User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
What We Know About Salmon Sperm in Dermatology
It may not have an aesthetic-sounding appeal to most people, but salmon sperm is indeed one of the novel ingredients featured in products for human skin. These products also reportedly enhance and promote skin regeneration.1 This column will focus on the innovative approach to skin care involving purified polynucleotides derived from salmon sperm.
The Properties and Activities of PDRNs, PNs
PDRNs contain DNA fragments primarily derived from Pacific or chum salmon (Oncorhynchus keta), and salmon trout (Oncorhynchus mykiss) sperm cells.2 Through preclinical and clinical trials, PDRN has demonstrated a wide range of salutary functions, including antiallodynic, antiapoptotic, anti-inflammatory, antimelanogenetic, antiosteonecrotic, antiosteoporotic, antiulcerative, bone-regenerative, tissue damage–preventive, and wound-healing activities through adenosine A2A receptor and salvage pathways activation. Indeed, PDRNs have been shown in vitro to spur the proliferation of preadipocytes and, in vivo, to be effective in treating wounds and ulcers.3,4 In particular, atrophic, hypertrophic, surgical, and various acne scars have been treated with such injections.2,5,6 PDRN is thought to affect cutaneous health more directly by facilitating angiogenesis, cellular functions, especially fibroblast stimulation, collagen production, soft-tissue regeneration, and skin revitalization. Further, it has been used successfully to treat hyperpigmentation.7
PNs, derived from the same fish species as PDRNs, have been used effectively to ameliorate skin elasticity, hydration, pore size, thickness, wrinkles, as well as pigmentation and, specifically, in treating periorbital rhytides and postsurgical scars.5,6,8 Beyond skin rejuvenation, PNs have been recognized for effectiveness in treating stretch marks and achieving vulvovaginal revitalization; guidelines for its use have been established and implemented in recent years.6,9,10 In South Korea, PNs have become a popular treatment for facial erythema even though preclinical and clinical data are sparse.11 Nevertheless, the use of these novel substances is thought to foster tissue regeneration and a more natural rejuvenation than achieved through more traditional fillers.6
Skin Rejuvenation
Park and colleagues conducted a small study with five patients in 2016 in which long-chain polynucleotide filler was used for skin rejuvenation. Over a 2-week period, five Korean women received four injections of the filler (0.05 mL) on one side of the face. No adverse side effects were reported. In the patients in their 30s, pore and skin thickness significantly improved with treatment. For patients in their 40s, observable improvements were noted in melanin, sagging, skin tone, and wrinkles. Despite the small study size, the investigators concluded that this intradermal injection material is a safe and effective product for skin rejuvenation therapy.1 The product is also available in Europe and reportedly spurs the regeneration of damaged tissues and yields a more natural appearance.1
A Hybrid HA-PN Filler
Given that the most common filling agent, hyaluronic acid (HA), is associated with multiple side effects, JH Kim and colleagues set out in 2020 to compare HA with a new HA-PN dermal filler that has displayed notable biocompatibility and promoted tissue regeneration. The investigators observed that the combination filler provoked greater cell migration in a wound healing assay and was more effective in promoting collagen production in human and mouse fibroblasts. To their knowledge, this was the first study showing the efficacy, safety, and durability of a hybrid HA-PN filler. They concluded that fillers containing both HA and PN were more effective than HA alone in suppressing cutaneous aging and may represent the next step in the evolution of dermal filling agents.12
Most Recent Findings
In August 2023, MJ Kim and colleagues became the first to report on the successful use of PNs derived from fish sperm as a volumizing treatment for fat atrophy in vivo (in the temple in one case, and the cheek in the other). Injections were made into the subcutaneous layer to treat iatrogenic volume loss resulting from lipolysis injections. In one case, a depression in the left temple of a 53-year-old female lipolysis patient was treated with a series of 1 cc PN injections in a 20 mg/mL concentration. At 1 month after the final series of injections (four treatments), significant clinical improvement was observed, with the result (barely visible depression) maintained at 11 months and 21 months after the last treatment. The second patient, a 34-year-old female, presented with two depressed areas on the left cheek 2 months after steroid injections for two acne lesions. A series of PN filler injections also with a concentration of 20 mg/mL was administered (four treatments) at 1-month intervals. Significant improvement was seen 2 months after the last treatment, with maintenance of complete healing noted at 5 months and 12 months after the final treatment. No adverse effects were reported in either case. The investigators concluded that long-chain PN fillers appear to be effective in treating depressions in the skin, but more data, particularly from controlled studies, is necessary to determine the safety and efficacy as a lone therapeutic approach for soft-tissue depression.6
A month later, Lee and colleagues reported on the results of their survey of clinicians in South Korea who use PNs in clinical practice. The goal was to understand current practices and perceptions of effectiveness in treating facial erythema. Of the 557 physicians who participated, 84.4% used PNs for facial erythema provoked by inflammatory facial dermatosis, 66.4% for facial erythema induced by repeated laser/microneedle radiofrequency, and 47.4% for facial erythema caused by steroid overuse. In these same classifications, 88.1%, 90%, and 83.7%, respectively, found PNs to be “highly effective” or “effective.” Survey respondents also characterized PNs as imparting wound healing/regeneration (95.8%), skin barrier protection (92.2%), hydration (90.5%), vascular stabilization (81.0%), and anti-inflammatory activity (79.5%).11
Conclusion
The use of salmon sperm cells is an example of the recent trend toward a cellular approach in which cutaneous components are activated with the intention of stimulating tissue regeneration. It is commonly used in Brazil and my Brazilian patients seem to know all about it. This innovative outlook is intriguing as are a spate of recently reported results. Nevertheless, much more evidence is required to ascertain safety and effectiveness in large sample sizes and, ideally, to establish maintenance of corrections over longer periods whether these ingredients are used in filling agents or topical formulations.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, a SaaS company used to generate skin care routines in office and as a e-commerce solution. Write to her at dermnews@mdedge.com.
References
1. Park KY et al. Dermatol Ther. 2016 Jan;29(1):37-40. .
2. Kim TH et al. Mar Drugs. 2021 May 22;19(6):296.
3. Raposio E et al. Cell Prolif. 2008 Oct;41(5):739-54.
4. Veronesi F et al. J Cell Physiol. 2017 Sep;232(9):2299-2307.
5. Kim JH et al. Lasers Surg Med. 2018 Mar 25.
6. Kim MJ et al. Skin Res Technol. 2023 Aug;29(8):e13439.
7. Khan A et al. Chinese Journal of Plastic and Reconstructive Surgery. 2022 Dec;4(4):187-193.
8. Lee YJ et al. J Dermatolog Treat. 2022 Feb;33(1):254-260.
9. De Caridi G et al. Int Wound J. 2016 Oct;13(5):754-8.
10. Cavallini M et al. J Cosmet Dermatol. 2021 Mar;20(3):922-928.
11. Lee D. Skin Res Technol. 2023 Sep;29(9):e13466. doi: 10.1111/srt.13466.
12. Kim JH et al. Sci Rep. 2020 Mar 20;10(1):5127. .
It may not have an aesthetic-sounding appeal to most people, but salmon sperm is indeed one of the novel ingredients featured in products for human skin. These products also reportedly enhance and promote skin regeneration.1 This column will focus on the innovative approach to skin care involving purified polynucleotides derived from salmon sperm.
The Properties and Activities of PDRNs, PNs
PDRNs contain DNA fragments primarily derived from Pacific or chum salmon (Oncorhynchus keta), and salmon trout (Oncorhynchus mykiss) sperm cells.2 Through preclinical and clinical trials, PDRN has demonstrated a wide range of salutary functions, including antiallodynic, antiapoptotic, anti-inflammatory, antimelanogenetic, antiosteonecrotic, antiosteoporotic, antiulcerative, bone-regenerative, tissue damage–preventive, and wound-healing activities through adenosine A2A receptor and salvage pathways activation. Indeed, PDRNs have been shown in vitro to spur the proliferation of preadipocytes and, in vivo, to be effective in treating wounds and ulcers.3,4 In particular, atrophic, hypertrophic, surgical, and various acne scars have been treated with such injections.2,5,6 PDRN is thought to affect cutaneous health more directly by facilitating angiogenesis, cellular functions, especially fibroblast stimulation, collagen production, soft-tissue regeneration, and skin revitalization. Further, it has been used successfully to treat hyperpigmentation.7
PNs, derived from the same fish species as PDRNs, have been used effectively to ameliorate skin elasticity, hydration, pore size, thickness, wrinkles, as well as pigmentation and, specifically, in treating periorbital rhytides and postsurgical scars.5,6,8 Beyond skin rejuvenation, PNs have been recognized for effectiveness in treating stretch marks and achieving vulvovaginal revitalization; guidelines for its use have been established and implemented in recent years.6,9,10 In South Korea, PNs have become a popular treatment for facial erythema even though preclinical and clinical data are sparse.11 Nevertheless, the use of these novel substances is thought to foster tissue regeneration and a more natural rejuvenation than achieved through more traditional fillers.6
Skin Rejuvenation
Park and colleagues conducted a small study with five patients in 2016 in which long-chain polynucleotide filler was used for skin rejuvenation. Over a 2-week period, five Korean women received four injections of the filler (0.05 mL) on one side of the face. No adverse side effects were reported. In the patients in their 30s, pore and skin thickness significantly improved with treatment. For patients in their 40s, observable improvements were noted in melanin, sagging, skin tone, and wrinkles. Despite the small study size, the investigators concluded that this intradermal injection material is a safe and effective product for skin rejuvenation therapy.1 The product is also available in Europe and reportedly spurs the regeneration of damaged tissues and yields a more natural appearance.1
A Hybrid HA-PN Filler
Given that the most common filling agent, hyaluronic acid (HA), is associated with multiple side effects, JH Kim and colleagues set out in 2020 to compare HA with a new HA-PN dermal filler that has displayed notable biocompatibility and promoted tissue regeneration. The investigators observed that the combination filler provoked greater cell migration in a wound healing assay and was more effective in promoting collagen production in human and mouse fibroblasts. To their knowledge, this was the first study showing the efficacy, safety, and durability of a hybrid HA-PN filler. They concluded that fillers containing both HA and PN were more effective than HA alone in suppressing cutaneous aging and may represent the next step in the evolution of dermal filling agents.12
Most Recent Findings
In August 2023, MJ Kim and colleagues became the first to report on the successful use of PNs derived from fish sperm as a volumizing treatment for fat atrophy in vivo (in the temple in one case, and the cheek in the other). Injections were made into the subcutaneous layer to treat iatrogenic volume loss resulting from lipolysis injections. In one case, a depression in the left temple of a 53-year-old female lipolysis patient was treated with a series of 1 cc PN injections in a 20 mg/mL concentration. At 1 month after the final series of injections (four treatments), significant clinical improvement was observed, with the result (barely visible depression) maintained at 11 months and 21 months after the last treatment. The second patient, a 34-year-old female, presented with two depressed areas on the left cheek 2 months after steroid injections for two acne lesions. A series of PN filler injections also with a concentration of 20 mg/mL was administered (four treatments) at 1-month intervals. Significant improvement was seen 2 months after the last treatment, with maintenance of complete healing noted at 5 months and 12 months after the final treatment. No adverse effects were reported in either case. The investigators concluded that long-chain PN fillers appear to be effective in treating depressions in the skin, but more data, particularly from controlled studies, is necessary to determine the safety and efficacy as a lone therapeutic approach for soft-tissue depression.6
A month later, Lee and colleagues reported on the results of their survey of clinicians in South Korea who use PNs in clinical practice. The goal was to understand current practices and perceptions of effectiveness in treating facial erythema. Of the 557 physicians who participated, 84.4% used PNs for facial erythema provoked by inflammatory facial dermatosis, 66.4% for facial erythema induced by repeated laser/microneedle radiofrequency, and 47.4% for facial erythema caused by steroid overuse. In these same classifications, 88.1%, 90%, and 83.7%, respectively, found PNs to be “highly effective” or “effective.” Survey respondents also characterized PNs as imparting wound healing/regeneration (95.8%), skin barrier protection (92.2%), hydration (90.5%), vascular stabilization (81.0%), and anti-inflammatory activity (79.5%).11
Conclusion
The use of salmon sperm cells is an example of the recent trend toward a cellular approach in which cutaneous components are activated with the intention of stimulating tissue regeneration. It is commonly used in Brazil and my Brazilian patients seem to know all about it. This innovative outlook is intriguing as are a spate of recently reported results. Nevertheless, much more evidence is required to ascertain safety and effectiveness in large sample sizes and, ideally, to establish maintenance of corrections over longer periods whether these ingredients are used in filling agents or topical formulations.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, a SaaS company used to generate skin care routines in office and as a e-commerce solution. Write to her at dermnews@mdedge.com.
