User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Black Children With Vitiligo at Increased Risk for Psychiatric Disorders: Study
TOPLINE:
Black children with vitiligo are significantly more likely to be diagnosed with psychiatric disorders, including depression, suicidal ideation, and disruptive behavior disorders, than matched controls who did not have vitiligo, according to a case-control study.
METHODOLOGY:
- Researchers conducted a retrospective, single-center, case-control study at Texas Children’s Hospital in Houston on 327 Black children with vitiligo and 981 matched controls without vitiligo.
- The average age of participants was 11.7 years, and 62% were girls.
- The study outcome was the prevalence of psychiatric conditions and rates of treatment (pharmacotherapy and/or psychotherapy) initiation for those conditions.
TAKEAWAY:
- Black children with vitiligo were more likely to be diagnosed with depression (odds ratio [OR], 3.63; P < .001), suicidal ideation (OR, 2.88; P = .005), disruptive behavior disorders (OR, 7.68; P < .001), eating disorders (OR, 15.22; P = .013), generalized anxiety disorder (OR, 2.61; P < .001), and substance abuse (OR, 2.67; P = .011).
- The likelihood of having a psychiatric comorbidity was not significantly different between children with segmental vitiligo and those with generalized vitiligo or between girls and boys.
- Among the patients with vitiligo and psychiatric comorbidities, treatment initiation rates were higher for depression (76.5%), disruptive behavior disorders (82.1%), and eating disorders (100%).
- Treatment initiation rates were lower in patients with vitiligo diagnosed with generalized anxiety disorder (55.3%) and substance abuse (61.5%). Treatment was not initiated in 14% patients with suicidal ideation.
IN PRACTICE:
“Pediatric dermatologists have an important role in screening for psychiatric comorbidities, and implementation of appropriate screening tools while treating vitiligo is likely to have a bidirectional positive impact,” the authors wrote, adding: “By better understanding psychiatric comorbidities of African American children with vitiligo, dermatologists can be more aware of pediatric mental health needs and provide appropriate referrals.”
SOURCE:
This study was led by Emily Strouphauer, BSA, Baylor College of Medicine, Houston, and was published online in JAAD International.
LIMITATIONS:
The study limitations were the retrospective design, small sample size, and heterogeneity in the control group.
DISCLOSURES:
The study did not receive any funding. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Black children with vitiligo are significantly more likely to be diagnosed with psychiatric disorders, including depression, suicidal ideation, and disruptive behavior disorders, than matched controls who did not have vitiligo, according to a case-control study.
METHODOLOGY:
- Researchers conducted a retrospective, single-center, case-control study at Texas Children’s Hospital in Houston on 327 Black children with vitiligo and 981 matched controls without vitiligo.
- The average age of participants was 11.7 years, and 62% were girls.
- The study outcome was the prevalence of psychiatric conditions and rates of treatment (pharmacotherapy and/or psychotherapy) initiation for those conditions.
TAKEAWAY:
- Black children with vitiligo were more likely to be diagnosed with depression (odds ratio [OR], 3.63; P < .001), suicidal ideation (OR, 2.88; P = .005), disruptive behavior disorders (OR, 7.68; P < .001), eating disorders (OR, 15.22; P = .013), generalized anxiety disorder (OR, 2.61; P < .001), and substance abuse (OR, 2.67; P = .011).
- The likelihood of having a psychiatric comorbidity was not significantly different between children with segmental vitiligo and those with generalized vitiligo or between girls and boys.
- Among the patients with vitiligo and psychiatric comorbidities, treatment initiation rates were higher for depression (76.5%), disruptive behavior disorders (82.1%), and eating disorders (100%).
- Treatment initiation rates were lower in patients with vitiligo diagnosed with generalized anxiety disorder (55.3%) and substance abuse (61.5%). Treatment was not initiated in 14% patients with suicidal ideation.
IN PRACTICE:
“Pediatric dermatologists have an important role in screening for psychiatric comorbidities, and implementation of appropriate screening tools while treating vitiligo is likely to have a bidirectional positive impact,” the authors wrote, adding: “By better understanding psychiatric comorbidities of African American children with vitiligo, dermatologists can be more aware of pediatric mental health needs and provide appropriate referrals.”
SOURCE:
This study was led by Emily Strouphauer, BSA, Baylor College of Medicine, Houston, and was published online in JAAD International.
LIMITATIONS:
The study limitations were the retrospective design, small sample size, and heterogeneity in the control group.
DISCLOSURES:
The study did not receive any funding. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Black children with vitiligo are significantly more likely to be diagnosed with psychiatric disorders, including depression, suicidal ideation, and disruptive behavior disorders, than matched controls who did not have vitiligo, according to a case-control study.
METHODOLOGY:
- Researchers conducted a retrospective, single-center, case-control study at Texas Children’s Hospital in Houston on 327 Black children with vitiligo and 981 matched controls without vitiligo.
- The average age of participants was 11.7 years, and 62% were girls.
- The study outcome was the prevalence of psychiatric conditions and rates of treatment (pharmacotherapy and/or psychotherapy) initiation for those conditions.
TAKEAWAY:
- Black children with vitiligo were more likely to be diagnosed with depression (odds ratio [OR], 3.63; P < .001), suicidal ideation (OR, 2.88; P = .005), disruptive behavior disorders (OR, 7.68; P < .001), eating disorders (OR, 15.22; P = .013), generalized anxiety disorder (OR, 2.61; P < .001), and substance abuse (OR, 2.67; P = .011).
- The likelihood of having a psychiatric comorbidity was not significantly different between children with segmental vitiligo and those with generalized vitiligo or between girls and boys.
- Among the patients with vitiligo and psychiatric comorbidities, treatment initiation rates were higher for depression (76.5%), disruptive behavior disorders (82.1%), and eating disorders (100%).
- Treatment initiation rates were lower in patients with vitiligo diagnosed with generalized anxiety disorder (55.3%) and substance abuse (61.5%). Treatment was not initiated in 14% patients with suicidal ideation.
IN PRACTICE:
“Pediatric dermatologists have an important role in screening for psychiatric comorbidities, and implementation of appropriate screening tools while treating vitiligo is likely to have a bidirectional positive impact,” the authors wrote, adding: “By better understanding psychiatric comorbidities of African American children with vitiligo, dermatologists can be more aware of pediatric mental health needs and provide appropriate referrals.”
SOURCE:
This study was led by Emily Strouphauer, BSA, Baylor College of Medicine, Houston, and was published online in JAAD International.
LIMITATIONS:
The study limitations were the retrospective design, small sample size, and heterogeneity in the control group.
DISCLOSURES:
The study did not receive any funding. The authors declared no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Neurofibromatosis: What Affects Quality of Life Most?
TOPLINE:
Mobile images may be reliable for assessing cutaneous neurofibroma (cNF) features in patients with neurofibromatosis type 1 (NF1), according to a crowd-sourced .
METHODOLOGY:
- To learn more about the association of cNFs with QoL, pain, and itch in patients with this rare disease, researchers enrolled 1016 individuals aged 40 years and older with NF1 who had at least one cNF, from May 2021 to December 2023, after reaching out to patient-led or NF1 advocacy organizations in 13 countries, including the United States.
- Participants provided demographic data, detailed photographs, and saliva samples for genetic sequencing, with 583 participants (mean age, 51.7 years; 65.9% women) submitting high-quality photographs from seven body regions at the time of the study analysis.
- A subset of 50 participants also underwent whole-body imaging.
- Four researchers independently rated the photographs for various cNF features, including general severity, number, size, facial severity, and subtypes.
TAKEAWAY:
- Based on evaluations by NF1 specialists, the agreement between mobile and whole-body images was “substantial” (74%-88% agreement) for the number of cNFs, general severity, and facial severity. Agreement between self-reported numbers of cNFs and investigator-rated numbers based on photographs was “minimal to fair.”
- Female sex, the number of cNFs, severity of cNFs on the face, and globular cNFs were associated with worse QoL (based on Skindex scores); severity of cNFs on the face had the strongest impact on overall QoL (P < .001).
- An increasing number of cNFs and worsening facial severity were strongly correlated with higher emotion subdomain scores.
- A higher number of cNFs, more severe cNFs on the face, and larger cNFs were all slightly associated with increased itch and pain (P < .01).
IN PRACTICE:
“To develop effective therapeutics, meaningful clinical outcomes that are tied with improvement in QoL for persons with NF1 must be clearly defined,” the authors wrote. The results of this study, they added, “suggested the benefit of this crowd-sourced resource by identifying the features of cNFs with the greatest association with QoL and symptoms of pain and itch in persons with NF1, highlighting new intervention strategies and features to target to most improve QoL in NF1.”
SOURCE:
The study was led by Michelle Jade Lin, BS, Stanford University School of Medicine, Redwood City, California, and was published online in JAMA Dermatology.
LIMITATIONS:
The study included only a small number of individuals from racial and ethnic minority groups and did not capture ethnicity information, which could have provided further insights into disease impact across different demographics.
DISCLOSURES:
This study was supported by Johns Hopkins University, Baltimore, and the Bloomberg Family Foundation. Ms. Lin reported support from the Stanford Medical Scholars Research Program. Three authors reported personal fees or grants outside this work. Other authors reported no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Mobile images may be reliable for assessing cutaneous neurofibroma (cNF) features in patients with neurofibromatosis type 1 (NF1), according to a crowd-sourced .
METHODOLOGY:
- To learn more about the association of cNFs with QoL, pain, and itch in patients with this rare disease, researchers enrolled 1016 individuals aged 40 years and older with NF1 who had at least one cNF, from May 2021 to December 2023, after reaching out to patient-led or NF1 advocacy organizations in 13 countries, including the United States.
- Participants provided demographic data, detailed photographs, and saliva samples for genetic sequencing, with 583 participants (mean age, 51.7 years; 65.9% women) submitting high-quality photographs from seven body regions at the time of the study analysis.
- A subset of 50 participants also underwent whole-body imaging.
- Four researchers independently rated the photographs for various cNF features, including general severity, number, size, facial severity, and subtypes.
TAKEAWAY:
- Based on evaluations by NF1 specialists, the agreement between mobile and whole-body images was “substantial” (74%-88% agreement) for the number of cNFs, general severity, and facial severity. Agreement between self-reported numbers of cNFs and investigator-rated numbers based on photographs was “minimal to fair.”
- Female sex, the number of cNFs, severity of cNFs on the face, and globular cNFs were associated with worse QoL (based on Skindex scores); severity of cNFs on the face had the strongest impact on overall QoL (P < .001).
- An increasing number of cNFs and worsening facial severity were strongly correlated with higher emotion subdomain scores.
- A higher number of cNFs, more severe cNFs on the face, and larger cNFs were all slightly associated with increased itch and pain (P < .01).
IN PRACTICE:
“To develop effective therapeutics, meaningful clinical outcomes that are tied with improvement in QoL for persons with NF1 must be clearly defined,” the authors wrote. The results of this study, they added, “suggested the benefit of this crowd-sourced resource by identifying the features of cNFs with the greatest association with QoL and symptoms of pain and itch in persons with NF1, highlighting new intervention strategies and features to target to most improve QoL in NF1.”
SOURCE:
The study was led by Michelle Jade Lin, BS, Stanford University School of Medicine, Redwood City, California, and was published online in JAMA Dermatology.
LIMITATIONS:
The study included only a small number of individuals from racial and ethnic minority groups and did not capture ethnicity information, which could have provided further insights into disease impact across different demographics.
DISCLOSURES:
This study was supported by Johns Hopkins University, Baltimore, and the Bloomberg Family Foundation. Ms. Lin reported support from the Stanford Medical Scholars Research Program. Three authors reported personal fees or grants outside this work. Other authors reported no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Mobile images may be reliable for assessing cutaneous neurofibroma (cNF) features in patients with neurofibromatosis type 1 (NF1), according to a crowd-sourced .
METHODOLOGY:
- To learn more about the association of cNFs with QoL, pain, and itch in patients with this rare disease, researchers enrolled 1016 individuals aged 40 years and older with NF1 who had at least one cNF, from May 2021 to December 2023, after reaching out to patient-led or NF1 advocacy organizations in 13 countries, including the United States.
- Participants provided demographic data, detailed photographs, and saliva samples for genetic sequencing, with 583 participants (mean age, 51.7 years; 65.9% women) submitting high-quality photographs from seven body regions at the time of the study analysis.
- A subset of 50 participants also underwent whole-body imaging.
- Four researchers independently rated the photographs for various cNF features, including general severity, number, size, facial severity, and subtypes.
TAKEAWAY:
- Based on evaluations by NF1 specialists, the agreement between mobile and whole-body images was “substantial” (74%-88% agreement) for the number of cNFs, general severity, and facial severity. Agreement between self-reported numbers of cNFs and investigator-rated numbers based on photographs was “minimal to fair.”
- Female sex, the number of cNFs, severity of cNFs on the face, and globular cNFs were associated with worse QoL (based on Skindex scores); severity of cNFs on the face had the strongest impact on overall QoL (P < .001).
- An increasing number of cNFs and worsening facial severity were strongly correlated with higher emotion subdomain scores.
- A higher number of cNFs, more severe cNFs on the face, and larger cNFs were all slightly associated with increased itch and pain (P < .01).
IN PRACTICE:
“To develop effective therapeutics, meaningful clinical outcomes that are tied with improvement in QoL for persons with NF1 must be clearly defined,” the authors wrote. The results of this study, they added, “suggested the benefit of this crowd-sourced resource by identifying the features of cNFs with the greatest association with QoL and symptoms of pain and itch in persons with NF1, highlighting new intervention strategies and features to target to most improve QoL in NF1.”
SOURCE:
The study was led by Michelle Jade Lin, BS, Stanford University School of Medicine, Redwood City, California, and was published online in JAMA Dermatology.
LIMITATIONS:
The study included only a small number of individuals from racial and ethnic minority groups and did not capture ethnicity information, which could have provided further insights into disease impact across different demographics.
DISCLOSURES:
This study was supported by Johns Hopkins University, Baltimore, and the Bloomberg Family Foundation. Ms. Lin reported support from the Stanford Medical Scholars Research Program. Three authors reported personal fees or grants outside this work. Other authors reported no competing interests.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Acute Tender Papules on the Arms and Legs
The Diagnosis: Erythema Nodosum Leprosum
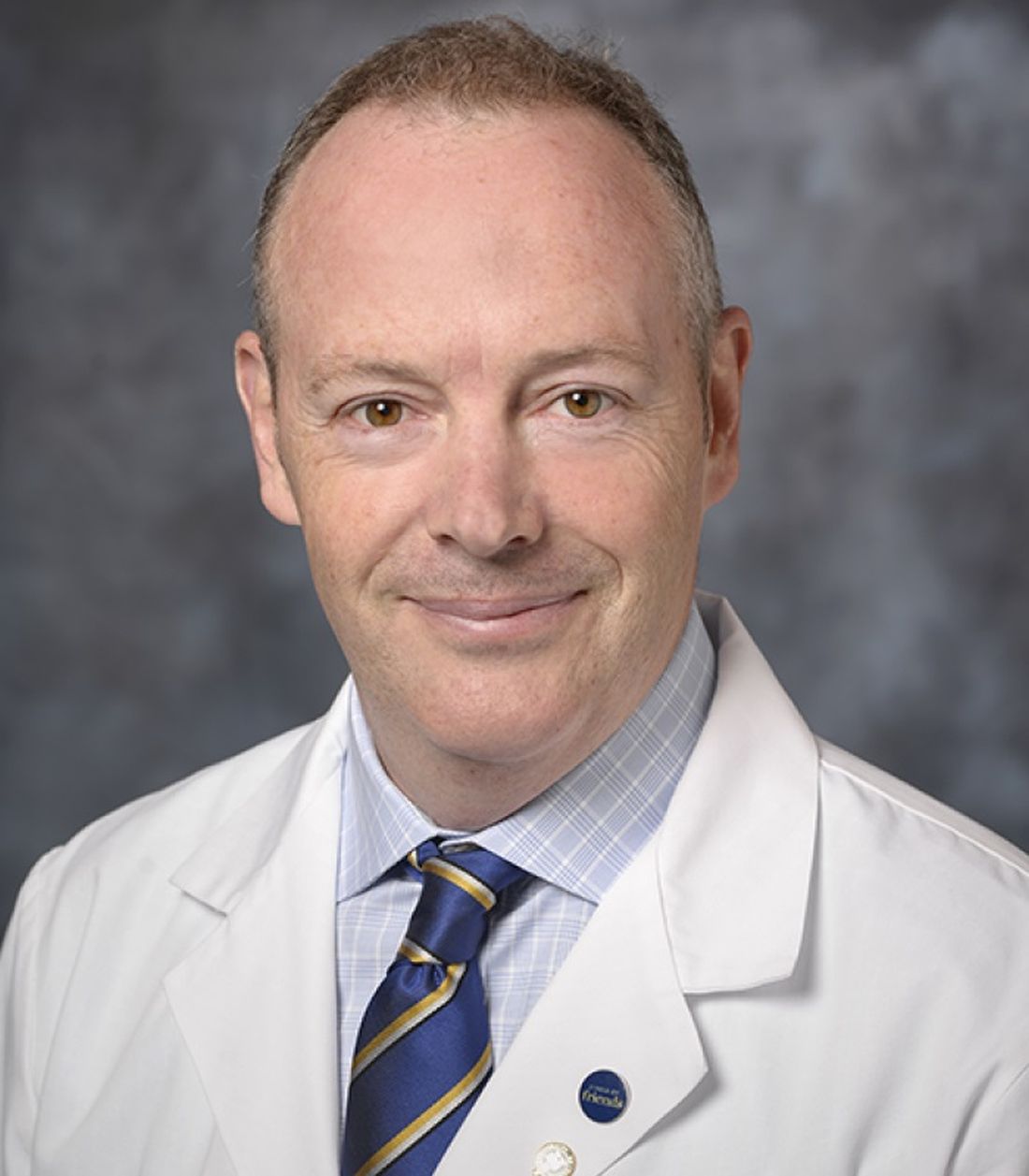
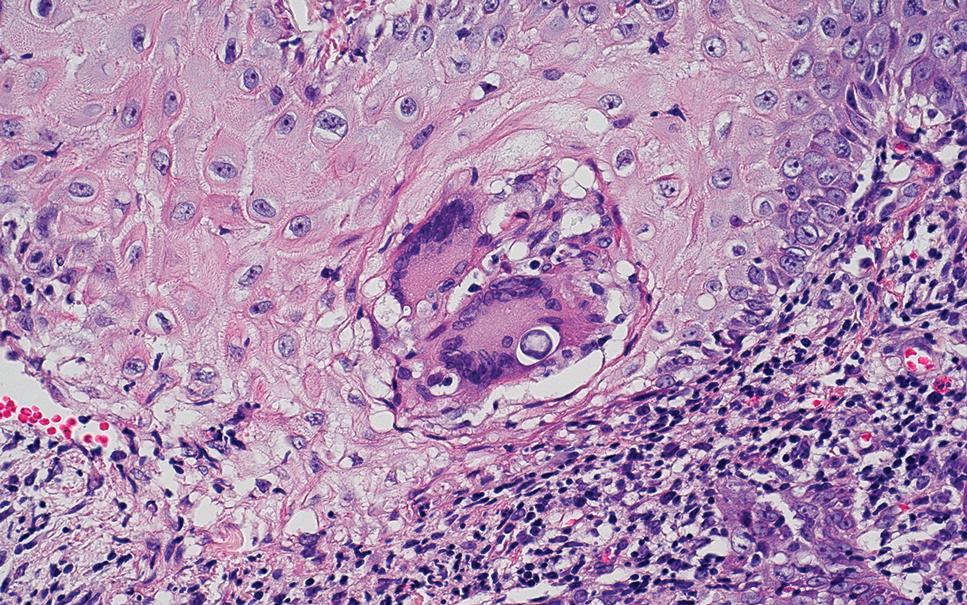
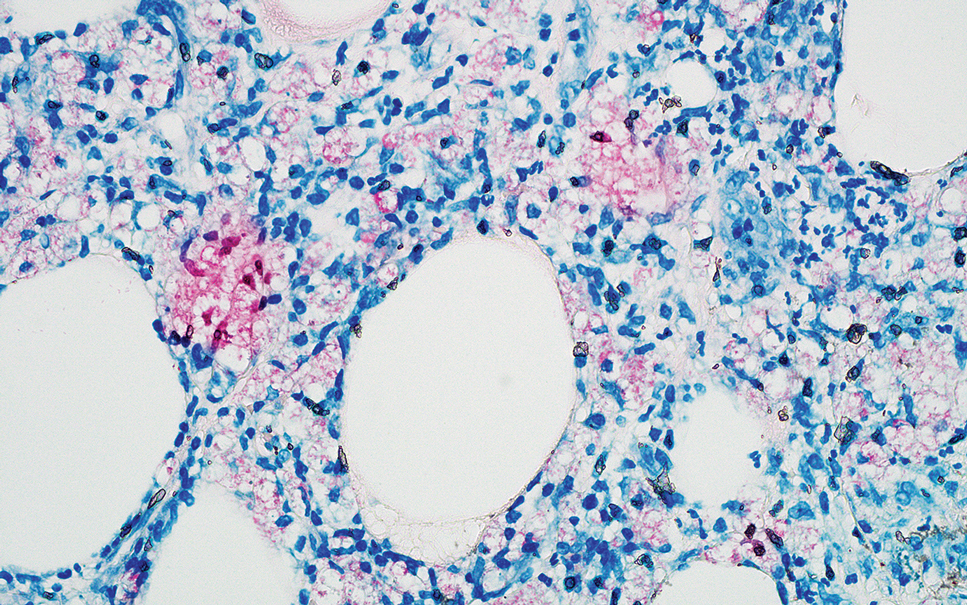
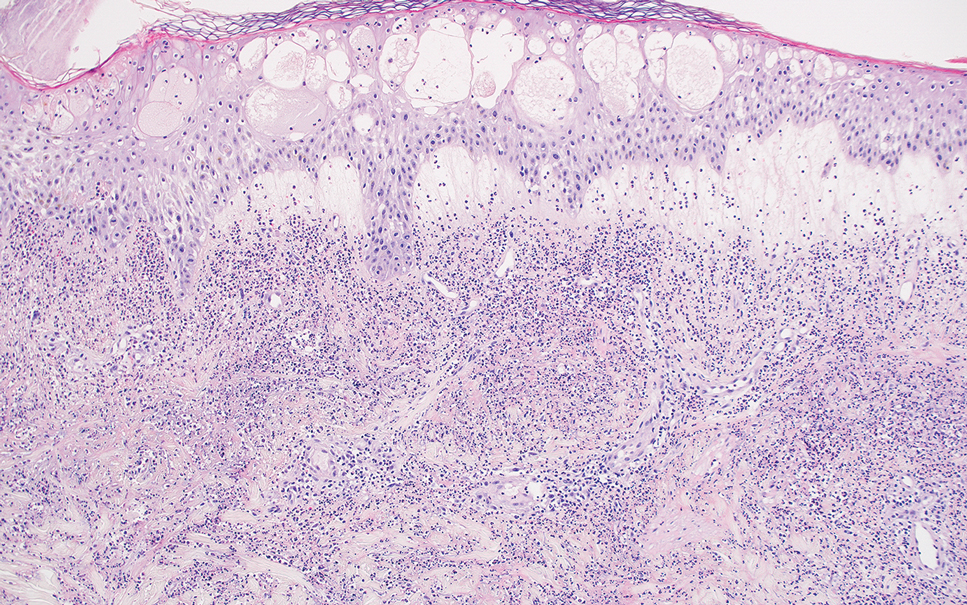
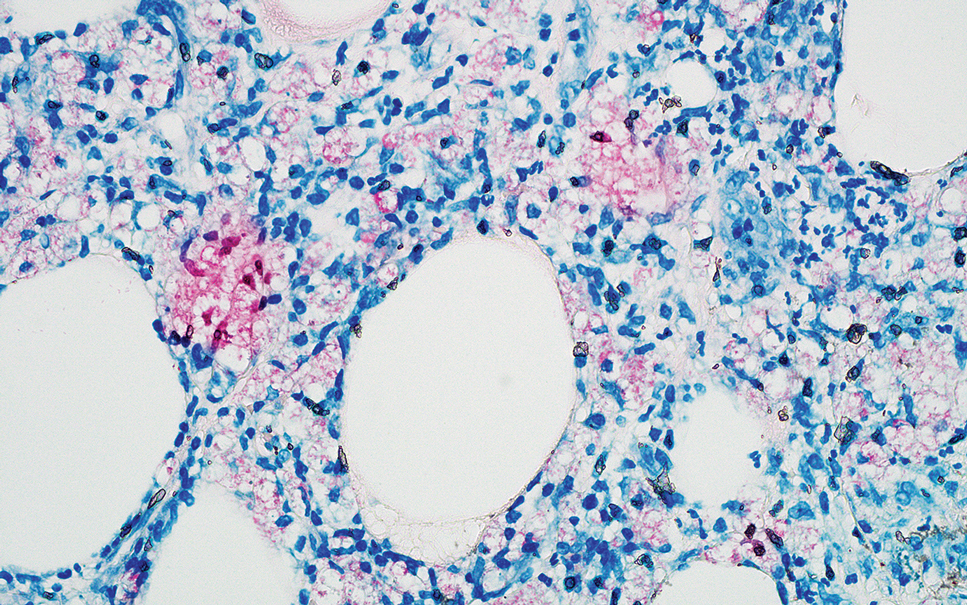
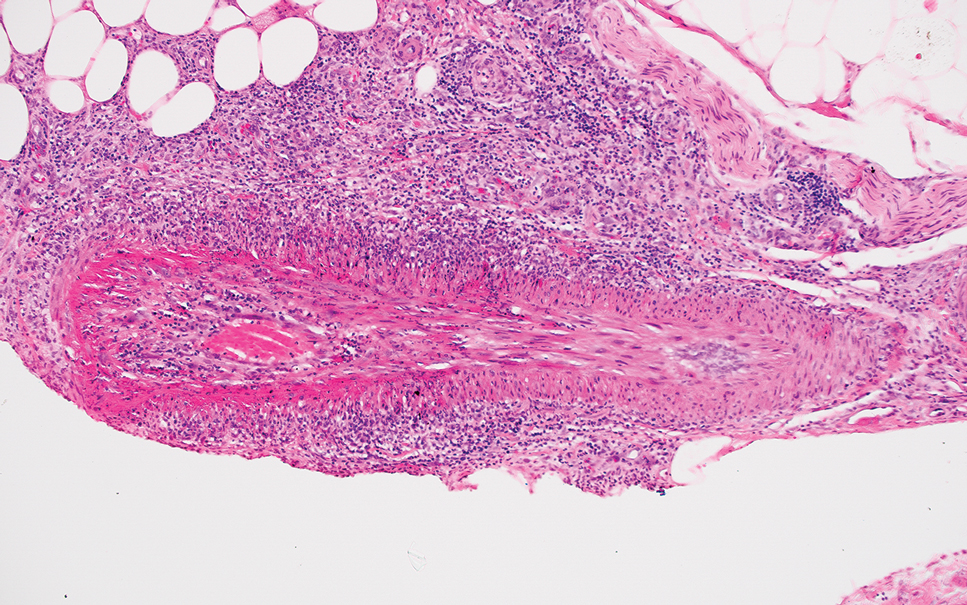
Erythema nodosum leprosum (ENL) is a type 2 reaction sometimes seen in patients infected with Mycobacterium leprae—primarily those with lepromatous or borderline lepromatous subtypes. Clinically, ENL manifests with abrupt onset of tender erythematous papules with associated fevers and general malaise. Studies have demonstrated a complex immune system reaction in ENL, but the detailed pathophysiology is not fully understood.1 Biopsies conducted within 24 hours of lesion formation are most elucidating. Foamy histiocytes admixed with neutrophils are seen in the subcutis, often causing a lobular panniculitis (quiz image).2 Neutrophils rarely are seen in other types of leprosy and thus are a useful diagnostic clue for ENL. Vasculitis of small- to medium-sized vessels can be seen but is not a necessary diagnostic criterion. Fite staining will highlight many acid-fast bacilli within the histiocytes (Figure 1).
Erythema nodosum leprosum is treated with a combination of immunosuppressants such as prednisone and thalidomide. Our patient was taking triple-antibiotic therapy—dapsone, rifampin, and clofazimine—for lepromatous leprosy when the erythematous papules developed on the arms and legs. After a skin biopsy confirmed the diagnosis of ENL, he was started on prednisone 20 mg daily with plans for close follow-up. Unfortunately, the patient was subsequently lost to follow-up.
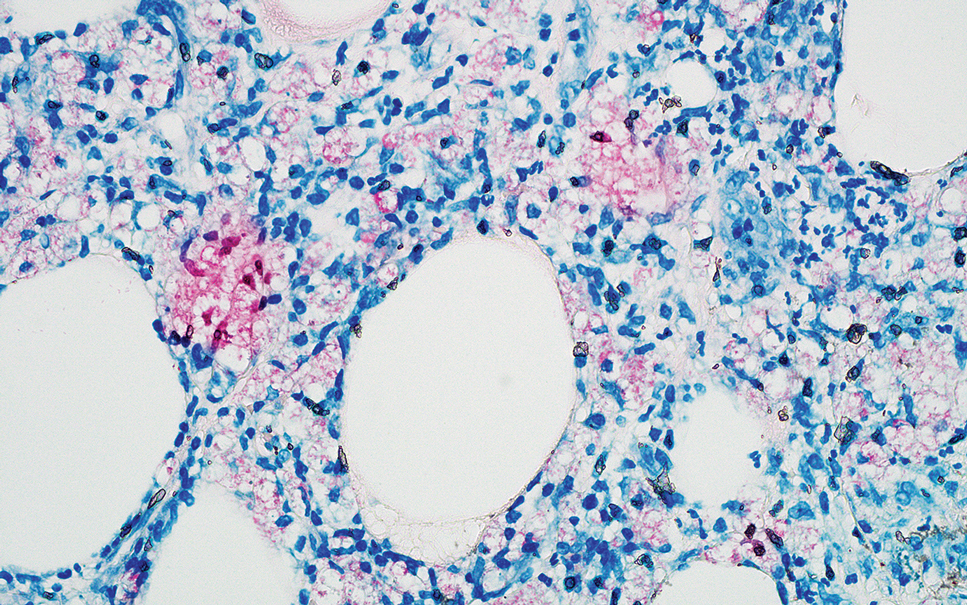
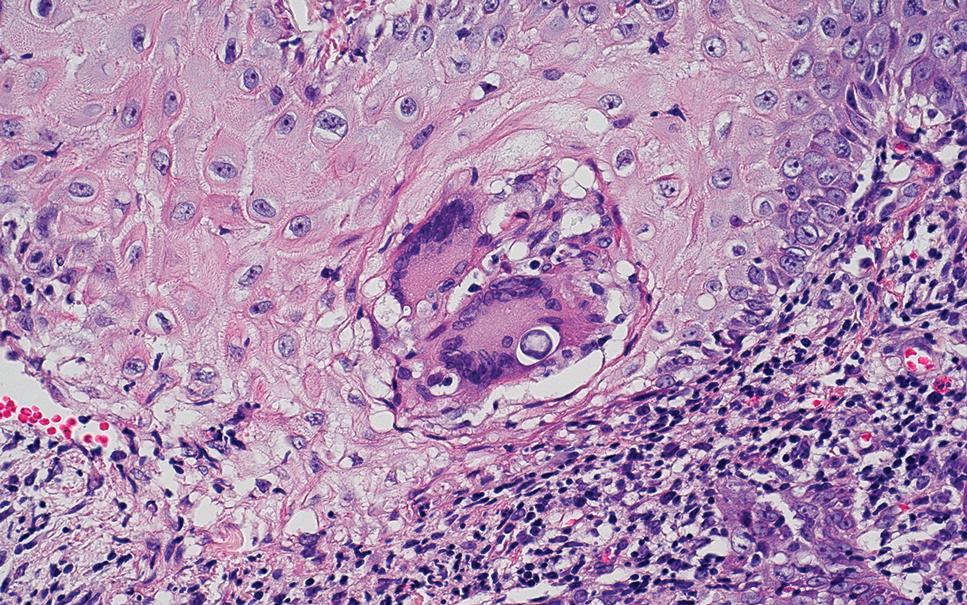
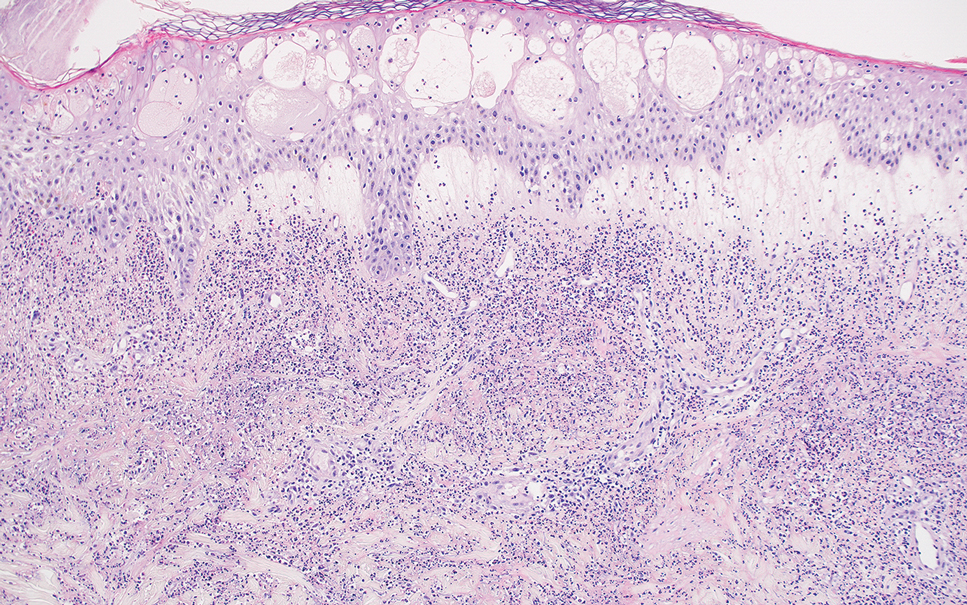
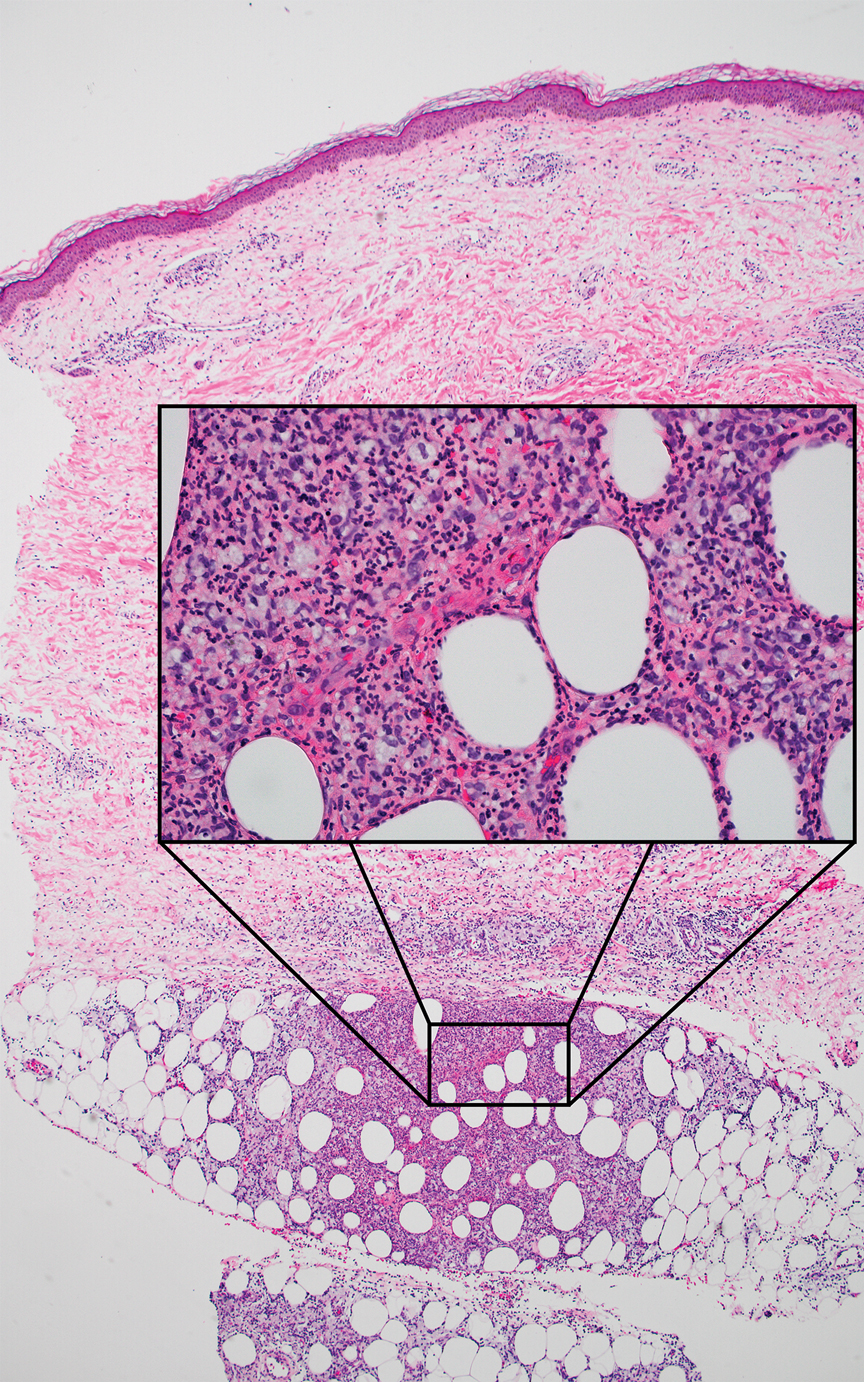
Acute febrile neutrophilic dermatosis (also known as Sweet syndrome) is an acute inflammatory disease characterized by abrupt onset of painful erythematous papules, plaques, or nodules on the skin. It often is seen in association with preceding infections (especially those in the upper respiratory or gastrointestinal tracts), hematologic malignancies, inflammatory bowel disease, or exposure to certain classes of medications (eg, granulocyte colony-stimulating factor, tyrosine kinase inhibitors, various antibiotics).3 Histologically, acute febrile neutrophilic dermatosis is characterized by dense neutrophilic infiltrates, often with notable dermal edema (Figure 2).4 Many cases also show leukocytoclastic vasculitis; however, foamy histiocytes are not a notable component of the inflammatory infiltrate, though a histiocytoid form of acute febrile neutrophilic dermatosis has been described.5 Infections must be rigorously ruled out prior to diagnosing a patient with acute febrile neutrophilic dermatosis, making it a diagnosis of exclusion.
