User login
-
DLBCL: Major new treatment breakthroughs
Significant breakthroughs have come in just the past few weeks and months, through the use of CAR T-cell and immunotherapies and with the approval in April by the Food and Drug Administration of polatuzumab for frontline DLBCL.
“Until the publishing of data from the POLARIX study (NCT03274492), which led to the approval of polatuzumab vedotin plus rituximab-cyclophosphamide, doxorubicin, and prednisone (pola + R-CHP), we had not had a breakthrough in frontline DLBCL therapies since the addition of rituximab 22 years ago,” said Dr. Charalambos Andreadis, MD, of the University of California at San Francisco’s Helen Diller Family Comprehensive Cancer Center.
“Pola + R-CHP is an improvement over the standard-of-care treatment, R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone), giving treatment naive patients an increase in PFS without an increase in side effects,” Dr. Andreadis said.
R-CHP-polatuzumab was approved only for patients with an International Prognostic Indices score between 2 and 5, leaving patients with IPI scores of 0 or 1 with the frontline standard of care (SoC) treatment of R-CHOP, which has a cure rate of between 60% and 70%.
“The highest likelihood of relapse is in the first year following treatment. After 2 years in remission, patients’ chance of relapsing is the same as the general populations’ chance of getting DLBCL for the first time. This is why even a slight increase in the progression-free survival rate with the addition of pola is so significant,” Dr. Andreadis noted.
Historically, patients with relapsed or refractory (RR) DLBCL who did not respond to R-CHOP or who experienced disease relapse less than a year after primary intervention were treated with alternative chemotherapy regimens, often followed by autologous stem cell transplants (ASCT). Randomized control studies have shown that CAR T-cell therapies yield higher success rates than chemotherapy and ASCT, leading to the SoC in RR patients being CAR-T cell therapy directly following failed primary treatment.
“There are many new CAR T-cell platforms in development, as well as novel combination strategies that aim to target critical genetic pathways,” Kieron Dunleavy, MD, professor of medicine at the Lombardi Comprehensive Cancer Center at Georgetown University Hospital, said in an interview. “While access to CAR T-cell therapies is becoming easier and more feasible in many centers, fast access continues to be an issue for many patients, often depending on geography and socioeconomic factors.”
Asked about the latest breakthroughs in treating DLBCL, Dr. Dunleavy said, “A significant proportion of patients with relapsed or refractory DLBCL do not have easy access to CAR T-cell therapies, so this needs to be addressed and improved. Sometimes the rapidity of clinical progression in DLBCL can make these therapies challenging to deliver, considering logistical issues like apheresis and insurance approvals, which are frequently complex. This highlights the need for alternative and ‘easier to deliver’ CAR-T cells and our continued prioritization of developing alternative effective agents for DLBCL.
“Currently, commercially approved CAR T-cells in DLBCL target the CD-19 marker on lymphoma cells but CAR T-cells targeting other and more than one antigen as well as alternative anti CD19 agents like loncastuximab and tafasitamab are similarly FDA approved and available for patients,” Dr. Dunleavy concluded.
Dr. Dunleavy is affiliated with the MedStar Georgetown Lymphoma group, where Rep. Raskin publicly announced that he had completed 4 months of chemotherapy treatment for DLBCL. On April 27, in an open letter to the U.S. public, he wrote that he rang the bell at MedStar to mark his preliminary diagnosis of being “in remission,” with a “90% prognosis of no relapse.”
Interviewed about the latest advances in treating DLBCL, Jason Westin, MD, associate professor of lymphoma and myeloma at the MD Anderson Cancer Center in Houston, said that even with improvements in overall survival possible with CAR T-cell therapies, “usually, a clinical trial should be considered strongly, as it is often the best option for patients, both in a newly diagnosed or in a relapsed setting, as they allow access to tomorrow’s breakthrough therapies today.”
Dr. Westin cited the example of bispecific T-cell engagers (BITE) as a promising therapy that is available to patients in clinical trials. These agents bind to one side to the lymphoma cell, but they also have a binding arm for T-cells, so they activate a patient’s own immune cells to kill lymphoma cells, in some cases offering a cure when CAR T-cell therapy has failed.
The first BITE to be approved, mosunetuzumab, is authorized only for the treatment of follicular lymphoma. However, data from a recent clinical study indicated that the agent yields complete responses in 24% of heavily pretreated patients with RR DLBCL.
Another BITE, glofitamab, was approved in Canada in March 2023 for use in RR DLBCL. Based on its high efficacy, it soon may be approved elsewhere.
Dr. Andreadis noted, “We are finally at a point where for both treatment naive and RR DLBCL patients, there are several promising options on the horizon that don’t involve ASCT. Furthermore, these breakthroughs reinforce each other, as there are studies in which therapies like BITE are being brought to the front line and pola to RR cases.”
The growing field of new frontline and RR DLBCL therapies lend credence to the optimism of specialists who treat DLBCL – and to the sanguine note that Congressman Raskin struck in published comments about his treatment for DLBCL.
Dr. Andreadis reported ties with BMS, Novartis, Roche, Genmab, Merck, Gilead, AbbVie, and J&J. Dr. Dunleavy disclosed relationships with ONO Pharmaceuticals, Kymera, Merck, Genentech, AstraZeneca, Amgen, ADC Therapeutics, MorphoSys and Incyte, Kite/Gilead, Cellectar. Dr. Westin reported ties with Kite/Gilead, BMS, Novartis, Genentech, AstraZeneca, Morphosys/Incyte, ADC Therapeutics, Kymera, Nurix, and MonteRosa.
Significant breakthroughs have come in just the past few weeks and months, through the use of CAR T-cell and immunotherapies and with the approval in April by the Food and Drug Administration of polatuzumab for frontline DLBCL.
“Until the publishing of data from the POLARIX study (NCT03274492), which led to the approval of polatuzumab vedotin plus rituximab-cyclophosphamide, doxorubicin, and prednisone (pola + R-CHP), we had not had a breakthrough in frontline DLBCL therapies since the addition of rituximab 22 years ago,” said Dr. Charalambos Andreadis, MD, of the University of California at San Francisco’s Helen Diller Family Comprehensive Cancer Center.
“Pola + R-CHP is an improvement over the standard-of-care treatment, R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone), giving treatment naive patients an increase in PFS without an increase in side effects,” Dr. Andreadis said.
R-CHP-polatuzumab was approved only for patients with an International Prognostic Indices score between 2 and 5, leaving patients with IPI scores of 0 or 1 with the frontline standard of care (SoC) treatment of R-CHOP, which has a cure rate of between 60% and 70%.
“The highest likelihood of relapse is in the first year following treatment. After 2 years in remission, patients’ chance of relapsing is the same as the general populations’ chance of getting DLBCL for the first time. This is why even a slight increase in the progression-free survival rate with the addition of pola is so significant,” Dr. Andreadis noted.
Historically, patients with relapsed or refractory (RR) DLBCL who did not respond to R-CHOP or who experienced disease relapse less than a year after primary intervention were treated with alternative chemotherapy regimens, often followed by autologous stem cell transplants (ASCT). Randomized control studies have shown that CAR T-cell therapies yield higher success rates than chemotherapy and ASCT, leading to the SoC in RR patients being CAR-T cell therapy directly following failed primary treatment.
“There are many new CAR T-cell platforms in development, as well as novel combination strategies that aim to target critical genetic pathways,” Kieron Dunleavy, MD, professor of medicine at the Lombardi Comprehensive Cancer Center at Georgetown University Hospital, said in an interview. “While access to CAR T-cell therapies is becoming easier and more feasible in many centers, fast access continues to be an issue for many patients, often depending on geography and socioeconomic factors.”
Asked about the latest breakthroughs in treating DLBCL, Dr. Dunleavy said, “A significant proportion of patients with relapsed or refractory DLBCL do not have easy access to CAR T-cell therapies, so this needs to be addressed and improved. Sometimes the rapidity of clinical progression in DLBCL can make these therapies challenging to deliver, considering logistical issues like apheresis and insurance approvals, which are frequently complex. This highlights the need for alternative and ‘easier to deliver’ CAR-T cells and our continued prioritization of developing alternative effective agents for DLBCL.
“Currently, commercially approved CAR T-cells in DLBCL target the CD-19 marker on lymphoma cells but CAR T-cells targeting other and more than one antigen as well as alternative anti CD19 agents like loncastuximab and tafasitamab are similarly FDA approved and available for patients,” Dr. Dunleavy concluded.
Dr. Dunleavy is affiliated with the MedStar Georgetown Lymphoma group, where Rep. Raskin publicly announced that he had completed 4 months of chemotherapy treatment for DLBCL. On April 27, in an open letter to the U.S. public, he wrote that he rang the bell at MedStar to mark his preliminary diagnosis of being “in remission,” with a “90% prognosis of no relapse.”
Interviewed about the latest advances in treating DLBCL, Jason Westin, MD, associate professor of lymphoma and myeloma at the MD Anderson Cancer Center in Houston, said that even with improvements in overall survival possible with CAR T-cell therapies, “usually, a clinical trial should be considered strongly, as it is often the best option for patients, both in a newly diagnosed or in a relapsed setting, as they allow access to tomorrow’s breakthrough therapies today.”
Dr. Westin cited the example of bispecific T-cell engagers (BITE) as a promising therapy that is available to patients in clinical trials. These agents bind to one side to the lymphoma cell, but they also have a binding arm for T-cells, so they activate a patient’s own immune cells to kill lymphoma cells, in some cases offering a cure when CAR T-cell therapy has failed.
The first BITE to be approved, mosunetuzumab, is authorized only for the treatment of follicular lymphoma. However, data from a recent clinical study indicated that the agent yields complete responses in 24% of heavily pretreated patients with RR DLBCL.
Another BITE, glofitamab, was approved in Canada in March 2023 for use in RR DLBCL. Based on its high efficacy, it soon may be approved elsewhere.
Dr. Andreadis noted, “We are finally at a point where for both treatment naive and RR DLBCL patients, there are several promising options on the horizon that don’t involve ASCT. Furthermore, these breakthroughs reinforce each other, as there are studies in which therapies like BITE are being brought to the front line and pola to RR cases.”
The growing field of new frontline and RR DLBCL therapies lend credence to the optimism of specialists who treat DLBCL – and to the sanguine note that Congressman Raskin struck in published comments about his treatment for DLBCL.
Dr. Andreadis reported ties with BMS, Novartis, Roche, Genmab, Merck, Gilead, AbbVie, and J&J. Dr. Dunleavy disclosed relationships with ONO Pharmaceuticals, Kymera, Merck, Genentech, AstraZeneca, Amgen, ADC Therapeutics, MorphoSys and Incyte, Kite/Gilead, Cellectar. Dr. Westin reported ties with Kite/Gilead, BMS, Novartis, Genentech, AstraZeneca, Morphosys/Incyte, ADC Therapeutics, Kymera, Nurix, and MonteRosa.
Significant breakthroughs have come in just the past few weeks and months, through the use of CAR T-cell and immunotherapies and with the approval in April by the Food and Drug Administration of polatuzumab for frontline DLBCL.
“Until the publishing of data from the POLARIX study (NCT03274492), which led to the approval of polatuzumab vedotin plus rituximab-cyclophosphamide, doxorubicin, and prednisone (pola + R-CHP), we had not had a breakthrough in frontline DLBCL therapies since the addition of rituximab 22 years ago,” said Dr. Charalambos Andreadis, MD, of the University of California at San Francisco’s Helen Diller Family Comprehensive Cancer Center.
“Pola + R-CHP is an improvement over the standard-of-care treatment, R-CHOP (rituximab-cyclophosphamide, doxorubicin, vincristine, and prednisone), giving treatment naive patients an increase in PFS without an increase in side effects,” Dr. Andreadis said.
R-CHP-polatuzumab was approved only for patients with an International Prognostic Indices score between 2 and 5, leaving patients with IPI scores of 0 or 1 with the frontline standard of care (SoC) treatment of R-CHOP, which has a cure rate of between 60% and 70%.
“The highest likelihood of relapse is in the first year following treatment. After 2 years in remission, patients’ chance of relapsing is the same as the general populations’ chance of getting DLBCL for the first time. This is why even a slight increase in the progression-free survival rate with the addition of pola is so significant,” Dr. Andreadis noted.
Historically, patients with relapsed or refractory (RR) DLBCL who did not respond to R-CHOP or who experienced disease relapse less than a year after primary intervention were treated with alternative chemotherapy regimens, often followed by autologous stem cell transplants (ASCT). Randomized control studies have shown that CAR T-cell therapies yield higher success rates than chemotherapy and ASCT, leading to the SoC in RR patients being CAR-T cell therapy directly following failed primary treatment.
“There are many new CAR T-cell platforms in development, as well as novel combination strategies that aim to target critical genetic pathways,” Kieron Dunleavy, MD, professor of medicine at the Lombardi Comprehensive Cancer Center at Georgetown University Hospital, said in an interview. “While access to CAR T-cell therapies is becoming easier and more feasible in many centers, fast access continues to be an issue for many patients, often depending on geography and socioeconomic factors.”