References
1. Park KY et al. Dermatol Ther. 2016 Jan;29(1):37-40. .
2. Kim TH et al. Mar Drugs. 2021 May 22;19(6):296.
3. Raposio E et al. Cell Prolif. 2008 Oct;41(5):739-54.
4. Veronesi F et al. J Cell Physiol. 2017 Sep;232(9):2299-2307.
5. Kim JH et al. Lasers Surg Med. 2018 Mar 25.
6. Kim MJ et al. Skin Res Technol. 2023 Aug;29(8):e13439.
7. Khan A et al. Chinese Journal of Plastic and Reconstructive Surgery. 2022 Dec;4(4):187-193.
8. Lee YJ et al. J Dermatolog Treat. 2022 Feb;33(1):254-260.
9. De Caridi G et al. Int Wound J. 2016 Oct;13(5):754-8.
10. Cavallini M et al. J Cosmet Dermatol. 2021 Mar;20(3):922-928.
11. Lee D. Skin Res Technol. 2023 Sep;29(9):e13466. doi: 10.1111/srt.13466.
12. Kim JH et al. Sci Rep. 2020 Mar 20;10(1):5127. .
It may not have an aesthetic-sounding appeal to most people, but salmon sperm is indeed one of the novel ingredients featured in products for human skin. These products also reportedly enhance and promote skin regeneration.1 This column will focus on the innovative approach to skin care involving purified polynucleotides derived from salmon sperm.
The Properties and Activities of PDRNs, PNs
PDRNs contain DNA fragments primarily derived from Pacific or chum salmon (Oncorhynchus keta), and salmon trout (Oncorhynchus mykiss) sperm cells.2 Through preclinical and clinical trials, PDRN has demonstrated a wide range of salutary functions, including antiallodynic, antiapoptotic, anti-inflammatory, antimelanogenetic, antiosteonecrotic, antiosteoporotic, antiulcerative, bone-regenerative, tissue damage–preventive, and wound-healing activities through adenosine A2A receptor and salvage pathways activation. Indeed, PDRNs have been shown in vitro to spur the proliferation of preadipocytes and, in vivo, to be effective in treating wounds and ulcers.3,4 In particular, atrophic, hypertrophic, surgical, and various acne scars have been treated with such injections.2,5,6 PDRN is thought to affect cutaneous health more directly by facilitating angiogenesis, cellular functions, especially fibroblast stimulation, collagen production, soft-tissue regeneration, and skin revitalization. Further, it has been used successfully to treat hyperpigmentation.7
PNs, derived from the same fish species as PDRNs, have been used effectively to ameliorate skin elasticity, hydration, pore size, thickness, wrinkles, as well as pigmentation and, specifically, in treating periorbital rhytides and postsurgical scars.5,6,8 Beyond skin rejuvenation, PNs have been recognized for effectiveness in treating stretch marks and achieving vulvovaginal revitalization; guidelines for its use have been established and implemented in recent years.6,9,10 In South Korea, PNs have become a popular treatment for facial erythema even though preclinical and clinical data are sparse.11 Nevertheless, the use of these novel substances is thought to foster tissue regeneration and a more natural rejuvenation than achieved through more traditional fillers.6
Skin Rejuvenation
Park and colleagues conducted a small study with five patients in 2016 in which long-chain polynucleotide filler was used for skin rejuvenation. Over a 2-week period, five Korean women received four injections of the filler (0.05 mL) on one side of the face. No adverse side effects were reported. In the patients in their 30s, pore and skin thickness significantly improved with treatment. For patients in their 40s, observable improvements were noted in melanin, sagging, skin tone, and wrinkles. Despite the small study size, the investigators concluded that this intradermal injection material is a safe and effective product for skin rejuvenation therapy.1 The product is also available in Europe and reportedly spurs the regeneration of damaged tissues and yields a more natural appearance.1
A Hybrid HA-PN Filler
Given that the most common filling agent, hyaluronic acid (HA), is associated with multiple side effects, JH Kim and colleagues set out in 2020 to compare HA with a new HA-PN dermal filler that has displayed notable biocompatibility and promoted tissue regeneration. The investigators observed that the combination filler provoked greater cell migration in a wound healing assay and was more effective in promoting collagen production in human and mouse fibroblasts. To their knowledge, this was the first study showing the efficacy, safety, and durability of a hybrid HA-PN filler. They concluded that fillers containing both HA and PN were more effective than HA alone in suppressing cutaneous aging and may represent the next step in the evolution of dermal filling agents.12
Most Recent Findings
In August 2023, MJ Kim and colleagues became the first to report on the successful use of PNs derived from fish sperm as a volumizing treatment for fat atrophy in vivo (in the temple in one case, and the cheek in the other). Injections were made into the subcutaneous layer to treat iatrogenic volume loss resulting from lipolysis injections. In one case, a depression in the left temple of a 53-year-old female lipolysis patient was treated with a series of 1 cc PN injections in a 20 mg/mL concentration. At 1 month after the final series of injections (four treatments), significant clinical improvement was observed, with the result (barely visible depression) maintained at 11 months and 21 months after the last treatment. The second patient, a 34-year-old female, presented with two depressed areas on the left cheek 2 months after steroid injections for two acne lesions. A series of PN filler injections also with a concentration of 20 mg/mL was administered (four treatments) at 1-month intervals. Significant improvement was seen 2 months after the last treatment, with maintenance of complete healing noted at 5 months and 12 months after the final treatment. No adverse effects were reported in either case. The investigators concluded that long-chain PN fillers appear to be effective in treating depressions in the skin, but more data, particularly from controlled studies, is necessary to determine the safety and efficacy as a lone therapeutic approach for soft-tissue depression.6
A month later, Lee and colleagues reported on the results of their survey of clinicians in South Korea who use PNs in clinical practice. The goal was to understand current practices and perceptions of effectiveness in treating facial erythema. Of the 557 physicians who participated, 84.4% used PNs for facial erythema provoked by inflammatory facial dermatosis, 66.4% for facial erythema induced by repeated laser/microneedle radiofrequency, and 47.4% for facial erythema caused by steroid overuse. In these same classifications, 88.1%, 90%, and 83.7%, respectively, found PNs to be “highly effective” or “effective.” Survey respondents also characterized PNs as imparting wound healing/regeneration (95.8%), skin barrier protection (92.2%), hydration (90.5%), vascular stabilization (81.0%), and anti-inflammatory activity (79.5%).11
Conclusion
The use of salmon sperm cells is an example of the recent trend toward a cellular approach in which cutaneous components are activated with the intention of stimulating tissue regeneration. It is commonly used in Brazil and my Brazilian patients seem to know all about it. This innovative outlook is intriguing as are a spate of recently reported results. Nevertheless, much more evidence is required to ascertain safety and effectiveness in large sample sizes and, ideally, to establish maintenance of corrections over longer periods whether these ingredients are used in filling agents or topical formulations.
Dr. Baumann is a private practice dermatologist, researcher, author, and entrepreneur in Miami. She founded the division of cosmetic dermatology at the University of Miami in 1997. The third edition of her bestselling textbook, “Cosmetic Dermatology,” was published in 2022. Dr. Baumann has received funding for advisory boards and/or clinical research trials from Allergan, Galderma, Johnson & Johnson, and Burt’s Bees. She is the CEO of Skin Type Solutions, a SaaS company used to generate skin care routines in office and as a e-commerce solution. Write to her at dermnews@mdedge.com.
References
1. Park KY et al. Dermatol Ther. 2016 Jan;29(1):37-40. .
2. Kim TH et al. Mar Drugs. 2021 May 22;19(6):296.
3. Raposio E et al. Cell Prolif. 2008 Oct;41(5):739-54.
4. Veronesi F et al. J Cell Physiol. 2017 Sep;232(9):2299-2307.
5. Kim JH et al. Lasers Surg Med. 2018 Mar 25.
6. Kim MJ et al. Skin Res Technol. 2023 Aug;29(8):e13439.
7. Khan A et al. Chinese Journal of Plastic and Reconstructive Surgery. 2022 Dec;4(4):187-193.
8. Lee YJ et al. J Dermatolog Treat. 2022 Feb;33(1):254-260.
9. De Caridi G et al. Int Wound J. 2016 Oct;13(5):754-8.
10. Cavallini M et al. J Cosmet Dermatol. 2021 Mar;20(3):922-928.
11. Lee D. Skin Res Technol. 2023 Sep;29(9):e13466. doi: 10.1111/srt.13466.
12. Kim JH et al. Sci Rep. 2020 Mar 20;10(1):5127. .
FDA’s Stricter Regulation of Lab-Developed Tests Faces Lawsuits and Lingering Concerns
The Food and Drug Administration (FDA) plans to scrutinize the safety and efficacy of lab-developed tests — those designed, manufactured, and used in a single laboratory — far more thoroughly in the future.
Under a rule finalized in April, the FDA will treat facilities that develop and use lab tests as manufacturers and regulate tests as medical devices. That means that most lab tests will need an FDA review before going on sale.
