User login
VA is a Leader in Mental Health and Social Service Research and Operations
VA is a Leader in Mental Health and Social Service Research and Operations
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
The US Department of Veterans Affairs (VA) mission is defined by President Abraham Lincoln’s promise “to care for him who shall have borne the battle, and for his widow, and his orphan.” Critically, the biopsychosocial needs of veterans differ from the needs of civilians due to the nature of military service.1 Veterans commonly experience traumatic brain injury (TBI) due to combat- or training-related injuries.2 Psychologically, veterans are disproportionately likely to be diagnosed with mental health conditions, such as posttraumatic stress disorder (PTSD), often linked to military exposures.3 Spiritually, veterans frequently express moral injury after living through circumstances when they perpetrate, fail to prevent, or witness events that contradict moral beliefs/ expectations.4 Veterans also have significant social challenges, including high rates of homelessness. 5 A critical strength of the VA mission is its awareness of these complex sequelae and its ability to provide well-informed treatment and social services to meet veterans’ unique needs.
Foundational to a well-informed health care system is a robust research and operational quality improvement infrastructure. The VA Office of Research and Development (ORD) has worked tirelessly to understand and address the unique, idiographic needs of veterans. In 2024 the ORD had a budget of $2.4 billion, excluding quality improvement initiatives enhancing VA operations.6
The integrated VA health care system is a major strength for providing state-of-the-science to inform veterans’ treatment and social service needs. The VA features medical centers and clinics capable of synergistically leveraging extant infrastructure to facilitate collaborations and centralized procedures across sites. The VA also has dedicated research centers, such as the National Center for PTSD, Centers of Excellence, Centers of Innovation, and Mental Illness, Research, Education and Clinical Centers that focus on PTSD, suicide prevention, TBI, and other high-priority areas. These centers recruit, train, and invest in experts dedicated to improving veterans’ lives. The VA Corporate Data Warehouse provides a national, system-wide repository for patient-level data, allowing for advanced analysis of large datasets.7
This special issue is a showcase of the strengths of VA mental health and social service research, aligning with the current strategic priorities of VA research. Topics focus on the unique needs of veterans, including sequelae (eg, PTSD, homelessness, moral injury), with particular attention to veterans. Manuscripts highlight the strengths of collaborations, including those between specialized research centers and national VA operational partners. Analyses highlight the VA research approach, leveraging data and perspectives from inside and outside the VA, and studying new and established approaches to care. This issue highlights the distinct advantages that VA research provides: experts with the tools, experience, and dedication to addressing the unique needs of veterans. Given the passion for veteran care among VA researchers, including those featured in this issue, we strongly believe the VA will continue to be a leader in this research.
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
- Oster C, Morello A, Venning A, Redpath P, Lawn S. The health and wellbeing needs of veterans: a rapid review. BMC Psychiatry. 2017;17(1):414. doi:10.1186/s12888-017-1547-0
- Cypel YS, Vogt D, Maguen S, et al. Physical health of Post- 9/11 U.S. military veterans in the context of Healthy People 2020 targeted topic areas: results from the Comparative Health Assessment Interview Research Study. Prev Med Rep. 2023;32:102122. doi:10.1016/j.pmedr.2023.102122
- Lehavot K, Katon JG, Chen JA, Fortney JC, Simpson TL. Post-traumatic stress disorder by gender and veteran Status. Am J Prev Med. 2018;54(1):e1-e9. doi:10.1016/j.amepre.2017.09.008
- Griffin BJ, Purcell N, Burkman K, et al. Moral injury: an integrative review. J Trauma Stress. 2019;32(3):350-362. doi:10.1002/jts.22362
- Tsai J, Pietrzak RH, Szymkowiak D. The problem of veteran homelessness: an update for the new decade. Am J Prev Med. 2021;60(6):774-780. doi:10.1016/j.amepre.2020.12.012
- US Department of Veterans Affairs, Office of Research and Development. About the office of research & development. Updated January 22, 2025. Accessed March 18, 2025. https://www.research.va.gov/about/default.cfm
- Fihn SD, Francis J, Clancy C, et al. Insights from advanced analytics at the Veterans Health Administration. Health Aff (Millwood). 2014;33(7):1203-1211. doi:10.1377/hlthaff.2014.0054
VA is a Leader in Mental Health and Social Service Research and Operations
VA is a Leader in Mental Health and Social Service Research and Operations
Severe anxiety and agitation
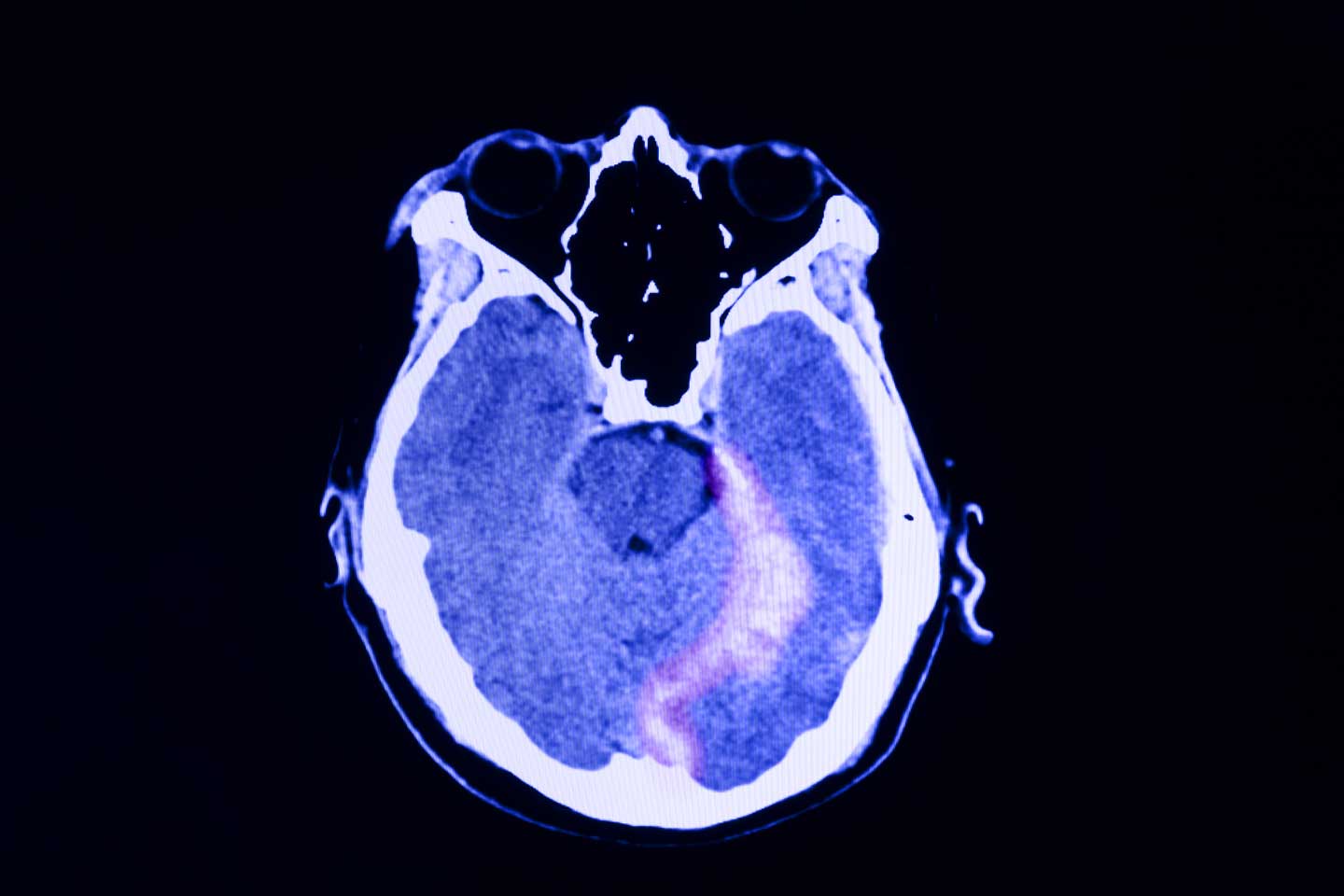
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis considering this patient’s symptoms of anxiety, hypervigilance, recurring nightmares, agitation, flashbacks, and violent outbursts. His experience of being robbed at gunpoint outside his gym seems to have been the triggering event for his PTSD, which may have also been influenced by his history of multiple concussions incurred in a fight setting in which he is forced to defend himself. His avoidance of continued training and appearing at scheduled fights further support this diagnosis. His CT scan, although not diagnostic for PTSD directly, does show evidence of minor brain injury, with the remaining hematomas.
Anxiety disorder may account for the patient’s severe anxiety, agitation, and headaches, but his symptoms are new and started after the robbery, which indicates PTSD and not a long-standing anxiety disorder.
Schizophrenia is an unlikely diagnosis for this patient. Although he is within the typical age range of symptom onset, has had violent outbursts, and is prone to vast changes in mood that come on quickly, he is not psychotic and does not experience any of the hallmark symptoms of schizophrenia: delusions, hallucinations, and disorganized speech/behavior, at least two of which would need to be present to support a diagnosis of schizophrenia.
Given this patient’s circumstances, post-traumatic epilepsy initially may be a potential diagnostic consideration. However, he is not experiencing seizures, but rather mood and behavioral disturbances, the onset of which occurred after a specific event. Additionally, posttraumatic epilepsy results from traumatic brain injury.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, an update to the 2017 clinical treatment guidelines published by the American Psychiatric Association (APA), the diagnostic criteria for PTSD in an individual older than 6 years are:
1. Exposure to actual or threatened death, serious injury or sexual assault
2. The traumatic event is persistently re-experienced via flashbacks, nightmares, and intrusive thoughts that cause strong emotional reactions and psychological distress
3. Avoidance behaviors either in thoughts or conversations about the event or of people and places associated with the event
4. At least two examples of negative alterations in cognition and mood
5. At least two examples of hyperarousal
6. Duration of symptoms > 1 month
7. Significant distress or impairment in function because of these symptoms
Trauma-focused therapy is the gold standard of treatment for patients with PTSD. A recent review of current treatment strategies for PTSD found that cognitive processing therapy, cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing, all with a strong trauma focus, are the most effective treatments for PTSD.