Asked about the latest breakthroughs in treating DLBCL, Dr. Dunleavy said, “A significant proportion of patients with relapsed or refractory DLBCL do not have easy access to CAR T-cell therapies, so this needs to be addressed and improved. Sometimes the rapidity of clinical progression in DLBCL can make these therapies challenging to deliver, considering logistical issues like apheresis and insurance approvals, which are frequently complex. This highlights the need for alternative and ‘easier to deliver’ CAR-T cells and our continued prioritization of developing alternative effective agents for DLBCL.
“Currently, commercially approved CAR T-cells in DLBCL target the CD-19 marker on lymphoma cells but CAR T-cells targeting other and more than one antigen as well as alternative anti CD19 agents like loncastuximab and tafasitamab are similarly FDA approved and available for patients,” Dr. Dunleavy concluded.
Dr. Dunleavy is affiliated with the MedStar Georgetown Lymphoma group, where Rep. Raskin publicly announced that he had completed 4 months of chemotherapy treatment for DLBCL. On April 27, in an open letter to the U.S. public, he wrote that he rang the bell at MedStar to mark his preliminary diagnosis of being “in remission,” with a “90% prognosis of no relapse.”
Interviewed about the latest advances in treating DLBCL, Jason Westin, MD, associate professor of lymphoma and myeloma at the MD Anderson Cancer Center in Houston, said that even with improvements in overall survival possible with CAR T-cell therapies, “usually, a clinical trial should be considered strongly, as it is often the best option for patients, both in a newly diagnosed or in a relapsed setting, as they allow access to tomorrow’s breakthrough therapies today.”
Dr. Westin cited the example of bispecific T-cell engagers (BITE) as a promising therapy that is available to patients in clinical trials. These agents bind to one side to the lymphoma cell, but they also have a binding arm for T-cells, so they activate a patient’s own immune cells to kill lymphoma cells, in some cases offering a cure when CAR T-cell therapy has failed.
The first BITE to be approved, mosunetuzumab, is authorized only for the treatment of follicular lymphoma. However, data from a recent clinical study indicated that the agent yields complete responses in 24% of heavily pretreated patients with RR DLBCL.
Another BITE, glofitamab, was approved in Canada in March 2023 for use in RR DLBCL. Based on its high efficacy, it soon may be approved elsewhere.
Dr. Andreadis noted, “We are finally at a point where for both treatment naive and RR DLBCL patients, there are several promising options on the horizon that don’t involve ASCT. Furthermore, these breakthroughs reinforce each other, as there are studies in which therapies like BITE are being brought to the front line and pola to RR cases.”
The growing field of new frontline and RR DLBCL therapies lend credence to the optimism of specialists who treat DLBCL – and to the sanguine note that Congressman Raskin struck in published comments about his treatment for DLBCL.
Dr. Andreadis reported ties with BMS, Novartis, Roche, Genmab, Merck, Gilead, AbbVie, and J&J. Dr. Dunleavy disclosed relationships with ONO Pharmaceuticals, Kymera, Merck, Genentech, AstraZeneca, Amgen, ADC Therapeutics, MorphoSys and Incyte, Kite/Gilead, Cellectar. Dr. Westin reported ties with Kite/Gilead, BMS, Novartis, Genentech, AstraZeneca, Morphosys/Incyte, ADC Therapeutics, Kymera, Nurix, and MonteRosa.
ASCO honors Hagop Kantarjian, MD, for leukemia research
This award is the society’s “highest scientific honor, and I am extremely happy and honored to receive it,” Dr. Kantarjian commented in an interview with this news organization.
Dr. Kantarjian serves as the chair of the department of leukemia and currently holds the Samsung Distinguished University Chair in Cancer Medicine at the University of Texas MD Anderson Cancer Center, Houston.
“No doubt that this is not an individual award. It represents an award for the accomplishments of all the leukemia faculty at MD Anderson across 4 decades. It’s really a teamwork effort that led to so many discoveries and improvements in treatment and care of patients with leukemia,” he commented.
The David A. Karnofsky Memorial Award has been presented annually since 1970 to recognize oncologists who have made outstanding contributions to cancer research, diagnosis, or treatment, ASCO noted.
From Lebanon to Texas
Dr. Kantarjian received his medical degree from the American University of Beirut, in Lebanon, in 1979 and completed his residency in internal medicine at the same institution in 1981.
It was his experience at MD Anderson as a young medical student and later as a fellow that fueled his interest and career in leukemia, he said.
“In 1978, I took a 4-month elective at MD Anderson, and I soon realized how different and innovative the atmosphere at MD Anderson was, compared to where I was training in Lebanon,” Dr. Kantarjian told this news organization.
Working with mentors that included MD Anderson heavyweights Emil Freireich, MD, Kenneth McCredie, MD, and Michael Keating, MD, helped shape his career and guide his leukemia research, he said.
Transformative impact on leukemia outcomes
The award citation notes that over the past 4 decades, Dr. Kantarjian’s research has transformed some standards of care and has dramatically improved survival in several leukemia subtypes, including chronic myeloid leukemia (CML), acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and acute lymphocytic leukemia (ALL).
“Four decades ago, most of the leukemias were incurable. Today, most of the leukemias are potentially curable with targeted therapies. That’s what I am most proud of,” Dr. Kantarjian told this news organization.
Among Dr. Kantarjian’s contributions to the field of leukemia:
- Developing the HYPER-CVAD regimen (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) as a standard-of-care, frontline therapy for adults with ALL.
- Establishing clinical biology parameters of CML, including definitions of CML phases and cytogenetic responses, and establishing new prognostic factors that were subsequently adopted in studies of tyrosine kinase inhibitors.
- Leading the development of decitabine and epigenetic hypomethylation therapy for MDS and for older/unfit patients with AML.
- Pioneering research with hypomethylating agents (HMAs) in combination with venetoclax, which led to FDA approval of HMA-venetoclax combinations for older/unfit patients with AML.
- Championing the development of clofarabine, conducting animal toxicology studies, and leading subsequent phase 1 and 2 trials and pivotal phase 3 and 4 trials that led to FDA approval of clofarabine for pediatric ALL.
- Developing several FLT3 inhibitors, isocitrate dehydrogenase inhibitors, and venetoclax, which all received FDA approval for the treatment of AML and its subsets.
- Developing regimens for inotuzumab and blinatumomab combined with chemotherapy for adults with pre-B ALL.
- Working on the development of imatinib, dasatinib, nilotinib, bosutinib, ponatinib, and omacetaxine, which all received FDA approval for CML therapy.
“Dr. Kantarjian’s long list of accomplishments and groundbreaking discoveries are a testament to his lifelong commitment to impactful cancer research and patient care,” Giulio Draetta, MD, PhD, chief scientific officer at MD Anderson, said in a statement.
Giving back
Dr. Kantarjian has written more than 2,200 peer-reviewed articles and more than 100 book chapters. In 2012, he cofounded the Society of Hematologic Oncology, which has now expanded worldwide.
He has served on multiple ASCO committees throughout the years and served on the ASCO board of directors from 2010 to 2015.
Dr. Kantarjian is passionately involved in mentoring and education. In 2000 he created the MD Anderson Leukemia Fellowship, which now trains about 10 fellows in leukemia annually.
He is a nonresident fellow in health care at the Rice Baker Institute and has written extensively on important health care issues in cancer, including the importance of universal equitable health care, health care safety nets, health care as a human right, and the problem of drug shortages.
Dr. Kantarjian is a strong advocate for more affordable drug therapies. For years he has been outspoken about the high price of leukemia drugs and has written high-profile articles in medical journals. He has even appeared on a popular television program to publicize the issue.
“Drug costs have been increasing over time. If you think about it, even if you discover a drug that cures cancer, but the drug is affordable for the 1% of the patients, then you have no cure for cancer,” Dr. Kantarjian told this news organization.
“I started speaking about the issue of the cancer drug costs in 2012. Unfortunately, we have not made progress simply because of the for-profit nature of health care and the strong lobbying by drug companies,” he added. Dr. Kantarjian hopes new legislation will eventually turn the tide.
Dr. Kantarjian has received many other honors throughout his distinguished career, including the American Lebanese Medical Association’s Lifetime Achievement Award, the American Association for Cancer Research’s Joseph H. Burchenal Memorial Award, and the Leukemia Society of America’s Outstanding Service to Mankind Award. He also was named an ASCO Fellow and a Leukemia Society of America Special Fellow and Scholar.
Dr. Kantarjian will be presented with the 2023 David A. Karnofsky Memorial Award, which includes a $25,000 honorarium, and will give a scientific lecture about his research at the ASCO annual meeting in Chicago in early June.
A version of this article originally appeared on Medscape.com.
This award is the society’s “highest scientific honor, and I am extremely happy and honored to receive it,” Dr. Kantarjian commented in an interview with this news organization.
Dr. Kantarjian serves as the chair of the department of leukemia and currently holds the Samsung Distinguished University Chair in Cancer Medicine at the University of Texas MD Anderson Cancer Center, Houston.
“No doubt that this is not an individual award. It represents an award for the accomplishments of all the leukemia faculty at MD Anderson across 4 decades. It’s really a teamwork effort that led to so many discoveries and improvements in treatment and care of patients with leukemia,” he commented.
The David A. Karnofsky Memorial Award has been presented annually since 1970 to recognize oncologists who have made outstanding contributions to cancer research, diagnosis, or treatment, ASCO noted.
From Lebanon to Texas
Dr. Kantarjian received his medical degree from the American University of Beirut, in Lebanon, in 1979 and completed his residency in internal medicine at the same institution in 1981.
It was his experience at MD Anderson as a young medical student and later as a fellow that fueled his interest and career in leukemia, he said.
“In 1978, I took a 4-month elective at MD Anderson, and I soon realized how different and innovative the atmosphere at MD Anderson was, compared to where I was training in Lebanon,” Dr. Kantarjian told this news organization.
Working with mentors that included MD Anderson heavyweights Emil Freireich, MD, Kenneth McCredie, MD, and Michael Keating, MD, helped shape his career and guide his leukemia research, he said.
Transformative impact on leukemia outcomes
The award citation notes that over the past 4 decades, Dr. Kantarjian’s research has transformed some standards of care and has dramatically improved survival in several leukemia subtypes, including chronic myeloid leukemia (CML), acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and acute lymphocytic leukemia (ALL).
“Four decades ago, most of the leukemias were incurable. Today, most of the leukemias are potentially curable with targeted therapies. That’s what I am most proud of,” Dr. Kantarjian told this news organization.
Among Dr. Kantarjian’s contributions to the field of leukemia:
- Developing the HYPER-CVAD regimen (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) as a standard-of-care, frontline therapy for adults with ALL.
- Establishing clinical biology parameters of CML, including definitions of CML phases and cytogenetic responses, and establishing new prognostic factors that were subsequently adopted in studies of tyrosine kinase inhibitors.
- Leading the development of decitabine and epigenetic hypomethylation therapy for MDS and for older/unfit patients with AML.
- Pioneering research with hypomethylating agents (HMAs) in combination with venetoclax, which led to FDA approval of HMA-venetoclax combinations for older/unfit patients with AML.
- Championing the development of clofarabine, conducting animal toxicology studies, and leading subsequent phase 1 and 2 trials and pivotal phase 3 and 4 trials that led to FDA approval of clofarabine for pediatric ALL.
- Developing several FLT3 inhibitors, isocitrate dehydrogenase inhibitors, and venetoclax, which all received FDA approval for the treatment of AML and its subsets.
- Developing regimens for inotuzumab and blinatumomab combined with chemotherapy for adults with pre-B ALL.
- Working on the development of imatinib, dasatinib, nilotinib, bosutinib, ponatinib, and omacetaxine, which all received FDA approval for CML therapy.
“Dr. Kantarjian’s long list of accomplishments and groundbreaking discoveries are a testament to his lifelong commitment to impactful cancer research and patient care,” Giulio Draetta, MD, PhD, chief scientific officer at MD Anderson, said in a statement.
Giving back
Dr. Kantarjian has written more than 2,200 peer-reviewed articles and more than 100 book chapters. In 2012, he cofounded the Society of Hematologic Oncology, which has now expanded worldwide.
He has served on multiple ASCO committees throughout the years and served on the ASCO board of directors from 2010 to 2015.
Dr. Kantarjian is passionately involved in mentoring and education. In 2000 he created the MD Anderson Leukemia Fellowship, which now trains about 10 fellows in leukemia annually.
He is a nonresident fellow in health care at the Rice Baker Institute and has written extensively on important health care issues in cancer, including the importance of universal equitable health care, health care safety nets, health care as a human right, and the problem of drug shortages.
Dr. Kantarjian is a strong advocate for more affordable drug therapies. For years he has been outspoken about the high price of leukemia drugs and has written high-profile articles in medical journals. He has even appeared on a popular television program to publicize the issue.
“Drug costs have been increasing over time. If you think about it, even if you discover a drug that cures cancer, but the drug is affordable for the 1% of the patients, then you have no cure for cancer,” Dr. Kantarjian told this news organization.
“I started speaking about the issue of the cancer drug costs in 2012. Unfortunately, we have not made progress simply because of the for-profit nature of health care and the strong lobbying by drug companies,” he added. Dr. Kantarjian hopes new legislation will eventually turn the tide.
Dr. Kantarjian has received many other honors throughout his distinguished career, including the American Lebanese Medical Association’s Lifetime Achievement Award, the American Association for Cancer Research’s Joseph H. Burchenal Memorial Award, and the Leukemia Society of America’s Outstanding Service to Mankind Award. He also was named an ASCO Fellow and a Leukemia Society of America Special Fellow and Scholar.
