User login
Pharmacist-Led Deprescribing of Aspirin for Primary Prevention of Cardiovascular Disease Among Geriatric Veterans
Pharmacist-Led Deprescribing of Aspirin for Primary Prevention of Cardiovascular Disease Among Geriatric Veterans
Low-dose aspirin commonly is used for the prevention of cardiovascular disease (CVD) but is associated with an increased risk of major bleeding.1 The use of aspirin for primary prevention is largely extrapolated from clinical trials showing benefit in the secondary prevention of myocardial infarction and ischemic stroke. However, results from the Aspirin in Reducing Events in the Elderly (ASPREE) trial challenged this practice.2 The ASPREE trial, conducted in the United States and Australia from 2010 to 2014, sought to determine whether daily 100 mg aspirin, was superior to placebo in promoting disability-free survival among older adults. Participants were aged ≥ 70 years (≥ 65 years for Hispanic and Black US participants), living in the community, and were free from preexisting CVD, cerebrovascular disease, or any chronic condition likely to limit survival to < 5 years. The study found no significant difference in the primary endpoints of death, dementia, or persistent physical disability, but there was a significantly higher risk of major hemorrhage in the aspirin group (3.8% vs 2.8%; hazard ratio, 1.38; 95% CI, 1.18-1.62; P < .001).
Several medical societies have updated their guideline recommendations for aspirin for primary prevention of CVD. The 2022 United States Public Service Task Force (USPSTF) provides a grade C recommendation (at least moderate certainty that the net benefit is small) to consider low-dose aspirin for the primary prevention of CVD on an individual patient basis for adults aged 40 to 59 years who have a ≥ 10% 10-year CVD risk. For adults aged ≥ 60 years, the USPSTF recommendation is grade D (moderate or high certainty that the practice has no net benefit or that harms outweigh the benefits) for low-dose aspirin use.1,3 The American College of Cardiology and American Heart Association (ACC/AHA) recommend considering low-dose aspirin for primary prevention of atherosclerotic cardiovascular disease (ASCVD) among select adults aged 40 to 70 years at higher CVD risk but not at increased risk of bleeding.4 The American Diabetes Association (ADA) recommends low-dose aspirin for primary prevention of CVD in patients with diabetes and additional risk factors such as family history of premature ASCVD, hypertension, dyslipidemia, smoking, or chronic kidney disease, and who are not at higher risk of bleeding.5 The ADA standards also caution against the use of aspirin as primary prevention in patients aged > 70 years. Low-dose aspirin use is not recommended for the primary prevention of CVD in older adults or adults of any age who are at increased risk of bleeding.
Recent literature using the US Department of Veterans Affairs (VA) Corporate Data Warehouse database confirms 86,555 of 1.8 million veterans aged > 70 years (5%) were taking low-dose aspirin for primary prevention of ASCVD despite guideline recommendations.6 Higher risk of gastrointestinal and other major bleeding from low-dose aspirin has been reported in the literature.1 Major bleeds represent a significant burden to the health care system with an estimated mean $13,093 cost for gastrointestinal bleed hospitalization.7
Considering the large scale aspirin use without appropriate indication within the veteran population, the risk of adverse effects, and the significant cost to patients and the health care system, it is imperative to determine the best approach to efficiently deprescribe aspirin for primary prevention among geriatric patients. Deprescribing refers to the systematic and supervised process of dose reduction or drug discontinuation with the goal of improving health and/or reducing the risk of adverse effects.8 During patient visits, primary care practitioners (PCPs) have opportunities to discontinue aspirin, but these encounters are time-limited and deprescribing might be secondary to more acute primary care needs. The shortage of PCPs is expected to worsen in coming years, which could further reduce their availability to assess inappropriate aspirin use.9
VA clinical pharmacist practitioners (CPPs) serve as medication experts and work autonomously under a broad scope of practice as part of the patient aligned care team.10-12 CPPs can free up time for PCPs and facilitate deprescribing efforts, especially for older adults. One retrospective cohort study conducted at a VA medical center found that CPPs deprescribed more potentially inappropriate medications among individuals aged ≥ 80 years compared with usual care with PCPs (26.8% vs 16.1%; P < .001).12,13 An aspirin deprescribing protocol conducted in 2022 resulted in nearly half of veterans aged ≥ 70 years contacted by phone agreeing to stop aspirin. Although this study supports the role pharmacists can play in reducing aspirin use in accordance with guidelines, the authors acknowledge that their interventions had a mean time of 12 minutes per patient and would require workflow changes.14 The purpose of this study is to evaluate the efficiency of aspirin deprescribing through 2 approaches: direct deprescribing by pharmacists using populationlevel review compared with clinicians following a pharmacist-led education.
Methods
This was a single-center quality improvement cohort study at the Durham VA Health Care System (DVAHCS) in North Carolina. Patients included were aged ≥ 70 years without known ASCVD who received care at any of 3 DVAHCS community-based outpatient clinics and prescribed aspirin. Patient data was obtained using the VIONE (Deprescribing Dashboard called Vital, Important, Optional, Not indicated, and Every medication has a specific indication or diagnosis) dashboard.15 VIONE was developed to identify potentially inappropriate medications (PIMs) that are eligible to deprescribe based on Beers Criteria, Screening Tool of Older Personsf Prescriptions criteria, and common clinical scenarios when clinicians determine the risk outweighs the benefit to continue a specific medication. 16,17 VIONE is used to reduce polypharmacy and improve patient safety, comfort, and medication adherence. Aspirin for patients aged ≥ 70 years without a history of ASCVD is a PIM identified by VIONE. Patients aged ≥ 70 years were chosen as an inclusion criteria in this study to match the ASPREE trial inclusion criteria and age inclusion criteria in the VIONE dashboard for aspirin deprescribing.2 Patient lists were generated for these potentially inappropriate aspirin prescriptions for 3 months before clinician staff education presentations, the day of the presentations, and 3 months after.
The primary endpoint was the number of veterans with aspirin deprescribed directly by 2 pharmacists over 12 weeks, divided by total patient care time spent, compared with the change in number of veterans with aspirin deprescribed by any DVAHCS physician, nurse practitioner, physician assistant, or CPP over 12 weeks, divided by the total pharmacist time spent on PCP education. Secondary endpoints were the number of aspirin orders discontinued by pharmacists and CPPs, the number of aspirin orders discontinued 12 weeks before pharmacist-led education compared with the number of aspirin orders discontinued 12 weeks after CPP-led education, average and median pharmacist time spent per patient encounter, and time of direct patient encounters vs time spent on PCP education.
Pharmacists reviewed each patient who met the inclusion criteria from the list generated by VIONE on December 1, 2022, for aspirin appropriateness according to the ACC/AHA and USPSTF guidelines, with the goal to discontinue aspirin for primary prevention of ASCVD and no other indications.1,4 Pharmacists documented their visits using VIONE methodology in the Computerized Patient Record System (CPRS) using a polypharmacy review note. CPPs contacted patients who were taking aspirin for primary prevention by unscheduled telephone call to assess for aspirin adherence, undocumented history of ASCVD, cardiovascular risk factors, and history of bleeding. Aspirin was discontinued if patients met guideline criteria recommendations and agreed to discontinuation. Risk-benefit discussions were completed when patients without known ASCVD were considered high risk because the ACC/AHA guidelines mention there is insufficient evidence of safety and efficacy of aspirin for primary prevention for patients with other known ASCVD risk factors (eg, strong family history of premature myocardial infarction, inability to achieve lipid, blood pressure, or glucose targets, or significant elevation in coronary artery calcium score).
High risk was defined as family history of premature ASCVD (in a male first-degree relative aged < 55 years or a female first-degree relative aged < 65 years), most recent blood pressure or 2 blood pressure results in the last 12 months > 160/100 mm Hg, recent hemoglobin A1c > 9%, and/or low-density lipoprotein > 190 mg/dL or not prescribed an indicated statin.3 Aspirin was continued or discontinued according to patient preference after the personalized risk-benefit discussion.
For patients with a clinical indication for aspirin use other than ASCVD (eg, atrial fibrillation not on anticoagulation, venous thromboembolism prophylaxis, carotid artery disease), CPPs documented their assessment and when appropriate deferred to the PCP for consideration of stopping aspirin. For patients with undocumented ASCVD, CPPs added their ASCVD history to their problem list and aspirin was continued. PCPs were notified by alert when aspirin was discontinued and when patients could not be reached by telephone.
presented a review of recent guideline updates and supporting literature at 2 online staff meetings. The education sessions lasted about 10 minutes and were presented to PCPs across 3 community-based outpatient clinics. An estimated 40 minutes were spent creating the PowerPoint education materials, seeking feedback, making edits, and answering questions or emails from PCPs after the presentation. During the presentation, pharmacists encouraged PCPs to discontinue aspirin (active VA prescriptions and reported over-the-counter use) for primary prevention of ASCVD in patients aged ≥ 70 years during their upcoming appointments and consider risk factors recommended by the ACC/AHA guidelines when applicable. PCPs were notified that CPPs planned to start a population review for discontinuing active VA aspirin prescriptions on December 1, 2022. The primary endpoint and secondary endpoints were analyzed using descriptive statistics. All data were analyzed using Microsoft Excel.
Results
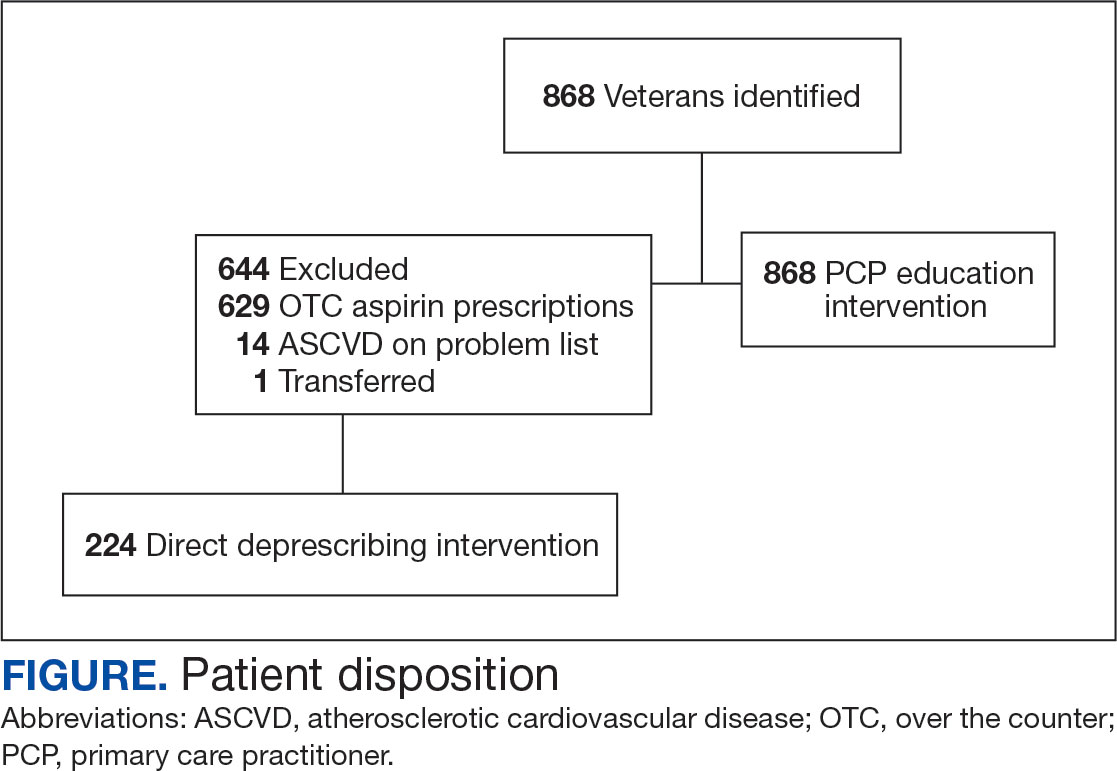
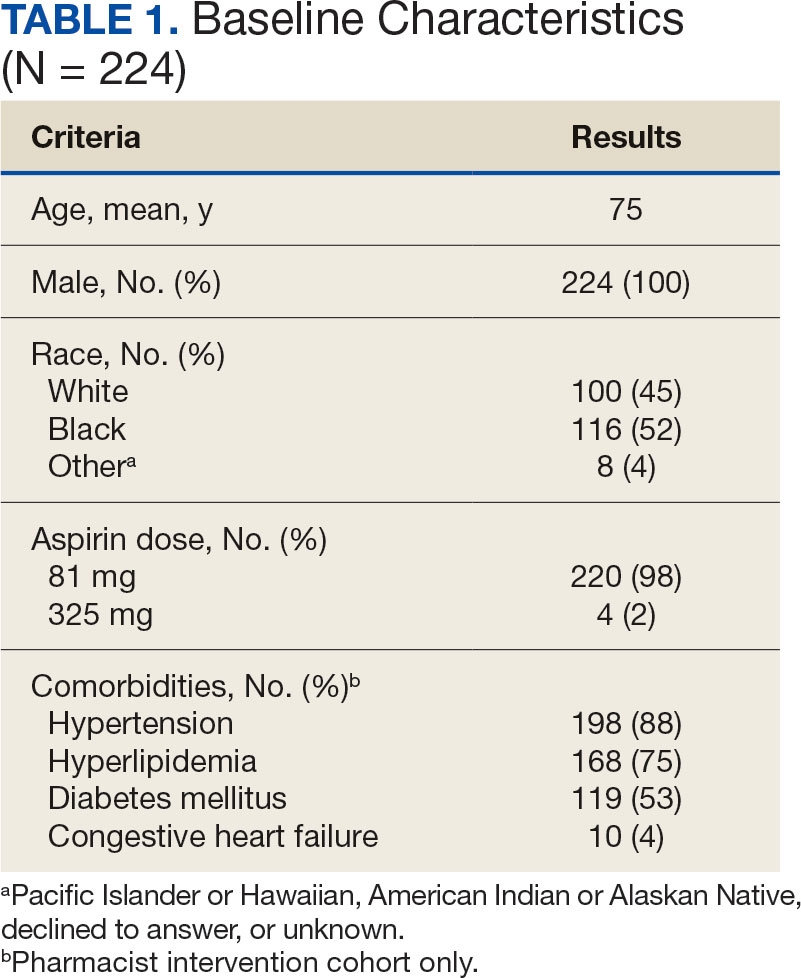
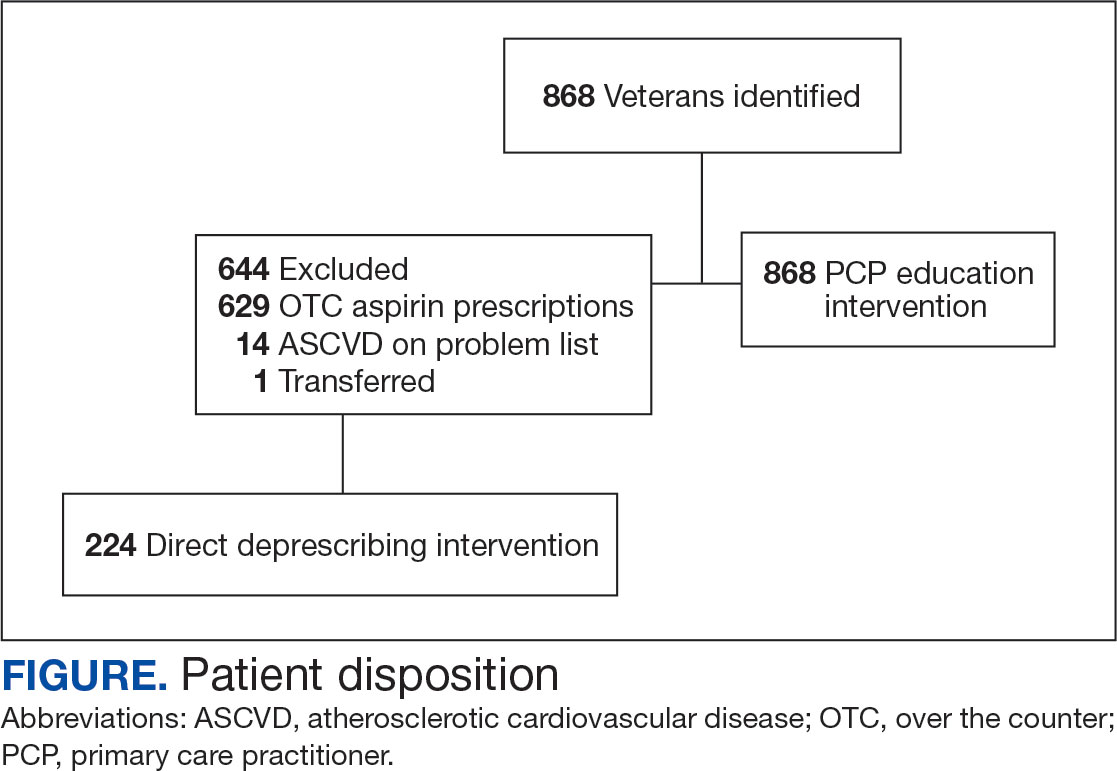
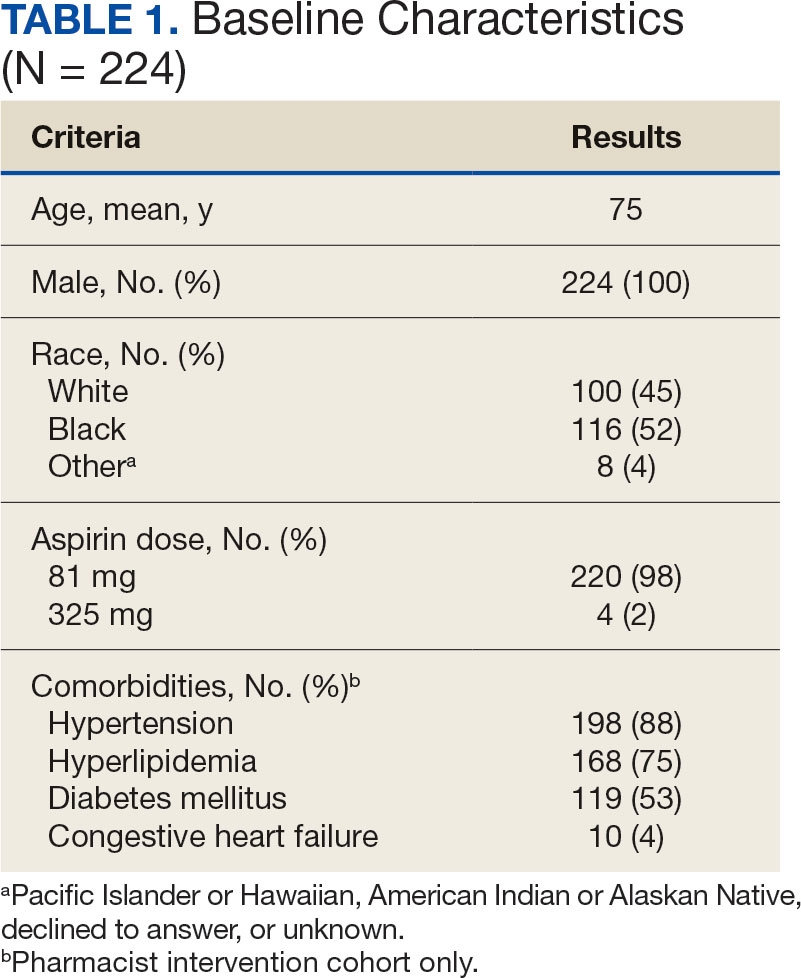
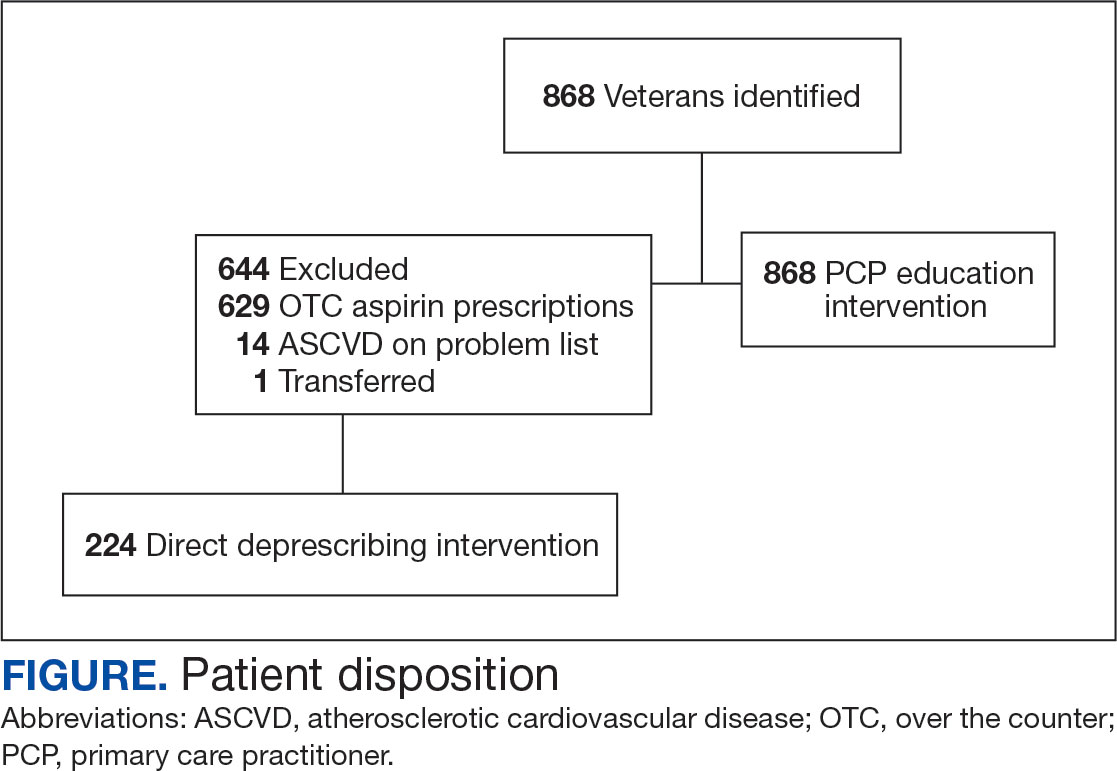
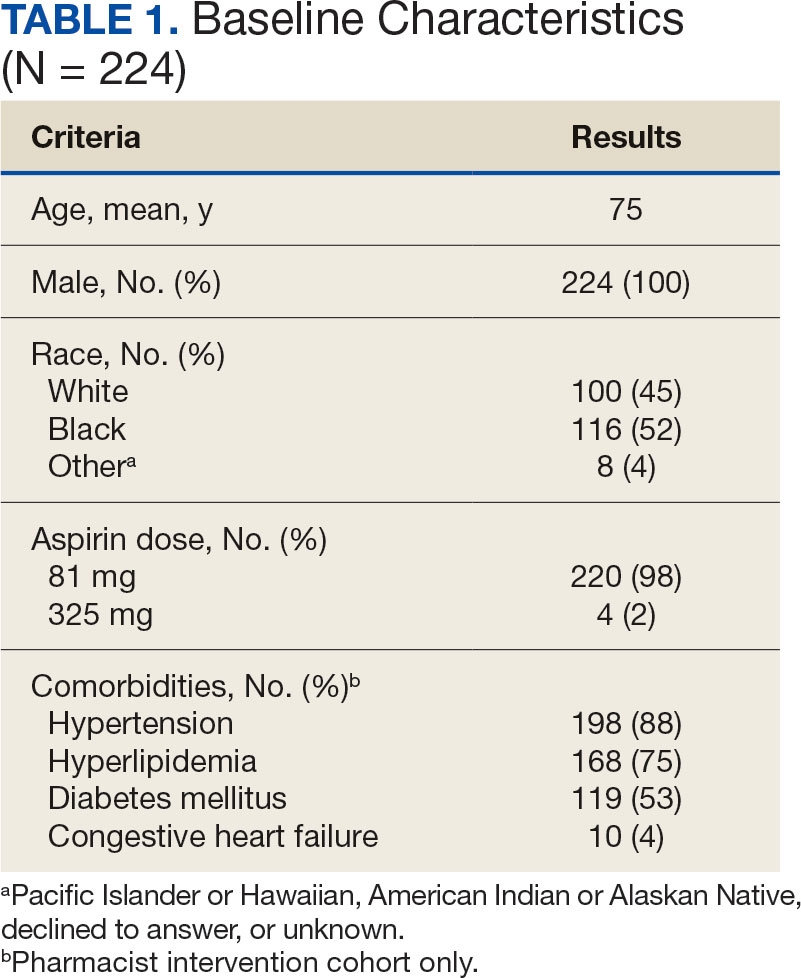
A total of 868 patients aged ≥ 70 years with active prescriptions for aspirin were identified on December 1, 2022. After applying inclusion and exclusion criteria for the pharmacist population review, 224 patients were included for cohort final analysis (Figure). All 868 patients were eligible for the CPP intervention. Primary reasons for exclusion from the CPP population included over-thecounter aspirin and a history of ASCVD in the patient’s problem list. All patients were male, with a mean (SD) age of 75 (4.4) years (Table 1). Most patients were prescribed aspirin, 81 mg daily (n = 220; 98%).
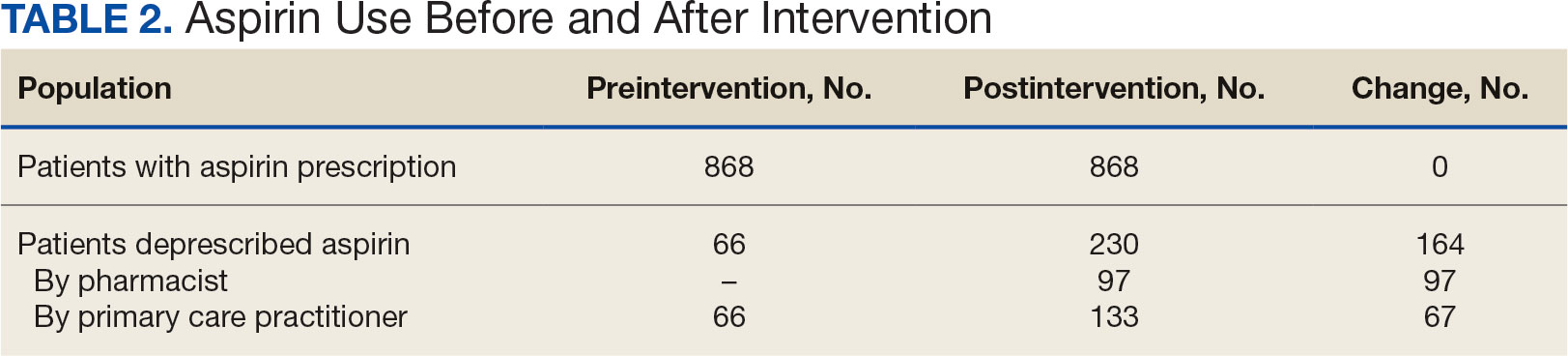
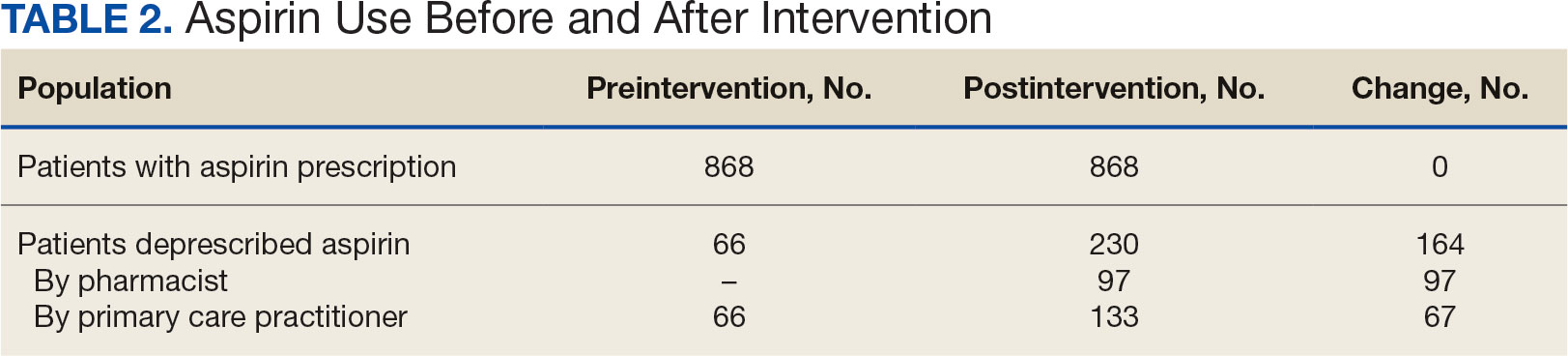
The direct CPP deprescribing intervention resulted in 2 aspirin prescriptions discontinued per hour of pharmacist time and 67 aspirin prescriptions discontinued per hour of pharmacist time via the PCP education intervention. CPPs discontinued 66 aspirin orders in the 12 weeks before the PCP education sessions. A total of 230 aspirin prescriptions were discontinued in the 12 weeks following the PCP education sessions, with 97 discontinued directly by CPPs and 133 discontinued by PCPs. The PCP education session yielded an additional 67 discontinued aspirin orders compared with the 12 weeks before the education sessions (Table 2).
