User login
Agitation and emotional lability
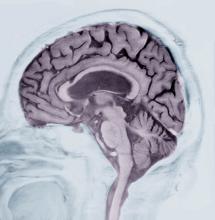
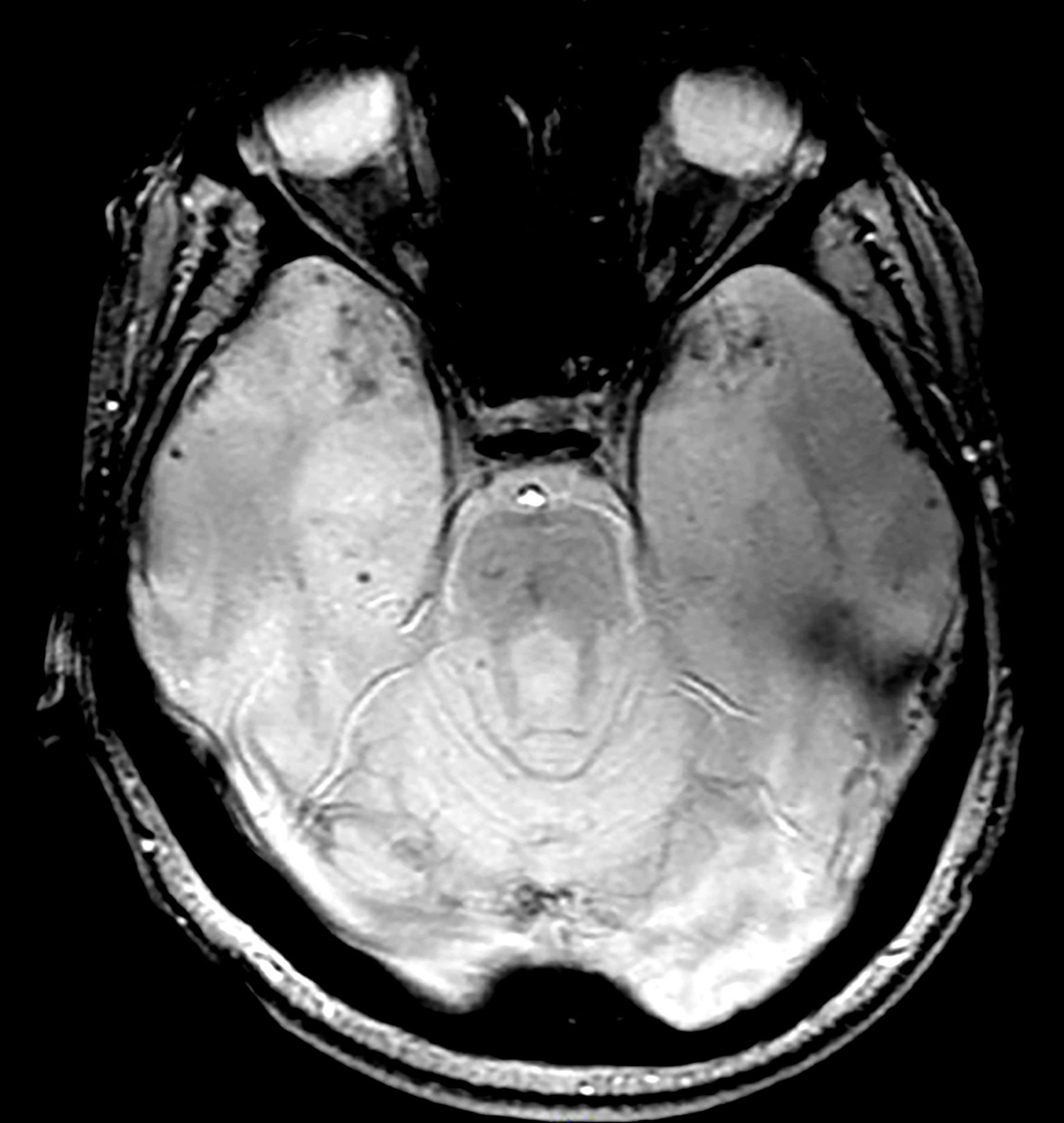
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 76-year-old Black woman presents to her physician. She is accompanied by her daughter who reports that, over the last 9 months, her mother has exhibited worsening memory loss, confusion, impaired judgment, agitation, and emotional lability. She is often unaware of where she is or how she got there. She sometimes does not recognize her family members or people who are familiar to her. Her appetite has been variable, and her sleep schedule is altered so that she often sleeps during the day and is awake at night. Sometimes, she is so irritable that she becomes aggressive and insists on situations that don’t exist. Her executive function is low. Her daughter reports that the patient had a fall 9 months ago and again 4 months ago, after which her symptoms became progressively worse.
The patient has complained about being forgetful and clumsy for much of the past 5 years, which she has attributed to old age. Until the last year or so, these have not greatly impaired her daily function and were not of great concern to her family or providers. She has a history of hypertension and diabetes, both of which are pharmacologically managed with mixed results due to variable adherence.
Physical exam confirms her daughter’s report. The patient appears thin, fatigued, and anxious. She has lost 20 lb since her last visit. She has great difficulty maintaining focus on what is being asked of her and in following the conversation. When she does speak, her speech is slow. She exhibits both motor deficits — in balance and coordination — and a bradykinetic gait.
Laboratory testing is performed: complete blood count w/diff, comprehensive metabolic panel, thyroid panel, cobalamin level, vitamin D screening. All results are within normal range for this patient. She was unable to complete the Geriatric Depression Scale on her own; direct questioning about whether she was feeling depressed is negative. Mini-Mental State Examination (MMSE) score is 18. MRI is performed; sagittal view reveals cortical atrophy.
Fatigue and brain fog
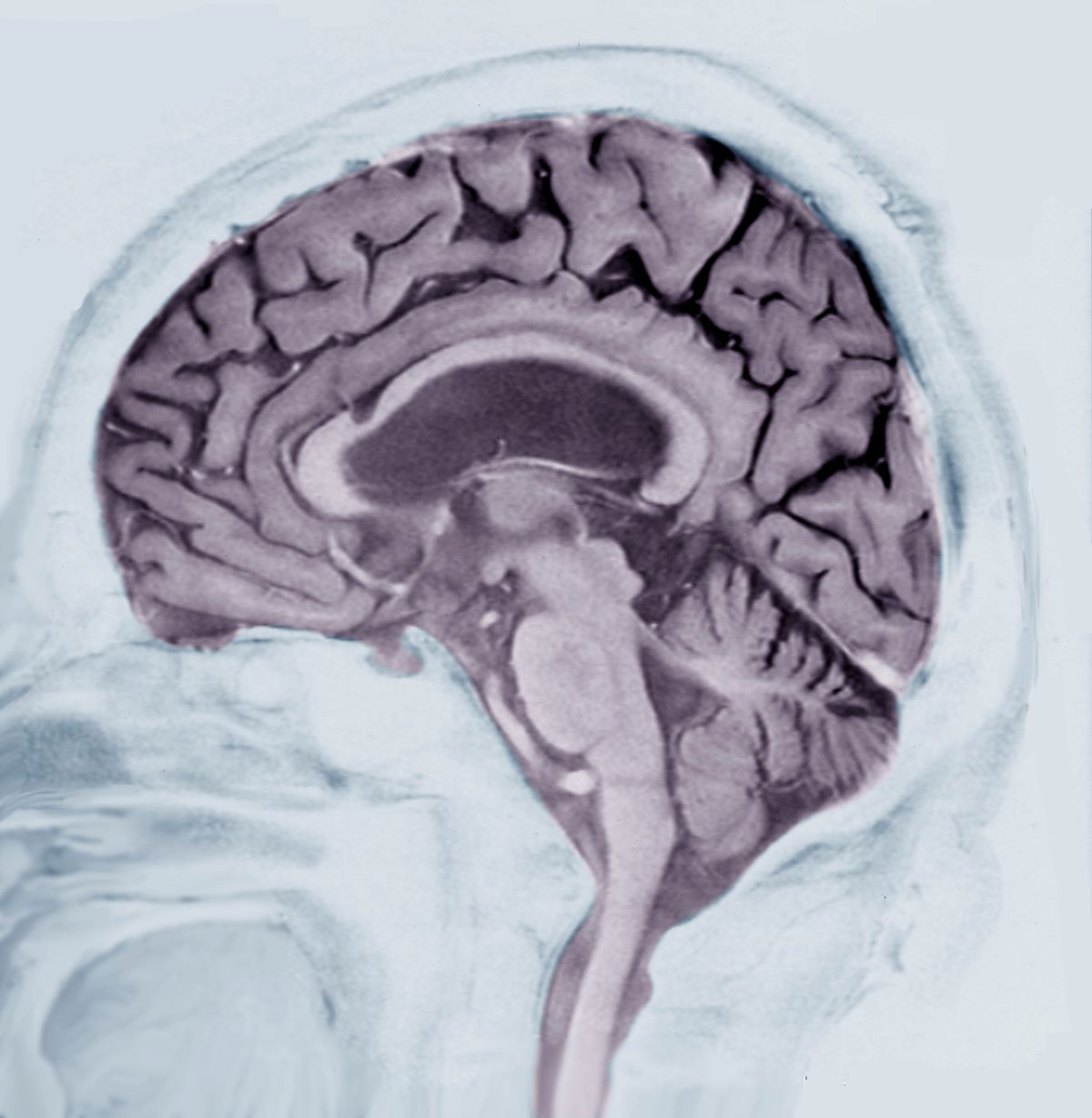
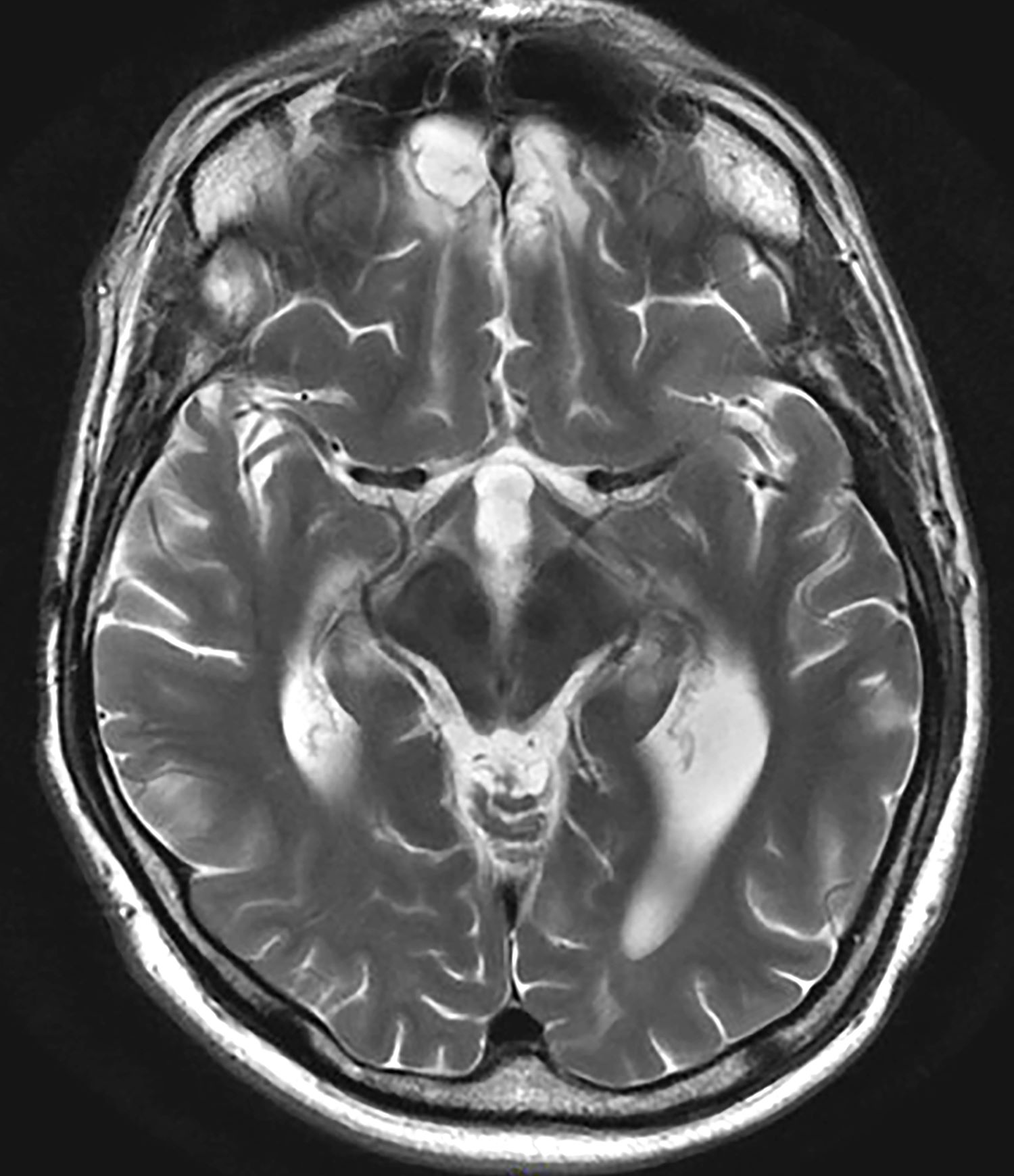
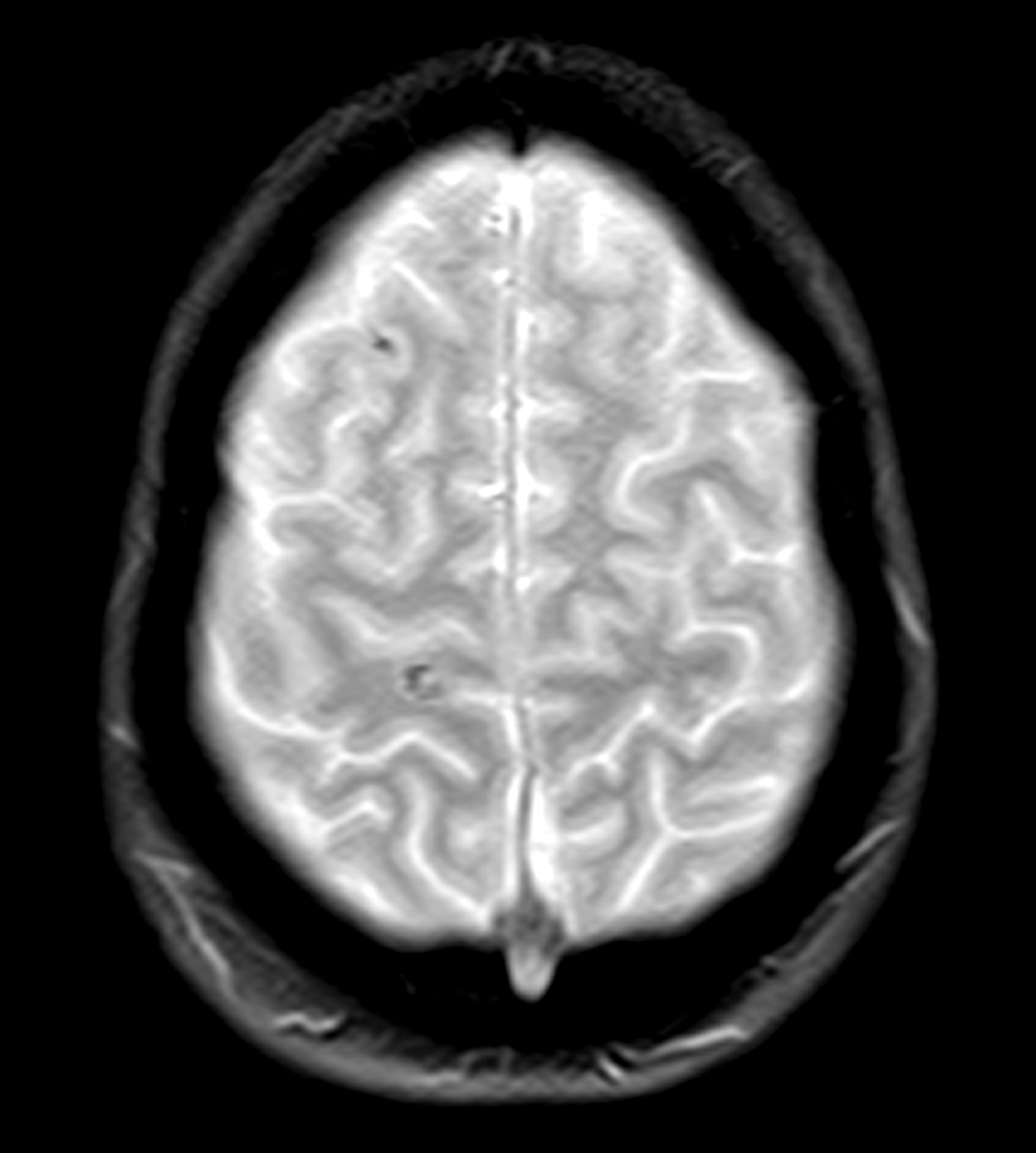
Early-onset AD (EOAD) is the most likely diagnosis for this patient. Her symptoms — cognitive decline, executive function deficits, and visuospatial dysfunction — and brain imaging results are consistent with EOAD. But importantly, her father’s diagnosis of EOAD at age 58 suggests a hereditary component, which greatly increases the genetic risk for this patient. Moreover, neuroimaging shows cortical atrophy in the temporal lobes. A key radiologic feature of AD in this patient is the large increase in the subarachnoid spaces affecting the parietal region.
Between one third to just over one half of patients with EOAD have at least one first-degree relative with the disease. Given the patient’s neuroimaging results and family history of EOAD, she was sent for genetic testing, which revealed mutations in the PSEN1 gene; one the most common genetic causes of EOAD (along with mutations in the APP gene). For those who do have an autosomal dominant familial form of EOAD, clinical presentation is often atypical and includes headaches, myoclonus, seizures, hyperreflexia, and gait abnormalities. This patient did experience headaches but not the other symptoms.
Traumatic brain injury (TBI) is an insult to the brain from an outside mechanical force. It is both non-congenital and non-degenerative but can lead to permanent physical, cognitive, and/or psychosocial functioning. Patients often experience an altered or diminished state of consciousness in the aftermath of such an event. TBI is a diagnostic consideration for this patient, given that she was in a car accident and has experienced unusual cognitive and behavioral symptoms — eg, memory loss and visuospatial dysfunction. However, imaging does not reveal evidence of TBI, with no concussion or cerebral hemorrhage. Thus, TBI is not an accurate diagnosis for this patient.
Parkinson’s disease (PD) is one of the most common neurologic disorders that is marked by three hallmark features: resting tremor, rigidity, and bradykinesia that generally affects people over the age of 60. Even though many patients with PD exhibit some measure of executive function impairment early in the course of the disease, substantial impairment and dementia usually manifest about 8 years after the onset of motor symptoms. Dementia occurs in approximately 20%-40% of patients with PD. Although patients with PD demonstrate executive function deficits, memory loss, and visuospatial dysfunction, they do not experience aphasia. This patient does not have any of the cardinal features of PD, which rules it out as a diagnosis.
Frontotemporal dementia is a progressive dysfunction of the frontal lobes of the brain, primarily manifesting as language abnormalities, including reduced speech, perseveration, mutism, and echolalia, also known as primary progressive aphasia (PPA). Over time, patients develop other psychiatric symptoms: disinhibition, impulsivity, loss of social awareness, neglect of personal hygiene, mental rigidity, and utilization behavior. Given the patient’s language difficulties, frontotemporal dementia may be an initial diagnostic consideration. However, per the neurologic imaging results, brain abnormalities are located in the temporal regions. Additionally, the patient does not exhibit any of the psychiatric symptoms associated with frontotemporal dementia but does experience short-term memory loss and visuospatial dysfunction, which are not typical of this diagnosis. This patient does not have frontotemporal dementia.
EOAD is characterized by deficits in language, visuospatial skills and executive function. Often, these patients do not exhibit amnestic disorder early in the disease. While their memory recognition and semantic memory is higher than for patients who present with late-onset (normal course) AD, their attention scores are typically lower. As a result of this atypical presentation, patients with EOAD tend to have a longer duration of disease before diagnosis (~1.6 years). They are also likely to have a history of TBI, which is a risk factor for dementia.
In comparison to late-onset AD (LOAD), EOAD has a larger genetic predisposition (92%-100% vs 70%-80%), a more aggressive course, a more frequent delay in initial diagnosis, higher prevalence of TBI, and less memory impairment. However, EOAD has greater decline in other cognitive domains, and because of the young age of onset, greater psychosocial impairment. Overall disease progression in these patients is much faster compared with patients who have LOAD. Neuroimaging in these patients generally features greater hippocampal sparing and posterior neocortical atrophy, with brain changes that affect the frontoparietal networks rather than the classic presentation found in LOAD.
