User login
What’s new in brain health?
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
This transcript has been edited for clarity.
Dear colleagues, I am Christoph Diener from the medical faculty of the University of Duisburg-Essen in Germany.
Treatment of tension-type headache
I would like to start with headache. You are all aware that we have several new studies regarding the prevention of migraine, but very few studies involving nondrug treatments for tension-type headache.
A working group in Göttingen, Germany, conducted a study in people with frequent episodic and chronic tension-type headache. The first of the four randomized groups received traditional Chinese acupuncture for 3 months. The second group received physical therapy and exercise for 1 hour per week for 12 weeks. The third group received a combination of acupuncture and exercise. The last was a control group that received only standard care.
The outcome parameters of tension-type headache were evaluated after 6 months and again after 12 months. Previously, these same researchers published that the intensity but not the frequency of tension-type headache was reduced by active therapy.
In Cephalalgia, they published the outcome for the endpoints of depression, anxiety, and quality of life. Acupuncture, exercise, and the combination of the two improved depression, anxiety, and quality of life. This shows that nonmedical treatment is effective in people with frequent episodic and chronic tension-type headache.
Headache after COVID-19
The next study was published in Headache and discusses headache after COVID-19. In this review of published studies, more than 50% of people with COVID-19 develop headache. It is more frequent in young patients and people with preexisting primary headaches, such as migraine and tension-type headache. Prognosis is usually good, but some patients develop new, daily persistent headache, which is a major problem because treatment is unclear. We desperately need studies investigating how to treat this new, daily persistent headache after COVID-19.
SSRIs during COVID-19 infection
The next study also focuses on COVID-19. We have conflicting results from several studies suggesting that selective serotonin reuptake inhibitors might be effective in people with mild COVID-19 infection. This hypothesis was tested in a study in Brazil and was published in JAMA, The study included 1,288 outpatients with mild COVID-19 who either received 50 mg of fluvoxamine twice daily for 10 days or placebo. There was no benefit of the treatment for any outcome.
Preventing dementia with antihypertensive treatment
The next study was published in the European Heart Journal and addresses the question of whether effective antihypertensive treatment in elderly persons can prevent dementia. This is a meta-analysis of five placebo-controlled trials with more than 28,000 patients. The meta-analysis clearly shows that treating hypertension in elderly patients does prevent dementia. The benefit is higher if the blood pressure is lowered by a larger amount which also stays true for elderly patients. There is no negative impact of lowering blood pressure in this population.
Antiplatelet therapy
The next study was published in Stroke and reexamines whether resumption of antiplatelet therapy should be early or late in people who had an intracerebral hemorrhage while on antiplatelet therapy. In the Taiwanese Health Registry, this was studied in 1,584 patients. The researchers divided participants into groups based on whether antiplatelet therapy was resumed within 30 days or after 30 days. In 1 year, the rate of recurrent intracerebral hemorrhage was 3.2%. There was no difference whether antiplatelet therapy was resumed early or late.
Regular exercise in Parkinson’s disease
The final study is a review of nonmedical therapy. This meta-analysis of 19 randomized trials looked at the benefit of regular exercise in patients with Parkinson’s disease and depression. The analysis clearly showed that rigorous and moderate exercise improved depression in patients with Parkinson’s disease. This is very important because exercise improves not only the symptoms of Parkinson’s disease but also comorbid depression while presenting no serious adverse events or side effects.
Dr. Diener is a professor in the department of neurology at Stroke Center–Headache Center, University Duisburg-Essen, Germany. He disclosed ties with Abbott, Addex Pharma, Alder, Allergan, Almirall, Amgen, Autonomic Technology, AstraZeneca, Bayer Vital, Berlin Chemie, Bristol-Myers Squibb, Boehringer Ingelheim, Chordate, CoAxia, Corimmun, Covidien, Coherex, CoLucid, Daiichi Sankyo, D-Pharm, Electrocore, Fresenius, GlaxoSmithKline, Grunenthal, Janssen-Cilag, Labrys Biologics Lilly, La Roche, Lundbeck, 3M Medica, MSD, Medtronic, Menarini, MindFrame, Minster, Neuroscore, Neurobiological Technologies, Novartis, Novo Nordisk, Johnson & Johnson, Knoll, Paion, Parke-Davis, Pierre Fabre, Pfizer Inc, Schaper and Brummer, Sanofi-Aventis, Schering-Plough, Servier, Solvay, St. Jude, Talecris, Thrombogenics, WebMD Global, Weber and Weber, Wyeth, and Yamanouchi. Dr. Diener has served as editor of Aktuelle Neurologie, Arzneimitteltherapie, Kopfschmerz News, Stroke News, and the Treatment Guidelines of the German Neurological Society; as co-editor of Cephalalgia; and on the editorial board of The Lancet Neurology, Stroke, European Neurology, and Cerebrovascular Disorders. The department of neurology in Essen is supported by the German Research Council, the German Ministry of Education and Research, European Union, National Institutes of Health, Bertelsmann Foundation, and Heinz Nixdorf Foundation. Dr. Diener has no ownership interest and does not own stocks in any pharmaceutical company. A version of this article originally appeared on Medscape.com.
A doctor must go to extremes to save a choking victim
Some time ago I was invited to join a bipartisan congressional task force on valley fever, also known as coccidioidomycosis. A large and diverse crowd attended the task force’s first meeting in Bakersfield, Calif. – a meeting for everyone: the medical profession, the public, it even included veterinarians.
The whole thing was a resounding success. Francis Collins was there, the just-retired director of the NIH. Tom Frieden, then-director of the Centers for Disease Control and Prevention was there, as were several congresspeople and also my college roommate, a retired Navy medical corps captain. I was enjoying it.
Afterward, we had a banquet dinner at a restaurant in downtown Bakersfield. One of the people there was a woman I knew well – her husband was a physician friend. The restaurant served steak and salmon, and this woman made the mistake of ordering the steak.
Not long after the entrees were served, I heard a commotion at the table just behind me. I turned around and saw that woman in distress. A piece of steak had wedged in her trachea and she couldn’t breathe.
Almost immediately, the chef showed up. I don’t know how he got there. The chef at this restaurant was a big guy. I mean, probably 6 feet, 5 inches tall and 275 pounds. He tried the Heimlich maneuver. It didn’t work.
At that point, I jumped up. I thought, “Well, maybe I know how to do this better than him.” Probably not, actually. I tried and couldn’t make it work either. So I knew we were going to have to do something.
Paul Krogstad, my friend and research partner who is a pediatric infectious disease physician, stepped up and tried to put his finger in her throat and dig it out. He couldn’t get it. The patient had lost consciousness.
So, I’m thinking, okay, there’s really only one choice. You have to get an airway surgically.
I said, “We have to put her down on the floor.” And then I said, “Knife!”
I was looking at the steak knives on the table and they weren’t to my liking for doing a procedure. My college roommate – the retired Navy man – whipped out this very good pocketknife.
I had never done this in my life.
While I was making the incision, somebody gave Paul a ballpoint pen and he broke it into pieces to make a tracheostomy tube. Once I’d made the little incision, I put the tube in. She wasn’t breathing, but she still had a pulse.
I leaned forward and blew into the tube and inflated her lungs. I could see her lungs balloon up. It was a nice feeling, because I knew I was clearly in the right place.
I can’t quite explain it, but while I was doing this, I was enormously calm and totally focused. I knew there was a crowd of people around me, all looking at me, but I wasn’t conscious of that.
It was really just the four of us: Paul and Tom and me and our patient. Those were the only people that I was really cognizant of. Paul and Tom were not panic stricken at all. I remember somebody shouting, “We have to start CPR!” and Frieden said, “No. We don’t.”
Moments later, she woke up, sat up, coughed, and shot the piece of steak across the room.
She was breathing on her own, but we still taped that tube into place. Somebody had already summoned an ambulance; they were there not very long after we completed this procedure. I got in the ambulance with her and we rode over to the emergency room at Mercy Truxtun.
She was stable and doing okay. I sat with her until a thoracic surgeon showed up. He checked out the situation and decided we didn’t need that tube and took it out. I didn’t want to take that out until I had a surgeon there who could do a formal tracheostomy.
They kept her in the hospital for 3 or 4 days. Now, this woman had always had difficulties swallowing, so steak may not have been the best choice. She still had trouble swallowing afterward but recovered.
I’ve known her and her husband a long time, so it was certainly rewarding to be able to provide this service. Years later, though, when her husband died, I spoke at his funeral. When she was speaking to the gathering, she said, “And oh, by the way, Royce, thanks for saving my life.”
That surprised me. I didn’t think we were going to go there.
I’d never tried to practice medicine “at the roadside” before. But that’s part of the career.
Royce Johnson, MD, is the chief of the division of infectious disease among other leadership positions at Kern Medical in Bakersfield, Calif., and the medical director of the Valley Fever Institute.
A version of this article first appeared on Medscape.com.
Some time ago I was invited to join a bipartisan congressional task force on valley fever, also known as coccidioidomycosis. A large and diverse crowd attended the task force’s first meeting in Bakersfield, Calif. – a meeting for everyone: the medical profession, the public, it even included veterinarians.
