User login
PTSD Boosts Risk of Violence, Legal and Financial Problems, and More
PTSD Boosts Risk of Violence, Legal and Financial Problems, and More
Veterans with posttraumatic stress disorder (PTSD) were much more likely than their counterparts to be a perpetrator or victim of violence and suffer from social, legal, and financial problems, a new retrospective analysis finds.
An analysis of 62,298 matched veterans found that those newly diagnosed with PTSD were more likely to be linked to violence (adjusted odds ratio [aOR], 3.98), social problems (aOR, 2.87) legal problems (aOR, 1.75), and financial problems (aOR, 2.01), reported Ouyang et al in the November 2025 issue of the Journal of Affective Disorders.
A separate analysis of 11,758 propensity-matched veterans found that those with PTSD were more likely to experience violence (50.15% vs 11.26%), social problems (64.44% vs 25.32%), legal problems (24.84% vs 8.07%), and financial problems (48.60% vs 19.21%).
The study does not prove that PTSD is directly linked to these problems. However, Ouyang told Federal Practitioner that the findings suggest "PTSD extends beyond psychiatric symptoms: It significantly impacts economic stability, housing security, and legal safety."
Clinicians should screen for various problems in patients with PTSD, Ouyang said, “particularly given that the risk is highest during the first year.” The study also sought to better understand the effects of PTSD over time.
“While it is established that PTSD creates serious challenges regarding employment, family dynamics, and substance use, most previous studies provided only a cross-sectional snapshot,” Ouyang said. “We aimed to understand the progression over a 10-year period.”
In addition, “previous studies relied heavily on standard diagnosis codes and missed a significant amount of unstructured data,” she said. The new study uses natural language processing, an artificial intelligence field that parses the words people use, to gain insight from clinical notes.
In the cross-sectional analysis of 62,298 veterans, including 31,149 diagnosed with PTSD in the 2011-2012 fiscal year and 31,149 without PTSD (average age 60, 91.49% male, 71.50% White and 19.27% Black), PTSD was linked to higher rates of housing instability (aOR, 1.65), barriers to care (aOR, 1.45), transitions of care (aOR, 1.58), food insecurity (aOR, 1.37), and nonspecific psychosocial needs (aOR, 1.31).
Why might PTSD be linked to violence, which was defined as perpetrated by or against the veteran?
“The primary theory centers on hyperarousal, a symptom of PTSD characterized by a state of constant high alert and anxiety,” Ouyang said. “This state creates difficulties in emotional regulation and impulse control, which can lead to aggressive reactions.”
Patients are also at risk of revictimization, Ouyang added, “where the erosion of social support networks leaves veterans more vulnerable to harm from others.”
Aspects of PTSD are also thought to contribute to problems other than violence, Ouyang said. For example, mental health struggles can make it hard to keep a job and stay financially stable “and veterans may be hesitant to seek help due to stigma until the situation becomes critical, potentially leading to housing loss.”
In terms of solutions, “clinical treatment alone is insufficient,” she said. “We recommend an integrated health care model that combines mental health treatment with referrals to social work and economic support services to address the broader determinants of well-being.”
Brian Klassen, PhD, an associate professor with the Department of Psychiatry and Behavioral Sciences at Rush University Medical Center, reviewed the study for Federal Practitioner.
The research “underscores how problematic the diagnosis of PTSD is for folks,” said Klassen, the director of Strategic Partnership for the Road Home Program/Center for Veterans and Their Families. “It plays out in lives in trouble with relationships, work, and housing, things like that.”
How PTSD cultivates a veteran’s everyday life is important for clinicians to understand, he said. “A lot of our treatments directly target symptoms: how to help people sleep better, manage their mood. This encourages practitioners to look at the whole person,” Klassen said. “What other kind of resource needs might this person have that are related to—or maybe caused by—their PTSD diagnosis?”
These resources can “include things like job training and housing and financial assistance, maybe help to get out in the community and form relationships with people.”
The US Department of Veterans Affairs and National Institutes of Health funded the study. The study authors and Klassen have no disclosures.
Veterans with posttraumatic stress disorder (PTSD) were much more likely than their counterparts to be a perpetrator or victim of violence and suffer from social, legal, and financial problems, a new retrospective analysis finds.
An analysis of 62,298 matched veterans found that those newly diagnosed with PTSD were more likely to be linked to violence (adjusted odds ratio [aOR], 3.98), social problems (aOR, 2.87) legal problems (aOR, 1.75), and financial problems (aOR, 2.01), reported Ouyang et al in the November 2025 issue of the Journal of Affective Disorders.
A separate analysis of 11,758 propensity-matched veterans found that those with PTSD were more likely to experience violence (50.15% vs 11.26%), social problems (64.44% vs 25.32%), legal problems (24.84% vs 8.07%), and financial problems (48.60% vs 19.21%).
The study does not prove that PTSD is directly linked to these problems. However, Ouyang told Federal Practitioner that the findings suggest "PTSD extends beyond psychiatric symptoms: It significantly impacts economic stability, housing security, and legal safety."
Clinicians should screen for various problems in patients with PTSD, Ouyang said, “particularly given that the risk is highest during the first year.” The study also sought to better understand the effects of PTSD over time.
“While it is established that PTSD creates serious challenges regarding employment, family dynamics, and substance use, most previous studies provided only a cross-sectional snapshot,” Ouyang said. “We aimed to understand the progression over a 10-year period.”
In addition, “previous studies relied heavily on standard diagnosis codes and missed a significant amount of unstructured data,” she said. The new study uses natural language processing, an artificial intelligence field that parses the words people use, to gain insight from clinical notes.
In the cross-sectional analysis of 62,298 veterans, including 31,149 diagnosed with PTSD in the 2011-2012 fiscal year and 31,149 without PTSD (average age 60, 91.49% male, 71.50% White and 19.27% Black), PTSD was linked to higher rates of housing instability (aOR, 1.65), barriers to care (aOR, 1.45), transitions of care (aOR, 1.58), food insecurity (aOR, 1.37), and nonspecific psychosocial needs (aOR, 1.31).
Why might PTSD be linked to violence, which was defined as perpetrated by or against the veteran?
“The primary theory centers on hyperarousal, a symptom of PTSD characterized by a state of constant high alert and anxiety,” Ouyang said. “This state creates difficulties in emotional regulation and impulse control, which can lead to aggressive reactions.”
Patients are also at risk of revictimization, Ouyang added, “where the erosion of social support networks leaves veterans more vulnerable to harm from others.”
Aspects of PTSD are also thought to contribute to problems other than violence, Ouyang said. For example, mental health struggles can make it hard to keep a job and stay financially stable “and veterans may be hesitant to seek help due to stigma until the situation becomes critical, potentially leading to housing loss.”
In terms of solutions, “clinical treatment alone is insufficient,” she said. “We recommend an integrated health care model that combines mental health treatment with referrals to social work and economic support services to address the broader determinants of well-being.”
Brian Klassen, PhD, an associate professor with the Department of Psychiatry and Behavioral Sciences at Rush University Medical Center, reviewed the study for Federal Practitioner.
The research “underscores how problematic the diagnosis of PTSD is for folks,” said Klassen, the director of Strategic Partnership for the Road Home Program/Center for Veterans and Their Families. “It plays out in lives in trouble with relationships, work, and housing, things like that.”
How PTSD cultivates a veteran’s everyday life is important for clinicians to understand, he said. “A lot of our treatments directly target symptoms: how to help people sleep better, manage their mood. This encourages practitioners to look at the whole person,” Klassen said. “What other kind of resource needs might this person have that are related to—or maybe caused by—their PTSD diagnosis?”
These resources can “include things like job training and housing and financial assistance, maybe help to get out in the community and form relationships with people.”
The US Department of Veterans Affairs and National Institutes of Health funded the study. The study authors and Klassen have no disclosures.
Veterans with posttraumatic stress disorder (PTSD) were much more likely than their counterparts to be a perpetrator or victim of violence and suffer from social, legal, and financial problems, a new retrospective analysis finds.
An analysis of 62,298 matched veterans found that those newly diagnosed with PTSD were more likely to be linked to violence (adjusted odds ratio [aOR], 3.98), social problems (aOR, 2.87) legal problems (aOR, 1.75), and financial problems (aOR, 2.01), reported Ouyang et al in the November 2025 issue of the Journal of Affective Disorders.
A separate analysis of 11,758 propensity-matched veterans found that those with PTSD were more likely to experience violence (50.15% vs 11.26%), social problems (64.44% vs 25.32%), legal problems (24.84% vs 8.07%), and financial problems (48.60% vs 19.21%).
The study does not prove that PTSD is directly linked to these problems. However, Ouyang told Federal Practitioner that the findings suggest "PTSD extends beyond psychiatric symptoms: It significantly impacts economic stability, housing security, and legal safety."
Clinicians should screen for various problems in patients with PTSD, Ouyang said, “particularly given that the risk is highest during the first year.” The study also sought to better understand the effects of PTSD over time.
“While it is established that PTSD creates serious challenges regarding employment, family dynamics, and substance use, most previous studies provided only a cross-sectional snapshot,” Ouyang said. “We aimed to understand the progression over a 10-year period.”
In addition, “previous studies relied heavily on standard diagnosis codes and missed a significant amount of unstructured data,” she said. The new study uses natural language processing, an artificial intelligence field that parses the words people use, to gain insight from clinical notes.
In the cross-sectional analysis of 62,298 veterans, including 31,149 diagnosed with PTSD in the 2011-2012 fiscal year and 31,149 without PTSD (average age 60, 91.49% male, 71.50% White and 19.27% Black), PTSD was linked to higher rates of housing instability (aOR, 1.65), barriers to care (aOR, 1.45), transitions of care (aOR, 1.58), food insecurity (aOR, 1.37), and nonspecific psychosocial needs (aOR, 1.31).
Why might PTSD be linked to violence, which was defined as perpetrated by or against the veteran?
“The primary theory centers on hyperarousal, a symptom of PTSD characterized by a state of constant high alert and anxiety,” Ouyang said. “This state creates difficulties in emotional regulation and impulse control, which can lead to aggressive reactions.”
Patients are also at risk of revictimization, Ouyang added, “where the erosion of social support networks leaves veterans more vulnerable to harm from others.”
Aspects of PTSD are also thought to contribute to problems other than violence, Ouyang said. For example, mental health struggles can make it hard to keep a job and stay financially stable “and veterans may be hesitant to seek help due to stigma until the situation becomes critical, potentially leading to housing loss.”
In terms of solutions, “clinical treatment alone is insufficient,” she said. “We recommend an integrated health care model that combines mental health treatment with referrals to social work and economic support services to address the broader determinants of well-being.”
Brian Klassen, PhD, an associate professor with the Department of Psychiatry and Behavioral Sciences at Rush University Medical Center, reviewed the study for Federal Practitioner.
The research “underscores how problematic the diagnosis of PTSD is for folks,” said Klassen, the director of Strategic Partnership for the Road Home Program/Center for Veterans and Their Families. “It plays out in lives in trouble with relationships, work, and housing, things like that.”
How PTSD cultivates a veteran’s everyday life is important for clinicians to understand, he said. “A lot of our treatments directly target symptoms: how to help people sleep better, manage their mood. This encourages practitioners to look at the whole person,” Klassen said. “What other kind of resource needs might this person have that are related to—or maybe caused by—their PTSD diagnosis?”
These resources can “include things like job training and housing and financial assistance, maybe help to get out in the community and form relationships with people.”
The US Department of Veterans Affairs and National Institutes of Health funded the study. The study authors and Klassen have no disclosures.
PTSD Boosts Risk of Violence, Legal and Financial Problems, and More
PTSD Boosts Risk of Violence, Legal and Financial Problems, and More
Research Focuses on Mental Health Needs of Women Veterans
The more than 2 million women US veterans are the fastest-growing military population. While research into women veterans has traditionally lagged, more recently studies have begun to focus on their needs impacts of combat and service on women. These studies have found that women veterans preferred tailored solutions focused on women veterans.
A November 2025 study is one of the first to examine the impact of combat on women veterans. It found that those in combat roles had higher levels of depression, posttraumatic stress disorder (PTSD), dissociation, and overall poorer health compared with civilians and noncombat women military personnel. Previous research had found that women veterans had higher rates of lifetime and past-year PTSD (13.4%) compared with female civilians (8.0%), male veterans (7.7%), and male civilians (3.4%). A 2020 US Department of Veterans (VA) study of 4,928,638 men and 448,455 women similarly found that women had nearly twice the rates of depression and anxiety compared with men.
For many veterans, mental health issues may develop or be exacerbated in their return to civilian life. That transition can be especially confusing and isolating for women veterans, according to a 2024 study: “They neither fit in the military due to gendered relations centered on masculinity, or civilian life where they are largely misunderstood as ‘veterans.’ This ‘no woman’s land’ is poorly understood.” Few programs for transitioning veterans have been found effective for women veterans because they’ve been developed for a largely male veteran population. That includes mental health support programs.
Some women may prefer women-only groups, and even that choice may be dependent on their background, service history, socioeconomic level, and other factors. They may feel more comfortable in women-only groups if they’ve experienced MST. Others who have served in combat may choose mixed-gender programs. One study found that some women benefited from being in a mixed-gender group because it enabled them to work on difficulties with men in a safe environment. Other research has found that women veterans with substance use disorders are reluctant to seek help alongside men in the same facilities.
Accessing care may be especially challenging for rural women veterans. However, separate facilities and women-only groups are not always available, particularly in rural areas where there may be very few women veterans. And even if they are available, rural women are often up against barriers that urban women do not face, such as having to travel long distances to get care. Clinicians also may be hard to find in rural areas. Some participants in a 2025 study were hampered not only by a lack of female practitioners, but practitioners who were well trained to understand and treat the unique needs of female veterans: “[It’s] incredibly difficult to find a mental health practitioner that understands a veteran’s unique experience as a woman,” a participant said.
The more than 2 million women US veterans are the fastest-growing military population. While research into women veterans has traditionally lagged, more recently studies have begun to focus on their needs impacts of combat and service on women. These studies have found that women veterans preferred tailored solutions focused on women veterans.
A November 2025 study is one of the first to examine the impact of combat on women veterans. It found that those in combat roles had higher levels of depression, posttraumatic stress disorder (PTSD), dissociation, and overall poorer health compared with civilians and noncombat women military personnel. Previous research had found that women veterans had higher rates of lifetime and past-year PTSD (13.4%) compared with female civilians (8.0%), male veterans (7.7%), and male civilians (3.4%). A 2020 US Department of Veterans (VA) study of 4,928,638 men and 448,455 women similarly found that women had nearly twice the rates of depression and anxiety compared with men.
For many veterans, mental health issues may develop or be exacerbated in their return to civilian life. That transition can be especially confusing and isolating for women veterans, according to a 2024 study: “They neither fit in the military due to gendered relations centered on masculinity, or civilian life where they are largely misunderstood as ‘veterans.’ This ‘no woman’s land’ is poorly understood.” Few programs for transitioning veterans have been found effective for women veterans because they’ve been developed for a largely male veteran population. That includes mental health support programs.
Some women may prefer women-only groups, and even that choice may be dependent on their background, service history, socioeconomic level, and other factors. They may feel more comfortable in women-only groups if they’ve experienced MST. Others who have served in combat may choose mixed-gender programs. One study found that some women benefited from being in a mixed-gender group because it enabled them to work on difficulties with men in a safe environment. Other research has found that women veterans with substance use disorders are reluctant to seek help alongside men in the same facilities.
Accessing care may be especially challenging for rural women veterans. However, separate facilities and women-only groups are not always available, particularly in rural areas where there may be very few women veterans. And even if they are available, rural women are often up against barriers that urban women do not face, such as having to travel long distances to get care. Clinicians also may be hard to find in rural areas. Some participants in a 2025 study were hampered not only by a lack of female practitioners, but practitioners who were well trained to understand and treat the unique needs of female veterans: “[It’s] incredibly difficult to find a mental health practitioner that understands a veteran’s unique experience as a woman,” a participant said.
The more than 2 million women US veterans are the fastest-growing military population. While research into women veterans has traditionally lagged, more recently studies have begun to focus on their needs impacts of combat and service on women. These studies have found that women veterans preferred tailored solutions focused on women veterans.
A November 2025 study is one of the first to examine the impact of combat on women veterans. It found that those in combat roles had higher levels of depression, posttraumatic stress disorder (PTSD), dissociation, and overall poorer health compared with civilians and noncombat women military personnel. Previous research had found that women veterans had higher rates of lifetime and past-year PTSD (13.4%) compared with female civilians (8.0%), male veterans (7.7%), and male civilians (3.4%). A 2020 US Department of Veterans (VA) study of 4,928,638 men and 448,455 women similarly found that women had nearly twice the rates of depression and anxiety compared with men.
For many veterans, mental health issues may develop or be exacerbated in their return to civilian life. That transition can be especially confusing and isolating for women veterans, according to a 2024 study: “They neither fit in the military due to gendered relations centered on masculinity, or civilian life where they are largely misunderstood as ‘veterans.’ This ‘no woman’s land’ is poorly understood.” Few programs for transitioning veterans have been found effective for women veterans because they’ve been developed for a largely male veteran population. That includes mental health support programs.
Some women may prefer women-only groups, and even that choice may be dependent on their background, service history, socioeconomic level, and other factors. They may feel more comfortable in women-only groups if they’ve experienced MST. Others who have served in combat may choose mixed-gender programs. One study found that some women benefited from being in a mixed-gender group because it enabled them to work on difficulties with men in a safe environment. Other research has found that women veterans with substance use disorders are reluctant to seek help alongside men in the same facilities.
Accessing care may be especially challenging for rural women veterans. However, separate facilities and women-only groups are not always available, particularly in rural areas where there may be very few women veterans. And even if they are available, rural women are often up against barriers that urban women do not face, such as having to travel long distances to get care. Clinicians also may be hard to find in rural areas. Some participants in a 2025 study were hampered not only by a lack of female practitioners, but practitioners who were well trained to understand and treat the unique needs of female veterans: “[It’s] incredibly difficult to find a mental health practitioner that understands a veteran’s unique experience as a woman,” a participant said.
Nine VA Facilities to Open Research Trials for Psychedelics
Nine VA Facilities to Open Research Trials for Psychedelics
On Nov. 22, 2014, 8 years after he came back from Iraq with “crippling” posttraumatic stress disorder (PTSD), Jonathan Lubecky took his first dose of the psychedelic compound methylenedioxymethamphetamine (MDMA). Lubecky, a Marine, Army, and National Guard veteran, described his path to MDMA therapy in in the New Horizons in Health podcast.
After 5 suicide attempts and “the hundreds of times I thought about it or stood on a bridge or had a plan,” he felt he had run out of options. Then, in a counseling session, a psychiatric intern slid a piece of paper across the table to him. It read “Google MDMA PTSD.”
Luckily for Lubecky, a space in a clinical trial opened up, in which he had 8 hours of talk therapy with specially trained therapists, combined with MDMA. “MDMA is a tool that opens up the mind, body and spirit,” he said, “so you can heal and process all those memories and traumas that are causing yourissues. It puts you in a middle place where you can talk about trauma without having panic attacks, without your body betraying you, and look at it from a different perspective.” said he added, “It’s like doing therapy while being hugged by everyone who loves you in a bathtub full of puppies licking your face.” In 2023, 9 years after that first dose, Lubecky said, “I’ve been PTSD free longer than I had it.”
And now, in 2025, the research into psychedelic therapy for veterans like Lubecky is taking another step forward according to a report by Military.com. Nine VA facilities, in the Bronx, Los Angeles, Omaha, Palo Alto, Portland (Oregon), San Diego, San Francisco, West Haven, and White River Junction, are participating in long-term studies to test the safety and clinical impact of psychedelic compounds for PTSD, treatment-resistant depression, and anxiety disorders.
Early trials from Johns Hopkins University, the Multidisciplinary Association for Psychedelic Studies (MAPS), and others found significant symptom reductions for some participants with chronic PTSD. MAPP2, the multisite phase 3 study that extended the findings of MAPP1, found that MDMA-assisted therapy significantly improved PTSD symptoms and functional impairment, compared with placebo-assisted therapy. Notably, of the 52 participants (including 16 veterans) 45 (86%) achieved a clinically meaningful benefit, and 37 (71%) no longer met criteria for PTSD by study end. Despite the promising findings, a US Food and Drug Administration (FDA) advisory panel recommended against approving the treatment.
In 2024 the VA issued a request for applications for proposals from its network of VA researchers and academic institutions to gather “definitive scientific evidence” on the potential efficacy and safety of psychedelic compounds, such as MDMA and psilocybin, when used in conjunction with psychotherapy. It would be the first time since the 1960s that the VA had funded research on such compounds.
Funding proposals for such research have cycled in and out of Congress for years, but have gathered more steam in the last few years. The 2024 National Defense Authorization Act directed the US Department of Defense to establish a process for funding clinical research into the use of certain psychedelic substances to treat PTSD and traumatic brain injury. In April 2024, Representatives Lou Correa (D-CA) and Jack Bergman (R-MI), cochairs of the Psychedelics Advancing Therapies (PATH) caucus, introduced the Innovative Therapies Centers of Excellence Act of 2025, bipartisan legislation that would increase federally funded research on innovative therapies to treat veterans with PTSD, substance use disorder, and depression. It would also, if enacted, direct the VA to create ≥ 5 dedicated centers of excellence to study the therapeutic uses of psychedelic substances. The bill has also been endorsed by the American Legion, Veterans of Foreign Wars, Iraq and Afghanistan Veterans of America, Disabled American Veterans, and the Wounded Warrior Project.
The current administration has two strong high-level supporters of psychedelics research: VA Secretary Doug Collins and US Department of Health and Human Service Secretary Robert F. Kennedy Jr. Sec. Kennedy has castigated the FDA for what he calls “aggressive suppression” of alternative and complementary treatments, including psychedelics. This, although the FDA granted breakthrough therapy status for MDMA for treating PTSD and psilocybin for treating depression in 2018 and 2019, respectively, as well a pivotal draft guidance in 2023 for the development of psychedelic drugs for psychiatric disorders, substance use disorders, and various medical conditions.
Collins, citing an “eye-opening” discussion with Kennedy, enthusiastically backs the research into psychedelics. In a May 2025 hearing that was mainly a series of testy exchanges about his proposed budget slashing, he emphasized the importance of keeping and expanding VA programs and studies on psychedelic treatments, something he has been advocating for since the beginning of his appointment. “We want to make sure we’re not closing off any outlet for a veteran who could be helped by these programs,” he said.
Taking the intern’s advice to look into MDMA, Jonathan Lubecky said, was one of the best decisions he’d ever made. But “it’s not the MDMA that fixes you,” he said. “It’s the therapy. It’s the therapist working with you and you doing the hard work.”
On Nov. 22, 2014, 8 years after he came back from Iraq with “crippling” posttraumatic stress disorder (PTSD), Jonathan Lubecky took his first dose of the psychedelic compound methylenedioxymethamphetamine (MDMA). Lubecky, a Marine, Army, and National Guard veteran, described his path to MDMA therapy in in the New Horizons in Health podcast.
After 5 suicide attempts and “the hundreds of times I thought about it or stood on a bridge or had a plan,” he felt he had run out of options. Then, in a counseling session, a psychiatric intern slid a piece of paper across the table to him. It read “Google MDMA PTSD.”
Luckily for Lubecky, a space in a clinical trial opened up, in which he had 8 hours of talk therapy with specially trained therapists, combined with MDMA. “MDMA is a tool that opens up the mind, body and spirit,” he said, “so you can heal and process all those memories and traumas that are causing yourissues. It puts you in a middle place where you can talk about trauma without having panic attacks, without your body betraying you, and look at it from a different perspective.” said he added, “It’s like doing therapy while being hugged by everyone who loves you in a bathtub full of puppies licking your face.” In 2023, 9 years after that first dose, Lubecky said, “I’ve been PTSD free longer than I had it.”
And now, in 2025, the research into psychedelic therapy for veterans like Lubecky is taking another step forward according to a report by Military.com. Nine VA facilities, in the Bronx, Los Angeles, Omaha, Palo Alto, Portland (Oregon), San Diego, San Francisco, West Haven, and White River Junction, are participating in long-term studies to test the safety and clinical impact of psychedelic compounds for PTSD, treatment-resistant depression, and anxiety disorders.