An important aspect of the workup of patients for whom EOAD is a diagnostic consideration is to thoroughly determine their family history and to perform genetic testing along with counseling.
The pharmacological treatment of patients with early-onset AD is identical to patients who have normal course or late-onset AD. Cholinesterase inhibitors (ChEIs) — eg, donepezil, galantamine, and rivastigmine, with the usual titration schedules — are indicated in these patients. Although these medications target memory, they also provide support to patients with other variants of EOAD — eg, logopenic variant PPA. However, it is imperative that providers monitor these patients carefully, as ChEIs may exacerbate some behaviors.
Management of patients with EOAD varies based on the patient's specific variant. It is vital for clinicians to coordinate patient-centered care individually. For example, patients with logopenic variant PPA should be referred for speech therapy assessment and treatment should focus on improving communication, while patients with posterior cortical atrophy benefit most from interventions for those who experience vision impairments. As this patient’s symptoms revolve primarily around cognition and visuospatial dysfunction, her treatment will focus on interventions to improve coordination, balance, and cognitive function.
Perhaps the most important part of managing a patient with EOAD is providing adequate and appropriate psychosocial support. These patients are most often in their most productive time of life, balancing careers and families. EOAD can bring about feelings of loss of independence, anticipatory grief, and anxiety about the future and the increased difficulty in managing the tasks of daily life. It is vital that these patients — and their families — receive adequate education and psychiatric support via therapists, support groups, and community resources that are age appropriate.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Early-onset AD (EOAD) is the most likely diagnosis for this patient. Her symptoms — cognitive decline, executive function deficits, and visuospatial dysfunction — and brain imaging results are consistent with EOAD. But importantly, her father’s diagnosis of EOAD at age 58 suggests a hereditary component, which greatly increases the genetic risk for this patient. Moreover, neuroimaging shows cortical atrophy in the temporal lobes. A key radiologic feature of AD in this patient is the large increase in the subarachnoid spaces affecting the parietal region.
Between one third to just over one half of patients with EOAD have at least one first-degree relative with the disease. Given the patient’s neuroimaging results and family history of EOAD, she was sent for genetic testing, which revealed mutations in the PSEN1 gene; one the most common genetic causes of EOAD (along with mutations in the APP gene). For those who do have an autosomal dominant familial form of EOAD, clinical presentation is often atypical and includes headaches, myoclonus, seizures, hyperreflexia, and gait abnormalities. This patient did experience headaches but not the other symptoms.
Traumatic brain injury (TBI) is an insult to the brain from an outside mechanical force. It is both non-congenital and non-degenerative but can lead to permanent physical, cognitive, and/or psychosocial functioning. Patients often experience an altered or diminished state of consciousness in the aftermath of such an event. TBI is a diagnostic consideration for this patient, given that she was in a car accident and has experienced unusual cognitive and behavioral symptoms — eg, memory loss and visuospatial dysfunction. However, imaging does not reveal evidence of TBI, with no concussion or cerebral hemorrhage. Thus, TBI is not an accurate diagnosis for this patient.
Parkinson’s disease (PD) is one of the most common neurologic disorders that is marked by three hallmark features: resting tremor, rigidity, and bradykinesia that generally affects people over the age of 60. Even though many patients with PD exhibit some measure of executive function impairment early in the course of the disease, substantial impairment and dementia usually manifest about 8 years after the onset of motor symptoms. Dementia occurs in approximately 20%-40% of patients with PD. Although patients with PD demonstrate executive function deficits, memory loss, and visuospatial dysfunction, they do not experience aphasia. This patient does not have any of the cardinal features of PD, which rules it out as a diagnosis.
Frontotemporal dementia is a progressive dysfunction of the frontal lobes of the brain, primarily manifesting as language abnormalities, including reduced speech, perseveration, mutism, and echolalia, also known as primary progressive aphasia (PPA). Over time, patients develop other psychiatric symptoms: disinhibition, impulsivity, loss of social awareness, neglect of personal hygiene, mental rigidity, and utilization behavior. Given the patient’s language difficulties, frontotemporal dementia may be an initial diagnostic consideration. However, per the neurologic imaging results, brain abnormalities are located in the temporal regions. Additionally, the patient does not exhibit any of the psychiatric symptoms associated with frontotemporal dementia but does experience short-term memory loss and visuospatial dysfunction, which are not typical of this diagnosis. This patient does not have frontotemporal dementia.
EOAD is characterized by deficits in language, visuospatial skills and executive function. Often, these patients do not exhibit amnestic disorder early in the disease. While their memory recognition and semantic memory is higher than for patients who present with late-onset (normal course) AD, their attention scores are typically lower. As a result of this atypical presentation, patients with EOAD tend to have a longer duration of disease before diagnosis (~1.6 years). They are also likely to have a history of TBI, which is a risk factor for dementia.
In comparison to late-onset AD (LOAD), EOAD has a larger genetic predisposition (92%-100% vs 70%-80%), a more aggressive course, a more frequent delay in initial diagnosis, higher prevalence of TBI, and less memory impairment. However, EOAD has greater decline in other cognitive domains, and because of the young age of onset, greater psychosocial impairment. Overall disease progression in these patients is much faster compared with patients who have LOAD. Neuroimaging in these patients generally features greater hippocampal sparing and posterior neocortical atrophy, with brain changes that affect the frontoparietal networks rather than the classic presentation found in LOAD.