The whole thing was a resounding success. Francis Collins was there, the just-retired director of the NIH. Tom Frieden, then-director of the Centers for Disease Control and Prevention was there, as were several congresspeople and also my college roommate, a retired Navy medical corps captain. I was enjoying it.
Afterward, we had a banquet dinner at a restaurant in downtown Bakersfield. One of the people there was a woman I knew well – her husband was a physician friend. The restaurant served steak and salmon, and this woman made the mistake of ordering the steak.
Not long after the entrees were served, I heard a commotion at the table just behind me. I turned around and saw that woman in distress. A piece of steak had wedged in her trachea and she couldn’t breathe.
Almost immediately, the chef showed up. I don’t know how he got there. The chef at this restaurant was a big guy. I mean, probably 6 feet, 5 inches tall and 275 pounds. He tried the Heimlich maneuver. It didn’t work.
At that point, I jumped up. I thought, “Well, maybe I know how to do this better than him.” Probably not, actually. I tried and couldn’t make it work either. So I knew we were going to have to do something.
Paul Krogstad, my friend and research partner who is a pediatric infectious disease physician, stepped up and tried to put his finger in her throat and dig it out. He couldn’t get it. The patient had lost consciousness.
So, I’m thinking, okay, there’s really only one choice. You have to get an airway surgically.
I said, “We have to put her down on the floor.” And then I said, “Knife!”
I was looking at the steak knives on the table and they weren’t to my liking for doing a procedure. My college roommate – the retired Navy man – whipped out this very good pocketknife.
I had never done this in my life.
While I was making the incision, somebody gave Paul a ballpoint pen and he broke it into pieces to make a tracheostomy tube. Once I’d made the little incision, I put the tube in. She wasn’t breathing, but she still had a pulse.
I leaned forward and blew into the tube and inflated her lungs. I could see her lungs balloon up. It was a nice feeling, because I knew I was clearly in the right place.
I can’t quite explain it, but while I was doing this, I was enormously calm and totally focused. I knew there was a crowd of people around me, all looking at me, but I wasn’t conscious of that.
It was really just the four of us: Paul and Tom and me and our patient. Those were the only people that I was really cognizant of. Paul and Tom were not panic stricken at all. I remember somebody shouting, “We have to start CPR!” and Frieden said, “No. We don’t.”
Moments later, she woke up, sat up, coughed, and shot the piece of steak across the room.
She was breathing on her own, but we still taped that tube into place. Somebody had already summoned an ambulance; they were there not very long after we completed this procedure. I got in the ambulance with her and we rode over to the emergency room at Mercy Truxtun.
She was stable and doing okay. I sat with her until a thoracic surgeon showed up. He checked out the situation and decided we didn’t need that tube and took it out. I didn’t want to take that out until I had a surgeon there who could do a formal tracheostomy.
They kept her in the hospital for 3 or 4 days. Now, this woman had always had difficulties swallowing, so steak may not have been the best choice. She still had trouble swallowing afterward but recovered.
I’ve known her and her husband a long time, so it was certainly rewarding to be able to provide this service. Years later, though, when her husband died, I spoke at his funeral. When she was speaking to the gathering, she said, “And oh, by the way, Royce, thanks for saving my life.”
That surprised me. I didn’t think we were going to go there.
I’d never tried to practice medicine “at the roadside” before. But that’s part of the career.
Royce Johnson, MD, is the chief of the division of infectious disease among other leadership positions at Kern Medical in Bakersfield, Calif., and the medical director of the Valley Fever Institute.
A version of this article first appeared on Medscape.com.
Some time ago I was invited to join a bipartisan congressional task force on valley fever, also known as coccidioidomycosis. A large and diverse crowd attended the task force’s first meeting in Bakersfield, Calif. – a meeting for everyone: the medical profession, the public, it even included veterinarians.
The whole thing was a resounding success. Francis Collins was there, the just-retired director of the NIH. Tom Frieden, then-director of the Centers for Disease Control and Prevention was there, as were several congresspeople and also my college roommate, a retired Navy medical corps captain. I was enjoying it.
Afterward, we had a banquet dinner at a restaurant in downtown Bakersfield. One of the people there was a woman I knew well – her husband was a physician friend. The restaurant served steak and salmon, and this woman made the mistake of ordering the steak.
Not long after the entrees were served, I heard a commotion at the table just behind me. I turned around and saw that woman in distress. A piece of steak had wedged in her trachea and she couldn’t breathe.
Almost immediately, the chef showed up. I don’t know how he got there. The chef at this restaurant was a big guy. I mean, probably 6 feet, 5 inches tall and 275 pounds. He tried the Heimlich maneuver. It didn’t work.
At that point, I jumped up. I thought, “Well, maybe I know how to do this better than him.” Probably not, actually. I tried and couldn’t make it work either. So I knew we were going to have to do something.
Paul Krogstad, my friend and research partner who is a pediatric infectious disease physician, stepped up and tried to put his finger in her throat and dig it out. He couldn’t get it. The patient had lost consciousness.
So, I’m thinking, okay, there’s really only one choice. You have to get an airway surgically.
I said, “We have to put her down on the floor.” And then I said, “Knife!”
I was looking at the steak knives on the table and they weren’t to my liking for doing a procedure. My college roommate – the retired Navy man – whipped out this very good pocketknife.
I had never done this in my life.
While I was making the incision, somebody gave Paul a ballpoint pen and he broke it into pieces to make a tracheostomy tube. Once I’d made the little incision, I put the tube in. She wasn’t breathing, but she still had a pulse.
I leaned forward and blew into the tube and inflated her lungs. I could see her lungs balloon up. It was a nice feeling, because I knew I was clearly in the right place.
I can’t quite explain it, but while I was doing this, I was enormously calm and totally focused. I knew there was a crowd of people around me, all looking at me, but I wasn’t conscious of that.
It was really just the four of us: Paul and Tom and me and our patient. Those were the only people that I was really cognizant of. Paul and Tom were not panic stricken at all. I remember somebody shouting, “We have to start CPR!” and Frieden said, “No. We don’t.”
Moments later, she woke up, sat up, coughed, and shot the piece of steak across the room.
She was breathing on her own, but we still taped that tube into place. Somebody had already summoned an ambulance; they were there not very long after we completed this procedure. I got in the ambulance with her and we rode over to the emergency room at Mercy Truxtun.
She was stable and doing okay. I sat with her until a thoracic surgeon showed up. He checked out the situation and decided we didn’t need that tube and took it out. I didn’t want to take that out until I had a surgeon there who could do a formal tracheostomy.
They kept her in the hospital for 3 or 4 days. Now, this woman had always had difficulties swallowing, so steak may not have been the best choice. She still had trouble swallowing afterward but recovered.
I’ve known her and her husband a long time, so it was certainly rewarding to be able to provide this service. Years later, though, when her husband died, I spoke at his funeral. When she was speaking to the gathering, she said, “And oh, by the way, Royce, thanks for saving my life.”
That surprised me. I didn’t think we were going to go there.
I’d never tried to practice medicine “at the roadside” before. But that’s part of the career.
Royce Johnson, MD, is the chief of the division of infectious disease among other leadership positions at Kern Medical in Bakersfield, Calif., and the medical director of the Valley Fever Institute.
A version of this article first appeared on Medscape.com.
COVID-19 shot appears to reduce diabetes risk, even after Omicron
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
new data suggest.
The findings, from more than 20,000 patients in the Cedars-Sinai Health System in Los Angeles, suggest that “continued efforts to prevent COVID-19 infection may be beneficial to patient health until we develop better understanding of the effects of potential long-term effects of COVID-19,” lead author Alan C. Kwan, MD, of the department of cardiology at Cedars Sinai’s Smidt Heart Institute, said in an interview.
Several studies conducted early in the pandemic suggested increased risks for both new-onset diabetes and cardiometabolic diseases following COVID-19 infection, possibly because of persistent inflammation contributing to insulin resistance.
However, it hasn’t been clear if those risks have persisted with the more recent predominance of the less-virulent Omicron variant or whether the COVID-19 vaccine influences the risk. This new study suggests that both are the case.
“Our results verify that the risk of developing type 2 diabetes after a COVID-19 infection was not just an early observation but, in fact, a real risk that has, unfortunately, persisted through the Omicron era,” Dr. Kwan noted.
“While the level of evidence by our study and others may not reach the degree needed to affect formal guidelines at this time, we believe it is reasonable to have increased clinical suspicion for diabetes after COVID-19 infection and a lower threshold for testing,” he added.
Moreover, “we believe that our study and others suggest the potential role of COVID-19 to affect cardiovascular risk, and so both prevention of COVID-19 infection, through reasonable personal practices and vaccination, and an increased attention to cardiovascular health after COVID-19 infection is warranted.”
The findings were published online in JAMA Network Open.
Dr. Kwan and colleagues analyzed data for a total of 23,709 patients treated (inpatient and outpatient) for at least one COVID-19 infection between March 2020 and June 2022.
