User login
PACIFIC: Durvalumab extends PFS in stage 3 NSCLC
MADRID – For patients with locally advanced, unresectable non-small cell lung cancer, consolidation therapy with the anti-programmed death ligand 1 (PD-L1) inhibitor durvalumab after chemoradiation was associated with significantly better progression-free survival (PFS) than placebo, results of an interim analysis of the phase 3 PACIFIC trial showed.
Among 713 patients with stage III NSCLC treated with definitive chemoradiotherapy, the median PFS from randomization was 16.8 months for patients assigned to durvalumab compared with 5.6 months for patients assigned to placebo, reported Luis Paz-Ares, MD, from the University of Madrid, Spain.
“Overall, we think durvalumab is a promising option for patients with stage III non-small cell lung cancer treated with chemoradiation,” he said at a briefing at the European Society of Medical Oncology (ESMO) Congress.
Approximately 25% to 30% of patients with NSCLC have locally advanced disease at the time of presentation. Patients with unresectable disease and good performance status are treated with chemoradiotheraoy consisting of a platinum doublet with concurrent radiation, but median PFS in these patients is generally short, on the order of 8 months. The 5-year overall survival (OS) rate is 15%, he said.
Given the lack of major advances in the care of patients with stage 3 disease, investigators have been looking to newer therapies such as immune checkpoint inhibitors to see whether they could improve outcomes.
PACIFIC is a phase 3 trial in which patients with stage III NSCLC who did not have disease progression after a minimum of two cycles of platinum-based chemotherapy were assigned on a 2:1 basis to receive intravenous durvalumab 10 mg/kg or placebo every 2 weeks for up to 12 months. Patients were stratified by age, sex, and smoking history.
Dr. Paz-Ares presented PFS results from the interim analysis, planned when about 367 events had occurred. Data on the co-primary endpoint of OS were not mature at the time of the data cutoff.
Median PFS from randomization according to blinded independent central review for 476 patients treated with durvalumab was 16.8 months, compared with 5.6 months for 237 patients who received the placebo. This translated into a stratified hazard ratio (HR) of 0.52 (P less than .0001).
The respective PFS rates for durvalumab and placebo, were 59.9% vs. 35.3% at 12 months, and 44.2% vs. 27% at 18 months.
Among 443 patients on durvalumab and 213 on placebo who were evaluable for objective responses (OR), the respective OR rates were 28.4% vs. 16.
There were 6 complete responses (CR), 120 partial responses (PR), and 233 cases of stable disease in the durvalumab arm, compared with one CR, 33 PR, and 119 cases of stable disease in the placebo arm. In the durvalumab arm, 73 patients (16.5%) had progressive disease, compared with 59 patients (27.7%) in the placebo arm.
The median duration of response was not reached in the durvalumab arm, compared with 13.8 months in the placebo arm.
The PD-L1 inhibitor was also associated with a lower incidence of any new lesion among the intention-to-treat population (20.4% vs. 32.1%).
Grade 3 or 4 toxicities from any cause were slightly higher with durvalumab, at 29.9% vs. 26.1%. Events leading to discontinuation were also higher with the active drug, at 15.4% vs. 9.8% for placebo.
There were 21 deaths (4.4%) of patients treated with durvalumab, and 13 deaths (5.6%) of patients treated with placebo.
“In my opinion, this is a very well-designed study, and the results are very promising,” commented Enriqueta Felip, MD, who was not involved in the PACIFIC trial.
“We need to wait for the overall survival results, but in my opinion this is a very valuable trial in a group of patients [for whom] we need new strategies,” she said.
Dr. Felip was invited to the briefing as an independent commentator.
Results of the interim analysis of the PACIFIC trial were also published online in the New England Journal of Medicine.
The PACIFIC trial was funded by AstraZeneca. Dr. Paz-Ares has received consultancy fees from the company. Dr. Felip disclosed financial relationships with multiple companies not including AstraZeneca.
MADRID – For patients with locally advanced, unresectable non-small cell lung cancer, consolidation therapy with the anti-programmed death ligand 1 (PD-L1) inhibitor durvalumab after chemoradiation was associated with significantly better progression-free survival (PFS) than placebo, results of an interim analysis of the phase 3 PACIFIC trial showed.
Among 713 patients with stage III NSCLC treated with definitive chemoradiotherapy, the median PFS from randomization was 16.8 months for patients assigned to durvalumab compared with 5.6 months for patients assigned to placebo, reported Luis Paz-Ares, MD, from the University of Madrid, Spain.
“Overall, we think durvalumab is a promising option for patients with stage III non-small cell lung cancer treated with chemoradiation,” he said at a briefing at the European Society of Medical Oncology (ESMO) Congress.
Approximately 25% to 30% of patients with NSCLC have locally advanced disease at the time of presentation. Patients with unresectable disease and good performance status are treated with chemoradiotheraoy consisting of a platinum doublet with concurrent radiation, but median PFS in these patients is generally short, on the order of 8 months. The 5-year overall survival (OS) rate is 15%, he said.
Given the lack of major advances in the care of patients with stage 3 disease, investigators have been looking to newer therapies such as immune checkpoint inhibitors to see whether they could improve outcomes.
PACIFIC is a phase 3 trial in which patients with stage III NSCLC who did not have disease progression after a minimum of two cycles of platinum-based chemotherapy were assigned on a 2:1 basis to receive intravenous durvalumab 10 mg/kg or placebo every 2 weeks for up to 12 months. Patients were stratified by age, sex, and smoking history.
Dr. Paz-Ares presented PFS results from the interim analysis, planned when about 367 events had occurred. Data on the co-primary endpoint of OS were not mature at the time of the data cutoff.
Median PFS from randomization according to blinded independent central review for 476 patients treated with durvalumab was 16.8 months, compared with 5.6 months for 237 patients who received the placebo. This translated into a stratified hazard ratio (HR) of 0.52 (P less than .0001).
The respective PFS rates for durvalumab and placebo, were 59.9% vs. 35.3% at 12 months, and 44.2% vs. 27% at 18 months.
Among 443 patients on durvalumab and 213 on placebo who were evaluable for objective responses (OR), the respective OR rates were 28.4% vs. 16.
There were 6 complete responses (CR), 120 partial responses (PR), and 233 cases of stable disease in the durvalumab arm, compared with one CR, 33 PR, and 119 cases of stable disease in the placebo arm. In the durvalumab arm, 73 patients (16.5%) had progressive disease, compared with 59 patients (27.7%) in the placebo arm.
The median duration of response was not reached in the durvalumab arm, compared with 13.8 months in the placebo arm.
The PD-L1 inhibitor was also associated with a lower incidence of any new lesion among the intention-to-treat population (20.4% vs. 32.1%).
Grade 3 or 4 toxicities from any cause were slightly higher with durvalumab, at 29.9% vs. 26.1%. Events leading to discontinuation were also higher with the active drug, at 15.4% vs. 9.8% for placebo.
There were 21 deaths (4.4%) of patients treated with durvalumab, and 13 deaths (5.6%) of patients treated with placebo.
“In my opinion, this is a very well-designed study, and the results are very promising,” commented Enriqueta Felip, MD, who was not involved in the PACIFIC trial.
“We need to wait for the overall survival results, but in my opinion this is a very valuable trial in a group of patients [for whom] we need new strategies,” she said.
Dr. Felip was invited to the briefing as an independent commentator.
Results of the interim analysis of the PACIFIC trial were also published online in the New England Journal of Medicine.
The PACIFIC trial was funded by AstraZeneca. Dr. Paz-Ares has received consultancy fees from the company. Dr. Felip disclosed financial relationships with multiple companies not including AstraZeneca.
MADRID – For patients with locally advanced, unresectable non-small cell lung cancer, consolidation therapy with the anti-programmed death ligand 1 (PD-L1) inhibitor durvalumab after chemoradiation was associated with significantly better progression-free survival (PFS) than placebo, results of an interim analysis of the phase 3 PACIFIC trial showed.
Among 713 patients with stage III NSCLC treated with definitive chemoradiotherapy, the median PFS from randomization was 16.8 months for patients assigned to durvalumab compared with 5.6 months for patients assigned to placebo, reported Luis Paz-Ares, MD, from the University of Madrid, Spain.
“Overall, we think durvalumab is a promising option for patients with stage III non-small cell lung cancer treated with chemoradiation,” he said at a briefing at the European Society of Medical Oncology (ESMO) Congress.
Approximately 25% to 30% of patients with NSCLC have locally advanced disease at the time of presentation. Patients with unresectable disease and good performance status are treated with chemoradiotheraoy consisting of a platinum doublet with concurrent radiation, but median PFS in these patients is generally short, on the order of 8 months. The 5-year overall survival (OS) rate is 15%, he said.
Given the lack of major advances in the care of patients with stage 3 disease, investigators have been looking to newer therapies such as immune checkpoint inhibitors to see whether they could improve outcomes.
PACIFIC is a phase 3 trial in which patients with stage III NSCLC who did not have disease progression after a minimum of two cycles of platinum-based chemotherapy were assigned on a 2:1 basis to receive intravenous durvalumab 10 mg/kg or placebo every 2 weeks for up to 12 months. Patients were stratified by age, sex, and smoking history.
Dr. Paz-Ares presented PFS results from the interim analysis, planned when about 367 events had occurred. Data on the co-primary endpoint of OS were not mature at the time of the data cutoff.
Median PFS from randomization according to blinded independent central review for 476 patients treated with durvalumab was 16.8 months, compared with 5.6 months for 237 patients who received the placebo. This translated into a stratified hazard ratio (HR) of 0.52 (P less than .0001).
The respective PFS rates for durvalumab and placebo, were 59.9% vs. 35.3% at 12 months, and 44.2% vs. 27% at 18 months.
Among 443 patients on durvalumab and 213 on placebo who were evaluable for objective responses (OR), the respective OR rates were 28.4% vs. 16.
There were 6 complete responses (CR), 120 partial responses (PR), and 233 cases of stable disease in the durvalumab arm, compared with one CR, 33 PR, and 119 cases of stable disease in the placebo arm. In the durvalumab arm, 73 patients (16.5%) had progressive disease, compared with 59 patients (27.7%) in the placebo arm.
The median duration of response was not reached in the durvalumab arm, compared with 13.8 months in the placebo arm.
The PD-L1 inhibitor was also associated with a lower incidence of any new lesion among the intention-to-treat population (20.4% vs. 32.1%).
Grade 3 or 4 toxicities from any cause were slightly higher with durvalumab, at 29.9% vs. 26.1%. Events leading to discontinuation were also higher with the active drug, at 15.4% vs. 9.8% for placebo.
There were 21 deaths (4.4%) of patients treated with durvalumab, and 13 deaths (5.6%) of patients treated with placebo.
“In my opinion, this is a very well-designed study, and the results are very promising,” commented Enriqueta Felip, MD, who was not involved in the PACIFIC trial.
“We need to wait for the overall survival results, but in my opinion this is a very valuable trial in a group of patients [for whom] we need new strategies,” she said.
Dr. Felip was invited to the briefing as an independent commentator.
Results of the interim analysis of the PACIFIC trial were also published online in the New England Journal of Medicine.
The PACIFIC trial was funded by AstraZeneca. Dr. Paz-Ares has received consultancy fees from the company. Dr. Felip disclosed financial relationships with multiple companies not including AstraZeneca.
AT ESMO 2017
Shinal v. Toms: It’s Now Harder to Get Informed Consent
Question: Which of the following statements regarding Shinal v. Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
On Nov. 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on Dec. 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On Jan. 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s neurosurgery clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On Jan. 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower-risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior Court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the court disagreed, citing their ruling in the 2002 case of Valles v. Albert Einstein Medical Center,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the court held that the duty to obtain a patient’s informed consent is a nondelegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.”
The court also held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives. ... Informed consent is a product of the physician-patient relationship.
"The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise," the court added. "It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the court’s decision is, however, another matter. The American Medical Association and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error Act, as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3
The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Shinal v. Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v. Albert Einstein Medical Center, 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.
Question: Which of the following statements regarding Shinal v. Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
On Nov. 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on Dec. 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On Jan. 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s neurosurgery clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On Jan. 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower-risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior Court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the court disagreed, citing their ruling in the 2002 case of Valles v. Albert Einstein Medical Center,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the court held that the duty to obtain a patient’s informed consent is a nondelegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.”
The court also held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives. ... Informed consent is a product of the physician-patient relationship.
"The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise," the court added. "It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the court’s decision is, however, another matter. The American Medical Association and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error Act, as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3
The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Shinal v. Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v. Albert Einstein Medical Center, 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.
Question: Which of the following statements regarding Shinal v. Toms, a recent landmark decision on informed consent, is correct?:
A. The case was heard in the Pennsylvania Supreme Court and its decision is binding only in that state.
B. It held that obtaining informed consent is a doctor’s duty that is non-delegable.
C. The decision reversed the lower courts, which had held that the defendant’s qualified assistant could obtain consent.
D. An earlier case heard by the same court had ruled that doctors, not hospitals, owe the legal duty to obtain informed consent.
E. All are correct.
Answer: E.
On Nov. 26, 2007, Megan Shinal and Dr. Steven Toms met for a 20-minute initial consultation to discuss removing a recurrent craniopharyngioma.1 Years earlier, a surgeon had performed a transsphenoidal resection, but was unable to remove all of it. The residual portion of the tumor had increased in size and extended into vital structures of the brain, jeopardizing Mrs. Shinal’s eyesight and her carotid artery, causing headaches, and threatening to impact her pituitary function.