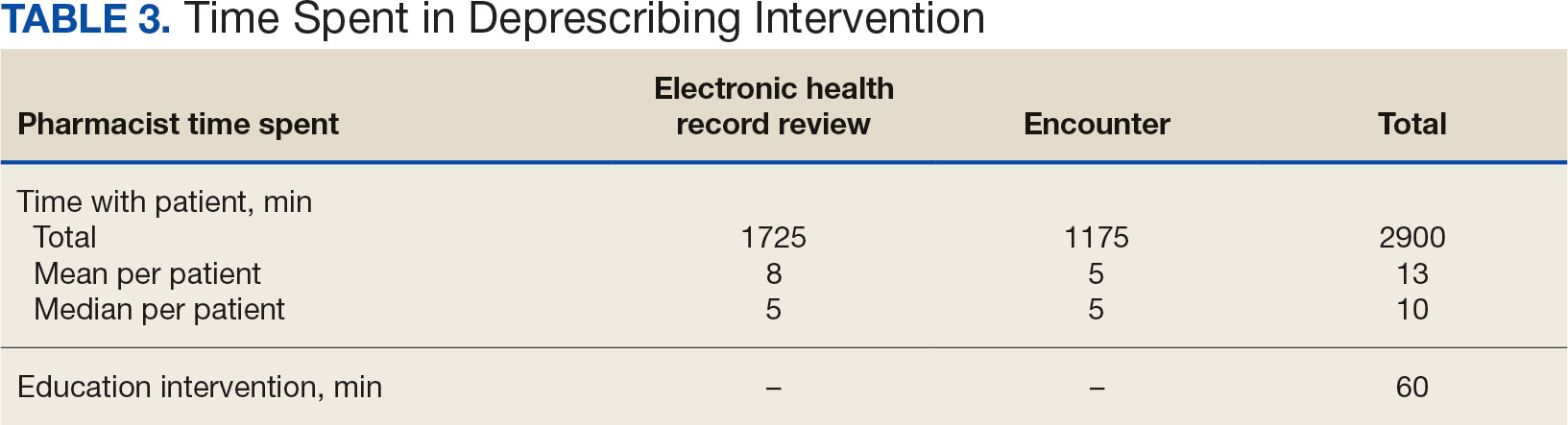
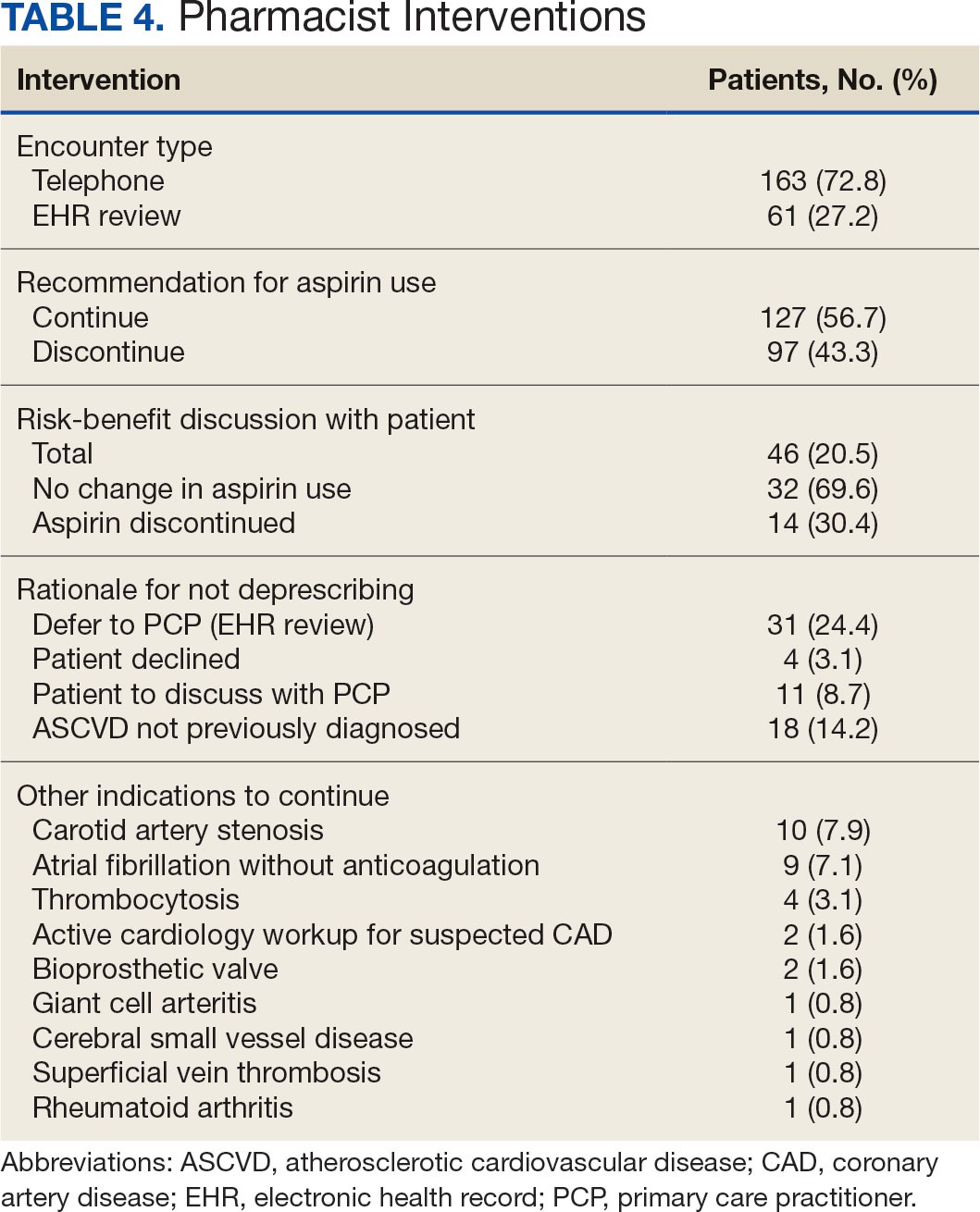
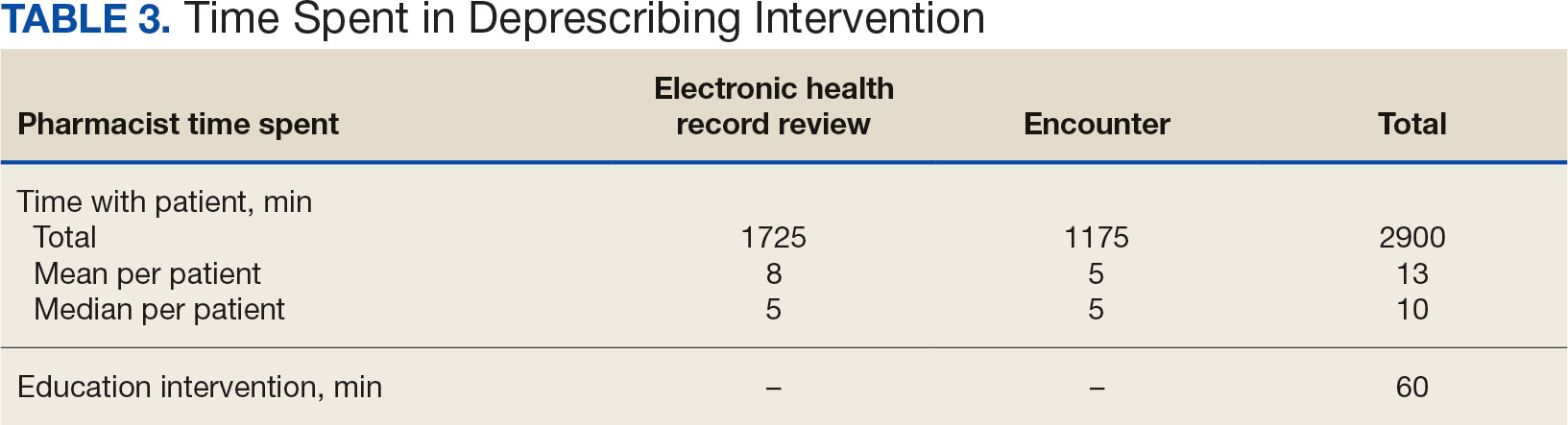
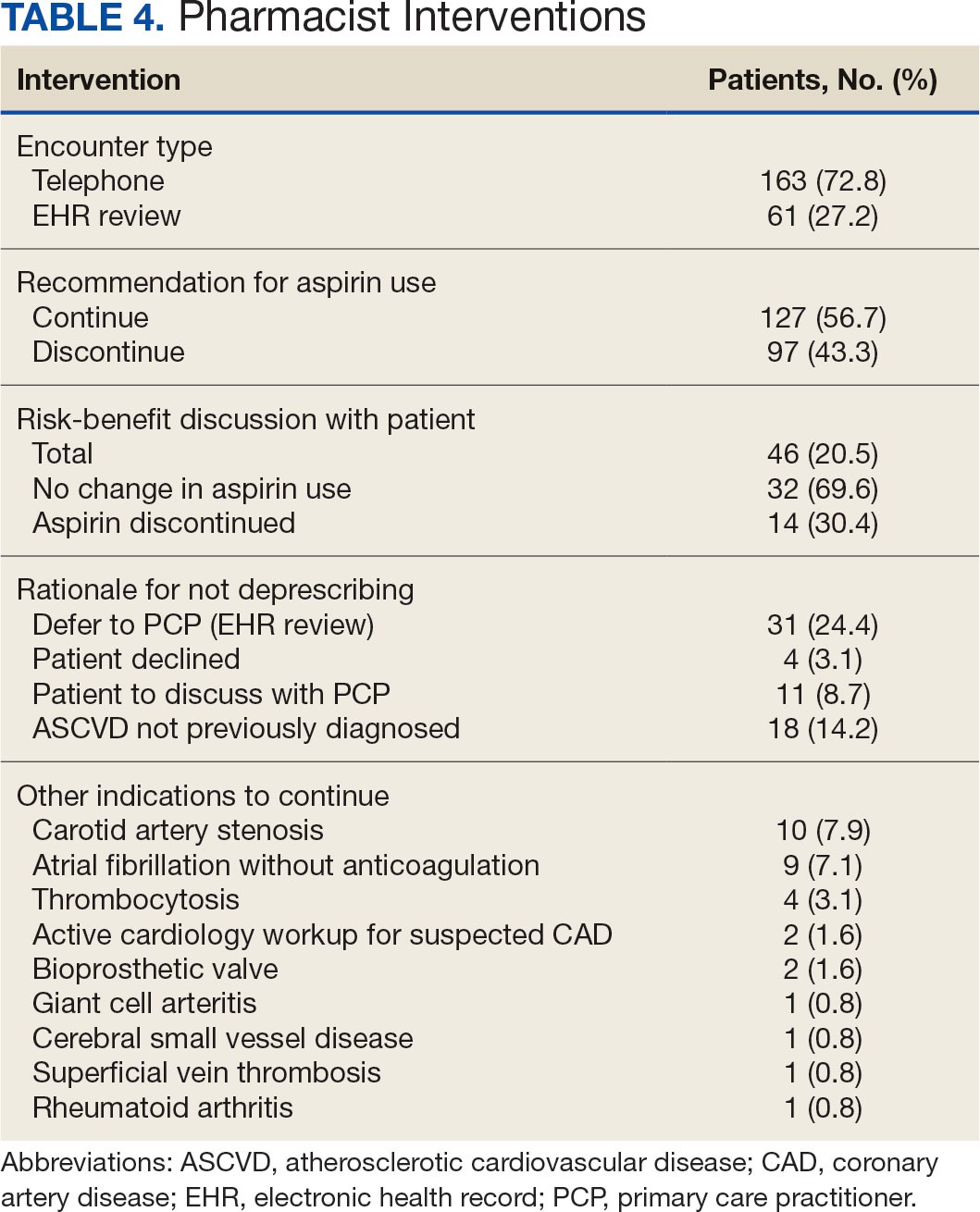
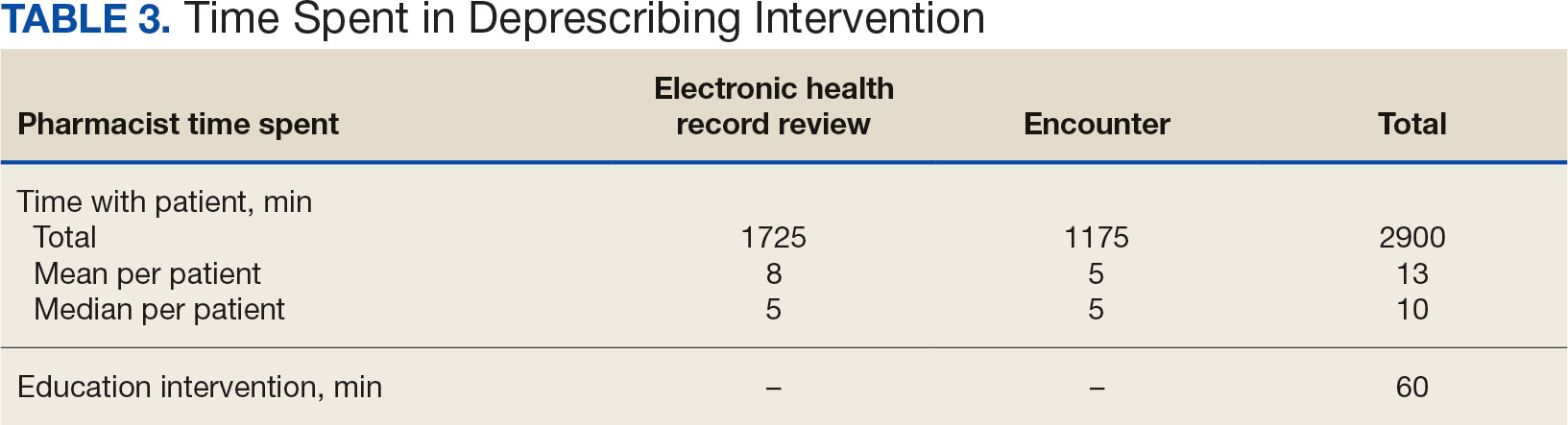
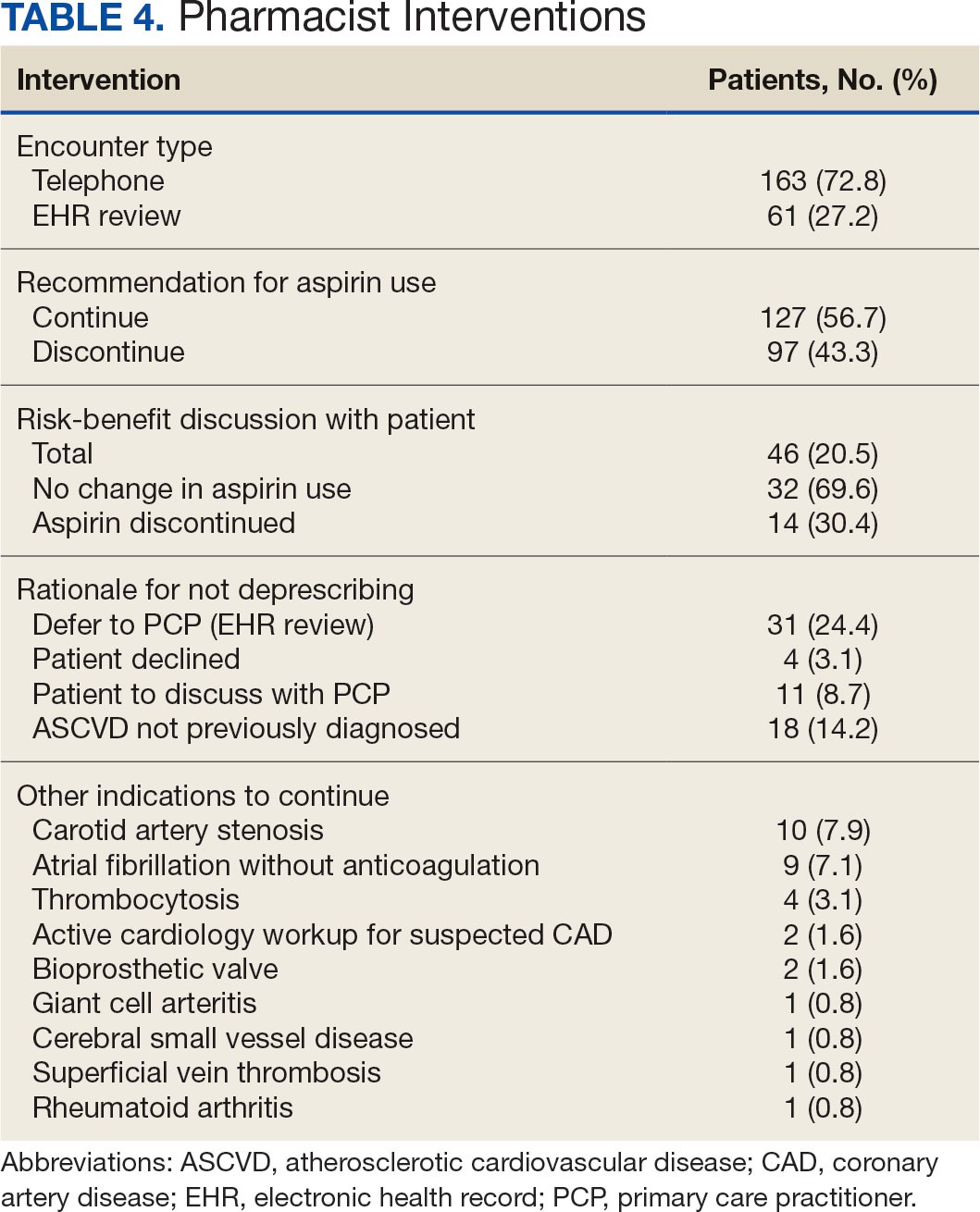
The CPP direct deprescribing intervention took about 48.3 hours, accounting for health record review and time interacting with patients. The PCP education intervention took about 60 minutes, which included time for preparing and delivering education materials (Table 3). CPP deprescribing encounter types, interventions, and related subcategories, and other identified indications to continue aspirin are listed in Table 4.
Discussion
Compared with direct deprescribing by pharmacists, the PCP education intervention was more efficient based on number of aspirin orders discontinued by pharmacist time. PCPs discontinued twice as many aspirin prescriptions in the 12 weeks after pharmacist-led education compared with the 12 weeks before.
Patients were primarily contacted by telephone (73%) for deprescribing. Among the 163 patients reached by phone and encouraged to discontinue aspirin, 97 patients (60%) accepted the recommendation, which was similar to the acceptance rates found in the literature (48% to 55%).14,18 Although many veterans continued taking aspirin (78%), most had indications for its continued use, such as a history of ASCVD, atrial fibrillation without anticoagulation, and carotid artery stenosis, and complex comorbidities that required further discussion with their PCP. Less common uses for aspirin were identified through CPRS review or patient reports included cerebral small vessel disease without history of ASCVD, subclavian artery stenosis, thrombocytosis, bioprosthetic valve replacement, giant cell arteritis, rheumatoid arthritis, and prevention of second eye involvement of ischemic optic neuropathy.
to describe the benefit of clinical pharmacy services for deprescribing aspirin for primary prevention of ASCVD through PCP education. Previously published literature has assessed alternative ways to identify or discontinue PIMs—including aspirin—among geriatric patients. One study evaluated the use of marking inappropriate aspirin prescriptions in the electronic health database, leading to a significant reduction in incidence of inappropriate aspirin prescribing; however, it did not assess changes in discontinuation rates of existing aspirin prescriptions.19 The previous VA pharmacist aspirin deprescribing protocol demonstrated pharmacists’ aptitude at discontinuing aspirin for primary prevention but only used direct patient contact and did not compare efficiency with other methods, including PCP education.14
This quality improvement project contributes new data to the existing literature to support the use of clinical pharmacists to discontinue aspirin for primary prevention and suggests a strong role for pharmacists as educators on clinical guidelines, in addition to their roles directly deprescribing PIMs in clinical practice. This study is further strengthened by its use of VIONE, which previously has demonstrated effectiveness in deprescribing a variety of PIMs in primary care settings.20
Despite using VIONE for generating a list of patients eligible for deprescription, our CPRS review found that this list was frequently inaccurate. For example, a small portion of patients were on the VIONE generated list indicating they had no ASCVD history, but had transient ischemic attack listed in their problem lists. Patient problem lists often were missing documented ASCVD history that was revealed by patient interview or CPRS review. It is possible that patients interviewed might have omitted relevant ASCVD history because of low health literacy, conditions affecting memory, or use of health care services outside the VA system.
There were several instances of aspirin used for other non-ASCVD indications, such as primary stroke prevention in atrial fibrillation. The ACC/AHA atrial fibrillation guidelines previously provided a Class IIb recommendation (benefit is greater than risk but additional studies are needed) for considering no antithrombic therapy or treatment with oral anticoagulant or aspirin for nonvalvular atrial fibrillation with CHA2DS2-VASc (Congestive heart failure, Hypertension, Age [> 65 y, 1 point; > 75 y, 2 points], Diabetes, previous Stroke/transient ischemic attack [2 points]) score of 1.21 The ACC/ AHA guidelines were updated in 2023 to recommend against antiplatelet therapy as an alternative to anticoagulation for reducing cardioembolic stroke risk among patients with atrial fibrillation with no indication for antiplatelet therapy because of risk of harm.22 If a patient has no risk factors for stroke, aspirin is not recommended to prevent thromboembolic events because of a lack of benefit. Interventions from this quality improvement study were completed before the 2023 atrial fibrillation guideline was published and therefore in this study aspirin was not discontinued when used for atrial fibrillation. Aspirin use for atrial fibrillation might benefit from similar discontinuation efforts analyzed within this study. Beyond atrial fibrillation, major guidelines do not comment on the use of aspirin for any other indications in the absence of clinical ASCVD.
Limitations
This study is limited by the lack of clinical consensus for complex patients and demonstrates the importance of individualized patient assessment when considering discontinuing aspirin. Because of the project’s relatively short intervention period, aspirin deprescribing rates could decrease over time and repeated education efforts might be necessary to see lasting impact. Health care professionals from services outside of primary care also might have discontinued aspirin during the study period unrelated to the education and these discontinued aspirin prescriptions could contribute to the higher rate observed among PCPs. This study included a specific population cohort of male, US veterans and might not reflect other populations where these interventions could be implemented.
The measurement of time spent by pharmacists and PCPs is an additional limitation. Although it is expected that PCPs attempt to discontinue aspirin during their existing patient care appointments, the time spent during visits was not measured or documented. Direct deprescribing by pharmacist CPRS review required a significant amount of time and could be a barrier to successful intervention by CPPs in patient aligned care teams.
To reduce the time pharmacists spent completing CPRS reviews, an aspirin deprescribing clinical reminder tool could be used to assess use and appropriate indication quickly during any primary care visit led by a PCP or CPP. In addition, it is recommended that pharmacists regularly educate health care professionals on guideline recommendations for aspirin use among geriatric patients. Future studies of the incidence of major cardiovascular events after aspirin deprescribing among geriatric patients and a longitudinal cost/benefit analysis could support these initiatives.
Conclusions
In this study, pharmacists successfully deprescribed inappropriate medications, such as aspirin. However, pharmacist-led PCP education is more efficient compared with direct deprescribing using a population-level review. PCP education requires less time and could allow ambulatory care pharmacists to spend more time on other direct patient care interventions to improve quality and access to care in primary care clinics. This study’s results further support the role of pharmacists in deprescribing PIMs for older adults and the use of a deprescribing tool, such as VIONE, in a primary care setting.
- US Preventive Services Task Force; Davidson KW, Barry MJ, et al. Aspirin use to prevent cardiovascular disease: US Preventive Services Task Force recommendation statement. JAMA. 2022;327(16):1577-1584. doi:10.1001/jama.2022.4983
- McNeil JJ, Nelson MR, Woods RL, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519-1528. doi:10.1056/NEJMoa1803955
- Barry MJ, Wolff TA, Pbert L, et al. Putting evidence into practice: an update on the US Preventive Services Task Force methods for developing recommendations for preventive services. Ann Fam Med. 2023;21(2):165-171. doi:10.1370/afm.2946
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/ AHA Guideline on the Primary Prevention of Cardiovascular Disease: A report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi:10.1161/CIR.0000000000000678
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: Standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S179-S218. doi:10.2337/dc24-S010
- Ong SY, Chui P, Bhargava A, Justice A, Hauser RG. Estimating aspirin overuse for primary prevention of atherosclerotic cardiovascular disease (from a nationwide healthcare system). Am J Cardiol. 2020;137:25-30. doi:10.1016/j.amjcard.2020.09.042
- Weiss AJ, Jiang HJ. Overview of clinical conditions with frequent and costly hospital readmissions by payer, 2018. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); July 20, 2021.
- Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol. 2019;73(20):2584-2595. doi:10.1016/j.jacc.2019.03.467
- Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2019 to 2034. Accessed March 17, 2024. https://www.aamc.org/media/54681/download
- US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1108.07(1): General pharmacy service requirements. November 28, 2022. Accessed March 17, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=10045
- US Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1108.11(3): Clinical pharmacy services. July 1, 2015. Accessed March 17, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3120
- US Department of Veterans Affairs. Clinical pharmacist practitioner (CPP) to improve access to and quality of care August 2021. August 2021. Accessed May 19, 2023. https://www.pbm.va.gov/PBM/CPPO/Documents/ExternalFactSheet_OptimizingtheCPPToImproveAccess_508.pdf
- Ammerman CA, Simpkins BA, Warman N, Downs TN. Potentially inappropriate medications in older adults: Deprescribing with a clinical pharmacist. J Am Geriatr Soc. 2019;67(1):115-118. doi:10.1111/jgs.15623
- Rothbauer K, Siodlak M, Dreischmeier E, Ranola TS, Welch L. Evaluation of a pharmacist-driven ambulatory aspirin deprescribing protocol. Fed Pract. 2022;39(suppl 5):S37- S41a. doi:10.12788/fp.0294
- US Department of Veterans Affairs. VIONE changes the way VA handles prescriptions. January 25, 2020. Accessed May 21, 2023. https://news.va.gov/70709/vione-changes-way-va-handles-prescriptions/
- 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052- 2081. doi:10.1111/jgs.18372
- O’Mahony D, Cherubini A, Guiteras AR, et al. STOPP/ START criteria for potentially inappropriate prescribing in older people: version 3. Eur Geriatr Med. 2023;14(4):625- 632. doi:10.1007/s41999-023-00777-y
- Draeger C, Lodhi F, Geissinger N, Larson T, Griesbach S. Interdisciplinary deprescribing of aspirin through prescriber education and provision of patient-specific recommendations. WMJ. 2022;121(3):220-225
- de Lusignan S, Hinton W, Seidu S, et al. Dashboards to reduce inappropriate prescribing of metformin and aspirin: A quality assurance programme in a primary care sentinel network. Prim Care Diabetes. 2021;15(6):1075-1079. doi:10.1016/j.pcd.2021.06.003
- Nelson MW, Downs TN, Puglisi GM, Simpkins BA, Collier AS. Use of a deprescribing tool in an interdisciplinary primary-care patient-aligned care team. Sr Care Pharm. 2022;37(1):34-43. doi:10.4140/TCP.n.2022.34
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199-e267. doi:10.1161/CIR.0000000000000041
- Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/ AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines Circulation. 2024;149(1):e1- e156. doi:10.1161/CIR.0000000000001193
Low-dose aspirin commonly is used for the prevention of cardiovascular disease (CVD) but is associated with an increased risk of major bleeding.1 The use of aspirin for primary prevention is largely extrapolated from clinical trials showing benefit in the secondary prevention of myocardial infarction and ischemic stroke. However, results from the Aspirin in Reducing Events in the Elderly (ASPREE) trial challenged this practice.2 The ASPREE trial, conducted in the United States and Australia from 2010 to 2014, sought to determine whether daily 100 mg aspirin, was superior to placebo in promoting disability-free survival among older adults. Participants were aged ≥ 70 years (≥ 65 years for Hispanic and Black US participants), living in the community, and were free from preexisting CVD, cerebrovascular disease, or any chronic condition likely to limit survival to < 5 years. The study found no significant difference in the primary endpoints of death, dementia, or persistent physical disability, but there was a significantly higher risk of major hemorrhage in the aspirin group (3.8% vs 2.8%; hazard ratio, 1.38; 95% CI, 1.18-1.62; P < .001).
Several medical societies have updated their guideline recommendations for aspirin for primary prevention of CVD. The 2022 United States Public Service Task Force (USPSTF) provides a grade C recommendation (at least moderate certainty that the net benefit is small) to consider low-dose aspirin for the primary prevention of CVD on an individual patient basis for adults aged 40 to 59 years who have a ≥ 10% 10-year CVD risk. For adults aged ≥ 60 years, the USPSTF recommendation is grade D (moderate or high certainty that the practice has no net benefit or that harms outweigh the benefits) for low-dose aspirin use.1,3 The American College of Cardiology and American Heart Association (ACC/AHA) recommend considering low-dose aspirin for primary prevention of atherosclerotic cardiovascular disease (ASCVD) among select adults aged 40 to 70 years at higher CVD risk but not at increased risk of bleeding.4 The American Diabetes Association (ADA) recommends low-dose aspirin for primary prevention of CVD in patients with diabetes and additional risk factors such as family history of premature ASCVD, hypertension, dyslipidemia, smoking, or chronic kidney disease, and who are not at higher risk of bleeding.5 The ADA standards also caution against the use of aspirin as primary prevention in patients aged > 70 years. Low-dose aspirin use is not recommended for the primary prevention of CVD in older adults or adults of any age who are at increased risk of bleeding.
Recent literature using the US Department of Veterans Affairs (VA) Corporate Data Warehouse database confirms 86,555 of 1.8 million veterans aged > 70 years (5%) were taking low-dose aspirin for primary prevention of ASCVD despite guideline recommendations.6 Higher risk of gastrointestinal and other major bleeding from low-dose aspirin has been reported in the literature.1 Major bleeds represent a significant burden to the health care system with an estimated mean $13,093 cost for gastrointestinal bleed hospitalization.7
Considering the large scale aspirin use without appropriate indication within the veteran population, the risk of adverse effects, and the significant cost to patients and the health care system, it is imperative to determine the best approach to efficiently deprescribe aspirin for primary prevention among geriatric patients. Deprescribing refers to the systematic and supervised process of dose reduction or drug discontinuation with the goal of improving health and/or reducing the risk of adverse effects.8 During patient visits, primary care practitioners (PCPs) have opportunities to discontinue aspirin, but these encounters are time-limited and deprescribing might be secondary to more acute primary care needs. The shortage of PCPs is expected to worsen in coming years, which could further reduce their availability to assess inappropriate aspirin use.9
VA clinical pharmacist practitioners (CPPs) serve as medication experts and work autonomously under a broad scope of practice as part of the patient aligned care team.10-12 CPPs can free up time for PCPs and facilitate deprescribing efforts, especially for older adults. One retrospective cohort study conducted at a VA medical center found that CPPs deprescribed more potentially inappropriate medications among individuals aged ≥ 80 years compared with usual care with PCPs (26.8% vs 16.1%; P < .001).12,13 An aspirin deprescribing protocol conducted in 2022 resulted in nearly half of veterans aged ≥ 70 years contacted by phone agreeing to stop aspirin. Although this study supports the role pharmacists can play in reducing aspirin use in accordance with guidelines, the authors acknowledge that their interventions had a mean time of 12 minutes per patient and would require workflow changes.14 The purpose of this study is to evaluate the efficiency of aspirin deprescribing through 2 approaches: direct deprescribing by pharmacists using populationlevel review compared with clinicians following a pharmacist-led education.
Methods
This was a single-center quality improvement cohort study at the Durham VA Health Care System (DVAHCS) in North Carolina. Patients included were aged ≥ 70 years without known ASCVD who received care at any of 3 DVAHCS community-based outpatient clinics and prescribed aspirin. Patient data was obtained using the VIONE (Deprescribing Dashboard called Vital, Important, Optional, Not indicated, and Every medication has a specific indication or diagnosis) dashboard.15 VIONE was developed to identify potentially inappropriate medications (PIMs) that are eligible to deprescribe based on Beers Criteria, Screening Tool of Older Personsf Prescriptions criteria, and common clinical scenarios when clinicians determine the risk outweighs the benefit to continue a specific medication. 16,17 VIONE is used to reduce polypharmacy and improve patient safety, comfort, and medication adherence. Aspirin for patients aged ≥ 70 years without a history of ASCVD is a PIM identified by VIONE. Patients aged ≥ 70 years were chosen as an inclusion criteria in this study to match the ASPREE trial inclusion criteria and age inclusion criteria in the VIONE dashboard for aspirin deprescribing.2 Patient lists were generated for these potentially inappropriate aspirin prescriptions for 3 months before clinician staff education presentations, the day of the presentations, and 3 months after.
The primary endpoint was the number of veterans with aspirin deprescribed directly by 2 pharmacists over 12 weeks, divided by total patient care time spent, compared with the change in number of veterans with aspirin deprescribed by any DVAHCS physician, nurse practitioner, physician assistant, or CPP over 12 weeks, divided by the total pharmacist time spent on PCP education. Secondary endpoints were the number of aspirin orders discontinued by pharmacists and CPPs, the number of aspirin orders discontinued 12 weeks before pharmacist-led education compared with the number of aspirin orders discontinued 12 weeks after CPP-led education, average and median pharmacist time spent per patient encounter, and time of direct patient encounters vs time spent on PCP education.
Pharmacists reviewed each patient who met the inclusion criteria from the list generated by VIONE on December 1, 2022, for aspirin appropriateness according to the ACC/AHA and USPSTF guidelines, with the goal to discontinue aspirin for primary prevention of ASCVD and no other indications.1,4 Pharmacists documented their visits using VIONE methodology in the Computerized Patient Record System (CPRS) using a polypharmacy review note. CPPs contacted patients who were taking aspirin for primary prevention by unscheduled telephone call to assess for aspirin adherence, undocumented history of ASCVD, cardiovascular risk factors, and history of bleeding. Aspirin was discontinued if patients met guideline criteria recommendations and agreed to discontinuation. Risk-benefit discussions were completed when patients without known ASCVD were considered high risk because the ACC/AHA guidelines mention there is insufficient evidence of safety and efficacy of aspirin for primary prevention for patients with other known ASCVD risk factors (eg, strong family history of premature myocardial infarction, inability to achieve lipid, blood pressure, or glucose targets, or significant elevation in coronary artery calcium score).
High risk was defined as family history of premature ASCVD (in a male first-degree relative aged < 55 years or a female first-degree relative aged < 65 years), most recent blood pressure or 2 blood pressure results in the last 12 months > 160/100 mm Hg, recent hemoglobin A1c > 9%, and/or low-density lipoprotein > 190 mg/dL or not prescribed an indicated statin.3 Aspirin was continued or discontinued according to patient preference after the personalized risk-benefit discussion.
For patients with a clinical indication for aspirin use other than ASCVD (eg, atrial fibrillation not on anticoagulation, venous thromboembolism prophylaxis, carotid artery disease), CPPs documented their assessment and when appropriate deferred to the PCP for consideration of stopping aspirin. For patients with undocumented ASCVD, CPPs added their ASCVD history to their problem list and aspirin was continued. PCPs were notified by alert when aspirin was discontinued and when patients could not be reached by telephone.
presented a review of recent guideline updates and supporting literature at 2 online staff meetings. The education sessions lasted about 10 minutes and were presented to PCPs across 3 community-based outpatient clinics. An estimated 40 minutes were spent creating the PowerPoint education materials, seeking feedback, making edits, and answering questions or emails from PCPs after the presentation. During the presentation, pharmacists encouraged PCPs to discontinue aspirin (active VA prescriptions and reported over-the-counter use) for primary prevention of ASCVD in patients aged ≥ 70 years during their upcoming appointments and consider risk factors recommended by the ACC/AHA guidelines when applicable. PCPs were notified that CPPs planned to start a population review for discontinuing active VA aspirin prescriptions on December 1, 2022. The primary endpoint and secondary endpoints were analyzed using descriptive statistics. All data were analyzed using Microsoft Excel.
Results
A total of 868 patients aged ≥ 70 years with active prescriptions for aspirin were identified on December 1, 2022. After applying inclusion and exclusion criteria for the pharmacist population review, 224 patients were included for cohort final analysis (Figure). All 868 patients were eligible for the CPP intervention. Primary reasons for exclusion from the CPP population included over-thecounter aspirin and a history of ASCVD in the patient’s problem list. All patients were male, with a mean (SD) age of 75 (4.4) years (Table 1). Most patients were prescribed aspirin, 81 mg daily (n = 220; 98%).
The direct CPP deprescribing intervention resulted in 2 aspirin prescriptions discontinued per hour of pharmacist time and 67 aspirin prescriptions discontinued per hour of pharmacist time via the PCP education intervention. CPPs discontinued 66 aspirin orders in the 12 weeks before the PCP education sessions. A total of 230 aspirin prescriptions were discontinued in the 12 weeks following the PCP education sessions, with 97 discontinued directly by CPPs and 133 discontinued by PCPs. The PCP education session yielded an additional 67 discontinued aspirin orders compared with the 12 weeks before the education sessions (Table 2).
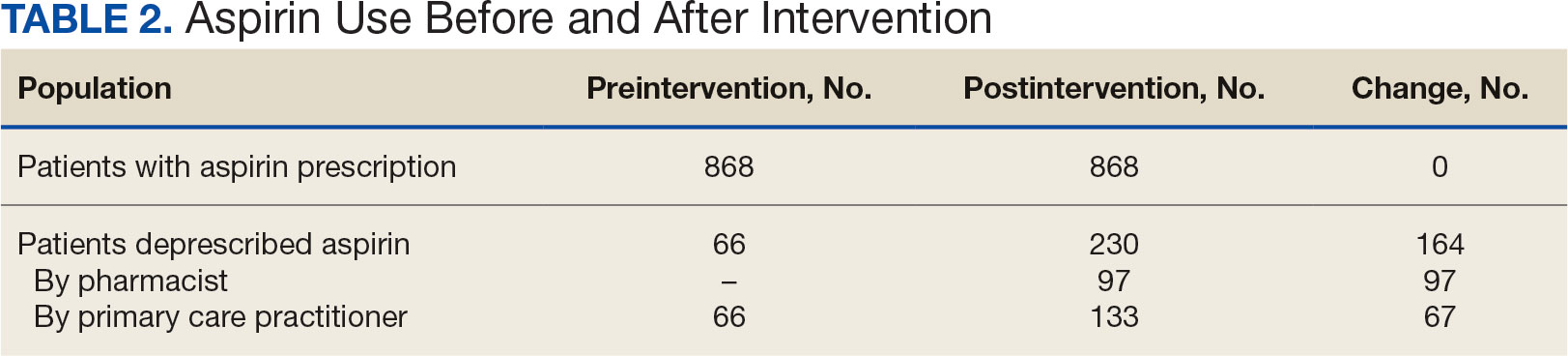
The CPP direct deprescribing intervention took about 48.3 hours, accounting for health record review and time interacting with patients. The PCP education intervention took about 60 minutes, which included time for preparing and delivering education materials (Table 3). CPP deprescribing encounter types, interventions, and related subcategories, and other identified indications to continue aspirin are listed in Table 4.
Discussion
Compared with direct deprescribing by pharmacists, the PCP education intervention was more efficient based on number of aspirin orders discontinued by pharmacist time. PCPs discontinued twice as many aspirin prescriptions in the 12 weeks after pharmacist-led education compared with the 12 weeks before.
Patients were primarily contacted by telephone (73%) for deprescribing. Among the 163 patients reached by phone and encouraged to discontinue aspirin, 97 patients (60%) accepted the recommendation, which was similar to the acceptance rates found in the literature (48% to 55%).14,18 Although many veterans continued taking aspirin (78%), most had indications for its continued use, such as a history of ASCVD, atrial fibrillation without anticoagulation, and carotid artery stenosis, and complex comorbidities that required further discussion with their PCP. Less common uses for aspirin were identified through CPRS review or patient reports included cerebral small vessel disease without history of ASCVD, subclavian artery stenosis, thrombocytosis, bioprosthetic valve replacement, giant cell arteritis, rheumatoid arthritis, and prevention of second eye involvement of ischemic optic neuropathy.
to describe the benefit of clinical pharmacy services for deprescribing aspirin for primary prevention of ASCVD through PCP education. Previously published literature has assessed alternative ways to identify or discontinue PIMs—including aspirin—among geriatric patients. One study evaluated the use of marking inappropriate aspirin prescriptions in the electronic health database, leading to a significant reduction in incidence of inappropriate aspirin prescribing; however, it did not assess changes in discontinuation rates of existing aspirin prescriptions.19 The previous VA pharmacist aspirin deprescribing protocol demonstrated pharmacists’ aptitude at discontinuing aspirin for primary prevention but only used direct patient contact and did not compare efficiency with other methods, including PCP education.14
This quality improvement project contributes new data to the existing literature to support the use of clinical pharmacists to discontinue aspirin for primary prevention and suggests a strong role for pharmacists as educators on clinical guidelines, in addition to their roles directly deprescribing PIMs in clinical practice. This study is further strengthened by its use of VIONE, which previously has demonstrated effectiveness in deprescribing a variety of PIMs in primary care settings.20
Despite using VIONE for generating a list of patients eligible for deprescription, our CPRS review found that this list was frequently inaccurate. For example, a small portion of patients were on the VIONE generated list indicating they had no ASCVD history, but had transient ischemic attack listed in their problem lists. Patient problem lists often were missing documented ASCVD history that was revealed by patient interview or CPRS review. It is possible that patients interviewed might have omitted relevant ASCVD history because of low health literacy, conditions affecting memory, or use of health care services outside the VA system.
There were several instances of aspirin used for other non-ASCVD indications, such as primary stroke prevention in atrial fibrillation. The ACC/AHA atrial fibrillation guidelines previously provided a Class IIb recommendation (benefit is greater than risk but additional studies are needed) for considering no antithrombic therapy or treatment with oral anticoagulant or aspirin for nonvalvular atrial fibrillation with CHA2DS2-VASc (Congestive heart failure, Hypertension, Age [> 65 y, 1 point; > 75 y, 2 points], Diabetes, previous Stroke/transient ischemic attack [2 points]) score of 1.21 The ACC/ AHA guidelines were updated in 2023 to recommend against antiplatelet therapy as an alternative to anticoagulation for reducing cardioembolic stroke risk among patients with atrial fibrillation with no indication for antiplatelet therapy because of risk of harm.22 If a patient has no risk factors for stroke, aspirin is not recommended to prevent thromboembolic events because of a lack of benefit. Interventions from this quality improvement study were completed before the 2023 atrial fibrillation guideline was published and therefore in this study aspirin was not discontinued when used for atrial fibrillation. Aspirin use for atrial fibrillation might benefit from similar discontinuation efforts analyzed within this study. Beyond atrial fibrillation, major guidelines do not comment on the use of aspirin for any other indications in the absence of clinical ASCVD.
Limitations
This study is limited by the lack of clinical consensus for complex patients and demonstrates the importance of individualized patient assessment when considering discontinuing aspirin. Because of the project’s relatively short intervention period, aspirin deprescribing rates could decrease over time and repeated education efforts might be necessary to see lasting impact. Health care professionals from services outside of primary care also might have discontinued aspirin during the study period unrelated to the education and these discontinued aspirin prescriptions could contribute to the higher rate observed among PCPs. This study included a specific population cohort of male, US veterans and might not reflect other populations where these interventions could be implemented.
The measurement of time spent by pharmacists and PCPs is an additional limitation. Although it is expected that PCPs attempt to discontinue aspirin during their existing patient care appointments, the time spent during visits was not measured or documented. Direct deprescribing by pharmacist CPRS review required a significant amount of time and could be a barrier to successful intervention by CPPs in patient aligned care teams.
To reduce the time pharmacists spent completing CPRS reviews, an aspirin deprescribing clinical reminder tool could be used to assess use and appropriate indication quickly during any primary care visit led by a PCP or CPP. In addition, it is recommended that pharmacists regularly educate health care professionals on guideline recommendations for aspirin use among geriatric patients. Future studies of the incidence of major cardiovascular events after aspirin deprescribing among geriatric patients and a longitudinal cost/benefit analysis could support these initiatives.
Conclusions
In this study, pharmacists successfully deprescribed inappropriate medications, such as aspirin. However, pharmacist-led PCP education is more efficient compared with direct deprescribing using a population-level review. PCP education requires less time and could allow ambulatory care pharmacists to spend more time on other direct patient care interventions to improve quality and access to care in primary care clinics. This study’s results further support the role of pharmacists in deprescribing PIMs for older adults and the use of a deprescribing tool, such as VIONE, in a primary care setting.
Low-dose aspirin commonly is used for the prevention of cardiovascular disease (CVD) but is associated with an increased risk of major bleeding.1 The use of aspirin for primary prevention is largely extrapolated from clinical trials showing benefit in the secondary prevention of myocardial infarction and ischemic stroke. However, results from the Aspirin in Reducing Events in the Elderly (ASPREE) trial challenged this practice.2 The ASPREE trial, conducted in the United States and Australia from 2010 to 2014, sought to determine whether daily 100 mg aspirin, was superior to placebo in promoting disability-free survival among older adults. Participants were aged ≥ 70 years (≥ 65 years for Hispanic and Black US participants), living in the community, and were free from preexisting CVD, cerebrovascular disease, or any chronic condition likely to limit survival to < 5 years. The study found no significant difference in the primary endpoints of death, dementia, or persistent physical disability, but there was a significantly higher risk of major hemorrhage in the aspirin group (3.8% vs 2.8%; hazard ratio, 1.38; 95% CI, 1.18-1.62; P < .001).
Several medical societies have updated their guideline recommendations for aspirin for primary prevention of CVD. The 2022 United States Public Service Task Force (USPSTF) provides a grade C recommendation (at least moderate certainty that the net benefit is small) to consider low-dose aspirin for the primary prevention of CVD on an individual patient basis for adults aged 40 to 59 years who have a ≥ 10% 10-year CVD risk. For adults aged ≥ 60 years, the USPSTF recommendation is grade D (moderate or high certainty that the practice has no net benefit or that harms outweigh the benefits) for low-dose aspirin use.1,3 The American College of Cardiology and American Heart Association (ACC/AHA) recommend considering low-dose aspirin for primary prevention of atherosclerotic cardiovascular disease (ASCVD) among select adults aged 40 to 70 years at higher CVD risk but not at increased risk of bleeding.4 The American Diabetes Association (ADA) recommends low-dose aspirin for primary prevention of CVD in patients with diabetes and additional risk factors such as family history of premature ASCVD, hypertension, dyslipidemia, smoking, or chronic kidney disease, and who are not at higher risk of bleeding.5 The ADA standards also caution against the use of aspirin as primary prevention in patients aged > 70 years. Low-dose aspirin use is not recommended for the primary prevention of CVD in older adults or adults of any age who are at increased risk of bleeding.
Recent literature using the US Department of Veterans Affairs (VA) Corporate Data Warehouse database confirms 86,555 of 1.8 million veterans aged > 70 years (5%) were taking low-dose aspirin for primary prevention of ASCVD despite guideline recommendations.6 Higher risk of gastrointestinal and other major bleeding from low-dose aspirin has been reported in the literature.1 Major bleeds represent a significant burden to the health care system with an estimated mean $13,093 cost for gastrointestinal bleed hospitalization.7
Considering the large scale aspirin use without appropriate indication within the veteran population, the risk of adverse effects, and the significant cost to patients and the health care system, it is imperative to determine the best approach to efficiently deprescribe aspirin for primary prevention among geriatric patients. Deprescribing refers to the systematic and supervised process of dose reduction or drug discontinuation with the goal of improving health and/or reducing the risk of adverse effects.8 During patient visits, primary care practitioners (PCPs) have opportunities to discontinue aspirin, but these encounters are time-limited and deprescribing might be secondary to more acute primary care needs. The shortage of PCPs is expected to worsen in coming years, which could further reduce their availability to assess inappropriate aspirin use.9
VA clinical pharmacist practitioners (CPPs) serve as medication experts and work autonomously under a broad scope of practice as part of the patient aligned care team.10-12 CPPs can free up time for PCPs and facilitate deprescribing efforts, especially for older adults. One retrospective cohort study conducted at a VA medical center found that CPPs deprescribed more potentially inappropriate medications among individuals aged ≥ 80 years compared with usual care with PCPs (26.8% vs 16.1%; P < .001).12,13 An aspirin deprescribing protocol conducted in 2022 resulted in nearly half of veterans aged ≥ 70 years contacted by phone agreeing to stop aspirin. Although this study supports the role pharmacists can play in reducing aspirin use in accordance with guidelines, the authors acknowledge that their interventions had a mean time of 12 minutes per patient and would require workflow changes.14 The purpose of this study is to evaluate the efficiency of aspirin deprescribing through 2 approaches: direct deprescribing by pharmacists using populationlevel review compared with clinicians following a pharmacist-led education.
Methods
This was a single-center quality improvement cohort study at the Durham VA Health Care System (DVAHCS) in North Carolina. Patients included were aged ≥ 70 years without known ASCVD who received care at any of 3 DVAHCS community-based outpatient clinics and prescribed aspirin. Patient data was obtained using the VIONE (Deprescribing Dashboard called Vital, Important, Optional, Not indicated, and Every medication has a specific indication or diagnosis) dashboard.15 VIONE was developed to identify potentially inappropriate medications (PIMs) that are eligible to deprescribe based on Beers Criteria, Screening Tool of Older Personsf Prescriptions criteria, and common clinical scenarios when clinicians determine the risk outweighs the benefit to continue a specific medication. 16,17 VIONE is used to reduce polypharmacy and improve patient safety, comfort, and medication adherence. Aspirin for patients aged ≥ 70 years without a history of ASCVD is a PIM identified by VIONE. Patients aged ≥ 70 years were chosen as an inclusion criteria in this study to match the ASPREE trial inclusion criteria and age inclusion criteria in the VIONE dashboard for aspirin deprescribing.2 Patient lists were generated for these potentially inappropriate aspirin prescriptions for 3 months before clinician staff education presentations, the day of the presentations, and 3 months after.
The primary endpoint was the number of veterans with aspirin deprescribed directly by 2 pharmacists over 12 weeks, divided by total patient care time spent, compared with the change in number of veterans with aspirin deprescribed by any DVAHCS physician, nurse practitioner, physician assistant, or CPP over 12 weeks, divided by the total pharmacist time spent on PCP education. Secondary endpoints were the number of aspirin orders discontinued by pharmacists and CPPs, the number of aspirin orders discontinued 12 weeks before pharmacist-led education compared with the number of aspirin orders discontinued 12 weeks after CPP-led education, average and median pharmacist time spent per patient encounter, and time of direct patient encounters vs time spent on PCP education.
Pharmacists reviewed each patient who met the inclusion criteria from the list generated by VIONE on December 1, 2022, for aspirin appropriateness according to the ACC/AHA and USPSTF guidelines, with the goal to discontinue aspirin for primary prevention of ASCVD and no other indications.1,4 Pharmacists documented their visits using VIONE methodology in the Computerized Patient Record System (CPRS) using a polypharmacy review note. CPPs contacted patients who were taking aspirin for primary prevention by unscheduled telephone call to assess for aspirin adherence, undocumented history of ASCVD, cardiovascular risk factors, and history of bleeding. Aspirin was discontinued if patients met guideline criteria recommendations and agreed to discontinuation. Risk-benefit discussions were completed when patients without known ASCVD were considered high risk because the ACC/AHA guidelines mention there is insufficient evidence of safety and efficacy of aspirin for primary prevention for patients with other known ASCVD risk factors (eg, strong family history of premature myocardial infarction, inability to achieve lipid, blood pressure, or glucose targets, or significant elevation in coronary artery calcium score).
High risk was defined as family history of premature ASCVD (in a male first-degree relative aged < 55 years or a female first-degree relative aged < 65 years), most recent blood pressure or 2 blood pressure results in the last 12 months > 160/100 mm Hg, recent hemoglobin A1c > 9%, and/or low-density lipoprotein > 190 mg/dL or not prescribed an indicated statin.3 Aspirin was continued or discontinued according to patient preference after the personalized risk-benefit discussion.