Rates of new-onset diabetes (using ICD-10 codes, primarily type 2 diabetes), hypertension, and hyperlipidemia were all elevated in the 90 days following COVID-19 infection compared with the 90 days prior. The same was true of two diagnoses unrelated to COVID-19, urinary tract infection and gastroesophageal reflux, used as benchmarks of health care engagement.
The highest odds for post versus preinfection were for diabetes (odds ratio, 2.35; P < .001), followed by hypertension (OR, 1.54; P < .001), the benchmark diagnoses (OR, 1.42; P < .001), and hyperlipidemia (OR, 1.22; P = .03).
Following adjustments, the risk versus the benchmark conditions for new-onset diabetes before versus after COVID-19 was significantly elevated (OR, 1.58; P < .001), while the risks for hypertension and hyperlipidemia versus benchmark diagnoses were not (OR, 1.06; P = .52 and 0.91, P = .43, respectively).
The diabetes risk after versus before COVID-19 infection was higher among those who had not been vaccinated (OR, 1.78; P < .001), compared with those who had received the vaccine (OR, 1.07; P = .80).
However, there was no significant interaction between vaccination and diabetes diagnosis (P = .08). “For this reason, we believe our data are suggestive of a protective effect in the population who received vaccination prior to infection, but [this is] not definitive,” Dr. Kwan said.
There were no apparent interactions by age, sex, or pre-existing cardiovascular risk factors, including hypertension or hyperlipidemia. Age, sex, and timing of index infection regarding the Omicron variant were not associated with an increased risk of a new cardiometabolic diagnosis before or after COVID-19 infection in any of the models.
Dr. Kwan said in an interview: “We have continued to be surprised by the evolving understanding of the SARS-CoV-2 virus and the effects on human health. In the beginning of the pandemic it was framed as a purely respiratory virus, which we now know to be a severely limited description of all of its potential effects on the human body. We believe that our research and others raise a concern for increased cardiometabolic risk after COVID infection.”
He added that, “while knowledge is incomplete on this topic, we believe that clinical providers may wish to have a higher degree of suspicion for both diabetes and risk of future cardiac events in patients after COVID infection, and that continued efforts to prevent COVID infection may be beneficial to patient health until we develop better understanding of the potential long-term effects of COVID.”
This study was funded by the Erika J. Glazer Family Foundation, the Doris Duke Charitable Foundation, and grants from the National Institutes of Health. Dr. Kwan reported receiving grants from the Doris Duke Charitable Foundation during the conduct of the study.
A version of this article originally appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Cardiac issues twice as likely with COVID plus high troponin
Hospitalized COVID-19 patients with high troponin levels are twice as likely to have cardiac abnormalities than those with normal troponin, with or without COVID-19, a multicenter U.K. study suggests.
The causes were diverse, myocarditis prevalence was lower than previously reported, and myocardial scar emerged as an independent risk factor for adverse cardiovascular outcomes at 12 months.
“We know that multiorgan involvement in hospitalized patients with COVID-19 is common ... and may result in acute myocardial injury, detected by an increase in cardiac troponin concentrations,” John P. Greenwood, PhD, of the University of Leeds (England), told this news organization. “Elevated cardiac troponin is associated with a worse prognosis.”
“Multiple mechanisms of myocardial injury have been proposed and ... mitigation or prevention strategies likely depend on the underpinning mechanisms,” he said. “The sequelae of scar may predispose to late events.”
The study, published online in Circulation, also identified a new pattern of microinfarction on cardiac magnetic resonance (CMR) imaging, highlighting the pro-thrombotic nature of SARS-CoV-2, Dr. Greenwood said.
Injury patterns different
Three hundred and forty-two patients with COVID-19 and elevated troponin levels (COVID+/troponin+) across 25 centers were enrolled between June 2020 and March 2021 in COVID-HEART, deemed an “urgent public health study” in the United Kingdom. The aim was to characterize myocardial injury and its associations and sequelae in convalescent patients after hospitalization with COVID-19.
Enrollment took place during the Wuhan and Alpha waves of COVID-19: before vaccination and when dexamethasone and anticoagulant protocols were emerging. All participants underwent CMR at a median of 21 days after discharge.
Two prospective control groups also were recruited: 64 patients with COVID-19 and normal troponin levels (COVID+/troponin−) and 113 without COVID-19 or elevated troponin matched by age and cardiovascular comorbidities (COVID−/comorbidity+).
Overall, participants’ median age was 61 years and 69% were men. Common comorbidities included hypertension (47%), obesity (43%), and diabetes (25%).
The frequency of any heart abnormality – for example, left or right ventricular impairment, scar, or pericardial disease – was twice as great (61%) in COVID+/troponin+ cases, compared with controls (36% for COVID+/troponin− patients versus 31% for COVID−/comorbidity+ patients).
Specifically, more cases than controls had ventricular impairment (17.2% vs. 3.1% and 7.1%) or scar (42% vs. 7% and 23%).
The myocardial injury pattern differed between cases and controls, with cases more likely to have infarction (13% vs. 2% and 7%) or microinfarction (9% vs. 0% and 1%).
However, there was no between-group difference in nonischemic scar (13% vs. 5% and 14%).
The prevalence of probable recent myocarditis was 6.7% in cases, compared with 1.7% in controls without COVID-19 – “much lower” than in previous studies, Dr. Greenwood noted.
During follow-up, four COVID+/troponin+ patients (1.2%) died, and 34 (10%) experienced a subsequent major adverse cardiovascular event (MACE; 10.2%), which was similar to controls (6.1%).
Myocardial scar, but not previous COVID-19 infection or troponin level, was an independent predictor of MACE (odds ratio, 2.25).
“These findings suggest that macroangiopathic and microangiopathic thrombosis may be the key pathologic process for myocardial injury in COVID-19 survivors,” the authors conclude.
Dr. Greenwood added, “We are currently analyzing the 6-month follow-up CMR scans, the quality-of-life questionnaires, and the 6-minute walk tests. These will give us great understanding of how the heart repairs after acute myocardial injury associated with COVID-19. It will also allow us to assess the impact on patient quality of life and functional capacity.”
‘Tour de force’
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and a professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said, “This is a tour de force collaboration – obtaining this many MRIs across multiple centers in the pandemic is quite remarkable. The study highlights the multiple different processes that lead to cardiac injury in COVID patients, complements autopsy studies and prior smaller MRI studies, [and] also provides the best data on the rate of myocarditis to date among the subset of COVID patients with cardiac injury.”
Overall, he said, the findings “do support closer follow-up for patients who had COVID and elevated troponins. We need to see follow-up MRI results in this cohort, as well as longer term outcomes. We also need studies on newer, more benign variants that are likely to have lower rates of cardiac injury and even fewer MRI abnormalities.”
Matthias Stuber, PhD, and Aaron L. Baggish, MD, both of Lausanne University Hospital and University of Lausanne, Switzerland, noted in a related editorial, “We are also reminded that the clinical severity of COVID-19 is most often dictated by the presence of pre-existing comorbidity, with antecedent ischemic scar now added to the long list of bad actors. Although not the primary focus of the COVID-HEART study, the question of whether cardiac troponin levels should be checked routinely and universally during the index admission for COVID-19 remains unresolved,” they noted.
“In general, we are most effective as clinicians when we use tests to confirm or rule out the specific disease processes suspected by careful basic clinical assessment rather than in a shotgun manner among undifferentiated all-comers,” they conclude.
No commercial funding or relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
Hospitalized COVID-19 patients with high troponin levels are twice as likely to have cardiac abnormalities than those with normal troponin, with or without COVID-19, a multicenter U.K. study suggests.
The causes were diverse, myocarditis prevalence was lower than previously reported, and myocardial scar emerged as an independent risk factor for adverse cardiovascular outcomes at 12 months.
“We know that multiorgan involvement in hospitalized patients with COVID-19 is common ... and may result in acute myocardial injury, detected by an increase in cardiac troponin concentrations,” John P. Greenwood, PhD, of the University of Leeds (England), told this news organization. “Elevated cardiac troponin is associated with a worse prognosis.”
“Multiple mechanisms of myocardial injury have been proposed and ... mitigation or prevention strategies likely depend on the underpinning mechanisms,” he said. “The sequelae of scar may predispose to late events.”
The study, published online in Circulation, also identified a new pattern of microinfarction on cardiac magnetic resonance (CMR) imaging, highlighting the pro-thrombotic nature of SARS-CoV-2, Dr. Greenwood said.
Injury patterns different
Three hundred and forty-two patients with COVID-19 and elevated troponin levels (COVID+/troponin+) across 25 centers were enrolled between June 2020 and March 2021 in COVID-HEART, deemed an “urgent public health study” in the United Kingdom. The aim was to characterize myocardial injury and its associations and sequelae in convalescent patients after hospitalization with COVID-19.
Enrollment took place during the Wuhan and Alpha waves of COVID-19: before vaccination and when dexamethasone and anticoagulant protocols were emerging. All participants underwent CMR at a median of 21 days after discharge.