Early trials from Johns Hopkins University, the Multidisciplinary Association for Psychedelic Studies (MAPS), and others found significant symptom reductions for some participants with chronic PTSD. MAPP2, the multisite phase 3 study that extended the findings of MAPP1, found that MDMA-assisted therapy significantly improved PTSD symptoms and functional impairment, compared with placebo-assisted therapy. Notably, of the 52 participants (including 16 veterans) 45 (86%) achieved a clinically meaningful benefit, and 37 (71%) no longer met criteria for PTSD by study end. Despite the promising findings, a US Food and Drug Administration (FDA) advisory panel recommended against approving the treatment.
In 2024 the VA issued a request for applications for proposals from its network of VA researchers and academic institutions to gather “definitive scientific evidence” on the potential efficacy and safety of psychedelic compounds, such as MDMA and psilocybin, when used in conjunction with psychotherapy. It would be the first time since the 1960s that the VA had funded research on such compounds.
Funding proposals for such research have cycled in and out of Congress for years, but have gathered more steam in the last few years. The 2024 National Defense Authorization Act directed the US Department of Defense to establish a process for funding clinical research into the use of certain psychedelic substances to treat PTSD and traumatic brain injury. In April 2024, Representatives Lou Correa (D-CA) and Jack Bergman (R-MI), cochairs of the Psychedelics Advancing Therapies (PATH) caucus, introduced the Innovative Therapies Centers of Excellence Act of 2025, bipartisan legislation that would increase federally funded research on innovative therapies to treat veterans with PTSD, substance use disorder, and depression. It would also, if enacted, direct the VA to create ≥ 5 dedicated centers of excellence to study the therapeutic uses of psychedelic substances. The bill has also been endorsed by the American Legion, Veterans of Foreign Wars, Iraq and Afghanistan Veterans of America, Disabled American Veterans, and the Wounded Warrior Project.
The current administration has two strong high-level supporters of psychedelics research: VA Secretary Doug Collins and US Department of Health and Human Service Secretary Robert F. Kennedy Jr. Sec. Kennedy has castigated the FDA for what he calls “aggressive suppression” of alternative and complementary treatments, including psychedelics. This, although the FDA granted breakthrough therapy status for MDMA for treating PTSD and psilocybin for treating depression in 2018 and 2019, respectively, as well a pivotal draft guidance in 2023 for the development of psychedelic drugs for psychiatric disorders, substance use disorders, and various medical conditions.
Collins, citing an “eye-opening” discussion with Kennedy, enthusiastically backs the research into psychedelics. In a May 2025 hearing that was mainly a series of testy exchanges about his proposed budget slashing, he emphasized the importance of keeping and expanding VA programs and studies on psychedelic treatments, something he has been advocating for since the beginning of his appointment. “We want to make sure we’re not closing off any outlet for a veteran who could be helped by these programs,” he said.
Taking the intern’s advice to look into MDMA, Jonathan Lubecky said, was one of the best decisions he’d ever made. But “it’s not the MDMA that fixes you,” he said. “It’s the therapy. It’s the therapist working with you and you doing the hard work.”
On Nov. 22, 2014, 8 years after he came back from Iraq with “crippling” posttraumatic stress disorder (PTSD), Jonathan Lubecky took his first dose of the psychedelic compound methylenedioxymethamphetamine (MDMA). Lubecky, a Marine, Army, and National Guard veteran, described his path to MDMA therapy in in the New Horizons in Health podcast.
After 5 suicide attempts and “the hundreds of times I thought about it or stood on a bridge or had a plan,” he felt he had run out of options. Then, in a counseling session, a psychiatric intern slid a piece of paper across the table to him. It read “Google MDMA PTSD.”
Luckily for Lubecky, a space in a clinical trial opened up, in which he had 8 hours of talk therapy with specially trained therapists, combined with MDMA. “MDMA is a tool that opens up the mind, body and spirit,” he said, “so you can heal and process all those memories and traumas that are causing yourissues. It puts you in a middle place where you can talk about trauma without having panic attacks, without your body betraying you, and look at it from a different perspective.” said he added, “It’s like doing therapy while being hugged by everyone who loves you in a bathtub full of puppies licking your face.” In 2023, 9 years after that first dose, Lubecky said, “I’ve been PTSD free longer than I had it.”
And now, in 2025, the research into psychedelic therapy for veterans like Lubecky is taking another step forward according to a report by Military.com. Nine VA facilities, in the Bronx, Los Angeles, Omaha, Palo Alto, Portland (Oregon), San Diego, San Francisco, West Haven, and White River Junction, are participating in long-term studies to test the safety and clinical impact of psychedelic compounds for PTSD, treatment-resistant depression, and anxiety disorders.
Early trials from Johns Hopkins University, the Multidisciplinary Association for Psychedelic Studies (MAPS), and others found significant symptom reductions for some participants with chronic PTSD. MAPP2, the multisite phase 3 study that extended the findings of MAPP1, found that MDMA-assisted therapy significantly improved PTSD symptoms and functional impairment, compared with placebo-assisted therapy. Notably, of the 52 participants (including 16 veterans) 45 (86%) achieved a clinically meaningful benefit, and 37 (71%) no longer met criteria for PTSD by study end. Despite the promising findings, a US Food and Drug Administration (FDA) advisory panel recommended against approving the treatment.
In 2024 the VA issued a request for applications for proposals from its network of VA researchers and academic institutions to gather “definitive scientific evidence” on the potential efficacy and safety of psychedelic compounds, such as MDMA and psilocybin, when used in conjunction with psychotherapy. It would be the first time since the 1960s that the VA had funded research on such compounds.
Funding proposals for such research have cycled in and out of Congress for years, but have gathered more steam in the last few years. The 2024 National Defense Authorization Act directed the US Department of Defense to establish a process for funding clinical research into the use of certain psychedelic substances to treat PTSD and traumatic brain injury. In April 2024, Representatives Lou Correa (D-CA) and Jack Bergman (R-MI), cochairs of the Psychedelics Advancing Therapies (PATH) caucus, introduced the Innovative Therapies Centers of Excellence Act of 2025, bipartisan legislation that would increase federally funded research on innovative therapies to treat veterans with PTSD, substance use disorder, and depression. It would also, if enacted, direct the VA to create ≥ 5 dedicated centers of excellence to study the therapeutic uses of psychedelic substances. The bill has also been endorsed by the American Legion, Veterans of Foreign Wars, Iraq and Afghanistan Veterans of America, Disabled American Veterans, and the Wounded Warrior Project.
The current administration has two strong high-level supporters of psychedelics research: VA Secretary Doug Collins and US Department of Health and Human Service Secretary Robert F. Kennedy Jr. Sec. Kennedy has castigated the FDA for what he calls “aggressive suppression” of alternative and complementary treatments, including psychedelics. This, although the FDA granted breakthrough therapy status for MDMA for treating PTSD and psilocybin for treating depression in 2018 and 2019, respectively, as well a pivotal draft guidance in 2023 for the development of psychedelic drugs for psychiatric disorders, substance use disorders, and various medical conditions.
Collins, citing an “eye-opening” discussion with Kennedy, enthusiastically backs the research into psychedelics. In a May 2025 hearing that was mainly a series of testy exchanges about his proposed budget slashing, he emphasized the importance of keeping and expanding VA programs and studies on psychedelic treatments, something he has been advocating for since the beginning of his appointment. “We want to make sure we’re not closing off any outlet for a veteran who could be helped by these programs,” he said.
Taking the intern’s advice to look into MDMA, Jonathan Lubecky said, was one of the best decisions he’d ever made. But “it’s not the MDMA that fixes you,” he said. “It’s the therapy. It’s the therapist working with you and you doing the hard work.”
Nine VA Facilities to Open Research Trials for Psychedelics
Nine VA Facilities to Open Research Trials for Psychedelics
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
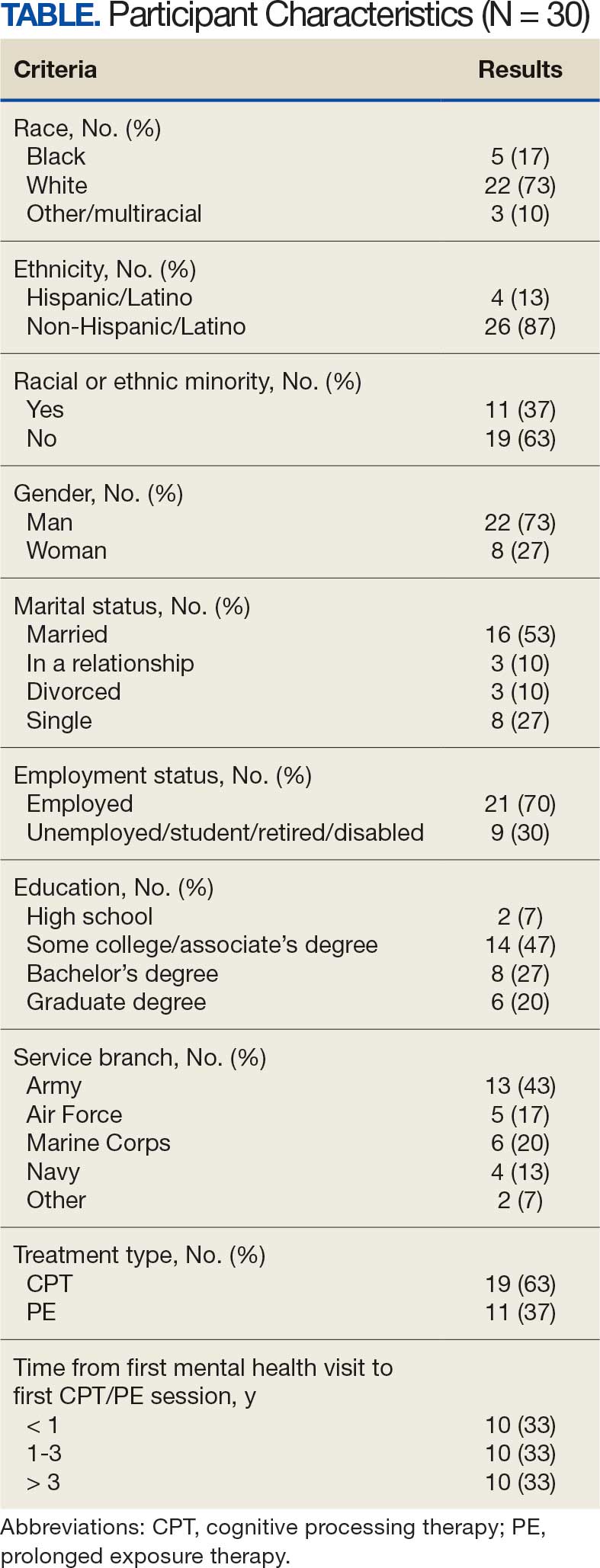
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
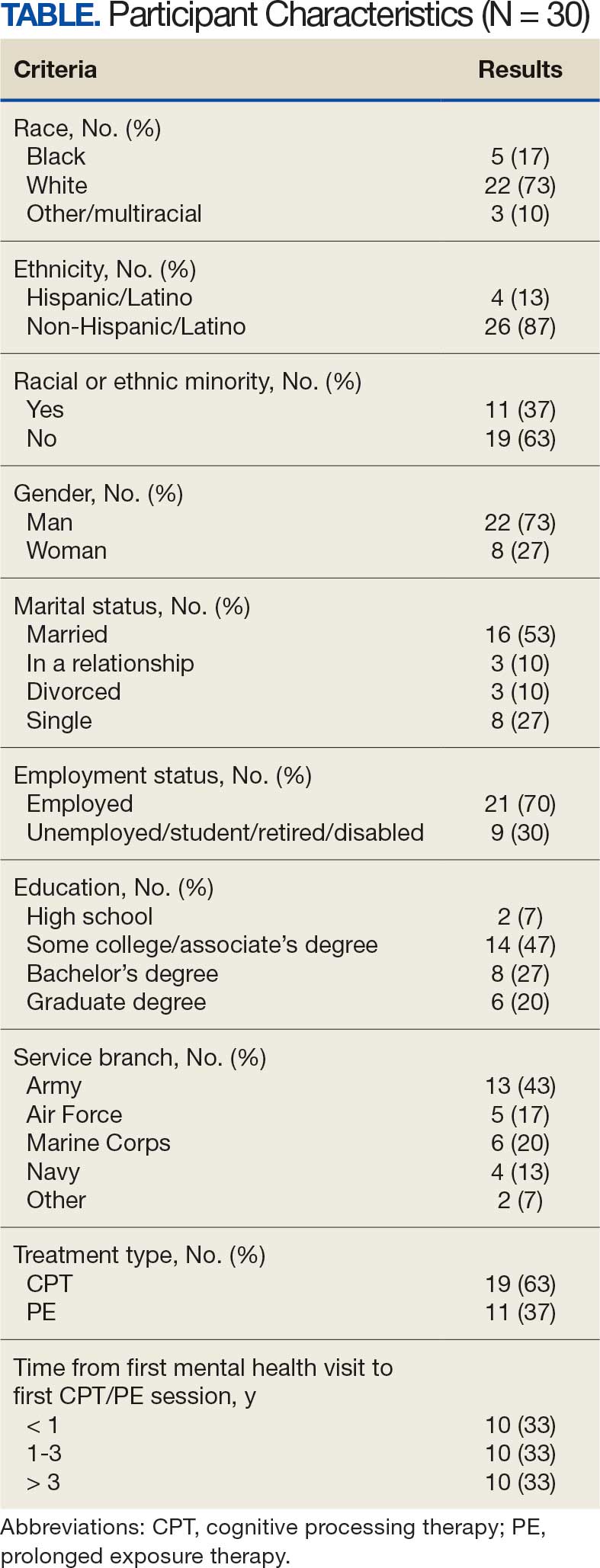
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
Trauma-focused evidence-based psychotherapies (TF-EBPs), including cognitive processing therapy (CPT) and prolonged exposure therapy (PE), are recommended treatments for posttraumatic stress disorder (PTSD) in clinical practice guidelines.1-3 To increase initiation of these treatments, the US Department of Veterans Affairs (VA) used a large-scale dissemination and implementation effort to improve access to TF-EBP.4,5 These efforts achieved modest success, increasing prevalence of TF-EBP from a handful of veterans in 2004 to an annual prevalence of 14.6% for CPT and 4.3% for PE in 2014.6
Throughout these efforts, qualitative studies have been used to better understand veterans’ perspectives on receiving TF-EBP care.7-18 Barriers to initiation of and engagement in TF-EBP and PTSD care have been identified from these qualitative studies. One identified barrier was lack of knowledge—particularly lack of knowledge about what is meant by a PTSD diagnosis and available treatments.7-10 Stigma (ie, automatic negative associations) toward mental health problems or seeking mental health care also has been identified as a barrier to initiation.7,10-14 Perceptions of poor alignment between treatment and veteran goals, including lack of buy-in for the rationale, served as barriers to initiation and engagement.8,15-18
Using prior qualitative work, numerous initiatives have been developed to reduce stigma, facilitate conversations about how treatment aligns with goals, and fill knowledge gaps, particularly through online resources and shared decision-making.19,20 To better inform the state of veterans’ experiences with TF-EBP, a qualitative investigation was conducted involving veterans who recently initiated TF-EBP. Themes directly related to transitions to TF-EBP were identified; however, all veterans interviewed also described their experiences with TFEBP engagement and mental health care. Consistent with recommendations for qualitative methods, this study extends prior work on transitions to TF-EBP by describing themes with a distinct focus on the experience of engaging with TF-EBP and mental health care.21,22
Methods
The experiences of veterans who were transitioning into TF-EBPs were collected in semistructured interviews and analyzed. The semistructured interview guide was developed and refined in consultation with both qualitative methods experts and PTSD treatment experts to ensure that 6 content domains were appropriately queried: PTSD treatment options, cultural sensitivity of treatment, PTSD treatment selection, transition criteria, beliefs about stabilization treatment, and treatment needs/preferences.
Participants were identified using the VA Corporate Data Warehouse and included post-9/11 veterans who had recently initiated CPT or PE for the first time between September 1, 2021, and September 1, 2022. More details of participant selection are available in Holder et al.21 From a population of 10,814 patients, stratified random sampling generated a recruitment pool of 200 veterans for further outreach. The strata were defined such that this recruitment pool had similar proportions of demographic characteristics (ie, gender, race, ethnicity) to the population of eligible veterans, equivalent distributions of time to CPT or PE initiation (ie, 33.3% < 1 year, 33.3% 1-3 years, and 33.3% > 3 years), and adequate variability in TF-EBP type (ie, 66.7% CPT, 33.3% PE). A manual chart review in the recruitment pool excluded 12 veterans who did not initiate CPT or PE, 1 veteran with evidence of current active psychosis and/or cognitive impairment that would likely preclude comprehension of study materials, and 1 who was deceased.
Eligible veterans from the recruitment pool were contacted in groups of 25. First, a recruitment letter with study information and instructions to opt-out of further contact was mailed or emailed to veterans. After 2 weeks, veterans who had not responded were contacted by phone up to 3 times. Veterans interested in participating were scheduled for a 1-time visit that included verbal consent and the qualitative interview. Metrics were established a priori to ensure an adequately diverse and inclusive sample. Specifically, a minimum number of racial and/or ethnic minority veterans (33%) and women veterans (20%) were sought. Equal distribution across the 3 categories of time from first mental health visit to CPT/PE initiation also was targeted. Throughout enrollment, recruitment efforts were adapted to meet these metrics in the emerging sample. While the goal was to generate a diverse and inclusive sample using these methods, the sample was not intended to be representative of the population.
Of the 186 eligible participants, 21 declined participation and 26 could not be reached. The targeted sample was reached after exhausting contact for 47 veterans and contacting 80 veterans for a final response rate of 40% among fully contacted veterans and 27% among veterans with any contact. The final sample included 30 veterans who received CPT or PE in VA facilities (Table).
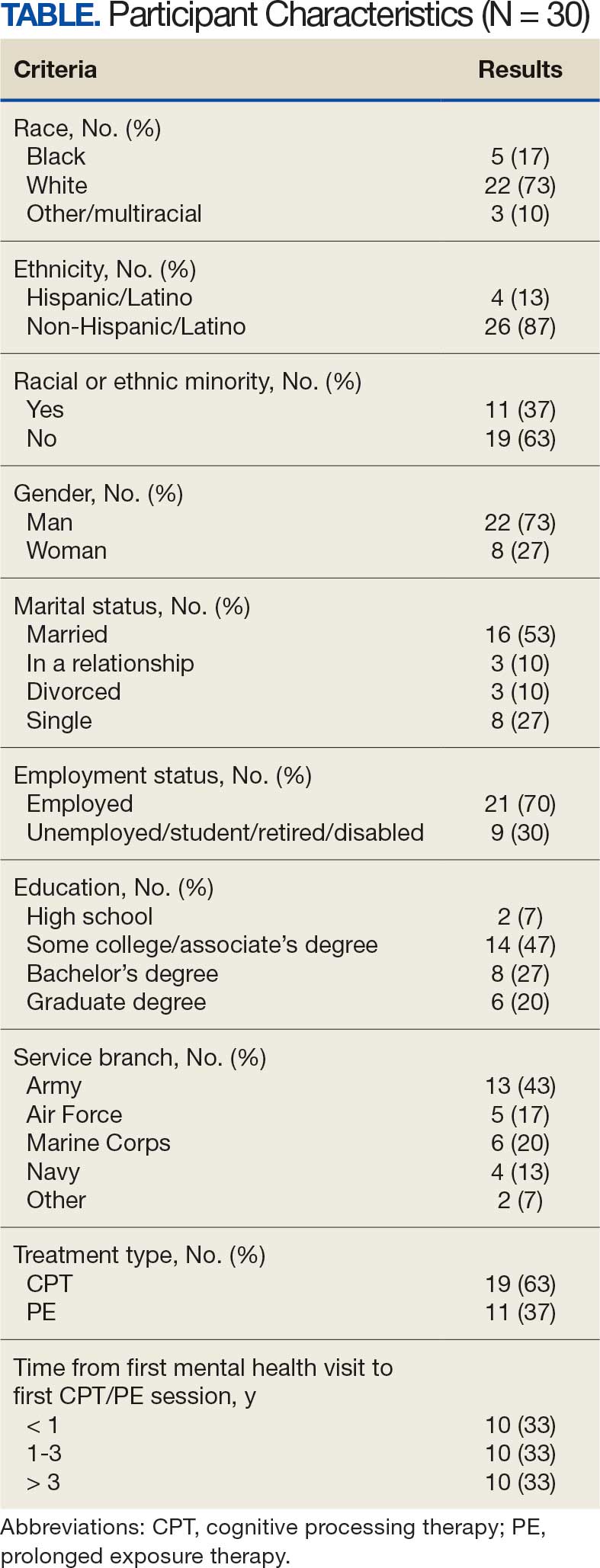
After veterans provided verbal consent for study participation, sociodemographic information was verbally reported, and a 30- to 60-minute semistructured qualitative phone interview was recorded and transcribed. Veterans received $40 for participation. All procedures were approved by the University of California San Francisco Institutional Review Board.
Qualitative Data Analysis
Rapid analysis procedures were used to analyze qualitative data. This approach is suitable for focused, moderately structured qualitative analyses in health services research and facilitates rapid dissemination to stakeholders.23 The qualitative analysts were 2 clinical psychologists with expertise in PTSD treatment (NH primary and RR secondary). Consistent with rapid analysis procedures, analysts prepared a templated summary (including relevant quotations) of each interview, organized by the prespecified content domains. Interviews were summarized independently, compared to ensure consistency, and discrepancies were resolved through review of the interview source materials. Individual summary templates were combined into a master analytic matrix to facilitate the identification of patterns and delineation of themes. Analysts routinely met to identify, discuss, and refine preliminary themes, revisiting source materials to reach consensus as needed.
Results
Fifteen themes were identified and organized into 2 distinct focus areas: themes directly related to the transition to TF-EBP (8 themes) and themes related to veterans’ experiences with TF-EBP and general mental health care with potential process-improvement implications (7 themes).21 Seven themes were identified related to experiences with TF-EBP engagement and VA mental health care. The 7 themes related to TF-EBP engagement and VA mental health care themes are summarized with exemplary quotations.
Veterans want a better understanding of psychotherapy and engaging with VA mental health. Veterans reported that they generally had a poor or “nebulous” understanding about the experience of psychotherapy. For example, veterans exhibited confusion about whether certain experiences were equivalent to participating in psychotherapy. They were sometimes unable to distinguish between interactions such as assessment, disability evaluations, peer support, and psychotherapy. One veteran described a conversation with a TFEBP therapist about prior treatment:
She [asked], have you ever been, or gone through a therapy to begin with? And I, I said, well I just chatted with somebody. And she said that’s not, that’s not therapy. So, I was like, oh, it’s not? That’s not what people do?
Veterans were surprised the VA offered a diverse range of psychotherapy interventions, rather than simply therapy. They did not realize there were different types of psychotherapy. As a result, veterans were not aware that some VA mental practitioners have specialty training and certification to provide treatment matched to specific diagnoses or needs. They thought that all clinicians could provide the same care. One veteran described their understanding:
I just figured all mental health people are mental health people. I didn’t have a better understanding of the system and all the different levels and how it plays out and specialties and things like that. Which, I guess, I should have because you have a primary care doctor, but then you have specialists in all these other different sectors that specialize in one particular area. I guess that should’ve been common sense, but it wasn’t.
Stigma was a barrier to seeking and engaging in mental health care. Veterans discovered they had to overcome stigma associated with seeking and engaging in mental health treatment. Military culture was often discussed as promoting stigma regarding mental health treatment. Specifically, veterans described that seeking treatment meant “either, I’m weak or I’m gonna be seen as weak.” In active-duty settings, the strategy for dealing with mental health symptoms was to “leave those feelings, you push ‘em aside,” an approach highly inconsistent with TF-EBP. In some cases, incorrect information about the VA and PTSD was presented as part of discharge from the military, leading to long-term skepticism of the VA and PTSD treatment. One veteran described his experience as part of a class on the VA compensation and pension assessment process for service-connected disabilities during his military discharge:
[A fellow discharging soldier asked] what about like PTSD, gettin’ rated for PTSD. I hear they take our weapons and stuff like we can’t own firearms and all that stuff. And [the instructor] was like, well, yes that’s a thing. He didn’t explain it like if you get compensated for PTSD you don’t lose your rights to carry a firearm or to have, to be able to go hunting.