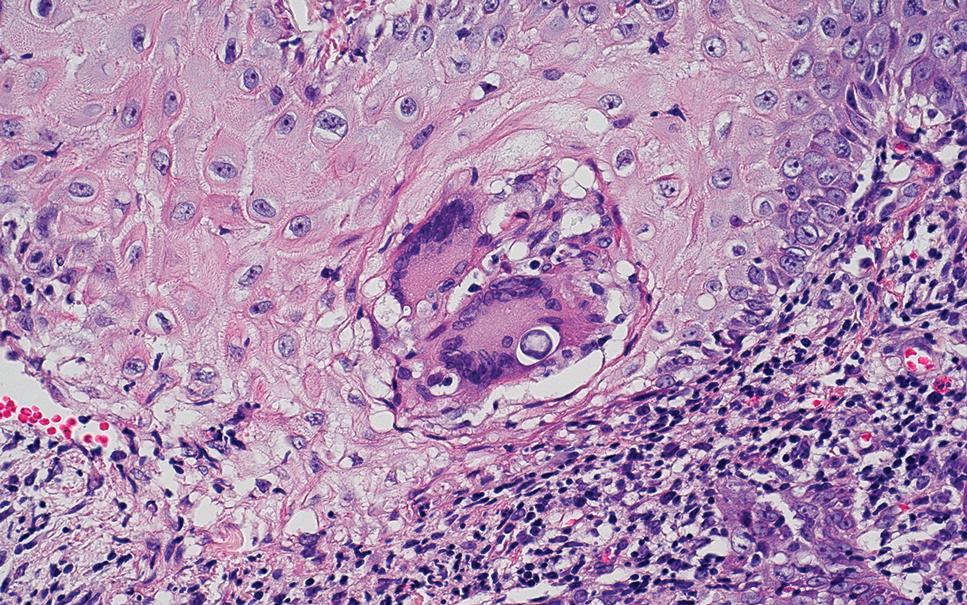
Cutaneous coccidioidomycosis is an infection caused by the dimorphic fungi Coccidioides immitis or Coccidioides posadasii. Cutaneous disease is rare but can occur from direct inoculation or dissemination from pulmonary disease in immunocompetent or immunocompromised patients. Papules, pustules, or plaques are seen clinically. Histologically, cutaneous coccidioidomycosis shows spherules that vary from 10 to 100 μm and are filled with multiple smaller endospores (Figure 3).6 Pseudoepitheliomatous hyperplasia with dense suppurative and granulomatous infiltrates also is seen.
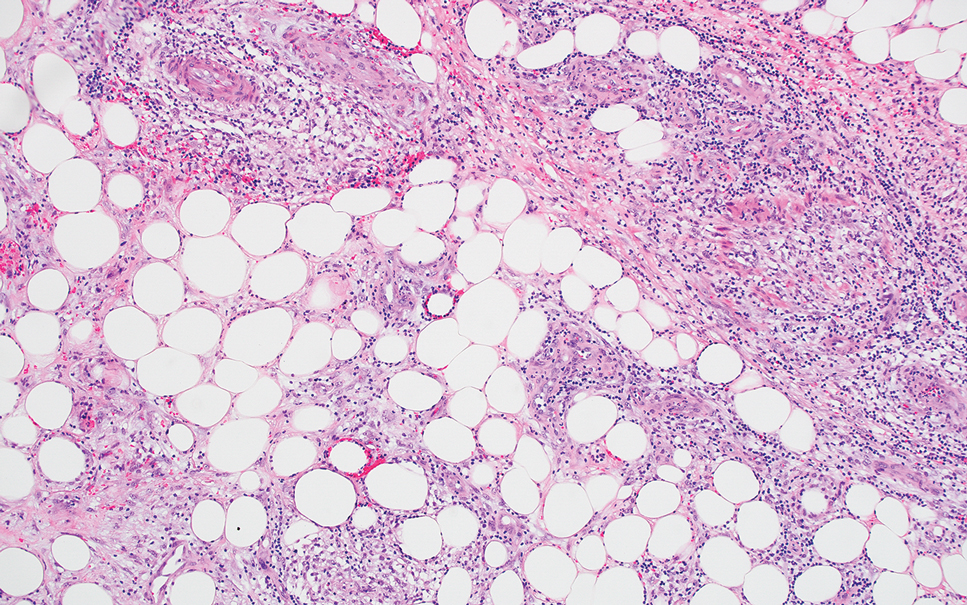
Erythema induratum is characterized by tender nodules on the lower extremities and has a substantial female predominance. Many cases are associated with Mycobacterium tuberculosis infection. The bacteria are not seen directly in the skin but are instead detectable through DNA polymerase chain reaction testing or investigation of other organ systems.7,8 Histologically, lesions show a lobular panniculitis with a mixed infiltrate. Vasculitis is seen in approximately 90% of erythema induratum cases vs approximately 25% of classic ENL cases (Figure 4),2,9 which has led some to use the term nodular vasculitis to describe this disease entity. Nodular vasculitis is considered by others to be a distinct disease entity in which there are clinical and histologic features similar to erythema induratum but no evidence of M tuberculosis infection.9
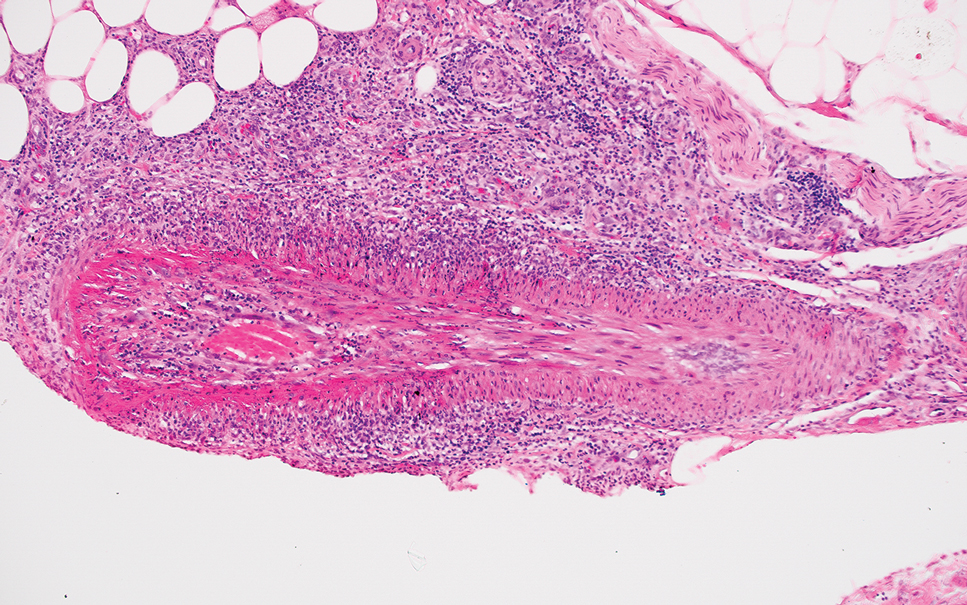
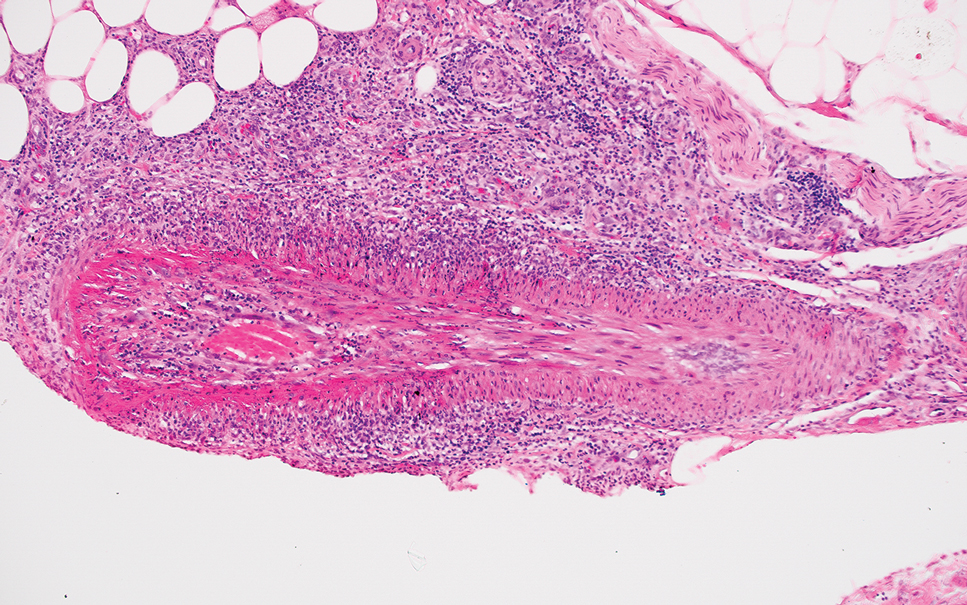
Polyarteritis nodosa is a vasculitis that affects medium- sized vessels of various organ systems. The presenting signs and symptoms vary based on the affected organ systems. Palpable to retiform purpura, livedo racemosa, subcutaneous nodules, or ulcers are seen when the skin is involved. The histologic hallmark is necrotizing vasculitis of medium-sized arterioles (Figure 5), although leukocytoclastic vasculitis of small-caliber vessels also can be seen in biopsies of affected skin.10 The vascular changes are said to be segmental, with uninvolved segments interspersed with involved segments. Antineutrophil cytoplasmic antibody (ANCA)– associated vasculitis also must be considered when one sees leukocytoclastic vasculitis of small-caliber vessels in the skin, as it can be distinguished most readily by detecting circulating antibodies specific for myeloperoxidase (MPO-ANCA) or proteinase 3 (PR3-ANCA).
- Polycarpou A, Walker SL, Lockwood DNJ. A systematic review of immunological studies of erythema nodosum leprosum. Front Immunol. 2017;8:233. doi:10.3389/fimmu.2017.00233
- Massone C, Belachew WA, Schettini A. Histopathology of the lepromatous skin biopsy. Clin Dermatol. 2015;33:38-45. doi:10.1016/j.clindermatol.2014.10.003
- Cohen PR. Sweet’s syndrome—a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:1-28. doi:10.1186/1750-1172-2-34
- Ratzinger G, Burgdorf W, Zelger BG, et al. Acute febrile neutrophilic dermatosis: a histopathologic study of 31 cases with review of literature. Am J Dermatopathol. 2007;29:125-133. doi:10.1097/01.dad.0000249887.59810.76
- Wilson TC, Stone MS, Swick BL. Histiocytoid Sweet syndrome with haloed myeloid cells masquerading as a cryptococcal infection. Am J Dermatopathology. 2014;36:264-269. doi:10.1097/DAD.0b013e31828b811b
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280. doi:10.1128/CMR.00053-10
- Schneider JW, Jordaan HF, Geiger DH, et al. Erythema induratum of Bazin: a clinicopathological study of 20 cases of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995;17:350-356. doi:10.1097/00000372-199508000-00008
- Boonchai W, Suthipinittharm P, Mahaisavariya P. Panniculitis in tuberculosis: a clinicopathologic study of nodular panniculitis associated with tuberculosis. Int J Dermatol. 1998;37:361-363. doi:10.1046/j.1365-4362.1998.00299.x
- Segura S, Pujol RM, Trindade F, et al. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008;59:839-851. doi:10.1016/j.jaad.2008.07.030
- Ishiguro N, Kawashima M. Cutaneous polyarteritis nodosa: a report of 16 cases with clinical and histopathological analysis and a review of the published work. J Dermatol. 2010;37:85-93. doi:10.1111/j.1346-8138.2009.00752.x
The Diagnosis: Erythema Nodosum Leprosum
Erythema nodosum leprosum (ENL) is a type 2 reaction sometimes seen in patients infected with Mycobacterium leprae—primarily those with lepromatous or borderline lepromatous subtypes. Clinically, ENL manifests with abrupt onset of tender erythematous papules with associated fevers and general malaise. Studies have demonstrated a complex immune system reaction in ENL, but the detailed pathophysiology is not fully understood.1 Biopsies conducted within 24 hours of lesion formation are most elucidating. Foamy histiocytes admixed with neutrophils are seen in the subcutis, often causing a lobular panniculitis (quiz image).2 Neutrophils rarely are seen in other types of leprosy and thus are a useful diagnostic clue for ENL. Vasculitis of small- to medium-sized vessels can be seen but is not a necessary diagnostic criterion. Fite staining will highlight many acid-fast bacilli within the histiocytes (Figure 1).
Erythema nodosum leprosum is treated with a combination of immunosuppressants such as prednisone and thalidomide. Our patient was taking triple-antibiotic therapy—dapsone, rifampin, and clofazimine—for lepromatous leprosy when the erythematous papules developed on the arms and legs. After a skin biopsy confirmed the diagnosis of ENL, he was started on prednisone 20 mg daily with plans for close follow-up. Unfortunately, the patient was subsequently lost to follow-up.
Acute febrile neutrophilic dermatosis (also known as Sweet syndrome) is an acute inflammatory disease characterized by abrupt onset of painful erythematous papules, plaques, or nodules on the skin. It often is seen in association with preceding infections (especially those in the upper respiratory or gastrointestinal tracts), hematologic malignancies, inflammatory bowel disease, or exposure to certain classes of medications (eg, granulocyte colony-stimulating factor, tyrosine kinase inhibitors, various antibiotics).3 Histologically, acute febrile neutrophilic dermatosis is characterized by dense neutrophilic infiltrates, often with notable dermal edema (Figure 2).4 Many cases also show leukocytoclastic vasculitis; however, foamy histiocytes are not a notable component of the inflammatory infiltrate, though a histiocytoid form of acute febrile neutrophilic dermatosis has been described.5 Infections must be rigorously ruled out prior to diagnosing a patient with acute febrile neutrophilic dermatosis, making it a diagnosis of exclusion.
Cutaneous coccidioidomycosis is an infection caused by the dimorphic fungi Coccidioides immitis or Coccidioides posadasii. Cutaneous disease is rare but can occur from direct inoculation or dissemination from pulmonary disease in immunocompetent or immunocompromised patients. Papules, pustules, or plaques are seen clinically. Histologically, cutaneous coccidioidomycosis shows spherules that vary from 10 to 100 μm and are filled with multiple smaller endospores (Figure 3).6 Pseudoepitheliomatous hyperplasia with dense suppurative and granulomatous infiltrates also is seen.
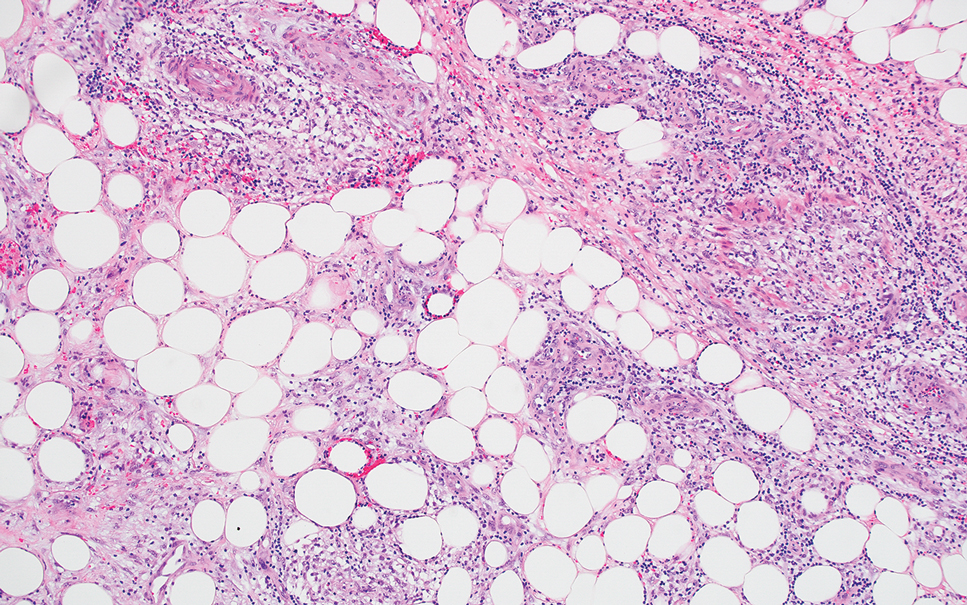
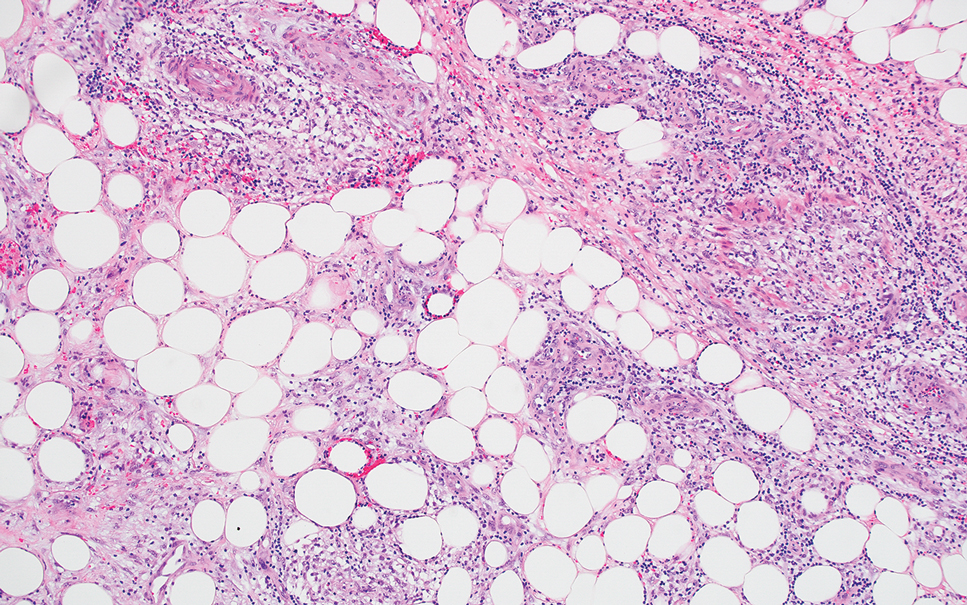
Erythema induratum is characterized by tender nodules on the lower extremities and has a substantial female predominance. Many cases are associated with Mycobacterium tuberculosis infection. The bacteria are not seen directly in the skin but are instead detectable through DNA polymerase chain reaction testing or investigation of other organ systems.7,8 Histologically, lesions show a lobular panniculitis with a mixed infiltrate. Vasculitis is seen in approximately 90% of erythema induratum cases vs approximately 25% of classic ENL cases (Figure 4),2,9 which has led some to use the term nodular vasculitis to describe this disease entity. Nodular vasculitis is considered by others to be a distinct disease entity in which there are clinical and histologic features similar to erythema induratum but no evidence of M tuberculosis infection.9
Polyarteritis nodosa is a vasculitis that affects medium- sized vessels of various organ systems. The presenting signs and symptoms vary based on the affected organ systems. Palpable to retiform purpura, livedo racemosa, subcutaneous nodules, or ulcers are seen when the skin is involved. The histologic hallmark is necrotizing vasculitis of medium-sized arterioles (Figure 5), although leukocytoclastic vasculitis of small-caliber vessels also can be seen in biopsies of affected skin.10 The vascular changes are said to be segmental, with uninvolved segments interspersed with involved segments. Antineutrophil cytoplasmic antibody (ANCA)– associated vasculitis also must be considered when one sees leukocytoclastic vasculitis of small-caliber vessels in the skin, as it can be distinguished most readily by detecting circulating antibodies specific for myeloperoxidase (MPO-ANCA) or proteinase 3 (PR3-ANCA).
The Diagnosis: Erythema Nodosum Leprosum
Erythema nodosum leprosum (ENL) is a type 2 reaction sometimes seen in patients infected with Mycobacterium leprae—primarily those with lepromatous or borderline lepromatous subtypes. Clinically, ENL manifests with abrupt onset of tender erythematous papules with associated fevers and general malaise. Studies have demonstrated a complex immune system reaction in ENL, but the detailed pathophysiology is not fully understood.1 Biopsies conducted within 24 hours of lesion formation are most elucidating. Foamy histiocytes admixed with neutrophils are seen in the subcutis, often causing a lobular panniculitis (quiz image).2 Neutrophils rarely are seen in other types of leprosy and thus are a useful diagnostic clue for ENL. Vasculitis of small- to medium-sized vessels can be seen but is not a necessary diagnostic criterion. Fite staining will highlight many acid-fast bacilli within the histiocytes (Figure 1).
Erythema nodosum leprosum is treated with a combination of immunosuppressants such as prednisone and thalidomide. Our patient was taking triple-antibiotic therapy—dapsone, rifampin, and clofazimine—for lepromatous leprosy when the erythematous papules developed on the arms and legs. After a skin biopsy confirmed the diagnosis of ENL, he was started on prednisone 20 mg daily with plans for close follow-up. Unfortunately, the patient was subsequently lost to follow-up.
Acute febrile neutrophilic dermatosis (also known as Sweet syndrome) is an acute inflammatory disease characterized by abrupt onset of painful erythematous papules, plaques, or nodules on the skin. It often is seen in association with preceding infections (especially those in the upper respiratory or gastrointestinal tracts), hematologic malignancies, inflammatory bowel disease, or exposure to certain classes of medications (eg, granulocyte colony-stimulating factor, tyrosine kinase inhibitors, various antibiotics).3 Histologically, acute febrile neutrophilic dermatosis is characterized by dense neutrophilic infiltrates, often with notable dermal edema (Figure 2).4 Many cases also show leukocytoclastic vasculitis; however, foamy histiocytes are not a notable component of the inflammatory infiltrate, though a histiocytoid form of acute febrile neutrophilic dermatosis has been described.5 Infections must be rigorously ruled out prior to diagnosing a patient with acute febrile neutrophilic dermatosis, making it a diagnosis of exclusion.
Cutaneous coccidioidomycosis is an infection caused by the dimorphic fungi Coccidioides immitis or Coccidioides posadasii. Cutaneous disease is rare but can occur from direct inoculation or dissemination from pulmonary disease in immunocompetent or immunocompromised patients. Papules, pustules, or plaques are seen clinically. Histologically, cutaneous coccidioidomycosis shows spherules that vary from 10 to 100 μm and are filled with multiple smaller endospores (Figure 3).6 Pseudoepitheliomatous hyperplasia with dense suppurative and granulomatous infiltrates also is seen.
Erythema induratum is characterized by tender nodules on the lower extremities and has a substantial female predominance. Many cases are associated with Mycobacterium tuberculosis infection. The bacteria are not seen directly in the skin but are instead detectable through DNA polymerase chain reaction testing or investigation of other organ systems.7,8 Histologically, lesions show a lobular panniculitis with a mixed infiltrate. Vasculitis is seen in approximately 90% of erythema induratum cases vs approximately 25% of classic ENL cases (Figure 4),2,9 which has led some to use the term nodular vasculitis to describe this disease entity. Nodular vasculitis is considered by others to be a distinct disease entity in which there are clinical and histologic features similar to erythema induratum but no evidence of M tuberculosis infection.9
Polyarteritis nodosa is a vasculitis that affects medium- sized vessels of various organ systems. The presenting signs and symptoms vary based on the affected organ systems. Palpable to retiform purpura, livedo racemosa, subcutaneous nodules, or ulcers are seen when the skin is involved. The histologic hallmark is necrotizing vasculitis of medium-sized arterioles (Figure 5), although leukocytoclastic vasculitis of small-caliber vessels also can be seen in biopsies of affected skin.10 The vascular changes are said to be segmental, with uninvolved segments interspersed with involved segments. Antineutrophil cytoplasmic antibody (ANCA)– associated vasculitis also must be considered when one sees leukocytoclastic vasculitis of small-caliber vessels in the skin, as it can be distinguished most readily by detecting circulating antibodies specific for myeloperoxidase (MPO-ANCA) or proteinase 3 (PR3-ANCA).
- Polycarpou A, Walker SL, Lockwood DNJ. A systematic review of immunological studies of erythema nodosum leprosum. Front Immunol. 2017;8:233. doi:10.3389/fimmu.2017.00233
- Massone C, Belachew WA, Schettini A. Histopathology of the lepromatous skin biopsy. Clin Dermatol. 2015;33:38-45. doi:10.1016/j.clindermatol.2014.10.003
- Cohen PR. Sweet’s syndrome—a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:1-28. doi:10.1186/1750-1172-2-34
- Ratzinger G, Burgdorf W, Zelger BG, et al. Acute febrile neutrophilic dermatosis: a histopathologic study of 31 cases with review of literature. Am J Dermatopathol. 2007;29:125-133. doi:10.1097/01.dad.0000249887.59810.76
- Wilson TC, Stone MS, Swick BL. Histiocytoid Sweet syndrome with haloed myeloid cells masquerading as a cryptococcal infection. Am J Dermatopathology. 2014;36:264-269. doi:10.1097/DAD.0b013e31828b811b
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280. doi:10.1128/CMR.00053-10
- Schneider JW, Jordaan HF, Geiger DH, et al. Erythema induratum of Bazin: a clinicopathological study of 20 cases of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995;17:350-356. doi:10.1097/00000372-199508000-00008
- Boonchai W, Suthipinittharm P, Mahaisavariya P. Panniculitis in tuberculosis: a clinicopathologic study of nodular panniculitis associated with tuberculosis. Int J Dermatol. 1998;37:361-363. doi:10.1046/j.1365-4362.1998.00299.x
- Segura S, Pujol RM, Trindade F, et al. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008;59:839-851. doi:10.1016/j.jaad.2008.07.030
- Ishiguro N, Kawashima M. Cutaneous polyarteritis nodosa: a report of 16 cases with clinical and histopathological analysis and a review of the published work. J Dermatol. 2010;37:85-93. doi:10.1111/j.1346-8138.2009.00752.x
- Polycarpou A, Walker SL, Lockwood DNJ. A systematic review of immunological studies of erythema nodosum leprosum. Front Immunol. 2017;8:233. doi:10.3389/fimmu.2017.00233
- Massone C, Belachew WA, Schettini A. Histopathology of the lepromatous skin biopsy. Clin Dermatol. 2015;33:38-45. doi:10.1016/j.clindermatol.2014.10.003
- Cohen PR. Sweet’s syndrome—a comprehensive review of an acute febrile neutrophilic dermatosis. Orphanet J Rare Dis. 2007;2:1-28. doi:10.1186/1750-1172-2-34
- Ratzinger G, Burgdorf W, Zelger BG, et al. Acute febrile neutrophilic dermatosis: a histopathologic study of 31 cases with review of literature. Am J Dermatopathol. 2007;29:125-133. doi:10.1097/01.dad.0000249887.59810.76
- Wilson TC, Stone MS, Swick BL. Histiocytoid Sweet syndrome with haloed myeloid cells masquerading as a cryptococcal infection. Am J Dermatopathology. 2014;36:264-269. doi:10.1097/DAD.0b013e31828b811b
- Guarner J, Brandt ME. Histopathologic diagnosis of fungal infections in the 21st century. Clin Microbiol Rev. 2011;24:247-280. doi:10.1128/CMR.00053-10
- Schneider JW, Jordaan HF, Geiger DH, et al. Erythema induratum of Bazin: a clinicopathological study of 20 cases of Mycobacterium tuberculosis DNA in skin lesions by polymerase chain reaction. Am J Dermatopathol. 1995;17:350-356. doi:10.1097/00000372-199508000-00008
- Boonchai W, Suthipinittharm P, Mahaisavariya P. Panniculitis in tuberculosis: a clinicopathologic study of nodular panniculitis associated with tuberculosis. Int J Dermatol. 1998;37:361-363. doi:10.1046/j.1365-4362.1998.00299.x
- Segura S, Pujol RM, Trindade F, et al. Vasculitis in erythema induratum of Bazin: a histopathologic study of 101 biopsy specimens from 86 patients. J Am Acad Dermatol. 2008;59:839-851. doi:10.1016/j.jaad.2008.07.030
- Ishiguro N, Kawashima M. Cutaneous polyarteritis nodosa: a report of 16 cases with clinical and histopathological analysis and a review of the published work. J Dermatol. 2010;37:85-93. doi:10.1111/j.1346-8138.2009.00752.x
A 66-year-old man presented with new tender erythematous papules scattered over the arms and legs. A biopsy of a lesion on the left thigh was performed.
Systemic Sclerosis Without Scleroderma Has Unique Severity, Prognosis
TOPLINE:
Systemic sclerosis sine scleroderma (ssSSc) affects nearly 10% of patients with systemic sclerosis (SSc), with substantial internal organ involvement. Despite lacking skin fibrosis, patients with ssSSc are at a risk for interstitial lung disease, pulmonary arterial hypertension, and cardiac dysfunction.
METHODOLOGY:
- Driven by a fatal case of ssSSc with cardiac involvement, researchers aimed to evaluate its prevalence, severity, and prognosis.
- They conducted a systematic literature and qualitative synthesis of 35 studies on SSc cohorts from databases published between 1976 and 2023 that comprised data on the prevalence of SSc with or without organ involvement.
- A total of 25,455 patients with SSc were included, with 2437 identified as having ssSSc.
- Studies used various classification criteria for SSc, including the 1980 American Rheumatism Association criteria, 2001 LeRoy and Medsger criteria, and 2013 American College of Rheumatology/European League Against Rheumatism criteria, while ssSSc was classified on the basis of the definitions provided by Rodnan and Fennell and also Poormoghim.
- The analysis focused on ssSSc prevalence, reclassification rates, and internal organ involvement, including interstitial lung disease, pulmonary arterial hypertension, scleroderma renal crisis, and cardiac dysfunction.
TAKEAWAY:
- The overall mean prevalence of ssSSc was 9.6%, with a range of 0%-22.9% across different studies.
- Reclassification rates of ssSSc into limited cutaneous SSc (lcSSc) or diffuse cutaneous SSc (dcSSc) varied substantially, with some studies reporting rates as high as 27.8% over a 4-year follow-up period.
- The mean frequency of internal organ involvement in patients with ssSSc was 46% for interstitial lung disease, 15% for pulmonary arterial hypertension, 5% for scleroderma renal crisis, and 26.5% for cardiac dysfunction — mainly diastolic dysfunction.
- The survival rates in patients with ssSSc were similar to those with lcSSc and better than those with dcSSc.
IN PRACTICE:
“The results presented herein suggest a slightly more severe yet similar clinical picture of ssSSc compared to lcSSc [limited cutaneous SSc], while dcSSc [diffuse cutaneous SSc] remains the most severe disease form,” the authors wrote. “Although classification criteria should not impact appropriate management of patients, updated ssSSc subclassification criteria, which will take into account time from disease onset, should be considered,” they further added.
SOURCE:
The study was led by Anastasios Makris, MD, First Department of Propaedeutic & Internal Medicine, National and Kapodistrian University of Athens, Medical School, Athens, Greece. It was published online on August 15, 2024, in The Journal of Rheumatology.
LIMITATIONS:
The variability in the classification criteria across different studies may affect the comparability of results. The included studies lacked data on cardiac MRI, restricting the identification of myocardial fibrosis patterns and characterization of cardiac disease activity.
DISCLOSURES:
The study did not receive any specific funding. Some authors disclosed having a consultancy relationship, serving as speakers, and receiving funding for research from multiple companies. One author reported having a patent and being a cofounder of CITUS AG.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Systemic sclerosis sine scleroderma (ssSSc) affects nearly 10% of patients with systemic sclerosis (SSc), with substantial internal organ involvement. Despite lacking skin fibrosis, patients with ssSSc are at a risk for interstitial lung disease, pulmonary arterial hypertension, and cardiac dysfunction.
METHODOLOGY:
- Driven by a fatal case of ssSSc with cardiac involvement, researchers aimed to evaluate its prevalence, severity, and prognosis.
- They conducted a systematic literature and qualitative synthesis of 35 studies on SSc cohorts from databases published between 1976 and 2023 that comprised data on the prevalence of SSc with or without organ involvement.
- A total of 25,455 patients with SSc were included, with 2437 identified as having ssSSc.
- Studies used various classification criteria for SSc, including the 1980 American Rheumatism Association criteria, 2001 LeRoy and Medsger criteria, and 2013 American College of Rheumatology/European League Against Rheumatism criteria, while ssSSc was classified on the basis of the definitions provided by Rodnan and Fennell and also Poormoghim.
- The analysis focused on ssSSc prevalence, reclassification rates, and internal organ involvement, including interstitial lung disease, pulmonary arterial hypertension, scleroderma renal crisis, and cardiac dysfunction.
TAKEAWAY:
- The overall mean prevalence of ssSSc was 9.6%, with a range of 0%-22.9% across different studies.
- Reclassification rates of ssSSc into limited cutaneous SSc (lcSSc) or diffuse cutaneous SSc (dcSSc) varied substantially, with some studies reporting rates as high as 27.8% over a 4-year follow-up period.
- The mean frequency of internal organ involvement in patients with ssSSc was 46% for interstitial lung disease, 15% for pulmonary arterial hypertension, 5% for scleroderma renal crisis, and 26.5% for cardiac dysfunction — mainly diastolic dysfunction.
- The survival rates in patients with ssSSc were similar to those with lcSSc and better than those with dcSSc.
IN PRACTICE:
“The results presented herein suggest a slightly more severe yet similar clinical picture of ssSSc compared to lcSSc [limited cutaneous SSc], while dcSSc [diffuse cutaneous SSc] remains the most severe disease form,” the authors wrote. “Although classification criteria should not impact appropriate management of patients, updated ssSSc subclassification criteria, which will take into account time from disease onset, should be considered,” they further added.
SOURCE:
The study was led by Anastasios Makris, MD, First Department of Propaedeutic & Internal Medicine, National and Kapodistrian University of Athens, Medical School, Athens, Greece. It was published online on August 15, 2024, in The Journal of Rheumatology.
LIMITATIONS:
The variability in the classification criteria across different studies may affect the comparability of results. The included studies lacked data on cardiac MRI, restricting the identification of myocardial fibrosis patterns and characterization of cardiac disease activity.
DISCLOSURES:
The study did not receive any specific funding. Some authors disclosed having a consultancy relationship, serving as speakers, and receiving funding for research from multiple companies. One author reported having a patent and being a cofounder of CITUS AG.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Systemic sclerosis sine scleroderma (ssSSc) affects nearly 10% of patients with systemic sclerosis (SSc), with substantial internal organ involvement. Despite lacking skin fibrosis, patients with ssSSc are at a risk for interstitial lung disease, pulmonary arterial hypertension, and cardiac dysfunction.