For patients with a clinical indication for aspirin use other than ASCVD (eg, atrial fibrillation not on anticoagulation, venous thromboembolism prophylaxis, carotid artery disease), CPPs documented their assessment and when appropriate deferred to the PCP for consideration of stopping aspirin. For patients with undocumented ASCVD, CPPs added their ASCVD history to their problem list and aspirin was continued. PCPs were notified by alert when aspirin was discontinued and when patients could not be reached by telephone.
presented a review of recent guideline updates and supporting literature at 2 online staff meetings. The education sessions lasted about 10 minutes and were presented to PCPs across 3 community-based outpatient clinics. An estimated 40 minutes were spent creating the PowerPoint education materials, seeking feedback, making edits, and answering questions or emails from PCPs after the presentation. During the presentation, pharmacists encouraged PCPs to discontinue aspirin (active VA prescriptions and reported over-the-counter use) for primary prevention of ASCVD in patients aged ≥ 70 years during their upcoming appointments and consider risk factors recommended by the ACC/AHA guidelines when applicable. PCPs were notified that CPPs planned to start a population review for discontinuing active VA aspirin prescriptions on December 1, 2022. The primary endpoint and secondary endpoints were analyzed using descriptive statistics. All data were analyzed using Microsoft Excel.
Results
A total of 868 patients aged ≥ 70 years with active prescriptions for aspirin were identified on December 1, 2022. After applying inclusion and exclusion criteria for the pharmacist population review, 224 patients were included for cohort final analysis (Figure). All 868 patients were eligible for the CPP intervention. Primary reasons for exclusion from the CPP population included over-thecounter aspirin and a history of ASCVD in the patient’s problem list. All patients were male, with a mean (SD) age of 75 (4.4) years (Table 1). Most patients were prescribed aspirin, 81 mg daily (n = 220; 98%).
The direct CPP deprescribing intervention resulted in 2 aspirin prescriptions discontinued per hour of pharmacist time and 67 aspirin prescriptions discontinued per hour of pharmacist time via the PCP education intervention. CPPs discontinued 66 aspirin orders in the 12 weeks before the PCP education sessions. A total of 230 aspirin prescriptions were discontinued in the 12 weeks following the PCP education sessions, with 97 discontinued directly by CPPs and 133 discontinued by PCPs. The PCP education session yielded an additional 67 discontinued aspirin orders compared with the 12 weeks before the education sessions (Table 2).
The CPP direct deprescribing intervention took about 48.3 hours, accounting for health record review and time interacting with patients. The PCP education intervention took about 60 minutes, which included time for preparing and delivering education materials (Table 3). CPP deprescribing encounter types, interventions, and related subcategories, and other identified indications to continue aspirin are listed in Table 4.
Discussion
Compared with direct deprescribing by pharmacists, the PCP education intervention was more efficient based on number of aspirin orders discontinued by pharmacist time. PCPs discontinued twice as many aspirin prescriptions in the 12 weeks after pharmacist-led education compared with the 12 weeks before.
Patients were primarily contacted by telephone (73%) for deprescribing. Among the 163 patients reached by phone and encouraged to discontinue aspirin, 97 patients (60%) accepted the recommendation, which was similar to the acceptance rates found in the literature (48% to 55%).14,18 Although many veterans continued taking aspirin (78%), most had indications for its continued use, such as a history of ASCVD, atrial fibrillation without anticoagulation, and carotid artery stenosis, and complex comorbidities that required further discussion with their PCP. Less common uses for aspirin were identified through CPRS review or patient reports included cerebral small vessel disease without history of ASCVD, subclavian artery stenosis, thrombocytosis, bioprosthetic valve replacement, giant cell arteritis, rheumatoid arthritis, and prevention of second eye involvement of ischemic optic neuropathy.
to describe the benefit of clinical pharmacy services for deprescribing aspirin for primary prevention of ASCVD through PCP education. Previously published literature has assessed alternative ways to identify or discontinue PIMs—including aspirin—among geriatric patients. One study evaluated the use of marking inappropriate aspirin prescriptions in the electronic health database, leading to a significant reduction in incidence of inappropriate aspirin prescribing; however, it did not assess changes in discontinuation rates of existing aspirin prescriptions.19 The previous VA pharmacist aspirin deprescribing protocol demonstrated pharmacists’ aptitude at discontinuing aspirin for primary prevention but only used direct patient contact and did not compare efficiency with other methods, including PCP education.14
This quality improvement project contributes new data to the existing literature to support the use of clinical pharmacists to discontinue aspirin for primary prevention and suggests a strong role for pharmacists as educators on clinical guidelines, in addition to their roles directly deprescribing PIMs in clinical practice. This study is further strengthened by its use of VIONE, which previously has demonstrated effectiveness in deprescribing a variety of PIMs in primary care settings.20
Despite using VIONE for generating a list of patients eligible for deprescription, our CPRS review found that this list was frequently inaccurate. For example, a small portion of patients were on the VIONE generated list indicating they had no ASCVD history, but had transient ischemic attack listed in their problem lists. Patient problem lists often were missing documented ASCVD history that was revealed by patient interview or CPRS review. It is possible that patients interviewed might have omitted relevant ASCVD history because of low health literacy, conditions affecting memory, or use of health care services outside the VA system.
There were several instances of aspirin used for other non-ASCVD indications, such as primary stroke prevention in atrial fibrillation. The ACC/AHA atrial fibrillation guidelines previously provided a Class IIb recommendation (benefit is greater than risk but additional studies are needed) for considering no antithrombic therapy or treatment with oral anticoagulant or aspirin for nonvalvular atrial fibrillation with CHA2DS2-VASc (Congestive heart failure, Hypertension, Age [> 65 y, 1 point; > 75 y, 2 points], Diabetes, previous Stroke/transient ischemic attack [2 points]) score of 1.21 The ACC/ AHA guidelines were updated in 2023 to recommend against antiplatelet therapy as an alternative to anticoagulation for reducing cardioembolic stroke risk among patients with atrial fibrillation with no indication for antiplatelet therapy because of risk of harm.22 If a patient has no risk factors for stroke, aspirin is not recommended to prevent thromboembolic events because of a lack of benefit. Interventions from this quality improvement study were completed before the 2023 atrial fibrillation guideline was published and therefore in this study aspirin was not discontinued when used for atrial fibrillation. Aspirin use for atrial fibrillation might benefit from similar discontinuation efforts analyzed within this study. Beyond atrial fibrillation, major guidelines do not comment on the use of aspirin for any other indications in the absence of clinical ASCVD.
Limitations
This study is limited by the lack of clinical consensus for complex patients and demonstrates the importance of individualized patient assessment when considering discontinuing aspirin. Because of the project’s relatively short intervention period, aspirin deprescribing rates could decrease over time and repeated education efforts might be necessary to see lasting impact. Health care professionals from services outside of primary care also might have discontinued aspirin during the study period unrelated to the education and these discontinued aspirin prescriptions could contribute to the higher rate observed among PCPs. This study included a specific population cohort of male, US veterans and might not reflect other populations where these interventions could be implemented.
The measurement of time spent by pharmacists and PCPs is an additional limitation. Although it is expected that PCPs attempt to discontinue aspirin during their existing patient care appointments, the time spent during visits was not measured or documented. Direct deprescribing by pharmacist CPRS review required a significant amount of time and could be a barrier to successful intervention by CPPs in patient aligned care teams.
To reduce the time pharmacists spent completing CPRS reviews, an aspirin deprescribing clinical reminder tool could be used to assess use and appropriate indication quickly during any primary care visit led by a PCP or CPP. In addition, it is recommended that pharmacists regularly educate health care professionals on guideline recommendations for aspirin use among geriatric patients. Future studies of the incidence of major cardiovascular events after aspirin deprescribing among geriatric patients and a longitudinal cost/benefit analysis could support these initiatives.
Conclusions
In this study, pharmacists successfully deprescribed inappropriate medications, such as aspirin. However, pharmacist-led PCP education is more efficient compared with direct deprescribing using a population-level review. PCP education requires less time and could allow ambulatory care pharmacists to spend more time on other direct patient care interventions to improve quality and access to care in primary care clinics. This study’s results further support the role of pharmacists in deprescribing PIMs for older adults and the use of a deprescribing tool, such as VIONE, in a primary care setting.
- US Preventive Services Task Force; Davidson KW, Barry MJ, et al. Aspirin use to prevent cardiovascular disease: US Preventive Services Task Force recommendation statement. JAMA. 2022;327(16):1577-1584. doi:10.1001/jama.2022.4983
- McNeil JJ, Nelson MR, Woods RL, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519-1528. doi:10.1056/NEJMoa1803955
- Barry MJ, Wolff TA, Pbert L, et al. Putting evidence into practice: an update on the US Preventive Services Task Force methods for developing recommendations for preventive services. Ann Fam Med. 2023;21(2):165-171. doi:10.1370/afm.2946
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/ AHA Guideline on the Primary Prevention of Cardiovascular Disease: A report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi:10.1161/CIR.0000000000000678
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: Standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S179-S218. doi:10.2337/dc24-S010
- Ong SY, Chui P, Bhargava A, Justice A, Hauser RG. Estimating aspirin overuse for primary prevention of atherosclerotic cardiovascular disease (from a nationwide healthcare system). Am J Cardiol. 2020;137:25-30. doi:10.1016/j.amjcard.2020.09.042
- Weiss AJ, Jiang HJ. Overview of clinical conditions with frequent and costly hospital readmissions by payer, 2018. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); July 20, 2021.
- Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol. 2019;73(20):2584-2595. doi:10.1016/j.jacc.2019.03.467
- Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2019 to 2034. Accessed March 17, 2024. https://www.aamc.org/media/54681/download
- US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1108.07(1): General pharmacy service requirements. November 28, 2022. Accessed March 17, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=10045
- US Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1108.11(3): Clinical pharmacy services. July 1, 2015. Accessed March 17, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3120
- US Department of Veterans Affairs. Clinical pharmacist practitioner (CPP) to improve access to and quality of care August 2021. August 2021. Accessed May 19, 2023. https://www.pbm.va.gov/PBM/CPPO/Documents/ExternalFactSheet_OptimizingtheCPPToImproveAccess_508.pdf
- Ammerman CA, Simpkins BA, Warman N, Downs TN. Potentially inappropriate medications in older adults: Deprescribing with a clinical pharmacist. J Am Geriatr Soc. 2019;67(1):115-118. doi:10.1111/jgs.15623
- Rothbauer K, Siodlak M, Dreischmeier E, Ranola TS, Welch L. Evaluation of a pharmacist-driven ambulatory aspirin deprescribing protocol. Fed Pract. 2022;39(suppl 5):S37- S41a. doi:10.12788/fp.0294
- US Department of Veterans Affairs. VIONE changes the way VA handles prescriptions. January 25, 2020. Accessed May 21, 2023. https://news.va.gov/70709/vione-changes-way-va-handles-prescriptions/
- 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052- 2081. doi:10.1111/jgs.18372
- O’Mahony D, Cherubini A, Guiteras AR, et al. STOPP/ START criteria for potentially inappropriate prescribing in older people: version 3. Eur Geriatr Med. 2023;14(4):625- 632. doi:10.1007/s41999-023-00777-y
- Draeger C, Lodhi F, Geissinger N, Larson T, Griesbach S. Interdisciplinary deprescribing of aspirin through prescriber education and provision of patient-specific recommendations. WMJ. 2022;121(3):220-225
- de Lusignan S, Hinton W, Seidu S, et al. Dashboards to reduce inappropriate prescribing of metformin and aspirin: A quality assurance programme in a primary care sentinel network. Prim Care Diabetes. 2021;15(6):1075-1079. doi:10.1016/j.pcd.2021.06.003
- Nelson MW, Downs TN, Puglisi GM, Simpkins BA, Collier AS. Use of a deprescribing tool in an interdisciplinary primary-care patient-aligned care team. Sr Care Pharm. 2022;37(1):34-43. doi:10.4140/TCP.n.2022.34
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199-e267. doi:10.1161/CIR.0000000000000041
- Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/ AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines Circulation. 2024;149(1):e1- e156. doi:10.1161/CIR.0000000000001193
- US Preventive Services Task Force; Davidson KW, Barry MJ, et al. Aspirin use to prevent cardiovascular disease: US Preventive Services Task Force recommendation statement. JAMA. 2022;327(16):1577-1584. doi:10.1001/jama.2022.4983
- McNeil JJ, Nelson MR, Woods RL, et al. Effect of aspirin on all-cause mortality in the healthy elderly. N Engl J Med. 2018;379(16):1519-1528. doi:10.1056/NEJMoa1803955
- Barry MJ, Wolff TA, Pbert L, et al. Putting evidence into practice: an update on the US Preventive Services Task Force methods for developing recommendations for preventive services. Ann Fam Med. 2023;21(2):165-171. doi:10.1370/afm.2946
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/ AHA Guideline on the Primary Prevention of Cardiovascular Disease: A report of the American College of Cardiology/ American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi:10.1161/CIR.0000000000000678
- American Diabetes Association Professional Practice Committee. 10. Cardiovascular disease and risk management: Standards of care in diabetes-2024. Diabetes Care. 2024;47(Suppl 1):S179-S218. doi:10.2337/dc24-S010
- Ong SY, Chui P, Bhargava A, Justice A, Hauser RG. Estimating aspirin overuse for primary prevention of atherosclerotic cardiovascular disease (from a nationwide healthcare system). Am J Cardiol. 2020;137:25-30. doi:10.1016/j.amjcard.2020.09.042
- Weiss AJ, Jiang HJ. Overview of clinical conditions with frequent and costly hospital readmissions by payer, 2018. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); July 20, 2021.
- Krishnaswami A, Steinman MA, Goyal P, et al. Deprescribing in older adults with cardiovascular disease. J Am Coll Cardiol. 2019;73(20):2584-2595. doi:10.1016/j.jacc.2019.03.467
- Association of American Medical Colleges. The complexities of physician supply and demand: projections from 2019 to 2034. Accessed March 17, 2024. https://www.aamc.org/media/54681/download
- US Department of Veterans Affairs, Veterans Health Administration. VHA Directive 1108.07(1): General pharmacy service requirements. November 28, 2022. Accessed March 17, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=10045
- US Department of Veterans Affairs, Veterans Health Administration. VHA Handbook 1108.11(3): Clinical pharmacy services. July 1, 2015. Accessed March 17, 2024. https://www.va.gov/vhapublications/ViewPublication.asp?pub_ID=3120
- US Department of Veterans Affairs. Clinical pharmacist practitioner (CPP) to improve access to and quality of care August 2021. August 2021. Accessed May 19, 2023. https://www.pbm.va.gov/PBM/CPPO/Documents/ExternalFactSheet_OptimizingtheCPPToImproveAccess_508.pdf
- Ammerman CA, Simpkins BA, Warman N, Downs TN. Potentially inappropriate medications in older adults: Deprescribing with a clinical pharmacist. J Am Geriatr Soc. 2019;67(1):115-118. doi:10.1111/jgs.15623
- Rothbauer K, Siodlak M, Dreischmeier E, Ranola TS, Welch L. Evaluation of a pharmacist-driven ambulatory aspirin deprescribing protocol. Fed Pract. 2022;39(suppl 5):S37- S41a. doi:10.12788/fp.0294
- US Department of Veterans Affairs. VIONE changes the way VA handles prescriptions. January 25, 2020. Accessed May 21, 2023. https://news.va.gov/70709/vione-changes-way-va-handles-prescriptions/
- 2023 American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2023;71(7):2052- 2081. doi:10.1111/jgs.18372
- O’Mahony D, Cherubini A, Guiteras AR, et al. STOPP/ START criteria for potentially inappropriate prescribing in older people: version 3. Eur Geriatr Med. 2023;14(4):625- 632. doi:10.1007/s41999-023-00777-y
- Draeger C, Lodhi F, Geissinger N, Larson T, Griesbach S. Interdisciplinary deprescribing of aspirin through prescriber education and provision of patient-specific recommendations. WMJ. 2022;121(3):220-225
- de Lusignan S, Hinton W, Seidu S, et al. Dashboards to reduce inappropriate prescribing of metformin and aspirin: A quality assurance programme in a primary care sentinel network. Prim Care Diabetes. 2021;15(6):1075-1079. doi:10.1016/j.pcd.2021.06.003
- Nelson MW, Downs TN, Puglisi GM, Simpkins BA, Collier AS. Use of a deprescribing tool in an interdisciplinary primary-care patient-aligned care team. Sr Care Pharm. 2022;37(1):34-43. doi:10.4140/TCP.n.2022.34
- January CT, Wann LS, Alpert JS, et al. 2014 AHA/ ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014;130(23):e199-e267. doi:10.1161/CIR.0000000000000041
- Joglar JA, Chung MK, Armbruster AL, et al. 2023 ACC/ AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines Circulation. 2024;149(1):e1- e156. doi:10.1161/CIR.0000000000001193
Pharmacist-Led Deprescribing of Aspirin for Primary Prevention of Cardiovascular Disease Among Geriatric Veterans
Pharmacist-Led Deprescribing of Aspirin for Primary Prevention of Cardiovascular Disease Among Geriatric Veterans
Loneliness, Isolation Affect One Third of US Adults Over 50
TOPLINE:
About one third of US adults aged 50-80 years report feeling lonely and socially isolated, a new study of data from 2018-2024 shows. While the levels have returned to the prepandemic range, investigators say the findings suggest clinicians should screen for loneliness and isolation.
METHODOLOGY:
- Researchers conducted a nationally representative survey of US adults aged 50-80 years through the University of Michigan National Poll on Healthy Aging at six timepoints between 2018 and 2024.
- Data collection involved online surveys conducted using the Ipsos KnowledgePanel from 2018 to 2021, transitioning to online and phone surveys conducted using the National Opinion Research Center AmeriSpeak panel from 2022 to 2024.
- Sample sizes ranged between 2051 and 2576 respondents, with completion rates ranging from 61% to 78% across the survey periods.
TAKEAWAY:
- Loneliness rates among adults aged 50-80 years showed notable fluctuation, starting at 34% (95% CI, 31.7%-36.2%) in 2018, rising to 41% (95% CI, 39.1%-43.7%) in 2020, and returning to 33% (95% CI, 31.7%-35.1%) by 2024.
- Social isolation showed a similar pattern in the study group, starting at 27% (95% CI, 24.5%-28.8%) in 2018, peaking at 56% (95% CI, 53.4%-58.1%) in 2020, and declining to 29% (95% CI, 27.5%-30.9%) by 2024.
- Higher loneliness and social isolation rates were frequently reported among individuals who did not work, lived alone, had lower household incomes, and had self-reported fair and poor physical and mental health than those who reported excellent, very good, or good health.
IN PRACTICE:
The findings suggest that “much like routinely asking about diet and exercise, clinicians should consider screening older adults for loneliness and social isolation and connect them with appropriate resources,” the investigators wrote.
SOURCE:
The study was led by Preeti N. Malani, MD, MSJ, University of Michigan Medical School, Ann Arbor. It was published online on December 9 in JAMA.
LIMITATIONS:
The study was limited by possible recall bias, reliance on self-reported data, lack of longitudinal results, and differences in survey timing, panels, and question framing across years. The findings may not have been applicable to excluded groups such as nursing home residents or individuals aged > 80 years, which limited their generalizability.
DISCLOSURES:
The study was supported by AARP and Michigan Medicine and the Department of Veterans Affairs, Veterans Health Administration, and Health Systems Research. One author reported receiving consulting fees and honoraria from various organizations. Details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
About one third of US adults aged 50-80 years report feeling lonely and socially isolated, a new study of data from 2018-2024 shows. While the levels have returned to the prepandemic range, investigators say the findings suggest clinicians should screen for loneliness and isolation.
METHODOLOGY:
- Researchers conducted a nationally representative survey of US adults aged 50-80 years through the University of Michigan National Poll on Healthy Aging at six timepoints between 2018 and 2024.
- Data collection involved online surveys conducted using the Ipsos KnowledgePanel from 2018 to 2021, transitioning to online and phone surveys conducted using the National Opinion Research Center AmeriSpeak panel from 2022 to 2024.
- Sample sizes ranged between 2051 and 2576 respondents, with completion rates ranging from 61% to 78% across the survey periods.
TAKEAWAY:
- Loneliness rates among adults aged 50-80 years showed notable fluctuation, starting at 34% (95% CI, 31.7%-36.2%) in 2018, rising to 41% (95% CI, 39.1%-43.7%) in 2020, and returning to 33% (95% CI, 31.7%-35.1%) by 2024.
- Social isolation showed a similar pattern in the study group, starting at 27% (95% CI, 24.5%-28.8%) in 2018, peaking at 56% (95% CI, 53.4%-58.1%) in 2020, and declining to 29% (95% CI, 27.5%-30.9%) by 2024.
- Higher loneliness and social isolation rates were frequently reported among individuals who did not work, lived alone, had lower household incomes, and had self-reported fair and poor physical and mental health than those who reported excellent, very good, or good health.
IN PRACTICE:
The findings suggest that “much like routinely asking about diet and exercise, clinicians should consider screening older adults for loneliness and social isolation and connect them with appropriate resources,” the investigators wrote.
SOURCE:
The study was led by Preeti N. Malani, MD, MSJ, University of Michigan Medical School, Ann Arbor. It was published online on December 9 in JAMA.
LIMITATIONS:
The study was limited by possible recall bias, reliance on self-reported data, lack of longitudinal results, and differences in survey timing, panels, and question framing across years. The findings may not have been applicable to excluded groups such as nursing home residents or individuals aged > 80 years, which limited their generalizability.
DISCLOSURES:
The study was supported by AARP and Michigan Medicine and the Department of Veterans Affairs, Veterans Health Administration, and Health Systems Research. One author reported receiving consulting fees and honoraria from various organizations. Details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
About one third of US adults aged 50-80 years report feeling lonely and socially isolated, a new study of data from 2018-2024 shows. While the levels have returned to the prepandemic range, investigators say the findings suggest clinicians should screen for loneliness and isolation.
METHODOLOGY:
- Researchers conducted a nationally representative survey of US adults aged 50-80 years through the University of Michigan National Poll on Healthy Aging at six timepoints between 2018 and 2024.
- Data collection involved online surveys conducted using the Ipsos KnowledgePanel from 2018 to 2021, transitioning to online and phone surveys conducted using the National Opinion Research Center AmeriSpeak panel from 2022 to 2024.
- Sample sizes ranged between 2051 and 2576 respondents, with completion rates ranging from 61% to 78% across the survey periods.
TAKEAWAY:
- Loneliness rates among adults aged 50-80 years showed notable fluctuation, starting at 34% (95% CI, 31.7%-36.2%) in 2018, rising to 41% (95% CI, 39.1%-43.7%) in 2020, and returning to 33% (95% CI, 31.7%-35.1%) by 2024.
- Social isolation showed a similar pattern in the study group, starting at 27% (95% CI, 24.5%-28.8%) in 2018, peaking at 56% (95% CI, 53.4%-58.1%) in 2020, and declining to 29% (95% CI, 27.5%-30.9%) by 2024.
- Higher loneliness and social isolation rates were frequently reported among individuals who did not work, lived alone, had lower household incomes, and had self-reported fair and poor physical and mental health than those who reported excellent, very good, or good health.
IN PRACTICE:
The findings suggest that “much like routinely asking about diet and exercise, clinicians should consider screening older adults for loneliness and social isolation and connect them with appropriate resources,” the investigators wrote.
SOURCE:
The study was led by Preeti N. Malani, MD, MSJ, University of Michigan Medical School, Ann Arbor. It was published online on December 9 in JAMA.
LIMITATIONS:
The study was limited by possible recall bias, reliance on self-reported data, lack of longitudinal results, and differences in survey timing, panels, and question framing across years. The findings may not have been applicable to excluded groups such as nursing home residents or individuals aged > 80 years, which limited their generalizability.
DISCLOSURES:
The study was supported by AARP and Michigan Medicine and the Department of Veterans Affairs, Veterans Health Administration, and Health Systems Research. One author reported receiving consulting fees and honoraria from various organizations. Details are provided in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Major Depression in Older Adults Tied to Risky Driving Behaviors
Older adults with major depressive disorder (MDD) exhibit riskier driving behaviors, compared with their nondepressed peers, including hard braking, cornering, and unpredictable driving patterns, new research showed.
Data for the study came from commercial vehicle data trackers installed in participants’ vehicles. After about a year of follow-up, the investigators found that MDD was associated with an increase in the amount and severity of risking driving, even after they controlled for antidepressant use.
Late-life depression often goes undiagnosed, and the new findings highlight the importance of routine depression screening and targeted interventions to ensure driving safety among older adults, the study team said.
“By using longitudinal, real-world driving data rather than controlled settings or self-reports, the study provides robust evidence of how MDD influences driving behaviors in day-to-day contexts,” first author Ganesh M. Babulal, PhD, OTD, with the Department of Neurology, Washington University School of Medicine in St Louis, Missouri, said in an interview.
“By analyzing the influence of antidepressant use and overall medication load, the study disentangles the effects of MDD from those of driver-impairing medications, further clarifying the unique contributions of depression to driving behaviors,” Babulal noted.
The study was published online in JAMA Network Open.
Road Risks
As the number of older adults grows, safe driving practices in this age group become increasingly crucial. By 2050, one quarter of drivers in the United States will be older than 65 years. MDD affects about 8% of US adults and is linked to cognitive impairments that may compromise driving safety.
Prior studies revealed a link between depression and increased car crash risk, regardless of age. And earlier research by Babulal and colleagues showed that older adults with depression were three times more likely to receive a marginal or failing score on a standardized road test.
To further study the issue, Babulal and colleagues examined the impact of MDD on naturalistic driving behaviors among older adults using longitudinal data.
Participants were recruited from the Driving Real-World In-Vehicle Evaluation System Project, where their daily driving behaviors were recorded using commercial vehicle data loggers installed in their personal vehicles.
The cohort included 85 adults with MDD (mean age, 69 years; 71% women) and 310 adults without MDD (mean age, 70 years; 49% women). The majority of participants in both groups were non-Hispanic White individuals.
Based on intercepts, adults with MDD had a propensity toward riskier driving habits with a higher frequency of speeding events and spending more time on the road than those without MDD, they found.
During a mean of 1.1 years of follow-up, compared with older adults without MDD, those with MDD exhibited significantly more hard braking (P < .001) and hard cornering events per trip (P = .04) over time. They also traveled farther from home and visited more unique destinations (P < .001 for both).
Over time, older adults also displayed increased entropy in driving patterns (P < .001), indicated less predictable driving routes.
“Driving unpredictability, as evidenced by increased random entropy, highlights the unique challenges posed by MDD in maintaining safe driving practices,” the researchers wrote.
Adjustment for antidepressant use, which could impair driving, or total medication burden did not change the findings, suggesting MDD independently affects driving.
“Most importantly, our findings demonstrate that MDD — a common and treatable illness in older adults — was associated with an increase in both the amount and magnitude of risky driving behaviors over time,” the researchers wrote.
The researchers noted that the study did not account for changes in depression severity over time and other psychiatric conditions co-occurring with MDD were not adjusted for. Also, situational factors like weather or traffic conditions were not assessed.
Clear Clinical Implications
There is a “pressing need” for targeted interventions to manage and mitigate the driving risks associated with late-life depression, the researchers wrote.
“The study emphasizes the need for interventions tailored to the mental health and driving behaviors of older adults. These could include cognitive retraining, driver rehabilitation programs, and routine depression screening to enhance road safety and preserve independence,” Babulal said.
“Encouraging older adults with MDD to self-regulate their driving habits (eg, avoiding night driving or high-traffic situations) and educating them about potential driving challenges related to their condition can enhance safety,” he added.