Two prospective control groups also were recruited: 64 patients with COVID-19 and normal troponin levels (COVID+/troponin−) and 113 without COVID-19 or elevated troponin matched by age and cardiovascular comorbidities (COVID−/comorbidity+).
Overall, participants’ median age was 61 years and 69% were men. Common comorbidities included hypertension (47%), obesity (43%), and diabetes (25%).
The frequency of any heart abnormality – for example, left or right ventricular impairment, scar, or pericardial disease – was twice as great (61%) in COVID+/troponin+ cases, compared with controls (36% for COVID+/troponin− patients versus 31% for COVID−/comorbidity+ patients).
Specifically, more cases than controls had ventricular impairment (17.2% vs. 3.1% and 7.1%) or scar (42% vs. 7% and 23%).
The myocardial injury pattern differed between cases and controls, with cases more likely to have infarction (13% vs. 2% and 7%) or microinfarction (9% vs. 0% and 1%).
However, there was no between-group difference in nonischemic scar (13% vs. 5% and 14%).
The prevalence of probable recent myocarditis was 6.7% in cases, compared with 1.7% in controls without COVID-19 – “much lower” than in previous studies, Dr. Greenwood noted.
During follow-up, four COVID+/troponin+ patients (1.2%) died, and 34 (10%) experienced a subsequent major adverse cardiovascular event (MACE; 10.2%), which was similar to controls (6.1%).
Myocardial scar, but not previous COVID-19 infection or troponin level, was an independent predictor of MACE (odds ratio, 2.25).
“These findings suggest that macroangiopathic and microangiopathic thrombosis may be the key pathologic process for myocardial injury in COVID-19 survivors,” the authors conclude.
Dr. Greenwood added, “We are currently analyzing the 6-month follow-up CMR scans, the quality-of-life questionnaires, and the 6-minute walk tests. These will give us great understanding of how the heart repairs after acute myocardial injury associated with COVID-19. It will also allow us to assess the impact on patient quality of life and functional capacity.”
‘Tour de force’
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and a professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said, “This is a tour de force collaboration – obtaining this many MRIs across multiple centers in the pandemic is quite remarkable. The study highlights the multiple different processes that lead to cardiac injury in COVID patients, complements autopsy studies and prior smaller MRI studies, [and] also provides the best data on the rate of myocarditis to date among the subset of COVID patients with cardiac injury.”
Overall, he said, the findings “do support closer follow-up for patients who had COVID and elevated troponins. We need to see follow-up MRI results in this cohort, as well as longer term outcomes. We also need studies on newer, more benign variants that are likely to have lower rates of cardiac injury and even fewer MRI abnormalities.”
Matthias Stuber, PhD, and Aaron L. Baggish, MD, both of Lausanne University Hospital and University of Lausanne, Switzerland, noted in a related editorial, “We are also reminded that the clinical severity of COVID-19 is most often dictated by the presence of pre-existing comorbidity, with antecedent ischemic scar now added to the long list of bad actors. Although not the primary focus of the COVID-HEART study, the question of whether cardiac troponin levels should be checked routinely and universally during the index admission for COVID-19 remains unresolved,” they noted.
“In general, we are most effective as clinicians when we use tests to confirm or rule out the specific disease processes suspected by careful basic clinical assessment rather than in a shotgun manner among undifferentiated all-comers,” they conclude.
No commercial funding or relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
Hospitalized COVID-19 patients with high troponin levels are twice as likely to have cardiac abnormalities than those with normal troponin, with or without COVID-19, a multicenter U.K. study suggests.
The causes were diverse, myocarditis prevalence was lower than previously reported, and myocardial scar emerged as an independent risk factor for adverse cardiovascular outcomes at 12 months.
“We know that multiorgan involvement in hospitalized patients with COVID-19 is common ... and may result in acute myocardial injury, detected by an increase in cardiac troponin concentrations,” John P. Greenwood, PhD, of the University of Leeds (England), told this news organization. “Elevated cardiac troponin is associated with a worse prognosis.”
“Multiple mechanisms of myocardial injury have been proposed and ... mitigation or prevention strategies likely depend on the underpinning mechanisms,” he said. “The sequelae of scar may predispose to late events.”
The study, published online in Circulation, also identified a new pattern of microinfarction on cardiac magnetic resonance (CMR) imaging, highlighting the pro-thrombotic nature of SARS-CoV-2, Dr. Greenwood said.
Injury patterns different
Three hundred and forty-two patients with COVID-19 and elevated troponin levels (COVID+/troponin+) across 25 centers were enrolled between June 2020 and March 2021 in COVID-HEART, deemed an “urgent public health study” in the United Kingdom. The aim was to characterize myocardial injury and its associations and sequelae in convalescent patients after hospitalization with COVID-19.
Enrollment took place during the Wuhan and Alpha waves of COVID-19: before vaccination and when dexamethasone and anticoagulant protocols were emerging. All participants underwent CMR at a median of 21 days after discharge.
Two prospective control groups also were recruited: 64 patients with COVID-19 and normal troponin levels (COVID+/troponin−) and 113 without COVID-19 or elevated troponin matched by age and cardiovascular comorbidities (COVID−/comorbidity+).
Overall, participants’ median age was 61 years and 69% were men. Common comorbidities included hypertension (47%), obesity (43%), and diabetes (25%).
The frequency of any heart abnormality – for example, left or right ventricular impairment, scar, or pericardial disease – was twice as great (61%) in COVID+/troponin+ cases, compared with controls (36% for COVID+/troponin− patients versus 31% for COVID−/comorbidity+ patients).
Specifically, more cases than controls had ventricular impairment (17.2% vs. 3.1% and 7.1%) or scar (42% vs. 7% and 23%).
The myocardial injury pattern differed between cases and controls, with cases more likely to have infarction (13% vs. 2% and 7%) or microinfarction (9% vs. 0% and 1%).
However, there was no between-group difference in nonischemic scar (13% vs. 5% and 14%).
The prevalence of probable recent myocarditis was 6.7% in cases, compared with 1.7% in controls without COVID-19 – “much lower” than in previous studies, Dr. Greenwood noted.
During follow-up, four COVID+/troponin+ patients (1.2%) died, and 34 (10%) experienced a subsequent major adverse cardiovascular event (MACE; 10.2%), which was similar to controls (6.1%).
Myocardial scar, but not previous COVID-19 infection or troponin level, was an independent predictor of MACE (odds ratio, 2.25).
“These findings suggest that macroangiopathic and microangiopathic thrombosis may be the key pathologic process for myocardial injury in COVID-19 survivors,” the authors conclude.
Dr. Greenwood added, “We are currently analyzing the 6-month follow-up CMR scans, the quality-of-life questionnaires, and the 6-minute walk tests. These will give us great understanding of how the heart repairs after acute myocardial injury associated with COVID-19. It will also allow us to assess the impact on patient quality of life and functional capacity.”
‘Tour de force’
James A. de Lemos, MD, co-chair of the American Heart Association’s COVID-19 CVD Registry Steering Committee and a professor of medicine at the University of Texas Southwestern Medical Center, Dallas, said, “This is a tour de force collaboration – obtaining this many MRIs across multiple centers in the pandemic is quite remarkable. The study highlights the multiple different processes that lead to cardiac injury in COVID patients, complements autopsy studies and prior smaller MRI studies, [and] also provides the best data on the rate of myocarditis to date among the subset of COVID patients with cardiac injury.”
Overall, he said, the findings “do support closer follow-up for patients who had COVID and elevated troponins. We need to see follow-up MRI results in this cohort, as well as longer term outcomes. We also need studies on newer, more benign variants that are likely to have lower rates of cardiac injury and even fewer MRI abnormalities.”
Matthias Stuber, PhD, and Aaron L. Baggish, MD, both of Lausanne University Hospital and University of Lausanne, Switzerland, noted in a related editorial, “We are also reminded that the clinical severity of COVID-19 is most often dictated by the presence of pre-existing comorbidity, with antecedent ischemic scar now added to the long list of bad actors. Although not the primary focus of the COVID-HEART study, the question of whether cardiac troponin levels should be checked routinely and universally during the index admission for COVID-19 remains unresolved,” they noted.
“In general, we are most effective as clinicians when we use tests to confirm or rule out the specific disease processes suspected by careful basic clinical assessment rather than in a shotgun manner among undifferentiated all-comers,” they conclude.
No commercial funding or relevant financial relationships were reported.
A version of this article originally appeared on Medscape.com.
New challenge for docs: End of COVID federal public health emergency
The Biden administration intends to end by May 11 certain COVID-19 emergency measures used to aid in the response to the pandemic, while many others will remain in place.
A separate declaration covers the Food and Drug Administration’s emergency use authorizations (EUAs) for COVID medicines and tests. That would not be affected by the May 11 deadline, the FDA said. In addition, Congress and state lawmakers have extended some COVID response measures.
The result is a patchwork of emergency COVID-19 measures with different end dates.
The American Medical Association and the American Academy of Family Physicians (AAFP) are assessing how best to advise their members about the end of the public health emergency.
Several waivers regarding copays and coverage and policies regarding controlled substances will expire, Claire Ernst, director of government affairs at the Medical Group Management Association, told this news organization.