Dr. Toms testified that he reviewed with Mrs. Shinal the alternatives, risks, and benefits of total versus subtotal resection, and shared his opinion that, although a less aggressive approach to removing the tumor was safer in the short term, such an approach would increase the likelihood that the tumor would regrow. Dr. Toms was unable to recall many of the specifics, but he testified that he advised Mrs. Shinal that total surgical resection offered the highest chance for long-term survival. By the end of the visit, Mrs. Shinal had decided to undergo surgery. However, the type of surgery had not yet been determined.
Shortly thereafter, on Dec. 19, 2007, Mrs. Shinal had a telephone conversation with Dr. Toms’ physician assistant. Mrs. Shinal later testified that she asked the physician assistant about scarring that would likely result from surgery, whether radiation would be necessary, and about the date of surgery. The medical record of this telephone call indicated that Dr. Toms’ physician assistant also answered questions about the craniotomy incision. On Jan. 17, 2008, Mrs. Shinal met with the physician assistant at the Geisinger Medical Center’s neurosurgery clinic. The assistant obtained Mrs. Shinal’s medical history, conducted a physical, and provided Mrs. Shinal with information relating to the surgery. Mrs. Shinal signed an informed consent form.
On Jan. 31, 2008, Mrs. Shinal underwent an open craniotomy for a total resection of the pituitary tumor at Geisinger Medical Center. During the operation, Dr. Toms perforated Mrs. Shinal’s carotid artery, which resulted in hemorrhage, stroke, brain injury, and partial blindness.
According to the Shinals’ complaint, Dr. Toms failed to explain the risks of surgery to Mrs. Shinal or to offer her the lower-risk surgical alternative of subtotal resection of the benign tumor, followed by radiation. At trial, Mrs. Shinal was unable to recall being informed of the relative risks of the surgery, other than coma and death. She testified that, had she known the alternative approaches to surgery, i.e., total versus subtotal resection, she would have chosen subtotal resection as the safer, less aggressive alternative.
The trial court instructed the jury with regard to Dr. Toms’ duty to obtain informed consent from Mrs. Shinal as follows: “[I]n considering whether [Dr. Toms] provided consent to [Mrs. Shinal], you may consider any relevant information you find was communicated to [Mrs. Shinal] by any qualified person acting as an assistant to [Dr. Toms].”
On April 21, 2014, the jury returned a verdict in favor of Dr. Toms.
The plaintiffs appealed to the Pennsylvania Superior Court, which affirmed the trial court’s judgment. It rejected the Shinals’ argument that the trial court’s informed consent charge, which permitted the jury to consider information provided by Dr. Toms’ physician assistant to Mrs. Shinal, was erroneous and prejudicial. The Superior Court relied upon two of its prior cases to opine that a qualified professional acting under the attending doctor’s supervision may convey information communicated to a patient for purposes of obtaining informed consent.
The trial court initially instructed the jury that, in assessing whether Dr. Toms obtained Mrs. Shinal’s informed consent, it could consider relevant information communicated by “any qualified person acting as an assistant” to Dr. Toms. The defendant doctor argued that while it is the physician’s duty to obtain the patient’s informed consent, the physician is not required to supply all of the information personally. It is the information conveyed, rather than the person conveying it that determines informed consent. Dr. Toms cited several older Pennsylvania Superior Court cases, which permitted a physician to fulfill through an intermediary the duty to provide sufficient information to obtain a patient’s informed consent.
The plaintiffs then appealed to the Pennsylvania Supreme Court, which led to a reversal. In a 4-3 decision, the court disagreed, citing their ruling in the 2002 case of Valles v. Albert Einstein Medical Center,2 where they held that the duty to obtain informed consent could not be imputed to a hospital. In Valles, the court held that the duty to obtain a patient’s informed consent is a nondelegable duty owed by the physician conducting the surgery or treatment, because obtaining informed consent results directly from the duty of disclosure, which lies solely with the physician, and a hospital therefore cannot be liable for a physician’s failure to obtain informed consent.
Reasoning by extension, the court accordingly ruled that a physician may not delegate to others his or her obligation to provide sufficient information in order to obtain a patient’s informed consent. It declared: “Informed consent requires direct communication between physician and patient, and contemplates a back-and-forth, face-to-face exchange, which might include questions that the patient feels the physician must answer personally before the patient feels informed and becomes willing to consent. The duty to obtain the patient’s informed consent belongs solely to the physician.”
The court also held that “a physician cannot rely upon a subordinate to disclose the information required to obtain informed consent. Without direct dialogue and a two-way exchange between the physician and patient, the physician cannot be confident that the patient comprehends the risks, benefits, likelihood of success, and alternatives. ... Informed consent is a product of the physician-patient relationship.
"The patient is in the vulnerable position of entrusting his or her care and well being to the physician based upon the physician’s education, training, and expertise," the court added. "It is incumbent upon the physician to cultivate a relationship with the patient and to familiarize himself or herself with the patient’s understanding and expectations. Were the law to permit physicians to delegate the provision of critical information to staff, it would undermine patient autonomy and bodily integrity by depriving the patient of the opportunity to engage in a dialogue with his or her chosen health care provider. A regime that would countenance delegation of the informed consent process would undermine the primacy of the physician-patient relationship. Only by personally satisfying the duty of disclosure may the physician ensure that consent truly is informed.”
The facts of the case appear straightforward, and its legal conclusion clear. Whether one agrees with the court’s decision is, however, another matter. The American Medical Association and the Pennsylvania Medical Society (PAMED) had submitted an amicus brief supporting Dr. Toms’ position, arguing that he had fulfilled his obligations under Pennsylvania’s Medical Care Availability and Reduction of Error Act, as well as common law established in previous Pennsylvania court rulings. The final appellate decision therefore came as a big disappointment. The PAMED website notes that the decision “could have significant ramifications for Pennsylvania physicians” in that they can “seemingly no longer rely on the aid of their qualified staff in the informed consent process.”3
The urgent question now is whether other jurisdictions will adopt this Pennsylvania rule that drastically changes the way doctors obtain informed consent from their patients.
Dr. Tan is emeritus professor of medicine and former adjunct professor of law at the University of Hawaii, Honolulu. This article is meant to be educational and does not constitute medical, ethical, or legal advice. For additional information, readers may contact the author at siang@hawaii.edu.
References
1. Shinal v. Toms, J-106-2016, Supreme Court of Pennsylvania, Decided: June 20, 2017.
2. Valles v. Albert Einstein Medical Center, 805 A.2d (PA, 2002).
3. Informed-consent ruling may have “far-reaching, negative impact.” AMA Wire, Aug 8, 2017.
Plerixafor doesn’t overcome HPC failure in R-hyperCVAD for mantle cell lymphoma
A commonly-used intensive induction regimen was associated with higher rates of hematopoietic progenitor cell mobilization failure in patients with mantle cell lymphoma, even when plerixafor rescue was attempted, based on a study by Amandeep Salhotra, MD, and his colleagues at City of Hope, Duarte, Calif.
Patients who received rituximab and hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-hyperCVAD) in the era after plerixafor came into use experienced significantly higher rates of peripheral blood stem cell (PBSC) collection failure than did patients receiving other induction regimens (17% vs. 4% failure rate, P = .04).
“Plerixafor does not overcome the negative impact of R-hyperCVAD on PBSC mobilization, and caution is warranted in using R-hyperCVAD in patients with newly diagnosed MCL who are candidates for ASCT (autologous stem cell transplant),” wrote Dr. Salhotra and his colleagues.
The higher rate of hematopoietic progenitor cell collection failure for R-hyperCVAD patients could not be attributed to their age at time of mantle cell lymphoma diagnosis or to the amount of time between diagnosis and collection.
Treatment records for 181 consecutive mantle cell lymphoma patients were examined for a 10 year period in the retrospective single-site study. Plerixafor, a C-X-C chemokine receptor agonist that reduces hematopoietic progenitor cells’ ability to bind to bone marrow stroma, was introduced on August 16, 2009; a total of 71 patients were treated before this point, and 110 were treated afterward.
The R-hyperCVAD regimen was received by 34 pre-plerixafor patients (45%) and by 42 of the post-plerixafor era patients (55%). Other regimens were received by 37 (35%) and 68 (65%) of the pre- and post-plerixafor era patients, respectively.
Before plerixafor came into use, Dr. Salhotra, of City of Hope’s department of hematology and hematopoietic cell transplantation, and his coinvestigators saw no significant difference among their study population in the rates of PBSC collection failure between those receiving R-hyperCVAD (11%) and those receiving other regimens (12%). The findings were reported in Biology of Blood and Marrow Transplantation.
The study was conducted in the context of other recent work that showed higher rates of PBSC collection failure and fewer CD34+ cells collected with the use of an R-hyperCVAD conditioning regimen. The fact that PBSC mobilization rates were significantly lower in R-hyperCVAD patients post-plerixafor surprised the investigators, who had hypothesized that the use of plerixafor would overcome PBSC mobilization failures without regard to the conditioning regimen used.
“It may be worthwhile to consider using a more aggressive strategy for [hematopoetic progenitor cell] mobilization in patients who have received R-hyperCVAD chemotherapy upfront or as salvage for aggressive lymphomas,” the researchers wrote. This might include the use of plerixafor upfront when patients have low CD34 counts before apheresis.
The researchers plan to examine their data to see how the choice of induction regimen and plerixafor usage impact patient survival.
The study authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
koakes@frontlinemedcom.com
SOURCE: Biol Blood Marrow Transplant 2017; 23:1264-1268. http://dx.doi.org/10.1016/j.bbmt.2017.04.011
A commonly-used intensive induction regimen was associated with higher rates of hematopoietic progenitor cell mobilization failure in patients with mantle cell lymphoma, even when plerixafor rescue was attempted, based on a study by Amandeep Salhotra, MD, and his colleagues at City of Hope, Duarte, Calif.
Patients who received rituximab and hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-hyperCVAD) in the era after plerixafor came into use experienced significantly higher rates of peripheral blood stem cell (PBSC) collection failure than did patients receiving other induction regimens (17% vs. 4% failure rate, P = .04).
“Plerixafor does not overcome the negative impact of R-hyperCVAD on PBSC mobilization, and caution is warranted in using R-hyperCVAD in patients with newly diagnosed MCL who are candidates for ASCT (autologous stem cell transplant),” wrote Dr. Salhotra and his colleagues.
The higher rate of hematopoietic progenitor cell collection failure for R-hyperCVAD patients could not be attributed to their age at time of mantle cell lymphoma diagnosis or to the amount of time between diagnosis and collection.
Treatment records for 181 consecutive mantle cell lymphoma patients were examined for a 10 year period in the retrospective single-site study. Plerixafor, a C-X-C chemokine receptor agonist that reduces hematopoietic progenitor cells’ ability to bind to bone marrow stroma, was introduced on August 16, 2009; a total of 71 patients were treated before this point, and 110 were treated afterward.
The R-hyperCVAD regimen was received by 34 pre-plerixafor patients (45%) and by 42 of the post-plerixafor era patients (55%). Other regimens were received by 37 (35%) and 68 (65%) of the pre- and post-plerixafor era patients, respectively.
Before plerixafor came into use, Dr. Salhotra, of City of Hope’s department of hematology and hematopoietic cell transplantation, and his coinvestigators saw no significant difference among their study population in the rates of PBSC collection failure between those receiving R-hyperCVAD (11%) and those receiving other regimens (12%). The findings were reported in Biology of Blood and Marrow Transplantation.
The study was conducted in the context of other recent work that showed higher rates of PBSC collection failure and fewer CD34+ cells collected with the use of an R-hyperCVAD conditioning regimen. The fact that PBSC mobilization rates were significantly lower in R-hyperCVAD patients post-plerixafor surprised the investigators, who had hypothesized that the use of plerixafor would overcome PBSC mobilization failures without regard to the conditioning regimen used.
“It may be worthwhile to consider using a more aggressive strategy for [hematopoetic progenitor cell] mobilization in patients who have received R-hyperCVAD chemotherapy upfront or as salvage for aggressive lymphomas,” the researchers wrote. This might include the use of plerixafor upfront when patients have low CD34 counts before apheresis.
The researchers plan to examine their data to see how the choice of induction regimen and plerixafor usage impact patient survival.
The study authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
koakes@frontlinemedcom.com
SOURCE: Biol Blood Marrow Transplant 2017; 23:1264-1268. http://dx.doi.org/10.1016/j.bbmt.2017.04.011
A commonly-used intensive induction regimen was associated with higher rates of hematopoietic progenitor cell mobilization failure in patients with mantle cell lymphoma, even when plerixafor rescue was attempted, based on a study by Amandeep Salhotra, MD, and his colleagues at City of Hope, Duarte, Calif.
Patients who received rituximab and hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone (R-hyperCVAD) in the era after plerixafor came into use experienced significantly higher rates of peripheral blood stem cell (PBSC) collection failure than did patients receiving other induction regimens (17% vs. 4% failure rate, P = .04).
“Plerixafor does not overcome the negative impact of R-hyperCVAD on PBSC mobilization, and caution is warranted in using R-hyperCVAD in patients with newly diagnosed MCL who are candidates for ASCT (autologous stem cell transplant),” wrote Dr. Salhotra and his colleagues.
The higher rate of hematopoietic progenitor cell collection failure for R-hyperCVAD patients could not be attributed to their age at time of mantle cell lymphoma diagnosis or to the amount of time between diagnosis and collection.
