Are they looking at you or at their phones? Do they seem bored? Do they laugh easily, even when you weren’t expecting them to? Observe what is happening and adjust your performance accordingly. Are you losing them? Pause. Let them catch up. Are you putting them to sleep? Pick up the pace. Try that bit of humor now.
Your delivery is critical to your success. If you’re on the dais and behind the podium of a large audience, then be big, Greek theatre big, which means bigger facial expressions and bigger arm and hand gestures. Vary the tone and pace of your voice. Speed it up to build excitement. Slow down and lower your pitch for gravity and authority. Pause for 3-4 seconds to create suspense and drama.
Leave time for discussion when possible. Invite the audience to engage by asking, What do you think? Finally, on the plane ride home, or even as you walk back from the auditorium to your clinic, think about your presentation: What worked? What fell flat? What roused the audience? How can you deliver it better next time?
Even if it didn’t go well, remember, there’s always next week. It’s on to Cincinnati.
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. Dr. Benabio is @Dermdoc on Twitter. Write to him at dermnews@frontlinemedcom.com.
GERD postop relapse rates highest in women, older adults
Healthy men younger than 45 years have the lowest risk of relapse after reflux surgery compared with other demographic subgroups, according to data from a population-based study of 2,655 adults in Sweden. The findings were published online in JAMA.
“Cohort studies have shown a high risk of recurrent symptoms of GERD after surgery, which may have contributed to the decline in the use of antireflux surgery,” but long-term reflux recurrence rates and potential risk factors have not been well studied, wrote John Maret-Ouda, MD, and colleagues at the Karolinska Institutet in Stockholm, Sweden.
Overall, 18% of the patients suffered a reflux relapse; 84% of these were prescribed long-term medication, and 16% underwent additional surgery.
The highest relapse rates occurred among women, older patients, and those with comorbid conditions. Reflux occurred in 22% of women vs. 14% of men (hazard ratio 1.57), and the hazard ratio was 1.41 for patients aged 61 years and older compared with those aged 45 years and younger. Patients with one or more comorbidities were approximately one-third more likely to have a recurrence of reflux, compared with those who had no comorbidities (hazard ratio 1.36).
Approximately 4% of patients reported complications; the most common complication was infection (1.1%), followed by bleeding (0.9%), and esophageal perforation (0.9%).
The recurrence rate of 18% is low compared with other studies, the researchers noted. Possible reasons for the difference include the population-based design of the current study, which meant that no patients were lost to follow-up, as well as the recent time period, “in which laparoscopic antireflux surgery has become more centralized to expert centers where selection of patients might be stricter and the quality of surgery might be higher,” they wrote.
The study findings were limited by several factors including clinical variations on coding, lack of data on certain confounding variables including body mass index and smoking, and a lack of control GERD patients who did not undergo antireflux surgery, the researchers said. The results suggest that the benefits of laparoscopic antireflux surgery may be diminished by the potential for recurrent GERD, they added.
The Swedish Research Council funded the study. The researchers had no financial conflicts to disclose.
“The operation can be performed with a relatively low rate of morbidity and a very low mortality rate,” Stuart J. Spechler, MD, wrote in an editorial. “Although findings regarding GERD symptom relief and patient satisfaction based on medication usage data should be interpreted with caution, the observation that more than 80% of patients did not restart antireflux medications after laparoscopic antireflux surgery suggests that the operation provided long-lasting relief of GERD symptoms for most patients,” he said. Although surgery is not a permanent cure for all patients with GERD, “the ever-increasing number of proposed [proton pump inhibitor] risks has caused the greatest concern among clinicians and their patients,” said Dr. Spechler. “Whether the greater than 80% possibility of long-term freedom from PPIs and their associated risks warrants the 4% risk of acute surgical complications and the 17.7% risk of GERD recurrence is a decision that individual patients should make after a detailed discussion of these risks and benefits with their physicians,” he said. However, the study findings suggest “that laparoscopic antireflux surgery might be an especially appealing option for young and otherwise healthy men, who seem to have the lowest rate of GERD recurrence after antireflux surgery and who otherwise would likely require decades of PPI treatment without the operation,” he wrote (JAMA 2017;318:913-5).
Dr. Spechler is affiliated with Baylor University in Dallas. He disclosed serving as a consultant for Ironwood Pharmaceuticals and Takeda Pharmaceuticals, and funding support from the National Institutes of Health.
“The operation can be performed with a relatively low rate of morbidity and a very low mortality rate,” Stuart J. Spechler, MD, wrote in an editorial. “Although findings regarding GERD symptom relief and patient satisfaction based on medication usage data should be interpreted with caution, the observation that more than 80% of patients did not restart antireflux medications after laparoscopic antireflux surgery suggests that the operation provided long-lasting relief of GERD symptoms for most patients,” he said. Although surgery is not a permanent cure for all patients with GERD, “the ever-increasing number of proposed [proton pump inhibitor] risks has caused the greatest concern among clinicians and their patients,” said Dr. Spechler. “Whether the greater than 80% possibility of long-term freedom from PPIs and their associated risks warrants the 4% risk of acute surgical complications and the 17.7% risk of GERD recurrence is a decision that individual patients should make after a detailed discussion of these risks and benefits with their physicians,” he said. However, the study findings suggest “that laparoscopic antireflux surgery might be an especially appealing option for young and otherwise healthy men, who seem to have the lowest rate of GERD recurrence after antireflux surgery and who otherwise would likely require decades of PPI treatment without the operation,” he wrote (JAMA 2017;318:913-5).
Dr. Spechler is affiliated with Baylor University in Dallas. He disclosed serving as a consultant for Ironwood Pharmaceuticals and Takeda Pharmaceuticals, and funding support from the National Institutes of Health.
“The operation can be performed with a relatively low rate of morbidity and a very low mortality rate,” Stuart J. Spechler, MD, wrote in an editorial. “Although findings regarding GERD symptom relief and patient satisfaction based on medication usage data should be interpreted with caution, the observation that more than 80% of patients did not restart antireflux medications after laparoscopic antireflux surgery suggests that the operation provided long-lasting relief of GERD symptoms for most patients,” he said. Although surgery is not a permanent cure for all patients with GERD, “the ever-increasing number of proposed [proton pump inhibitor] risks has caused the greatest concern among clinicians and their patients,” said Dr. Spechler. “Whether the greater than 80% possibility of long-term freedom from PPIs and their associated risks warrants the 4% risk of acute surgical complications and the 17.7% risk of GERD recurrence is a decision that individual patients should make after a detailed discussion of these risks and benefits with their physicians,” he said. However, the study findings suggest “that laparoscopic antireflux surgery might be an especially appealing option for young and otherwise healthy men, who seem to have the lowest rate of GERD recurrence after antireflux surgery and who otherwise would likely require decades of PPI treatment without the operation,” he wrote (JAMA 2017;318:913-5).
Dr. Spechler is affiliated with Baylor University in Dallas. He disclosed serving as a consultant for Ironwood Pharmaceuticals and Takeda Pharmaceuticals, and funding support from the National Institutes of Health.
Healthy men younger than 45 years have the lowest risk of relapse after reflux surgery compared with other demographic subgroups, according to data from a population-based study of 2,655 adults in Sweden. The findings were published online in JAMA.
“Cohort studies have shown a high risk of recurrent symptoms of GERD after surgery, which may have contributed to the decline in the use of antireflux surgery,” but long-term reflux recurrence rates and potential risk factors have not been well studied, wrote John Maret-Ouda, MD, and colleagues at the Karolinska Institutet in Stockholm, Sweden.
Overall, 18% of the patients suffered a reflux relapse; 84% of these were prescribed long-term medication, and 16% underwent additional surgery.
The highest relapse rates occurred among women, older patients, and those with comorbid conditions. Reflux occurred in 22% of women vs. 14% of men (hazard ratio 1.57), and the hazard ratio was 1.41 for patients aged 61 years and older compared with those aged 45 years and younger. Patients with one or more comorbidities were approximately one-third more likely to have a recurrence of reflux, compared with those who had no comorbidities (hazard ratio 1.36).
Approximately 4% of patients reported complications; the most common complication was infection (1.1%), followed by bleeding (0.9%), and esophageal perforation (0.9%).
The recurrence rate of 18% is low compared with other studies, the researchers noted. Possible reasons for the difference include the population-based design of the current study, which meant that no patients were lost to follow-up, as well as the recent time period, “in which laparoscopic antireflux surgery has become more centralized to expert centers where selection of patients might be stricter and the quality of surgery might be higher,” they wrote.
The study findings were limited by several factors including clinical variations on coding, lack of data on certain confounding variables including body mass index and smoking, and a lack of control GERD patients who did not undergo antireflux surgery, the researchers said. The results suggest that the benefits of laparoscopic antireflux surgery may be diminished by the potential for recurrent GERD, they added.
The Swedish Research Council funded the study. The researchers had no financial conflicts to disclose.
Healthy men younger than 45 years have the lowest risk of relapse after reflux surgery compared with other demographic subgroups, according to data from a population-based study of 2,655 adults in Sweden. The findings were published online in JAMA.
“Cohort studies have shown a high risk of recurrent symptoms of GERD after surgery, which may have contributed to the decline in the use of antireflux surgery,” but long-term reflux recurrence rates and potential risk factors have not been well studied, wrote John Maret-Ouda, MD, and colleagues at the Karolinska Institutet in Stockholm, Sweden.
Overall, 18% of the patients suffered a reflux relapse; 84% of these were prescribed long-term medication, and 16% underwent additional surgery.
The highest relapse rates occurred among women, older patients, and those with comorbid conditions. Reflux occurred in 22% of women vs. 14% of men (hazard ratio 1.57), and the hazard ratio was 1.41 for patients aged 61 years and older compared with those aged 45 years and younger. Patients with one or more comorbidities were approximately one-third more likely to have a recurrence of reflux, compared with those who had no comorbidities (hazard ratio 1.36).
Approximately 4% of patients reported complications; the most common complication was infection (1.1%), followed by bleeding (0.9%), and esophageal perforation (0.9%).
The recurrence rate of 18% is low compared with other studies, the researchers noted. Possible reasons for the difference include the population-based design of the current study, which meant that no patients were lost to follow-up, as well as the recent time period, “in which laparoscopic antireflux surgery has become more centralized to expert centers where selection of patients might be stricter and the quality of surgery might be higher,” they wrote.
The study findings were limited by several factors including clinical variations on coding, lack of data on certain confounding variables including body mass index and smoking, and a lack of control GERD patients who did not undergo antireflux surgery, the researchers said. The results suggest that the benefits of laparoscopic antireflux surgery may be diminished by the potential for recurrent GERD, they added.
The Swedish Research Council funded the study. The researchers had no financial conflicts to disclose.
FROM JAMA
Key clinical point: Young men were less likely than were other demographic groups to experience recurrence of gastroesophageal reflux after surgery.
Major finding: Overall, 18% of 2,655 adults who underwent reflux surgery experienced recurrent reflux requiring long-term medication or additional surgery.
Data source: A population-based, retrospective cohort study of reflux surgery patients in Sweden.
Disclosures: The Swedish Research Council supported the study.
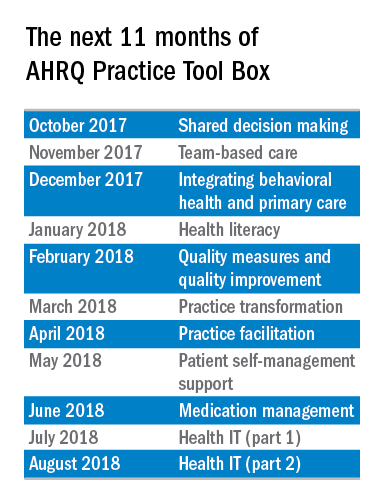
The AHRQ Practice Tool Box
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
This is the first in a series of articles from the National Center for Excellence in Primary Care Research (NCEPCR) in the Agency for Healthcare Research and Quality (AHRQ). This series introduces sets of tools and resources designed to help your practice.
Primary care providers deal with a multitude of challenging clinical issues (e.g., providing first contact and preventive care, diagnosis in the undifferentiated patient, care of patients with chronic illness and multiple chronic conditions, keeping up with the literature) while managing a rapidly changing and often difficult health care environment. Despite this complexity and these challenges, primary care clinicians and health care systems strive to provide high-quality health care – i.e., care that is safe, effective, patient centered, timely, efficient, and equitable.
The Agency for Healthcare Research and Quality (AHRQ), a subdivision of the U.S. Department of Health & Human Services, recognizes that revitalizing this nation’s primary care system is critical to achieving quality health care. To that end, the agency is committed to helping you improve the care you deliver by offering the latest information, providing evidence syntheses, developing tools for improving primary care practice, and generating data and measures to track and improve performance in primary care.
AHRQ established the National Center for Excellence in Primary Care Research (NCEPCR) to be its intellectual home for primary care research. It is the agency’s vehicle for communicating the evidence from AHRQ’s research – and information about how this evidence can be used to improve health and primary health care – to researchers, primary care professionals, health care decision makers, patients, and families.
Electronic resources for daily practice
Every day you rely on guidelines for handling issues that range from prevention to caring for those with multiple chronic conditions. Two of AHRQ’s tools make the use of these guidelines easier.
First, the Electronic Prevention Services Selector (ePSS) is a free application that allows you to search or browse U.S. Preventive Services Task Force recommendations on the Web, a PDA, or a mobile device. You can enter patient-specific information (for example, age, sex, smoking status) to get customized information for your patient. The ePSS brings information on clinical preventive services – recommendations, clinical considerations, and selected practice tools – to the point of care. You can sign up for notifications when there are updates.
The National Guideline Clearinghouse (NGC) provides health professionals with a tool for obtaining objective, detailed information on evidence-based clinical practice guidelines. After you enter a condition onto the webpage, the site offers key information on guidelines related to that condition – including relevant FDA drug safety alerts – and flags guidelines addressing multiple chronic conditions. The site lets you readily compare different guidelines on the same topic.
Like all of AHRQ’s tools and resources, the ePSS and NGC are freely available. These and other tools can be found at the NCEPCR website.
Dr. Bierman is the director of the Center for Evidence and Practice Improvement at AHRQ. Dr. Ganiats is the director for the National Center for Excellence in Primary Care Research at AHRQ.
Statins linked to lower death rates in COPD
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Despite [its] limitations, the study results are intriguing and in line with findings from other retrospective cohorts. How then can we reconcile the apparent benefits observed in retrospective studies with the lack of clinical effect seen in prospective trials, particularly the Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) study? Could it be that both negative and positive studies are “correct”? Prospective studies have thus far not been adequately powered for mortality as an endpoint. Perhaps the choice of the particular statin matters? While STATCOPE involved simvastatin, the majority of the cohort reported by Raymakers et al. received atorvastatin. [Or perhaps] the negative results of STATCOPE could be related to careful selection of study participants with a low burden of systemic inflammation.
This most recent study reinforces the idea that statins may play a beneficial role in COPD, but it isn’t clear which patients to target for therapy. It is unlikely that the findings by Raymakers et al. will reverse recent recommendations by the American College of Chest Physicians and Canadian Thoracic Society against the use of statins for the purpose of prevention of COPD exacerbations, but the suggestion of survival advantage related to statins certainly may breathe new life into an enthusiasm greatly tempered by STATCOPE.
