User login
CMT provides survival benefit in young HL patients
Combined modality therapy (CMT) can improve survival in young patients with early stage Hodgkin lymphoma (HL), according to research published in JAMA Oncology.
In a retrospective study, researchers compared chemotherapy followed by radiotherapy—CMT—to chemotherapy alone in more than 5,600 HL patients age 21 and younger.
There was a significant improvement in 5-year overall survival (OS) among patients who received CMT.
The treatment appeared particularly beneficial for adolescents and young adults as well as patients with low-risk disease.
However, the researchers observed a nearly 25% decrease in the use of CMT over the period studied.
“Nationwide, there has been a notable decrease in combined modality therapy, especially in clinical trials, many of which are designed to avoid this strategy,” said Rahul Parikh, MD, of Rutgers Cancer Institute of New Jersey in New Brunswick.
“This form of treatment has shown to be effective, with event-free survival rates greater than 80% and overall survival rates greater than 95%. The question then becomes, ‘does treatment benefit outweigh the risk of long-term side effects?”
With this in mind, Dr. Parikh and his colleagues compared CMT to chemotherapy alone using data from the National Cancer Database spanning the period from 2004 to 2015.
The researchers analyzed 5,657 patients with stage I/II classical HL who had a mean age of 17.1.
Roughly half of patients received CMT (50.3%, n=2845), and the other half received chemotherapy alone (49.7%, n=2812).
The median radiotherapy dose was 21.0 Gy, and the most common modality was photon therapy (59.0%).
Patients who received CMT were significantly more likely to be younger than 16 (P<0.001), be male (P<0.001), have stage II disease (P=0.02), and have private health insurance (P=0.002).
Results
The median follow-up was 5.1 years.
The 5-year OS was 94.5% for patients who received chemotherapy alone and 97.3% for patients treated with CMT.
CMT was significantly associated with improved OS in both univariate (hazard ratio [HR]=0.58, P<0.001) and multivariate analyses (HR=0.57, P<0.001).
In a sensitivity analysis, the researchers found the greatest benefits of CMT were in adolescents and young adults (age 14 and older, adjusted HR=0.47) and patients with low-risk disease (stage I-IIA, adjusted HR=0.59).
The researchers noted that this study was limited by their inability to control for unreported prognostic factors, such as the number of nodal sites and bulk of disease.
Another limitation was the duration of follow-up, which did not allow the researchers to fully assess secondary late effects of CMT and their potential impact on survival.
Still, Dr. Parikh said this study demonstrates a survival benefit for young HL patients treated with CMT.
“With that, physicians should be encouraged to discuss combined modality therapy as one of the many treatment options [for young HL patients],” he said.
“Investigators may also consider designing future clinical trials for this population to include combined modality therapy as a standard arm with the inclusion of interim treatment response assessment (PET scans, etc.). And as multiple disparities to the use of combined modality therapy have been identified through this work, future studies should address improving access to care for all pediatric patients.”
Dr. Parikh and his colleagues declared no conflicts of interest for the current study.
Combined modality therapy (CMT) can improve survival in young patients with early stage Hodgkin lymphoma (HL), according to research published in JAMA Oncology.
In a retrospective study, researchers compared chemotherapy followed by radiotherapy—CMT—to chemotherapy alone in more than 5,600 HL patients age 21 and younger.
There was a significant improvement in 5-year overall survival (OS) among patients who received CMT.
The treatment appeared particularly beneficial for adolescents and young adults as well as patients with low-risk disease.
However, the researchers observed a nearly 25% decrease in the use of CMT over the period studied.
“Nationwide, there has been a notable decrease in combined modality therapy, especially in clinical trials, many of which are designed to avoid this strategy,” said Rahul Parikh, MD, of Rutgers Cancer Institute of New Jersey in New Brunswick.
“This form of treatment has shown to be effective, with event-free survival rates greater than 80% and overall survival rates greater than 95%. The question then becomes, ‘does treatment benefit outweigh the risk of long-term side effects?”
With this in mind, Dr. Parikh and his colleagues compared CMT to chemotherapy alone using data from the National Cancer Database spanning the period from 2004 to 2015.
The researchers analyzed 5,657 patients with stage I/II classical HL who had a mean age of 17.1.
Roughly half of patients received CMT (50.3%, n=2845), and the other half received chemotherapy alone (49.7%, n=2812).
The median radiotherapy dose was 21.0 Gy, and the most common modality was photon therapy (59.0%).
Patients who received CMT were significantly more likely to be younger than 16 (P<0.001), be male (P<0.001), have stage II disease (P=0.02), and have private health insurance (P=0.002).
Results
The median follow-up was 5.1 years.
The 5-year OS was 94.5% for patients who received chemotherapy alone and 97.3% for patients treated with CMT.
CMT was significantly associated with improved OS in both univariate (hazard ratio [HR]=0.58, P<0.001) and multivariate analyses (HR=0.57, P<0.001).
In a sensitivity analysis, the researchers found the greatest benefits of CMT were in adolescents and young adults (age 14 and older, adjusted HR=0.47) and patients with low-risk disease (stage I-IIA, adjusted HR=0.59).
The researchers noted that this study was limited by their inability to control for unreported prognostic factors, such as the number of nodal sites and bulk of disease.
Another limitation was the duration of follow-up, which did not allow the researchers to fully assess secondary late effects of CMT and their potential impact on survival.
Still, Dr. Parikh said this study demonstrates a survival benefit for young HL patients treated with CMT.
“With that, physicians should be encouraged to discuss combined modality therapy as one of the many treatment options [for young HL patients],” he said.
“Investigators may also consider designing future clinical trials for this population to include combined modality therapy as a standard arm with the inclusion of interim treatment response assessment (PET scans, etc.). And as multiple disparities to the use of combined modality therapy have been identified through this work, future studies should address improving access to care for all pediatric patients.”
Dr. Parikh and his colleagues declared no conflicts of interest for the current study.
Combined modality therapy (CMT) can improve survival in young patients with early stage Hodgkin lymphoma (HL), according to research published in JAMA Oncology.
In a retrospective study, researchers compared chemotherapy followed by radiotherapy—CMT—to chemotherapy alone in more than 5,600 HL patients age 21 and younger.
There was a significant improvement in 5-year overall survival (OS) among patients who received CMT.
The treatment appeared particularly beneficial for adolescents and young adults as well as patients with low-risk disease.
However, the researchers observed a nearly 25% decrease in the use of CMT over the period studied.
“Nationwide, there has been a notable decrease in combined modality therapy, especially in clinical trials, many of which are designed to avoid this strategy,” said Rahul Parikh, MD, of Rutgers Cancer Institute of New Jersey in New Brunswick.
“This form of treatment has shown to be effective, with event-free survival rates greater than 80% and overall survival rates greater than 95%. The question then becomes, ‘does treatment benefit outweigh the risk of long-term side effects?”
With this in mind, Dr. Parikh and his colleagues compared CMT to chemotherapy alone using data from the National Cancer Database spanning the period from 2004 to 2015.
The researchers analyzed 5,657 patients with stage I/II classical HL who had a mean age of 17.1.
Roughly half of patients received CMT (50.3%, n=2845), and the other half received chemotherapy alone (49.7%, n=2812).
The median radiotherapy dose was 21.0 Gy, and the most common modality was photon therapy (59.0%).
Patients who received CMT were significantly more likely to be younger than 16 (P<0.001), be male (P<0.001), have stage II disease (P=0.02), and have private health insurance (P=0.002).
Results
The median follow-up was 5.1 years.
The 5-year OS was 94.5% for patients who received chemotherapy alone and 97.3% for patients treated with CMT.
CMT was significantly associated with improved OS in both univariate (hazard ratio [HR]=0.58, P<0.001) and multivariate analyses (HR=0.57, P<0.001).
In a sensitivity analysis, the researchers found the greatest benefits of CMT were in adolescents and young adults (age 14 and older, adjusted HR=0.47) and patients with low-risk disease (stage I-IIA, adjusted HR=0.59).
The researchers noted that this study was limited by their inability to control for unreported prognostic factors, such as the number of nodal sites and bulk of disease.
Another limitation was the duration of follow-up, which did not allow the researchers to fully assess secondary late effects of CMT and their potential impact on survival.
Still, Dr. Parikh said this study demonstrates a survival benefit for young HL patients treated with CMT.
“With that, physicians should be encouraged to discuss combined modality therapy as one of the many treatment options [for young HL patients],” he said.
“Investigators may also consider designing future clinical trials for this population to include combined modality therapy as a standard arm with the inclusion of interim treatment response assessment (PET scans, etc.). And as multiple disparities to the use of combined modality therapy have been identified through this work, future studies should address improving access to care for all pediatric patients.”
Dr. Parikh and his colleagues declared no conflicts of interest for the current study.
EC approves split dosing regimen for daratumumab
The European Commission (EC) has granted marketing authorization for a split dosing regimen for daratumumab (Darzalex®).
The approval provides healthcare professionals with the option to split the first infusion of daratumumab over 2 consecutive days.
“We are hopeful that the availability of this more flexible dosing option will make the first infusion of Darzalex more convenient for European multiple myeloma patients,” said Jan van de Winkel, PhD, chief executive officer of Genmab, which licensed daratumumab to Janssen Biotech, Inc.
Daratumumab is currently EC-approved for the following indications:
- For use in combination with bortezomib, melphalan, and prednisone to treat adults with newly diagnosed multiple myeloma (MM) who are ineligible for autologous stem cell transplant
- For use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for the treatment of adults with MM who have received at least one prior therapy
- As monotherapy for adults with relapsed and refractory MM whose prior therapy included a proteasome inhibitor and an immunomodulatory agent and who have demonstrated disease progression on their last therapy.
The EC’s approval of a split dosing regimen for daratumumab was based on data from the phase 1b EQUULEUS trial (MMY1001, NCT01998971), which was sponsored by Janssen.