Treatment records for 181 consecutive mantle cell lymphoma patients were examined for a 10 year period in the retrospective single-site study. Plerixafor, a C-X-C chemokine receptor agonist that reduces hematopoietic progenitor cells’ ability to bind to bone marrow stroma, was introduced on August 16, 2009; a total of 71 patients were treated before this point, and 110 were treated afterward.
The R-hyperCVAD regimen was received by 34 pre-plerixafor patients (45%) and by 42 of the post-plerixafor era patients (55%). Other regimens were received by 37 (35%) and 68 (65%) of the pre- and post-plerixafor era patients, respectively.
Before plerixafor came into use, Dr. Salhotra, of City of Hope’s department of hematology and hematopoietic cell transplantation, and his coinvestigators saw no significant difference among their study population in the rates of PBSC collection failure between those receiving R-hyperCVAD (11%) and those receiving other regimens (12%). The findings were reported in Biology of Blood and Marrow Transplantation.
The study was conducted in the context of other recent work that showed higher rates of PBSC collection failure and fewer CD34+ cells collected with the use of an R-hyperCVAD conditioning regimen. The fact that PBSC mobilization rates were significantly lower in R-hyperCVAD patients post-plerixafor surprised the investigators, who had hypothesized that the use of plerixafor would overcome PBSC mobilization failures without regard to the conditioning regimen used.
“It may be worthwhile to consider using a more aggressive strategy for [hematopoetic progenitor cell] mobilization in patients who have received R-hyperCVAD chemotherapy upfront or as salvage for aggressive lymphomas,” the researchers wrote. This might include the use of plerixafor upfront when patients have low CD34 counts before apheresis.
The researchers plan to examine their data to see how the choice of induction regimen and plerixafor usage impact patient survival.
The study authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
koakes@frontlinemedcom.com
SOURCE: Biol Blood Marrow Transplant 2017; 23:1264-1268. http://dx.doi.org/10.1016/j.bbmt.2017.04.011
FROM BIOLOGY OF BLOOD AND MARROW TRANSPLANTATION
Key clinical point: R-hyperCVAD was associated with increased peripheral blood stem cell (PBSC) collection failure in the post-plerixafor era.
Major finding: Patients receiving R-hyperCVAD in the post-plerixafor era had a 17% PBSC collection failure rate, compared to a 4% rate for those receiving other chemotherapy (P = 0.04).
Study details: Single-center retrospective study of 181 consecutive patients with mantle cell lymphoma over a 10-year period spanning the introduction of plerixafor.
Disclosures: The study was sponsored by City of Hope and the National Cancer Institute; the authors reported no conflicts of interest.
Source: Amandeep Salhotra, et al. Hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone chemotherapy in mantle cell lymphoma patients is associated with higher rates of hematopoietic progenitor cell mobilization failure despite plerixafor rescue. Biol Blood Marrow Transplant 2017; 23:1264-1268.
Alcohol misuse universal screening effective and efficient
Universal screening for alcohol misuse in acute medical admissions is feasible and can reduce readmissions for liver disease, according to a new study.
Detecting patients’ alcohol misuse early can help treat or prevent alcohol-related liver disease, such as cirrhosis; however, screening is not being used in a routine, effective way, according to Greta Westwood, PhD, head of Nursing, Midwifery, and AHP Research at Portsmouth (England) Hospitals and her fellow investigators.
“In primary care, screening is highly variable, and treatment rates are low, often focusing on patients who already have advanced psychiatric or physical illness,” Dr. Westwood and her colleagues wrote. “In addition, many patients with alcohol use disorders do not fully engage with primary care services for a variety of reasons, often leading to excessive use of the hospital ED as the first point of contact.”
Investigators conducted a retrospective, observational study of 53,165 patients who were admitted to the acute medical unit at Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014 (J Hepatol. 2017 Sep;67[3]:559-67).
More than half of patients were male (52%), the average patient age was 67 years, and the patients had an average of three previous hospital admissions.
Of the patients observed, 48,211 (90.68%) completed the screening test, while the remaining 4,934 (9.32%) did not.
Those who were not screened had a higher mortality rate than did those who were (8.30% vs 6.17%; P less than .001), were more likely to be discharged the same day (3.37% vs. 1.87%; P less than .001), and were more likely to discharge themselves (29.67% vs. 13.31%; P less than .001).
The screening process, an electronic modified version of the Paddington Alcohol Test, consisted of the nurses’ asking a series of questions about types of alcohol consumed, frequency and maximum daily amount, whether the admission was considered alcohol related, and they documented signs of alcohol withdrawal.
Patients were then given a score based on how the answers compared with the healthy level of alcohol consumption, with 0-2 points considered “low risk,” 3-5 points considered “increasing risk,” and 6-10 points considered “high risk.”
Those assigned a low-risk status were not referred to intervention, but doctors recommended increasing-risk patients attend a community alcohol intervention team for brief intervention, while high-risk patients were automatically referred to an Alcohol Specialist Nursing Service (ASNS).
Of those screened, there were 1,135 patients (2.33%) considered at increasing risk of alcohol misuse and 1,921 (3.98%) at high risk.
While 68.5% of patients with a high-risk score were referred to the ASNS, all those who were referred completed the medical detoxification course, according to investigators.
High-risk patients were found to have had, on average, more hospital visits than increasing- and low-risk patients – 4.74 visits, compared with 2.92 and 3.00, respectively; they also reported more ED trips – 7.68 visits, compared with 3.81 and 2.64, respectively.
Dr. Westwood and her colleagues found that, when using the screening tool, investigators were more likely to find signs of alcohol-related liver disease among those with higher scores.
Liver, pancreatic, and digestive disorders accounted for 22.1% of primary admission codes of high-risk patients, compared with 3.2% of low-risk patients.
Investigators wrote that this tool can help doctors identify at-risk patients early and attack the problem of alcohol misuse head on and in a timely manner.
“It is vital that patients with cirrhosis who continue to drink are identified and referred to dedicated hospital alcohol care teams,” Dr. Westwood and her colleagues wrote. “Screening can identify patients at an increased risk of alcohol-related harm whose range of diagnoses is not dissimilar to lower-risk patients and whose misuse of alcohol might otherwise have not been identified.”
Investigators did not account for decreased scores or testing effectiveness in patients readmitted and retested. Additionally, the long-term impact of ASNS care is still being studied.
Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
Universal screening for alcohol misuse in acute medical admissions is feasible and can reduce readmissions for liver disease, according to a new study.
Detecting patients’ alcohol misuse early can help treat or prevent alcohol-related liver disease, such as cirrhosis; however, screening is not being used in a routine, effective way, according to Greta Westwood, PhD, head of Nursing, Midwifery, and AHP Research at Portsmouth (England) Hospitals and her fellow investigators.
“In primary care, screening is highly variable, and treatment rates are low, often focusing on patients who already have advanced psychiatric or physical illness,” Dr. Westwood and her colleagues wrote. “In addition, many patients with alcohol use disorders do not fully engage with primary care services for a variety of reasons, often leading to excessive use of the hospital ED as the first point of contact.”
Investigators conducted a retrospective, observational study of 53,165 patients who were admitted to the acute medical unit at Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014 (J Hepatol. 2017 Sep;67[3]:559-67).
More than half of patients were male (52%), the average patient age was 67 years, and the patients had an average of three previous hospital admissions.
Of the patients observed, 48,211 (90.68%) completed the screening test, while the remaining 4,934 (9.32%) did not.
Those who were not screened had a higher mortality rate than did those who were (8.30% vs 6.17%; P less than .001), were more likely to be discharged the same day (3.37% vs. 1.87%; P less than .001), and were more likely to discharge themselves (29.67% vs. 13.31%; P less than .001).
The screening process, an electronic modified version of the Paddington Alcohol Test, consisted of the nurses’ asking a series of questions about types of alcohol consumed, frequency and maximum daily amount, whether the admission was considered alcohol related, and they documented signs of alcohol withdrawal.
Patients were then given a score based on how the answers compared with the healthy level of alcohol consumption, with 0-2 points considered “low risk,” 3-5 points considered “increasing risk,” and 6-10 points considered “high risk.”
Those assigned a low-risk status were not referred to intervention, but doctors recommended increasing-risk patients attend a community alcohol intervention team for brief intervention, while high-risk patients were automatically referred to an Alcohol Specialist Nursing Service (ASNS).
Of those screened, there were 1,135 patients (2.33%) considered at increasing risk of alcohol misuse and 1,921 (3.98%) at high risk.
While 68.5% of patients with a high-risk score were referred to the ASNS, all those who were referred completed the medical detoxification course, according to investigators.
High-risk patients were found to have had, on average, more hospital visits than increasing- and low-risk patients – 4.74 visits, compared with 2.92 and 3.00, respectively; they also reported more ED trips – 7.68 visits, compared with 3.81 and 2.64, respectively.
Dr. Westwood and her colleagues found that, when using the screening tool, investigators were more likely to find signs of alcohol-related liver disease among those with higher scores.
Liver, pancreatic, and digestive disorders accounted for 22.1% of primary admission codes of high-risk patients, compared with 3.2% of low-risk patients.
Investigators wrote that this tool can help doctors identify at-risk patients early and attack the problem of alcohol misuse head on and in a timely manner.
“It is vital that patients with cirrhosis who continue to drink are identified and referred to dedicated hospital alcohol care teams,” Dr. Westwood and her colleagues wrote. “Screening can identify patients at an increased risk of alcohol-related harm whose range of diagnoses is not dissimilar to lower-risk patients and whose misuse of alcohol might otherwise have not been identified.”
Investigators did not account for decreased scores or testing effectiveness in patients readmitted and retested. Additionally, the long-term impact of ASNS care is still being studied.
Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
Universal screening for alcohol misuse in acute medical admissions is feasible and can reduce readmissions for liver disease, according to a new study.
Detecting patients’ alcohol misuse early can help treat or prevent alcohol-related liver disease, such as cirrhosis; however, screening is not being used in a routine, effective way, according to Greta Westwood, PhD, head of Nursing, Midwifery, and AHP Research at Portsmouth (England) Hospitals and her fellow investigators.
“In primary care, screening is highly variable, and treatment rates are low, often focusing on patients who already have advanced psychiatric or physical illness,” Dr. Westwood and her colleagues wrote. “In addition, many patients with alcohol use disorders do not fully engage with primary care services for a variety of reasons, often leading to excessive use of the hospital ED as the first point of contact.”
Investigators conducted a retrospective, observational study of 53,165 patients who were admitted to the acute medical unit at Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014 (J Hepatol. 2017 Sep;67[3]:559-67).
More than half of patients were male (52%), the average patient age was 67 years, and the patients had an average of three previous hospital admissions.
Of the patients observed, 48,211 (90.68%) completed the screening test, while the remaining 4,934 (9.32%) did not.
Those who were not screened had a higher mortality rate than did those who were (8.30% vs 6.17%; P less than .001), were more likely to be discharged the same day (3.37% vs. 1.87%; P less than .001), and were more likely to discharge themselves (29.67% vs. 13.31%; P less than .001).
The screening process, an electronic modified version of the Paddington Alcohol Test, consisted of the nurses’ asking a series of questions about types of alcohol consumed, frequency and maximum daily amount, whether the admission was considered alcohol related, and they documented signs of alcohol withdrawal.
Patients were then given a score based on how the answers compared with the healthy level of alcohol consumption, with 0-2 points considered “low risk,” 3-5 points considered “increasing risk,” and 6-10 points considered “high risk.”
Those assigned a low-risk status were not referred to intervention, but doctors recommended increasing-risk patients attend a community alcohol intervention team for brief intervention, while high-risk patients were automatically referred to an Alcohol Specialist Nursing Service (ASNS).
Of those screened, there were 1,135 patients (2.33%) considered at increasing risk of alcohol misuse and 1,921 (3.98%) at high risk.
While 68.5% of patients with a high-risk score were referred to the ASNS, all those who were referred completed the medical detoxification course, according to investigators.
High-risk patients were found to have had, on average, more hospital visits than increasing- and low-risk patients – 4.74 visits, compared with 2.92 and 3.00, respectively; they also reported more ED trips – 7.68 visits, compared with 3.81 and 2.64, respectively.
Dr. Westwood and her colleagues found that, when using the screening tool, investigators were more likely to find signs of alcohol-related liver disease among those with higher scores.
Liver, pancreatic, and digestive disorders accounted for 22.1% of primary admission codes of high-risk patients, compared with 3.2% of low-risk patients.
Investigators wrote that this tool can help doctors identify at-risk patients early and attack the problem of alcohol misuse head on and in a timely manner.
“It is vital that patients with cirrhosis who continue to drink are identified and referred to dedicated hospital alcohol care teams,” Dr. Westwood and her colleagues wrote. “Screening can identify patients at an increased risk of alcohol-related harm whose range of diagnoses is not dissimilar to lower-risk patients and whose misuse of alcohol might otherwise have not been identified.”
Investigators did not account for decreased scores or testing effectiveness in patients readmitted and retested. Additionally, the long-term impact of ASNS care is still being studied.
Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
ezimmerman@frontlinemedcom.com
On Twitter @eaztweets
FROM JOURNAL OF HEPATOLOGY
Key clinical point:
Major finding: Patients who were admitted and were not screened for alcohol misuse risk had a higher mortality rate, compared with those who were screened (8.3% vs. 6.17%; P less than .001).
Data source: Retrospective observational study of 53,165 patients admitted to the acute medical clinic of the Queen Alexandra Hospital, Portsmouth, England, between July 2011 and March 2014.