The impact of the unwinding “will vary based on some factors, such as what state the practice resides in,” Ms. Ernst said. “Fortunately, Congress provided some predictability for practices by extending many of the telehealth waivers through the end of 2024.”
The AAFP told this news organization that it has joined several other groups in calling for the release of proposed Drug Enforcement Administration (DEA) regulations meant to permanently allow prescriptions of buprenorphine treatment for opioid use disorder via telehealth. The AAFP and other groups want to review these proposals and, if needed, urge the DEA to modify or finalize before there are any disruptions in access to medications for opioid use disorder.
Patients’ questions
Clinicians can expect to field patients’ questions about their insurance coverage and what they need to pay, said Nancy Foster, vice president for quality and patient safety policy at the American Hospital Association (AHA).
“Your doctor’s office, that clinic you typically get care at, that is the face of medicine to you,” Ms. Foster told this news organization. “Many doctors and their staff will be asked, ‘What’s happening with Medicaid?’ ‘What about my Medicare coverage?’ ‘Can I still access care in the same way that I did before?’ ”
Physicians will need to be ready to answers those question, or point patients to where they can get answers, Ms. Foster said.
For example, Medicaid will no longer cover postpartum care for some enrollees after giving birth, said Taylor Platt, health policy manager for the American College of Obstetricians and Gynecologists.
The federal response to the pandemic created “a de facto postpartum coverage extension for Medicaid enrollees,” which will be lost in some states, Ms. Platt told this news organization. However, 28 states and the District of Columbia have taken separate measures to extend postpartum coverage to 1 year.
“This coverage has been critical for postpartum individuals to address health needs like substance use and mental health treatment and chronic conditions,” Ms. Platt said.
States significantly changed Medicaid policy to expand access to care during the pandemic.
All 50 states and the District of Columbia, for example, expanded coverage or access to telehealth services in Medicaid during the pandemic, according to a Jan. 31 report from the Kaiser Family Foundation (KFF). These expansions expire under various deadlines, although most states have made or are planning to make some Medicaid telehealth flexibilities permanent, KFF said.
The KFF report notes that all states and the District of Columbia temporarily waived some aspects of state licensure requirements, so that clinicians with equivalent licenses in other states could practice via telehealth.
In some states, these waivers are still active and are tied to the end of the federal emergency declaration. In others, they expired, with some states allowing for long-term or permanent interstate telemedicine, KFF said. (The Federation of State Medical Boards has a detailed summary of these modifications.)
The end of free COVID vaccines, testing for some patients
The AAFP has also raised concerns about continued access to COVID-19 vaccines, particularly for uninsured adults. Ashish Jha, MD, MPH, the White House COVID-19 Response Coordinator, said in a tweet that this transition, however, wouldn’t happen until a few months after the public health emergency ends.
After those few months, there will be a transition from U.S. government–distributed vaccines and treatments to ones purchased through the regular health care system, the “way we do for every other vaccine and treatment,” Dr. Jha added.
But that raises the same kind of difficult questions that permeate U.S. health care, with a potential to keep COVID active, said Patricia Jackson, RN, president of the Association for Professionals in Infection Control and Epidemiology (APIC).
People who don’t have insurance may lose access to COVID testing and vaccines.
“Will that lead to increases in transmission? Who knows,” Ms. Jackson told this news organization. “We will have to see. There are some health equity issues that potentially arise.”
Future FDA actions
Biden’s May 11 deadline applies to emergency provisions made under a Section 319 declaration, which allow the Department of Health and Human Services to respond to crises.
But a separate flexibility, known as a Section 564 declaration, covers the FDA’s EUAs, which can remain in effect even as the other declarations end.
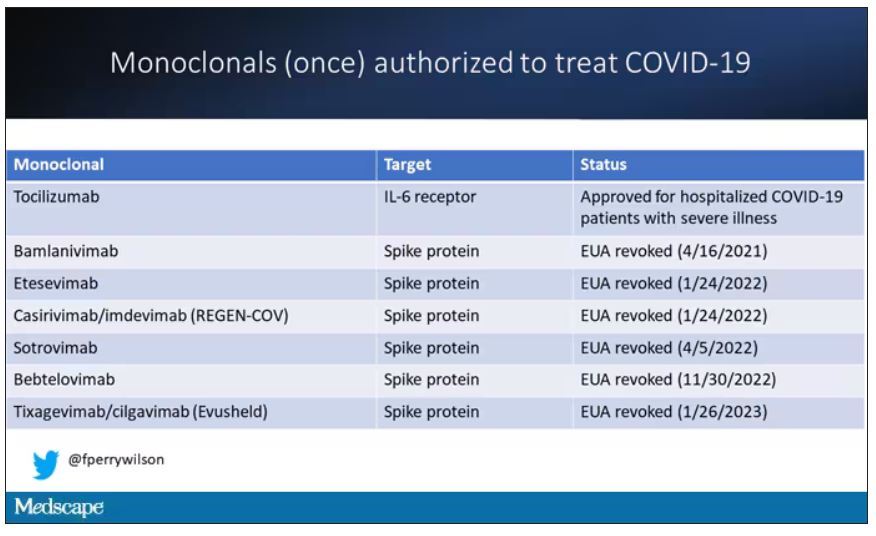
The best-known EUAs for the pandemic were used to bring COVID vaccines and treatments to market. Many of these have since been converted to normal approvals as companies presented more evidence to support the initial emergency approvals. In other cases, EUAs have been withdrawn owing to disappointing research results, changing virus strains, and evolving medical treatments.
The FDA also used many EUAs to cover new uses of ventilators and other hospital equipment and expand these supplies in response to the pandemic, said Mark Howell, AHA’s director of policy and patient safety.
The FDA should examine the EUAs issued during the pandemic to see what greater flexibilities might be used to deal with future serious shortages of critical supplies. International incidents such as the war in Ukraine show how fragile the supply chain can be. The FDA should consider its recent experience with EUAs to address this, Mr. Howell said.
“What do we do coming out of the pandemic? And how do we think about being more proactive in this space to ensure that our supply doesn’t bottleneck, that we continue to make sure that providers have access to supply that’s not only safe and effective, but that they can use?” Mr. Howell told this news organization.
Such planning might also help prepare the country for the next pandemic, which is a near certainty, APIC’s Ms. Jackson said. The nation needs a nimbler response to the next major outbreak of an infectious disease, she said.
“There is going to be a next time,” Ms. Jackson said. “We are going to have another pandemic.”
A version of this article first appeared on Medscape.com.
The Biden administration intends to end by May 11 certain COVID-19 emergency measures used to aid in the response to the pandemic, while many others will remain in place.
A separate declaration covers the Food and Drug Administration’s emergency use authorizations (EUAs) for COVID medicines and tests. That would not be affected by the May 11 deadline, the FDA said. In addition, Congress and state lawmakers have extended some COVID response measures.
The result is a patchwork of emergency COVID-19 measures with different end dates.
The American Medical Association and the American Academy of Family Physicians (AAFP) are assessing how best to advise their members about the end of the public health emergency.
Several waivers regarding copays and coverage and policies regarding controlled substances will expire, Claire Ernst, director of government affairs at the Medical Group Management Association, told this news organization.
The impact of the unwinding “will vary based on some factors, such as what state the practice resides in,” Ms. Ernst said. “Fortunately, Congress provided some predictability for practices by extending many of the telehealth waivers through the end of 2024.”
The AAFP told this news organization that it has joined several other groups in calling for the release of proposed Drug Enforcement Administration (DEA) regulations meant to permanently allow prescriptions of buprenorphine treatment for opioid use disorder via telehealth. The AAFP and other groups want to review these proposals and, if needed, urge the DEA to modify or finalize before there are any disruptions in access to medications for opioid use disorder.
Patients’ questions
Clinicians can expect to field patients’ questions about their insurance coverage and what they need to pay, said Nancy Foster, vice president for quality and patient safety policy at the American Hospital Association (AHA).
“Your doctor’s office, that clinic you typically get care at, that is the face of medicine to you,” Ms. Foster told this news organization. “Many doctors and their staff will be asked, ‘What’s happening with Medicaid?’ ‘What about my Medicare coverage?’ ‘Can I still access care in the same way that I did before?’ ”
Physicians will need to be ready to answers those question, or point patients to where they can get answers, Ms. Foster said.
For example, Medicaid will no longer cover postpartum care for some enrollees after giving birth, said Taylor Platt, health policy manager for the American College of Obstetricians and Gynecologists.
The federal response to the pandemic created “a de facto postpartum coverage extension for Medicaid enrollees,” which will be lost in some states, Ms. Platt told this news organization. However, 28 states and the District of Columbia have taken separate measures to extend postpartum coverage to 1 year.
“This coverage has been critical for postpartum individuals to address health needs like substance use and mental health treatment and chronic conditions,” Ms. Platt said.
States significantly changed Medicaid policy to expand access to care during the pandemic.
All 50 states and the District of Columbia, for example, expanded coverage or access to telehealth services in Medicaid during the pandemic, according to a Jan. 31 report from the Kaiser Family Foundation (KFF). These expansions expire under various deadlines, although most states have made or are planning to make some Medicaid telehealth flexibilities permanent, KFF said.