An important aspect of the workup of patients for whom EOAD is a diagnostic consideration is to thoroughly determine their family history and to perform genetic testing along with counseling.
The pharmacological treatment of patients with early-onset AD is identical to patients who have normal course or late-onset AD. Cholinesterase inhibitors (ChEIs) — eg, donepezil, galantamine, and rivastigmine, with the usual titration schedules — are indicated in these patients. Although these medications target memory, they also provide support to patients with other variants of EOAD — eg, logopenic variant PPA. However, it is imperative that providers monitor these patients carefully, as ChEIs may exacerbate some behaviors.
Management of patients with EOAD varies based on the patient's specific variant. It is vital for clinicians to coordinate patient-centered care individually. For example, patients with logopenic variant PPA should be referred for speech therapy assessment and treatment should focus on improving communication, while patients with posterior cortical atrophy benefit most from interventions for those who experience vision impairments. As this patient’s symptoms revolve primarily around cognition and visuospatial dysfunction, her treatment will focus on interventions to improve coordination, balance, and cognitive function.
Perhaps the most important part of managing a patient with EOAD is providing adequate and appropriate psychosocial support. These patients are most often in their most productive time of life, balancing careers and families. EOAD can bring about feelings of loss of independence, anticipatory grief, and anxiety about the future and the increased difficulty in managing the tasks of daily life. It is vital that these patients — and their families — receive adequate education and psychiatric support via therapists, support groups, and community resources that are age appropriate.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Early-onset AD (EOAD) is the most likely diagnosis for this patient. Her symptoms — cognitive decline, executive function deficits, and visuospatial dysfunction — and brain imaging results are consistent with EOAD. But importantly, her father’s diagnosis of EOAD at age 58 suggests a hereditary component, which greatly increases the genetic risk for this patient. Moreover, neuroimaging shows cortical atrophy in the temporal lobes. A key radiologic feature of AD in this patient is the large increase in the subarachnoid spaces affecting the parietal region.
Between one third to just over one half of patients with EOAD have at least one first-degree relative with the disease. Given the patient’s neuroimaging results and family history of EOAD, she was sent for genetic testing, which revealed mutations in the PSEN1 gene; one the most common genetic causes of EOAD (along with mutations in the APP gene). For those who do have an autosomal dominant familial form of EOAD, clinical presentation is often atypical and includes headaches, myoclonus, seizures, hyperreflexia, and gait abnormalities. This patient did experience headaches but not the other symptoms.
Traumatic brain injury (TBI) is an insult to the brain from an outside mechanical force. It is both non-congenital and non-degenerative but can lead to permanent physical, cognitive, and/or psychosocial functioning. Patients often experience an altered or diminished state of consciousness in the aftermath of such an event. TBI is a diagnostic consideration for this patient, given that she was in a car accident and has experienced unusual cognitive and behavioral symptoms — eg, memory loss and visuospatial dysfunction. However, imaging does not reveal evidence of TBI, with no concussion or cerebral hemorrhage. Thus, TBI is not an accurate diagnosis for this patient.
Parkinson’s disease (PD) is one of the most common neurologic disorders that is marked by three hallmark features: resting tremor, rigidity, and bradykinesia that generally affects people over the age of 60. Even though many patients with PD exhibit some measure of executive function impairment early in the course of the disease, substantial impairment and dementia usually manifest about 8 years after the onset of motor symptoms. Dementia occurs in approximately 20%-40% of patients with PD. Although patients with PD demonstrate executive function deficits, memory loss, and visuospatial dysfunction, they do not experience aphasia. This patient does not have any of the cardinal features of PD, which rules it out as a diagnosis.
Frontotemporal dementia is a progressive dysfunction of the frontal lobes of the brain, primarily manifesting as language abnormalities, including reduced speech, perseveration, mutism, and echolalia, also known as primary progressive aphasia (PPA). Over time, patients develop other psychiatric symptoms: disinhibition, impulsivity, loss of social awareness, neglect of personal hygiene, mental rigidity, and utilization behavior. Given the patient’s language difficulties, frontotemporal dementia may be an initial diagnostic consideration. However, per the neurologic imaging results, brain abnormalities are located in the temporal regions. Additionally, the patient does not exhibit any of the psychiatric symptoms associated with frontotemporal dementia but does experience short-term memory loss and visuospatial dysfunction, which are not typical of this diagnosis. This patient does not have frontotemporal dementia.
EOAD is characterized by deficits in language, visuospatial skills and executive function. Often, these patients do not exhibit amnestic disorder early in the disease. While their memory recognition and semantic memory is higher than for patients who present with late-onset (normal course) AD, their attention scores are typically lower. As a result of this atypical presentation, patients with EOAD tend to have a longer duration of disease before diagnosis (~1.6 years). They are also likely to have a history of TBI, which is a risk factor for dementia.
In comparison to late-onset AD (LOAD), EOAD has a larger genetic predisposition (92%-100% vs 70%-80%), a more aggressive course, a more frequent delay in initial diagnosis, higher prevalence of TBI, and less memory impairment. However, EOAD has greater decline in other cognitive domains, and because of the young age of onset, greater psychosocial impairment. Overall disease progression in these patients is much faster compared with patients who have LOAD. Neuroimaging in these patients generally features greater hippocampal sparing and posterior neocortical atrophy, with brain changes that affect the frontoparietal networks rather than the classic presentation found in LOAD.
An important aspect of the workup of patients for whom EOAD is a diagnostic consideration is to thoroughly determine their family history and to perform genetic testing along with counseling.
The pharmacological treatment of patients with early-onset AD is identical to patients who have normal course or late-onset AD. Cholinesterase inhibitors (ChEIs) — eg, donepezil, galantamine, and rivastigmine, with the usual titration schedules — are indicated in these patients. Although these medications target memory, they also provide support to patients with other variants of EOAD — eg, logopenic variant PPA. However, it is imperative that providers monitor these patients carefully, as ChEIs may exacerbate some behaviors.
Management of patients with EOAD varies based on the patient's specific variant. It is vital for clinicians to coordinate patient-centered care individually. For example, patients with logopenic variant PPA should be referred for speech therapy assessment and treatment should focus on improving communication, while patients with posterior cortical atrophy benefit most from interventions for those who experience vision impairments. As this patient’s symptoms revolve primarily around cognition and visuospatial dysfunction, her treatment will focus on interventions to improve coordination, balance, and cognitive function.
Perhaps the most important part of managing a patient with EOAD is providing adequate and appropriate psychosocial support. These patients are most often in their most productive time of life, balancing careers and families. EOAD can bring about feelings of loss of independence, anticipatory grief, and anxiety about the future and the increased difficulty in managing the tasks of daily life. It is vital that these patients — and their families — receive adequate education and psychiatric support via therapists, support groups, and community resources that are age appropriate.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 52-year-old female presents complaining of fatigue, brain fog, and headaches. She reports that, over the last year, she feels increasingly more irritable, anxious, overwhelmed, and sometimes disoriented. When prompted, she admits to having trouble keeping track of things — dates, important deadlines, objects like her keys, and things she uses each day. She needs multiple reminder events or tasks and must write everything down. She also reports that she often loses her train of thought and sometimes struggles to find words. She works in a medical office, is married, and has two children in college. She helps with caring for her in-laws on the weekend by doing their bills and grocery shopping. She admits to being moody and does not want to socialize, which she attributes to fatigue and having a busy life. She also complains of muscle stiffness and general clumsiness. Eight months ago, the patient was in an automobile accident in which her car was totaled, but she did not sustain serious injury and opted not to seek medical evaluation.
Physical exam reveals slight visuospatial dysfunction, with issues with both coordination and balance. The patient appears fatigued and has some trouble maintaining her attention during the conversation. Further questioning reveals mild anomic aphasia and some lapses in recent memory. Her reflexes are otherwise normal, as are heart, lung, and breath sounds. All systemic lymph nodes are normal as are liver and spleen on palpation. The patient recently discovered that her estranged father had been diagnosed with Alzheimer’s disease (AD) at 58 years of age and passed away 5 years later.
Laboratory testing is performed and reveals nothing remarkable. Considering the car accident and new cognitive/behavioral changes experienced by the patient, a CT of the brain is ordered. Results are negative for concussion and cerebral hemorrhage but show cortical atrophy of the temporal territories and a large increase in the size of the subarachnoid spaces predominantly affecting the parietal region.