The use of pharmacology to treat PTSD is controversial and varies by guideline. The APA and US Department of Veterans Affairs both recommend the use of antidepressants, particularly selective serotonin reuptake inhibitors, as a first-line treatment of PTSD. This is particularly important for patients who have psychiatric comorbid conditions, such as depression, who may not be able to effectively engage in cognitive- behavioral therapy. However, use of benzodiazepines or hypnotics should be strictly avoided in these patients because these drugs increase intrusive and avoidance symptoms over time. Medication should be continued for 6 to 12 months to help prevent relapse.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 28-year-old professional boxer presents with severe anxiety, agitation, headaches, and insomnia with recurring nightmares and flashbacks. His symptoms began after he was robbed at gunpoint in the gym parking lot as he was getting into his car about 6 months ago. Since that time, he has had to postpone several fights because he is unable to maintain his training schedule and reports feeling depressed as a result. He is also at risk for suspension from his regular gym because he has gotten into several violent, unprovoked altercations with fellow boxers, and he has also had multiple violent outbursts outside of the gym. He has a history of concussion.
Physical exam reveals increased heart rate and hypervigilance. The patient is administered the Patient Health Questionnaire and has a score of 14 out of a possible 27. Zero to 4 indicates no depression, whereas 14 falls within the range of moderate depression. A brain CT scan (Figure) is ordered because of his history of concussion and his chronic symptoms. The scan reveals two subacute hematomas in the left hemisphere, one in the frontal lobe and the other in the temporal lobe. Additional tests are ordered: laboratory testing, to rule out organic or infectious causes of symptoms and electroencephalography, to assess for a possible seizure focus; both tests reveal nothing remarkable. The hematomas were noted at the time of a previous head injury 2 years ago.
PTSD Guidelines
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Finally, a New Drug for Posttraumatic Stress Disorder?
A drug that combines the atypical antipsychotic brexpiprazole and the selective serotonin reuptake inhibitor sertraline provides significantly greater relief of posttraumatic stress disorder (PTSD) symptoms than sertraline plus placebo, results of a phase 3 trial showed.
The medication is currently under review by the Food and Drug Administration (FDA) and if approved, will be the first pharmacologic option for PTSD in more than 20 years.
The trial met its primary endpoint of change in the Clinician Administered PTSD Scale for Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) (CAPS-5) total score at week 10 and secondary patient-reported outcomes of PTSD symptoms, anxiety, and depression.
“And what is really cool, what’s really impactful is the combination worked better than sertraline plus placebo on a brief inventory of psychosocial functioning,” study investigator Lori L. Davis, a senior research psychiatrist, Birmingham Veterans Affairs Health Care System in Alabama, said in an interview.
“We can treat symptoms but that’s where the rubber meets the road, in terms of are they functioning better,” added Davis, who is also an adjunct professor of psychiatry, Heersink School of Medicine, University of Alabama at Birmingham.
The findings were published online on December 18 in JAMA Psychiatry and reported in May 2024 as part of a trio of trials conducted by Otsuka Pharmaceutical and Lundbeck Pharmaceuticals, codevelopers of the drug.
Clinically Meaningful
“This study provides promising results for a medication that may be an important new option for PTSD,” John Krystal, MD, director, Clinical Neuroscience Division, National Center for PTSD, US Department of Veterans Affairs, who was not involved in the research, said in an interview. “New PTSD treatments are a high priority.”
Currently, there are two FDA-approved medication treatments for PTSD — sertraline and paroxetine.
“They are helpful for many people, but patients are often left with residual symptoms or tolerability issues,” noted Krystal, who is also professor and chair of psychiatry, Yale University, New Haven, Connecticut.
“New medications that might address the important ‘effectiveness gap’ in PTSD could help to reduce the remaining distress, disability, and suicide risk associated with PTSD.”
The double-blind, phase 3 trial included 416 adults aged 18-65 years with a DSM-5 diagnosis of PTSD and symptoms for at least 6 months prior to screening. Patients underwent a 1-week placebo-run in period followed by randomization to daily oral brexpiprazole 2-3 mg plus sertraline 150 mg or daily sertraline 150 mg plus placebo for 11 weeks.
Participants’ mean age was 37.4 years, 74.5% were women, and mean CAPS-5 total score was 38.4, suggesting moderate to high severity PTSD, Davis said. The average time from the index traumatic event was 4 years and three fourths had no prior exposure to PTSD prescription medications.
At week 10, the mean change in CAPS-5 score from randomization was –19.2 points in the brexpiprazole plus sertraline group and –13.6 points in the sertraline plus placebo group (95% CI, –8.79 to –2.38; P < .001).
Asked whether the 5.59-point treatment difference is clinically meaningful, Davis said there is no widely agreed definition for change in CAPS-5 total score but that a within-group reduction of more than 10-13 points is most-often cited as being clinically meaningful.
The key secondary endpoint of least square mean change in the patient-reported Brief Inventory of Psychosocial Function total score from baseline to week 12 was –33.8 with the combination vs –21.8 with sertraline plus placebo (95% CI, –19.4 to –4.62; P = .002).
“That’s clinically meaningful for me as a provider and a clinician and a researcher when you’re getting the PTSD symptom change differences in parallel with the improvement in functional outcome,” she said. “I see that as the clinically meaningful gauge.”
In terms of safety, 3.9% of the participants in the brexpiprazole/sertraline group and 10.2% of those in the sertraline/placebo group discontinued treatment because of adverse events.
In both the combination and control groups, the only treatment-emergent adverse event with an incidence of more than 10% was nausea (12.2% vs 11.7%, respectively).
At the last visit, the mean change in body weight from baseline was an increase of 1.3 kg for brexpiprazole plus sertraline vs 0 kg for sertraline alone. Rates of fatigue (6.8% vs 4.1%) and somnolence (5.4% vs 2.6%) were also higher with brexpiprazole plus sertraline.
A Trio of Clinical Trials
The findings are part of a larger program reported by the drug makers that includes a flexible-dose brexpiprazole phase 2 trial that met the same CAPS-5 primary endpoint and a second phase 3 trial (072 study) that did not.
“We’ve looked at that data and the sertraline/placebo response was a lot higher, so it was not due to a lack of response with the combination but due to a more robust response with the active control,” Davis said. “But we want to point out for that 072 study, there was still important separation between the combination and sertraline plus placebo on the functional outcome.”
All three trials ran for 12 weeks, so longer-term efficacy and safety data are needed, she said. Other limitations of the published phase 3 study are the patient eligibility criteria, restrictions on concomitant therapy, and lack of non-US sites, which many limit generalizability, the authors noted.
“Specifically, the exclusion of patients with a current major depressive episode is both a strength (to show a specific effect on PTSD) and a limitation (given the high prevalence of comorbid depression in PTSD),” they added.
Kudos, Caveats
Reached for comment, Vincent F. Capaldi, II, MD, ScM, professor and chair, department of psychiatry, Uniformed Services University of the Health Sciences School of Medicine, Bethesda, Maryland, said the exclusion of these patients is a limitation but that the study was well designed and conducted in a large sample across the United States.
“The findings suggest that brexpiprazole plus sertraline is a more effective treatment for PTSD than sertraline alone,” he said. “This finding is significant for our service members, who suffer from PTSD at higher rates than the general population.”
Additionally, the significant improvement in psychosocial functioning at week 12 “is important because PTSD is known to cause significant social and occupational disability, as well as quality-of-life issues,” he said.
Capaldi pointed out, however, that the study was conducted only at US sites and did not specifically target military/veteran persons, which may limit applicability to these unique populations.
“While subgroup analyses were generally consistent with the primary analysis, the study was not powered to detect differences between subgroups,” he added. “These subgroup analyses are quite important when considering military and veteran populations.”
Further research is needed to explore whether certain traumas are more responsive to combination treatment, the efficacy of augmenting existing sertraline therapy, and the specific mechanisms of brexpiprazole driving the improved outcomes, Capaldi said.
This study was funded by Otsuka Pharmaceutical Development & Commercialization, which was involved in the design, conduct, and data analysis. Davis reported receiving advisory board fees from Otsuka and Boehringer Ingelheim; lecture fees from Clinical Care Options; and grants from Alkermes, the Veterans Affairs, Patient-Centered Outcomes Research Institute, Department of Defense, and Social Finance. Several coauthors are employees of Otsuka. Krystal reported serving as a consultant for Otsuka America Pharmaceutical, Aptinyx, Biogen, IDEC, Bionomics, Boehringer Ingelheim International, Clearmind Medicine, Cybin IRL, Enveric Biosciences, Epiodyne, EpiVario, Janssen, Jazz Pharmaceuticals, Perception Neuroscience, Praxis Precision Medicines, Springcare, and Sunovion Pharmaceuticals. Krystal also reported serving as a scientific advisory board member for several companies and holding several patents.
A version of this article appeared on Medscape.com.
A drug that combines the atypical antipsychotic brexpiprazole and the selective serotonin reuptake inhibitor sertraline provides significantly greater relief of posttraumatic stress disorder (PTSD) symptoms than sertraline plus placebo, results of a phase 3 trial showed.
The medication is currently under review by the Food and Drug Administration (FDA) and if approved, will be the first pharmacologic option for PTSD in more than 20 years.
The trial met its primary endpoint of change in the Clinician Administered PTSD Scale for Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) (CAPS-5) total score at week 10 and secondary patient-reported outcomes of PTSD symptoms, anxiety, and depression.
“And what is really cool, what’s really impactful is the combination worked better than sertraline plus placebo on a brief inventory of psychosocial functioning,” study investigator Lori L. Davis, a senior research psychiatrist, Birmingham Veterans Affairs Health Care System in Alabama, said in an interview.
“We can treat symptoms but that’s where the rubber meets the road, in terms of are they functioning better,” added Davis, who is also an adjunct professor of psychiatry, Heersink School of Medicine, University of Alabama at Birmingham.
The findings were published online on December 18 in JAMA Psychiatry and reported in May 2024 as part of a trio of trials conducted by Otsuka Pharmaceutical and Lundbeck Pharmaceuticals, codevelopers of the drug.
Clinically Meaningful
“This study provides promising results for a medication that may be an important new option for PTSD,” John Krystal, MD, director, Clinical Neuroscience Division, National Center for PTSD, US Department of Veterans Affairs, who was not involved in the research, said in an interview. “New PTSD treatments are a high priority.”
Currently, there are two FDA-approved medication treatments for PTSD — sertraline and paroxetine.
