User login
The three pillars of perinatal care: Babies, parents, dyadic relationships
Perinatal depression (PND) is the most common obstetric complication in the United States. Even when screening results are positive, mothers often do not receive further evaluation, and even when PND is diagnosed, mothers do not receive evidence-based treatments.
Meta-analytic estimates show that pregnant women suffer from PND at rates from 6.5% to 12.9% across pregnancy to 3-months post partum.1 Women from low-income families and adolescent mothers are at highest risk, where rates are double and triple respectively.
Fathers also suffer from PND, with a prevalence rate from 2% to 25%, increasing to 50% when the mother experiences PND.
The American Academy of Pediatrics issued a Policy Statement (January 2019) about the need to recognize and manage PND. They recommended that pediatric medical homes establish a system to implement the screening of mothers at the 1-, 2-, 4-, and 6-month well-child visits, to use community resources for the treatment and referral of the mother with depression, and to provide support for the maternal-child relationship.2
The American Academy of Pediatrics also recommends advocacy for workforce development for mental health professionals who care for young children and mother-infant dyads, and for promotion of evidence-based interventions focused on healthy attachment and parent-child relationships.
Family research
There is a bidirectional association between family relational stress and PND. Lack of family support is both a predictor and a consequence of perinatal depression. Frequent arguments, conflict because one or both partners did not want the pregnancy, division of labor, poor support following stressful life events, lack of partner availability, and low intimacy are associated with increased perinatal depressive symptoms.
Gender role stress is also included as a risk factor. For example, men may fear performance failure related to work and sex, and women may fear disruption in the couple relationship due to the introduction of a child.
When depressed and nondepressed women at 2 months post delivery were compared, the women with depressive symptoms perceived that their partners did not share similar interests, provided little companionship, expressed disinterest in infant care, did not provide a feeling of connection, did not encourage them to get assistance to cope with difficulties, and expressed disagreement in infant care.3
A high-quality intimate relationship is protective for many illnesses and PND is no exception.4
Assessment
Despite the availability of effective treatments, perinatal mental health utilization rates are strikingly low. There are limited providers and a general lack of awareness of the need for this care. The stigma for assessing and treating PND is high because the perception is that pregnancy is supposed to be a joyous time and with time, PND will pass.
The first step is a timely and accurate assessment of the mother, which should, if possible, include the father and other family support people. The preferred standard for women is the Edinburgh Postnatal Depression Scale (EPDS), a checklist of 10 items (listed below) with a maximum score of 30, and any score over 10 warrants further assessment.5 This scale is used worldwide in obstetric clinics and has been used to identify PND in fathers.
- I have been able to laugh and see the funny side of things.
- I have looked forward with enjoyment to things.
- I have blamed myself unnecessarily when things went wrong.
- I have been anxious or worried for no good reason.
- I have felt scared or panicky for no good reason.
- Things have been getting to me.
- I have been so unhappy that I have had difficulty sleeping.
- I have felt sad or miserable.
- I have been so unhappy that I have been crying.
- The thought of harming myself has occurred to me.
A new ultrabrief tool with only four questions is the Brief Multidimensional Assessment Scale (BMAS), which measures the ability to get things done, emotional support in important relationships, quality of life, and sense of purpose in life. It demonstrates concurrent validity with other measures and discriminates between nonclinical participants and participants from most clinical contexts.6
For those interested in assessing family health, an easy-to-use assessment tool is the 12-item Family Assessment Device (FAD).7
Family therapy interventions
A systematic review and meta-analysis of the current evidence on the usefulness of family therapy interventions in the prevention and treatment of PND identified seven studies.
In these studies, there were statistically significant reductions in depressive symptoms at postintervention in intervention group mothers. Intervention intensity and level of family involvement moderated the impacts of intervention on maternal depression, and there was a trend in improved family functioning in intervention group couples.8
Evidence-based interventions are usually psychoeducational or cognitive-behavioral family therapy models where focused interventions target the following three areas:
- Communication skills related to expectations (including those that pertain to gender roles and the transition to parenthood) and emotional support.
- Conflict management.
- Problem-solving skills related to shared responsibility in infant care and household activities.
Intensive day program for mothers and babies
There is a growing awareness of the effectiveness of specialized mother-baby day hospital programs for women with psychiatric distress during the peripartum period.9
The Women & Infants’ Hospital (WIH) in Providence, R.I., established a mother-baby postpartum depression day program in 2000, adjacent to the obstetrical hospital, the ninth largest obstetrical service in the United States. The day program is integrated with the hospital’s obstetric medicine team and referrals are also accepted from the perinatal practices in the surrounding community. The treatment day includes group, individual, and milieu treatment, as well as consultation with psychiatrists, nutritionists, social workers, lactation specialists and others.
The primary theoretical model utilized by the program is interpersonal psychotherapy (IPT), with essential elements of the program incorporating cognitive behavioral therapy (CBT), and experiential strategies (for instance, mindfulness, breathing, progressive muscle relaxation) to improve self-care and relaxation skills. Patient satisfaction surveys collected from 800 women, (54% identified as White) treated at the program between 2007 and 2012 found that women were highly satisfied with the treatment received, noting that the inclusion of the baby in their treatment is a highly valued aspect of care.
A similar program in Minnesota reported that 328 women who consented to participation in research had significant improvements (P < .001) in self-report scales assessing depression, anxiety, and maternal functioning, improving mental health and parenting functioning.10
Lastly, a recent study out of Brussels, on the benefit of a mother-baby day program analyzed patient data from 2015 and 2020. This clinical population of 92 patients (43% identifying as North African) was comparable to the population of the inpatient mother-baby units in terms of psychosocial fragility except that the parents entering the day program had less severe illnesses, more anxiety disorder, and less postpartum psychosis. In the day program, all the babies improved in terms of symptoms and relationships, except for those with significant developmental difficulties.
The dyadic relationship was measured using “levels of adaptation of the parent–child relationship” scale which has four general levels of adjustment, from well-adjusted to troubled or dangerous relationship. Unlike programs in the United States, this program takes children up to 2.5 years old and the assessment period is up to 8 weeks.11
Prevention of mental illness is best achieved by reducing the known determinants of illness. For PND, the research is clear, so why not start at the earliest possible stage, when we know that change is possible? Pushing health care systems to change is not easy, but as the research accumulates and the positive results grow, our arguments become stronger.
Dr. Heru is a psychiatrist in Aurora, Colo. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Gavin NI et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1071-83. doi: 10.1097/01.AOG.0000183597.31630.db.
2. Rafferty J et al. Incorporating recognition and management of perinatal depression into pediatric practice. Pediatrics. 2019 Jan;143(1):e20183260. doi: 10.1542/peds.2018-3260.
3. Cluxton-Keller F, Bruce ML. Clinical effectiveness of family therapeutic interventions in the prevention and treatment of perinatal depression: A systematic review and meta-analysis. PLoS One. 2018 Jun 14;13(6):e0198730. doi: 10.1371/journal.pone.0198730.
4. Kumar SA et al. Promoting resilience to depression among couples during pregnancy: The protective functions of intimate relationship satisfaction and self-compassion. Family Process. 2022 May;62(1):387-405. doi: 10.1111/famp.12788.
5. Cox JL et al. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987 Jun;150:782-6. doi: 10.1192/bjp.150.6.782.
6. Keitner GI et al. The Brief Multidimensional Assessment Scale (BMAS): A broad measure of patient well-being. Am J Psychother. 2023 Feb 1;76(2):75-81. doi: 10.1176/appi.psychotherapy.20220032.
7. Boterhoven de Haan KL et al. Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 2015 Mar;54(1):116-23. doi: 10.1111/famp.12113.
8. Cluxton-Keller F, Bruce ML. Clinical effectiveness of family therapeutic interventions in the prevention and treatment of perinatal depression: A systematic review and meta-analysis. PLoS One. 2018 Jun 14;13(6):e0198730. doi: 10.1371/journal.pone.0198730.
9. Battle CL, Howard MM. A mother-baby psychiatric day hospital: History, rationale, and why perinatal mental health is important for obstetric medicine. Obstet Med. 2014 Jun;7(2):66-70. doi: 10.1177/1753495X13514402.
10. Kim HG et al. Keeping Parent, Child, and Relationship in Mind: Clinical Effectiveness of a Trauma-informed, Multigenerational, Attachment-Based, Mother-Baby Partial Hospital Program in an Urban Safety Net Hospital. Matern Child Health J. 2021 Nov;25(11):1776-86. doi: 10.1007/s10995-021-03221-4.
11. Moureau A et al. A 5 years’ experience of a parent-baby day unit: impact on baby’s development. Front Psychiatry. 2023 June 15;14. doi: 10.3389/fpsyt.2023.1121894.
Perinatal depression (PND) is the most common obstetric complication in the United States. Even when screening results are positive, mothers often do not receive further evaluation, and even when PND is diagnosed, mothers do not receive evidence-based treatments.
Meta-analytic estimates show that pregnant women suffer from PND at rates from 6.5% to 12.9% across pregnancy to 3-months post partum.1 Women from low-income families and adolescent mothers are at highest risk, where rates are double and triple respectively.
Fathers also suffer from PND, with a prevalence rate from 2% to 25%, increasing to 50% when the mother experiences PND.
The American Academy of Pediatrics issued a Policy Statement (January 2019) about the need to recognize and manage PND. They recommended that pediatric medical homes establish a system to implement the screening of mothers at the 1-, 2-, 4-, and 6-month well-child visits, to use community resources for the treatment and referral of the mother with depression, and to provide support for the maternal-child relationship.2
The American Academy of Pediatrics also recommends advocacy for workforce development for mental health professionals who care for young children and mother-infant dyads, and for promotion of evidence-based interventions focused on healthy attachment and parent-child relationships.
Family research
There is a bidirectional association between family relational stress and PND. Lack of family support is both a predictor and a consequence of perinatal depression. Frequent arguments, conflict because one or both partners did not want the pregnancy, division of labor, poor support following stressful life events, lack of partner availability, and low intimacy are associated with increased perinatal depressive symptoms.
Gender role stress is also included as a risk factor. For example, men may fear performance failure related to work and sex, and women may fear disruption in the couple relationship due to the introduction of a child.
When depressed and nondepressed women at 2 months post delivery were compared, the women with depressive symptoms perceived that their partners did not share similar interests, provided little companionship, expressed disinterest in infant care, did not provide a feeling of connection, did not encourage them to get assistance to cope with difficulties, and expressed disagreement in infant care.3
A high-quality intimate relationship is protective for many illnesses and PND is no exception.4
Assessment
Despite the availability of effective treatments, perinatal mental health utilization rates are strikingly low. There are limited providers and a general lack of awareness of the need for this care. The stigma for assessing and treating PND is high because the perception is that pregnancy is supposed to be a joyous time and with time, PND will pass.
The first step is a timely and accurate assessment of the mother, which should, if possible, include the father and other family support people. The preferred standard for women is the Edinburgh Postnatal Depression Scale (EPDS), a checklist of 10 items (listed below) with a maximum score of 30, and any score over 10 warrants further assessment.5 This scale is used worldwide in obstetric clinics and has been used to identify PND in fathers.
- I have been able to laugh and see the funny side of things.
- I have looked forward with enjoyment to things.
- I have blamed myself unnecessarily when things went wrong.
- I have been anxious or worried for no good reason.
- I have felt scared or panicky for no good reason.
- Things have been getting to me.
- I have been so unhappy that I have had difficulty sleeping.
- I have felt sad or miserable.
- I have been so unhappy that I have been crying.
- The thought of harming myself has occurred to me.
A new ultrabrief tool with only four questions is the Brief Multidimensional Assessment Scale (BMAS), which measures the ability to get things done, emotional support in important relationships, quality of life, and sense of purpose in life. It demonstrates concurrent validity with other measures and discriminates between nonclinical participants and participants from most clinical contexts.6
For those interested in assessing family health, an easy-to-use assessment tool is the 12-item Family Assessment Device (FAD).7
Family therapy interventions
A systematic review and meta-analysis of the current evidence on the usefulness of family therapy interventions in the prevention and treatment of PND identified seven studies.
In these studies, there were statistically significant reductions in depressive symptoms at postintervention in intervention group mothers. Intervention intensity and level of family involvement moderated the impacts of intervention on maternal depression, and there was a trend in improved family functioning in intervention group couples.8
Evidence-based interventions are usually psychoeducational or cognitive-behavioral family therapy models where focused interventions target the following three areas:
- Communication skills related to expectations (including those that pertain to gender roles and the transition to parenthood) and emotional support.
- Conflict management.
- Problem-solving skills related to shared responsibility in infant care and household activities.
Intensive day program for mothers and babies
There is a growing awareness of the effectiveness of specialized mother-baby day hospital programs for women with psychiatric distress during the peripartum period.9
The Women & Infants’ Hospital (WIH) in Providence, R.I., established a mother-baby postpartum depression day program in 2000, adjacent to the obstetrical hospital, the ninth largest obstetrical service in the United States. The day program is integrated with the hospital’s obstetric medicine team and referrals are also accepted from the perinatal practices in the surrounding community. The treatment day includes group, individual, and milieu treatment, as well as consultation with psychiatrists, nutritionists, social workers, lactation specialists and others.
The primary theoretical model utilized by the program is interpersonal psychotherapy (IPT), with essential elements of the program incorporating cognitive behavioral therapy (CBT), and experiential strategies (for instance, mindfulness, breathing, progressive muscle relaxation) to improve self-care and relaxation skills. Patient satisfaction surveys collected from 800 women, (54% identified as White) treated at the program between 2007 and 2012 found that women were highly satisfied with the treatment received, noting that the inclusion of the baby in their treatment is a highly valued aspect of care.
A similar program in Minnesota reported that 328 women who consented to participation in research had significant improvements (P < .001) in self-report scales assessing depression, anxiety, and maternal functioning, improving mental health and parenting functioning.10
Lastly, a recent study out of Brussels, on the benefit of a mother-baby day program analyzed patient data from 2015 and 2020. This clinical population of 92 patients (43% identifying as North African) was comparable to the population of the inpatient mother-baby units in terms of psychosocial fragility except that the parents entering the day program had less severe illnesses, more anxiety disorder, and less postpartum psychosis. In the day program, all the babies improved in terms of symptoms and relationships, except for those with significant developmental difficulties.
The dyadic relationship was measured using “levels of adaptation of the parent–child relationship” scale which has four general levels of adjustment, from well-adjusted to troubled or dangerous relationship. Unlike programs in the United States, this program takes children up to 2.5 years old and the assessment period is up to 8 weeks.11
Prevention of mental illness is best achieved by reducing the known determinants of illness. For PND, the research is clear, so why not start at the earliest possible stage, when we know that change is possible? Pushing health care systems to change is not easy, but as the research accumulates and the positive results grow, our arguments become stronger.
Dr. Heru is a psychiatrist in Aurora, Colo. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Gavin NI et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1071-83. doi: 10.1097/01.AOG.0000183597.31630.db.
2. Rafferty J et al. Incorporating recognition and management of perinatal depression into pediatric practice. Pediatrics. 2019 Jan;143(1):e20183260. doi: 10.1542/peds.2018-3260.
3. Cluxton-Keller F, Bruce ML. Clinical effectiveness of family therapeutic interventions in the prevention and treatment of perinatal depression: A systematic review and meta-analysis. PLoS One. 2018 Jun 14;13(6):e0198730. doi: 10.1371/journal.pone.0198730.
4. Kumar SA et al. Promoting resilience to depression among couples during pregnancy: The protective functions of intimate relationship satisfaction and self-compassion. Family Process. 2022 May;62(1):387-405. doi: 10.1111/famp.12788.
5. Cox JL et al. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987 Jun;150:782-6. doi: 10.1192/bjp.150.6.782.
6. Keitner GI et al. The Brief Multidimensional Assessment Scale (BMAS): A broad measure of patient well-being. Am J Psychother. 2023 Feb 1;76(2):75-81. doi: 10.1176/appi.psychotherapy.20220032.
7. Boterhoven de Haan KL et al. Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 2015 Mar;54(1):116-23. doi: 10.1111/famp.12113.
8. Cluxton-Keller F, Bruce ML. Clinical effectiveness of family therapeutic interventions in the prevention and treatment of perinatal depression: A systematic review and meta-analysis. PLoS One. 2018 Jun 14;13(6):e0198730. doi: 10.1371/journal.pone.0198730.
9. Battle CL, Howard MM. A mother-baby psychiatric day hospital: History, rationale, and why perinatal mental health is important for obstetric medicine. Obstet Med. 2014 Jun;7(2):66-70. doi: 10.1177/1753495X13514402.
10. Kim HG et al. Keeping Parent, Child, and Relationship in Mind: Clinical Effectiveness of a Trauma-informed, Multigenerational, Attachment-Based, Mother-Baby Partial Hospital Program in an Urban Safety Net Hospital. Matern Child Health J. 2021 Nov;25(11):1776-86. doi: 10.1007/s10995-021-03221-4.
11. Moureau A et al. A 5 years’ experience of a parent-baby day unit: impact on baby’s development. Front Psychiatry. 2023 June 15;14. doi: 10.3389/fpsyt.2023.1121894.
Perinatal depression (PND) is the most common obstetric complication in the United States. Even when screening results are positive, mothers often do not receive further evaluation, and even when PND is diagnosed, mothers do not receive evidence-based treatments.
Meta-analytic estimates show that pregnant women suffer from PND at rates from 6.5% to 12.9% across pregnancy to 3-months post partum.1 Women from low-income families and adolescent mothers are at highest risk, where rates are double and triple respectively.
Fathers also suffer from PND, with a prevalence rate from 2% to 25%, increasing to 50% when the mother experiences PND.
The American Academy of Pediatrics issued a Policy Statement (January 2019) about the need to recognize and manage PND. They recommended that pediatric medical homes establish a system to implement the screening of mothers at the 1-, 2-, 4-, and 6-month well-child visits, to use community resources for the treatment and referral of the mother with depression, and to provide support for the maternal-child relationship.2
The American Academy of Pediatrics also recommends advocacy for workforce development for mental health professionals who care for young children and mother-infant dyads, and for promotion of evidence-based interventions focused on healthy attachment and parent-child relationships.
Family research
There is a bidirectional association between family relational stress and PND. Lack of family support is both a predictor and a consequence of perinatal depression. Frequent arguments, conflict because one or both partners did not want the pregnancy, division of labor, poor support following stressful life events, lack of partner availability, and low intimacy are associated with increased perinatal depressive symptoms.
Gender role stress is also included as a risk factor. For example, men may fear performance failure related to work and sex, and women may fear disruption in the couple relationship due to the introduction of a child.
When depressed and nondepressed women at 2 months post delivery were compared, the women with depressive symptoms perceived that their partners did not share similar interests, provided little companionship, expressed disinterest in infant care, did not provide a feeling of connection, did not encourage them to get assistance to cope with difficulties, and expressed disagreement in infant care.3
A high-quality intimate relationship is protective for many illnesses and PND is no exception.4
Assessment
Despite the availability of effective treatments, perinatal mental health utilization rates are strikingly low. There are limited providers and a general lack of awareness of the need for this care. The stigma for assessing and treating PND is high because the perception is that pregnancy is supposed to be a joyous time and with time, PND will pass.
The first step is a timely and accurate assessment of the mother, which should, if possible, include the father and other family support people. The preferred standard for women is the Edinburgh Postnatal Depression Scale (EPDS), a checklist of 10 items (listed below) with a maximum score of 30, and any score over 10 warrants further assessment.5 This scale is used worldwide in obstetric clinics and has been used to identify PND in fathers.
- I have been able to laugh and see the funny side of things.
- I have looked forward with enjoyment to things.
- I have blamed myself unnecessarily when things went wrong.
- I have been anxious or worried for no good reason.
- I have felt scared or panicky for no good reason.
- Things have been getting to me.
- I have been so unhappy that I have had difficulty sleeping.
- I have felt sad or miserable.
- I have been so unhappy that I have been crying.
- The thought of harming myself has occurred to me.
A new ultrabrief tool with only four questions is the Brief Multidimensional Assessment Scale (BMAS), which measures the ability to get things done, emotional support in important relationships, quality of life, and sense of purpose in life. It demonstrates concurrent validity with other measures and discriminates between nonclinical participants and participants from most clinical contexts.6
For those interested in assessing family health, an easy-to-use assessment tool is the 12-item Family Assessment Device (FAD).7
Family therapy interventions
A systematic review and meta-analysis of the current evidence on the usefulness of family therapy interventions in the prevention and treatment of PND identified seven studies.
In these studies, there were statistically significant reductions in depressive symptoms at postintervention in intervention group mothers. Intervention intensity and level of family involvement moderated the impacts of intervention on maternal depression, and there was a trend in improved family functioning in intervention group couples.8
Evidence-based interventions are usually psychoeducational or cognitive-behavioral family therapy models where focused interventions target the following three areas:
- Communication skills related to expectations (including those that pertain to gender roles and the transition to parenthood) and emotional support.
- Conflict management.
- Problem-solving skills related to shared responsibility in infant care and household activities.
Intensive day program for mothers and babies
There is a growing awareness of the effectiveness of specialized mother-baby day hospital programs for women with psychiatric distress during the peripartum period.9
The Women & Infants’ Hospital (WIH) in Providence, R.I., established a mother-baby postpartum depression day program in 2000, adjacent to the obstetrical hospital, the ninth largest obstetrical service in the United States. The day program is integrated with the hospital’s obstetric medicine team and referrals are also accepted from the perinatal practices in the surrounding community. The treatment day includes group, individual, and milieu treatment, as well as consultation with psychiatrists, nutritionists, social workers, lactation specialists and others.