Progressive cognitive decline
Individuals with DS are at significantly increased risk of developing Alzheimer’s disease (AD) because of the overexpression of the amyloid precursor protein (APP) gene on chromosome 21.
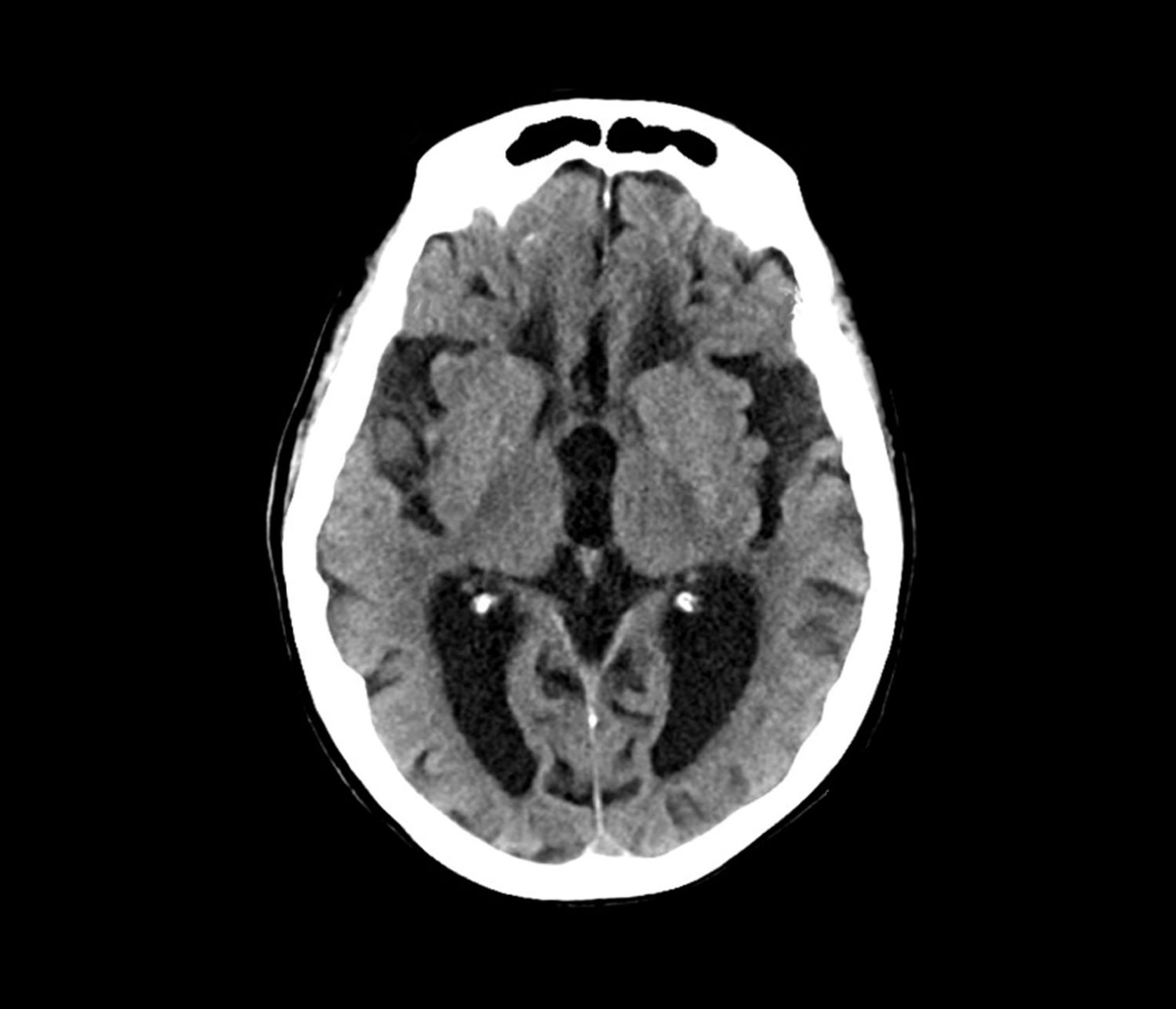
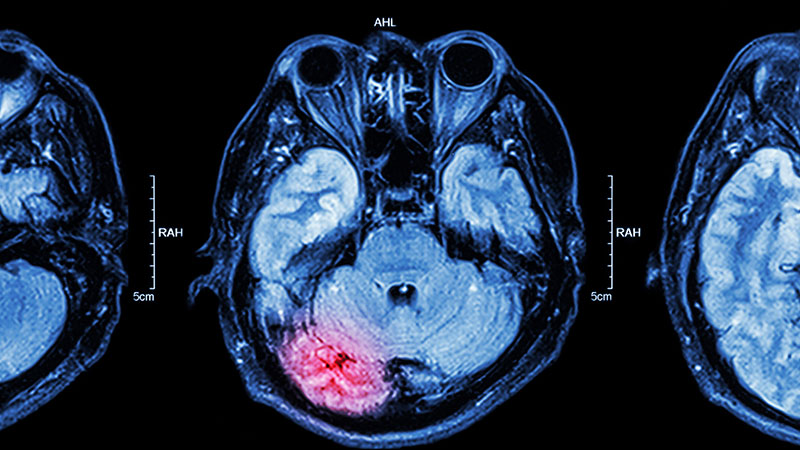
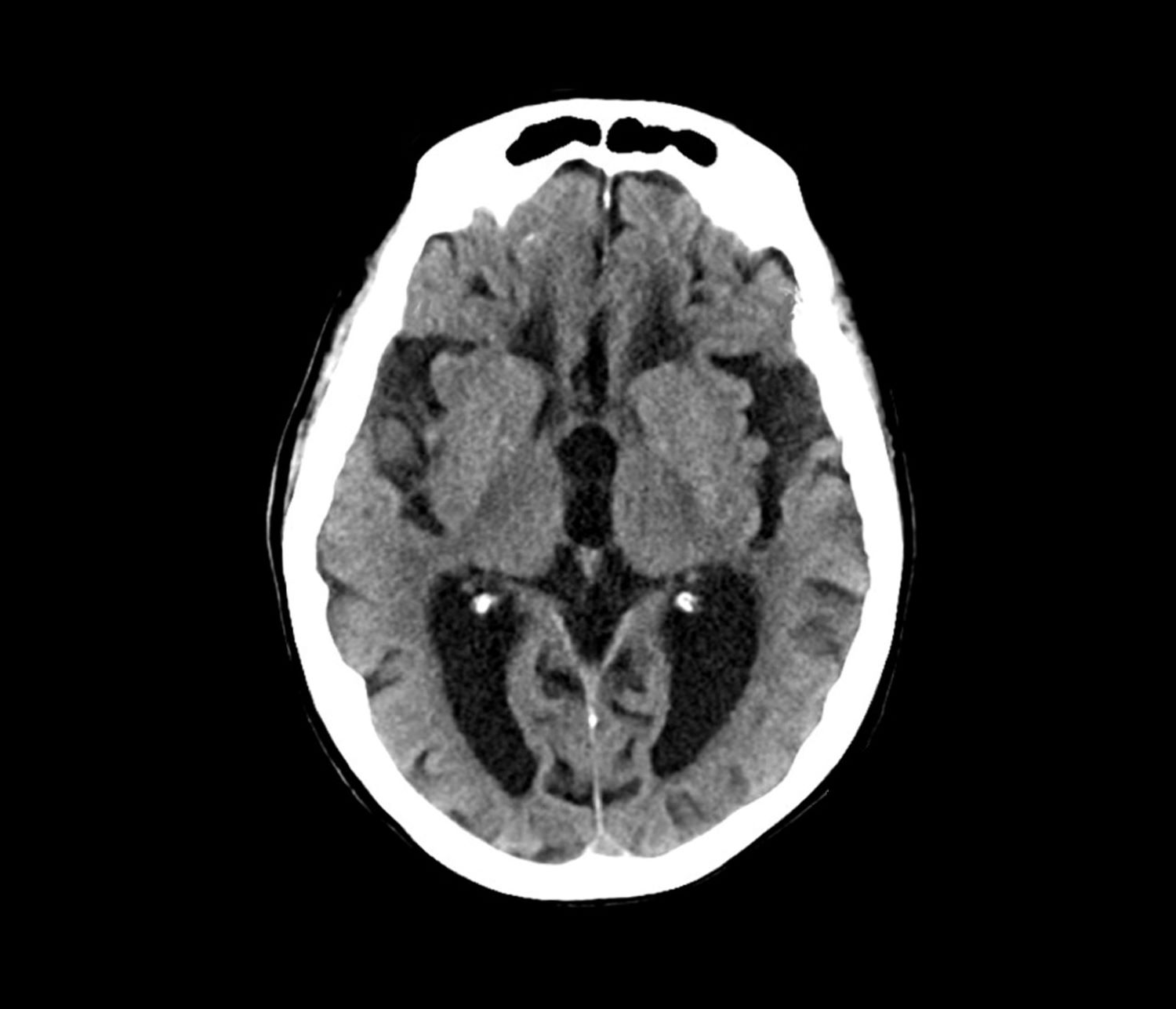
The patient exhibits hallmark symptoms of AD, including progressive memory loss, disorientation, difficulty performing daily tasks, and behavioral changes such as irritability and social withdrawal. The MRI findings of ventricular enlargement and cortical atrophy are consistent with brain changes commonly seen in AD, particularly in individuals with DS who often develop these changes earlier in life (typically in their thirties or forties).
Frontotemporal dementia primarily causes behavioral and language changes with relative memory sparing early on, making it inconsistent with this patient's prominent memory loss, disorientation, and generalized cortical atrophy — features more typical of AD.
Vascular dementia often presents with stepwise decline and focal neurologic deficits; it is unlikely in this patient, given the absence of cerebrovascular events or risk factors like hypertension or diabetes.
While normal pressure hydrocephalus can cause ventricular enlargement, its classic triad of gait disturbance, urinary incontinence, and dementia is incomplete here, making this answer unlikely.
DS is the most common genetic cause of intellectual disability, occurring in approximately 1 in 700 live births worldwide. Nearly all adults with DS develop neuropathologic changes associated with AD by age 40, and the lifetime risk of developing dementia exceeds 90%; by the age of 55-60, at least 70% of individuals with DS exhibit clinical signs of dementia.
The link between DS and neurodegeneration is largely attributed to the triplication of chromosome 21, which includes the APP gene. Overexpression of APP leads to excessive production and accumulation of amyloid-β (Aβ), which forms the hallmark plaques seen in AD. In DS, amyloid plaques begin to form as early as the teenage years, and by the fourth decade, neurofibrillary tangles (tau protein aggregates) and widespread neurodegeneration are nearly universal.
Initial symptoms of AD often include memory impairment, particularly short-term memory deficits, and executive dysfunction, difficulty with planning and problem-solving, and visuospatial deficits. Behavioral and personality changes, such as irritability, withdrawal, or apathy, are also commonly reported. Compared with sporadic AD, individuals with DS often show earlier behavioral symptoms, including impulsivity and changes in social interactions, which may precede noticeable memory deficits. Additionally, late-onset myoclonic epilepsy is common in individuals with DS and dementia, further complicating diagnosis and care.
The diagnosis of dementia in DS is challenging because of baseline intellectual disability, which makes it difficult to assess cognitive decline using standard neuropsychological tests. However, a combination of clinical history, caregiver reports, neuroimaging, and biomarker analysis can aid in early detection. Structural MRI of the brain often reveals ventricular enlargement and cortical atrophy, while PET imaging can detect early amyloid and tau accumulation.
Because AD is now the leading cause of death in individuals with DS, the lack of effective disease-modifying treatments highlights an important need for clinical trials focused on this population. Current research aims to explore the role of anti-amyloid monoclonal antibodies, neuroprotective agents, and lifestyle interventions to delay or prevent neurodegeneration.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Individuals with DS are at significantly increased risk of developing Alzheimer’s disease (AD) because of the overexpression of the amyloid precursor protein (APP) gene on chromosome 21.
The patient exhibits hallmark symptoms of AD, including progressive memory loss, disorientation, difficulty performing daily tasks, and behavioral changes such as irritability and social withdrawal. The MRI findings of ventricular enlargement and cortical atrophy are consistent with brain changes commonly seen in AD, particularly in individuals with DS who often develop these changes earlier in life (typically in their thirties or forties).
Frontotemporal dementia primarily causes behavioral and language changes with relative memory sparing early on, making it inconsistent with this patient's prominent memory loss, disorientation, and generalized cortical atrophy — features more typical of AD.
Vascular dementia often presents with stepwise decline and focal neurologic deficits; it is unlikely in this patient, given the absence of cerebrovascular events or risk factors like hypertension or diabetes.
While normal pressure hydrocephalus can cause ventricular enlargement, its classic triad of gait disturbance, urinary incontinence, and dementia is incomplete here, making this answer unlikely.
DS is the most common genetic cause of intellectual disability, occurring in approximately 1 in 700 live births worldwide. Nearly all adults with DS develop neuropathologic changes associated with AD by age 40, and the lifetime risk of developing dementia exceeds 90%; by the age of 55-60, at least 70% of individuals with DS exhibit clinical signs of dementia.
The link between DS and neurodegeneration is largely attributed to the triplication of chromosome 21, which includes the APP gene. Overexpression of APP leads to excessive production and accumulation of amyloid-β (Aβ), which forms the hallmark plaques seen in AD. In DS, amyloid plaques begin to form as early as the teenage years, and by the fourth decade, neurofibrillary tangles (tau protein aggregates) and widespread neurodegeneration are nearly universal.
Initial symptoms of AD often include memory impairment, particularly short-term memory deficits, and executive dysfunction, difficulty with planning and problem-solving, and visuospatial deficits. Behavioral and personality changes, such as irritability, withdrawal, or apathy, are also commonly reported. Compared with sporadic AD, individuals with DS often show earlier behavioral symptoms, including impulsivity and changes in social interactions, which may precede noticeable memory deficits. Additionally, late-onset myoclonic epilepsy is common in individuals with DS and dementia, further complicating diagnosis and care.
The diagnosis of dementia in DS is challenging because of baseline intellectual disability, which makes it difficult to assess cognitive decline using standard neuropsychological tests. However, a combination of clinical history, caregiver reports, neuroimaging, and biomarker analysis can aid in early detection. Structural MRI of the brain often reveals ventricular enlargement and cortical atrophy, while PET imaging can detect early amyloid and tau accumulation.
Because AD is now the leading cause of death in individuals with DS, the lack of effective disease-modifying treatments highlights an important need for clinical trials focused on this population. Current research aims to explore the role of anti-amyloid monoclonal antibodies, neuroprotective agents, and lifestyle interventions to delay or prevent neurodegeneration.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Individuals with DS are at significantly increased risk of developing Alzheimer’s disease (AD) because of the overexpression of the amyloid precursor protein (APP) gene on chromosome 21.
The patient exhibits hallmark symptoms of AD, including progressive memory loss, disorientation, difficulty performing daily tasks, and behavioral changes such as irritability and social withdrawal. The MRI findings of ventricular enlargement and cortical atrophy are consistent with brain changes commonly seen in AD, particularly in individuals with DS who often develop these changes earlier in life (typically in their thirties or forties).
Frontotemporal dementia primarily causes behavioral and language changes with relative memory sparing early on, making it inconsistent with this patient's prominent memory loss, disorientation, and generalized cortical atrophy — features more typical of AD.
Vascular dementia often presents with stepwise decline and focal neurologic deficits; it is unlikely in this patient, given the absence of cerebrovascular events or risk factors like hypertension or diabetes.
While normal pressure hydrocephalus can cause ventricular enlargement, its classic triad of gait disturbance, urinary incontinence, and dementia is incomplete here, making this answer unlikely.
DS is the most common genetic cause of intellectual disability, occurring in approximately 1 in 700 live births worldwide. Nearly all adults with DS develop neuropathologic changes associated with AD by age 40, and the lifetime risk of developing dementia exceeds 90%; by the age of 55-60, at least 70% of individuals with DS exhibit clinical signs of dementia.
The link between DS and neurodegeneration is largely attributed to the triplication of chromosome 21, which includes the APP gene. Overexpression of APP leads to excessive production and accumulation of amyloid-β (Aβ), which forms the hallmark plaques seen in AD. In DS, amyloid plaques begin to form as early as the teenage years, and by the fourth decade, neurofibrillary tangles (tau protein aggregates) and widespread neurodegeneration are nearly universal.
Initial symptoms of AD often include memory impairment, particularly short-term memory deficits, and executive dysfunction, difficulty with planning and problem-solving, and visuospatial deficits. Behavioral and personality changes, such as irritability, withdrawal, or apathy, are also commonly reported. Compared with sporadic AD, individuals with DS often show earlier behavioral symptoms, including impulsivity and changes in social interactions, which may precede noticeable memory deficits. Additionally, late-onset myoclonic epilepsy is common in individuals with DS and dementia, further complicating diagnosis and care.
The diagnosis of dementia in DS is challenging because of baseline intellectual disability, which makes it difficult to assess cognitive decline using standard neuropsychological tests. However, a combination of clinical history, caregiver reports, neuroimaging, and biomarker analysis can aid in early detection. Structural MRI of the brain often reveals ventricular enlargement and cortical atrophy, while PET imaging can detect early amyloid and tau accumulation.