Commenting on this study, Ipsit Vahia, MD, McLean Hospital, Belmont, Massachusetts, and Harvard Medical School, Boston, Massachusetts, said it “adds nuance to our understanding of how depression can impact driving among older adults.
“While the connection between depression and a higher incident of crashes is known, this study demonstrates an association with riskier driving behaviors such as speeding,” Vahia said. “It highlights the importance of clinicians proactively initiating discussion of driving and safety when working with older adults with depressive symptoms.”
This work was funded by grants from the National Institutes of Health and National Institute on Aging. Babulal had no relevant disclosures. Vahia had served as a consultant for Otsuka.
A version of this article appeared on Medscape.com.
Older adults with major depressive disorder (MDD) exhibit riskier driving behaviors, compared with their nondepressed peers, including hard braking, cornering, and unpredictable driving patterns, new research showed.
Data for the study came from commercial vehicle data trackers installed in participants’ vehicles. After about a year of follow-up, the investigators found that MDD was associated with an increase in the amount and severity of risking driving, even after they controlled for antidepressant use.
Late-life depression often goes undiagnosed, and the new findings highlight the importance of routine depression screening and targeted interventions to ensure driving safety among older adults, the study team said.
“By using longitudinal, real-world driving data rather than controlled settings or self-reports, the study provides robust evidence of how MDD influences driving behaviors in day-to-day contexts,” first author Ganesh M. Babulal, PhD, OTD, with the Department of Neurology, Washington University School of Medicine in St Louis, Missouri, said in an interview.
“By analyzing the influence of antidepressant use and overall medication load, the study disentangles the effects of MDD from those of driver-impairing medications, further clarifying the unique contributions of depression to driving behaviors,” Babulal noted.
The study was published online in JAMA Network Open.
Road Risks
As the number of older adults grows, safe driving practices in this age group become increasingly crucial. By 2050, one quarter of drivers in the United States will be older than 65 years. MDD affects about 8% of US adults and is linked to cognitive impairments that may compromise driving safety.
Prior studies revealed a link between depression and increased car crash risk, regardless of age. And earlier research by Babulal and colleagues showed that older adults with depression were three times more likely to receive a marginal or failing score on a standardized road test.
To further study the issue, Babulal and colleagues examined the impact of MDD on naturalistic driving behaviors among older adults using longitudinal data.
Participants were recruited from the Driving Real-World In-Vehicle Evaluation System Project, where their daily driving behaviors were recorded using commercial vehicle data loggers installed in their personal vehicles.
The cohort included 85 adults with MDD (mean age, 69 years; 71% women) and 310 adults without MDD (mean age, 70 years; 49% women). The majority of participants in both groups were non-Hispanic White individuals.
Based on intercepts, adults with MDD had a propensity toward riskier driving habits with a higher frequency of speeding events and spending more time on the road than those without MDD, they found.
During a mean of 1.1 years of follow-up, compared with older adults without MDD, those with MDD exhibited significantly more hard braking (P < .001) and hard cornering events per trip (P = .04) over time. They also traveled farther from home and visited more unique destinations (P < .001 for both).
Over time, older adults also displayed increased entropy in driving patterns (P < .001), indicated less predictable driving routes.
“Driving unpredictability, as evidenced by increased random entropy, highlights the unique challenges posed by MDD in maintaining safe driving practices,” the researchers wrote.
Adjustment for antidepressant use, which could impair driving, or total medication burden did not change the findings, suggesting MDD independently affects driving.
“Most importantly, our findings demonstrate that MDD — a common and treatable illness in older adults — was associated with an increase in both the amount and magnitude of risky driving behaviors over time,” the researchers wrote.
The researchers noted that the study did not account for changes in depression severity over time and other psychiatric conditions co-occurring with MDD were not adjusted for. Also, situational factors like weather or traffic conditions were not assessed.
Clear Clinical Implications
There is a “pressing need” for targeted interventions to manage and mitigate the driving risks associated with late-life depression, the researchers wrote.
“The study emphasizes the need for interventions tailored to the mental health and driving behaviors of older adults. These could include cognitive retraining, driver rehabilitation programs, and routine depression screening to enhance road safety and preserve independence,” Babulal said.
“Encouraging older adults with MDD to self-regulate their driving habits (eg, avoiding night driving or high-traffic situations) and educating them about potential driving challenges related to their condition can enhance safety,” he added.
Commenting on this study, Ipsit Vahia, MD, McLean Hospital, Belmont, Massachusetts, and Harvard Medical School, Boston, Massachusetts, said it “adds nuance to our understanding of how depression can impact driving among older adults.
“While the connection between depression and a higher incident of crashes is known, this study demonstrates an association with riskier driving behaviors such as speeding,” Vahia said. “It highlights the importance of clinicians proactively initiating discussion of driving and safety when working with older adults with depressive symptoms.”
This work was funded by grants from the National Institutes of Health and National Institute on Aging. Babulal had no relevant disclosures. Vahia had served as a consultant for Otsuka.
A version of this article appeared on Medscape.com.
Older adults with major depressive disorder (MDD) exhibit riskier driving behaviors, compared with their nondepressed peers, including hard braking, cornering, and unpredictable driving patterns, new research showed.
Data for the study came from commercial vehicle data trackers installed in participants’ vehicles. After about a year of follow-up, the investigators found that MDD was associated with an increase in the amount and severity of risking driving, even after they controlled for antidepressant use.
Late-life depression often goes undiagnosed, and the new findings highlight the importance of routine depression screening and targeted interventions to ensure driving safety among older adults, the study team said.
“By using longitudinal, real-world driving data rather than controlled settings or self-reports, the study provides robust evidence of how MDD influences driving behaviors in day-to-day contexts,” first author Ganesh M. Babulal, PhD, OTD, with the Department of Neurology, Washington University School of Medicine in St Louis, Missouri, said in an interview.
“By analyzing the influence of antidepressant use and overall medication load, the study disentangles the effects of MDD from those of driver-impairing medications, further clarifying the unique contributions of depression to driving behaviors,” Babulal noted.
The study was published online in JAMA Network Open.
Road Risks
As the number of older adults grows, safe driving practices in this age group become increasingly crucial. By 2050, one quarter of drivers in the United States will be older than 65 years. MDD affects about 8% of US adults and is linked to cognitive impairments that may compromise driving safety.
Prior studies revealed a link between depression and increased car crash risk, regardless of age. And earlier research by Babulal and colleagues showed that older adults with depression were three times more likely to receive a marginal or failing score on a standardized road test.
To further study the issue, Babulal and colleagues examined the impact of MDD on naturalistic driving behaviors among older adults using longitudinal data.
Participants were recruited from the Driving Real-World In-Vehicle Evaluation System Project, where their daily driving behaviors were recorded using commercial vehicle data loggers installed in their personal vehicles.
The cohort included 85 adults with MDD (mean age, 69 years; 71% women) and 310 adults without MDD (mean age, 70 years; 49% women). The majority of participants in both groups were non-Hispanic White individuals.
Based on intercepts, adults with MDD had a propensity toward riskier driving habits with a higher frequency of speeding events and spending more time on the road than those without MDD, they found.
During a mean of 1.1 years of follow-up, compared with older adults without MDD, those with MDD exhibited significantly more hard braking (P < .001) and hard cornering events per trip (P = .04) over time. They also traveled farther from home and visited more unique destinations (P < .001 for both).
Over time, older adults also displayed increased entropy in driving patterns (P < .001), indicated less predictable driving routes.
“Driving unpredictability, as evidenced by increased random entropy, highlights the unique challenges posed by MDD in maintaining safe driving practices,” the researchers wrote.
Adjustment for antidepressant use, which could impair driving, or total medication burden did not change the findings, suggesting MDD independently affects driving.
“Most importantly, our findings demonstrate that MDD — a common and treatable illness in older adults — was associated with an increase in both the amount and magnitude of risky driving behaviors over time,” the researchers wrote.
The researchers noted that the study did not account for changes in depression severity over time and other psychiatric conditions co-occurring with MDD were not adjusted for. Also, situational factors like weather or traffic conditions were not assessed.
Clear Clinical Implications
There is a “pressing need” for targeted interventions to manage and mitigate the driving risks associated with late-life depression, the researchers wrote.
“The study emphasizes the need for interventions tailored to the mental health and driving behaviors of older adults. These could include cognitive retraining, driver rehabilitation programs, and routine depression screening to enhance road safety and preserve independence,” Babulal said.
“Encouraging older adults with MDD to self-regulate their driving habits (eg, avoiding night driving or high-traffic situations) and educating them about potential driving challenges related to their condition can enhance safety,” he added.
Commenting on this study, Ipsit Vahia, MD, McLean Hospital, Belmont, Massachusetts, and Harvard Medical School, Boston, Massachusetts, said it “adds nuance to our understanding of how depression can impact driving among older adults.
“While the connection between depression and a higher incident of crashes is known, this study demonstrates an association with riskier driving behaviors such as speeding,” Vahia said. “It highlights the importance of clinicians proactively initiating discussion of driving and safety when working with older adults with depressive symptoms.”
This work was funded by grants from the National Institutes of Health and National Institute on Aging. Babulal had no relevant disclosures. Vahia had served as a consultant for Otsuka.
A version of this article appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Geriatric Dermatology: Q&A With Daniel C. Butler, MD
Daniel C. Butler, MD, is associate professor of dermatology and director of the new Inflammatory and Aging Skin Research Program in the Division of Dermatology at the University of Arizona College of Medicine, Tucson, Arizona. Before returning to Arizona, where he had attended medical school, Butler practiced and was a researcher at the University of California, San Francisco, and its geriatric dermatology clinic. He is a co-founder and continues to co-lead the American Academy of Dermatology (AAD) Geriatric Dermatology Expert Resource Group (ERG).
Butler’s interest in geriatric dermatology is rooted in his experience growing up with four grandparents and witnessing their wisdom, relationships, moments with loved ones, and other unique and desirable parts of growing old. “When I looked later at how aging was perceived in dermatology, I found it was a lot about ‘antiaging,’” he told this news organization. “I thought there was a needed voice in dermatology for healthy aging, for all the desirable things that only growing old can provide, along with all the incredible ‘antiaging’ things we can do.”
In interviews, Butler spoke about research priorities in geriatric dermatology, how the “4M” model of geriatrics should be applied within dermatology, how dermatologists can best work with older complex patients, and more. The conversation was edited for clarity and length.
What is geriatric dermatology? It is described by the AAD’s Geriatric Dermatology ERG as “an emerging subspecialty.” Yet it’s also viewed more broadly. Please speak about its various identities and meanings and its importance for dermatology.
If you’re a Mohs surgeon, you’re seeing a strong majority of over 65 patients. And in various specialty clinics, such as inflammatory skin disease, geriatric dermatology pertains to you. In many ways, it can be viewed as a mindset.
From a framework standpoint, and as a field, geriatric dermatology is a basic science initiative, a clinical initiative, an educational initiative, and an advocacy initiative. The goal is to be able to influence, grow, and learn in each of these categories for our older patients. This is happening: Research in this field has progressed, and education has progressed, which has driven some progress in clinical care.
How has research progressed in the basic science of aging skin? What are key questions for dermatology?
There has been a lot of basic science research on aging skin and on how an aging immune system, for instance, is reflected in conditions such as bullous pemphigoid, atopic dermatitis (AD), and chronic itch. But aging involves more than immunosenescence. I think of aging skin as a three-headed monster that involves changes in the skin barrier and the microbiome as well. But is there a primary piece of aging in the skin? What comes first or influences the other? More research on these questions can potentially influence our treatments.
With respect to the immune system, what we’re finding in the skin is that age-related change is not a decline in the immune system per se, but rather aberrance in response. Parts of the system tend to become overactive, with a skew toward overexpression of type 2 inflammation. This can be problematic, driving conditions such as chronic itch.
With respect to the skin barrier, we lose essential fatty acids, and we lose a lot of our recovery ability and our ability to respond quickly to environmental stressors. But are barrier changes triggering the immune system? Or is it the other way around?
The microbiome, which is a big focus of research, involves similar chicken-and-egg discussions. Is it the microbiome that changes and alters the barrier, which then entices the immune system? Which one happens first? We have a lot to learn, and there’s probably not one answer for every patient.
Please speak about research more broadly. What questions and issues need to be answered and addressed to improve the dermatologic care of older adults?
In general, research in dermatology is very disease-specific and not particularly conducive to looking at the larger demographic populations. We have a huge opportunity, therefore, to break the mold and grow geriatric dermatology as an area of population-based research — so that geriatric dermatology research encompasses not only the melanoma researcher who’s trying to understand how aging influences the melanocytes but also the epidemiologic researcher looking at how our diagnoses and coding and prescription practices are different in the 65-plus age group.
Clinically speaking, researchers want to better understand how aging influences the clinical presentations of our diseases. And there’s research to be done on best practices. For example, what are the best practices for treating basal cell carcinomas in patients with mild cognitive impairment? How should we consider the use of topicals in a patient who has severe arthritis or who lives alone? And then how should we teach practical approaches to help providers meet people where they are?
Looking at it from a healthcare system standpoint, there are many care delivery and access issues — practical pieces — to research, and we’re getting a lot better with this. We’re also advocating not only for more inclusion of older adults in clinical trials of treatments but also for the use of evaluations and outcomes that are relevant and important for older adults.
One piece of good news is that we’re seeing safer treatment options with tremendous efficacy that target known pathways for diseases like AD and chronic itch that affect older adults. Again, now we must find ways to improve access to these novel, safe options.
Our research program at the University of Arizona College of Medicine, which we’re just getting off the ground, aims to be dual-sided, looking both at the basic science of aging skin and at access and care delivery issues, such as how to ensure that patients on Medicare have access to medications that are at least on par with others with private insurance.
What are the most common dermatologic problems experienced by older adults?
Based on my experience and on research that we expect to be published soon, it’s absolutely nonmelanoma skin cancers, precancers like actinic keratoses — and on the inflammatory disease side, itch, AD, and psoriasis. Of course, also common are the age-related changes to the skin that we put in the benign category, such as solar lentigines.
How does age influence dermatologic diseases from a pathophysiological and clinical standpoint?
Diseases overall are very similar and respond to the same treatments, but age in and of itself does influence little pieces. For example, there is more crossover in the presentation of psoriasis and AD in older adults, leading to delays in the diagnosis of psoriasis.
With AD, we’ve found that itch is the predominant symptom for older adults rather than the red rash. We see higher or more severe itch scores in older adults with AD with less visual changes on the skin than in younger cohorts. And rash occurs in different locations than in young patients. Older adults typically present with it on their chest, back, and across the trunk, rather than in folded areas. They’re also more likely to get it on their legs in a nummular pattern as opposed to the more traditional flexural area presentation.
What unique considerations need to be made in treating older adults? How should the 4M model of geriatrics be applied to dermatologic care?
Our care model pushes us to be very algorithmic, but at the end of the day, what’s really important are the 4Ms: Mobility, medication, mentation, and “what matters most.” As you’re having your shared decision-making conversations with your patients and their families, these should be your priorities.
A patient with physical limitations, for instance, may not be able to apply a topical cream twice a day all over the body. They may have comorbidities and treatments for these comorbidities that may conflict with medications you’re considering.
And then mentation is so important. For a long time, we used antihistamines for older adults, but this has been proven to be bad for their mentation and risky in other ways. We need to be sure we’re prioritizing their ability to be clear mentally when we’re prescribing medications and even when we’re considering surgical approaches. Do they show capacity for that procedure or treatment, and how will they respond to that treatment later on?
Using the 4M model to drive conversations is a way to get all of us to connect to the patient and learn about what’s most important for them. In many ways, geriatrics is about taking a step back from your specialist skills and thinking about how you would want a family member treated.
We want to avoid treating just the lesion or the pathologic diagnosis. We want to avoid the “conveyor belt” from a biopsy to Mohs. I have 95-year-olds who say, “Heck yeah, if Mohs is the best treatment, that’s what I want.” And I have 70-year-olds who say, “I think I’ll go with another option,” and that’s the right decision for them. It’s having the conversation that matters.
In practice, given time constraints and other confines, how can dermatologists best work with more complex older patients? What are your practical tips?
People talk about having 45-minute “golden year” conversations with their older patients, but it doesn’t have to be this way. In pursuing geriatric dermatology, I decided early on that I wanted to make sure it was practical, so I’ve focused on maximizing shorter visits and on embracing the concept that relationships can be developed over time. Each time we meet with someone, we’re building equity to have bigger conversations later on.
I can have a 15-minute conversation about whether my patient may want to have Mohs surgery, for instance, or escalate treatment to a systemic agent for their chronic inflammatory disease. If that time isn’t enough, I can encourage further thought about treatment options, acknowledge that decisions aren’t necessarily easy, and schedule a follow-up or offer to call the patient after clinic to continue the conversation.
Sometimes, when I’m at an impasse and my patient is unsure how to proceed, I’ll use clear metrics relevant to older adults — sleep, activity level, and caregiver burden — to help my patient. If someone is not sleeping because of their lesion — if they’re so itchy or their inflammatory disease is uncontrolled, for instance — I’ll point out that the side effects of not sleeping are worse than the medications or surgery we’d pursue. If someone removes themselves from an activity due to their skin condition, that’s a red flag. And if the caregiver in the room is overwhelmed or frustrated by having to put cream on twice a day, I’ll use this to advance treatment.
What resources are available for dermatologists interested in improving their geriatric dermatology skills or advancing the area?
For those interested in investigating these issues or improving their practices, the AAD’s Geriatric Dermatology ERG is always welcoming of new members. The ERG will have an all-inclusive meeting at the 2025 annual AAD meeting in March.
The AAD also has educational modules on geriatric dermatology that were recently published as an initiative of our ERG. More information is available on the website. Also valuable is the ElderDerm conference hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC; the second such conference takes place in May 2025.
Butler reported that he had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Daniel C. Butler, MD, is associate professor of dermatology and director of the new Inflammatory and Aging Skin Research Program in the Division of Dermatology at the University of Arizona College of Medicine, Tucson, Arizona. Before returning to Arizona, where he had attended medical school, Butler practiced and was a researcher at the University of California, San Francisco, and its geriatric dermatology clinic. He is a co-founder and continues to co-lead the American Academy of Dermatology (AAD) Geriatric Dermatology Expert Resource Group (ERG).
Butler’s interest in geriatric dermatology is rooted in his experience growing up with four grandparents and witnessing their wisdom, relationships, moments with loved ones, and other unique and desirable parts of growing old. “When I looked later at how aging was perceived in dermatology, I found it was a lot about ‘antiaging,’” he told this news organization. “I thought there was a needed voice in dermatology for healthy aging, for all the desirable things that only growing old can provide, along with all the incredible ‘antiaging’ things we can do.”
In interviews, Butler spoke about research priorities in geriatric dermatology, how the “4M” model of geriatrics should be applied within dermatology, how dermatologists can best work with older complex patients, and more. The conversation was edited for clarity and length.
What is geriatric dermatology? It is described by the AAD’s Geriatric Dermatology ERG as “an emerging subspecialty.” Yet it’s also viewed more broadly. Please speak about its various identities and meanings and its importance for dermatology.
If you’re a Mohs surgeon, you’re seeing a strong majority of over 65 patients. And in various specialty clinics, such as inflammatory skin disease, geriatric dermatology pertains to you. In many ways, it can be viewed as a mindset.
From a framework standpoint, and as a field, geriatric dermatology is a basic science initiative, a clinical initiative, an educational initiative, and an advocacy initiative. The goal is to be able to influence, grow, and learn in each of these categories for our older patients. This is happening: Research in this field has progressed, and education has progressed, which has driven some progress in clinical care.
How has research progressed in the basic science of aging skin? What are key questions for dermatology?
There has been a lot of basic science research on aging skin and on how an aging immune system, for instance, is reflected in conditions such as bullous pemphigoid, atopic dermatitis (AD), and chronic itch. But aging involves more than immunosenescence. I think of aging skin as a three-headed monster that involves changes in the skin barrier and the microbiome as well. But is there a primary piece of aging in the skin? What comes first or influences the other? More research on these questions can potentially influence our treatments.
With respect to the immune system, what we’re finding in the skin is that age-related change is not a decline in the immune system per se, but rather aberrance in response. Parts of the system tend to become overactive, with a skew toward overexpression of type 2 inflammation. This can be problematic, driving conditions such as chronic itch.
With respect to the skin barrier, we lose essential fatty acids, and we lose a lot of our recovery ability and our ability to respond quickly to environmental stressors. But are barrier changes triggering the immune system? Or is it the other way around?
The microbiome, which is a big focus of research, involves similar chicken-and-egg discussions. Is it the microbiome that changes and alters the barrier, which then entices the immune system? Which one happens first? We have a lot to learn, and there’s probably not one answer for every patient.
Please speak about research more broadly. What questions and issues need to be answered and addressed to improve the dermatologic care of older adults?
In general, research in dermatology is very disease-specific and not particularly conducive to looking at the larger demographic populations. We have a huge opportunity, therefore, to break the mold and grow geriatric dermatology as an area of population-based research — so that geriatric dermatology research encompasses not only the melanoma researcher who’s trying to understand how aging influences the melanocytes but also the epidemiologic researcher looking at how our diagnoses and coding and prescription practices are different in the 65-plus age group.
Clinically speaking, researchers want to better understand how aging influences the clinical presentations of our diseases. And there’s research to be done on best practices. For example, what are the best practices for treating basal cell carcinomas in patients with mild cognitive impairment? How should we consider the use of topicals in a patient who has severe arthritis or who lives alone? And then how should we teach practical approaches to help providers meet people where they are?
Looking at it from a healthcare system standpoint, there are many care delivery and access issues — practical pieces — to research, and we’re getting a lot better with this. We’re also advocating not only for more inclusion of older adults in clinical trials of treatments but also for the use of evaluations and outcomes that are relevant and important for older adults.
One piece of good news is that we’re seeing safer treatment options with tremendous efficacy that target known pathways for diseases like AD and chronic itch that affect older adults. Again, now we must find ways to improve access to these novel, safe options.
Our research program at the University of Arizona College of Medicine, which we’re just getting off the ground, aims to be dual-sided, looking both at the basic science of aging skin and at access and care delivery issues, such as how to ensure that patients on Medicare have access to medications that are at least on par with others with private insurance.
What are the most common dermatologic problems experienced by older adults?
Based on my experience and on research that we expect to be published soon, it’s absolutely nonmelanoma skin cancers, precancers like actinic keratoses — and on the inflammatory disease side, itch, AD, and psoriasis. Of course, also common are the age-related changes to the skin that we put in the benign category, such as solar lentigines.
How does age influence dermatologic diseases from a pathophysiological and clinical standpoint?
Diseases overall are very similar and respond to the same treatments, but age in and of itself does influence little pieces. For example, there is more crossover in the presentation of psoriasis and AD in older adults, leading to delays in the diagnosis of psoriasis.
With AD, we’ve found that itch is the predominant symptom for older adults rather than the red rash. We see higher or more severe itch scores in older adults with AD with less visual changes on the skin than in younger cohorts. And rash occurs in different locations than in young patients. Older adults typically present with it on their chest, back, and across the trunk, rather than in folded areas. They’re also more likely to get it on their legs in a nummular pattern as opposed to the more traditional flexural area presentation.
What unique considerations need to be made in treating older adults? How should the 4M model of geriatrics be applied to dermatologic care?
Our care model pushes us to be very algorithmic, but at the end of the day, what’s really important are the 4Ms: Mobility, medication, mentation, and “what matters most.” As you’re having your shared decision-making conversations with your patients and their families, these should be your priorities.
A patient with physical limitations, for instance, may not be able to apply a topical cream twice a day all over the body. They may have comorbidities and treatments for these comorbidities that may conflict with medications you’re considering.
And then mentation is so important. For a long time, we used antihistamines for older adults, but this has been proven to be bad for their mentation and risky in other ways. We need to be sure we’re prioritizing their ability to be clear mentally when we’re prescribing medications and even when we’re considering surgical approaches. Do they show capacity for that procedure or treatment, and how will they respond to that treatment later on?
Using the 4M model to drive conversations is a way to get all of us to connect to the patient and learn about what’s most important for them. In many ways, geriatrics is about taking a step back from your specialist skills and thinking about how you would want a family member treated.
We want to avoid treating just the lesion or the pathologic diagnosis. We want to avoid the “conveyor belt” from a biopsy to Mohs. I have 95-year-olds who say, “Heck yeah, if Mohs is the best treatment, that’s what I want.” And I have 70-year-olds who say, “I think I’ll go with another option,” and that’s the right decision for them. It’s having the conversation that matters.
In practice, given time constraints and other confines, how can dermatologists best work with more complex older patients? What are your practical tips?
People talk about having 45-minute “golden year” conversations with their older patients, but it doesn’t have to be this way. In pursuing geriatric dermatology, I decided early on that I wanted to make sure it was practical, so I’ve focused on maximizing shorter visits and on embracing the concept that relationships can be developed over time. Each time we meet with someone, we’re building equity to have bigger conversations later on.
I can have a 15-minute conversation about whether my patient may want to have Mohs surgery, for instance, or escalate treatment to a systemic agent for their chronic inflammatory disease. If that time isn’t enough, I can encourage further thought about treatment options, acknowledge that decisions aren’t necessarily easy, and schedule a follow-up or offer to call the patient after clinic to continue the conversation.
Sometimes, when I’m at an impasse and my patient is unsure how to proceed, I’ll use clear metrics relevant to older adults — sleep, activity level, and caregiver burden — to help my patient. If someone is not sleeping because of their lesion — if they’re so itchy or their inflammatory disease is uncontrolled, for instance — I’ll point out that the side effects of not sleeping are worse than the medications or surgery we’d pursue. If someone removes themselves from an activity due to their skin condition, that’s a red flag. And if the caregiver in the room is overwhelmed or frustrated by having to put cream on twice a day, I’ll use this to advance treatment.
What resources are available for dermatologists interested in improving their geriatric dermatology skills or advancing the area?
For those interested in investigating these issues or improving their practices, the AAD’s Geriatric Dermatology ERG is always welcoming of new members. The ERG will have an all-inclusive meeting at the 2025 annual AAD meeting in March.
The AAD also has educational modules on geriatric dermatology that were recently published as an initiative of our ERG. More information is available on the website. Also valuable is the ElderDerm conference hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC; the second such conference takes place in May 2025.
Butler reported that he had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Daniel C. Butler, MD, is associate professor of dermatology and director of the new Inflammatory and Aging Skin Research Program in the Division of Dermatology at the University of Arizona College of Medicine, Tucson, Arizona. Before returning to Arizona, where he had attended medical school, Butler practiced and was a researcher at the University of California, San Francisco, and its geriatric dermatology clinic. He is a co-founder and continues to co-lead the American Academy of Dermatology (AAD) Geriatric Dermatology Expert Resource Group (ERG).
Butler’s interest in geriatric dermatology is rooted in his experience growing up with four grandparents and witnessing their wisdom, relationships, moments with loved ones, and other unique and desirable parts of growing old. “When I looked later at how aging was perceived in dermatology, I found it was a lot about ‘antiaging,’” he told this news organization. “I thought there was a needed voice in dermatology for healthy aging, for all the desirable things that only growing old can provide, along with all the incredible ‘antiaging’ things we can do.”
In interviews, Butler spoke about research priorities in geriatric dermatology, how the “4M” model of geriatrics should be applied within dermatology, how dermatologists can best work with older complex patients, and more. The conversation was edited for clarity and length.