The FDA will also impose new quality standards, requiring test manufacturers to report adverse events and create a registry of lab tests under the new rule, which will be phased in over 4 years.
FDA officials have been concerned for years about the reliability of commercial lab tests, which have ballooned into a multibillion-dollar industry.
Consumer groups have long urged the FDA to regulate lab tests more strictly, arguing that the lack of scrutiny allows doctors and patients to be exploited by bad actors such as Theranos, which falsely claimed that its tests could diagnose multiple diseases with a single drop of blood.
“When it comes to some of these tests that doctors are recommending for patients, many doctors are just crossing their fingers and relying on the representation of the company because nobody is checking” to verify a manufacturer’s claims, said Joshua Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland.
Nearly 12,000 Labs Making Medical Tests
Although the FDA estimates there are nearly 12,000 labs manufacturing medical tests, agency officials said they don’t know how many tests are being marketed. The FDA already requires that home test kits marketed directly to consumers, such as those used to detect COVID-19, get clearance from the agency before being sold.
“There’s plenty of time for industry to get its act together to develop the data that it might need to make a premarket application,” said Peter Lurie, MD, PhD, a former associate commissioner at the FDA. In 2015, Dr. Lurie led a report outlining some of the dangers of unregulated lab tests.
For the average physician who orders lab tests, nothing is going to immediately change because of the final rule, said Dr. Lurie, now president of the Center for Science in the Public Interest, a nonprofit consumer watchdog.
“Tomorrow, this will look just the same as it does today,” Dr. Lurie said. “For the next 3 years, the companies will be scurrying behind the scenes to comply with the early stages of implementation. But most of that will be invisible to the average practitioner.”
Dr. Lurie predicted the FDA will focus its scrutiny on tests that pose the greatest potential risk to patients, such as ones used to diagnose serious diseases or guide treatment for life-threatening conditions. “The least significant tests will likely get very limited, if any, scrutiny,” said Dr. Lurie, adding that the FDA will likely issue guidance about how it plans to define low- and high-risk tests. “My suspicion is that it will be probably a small minority of products that are subject to full premarket approval.”
Lab Industry Groups Push Back
But imposing new rules with the potential to affect an industry’s bottom line is no easy task.
The American Clinical Laboratory Association, which represents the lab industry, said in a statement that the FDA rule will “limit access to scores of critical tests, increase healthcare costs, and undermine innovation in new diagnostics.” Another industry group, the Association for Molecular Pathology, has warned of “significant and harmful disruption to laboratory medicine.”
The two associations have filed separate lawsuits, charging that the FDA overstepped the authority granted by Congress. In their lawsuits, groups claim that lab tests are professional services, not manufactured products. The groups noted that the Centers for Medicare & Medicaid Services (CMS) already inspects lab facilities. CMS does not assess the tests’ quality or reliability.
A recent Supreme Court decision could make those lawsuits more likely to succeed, said David Simon, JD, LLM, PhD, an assistant professor of law at the Northeastern University School of Law, Boston, Massachusetts.
In the case of Loper Bright Enterprises v. Raimondo, decided in June, justices overturned a long-standing precedent known as Chevron deference, which required courts to defer to federal agencies when interpreting ambiguous laws. That means that courts no longer have to accept the FDA’s definition of a device, Dr. Simon said.
“Because judges may have more active roles in defining agency authority, federal agencies may have correspondingly less robust roles in policymaking,” Dr. Simon wrote in an editorial coauthored with Michael J. Young, MD, MPhil, of Harvard Medical School, Boston.
The Supreme Court ruling could pressure Congress to more clearly define FDA’s ruling in regulating lab tests, Dr. Simon and Dr. Young wrote.
Members of Congress first introduced a bill to clarify the FDA’s role in regulating lab tests, called the VALID Act, in 2020. The bill stalled and, despite efforts to revive it, still hasn’t passed.
FDA officials have said they remain “open to working with Congress,” noting that any future legislation about lab-developed tests would supersede their current policy.
In an interview, Dr. Simon noted the FDA significantly narrowed the scope of the final rule in response to comments from critics who objected to an earlier version of the policy proposed in 2023. The final rule carves out several categories of tests that won’t need to apply for “premarket review.”
Notably, a “grandfather clause” will allow some lab tests already on the market to continue being sold without undergoing FDA’s premarket review process. In explaining the exemption, FDA officials said they did not want doctors and patients to lose access to tests on which they rely. But Dr. Lurie noted that because the FDA views all these tests as under its jurisdiction, the agency could opt to take a closer look “at a very old device that is causing a problem today.”
The FDA also will exempt tests approved by New York State’s Clinical Laboratory Evaluation Program, which conducts its own stringent reviews. And the FDA will continue to allow hospitals to develop tests for patients within their healthcare system without going through the FDA approval process, if no FDA-approved tests are available.
Hospital-based tests play a critical role in treating infectious diseases, said Amesh Adalja, MD, an infectious diseases specialist and senior scholar at the Johns Hopkins Center for Health Security. For example, a large research hospital treating a patient with cytomegalovirus may need to develop its own test to determine whether the infection is resistant to antiviral drugs, Dr. Adalja said.
“With novel infectious disease outbreaks, researchers are able to move quickly to make diagnostic tests months and months before commercial laboratories are able to get through regulatory processes,” Dr. Adalja said.
To help scientists respond quickly to emergencies, the FDA published special guidance for labs that develop unauthorized lab tests for disease outbreaks.
Medical groups such as the American Hospital Association and Infectious Diseases Society of America remain concerned about the burden of complying with new regulations.
“Many vital tests developed in hospitals and health systems may be subjected to unnecessary and costly paperwork,” said Stacey Hughes, executive vice president of the American Hospital Association, in a statement.
Other groups, such as the American Society of Clinical Oncology, praised the new FDA policy. In comments submitted to the FDA in 2023, the cancer group said it “emphatically supports” requiring lab tests to undergo FDA review.
“We appreciate FDA action to modernize oversight of these tests and are hopeful this rule will increase focus on the need to balance rapid diagnostic innovation with patient safety and access” Everett Vokes, MD, the group’s board chair, said in a statement released after the FDA’s final rule was published.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) plans to scrutinize the safety and efficacy of lab-developed tests — those designed, manufactured, and used in a single laboratory — far more thoroughly in the future.
Under a rule finalized in April, the FDA will treat facilities that develop and use lab tests as manufacturers and regulate tests as medical devices. That means that most lab tests will need an FDA review before going on sale.
The FDA will also impose new quality standards, requiring test manufacturers to report adverse events and create a registry of lab tests under the new rule, which will be phased in over 4 years.
FDA officials have been concerned for years about the reliability of commercial lab tests, which have ballooned into a multibillion-dollar industry.
Consumer groups have long urged the FDA to regulate lab tests more strictly, arguing that the lack of scrutiny allows doctors and patients to be exploited by bad actors such as Theranos, which falsely claimed that its tests could diagnose multiple diseases with a single drop of blood.
“When it comes to some of these tests that doctors are recommending for patients, many doctors are just crossing their fingers and relying on the representation of the company because nobody is checking” to verify a manufacturer’s claims, said Joshua Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland.
Nearly 12,000 Labs Making Medical Tests
Although the FDA estimates there are nearly 12,000 labs manufacturing medical tests, agency officials said they don’t know how many tests are being marketed. The FDA already requires that home test kits marketed directly to consumers, such as those used to detect COVID-19, get clearance from the agency before being sold.
“There’s plenty of time for industry to get its act together to develop the data that it might need to make a premarket application,” said Peter Lurie, MD, PhD, a former associate commissioner at the FDA. In 2015, Dr. Lurie led a report outlining some of the dangers of unregulated lab tests.
For the average physician who orders lab tests, nothing is going to immediately change because of the final rule, said Dr. Lurie, now president of the Center for Science in the Public Interest, a nonprofit consumer watchdog.
“Tomorrow, this will look just the same as it does today,” Dr. Lurie said. “For the next 3 years, the companies will be scurrying behind the scenes to comply with the early stages of implementation. But most of that will be invisible to the average practitioner.”
Dr. Lurie predicted the FDA will focus its scrutiny on tests that pose the greatest potential risk to patients, such as ones used to diagnose serious diseases or guide treatment for life-threatening conditions. “The least significant tests will likely get very limited, if any, scrutiny,” said Dr. Lurie, adding that the FDA will likely issue guidance about how it plans to define low- and high-risk tests. “My suspicion is that it will be probably a small minority of products that are subject to full premarket approval.”
Lab Industry Groups Push Back
But imposing new rules with the potential to affect an industry’s bottom line is no easy task.
The American Clinical Laboratory Association, which represents the lab industry, said in a statement that the FDA rule will “limit access to scores of critical tests, increase healthcare costs, and undermine innovation in new diagnostics.” Another industry group, the Association for Molecular Pathology, has warned of “significant and harmful disruption to laboratory medicine.”
The two associations have filed separate lawsuits, charging that the FDA overstepped the authority granted by Congress. In their lawsuits, groups claim that lab tests are professional services, not manufactured products. The groups noted that the Centers for Medicare & Medicaid Services (CMS) already inspects lab facilities. CMS does not assess the tests’ quality or reliability.
A recent Supreme Court decision could make those lawsuits more likely to succeed, said David Simon, JD, LLM, PhD, an assistant professor of law at the Northeastern University School of Law, Boston, Massachusetts.
In the case of Loper Bright Enterprises v. Raimondo, decided in June, justices overturned a long-standing precedent known as Chevron deference, which required courts to defer to federal agencies when interpreting ambiguous laws. That means that courts no longer have to accept the FDA’s definition of a device, Dr. Simon said.
“Because judges may have more active roles in defining agency authority, federal agencies may have correspondingly less robust roles in policymaking,” Dr. Simon wrote in an editorial coauthored with Michael J. Young, MD, MPhil, of Harvard Medical School, Boston.
The Supreme Court ruling could pressure Congress to more clearly define FDA’s ruling in regulating lab tests, Dr. Simon and Dr. Young wrote.
Members of Congress first introduced a bill to clarify the FDA’s role in regulating lab tests, called the VALID Act, in 2020. The bill stalled and, despite efforts to revive it, still hasn’t passed.
FDA officials have said they remain “open to working with Congress,” noting that any future legislation about lab-developed tests would supersede their current policy.
In an interview, Dr. Simon noted the FDA significantly narrowed the scope of the final rule in response to comments from critics who objected to an earlier version of the policy proposed in 2023. The final rule carves out several categories of tests that won’t need to apply for “premarket review.”
Notably, a “grandfather clause” will allow some lab tests already on the market to continue being sold without undergoing FDA’s premarket review process. In explaining the exemption, FDA officials said they did not want doctors and patients to lose access to tests on which they rely. But Dr. Lurie noted that because the FDA views all these tests as under its jurisdiction, the agency could opt to take a closer look “at a very old device that is causing a problem today.”