The primary theoretical model utilized by the program is interpersonal psychotherapy (IPT), with essential elements of the program incorporating cognitive behavioral therapy (CBT), and experiential strategies (for instance, mindfulness, breathing, progressive muscle relaxation) to improve self-care and relaxation skills. Patient satisfaction surveys collected from 800 women, (54% identified as White) treated at the program between 2007 and 2012 found that women were highly satisfied with the treatment received, noting that the inclusion of the baby in their treatment is a highly valued aspect of care.
A similar program in Minnesota reported that 328 women who consented to participation in research had significant improvements (P < .001) in self-report scales assessing depression, anxiety, and maternal functioning, improving mental health and parenting functioning.10
Lastly, a recent study out of Brussels, on the benefit of a mother-baby day program analyzed patient data from 2015 and 2020. This clinical population of 92 patients (43% identifying as North African) was comparable to the population of the inpatient mother-baby units in terms of psychosocial fragility except that the parents entering the day program had less severe illnesses, more anxiety disorder, and less postpartum psychosis. In the day program, all the babies improved in terms of symptoms and relationships, except for those with significant developmental difficulties.
The dyadic relationship was measured using “levels of adaptation of the parent–child relationship” scale which has four general levels of adjustment, from well-adjusted to troubled or dangerous relationship. Unlike programs in the United States, this program takes children up to 2.5 years old and the assessment period is up to 8 weeks.11
Prevention of mental illness is best achieved by reducing the known determinants of illness. For PND, the research is clear, so why not start at the earliest possible stage, when we know that change is possible? Pushing health care systems to change is not easy, but as the research accumulates and the positive results grow, our arguments become stronger.
Dr. Heru is a psychiatrist in Aurora, Colo. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Gavin NI et al. Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol. 2005 Nov;106(5 Pt 1):1071-83. doi: 10.1097/01.AOG.0000183597.31630.db.
2. Rafferty J et al. Incorporating recognition and management of perinatal depression into pediatric practice. Pediatrics. 2019 Jan;143(1):e20183260. doi: 10.1542/peds.2018-3260.
3. Cluxton-Keller F, Bruce ML. Clinical effectiveness of family therapeutic interventions in the prevention and treatment of perinatal depression: A systematic review and meta-analysis. PLoS One. 2018 Jun 14;13(6):e0198730. doi: 10.1371/journal.pone.0198730.
4. Kumar SA et al. Promoting resilience to depression among couples during pregnancy: The protective functions of intimate relationship satisfaction and self-compassion. Family Process. 2022 May;62(1):387-405. doi: 10.1111/famp.12788.
5. Cox JL et al. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987 Jun;150:782-6. doi: 10.1192/bjp.150.6.782.
6. Keitner GI et al. The Brief Multidimensional Assessment Scale (BMAS): A broad measure of patient well-being. Am J Psychother. 2023 Feb 1;76(2):75-81. doi: 10.1176/appi.psychotherapy.20220032.
7. Boterhoven de Haan KL et al. Reliability and validity of a short version of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 2015 Mar;54(1):116-23. doi: 10.1111/famp.12113.
8. Cluxton-Keller F, Bruce ML. Clinical effectiveness of family therapeutic interventions in the prevention and treatment of perinatal depression: A systematic review and meta-analysis. PLoS One. 2018 Jun 14;13(6):e0198730. doi: 10.1371/journal.pone.0198730.
9. Battle CL, Howard MM. A mother-baby psychiatric day hospital: History, rationale, and why perinatal mental health is important for obstetric medicine. Obstet Med. 2014 Jun;7(2):66-70. doi: 10.1177/1753495X13514402.
10. Kim HG et al. Keeping Parent, Child, and Relationship in Mind: Clinical Effectiveness of a Trauma-informed, Multigenerational, Attachment-Based, Mother-Baby Partial Hospital Program in an Urban Safety Net Hospital. Matern Child Health J. 2021 Nov;25(11):1776-86. doi: 10.1007/s10995-021-03221-4.
11. Moureau A et al. A 5 years’ experience of a parent-baby day unit: impact on baby’s development. Front Psychiatry. 2023 June 15;14. doi: 10.3389/fpsyt.2023.1121894.
Family violence after COVID: Understanding coercive relationships
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
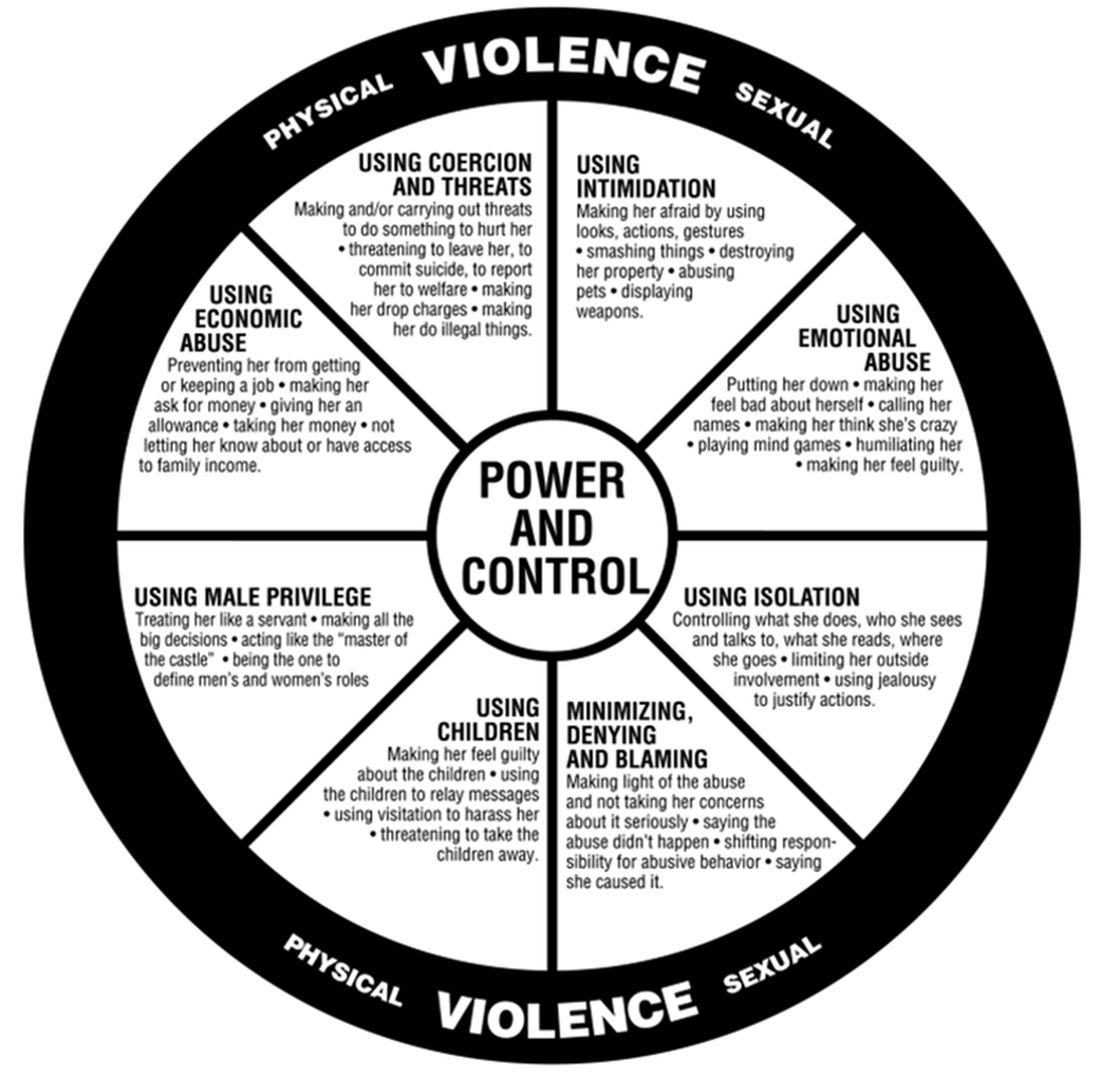
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
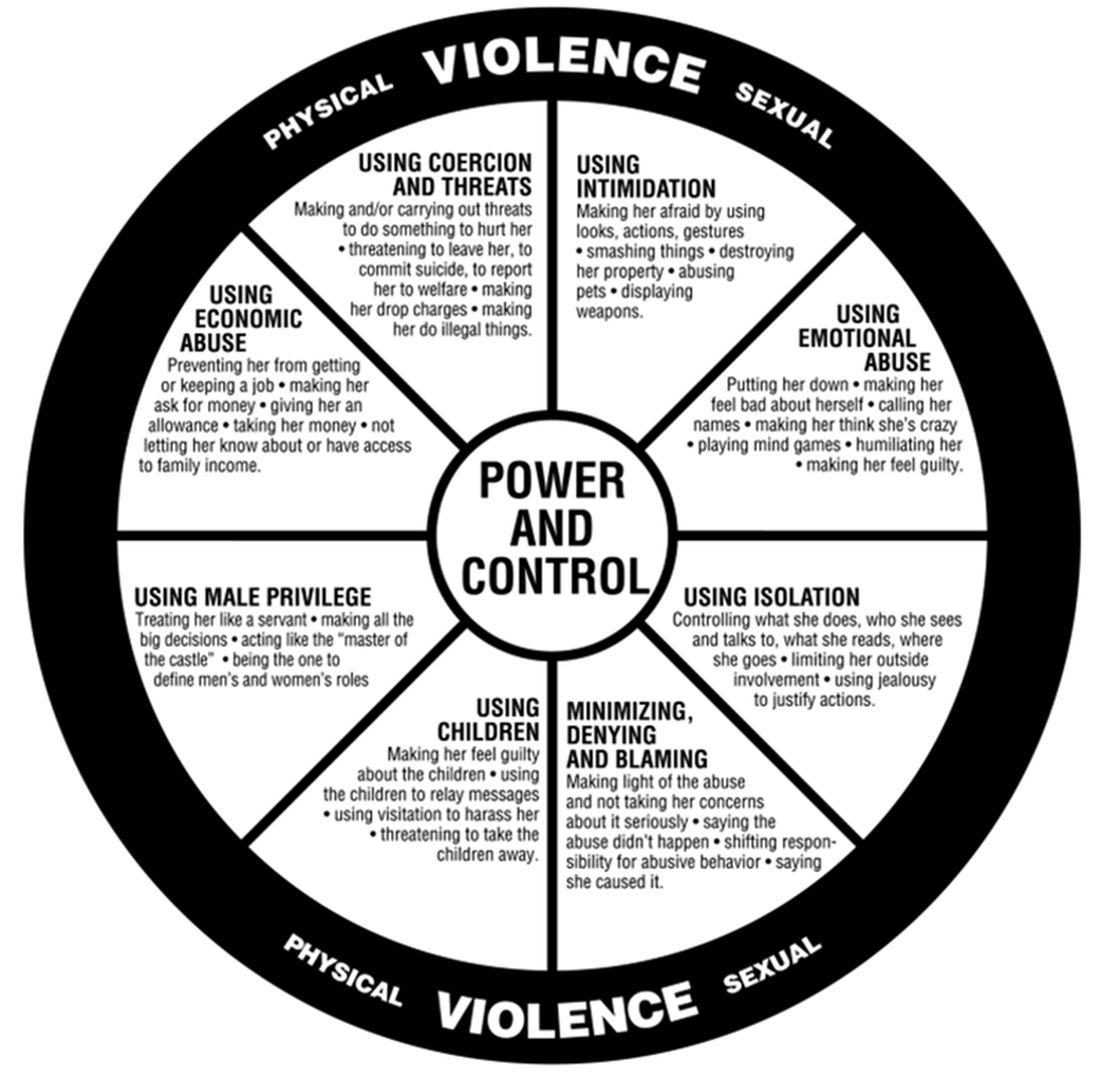
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Despite the ability of some couples to pull together and manage through the COVID-19 pandemic, other couples and families failed to thrive. Increasing divorce rates have been noted nationwide with many disagreements being specifically about COVID.1
A review of over 1 million tweets, between April 12 and July 16, 2020, found an increase in calls to hotlines and increased reports of a variety of types of family violence. There were also more inquiries about social services for family violence, an increased presence from social movements, and more domestic violence-related news.2
The literature addressing family violence uses a variety of terms, so here are some definitions.
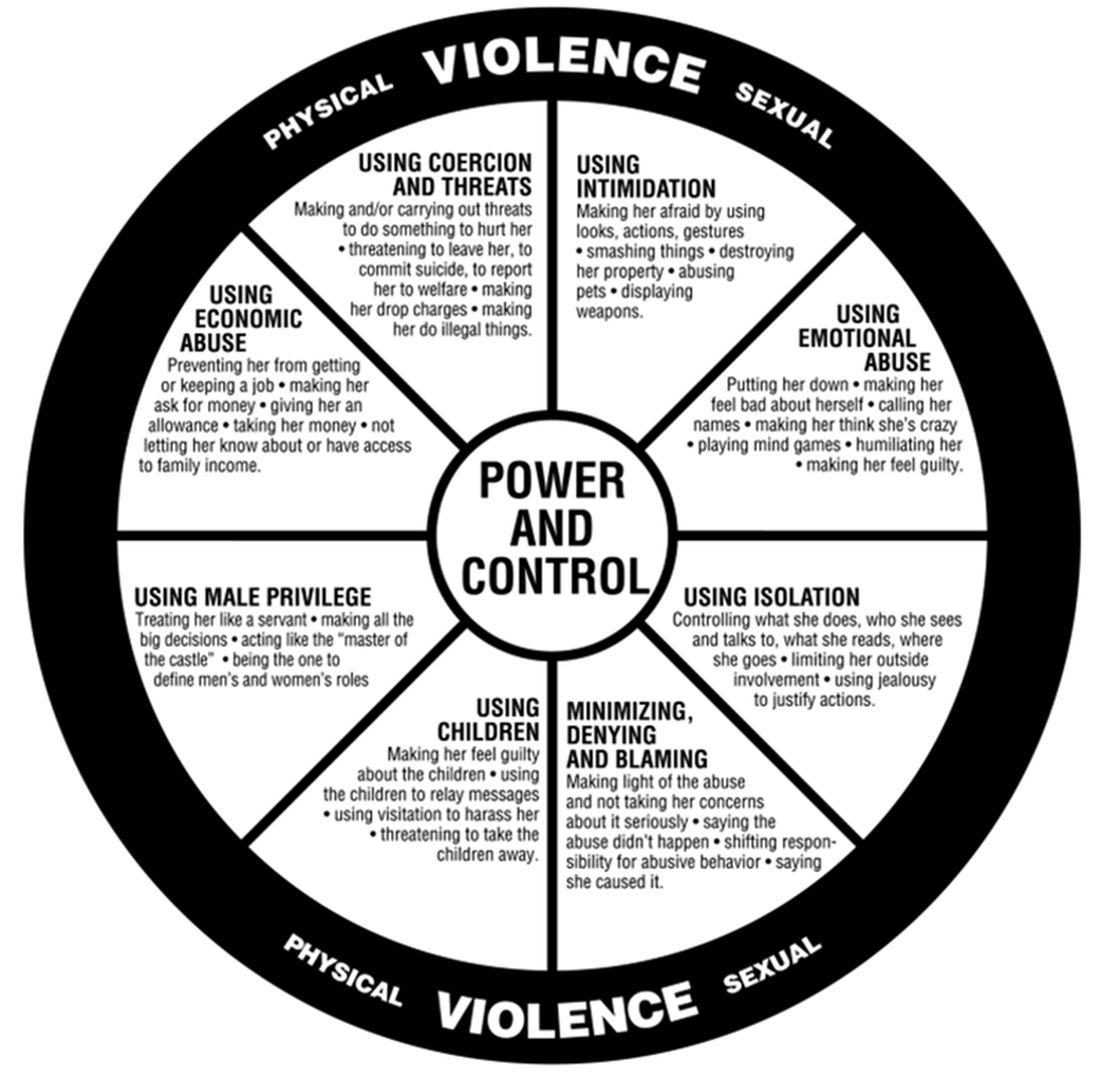
Domestic violence is defined as a pattern of behaviors used to gain or maintain power and control. Broadly speaking, domestic violence includes elder abuse, sibling abuse, child abuse, intimate partner abuse, parent abuse, and can also include people who don’t necessarily live together but who have an intimate relationship. Domestic violence centers use the Power and Control Wheel (see graphic) developed by the Domestic Abuse Intervention Project in Duluth, Minn., to describe how domestic violence occurs.
Intimate partner violence is more specific, referring to violence that happens between people in an ongoing or former intimate or romantic relationship, and is a subcategory of domestic violence.
Coercive control is the use of power for control and compliance. It is a dynamic and systematic process described in the top left corner of the Power and Control Wheel. Overt control occurs with the implication that “if you don’t follow the rules, I’ll kill you.” More subtle control is when obedience is forced through monopolizing resources, dictating preferred choices, microregulating a partner’s behavior, and deprivation of supports needed to exercise independent judgment.
All interpersonal relationships have elements of persuasion and influence; however, the goal of coercive relationships is to maintain power and control. It is a dynamic of the relationship. Coercive control emphasizes the systematic, organized, multifaceted, and patterned nature of this interpersonal dynamic and can be considered to originate in the patriarchal dynamic where men control women.
Most professionals who work in this interdisciplinary area now refer to domestic violence as coercive control. Victimizers target women whom they sense they can control to get their own needs met. They are disinclined to invest in relationships with women who stress their own points of view, who do not readily accept blame when there is a disagreement, and who offer nurturing only when it is reciprocated.
In my office, if I think there are elements of coercion in a relationship, I bring out the Power and Control Wheel and the patient and I go over it. Good education is our responsibility. However, we all have met women who decide to stay in unhealthy relationships.
Assessing people who stay in coercive relationships
Fear
The most important first step is to assess safety. Are they afraid of increased violence if they challenge their partner? Restraining orders or other legal deterrents may not offer solace, as many women are clear that their spouse will come after them, if not tomorrow, then next week, or even next month. They are sure that they will not be safe.
In these cases, I go over safety steps with them so that if they decide to go, they will be prepared. I bring out the “safety box,” which includes the following action steps:
- Memorize important phone numbers of people to call in an emergency.
- If your children are old enough, teach them important phone numbers, including when to dial 911.
- If you can, open your own bank account.
- Stay in touch with friends. Get to know your neighbors. Don’t cut yourself off from people, even if you feel like you want to be alone.
- Rehearse your escape plan until you know it by heart.
- Leave a set of car keys, extra money, a change of clothes and copies of important documents with a trusted friend or relative: your own and your children’s birth certificates, children’s school and medical records, bank books, welfare identification, passport/green card, immigration papers, social security card, lease agreements or mortgage payment books, insurance papers, important addresses, and telephone numbers.
- Keep information about domestic violence in a safe place, where your abuser won’t find it, but where you can get it when you need to review it.
Some women may acknowledge that the risk of physical violence is not the determining factor in their decision to stay and have difficulty explaining why they choose to stay. I suggest that we then consider the following frames that have their origin in the study of the impact of trauma.
Shame
From this lens, abusive events are humiliating experiences, now represented as shame experiences. Humiliation and shame hide hostile feelings that the patient is not able to acknowledge.
“In shame, the self is the failure and others may reject or be critical of this exposed, flawed self.”3 Women will therefore remain attached to an abuser to avoid the exposure of their defective self.
Action steps: Empathic engagement and acknowledgment of shame and humiliation are key. For someone to overcome shame, they must face their sense of their defective self and have strategies to manage these feelings. The development of such strategies is the next step.
Trauma repetition and trauma bonding
Women subjected to domestic violence often respond with incapacitating traumatic syndromes. The concept of “trauma repetition” is suggested as a cause of vulnerability to repeated abuse, and “trauma bonding” is the term for the intense and tenacious bond that can form between abusers and victims.4
Trauma bonding implies that a sense of safety and closeness and secure attachment can only be reached through highly abusive engagement; anything else is experienced as “superficial, cold, or irrelevant.”5 Trauma bonding may have its origins in emotional neglect, according to self reports of 116 women.6Action steps: The literature on trauma is growing and many patients will benefit from good curated sources. Having a good list of books and website on hand is important. Discussion and exploration of the impact of trauma will be needed, and can be provided by someone who is available on a consistent and frequent basis. This work may be time consuming and difficult.
Some asides
1. Some psychiatrists proffer the explanation that these women who stay must be masochistic. The misogynistic concept of masochism still haunts the halls of psychiatry. It is usually offered as a way to dismiss these women’s concerns.
2. One of the obstacles to recognizing chronic mistreatment in relationships is that most abusive men simply “do not seem like abusers.” They have many good qualities, including times of kindness, warmth, and humor, especially in the initial period of a relationship. An abuser’s friends may think the world of him. He may have a successful work life and have no problems with drugs or alcohol. He may simply not fit anyone’s image of a cruel or intimidating person. So, when a woman feels her relationship spinning out of control, it may not occur to her that her partner is an abuser. Even if she does consider her partner to be overly controlling, others may question her perception.