What is geriatric dermatology? It is described by the AAD’s Geriatric Dermatology ERG as “an emerging subspecialty.” Yet it’s also viewed more broadly. Please speak about its various identities and meanings and its importance for dermatology.
If you’re a Mohs surgeon, you’re seeing a strong majority of over 65 patients. And in various specialty clinics, such as inflammatory skin disease, geriatric dermatology pertains to you. In many ways, it can be viewed as a mindset.
From a framework standpoint, and as a field, geriatric dermatology is a basic science initiative, a clinical initiative, an educational initiative, and an advocacy initiative. The goal is to be able to influence, grow, and learn in each of these categories for our older patients. This is happening: Research in this field has progressed, and education has progressed, which has driven some progress in clinical care.
How has research progressed in the basic science of aging skin? What are key questions for dermatology?
There has been a lot of basic science research on aging skin and on how an aging immune system, for instance, is reflected in conditions such as bullous pemphigoid, atopic dermatitis (AD), and chronic itch. But aging involves more than immunosenescence. I think of aging skin as a three-headed monster that involves changes in the skin barrier and the microbiome as well. But is there a primary piece of aging in the skin? What comes first or influences the other? More research on these questions can potentially influence our treatments.
With respect to the immune system, what we’re finding in the skin is that age-related change is not a decline in the immune system per se, but rather aberrance in response. Parts of the system tend to become overactive, with a skew toward overexpression of type 2 inflammation. This can be problematic, driving conditions such as chronic itch.
With respect to the skin barrier, we lose essential fatty acids, and we lose a lot of our recovery ability and our ability to respond quickly to environmental stressors. But are barrier changes triggering the immune system? Or is it the other way around?
The microbiome, which is a big focus of research, involves similar chicken-and-egg discussions. Is it the microbiome that changes and alters the barrier, which then entices the immune system? Which one happens first? We have a lot to learn, and there’s probably not one answer for every patient.
Please speak about research more broadly. What questions and issues need to be answered and addressed to improve the dermatologic care of older adults?
In general, research in dermatology is very disease-specific and not particularly conducive to looking at the larger demographic populations. We have a huge opportunity, therefore, to break the mold and grow geriatric dermatology as an area of population-based research — so that geriatric dermatology research encompasses not only the melanoma researcher who’s trying to understand how aging influences the melanocytes but also the epidemiologic researcher looking at how our diagnoses and coding and prescription practices are different in the 65-plus age group.
Clinically speaking, researchers want to better understand how aging influences the clinical presentations of our diseases. And there’s research to be done on best practices. For example, what are the best practices for treating basal cell carcinomas in patients with mild cognitive impairment? How should we consider the use of topicals in a patient who has severe arthritis or who lives alone? And then how should we teach practical approaches to help providers meet people where they are?
Looking at it from a healthcare system standpoint, there are many care delivery and access issues — practical pieces — to research, and we’re getting a lot better with this. We’re also advocating not only for more inclusion of older adults in clinical trials of treatments but also for the use of evaluations and outcomes that are relevant and important for older adults.
One piece of good news is that we’re seeing safer treatment options with tremendous efficacy that target known pathways for diseases like AD and chronic itch that affect older adults. Again, now we must find ways to improve access to these novel, safe options.
Our research program at the University of Arizona College of Medicine, which we’re just getting off the ground, aims to be dual-sided, looking both at the basic science of aging skin and at access and care delivery issues, such as how to ensure that patients on Medicare have access to medications that are at least on par with others with private insurance.
What are the most common dermatologic problems experienced by older adults?
Based on my experience and on research that we expect to be published soon, it’s absolutely nonmelanoma skin cancers, precancers like actinic keratoses — and on the inflammatory disease side, itch, AD, and psoriasis. Of course, also common are the age-related changes to the skin that we put in the benign category, such as solar lentigines.
How does age influence dermatologic diseases from a pathophysiological and clinical standpoint?
Diseases overall are very similar and respond to the same treatments, but age in and of itself does influence little pieces. For example, there is more crossover in the presentation of psoriasis and AD in older adults, leading to delays in the diagnosis of psoriasis.
With AD, we’ve found that itch is the predominant symptom for older adults rather than the red rash. We see higher or more severe itch scores in older adults with AD with less visual changes on the skin than in younger cohorts. And rash occurs in different locations than in young patients. Older adults typically present with it on their chest, back, and across the trunk, rather than in folded areas. They’re also more likely to get it on their legs in a nummular pattern as opposed to the more traditional flexural area presentation.
What unique considerations need to be made in treating older adults? How should the 4M model of geriatrics be applied to dermatologic care?
Our care model pushes us to be very algorithmic, but at the end of the day, what’s really important are the 4Ms: Mobility, medication, mentation, and “what matters most.” As you’re having your shared decision-making conversations with your patients and their families, these should be your priorities.
A patient with physical limitations, for instance, may not be able to apply a topical cream twice a day all over the body. They may have comorbidities and treatments for these comorbidities that may conflict with medications you’re considering.
And then mentation is so important. For a long time, we used antihistamines for older adults, but this has been proven to be bad for their mentation and risky in other ways. We need to be sure we’re prioritizing their ability to be clear mentally when we’re prescribing medications and even when we’re considering surgical approaches. Do they show capacity for that procedure or treatment, and how will they respond to that treatment later on?
Using the 4M model to drive conversations is a way to get all of us to connect to the patient and learn about what’s most important for them. In many ways, geriatrics is about taking a step back from your specialist skills and thinking about how you would want a family member treated.
We want to avoid treating just the lesion or the pathologic diagnosis. We want to avoid the “conveyor belt” from a biopsy to Mohs. I have 95-year-olds who say, “Heck yeah, if Mohs is the best treatment, that’s what I want.” And I have 70-year-olds who say, “I think I’ll go with another option,” and that’s the right decision for them. It’s having the conversation that matters.
In practice, given time constraints and other confines, how can dermatologists best work with more complex older patients? What are your practical tips?
People talk about having 45-minute “golden year” conversations with their older patients, but it doesn’t have to be this way. In pursuing geriatric dermatology, I decided early on that I wanted to make sure it was practical, so I’ve focused on maximizing shorter visits and on embracing the concept that relationships can be developed over time. Each time we meet with someone, we’re building equity to have bigger conversations later on.
I can have a 15-minute conversation about whether my patient may want to have Mohs surgery, for instance, or escalate treatment to a systemic agent for their chronic inflammatory disease. If that time isn’t enough, I can encourage further thought about treatment options, acknowledge that decisions aren’t necessarily easy, and schedule a follow-up or offer to call the patient after clinic to continue the conversation.
Sometimes, when I’m at an impasse and my patient is unsure how to proceed, I’ll use clear metrics relevant to older adults — sleep, activity level, and caregiver burden — to help my patient. If someone is not sleeping because of their lesion — if they’re so itchy or their inflammatory disease is uncontrolled, for instance — I’ll point out that the side effects of not sleeping are worse than the medications or surgery we’d pursue. If someone removes themselves from an activity due to their skin condition, that’s a red flag. And if the caregiver in the room is overwhelmed or frustrated by having to put cream on twice a day, I’ll use this to advance treatment.
What resources are available for dermatologists interested in improving their geriatric dermatology skills or advancing the area?
For those interested in investigating these issues or improving their practices, the AAD’s Geriatric Dermatology ERG is always welcoming of new members. The ERG will have an all-inclusive meeting at the 2025 annual AAD meeting in March.
The AAD also has educational modules on geriatric dermatology that were recently published as an initiative of our ERG. More information is available on the website. Also valuable is the ElderDerm conference hosted by the George Washington University School of Medicine and Health Sciences, Washington, DC; the second such conference takes place in May 2025.
Butler reported that he had no relevant financial disclosures.
A version of this article appeared on Medscape.com.
Transdermal Beats Oral Estrogen for CVD Safety of Hormone Therapy
I’d like to talk with you about a recent report in the British Medical Journal (BMJ) on different forms of contemporary menopausal hormone therapy and risks for cardiovascular disease (CVD).
This is a very large-scale and comprehensive study from Sweden that looked at more than 900,000 women, including more than 77,000 users of hormone therapy. The women were aged 50-58 years and the study leveraged the nationwide register system, where they have information on prescription medications as well as health outcomes that can be linked.
This study looked at the different forms of hormone therapy: oral vs transdermal, estrogen with and without a progestogen, and also tibolone (which is not available in the United States). The endpoints included myocardial infarction (MI), total ischemic heart disease, stroke, a composite of CVD, as well as venous thromboembolism (VTE).
They found that tibolone was associated with the greatest increased risk for CVD; there was actually an increase in both ischemic heart disease and stroke as well as composite CVD. They did not see an increased risk for VTE. This may be related to the unique pharmacologic profile of tibolone, which has estrogenic, progestogenic, and androgenic properties.
The estrogens tested in the estrogen plus progestin and estrogen alone formulations were not conjugated equine estrogen as tested in the Women’s Health Initiative (WHI) and HERS trials, but mostly oral or transdermal estradiol. With combination estrogen plus progestin, they saw a small (about 20%) increase in ischemic heart disease, similar to what was seen in the WHI. And they saw about a doubling in the risk for VTE, also similar to what was seen in the WHI. With estrogen alone there was no increase in ischemic heart disease or MI, but there was about a 50% increase in VTE — again, similar to the WHI findings.
With transdermal estradiol (transdermal forms of estrogen), in contrast, there was no clear increase in any of these CVD outcomes. In fact, there was a borderline reduction in both MI and composite CVD.
So overall, this study suggests greater cardiovascular safety with transdermal compared with oral estrogen. This would be expected, given the first-pass metabolism and increased clotting associated with oral estrogens.
On the basis of a large body of evidence, we know that for women in early menopause who have bothersome vasomotor symptoms, if they’re healthy, oral or transdermal estrogen could be used according to the preference of the woman. But this study suggests that, especially in women who do have cardiovascular risk factors, it may be very reasonable to lean toward the use of transdermal over oral estrogen among those who are choosing to use hormone therapy.
We certainly need more research on transdermal estradiol, micronized progesterone, and these contemporary formulations that are being used. But in the meantime, this study in the BMJ does provide very useful information for women and their clinicians.
Dr Manson, Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School; Chief, Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston, Massachusetts; Past President, North American Menopause Society, 2011-2012, has disclosed receiving study pill donation and infrastructure support from Mars Symbioscience (for the COSMOS trial).
A version of this article appeared on Medscape.com.
I’d like to talk with you about a recent report in the British Medical Journal (BMJ) on different forms of contemporary menopausal hormone therapy and risks for cardiovascular disease (CVD).
This is a very large-scale and comprehensive study from Sweden that looked at more than 900,000 women, including more than 77,000 users of hormone therapy. The women were aged 50-58 years and the study leveraged the nationwide register system, where they have information on prescription medications as well as health outcomes that can be linked.
This study looked at the different forms of hormone therapy: oral vs transdermal, estrogen with and without a progestogen, and also tibolone (which is not available in the United States). The endpoints included myocardial infarction (MI), total ischemic heart disease, stroke, a composite of CVD, as well as venous thromboembolism (VTE).
They found that tibolone was associated with the greatest increased risk for CVD; there was actually an increase in both ischemic heart disease and stroke as well as composite CVD. They did not see an increased risk for VTE. This may be related to the unique pharmacologic profile of tibolone, which has estrogenic, progestogenic, and androgenic properties.
The estrogens tested in the estrogen plus progestin and estrogen alone formulations were not conjugated equine estrogen as tested in the Women’s Health Initiative (WHI) and HERS trials, but mostly oral or transdermal estradiol. With combination estrogen plus progestin, they saw a small (about 20%) increase in ischemic heart disease, similar to what was seen in the WHI. And they saw about a doubling in the risk for VTE, also similar to what was seen in the WHI. With estrogen alone there was no increase in ischemic heart disease or MI, but there was about a 50% increase in VTE — again, similar to the WHI findings.
With transdermal estradiol (transdermal forms of estrogen), in contrast, there was no clear increase in any of these CVD outcomes. In fact, there was a borderline reduction in both MI and composite CVD.
So overall, this study suggests greater cardiovascular safety with transdermal compared with oral estrogen. This would be expected, given the first-pass metabolism and increased clotting associated with oral estrogens.
On the basis of a large body of evidence, we know that for women in early menopause who have bothersome vasomotor symptoms, if they’re healthy, oral or transdermal estrogen could be used according to the preference of the woman. But this study suggests that, especially in women who do have cardiovascular risk factors, it may be very reasonable to lean toward the use of transdermal over oral estrogen among those who are choosing to use hormone therapy.
We certainly need more research on transdermal estradiol, micronized progesterone, and these contemporary formulations that are being used. But in the meantime, this study in the BMJ does provide very useful information for women and their clinicians.
Dr Manson, Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School; Chief, Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston, Massachusetts; Past President, North American Menopause Society, 2011-2012, has disclosed receiving study pill donation and infrastructure support from Mars Symbioscience (for the COSMOS trial).
A version of this article appeared on Medscape.com.
I’d like to talk with you about a recent report in the British Medical Journal (BMJ) on different forms of contemporary menopausal hormone therapy and risks for cardiovascular disease (CVD).
This is a very large-scale and comprehensive study from Sweden that looked at more than 900,000 women, including more than 77,000 users of hormone therapy. The women were aged 50-58 years and the study leveraged the nationwide register system, where they have information on prescription medications as well as health outcomes that can be linked.
This study looked at the different forms of hormone therapy: oral vs transdermal, estrogen with and without a progestogen, and also tibolone (which is not available in the United States). The endpoints included myocardial infarction (MI), total ischemic heart disease, stroke, a composite of CVD, as well as venous thromboembolism (VTE).
They found that tibolone was associated with the greatest increased risk for CVD; there was actually an increase in both ischemic heart disease and stroke as well as composite CVD. They did not see an increased risk for VTE. This may be related to the unique pharmacologic profile of tibolone, which has estrogenic, progestogenic, and androgenic properties.
The estrogens tested in the estrogen plus progestin and estrogen alone formulations were not conjugated equine estrogen as tested in the Women’s Health Initiative (WHI) and HERS trials, but mostly oral or transdermal estradiol. With combination estrogen plus progestin, they saw a small (about 20%) increase in ischemic heart disease, similar to what was seen in the WHI. And they saw about a doubling in the risk for VTE, also similar to what was seen in the WHI. With estrogen alone there was no increase in ischemic heart disease or MI, but there was about a 50% increase in VTE — again, similar to the WHI findings.
With transdermal estradiol (transdermal forms of estrogen), in contrast, there was no clear increase in any of these CVD outcomes. In fact, there was a borderline reduction in both MI and composite CVD.
So overall, this study suggests greater cardiovascular safety with transdermal compared with oral estrogen. This would be expected, given the first-pass metabolism and increased clotting associated with oral estrogens.
On the basis of a large body of evidence, we know that for women in early menopause who have bothersome vasomotor symptoms, if they’re healthy, oral or transdermal estrogen could be used according to the preference of the woman. But this study suggests that, especially in women who do have cardiovascular risk factors, it may be very reasonable to lean toward the use of transdermal over oral estrogen among those who are choosing to use hormone therapy.
We certainly need more research on transdermal estradiol, micronized progesterone, and these contemporary formulations that are being used. But in the meantime, this study in the BMJ does provide very useful information for women and their clinicians.
Dr Manson, Professor of Medicine and the Michael and Lee Bell Professor of Women’s Health, Harvard Medical School; Chief, Division of Preventive Medicine, Brigham and Women’s Hospital, both in Boston, Massachusetts; Past President, North American Menopause Society, 2011-2012, has disclosed receiving study pill donation and infrastructure support from Mars Symbioscience (for the COSMOS trial).
A version of this article appeared on Medscape.com.
Is Vitamin E Beneficial for Bone Health?
Vitamin E may be best known for boosting skin and eye health as well as immune function. In recent years, researchers have explored the potential benefits of vitamin E on bone loss, especially in women with menopause-related osteoporosis. While data are beginning to roll in from these studies, evidence supporting a positive impact of vitamin E on osteoporosis and hip fracture risk in perimenopausal women remains elusive.
For osteoporosis, the rationale for using vitamin E is based on its antioxidant activity, which can scavenge potentially damaging free radicals. Researchers have asked whether vitamin E can help maintain the integrity of bone matrix and stimulate bone formation while minimizing bone resorption, particularly in trabecular (spongy) bone, the bone compartment preferentially affected in perimenopausal bone loss.
Vitamin E mostly consists of two isomers: alpha-tocopherol and gamma-tocopherol. Alpha-tocopherol has higher antioxidant activity and is found in nuts, seeds, vegetable oils, green leafy vegetables, fortified cereals, and vitamin E supplements. Gamma-tocopherol is known for its superior anti-inflammatory properties and accounts for about 70% of the total vitamin E intake in a typical American diet, largely sourced from soybean and other vegetable oils.
Benefits and Risks in Bone Loss Studies
Perimenopausal bone loss is caused, to a great extent, by the decrease in sex hormones. Studies of vitamin E in ovariectomized rats have yielded mixed results. This animal model lacks sex hormones and has similar bone changes to those of postmenopausal women. Some animal studies have suggested a positive effect of vitamin E on bone while others have reported no effect.
Studies in humans also have produced conflicting reports of positive, neutral, and negative associations of vitamin E with bone health. For example, the Women’s Health Initiative examined the relationship between vitamin and mineral antioxidants and bone health in postmenopausal women and found no significant association between antioxidants and bone mineral density.
Another study examining data from children and adolescents enrolled in the National Health and Nutrition Examination Survey (NHANES) database found an inverse association between alpha-tocopherol and lumbar spine bone density, suggesting a deleterious effect on bone. Inverse associations also have been reported in certain studies of postmenopausal women.
High doses of alpha-tocopherol have been linked to a risk for impaired bone health through a variety of mechanisms, such as interference with vitamin K metabolism; competitive binding for alpha-tocopherol transfer protein, inhibiting the entry of beneficial vitamin E isomers, including gamma-tocopherol; and pro-oxidant effects that harm bone. Thus, postmenopausal women taking vitamin E supplements primarily as high doses of alpha-tocopherol might be hindering their bone health.
Data for gamma-tocopherol are more promising. Some studies hypothesize that gamma-tocopherol might uncouple bone turnover, leading to increased bone formation without affecting bone resorption. Further, a randomized controlled study of mixed tocopherols (rather than alpha-tocopherol) vs placebo reported a protective effect of this preparation on bone outcomes by suppressing bone resorption. This raises the importance of considering the specific forms of vitamin E when evaluating its role in bone health.
Limitations of Current Studies
Researchers acknowledge several limitations in studies to date. For example, there are very few randomized controlled trials assessing the impact of vitamin E on bone health. Most studies are cross-sectional or observational, even when longitudinal. Cross-sectional and observational designs prevent us from establishing a causal relationship between vitamin E and bone endpoints.
Such designs also run the risk of additional confounders that may affect associations between vitamin E and bone, or the lack thereof. These could include both known and unknown confounders. Of note, gamma-tocopherol intake data were not available for certain NHANES studies.
Further, people often consume multiple nutrients and supplements, complicating the identification of specific nutrient-disease associations. Most human studies estimate tocopherol intake by dietary questionnaires or measure serum tocopherol levels, which reflect short-term dietary intake, while bone mineral density is probably influenced by long-term dietary patterns.
Too Soon to Prescribe Vitamin E for Bone Health
Some nutrition experts advocate for vitamin E supplements containing mixed tocopherols, specifically suggesting a ratio of 50-100 IU of gamma-tocopherol per 400 IU of D-alpha-tocopherol. Additional research is essential to confirm and further clarify the role of gamma-tocopherol in bone formation and resorption. In fact, it is also important to explore the influence of other compounds in the vitamin E family on skeletal health.
Until more data are available, we would recommend following the Institute of Medicine’s guidelines for the recommended daily allowance (RDA) of vitamin E. This is age dependent, ranging from 4 to 11 mg/d between the ages of 0 and 13 years, and 15 mg/d thereafter.
Overall, evidence of vitamin E’s impact on osteoporosis and hip fracture risk in perimenopausal women remains inconclusive. Although some observational and interventional studies suggest potential benefits, more interventional studies, particularly randomized controlled trials, are necessary to explore the risks and benefits of vitamin E supplementation and serum vitamin E levels on bone density and fracture risk more thoroughly.
Dr. Pani, Assistant Professor, Department of Internal Medicine, UVA School of Medicine; Medical Director, Department of General Medicine, Same Day Care Clinic, both in Charlottesville, has disclosed no relevant financial relationships. Dr. Misra, Professor, Chair, Physician-in-Chief, Department of Pediatrics, University of Virginia, and UVA Health Children’s, Charlottesville, has disclosed being a key opinion leader for Lumos Pharma.
A version of this article appeared on Medscape.com.
Vitamin E may be best known for boosting skin and eye health as well as immune function. In recent years, researchers have explored the potential benefits of vitamin E on bone loss, especially in women with menopause-related osteoporosis. While data are beginning to roll in from these studies, evidence supporting a positive impact of vitamin E on osteoporosis and hip fracture risk in perimenopausal women remains elusive.
For osteoporosis, the rationale for using vitamin E is based on its antioxidant activity, which can scavenge potentially damaging free radicals. Researchers have asked whether vitamin E can help maintain the integrity of bone matrix and stimulate bone formation while minimizing bone resorption, particularly in trabecular (spongy) bone, the bone compartment preferentially affected in perimenopausal bone loss.
Vitamin E mostly consists of two isomers: alpha-tocopherol and gamma-tocopherol. Alpha-tocopherol has higher antioxidant activity and is found in nuts, seeds, vegetable oils, green leafy vegetables, fortified cereals, and vitamin E supplements. Gamma-tocopherol is known for its superior anti-inflammatory properties and accounts for about 70% of the total vitamin E intake in a typical American diet, largely sourced from soybean and other vegetable oils.
Benefits and Risks in Bone Loss Studies
Perimenopausal bone loss is caused, to a great extent, by the decrease in sex hormones. Studies of vitamin E in ovariectomized rats have yielded mixed results. This animal model lacks sex hormones and has similar bone changes to those of postmenopausal women. Some animal studies have suggested a positive effect of vitamin E on bone while others have reported no effect.
Studies in humans also have produced conflicting reports of positive, neutral, and negative associations of vitamin E with bone health. For example, the Women’s Health Initiative examined the relationship between vitamin and mineral antioxidants and bone health in postmenopausal women and found no significant association between antioxidants and bone mineral density.
Another study examining data from children and adolescents enrolled in the National Health and Nutrition Examination Survey (NHANES) database found an inverse association between alpha-tocopherol and lumbar spine bone density, suggesting a deleterious effect on bone. Inverse associations also have been reported in certain studies of postmenopausal women.
High doses of alpha-tocopherol have been linked to a risk for impaired bone health through a variety of mechanisms, such as interference with vitamin K metabolism; competitive binding for alpha-tocopherol transfer protein, inhibiting the entry of beneficial vitamin E isomers, including gamma-tocopherol; and pro-oxidant effects that harm bone. Thus, postmenopausal women taking vitamin E supplements primarily as high doses of alpha-tocopherol might be hindering their bone health.
Data for gamma-tocopherol are more promising. Some studies hypothesize that gamma-tocopherol might uncouple bone turnover, leading to increased bone formation without affecting bone resorption. Further, a randomized controlled study of mixed tocopherols (rather than alpha-tocopherol) vs placebo reported a protective effect of this preparation on bone outcomes by suppressing bone resorption. This raises the importance of considering the specific forms of vitamin E when evaluating its role in bone health.
Limitations of Current Studies
Researchers acknowledge several limitations in studies to date. For example, there are very few randomized controlled trials assessing the impact of vitamin E on bone health. Most studies are cross-sectional or observational, even when longitudinal. Cross-sectional and observational designs prevent us from establishing a causal relationship between vitamin E and bone endpoints.
Such designs also run the risk of additional confounders that may affect associations between vitamin E and bone, or the lack thereof. These could include both known and unknown confounders. Of note, gamma-tocopherol intake data were not available for certain NHANES studies.
Further, people often consume multiple nutrients and supplements, complicating the identification of specific nutrient-disease associations. Most human studies estimate tocopherol intake by dietary questionnaires or measure serum tocopherol levels, which reflect short-term dietary intake, while bone mineral density is probably influenced by long-term dietary patterns.
Too Soon to Prescribe Vitamin E for Bone Health
Some nutrition experts advocate for vitamin E supplements containing mixed tocopherols, specifically suggesting a ratio of 50-100 IU of gamma-tocopherol per 400 IU of D-alpha-tocopherol. Additional research is essential to confirm and further clarify the role of gamma-tocopherol in bone formation and resorption. In fact, it is also important to explore the influence of other compounds in the vitamin E family on skeletal health.
Until more data are available, we would recommend following the Institute of Medicine’s guidelines for the recommended daily allowance (RDA) of vitamin E. This is age dependent, ranging from 4 to 11 mg/d between the ages of 0 and 13 years, and 15 mg/d thereafter.
Overall, evidence of vitamin E’s impact on osteoporosis and hip fracture risk in perimenopausal women remains inconclusive. Although some observational and interventional studies suggest potential benefits, more interventional studies, particularly randomized controlled trials, are necessary to explore the risks and benefits of vitamin E supplementation and serum vitamin E levels on bone density and fracture risk more thoroughly.
Dr. Pani, Assistant Professor, Department of Internal Medicine, UVA School of Medicine; Medical Director, Department of General Medicine, Same Day Care Clinic, both in Charlottesville, has disclosed no relevant financial relationships. Dr. Misra, Professor, Chair, Physician-in-Chief, Department of Pediatrics, University of Virginia, and UVA Health Children’s, Charlottesville, has disclosed being a key opinion leader for Lumos Pharma.
A version of this article appeared on Medscape.com.
Vitamin E may be best known for boosting skin and eye health as well as immune function. In recent years, researchers have explored the potential benefits of vitamin E on bone loss, especially in women with menopause-related osteoporosis. While data are beginning to roll in from these studies, evidence supporting a positive impact of vitamin E on osteoporosis and hip fracture risk in perimenopausal women remains elusive.
For osteoporosis, the rationale for using vitamin E is based on its antioxidant activity, which can scavenge potentially damaging free radicals. Researchers have asked whether vitamin E can help maintain the integrity of bone matrix and stimulate bone formation while minimizing bone resorption, particularly in trabecular (spongy) bone, the bone compartment preferentially affected in perimenopausal bone loss.
Vitamin E mostly consists of two isomers: alpha-tocopherol and gamma-tocopherol. Alpha-tocopherol has higher antioxidant activity and is found in nuts, seeds, vegetable oils, green leafy vegetables, fortified cereals, and vitamin E supplements. Gamma-tocopherol is known for its superior anti-inflammatory properties and accounts for about 70% of the total vitamin E intake in a typical American diet, largely sourced from soybean and other vegetable oils.
Benefits and Risks in Bone Loss Studies
Perimenopausal bone loss is caused, to a great extent, by the decrease in sex hormones. Studies of vitamin E in ovariectomized rats have yielded mixed results. This animal model lacks sex hormones and has similar bone changes to those of postmenopausal women. Some animal studies have suggested a positive effect of vitamin E on bone while others have reported no effect.
Studies in humans also have produced conflicting reports of positive, neutral, and negative associations of vitamin E with bone health. For example, the Women’s Health Initiative examined the relationship between vitamin and mineral antioxidants and bone health in postmenopausal women and found no significant association between antioxidants and bone mineral density.