The FDA also will exempt tests approved by New York State’s Clinical Laboratory Evaluation Program, which conducts its own stringent reviews. And the FDA will continue to allow hospitals to develop tests for patients within their healthcare system without going through the FDA approval process, if no FDA-approved tests are available.
Hospital-based tests play a critical role in treating infectious diseases, said Amesh Adalja, MD, an infectious diseases specialist and senior scholar at the Johns Hopkins Center for Health Security. For example, a large research hospital treating a patient with cytomegalovirus may need to develop its own test to determine whether the infection is resistant to antiviral drugs, Dr. Adalja said.
“With novel infectious disease outbreaks, researchers are able to move quickly to make diagnostic tests months and months before commercial laboratories are able to get through regulatory processes,” Dr. Adalja said.
To help scientists respond quickly to emergencies, the FDA published special guidance for labs that develop unauthorized lab tests for disease outbreaks.
Medical groups such as the American Hospital Association and Infectious Diseases Society of America remain concerned about the burden of complying with new regulations.
“Many vital tests developed in hospitals and health systems may be subjected to unnecessary and costly paperwork,” said Stacey Hughes, executive vice president of the American Hospital Association, in a statement.
Other groups, such as the American Society of Clinical Oncology, praised the new FDA policy. In comments submitted to the FDA in 2023, the cancer group said it “emphatically supports” requiring lab tests to undergo FDA review.
“We appreciate FDA action to modernize oversight of these tests and are hopeful this rule will increase focus on the need to balance rapid diagnostic innovation with patient safety and access” Everett Vokes, MD, the group’s board chair, said in a statement released after the FDA’s final rule was published.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration (FDA) plans to scrutinize the safety and efficacy of lab-developed tests — those designed, manufactured, and used in a single laboratory — far more thoroughly in the future.
Under a rule finalized in April, the FDA will treat facilities that develop and use lab tests as manufacturers and regulate tests as medical devices. That means that most lab tests will need an FDA review before going on sale.
The FDA will also impose new quality standards, requiring test manufacturers to report adverse events and create a registry of lab tests under the new rule, which will be phased in over 4 years.
FDA officials have been concerned for years about the reliability of commercial lab tests, which have ballooned into a multibillion-dollar industry.
Consumer groups have long urged the FDA to regulate lab tests more strictly, arguing that the lack of scrutiny allows doctors and patients to be exploited by bad actors such as Theranos, which falsely claimed that its tests could diagnose multiple diseases with a single drop of blood.
“When it comes to some of these tests that doctors are recommending for patients, many doctors are just crossing their fingers and relying on the representation of the company because nobody is checking” to verify a manufacturer’s claims, said Joshua Sharfstein, MD, vice dean for public health practice and community engagement at the Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland.
Nearly 12,000 Labs Making Medical Tests
Although the FDA estimates there are nearly 12,000 labs manufacturing medical tests, agency officials said they don’t know how many tests are being marketed. The FDA already requires that home test kits marketed directly to consumers, such as those used to detect COVID-19, get clearance from the agency before being sold.
“There’s plenty of time for industry to get its act together to develop the data that it might need to make a premarket application,” said Peter Lurie, MD, PhD, a former associate commissioner at the FDA. In 2015, Dr. Lurie led a report outlining some of the dangers of unregulated lab tests.
For the average physician who orders lab tests, nothing is going to immediately change because of the final rule, said Dr. Lurie, now president of the Center for Science in the Public Interest, a nonprofit consumer watchdog.
“Tomorrow, this will look just the same as it does today,” Dr. Lurie said. “For the next 3 years, the companies will be scurrying behind the scenes to comply with the early stages of implementation. But most of that will be invisible to the average practitioner.”
Dr. Lurie predicted the FDA will focus its scrutiny on tests that pose the greatest potential risk to patients, such as ones used to diagnose serious diseases or guide treatment for life-threatening conditions. “The least significant tests will likely get very limited, if any, scrutiny,” said Dr. Lurie, adding that the FDA will likely issue guidance about how it plans to define low- and high-risk tests. “My suspicion is that it will be probably a small minority of products that are subject to full premarket approval.”
Lab Industry Groups Push Back
But imposing new rules with the potential to affect an industry’s bottom line is no easy task.
The American Clinical Laboratory Association, which represents the lab industry, said in a statement that the FDA rule will “limit access to scores of critical tests, increase healthcare costs, and undermine innovation in new diagnostics.” Another industry group, the Association for Molecular Pathology, has warned of “significant and harmful disruption to laboratory medicine.”
The two associations have filed separate lawsuits, charging that the FDA overstepped the authority granted by Congress. In their lawsuits, groups claim that lab tests are professional services, not manufactured products. The groups noted that the Centers for Medicare & Medicaid Services (CMS) already inspects lab facilities. CMS does not assess the tests’ quality or reliability.
A recent Supreme Court decision could make those lawsuits more likely to succeed, said David Simon, JD, LLM, PhD, an assistant professor of law at the Northeastern University School of Law, Boston, Massachusetts.
In the case of Loper Bright Enterprises v. Raimondo, decided in June, justices overturned a long-standing precedent known as Chevron deference, which required courts to defer to federal agencies when interpreting ambiguous laws. That means that courts no longer have to accept the FDA’s definition of a device, Dr. Simon said.
“Because judges may have more active roles in defining agency authority, federal agencies may have correspondingly less robust roles in policymaking,” Dr. Simon wrote in an editorial coauthored with Michael J. Young, MD, MPhil, of Harvard Medical School, Boston.
The Supreme Court ruling could pressure Congress to more clearly define FDA’s ruling in regulating lab tests, Dr. Simon and Dr. Young wrote.
Members of Congress first introduced a bill to clarify the FDA’s role in regulating lab tests, called the VALID Act, in 2020. The bill stalled and, despite efforts to revive it, still hasn’t passed.
FDA officials have said they remain “open to working with Congress,” noting that any future legislation about lab-developed tests would supersede their current policy.
In an interview, Dr. Simon noted the FDA significantly narrowed the scope of the final rule in response to comments from critics who objected to an earlier version of the policy proposed in 2023. The final rule carves out several categories of tests that won’t need to apply for “premarket review.”
Notably, a “grandfather clause” will allow some lab tests already on the market to continue being sold without undergoing FDA’s premarket review process. In explaining the exemption, FDA officials said they did not want doctors and patients to lose access to tests on which they rely. But Dr. Lurie noted that because the FDA views all these tests as under its jurisdiction, the agency could opt to take a closer look “at a very old device that is causing a problem today.”
The FDA also will exempt tests approved by New York State’s Clinical Laboratory Evaluation Program, which conducts its own stringent reviews. And the FDA will continue to allow hospitals to develop tests for patients within their healthcare system without going through the FDA approval process, if no FDA-approved tests are available.
Hospital-based tests play a critical role in treating infectious diseases, said Amesh Adalja, MD, an infectious diseases specialist and senior scholar at the Johns Hopkins Center for Health Security. For example, a large research hospital treating a patient with cytomegalovirus may need to develop its own test to determine whether the infection is resistant to antiviral drugs, Dr. Adalja said.
“With novel infectious disease outbreaks, researchers are able to move quickly to make diagnostic tests months and months before commercial laboratories are able to get through regulatory processes,” Dr. Adalja said.
To help scientists respond quickly to emergencies, the FDA published special guidance for labs that develop unauthorized lab tests for disease outbreaks.
Medical groups such as the American Hospital Association and Infectious Diseases Society of America remain concerned about the burden of complying with new regulations.
“Many vital tests developed in hospitals and health systems may be subjected to unnecessary and costly paperwork,” said Stacey Hughes, executive vice president of the American Hospital Association, in a statement.
Other groups, such as the American Society of Clinical Oncology, praised the new FDA policy. In comments submitted to the FDA in 2023, the cancer group said it “emphatically supports” requiring lab tests to undergo FDA review.
“We appreciate FDA action to modernize oversight of these tests and are hopeful this rule will increase focus on the need to balance rapid diagnostic innovation with patient safety and access” Everett Vokes, MD, the group’s board chair, said in a statement released after the FDA’s final rule was published.
A version of this article first appeared on Medscape.com.
A 71-year-old White female developed erosions after hip replacement surgery 2 months prior to presentation
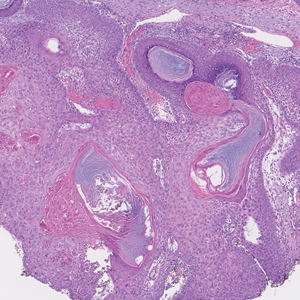
The patient had been diagnosed with pemphigus vulgaris (PV) 1 year prior to presentation with erosions on the axilla. Biopsy at that time revealed intraepithelial acantholytic blistering with areas of suprabasilar and subcorneal clefting. Direct immunofluorescence was positive for linear/granular IgG deposition throughout the epithelial cell surfaces, as well as linear/granular C3 deposits of the lower two thirds of the epithelial strata, consistent for pemphigus vulgaris.
There is likely a genetic predisposition. Medications that may induce pemphigus include penicillamine, nifedipine, or captopril.
Clinically, PV presents with flaccid blistering lesions that may be cutaneous and/or mucosal. Bullae can progress to erosions and crusting, which then heal with pigment alteration but not scarring. The most commonly affected sites are the mouth, intertriginous areas, face, and neck. Mucosal lesions can involve the lips, esophagus, conjunctiva, and genitals.
Biopsy for histology and direct immunofluorescence is important in distinguishing between PV and other blistering disorders. Up to 75% of patients with active disease also have a positive indirect immunofluorescence with circulating IgG.
There are numerous reports in the literature of PV occurring in previous surgical scars, and areas of friction or trauma. This so-called Koebner’s phenomenon is seen more commonly in several dermatologic conditions, such as psoriasis, lichen planus, verruca vulgaris, and vitiligo.
Treatment for PV is generally immunosuppressive. Systemic therapy usually begins with prednisone and then is transitioned to a steroid sparing agent such as mycophenolate mofetil. Other steroid sparing agents include azathioprine, methotrexate, cyclophosphamide, and intravenous immunoglobulin. Secondary infections are possible and should be treated. Topical therapies aimed at reducing pain, especially in mucosal lesions, can be beneficial.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Cerottini JP et al. Eur J Dermatol. 2000 Oct-Nov;10(7):546-7.
Reichert-Penetrat S et al. Eur J Dermatol. 1998 Jan-Feb;8(1):60-2.
Saini P et al. Skinmed. 2020 Aug 1;18(4):252-253.
The patient had been diagnosed with pemphigus vulgaris (PV) 1 year prior to presentation with erosions on the axilla. Biopsy at that time revealed intraepithelial acantholytic blistering with areas of suprabasilar and subcorneal clefting. Direct immunofluorescence was positive for linear/granular IgG deposition throughout the epithelial cell surfaces, as well as linear/granular C3 deposits of the lower two thirds of the epithelial strata, consistent for pemphigus vulgaris.