3. Neutrality in family courts is systemic sexism/misogyny. When it comes to domestic violence, family courts tend to split the difference. Stephanie Brandt, MD, notes that The assumption that it is violence alone that matters has formed the basis of much clinical and legal confusion.7 As an analyst, she has gone against the grain of a favored neutrality and become active in the courts, noting the secondary victimization that occurs when a woman enters the legal system.
In summary, psychiatrists must reclaim our expertise in systemic dynamics and point out the role of systemic misogyny. Justices and other court officials need to be educated. Ideally, justice should be based on the equality of men and women in a society free of systemic misogyny. Unfortunately our society has not yet reached this position. In the meanwhile, we must think systemically about interpersonal dynamics. This is our lane. This should not be controversial.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com. Dr. Heru would like to thank Dr. Stephanie Brandt for discussing this topic with her and supporting this work.
References
1. Ellyatt H. Arguing with your partner over Covid? You’re not alone, with the pandemic straining many relationships. 2022 Jan 21. https://www.cnbc.com/2022/01/21/covid-has-put-pressures-and-strains-on-relationships.html
2. Xue J et al. J Med Internet Res. 2020 Nov 6;22(11):e24361. doi: 10.2196/24361.
3. Dorahy MJ. J Trauma Dissociation. 2017 May-Jun;18(3):383-96. doi: 10.1080/15299732.2017.1295422.
4. Dutton DG and Painter SL. Victimology. 1981 Jan;6(1):139-55.
5. Sachs A. J Trauma Dissociation. 2017 May-Jun;18(3):319-39. doi: 10.1080/15299732.2017.1295400.
6. Krüger C and Fletcher L. J Trauma Dissociation. 2017 May-Jun;18(3):356-72. doi: 10.1080/15299732.2017.1295420.
7. Brandt S and Rudden M. Int J Appl Psychoanal Studies. 2020 Sept;17(3):215-31. doi: 10.1002/aps.1671.
Me, my spouse, and COVID
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
Managing family conflict and cohesion
Managing family conflict and cohesion
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
I watched you in the garage, with your wipes and your mask, your gloves and bottles of sprays and potions. I admired your fealty to CNN’s Dr. Sanjay Gupta as he demonstrated the proper technique for disinfecting groceries. I watched sterile protocol being broken and quietly closed the garage door.
I listened to your descriptions of the agility of the virus with each exhalation of breath, and how far the virus could travel with a tailwind and in cold dry air. I listen as closely and with the same intention as I listen to my yoga teacher’s explication of the benefits of attention to the breath.
Relatives and friends came prepared to be entertained outdoors. Even masked, you eschewed the world. Your version of science clashes with my laissez-faire attitude. We blow up as a couple. Then we settle down and learn how to cope with the stress, as a team, together.
The COVID factor
In the first few months of any stressor, family and couple functioning must reorganize to manage well.
During lockdown, social scientists accessed an eager public ready to participate in their studies. With nowhere to go, many people, especially women, completed online COVID surveys. Community-based tools such as the Centers for Disease Control and Prevention’s Social Vulnerability Index identified populations of high social vulnerability (as caused by external stresses on human health, such as unemployment, overcrowding, presence of an individual with caregiving needs, and low educational attainment). It is assumed that such populations will experience more stress and have more difficulty coping and adjusting.
In a study by a team at the University of Miami, social vulnerability was associated with more disrupted family functioning, except when households with children (n = 2,666) were compared to households without children (n = 1,456).1 What allowed these families with children to enjoy better functioning?
Looking more closely at the Miami study, what can we find? It is a large survey study (n = 4,122), disseminated through professional networks and social media via purchased Facebook and Instagram ads. Data were logged in REDCap, and participants had the option of taking the survey in English or Spanish. Most participants were female (93.5%), 55.7% responded in English, and 44.3% in Spanish. There were few differences between the women who had and did not have children, in terms of their age, employment status, and education level. The number of children in the household did not affect the results.
This study used a new tool called the COVID-19 Household Environment Scale. This tool has 25 items measuring individual and household characteristics, and associated COVID-19 stressors. This tool also includes two family functioning measures: conflict and cohesion, asking the respondent to reflect on the change in “conflict” or “togetherness,” as it relates to household experiences and activities, compared with the period before social distancing.
The surprising finding was that even though households with children reported more conflict than before the start of the pandemic, they also reported more cohesion. This syncs with my experience. My niece and nephew found that having their teenage children at home brought them closer as a family, cut down on some of the extracurricular activities they did not support, and generally “slowed the world down.”
However, in a study in Germany, survey respondents (n = 1,042) noted that having children up to 17 years old was associated with decreases in satisfaction with family life, although this was not related to changes in family demands. The study assessed changes over 6 months and underscores the fact that perceptions of family demands and family well-being are independent of each other.2
These findings also resonate with prior research that measured burden and reward in couples. High burden is not associated with low reward; these two constructs are independent of each other.3
What about couples?
It is no surprise that poor relationships begat poor coping. In an online Belgian survey of 1,491 cohabiting couples during the shutdown, both men and women felt significantly more stress than before, because they felt restricted in their relationship.4
However, only women reported significantly more stress during the lockdown than before, because of relationship conflicts, such as feeling neglected by their partner. These feelings had predated lockdown.
In another lockdown online survey of 782 U.S. adults (89.8% White, 84.5% female), cohabitating intimate partners reported that there were higher thoughts of separation if the participants were younger, or if there was higher verbal aggression, higher relationship invalidation, and lower relationship satisfaction. Higher relationship satisfaction was reported when there was lower money stress, higher sexual fulfillment, lower relationship invalidation, and higher perceived fairness of relationship power. High relationship satisfaction was also reported where there were no children in the home.5
It should be noted that none of these relationship variables was measured in the Miami study discussed above, and this study did not measure perceived conflict or perceived cohesion, so we know less about these aspects of the family unit.
What about teens?
The COVID-19 lockdown had a positive effect on the dynamics in some families, according to a naturalistic study of adolescents (n = 155) who completed surveys at two time periods (initial and 8 weeks).6
These adolescents reported a reduction in perceived psychological control by their mothers, and no change in autonomy support. The changes did not vary according to gender or the mother’s employment situation. The decrease in psychological control was greater with higher initial levels of satisfaction with the mother, and lower levels of the teens disobeying their parents.
What about hospital settings?
The worst of the COVID experience was in the hospital. The pain was displayed on the faces of the staff as they labored to figure out how to care for the dying patients who had no contact with their families. Hospitals, out of fear of contamination and viral dissemination, excluded visitors. In those early days of uncertainty, the stress among staff, patients, and family members was high.
In response to family members feeling disconnected from the health care team and the psychological and moral distress of the staff, Nadine J. Kaslow and colleagues revised policies and procedures at Emory University, Atlanta, facilities to reprioritize patient- and family-centered care.7
The guiding principles focus on providing safe yet compassionate and ethical care, balancing community health and the mitigation of viral transmission, while appreciating family members as essential partners in care; fostering communication between patients and their families; and promoting interactions and decision-making among health care providers, patients, and families.
COVID continues to intrude in many of our lives. Many people are mourning family members and friends who died after contracting the disease. Many people choose to ignore their risk and live their lives as before. Many people, like my spouse and me, continue to debate the merits of venturing into public spaces. Personally, COVID has given me time to read many more books than I could ever have imagined and allowed my spouse to explore the delicate nuances of cooking.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alisonheru@gmail.com.
References
1. Chavez JV et al. Assessing the impact of COVID-19 social distancing and social vulnerability on family functioning in an international sample of households with and without children. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 233-48. doi: 10.1037/cfp0000166.
2. Rudolph CW, Zacher H. Family demands and satisfaction with family life during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 249-59. doi: 10.1037/cfp0000170.
3. Heru AM et al. Family functioning in the caregivers of patients with dementia. Int J Geriatr Psychiatry. 2004 Jun;19(6):533-7. doi: 10.1002/gps.1119.
4. Schokkenbroek JM et al. Partners in lockdown: Relationship stress in men and women during the COVID-19 pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 149-57. doi: 10.1037/cfp0000172.
5. Eubanks Fleming CJ, Franzese AT. Should I stay or should I go? Evaluating intimate relationship outcomes during the 2020 pandemic shutdown. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 158-67. doi: 10.1037/cfp0000169.
6. Bacikova-Sleskova M,et al. Did perceived parenting in adolescence change as a result of the COVID-19 lockdown? A natural experiment. Couple Fam Psychol: Res Pract. 2021 Dec;10(4): 271-80. doi: 10.1037/cfp0000167.
7. Kaslow NJ et al. A roadmap for patient- and family-centered care during the pandemic. Couple Fam Psychol: Res Pract. 2021 Sept;10(3): 223-32. doi: 10.1037/cfp0000176.
The mother’s double jeopardy
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
Jamestown, Colo., is a small mountain town several miles up through Lefthand Canyon out of Boulder, in the Rocky Mountains. The canyon roads are steep, winding, and narrow, and peopled by brightly clad cyclists struggling up the hill and flying down faster than the cars. The road through Jamestown is dusty in the summer with brightly colored oil barrels strategically placed in the middle of the single road through town. Slashed across their sides: “SLOW DOWN! Watch out for our feral children!”
Wild child or hothouse child? What is the best choice? Women bear the brunt of this deciding, whether they are working outside of the home, or stay-at-home caregivers, or both. Women know they will be blamed if they get it wrong.
Society has exacted a tall order on women who choose to have children. Patriarchal norms ask (White) women who choose both to work and have children, if they are really a “stay-at-home” mother who must work, or a “working” mother who prefers work over their children. The underlying attitude can be read as: “Are you someone who prioritizes paid work over caregiving, or are you someone who prioritizes caregiving over work?” You may be seen as a bad mother if you prioritize work over the welfare of your child. If you prioritize your child over your work, then you are not a reliable, dedicated worker. The working mother can’t win.
Woman’s central question is what kind of mother should I be? Mothers struggle with this question all their lives; when their child has difficulties, society’s question is what did you do wrong with your child? Mothers internalize the standard of the “good mother” and are aware of each minor transgression that depicts them as the “bad mother.” It is hard to escape the impossible perfectionistic standard of the good mother. But perhaps it has come time to push back on the moral imbalance.
Internalized sexism
As women move out of the home into the workplace, the societal pressures to maintain the status quo bear down on women, trying to keep them in their place.
Social pressures employ subtle “technologies of the self,” so that women – as any oppressed group – learn to internalize these technologies, and monitor themselves.1 This is now widely accepted as internalized sexism, whereby women feel that they are not good enough, do not have the right qualifications, and are “less” than the dominant group (men). This phenomenon is also recognized when racial and ethnic biases are assimilated unconsciously, as internalized racism. Should we also have internalized “momism”?
Women are caught between trying to claim their individualism as well as feeling the responsibility to be the self-denying mother. Everyone has an opinion about the place of women. Conservative activist Phyllis Schlafly considered “women’s lib” to be un-American, citing women in the military and the establishment of federal day care centers as actions of a communist state. A similar ideology helped form the antifeminist organization Concerned Women for America, which self-reports that it is the largest American public policy women’s organization. Formed in opposition to the National Organization for Women, CWA is focused on maintaining the traditional family, as understood by (White) evangelical Christians.
An example similar to CWA is the Council of Biblical Manhood and Womanhood. It was established to help evangelical Christian churches defend themselves against an accommodation of secular feminism and also against evangelical feminism (which pushes for more equality in the church). It promotes complementarianism – the idea that masculinity and femininity are ordained by God and that men and women are created to complement each other.
At the other extreme, the most radical of feminists believe in the need to create a women-only society where women would be free from the patriarchy. Less angry but decidedly weirder are the feminists called “FEMEN” who once staged a protest at the Vatican where topless women feigned intercourse with crucifixes, chanting slogans against the pope and religion.
Most women tread a path between extremes, a path which is difficult and lonely. Without a firm ideology, this path is strewn with doubts and pitfalls. Some career-oriented women who have delayed motherhood, knowing that they will soon be biologically past their peak and possibly also without a partner, wonder if they should become single mothers using sperm donation. For many women, the workplace does not offer much help with maternity leave or childcare. Even when maternity leave is available, there is a still a lack of understanding about what is needed.
“Think of it as caregiver bias. If you just extend maternity leave, what is implied is that you’re still expecting me to be the primary source of care for my child, when in fact my partner wants to share the load and will need support to do so as well,” said Pamela Culpepper, an expert in corporate diversity and inclusion.2
Intensive mothering
When the glamor of the workplace wears off and/or when the misogyny and the harassment become too much, women who have the financial stability may decide to return to the role of the stay-at-home mother. Perhaps, in the home, she can feel fulfilled. Yet, young American urban and suburban mothers now parent under a new name – “intensive mothering.”
Conducting in-depth interviews of 38 women of diverse backgrounds in the United States, Sharon Hays found women describing their 2- to 4-year-old children as innocent and priceless, and believing that they – the mothers – should be primarily responsible for rearing their children, using “child-rearing methods that are child centered, expert guided, emotionally absorbing, labor intensive, and financially expensive.”3 Ms. Hays clarified four beliefs that were common to all the women in the study: mothers are more suitable caregivers than fathers; mothering should be child centered; parenting consists of a set of skills that need to be learned; and parenting is labor-intensive but an emotionally fulfilling activity.
Hays wondered if this type of mothering developed as the last defense against “the impoverishment of social ties, communal obligations and unremunerated commitments.”3 She suggested that women succumbing to social pressures to return to the home is yet another example of how society is set up to benefit men, capitalism, political leaders, and those who try to maintain a “traditional” form of family life.3 Ms. Hays concluded that the practice of intensive mothering is a class-based practice of privileged white women, entangled with capitalism in that the buying of “essential” baby products is equated with good mothering. She found this ideology to be oppressive of all women, regardless of their social class, ethnic background, household composition, and financial situation. Ms. Hays noted that many women experience guilt for not matching up to these ideals.
In “Dead End Feminism,” Elisabeth Badinter asks if the upheaval in the role of women has caused so much uncertainty that it is easier for women to regress to a time when they were in the home and knew themselves as mothers. They ask if this has been reinforced by the movement to embrace all things natural, eschewing the falseness of chemicals and other things that threaten Mother Earth.4
There is no escaping the power of the mother: she will continue to symbolize all that is good and bad as the embodiment of the Mother Archetype. All of this is the background against which you will see the new mother in the family. She will not articulate her dilemma, that is your role as the family psychiatrist.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Martin LH et al (eds.). Technologies of the Self: A Seminar with Michel Foucault. University of Massachusetts Press: Amherst, Mass.: University of Massachusetts Press, 2022.
2. How Pamela Culpepper Is Changing The Narrative Of Women In The Workplace. Huffpost. 2020 Mar 6. https://www.huffpost.com/entry/pamela-culpepper-diversity-inclusion-empowerment_n_5e56b6ffc5b62e9dc7dbc307.
3. Hays S. Cultural Contradictions of Motherhood. Yale University Press: New Haven, Conn.: Yale University Press, 1996.
4. Badinter E. (translated by Borossa J). Dead End Feminism. Malden, Mass.: Polity Press, 2006.
The context of our lives
Neuroscience expands our knowledge of relational and social worlds
Psychiatry may be emerging from the era of psychopharmacology and entering the era of the brain, but these reductionist, jingoistic labels do little justice to the need to acknowledge and incorporate the context of our lives into our theories and treatments. Yet psychiatrists who embrace context have much to celebrate in evolving neuroscience research.
One aptly named article – ’Families that fire together smile together’ – illustrates the fundamental connection between parent and child.1 In the functional MRIs (fMRIs) taken of these parent-child dyads (n = 76), the dyads with similar resting state connectomes also have similar day-to-day emotional states, as reflected in their diary entries. Their empathic states were identified in the multivoxel patterns in the fusiform face area of the brain.2 Another study of fMRIs and parent-child dyads (n = 93) found that the parental functional connectomes (fbc) predicted their children’s externalizing and internalizing problems. The maternal fbcs were correlated with the daughter-mother relationship, and to the daughter’s internalizing problems, suggesting a potential future focus on gendered relationships.3
The implications for psychotherapy are clear: These studies show that empathic connection between parent and child results in a better outcome for the child. Patient and psychotherapist can choose from a range of psychotherapeutic interventions that promote empathy, from providing behavioral tasks that support connection between parent and child to more in-depth family interventions. Family interventions that promote empathy include increasing the family’s understanding of the importance of empathic connection and providing a safe space to help establish empathic connection.
Studying prosocial behavior, Lukas Lengersdorff and colleagues found that fMRIs of male participants (n = 96) reflected stronger activity when they were acting on behalf of the other, rather than when acting for themselves.4 During this prosocial learning fMRI study, there was stronger engagement of the ventromedial prefrontal cortex (PFC) and higher connectivity between the ventromedial PFC and the right temporoparietal junction (rTPJ). Protecting others from harm appears to be associated with neural mechanisms that support self-relevant learning, but with the added recruitment of structures associated with the social brain. This study shows what we already know – that our brains are wired for social context. This research supports psychotherapeutic interventions aimed at creating interpersonal connection, not just at an intimate level, but also at the prosocial level, such as caring and helping others.
When social interactions are coded, the default mode network (DMN) shows increased activity. Participants (n = 11) in another study had heightened medial PFC–rTPJ connectivity, not only during rest that followed the experimental social encoding, but also during rest that followed a subsequent, nonsocial task.5 Engaging portions of the DMN during live social interactions when actively decoding the social environment, and later engaging these regions when relaxing after the social interaction, appears to facilitate social functioning. Our brains are wired to respond to context. This research underscores the positive impact of interventions such as group therapy and support groups, two underutilized modalities.
Neuroscience evaluation of our relationships provides depth to studies that fall under the medical paradigm of the gene/environment interaction. One of the most elegant in psychiatry is the Finnish study of a sample of offspring of mothers with schizophrenia who gave their children up for adoption.6 This sample of index offspring (n = 155) was compared blindly with matched controls (n = 186) of adopted/away offspring of parents without schizophrenia. The genetic effect manifested only as a psychiatric disorder in the presence of a disturbed family environment. We can now extrapolate certain possible mechanisms from the studies mentioned above: That the deficits lie in the activity or lack of activity in the DMN and associated areas, and in the generation of connectomes responsible for empathic connections.
Neuroscience expands our knowledge of our relational and social worlds, but can psychiatry make the case for inclusion of context in our conceptualization of psychiatric distress? From time to time, inroads are made, for example, the Global Assessment of Relational Functioning was incorporated into the DSM-IV-R and the Cultural Formulation Interview is in the DSM-5. However, without a sustained paradigm shift that places the gene/environment paradigm at the core of psychiatry, these efforts will rise and fall as the pioneers in these fields rise and fall.
A major barrier to moving the gene/environment paradigm more centrally in psychiatry is the prominence of individualism as an American ideal. As the neuroscience of context develops, we will be able to argue more robustly for a contextual approach to patient care.
A second barrier is the difficulty of teaching and learning about complexity. It is easy to learn how to use the DSM to make a diagnosis, to understand when and how to prescribe medications, but it is much more difficult to understand how to incorporate the complexity of life and the context within which we live, into our lexicon of psychiatric theories and treatments. As Tanya Luhrmann, PhD, points out in her study of the process of psychiatric training, residents are intimidated by the need to learn the many psychological theories and their practice; learning about medications is much simpler and takes much less time and effort.7
Nevertheless, context is embraced by several psychiatric subspecialties. Family psychiatrists recognize the power of relational dynamics in the family, and their role in shaping the individual. From understanding family communication patterns, to understanding how roles in the family get allocated, family psychiatry has well established tools for assessment and many evidence-based treatments that focus on changing relational dynamics. Social and community psychiatrists emphasize the role of race, poverty, and access, and support the assessment and treatment of the underprivileged. Cultural psychiatrists recognize that each culture has its own way of constructing identities and shaping our experiences, its own conceptualization of illness and specific idioms of distress. Cultural psychiatrists focus on sensitizing the general psychiatrist to these nuances. Child psychiatrists involve parents, and geriatric psychiatrists involve guardians. General psychiatrists understand context when, for example, understanding the role of trauma in the development of an individual, recognizing that its impact is contingent on the context within which the trauma occurs.
Neuroscience clarifies the neural pathways involved in the development of empathic and social behaviors. Our psychological theories and practice must reflect this advancement. We can teach the relevant neuroscience along with basic concepts such as child-parent relationships. We must assess an individual’s degree of fit within their family and community. Apart from asking relational questions, such as who in your world is important to you, we can use well recognized tools to help us bring context to the forefront. An easy tool is the three generational genogram, or an ecomap, which allows each individual to see where they sit in the context of their world.8 Cultural influences, societal, religious, and family influences can be drawn on the genogram, highlighting both formal and hidden family narratives. In addition, we can share how the brain works with our patients; the science of empathy and social behaviors shows us that our need for interpersonal connection is hardwired.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Lee TH et al. Families that fire together smile together: Resting state connectome similarity and daily emotional synchrony in parent-child dyads. Neuroimage. 2017 May 15;152:31-37. doi: 10.1016/j.neuroimage.2017.02.078.
2. Lee TH et al. Love flows downstream: Mothers’ and children’s neural representation similarity in perceiving distress of self and family. Soc Cogn Affect Neurosci. 2017 Dec 1;12(12):1916-27. doi: 10.1093/scan/nsx125.
3. Itahashi T et al. Functional connectomes linking child-parent relationships with psychological problems in adolescence. Neuroimage. 2020 Oct 1;219:117013. doi: 10.1016/j.neuroimage.2020.117013.