Dr. Kantarjian will be presented with the 2023 David A. Karnofsky Memorial Award, which includes a $25,000 honorarium, and will give a scientific lecture about his research at the ASCO annual meeting in Chicago in early June.
A version of this article originally appeared on Medscape.com.
This award is the society’s “highest scientific honor, and I am extremely happy and honored to receive it,” Dr. Kantarjian commented in an interview with this news organization.
Dr. Kantarjian serves as the chair of the department of leukemia and currently holds the Samsung Distinguished University Chair in Cancer Medicine at the University of Texas MD Anderson Cancer Center, Houston.
“No doubt that this is not an individual award. It represents an award for the accomplishments of all the leukemia faculty at MD Anderson across 4 decades. It’s really a teamwork effort that led to so many discoveries and improvements in treatment and care of patients with leukemia,” he commented.
The David A. Karnofsky Memorial Award has been presented annually since 1970 to recognize oncologists who have made outstanding contributions to cancer research, diagnosis, or treatment, ASCO noted.
From Lebanon to Texas
Dr. Kantarjian received his medical degree from the American University of Beirut, in Lebanon, in 1979 and completed his residency in internal medicine at the same institution in 1981.
It was his experience at MD Anderson as a young medical student and later as a fellow that fueled his interest and career in leukemia, he said.
“In 1978, I took a 4-month elective at MD Anderson, and I soon realized how different and innovative the atmosphere at MD Anderson was, compared to where I was training in Lebanon,” Dr. Kantarjian told this news organization.
Working with mentors that included MD Anderson heavyweights Emil Freireich, MD, Kenneth McCredie, MD, and Michael Keating, MD, helped shape his career and guide his leukemia research, he said.
Transformative impact on leukemia outcomes
The award citation notes that over the past 4 decades, Dr. Kantarjian’s research has transformed some standards of care and has dramatically improved survival in several leukemia subtypes, including chronic myeloid leukemia (CML), acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and acute lymphocytic leukemia (ALL).
“Four decades ago, most of the leukemias were incurable. Today, most of the leukemias are potentially curable with targeted therapies. That’s what I am most proud of,” Dr. Kantarjian told this news organization.
Among Dr. Kantarjian’s contributions to the field of leukemia:
- Developing the HYPER-CVAD regimen (hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone) as a standard-of-care, frontline therapy for adults with ALL.
- Establishing clinical biology parameters of CML, including definitions of CML phases and cytogenetic responses, and establishing new prognostic factors that were subsequently adopted in studies of tyrosine kinase inhibitors.
- Leading the development of decitabine and epigenetic hypomethylation therapy for MDS and for older/unfit patients with AML.
- Pioneering research with hypomethylating agents (HMAs) in combination with venetoclax, which led to FDA approval of HMA-venetoclax combinations for older/unfit patients with AML.
- Championing the development of clofarabine, conducting animal toxicology studies, and leading subsequent phase 1 and 2 trials and pivotal phase 3 and 4 trials that led to FDA approval of clofarabine for pediatric ALL.
- Developing several FLT3 inhibitors, isocitrate dehydrogenase inhibitors, and venetoclax, which all received FDA approval for the treatment of AML and its subsets.
- Developing regimens for inotuzumab and blinatumomab combined with chemotherapy for adults with pre-B ALL.
- Working on the development of imatinib, dasatinib, nilotinib, bosutinib, ponatinib, and omacetaxine, which all received FDA approval for CML therapy.
“Dr. Kantarjian’s long list of accomplishments and groundbreaking discoveries are a testament to his lifelong commitment to impactful cancer research and patient care,” Giulio Draetta, MD, PhD, chief scientific officer at MD Anderson, said in a statement.
Giving back
Dr. Kantarjian has written more than 2,200 peer-reviewed articles and more than 100 book chapters. In 2012, he cofounded the Society of Hematologic Oncology, which has now expanded worldwide.
He has served on multiple ASCO committees throughout the years and served on the ASCO board of directors from 2010 to 2015.
Dr. Kantarjian is passionately involved in mentoring and education. In 2000 he created the MD Anderson Leukemia Fellowship, which now trains about 10 fellows in leukemia annually.
He is a nonresident fellow in health care at the Rice Baker Institute and has written extensively on important health care issues in cancer, including the importance of universal equitable health care, health care safety nets, health care as a human right, and the problem of drug shortages.
Dr. Kantarjian is a strong advocate for more affordable drug therapies. For years he has been outspoken about the high price of leukemia drugs and has written high-profile articles in medical journals. He has even appeared on a popular television program to publicize the issue.
“Drug costs have been increasing over time. If you think about it, even if you discover a drug that cures cancer, but the drug is affordable for the 1% of the patients, then you have no cure for cancer,” Dr. Kantarjian told this news organization.
“I started speaking about the issue of the cancer drug costs in 2012. Unfortunately, we have not made progress simply because of the for-profit nature of health care and the strong lobbying by drug companies,” he added. Dr. Kantarjian hopes new legislation will eventually turn the tide.
Dr. Kantarjian has received many other honors throughout his distinguished career, including the American Lebanese Medical Association’s Lifetime Achievement Award, the American Association for Cancer Research’s Joseph H. Burchenal Memorial Award, and the Leukemia Society of America’s Outstanding Service to Mankind Award. He also was named an ASCO Fellow and a Leukemia Society of America Special Fellow and Scholar.
Dr. Kantarjian will be presented with the 2023 David A. Karnofsky Memorial Award, which includes a $25,000 honorarium, and will give a scientific lecture about his research at the ASCO annual meeting in Chicago in early June.
A version of this article originally appeared on Medscape.com.
CLL: Venetoclax combos top first-line chemoimmunotherapy
according to a phase 3 trial published in the New England Journal of Medicine.
The trial, dubbed GAIA–CLL13, “is a remarkable demonstration of the quality of fixed-duration therapies for younger, fit patients, and it challenges us to continue to work to develop therapeutic strategies that will ultimately cure patients with CLL,” two hematologic cancer specialists said in an accompanying editorial.
In short, “venetoclax-obinutuzumab and venetoclax-obinutuzumab-ibrutinib were superior to chemoimmunotherapy with respect to both the minimal residual disease end point and progression-free survival, but venetoclax-rituximab was not,” Jennifer Woyach, MD, of Ohio State University, Columbus, and John Byrd, MD, University of Cincinnati, said in their commentary.
Noting that randomized trials involving venetoclax combinations in fit CLL patients “have been lacking,” the investigators compared 6 cycles of chemoimmunotherapy (fludarabine-cyclophosphamide-rituximab or bendamustine-rituximab) with 12 cycles of venetoclax plus the anti-CD20 antibody rituximab, venetoclax plus the third generation anti-CD20 antibody obinutuzumab, and venetoclax combined with both obinutuzumab and the Bruton’s tyrosine kinase inhibitor ibrutinib in a novel triple-therapy regimen.
The 926 patients in the study were a mean of 61 years old and split about evenly among the four treatment arms. Ibrutinib was discontinued after two consecutive measurements if patients had undetectable minimal residual disease (uMRD). Subjects did not have TP53 aberrations, a marker of poor prognosis in CLL.
At 15 months, the percentage of patients with uMRD was significantly higher in the triple-therapy arm (92.2%) and the venetoclax-obinutuzumab group (86.5%) than in the chemoimmunotherapy group (52.0%), but there was no statistical difference with venetoclax-rituximab (57%, P = .32).
The three-year progression-free survival (PFS) was 90.5% in the triple-therapy arm versus 87.7% with venetoclax-obinutuzumab. The 3-year PFS with venetoclax-rituximab (80.8%) was again not statistically different than the 75.5% with chemoimmunotherapy (P = .18).
Not ready for prime time
The benefits of triple therapy and venetoclax-obinutuzumab held only in patients with unmutated IgVH. “The high efficacy of the fludarabine, cyclophosphamide, and rituximab regimen in young, fit patients with mutated IgVH may be difficult to improve on,” noted the investigators, led by Barbara Eichhorst, MD, a hematologic malignancy specialist at the University of Cologne (Germany).
Also, although triple-therapy results were impressive, some of the benefits “are neutralized by the need for dose reductions and early treatment discontinuation owing to adverse events,” they said.
For instance, triple therapy had the highest incidence of both grade 3 and 4 infections (21.2%) and atrial fibrillation (7.8%).
The editorialists noted that there has been “a flurry of interest” in trials combining ibrutinib and venetoclax – as was done in the triple-therapy arm – since both emerged as powerful tools against CLL in recent years. However, even with the study results, they said “the use of triplet therapy should be viewed as investigational.”
For one thing, rates of uMRD were not “dramatically different” between triple therapy and venetoclax-obinutuzumab, and longer follow-up is better gauge differences in PFS and long-term toxicities.
Also, ibrutinib is being eclipsed by the second-generation Bruton’s tyrosine kinase inhibitors acalabrutinib and zanubrutinib, because they have better safety profiles, and they are being assessed in CLL combination trials. For now, there are too many unknowns for routine use of triple therapy in fit CLL patients, they said.
The investigators and editorialists both noted that improved uMRD in the study translated into superior PFS, raising the possibility that uMRD might be a valid alternative endpoint to PFS in CLL trials.
With “median remissions in CLL lasting far in excess of 5 years, designing studies that take 8-10 years” to reach a PFS endpoint is simply too slow. Moving to an alternative endpoint such a uMRD would preserve “the momentum that has been generated” with recent advances, Dr. Woyach and Dr. Byrd said.
The work was funded by the companies that market venetoclax, ibrutinib, and obinutuzumab: AbbVie, Janssen, and Roche. Dr. Eichhorst is a consultant and/or speaker for the companies and also reported grants from them. Dr. Byrd is a consultant/adviser for Eilean Therapeutics, Kurome Therapeutics, Newave, and Orbimed. Dr. Woyach disclosed ties with AbbVie, AstraZeneca, Lilly, and other companies.
according to a phase 3 trial published in the New England Journal of Medicine.
The trial, dubbed GAIA–CLL13, “is a remarkable demonstration of the quality of fixed-duration therapies for younger, fit patients, and it challenges us to continue to work to develop therapeutic strategies that will ultimately cure patients with CLL,” two hematologic cancer specialists said in an accompanying editorial.
In short, “venetoclax-obinutuzumab and venetoclax-obinutuzumab-ibrutinib were superior to chemoimmunotherapy with respect to both the minimal residual disease end point and progression-free survival, but venetoclax-rituximab was not,” Jennifer Woyach, MD, of Ohio State University, Columbus, and John Byrd, MD, University of Cincinnati, said in their commentary.
Noting that randomized trials involving venetoclax combinations in fit CLL patients “have been lacking,” the investigators compared 6 cycles of chemoimmunotherapy (fludarabine-cyclophosphamide-rituximab or bendamustine-rituximab) with 12 cycles of venetoclax plus the anti-CD20 antibody rituximab, venetoclax plus the third generation anti-CD20 antibody obinutuzumab, and venetoclax combined with both obinutuzumab and the Bruton’s tyrosine kinase inhibitor ibrutinib in a novel triple-therapy regimen.
The 926 patients in the study were a mean of 61 years old and split about evenly among the four treatment arms. Ibrutinib was discontinued after two consecutive measurements if patients had undetectable minimal residual disease (uMRD). Subjects did not have TP53 aberrations, a marker of poor prognosis in CLL.
At 15 months, the percentage of patients with uMRD was significantly higher in the triple-therapy arm (92.2%) and the venetoclax-obinutuzumab group (86.5%) than in the chemoimmunotherapy group (52.0%), but there was no statistical difference with venetoclax-rituximab (57%, P = .32).
The three-year progression-free survival (PFS) was 90.5% in the triple-therapy arm versus 87.7% with venetoclax-obinutuzumab. The 3-year PFS with venetoclax-rituximab (80.8%) was again not statistically different than the 75.5% with chemoimmunotherapy (P = .18).
Not ready for prime time
The benefits of triple therapy and venetoclax-obinutuzumab held only in patients with unmutated IgVH. “The high efficacy of the fludarabine, cyclophosphamide, and rituximab regimen in young, fit patients with mutated IgVH may be difficult to improve on,” noted the investigators, led by Barbara Eichhorst, MD, a hematologic malignancy specialist at the University of Cologne (Germany).
Also, although triple-therapy results were impressive, some of the benefits “are neutralized by the need for dose reductions and early treatment discontinuation owing to adverse events,” they said.
For instance, triple therapy had the highest incidence of both grade 3 and 4 infections (21.2%) and atrial fibrillation (7.8%).
The editorialists noted that there has been “a flurry of interest” in trials combining ibrutinib and venetoclax – as was done in the triple-therapy arm – since both emerged as powerful tools against CLL in recent years. However, even with the study results, they said “the use of triplet therapy should be viewed as investigational.”
For one thing, rates of uMRD were not “dramatically different” between triple therapy and venetoclax-obinutuzumab, and longer follow-up is better gauge differences in PFS and long-term toxicities.
Also, ibrutinib is being eclipsed by the second-generation Bruton’s tyrosine kinase inhibitors acalabrutinib and zanubrutinib, because they have better safety profiles, and they are being assessed in CLL combination trials. For now, there are too many unknowns for routine use of triple therapy in fit CLL patients, they said.