Because AD is now the leading cause of death in individuals with DS, the lack of effective disease-modifying treatments highlights an important need for clinical trials focused on this population. Current research aims to explore the role of anti-amyloid monoclonal antibodies, neuroprotective agents, and lifestyle interventions to delay or prevent neurodegeneration.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 40-year-old man with Down syndrome (DS) presented with progressive cognitive decline over 2 years, characterized by memory impairment, difficulty performing familiar tasks, and increasing disorientation. His caregivers noted mood changes, including irritability and withdrawal, and occasional episodes of agitation. Clinical history revealed congenital heart disease (surgically repaired in childhood) and hypothyroidism, which was well controlled with levothyroxine. Physical examination showed no focal neurologic deficits, but he exhibited mild hypotonia, a characteristic feature of DS, and a shuffling gait. Routine blood tests revealed normal thyroid function, no evidence of vitamin B12 deficiency, and unremarkable metabolic panels. An MRI scan (as shown in the image) demonstrated marked ventricular enlargement and generalized cortical atrophy.
Severe anxiety and agitation
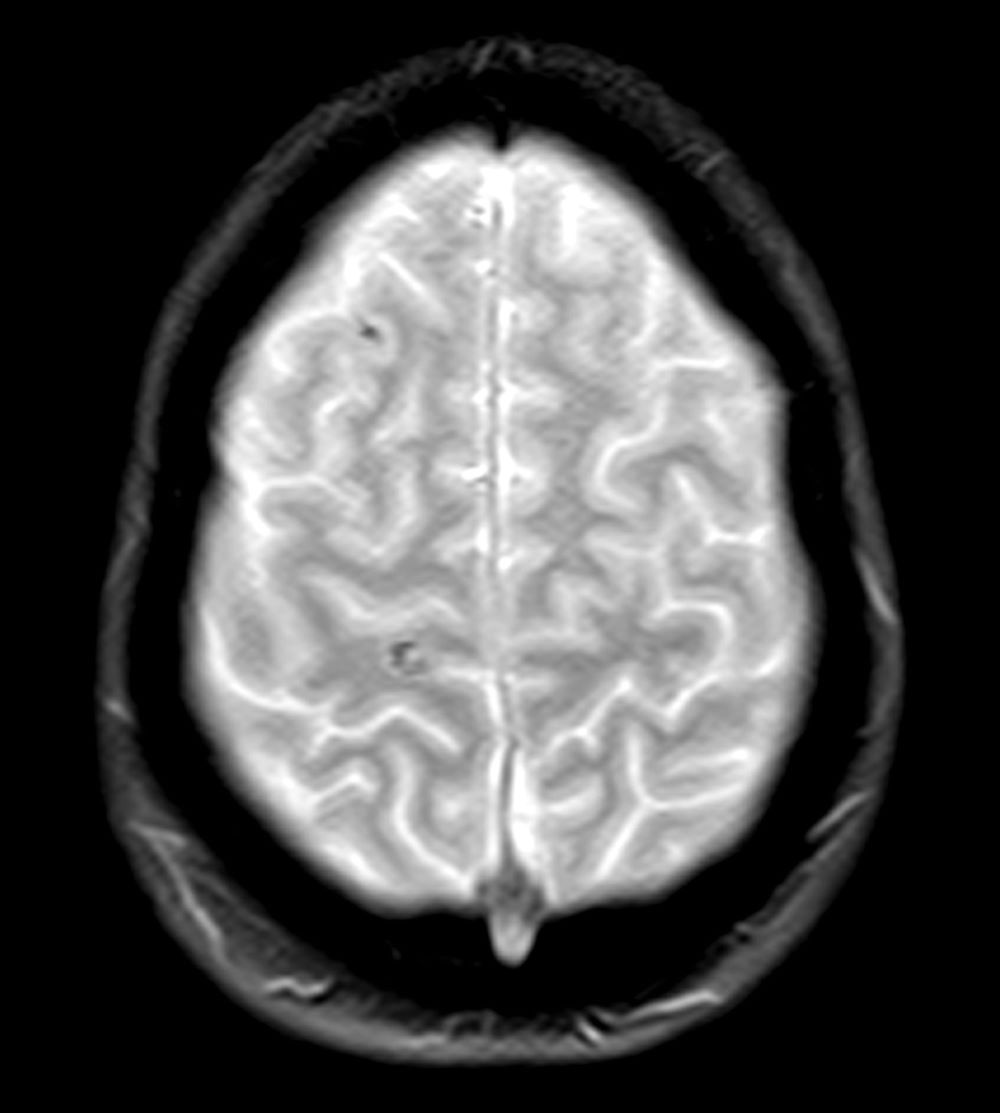
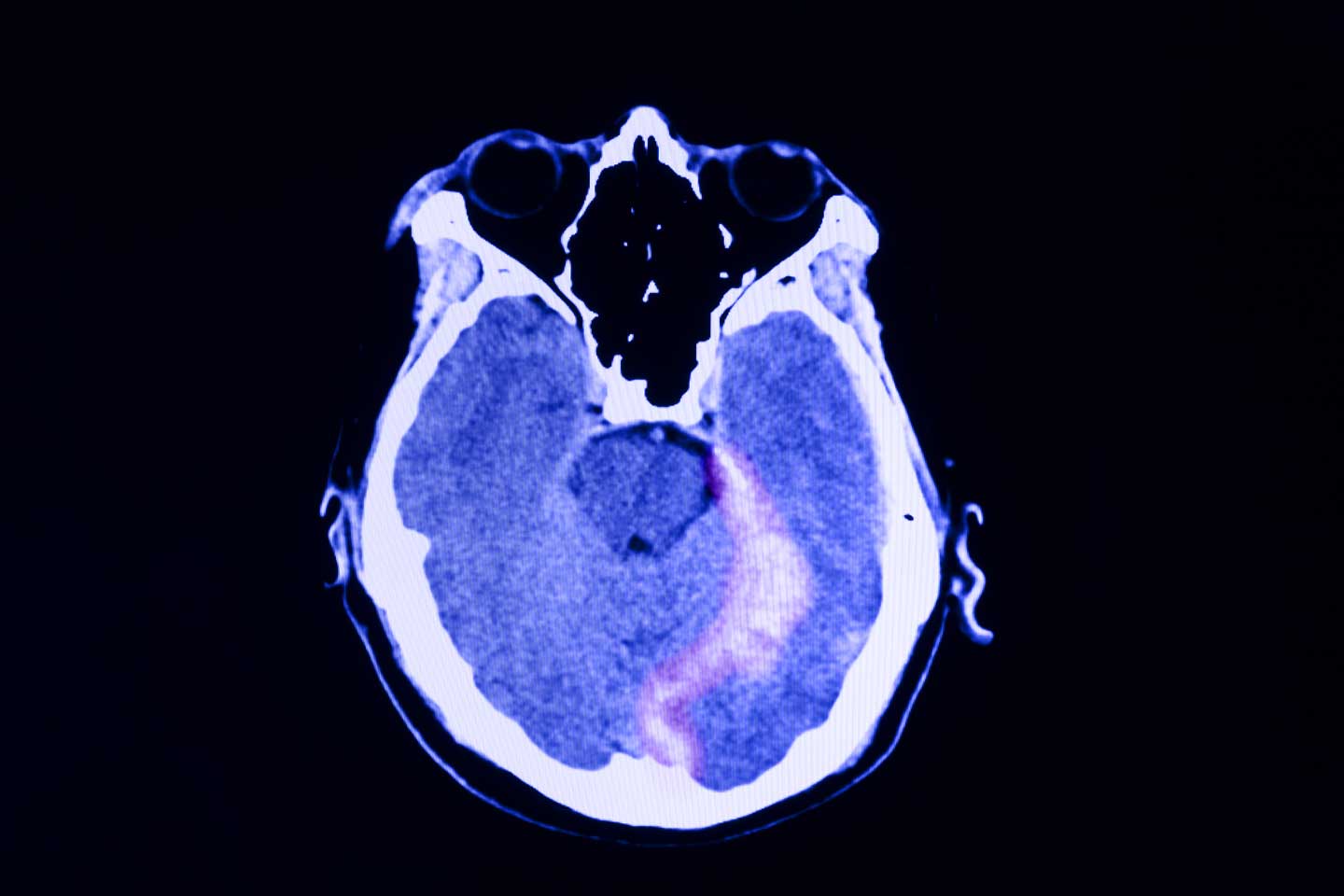
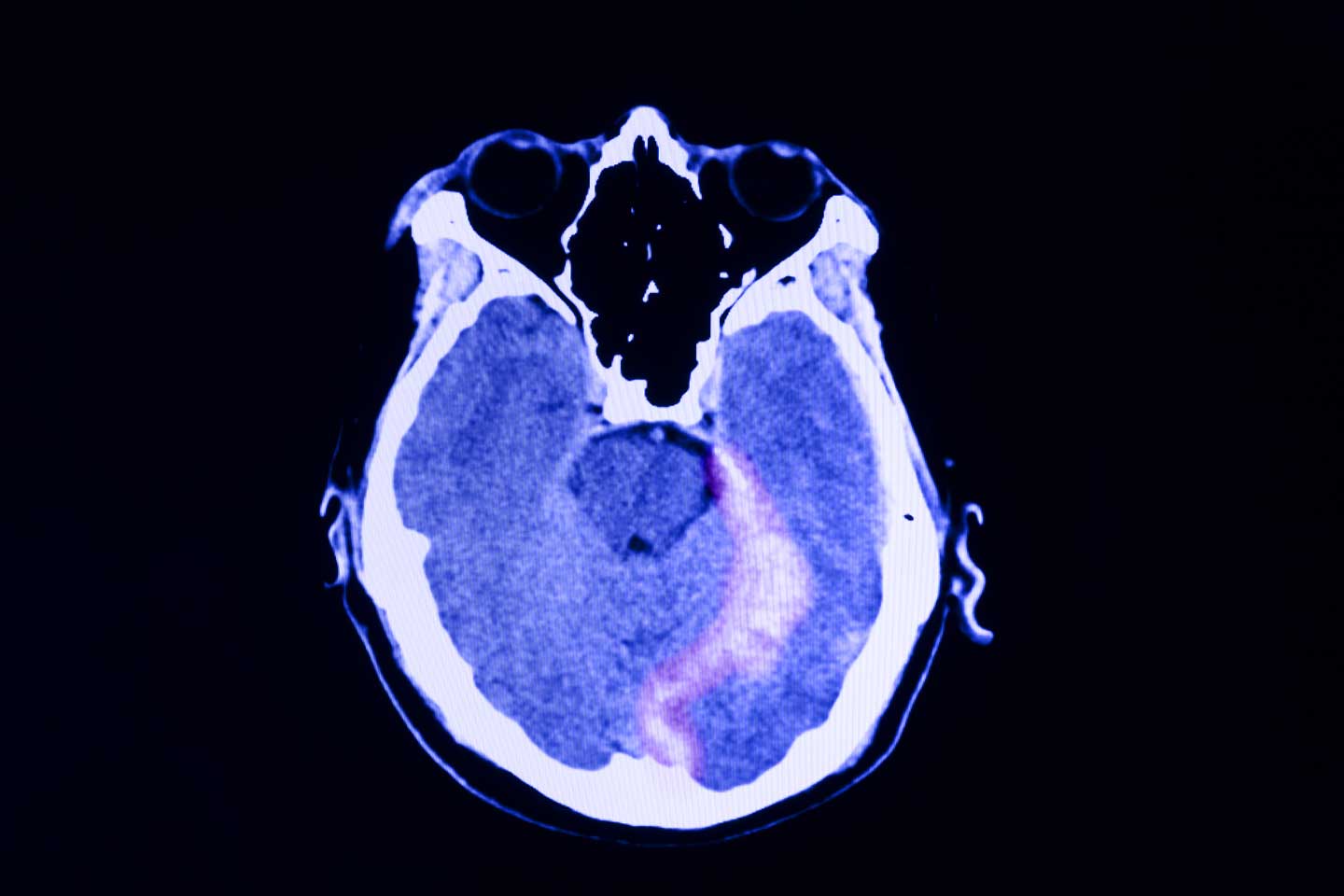
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 28-year-old professional boxer presents with severe anxiety, agitation, headaches, and insomnia with recurring nightmares and flashbacks. His symptoms began after he was robbed at gunpoint in the gym parking lot as he was getting into his car about 6 months ago. Since that time, he has had to postpone several fights because he is unable to maintain his training schedule and reports feeling depressed as a result. He is also at risk for suspension from his regular gym because he has gotten into several violent, unprovoked altercations with fellow boxers, and he has also had multiple violent outbursts outside of the gym. He has a history of concussion.
Physical exam reveals increased heart rate and hypervigilance. The patient is administered the Patient Health Questionnaire and has a score of 14 out of a possible 27. Zero to 4 indicates no depression, whereas 14 falls within the range of moderate depression. A brain CT scan (Figure) is ordered because of his history of concussion and his chronic symptoms. The scan reveals two subacute hematomas in the left hemisphere, one in the frontal lobe and the other in the temporal lobe. Additional tests are ordered: laboratory testing, to rule out organic or infectious causes of symptoms and electroencephalography, to assess for a possible seizure focus; both tests reveal nothing remarkable. The hematomas were noted at the time of a previous head injury 2 years ago.