This trial was designed to evaluate daratumumab in combination with bortezomib-dexamethasone, bortezomib-melphalan-prednisone, bortezomib-thalidomide-dexamethasone, pomalidomide-dexamethasone, carfilzomib-dexamethasone, and carfilzomib-lenalidomide-dexamethasone.
At the 2018 ASH Annual Meeting (abstract 1970), researchers presented data from this trial in MM patients who received their first 16 mg/kg daratumumab dose as a split dose of 8 mg/kg on day 1 of cycle 1 and 8 mg/kg on day 2 of cycle 1, compared to patients who received the full 16 mg/kg dose on day 1 of cycle 1.
The researchers said they observed “virtually identical” pharmacokinetics between the dosing groups.
Cmax on the first day of cycle 1 was lower in the split-dose group than in the full-dose group. However, after patients in the split-dose group received the second 8 mg/kg dose on day 2, concentrations were similar between the groups.
The researchers said they do not expect the initial difference they observed to have any impact on clinical outcomes.
The team also pointed out that there was no increase in infusion-related reactions among patients who received the split dose.
The researchers said split dosing of daratumumab is still being investigated in ongoing studies of MM patients, including CANDOR (NCT03158688) and LYRA (NCT02951819).
The European Commission (EC) has granted marketing authorization for a split dosing regimen for daratumumab (Darzalex®).
The approval provides healthcare professionals with the option to split the first infusion of daratumumab over 2 consecutive days.
“We are hopeful that the availability of this more flexible dosing option will make the first infusion of Darzalex more convenient for European multiple myeloma patients,” said Jan van de Winkel, PhD, chief executive officer of Genmab, which licensed daratumumab to Janssen Biotech, Inc.
Daratumumab is currently EC-approved for the following indications:
- For use in combination with bortezomib, melphalan, and prednisone to treat adults with newly diagnosed multiple myeloma (MM) who are ineligible for autologous stem cell transplant
- For use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for the treatment of adults with MM who have received at least one prior therapy
- As monotherapy for adults with relapsed and refractory MM whose prior therapy included a proteasome inhibitor and an immunomodulatory agent and who have demonstrated disease progression on their last therapy.
The EC’s approval of a split dosing regimen for daratumumab was based on data from the phase 1b EQUULEUS trial (MMY1001, NCT01998971), which was sponsored by Janssen.
This trial was designed to evaluate daratumumab in combination with bortezomib-dexamethasone, bortezomib-melphalan-prednisone, bortezomib-thalidomide-dexamethasone, pomalidomide-dexamethasone, carfilzomib-dexamethasone, and carfilzomib-lenalidomide-dexamethasone.
At the 2018 ASH Annual Meeting (abstract 1970), researchers presented data from this trial in MM patients who received their first 16 mg/kg daratumumab dose as a split dose of 8 mg/kg on day 1 of cycle 1 and 8 mg/kg on day 2 of cycle 1, compared to patients who received the full 16 mg/kg dose on day 1 of cycle 1.
The researchers said they observed “virtually identical” pharmacokinetics between the dosing groups.
Cmax on the first day of cycle 1 was lower in the split-dose group than in the full-dose group. However, after patients in the split-dose group received the second 8 mg/kg dose on day 2, concentrations were similar between the groups.
The researchers said they do not expect the initial difference they observed to have any impact on clinical outcomes.
The team also pointed out that there was no increase in infusion-related reactions among patients who received the split dose.
The researchers said split dosing of daratumumab is still being investigated in ongoing studies of MM patients, including CANDOR (NCT03158688) and LYRA (NCT02951819).
The European Commission (EC) has granted marketing authorization for a split dosing regimen for daratumumab (Darzalex®).
The approval provides healthcare professionals with the option to split the first infusion of daratumumab over 2 consecutive days.
“We are hopeful that the availability of this more flexible dosing option will make the first infusion of Darzalex more convenient for European multiple myeloma patients,” said Jan van de Winkel, PhD, chief executive officer of Genmab, which licensed daratumumab to Janssen Biotech, Inc.
Daratumumab is currently EC-approved for the following indications:
- For use in combination with bortezomib, melphalan, and prednisone to treat adults with newly diagnosed multiple myeloma (MM) who are ineligible for autologous stem cell transplant
- For use in combination with lenalidomide and dexamethasone, or bortezomib and dexamethasone, for the treatment of adults with MM who have received at least one prior therapy
- As monotherapy for adults with relapsed and refractory MM whose prior therapy included a proteasome inhibitor and an immunomodulatory agent and who have demonstrated disease progression on their last therapy.
The EC’s approval of a split dosing regimen for daratumumab was based on data from the phase 1b EQUULEUS trial (MMY1001, NCT01998971), which was sponsored by Janssen.
This trial was designed to evaluate daratumumab in combination with bortezomib-dexamethasone, bortezomib-melphalan-prednisone, bortezomib-thalidomide-dexamethasone, pomalidomide-dexamethasone, carfilzomib-dexamethasone, and carfilzomib-lenalidomide-dexamethasone.
At the 2018 ASH Annual Meeting (abstract 1970), researchers presented data from this trial in MM patients who received their first 16 mg/kg daratumumab dose as a split dose of 8 mg/kg on day 1 of cycle 1 and 8 mg/kg on day 2 of cycle 1, compared to patients who received the full 16 mg/kg dose on day 1 of cycle 1.
The researchers said they observed “virtually identical” pharmacokinetics between the dosing groups.
Cmax on the first day of cycle 1 was lower in the split-dose group than in the full-dose group. However, after patients in the split-dose group received the second 8 mg/kg dose on day 2, concentrations were similar between the groups.
The researchers said they do not expect the initial difference they observed to have any impact on clinical outcomes.
The team also pointed out that there was no increase in infusion-related reactions among patients who received the split dose.
The researchers said split dosing of daratumumab is still being investigated in ongoing studies of MM patients, including CANDOR (NCT03158688) and LYRA (NCT02951819).
Potential treatment on the horizon for cold agglutinin disease
In a first-in-human trial, sutimlimab rapidly halted hemolysis, corrected anemia, precluded the need for transfusion, and caused no serious adverse effects in patients with cold agglutinin disease.
Sutimlimab also “induced clinically meaningful increases in hemoglobin levels, even in patients with multiple previous lines of therapy,” according to investigators.
The European Medicines Agency and the U.S. Food and Drug Administration (FDA) awarded sutimlimab orphan drug status based on these results. The FDA also granted sutimlimab breakthrough therapy designation.
Sutimlimab is a humanized anti-C1s IgG4 monoclonal antibody that blocks the classical complement pathway–specific protease C1s and prevents further hemolysis in patients with cold agglutinin disease.
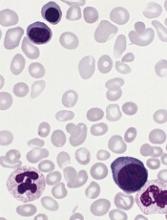
Cold agglutinin disease is a rare, acquired chronic autoimmune hemolytic condition that destroys red blood cells. It leads to chronic anemia, severe fatigue, and potentially fatal thrombotic events. No drug has yet been approved to treat cold agglutinin disease.
The phase 1 trial of sutimlimab (formerly BIVV009 and TNT009) in cold agglutinin disease was conducted at the Medical University of Vienna in Austria and reported in Blood.
The study (NCT02502903) involved 10 patients, ages 56 to 76, who were previously treated with multiple lines of therapy, including two patients who failed treatment with eculizumab.
Of the 10 patients, eight were female, eight were Caucasian, one was Asian, and one was Hispanic. Patients had cold agglutinin disease for a median of 5 years (range, 1 – 20).
At baseline, the median hemoglobin level was 7.8 g/dL, the median number of reticulocytes was 133 x 109/L, the median bilirubin was 2.0 mg/dL, and the median haptoglobin was less than 12 mg/dL.
The patients received an initial dose of 10 mg/kg intravenous sutimlimab as a test dose to allow rapid wash-out of the drug if unforeseen adverse effects occurred with the first infusion.
One to 4 days later, they received the full dose of 60 mg/kg, followed by three additional weekly doses.
Investigators observed the patients for 49 to 53 days.
Results
Within the first week, patients’ median hemoglobin levels increased by 1.6 g/dL (P=0.007), and the median best response was an increase of 3.9 g/dL (P=0.005) after 6 weeks.
Seven patients had increased hemoglobin levels by more than 2 g/dL, and this included those who recently failed to respond or relapsed after rituximab, rituximab plus bendamustine, or eculizumab.
In five patients, hemoglobin increased by 4 g/dL or more. In four patients, it completely normalized to 12 g/dL.
In the first 24 hours after sutimlimab infusion, reticulocyte counts increased by a median of 41% and then gradually declined as hemoglobin levels rose.
In four patients, haptoglobin levels normalized within 1 to 2 weeks. In eight patients who had abnormal bilirubin levels at baseline, sutimlimab decreased the median bilirubin levels by 61%, normalizing levels in most patients within 24 hours of the first infusion (P=0.007).
When sutimlimab was washed out, bilirubin levels increased again, which demonstrated the recurrence of hemolysis.
Approximately 3 to 4 weeks after the last dose of sutimlimab, hemolysis and anemia recurred in all responders.
When patients were re-exposed to sutimlimab, rapid and complete inhibition of hemolysis occurred once again.
None of the patients required packed red blood cell transfusions during treatment.
Safety
The investigators reported that all infusions were well tolerated without premedication and without relevant drug-related adverse effects.
They reported few adverse events during the trial. All were mild or moderate in severity, and most were considered unrelated or unlikely related to sutimlimab.
Two adverse events—one mild purpural rash on both hands and one case of moderate hair loss (each occurring in one patient)—were possibly related to sutimlimab.
While the investigators considered the safety data encouraging, they recommended interpreting the data “cautiously in light of the limited duration of the trial.”
“Provided that safety results remain positive, sutimlimab could become the first approved treatment for cold agglutinin disease,” said corresponding author Bernd Jilma, MD, of the Medical University of Vienna in Austria.
“The drug clearly addresses an unmet medical need, as we have seen rapid, strong responses in patients for whom multiple prior therapies have failed.”