There is likely a genetic predisposition. Medications that may induce pemphigus include penicillamine, nifedipine, or captopril.
Clinically, PV presents with flaccid blistering lesions that may be cutaneous and/or mucosal. Bullae can progress to erosions and crusting, which then heal with pigment alteration but not scarring. The most commonly affected sites are the mouth, intertriginous areas, face, and neck. Mucosal lesions can involve the lips, esophagus, conjunctiva, and genitals.
Biopsy for histology and direct immunofluorescence is important in distinguishing between PV and other blistering disorders. Up to 75% of patients with active disease also have a positive indirect immunofluorescence with circulating IgG.
There are numerous reports in the literature of PV occurring in previous surgical scars, and areas of friction or trauma. This so-called Koebner’s phenomenon is seen more commonly in several dermatologic conditions, such as psoriasis, lichen planus, verruca vulgaris, and vitiligo.
Treatment for PV is generally immunosuppressive. Systemic therapy usually begins with prednisone and then is transitioned to a steroid sparing agent such as mycophenolate mofetil. Other steroid sparing agents include azathioprine, methotrexate, cyclophosphamide, and intravenous immunoglobulin. Secondary infections are possible and should be treated. Topical therapies aimed at reducing pain, especially in mucosal lesions, can be beneficial.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Cerottini JP et al. Eur J Dermatol. 2000 Oct-Nov;10(7):546-7.
Reichert-Penetrat S et al. Eur J Dermatol. 1998 Jan-Feb;8(1):60-2.
Saini P et al. Skinmed. 2020 Aug 1;18(4):252-253.
The patient had been diagnosed with pemphigus vulgaris (PV) 1 year prior to presentation with erosions on the axilla. Biopsy at that time revealed intraepithelial acantholytic blistering with areas of suprabasilar and subcorneal clefting. Direct immunofluorescence was positive for linear/granular IgG deposition throughout the epithelial cell surfaces, as well as linear/granular C3 deposits of the lower two thirds of the epithelial strata, consistent for pemphigus vulgaris.
There is likely a genetic predisposition. Medications that may induce pemphigus include penicillamine, nifedipine, or captopril.
Clinically, PV presents with flaccid blistering lesions that may be cutaneous and/or mucosal. Bullae can progress to erosions and crusting, which then heal with pigment alteration but not scarring. The most commonly affected sites are the mouth, intertriginous areas, face, and neck. Mucosal lesions can involve the lips, esophagus, conjunctiva, and genitals.
Biopsy for histology and direct immunofluorescence is important in distinguishing between PV and other blistering disorders. Up to 75% of patients with active disease also have a positive indirect immunofluorescence with circulating IgG.
There are numerous reports in the literature of PV occurring in previous surgical scars, and areas of friction or trauma. This so-called Koebner’s phenomenon is seen more commonly in several dermatologic conditions, such as psoriasis, lichen planus, verruca vulgaris, and vitiligo.
Treatment for PV is generally immunosuppressive. Systemic therapy usually begins with prednisone and then is transitioned to a steroid sparing agent such as mycophenolate mofetil. Other steroid sparing agents include azathioprine, methotrexate, cyclophosphamide, and intravenous immunoglobulin. Secondary infections are possible and should be treated. Topical therapies aimed at reducing pain, especially in mucosal lesions, can be beneficial.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Florida. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
Cerottini JP et al. Eur J Dermatol. 2000 Oct-Nov;10(7):546-7.
Reichert-Penetrat S et al. Eur J Dermatol. 1998 Jan-Feb;8(1):60-2.
Saini P et al. Skinmed. 2020 Aug 1;18(4):252-253.
Bimekizumab Gains FDA Approval for Psoriatic Arthritis, Axial Spondyloarthritis
The Food and Drug Administration has approved bimekizumab-bkzx (Bimzelx; UCB) for adult patients with active psoriatic arthritis (PsA), active nonradiographic axial spondyloarthritis (nr-axSpA) with objective signs of inflammation, and active ankylosing spondylitis (AS).
The drug, an interleukin (IL)–17A and IL-17F inhibitor, was first approved in October 2023 for treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
“In psoriatic arthritis and across the spectrum of axSpA, clinical study results and real-world experience outside the US have highlighted that Bimzelx can help patients achieve high thresholds of clinical response that are rapid in onset and sustained up to 2 years,” said Emmanuel Caeymaex, executive vice president, head of patient impact, and chief commercial officer of UCB in a press release.
The recommended dosage of bimekizumab for adult patients with active PsA, nr-axSpA, or AS is 160 mg by subcutaneous injection every 4 weeks. For patients with PsA and coexistent moderate to severe plaque psoriasis, the dosage is the same as for patients with plaque psoriasis. The dosing for plaque psoriasis is to administer 320 mg (two 160-mg injections) by subcutaneous injection at weeks 0, 4, 8, 12, and 16, then every 8 weeks thereafter. For patients weighing ≥ 120 kg, consider a dose of 320 mg every 4 weeks after week 16.
PsA Clinical Trials
The approval for PsA was based on data from two phase 3 clinical trials, including 852 participants naive to biologics (BE OPTIMAL) and 400 participants with inadequate response to treatment with one or two tumor necrosis factor (TNF) inhibitors (BE COMPLETE). Both studies met their primary endpoint, 50% improvement in American College of Rheumatology response criteria (ACR50) at 16 weeks, as well as ranked secondary endpoints. Secondary endpoints included minimal disease activity (MDA) and Psoriasis Area and Severity Index 100 (complete skin clearance) at week 16.
At 16 weeks:
- About 44% of both the biologic-naive (189 of 431) and TNF inhibitor–resistant (116 of 267) groups receiving bimekizumab achieved ACR50 response, compared with 10% (28 of 281) and 7% (9 of 133) receiving placebo, respectively.
- About 45% of all patients treated with bimekizumab achieved MDA.
- Nearly 60% of TNF inhibitor–resistant patients had complete skin clearance.
These responses generally were sustained for 1 year. The most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, and urinary tract infection.
NR-axSpA and AS Clinical Trials
The approval for active nr-axSpA and active AS was based on data from two clinical studies, BE MOBILE 1 (nr-axSpA) and BE MOBILE 2 (AS). Both studies met their primary endpoint, 40% improvement in Assessment of Spondyloarthritis International Society response criteria (ASAS40) at 16 weeks.
Key findings included:
- In nr-axSpA patients, 47.7% (61 of 128) receiving bimekizumab achieved ASAS40 at week 16, compared with 21.4% (27 of 126) receiving placebo.
- In AS patients, 44.8% (99 of 221) in the bimekizumab group achieved ASAS40 response at week 16 vs 22.5% (25 of 111) receiving placebo.
- At 1 year in both groups, 60% treated with bimekizumab achieved an Ankylosing Spondylitis Disease Activity Score < 2.1.
In nr-axSpA, the most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, cough, fatigue, musculoskeletal pain, myalgia, tonsillitis, increase in transaminase, and urinary tract infection. In AS, the most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, injection-site pain, rash, and vulvovaginal mycotic infection.
Bimekizumab was approved by the European Commission for the same rheumatologic indications in June 2023.
Bimekizumab is currently available to eligible patients in the United States, according to the press release.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved bimekizumab-bkzx (Bimzelx; UCB) for adult patients with active psoriatic arthritis (PsA), active nonradiographic axial spondyloarthritis (nr-axSpA) with objective signs of inflammation, and active ankylosing spondylitis (AS).
The drug, an interleukin (IL)–17A and IL-17F inhibitor, was first approved in October 2023 for treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
“In psoriatic arthritis and across the spectrum of axSpA, clinical study results and real-world experience outside the US have highlighted that Bimzelx can help patients achieve high thresholds of clinical response that are rapid in onset and sustained up to 2 years,” said Emmanuel Caeymaex, executive vice president, head of patient impact, and chief commercial officer of UCB in a press release.
The recommended dosage of bimekizumab for adult patients with active PsA, nr-axSpA, or AS is 160 mg by subcutaneous injection every 4 weeks. For patients with PsA and coexistent moderate to severe plaque psoriasis, the dosage is the same as for patients with plaque psoriasis. The dosing for plaque psoriasis is to administer 320 mg (two 160-mg injections) by subcutaneous injection at weeks 0, 4, 8, 12, and 16, then every 8 weeks thereafter. For patients weighing ≥ 120 kg, consider a dose of 320 mg every 4 weeks after week 16.
PsA Clinical Trials
The approval for PsA was based on data from two phase 3 clinical trials, including 852 participants naive to biologics (BE OPTIMAL) and 400 participants with inadequate response to treatment with one or two tumor necrosis factor (TNF) inhibitors (BE COMPLETE). Both studies met their primary endpoint, 50% improvement in American College of Rheumatology response criteria (ACR50) at 16 weeks, as well as ranked secondary endpoints. Secondary endpoints included minimal disease activity (MDA) and Psoriasis Area and Severity Index 100 (complete skin clearance) at week 16.
At 16 weeks:
- About 44% of both the biologic-naive (189 of 431) and TNF inhibitor–resistant (116 of 267) groups receiving bimekizumab achieved ACR50 response, compared with 10% (28 of 281) and 7% (9 of 133) receiving placebo, respectively.
- About 45% of all patients treated with bimekizumab achieved MDA.
- Nearly 60% of TNF inhibitor–resistant patients had complete skin clearance.
These responses generally were sustained for 1 year. The most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, and urinary tract infection.
NR-axSpA and AS Clinical Trials
The approval for active nr-axSpA and active AS was based on data from two clinical studies, BE MOBILE 1 (nr-axSpA) and BE MOBILE 2 (AS). Both studies met their primary endpoint, 40% improvement in Assessment of Spondyloarthritis International Society response criteria (ASAS40) at 16 weeks.
Key findings included:
- In nr-axSpA patients, 47.7% (61 of 128) receiving bimekizumab achieved ASAS40 at week 16, compared with 21.4% (27 of 126) receiving placebo.
- In AS patients, 44.8% (99 of 221) in the bimekizumab group achieved ASAS40 response at week 16 vs 22.5% (25 of 111) receiving placebo.
- At 1 year in both groups, 60% treated with bimekizumab achieved an Ankylosing Spondylitis Disease Activity Score < 2.1.
In nr-axSpA, the most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, cough, fatigue, musculoskeletal pain, myalgia, tonsillitis, increase in transaminase, and urinary tract infection. In AS, the most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, injection-site pain, rash, and vulvovaginal mycotic infection.
Bimekizumab was approved by the European Commission for the same rheumatologic indications in June 2023.
Bimekizumab is currently available to eligible patients in the United States, according to the press release.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved bimekizumab-bkzx (Bimzelx; UCB) for adult patients with active psoriatic arthritis (PsA), active nonradiographic axial spondyloarthritis (nr-axSpA) with objective signs of inflammation, and active ankylosing spondylitis (AS).