Flashbacks triggered by loud noises
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 48-year-old male construction worker presented with worsening symptoms over the past year, including recurrent nightmares, heightened anxiety, and flashbacks triggered by loud noises such as those heard on job sites. These symptoms have begun to interfere with his daily functioning, particularly affecting his work and family life. The patient has a history of multiple traumatic experiences at work, including witnessing a fatal accident involving a coworker. On neurologic examination, he appeared highly agitated and displayed signs of hypervigilance. A brain CT scan (as shown in the image) was ordered because of the chronic nature of his symptoms and the potential for neurologic causes—such as traumatic brain injury—to contribute to his condition. The scan revealed an abnormality on the left side, prompting further investigation to determine whether the lesion is related to his symptoms or indicative of another underlying condition. Additional tests were ordered to further characterize the lesion: electroencephalography to assess for any associated seizure activity, and blood tests and a lumbar puncture to rule out infection or inflammatory processes. These additional tests came back negative, and the abnormality was later diagnosed as artifact.
Persistent headaches and nightmares
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
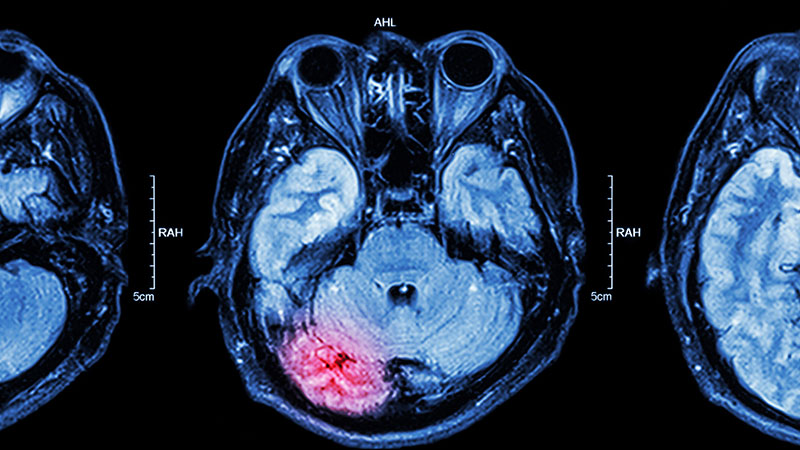
A 15-year-old girl presented to the emergency department with complaints of persistent headaches, nightmares, and difficulty concentrating in school over the past 3 months. The patient had recently experienced a traumatic event, a severe car accident in which a close friend was critically injured. Since the incident, the patient has been exhibiting increased irritability, avoidance of activities that she previously enjoyed, and a noticeable withdrawal from social interactions. Additionally, she reported recurrent flashbacks to the accident, often triggered by sounds resembling car engines. On physical examination, the patient appeared anxious and exhibited hypervigilance. An MRI of the brain was performed to rule out any organic causes of her symptoms, revealing an area of increased signal intensity in the left cerebellar hemisphere (as highlighted in the image).
Swollen elbow and knee joints
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Obesity is a chronic disease affecting more than 20% of adults in the United States. In 2022, prevalence was 20.5% among those aged 18 to 24 and 39.9% among those aged 45 to 54 years. This patient meets criteria for obesity (BMI ≥ 30), and it is likely that her obesity contributed to development of T2D, hypertension, osteoarthritis, and joint edema (as shown in the image).
Patients with obesity are at high risk of developing cardiometabolic disease and osteoarthritis. Obesity is a key driver of T2D and cardiovascular disease development through its influence on insulin and lipid metabolism and proinflammatory changes. Factors associated with obesity that foster arthritis development include the erosive effects of adiponectin and leptin on cartilage and direct inflammation in joint tissues.
It is important for patients with obesity and comorbid T2D and hypertension to receive multidisciplinary care designed to address all aspects of their health and minimize their risk for progression. The primary goal for this patient should be to promote weight loss safely while also improving her glycemic control and blood pressure. For patients with obesity and comorbid T2D, the American Diabetes Association recommends glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide or liraglutide) or the dual gastric inhibitory polypeptide (GIP)/GLP-1 RA tirzepatide. The GLP-1 RA drugs reduce the risk for major cardiovascular events for patients with T2D while also providing substantial reductions in glucose levels without increasing hypoglycemia risk. They are available in higher doses (semaglutide 2.4 mg weekly, liraglutide 3.0 mg daily) for patients with obesity. These drugs also have salubrious effects on cardiorenal health and reduce progression of kidney disease. Tirzepatide produced greater reductions in A1c vs semaglutide in patients with T2D in the SURPASS-2 trial. It also has been shown to reduce atherosclerotic cardiovascular events in patients with overweight or obesity (without diabetes) in a post hoc analysis of the SURMOUNT-1 trial. Its effect on a broad set of cardiac, renal, and metabolic outcomes is being studied in the ongoing SURMOUNT-MMO trial. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27).
Pharmacologic interventions for osteoarthritis include nonsteroidal anti-inflammatory drugs, including ibuprofen, naproxen, meloxicam, diclofenac, or celecoxib. These may be used with regular follow-up to assess cardiovascular and gastrointestinal health. Topical nonsteroidal anti-inflammatory drugs also may be useful. For more intractable joint pain, options include injecting corticosteroid or sodium hyaluronate into the affected joints or joint replacement.
In addition, comprehensive care includes lifestyle modifications designed to promote weight loss, reduce sodium, and increase exercise and intake of healthy foods. While maintaining intensive lifestyle modifications can be challenging, achieving weight loss of ≥ 5% can improve cardiometabolic risk factors in patients with obesity and T2D. Greater benefit is seen with greater reductions in body weight. Other interventions include behavioral modification and encouragement of increased physical activity to the extent of the patient's ability. Achieving substantial weight loss also could help relieve stress on the patient's joints, improve physical function, and mitigate osteoarthritis-related pain. The patient also may benefit from nonpharmacologic approaches to joint pain, including hot or cold compresses, physical therapy, and strength and resistance training to improve the strength of muscles supporting the joints.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 24-year-old woman presents for swollen and painful elbow and knee joints. The patient is 5 ft 7 in tall and weighs 235 lb (BMI 36.8). The patient says she has been overweight since her preteen years and has never been involved in sports or exercise activities. She has gained a significant amount of weight in the past 2 years since beginning work in an insurance office. She has lived at home with her parents since graduating from college.
Her elbows are tender to the touch; further examination reveals tender joints at her wrists, knees, and hips as well. Extremities are thick because of obesity.
Medical history includes diagnosis of type 2 diabetes (T2D) at age 22. In the office, her blood pressure is elevated (150/85 mm Hg), heart rate is 110 beats/min, and respiratory rate is 18 breaths/min. Lab results indicate A1c = 8.5%, low-density lipoprotein cholesterol = 145 mg/dL, and estimated glomerular filtration rate = 90 mL/min/1.73 m2; all other results are within normal range. Her only current medication is metformin 1000 mg daily.
In-office radiography reveals no obvious bone or joint damage.
Involuntary flashbacks
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is posttraumatic stress disorder (PTSD). The patient's anxiety, irritability, sleep difficulties, and other symptoms are directly related to the recent traumatic event (car crash), and he has no significant physical injuries or neurologic abnormalities.
Generalized anxiety disorder is incorrect because it involves chronic worry about various life aspects for at least 6 months, unrelated to a specific trauma.
Postconcussion syndrome is not applicable because of the lack of concussion evidence and other symptoms, such as headaches or dizziness.
Acute stress disorder is similar to PTSD but is diagnosed when symptoms occur within 3 days to 1 month after a trauma. Because this patient's symptoms have persisted beyond 1 month, PTSD is the most likely diagnosis.
Patients with PTSD exhibit pronounced cognitive, affective, or behavioral responses to trauma reminders; these responses may include severe anxiety, dissociative episodes, flashbacks, and hyperreactive behaviors. The intensity of these symptoms and the resulting psychosocial impairment are more severe in individuals with PTSD compared with people who experience trauma without developing the disorder. To manage such heightened arousal, individuals with PTSD often engage in avoidance behaviors, leading to emotional numbing; reduced interest in daily activities; and, in severe cases, detachment from others.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals older than 6 years. These criteria include: (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the traumatic event; (C) persistent avoidance of stimuli associated with the trauma; (D) negative alterations in cognitions and mood related to the trauma; and (E) marked alterations in arousal and reactivity, evidenced by two or more specific symptoms.
Early intervention is key in the treatment of PTSD to prevent the condition from becoming chronic. Although more empirical data are needed, especially regarding pharmacotherapy, early supportive interventions such as psychoeducation and case management have shown promise in acutely traumatized individuals.
Trauma-focused psychotherapy is recommended as the first-line treatment for most adults with PTSD. This approach, which includes exposure-based therapies, is generally preferred over other therapies or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions (eg, depression, psychosis) that impair their ability to engage in trauma-focused therapy, initial pharmacologic management is advised until symptoms stabilize, after which psychotherapy can be introduced.
Clinical trials and meta-analyses have demonstrated the efficacy of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. The treatment choice should be collaborative, based on patient presentation, preference, and therapist expertise.
For individuals with PTSD experiencing significant sleep disturbances, particularly nightmares, prazosin is suggested. Clinical studies demonstrate that prazosin effectively reduces overall PTSD symptoms, nightmares, and sleep disturbances in approximately half of the patients treated.
Medication regimens effective for PTSD should be continued for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials in patients with PTSD who completed acute treatment with SSRIs have demonstrated that those who continued with SSRIs were less likely to have relapse compared with those receiving placebo.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
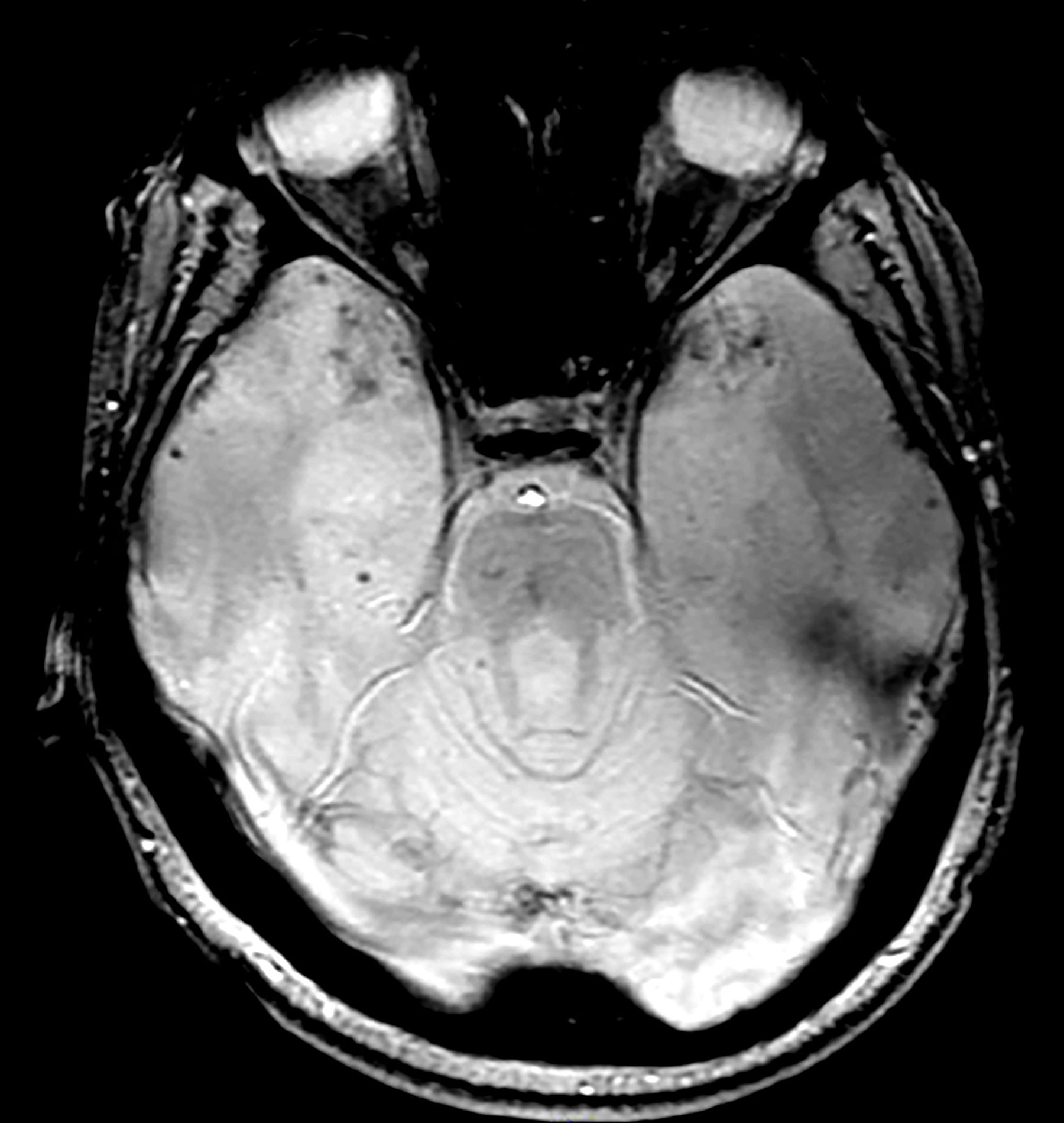
A 28-year-old man presented to the emergency department following a high-speed motor vehicle accident 2 months ago. He sustained no major physical injuries but had minor lacerations and bruising. The patient reported feeling unusually irritable and having difficulty sleeping since the accident, citing frequent flashbacks to the accident and occasional nightmares. He has started to feel more anxious and withdrawn, losing interest in hobbies such as swimming and biking that he previously enjoyed.