Importantly, veterans often described how other identities (eg, race, ethnicity, gender, region of origin) interacted with military culture to enhance stigma. Hearing messaging from multiple sources reinforced beliefs that mental health treatment is inappropriate or is associated with weakness:
As a first-generation Italian, I was always taught keep your feelings to yourself. Never talk outside your family. Never bring up problems to other people and stuff like that. Same with the military. And then the old stigma working in [emergency medical services] and public safety, you’re weak if you get help.
The fundamentals of therapy, including rapport and flexibility, were important. Veterans valued nonspecific therapy factors, genuine empathy, building trust, being honest about treatment, personality, and rapport. These characteristics were almost universally described as particularly important:
I liked the fact that she made it personable and she cared. It wasn’t just like, here, we’re gonna start this. She explained it in the ways I could understand, not in medical terms, so to speak, but that’s what I liked about her. She really cared about what she did and helping me.
Flexibility was viewed as an asset, particularly when clinicians acknowledged veteran autonomy. A consistent example was when veterans were able to titrate trauma disclosure. One veteran described this flexible treatment experience: “She was right there in the room, she said, you know, at any time, you know, we could stop, we could debrief.”
Experiences of clinician flexibility and personalization of therapy were contrasted with experiences of overly rigid therapy. Overemphasis on protocols created barriers, often because treatment did not feel personalized. One veteran described how a clinician’s task-oriented approach interfered with their ability to engage in TF-EBP:
They listened, but it just didn’t seem like they were listening, because they really wanted to stay on task… So, I felt like if the person was more concerned, or more sympathetic to the things that was also going on in my life at that present time, I think I would’ve felt more comfortable talking about what was the PTSD part, too.
Veterans valued shared decision-making prior to TF-EBP initiation. Veterans typically described being involved in a shared decision-making process prior to initiating TF-EBP. During these sessions, clinicians discussed treatment options and provided veterans with a variety of materials describing treatments (eg, pamphlets, websites, videos, statistics). Most veterans appreciated being able to reflect on and discuss treatment options with their clinicians. Being given time in and out of session to review was viewed as valuable and increased confidence in treatment choice. One veteran described their experience:
I was given the information, you know, they gave me handouts, PDFs, whatever was available, and let me read over it. I didn’t have to choose anything right then and there, you know, they let me sleep on it. And I got back to them after some thought.
However, some veterans felt overwhelmed by being presented with too much information and did not believe they knew enough to make a final treatment decision. One veteran described being asked to contribute to the treatment decision:
I definitely asked [the clinician] to weigh in on maybe what he thought was best, because—I mean, I don’t know… I’m not necessarily sure I know what I think is best. I think we’re just lucky I’m here, so if you can give me a solid and help me out here by telling me just based on what I’ve said to you and the things that I’ve gone through, what do you think?
Veterans who perceived that their treatment preferences were respected had a positive outlook on TF-EBP. As part of the shared-decision making process, veterans typically described being given choices among PTSD treatments. One way that preferences were respected was through clinicians tailoring treatment descriptions to a veteran’s unique symptoms, experiences, and values. In these cases, clinicians observed specific concerns and clearly linked treatment principles to those concerns. For example, one veteran described their clinician’s recommendation for PE: “The hardest thing for me is to do the normal things like grocery store or getting on a train or anything like that. And so, he suggested that [PE] would be a good idea.”
In other cases, veterans wanted the highest quality of treatment rather than a match between treatment principles and the veteran’s presentation, goals, or strengths. These veterans wanted the best treatment available for PTSD and valued research support, recommendations from clinical practice guidelines, or clinician confidence in the effectiveness of the treatment. One veteran described this perspective:
I just wanted to be able to really tackle it in the best way possible and in the most like aggressive way possible. And it seemed like PE really was going to, they said that it’s a difficult type of therapy, but I really just wanted to kind of do the best that I could to eradicate some of the issues that I was having.
When veterans perceived a lack of respect for their preferences, they were hesitant about TF-EBP. For some veterans, a generic pitch for a TF-EBP was detrimental in the absence of the personal connection between the treatment and their own symptoms, goals, or strengths. These veterans did not question whether the treatment was effective in general but did question whether the treatment was best for them. One veteran described the contrast between their clinician’s perspective and their own.
I felt like they felt very comfortable, very confident in [CPT] being the program, because it was comfortable for them. Because they did it several times. And maybe they had a lot of success with other individuals... but they were very comfortable with that one, as a provider, more than: Is this the best fit for [me]?
Some veterans perceived little concern for their preferences and a lack of choice in available treatments, which tended to perpetuate negative perceptions of TFEBP. These veterans described their lack of choices with frustration. Alternatives to TFEBP were described by these veterans as so undesirable that they did not believe they had a real choice:
[CPT] was the only decision they had. There was nothing else for PTSD. They didn’t offer anything else. So, I mean it wasn’t a decision. It was either … take treatment or don’t take treatment at all… Actually, I need to correct myself. So, there were 2 options, group therapy or CPT. I forgot about that. I’m not a big group guy so I chose the CPT.
Another veteran was offered a choice between therapeutic approaches, but all were delivered via telehealth (consistent with the transition to virtual services during the COVID-19 pandemic). For this veteran, not only was the distinction between approaches unclear, but the choice between approaches was unimportant compared to the mode of delivery.
This happened during COVID-19 and VA stopped seeing anybody physically, face-to-face. So my only option for therapy was [telehealth]… There was like 3 of them, and I tried to figure out, you know, from the layperson’s perspective, like: I don’t know which one to go with.
Veterans wanted to be asked about their cultural identity. Veterans valued when clinicians asked questions about cultural identity as part of their mental health treatment and listened to their cultural context. Cultural identity factors extended beyond factors such as race, ethnicity, gender, and sexual orientation to religion, military culture, and regionality. Veterans often described situations where they wished clinicians would ask the question or initiate conversations about culture. A veteran highlighted the importance of their faith but noted that it was a taboo topic. Their clinician did not say “we don’t go there,” but they “never dove into it either.” Another veteran expressed a desire for their clinician to ask questions about experiences in the National Guard and as an African American veteran:
If a provider was to say like: Oh, you know, it’s a stressful situation being a part of the military, being in the National Guard. You know, just asking questions about that. I think that would really go a long way… Being African American was difficult as well. And more so because of my region, I think… I felt like it would probably be an uncomfortable subject to speak on… I mean, it wasn’t anything that my providers necessarily did, it was more so just because it wasn’t brought up.
One common area of concern for veterans was a match between veteran and therapist demographics. When asked about how their cultural identity influenced treatment, several veterans described the relevance of therapist match. Much like questions about their own cultural identity, veterans valued being asked about identity preferences in clinicians (eg, gender or race matching), rather than having to bring up the preference themselves. One veteran described relief at this question being asked directly: “I was relieved when she had asked [whether I wanted a male or female clinician] primarily because I was going to ask that or bring that up somehow. But her asking that before me was a weight off my shoulders.”
Discussing cultural identity through treatment strengthened veterans’ engagement in therapy. Many veterans appreciated when analogies used in therapy were relevant to their cultural experiences and when clinicians understood their culture (eg, military culture, race, ethnicity, religious beliefs, sexual orientation). One veteran described how their clinician understood military culture and made connections between military culture and the rationale for TF-EBP, which strengthened the veteran’s buy-in for the treatment and alliance with the clinician:
At the beginning when she was explaining PTSD, and I remember she said that your brain needed to think this way when you were in the military because it was a way of protecting and surviving, so your brain was doing that in order for you to survive in whatever areas you were because there was danger. So, your brain had you thinking that way. But now, you’re not in those situations anymore. You’re not in danger. You’re not in the military, but your brain is still thinking you are, and that’s what PTSD generally does to you.
Specific elements of TF-EBP also provided opportunities to discuss and integrate important aspects of identity. This is accomplished in PE by assigning relevant in vivo exercises. In CPT, “connecting the dots” on how prior experiences influenced trauma-related stuck points achieved this element. One veteran described their experience with a clinician who was comfortable discussing the veteran’s sexual orientation and recognized the impacts of prior trauma on intimacy:
They’re very different, and there’s a lot of things that can be accepted in gay relationships that are not in straight ones. With all that said, I think [the PE therapist] did a fantastic job being not—like never once did she laugh or make an uncomfortable comment or say she didn’t wanna talk about something when like part of the reason I wanted to get into therapy is that my partner and I weren’t having sex unless I used alcohol.
Discussion
As part of a larger national qualitative investigation of the experiences of veterans who recently initiated TF-EBP, veterans discussed their experiences with therapy and mental health care that have important implications for continued process improvement.21 Three key areas for continued process improvement were identified: (1) providing information about the diverse range of mental health care services at the VA and the implications of this continuum of care; (2) consideration of veteran preferences in treatment decision-making, including the importance of perceived choice; and (3) incorporating cultural assessment and cultural responsiveness into case conceptualization and treatment.
One area of process improvement identified was increasing knowledge about different types of psychotherapy and the continuum of care available at the VA. Veterans in this study confused or conflated participating in psychotherapy with talking about mental health symptoms with a clinician (eg, assessment, disability evaluation). They were sometimes surprised that psychotherapy is an umbrella term referring to a variety of different modalities. The downstream impact of these misunderstandings was a perception of VA mental health care as nebulous. Veterans were surprised that all mental health practitioners were unable to provide the same care. Confusion may have been compounded by highly variable referral processes across VA.24 To address this, clinicians have developed local educational resources and handouts for both veterans and referring clinicians from nonmental health and general mental health specialties.25 Given the variability in referral processes both between and within VA medical centers, national dissemination of these educational materials may be more difficult compared to materials for TF-EBPs.24 The VA started to use behavioral health interdisciplinary program (BHIP) teams, which are designed to be clinical homes for veterans connected with a central clinician who can explain and coordinate their mental health care as well as bring more consistency to the referral process.26 The ongoing transition toward the BHIP model of mental health care at VA may provide the opportunity to consolidate and integrate knowledge about the VA approach to mental health care, potentially filling knowledge gaps.
A second area of process improvement focused on the shared decision-making process. Consistent with mental health initiatives, veterans generally believed they had received sufficient information about TF-EBP and engaged in shared decision-making with clinicians.20,27 Veterans were given educational materials to review and had the opportunity to discuss these materials with clinicians. However, veterans described variability in the success of shared decision-making. Although veterans valued receiving accurate, comprehensible information to support treatment decisions, some preferred to defer to clinicians’ expertise regarding which treatment to pursue. While these veterans valued information, they also valued the expertise of clinicians in explaining why specific treatments would be beneficial. A key contributor to veterans satisfaction was assessing how veterans wanted to engage in the decision-making process and respecting those preferences.28 Veterans approached shared decision-making differently, from making decisions independently after receiving information to relying solely on clinician recommendation. The process was most successful when clinicians articulated how their recommended treatment aligned with a veteran’s preferences, including recommendations based on specific values (eg, personalized match vs being the best). Another important consideration is ensuring veterans know they can receive a variety of different types of mental health services available in different modalities (eg, virtual vs in-person; group vs individual). When veterans did not perceive choice in treatment aspects important to them (typically despite having choices), they were less satisfied with their TF-EBP experience.
A final area of process improvement identified involves how therapists address important aspects of culture. Veterans often described mental health stigma coming from intersecting cultural identities and expressed appreciation when therapists helped them recognize the impact of these beliefs on treatment. Some veterans did not discuss important aspects of their identity with clinicians, including race/ethnicity, religion, and military culture. Veterans did not report negative interactions with clinicians or experiences suggesting it was inappropriate to discuss identity; however, they were reluctant to independently raise these identity factors. Strategies such as the ADDRESSING framework, a mnemonic acronym that describes a series of potentially relevant characteristics, can help clinicians comprehensively consider different aspects that may be relevant to veterans, modeling that discussion of relevant these characteristics is welcome in TF-EBP.29 Veterans reported that making culturally relevant connections enhanced the TF-EBP experience, most commonly with military culture. These data support that TF-EBP delivery with attention to culture should be an integrated part of treatment, supporting engagement and therapeutic alliance.30 The VA National Center for PTSD consultation program is a resource to support clinicians in assessing and incorporating relevant aspects of cultural identity.31 For example, the National Center for PTSD provides a guide for using case conceptualization to address patient reactions to race-based violence during PTSD treatment.32 Both manualized design and therapist certification training can reinforce that assessing and attending to case conceptualization (including identity factors) is an integral component of TF-EBP.33,34
Limitations
While the current study has numerous strengths (eg, national veteran sampling, robust qualitative methods), results should be considered within the context of study limitations. First, veteran participants all received TF-EBP, and the perspectives of veterans who never initiate TF-EBP may differ. Despite the strong sampling approach, the study design is not intended to be generalizable to all veterans receiving TF-EBP for PTSD. Qualitative analysis yielded 15 themes, described in this study and prior research, consistent with recommendations.21,22 This approach allows rich description of distinct focus areas that would not be possible in a single manuscript. Nonetheless, all veterans interviewed described their experiences in TF-EBP and general mental health care, the focus of the semistructured interview guide was on the experience of transitioning from other treatment to TF-EBP.
Conclusion
This study describes themes related to general mental health and TF-EBP process improvement as part of a larger study on transitions in PTSD care.21,22 Veterans valued the fundamentals of therapy, including rapport and flexibility. Treatment-specific rapport (eg, pointing out treatment progress and effort in completing treatment components) and flexibility within the context of fidelity (ie, personalizing treatment while maintaining core treatment elements) may be most effective at engaging veterans in recommended PTSD treatments.18,34 In addition to successes, themes suggest multiple opportunities for process improvement. Ongoing VA initiatives and priorities (ie, BHIP, shared decision-making, consultation services) aim to improve processes consistent with veteran recommendations. Future research is needed to evaluate the success of these and other programs to optimize access to and engagement in recommended PTSD treatments.
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
- US Department of Veterans Affairs; US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. 2023. Updated August 20, 2025. Accessed October 17, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/
- International Society for Traumatic Stress Studies. ISTSS PTSD prevention and treatment guidelines: methodology and recommendations. Accessed August 13, 2025. http://www.istss.org/getattachment/Treating-Trauma/New-ISTSS-Prevention-and-TreatmentGuidelines/ISTSS_PreventionTreatmentGuidelines_FNL-March-19-2019.pdf.aspx
- American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. Accessed August 13, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- Karlin BE, Cross G. From the laboratory to the therapy room: National dissemination and implementation of evidence- based psychotherapies in the U.S. Department of Veterans Affairs Health Care System. Am Psychol. 2014;69:19-33. doi:10.1037/a0033888
- Rosen CS, Matthieu MM, Wiltsey Stirman S, et al. A review of studies on the system-wide implementation of evidencebased psychotherapies for posttraumatic stress disorder in the Veterans Health Administration. Adm Policy Ment Health. 2016;43:957-977. doi:10.1007/s10488-016-0755-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37:356-364. doi:10.1002/da.22983
- Cheney AM, Koenig CJ, Miller CJ, et al. Veteran-centered barriers to VA mental healthcare services use. BMC Health Serv Res. 2018;18:591. doi:10.1186/s12913-018-3346-9
- Hundt NE, Mott JM, Miles SR, et al. Veterans’ perspectives on initiating evidence-based psychotherapy for posttraumatic stress disorder. Psychol Trauma. 2015;7:539-546. doi:10.1037/tra0000035
- Hundt NE, Helm A, Smith TL, et al. Failure to engage: a qualitative study of veterans who decline evidence-based psychotherapies for PTSD. Psychol Serv. 2018;15:536- 542. doi:10.1037/ser0000212
- Sayer NA, Friedemann-Sanchez G, Spoont M, et al. A qualitative study of determinants of PTSD treatment initiation in veterans. Psychiatry. 2009;72:238-255. doi:10.1521/psyc.2009.72.3.238
- Mittal D, Drummond KL, Blevins D, et al. Stigma associated with PTSD: perceptions of treatment seeking combat veterans. Psychiatr Rehabil J. 2013;36:86-92. doi:10.1037/h0094976
- Possemato K, Wray LO, Johnson E, et al. Facilitators and barriers to seeking mental health care among primary care veterans with posttraumatic stress disorder. J Trauma Stress. 2018;31:742-752. doi:10.1002/jts.22327
- Silvestrini M, Chen JA. “It’s a sign of weakness”: Masculinity and help-seeking behaviors among male veterans accessing posttraumatic stress disorder care. Psychol Trauma. 2023;15:665-671. doi:10.1037/tra0001382
- Stecker T, Shiner B, Watts BV, et al. Treatment-seeking barriers for veterans of the Iraq and Afghanistan conflicts who screen positive for PTSD. Psychiatr Serv. 2013;64:280-283. doi:10.1176/appi.ps.001372012
- Etingen B, Grubbs KM, Harik JM. Drivers of preference for evidence-based PTSD treatment: a qualitative assessment. Mil Med. 2020;185:303-310. doi:10.1093/milmed/usz220
- Hundt NE, Ecker AH, Thompson K, et al. “It didn’t fit for me:” A qualitative examination of dropout from prolonged exposure and cognitive processing therapy in veterans. Psychol Serv. 2020;17:414-421. doi:10.1037/ser0000316
- Kehle-Forbes SM, Gerould H, Polusny MA, et al. “It leaves me very skeptical” messaging in marketing prolonged exposure and cognitive processing therapy to veterans with PTSD. Psychol Trauma. 2022;14:849-852. doi:10.1037/tra0000550
- Kehle-Forbes SM, Ackland PE, Spoont MR, et al. Divergent experiences of U.S. veterans who did and did not complete trauma-focused therapies for PTSD: a national qualitative study of treatment dropout. Behav Res Ther. 2022;154:104123. doi:10.1016/j.brat.2022.104123
- Hessinger JD, London MJ, Baer SM. Evaluation of a shared decision-making intervention on the utilization of evidence-based psychotherapy in a VA outpatient PTSD clinic. Psychol Serv. 2018;15:437-441. doi:10.1037/ser0000141
- Hamblen JL, Grubbs KM, Cole B, et al. “Will it work for me?” Developing patient-friendly graphical displays of posttraumatic stress disorder treatment effectiveness. J Trauma Stress. 2022;35:999-1010. doi:10.1002/jts.22808
- Holder N, Ranney RM, Delgado AK, et al. Transitioning into trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatments: a qualitative investigation. Cogn Behav Ther. 2025;54:391-407. doi:10.1080/16506073.2024.2408386
- Levitt HM, Bamberg M, Creswell JW, et al. Journal article reporting standards for qualitative primary, qualitative meta-analytic, and mixed methods research in psychology: The APA Publications and Communications Board task force report. Am Psychol. 2018;73:26-46. doi:10.1037/amp0000151
- Palinkas LA, Mendon SJ, Hamilton AB. Innovations in mixed methods evaluations. Annu Rev Public Health. 2019;40:423- 442. doi:10.1146/annurev-publhealth-040218-044215
- Ranney RM, Cordova MJ, Maguen S. A review of the referral process for evidence-based psychotherapies for PTSD among veterans. Prof Psychol Res Pr. 2022;53:276-285. doi:10.1037/pro0000463
- Holder N, Ranney RM, Delgado AK, et al. Transitions to trauma-focused evidence-based psychotherapy for posttraumatic stress disorder from other treatment: a qualitative investigation of clinician’s perspectives. Cogn Behav Ther. 2025;1-19. doi:10.1080/16506073.2025.2481475
- Barry CN, Abraham KM, Weaver KR, et al. Innovating team-based outpatient mental health care in the Veterans Health Administration: staff-perceived benefits and challenges to pilot implementation of the Behavioral Health Interdisciplinary Program (BHIP). Psychol Serv. 2016;13:148-155. doi:10.1037/ser0000072
- Harik JM, Hundt NE, Bernardy NC, et al. Desired involvement in treatment decisions among adults with PTSD symptoms. J Trauma Stress. 2016;29:221-228. doi:10.1002/jts.22102
- Larsen SE, Hooyer K, Kehle-Forbes SM, et al. Patient experiences in making PTSD treatment decisions. Psychol Serv. 2024;21:529-537. doi:10.1037/ser0000817
- Hays PA. Four steps toward intersectionality in psychotherapy using the ADDRESSING framework. Prof Psychol Res Pr. 2024;55:454-462. doi:10.1037/pro0000577
- Galovski TE, Nixon RDV, Kaysen D. Flexible Applications of Cognitive Processing Therapy: Evidence-Based Treatment Methods. Academic Press; 2020.
- Larsen SE, McKee T, Fielstein E, et al. The development of a posttraumatic stress disorder (PTSD) consultation program to support system-wide implementation of high-quality PTSD care for veterans. Psychol Serv. 2025;22:342-348. doi:10.1037/ser0000867
- Galovski T, Kaysen D, McClendon J, et al. Provider guide to addressing patient reactions to race-based violence during PTSD treatment. PTSD.va.gov. Accessed August 3, 2025. www.ptsd.va.gov/professional/treat/specific/patient_reactions_race_violence.asp
- Galovski TE, Nixon RDV, Kehle-Forbes S. Walking the line between fidelity and flexibility: a conceptual review of personalized approaches to manualized treatments for posttraumatic stress disorder. J Trauma Stress. 2024;37:768-774. doi:10.1002/jts.23073
- Galovski TE, McSweeney LB, Nixon RDV, et al. Personalizing cognitive processing therapy with a case formulation approach to intentionally target impairment in psychosocial functioning associated with PTSD. Contemp Clin Trials Commun. 2024;42:101385. doi:10.1016/j.conctc.2024.101385
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Process Improvement for Engaging With Trauma-Focused Evidence-Based Psychotherapy for PTSD
Veterans and Loneliness: More Than Just Isolation
According to the National Institute on Drug Abuse, > 1 in 10 veterans have been diagnosed with substance use disorder (SUD). Additionally, 7 out of every 100 veterans will have posttraumatic stress disorder (PTSD) at some point in their life, per research from the US Department of Veterans Affairs (VA). However, a common and perhaps unsuspected parallel is found in those statistics: loneliness.
Of the 4069 veterans who participated in the 2019-2020 National Health and Resilience in Veterans Survey, 56.9% reported they felt lonely sometimes or often, while 1 in 5 reported feeling lonely often.
An Epidemic
In his 2023 advisory, Former US Surgeon General Vivek Murthy called it an epidemic noting that when he spoke with veterans during a cross-country listening tour, he heard how they felt “isolated, invisible, and insignificant.” About 1 in 2 adults in America experience loneliness, even before the COVID-19 pandemic isolation.
Loneliness can have individual and synergistic ill effects, including a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. It also can both trigger and exacerbate substance use and PTSD.
A study using data from the RAND Health and Retirement Study Longitudinal File 2020 (N = 5259) found significant associations between loneliness and being unmarried/unpartnered, and greater depressive symptoms for both veterans and civilians, as well as significant negative associations between loneliness and greater life satisfaction and positive affect. Health conditions that limited an individual's ability to work was a “unique risk factor for loneliness among veterans.”
The National Health and Resilience in Veterans Study found that those aged ≤ 50 years were 3 times more likely to screen positive for PTSD compared to older veterans. In a survey of 409 veterans, many who engaged in problematic substance use during the COVID-19 pandemic reported that despite having social supports they still felt lonely. In regression analyses, higher levels of loneliness were associated with more negative impacts of the pandemic, greater substance use, and poorer physical and mental health functioning.
Addressing Loneliness
Researchers believe an answer to some mental health and substance abuse problems may lie in addressing loneliness. Positive psychology is providing promising results in the treatment of SUD. Bryant Stone, from the Johns Hopkins Bloomberg School of Public Health, emphasizes focusing on well-being and quality of life rather than solely on abstinence with “positive psychological interventions,” or activities and behavioral interventions that target positive variables to promote adaptive functioning.
Veterans can face tough challenges as they rejoin civilian life. How successfully they meet and conquer those challenges, especially if they include drug problems, may directly relate to their general feeling of well-being.