The drug, an interleukin (IL)–17A and IL-17F inhibitor, was first approved in October 2023 for treatment of moderate to severe plaque psoriasis in adults who are candidates for systemic therapy or phototherapy.
“In psoriatic arthritis and across the spectrum of axSpA, clinical study results and real-world experience outside the US have highlighted that Bimzelx can help patients achieve high thresholds of clinical response that are rapid in onset and sustained up to 2 years,” said Emmanuel Caeymaex, executive vice president, head of patient impact, and chief commercial officer of UCB in a press release.
The recommended dosage of bimekizumab for adult patients with active PsA, nr-axSpA, or AS is 160 mg by subcutaneous injection every 4 weeks. For patients with PsA and coexistent moderate to severe plaque psoriasis, the dosage is the same as for patients with plaque psoriasis. The dosing for plaque psoriasis is to administer 320 mg (two 160-mg injections) by subcutaneous injection at weeks 0, 4, 8, 12, and 16, then every 8 weeks thereafter. For patients weighing ≥ 120 kg, consider a dose of 320 mg every 4 weeks after week 16.
PsA Clinical Trials
The approval for PsA was based on data from two phase 3 clinical trials, including 852 participants naive to biologics (BE OPTIMAL) and 400 participants with inadequate response to treatment with one or two tumor necrosis factor (TNF) inhibitors (BE COMPLETE). Both studies met their primary endpoint, 50% improvement in American College of Rheumatology response criteria (ACR50) at 16 weeks, as well as ranked secondary endpoints. Secondary endpoints included minimal disease activity (MDA) and Psoriasis Area and Severity Index 100 (complete skin clearance) at week 16.
At 16 weeks:
- About 44% of both the biologic-naive (189 of 431) and TNF inhibitor–resistant (116 of 267) groups receiving bimekizumab achieved ACR50 response, compared with 10% (28 of 281) and 7% (9 of 133) receiving placebo, respectively.
- About 45% of all patients treated with bimekizumab achieved MDA.
- Nearly 60% of TNF inhibitor–resistant patients had complete skin clearance.
These responses generally were sustained for 1 year. The most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, and urinary tract infection.
NR-axSpA and AS Clinical Trials
The approval for active nr-axSpA and active AS was based on data from two clinical studies, BE MOBILE 1 (nr-axSpA) and BE MOBILE 2 (AS). Both studies met their primary endpoint, 40% improvement in Assessment of Spondyloarthritis International Society response criteria (ASAS40) at 16 weeks.
Key findings included:
- In nr-axSpA patients, 47.7% (61 of 128) receiving bimekizumab achieved ASAS40 at week 16, compared with 21.4% (27 of 126) receiving placebo.
- In AS patients, 44.8% (99 of 221) in the bimekizumab group achieved ASAS40 response at week 16 vs 22.5% (25 of 111) receiving placebo.
- At 1 year in both groups, 60% treated with bimekizumab achieved an Ankylosing Spondylitis Disease Activity Score < 2.1.
In nr-axSpA, the most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, cough, fatigue, musculoskeletal pain, myalgia, tonsillitis, increase in transaminase, and urinary tract infection. In AS, the most common adverse reactions are upper respiratory tract infections, oral candidiasis, headache, diarrhea, injection-site pain, rash, and vulvovaginal mycotic infection.
Bimekizumab was approved by the European Commission for the same rheumatologic indications in June 2023.
Bimekizumab is currently available to eligible patients in the United States, according to the press release.
A version of this article first appeared on Medscape.com.
Biomarkers in Cord Blood May Predict AD Onset in Newborns, Study Suggests
TOPLINE:
and interleukin (IL) 31.
METHODOLOGY:
- Researchers conducted a prospective study to evaluate the predictive role of serologic biomarkers and cutaneous markers and the development of AD in 40 full-term newborns from a university hospital in Italy.
- Cord blood was collected at birth and analyzed for serum biomarkers such as CCL17/TARC and IL-31.
- TEWL and skin hydration rates were measured at 1, 6, and 12 months, and dermatological features such as dryness, cradle cap, and eczematous lesions were also monitored during visits.
TAKEAWAY:
- At 6 months, 16 infants had symptoms of AD, which included dry skin, pruritus, and keratosis pilaris, which persisted at 12 months. Their mean Eczema Area and Severity Index score was 6.6 at 6 months and 2.9 at 12 months.
- Infants with signs of AD had significantly higher TEWL levels at the anterior cubital fossa at 1, 6, and 12 months than those without AD.
- Cord blood levels of CCL17/TARC and IL-31 were significantly higher in infants with AD.
- A correlation was found between TEWL values and CCL17 levels at 1, 6, and 12 months.
IN PRACTICE:
“,” the authors wrote. “Stratified interventions based on these variables, family history, FLG [filaggrin] variations, and other biomarkers could offer more targeted approaches to AD prevention and management, especially during the first year of life,” they added.
SOURCE:
The study was led by Angelo Massimiliano D’Erme, MD, PhD, of the Dermatology Unit, in the Department of Medical and Oncology, University of Pisa, Pisa, Italy, and was published online in JAMA Dermatology.
LIMITATIONS:
The limitations included the observational design and small sample size, and it was a single-center study.
DISCLOSURES:
The authors did not disclose any funding information. One author disclosed receiving personal fees from various pharmaceutical companies and serving as a founder and chairman of a nonprofit organization.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.A version of this article appeared on Medscape.com.
TOPLINE:
and interleukin (IL) 31.
METHODOLOGY:
- Researchers conducted a prospective study to evaluate the predictive role of serologic biomarkers and cutaneous markers and the development of AD in 40 full-term newborns from a university hospital in Italy.
- Cord blood was collected at birth and analyzed for serum biomarkers such as CCL17/TARC and IL-31.
- TEWL and skin hydration rates were measured at 1, 6, and 12 months, and dermatological features such as dryness, cradle cap, and eczematous lesions were also monitored during visits.
TAKEAWAY:
- At 6 months, 16 infants had symptoms of AD, which included dry skin, pruritus, and keratosis pilaris, which persisted at 12 months. Their mean Eczema Area and Severity Index score was 6.6 at 6 months and 2.9 at 12 months.
- Infants with signs of AD had significantly higher TEWL levels at the anterior cubital fossa at 1, 6, and 12 months than those without AD.
- Cord blood levels of CCL17/TARC and IL-31 were significantly higher in infants with AD.
- A correlation was found between TEWL values and CCL17 levels at 1, 6, and 12 months.
IN PRACTICE:
“,” the authors wrote. “Stratified interventions based on these variables, family history, FLG [filaggrin] variations, and other biomarkers could offer more targeted approaches to AD prevention and management, especially during the first year of life,” they added.
SOURCE:
The study was led by Angelo Massimiliano D’Erme, MD, PhD, of the Dermatology Unit, in the Department of Medical and Oncology, University of Pisa, Pisa, Italy, and was published online in JAMA Dermatology.
LIMITATIONS:
The limitations included the observational design and small sample size, and it was a single-center study.
DISCLOSURES:
The authors did not disclose any funding information. One author disclosed receiving personal fees from various pharmaceutical companies and serving as a founder and chairman of a nonprofit organization.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.A version of this article appeared on Medscape.com.
TOPLINE:
and interleukin (IL) 31.
METHODOLOGY:
- Researchers conducted a prospective study to evaluate the predictive role of serologic biomarkers and cutaneous markers and the development of AD in 40 full-term newborns from a university hospital in Italy.
- Cord blood was collected at birth and analyzed for serum biomarkers such as CCL17/TARC and IL-31.
- TEWL and skin hydration rates were measured at 1, 6, and 12 months, and dermatological features such as dryness, cradle cap, and eczematous lesions were also monitored during visits.
TAKEAWAY:
- At 6 months, 16 infants had symptoms of AD, which included dry skin, pruritus, and keratosis pilaris, which persisted at 12 months. Their mean Eczema Area and Severity Index score was 6.6 at 6 months and 2.9 at 12 months.
- Infants with signs of AD had significantly higher TEWL levels at the anterior cubital fossa at 1, 6, and 12 months than those without AD.
- Cord blood levels of CCL17/TARC and IL-31 were significantly higher in infants with AD.
- A correlation was found between TEWL values and CCL17 levels at 1, 6, and 12 months.
IN PRACTICE:
“,” the authors wrote. “Stratified interventions based on these variables, family history, FLG [filaggrin] variations, and other biomarkers could offer more targeted approaches to AD prevention and management, especially during the first year of life,” they added.
SOURCE:
The study was led by Angelo Massimiliano D’Erme, MD, PhD, of the Dermatology Unit, in the Department of Medical and Oncology, University of Pisa, Pisa, Italy, and was published online in JAMA Dermatology.
LIMITATIONS:
The limitations included the observational design and small sample size, and it was a single-center study.
DISCLOSURES:
The authors did not disclose any funding information. One author disclosed receiving personal fees from various pharmaceutical companies and serving as a founder and chairman of a nonprofit organization.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.A version of this article appeared on Medscape.com.
Trial Looks at Early Use of Mycophenolate to Reduce Flares, Nephritis
Early use of mycophenolate mofetil (MMF), a drug used to dampen the immune system in organ transplant recipients, may reduce the risk for severe flares in patients with newly diagnosed systemic lupus erythematosus (SLE), according to results from a randomized, open-label, observer-blinded clinical trial.
In interviews, two SLE specialists who were not involved with the study said the research is preliminary but promising. However, another specialist criticized the paper’s reliance on unusual doses of prednisone and MMF, saying it “puts people on a treatment regimen that nobody ever uses.”
The Lupus Foundation of America estimates that about 16,000 people in the United States are diagnosed with lupus each year. “Our current treatment paradigm is to go pretty slowly and start treatment for new-onset, mild SLE with glucocorticoids, if necessary, and hydroxychloroquine,” said Karen H. Costenbader, MD, MPH, of Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts.
Stronger immunosuppressive agents may be added as patients progress, she said.
Off-label use of MMF, which is approved by the Food and Drug Administration only for patients with certain organ transplants, may be appropriate in some cases, she said. “There is a big push to start immunosuppressives earlier, but we currently would reserve mycophenolate for those with severe manifestations — lupus nephritis; vasculitis; or lung, brain, or heart inflammation.”
In the trial, adult patients who received oral prednisone (starting at 0.5 mg/kg per day) and hydroxychloroquine sulfate (5 mg/kg per day) plus MMF (500 mg twice daily) for 96 weeks were less likely to develop severe flares than those who took the regimen without MMF (relative risk [RR], 0.39; 95% CI, 0.17-0.87; P = .01). Severe flares occurred in 10.8% of the MMF group (7 of 65 patients) and in 27.7% of the control group (18 of 65), Yijun You, MD, of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, and colleagues reported in JAMA Network Open.