The patient's medical history is unremarkable, with no previous psychiatric or neurologic conditions. His neurologic examination was normal. An initial axial T2-weighted brain MRI demonstrated multiple small areas of hemorrhage, indicative of a diffuse axonal injury or shear-type injury. Despite the lack of significant physical injuries, the patient expressed ongoing distress related to the traumatic event.
Persistent mood swings
The most likely diagnosis for this patient is veteran posttraumatic stress disorder (PTSD), given his history of combat exposure and symptoms, such as severe headaches, difficulty concentrating, mood swings, nightmares, flashbacks, increased startle response, and hypervigilance. MRI findings showing significant changes in the limbic system and hippocampal regions support this diagnosis. Other potential diagnoses, like traumatic brain injury, chronic migraine, and major depressive disorder, are less likely because of their inability to account for the full range of his symptoms and specific MRI abnormalities.
PTSD, experienced by a subset of individuals after exposure to life-threatening events, has a lifetime prevalence of 4%-7% and a current prevalence of 1%-3%, with higher rates in older women, those with more trauma, and combat veterans. Nearly half of US veterans are aged 65 or older, many being Vietnam-era veterans at elevated risk for PTSD. Prevalence rates in older veterans range between 1% and 22%.
PTSD is characterized by intrusive thoughts, flashbacks, nightmares, avoidance of reminders, hypervigilance, and sleep difficulties, significantly disrupting interpersonal and occupational functioning. Screening tools like the primary care (PC) PTSD-5 and PCL-5, used in primary care settings, are effective for early detection, provisional diagnosis, and monitoring of symptom changes. The clinician-administered PTSD scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 (CAPS-5) is the gold standard for diagnosis, particularly among veterans, with multimethod assessments combining self-report measures and semi-structured interviews recommended for accuracy. The DSM-5 criteria for PTSD diagnosis describe exposure to traumatic events, intrusion symptoms, avoidance behaviors, negative mood, and altered arousal, with symptoms persisting for over a month and causing significant distress or functional impairment.
Research has identified consistent anatomical and functional changes in PTSD patients, such as smaller hippocampi, decreased corpus callosum and prefrontal cortex, increased amygdala reactivity, and decreased prefrontal cortex activity. PTSD, linked to alterations in brain regions involved in fear learning and memory, shows diminished structural integrity in executive function areas, reduced cortical volumes in the cingulate brain cortex and frontal regions, and reduced white matter integrity in key brain pathways. Neuroimaging findings, however, are primarily used for research currently and have yet to be widely implemented in clinical guidelines.
International PTSD treatment guidelines consistently recognize trauma-focused cognitive-behavioral therapies (CBTs), such as cognitive processing therapy (CPT), prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) as the gold standard. Recent guidelines have expanded the list of recommended treatments: The 2023 Department of Veterans Affairs and Department of Defense guidelines in the United States also endorse therapies like written narrative exposure and brief eclectic therapy. Internationally, guidelines do not perfectly coincide, as the 2018 update from the United Kingdom's National Institute for Health and Care Excellence (NICE) gives the highest recommendations to PE and CPT but rates EMDR slightly lower for military veterans because of limited evidence. Overall, guidelines consistently advocate for trauma-focused psychological interventions as the primary treatment for PTSD.
Guidelines from NICE and the World Health Organization do not recommend medications as the primary treatment; the American Psychiatric Association and the US Department of Veterans Affairs support selective serotonin reuptake inhibitors and prazosin but advise against benzodiazepines. Inpatient care may be necessary for individuals who pose a danger to themselves or others, or for those with severe PTSD from childhood abuse, to aid in emotional regulation and treatment.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The most likely diagnosis for this patient is veteran posttraumatic stress disorder (PTSD), given his history of combat exposure and symptoms, such as severe headaches, difficulty concentrating, mood swings, nightmares, flashbacks, increased startle response, and hypervigilance. MRI findings showing significant changes in the limbic system and hippocampal regions support this diagnosis. Other potential diagnoses, like traumatic brain injury, chronic migraine, and major depressive disorder, are less likely because of their inability to account for the full range of his symptoms and specific MRI abnormalities.
PTSD, experienced by a subset of individuals after exposure to life-threatening events, has a lifetime prevalence of 4%-7% and a current prevalence of 1%-3%, with higher rates in older women, those with more trauma, and combat veterans. Nearly half of US veterans are aged 65 or older, many being Vietnam-era veterans at elevated risk for PTSD. Prevalence rates in older veterans range between 1% and 22%.
PTSD is characterized by intrusive thoughts, flashbacks, nightmares, avoidance of reminders, hypervigilance, and sleep difficulties, significantly disrupting interpersonal and occupational functioning. Screening tools like the primary care (PC) PTSD-5 and PCL-5, used in primary care settings, are effective for early detection, provisional diagnosis, and monitoring of symptom changes. The clinician-administered PTSD scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 (CAPS-5) is the gold standard for diagnosis, particularly among veterans, with multimethod assessments combining self-report measures and semi-structured interviews recommended for accuracy. The DSM-5 criteria for PTSD diagnosis describe exposure to traumatic events, intrusion symptoms, avoidance behaviors, negative mood, and altered arousal, with symptoms persisting for over a month and causing significant distress or functional impairment.
Research has identified consistent anatomical and functional changes in PTSD patients, such as smaller hippocampi, decreased corpus callosum and prefrontal cortex, increased amygdala reactivity, and decreased prefrontal cortex activity. PTSD, linked to alterations in brain regions involved in fear learning and memory, shows diminished structural integrity in executive function areas, reduced cortical volumes in the cingulate brain cortex and frontal regions, and reduced white matter integrity in key brain pathways. Neuroimaging findings, however, are primarily used for research currently and have yet to be widely implemented in clinical guidelines.
International PTSD treatment guidelines consistently recognize trauma-focused cognitive-behavioral therapies (CBTs), such as cognitive processing therapy (CPT), prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) as the gold standard. Recent guidelines have expanded the list of recommended treatments: The 2023 Department of Veterans Affairs and Department of Defense guidelines in the United States also endorse therapies like written narrative exposure and brief eclectic therapy. Internationally, guidelines do not perfectly coincide, as the 2018 update from the United Kingdom's National Institute for Health and Care Excellence (NICE) gives the highest recommendations to PE and CPT but rates EMDR slightly lower for military veterans because of limited evidence. Overall, guidelines consistently advocate for trauma-focused psychological interventions as the primary treatment for PTSD.
Guidelines from NICE and the World Health Organization do not recommend medications as the primary treatment; the American Psychiatric Association and the US Department of Veterans Affairs support selective serotonin reuptake inhibitors and prazosin but advise against benzodiazepines. Inpatient care may be necessary for individuals who pose a danger to themselves or others, or for those with severe PTSD from childhood abuse, to aid in emotional regulation and treatment.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The most likely diagnosis for this patient is veteran posttraumatic stress disorder (PTSD), given his history of combat exposure and symptoms, such as severe headaches, difficulty concentrating, mood swings, nightmares, flashbacks, increased startle response, and hypervigilance. MRI findings showing significant changes in the limbic system and hippocampal regions support this diagnosis. Other potential diagnoses, like traumatic brain injury, chronic migraine, and major depressive disorder, are less likely because of their inability to account for the full range of his symptoms and specific MRI abnormalities.
PTSD, experienced by a subset of individuals after exposure to life-threatening events, has a lifetime prevalence of 4%-7% and a current prevalence of 1%-3%, with higher rates in older women, those with more trauma, and combat veterans. Nearly half of US veterans are aged 65 or older, many being Vietnam-era veterans at elevated risk for PTSD. Prevalence rates in older veterans range between 1% and 22%.
PTSD is characterized by intrusive thoughts, flashbacks, nightmares, avoidance of reminders, hypervigilance, and sleep difficulties, significantly disrupting interpersonal and occupational functioning. Screening tools like the primary care (PC) PTSD-5 and PCL-5, used in primary care settings, are effective for early detection, provisional diagnosis, and monitoring of symptom changes. The clinician-administered PTSD scale for Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition DSM-5 (CAPS-5) is the gold standard for diagnosis, particularly among veterans, with multimethod assessments combining self-report measures and semi-structured interviews recommended for accuracy. The DSM-5 criteria for PTSD diagnosis describe exposure to traumatic events, intrusion symptoms, avoidance behaviors, negative mood, and altered arousal, with symptoms persisting for over a month and causing significant distress or functional impairment.
Research has identified consistent anatomical and functional changes in PTSD patients, such as smaller hippocampi, decreased corpus callosum and prefrontal cortex, increased amygdala reactivity, and decreased prefrontal cortex activity. PTSD, linked to alterations in brain regions involved in fear learning and memory, shows diminished structural integrity in executive function areas, reduced cortical volumes in the cingulate brain cortex and frontal regions, and reduced white matter integrity in key brain pathways. Neuroimaging findings, however, are primarily used for research currently and have yet to be widely implemented in clinical guidelines.
International PTSD treatment guidelines consistently recognize trauma-focused cognitive-behavioral therapies (CBTs), such as cognitive processing therapy (CPT), prolonged exposure (PE), and eye movement desensitization and reprocessing (EMDR) as the gold standard. Recent guidelines have expanded the list of recommended treatments: The 2023 Department of Veterans Affairs and Department of Defense guidelines in the United States also endorse therapies like written narrative exposure and brief eclectic therapy. Internationally, guidelines do not perfectly coincide, as the 2018 update from the United Kingdom's National Institute for Health and Care Excellence (NICE) gives the highest recommendations to PE and CPT but rates EMDR slightly lower for military veterans because of limited evidence. Overall, guidelines consistently advocate for trauma-focused psychological interventions as the primary treatment for PTSD.
Guidelines from NICE and the World Health Organization do not recommend medications as the primary treatment; the American Psychiatric Association and the US Department of Veterans Affairs support selective serotonin reuptake inhibitors and prazosin but advise against benzodiazepines. Inpatient care may be necessary for individuals who pose a danger to themselves or others, or for those with severe PTSD from childhood abuse, to aid in emotional regulation and treatment.
Jasvinder Chawla, MD, Professor of Neurology, Loyola University Medical Center, Maywood; Director, Clinical Neurophysiology Lab, Department of Neurology, Hines VA Hospital, Hines, IL.