Or Kalchiem-Dekel, MD, and Robert M. Reed, MD, are at the pulmonary and critical care medicine division, University of Maryland, Baltimore. Neither editorialist had conflicts of interest (Chest. 2017;152:456-7. doi: 10.1016/j.chest.2017.04.156).
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Receiving a statin prescription within a year after diagnosis of chronic obstructive pulmonary disease was associated with a 21% decrease in the subsequent risk of all-cause mortality and a 45% drop in risk of pulmonary mortality, according to the results of a large retrospective administrative database study.
The findings belie those of the recent Simvastatin in the Prevention of COPD Exacerbation (STATCOPE) trial, in which daily simvastatin (40 mg) did not affect exacerbation rates or time to first exacerbation in high-risk COPD patients, wrote Adam Raymakers, MSc, a doctoral candidate at the University of British Columbia, Vancouver, and his associates. Their study was observational, but the association between statin use and decreased mortality “persisted across several measures of statin exposure,” they wrote. “Our findings, in conjunction with previously reported evidence, suggests that there may be a specific subtype of COPD patients that may benefit from statin use.” The study appears in the September issue of Chest (2017;152;486-93).
To further explore the question, the researchers analyzed linked health databases from nearly 40,000 patients aged 50 years and older who had received at least three prescriptions for an anticholinergic or a short-acting beta agonist in 12 months some time between 1998 and 2007. The first prescription was considered the date of COPD “diagnosis.” The average age of the patients was 71 years; 55% were female.
A total of 7,775 patients (19.6%) who met this definition of incident COPD were prescribed a statin at least once during the subsequent year. These patients had a significantly reduced risk of subsequent all-cause mortality in univariate and multivariate analyses, with hazard ratios of 0.79 (95% confidence intervals, 0.68 to 0.91; P less than .002). Statins also showed a protective effect against pulmonary mortality, with univariate and multivariate hazard ratios of 0.52 (P = .01) and 0.55 (P = .03), respectively.
The protective effect of statins held up when the investigators narrowed the exposure period to 6 months after COPD diagnosis and when they expanded it to 18 months. Exposure to statins for 80% of the 1-year window after COPD diagnosis – a proxy for statin adherence – also led to a reduced risk of all-cause mortality, but the 95% confidence interval for the hazard ratio did not reach statistical significance (0.71 to 1.01; P = .06).
The most common prescription was for atorvastatin (49%), usually for 90 days (23%), 100 days (20%), or 30 days (15%), the researchers said. While the “possibility of the ‘healthy user’ or the ‘healthy adherer’ cannot be ignored,” they adjusted for other prescriptions, comorbidities, and income level, which should have helped eliminate this effect, they added. However, they lacked data on smoking and lung function assessments, both of which are “important confounders and contributors to mortality,” they acknowledged.
Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
FROM CHEST
Key clinical point: Statins might reduce the risk of death among patients with chronic obstructive pulmonary disease.
Major finding: Statin use was associated with a 21% decrease in risk of all-cause mortality and a 45% decrease in risk of pulmonary mortality.
Data source: A retrospective cohort study of 39,678 patients with COPD, including 7,775 prescribed statins.
Disclosures: Canadian Institutes of Health Research supported the study. One coinvestigator disclosed consulting relationships with Teva, Pfizer, and Novartis. The others had no conflicts of interest.
Palliative care for patients suffering from severe persistent mental illness
While palliative care grows as an interdisciplinary specialty, more clinicians are asking how it can benefit certain patients with severe mental illness.
Palliative care, which developed with the founding of hospices in the 1960s, initially focused on patients who were dying from cancer. The specialty – which emphasizes improving patients’ quality of life rather than finding a cure, and which is different from hospice – can now be used for patients with noncancer diagnoses such as dementia and HIV/AIDS (Psychiatry. 2009 Jun;8[6]:212-15).
Some psychiatrists think that certain patients with another diagnosis would benefit from palliative care: those with severe persistent mental illness.
In fact, this approach might apply to psychiatric patients who are in long-term residential care with “severe/chronic schizophrenia and insufficient quality of life, those with therapy-refractory depressions and repeated suicide attempts, and those with severe long-standing therapy-refractory anorexia nervosa,” wrote Manuel Trachsel, MD, PhD, and his colleagues (BMC Psychiatry (2016 Jul 14:1-9).
Scott A. Irwin, MD, PhD, who coauthored that article and a letter examining these issues, said Dr. Trachsel’s theories lie on the frontiers of current thinking about incorporating palliative care and psychiatric medicine.
Meanwhile, both Dr. Irwin and Maria I. Lapid, MD, another psychiatrist with expertise in palliative care, said that in many ways, the field of psychiatry is inherently palliative in nature.
Palliative ‘approach’ in SPMI
Dr. Trachsel presented unpublished results from a survey of U.S. psychiatrists at the annual meeting of the American Psychiatric Association in May that sought to discern whether they favored supporting short-term quality of life rather than long-term disease modification in certain patients with severe and persistent mental illness (SPMI) – defined as mental illness that is chronic or recurring, requires ongoing intensive psychiatric treatment, and seriously impairs functioning.

Specifically, a palliative care approach to SPMI could include a more relaxed use of agents considered potentially addictive or problematic long term, such as benzodiazepines, Dr. Trachsel said. For patients with medical decision-making capacity, it could 1) include withdrawal of care at a patient’s insistence or periods of intermittent sedation – which is used in palliative medicine for patients with intractable pain; or 2) mean switching a patient with end-stage anorexia and multiple failed treatment attempts to hospice care rather than force feeding, Dr. Trachsel said.
Neither Dr. Trachsel’s survey respondents nor those who attended his presentation seemed comfortable with the idea of extending the term “palliative care” – which is often and incorrectly associated with well-defined end-of-life scenarios – to serious, treatment-refractory mental illness. In those illnesses, disease trajectories may be less certain and futility is harder to define. They and other clinicians, however, did voice general support for the underlying concepts of promoting quality of life and decision-making autonomy for patients with SPMI, as well as palliative care targeted at the medical illnesses often acquired by those with SPMI.
According to Dr. Irwin and Dr. Lapid, reducing symptoms, acknowledging that there is no cure for SPMI, and focusing on optimizing patients’ quality of life would be core components of palliative care.
Futility difficult to define
Dr. Irwin said in an interview that the ideas in the letter (Lancet Psychiatry. 2016 Mar;3[3]:200) in which he and a few other colleagues collaborated with Dr. Trachsel were essentially “a thought experiment and very philosophical.” In addition, the letter, which proposed palliative psychiatry “as a means to improve quality of care, person-centeredness, and autonomy” for patients with SPMI, was supported by a handful of case studies, most of them in patients with end-stage anorexia, he said. Furthermore, end-of-life interventions are only a subset of what palliative care brings to the table, said Dr. Irwin, palliative care psychiatrist at Cedars-Sinai Health System’s Samuel Oschin Comprehensive Cancer Center in Los Angeles.
With a psychiatric illness, the goals are usually around symptom management and quality of life, and for certain palliative care interventions reserved for end-of-life situations, “there’s usually not something knocking at the door that’s putting that end-of-life question into focus,” Dr. Irwin said. To create end-of-life protocols for SPMI, “you would need to know what the prognosis and trajectory are of each stage of these illnesses. And we don’t have good evidence guiding us.
“If we have a patient who is depressed and wants to commit suicide, who knows how many years they could have left if we intervene?” said Dr. Irwin, who has mentored Dr. Trachsel. “If we had the data that this person’s 90% likely to complete a suicide within the next year, it might change the conversation and treatment decisions.”
Dr. Lapid, a board-certified practitioner of palliative and hospice medicine and geriatric psychiatry at the Mayo Clinic in Rochester, Minn., agreed in an interview that for patients with an SPMI and no life-limiting comorbidity, it becomes complicated to attempt to define futility.
Moreover, while Medicare and insurance have precisely detailed guidelines for hospice, which provides palliative care for those with a prognosis of 6 months or less, “there’s no psychiatric illness currently considered a terminal disease eligible for hospice care,” Dr. Lapid said.
Obstacles to access
Patients with SPMI die 25 years earlier than do their peers without SPMI. Most of the premature mortality associated with SPMI, which cuts across age groups, is attributable to chronic diseases rather than to violence or suicide. Less overall engagement with the health care system, leading to late treatment or undertreatment of disease, is one explanation for the premature mortality found among some people in this demographic.
In addition, studies have shown that individuals with SPMI have less access to palliative and hospice care. One study, for example, found that people with schizophrenia and a terminal illness went into hospice half as often as did people without SPMI (Schizophr Res. 2012 Nov;141:241-6). In a recent editorial, a team of psychiatrists and pain specialists called such disparities “unacceptable” and demanded cross-collaboration to resolve them (Gen Hospital Psych. 2017 Jan-Feb;44:1-3).
Dr. Lapid said one reason people with SPMI – with or without a life-limiting comorbidity – end up with less access to palliative and hospice care is that “the art of what we do in hospice and palliative care, advanced planning – is not something we do well or routinely in psychiatry.”
And palliative care specialists may find that for some people with severe mental illness, “it can be hard to really palliate their symptoms,” Dr. Lapid said.
Dr. Irwin noted that patients with SPMI and a terminal illness generally are not extended the same level of agency over their treatment choices as are people without it. Cancer patients, for example, can elect not to receive a treatment even when their prognosis is good. People with serious mental illness – even when they have life-limiting medical comorbidities – may not be given the option of deciding whether to opt for treatment.
Rebecca L. Bauer, MD, a psychosomatic medicine fellow at the Medical College of Wisconsin in Milwaukee, said that psychiatrists, including those with outpatient practices, are well positioned to help patients gain greater access to palliative care and end-of-life planning.
These patients’ medical needs become so pressing at the end of life that psychiatric disease and the distress it inflicts end up a secondary concern, she said, resulting in the patient suffering.
Psychiatrists “can play an important role in removing some of these barriers,” Dr. Bauer said, especially on multidisciplinary teams. For one thing, psychiatrists are adept at prescribing medications aimed at treating concurrent psychiatric symptoms. In addition, they are more likely than are other clinicians to have experience in communicating with patients with psychosis or other thought disorders.
Another important way psychiatrists can help secure access to palliative care for their patients who need it, she said, is to engage patients during times of relative wellness by encouraging them to discuss end-of-life desires and plans, and help them create formal health care directives.
“We know that sometimes patients [with SPMI] are not as engaged in their primary and medical care, and sometimes the psychiatrist is the only provider they consistently follow up with,” Dr. Bauer said.
All the clinicians interviewed acknowledged that, regardless of the feasibility or ethical viability of any single approach, the idea of incorporating some of the pillars of palliative care for patients with SPMI merits more consideration.
The approach used by psychiatrists treating patients with SPMI is very palliative in approach, Dr. Irwin and Dr. Lapid said. Psychiatrists reduce symptoms and acknowledge that SPMIs are chronic diseases for which there is no cure. To palliate is to make comfortable, to reduce symptoms, to reduce distress and pain, and to relieve suffering and optimize quality of life.
“In cancer, we’ve been telling people for 30 years, ‘keep fighting, because tomorrow there could be a new cure.’ But there’ve been very few new cures,” Dr. Irwin said. “And while some people want to fight to the end in case that cure comes, there are many who would have rather known that there really was little chance and might have made different choices.” In psychiatry, for psychiatric illnesses, he continued, “we need to really start thinking about the course of a person’s life, their quality of life, and the likelihood that they will get better or meet their goals, and what is a tolerable symptom burden for them. Because in the end, these questions apply to all patients.”
While palliative care grows as an interdisciplinary specialty, more clinicians are asking how it can benefit certain patients with severe mental illness.
Palliative care, which developed with the founding of hospices in the 1960s, initially focused on patients who were dying from cancer. The specialty – which emphasizes improving patients’ quality of life rather than finding a cure, and which is different from hospice – can now be used for patients with noncancer diagnoses such as dementia and HIV/AIDS (Psychiatry. 2009 Jun;8[6]:212-15).
Some psychiatrists think that certain patients with another diagnosis would benefit from palliative care: those with severe persistent mental illness.
In fact, this approach might apply to psychiatric patients who are in long-term residential care with “severe/chronic schizophrenia and insufficient quality of life, those with therapy-refractory depressions and repeated suicide attempts, and those with severe long-standing therapy-refractory anorexia nervosa,” wrote Manuel Trachsel, MD, PhD, and his colleagues (BMC Psychiatry (2016 Jul 14:1-9).
Scott A. Irwin, MD, PhD, who coauthored that article and a letter examining these issues, said Dr. Trachsel’s theories lie on the frontiers of current thinking about incorporating palliative care and psychiatric medicine.
Meanwhile, both Dr. Irwin and Maria I. Lapid, MD, another psychiatrist with expertise in palliative care, said that in many ways, the field of psychiatry is inherently palliative in nature.
Palliative ‘approach’ in SPMI
Dr. Trachsel presented unpublished results from a survey of U.S. psychiatrists at the annual meeting of the American Psychiatric Association in May that sought to discern whether they favored supporting short-term quality of life rather than long-term disease modification in certain patients with severe and persistent mental illness (SPMI) – defined as mental illness that is chronic or recurring, requires ongoing intensive psychiatric treatment, and seriously impairs functioning.

Specifically, a palliative care approach to SPMI could include a more relaxed use of agents considered potentially addictive or problematic long term, such as benzodiazepines, Dr. Trachsel said. For patients with medical decision-making capacity, it could 1) include withdrawal of care at a patient’s insistence or periods of intermittent sedation – which is used in palliative medicine for patients with intractable pain; or 2) mean switching a patient with end-stage anorexia and multiple failed treatment attempts to hospice care rather than force feeding, Dr. Trachsel said.
Neither Dr. Trachsel’s survey respondents nor those who attended his presentation seemed comfortable with the idea of extending the term “palliative care” – which is often and incorrectly associated with well-defined end-of-life scenarios – to serious, treatment-refractory mental illness. In those illnesses, disease trajectories may be less certain and futility is harder to define. They and other clinicians, however, did voice general support for the underlying concepts of promoting quality of life and decision-making autonomy for patients with SPMI, as well as palliative care targeted at the medical illnesses often acquired by those with SPMI.
According to Dr. Irwin and Dr. Lapid, reducing symptoms, acknowledging that there is no cure for SPMI, and focusing on optimizing patients’ quality of life would be core components of palliative care.
Futility difficult to define
Dr. Irwin said in an interview that the ideas in the letter (Lancet Psychiatry. 2016 Mar;3[3]:200) in which he and a few other colleagues collaborated with Dr. Trachsel were essentially “a thought experiment and very philosophical.” In addition, the letter, which proposed palliative psychiatry “as a means to improve quality of care, person-centeredness, and autonomy” for patients with SPMI, was supported by a handful of case studies, most of them in patients with end-stage anorexia, he said. Furthermore, end-of-life interventions are only a subset of what palliative care brings to the table, said Dr. Irwin, palliative care psychiatrist at Cedars-Sinai Health System’s Samuel Oschin Comprehensive Cancer Center in Los Angeles.