The KFF report notes that all states and the District of Columbia temporarily waived some aspects of state licensure requirements, so that clinicians with equivalent licenses in other states could practice via telehealth.
In some states, these waivers are still active and are tied to the end of the federal emergency declaration. In others, they expired, with some states allowing for long-term or permanent interstate telemedicine, KFF said. (The Federation of State Medical Boards has a detailed summary of these modifications.)
The end of free COVID vaccines, testing for some patients
The AAFP has also raised concerns about continued access to COVID-19 vaccines, particularly for uninsured adults. Ashish Jha, MD, MPH, the White House COVID-19 Response Coordinator, said in a tweet that this transition, however, wouldn’t happen until a few months after the public health emergency ends.
After those few months, there will be a transition from U.S. government–distributed vaccines and treatments to ones purchased through the regular health care system, the “way we do for every other vaccine and treatment,” Dr. Jha added.
But that raises the same kind of difficult questions that permeate U.S. health care, with a potential to keep COVID active, said Patricia Jackson, RN, president of the Association for Professionals in Infection Control and Epidemiology (APIC).
People who don’t have insurance may lose access to COVID testing and vaccines.
“Will that lead to increases in transmission? Who knows,” Ms. Jackson told this news organization. “We will have to see. There are some health equity issues that potentially arise.”
Future FDA actions
Biden’s May 11 deadline applies to emergency provisions made under a Section 319 declaration, which allow the Department of Health and Human Services to respond to crises.
But a separate flexibility, known as a Section 564 declaration, covers the FDA’s EUAs, which can remain in effect even as the other declarations end.
The best-known EUAs for the pandemic were used to bring COVID vaccines and treatments to market. Many of these have since been converted to normal approvals as companies presented more evidence to support the initial emergency approvals. In other cases, EUAs have been withdrawn owing to disappointing research results, changing virus strains, and evolving medical treatments.
The FDA also used many EUAs to cover new uses of ventilators and other hospital equipment and expand these supplies in response to the pandemic, said Mark Howell, AHA’s director of policy and patient safety.
The FDA should examine the EUAs issued during the pandemic to see what greater flexibilities might be used to deal with future serious shortages of critical supplies. International incidents such as the war in Ukraine show how fragile the supply chain can be. The FDA should consider its recent experience with EUAs to address this, Mr. Howell said.
“What do we do coming out of the pandemic? And how do we think about being more proactive in this space to ensure that our supply doesn’t bottleneck, that we continue to make sure that providers have access to supply that’s not only safe and effective, but that they can use?” Mr. Howell told this news organization.
Such planning might also help prepare the country for the next pandemic, which is a near certainty, APIC’s Ms. Jackson said. The nation needs a nimbler response to the next major outbreak of an infectious disease, she said.
“There is going to be a next time,” Ms. Jackson said. “We are going to have another pandemic.”
A version of this article first appeared on Medscape.com.
The Biden administration intends to end by May 11 certain COVID-19 emergency measures used to aid in the response to the pandemic, while many others will remain in place.
A separate declaration covers the Food and Drug Administration’s emergency use authorizations (EUAs) for COVID medicines and tests. That would not be affected by the May 11 deadline, the FDA said. In addition, Congress and state lawmakers have extended some COVID response measures.
The result is a patchwork of emergency COVID-19 measures with different end dates.
The American Medical Association and the American Academy of Family Physicians (AAFP) are assessing how best to advise their members about the end of the public health emergency.
Several waivers regarding copays and coverage and policies regarding controlled substances will expire, Claire Ernst, director of government affairs at the Medical Group Management Association, told this news organization.
The impact of the unwinding “will vary based on some factors, such as what state the practice resides in,” Ms. Ernst said. “Fortunately, Congress provided some predictability for practices by extending many of the telehealth waivers through the end of 2024.”
The AAFP told this news organization that it has joined several other groups in calling for the release of proposed Drug Enforcement Administration (DEA) regulations meant to permanently allow prescriptions of buprenorphine treatment for opioid use disorder via telehealth. The AAFP and other groups want to review these proposals and, if needed, urge the DEA to modify or finalize before there are any disruptions in access to medications for opioid use disorder.
Patients’ questions
Clinicians can expect to field patients’ questions about their insurance coverage and what they need to pay, said Nancy Foster, vice president for quality and patient safety policy at the American Hospital Association (AHA).
“Your doctor’s office, that clinic you typically get care at, that is the face of medicine to you,” Ms. Foster told this news organization. “Many doctors and their staff will be asked, ‘What’s happening with Medicaid?’ ‘What about my Medicare coverage?’ ‘Can I still access care in the same way that I did before?’ ”
Physicians will need to be ready to answers those question, or point patients to where they can get answers, Ms. Foster said.
For example, Medicaid will no longer cover postpartum care for some enrollees after giving birth, said Taylor Platt, health policy manager for the American College of Obstetricians and Gynecologists.
The federal response to the pandemic created “a de facto postpartum coverage extension for Medicaid enrollees,” which will be lost in some states, Ms. Platt told this news organization. However, 28 states and the District of Columbia have taken separate measures to extend postpartum coverage to 1 year.
“This coverage has been critical for postpartum individuals to address health needs like substance use and mental health treatment and chronic conditions,” Ms. Platt said.
States significantly changed Medicaid policy to expand access to care during the pandemic.
All 50 states and the District of Columbia, for example, expanded coverage or access to telehealth services in Medicaid during the pandemic, according to a Jan. 31 report from the Kaiser Family Foundation (KFF). These expansions expire under various deadlines, although most states have made or are planning to make some Medicaid telehealth flexibilities permanent, KFF said.
The KFF report notes that all states and the District of Columbia temporarily waived some aspects of state licensure requirements, so that clinicians with equivalent licenses in other states could practice via telehealth.
In some states, these waivers are still active and are tied to the end of the federal emergency declaration. In others, they expired, with some states allowing for long-term or permanent interstate telemedicine, KFF said. (The Federation of State Medical Boards has a detailed summary of these modifications.)
The end of free COVID vaccines, testing for some patients
The AAFP has also raised concerns about continued access to COVID-19 vaccines, particularly for uninsured adults. Ashish Jha, MD, MPH, the White House COVID-19 Response Coordinator, said in a tweet that this transition, however, wouldn’t happen until a few months after the public health emergency ends.
After those few months, there will be a transition from U.S. government–distributed vaccines and treatments to ones purchased through the regular health care system, the “way we do for every other vaccine and treatment,” Dr. Jha added.
But that raises the same kind of difficult questions that permeate U.S. health care, with a potential to keep COVID active, said Patricia Jackson, RN, president of the Association for Professionals in Infection Control and Epidemiology (APIC).
People who don’t have insurance may lose access to COVID testing and vaccines.
“Will that lead to increases in transmission? Who knows,” Ms. Jackson told this news organization. “We will have to see. There are some health equity issues that potentially arise.”
Future FDA actions
Biden’s May 11 deadline applies to emergency provisions made under a Section 319 declaration, which allow the Department of Health and Human Services to respond to crises.
But a separate flexibility, known as a Section 564 declaration, covers the FDA’s EUAs, which can remain in effect even as the other declarations end.
The best-known EUAs for the pandemic were used to bring COVID vaccines and treatments to market. Many of these have since been converted to normal approvals as companies presented more evidence to support the initial emergency approvals. In other cases, EUAs have been withdrawn owing to disappointing research results, changing virus strains, and evolving medical treatments.
The FDA also used many EUAs to cover new uses of ventilators and other hospital equipment and expand these supplies in response to the pandemic, said Mark Howell, AHA’s director of policy and patient safety.
The FDA should examine the EUAs issued during the pandemic to see what greater flexibilities might be used to deal with future serious shortages of critical supplies. International incidents such as the war in Ukraine show how fragile the supply chain can be. The FDA should consider its recent experience with EUAs to address this, Mr. Howell said.
“What do we do coming out of the pandemic? And how do we think about being more proactive in this space to ensure that our supply doesn’t bottleneck, that we continue to make sure that providers have access to supply that’s not only safe and effective, but that they can use?” Mr. Howell told this news organization.
Such planning might also help prepare the country for the next pandemic, which is a near certainty, APIC’s Ms. Jackson said. The nation needs a nimbler response to the next major outbreak of an infectious disease, she said.
“There is going to be a next time,” Ms. Jackson said. “We are going to have another pandemic.”
A version of this article first appeared on Medscape.com.
New report says suicide rates rising among young Black people
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Significant increases in suicide occurred among Native American, Black and Hispanic people, with a startling rise among young Black people. Meanwhile, the rate of suicide among older people declined between 2018 and 2021, the Centers for Disease Control and Prevention has reported.
In 2021, 48,183 people died by suicide in the United States, which equates to a suicide rate of 14.1 per 100,000 people. That level equals the 2018 suicide rate, which had seen a peak that was followed by declines associated with the pandemic.
