User login
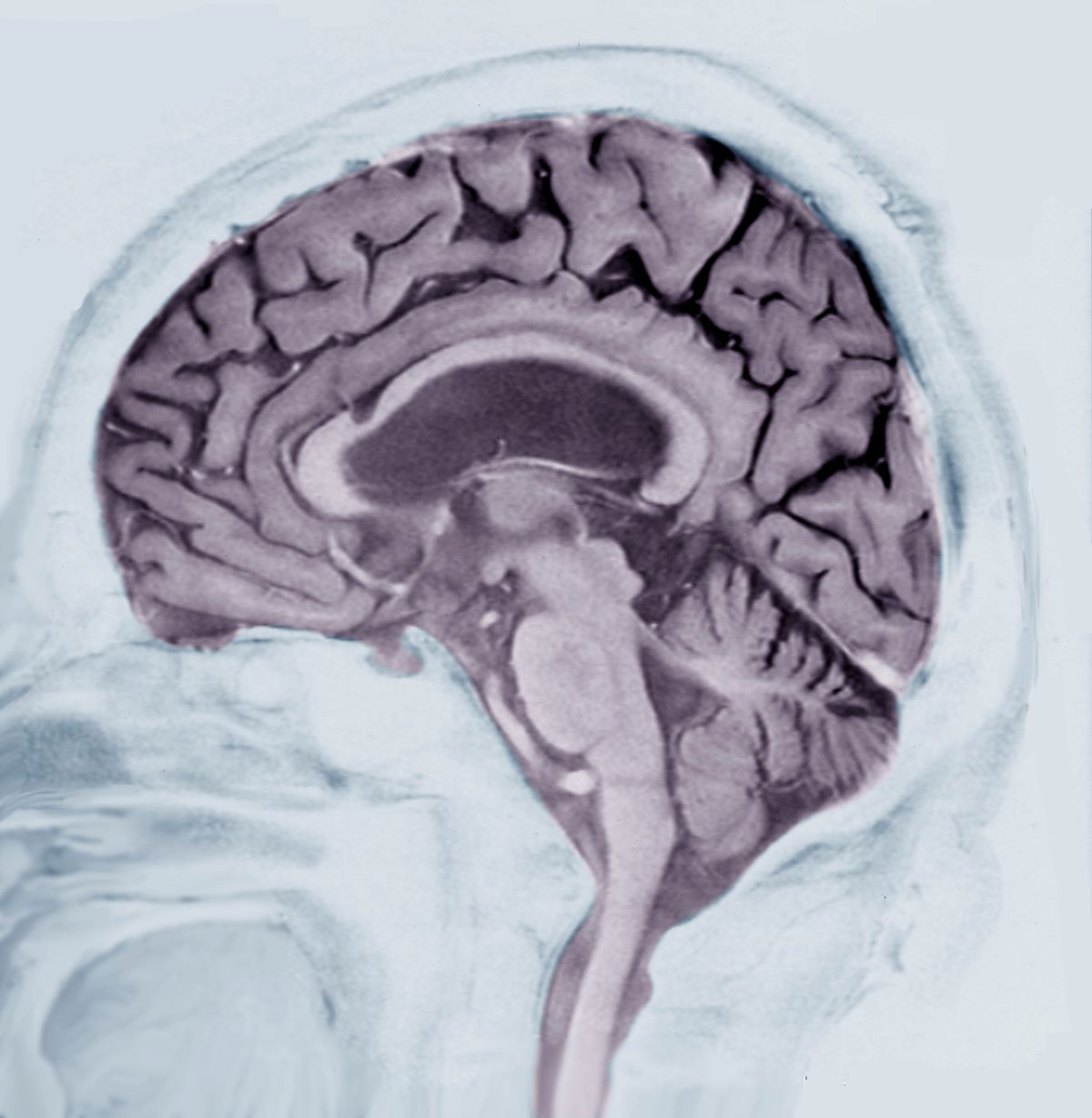
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
This patient’s presentation is indicative of moderate-stage Alzheimer’s disease (AD), which is confirmed by physical exam and testing; most notably, her MMSE score of 18 (a score of ≥ 25 is considered normal) and MRI results showing distinct cortical atrophy. At this stage of disease, signs and symptoms become more pronounced and widespread to include not only language deficiencies, prominent memory loss, and sensory processing, but also motor deficits and behavioral issues, all of which are clearly present in this patient.