4. Lengersdorff LL et al. When implicit prosociality trumps selfishness: The neural valuation system underpins more optimal choices when learning to avoid harm to others than to oneself. J Neurosci. 2020 Sep 16;40(38):7286-99. doi: 10.1523/JNEUROSCI.0842-20.2020.
5. Meyer ML et al. Evidence that default network connectivity during rest consolidates social information. Cereb Cortex. 2019 May 1;29(5):1910-20. doi: 10.1093/cercor/bhy071.
6. Tienari P et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br J Psychiatry Suppl. 1994 Apr;(23):20-6.
7. Luhrmann, TM. Of two minds: The growing disorder in American psychiatry. New York, NY: Alfred A. Knopf, 2000.
8. Libbon R et al. Family skills for the resident toolbox: The 10-min. Genogram, Ecomap, and Prescribing Homework. Acad Psychiatry. 2019 Aug;43(4):435-439. doi: 10.1007/s40596-019-01054-6.
Neuroscience expands our knowledge of relational and social worlds
Neuroscience expands our knowledge of relational and social worlds
Psychiatry may be emerging from the era of psychopharmacology and entering the era of the brain, but these reductionist, jingoistic labels do little justice to the need to acknowledge and incorporate the context of our lives into our theories and treatments. Yet psychiatrists who embrace context have much to celebrate in evolving neuroscience research.
One aptly named article – ’Families that fire together smile together’ – illustrates the fundamental connection between parent and child.1 In the functional MRIs (fMRIs) taken of these parent-child dyads (n = 76), the dyads with similar resting state connectomes also have similar day-to-day emotional states, as reflected in their diary entries. Their empathic states were identified in the multivoxel patterns in the fusiform face area of the brain.2 Another study of fMRIs and parent-child dyads (n = 93) found that the parental functional connectomes (fbc) predicted their children’s externalizing and internalizing problems. The maternal fbcs were correlated with the daughter-mother relationship, and to the daughter’s internalizing problems, suggesting a potential future focus on gendered relationships.3
The implications for psychotherapy are clear: These studies show that empathic connection between parent and child results in a better outcome for the child. Patient and psychotherapist can choose from a range of psychotherapeutic interventions that promote empathy, from providing behavioral tasks that support connection between parent and child to more in-depth family interventions. Family interventions that promote empathy include increasing the family’s understanding of the importance of empathic connection and providing a safe space to help establish empathic connection.
Studying prosocial behavior, Lukas Lengersdorff and colleagues found that fMRIs of male participants (n = 96) reflected stronger activity when they were acting on behalf of the other, rather than when acting for themselves.4 During this prosocial learning fMRI study, there was stronger engagement of the ventromedial prefrontal cortex (PFC) and higher connectivity between the ventromedial PFC and the right temporoparietal junction (rTPJ). Protecting others from harm appears to be associated with neural mechanisms that support self-relevant learning, but with the added recruitment of structures associated with the social brain. This study shows what we already know – that our brains are wired for social context. This research supports psychotherapeutic interventions aimed at creating interpersonal connection, not just at an intimate level, but also at the prosocial level, such as caring and helping others.
When social interactions are coded, the default mode network (DMN) shows increased activity. Participants (n = 11) in another study had heightened medial PFC–rTPJ connectivity, not only during rest that followed the experimental social encoding, but also during rest that followed a subsequent, nonsocial task.5 Engaging portions of the DMN during live social interactions when actively decoding the social environment, and later engaging these regions when relaxing after the social interaction, appears to facilitate social functioning. Our brains are wired to respond to context. This research underscores the positive impact of interventions such as group therapy and support groups, two underutilized modalities.
Neuroscience evaluation of our relationships provides depth to studies that fall under the medical paradigm of the gene/environment interaction. One of the most elegant in psychiatry is the Finnish study of a sample of offspring of mothers with schizophrenia who gave their children up for adoption.6 This sample of index offspring (n = 155) was compared blindly with matched controls (n = 186) of adopted/away offspring of parents without schizophrenia. The genetic effect manifested only as a psychiatric disorder in the presence of a disturbed family environment. We can now extrapolate certain possible mechanisms from the studies mentioned above: That the deficits lie in the activity or lack of activity in the DMN and associated areas, and in the generation of connectomes responsible for empathic connections.
Neuroscience expands our knowledge of our relational and social worlds, but can psychiatry make the case for inclusion of context in our conceptualization of psychiatric distress? From time to time, inroads are made, for example, the Global Assessment of Relational Functioning was incorporated into the DSM-IV-R and the Cultural Formulation Interview is in the DSM-5. However, without a sustained paradigm shift that places the gene/environment paradigm at the core of psychiatry, these efforts will rise and fall as the pioneers in these fields rise and fall.
A major barrier to moving the gene/environment paradigm more centrally in psychiatry is the prominence of individualism as an American ideal. As the neuroscience of context develops, we will be able to argue more robustly for a contextual approach to patient care.
A second barrier is the difficulty of teaching and learning about complexity. It is easy to learn how to use the DSM to make a diagnosis, to understand when and how to prescribe medications, but it is much more difficult to understand how to incorporate the complexity of life and the context within which we live, into our lexicon of psychiatric theories and treatments. As Tanya Luhrmann, PhD, points out in her study of the process of psychiatric training, residents are intimidated by the need to learn the many psychological theories and their practice; learning about medications is much simpler and takes much less time and effort.7
Nevertheless, context is embraced by several psychiatric subspecialties. Family psychiatrists recognize the power of relational dynamics in the family, and their role in shaping the individual. From understanding family communication patterns, to understanding how roles in the family get allocated, family psychiatry has well established tools for assessment and many evidence-based treatments that focus on changing relational dynamics. Social and community psychiatrists emphasize the role of race, poverty, and access, and support the assessment and treatment of the underprivileged. Cultural psychiatrists recognize that each culture has its own way of constructing identities and shaping our experiences, its own conceptualization of illness and specific idioms of distress. Cultural psychiatrists focus on sensitizing the general psychiatrist to these nuances. Child psychiatrists involve parents, and geriatric psychiatrists involve guardians. General psychiatrists understand context when, for example, understanding the role of trauma in the development of an individual, recognizing that its impact is contingent on the context within which the trauma occurs.
Neuroscience clarifies the neural pathways involved in the development of empathic and social behaviors. Our psychological theories and practice must reflect this advancement. We can teach the relevant neuroscience along with basic concepts such as child-parent relationships. We must assess an individual’s degree of fit within their family and community. Apart from asking relational questions, such as who in your world is important to you, we can use well recognized tools to help us bring context to the forefront. An easy tool is the three generational genogram, or an ecomap, which allows each individual to see where they sit in the context of their world.8 Cultural influences, societal, religious, and family influences can be drawn on the genogram, highlighting both formal and hidden family narratives. In addition, we can share how the brain works with our patients; the science of empathy and social behaviors shows us that our need for interpersonal connection is hardwired.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Lee TH et al. Families that fire together smile together: Resting state connectome similarity and daily emotional synchrony in parent-child dyads. Neuroimage. 2017 May 15;152:31-37. doi: 10.1016/j.neuroimage.2017.02.078.
2. Lee TH et al. Love flows downstream: Mothers’ and children’s neural representation similarity in perceiving distress of self and family. Soc Cogn Affect Neurosci. 2017 Dec 1;12(12):1916-27. doi: 10.1093/scan/nsx125.
3. Itahashi T et al. Functional connectomes linking child-parent relationships with psychological problems in adolescence. Neuroimage. 2020 Oct 1;219:117013. doi: 10.1016/j.neuroimage.2020.117013.
4. Lengersdorff LL et al. When implicit prosociality trumps selfishness: The neural valuation system underpins more optimal choices when learning to avoid harm to others than to oneself. J Neurosci. 2020 Sep 16;40(38):7286-99. doi: 10.1523/JNEUROSCI.0842-20.2020.
5. Meyer ML et al. Evidence that default network connectivity during rest consolidates social information. Cereb Cortex. 2019 May 1;29(5):1910-20. doi: 10.1093/cercor/bhy071.
6. Tienari P et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br J Psychiatry Suppl. 1994 Apr;(23):20-6.
7. Luhrmann, TM. Of two minds: The growing disorder in American psychiatry. New York, NY: Alfred A. Knopf, 2000.
8. Libbon R et al. Family skills for the resident toolbox: The 10-min. Genogram, Ecomap, and Prescribing Homework. Acad Psychiatry. 2019 Aug;43(4):435-439. doi: 10.1007/s40596-019-01054-6.
Psychiatry may be emerging from the era of psychopharmacology and entering the era of the brain, but these reductionist, jingoistic labels do little justice to the need to acknowledge and incorporate the context of our lives into our theories and treatments. Yet psychiatrists who embrace context have much to celebrate in evolving neuroscience research.
One aptly named article – ’Families that fire together smile together’ – illustrates the fundamental connection between parent and child.1 In the functional MRIs (fMRIs) taken of these parent-child dyads (n = 76), the dyads with similar resting state connectomes also have similar day-to-day emotional states, as reflected in their diary entries. Their empathic states were identified in the multivoxel patterns in the fusiform face area of the brain.2 Another study of fMRIs and parent-child dyads (n = 93) found that the parental functional connectomes (fbc) predicted their children’s externalizing and internalizing problems. The maternal fbcs were correlated with the daughter-mother relationship, and to the daughter’s internalizing problems, suggesting a potential future focus on gendered relationships.3
The implications for psychotherapy are clear: These studies show that empathic connection between parent and child results in a better outcome for the child. Patient and psychotherapist can choose from a range of psychotherapeutic interventions that promote empathy, from providing behavioral tasks that support connection between parent and child to more in-depth family interventions. Family interventions that promote empathy include increasing the family’s understanding of the importance of empathic connection and providing a safe space to help establish empathic connection.
Studying prosocial behavior, Lukas Lengersdorff and colleagues found that fMRIs of male participants (n = 96) reflected stronger activity when they were acting on behalf of the other, rather than when acting for themselves.4 During this prosocial learning fMRI study, there was stronger engagement of the ventromedial prefrontal cortex (PFC) and higher connectivity between the ventromedial PFC and the right temporoparietal junction (rTPJ). Protecting others from harm appears to be associated with neural mechanisms that support self-relevant learning, but with the added recruitment of structures associated with the social brain. This study shows what we already know – that our brains are wired for social context. This research supports psychotherapeutic interventions aimed at creating interpersonal connection, not just at an intimate level, but also at the prosocial level, such as caring and helping others.
When social interactions are coded, the default mode network (DMN) shows increased activity. Participants (n = 11) in another study had heightened medial PFC–rTPJ connectivity, not only during rest that followed the experimental social encoding, but also during rest that followed a subsequent, nonsocial task.5 Engaging portions of the DMN during live social interactions when actively decoding the social environment, and later engaging these regions when relaxing after the social interaction, appears to facilitate social functioning. Our brains are wired to respond to context. This research underscores the positive impact of interventions such as group therapy and support groups, two underutilized modalities.
Neuroscience evaluation of our relationships provides depth to studies that fall under the medical paradigm of the gene/environment interaction. One of the most elegant in psychiatry is the Finnish study of a sample of offspring of mothers with schizophrenia who gave their children up for adoption.6 This sample of index offspring (n = 155) was compared blindly with matched controls (n = 186) of adopted/away offspring of parents without schizophrenia. The genetic effect manifested only as a psychiatric disorder in the presence of a disturbed family environment. We can now extrapolate certain possible mechanisms from the studies mentioned above: That the deficits lie in the activity or lack of activity in the DMN and associated areas, and in the generation of connectomes responsible for empathic connections.
Neuroscience expands our knowledge of our relational and social worlds, but can psychiatry make the case for inclusion of context in our conceptualization of psychiatric distress? From time to time, inroads are made, for example, the Global Assessment of Relational Functioning was incorporated into the DSM-IV-R and the Cultural Formulation Interview is in the DSM-5. However, without a sustained paradigm shift that places the gene/environment paradigm at the core of psychiatry, these efforts will rise and fall as the pioneers in these fields rise and fall.
A major barrier to moving the gene/environment paradigm more centrally in psychiatry is the prominence of individualism as an American ideal. As the neuroscience of context develops, we will be able to argue more robustly for a contextual approach to patient care.
A second barrier is the difficulty of teaching and learning about complexity. It is easy to learn how to use the DSM to make a diagnosis, to understand when and how to prescribe medications, but it is much more difficult to understand how to incorporate the complexity of life and the context within which we live, into our lexicon of psychiatric theories and treatments. As Tanya Luhrmann, PhD, points out in her study of the process of psychiatric training, residents are intimidated by the need to learn the many psychological theories and their practice; learning about medications is much simpler and takes much less time and effort.7
Nevertheless, context is embraced by several psychiatric subspecialties. Family psychiatrists recognize the power of relational dynamics in the family, and their role in shaping the individual. From understanding family communication patterns, to understanding how roles in the family get allocated, family psychiatry has well established tools for assessment and many evidence-based treatments that focus on changing relational dynamics. Social and community psychiatrists emphasize the role of race, poverty, and access, and support the assessment and treatment of the underprivileged. Cultural psychiatrists recognize that each culture has its own way of constructing identities and shaping our experiences, its own conceptualization of illness and specific idioms of distress. Cultural psychiatrists focus on sensitizing the general psychiatrist to these nuances. Child psychiatrists involve parents, and geriatric psychiatrists involve guardians. General psychiatrists understand context when, for example, understanding the role of trauma in the development of an individual, recognizing that its impact is contingent on the context within which the trauma occurs.
Neuroscience clarifies the neural pathways involved in the development of empathic and social behaviors. Our psychological theories and practice must reflect this advancement. We can teach the relevant neuroscience along with basic concepts such as child-parent relationships. We must assess an individual’s degree of fit within their family and community. Apart from asking relational questions, such as who in your world is important to you, we can use well recognized tools to help us bring context to the forefront. An easy tool is the three generational genogram, or an ecomap, which allows each individual to see where they sit in the context of their world.8 Cultural influences, societal, religious, and family influences can be drawn on the genogram, highlighting both formal and hidden family narratives. In addition, we can share how the brain works with our patients; the science of empathy and social behaviors shows us that our need for interpersonal connection is hardwired.
Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
References
1. Lee TH et al. Families that fire together smile together: Resting state connectome similarity and daily emotional synchrony in parent-child dyads. Neuroimage. 2017 May 15;152:31-37. doi: 10.1016/j.neuroimage.2017.02.078.
2. Lee TH et al. Love flows downstream: Mothers’ and children’s neural representation similarity in perceiving distress of self and family. Soc Cogn Affect Neurosci. 2017 Dec 1;12(12):1916-27. doi: 10.1093/scan/nsx125.
3. Itahashi T et al. Functional connectomes linking child-parent relationships with psychological problems in adolescence. Neuroimage. 2020 Oct 1;219:117013. doi: 10.1016/j.neuroimage.2020.117013.
4. Lengersdorff LL et al. When implicit prosociality trumps selfishness: The neural valuation system underpins more optimal choices when learning to avoid harm to others than to oneself. J Neurosci. 2020 Sep 16;40(38):7286-99. doi: 10.1523/JNEUROSCI.0842-20.2020.
5. Meyer ML et al. Evidence that default network connectivity during rest consolidates social information. Cereb Cortex. 2019 May 1;29(5):1910-20. doi: 10.1093/cercor/bhy071.
6. Tienari P et al. The Finnish adoptive family study of schizophrenia. Implications for family research. Br J Psychiatry Suppl. 1994 Apr;(23):20-6.
7. Luhrmann, TM. Of two minds: The growing disorder in American psychiatry. New York, NY: Alfred A. Knopf, 2000.
8. Libbon R et al. Family skills for the resident toolbox: The 10-min. Genogram, Ecomap, and Prescribing Homework. Acad Psychiatry. 2019 Aug;43(4):435-439. doi: 10.1007/s40596-019-01054-6.
Family-oriented care in adult psychiatric residency
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
The Group for the Advancement of Psychiatry’s Committee on the Family published an updated curriculum in October 2021 on family-oriented care. The first curriculum, published in 2006, was nominated as the American Association of Directors of Psychiatric Residency Training model curriculum for family-oriented care. The updated curriculum, produced by the GAP family committee and guests, is shorter and more focused.
The following is a summary of the introduction and the highlights.
Introduction
Use of family systems–based techniques in the diagnosis and care of patients is a key evidence-based tool for psychiatric disorders. However, it is not a current Accreditation Council for Graduate Medical Education Training training requirement, and it is possible to complete psychiatry residency without exposure to this key framework.
Here, we highlight the importance of considering patients through a “family systems” lens and the incorporation of multiple individuals from an individual patient’s identified system in their care.
Current medicine curricula emphasize patient autonomy, one of the core pillars of ethics. Autonomy is the cornerstone of the everyday practice within medicine of communicating all risks, benefits, and alternatives of a proposed treatment to a patient making decisions about desired paths forward. This prevents paternalistic care in which the doctor “knows best” and makes decisions for the patient. Unfortunately, the emphasis of this pillar has morphed over time into the idea that the individual patient is the only person to whom this information should be provided or from whom information should be obtained.
Extensive research proves conclusively that family support, education, and psychoeducation improve both patient and family functioning in medical and psychiatric illness. as well as overlook the opportunity to use the structure and support system around a patient to strengthen their care and improve treatment outcomes.
The network and family dynamics around a patient can be critical to providing accurate information on medication adherence and symptoms, supporting recovery, and handling emergencies. Markedly improved patient outcomes occur when family members are seen as allies and offered support, assessment, and psychoeducation. In fact, the American Psychiatric Association’s Practice Guidelines on the treatment of schizophrenia (2020), major depressive disorder (2010), and bipolar disorder (2002) include the expectation that patients’ family members will be involved in the assessment and treatment of patients. Yet, training in how to incorporate these practices is often minimal or nonexistent during residency.
A family systems orientation is distinguished by its view of the family as a transactional system. Stressful events and problems of an individual member affect the whole family as a functional unit, with ripple effects for all members and their relationships. In turn, the family response – how the family handles problems – contributes significantly to positive adaptation or to individual and relational dysfunction. Thus, individual problems are assessed and addressed in the context of the family, with attention to socioeconomic and other environmental stressors.
A family systems approach is distinguished less by who is in the room and more by the clinician’s attention to relationship systems in assessment and treatment planning. We need to consider how family members may contribute to – and be affected by – problem situations. Most importantly, regardless of the source of difficulties, we involve key family members who can contribute to needed changes. Interventions are aimed at modifying dysfunctional patterns, tapping family resources, and strengthening both individual and family functioning.
A family systemic lens is useful for working with all types of families, for example: refugee families, thinking through child adoption processes, working with families with specific social disadvantages, etc. Incorporating issues of race, gender, and sexual orientation is important in this work, as is working with larger systems such as schools, workplaces, and health care settings.
As opposed to previous viewpoints that family therapy is the only “family” skill to be taught during residency, the GAP committee proposes that psychiatric residents should be trained in skills of family inclusion, support, and psychoeducation, and that these skills should be taught throughout the residency. Our goal is to have residents be able to consider any case through a family systems lens, to understand how patients’ illnesses and their family systems have bidirectional effects on each other, to perform a basic assessment of family system functioning, and to use this information in diagnostic and treatment planning.
Training goals
Systems-based thinking will enable trainees to:
1. Ally with family members to work with the patient to comply with goals of care (for example, taking medications, complying with lifestyle changes, and maintaining sobriety).
- Teachers focus on engagement, joining with families.
2. Help patients understand the influences of their families in their own lives, such as intergenerational transmission of trauma and resilience.
- Teachers focus on the creation of a genogram, and the location of the individual within their family system.
3. Understand that mental health includes the creation and maintenance of healthy relationships.
- Teachers focus on assessing a willingness to listen to others’ points of view and the cocreation of a shared reality and belief system: a belief that relationships can change over time and how to create new family narratives.
4. Understand the impact of illness on the family unit and the impact of the family unit on illness.
- Teachers focus on the concept of a family system, clarifying the roles within the family, including caregiving responsibilities.
5. Assess the family for strengths and weaknesses.
- Teachers focus on how families maintain a healthy emotional climate, allocate roles, decide on rules, problem-solving abilities, and so on.
6. Gather information from multiple informants in the same room.
- Teachers focus on using communication techniques to elicit, guide, and redirect information from multiple individuals of a system with varying perspectives in the same room. Teachers help students understand that there are multiple realities in families and learn how to maintain multidirectional partiality.
Knowledge, skills, and attitudes across all treatment settings
Knowledge: Beginning level
- Healthy family functioning at the various phases of the family life cycle. Systems concepts are applicable to families, multidisciplinary teams in clinical settings, and medical/government organizations. However, family systems are distinguished by deep attachment bonds, specific generational hierarchy, goals of emotional safety and, for many families, child rearing.
- Systemic thinking, unlike a linear cause and effect model, examines the feedback loops by which multiple persons or groups arrive at a specific way of functioning.
- Understanding boundaries, subsystems, and feedback loops is critical to understanding interpersonal connections. Understand how the family affects and is affected by psychiatric and medical illnesses. Impact of interpersonal stress on biological systems. The role of expressed emotion (EE) in psychiatric illness. EE describes the level of criticism, hostility, and emotional overinvolvement in families. It has been studied extensively across the health care spectrum, and cultural variance is significant.
- The components of family psychoeducation, and its associated research in improving patient and family outcomes.
Knowledge: Advanced level
- Principles of adaptive and maladaptive relational functioning in family life and family organization, communication, problem solving, and emotional regulation. Role of family strengths, resilience in reducing vulnerability.