Disclosures: Two investigators reported affiliations with the Learning Clinic, which created and licensed the analysis program that is part of the screening tool. All other investigators, including Dr. Westwood, reported no relevant financial disclosures.
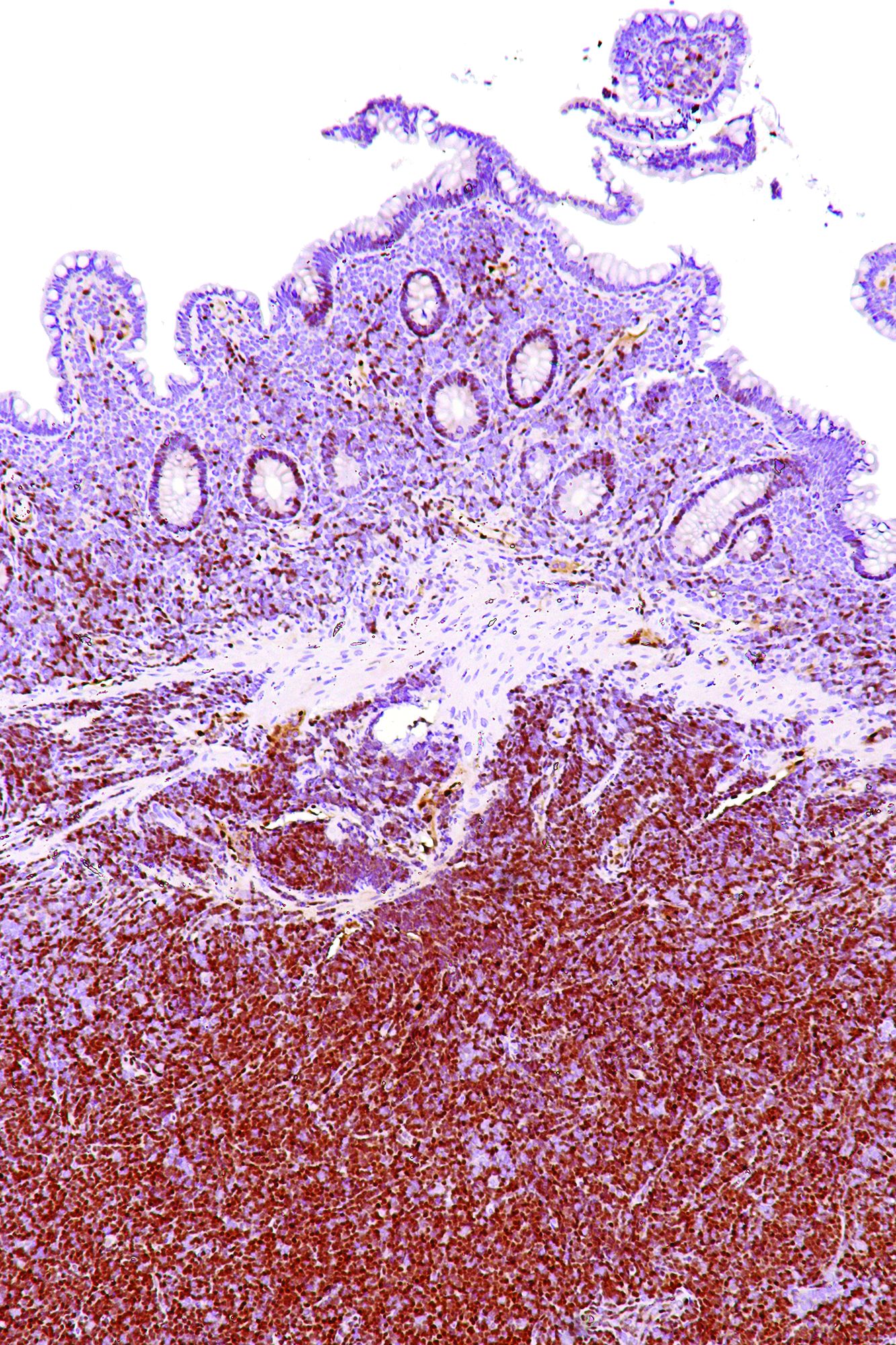
Team identifies mutation that causes EPP
Researchers say they have discovered a genetic mutation that triggers erythropoietic protoporphyria (EPP).
The team performed genetic sequencing on members of a family from Northern France who had EPP of a previously unknown genetic signature.
The sequencing revealed a mutation in the gene CLPX that promotes EPP.
Barry Paw MD, PhD, of the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center in Massachusetts, and his colleagues reported this discovery in PNAS.
About EPP
To produce heme, the body goes through porphyrin synthesis, which mainly occurs in the liver and bone marrow. Genetic defects can hinder the body’s ability to produce heme, and a decrease in heme production leads to a buildup of protoporphyrin components.
In the case of EPP, protoporphyrin IX accumulates in the red blood cells, plasma, and sometimes the liver.
When protoporphyrin IX is exposed to light, it produces chemicals that damage surrounding cells. As a result, people with EPP experience swelling, burning, and redness of the skin after exposure to sunlight.
“People with EPP are chronically anemic, which makes them feel very tired and look very pale, with increased photosensitivity because they can’t come out in the daylight,” Dr Paw said. “Even on a cloudy day, there’s enough ultraviolet light to cause blistering and disfigurement of the exposed body parts, ears, and nose.”
Although some genetic pathways leading to the build-up of protoporphyrin IX have already been described, many cases of EPP remain unexplained.
New discovery
Dr Paw and his colleagues noted that heme synthesis is controlled by the mitochondrial AAA+ unfoldase ClpX, which participates in the degradation and activation of δ-aminolevulinate synthase (ALAS).
In their analysis of the French family with EPP, the researchers discovered a dominant mutation in the ATPase active site of CLPX. This mutation—p.Gly298Asp—prompts the accumulation of protoporphyrin IX.
The researchers said the mutation partially inactivates CLPX, which increases the post-translational stability of ALAS. This increases ALAS protein and ALA levels and leads to the accumulation of protoporphyrin IX.
“This newly discovered mutation really highlights the complex genetic network that underpins heme metabolism,” Dr Paw said. “Loss-of-function mutations in any number of genes that are part of this network can result in devastating, disfiguring disorders.”
Dr Paw also noted that identifying the mutations that contribute to EPP and other porphyrias could pave the way for new methods of treating these disorders. ![]()
Researchers say they have discovered a genetic mutation that triggers erythropoietic protoporphyria (EPP).
The team performed genetic sequencing on members of a family from Northern France who had EPP of a previously unknown genetic signature.
The sequencing revealed a mutation in the gene CLPX that promotes EPP.
Barry Paw MD, PhD, of the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center in Massachusetts, and his colleagues reported this discovery in PNAS.
About EPP
To produce heme, the body goes through porphyrin synthesis, which mainly occurs in the liver and bone marrow. Genetic defects can hinder the body’s ability to produce heme, and a decrease in heme production leads to a buildup of protoporphyrin components.
In the case of EPP, protoporphyrin IX accumulates in the red blood cells, plasma, and sometimes the liver.
When protoporphyrin IX is exposed to light, it produces chemicals that damage surrounding cells. As a result, people with EPP experience swelling, burning, and redness of the skin after exposure to sunlight.
“People with EPP are chronically anemic, which makes them feel very tired and look very pale, with increased photosensitivity because they can’t come out in the daylight,” Dr Paw said. “Even on a cloudy day, there’s enough ultraviolet light to cause blistering and disfigurement of the exposed body parts, ears, and nose.”
Although some genetic pathways leading to the build-up of protoporphyrin IX have already been described, many cases of EPP remain unexplained.
New discovery
Dr Paw and his colleagues noted that heme synthesis is controlled by the mitochondrial AAA+ unfoldase ClpX, which participates in the degradation and activation of δ-aminolevulinate synthase (ALAS).
In their analysis of the French family with EPP, the researchers discovered a dominant mutation in the ATPase active site of CLPX. This mutation—p.Gly298Asp—prompts the accumulation of protoporphyrin IX.
The researchers said the mutation partially inactivates CLPX, which increases the post-translational stability of ALAS. This increases ALAS protein and ALA levels and leads to the accumulation of protoporphyrin IX.
“This newly discovered mutation really highlights the complex genetic network that underpins heme metabolism,” Dr Paw said. “Loss-of-function mutations in any number of genes that are part of this network can result in devastating, disfiguring disorders.”
Dr Paw also noted that identifying the mutations that contribute to EPP and other porphyrias could pave the way for new methods of treating these disorders. ![]()
Researchers say they have discovered a genetic mutation that triggers erythropoietic protoporphyria (EPP).
The team performed genetic sequencing on members of a family from Northern France who had EPP of a previously unknown genetic signature.
The sequencing revealed a mutation in the gene CLPX that promotes EPP.
Barry Paw MD, PhD, of the Dana-Farber/Boston Children’s Cancer and Blood Disorders Center in Massachusetts, and his colleagues reported this discovery in PNAS.
About EPP
To produce heme, the body goes through porphyrin synthesis, which mainly occurs in the liver and bone marrow. Genetic defects can hinder the body’s ability to produce heme, and a decrease in heme production leads to a buildup of protoporphyrin components.
In the case of EPP, protoporphyrin IX accumulates in the red blood cells, plasma, and sometimes the liver.
When protoporphyrin IX is exposed to light, it produces chemicals that damage surrounding cells. As a result, people with EPP experience swelling, burning, and redness of the skin after exposure to sunlight.
“People with EPP are chronically anemic, which makes them feel very tired and look very pale, with increased photosensitivity because they can’t come out in the daylight,” Dr Paw said. “Even on a cloudy day, there’s enough ultraviolet light to cause blistering and disfigurement of the exposed body parts, ears, and nose.”
Although some genetic pathways leading to the build-up of protoporphyrin IX have already been described, many cases of EPP remain unexplained.
New discovery
Dr Paw and his colleagues noted that heme synthesis is controlled by the mitochondrial AAA+ unfoldase ClpX, which participates in the degradation and activation of δ-aminolevulinate synthase (ALAS).
In their analysis of the French family with EPP, the researchers discovered a dominant mutation in the ATPase active site of CLPX. This mutation—p.Gly298Asp—prompts the accumulation of protoporphyrin IX.
The researchers said the mutation partially inactivates CLPX, which increases the post-translational stability of ALAS. This increases ALAS protein and ALA levels and leads to the accumulation of protoporphyrin IX.
“This newly discovered mutation really highlights the complex genetic network that underpins heme metabolism,” Dr Paw said. “Loss-of-function mutations in any number of genes that are part of this network can result in devastating, disfiguring disorders.”
Dr Paw also noted that identifying the mutations that contribute to EPP and other porphyrias could pave the way for new methods of treating these disorders. ![]()
Minimally invasive esophagectomy may mean less major morbidity
COLORADO SPRINGS – Minimally invasive esophagectomy was associated with a significantly lower rate of postoperative major morbidity as well as a mean 1-day briefer length of stay than open esophagectomy in a propensity-matched analysis of the real-world American College of Surgeons-National Quality Improvement Program database, Mark F. Berry, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
However, both of the study’s discussants questioned whether the reported modest absolute reduction in major morbidity was really attributable to the minimally invasive approach or could instead have resulted from one of several potential confounders that couldn’t be fully adjusted for, given inherent limitations of the ACS-NSQIP database.
“There was a statistically significant difference in morbidity,” replied Dr. Berry of Stanford (Calif.) University. “It was a 4% absolute difference, which I think is probably clinically meaningful, but certainly it’s not really, really dramatic.”
“What I think we found is that it’s safe to do a minimally invasive esophagectomy and safe for people to introduce it into their practice. But it’s not necessarily something that’s a game changer, unlike what’s been seen with minimally invasive approaches for some other things,” said Dr. Berry, who added that he didn’t wish to overstate the importance of the observed difference in morbidity.
Studies from high-volume centers show that minimally-invasive esophagectomy (MIE) reduces length of stay, postoperative major morbidity, and features equivalent or even slightly lower mortality than traditional open esophagectomy, the generalizability of these findings beyond such centers is questionable. That’s why Dr. Berry and his coinvestigators turned to the ACS-NSQIP database, which includes all esophagectomies performed for esophageal cancer at roughly 700 U.S. hospitals, not just those done by board-certified thoracic surgeons.
He presented a retrospective cohort study of 3,901 esophagectomy patients during 2005-2013 who met study criteria, 16.4% of whom had MIE. The use of this approach increased steadily from 6.5% of all esophagectomies in 2005 to 22.3% in 2013. A propensity-matched analysis designed to neutralize potentially confounding differences included 638 MIE and 1,914 open esophagectomy patients.
The primary outcome was the 30-day rate of composite major morbidity in the realms of various wound, respiratory, renal, and cardiovascular complications. The rate was 36.1% in the MIE group and 40.5% with open esophagectomy in the propensity-matched analysis, an absolute risk reduction of 4.4% and a relative risk reduction of 17%. Although rates were consistently slightly lower in each of the categories of major morbidity, those individual differences didn’t achieve statistical significance. The difference in major morbidity became significant only when major morbidity was considered as a whole.
Mean length of stay was 9 days with MIE and 10 days with open surgery.
There was no significant difference between the two study groups in 30-day rates of readmission, reoperation, or mortality.
Discussant Donald E. Low said “esophagectomy is being analysed regarding its place in all sorts of presentations, stages, and situations, so the aspect of making sure that we’re delivering the services as efficiently as possible is going to become more important, not less important.”
That being said, he noted that there is no specific CPT code for MIE. That raises the possibility of an uncertain amount of procedural misclassification in the ACS-NSQIP database.