The investigators and editorialists both noted that improved uMRD in the study translated into superior PFS, raising the possibility that uMRD might be a valid alternative endpoint to PFS in CLL trials.
With “median remissions in CLL lasting far in excess of 5 years, designing studies that take 8-10 years” to reach a PFS endpoint is simply too slow. Moving to an alternative endpoint such a uMRD would preserve “the momentum that has been generated” with recent advances, Dr. Woyach and Dr. Byrd said.
The work was funded by the companies that market venetoclax, ibrutinib, and obinutuzumab: AbbVie, Janssen, and Roche. Dr. Eichhorst is a consultant and/or speaker for the companies and also reported grants from them. Dr. Byrd is a consultant/adviser for Eilean Therapeutics, Kurome Therapeutics, Newave, and Orbimed. Dr. Woyach disclosed ties with AbbVie, AstraZeneca, Lilly, and other companies.
according to a phase 3 trial published in the New England Journal of Medicine.
The trial, dubbed GAIA–CLL13, “is a remarkable demonstration of the quality of fixed-duration therapies for younger, fit patients, and it challenges us to continue to work to develop therapeutic strategies that will ultimately cure patients with CLL,” two hematologic cancer specialists said in an accompanying editorial.
In short, “venetoclax-obinutuzumab and venetoclax-obinutuzumab-ibrutinib were superior to chemoimmunotherapy with respect to both the minimal residual disease end point and progression-free survival, but venetoclax-rituximab was not,” Jennifer Woyach, MD, of Ohio State University, Columbus, and John Byrd, MD, University of Cincinnati, said in their commentary.
Noting that randomized trials involving venetoclax combinations in fit CLL patients “have been lacking,” the investigators compared 6 cycles of chemoimmunotherapy (fludarabine-cyclophosphamide-rituximab or bendamustine-rituximab) with 12 cycles of venetoclax plus the anti-CD20 antibody rituximab, venetoclax plus the third generation anti-CD20 antibody obinutuzumab, and venetoclax combined with both obinutuzumab and the Bruton’s tyrosine kinase inhibitor ibrutinib in a novel triple-therapy regimen.
The 926 patients in the study were a mean of 61 years old and split about evenly among the four treatment arms. Ibrutinib was discontinued after two consecutive measurements if patients had undetectable minimal residual disease (uMRD). Subjects did not have TP53 aberrations, a marker of poor prognosis in CLL.
At 15 months, the percentage of patients with uMRD was significantly higher in the triple-therapy arm (92.2%) and the venetoclax-obinutuzumab group (86.5%) than in the chemoimmunotherapy group (52.0%), but there was no statistical difference with venetoclax-rituximab (57%, P = .32).
The three-year progression-free survival (PFS) was 90.5% in the triple-therapy arm versus 87.7% with venetoclax-obinutuzumab. The 3-year PFS with venetoclax-rituximab (80.8%) was again not statistically different than the 75.5% with chemoimmunotherapy (P = .18).
Not ready for prime time
The benefits of triple therapy and venetoclax-obinutuzumab held only in patients with unmutated IgVH. “The high efficacy of the fludarabine, cyclophosphamide, and rituximab regimen in young, fit patients with mutated IgVH may be difficult to improve on,” noted the investigators, led by Barbara Eichhorst, MD, a hematologic malignancy specialist at the University of Cologne (Germany).
Also, although triple-therapy results were impressive, some of the benefits “are neutralized by the need for dose reductions and early treatment discontinuation owing to adverse events,” they said.
For instance, triple therapy had the highest incidence of both grade 3 and 4 infections (21.2%) and atrial fibrillation (7.8%).
The editorialists noted that there has been “a flurry of interest” in trials combining ibrutinib and venetoclax – as was done in the triple-therapy arm – since both emerged as powerful tools against CLL in recent years. However, even with the study results, they said “the use of triplet therapy should be viewed as investigational.”
For one thing, rates of uMRD were not “dramatically different” between triple therapy and venetoclax-obinutuzumab, and longer follow-up is better gauge differences in PFS and long-term toxicities.
Also, ibrutinib is being eclipsed by the second-generation Bruton’s tyrosine kinase inhibitors acalabrutinib and zanubrutinib, because they have better safety profiles, and they are being assessed in CLL combination trials. For now, there are too many unknowns for routine use of triple therapy in fit CLL patients, they said.
The investigators and editorialists both noted that improved uMRD in the study translated into superior PFS, raising the possibility that uMRD might be a valid alternative endpoint to PFS in CLL trials.
With “median remissions in CLL lasting far in excess of 5 years, designing studies that take 8-10 years” to reach a PFS endpoint is simply too slow. Moving to an alternative endpoint such a uMRD would preserve “the momentum that has been generated” with recent advances, Dr. Woyach and Dr. Byrd said.
The work was funded by the companies that market venetoclax, ibrutinib, and obinutuzumab: AbbVie, Janssen, and Roche. Dr. Eichhorst is a consultant and/or speaker for the companies and also reported grants from them. Dr. Byrd is a consultant/adviser for Eilean Therapeutics, Kurome Therapeutics, Newave, and Orbimed. Dr. Woyach disclosed ties with AbbVie, AstraZeneca, Lilly, and other companies.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Number of cancer survivors with functional limitations doubled in 20 years
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
Vishal Patel, BS, a student at the Dell Medical School at The University of Texas at Austin, and colleagues identified 51,258 cancer survivors from the National Health Interview Survey, representing a weighted population of approximately 178.8 million from 1999 to 2018.
Most survivors were women (60.2%) and were at least 65 years old (55.4%). In 1999, 3.6 million weighted survivors reported functional limitation. In 2018, the number increased to 8.2 million, a 2.25-fold increase.
The number of survivors who reported no limitations also increased, but not by as much. That group grew 1.34-fold during the study period.
For context, “the 70% prevalence of functional limitation among survivors in 2018 is nearly twice that of the general population,” the authors wrote.
Patients surveyed on function
Functional limitation was defined as “self-reported difficulty performing any of 12 routine physical or social activities without assistance.” Examples of the activities included difficulty sitting for more than 2 hours, difficulty participating in social activities or difficulty pushing or pulling an object the size of a living room chair.
Over the 2 decades analyzed, the adjusted prevalence of functional limitation was highest among survivors of pancreatic cancer (80.3%) and lung cancer (76.5%). Prevalence was lowest for survivors of melanoma (62.2%), breast (61.8%) and prostate (59.5%) cancers.
Not just a result of living longer
Mr. Patel told this publication that one assumption people might make when they read these results is that people are just living longer with cancer and losing functional ability accordingly.
“But, in fact, we found that the youngest [– those less than 65 years–] actually contributed to this trend more than the oldest people, which means it’s not just [happening], because people are getting older,” he said.
Hispanic and Black individuals had disproportionately higher increases in functional limitation; percentage point increases over the 2 decades were 19.5 for Black people, 25.1 for Hispanic people and 12.5 for White people. There may be a couple of reasons for that, Mr. Patel noted.
Those who are Black or Hispanic tend to have less access to cancer survivorship care for reasons including insurance status and historic health care inequities, he noted.
“The other potential reason is that they have had less access to cancer care historically. And if, 20 years ago Black and Hispanic individuals didn’t have access to some chemotherapies, and now they do, maybe it’s the increased access to care that’s causing these functional limitations. Because chemotherapy can sometimes be very toxic. It may be sort of a catch-up toxicity,” he said.
Quality of life beyond survivorship
Mr. Patel said the results seem to call for building on improved survival rates by tracking and improving function.
“It’s good to celebrate that there are more survivors. But now that we can keep people alive longer, maybe we can shift gears to improving their quality of life,” he said.
The more-than-doubling of functional limitations over 2 decades “is a very sobering trend,” he noted, while pointing out that the functional limitations applied to 8 million people in the United States – people whose needs are not being met.
There’s no sign of the trend stopping, he continued. “We saw no downward trend, only an upward trend.”
Increasingly, including functionality as an endpoint in cancer trials, in addition to improvements in mortality, is one place to start, he added.
“Our findings suggest an urgent need for care teams to understand and address function, for researchers to evaluate function as a core outcome in trials, and for health systems and policy makers to reimagine survivorship care, recognizing the burden of cancer and its treatment on physical, psychosocial, and cognitive function,” the authors wrote in their paper. Limitations of the study include the potential for recall bias, lack of cancer staging or treatment information, and the subjective perception of function.
A coauthor reported personal fees from Astellas, AstraZeneca, AAA, Blue Earth, Janssen, Lantheus, Myovant, Myriad Genetics, Novartis, Telix, and Sanofi, as well as grants from Pfizer and Bayer during the conduct of the study. No other disclosures were reported.
FROM JAMA ONCOLOGY
Boys may carry the weight, or overweight, of adults’ infertility
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
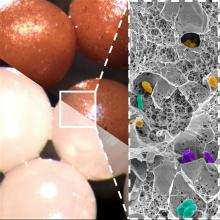
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
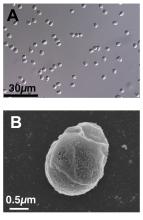
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
Overweight boy, infertile man?
When it comes to causes of infertility, history and science have generally focused on women. A lot of the research overlooks men, but some previous studies have suggested that male infertility contributes to about half of the cases of couple infertility. The reason for much of that male infertility, however, has been a mystery. Until now.
A group of Italian investigators looked at the declining trend in sperm counts over the past 40 years and the increase of childhood obesity. Is there a correlation? The researchers think so. Childhood obesity can be linked to multiple causes, but the researchers zeroed in on the effect that obesity has on metabolic rates and, therefore, testicular growth.
Collecting data on testicular volume, body mass index (BMI), and insulin resistance from 268 boys aged 2-18 years, the researchers discovered that those with normal weight and normal insulin levels had testicular volumes 1.5 times higher than their overweight counterparts and 1.5-2 times higher than those with hyperinsulinemia, building a case for obesity being a factor for infertility later in life.
Since low testicular volume is associated with lower sperm count and production as an adult, putting two and two together makes a compelling argument for childhood obesity being a major male infertility culprit. It also creates even more urgency for the health care industry and community decision makers to focus on childhood obesity.
It sure would be nice to be able to take one of the many risk factors for future human survival off the table. Maybe by taking something, like cake, off the table.
Fecal transplantation moves to the kitchen
Fecal microbiota transplantation is an effective way to treat Clostridioides difficile infection, but, in the end, it’s still a transplantation procedure involving a nasogastric or colorectal tube or rather large oral capsules with a demanding (30-40 capsules over 2 days) dosage. Please, Science, tell us there’s a better way.
Science, in the form of investigators at the University of Geneva and Lausanne University Hospital in Switzerland, has spoken, and there may be a better way. Presenting fecal beads: All the bacterial goodness of donor stool without the tubal insertions or massive quantities of giant capsules.
We know you’re scoffing out there, but it’s true. All you need is a little alginate, which is a “biocompatible polysaccharide isolated from brown algae” of the Phaeophyceae family. The donor feces is microencapsulated by mixing it with the alginate, dropping that mixture into water containing calcium chloride, turning it into a gel, and then freeze-drying the gel into small (just 2 mm), solid beads.
Sounds plausible enough, but what do you do with them? “These brownish beads can be easily dispersed in a liquid or food that is pleasant to eat. They also have no taste,” senior author Eric Allémann, PhD, said in a statement released by the University of Geneva.
Pleasant to eat? No taste? So which is it? If you really want to know, watch fecal beads week on the new season of “The Great British Baking Show,” when Paul and Prue judge poop baked into crumpets, crepes, and crostatas. Yum.
We’re on the low-oxygen diet
Nine out of ten doctors agree: Oxygen is more important to your continued well-being than food. After all, a human can go weeks without food, but just minutes without oxygen. However, ten out of ten doctors agree that the United States has an obesity problem. They all also agree that previous research has shown soldiers who train at high altitudes lose more weight than those training at lower altitudes.
So, on the one hand, we have a country full of overweight people, and on the other, we have low oxygen levels causing weight loss. The solution, then, is obvious: Stop breathing.
More specifically (and somewhat less facetiously), researchers from Louisiana have launched the Low Oxygen and Weight Status trial and are currently recruiting individuals with BMIs of 30-40 to, uh, suffocate themselves. No, no, it’s okay, it’s just when they’re sleeping.
Fine, straight face. Participants in the LOWS trial will undergo an 8-week period when they will consume a controlled weight-loss diet and spend their nights in a hypoxic sealed tent, where they will sleep in an environment with an oxygen level equivalent to 8,500 feet above sea level (roughly equivalent to Aspen, Colo.). They will be compared with people on the same diet who sleep in a normal, sea-level oxygen environment.
The study’s goal is to determine whether or not spending time in a low-oxygen environment will suppress appetite, increase energy expenditure, and improve weight loss and insulin sensitivity. Excessive weight loss in high-altitude environments isn’t a good thing for soldiers – they kind of need their muscles and body weight to do the whole soldiering thing – but it could be great for people struggling to lose those last few pounds. And it also may prove LOTME’s previous thesis: Air is not good.