The PERMA model outlines 5 core elements to assess well-being: Positive emotions, Engagement, Relationships, Meaning, and Accomplishment. A study based on that model found loneliness to be a “particularly significant factor” among key variables influencing the prevention and treatment of SUDs. The study of 156 veterans with self-reported mental health conditions found the ability to engage in social roles and activities was positively correlated with overall well-being and negatively correlated with degree of problems related to drug abuse.
Rural Veterans
The estimated 4.4 million veterans living in rural communities may benefit most from interventions that tackle isolation. Compared with urban counterparts, they’re more likely to be older, have more complex medical issues, have a service-connected disability, and be unemployed. Those factors, compounded by geographical and social isolation, can have a substantial impact on well-being.
A study centered on the initial validation of a short (5-item) version of PERMA found that individuals who scored higher on the short form tended to report higher levels of optimism, resilience, and happiness. Thus, the short form may be particularly useful for rural veterans who do not always have easy access to health care.
VA has instituted a variety of programs to encourage and support social connection. During the COVID-19 pandemic, telehealth interventions targeted social support and loneliness among veterans—albeit with mixed results. VA CONNECT, a 10-session group telehealth intervention that integrated peer support, did not show significant changes in loneliness, but did significantly reduce perceived stress.
Another initiative, Compassionate Contact Corps, trained volunteers made weekly phone calls aimed at reducing loneliness and fostering social connection. Started in Columbus, Ohio, in 2020, > 80 sites had adopted the initiative by 2021, with 310 volunteers, 5320 visits, and 4757 hours spent with veterans.
In 2014, VA peer specialists developed and co-hosted Veterans Socials through community partnerships between VA, veteran-serving organizations, and veteran community leaders. As of 2025, 178 known Veterans Socials were spread across 26 states and territories.
The researchers say their case examples collectively demonstrate that Veterans Socials have the potential to serve as a vital platform for peer support, resource sharing, and health service use among veterans. Virtual Veterans Socials also provided hosts with a channel to reach potentially isolated veterans who might not otherwise access services while simultaneously offering veterans an opportunity for social connection.
According to the National Institute on Drug Abuse, > 1 in 10 veterans have been diagnosed with substance use disorder (SUD). Additionally, 7 out of every 100 veterans will have posttraumatic stress disorder (PTSD) at some point in their life, per research from the US Department of Veterans Affairs (VA). However, a common and perhaps unsuspected parallel is found in those statistics: loneliness.
Of the 4069 veterans who participated in the 2019-2020 National Health and Resilience in Veterans Survey, 56.9% reported they felt lonely sometimes or often, while 1 in 5 reported feeling lonely often.
An Epidemic
In his 2023 advisory, Former US Surgeon General Vivek Murthy called it an epidemic noting that when he spoke with veterans during a cross-country listening tour, he heard how they felt “isolated, invisible, and insignificant.” About 1 in 2 adults in America experience loneliness, even before the COVID-19 pandemic isolation.
Loneliness can have individual and synergistic ill effects, including a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. It also can both trigger and exacerbate substance use and PTSD.
A study using data from the RAND Health and Retirement Study Longitudinal File 2020 (N = 5259) found significant associations between loneliness and being unmarried/unpartnered, and greater depressive symptoms for both veterans and civilians, as well as significant negative associations between loneliness and greater life satisfaction and positive affect. Health conditions that limited an individual's ability to work was a “unique risk factor for loneliness among veterans.”
The National Health and Resilience in Veterans Study found that those aged ≤ 50 years were 3 times more likely to screen positive for PTSD compared to older veterans. In a survey of 409 veterans, many who engaged in problematic substance use during the COVID-19 pandemic reported that despite having social supports they still felt lonely. In regression analyses, higher levels of loneliness were associated with more negative impacts of the pandemic, greater substance use, and poorer physical and mental health functioning.
Addressing Loneliness
Researchers believe an answer to some mental health and substance abuse problems may lie in addressing loneliness. Positive psychology is providing promising results in the treatment of SUD. Bryant Stone, from the Johns Hopkins Bloomberg School of Public Health, emphasizes focusing on well-being and quality of life rather than solely on abstinence with “positive psychological interventions,” or activities and behavioral interventions that target positive variables to promote adaptive functioning.
Veterans can face tough challenges as they rejoin civilian life. How successfully they meet and conquer those challenges, especially if they include drug problems, may directly relate to their general feeling of well-being.
The PERMA model outlines 5 core elements to assess well-being: Positive emotions, Engagement, Relationships, Meaning, and Accomplishment. A study based on that model found loneliness to be a “particularly significant factor” among key variables influencing the prevention and treatment of SUDs. The study of 156 veterans with self-reported mental health conditions found the ability to engage in social roles and activities was positively correlated with overall well-being and negatively correlated with degree of problems related to drug abuse.
Rural Veterans
The estimated 4.4 million veterans living in rural communities may benefit most from interventions that tackle isolation. Compared with urban counterparts, they’re more likely to be older, have more complex medical issues, have a service-connected disability, and be unemployed. Those factors, compounded by geographical and social isolation, can have a substantial impact on well-being.
A study centered on the initial validation of a short (5-item) version of PERMA found that individuals who scored higher on the short form tended to report higher levels of optimism, resilience, and happiness. Thus, the short form may be particularly useful for rural veterans who do not always have easy access to health care.
VA has instituted a variety of programs to encourage and support social connection. During the COVID-19 pandemic, telehealth interventions targeted social support and loneliness among veterans—albeit with mixed results. VA CONNECT, a 10-session group telehealth intervention that integrated peer support, did not show significant changes in loneliness, but did significantly reduce perceived stress.
Another initiative, Compassionate Contact Corps, trained volunteers made weekly phone calls aimed at reducing loneliness and fostering social connection. Started in Columbus, Ohio, in 2020, > 80 sites had adopted the initiative by 2021, with 310 volunteers, 5320 visits, and 4757 hours spent with veterans.
In 2014, VA peer specialists developed and co-hosted Veterans Socials through community partnerships between VA, veteran-serving organizations, and veteran community leaders. As of 2025, 178 known Veterans Socials were spread across 26 states and territories.
The researchers say their case examples collectively demonstrate that Veterans Socials have the potential to serve as a vital platform for peer support, resource sharing, and health service use among veterans. Virtual Veterans Socials also provided hosts with a channel to reach potentially isolated veterans who might not otherwise access services while simultaneously offering veterans an opportunity for social connection.
According to the National Institute on Drug Abuse, > 1 in 10 veterans have been diagnosed with substance use disorder (SUD). Additionally, 7 out of every 100 veterans will have posttraumatic stress disorder (PTSD) at some point in their life, per research from the US Department of Veterans Affairs (VA). However, a common and perhaps unsuspected parallel is found in those statistics: loneliness.
Of the 4069 veterans who participated in the 2019-2020 National Health and Resilience in Veterans Survey, 56.9% reported they felt lonely sometimes or often, while 1 in 5 reported feeling lonely often.
An Epidemic
In his 2023 advisory, Former US Surgeon General Vivek Murthy called it an epidemic noting that when he spoke with veterans during a cross-country listening tour, he heard how they felt “isolated, invisible, and insignificant.” About 1 in 2 adults in America experience loneliness, even before the COVID-19 pandemic isolation.
Loneliness can have individual and synergistic ill effects, including a greater risk of cardiovascular disease, dementia, stroke, depression, anxiety, and premature death. It also can both trigger and exacerbate substance use and PTSD.
A study using data from the RAND Health and Retirement Study Longitudinal File 2020 (N = 5259) found significant associations between loneliness and being unmarried/unpartnered, and greater depressive symptoms for both veterans and civilians, as well as significant negative associations between loneliness and greater life satisfaction and positive affect. Health conditions that limited an individual's ability to work was a “unique risk factor for loneliness among veterans.”
The National Health and Resilience in Veterans Study found that those aged ≤ 50 years were 3 times more likely to screen positive for PTSD compared to older veterans. In a survey of 409 veterans, many who engaged in problematic substance use during the COVID-19 pandemic reported that despite having social supports they still felt lonely. In regression analyses, higher levels of loneliness were associated with more negative impacts of the pandemic, greater substance use, and poorer physical and mental health functioning.
Addressing Loneliness
Researchers believe an answer to some mental health and substance abuse problems may lie in addressing loneliness. Positive psychology is providing promising results in the treatment of SUD. Bryant Stone, from the Johns Hopkins Bloomberg School of Public Health, emphasizes focusing on well-being and quality of life rather than solely on abstinence with “positive psychological interventions,” or activities and behavioral interventions that target positive variables to promote adaptive functioning.
Veterans can face tough challenges as they rejoin civilian life. How successfully they meet and conquer those challenges, especially if they include drug problems, may directly relate to their general feeling of well-being.
The PERMA model outlines 5 core elements to assess well-being: Positive emotions, Engagement, Relationships, Meaning, and Accomplishment. A study based on that model found loneliness to be a “particularly significant factor” among key variables influencing the prevention and treatment of SUDs. The study of 156 veterans with self-reported mental health conditions found the ability to engage in social roles and activities was positively correlated with overall well-being and negatively correlated with degree of problems related to drug abuse.
Rural Veterans
The estimated 4.4 million veterans living in rural communities may benefit most from interventions that tackle isolation. Compared with urban counterparts, they’re more likely to be older, have more complex medical issues, have a service-connected disability, and be unemployed. Those factors, compounded by geographical and social isolation, can have a substantial impact on well-being.
A study centered on the initial validation of a short (5-item) version of PERMA found that individuals who scored higher on the short form tended to report higher levels of optimism, resilience, and happiness. Thus, the short form may be particularly useful for rural veterans who do not always have easy access to health care.
VA has instituted a variety of programs to encourage and support social connection. During the COVID-19 pandemic, telehealth interventions targeted social support and loneliness among veterans—albeit with mixed results. VA CONNECT, a 10-session group telehealth intervention that integrated peer support, did not show significant changes in loneliness, but did significantly reduce perceived stress.
Another initiative, Compassionate Contact Corps, trained volunteers made weekly phone calls aimed at reducing loneliness and fostering social connection. Started in Columbus, Ohio, in 2020, > 80 sites had adopted the initiative by 2021, with 310 volunteers, 5320 visits, and 4757 hours spent with veterans.
In 2014, VA peer specialists developed and co-hosted Veterans Socials through community partnerships between VA, veteran-serving organizations, and veteran community leaders. As of 2025, 178 known Veterans Socials were spread across 26 states and territories.
The researchers say their case examples collectively demonstrate that Veterans Socials have the potential to serve as a vital platform for peer support, resource sharing, and health service use among veterans. Virtual Veterans Socials also provided hosts with a channel to reach potentially isolated veterans who might not otherwise access services while simultaneously offering veterans an opportunity for social connection.
PET and CPT Show Promise in Veteran PTSD Treatment
Posttraumatic stress disorder (PTSD) guidelines increasingly are recommending prolonged exposure therapy (PET) and cognitive processing therapy (CPT) as first-line treatments, including the 2023 US Department of Veterans Affairs (VA) and US Department of Defense clinical practice guideline.
Since 2006, > 6000 VA therapists have been trained in PET and CPT; the VA requires all veterans to have access to these treatments. However, despite strong clinical trial evidence supporting PET and CPT for the treatment of PTSD, a 2023 study found that only 11.6% of veterans who received a PTSD diagnosis between 2017 and 2019 initiated Trauma-Focused Evidence-Based Psychotherapy (TF-EBP) in their first year of treatment. Of those who initiated TF-EBP, 67% dropped out. Recent VA programs have attempted to expand the reach of PET with video telehealth to reach rural and remote veterans through virtual group programs.
Recent research has suggested ways to maximize the effectiveness of the programs and assist veterans in receiving the full benefits. Studies have found that swapping traditional longer-term treatments (usually spanning 8 to 15 weeks) for intensified, shorter versions (eg, 6 sessions) may enhance engagement and retention.
Intensive PET for PTSD is safe and highly effective. A study involving patients with chronic PTSD and complex trauma showed significant reductions in PTSD symptom severity, with large effect sizes and sustained improvements at 3 and 6 months. Multiple 90-minute sessions over consecutive days, supplemented with in vivo exposure or followed by weekly booster sessions, were found to minimize treatment disruptions.
PET is among the most extensively studied treatments for PTSD and is supported by dozens of clinical trials involving thousands of patients. The intervention was originally developed and validated in civilian samples and includes psychoeducation, relaxation through breathing retraining, and in vivo and imaginal exposure to traumatic memories.
A recent study compared treatment outcomes among military veterans and civilian patients receiving treatment in a community setting. Although some studies have compared PET outcomes for military veterans and civilian participants in community settings, none have directly compared outcomes across trauma type (combat, terror, or civilian trauma) and veteran status (military vs civilian) within the same framework. The study notes that combat-related trauma significantly differs from other forms of trauma exposure, as it is typically more prolonged and severe and therefore is more often resistant to treatment. Military personnel also often find themselves both victims and aggressors, a duality that can intensify guilt, shame, anger, disgust, and emotional reactions to moral injury, complicating treatment.
The study assessed the effects of 8 to 15 PET sessions on PTSD symptoms in 55 civilians and 43 veterans using the PTSD Symptom Scale–Interview Version (PSS-I). Participants showed significant symptom reductions across all trauma types and veteran statuses.
Although veterans and participants in the combat trauma subgroup showed higher levels of baseline symptom severity compared with civilians, all groups experienced similar symptom reductions. These findings differ from some meta-analyses, which have found that PET often produces smaller effect sizes in combat-related PTSD compared to civilian trauma samples.
The study compared treatment outcomes across different groups within the same treatment centers and under consistent supervision. The PET intervention was delivered in community mental health centers to all patients regardless of background. Only 2 prior studies have compared civilian and military veterans within the same locations.
Although the “traditional” number of PET sessions produce evidence-based outcomes, high dropout rates and relapses have catalyzed interest in approaches that boost the power of therapy, such as delivering PET in ever-shorter sequences.
A study in a Swedish psychiatric outpatient clinic compared the effect of an 8-day intensified treatment program with traditionally spaced treatments on 101 participants with PTSD or complex PTSD. The study reported a significant reduction in PTSD symptoms at posttreatment, with large effect sizes in both conditions. Moreover, symptom reduction was maintained at follow-up. Dropout rates were significantly different between treatment groups: 4.3% in the intensified treatment program and 24.1% in the traditional group.
Another study used VA administrative data to assess the impact of sequenced psychotherapy (≥ 8 sessions of not trauma-focused individual or group psychotherapy delivered before trauma-focused care) on initiation and retention in CPT and PET over 2 years. Roughly 13% of 490,097 veterans who entered care for PTSD between 2014 and 2020 initiated VA-disseminated evidence-based treatment within 21 months (9.5% CPT, 3.4% PE). Among those who initiated treatment, retention was 46% and 42%, respectively. Individual therapy was associated with increased CPT and PET retention of 8.0% and 8.2%. For group therapy, retention increases were 3.4% and 8.7%.
Another recent study examined the RESET (Reconsolidation, Exposure, and Short-term Emotional Transformation) clinical protocol, an intensive, structured trauma-focused intervention designed to treat PTSD within 6 daily sessions. The protocol includes psychoeducation, targeted exposure, dynamic case formulation, and guided trauma processing. This novel framework ensures therapy moves beyond symptom reduction, fostering a deep understanding of the patient’s core struggles and their broader psychological patterns, and integrates it with the reconsolidation of the index trauma narrative to form a more cohesive sense of self.”
Clinical studies are ongoing to refine and enhance PET and CPT. They may serve to make therapy more useful and effective in easing—maybe erasing—veterans’ traumatic memories.
Posttraumatic stress disorder (PTSD) guidelines increasingly are recommending prolonged exposure therapy (PET) and cognitive processing therapy (CPT) as first-line treatments, including the 2023 US Department of Veterans Affairs (VA) and US Department of Defense clinical practice guideline.
Since 2006, > 6000 VA therapists have been trained in PET and CPT; the VA requires all veterans to have access to these treatments. However, despite strong clinical trial evidence supporting PET and CPT for the treatment of PTSD, a 2023 study found that only 11.6% of veterans who received a PTSD diagnosis between 2017 and 2019 initiated Trauma-Focused Evidence-Based Psychotherapy (TF-EBP) in their first year of treatment. Of those who initiated TF-EBP, 67% dropped out. Recent VA programs have attempted to expand the reach of PET with video telehealth to reach rural and remote veterans through virtual group programs.
Recent research has suggested ways to maximize the effectiveness of the programs and assist veterans in receiving the full benefits. Studies have found that swapping traditional longer-term treatments (usually spanning 8 to 15 weeks) for intensified, shorter versions (eg, 6 sessions) may enhance engagement and retention.
Intensive PET for PTSD is safe and highly effective. A study involving patients with chronic PTSD and complex trauma showed significant reductions in PTSD symptom severity, with large effect sizes and sustained improvements at 3 and 6 months. Multiple 90-minute sessions over consecutive days, supplemented with in vivo exposure or followed by weekly booster sessions, were found to minimize treatment disruptions.
PET is among the most extensively studied treatments for PTSD and is supported by dozens of clinical trials involving thousands of patients. The intervention was originally developed and validated in civilian samples and includes psychoeducation, relaxation through breathing retraining, and in vivo and imaginal exposure to traumatic memories.
A recent study compared treatment outcomes among military veterans and civilian patients receiving treatment in a community setting. Although some studies have compared PET outcomes for military veterans and civilian participants in community settings, none have directly compared outcomes across trauma type (combat, terror, or civilian trauma) and veteran status (military vs civilian) within the same framework. The study notes that combat-related trauma significantly differs from other forms of trauma exposure, as it is typically more prolonged and severe and therefore is more often resistant to treatment. Military personnel also often find themselves both victims and aggressors, a duality that can intensify guilt, shame, anger, disgust, and emotional reactions to moral injury, complicating treatment.
The study assessed the effects of 8 to 15 PET sessions on PTSD symptoms in 55 civilians and 43 veterans using the PTSD Symptom Scale–Interview Version (PSS-I). Participants showed significant symptom reductions across all trauma types and veteran statuses.
Although veterans and participants in the combat trauma subgroup showed higher levels of baseline symptom severity compared with civilians, all groups experienced similar symptom reductions. These findings differ from some meta-analyses, which have found that PET often produces smaller effect sizes in combat-related PTSD compared to civilian trauma samples.
The study compared treatment outcomes across different groups within the same treatment centers and under consistent supervision. The PET intervention was delivered in community mental health centers to all patients regardless of background. Only 2 prior studies have compared civilian and military veterans within the same locations.
Although the “traditional” number of PET sessions produce evidence-based outcomes, high dropout rates and relapses have catalyzed interest in approaches that boost the power of therapy, such as delivering PET in ever-shorter sequences.
A study in a Swedish psychiatric outpatient clinic compared the effect of an 8-day intensified treatment program with traditionally spaced treatments on 101 participants with PTSD or complex PTSD. The study reported a significant reduction in PTSD symptoms at posttreatment, with large effect sizes in both conditions. Moreover, symptom reduction was maintained at follow-up. Dropout rates were significantly different between treatment groups: 4.3% in the intensified treatment program and 24.1% in the traditional group.
Another study used VA administrative data to assess the impact of sequenced psychotherapy (≥ 8 sessions of not trauma-focused individual or group psychotherapy delivered before trauma-focused care) on initiation and retention in CPT and PET over 2 years. Roughly 13% of 490,097 veterans who entered care for PTSD between 2014 and 2020 initiated VA-disseminated evidence-based treatment within 21 months (9.5% CPT, 3.4% PE). Among those who initiated treatment, retention was 46% and 42%, respectively. Individual therapy was associated with increased CPT and PET retention of 8.0% and 8.2%. For group therapy, retention increases were 3.4% and 8.7%.
Another recent study examined the RESET (Reconsolidation, Exposure, and Short-term Emotional Transformation) clinical protocol, an intensive, structured trauma-focused intervention designed to treat PTSD within 6 daily sessions. The protocol includes psychoeducation, targeted exposure, dynamic case formulation, and guided trauma processing. This novel framework ensures therapy moves beyond symptom reduction, fostering a deep understanding of the patient’s core struggles and their broader psychological patterns, and integrates it with the reconsolidation of the index trauma narrative to form a more cohesive sense of self.”
Clinical studies are ongoing to refine and enhance PET and CPT. They may serve to make therapy more useful and effective in easing—maybe erasing—veterans’ traumatic memories.
Posttraumatic stress disorder (PTSD) guidelines increasingly are recommending prolonged exposure therapy (PET) and cognitive processing therapy (CPT) as first-line treatments, including the 2023 US Department of Veterans Affairs (VA) and US Department of Defense clinical practice guideline.
Since 2006, > 6000 VA therapists have been trained in PET and CPT; the VA requires all veterans to have access to these treatments. However, despite strong clinical trial evidence supporting PET and CPT for the treatment of PTSD, a 2023 study found that only 11.6% of veterans who received a PTSD diagnosis between 2017 and 2019 initiated Trauma-Focused Evidence-Based Psychotherapy (TF-EBP) in their first year of treatment. Of those who initiated TF-EBP, 67% dropped out. Recent VA programs have attempted to expand the reach of PET with video telehealth to reach rural and remote veterans through virtual group programs.
Recent research has suggested ways to maximize the effectiveness of the programs and assist veterans in receiving the full benefits. Studies have found that swapping traditional longer-term treatments (usually spanning 8 to 15 weeks) for intensified, shorter versions (eg, 6 sessions) may enhance engagement and retention.
Intensive PET for PTSD is safe and highly effective. A study involving patients with chronic PTSD and complex trauma showed significant reductions in PTSD symptom severity, with large effect sizes and sustained improvements at 3 and 6 months. Multiple 90-minute sessions over consecutive days, supplemented with in vivo exposure or followed by weekly booster sessions, were found to minimize treatment disruptions.
PET is among the most extensively studied treatments for PTSD and is supported by dozens of clinical trials involving thousands of patients. The intervention was originally developed and validated in civilian samples and includes psychoeducation, relaxation through breathing retraining, and in vivo and imaginal exposure to traumatic memories.
A recent study compared treatment outcomes among military veterans and civilian patients receiving treatment in a community setting. Although some studies have compared PET outcomes for military veterans and civilian participants in community settings, none have directly compared outcomes across trauma type (combat, terror, or civilian trauma) and veteran status (military vs civilian) within the same framework. The study notes that combat-related trauma significantly differs from other forms of trauma exposure, as it is typically more prolonged and severe and therefore is more often resistant to treatment. Military personnel also often find themselves both victims and aggressors, a duality that can intensify guilt, shame, anger, disgust, and emotional reactions to moral injury, complicating treatment.
The study assessed the effects of 8 to 15 PET sessions on PTSD symptoms in 55 civilians and 43 veterans using the PTSD Symptom Scale–Interview Version (PSS-I). Participants showed significant symptom reductions across all trauma types and veteran statuses.
Although veterans and participants in the combat trauma subgroup showed higher levels of baseline symptom severity compared with civilians, all groups experienced similar symptom reductions. These findings differ from some meta-analyses, which have found that PET often produces smaller effect sizes in combat-related PTSD compared to civilian trauma samples.
The study compared treatment outcomes across different groups within the same treatment centers and under consistent supervision. The PET intervention was delivered in community mental health centers to all patients regardless of background. Only 2 prior studies have compared civilian and military veterans within the same locations.
Although the “traditional” number of PET sessions produce evidence-based outcomes, high dropout rates and relapses have catalyzed interest in approaches that boost the power of therapy, such as delivering PET in ever-shorter sequences.
A study in a Swedish psychiatric outpatient clinic compared the effect of an 8-day intensified treatment program with traditionally spaced treatments on 101 participants with PTSD or complex PTSD. The study reported a significant reduction in PTSD symptoms at posttreatment, with large effect sizes in both conditions. Moreover, symptom reduction was maintained at follow-up. Dropout rates were significantly different between treatment groups: 4.3% in the intensified treatment program and 24.1% in the traditional group.