Also, the only significant difference in major morbidity between the two study groups was in the subcategory of intra- or postoperative bleeding requiring transfusion, which occurred in 10.8% of the MIE and 16.7% of the open esophagectomy groups, observed Dr. Low, director of the Esophageal Center of Excellence at Virginia Mason Medical Center, Seattle.
“Some of us believe that blood utilization and transfusion requirement is really a quality measure and not a complication,” the surgeon said. And if that outcome is excluded from consideration, then there is no significant difference in major morbidity.
Discussant Douglas E. Wood, MD, professor and chair of the department of surgery at the University of Washington, Seattle, took the opportunity to share a self-described “pet peeve” about analyses of national surgical databases: these databases typically don’t contain key details necessary to correct for provider and hospital characteristics.
“The small differences that you demonstrate could easily have been completely driven by providers who choose to do minimally invasive esophagectomy and are in higher-volume, more specialized centers,” he said. “I’m not convinced of your conclusion that MIE produces less morbidity based on a 4% difference and no analysis of provider characteristics.”
COLORADO SPRINGS – Minimally invasive esophagectomy was associated with a significantly lower rate of postoperative major morbidity as well as a mean 1-day briefer length of stay than open esophagectomy in a propensity-matched analysis of the real-world American College of Surgeons-National Quality Improvement Program database, Mark F. Berry, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
However, both of the study’s discussants questioned whether the reported modest absolute reduction in major morbidity was really attributable to the minimally invasive approach or could instead have resulted from one of several potential confounders that couldn’t be fully adjusted for, given inherent limitations of the ACS-NSQIP database.
“There was a statistically significant difference in morbidity,” replied Dr. Berry of Stanford (Calif.) University. “It was a 4% absolute difference, which I think is probably clinically meaningful, but certainly it’s not really, really dramatic.”
“What I think we found is that it’s safe to do a minimally invasive esophagectomy and safe for people to introduce it into their practice. But it’s not necessarily something that’s a game changer, unlike what’s been seen with minimally invasive approaches for some other things,” said Dr. Berry, who added that he didn’t wish to overstate the importance of the observed difference in morbidity.
Studies from high-volume centers show that minimally-invasive esophagectomy (MIE) reduces length of stay, postoperative major morbidity, and features equivalent or even slightly lower mortality than traditional open esophagectomy, the generalizability of these findings beyond such centers is questionable. That’s why Dr. Berry and his coinvestigators turned to the ACS-NSQIP database, which includes all esophagectomies performed for esophageal cancer at roughly 700 U.S. hospitals, not just those done by board-certified thoracic surgeons.
He presented a retrospective cohort study of 3,901 esophagectomy patients during 2005-2013 who met study criteria, 16.4% of whom had MIE. The use of this approach increased steadily from 6.5% of all esophagectomies in 2005 to 22.3% in 2013. A propensity-matched analysis designed to neutralize potentially confounding differences included 638 MIE and 1,914 open esophagectomy patients.
The primary outcome was the 30-day rate of composite major morbidity in the realms of various wound, respiratory, renal, and cardiovascular complications. The rate was 36.1% in the MIE group and 40.5% with open esophagectomy in the propensity-matched analysis, an absolute risk reduction of 4.4% and a relative risk reduction of 17%. Although rates were consistently slightly lower in each of the categories of major morbidity, those individual differences didn’t achieve statistical significance. The difference in major morbidity became significant only when major morbidity was considered as a whole.
Mean length of stay was 9 days with MIE and 10 days with open surgery.
There was no significant difference between the two study groups in 30-day rates of readmission, reoperation, or mortality.
Discussant Donald E. Low said “esophagectomy is being analysed regarding its place in all sorts of presentations, stages, and situations, so the aspect of making sure that we’re delivering the services as efficiently as possible is going to become more important, not less important.”
That being said, he noted that there is no specific CPT code for MIE. That raises the possibility of an uncertain amount of procedural misclassification in the ACS-NSQIP database.
Also, the only significant difference in major morbidity between the two study groups was in the subcategory of intra- or postoperative bleeding requiring transfusion, which occurred in 10.8% of the MIE and 16.7% of the open esophagectomy groups, observed Dr. Low, director of the Esophageal Center of Excellence at Virginia Mason Medical Center, Seattle.
“Some of us believe that blood utilization and transfusion requirement is really a quality measure and not a complication,” the surgeon said. And if that outcome is excluded from consideration, then there is no significant difference in major morbidity.
Discussant Douglas E. Wood, MD, professor and chair of the department of surgery at the University of Washington, Seattle, took the opportunity to share a self-described “pet peeve” about analyses of national surgical databases: these databases typically don’t contain key details necessary to correct for provider and hospital characteristics.
“The small differences that you demonstrate could easily have been completely driven by providers who choose to do minimally invasive esophagectomy and are in higher-volume, more specialized centers,” he said. “I’m not convinced of your conclusion that MIE produces less morbidity based on a 4% difference and no analysis of provider characteristics.”
COLORADO SPRINGS – Minimally invasive esophagectomy was associated with a significantly lower rate of postoperative major morbidity as well as a mean 1-day briefer length of stay than open esophagectomy in a propensity-matched analysis of the real-world American College of Surgeons-National Quality Improvement Program database, Mark F. Berry, MD, reported at the annual meeting of the Western Thoracic Surgical Association.
However, both of the study’s discussants questioned whether the reported modest absolute reduction in major morbidity was really attributable to the minimally invasive approach or could instead have resulted from one of several potential confounders that couldn’t be fully adjusted for, given inherent limitations of the ACS-NSQIP database.
“There was a statistically significant difference in morbidity,” replied Dr. Berry of Stanford (Calif.) University. “It was a 4% absolute difference, which I think is probably clinically meaningful, but certainly it’s not really, really dramatic.”
“What I think we found is that it’s safe to do a minimally invasive esophagectomy and safe for people to introduce it into their practice. But it’s not necessarily something that’s a game changer, unlike what’s been seen with minimally invasive approaches for some other things,” said Dr. Berry, who added that he didn’t wish to overstate the importance of the observed difference in morbidity.
Studies from high-volume centers show that minimally-invasive esophagectomy (MIE) reduces length of stay, postoperative major morbidity, and features equivalent or even slightly lower mortality than traditional open esophagectomy, the generalizability of these findings beyond such centers is questionable. That’s why Dr. Berry and his coinvestigators turned to the ACS-NSQIP database, which includes all esophagectomies performed for esophageal cancer at roughly 700 U.S. hospitals, not just those done by board-certified thoracic surgeons.
He presented a retrospective cohort study of 3,901 esophagectomy patients during 2005-2013 who met study criteria, 16.4% of whom had MIE. The use of this approach increased steadily from 6.5% of all esophagectomies in 2005 to 22.3% in 2013. A propensity-matched analysis designed to neutralize potentially confounding differences included 638 MIE and 1,914 open esophagectomy patients.
The primary outcome was the 30-day rate of composite major morbidity in the realms of various wound, respiratory, renal, and cardiovascular complications. The rate was 36.1% in the MIE group and 40.5% with open esophagectomy in the propensity-matched analysis, an absolute risk reduction of 4.4% and a relative risk reduction of 17%. Although rates were consistently slightly lower in each of the categories of major morbidity, those individual differences didn’t achieve statistical significance. The difference in major morbidity became significant only when major morbidity was considered as a whole.
Mean length of stay was 9 days with MIE and 10 days with open surgery.
There was no significant difference between the two study groups in 30-day rates of readmission, reoperation, or mortality.
Discussant Donald E. Low said “esophagectomy is being analysed regarding its place in all sorts of presentations, stages, and situations, so the aspect of making sure that we’re delivering the services as efficiently as possible is going to become more important, not less important.”
That being said, he noted that there is no specific CPT code for MIE. That raises the possibility of an uncertain amount of procedural misclassification in the ACS-NSQIP database.
Also, the only significant difference in major morbidity between the two study groups was in the subcategory of intra- or postoperative bleeding requiring transfusion, which occurred in 10.8% of the MIE and 16.7% of the open esophagectomy groups, observed Dr. Low, director of the Esophageal Center of Excellence at Virginia Mason Medical Center, Seattle.
“Some of us believe that blood utilization and transfusion requirement is really a quality measure and not a complication,” the surgeon said. And if that outcome is excluded from consideration, then there is no significant difference in major morbidity.
Discussant Douglas E. Wood, MD, professor and chair of the department of surgery at the University of Washington, Seattle, took the opportunity to share a self-described “pet peeve” about analyses of national surgical databases: these databases typically don’t contain key details necessary to correct for provider and hospital characteristics.
“The small differences that you demonstrate could easily have been completely driven by providers who choose to do minimally invasive esophagectomy and are in higher-volume, more specialized centers,” he said. “I’m not convinced of your conclusion that MIE produces less morbidity based on a 4% difference and no analysis of provider characteristics.”
AT WTSA 2017
Key clinical point:
Major finding: The 30-day rate of major morbidity was 36.1% in patients who underwent minimally invasive esophagectomy, significantly lower than the 40.5% rate with open esophagectomy in a propensity-matched analysis.
Data source: This retrospective cohort study included 3,901 patients who underwent esophagectomy for esophageal cancer as recorded in the American College of Surgeons-National Quality Improvement Program database for 2005-2013.
Disclosures: The study presenter reported having no financial conflicts of interest.
Medical abortions provided via telemedicine appear safe
Medical abortions using mifepristone and misoprostol to terminate a pregnancy up to 10 weeks of gestation were associated with similar rates of clinically significant adverse events whether the patient encounters occurred via telemedicine or in-office appointments, according to a retrospective cohort study published online in Obstetrics & Gynecology.
Among the 8,765 medical abortions associated with telemedicine visits and the 10,405 associated with in-person visits at Planned Parenthood of the Heartland clinics in Iowa during the 7-year study period, a total of 49 clinically significant adverse events (hospital admission, blood transfusion, treatment given in an emergency department) were reported. There were no surgeries or deaths in the cohort. Of telemedicine patients, 0.18% had any clinically adverse event (95% confidence interval, 0.11%-0.29%), compared with 0.32% of in-person patients (95% CI, 0.23%-0.45%), wrote Daniel Grossman, MD, of Advancing New Standards in Reproductive Health (ANSIRH), Bixby Center for Global Reproductive Health, Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Francisco, and Kate Grindlay, MSPH, of IBIS Reproductive Health, Cambridge, Mass.
“In the 2 years after telemedicine was introduced at [these] clinics, women had an almost 50% higher adjusted odds of obtaining a first trimester abortion instead of a second-trimester abortion, [which] is associated with a higher risk of complications,” Dr. Grossman and Dr. Grindlay wrote. “Rather than increasing risks of abortion, it may be that telemedicine provision of medical abortion helps to reduce such risks by improving access to early abortion.”
Dr. Grossman has served as a consultant to the Planned Parenthood Federation of America, providing input on the implementation of telemedicine services. Dr. Grindlay reported no financial disclosures.
Medical abortions using mifepristone and misoprostol to terminate a pregnancy up to 10 weeks of gestation were associated with similar rates of clinically significant adverse events whether the patient encounters occurred via telemedicine or in-office appointments, according to a retrospective cohort study published online in Obstetrics & Gynecology.
Among the 8,765 medical abortions associated with telemedicine visits and the 10,405 associated with in-person visits at Planned Parenthood of the Heartland clinics in Iowa during the 7-year study period, a total of 49 clinically significant adverse events (hospital admission, blood transfusion, treatment given in an emergency department) were reported. There were no surgeries or deaths in the cohort. Of telemedicine patients, 0.18% had any clinically adverse event (95% confidence interval, 0.11%-0.29%), compared with 0.32% of in-person patients (95% CI, 0.23%-0.45%), wrote Daniel Grossman, MD, of Advancing New Standards in Reproductive Health (ANSIRH), Bixby Center for Global Reproductive Health, Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Francisco, and Kate Grindlay, MSPH, of IBIS Reproductive Health, Cambridge, Mass.
“In the 2 years after telemedicine was introduced at [these] clinics, women had an almost 50% higher adjusted odds of obtaining a first trimester abortion instead of a second-trimester abortion, [which] is associated with a higher risk of complications,” Dr. Grossman and Dr. Grindlay wrote. “Rather than increasing risks of abortion, it may be that telemedicine provision of medical abortion helps to reduce such risks by improving access to early abortion.”
Dr. Grossman has served as a consultant to the Planned Parenthood Federation of America, providing input on the implementation of telemedicine services. Dr. Grindlay reported no financial disclosures.
Medical abortions using mifepristone and misoprostol to terminate a pregnancy up to 10 weeks of gestation were associated with similar rates of clinically significant adverse events whether the patient encounters occurred via telemedicine or in-office appointments, according to a retrospective cohort study published online in Obstetrics & Gynecology.
Among the 8,765 medical abortions associated with telemedicine visits and the 10,405 associated with in-person visits at Planned Parenthood of the Heartland clinics in Iowa during the 7-year study period, a total of 49 clinically significant adverse events (hospital admission, blood transfusion, treatment given in an emergency department) were reported. There were no surgeries or deaths in the cohort. Of telemedicine patients, 0.18% had any clinically adverse event (95% confidence interval, 0.11%-0.29%), compared with 0.32% of in-person patients (95% CI, 0.23%-0.45%), wrote Daniel Grossman, MD, of Advancing New Standards in Reproductive Health (ANSIRH), Bixby Center for Global Reproductive Health, Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Francisco, and Kate Grindlay, MSPH, of IBIS Reproductive Health, Cambridge, Mass.