“They are helpful for many people, but patients are often left with residual symptoms or tolerability issues,” noted Krystal, who is also professor and chair of psychiatry, Yale University, New Haven, Connecticut.
“New medications that might address the important ‘effectiveness gap’ in PTSD could help to reduce the remaining distress, disability, and suicide risk associated with PTSD.”
The double-blind, phase 3 trial included 416 adults aged 18-65 years with a DSM-5 diagnosis of PTSD and symptoms for at least 6 months prior to screening. Patients underwent a 1-week placebo-run in period followed by randomization to daily oral brexpiprazole 2-3 mg plus sertraline 150 mg or daily sertraline 150 mg plus placebo for 11 weeks.
Participants’ mean age was 37.4 years, 74.5% were women, and mean CAPS-5 total score was 38.4, suggesting moderate to high severity PTSD, Davis said. The average time from the index traumatic event was 4 years and three fourths had no prior exposure to PTSD prescription medications.
At week 10, the mean change in CAPS-5 score from randomization was –19.2 points in the brexpiprazole plus sertraline group and –13.6 points in the sertraline plus placebo group (95% CI, –8.79 to –2.38; P < .001).
Asked whether the 5.59-point treatment difference is clinically meaningful, Davis said there is no widely agreed definition for change in CAPS-5 total score but that a within-group reduction of more than 10-13 points is most-often cited as being clinically meaningful.
The key secondary endpoint of least square mean change in the patient-reported Brief Inventory of Psychosocial Function total score from baseline to week 12 was –33.8 with the combination vs –21.8 with sertraline plus placebo (95% CI, –19.4 to –4.62; P = .002).
“That’s clinically meaningful for me as a provider and a clinician and a researcher when you’re getting the PTSD symptom change differences in parallel with the improvement in functional outcome,” she said. “I see that as the clinically meaningful gauge.”
In terms of safety, 3.9% of the participants in the brexpiprazole/sertraline group and 10.2% of those in the sertraline/placebo group discontinued treatment because of adverse events.
In both the combination and control groups, the only treatment-emergent adverse event with an incidence of more than 10% was nausea (12.2% vs 11.7%, respectively).
At the last visit, the mean change in body weight from baseline was an increase of 1.3 kg for brexpiprazole plus sertraline vs 0 kg for sertraline alone. Rates of fatigue (6.8% vs 4.1%) and somnolence (5.4% vs 2.6%) were also higher with brexpiprazole plus sertraline.
A Trio of Clinical Trials
The findings are part of a larger program reported by the drug makers that includes a flexible-dose brexpiprazole phase 2 trial that met the same CAPS-5 primary endpoint and a second phase 3 trial (072 study) that did not.
“We’ve looked at that data and the sertraline/placebo response was a lot higher, so it was not due to a lack of response with the combination but due to a more robust response with the active control,” Davis said. “But we want to point out for that 072 study, there was still important separation between the combination and sertraline plus placebo on the functional outcome.”
All three trials ran for 12 weeks, so longer-term efficacy and safety data are needed, she said. Other limitations of the published phase 3 study are the patient eligibility criteria, restrictions on concomitant therapy, and lack of non-US sites, which many limit generalizability, the authors noted.
“Specifically, the exclusion of patients with a current major depressive episode is both a strength (to show a specific effect on PTSD) and a limitation (given the high prevalence of comorbid depression in PTSD),” they added.
Kudos, Caveats
Reached for comment, Vincent F. Capaldi, II, MD, ScM, professor and chair, department of psychiatry, Uniformed Services University of the Health Sciences School of Medicine, Bethesda, Maryland, said the exclusion of these patients is a limitation but that the study was well designed and conducted in a large sample across the United States.
“The findings suggest that brexpiprazole plus sertraline is a more effective treatment for PTSD than sertraline alone,” he said. “This finding is significant for our service members, who suffer from PTSD at higher rates than the general population.”
Additionally, the significant improvement in psychosocial functioning at week 12 “is important because PTSD is known to cause significant social and occupational disability, as well as quality-of-life issues,” he said.
Capaldi pointed out, however, that the study was conducted only at US sites and did not specifically target military/veteran persons, which may limit applicability to these unique populations.
“While subgroup analyses were generally consistent with the primary analysis, the study was not powered to detect differences between subgroups,” he added. “These subgroup analyses are quite important when considering military and veteran populations.”
Further research is needed to explore whether certain traumas are more responsive to combination treatment, the efficacy of augmenting existing sertraline therapy, and the specific mechanisms of brexpiprazole driving the improved outcomes, Capaldi said.
This study was funded by Otsuka Pharmaceutical Development & Commercialization, which was involved in the design, conduct, and data analysis. Davis reported receiving advisory board fees from Otsuka and Boehringer Ingelheim; lecture fees from Clinical Care Options; and grants from Alkermes, the Veterans Affairs, Patient-Centered Outcomes Research Institute, Department of Defense, and Social Finance. Several coauthors are employees of Otsuka. Krystal reported serving as a consultant for Otsuka America Pharmaceutical, Aptinyx, Biogen, IDEC, Bionomics, Boehringer Ingelheim International, Clearmind Medicine, Cybin IRL, Enveric Biosciences, Epiodyne, EpiVario, Janssen, Jazz Pharmaceuticals, Perception Neuroscience, Praxis Precision Medicines, Springcare, and Sunovion Pharmaceuticals. Krystal also reported serving as a scientific advisory board member for several companies and holding several patents.
A version of this article appeared on Medscape.com.
A drug that combines the atypical antipsychotic brexpiprazole and the selective serotonin reuptake inhibitor sertraline provides significantly greater relief of posttraumatic stress disorder (PTSD) symptoms than sertraline plus placebo, results of a phase 3 trial showed.
The medication is currently under review by the Food and Drug Administration (FDA) and if approved, will be the first pharmacologic option for PTSD in more than 20 years.
The trial met its primary endpoint of change in the Clinician Administered PTSD Scale for Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) (CAPS-5) total score at week 10 and secondary patient-reported outcomes of PTSD symptoms, anxiety, and depression.
“And what is really cool, what’s really impactful is the combination worked better than sertraline plus placebo on a brief inventory of psychosocial functioning,” study investigator Lori L. Davis, a senior research psychiatrist, Birmingham Veterans Affairs Health Care System in Alabama, said in an interview.
“We can treat symptoms but that’s where the rubber meets the road, in terms of are they functioning better,” added Davis, who is also an adjunct professor of psychiatry, Heersink School of Medicine, University of Alabama at Birmingham.
The findings were published online on December 18 in JAMA Psychiatry and reported in May 2024 as part of a trio of trials conducted by Otsuka Pharmaceutical and Lundbeck Pharmaceuticals, codevelopers of the drug.
Clinically Meaningful
“This study provides promising results for a medication that may be an important new option for PTSD,” John Krystal, MD, director, Clinical Neuroscience Division, National Center for PTSD, US Department of Veterans Affairs, who was not involved in the research, said in an interview. “New PTSD treatments are a high priority.”
Currently, there are two FDA-approved medication treatments for PTSD — sertraline and paroxetine.
“They are helpful for many people, but patients are often left with residual symptoms or tolerability issues,” noted Krystal, who is also professor and chair of psychiatry, Yale University, New Haven, Connecticut.
“New medications that might address the important ‘effectiveness gap’ in PTSD could help to reduce the remaining distress, disability, and suicide risk associated with PTSD.”
The double-blind, phase 3 trial included 416 adults aged 18-65 years with a DSM-5 diagnosis of PTSD and symptoms for at least 6 months prior to screening. Patients underwent a 1-week placebo-run in period followed by randomization to daily oral brexpiprazole 2-3 mg plus sertraline 150 mg or daily sertraline 150 mg plus placebo for 11 weeks.
Participants’ mean age was 37.4 years, 74.5% were women, and mean CAPS-5 total score was 38.4, suggesting moderate to high severity PTSD, Davis said. The average time from the index traumatic event was 4 years and three fourths had no prior exposure to PTSD prescription medications.
At week 10, the mean change in CAPS-5 score from randomization was –19.2 points in the brexpiprazole plus sertraline group and –13.6 points in the sertraline plus placebo group (95% CI, –8.79 to –2.38; P < .001).
Asked whether the 5.59-point treatment difference is clinically meaningful, Davis said there is no widely agreed definition for change in CAPS-5 total score but that a within-group reduction of more than 10-13 points is most-often cited as being clinically meaningful.
The key secondary endpoint of least square mean change in the patient-reported Brief Inventory of Psychosocial Function total score from baseline to week 12 was –33.8 with the combination vs –21.8 with sertraline plus placebo (95% CI, –19.4 to –4.62; P = .002).
“That’s clinically meaningful for me as a provider and a clinician and a researcher when you’re getting the PTSD symptom change differences in parallel with the improvement in functional outcome,” she said. “I see that as the clinically meaningful gauge.”
In terms of safety, 3.9% of the participants in the brexpiprazole/sertraline group and 10.2% of those in the sertraline/placebo group discontinued treatment because of adverse events.
In both the combination and control groups, the only treatment-emergent adverse event with an incidence of more than 10% was nausea (12.2% vs 11.7%, respectively).
At the last visit, the mean change in body weight from baseline was an increase of 1.3 kg for brexpiprazole plus sertraline vs 0 kg for sertraline alone. Rates of fatigue (6.8% vs 4.1%) and somnolence (5.4% vs 2.6%) were also higher with brexpiprazole plus sertraline.
A Trio of Clinical Trials
The findings are part of a larger program reported by the drug makers that includes a flexible-dose brexpiprazole phase 2 trial that met the same CAPS-5 primary endpoint and a second phase 3 trial (072 study) that did not.
“We’ve looked at that data and the sertraline/placebo response was a lot higher, so it was not due to a lack of response with the combination but due to a more robust response with the active control,” Davis said. “But we want to point out for that 072 study, there was still important separation between the combination and sertraline plus placebo on the functional outcome.”
All three trials ran for 12 weeks, so longer-term efficacy and safety data are needed, she said. Other limitations of the published phase 3 study are the patient eligibility criteria, restrictions on concomitant therapy, and lack of non-US sites, which many limit generalizability, the authors noted.
“Specifically, the exclusion of patients with a current major depressive episode is both a strength (to show a specific effect on PTSD) and a limitation (given the high prevalence of comorbid depression in PTSD),” they added.