This study was funded by True North Therapeutics, Inc, now part of Bioverativ, a Sanofi company.
Some of the authors disclosed financial relationships, including employment, with True North Therapeutics and Bioverativ.
A phase 3 trial of sutimlimab is underway with top-line results due in 2019.
In a first-in-human trial, sutimlimab rapidly halted hemolysis, corrected anemia, precluded the need for transfusion, and caused no serious adverse effects in patients with cold agglutinin disease.
Sutimlimab also “induced clinically meaningful increases in hemoglobin levels, even in patients with multiple previous lines of therapy,” according to investigators.
The European Medicines Agency and the U.S. Food and Drug Administration (FDA) awarded sutimlimab orphan drug status based on these results. The FDA also granted sutimlimab breakthrough therapy designation.
Sutimlimab is a humanized anti-C1s IgG4 monoclonal antibody that blocks the classical complement pathway–specific protease C1s and prevents further hemolysis in patients with cold agglutinin disease.
Cold agglutinin disease is a rare, acquired chronic autoimmune hemolytic condition that destroys red blood cells. It leads to chronic anemia, severe fatigue, and potentially fatal thrombotic events. No drug has yet been approved to treat cold agglutinin disease.
The phase 1 trial of sutimlimab (formerly BIVV009 and TNT009) in cold agglutinin disease was conducted at the Medical University of Vienna in Austria and reported in Blood.
The study (NCT02502903) involved 10 patients, ages 56 to 76, who were previously treated with multiple lines of therapy, including two patients who failed treatment with eculizumab.
Of the 10 patients, eight were female, eight were Caucasian, one was Asian, and one was Hispanic. Patients had cold agglutinin disease for a median of 5 years (range, 1 – 20).
At baseline, the median hemoglobin level was 7.8 g/dL, the median number of reticulocytes was 133 x 109/L, the median bilirubin was 2.0 mg/dL, and the median haptoglobin was less than 12 mg/dL.
The patients received an initial dose of 10 mg/kg intravenous sutimlimab as a test dose to allow rapid wash-out of the drug if unforeseen adverse effects occurred with the first infusion.
One to 4 days later, they received the full dose of 60 mg/kg, followed by three additional weekly doses.
Investigators observed the patients for 49 to 53 days.
Results
Within the first week, patients’ median hemoglobin levels increased by 1.6 g/dL (P=0.007), and the median best response was an increase of 3.9 g/dL (P=0.005) after 6 weeks.
Seven patients had increased hemoglobin levels by more than 2 g/dL, and this included those who recently failed to respond or relapsed after rituximab, rituximab plus bendamustine, or eculizumab.
In five patients, hemoglobin increased by 4 g/dL or more. In four patients, it completely normalized to 12 g/dL.
In the first 24 hours after sutimlimab infusion, reticulocyte counts increased by a median of 41% and then gradually declined as hemoglobin levels rose.
In four patients, haptoglobin levels normalized within 1 to 2 weeks. In eight patients who had abnormal bilirubin levels at baseline, sutimlimab decreased the median bilirubin levels by 61%, normalizing levels in most patients within 24 hours of the first infusion (P=0.007).
When sutimlimab was washed out, bilirubin levels increased again, which demonstrated the recurrence of hemolysis.
Approximately 3 to 4 weeks after the last dose of sutimlimab, hemolysis and anemia recurred in all responders.
When patients were re-exposed to sutimlimab, rapid and complete inhibition of hemolysis occurred once again.
None of the patients required packed red blood cell transfusions during treatment.
Safety
The investigators reported that all infusions were well tolerated without premedication and without relevant drug-related adverse effects.
They reported few adverse events during the trial. All were mild or moderate in severity, and most were considered unrelated or unlikely related to sutimlimab.
Two adverse events—one mild purpural rash on both hands and one case of moderate hair loss (each occurring in one patient)—were possibly related to sutimlimab.
While the investigators considered the safety data encouraging, they recommended interpreting the data “cautiously in light of the limited duration of the trial.”
“Provided that safety results remain positive, sutimlimab could become the first approved treatment for cold agglutinin disease,” said corresponding author Bernd Jilma, MD, of the Medical University of Vienna in Austria.
“The drug clearly addresses an unmet medical need, as we have seen rapid, strong responses in patients for whom multiple prior therapies have failed.”
This study was funded by True North Therapeutics, Inc, now part of Bioverativ, a Sanofi company.
Some of the authors disclosed financial relationships, including employment, with True North Therapeutics and Bioverativ.
A phase 3 trial of sutimlimab is underway with top-line results due in 2019.
In a first-in-human trial, sutimlimab rapidly halted hemolysis, corrected anemia, precluded the need for transfusion, and caused no serious adverse effects in patients with cold agglutinin disease.
Sutimlimab also “induced clinically meaningful increases in hemoglobin levels, even in patients with multiple previous lines of therapy,” according to investigators.
The European Medicines Agency and the U.S. Food and Drug Administration (FDA) awarded sutimlimab orphan drug status based on these results. The FDA also granted sutimlimab breakthrough therapy designation.
Sutimlimab is a humanized anti-C1s IgG4 monoclonal antibody that blocks the classical complement pathway–specific protease C1s and prevents further hemolysis in patients with cold agglutinin disease.
Cold agglutinin disease is a rare, acquired chronic autoimmune hemolytic condition that destroys red blood cells. It leads to chronic anemia, severe fatigue, and potentially fatal thrombotic events. No drug has yet been approved to treat cold agglutinin disease.
The phase 1 trial of sutimlimab (formerly BIVV009 and TNT009) in cold agglutinin disease was conducted at the Medical University of Vienna in Austria and reported in Blood.
The study (NCT02502903) involved 10 patients, ages 56 to 76, who were previously treated with multiple lines of therapy, including two patients who failed treatment with eculizumab.
Of the 10 patients, eight were female, eight were Caucasian, one was Asian, and one was Hispanic. Patients had cold agglutinin disease for a median of 5 years (range, 1 – 20).
At baseline, the median hemoglobin level was 7.8 g/dL, the median number of reticulocytes was 133 x 109/L, the median bilirubin was 2.0 mg/dL, and the median haptoglobin was less than 12 mg/dL.
The patients received an initial dose of 10 mg/kg intravenous sutimlimab as a test dose to allow rapid wash-out of the drug if unforeseen adverse effects occurred with the first infusion.
One to 4 days later, they received the full dose of 60 mg/kg, followed by three additional weekly doses.
Investigators observed the patients for 49 to 53 days.
Results
Within the first week, patients’ median hemoglobin levels increased by 1.6 g/dL (P=0.007), and the median best response was an increase of 3.9 g/dL (P=0.005) after 6 weeks.
Seven patients had increased hemoglobin levels by more than 2 g/dL, and this included those who recently failed to respond or relapsed after rituximab, rituximab plus bendamustine, or eculizumab.
In five patients, hemoglobin increased by 4 g/dL or more. In four patients, it completely normalized to 12 g/dL.
In the first 24 hours after sutimlimab infusion, reticulocyte counts increased by a median of 41% and then gradually declined as hemoglobin levels rose.
In four patients, haptoglobin levels normalized within 1 to 2 weeks. In eight patients who had abnormal bilirubin levels at baseline, sutimlimab decreased the median bilirubin levels by 61%, normalizing levels in most patients within 24 hours of the first infusion (P=0.007).
When sutimlimab was washed out, bilirubin levels increased again, which demonstrated the recurrence of hemolysis.
Approximately 3 to 4 weeks after the last dose of sutimlimab, hemolysis and anemia recurred in all responders.
When patients were re-exposed to sutimlimab, rapid and complete inhibition of hemolysis occurred once again.
None of the patients required packed red blood cell transfusions during treatment.
Safety
The investigators reported that all infusions were well tolerated without premedication and without relevant drug-related adverse effects.
They reported few adverse events during the trial. All were mild or moderate in severity, and most were considered unrelated or unlikely related to sutimlimab.
Two adverse events—one mild purpural rash on both hands and one case of moderate hair loss (each occurring in one patient)—were possibly related to sutimlimab.
While the investigators considered the safety data encouraging, they recommended interpreting the data “cautiously in light of the limited duration of the trial.”
“Provided that safety results remain positive, sutimlimab could become the first approved treatment for cold agglutinin disease,” said corresponding author Bernd Jilma, MD, of the Medical University of Vienna in Austria.
“The drug clearly addresses an unmet medical need, as we have seen rapid, strong responses in patients for whom multiple prior therapies have failed.”
This study was funded by True North Therapeutics, Inc, now part of Bioverativ, a Sanofi company.
Some of the authors disclosed financial relationships, including employment, with True North Therapeutics and Bioverativ.
A phase 3 trial of sutimlimab is underway with top-line results due in 2019.
FDA approves first treatment for BPDCN
The U.S. Food and Drug Administration (FDA) has approved tagraxofusp-erzs (Elzonris) to treat patients age 2 and older who have blastic plasmacytoid dendritic cell neoplasm (BPDCN).
Tagraxofusp-erzs (formerly SL-401) is a CD123-directed cytotoxin that is the first FDA-approved treatment for BPDCN.
Tagraxofusp-erzs will be commercially available in early 2019, according to Stemline Therapeutics, makers of the drug.
The prescribing information for tagraxofusp-erzs contains a boxed warning noting that the drug is associated with an increased risk of capillary leak syndrome (CLS), which may be life-threatening or fatal.
The FDA previously granted tagraxofusp-erzs breakthrough therapy and orphan drug designations and assessed the drug under priority review.
The FDA’s approval of tagraxofusp-erzs was based on a phase 1 trial (STML-401-0114; NCT02113982).
The trial enrolled 47 patients with BPDCN, including 32 who were treatment-naïve and 15 who were previously treated.
Patients received tagraxofusp-erzs intravenously on days 1-5 of a 21-day cycle for multiple consecutive cycles. The trial had a dose-escalation stage (stage 1), an expansion stage (stage 2), a confirmatory stage (stage 3), and a stage that enabled uninterrupted access to tagraxofusp-erzs (stage 4).