Another study used VA administrative data to assess the impact of sequenced psychotherapy (≥ 8 sessions of not trauma-focused individual or group psychotherapy delivered before trauma-focused care) on initiation and retention in CPT and PET over 2 years. Roughly 13% of 490,097 veterans who entered care for PTSD between 2014 and 2020 initiated VA-disseminated evidence-based treatment within 21 months (9.5% CPT, 3.4% PE). Among those who initiated treatment, retention was 46% and 42%, respectively. Individual therapy was associated with increased CPT and PET retention of 8.0% and 8.2%. For group therapy, retention increases were 3.4% and 8.7%.
Another recent study examined the RESET (Reconsolidation, Exposure, and Short-term Emotional Transformation) clinical protocol, an intensive, structured trauma-focused intervention designed to treat PTSD within 6 daily sessions. The protocol includes psychoeducation, targeted exposure, dynamic case formulation, and guided trauma processing. This novel framework ensures therapy moves beyond symptom reduction, fostering a deep understanding of the patient’s core struggles and their broader psychological patterns, and integrates it with the reconsolidation of the index trauma narrative to form a more cohesive sense of self.”
Clinical studies are ongoing to refine and enhance PET and CPT. They may serve to make therapy more useful and effective in easing—maybe erasing—veterans’ traumatic memories.
Moral Injury-informed Interventions May Enhance Treatment for Combat Veterans
“Moral and mortal stressors may be intertwined in their contribution to the complex symptomatic outcomes” of combat exposure according to a recent study in the European Journal of Psychotraumatology. The study examined the effect moral injury has on Israel Defense Forces (IDF) combat veterans. The resulting trauma may be consolidated in a single category, such as posttraumatic stress disorder (PTSD), but stressors leading to that diagnosis may have been quite different. Properly defining the stressors to assist in better targeted treatment is a challenge.
Moral injury is the emotional distress of being involved in or witnessing actions that conflict with deeply held beliefs. Such experiences could be committing or failing to prevent a transgressive act or learning about or surviving a transgressive act.
The study defines moral injury outcomes as the psychological and emotional consequences that result from exposure to potentially morally injurious events (PMIEs): “This terminology is intended to distinguish the outcomes of moral injury from the broader and sometimes ambiguous use of ‘moral injury’ in the literature, which can refer to either the event, the experience, or the resulting symptoms.”
The study followed 374 male combat veterans for 5 years. Veterans served in the Israel Defense Forces (IDF) in 4 primary combat roles: infantry, armored corps, special forces, and combat engineering. Psychological characteristics were measured 12 months prior to enlistment. PMIE exposure was measured during the final month of military service using the Moral Injury Events Scale. Moral injury outcomes were assessed 6 months postdischarge using the Expressions of Moral Injury Scale-Military Version-Short Form. Posttraumatic stress symptom (PTSS) clusters were evaluated 1 year postdischarge using the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Nearly half (49%) of participants reported exposure to PMIEs, while 8% met criteria for probable PTSD. The researchers say elevated PMIE rates observed in their sample may be attributed, in part, to participants’ extended deployments in densely populated urban areas, carrying out operations in close proximity to civilians, where it is difficult to distinguish between combatants and noncombatants. PTSD rates were somewhat lower than those reported in US studies (10% to 30%) among veterans; this may be attributed to the cohort not being engaged in a full-scale war, but deployed mostly in peacekeeping missions.
Longitudinal studies have described the effects of wartime atrocities on PTSD symptom severity. Studies have also linked moral injury outcomes and PTSS clusters (including negative alterations in cognition and mood [NACM]), depression, anxiety, and substance abuse. PMIEs can also include perceptions of betrayal from leaders, colleagues, or trusted others. The study of 374 male combat veterans found a direct effect of PMIE-betrayal on arousal and reactivity as well as NACM clusters. Results also showed indirect associations between exposure to all PMIE dimensions and PTSS clusters via moral injury outcomes. Combat exposure and experiencing PMIEs during military service significantly contributed to the emergence of PTSS during the first year after discharge. The study found 2 distinct paths PMIEs may lead to PTSS among veterans: experiencing acts of transgression and encountering betrayal.
Betrayal has been linked to feelings of anger and humiliation, emotions thought to have evolved to trigger adaptive behavioral responses, such as aggression and revenge, to threats or transgressions by others. PMIE-betrayal also demonstrated direct effects on the arousal and reactivity and NACM symptom clusters, suggesting partial mediation. Another study (also on IDF veterans) found significant positive correlations between PMIE-betrayal and the NACM cluster, suggesting PMIE-betrayal as a link between PTSD and moral injury. While the link between betrayal and NACM is readily apparent, its connection to arousal and reactivity, a fear-based physiological symptom, is less evident.
The findings of the study point to the need for assessment tools that separately measure exposure to PMIEs and individual reactions to them. A recent Federal Practitioner study of 100 veterans with a history of incarceration completed the Moral Injury Events Scale and an adapted version for legal-involved persons (MIES-LIP). The authors found that MIES-LIP demonstrated strong psychometric properties, including good reliability and convergent validity for legal-related moral injury.
The study cites a recent review of cognitive-behavioral psychotherapies for individuals experiencing moral injury that challenges the adequacy of existing evidence-based treatments for PTSD for addressing moral injury and its associated symptoms. It is important to evaluate individuals who express feelings of betrayal with tailored, evidence-based interventions such as adaptive disclosure or cognitive-processing therapy. Acceptance and commitment therapy may also help individuals experiencing emotions such as shame, humiliation, guilt, and anger following morally injurious events.
Newer therapy models like Multi-Modal Motion-Assisted Memory Desensitization and Reconsolidation allow clinicians to use personalized trauma cues to facilitate memory processing, reduce avoidance, and aid in emotional reconsolidation. Clinical research has demonstrated this model’s efficacy in reducing PTSD symptoms, depression, and anxiety, with high acceptability and low dropout rates among military personnel, veterans, and first responders.
Regardless of the treatment, the researchers encourage mental health professionals to approach veterans seeking help with the “utmost sensitivity and attentiveness to any expressions of (moral injury) outcomes.”
“Moral and mortal stressors may be intertwined in their contribution to the complex symptomatic outcomes” of combat exposure according to a recent study in the European Journal of Psychotraumatology. The study examined the effect moral injury has on Israel Defense Forces (IDF) combat veterans. The resulting trauma may be consolidated in a single category, such as posttraumatic stress disorder (PTSD), but stressors leading to that diagnosis may have been quite different. Properly defining the stressors to assist in better targeted treatment is a challenge.
Moral injury is the emotional distress of being involved in or witnessing actions that conflict with deeply held beliefs. Such experiences could be committing or failing to prevent a transgressive act or learning about or surviving a transgressive act.
The study defines moral injury outcomes as the psychological and emotional consequences that result from exposure to potentially morally injurious events (PMIEs): “This terminology is intended to distinguish the outcomes of moral injury from the broader and sometimes ambiguous use of ‘moral injury’ in the literature, which can refer to either the event, the experience, or the resulting symptoms.”
The study followed 374 male combat veterans for 5 years. Veterans served in the Israel Defense Forces (IDF) in 4 primary combat roles: infantry, armored corps, special forces, and combat engineering. Psychological characteristics were measured 12 months prior to enlistment. PMIE exposure was measured during the final month of military service using the Moral Injury Events Scale. Moral injury outcomes were assessed 6 months postdischarge using the Expressions of Moral Injury Scale-Military Version-Short Form. Posttraumatic stress symptom (PTSS) clusters were evaluated 1 year postdischarge using the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Nearly half (49%) of participants reported exposure to PMIEs, while 8% met criteria for probable PTSD. The researchers say elevated PMIE rates observed in their sample may be attributed, in part, to participants’ extended deployments in densely populated urban areas, carrying out operations in close proximity to civilians, where it is difficult to distinguish between combatants and noncombatants. PTSD rates were somewhat lower than those reported in US studies (10% to 30%) among veterans; this may be attributed to the cohort not being engaged in a full-scale war, but deployed mostly in peacekeeping missions.
Longitudinal studies have described the effects of wartime atrocities on PTSD symptom severity. Studies have also linked moral injury outcomes and PTSS clusters (including negative alterations in cognition and mood [NACM]), depression, anxiety, and substance abuse. PMIEs can also include perceptions of betrayal from leaders, colleagues, or trusted others. The study of 374 male combat veterans found a direct effect of PMIE-betrayal on arousal and reactivity as well as NACM clusters. Results also showed indirect associations between exposure to all PMIE dimensions and PTSS clusters via moral injury outcomes. Combat exposure and experiencing PMIEs during military service significantly contributed to the emergence of PTSS during the first year after discharge. The study found 2 distinct paths PMIEs may lead to PTSS among veterans: experiencing acts of transgression and encountering betrayal.
Betrayal has been linked to feelings of anger and humiliation, emotions thought to have evolved to trigger adaptive behavioral responses, such as aggression and revenge, to threats or transgressions by others. PMIE-betrayal also demonstrated direct effects on the arousal and reactivity and NACM symptom clusters, suggesting partial mediation. Another study (also on IDF veterans) found significant positive correlations between PMIE-betrayal and the NACM cluster, suggesting PMIE-betrayal as a link between PTSD and moral injury. While the link between betrayal and NACM is readily apparent, its connection to arousal and reactivity, a fear-based physiological symptom, is less evident.
The findings of the study point to the need for assessment tools that separately measure exposure to PMIEs and individual reactions to them. A recent Federal Practitioner study of 100 veterans with a history of incarceration completed the Moral Injury Events Scale and an adapted version for legal-involved persons (MIES-LIP). The authors found that MIES-LIP demonstrated strong psychometric properties, including good reliability and convergent validity for legal-related moral injury.
The study cites a recent review of cognitive-behavioral psychotherapies for individuals experiencing moral injury that challenges the adequacy of existing evidence-based treatments for PTSD for addressing moral injury and its associated symptoms. It is important to evaluate individuals who express feelings of betrayal with tailored, evidence-based interventions such as adaptive disclosure or cognitive-processing therapy. Acceptance and commitment therapy may also help individuals experiencing emotions such as shame, humiliation, guilt, and anger following morally injurious events.
Newer therapy models like Multi-Modal Motion-Assisted Memory Desensitization and Reconsolidation allow clinicians to use personalized trauma cues to facilitate memory processing, reduce avoidance, and aid in emotional reconsolidation. Clinical research has demonstrated this model’s efficacy in reducing PTSD symptoms, depression, and anxiety, with high acceptability and low dropout rates among military personnel, veterans, and first responders.
Regardless of the treatment, the researchers encourage mental health professionals to approach veterans seeking help with the “utmost sensitivity and attentiveness to any expressions of (moral injury) outcomes.”
“Moral and mortal stressors may be intertwined in their contribution to the complex symptomatic outcomes” of combat exposure according to a recent study in the European Journal of Psychotraumatology. The study examined the effect moral injury has on Israel Defense Forces (IDF) combat veterans. The resulting trauma may be consolidated in a single category, such as posttraumatic stress disorder (PTSD), but stressors leading to that diagnosis may have been quite different. Properly defining the stressors to assist in better targeted treatment is a challenge.
Moral injury is the emotional distress of being involved in or witnessing actions that conflict with deeply held beliefs. Such experiences could be committing or failing to prevent a transgressive act or learning about or surviving a transgressive act.
The study defines moral injury outcomes as the psychological and emotional consequences that result from exposure to potentially morally injurious events (PMIEs): “This terminology is intended to distinguish the outcomes of moral injury from the broader and sometimes ambiguous use of ‘moral injury’ in the literature, which can refer to either the event, the experience, or the resulting symptoms.”
The study followed 374 male combat veterans for 5 years. Veterans served in the Israel Defense Forces (IDF) in 4 primary combat roles: infantry, armored corps, special forces, and combat engineering. Psychological characteristics were measured 12 months prior to enlistment. PMIE exposure was measured during the final month of military service using the Moral Injury Events Scale. Moral injury outcomes were assessed 6 months postdischarge using the Expressions of Moral Injury Scale-Military Version-Short Form. Posttraumatic stress symptom (PTSS) clusters were evaluated 1 year postdischarge using the PTSD Checklist for the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition.
Nearly half (49%) of participants reported exposure to PMIEs, while 8% met criteria for probable PTSD. The researchers say elevated PMIE rates observed in their sample may be attributed, in part, to participants’ extended deployments in densely populated urban areas, carrying out operations in close proximity to civilians, where it is difficult to distinguish between combatants and noncombatants. PTSD rates were somewhat lower than those reported in US studies (10% to 30%) among veterans; this may be attributed to the cohort not being engaged in a full-scale war, but deployed mostly in peacekeeping missions.
Longitudinal studies have described the effects of wartime atrocities on PTSD symptom severity. Studies have also linked moral injury outcomes and PTSS clusters (including negative alterations in cognition and mood [NACM]), depression, anxiety, and substance abuse. PMIEs can also include perceptions of betrayal from leaders, colleagues, or trusted others. The study of 374 male combat veterans found a direct effect of PMIE-betrayal on arousal and reactivity as well as NACM clusters. Results also showed indirect associations between exposure to all PMIE dimensions and PTSS clusters via moral injury outcomes. Combat exposure and experiencing PMIEs during military service significantly contributed to the emergence of PTSS during the first year after discharge. The study found 2 distinct paths PMIEs may lead to PTSS among veterans: experiencing acts of transgression and encountering betrayal.
Betrayal has been linked to feelings of anger and humiliation, emotions thought to have evolved to trigger adaptive behavioral responses, such as aggression and revenge, to threats or transgressions by others. PMIE-betrayal also demonstrated direct effects on the arousal and reactivity and NACM symptom clusters, suggesting partial mediation. Another study (also on IDF veterans) found significant positive correlations between PMIE-betrayal and the NACM cluster, suggesting PMIE-betrayal as a link between PTSD and moral injury. While the link between betrayal and NACM is readily apparent, its connection to arousal and reactivity, a fear-based physiological symptom, is less evident.
The findings of the study point to the need for assessment tools that separately measure exposure to PMIEs and individual reactions to them. A recent Federal Practitioner study of 100 veterans with a history of incarceration completed the Moral Injury Events Scale and an adapted version for legal-involved persons (MIES-LIP). The authors found that MIES-LIP demonstrated strong psychometric properties, including good reliability and convergent validity for legal-related moral injury.
The study cites a recent review of cognitive-behavioral psychotherapies for individuals experiencing moral injury that challenges the adequacy of existing evidence-based treatments for PTSD for addressing moral injury and its associated symptoms. It is important to evaluate individuals who express feelings of betrayal with tailored, evidence-based interventions such as adaptive disclosure or cognitive-processing therapy. Acceptance and commitment therapy may also help individuals experiencing emotions such as shame, humiliation, guilt, and anger following morally injurious events.
Newer therapy models like Multi-Modal Motion-Assisted Memory Desensitization and Reconsolidation allow clinicians to use personalized trauma cues to facilitate memory processing, reduce avoidance, and aid in emotional reconsolidation. Clinical research has demonstrated this model’s efficacy in reducing PTSD symptoms, depression, and anxiety, with high acceptability and low dropout rates among military personnel, veterans, and first responders.
Regardless of the treatment, the researchers encourage mental health professionals to approach veterans seeking help with the “utmost sensitivity and attentiveness to any expressions of (moral injury) outcomes.”
Accelerated Prolonged Exposure Therapy for Posttraumatic Stress Disorder in a Veterans Health Administration System
Accelerated Prolonged Exposure Therapy for Posttraumatic Stress Disorder in a Veterans Health Administration System
Evidence-based psychotherapy (EBP) for posttraumatic stress disorder (PTSD), such as prolonged exposure (PE), is supported by multiple clinical practice guidelines and is expected to be available to veterans served by the Veterans Health Administration (VHA).1-5 However, traditional models of EBP delivery with 1 or 2 sessions weekly have high dropout rates.6,7 Few veterans who could benefit from such EBPs receive them, and those who do have low completion rates.8,9 Over a 15-year period, VHA records review of > 265,500 veterans with PTSD showed only 9.1% completed EBP treatment that included but was not limited to PE.10
One empirically supported solution that has yet to be widely implemented is delivering EBPs for PTSD in a massed or accelerated format of ≥ 3 sessions weekly.11 While these massed models of EBP delivery for PTSD are promising, their implementation is limited in federal health care settings, such as the VHA.12 PE therapy is a first-line treatment for PTSD that has been evaluated in numerous clinical trials since the early 1990s and in a wide range of trauma populations.13,14 Massed PE is effective and PE has been found to be effective both in-person and via telehealth.11,15,16
Another approach to accelerated PE is the inclusion of a massed PE course within a broader treatment context that includes augmentation of the massed PE with additional services, this is referred to as an intensive outpatient model (IOP).17 PE-IOP has also been shown to be feasible, acceptable, and effective with increased completion rates in comparison to the traditional (1 or 2 sessions weekly) model of PE.12,16,18,19 Ragsdale et al describe a 2-week IOP with multiple treatment tracks, including a PTSD track. The PTSD treatment track includes massed PE and additional standard services including case management, wellness services, family services, and a single session effective behaviors group. Additional augmentation services are available when clinically indicated (eg, repetitive transcranial magnetic stimulation, transcranial direct current stimulation treatment, psychoeducation, motivational interviewing, and/or relapse prevention).17
Rauch et al studied the first 80 patients completing an IOP program that consisted of PE (5 sessions weekly) and complementary interventions (eg, mindfulness and yoga) and reported a 96% retention rate, significant reductions of self-reported PTSD symptoms, significant reduction in self-reported co-occurring depression symptoms, and significant increase in self-reported satisfaction with social functioning. 18 In another study, Sherril et al explored patient reactions to participation in massed PE (5 sessions weekly) and found that patients reported significantly more positive than negative reactions. Sherrill et al noted that according to patients, the benefits of massed PE included a structured format that limits avoidance and distraction. The resulting fast pace of progress enhanced motivation; however, drawbacks included short-term discomfort and time demands.19 Yamokoski et al explored the feasibility of massed PE in a larger study of PTSD treatment in an intensive outpatient track (IOT) in a VHA PTSD clinic with minimal staffing. The 48 patients who completed IOT PTSD treatment in 2 or 4 weeks (including 35 patients who received massed PE) had high retention rates (85%), reported high satisfaction, and had significantly reduced PTSD and depression symptoms.12
The massed IOT PE model implemented by Yamokoski et al included the primary EBP intervention of massed PE with adjunctive groups. The addition of these groups increased both retention and patient-reported satisfaction. The PE-IOP model implemented by Rauch et al and Sherrill et al also included wellness and educational groups, as well as access to complementary interventions such as mindfulness and yoga.18,19 The addition of wellness education along with a primary EBP aligned with the VHA focus on whole health well-being and wellness. The whole health approach includes understanding the factors that motivate a patient toward health and well-being, provision of health education, and providing access to complementary interventions such as mindfulness.20 Dryden et al describe the whole health transformation within VHA as a proactive approach to addressing employee and patient wellness and health. Their research found that the whole health model promoted well-being in patients and staff and was sustained even during the COVID-19 pandemic.21 Dryden et al also noted that use of virtual technologies facilitated and promoted continued whole health implementation. The literature illustrates that: (1) massed PE can be provided with complementary education and wellness offerings, and that such offerings may increase both retention and satisfaction by enriching the massed PE treatment (eg, delivering PE-IOP); (2) whole health including wellness education and complementary interventions (eg, mindfulness, motivational enhancement) promotes well-being in both patients and mental health professionals; and (3) whole health education and complementary interventions can be delivered virtually.
Health Care Need
Prior to the implementation of a massed EBP for PTSD program at US Department of Veterans Affairs (VA) Pacific Islands Health Care System (VAPIHCS), our setting included a traditional outpatient program for treatment of PTSD and a 12- bed residential program for treatment of PTSD for male-identified (self-identified and identified as male in the electronic medical record) veterans via a cohort model with an 8- or 9-week length of stay. Both programs were located on Oahu. Thus, veterans who received care at VAPIHCS had access to PE in both outpatient and residential settings and via in-person and telehealth modalities. However, their access to PE was limited to the traditional models of PE delivery (eg, 1 or 2 session per week) and very few veterans outside of the island of Oahu had accessed PE treatment for PTSD. Moreover, when looking at PE reach within VAPIHCS, in the fiscal year prior to the implementation of the massed EBP program, only 32 of the > 5000 eligible veterans with a PTSD diagnosis had received PE. VAPIHCS serves veterans in a catchment area across the Pacific Basin which includes 3 time zones: Hawaii Standard Time (HST), Chamorro Standard Time (ChST), and Samoa Standard Time (SST). ChST is 20 hours ahead of HST, making service delivery that is inclusive for patients in Guam and Saipan especially challenging when providing care from Hawaii or other US states or territories. Given all of this, implementation of a new program offering accelerated PE virtually to any veterans with PTSD within the VAPIHCS would increase access to and reduce barriers to receiving PE.
PROGRAM DESCRIPTION
The Intensive Virtual EBP Team (iVET) for PTSD consists of an accelerated course of PE therapy and whole health education provided via VA Video Connect (VVC). iVET is a 3-week program and includes 3 parts: (1) massed individual PE therapy for PTSD; (2) group whole health and wellness classes; and (3) individual health coaching to address personal wellness goals. Programming is offered over 10-hour days to increase access across multiple time zones, especially to allow for participation in Guam and Saipan.
When a patient is referred to the iVET, their first contact is a video (or telephone) appointment with a registered nurse (RN) for a screening session. The screening session is designed to educate the patient about the program, including interventions, time commitment, and resources required for participation. In addition, following the educational discussion, the RN completes screening for safety with the patient including suicidal ideation and risk, as well as intimate partner violence risk. If urgent safety concerns are present, a licensed social worker or psychologist will join the screening to complete further assessment of risk and to address any safety concerns. Following screening, patients are scheduled for a VVC intake with a licensed therapist (social worker or psychologist) to complete the Clinician-Administered PTSD Scale (CAPS-5) for the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition), a clinical interview for PTSD assessment. Patients are also sent a secure link to complete a measurement-based care (MBC) battery of self-report measures including measures assessing demographics, PTSD symptoms, anxiety symptoms, depression symptoms, substance use, quality of life (QOL), and satisfaction with mental health care. The results of the CAPS-5 and self-report measures are discussed with the patient during the intake session when planning next steps and engaging in shared decision-making. This initial VVC intake not only allows for diagnostic goodness of fit but also provides the opportunity to troubleshoot any technical difficulties the patients might have with the virtual platforms.
There are minimal exclusion criteria for participation in iVET, which include active unmanaged psychosis or manic symptoms, recent suicidal crises (attempt within 8 weeks), active nonsuicidal self-injurious behaviors (within 8 weeks), and moderate-to-severe cognitive impairment. Following intake, patients are scheduled to begin their course of care with iVET. Upon completion of intake, patients are sent program materials for their individual and group classes, asked to obtain or request a recording device, and told they will receive email links for all VVC appointments. Patients are admitted to the iVET in a rolling admission fashion, thereby increasing access when compared to closed group and/or cohort models of care.
Patients receiving care in iVET attend 2 or 3 telehealth appointments daily with practice exercises daily between telehealth sessions. The primary EBP intervention in the iVET for PTSD program is a massed or accelerated course of PE, which includes 4 primary components: psychoeducation, in-vivo exposure, imaginal exposure, and breathing retraining. Specifically, PE is delivered in 4 90-minute individual sessions weekly allowing completion of the full PE protocol, to fidelity, in 3 weeks. In addition to receiving this primary intervention, patients also participate in four 50-minute group sessions per week of a whole health and wellness education class and have access to one 30- to 60-minute session weekly of individual health coaching should they wish to set wellness goals and receive coaching in support of attaining wellness goals. During iVET, patients are invited to complete MBC batteries of selfreport measures including measures assessing PTSD symptoms, anxiety symptoms, depression symptoms, substance use, QOL, and satisfaction with mental health care at sessions 1, 5, 9, and the final session of PE. Following discharge from the iVET, patients are offered 1-month, 3-month, and 6-month individual postdischarge check-up sessions with a therapist where they are invited to complete MBC measures and review relapse prevention and maintenance of treatment gains. Likewise, they are offered 1-month, 3-month, and 6-month postdischarge check-up sessions with an RN focused on maintaining wellness gains.