METHODOLOGY:
- Driven by a fatal case of ssSSc with cardiac involvement, researchers aimed to evaluate its prevalence, severity, and prognosis.
- They conducted a systematic literature and qualitative synthesis of 35 studies on SSc cohorts from databases published between 1976 and 2023 that comprised data on the prevalence of SSc with or without organ involvement.
- A total of 25,455 patients with SSc were included, with 2437 identified as having ssSSc.
- Studies used various classification criteria for SSc, including the 1980 American Rheumatism Association criteria, 2001 LeRoy and Medsger criteria, and 2013 American College of Rheumatology/European League Against Rheumatism criteria, while ssSSc was classified on the basis of the definitions provided by Rodnan and Fennell and also Poormoghim.
- The analysis focused on ssSSc prevalence, reclassification rates, and internal organ involvement, including interstitial lung disease, pulmonary arterial hypertension, scleroderma renal crisis, and cardiac dysfunction.
TAKEAWAY:
- The overall mean prevalence of ssSSc was 9.6%, with a range of 0%-22.9% across different studies.
- Reclassification rates of ssSSc into limited cutaneous SSc (lcSSc) or diffuse cutaneous SSc (dcSSc) varied substantially, with some studies reporting rates as high as 27.8% over a 4-year follow-up period.
- The mean frequency of internal organ involvement in patients with ssSSc was 46% for interstitial lung disease, 15% for pulmonary arterial hypertension, 5% for scleroderma renal crisis, and 26.5% for cardiac dysfunction — mainly diastolic dysfunction.
- The survival rates in patients with ssSSc were similar to those with lcSSc and better than those with dcSSc.
IN PRACTICE:
“The results presented herein suggest a slightly more severe yet similar clinical picture of ssSSc compared to lcSSc [limited cutaneous SSc], while dcSSc [diffuse cutaneous SSc] remains the most severe disease form,” the authors wrote. “Although classification criteria should not impact appropriate management of patients, updated ssSSc subclassification criteria, which will take into account time from disease onset, should be considered,” they further added.
SOURCE:
The study was led by Anastasios Makris, MD, First Department of Propaedeutic & Internal Medicine, National and Kapodistrian University of Athens, Medical School, Athens, Greece. It was published online on August 15, 2024, in The Journal of Rheumatology.
LIMITATIONS:
The variability in the classification criteria across different studies may affect the comparability of results. The included studies lacked data on cardiac MRI, restricting the identification of myocardial fibrosis patterns and characterization of cardiac disease activity.
DISCLOSURES:
The study did not receive any specific funding. Some authors disclosed having a consultancy relationship, serving as speakers, and receiving funding for research from multiple companies. One author reported having a patent and being a cofounder of CITUS AG.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Ustekinumab’s ‘Egregious’ Medicare Part B and D Pricing Differences Led to Federal Intervention
A US government report showed how a Medicare policy change made the drug ustekinumab (Stelara) for autoimmune diseases much more expensive, a finding that experts say illustrates the need for reforms created by the Inflation Reduction Act of 2022 (IRA).
The topline findings of an August report from the Department of Health and Human Services (HHS) about ustekinumab may seem somewhat surprising and a bit counterintuitive.
Ustekinumab costs spiked as Medicare pushed patients to get their supply through the Part D pharmacy program. The aim of Part D is to make medicines more affordable and accessible for patients. It runs on a model of insurers to negotiate deals for pharmaceuticals.
Earlier, many patients who needed ustekinumab had the drug covered by Medicare Part B. For many years, Medicare Part B has been largely a passive purchaser of medicines. Part B covers drugs administered by physicians. Its longtime model has been to add a premium of 6% to the reported average sales price to reimburse physicians who buy and administer the drug for patients.
But it was Part D, the Medicare program based on insurers’ negotiating clout, that saw a spike in ustekinumab costs after patients were shifted out of Part B coverage, where the cost of the medicine fell.
The average reported Part B cost for an ustekinumab injection slipped from $14,450 in 2016 to $12,912 by 2023, according to the report from HHS’ Office of Inspector General (OIG).
The Part D cost jumped in the same period. It rose by 84% from $17,717 in 2016 to $32,559 by 2023.
The IRA is intended to curb these kinds of increases in the future for drugs covered by Medicare, said Stacie B. Dusetzina, PhD, professor of health policy at Vanderbilt University School of Medicine, Nashville, Tennessee. The law demands companies pay rebates to Medicare if they increase drug prices faster than consumer inflation.
“That should at least help with some of this price growth that over time has seemed quite egregious,” Dr. Dusetzina told this news organization.
The IRA contains several provisions intended to curb rising drug costs for people enrolled in Medicare, including allowing the federal government to directly negotiate on some medicines.
Ustekinumab is one of the first 10 medicines that are subject to negotiations. Medicare will select as many as 15 additional drugs covered under Part D for negotiation in 2025, another 15 Part B and D drugs in 2026, and up to 20 drugs every year after that.
Earlier in August, the Centers for Medicare & Medicaid Services (CMS) announced the results of its first drug negotiations, with prices set to take effect in 2026. The Part D price for a 30-day supply of ustekinumab will be $4695 in 2026, a 66% reduction from the list price last year of $13,836.
Even at the negotiated price, ustekinumab’s cost will be high enough to trigger a new cap on out-of-pocket Part D spending, Dr. Dusetzina said.
Starting in 2025, Part D will have a cap of $2000 on individuals’ out-of-pocket costs, with annual adjustments in future years.
“It may not be better for someone who was filling this on Part B, who had a supplement [that covered their share of the ustekinumab cost], but it will be better for a lot of people that it’s covered under Part D,” Dr. Dusetzina said. “The good news is that at least from a beneficiary affordability standpoint, they’re going to have some price protection.”
OIG noted that the US Food and Drug Administration has approved three competing biosimilar versions of ustekinumab. These could also potentially work to lower costs.
‘A Complicated and Not Particularly Transparent Process’
OIG said it expects to release a report later this year with more detail about the decision that shifted ustekinumab coverage from Part B to Part D.
First cleared for US sales in 2009, ustekinumab is approved for psoriasis, psoriatic arthritis, Crohn’s disease, and ulcerative colitis. It can be given subcutaneously or intravenously.
Part B does not generally cover self-administered drugs. The infused version of ustekinumab has been covered under Medicare Part B since it reached the market.
“However, Part B coverage of the subcutaneous versions has been less straightforward,” OIG said in the report.
In 2020, Medicare administrative contractors — the units or affiliates of insurers that for decades have processed Part B claims for the traditional Medicare programs — determined that subcutaneous ustekinumab did not meet the criteria for coverage under Part B. Implementation of this change was delayed due to the COVID public health emergency but has since taken effect.
The shift in ustekinumab coverage to Part D eroded financial protections of many people on Medicare when Part B covered the drug.
Almost 9 in 10 people enrolled in Medicare Part B have supplemental insurance such as Medigap, employer coverage, or Medicaid to fully or partially cover their cost-sharing requirements, the OIG report said. That means Part B coverage shielded many patients from high ustekinumab costs.
In contrast, patients who self-administered the drug at home under Part D coverage paid an average of almost $6000 out of pocket if they did not receive any type of financial assistance, OIG said.
“From a financial standpoint, as long as you have Part B coinsurance, it would be much cheaper to get the drug in your doctor’s office than getting it through a pharmacy, unless you qualify for the low-income subsidy,” OIG Regional Inspector General David Tawes, who supervised the team that produced the report, told this news organization.
OIG has previously reported that post–point-of-sale rebates paid by manufacturers sometimes lower the costs incurred by Part D plans by a significant margin. But this was not the case with ustekinumab. Instead, OIG said the gap between initial and actual costs of ustekinumab was reduced by less than one third even with rebates. Rebate information is considered confidential.
“The whole negotiation structure is a complicated and not particularly transparent process,” Mr. Tawes said.
Backchannel Discounts, Top-Line Prices
The IRA is bringing some more transparency to the process through negotiations, said Mariana P. Socal, MD, associate professor at the Johns Hopkins Bloomberg School of Public Health in Baltimore. Patients who buy medicines that have been through the CMS negotiation process will be able to see if they are being charged correctly.
Dr. Socal noted that there’s something of a disconnect in discussions of Part D between how insurers and consumers view prices.
For Part D plans, the list prices represent the beginning of negotiations. They get rebates from drugmakers’ list prices for medicines, which insurers say work to lower premium costs.
“For plans, those prices are unrealistic. They are simply a sticker price. But for patients, for the Medicare beneficiaries, these prices are very real” because they are used to set copays, Dr. Socal said.
Dr. Dusetzina reported receiving funding from Arnold Ventures and the Commonwealth Fund for research related to drug pricing. Dr. Socal reported receiving funding from Arnold Ventures.
A version of this article first appeared on Medscape.com.
A US government report showed how a Medicare policy change made the drug ustekinumab (Stelara) for autoimmune diseases much more expensive, a finding that experts say illustrates the need for reforms created by the Inflation Reduction Act of 2022 (IRA).
The topline findings of an August report from the Department of Health and Human Services (HHS) about ustekinumab may seem somewhat surprising and a bit counterintuitive.
Ustekinumab costs spiked as Medicare pushed patients to get their supply through the Part D pharmacy program. The aim of Part D is to make medicines more affordable and accessible for patients. It runs on a model of insurers to negotiate deals for pharmaceuticals.
Earlier, many patients who needed ustekinumab had the drug covered by Medicare Part B. For many years, Medicare Part B has been largely a passive purchaser of medicines. Part B covers drugs administered by physicians. Its longtime model has been to add a premium of 6% to the reported average sales price to reimburse physicians who buy and administer the drug for patients.
But it was Part D, the Medicare program based on insurers’ negotiating clout, that saw a spike in ustekinumab costs after patients were shifted out of Part B coverage, where the cost of the medicine fell.
The average reported Part B cost for an ustekinumab injection slipped from $14,450 in 2016 to $12,912 by 2023, according to the report from HHS’ Office of Inspector General (OIG).
The Part D cost jumped in the same period. It rose by 84% from $17,717 in 2016 to $32,559 by 2023.
The IRA is intended to curb these kinds of increases in the future for drugs covered by Medicare, said Stacie B. Dusetzina, PhD, professor of health policy at Vanderbilt University School of Medicine, Nashville, Tennessee. The law demands companies pay rebates to Medicare if they increase drug prices faster than consumer inflation.
“That should at least help with some of this price growth that over time has seemed quite egregious,” Dr. Dusetzina told this news organization.
The IRA contains several provisions intended to curb rising drug costs for people enrolled in Medicare, including allowing the federal government to directly negotiate on some medicines.
Ustekinumab is one of the first 10 medicines that are subject to negotiations. Medicare will select as many as 15 additional drugs covered under Part D for negotiation in 2025, another 15 Part B and D drugs in 2026, and up to 20 drugs every year after that.
Earlier in August, the Centers for Medicare & Medicaid Services (CMS) announced the results of its first drug negotiations, with prices set to take effect in 2026. The Part D price for a 30-day supply of ustekinumab will be $4695 in 2026, a 66% reduction from the list price last year of $13,836.
Even at the negotiated price, ustekinumab’s cost will be high enough to trigger a new cap on out-of-pocket Part D spending, Dr. Dusetzina said.
Starting in 2025, Part D will have a cap of $2000 on individuals’ out-of-pocket costs, with annual adjustments in future years.
“It may not be better for someone who was filling this on Part B, who had a supplement [that covered their share of the ustekinumab cost], but it will be better for a lot of people that it’s covered under Part D,” Dr. Dusetzina said. “The good news is that at least from a beneficiary affordability standpoint, they’re going to have some price protection.”
OIG noted that the US Food and Drug Administration has approved three competing biosimilar versions of ustekinumab. These could also potentially work to lower costs.
‘A Complicated and Not Particularly Transparent Process’
OIG said it expects to release a report later this year with more detail about the decision that shifted ustekinumab coverage from Part B to Part D.
First cleared for US sales in 2009, ustekinumab is approved for psoriasis, psoriatic arthritis, Crohn’s disease, and ulcerative colitis. It can be given subcutaneously or intravenously.
Part B does not generally cover self-administered drugs. The infused version of ustekinumab has been covered under Medicare Part B since it reached the market.
“However, Part B coverage of the subcutaneous versions has been less straightforward,” OIG said in the report.
In 2020, Medicare administrative contractors — the units or affiliates of insurers that for decades have processed Part B claims for the traditional Medicare programs — determined that subcutaneous ustekinumab did not meet the criteria for coverage under Part B. Implementation of this change was delayed due to the COVID public health emergency but has since taken effect.
The shift in ustekinumab coverage to Part D eroded financial protections of many people on Medicare when Part B covered the drug.
Almost 9 in 10 people enrolled in Medicare Part B have supplemental insurance such as Medigap, employer coverage, or Medicaid to fully or partially cover their cost-sharing requirements, the OIG report said. That means Part B coverage shielded many patients from high ustekinumab costs.
In contrast, patients who self-administered the drug at home under Part D coverage paid an average of almost $6000 out of pocket if they did not receive any type of financial assistance, OIG said.
“From a financial standpoint, as long as you have Part B coinsurance, it would be much cheaper to get the drug in your doctor’s office than getting it through a pharmacy, unless you qualify for the low-income subsidy,” OIG Regional Inspector General David Tawes, who supervised the team that produced the report, told this news organization.
OIG has previously reported that post–point-of-sale rebates paid by manufacturers sometimes lower the costs incurred by Part D plans by a significant margin. But this was not the case with ustekinumab. Instead, OIG said the gap between initial and actual costs of ustekinumab was reduced by less than one third even with rebates. Rebate information is considered confidential.
“The whole negotiation structure is a complicated and not particularly transparent process,” Mr. Tawes said.
Backchannel Discounts, Top-Line Prices
The IRA is bringing some more transparency to the process through negotiations, said Mariana P. Socal, MD, associate professor at the Johns Hopkins Bloomberg School of Public Health in Baltimore. Patients who buy medicines that have been through the CMS negotiation process will be able to see if they are being charged correctly.
Dr. Socal noted that there’s something of a disconnect in discussions of Part D between how insurers and consumers view prices.
For Part D plans, the list prices represent the beginning of negotiations. They get rebates from drugmakers’ list prices for medicines, which insurers say work to lower premium costs.
“For plans, those prices are unrealistic. They are simply a sticker price. But for patients, for the Medicare beneficiaries, these prices are very real” because they are used to set copays, Dr. Socal said.
Dr. Dusetzina reported receiving funding from Arnold Ventures and the Commonwealth Fund for research related to drug pricing. Dr. Socal reported receiving funding from Arnold Ventures.
A version of this article first appeared on Medscape.com.
A US government report showed how a Medicare policy change made the drug ustekinumab (Stelara) for autoimmune diseases much more expensive, a finding that experts say illustrates the need for reforms created by the Inflation Reduction Act of 2022 (IRA).
The topline findings of an August report from the Department of Health and Human Services (HHS) about ustekinumab may seem somewhat surprising and a bit counterintuitive.
Ustekinumab costs spiked as Medicare pushed patients to get their supply through the Part D pharmacy program. The aim of Part D is to make medicines more affordable and accessible for patients. It runs on a model of insurers to negotiate deals for pharmaceuticals.
Earlier, many patients who needed ustekinumab had the drug covered by Medicare Part B. For many years, Medicare Part B has been largely a passive purchaser of medicines. Part B covers drugs administered by physicians. Its longtime model has been to add a premium of 6% to the reported average sales price to reimburse physicians who buy and administer the drug for patients.
But it was Part D, the Medicare program based on insurers’ negotiating clout, that saw a spike in ustekinumab costs after patients were shifted out of Part B coverage, where the cost of the medicine fell.
The average reported Part B cost for an ustekinumab injection slipped from $14,450 in 2016 to $12,912 by 2023, according to the report from HHS’ Office of Inspector General (OIG).
The Part D cost jumped in the same period. It rose by 84% from $17,717 in 2016 to $32,559 by 2023.
The IRA is intended to curb these kinds of increases in the future for drugs covered by Medicare, said Stacie B. Dusetzina, PhD, professor of health policy at Vanderbilt University School of Medicine, Nashville, Tennessee. The law demands companies pay rebates to Medicare if they increase drug prices faster than consumer inflation.
“That should at least help with some of this price growth that over time has seemed quite egregious,” Dr. Dusetzina told this news organization.
The IRA contains several provisions intended to curb rising drug costs for people enrolled in Medicare, including allowing the federal government to directly negotiate on some medicines.
Ustekinumab is one of the first 10 medicines that are subject to negotiations. Medicare will select as many as 15 additional drugs covered under Part D for negotiation in 2025, another 15 Part B and D drugs in 2026, and up to 20 drugs every year after that.
Earlier in August, the Centers for Medicare & Medicaid Services (CMS) announced the results of its first drug negotiations, with prices set to take effect in 2026. The Part D price for a 30-day supply of ustekinumab will be $4695 in 2026, a 66% reduction from the list price last year of $13,836.
Even at the negotiated price, ustekinumab’s cost will be high enough to trigger a new cap on out-of-pocket Part D spending, Dr. Dusetzina said.
Starting in 2025, Part D will have a cap of $2000 on individuals’ out-of-pocket costs, with annual adjustments in future years.
“It may not be better for someone who was filling this on Part B, who had a supplement [that covered their share of the ustekinumab cost], but it will be better for a lot of people that it’s covered under Part D,” Dr. Dusetzina said. “The good news is that at least from a beneficiary affordability standpoint, they’re going to have some price protection.”
OIG noted that the US Food and Drug Administration has approved three competing biosimilar versions of ustekinumab. These could also potentially work to lower costs.
‘A Complicated and Not Particularly Transparent Process’
OIG said it expects to release a report later this year with more detail about the decision that shifted ustekinumab coverage from Part B to Part D.
First cleared for US sales in 2009, ustekinumab is approved for psoriasis, psoriatic arthritis, Crohn’s disease, and ulcerative colitis. It can be given subcutaneously or intravenously.
Part B does not generally cover self-administered drugs. The infused version of ustekinumab has been covered under Medicare Part B since it reached the market.
“However, Part B coverage of the subcutaneous versions has been less straightforward,” OIG said in the report.
In 2020, Medicare administrative contractors — the units or affiliates of insurers that for decades have processed Part B claims for the traditional Medicare programs — determined that subcutaneous ustekinumab did not meet the criteria for coverage under Part B. Implementation of this change was delayed due to the COVID public health emergency but has since taken effect.
The shift in ustekinumab coverage to Part D eroded financial protections of many people on Medicare when Part B covered the drug.
Almost 9 in 10 people enrolled in Medicare Part B have supplemental insurance such as Medigap, employer coverage, or Medicaid to fully or partially cover their cost-sharing requirements, the OIG report said. That means Part B coverage shielded many patients from high ustekinumab costs.
In contrast, patients who self-administered the drug at home under Part D coverage paid an average of almost $6000 out of pocket if they did not receive any type of financial assistance, OIG said.
“From a financial standpoint, as long as you have Part B coinsurance, it would be much cheaper to get the drug in your doctor’s office than getting it through a pharmacy, unless you qualify for the low-income subsidy,” OIG Regional Inspector General David Tawes, who supervised the team that produced the report, told this news organization.
OIG has previously reported that post–point-of-sale rebates paid by manufacturers sometimes lower the costs incurred by Part D plans by a significant margin. But this was not the case with ustekinumab. Instead, OIG said the gap between initial and actual costs of ustekinumab was reduced by less than one third even with rebates. Rebate information is considered confidential.
“The whole negotiation structure is a complicated and not particularly transparent process,” Mr. Tawes said.
Backchannel Discounts, Top-Line Prices
The IRA is bringing some more transparency to the process through negotiations, said Mariana P. Socal, MD, associate professor at the Johns Hopkins Bloomberg School of Public Health in Baltimore. Patients who buy medicines that have been through the CMS negotiation process will be able to see if they are being charged correctly.
Dr. Socal noted that there’s something of a disconnect in discussions of Part D between how insurers and consumers view prices.
For Part D plans, the list prices represent the beginning of negotiations. They get rebates from drugmakers’ list prices for medicines, which insurers say work to lower premium costs.
“For plans, those prices are unrealistic. They are simply a sticker price. But for patients, for the Medicare beneficiaries, these prices are very real” because they are used to set copays, Dr. Socal said.
Dr. Dusetzina reported receiving funding from Arnold Ventures and the Commonwealth Fund for research related to drug pricing. Dr. Socal reported receiving funding from Arnold Ventures.
A version of this article first appeared on Medscape.com.
More Than the Paycheck: Top Non-Salary Perks for Doctors
Holly Wyatt, MD, had spent 20 years in UCHealth with no plans to leave. Her home, support system, and lifestyle were all rooted in Denver. But in 2020, The University of Alabama at Birmingham (UAB) made the endocrinologist an offer she couldn’t resist.
The pay increase and a bump to full professorship weren’t enough to lure her across the country. But then UAB sweetened the deal with fewer clinic hours and paid time to create. “I didn’t have to fit into the typical ‘see patients 5 days a week, bill this many dollars,’ ” she said.
With no minimum billable hours, she could spend her time on clinical trials, designing programs, and recording podcasts. “When they offered that, I said, ‘Ooh, that’s enticing.’ ”
After a couple of visits to the campus, she began the job transition.
Doctors are looking for more than base pay. For many physicians, like Dr. Wyatt, non-salary incentives carry a lot of weight in the recruitment and job-hunting process.
“Some of the usual suspects are CME [continuing medical education] budget, signing bonuses, relocation assistance, loan repayment programs, and housing allowances,” said Jake Jorgovan, partner at Alpha Apex Group, a physician recruiting firm in Denver.
Post pandemic, doctors are vying for other benefits, perks that support their interests, work-life balance, and financial stability. “We’ve come across offers like sabbatical opportunities, paid time for research or personal projects, and even concierge services that handle things like grocery shopping or pet care,” said Mr. Jorgovan.
Amid physician shortages, doctors have more bargaining power than ever.
Money Still Talks
Financial perks are still the premiere portion of a benefits package, according to Marc Adam, physician recruiter at MASC Medical, a medical recruitment firm in Fort Lauderdale, Florida.
New data from the medical staffing company AMN Healthcare reported that the average signing bonus for physicians is $31,103. The average relocation allowance is $11,000, and the average CME allowance is $4000.
“CME budget and loan repayment programs are big because they directly impact career advancement and financial well-being,” Mr. Jorgovan said. Employers have historically been hesitant to offer these kinds of long-term benefits because of the financial commitment and planning involved, but that’s changing.
Mr. Adam said that short-term financial perks, like relocation assistance and signing bonuses, tend to be more important for younger doctors. They’re not yet financially established, so the relocation support and bonus funds have more impact as they take on a new role, he said.
Mid- and late-career doctors, on the other hand, are less beholden to these types of bonuses. Mr. Adam has recruited established doctors from across the country to Florida, and he said that the relocation allowance and singing bonus didn’t even rank in their top five priorities. Similarly, in Birmingham, Dr. Wyatt recently reread her offer letter from UAB and was surprised to find a relocation stipend that she never used. “I had no idea,” she said.
Vying for Time
Mid- and late-career doctors who have a better financial safety net tend to seek benefits that boost their quality of life.
One of Mr. Adam’s recent job-searching clients was unwilling to compromise on priorities like specific location and a 4-day workweek.
Four-day workweeks, flexible scheduling, and options for remote work are increasingly popular, especially since the pandemic. Some physicians, like those in primary care, are looking for dedicated charting hours — paid days or half-days set aside for updating the electronic medical records. Other doctors are negotiating multistate telehealth licensing paid by their employer and work-from-home telehealth hours.
“Work life has been slowly increasing over the 14 years I’ve been doing this. And post COVID, the employer’s willingness to be flexible with those types of accommodations increased,” said Mr. Adam.
Priya Jaisinghani, MD, an endocrinologist and obesity medicine specialist in her second year of practice, NYU Langone Health, New York City, said work-life balance can be a priority for young doctors, too. After training in New York during the pandemic, Dr. Jaisinghani was all too aware of the risk for burnout. So she negotiated a 4-day workweek when she took her first job out of fellowship in 2022. “I was able to prioritize work-life balance from the start,” she said.
Support for the Career You Want
When Dr. Jaisinghani signed her first contract in 2022 with NYU, her move from New Jersey to New York wasn’t far enough to warrant a relocation allowance. “There was a signing bonus, sure,” she said. But what really grabbed her attention were perks like mentorship, access to trainees, and autonomy.
Perks that support long-term growth — like CME allowance, teaching opportunities, or access to leadership tracks — are especially important to young doctors. “After dedicating so many years to medical training, you want to look for some degree of autonomy in building your practice,” she said. NYU offered her that kind of freedom and support.
On top of personal growth, young physicians are looking for perks that will allow them to build the practice they want for their patients,Dr. Jaisinghani told this news organization. A lot of young doctors don’t know that they can negotiate for schedule preferences, office space, their own exam room, and dedicated support staff. However, they can and should because these factors influence their daily work life and patient experience.
Experienced doctors are also looking for perks that support the career they want. Recruitment experts say that doctors tend to look for opportunities that accommodate their interests. One of Mr. Jorgovan’s recent clients took a position because it offered a generous CME budget and dedicated research hours. Similarly, Dr. Wyatt at UAB moved because her contract included paid time to create.
“It really comes down to the need for balance — being able to keep learning while also having time for personal life and family,” Mr. Jorgovan said.
Making and Meeting Demand
Thanks to the rising demand, doctors have more power than ever to negotiate the perks they want and need.
The existing physician shortage — driven by retiring doctors and an aging patient population — was only exacerbated by the pandemic. Now, a number of new market entries are further increasing competition for talent, according to AMN Healthcare’s report. Retail clinics, urgent care, telehealth companies, and private equity firms compete for the same doctors, driving up salaries and doctor bargaining power.
“Physicians were always in the driver’s seat, and their bargaining power has only increased,” Mr. Adam said. Healthcare systems, once reticent about flexible working arrangements or loan repayment, are reconsidering.
Even young doctors have more negotiating power than they realize, but they might need help. “It’s underrated to get a contracts lawyer as a young doctor, but I think it’s smart,” Dr. Jaisinghani said. They’re often more familiar with salaries in the area, flexibility options, and potential benefits, none of which doctors are taught in training, she said.
Mr. Adam said that the pandemic opened employers’ eyes to the fact that doctors have the bargaining power. There’s a stark need for their talent and a lot of public support for their service. So hiring managers are listening and are ready to offer “creative benefits to accommodate the market demand,” he said.
In her new position at UAB, Dr. Wyatt said that money will always matter. “When your salary is low, bumping that salary will make you happier.” But after a certain point, she said, other things become more important — like your time, the work you do, and the people you work with. Her perks at UAB offer more than money can. “I get up in the morning, and I’m excited — [the work] excites me,” she said.
A version of this article first appeared on Medscape.com.
Holly Wyatt, MD, had spent 20 years in UCHealth with no plans to leave. Her home, support system, and lifestyle were all rooted in Denver. But in 2020, The University of Alabama at Birmingham (UAB) made the endocrinologist an offer she couldn’t resist.
The pay increase and a bump to full professorship weren’t enough to lure her across the country. But then UAB sweetened the deal with fewer clinic hours and paid time to create. “I didn’t have to fit into the typical ‘see patients 5 days a week, bill this many dollars,’ ” she said.
With no minimum billable hours, she could spend her time on clinical trials, designing programs, and recording podcasts. “When they offered that, I said, ‘Ooh, that’s enticing.’ ”
After a couple of visits to the campus, she began the job transition.
Doctors are looking for more than base pay. For many physicians, like Dr. Wyatt, non-salary incentives carry a lot of weight in the recruitment and job-hunting process.
“Some of the usual suspects are CME [continuing medical education] budget, signing bonuses, relocation assistance, loan repayment programs, and housing allowances,” said Jake Jorgovan, partner at Alpha Apex Group, a physician recruiting firm in Denver.
Post pandemic, doctors are vying for other benefits, perks that support their interests, work-life balance, and financial stability. “We’ve come across offers like sabbatical opportunities, paid time for research or personal projects, and even concierge services that handle things like grocery shopping or pet care,” said Mr. Jorgovan.
Amid physician shortages, doctors have more bargaining power than ever.
Money Still Talks
Financial perks are still the premiere portion of a benefits package, according to Marc Adam, physician recruiter at MASC Medical, a medical recruitment firm in Fort Lauderdale, Florida.
New data from the medical staffing company AMN Healthcare reported that the average signing bonus for physicians is $31,103. The average relocation allowance is $11,000, and the average CME allowance is $4000.
“CME budget and loan repayment programs are big because they directly impact career advancement and financial well-being,” Mr. Jorgovan said. Employers have historically been hesitant to offer these kinds of long-term benefits because of the financial commitment and planning involved, but that’s changing.
Mr. Adam said that short-term financial perks, like relocation assistance and signing bonuses, tend to be more important for younger doctors. They’re not yet financially established, so the relocation support and bonus funds have more impact as they take on a new role, he said.
Mid- and late-career doctors, on the other hand, are less beholden to these types of bonuses. Mr. Adam has recruited established doctors from across the country to Florida, and he said that the relocation allowance and singing bonus didn’t even rank in their top five priorities. Similarly, in Birmingham, Dr. Wyatt recently reread her offer letter from UAB and was surprised to find a relocation stipend that she never used. “I had no idea,” she said.
Vying for Time
Mid- and late-career doctors who have a better financial safety net tend to seek benefits that boost their quality of life.
One of Mr. Adam’s recent job-searching clients was unwilling to compromise on priorities like specific location and a 4-day workweek.
Four-day workweeks, flexible scheduling, and options for remote work are increasingly popular, especially since the pandemic. Some physicians, like those in primary care, are looking for dedicated charting hours — paid days or half-days set aside for updating the electronic medical records. Other doctors are negotiating multistate telehealth licensing paid by their employer and work-from-home telehealth hours.
“Work life has been slowly increasing over the 14 years I’ve been doing this. And post COVID, the employer’s willingness to be flexible with those types of accommodations increased,” said Mr. Adam.
Priya Jaisinghani, MD, an endocrinologist and obesity medicine specialist in her second year of practice, NYU Langone Health, New York City, said work-life balance can be a priority for young doctors, too. After training in New York during the pandemic, Dr. Jaisinghani was all too aware of the risk for burnout. So she negotiated a 4-day workweek when she took her first job out of fellowship in 2022. “I was able to prioritize work-life balance from the start,” she said.
Support for the Career You Want
When Dr. Jaisinghani signed her first contract in 2022 with NYU, her move from New Jersey to New York wasn’t far enough to warrant a relocation allowance. “There was a signing bonus, sure,” she said. But what really grabbed her attention were perks like mentorship, access to trainees, and autonomy.
Perks that support long-term growth — like CME allowance, teaching opportunities, or access to leadership tracks — are especially important to young doctors. “After dedicating so many years to medical training, you want to look for some degree of autonomy in building your practice,” she said. NYU offered her that kind of freedom and support.
On top of personal growth, young physicians are looking for perks that will allow them to build the practice they want for their patients,Dr. Jaisinghani told this news organization. A lot of young doctors don’t know that they can negotiate for schedule preferences, office space, their own exam room, and dedicated support staff. However, they can and should because these factors influence their daily work life and patient experience.
Experienced doctors are also looking for perks that support the career they want. Recruitment experts say that doctors tend to look for opportunities that accommodate their interests. One of Mr. Jorgovan’s recent clients took a position because it offered a generous CME budget and dedicated research hours. Similarly, Dr. Wyatt at UAB moved because her contract included paid time to create.
“It really comes down to the need for balance — being able to keep learning while also having time for personal life and family,” Mr. Jorgovan said.
Making and Meeting Demand
Thanks to the rising demand, doctors have more power than ever to negotiate the perks they want and need.
The existing physician shortage — driven by retiring doctors and an aging patient population — was only exacerbated by the pandemic. Now, a number of new market entries are further increasing competition for talent, according to AMN Healthcare’s report. Retail clinics, urgent care, telehealth companies, and private equity firms compete for the same doctors, driving up salaries and doctor bargaining power.
“Physicians were always in the driver’s seat, and their bargaining power has only increased,” Mr. Adam said. Healthcare systems, once reticent about flexible working arrangements or loan repayment, are reconsidering.
Even young doctors have more negotiating power than they realize, but they might need help. “It’s underrated to get a contracts lawyer as a young doctor, but I think it’s smart,” Dr. Jaisinghani said. They’re often more familiar with salaries in the area, flexibility options, and potential benefits, none of which doctors are taught in training, she said.
Mr. Adam said that the pandemic opened employers’ eyes to the fact that doctors have the bargaining power. There’s a stark need for their talent and a lot of public support for their service. So hiring managers are listening and are ready to offer “creative benefits to accommodate the market demand,” he said.
In her new position at UAB, Dr. Wyatt said that money will always matter. “When your salary is low, bumping that salary will make you happier.” But after a certain point, she said, other things become more important — like your time, the work you do, and the people you work with. Her perks at UAB offer more than money can. “I get up in the morning, and I’m excited — [the work] excites me,” she said.
A version of this article first appeared on Medscape.com.
Holly Wyatt, MD, had spent 20 years in UCHealth with no plans to leave. Her home, support system, and lifestyle were all rooted in Denver. But in 2020, The University of Alabama at Birmingham (UAB) made the endocrinologist an offer she couldn’t resist.
The pay increase and a bump to full professorship weren’t enough to lure her across the country. But then UAB sweetened the deal with fewer clinic hours and paid time to create. “I didn’t have to fit into the typical ‘see patients 5 days a week, bill this many dollars,’ ” she said.
With no minimum billable hours, she could spend her time on clinical trials, designing programs, and recording podcasts. “When they offered that, I said, ‘Ooh, that’s enticing.’ ”
After a couple of visits to the campus, she began the job transition.
Doctors are looking for more than base pay. For many physicians, like Dr. Wyatt, non-salary incentives carry a lot of weight in the recruitment and job-hunting process.
“Some of the usual suspects are CME [continuing medical education] budget, signing bonuses, relocation assistance, loan repayment programs, and housing allowances,” said Jake Jorgovan, partner at Alpha Apex Group, a physician recruiting firm in Denver.
Post pandemic, doctors are vying for other benefits, perks that support their interests, work-life balance, and financial stability. “We’ve come across offers like sabbatical opportunities, paid time for research or personal projects, and even concierge services that handle things like grocery shopping or pet care,” said Mr. Jorgovan.
Amid physician shortages, doctors have more bargaining power than ever.
Money Still Talks
Financial perks are still the premiere portion of a benefits package, according to Marc Adam, physician recruiter at MASC Medical, a medical recruitment firm in Fort Lauderdale, Florida.
New data from the medical staffing company AMN Healthcare reported that the average signing bonus for physicians is $31,103. The average relocation allowance is $11,000, and the average CME allowance is $4000.
“CME budget and loan repayment programs are big because they directly impact career advancement and financial well-being,” Mr. Jorgovan said. Employers have historically been hesitant to offer these kinds of long-term benefits because of the financial commitment and planning involved, but that’s changing.
Mr. Adam said that short-term financial perks, like relocation assistance and signing bonuses, tend to be more important for younger doctors. They’re not yet financially established, so the relocation support and bonus funds have more impact as they take on a new role, he said.
Mid- and late-career doctors, on the other hand, are less beholden to these types of bonuses. Mr. Adam has recruited established doctors from across the country to Florida, and he said that the relocation allowance and singing bonus didn’t even rank in their top five priorities. Similarly, in Birmingham, Dr. Wyatt recently reread her offer letter from UAB and was surprised to find a relocation stipend that she never used. “I had no idea,” she said.
Vying for Time
Mid- and late-career doctors who have a better financial safety net tend to seek benefits that boost their quality of life.
One of Mr. Adam’s recent job-searching clients was unwilling to compromise on priorities like specific location and a 4-day workweek.
Four-day workweeks, flexible scheduling, and options for remote work are increasingly popular, especially since the pandemic. Some physicians, like those in primary care, are looking for dedicated charting hours — paid days or half-days set aside for updating the electronic medical records. Other doctors are negotiating multistate telehealth licensing paid by their employer and work-from-home telehealth hours.
“Work life has been slowly increasing over the 14 years I’ve been doing this. And post COVID, the employer’s willingness to be flexible with those types of accommodations increased,” said Mr. Adam.
Priya Jaisinghani, MD, an endocrinologist and obesity medicine specialist in her second year of practice, NYU Langone Health, New York City, said work-life balance can be a priority for young doctors, too. After training in New York during the pandemic, Dr. Jaisinghani was all too aware of the risk for burnout. So she negotiated a 4-day workweek when she took her first job out of fellowship in 2022. “I was able to prioritize work-life balance from the start,” she said.