With a psychiatric illness, the goals are usually around symptom management and quality of life, and for certain palliative care interventions reserved for end-of-life situations, “there’s usually not something knocking at the door that’s putting that end-of-life question into focus,” Dr. Irwin said. To create end-of-life protocols for SPMI, “you would need to know what the prognosis and trajectory are of each stage of these illnesses. And we don’t have good evidence guiding us.
“If we have a patient who is depressed and wants to commit suicide, who knows how many years they could have left if we intervene?” said Dr. Irwin, who has mentored Dr. Trachsel. “If we had the data that this person’s 90% likely to complete a suicide within the next year, it might change the conversation and treatment decisions.”
Dr. Lapid, a board-certified practitioner of palliative and hospice medicine and geriatric psychiatry at the Mayo Clinic in Rochester, Minn., agreed in an interview that for patients with an SPMI and no life-limiting comorbidity, it becomes complicated to attempt to define futility.
Moreover, while Medicare and insurance have precisely detailed guidelines for hospice, which provides palliative care for those with a prognosis of 6 months or less, “there’s no psychiatric illness currently considered a terminal disease eligible for hospice care,” Dr. Lapid said.
Obstacles to access
Patients with SPMI die 25 years earlier than do their peers without SPMI. Most of the premature mortality associated with SPMI, which cuts across age groups, is attributable to chronic diseases rather than to violence or suicide. Less overall engagement with the health care system, leading to late treatment or undertreatment of disease, is one explanation for the premature mortality found among some people in this demographic.
In addition, studies have shown that individuals with SPMI have less access to palliative and hospice care. One study, for example, found that people with schizophrenia and a terminal illness went into hospice half as often as did people without SPMI (Schizophr Res. 2012 Nov;141:241-6). In a recent editorial, a team of psychiatrists and pain specialists called such disparities “unacceptable” and demanded cross-collaboration to resolve them (Gen Hospital Psych. 2017 Jan-Feb;44:1-3).
Dr. Lapid said one reason people with SPMI – with or without a life-limiting comorbidity – end up with less access to palliative and hospice care is that “the art of what we do in hospice and palliative care, advanced planning – is not something we do well or routinely in psychiatry.”
And palliative care specialists may find that for some people with severe mental illness, “it can be hard to really palliate their symptoms,” Dr. Lapid said.
Dr. Irwin noted that patients with SPMI and a terminal illness generally are not extended the same level of agency over their treatment choices as are people without it. Cancer patients, for example, can elect not to receive a treatment even when their prognosis is good. People with serious mental illness – even when they have life-limiting medical comorbidities – may not be given the option of deciding whether to opt for treatment.
Rebecca L. Bauer, MD, a psychosomatic medicine fellow at the Medical College of Wisconsin in Milwaukee, said that psychiatrists, including those with outpatient practices, are well positioned to help patients gain greater access to palliative care and end-of-life planning.
These patients’ medical needs become so pressing at the end of life that psychiatric disease and the distress it inflicts end up a secondary concern, she said, resulting in the patient suffering.
Psychiatrists “can play an important role in removing some of these barriers,” Dr. Bauer said, especially on multidisciplinary teams. For one thing, psychiatrists are adept at prescribing medications aimed at treating concurrent psychiatric symptoms. In addition, they are more likely than are other clinicians to have experience in communicating with patients with psychosis or other thought disorders.
Another important way psychiatrists can help secure access to palliative care for their patients who need it, she said, is to engage patients during times of relative wellness by encouraging them to discuss end-of-life desires and plans, and help them create formal health care directives.
“We know that sometimes patients [with SPMI] are not as engaged in their primary and medical care, and sometimes the psychiatrist is the only provider they consistently follow up with,” Dr. Bauer said.
All the clinicians interviewed acknowledged that, regardless of the feasibility or ethical viability of any single approach, the idea of incorporating some of the pillars of palliative care for patients with SPMI merits more consideration.
The approach used by psychiatrists treating patients with SPMI is very palliative in approach, Dr. Irwin and Dr. Lapid said. Psychiatrists reduce symptoms and acknowledge that SPMIs are chronic diseases for which there is no cure. To palliate is to make comfortable, to reduce symptoms, to reduce distress and pain, and to relieve suffering and optimize quality of life.
“In cancer, we’ve been telling people for 30 years, ‘keep fighting, because tomorrow there could be a new cure.’ But there’ve been very few new cures,” Dr. Irwin said. “And while some people want to fight to the end in case that cure comes, there are many who would have rather known that there really was little chance and might have made different choices.” In psychiatry, for psychiatric illnesses, he continued, “we need to really start thinking about the course of a person’s life, their quality of life, and the likelihood that they will get better or meet their goals, and what is a tolerable symptom burden for them. Because in the end, these questions apply to all patients.”
While palliative care grows as an interdisciplinary specialty, more clinicians are asking how it can benefit certain patients with severe mental illness.
Palliative care, which developed with the founding of hospices in the 1960s, initially focused on patients who were dying from cancer. The specialty – which emphasizes improving patients’ quality of life rather than finding a cure, and which is different from hospice – can now be used for patients with noncancer diagnoses such as dementia and HIV/AIDS (Psychiatry. 2009 Jun;8[6]:212-15).
Some psychiatrists think that certain patients with another diagnosis would benefit from palliative care: those with severe persistent mental illness.
In fact, this approach might apply to psychiatric patients who are in long-term residential care with “severe/chronic schizophrenia and insufficient quality of life, those with therapy-refractory depressions and repeated suicide attempts, and those with severe long-standing therapy-refractory anorexia nervosa,” wrote Manuel Trachsel, MD, PhD, and his colleagues (BMC Psychiatry (2016 Jul 14:1-9).
Scott A. Irwin, MD, PhD, who coauthored that article and a letter examining these issues, said Dr. Trachsel’s theories lie on the frontiers of current thinking about incorporating palliative care and psychiatric medicine.
Meanwhile, both Dr. Irwin and Maria I. Lapid, MD, another psychiatrist with expertise in palliative care, said that in many ways, the field of psychiatry is inherently palliative in nature.
Palliative ‘approach’ in SPMI
Dr. Trachsel presented unpublished results from a survey of U.S. psychiatrists at the annual meeting of the American Psychiatric Association in May that sought to discern whether they favored supporting short-term quality of life rather than long-term disease modification in certain patients with severe and persistent mental illness (SPMI) – defined as mental illness that is chronic or recurring, requires ongoing intensive psychiatric treatment, and seriously impairs functioning.

Specifically, a palliative care approach to SPMI could include a more relaxed use of agents considered potentially addictive or problematic long term, such as benzodiazepines, Dr. Trachsel said. For patients with medical decision-making capacity, it could 1) include withdrawal of care at a patient’s insistence or periods of intermittent sedation – which is used in palliative medicine for patients with intractable pain; or 2) mean switching a patient with end-stage anorexia and multiple failed treatment attempts to hospice care rather than force feeding, Dr. Trachsel said.
Neither Dr. Trachsel’s survey respondents nor those who attended his presentation seemed comfortable with the idea of extending the term “palliative care” – which is often and incorrectly associated with well-defined end-of-life scenarios – to serious, treatment-refractory mental illness. In those illnesses, disease trajectories may be less certain and futility is harder to define. They and other clinicians, however, did voice general support for the underlying concepts of promoting quality of life and decision-making autonomy for patients with SPMI, as well as palliative care targeted at the medical illnesses often acquired by those with SPMI.
According to Dr. Irwin and Dr. Lapid, reducing symptoms, acknowledging that there is no cure for SPMI, and focusing on optimizing patients’ quality of life would be core components of palliative care.
Futility difficult to define
Dr. Irwin said in an interview that the ideas in the letter (Lancet Psychiatry. 2016 Mar;3[3]:200) in which he and a few other colleagues collaborated with Dr. Trachsel were essentially “a thought experiment and very philosophical.” In addition, the letter, which proposed palliative psychiatry “as a means to improve quality of care, person-centeredness, and autonomy” for patients with SPMI, was supported by a handful of case studies, most of them in patients with end-stage anorexia, he said. Furthermore, end-of-life interventions are only a subset of what palliative care brings to the table, said Dr. Irwin, palliative care psychiatrist at Cedars-Sinai Health System’s Samuel Oschin Comprehensive Cancer Center in Los Angeles.
With a psychiatric illness, the goals are usually around symptom management and quality of life, and for certain palliative care interventions reserved for end-of-life situations, “there’s usually not something knocking at the door that’s putting that end-of-life question into focus,” Dr. Irwin said. To create end-of-life protocols for SPMI, “you would need to know what the prognosis and trajectory are of each stage of these illnesses. And we don’t have good evidence guiding us.
“If we have a patient who is depressed and wants to commit suicide, who knows how many years they could have left if we intervene?” said Dr. Irwin, who has mentored Dr. Trachsel. “If we had the data that this person’s 90% likely to complete a suicide within the next year, it might change the conversation and treatment decisions.”
Dr. Lapid, a board-certified practitioner of palliative and hospice medicine and geriatric psychiatry at the Mayo Clinic in Rochester, Minn., agreed in an interview that for patients with an SPMI and no life-limiting comorbidity, it becomes complicated to attempt to define futility.
Moreover, while Medicare and insurance have precisely detailed guidelines for hospice, which provides palliative care for those with a prognosis of 6 months or less, “there’s no psychiatric illness currently considered a terminal disease eligible for hospice care,” Dr. Lapid said.
Obstacles to access
Patients with SPMI die 25 years earlier than do their peers without SPMI. Most of the premature mortality associated with SPMI, which cuts across age groups, is attributable to chronic diseases rather than to violence or suicide. Less overall engagement with the health care system, leading to late treatment or undertreatment of disease, is one explanation for the premature mortality found among some people in this demographic.
In addition, studies have shown that individuals with SPMI have less access to palliative and hospice care. One study, for example, found that people with schizophrenia and a terminal illness went into hospice half as often as did people without SPMI (Schizophr Res. 2012 Nov;141:241-6). In a recent editorial, a team of psychiatrists and pain specialists called such disparities “unacceptable” and demanded cross-collaboration to resolve them (Gen Hospital Psych. 2017 Jan-Feb;44:1-3).
Dr. Lapid said one reason people with SPMI – with or without a life-limiting comorbidity – end up with less access to palliative and hospice care is that “the art of what we do in hospice and palliative care, advanced planning – is not something we do well or routinely in psychiatry.”
And palliative care specialists may find that for some people with severe mental illness, “it can be hard to really palliate their symptoms,” Dr. Lapid said.
Dr. Irwin noted that patients with SPMI and a terminal illness generally are not extended the same level of agency over their treatment choices as are people without it. Cancer patients, for example, can elect not to receive a treatment even when their prognosis is good. People with serious mental illness – even when they have life-limiting medical comorbidities – may not be given the option of deciding whether to opt for treatment.
Rebecca L. Bauer, MD, a psychosomatic medicine fellow at the Medical College of Wisconsin in Milwaukee, said that psychiatrists, including those with outpatient practices, are well positioned to help patients gain greater access to palliative care and end-of-life planning.
These patients’ medical needs become so pressing at the end of life that psychiatric disease and the distress it inflicts end up a secondary concern, she said, resulting in the patient suffering.
Psychiatrists “can play an important role in removing some of these barriers,” Dr. Bauer said, especially on multidisciplinary teams. For one thing, psychiatrists are adept at prescribing medications aimed at treating concurrent psychiatric symptoms. In addition, they are more likely than are other clinicians to have experience in communicating with patients with psychosis or other thought disorders.
Another important way psychiatrists can help secure access to palliative care for their patients who need it, she said, is to engage patients during times of relative wellness by encouraging them to discuss end-of-life desires and plans, and help them create formal health care directives.
“We know that sometimes patients [with SPMI] are not as engaged in their primary and medical care, and sometimes the psychiatrist is the only provider they consistently follow up with,” Dr. Bauer said.
All the clinicians interviewed acknowledged that, regardless of the feasibility or ethical viability of any single approach, the idea of incorporating some of the pillars of palliative care for patients with SPMI merits more consideration.
The approach used by psychiatrists treating patients with SPMI is very palliative in approach, Dr. Irwin and Dr. Lapid said. Psychiatrists reduce symptoms and acknowledge that SPMIs are chronic diseases for which there is no cure. To palliate is to make comfortable, to reduce symptoms, to reduce distress and pain, and to relieve suffering and optimize quality of life.
“In cancer, we’ve been telling people for 30 years, ‘keep fighting, because tomorrow there could be a new cure.’ But there’ve been very few new cures,” Dr. Irwin said. “And while some people want to fight to the end in case that cure comes, there are many who would have rather known that there really was little chance and might have made different choices.” In psychiatry, for psychiatric illnesses, he continued, “we need to really start thinking about the course of a person’s life, their quality of life, and the likelihood that they will get better or meet their goals, and what is a tolerable symptom burden for them. Because in the end, these questions apply to all patients.”
Changing the dance
I supervise the family clinic in the outpatient psychiatry resident-run clinic. The Suttons are a typical couple, encountered by the new resident, whom I will call Dr. Suraj. Initially, Dr. Suraj is enthusiastic in his meeting with the Suttons, but soon enters into a conundrum and brings the case to supervision. The couple has an intricate inexplicable dance, leaving the resident baffled. Let’s review the case. (I have changed several key details to protect the couple’s confidentiality.)
Ms. Sutton presents with complaints of “depression,” and slowly, it becomes clear that her complaints center on her spouse’s deficiencies. “He doesn’t understand me; he doesn’t know what it is like being depressed.”
Other complaints follow; some are practical, such as: “He doesn’t help around the house.” Ms. Sutton’s complaints mostly reflect her perception that either her spouse does not care for her adequately, he has lost interest in her, or he is fundamentally unable to respond adequately to her needs. “He says bad things to me, like ‘Just get over it,’ or ‘Don’t make such a fuss about things.’ ”
After three further sessions of listening to her complaints, and a general lack of response to prior and current medications, Dr. Suraj decides that Mr. Sutton needs to come in. Dr. Suraj follows what he has been taught so far: Get a history from the partner to validate symptoms, functioning, and quality of life. Mostly, the session goes as predicted, ending with Dr. Suraj’s attempt to educate Mr. Sutton about the signs and symptoms of depression. It doesn’t come out right, because the impression that Mr. Sutton gets is that Dr. Suraj is siding with his wife. This seems to make things worse, as Mr. Sutton then complains to his wife that “The doctor doesn’t know what he’s talking about,” “is too young to understand,” or a myriad of other put-downs. Ms. Sutton, of course, tells Dr. Suraj about all of this, following it up with “Don’t worry Doc; you are doing a great job.” Other comments are more in the way of commentary: “I told my husband what you said last week, and he disagrees with you.”
Dr. Suraj realizes that “something is amiss;” the case is stuck, and worse, he is stuck in the middle. The general impression, says Dr. Suraj, “is of a woman who feels victimized, neglected, or overlooked, but somehow, she has the power. She presents as the victim but also is the victimizer. He seems to be the victimizer and tormenter, but all in all, just as much the victim of her torments! I do not know how to think about this couple: They seem stuck, unhappily but inexorably stuck together in perpetuity.” Can anything be done to change this relationship?