- Couple and family development over the life cycle.
- Understanding multigenerational patterns.
- How age, gender, class, culture, and spirituality affect family life.
- The variety of family forms (for example, single parent, stepfamilies, same-sex parents).
- Special issues in couples and families, including loss, divorce and remarriage, immigration, illness, secrets, affairs, violence, alcohol and substance abuse, sexuality, including LGBTQi. Relationship of families to larger systems, for example, schools, work, health care systems, government agencies.
Skills
- Family-interviewing skills, especially managing high levels of emotion and making room for multiple points of view.
- Promoting resilience, hope, and strength.
- Basic psychoeducation techniques, which includes providing a therapeutic space for emotional processing, providing information about the illness, skills such as better communication, problem-solving, and relapse drill and support.
- Collaborative treatment planning with family members and other helping professionals. Treatment planning should include all members of the system: patient, family members, and members of the treatment team. Good planning establishes a role for family members, helps define criteria for managing emergencies, looks for areas of strength and resilience and provides clear and realistic goals for treatment.
- Knowledge of, and referral to, local and national resources, both in the community and online.
Attitudes
- Appreciate the multiple points of view in a family.
- Interest in family members as people with their own needs and history.
- Including family members as a resource in recovery.
- Understand caregiver burden and rewards and that stress extends to all family members.
Training techniques
Most learning takes place at the level of patient, supervisor, and resident. It is critical that the resident sees faculty members dealing with patients in observed or shared family sessions, and /or sees videos made by faculty or professionally made videos. Attitudes are best learned by modeling.
Areas of focus can include time management, addressing the fear that family sessions may get out of control, and the influence of the residents’ own life experiences and background including potential generational or cultural differences on their assessment and interactions with patient family dynamics. In skill development, our goal is efficient interviewing, history taking, and support in controlling sessions.
It is difficult to specify which techniques are most useful in didactic sessions as each presenter will have a different skill set for engaging the class. The techniques that work best are the ones most comfortable to the presenter. Any technique that gets emotions involved, such as role play, sculpting, discussing movie clips, bringing in family members to discuss their experiences, or self-exploration, will generate the most powerful learning. If time permits, exploration of the resident’s own family, including a genogram, is an exceptionally helpful technique, especially if accompanied by asking the residents to interview their own families.
Adult didactic curriculum
The curriculum represents basic concepts. We have vignettes by the authors, if needed, but it is best if the class, including the supervisor, uses vignettes from their own experiences. Material for use in class is in references, but the class is urged to draw on their own experiences as this supports strength-based teaching. The following are key topics and concepts for each of the training years.
Basic concepts for PGY1 and PGY2
1. Where are you in the family and individual life cycles? What are your experiences with psychiatric illness in family/friends? Open discussion about how individual and family life cycles interact. Draw genograms of s/o in the class or with the supervisor.
2. Healthy family functioning and family resilience. Recommend asking residents to talk to their parents/elders about their lives and family life cycle when they were your age. Open discussion about what makes a healthy resilient family.
3. How do I connect with the family rather than just one person? How do you learn to hold multiple perspectives? How do I try not to take sides/multidirectional partiality? How do I see each person in a positive way? How do I focus on family strengths, rather than focusing on someone behaving badly (which is really hard because it is overlearned in individual therapy).
4. What are the common factors used across all therapies, both individual and family? When is it best to use an individual relational approach versus a family systemic approach?
5. How do I decide if a family needs support or education or family therapy?
6. Psychoeducation: Research, current use and cultural adaptations.
7. Attachment styles and couples therapy.
8. What is the evidence base behind our work?
System practice for PGY 3 and 4
These seminars follow the basic seminars. The focus is on clarification of what systems thinking means. Systems thinking or relational thinking is to be differentiated from systems-based practice. These lectures require knowledge of systemic practice. If there are no local experts, residency programs can reach out to national experts at the Association of Family Psychiatrists, for help with virtual/remote or in-person teaching.
Here is a list of other topics that should be covered:
- Relational formulation, nested subsystems, boundaries, history of these concepts, contributions to the development of family therapy.
- How to define and identify common systems concepts, such as circular patterns, feedback loops, and triangulation. Teach circular questioning. Framing. This concept is the family systems equivalent of insight. How to intervene to effect communication change and behavior change?
- Working at interfaces: community, legal, government, agencies, and so on, and other treaters, consultation. Include systemic and individual racism.
- Understanding the complexity of intimacy.
- Emergency situations. When to report regarding abuse. Dealing with family trauma.
- Varieties of family therapy; assumptions and major concepts.
*The new curriculum was written by The GAP Committee on the Family: Ellen Berman, MD; John Rolland, MD, MPH; John Sargent, MD; and me, and with guests Chayanin Foongsathaporn, MD; Sarah Nguyen, MD, MPH; Neha Sharma, DO; and Jodi Zik, MD. For the full curriculum, which includes residency milestones, site-specific training goals, references, and case studies, please access the Association of Family Psychiatry’s website: www.familypsychiatrists.org.Dr. Heru is professor of psychiatry at the University of Colorado Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest to disclose. Contact Dr. Heru at alison.heru@ucdenver.edu.
Old wives’ tales, traditional medicine, and science
Sixteen-year-old Ana and is sitting on the bench with her science teacher, Ms. Tehrani, waiting for the bus to take them back to their village after school. Ana wants to hear her science teacher’s opinion about her grandmother.
Do you respect your grandmother?
Why yes, of course, why to do you ask?
So you think my grandmother is wise when she tells me old wife tales?
Like what?
Well, she says not to take my medicine because it will have bad effects and that I should take her remedies instead.
What else does she tell you?
Well, she says that people are born how they are and that they belong to either God or the Devil, not to their parents.
What else?
She thinks I am a fay child; she has always said that about me.
What does that mean?
It means that I have my own ways, fairy ways, and that I should go out in the forest and listen.
Do you?
Yes.
What do you hear?
I hear about my destiny.
What do you hear?
I hear that I must wash in witch hazel. My grandmother taught me how to find it and how to prepare it. She said I should sit in the forest and wait for a sign.
What sign?
I don’t know.
Well, what do you think about your grandmother?
I love her but …
But what?
I think she might be wrong about all of this, you know, science and all that.
But you do it, anyway?
Yes.
Why?
Aren’t we supposed to respect our elders, and aren’t they supposed to be wise?
Ms. Tehrani is in a bind. What to say? She has no ready answer, feeling caught between two beliefs: the unscientific basis of ineffective old wives’ treatments and the purported wisdom of our elders. She knows Ana’s family and that there are women in that family going back generations who are identified as medicine women or women with the special powers of the forest.
Ana wants to study science but she is being groomed as the family wise mother. Ana is caught between the ways of the past and the ways of the future. She sees that to go with the future is to devalue her family tradition. If she chooses to study medicine, can she keep the balance between magical ways and the ways of science?
Ms. Tehrani decides to expose her class to Indigenous and preindustrial cultural practices and what science has to say. She describes how knowledge is passed down through the generations, and how some of this knowledge has now been proved correct by science, such as the use of opium for pain management and how some knowledge has been corrected by science. She asks the class: What myths have been passed down in your family that science has shown to be effective or ineffective? What does science have to say about how we live our lives?
After a baby in the village dies, Ms. Tehrani asks the local health center to think about implementing a teaching course on caring for babies, a course that will discuss tradition and science. She is well aware of the fact that Black mothers tend not to follow the advice of the pediatricians who now recommend that parents put babies to sleep on their backs. Black women trust the advice of their paternal and maternal grandmothers more than the advice of health care providers, research by Deborah Stiffler, PhD, RN, CNM, shows (J Spec Pediatr Nurs. 2018 Apr;23[2]:e12213). While new Black mothers feel that they have limited knowledge and are eager to learn about safe sleep practices, their grandmothers were skeptical – and the grandmothers often won that argument. Black mothers believed that their own mothers knew best, based on their experience raising infants.
In Dr. Stiffler’s study, one grandmother commented: “Girls today need a mother to help them take care of their babies. They don’t know how to do anything. When I was growing up, our moms helped us.”
One new mother said: I “listen more to the elderly people because like the social workers and stuff some of them don’t have kids. They just go by the book … so I feel like I listen more to like my grandparents.”
Integrating traditions
When Ana enters medical school she is faced with the task of integration of traditional practice and Western medicine. Ana looks to the National Center for Complementary and Integrative Health (NCCIH), the U.S. government’s lead agency for scientific research on complementary and integrative health approaches for support in her task. The NCCIH was established in 1998 with the mission of determining the usefulness and safety of complementary and integrative health approaches, and their roles in improving health and health care.
The NCCIH notes that more than 30% of adults use health care approaches that are not part of conventional medical care or that have origins outside of usual Western practice, and 17.7% of American adults had used a dietary supplement other than vitamins and minerals in the past year, most commonly fish oil. This agency notes that large rigorous research studies extend to only a few dietary supplements, with results showing that the products didn’t work for the conditions studied. The work of the NCCIH is mirrored worldwide.
The 2008 Beijing Declaration called on World Health Organization member states and other stakeholders to integrate traditional medicine and complementary alternative medicines into national health care systems. The WHO Congress on Traditional Medicine recognizes that traditional medicine (TM) may be more affordable and accessible than Western medicine, and that it plays an important role in meeting the demands of primary health care in many developing countries. From 70% to 80% of the population in India and Ethiopia depend on TM for primary health care, and 70% of the population in Canada and 80% in Germany are reported to have used TM as complementary and/or alternative medical treatment.
After graduation and residency, Ana returns to her village and helps her science teacher consider how best to shape the intergenerational transmission of knowledge, so that it is both honored by the elders and also shaped by the science of medicine.
Every village, regardless of where it is in the world, has to contend with finding the balance between the traditional medical knowledge that is passed down through the family and the discoveries of science. When it comes to practicing medicine and psychiatry, a respect for family tradition must be weighed against the application of science: this is a long conversation that is well worth its time.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). Dr. Heru has no conflicts of interest. Contact Dr. Heru at alison.heru@cuanschutz.edu.
Sixteen-year-old Ana and is sitting on the bench with her science teacher, Ms. Tehrani, waiting for the bus to take them back to their village after school. Ana wants to hear her science teacher’s opinion about her grandmother.
Do you respect your grandmother?
Why yes, of course, why to do you ask?
So you think my grandmother is wise when she tells me old wife tales?
Like what?
Well, she says not to take my medicine because it will have bad effects and that I should take her remedies instead.
What else does she tell you?
Well, she says that people are born how they are and that they belong to either God or the Devil, not to their parents.
What else?
She thinks I am a fay child; she has always said that about me.
What does that mean?
It means that I have my own ways, fairy ways, and that I should go out in the forest and listen.
Do you?
Yes.
What do you hear?
I hear about my destiny.
What do you hear?
I hear that I must wash in witch hazel. My grandmother taught me how to find it and how to prepare it. She said I should sit in the forest and wait for a sign.
What sign?
I don’t know.
Well, what do you think about your grandmother?
I love her but …
But what?
I think she might be wrong about all of this, you know, science and all that.
But you do it, anyway?
Yes.
Why?
Aren’t we supposed to respect our elders, and aren’t they supposed to be wise?
Ms. Tehrani is in a bind. What to say? She has no ready answer, feeling caught between two beliefs: the unscientific basis of ineffective old wives’ treatments and the purported wisdom of our elders. She knows Ana’s family and that there are women in that family going back generations who are identified as medicine women or women with the special powers of the forest.
Ana wants to study science but she is being groomed as the family wise mother. Ana is caught between the ways of the past and the ways of the future. She sees that to go with the future is to devalue her family tradition. If she chooses to study medicine, can she keep the balance between magical ways and the ways of science?
Ms. Tehrani decides to expose her class to Indigenous and preindustrial cultural practices and what science has to say. She describes how knowledge is passed down through the generations, and how some of this knowledge has now been proved correct by science, such as the use of opium for pain management and how some knowledge has been corrected by science. She asks the class: What myths have been passed down in your family that science has shown to be effective or ineffective? What does science have to say about how we live our lives?
After a baby in the village dies, Ms. Tehrani asks the local health center to think about implementing a teaching course on caring for babies, a course that will discuss tradition and science. She is well aware of the fact that Black mothers tend not to follow the advice of the pediatricians who now recommend that parents put babies to sleep on their backs. Black women trust the advice of their paternal and maternal grandmothers more than the advice of health care providers, research by Deborah Stiffler, PhD, RN, CNM, shows (J Spec Pediatr Nurs. 2018 Apr;23[2]:e12213). While new Black mothers feel that they have limited knowledge and are eager to learn about safe sleep practices, their grandmothers were skeptical – and the grandmothers often won that argument. Black mothers believed that their own mothers knew best, based on their experience raising infants.
In Dr. Stiffler’s study, one grandmother commented: “Girls today need a mother to help them take care of their babies. They don’t know how to do anything. When I was growing up, our moms helped us.”
One new mother said: I “listen more to the elderly people because like the social workers and stuff some of them don’t have kids. They just go by the book … so I feel like I listen more to like my grandparents.”
Integrating traditions
When Ana enters medical school she is faced with the task of integration of traditional practice and Western medicine. Ana looks to the National Center for Complementary and Integrative Health (NCCIH), the U.S. government’s lead agency for scientific research on complementary and integrative health approaches for support in her task. The NCCIH was established in 1998 with the mission of determining the usefulness and safety of complementary and integrative health approaches, and their roles in improving health and health care.
The NCCIH notes that more than 30% of adults use health care approaches that are not part of conventional medical care or that have origins outside of usual Western practice, and 17.7% of American adults had used a dietary supplement other than vitamins and minerals in the past year, most commonly fish oil. This agency notes that large rigorous research studies extend to only a few dietary supplements, with results showing that the products didn’t work for the conditions studied. The work of the NCCIH is mirrored worldwide.
The 2008 Beijing Declaration called on World Health Organization member states and other stakeholders to integrate traditional medicine and complementary alternative medicines into national health care systems. The WHO Congress on Traditional Medicine recognizes that traditional medicine (TM) may be more affordable and accessible than Western medicine, and that it plays an important role in meeting the demands of primary health care in many developing countries. From 70% to 80% of the population in India and Ethiopia depend on TM for primary health care, and 70% of the population in Canada and 80% in Germany are reported to have used TM as complementary and/or alternative medical treatment.
After graduation and residency, Ana returns to her village and helps her science teacher consider how best to shape the intergenerational transmission of knowledge, so that it is both honored by the elders and also shaped by the science of medicine.
Every village, regardless of where it is in the world, has to contend with finding the balance between the traditional medical knowledge that is passed down through the family and the discoveries of science. When it comes to practicing medicine and psychiatry, a respect for family tradition must be weighed against the application of science: this is a long conversation that is well worth its time.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). Dr. Heru has no conflicts of interest. Contact Dr. Heru at alison.heru@cuanschutz.edu.
Sixteen-year-old Ana and is sitting on the bench with her science teacher, Ms. Tehrani, waiting for the bus to take them back to their village after school. Ana wants to hear her science teacher’s opinion about her grandmother.
Do you respect your grandmother?
Why yes, of course, why to do you ask?
So you think my grandmother is wise when she tells me old wife tales?
Like what?
Well, she says not to take my medicine because it will have bad effects and that I should take her remedies instead.
What else does she tell you?
Well, she says that people are born how they are and that they belong to either God or the Devil, not to their parents.
What else?
She thinks I am a fay child; she has always said that about me.
What does that mean?
It means that I have my own ways, fairy ways, and that I should go out in the forest and listen.
Do you?
Yes.
What do you hear?
I hear about my destiny.
What do you hear?
I hear that I must wash in witch hazel. My grandmother taught me how to find it and how to prepare it. She said I should sit in the forest and wait for a sign.
What sign?
I don’t know.
Well, what do you think about your grandmother?
I love her but …
But what?
I think she might be wrong about all of this, you know, science and all that.
But you do it, anyway?
Yes.
Why?
Aren’t we supposed to respect our elders, and aren’t they supposed to be wise?
Ms. Tehrani is in a bind. What to say? She has no ready answer, feeling caught between two beliefs: the unscientific basis of ineffective old wives’ treatments and the purported wisdom of our elders. She knows Ana’s family and that there are women in that family going back generations who are identified as medicine women or women with the special powers of the forest.
Ana wants to study science but she is being groomed as the family wise mother. Ana is caught between the ways of the past and the ways of the future. She sees that to go with the future is to devalue her family tradition. If she chooses to study medicine, can she keep the balance between magical ways and the ways of science?
Ms. Tehrani decides to expose her class to Indigenous and preindustrial cultural practices and what science has to say. She describes how knowledge is passed down through the generations, and how some of this knowledge has now been proved correct by science, such as the use of opium for pain management and how some knowledge has been corrected by science. She asks the class: What myths have been passed down in your family that science has shown to be effective or ineffective? What does science have to say about how we live our lives?
After a baby in the village dies, Ms. Tehrani asks the local health center to think about implementing a teaching course on caring for babies, a course that will discuss tradition and science. She is well aware of the fact that Black mothers tend not to follow the advice of the pediatricians who now recommend that parents put babies to sleep on their backs. Black women trust the advice of their paternal and maternal grandmothers more than the advice of health care providers, research by Deborah Stiffler, PhD, RN, CNM, shows (J Spec Pediatr Nurs. 2018 Apr;23[2]:e12213). While new Black mothers feel that they have limited knowledge and are eager to learn about safe sleep practices, their grandmothers were skeptical – and the grandmothers often won that argument. Black mothers believed that their own mothers knew best, based on their experience raising infants.
In Dr. Stiffler’s study, one grandmother commented: “Girls today need a mother to help them take care of their babies. They don’t know how to do anything. When I was growing up, our moms helped us.”
One new mother said: I “listen more to the elderly people because like the social workers and stuff some of them don’t have kids. They just go by the book … so I feel like I listen more to like my grandparents.”
Integrating traditions
When Ana enters medical school she is faced with the task of integration of traditional practice and Western medicine. Ana looks to the National Center for Complementary and Integrative Health (NCCIH), the U.S. government’s lead agency for scientific research on complementary and integrative health approaches for support in her task. The NCCIH was established in 1998 with the mission of determining the usefulness and safety of complementary and integrative health approaches, and their roles in improving health and health care.
The NCCIH notes that more than 30% of adults use health care approaches that are not part of conventional medical care or that have origins outside of usual Western practice, and 17.7% of American adults had used a dietary supplement other than vitamins and minerals in the past year, most commonly fish oil. This agency notes that large rigorous research studies extend to only a few dietary supplements, with results showing that the products didn’t work for the conditions studied. The work of the NCCIH is mirrored worldwide.
The 2008 Beijing Declaration called on World Health Organization member states and other stakeholders to integrate traditional medicine and complementary alternative medicines into national health care systems. The WHO Congress on Traditional Medicine recognizes that traditional medicine (TM) may be more affordable and accessible than Western medicine, and that it plays an important role in meeting the demands of primary health care in many developing countries. From 70% to 80% of the population in India and Ethiopia depend on TM for primary health care, and 70% of the population in Canada and 80% in Germany are reported to have used TM as complementary and/or alternative medical treatment.
After graduation and residency, Ana returns to her village and helps her science teacher consider how best to shape the intergenerational transmission of knowledge, so that it is both honored by the elders and also shaped by the science of medicine.
Every village, regardless of where it is in the world, has to contend with finding the balance between the traditional medical knowledge that is passed down through the family and the discoveries of science. When it comes to practicing medicine and psychiatry, a respect for family tradition must be weighed against the application of science: this is a long conversation that is well worth its time.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). Dr. Heru has no conflicts of interest. Contact Dr. Heru at alison.heru@cuanschutz.edu.
Grandmothers, the Friendship Bench, and wisdom
Is this model a blueprint for delivering mental health care?
The 4-year-old boy and his grandmother are out for stroll around the neighborhood, walking hand in hand.
“Let’s sit on the bench and talk,” the boy says.
“Okay,” says the grandmother and they climb up onto the high bench and look out across the quiet road to a small garden beyond.
“What would you like to talk about?” his grandmother asks.
“You first,” he says.
“Okay, let’s see ... the grandmother and the grandson are out for a walk and they see a bench to sit on. They climb up and look around. They see the daffodils and the white clouds in the blue sky. The breeze is blowing gently. It is a happy day. Your turn; what would you like to talk about?”
“Nanna and Papa.”
“Do you miss Papa?”
“Yes.”
“It has been a whole year since he died.”
“A long, long time.”
“He loved you very much.”
“Yes,” the boy replies.
“Nanna must miss him very much. She must be lonely without him.”
The boy nods.
They sit on for a while, watching the occasional car and the occasional bird pass by. The boy and the grandmother are quiet and contemplative.
“Okay, let’s go,” he says and jumps down, ready to continue their walk.
The Friendship Bench
It must have been such an experience that gave Dixon Chibanda, MD, MPH, PhD, a psychiatrist from Zimbabwe, his brilliant idea. He trained grandmothers in evidence-based talk therapy and sat them on a bench in the park with his patients.1,2 He founded the Friendship Bench in 2006 in the Harare township of Mbare with 14 grandmothers. There are more than 300 grandmothers sitting on benches, listening, and providing cognitive-behavioral therapy–informed interventions because he could find no therapists in the community and he found that, with a little training, these grandmothers could provide effective culturally sensitive interventions.