Kudos, Caveats
Reached for comment, Vincent F. Capaldi, II, MD, ScM, professor and chair, department of psychiatry, Uniformed Services University of the Health Sciences School of Medicine, Bethesda, Maryland, said the exclusion of these patients is a limitation but that the study was well designed and conducted in a large sample across the United States.
“The findings suggest that brexpiprazole plus sertraline is a more effective treatment for PTSD than sertraline alone,” he said. “This finding is significant for our service members, who suffer from PTSD at higher rates than the general population.”
Additionally, the significant improvement in psychosocial functioning at week 12 “is important because PTSD is known to cause significant social and occupational disability, as well as quality-of-life issues,” he said.
Capaldi pointed out, however, that the study was conducted only at US sites and did not specifically target military/veteran persons, which may limit applicability to these unique populations.
“While subgroup analyses were generally consistent with the primary analysis, the study was not powered to detect differences between subgroups,” he added. “These subgroup analyses are quite important when considering military and veteran populations.”
Further research is needed to explore whether certain traumas are more responsive to combination treatment, the efficacy of augmenting existing sertraline therapy, and the specific mechanisms of brexpiprazole driving the improved outcomes, Capaldi said.
This study was funded by Otsuka Pharmaceutical Development & Commercialization, which was involved in the design, conduct, and data analysis. Davis reported receiving advisory board fees from Otsuka and Boehringer Ingelheim; lecture fees from Clinical Care Options; and grants from Alkermes, the Veterans Affairs, Patient-Centered Outcomes Research Institute, Department of Defense, and Social Finance. Several coauthors are employees of Otsuka. Krystal reported serving as a consultant for Otsuka America Pharmaceutical, Aptinyx, Biogen, IDEC, Bionomics, Boehringer Ingelheim International, Clearmind Medicine, Cybin IRL, Enveric Biosciences, Epiodyne, EpiVario, Janssen, Jazz Pharmaceuticals, Perception Neuroscience, Praxis Precision Medicines, Springcare, and Sunovion Pharmaceuticals. Krystal also reported serving as a scientific advisory board member for several companies and holding several patents.
A version of this article appeared on Medscape.com.
Veterans Enroll in VA MDMA and PTSD Phase 2 Trial
The first study funded by the US Department of Veterans Affairs (VA) for psychedelic-assisted therapy since the 1960s is currently enrolling veterans. Researchers are set to evaluate the potential of methylenedioxymethamphetamine (MDMA) for veterans with posttraumatic stress disorder (PTSD) and alcohol use disorder.
The grant—about $1.5 million over 5 years—will fund a randomized, placebo-controlled trial at the Providence VA Medical Center in Rhode Island and the West Haven VA Medical Center in Connecticut by VA researchers affiliated with Brown University and Yale University. Pharmaceutical-grade MDMA will be used, and some participants will be randomly selected to receive an active placebo (lower dose of MDMA). MDMA is a psychedelic compound believed to increase emotional openness, reduce fear, and promote introspection during therapy.
The study is part of the VA’s broader effort to gather definitive scientific evidence on the potential efficacy and safety of psychedelic compounds used in conjunction with psychotherapy to treat PTSD, depression, and related mental health conditions. Veterans service organizations like the American Legion and Disabled American Veterans in addition to mental health clinician groups have also called for expanded research into psychedelic compounds. The National Defense Authorization Act for fiscal year 2024 also authorized the US Department of Defense to perform research on psychedelics within military populations.
In September 2023, VA and other federal clinicians, scientists, and policy makers assessed the state of scientific evidence regarding psychedelic-assisted therapies. The working groups provided advice to VA leadership, including the recommendation for the VA to begin funding its own research into these areas of care.
The guidance was based on previously published studies that have found encouraging results but included few or no veteran participants. For example, a confirmatory phase 3 study by the MAPP2 Study Collaborator Group involved 104 patients, of whom only 16 were veterans.
However, the findings of that study underscored the potential of the treatment: MDMA significantly improved PTSD symptoms and functional impairment, compared with placebo with therapy over 18 weeks. Notably, 45 of 52 (86%) participants treated with MDMA achieved a clinically meaningful benefit, and 37 of 52 (71%) participants no longer met criteria for PTSD by the end of the study. Consistent with an earlier study, no new major safety issues were reported. Common treatment-emergent adverse effects were like those of previous research and consistent with expected effects of MDMA. MDMA did not appear to increase the risk of suicidal ideation, and no suicidal behavior was observed.
The VA researchers has conducted a limited number of small studies on psychedelics in VA facilities using non-VA funding. “VA is on the cutting edge of clinical research for veteran health, including in the investigation of psychedelics for mental health,” said Under Secretary for Health Shereef Elnahal, MD.
The FDA granted breakthrough therapy status for MDMA in the treatment of PTSD and psilocybin for the treatment of depression in 2017 and 2018, respectively, based on promising preliminary research evidence. However, in June 2024 an FDA panel voted against approving a MDMA therapy for PTSD, citing concerns about research practices, a lack of diversity in the trials, and a failure to provide data on adverse effects such as potential for abuse.
In August, the FDA formally rejected the treatment and called for another phase 3 study. “The FDA’s decision is disgraceful,” said Heroic Hearts Project, a veterans organization that had lobbied for FDA approval citing the many veteran suicides in a statement. “This is the epitome of bureaucratic red tape—and the result is people will keep dying.”
Meanwhile, VA Press Secretary Terrence Hayes said in a statement: “VA is committed to high-quality research that safely promotes the health of our nation’s Veterans … VA anticipates that additional insights on the efficacy and safety of these therapies will add to the broader body of knowledge on MDMA-assisted psychotherapy.”
The first study funded by the US Department of Veterans Affairs (VA) for psychedelic-assisted therapy since the 1960s is currently enrolling veterans. Researchers are set to evaluate the potential of methylenedioxymethamphetamine (MDMA) for veterans with posttraumatic stress disorder (PTSD) and alcohol use disorder.
The grant—about $1.5 million over 5 years—will fund a randomized, placebo-controlled trial at the Providence VA Medical Center in Rhode Island and the West Haven VA Medical Center in Connecticut by VA researchers affiliated with Brown University and Yale University. Pharmaceutical-grade MDMA will be used, and some participants will be randomly selected to receive an active placebo (lower dose of MDMA). MDMA is a psychedelic compound believed to increase emotional openness, reduce fear, and promote introspection during therapy.
The study is part of the VA’s broader effort to gather definitive scientific evidence on the potential efficacy and safety of psychedelic compounds used in conjunction with psychotherapy to treat PTSD, depression, and related mental health conditions. Veterans service organizations like the American Legion and Disabled American Veterans in addition to mental health clinician groups have also called for expanded research into psychedelic compounds. The National Defense Authorization Act for fiscal year 2024 also authorized the US Department of Defense to perform research on psychedelics within military populations.
In September 2023, VA and other federal clinicians, scientists, and policy makers assessed the state of scientific evidence regarding psychedelic-assisted therapies. The working groups provided advice to VA leadership, including the recommendation for the VA to begin funding its own research into these areas of care.
The guidance was based on previously published studies that have found encouraging results but included few or no veteran participants. For example, a confirmatory phase 3 study by the MAPP2 Study Collaborator Group involved 104 patients, of whom only 16 were veterans.
However, the findings of that study underscored the potential of the treatment: MDMA significantly improved PTSD symptoms and functional impairment, compared with placebo with therapy over 18 weeks. Notably, 45 of 52 (86%) participants treated with MDMA achieved a clinically meaningful benefit, and 37 of 52 (71%) participants no longer met criteria for PTSD by the end of the study. Consistent with an earlier study, no new major safety issues were reported. Common treatment-emergent adverse effects were like those of previous research and consistent with expected effects of MDMA. MDMA did not appear to increase the risk of suicidal ideation, and no suicidal behavior was observed.
The VA researchers has conducted a limited number of small studies on psychedelics in VA facilities using non-VA funding. “VA is on the cutting edge of clinical research for veteran health, including in the investigation of psychedelics for mental health,” said Under Secretary for Health Shereef Elnahal, MD.
The FDA granted breakthrough therapy status for MDMA in the treatment of PTSD and psilocybin for the treatment of depression in 2017 and 2018, respectively, based on promising preliminary research evidence. However, in June 2024 an FDA panel voted against approving a MDMA therapy for PTSD, citing concerns about research practices, a lack of diversity in the trials, and a failure to provide data on adverse effects such as potential for abuse.
In August, the FDA formally rejected the treatment and called for another phase 3 study. “The FDA’s decision is disgraceful,” said Heroic Hearts Project, a veterans organization that had lobbied for FDA approval citing the many veteran suicides in a statement. “This is the epitome of bureaucratic red tape—and the result is people will keep dying.”
Meanwhile, VA Press Secretary Terrence Hayes said in a statement: “VA is committed to high-quality research that safely promotes the health of our nation’s Veterans … VA anticipates that additional insights on the efficacy and safety of these therapies will add to the broader body of knowledge on MDMA-assisted psychotherapy.”
The first study funded by the US Department of Veterans Affairs (VA) for psychedelic-assisted therapy since the 1960s is currently enrolling veterans. Researchers are set to evaluate the potential of methylenedioxymethamphetamine (MDMA) for veterans with posttraumatic stress disorder (PTSD) and alcohol use disorder.
The grant—about $1.5 million over 5 years—will fund a randomized, placebo-controlled trial at the Providence VA Medical Center in Rhode Island and the West Haven VA Medical Center in Connecticut by VA researchers affiliated with Brown University and Yale University. Pharmaceutical-grade MDMA will be used, and some participants will be randomly selected to receive an active placebo (lower dose of MDMA). MDMA is a psychedelic compound believed to increase emotional openness, reduce fear, and promote introspection during therapy.
The study is part of the VA’s broader effort to gather definitive scientific evidence on the potential efficacy and safety of psychedelic compounds used in conjunction with psychotherapy to treat PTSD, depression, and related mental health conditions. Veterans service organizations like the American Legion and Disabled American Veterans in addition to mental health clinician groups have also called for expanded research into psychedelic compounds. The National Defense Authorization Act for fiscal year 2024 also authorized the US Department of Defense to perform research on psychedelics within military populations.
In September 2023, VA and other federal clinicians, scientists, and policy makers assessed the state of scientific evidence regarding psychedelic-assisted therapies. The working groups provided advice to VA leadership, including the recommendation for the VA to begin funding its own research into these areas of care.
The guidance was based on previously published studies that have found encouraging results but included few or no veteran participants. For example, a confirmatory phase 3 study by the MAPP2 Study Collaborator Group involved 104 patients, of whom only 16 were veterans.