“In the 2 years after telemedicine was introduced at [these] clinics, women had an almost 50% higher adjusted odds of obtaining a first trimester abortion instead of a second-trimester abortion, [which] is associated with a higher risk of complications,” Dr. Grossman and Dr. Grindlay wrote. “Rather than increasing risks of abortion, it may be that telemedicine provision of medical abortion helps to reduce such risks by improving access to early abortion.”
Dr. Grossman has served as a consultant to the Planned Parenthood Federation of America, providing input on the implementation of telemedicine services. Dr. Grindlay reported no financial disclosures.
FROM OBSTETRICS AND GYNECOLOGY
Key clinical point:
Major finding: Of patients seen via telemedicine, 0.18% had any clinically significant adverse event (95% confidence interval, 0.11%-0.29%), compared with 0.32% of in-person patients (95% CI, 0.23%-0.45%).
Data source: A retrospective cohort study of 19,170 women who had received medical abortions at Planned Parenthood of the Heartland clinics in Iowa.
Disclosures: Dr. Grossman has served as a consultant to the Planned Parenthood Federation of America, providing input on the implementation of telemedicine services. Dr. Grindlay reported no financial disclosures.
For interstitial cystitis, restrictive diet pays off
ESTES PARK, CO. – When patients with interstitial cystitis (IC) learn that first-line therapy is a rigorous diet designed to eliminate common bladder irritants, they tend to react in one of two ways, according to Julie A. Chacko, MD, a urologist in private practice in Santa Barbara, Calif.
Some “are just so grateful that they’re not crazy, which is what they’ve been told after 15 negative urine cultures. (Others) “look at the diet and think I’m sentencing them to death,” she said.
The sole medication approved by the Food and Drug Administration for IC is pentosan polysulfate sodium (Elmiron), and it should be reserved for the minority of patients who don’t experience significant improvement after giving the diet a reasonable shot, Dr. Chako advised. “When Elmiron works it’s great, but it’s not usually my go-to agent because it’s very expensive, you have to take it for 3-6 months to know for sure if it’s efficacious, and it has to be taken on an empty stomach. It’s a difficult medication.”
She advises patients to work with the diet. “Over time, they’re going to be able to find what I call their island – a point where they know very well their limitations and become quite comfortable with them,” she said at a conference on internal medicine sponsored by the University of Colorado.
A poorly understood yet common disorder, IC has a prevalence estimated at 0.5%-4% in women, less in men. Although typically diagnosed in the fourth decade or later, IC occurs at all ages. In some studies, the delay from first appearance of symptoms to arrival at a diagnosis is up to 8 years.
Interstitial cystitis is increasingly being called bladder pain syndrome in the literature, said Dr. Chako, who added, “I personally don’t love bladder pain syndrome as a description for this process. This syndrome has variable symptoms, and patients can have no pain at all.”
The mechanisms that result in IC are a mystery. The leading theory is that a bladder permeability problem allows urinary irritants to reach the interstitium. Nearly 80% of patients with IC can, with coaxing, identify dietary triggers for their symptoms, thereby basically establishing the diagnosis.
Other proposed mechanisms include an infectious agent that’s yet to be identified, allergic reaction, and neuromodulatory dysfunction. Common triggers other than foods include menses, copulation, emotional distress, and bladder trauma, including transvaginal ultrasound.
Conditions commonly associated with IC include fibromyalgia, irritable bowel syndrome, chronic fatigue, vulvodynia, migraines, depression, and anxiety.
The most common symptoms of IC are urinary urgency and frequency. Many affected patients have dysuria. Some have pain, which is typically suprapubic. However, pain can be present anywhere in a band circumscribing the whole central section of the torso, including the lower back, lower abdomen, urethra, vagina, and vulva. Patients describe a range of pain – burning, aching, stabbing, itching, buzzing, or a feeling of pressure.
“Most women who come in with IC are married to the idea that they’re having recurrent UTIs. They’re going to get antibiotics any way they can for their UTIs: over the phone, at urgent care. You need to get them to buy into the idea that even though UTIs are common, maybe not all of their flares are infections. They ask, ‘Then why do I feel better when I’m on antibiotics for recurrent UTI even though the cultures are negative?’ I say, ‘You feel less stress and anxiety because you think you’re on effective treatment,” Dr. Chacko said.
The diagnosis of IC is one of exclusions. Diagnoses to rule out before arriving at IC include recurrent UTI; overactive bladder, which should present with pure urge frequency and respond to medications for that condition; kidney stone disease present at the end of the ureter where it enters the bladder; gastrointestinal pathology; bladder cancer; and ovarian or uterine pathology.
Referral to a urologist for cystoscopy and cytology is appropriate in patients with microscopic hematuria, a significant smoking history predisposing to bladder cancer, or severe pain with severe frequency, which raises the possibility of Hunner’s ulcers, considered pathognomic for IC, respond “beautifully” to fulguration, she said.
Otherwise, IC can readily be managed by interested primary care physicians. The IC diet initially calls for 2 weeks of strict avoidance of all high-risk foods, most of which are acidic foods. These include fruits and fruit juices, especially citrus and cranberry juices; tomatoes and tomato products, including ketchup; yogurt; chocolate; coffee and tea, including decaf; vinegar; spicy foods; and carbonated beverages, water included.
These foods can later be added back one at a time to the diet while watching for IC flares, which typically occur within hours to several days of re-introducing the food. The return to coffee consumption, if that’s something important to the patient, should be with low-acid coffee. If that triggers an IC flare, try decaf. In time, many patients find they can consume some trigger foods in modest amounts.
“I tell patients it will take 12-18 months to get a good handle on their IC,” Dr. Chacko noted.
The use of OTC alkalizing agents such as Prelief may diffuse dietary triggers. A teaspoon of baking soda in water is also effective.
Second-line treatments include oral hydroxyzine 10-20 mg at bedtime; amitriptyline 10-20 mg at bedtime, mainly for patients with predominant pain symptoms; cimeditine; and pentosan polysulfate at 100 mg TID.
For IC patients with pelvic muscle tightness on pelvic examination, referral to a physical therapist adept at pelvic floor trigger point release can work wonders, she added.
One second-line option is bladder instillations of dimethyl sulfoxide weekly for 6 weeks, cutting back to once monthly maintenance therapy if the more intensive regimen is effective. Instillation of “heparin with lidocaine is a rescue solution. If it’s going to work, it kicks in within a few hours and usually lasts for 24-72 hours. It gets patients through a weekend, a wedding, or a funeral. A response can help make the IC diagnosis, too,” Dr. Chacko said.
She reported having no financial conflicts of interest regarding her presentation.
bjancin@frontlinemedcom.com
ESTES PARK, CO. – When patients with interstitial cystitis (IC) learn that first-line therapy is a rigorous diet designed to eliminate common bladder irritants, they tend to react in one of two ways, according to Julie A. Chacko, MD, a urologist in private practice in Santa Barbara, Calif.
Some “are just so grateful that they’re not crazy, which is what they’ve been told after 15 negative urine cultures. (Others) “look at the diet and think I’m sentencing them to death,” she said.
The sole medication approved by the Food and Drug Administration for IC is pentosan polysulfate sodium (Elmiron), and it should be reserved for the minority of patients who don’t experience significant improvement after giving the diet a reasonable shot, Dr. Chako advised. “When Elmiron works it’s great, but it’s not usually my go-to agent because it’s very expensive, you have to take it for 3-6 months to know for sure if it’s efficacious, and it has to be taken on an empty stomach. It’s a difficult medication.”
She advises patients to work with the diet. “Over time, they’re going to be able to find what I call their island – a point where they know very well their limitations and become quite comfortable with them,” she said at a conference on internal medicine sponsored by the University of Colorado.
A poorly understood yet common disorder, IC has a prevalence estimated at 0.5%-4% in women, less in men. Although typically diagnosed in the fourth decade or later, IC occurs at all ages. In some studies, the delay from first appearance of symptoms to arrival at a diagnosis is up to 8 years.
Interstitial cystitis is increasingly being called bladder pain syndrome in the literature, said Dr. Chako, who added, “I personally don’t love bladder pain syndrome as a description for this process. This syndrome has variable symptoms, and patients can have no pain at all.”
The mechanisms that result in IC are a mystery. The leading theory is that a bladder permeability problem allows urinary irritants to reach the interstitium. Nearly 80% of patients with IC can, with coaxing, identify dietary triggers for their symptoms, thereby basically establishing the diagnosis.
Other proposed mechanisms include an infectious agent that’s yet to be identified, allergic reaction, and neuromodulatory dysfunction. Common triggers other than foods include menses, copulation, emotional distress, and bladder trauma, including transvaginal ultrasound.
Conditions commonly associated with IC include fibromyalgia, irritable bowel syndrome, chronic fatigue, vulvodynia, migraines, depression, and anxiety.
The most common symptoms of IC are urinary urgency and frequency. Many affected patients have dysuria. Some have pain, which is typically suprapubic. However, pain can be present anywhere in a band circumscribing the whole central section of the torso, including the lower back, lower abdomen, urethra, vagina, and vulva. Patients describe a range of pain – burning, aching, stabbing, itching, buzzing, or a feeling of pressure.
“Most women who come in with IC are married to the idea that they’re having recurrent UTIs. They’re going to get antibiotics any way they can for their UTIs: over the phone, at urgent care. You need to get them to buy into the idea that even though UTIs are common, maybe not all of their flares are infections. They ask, ‘Then why do I feel better when I’m on antibiotics for recurrent UTI even though the cultures are negative?’ I say, ‘You feel less stress and anxiety because you think you’re on effective treatment,” Dr. Chacko said.
The diagnosis of IC is one of exclusions. Diagnoses to rule out before arriving at IC include recurrent UTI; overactive bladder, which should present with pure urge frequency and respond to medications for that condition; kidney stone disease present at the end of the ureter where it enters the bladder; gastrointestinal pathology; bladder cancer; and ovarian or uterine pathology.
Referral to a urologist for cystoscopy and cytology is appropriate in patients with microscopic hematuria, a significant smoking history predisposing to bladder cancer, or severe pain with severe frequency, which raises the possibility of Hunner’s ulcers, considered pathognomic for IC, respond “beautifully” to fulguration, she said.
Otherwise, IC can readily be managed by interested primary care physicians. The IC diet initially calls for 2 weeks of strict avoidance of all high-risk foods, most of which are acidic foods. These include fruits and fruit juices, especially citrus and cranberry juices; tomatoes and tomato products, including ketchup; yogurt; chocolate; coffee and tea, including decaf; vinegar; spicy foods; and carbonated beverages, water included.
These foods can later be added back one at a time to the diet while watching for IC flares, which typically occur within hours to several days of re-introducing the food. The return to coffee consumption, if that’s something important to the patient, should be with low-acid coffee. If that triggers an IC flare, try decaf. In time, many patients find they can consume some trigger foods in modest amounts.
“I tell patients it will take 12-18 months to get a good handle on their IC,” Dr. Chacko noted.
The use of OTC alkalizing agents such as Prelief may diffuse dietary triggers. A teaspoon of baking soda in water is also effective.
Second-line treatments include oral hydroxyzine 10-20 mg at bedtime; amitriptyline 10-20 mg at bedtime, mainly for patients with predominant pain symptoms; cimeditine; and pentosan polysulfate at 100 mg TID.
For IC patients with pelvic muscle tightness on pelvic examination, referral to a physical therapist adept at pelvic floor trigger point release can work wonders, she added.
One second-line option is bladder instillations of dimethyl sulfoxide weekly for 6 weeks, cutting back to once monthly maintenance therapy if the more intensive regimen is effective. Instillation of “heparin with lidocaine is a rescue solution. If it’s going to work, it kicks in within a few hours and usually lasts for 24-72 hours. It gets patients through a weekend, a wedding, or a funeral. A response can help make the IC diagnosis, too,” Dr. Chacko said.
She reported having no financial conflicts of interest regarding her presentation.
bjancin@frontlinemedcom.com
ESTES PARK, CO. – When patients with interstitial cystitis (IC) learn that first-line therapy is a rigorous diet designed to eliminate common bladder irritants, they tend to react in one of two ways, according to Julie A. Chacko, MD, a urologist in private practice in Santa Barbara, Calif.
Some “are just so grateful that they’re not crazy, which is what they’ve been told after 15 negative urine cultures. (Others) “look at the diet and think I’m sentencing them to death,” she said.
The sole medication approved by the Food and Drug Administration for IC is pentosan polysulfate sodium (Elmiron), and it should be reserved for the minority of patients who don’t experience significant improvement after giving the diet a reasonable shot, Dr. Chako advised. “When Elmiron works it’s great, but it’s not usually my go-to agent because it’s very expensive, you have to take it for 3-6 months to know for sure if it’s efficacious, and it has to be taken on an empty stomach. It’s a difficult medication.”
She advises patients to work with the diet. “Over time, they’re going to be able to find what I call their island – a point where they know very well their limitations and become quite comfortable with them,” she said at a conference on internal medicine sponsored by the University of Colorado.
A poorly understood yet common disorder, IC has a prevalence estimated at 0.5%-4% in women, less in men. Although typically diagnosed in the fourth decade or later, IC occurs at all ages. In some studies, the delay from first appearance of symptoms to arrival at a diagnosis is up to 8 years.
Interstitial cystitis is increasingly being called bladder pain syndrome in the literature, said Dr. Chako, who added, “I personally don’t love bladder pain syndrome as a description for this process. This syndrome has variable symptoms, and patients can have no pain at all.”