Originally, the sessions were conducted in Shona, the predominant native language in Zimbabwe, but since 2017, the sessions are also in English. By 2017, the Friendship Bench had helped more than 30,000 people. The method has been empirically vetted and expanded to countries beyond, including the United States. Dr. Chibanda’s Friendship Bench serves as a blueprint for any community interested in bringing affordable, accessible, and highly effective mental health services to its residents. Dr. Chibanda said: “Imagine if we could create a global network of grandmothers in every major city in the world.”3 Participants in this study reported that the Friendship Bench had a critical role in helping them accept their HIV status, citing the grandmothers’ empathic attitude, their normalization of the reality of living with HIV, and their encouragement of young people to socialize with peers and be free of guilt. Many recipients also described enhanced health and well-being.
Why grandmothers?
Have you heard of the evolutionary importance of grandmothers? The grandmother hypothesis is an adaptationist explanation for the fact that the human female lifespan extends beyond the period of fertility. A third of the average human female life span is post menopause. Does such a long female postreproductive life span have a reason, inquired Mwenza Blell, PhD.5
Peter B. Medawar, PhD,6 and Kristen Hawkes, PhD,7 suggested that grandparents influence their own fitness by their actions toward their grandchildren. International fieldwork has revealed that the situation is less clear than their hypothesis. In industrialized countries, grandmaternal support is often financial or emotional. Two meta-analyses of largely the same group of studies investigating grandmother effects have come up with differing conclusions. Rebecca Sear, PhD, and Ruth Mace, PhD, conclude that grandmothers are “almost universally” beneficial, while acknowledging some variation in the effects of paternal grandmothers.8 Maternal grandparents appear to invest more in their grandchildren than paternal grandparents. Beverly I. Strassmann, PhD, and Wendy M. Garrard, PhD, concluded that, in patrilineal societies, survival of maternal grandparents is associated with survival of grandchildren and suggest this may represent covert matriliny.9
Examining specific time periods, maternal grandmothers may have greatest effect on survival of grandchildren at the time of weaning, a time when increased pathogenic exposure is a threat to survival. Paternal grandmothers may influence the survival of grandchildren during the early period of life (1-12 months) and to influence the condition of their daughters-in-law during pregnancy. The fact that grandmothers share one X chromosome with their sons’ daughters, none with their sons’ sons, and have a 50% chance of sharing an X chromosome with their daughters’ children is suggested to explain the patterns of survival observed in these studies than a simple maternal/paternal division.
In low- and middle-income countries, grandmothers and older women are seen as owners of traditional knowledge, and influence many decisions about childcare, help with domestic work, and emotional support and advice.10 Studies find a significant positive impact on breastfeeding when grandmothers of the infants had their own breastfeeding experience or were positively inclined toward breastfeeding, although one Chinese study found that highly educated grandmothers were associated with decreased exclusive breastfeeding.11 Despite this, most health programs target individual new mothers, without an understanding of the family and who else influences decisions.
Grandchildren and grandparents benefit from intergenerational activities with improved health and well-being of both generations. When older adults are involved in raising children, there is a significant reduction in the incidence of behavioral problems in childhood and adolescence. Grandparents improve grandchild outcomes, when measured by coresidence, caregiving, financial, and other support. The grandchild outcomes include physical health, socioemotional well-being, and cognitive development.12
Are there ‘grandparent genes?’
Flavio Schwarz, PhD, and colleagues think that variants of APOE and CD33 protect against heart disease and Alzheimer’s disease, allowing older people to live longer with better functioning hearts and brains – thus enabling transfer of wisdom from older to younger generations.13 While this logic may be a bit of a stretch, it does lead to a more interesting question: What has wisdom got to do with it?
When I ask psychiatrists what they think about wisdom, they give a variety of answers. Dilip Jeste, MD, a geriatric psychiatrist who studies successful aging, helped develop a measurable vision of wisdom.14 Wisdom is defined as a “multidimensional human trait that includes good social decision-making and pragmatic knowledge of life, prosocial attitudes and behaviors such as empathy and compassion, emotional homeostasis with a tendency to favor positive emotions, reflection and self-understanding, acknowledgment of and coping effectively with uncertainty, and decisiveness.”15 Others suggest that they include spirituality, openness to new experience, and a sense of humor.16 A scale called the San Diego Wisdom scale (SD-WISE) was created, using 524 community-dwelling adults aged 25-104 years. These subjects comprised a high proportion of White adults and individuals with a higher education, thus lacking diversity. Lack of diversity perpetuates generalizations, and like all sociocultural constructs, truth is specific to the population studied. High scores on the SD-WISE are positively correlated with good mental health, self-ratings of successful aging, mastery, resilience, happiness, and satisfaction with life.
Which brings us back to the grandmothers on the bench: Can someone please give them the SD-WISE scale and confirm several hypotheses? I would like to know whether a pragmatic knowledge of life is a recognized grandmotherly quality, suitable for the bench.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
References
1. Chibanda D. Bull World Health Organ. 2018 Jun 196(6):376-7.
2. Cavanaugh R. Lancet Psychiatry. 2017 Nov. doi: 10.1016/S2215-0366(17)30420-0.
3. Nuwer R. “How a bench and a team of grandmothers can tackle depression.” BBC. 2020 May 27.
4. Ouansafi I et al. PLoS One. 2021 Apr 22;16(4):e0250074.
5. Blell M. “Grandmother hypothesis, grandmother effect, and residence patterns.” Int Encyclopedia Anthropol. John Wiley & Sons, 2018.
6. Medawar PB. An Unsolved Problem of Biology. Routledge, 1957.
7. Hawkes K et al. Proc Nat Acad Sci. 1998 Feb 395(3):1336-9.
8. Sear R and Mace R. Evol Hum Behav. 2008;29(1):1-18.
9. Strassmann B and Garrard WM. Hum Nat. 2011 Jul;22(1-2):201-22.
10. Aubel J. BMJ Glob Health. 2021;6(2). doi 10.1136/bmjgh-2020-003808.
11. Negin J et al. BMJ Pregnancy Childbirth. 2016 Apr 7. doi: 10.1186/s12884-016-0880-5.
12. Sadruddin AFA. Soc Sci Med. 2019 Aug;239(4):112476.
13. Schwarz F et al. Proc Nat Acad Sci. 2016 Jan 5;113(1):74-9.
14. Jeste DV et al. Psychol Inquiry. 2020 Jun 22;31(2):134-43.
15. Meeks TW and Jeste DV. Arch Gen Psychiatry. 2009 Apr;66(4):355-65.
16. Bangen KJ et al. Am J Geriatr Psychiatry. 2013 Dec;21(12):1254-66.
Is this model a blueprint for delivering mental health care?
Is this model a blueprint for delivering mental health care?
The 4-year-old boy and his grandmother are out for stroll around the neighborhood, walking hand in hand.
“Let’s sit on the bench and talk,” the boy says.
“Okay,” says the grandmother and they climb up onto the high bench and look out across the quiet road to a small garden beyond.
“What would you like to talk about?” his grandmother asks.
“You first,” he says.
“Okay, let’s see ... the grandmother and the grandson are out for a walk and they see a bench to sit on. They climb up and look around. They see the daffodils and the white clouds in the blue sky. The breeze is blowing gently. It is a happy day. Your turn; what would you like to talk about?”
“Nanna and Papa.”
“Do you miss Papa?”
“Yes.”
“It has been a whole year since he died.”
“A long, long time.”
“He loved you very much.”
“Yes,” the boy replies.
“Nanna must miss him very much. She must be lonely without him.”
The boy nods.
They sit on for a while, watching the occasional car and the occasional bird pass by. The boy and the grandmother are quiet and contemplative.
“Okay, let’s go,” he says and jumps down, ready to continue their walk.
The Friendship Bench
It must have been such an experience that gave Dixon Chibanda, MD, MPH, PhD, a psychiatrist from Zimbabwe, his brilliant idea. He trained grandmothers in evidence-based talk therapy and sat them on a bench in the park with his patients.1,2 He founded the Friendship Bench in 2006 in the Harare township of Mbare with 14 grandmothers. There are more than 300 grandmothers sitting on benches, listening, and providing cognitive-behavioral therapy–informed interventions because he could find no therapists in the community and he found that, with a little training, these grandmothers could provide effective culturally sensitive interventions.
Originally, the sessions were conducted in Shona, the predominant native language in Zimbabwe, but since 2017, the sessions are also in English. By 2017, the Friendship Bench had helped more than 30,000 people. The method has been empirically vetted and expanded to countries beyond, including the United States. Dr. Chibanda’s Friendship Bench serves as a blueprint for any community interested in bringing affordable, accessible, and highly effective mental health services to its residents. Dr. Chibanda said: “Imagine if we could create a global network of grandmothers in every major city in the world.”3 Participants in this study reported that the Friendship Bench had a critical role in helping them accept their HIV status, citing the grandmothers’ empathic attitude, their normalization of the reality of living with HIV, and their encouragement of young people to socialize with peers and be free of guilt. Many recipients also described enhanced health and well-being.
Why grandmothers?
Have you heard of the evolutionary importance of grandmothers? The grandmother hypothesis is an adaptationist explanation for the fact that the human female lifespan extends beyond the period of fertility. A third of the average human female life span is post menopause. Does such a long female postreproductive life span have a reason, inquired Mwenza Blell, PhD.5
Peter B. Medawar, PhD,6 and Kristen Hawkes, PhD,7 suggested that grandparents influence their own fitness by their actions toward their grandchildren. International fieldwork has revealed that the situation is less clear than their hypothesis. In industrialized countries, grandmaternal support is often financial or emotional. Two meta-analyses of largely the same group of studies investigating grandmother effects have come up with differing conclusions. Rebecca Sear, PhD, and Ruth Mace, PhD, conclude that grandmothers are “almost universally” beneficial, while acknowledging some variation in the effects of paternal grandmothers.8 Maternal grandparents appear to invest more in their grandchildren than paternal grandparents. Beverly I. Strassmann, PhD, and Wendy M. Garrard, PhD, concluded that, in patrilineal societies, survival of maternal grandparents is associated with survival of grandchildren and suggest this may represent covert matriliny.9
Examining specific time periods, maternal grandmothers may have greatest effect on survival of grandchildren at the time of weaning, a time when increased pathogenic exposure is a threat to survival. Paternal grandmothers may influence the survival of grandchildren during the early period of life (1-12 months) and to influence the condition of their daughters-in-law during pregnancy. The fact that grandmothers share one X chromosome with their sons’ daughters, none with their sons’ sons, and have a 50% chance of sharing an X chromosome with their daughters’ children is suggested to explain the patterns of survival observed in these studies than a simple maternal/paternal division.
In low- and middle-income countries, grandmothers and older women are seen as owners of traditional knowledge, and influence many decisions about childcare, help with domestic work, and emotional support and advice.10 Studies find a significant positive impact on breastfeeding when grandmothers of the infants had their own breastfeeding experience or were positively inclined toward breastfeeding, although one Chinese study found that highly educated grandmothers were associated with decreased exclusive breastfeeding.11 Despite this, most health programs target individual new mothers, without an understanding of the family and who else influences decisions.
Grandchildren and grandparents benefit from intergenerational activities with improved health and well-being of both generations. When older adults are involved in raising children, there is a significant reduction in the incidence of behavioral problems in childhood and adolescence. Grandparents improve grandchild outcomes, when measured by coresidence, caregiving, financial, and other support. The grandchild outcomes include physical health, socioemotional well-being, and cognitive development.12
Are there ‘grandparent genes?’
Flavio Schwarz, PhD, and colleagues think that variants of APOE and CD33 protect against heart disease and Alzheimer’s disease, allowing older people to live longer with better functioning hearts and brains – thus enabling transfer of wisdom from older to younger generations.13 While this logic may be a bit of a stretch, it does lead to a more interesting question: What has wisdom got to do with it?
When I ask psychiatrists what they think about wisdom, they give a variety of answers. Dilip Jeste, MD, a geriatric psychiatrist who studies successful aging, helped develop a measurable vision of wisdom.14 Wisdom is defined as a “multidimensional human trait that includes good social decision-making and pragmatic knowledge of life, prosocial attitudes and behaviors such as empathy and compassion, emotional homeostasis with a tendency to favor positive emotions, reflection and self-understanding, acknowledgment of and coping effectively with uncertainty, and decisiveness.”15 Others suggest that they include spirituality, openness to new experience, and a sense of humor.16 A scale called the San Diego Wisdom scale (SD-WISE) was created, using 524 community-dwelling adults aged 25-104 years. These subjects comprised a high proportion of White adults and individuals with a higher education, thus lacking diversity. Lack of diversity perpetuates generalizations, and like all sociocultural constructs, truth is specific to the population studied. High scores on the SD-WISE are positively correlated with good mental health, self-ratings of successful aging, mastery, resilience, happiness, and satisfaction with life.
Which brings us back to the grandmothers on the bench: Can someone please give them the SD-WISE scale and confirm several hypotheses? I would like to know whether a pragmatic knowledge of life is a recognized grandmotherly quality, suitable for the bench.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
References
1. Chibanda D. Bull World Health Organ. 2018 Jun 196(6):376-7.
2. Cavanaugh R. Lancet Psychiatry. 2017 Nov. doi: 10.1016/S2215-0366(17)30420-0.
3. Nuwer R. “How a bench and a team of grandmothers can tackle depression.” BBC. 2020 May 27.
4. Ouansafi I et al. PLoS One. 2021 Apr 22;16(4):e0250074.
5. Blell M. “Grandmother hypothesis, grandmother effect, and residence patterns.” Int Encyclopedia Anthropol. John Wiley & Sons, 2018.
6. Medawar PB. An Unsolved Problem of Biology. Routledge, 1957.
7. Hawkes K et al. Proc Nat Acad Sci. 1998 Feb 395(3):1336-9.
8. Sear R and Mace R. Evol Hum Behav. 2008;29(1):1-18.
9. Strassmann B and Garrard WM. Hum Nat. 2011 Jul;22(1-2):201-22.
10. Aubel J. BMJ Glob Health. 2021;6(2). doi 10.1136/bmjgh-2020-003808.
11. Negin J et al. BMJ Pregnancy Childbirth. 2016 Apr 7. doi: 10.1186/s12884-016-0880-5.
12. Sadruddin AFA. Soc Sci Med. 2019 Aug;239(4):112476.
13. Schwarz F et al. Proc Nat Acad Sci. 2016 Jan 5;113(1):74-9.
14. Jeste DV et al. Psychol Inquiry. 2020 Jun 22;31(2):134-43.
15. Meeks TW and Jeste DV. Arch Gen Psychiatry. 2009 Apr;66(4):355-65.
16. Bangen KJ et al. Am J Geriatr Psychiatry. 2013 Dec;21(12):1254-66.
The 4-year-old boy and his grandmother are out for stroll around the neighborhood, walking hand in hand.
“Let’s sit on the bench and talk,” the boy says.
“Okay,” says the grandmother and they climb up onto the high bench and look out across the quiet road to a small garden beyond.
“What would you like to talk about?” his grandmother asks.
“You first,” he says.
“Okay, let’s see ... the grandmother and the grandson are out for a walk and they see a bench to sit on. They climb up and look around. They see the daffodils and the white clouds in the blue sky. The breeze is blowing gently. It is a happy day. Your turn; what would you like to talk about?”
“Nanna and Papa.”
“Do you miss Papa?”
“Yes.”
“It has been a whole year since he died.”
“A long, long time.”
“He loved you very much.”
“Yes,” the boy replies.
“Nanna must miss him very much. She must be lonely without him.”
The boy nods.
They sit on for a while, watching the occasional car and the occasional bird pass by. The boy and the grandmother are quiet and contemplative.
“Okay, let’s go,” he says and jumps down, ready to continue their walk.
The Friendship Bench
It must have been such an experience that gave Dixon Chibanda, MD, MPH, PhD, a psychiatrist from Zimbabwe, his brilliant idea. He trained grandmothers in evidence-based talk therapy and sat them on a bench in the park with his patients.1,2 He founded the Friendship Bench in 2006 in the Harare township of Mbare with 14 grandmothers. There are more than 300 grandmothers sitting on benches, listening, and providing cognitive-behavioral therapy–informed interventions because he could find no therapists in the community and he found that, with a little training, these grandmothers could provide effective culturally sensitive interventions.
Originally, the sessions were conducted in Shona, the predominant native language in Zimbabwe, but since 2017, the sessions are also in English. By 2017, the Friendship Bench had helped more than 30,000 people. The method has been empirically vetted and expanded to countries beyond, including the United States. Dr. Chibanda’s Friendship Bench serves as a blueprint for any community interested in bringing affordable, accessible, and highly effective mental health services to its residents. Dr. Chibanda said: “Imagine if we could create a global network of grandmothers in every major city in the world.”3 Participants in this study reported that the Friendship Bench had a critical role in helping them accept their HIV status, citing the grandmothers’ empathic attitude, their normalization of the reality of living with HIV, and their encouragement of young people to socialize with peers and be free of guilt. Many recipients also described enhanced health and well-being.
Why grandmothers?
Have you heard of the evolutionary importance of grandmothers? The grandmother hypothesis is an adaptationist explanation for the fact that the human female lifespan extends beyond the period of fertility. A third of the average human female life span is post menopause. Does such a long female postreproductive life span have a reason, inquired Mwenza Blell, PhD.5
Peter B. Medawar, PhD,6 and Kristen Hawkes, PhD,7 suggested that grandparents influence their own fitness by their actions toward their grandchildren. International fieldwork has revealed that the situation is less clear than their hypothesis. In industrialized countries, grandmaternal support is often financial or emotional. Two meta-analyses of largely the same group of studies investigating grandmother effects have come up with differing conclusions. Rebecca Sear, PhD, and Ruth Mace, PhD, conclude that grandmothers are “almost universally” beneficial, while acknowledging some variation in the effects of paternal grandmothers.8 Maternal grandparents appear to invest more in their grandchildren than paternal grandparents. Beverly I. Strassmann, PhD, and Wendy M. Garrard, PhD, concluded that, in patrilineal societies, survival of maternal grandparents is associated with survival of grandchildren and suggest this may represent covert matriliny.9
Examining specific time periods, maternal grandmothers may have greatest effect on survival of grandchildren at the time of weaning, a time when increased pathogenic exposure is a threat to survival. Paternal grandmothers may influence the survival of grandchildren during the early period of life (1-12 months) and to influence the condition of their daughters-in-law during pregnancy. The fact that grandmothers share one X chromosome with their sons’ daughters, none with their sons’ sons, and have a 50% chance of sharing an X chromosome with their daughters’ children is suggested to explain the patterns of survival observed in these studies than a simple maternal/paternal division.
In low- and middle-income countries, grandmothers and older women are seen as owners of traditional knowledge, and influence many decisions about childcare, help with domestic work, and emotional support and advice.10 Studies find a significant positive impact on breastfeeding when grandmothers of the infants had their own breastfeeding experience or were positively inclined toward breastfeeding, although one Chinese study found that highly educated grandmothers were associated with decreased exclusive breastfeeding.11 Despite this, most health programs target individual new mothers, without an understanding of the family and who else influences decisions.
Grandchildren and grandparents benefit from intergenerational activities with improved health and well-being of both generations. When older adults are involved in raising children, there is a significant reduction in the incidence of behavioral problems in childhood and adolescence. Grandparents improve grandchild outcomes, when measured by coresidence, caregiving, financial, and other support. The grandchild outcomes include physical health, socioemotional well-being, and cognitive development.12
Are there ‘grandparent genes?’
Flavio Schwarz, PhD, and colleagues think that variants of APOE and CD33 protect against heart disease and Alzheimer’s disease, allowing older people to live longer with better functioning hearts and brains – thus enabling transfer of wisdom from older to younger generations.13 While this logic may be a bit of a stretch, it does lead to a more interesting question: What has wisdom got to do with it?
When I ask psychiatrists what they think about wisdom, they give a variety of answers. Dilip Jeste, MD, a geriatric psychiatrist who studies successful aging, helped develop a measurable vision of wisdom.14 Wisdom is defined as a “multidimensional human trait that includes good social decision-making and pragmatic knowledge of life, prosocial attitudes and behaviors such as empathy and compassion, emotional homeostasis with a tendency to favor positive emotions, reflection and self-understanding, acknowledgment of and coping effectively with uncertainty, and decisiveness.”15 Others suggest that they include spirituality, openness to new experience, and a sense of humor.16 A scale called the San Diego Wisdom scale (SD-WISE) was created, using 524 community-dwelling adults aged 25-104 years. These subjects comprised a high proportion of White adults and individuals with a higher education, thus lacking diversity. Lack of diversity perpetuates generalizations, and like all sociocultural constructs, truth is specific to the population studied. High scores on the SD-WISE are positively correlated with good mental health, self-ratings of successful aging, mastery, resilience, happiness, and satisfaction with life.
Which brings us back to the grandmothers on the bench: Can someone please give them the SD-WISE scale and confirm several hypotheses? I would like to know whether a pragmatic knowledge of life is a recognized grandmotherly quality, suitable for the bench.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest.
References
1. Chibanda D. Bull World Health Organ. 2018 Jun 196(6):376-7.
2. Cavanaugh R. Lancet Psychiatry. 2017 Nov. doi: 10.1016/S2215-0366(17)30420-0.
3. Nuwer R. “How a bench and a team of grandmothers can tackle depression.” BBC. 2020 May 27.
4. Ouansafi I et al. PLoS One. 2021 Apr 22;16(4):e0250074.
5. Blell M. “Grandmother hypothesis, grandmother effect, and residence patterns.” Int Encyclopedia Anthropol. John Wiley & Sons, 2018.