Patients in the MMF group also had 89% lower risk for lupus nephritis than those in the control group (RR, 0.11; 95% CI, 0.01-0.85; P = .008), with kidney involvement occurring in 1.5% (1 of 65) vs 13.8% (9 of 65).
During 2018-2021, researchers recruited 130 patients in China aged 18-65 years with newly diagnosed SLE, a high titer of anti–double-stranded DNA (dsDNA) antibodies, and no major organ involvement (mean age, 34.5 years; 86.2% women). Patients’ initial 0.5–mg/kg per day prednisone dose was maintained for 4 weeks, then tapered by 5.0 mg every 2 weeks, and when the dose had been reduced to 20.0 mg/day, it was tapered by 5 mg every month and then gradually to 0.1-0.2 mg/kg per day. If patients had severe flares, they stopped taking MMF. (The study authors did not respond to requests for comment on the study.)
‘A Treatment Regimen That Nobody Ever Uses’
While Dr. Costenbader called the study “very interesting” and said “every person diagnosing or taking care of patients with lupus should be familiar” with it, she noted that the prednisone doses were high. “I am wondering why they used quite so much glucocorticoid for everyone. This may have masked some of the MMF effect and biased toward the null. They also used a low dose of MMF and did not ramp it up as we would normally to a full dose. That being said, it is remarkable that it was well-tolerated and resulted in better outcomes over the period of the trial.”
Daniel J. Wallace, MD, of Cedars-Sinai Medical Center, Los Angeles, California, and the University of California, Los Angeles, also highlighted the high doses of prednisone and low doses of MMF. “It’s a useless paper that puts people on a treatment regimen that nobody ever uses,” he said.
The rates of mild to moderate flares were similar between the control and intervention groups (38.5% vs 36.9%, respectively; RR, 0.96; P = .90). This finding is surprising, said Judith A. James, MD, PhD, executive vice president, chief medical officer, and head of the rheumatology clinic and Arthritis and Clinical Immunology Research Program at the Oklahoma Medical Research Foundation in Oklahoma City and also the Associate Vice Provost of Clinical & Translational Science, professor of medicine, and George Lynn Cross Research Professor at the University of Oklahoma Health Sciences Center in Oklahoma City. “It may be that mild flares have a different mechanism or are caused by noninflammatory endotypes that don’t respond to MMF.”
Dr. Costenbader noted that a risk-benefit analysis will need to be done to take the risks of MMF into account. “However, every time that a person flares or is not in lupus low-disease activity state, potentially permanent organ damage is done and the patient suffers,” she said. “Preventing lupus nephritis de novo was also seen — nine cases potentially prevented — and that is also really interesting. It would be amazing if we could completely avoid that life-threatening complication.”
MMF can cause miscarriage and boost the risk for birth defects, and the manufacturer says it can lower the effectiveness of birth control pills. It can also boost the risk for some cancers such as lymphoma and increase the risk for infections.
Surprisingly, the number of adverse events in the control and intervention groups were similar (35.4% vs 46.2%, respectively; RR, 1.30; 95% CI, 0.86-1.99; P = .20). They included infection (30.8% vs 33.8%, respectively; P = .70) and gastrointestinal tract events (16.9% for both; P > .99).
“There were overall pretty similar rates of side effects, but maybe this was because MMF dose was pretty low in the treated group, or the glucocorticoid dose was not so low in both groups,” Dr. Costenbader said. She also noted that “the risk of malignancy with MMF is longer term than this study. It may not show up for 5-10 or even more years, but we know it exists. Infections are also increased with MMF — some of which can be avoided with vaccines for COVID, pneumonia, influenza, shingles, etc. MMF also causes gastrointestinal intolerance, and people often are not able to take it because of nausea, vomiting, diarrhea, and elevated liver function tests.”
Dr. James said the infection rates “may be due to the higher doses of steroids patients in both groups are on for several months at the beginning of the study.”
A total of 12 patients in the MMF group discontinued the intervention for various reasons, and 6 were lost to follow-up. In the control group, 20 discontinued the intervention and two were lost to follow-up. However, all 130 patients in the trial were included in the primary and secondary outcome analyses.
Should clinicians consider prescribing MMF to patients with new-onset SLE? “We usually wait until later when there are indications of more severe disease, but here they started it from the time of diagnosis if the patient was anti-dsDNA positive. Given insurance restrictions in this country, we would be unlikely to be able to do that for many patients,” Dr. Costenbader said. “They likely also overtreated a lot of patients who didn’t need it. Due to our lack of more specific biomarkers and precision medicine for lupus, we do currently undertreat a lot of patients, as this study highlights, as well as overtreat others.”
How Much Might Cost Factor Into Treatment Decisions?
The study did not examine cost. Prednisone and hydroxychloroquine sulfate are inexpensive, but Dr. James said MMF can cost about $450 a month at the study dosage. However, “the average hospitalization without an ICU [intensive care unit] visit for an SLE patient is about $15,000-$20,000. If you can avoid one hospitalization, you can pay for nearly 4 years of MMF. More importantly, from a financial perspective, if you can convert a severe lupus patient to a mild/moderate lupus patient, then the annual costs of lupus decrease nearly by half, from about $52,000 per year to $25,000 per year.”
The study authors noted various limitations such as the small number of subjects, the need for a longer trial “to determine the advantages and disadvantages of early application of MMF,” and the fact that all subjects were Asian. The authors also called for confirmation via a double-blind, placebo-controlled study.
The study was funded by grants to the authors by the National Natural Science Foundation of China, Shanghai Rising-Star Program, Natural Science Foundation of Shanghai, Five-Year National Key R&D Program, and Ruijin–Zhongmei Huadong Lupus Funding. The authors had no disclosures. Dr. Costenbader disclosed consulting/research collaboration relationships with AstraZeneca, Amgen, Biogen, Bristol-Myers Squibb, GSK, Merck, Gilead, and Cabaletta. Dr. James and Dr. Wallace had no disclosures.
A version of this article first appeared on Medscape.com.
Early use of mycophenolate mofetil (MMF), a drug used to dampen the immune system in organ transplant recipients, may reduce the risk for severe flares in patients with newly diagnosed systemic lupus erythematosus (SLE), according to results from a randomized, open-label, observer-blinded clinical trial.
In interviews, two SLE specialists who were not involved with the study said the research is preliminary but promising. However, another specialist criticized the paper’s reliance on unusual doses of prednisone and MMF, saying it “puts people on a treatment regimen that nobody ever uses.”
The Lupus Foundation of America estimates that about 16,000 people in the United States are diagnosed with lupus each year. “Our current treatment paradigm is to go pretty slowly and start treatment for new-onset, mild SLE with glucocorticoids, if necessary, and hydroxychloroquine,” said Karen H. Costenbader, MD, MPH, of Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts.
Stronger immunosuppressive agents may be added as patients progress, she said.
Off-label use of MMF, which is approved by the Food and Drug Administration only for patients with certain organ transplants, may be appropriate in some cases, she said. “There is a big push to start immunosuppressives earlier, but we currently would reserve mycophenolate for those with severe manifestations — lupus nephritis; vasculitis; or lung, brain, or heart inflammation.”
In the trial, adult patients who received oral prednisone (starting at 0.5 mg/kg per day) and hydroxychloroquine sulfate (5 mg/kg per day) plus MMF (500 mg twice daily) for 96 weeks were less likely to develop severe flares than those who took the regimen without MMF (relative risk [RR], 0.39; 95% CI, 0.17-0.87; P = .01). Severe flares occurred in 10.8% of the MMF group (7 of 65 patients) and in 27.7% of the control group (18 of 65), Yijun You, MD, of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, and colleagues reported in JAMA Network Open.
Patients in the MMF group also had 89% lower risk for lupus nephritis than those in the control group (RR, 0.11; 95% CI, 0.01-0.85; P = .008), with kidney involvement occurring in 1.5% (1 of 65) vs 13.8% (9 of 65).
During 2018-2021, researchers recruited 130 patients in China aged 18-65 years with newly diagnosed SLE, a high titer of anti–double-stranded DNA (dsDNA) antibodies, and no major organ involvement (mean age, 34.5 years; 86.2% women). Patients’ initial 0.5–mg/kg per day prednisone dose was maintained for 4 weeks, then tapered by 5.0 mg every 2 weeks, and when the dose had been reduced to 20.0 mg/day, it was tapered by 5 mg every month and then gradually to 0.1-0.2 mg/kg per day. If patients had severe flares, they stopped taking MMF. (The study authors did not respond to requests for comment on the study.)
‘A Treatment Regimen That Nobody Ever Uses’
While Dr. Costenbader called the study “very interesting” and said “every person diagnosing or taking care of patients with lupus should be familiar” with it, she noted that the prednisone doses were high. “I am wondering why they used quite so much glucocorticoid for everyone. This may have masked some of the MMF effect and biased toward the null. They also used a low dose of MMF and did not ramp it up as we would normally to a full dose. That being said, it is remarkable that it was well-tolerated and resulted in better outcomes over the period of the trial.”
Daniel J. Wallace, MD, of Cedars-Sinai Medical Center, Los Angeles, California, and the University of California, Los Angeles, also highlighted the high doses of prednisone and low doses of MMF. “It’s a useless paper that puts people on a treatment regimen that nobody ever uses,” he said.
The rates of mild to moderate flares were similar between the control and intervention groups (38.5% vs 36.9%, respectively; RR, 0.96; P = .90). This finding is surprising, said Judith A. James, MD, PhD, executive vice president, chief medical officer, and head of the rheumatology clinic and Arthritis and Clinical Immunology Research Program at the Oklahoma Medical Research Foundation in Oklahoma City and also the Associate Vice Provost of Clinical & Translational Science, professor of medicine, and George Lynn Cross Research Professor at the University of Oklahoma Health Sciences Center in Oklahoma City. “It may be that mild flares have a different mechanism or are caused by noninflammatory endotypes that don’t respond to MMF.”
Dr. Costenbader noted that a risk-benefit analysis will need to be done to take the risks of MMF into account. “However, every time that a person flares or is not in lupus low-disease activity state, potentially permanent organ damage is done and the patient suffers,” she said. “Preventing lupus nephritis de novo was also seen — nine cases potentially prevented — and that is also really interesting. It would be amazing if we could completely avoid that life-threatening complication.”
MMF can cause miscarriage and boost the risk for birth defects, and the manufacturer says it can lower the effectiveness of birth control pills. It can also boost the risk for some cancers such as lymphoma and increase the risk for infections.
Surprisingly, the number of adverse events in the control and intervention groups were similar (35.4% vs 46.2%, respectively; RR, 1.30; 95% CI, 0.86-1.99; P = .20). They included infection (30.8% vs 33.8%, respectively; P = .70) and gastrointestinal tract events (16.9% for both; P > .99).