Support for the Career You Want
When Dr. Jaisinghani signed her first contract in 2022 with NYU, her move from New Jersey to New York wasn’t far enough to warrant a relocation allowance. “There was a signing bonus, sure,” she said. But what really grabbed her attention were perks like mentorship, access to trainees, and autonomy.
Perks that support long-term growth — like CME allowance, teaching opportunities, or access to leadership tracks — are especially important to young doctors. “After dedicating so many years to medical training, you want to look for some degree of autonomy in building your practice,” she said. NYU offered her that kind of freedom and support.
On top of personal growth, young physicians are looking for perks that will allow them to build the practice they want for their patients,Dr. Jaisinghani told this news organization. A lot of young doctors don’t know that they can negotiate for schedule preferences, office space, their own exam room, and dedicated support staff. However, they can and should because these factors influence their daily work life and patient experience.
Experienced doctors are also looking for perks that support the career they want. Recruitment experts say that doctors tend to look for opportunities that accommodate their interests. One of Mr. Jorgovan’s recent clients took a position because it offered a generous CME budget and dedicated research hours. Similarly, Dr. Wyatt at UAB moved because her contract included paid time to create.
“It really comes down to the need for balance — being able to keep learning while also having time for personal life and family,” Mr. Jorgovan said.
Making and Meeting Demand
Thanks to the rising demand, doctors have more power than ever to negotiate the perks they want and need.
The existing physician shortage — driven by retiring doctors and an aging patient population — was only exacerbated by the pandemic. Now, a number of new market entries are further increasing competition for talent, according to AMN Healthcare’s report. Retail clinics, urgent care, telehealth companies, and private equity firms compete for the same doctors, driving up salaries and doctor bargaining power.
“Physicians were always in the driver’s seat, and their bargaining power has only increased,” Mr. Adam said. Healthcare systems, once reticent about flexible working arrangements or loan repayment, are reconsidering.
Even young doctors have more negotiating power than they realize, but they might need help. “It’s underrated to get a contracts lawyer as a young doctor, but I think it’s smart,” Dr. Jaisinghani said. They’re often more familiar with salaries in the area, flexibility options, and potential benefits, none of which doctors are taught in training, she said.
Mr. Adam said that the pandemic opened employers’ eyes to the fact that doctors have the bargaining power. There’s a stark need for their talent and a lot of public support for their service. So hiring managers are listening and are ready to offer “creative benefits to accommodate the market demand,” he said.
In her new position at UAB, Dr. Wyatt said that money will always matter. “When your salary is low, bumping that salary will make you happier.” But after a certain point, she said, other things become more important — like your time, the work you do, and the people you work with. Her perks at UAB offer more than money can. “I get up in the morning, and I’m excited — [the work] excites me,” she said.
A version of this article first appeared on Medscape.com.
Seated Doctors Better Satisfy Patients, Communication
During a busy day of consultations, however, it can be difficult for healthcare professionals to sit regularly with patients. Previous studies have revealed that hospital doctors sit during one out of every five meetings with patients.
A recent US study evaluated the impact of the practitioner’s seated position next to the patient on the quality of the doctor-patient interaction in an internal medicine department. This research involved a sample of 51 doctors (average age, 35 years; 51% men) and analyzed 125 clinical interviews (n = 125 patients; average age, 53 years; 55% men). Participants were not informed of the real objective of the study. The patient’s perception of medical care was also solicited.
The experimental protocol involved two distinct configurations. Either the chair was positioned near the bed (within 90 cm) before the doctor arrived or it remained visible in its usual place. Each meeting with a patient was randomized according to the chair location (intervention group: n = 60; control group: n = 65).
The primary criterion was the doctor’s binary decision to sit or not at a given moment during a meeting with a patient. Secondary criteria included patient satisfaction, time spent in the room, and the perception of time spent in the room by doctors and patients.
The chair’s location had no effect on the average duration of the interview, whether actual or estimated. When a chair was placed near the bed, the doctor sat in more than six out of 10 cases (63%), compared with fewer than one case out of 10 (8%) when the chair was less easily accessible (odds ratio, 20.7; 95% CI, 7.2-59.4; P < .001).
The chair arrangement did not lead to a significant difference in the average duration of presence in the room (10.6 min for both groups). Likewise, no notable difference was observed regarding the subjective estimation of this duration from the practitioners’ point of view (9.4 min vs 9.8 min) or from the patients’ point of view (13.1 min vs 13.5 min).
In the group in which the doctor sat to converse, patient satisfaction was significantly higher, with an overall difference of 3.9% (P = .02). Patients felt that the information provided was better (72% vs 52%; P =.03), and their confidence in the proposed care was also higher (58% vs 35%; P = .01). On the other hand, no significant difference appeared between the two groups regarding the information retained by the patient (doctor’s name and reason for hospitalization) or the doctor’s behavior.
The study authors acknowledged the study’s methodological limitations, which included a sample size that was lower than initially projected and the restriction to a single hospital setting. In addition, they noted that all patients were housed in individual rooms, which could be a source of bias. Despite these reservations, they suggested that even minimal environmental changes, such as the thoughtful placement of a chair, can significantly affect patients’ perceptions of the quality of care provided.
This story was translated from JIM, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
During a busy day of consultations, however, it can be difficult for healthcare professionals to sit regularly with patients. Previous studies have revealed that hospital doctors sit during one out of every five meetings with patients.
A recent US study evaluated the impact of the practitioner’s seated position next to the patient on the quality of the doctor-patient interaction in an internal medicine department. This research involved a sample of 51 doctors (average age, 35 years; 51% men) and analyzed 125 clinical interviews (n = 125 patients; average age, 53 years; 55% men). Participants were not informed of the real objective of the study. The patient’s perception of medical care was also solicited.
The experimental protocol involved two distinct configurations. Either the chair was positioned near the bed (within 90 cm) before the doctor arrived or it remained visible in its usual place. Each meeting with a patient was randomized according to the chair location (intervention group: n = 60; control group: n = 65).
The primary criterion was the doctor’s binary decision to sit or not at a given moment during a meeting with a patient. Secondary criteria included patient satisfaction, time spent in the room, and the perception of time spent in the room by doctors and patients.
The chair’s location had no effect on the average duration of the interview, whether actual or estimated. When a chair was placed near the bed, the doctor sat in more than six out of 10 cases (63%), compared with fewer than one case out of 10 (8%) when the chair was less easily accessible (odds ratio, 20.7; 95% CI, 7.2-59.4; P < .001).
The chair arrangement did not lead to a significant difference in the average duration of presence in the room (10.6 min for both groups). Likewise, no notable difference was observed regarding the subjective estimation of this duration from the practitioners’ point of view (9.4 min vs 9.8 min) or from the patients’ point of view (13.1 min vs 13.5 min).
In the group in which the doctor sat to converse, patient satisfaction was significantly higher, with an overall difference of 3.9% (P = .02). Patients felt that the information provided was better (72% vs 52%; P =.03), and their confidence in the proposed care was also higher (58% vs 35%; P = .01). On the other hand, no significant difference appeared between the two groups regarding the information retained by the patient (doctor’s name and reason for hospitalization) or the doctor’s behavior.
The study authors acknowledged the study’s methodological limitations, which included a sample size that was lower than initially projected and the restriction to a single hospital setting. In addition, they noted that all patients were housed in individual rooms, which could be a source of bias. Despite these reservations, they suggested that even minimal environmental changes, such as the thoughtful placement of a chair, can significantly affect patients’ perceptions of the quality of care provided.
This story was translated from JIM, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
During a busy day of consultations, however, it can be difficult for healthcare professionals to sit regularly with patients. Previous studies have revealed that hospital doctors sit during one out of every five meetings with patients.
A recent US study evaluated the impact of the practitioner’s seated position next to the patient on the quality of the doctor-patient interaction in an internal medicine department. This research involved a sample of 51 doctors (average age, 35 years; 51% men) and analyzed 125 clinical interviews (n = 125 patients; average age, 53 years; 55% men). Participants were not informed of the real objective of the study. The patient’s perception of medical care was also solicited.
The experimental protocol involved two distinct configurations. Either the chair was positioned near the bed (within 90 cm) before the doctor arrived or it remained visible in its usual place. Each meeting with a patient was randomized according to the chair location (intervention group: n = 60; control group: n = 65).
The primary criterion was the doctor’s binary decision to sit or not at a given moment during a meeting with a patient. Secondary criteria included patient satisfaction, time spent in the room, and the perception of time spent in the room by doctors and patients.
The chair’s location had no effect on the average duration of the interview, whether actual or estimated. When a chair was placed near the bed, the doctor sat in more than six out of 10 cases (63%), compared with fewer than one case out of 10 (8%) when the chair was less easily accessible (odds ratio, 20.7; 95% CI, 7.2-59.4; P < .001).
The chair arrangement did not lead to a significant difference in the average duration of presence in the room (10.6 min for both groups). Likewise, no notable difference was observed regarding the subjective estimation of this duration from the practitioners’ point of view (9.4 min vs 9.8 min) or from the patients’ point of view (13.1 min vs 13.5 min).
In the group in which the doctor sat to converse, patient satisfaction was significantly higher, with an overall difference of 3.9% (P = .02). Patients felt that the information provided was better (72% vs 52%; P =.03), and their confidence in the proposed care was also higher (58% vs 35%; P = .01). On the other hand, no significant difference appeared between the two groups regarding the information retained by the patient (doctor’s name and reason for hospitalization) or the doctor’s behavior.
The study authors acknowledged the study’s methodological limitations, which included a sample size that was lower than initially projected and the restriction to a single hospital setting. In addition, they noted that all patients were housed in individual rooms, which could be a source of bias. Despite these reservations, they suggested that even minimal environmental changes, such as the thoughtful placement of a chair, can significantly affect patients’ perceptions of the quality of care provided.
This story was translated from JIM, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Cancer Cases, Deaths in Men Predicted to Surge by 2050
TOPLINE:
— with substantial disparities in cancer cases and deaths by age and region of the world, a recent analysis found.
METHODOLOGY:
- Overall, men have higher cancer incidence and mortality rates, which can be largely attributed to a higher prevalence of modifiable risk factors such as smoking, alcohol consumption, and occupational carcinogens, as well as the underuse of cancer prevention, screening, and treatment services.
- To assess the burden of cancer in men of different ages and from different regions of the world, researchers analyzed data from the 2022 Global Cancer Observatory (GLOBOCAN), which provides national-level estimates for cancer cases and deaths.
- Study outcomes included the incidence, mortality, and prevalence of cancer among men in 2022, along with projections for 2050. Estimates were stratified by several factors, including age; region; and Human Development Index (HDI), a composite score for health, education, and standard of living.
- Researchers also calculated mortality-to-incidence ratios (MIRs) for various cancer types, where higher values indicate worse survival.
TAKEAWAY:
- The researchers reported an estimated 10.3 million cancer cases and 5.4 million deaths globally in 2022, with almost two thirds of cases and deaths occurring in men aged 65 years or older.
- By 2050, cancer cases and deaths were projected to increase by 84.3% (to 19 million) and 93.2% (to 10.5 million), respectively. The increase from 2022 to 2050 was more than twofold higher for older men and countries with low and medium HDI.
- In 2022, the estimated global cancer MIR among men was nearly 55%, with variations by cancer types, age, and HDI. The MIR was lowest for thyroid cancer (7.6%) and highest for pancreatic cancer (90.9%); among World Health Organization regions, Africa had the highest MIR (72.6%), while the Americas had the lowest MIR (39.1%); countries with the lowest HDI had the highest MIR (73.5% vs 41.1% for very high HDI).
- Lung cancer was the leading cause for cases and deaths in 2022 and was projected to remain the leading cause in 2050.
IN PRACTICE:
“Disparities in cancer incidence and mortality among men were observed across age groups, countries/territories, and HDI in 2022, with these disparities projected to widen further by 2050,” according to the authors, who called for efforts to “reduce disparities in cancer burden and ensure equity in cancer prevention and care for men across the globe.”
SOURCE:
The study, led by Habtamu Mellie Bizuayehu, PhD, School of Public Health, Faculty of Medicine, The University of Queensland, Brisbane, Australia, was published online in Cancer.
LIMITATIONS:
The findings may be influenced by the quality of GLOBOCAN data. Interpretation should be cautious as MIR may not fully reflect cancer outcome inequalities. The study did not include other measures of cancer burden, such as years of life lost or years lived with disability, which were unavailable from the data source.
DISCLOSURES:
The authors did not disclose any funding information. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
— with substantial disparities in cancer cases and deaths by age and region of the world, a recent analysis found.
METHODOLOGY:
- Overall, men have higher cancer incidence and mortality rates, which can be largely attributed to a higher prevalence of modifiable risk factors such as smoking, alcohol consumption, and occupational carcinogens, as well as the underuse of cancer prevention, screening, and treatment services.
- To assess the burden of cancer in men of different ages and from different regions of the world, researchers analyzed data from the 2022 Global Cancer Observatory (GLOBOCAN), which provides national-level estimates for cancer cases and deaths.
- Study outcomes included the incidence, mortality, and prevalence of cancer among men in 2022, along with projections for 2050. Estimates were stratified by several factors, including age; region; and Human Development Index (HDI), a composite score for health, education, and standard of living.
- Researchers also calculated mortality-to-incidence ratios (MIRs) for various cancer types, where higher values indicate worse survival.
TAKEAWAY:
- The researchers reported an estimated 10.3 million cancer cases and 5.4 million deaths globally in 2022, with almost two thirds of cases and deaths occurring in men aged 65 years or older.
- By 2050, cancer cases and deaths were projected to increase by 84.3% (to 19 million) and 93.2% (to 10.5 million), respectively. The increase from 2022 to 2050 was more than twofold higher for older men and countries with low and medium HDI.
- In 2022, the estimated global cancer MIR among men was nearly 55%, with variations by cancer types, age, and HDI. The MIR was lowest for thyroid cancer (7.6%) and highest for pancreatic cancer (90.9%); among World Health Organization regions, Africa had the highest MIR (72.6%), while the Americas had the lowest MIR (39.1%); countries with the lowest HDI had the highest MIR (73.5% vs 41.1% for very high HDI).
- Lung cancer was the leading cause for cases and deaths in 2022 and was projected to remain the leading cause in 2050.
IN PRACTICE:
“Disparities in cancer incidence and mortality among men were observed across age groups, countries/territories, and HDI in 2022, with these disparities projected to widen further by 2050,” according to the authors, who called for efforts to “reduce disparities in cancer burden and ensure equity in cancer prevention and care for men across the globe.”
SOURCE:
The study, led by Habtamu Mellie Bizuayehu, PhD, School of Public Health, Faculty of Medicine, The University of Queensland, Brisbane, Australia, was published online in Cancer.
LIMITATIONS:
The findings may be influenced by the quality of GLOBOCAN data. Interpretation should be cautious as MIR may not fully reflect cancer outcome inequalities. The study did not include other measures of cancer burden, such as years of life lost or years lived with disability, which were unavailable from the data source.
DISCLOSURES:
The authors did not disclose any funding information. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
— with substantial disparities in cancer cases and deaths by age and region of the world, a recent analysis found.
METHODOLOGY:
- Overall, men have higher cancer incidence and mortality rates, which can be largely attributed to a higher prevalence of modifiable risk factors such as smoking, alcohol consumption, and occupational carcinogens, as well as the underuse of cancer prevention, screening, and treatment services.
- To assess the burden of cancer in men of different ages and from different regions of the world, researchers analyzed data from the 2022 Global Cancer Observatory (GLOBOCAN), which provides national-level estimates for cancer cases and deaths.
- Study outcomes included the incidence, mortality, and prevalence of cancer among men in 2022, along with projections for 2050. Estimates were stratified by several factors, including age; region; and Human Development Index (HDI), a composite score for health, education, and standard of living.
- Researchers also calculated mortality-to-incidence ratios (MIRs) for various cancer types, where higher values indicate worse survival.
TAKEAWAY:
- The researchers reported an estimated 10.3 million cancer cases and 5.4 million deaths globally in 2022, with almost two thirds of cases and deaths occurring in men aged 65 years or older.
- By 2050, cancer cases and deaths were projected to increase by 84.3% (to 19 million) and 93.2% (to 10.5 million), respectively. The increase from 2022 to 2050 was more than twofold higher for older men and countries with low and medium HDI.
- In 2022, the estimated global cancer MIR among men was nearly 55%, with variations by cancer types, age, and HDI. The MIR was lowest for thyroid cancer (7.6%) and highest for pancreatic cancer (90.9%); among World Health Organization regions, Africa had the highest MIR (72.6%), while the Americas had the lowest MIR (39.1%); countries with the lowest HDI had the highest MIR (73.5% vs 41.1% for very high HDI).
- Lung cancer was the leading cause for cases and deaths in 2022 and was projected to remain the leading cause in 2050.
IN PRACTICE:
“Disparities in cancer incidence and mortality among men were observed across age groups, countries/territories, and HDI in 2022, with these disparities projected to widen further by 2050,” according to the authors, who called for efforts to “reduce disparities in cancer burden and ensure equity in cancer prevention and care for men across the globe.”
SOURCE:
The study, led by Habtamu Mellie Bizuayehu, PhD, School of Public Health, Faculty of Medicine, The University of Queensland, Brisbane, Australia, was published online in Cancer.
LIMITATIONS:
The findings may be influenced by the quality of GLOBOCAN data. Interpretation should be cautious as MIR may not fully reflect cancer outcome inequalities. The study did not include other measures of cancer burden, such as years of life lost or years lived with disability, which were unavailable from the data source.
DISCLOSURES:
The authors did not disclose any funding information. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Prurigo Nodularis Mechanisms and Current Management Options
Prurigo nodularis (PN)(also called chronic nodular prurigo, prurigo nodularis of Hyde, or picker’s nodules) was first characterized by James Hyde in 1909.1-3 Prurigo nodularis manifests with symmetrical, intensely pruritic, eroded, or hyperkeratotic nodules or papules on the extremities and trunk.1,2,4,5 Studies have shown that individuals with PN experience pruritus, sleep loss, decreased social functioning from the appearance of the nodules, and a higher incidence of anxiety and depression, causing a negative impact on their quality of life.2,6 In addition, the manifestation of PN has been linked to neurologic and psychiatric disorders; however, PN also can be idiopathic and manifest without underlying illnesses.2,6,7
Prurigo nodularis has been associated with other dermatologic conditions such as atopic dermatitis (up to 50%), lichen planus, keratoacanthomas (KAs), and bullous pemphigoid.7-9 It also has been linked to systemic diseases in 38% to 50% of cases, including chronic kidney disease, liver disease, type 2 diabetes mellitus, malignancies (hematopoietic, liver, and skin), and HIV infection.6,8,10
The pathophysiology of PN is highly complex and has yet to be fully elucidated. It is thought to be due to dysregulation and interaction of the increase in neural and immunologic responses of proinflammatory and pruritogenic cytokines.2,11 Treatments aim to break the itch-scratch cycle that perpetuates this disorder; however, this proves difficult, as PN is associated with a higher itch intensity than atopic dermatitis and psoriasis.10 Therefore, most patients attempt multiple forms of treatment for PN, ranging from topical therapies, oral immunosuppressants, and phototherapy to the newest and only medication approved by the US Food and Drug Administration for the treatment of PN—dupilumab.1,7,11 Herein, we provide an updated review of PN with a focus on its epidemiology, histopathology and pathophysiology, comorbidities, clinical presentation, differential diagnosis, and current treatment options.
Epidemiology
There are few studies on the epidemiology of PN; however, middle-aged populations with underlying dermatologic or psychiatric disorders tend to be impacted most frequently.2,12,13 In 2016, it was estimated that almost 88,000 individuals had PN in the United States, with the majority being female; however, this estimate only took into account those aged 18 to 64 years and utilized data from IBM MarketScan Commercial Claims and Encounters Database (IBM Watson Health) from October 2015 to December 2016.14 More recently, a retrospective database analysis estimated the prevalence of PN in the United States to be anywhere from 36.7 to 43.9 cases per 100,000 individuals. However, this retrospective review utilized the International Classification of Diseases, Tenth Revision code; PN has 2 codes associated with the diagnosis, and the coding accuracy is unknown.15 Sutaria et al16 looked at racial disparities in patients with PN utilizing data from TriNetX and found that patients who received a diagnosis of PN were more likely to be women, non-Hispanic, and Black compared with control patients. However, these estimates are restricted to the health care organizations within this database.
In 2018, Poland reported an annual prevalence of 6.52 cases per 100,000 individuals,17 while England reported a yearly prevalence of 3.27 cases per 100,000 individuals.18 Both countries reported most cases were female. However, these studies are not without limitations. Poland only uses the primary diagnosis code for medical billing to simplify clinical coding, thus underestimating the actual prevalence; furthermore, clinical codes more often than not are assigned by someone other than the diagnosing physician, leaving room for error.17 In addition, England’s PN estimate utilized diagnosis data from primary care and inpatient datasets, leaving out outpatient datasets in which patients with PN may have been referred and obtained the diagnosis, potentially underestimating the prevalence in this population.18
In contrast, Korea estimated the annual prevalence of PN to be 4.82 cases per 1000 dermatology outpatients, with the majority being men, based on results from a cross-sectional study among outpatients from the Catholic Medical Center. Although this is the largest health organization in Korea, the scope of this study is limited and lacks data from other medical centers in Korea.19
Histopathology and Pathophysiology
Almost all cells in the skin are involved in PN: keratinocytes, mast cells, dendritic cells, endothelial cells, lymphocytes, eosinophils, collagen fibers, and nerve fibers.11,20 Classically, PN manifests as a dome-shaped lesion with hyperkeratosis, hypergranulosis, and psoriasiform epidermal hyperplasia with increased thickness of the papillary dermis consisting of coarse collagen with compact interstitial and circumvascular infiltration as well as increased lymphocytes and histocytes in the superficial dermis (Figure 1).20 Hyperkeratosis is thought to be due to either the alteration of keratinocyte structures from scratching or keratinocyte abnormalities triggering PN.21 However, the increase in keratinocytes, which secrete nerve growth factor, allows for neuronal hyperplasia within the dermis.22 Nerve growth factor can stimulate keratinocyte proliferation23 in addition to the upregulation of substance P (SP), a tachykinin that triggers vascular dilation and pruritus in the skin.24 The density of SP nerve fibers in the dermis increases in PN, causing proinflammatory effects, upregulating the immune response to promote endothelial hyperplasia and increased vascularization.25 The increase in these fibers may lead to pruritus associated with PN.2,26
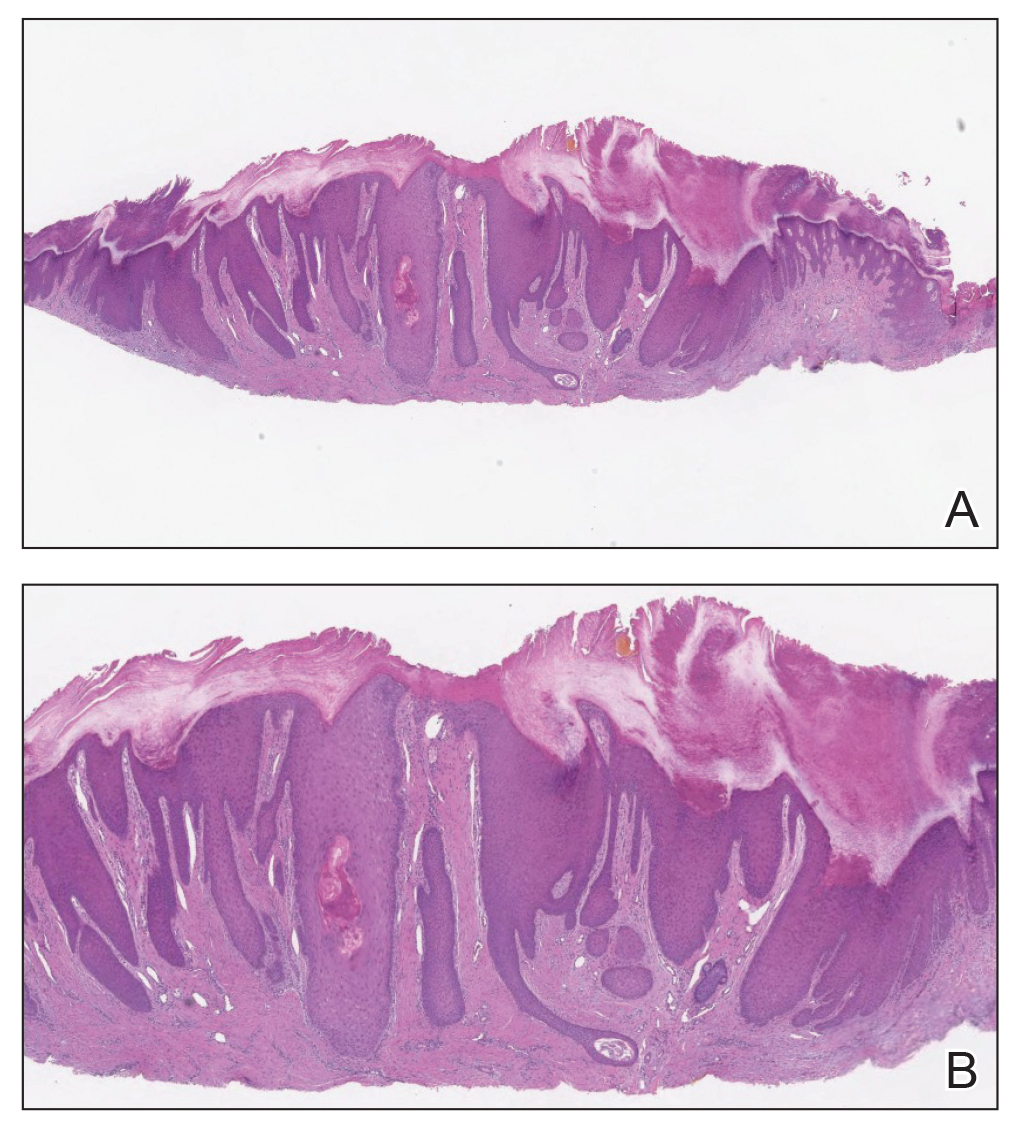
Many inflammatory cytokines and mediators also have been implicated in PN. Increased messenger RNA expression of IL-4, IL-17, IL-22, and IL-31 has been described in PN lesions.3,27 Furthermore, studies also have reported increased helper T cell (TH2) cytokines, including IL-4, IL-5, IL-10, and IL-13, in the dermis of PN lesions in patients without a history of atopy.3,28 These pruritogenic cytokines in conjunction with the SP fibers may create an intractable itch for those with PN. The interaction and culmination of the neural and immune responses make PN a complex condition to treat with the multifactorial interaction of systems.
Comorbidities
Prurigo nodularis has been associated with a wide array of comorbidities; however, the direction of the relationship between PN and these conditions makes it difficult to discern if PN is a primary or secondary condition.29 Prurigo nodularis commonly has been connected to other inflammatory dermatoses, with a link to atopic dermatitis being the strongest.5,29 However, PN also has been linked to other pruritic inflammatory cutaneous disorders, including psoriasis, cutaneous T-cell lymphoma, lichen planus, and dermatitis herpetiformis.14,29
Huang et al14 found an increased likelihood of psychiatric illnesses in patients with PN, including eating disorders, nonsuicidal self-injury disorder, attention-deficit/hyperactivity disorder, schizophrenia, mood disorders, anxiety, and substance abuse disorders. Treatments directed at the neural aspect of PN have included selective serotonin reuptake inhibitors (SSRIs), which also are utilized to treat these mental health disorders.
Furthermore, systemic diseases also have been found to be associated with PN, including hypertension, type 2 diabetes mellitus, chronic kidney disease, heart failure, cerebrovascular disease, coronary heart disease, and chronic obstructive pulmonary disease.14 The relationship between PN and systemic conditions may be due to increased systemic inflammation and dysregulation of neural and metabolic functions implicated in these conditions from increased pruritic manifestations.29,30 However, studies also have connected PN to infectious conditions such as HIV. One study found that patients with PN had 2.68 higher odds of infection with HIV compared to age- and sex-matched controls.14 It is unknown if these conditions contributed to the development of PN or PN contributed to the development of these disorders.
Clinical Presentations
Prurigo nodularis is a chronic inflammatory skin disease that typically manifests with multiple severely pruritic, dome-shaped, firm, hyperpigmented papulonodules with central scale or crust, often with erosion, due to chronic repetitive scratching and picking secondary to pruritic systemic or dermatologic diseases or psychological disorders (Figure 2).1,2,4,5,8,31 Most often, diagnosis of PN is based on history and physical examination of the lesion; however, biopsies may be performed. These nodules commonly manifest with ulceration distributed symmetrically on extensor extremities in easy-to-reach places, sparing the mid back (called the butterfly sign).8 Lesions—either a few or hundreds—can range from a few millimeters to 2 to 3 cm.8,32 The lesions differ in appearance depending on the pigment in the patient’s skin. In patients with darker skin tones, hyperpigmented or hypopigmented papulonodules are not uncommon, while those with fairer skin tones tend to present with erythema.31
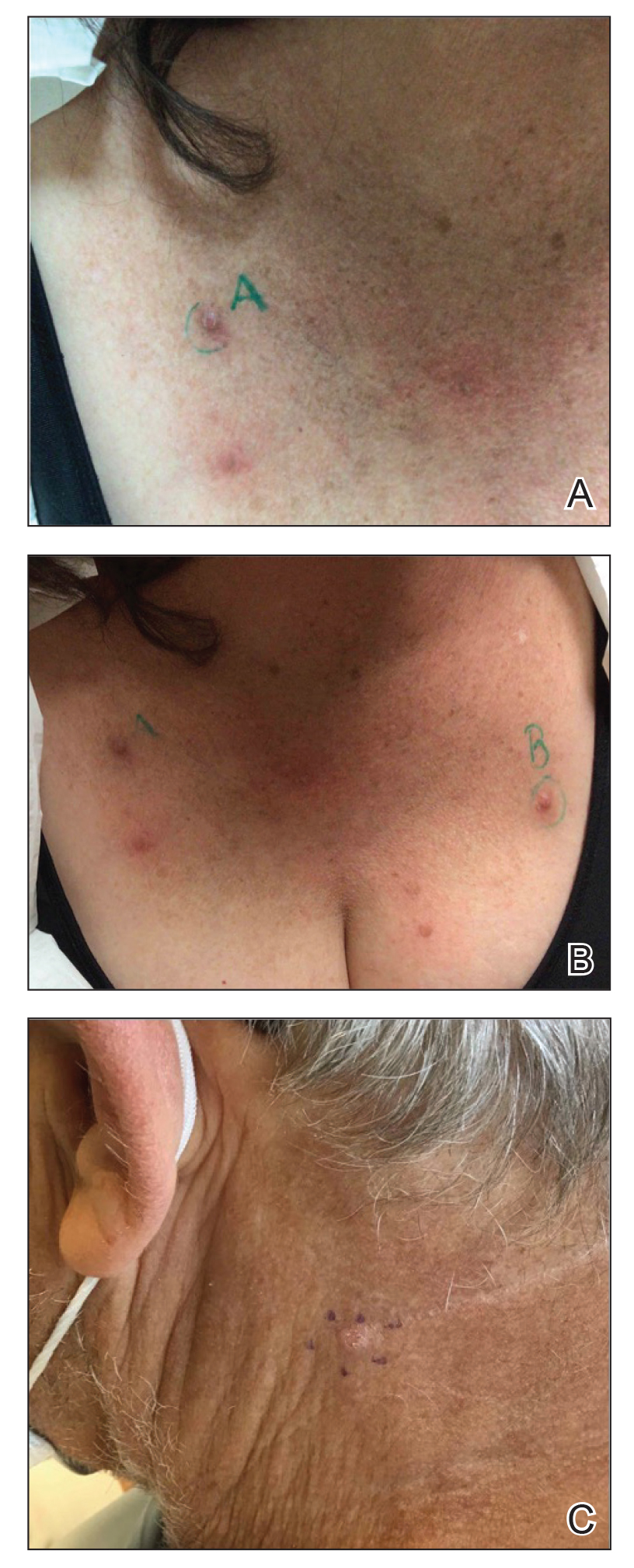
Differential Diagnosis
Because of the variation in manifestation of PN, these lesions may resemble other cutaneous conditions. If the lesions are hyperkeratotic, they can mimic hypertrophic lichen planus, which mainfests with hyperkeratotic plaques or nodules on the lower extremities.8,29 In addition, the histopathology of lichen planus resembles the appearance of PN, with epidermal hyperplasia, hypergranulosis, hyperkeratosis, and increased fibroblasts and capillaries.8,29
Pemphigoid nodularis is a rare subtype of bullous pemphigoid that exhibits characteristics of PN with pruritic plaques and erosions.8,29,33 The patient population for pemphigoid nodularis tends to be aged 50 to 60 years, and females are affected more frequently than males. However, pemphigoid nodularis may manifest with blistering and large plaques, which are not seen commonly with PN.29 On histopathology, pemphigoid nodularis deposits IgG and C3 on the basement membrane and has subepidermal clefting, unlike PN.7,29
Actinic prurigo manifests with pruritic papules or nodules post–UV exposure to unprotected skin.8,29,33 This rare condition usually manifests with cheilitis and conjunctivitis. Unlike PN, which commonly affects elderly populations, actinic prurigo typically is found in young females.8,29 Cytologic examination shows hyperkeratosis, spongiosis, and acanthosis of the epidermis with lymphocytic perivascular infiltration of the dermis.34
Neurotic excoriations also tend to mimic PN with raised excoriated lesions; however, this disorder is due to neurotic picking of the skin without associated pruritus or true hyperkeratosis.8,29,33 Histopathology shows epidermal crusting with inflammation of the upper dermis.35
Infiltrative cutaneous squamous cell carcinoma (SCC) may imitate PN in appearance. It manifests as tender, ulcerated, scaly plaques or nodules. Histopathology shows cytologic atypia with an infiltrative architectural pattern and presence of collections of compact keratin and parakeratin (called keratin pearls).
Keratoacanthomas can resemble PN lesions. They usually manifest as nodules measuring 1 to 2 cm in diameter and 0.5 cm thick, resembling crateriform tumors.36 On histopathology, KAs can resemble SCCs; however, KAs tend to manifest more frequently with a keratin-filled crater with a ground-glass appearance.36
Inverted follicular keratosis commonly manifests on the face in elderly men as a single, flesh-colored, verrucous papule that may resemble PN. However, cytology of inverted follicular keratosis is characterized by proliferation and squamous eddies.37 Consideration of the histologic findings and clinical appearance are important to differentiate between PN and cutaneous SCC.
Pseudoepitheliomatous hyperplasia is a benign condition that manifests as a plaque or nodule with crust, scale, or ulceration. Histologically, this condition presents with hyperplastic proliferation of the epidermis and adnexal epithelium.38 The clinical and histologic appearance can mimic PN and other cutaneous eruptions with epidermal hyperplasia.
In clinical cases that are resistant to treatment, biopsy is the best approach to diagnose the lesion. Due to similarities in physical appearance and superficial histologic presentation of PN, KAs from SCC, hypertrophic lichen planus, and other hyperkeratotic lesions, the biopsy should be taken at the base of the lesion to sample deeper layers of skin to differentiate these dermatologic disorders.
Management
Current treatments for PN yield varied results. Many patients with moderate to severe PN attempt multiple therapies before seeing improvement.31 Treatments include topical, oral, and injectable medications and are either directed at the neural or immune components of PN due to the interplay between increased nerve fibers in the lesions (neural axis) as well as increases in cytokines and other immunologic mediators (immune axis) of this condition. However, the FDA recently approved the first treatment for PN—dupilumab—which is an injectable IL-4 receptor antagonist directed at the immunologic interactions affiliated with PN.