6. Medawar PB. An Unsolved Problem of Biology. Routledge, 1957.
7. Hawkes K et al. Proc Nat Acad Sci. 1998 Feb 395(3):1336-9.
8. Sear R and Mace R. Evol Hum Behav. 2008;29(1):1-18.
9. Strassmann B and Garrard WM. Hum Nat. 2011 Jul;22(1-2):201-22.
10. Aubel J. BMJ Glob Health. 2021;6(2). doi 10.1136/bmjgh-2020-003808.
11. Negin J et al. BMJ Pregnancy Childbirth. 2016 Apr 7. doi: 10.1186/s12884-016-0880-5.
12. Sadruddin AFA. Soc Sci Med. 2019 Aug;239(4):112476.
13. Schwarz F et al. Proc Nat Acad Sci. 2016 Jan 5;113(1):74-9.
14. Jeste DV et al. Psychol Inquiry. 2020 Jun 22;31(2):134-43.
15. Meeks TW and Jeste DV. Arch Gen Psychiatry. 2009 Apr;66(4):355-65.
16. Bangen KJ et al. Am J Geriatr Psychiatry. 2013 Dec;21(12):1254-66.
Family psychoeducation is critical in care of children with disabilities
Dr. Margaret G. Klitzke is a board-certified child and adolescent psychiatrist who has worked across all settings of the Center for Autism and Developmental Disabilities at Bradley Hospital in East Providence, R.I.
I spoke with Dr. Klitzke recently about her work as an outpatient psychiatrist at the center and about the important role of families in the treatment it provides. The center offers highly specialized clinical services for children and adolescents between the ages of 2 and 18 who show signs of serious emotional and behavioral problems in addition to a developmental disability, such as autism, Asperger’s, or intellectual disability.
The center’s model of care emphasizes family involvement. Dr. Klitzke was trained in family interventions by Nathan B. Epstein, MD, and Duane S. Bishop, MD, the originators of the McMaster approach and the problem-centered systems therapy of the family. This training informs much of her work with families.
ALISON M. HERU, MD: Hello, Dr. Klitzke and thank you for agreeing to this interview.
MARGARET G. KLITZKE, DO: My pleasure.
AMH: I admire your dedication to this population of children and adolescents. To me, it seems very hard to work with patients and families where there is significant disability and there is little hope of the patient “getting better.”
MGK: When parents come to us, they have great hopes their children can be helped. They often express understanding and acceptance of the child’s disability, and seek to understand the psychiatric or behavioral issues. These parents are often very dedicated to their children, giving up careers to care for them. But as professionals, we must be sensitive to the role each parent can play and how they can support each other and the family.
AMH: So much of your work focuses on family inclusion and family psychoeducation?
MGK: Yes. An example that stands out is a couple where the mother had become the voice for the family in dealing with professionals, but she was overwhelmed in this role. So, we invited the father in. He explained that medical professionals and school personnel would address their remarks to his wife and that he felt marginalized. We worked with the couple, now always including the father, and he has gone on to become a vocal advocate for children with disabilities. It is inspiring to watch families become advocates – to insist that others see the child’s strengths – not just weaknesses.
AMH: Do you feel that the families ever come to you with too high expectations of what you can do to help their child?
MGK: As a child psychiatrist, one must put oneself in the parents’ shoes. Charlie Zeanah Jr., MD, and others have done wonderful work in attachment. They have identified that parents have fantasies and beliefs about what the child will be like before the child is born. We all have fantasies about our babies before they come to us! For many families, they quickly come to understand that their child is not like other children. This new world of parenting is not what they expected. A mother once gave me a short piece called “Welcome to Holland,” written by a mother whose child has Down syndrome.
AMH: How do you begin to work with these families? There must be such a sense of loss and tragedy in their lives.
MGK: My first goal is to understand what it is like to have a child with developmental disability, not just for the parents but for the siblings, too. I strive to understand what the parents want for their child and how they see themselves as a family. I see us, the health care team, as agents to help the child and the family be the very best they can be.
AMH: How do you deal with parents who are not be on the same page?
MGK: It is important that parents are consistent and are able to work together. Even if they are divorced, I have seen families able to unite around the care of their child with a disability. This is quite an achievement given the high rates of divorce – although most of the families that I have worked with are intact. As in all families, each member has a role in helping the family function well. It means using the strength of each parent to help them become a parenting team.
AMH: What if the parents have unrealistic expectations of their child?
MGK: Yes, there are parents who come to us with unrealistic expectations, such as believing their nonverbal child will talk some day. In such a case, we must be certain that we have exhausted all methods to help this child communicate, and once we have done all we can, then we must accept where that child is; to accept and help the family accept, the child’s weaknesses and acknowledge their strengths. Change what you can and be a support for everything else.
AMH: I find it hard to imagine caring for a severely disabled child. How do these parents do this?
MGK: These are children who are nonverbal, and children who can be very fragile, even medically. What I see are parents who want to connect, who want to find that something inside that child, that special place where there is connection. That place of reciprocity. That is important to us all, helping the family find that place of reciprocal connection.
AMH: What language do you use to discuss this with families?
MGK: I say, “This is the child’s strength and this is the child’s weakness; capitalize on the strengths and let’s shore up their weaknesses.”
AMH: How do you approach the families? Where do you start?
MGK: I meet the family where they are. One cannot with these families or any families stand rigidly 10 feet away, and demand that they change. This never works, and we will be of no help to them. We must understand the family system and how they have arrived at their current place of functioning.
AMH: Can you give an example?
MGK: Yes, for example if a parent is drinking excessively, I help them understand why they are coping that way and see if they are willing to change.
AMH: What keeps you going ?
MGK: I think it comes back to the family work. For me, I believe the families are doing the very best they can. If the family is really impaired in some way, I see it as my job to figure out why that is their pattern of behavior, and I do what I can to help them facilitate change.
AMH: What inspires you about these families?
MGK: These families are able to recognize the strengths and beauty that their children bring them – the strength of these children, their personalities and their wills of steel! They are able to communicate what they need. Siblings, too, make life decisions based on their experiences. They often end up going down the path of caring for such children as professionals.
AMH: Do you have any recommendations for a young child psychiatrist who might be considering working with this population?
MGK: Developmental disabilities in child psychiatry is where medicine, neurology, and child development meet. The advances in genetics and neurology are major gifts to the field. It used to be that I would have to sell the field to medical students and residents. Now they are coming to me saying that they want to work in this area. It is an intellectually rich field in which to work. There is a real change happening. But the place where it becomes really magical is in working with the families.
AMH: What other changes have you seen?
MGK: With the closure of big institutions, it is less of an option for families to walk away. The families now feel that they need to take care of the child.
AMH: What has your career taught you?
MGK: It has taught me patience, to enter every situation without preconceived notions, and that there is something new to learn every day.
References
J Child Adolesc Psychiatry. 1975 Jun 1;14(3):387-421.
Evaluation and Treating Families: The McMaster Approach. Routledge/Taylor & Francis Group, 2005.
Movies to watch
Lorenzo’s Oil, 1992.
My Left Foot, 1989.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest.
Dr. Klitkze is a 1983 graduate of the Texas College of Osteopathic Medicine, and completed her residency and fellowship training at Brown University, Providence, R.I. She is a member of the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the Rhode Island Medical Society, where she serves on the Physicians’ Health Committee. She is actively involved in teaching medical students, residents, and fellows, and has received several teaching awards from the department of psychiatry and human behavior at Brown.
Dr. Margaret G. Klitzke is a board-certified child and adolescent psychiatrist who has worked across all settings of the Center for Autism and Developmental Disabilities at Bradley Hospital in East Providence, R.I.
I spoke with Dr. Klitzke recently about her work as an outpatient psychiatrist at the center and about the important role of families in the treatment it provides. The center offers highly specialized clinical services for children and adolescents between the ages of 2 and 18 who show signs of serious emotional and behavioral problems in addition to a developmental disability, such as autism, Asperger’s, or intellectual disability.
The center’s model of care emphasizes family involvement. Dr. Klitzke was trained in family interventions by Nathan B. Epstein, MD, and Duane S. Bishop, MD, the originators of the McMaster approach and the problem-centered systems therapy of the family. This training informs much of her work with families.
ALISON M. HERU, MD: Hello, Dr. Klitzke and thank you for agreeing to this interview.
MARGARET G. KLITZKE, DO: My pleasure.
AMH: I admire your dedication to this population of children and adolescents. To me, it seems very hard to work with patients and families where there is significant disability and there is little hope of the patient “getting better.”
MGK: When parents come to us, they have great hopes their children can be helped. They often express understanding and acceptance of the child’s disability, and seek to understand the psychiatric or behavioral issues. These parents are often very dedicated to their children, giving up careers to care for them. But as professionals, we must be sensitive to the role each parent can play and how they can support each other and the family.
AMH: So much of your work focuses on family inclusion and family psychoeducation?
MGK: Yes. An example that stands out is a couple where the mother had become the voice for the family in dealing with professionals, but she was overwhelmed in this role. So, we invited the father in. He explained that medical professionals and school personnel would address their remarks to his wife and that he felt marginalized. We worked with the couple, now always including the father, and he has gone on to become a vocal advocate for children with disabilities. It is inspiring to watch families become advocates – to insist that others see the child’s strengths – not just weaknesses.
AMH: Do you feel that the families ever come to you with too high expectations of what you can do to help their child?
MGK: As a child psychiatrist, one must put oneself in the parents’ shoes. Charlie Zeanah Jr., MD, and others have done wonderful work in attachment. They have identified that parents have fantasies and beliefs about what the child will be like before the child is born. We all have fantasies about our babies before they come to us! For many families, they quickly come to understand that their child is not like other children. This new world of parenting is not what they expected. A mother once gave me a short piece called “Welcome to Holland,” written by a mother whose child has Down syndrome.
AMH: How do you begin to work with these families? There must be such a sense of loss and tragedy in their lives.
MGK: My first goal is to understand what it is like to have a child with developmental disability, not just for the parents but for the siblings, too. I strive to understand what the parents want for their child and how they see themselves as a family. I see us, the health care team, as agents to help the child and the family be the very best they can be.
AMH: How do you deal with parents who are not be on the same page?
MGK: It is important that parents are consistent and are able to work together. Even if they are divorced, I have seen families able to unite around the care of their child with a disability. This is quite an achievement given the high rates of divorce – although most of the families that I have worked with are intact. As in all families, each member has a role in helping the family function well. It means using the strength of each parent to help them become a parenting team.
AMH: What if the parents have unrealistic expectations of their child?
MGK: Yes, there are parents who come to us with unrealistic expectations, such as believing their nonverbal child will talk some day. In such a case, we must be certain that we have exhausted all methods to help this child communicate, and once we have done all we can, then we must accept where that child is; to accept and help the family accept, the child’s weaknesses and acknowledge their strengths. Change what you can and be a support for everything else.
AMH: I find it hard to imagine caring for a severely disabled child. How do these parents do this?
MGK: These are children who are nonverbal, and children who can be very fragile, even medically. What I see are parents who want to connect, who want to find that something inside that child, that special place where there is connection. That place of reciprocity. That is important to us all, helping the family find that place of reciprocal connection.
AMH: What language do you use to discuss this with families?
MGK: I say, “This is the child’s strength and this is the child’s weakness; capitalize on the strengths and let’s shore up their weaknesses.”
AMH: How do you approach the families? Where do you start?
MGK: I meet the family where they are. One cannot with these families or any families stand rigidly 10 feet away, and demand that they change. This never works, and we will be of no help to them. We must understand the family system and how they have arrived at their current place of functioning.
AMH: Can you give an example?
MGK: Yes, for example if a parent is drinking excessively, I help them understand why they are coping that way and see if they are willing to change.
AMH: What keeps you going ?
MGK: I think it comes back to the family work. For me, I believe the families are doing the very best they can. If the family is really impaired in some way, I see it as my job to figure out why that is their pattern of behavior, and I do what I can to help them facilitate change.
AMH: What inspires you about these families?
MGK: These families are able to recognize the strengths and beauty that their children bring them – the strength of these children, their personalities and their wills of steel! They are able to communicate what they need. Siblings, too, make life decisions based on their experiences. They often end up going down the path of caring for such children as professionals.
AMH: Do you have any recommendations for a young child psychiatrist who might be considering working with this population?
MGK: Developmental disabilities in child psychiatry is where medicine, neurology, and child development meet. The advances in genetics and neurology are major gifts to the field. It used to be that I would have to sell the field to medical students and residents. Now they are coming to me saying that they want to work in this area. It is an intellectually rich field in which to work. There is a real change happening. But the place where it becomes really magical is in working with the families.
AMH: What other changes have you seen?
MGK: With the closure of big institutions, it is less of an option for families to walk away. The families now feel that they need to take care of the child.
AMH: What has your career taught you?
MGK: It has taught me patience, to enter every situation without preconceived notions, and that there is something new to learn every day.
References
J Child Adolesc Psychiatry. 1975 Jun 1;14(3):387-421.
Evaluation and Treating Families: The McMaster Approach. Routledge/Taylor & Francis Group, 2005.
Movies to watch
Lorenzo’s Oil, 1992.
My Left Foot, 1989.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest.
Dr. Klitkze is a 1983 graduate of the Texas College of Osteopathic Medicine, and completed her residency and fellowship training at Brown University, Providence, R.I. She is a member of the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the Rhode Island Medical Society, where she serves on the Physicians’ Health Committee. She is actively involved in teaching medical students, residents, and fellows, and has received several teaching awards from the department of psychiatry and human behavior at Brown.
Dr. Margaret G. Klitzke is a board-certified child and adolescent psychiatrist who has worked across all settings of the Center for Autism and Developmental Disabilities at Bradley Hospital in East Providence, R.I.
I spoke with Dr. Klitzke recently about her work as an outpatient psychiatrist at the center and about the important role of families in the treatment it provides. The center offers highly specialized clinical services for children and adolescents between the ages of 2 and 18 who show signs of serious emotional and behavioral problems in addition to a developmental disability, such as autism, Asperger’s, or intellectual disability.
The center’s model of care emphasizes family involvement. Dr. Klitzke was trained in family interventions by Nathan B. Epstein, MD, and Duane S. Bishop, MD, the originators of the McMaster approach and the problem-centered systems therapy of the family. This training informs much of her work with families.
ALISON M. HERU, MD: Hello, Dr. Klitzke and thank you for agreeing to this interview.
MARGARET G. KLITZKE, DO: My pleasure.
AMH: I admire your dedication to this population of children and adolescents. To me, it seems very hard to work with patients and families where there is significant disability and there is little hope of the patient “getting better.”
MGK: When parents come to us, they have great hopes their children can be helped. They often express understanding and acceptance of the child’s disability, and seek to understand the psychiatric or behavioral issues. These parents are often very dedicated to their children, giving up careers to care for them. But as professionals, we must be sensitive to the role each parent can play and how they can support each other and the family.
AMH: So much of your work focuses on family inclusion and family psychoeducation?
MGK: Yes. An example that stands out is a couple where the mother had become the voice for the family in dealing with professionals, but she was overwhelmed in this role. So, we invited the father in. He explained that medical professionals and school personnel would address their remarks to his wife and that he felt marginalized. We worked with the couple, now always including the father, and he has gone on to become a vocal advocate for children with disabilities. It is inspiring to watch families become advocates – to insist that others see the child’s strengths – not just weaknesses.
AMH: Do you feel that the families ever come to you with too high expectations of what you can do to help their child?
MGK: As a child psychiatrist, one must put oneself in the parents’ shoes. Charlie Zeanah Jr., MD, and others have done wonderful work in attachment. They have identified that parents have fantasies and beliefs about what the child will be like before the child is born. We all have fantasies about our babies before they come to us! For many families, they quickly come to understand that their child is not like other children. This new world of parenting is not what they expected. A mother once gave me a short piece called “Welcome to Holland,” written by a mother whose child has Down syndrome.
AMH: How do you begin to work with these families? There must be such a sense of loss and tragedy in their lives.
MGK: My first goal is to understand what it is like to have a child with developmental disability, not just for the parents but for the siblings, too. I strive to understand what the parents want for their child and how they see themselves as a family. I see us, the health care team, as agents to help the child and the family be the very best they can be.
AMH: How do you deal with parents who are not be on the same page?
MGK: It is important that parents are consistent and are able to work together. Even if they are divorced, I have seen families able to unite around the care of their child with a disability. This is quite an achievement given the high rates of divorce – although most of the families that I have worked with are intact. As in all families, each member has a role in helping the family function well. It means using the strength of each parent to help them become a parenting team.
AMH: What if the parents have unrealistic expectations of their child?
MGK: Yes, there are parents who come to us with unrealistic expectations, such as believing their nonverbal child will talk some day. In such a case, we must be certain that we have exhausted all methods to help this child communicate, and once we have done all we can, then we must accept where that child is; to accept and help the family accept, the child’s weaknesses and acknowledge their strengths. Change what you can and be a support for everything else.
AMH: I find it hard to imagine caring for a severely disabled child. How do these parents do this?
MGK: These are children who are nonverbal, and children who can be very fragile, even medically. What I see are parents who want to connect, who want to find that something inside that child, that special place where there is connection. That place of reciprocity. That is important to us all, helping the family find that place of reciprocal connection.
AMH: What language do you use to discuss this with families?
MGK: I say, “This is the child’s strength and this is the child’s weakness; capitalize on the strengths and let’s shore up their weaknesses.”
AMH: How do you approach the families? Where do you start?
MGK: I meet the family where they are. One cannot with these families or any families stand rigidly 10 feet away, and demand that they change. This never works, and we will be of no help to them. We must understand the family system and how they have arrived at their current place of functioning.
AMH: Can you give an example?
MGK: Yes, for example if a parent is drinking excessively, I help them understand why they are coping that way and see if they are willing to change.
AMH: What keeps you going ?
MGK: I think it comes back to the family work. For me, I believe the families are doing the very best they can. If the family is really impaired in some way, I see it as my job to figure out why that is their pattern of behavior, and I do what I can to help them facilitate change.
AMH: What inspires you about these families?
MGK: These families are able to recognize the strengths and beauty that their children bring them – the strength of these children, their personalities and their wills of steel! They are able to communicate what they need. Siblings, too, make life decisions based on their experiences. They often end up going down the path of caring for such children as professionals.
AMH: Do you have any recommendations for a young child psychiatrist who might be considering working with this population?
MGK: Developmental disabilities in child psychiatry is where medicine, neurology, and child development meet. The advances in genetics and neurology are major gifts to the field. It used to be that I would have to sell the field to medical students and residents. Now they are coming to me saying that they want to work in this area. It is an intellectually rich field in which to work. There is a real change happening. But the place where it becomes really magical is in working with the families.
AMH: What other changes have you seen?
MGK: With the closure of big institutions, it is less of an option for families to walk away. The families now feel that they need to take care of the child.
AMH: What has your career taught you?
MGK: It has taught me patience, to enter every situation without preconceived notions, and that there is something new to learn every day.
References
J Child Adolesc Psychiatry. 1975 Jun 1;14(3):387-421.
Evaluation and Treating Families: The McMaster Approach. Routledge/Taylor & Francis Group, 2005.
Movies to watch
Lorenzo’s Oil, 1992.
My Left Foot, 1989.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (Routledge, 2013). She has no conflicts of interest.
Dr. Klitkze is a 1983 graduate of the Texas College of Osteopathic Medicine, and completed her residency and fellowship training at Brown University, Providence, R.I. She is a member of the American Psychiatric Association, the American Academy of Child and Adolescent Psychiatry, and the Rhode Island Medical Society, where she serves on the Physicians’ Health Committee. She is actively involved in teaching medical students, residents, and fellows, and has received several teaching awards from the department of psychiatry and human behavior at Brown.
Helping interracial couples navigate racism
Joe and Esi were in the therapist’s office wanting help with their relationship. The therapist had just asked the BIG question: How does race impact your lives?”
Esi began with her story about her ethics class, a story that was at sufficient distance from her life. Depending on her husband’s response, she would move in closer. His somewhat patronizing response made her feel both angry and that he lacked any real understanding.
“Me and a mulatto girl were in ethics class,” said Esi, who grew in Kenya. We had a White professor. He seemed to think I had no education. If you are a woman of color, you are automatically thought to have no education and that you don’t know what you are talking about. He tried to shut me up. When I persisted, I know he thought from the tone of my voice that I was an angry Black woman, even although I am not Black and I am not angry! In this country, if you have any color to your skin, you are called Black and relegated to a certain place: The bottom. I was excited about what he was teaching us, but when everyone looked at me with a certain gaze, like something bad was going to happen, all those White people, just looking, I tightened up inside and sat back down.”
Esi looked down at her folded hands. Her husband, who was White, reached over and reassuringly patted her hands.
“Yes, Esi, they are wrong. They shouldn’t have treated you that way. White people can be insensitive.”
Then, she continued, “Joe, you do the same to me!”
“What do you mean, Esi?” responded Joe, with an innocent and anxious look scanning back and forth between her and the White male therapist.
“Well, Joe, do you really want to hear how I felt last week after we came back from that party at your sister’s house?”
“Yes, Esi.”
“But do you really? Are you sure you want to hear this?”
“Yes, Esi.”
“Remember when we went over, me and the kids sat with the other people of color and you sat with your sister and her side of the family?