CLL: Black patients die sooner than Whites
The findings, published in the American Journal of Hematology, hint that the racial disparity has shrunk over time, especially within the first few years of the targeted-therapy era. Still, “Black patients had a shorter median overall survival of 7 years compared to 9 years for White patients,” study coauthor Deborah Stephens, DO, of the University of Utah Huntsman Cancer Institute, said in an interview. “Clearly, more research is needed to tease out the biologic or economic barriers to achieving prolonged survival.”
As the researchers noted, CLL is far more common among White patients (5.1 cases per 100,000) than other races (Black patients: 3.2 cases per 100,000; Hispanic patients: 2.1 cases per 100,000; Asian American patients: 1.1 per 100,000). In total, non-White patients make up just 11%-13% of CLL cases in the United States.
According to Dr. Stephens, “little is known or published” about Black patients with CLL, “and it is still a mystery why fewer patients that are Black develop CLL and why this group would have shorter survival.”
Dr. Stephens and colleagues launched the new study – the largest of its kind to date – to understand disparities between White and Black patients over most of the past 20 years. The researchers especially wanted to analyze trends during the last decade, when targeted therapies revolutionized treatment of the disease.
The study authors analyzed data in the National Cancer Database for 97,804 patients diagnosed from 2004 to 2018 (90.7% White, 7.6% Black, 0.6% Asian, 1.1% other). Of patients who reported ethnicity (n = 93,555), 2.6% were Hispanic.
Black patients were more likely to have begun CLL therapy at diagnosis (35.9%) than were White patients (23.6%), a sign that Black patients had more advanced disease. Black patients also had shorter overall survival (7.0 years, 95% confidence interval [CI], 6.7–7.3 years) vs. White patients (9.1 years, 95% CI, 9.0–9.3 years, P < .001).
“This finding could be due to underlying biologic differences in the pathology of CLL, when comparing patients across racial groups,” Dr. Stephens said. “Additionally, there could be differences in access to care. Notably, there are fewer racial minorities enrolled in clinical trials, and perhaps we are not individualizing therapy for unique biologic factors seen in CLL affecting racial minorities.”
Other factors also could be at play. Black patients were more likely than were White patients to have one or more comorbidities (27.9% vs. 21.3%, P < .001), lack insurance (6.6% vs. 2.1%, P < .001) and live in lower-income neighborhoods (47.7% vs. 13.1%, P < .001).
What explains the gap in outcomes? In an interview, study lead author Victoria Vardell, MD, of the University of Utah, Salt Lake City, noted that researchers often attribute worse medical outcomes in Black patients to economic and social disparities.
“However, when we adjusted for a number of surrogate markers of health care access, including income, comorbidities, and location, among others, this disparity remained. That indicates that this may be a more complex problem in CLL in particular. Certainly, we cannot adjust for all the socioeconomic strain placed on Black Americans, including those with CLL, but there may be molecular features related to ancestry or environmental exposures that also play a role,” Dr. Vardell said.
She added that “the high cost and difficulty obtaining many novel therapies, particularly in the clinical trial setting, places significantly higher burdens on already disadvantaged populations.”
There is some good news in the new report. “Promisingly, our data suggest that the survival disparity between White and Black patients with CLL may be improving, particularly within the last 5 years, though longer follow-up is needed to confirm significance,” the researchers reported.
Alessandra Ferrajoli, MD, of M.D. Anderson Cancer Center, Houston, who has studied racial disparities in CLL, praised the study in an interview. As she noted, it examines an impressively large population.
The explanations for the disparities are still elusive, she said, although it seems clear there are multiple factors at play. “We don’t know if the disease has the same characteristics in African-Americans as in Whites,” Dr. Ferrajoli said. However, she noted, there’s “no indication that the response to treatment is different according to race.”
Moving forward, she said, the study findings “reinforce the fact that we need to pay attention to this population and be quite attentive to their characteristics.”
No study funding was reported. The authors and Dr. Ferrajoli have no disclosures.
The findings, published in the American Journal of Hematology, hint that the racial disparity has shrunk over time, especially within the first few years of the targeted-therapy era. Still, “Black patients had a shorter median overall survival of 7 years compared to 9 years for White patients,” study coauthor Deborah Stephens, DO, of the University of Utah Huntsman Cancer Institute, said in an interview. “Clearly, more research is needed to tease out the biologic or economic barriers to achieving prolonged survival.”
As the researchers noted, CLL is far more common among White patients (5.1 cases per 100,000) than other races (Black patients: 3.2 cases per 100,000; Hispanic patients: 2.1 cases per 100,000; Asian American patients: 1.1 per 100,000). In total, non-White patients make up just 11%-13% of CLL cases in the United States.
According to Dr. Stephens, “little is known or published” about Black patients with CLL, “and it is still a mystery why fewer patients that are Black develop CLL and why this group would have shorter survival.”
Dr. Stephens and colleagues launched the new study – the largest of its kind to date – to understand disparities between White and Black patients over most of the past 20 years. The researchers especially wanted to analyze trends during the last decade, when targeted therapies revolutionized treatment of the disease.
The study authors analyzed data in the National Cancer Database for 97,804 patients diagnosed from 2004 to 2018 (90.7% White, 7.6% Black, 0.6% Asian, 1.1% other). Of patients who reported ethnicity (n = 93,555), 2.6% were Hispanic.
Black patients were more likely to have begun CLL therapy at diagnosis (35.9%) than were White patients (23.6%), a sign that Black patients had more advanced disease. Black patients also had shorter overall survival (7.0 years, 95% confidence interval [CI], 6.7–7.3 years) vs. White patients (9.1 years, 95% CI, 9.0–9.3 years, P < .001).
“This finding could be due to underlying biologic differences in the pathology of CLL, when comparing patients across racial groups,” Dr. Stephens said. “Additionally, there could be differences in access to care. Notably, there are fewer racial minorities enrolled in clinical trials, and perhaps we are not individualizing therapy for unique biologic factors seen in CLL affecting racial minorities.”
Other factors also could be at play. Black patients were more likely than were White patients to have one or more comorbidities (27.9% vs. 21.3%, P < .001), lack insurance (6.6% vs. 2.1%, P < .001) and live in lower-income neighborhoods (47.7% vs. 13.1%, P < .001).
What explains the gap in outcomes? In an interview, study lead author Victoria Vardell, MD, of the University of Utah, Salt Lake City, noted that researchers often attribute worse medical outcomes in Black patients to economic and social disparities.
“However, when we adjusted for a number of surrogate markers of health care access, including income, comorbidities, and location, among others, this disparity remained. That indicates that this may be a more complex problem in CLL in particular. Certainly, we cannot adjust for all the socioeconomic strain placed on Black Americans, including those with CLL, but there may be molecular features related to ancestry or environmental exposures that also play a role,” Dr. Vardell said.
She added that “the high cost and difficulty obtaining many novel therapies, particularly in the clinical trial setting, places significantly higher burdens on already disadvantaged populations.”
There is some good news in the new report. “Promisingly, our data suggest that the survival disparity between White and Black patients with CLL may be improving, particularly within the last 5 years, though longer follow-up is needed to confirm significance,” the researchers reported.
Alessandra Ferrajoli, MD, of M.D. Anderson Cancer Center, Houston, who has studied racial disparities in CLL, praised the study in an interview. As she noted, it examines an impressively large population.
The explanations for the disparities are still elusive, she said, although it seems clear there are multiple factors at play. “We don’t know if the disease has the same characteristics in African-Americans as in Whites,” Dr. Ferrajoli said. However, she noted, there’s “no indication that the response to treatment is different according to race.”
Moving forward, she said, the study findings “reinforce the fact that we need to pay attention to this population and be quite attentive to their characteristics.”
No study funding was reported. The authors and Dr. Ferrajoli have no disclosures.
The findings, published in the American Journal of Hematology, hint that the racial disparity has shrunk over time, especially within the first few years of the targeted-therapy era. Still, “Black patients had a shorter median overall survival of 7 years compared to 9 years for White patients,” study coauthor Deborah Stephens, DO, of the University of Utah Huntsman Cancer Institute, said in an interview. “Clearly, more research is needed to tease out the biologic or economic barriers to achieving prolonged survival.”
As the researchers noted, CLL is far more common among White patients (5.1 cases per 100,000) than other races (Black patients: 3.2 cases per 100,000; Hispanic patients: 2.1 cases per 100,000; Asian American patients: 1.1 per 100,000). In total, non-White patients make up just 11%-13% of CLL cases in the United States.
According to Dr. Stephens, “little is known or published” about Black patients with CLL, “and it is still a mystery why fewer patients that are Black develop CLL and why this group would have shorter survival.”
Dr. Stephens and colleagues launched the new study – the largest of its kind to date – to understand disparities between White and Black patients over most of the past 20 years. The researchers especially wanted to analyze trends during the last decade, when targeted therapies revolutionized treatment of the disease.
The study authors analyzed data in the National Cancer Database for 97,804 patients diagnosed from 2004 to 2018 (90.7% White, 7.6% Black, 0.6% Asian, 1.1% other). Of patients who reported ethnicity (n = 93,555), 2.6% were Hispanic.
Black patients were more likely to have begun CLL therapy at diagnosis (35.9%) than were White patients (23.6%), a sign that Black patients had more advanced disease. Black patients also had shorter overall survival (7.0 years, 95% confidence interval [CI], 6.7–7.3 years) vs. White patients (9.1 years, 95% CI, 9.0–9.3 years, P < .001).
“This finding could be due to underlying biologic differences in the pathology of CLL, when comparing patients across racial groups,” Dr. Stephens said. “Additionally, there could be differences in access to care. Notably, there are fewer racial minorities enrolled in clinical trials, and perhaps we are not individualizing therapy for unique biologic factors seen in CLL affecting racial minorities.”
Other factors also could be at play. Black patients were more likely than were White patients to have one or more comorbidities (27.9% vs. 21.3%, P < .001), lack insurance (6.6% vs. 2.1%, P < .001) and live in lower-income neighborhoods (47.7% vs. 13.1%, P < .001).
What explains the gap in outcomes? In an interview, study lead author Victoria Vardell, MD, of the University of Utah, Salt Lake City, noted that researchers often attribute worse medical outcomes in Black patients to economic and social disparities.
“However, when we adjusted for a number of surrogate markers of health care access, including income, comorbidities, and location, among others, this disparity remained. That indicates that this may be a more complex problem in CLL in particular. Certainly, we cannot adjust for all the socioeconomic strain placed on Black Americans, including those with CLL, but there may be molecular features related to ancestry or environmental exposures that also play a role,” Dr. Vardell said.
She added that “the high cost and difficulty obtaining many novel therapies, particularly in the clinical trial setting, places significantly higher burdens on already disadvantaged populations.”
There is some good news in the new report. “Promisingly, our data suggest that the survival disparity between White and Black patients with CLL may be improving, particularly within the last 5 years, though longer follow-up is needed to confirm significance,” the researchers reported.
Alessandra Ferrajoli, MD, of M.D. Anderson Cancer Center, Houston, who has studied racial disparities in CLL, praised the study in an interview. As she noted, it examines an impressively large population.
The explanations for the disparities are still elusive, she said, although it seems clear there are multiple factors at play. “We don’t know if the disease has the same characteristics in African-Americans as in Whites,” Dr. Ferrajoli said. However, she noted, there’s “no indication that the response to treatment is different according to race.”
Moving forward, she said, the study findings “reinforce the fact that we need to pay attention to this population and be quite attentive to their characteristics.”
No study funding was reported. The authors and Dr. Ferrajoli have no disclosures.
FROM AMERICAN JOURNAL OF HEMATOLOGY
Phase 3 trial: Maribavir yields post-transplant benefits
Overall mortality in the 109 patients from these subcohorts from SOLSTICE was lower, compared with mortality reported for similar populations treated with conventional therapies used to treat relapsed or refractory (R/R) CMV, according to findings presented in April at the annual meeting of the European Society for Bone and Marrow Transplantation.
“These results, in addition to the superior efficacy in CMV clearance observed for maribavir in SOLSTICE provide supportive evidence of the potential for the long-term benefit of maribavir treatment for post-transplant CMV infection,” Ishan Hirji, of Takeda Development Center Americas, and colleagues reported during a poster session at the meeting.
A retrospective chart review of the 41 hematopoietic stem cell transplant (HSCT) patients and 68 solid organ transplant (SOT) patients randomized to receive maribavir showed an overall mortality rate of 15.6% at 52 weeks after initiation of treatment with the antiviral agent. Among the HSCT patients, 14 deaths occurred (34.1%), with 8 occurring during the study periods and 6 occurring during follow-up. Among the SOT patients, three deaths occurred (4.4%), all during follow-up chart review.
Causes of death included underlying disease relapse in four patients, infection other than CMV in six patients, and one case each of CMV-related factors, transplant-related factors, acute lymphoblastic leukemia, and septic shock. Causes of death in the SOT patients included one case each of CMV-related factors, anemia, and renal failure.
“No patients had new graft loss or retransplantation during the chart review period,” the investigators noted.
The findings are notable as CMV infection occurs in 30%-70% of HSCT recipients and 16%-56% of SOT recipients and can lead to complications, including transplant failure and death. Reported 1-year mortality rates following standard therapies for CMV range from 31% to 50%, they explained.