The iVET for PTSD staff includes 3 therapists (psychologists or social workers) and an RN. Additionally, the iVET for PTSD is supported by a program manager and a program support assistant. The primary cost of the program is salary for staff. Additional iVET for PTSD resources included computer equipment for staff and minimal supplies. Due to the virtual environment of care, iVET staff telework and do not require physical space within VAPIHCS.
OUTCOMES
All veterans receiving care in iVET for PTSD are invited to complete a MBC at multiple timepoints including pretreatment, during PE treatment, and posttreatment. The MBC measures included self-reported demographics, a 2-item measure of satisfaction with mental health services, the Brief Addiction Monitor-Intensive Outpatient Program questionnaire,22 the Generalized Anxiety Disorder-7 scale,23, the Patient Health Questionnaire (PHQ-9),24 the QOL Enjoyment and Satisfaction Questionnaire- Short Form,25 and the PTSD Checklist for DSM-5 (PCL-5), both weekly and monthly versions. 26,27
The retention rate has averaged 81% since the iVET for PTSD opened in 2022. To date, 132 veterans have completed the iVET for PTSD program, including a full course of massed PE (Table 1). Veterans experienced reduced PTSD (P < .005), depression (P < .005), anxiety (P < .005), and substance use risk (P < .005). Veterans experienced improved QOL (P < .005) and reported high satisfaction with mental health care in iVET for PTSD (Table 2). Veterans also experienced reduced thoughts of death or suicidal ideation (SI) based on PHQ-9 item 9 responses. When looking categorically at presence or absence of SI on PHQ-9 item 9, a significant relationship was found between the absence of suicidal ideation and completion of a course of massed PE: X2 (1, N = 132) = 13.75, P < .001. In addition, veterans who completed the program showed a significant decrease in severity of SI as measured continuously (range, 0-3) on PHQ-9 item 9 (P < .005).
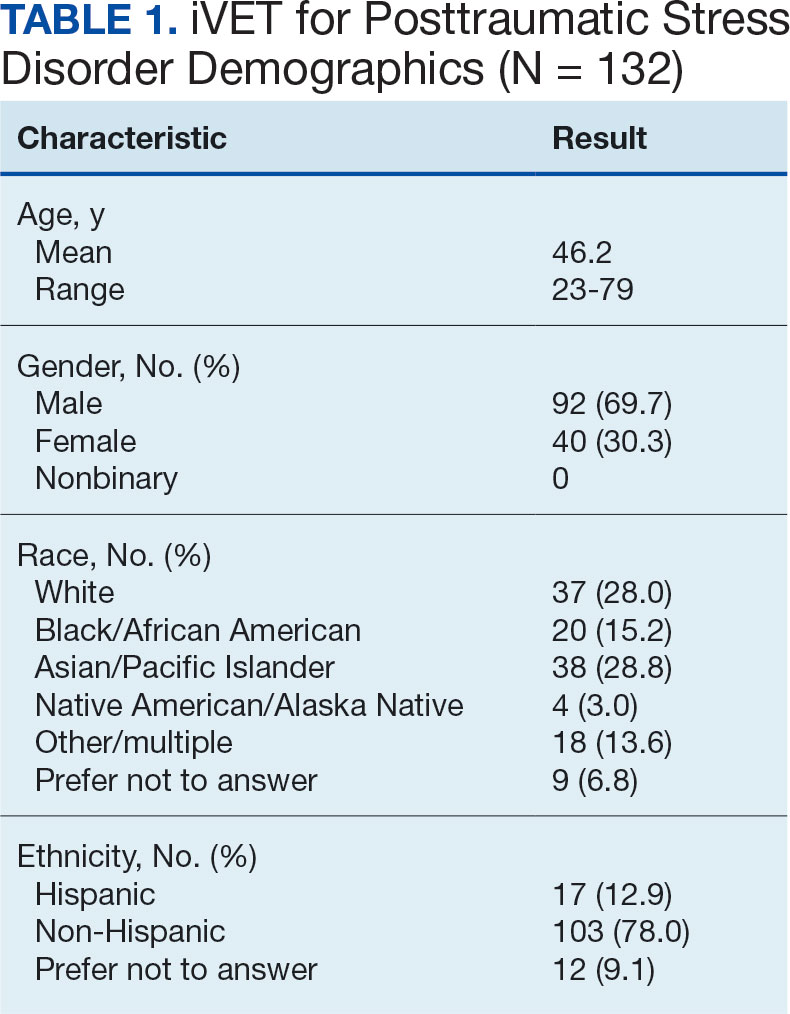
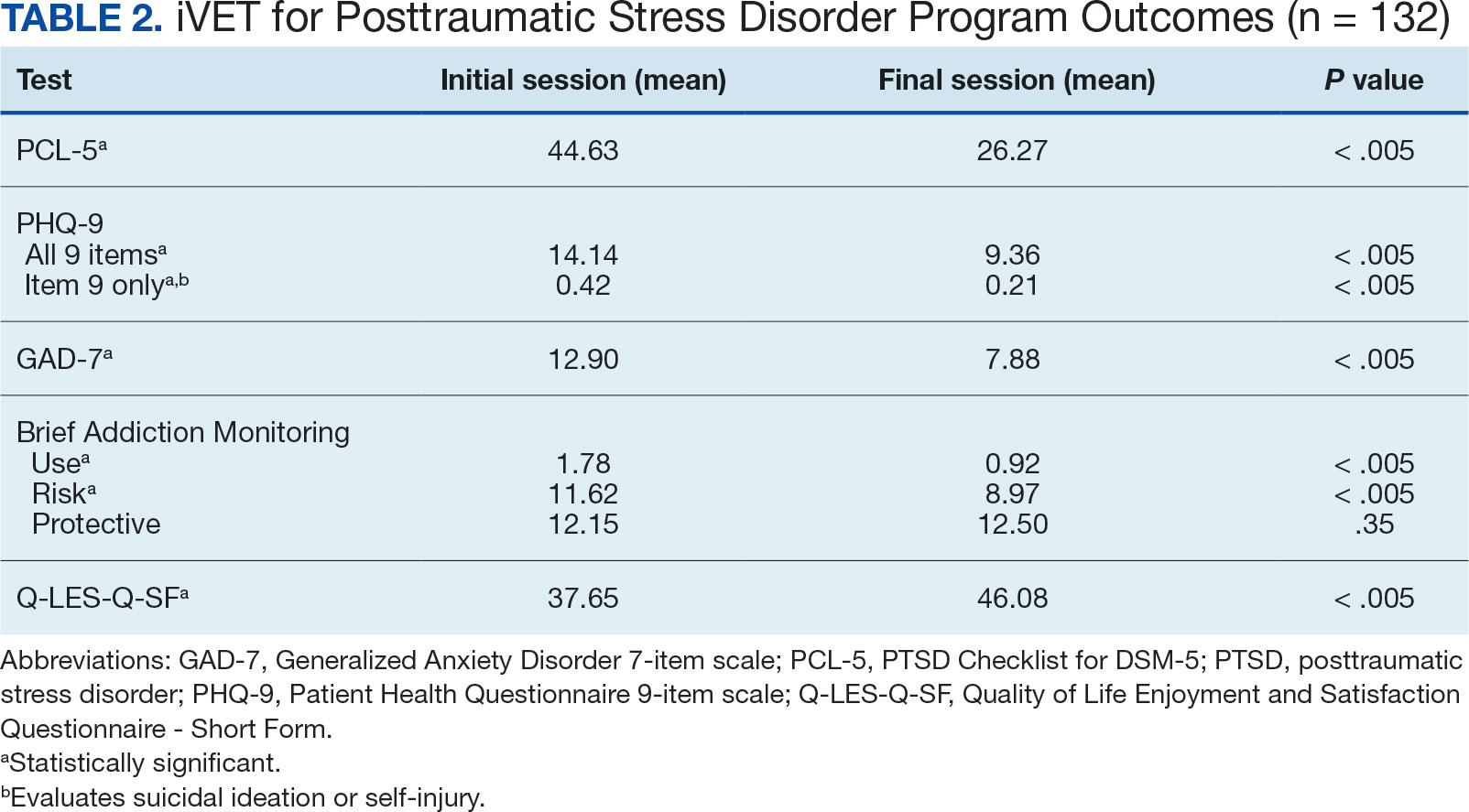
Another important aspect to consider when implementing massed models of EBP is the impact on employee well-being and job satisfaction. The impact of EBP on staff was assessed following the initial EBP project. To explore this further, all staff members in the iVET for PTSD were invited to engage in a small program evaluation. iVET staff were guided through a visualization meditation intended to recall a typical workday 1 month prior to starting their new position with iVET. After the visualization meditation, staff completed the Professional Quality of Life (ProQOL) scale, a 30-item, self-reported questionnaire for health care workers that evaluates compassion satisfaction, perceived support, burnout, secondary traumatic stress, and moral distress.28 One week later, staff were asked to complete the ProQOL again to capture their state after the first 6 months into their tenure as iVET staff. iVET employees experienced significantly increased perceived support (P < .05), reduced burnout (P < .05), reduced secondary traumatic stress (P < .05), and reduced moral distress (P < .05). Team members also remarked on the rewarding nature of the work and care model.
Future Directions
Future research should aim to sustain these outcomes as the iVET program continues to serve more veterans. Another important line of inquiry is longer-term follow-up, as exploring if outcomes are maintained over time is an important question that has not been answered in this article. In addition, we hope to see the accelerated model of care applied to treatment of other presenting concerns in mental health treatment (eg, anxiety, depression, insomnia). Expansion of accelerated mental health treatment into other federal and non-federal health care settings is another worthy direction. Finally, while short term (6 months) assessment of staff satisfaction in iVET was promising, ongoing assessment staff satisfaction over a longer timeframe (1-5 years) is also important.
CONCLUSIONS
PE for PTSD has been demonstrated to be effective and improve functioning and is supported by multiple clinical practice guidelines.1-5 However, as federal practitioners, we must consider the reality that many of the individuals who could benefit are not engaging in PE and there is a high dropout rate for those that do. It is vital that we envision a future state where access to PE for PTSD is equitable and inclusive, retention rates are dramatically improved, and clinicians providing PE do not experience high rates of burnout.
We must continue exploring how we can better care for our patients and colleagues. We posit that the development of programs, or tracks within existing programs, that provide massed or accelerated PE for PTSD with virtual delivery options is an imperative step toward improved care. Federal health care settings treating trauma-exposed patients with PTSD, such as those within the US Department of Defense, Indian Health Services, Federal Bureau of Prisons, and VA, are well positioned to implement programs like iVET. We believe this model of care has great merit and foresee a future where all patients seeking PTSD treatment have the option to complete an accelerated or massed course of PE should they so desire. The experiences outlined in this article illustrate the feasibility, acceptability, and sustainability of such programs without requiring substantial staffing and financial resources.
- American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. February 24, 2017. Accessed February 27, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- US Department of Veterans Affairs, Veterans Health Administration. Uniform mental health services in VA medical centers and clinics. Veterans Health Administration (VHA) Handbook 1160.01. September 11, 2008. Accessed February 27, 2025. https://www.mentalhealth.va.gov/providers/sud/docs/UniformServicesHandbook1160-01.pdf
- US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Version 3. 2017. Accessed February 27, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DoD-CPG-PTSD-Full-CPG-Edited-11162024.pdf
- Hamblen JL, Bernardy NC, Sherrieb K, et al. VA PTSD clinic director perspectives: How perceptions of readiness influence delivery of evidence-based PTSD treatment. Prof Psychol Res Pract. 2015;46(2): 90-96. doi:10.1037/a0038535
- Schnurr PP, Chard KM, Ruzek JI, et al. Comparison of prolonged exposure vs cognitive processing therapy for treatment of posttraumatic stress disorder among US veterans: a randomized clinical trial. JAMA Netw Open. 2022;5(1):e2136921. doi:10.1001/jamanetworkopen. 2021.36921
- Kehle-Forbes SM, Meis LA, Spoont MR, Polusny MA. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol Trauma. 2016;8(1):107-114. doi:10.1037/tra0000065
- Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, Teng EJ. Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. J Trauma Stress. 2014;27(3):265-273. doi:10.1002/jts.21927
- Shiner B, D’Avolio LW, Nguyen TM, et al. Measuring use of evidence based psychotherapy for posttraumatic stress disorder. Adm Policy Ment Health. 2013;40(4):311-318. doi:10.1007/s10488-012-0421-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37(4):356-364. doi:10.1002/da.22983
- Maguen S, Li Y, Madden E, et al. Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Res. 2019;274:112-128. doi:10.1016/j.psychres.2019.02.027
- Foa EB, McLean CP, Zang Y, et al. Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: a randomized clinical trial. JAMA. 2018;319(4):354-364. doi:10.1001/jama.2017.21242
- Yamokoski C, Flores H, Facemire V, Maieritsch K, Perez S, Fedynich A. Feasibility of an intensive outpatient treatment program for posttraumatic stress disorder within the veterans health care administration. Psychol Serv. 2023;20(3):506-515. doi:10.1037/ser0000628
- McLean CP, Foa EB. State of the Science: Prolonged exposure therapy for the treatment of posttraumatic stress disorder. J Trauma Stress. 2024;37(4):535-550. doi:10.1002/jts.23046
- McLean CP, Levy HC, Miller ML, Tolin DF. Exposure therapy for PTSD: A meta-analysis. Clin Psychol Rev. 2022;91:102115. doi:10.1016/j.cpr.2021.102115
- Wells SY, Morland LA, Wilhite ER, et al. Delivering Prolonged Exposure Therapy via Videoconferencing During the COVID-19 Pandemic: An Overview of the Research and Special Considerations for Providers. J Trauma Stress. 2020;33(4):380-390. doi:10.1002/jts.22573
- Peterson AL, Blount TH, Foa EB, et al. Massed vs intensive outpatient prolonged exposure for combat-related posttraumatic stress disorder: a randomized clinical trial. JAMA Netw Open. 2023;6(1):e2249422. Published 2023 Jan 3. doi:10.1001/jamanetworkopen.2022.49422
- Ragsdale KA, Nichols AA, Mehta M, et al. Comorbid treatment of traumatic brain injury and mental health disorders. NeuroRehabilitation. 2024;55(3):375-384. doi:10.3233/NRE-230235
- Rauch SAM, Yasinski CW, Post LM, et al. An intensive outpatient program with prolonged exposure for veterans with posttraumatic stress disorder: retention, predictors, and patterns of change. Psychol Serv. 2021;18(4):606-618. doi:10.1037/ser0000422
- Sherrill AM, Maples-Keller JL, Yasinski CW, Loucks LA, Rothbaum BO, Rauch SAM. Perceived benefits and drawbacks of massed prolonged exposure: qualitative thematic analysis of reactions from treatment completers. Psychol Trauma. 2022;14(5):862-870. doi:10.1037/tra0000548
- Gaudet T, Kligler B. Whole health in the whole system of the Veterans Administration: how will we know we have reached this future state? J Altern Complement Med. 2019;25(S1):S7-S11. doi:10.1089/acm.2018.29061.gau
- Dryden EM, Bolton RE, Bokhour BG, et al. Leaning Into whole health: sustaining system transformation while supporting patients and employees during COVID-19. Glob Adv Health Med. 2021;10:21649561211021047. doi:10.1177/21649561211021047
- Cacciola JS, Alterman AI, Dephilippis D, et al. Development and initial evaluation of the Brief Addiction Monitor (BAM). J Subst Abuse Treat. 2013;44(3):256-263. doi:10.1016/j.jsat.2012.07.013
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097. doi:10.1001/archinte.166.10.1092
- Kroenke K, Spi tze r RL , Wi l l i ams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Stevanovic D. Quality of Life Enjoyment and Satisfaction Questionnaire-short form for quality of life assessments in clinical practice: a psychometric study. J Psychiatr Ment Health Nurs. 2011;18(8):744-750. doi:10.1111/j.1365-2850.2011.01735.x
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL- 5). National Center for PTSD. Updated August 29, 2023. Accessed February 27, 2025. https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.pdf
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi:10.1002/jts.22059
- Stamm BH. The Concise ProQOL Manual. 2nd ed. Pro- QOL.org; 2010.
Evidence-based psychotherapy (EBP) for posttraumatic stress disorder (PTSD), such as prolonged exposure (PE), is supported by multiple clinical practice guidelines and is expected to be available to veterans served by the Veterans Health Administration (VHA).1-5 However, traditional models of EBP delivery with 1 or 2 sessions weekly have high dropout rates.6,7 Few veterans who could benefit from such EBPs receive them, and those who do have low completion rates.8,9 Over a 15-year period, VHA records review of > 265,500 veterans with PTSD showed only 9.1% completed EBP treatment that included but was not limited to PE.10
One empirically supported solution that has yet to be widely implemented is delivering EBPs for PTSD in a massed or accelerated format of ≥ 3 sessions weekly.11 While these massed models of EBP delivery for PTSD are promising, their implementation is limited in federal health care settings, such as the VHA.12 PE therapy is a first-line treatment for PTSD that has been evaluated in numerous clinical trials since the early 1990s and in a wide range of trauma populations.13,14 Massed PE is effective and PE has been found to be effective both in-person and via telehealth.11,15,16
Another approach to accelerated PE is the inclusion of a massed PE course within a broader treatment context that includes augmentation of the massed PE with additional services, this is referred to as an intensive outpatient model (IOP).17 PE-IOP has also been shown to be feasible, acceptable, and effective with increased completion rates in comparison to the traditional (1 or 2 sessions weekly) model of PE.12,16,18,19 Ragsdale et al describe a 2-week IOP with multiple treatment tracks, including a PTSD track. The PTSD treatment track includes massed PE and additional standard services including case management, wellness services, family services, and a single session effective behaviors group. Additional augmentation services are available when clinically indicated (eg, repetitive transcranial magnetic stimulation, transcranial direct current stimulation treatment, psychoeducation, motivational interviewing, and/or relapse prevention).17
Rauch et al studied the first 80 patients completing an IOP program that consisted of PE (5 sessions weekly) and complementary interventions (eg, mindfulness and yoga) and reported a 96% retention rate, significant reductions of self-reported PTSD symptoms, significant reduction in self-reported co-occurring depression symptoms, and significant increase in self-reported satisfaction with social functioning. 18 In another study, Sherril et al explored patient reactions to participation in massed PE (5 sessions weekly) and found that patients reported significantly more positive than negative reactions. Sherrill et al noted that according to patients, the benefits of massed PE included a structured format that limits avoidance and distraction. The resulting fast pace of progress enhanced motivation; however, drawbacks included short-term discomfort and time demands.19 Yamokoski et al explored the feasibility of massed PE in a larger study of PTSD treatment in an intensive outpatient track (IOT) in a VHA PTSD clinic with minimal staffing. The 48 patients who completed IOT PTSD treatment in 2 or 4 weeks (including 35 patients who received massed PE) had high retention rates (85%), reported high satisfaction, and had significantly reduced PTSD and depression symptoms.12
The massed IOT PE model implemented by Yamokoski et al included the primary EBP intervention of massed PE with adjunctive groups. The addition of these groups increased both retention and patient-reported satisfaction. The PE-IOP model implemented by Rauch et al and Sherrill et al also included wellness and educational groups, as well as access to complementary interventions such as mindfulness and yoga.18,19 The addition of wellness education along with a primary EBP aligned with the VHA focus on whole health well-being and wellness. The whole health approach includes understanding the factors that motivate a patient toward health and well-being, provision of health education, and providing access to complementary interventions such as mindfulness.20 Dryden et al describe the whole health transformation within VHA as a proactive approach to addressing employee and patient wellness and health. Their research found that the whole health model promoted well-being in patients and staff and was sustained even during the COVID-19 pandemic.21 Dryden et al also noted that use of virtual technologies facilitated and promoted continued whole health implementation. The literature illustrates that: (1) massed PE can be provided with complementary education and wellness offerings, and that such offerings may increase both retention and satisfaction by enriching the massed PE treatment (eg, delivering PE-IOP); (2) whole health including wellness education and complementary interventions (eg, mindfulness, motivational enhancement) promotes well-being in both patients and mental health professionals; and (3) whole health education and complementary interventions can be delivered virtually.
Health Care Need
Prior to the implementation of a massed EBP for PTSD program at US Department of Veterans Affairs (VA) Pacific Islands Health Care System (VAPIHCS), our setting included a traditional outpatient program for treatment of PTSD and a 12- bed residential program for treatment of PTSD for male-identified (self-identified and identified as male in the electronic medical record) veterans via a cohort model with an 8- or 9-week length of stay. Both programs were located on Oahu. Thus, veterans who received care at VAPIHCS had access to PE in both outpatient and residential settings and via in-person and telehealth modalities. However, their access to PE was limited to the traditional models of PE delivery (eg, 1 or 2 session per week) and very few veterans outside of the island of Oahu had accessed PE treatment for PTSD. Moreover, when looking at PE reach within VAPIHCS, in the fiscal year prior to the implementation of the massed EBP program, only 32 of the > 5000 eligible veterans with a PTSD diagnosis had received PE. VAPIHCS serves veterans in a catchment area across the Pacific Basin which includes 3 time zones: Hawaii Standard Time (HST), Chamorro Standard Time (ChST), and Samoa Standard Time (SST). ChST is 20 hours ahead of HST, making service delivery that is inclusive for patients in Guam and Saipan especially challenging when providing care from Hawaii or other US states or territories. Given all of this, implementation of a new program offering accelerated PE virtually to any veterans with PTSD within the VAPIHCS would increase access to and reduce barriers to receiving PE.
PROGRAM DESCRIPTION
The Intensive Virtual EBP Team (iVET) for PTSD consists of an accelerated course of PE therapy and whole health education provided via VA Video Connect (VVC). iVET is a 3-week program and includes 3 parts: (1) massed individual PE therapy for PTSD; (2) group whole health and wellness classes; and (3) individual health coaching to address personal wellness goals. Programming is offered over 10-hour days to increase access across multiple time zones, especially to allow for participation in Guam and Saipan.
When a patient is referred to the iVET, their first contact is a video (or telephone) appointment with a registered nurse (RN) for a screening session. The screening session is designed to educate the patient about the program, including interventions, time commitment, and resources required for participation. In addition, following the educational discussion, the RN completes screening for safety with the patient including suicidal ideation and risk, as well as intimate partner violence risk. If urgent safety concerns are present, a licensed social worker or psychologist will join the screening to complete further assessment of risk and to address any safety concerns. Following screening, patients are scheduled for a VVC intake with a licensed therapist (social worker or psychologist) to complete the Clinician-Administered PTSD Scale (CAPS-5) for the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition), a clinical interview for PTSD assessment. Patients are also sent a secure link to complete a measurement-based care (MBC) battery of self-report measures including measures assessing demographics, PTSD symptoms, anxiety symptoms, depression symptoms, substance use, quality of life (QOL), and satisfaction with mental health care. The results of the CAPS-5 and self-report measures are discussed with the patient during the intake session when planning next steps and engaging in shared decision-making. This initial VVC intake not only allows for diagnostic goodness of fit but also provides the opportunity to troubleshoot any technical difficulties the patients might have with the virtual platforms.
There are minimal exclusion criteria for participation in iVET, which include active unmanaged psychosis or manic symptoms, recent suicidal crises (attempt within 8 weeks), active nonsuicidal self-injurious behaviors (within 8 weeks), and moderate-to-severe cognitive impairment. Following intake, patients are scheduled to begin their course of care with iVET. Upon completion of intake, patients are sent program materials for their individual and group classes, asked to obtain or request a recording device, and told they will receive email links for all VVC appointments. Patients are admitted to the iVET in a rolling admission fashion, thereby increasing access when compared to closed group and/or cohort models of care.