Another study examining data from children and adolescents enrolled in the National Health and Nutrition Examination Survey (NHANES) database found an inverse association between alpha-tocopherol and lumbar spine bone density, suggesting a deleterious effect on bone. Inverse associations also have been reported in certain studies of postmenopausal women.
High doses of alpha-tocopherol have been linked to a risk for impaired bone health through a variety of mechanisms, such as interference with vitamin K metabolism; competitive binding for alpha-tocopherol transfer protein, inhibiting the entry of beneficial vitamin E isomers, including gamma-tocopherol; and pro-oxidant effects that harm bone. Thus, postmenopausal women taking vitamin E supplements primarily as high doses of alpha-tocopherol might be hindering their bone health.
Data for gamma-tocopherol are more promising. Some studies hypothesize that gamma-tocopherol might uncouple bone turnover, leading to increased bone formation without affecting bone resorption. Further, a randomized controlled study of mixed tocopherols (rather than alpha-tocopherol) vs placebo reported a protective effect of this preparation on bone outcomes by suppressing bone resorption. This raises the importance of considering the specific forms of vitamin E when evaluating its role in bone health.
Limitations of Current Studies
Researchers acknowledge several limitations in studies to date. For example, there are very few randomized controlled trials assessing the impact of vitamin E on bone health. Most studies are cross-sectional or observational, even when longitudinal. Cross-sectional and observational designs prevent us from establishing a causal relationship between vitamin E and bone endpoints.
Such designs also run the risk of additional confounders that may affect associations between vitamin E and bone, or the lack thereof. These could include both known and unknown confounders. Of note, gamma-tocopherol intake data were not available for certain NHANES studies.
Further, people often consume multiple nutrients and supplements, complicating the identification of specific nutrient-disease associations. Most human studies estimate tocopherol intake by dietary questionnaires or measure serum tocopherol levels, which reflect short-term dietary intake, while bone mineral density is probably influenced by long-term dietary patterns.
Too Soon to Prescribe Vitamin E for Bone Health
Some nutrition experts advocate for vitamin E supplements containing mixed tocopherols, specifically suggesting a ratio of 50-100 IU of gamma-tocopherol per 400 IU of D-alpha-tocopherol. Additional research is essential to confirm and further clarify the role of gamma-tocopherol in bone formation and resorption. In fact, it is also important to explore the influence of other compounds in the vitamin E family on skeletal health.
Until more data are available, we would recommend following the Institute of Medicine’s guidelines for the recommended daily allowance (RDA) of vitamin E. This is age dependent, ranging from 4 to 11 mg/d between the ages of 0 and 13 years, and 15 mg/d thereafter.
Overall, evidence of vitamin E’s impact on osteoporosis and hip fracture risk in perimenopausal women remains inconclusive. Although some observational and interventional studies suggest potential benefits, more interventional studies, particularly randomized controlled trials, are necessary to explore the risks and benefits of vitamin E supplementation and serum vitamin E levels on bone density and fracture risk more thoroughly.
Dr. Pani, Assistant Professor, Department of Internal Medicine, UVA School of Medicine; Medical Director, Department of General Medicine, Same Day Care Clinic, both in Charlottesville, has disclosed no relevant financial relationships. Dr. Misra, Professor, Chair, Physician-in-Chief, Department of Pediatrics, University of Virginia, and UVA Health Children’s, Charlottesville, has disclosed being a key opinion leader for Lumos Pharma.
A version of this article appeared on Medscape.com.
Internet Use May Boost Mental Health in Later Life
TOPLINE:
and better self-reported health among adults aged 50 years or older across 23 countries than nonuse, a new cohort study suggests.
METHODOLOGY:
- Data were examined for more than 87,000 adults aged 50 years or older across 23 countries and from six aging cohorts.
- Researchers examined the potential association between internet use and mental health outcomes, including depressive symptoms, life satisfaction, and self-reported health.
- Polygenic scores were used for subset analysis to stratify participants from England and the United States according to their genetic risk for depression.
- Participants were followed up for a median of 6 years.
TAKEAWAY:
- Internet use was linked to consistent benefits across countries, including lower depressive symptoms (pooled average marginal effect [AME], –0.09; 95% CI, –0.12 to –0.07), higher life satisfaction (pooled AME, 0.07; 95% CI, 0.05-0.10), and better self-reported health (pooled AME, 0.15; 95% CI, 0.12-0.17).
- Frequent internet users showed better mental health outcomes than nonusers, and daily internet users showed significant improvements in depressive symptoms and self-reported health in England and the United States.
- Each additional wave of internet use was associated with reduced depressive symptoms (pooled AME, –0.06; 95% CI, –0.09 to –0.04) and improved life satisfaction (pooled AME, 0.05; 95% CI, 0.03-0.07).
- Benefits of internet use were observed across all genetic risk categories for depression in England and the United States, suggesting potential utility regardless of genetic predisposition.
IN PRACTICE:
“Our findings are relevant to public health policies and practices in promoting mental health in later life through the internet, especially in countries with limited internet access and mental health services,” the investigators wrote.
SOURCE:
The study was led by Yan Luo, Department of Data Science, City University of Hong Kong, Hong Kong, China. It was published online November 18 in Nature Human Behaviour.
LIMITATIONS:
The possibility of residual confounding and reverse causation prevented the establishment of direct causality between internet use and mental health. Selection bias may have also existed due to differences in baseline characteristics between the analytic samples and entire populations. Internet use was assessed through self-reported items, which could have led to recall and information bias. Additionally, genetic data were available for participants only from England and the United States.
DISCLOSURES:
The study was funded in part by the National Natural Science Foundation of China. The investigators reported no conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
and better self-reported health among adults aged 50 years or older across 23 countries than nonuse, a new cohort study suggests.
METHODOLOGY:
- Data were examined for more than 87,000 adults aged 50 years or older across 23 countries and from six aging cohorts.
- Researchers examined the potential association between internet use and mental health outcomes, including depressive symptoms, life satisfaction, and self-reported health.
- Polygenic scores were used for subset analysis to stratify participants from England and the United States according to their genetic risk for depression.
- Participants were followed up for a median of 6 years.
TAKEAWAY:
- Internet use was linked to consistent benefits across countries, including lower depressive symptoms (pooled average marginal effect [AME], –0.09; 95% CI, –0.12 to –0.07), higher life satisfaction (pooled AME, 0.07; 95% CI, 0.05-0.10), and better self-reported health (pooled AME, 0.15; 95% CI, 0.12-0.17).
- Frequent internet users showed better mental health outcomes than nonusers, and daily internet users showed significant improvements in depressive symptoms and self-reported health in England and the United States.
- Each additional wave of internet use was associated with reduced depressive symptoms (pooled AME, –0.06; 95% CI, –0.09 to –0.04) and improved life satisfaction (pooled AME, 0.05; 95% CI, 0.03-0.07).
- Benefits of internet use were observed across all genetic risk categories for depression in England and the United States, suggesting potential utility regardless of genetic predisposition.
IN PRACTICE:
“Our findings are relevant to public health policies and practices in promoting mental health in later life through the internet, especially in countries with limited internet access and mental health services,” the investigators wrote.
SOURCE:
The study was led by Yan Luo, Department of Data Science, City University of Hong Kong, Hong Kong, China. It was published online November 18 in Nature Human Behaviour.
LIMITATIONS:
The possibility of residual confounding and reverse causation prevented the establishment of direct causality between internet use and mental health. Selection bias may have also existed due to differences in baseline characteristics between the analytic samples and entire populations. Internet use was assessed through self-reported items, which could have led to recall and information bias. Additionally, genetic data were available for participants only from England and the United States.
DISCLOSURES:
The study was funded in part by the National Natural Science Foundation of China. The investigators reported no conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
and better self-reported health among adults aged 50 years or older across 23 countries than nonuse, a new cohort study suggests.
METHODOLOGY:
- Data were examined for more than 87,000 adults aged 50 years or older across 23 countries and from six aging cohorts.
- Researchers examined the potential association between internet use and mental health outcomes, including depressive symptoms, life satisfaction, and self-reported health.
- Polygenic scores were used for subset analysis to stratify participants from England and the United States according to their genetic risk for depression.
- Participants were followed up for a median of 6 years.
TAKEAWAY:
- Internet use was linked to consistent benefits across countries, including lower depressive symptoms (pooled average marginal effect [AME], –0.09; 95% CI, –0.12 to –0.07), higher life satisfaction (pooled AME, 0.07; 95% CI, 0.05-0.10), and better self-reported health (pooled AME, 0.15; 95% CI, 0.12-0.17).
- Frequent internet users showed better mental health outcomes than nonusers, and daily internet users showed significant improvements in depressive symptoms and self-reported health in England and the United States.
- Each additional wave of internet use was associated with reduced depressive symptoms (pooled AME, –0.06; 95% CI, –0.09 to –0.04) and improved life satisfaction (pooled AME, 0.05; 95% CI, 0.03-0.07).
- Benefits of internet use were observed across all genetic risk categories for depression in England and the United States, suggesting potential utility regardless of genetic predisposition.
IN PRACTICE:
“Our findings are relevant to public health policies and practices in promoting mental health in later life through the internet, especially in countries with limited internet access and mental health services,” the investigators wrote.
SOURCE:
The study was led by Yan Luo, Department of Data Science, City University of Hong Kong, Hong Kong, China. It was published online November 18 in Nature Human Behaviour.
LIMITATIONS:
The possibility of residual confounding and reverse causation prevented the establishment of direct causality between internet use and mental health. Selection bias may have also existed due to differences in baseline characteristics between the analytic samples and entire populations. Internet use was assessed through self-reported items, which could have led to recall and information bias. Additionally, genetic data were available for participants only from England and the United States.
DISCLOSURES:
The study was funded in part by the National Natural Science Foundation of China. The investigators reported no conflicts of interest.
This article was created using several editorial tools, including artificial intelligence, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
New Approaches to Research Beyond Massive Clinical Trials
This transcript has been edited for clarity.
I want to briefly present a fascinating effort, one that needs to be applauded and applauded again, and then we need to scratch our collective heads and ask, why did we do it and what did we learn?
I’m referring to a report recently published in Annals of Internal Medicine, “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women: Postintervention Follow-up of a Randomized Clinical Trial.” The title of this report does not do it justice. This was a massive effort — one could, I believe, even use the term Herculean — to ask an important question that was asked more than 20 years ago.
This was a national women’s health initiative to answer these questions. The study looked at 36,282 postmenopausal women who, at the time of agreeing to be randomized in this trial, had no history of breast or colorectal cancer. This was a 7-year randomized intervention effort, and 40 centers across the United States participated, obviously funded by the government. Randomization was one-to-one to placebo or 1000 mg calcium and 400 international units of vitamin D3 daily.
They looked at the incidence of colorectal cancer, breast cancer, and total cancer, and importantly as an endpoint, total cardiovascular disease and hip fractures. They didn’t comment on hip fractures in this particular analysis. Obviously, hip fractures relate to this question of osteoporosis in postmenopausal women.
Here’s the bottom line: With a median follow-up now of 22.3 years — that’s not 2 years, but 22.3 years — there was a 7% decrease in cancer mortality in the population that received the calcium and vitamin D3. This is nothing to snicker at, and nothing at which to say, “Wow. That’s not important.”
However, in this analysis involving several tens of thousands of women, there was a 6% increase in cardiovascular disease mortality noted and reported. Overall, there was no effect on all-cause mortality of this intervention, with a hazard ratio — you rarely see this — of 1.00.
There is much that can be said, but I will summarize my comments very briefly. Criticize this if you want. It’s not inappropriate to criticize, but what was the individual impact of the calcium vs vitamin D? If they had only used one vs the other, or used both but in separate arms of the trial, and you could have separated what might have caused the decrease in cancer mortality and not the increased cardiovascular disease… This was designed more than 20 years ago. That’s one point.
The second is, how many more tens of thousands of patients would they have had to add to do this, and at what cost? This was a massive study, a national study, and a simple study in terms of the intervention. It was low risk except if you look at the long-term outcome. You can only imagine how much it would cost to do that study today — not the cost of the calcium, the vitamin D3, but the cost of doing the trial that was concluded to have no impact.
From a societal perspective, this was an important question to answer, certainly then. What did we learn and at what cost? The bottom line is that we have to figure out a way of answering these kinds of questions.
Perhaps now they should be from real-world data, looking at electronic medical records or at a variety of other population-based data so that we can get the answer — not in 20 years but in perhaps 2 months, because we’ve looked at the data using artificial intelligence to help us to answer these questions; and maybe not 36,000 patients but 360,000 individuals looked at over this period of time.
Again, I’m proposing an alternative solution because the questions that were asked 20 years ago remain important today. This cannot be the way that we, in the future, try to answer them, certainly from the perspective of cost and also the perspective of time to get the answers.
Let me conclude by, again, applauding these researchers because of the quality of the work they started out doing and ended up doing and reporting. Also, I think we’ve learned that we have to come up with alternative ways to answer what were important questions then and are important questions today.
Dr. Markman, Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix, disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly present a fascinating effort, one that needs to be applauded and applauded again, and then we need to scratch our collective heads and ask, why did we do it and what did we learn?
I’m referring to a report recently published in Annals of Internal Medicine, “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women: Postintervention Follow-up of a Randomized Clinical Trial.” The title of this report does not do it justice. This was a massive effort — one could, I believe, even use the term Herculean — to ask an important question that was asked more than 20 years ago.
This was a national women’s health initiative to answer these questions. The study looked at 36,282 postmenopausal women who, at the time of agreeing to be randomized in this trial, had no history of breast or colorectal cancer. This was a 7-year randomized intervention effort, and 40 centers across the United States participated, obviously funded by the government. Randomization was one-to-one to placebo or 1000 mg calcium and 400 international units of vitamin D3 daily.
They looked at the incidence of colorectal cancer, breast cancer, and total cancer, and importantly as an endpoint, total cardiovascular disease and hip fractures. They didn’t comment on hip fractures in this particular analysis. Obviously, hip fractures relate to this question of osteoporosis in postmenopausal women.
Here’s the bottom line: With a median follow-up now of 22.3 years — that’s not 2 years, but 22.3 years — there was a 7% decrease in cancer mortality in the population that received the calcium and vitamin D3. This is nothing to snicker at, and nothing at which to say, “Wow. That’s not important.”
However, in this analysis involving several tens of thousands of women, there was a 6% increase in cardiovascular disease mortality noted and reported. Overall, there was no effect on all-cause mortality of this intervention, with a hazard ratio — you rarely see this — of 1.00.
There is much that can be said, but I will summarize my comments very briefly. Criticize this if you want. It’s not inappropriate to criticize, but what was the individual impact of the calcium vs vitamin D? If they had only used one vs the other, or used both but in separate arms of the trial, and you could have separated what might have caused the decrease in cancer mortality and not the increased cardiovascular disease… This was designed more than 20 years ago. That’s one point.
The second is, how many more tens of thousands of patients would they have had to add to do this, and at what cost? This was a massive study, a national study, and a simple study in terms of the intervention. It was low risk except if you look at the long-term outcome. You can only imagine how much it would cost to do that study today — not the cost of the calcium, the vitamin D3, but the cost of doing the trial that was concluded to have no impact.
From a societal perspective, this was an important question to answer, certainly then. What did we learn and at what cost? The bottom line is that we have to figure out a way of answering these kinds of questions.
Perhaps now they should be from real-world data, looking at electronic medical records or at a variety of other population-based data so that we can get the answer — not in 20 years but in perhaps 2 months, because we’ve looked at the data using artificial intelligence to help us to answer these questions; and maybe not 36,000 patients but 360,000 individuals looked at over this period of time.
Again, I’m proposing an alternative solution because the questions that were asked 20 years ago remain important today. This cannot be the way that we, in the future, try to answer them, certainly from the perspective of cost and also the perspective of time to get the answers.
Let me conclude by, again, applauding these researchers because of the quality of the work they started out doing and ended up doing and reporting. Also, I think we’ve learned that we have to come up with alternative ways to answer what were important questions then and are important questions today.
Dr. Markman, Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix, disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
I want to briefly present a fascinating effort, one that needs to be applauded and applauded again, and then we need to scratch our collective heads and ask, why did we do it and what did we learn?
I’m referring to a report recently published in Annals of Internal Medicine, “Long-Term Effect of Randomization to Calcium and Vitamin D Supplementation on Health in Older Women: Postintervention Follow-up of a Randomized Clinical Trial.” The title of this report does not do it justice. This was a massive effort — one could, I believe, even use the term Herculean — to ask an important question that was asked more than 20 years ago.
This was a national women’s health initiative to answer these questions. The study looked at 36,282 postmenopausal women who, at the time of agreeing to be randomized in this trial, had no history of breast or colorectal cancer. This was a 7-year randomized intervention effort, and 40 centers across the United States participated, obviously funded by the government. Randomization was one-to-one to placebo or 1000 mg calcium and 400 international units of vitamin D3 daily.
They looked at the incidence of colorectal cancer, breast cancer, and total cancer, and importantly as an endpoint, total cardiovascular disease and hip fractures. They didn’t comment on hip fractures in this particular analysis. Obviously, hip fractures relate to this question of osteoporosis in postmenopausal women.
Here’s the bottom line: With a median follow-up now of 22.3 years — that’s not 2 years, but 22.3 years — there was a 7% decrease in cancer mortality in the population that received the calcium and vitamin D3. This is nothing to snicker at, and nothing at which to say, “Wow. That’s not important.”
However, in this analysis involving several tens of thousands of women, there was a 6% increase in cardiovascular disease mortality noted and reported. Overall, there was no effect on all-cause mortality of this intervention, with a hazard ratio — you rarely see this — of 1.00.
There is much that can be said, but I will summarize my comments very briefly. Criticize this if you want. It’s not inappropriate to criticize, but what was the individual impact of the calcium vs vitamin D? If they had only used one vs the other, or used both but in separate arms of the trial, and you could have separated what might have caused the decrease in cancer mortality and not the increased cardiovascular disease… This was designed more than 20 years ago. That’s one point.
The second is, how many more tens of thousands of patients would they have had to add to do this, and at what cost? This was a massive study, a national study, and a simple study in terms of the intervention. It was low risk except if you look at the long-term outcome. You can only imagine how much it would cost to do that study today — not the cost of the calcium, the vitamin D3, but the cost of doing the trial that was concluded to have no impact.
From a societal perspective, this was an important question to answer, certainly then. What did we learn and at what cost? The bottom line is that we have to figure out a way of answering these kinds of questions.
Perhaps now they should be from real-world data, looking at electronic medical records or at a variety of other population-based data so that we can get the answer — not in 20 years but in perhaps 2 months, because we’ve looked at the data using artificial intelligence to help us to answer these questions; and maybe not 36,000 patients but 360,000 individuals looked at over this period of time.
Again, I’m proposing an alternative solution because the questions that were asked 20 years ago remain important today. This cannot be the way that we, in the future, try to answer them, certainly from the perspective of cost and also the perspective of time to get the answers.
Let me conclude by, again, applauding these researchers because of the quality of the work they started out doing and ended up doing and reporting. Also, I think we’ve learned that we have to come up with alternative ways to answer what were important questions then and are important questions today.
Dr. Markman, Professor of Medical Oncology and Therapeutics Research, City of Hope Comprehensive Cancer Center; President, Medicine & Science, City of Hope Atlanta, Chicago, Phoenix, disclosed ties with GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
Watch That Attitude: Is There Ageism in Healthcare?
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
People are living longer in Europe. Life expectancy increased on the continent by around 12 years between 1960 and 2022. And despite slower progress during the COVID-19 pandemic, the trend appears to be continuing.
Not only are Europeans living longer, their fertility rates are declining. This means that the number of people aged 75-84 years is projected to grow in Europe a full 56.1% by 2050, while the population younger than 55 years is expected to fall by 13.5%.
This means that attitudes toward age need to change, and fast — even among healthcare professionals.
Healthcare Is Not Exempt From Ageist Attitudes
A systematic review published in the journal PLOS ONE in 2020 found that age was a determinant factor in dictating who received certain medical procedures or treatments. For example, a study of 9105 hospitalized patients found that healthcare providers were significantly more likely to withhold life-sustaining treatments from older patients. Another study found evidence that older people are excluded from clinical trials, even when the trials are for diseases that appear later in life, like Parkinson’s.
“In healthcare, there are different levels of ageism,” explained Hannah Swift, PhD, reader in social and organizational psychology at the University of Kent in the United Kingdom.
Ageism is embedded in the laws, rules, and practices of institutions, she explained. This became especially obvious during the pandemic, when health professionals had to decide who to treat, possibly using age as a proxy for making some of these decisions, she said.
“When you categorize people, you might be using stereotypes, assumptions, and expectations about age and that age group to make those decisions, and that’s where errors can occur.”
She added that ageist attitudes also become apparent at the interpersonal level by using patronizing language or offering unnecessary help to older people based on assumptions about their cognitive and physical abilities.
“Older age is often wrongly associated with declining levels of health and activity,” said Ittay Mannheim, PhD, guest postdoctoral researcher on aging and ageism at the Open University of the Netherlands. “However, older adults are a very diverse group, varying widely in many aspects, including health conditions. This stereotype can influence how healthcare professionals interact with them, assuming frailty or memory issues simply based on age. It’s important to recognize that being older doesn’t necessarily mean being ill.”
Mannheim’s research found that healthcare professionals often stand in the way of older people using technology-based treatments due to negative attitudes towards age. “So, actually, a barrier to using these technologies could be that healthcare professionals don’t think that someone can use it or won’t even offer it because someone looks old or is old,” he said.
The Impacts
Discrimination impacts the physical, mental, and social well-being of its victims. This includes attitudes towards age.
The PLOS ONE review of research on the global reach of ageism found that experienced or self-determined ageism was associated with significantly worse health outcomes across all countries examined. The same research team calculated that an estimated 6.3 million cases of depression worldwide are linked to ageism.
Other research has found that exposure to negative age stereotyping impacts willingness to adopt a healthy lifestyle in addition to increasing the risk for cardiovascular events.
What Can Be Done?
“Healthcare professionals frequently interact with older adults at their most vulnerable, which can reinforce negative stereotypes of older people being vulnerable or ill,” said Swift. “However, not all older adults fit these stereotypes. Many can live well and independently. Perhaps healthcare education should include reminders of the diverse experiences of older individuals rather than solely focusing on the moments when they require help.”
Research indicates that although progress has been made in geriatric training and the care of older individuals by healthcare education institutions, improved education and training are still needed at all levels of geriatric healthcare, including hospital administrators, physicians, nurses, personal caregivers, and associated health professions.
“Generally speaking, what healthcare professionals learn about aging tends to focus more on the biological aspects,” said Mannheim. “However, they may not fully understand what it means to be old or how to interact with older individuals, especially regarding technology. It is important to raise awareness about ageism because, in my experience working with healthcare professionals, even a single workshop on ageism can have a profound impact. Participants often respond with surprise, saying something like, ‘Wow, I never thought about this before.’”
Mannheim said that training healthcare providers to understand the aging process better could help to reduce any biases they might have and better prepare them to respond more adequately to the needs of older patients.
“We cannot devalue the lives of older people simply because they are older. It is crucial for all of us, especially governments, to acknowledge our responsibility to protect and promote human rights for individuals of all ages. If we fail to do this, the strategies we’ve witnessed during this pandemic will be repeated in the future,” said Nena Georgantzi, PhD, Barcelona-based human rights manager at AGE Platform Europe, an EU network of organizations of and for older people.
A version of this article appeared on Medscape.com.
Hoarding Disorder: A Looming National Crisis?
A report published in July 2024 by the US Senate Special Committee on Aging is calling for a national coordinated response to what the authors claim may be an emerging hoarding disorder (HD) crisis.
While millions of US adults are estimated to have HD, it is the disorder’s prevalence and severity among older adults that sounded the alarm for the Committee Chair Sen. Bob Casey (D-PA).
the report stated. Older adults made up about 16% of the US population in 2019. By 2060, that proportion is projected to soar to 25%.
The country’s aging population alone “could fuel a rise in hoarding in the coming decades,” the report authors noted.
These findings underscore the pressing need for a deeper understanding of HD, particularly as reports of its impact continue to rise. The Senate report also raises critical questions about the nature of HD: What is known about the condition? What evidence-based treatments are currently available, and are there national strategies that will prevent it from becoming a systemic crisis?
Why the Urgency?
An increase in anecdotal reports of HD in his home state prompted Casey, chair of the Senate Committee on Aging, to launch the investigation into the incidence and consequences of HD. Soon after the committee began its work, it became evident that the problem was not unique to communities in Pennsylvania. It was a nationwide issue.
“Communities throughout the United States are already grappling with HD,” the report noted.
HD is characterized by persistent difficulty discarding possessions, regardless of their monetary value. For individuals with HD, such items frequently hold meaningful reminders of past events and provide a sense of security. Difficulties with emotional regulation, executive functioning, and impulse control all contribute to the excessive buildup of clutter. Problems with attention, organization, and problem-solving are also common.
As individuals with HD age, physical limitations or disabilities may hinder their ability to discard clutter. As the accumulation increases, it can pose serious risks not only to their safety but also to public health.
Dozens of statements submitted to the Senate committee by those with HD, clinicians and social workers, first responders, social service organizations, state and federal agencies, and professional societies paint a concerning picture about the impact of hoarding on emergency and community services.
Data from the National Fire Incident Reporting System show the number of hoarding-related residential structural fires increased 26% between 2014 and 2022. Some 5242 residential fires connected to cluttered environments during that time resulted in 1367 fire service injuries, 1119 civilian injuries, and over $396 million in damages.
“For older adults, those consequences include health and safety risks, social isolation, eviction, and homelessness,” the report authors noted. “For communities, those consequences include public health concerns, increased risk of fire, and dangers to emergency responders.”
What Causes HD?
HD was once classified as a symptom of obsessive-compulsive personality disorder, with extreme causes meeting the diagnostic criteria for obsessive-compulsive disorder. That changed in 2010 when a working group recommended that HD be added to the Diagnostic and Statistical Manual of Mental Disorders (DSM), Fifth Edition, as a stand-alone disorder. That recommendation was approved in 2012.
However, a decade later, much about HD’s etiology remains unknown.
Often beginning in early adolescence, HD is a chronic and progressive condition, with genetics and trauma playing a role in its onset and course, Sanjaya Saxena, MD, director of Clinical and Research Affairs at the International OCD Foundation, said in an interview.
Between 50% and 85% of people with HD symptoms have family members with similar behavior. HD is often comorbid with other psychiatric and medical disorders, which can complicate treatment.
Results of a 2022 study showed that, compared with healthy control individuals, people with HD had widespread abnormalities in the prefrontal white matter tract which connects cortical regions involved in executive functioning, including working memory, attention, reward processing, and decision-making.
Some research also suggests that dysregulation of serotonin transmission may contribute to compulsive behaviors and the difficulty in letting go of possessions.
“We do know that there are factors that contribute to worsening of hoarding symptoms, but that’s not the same thing as what really causes it. So unfortunately, it’s still very understudied, and we don’t have great knowledge of what causes it,” Saxena said.
What Treatments Are Available?
There are currently no Food and Drug Administration–approved medications to treat HD, although some research has shown antidepressants paroxetine and venlafaxine may have some benefit. Methylphenidate and atomoxetine are also under study for HD.