However, the findings of that study underscored the potential of the treatment: MDMA significantly improved PTSD symptoms and functional impairment, compared with placebo with therapy over 18 weeks. Notably, 45 of 52 (86%) participants treated with MDMA achieved a clinically meaningful benefit, and 37 of 52 (71%) participants no longer met criteria for PTSD by the end of the study. Consistent with an earlier study, no new major safety issues were reported. Common treatment-emergent adverse effects were like those of previous research and consistent with expected effects of MDMA. MDMA did not appear to increase the risk of suicidal ideation, and no suicidal behavior was observed.
The VA researchers has conducted a limited number of small studies on psychedelics in VA facilities using non-VA funding. “VA is on the cutting edge of clinical research for veteran health, including in the investigation of psychedelics for mental health,” said Under Secretary for Health Shereef Elnahal, MD.
The FDA granted breakthrough therapy status for MDMA in the treatment of PTSD and psilocybin for the treatment of depression in 2017 and 2018, respectively, based on promising preliminary research evidence. However, in June 2024 an FDA panel voted against approving a MDMA therapy for PTSD, citing concerns about research practices, a lack of diversity in the trials, and a failure to provide data on adverse effects such as potential for abuse.
In August, the FDA formally rejected the treatment and called for another phase 3 study. “The FDA’s decision is disgraceful,” said Heroic Hearts Project, a veterans organization that had lobbied for FDA approval citing the many veteran suicides in a statement. “This is the epitome of bureaucratic red tape—and the result is people will keep dying.”
Meanwhile, VA Press Secretary Terrence Hayes said in a statement: “VA is committed to high-quality research that safely promotes the health of our nation’s Veterans … VA anticipates that additional insights on the efficacy and safety of these therapies will add to the broader body of knowledge on MDMA-assisted psychotherapy.”
Flashbacks triggered by loud noises
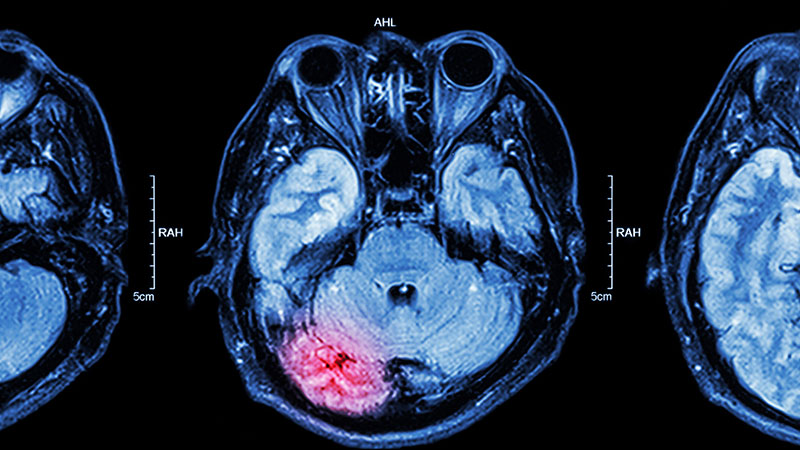
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Posttraumatic stress disorder (PTSD) is the most likely diagnosis given the patient's symptoms — recurrent nightmares, flashbacks, and anxiety triggered by trauma-related noises, all of which are classic indicators of the disorder. His history of witnessing traumatic events at work, including a fatal accident, further reinforces this diagnosis and strongly suggests PTSD as the most fitting explanation. Although the brain scan does not diagnose PTSD directly, it plays an important role in ruling out other potential causes, such as structural brain damage, that could be contributing to his symptoms. Thus, the patient's symptoms are more likely a result of PTSD rather than an underlying organic brain injury.
Although major depressive disorder could explain some of the patient's symptoms, such as impaired daily functioning and withdrawal, the presence of recurrent nightmares, flashbacks, and trauma-specific triggers are more indicative of PTSD.
Generalized anxiety disorder might account for the patient's heightened anxiety, but it typically involves chronic, pervasive worry rather than the trauma-specific symptoms seen here.
Chronic traumatic encephalopathy (CTE) is a possible concern given the patient's occupation and the findings on the CT scan. However, CTE generally presents with cognitive and behavioral changes over time, such as memory loss and aggression, rather than the distinctive trauma-related symptoms characteristic of PTSD.
Individuals with PTSD often display heightened emotional, cognitive, and behavioral responses when exposed to trauma-related cues; these responses include severe anxiety, dissociative episodes, flashbacks, and heightened reactivity. To manage their increased arousal, individuals with PTSD frequently engage in avoidance behaviors, which can result in emotional numbing, diminished interest in daily activities, and, in more severe cases, social withdrawal.
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR), the diagnostic criteria for PTSD in individuals older than 6 years include (A) exposure to actual or threatened death, serious injury, or sexual violence; (B) the presence of one or more intrusion symptoms related to the trauma; (C) persistent avoidance of trauma-related stimuli; (D) negative changes in cognition and mood associated with the trauma; and (E) marked alterations in arousal and reactivity, with at least two specific symptoms.
Trauma-focused psychotherapy is generally recommended as the first-line treatment for most adults with PTSD, with exposure-based therapies often preferred over other therapeutic approaches or pharmacologic treatments, such as selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors. However, in patients with comorbid conditions such as depression or psychosis that hinder their ability to engage in trauma-focused therapy, initial pharmacologic management is recommended until symptoms stabilize, allowing for the later introduction of psychotherapy. Clinical trials and meta-analyses have demonstrated the effectiveness of various trauma-focused therapies, including trauma-focused cognitive-behavioral therapy, prolonged exposure therapy, and eye movement desensitization and reprocessing. Treatment selection should be made collaboratively, considering the patient's presentation and preferences and the therapist's expertise.
For effective management of PTSD, medication regimens should be maintained for at least 6 months to 1 year to prevent relapse or recurrence. Multiple clinical trials have shown that patients who continue SSRIs after acute treatment are less likely to experience a relapse than those who switch to placebo.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
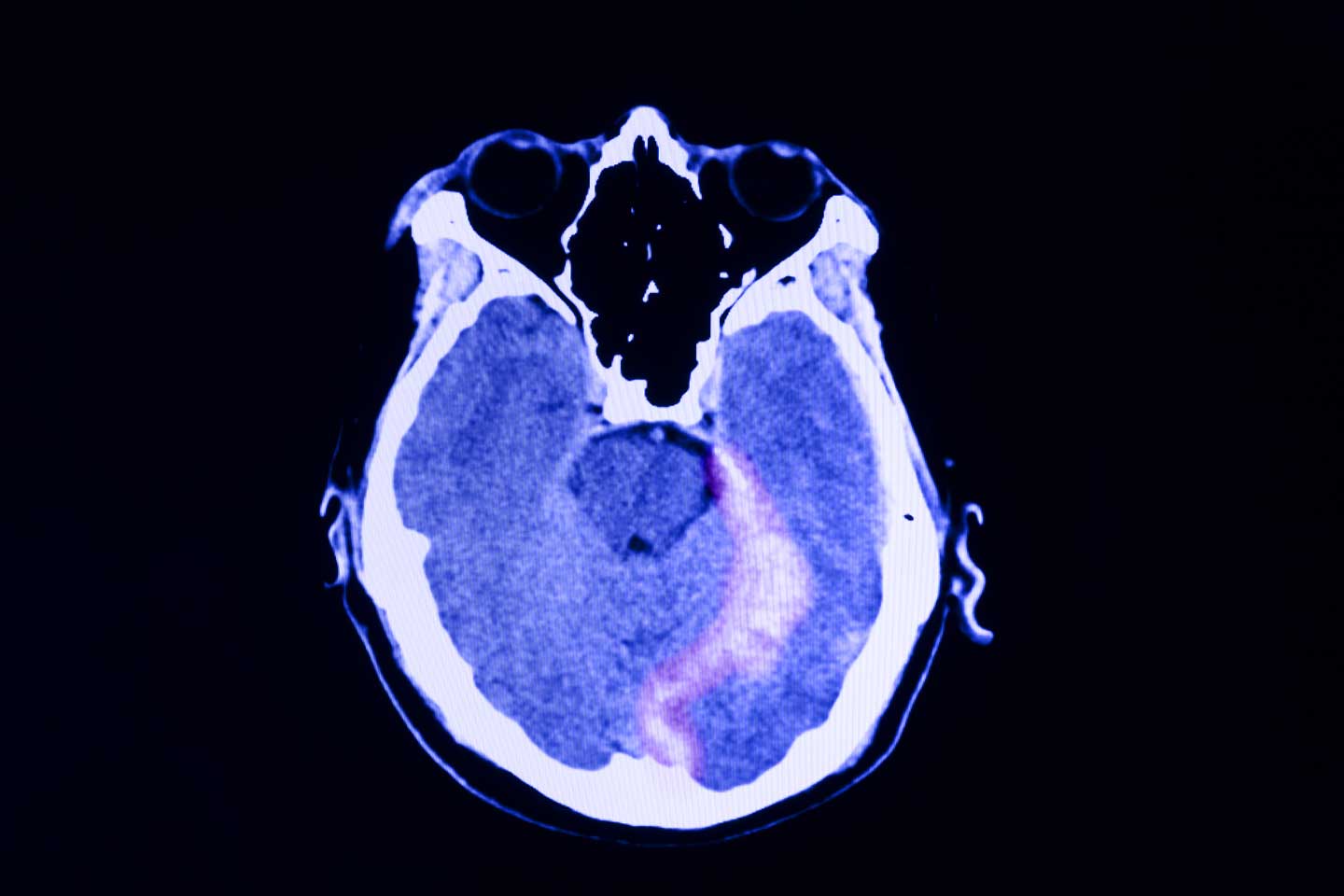
A 48-year-old male construction worker presented with worsening symptoms over the past year, including recurrent nightmares, heightened anxiety, and flashbacks triggered by loud noises such as those heard on job sites. These symptoms have begun to interfere with his daily functioning, particularly affecting his work and family life. The patient has a history of multiple traumatic experiences at work, including witnessing a fatal accident involving a coworker. On neurologic examination, he appeared highly agitated and displayed signs of hypervigilance. A brain CT scan (as shown in the image) was ordered because of the chronic nature of his symptoms and the potential for neurologic causes—such as traumatic brain injury—to contribute to his condition. The scan revealed an abnormality on the left side, prompting further investigation to determine whether the lesion is related to his symptoms or indicative of another underlying condition. Additional tests were ordered to further characterize the lesion: electroencephalography to assess for any associated seizure activity, and blood tests and a lumbar puncture to rule out infection or inflammatory processes. These additional tests came back negative, and the abnormality was later diagnosed as artifact.