Patients receiving care in iVET attend 2 or 3 telehealth appointments daily with practice exercises daily between telehealth sessions. The primary EBP intervention in the iVET for PTSD program is a massed or accelerated course of PE, which includes 4 primary components: psychoeducation, in-vivo exposure, imaginal exposure, and breathing retraining. Specifically, PE is delivered in 4 90-minute individual sessions weekly allowing completion of the full PE protocol, to fidelity, in 3 weeks. In addition to receiving this primary intervention, patients also participate in four 50-minute group sessions per week of a whole health and wellness education class and have access to one 30- to 60-minute session weekly of individual health coaching should they wish to set wellness goals and receive coaching in support of attaining wellness goals. During iVET, patients are invited to complete MBC batteries of selfreport measures including measures assessing PTSD symptoms, anxiety symptoms, depression symptoms, substance use, QOL, and satisfaction with mental health care at sessions 1, 5, 9, and the final session of PE. Following discharge from the iVET, patients are offered 1-month, 3-month, and 6-month individual postdischarge check-up sessions with a therapist where they are invited to complete MBC measures and review relapse prevention and maintenance of treatment gains. Likewise, they are offered 1-month, 3-month, and 6-month postdischarge check-up sessions with an RN focused on maintaining wellness gains.
The iVET for PTSD staff includes 3 therapists (psychologists or social workers) and an RN. Additionally, the iVET for PTSD is supported by a program manager and a program support assistant. The primary cost of the program is salary for staff. Additional iVET for PTSD resources included computer equipment for staff and minimal supplies. Due to the virtual environment of care, iVET staff telework and do not require physical space within VAPIHCS.
OUTCOMES
All veterans receiving care in iVET for PTSD are invited to complete a MBC at multiple timepoints including pretreatment, during PE treatment, and posttreatment. The MBC measures included self-reported demographics, a 2-item measure of satisfaction with mental health services, the Brief Addiction Monitor-Intensive Outpatient Program questionnaire,22 the Generalized Anxiety Disorder-7 scale,23, the Patient Health Questionnaire (PHQ-9),24 the QOL Enjoyment and Satisfaction Questionnaire- Short Form,25 and the PTSD Checklist for DSM-5 (PCL-5), both weekly and monthly versions. 26,27
The retention rate has averaged 81% since the iVET for PTSD opened in 2022. To date, 132 veterans have completed the iVET for PTSD program, including a full course of massed PE (Table 1). Veterans experienced reduced PTSD (P < .005), depression (P < .005), anxiety (P < .005), and substance use risk (P < .005). Veterans experienced improved QOL (P < .005) and reported high satisfaction with mental health care in iVET for PTSD (Table 2). Veterans also experienced reduced thoughts of death or suicidal ideation (SI) based on PHQ-9 item 9 responses. When looking categorically at presence or absence of SI on PHQ-9 item 9, a significant relationship was found between the absence of suicidal ideation and completion of a course of massed PE: X2 (1, N = 132) = 13.75, P < .001. In addition, veterans who completed the program showed a significant decrease in severity of SI as measured continuously (range, 0-3) on PHQ-9 item 9 (P < .005).
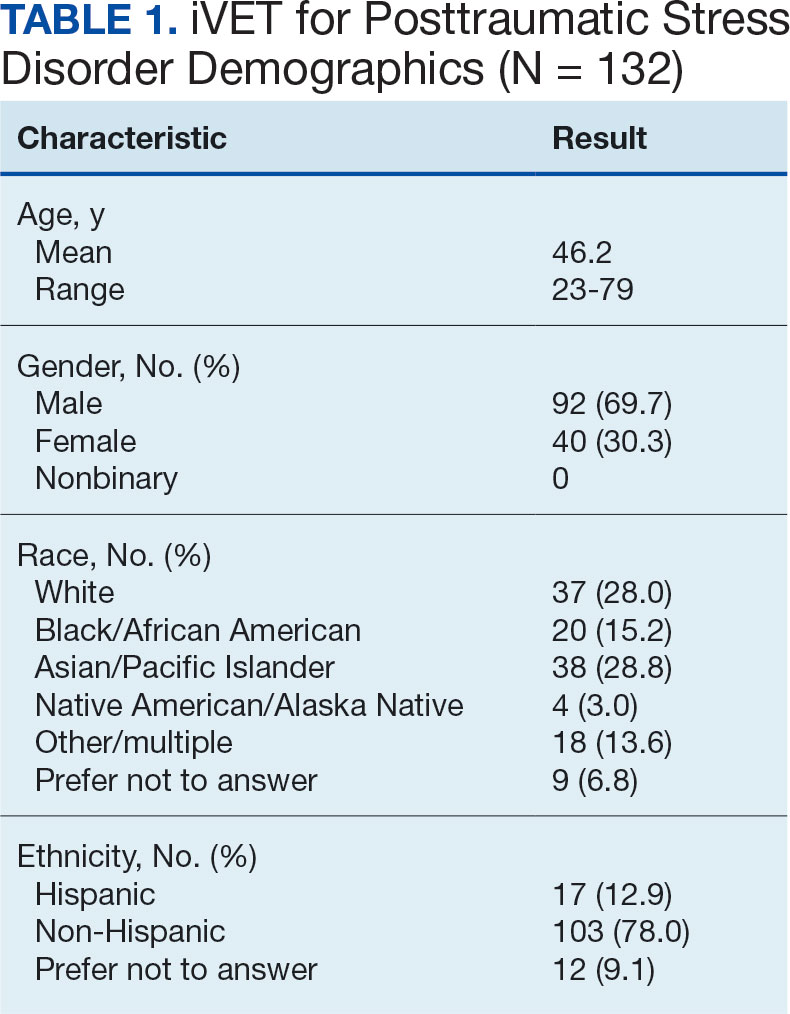
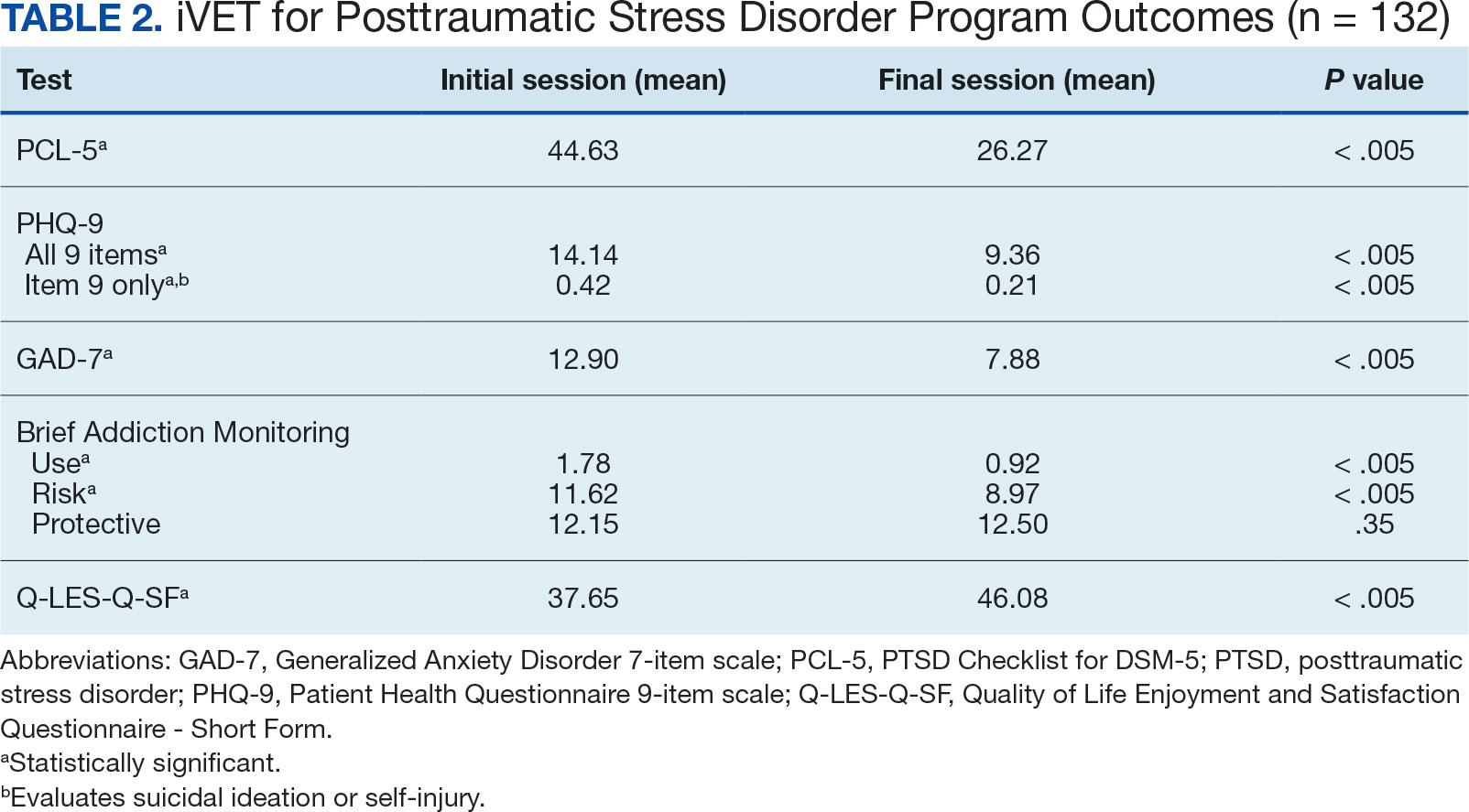
Another important aspect to consider when implementing massed models of EBP is the impact on employee well-being and job satisfaction. The impact of EBP on staff was assessed following the initial EBP project. To explore this further, all staff members in the iVET for PTSD were invited to engage in a small program evaluation. iVET staff were guided through a visualization meditation intended to recall a typical workday 1 month prior to starting their new position with iVET. After the visualization meditation, staff completed the Professional Quality of Life (ProQOL) scale, a 30-item, self-reported questionnaire for health care workers that evaluates compassion satisfaction, perceived support, burnout, secondary traumatic stress, and moral distress.28 One week later, staff were asked to complete the ProQOL again to capture their state after the first 6 months into their tenure as iVET staff. iVET employees experienced significantly increased perceived support (P < .05), reduced burnout (P < .05), reduced secondary traumatic stress (P < .05), and reduced moral distress (P < .05). Team members also remarked on the rewarding nature of the work and care model.
Future Directions
Future research should aim to sustain these outcomes as the iVET program continues to serve more veterans. Another important line of inquiry is longer-term follow-up, as exploring if outcomes are maintained over time is an important question that has not been answered in this article. In addition, we hope to see the accelerated model of care applied to treatment of other presenting concerns in mental health treatment (eg, anxiety, depression, insomnia). Expansion of accelerated mental health treatment into other federal and non-federal health care settings is another worthy direction. Finally, while short term (6 months) assessment of staff satisfaction in iVET was promising, ongoing assessment staff satisfaction over a longer timeframe (1-5 years) is also important.
CONCLUSIONS
PE for PTSD has been demonstrated to be effective and improve functioning and is supported by multiple clinical practice guidelines.1-5 However, as federal practitioners, we must consider the reality that many of the individuals who could benefit are not engaging in PE and there is a high dropout rate for those that do. It is vital that we envision a future state where access to PE for PTSD is equitable and inclusive, retention rates are dramatically improved, and clinicians providing PE do not experience high rates of burnout.
We must continue exploring how we can better care for our patients and colleagues. We posit that the development of programs, or tracks within existing programs, that provide massed or accelerated PE for PTSD with virtual delivery options is an imperative step toward improved care. Federal health care settings treating trauma-exposed patients with PTSD, such as those within the US Department of Defense, Indian Health Services, Federal Bureau of Prisons, and VA, are well positioned to implement programs like iVET. We believe this model of care has great merit and foresee a future where all patients seeking PTSD treatment have the option to complete an accelerated or massed course of PE should they so desire. The experiences outlined in this article illustrate the feasibility, acceptability, and sustainability of such programs without requiring substantial staffing and financial resources.
Evidence-based psychotherapy (EBP) for posttraumatic stress disorder (PTSD), such as prolonged exposure (PE), is supported by multiple clinical practice guidelines and is expected to be available to veterans served by the Veterans Health Administration (VHA).1-5 However, traditional models of EBP delivery with 1 or 2 sessions weekly have high dropout rates.6,7 Few veterans who could benefit from such EBPs receive them, and those who do have low completion rates.8,9 Over a 15-year period, VHA records review of > 265,500 veterans with PTSD showed only 9.1% completed EBP treatment that included but was not limited to PE.10
One empirically supported solution that has yet to be widely implemented is delivering EBPs for PTSD in a massed or accelerated format of ≥ 3 sessions weekly.11 While these massed models of EBP delivery for PTSD are promising, their implementation is limited in federal health care settings, such as the VHA.12 PE therapy is a first-line treatment for PTSD that has been evaluated in numerous clinical trials since the early 1990s and in a wide range of trauma populations.13,14 Massed PE is effective and PE has been found to be effective both in-person and via telehealth.11,15,16
Another approach to accelerated PE is the inclusion of a massed PE course within a broader treatment context that includes augmentation of the massed PE with additional services, this is referred to as an intensive outpatient model (IOP).17 PE-IOP has also been shown to be feasible, acceptable, and effective with increased completion rates in comparison to the traditional (1 or 2 sessions weekly) model of PE.12,16,18,19 Ragsdale et al describe a 2-week IOP with multiple treatment tracks, including a PTSD track. The PTSD treatment track includes massed PE and additional standard services including case management, wellness services, family services, and a single session effective behaviors group. Additional augmentation services are available when clinically indicated (eg, repetitive transcranial magnetic stimulation, transcranial direct current stimulation treatment, psychoeducation, motivational interviewing, and/or relapse prevention).17
Rauch et al studied the first 80 patients completing an IOP program that consisted of PE (5 sessions weekly) and complementary interventions (eg, mindfulness and yoga) and reported a 96% retention rate, significant reductions of self-reported PTSD symptoms, significant reduction in self-reported co-occurring depression symptoms, and significant increase in self-reported satisfaction with social functioning. 18 In another study, Sherril et al explored patient reactions to participation in massed PE (5 sessions weekly) and found that patients reported significantly more positive than negative reactions. Sherrill et al noted that according to patients, the benefits of massed PE included a structured format that limits avoidance and distraction. The resulting fast pace of progress enhanced motivation; however, drawbacks included short-term discomfort and time demands.19 Yamokoski et al explored the feasibility of massed PE in a larger study of PTSD treatment in an intensive outpatient track (IOT) in a VHA PTSD clinic with minimal staffing. The 48 patients who completed IOT PTSD treatment in 2 or 4 weeks (including 35 patients who received massed PE) had high retention rates (85%), reported high satisfaction, and had significantly reduced PTSD and depression symptoms.12
The massed IOT PE model implemented by Yamokoski et al included the primary EBP intervention of massed PE with adjunctive groups. The addition of these groups increased both retention and patient-reported satisfaction. The PE-IOP model implemented by Rauch et al and Sherrill et al also included wellness and educational groups, as well as access to complementary interventions such as mindfulness and yoga.18,19 The addition of wellness education along with a primary EBP aligned with the VHA focus on whole health well-being and wellness. The whole health approach includes understanding the factors that motivate a patient toward health and well-being, provision of health education, and providing access to complementary interventions such as mindfulness.20 Dryden et al describe the whole health transformation within VHA as a proactive approach to addressing employee and patient wellness and health. Their research found that the whole health model promoted well-being in patients and staff and was sustained even during the COVID-19 pandemic.21 Dryden et al also noted that use of virtual technologies facilitated and promoted continued whole health implementation. The literature illustrates that: (1) massed PE can be provided with complementary education and wellness offerings, and that such offerings may increase both retention and satisfaction by enriching the massed PE treatment (eg, delivering PE-IOP); (2) whole health including wellness education and complementary interventions (eg, mindfulness, motivational enhancement) promotes well-being in both patients and mental health professionals; and (3) whole health education and complementary interventions can be delivered virtually.
Health Care Need
Prior to the implementation of a massed EBP for PTSD program at US Department of Veterans Affairs (VA) Pacific Islands Health Care System (VAPIHCS), our setting included a traditional outpatient program for treatment of PTSD and a 12- bed residential program for treatment of PTSD for male-identified (self-identified and identified as male in the electronic medical record) veterans via a cohort model with an 8- or 9-week length of stay. Both programs were located on Oahu. Thus, veterans who received care at VAPIHCS had access to PE in both outpatient and residential settings and via in-person and telehealth modalities. However, their access to PE was limited to the traditional models of PE delivery (eg, 1 or 2 session per week) and very few veterans outside of the island of Oahu had accessed PE treatment for PTSD. Moreover, when looking at PE reach within VAPIHCS, in the fiscal year prior to the implementation of the massed EBP program, only 32 of the > 5000 eligible veterans with a PTSD diagnosis had received PE. VAPIHCS serves veterans in a catchment area across the Pacific Basin which includes 3 time zones: Hawaii Standard Time (HST), Chamorro Standard Time (ChST), and Samoa Standard Time (SST). ChST is 20 hours ahead of HST, making service delivery that is inclusive for patients in Guam and Saipan especially challenging when providing care from Hawaii or other US states or territories. Given all of this, implementation of a new program offering accelerated PE virtually to any veterans with PTSD within the VAPIHCS would increase access to and reduce barriers to receiving PE.
PROGRAM DESCRIPTION
The Intensive Virtual EBP Team (iVET) for PTSD consists of an accelerated course of PE therapy and whole health education provided via VA Video Connect (VVC). iVET is a 3-week program and includes 3 parts: (1) massed individual PE therapy for PTSD; (2) group whole health and wellness classes; and (3) individual health coaching to address personal wellness goals. Programming is offered over 10-hour days to increase access across multiple time zones, especially to allow for participation in Guam and Saipan.
When a patient is referred to the iVET, their first contact is a video (or telephone) appointment with a registered nurse (RN) for a screening session. The screening session is designed to educate the patient about the program, including interventions, time commitment, and resources required for participation. In addition, following the educational discussion, the RN completes screening for safety with the patient including suicidal ideation and risk, as well as intimate partner violence risk. If urgent safety concerns are present, a licensed social worker or psychologist will join the screening to complete further assessment of risk and to address any safety concerns. Following screening, patients are scheduled for a VVC intake with a licensed therapist (social worker or psychologist) to complete the Clinician-Administered PTSD Scale (CAPS-5) for the Diagnostic and Statistical Manual of Mental Disorders (Fifth Edition), a clinical interview for PTSD assessment. Patients are also sent a secure link to complete a measurement-based care (MBC) battery of self-report measures including measures assessing demographics, PTSD symptoms, anxiety symptoms, depression symptoms, substance use, quality of life (QOL), and satisfaction with mental health care. The results of the CAPS-5 and self-report measures are discussed with the patient during the intake session when planning next steps and engaging in shared decision-making. This initial VVC intake not only allows for diagnostic goodness of fit but also provides the opportunity to troubleshoot any technical difficulties the patients might have with the virtual platforms.
There are minimal exclusion criteria for participation in iVET, which include active unmanaged psychosis or manic symptoms, recent suicidal crises (attempt within 8 weeks), active nonsuicidal self-injurious behaviors (within 8 weeks), and moderate-to-severe cognitive impairment. Following intake, patients are scheduled to begin their course of care with iVET. Upon completion of intake, patients are sent program materials for their individual and group classes, asked to obtain or request a recording device, and told they will receive email links for all VVC appointments. Patients are admitted to the iVET in a rolling admission fashion, thereby increasing access when compared to closed group and/or cohort models of care.
Patients receiving care in iVET attend 2 or 3 telehealth appointments daily with practice exercises daily between telehealth sessions. The primary EBP intervention in the iVET for PTSD program is a massed or accelerated course of PE, which includes 4 primary components: psychoeducation, in-vivo exposure, imaginal exposure, and breathing retraining. Specifically, PE is delivered in 4 90-minute individual sessions weekly allowing completion of the full PE protocol, to fidelity, in 3 weeks. In addition to receiving this primary intervention, patients also participate in four 50-minute group sessions per week of a whole health and wellness education class and have access to one 30- to 60-minute session weekly of individual health coaching should they wish to set wellness goals and receive coaching in support of attaining wellness goals. During iVET, patients are invited to complete MBC batteries of selfreport measures including measures assessing PTSD symptoms, anxiety symptoms, depression symptoms, substance use, QOL, and satisfaction with mental health care at sessions 1, 5, 9, and the final session of PE. Following discharge from the iVET, patients are offered 1-month, 3-month, and 6-month individual postdischarge check-up sessions with a therapist where they are invited to complete MBC measures and review relapse prevention and maintenance of treatment gains. Likewise, they are offered 1-month, 3-month, and 6-month postdischarge check-up sessions with an RN focused on maintaining wellness gains.
The iVET for PTSD staff includes 3 therapists (psychologists or social workers) and an RN. Additionally, the iVET for PTSD is supported by a program manager and a program support assistant. The primary cost of the program is salary for staff. Additional iVET for PTSD resources included computer equipment for staff and minimal supplies. Due to the virtual environment of care, iVET staff telework and do not require physical space within VAPIHCS.
OUTCOMES
All veterans receiving care in iVET for PTSD are invited to complete a MBC at multiple timepoints including pretreatment, during PE treatment, and posttreatment. The MBC measures included self-reported demographics, a 2-item measure of satisfaction with mental health services, the Brief Addiction Monitor-Intensive Outpatient Program questionnaire,22 the Generalized Anxiety Disorder-7 scale,23, the Patient Health Questionnaire (PHQ-9),24 the QOL Enjoyment and Satisfaction Questionnaire- Short Form,25 and the PTSD Checklist for DSM-5 (PCL-5), both weekly and monthly versions. 26,27
The retention rate has averaged 81% since the iVET for PTSD opened in 2022. To date, 132 veterans have completed the iVET for PTSD program, including a full course of massed PE (Table 1). Veterans experienced reduced PTSD (P < .005), depression (P < .005), anxiety (P < .005), and substance use risk (P < .005). Veterans experienced improved QOL (P < .005) and reported high satisfaction with mental health care in iVET for PTSD (Table 2). Veterans also experienced reduced thoughts of death or suicidal ideation (SI) based on PHQ-9 item 9 responses. When looking categorically at presence or absence of SI on PHQ-9 item 9, a significant relationship was found between the absence of suicidal ideation and completion of a course of massed PE: X2 (1, N = 132) = 13.75, P < .001. In addition, veterans who completed the program showed a significant decrease in severity of SI as measured continuously (range, 0-3) on PHQ-9 item 9 (P < .005).