In the confirmatory stage, 13 patients with treatment-naïve BPDCN received tagraxofusp-erzs at the recommended dose and schedule—12 mcg/kg daily for 5 days of a 21-day cycle.
Efficacy was based on the rate of complete response (CR) or clinical complete response (CRc). CRc was defined as CR with residual skin abnormality not indicative of active disease.
The CR/CRc rate was 53.8% (7/13), and the median duration of CR/CRc was not reached (range, 3.9 to 12.2 months).
The safety of tagraxofusp-erzs was assessed in 94 adults with treatment-naïve or previously treated myeloid malignancies, including 58 patients with BPDCN, who were treated at the recommended dose and schedule.
There were two fatal adverse events—both CLS. Eleven percent of patients discontinued treatment with tagraxofusp-erzs due to an adverse event. The most common of these were hepatic toxicities and CLS.
The most common adverse events overall were CLS (55%), nausea (49%), fatigue (45%), peripheral edema (43%), pyrexia (43%), and weight increase (31%).
The most common laboratory abnormalities were decreases in albumin (77%), platelets (67%), hemoglobin (60%), calcium (57%), and sodium (50%), as well as increases in glucose (87%), alanine aminotransferase (82%), and aspartate aminotransferase (79%).
The U.S. Food and Drug Administration (FDA) has approved tagraxofusp-erzs (Elzonris) to treat patients age 2 and older who have blastic plasmacytoid dendritic cell neoplasm (BPDCN).
Tagraxofusp-erzs (formerly SL-401) is a CD123-directed cytotoxin that is the first FDA-approved treatment for BPDCN.
Tagraxofusp-erzs will be commercially available in early 2019, according to Stemline Therapeutics, makers of the drug.
The prescribing information for tagraxofusp-erzs contains a boxed warning noting that the drug is associated with an increased risk of capillary leak syndrome (CLS), which may be life-threatening or fatal.
The FDA previously granted tagraxofusp-erzs breakthrough therapy and orphan drug designations and assessed the drug under priority review.
The FDA’s approval of tagraxofusp-erzs was based on a phase 1 trial (STML-401-0114; NCT02113982).
The trial enrolled 47 patients with BPDCN, including 32 who were treatment-naïve and 15 who were previously treated.
Patients received tagraxofusp-erzs intravenously on days 1-5 of a 21-day cycle for multiple consecutive cycles. The trial had a dose-escalation stage (stage 1), an expansion stage (stage 2), a confirmatory stage (stage 3), and a stage that enabled uninterrupted access to tagraxofusp-erzs (stage 4).
In the confirmatory stage, 13 patients with treatment-naïve BPDCN received tagraxofusp-erzs at the recommended dose and schedule—12 mcg/kg daily for 5 days of a 21-day cycle.
Efficacy was based on the rate of complete response (CR) or clinical complete response (CRc). CRc was defined as CR with residual skin abnormality not indicative of active disease.
The CR/CRc rate was 53.8% (7/13), and the median duration of CR/CRc was not reached (range, 3.9 to 12.2 months).
The safety of tagraxofusp-erzs was assessed in 94 adults with treatment-naïve or previously treated myeloid malignancies, including 58 patients with BPDCN, who were treated at the recommended dose and schedule.
There were two fatal adverse events—both CLS. Eleven percent of patients discontinued treatment with tagraxofusp-erzs due to an adverse event. The most common of these were hepatic toxicities and CLS.
The most common adverse events overall were CLS (55%), nausea (49%), fatigue (45%), peripheral edema (43%), pyrexia (43%), and weight increase (31%).
The most common laboratory abnormalities were decreases in albumin (77%), platelets (67%), hemoglobin (60%), calcium (57%), and sodium (50%), as well as increases in glucose (87%), alanine aminotransferase (82%), and aspartate aminotransferase (79%).
The U.S. Food and Drug Administration (FDA) has approved tagraxofusp-erzs (Elzonris) to treat patients age 2 and older who have blastic plasmacytoid dendritic cell neoplasm (BPDCN).
Tagraxofusp-erzs (formerly SL-401) is a CD123-directed cytotoxin that is the first FDA-approved treatment for BPDCN.
Tagraxofusp-erzs will be commercially available in early 2019, according to Stemline Therapeutics, makers of the drug.
The prescribing information for tagraxofusp-erzs contains a boxed warning noting that the drug is associated with an increased risk of capillary leak syndrome (CLS), which may be life-threatening or fatal.
The FDA previously granted tagraxofusp-erzs breakthrough therapy and orphan drug designations and assessed the drug under priority review.
The FDA’s approval of tagraxofusp-erzs was based on a phase 1 trial (STML-401-0114; NCT02113982).
The trial enrolled 47 patients with BPDCN, including 32 who were treatment-naïve and 15 who were previously treated.
Patients received tagraxofusp-erzs intravenously on days 1-5 of a 21-day cycle for multiple consecutive cycles. The trial had a dose-escalation stage (stage 1), an expansion stage (stage 2), a confirmatory stage (stage 3), and a stage that enabled uninterrupted access to tagraxofusp-erzs (stage 4).
In the confirmatory stage, 13 patients with treatment-naïve BPDCN received tagraxofusp-erzs at the recommended dose and schedule—12 mcg/kg daily for 5 days of a 21-day cycle.
Efficacy was based on the rate of complete response (CR) or clinical complete response (CRc). CRc was defined as CR with residual skin abnormality not indicative of active disease.
The CR/CRc rate was 53.8% (7/13), and the median duration of CR/CRc was not reached (range, 3.9 to 12.2 months).
The safety of tagraxofusp-erzs was assessed in 94 adults with treatment-naïve or previously treated myeloid malignancies, including 58 patients with BPDCN, who were treated at the recommended dose and schedule.
There were two fatal adverse events—both CLS. Eleven percent of patients discontinued treatment with tagraxofusp-erzs due to an adverse event. The most common of these were hepatic toxicities and CLS.
The most common adverse events overall were CLS (55%), nausea (49%), fatigue (45%), peripheral edema (43%), pyrexia (43%), and weight increase (31%).
The most common laboratory abnormalities were decreases in albumin (77%), platelets (67%), hemoglobin (60%), calcium (57%), and sodium (50%), as well as increases in glucose (87%), alanine aminotransferase (82%), and aspartate aminotransferase (79%).
FDA approves ravulizumab for PNH
The U.S. Food and Drug Administration (FDA) has approved ravulizumab-cwvz (Ultomiris) to treat adults with paroxysmal nocturnal hemoglobinuria (PNH).
Ravulizumab is a long-acting C5 complement inhibitor, administered every 8 weeks, that has been shown to prevent hemolysis.
The prescribing information for ravulizumab includes a boxed warning stating that meningococcal infections/sepsis have occurred in patients treated with the drug, and these adverse effects can become life-threatening or fatal if not recognized and treated early.
Ravulizumab is available only through a restricted program under a Risk Evaluation and Mitigation Strategy.
The FDA previously granted the application for ravulizumab priority review, and the product received orphan drug designation from the FDA.
The FDA granted the approval of ravulizumab to Alexion Pharmaceuticals.
The FDA’s approval of ravulizumab is based on results from two phase 3 studies, one in patients who had previously received treatment with a complement inhibitor and one in patients who were complement-inhibitor-naïve. Both studies were recently published in Blood.
Efficacy in inhibitor-experienced patients
In one study (NCT03056040), researchers compared ravulizumab administered every 8 weeks to eculizumab administered every 2 weeks in complement-inhibitor-experienced patients.
The trial included 195 PNH patients who were taking eculizumab for more than 6 months. They were randomized to switch to ravulizumab (n=97) or continue on eculizumab (n=98).
Ravulizumab proved noninferior to eculizumab for all endpoints studied (P<0.0006), including:
- Percentage change in lactate dehydrogenase (LDH): difference, 9.21% (95% CI: -0.42 to 18.84; P=0.058 for superiority)
- Breakthrough hemolysis: difference, 5.1 (95% CI: -8.89 to 18.99)
- Change in FACIT-Fatigue score: difference, 1.47 (95% CI: -0.21 to 3.15)
- Transfusion avoidance: difference, 5.5 (95% CI: -4.27 to 15.68)
- Stabilized hemoglobin: difference, 1.4 (95% CI: -10.41 to 13.31).
Efficacy in inhibitor-naïve patients
In another study (NCT02946463), researchers compared ravulizumab and eculizumab in 246 PNH patients who had not previously received a complement inhibitor.
Ravulizumab was noninferior to eculizumab for all endpoints (P<0.0001), including:
- Transfusion avoidance: 73.6% vs 66.1%; difference of 6.8% (95% CI: -4.66 to 18.14)
- LDH normalization: 53.6% vs 49.4%; odds ratio=1.19 (95% CI: 0.80 to 1.77)
- Percent reduction in LDH: -76.8% vs -76.0%; difference of -0.83% (95% CI: -5.21 to 3.56)
- Change in FACIT-Fatigue score: 7.07 vs 6.40; difference of 0.67 (95% CI: -1.21 to 2.55)
- Breakthrough hemolysis: 4.0% vs 10.7%; difference of -6.7% (95% CI: -14.21 to 0.18)
- Stabilized hemoglobin: 68.0% vs 64.5%; difference of 2.9 (95% CI: -8.80 to 14.64).
Safety in both trials
The safety data from both trials included 441 adults who received ravulizumab (n=222) or eculizumab (n=219) for a median of 6 months.
The most frequent adverse events in both arms (ravulizumab and eculizumab, respectively) were upper respiratory tract infection (39% and 39%) and headache (32% and 26%).
Serious adverse events occurred in 15 (6.8%) patients treated with ravulizumab. These events included hyperthermia and pyrexia.
There was one fatal case of sepsis in a patient treated with ravulizumab.