Dr. Suraj’s uncensored thoughts: Perhaps they should break up or at least stop complaining. What is it that makes people keep complaining about their relationships? Either they accept it or they leave.
Initial areas of focus
Interpersonal violence. The archetypal extreme is that of an abusive relationship, where the victim is subjected to domestic violence. As I wrote in Advances in Psychiatric Treatment, many relationships where violence is present are bidirectional (2007;13[5]:376-83). Couples may not voice this concern for fear of the spouse being turned over to the police. I usually include a question such as: “How many times do your arguments include pushing or shoving or things like that?”
Asking about income, specifically, who controls the finances and how money is spent, clarifies whether one person feels that he or she has no option but to stay in the relationship.
If intimate partner violence (IPV) exists, there are typical protocols for helping the victim leave. When IPV is not a consideration, the resident wonders about the Suttons, when the victim and abuser change or share roles. Why do they keep up this struggle if they are unhappy?
Life expectations. Many couples do not discuss their expectations or what they imagine will happen when they get married. There may be unspoken fantasies such as “I always assumed that you would retire at 65, and we would go traveling together.” People may change their minds, or life circumstances change so that expectations and fantasies about their life together can no longer be sustained. Are there goals that have changed? Are there dependent relatives that prevent marital goals from being achieved? Is there a lack of agreement about what are important life goals?
Change! One spouse may try to make the other person change, according to his or her preferences. In the psychiatrist’s office, this can take the form of pathologizing: He just wasn’t brought up to talk about feelings, meaning he needs to talk about feelings. We hear questions such as: “Can you take him on in therapy?”; “He doesn’t listen ... can you check him for hearing loss?”; “She doesn’t remember what I said: Can you check her for dementia?” These complaints may come up at the beginning of a relationship or later in life, for example, after retirement when the couple is home together for extended periods of time. Is the expectation that each person should be able to fulfill the partner’s every wish and desire? Be all things? That is a tough order.
The Suttons report that change is the main thing they want from each other. After a full family assessment, it is clear that roles are evenly and acceptably shared; they have no differences in family rules; they both enjoy the same hobbies, care for each other, and work together to solve family crises. However, they cannot accept each other the way they are. When the children were young, she said: “I was too busy to get depressed.” Mr. Sutton states that she now wants him to be attentive to her but he is too tired after a lifetime of work, and anyway, she is so whiny he does not want to be around her. So they bicker back and forth, neither giving an inch.
Useful theories
A. Dr. Gottman’s typology. John Gottman, PhD, categorizes couples into five types: Conflict-Avoiding, Validating, Volatile, Hostile, and Hostile-Detached. The three happy couple types (Conflict-Avoiding, Validating, and Volatile) are very different from one another, and each type has its own benefits and risks. Of the two unhappy couple types, hostile couples stayed unhappily married. He derived this categorization from observations of couples in his lab (https://www.gottman.com).
Conflict-Avoiding: Conflict avoiders minimize persuasion attempts and instead emphasize their areas of common ground. They avoid conflict, avoid expressing what they need from one another, and congratulate their relationship for being generally happy. Conflict-avoiding couples balance independence and interdependence. They have clear boundaries, and are separate people with separate interests. They can be connected and caring in areas of overlap where they are interdependent. While they are minimally emotionally expressive, they maintain a ratio of positive-to-negative affect around 5 to 1. Their interaction is good enough for them.
Validating: The interaction of these couples is characterized by ease and calm. They are somewhat expressive but mostly neutral. They are intermediate between avoiders and the volatile couples. They put a lot of emphasis on supporting and understanding their partner’s point of view, and are often empathetic about their partner’s feelings. They will confront their differences, but only on some topics and not on others. They can become highly competitive on some issues, which can turn into a power struggle, but they usually calm down and compromise. The ratio of positive-to-negative comments is 5 to 1.
Volatile: Volatile couples are intensely emotional. During a conflict discussion, they begin persuasion immediately, and they debate with laughter and humor. They are not disrespectful or insulting. Their positive-to-negative comments ratio is 5 to 1. Anger and feelings of insecurity are expressed, but not contempt. They have no clear boundaries around their individual worlds. While they argue about their roles, they emphasize connection and honesty in their communication.
Hostile: Hostile couples are like validators, except there are high levels of defensiveness on the part of both partners. In Dr. Gottman’s lab, the husband was usually the validator and the wife was the avoider.
Hostile-Detached: These couples are like two armies engaged in a standoff. They snipe at one another during conflict, although the air is one of emotional detachment and resignation. In Dr. Gottman’s lab, usually there was a validator husband with a volatile wife. Escalating conflict will occur between two validators, but then one of them will back down. But the volatile will not let the validator withdraw. Dr. Gottman notes that there is a superiority involved in the woman: that the man needs to be taught the right way to be. The woman does not see the need to change.
B. The approach/avoidance dance
The approach/avoidance dance is based on the motivation of each person (Psychol Sci. 2008 Oct 19;[10]:1030-6). A partner with approach goals focuses on attaining positive outcomes, such as intimacy and growth. A partner with avoidance goals focuses away from negative outcomes, such as conflict and rejection (Educational Psychologist. 1999;34:169-89). For example, in a discussion about child care, a husband who has strong approach goals may be concerned with wanting the discussion to go smoothly and wanting both partners to be happy with the outcome. In contrast, a husband with strong avoidance goals may be more concerned with avoiding conflict about child care and preventing both partners from being unhappy with the outcome. People who are not motivated by approach goals are not particularly interested in pursuing positive experiences in their relationships, such as bonding, intimacy, or fun activities. In contrast, people who are motivated by avoidance goals are interested in avoiding negative experiences, such as conflict, betrayal, or rejection by a romantic partner.
C. Attachment
Both of the previously discussed theories have attachment theory at their core, and are organized around anxiety and avoidance. The anxiety would be tied to concern that the partner may not be available or supportive in times of need, and the avoidance piece would be tied to worry that the partner cannot be fully trusted (Fam Process. 2002 Fall;41[3]:546-50). A low score on both of these indices means a secure attachment style. For unhappy couples with cemented attachments, there is no thought that one would leave. They are bound together in unhappiness (Current Opin Psychol. 2017 Feb;13:60-4).
Nice guy husband/borderline wife relationship or hysterical wife/obsessive-compulsive husband: These relationship can be explained using an attachment framework. This male personality type truly enjoys giving and often finds that he needs nothing more in return than a feeling of being appreciated.
D. Emotionally focused therapy
Sue Johnson, EdD, has an evidence-based couples therapy called emotionally focused couples and family therapy. She would interpret the Suttons as a couple caught in a dance of negativity. The goal of therapy is to help couples let down defenses enough to be vulnerable and then to help them express emotional needs to each other. Dr. Johnson helps each person meet the emotional needs of the other. (See http://drsuejohnson.com/)
E. The game of struggle for power and control
In most relationships, there is a minimizer and a maximizer. The minimizer is more subdued within the relationship, while the maximizer is more evocative. When this turns into a game of “Who has the power,” then minimizing and maximizing turns into submission and dominance. Typically, the minimizer becomes dominant, and the maximizer becomes submissive. One partner can become parentalized and the other infantilized. Most often, the maximizer, being more emotional, tends to become infantilized and submissive for fear of angering or disappointing his or her partner. The minimizer, being more contained, tends to gather the power in the relationship, whether by intention or default, and, in this way, becomes parentalized.
Is this power struggle similar to the developmental challenges faced by toddlers? Being in a growth-supporting relationship means that the relationship helps people develop a more mature interpersonal relationship. It is this notion that supports the theory that people at the same developmental level find each other compatible, as they both face the same challenges in life.
So what happened to the Suttons? The resident referred the patient to the outpatient couples therapist, who treated them for six sessions. The assessment revealed that they had played this dance for decades, but it had intensified after Mr. Sutton retired and was available as a daily target for Ms. Sutton’s unhappiness with the way that life had treated her. The mutual negative impact of their interactions was ameliorated to some extent, by helping the couple develop individual interests. They moved from being hostile-detached to conflict-avoiding. The Suttons moved from waltzing to circle dancing.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
I supervise the family clinic in the outpatient psychiatry resident-run clinic. The Suttons are a typical couple, encountered by the new resident, whom I will call Dr. Suraj. Initially, Dr. Suraj is enthusiastic in his meeting with the Suttons, but soon enters into a conundrum and brings the case to supervision. The couple has an intricate inexplicable dance, leaving the resident baffled. Let’s review the case. (I have changed several key details to protect the couple’s confidentiality.)
Ms. Sutton presents with complaints of “depression,” and slowly, it becomes clear that her complaints center on her spouse’s deficiencies. “He doesn’t understand me; he doesn’t know what it is like being depressed.”
Other complaints follow; some are practical, such as: “He doesn’t help around the house.” Ms. Sutton’s complaints mostly reflect her perception that either her spouse does not care for her adequately, he has lost interest in her, or he is fundamentally unable to respond adequately to her needs. “He says bad things to me, like ‘Just get over it,’ or ‘Don’t make such a fuss about things.’ ”
After three further sessions of listening to her complaints, and a general lack of response to prior and current medications, Dr. Suraj decides that Mr. Sutton needs to come in. Dr. Suraj follows what he has been taught so far: Get a history from the partner to validate symptoms, functioning, and quality of life. Mostly, the session goes as predicted, ending with Dr. Suraj’s attempt to educate Mr. Sutton about the signs and symptoms of depression. It doesn’t come out right, because the impression that Mr. Sutton gets is that Dr. Suraj is siding with his wife. This seems to make things worse, as Mr. Sutton then complains to his wife that “The doctor doesn’t know what he’s talking about,” “is too young to understand,” or a myriad of other put-downs. Ms. Sutton, of course, tells Dr. Suraj about all of this, following it up with “Don’t worry Doc; you are doing a great job.” Other comments are more in the way of commentary: “I told my husband what you said last week, and he disagrees with you.”
Dr. Suraj realizes that “something is amiss;” the case is stuck, and worse, he is stuck in the middle. The general impression, says Dr. Suraj, “is of a woman who feels victimized, neglected, or overlooked, but somehow, she has the power. She presents as the victim but also is the victimizer. He seems to be the victimizer and tormenter, but all in all, just as much the victim of her torments! I do not know how to think about this couple: They seem stuck, unhappily but inexorably stuck together in perpetuity.” Can anything be done to change this relationship?
Dr. Suraj’s uncensored thoughts: Perhaps they should break up or at least stop complaining. What is it that makes people keep complaining about their relationships? Either they accept it or they leave.
Initial areas of focus
Interpersonal violence. The archetypal extreme is that of an abusive relationship, where the victim is subjected to domestic violence. As I wrote in Advances in Psychiatric Treatment, many relationships where violence is present are bidirectional (2007;13[5]:376-83). Couples may not voice this concern for fear of the spouse being turned over to the police. I usually include a question such as: “How many times do your arguments include pushing or shoving or things like that?”
Asking about income, specifically, who controls the finances and how money is spent, clarifies whether one person feels that he or she has no option but to stay in the relationship.
If intimate partner violence (IPV) exists, there are typical protocols for helping the victim leave. When IPV is not a consideration, the resident wonders about the Suttons, when the victim and abuser change or share roles. Why do they keep up this struggle if they are unhappy?
Life expectations. Many couples do not discuss their expectations or what they imagine will happen when they get married. There may be unspoken fantasies such as “I always assumed that you would retire at 65, and we would go traveling together.” People may change their minds, or life circumstances change so that expectations and fantasies about their life together can no longer be sustained. Are there goals that have changed? Are there dependent relatives that prevent marital goals from being achieved? Is there a lack of agreement about what are important life goals?
Change! One spouse may try to make the other person change, according to his or her preferences. In the psychiatrist’s office, this can take the form of pathologizing: He just wasn’t brought up to talk about feelings, meaning he needs to talk about feelings. We hear questions such as: “Can you take him on in therapy?”; “He doesn’t listen ... can you check him for hearing loss?”; “She doesn’t remember what I said: Can you check her for dementia?” These complaints may come up at the beginning of a relationship or later in life, for example, after retirement when the couple is home together for extended periods of time. Is the expectation that each person should be able to fulfill the partner’s every wish and desire? Be all things? That is a tough order.
The Suttons report that change is the main thing they want from each other. After a full family assessment, it is clear that roles are evenly and acceptably shared; they have no differences in family rules; they both enjoy the same hobbies, care for each other, and work together to solve family crises. However, they cannot accept each other the way they are. When the children were young, she said: “I was too busy to get depressed.” Mr. Sutton states that she now wants him to be attentive to her but he is too tired after a lifetime of work, and anyway, she is so whiny he does not want to be around her. So they bicker back and forth, neither giving an inch.
Useful theories
A. Dr. Gottman’s typology. John Gottman, PhD, categorizes couples into five types: Conflict-Avoiding, Validating, Volatile, Hostile, and Hostile-Detached. The three happy couple types (Conflict-Avoiding, Validating, and Volatile) are very different from one another, and each type has its own benefits and risks. Of the two unhappy couple types, hostile couples stayed unhappily married. He derived this categorization from observations of couples in his lab (https://www.gottman.com).
Conflict-Avoiding: Conflict avoiders minimize persuasion attempts and instead emphasize their areas of common ground. They avoid conflict, avoid expressing what they need from one another, and congratulate their relationship for being generally happy. Conflict-avoiding couples balance independence and interdependence. They have clear boundaries, and are separate people with separate interests. They can be connected and caring in areas of overlap where they are interdependent. While they are minimally emotionally expressive, they maintain a ratio of positive-to-negative affect around 5 to 1. Their interaction is good enough for them.
Validating: The interaction of these couples is characterized by ease and calm. They are somewhat expressive but mostly neutral. They are intermediate between avoiders and the volatile couples. They put a lot of emphasis on supporting and understanding their partner’s point of view, and are often empathetic about their partner’s feelings. They will confront their differences, but only on some topics and not on others. They can become highly competitive on some issues, which can turn into a power struggle, but they usually calm down and compromise. The ratio of positive-to-negative comments is 5 to 1.
Volatile: Volatile couples are intensely emotional. During a conflict discussion, they begin persuasion immediately, and they debate with laughter and humor. They are not disrespectful or insulting. Their positive-to-negative comments ratio is 5 to 1. Anger and feelings of insecurity are expressed, but not contempt. They have no clear boundaries around their individual worlds. While they argue about their roles, they emphasize connection and honesty in their communication.
Hostile: Hostile couples are like validators, except there are high levels of defensiveness on the part of both partners. In Dr. Gottman’s lab, the husband was usually the validator and the wife was the avoider.
Hostile-Detached: These couples are like two armies engaged in a standoff. They snipe at one another during conflict, although the air is one of emotional detachment and resignation. In Dr. Gottman’s lab, usually there was a validator husband with a volatile wife. Escalating conflict will occur between two validators, but then one of them will back down. But the volatile will not let the validator withdraw. Dr. Gottman notes that there is a superiority involved in the woman: that the man needs to be taught the right way to be. The woman does not see the need to change.