Immune-Mediated Topical Therapies—Immunologic topical therapies include corticosteroids, calcipotriol, and calcineurin inhibitors. Studies that have analyzed these treatments are limited to case reports and small intraindividual and randomized controlled trials (Table 1). Topical therapies usually are first-line agents for most patients. Adverse effects include transient irritation of the skin.40,42,43
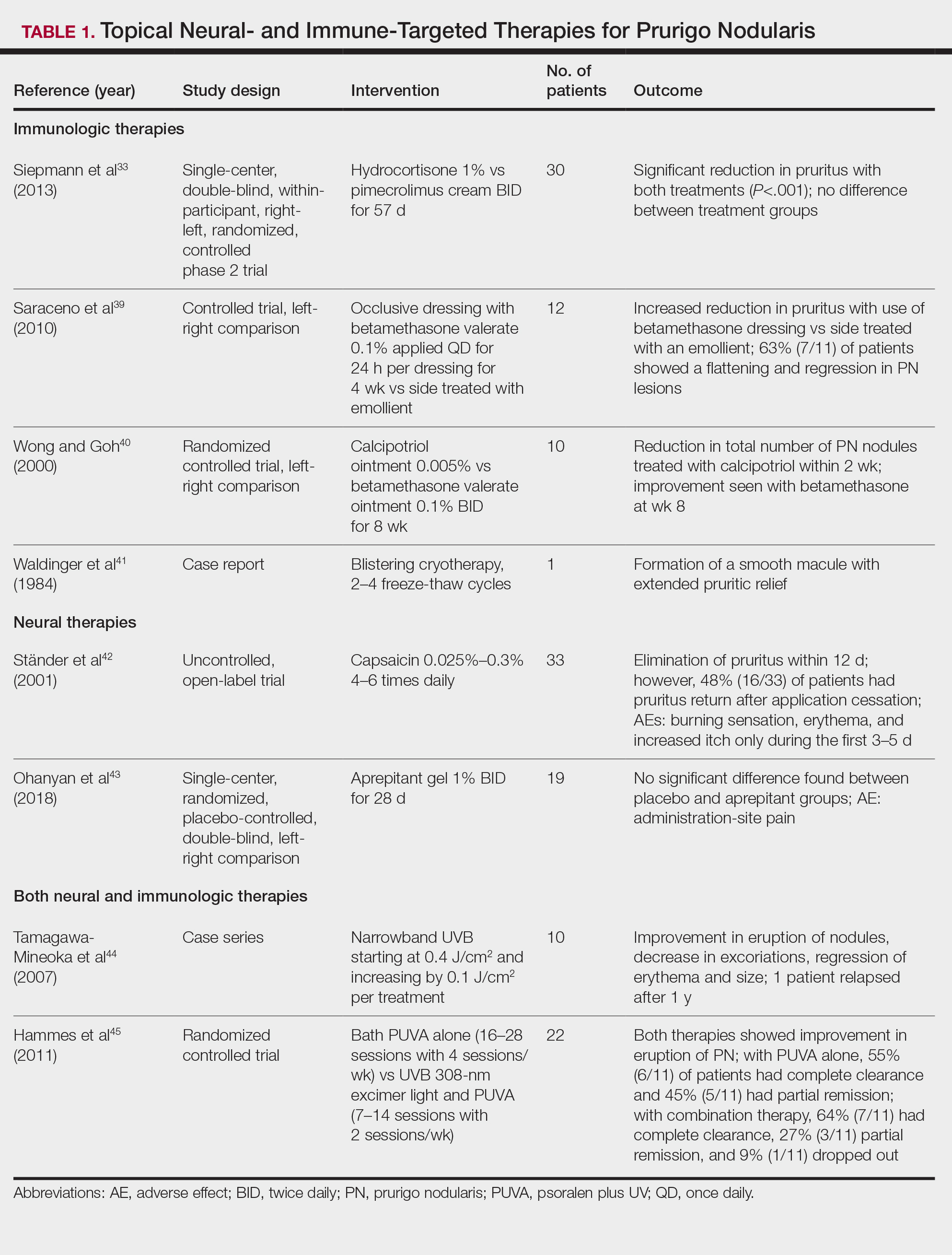
Cryotherapy is another topical and immunologic therapy for those with PN; however, this treatment is more appropriate for patients with fewer lesions due to the pain that accompanies lesions treated with liquid nitrogen. In addition, this therapy can cause dyspigmentation of the skin in the treated areas.41
Similar to cryotherapy, intralesional corticosteroid injections are appropriate for patients with few PN lesions. A recent report described intralesional corticosteroid injections of 2.5 mg/mL for a PN nodule with high efficacy.46,47 This treatment has not undergone trials, but success with this modality has been documented, with adverse effects including hyperpigmentation or hypopigmentation in the treated area and transient pain.46
Neural-Mediated Topical Therapies—Neural topical therapies include capsaicin and neurokinin-1 receptor antagonists, aprepitant43 and serlopitant. These treatment studies are limited to small open-label and randomized controlled trials. Adverse effects of these treatments include transient cutaneous pain at the site of topical administration. In addition, neural-mediated topical therapies have shown either limited improvements from baseline or return of symptoms after treatment cessation.42,43
Supplements—N-acetyl cysteine is an over-the-counter supplement that has been reported to improve symptoms in patients with skin-picking disorders.48 The mechanism of action includes antioxidant effects such as decreasing reactive oxygen species, decreasing inflammatory markers, regulating neurotransmitters, and inhibiting hyperkeratosis.49 N-acetyl cysteine has been poorly studied for its application in PN. A small study of 3 patients with subacute PN receiving 1200 mg of oral N-acetyl cysteine reported varying levels of improvement in skin appearance and reduction in skin picking.50
Phototherapy—Phototherapy, a typical first- or second-line treatment modality for PN, targets both the neural- and immune-mediated aspects associated with pruritus in PN (Table 1).51 UV light can penetrate through the epidermal layer of the skin and reach the keratinocytes, which play a role in the immune-related response of PN. In addition, the cutaneous sensory nerves are located in the upper dermal layer, from which nerve fibers grow and penetrate into the epidermis, thereby interacting with the keratinocytes where pruritic signals are transmitted from the periphery up to the brain.51
Studies analyzing the effects of phototherapy on PN are limited to case series and a small randomized controlled trial. However, this trial has shown improvements in pruritus in the participants. Adverse effects include transient burning and erythema at the treated sites.44,45
Immune-Mediated Oral Therapies—Immunologic-targeted oral therapies include bilastine, methotrexate, and cyclosporine (Table 2).52,53 Bilastine efficacy was analyzed in a small phase 3, open-label, multicenter study in Japan; however, patients were allowed to use topical steroids in conjunction with the oral antihistamine.54 Methotrexate and cyclosporine are immunosuppressive medications and were analyzed in small retrospective studies. Both treatments yielded notable relief for patients; however, 38.5% (15/39) of patients receiving methotrexate experienced adverse events, and 50.0% (4/8) experienced adverse events with cyclosporine.52,53
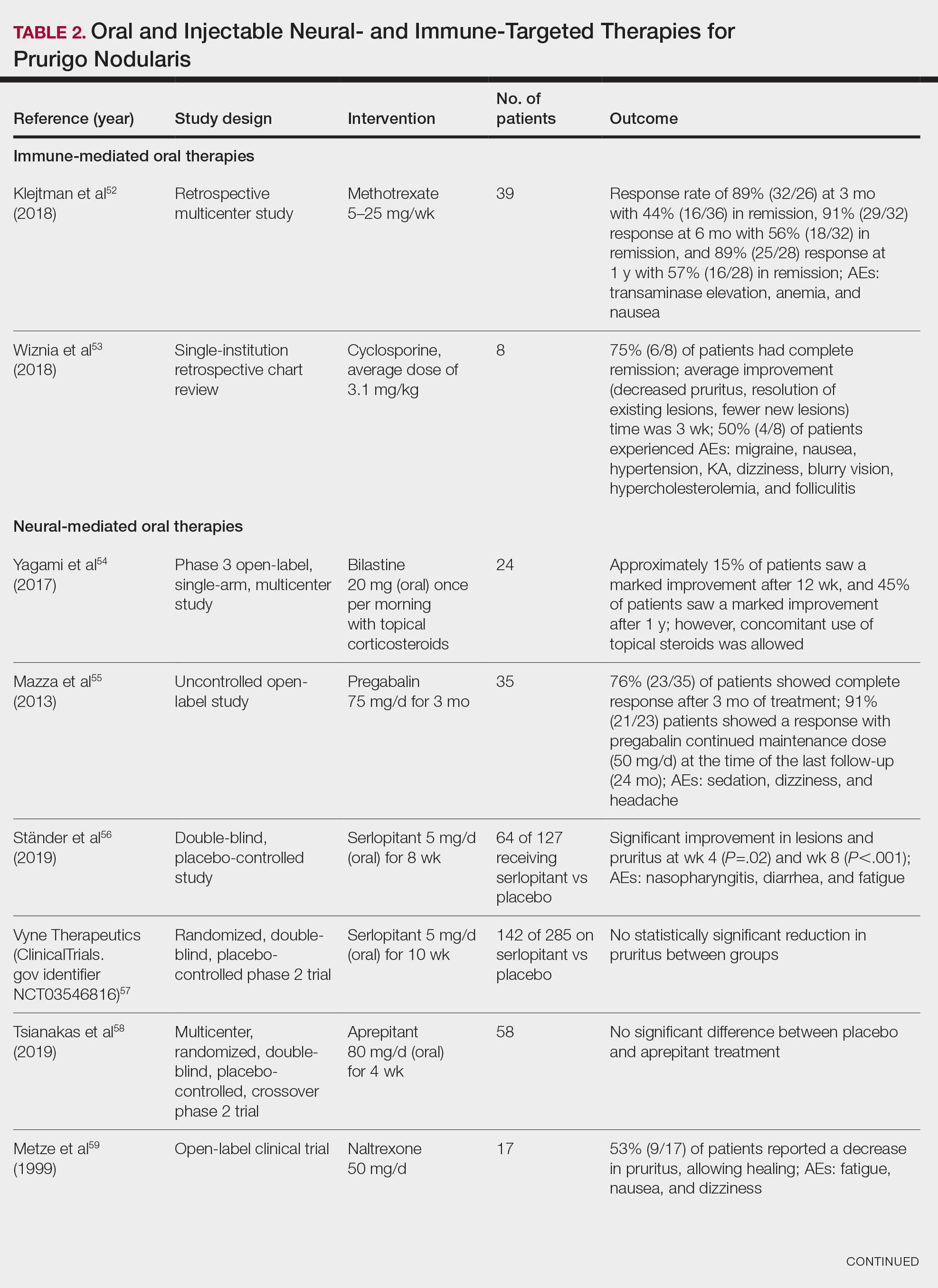
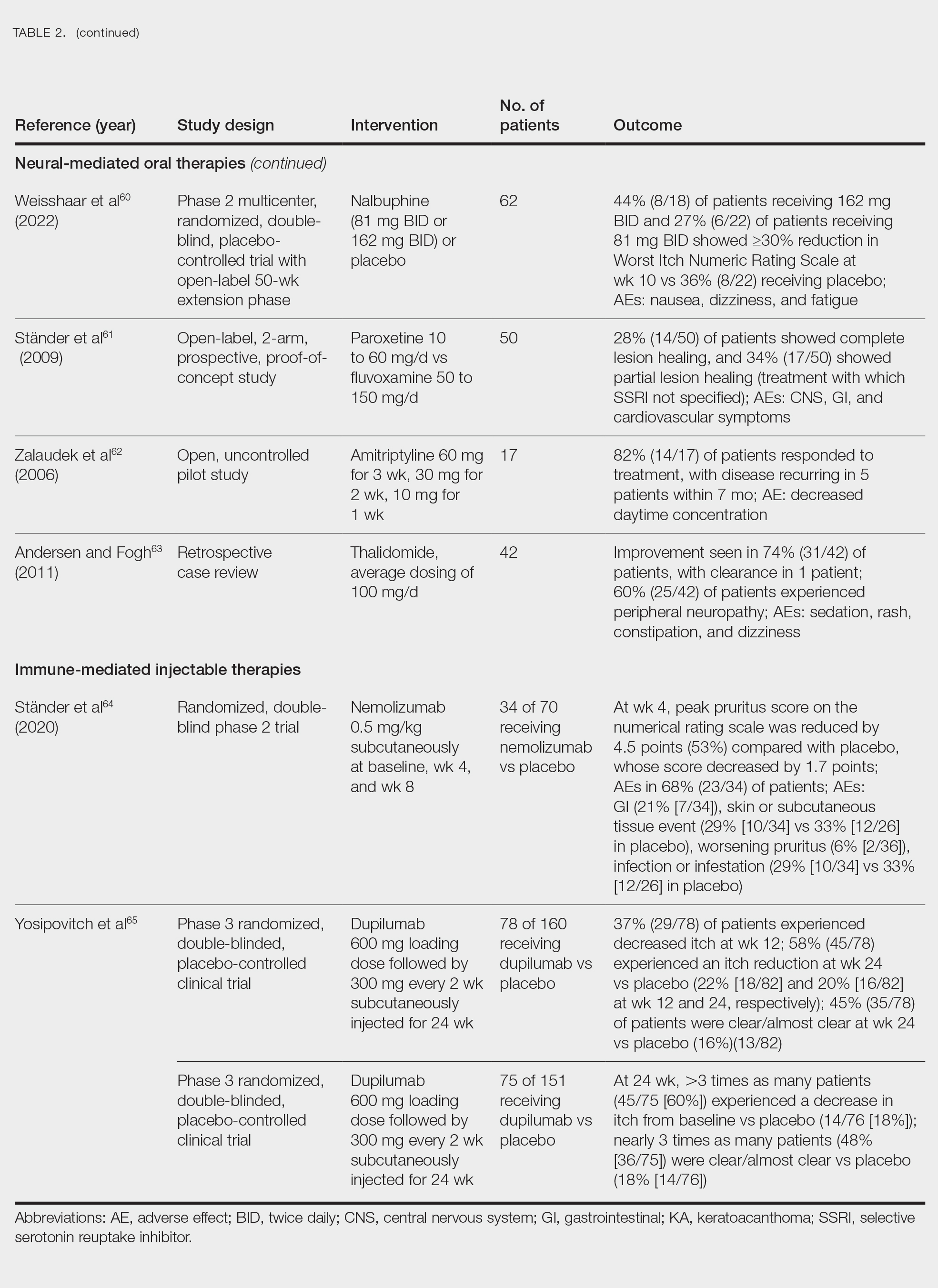
Neural-Mediated Oral Therapies—Neural-targeted oral therapies include pregabalin, serlopitant, aprepitant, naltrexone, nalbuphine, SSRIs (paroxetine and fluvoxamine), amitriptyline, and thalidomide. The research on these treatments ranges from case reviews to randomized controlled trials and open-label trials (Table 2).55-63
Thalidomide was studied in a small retrospective case review that showed notable improvement in PN. Dosages of thalidomide varied, but on average the dose was 100 mg/d. However, greater than 50% of patients experienced at least 1 adverse effect with this treatment.63
A study performed in Italy showed promising results for patients treated with pregabalin, with 70.0% (21/30) continuing to take pregabalin for almost 2 years following completion of the initial 3-month trial.55 Naltrexone decreased pruritus in more than half of patients (9/17).59 Amitriptyline yielded improvements in patients with PN; however, disease recurred in 5 patients (29%) after 7 months.62 A study performed in Germany reported promising results for paroxetine and fluvoxamine; however, some patients enrolled in the study had some form of psychiatric disorder.61
Serlopitant, aprepitant, and nalbuphine were studied in randomized controlled trials. The serlopitant trials were the largest of the neurally mediated oral medication studies; one showed substantial improvement in patients with PN,56 while the most recent trial did not show significant improvement (ClinicalTrials.gov identifier NCT03546816).57 On the other hand, aprepitant showed no major difference between the experimental and placebo groups.58 Nalbuphine 162 mg twice daily showed greater improvement in PN than nalbuphine 81 mg twice daily.60
Immune-Mediated Injectable Therapies—Immune-targeted injectables include nemolizumab and dupilumab (Table 2). Nemolizumab is an IL-31 antagonist that has been studied in a small randomized controlled trial that showed great success in decreasing pruritus associated with PN.64 IL-31 has been implicated in PN, and inhibition of the IL-31 receptor has been shown to disrupt the itch-scratch cycle of PN. Dupilumab is a monoclonal antibody against the IL-4 and IL-13 receptors, and it is the only FDA-approved treatment for PN.65 Blockage of these protein receptors decreases type 2 inflammation and chronic pruritus.66,67 Dupilumab is FDA approved for the treatment of atopic dermatitis and recently was approved for adults with PN. Dupilumab acts to block the shared α-subunit of the pruritogenic cytokines IL-4 and IL-13 pathways,29 thereby breaking the itch-scratch cycle associated with PN and allowing for the healing of these lesions. Results from 2 clinical trials showed substantially reduced itch in patients with PN.65 Dupilumab also was approved by the European Medicines Agency for moderate to severe PN.68
Conclusion
Prurigo nodularis is a chronic condition that affects patient quality of life and can mimic various dermatologic conditions. The epidemiology and pathophysiology of PN have not been fully expounded. More research should be conducted to determine the underpinnings of PN to help identify more consistently effective therapies for this complex condition.
- Durmaz K, Ataseven A, Ozer I, et al. Prurigo nodularis responding to intravenous immunoglobulins. Przegl Dermatol. 2022;109:159-162. doi:10.5114/dr.2022.117988
- Kowalski EH, Kneiber D, Valdebran M, et al. Treatment-resistant prurigo nodularis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:163-172. doi:10.2147/CCID.S188070
- Wong LS, Yen YT. Chronic nodular prurigo: an update on the pathogenesis and treatment. Int J Mol Sci. 2022;23:12390. doi:10.3390/ijms232012390
- Janmohamed SR, Gwillim EC, Yousaf M, et al. The impact of prurigo nodularis on quality of life: a systematic review and meta-analysis. Arch Dermatol Res. 2021;313:669-677. doi:10.1007/s00403-020-02148-0
- Zeidler C, Ständer S. The pathogenesis of prurigo nodularis - ‘super-itch’ in exploration. Eur J Pain. 2016;20:37-40. doi:10.1002/ejp.767
- Kwatra SG. Breaking the itch–scratch cycle in prurigo nodularis. N Engl J Med. 2020;382:757-758. doi:10.1056/NEJMe1916733
- Frølunde AS, Wiis MAK, Ben Abdallah H, et al. Non-atopic chronic nodular prurigo (prurigo nodularis hyde): a systematic review of best-evidenced treatment options. Dermatology. 2022;238:950-960. doi:10.1159/000523700
- Kwon CD, Khanna R, Williams KA, et al. Diagnostic workup and evaluation of patients with prurigo nodularis. Medicines (Basel). 2019;6:97. doi:10.3390/medicines6040097
- Kowalski EH, Kneiber D, Valdebran M, et al. Distinguishing truly recalcitrant prurigo nodularis from poor treatment adherence: a response to treatment-resistant prurigo nodularis [Response to letter]. Clin Cosmet Investig Dermatol. 2019;12:371-372. doi:10.2147/CCID.S214195
- Whang KA, Le TK, Khanna R, et al. Health-related quality of life and economic burden of prurigo nodularis. J Am Acad Dermatol. 2022;86:573-580. doi:10.1016/j.jaad.2021.05.036
- Labib A, Ju T, Vander Does A, et al. Immunotargets and therapy for prurigo nodularis. Immunotargets Ther. 2022;11:11-21. doi:10.2147/ITT.S316602
- Belzberg M, Alphonse MP, Brown I, et al. Prurigo nodularis is characterized by systemic and cutaneous T helper 22 immune polarization. J Invest Dermatol. 2021;141:2208-2218.e14. doi:10.1016/j.jid.2021.02.749
- Ständer S, Pereira MP, Berger T, et al. IFSI-guideline on chronic prurigo including prurigo nodularis. Itch. 2020;5:e42. doi:10.1097/itx.0000000000000042
- Huang AH, Canner JK, Khanna R, et al. Real-world prevalence of prurigo nodularis and burden of associated diseases. J Invest Dermatol. 2020;140:480-483.e4. doi:10.1016/j.jid.2019.07.697
- Ständer S, Augustin M, Berger T, et al. Prevalence of prurigo nodularis in the United States of America: a retrospective database analysis. JAAD Int. 2021;2:28-30. doi:10.1016/j.jdin.2020.10.009
- Sutaria N, Adawi W, Brown I, et al. Racial disparities in mortality among patients with prurigo nodularis: a multi-center cohort study. J Am Acad Dermatol. 2022;86:487-490. doi:10.1016/j.jaad.2021.09.028
- Ryczek A, Reich A. Prevalence of prurigo nodularis in Poland. Acta Derm Venereol. 2020;100:adv00155. doi:10.2340/00015555-3518
- Morgan CL, Thomas M, Ständer S, et al. Epidemiology of prurigo nodularis in England: a retrospective database analysis. Br J Dermatol. 2022;187:188-195. doi:10.1111/bjd.21032
- Woo YR, Wang S, Sohn KA, et al. Epidemiology, comorbidities, and prescription patterns of Korean prurigo nodularis patients: a multi-institution study. J Clin Med Res. 2021;11:95. doi:10.3390/jcm11010095
- Weigelt N, Metze D, Ständer S. Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37:578-586. doi:10.1111/j.1600-0560.2009.01484.x
- Yang LL, Jiang B, Chen SH, et al. Abnormal keratin expression pattern in prurigo nodularis epidermis. Skin Health Dis. 2022;2:e75. doi:10.1002/ski2.75
- Nockher WA, Renz H. Neurotrophins in allergic diseases: from neuronal growth factors to intercellular signaling molecules. J Allergy Clin Immunol. 2006;117:583-589. doi:10.1016/j.jaci.2005.11.049
- Di Marco E, Mathor M, Bondanza S, et al. Nerve growth factor binds to normal human keratinocytes through high and low affinity receptors and stimulates their growth by a novel autocrine loop. J Biol Chem. 1993;268:22838-22846.
- Hägermark O, Hökfelt T, Pernow B. Flare and itch induced by substance P in human skin. J Invest Dermatol. 1978;71:233-235. doi:10.1111/1523-1747.ep12515092
- Choi JE, Di Nardo A. Skin neurogenic inflammation. Semin Immunopathol. 2018;40:249-259. doi:10.1007/s00281-018-0675-z
- Haas S, Capellino S, Phan NQ, et al. Low density of sympathetic nerve fibers relative to substance P-positive nerve fibers in lesional skin of chronic pruritus and prurigo nodularis. J Dermatol Sci. 2010;58:193-197. doi:10.1016/j.jdermsci.2010.03.020
- Park K, Mori T, Nakamura M, et al. Increased expression of mRNAs for IL-4, IL-17, IL-22 and IL-31 in skin lesions of subacute and chronic forms of prurigo. Eur J Dermatol. 2011;21:135-136.
- Tokura Y, Yagi H, Hanaoka K, et al. Subacute and chronic prurigo effectively treated with recombination interferon-gamma: implications for participation of Th2 cells in the pathogenesis of prurigo. Acta Derm Venereol. 1997;77:231-234. doi:10.2340/0001555577231234
- Williams KA, Roh YS, Brown I, et al. Pathophysiology, diagnosis, and pharmacological treatment of prurigo nodularis. Expert Rev Clin Pharmacol. 2021;14:67-77. doi:10.1080/17512433.2021.1852080
- Huang AH, Williams KA, Kwatra SG. Prurigo nodularis: epidemiology and clinical features. J Am Acad Dermatol. 2020;83:1559-1565. doi:10.1016/j.jaad.2020.04.183
- Bewley A, Homey B, Pink A. Prurigo nodularis: a review of IL-31RA blockade and other potential treatments. Dermatol Ther. 2022;12:2039-2048. doi:10.1007/s13555-022-00782-2
- Zeidler C, Yosipovitch G, Ständer S. Prurigo nodularis and its management. Dermatol Clin. 2018;36:189-197. doi:10.1016/j.det.2018.02.003
- Siepmann D, Lotts T, Blome C, et al. Evaluation of the antipruritic effects of topical pimecrolimus in non-atopic prurigo nodularis: results of a randomized, hydrocortisone-controlled, double-blind phase II trial. Dermatology. 2013;227:353-360. doi:10.1159/000355671
- Valbuena MC, Muvdi S, Lim HW. Actinic prurigo. Dermatol Clin. 2014;32:335-344, viii. doi:10.1016/j.det.2014.03.010
- Aldhahwani R, Al Hawsawi KA. Neurotic excoriation presenting as solitary papule: case report. J Dermatol Dermatolog Surg. 2022;26:45. doi:10.4103/jdds.jdds_59_21
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74:1220-1233. doi:10.1016/j.jaad.2015.11.033
- Karadag AS, Ozlu E, Uzuncakmak TK, et al. Inverted follicular keratosis successfully treated with imiquimod. Indian Dermatol Online J. 2016;7:177-179. doi:10.4103/2229-5178.182354
- Nayak VN, Uma K, Girish HC, et al. Pseudoepitheliomatous hyperplasia in oral lesions: a review. J Int Oral Health. 2015;7:148-152.
- Saraceno R, Chiricozzi A, Nisticò SP, et al. An occlusive dressing containing betamethasone valerate 0.1% for the treatment of prurigo nodularis. J Dermatolog Treat. 2010;21:363-366. doi:10.3109/09546630903386606
- Wong SS, Goh CL. Double-blind, right/left comparison of calcipotriol ointment and betamethasone ointment in the treatment of prurigo nodularis. Arch Dermatol. 2000;136:807-808. doi:10.1001/archderm.136.6.807
- Waldinger TP, Wong RC, Taylor WB, et al. Cryotherapy improves prurigo nodularis. Arch Dermatol. 1984;120:1598-1600.
- Ständer S, Luger T, Metze D. Treatment of prurigo nodularis with topical capsaicin. J Am Acad Dermatol. 2001;44:471-478. doi:10.1067/mjd.2001.110059
- Ohanyan T, Schoepke N, Eirefelt S, et al. Role of substance P and its receptor neurokinin 1 in chronic prurigo: a randomized, proof-of-concept, controlled trial with topical aprepitant. Acta Derm Venereol. 2018;98:26-31. doi:10.2340/00015555-2780
- Tamagawa-Mineoka R, Katoh N, Ueda E, et al. Narrow-band ultraviolet B phototherapy in patients with recalcitrant nodular prurigo. J Dermatol. 2007;34:691-695. doi:10.1111/j.1346-8138.2007.00360.x
- Hammes S, Hermann J, Roos S, et al. UVB 308-nm excimer light and bath PUVA: combination therapy is very effective in the treatment of prurigo nodularis. J Eur Acad Dermatol Venereol. 2011;25:799-803. doi:10.1111/j.1468-3083.2010.03865.x
- Richards RN. Update on intralesional steroid: focus on dermatoses. J Cutan Med Surg. 2010;14:19-23. doi:10.2310/7750.2009.08082
- Elmariah S, Kim B, Berger T, et al. Practical approaches for diagnosis and management of prurigo nodularis: United States expert panel consensus. J Am Acad Dermatol. 2021;84:747-760. doi:10.1016/j.jaad.2020.07.025
- Grant JE Chamberlain SR Redden SA et al. N-Acetylcysteine in the treatment of excoriation disorder: a randomized clinical trial. JAMA Psychiatry. 2016;73:490-496. doi:10.1001/jamapsychiatry.2016.0060
- Adil M, Amin SS, Mohtashim M. N-acetylcysteine in dermatology. Indian J Dermatol Venereol Leprol. 2018;84:652-659. doi: 10.4103/ijdvl.IJDVL_33_18.
- Taylor M, Bhagwandas K. Trichotillosis, skin picking and N-acetylcysteine. J Am Acad Dermatol. 2015;72(suppl 1):AB117. https://doi.org/10.1016/j.jaad.2015.02.482
- Legat FJ. The antipruritic effect of phototherapy. Front Med (Lausanne). 2018;5:333. doi:10.3389/fmed.2018.00333
- Klejtman T, Beylot-Barry M, Joly P, et al. Treatment of prurigo with methotrexate: a multicentre retrospective study of 39 cases. J Eur Acad Dermatol Venereol. 2018;32:437-440. doi:10.1111/jdv.14646
- Wiznia LE, Callahan SW, Cohen DE, et al. Rapid improvement of prurigo nodularis with cyclosporine treatment. J Am Acad Dermatol. 2018;78:1209-1211. doi:10.1016/j.jaad.2018.02.024
- Yagami A, Furue M, Togawa M, et al. One-year safety and efficacy study of bilastine treatment in Japanese patients with chronic spontaneous urticaria or pruritus associated with skin diseases. J Dermatol. 2017;44:375-385. doi:10.1111/1346-8138.13644
- Mazza M, Guerriero G, Marano G, et al. Treatment of prurigo nodularis with pregabalin. J Clin Pharm Ther. 2013;38:16-18. doi:10.1111/jcpt.12005
- Ständer S, Kwon P, Hirman J, et al. Serlopitant reduced pruritus in patients with prurigo nodularis in a phase 2, randomized, placebo-controlled trial. J Am Acad Dermatol. 2019;80:1395-1402. doi:10.1016/j.jaad.2019.01.052
- Study of the efficacy, safety and tolerability of serlopitant for the treatment of pruritus (itch) with prurigo nodularis. ClinicalTrials.gov identifier: NCT03546816. Updated May 20, 2021. Accessed August 8, 2024. https://clinicaltrials.gov/study/NCT03546816
- Tsianakas A, Zeidler C, Riepe C, et al. Aprepitant in anti-histamine-refractory chronic nodular prurigo: a multicentre, randomized, double-blind, placebo-controlled, cross-over, phase-II trial (APREPRU). Acta Derm Venereol. 2019;99:379-385. doi:10.2340/00015555-3120
- Metze D, Reimann S, Beissert S, et al. Efficacy and safety of naltrexone, an oral opiate receptor antagonist, in the treatment of pruritus in internal and dermatological diseases. J Am Acad Dermatol. 1999;41:533-539.
- Weisshaar E, Szepietowski JC, Bernhard JD, et al. Efficacy and safety of oral nalbuphine extended release in prurigo nodularis: results of a phase 2 randomized controlled trial with an open‐label extension phase. J Eur Acad Dermatol Venereol. 2022;36:453-461. doi:10.1111/jdv.17816
- Ständer S, Böckenholt B, Schürmeyer-Horst F, et al. Treatment of chronic pruritus with the selective serotonin re-uptake inhibitors paroxetine and fluvoxamine: results of an open-labelled, two-arm proof-of-concept study. Acta Derm Venereol. 2009;89:45-51. doi:10.2340/00015555-0553
- Zalaudek I, Petrillo G, Baldassarre MA, et al. Amitriptyline as therapeutic and not symptomatic approach in the treatment of prurigo nodularis. G Ital Dermatol Venereol. 2006;141:433-437.
- Andersen TP, Fogh K. Thalidomide in 42 patients with prurigo nodularis Hyde. Dermatology. 2011;223:107-112. doi:10.1159/000331577
- Ständer S, Yosipovitch G, Legat FJ, et al. Trial of nemolizumab in moderate-to-severe prurigo nodularis. N Engl J Med. 2020;382:706-716. doi:10.1056/NEJMoa1908316
- Yosipovitch G, Mollanazar N, Ständer S, et al. Dupilumab in patients with prurigo nodularis: two randomized, double-blind, placebo-controlled phase 3 trials. Nat Med. 2023;29:1180-1190. doi:10.1038/s41591-023-02320-9
- Mastorino L, Rosset F, Gelato F, et al. Chronic pruritus in atopic patients treated with dupilumab: real life response and related parameters in 354 patients. Pharmaceuticals (Basel). 2022;15:883. doi: 10.3390/ph15070883
- Kishi R, Toyama S, Tominaga M, et al. Effects of dupilumab on itch-related events in atopic dermatitis: implications for assessing treatment efficacy in clinical practice. Cells. 2023;12:239. doi: 10.3390/cells12020239
- Dupixent. European Medicines Agency website. Updated July 15, 2024. Accessed August 27, 2024. https://www.ema.europa.eu/en/medicines/human/EPAR/dupixent
Prurigo nodularis (PN)(also called chronic nodular prurigo, prurigo nodularis of Hyde, or picker’s nodules) was first characterized by James Hyde in 1909.1-3 Prurigo nodularis manifests with symmetrical, intensely pruritic, eroded, or hyperkeratotic nodules or papules on the extremities and trunk.1,2,4,5 Studies have shown that individuals with PN experience pruritus, sleep loss, decreased social functioning from the appearance of the nodules, and a higher incidence of anxiety and depression, causing a negative impact on their quality of life.2,6 In addition, the manifestation of PN has been linked to neurologic and psychiatric disorders; however, PN also can be idiopathic and manifest without underlying illnesses.2,6,7
Prurigo nodularis has been associated with other dermatologic conditions such as atopic dermatitis (up to 50%), lichen planus, keratoacanthomas (KAs), and bullous pemphigoid.7-9 It also has been linked to systemic diseases in 38% to 50% of cases, including chronic kidney disease, liver disease, type 2 diabetes mellitus, malignancies (hematopoietic, liver, and skin), and HIV infection.6,8,10
The pathophysiology of PN is highly complex and has yet to be fully elucidated. It is thought to be due to dysregulation and interaction of the increase in neural and immunologic responses of proinflammatory and pruritogenic cytokines.2,11 Treatments aim to break the itch-scratch cycle that perpetuates this disorder; however, this proves difficult, as PN is associated with a higher itch intensity than atopic dermatitis and psoriasis.10 Therefore, most patients attempt multiple forms of treatment for PN, ranging from topical therapies, oral immunosuppressants, and phototherapy to the newest and only medication approved by the US Food and Drug Administration for the treatment of PN—dupilumab.1,7,11 Herein, we provide an updated review of PN with a focus on its epidemiology, histopathology and pathophysiology, comorbidities, clinical presentation, differential diagnosis, and current treatment options.
Epidemiology
There are few studies on the epidemiology of PN; however, middle-aged populations with underlying dermatologic or psychiatric disorders tend to be impacted most frequently.2,12,13 In 2016, it was estimated that almost 88,000 individuals had PN in the United States, with the majority being female; however, this estimate only took into account those aged 18 to 64 years and utilized data from IBM MarketScan Commercial Claims and Encounters Database (IBM Watson Health) from October 2015 to December 2016.14 More recently, a retrospective database analysis estimated the prevalence of PN in the United States to be anywhere from 36.7 to 43.9 cases per 100,000 individuals. However, this retrospective review utilized the International Classification of Diseases, Tenth Revision code; PN has 2 codes associated with the diagnosis, and the coding accuracy is unknown.15 Sutaria et al16 looked at racial disparities in patients with PN utilizing data from TriNetX and found that patients who received a diagnosis of PN were more likely to be women, non-Hispanic, and Black compared with control patients. However, these estimates are restricted to the health care organizations within this database.