Patients in the SOLSTICE trial received 8 weeks of treatment and were followed for 12 additional weeks. CMV clearance at the end of treatment was 55.7% in the maribavir treatment arm versus 23.9% in a control group of patients treated with investigator choice of therapy. As reported by this news organization, the findings formed the basis for U.S. Food and Drug Administration approval of maribavir in November 2021.
The current analysis included a chart review period that started 1 day after the SOLSTICE trial period and continued for 32 additional weeks.
These long-term follow-up data confirm the benefits of maribavir for the treatment of post-transplant CMV, according to the investigators, and findings from a separate study reported at the ESBMT meeting underscore the importance of the durable benefits observed with maribavir treatment.
For that retrospective study, Maria Laura Fox, of Vall d’Hebron Institute of Oncology, Barcelona, and colleagues pooled de-identified data from 250 adult HSCT recipients with R/R CMV who were treated with agents other than maribavir at transplant centers in the United States or Europe. They aimed to “generate real-world evidence on the burden of CMV infection/disease in HSCT recipients who had refractory/resistant CMV or were intolerant to current treatments.”
Nearly 92% of patients received two or more therapies to treat CMV, and 92.2% discontinued treatment or had one or more therapy dose changes or discontinuation, and 42 patients failed to achieve clearance of the CMV index episode.
CMV recurred in 35.2% of patients, and graft failure occurred in 4% of patients, the investigators reported.
All-cause mortality was 56.0%, and mortality at 1 year after identification of R/R disease or treatment intolerance was 45.2%, they noted, adding that the study results “highlight the real-world complexities and high burden of CMV infection for HSCT recipients.”
“With available anti-CMV agents [excluding maribavir], a notable proportion of patients failed to achieve viremia clearance once developing RRI [resistant, refractory, or intolerant] CMV and/or experienced recurrence, and were at risk of adverse outcomes, including myelosuppression and mortality. There is a need for therapies that achieve and maintain CMV clearance with improved safety profiles,” they concluded.
Both studies were funded by Takeda Development Center Americas, the maker of Levtencity. Ms. Hirji is an employee of Takeda and reported stock ownership. Ms. Fox reported relationships with Sierra Oncology, GlaxoSmithKline, Bristol Myers Squibb, Novartis, and AbbVie.
Overall mortality in the 109 patients from these subcohorts from SOLSTICE was lower, compared with mortality reported for similar populations treated with conventional therapies used to treat relapsed or refractory (R/R) CMV, according to findings presented in April at the annual meeting of the European Society for Bone and Marrow Transplantation.
“These results, in addition to the superior efficacy in CMV clearance observed for maribavir in SOLSTICE provide supportive evidence of the potential for the long-term benefit of maribavir treatment for post-transplant CMV infection,” Ishan Hirji, of Takeda Development Center Americas, and colleagues reported during a poster session at the meeting.
A retrospective chart review of the 41 hematopoietic stem cell transplant (HSCT) patients and 68 solid organ transplant (SOT) patients randomized to receive maribavir showed an overall mortality rate of 15.6% at 52 weeks after initiation of treatment with the antiviral agent. Among the HSCT patients, 14 deaths occurred (34.1%), with 8 occurring during the study periods and 6 occurring during follow-up. Among the SOT patients, three deaths occurred (4.4%), all during follow-up chart review.
Causes of death included underlying disease relapse in four patients, infection other than CMV in six patients, and one case each of CMV-related factors, transplant-related factors, acute lymphoblastic leukemia, and septic shock. Causes of death in the SOT patients included one case each of CMV-related factors, anemia, and renal failure.
“No patients had new graft loss or retransplantation during the chart review period,” the investigators noted.
The findings are notable as CMV infection occurs in 30%-70% of HSCT recipients and 16%-56% of SOT recipients and can lead to complications, including transplant failure and death. Reported 1-year mortality rates following standard therapies for CMV range from 31% to 50%, they explained.
Patients in the SOLSTICE trial received 8 weeks of treatment and were followed for 12 additional weeks. CMV clearance at the end of treatment was 55.7% in the maribavir treatment arm versus 23.9% in a control group of patients treated with investigator choice of therapy. As reported by this news organization, the findings formed the basis for U.S. Food and Drug Administration approval of maribavir in November 2021.
The current analysis included a chart review period that started 1 day after the SOLSTICE trial period and continued for 32 additional weeks.
These long-term follow-up data confirm the benefits of maribavir for the treatment of post-transplant CMV, according to the investigators, and findings from a separate study reported at the ESBMT meeting underscore the importance of the durable benefits observed with maribavir treatment.
For that retrospective study, Maria Laura Fox, of Vall d’Hebron Institute of Oncology, Barcelona, and colleagues pooled de-identified data from 250 adult HSCT recipients with R/R CMV who were treated with agents other than maribavir at transplant centers in the United States or Europe. They aimed to “generate real-world evidence on the burden of CMV infection/disease in HSCT recipients who had refractory/resistant CMV or were intolerant to current treatments.”
Nearly 92% of patients received two or more therapies to treat CMV, and 92.2% discontinued treatment or had one or more therapy dose changes or discontinuation, and 42 patients failed to achieve clearance of the CMV index episode.
CMV recurred in 35.2% of patients, and graft failure occurred in 4% of patients, the investigators reported.
All-cause mortality was 56.0%, and mortality at 1 year after identification of R/R disease or treatment intolerance was 45.2%, they noted, adding that the study results “highlight the real-world complexities and high burden of CMV infection for HSCT recipients.”
“With available anti-CMV agents [excluding maribavir], a notable proportion of patients failed to achieve viremia clearance once developing RRI [resistant, refractory, or intolerant] CMV and/or experienced recurrence, and were at risk of adverse outcomes, including myelosuppression and mortality. There is a need for therapies that achieve and maintain CMV clearance with improved safety profiles,” they concluded.
Both studies were funded by Takeda Development Center Americas, the maker of Levtencity. Ms. Hirji is an employee of Takeda and reported stock ownership. Ms. Fox reported relationships with Sierra Oncology, GlaxoSmithKline, Bristol Myers Squibb, Novartis, and AbbVie.
Overall mortality in the 109 patients from these subcohorts from SOLSTICE was lower, compared with mortality reported for similar populations treated with conventional therapies used to treat relapsed or refractory (R/R) CMV, according to findings presented in April at the annual meeting of the European Society for Bone and Marrow Transplantation.
“These results, in addition to the superior efficacy in CMV clearance observed for maribavir in SOLSTICE provide supportive evidence of the potential for the long-term benefit of maribavir treatment for post-transplant CMV infection,” Ishan Hirji, of Takeda Development Center Americas, and colleagues reported during a poster session at the meeting.
A retrospective chart review of the 41 hematopoietic stem cell transplant (HSCT) patients and 68 solid organ transplant (SOT) patients randomized to receive maribavir showed an overall mortality rate of 15.6% at 52 weeks after initiation of treatment with the antiviral agent. Among the HSCT patients, 14 deaths occurred (34.1%), with 8 occurring during the study periods and 6 occurring during follow-up. Among the SOT patients, three deaths occurred (4.4%), all during follow-up chart review.
Causes of death included underlying disease relapse in four patients, infection other than CMV in six patients, and one case each of CMV-related factors, transplant-related factors, acute lymphoblastic leukemia, and septic shock. Causes of death in the SOT patients included one case each of CMV-related factors, anemia, and renal failure.
“No patients had new graft loss or retransplantation during the chart review period,” the investigators noted.
The findings are notable as CMV infection occurs in 30%-70% of HSCT recipients and 16%-56% of SOT recipients and can lead to complications, including transplant failure and death. Reported 1-year mortality rates following standard therapies for CMV range from 31% to 50%, they explained.
Patients in the SOLSTICE trial received 8 weeks of treatment and were followed for 12 additional weeks. CMV clearance at the end of treatment was 55.7% in the maribavir treatment arm versus 23.9% in a control group of patients treated with investigator choice of therapy. As reported by this news organization, the findings formed the basis for U.S. Food and Drug Administration approval of maribavir in November 2021.
The current analysis included a chart review period that started 1 day after the SOLSTICE trial period and continued for 32 additional weeks.
These long-term follow-up data confirm the benefits of maribavir for the treatment of post-transplant CMV, according to the investigators, and findings from a separate study reported at the ESBMT meeting underscore the importance of the durable benefits observed with maribavir treatment.
For that retrospective study, Maria Laura Fox, of Vall d’Hebron Institute of Oncology, Barcelona, and colleagues pooled de-identified data from 250 adult HSCT recipients with R/R CMV who were treated with agents other than maribavir at transplant centers in the United States or Europe. They aimed to “generate real-world evidence on the burden of CMV infection/disease in HSCT recipients who had refractory/resistant CMV or were intolerant to current treatments.”
Nearly 92% of patients received two or more therapies to treat CMV, and 92.2% discontinued treatment or had one or more therapy dose changes or discontinuation, and 42 patients failed to achieve clearance of the CMV index episode.
CMV recurred in 35.2% of patients, and graft failure occurred in 4% of patients, the investigators reported.
All-cause mortality was 56.0%, and mortality at 1 year after identification of R/R disease or treatment intolerance was 45.2%, they noted, adding that the study results “highlight the real-world complexities and high burden of CMV infection for HSCT recipients.”
“With available anti-CMV agents [excluding maribavir], a notable proportion of patients failed to achieve viremia clearance once developing RRI [resistant, refractory, or intolerant] CMV and/or experienced recurrence, and were at risk of adverse outcomes, including myelosuppression and mortality. There is a need for therapies that achieve and maintain CMV clearance with improved safety profiles,” they concluded.
Both studies were funded by Takeda Development Center Americas, the maker of Levtencity. Ms. Hirji is an employee of Takeda and reported stock ownership. Ms. Fox reported relationships with Sierra Oncology, GlaxoSmithKline, Bristol Myers Squibb, Novartis, and AbbVie.
FROM ESBMT 2023
“Terrific progress”: Adding blinatumomab for infant leukemia
.
Two-year disease-free and overall survival measures, as well as the percentage of children who had complete minimal residual disease (MRD) responses, were substantially higher among the 30 infants in the study than in historical controls treated with the same chemotherapy backbone in an earlier trial, Interfant-06.
“These outcome data are very promising, given the poor survival and lack of improvements in outcomes among infants with KMT2A-rearranged ALL in recent decades,” said the investigators, led by Inge M. van der Sluis, MD, PhD, a hematologist-oncologist at Princess Maxima Center for Pediatric Oncology in Utrecht, the Netherlands.
“The low incidence of relapse after treatment with blinatumomab is remarkable, given that in historical controls relapses occur frequently and early during therapy,” the investigators stated. Although the “follow-up time was relatively short” in the study, “it included the period historically defined” as being at high risk of relapse, they said.
The team suggested that future research should assess whether infants benefit from multiple courses of blinatumomab, rather than the one course used in the study, and whether blinatumomab plus chemotherapy can replace stem cell transplants for high-risk infants.
Pediatric community responds
There was excitement on Twitter about the results; a number of pediatric blood cancer specialists were impressed and posted the study on that platform. Comments included, “Wow! After years of stagnation, a huge step forward for infant leukemia” and “great news for infant lymphoblastic leukemia.”
Akshay Sharma, MBBS, a pediatric bone marrow transplant and cellular therapy specialist at St. Jude Children’s Research Hospital, Memphis, also posted. He said in an interview that the findings are “very exciting.”
The “outcomes of children diagnosed with leukemia in their infancy, particularly if they have a KMT2A rearrangement, have been dismal. This is terrific progress and a testament to the role that immunotherapy and novel agents will be playing in treatment of several malignant diseases in the decade to come,” he said.
Another poster, Pratik “Tik” Patel, MD, a pediatric hematology/oncology fellow at Emory University in Atlanta, told this news organization that the study “is welcome news to pediatric oncologists” and highlights “the success in incorporating newer immune-based therapeutics upfront in treatment rather than in relapsed/refractory settings.”
The National Cancer Institute–funded Children’s Oncology Group is thinking the same way. The group is launching a large, randomized trial to test if adding blinatumomab to chemotherapy upfront for B-cell acute lymphoblastic leukemia and lymphoblastic lymphoma improves outcomes in children and young adults aged 1-31 years. Results are due after 2029.
Study details
Blinatumomab is an expensive “T-cell engager” that helps cytotoxic CD3+T cells link to and destroy leukemic CD19+ B cells. Past studies have shown that it’s safe and works in older children and adults with B-lineage ALL after intensive chemotherapy, but until now the approach hadn’t been tested in infants, the investigators said.
The 30 subjects in the study were under a year old and newly diagnosed with KMT2A-rearranged ALL. They were treated with the Interfant-06 chemotherapy regimen – cytosine arabinoside and other agents – plus one postinduction course of blinatumomab at 15 micrograms/m2 per day as a 4-week continuous infusion. Eight of nine high-risk patients had allogeneic hematopoietic stem cell transplants.
Overall survival was 93.3% over a median follow up of 26.3 months, substantially higher than the 65.8% in the Interfant-06 trial. Two-year disease-free survival was 81.6% versus 49.4% in Interfant-06.
Sixteen patients (53%) were MRD negative after blinatumomab infusion and 12 (40%) had low levels of MRD. All of the children who continued chemotherapy went on to become MRD negative.
There were no permanent blinatumomab discontinuations and no treatment related deaths. Serious toxic effects were consistent with those in older patients and included four fevers, four infections, and one case each of hypertension and vomiting.