The U.S. Food and Drug Administration (FDA) has approved ravulizumab-cwvz (Ultomiris) to treat adults with paroxysmal nocturnal hemoglobinuria (PNH).
Ravulizumab is a long-acting C5 complement inhibitor, administered every 8 weeks, that has been shown to prevent hemolysis.
The prescribing information for ravulizumab includes a boxed warning stating that meningococcal infections/sepsis have occurred in patients treated with the drug, and these adverse effects can become life-threatening or fatal if not recognized and treated early.
Ravulizumab is available only through a restricted program under a Risk Evaluation and Mitigation Strategy.
The FDA previously granted the application for ravulizumab priority review, and the product received orphan drug designation from the FDA.
The FDA granted the approval of ravulizumab to Alexion Pharmaceuticals.
The FDA’s approval of ravulizumab is based on results from two phase 3 studies, one in patients who had previously received treatment with a complement inhibitor and one in patients who were complement-inhibitor-naïve. Both studies were recently published in Blood.
Efficacy in inhibitor-experienced patients
In one study (NCT03056040), researchers compared ravulizumab administered every 8 weeks to eculizumab administered every 2 weeks in complement-inhibitor-experienced patients.
The trial included 195 PNH patients who were taking eculizumab for more than 6 months. They were randomized to switch to ravulizumab (n=97) or continue on eculizumab (n=98).
Ravulizumab proved noninferior to eculizumab for all endpoints studied (P<0.0006), including:
- Percentage change in lactate dehydrogenase (LDH): difference, 9.21% (95% CI: -0.42 to 18.84; P=0.058 for superiority)
- Breakthrough hemolysis: difference, 5.1 (95% CI: -8.89 to 18.99)
- Change in FACIT-Fatigue score: difference, 1.47 (95% CI: -0.21 to 3.15)
- Transfusion avoidance: difference, 5.5 (95% CI: -4.27 to 15.68)
- Stabilized hemoglobin: difference, 1.4 (95% CI: -10.41 to 13.31).
Efficacy in inhibitor-naïve patients
In another study (NCT02946463), researchers compared ravulizumab and eculizumab in 246 PNH patients who had not previously received a complement inhibitor.
Ravulizumab was noninferior to eculizumab for all endpoints (P<0.0001), including:
- Transfusion avoidance: 73.6% vs 66.1%; difference of 6.8% (95% CI: -4.66 to 18.14)
- LDH normalization: 53.6% vs 49.4%; odds ratio=1.19 (95% CI: 0.80 to 1.77)
- Percent reduction in LDH: -76.8% vs -76.0%; difference of -0.83% (95% CI: -5.21 to 3.56)
- Change in FACIT-Fatigue score: 7.07 vs 6.40; difference of 0.67 (95% CI: -1.21 to 2.55)
- Breakthrough hemolysis: 4.0% vs 10.7%; difference of -6.7% (95% CI: -14.21 to 0.18)
- Stabilized hemoglobin: 68.0% vs 64.5%; difference of 2.9 (95% CI: -8.80 to 14.64).
Safety in both trials
The safety data from both trials included 441 adults who received ravulizumab (n=222) or eculizumab (n=219) for a median of 6 months.
The most frequent adverse events in both arms (ravulizumab and eculizumab, respectively) were upper respiratory tract infection (39% and 39%) and headache (32% and 26%).
Serious adverse events occurred in 15 (6.8%) patients treated with ravulizumab. These events included hyperthermia and pyrexia.
There was one fatal case of sepsis in a patient treated with ravulizumab.
The U.S. Food and Drug Administration (FDA) has approved ravulizumab-cwvz (Ultomiris) to treat adults with paroxysmal nocturnal hemoglobinuria (PNH).
Ravulizumab is a long-acting C5 complement inhibitor, administered every 8 weeks, that has been shown to prevent hemolysis.
The prescribing information for ravulizumab includes a boxed warning stating that meningococcal infections/sepsis have occurred in patients treated with the drug, and these adverse effects can become life-threatening or fatal if not recognized and treated early.
Ravulizumab is available only through a restricted program under a Risk Evaluation and Mitigation Strategy.
The FDA previously granted the application for ravulizumab priority review, and the product received orphan drug designation from the FDA.
The FDA granted the approval of ravulizumab to Alexion Pharmaceuticals.
The FDA’s approval of ravulizumab is based on results from two phase 3 studies, one in patients who had previously received treatment with a complement inhibitor and one in patients who were complement-inhibitor-naïve. Both studies were recently published in Blood.
Efficacy in inhibitor-experienced patients
In one study (NCT03056040), researchers compared ravulizumab administered every 8 weeks to eculizumab administered every 2 weeks in complement-inhibitor-experienced patients.
The trial included 195 PNH patients who were taking eculizumab for more than 6 months. They were randomized to switch to ravulizumab (n=97) or continue on eculizumab (n=98).
Ravulizumab proved noninferior to eculizumab for all endpoints studied (P<0.0006), including:
- Percentage change in lactate dehydrogenase (LDH): difference, 9.21% (95% CI: -0.42 to 18.84; P=0.058 for superiority)
- Breakthrough hemolysis: difference, 5.1 (95% CI: -8.89 to 18.99)
- Change in FACIT-Fatigue score: difference, 1.47 (95% CI: -0.21 to 3.15)
- Transfusion avoidance: difference, 5.5 (95% CI: -4.27 to 15.68)
- Stabilized hemoglobin: difference, 1.4 (95% CI: -10.41 to 13.31).
Efficacy in inhibitor-naïve patients
In another study (NCT02946463), researchers compared ravulizumab and eculizumab in 246 PNH patients who had not previously received a complement inhibitor.
Ravulizumab was noninferior to eculizumab for all endpoints (P<0.0001), including:
- Transfusion avoidance: 73.6% vs 66.1%; difference of 6.8% (95% CI: -4.66 to 18.14)
- LDH normalization: 53.6% vs 49.4%; odds ratio=1.19 (95% CI: 0.80 to 1.77)
- Percent reduction in LDH: -76.8% vs -76.0%; difference of -0.83% (95% CI: -5.21 to 3.56)
- Change in FACIT-Fatigue score: 7.07 vs 6.40; difference of 0.67 (95% CI: -1.21 to 2.55)
- Breakthrough hemolysis: 4.0% vs 10.7%; difference of -6.7% (95% CI: -14.21 to 0.18)
- Stabilized hemoglobin: 68.0% vs 64.5%; difference of 2.9 (95% CI: -8.80 to 14.64).
Safety in both trials
The safety data from both trials included 441 adults who received ravulizumab (n=222) or eculizumab (n=219) for a median of 6 months.
The most frequent adverse events in both arms (ravulizumab and eculizumab, respectively) were upper respiratory tract infection (39% and 39%) and headache (32% and 26%).
Serious adverse events occurred in 15 (6.8%) patients treated with ravulizumab. These events included hyperthermia and pyrexia.
There was one fatal case of sepsis in a patient treated with ravulizumab.
FDA approves calaspargase pegol-mknl for ALL
The U.S. Food and Drug Administration (FDA) has approved calaspargase pegol-mknl (Asparlas) as a component of a multi-agent chemotherapeutic regimen to treat acute lymphoblastic leukemia (ALL) in pediatric and young adult patients age 1 month to 21 years.
Calaspargase pegol-mknl is an asparagine-specific enzyme intended to provide a longer interval between doses compared to other available pegaspargase products.
The recommended dosage of calaspargase pegol-mknl is 2,500 U/m2 given no more frequently than every 21 days.
The FDA said it approved calaspargase pegol-mknl because the drug maintained nadir serum asparaginase activity above the level of 0.1 U/mL when given at 2,500 U/m2 every 3 weeks.
Calaspargase pegol-mknl was evaluated in Study DFCI 11-001, a trial of 237 children and adolescents with newly diagnosed ALL or lymphoblastic lymphoma. The patients’ median age was 5 years (range, 1 to 20 years).
They received calaspargase pegol-mknl at 2,500 U/m2 (n=118) or pegaspargase at 2,500 U/m2 (n=119) as part of a Dana-Farber Cancer Institute (DFCI) ALL Consortium backbone therapy.
The median duration of exposure was 8 months for both calaspargase pegol-mknl and pegaspargase.
Among the patients with B-cell lineage ALL, the complete remission rate was 98% in the calaspargase pegol-mknl arm and 99% in the pegaspargase arm. Estimated overall survival rates were comparable between the arms.
Common grade 3 or higher adverse events (in the calaspargase pegol-mknl and pegaspargase arms, respectively) included elevated transaminase (52% and 66%), bilirubin increase (20% and 25%), pancreatitis (18% and 24%), and abnormal clotting studies (14% and 21%).
There was one fatal adverse event among patients on calaspargase pegol-mknl—multi-organ failure in the setting of chronic pancreatitis associated with a pancreatic pseudocyst.
The safety of calaspargase pegol-mknl was also evaluated in Study AALL07P4, a trial of patients with newly diagnosed, high-risk B-precursor ALL.
The patients received calaspargase pegol-mknl at 2,500 U/m2 (n=43) or 2,100 U/m2 (n=68) or pegaspargase at 2,500 U/m2 (n=52) as a component of an augmented Berlin-Frankfurt-Münster regimen.
The patients’ median age was 11 years (range, 1 to 26 years). The median duration of exposure was 7 months for both calaspargase pegol-mknl and pegaspargase.
There were three induction deaths among the 111 patients who received calaspargase pegol-mknl (2.8%) but no induction deaths among the 52 patients treated with pegaspargase.
Additional details on these studies and calaspargase pegol-mknl can be found in the drug’s prescribing information.
Calaspargase pegol-mknl is a product of Servier Pharmaceuticals LLC.
The U.S. Food and Drug Administration (FDA) has approved calaspargase pegol-mknl (Asparlas) as a component of a multi-agent chemotherapeutic regimen to treat acute lymphoblastic leukemia (ALL) in pediatric and young adult patients age 1 month to 21 years.