In 2018, Poland reported an annual prevalence of 6.52 cases per 100,000 individuals,17 while England reported a yearly prevalence of 3.27 cases per 100,000 individuals.18 Both countries reported most cases were female. However, these studies are not without limitations. Poland only uses the primary diagnosis code for medical billing to simplify clinical coding, thus underestimating the actual prevalence; furthermore, clinical codes more often than not are assigned by someone other than the diagnosing physician, leaving room for error.17 In addition, England’s PN estimate utilized diagnosis data from primary care and inpatient datasets, leaving out outpatient datasets in which patients with PN may have been referred and obtained the diagnosis, potentially underestimating the prevalence in this population.18
In contrast, Korea estimated the annual prevalence of PN to be 4.82 cases per 1000 dermatology outpatients, with the majority being men, based on results from a cross-sectional study among outpatients from the Catholic Medical Center. Although this is the largest health organization in Korea, the scope of this study is limited and lacks data from other medical centers in Korea.19
Histopathology and Pathophysiology
Almost all cells in the skin are involved in PN: keratinocytes, mast cells, dendritic cells, endothelial cells, lymphocytes, eosinophils, collagen fibers, and nerve fibers.11,20 Classically, PN manifests as a dome-shaped lesion with hyperkeratosis, hypergranulosis, and psoriasiform epidermal hyperplasia with increased thickness of the papillary dermis consisting of coarse collagen with compact interstitial and circumvascular infiltration as well as increased lymphocytes and histocytes in the superficial dermis (Figure 1).20 Hyperkeratosis is thought to be due to either the alteration of keratinocyte structures from scratching or keratinocyte abnormalities triggering PN.21 However, the increase in keratinocytes, which secrete nerve growth factor, allows for neuronal hyperplasia within the dermis.22 Nerve growth factor can stimulate keratinocyte proliferation23 in addition to the upregulation of substance P (SP), a tachykinin that triggers vascular dilation and pruritus in the skin.24 The density of SP nerve fibers in the dermis increases in PN, causing proinflammatory effects, upregulating the immune response to promote endothelial hyperplasia and increased vascularization.25 The increase in these fibers may lead to pruritus associated with PN.2,26
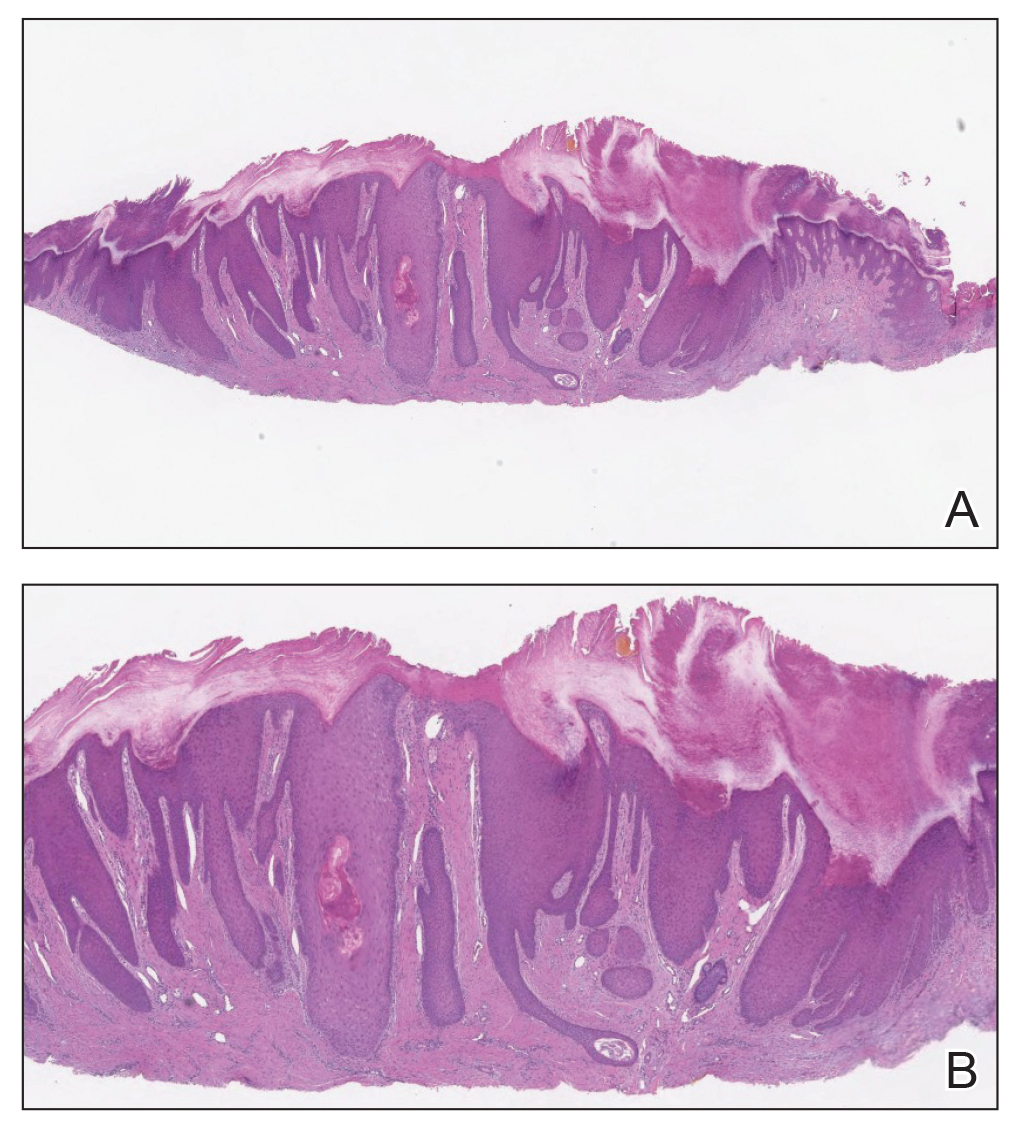
Many inflammatory cytokines and mediators also have been implicated in PN. Increased messenger RNA expression of IL-4, IL-17, IL-22, and IL-31 has been described in PN lesions.3,27 Furthermore, studies also have reported increased helper T cell (TH2) cytokines, including IL-4, IL-5, IL-10, and IL-13, in the dermis of PN lesions in patients without a history of atopy.3,28 These pruritogenic cytokines in conjunction with the SP fibers may create an intractable itch for those with PN. The interaction and culmination of the neural and immune responses make PN a complex condition to treat with the multifactorial interaction of systems.
Comorbidities
Prurigo nodularis has been associated with a wide array of comorbidities; however, the direction of the relationship between PN and these conditions makes it difficult to discern if PN is a primary or secondary condition.29 Prurigo nodularis commonly has been connected to other inflammatory dermatoses, with a link to atopic dermatitis being the strongest.5,29 However, PN also has been linked to other pruritic inflammatory cutaneous disorders, including psoriasis, cutaneous T-cell lymphoma, lichen planus, and dermatitis herpetiformis.14,29
Huang et al14 found an increased likelihood of psychiatric illnesses in patients with PN, including eating disorders, nonsuicidal self-injury disorder, attention-deficit/hyperactivity disorder, schizophrenia, mood disorders, anxiety, and substance abuse disorders. Treatments directed at the neural aspect of PN have included selective serotonin reuptake inhibitors (SSRIs), which also are utilized to treat these mental health disorders.
Furthermore, systemic diseases also have been found to be associated with PN, including hypertension, type 2 diabetes mellitus, chronic kidney disease, heart failure, cerebrovascular disease, coronary heart disease, and chronic obstructive pulmonary disease.14 The relationship between PN and systemic conditions may be due to increased systemic inflammation and dysregulation of neural and metabolic functions implicated in these conditions from increased pruritic manifestations.29,30 However, studies also have connected PN to infectious conditions such as HIV. One study found that patients with PN had 2.68 higher odds of infection with HIV compared to age- and sex-matched controls.14 It is unknown if these conditions contributed to the development of PN or PN contributed to the development of these disorders.
Clinical Presentations
Prurigo nodularis is a chronic inflammatory skin disease that typically manifests with multiple severely pruritic, dome-shaped, firm, hyperpigmented papulonodules with central scale or crust, often with erosion, due to chronic repetitive scratching and picking secondary to pruritic systemic or dermatologic diseases or psychological disorders (Figure 2).1,2,4,5,8,31 Most often, diagnosis of PN is based on history and physical examination of the lesion; however, biopsies may be performed. These nodules commonly manifest with ulceration distributed symmetrically on extensor extremities in easy-to-reach places, sparing the mid back (called the butterfly sign).8 Lesions—either a few or hundreds—can range from a few millimeters to 2 to 3 cm.8,32 The lesions differ in appearance depending on the pigment in the patient’s skin. In patients with darker skin tones, hyperpigmented or hypopigmented papulonodules are not uncommon, while those with fairer skin tones tend to present with erythema.31
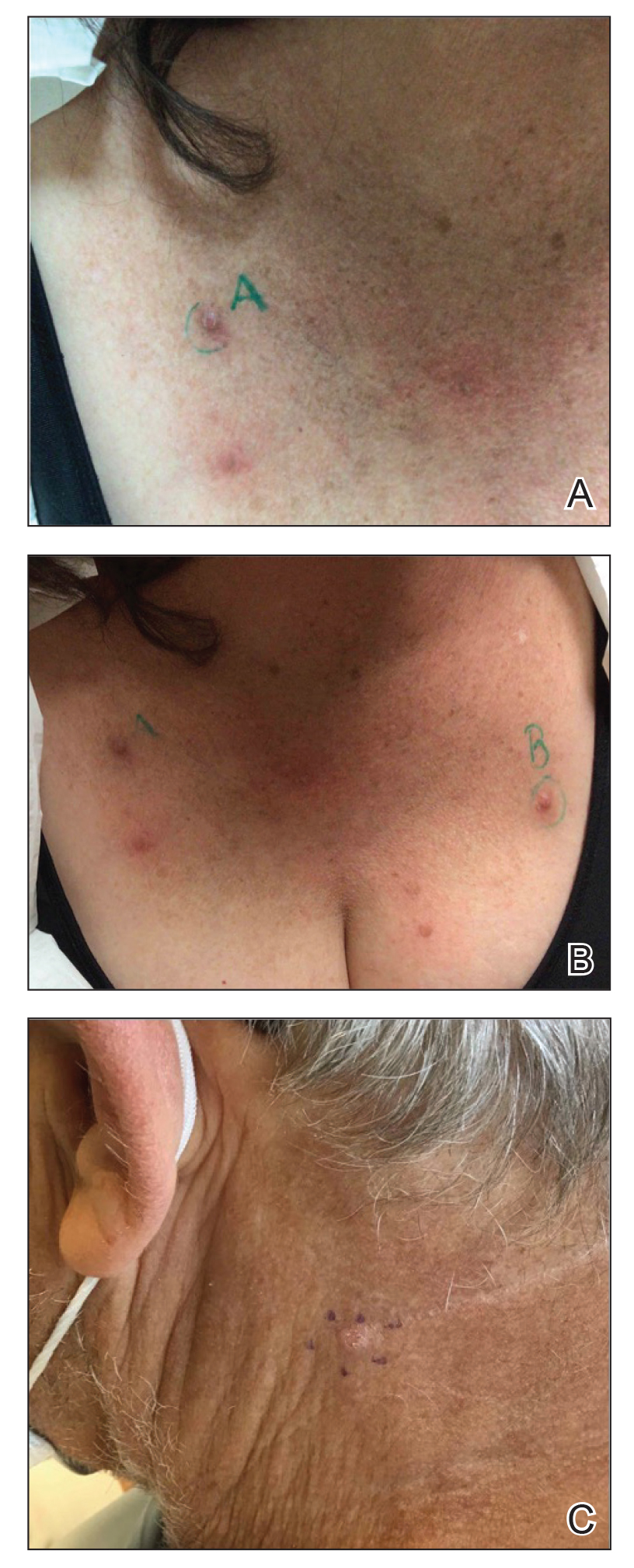
Differential Diagnosis
Because of the variation in manifestation of PN, these lesions may resemble other cutaneous conditions. If the lesions are hyperkeratotic, they can mimic hypertrophic lichen planus, which mainfests with hyperkeratotic plaques or nodules on the lower extremities.8,29 In addition, the histopathology of lichen planus resembles the appearance of PN, with epidermal hyperplasia, hypergranulosis, hyperkeratosis, and increased fibroblasts and capillaries.8,29
Pemphigoid nodularis is a rare subtype of bullous pemphigoid that exhibits characteristics of PN with pruritic plaques and erosions.8,29,33 The patient population for pemphigoid nodularis tends to be aged 50 to 60 years, and females are affected more frequently than males. However, pemphigoid nodularis may manifest with blistering and large plaques, which are not seen commonly with PN.29 On histopathology, pemphigoid nodularis deposits IgG and C3 on the basement membrane and has subepidermal clefting, unlike PN.7,29
Actinic prurigo manifests with pruritic papules or nodules post–UV exposure to unprotected skin.8,29,33 This rare condition usually manifests with cheilitis and conjunctivitis. Unlike PN, which commonly affects elderly populations, actinic prurigo typically is found in young females.8,29 Cytologic examination shows hyperkeratosis, spongiosis, and acanthosis of the epidermis with lymphocytic perivascular infiltration of the dermis.34
Neurotic excoriations also tend to mimic PN with raised excoriated lesions; however, this disorder is due to neurotic picking of the skin without associated pruritus or true hyperkeratosis.8,29,33 Histopathology shows epidermal crusting with inflammation of the upper dermis.35
Infiltrative cutaneous squamous cell carcinoma (SCC) may imitate PN in appearance. It manifests as tender, ulcerated, scaly plaques or nodules. Histopathology shows cytologic atypia with an infiltrative architectural pattern and presence of collections of compact keratin and parakeratin (called keratin pearls).
Keratoacanthomas can resemble PN lesions. They usually manifest as nodules measuring 1 to 2 cm in diameter and 0.5 cm thick, resembling crateriform tumors.36 On histopathology, KAs can resemble SCCs; however, KAs tend to manifest more frequently with a keratin-filled crater with a ground-glass appearance.36
Inverted follicular keratosis commonly manifests on the face in elderly men as a single, flesh-colored, verrucous papule that may resemble PN. However, cytology of inverted follicular keratosis is characterized by proliferation and squamous eddies.37 Consideration of the histologic findings and clinical appearance are important to differentiate between PN and cutaneous SCC.
Pseudoepitheliomatous hyperplasia is a benign condition that manifests as a plaque or nodule with crust, scale, or ulceration. Histologically, this condition presents with hyperplastic proliferation of the epidermis and adnexal epithelium.38 The clinical and histologic appearance can mimic PN and other cutaneous eruptions with epidermal hyperplasia.
In clinical cases that are resistant to treatment, biopsy is the best approach to diagnose the lesion. Due to similarities in physical appearance and superficial histologic presentation of PN, KAs from SCC, hypertrophic lichen planus, and other hyperkeratotic lesions, the biopsy should be taken at the base of the lesion to sample deeper layers of skin to differentiate these dermatologic disorders.
Management
Current treatments for PN yield varied results. Many patients with moderate to severe PN attempt multiple therapies before seeing improvement.31 Treatments include topical, oral, and injectable medications and are either directed at the neural or immune components of PN due to the interplay between increased nerve fibers in the lesions (neural axis) as well as increases in cytokines and other immunologic mediators (immune axis) of this condition. However, the FDA recently approved the first treatment for PN—dupilumab—which is an injectable IL-4 receptor antagonist directed at the immunologic interactions affiliated with PN.
Immune-Mediated Topical Therapies—Immunologic topical therapies include corticosteroids, calcipotriol, and calcineurin inhibitors. Studies that have analyzed these treatments are limited to case reports and small intraindividual and randomized controlled trials (Table 1). Topical therapies usually are first-line agents for most patients. Adverse effects include transient irritation of the skin.40,42,43
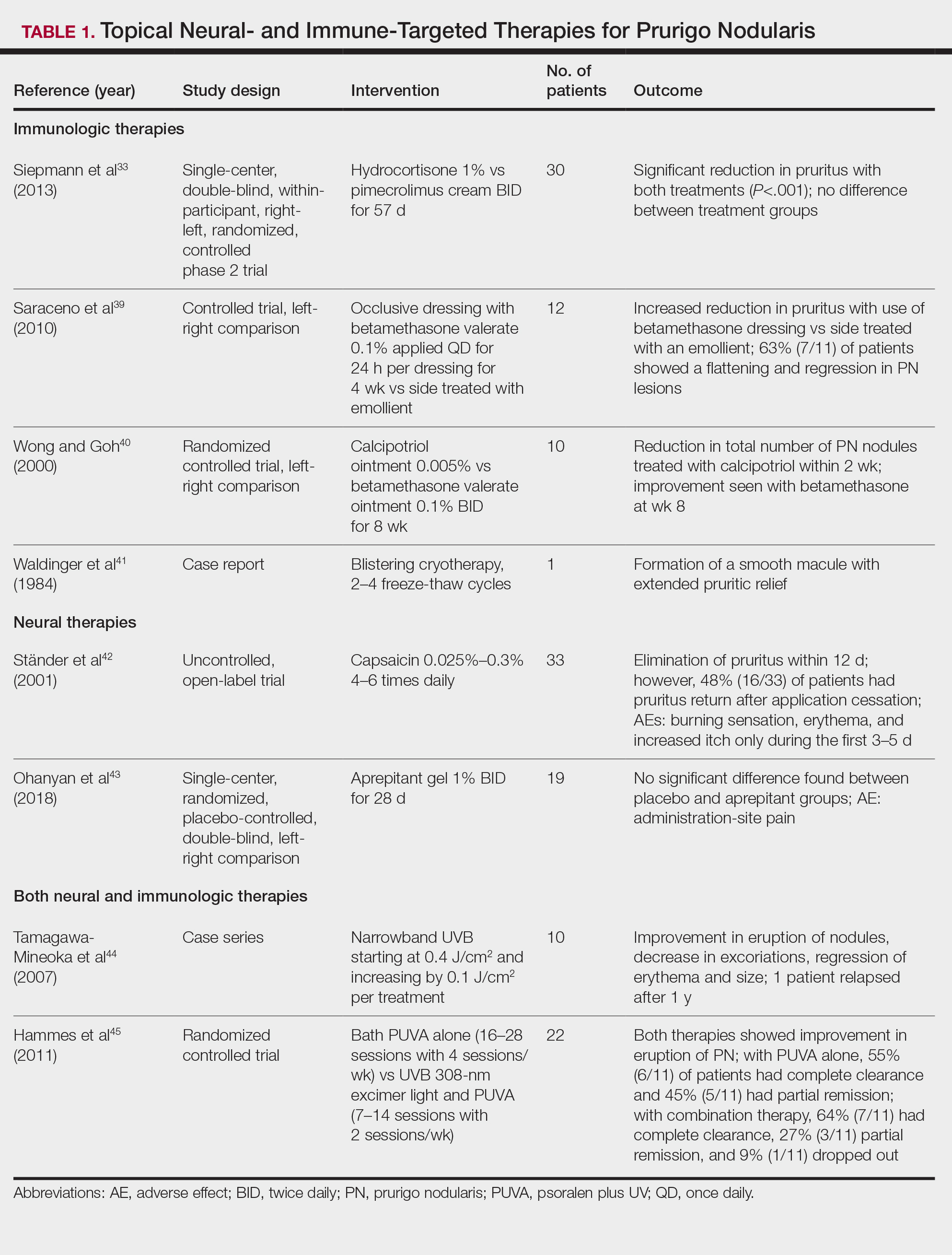
Cryotherapy is another topical and immunologic therapy for those with PN; however, this treatment is more appropriate for patients with fewer lesions due to the pain that accompanies lesions treated with liquid nitrogen. In addition, this therapy can cause dyspigmentation of the skin in the treated areas.41
Similar to cryotherapy, intralesional corticosteroid injections are appropriate for patients with few PN lesions. A recent report described intralesional corticosteroid injections of 2.5 mg/mL for a PN nodule with high efficacy.46,47 This treatment has not undergone trials, but success with this modality has been documented, with adverse effects including hyperpigmentation or hypopigmentation in the treated area and transient pain.46
Neural-Mediated Topical Therapies—Neural topical therapies include capsaicin and neurokinin-1 receptor antagonists, aprepitant43 and serlopitant. These treatment studies are limited to small open-label and randomized controlled trials. Adverse effects of these treatments include transient cutaneous pain at the site of topical administration. In addition, neural-mediated topical therapies have shown either limited improvements from baseline or return of symptoms after treatment cessation.42,43
Supplements—N-acetyl cysteine is an over-the-counter supplement that has been reported to improve symptoms in patients with skin-picking disorders.48 The mechanism of action includes antioxidant effects such as decreasing reactive oxygen species, decreasing inflammatory markers, regulating neurotransmitters, and inhibiting hyperkeratosis.49 N-acetyl cysteine has been poorly studied for its application in PN. A small study of 3 patients with subacute PN receiving 1200 mg of oral N-acetyl cysteine reported varying levels of improvement in skin appearance and reduction in skin picking.50
Phototherapy—Phototherapy, a typical first- or second-line treatment modality for PN, targets both the neural- and immune-mediated aspects associated with pruritus in PN (Table 1).51 UV light can penetrate through the epidermal layer of the skin and reach the keratinocytes, which play a role in the immune-related response of PN. In addition, the cutaneous sensory nerves are located in the upper dermal layer, from which nerve fibers grow and penetrate into the epidermis, thereby interacting with the keratinocytes where pruritic signals are transmitted from the periphery up to the brain.51
Studies analyzing the effects of phototherapy on PN are limited to case series and a small randomized controlled trial. However, this trial has shown improvements in pruritus in the participants. Adverse effects include transient burning and erythema at the treated sites.44,45
Immune-Mediated Oral Therapies—Immunologic-targeted oral therapies include bilastine, methotrexate, and cyclosporine (Table 2).52,53 Bilastine efficacy was analyzed in a small phase 3, open-label, multicenter study in Japan; however, patients were allowed to use topical steroids in conjunction with the oral antihistamine.54 Methotrexate and cyclosporine are immunosuppressive medications and were analyzed in small retrospective studies. Both treatments yielded notable relief for patients; however, 38.5% (15/39) of patients receiving methotrexate experienced adverse events, and 50.0% (4/8) experienced adverse events with cyclosporine.52,53
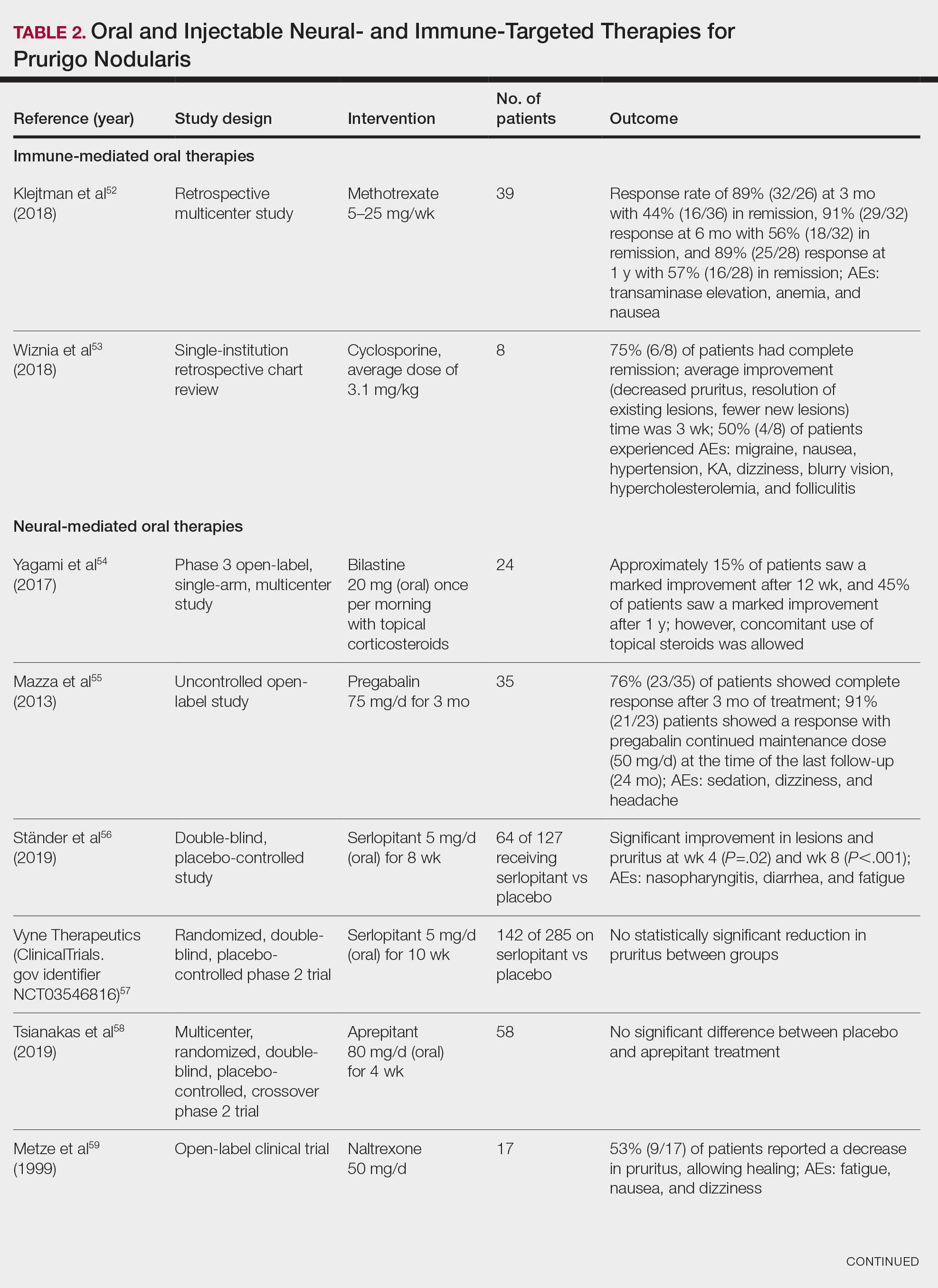
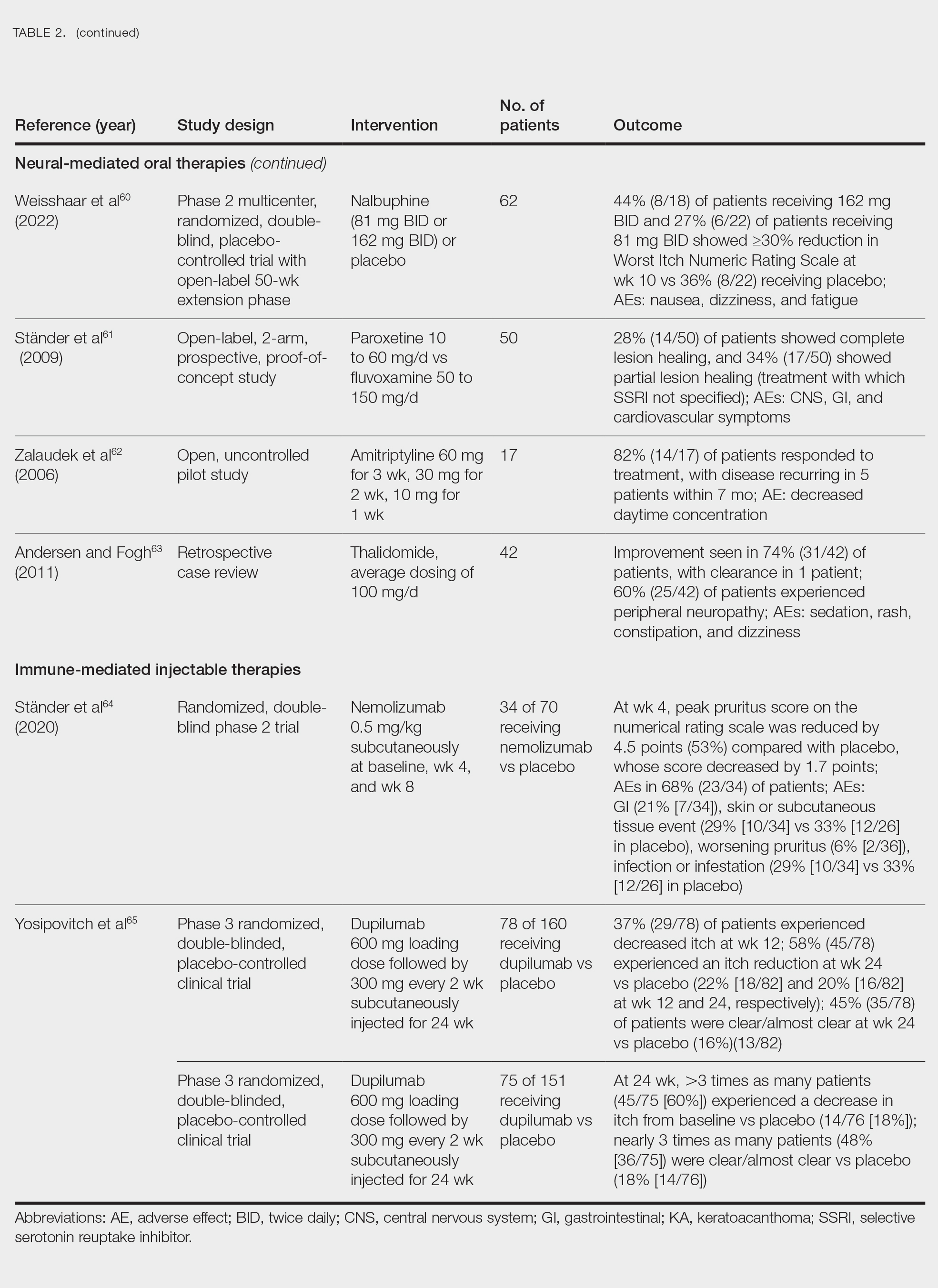
Neural-Mediated Oral Therapies—Neural-targeted oral therapies include pregabalin, serlopitant, aprepitant, naltrexone, nalbuphine, SSRIs (paroxetine and fluvoxamine), amitriptyline, and thalidomide. The research on these treatments ranges from case reviews to randomized controlled trials and open-label trials (Table 2).55-63
Thalidomide was studied in a small retrospective case review that showed notable improvement in PN. Dosages of thalidomide varied, but on average the dose was 100 mg/d. However, greater than 50% of patients experienced at least 1 adverse effect with this treatment.63
A study performed in Italy showed promising results for patients treated with pregabalin, with 70.0% (21/30) continuing to take pregabalin for almost 2 years following completion of the initial 3-month trial.55 Naltrexone decreased pruritus in more than half of patients (9/17).59 Amitriptyline yielded improvements in patients with PN; however, disease recurred in 5 patients (29%) after 7 months.62 A study performed in Germany reported promising results for paroxetine and fluvoxamine; however, some patients enrolled in the study had some form of psychiatric disorder.61
Serlopitant, aprepitant, and nalbuphine were studied in randomized controlled trials. The serlopitant trials were the largest of the neurally mediated oral medication studies; one showed substantial improvement in patients with PN,56 while the most recent trial did not show significant improvement (ClinicalTrials.gov identifier NCT03546816).57 On the other hand, aprepitant showed no major difference between the experimental and placebo groups.58 Nalbuphine 162 mg twice daily showed greater improvement in PN than nalbuphine 81 mg twice daily.60
Immune-Mediated Injectable Therapies—Immune-targeted injectables include nemolizumab and dupilumab (Table 2). Nemolizumab is an IL-31 antagonist that has been studied in a small randomized controlled trial that showed great success in decreasing pruritus associated with PN.64 IL-31 has been implicated in PN, and inhibition of the IL-31 receptor has been shown to disrupt the itch-scratch cycle of PN. Dupilumab is a monoclonal antibody against the IL-4 and IL-13 receptors, and it is the only FDA-approved treatment for PN.65 Blockage of these protein receptors decreases type 2 inflammation and chronic pruritus.66,67 Dupilumab is FDA approved for the treatment of atopic dermatitis and recently was approved for adults with PN. Dupilumab acts to block the shared α-subunit of the pruritogenic cytokines IL-4 and IL-13 pathways,29 thereby breaking the itch-scratch cycle associated with PN and allowing for the healing of these lesions. Results from 2 clinical trials showed substantially reduced itch in patients with PN.65 Dupilumab also was approved by the European Medicines Agency for moderate to severe PN.68
Conclusion
Prurigo nodularis is a chronic condition that affects patient quality of life and can mimic various dermatologic conditions. The epidemiology and pathophysiology of PN have not been fully expounded. More research should be conducted to determine the underpinnings of PN to help identify more consistently effective therapies for this complex condition.
Prurigo nodularis (PN)(also called chronic nodular prurigo, prurigo nodularis of Hyde, or picker’s nodules) was first characterized by James Hyde in 1909.1-3 Prurigo nodularis manifests with symmetrical, intensely pruritic, eroded, or hyperkeratotic nodules or papules on the extremities and trunk.1,2,4,5 Studies have shown that individuals with PN experience pruritus, sleep loss, decreased social functioning from the appearance of the nodules, and a higher incidence of anxiety and depression, causing a negative impact on their quality of life.2,6 In addition, the manifestation of PN has been linked to neurologic and psychiatric disorders; however, PN also can be idiopathic and manifest without underlying illnesses.2,6,7
Prurigo nodularis has been associated with other dermatologic conditions such as atopic dermatitis (up to 50%), lichen planus, keratoacanthomas (KAs), and bullous pemphigoid.7-9 It also has been linked to systemic diseases in 38% to 50% of cases, including chronic kidney disease, liver disease, type 2 diabetes mellitus, malignancies (hematopoietic, liver, and skin), and HIV infection.6,8,10
The pathophysiology of PN is highly complex and has yet to be fully elucidated. It is thought to be due to dysregulation and interaction of the increase in neural and immunologic responses of proinflammatory and pruritogenic cytokines.2,11 Treatments aim to break the itch-scratch cycle that perpetuates this disorder; however, this proves difficult, as PN is associated with a higher itch intensity than atopic dermatitis and psoriasis.10 Therefore, most patients attempt multiple forms of treatment for PN, ranging from topical therapies, oral immunosuppressants, and phototherapy to the newest and only medication approved by the US Food and Drug Administration for the treatment of PN—dupilumab.1,7,11 Herein, we provide an updated review of PN with a focus on its epidemiology, histopathology and pathophysiology, comorbidities, clinical presentation, differential diagnosis, and current treatment options.
Epidemiology
There are few studies on the epidemiology of PN; however, middle-aged populations with underlying dermatologic or psychiatric disorders tend to be impacted most frequently.2,12,13 In 2016, it was estimated that almost 88,000 individuals had PN in the United States, with the majority being female; however, this estimate only took into account those aged 18 to 64 years and utilized data from IBM MarketScan Commercial Claims and Encounters Database (IBM Watson Health) from October 2015 to December 2016.14 More recently, a retrospective database analysis estimated the prevalence of PN in the United States to be anywhere from 36.7 to 43.9 cases per 100,000 individuals. However, this retrospective review utilized the International Classification of Diseases, Tenth Revision code; PN has 2 codes associated with the diagnosis, and the coding accuracy is unknown.15 Sutaria et al16 looked at racial disparities in patients with PN utilizing data from TriNetX and found that patients who received a diagnosis of PN were more likely to be women, non-Hispanic, and Black compared with control patients. However, these estimates are restricted to the health care organizations within this database.
In 2018, Poland reported an annual prevalence of 6.52 cases per 100,000 individuals,17 while England reported a yearly prevalence of 3.27 cases per 100,000 individuals.18 Both countries reported most cases were female. However, these studies are not without limitations. Poland only uses the primary diagnosis code for medical billing to simplify clinical coding, thus underestimating the actual prevalence; furthermore, clinical codes more often than not are assigned by someone other than the diagnosing physician, leaving room for error.17 In addition, England’s PN estimate utilized diagnosis data from primary care and inpatient datasets, leaving out outpatient datasets in which patients with PN may have been referred and obtained the diagnosis, potentially underestimating the prevalence in this population.18
In contrast, Korea estimated the annual prevalence of PN to be 4.82 cases per 1000 dermatology outpatients, with the majority being men, based on results from a cross-sectional study among outpatients from the Catholic Medical Center. Although this is the largest health organization in Korea, the scope of this study is limited and lacks data from other medical centers in Korea.19
Histopathology and Pathophysiology
Almost all cells in the skin are involved in PN: keratinocytes, mast cells, dendritic cells, endothelial cells, lymphocytes, eosinophils, collagen fibers, and nerve fibers.11,20 Classically, PN manifests as a dome-shaped lesion with hyperkeratosis, hypergranulosis, and psoriasiform epidermal hyperplasia with increased thickness of the papillary dermis consisting of coarse collagen with compact interstitial and circumvascular infiltration as well as increased lymphocytes and histocytes in the superficial dermis (Figure 1).20 Hyperkeratosis is thought to be due to either the alteration of keratinocyte structures from scratching or keratinocyte abnormalities triggering PN.21 However, the increase in keratinocytes, which secrete nerve growth factor, allows for neuronal hyperplasia within the dermis.22 Nerve growth factor can stimulate keratinocyte proliferation23 in addition to the upregulation of substance P (SP), a tachykinin that triggers vascular dilation and pruritus in the skin.24 The density of SP nerve fibers in the dermis increases in PN, causing proinflammatory effects, upregulating the immune response to promote endothelial hyperplasia and increased vascularization.25 The increase in these fibers may lead to pruritus associated with PN.2,26
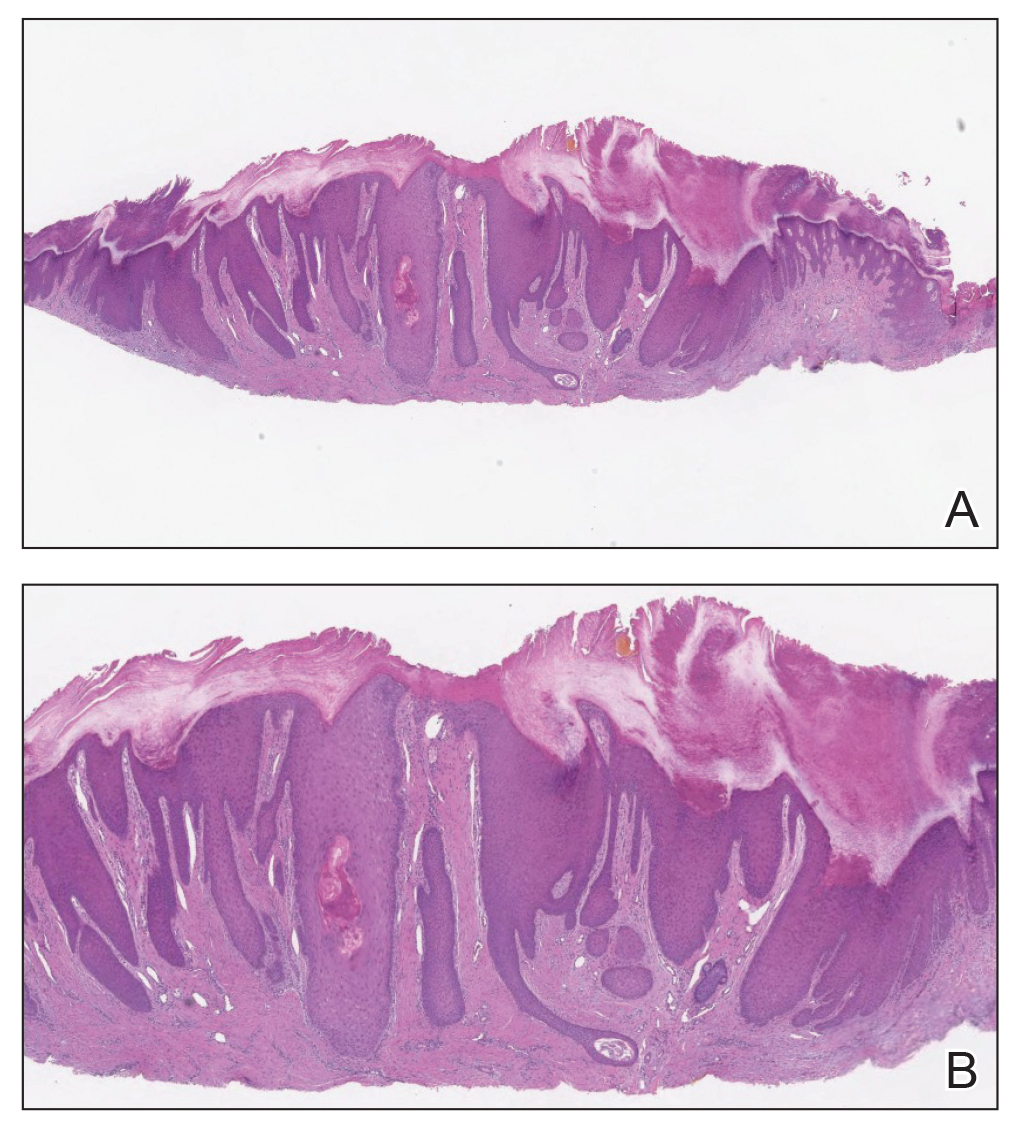
Many inflammatory cytokines and mediators also have been implicated in PN. Increased messenger RNA expression of IL-4, IL-17, IL-22, and IL-31 has been described in PN lesions.3,27 Furthermore, studies also have reported increased helper T cell (TH2) cytokines, including IL-4, IL-5, IL-10, and IL-13, in the dermis of PN lesions in patients without a history of atopy.3,28 These pruritogenic cytokines in conjunction with the SP fibers may create an intractable itch for those with PN. The interaction and culmination of the neural and immune responses make PN a complex condition to treat with the multifactorial interaction of systems.