There were no cases of severe cytokine release syndrome (CRS) because of the low tumor burden of the subjects. Likewise, there were no obvious neurologic adverse events – like CRS, a particular concern with blinatumomab – but “we cannot rule out underreporting of mild neurologic symptoms that may have been unrecognized in infants,” the investigators said.
Patients who relapsed in the study had CNS involvement at relapse. “This underscores the need for adequate intrathecal chemotherapy during the blinatumomab infusion, because the efficacy of blinatumomab for the treatment of CNS leukemia may be limited,” they said.
The work was supported by Amgen, the maker of blinatumomab, as well as the Princess Maxima Center Foundation, the Danish Childhood Cancer Foundation, and others. Dr. Sluis is a consultant and researcher for Amgen. Five other authors were also consultants/advisers/researchers for the company. Dr. Sharma and Dr. Patel didn’t have any relevant disclosures.
.
Two-year disease-free and overall survival measures, as well as the percentage of children who had complete minimal residual disease (MRD) responses, were substantially higher among the 30 infants in the study than in historical controls treated with the same chemotherapy backbone in an earlier trial, Interfant-06.
“These outcome data are very promising, given the poor survival and lack of improvements in outcomes among infants with KMT2A-rearranged ALL in recent decades,” said the investigators, led by Inge M. van der Sluis, MD, PhD, a hematologist-oncologist at Princess Maxima Center for Pediatric Oncology in Utrecht, the Netherlands.
“The low incidence of relapse after treatment with blinatumomab is remarkable, given that in historical controls relapses occur frequently and early during therapy,” the investigators stated. Although the “follow-up time was relatively short” in the study, “it included the period historically defined” as being at high risk of relapse, they said.
The team suggested that future research should assess whether infants benefit from multiple courses of blinatumomab, rather than the one course used in the study, and whether blinatumomab plus chemotherapy can replace stem cell transplants for high-risk infants.
Pediatric community responds
There was excitement on Twitter about the results; a number of pediatric blood cancer specialists were impressed and posted the study on that platform. Comments included, “Wow! After years of stagnation, a huge step forward for infant leukemia” and “great news for infant lymphoblastic leukemia.”
Akshay Sharma, MBBS, a pediatric bone marrow transplant and cellular therapy specialist at St. Jude Children’s Research Hospital, Memphis, also posted. He said in an interview that the findings are “very exciting.”
The “outcomes of children diagnosed with leukemia in their infancy, particularly if they have a KMT2A rearrangement, have been dismal. This is terrific progress and a testament to the role that immunotherapy and novel agents will be playing in treatment of several malignant diseases in the decade to come,” he said.
Another poster, Pratik “Tik” Patel, MD, a pediatric hematology/oncology fellow at Emory University in Atlanta, told this news organization that the study “is welcome news to pediatric oncologists” and highlights “the success in incorporating newer immune-based therapeutics upfront in treatment rather than in relapsed/refractory settings.”
The National Cancer Institute–funded Children’s Oncology Group is thinking the same way. The group is launching a large, randomized trial to test if adding blinatumomab to chemotherapy upfront for B-cell acute lymphoblastic leukemia and lymphoblastic lymphoma improves outcomes in children and young adults aged 1-31 years. Results are due after 2029.
Study details
Blinatumomab is an expensive “T-cell engager” that helps cytotoxic CD3+T cells link to and destroy leukemic CD19+ B cells. Past studies have shown that it’s safe and works in older children and adults with B-lineage ALL after intensive chemotherapy, but until now the approach hadn’t been tested in infants, the investigators said.
The 30 subjects in the study were under a year old and newly diagnosed with KMT2A-rearranged ALL. They were treated with the Interfant-06 chemotherapy regimen – cytosine arabinoside and other agents – plus one postinduction course of blinatumomab at 15 micrograms/m2 per day as a 4-week continuous infusion. Eight of nine high-risk patients had allogeneic hematopoietic stem cell transplants.
Overall survival was 93.3% over a median follow up of 26.3 months, substantially higher than the 65.8% in the Interfant-06 trial. Two-year disease-free survival was 81.6% versus 49.4% in Interfant-06.
Sixteen patients (53%) were MRD negative after blinatumomab infusion and 12 (40%) had low levels of MRD. All of the children who continued chemotherapy went on to become MRD negative.
There were no permanent blinatumomab discontinuations and no treatment related deaths. Serious toxic effects were consistent with those in older patients and included four fevers, four infections, and one case each of hypertension and vomiting.
There were no cases of severe cytokine release syndrome (CRS) because of the low tumor burden of the subjects. Likewise, there were no obvious neurologic adverse events – like CRS, a particular concern with blinatumomab – but “we cannot rule out underreporting of mild neurologic symptoms that may have been unrecognized in infants,” the investigators said.
Patients who relapsed in the study had CNS involvement at relapse. “This underscores the need for adequate intrathecal chemotherapy during the blinatumomab infusion, because the efficacy of blinatumomab for the treatment of CNS leukemia may be limited,” they said.
The work was supported by Amgen, the maker of blinatumomab, as well as the Princess Maxima Center Foundation, the Danish Childhood Cancer Foundation, and others. Dr. Sluis is a consultant and researcher for Amgen. Five other authors were also consultants/advisers/researchers for the company. Dr. Sharma and Dr. Patel didn’t have any relevant disclosures.
.
Two-year disease-free and overall survival measures, as well as the percentage of children who had complete minimal residual disease (MRD) responses, were substantially higher among the 30 infants in the study than in historical controls treated with the same chemotherapy backbone in an earlier trial, Interfant-06.
“These outcome data are very promising, given the poor survival and lack of improvements in outcomes among infants with KMT2A-rearranged ALL in recent decades,” said the investigators, led by Inge M. van der Sluis, MD, PhD, a hematologist-oncologist at Princess Maxima Center for Pediatric Oncology in Utrecht, the Netherlands.
“The low incidence of relapse after treatment with blinatumomab is remarkable, given that in historical controls relapses occur frequently and early during therapy,” the investigators stated. Although the “follow-up time was relatively short” in the study, “it included the period historically defined” as being at high risk of relapse, they said.
The team suggested that future research should assess whether infants benefit from multiple courses of blinatumomab, rather than the one course used in the study, and whether blinatumomab plus chemotherapy can replace stem cell transplants for high-risk infants.
Pediatric community responds
There was excitement on Twitter about the results; a number of pediatric blood cancer specialists were impressed and posted the study on that platform. Comments included, “Wow! After years of stagnation, a huge step forward for infant leukemia” and “great news for infant lymphoblastic leukemia.”
Akshay Sharma, MBBS, a pediatric bone marrow transplant and cellular therapy specialist at St. Jude Children’s Research Hospital, Memphis, also posted. He said in an interview that the findings are “very exciting.”
The “outcomes of children diagnosed with leukemia in their infancy, particularly if they have a KMT2A rearrangement, have been dismal. This is terrific progress and a testament to the role that immunotherapy and novel agents will be playing in treatment of several malignant diseases in the decade to come,” he said.
Another poster, Pratik “Tik” Patel, MD, a pediatric hematology/oncology fellow at Emory University in Atlanta, told this news organization that the study “is welcome news to pediatric oncologists” and highlights “the success in incorporating newer immune-based therapeutics upfront in treatment rather than in relapsed/refractory settings.”
The National Cancer Institute–funded Children’s Oncology Group is thinking the same way. The group is launching a large, randomized trial to test if adding blinatumomab to chemotherapy upfront for B-cell acute lymphoblastic leukemia and lymphoblastic lymphoma improves outcomes in children and young adults aged 1-31 years. Results are due after 2029.
Study details
Blinatumomab is an expensive “T-cell engager” that helps cytotoxic CD3+T cells link to and destroy leukemic CD19+ B cells. Past studies have shown that it’s safe and works in older children and adults with B-lineage ALL after intensive chemotherapy, but until now the approach hadn’t been tested in infants, the investigators said.
The 30 subjects in the study were under a year old and newly diagnosed with KMT2A-rearranged ALL. They were treated with the Interfant-06 chemotherapy regimen – cytosine arabinoside and other agents – plus one postinduction course of blinatumomab at 15 micrograms/m2 per day as a 4-week continuous infusion. Eight of nine high-risk patients had allogeneic hematopoietic stem cell transplants.
Overall survival was 93.3% over a median follow up of 26.3 months, substantially higher than the 65.8% in the Interfant-06 trial. Two-year disease-free survival was 81.6% versus 49.4% in Interfant-06.
Sixteen patients (53%) were MRD negative after blinatumomab infusion and 12 (40%) had low levels of MRD. All of the children who continued chemotherapy went on to become MRD negative.
There were no permanent blinatumomab discontinuations and no treatment related deaths. Serious toxic effects were consistent with those in older patients and included four fevers, four infections, and one case each of hypertension and vomiting.
There were no cases of severe cytokine release syndrome (CRS) because of the low tumor burden of the subjects. Likewise, there were no obvious neurologic adverse events – like CRS, a particular concern with blinatumomab – but “we cannot rule out underreporting of mild neurologic symptoms that may have been unrecognized in infants,” the investigators said.
Patients who relapsed in the study had CNS involvement at relapse. “This underscores the need for adequate intrathecal chemotherapy during the blinatumomab infusion, because the efficacy of blinatumomab for the treatment of CNS leukemia may be limited,” they said.
The work was supported by Amgen, the maker of blinatumomab, as well as the Princess Maxima Center Foundation, the Danish Childhood Cancer Foundation, and others. Dr. Sluis is a consultant and researcher for Amgen. Five other authors were also consultants/advisers/researchers for the company. Dr. Sharma and Dr. Patel didn’t have any relevant disclosures.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Medical-level empathy? Yup, ChatGPT can fake that
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Caution: Robotic uprisings in the rearview mirror are closer than they appear
ChatGPT. If you’ve been even in the proximity of the Internet lately, you may have heard of it. It’s quite an incredible piece of technology, an artificial intelligence that really could up-end a lot of industries. And lest doctors believe they’re safe from robotic replacement, consider this: ChatGPT took a test commonly used as a study resource by ophthalmologists and scored a 46%. Obviously, that’s not a passing grade. Job safe, right?
A month later, the researchers tried again. This time, ChatGPT got a 58%. Still not passing, and ChatGPT did especially poorly on ophthalmology specialty questions (it got 80% of general medicine questions right), but still, the jump in quality after just a month is ... concerning. It’s not like an AI will forget things. That score can only go up, and it’ll go up faster than you think.
“Sure, the robot is smart,” the doctors out there are thinking, “but how can an AI compete with human compassion, understanding, and bedside manner?”
And they’d be right. When it comes to bedside manner, there’s no competition between man and bot. ChatGPT is already winning.
In another study, researchers sampled nearly 200 questions from the subreddit r/AskDocs, which received verified physician responses. The researchers fed ChatGPT the questions – without the doctor’s answer – and a panel of health care professionals evaluated both the human doctor and ChatGPT in terms of quality and empathy.
Perhaps not surprisingly, the robot did better when it came to quality, providing a high-quality response 79% of the time, versus 22% for the human. But empathy? It was a bloodbath. ChatGPT provided an empathetic or very empathetic response 45% of the time, while humans could only do so 4.6% of the time. So much for bedside manner.
The researchers were suspiciously quick to note that ChatGPT isn’t a legitimate replacement for physicians, but could represent a tool to better provide care for patients. But let’s be honest, given ChatGPT’s quick advancement, how long before some intrepid stockholder says: “Hey, instead of paying doctors, why don’t we just use the free robot instead?” We give it a week. Or 11 minutes.
This week, on ‘As the sperm turns’
We’ve got a lot of spermy ground to cover, so let’s get right to it, starting with the small and working our way up.
We’re all pretty familiar with the basic structure of a sperm cell, yes? Bulbous head that contains all the important genetic information and a tail-like flagellum to propel it to its ultimate destination. Not much to work with there, you’d think, but what if Mother Nature, who clearly has a robust sense of humor, had something else in mind?
We present exhibit A, Paramormyorps kingsleyae, also known as the electric elephantfish, which happens to be the only known vertebrate species with tailless sperm. Sounds crazy to us, too, but Jason Gallant, PhD, of
Michigan State University, Lansing, has a theory: “A general notion in biology is that sperm are cheap, and eggs are expensive – but these fish may be telling us that sperm are more expensive than we might think. They could be saving energy by cutting back on sperm tails.”
He and his team think that finding the gene that turns off development of the flagellum in the elephant fish could benefit humans, specifically those with a genetic disorder called primary ciliary dyskinesia, whose lack of normally functioning cilia and flagella leads to chronic respiratory infection, abnormally positioned organs, fluid on the brain, and infertility.
And that – with “that” being infertility – brings us to exhibit B, a 41-year-old Dutch man named Jonathan Meijer who clearly has too much time on his hands.
A court in the Netherlands recently ordered him, and not for the first time, to stop donating sperm to fertility clinics after it was discovered that he had fathered between 500 and 600 children around the world. He had been banned from donating to Dutch clinics in 2017, at which point he had already fathered 100 children, but managed a workaround by donating internationally and online, sometimes using another name.
The judge ordered Mr. Meijer to contact all of the clinics abroad and ask them to destroy any of his sperm they still had in stock and threatened to fine him over $100,000 for each future violation.