Calaspargase pegol-mknl is an asparagine-specific enzyme intended to provide a longer interval between doses compared to other available pegaspargase products.
The recommended dosage of calaspargase pegol-mknl is 2,500 U/m2 given no more frequently than every 21 days.
The FDA said it approved calaspargase pegol-mknl because the drug maintained nadir serum asparaginase activity above the level of 0.1 U/mL when given at 2,500 U/m2 every 3 weeks.
Calaspargase pegol-mknl was evaluated in Study DFCI 11-001, a trial of 237 children and adolescents with newly diagnosed ALL or lymphoblastic lymphoma. The patients’ median age was 5 years (range, 1 to 20 years).
They received calaspargase pegol-mknl at 2,500 U/m2 (n=118) or pegaspargase at 2,500 U/m2 (n=119) as part of a Dana-Farber Cancer Institute (DFCI) ALL Consortium backbone therapy.
The median duration of exposure was 8 months for both calaspargase pegol-mknl and pegaspargase.
Among the patients with B-cell lineage ALL, the complete remission rate was 98% in the calaspargase pegol-mknl arm and 99% in the pegaspargase arm. Estimated overall survival rates were comparable between the arms.
Common grade 3 or higher adverse events (in the calaspargase pegol-mknl and pegaspargase arms, respectively) included elevated transaminase (52% and 66%), bilirubin increase (20% and 25%), pancreatitis (18% and 24%), and abnormal clotting studies (14% and 21%).
There was one fatal adverse event among patients on calaspargase pegol-mknl—multi-organ failure in the setting of chronic pancreatitis associated with a pancreatic pseudocyst.
The safety of calaspargase pegol-mknl was also evaluated in Study AALL07P4, a trial of patients with newly diagnosed, high-risk B-precursor ALL.
The patients received calaspargase pegol-mknl at 2,500 U/m2 (n=43) or 2,100 U/m2 (n=68) or pegaspargase at 2,500 U/m2 (n=52) as a component of an augmented Berlin-Frankfurt-Münster regimen.
The patients’ median age was 11 years (range, 1 to 26 years). The median duration of exposure was 7 months for both calaspargase pegol-mknl and pegaspargase.
There were three induction deaths among the 111 patients who received calaspargase pegol-mknl (2.8%) but no induction deaths among the 52 patients treated with pegaspargase.
Additional details on these studies and calaspargase pegol-mknl can be found in the drug’s prescribing information.
Calaspargase pegol-mknl is a product of Servier Pharmaceuticals LLC.
The U.S. Food and Drug Administration (FDA) has approved calaspargase pegol-mknl (Asparlas) as a component of a multi-agent chemotherapeutic regimen to treat acute lymphoblastic leukemia (ALL) in pediatric and young adult patients age 1 month to 21 years.
Calaspargase pegol-mknl is an asparagine-specific enzyme intended to provide a longer interval between doses compared to other available pegaspargase products.
The recommended dosage of calaspargase pegol-mknl is 2,500 U/m2 given no more frequently than every 21 days.
The FDA said it approved calaspargase pegol-mknl because the drug maintained nadir serum asparaginase activity above the level of 0.1 U/mL when given at 2,500 U/m2 every 3 weeks.
Calaspargase pegol-mknl was evaluated in Study DFCI 11-001, a trial of 237 children and adolescents with newly diagnosed ALL or lymphoblastic lymphoma. The patients’ median age was 5 years (range, 1 to 20 years).
They received calaspargase pegol-mknl at 2,500 U/m2 (n=118) or pegaspargase at 2,500 U/m2 (n=119) as part of a Dana-Farber Cancer Institute (DFCI) ALL Consortium backbone therapy.
The median duration of exposure was 8 months for both calaspargase pegol-mknl and pegaspargase.
Among the patients with B-cell lineage ALL, the complete remission rate was 98% in the calaspargase pegol-mknl arm and 99% in the pegaspargase arm. Estimated overall survival rates were comparable between the arms.
Common grade 3 or higher adverse events (in the calaspargase pegol-mknl and pegaspargase arms, respectively) included elevated transaminase (52% and 66%), bilirubin increase (20% and 25%), pancreatitis (18% and 24%), and abnormal clotting studies (14% and 21%).
There was one fatal adverse event among patients on calaspargase pegol-mknl—multi-organ failure in the setting of chronic pancreatitis associated with a pancreatic pseudocyst.
The safety of calaspargase pegol-mknl was also evaluated in Study AALL07P4, a trial of patients with newly diagnosed, high-risk B-precursor ALL.
The patients received calaspargase pegol-mknl at 2,500 U/m2 (n=43) or 2,100 U/m2 (n=68) or pegaspargase at 2,500 U/m2 (n=52) as a component of an augmented Berlin-Frankfurt-Münster regimen.
The patients’ median age was 11 years (range, 1 to 26 years). The median duration of exposure was 7 months for both calaspargase pegol-mknl and pegaspargase.
There were three induction deaths among the 111 patients who received calaspargase pegol-mknl (2.8%) but no induction deaths among the 52 patients treated with pegaspargase.
Additional details on these studies and calaspargase pegol-mknl can be found in the drug’s prescribing information.
Calaspargase pegol-mknl is a product of Servier Pharmaceuticals LLC.
CHMP recommends treosulfan for allo-HSCT conditioning
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for treosulfan (Trecondi) as part of conditioning prior to allogeneic hematopoietic stem cell transplant (allo-HSCT).
The full indication is for treosulfan to be used in combination with fludarabine for conditioning prior to allo-HSCT in adults with malignant and non-malignant diseases and in pediatric patients older than 1 month who have malignant diseases.
The CHMP’s recommendation for treosulfan will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s opinion of treosulfan is supported by results from a phase 3 trial (NCT00822393), which were presented at the 2017 ASH Annual Meeting.
In this trial, investigators compared two conditioning regimens, treosulfan-fludarabine and busulfan-fludarabine, in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes who were undergoing allo-HSCT.
The ASH data included 476 patients from the final analysis.
Investigators said safety results between day -6 and day +28 were similar with the two regimens.
The same was true for trilineage engraftment and the cumulative incidence of relapse/progression at 24 months after allo-HSCT.
However, survival rates were higher in the treosulfan arm.
The event-free survival at 24 months was 64.0% in the treosulfan arm and 50.4% in the busulfan arm (P=0.0000164). The overall survival at 24 months was 72.5% and 56.4%, respectively (P=0.0082).
Transplant-related mortality at 24 months was 11.3% in the treosulfan arm and 28.2% in the busulfan arm (P=0.0201).
This trial was sponsored by medac GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for treosulfan (Trecondi) as part of conditioning prior to allogeneic hematopoietic stem cell transplant (allo-HSCT).
The full indication is for treosulfan to be used in combination with fludarabine for conditioning prior to allo-HSCT in adults with malignant and non-malignant diseases and in pediatric patients older than 1 month who have malignant diseases.
The CHMP’s recommendation for treosulfan will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s opinion of treosulfan is supported by results from a phase 3 trial (NCT00822393), which were presented at the 2017 ASH Annual Meeting.
In this trial, investigators compared two conditioning regimens, treosulfan-fludarabine and busulfan-fludarabine, in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes who were undergoing allo-HSCT.
The ASH data included 476 patients from the final analysis.
Investigators said safety results between day -6 and day +28 were similar with the two regimens.
The same was true for trilineage engraftment and the cumulative incidence of relapse/progression at 24 months after allo-HSCT.
However, survival rates were higher in the treosulfan arm.
The event-free survival at 24 months was 64.0% in the treosulfan arm and 50.4% in the busulfan arm (P=0.0000164). The overall survival at 24 months was 72.5% and 56.4%, respectively (P=0.0082).
Transplant-related mortality at 24 months was 11.3% in the treosulfan arm and 28.2% in the busulfan arm (P=0.0201).
This trial was sponsored by medac GmbH.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for treosulfan (Trecondi) as part of conditioning prior to allogeneic hematopoietic stem cell transplant (allo-HSCT).
The full indication is for treosulfan to be used in combination with fludarabine for conditioning prior to allo-HSCT in adults with malignant and non-malignant diseases and in pediatric patients older than 1 month who have malignant diseases.
The CHMP’s recommendation for treosulfan will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s opinion of treosulfan is supported by results from a phase 3 trial (NCT00822393), which were presented at the 2017 ASH Annual Meeting.
In this trial, investigators compared two conditioning regimens, treosulfan-fludarabine and busulfan-fludarabine, in elderly or comorbid patients with acute myeloid leukemia or myelodysplastic syndromes who were undergoing allo-HSCT.
The ASH data included 476 patients from the final analysis.
Investigators said safety results between day -6 and day +28 were similar with the two regimens.
The same was true for trilineage engraftment and the cumulative incidence of relapse/progression at 24 months after allo-HSCT.
However, survival rates were higher in the treosulfan arm.
The event-free survival at 24 months was 64.0% in the treosulfan arm and 50.4% in the busulfan arm (P=0.0000164). The overall survival at 24 months was 72.5% and 56.4%, respectively (P=0.0082).
Transplant-related mortality at 24 months was 11.3% in the treosulfan arm and 28.2% in the busulfan arm (P=0.0201).
This trial was sponsored by medac GmbH.
CHMP backs lusutrombopag for severe thrombocytopenia
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for lusutrombopag to treat severe thrombocytopenia in adults with chronic liver disease who are undergoing invasive procedures.
Lusutrombopag is a thrombopoietin (TPO) receptor agonist that acts on the transmembrane domain of TPO receptors to induce proliferation and differentiation of megakaryocyte progenitor cells, thus leading to thrombocytopoiesis.
Lusutrombopag is intended to reduce the need for platelet transfusions before an invasive procedure and for rescue therapy for bleeding in the 7 days after the procedure.
The CHMP’s recommendation for lusutrombopag will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
Lusutrombopag trials
The efficacy of lusutrombopag was evaluated in two phase 3 trials—L-PLUS1 (1304M0631) and L-PLUS2 (1423M0634, NCT02389621).