Comorbidities
Prurigo nodularis has been associated with a wide array of comorbidities; however, the direction of the relationship between PN and these conditions makes it difficult to discern if PN is a primary or secondary condition.29 Prurigo nodularis commonly has been connected to other inflammatory dermatoses, with a link to atopic dermatitis being the strongest.5,29 However, PN also has been linked to other pruritic inflammatory cutaneous disorders, including psoriasis, cutaneous T-cell lymphoma, lichen planus, and dermatitis herpetiformis.14,29
Huang et al14 found an increased likelihood of psychiatric illnesses in patients with PN, including eating disorders, nonsuicidal self-injury disorder, attention-deficit/hyperactivity disorder, schizophrenia, mood disorders, anxiety, and substance abuse disorders. Treatments directed at the neural aspect of PN have included selective serotonin reuptake inhibitors (SSRIs), which also are utilized to treat these mental health disorders.
Furthermore, systemic diseases also have been found to be associated with PN, including hypertension, type 2 diabetes mellitus, chronic kidney disease, heart failure, cerebrovascular disease, coronary heart disease, and chronic obstructive pulmonary disease.14 The relationship between PN and systemic conditions may be due to increased systemic inflammation and dysregulation of neural and metabolic functions implicated in these conditions from increased pruritic manifestations.29,30 However, studies also have connected PN to infectious conditions such as HIV. One study found that patients with PN had 2.68 higher odds of infection with HIV compared to age- and sex-matched controls.14 It is unknown if these conditions contributed to the development of PN or PN contributed to the development of these disorders.
Clinical Presentations
Prurigo nodularis is a chronic inflammatory skin disease that typically manifests with multiple severely pruritic, dome-shaped, firm, hyperpigmented papulonodules with central scale or crust, often with erosion, due to chronic repetitive scratching and picking secondary to pruritic systemic or dermatologic diseases or psychological disorders (Figure 2).1,2,4,5,8,31 Most often, diagnosis of PN is based on history and physical examination of the lesion; however, biopsies may be performed. These nodules commonly manifest with ulceration distributed symmetrically on extensor extremities in easy-to-reach places, sparing the mid back (called the butterfly sign).8 Lesions—either a few or hundreds—can range from a few millimeters to 2 to 3 cm.8,32 The lesions differ in appearance depending on the pigment in the patient’s skin. In patients with darker skin tones, hyperpigmented or hypopigmented papulonodules are not uncommon, while those with fairer skin tones tend to present with erythema.31
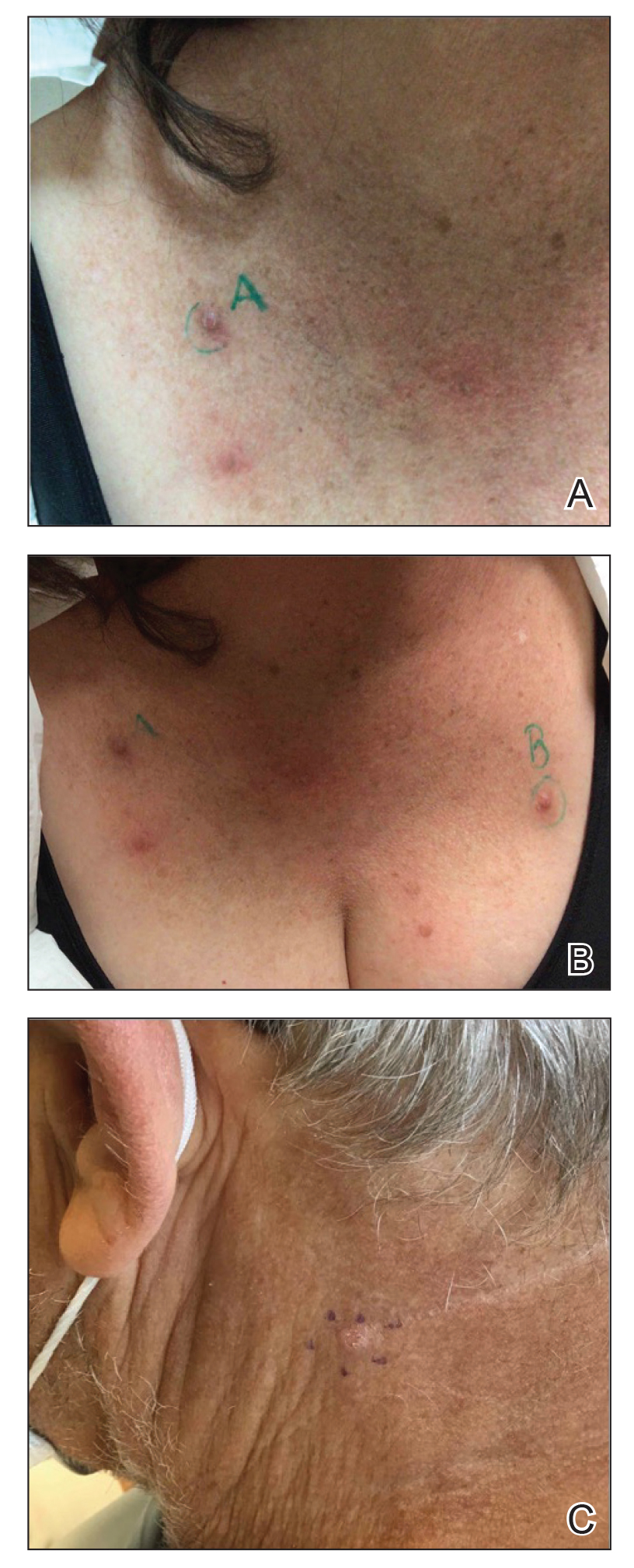
Differential Diagnosis
Because of the variation in manifestation of PN, these lesions may resemble other cutaneous conditions. If the lesions are hyperkeratotic, they can mimic hypertrophic lichen planus, which mainfests with hyperkeratotic plaques or nodules on the lower extremities.8,29 In addition, the histopathology of lichen planus resembles the appearance of PN, with epidermal hyperplasia, hypergranulosis, hyperkeratosis, and increased fibroblasts and capillaries.8,29
Pemphigoid nodularis is a rare subtype of bullous pemphigoid that exhibits characteristics of PN with pruritic plaques and erosions.8,29,33 The patient population for pemphigoid nodularis tends to be aged 50 to 60 years, and females are affected more frequently than males. However, pemphigoid nodularis may manifest with blistering and large plaques, which are not seen commonly with PN.29 On histopathology, pemphigoid nodularis deposits IgG and C3 on the basement membrane and has subepidermal clefting, unlike PN.7,29
Actinic prurigo manifests with pruritic papules or nodules post–UV exposure to unprotected skin.8,29,33 This rare condition usually manifests with cheilitis and conjunctivitis. Unlike PN, which commonly affects elderly populations, actinic prurigo typically is found in young females.8,29 Cytologic examination shows hyperkeratosis, spongiosis, and acanthosis of the epidermis with lymphocytic perivascular infiltration of the dermis.34
Neurotic excoriations also tend to mimic PN with raised excoriated lesions; however, this disorder is due to neurotic picking of the skin without associated pruritus or true hyperkeratosis.8,29,33 Histopathology shows epidermal crusting with inflammation of the upper dermis.35
Infiltrative cutaneous squamous cell carcinoma (SCC) may imitate PN in appearance. It manifests as tender, ulcerated, scaly plaques or nodules. Histopathology shows cytologic atypia with an infiltrative architectural pattern and presence of collections of compact keratin and parakeratin (called keratin pearls).
Keratoacanthomas can resemble PN lesions. They usually manifest as nodules measuring 1 to 2 cm in diameter and 0.5 cm thick, resembling crateriform tumors.36 On histopathology, KAs can resemble SCCs; however, KAs tend to manifest more frequently with a keratin-filled crater with a ground-glass appearance.36
Inverted follicular keratosis commonly manifests on the face in elderly men as a single, flesh-colored, verrucous papule that may resemble PN. However, cytology of inverted follicular keratosis is characterized by proliferation and squamous eddies.37 Consideration of the histologic findings and clinical appearance are important to differentiate between PN and cutaneous SCC.
Pseudoepitheliomatous hyperplasia is a benign condition that manifests as a plaque or nodule with crust, scale, or ulceration. Histologically, this condition presents with hyperplastic proliferation of the epidermis and adnexal epithelium.38 The clinical and histologic appearance can mimic PN and other cutaneous eruptions with epidermal hyperplasia.
In clinical cases that are resistant to treatment, biopsy is the best approach to diagnose the lesion. Due to similarities in physical appearance and superficial histologic presentation of PN, KAs from SCC, hypertrophic lichen planus, and other hyperkeratotic lesions, the biopsy should be taken at the base of the lesion to sample deeper layers of skin to differentiate these dermatologic disorders.
Management
Current treatments for PN yield varied results. Many patients with moderate to severe PN attempt multiple therapies before seeing improvement.31 Treatments include topical, oral, and injectable medications and are either directed at the neural or immune components of PN due to the interplay between increased nerve fibers in the lesions (neural axis) as well as increases in cytokines and other immunologic mediators (immune axis) of this condition. However, the FDA recently approved the first treatment for PN—dupilumab—which is an injectable IL-4 receptor antagonist directed at the immunologic interactions affiliated with PN.
Immune-Mediated Topical Therapies—Immunologic topical therapies include corticosteroids, calcipotriol, and calcineurin inhibitors. Studies that have analyzed these treatments are limited to case reports and small intraindividual and randomized controlled trials (Table 1). Topical therapies usually are first-line agents for most patients. Adverse effects include transient irritation of the skin.40,42,43
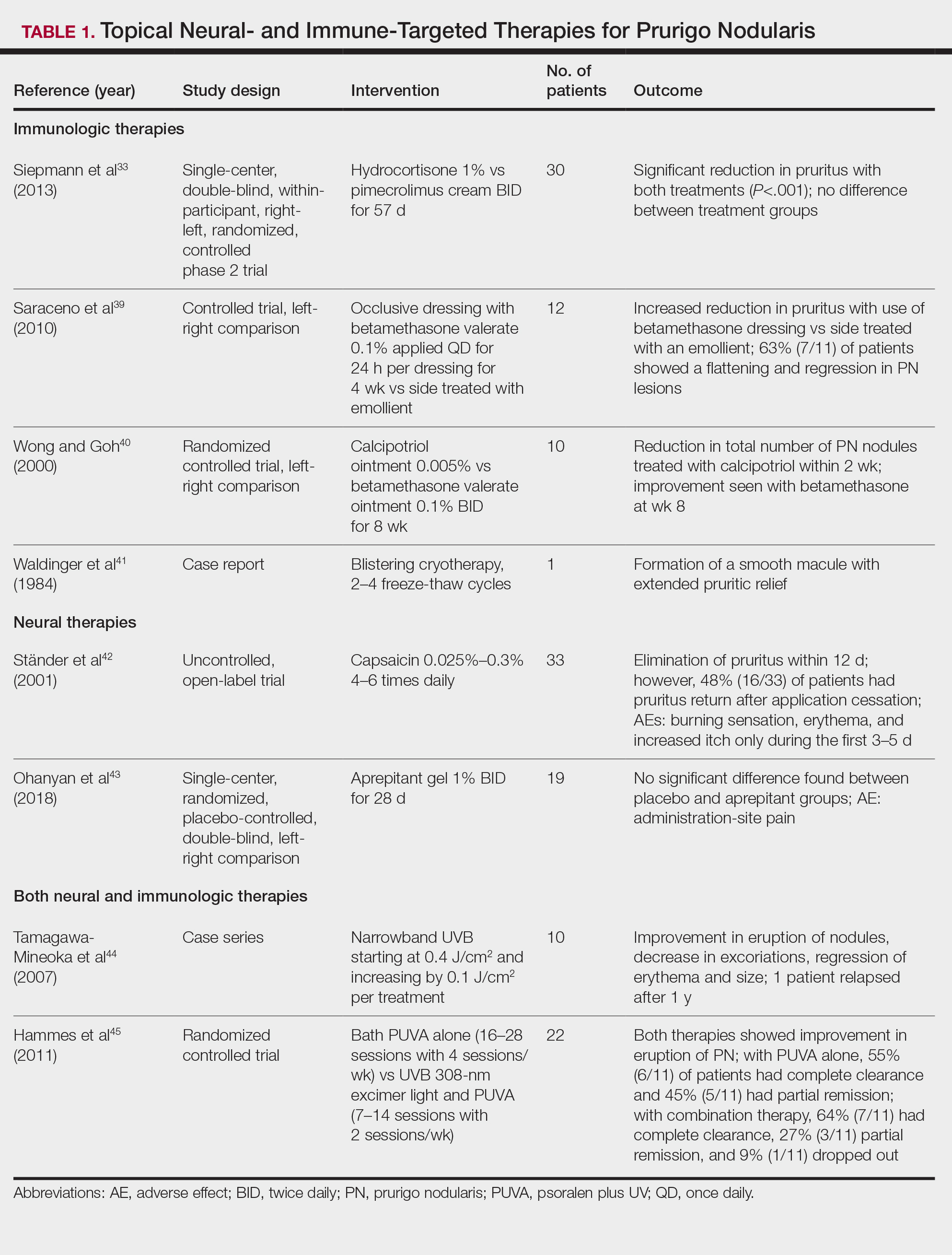
Cryotherapy is another topical and immunologic therapy for those with PN; however, this treatment is more appropriate for patients with fewer lesions due to the pain that accompanies lesions treated with liquid nitrogen. In addition, this therapy can cause dyspigmentation of the skin in the treated areas.41
Similar to cryotherapy, intralesional corticosteroid injections are appropriate for patients with few PN lesions. A recent report described intralesional corticosteroid injections of 2.5 mg/mL for a PN nodule with high efficacy.46,47 This treatment has not undergone trials, but success with this modality has been documented, with adverse effects including hyperpigmentation or hypopigmentation in the treated area and transient pain.46
Neural-Mediated Topical Therapies—Neural topical therapies include capsaicin and neurokinin-1 receptor antagonists, aprepitant43 and serlopitant. These treatment studies are limited to small open-label and randomized controlled trials. Adverse effects of these treatments include transient cutaneous pain at the site of topical administration. In addition, neural-mediated topical therapies have shown either limited improvements from baseline or return of symptoms after treatment cessation.42,43
Supplements—N-acetyl cysteine is an over-the-counter supplement that has been reported to improve symptoms in patients with skin-picking disorders.48 The mechanism of action includes antioxidant effects such as decreasing reactive oxygen species, decreasing inflammatory markers, regulating neurotransmitters, and inhibiting hyperkeratosis.49 N-acetyl cysteine has been poorly studied for its application in PN. A small study of 3 patients with subacute PN receiving 1200 mg of oral N-acetyl cysteine reported varying levels of improvement in skin appearance and reduction in skin picking.50
Phototherapy—Phototherapy, a typical first- or second-line treatment modality for PN, targets both the neural- and immune-mediated aspects associated with pruritus in PN (Table 1).51 UV light can penetrate through the epidermal layer of the skin and reach the keratinocytes, which play a role in the immune-related response of PN. In addition, the cutaneous sensory nerves are located in the upper dermal layer, from which nerve fibers grow and penetrate into the epidermis, thereby interacting with the keratinocytes where pruritic signals are transmitted from the periphery up to the brain.51
Studies analyzing the effects of phototherapy on PN are limited to case series and a small randomized controlled trial. However, this trial has shown improvements in pruritus in the participants. Adverse effects include transient burning and erythema at the treated sites.44,45
Immune-Mediated Oral Therapies—Immunologic-targeted oral therapies include bilastine, methotrexate, and cyclosporine (Table 2).52,53 Bilastine efficacy was analyzed in a small phase 3, open-label, multicenter study in Japan; however, patients were allowed to use topical steroids in conjunction with the oral antihistamine.54 Methotrexate and cyclosporine are immunosuppressive medications and were analyzed in small retrospective studies. Both treatments yielded notable relief for patients; however, 38.5% (15/39) of patients receiving methotrexate experienced adverse events, and 50.0% (4/8) experienced adverse events with cyclosporine.52,53
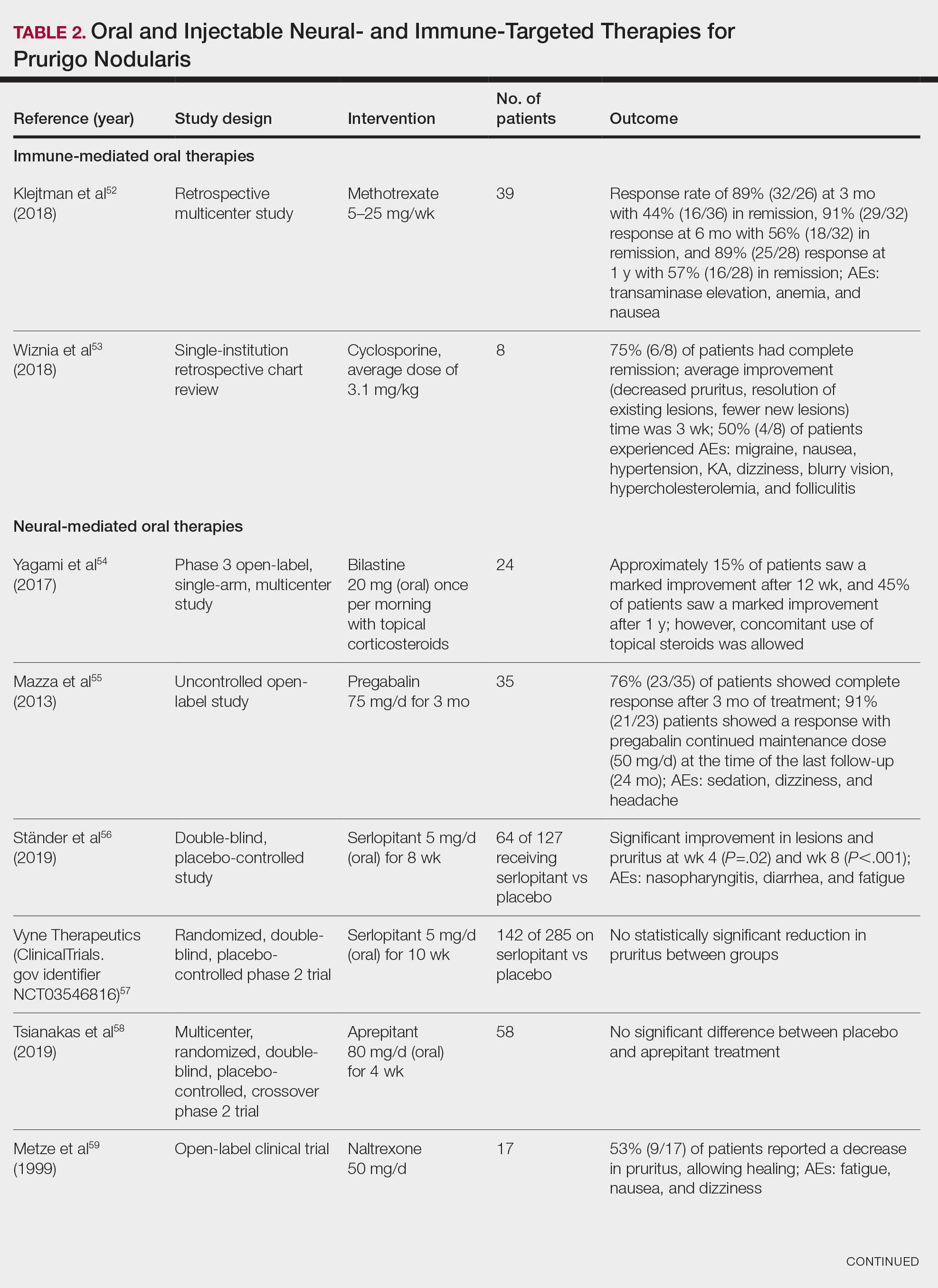
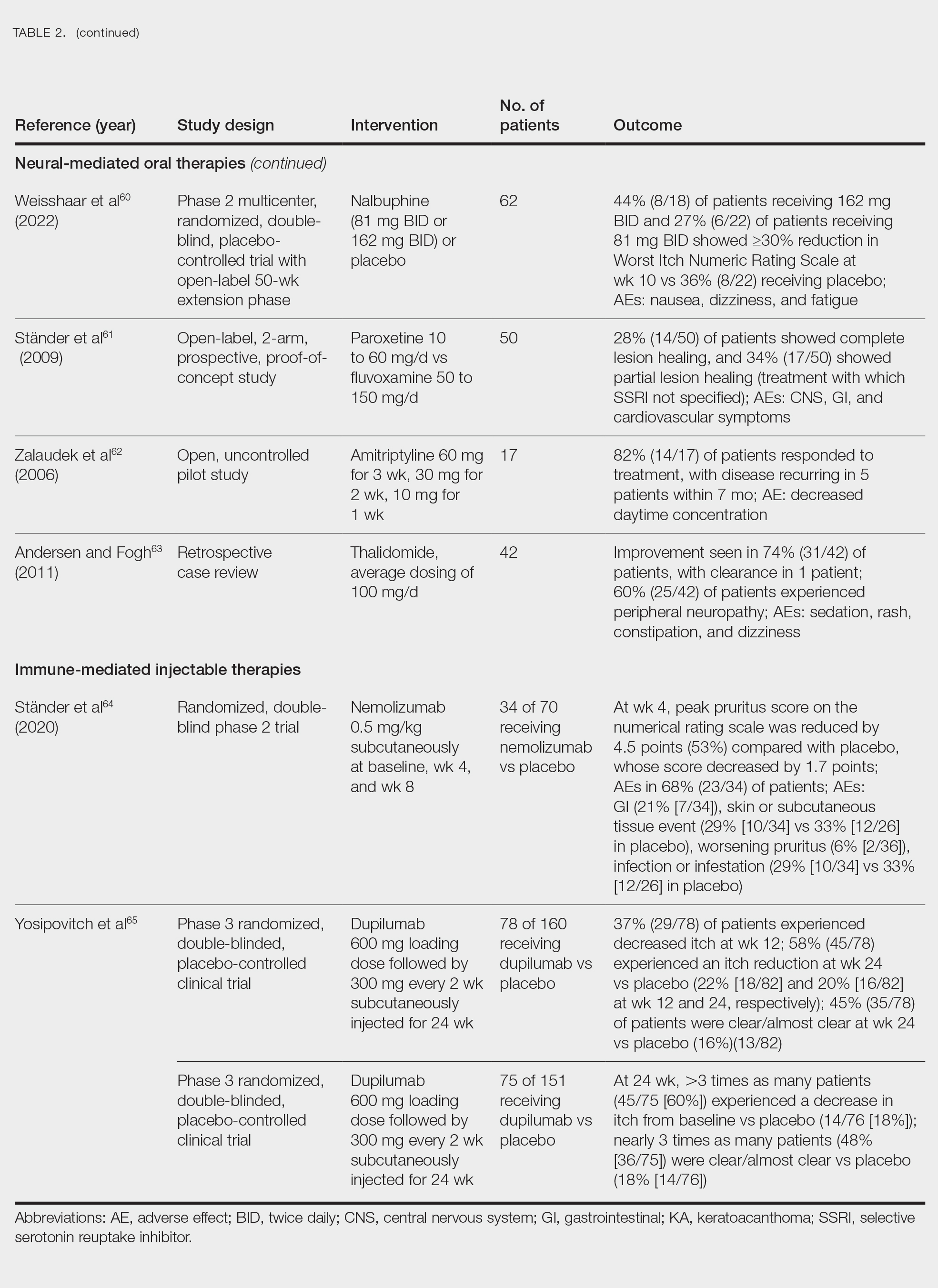
Neural-Mediated Oral Therapies—Neural-targeted oral therapies include pregabalin, serlopitant, aprepitant, naltrexone, nalbuphine, SSRIs (paroxetine and fluvoxamine), amitriptyline, and thalidomide. The research on these treatments ranges from case reviews to randomized controlled trials and open-label trials (Table 2).55-63
Thalidomide was studied in a small retrospective case review that showed notable improvement in PN. Dosages of thalidomide varied, but on average the dose was 100 mg/d. However, greater than 50% of patients experienced at least 1 adverse effect with this treatment.63
A study performed in Italy showed promising results for patients treated with pregabalin, with 70.0% (21/30) continuing to take pregabalin for almost 2 years following completion of the initial 3-month trial.55 Naltrexone decreased pruritus in more than half of patients (9/17).59 Amitriptyline yielded improvements in patients with PN; however, disease recurred in 5 patients (29%) after 7 months.62 A study performed in Germany reported promising results for paroxetine and fluvoxamine; however, some patients enrolled in the study had some form of psychiatric disorder.61
Serlopitant, aprepitant, and nalbuphine were studied in randomized controlled trials. The serlopitant trials were the largest of the neurally mediated oral medication studies; one showed substantial improvement in patients with PN,56 while the most recent trial did not show significant improvement (ClinicalTrials.gov identifier NCT03546816).57 On the other hand, aprepitant showed no major difference between the experimental and placebo groups.58 Nalbuphine 162 mg twice daily showed greater improvement in PN than nalbuphine 81 mg twice daily.60
Immune-Mediated Injectable Therapies—Immune-targeted injectables include nemolizumab and dupilumab (Table 2). Nemolizumab is an IL-31 antagonist that has been studied in a small randomized controlled trial that showed great success in decreasing pruritus associated with PN.64 IL-31 has been implicated in PN, and inhibition of the IL-31 receptor has been shown to disrupt the itch-scratch cycle of PN. Dupilumab is a monoclonal antibody against the IL-4 and IL-13 receptors, and it is the only FDA-approved treatment for PN.65 Blockage of these protein receptors decreases type 2 inflammation and chronic pruritus.66,67 Dupilumab is FDA approved for the treatment of atopic dermatitis and recently was approved for adults with PN. Dupilumab acts to block the shared α-subunit of the pruritogenic cytokines IL-4 and IL-13 pathways,29 thereby breaking the itch-scratch cycle associated with PN and allowing for the healing of these lesions. Results from 2 clinical trials showed substantially reduced itch in patients with PN.65 Dupilumab also was approved by the European Medicines Agency for moderate to severe PN.68
Conclusion
Prurigo nodularis is a chronic condition that affects patient quality of life and can mimic various dermatologic conditions. The epidemiology and pathophysiology of PN have not been fully expounded. More research should be conducted to determine the underpinnings of PN to help identify more consistently effective therapies for this complex condition.
- Durmaz K, Ataseven A, Ozer I, et al. Prurigo nodularis responding to intravenous immunoglobulins. Przegl Dermatol. 2022;109:159-162. doi:10.5114/dr.2022.117988
- Kowalski EH, Kneiber D, Valdebran M, et al. Treatment-resistant prurigo nodularis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:163-172. doi:10.2147/CCID.S188070
- Wong LS, Yen YT. Chronic nodular prurigo: an update on the pathogenesis and treatment. Int J Mol Sci. 2022;23:12390. doi:10.3390/ijms232012390
- Janmohamed SR, Gwillim EC, Yousaf M, et al. The impact of prurigo nodularis on quality of life: a systematic review and meta-analysis. Arch Dermatol Res. 2021;313:669-677. doi:10.1007/s00403-020-02148-0
- Zeidler C, Ständer S. The pathogenesis of prurigo nodularis - ‘super-itch’ in exploration. Eur J Pain. 2016;20:37-40. doi:10.1002/ejp.767
- Kwatra SG. Breaking the itch–scratch cycle in prurigo nodularis. N Engl J Med. 2020;382:757-758. doi:10.1056/NEJMe1916733
- Frølunde AS, Wiis MAK, Ben Abdallah H, et al. Non-atopic chronic nodular prurigo (prurigo nodularis hyde): a systematic review of best-evidenced treatment options. Dermatology. 2022;238:950-960. doi:10.1159/000523700
- Kwon CD, Khanna R, Williams KA, et al. Diagnostic workup and evaluation of patients with prurigo nodularis. Medicines (Basel). 2019;6:97. doi:10.3390/medicines6040097
- Kowalski EH, Kneiber D, Valdebran M, et al. Distinguishing truly recalcitrant prurigo nodularis from poor treatment adherence: a response to treatment-resistant prurigo nodularis [Response to letter]. Clin Cosmet Investig Dermatol. 2019;12:371-372. doi:10.2147/CCID.S214195
- Whang KA, Le TK, Khanna R, et al. Health-related quality of life and economic burden of prurigo nodularis. J Am Acad Dermatol. 2022;86:573-580. doi:10.1016/j.jaad.2021.05.036
- Labib A, Ju T, Vander Does A, et al. Immunotargets and therapy for prurigo nodularis. Immunotargets Ther. 2022;11:11-21. doi:10.2147/ITT.S316602
- Belzberg M, Alphonse MP, Brown I, et al. Prurigo nodularis is characterized by systemic and cutaneous T helper 22 immune polarization. J Invest Dermatol. 2021;141:2208-2218.e14. doi:10.1016/j.jid.2021.02.749
- Ständer S, Pereira MP, Berger T, et al. IFSI-guideline on chronic prurigo including prurigo nodularis. Itch. 2020;5:e42. doi:10.1097/itx.0000000000000042
- Huang AH, Canner JK, Khanna R, et al. Real-world prevalence of prurigo nodularis and burden of associated diseases. J Invest Dermatol. 2020;140:480-483.e4. doi:10.1016/j.jid.2019.07.697
- Ständer S, Augustin M, Berger T, et al. Prevalence of prurigo nodularis in the United States of America: a retrospective database analysis. JAAD Int. 2021;2:28-30. doi:10.1016/j.jdin.2020.10.009
- Sutaria N, Adawi W, Brown I, et al. Racial disparities in mortality among patients with prurigo nodularis: a multi-center cohort study. J Am Acad Dermatol. 2022;86:487-490. doi:10.1016/j.jaad.2021.09.028
- Ryczek A, Reich A. Prevalence of prurigo nodularis in Poland. Acta Derm Venereol. 2020;100:adv00155. doi:10.2340/00015555-3518
- Morgan CL, Thomas M, Ständer S, et al. Epidemiology of prurigo nodularis in England: a retrospective database analysis. Br J Dermatol. 2022;187:188-195. doi:10.1111/bjd.21032
- Woo YR, Wang S, Sohn KA, et al. Epidemiology, comorbidities, and prescription patterns of Korean prurigo nodularis patients: a multi-institution study. J Clin Med Res. 2021;11:95. doi:10.3390/jcm11010095
- Weigelt N, Metze D, Ständer S. Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37:578-586. doi:10.1111/j.1600-0560.2009.01484.x
- Yang LL, Jiang B, Chen SH, et al. Abnormal keratin expression pattern in prurigo nodularis epidermis. Skin Health Dis. 2022;2:e75. doi:10.1002/ski2.75
- Nockher WA, Renz H. Neurotrophins in allergic diseases: from neuronal growth factors to intercellular signaling molecules. J Allergy Clin Immunol. 2006;117:583-589. doi:10.1016/j.jaci.2005.11.049
- Di Marco E, Mathor M, Bondanza S, et al. Nerve growth factor binds to normal human keratinocytes through high and low affinity receptors and stimulates their growth by a novel autocrine loop. J Biol Chem. 1993;268:22838-22846.
- Hägermark O, Hökfelt T, Pernow B. Flare and itch induced by substance P in human skin. J Invest Dermatol. 1978;71:233-235. doi:10.1111/1523-1747.ep12515092
- Choi JE, Di Nardo A. Skin neurogenic inflammation. Semin Immunopathol. 2018;40:249-259. doi:10.1007/s00281-018-0675-z
- Haas S, Capellino S, Phan NQ, et al. Low density of sympathetic nerve fibers relative to substance P-positive nerve fibers in lesional skin of chronic pruritus and prurigo nodularis. J Dermatol Sci. 2010;58:193-197. doi:10.1016/j.jdermsci.2010.03.020
- Park K, Mori T, Nakamura M, et al. Increased expression of mRNAs for IL-4, IL-17, IL-22 and IL-31 in skin lesions of subacute and chronic forms of prurigo. Eur J Dermatol. 2011;21:135-136.
- Tokura Y, Yagi H, Hanaoka K, et al. Subacute and chronic prurigo effectively treated with recombination interferon-gamma: implications for participation of Th2 cells in the pathogenesis of prurigo. Acta Derm Venereol. 1997;77:231-234. doi:10.2340/0001555577231234
- Williams KA, Roh YS, Brown I, et al. Pathophysiology, diagnosis, and pharmacological treatment of prurigo nodularis. Expert Rev Clin Pharmacol. 2021;14:67-77. doi:10.1080/17512433.2021.1852080
- Huang AH, Williams KA, Kwatra SG. Prurigo nodularis: epidemiology and clinical features. J Am Acad Dermatol. 2020;83:1559-1565. doi:10.1016/j.jaad.2020.04.183
- Bewley A, Homey B, Pink A. Prurigo nodularis: a review of IL-31RA blockade and other potential treatments. Dermatol Ther. 2022;12:2039-2048. doi:10.1007/s13555-022-00782-2
- Zeidler C, Yosipovitch G, Ständer S. Prurigo nodularis and its management. Dermatol Clin. 2018;36:189-197. doi:10.1016/j.det.2018.02.003
- Siepmann D, Lotts T, Blome C, et al. Evaluation of the antipruritic effects of topical pimecrolimus in non-atopic prurigo nodularis: results of a randomized, hydrocortisone-controlled, double-blind phase II trial. Dermatology. 2013;227:353-360. doi:10.1159/000355671
- Valbuena MC, Muvdi S, Lim HW. Actinic prurigo. Dermatol Clin. 2014;32:335-344, viii. doi:10.1016/j.det.2014.03.010
- Aldhahwani R, Al Hawsawi KA. Neurotic excoriation presenting as solitary papule: case report. J Dermatol Dermatolog Surg. 2022;26:45. doi:10.4103/jdds.jdds_59_21
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74:1220-1233. doi:10.1016/j.jaad.2015.11.033
- Karadag AS, Ozlu E, Uzuncakmak TK, et al. Inverted follicular keratosis successfully treated with imiquimod. Indian Dermatol Online J. 2016;7:177-179. doi:10.4103/2229-5178.182354
- Nayak VN, Uma K, Girish HC, et al. Pseudoepitheliomatous hyperplasia in oral lesions: a review. J Int Oral Health. 2015;7:148-152.