Jasvinder Chawla, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
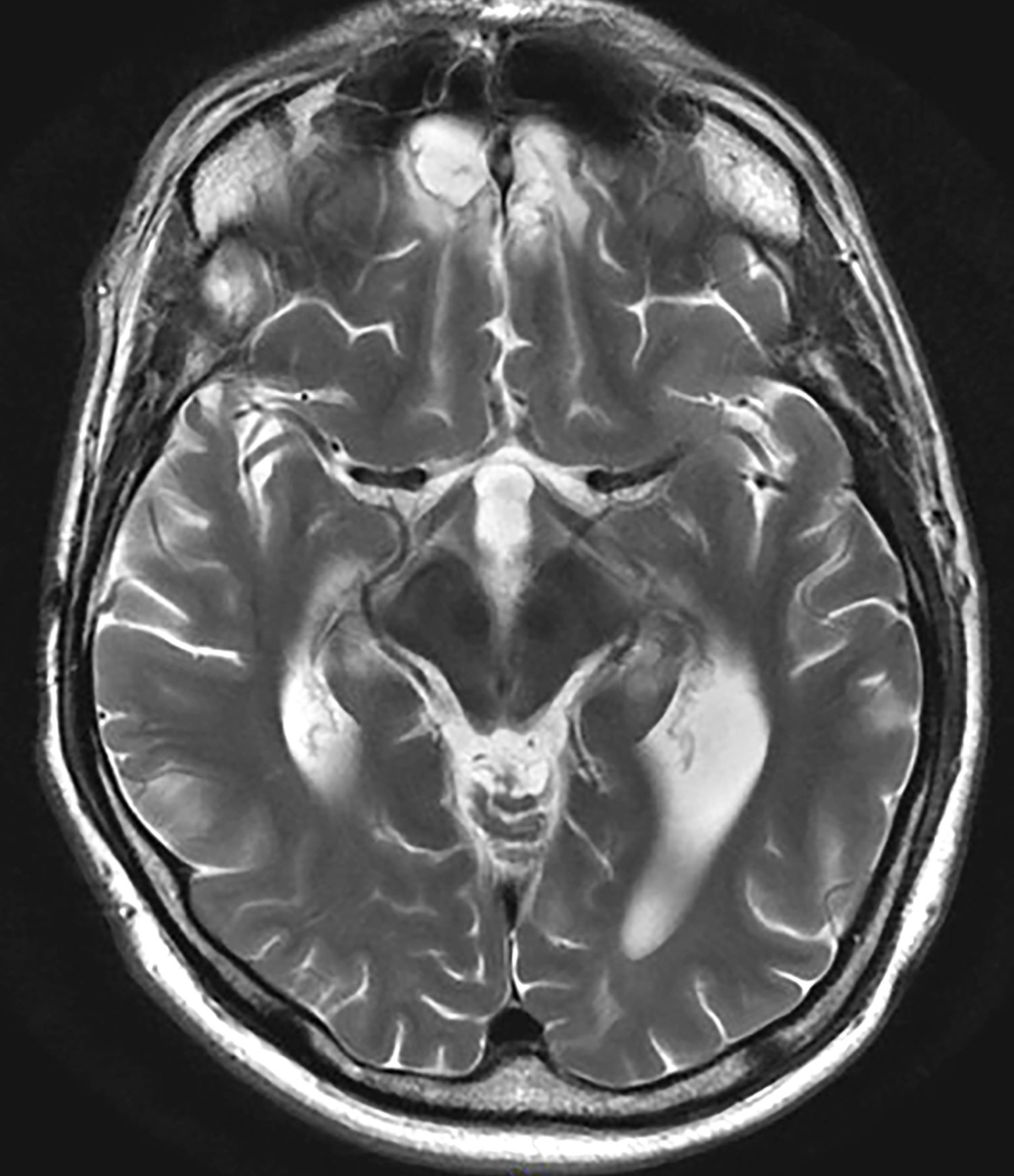
A 35-year-old male veteran presents with a history of severe headaches, difficulty concentrating, and persistent mood swings. He served multiple tours in a combat zone, where he was exposed to several traumatic events, including the loss of close friends. His medical history reveals previous diagnoses of insomnia and anxiety, for which he has been prescribed various medications over the years with limited success. During his clinical evaluation, he describes frequent nightmares and flashbacks related to his time in service. He reports an increased startle response and hypervigilance, often feeling on edge and irritable. A recent MRI of the brain, as shown in the image here, reveals significant changes in the limbic system, with abnormalities in the hippocampal regions. Laboratory tests and physical exams are otherwise unremarkable, but his mental health assessment indicates severe distress, which is affecting his daily functioning and interpersonal relationships.
Weight gain despite dieting
Binge-eating disorder is more prevalent in women than men and has one of the strongest associations with obesity; among patients with obesity, lifetime prevalence of binge eating is approximately 5.5%. Large population studies suggest that binge-eating disorder may be present in 2%-4% of adolescents, with a mean age of onset of 12-13 years. This patient probably had milder binge-eating disorder as an adolescent and young adult, which was exacerbated by the pandemic.
Both new diagnoses and reports of clinical worsening in patients with preexisting diagnoses of binge-eating disorder during the pandemic have been documented. Food insecurity has been associated with binge eating, consistent with this patient's anxiety over food and grocery availability during the pandemic. The definition of binge-eating disorder includes recurrent specific episodes of overeating that are not consistent with the patient's usual behavior, eating to the point of being uncomfortably full, eating more quickly or when not hungry, and having feelings of loss of control during episodes and of guilt or disgust afterward.
Obesity and eating disorders share some common risk factors and approaches to management. Binge eating has been associated with type 2 diabetes, hypertension, asthma, sleep disorders, and menstrual disorders, all of which are also affected by obesity. The presence of both conditions increases the adverse outcomes associated with each, including negative impacts on cardiometabolic and psychological health. Workup of patients presenting with binge eating and obesity should always include complete blood/metabolic panels and cardiovascular and renal health, as well as assessments of nutrition status, electrolyte imbalances, gastrointestinal reflux disease, and chronic pain.
In general, where binge-eating disorder and obesity are concurrent, cognitive-behavioral therapy (CBT) for binge-eating disorder should be the first priority, with obesity management (medication or surgery) to follow. CBT has the strongest evidence of benefit for patients with binge-eating disorder and is the recommended treatment approach. Other psychotherapeutic interventions that may be of benefit include dialectical behavioral therapy (to reduce binge-eating frequency), technology-based options, and family-based therapy when symptoms are recognized in children or adolescents. Structured behavioral weight management strategies for management of obesity and overweight do not increase symptoms of eating disorders and may instead relieve some symptoms. An emerging approach to binge eating in patients with obesity is CBT that integrates therapeutic approaches to both issues.
Medications to treat binge-eating disorder are limited and should not be used without concurrent psychotherapy; lisdexamfetamine has demonstrated benefit, is recommended by the American Psychiatric Association, and is approved by the US Food and Drug Administration specifically to treat adults with binge-eating disorder.
The success of psychological interventions and lifestyle modifications for obesity is heavily dependent on the individual's ability and motivation to comply with recommended interventions. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27). Recommended medications include phentermine-topiramate and bupropion-naltrexone (which may benefit those with binge-eating disorder), as well as injectable glucagon-like peptide receptor agonists (GLP-1 RAs) at the approved dosage for obesity management (semaglutide 2.4 mg weekly or liraglutide 3.0 mg daily). Orlistat is not recommended. Ongoing research on the potential benefit of GLP-1 RAs in management of binge eating offers additional support for a role in patients, like this one, with binge-eating disorder and obesity.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Binge-eating disorder is more prevalent in women than men and has one of the strongest associations with obesity; among patients with obesity, lifetime prevalence of binge eating is approximately 5.5%. Large population studies suggest that binge-eating disorder may be present in 2%-4% of adolescents, with a mean age of onset of 12-13 years. This patient probably had milder binge-eating disorder as an adolescent and young adult, which was exacerbated by the pandemic.
Both new diagnoses and reports of clinical worsening in patients with preexisting diagnoses of binge-eating disorder during the pandemic have been documented. Food insecurity has been associated with binge eating, consistent with this patient's anxiety over food and grocery availability during the pandemic. The definition of binge-eating disorder includes recurrent specific episodes of overeating that are not consistent with the patient's usual behavior, eating to the point of being uncomfortably full, eating more quickly or when not hungry, and having feelings of loss of control during episodes and of guilt or disgust afterward.
Obesity and eating disorders share some common risk factors and approaches to management. Binge eating has been associated with type 2 diabetes, hypertension, asthma, sleep disorders, and menstrual disorders, all of which are also affected by obesity. The presence of both conditions increases the adverse outcomes associated with each, including negative impacts on cardiometabolic and psychological health. Workup of patients presenting with binge eating and obesity should always include complete blood/metabolic panels and cardiovascular and renal health, as well as assessments of nutrition status, electrolyte imbalances, gastrointestinal reflux disease, and chronic pain.
In general, where binge-eating disorder and obesity are concurrent, cognitive-behavioral therapy (CBT) for binge-eating disorder should be the first priority, with obesity management (medication or surgery) to follow. CBT has the strongest evidence of benefit for patients with binge-eating disorder and is the recommended treatment approach. Other psychotherapeutic interventions that may be of benefit include dialectical behavioral therapy (to reduce binge-eating frequency), technology-based options, and family-based therapy when symptoms are recognized in children or adolescents. Structured behavioral weight management strategies for management of obesity and overweight do not increase symptoms of eating disorders and may instead relieve some symptoms. An emerging approach to binge eating in patients with obesity is CBT that integrates therapeutic approaches to both issues.
Medications to treat binge-eating disorder are limited and should not be used without concurrent psychotherapy; lisdexamfetamine has demonstrated benefit, is recommended by the American Psychiatric Association, and is approved by the US Food and Drug Administration specifically to treat adults with binge-eating disorder.
The success of psychological interventions and lifestyle modifications for obesity is heavily dependent on the individual's ability and motivation to comply with recommended interventions. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27). Recommended medications include phentermine-topiramate and bupropion-naltrexone (which may benefit those with binge-eating disorder), as well as injectable glucagon-like peptide receptor agonists (GLP-1 RAs) at the approved dosage for obesity management (semaglutide 2.4 mg weekly or liraglutide 3.0 mg daily). Orlistat is not recommended. Ongoing research on the potential benefit of GLP-1 RAs in management of binge eating offers additional support for a role in patients, like this one, with binge-eating disorder and obesity.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Binge-eating disorder is more prevalent in women than men and has one of the strongest associations with obesity; among patients with obesity, lifetime prevalence of binge eating is approximately 5.5%. Large population studies suggest that binge-eating disorder may be present in 2%-4% of adolescents, with a mean age of onset of 12-13 years. This patient probably had milder binge-eating disorder as an adolescent and young adult, which was exacerbated by the pandemic.
Both new diagnoses and reports of clinical worsening in patients with preexisting diagnoses of binge-eating disorder during the pandemic have been documented. Food insecurity has been associated with binge eating, consistent with this patient's anxiety over food and grocery availability during the pandemic. The definition of binge-eating disorder includes recurrent specific episodes of overeating that are not consistent with the patient's usual behavior, eating to the point of being uncomfortably full, eating more quickly or when not hungry, and having feelings of loss of control during episodes and of guilt or disgust afterward.
Obesity and eating disorders share some common risk factors and approaches to management. Binge eating has been associated with type 2 diabetes, hypertension, asthma, sleep disorders, and menstrual disorders, all of which are also affected by obesity. The presence of both conditions increases the adverse outcomes associated with each, including negative impacts on cardiometabolic and psychological health. Workup of patients presenting with binge eating and obesity should always include complete blood/metabolic panels and cardiovascular and renal health, as well as assessments of nutrition status, electrolyte imbalances, gastrointestinal reflux disease, and chronic pain.
In general, where binge-eating disorder and obesity are concurrent, cognitive-behavioral therapy (CBT) for binge-eating disorder should be the first priority, with obesity management (medication or surgery) to follow. CBT has the strongest evidence of benefit for patients with binge-eating disorder and is the recommended treatment approach. Other psychotherapeutic interventions that may be of benefit include dialectical behavioral therapy (to reduce binge-eating frequency), technology-based options, and family-based therapy when symptoms are recognized in children or adolescents. Structured behavioral weight management strategies for management of obesity and overweight do not increase symptoms of eating disorders and may instead relieve some symptoms. An emerging approach to binge eating in patients with obesity is CBT that integrates therapeutic approaches to both issues.
Medications to treat binge-eating disorder are limited and should not be used without concurrent psychotherapy; lisdexamfetamine has demonstrated benefit, is recommended by the American Psychiatric Association, and is approved by the US Food and Drug Administration specifically to treat adults with binge-eating disorder.
The success of psychological interventions and lifestyle modifications for obesity is heavily dependent on the individual's ability and motivation to comply with recommended interventions. The American Gastroenterological Association and other organizations recommend treatment with antiobesity medications along with lifestyle modifications for patients with obesity (BMI ≥ 30) and weight-related complications (BMI > 27). Recommended medications include phentermine-topiramate and bupropion-naltrexone (which may benefit those with binge-eating disorder), as well as injectable glucagon-like peptide receptor agonists (GLP-1 RAs) at the approved dosage for obesity management (semaglutide 2.4 mg weekly or liraglutide 3.0 mg daily). Orlistat is not recommended. Ongoing research on the potential benefit of GLP-1 RAs in management of binge eating offers additional support for a role in patients, like this one, with binge-eating disorder and obesity.
Carolyn Newberry, MD, Assistant Professor of Medicine, Director of GI Nutrition, Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE), Division of Gastroenterology, Weill Cornell Medical Center, New York, NY.
Disclosure: Carolyn Newberry, MD, has disclosed the following relevant financial relationships:
Serve(d) as a speaker or a member of a speakers bureau for: Baster International; InBody.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 28-year-old woman presents with concerns about weight gain despite dieting. She is 5 ft 4 in and weighs 180 lb (BMI 30.9). The patient lives alone and says she often feels isolated and has ongoing anxiety. She states that she has been overweight since her early teen years and had rare episodes of overeating. As an adult, her weight remained relatively stable (BMI ~26) until she began working remotely because of the COVID-19 pandemic in March 2020. She admits to becoming increasingly anxious and worried about food availability and grocery shopping during the early pandemic closures, feelings that have not completely resolved. While working from home, she has had more days where she compulsively overeats, even while trying to diet or use supplements she saw on TV or the internet. She stopped participating in a regular exercise walking group in mid-2020 and has not returned to it.
At presentation, she appears anxious and nervous. Her blood pressure is elevated (140/90 mm Hg), heart rate is 110 beats/min, and respiratory rate is 18 breaths/min. Her results on the Generalized Anxiety Disorder assessment indicate moderate symptoms of anxiety. Lab results indicate A1c = 6.5%, low-density lipoprotein cholesterol = 105 mg/dL, and estimated glomerular filtration rate = 90 mL/min/1.73 m2; all other results are within normal.