B. The approach/avoidance dance
The approach/avoidance dance is based on the motivation of each person (Psychol Sci. 2008 Oct 19;[10]:1030-6). A partner with approach goals focuses on attaining positive outcomes, such as intimacy and growth. A partner with avoidance goals focuses away from negative outcomes, such as conflict and rejection (Educational Psychologist. 1999;34:169-89). For example, in a discussion about child care, a husband who has strong approach goals may be concerned with wanting the discussion to go smoothly and wanting both partners to be happy with the outcome. In contrast, a husband with strong avoidance goals may be more concerned with avoiding conflict about child care and preventing both partners from being unhappy with the outcome. People who are not motivated by approach goals are not particularly interested in pursuing positive experiences in their relationships, such as bonding, intimacy, or fun activities. In contrast, people who are motivated by avoidance goals are interested in avoiding negative experiences, such as conflict, betrayal, or rejection by a romantic partner.
C. Attachment
Both of the previously discussed theories have attachment theory at their core, and are organized around anxiety and avoidance. The anxiety would be tied to concern that the partner may not be available or supportive in times of need, and the avoidance piece would be tied to worry that the partner cannot be fully trusted (Fam Process. 2002 Fall;41[3]:546-50). A low score on both of these indices means a secure attachment style. For unhappy couples with cemented attachments, there is no thought that one would leave. They are bound together in unhappiness (Current Opin Psychol. 2017 Feb;13:60-4).
Nice guy husband/borderline wife relationship or hysterical wife/obsessive-compulsive husband: These relationship can be explained using an attachment framework. This male personality type truly enjoys giving and often finds that he needs nothing more in return than a feeling of being appreciated.
D. Emotionally focused therapy
Sue Johnson, EdD, has an evidence-based couples therapy called emotionally focused couples and family therapy. She would interpret the Suttons as a couple caught in a dance of negativity. The goal of therapy is to help couples let down defenses enough to be vulnerable and then to help them express emotional needs to each other. Dr. Johnson helps each person meet the emotional needs of the other. (See http://drsuejohnson.com/)
E. The game of struggle for power and control
In most relationships, there is a minimizer and a maximizer. The minimizer is more subdued within the relationship, while the maximizer is more evocative. When this turns into a game of “Who has the power,” then minimizing and maximizing turns into submission and dominance. Typically, the minimizer becomes dominant, and the maximizer becomes submissive. One partner can become parentalized and the other infantilized. Most often, the maximizer, being more emotional, tends to become infantilized and submissive for fear of angering or disappointing his or her partner. The minimizer, being more contained, tends to gather the power in the relationship, whether by intention or default, and, in this way, becomes parentalized.
Is this power struggle similar to the developmental challenges faced by toddlers? Being in a growth-supporting relationship means that the relationship helps people develop a more mature interpersonal relationship. It is this notion that supports the theory that people at the same developmental level find each other compatible, as they both face the same challenges in life.
So what happened to the Suttons? The resident referred the patient to the outpatient couples therapist, who treated them for six sessions. The assessment revealed that they had played this dance for decades, but it had intensified after Mr. Sutton retired and was available as a daily target for Ms. Sutton’s unhappiness with the way that life had treated her. The mutual negative impact of their interactions was ameliorated to some extent, by helping the couple develop individual interests. They moved from being hostile-detached to conflict-avoiding. The Suttons moved from waltzing to circle dancing.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
I supervise the family clinic in the outpatient psychiatry resident-run clinic. The Suttons are a typical couple, encountered by the new resident, whom I will call Dr. Suraj. Initially, Dr. Suraj is enthusiastic in his meeting with the Suttons, but soon enters into a conundrum and brings the case to supervision. The couple has an intricate inexplicable dance, leaving the resident baffled. Let’s review the case. (I have changed several key details to protect the couple’s confidentiality.)
Ms. Sutton presents with complaints of “depression,” and slowly, it becomes clear that her complaints center on her spouse’s deficiencies. “He doesn’t understand me; he doesn’t know what it is like being depressed.”
Other complaints follow; some are practical, such as: “He doesn’t help around the house.” Ms. Sutton’s complaints mostly reflect her perception that either her spouse does not care for her adequately, he has lost interest in her, or he is fundamentally unable to respond adequately to her needs. “He says bad things to me, like ‘Just get over it,’ or ‘Don’t make such a fuss about things.’ ”
After three further sessions of listening to her complaints, and a general lack of response to prior and current medications, Dr. Suraj decides that Mr. Sutton needs to come in. Dr. Suraj follows what he has been taught so far: Get a history from the partner to validate symptoms, functioning, and quality of life. Mostly, the session goes as predicted, ending with Dr. Suraj’s attempt to educate Mr. Sutton about the signs and symptoms of depression. It doesn’t come out right, because the impression that Mr. Sutton gets is that Dr. Suraj is siding with his wife. This seems to make things worse, as Mr. Sutton then complains to his wife that “The doctor doesn’t know what he’s talking about,” “is too young to understand,” or a myriad of other put-downs. Ms. Sutton, of course, tells Dr. Suraj about all of this, following it up with “Don’t worry Doc; you are doing a great job.” Other comments are more in the way of commentary: “I told my husband what you said last week, and he disagrees with you.”
Dr. Suraj realizes that “something is amiss;” the case is stuck, and worse, he is stuck in the middle. The general impression, says Dr. Suraj, “is of a woman who feels victimized, neglected, or overlooked, but somehow, she has the power. She presents as the victim but also is the victimizer. He seems to be the victimizer and tormenter, but all in all, just as much the victim of her torments! I do not know how to think about this couple: They seem stuck, unhappily but inexorably stuck together in perpetuity.” Can anything be done to change this relationship?
Dr. Suraj’s uncensored thoughts: Perhaps they should break up or at least stop complaining. What is it that makes people keep complaining about their relationships? Either they accept it or they leave.
Initial areas of focus
Interpersonal violence. The archetypal extreme is that of an abusive relationship, where the victim is subjected to domestic violence. As I wrote in Advances in Psychiatric Treatment, many relationships where violence is present are bidirectional (2007;13[5]:376-83). Couples may not voice this concern for fear of the spouse being turned over to the police. I usually include a question such as: “How many times do your arguments include pushing or shoving or things like that?”
Asking about income, specifically, who controls the finances and how money is spent, clarifies whether one person feels that he or she has no option but to stay in the relationship.
If intimate partner violence (IPV) exists, there are typical protocols for helping the victim leave. When IPV is not a consideration, the resident wonders about the Suttons, when the victim and abuser change or share roles. Why do they keep up this struggle if they are unhappy?
Life expectations. Many couples do not discuss their expectations or what they imagine will happen when they get married. There may be unspoken fantasies such as “I always assumed that you would retire at 65, and we would go traveling together.” People may change their minds, or life circumstances change so that expectations and fantasies about their life together can no longer be sustained. Are there goals that have changed? Are there dependent relatives that prevent marital goals from being achieved? Is there a lack of agreement about what are important life goals?
Change! One spouse may try to make the other person change, according to his or her preferences. In the psychiatrist’s office, this can take the form of pathologizing: He just wasn’t brought up to talk about feelings, meaning he needs to talk about feelings. We hear questions such as: “Can you take him on in therapy?”; “He doesn’t listen ... can you check him for hearing loss?”; “She doesn’t remember what I said: Can you check her for dementia?” These complaints may come up at the beginning of a relationship or later in life, for example, after retirement when the couple is home together for extended periods of time. Is the expectation that each person should be able to fulfill the partner’s every wish and desire? Be all things? That is a tough order.
The Suttons report that change is the main thing they want from each other. After a full family assessment, it is clear that roles are evenly and acceptably shared; they have no differences in family rules; they both enjoy the same hobbies, care for each other, and work together to solve family crises. However, they cannot accept each other the way they are. When the children were young, she said: “I was too busy to get depressed.” Mr. Sutton states that she now wants him to be attentive to her but he is too tired after a lifetime of work, and anyway, she is so whiny he does not want to be around her. So they bicker back and forth, neither giving an inch.
Useful theories
A. Dr. Gottman’s typology. John Gottman, PhD, categorizes couples into five types: Conflict-Avoiding, Validating, Volatile, Hostile, and Hostile-Detached. The three happy couple types (Conflict-Avoiding, Validating, and Volatile) are very different from one another, and each type has its own benefits and risks. Of the two unhappy couple types, hostile couples stayed unhappily married. He derived this categorization from observations of couples in his lab (https://www.gottman.com).
Conflict-Avoiding: Conflict avoiders minimize persuasion attempts and instead emphasize their areas of common ground. They avoid conflict, avoid expressing what they need from one another, and congratulate their relationship for being generally happy. Conflict-avoiding couples balance independence and interdependence. They have clear boundaries, and are separate people with separate interests. They can be connected and caring in areas of overlap where they are interdependent. While they are minimally emotionally expressive, they maintain a ratio of positive-to-negative affect around 5 to 1. Their interaction is good enough for them.
Validating: The interaction of these couples is characterized by ease and calm. They are somewhat expressive but mostly neutral. They are intermediate between avoiders and the volatile couples. They put a lot of emphasis on supporting and understanding their partner’s point of view, and are often empathetic about their partner’s feelings. They will confront their differences, but only on some topics and not on others. They can become highly competitive on some issues, which can turn into a power struggle, but they usually calm down and compromise. The ratio of positive-to-negative comments is 5 to 1.
Volatile: Volatile couples are intensely emotional. During a conflict discussion, they begin persuasion immediately, and they debate with laughter and humor. They are not disrespectful or insulting. Their positive-to-negative comments ratio is 5 to 1. Anger and feelings of insecurity are expressed, but not contempt. They have no clear boundaries around their individual worlds. While they argue about their roles, they emphasize connection and honesty in their communication.
Hostile: Hostile couples are like validators, except there are high levels of defensiveness on the part of both partners. In Dr. Gottman’s lab, the husband was usually the validator and the wife was the avoider.
Hostile-Detached: These couples are like two armies engaged in a standoff. They snipe at one another during conflict, although the air is one of emotional detachment and resignation. In Dr. Gottman’s lab, usually there was a validator husband with a volatile wife. Escalating conflict will occur between two validators, but then one of them will back down. But the volatile will not let the validator withdraw. Dr. Gottman notes that there is a superiority involved in the woman: that the man needs to be taught the right way to be. The woman does not see the need to change.
B. The approach/avoidance dance
The approach/avoidance dance is based on the motivation of each person (Psychol Sci. 2008 Oct 19;[10]:1030-6). A partner with approach goals focuses on attaining positive outcomes, such as intimacy and growth. A partner with avoidance goals focuses away from negative outcomes, such as conflict and rejection (Educational Psychologist. 1999;34:169-89). For example, in a discussion about child care, a husband who has strong approach goals may be concerned with wanting the discussion to go smoothly and wanting both partners to be happy with the outcome. In contrast, a husband with strong avoidance goals may be more concerned with avoiding conflict about child care and preventing both partners from being unhappy with the outcome. People who are not motivated by approach goals are not particularly interested in pursuing positive experiences in their relationships, such as bonding, intimacy, or fun activities. In contrast, people who are motivated by avoidance goals are interested in avoiding negative experiences, such as conflict, betrayal, or rejection by a romantic partner.
C. Attachment
Both of the previously discussed theories have attachment theory at their core, and are organized around anxiety and avoidance. The anxiety would be tied to concern that the partner may not be available or supportive in times of need, and the avoidance piece would be tied to worry that the partner cannot be fully trusted (Fam Process. 2002 Fall;41[3]:546-50). A low score on both of these indices means a secure attachment style. For unhappy couples with cemented attachments, there is no thought that one would leave. They are bound together in unhappiness (Current Opin Psychol. 2017 Feb;13:60-4).
Nice guy husband/borderline wife relationship or hysterical wife/obsessive-compulsive husband: These relationship can be explained using an attachment framework. This male personality type truly enjoys giving and often finds that he needs nothing more in return than a feeling of being appreciated.
D. Emotionally focused therapy
Sue Johnson, EdD, has an evidence-based couples therapy called emotionally focused couples and family therapy. She would interpret the Suttons as a couple caught in a dance of negativity. The goal of therapy is to help couples let down defenses enough to be vulnerable and then to help them express emotional needs to each other. Dr. Johnson helps each person meet the emotional needs of the other. (See http://drsuejohnson.com/)
E. The game of struggle for power and control
In most relationships, there is a minimizer and a maximizer. The minimizer is more subdued within the relationship, while the maximizer is more evocative. When this turns into a game of “Who has the power,” then minimizing and maximizing turns into submission and dominance. Typically, the minimizer becomes dominant, and the maximizer becomes submissive. One partner can become parentalized and the other infantilized. Most often, the maximizer, being more emotional, tends to become infantilized and submissive for fear of angering or disappointing his or her partner. The minimizer, being more contained, tends to gather the power in the relationship, whether by intention or default, and, in this way, becomes parentalized.
Is this power struggle similar to the developmental challenges faced by toddlers? Being in a growth-supporting relationship means that the relationship helps people develop a more mature interpersonal relationship. It is this notion that supports the theory that people at the same developmental level find each other compatible, as they both face the same challenges in life.
So what happened to the Suttons? The resident referred the patient to the outpatient couples therapist, who treated them for six sessions. The assessment revealed that they had played this dance for decades, but it had intensified after Mr. Sutton retired and was available as a daily target for Ms. Sutton’s unhappiness with the way that life had treated her. The mutual negative impact of their interactions was ameliorated to some extent, by helping the couple develop individual interests. They moved from being hostile-detached to conflict-avoiding. The Suttons moved from waltzing to circle dancing.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose.
Hospital readmissions penalties now in 5th year
With the Hospital Readmissions Reduction Program (HRRP) in its 5th year, what has been the impact on hospitals and on hospitalists?
First of all, a lot of penalties have been paid by hospitals. According to an analysis by Kaiser Health News,1 the Centers for Medicare and Medicaid Services will withhold $528 million from 2,597 hospitals in the current fiscal year, Oct. 1, 2016 to Sept. 30, 2017, for readmissions for six diagnoses that occurred between July 2012 and June 2015. The number of penalized hospitals is down slightly from 2,665 the year before, but the total annual withhold will go up by $108 million.
HRRP exacts Medicare payment penalties from hospitals that have rates of readmissions – within 30 days of discharge – that are higher than expected, based on national rates and the health of their patient population. The maximum penalty is now up to 3% of a hospital’s Medicare reimbursement. Hospitals are being penalized an average of 0.73% of their annual Medicare reimbursement, and cumulative HRRP penalties will reach nearly $1.9 billion by the end of the fiscal year, Kaiser Health News reports.2
“Basically, we chose to introduce the idea of measuring readmissions because we felt it represented an adverse outcome for many people that was being ignored; that risk could be reduced; and improvements would yield benefits for people as well as save money for the health care system,” he told The Hospitalist.
“More than anything, HRRP has sharpened the focus on considering the episode of care from the patient’s perspective – rather than just focusing on venues of care like the hospitalization alone,” Dr. Krumholz said. “The focus on readmission forced many of us in the health professions to consider what the experience was like to leave the acute setting – how information flowed, what kind of concerns people had, the degree to which they understood what had happened to them, the extent to which they were prepared for the next steps.”