Experts said rebounding suicide rates are common following times of crisis, such as the COVID-19 pandemic. Suicide declines have also occurred during times of war and natural disaster, when psychological resilience tends to increase and people work together to overcome shared adversity.
“That will wane, and then you will see rebounding in suicide rates. That is, in fact, what we feared would happen. And it has happened, at least in 2021,” Christine Moutier, MD, chief medical officer of the American Foundation for Suicide Prevention, told the New York Times.
The new CDC report found that the largest increase was among Black people aged 10-24 years, who experienced a 36.6% increase in suicide rate between 2018 and 2021. While Black people experience mental illness at the same rates as that of the general population, historically they have disproportionately limited access to mental health care, according to the American Psychiatric Association.
CDC report authors noted that some of the biggest increases in suicide rates occurred among groups most affected by the pandemic.
From 2018 to 2021, the suicide rate for people aged 25-44 increased among Native Americans by 33.7% and among Black people by 22.9%. Suicide increased among multiracial people by 20.6% and among Hispanic or Latinx people by 19.4%. Among White people of all ages, the suicide rate declined or remained steady.
“As the nation continues to respond to the short- and long-term impacts of the COVID-19 pandemic, remaining vigilant in prevention efforts is critical, especially among disproportionately affected populations where longer-term impacts might compound preexisting inequities in suicide risk,” the CDC researchers wrote.
A version of this article first appeared on WebMD.com.
Prehospital COVID therapy effective in rheumatic disease patients
Outpatient COVID-19 treatment with monoclonal antibodies or antiretroviral medications such as nirmatrelvir-ritonavir (Paxlovid) administered to patients with systemic autoimmune rheumatic disease led to lower odds of having severe outcomes when compared with similar patients who received no outpatient treatment in a real-world, retrospective analysis of cases.
The investigators found that there were nine hospitalizations or deaths (2.1%) among 426 patients who received outpatient treatment, compared with 49 (17.6%) among 278 who did not receive outpatient treatment, yielding an odds ratio of 0.12 (95% confidence interval, 0.05-0.25), after adjusting for age, sex, race, comorbidities, and kidney function. The study was published in Lancet Rheumatology.
“Across the board, there was a really strong association with receiving outpatient treatment and lower risk of severe COVID-19,” senior author Jeffrey A. Sparks, MD, MMSc, assistant professor of medicine, Harvard Medical School and Brigham and Women’s Hospital, Boston, said in an interview. “It is pretty powerful evidence that, in this high-risk group, that treatment still matters related to preventing severe COVID. We found almost all patients who had severe COVID-19, either hospitalized or who had died, were in the untreated group.”
Early outpatient treatment an important tool in patients with rheumatic disease
Dr. Sparks noted that he and his coinvestigators conducted the study because the benefit of outpatient COVID-19 treatments in individuals with systemic autoimmune rheumatic disease was not adequately determined in clinical trials because they had infrequent enrollment of such patients.
The analysis included 704 patients with a mean age of 58.4 years who were seen at Mass General Brigham Integrated Health Care System, a multicenter health care system that includes 14 hospitals and primary care or specialty outpatient centers in the Boston area. A majority were female (76%) and White (84%). Nearly half had rheumatoid arthritis. Of the 704, 426 (61%) received outpatient treatment, which included nirmatrelvir-ritonavir (n = 307), monoclonal antibodies (n = 105), molnupiravir (n = 5), remdesivir (n = 3), and combination treatment (n = 6).
The findings underline the need to individualize approaches to outpatient treatment in those who test positive for SARS-CoV-2 to fend off severe COVID-19, according to Dr. Sparks. “It seems if you are vaccinated and in the general population that you are way less likely to have severe COVID-19 in the current environment, but that doesn’t necessarily apply to some high-risk groups like patients on immunosuppression. There are still patients at risk of severe COVID-19, and some of them are in this group of rheumatic patients. This should be part of the discussion related to deciding whether or not to treat.”
Dr. Sparks noted that vaccination against COVID-19 confers protection against developing severe COVID-19 in patients with rheumatic disease as it does in the general population, but patients with rheumatic diseases remain at increased risk for severe presentation. “Certainly, the vaccines really help our patients too, but there’s still a bit of a gap between the risk for our patients with rheumatic diseases and the general population” in developing severe COVID-19.
Dr. Sparks said he hopes the results represent a “call to action” that even among vaccinated patients there are still some who have poor outcomes, and that early outpatient treatment appears to be an important tool in the fight against poor outcomes from SARS-CoV-2 infection.
COVID-19 rebound
The study also reported on the phenomenon of COVID-19 rebound (recurrence of symptoms and test positivity after regimen completion) after oral outpatient SARS-CoV-2 treatment. “This [COVID-19 rebound] is a downside to treatment,” he said. COVID rebound was not infrequent: A total of 25 (8%) of 318 patients who received oral outpatient treatment had documented COVID-19 rebound.
“It was reassuring because we found no one who had rebound progressed to have severe COVID-19,” Dr. Sparks said. “On the other hand, [rebound] happened pretty frequently in our data, as 8% of patients are documented to have it.”
Dr. Sparks said he and coinvestigators speculate that more patients in the cohort may have experienced COVID-19 rebound but did not communicate this to their health care providers, and, as such, it was not documented in the medical record. The potential development of COVID-19 rebound “is something to counsel your patients about.” COVID-19 rebound is a phenomenon that is being most commonly observed with nirmatrelvir-ritonavir as outpatient treatment.
Possible confounding factors in study
Katie Bechman, MBChB, clinical lecturer in rheumatology at King’s College London, who coauthored an accompanying editorial about the study and its findings, pointed out that the study is limited by its observational design.
“With any study that looks at the efficacy of treatment, especially in an observational cohort, you’re going to have to consider the unmeasured confounding and the difference between these two groups,” Dr. Bechman said. “I know that they did try to adjust for that in this study, but there’s always going to be factors that we can’t [control for]. That is something that needs to be considered. I think that’s always something we need to consider when we’re looking at observational data.”
In lieu of a randomized, controlled trial, Dr. Bechman noted that the study and its associated findings serve as “the best data we have,” and she described the results as “very informative and positive.”
She added that the large number of patients represents a strength of the study, as does the robust method employed for identifying which patients had COVID-19.
The learnings from this study with respect to outpatient treatment can be applied to more common illnesses that patients with rheumatic disease may develop, such as the flu, according to Dr. Bechman.
“One of the positive aspects from this pandemic is that we’ve learned a huge amount about how best to treat certain viruses and prevent them in patients,” she said. “It would be worth thinking towards the future, what we can do for illnesses that we see very commonly in these populations. There may be treatment regimens that we haven’t really considered until now. You could hypothesize that in the next couple of years, if we have an influenza breakout, that we should be providing some prehospital antiviral treatment to patients, especially the ones that are at high risk.”
The study was conducted without outside funding. Dr. Sparks has received research support from Bristol-Myers Squibb and consulted for AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer unrelated to this work. Dr. Bechman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Outpatient COVID-19 treatment with monoclonal antibodies or antiretroviral medications such as nirmatrelvir-ritonavir (Paxlovid) administered to patients with systemic autoimmune rheumatic disease led to lower odds of having severe outcomes when compared with similar patients who received no outpatient treatment in a real-world, retrospective analysis of cases.
The investigators found that there were nine hospitalizations or deaths (2.1%) among 426 patients who received outpatient treatment, compared with 49 (17.6%) among 278 who did not receive outpatient treatment, yielding an odds ratio of 0.12 (95% confidence interval, 0.05-0.25), after adjusting for age, sex, race, comorbidities, and kidney function. The study was published in Lancet Rheumatology.
“Across the board, there was a really strong association with receiving outpatient treatment and lower risk of severe COVID-19,” senior author Jeffrey A. Sparks, MD, MMSc, assistant professor of medicine, Harvard Medical School and Brigham and Women’s Hospital, Boston, said in an interview. “It is pretty powerful evidence that, in this high-risk group, that treatment still matters related to preventing severe COVID. We found almost all patients who had severe COVID-19, either hospitalized or who had died, were in the untreated group.”
Early outpatient treatment an important tool in patients with rheumatic disease
Dr. Sparks noted that he and his coinvestigators conducted the study because the benefit of outpatient COVID-19 treatments in individuals with systemic autoimmune rheumatic disease was not adequately determined in clinical trials because they had infrequent enrollment of such patients.
The analysis included 704 patients with a mean age of 58.4 years who were seen at Mass General Brigham Integrated Health Care System, a multicenter health care system that includes 14 hospitals and primary care or specialty outpatient centers in the Boston area. A majority were female (76%) and White (84%). Nearly half had rheumatoid arthritis. Of the 704, 426 (61%) received outpatient treatment, which included nirmatrelvir-ritonavir (n = 307), monoclonal antibodies (n = 105), molnupiravir (n = 5), remdesivir (n = 3), and combination treatment (n = 6).