PTSD in Children
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
MDMA Is Off the Table, So What’s Next for PTSD?
It has been 24 years since a pharmaceutical was last approved for posttraumatic stress disorder (PTSD). The condition is notoriously difficult to treat, with up to 40% patients finding no relief from symptoms through psychotherapy or current medications.
Many clinicians, advocates, and patients had pinned their hopes on the psychedelic drug midomafetamine with assisted therapy (MDMA-AT). However, in August, the US Food and Drug Administration (FDA) rejected it. At this point, it’s unclear when the therapy will be available, if ever.
“Not getting the FDA approval of any drug at this point is a setback for the field,” Lori Davis, MD, a senior research psychiatrist at the Birmingham Veterans Affairs (VA) Health Care System in Birmingham, Alabama, told Medscape Medical News.
Having an FDA-approved product would have helped increase public awareness of PTSD and driven interest in developing new therapies, said Davis, who is also adjunct professor of psychiatry at the Heersink School of Medicine, University of Alabama at Birmingham.
A Treatable Condition
So with MDMA-AT off the table, where does the field go next?
A public meeting in September hosted by the Reagan-Udall Foundation for the FDA in sought to answer that question. Agency officials joined representatives from the Department of Defense (DoD) and VA, patients, advocates, and industry representatives to discuss the current treatment landscape and what can be done to accelerate development of PTSD treatment.
Despite the common belief that PTSD is intractable, it “is a treatable condition,” Paula P. Schnurr, PhD, executive director of the VA National Center for PTSD, said at the meeting.
“There are effective treatments that work well for a lot of people, although not everyone has a satisfactory response,” she added.
The most effective psychotherapies are “trauma-focused,” and include cognitive processing therapy, eye movement desensitization and reprocessing, and prolonged exposure, according to the VA National Center for PTSD.
Three drugs have been approved by the FDA for PTSD: Venlafaxine (Effexor) in 1993, sertraline (Zoloft) in 1999, and paroxetine (Paxil) in 2000.
However, as the September meeting demonstrated, more therapies are needed.
“It’s clear to FDA and the federal government at large that there is an unmet need for safe and effective therapies to treat PTSD,” Bernard Fischer, MD, deputy director of the Division of Psychiatry in the Office of New Drugs at FDA’s Center for Drug Evaluation and Research, said at the meeting.
There is no shortage of research, Fischer added. Nearly 500 trials focused on PTSD are listed on clinicaltrials.gov are recruiting participants now or plan to soon.
Unsurprisingly, one of the primary drivers of PTSD therapeutics research is the VA. About 14% of the 5.7 million veterans who received care through the VA in 2023 had a diagnosis of PTSD.
“The US military is currently losing thousands of service members each year to PTSD- related disability discharges,” US Army Maj. Aaron Wolfgang, MD, a psychiatrist at the Walter Reed National Military Medical Center, said at the meeting. Only about 12%-20% of patients achieve remission with conventional therapies, added Wolfgang, who also is an assistant professor at the Uniformed Services University.
“For these reasons, establishing better treatments for PTSD is not only a matter of humanitarianism but also a pressing matter of national security,” he said.
The VA has committed at least $230 million to more than 140 active research projects in PTSD, Miriam J. Smyth, PhD, acting director of the clinical science, research and development service at the VA, said at the Reagan-Udall meeting.
One of the VA projects is the PTSD psychopharmacology initiative, which began in 2017 and now has 14 active clinical trials, said Smyth, who is also acting director for brain behavior and mental health at the VA. The first study should be finished by 2025.
The Million Veteran Program, with more than 1 million enrollees, has led to the discovery of genes related to re-experiencing traumatic memories and has confirmed that both PTSD and traumatic brain injury are risk factors for dementia, Smyth said.
The DoD has created a novel platform that establishes a common infrastructure for testing multiple drugs, called M-PACT. The platform allows sharing of placebo data across treatment arms. Drugs cycle off the platform if evidence indicates probability of success or failure.
Four trials are actively recruiting veterans and current service members. One is looking at vilazodone, approved in 2011 for major depressive disorder. It is being compared with placebo and fluoxetine in a trial that is currently recruiting.
Another trial will study daridorexant (sold as Quviviq), an orexin receptor antagonist, against placebo. The FDA approved daridorexant in 2022 as an insomnia treatment. A core issue in PTSD is sleep disruption, noted Davis.
New Therapies on the Way
Separately, Davis and colleagues are also studying methylphenidate, the stimulant used for attention-deficit/hyperactivity disorder. It may help with neurocognitive complaints and reduce PTSD symptoms, said Davis.
Because it is generic, few pharmaceutical manufacturers are likely to test it for PTSD, she said. But eventually, their work may lead a company to test newer stimulants for PTSD, she said.
Another potential therapeutic, BNC210, received Fast Track designation for PTSD from the FDA in 2019. Bionomics Limited in Australia will soon launch phase 3 trials of the investigational oral drug, which is a negative allosteric modulator of the alpha-7 nicotinic acetylcholine receptor. In late July, the company announced “ favorable feedback” from the agency on its phase 2 study, which led to the decision to move forward with larger trials.
Researchers at Brigham and Women’s Hospital have just reported that they may have found a target within the brain that will allow for transcranial magnetic stimulation (TMS) to ameliorate PTSD symptoms. They published results of a mapping effort in Nature Neuroscience and reported on one patient who had improved symptoms after receiving TMS for severe PTSD.
But perhaps one of the most promising treatments is a combination of sertraline and the new psychiatric medication brexpiprazole.
Brexpiprazole was developed by Otsuka Pharmaceutical and approved in the United States in 2015 as an adjunctive therapy to antidepressants for major depressive disorder and as a treatment for schizophrenia. In 2023, the FDA approved it for Alzheimer’s-related agitation. However, according to Otsuka, its mechanism of action is unknown.
Its efficacy may be mediated through a combination of partial agonist activity at serotonin 5-HT1A and dopamine D2 receptors, antagonist activity at serotonin 5-HT2A receptors, as well as antagonism of alpha-1B/2C receptors, said the company.
“It is the combination, rather than either alone, that’s going to have that broad synergistic pharmacology that is obviously potent for ameliorating the symptoms of PTSD,” said Davis, who has received consulting fees from Otsuka. “That’s an exciting development.”
Otsuka and partner Lundbeck Pharmaceuticals reported results in May from the companies’ phase 2 and 3 randomized clinical trials. The therapy achieved a statistically significant reduction (P <.05) in PTSD symptoms compared with sertraline plus placebo. This was without any supplemental psychotherapy.
The FDA accepted the companies’ new drug application in June and is expected to make a decision on approval in February 2025.
The Potential of Psychedelics
Though Lykos Therapeutics may have to go back to the drawing board on its MDMA-AT, psychedelics still have potential as PTSD therapies, Smyth said, who added that the VA is continuing to encourage study of MDMA and other psychedelic agents.
The VA issued a call for proposals for research on psychedelics in January, focused on MDMA or psilocybin in combination with psychotherapy. The administration received the first wave of applications early in the summer.
Scientific peer review panels made up of research experts from within and outside the VA have reviewed the applications and funding announcements are expected this fall, Smyth said.
Wolfgang, the Army psychiatrist, said, “Under the psychedelic treatment research clinical trial award, we welcome investigators to apply to what we anticipate will usher in a new era of innovation and hope for service members and their families who need it the most.”
Psychedelic studies are also proceeding without VA funding, as they have for years, when most of the trials were backed by universities or foundations or other private money. Johns Hopkins University is recruiting for a study in which patients would receive psilocybin along with trauma-focused psychotherapy, as is Ohio State University.
London-based Compass Pathways said in May that it successfully completed a phase 2 trial of Comp360, its synthetic psilocybin, in PTSD. The company has started a phase 3 study in treatment-resistant depression but has not given any further updates on PTSD.
Davis said that she believes that the FDA’s rejection of Lykos won’t lead to a shutdown of exploration of psychedelics.
“I think it informs these designs going forward, but it doesn’t eliminate that whole field of research,” she said.
Davis reported receiving consulting fees from Boehringer Ingelheim and Otsuka and research funding from Alkermes, the Patient-Centered Outcomes Research Institute, and the VA. Schnurr, Fischer, Smyth, and Wolfgang reported no relevant disclosures.
A version of this article appeared on Medscape.com.
It has been 24 years since a pharmaceutical was last approved for posttraumatic stress disorder (PTSD). The condition is notoriously difficult to treat, with up to 40% patients finding no relief from symptoms through psychotherapy or current medications.
Many clinicians, advocates, and patients had pinned their hopes on the psychedelic drug midomafetamine with assisted therapy (MDMA-AT). However, in August, the US Food and Drug Administration (FDA) rejected it. At this point, it’s unclear when the therapy will be available, if ever.
“Not getting the FDA approval of any drug at this point is a setback for the field,” Lori Davis, MD, a senior research psychiatrist at the Birmingham Veterans Affairs (VA) Health Care System in Birmingham, Alabama, told Medscape Medical News.
Having an FDA-approved product would have helped increase public awareness of PTSD and driven interest in developing new therapies, said Davis, who is also adjunct professor of psychiatry at the Heersink School of Medicine, University of Alabama at Birmingham.
A Treatable Condition
So with MDMA-AT off the table, where does the field go next?
A public meeting in September hosted by the Reagan-Udall Foundation for the FDA in sought to answer that question. Agency officials joined representatives from the Department of Defense (DoD) and VA, patients, advocates, and industry representatives to discuss the current treatment landscape and what can be done to accelerate development of PTSD treatment.
Despite the common belief that PTSD is intractable, it “is a treatable condition,” Paula P. Schnurr, PhD, executive director of the VA National Center for PTSD, said at the meeting.
“There are effective treatments that work well for a lot of people, although not everyone has a satisfactory response,” she added.
The most effective psychotherapies are “trauma-focused,” and include cognitive processing therapy, eye movement desensitization and reprocessing, and prolonged exposure, according to the VA National Center for PTSD.