The trials included 312 patients with chronic liver disease, severe thrombocytopenia (platelet counts below 50,000/μL), and a scheduled invasive procedure. The patients received lusutrombopag or placebo once daily for up to 7 days.
In L-PLUS1, 78% (38/49) of patients receiving lusutrombopag did not require platelet transfusions prior to the primary invasive procedure. The same was true for 13% (6/48) of patients who received placebo (P<0.0001).
In L-PLUS2 , 65% (70/108) of patients who received lusutrombopag did not require platelet transfusions prior to the primary invasive procedure or rescue therapy for bleeding in the 7 days after the procedure. The same was true for 29% (31/107) of patients receiving placebo (P<0.0001).
The safety of lusutrombopag was evaluated in three trials—L‐PLUS 1, L‐PLUS 2, and M0626 (1208M062).
The most common adverse event (AE) in these trials (n=341) was headache, which occurred in 5% of patients on lusutrombopag and 4% of patients on placebo.
Serious AEs occurred in 5% of patients on lusutrombopag and 7% of patients on placebo. The most common serious AE was portal vein thrombosis, which occurred in 1% of patients in both treatment groups.
None of the patients discontinued lusutrombopag due to AEs.
The trials were sponsored by Shionogi & Co., Ltd.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for lusutrombopag to treat severe thrombocytopenia in adults with chronic liver disease who are undergoing invasive procedures.
Lusutrombopag is a thrombopoietin (TPO) receptor agonist that acts on the transmembrane domain of TPO receptors to induce proliferation and differentiation of megakaryocyte progenitor cells, thus leading to thrombocytopoiesis.
Lusutrombopag is intended to reduce the need for platelet transfusions before an invasive procedure and for rescue therapy for bleeding in the 7 days after the procedure.
The CHMP’s recommendation for lusutrombopag will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
Lusutrombopag trials
The efficacy of lusutrombopag was evaluated in two phase 3 trials—L-PLUS1 (1304M0631) and L-PLUS2 (1423M0634, NCT02389621).
The trials included 312 patients with chronic liver disease, severe thrombocytopenia (platelet counts below 50,000/μL), and a scheduled invasive procedure. The patients received lusutrombopag or placebo once daily for up to 7 days.
In L-PLUS1, 78% (38/49) of patients receiving lusutrombopag did not require platelet transfusions prior to the primary invasive procedure. The same was true for 13% (6/48) of patients who received placebo (P<0.0001).
In L-PLUS2 , 65% (70/108) of patients who received lusutrombopag did not require platelet transfusions prior to the primary invasive procedure or rescue therapy for bleeding in the 7 days after the procedure. The same was true for 29% (31/107) of patients receiving placebo (P<0.0001).
The safety of lusutrombopag was evaluated in three trials—L‐PLUS 1, L‐PLUS 2, and M0626 (1208M062).
The most common adverse event (AE) in these trials (n=341) was headache, which occurred in 5% of patients on lusutrombopag and 4% of patients on placebo.
Serious AEs occurred in 5% of patients on lusutrombopag and 7% of patients on placebo. The most common serious AE was portal vein thrombosis, which occurred in 1% of patients in both treatment groups.
None of the patients discontinued lusutrombopag due to AEs.
The trials were sponsored by Shionogi & Co., Ltd.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for lusutrombopag to treat severe thrombocytopenia in adults with chronic liver disease who are undergoing invasive procedures.
Lusutrombopag is a thrombopoietin (TPO) receptor agonist that acts on the transmembrane domain of TPO receptors to induce proliferation and differentiation of megakaryocyte progenitor cells, thus leading to thrombocytopoiesis.
Lusutrombopag is intended to reduce the need for platelet transfusions before an invasive procedure and for rescue therapy for bleeding in the 7 days after the procedure.
The CHMP’s recommendation for lusutrombopag will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
Lusutrombopag trials
The efficacy of lusutrombopag was evaluated in two phase 3 trials—L-PLUS1 (1304M0631) and L-PLUS2 (1423M0634, NCT02389621).
The trials included 312 patients with chronic liver disease, severe thrombocytopenia (platelet counts below 50,000/μL), and a scheduled invasive procedure. The patients received lusutrombopag or placebo once daily for up to 7 days.
In L-PLUS1, 78% (38/49) of patients receiving lusutrombopag did not require platelet transfusions prior to the primary invasive procedure. The same was true for 13% (6/48) of patients who received placebo (P<0.0001).
In L-PLUS2 , 65% (70/108) of patients who received lusutrombopag did not require platelet transfusions prior to the primary invasive procedure or rescue therapy for bleeding in the 7 days after the procedure. The same was true for 29% (31/107) of patients receiving placebo (P<0.0001).
The safety of lusutrombopag was evaluated in three trials—L‐PLUS 1, L‐PLUS 2, and M0626 (1208M062).
The most common adverse event (AE) in these trials (n=341) was headache, which occurred in 5% of patients on lusutrombopag and 4% of patients on placebo.
Serious AEs occurred in 5% of patients on lusutrombopag and 7% of patients on placebo. The most common serious AE was portal vein thrombosis, which occurred in 1% of patients in both treatment groups.
None of the patients discontinued lusutrombopag due to AEs.
The trials were sponsored by Shionogi & Co., Ltd.
Long-acting interferon recommended for PV
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for ropeginterferon alfa-2b (BESREMi®) to treat adults who have polycythemia vera (PV) without symptomatic splenomegaly.
Ropeginterferon alfa-2b is a long-acting interferon, which is administered once every 2 weeks or monthly after stabilization of hematological parameters.
The CHMP’s recommendation for ropeginterferon alfa-2b will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s positive opinion of ropeginterferon alfa-2b is supported by data from CONTINUATION-PV (NCT02218047), a phase 3b extension trial of PROUD-PV (NCT01949805).
Results from the PROUD-PV study were presented at the 2016 ASH Annual Meeting. The latest data from CONTINUATION-PV were presented at the 2018 ASH Annual Meeting.
PROUD-PV enrolled 254 PV patients who were treatment-naive or pretreated with hydroxyurea (HU). They were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127).
The latest analysis of CONTINUATION-PV included 83 of the patients on ropeginterferon alfa-2b and 70 of the patients who either remained on HU or switched to best available therapy (BAT) as selected by investigators.
At 24 months, the complete hematologic response (CHR) rate was 70.5% with ropeginterferon alfa-2b and 49.3% with HU/BAT (P=0.0101).
At 36 months, the CHR rate was 70.5% with ropeginterferon alfa-2b and 51.4% with HU/BAT (P=0.0122).
A composite endpoint of CHR plus symptom improvement occurred in 52.6% of patients treated with ropeginterferon alfa-2b and 37.8% of patients on HU/BAT (P=0.0437).
Disease- or treatment-related secondary malignancies in patients receiving HU/BAT included two cases of acute myeloid leukemia, one melanoma, and two basaliomas.
There were three malignancies—glioblastoma, seminoma, and adrenal neoplasm—reported in patients treated with ropeginterferon alfa-2b. Investigators said these malignancies were most likely unrelated to treatment.
The rate of adverse events was 89.8% in the ropeginterferon alfa-2b arm and 90.6% in the HU/BAT arm. Treatment-related adverse events occurred in 74.8% and 78.7% of patients, respectively.
Anemia, thrombocytopenia, and leukopenia occurred more frequently with HU/BAT, whereas liver enzyme increase was mainly observed with ropeginterferon alfa-2b.
CONTINUATION-PV was sponsored by AOP Orphan Pharmaceuticals AG in collaboration with PharmaEssentia.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for ropeginterferon alfa-2b (BESREMi®) to treat adults who have polycythemia vera (PV) without symptomatic splenomegaly.
Ropeginterferon alfa-2b is a long-acting interferon, which is administered once every 2 weeks or monthly after stabilization of hematological parameters.
The CHMP’s recommendation for ropeginterferon alfa-2b will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s positive opinion of ropeginterferon alfa-2b is supported by data from CONTINUATION-PV (NCT02218047), a phase 3b extension trial of PROUD-PV (NCT01949805).
Results from the PROUD-PV study were presented at the 2016 ASH Annual Meeting. The latest data from CONTINUATION-PV were presented at the 2018 ASH Annual Meeting.
PROUD-PV enrolled 254 PV patients who were treatment-naive or pretreated with hydroxyurea (HU). They were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127).
The latest analysis of CONTINUATION-PV included 83 of the patients on ropeginterferon alfa-2b and 70 of the patients who either remained on HU or switched to best available therapy (BAT) as selected by investigators.
At 24 months, the complete hematologic response (CHR) rate was 70.5% with ropeginterferon alfa-2b and 49.3% with HU/BAT (P=0.0101).
At 36 months, the CHR rate was 70.5% with ropeginterferon alfa-2b and 51.4% with HU/BAT (P=0.0122).
A composite endpoint of CHR plus symptom improvement occurred in 52.6% of patients treated with ropeginterferon alfa-2b and 37.8% of patients on HU/BAT (P=0.0437).
Disease- or treatment-related secondary malignancies in patients receiving HU/BAT included two cases of acute myeloid leukemia, one melanoma, and two basaliomas.
There were three malignancies—glioblastoma, seminoma, and adrenal neoplasm—reported in patients treated with ropeginterferon alfa-2b. Investigators said these malignancies were most likely unrelated to treatment.
The rate of adverse events was 89.8% in the ropeginterferon alfa-2b arm and 90.6% in the HU/BAT arm. Treatment-related adverse events occurred in 74.8% and 78.7% of patients, respectively.
Anemia, thrombocytopenia, and leukopenia occurred more frequently with HU/BAT, whereas liver enzyme increase was mainly observed with ropeginterferon alfa-2b.
CONTINUATION-PV was sponsored by AOP Orphan Pharmaceuticals AG in collaboration with PharmaEssentia.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended approval for ropeginterferon alfa-2b (BESREMi®) to treat adults who have polycythemia vera (PV) without symptomatic splenomegaly.