“Yes, I remember. What is wrong with that?”
“Well, me and my colored friends got loud and excited, and you shot me a look, like ‘pipe down over there.’ THEN, after we got home, the next day, your sister called you and said that you had better control your wife; she is too loud. Do you remember all that?
“Yes, well you do get loud – especially when you are around your people.”
“So why is it I have to fit in with your relatives and not the other way round? Why do I have to conform to the whiteness in your sister’s world, not the other way round?”
“Well, we were in her house.”
“So if they came to our house and were too quiet, how would you feel if I called them up and said they needed to participate with more enthusiasm?”
“Esi, that’s not fair, and you know it isn’t.”
Esi stops and looks at the therapist.
“So I check myself. It is the same all over, White people imposing their values and beliefs on me, on us. I am not an angry Black woman. I am just frustrated. People, White people, always want an explanation for what they think is my loss of control. You can see when their demeanor changes, they pull back, sit up, back away, fidget, and won’t look you in the eye. All these little tics that show that they are trying to get out of the situation.”
Esi took a breath and saw that her husband and the therapist were listening.
“These signs are ingrained in your brain ... these signs ... I saw it when I first came here to this country. The first time I had a good dose of it ... was in that ethics class in college. You can’t use words that you are accustomed to, ’cause they mean something else here, something bad.”
“Oh, Esi, I am so sorry,” said Joe, looking concerned.
“You may be sorry but you are not willing to stand up for me against your sister and her White values. You want me to conform.”
“What do you want me to do?”
“I want you to call your sister out.”
“But she may not ever speak to me again!”
“OK, don’t then,” and Esi looked down at her hands. She was finished talking. Joe looked at the therapist, waiting for something.
The therapist resisted intervening on the issue. “Keep talking this through,” he instructed them.
Joe could see that Esi had done talking and that it was his move.
“Do you really want me to call my sister out, even if it means that she will not talk to me again?”
“Yes.”
“I don’t know if I can do that.”
The therapist now intervened: “What does that mean to you, Esi, that he doesn’t know if he can do that.”
“It means he doesn’t really love me or value me or even value our mulatto children. What do think our daughter is learning?”
“That’s not true, Esi.”
The therapist, Dr. Swarthmore, watched Esi, who has very a dark, blue-black skin tone, with a flawless complexion and a shapely body. She wears her hair cropped and she looks like that Black model, what’s her name. Joe was short, a little plump with ultra White skin and freckles on his nose. He had been brought up in the Midwest and had had little exposure to Africans before his internship abroad in Kenya. Dr. S. thought he had probably not really thought much about Esi’s dilemma.
Dr. Swarthmore encouraged Esi to talk about her immigration experience.
“Esi, can you talk more about what it is like to be an immigrant from Africa?”
“Well, I just have to check myself so that I can fit in with this White culture. If you want to see how I feel about it, you will have to see an angry Black woman and I have learned not to give you that satisfaction. You will just dismiss me. Please Dr. Swarthmore, can we move on?”
Dr. Swarthmore was caught between his desire to accept her wish to move on and his wish to have her express herself fully. He realized that it was not his desire that mattered; that the couple had to work this out between them if they were going to move forward. So he punted it back to them.
“Esi and Joe, you are both caught in an important dilemma. Esi, you want more respect from your husband and his family. Joe, you do not want to upset your family by confronting them. Is that right? You are both dammed if you do and dammed if you don’t.”
“I agree,” Joe and Esi both said, nodding.
“Do you want to work on this issue?”
They both agreed with equal enthusiasm.
“Ok, can you spend the next 10 minutes to work on this?”
They agreed.
“Ok, let’s start. What skills do you have that can help you resolve this important issue?”
Dr. Swarthmore framed the issue as one to be solved by the couple. The couple discussed that they are usually good at communication and solving problems. This problem is about whether or not Joe is more aligned with his White family than with Esi and their children.
Dr. Swarthmore encouraged them to think about this more deeply and over time; that this is such an important issue that it requires time and deep conversation.
“How do you think you can educate yourselves about the issues at hand?”
Esi’s reading list
1. “Why I’m No Longer Talking to White People About Race” by Reni Eddo-Lodge (London: Bloomsbury, 2018).
2. “Americanah” by Chimamanda Ngozi Adichie (New York: Alfred A. Knopf, 2013).
3. “How to be an Antiracist” by Ibram X. Kendi (New York: Random House, 2019).
Joe suggests that Esi think about what it might mean if his sister and their children were no longer part of their lives. She agrees to do this.
Dr. Swarthmore asks if they can each do their homework before they come back. They agree and thought they could manage that and the book for 2 weeks out.
Dr. Swarthmore decides that he will read one of the books Esi suggested, as he does not know much about racism and White privilege and he wants to learn more. Dr. Swarthmore demonstrates his desire to become more racially sensitive. The following steps can be taken by therapists who want to become more racially sensitive, according to TA Laszloffy and KV Hardy (Fam Process. 2000 Spring;39[1]:35-50):
1. Read and watch movies that address the experience of other cultural groups.
2. Go to and participate in cross-cultural events.
3. Engage in a racial self-exploration process. The following questions can begin the racial identity exploration process:
- How do I define myself racially?
- When did I first become aware of race/skin color in general, and mine in particular?
- What messages did I learn about race/skin color based on that first experience?
- What direct and indirect messages did I receive about race/skin color?
- How did the messages that I received about race/skin color affect how I thought and felt about myself racially?
- What benefits did I gain because of my race/skin color?
- What did I lose because of my race/skin?
- Have I ever dated cross-racially? Why or why not?
- How many friends of a different race do I have?
4. Internal commitment. This means committing to addressing racism in therapeutic encounters.
Lessons learned for psychiatrists
1. Therapeutic space is allocated to discuss the issue.
2. The time is strictly limited to 10 minutes, so the couple won’t feel that their emotions will overwhelm them.
3. The space is to focus on the strengths that they can bring to resolving the issue.
4. Give patients the impression that they can solve this and that it is an important issue.
5. Do not put yourself in the patients’ argument; take neither side.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest. Dr. Heru wrote the article in collaboration with Lynette Ramsingh Barros, artist and social commentator.
Joe and Esi were in the therapist’s office wanting help with their relationship. The therapist had just asked the BIG question: How does race impact your lives?”
Esi began with her story about her ethics class, a story that was at sufficient distance from her life. Depending on her husband’s response, she would move in closer. His somewhat patronizing response made her feel both angry and that he lacked any real understanding.
“Me and a mulatto girl were in ethics class,” said Esi, who grew in Kenya. We had a White professor. He seemed to think I had no education. If you are a woman of color, you are automatically thought to have no education and that you don’t know what you are talking about. He tried to shut me up. When I persisted, I know he thought from the tone of my voice that I was an angry Black woman, even although I am not Black and I am not angry! In this country, if you have any color to your skin, you are called Black and relegated to a certain place: The bottom. I was excited about what he was teaching us, but when everyone looked at me with a certain gaze, like something bad was going to happen, all those White people, just looking, I tightened up inside and sat back down.”
Esi looked down at her folded hands. Her husband, who was White, reached over and reassuringly patted her hands.
“Yes, Esi, they are wrong. They shouldn’t have treated you that way. White people can be insensitive.”
Then, she continued, “Joe, you do the same to me!”
“What do you mean, Esi?” responded Joe, with an innocent and anxious look scanning back and forth between her and the White male therapist.
“Well, Joe, do you really want to hear how I felt last week after we came back from that party at your sister’s house?”
“Yes, Esi.”
“But do you really? Are you sure you want to hear this?”
“Yes, Esi.”
“Remember when we went over, me and the kids sat with the other people of color and you sat with your sister and her side of the family?
“Yes, I remember. What is wrong with that?”
“Well, me and my colored friends got loud and excited, and you shot me a look, like ‘pipe down over there.’ THEN, after we got home, the next day, your sister called you and said that you had better control your wife; she is too loud. Do you remember all that?
“Yes, well you do get loud – especially when you are around your people.”
“So why is it I have to fit in with your relatives and not the other way round? Why do I have to conform to the whiteness in your sister’s world, not the other way round?”
“Well, we were in her house.”
“So if they came to our house and were too quiet, how would you feel if I called them up and said they needed to participate with more enthusiasm?”
“Esi, that’s not fair, and you know it isn’t.”
Esi stops and looks at the therapist.
“So I check myself. It is the same all over, White people imposing their values and beliefs on me, on us. I am not an angry Black woman. I am just frustrated. People, White people, always want an explanation for what they think is my loss of control. You can see when their demeanor changes, they pull back, sit up, back away, fidget, and won’t look you in the eye. All these little tics that show that they are trying to get out of the situation.”
Esi took a breath and saw that her husband and the therapist were listening.
“These signs are ingrained in your brain ... these signs ... I saw it when I first came here to this country. The first time I had a good dose of it ... was in that ethics class in college. You can’t use words that you are accustomed to, ’cause they mean something else here, something bad.”
“Oh, Esi, I am so sorry,” said Joe, looking concerned.
“You may be sorry but you are not willing to stand up for me against your sister and her White values. You want me to conform.”
“What do you want me to do?”
“I want you to call your sister out.”
“But she may not ever speak to me again!”
“OK, don’t then,” and Esi looked down at her hands. She was finished talking. Joe looked at the therapist, waiting for something.
The therapist resisted intervening on the issue. “Keep talking this through,” he instructed them.
Joe could see that Esi had done talking and that it was his move.
“Do you really want me to call my sister out, even if it means that she will not talk to me again?”
“Yes.”
“I don’t know if I can do that.”
The therapist now intervened: “What does that mean to you, Esi, that he doesn’t know if he can do that.”
“It means he doesn’t really love me or value me or even value our mulatto children. What do think our daughter is learning?”
“That’s not true, Esi.”
The therapist, Dr. Swarthmore, watched Esi, who has very a dark, blue-black skin tone, with a flawless complexion and a shapely body. She wears her hair cropped and she looks like that Black model, what’s her name. Joe was short, a little plump with ultra White skin and freckles on his nose. He had been brought up in the Midwest and had had little exposure to Africans before his internship abroad in Kenya. Dr. S. thought he had probably not really thought much about Esi’s dilemma.
Dr. Swarthmore encouraged Esi to talk about her immigration experience.
“Esi, can you talk more about what it is like to be an immigrant from Africa?”
“Well, I just have to check myself so that I can fit in with this White culture. If you want to see how I feel about it, you will have to see an angry Black woman and I have learned not to give you that satisfaction. You will just dismiss me. Please Dr. Swarthmore, can we move on?”
Dr. Swarthmore was caught between his desire to accept her wish to move on and his wish to have her express herself fully. He realized that it was not his desire that mattered; that the couple had to work this out between them if they were going to move forward. So he punted it back to them.
“Esi and Joe, you are both caught in an important dilemma. Esi, you want more respect from your husband and his family. Joe, you do not want to upset your family by confronting them. Is that right? You are both dammed if you do and dammed if you don’t.”
“I agree,” Joe and Esi both said, nodding.
“Do you want to work on this issue?”
They both agreed with equal enthusiasm.
“Ok, can you spend the next 10 minutes to work on this?”
They agreed.
“Ok, let’s start. What skills do you have that can help you resolve this important issue?”
Dr. Swarthmore framed the issue as one to be solved by the couple. The couple discussed that they are usually good at communication and solving problems. This problem is about whether or not Joe is more aligned with his White family than with Esi and their children.
Dr. Swarthmore encouraged them to think about this more deeply and over time; that this is such an important issue that it requires time and deep conversation.
“How do you think you can educate yourselves about the issues at hand?”
Esi’s reading list
1. “Why I’m No Longer Talking to White People About Race” by Reni Eddo-Lodge (London: Bloomsbury, 2018).
2. “Americanah” by Chimamanda Ngozi Adichie (New York: Alfred A. Knopf, 2013).
3. “How to be an Antiracist” by Ibram X. Kendi (New York: Random House, 2019).
Joe suggests that Esi think about what it might mean if his sister and their children were no longer part of their lives. She agrees to do this.
Dr. Swarthmore asks if they can each do their homework before they come back. They agree and thought they could manage that and the book for 2 weeks out.
Dr. Swarthmore decides that he will read one of the books Esi suggested, as he does not know much about racism and White privilege and he wants to learn more. Dr. Swarthmore demonstrates his desire to become more racially sensitive. The following steps can be taken by therapists who want to become more racially sensitive, according to TA Laszloffy and KV Hardy (Fam Process. 2000 Spring;39[1]:35-50):
1. Read and watch movies that address the experience of other cultural groups.
2. Go to and participate in cross-cultural events.
3. Engage in a racial self-exploration process. The following questions can begin the racial identity exploration process:
- How do I define myself racially?
- When did I first become aware of race/skin color in general, and mine in particular?
- What messages did I learn about race/skin color based on that first experience?
- What direct and indirect messages did I receive about race/skin color?
- How did the messages that I received about race/skin color affect how I thought and felt about myself racially?
- What benefits did I gain because of my race/skin color?
- What did I lose because of my race/skin?
- Have I ever dated cross-racially? Why or why not?
- How many friends of a different race do I have?
4. Internal commitment. This means committing to addressing racism in therapeutic encounters.
Lessons learned for psychiatrists
1. Therapeutic space is allocated to discuss the issue.
2. The time is strictly limited to 10 minutes, so the couple won’t feel that their emotions will overwhelm them.
3. The space is to focus on the strengths that they can bring to resolving the issue.
4. Give patients the impression that they can solve this and that it is an important issue.
5. Do not put yourself in the patients’ argument; take neither side.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest. Dr. Heru wrote the article in collaboration with Lynette Ramsingh Barros, artist and social commentator.
Joe and Esi were in the therapist’s office wanting help with their relationship. The therapist had just asked the BIG question: How does race impact your lives?”
Esi began with her story about her ethics class, a story that was at sufficient distance from her life. Depending on her husband’s response, she would move in closer. His somewhat patronizing response made her feel both angry and that he lacked any real understanding.
“Me and a mulatto girl were in ethics class,” said Esi, who grew in Kenya. We had a White professor. He seemed to think I had no education. If you are a woman of color, you are automatically thought to have no education and that you don’t know what you are talking about. He tried to shut me up. When I persisted, I know he thought from the tone of my voice that I was an angry Black woman, even although I am not Black and I am not angry! In this country, if you have any color to your skin, you are called Black and relegated to a certain place: The bottom. I was excited about what he was teaching us, but when everyone looked at me with a certain gaze, like something bad was going to happen, all those White people, just looking, I tightened up inside and sat back down.”
Esi looked down at her folded hands. Her husband, who was White, reached over and reassuringly patted her hands.
“Yes, Esi, they are wrong. They shouldn’t have treated you that way. White people can be insensitive.”
Then, she continued, “Joe, you do the same to me!”
“What do you mean, Esi?” responded Joe, with an innocent and anxious look scanning back and forth between her and the White male therapist.
“Well, Joe, do you really want to hear how I felt last week after we came back from that party at your sister’s house?”
“Yes, Esi.”
“But do you really? Are you sure you want to hear this?”
“Yes, Esi.”
“Remember when we went over, me and the kids sat with the other people of color and you sat with your sister and her side of the family?
“Yes, I remember. What is wrong with that?”
“Well, me and my colored friends got loud and excited, and you shot me a look, like ‘pipe down over there.’ THEN, after we got home, the next day, your sister called you and said that you had better control your wife; she is too loud. Do you remember all that?
“Yes, well you do get loud – especially when you are around your people.”
“So why is it I have to fit in with your relatives and not the other way round? Why do I have to conform to the whiteness in your sister’s world, not the other way round?”
“Well, we were in her house.”
“So if they came to our house and were too quiet, how would you feel if I called them up and said they needed to participate with more enthusiasm?”
“Esi, that’s not fair, and you know it isn’t.”
Esi stops and looks at the therapist.
“So I check myself. It is the same all over, White people imposing their values and beliefs on me, on us. I am not an angry Black woman. I am just frustrated. People, White people, always want an explanation for what they think is my loss of control. You can see when their demeanor changes, they pull back, sit up, back away, fidget, and won’t look you in the eye. All these little tics that show that they are trying to get out of the situation.”
Esi took a breath and saw that her husband and the therapist were listening.
“These signs are ingrained in your brain ... these signs ... I saw it when I first came here to this country. The first time I had a good dose of it ... was in that ethics class in college. You can’t use words that you are accustomed to, ’cause they mean something else here, something bad.”
“Oh, Esi, I am so sorry,” said Joe, looking concerned.
“You may be sorry but you are not willing to stand up for me against your sister and her White values. You want me to conform.”
“What do you want me to do?”
“I want you to call your sister out.”
“But she may not ever speak to me again!”
“OK, don’t then,” and Esi looked down at her hands. She was finished talking. Joe looked at the therapist, waiting for something.
The therapist resisted intervening on the issue. “Keep talking this through,” he instructed them.
Joe could see that Esi had done talking and that it was his move.
“Do you really want me to call my sister out, even if it means that she will not talk to me again?”
“Yes.”
“I don’t know if I can do that.”
The therapist now intervened: “What does that mean to you, Esi, that he doesn’t know if he can do that.”
“It means he doesn’t really love me or value me or even value our mulatto children. What do think our daughter is learning?”
“That’s not true, Esi.”
The therapist, Dr. Swarthmore, watched Esi, who has very a dark, blue-black skin tone, with a flawless complexion and a shapely body. She wears her hair cropped and she looks like that Black model, what’s her name. Joe was short, a little plump with ultra White skin and freckles on his nose. He had been brought up in the Midwest and had had little exposure to Africans before his internship abroad in Kenya. Dr. S. thought he had probably not really thought much about Esi’s dilemma.
Dr. Swarthmore encouraged Esi to talk about her immigration experience.
“Esi, can you talk more about what it is like to be an immigrant from Africa?”
“Well, I just have to check myself so that I can fit in with this White culture. If you want to see how I feel about it, you will have to see an angry Black woman and I have learned not to give you that satisfaction. You will just dismiss me. Please Dr. Swarthmore, can we move on?”
Dr. Swarthmore was caught between his desire to accept her wish to move on and his wish to have her express herself fully. He realized that it was not his desire that mattered; that the couple had to work this out between them if they were going to move forward. So he punted it back to them.
“Esi and Joe, you are both caught in an important dilemma. Esi, you want more respect from your husband and his family. Joe, you do not want to upset your family by confronting them. Is that right? You are both dammed if you do and dammed if you don’t.”
“I agree,” Joe and Esi both said, nodding.
“Do you want to work on this issue?”
They both agreed with equal enthusiasm.
“Ok, can you spend the next 10 minutes to work on this?”
They agreed.
“Ok, let’s start. What skills do you have that can help you resolve this important issue?”
Dr. Swarthmore framed the issue as one to be solved by the couple. The couple discussed that they are usually good at communication and solving problems. This problem is about whether or not Joe is more aligned with his White family than with Esi and their children.
Dr. Swarthmore encouraged them to think about this more deeply and over time; that this is such an important issue that it requires time and deep conversation.
“How do you think you can educate yourselves about the issues at hand?”
Esi’s reading list
1. “Why I’m No Longer Talking to White People About Race” by Reni Eddo-Lodge (London: Bloomsbury, 2018).
2. “Americanah” by Chimamanda Ngozi Adichie (New York: Alfred A. Knopf, 2013).
3. “How to be an Antiracist” by Ibram X. Kendi (New York: Random House, 2019).
Joe suggests that Esi think about what it might mean if his sister and their children were no longer part of their lives. She agrees to do this.
Dr. Swarthmore asks if they can each do their homework before they come back. They agree and thought they could manage that and the book for 2 weeks out.
Dr. Swarthmore decides that he will read one of the books Esi suggested, as he does not know much about racism and White privilege and he wants to learn more. Dr. Swarthmore demonstrates his desire to become more racially sensitive. The following steps can be taken by therapists who want to become more racially sensitive, according to TA Laszloffy and KV Hardy (Fam Process. 2000 Spring;39[1]:35-50):
1. Read and watch movies that address the experience of other cultural groups.
2. Go to and participate in cross-cultural events.
3. Engage in a racial self-exploration process. The following questions can begin the racial identity exploration process:
- How do I define myself racially?
- When did I first become aware of race/skin color in general, and mine in particular?
- What messages did I learn about race/skin color based on that first experience?
- What direct and indirect messages did I receive about race/skin color?
- How did the messages that I received about race/skin color affect how I thought and felt about myself racially?
- What benefits did I gain because of my race/skin color?
- What did I lose because of my race/skin?
- Have I ever dated cross-racially? Why or why not?
- How many friends of a different race do I have?
4. Internal commitment. This means committing to addressing racism in therapeutic encounters.
Lessons learned for psychiatrists
1. Therapeutic space is allocated to discuss the issue.
2. The time is strictly limited to 10 minutes, so the couple won’t feel that their emotions will overwhelm them.
3. The space is to focus on the strengths that they can bring to resolving the issue.
4. Give patients the impression that they can solve this and that it is an important issue.
5. Do not put yourself in the patients’ argument; take neither side.
Dr. Heru is professor of psychiatry at the University of Colorado at Denver, Aurora. She is editor of “Working With Families in Medical Settings: A Multidisciplinary Guide for Psychiatrists and Other Health Professionals” (New York: Routledge, 2013). She has no conflicts of interest. Dr. Heru wrote the article in collaboration with Lynette Ramsingh Barros, artist and social commentator.