Once the patient leaves the hospital, there are myriad factors that will influence their likelihood of returning, notes researcher Karen Joynt, MD, MPH, of the Department of Health Policy and Management at Harvard’s School of Public Health, Boston. “The proportion of patients readmitted to the hospital because of gross error is low, but sometimes we’re too optimistic about our patients’ ability to manage postdischarge,” she said.
“We all know we can do better at providing softer landings, and anyone who’s ever been a hospital patient or a family member of one knows that leaving the hospital is incredibly tumultuous. I experienced that with my own parents, and it’s frightening, even if everything is done right. It’s still a very vulnerable time.”
HRRP has fundamentally changed the conversation about hospital care, Dr. Joynt said. “I think we need to change the conversation even more and talk more about how to prevent admissions in the first place. As a clinician, I think we need to be more innovative, recognizing that the ways we’ll make a real difference probably has more to do with what happens outside of the hospital. My personal hope is that new alternate payment models like accountable care organizations will lead to more creative partnerships with other providers.”
What have we learned about readmissions in 5 years?
A lot of recently published research about readmissions has documented modest decreases in overall readmissions nationally, from over 21% to under 18% between 2007 and 2014, although most of the reduction occurred in the first couple of years after HRRP was announced and it has since largely leveled off.
Other research has tried to explore the relationship between readmissions rates and other outcomes that might matter more to patients or that might be better proxies for the quality of the hospital experience. Is readmission rate a true measure of quality, or just a utilization measure? Research has also tried to document what works: what are the best strategies for preventing avoidable readmissions by improving the discharge process, care transitions, and the coordination of care postdischarge in the community – although no silver bullet has yet been identified.
A recent effort to inject more equity into the penalties program, contained in the wide-ranging 21st Century Cures Act signed into law by President Obama in December 2016, requires Medicare to account for patients’ socio-economic backgrounds when it calculates reductions in its payments to hospitals under HRRP. The law directs the government to change the way pay for performance is applied to safety net hospitals by setting different penalty thresholds for hospitals based on the proportion of their patients who are dually eligible for Medicare and Medicaid.
It remains to be seen how this will be implemented and with what impact. But some critics have continued to question whether hospitals should be held accountable for readmissions, whether 30 days is the correct time frame for that accountability, and whether some hospitals might be simply taking the penalty hit rather than investing in the hard work of care transitions.
Impact on working hospitalists
One expert, Ashish Jha, MD, MPH, director of Harvard’s Global Health Institute, wants to see hospitalists get more engaged in the conversation about how to improve hospital care overall.
Experts say there aren’t metrics available that could allocate penalties to individual hospitalists for their performance in readmissions prevention. But hospitals, clearly, are paying attention, and hospitalist groups may find that part of their negotiation of quality and performance incentives with the hospital includes readmissions.
“There are so many other variables that go into transitions of care, and it would be unreasonable to try to hold the individual doctor responsible for all of them,” he said. But accountability can be passed on to the hospitalist group. “My hospital contracts with a national hospitalist company and our agreement has quality measures that we review with them. We ask them to focus on readmissions.”
Dr. Harte said that when patients are discharged from the hospital, they go from an environment where everything is taken care of for them, to total responsibility for their self-care. Yet we are asking ever more from patients in terms of self-management.
“We need to focus on the human side of the experience. The hospital is a place to be avoided wherever possible,” he said. Yet some readmissions are largely unpreventable. Hospitalists should focus on the patient’s greatest risk of preventable readmission. “Is it health literacy? Is it transportation?”
Readmissions at the front lines
Preetham Talari, MD, FACP, FHM, hospitalist at University of Kentucky HealthCare in Lexington, has an interest in health care safety, quality improvement, and value. He has led the university’s site participation in Project BOOST, the Society of Hospital Medicine’s national mentored quality improvement initiative for care transitions. Dr. Talari also led a quality initiative at the university called the Interprofessional Teamwork Innovation Model to systematize teamwork, first piloted on a 30-bed hospitalist unit where he is medical director.
“Readmissions are not just about doctors, they are more about patient factors, socioeconomic factors, where they live,” Dr. Talari said. “Those are harder to impact, but in my experience, it comes down to thinking about the patient’s needs before discharge – really from the time of admission: What are all the things we can do in the hospital to make sure the patient is safely transitioned home?”
According to Dr. Talari, complex issues like readmissions don’t depend on just one, two, or three factors. “But we do the interventions believing that it will improve processes and outcomes, and then add another intervention and another,” he said. “All of these interventions will add up like a jigsaw puzzle to achieve a final, sustainable outcome. One thing I believe is hospitalists should be leading these efforts.”
Better interventions, better infrastructure
Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University School of Public Health, says the biggest change she has seen resulting from readmissions penalties is that transitions of care are now understood to be both important and the responsibility of front line hospitalists. “That was not true 5 or 10 years ago. We used to spend hours admitting patients to the hospital and then 5 minutes on their discharge.”
“We’ve also learned that the infrastructure can be built better. Historically, hospital discharge summaries have been abysmal. But we can automate the importation of pending labs into the electronic health record. These are things you can change for everybody by changing your template. Sit down in a room together every afternoon to talk about what will happen to the patients when they go home. That’s become standard at our hospital. That was never done before.”
Evidence for improved outcomes is mixed, Dr. Horwitz noted. However, she pointed out, is there any evidence that readmissions penalties have produced adverse outcomes? Did they increase mortality, or length of stay? “So far the evidence suggests that they did not,” she said.
“I think it’s generally likely that the work we have done has resulted in better care. Thousands of people haven’t had to go back to the hospital, and that’s a good thing.”
Recent research on readmissions penalties
A survey by Yale researchers, published in JAMA in December 2016, found that hospitals financially penalized under HRRP reduced their readmissions rates at a higher rate than nonpenalized hospitals, “which implies that penalties can improve quality and readmission performance for hospitals with the most room for improvement,” coauthor Kumar Dharmarajan, MD, MBA, said in a statement.4 The hospitals responded to external pressures – in other words, financial penalties worked. But most of the reduction happened in the 2 years before actual penalties went into effect, which suggests that further improvement will not be easy, the authors note.
A survey of the attitudes of hospital leaders on the HRRP found that it has had a major impact on their efforts to reduce readmissions rates, although the failure to take sociodemographic factors into account was a major complaint for these leaders.5 Most said the penalties were too large, but 42.5% believed HRRP was likely to improve quality.
Some have questioned whether readmissions penalties were just encouraging hospitals to reduce their rates by keeping returning patients in observation units rather than formally readmitting them. Zuckerman et al. in the New England Journal of Medicine found no evidence that changes in observation unit stays accounted for the documented decrease in readmissions.6
But according to Papanicolas et al. in Health Affairs, patient hospital experience has improved only modestly under hospital value-based purchasing for U.S. hospitals, with no evidence that the program has had a beneficial effect on overall patient experience.7 Another study from Harvard by Figueroa et al. found that evidence is lacking that hospital value-based purchasing leads to lower mortality rates.8
“Patients and caregivers tell us: Hey, you people are the experts. You’ve taken care of lots of people with my medical condition before. You should know what my needs are going to be postdischarge and help me anticipate them,” he said.
References
1. Rau J. Medicare’s Readmission Penalties Hit New High. Kaiser Health News. 2016 Aug 2.
2. Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Kaiser Health News, 2016 Sep 30.
3. Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29-37.
4. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016 Dec 27;316(24):2647-56.
5. Joynt KE, Figueroa JF, Orav EJ, Jha AK. Opinions on the Hospital Readmissions Reduction Program: Results of a national survey of hospital leaders. Am J Manag Care. 2016 Aug 1;222(8):e287-94.
6. Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 Apr 21;374(16):1543-51.
7. Papanicolas I, Figueroa JF, Orav EJ, Jha AK. Patient hospital experience improved modestly, but no evidence Medicare incentives promoted meaningful gain. Health Aff (Millwood). 2017 Jan;36(1):133-40.
8. Figueroa JF, Tsugawa Y, Zheng J, et al. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214.
With the Hospital Readmissions Reduction Program (HRRP) in its 5th year, what has been the impact on hospitals and on hospitalists?
First of all, a lot of penalties have been paid by hospitals. According to an analysis by Kaiser Health News,1 the Centers for Medicare and Medicaid Services will withhold $528 million from 2,597 hospitals in the current fiscal year, Oct. 1, 2016 to Sept. 30, 2017, for readmissions for six diagnoses that occurred between July 2012 and June 2015. The number of penalized hospitals is down slightly from 2,665 the year before, but the total annual withhold will go up by $108 million.
HRRP exacts Medicare payment penalties from hospitals that have rates of readmissions – within 30 days of discharge – that are higher than expected, based on national rates and the health of their patient population. The maximum penalty is now up to 3% of a hospital’s Medicare reimbursement. Hospitals are being penalized an average of 0.73% of their annual Medicare reimbursement, and cumulative HRRP penalties will reach nearly $1.9 billion by the end of the fiscal year, Kaiser Health News reports.2
“Basically, we chose to introduce the idea of measuring readmissions because we felt it represented an adverse outcome for many people that was being ignored; that risk could be reduced; and improvements would yield benefits for people as well as save money for the health care system,” he told The Hospitalist.
“More than anything, HRRP has sharpened the focus on considering the episode of care from the patient’s perspective – rather than just focusing on venues of care like the hospitalization alone,” Dr. Krumholz said. “The focus on readmission forced many of us in the health professions to consider what the experience was like to leave the acute setting – how information flowed, what kind of concerns people had, the degree to which they understood what had happened to them, the extent to which they were prepared for the next steps.”
Once the patient leaves the hospital, there are myriad factors that will influence their likelihood of returning, notes researcher Karen Joynt, MD, MPH, of the Department of Health Policy and Management at Harvard’s School of Public Health, Boston. “The proportion of patients readmitted to the hospital because of gross error is low, but sometimes we’re too optimistic about our patients’ ability to manage postdischarge,” she said.
“We all know we can do better at providing softer landings, and anyone who’s ever been a hospital patient or a family member of one knows that leaving the hospital is incredibly tumultuous. I experienced that with my own parents, and it’s frightening, even if everything is done right. It’s still a very vulnerable time.”
HRRP has fundamentally changed the conversation about hospital care, Dr. Joynt said. “I think we need to change the conversation even more and talk more about how to prevent admissions in the first place. As a clinician, I think we need to be more innovative, recognizing that the ways we’ll make a real difference probably has more to do with what happens outside of the hospital. My personal hope is that new alternate payment models like accountable care organizations will lead to more creative partnerships with other providers.”
What have we learned about readmissions in 5 years?
A lot of recently published research about readmissions has documented modest decreases in overall readmissions nationally, from over 21% to under 18% between 2007 and 2014, although most of the reduction occurred in the first couple of years after HRRP was announced and it has since largely leveled off.
Other research has tried to explore the relationship between readmissions rates and other outcomes that might matter more to patients or that might be better proxies for the quality of the hospital experience. Is readmission rate a true measure of quality, or just a utilization measure? Research has also tried to document what works: what are the best strategies for preventing avoidable readmissions by improving the discharge process, care transitions, and the coordination of care postdischarge in the community – although no silver bullet has yet been identified.
A recent effort to inject more equity into the penalties program, contained in the wide-ranging 21st Century Cures Act signed into law by President Obama in December 2016, requires Medicare to account for patients’ socio-economic backgrounds when it calculates reductions in its payments to hospitals under HRRP. The law directs the government to change the way pay for performance is applied to safety net hospitals by setting different penalty thresholds for hospitals based on the proportion of their patients who are dually eligible for Medicare and Medicaid.
It remains to be seen how this will be implemented and with what impact. But some critics have continued to question whether hospitals should be held accountable for readmissions, whether 30 days is the correct time frame for that accountability, and whether some hospitals might be simply taking the penalty hit rather than investing in the hard work of care transitions.
Impact on working hospitalists
One expert, Ashish Jha, MD, MPH, director of Harvard’s Global Health Institute, wants to see hospitalists get more engaged in the conversation about how to improve hospital care overall.
Experts say there aren’t metrics available that could allocate penalties to individual hospitalists for their performance in readmissions prevention. But hospitals, clearly, are paying attention, and hospitalist groups may find that part of their negotiation of quality and performance incentives with the hospital includes readmissions.
“There are so many other variables that go into transitions of care, and it would be unreasonable to try to hold the individual doctor responsible for all of them,” he said. But accountability can be passed on to the hospitalist group. “My hospital contracts with a national hospitalist company and our agreement has quality measures that we review with them. We ask them to focus on readmissions.”
Dr. Harte said that when patients are discharged from the hospital, they go from an environment where everything is taken care of for them, to total responsibility for their self-care. Yet we are asking ever more from patients in terms of self-management.
“We need to focus on the human side of the experience. The hospital is a place to be avoided wherever possible,” he said. Yet some readmissions are largely unpreventable. Hospitalists should focus on the patient’s greatest risk of preventable readmission. “Is it health literacy? Is it transportation?”
Readmissions at the front lines
Preetham Talari, MD, FACP, FHM, hospitalist at University of Kentucky HealthCare in Lexington, has an interest in health care safety, quality improvement, and value. He has led the university’s site participation in Project BOOST, the Society of Hospital Medicine’s national mentored quality improvement initiative for care transitions. Dr. Talari also led a quality initiative at the university called the Interprofessional Teamwork Innovation Model to systematize teamwork, first piloted on a 30-bed hospitalist unit where he is medical director.
“Readmissions are not just about doctors, they are more about patient factors, socioeconomic factors, where they live,” Dr. Talari said. “Those are harder to impact, but in my experience, it comes down to thinking about the patient’s needs before discharge – really from the time of admission: What are all the things we can do in the hospital to make sure the patient is safely transitioned home?”
According to Dr. Talari, complex issues like readmissions don’t depend on just one, two, or three factors. “But we do the interventions believing that it will improve processes and outcomes, and then add another intervention and another,” he said. “All of these interventions will add up like a jigsaw puzzle to achieve a final, sustainable outcome. One thing I believe is hospitalists should be leading these efforts.”
Better interventions, better infrastructure
Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University School of Public Health, says the biggest change she has seen resulting from readmissions penalties is that transitions of care are now understood to be both important and the responsibility of front line hospitalists. “That was not true 5 or 10 years ago. We used to spend hours admitting patients to the hospital and then 5 minutes on their discharge.”
“We’ve also learned that the infrastructure can be built better. Historically, hospital discharge summaries have been abysmal. But we can automate the importation of pending labs into the electronic health record. These are things you can change for everybody by changing your template. Sit down in a room together every afternoon to talk about what will happen to the patients when they go home. That’s become standard at our hospital. That was never done before.”
Evidence for improved outcomes is mixed, Dr. Horwitz noted. However, she pointed out, is there any evidence that readmissions penalties have produced adverse outcomes? Did they increase mortality, or length of stay? “So far the evidence suggests that they did not,” she said.
“I think it’s generally likely that the work we have done has resulted in better care. Thousands of people haven’t had to go back to the hospital, and that’s a good thing.”