Three drugs have been approved by the FDA for PTSD: Venlafaxine (Effexor) in 1993, sertraline (Zoloft) in 1999, and paroxetine (Paxil) in 2000.
However, as the September meeting demonstrated, more therapies are needed.
“It’s clear to FDA and the federal government at large that there is an unmet need for safe and effective therapies to treat PTSD,” Bernard Fischer, MD, deputy director of the Division of Psychiatry in the Office of New Drugs at FDA’s Center for Drug Evaluation and Research, said at the meeting.
There is no shortage of research, Fischer added. Nearly 500 trials focused on PTSD are listed on clinicaltrials.gov are recruiting participants now or plan to soon.
Unsurprisingly, one of the primary drivers of PTSD therapeutics research is the VA. About 14% of the 5.7 million veterans who received care through the VA in 2023 had a diagnosis of PTSD.
“The US military is currently losing thousands of service members each year to PTSD- related disability discharges,” US Army Maj. Aaron Wolfgang, MD, a psychiatrist at the Walter Reed National Military Medical Center, said at the meeting. Only about 12%-20% of patients achieve remission with conventional therapies, added Wolfgang, who also is an assistant professor at the Uniformed Services University.
“For these reasons, establishing better treatments for PTSD is not only a matter of humanitarianism but also a pressing matter of national security,” he said.
The VA has committed at least $230 million to more than 140 active research projects in PTSD, Miriam J. Smyth, PhD, acting director of the clinical science, research and development service at the VA, said at the Reagan-Udall meeting.
One of the VA projects is the PTSD psychopharmacology initiative, which began in 2017 and now has 14 active clinical trials, said Smyth, who is also acting director for brain behavior and mental health at the VA. The first study should be finished by 2025.
The Million Veteran Program, with more than 1 million enrollees, has led to the discovery of genes related to re-experiencing traumatic memories and has confirmed that both PTSD and traumatic brain injury are risk factors for dementia, Smyth said.
The DoD has created a novel platform that establishes a common infrastructure for testing multiple drugs, called M-PACT. The platform allows sharing of placebo data across treatment arms. Drugs cycle off the platform if evidence indicates probability of success or failure.
Four trials are actively recruiting veterans and current service members. One is looking at vilazodone, approved in 2011 for major depressive disorder. It is being compared with placebo and fluoxetine in a trial that is currently recruiting.
Another trial will study daridorexant (sold as Quviviq), an orexin receptor antagonist, against placebo. The FDA approved daridorexant in 2022 as an insomnia treatment. A core issue in PTSD is sleep disruption, noted Davis.
New Therapies on the Way
Separately, Davis and colleagues are also studying methylphenidate, the stimulant used for attention-deficit/hyperactivity disorder. It may help with neurocognitive complaints and reduce PTSD symptoms, said Davis.
Because it is generic, few pharmaceutical manufacturers are likely to test it for PTSD, she said. But eventually, their work may lead a company to test newer stimulants for PTSD, she said.
Another potential therapeutic, BNC210, received Fast Track designation for PTSD from the FDA in 2019. Bionomics Limited in Australia will soon launch phase 3 trials of the investigational oral drug, which is a negative allosteric modulator of the alpha-7 nicotinic acetylcholine receptor. In late July, the company announced “ favorable feedback” from the agency on its phase 2 study, which led to the decision to move forward with larger trials.
Researchers at Brigham and Women’s Hospital have just reported that they may have found a target within the brain that will allow for transcranial magnetic stimulation (TMS) to ameliorate PTSD symptoms. They published results of a mapping effort in Nature Neuroscience and reported on one patient who had improved symptoms after receiving TMS for severe PTSD.
But perhaps one of the most promising treatments is a combination of sertraline and the new psychiatric medication brexpiprazole.
Brexpiprazole was developed by Otsuka Pharmaceutical and approved in the United States in 2015 as an adjunctive therapy to antidepressants for major depressive disorder and as a treatment for schizophrenia. In 2023, the FDA approved it for Alzheimer’s-related agitation. However, according to Otsuka, its mechanism of action is unknown.
Its efficacy may be mediated through a combination of partial agonist activity at serotonin 5-HT1A and dopamine D2 receptors, antagonist activity at serotonin 5-HT2A receptors, as well as antagonism of alpha-1B/2C receptors, said the company.
“It is the combination, rather than either alone, that’s going to have that broad synergistic pharmacology that is obviously potent for ameliorating the symptoms of PTSD,” said Davis, who has received consulting fees from Otsuka. “That’s an exciting development.”
Otsuka and partner Lundbeck Pharmaceuticals reported results in May from the companies’ phase 2 and 3 randomized clinical trials. The therapy achieved a statistically significant reduction (P <.05) in PTSD symptoms compared with sertraline plus placebo. This was without any supplemental psychotherapy.
The FDA accepted the companies’ new drug application in June and is expected to make a decision on approval in February 2025.
The Potential of Psychedelics
Though Lykos Therapeutics may have to go back to the drawing board on its MDMA-AT, psychedelics still have potential as PTSD therapies, Smyth said, who added that the VA is continuing to encourage study of MDMA and other psychedelic agents.
The VA issued a call for proposals for research on psychedelics in January, focused on MDMA or psilocybin in combination with psychotherapy. The administration received the first wave of applications early in the summer.
Scientific peer review panels made up of research experts from within and outside the VA have reviewed the applications and funding announcements are expected this fall, Smyth said.
Wolfgang, the Army psychiatrist, said, “Under the psychedelic treatment research clinical trial award, we welcome investigators to apply to what we anticipate will usher in a new era of innovation and hope for service members and their families who need it the most.”
Psychedelic studies are also proceeding without VA funding, as they have for years, when most of the trials were backed by universities or foundations or other private money. Johns Hopkins University is recruiting for a study in which patients would receive psilocybin along with trauma-focused psychotherapy, as is Ohio State University.
London-based Compass Pathways said in May that it successfully completed a phase 2 trial of Comp360, its synthetic psilocybin, in PTSD. The company has started a phase 3 study in treatment-resistant depression but has not given any further updates on PTSD.
Davis said that she believes that the FDA’s rejection of Lykos won’t lead to a shutdown of exploration of psychedelics.
“I think it informs these designs going forward, but it doesn’t eliminate that whole field of research,” she said.
Davis reported receiving consulting fees from Boehringer Ingelheim and Otsuka and research funding from Alkermes, the Patient-Centered Outcomes Research Institute, and the VA. Schnurr, Fischer, Smyth, and Wolfgang reported no relevant disclosures.
A version of this article appeared on Medscape.com.
It has been 24 years since a pharmaceutical was last approved for posttraumatic stress disorder (PTSD). The condition is notoriously difficult to treat, with up to 40% patients finding no relief from symptoms through psychotherapy or current medications.
Many clinicians, advocates, and patients had pinned their hopes on the psychedelic drug midomafetamine with assisted therapy (MDMA-AT). However, in August, the US Food and Drug Administration (FDA) rejected it. At this point, it’s unclear when the therapy will be available, if ever.
“Not getting the FDA approval of any drug at this point is a setback for the field,” Lori Davis, MD, a senior research psychiatrist at the Birmingham Veterans Affairs (VA) Health Care System in Birmingham, Alabama, told Medscape Medical News.
Having an FDA-approved product would have helped increase public awareness of PTSD and driven interest in developing new therapies, said Davis, who is also adjunct professor of psychiatry at the Heersink School of Medicine, University of Alabama at Birmingham.
A Treatable Condition
So with MDMA-AT off the table, where does the field go next?
A public meeting in September hosted by the Reagan-Udall Foundation for the FDA in sought to answer that question. Agency officials joined representatives from the Department of Defense (DoD) and VA, patients, advocates, and industry representatives to discuss the current treatment landscape and what can be done to accelerate development of PTSD treatment.
Despite the common belief that PTSD is intractable, it “is a treatable condition,” Paula P. Schnurr, PhD, executive director of the VA National Center for PTSD, said at the meeting.
“There are effective treatments that work well for a lot of people, although not everyone has a satisfactory response,” she added.
The most effective psychotherapies are “trauma-focused,” and include cognitive processing therapy, eye movement desensitization and reprocessing, and prolonged exposure, according to the VA National Center for PTSD.
Three drugs have been approved by the FDA for PTSD: Venlafaxine (Effexor) in 1993, sertraline (Zoloft) in 1999, and paroxetine (Paxil) in 2000.
However, as the September meeting demonstrated, more therapies are needed.
“It’s clear to FDA and the federal government at large that there is an unmet need for safe and effective therapies to treat PTSD,” Bernard Fischer, MD, deputy director of the Division of Psychiatry in the Office of New Drugs at FDA’s Center for Drug Evaluation and Research, said at the meeting.
There is no shortage of research, Fischer added. Nearly 500 trials focused on PTSD are listed on clinicaltrials.gov are recruiting participants now or plan to soon.
Unsurprisingly, one of the primary drivers of PTSD therapeutics research is the VA. About 14% of the 5.7 million veterans who received care through the VA in 2023 had a diagnosis of PTSD.
“The US military is currently losing thousands of service members each year to PTSD- related disability discharges,” US Army Maj. Aaron Wolfgang, MD, a psychiatrist at the Walter Reed National Military Medical Center, said at the meeting. Only about 12%-20% of patients achieve remission with conventional therapies, added Wolfgang, who also is an assistant professor at the Uniformed Services University.
“For these reasons, establishing better treatments for PTSD is not only a matter of humanitarianism but also a pressing matter of national security,” he said.
The VA has committed at least $230 million to more than 140 active research projects in PTSD, Miriam J. Smyth, PhD, acting director of the clinical science, research and development service at the VA, said at the Reagan-Udall meeting.
One of the VA projects is the PTSD psychopharmacology initiative, which began in 2017 and now has 14 active clinical trials, said Smyth, who is also acting director for brain behavior and mental health at the VA. The first study should be finished by 2025.
The Million Veteran Program, with more than 1 million enrollees, has led to the discovery of genes related to re-experiencing traumatic memories and has confirmed that both PTSD and traumatic brain injury are risk factors for dementia, Smyth said.
The DoD has created a novel platform that establishes a common infrastructure for testing multiple drugs, called M-PACT. The platform allows sharing of placebo data across treatment arms. Drugs cycle off the platform if evidence indicates probability of success or failure.
Four trials are actively recruiting veterans and current service members. One is looking at vilazodone, approved in 2011 for major depressive disorder. It is being compared with placebo and fluoxetine in a trial that is currently recruiting.