The mechanisms that result in IC are a mystery. The leading theory is that a bladder permeability problem allows urinary irritants to reach the interstitium. Nearly 80% of patients with IC can, with coaxing, identify dietary triggers for their symptoms, thereby basically establishing the diagnosis.
Other proposed mechanisms include an infectious agent that’s yet to be identified, allergic reaction, and neuromodulatory dysfunction. Common triggers other than foods include menses, copulation, emotional distress, and bladder trauma, including transvaginal ultrasound.
Conditions commonly associated with IC include fibromyalgia, irritable bowel syndrome, chronic fatigue, vulvodynia, migraines, depression, and anxiety.
The most common symptoms of IC are urinary urgency and frequency. Many affected patients have dysuria. Some have pain, which is typically suprapubic. However, pain can be present anywhere in a band circumscribing the whole central section of the torso, including the lower back, lower abdomen, urethra, vagina, and vulva. Patients describe a range of pain – burning, aching, stabbing, itching, buzzing, or a feeling of pressure.
“Most women who come in with IC are married to the idea that they’re having recurrent UTIs. They’re going to get antibiotics any way they can for their UTIs: over the phone, at urgent care. You need to get them to buy into the idea that even though UTIs are common, maybe not all of their flares are infections. They ask, ‘Then why do I feel better when I’m on antibiotics for recurrent UTI even though the cultures are negative?’ I say, ‘You feel less stress and anxiety because you think you’re on effective treatment,” Dr. Chacko said.
The diagnosis of IC is one of exclusions. Diagnoses to rule out before arriving at IC include recurrent UTI; overactive bladder, which should present with pure urge frequency and respond to medications for that condition; kidney stone disease present at the end of the ureter where it enters the bladder; gastrointestinal pathology; bladder cancer; and ovarian or uterine pathology.
Referral to a urologist for cystoscopy and cytology is appropriate in patients with microscopic hematuria, a significant smoking history predisposing to bladder cancer, or severe pain with severe frequency, which raises the possibility of Hunner’s ulcers, considered pathognomic for IC, respond “beautifully” to fulguration, she said.
Otherwise, IC can readily be managed by interested primary care physicians. The IC diet initially calls for 2 weeks of strict avoidance of all high-risk foods, most of which are acidic foods. These include fruits and fruit juices, especially citrus and cranberry juices; tomatoes and tomato products, including ketchup; yogurt; chocolate; coffee and tea, including decaf; vinegar; spicy foods; and carbonated beverages, water included.
These foods can later be added back one at a time to the diet while watching for IC flares, which typically occur within hours to several days of re-introducing the food. The return to coffee consumption, if that’s something important to the patient, should be with low-acid coffee. If that triggers an IC flare, try decaf. In time, many patients find they can consume some trigger foods in modest amounts.
“I tell patients it will take 12-18 months to get a good handle on their IC,” Dr. Chacko noted.
The use of OTC alkalizing agents such as Prelief may diffuse dietary triggers. A teaspoon of baking soda in water is also effective.
Second-line treatments include oral hydroxyzine 10-20 mg at bedtime; amitriptyline 10-20 mg at bedtime, mainly for patients with predominant pain symptoms; cimeditine; and pentosan polysulfate at 100 mg TID.
For IC patients with pelvic muscle tightness on pelvic examination, referral to a physical therapist adept at pelvic floor trigger point release can work wonders, she added.
One second-line option is bladder instillations of dimethyl sulfoxide weekly for 6 weeks, cutting back to once monthly maintenance therapy if the more intensive regimen is effective. Instillation of “heparin with lidocaine is a rescue solution. If it’s going to work, it kicks in within a few hours and usually lasts for 24-72 hours. It gets patients through a weekend, a wedding, or a funeral. A response can help make the IC diagnosis, too,” Dr. Chacko said.
She reported having no financial conflicts of interest regarding her presentation.
bjancin@frontlinemedcom.com
EXPERT ANALYSIS FROM THE ANNUAL INTERNAL MEDICINE PROGRAM
Opioid use disorder: Simplifying diagnosis and treatment in primary care
ESTES PARK, COLO. – Have a low threshold for diagnosing opioid use disorder in chronic pain patients, Joshua Blum, MD, advised at a conference on internal medicine sponsored by the University of Colorado.
Be alert to so-called ‘chemical copers’ as they skate through your practice, he said. “Maybe they call in here and there for an early refill; maybe they go to the ER and get a few pills here and there. But they never really surface to the level where we recognize them as an opioid use disorder patient.
“Some of them cross that line where they go from use and maybe intermittent misuse to meeting the criteria for opioid use disorder. I think we underdiagnose this in our chronic pain patients. I spend a lot of time trying to convince patients who tell me I just need to take their pain seriously that, yes, you’re in pain, and you have a pain diagnosis, but you also have an opioid use disorder. Medicalizing it makes things a lot easier for them; it helps take away the blame,” said Dr. Blum, program coordinator for the HIV primary care clinic at Denver Health.
Chemical copers, a well-established term in addiction medicine, are not the glaringly obvious substance abusers or addicts. “They’re the ones in your practice who are on four or five different psychoactive drugs. They’ve never met a psychoactive drug they didn’t like. When they hurt their back, they’re on Flexoril [cyclobenzaprine]; they’re on an antidepressant, a neuropathic pain agent; they’re on a sedative or sleeping agent or trazadone. If you took the five pills they’re on, you’d be knocked out for 2 days. And they always go to the maximum dose,” he said.
As newly described in the the Diagnostic and Statistical Manual of Mental Disorders, DSM-5, the diagnosis of opioid use disorder (OUD) requires that any 2 of the following 11 criteria be met:
- Taking more opioids than intended.
- Unsuccessful efforts to control opioid use.
- Spending a great deal of time in activities aimed at obtaining, using, or recovering from the effects of opioids.
- Craving opioids.
- Failure to fulfill major work, school, or home obligations because of opioid use.
- Worsening interpersonal problems related to opioid use.
- Giving up or reducing involvement in important social, recreational, or occupational activities because of opioid use.
- Recurrent use in situations where it’s physically hazardous, such as driving under the influence.
- Continued use despite physical or psychological problems stemming from opioid use.
- And finally, two special criteria applicable only if the opioid wasn’t prescribed and therefore isn’t being used under medical supervision: tolerance for opioids and withdrawal symptoms when they aren’t taken.
“Even if you can’t remember all these criteria, all you basically have to remember is ‘control.’ Many of these criteria describe situations where the patient is losing control of the drug. When they’re not controlling their drug use, the drug use is controlling them – and that’s addiction. All you need is for a patient to tell you ‘I tried to cut back on these drugs and I couldn’t,’ and that they’re experiencing some health consequences related to use yet still want to stay on the drugs, and, boom, they meet criteria for at least mild opioid use disorder,” he explained.
The standard treatment for OUD is opioid replacement therapy using methadone or buprenorphine (Subutex).
This approach is evidence-based therapy, Dr. Blum said, citing a recent meta-analysis of studies totaling nearly 123,000 opioid-dependent patients treated long-term with methadone and 16,000 treated with buprenorphine. The risk of all-cause mortality dropped by two-thirds when patients went on methadone, from 36.1% while out of treatment to 11.3% while on treatment. Similarly, all-cause mortality was 4.3% in patients on buprenorphine, compared with 9.5% in those out of treatment (BMJ. 2017 Apr 26;357:j1550. doi: 10.1136/bmj.j1550).
Access to methadone for treatment of OUD is available only through authorized methadone clinics, typically found only in big cities. But buprenorphine is a very useful alternative to methodone, Dr. Blum said.
“Buprenorphine is a schedule III drug that’s safe to prescribe in an office-based setting. It’s a partial mu opioid agonist with a ceiling effect, so people using buprenorphine can’t die from taking excessive amounts of it. You can even write refills on the prescription. And in head-to-head studies, it looks about as effective as moderate-dose methodone at 60 mg/day,” he said.
Opioid replacement therapy reduces euphoria and extinguishes craving. When methadone or buprenorphine is on board, saturating the opioid receptors, patients can use prescription or illicit opioids, but they won’t get high.
“People can really get their brains back online again,” Dr. Blum said.
Opioid maintenance therapy is consistent with the principles of harm reduction, a philosophy Dr. Blum said he embraces. Harm reduction can be summarized as “a set of practical strategies that reduce negative consequences of drug use, incorporating a spectrum of strategies from safer use, to managed use, to abstinence,” according to the Harm Reduction Coalition.
“Primary care doctors are very used to meeting patients where they are. We don’t require perfectionism from our patients. We don’t withhold insulin from diabetic patients because they’re not exercising, for example. In the case of drug use, there is complete abstinence on one end and really severe misuse on the other, and there’s a whole lot of life that happens in the middle. We’re addressing that part in the middle,” Dr. Blum said.
Dr. Blum reported having no financial conflicts of interest regarding his presentation.
ESTES PARK, COLO. – Have a low threshold for diagnosing opioid use disorder in chronic pain patients, Joshua Blum, MD, advised at a conference on internal medicine sponsored by the University of Colorado.
Be alert to so-called ‘chemical copers’ as they skate through your practice, he said. “Maybe they call in here and there for an early refill; maybe they go to the ER and get a few pills here and there. But they never really surface to the level where we recognize them as an opioid use disorder patient.
“Some of them cross that line where they go from use and maybe intermittent misuse to meeting the criteria for opioid use disorder. I think we underdiagnose this in our chronic pain patients. I spend a lot of time trying to convince patients who tell me I just need to take their pain seriously that, yes, you’re in pain, and you have a pain diagnosis, but you also have an opioid use disorder. Medicalizing it makes things a lot easier for them; it helps take away the blame,” said Dr. Blum, program coordinator for the HIV primary care clinic at Denver Health.
Chemical copers, a well-established term in addiction medicine, are not the glaringly obvious substance abusers or addicts. “They’re the ones in your practice who are on four or five different psychoactive drugs. They’ve never met a psychoactive drug they didn’t like. When they hurt their back, they’re on Flexoril [cyclobenzaprine]; they’re on an antidepressant, a neuropathic pain agent; they’re on a sedative or sleeping agent or trazadone. If you took the five pills they’re on, you’d be knocked out for 2 days. And they always go to the maximum dose,” he said.
As newly described in the the Diagnostic and Statistical Manual of Mental Disorders, DSM-5, the diagnosis of opioid use disorder (OUD) requires that any 2 of the following 11 criteria be met:
- Taking more opioids than intended.
- Unsuccessful efforts to control opioid use.
- Spending a great deal of time in activities aimed at obtaining, using, or recovering from the effects of opioids.
- Craving opioids.
- Failure to fulfill major work, school, or home obligations because of opioid use.
- Worsening interpersonal problems related to opioid use.
- Giving up or reducing involvement in important social, recreational, or occupational activities because of opioid use.
- Recurrent use in situations where it’s physically hazardous, such as driving under the influence.
- Continued use despite physical or psychological problems stemming from opioid use.
- And finally, two special criteria applicable only if the opioid wasn’t prescribed and therefore isn’t being used under medical supervision: tolerance for opioids and withdrawal symptoms when they aren’t taken.
“Even if you can’t remember all these criteria, all you basically have to remember is ‘control.’ Many of these criteria describe situations where the patient is losing control of the drug. When they’re not controlling their drug use, the drug use is controlling them – and that’s addiction. All you need is for a patient to tell you ‘I tried to cut back on these drugs and I couldn’t,’ and that they’re experiencing some health consequences related to use yet still want to stay on the drugs, and, boom, they meet criteria for at least mild opioid use disorder,” he explained.
The standard treatment for OUD is opioid replacement therapy using methadone or buprenorphine (Subutex).
This approach is evidence-based therapy, Dr. Blum said, citing a recent meta-analysis of studies totaling nearly 123,000 opioid-dependent patients treated long-term with methadone and 16,000 treated with buprenorphine. The risk of all-cause mortality dropped by two-thirds when patients went on methadone, from 36.1% while out of treatment to 11.3% while on treatment. Similarly, all-cause mortality was 4.3% in patients on buprenorphine, compared with 9.5% in those out of treatment (BMJ. 2017 Apr 26;357:j1550. doi: 10.1136/bmj.j1550).
Access to methadone for treatment of OUD is available only through authorized methadone clinics, typically found only in big cities. But buprenorphine is a very useful alternative to methodone, Dr. Blum said.
“Buprenorphine is a schedule III drug that’s safe to prescribe in an office-based setting. It’s a partial mu opioid agonist with a ceiling effect, so people using buprenorphine can’t die from taking excessive amounts of it. You can even write refills on the prescription. And in head-to-head studies, it looks about as effective as moderate-dose methodone at 60 mg/day,” he said.
Opioid replacement therapy reduces euphoria and extinguishes craving. When methadone or buprenorphine is on board, saturating the opioid receptors, patients can use prescription or illicit opioids, but they won’t get high.
“People can really get their brains back online again,” Dr. Blum said.
Opioid maintenance therapy is consistent with the principles of harm reduction, a philosophy Dr. Blum said he embraces. Harm reduction can be summarized as “a set of practical strategies that reduce negative consequences of drug use, incorporating a spectrum of strategies from safer use, to managed use, to abstinence,” according to the Harm Reduction Coalition.
“Primary care doctors are very used to meeting patients where they are. We don’t require perfectionism from our patients. We don’t withhold insulin from diabetic patients because they’re not exercising, for example. In the case of drug use, there is complete abstinence on one end and really severe misuse on the other, and there’s a whole lot of life that happens in the middle. We’re addressing that part in the middle,” Dr. Blum said.