Recent research on readmissions penalties
A survey by Yale researchers, published in JAMA in December 2016, found that hospitals financially penalized under HRRP reduced their readmissions rates at a higher rate than nonpenalized hospitals, “which implies that penalties can improve quality and readmission performance for hospitals with the most room for improvement,” coauthor Kumar Dharmarajan, MD, MBA, said in a statement.4 The hospitals responded to external pressures – in other words, financial penalties worked. But most of the reduction happened in the 2 years before actual penalties went into effect, which suggests that further improvement will not be easy, the authors note.
A survey of the attitudes of hospital leaders on the HRRP found that it has had a major impact on their efforts to reduce readmissions rates, although the failure to take sociodemographic factors into account was a major complaint for these leaders.5 Most said the penalties were too large, but 42.5% believed HRRP was likely to improve quality.
Some have questioned whether readmissions penalties were just encouraging hospitals to reduce their rates by keeping returning patients in observation units rather than formally readmitting them. Zuckerman et al. in the New England Journal of Medicine found no evidence that changes in observation unit stays accounted for the documented decrease in readmissions.6
But according to Papanicolas et al. in Health Affairs, patient hospital experience has improved only modestly under hospital value-based purchasing for U.S. hospitals, with no evidence that the program has had a beneficial effect on overall patient experience.7 Another study from Harvard by Figueroa et al. found that evidence is lacking that hospital value-based purchasing leads to lower mortality rates.8
“Patients and caregivers tell us: Hey, you people are the experts. You’ve taken care of lots of people with my medical condition before. You should know what my needs are going to be postdischarge and help me anticipate them,” he said.
References
1. Rau J. Medicare’s Readmission Penalties Hit New High. Kaiser Health News. 2016 Aug 2.
2. Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Kaiser Health News, 2016 Sep 30.
3. Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29-37.
4. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016 Dec 27;316(24):2647-56.
5. Joynt KE, Figueroa JF, Orav EJ, Jha AK. Opinions on the Hospital Readmissions Reduction Program: Results of a national survey of hospital leaders. Am J Manag Care. 2016 Aug 1;222(8):e287-94.
6. Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 Apr 21;374(16):1543-51.
7. Papanicolas I, Figueroa JF, Orav EJ, Jha AK. Patient hospital experience improved modestly, but no evidence Medicare incentives promoted meaningful gain. Health Aff (Millwood). 2017 Jan;36(1):133-40.
8. Figueroa JF, Tsugawa Y, Zheng J, et al. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214.
With the Hospital Readmissions Reduction Program (HRRP) in its 5th year, what has been the impact on hospitals and on hospitalists?
First of all, a lot of penalties have been paid by hospitals. According to an analysis by Kaiser Health News,1 the Centers for Medicare and Medicaid Services will withhold $528 million from 2,597 hospitals in the current fiscal year, Oct. 1, 2016 to Sept. 30, 2017, for readmissions for six diagnoses that occurred between July 2012 and June 2015. The number of penalized hospitals is down slightly from 2,665 the year before, but the total annual withhold will go up by $108 million.
HRRP exacts Medicare payment penalties from hospitals that have rates of readmissions – within 30 days of discharge – that are higher than expected, based on national rates and the health of their patient population. The maximum penalty is now up to 3% of a hospital’s Medicare reimbursement. Hospitals are being penalized an average of 0.73% of their annual Medicare reimbursement, and cumulative HRRP penalties will reach nearly $1.9 billion by the end of the fiscal year, Kaiser Health News reports.2
“Basically, we chose to introduce the idea of measuring readmissions because we felt it represented an adverse outcome for many people that was being ignored; that risk could be reduced; and improvements would yield benefits for people as well as save money for the health care system,” he told The Hospitalist.
“More than anything, HRRP has sharpened the focus on considering the episode of care from the patient’s perspective – rather than just focusing on venues of care like the hospitalization alone,” Dr. Krumholz said. “The focus on readmission forced many of us in the health professions to consider what the experience was like to leave the acute setting – how information flowed, what kind of concerns people had, the degree to which they understood what had happened to them, the extent to which they were prepared for the next steps.”
Once the patient leaves the hospital, there are myriad factors that will influence their likelihood of returning, notes researcher Karen Joynt, MD, MPH, of the Department of Health Policy and Management at Harvard’s School of Public Health, Boston. “The proportion of patients readmitted to the hospital because of gross error is low, but sometimes we’re too optimistic about our patients’ ability to manage postdischarge,” she said.
“We all know we can do better at providing softer landings, and anyone who’s ever been a hospital patient or a family member of one knows that leaving the hospital is incredibly tumultuous. I experienced that with my own parents, and it’s frightening, even if everything is done right. It’s still a very vulnerable time.”
HRRP has fundamentally changed the conversation about hospital care, Dr. Joynt said. “I think we need to change the conversation even more and talk more about how to prevent admissions in the first place. As a clinician, I think we need to be more innovative, recognizing that the ways we’ll make a real difference probably has more to do with what happens outside of the hospital. My personal hope is that new alternate payment models like accountable care organizations will lead to more creative partnerships with other providers.”
What have we learned about readmissions in 5 years?
A lot of recently published research about readmissions has documented modest decreases in overall readmissions nationally, from over 21% to under 18% between 2007 and 2014, although most of the reduction occurred in the first couple of years after HRRP was announced and it has since largely leveled off.
Other research has tried to explore the relationship between readmissions rates and other outcomes that might matter more to patients or that might be better proxies for the quality of the hospital experience. Is readmission rate a true measure of quality, or just a utilization measure? Research has also tried to document what works: what are the best strategies for preventing avoidable readmissions by improving the discharge process, care transitions, and the coordination of care postdischarge in the community – although no silver bullet has yet been identified.
A recent effort to inject more equity into the penalties program, contained in the wide-ranging 21st Century Cures Act signed into law by President Obama in December 2016, requires Medicare to account for patients’ socio-economic backgrounds when it calculates reductions in its payments to hospitals under HRRP. The law directs the government to change the way pay for performance is applied to safety net hospitals by setting different penalty thresholds for hospitals based on the proportion of their patients who are dually eligible for Medicare and Medicaid.
It remains to be seen how this will be implemented and with what impact. But some critics have continued to question whether hospitals should be held accountable for readmissions, whether 30 days is the correct time frame for that accountability, and whether some hospitals might be simply taking the penalty hit rather than investing in the hard work of care transitions.
Impact on working hospitalists
One expert, Ashish Jha, MD, MPH, director of Harvard’s Global Health Institute, wants to see hospitalists get more engaged in the conversation about how to improve hospital care overall.
Experts say there aren’t metrics available that could allocate penalties to individual hospitalists for their performance in readmissions prevention. But hospitals, clearly, are paying attention, and hospitalist groups may find that part of their negotiation of quality and performance incentives with the hospital includes readmissions.
“There are so many other variables that go into transitions of care, and it would be unreasonable to try to hold the individual doctor responsible for all of them,” he said. But accountability can be passed on to the hospitalist group. “My hospital contracts with a national hospitalist company and our agreement has quality measures that we review with them. We ask them to focus on readmissions.”
Dr. Harte said that when patients are discharged from the hospital, they go from an environment where everything is taken care of for them, to total responsibility for their self-care. Yet we are asking ever more from patients in terms of self-management.
“We need to focus on the human side of the experience. The hospital is a place to be avoided wherever possible,” he said. Yet some readmissions are largely unpreventable. Hospitalists should focus on the patient’s greatest risk of preventable readmission. “Is it health literacy? Is it transportation?”
Readmissions at the front lines
Preetham Talari, MD, FACP, FHM, hospitalist at University of Kentucky HealthCare in Lexington, has an interest in health care safety, quality improvement, and value. He has led the university’s site participation in Project BOOST, the Society of Hospital Medicine’s national mentored quality improvement initiative for care transitions. Dr. Talari also led a quality initiative at the university called the Interprofessional Teamwork Innovation Model to systematize teamwork, first piloted on a 30-bed hospitalist unit where he is medical director.
“Readmissions are not just about doctors, they are more about patient factors, socioeconomic factors, where they live,” Dr. Talari said. “Those are harder to impact, but in my experience, it comes down to thinking about the patient’s needs before discharge – really from the time of admission: What are all the things we can do in the hospital to make sure the patient is safely transitioned home?”
According to Dr. Talari, complex issues like readmissions don’t depend on just one, two, or three factors. “But we do the interventions believing that it will improve processes and outcomes, and then add another intervention and another,” he said. “All of these interventions will add up like a jigsaw puzzle to achieve a final, sustainable outcome. One thing I believe is hospitalists should be leading these efforts.”
Better interventions, better infrastructure
Leora Horwitz, MD, MHS, director of the Center for Healthcare Innovation and Delivery Science at New York University School of Public Health, says the biggest change she has seen resulting from readmissions penalties is that transitions of care are now understood to be both important and the responsibility of front line hospitalists. “That was not true 5 or 10 years ago. We used to spend hours admitting patients to the hospital and then 5 minutes on their discharge.”
“We’ve also learned that the infrastructure can be built better. Historically, hospital discharge summaries have been abysmal. But we can automate the importation of pending labs into the electronic health record. These are things you can change for everybody by changing your template. Sit down in a room together every afternoon to talk about what will happen to the patients when they go home. That’s become standard at our hospital. That was never done before.”
Evidence for improved outcomes is mixed, Dr. Horwitz noted. However, she pointed out, is there any evidence that readmissions penalties have produced adverse outcomes? Did they increase mortality, or length of stay? “So far the evidence suggests that they did not,” she said.
“I think it’s generally likely that the work we have done has resulted in better care. Thousands of people haven’t had to go back to the hospital, and that’s a good thing.”
Recent research on readmissions penalties
A survey by Yale researchers, published in JAMA in December 2016, found that hospitals financially penalized under HRRP reduced their readmissions rates at a higher rate than nonpenalized hospitals, “which implies that penalties can improve quality and readmission performance for hospitals with the most room for improvement,” coauthor Kumar Dharmarajan, MD, MBA, said in a statement.4 The hospitals responded to external pressures – in other words, financial penalties worked. But most of the reduction happened in the 2 years before actual penalties went into effect, which suggests that further improvement will not be easy, the authors note.
A survey of the attitudes of hospital leaders on the HRRP found that it has had a major impact on their efforts to reduce readmissions rates, although the failure to take sociodemographic factors into account was a major complaint for these leaders.5 Most said the penalties were too large, but 42.5% believed HRRP was likely to improve quality.
Some have questioned whether readmissions penalties were just encouraging hospitals to reduce their rates by keeping returning patients in observation units rather than formally readmitting them. Zuckerman et al. in the New England Journal of Medicine found no evidence that changes in observation unit stays accounted for the documented decrease in readmissions.6
But according to Papanicolas et al. in Health Affairs, patient hospital experience has improved only modestly under hospital value-based purchasing for U.S. hospitals, with no evidence that the program has had a beneficial effect on overall patient experience.7 Another study from Harvard by Figueroa et al. found that evidence is lacking that hospital value-based purchasing leads to lower mortality rates.8
“Patients and caregivers tell us: Hey, you people are the experts. You’ve taken care of lots of people with my medical condition before. You should know what my needs are going to be postdischarge and help me anticipate them,” he said.
References
1. Rau J. Medicare’s Readmission Penalties Hit New High. Kaiser Health News. 2016 Aug 2.
2. Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Kaiser Health News, 2016 Sep 30.
3. Keenan PS, Normand SLT, Lin Z, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008;1:29-37.
4. Desai NR, Ross JS, Kwon JY, et al. Association between hospital penalty status under the Hospital Readmission Reduction Program and readmission rates for target and nontarget conditions. JAMA. 2016 Dec 27;316(24):2647-56.
5. Joynt KE, Figueroa JF, Orav EJ, Jha AK. Opinions on the Hospital Readmissions Reduction Program: Results of a national survey of hospital leaders. Am J Manag Care. 2016 Aug 1;222(8):e287-94.
6. Zuckerman RB, Sheingold SH, Orav EJ, et al. Readmissions, observation, and the Hospital Readmissions Reduction Program. N Engl J Med. 2016 Apr 21;374(16):1543-51.
7. Papanicolas I, Figueroa JF, Orav EJ, Jha AK. Patient hospital experience improved modestly, but no evidence Medicare incentives promoted meaningful gain. Health Aff (Millwood). 2017 Jan;36(1):133-40.
8. Figueroa JF, Tsugawa Y, Zheng J, et al. Association between the value-based purchasing pay for performance program and patient mortality in US hospitals: observational study. BMJ. 2016;353:i2214.
Murine study provides new insight into hematopoiesis
Life-long hematopoiesis relies on hundreds more blood progenitors than previously reported, according to preclinical research published in Nature Cell Biology.
Previous studies linked life-long mammalian blood production to just a handful of precursor cells that emerge during prenatal development.
In the current study, researchers found that, in mice, roughly 600 to 700 developmental precursors contribute to life-long hematopoiesis.
The number of precursor cells in humans is likely at least 10 times greater, according to researchers.
“All previous studies had reported that very few precursor cells are involved in establishing the blood system,” said study author Shannon McKinney-Freeman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“But data in this study show that, actually, hundreds of cells are involved and that the developing blood system is more complex and may be shaped, in part, by regulatory bottlenecks that occur late in development and serve to restrict the number of blood-forming stem cells.”
For this study, Miguel Ganuza, PhD, a fellow in Dr McKinney-Freeman’s lab, adapted a system used to study the cellular makeup of solid tumors. The multi-colored labeling system is activated by genes expressed during specific windows of development.
Dr Ganuza used the system to label and track the fate of precursor cells from various developmental stages in mice.
“We wanted to understand what was happening with different progenitor cells at different stages of development when we knew important decisions on the fate of cells occurred,” Dr Ganuza said.
David Finkelstein, PhD, of the St. Jude Department of Computational Biology, then used mathematical modeling to work backward from peripheral blood in adult mice to track the contribution of precursor cells from the early, middle, and late stages of prenatal development.
The results showed that far more precursor cells than expected contribute to life-long hematopoiesis in adult mice.
The researchers found about 719 Flk1+ mesodermal precursors emerged at embryonic days 7 to 8.5, 633 VE-cadherin+ endothelial precursors emerged at embryonic days 8.5 to 11.5, and 545 Vav1+ nascent hematopoietic stem and progenitor cells emerged at embryonic days 11.5 to 14.5.
The team also said specification of hemogenic endothelial cells begins at embryonic day 8.5 and ends by embryonic day 10.5. After that, it cannot be reactivated.
Finally, the researchers found that intra-aortic hematopoietic clusters are polyclonal in origin.
The team said these findings raised questions about the role of the fetal liver in hematopoiesis.
“For decades, the fetal liver was thought to be where the number of blood stem cells expanded dramatically,” Dr McKinney-Freeman said.
“The results in this study raise questions about that model and even suggest the presence of developmental bottlenecks in the fetal liver or at later stages of development that restrict the blood stem cell population. This is when science is most interesting, when you see things you didn’t expect.”
While unexpected, the newly revealed size and complexity of the emerging blood system make sense developmentally, Dr McKinney-Freeman said.
“Producing hundreds of progenitor cells during different developmental stages means the organism has greater flexibility to adapt to issues and problems that might emerge as development progresses,” she noted.
The findings also have clinical implications, according to Dr McKinney-Freeman.