Another trial will study daridorexant (sold as Quviviq), an orexin receptor antagonist, against placebo. The FDA approved daridorexant in 2022 as an insomnia treatment. A core issue in PTSD is sleep disruption, noted Davis.
New Therapies on the Way
Separately, Davis and colleagues are also studying methylphenidate, the stimulant used for attention-deficit/hyperactivity disorder. It may help with neurocognitive complaints and reduce PTSD symptoms, said Davis.
Because it is generic, few pharmaceutical manufacturers are likely to test it for PTSD, she said. But eventually, their work may lead a company to test newer stimulants for PTSD, she said.
Another potential therapeutic, BNC210, received Fast Track designation for PTSD from the FDA in 2019. Bionomics Limited in Australia will soon launch phase 3 trials of the investigational oral drug, which is a negative allosteric modulator of the alpha-7 nicotinic acetylcholine receptor. In late July, the company announced “ favorable feedback” from the agency on its phase 2 study, which led to the decision to move forward with larger trials.
Researchers at Brigham and Women’s Hospital have just reported that they may have found a target within the brain that will allow for transcranial magnetic stimulation (TMS) to ameliorate PTSD symptoms. They published results of a mapping effort in Nature Neuroscience and reported on one patient who had improved symptoms after receiving TMS for severe PTSD.
But perhaps one of the most promising treatments is a combination of sertraline and the new psychiatric medication brexpiprazole.
Brexpiprazole was developed by Otsuka Pharmaceutical and approved in the United States in 2015 as an adjunctive therapy to antidepressants for major depressive disorder and as a treatment for schizophrenia. In 2023, the FDA approved it for Alzheimer’s-related agitation. However, according to Otsuka, its mechanism of action is unknown.
Its efficacy may be mediated through a combination of partial agonist activity at serotonin 5-HT1A and dopamine D2 receptors, antagonist activity at serotonin 5-HT2A receptors, as well as antagonism of alpha-1B/2C receptors, said the company.
“It is the combination, rather than either alone, that’s going to have that broad synergistic pharmacology that is obviously potent for ameliorating the symptoms of PTSD,” said Davis, who has received consulting fees from Otsuka. “That’s an exciting development.”
Otsuka and partner Lundbeck Pharmaceuticals reported results in May from the companies’ phase 2 and 3 randomized clinical trials. The therapy achieved a statistically significant reduction (P <.05) in PTSD symptoms compared with sertraline plus placebo. This was without any supplemental psychotherapy.
The FDA accepted the companies’ new drug application in June and is expected to make a decision on approval in February 2025.
The Potential of Psychedelics
Though Lykos Therapeutics may have to go back to the drawing board on its MDMA-AT, psychedelics still have potential as PTSD therapies, Smyth said, who added that the VA is continuing to encourage study of MDMA and other psychedelic agents.
The VA issued a call for proposals for research on psychedelics in January, focused on MDMA or psilocybin in combination with psychotherapy. The administration received the first wave of applications early in the summer.
Scientific peer review panels made up of research experts from within and outside the VA have reviewed the applications and funding announcements are expected this fall, Smyth said.
Wolfgang, the Army psychiatrist, said, “Under the psychedelic treatment research clinical trial award, we welcome investigators to apply to what we anticipate will usher in a new era of innovation and hope for service members and their families who need it the most.”
Psychedelic studies are also proceeding without VA funding, as they have for years, when most of the trials were backed by universities or foundations or other private money. Johns Hopkins University is recruiting for a study in which patients would receive psilocybin along with trauma-focused psychotherapy, as is Ohio State University.
London-based Compass Pathways said in May that it successfully completed a phase 2 trial of Comp360, its synthetic psilocybin, in PTSD. The company has started a phase 3 study in treatment-resistant depression but has not given any further updates on PTSD.
Davis said that she believes that the FDA’s rejection of Lykos won’t lead to a shutdown of exploration of psychedelics.
“I think it informs these designs going forward, but it doesn’t eliminate that whole field of research,” she said.
Davis reported receiving consulting fees from Boehringer Ingelheim and Otsuka and research funding from Alkermes, the Patient-Centered Outcomes Research Institute, and the VA. Schnurr, Fischer, Smyth, and Wolfgang reported no relevant disclosures.
A version of this article appeared on Medscape.com.
PTSD Comorbidities
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Editor's Note: This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
Persistent headaches and nightmares
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
The correct diagnosis is adolescent posttraumatic stress disorder (PTSD), as the patient's symptoms — recurrent nightmares, flashbacks, hypervigilance, and avoidance behaviors — are closely linked to her recent traumatic experience, fitting the clinical profile of PTSD. The MRI finding, although abnormal, does not correlate with a neurologic cause for her symptoms and may be incidental.
Temporal lobe epilepsy can cause behavioral changes but does not explain the specific PTSD symptoms like flashbacks and nightmares.
Chronic migraine could explain the headaches but not the full spectrum of PTSD symptoms.
Major depressive disorder could account for some of the emotional and social symptoms but lacks the characteristic re-experiencing and avoidance behaviors typical of PTSD.
Adolescent PTSD is a significant public health concern, causing significant distress to a small portion of the youth population. By late adolescence, approximately two thirds of youths have been exposed to trauma, and 8% of these individuals meet the criteria for PTSD by age 18. The incidence is exceptionally high in cases of sexual abuse and assault, with rates reaching up to 40%. PTSD in adolescents is associated with severe psychological distress, reduced academic performance, and a high rate of comorbidities, including anxiety and depression. There are specific populations (including children who are evacuated from home, asylum seekers, etc.) that show higher rates of PTSD.
PTSD can lead to chronic impairments, comorbid psychiatric disorders, and an increased risk for suicide, with cases documented in toddlers as young as 1 year old. Thus, it is important to consider the individual's background and social history, as older children with PTSD may present with symptoms from early childhood trauma, often distant from the time of clinical evaluation.
Intrusion symptoms are a hallmark of PTSD, characterized by persistent and uncontrollable thoughts, dreams, and emotional reactions related to the traumatic event. These symptoms distinguish PTSD from other anxiety and mood disorders. Children with PTSD often experience involuntary, distressing thoughts and memories triggered by trauma cues, such as sights, sounds, or smells associated with the traumatic event. In younger children, these intrusive thoughts may manifest through repetitive play that re-enacts aspects of the trauma.
Nightmares are also common, although in children the content may not always directly relate to the traumatic event. Chronic nightmares contribute to sleep disturbances, exacerbating PTSD symptoms. Trauma reminders, which can be both internal (thoughts, memories) and external (places, sensory experiences), can provoke severe distress and physiologic reactions.
Avoidance symptoms often develop as a coping mechanism in response to distressing re-experiencing symptoms. Children may avoid thoughts, feelings, and memories of the traumatic event or people, places, and activities associated with the trauma. In young children, avoidance may manifest as restricted play or reduced exploration of their environment.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR) outlines specific criteria for diagnosing PTSD in individuals over 6 years old, which includes exposure to actual or threatened death, serious injury, or sexual violence, and the presence of symptoms such as intrusion, avoidance, negative mood alterations, and heightened arousal. The DSM-5-TR provides tailored diagnostic criteria for developmental differences in symptom expression for children under 6.
Managing PTSD in children requires a patient-specific approach, with an emphasis on obtaining consent from both the patient and guardian. The American Academy of Child and Adolescent Psychiatry (AACAP) recommends psychotherapy as the first-line treatment for pediatric PTSD. However, patients with severe symptoms or comorbidities may initially be unable to engage in meaningful therapy and may require medication to stabilize symptoms before starting psychotherapy.
Trauma-focused psychotherapy, including cognitive-behavioral therapy (CBT), exposure-based therapy, and eye movement desensitization and reprocessing (EMDR) therapy, is the preferred treatment for PTSD. Clinical studies have shown that patients receiving trauma-focused psychotherapy experience more remarkable symptom improvement than those who do not receive treatment and, in children, psychotherapy generally yields better outcomes than pharmacotherapy.
While selective serotonin reuptake inhibitors like sertraline and paroxetine are FDA-approved for PTSD treatment in adults, their efficacy in children often produces outcomes similar to those of placebo. Medications are typically reserved for severe symptoms and are used as an off-label treatment in pediatric cases. Pharmacologic management may be necessary when the severity of symptoms prevents the use of trauma-focused psychotherapy or requires immediate stabilization.
Heidi Moawad, MD, Clinical Assistant Professor, Department of Medical Education, Case Western Reserve University School of Medicine, Cleveland, Ohio.
Heidi Moawad, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
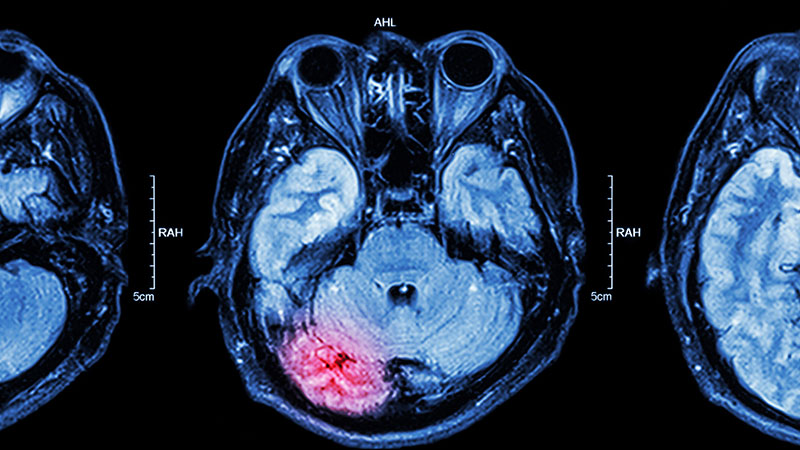
A 15-year-old girl presented to the emergency department with complaints of persistent headaches, nightmares, and difficulty concentrating in school over the past 3 months. The patient had recently experienced a traumatic event, a severe car accident in which a close friend was critically injured. Since the incident, the patient has been exhibiting increased irritability, avoidance of activities that she previously enjoyed, and a noticeable withdrawal from social interactions. Additionally, she reported recurrent flashbacks to the accident, often triggered by sounds resembling car engines. On physical examination, the patient appeared anxious and exhibited hypervigilance. An MRI of the brain was performed to rule out any organic causes of her symptoms, revealing an area of increased signal intensity in the left cerebellar hemisphere (as highlighted in the image).