User login
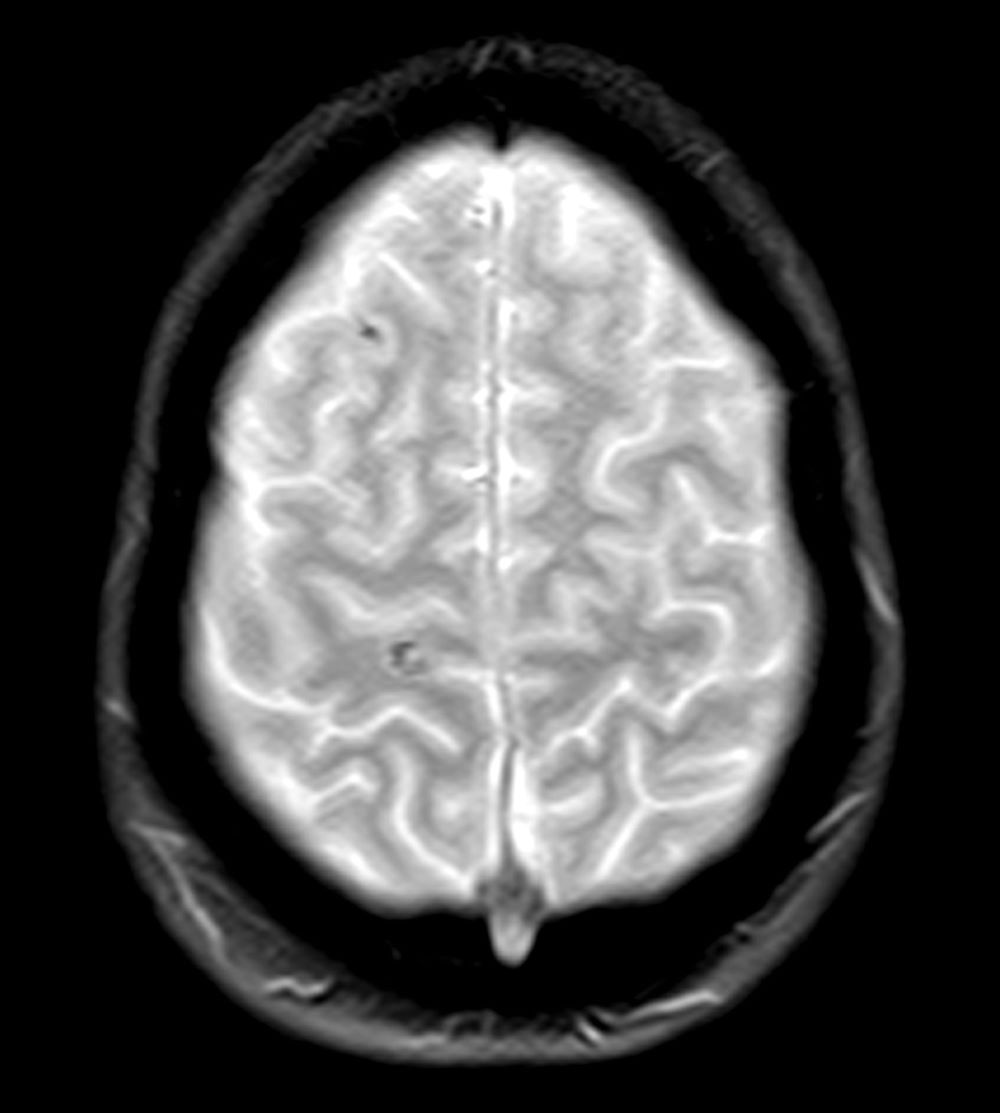
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
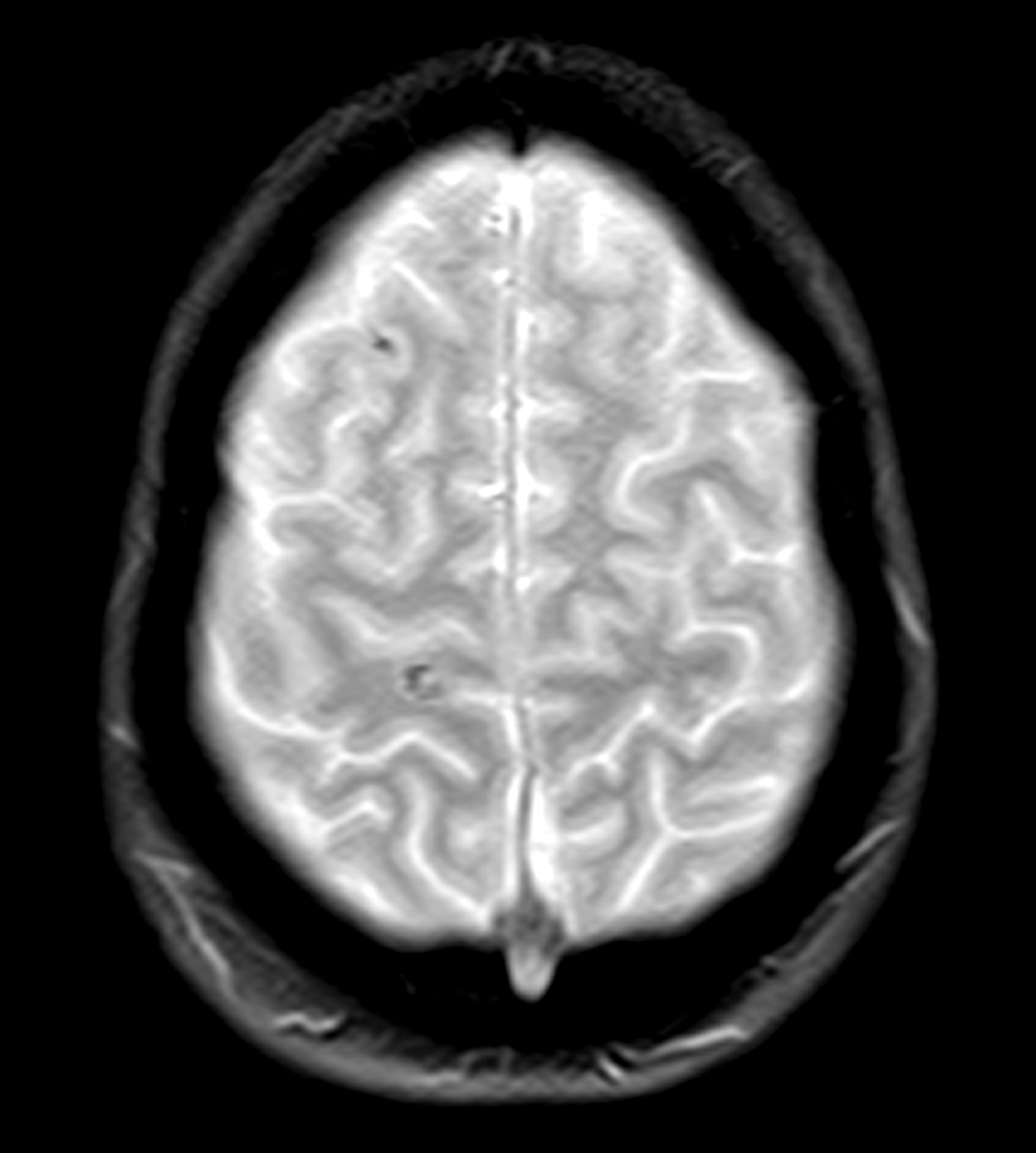
A 28-year-old professional boxer presents with severe anxiety, agitation, headaches, and insomnia with recurring nightmares and flashbacks. His symptoms began after he was robbed at gunpoint in the gym parking lot as he was getting into his car about 6 months ago. Since that time, he has had to postpone several fights because he is unable to maintain his training schedule and reports feeling depressed as a result. He is also at risk for suspension from his regular gym because he has gotten into several violent, unprovoked altercations with fellow boxers, and he has also had multiple violent outbursts outside of the gym. He has a history of concussion.
Physical exam reveals increased heart rate and hypervigilance. The patient is administered the Patient Health Questionnaire and has a score of 14 out of a possible 27. Zero to 4 indicates no depression, whereas 14 falls within the range of moderate depression. A brain CT scan (Figure) is ordered because of his history of concussion and his chronic symptoms. The scan reveals two subacute hematomas in the left hemisphere, one in the frontal lobe and the other in the temporal lobe. Additional tests are ordered: laboratory testing, to rule out organic or infectious causes of symptoms and electroencephalography, to assess for a possible seizure focus; both tests reveal nothing remarkable. The hematomas were noted at the time of a previous head injury 2 years ago.