“Understanding how the blood system emerges, including the number and complexity of the progenitor cells involved, will help us unravel the origins of disease and identify cells that might be susceptible to disease-causing mutations,” she concluded. ![]()
Life-long hematopoiesis relies on hundreds more blood progenitors than previously reported, according to preclinical research published in Nature Cell Biology.
Previous studies linked life-long mammalian blood production to just a handful of precursor cells that emerge during prenatal development.
In the current study, researchers found that, in mice, roughly 600 to 700 developmental precursors contribute to life-long hematopoiesis.
The number of precursor cells in humans is likely at least 10 times greater, according to researchers.
“All previous studies had reported that very few precursor cells are involved in establishing the blood system,” said study author Shannon McKinney-Freeman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“But data in this study show that, actually, hundreds of cells are involved and that the developing blood system is more complex and may be shaped, in part, by regulatory bottlenecks that occur late in development and serve to restrict the number of blood-forming stem cells.”
For this study, Miguel Ganuza, PhD, a fellow in Dr McKinney-Freeman’s lab, adapted a system used to study the cellular makeup of solid tumors. The multi-colored labeling system is activated by genes expressed during specific windows of development.
Dr Ganuza used the system to label and track the fate of precursor cells from various developmental stages in mice.
“We wanted to understand what was happening with different progenitor cells at different stages of development when we knew important decisions on the fate of cells occurred,” Dr Ganuza said.
David Finkelstein, PhD, of the St. Jude Department of Computational Biology, then used mathematical modeling to work backward from peripheral blood in adult mice to track the contribution of precursor cells from the early, middle, and late stages of prenatal development.
The results showed that far more precursor cells than expected contribute to life-long hematopoiesis in adult mice.
The researchers found about 719 Flk1+ mesodermal precursors emerged at embryonic days 7 to 8.5, 633 VE-cadherin+ endothelial precursors emerged at embryonic days 8.5 to 11.5, and 545 Vav1+ nascent hematopoietic stem and progenitor cells emerged at embryonic days 11.5 to 14.5.
The team also said specification of hemogenic endothelial cells begins at embryonic day 8.5 and ends by embryonic day 10.5. After that, it cannot be reactivated.
Finally, the researchers found that intra-aortic hematopoietic clusters are polyclonal in origin.
The team said these findings raised questions about the role of the fetal liver in hematopoiesis.
“For decades, the fetal liver was thought to be where the number of blood stem cells expanded dramatically,” Dr McKinney-Freeman said.
“The results in this study raise questions about that model and even suggest the presence of developmental bottlenecks in the fetal liver or at later stages of development that restrict the blood stem cell population. This is when science is most interesting, when you see things you didn’t expect.”
While unexpected, the newly revealed size and complexity of the emerging blood system make sense developmentally, Dr McKinney-Freeman said.
“Producing hundreds of progenitor cells during different developmental stages means the organism has greater flexibility to adapt to issues and problems that might emerge as development progresses,” she noted.
The findings also have clinical implications, according to Dr McKinney-Freeman.
“Understanding how the blood system emerges, including the number and complexity of the progenitor cells involved, will help us unravel the origins of disease and identify cells that might be susceptible to disease-causing mutations,” she concluded. ![]()
Life-long hematopoiesis relies on hundreds more blood progenitors than previously reported, according to preclinical research published in Nature Cell Biology.
Previous studies linked life-long mammalian blood production to just a handful of precursor cells that emerge during prenatal development.
In the current study, researchers found that, in mice, roughly 600 to 700 developmental precursors contribute to life-long hematopoiesis.
The number of precursor cells in humans is likely at least 10 times greater, according to researchers.
“All previous studies had reported that very few precursor cells are involved in establishing the blood system,” said study author Shannon McKinney-Freeman, PhD, of St. Jude Children’s Research Hospital in Memphis, Tennessee.
“But data in this study show that, actually, hundreds of cells are involved and that the developing blood system is more complex and may be shaped, in part, by regulatory bottlenecks that occur late in development and serve to restrict the number of blood-forming stem cells.”
For this study, Miguel Ganuza, PhD, a fellow in Dr McKinney-Freeman’s lab, adapted a system used to study the cellular makeup of solid tumors. The multi-colored labeling system is activated by genes expressed during specific windows of development.
Dr Ganuza used the system to label and track the fate of precursor cells from various developmental stages in mice.
“We wanted to understand what was happening with different progenitor cells at different stages of development when we knew important decisions on the fate of cells occurred,” Dr Ganuza said.
David Finkelstein, PhD, of the St. Jude Department of Computational Biology, then used mathematical modeling to work backward from peripheral blood in adult mice to track the contribution of precursor cells from the early, middle, and late stages of prenatal development.
The results showed that far more precursor cells than expected contribute to life-long hematopoiesis in adult mice.
The researchers found about 719 Flk1+ mesodermal precursors emerged at embryonic days 7 to 8.5, 633 VE-cadherin+ endothelial precursors emerged at embryonic days 8.5 to 11.5, and 545 Vav1+ nascent hematopoietic stem and progenitor cells emerged at embryonic days 11.5 to 14.5.
The team also said specification of hemogenic endothelial cells begins at embryonic day 8.5 and ends by embryonic day 10.5. After that, it cannot be reactivated.
Finally, the researchers found that intra-aortic hematopoietic clusters are polyclonal in origin.
The team said these findings raised questions about the role of the fetal liver in hematopoiesis.
“For decades, the fetal liver was thought to be where the number of blood stem cells expanded dramatically,” Dr McKinney-Freeman said.
“The results in this study raise questions about that model and even suggest the presence of developmental bottlenecks in the fetal liver or at later stages of development that restrict the blood stem cell population. This is when science is most interesting, when you see things you didn’t expect.”
While unexpected, the newly revealed size and complexity of the emerging blood system make sense developmentally, Dr McKinney-Freeman said.
“Producing hundreds of progenitor cells during different developmental stages means the organism has greater flexibility to adapt to issues and problems that might emerge as development progresses,” she noted.
The findings also have clinical implications, according to Dr McKinney-Freeman.
“Understanding how the blood system emerges, including the number and complexity of the progenitor cells involved, will help us unravel the origins of disease and identify cells that might be susceptible to disease-causing mutations,” she concluded. ![]()
Trials of atezolizumab placed on partial hold
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
Roche has announced a partial clinical hold on 2 trials of the anti-PD-L1 antibody atezolizumab (Tecentriq).
One is a phase 1b/2 study (NCT02631577) in which researchers are evaluating atezolizumab in combination with obinutuzumab plus lenalidomide in patients with relapsed or refractory follicular lymphoma.
The other is a phase 1b study (NCT02431208) of atezolizumab alone or in combination with an immunomodulatory drug and/or daratumumab in patients with multiple myeloma (MM).
The partial clinical hold on these trials means patients who are currently enrolled and are deriving clinical benefit may continue to receive treatment, but no additional patients will be enrolled.
The decision to place these trials on hold is related to risks identified in 2 trials of the anti-PD-1 agent pembrolizumab. Results from these trials showed that combining pembrolizumab with dexamethasone and an immunomodulatory agent (lenalidomide or pomalidomide) increases the risk of death in patients with MM.
The results led to clinical holds on these trials (and a third trial of pembrolizumab) as well as an investigation by the US Food and Drug Administration (FDA).
The FDA has stressed its belief that the benefits of taking pembrolizumab and other PD-1/PD-L1 inhibitors for their approved uses continue to outweigh the risks.
However, the agency also thinks there may be an unfavorable risk-benefit ratio for patients receiving PD-1/PD-L1 treatment alone or in other combinations in unapproved indications.
Therefore, the FDA is investigating trials of PD-1/PD-L1 inhibitors being studied in combination with immunomodulatory agents or other classes of drugs in patients with hematologic malignancies.
In the course of this investigation, the FDA has placed holds on trials of nivolumab and durvalumab as well as atezolizumab.
According to Roche, there is no evidence of an increased risk of death or serious events with the use of atezolizumab in combination with immunomodulatory agents. ![]()
EMA issues final opinion on FVIII products
The European Medicines Agency (EMA) has concluded there is “no clear and consistent evidence” of a difference in inhibitor development between the 2 classes of factor VIII (FVIII) products.
A review of data from several studies has suggested that hemophilia A patients are no more likely to develop inhibitors if they receive a recombinant FVIII product rather than a plasma-derived FVIII product.
The review began after publication of the SIPPET study1, which suggested that patients who received plasma-derived FVIII had a lower incidence of inhibitors than patients treated with recombinant FVIII.
To test this conclusion, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data on all FVIII products authorized for use in the European Union. This includes products containing the active substances human coagulation FVIII, efmoroctocog alfa, moroctocog alfa, octocog alfa, simoctocog alfa, susoctocog alfa, and turoctocog alfa.
The PRAC examined data from the SIPPET study and additional clinical trials and observational studies.2-5
The data did not show any statistically significant or clinically meaningful difference in inhibitor risk between FVIII classes.
The PRAC said results of the SIPPET study cannot be extrapolated to individual products, as the study only included a small number of FVIII products.
The PRAC’s conclusion was sent to the EMA’s Committee for Medicinal Products for Human Use (CHMP) for adoption of the EMA’s final opinion. And the CHMP has adopted the opinion that there is “no clear and consistent evidence” of a difference in inhibitor development.
The CHMP’s opinion will be forwarded to the European Commission, which will issue a final, legally binding decision applicable in all European Union member states. The European Commission typically adheres to the CHMP’s recommendations.
The EMA said prescribing information for FVIII products will be updated as appropriate to add inhibitor development as a very common side effect in previously untreated patients and as uncommon in previously treated patients.
The warning on inhibitor development will be amended to state that low titers of inhibitors pose less risk of insufficient response than high titers. ![]()
1. Peyvandi F, Mannucci PM, Garagiola I et al. A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N Engl J Med (2016), 374:2054-64.
2. Gouw SC et al. Treatment-related risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood (2007), 109:4648-54.
3. Gouw SC et al. PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med (2013), 368:231-9.
4. Iorio A et al. Natural history and clinical characteristics of inhibitors in previously treated haemophilia A patients: a case series. Haemophilia (2017), 23:255-63.
5. Fischer K et al. Inhibitor development in haemophilia according to concentrate. Four-year results from the European HAemophilia Safety Surveillance (EUHASS) project. Thromb Haemost (2015) 113:968-75.
The European Medicines Agency (EMA) has concluded there is “no clear and consistent evidence” of a difference in inhibitor development between the 2 classes of factor VIII (FVIII) products.
A review of data from several studies has suggested that hemophilia A patients are no more likely to develop inhibitors if they receive a recombinant FVIII product rather than a plasma-derived FVIII product.
The review began after publication of the SIPPET study1, which suggested that patients who received plasma-derived FVIII had a lower incidence of inhibitors than patients treated with recombinant FVIII.
To test this conclusion, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data on all FVIII products authorized for use in the European Union. This includes products containing the active substances human coagulation FVIII, efmoroctocog alfa, moroctocog alfa, octocog alfa, simoctocog alfa, susoctocog alfa, and turoctocog alfa.
The PRAC examined data from the SIPPET study and additional clinical trials and observational studies.2-5
The data did not show any statistically significant or clinically meaningful difference in inhibitor risk between FVIII classes.
The PRAC said results of the SIPPET study cannot be extrapolated to individual products, as the study only included a small number of FVIII products.
The PRAC’s conclusion was sent to the EMA’s Committee for Medicinal Products for Human Use (CHMP) for adoption of the EMA’s final opinion. And the CHMP has adopted the opinion that there is “no clear and consistent evidence” of a difference in inhibitor development.
The CHMP’s opinion will be forwarded to the European Commission, which will issue a final, legally binding decision applicable in all European Union member states. The European Commission typically adheres to the CHMP’s recommendations.
The EMA said prescribing information for FVIII products will be updated as appropriate to add inhibitor development as a very common side effect in previously untreated patients and as uncommon in previously treated patients.
The warning on inhibitor development will be amended to state that low titers of inhibitors pose less risk of insufficient response than high titers. ![]()
1. Peyvandi F, Mannucci PM, Garagiola I et al. A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N Engl J Med (2016), 374:2054-64.
2. Gouw SC et al. Treatment-related risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood (2007), 109:4648-54.
3. Gouw SC et al. PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med (2013), 368:231-9.
4. Iorio A et al. Natural history and clinical characteristics of inhibitors in previously treated haemophilia A patients: a case series. Haemophilia (2017), 23:255-63.
5. Fischer K et al. Inhibitor development in haemophilia according to concentrate. Four-year results from the European HAemophilia Safety Surveillance (EUHASS) project. Thromb Haemost (2015) 113:968-75.
The European Medicines Agency (EMA) has concluded there is “no clear and consistent evidence” of a difference in inhibitor development between the 2 classes of factor VIII (FVIII) products.
A review of data from several studies has suggested that hemophilia A patients are no more likely to develop inhibitors if they receive a recombinant FVIII product rather than a plasma-derived FVIII product.
The review began after publication of the SIPPET study1, which suggested that patients who received plasma-derived FVIII had a lower incidence of inhibitors than patients treated with recombinant FVIII.
To test this conclusion, the EMA’s Pharmacovigilance Risk Assessment Committee (PRAC) reviewed data on all FVIII products authorized for use in the European Union. This includes products containing the active substances human coagulation FVIII, efmoroctocog alfa, moroctocog alfa, octocog alfa, simoctocog alfa, susoctocog alfa, and turoctocog alfa.
The PRAC examined data from the SIPPET study and additional clinical trials and observational studies.2-5
The data did not show any statistically significant or clinically meaningful difference in inhibitor risk between FVIII classes.
The PRAC said results of the SIPPET study cannot be extrapolated to individual products, as the study only included a small number of FVIII products.
The PRAC’s conclusion was sent to the EMA’s Committee for Medicinal Products for Human Use (CHMP) for adoption of the EMA’s final opinion. And the CHMP has adopted the opinion that there is “no clear and consistent evidence” of a difference in inhibitor development.
The CHMP’s opinion will be forwarded to the European Commission, which will issue a final, legally binding decision applicable in all European Union member states. The European Commission typically adheres to the CHMP’s recommendations.
The EMA said prescribing information for FVIII products will be updated as appropriate to add inhibitor development as a very common side effect in previously untreated patients and as uncommon in previously treated patients.
The warning on inhibitor development will be amended to state that low titers of inhibitors pose less risk of insufficient response than high titers. ![]()
1. Peyvandi F, Mannucci PM, Garagiola I et al. A Randomized Trial of Factor VIII and Neutralizing Antibodies in Hemophilia A. N Engl J Med (2016), 374:2054-64.
2. Gouw SC et al. Treatment-related risk factors of inhibitor development in previously untreated patients with hemophilia A: the CANAL cohort study. Blood (2007), 109:4648-54.
3. Gouw SC et al. PedNet and RODIN Study Group. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med (2013), 368:231-9.
4. Iorio A et al. Natural history and clinical characteristics of inhibitors in previously treated haemophilia A patients: a case series. Haemophilia (2017), 23:255-63.
5. Fischer K et al. Inhibitor development in haemophilia according to concentrate. Four-year results from the European HAemophilia Safety Surveillance (EUHASS) project. Thromb Haemost (2015) 113:968-75.