- Saraceno R, Chiricozzi A, Nisticò SP, et al. An occlusive dressing containing betamethasone valerate 0.1% for the treatment of prurigo nodularis. J Dermatolog Treat. 2010;21:363-366. doi:10.3109/09546630903386606
- Wong SS, Goh CL. Double-blind, right/left comparison of calcipotriol ointment and betamethasone ointment in the treatment of prurigo nodularis. Arch Dermatol. 2000;136:807-808. doi:10.1001/archderm.136.6.807
- Waldinger TP, Wong RC, Taylor WB, et al. Cryotherapy improves prurigo nodularis. Arch Dermatol. 1984;120:1598-1600.
- Ständer S, Luger T, Metze D. Treatment of prurigo nodularis with topical capsaicin. J Am Acad Dermatol. 2001;44:471-478. doi:10.1067/mjd.2001.110059
- Ohanyan T, Schoepke N, Eirefelt S, et al. Role of substance P and its receptor neurokinin 1 in chronic prurigo: a randomized, proof-of-concept, controlled trial with topical aprepitant. Acta Derm Venereol. 2018;98:26-31. doi:10.2340/00015555-2780
- Tamagawa-Mineoka R, Katoh N, Ueda E, et al. Narrow-band ultraviolet B phototherapy in patients with recalcitrant nodular prurigo. J Dermatol. 2007;34:691-695. doi:10.1111/j.1346-8138.2007.00360.x
- Hammes S, Hermann J, Roos S, et al. UVB 308-nm excimer light and bath PUVA: combination therapy is very effective in the treatment of prurigo nodularis. J Eur Acad Dermatol Venereol. 2011;25:799-803. doi:10.1111/j.1468-3083.2010.03865.x
- Richards RN. Update on intralesional steroid: focus on dermatoses. J Cutan Med Surg. 2010;14:19-23. doi:10.2310/7750.2009.08082
- Elmariah S, Kim B, Berger T, et al. Practical approaches for diagnosis and management of prurigo nodularis: United States expert panel consensus. J Am Acad Dermatol. 2021;84:747-760. doi:10.1016/j.jaad.2020.07.025
- Grant JE Chamberlain SR Redden SA et al. N-Acetylcysteine in the treatment of excoriation disorder: a randomized clinical trial. JAMA Psychiatry. 2016;73:490-496. doi:10.1001/jamapsychiatry.2016.0060
- Adil M, Amin SS, Mohtashim M. N-acetylcysteine in dermatology. Indian J Dermatol Venereol Leprol. 2018;84:652-659. doi: 10.4103/ijdvl.IJDVL_33_18.
- Taylor M, Bhagwandas K. Trichotillosis, skin picking and N-acetylcysteine. J Am Acad Dermatol. 2015;72(suppl 1):AB117. https://doi.org/10.1016/j.jaad.2015.02.482
- Legat FJ. The antipruritic effect of phototherapy. Front Med (Lausanne). 2018;5:333. doi:10.3389/fmed.2018.00333
- Klejtman T, Beylot-Barry M, Joly P, et al. Treatment of prurigo with methotrexate: a multicentre retrospective study of 39 cases. J Eur Acad Dermatol Venereol. 2018;32:437-440. doi:10.1111/jdv.14646
- Wiznia LE, Callahan SW, Cohen DE, et al. Rapid improvement of prurigo nodularis with cyclosporine treatment. J Am Acad Dermatol. 2018;78:1209-1211. doi:10.1016/j.jaad.2018.02.024
- Yagami A, Furue M, Togawa M, et al. One-year safety and efficacy study of bilastine treatment in Japanese patients with chronic spontaneous urticaria or pruritus associated with skin diseases. J Dermatol. 2017;44:375-385. doi:10.1111/1346-8138.13644
- Mazza M, Guerriero G, Marano G, et al. Treatment of prurigo nodularis with pregabalin. J Clin Pharm Ther. 2013;38:16-18. doi:10.1111/jcpt.12005
- Ständer S, Kwon P, Hirman J, et al. Serlopitant reduced pruritus in patients with prurigo nodularis in a phase 2, randomized, placebo-controlled trial. J Am Acad Dermatol. 2019;80:1395-1402. doi:10.1016/j.jaad.2019.01.052
- Study of the efficacy, safety and tolerability of serlopitant for the treatment of pruritus (itch) with prurigo nodularis. ClinicalTrials.gov identifier: NCT03546816. Updated May 20, 2021. Accessed August 8, 2024. https://clinicaltrials.gov/study/NCT03546816
- Tsianakas A, Zeidler C, Riepe C, et al. Aprepitant in anti-histamine-refractory chronic nodular prurigo: a multicentre, randomized, double-blind, placebo-controlled, cross-over, phase-II trial (APREPRU). Acta Derm Venereol. 2019;99:379-385. doi:10.2340/00015555-3120
- Metze D, Reimann S, Beissert S, et al. Efficacy and safety of naltrexone, an oral opiate receptor antagonist, in the treatment of pruritus in internal and dermatological diseases. J Am Acad Dermatol. 1999;41:533-539.
- Weisshaar E, Szepietowski JC, Bernhard JD, et al. Efficacy and safety of oral nalbuphine extended release in prurigo nodularis: results of a phase 2 randomized controlled trial with an open‐label extension phase. J Eur Acad Dermatol Venereol. 2022;36:453-461. doi:10.1111/jdv.17816
- Ständer S, Böckenholt B, Schürmeyer-Horst F, et al. Treatment of chronic pruritus with the selective serotonin re-uptake inhibitors paroxetine and fluvoxamine: results of an open-labelled, two-arm proof-of-concept study. Acta Derm Venereol. 2009;89:45-51. doi:10.2340/00015555-0553
- Zalaudek I, Petrillo G, Baldassarre MA, et al. Amitriptyline as therapeutic and not symptomatic approach in the treatment of prurigo nodularis. G Ital Dermatol Venereol. 2006;141:433-437.
- Andersen TP, Fogh K. Thalidomide in 42 patients with prurigo nodularis Hyde. Dermatology. 2011;223:107-112. doi:10.1159/000331577
- Ständer S, Yosipovitch G, Legat FJ, et al. Trial of nemolizumab in moderate-to-severe prurigo nodularis. N Engl J Med. 2020;382:706-716. doi:10.1056/NEJMoa1908316
- Yosipovitch G, Mollanazar N, Ständer S, et al. Dupilumab in patients with prurigo nodularis: two randomized, double-blind, placebo-controlled phase 3 trials. Nat Med. 2023;29:1180-1190. doi:10.1038/s41591-023-02320-9
- Mastorino L, Rosset F, Gelato F, et al. Chronic pruritus in atopic patients treated with dupilumab: real life response and related parameters in 354 patients. Pharmaceuticals (Basel). 2022;15:883. doi: 10.3390/ph15070883
- Kishi R, Toyama S, Tominaga M, et al. Effects of dupilumab on itch-related events in atopic dermatitis: implications for assessing treatment efficacy in clinical practice. Cells. 2023;12:239. doi: 10.3390/cells12020239
- Dupixent. European Medicines Agency website. Updated July 15, 2024. Accessed August 27, 2024. https://www.ema.europa.eu/en/medicines/human/EPAR/dupixent
- Durmaz K, Ataseven A, Ozer I, et al. Prurigo nodularis responding to intravenous immunoglobulins. Przegl Dermatol. 2022;109:159-162. doi:10.5114/dr.2022.117988
- Kowalski EH, Kneiber D, Valdebran M, et al. Treatment-resistant prurigo nodularis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:163-172. doi:10.2147/CCID.S188070
- Wong LS, Yen YT. Chronic nodular prurigo: an update on the pathogenesis and treatment. Int J Mol Sci. 2022;23:12390. doi:10.3390/ijms232012390
- Janmohamed SR, Gwillim EC, Yousaf M, et al. The impact of prurigo nodularis on quality of life: a systematic review and meta-analysis. Arch Dermatol Res. 2021;313:669-677. doi:10.1007/s00403-020-02148-0
- Zeidler C, Ständer S. The pathogenesis of prurigo nodularis - ‘super-itch’ in exploration. Eur J Pain. 2016;20:37-40. doi:10.1002/ejp.767
- Kwatra SG. Breaking the itch–scratch cycle in prurigo nodularis. N Engl J Med. 2020;382:757-758. doi:10.1056/NEJMe1916733
- Frølunde AS, Wiis MAK, Ben Abdallah H, et al. Non-atopic chronic nodular prurigo (prurigo nodularis hyde): a systematic review of best-evidenced treatment options. Dermatology. 2022;238:950-960. doi:10.1159/000523700
- Kwon CD, Khanna R, Williams KA, et al. Diagnostic workup and evaluation of patients with prurigo nodularis. Medicines (Basel). 2019;6:97. doi:10.3390/medicines6040097
- Kowalski EH, Kneiber D, Valdebran M, et al. Distinguishing truly recalcitrant prurigo nodularis from poor treatment adherence: a response to treatment-resistant prurigo nodularis [Response to letter]. Clin Cosmet Investig Dermatol. 2019;12:371-372. doi:10.2147/CCID.S214195
- Whang KA, Le TK, Khanna R, et al. Health-related quality of life and economic burden of prurigo nodularis. J Am Acad Dermatol. 2022;86:573-580. doi:10.1016/j.jaad.2021.05.036
- Labib A, Ju T, Vander Does A, et al. Immunotargets and therapy for prurigo nodularis. Immunotargets Ther. 2022;11:11-21. doi:10.2147/ITT.S316602
- Belzberg M, Alphonse MP, Brown I, et al. Prurigo nodularis is characterized by systemic and cutaneous T helper 22 immune polarization. J Invest Dermatol. 2021;141:2208-2218.e14. doi:10.1016/j.jid.2021.02.749
- Ständer S, Pereira MP, Berger T, et al. IFSI-guideline on chronic prurigo including prurigo nodularis. Itch. 2020;5:e42. doi:10.1097/itx.0000000000000042
- Huang AH, Canner JK, Khanna R, et al. Real-world prevalence of prurigo nodularis and burden of associated diseases. J Invest Dermatol. 2020;140:480-483.e4. doi:10.1016/j.jid.2019.07.697
- Ständer S, Augustin M, Berger T, et al. Prevalence of prurigo nodularis in the United States of America: a retrospective database analysis. JAAD Int. 2021;2:28-30. doi:10.1016/j.jdin.2020.10.009
- Sutaria N, Adawi W, Brown I, et al. Racial disparities in mortality among patients with prurigo nodularis: a multi-center cohort study. J Am Acad Dermatol. 2022;86:487-490. doi:10.1016/j.jaad.2021.09.028
- Ryczek A, Reich A. Prevalence of prurigo nodularis in Poland. Acta Derm Venereol. 2020;100:adv00155. doi:10.2340/00015555-3518
- Morgan CL, Thomas M, Ständer S, et al. Epidemiology of prurigo nodularis in England: a retrospective database analysis. Br J Dermatol. 2022;187:188-195. doi:10.1111/bjd.21032
- Woo YR, Wang S, Sohn KA, et al. Epidemiology, comorbidities, and prescription patterns of Korean prurigo nodularis patients: a multi-institution study. J Clin Med Res. 2021;11:95. doi:10.3390/jcm11010095
- Weigelt N, Metze D, Ständer S. Prurigo nodularis: systematic analysis of 58 histological criteria in 136 patients. J Cutan Pathol. 2010;37:578-586. doi:10.1111/j.1600-0560.2009.01484.x
- Yang LL, Jiang B, Chen SH, et al. Abnormal keratin expression pattern in prurigo nodularis epidermis. Skin Health Dis. 2022;2:e75. doi:10.1002/ski2.75
- Nockher WA, Renz H. Neurotrophins in allergic diseases: from neuronal growth factors to intercellular signaling molecules. J Allergy Clin Immunol. 2006;117:583-589. doi:10.1016/j.jaci.2005.11.049
- Di Marco E, Mathor M, Bondanza S, et al. Nerve growth factor binds to normal human keratinocytes through high and low affinity receptors and stimulates their growth by a novel autocrine loop. J Biol Chem. 1993;268:22838-22846.
- Hägermark O, Hökfelt T, Pernow B. Flare and itch induced by substance P in human skin. J Invest Dermatol. 1978;71:233-235. doi:10.1111/1523-1747.ep12515092
- Choi JE, Di Nardo A. Skin neurogenic inflammation. Semin Immunopathol. 2018;40:249-259. doi:10.1007/s00281-018-0675-z
- Haas S, Capellino S, Phan NQ, et al. Low density of sympathetic nerve fibers relative to substance P-positive nerve fibers in lesional skin of chronic pruritus and prurigo nodularis. J Dermatol Sci. 2010;58:193-197. doi:10.1016/j.jdermsci.2010.03.020
- Park K, Mori T, Nakamura M, et al. Increased expression of mRNAs for IL-4, IL-17, IL-22 and IL-31 in skin lesions of subacute and chronic forms of prurigo. Eur J Dermatol. 2011;21:135-136.
- Tokura Y, Yagi H, Hanaoka K, et al. Subacute and chronic prurigo effectively treated with recombination interferon-gamma: implications for participation of Th2 cells in the pathogenesis of prurigo. Acta Derm Venereol. 1997;77:231-234. doi:10.2340/0001555577231234
- Williams KA, Roh YS, Brown I, et al. Pathophysiology, diagnosis, and pharmacological treatment of prurigo nodularis. Expert Rev Clin Pharmacol. 2021;14:67-77. doi:10.1080/17512433.2021.1852080
- Huang AH, Williams KA, Kwatra SG. Prurigo nodularis: epidemiology and clinical features. J Am Acad Dermatol. 2020;83:1559-1565. doi:10.1016/j.jaad.2020.04.183
- Bewley A, Homey B, Pink A. Prurigo nodularis: a review of IL-31RA blockade and other potential treatments. Dermatol Ther. 2022;12:2039-2048. doi:10.1007/s13555-022-00782-2
- Zeidler C, Yosipovitch G, Ständer S. Prurigo nodularis and its management. Dermatol Clin. 2018;36:189-197. doi:10.1016/j.det.2018.02.003
- Siepmann D, Lotts T, Blome C, et al. Evaluation of the antipruritic effects of topical pimecrolimus in non-atopic prurigo nodularis: results of a randomized, hydrocortisone-controlled, double-blind phase II trial. Dermatology. 2013;227:353-360. doi:10.1159/000355671
- Valbuena MC, Muvdi S, Lim HW. Actinic prurigo. Dermatol Clin. 2014;32:335-344, viii. doi:10.1016/j.det.2014.03.010
- Aldhahwani R, Al Hawsawi KA. Neurotic excoriation presenting as solitary papule: case report. J Dermatol Dermatolog Surg. 2022;26:45. doi:10.4103/jdds.jdds_59_21
- Kwiek B, Schwartz RA. Keratoacanthoma (KA): an update and review. J Am Acad Dermatol. 2016;74:1220-1233. doi:10.1016/j.jaad.2015.11.033
- Karadag AS, Ozlu E, Uzuncakmak TK, et al. Inverted follicular keratosis successfully treated with imiquimod. Indian Dermatol Online J. 2016;7:177-179. doi:10.4103/2229-5178.182354
- Nayak VN, Uma K, Girish HC, et al. Pseudoepitheliomatous hyperplasia in oral lesions: a review. J Int Oral Health. 2015;7:148-152.
- Saraceno R, Chiricozzi A, Nisticò SP, et al. An occlusive dressing containing betamethasone valerate 0.1% for the treatment of prurigo nodularis. J Dermatolog Treat. 2010;21:363-366. doi:10.3109/09546630903386606
- Wong SS, Goh CL. Double-blind, right/left comparison of calcipotriol ointment and betamethasone ointment in the treatment of prurigo nodularis. Arch Dermatol. 2000;136:807-808. doi:10.1001/archderm.136.6.807
- Waldinger TP, Wong RC, Taylor WB, et al. Cryotherapy improves prurigo nodularis. Arch Dermatol. 1984;120:1598-1600.
- Ständer S, Luger T, Metze D. Treatment of prurigo nodularis with topical capsaicin. J Am Acad Dermatol. 2001;44:471-478. doi:10.1067/mjd.2001.110059
- Ohanyan T, Schoepke N, Eirefelt S, et al. Role of substance P and its receptor neurokinin 1 in chronic prurigo: a randomized, proof-of-concept, controlled trial with topical aprepitant. Acta Derm Venereol. 2018;98:26-31. doi:10.2340/00015555-2780
- Tamagawa-Mineoka R, Katoh N, Ueda E, et al. Narrow-band ultraviolet B phototherapy in patients with recalcitrant nodular prurigo. J Dermatol. 2007;34:691-695. doi:10.1111/j.1346-8138.2007.00360.x
- Hammes S, Hermann J, Roos S, et al. UVB 308-nm excimer light and bath PUVA: combination therapy is very effective in the treatment of prurigo nodularis. J Eur Acad Dermatol Venereol. 2011;25:799-803. doi:10.1111/j.1468-3083.2010.03865.x
- Richards RN. Update on intralesional steroid: focus on dermatoses. J Cutan Med Surg. 2010;14:19-23. doi:10.2310/7750.2009.08082
- Elmariah S, Kim B, Berger T, et al. Practical approaches for diagnosis and management of prurigo nodularis: United States expert panel consensus. J Am Acad Dermatol. 2021;84:747-760. doi:10.1016/j.jaad.2020.07.025
- Grant JE Chamberlain SR Redden SA et al. N-Acetylcysteine in the treatment of excoriation disorder: a randomized clinical trial. JAMA Psychiatry. 2016;73:490-496. doi:10.1001/jamapsychiatry.2016.0060
- Adil M, Amin SS, Mohtashim M. N-acetylcysteine in dermatology. Indian J Dermatol Venereol Leprol. 2018;84:652-659. doi: 10.4103/ijdvl.IJDVL_33_18.
- Taylor M, Bhagwandas K. Trichotillosis, skin picking and N-acetylcysteine. J Am Acad Dermatol. 2015;72(suppl 1):AB117. https://doi.org/10.1016/j.jaad.2015.02.482
- Legat FJ. The antipruritic effect of phototherapy. Front Med (Lausanne). 2018;5:333. doi:10.3389/fmed.2018.00333
- Klejtman T, Beylot-Barry M, Joly P, et al. Treatment of prurigo with methotrexate: a multicentre retrospective study of 39 cases. J Eur Acad Dermatol Venereol. 2018;32:437-440. doi:10.1111/jdv.14646
- Wiznia LE, Callahan SW, Cohen DE, et al. Rapid improvement of prurigo nodularis with cyclosporine treatment. J Am Acad Dermatol. 2018;78:1209-1211. doi:10.1016/j.jaad.2018.02.024
- Yagami A, Furue M, Togawa M, et al. One-year safety and efficacy study of bilastine treatment in Japanese patients with chronic spontaneous urticaria or pruritus associated with skin diseases. J Dermatol. 2017;44:375-385. doi:10.1111/1346-8138.13644
- Mazza M, Guerriero G, Marano G, et al. Treatment of prurigo nodularis with pregabalin. J Clin Pharm Ther. 2013;38:16-18. doi:10.1111/jcpt.12005
- Ständer S, Kwon P, Hirman J, et al. Serlopitant reduced pruritus in patients with prurigo nodularis in a phase 2, randomized, placebo-controlled trial. J Am Acad Dermatol. 2019;80:1395-1402. doi:10.1016/j.jaad.2019.01.052
- Study of the efficacy, safety and tolerability of serlopitant for the treatment of pruritus (itch) with prurigo nodularis. ClinicalTrials.gov identifier: NCT03546816. Updated May 20, 2021. Accessed August 8, 2024. https://clinicaltrials.gov/study/NCT03546816
- Tsianakas A, Zeidler C, Riepe C, et al. Aprepitant in anti-histamine-refractory chronic nodular prurigo: a multicentre, randomized, double-blind, placebo-controlled, cross-over, phase-II trial (APREPRU). Acta Derm Venereol. 2019;99:379-385. doi:10.2340/00015555-3120
- Metze D, Reimann S, Beissert S, et al. Efficacy and safety of naltrexone, an oral opiate receptor antagonist, in the treatment of pruritus in internal and dermatological diseases. J Am Acad Dermatol. 1999;41:533-539.
- Weisshaar E, Szepietowski JC, Bernhard JD, et al. Efficacy and safety of oral nalbuphine extended release in prurigo nodularis: results of a phase 2 randomized controlled trial with an open‐label extension phase. J Eur Acad Dermatol Venereol. 2022;36:453-461. doi:10.1111/jdv.17816
- Ständer S, Böckenholt B, Schürmeyer-Horst F, et al. Treatment of chronic pruritus with the selective serotonin re-uptake inhibitors paroxetine and fluvoxamine: results of an open-labelled, two-arm proof-of-concept study. Acta Derm Venereol. 2009;89:45-51. doi:10.2340/00015555-0553
- Zalaudek I, Petrillo G, Baldassarre MA, et al. Amitriptyline as therapeutic and not symptomatic approach in the treatment of prurigo nodularis. G Ital Dermatol Venereol. 2006;141:433-437.
- Andersen TP, Fogh K. Thalidomide in 42 patients with prurigo nodularis Hyde. Dermatology. 2011;223:107-112. doi:10.1159/000331577
- Ständer S, Yosipovitch G, Legat FJ, et al. Trial of nemolizumab in moderate-to-severe prurigo nodularis. N Engl J Med. 2020;382:706-716. doi:10.1056/NEJMoa1908316
- Yosipovitch G, Mollanazar N, Ständer S, et al. Dupilumab in patients with prurigo nodularis: two randomized, double-blind, placebo-controlled phase 3 trials. Nat Med. 2023;29:1180-1190. doi:10.1038/s41591-023-02320-9
- Mastorino L, Rosset F, Gelato F, et al. Chronic pruritus in atopic patients treated with dupilumab: real life response and related parameters in 354 patients. Pharmaceuticals (Basel). 2022;15:883. doi: 10.3390/ph15070883
- Kishi R, Toyama S, Tominaga M, et al. Effects of dupilumab on itch-related events in atopic dermatitis: implications for assessing treatment efficacy in clinical practice. Cells. 2023;12:239. doi: 10.3390/cells12020239
- Dupixent. European Medicines Agency website. Updated July 15, 2024. Accessed August 27, 2024. https://www.ema.europa.eu/en/medicines/human/EPAR/dupixent
Practice Points
- Clinically, prurigo nodularis can mimic an array of dermatologic skin conditions and may be diagnosed more frequently in patients with comorbidities.
- Dupilumab is the first and only treatment for prurigo nodularis approved by the US Food and Drug Administration; however, many topical treatments are currently used as first-line therapies.
New Associations Identified Between IBD and Extraintestinal Manifestations
, according to a recent study.
For instance, antinuclear cytoplastic antibody is associated with primary sclerosing cholangitis (PSC) in Crohn’s disease, and CPEB4 genetic variation is associated with skin manifestations.
“Up to 40% of people with IBD suffer with symptoms from inflammation that occurs outside the gut, particularly affecting the liver, skin, and joints. These symptoms can often have a bigger impact on quality of life than the gut inflammation itself and can actually be life-threatening,” said senior author Dermot McGovern, MD, PhD, AGAF, director of translational medicine at the F. Widjaja Foundation Inflammatory Bowel Disease and Immunobiology Research Institute at Cedars-Sinai Medical Center, Los Angeles.
“With the advances in therapies for IBD, including availability of gut-selective agents, treatment choices often incorporate whether a patient has one of these manifestations or not,” he said. “We need to understand who is at increased risk of these and why.”
The study was published in Gastroenterology .
Analyzing Associations
Dr. McGovern and colleagues analyzed data for 12,083 unrelated European ancestry IBD cases with presence or absence of EIMs across four cohorts in the Cedars-Sinai Medical Center IBD Research Repository, National Institute for Diabetes and Digestive and Kidney Diseases IBD Genetics Consortium, Sinai Helmsley Alliance for Research Excellence Consortium, and Risk Stratification and Identification of Immunogenetic and Microbial Markers of Rapid Disease Progression in Children with Crohn’s Disease.
In particular, the researchers looked at EIM phenotypes such as ankylosing spondylitis and sacroiliitis, PSC, peripheral arthritis, and skin and ocular manifestations. They analyzed clinical and serologic parameters through regression analyses using a mixed-effects model, as well as within-case logistic regression for genetic associations.
Overall, 14% of patients had at least one EIM. Contrary to previous reports, only 2% had multiple EIMs, and most co-occurrences were negatively correlated. Nearly all EIMs were more common in Crohn’s disease, except for PSC, which was more common in ulcerative colitis.
In general, EIMs occurred more often in women, particularly with Crohn’s disease and colonic disease location, and in patients who required surgery. Jewish ancestry was associated with psoriasis and overall skin manifestations.
Smoking increased the risk for multiple EIMs, except for PSC, where there appeared to be a “protective” effect. Older age at diagnosis and a family history of IBD were associated with increased risk for certain EIMs as well.
In addition, the research team noted multiple serologic associations, such as immunoglobulin (Ig) G and IgA, perinuclear antinuclear cytoplastic antibodies, and anti–Pseudomonas fluorescens–associated sequences with any EIM, as well as particular associations with PSC, such as anti-Saccharomyces cerevisiae antibodies and anti-flagellin.
There were also genome-wide significant associations within the major histocompatibility complex and CPEB4. Genetic associations implicated tumor necrosis factor, Janus kinase-signal transducer and activator of transcription, and interleukin 6 as potential targets for EIMs.
“We are working with colleagues across the world to increase the sample size, as we believe there is more to find,” Dr. McGovern said. “Importantly, this includes non-European ancestry subjects, as there is an urgent need to increase the diversity of populations we study so advances in clinical care are available to all communities.”
Considering Target Therapies
As medicine becomes more specialized, physicians should remember to consider the whole patient while choosing treatment strategies.
“Sometimes doctors wear blinders to the whole person, and it’s important to be aware of a holistic approach, where a gastroenterologist also asks about potential joint inflammation or a rheumatologist asks about bowel inflammation,” said David Rubin, MD, AGAF, chief of the Section of Gastroenterology, Hepatology and Nutrition at the University of Chicago Medicine, Chicago.
Dr. Rubin, who wasn’t involved with this study, has researched and published on EIMs in IBD. He and colleagues analyzed the prevalence, pathophysiology, and clinical presentation of EIMs to better understand possibilities for disease management.
“As we’ve gotten a better understanding of the immune system, we’ve learned that an EIM can sometimes provide a clue to the treatment we might use,” he said. “Given a similar amount of bowel inflammation, if one patient also has joint pain and another doesn’t, we might choose different treatments based on the immune pathway that might be involved.”
In future studies, researchers may consider whether these genetic or serologic markers could predict EIM manifestation before it occurs clinically, Dr. Rubin said. He and colleagues are also studying the links between IBD and mental health associations.
“So far, we don’t have a blood test or biopsy test that tells you which treatment is more or less likely to work, so we need to think carefully as clinicians and look to other organ systems for clues,” he said. “It’s not only more efficient to pick a single therapy to treat both the skin and bowel, but it may actually be more effective if both have a particular dominant pathway.”
The study was supported by internal funds from the F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute. Several authors reported consultant roles or other associations with pharmaceutical companies. Dr. Rubin reported no relevant disclosures.
A version of this article appeared on Medscape.com.
, according to a recent study.
For instance, antinuclear cytoplastic antibody is associated with primary sclerosing cholangitis (PSC) in Crohn’s disease, and CPEB4 genetic variation is associated with skin manifestations.
“Up to 40% of people with IBD suffer with symptoms from inflammation that occurs outside the gut, particularly affecting the liver, skin, and joints. These symptoms can often have a bigger impact on quality of life than the gut inflammation itself and can actually be life-threatening,” said senior author Dermot McGovern, MD, PhD, AGAF, director of translational medicine at the F. Widjaja Foundation Inflammatory Bowel Disease and Immunobiology Research Institute at Cedars-Sinai Medical Center, Los Angeles.
“With the advances in therapies for IBD, including availability of gut-selective agents, treatment choices often incorporate whether a patient has one of these manifestations or not,” he said. “We need to understand who is at increased risk of these and why.”
The study was published in Gastroenterology .
Analyzing Associations
Dr. McGovern and colleagues analyzed data for 12,083 unrelated European ancestry IBD cases with presence or absence of EIMs across four cohorts in the Cedars-Sinai Medical Center IBD Research Repository, National Institute for Diabetes and Digestive and Kidney Diseases IBD Genetics Consortium, Sinai Helmsley Alliance for Research Excellence Consortium, and Risk Stratification and Identification of Immunogenetic and Microbial Markers of Rapid Disease Progression in Children with Crohn’s Disease.
In particular, the researchers looked at EIM phenotypes such as ankylosing spondylitis and sacroiliitis, PSC, peripheral arthritis, and skin and ocular manifestations. They analyzed clinical and serologic parameters through regression analyses using a mixed-effects model, as well as within-case logistic regression for genetic associations.
Overall, 14% of patients had at least one EIM. Contrary to previous reports, only 2% had multiple EIMs, and most co-occurrences were negatively correlated. Nearly all EIMs were more common in Crohn’s disease, except for PSC, which was more common in ulcerative colitis.
In general, EIMs occurred more often in women, particularly with Crohn’s disease and colonic disease location, and in patients who required surgery. Jewish ancestry was associated with psoriasis and overall skin manifestations.
Smoking increased the risk for multiple EIMs, except for PSC, where there appeared to be a “protective” effect. Older age at diagnosis and a family history of IBD were associated with increased risk for certain EIMs as well.
In addition, the research team noted multiple serologic associations, such as immunoglobulin (Ig) G and IgA, perinuclear antinuclear cytoplastic antibodies, and anti–Pseudomonas fluorescens–associated sequences with any EIM, as well as particular associations with PSC, such as anti-Saccharomyces cerevisiae antibodies and anti-flagellin.
There were also genome-wide significant associations within the major histocompatibility complex and CPEB4. Genetic associations implicated tumor necrosis factor, Janus kinase-signal transducer and activator of transcription, and interleukin 6 as potential targets for EIMs.
“We are working with colleagues across the world to increase the sample size, as we believe there is more to find,” Dr. McGovern said. “Importantly, this includes non-European ancestry subjects, as there is an urgent need to increase the diversity of populations we study so advances in clinical care are available to all communities.”
Considering Target Therapies
As medicine becomes more specialized, physicians should remember to consider the whole patient while choosing treatment strategies.
“Sometimes doctors wear blinders to the whole person, and it’s important to be aware of a holistic approach, where a gastroenterologist also asks about potential joint inflammation or a rheumatologist asks about bowel inflammation,” said David Rubin, MD, AGAF, chief of the Section of Gastroenterology, Hepatology and Nutrition at the University of Chicago Medicine, Chicago.
Dr. Rubin, who wasn’t involved with this study, has researched and published on EIMs in IBD. He and colleagues analyzed the prevalence, pathophysiology, and clinical presentation of EIMs to better understand possibilities for disease management.
“As we’ve gotten a better understanding of the immune system, we’ve learned that an EIM can sometimes provide a clue to the treatment we might use,” he said. “Given a similar amount of bowel inflammation, if one patient also has joint pain and another doesn’t, we might choose different treatments based on the immune pathway that might be involved.”
In future studies, researchers may consider whether these genetic or serologic markers could predict EIM manifestation before it occurs clinically, Dr. Rubin said. He and colleagues are also studying the links between IBD and mental health associations.
“So far, we don’t have a blood test or biopsy test that tells you which treatment is more or less likely to work, so we need to think carefully as clinicians and look to other organ systems for clues,” he said. “It’s not only more efficient to pick a single therapy to treat both the skin and bowel, but it may actually be more effective if both have a particular dominant pathway.”
The study was supported by internal funds from the F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute. Several authors reported consultant roles or other associations with pharmaceutical companies. Dr. Rubin reported no relevant disclosures.
A version of this article appeared on Medscape.com.
, according to a recent study.
For instance, antinuclear cytoplastic antibody is associated with primary sclerosing cholangitis (PSC) in Crohn’s disease, and CPEB4 genetic variation is associated with skin manifestations.
“Up to 40% of people with IBD suffer with symptoms from inflammation that occurs outside the gut, particularly affecting the liver, skin, and joints. These symptoms can often have a bigger impact on quality of life than the gut inflammation itself and can actually be life-threatening,” said senior author Dermot McGovern, MD, PhD, AGAF, director of translational medicine at the F. Widjaja Foundation Inflammatory Bowel Disease and Immunobiology Research Institute at Cedars-Sinai Medical Center, Los Angeles.
“With the advances in therapies for IBD, including availability of gut-selective agents, treatment choices often incorporate whether a patient has one of these manifestations or not,” he said. “We need to understand who is at increased risk of these and why.”
The study was published in Gastroenterology .
Analyzing Associations
Dr. McGovern and colleagues analyzed data for 12,083 unrelated European ancestry IBD cases with presence or absence of EIMs across four cohorts in the Cedars-Sinai Medical Center IBD Research Repository, National Institute for Diabetes and Digestive and Kidney Diseases IBD Genetics Consortium, Sinai Helmsley Alliance for Research Excellence Consortium, and Risk Stratification and Identification of Immunogenetic and Microbial Markers of Rapid Disease Progression in Children with Crohn’s Disease.
In particular, the researchers looked at EIM phenotypes such as ankylosing spondylitis and sacroiliitis, PSC, peripheral arthritis, and skin and ocular manifestations. They analyzed clinical and serologic parameters through regression analyses using a mixed-effects model, as well as within-case logistic regression for genetic associations.
Overall, 14% of patients had at least one EIM. Contrary to previous reports, only 2% had multiple EIMs, and most co-occurrences were negatively correlated. Nearly all EIMs were more common in Crohn’s disease, except for PSC, which was more common in ulcerative colitis.
In general, EIMs occurred more often in women, particularly with Crohn’s disease and colonic disease location, and in patients who required surgery. Jewish ancestry was associated with psoriasis and overall skin manifestations.
Smoking increased the risk for multiple EIMs, except for PSC, where there appeared to be a “protective” effect. Older age at diagnosis and a family history of IBD were associated with increased risk for certain EIMs as well.
In addition, the research team noted multiple serologic associations, such as immunoglobulin (Ig) G and IgA, perinuclear antinuclear cytoplastic antibodies, and anti–Pseudomonas fluorescens–associated sequences with any EIM, as well as particular associations with PSC, such as anti-Saccharomyces cerevisiae antibodies and anti-flagellin.
There were also genome-wide significant associations within the major histocompatibility complex and CPEB4. Genetic associations implicated tumor necrosis factor, Janus kinase-signal transducer and activator of transcription, and interleukin 6 as potential targets for EIMs.
“We are working with colleagues across the world to increase the sample size, as we believe there is more to find,” Dr. McGovern said. “Importantly, this includes non-European ancestry subjects, as there is an urgent need to increase the diversity of populations we study so advances in clinical care are available to all communities.”
Considering Target Therapies
As medicine becomes more specialized, physicians should remember to consider the whole patient while choosing treatment strategies.
“Sometimes doctors wear blinders to the whole person, and it’s important to be aware of a holistic approach, where a gastroenterologist also asks about potential joint inflammation or a rheumatologist asks about bowel inflammation,” said David Rubin, MD, AGAF, chief of the Section of Gastroenterology, Hepatology and Nutrition at the University of Chicago Medicine, Chicago.
Dr. Rubin, who wasn’t involved with this study, has researched and published on EIMs in IBD. He and colleagues analyzed the prevalence, pathophysiology, and clinical presentation of EIMs to better understand possibilities for disease management.
“As we’ve gotten a better understanding of the immune system, we’ve learned that an EIM can sometimes provide a clue to the treatment we might use,” he said. “Given a similar amount of bowel inflammation, if one patient also has joint pain and another doesn’t, we might choose different treatments based on the immune pathway that might be involved.”
In future studies, researchers may consider whether these genetic or serologic markers could predict EIM manifestation before it occurs clinically, Dr. Rubin said. He and colleagues are also studying the links between IBD and mental health associations.
“So far, we don’t have a blood test or biopsy test that tells you which treatment is more or less likely to work, so we need to think carefully as clinicians and look to other organ systems for clues,” he said. “It’s not only more efficient to pick a single therapy to treat both the skin and bowel, but it may actually be more effective if both have a particular dominant pathway.”
The study was supported by internal funds from the F. Widjaja Foundation Inflammatory Bowel and Immunobiology Research Institute. Several authors reported consultant roles or other associations with pharmaceutical companies. Dr. Rubin reported no relevant disclosures.
A version of this article appeared on Medscape.com.