Nonpharmacological therapies have shown more promising results. Among the first was a specialized cognitive-behavioral therapy (CBT) program developed by Randy Frost, PhD, professor emeritus of psychology at Smith College in Northampton, Massachusetts, and Gail Steketee, PhD, dean emerita and professor emerita of social work at Boston University in Massachusetts.
First published in 2007 and the subject of many clinical trials and studies since, the 26-session program has served as a model for psychosocial treatments for HD. The evidence-based therapy addresses various symptoms, including impulse control. One module encourages participants to develop a set of questions to consider before acquiring new items, gradually helping them build resistance to the urge to accumulate more possessions, said Frost, whose early work on HD was cited by those who supported adding the condition to the DSM in 2012.
“There are several features that I think are important including exercises in resisting acquiring and processing information when making decisions about discarding,” Frost said in an interview.
A number of studies have demonstrated the efficacy of CBT for HD, including a 2015 meta-analysis coauthored by Frost. The research showed symptom severity decreased significantly following CBT, with the largest gains in difficulty discarding and moderate improvements in clutter and acquiring.
Responses were better among women and younger patients, and although symptoms improved, posttreatment scores remained closer to the clinical range, researchers noted. It’s possible that more intervention beyond what is usually included in clinical trials — such as more sessions or adding home decluttering visits — could improve treatment response, they added.
A workshop based on the specialized CBT program has expanded the reach of the treatment. The group therapy project, Buried in Treasures (BiT), was developed by Frost, Steketee, and David Tolin, PhD, founder and director of the Anxiety Disorders Center at the Institute of Living, Hartford, and an adjunct professor of psychiatry at Yale School of Medicine, New Haven, Connecticut. The workshop is designed as a facilitated treatment that can be delivered by clinicians or trained nonclinician facilitators.
A study published in May found that more than half the participants with HD responded to the treatment, and of those, 39% reported significant reductions in HD symptoms. BiT sessions were led by trained facilitators, and the study included in-home decluttering sessions, also led by trained volunteers. Researchers said adding the home intervention could increase engagement with the group therapy.
Another study of a modified version of BiT found a 32% decrease in HD symptoms after 15 weeks of treatment delivered via video teleconference.
“The BiT workshop has been expanding around the world and has the advantage of being relatively inexpensive,” Frost said. Another advantage is that it can be run by nonclinicians, which expands treatment options in areas where mental health professionals trained to treat HD are in short supply.
However, the workshop “is not perfect, and clients usually still have symptoms at the end of the workshop,” Frost noted.
“The point is that the BiT workshop is the first step in changing a lifestyle related to possessions,” he continued. “We do certainly need to train more people in how to treat hoarding, and we need to facilitate research to make our treatments more effective.”
What’s New in the Field?
One novel program currently under study combines CBT with a cognitive rehabilitation protocol. Called Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST), the program has been shown to help older adults with HD who don’t respond to traditional CBT for HD.
The program, led by Catherine Ayers, PhD, professor of clinical psychiatry at University of California, San Diego, involves memory training and problem-solving combined with exposure therapy to help participants learn how to tolerate distress associated with discarding their possessions.
Early findings pointed to symptom improvement in older adults following 24 sessions with CREST. The program fared better than geriatric case management in a 2018 study — the first randomized controlled trial of a treatment for HD in older adults — and offered additional benefits compared with exposure therapy in a study published in February 2024.
Virtual reality is also helping people with HD. A program developed at Stanford University in California, allows people with HD to work with a therapist as they practice decluttering in a three-dimensional virtual environment created using photographs and videos of actual hoarded objects and cluttered rooms in patients’ homes.
In a small pilot study, nine people older than 55 years with HD attended 16 weeks of online facilitated therapy where they learned to better understand their attachment to those items. They practiced decluttering by selecting virtual items for recycling, donation, or trash. A virtual garbage truck even hauled away the items they had placed in the trash.
Participants were then asked to discard the actual items at home. Most participants reported a decrease in hoarding symptoms, which was confirmed following a home assessment by a clinician.
“When you pick up an object from a loved one, it still maybe has the scent of the loved one. It has these tactile cues, colors. But in the virtual world, you can take a little bit of a step back,” lead researchers Carolyn Rodriguez, MD, PhD, director of Stanford’s Hoarding Disorders Research Program, said in an interview.
“It’s a little ramp to help people practice these skills. And then what we find is that it actually translated really well. They were able to go home and actually do the real uncluttering,” Rodriguez added.
What Else Can Be Done?
While researchers like Rodriguez continue studies of new and existing treatments, the Senate report draws attention to other responses that could aid people with HD. Because of its significant impact on emergency responders, adult protective services, aging services, and housing providers, the report recommends a nationwide response to older adults with HD.
Currently, federal agencies in charge of mental and community health are not doing enough to address HD, the report’s authors noted.
The report demonstrates “the scope and severity of these challenges and offers a path forward for how we can help people, communities, and local governments contend with this condition,” Casey said.
Specifically, the document cites a lack of HD services and tracking by the Substance Abuse and Mental Health Services Administration, the Administration for Community Living, and the Centers for Disease Control and Prevention.
The committee recommended these agencies collaborate to improve HD data collection, which will be critical to managing a potential spike in cases as the population ages. The committee also suggested awareness and training campaigns to better educate clinicians, social service providers, court officials, and first responders about HD.
Further, the report’s authors called for the Department of Housing and Urban Development to provide guidance and technical assistance on HD for landlords and housing assistance programs and urged Congress to collaborate with the Centers for Medicare & Medicaid Services to expand coverage for hoarding treatments.
Finally, the committee encouraged policymakers to engage directly with individuals affected by HD and their families to better understand the impact of the disorder and inform policy development.
“I think the Senate report focuses on education, not just for therapists, but other stakeholders too,” Frost said. “There are lots of other professionals who have a stake in this process, housing specialists, elder service folks, health and human services. Awareness of this problem is something that’s important for them as well.”
Rodriguez characterized the report’s recommendations as “potentially lifesaving” for individuals with HD. She added that it represents the first step in an ongoing effort to address an impending public health crisis related to HD in older adults and its broader impact on communities.
A spokesperson with Casey’s office said it’s unclear whether any federal agencies have acted on the report recommendations since it was released in June. It’s also unknown whether the Senate Committee on Aging will pursue any additional work on HD when new committee leaders are appointed in 2025.
“Although some federal agencies have taken steps to address HD, those steps are frequently limited. Other relevant agencies have not addressed HD at all in recent years,” report authors wrote. “The federal government can, and should, do more to bolster the response to HD.”
Frost agreed.
“I think federal agencies can have a positive effect by promoting, supporting, and tracking local efforts in dealing with this problem,” he said.
With reporting from Eve Bender.
A version of this article appeared on Medscape.com.
A report published in July 2024 by the US Senate Special Committee on Aging is calling for a national coordinated response to what the authors claim may be an emerging hoarding disorder (HD) crisis.
While millions of US adults are estimated to have HD, it is the disorder’s prevalence and severity among older adults that sounded the alarm for the Committee Chair Sen. Bob Casey (D-PA).
the report stated. Older adults made up about 16% of the US population in 2019. By 2060, that proportion is projected to soar to 25%.
The country’s aging population alone “could fuel a rise in hoarding in the coming decades,” the report authors noted.
These findings underscore the pressing need for a deeper understanding of HD, particularly as reports of its impact continue to rise. The Senate report also raises critical questions about the nature of HD: What is known about the condition? What evidence-based treatments are currently available, and are there national strategies that will prevent it from becoming a systemic crisis?
Why the Urgency?
An increase in anecdotal reports of HD in his home state prompted Casey, chair of the Senate Committee on Aging, to launch the investigation into the incidence and consequences of HD. Soon after the committee began its work, it became evident that the problem was not unique to communities in Pennsylvania. It was a nationwide issue.
“Communities throughout the United States are already grappling with HD,” the report noted.
HD is characterized by persistent difficulty discarding possessions, regardless of their monetary value. For individuals with HD, such items frequently hold meaningful reminders of past events and provide a sense of security. Difficulties with emotional regulation, executive functioning, and impulse control all contribute to the excessive buildup of clutter. Problems with attention, organization, and problem-solving are also common.
As individuals with HD age, physical limitations or disabilities may hinder their ability to discard clutter. As the accumulation increases, it can pose serious risks not only to their safety but also to public health.
Dozens of statements submitted to the Senate committee by those with HD, clinicians and social workers, first responders, social service organizations, state and federal agencies, and professional societies paint a concerning picture about the impact of hoarding on emergency and community services.
Data from the National Fire Incident Reporting System show the number of hoarding-related residential structural fires increased 26% between 2014 and 2022. Some 5242 residential fires connected to cluttered environments during that time resulted in 1367 fire service injuries, 1119 civilian injuries, and over $396 million in damages.
“For older adults, those consequences include health and safety risks, social isolation, eviction, and homelessness,” the report authors noted. “For communities, those consequences include public health concerns, increased risk of fire, and dangers to emergency responders.”
What Causes HD?
HD was once classified as a symptom of obsessive-compulsive personality disorder, with extreme causes meeting the diagnostic criteria for obsessive-compulsive disorder. That changed in 2010 when a working group recommended that HD be added to the Diagnostic and Statistical Manual of Mental Disorders (DSM), Fifth Edition, as a stand-alone disorder. That recommendation was approved in 2012.
However, a decade later, much about HD’s etiology remains unknown.
Often beginning in early adolescence, HD is a chronic and progressive condition, with genetics and trauma playing a role in its onset and course, Sanjaya Saxena, MD, director of Clinical and Research Affairs at the International OCD Foundation, said in an interview.
Between 50% and 85% of people with HD symptoms have family members with similar behavior. HD is often comorbid with other psychiatric and medical disorders, which can complicate treatment.
Results of a 2022 study showed that, compared with healthy control individuals, people with HD had widespread abnormalities in the prefrontal white matter tract which connects cortical regions involved in executive functioning, including working memory, attention, reward processing, and decision-making.
Some research also suggests that dysregulation of serotonin transmission may contribute to compulsive behaviors and the difficulty in letting go of possessions.
“We do know that there are factors that contribute to worsening of hoarding symptoms, but that’s not the same thing as what really causes it. So unfortunately, it’s still very understudied, and we don’t have great knowledge of what causes it,” Saxena said.
What Treatments Are Available?
There are currently no Food and Drug Administration–approved medications to treat HD, although some research has shown antidepressants paroxetine and venlafaxine may have some benefit. Methylphenidate and atomoxetine are also under study for HD.
Nonpharmacological therapies have shown more promising results. Among the first was a specialized cognitive-behavioral therapy (CBT) program developed by Randy Frost, PhD, professor emeritus of psychology at Smith College in Northampton, Massachusetts, and Gail Steketee, PhD, dean emerita and professor emerita of social work at Boston University in Massachusetts.
First published in 2007 and the subject of many clinical trials and studies since, the 26-session program has served as a model for psychosocial treatments for HD. The evidence-based therapy addresses various symptoms, including impulse control. One module encourages participants to develop a set of questions to consider before acquiring new items, gradually helping them build resistance to the urge to accumulate more possessions, said Frost, whose early work on HD was cited by those who supported adding the condition to the DSM in 2012.
“There are several features that I think are important including exercises in resisting acquiring and processing information when making decisions about discarding,” Frost said in an interview.
A number of studies have demonstrated the efficacy of CBT for HD, including a 2015 meta-analysis coauthored by Frost. The research showed symptom severity decreased significantly following CBT, with the largest gains in difficulty discarding and moderate improvements in clutter and acquiring.
Responses were better among women and younger patients, and although symptoms improved, posttreatment scores remained closer to the clinical range, researchers noted. It’s possible that more intervention beyond what is usually included in clinical trials — such as more sessions or adding home decluttering visits — could improve treatment response, they added.
A workshop based on the specialized CBT program has expanded the reach of the treatment. The group therapy project, Buried in Treasures (BiT), was developed by Frost, Steketee, and David Tolin, PhD, founder and director of the Anxiety Disorders Center at the Institute of Living, Hartford, and an adjunct professor of psychiatry at Yale School of Medicine, New Haven, Connecticut. The workshop is designed as a facilitated treatment that can be delivered by clinicians or trained nonclinician facilitators.
A study published in May found that more than half the participants with HD responded to the treatment, and of those, 39% reported significant reductions in HD symptoms. BiT sessions were led by trained facilitators, and the study included in-home decluttering sessions, also led by trained volunteers. Researchers said adding the home intervention could increase engagement with the group therapy.
Another study of a modified version of BiT found a 32% decrease in HD symptoms after 15 weeks of treatment delivered via video teleconference.
“The BiT workshop has been expanding around the world and has the advantage of being relatively inexpensive,” Frost said. Another advantage is that it can be run by nonclinicians, which expands treatment options in areas where mental health professionals trained to treat HD are in short supply.
However, the workshop “is not perfect, and clients usually still have symptoms at the end of the workshop,” Frost noted.
“The point is that the BiT workshop is the first step in changing a lifestyle related to possessions,” he continued. “We do certainly need to train more people in how to treat hoarding, and we need to facilitate research to make our treatments more effective.”
What’s New in the Field?
One novel program currently under study combines CBT with a cognitive rehabilitation protocol. Called Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST), the program has been shown to help older adults with HD who don’t respond to traditional CBT for HD.
The program, led by Catherine Ayers, PhD, professor of clinical psychiatry at University of California, San Diego, involves memory training and problem-solving combined with exposure therapy to help participants learn how to tolerate distress associated with discarding their possessions.
Early findings pointed to symptom improvement in older adults following 24 sessions with CREST. The program fared better than geriatric case management in a 2018 study — the first randomized controlled trial of a treatment for HD in older adults — and offered additional benefits compared with exposure therapy in a study published in February 2024.
Virtual reality is also helping people with HD. A program developed at Stanford University in California, allows people with HD to work with a therapist as they practice decluttering in a three-dimensional virtual environment created using photographs and videos of actual hoarded objects and cluttered rooms in patients’ homes.
In a small pilot study, nine people older than 55 years with HD attended 16 weeks of online facilitated therapy where they learned to better understand their attachment to those items. They practiced decluttering by selecting virtual items for recycling, donation, or trash. A virtual garbage truck even hauled away the items they had placed in the trash.
Participants were then asked to discard the actual items at home. Most participants reported a decrease in hoarding symptoms, which was confirmed following a home assessment by a clinician.
“When you pick up an object from a loved one, it still maybe has the scent of the loved one. It has these tactile cues, colors. But in the virtual world, you can take a little bit of a step back,” lead researchers Carolyn Rodriguez, MD, PhD, director of Stanford’s Hoarding Disorders Research Program, said in an interview.
“It’s a little ramp to help people practice these skills. And then what we find is that it actually translated really well. They were able to go home and actually do the real uncluttering,” Rodriguez added.
What Else Can Be Done?
While researchers like Rodriguez continue studies of new and existing treatments, the Senate report draws attention to other responses that could aid people with HD. Because of its significant impact on emergency responders, adult protective services, aging services, and housing providers, the report recommends a nationwide response to older adults with HD.
Currently, federal agencies in charge of mental and community health are not doing enough to address HD, the report’s authors noted.
The report demonstrates “the scope and severity of these challenges and offers a path forward for how we can help people, communities, and local governments contend with this condition,” Casey said.
Specifically, the document cites a lack of HD services and tracking by the Substance Abuse and Mental Health Services Administration, the Administration for Community Living, and the Centers for Disease Control and Prevention.
The committee recommended these agencies collaborate to improve HD data collection, which will be critical to managing a potential spike in cases as the population ages. The committee also suggested awareness and training campaigns to better educate clinicians, social service providers, court officials, and first responders about HD.
Further, the report’s authors called for the Department of Housing and Urban Development to provide guidance and technical assistance on HD for landlords and housing assistance programs and urged Congress to collaborate with the Centers for Medicare & Medicaid Services to expand coverage for hoarding treatments.
Finally, the committee encouraged policymakers to engage directly with individuals affected by HD and their families to better understand the impact of the disorder and inform policy development.
“I think the Senate report focuses on education, not just for therapists, but other stakeholders too,” Frost said. “There are lots of other professionals who have a stake in this process, housing specialists, elder service folks, health and human services. Awareness of this problem is something that’s important for them as well.”
Rodriguez characterized the report’s recommendations as “potentially lifesaving” for individuals with HD. She added that it represents the first step in an ongoing effort to address an impending public health crisis related to HD in older adults and its broader impact on communities.
A spokesperson with Casey’s office said it’s unclear whether any federal agencies have acted on the report recommendations since it was released in June. It’s also unknown whether the Senate Committee on Aging will pursue any additional work on HD when new committee leaders are appointed in 2025.
“Although some federal agencies have taken steps to address HD, those steps are frequently limited. Other relevant agencies have not addressed HD at all in recent years,” report authors wrote. “The federal government can, and should, do more to bolster the response to HD.”
Frost agreed.
“I think federal agencies can have a positive effect by promoting, supporting, and tracking local efforts in dealing with this problem,” he said.
With reporting from Eve Bender.
A version of this article appeared on Medscape.com.
A report published in July 2024 by the US Senate Special Committee on Aging is calling for a national coordinated response to what the authors claim may be an emerging hoarding disorder (HD) crisis.
While millions of US adults are estimated to have HD, it is the disorder’s prevalence and severity among older adults that sounded the alarm for the Committee Chair Sen. Bob Casey (D-PA).
the report stated. Older adults made up about 16% of the US population in 2019. By 2060, that proportion is projected to soar to 25%.
The country’s aging population alone “could fuel a rise in hoarding in the coming decades,” the report authors noted.
These findings underscore the pressing need for a deeper understanding of HD, particularly as reports of its impact continue to rise. The Senate report also raises critical questions about the nature of HD: What is known about the condition? What evidence-based treatments are currently available, and are there national strategies that will prevent it from becoming a systemic crisis?
Why the Urgency?
An increase in anecdotal reports of HD in his home state prompted Casey, chair of the Senate Committee on Aging, to launch the investigation into the incidence and consequences of HD. Soon after the committee began its work, it became evident that the problem was not unique to communities in Pennsylvania. It was a nationwide issue.
“Communities throughout the United States are already grappling with HD,” the report noted.
HD is characterized by persistent difficulty discarding possessions, regardless of their monetary value. For individuals with HD, such items frequently hold meaningful reminders of past events and provide a sense of security. Difficulties with emotional regulation, executive functioning, and impulse control all contribute to the excessive buildup of clutter. Problems with attention, organization, and problem-solving are also common.
As individuals with HD age, physical limitations or disabilities may hinder their ability to discard clutter. As the accumulation increases, it can pose serious risks not only to their safety but also to public health.
Dozens of statements submitted to the Senate committee by those with HD, clinicians and social workers, first responders, social service organizations, state and federal agencies, and professional societies paint a concerning picture about the impact of hoarding on emergency and community services.
Data from the National Fire Incident Reporting System show the number of hoarding-related residential structural fires increased 26% between 2014 and 2022. Some 5242 residential fires connected to cluttered environments during that time resulted in 1367 fire service injuries, 1119 civilian injuries, and over $396 million in damages.
“For older adults, those consequences include health and safety risks, social isolation, eviction, and homelessness,” the report authors noted. “For communities, those consequences include public health concerns, increased risk of fire, and dangers to emergency responders.”
What Causes HD?
HD was once classified as a symptom of obsessive-compulsive personality disorder, with extreme causes meeting the diagnostic criteria for obsessive-compulsive disorder. That changed in 2010 when a working group recommended that HD be added to the Diagnostic and Statistical Manual of Mental Disorders (DSM), Fifth Edition, as a stand-alone disorder. That recommendation was approved in 2012.
However, a decade later, much about HD’s etiology remains unknown.
Often beginning in early adolescence, HD is a chronic and progressive condition, with genetics and trauma playing a role in its onset and course, Sanjaya Saxena, MD, director of Clinical and Research Affairs at the International OCD Foundation, said in an interview.
Between 50% and 85% of people with HD symptoms have family members with similar behavior. HD is often comorbid with other psychiatric and medical disorders, which can complicate treatment.
Results of a 2022 study showed that, compared with healthy control individuals, people with HD had widespread abnormalities in the prefrontal white matter tract which connects cortical regions involved in executive functioning, including working memory, attention, reward processing, and decision-making.
Some research also suggests that dysregulation of serotonin transmission may contribute to compulsive behaviors and the difficulty in letting go of possessions.
“We do know that there are factors that contribute to worsening of hoarding symptoms, but that’s not the same thing as what really causes it. So unfortunately, it’s still very understudied, and we don’t have great knowledge of what causes it,” Saxena said.
What Treatments Are Available?
There are currently no Food and Drug Administration–approved medications to treat HD, although some research has shown antidepressants paroxetine and venlafaxine may have some benefit. Methylphenidate and atomoxetine are also under study for HD.
Nonpharmacological therapies have shown more promising results. Among the first was a specialized cognitive-behavioral therapy (CBT) program developed by Randy Frost, PhD, professor emeritus of psychology at Smith College in Northampton, Massachusetts, and Gail Steketee, PhD, dean emerita and professor emerita of social work at Boston University in Massachusetts.
First published in 2007 and the subject of many clinical trials and studies since, the 26-session program has served as a model for psychosocial treatments for HD. The evidence-based therapy addresses various symptoms, including impulse control. One module encourages participants to develop a set of questions to consider before acquiring new items, gradually helping them build resistance to the urge to accumulate more possessions, said Frost, whose early work on HD was cited by those who supported adding the condition to the DSM in 2012.
“There are several features that I think are important including exercises in resisting acquiring and processing information when making decisions about discarding,” Frost said in an interview.
A number of studies have demonstrated the efficacy of CBT for HD, including a 2015 meta-analysis coauthored by Frost. The research showed symptom severity decreased significantly following CBT, with the largest gains in difficulty discarding and moderate improvements in clutter and acquiring.
Responses were better among women and younger patients, and although symptoms improved, posttreatment scores remained closer to the clinical range, researchers noted. It’s possible that more intervention beyond what is usually included in clinical trials — such as more sessions or adding home decluttering visits — could improve treatment response, they added.
A workshop based on the specialized CBT program has expanded the reach of the treatment. The group therapy project, Buried in Treasures (BiT), was developed by Frost, Steketee, and David Tolin, PhD, founder and director of the Anxiety Disorders Center at the Institute of Living, Hartford, and an adjunct professor of psychiatry at Yale School of Medicine, New Haven, Connecticut. The workshop is designed as a facilitated treatment that can be delivered by clinicians or trained nonclinician facilitators.
A study published in May found that more than half the participants with HD responded to the treatment, and of those, 39% reported significant reductions in HD symptoms. BiT sessions were led by trained facilitators, and the study included in-home decluttering sessions, also led by trained volunteers. Researchers said adding the home intervention could increase engagement with the group therapy.
Another study of a modified version of BiT found a 32% decrease in HD symptoms after 15 weeks of treatment delivered via video teleconference.
“The BiT workshop has been expanding around the world and has the advantage of being relatively inexpensive,” Frost said. Another advantage is that it can be run by nonclinicians, which expands treatment options in areas where mental health professionals trained to treat HD are in short supply.
However, the workshop “is not perfect, and clients usually still have symptoms at the end of the workshop,” Frost noted.
“The point is that the BiT workshop is the first step in changing a lifestyle related to possessions,” he continued. “We do certainly need to train more people in how to treat hoarding, and we need to facilitate research to make our treatments more effective.”
What’s New in the Field?
One novel program currently under study combines CBT with a cognitive rehabilitation protocol. Called Cognitive Rehabilitation and Exposure/Sorting Therapy (CREST), the program has been shown to help older adults with HD who don’t respond to traditional CBT for HD.
The program, led by Catherine Ayers, PhD, professor of clinical psychiatry at University of California, San Diego, involves memory training and problem-solving combined with exposure therapy to help participants learn how to tolerate distress associated with discarding their possessions.
Early findings pointed to symptom improvement in older adults following 24 sessions with CREST. The program fared better than geriatric case management in a 2018 study — the first randomized controlled trial of a treatment for HD in older adults — and offered additional benefits compared with exposure therapy in a study published in February 2024.
Virtual reality is also helping people with HD. A program developed at Stanford University in California, allows people with HD to work with a therapist as they practice decluttering in a three-dimensional virtual environment created using photographs and videos of actual hoarded objects and cluttered rooms in patients’ homes.
In a small pilot study, nine people older than 55 years with HD attended 16 weeks of online facilitated therapy where they learned to better understand their attachment to those items. They practiced decluttering by selecting virtual items for recycling, donation, or trash. A virtual garbage truck even hauled away the items they had placed in the trash.
Participants were then asked to discard the actual items at home. Most participants reported a decrease in hoarding symptoms, which was confirmed following a home assessment by a clinician.
“When you pick up an object from a loved one, it still maybe has the scent of the loved one. It has these tactile cues, colors. But in the virtual world, you can take a little bit of a step back,” lead researchers Carolyn Rodriguez, MD, PhD, director of Stanford’s Hoarding Disorders Research Program, said in an interview.
“It’s a little ramp to help people practice these skills. And then what we find is that it actually translated really well. They were able to go home and actually do the real uncluttering,” Rodriguez added.
What Else Can Be Done?
While researchers like Rodriguez continue studies of new and existing treatments, the Senate report draws attention to other responses that could aid people with HD. Because of its significant impact on emergency responders, adult protective services, aging services, and housing providers, the report recommends a nationwide response to older adults with HD.
Currently, federal agencies in charge of mental and community health are not doing enough to address HD, the report’s authors noted.
The report demonstrates “the scope and severity of these challenges and offers a path forward for how we can help people, communities, and local governments contend with this condition,” Casey said.
Specifically, the document cites a lack of HD services and tracking by the Substance Abuse and Mental Health Services Administration, the Administration for Community Living, and the Centers for Disease Control and Prevention.
The committee recommended these agencies collaborate to improve HD data collection, which will be critical to managing a potential spike in cases as the population ages. The committee also suggested awareness and training campaigns to better educate clinicians, social service providers, court officials, and first responders about HD.
Further, the report’s authors called for the Department of Housing and Urban Development to provide guidance and technical assistance on HD for landlords and housing assistance programs and urged Congress to collaborate with the Centers for Medicare & Medicaid Services to expand coverage for hoarding treatments.
Finally, the committee encouraged policymakers to engage directly with individuals affected by HD and their families to better understand the impact of the disorder and inform policy development.
“I think the Senate report focuses on education, not just for therapists, but other stakeholders too,” Frost said. “There are lots of other professionals who have a stake in this process, housing specialists, elder service folks, health and human services. Awareness of this problem is something that’s important for them as well.”
Rodriguez characterized the report’s recommendations as “potentially lifesaving” for individuals with HD. She added that it represents the first step in an ongoing effort to address an impending public health crisis related to HD in older adults and its broader impact on communities.
A spokesperson with Casey’s office said it’s unclear whether any federal agencies have acted on the report recommendations since it was released in June. It’s also unknown whether the Senate Committee on Aging will pursue any additional work on HD when new committee leaders are appointed in 2025.
“Although some federal agencies have taken steps to address HD, those steps are frequently limited. Other relevant agencies have not addressed HD at all in recent years,” report authors wrote. “The federal government can, and should, do more to bolster the response to HD.”
Frost agreed.
“I think federal agencies can have a positive effect by promoting, supporting, and tracking local efforts in dealing with this problem,” he said.
With reporting from Eve Bender.
A version of this article appeared on Medscape.com.