The findings underline the need to individualize approaches to outpatient treatment in those who test positive for SARS-CoV-2 to fend off severe COVID-19, according to Dr. Sparks. “It seems if you are vaccinated and in the general population that you are way less likely to have severe COVID-19 in the current environment, but that doesn’t necessarily apply to some high-risk groups like patients on immunosuppression. There are still patients at risk of severe COVID-19, and some of them are in this group of rheumatic patients. This should be part of the discussion related to deciding whether or not to treat.”
Dr. Sparks noted that vaccination against COVID-19 confers protection against developing severe COVID-19 in patients with rheumatic disease as it does in the general population, but patients with rheumatic diseases remain at increased risk for severe presentation. “Certainly, the vaccines really help our patients too, but there’s still a bit of a gap between the risk for our patients with rheumatic diseases and the general population” in developing severe COVID-19.
Dr. Sparks said he hopes the results represent a “call to action” that even among vaccinated patients there are still some who have poor outcomes, and that early outpatient treatment appears to be an important tool in the fight against poor outcomes from SARS-CoV-2 infection.
COVID-19 rebound
The study also reported on the phenomenon of COVID-19 rebound (recurrence of symptoms and test positivity after regimen completion) after oral outpatient SARS-CoV-2 treatment. “This [COVID-19 rebound] is a downside to treatment,” he said. COVID rebound was not infrequent: A total of 25 (8%) of 318 patients who received oral outpatient treatment had documented COVID-19 rebound.
“It was reassuring because we found no one who had rebound progressed to have severe COVID-19,” Dr. Sparks said. “On the other hand, [rebound] happened pretty frequently in our data, as 8% of patients are documented to have it.”
Dr. Sparks said he and coinvestigators speculate that more patients in the cohort may have experienced COVID-19 rebound but did not communicate this to their health care providers, and, as such, it was not documented in the medical record. The potential development of COVID-19 rebound “is something to counsel your patients about.” COVID-19 rebound is a phenomenon that is being most commonly observed with nirmatrelvir-ritonavir as outpatient treatment.
Possible confounding factors in study
Katie Bechman, MBChB, clinical lecturer in rheumatology at King’s College London, who coauthored an accompanying editorial about the study and its findings, pointed out that the study is limited by its observational design.
“With any study that looks at the efficacy of treatment, especially in an observational cohort, you’re going to have to consider the unmeasured confounding and the difference between these two groups,” Dr. Bechman said. “I know that they did try to adjust for that in this study, but there’s always going to be factors that we can’t [control for]. That is something that needs to be considered. I think that’s always something we need to consider when we’re looking at observational data.”
In lieu of a randomized, controlled trial, Dr. Bechman noted that the study and its associated findings serve as “the best data we have,” and she described the results as “very informative and positive.”
She added that the large number of patients represents a strength of the study, as does the robust method employed for identifying which patients had COVID-19.
The learnings from this study with respect to outpatient treatment can be applied to more common illnesses that patients with rheumatic disease may develop, such as the flu, according to Dr. Bechman.
“One of the positive aspects from this pandemic is that we’ve learned a huge amount about how best to treat certain viruses and prevent them in patients,” she said. “It would be worth thinking towards the future, what we can do for illnesses that we see very commonly in these populations. There may be treatment regimens that we haven’t really considered until now. You could hypothesize that in the next couple of years, if we have an influenza breakout, that we should be providing some prehospital antiviral treatment to patients, especially the ones that are at high risk.”
The study was conducted without outside funding. Dr. Sparks has received research support from Bristol-Myers Squibb and consulted for AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer unrelated to this work. Dr. Bechman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Outpatient COVID-19 treatment with monoclonal antibodies or antiretroviral medications such as nirmatrelvir-ritonavir (Paxlovid) administered to patients with systemic autoimmune rheumatic disease led to lower odds of having severe outcomes when compared with similar patients who received no outpatient treatment in a real-world, retrospective analysis of cases.
The investigators found that there were nine hospitalizations or deaths (2.1%) among 426 patients who received outpatient treatment, compared with 49 (17.6%) among 278 who did not receive outpatient treatment, yielding an odds ratio of 0.12 (95% confidence interval, 0.05-0.25), after adjusting for age, sex, race, comorbidities, and kidney function. The study was published in Lancet Rheumatology.
“Across the board, there was a really strong association with receiving outpatient treatment and lower risk of severe COVID-19,” senior author Jeffrey A. Sparks, MD, MMSc, assistant professor of medicine, Harvard Medical School and Brigham and Women’s Hospital, Boston, said in an interview. “It is pretty powerful evidence that, in this high-risk group, that treatment still matters related to preventing severe COVID. We found almost all patients who had severe COVID-19, either hospitalized or who had died, were in the untreated group.”
Early outpatient treatment an important tool in patients with rheumatic disease
Dr. Sparks noted that he and his coinvestigators conducted the study because the benefit of outpatient COVID-19 treatments in individuals with systemic autoimmune rheumatic disease was not adequately determined in clinical trials because they had infrequent enrollment of such patients.
The analysis included 704 patients with a mean age of 58.4 years who were seen at Mass General Brigham Integrated Health Care System, a multicenter health care system that includes 14 hospitals and primary care or specialty outpatient centers in the Boston area. A majority were female (76%) and White (84%). Nearly half had rheumatoid arthritis. Of the 704, 426 (61%) received outpatient treatment, which included nirmatrelvir-ritonavir (n = 307), monoclonal antibodies (n = 105), molnupiravir (n = 5), remdesivir (n = 3), and combination treatment (n = 6).
The findings underline the need to individualize approaches to outpatient treatment in those who test positive for SARS-CoV-2 to fend off severe COVID-19, according to Dr. Sparks. “It seems if you are vaccinated and in the general population that you are way less likely to have severe COVID-19 in the current environment, but that doesn’t necessarily apply to some high-risk groups like patients on immunosuppression. There are still patients at risk of severe COVID-19, and some of them are in this group of rheumatic patients. This should be part of the discussion related to deciding whether or not to treat.”
Dr. Sparks noted that vaccination against COVID-19 confers protection against developing severe COVID-19 in patients with rheumatic disease as it does in the general population, but patients with rheumatic diseases remain at increased risk for severe presentation. “Certainly, the vaccines really help our patients too, but there’s still a bit of a gap between the risk for our patients with rheumatic diseases and the general population” in developing severe COVID-19.
Dr. Sparks said he hopes the results represent a “call to action” that even among vaccinated patients there are still some who have poor outcomes, and that early outpatient treatment appears to be an important tool in the fight against poor outcomes from SARS-CoV-2 infection.
COVID-19 rebound
The study also reported on the phenomenon of COVID-19 rebound (recurrence of symptoms and test positivity after regimen completion) after oral outpatient SARS-CoV-2 treatment. “This [COVID-19 rebound] is a downside to treatment,” he said. COVID rebound was not infrequent: A total of 25 (8%) of 318 patients who received oral outpatient treatment had documented COVID-19 rebound.
“It was reassuring because we found no one who had rebound progressed to have severe COVID-19,” Dr. Sparks said. “On the other hand, [rebound] happened pretty frequently in our data, as 8% of patients are documented to have it.”
Dr. Sparks said he and coinvestigators speculate that more patients in the cohort may have experienced COVID-19 rebound but did not communicate this to their health care providers, and, as such, it was not documented in the medical record. The potential development of COVID-19 rebound “is something to counsel your patients about.” COVID-19 rebound is a phenomenon that is being most commonly observed with nirmatrelvir-ritonavir as outpatient treatment.
Possible confounding factors in study
Katie Bechman, MBChB, clinical lecturer in rheumatology at King’s College London, who coauthored an accompanying editorial about the study and its findings, pointed out that the study is limited by its observational design.
“With any study that looks at the efficacy of treatment, especially in an observational cohort, you’re going to have to consider the unmeasured confounding and the difference between these two groups,” Dr. Bechman said. “I know that they did try to adjust for that in this study, but there’s always going to be factors that we can’t [control for]. That is something that needs to be considered. I think that’s always something we need to consider when we’re looking at observational data.”
In lieu of a randomized, controlled trial, Dr. Bechman noted that the study and its associated findings serve as “the best data we have,” and she described the results as “very informative and positive.”
She added that the large number of patients represents a strength of the study, as does the robust method employed for identifying which patients had COVID-19.
The learnings from this study with respect to outpatient treatment can be applied to more common illnesses that patients with rheumatic disease may develop, such as the flu, according to Dr. Bechman.
“One of the positive aspects from this pandemic is that we’ve learned a huge amount about how best to treat certain viruses and prevent them in patients,” she said. “It would be worth thinking towards the future, what we can do for illnesses that we see very commonly in these populations. There may be treatment regimens that we haven’t really considered until now. You could hypothesize that in the next couple of years, if we have an influenza breakout, that we should be providing some prehospital antiviral treatment to patients, especially the ones that are at high risk.”
The study was conducted without outside funding. Dr. Sparks has received research support from Bristol-Myers Squibb and consulted for AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer unrelated to this work. Dr. Bechman reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE LANCET RHEUMATOLOGY
The five biggest changes in the 2023 adult vaccine schedules
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
AAP approves 2023 child and adolescent immunization schedule
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
A new (old) drug joins the COVID fray, and guess what? It works
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.