Okay, so here’s the thing. We have been, um, let’s call it ... warned, about the evils of tastelessness in journalism, so we’re going to do what Mr. Meijer should have done and abstain. And we can last for longer than 11 minutes.
The realm of lost luggage and lost sleep
It may be convenient to live near an airport if you’re a frequent flyer, but it really doesn’t help your sleep numbers.
The first look at how such a common sound affects sleep duration showed that people exposed to even 45 decibels of airplane noise were less likely to get the 7-9 hours of sleep needed for healthy functioning, investigators said in Environmental Health Perspectives.
How loud is 45 dB exactly? A normal conversation is about 50 dB, while a whisper is 30 dB, to give you an idea. Airplane noise at 45 dB? You might not even notice it amongst the other noises in daily life.
The researchers looked at data from about 35,000 participants in the Nurses’ Health Study who live around 90 major U.S. airports. They examined plane noise every 5 years between 1995 and 2005, focusing on estimates of nighttime and daytime levels. Short sleep was most common among the nurses who lived on the West Coast, near major cargo airports or large bodies of water, and also among those who reported no hearing loss.
The investigators noted, however, that there was no consistent association between airplane noise and quality of sleep and stopped short of making any policy recommendations. Still, sleep is a very important, yet slept-on (pun intended) factor for our overall health, so it’s good to know if anything has the potential to cause disruption.
Experts debate reducing ASCT for multiple myeloma
NEW YORK –
Hematologist-oncologists whose top priority is ensuring that patients have the best chance of progression-free survival (PFS) will continue to choose ASCT as a best practice, argued Amrita Krishnan, MD, hematologist at the Judy and Bernard Briskin Center for Multiple Myeloma Research, City of Hope Comprehensive Cancer Center, Duarte, Calif.
A differing perspective was presented by C. Ola Landgren, MD, PhD, hematologist at the Sylvester Comprehensive Cancer Center at the University of Miami. Dr. Landgren cited evidence that, for newly diagnosed MM patients treated successfully with modern combination therapies, ASCT is not a mandatory treatment step before starting maintenance therapy.
Making a case for ASCT as the SoC, Dr. Krishnan noted, “based on the DETERMINATION trial [DT], there is far superior rate of PFS with patients who get ASCT up front, compared patients who got only conventional chemotherapy with lenalidomide, bortezomib, and dexamethasone [RVd]. PFS is the endpoint we look for in our treatment regimens.
“If you don’t use ASCT up front, you may lose the opportunity at later relapse. This is not to say that transplant is the only tool at our disposal. It is just an indispensable one. The GRIFFIN trial [GT] has shown us that robust combinations of drugs [both RVd and dexamethasone +RVd] can improve patient outcomes both before and after ASCT,” Dr. Krishnan concluded.
In his presentation, Dr. Landgren stated that, in the DT, while PFS is prolonged by the addition of ASCT to RVd, adding ASCT did not significantly increase overall survival (OS) rates. He added that treatment-related AEs of grade 3+ occurred in only 78.2% of patients on RVd versus 94.2% of RVd + ASCT patients.
“ASCT should not be the SoC frontline treatment in MM because it does not prolong OS. The IFM trial and the DT both show that there is no difference in OS between drug combination therapy followed by transplant and maintenance versus combination therapy alone, followed by transplant and maintenance. Furthermore, patients who get ASCT have higher risk of developing secondary malignancies, worse quality of life, and higher long-term morbidity with other conditions,” Dr. Landgren said.
He cited the MAIA trial administered daratumumab and lenalidomide plus dexamethasone (DRd) to patients who were too old or too frail to qualify for ASCT. Over half of patients in the DRd arm of MAIA had an estimated progression-free survival rate at 60 months.
“Furthermore, GT and the MANHATTAN clinical trials showed that we can safely add CD38-targeted monoclonal antibodies to standard combination therapies [lenalidomide, bortezomib, and dexamethasone (KRd)], resulting in higher rates of minimal-residual-disease (MRD) negativity. That means modern four-drug combination therapies [DR-RVd and DR-KRd] will allow more [and more newly diagnosed] MM patients to achieve MRD negativity in the absence of ASCT,” Dr. Landgren concluded.
Asked to comment on the two viewpoints, Joshua Richter, MD, director of myeloma treatment at the Blavatnik Family Center at Chelsea Mount Sinai, New York, said: “With some patients, we can get similar outcomes, whether or not we do a transplant. Doctors need to be better at choosing who really needs ASCT. Older people with standard-risk disease or people who achieve MRD-negative status after pharmacological treatment might not need to receive a transplant as much as those who have bulk disease or high-risk cytogenetics.
“Although ASCT might not be the best frontline option for everyone, collecting cells from most patients and storing them has many advantages. It allows us to do have the option of ASCT in later lines of therapy. In some patients with low blood counts, we can use stored cells to reboot their marrow and make them eligible for trials of promising new drugs,” Dr. Richter said.
Dr. Krishnan disclosed relationships with Takeda, Amgen, GlaxoSmithKline, Bristol-Myers Squibb, Sanofi, Pfizer, Adaptive, Regeneron, Janssen, AstraZeneca, Artiva, and Sutro. Dr. Landgren reported ties with Amgen, BMS, Celgene, Janssen, Takedam Glenmark, Juno, Pfizer, Merck, and others. Dr. Richter disclosed relationships with Janssen, BMS, and Takeda.
NEW YORK –
Hematologist-oncologists whose top priority is ensuring that patients have the best chance of progression-free survival (PFS) will continue to choose ASCT as a best practice, argued Amrita Krishnan, MD, hematologist at the Judy and Bernard Briskin Center for Multiple Myeloma Research, City of Hope Comprehensive Cancer Center, Duarte, Calif.
A differing perspective was presented by C. Ola Landgren, MD, PhD, hematologist at the Sylvester Comprehensive Cancer Center at the University of Miami. Dr. Landgren cited evidence that, for newly diagnosed MM patients treated successfully with modern combination therapies, ASCT is not a mandatory treatment step before starting maintenance therapy.
Making a case for ASCT as the SoC, Dr. Krishnan noted, “based on the DETERMINATION trial [DT], there is far superior rate of PFS with patients who get ASCT up front, compared patients who got only conventional chemotherapy with lenalidomide, bortezomib, and dexamethasone [RVd]. PFS is the endpoint we look for in our treatment regimens.
“If you don’t use ASCT up front, you may lose the opportunity at later relapse. This is not to say that transplant is the only tool at our disposal. It is just an indispensable one. The GRIFFIN trial [GT] has shown us that robust combinations of drugs [both RVd and dexamethasone +RVd] can improve patient outcomes both before and after ASCT,” Dr. Krishnan concluded.
In his presentation, Dr. Landgren stated that, in the DT, while PFS is prolonged by the addition of ASCT to RVd, adding ASCT did not significantly increase overall survival (OS) rates. He added that treatment-related AEs of grade 3+ occurred in only 78.2% of patients on RVd versus 94.2% of RVd + ASCT patients.
“ASCT should not be the SoC frontline treatment in MM because it does not prolong OS. The IFM trial and the DT both show that there is no difference in OS between drug combination therapy followed by transplant and maintenance versus combination therapy alone, followed by transplant and maintenance. Furthermore, patients who get ASCT have higher risk of developing secondary malignancies, worse quality of life, and higher long-term morbidity with other conditions,” Dr. Landgren said.
He cited the MAIA trial administered daratumumab and lenalidomide plus dexamethasone (DRd) to patients who were too old or too frail to qualify for ASCT. Over half of patients in the DRd arm of MAIA had an estimated progression-free survival rate at 60 months.
“Furthermore, GT and the MANHATTAN clinical trials showed that we can safely add CD38-targeted monoclonal antibodies to standard combination therapies [lenalidomide, bortezomib, and dexamethasone (KRd)], resulting in higher rates of minimal-residual-disease (MRD) negativity. That means modern four-drug combination therapies [DR-RVd and DR-KRd] will allow more [and more newly diagnosed] MM patients to achieve MRD negativity in the absence of ASCT,” Dr. Landgren concluded.
Asked to comment on the two viewpoints, Joshua Richter, MD, director of myeloma treatment at the Blavatnik Family Center at Chelsea Mount Sinai, New York, said: “With some patients, we can get similar outcomes, whether or not we do a transplant. Doctors need to be better at choosing who really needs ASCT. Older people with standard-risk disease or people who achieve MRD-negative status after pharmacological treatment might not need to receive a transplant as much as those who have bulk disease or high-risk cytogenetics.
“Although ASCT might not be the best frontline option for everyone, collecting cells from most patients and storing them has many advantages. It allows us to do have the option of ASCT in later lines of therapy. In some patients with low blood counts, we can use stored cells to reboot their marrow and make them eligible for trials of promising new drugs,” Dr. Richter said.
Dr. Krishnan disclosed relationships with Takeda, Amgen, GlaxoSmithKline, Bristol-Myers Squibb, Sanofi, Pfizer, Adaptive, Regeneron, Janssen, AstraZeneca, Artiva, and Sutro. Dr. Landgren reported ties with Amgen, BMS, Celgene, Janssen, Takedam Glenmark, Juno, Pfizer, Merck, and others. Dr. Richter disclosed relationships with Janssen, BMS, and Takeda.
NEW YORK –
Hematologist-oncologists whose top priority is ensuring that patients have the best chance of progression-free survival (PFS) will continue to choose ASCT as a best practice, argued Amrita Krishnan, MD, hematologist at the Judy and Bernard Briskin Center for Multiple Myeloma Research, City of Hope Comprehensive Cancer Center, Duarte, Calif.
A differing perspective was presented by C. Ola Landgren, MD, PhD, hematologist at the Sylvester Comprehensive Cancer Center at the University of Miami. Dr. Landgren cited evidence that, for newly diagnosed MM patients treated successfully with modern combination therapies, ASCT is not a mandatory treatment step before starting maintenance therapy.
Making a case for ASCT as the SoC, Dr. Krishnan noted, “based on the DETERMINATION trial [DT], there is far superior rate of PFS with patients who get ASCT up front, compared patients who got only conventional chemotherapy with lenalidomide, bortezomib, and dexamethasone [RVd]. PFS is the endpoint we look for in our treatment regimens.
“If you don’t use ASCT up front, you may lose the opportunity at later relapse. This is not to say that transplant is the only tool at our disposal. It is just an indispensable one. The GRIFFIN trial [GT] has shown us that robust combinations of drugs [both RVd and dexamethasone +RVd] can improve patient outcomes both before and after ASCT,” Dr. Krishnan concluded.
In his presentation, Dr. Landgren stated that, in the DT, while PFS is prolonged by the addition of ASCT to RVd, adding ASCT did not significantly increase overall survival (OS) rates. He added that treatment-related AEs of grade 3+ occurred in only 78.2% of patients on RVd versus 94.2% of RVd + ASCT patients.
“ASCT should not be the SoC frontline treatment in MM because it does not prolong OS. The IFM trial and the DT both show that there is no difference in OS between drug combination therapy followed by transplant and maintenance versus combination therapy alone, followed by transplant and maintenance. Furthermore, patients who get ASCT have higher risk of developing secondary malignancies, worse quality of life, and higher long-term morbidity with other conditions,” Dr. Landgren said.
He cited the MAIA trial administered daratumumab and lenalidomide plus dexamethasone (DRd) to patients who were too old or too frail to qualify for ASCT. Over half of patients in the DRd arm of MAIA had an estimated progression-free survival rate at 60 months.
“Furthermore, GT and the MANHATTAN clinical trials showed that we can safely add CD38-targeted monoclonal antibodies to standard combination therapies [lenalidomide, bortezomib, and dexamethasone (KRd)], resulting in higher rates of minimal-residual-disease (MRD) negativity. That means modern four-drug combination therapies [DR-RVd and DR-KRd] will allow more [and more newly diagnosed] MM patients to achieve MRD negativity in the absence of ASCT,” Dr. Landgren concluded.
Asked to comment on the two viewpoints, Joshua Richter, MD, director of myeloma treatment at the Blavatnik Family Center at Chelsea Mount Sinai, New York, said: “With some patients, we can get similar outcomes, whether or not we do a transplant. Doctors need to be better at choosing who really needs ASCT. Older people with standard-risk disease or people who achieve MRD-negative status after pharmacological treatment might not need to receive a transplant as much as those who have bulk disease or high-risk cytogenetics.
“Although ASCT might not be the best frontline option for everyone, collecting cells from most patients and storing them has many advantages. It allows us to do have the option of ASCT in later lines of therapy. In some patients with low blood counts, we can use stored cells to reboot their marrow and make them eligible for trials of promising new drugs,” Dr. Richter said.
Dr. Krishnan disclosed relationships with Takeda, Amgen, GlaxoSmithKline, Bristol-Myers Squibb, Sanofi, Pfizer, Adaptive, Regeneron, Janssen, AstraZeneca, Artiva, and Sutro. Dr. Landgren reported ties with Amgen, BMS, Celgene, Janssen, Takedam Glenmark, Juno, Pfizer, Merck, and others. Dr. Richter disclosed relationships with Janssen, BMS, and Takeda.
AT 2023 GREAT DEBATES AND UPDATES HEMATOLOGIC MALIGNANCIES CONFERENCE