A very important clinical consideration is a possible delay in diagnosis. It is atypical for an initial diagnosis of AD to be made when a patient is in the moderate stage of disease. This patient’s history over 5 years before her diagnosis included complaints of forgetfulness and low-level dyspraxia, which were not pursued. Reasons for this can vary. Broadly, patient interactions in a primary care setting tend to be brief, thus, many patients are not engaged in their care. Early symptoms — eg, memory impairment — can be missed during routine office visits.
There are also significant racial disparities in the diagnosis of dementia. According to National Institute of Aging-funded studies that were conducted in 39 AD Research Centers, White patients > 65 years old had a significantly higher prevalence of dementia diagnoses at baseline visits than Black patients in the same age group. Black patients, especially Black women, tend not to be diagnosed with AD until it has progressed. Conversely, Black patients had more risk factors for AD, greater cognitive impairment, and more severe neuropsychiatric symptoms (delusions and hallucinations) than those of other races and ethnicities.
Another barrier to timely diagnosis in Black patients is disparity in access to neuroimaging. In a study conducted by Wibecan and colleagues at Boston Medical Center, researchers found that among neuroimaging assessments conducted at the facility, Black patients who received MRI or CT scan for the diagnosis of cognitive impairment were older than White patients (72.5 years vs 67 years). Additionally, Black patients were significantly less likely to undergo MRI (the gold standard of care for dementia diagnosis) than CT scan.
Hypothyroidism is an endocrine disorder that occurs because of a deficiency in thyroid hormone. Symptoms tend to be subtle and non-specific but vary greatly. Some of the hallmark symptoms are fatigue, weight gain, cold intolerance, dry skin, and hair loss. Additionally, emotional lability and depressed mood with mental impairment, slowed speech, and movement, as evident in this patient. However, hypothyroidism was ruled out when her laboratory results returned with all values within normal range.
Vascular dementia is the second-most prevalent form of dementia after AD. It is characterized as cognitive impairment that occurs after one, or a series of, neurologic events and does not refer to a single disease but to a variety of vascular disorders. Patients with vascular dementia often exhibit mood and behavioral changes, deficits in executive function, and severe memory loss, all of which are present in this patient. However, as there were no (known) neurologic events in this patient — and no evidence thereof on imaging — and her hypertension is relatively well controlled, this is not a diagnostic consideration for this patient.
Normal pressure hydrocephalus (NPH) is caused by the build-up of cerebrospinal fluid in the brain. It is characterized by abnormal gait, dementia, and urinary incontinence. Patients with NPH experience decreased attention, significant memory loss, bradyphrenia, bradykinesia, and broad-based gait, all of which feature in this patient. However, brain MRI was negative for structural abnormalities of this type, and there was no indication of NPH, which rules it out as a potential diagnosis.
Shaheen E. Lakhan, MD, PhD, MS, MEd, Chief of Pain Management, Carilion Clinic and Virginia Tech Carilion School of Medicine, Roanoke, Virginia.
Disclosure: Shaheen E. Lakhan, MD, PhD, MS, MEd, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 76-year-old Black woman presents to her physician. She is accompanied by her daughter who reports that, over the last 9 months, her mother has exhibited worsening memory loss, confusion, impaired judgment, agitation, and emotional lability. She is often unaware of where she is or how she got there. She sometimes does not recognize her family members or people who are familiar to her. Her appetite has been variable, and her sleep schedule is altered so that she often sleeps during the day and is awake at night. Sometimes, she is so irritable that she becomes aggressive and insists on situations that don’t exist. Her executive function is low. Her daughter reports that the patient had a fall 9 months ago and again 4 months ago, after which her symptoms became progressively worse.
The patient has complained about being forgetful and clumsy for much of the past 5 years, which she has attributed to old age. Until the last year or so, these have not greatly impaired her daily function and were not of great concern to her family or providers. She has a history of hypertension and diabetes, both of which are pharmacologically managed with mixed results due to variable adherence.
Physical exam confirms her daughter’s report. The patient appears thin, fatigued, and anxious. She has lost 20 lb since her last visit. She has great difficulty maintaining focus on what is being asked of her and in following the conversation. When she does speak, her speech is slow. She exhibits both motor deficits — in balance and coordination — and a bradykinetic gait.
Laboratory testing is performed: complete blood count w/diff, comprehensive metabolic panel, thyroid panel, cobalamin level, vitamin D screening. All results are within normal range for this patient. She was unable to complete the Geriatric Depression Scale on her own; direct questioning about whether she was feeling depressed is negative. Mini-Mental State Examination (MMSE) score is 18. MRI is performed; sagittal view reveals cortical atrophy.