Ropeginterferon alfa-2b is a long-acting interferon, which is administered once every 2 weeks or monthly after stabilization of hematological parameters.
The CHMP’s recommendation for ropeginterferon alfa-2b will be reviewed by the European Commission, which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The European Commission usually makes a decision within 67 days of a CHMP recommendation.
The CHMP’s positive opinion of ropeginterferon alfa-2b is supported by data from CONTINUATION-PV (NCT02218047), a phase 3b extension trial of PROUD-PV (NCT01949805).
Results from the PROUD-PV study were presented at the 2016 ASH Annual Meeting. The latest data from CONTINUATION-PV were presented at the 2018 ASH Annual Meeting.
PROUD-PV enrolled 254 PV patients who were treatment-naive or pretreated with hydroxyurea (HU). They were randomized to receive ropeginterferon alfa-2b (n=127) or HU (n=127).
The latest analysis of CONTINUATION-PV included 83 of the patients on ropeginterferon alfa-2b and 70 of the patients who either remained on HU or switched to best available therapy (BAT) as selected by investigators.
At 24 months, the complete hematologic response (CHR) rate was 70.5% with ropeginterferon alfa-2b and 49.3% with HU/BAT (P=0.0101).
At 36 months, the CHR rate was 70.5% with ropeginterferon alfa-2b and 51.4% with HU/BAT (P=0.0122).
A composite endpoint of CHR plus symptom improvement occurred in 52.6% of patients treated with ropeginterferon alfa-2b and 37.8% of patients on HU/BAT (P=0.0437).
Disease- or treatment-related secondary malignancies in patients receiving HU/BAT included two cases of acute myeloid leukemia, one melanoma, and two basaliomas.
There were three malignancies—glioblastoma, seminoma, and adrenal neoplasm—reported in patients treated with ropeginterferon alfa-2b. Investigators said these malignancies were most likely unrelated to treatment.
The rate of adverse events was 89.8% in the ropeginterferon alfa-2b arm and 90.6% in the HU/BAT arm. Treatment-related adverse events occurred in 74.8% and 78.7% of patients, respectively.
Anemia, thrombocytopenia, and leukopenia occurred more frequently with HU/BAT, whereas liver enzyme increase was mainly observed with ropeginterferon alfa-2b.
CONTINUATION-PV was sponsored by AOP Orphan Pharmaceuticals AG in collaboration with PharmaEssentia.
CHMP backs dasatinib for kids with newly diagnosed ALL
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for dasatinib (Sprycel).
The CHMP’s recommendation is to approve dasatinib in combination with chemotherapy to treat pediatric patients with newly diagnosed, Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of a CHMP recommendation.
Dasatinib is already EC-approved to treat:
- Adults with newly diagnosed, Ph+ chronic myelogenous leukemia (CML) in the chronic phase
- Adults with chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy including imatinib
- Adults with Ph+ ALL and lymphoid blast CML with resistance or intolerance to prior therapy
- Pediatric patients with newly diagnosed, Ph+ CML in chronic phase
- Pediatric patients with Ph+ CML in chronic phase that is resistant or intolerant to prior therapy including imatinib.
Phase 2 trial
The CHMP’s recommendation to approve dasatinib in pediatric patients with newly diagnosed, Ph+ ALL is based on data from a phase 2 trial (NCT01460160). In this trial, researchers are evaluating dasatinib in combination with a chemotherapy regimen modeled on a Berlin-Frankfurt-Munster high-risk backbone.
Results from the trial were presented at the 2017 ASH Annual Meeting.
At that time, 106 patients had been treated. They received continuous daily dasatinib (60 mg/m2) beginning at day 15 of induction chemotherapy. All treated patients achieved complete remission.
Patients who had evidence of minimal residual disease (MRD) ≥ 0.05% at the end of the first block of treatment (day 78) and those with MRD 0.005% to 0.05% who remained MRD-positive at any detectable level after three additional high-risk chemotherapy blocks were eligible for hematopoietic stem cell transplant (HSCT) in first remission.
Nineteen patients met these criteria, and 15 (14.2%) received HSCT. The remaining 85.8% of patients received dasatinib plus chemotherapy for two years.
The 3-year event-free survival rate was 65.5%, and the 3-year overall survival rate was 91.5%.
Two patients discontinued dasatinib due to toxicity—one due to allergy and one due to prolonged thrombocytopenia.
Grade 3/4 adverse events attributed to dasatinib included elevated alanine aminotransferase (21.7%), elevated aspartate transaminase (10.4%), pleural effusion (3.8%), edema (2.8%), hemorrhage (5.7%), and cardiac failure (0.8%).
Five patients died while receiving chemotherapy (three from sepsis, one due to pneumonia, and one of an unknown cause). Two deaths were HSCT-related.
This trial was sponsored by Bristol-Myers Squibb.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for dasatinib (Sprycel).
The CHMP’s recommendation is to approve dasatinib in combination with chemotherapy to treat pediatric patients with newly diagnosed, Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of a CHMP recommendation.
Dasatinib is already EC-approved to treat:
- Adults with newly diagnosed, Ph+ chronic myelogenous leukemia (CML) in the chronic phase
- Adults with chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy including imatinib
- Adults with Ph+ ALL and lymphoid blast CML with resistance or intolerance to prior therapy
- Pediatric patients with newly diagnosed, Ph+ CML in chronic phase
- Pediatric patients with Ph+ CML in chronic phase that is resistant or intolerant to prior therapy including imatinib.
Phase 2 trial
The CHMP’s recommendation to approve dasatinib in pediatric patients with newly diagnosed, Ph+ ALL is based on data from a phase 2 trial (NCT01460160). In this trial, researchers are evaluating dasatinib in combination with a chemotherapy regimen modeled on a Berlin-Frankfurt-Munster high-risk backbone.
Results from the trial were presented at the 2017 ASH Annual Meeting.
At that time, 106 patients had been treated. They received continuous daily dasatinib (60 mg/m2) beginning at day 15 of induction chemotherapy. All treated patients achieved complete remission.
Patients who had evidence of minimal residual disease (MRD) ≥ 0.05% at the end of the first block of treatment (day 78) and those with MRD 0.005% to 0.05% who remained MRD-positive at any detectable level after three additional high-risk chemotherapy blocks were eligible for hematopoietic stem cell transplant (HSCT) in first remission.
Nineteen patients met these criteria, and 15 (14.2%) received HSCT. The remaining 85.8% of patients received dasatinib plus chemotherapy for two years.
The 3-year event-free survival rate was 65.5%, and the 3-year overall survival rate was 91.5%.
Two patients discontinued dasatinib due to toxicity—one due to allergy and one due to prolonged thrombocytopenia.
Grade 3/4 adverse events attributed to dasatinib included elevated alanine aminotransferase (21.7%), elevated aspartate transaminase (10.4%), pleural effusion (3.8%), edema (2.8%), hemorrhage (5.7%), and cardiac failure (0.8%).
Five patients died while receiving chemotherapy (three from sepsis, one due to pneumonia, and one of an unknown cause). Two deaths were HSCT-related.
This trial was sponsored by Bristol-Myers Squibb.
The European Medicines Agency’s Committee for Medicinal Products for Human Use (CHMP) has recommended expanding the marketing authorization for dasatinib (Sprycel).
The CHMP’s recommendation is to approve dasatinib in combination with chemotherapy to treat pediatric patients with newly diagnosed, Philadelphia chromosome-positive (Ph+) acute lymphoblastic leukemia (ALL).
The CHMP’s recommendation will be reviewed by the European Commission (EC), which has the authority to approve medicines for use in the European Union, Norway, Iceland, and Liechtenstein.
The EC usually makes a decision within 67 days of a CHMP recommendation.
Dasatinib is already EC-approved to treat:
- Adults with newly diagnosed, Ph+ chronic myelogenous leukemia (CML) in the chronic phase
- Adults with chronic, accelerated, or blast phase CML with resistance or intolerance to prior therapy including imatinib
- Adults with Ph+ ALL and lymphoid blast CML with resistance or intolerance to prior therapy
- Pediatric patients with newly diagnosed, Ph+ CML in chronic phase
- Pediatric patients with Ph+ CML in chronic phase that is resistant or intolerant to prior therapy including imatinib.
Phase 2 trial
The CHMP’s recommendation to approve dasatinib in pediatric patients with newly diagnosed, Ph+ ALL is based on data from a phase 2 trial (NCT01460160). In this trial, researchers are evaluating dasatinib in combination with a chemotherapy regimen modeled on a Berlin-Frankfurt-Munster high-risk backbone.
Results from the trial were presented at the 2017 ASH Annual Meeting.
At that time, 106 patients had been treated. They received continuous daily dasatinib (60 mg/m2) beginning at day 15 of induction chemotherapy. All treated patients achieved complete remission.
Patients who had evidence of minimal residual disease (MRD) ≥ 0.05% at the end of the first block of treatment (day 78) and those with MRD 0.005% to 0.05% who remained MRD-positive at any detectable level after three additional high-risk chemotherapy blocks were eligible for hematopoietic stem cell transplant (HSCT) in first remission.
Nineteen patients met these criteria, and 15 (14.2%) received HSCT. The remaining 85.8% of patients received dasatinib plus chemotherapy for two years.
The 3-year event-free survival rate was 65.5%, and the 3-year overall survival rate was 91.5%.
Two patients discontinued dasatinib due to toxicity—one due to allergy and one due to prolonged thrombocytopenia.
Grade 3/4 adverse events attributed to dasatinib included elevated alanine aminotransferase (21.7%), elevated aspartate transaminase (10.4%), pleural effusion (3.8%), edema (2.8%), hemorrhage (5.7%), and cardiac failure (0.8%).
Five patients died while receiving chemotherapy (three from sepsis, one due to pneumonia, and one of an unknown cause). Two deaths were HSCT-related.
This trial was sponsored by Bristol-Myers Squibb.