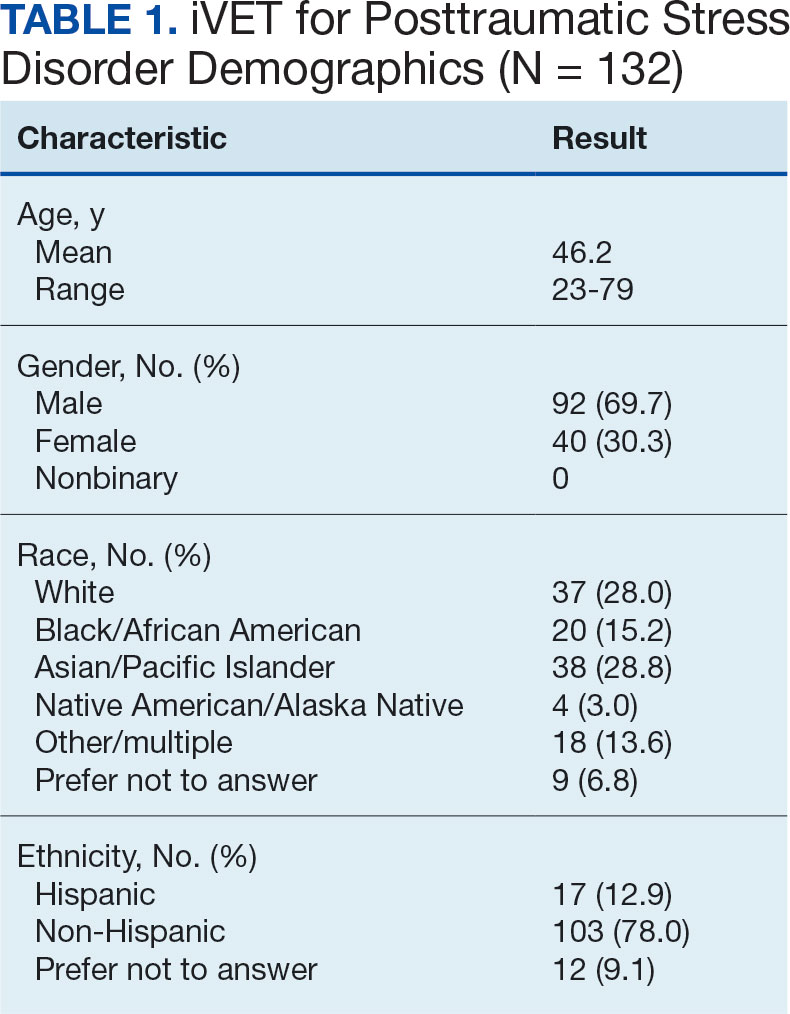
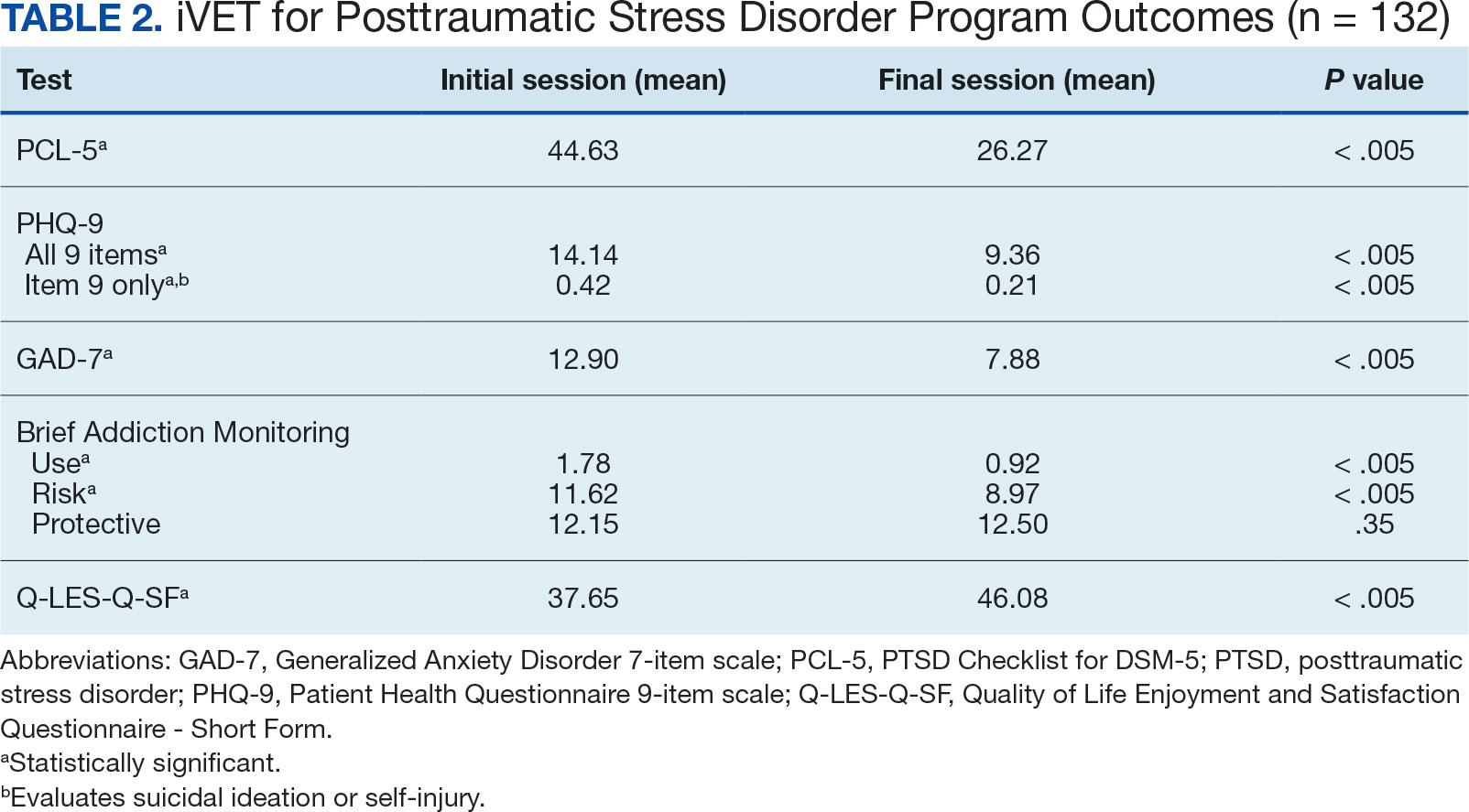
Another important aspect to consider when implementing massed models of EBP is the impact on employee well-being and job satisfaction. The impact of EBP on staff was assessed following the initial EBP project. To explore this further, all staff members in the iVET for PTSD were invited to engage in a small program evaluation. iVET staff were guided through a visualization meditation intended to recall a typical workday 1 month prior to starting their new position with iVET. After the visualization meditation, staff completed the Professional Quality of Life (ProQOL) scale, a 30-item, self-reported questionnaire for health care workers that evaluates compassion satisfaction, perceived support, burnout, secondary traumatic stress, and moral distress.28 One week later, staff were asked to complete the ProQOL again to capture their state after the first 6 months into their tenure as iVET staff. iVET employees experienced significantly increased perceived support (P < .05), reduced burnout (P < .05), reduced secondary traumatic stress (P < .05), and reduced moral distress (P < .05). Team members also remarked on the rewarding nature of the work and care model.
Future Directions
Future research should aim to sustain these outcomes as the iVET program continues to serve more veterans. Another important line of inquiry is longer-term follow-up, as exploring if outcomes are maintained over time is an important question that has not been answered in this article. In addition, we hope to see the accelerated model of care applied to treatment of other presenting concerns in mental health treatment (eg, anxiety, depression, insomnia). Expansion of accelerated mental health treatment into other federal and non-federal health care settings is another worthy direction. Finally, while short term (6 months) assessment of staff satisfaction in iVET was promising, ongoing assessment staff satisfaction over a longer timeframe (1-5 years) is also important.
CONCLUSIONS
PE for PTSD has been demonstrated to be effective and improve functioning and is supported by multiple clinical practice guidelines.1-5 However, as federal practitioners, we must consider the reality that many of the individuals who could benefit are not engaging in PE and there is a high dropout rate for those that do. It is vital that we envision a future state where access to PE for PTSD is equitable and inclusive, retention rates are dramatically improved, and clinicians providing PE do not experience high rates of burnout.
We must continue exploring how we can better care for our patients and colleagues. We posit that the development of programs, or tracks within existing programs, that provide massed or accelerated PE for PTSD with virtual delivery options is an imperative step toward improved care. Federal health care settings treating trauma-exposed patients with PTSD, such as those within the US Department of Defense, Indian Health Services, Federal Bureau of Prisons, and VA, are well positioned to implement programs like iVET. We believe this model of care has great merit and foresee a future where all patients seeking PTSD treatment have the option to complete an accelerated or massed course of PE should they so desire. The experiences outlined in this article illustrate the feasibility, acceptability, and sustainability of such programs without requiring substantial staffing and financial resources.
- American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. February 24, 2017. Accessed February 27, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- US Department of Veterans Affairs, Veterans Health Administration. Uniform mental health services in VA medical centers and clinics. Veterans Health Administration (VHA) Handbook 1160.01. September 11, 2008. Accessed February 27, 2025. https://www.mentalhealth.va.gov/providers/sud/docs/UniformServicesHandbook1160-01.pdf
- US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Version 3. 2017. Accessed February 27, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DoD-CPG-PTSD-Full-CPG-Edited-11162024.pdf
- Hamblen JL, Bernardy NC, Sherrieb K, et al. VA PTSD clinic director perspectives: How perceptions of readiness influence delivery of evidence-based PTSD treatment. Prof Psychol Res Pract. 2015;46(2): 90-96. doi:10.1037/a0038535
- Schnurr PP, Chard KM, Ruzek JI, et al. Comparison of prolonged exposure vs cognitive processing therapy for treatment of posttraumatic stress disorder among US veterans: a randomized clinical trial. JAMA Netw Open. 2022;5(1):e2136921. doi:10.1001/jamanetworkopen. 2021.36921
- Kehle-Forbes SM, Meis LA, Spoont MR, Polusny MA. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol Trauma. 2016;8(1):107-114. doi:10.1037/tra0000065
- Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, Teng EJ. Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. J Trauma Stress. 2014;27(3):265-273. doi:10.1002/jts.21927
- Shiner B, D’Avolio LW, Nguyen TM, et al. Measuring use of evidence based psychotherapy for posttraumatic stress disorder. Adm Policy Ment Health. 2013;40(4):311-318. doi:10.1007/s10488-012-0421-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37(4):356-364. doi:10.1002/da.22983
- Maguen S, Li Y, Madden E, et al. Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Res. 2019;274:112-128. doi:10.1016/j.psychres.2019.02.027
- Foa EB, McLean CP, Zang Y, et al. Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: a randomized clinical trial. JAMA. 2018;319(4):354-364. doi:10.1001/jama.2017.21242
- Yamokoski C, Flores H, Facemire V, Maieritsch K, Perez S, Fedynich A. Feasibility of an intensive outpatient treatment program for posttraumatic stress disorder within the veterans health care administration. Psychol Serv. 2023;20(3):506-515. doi:10.1037/ser0000628
- McLean CP, Foa EB. State of the Science: Prolonged exposure therapy for the treatment of posttraumatic stress disorder. J Trauma Stress. 2024;37(4):535-550. doi:10.1002/jts.23046
- McLean CP, Levy HC, Miller ML, Tolin DF. Exposure therapy for PTSD: A meta-analysis. Clin Psychol Rev. 2022;91:102115. doi:10.1016/j.cpr.2021.102115
- Wells SY, Morland LA, Wilhite ER, et al. Delivering Prolonged Exposure Therapy via Videoconferencing During the COVID-19 Pandemic: An Overview of the Research and Special Considerations for Providers. J Trauma Stress. 2020;33(4):380-390. doi:10.1002/jts.22573
- Peterson AL, Blount TH, Foa EB, et al. Massed vs intensive outpatient prolonged exposure for combat-related posttraumatic stress disorder: a randomized clinical trial. JAMA Netw Open. 2023;6(1):e2249422. Published 2023 Jan 3. doi:10.1001/jamanetworkopen.2022.49422
- Ragsdale KA, Nichols AA, Mehta M, et al. Comorbid treatment of traumatic brain injury and mental health disorders. NeuroRehabilitation. 2024;55(3):375-384. doi:10.3233/NRE-230235
- Rauch SAM, Yasinski CW, Post LM, et al. An intensive outpatient program with prolonged exposure for veterans with posttraumatic stress disorder: retention, predictors, and patterns of change. Psychol Serv. 2021;18(4):606-618. doi:10.1037/ser0000422
- Sherrill AM, Maples-Keller JL, Yasinski CW, Loucks LA, Rothbaum BO, Rauch SAM. Perceived benefits and drawbacks of massed prolonged exposure: qualitative thematic analysis of reactions from treatment completers. Psychol Trauma. 2022;14(5):862-870. doi:10.1037/tra0000548
- Gaudet T, Kligler B. Whole health in the whole system of the Veterans Administration: how will we know we have reached this future state? J Altern Complement Med. 2019;25(S1):S7-S11. doi:10.1089/acm.2018.29061.gau
- Dryden EM, Bolton RE, Bokhour BG, et al. Leaning Into whole health: sustaining system transformation while supporting patients and employees during COVID-19. Glob Adv Health Med. 2021;10:21649561211021047. doi:10.1177/21649561211021047
- Cacciola JS, Alterman AI, Dephilippis D, et al. Development and initial evaluation of the Brief Addiction Monitor (BAM). J Subst Abuse Treat. 2013;44(3):256-263. doi:10.1016/j.jsat.2012.07.013
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097. doi:10.1001/archinte.166.10.1092
- Kroenke K, Spi tze r RL , Wi l l i ams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Stevanovic D. Quality of Life Enjoyment and Satisfaction Questionnaire-short form for quality of life assessments in clinical practice: a psychometric study. J Psychiatr Ment Health Nurs. 2011;18(8):744-750. doi:10.1111/j.1365-2850.2011.01735.x
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL- 5). National Center for PTSD. Updated August 29, 2023. Accessed February 27, 2025. https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.pdf
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi:10.1002/jts.22059
- Stamm BH. The Concise ProQOL Manual. 2nd ed. Pro- QOL.org; 2010.
- American Psychological Association. Clinical Practice Guideline for the Treatment of Posttraumatic Stress Disorder (PTSD) in Adults. February 24, 2017. Accessed February 27, 2025. https://www.apa.org/ptsd-guideline/ptsd.pdf
- US Department of Veterans Affairs, Veterans Health Administration. Uniform mental health services in VA medical centers and clinics. Veterans Health Administration (VHA) Handbook 1160.01. September 11, 2008. Accessed February 27, 2025. https://www.mentalhealth.va.gov/providers/sud/docs/UniformServicesHandbook1160-01.pdf
- US Department of Veterans Affairs, US Department of Defense. VA/DoD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder. Version 3. 2017. Accessed February 27, 2025. https://www.healthquality.va.gov/guidelines/MH/ptsd/VA-DoD-CPG-PTSD-Full-CPG-Edited-11162024.pdf
- Hamblen JL, Bernardy NC, Sherrieb K, et al. VA PTSD clinic director perspectives: How perceptions of readiness influence delivery of evidence-based PTSD treatment. Prof Psychol Res Pract. 2015;46(2): 90-96. doi:10.1037/a0038535
- Schnurr PP, Chard KM, Ruzek JI, et al. Comparison of prolonged exposure vs cognitive processing therapy for treatment of posttraumatic stress disorder among US veterans: a randomized clinical trial. JAMA Netw Open. 2022;5(1):e2136921. doi:10.1001/jamanetworkopen. 2021.36921
- Kehle-Forbes SM, Meis LA, Spoont MR, Polusny MA. Treatment initiation and dropout from prolonged exposure and cognitive processing therapy in a VA outpatient clinic. Psychol Trauma. 2016;8(1):107-114. doi:10.1037/tra0000065
- Mott JM, Mondragon S, Hundt NE, Beason-Smith M, Grady RH, Teng EJ. Characteristics of U.S. veterans who begin and complete prolonged exposure and cognitive processing therapy for PTSD. J Trauma Stress. 2014;27(3):265-273. doi:10.1002/jts.21927
- Shiner B, D’Avolio LW, Nguyen TM, et al. Measuring use of evidence based psychotherapy for posttraumatic stress disorder. Adm Policy Ment Health. 2013;40(4):311-318. doi:10.1007/s10488-012-0421-0
- Maguen S, Holder N, Madden E, et al. Evidence-based psychotherapy trends among posttraumatic stress disorder patients in a national healthcare system, 2001-2014. Depress Anxiety. 2020;37(4):356-364. doi:10.1002/da.22983
- Maguen S, Li Y, Madden E, et al. Factors associated with completing evidence-based psychotherapy for PTSD among veterans in a national healthcare system. Psychiatry Res. 2019;274:112-128. doi:10.1016/j.psychres.2019.02.027
- Foa EB, McLean CP, Zang Y, et al. Effect of prolonged exposure therapy delivered over 2 weeks vs 8 weeks vs present-centered therapy on PTSD symptom severity in military personnel: a randomized clinical trial. JAMA. 2018;319(4):354-364. doi:10.1001/jama.2017.21242
- Yamokoski C, Flores H, Facemire V, Maieritsch K, Perez S, Fedynich A. Feasibility of an intensive outpatient treatment program for posttraumatic stress disorder within the veterans health care administration. Psychol Serv. 2023;20(3):506-515. doi:10.1037/ser0000628
- McLean CP, Foa EB. State of the Science: Prolonged exposure therapy for the treatment of posttraumatic stress disorder. J Trauma Stress. 2024;37(4):535-550. doi:10.1002/jts.23046
- McLean CP, Levy HC, Miller ML, Tolin DF. Exposure therapy for PTSD: A meta-analysis. Clin Psychol Rev. 2022;91:102115. doi:10.1016/j.cpr.2021.102115
- Wells SY, Morland LA, Wilhite ER, et al. Delivering Prolonged Exposure Therapy via Videoconferencing During the COVID-19 Pandemic: An Overview of the Research and Special Considerations for Providers. J Trauma Stress. 2020;33(4):380-390. doi:10.1002/jts.22573
- Peterson AL, Blount TH, Foa EB, et al. Massed vs intensive outpatient prolonged exposure for combat-related posttraumatic stress disorder: a randomized clinical trial. JAMA Netw Open. 2023;6(1):e2249422. Published 2023 Jan 3. doi:10.1001/jamanetworkopen.2022.49422
- Ragsdale KA, Nichols AA, Mehta M, et al. Comorbid treatment of traumatic brain injury and mental health disorders. NeuroRehabilitation. 2024;55(3):375-384. doi:10.3233/NRE-230235
- Rauch SAM, Yasinski CW, Post LM, et al. An intensive outpatient program with prolonged exposure for veterans with posttraumatic stress disorder: retention, predictors, and patterns of change. Psychol Serv. 2021;18(4):606-618. doi:10.1037/ser0000422
- Sherrill AM, Maples-Keller JL, Yasinski CW, Loucks LA, Rothbaum BO, Rauch SAM. Perceived benefits and drawbacks of massed prolonged exposure: qualitative thematic analysis of reactions from treatment completers. Psychol Trauma. 2022;14(5):862-870. doi:10.1037/tra0000548
- Gaudet T, Kligler B. Whole health in the whole system of the Veterans Administration: how will we know we have reached this future state? J Altern Complement Med. 2019;25(S1):S7-S11. doi:10.1089/acm.2018.29061.gau
- Dryden EM, Bolton RE, Bokhour BG, et al. Leaning Into whole health: sustaining system transformation while supporting patients and employees during COVID-19. Glob Adv Health Med. 2021;10:21649561211021047. doi:10.1177/21649561211021047
- Cacciola JS, Alterman AI, Dephilippis D, et al. Development and initial evaluation of the Brief Addiction Monitor (BAM). J Subst Abuse Treat. 2013;44(3):256-263. doi:10.1016/j.jsat.2012.07.013
- Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092-1097. doi:10.1001/archinte.166.10.1092
- Kroenke K, Spi tze r RL , Wi l l i ams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. doi:10.1046/j.1525-1497.2001.016009606.x
- Stevanovic D. Quality of Life Enjoyment and Satisfaction Questionnaire-short form for quality of life assessments in clinical practice: a psychometric study. J Psychiatr Ment Health Nurs. 2011;18(8):744-750. doi:10.1111/j.1365-2850.2011.01735.x
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, Schnurr PP. The PTSD Checklist for DSM-5 (PCL- 5). National Center for PTSD. Updated August 29, 2023. Accessed February 27, 2025. https://www.ptsd.va.gov/professional/assessment/documents/PCL5_Standard_form.pdf
- Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489-498. doi:10.1002/jts.22059
- Stamm BH. The Concise ProQOL Manual. 2nd ed. Pro- QOL.org; 2010.
Accelerated Prolonged Exposure Therapy for Posttraumatic Stress Disorder in a Veterans Health Administration System
Accelerated Prolonged Exposure Therapy for Posttraumatic Stress Disorder in a Veterans Health Administration System
VA is a Leader in Mental Health and Social Service Research and Operations
VA is a Leader in Mental Health and Social Service Research and Operations
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
VA is a Leader in Mental Health and Social Service Research and Operations
VA is a Leader in Mental Health and Social Service Research and Operations
Severe anxiety and agitation
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
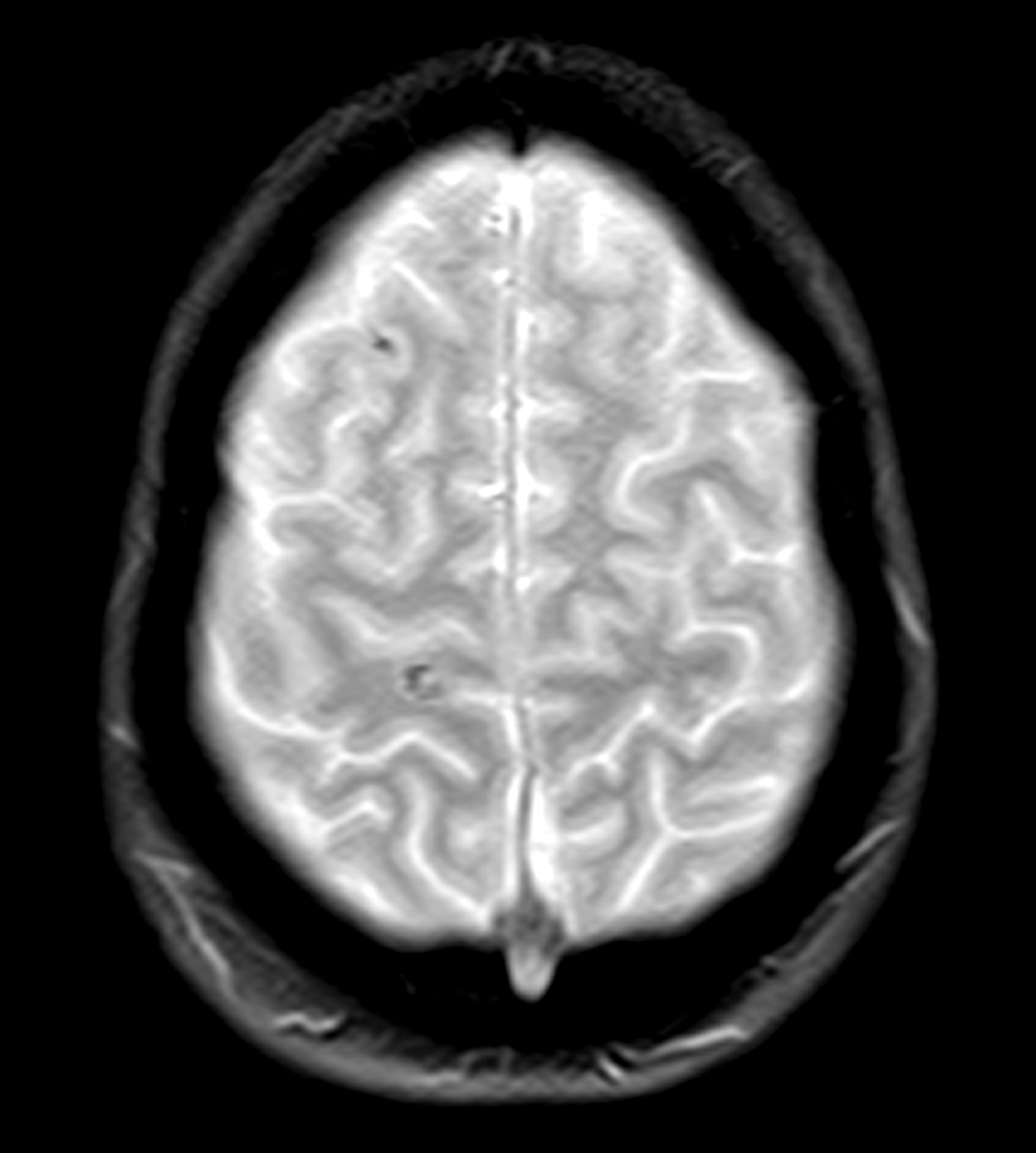
A 28-year-old professional boxer presents with severe anxiety, agitation, headaches, and insomnia with recurring nightmares and flashbacks. His symptoms began after he was robbed at gunpoint in the gym parking lot as he was getting into his car about 6 months ago. Since that time, he has had to postpone several fights because he is unable to maintain his training schedule and reports feeling depressed as a result. He is also at risk for suspension from his regular gym because he has gotten into several violent, unprovoked altercations with fellow boxers, and he has also had multiple violent outbursts outside of the gym. He has a history of concussion.
Physical exam reveals increased heart rate and hypervigilance. The patient is administered the Patient Health Questionnaire and has a score of 14 out of a possible 27. Zero to 4 indicates no depression, whereas 14 falls within the range of moderate depression. A brain CT scan (Figure) is ordered because of his history of concussion and his chronic symptoms. The scan reveals two subacute hematomas in the left hemisphere, one in the frontal lobe and the other in the temporal lobe. Additional tests are ordered: laboratory testing, to rule out organic or infectious causes of symptoms and electroencephalography, to assess for a possible seizure focus; both tests reveal nothing remarkable. The hematomas were noted at the time of a previous head injury 2 years ago.