Dr. Blum reported having no financial conflicts of interest regarding his presentation.
ESTES PARK, COLO. – Have a low threshold for diagnosing opioid use disorder in chronic pain patients, Joshua Blum, MD, advised at a conference on internal medicine sponsored by the University of Colorado.
Be alert to so-called ‘chemical copers’ as they skate through your practice, he said. “Maybe they call in here and there for an early refill; maybe they go to the ER and get a few pills here and there. But they never really surface to the level where we recognize them as an opioid use disorder patient.
“Some of them cross that line where they go from use and maybe intermittent misuse to meeting the criteria for opioid use disorder. I think we underdiagnose this in our chronic pain patients. I spend a lot of time trying to convince patients who tell me I just need to take their pain seriously that, yes, you’re in pain, and you have a pain diagnosis, but you also have an opioid use disorder. Medicalizing it makes things a lot easier for them; it helps take away the blame,” said Dr. Blum, program coordinator for the HIV primary care clinic at Denver Health.
Chemical copers, a well-established term in addiction medicine, are not the glaringly obvious substance abusers or addicts. “They’re the ones in your practice who are on four or five different psychoactive drugs. They’ve never met a psychoactive drug they didn’t like. When they hurt their back, they’re on Flexoril [cyclobenzaprine]; they’re on an antidepressant, a neuropathic pain agent; they’re on a sedative or sleeping agent or trazadone. If you took the five pills they’re on, you’d be knocked out for 2 days. And they always go to the maximum dose,” he said.
As newly described in the the Diagnostic and Statistical Manual of Mental Disorders, DSM-5, the diagnosis of opioid use disorder (OUD) requires that any 2 of the following 11 criteria be met:
- Taking more opioids than intended.
- Unsuccessful efforts to control opioid use.
- Spending a great deal of time in activities aimed at obtaining, using, or recovering from the effects of opioids.
- Craving opioids.
- Failure to fulfill major work, school, or home obligations because of opioid use.
- Worsening interpersonal problems related to opioid use.
- Giving up or reducing involvement in important social, recreational, or occupational activities because of opioid use.
- Recurrent use in situations where it’s physically hazardous, such as driving under the influence.
- Continued use despite physical or psychological problems stemming from opioid use.
- And finally, two special criteria applicable only if the opioid wasn’t prescribed and therefore isn’t being used under medical supervision: tolerance for opioids and withdrawal symptoms when they aren’t taken.
“Even if you can’t remember all these criteria, all you basically have to remember is ‘control.’ Many of these criteria describe situations where the patient is losing control of the drug. When they’re not controlling their drug use, the drug use is controlling them – and that’s addiction. All you need is for a patient to tell you ‘I tried to cut back on these drugs and I couldn’t,’ and that they’re experiencing some health consequences related to use yet still want to stay on the drugs, and, boom, they meet criteria for at least mild opioid use disorder,” he explained.
The standard treatment for OUD is opioid replacement therapy using methadone or buprenorphine (Subutex).
This approach is evidence-based therapy, Dr. Blum said, citing a recent meta-analysis of studies totaling nearly 123,000 opioid-dependent patients treated long-term with methadone and 16,000 treated with buprenorphine. The risk of all-cause mortality dropped by two-thirds when patients went on methadone, from 36.1% while out of treatment to 11.3% while on treatment. Similarly, all-cause mortality was 4.3% in patients on buprenorphine, compared with 9.5% in those out of treatment (BMJ. 2017 Apr 26;357:j1550. doi: 10.1136/bmj.j1550).
Access to methadone for treatment of OUD is available only through authorized methadone clinics, typically found only in big cities. But buprenorphine is a very useful alternative to methodone, Dr. Blum said.
“Buprenorphine is a schedule III drug that’s safe to prescribe in an office-based setting. It’s a partial mu opioid agonist with a ceiling effect, so people using buprenorphine can’t die from taking excessive amounts of it. You can even write refills on the prescription. And in head-to-head studies, it looks about as effective as moderate-dose methodone at 60 mg/day,” he said.
Opioid replacement therapy reduces euphoria and extinguishes craving. When methadone or buprenorphine is on board, saturating the opioid receptors, patients can use prescription or illicit opioids, but they won’t get high.
“People can really get their brains back online again,” Dr. Blum said.
Opioid maintenance therapy is consistent with the principles of harm reduction, a philosophy Dr. Blum said he embraces. Harm reduction can be summarized as “a set of practical strategies that reduce negative consequences of drug use, incorporating a spectrum of strategies from safer use, to managed use, to abstinence,” according to the Harm Reduction Coalition.
“Primary care doctors are very used to meeting patients where they are. We don’t require perfectionism from our patients. We don’t withhold insulin from diabetic patients because they’re not exercising, for example. In the case of drug use, there is complete abstinence on one end and really severe misuse on the other, and there’s a whole lot of life that happens in the middle. We’re addressing that part in the middle,” Dr. Blum said.
Dr. Blum reported having no financial conflicts of interest regarding his presentation.
EXPERT ANALYSIS AT THE ANNUAL INTERNAL MEDICINE PROGRAM
Poor smell predicts 6-year risk of Parkinson’s
Poor olfaction is a predictor of Parkinson’s disease (PD) in both the short and immediate term, with accuracy out to at least 6 years, especially in white men, according to a retrospective case adjudication of the Health ABC study published in Neurology.
Of 2,462 study participants, 42 were found to have PD during an average of 9.8 years of follow-up, Honglei Chen, MD, PhD, of the department of epidemiology and biostatistics at Michigan State University, East Lansing, and his coauthors wrote. Of those cases, 26 (62%) were associated with a poor Brief Smell Identification Test (BSIT) score of 0-8 out of 12 (hazard ratio, 5.1; 95% confidence interval, 2.1-11.9), supporting other studies that indicate that olfactory impairment is one of the early symptoms of PD.
In contrast to previous studies, however, “the current study has longer follow-up and showed that poor olfaction was associated with PD beyond the first [4] years of follow-up, although the association was somewhat attenuated,” the researchers said. Both before and after the first 5 years of follow-up, 13 people in the lowest BSIT tertile were diagnosed with PD (HR, 4.2; 95% CI, 1.7-10.8 vs. HR, 4.1; 95% CI, 1.7-9.8, respectively),
In addition, poor sense of smell was more clearly associated with PD diagnosis in white patients, Dr. Chen and her coauthors said. Of 30 PD diagnoses in white participants, 19 were associated with poor smell (HR, 4.9; 95% CI, 2.3-10.5), compared with 7 out of 12 diagnoses in black participants (HR, 2.5; 95% CI, 0.8-8.1; P = .3). Similarly, 19 out of 26 diagnoses in men were associated with poor smell (HR, 5.4; 95% CI, 2.3-12.9), compared with 7 out of 16 diagnoses in women (HR, 2.9; 95% CI, 1.1-7.8; P = .4).
Future studies should confirm these stratified findings. Olfactory dysfunction’s “potential usefulness as a screening tool for prodromal or undiagnosed PD in other general population awaits further investigations,” the authors said.
Dr. Chen reported editorial roles for a number of medical journals. None of the authors reported any financial disclosures.
email address
Olfactory dysfunction is high in Parkinson’s disease, and the study by Chen et al. is the first to describe the natural history of olfactory dysfunction in the evolution of PD prior to diagnosis in diverse populations with extended periods of follow-up.
The length of follow-up is the longest to date, and includes important data on a large cohort of black participants. The results are a start for creating a much needed preventional paradigm, but more granularity will be needed to determine how poor smell, especially as stratified by race and sex, might help in prevention and treatment of PD.
Gene L. Bowman, ND, MPH, is a physician in the department of neurology at Oregon Health & Science University, Portland. His editorial comments accompanied the Chen et al. article in Neurology. He reported no financial disclosures.
Olfactory dysfunction is high in Parkinson’s disease, and the study by Chen et al. is the first to describe the natural history of olfactory dysfunction in the evolution of PD prior to diagnosis in diverse populations with extended periods of follow-up.
The length of follow-up is the longest to date, and includes important data on a large cohort of black participants. The results are a start for creating a much needed preventional paradigm, but more granularity will be needed to determine how poor smell, especially as stratified by race and sex, might help in prevention and treatment of PD.
Gene L. Bowman, ND, MPH, is a physician in the department of neurology at Oregon Health & Science University, Portland. His editorial comments accompanied the Chen et al. article in Neurology. He reported no financial disclosures.
Olfactory dysfunction is high in Parkinson’s disease, and the study by Chen et al. is the first to describe the natural history of olfactory dysfunction in the evolution of PD prior to diagnosis in diverse populations with extended periods of follow-up.
The length of follow-up is the longest to date, and includes important data on a large cohort of black participants. The results are a start for creating a much needed preventional paradigm, but more granularity will be needed to determine how poor smell, especially as stratified by race and sex, might help in prevention and treatment of PD.
Gene L. Bowman, ND, MPH, is a physician in the department of neurology at Oregon Health & Science University, Portland. His editorial comments accompanied the Chen et al. article in Neurology. He reported no financial disclosures.
Poor olfaction is a predictor of Parkinson’s disease (PD) in both the short and immediate term, with accuracy out to at least 6 years, especially in white men, according to a retrospective case adjudication of the Health ABC study published in Neurology.
Of 2,462 study participants, 42 were found to have PD during an average of 9.8 years of follow-up, Honglei Chen, MD, PhD, of the department of epidemiology and biostatistics at Michigan State University, East Lansing, and his coauthors wrote. Of those cases, 26 (62%) were associated with a poor Brief Smell Identification Test (BSIT) score of 0-8 out of 12 (hazard ratio, 5.1; 95% confidence interval, 2.1-11.9), supporting other studies that indicate that olfactory impairment is one of the early symptoms of PD.
In contrast to previous studies, however, “the current study has longer follow-up and showed that poor olfaction was associated with PD beyond the first [4] years of follow-up, although the association was somewhat attenuated,” the researchers said. Both before and after the first 5 years of follow-up, 13 people in the lowest BSIT tertile were diagnosed with PD (HR, 4.2; 95% CI, 1.7-10.8 vs. HR, 4.1; 95% CI, 1.7-9.8, respectively),
In addition, poor sense of smell was more clearly associated with PD diagnosis in white patients, Dr. Chen and her coauthors said. Of 30 PD diagnoses in white participants, 19 were associated with poor smell (HR, 4.9; 95% CI, 2.3-10.5), compared with 7 out of 12 diagnoses in black participants (HR, 2.5; 95% CI, 0.8-8.1; P = .3). Similarly, 19 out of 26 diagnoses in men were associated with poor smell (HR, 5.4; 95% CI, 2.3-12.9), compared with 7 out of 16 diagnoses in women (HR, 2.9; 95% CI, 1.1-7.8; P = .4).
Future studies should confirm these stratified findings. Olfactory dysfunction’s “potential usefulness as a screening tool for prodromal or undiagnosed PD in other general population awaits further investigations,” the authors said.
Dr. Chen reported editorial roles for a number of medical journals. None of the authors reported any financial disclosures.
email address
Poor olfaction is a predictor of Parkinson’s disease (PD) in both the short and immediate term, with accuracy out to at least 6 years, especially in white men, according to a retrospective case adjudication of the Health ABC study published in Neurology.
Of 2,462 study participants, 42 were found to have PD during an average of 9.8 years of follow-up, Honglei Chen, MD, PhD, of the department of epidemiology and biostatistics at Michigan State University, East Lansing, and his coauthors wrote. Of those cases, 26 (62%) were associated with a poor Brief Smell Identification Test (BSIT) score of 0-8 out of 12 (hazard ratio, 5.1; 95% confidence interval, 2.1-11.9), supporting other studies that indicate that olfactory impairment is one of the early symptoms of PD.
In contrast to previous studies, however, “the current study has longer follow-up and showed that poor olfaction was associated with PD beyond the first [4] years of follow-up, although the association was somewhat attenuated,” the researchers said. Both before and after the first 5 years of follow-up, 13 people in the lowest BSIT tertile were diagnosed with PD (HR, 4.2; 95% CI, 1.7-10.8 vs. HR, 4.1; 95% CI, 1.7-9.8, respectively),
In addition, poor sense of smell was more clearly associated with PD diagnosis in white patients, Dr. Chen and her coauthors said. Of 30 PD diagnoses in white participants, 19 were associated with poor smell (HR, 4.9; 95% CI, 2.3-10.5), compared with 7 out of 12 diagnoses in black participants (HR, 2.5; 95% CI, 0.8-8.1; P = .3). Similarly, 19 out of 26 diagnoses in men were associated with poor smell (HR, 5.4; 95% CI, 2.3-12.9), compared with 7 out of 16 diagnoses in women (HR, 2.9; 95% CI, 1.1-7.8; P = .4).
Future studies should confirm these stratified findings. Olfactory dysfunction’s “potential usefulness as a screening tool for prodromal or undiagnosed PD in other general population awaits further investigations,” the authors said.
Dr. Chen reported editorial roles for a number of medical journals. None of the authors reported any financial disclosures.
email address
FROM NEUROLOGY
Key clinical point:
Major finding: Both before and after the first 5 years of follow-up, 13 people in the lowest BSIT tertile were diagnosed with PD (HR, 4.2; 95% CI, 1.7-10.8 vs. HR, 4.1; 95% CI, 1.7-9.8, respectively).
Data source: A retrospective case adjudication of PD cases diagnosed in the Health ABC study.
Disclosures: Dr. Chen reported editorial roles for a number of medical journals. None of the authors reported any financial disclosures.