“There were overall pretty similar rates of side effects, but maybe this was because MMF dose was pretty low in the treated group, or the glucocorticoid dose was not so low in both groups,” Dr. Costenbader said. She also noted that “the risk of malignancy with MMF is longer term than this study. It may not show up for 5-10 or even more years, but we know it exists. Infections are also increased with MMF — some of which can be avoided with vaccines for COVID, pneumonia, influenza, shingles, etc. MMF also causes gastrointestinal intolerance, and people often are not able to take it because of nausea, vomiting, diarrhea, and elevated liver function tests.”
Dr. James said the infection rates “may be due to the higher doses of steroids patients in both groups are on for several months at the beginning of the study.”
A total of 12 patients in the MMF group discontinued the intervention for various reasons, and 6 were lost to follow-up. In the control group, 20 discontinued the intervention and two were lost to follow-up. However, all 130 patients in the trial were included in the primary and secondary outcome analyses.
Should clinicians consider prescribing MMF to patients with new-onset SLE? “We usually wait until later when there are indications of more severe disease, but here they started it from the time of diagnosis if the patient was anti-dsDNA positive. Given insurance restrictions in this country, we would be unlikely to be able to do that for many patients,” Dr. Costenbader said. “They likely also overtreated a lot of patients who didn’t need it. Due to our lack of more specific biomarkers and precision medicine for lupus, we do currently undertreat a lot of patients, as this study highlights, as well as overtreat others.”
How Much Might Cost Factor Into Treatment Decisions?
The study did not examine cost. Prednisone and hydroxychloroquine sulfate are inexpensive, but Dr. James said MMF can cost about $450 a month at the study dosage. However, “the average hospitalization without an ICU [intensive care unit] visit for an SLE patient is about $15,000-$20,000. If you can avoid one hospitalization, you can pay for nearly 4 years of MMF. More importantly, from a financial perspective, if you can convert a severe lupus patient to a mild/moderate lupus patient, then the annual costs of lupus decrease nearly by half, from about $52,000 per year to $25,000 per year.”
The study authors noted various limitations such as the small number of subjects, the need for a longer trial “to determine the advantages and disadvantages of early application of MMF,” and the fact that all subjects were Asian. The authors also called for confirmation via a double-blind, placebo-controlled study.
The study was funded by grants to the authors by the National Natural Science Foundation of China, Shanghai Rising-Star Program, Natural Science Foundation of Shanghai, Five-Year National Key R&D Program, and Ruijin–Zhongmei Huadong Lupus Funding. The authors had no disclosures. Dr. Costenbader disclosed consulting/research collaboration relationships with AstraZeneca, Amgen, Biogen, Bristol-Myers Squibb, GSK, Merck, Gilead, and Cabaletta. Dr. James and Dr. Wallace had no disclosures.
A version of this article first appeared on Medscape.com.
Early use of mycophenolate mofetil (MMF), a drug used to dampen the immune system in organ transplant recipients, may reduce the risk for severe flares in patients with newly diagnosed systemic lupus erythematosus (SLE), according to results from a randomized, open-label, observer-blinded clinical trial.
In interviews, two SLE specialists who were not involved with the study said the research is preliminary but promising. However, another specialist criticized the paper’s reliance on unusual doses of prednisone and MMF, saying it “puts people on a treatment regimen that nobody ever uses.”
The Lupus Foundation of America estimates that about 16,000 people in the United States are diagnosed with lupus each year. “Our current treatment paradigm is to go pretty slowly and start treatment for new-onset, mild SLE with glucocorticoids, if necessary, and hydroxychloroquine,” said Karen H. Costenbader, MD, MPH, of Harvard Medical School and Harvard School of Public Health, Boston, Massachusetts.
Stronger immunosuppressive agents may be added as patients progress, she said.
Off-label use of MMF, which is approved by the Food and Drug Administration only for patients with certain organ transplants, may be appropriate in some cases, she said. “There is a big push to start immunosuppressives earlier, but we currently would reserve mycophenolate for those with severe manifestations — lupus nephritis; vasculitis; or lung, brain, or heart inflammation.”
In the trial, adult patients who received oral prednisone (starting at 0.5 mg/kg per day) and hydroxychloroquine sulfate (5 mg/kg per day) plus MMF (500 mg twice daily) for 96 weeks were less likely to develop severe flares than those who took the regimen without MMF (relative risk [RR], 0.39; 95% CI, 0.17-0.87; P = .01). Severe flares occurred in 10.8% of the MMF group (7 of 65 patients) and in 27.7% of the control group (18 of 65), Yijun You, MD, of Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China, and colleagues reported in JAMA Network Open.
Patients in the MMF group also had 89% lower risk for lupus nephritis than those in the control group (RR, 0.11; 95% CI, 0.01-0.85; P = .008), with kidney involvement occurring in 1.5% (1 of 65) vs 13.8% (9 of 65).
During 2018-2021, researchers recruited 130 patients in China aged 18-65 years with newly diagnosed SLE, a high titer of anti–double-stranded DNA (dsDNA) antibodies, and no major organ involvement (mean age, 34.5 years; 86.2% women). Patients’ initial 0.5–mg/kg per day prednisone dose was maintained for 4 weeks, then tapered by 5.0 mg every 2 weeks, and when the dose had been reduced to 20.0 mg/day, it was tapered by 5 mg every month and then gradually to 0.1-0.2 mg/kg per day. If patients had severe flares, they stopped taking MMF. (The study authors did not respond to requests for comment on the study.)
‘A Treatment Regimen That Nobody Ever Uses’
While Dr. Costenbader called the study “very interesting” and said “every person diagnosing or taking care of patients with lupus should be familiar” with it, she noted that the prednisone doses were high. “I am wondering why they used quite so much glucocorticoid for everyone. This may have masked some of the MMF effect and biased toward the null. They also used a low dose of MMF and did not ramp it up as we would normally to a full dose. That being said, it is remarkable that it was well-tolerated and resulted in better outcomes over the period of the trial.”
Daniel J. Wallace, MD, of Cedars-Sinai Medical Center, Los Angeles, California, and the University of California, Los Angeles, also highlighted the high doses of prednisone and low doses of MMF. “It’s a useless paper that puts people on a treatment regimen that nobody ever uses,” he said.
The rates of mild to moderate flares were similar between the control and intervention groups (38.5% vs 36.9%, respectively; RR, 0.96; P = .90). This finding is surprising, said Judith A. James, MD, PhD, executive vice president, chief medical officer, and head of the rheumatology clinic and Arthritis and Clinical Immunology Research Program at the Oklahoma Medical Research Foundation in Oklahoma City and also the Associate Vice Provost of Clinical & Translational Science, professor of medicine, and George Lynn Cross Research Professor at the University of Oklahoma Health Sciences Center in Oklahoma City. “It may be that mild flares have a different mechanism or are caused by noninflammatory endotypes that don’t respond to MMF.”
Dr. Costenbader noted that a risk-benefit analysis will need to be done to take the risks of MMF into account. “However, every time that a person flares or is not in lupus low-disease activity state, potentially permanent organ damage is done and the patient suffers,” she said. “Preventing lupus nephritis de novo was also seen — nine cases potentially prevented — and that is also really interesting. It would be amazing if we could completely avoid that life-threatening complication.”
MMF can cause miscarriage and boost the risk for birth defects, and the manufacturer says it can lower the effectiveness of birth control pills. It can also boost the risk for some cancers such as lymphoma and increase the risk for infections.
Surprisingly, the number of adverse events in the control and intervention groups were similar (35.4% vs 46.2%, respectively; RR, 1.30; 95% CI, 0.86-1.99; P = .20). They included infection (30.8% vs 33.8%, respectively; P = .70) and gastrointestinal tract events (16.9% for both; P > .99).
“There were overall pretty similar rates of side effects, but maybe this was because MMF dose was pretty low in the treated group, or the glucocorticoid dose was not so low in both groups,” Dr. Costenbader said. She also noted that “the risk of malignancy with MMF is longer term than this study. It may not show up for 5-10 or even more years, but we know it exists. Infections are also increased with MMF — some of which can be avoided with vaccines for COVID, pneumonia, influenza, shingles, etc. MMF also causes gastrointestinal intolerance, and people often are not able to take it because of nausea, vomiting, diarrhea, and elevated liver function tests.”
Dr. James said the infection rates “may be due to the higher doses of steroids patients in both groups are on for several months at the beginning of the study.”
A total of 12 patients in the MMF group discontinued the intervention for various reasons, and 6 were lost to follow-up. In the control group, 20 discontinued the intervention and two were lost to follow-up. However, all 130 patients in the trial were included in the primary and secondary outcome analyses.
Should clinicians consider prescribing MMF to patients with new-onset SLE? “We usually wait until later when there are indications of more severe disease, but here they started it from the time of diagnosis if the patient was anti-dsDNA positive. Given insurance restrictions in this country, we would be unlikely to be able to do that for many patients,” Dr. Costenbader said. “They likely also overtreated a lot of patients who didn’t need it. Due to our lack of more specific biomarkers and precision medicine for lupus, we do currently undertreat a lot of patients, as this study highlights, as well as overtreat others.”
How Much Might Cost Factor Into Treatment Decisions?
The study did not examine cost. Prednisone and hydroxychloroquine sulfate are inexpensive, but Dr. James said MMF can cost about $450 a month at the study dosage. However, “the average hospitalization without an ICU [intensive care unit] visit for an SLE patient is about $15,000-$20,000. If you can avoid one hospitalization, you can pay for nearly 4 years of MMF. More importantly, from a financial perspective, if you can convert a severe lupus patient to a mild/moderate lupus patient, then the annual costs of lupus decrease nearly by half, from about $52,000 per year to $25,000 per year.”
The study authors noted various limitations such as the small number of subjects, the need for a longer trial “to determine the advantages and disadvantages of early application of MMF,” and the fact that all subjects were Asian. The authors also called for confirmation via a double-blind, placebo-controlled study.
The study was funded by grants to the authors by the National Natural Science Foundation of China, Shanghai Rising-Star Program, Natural Science Foundation of Shanghai, Five-Year National Key R&D Program, and Ruijin–Zhongmei Huadong Lupus Funding. The authors had no disclosures. Dr. Costenbader disclosed consulting/research collaboration relationships with AstraZeneca, Amgen, Biogen, Bristol-Myers Squibb, GSK, Merck, Gilead, and Cabaletta. Dr. James and Dr. Wallace had no disclosures.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Inspection of Deep Tumor Margins for Accurate Cutaneous Squamous Cell Carcinoma Staging
To the Editor:
Histopathologic analysis of debulk specimens in Mohs micrographic surgery (MMS) may augment identification of high-risk factors in cutaneous squamous cell carcinoma (cSCC), which may warrant tumor upstaging.1 Intratumor location has not been studied when looking at these high-risk factors. Herein, we report 4 cSCCs initially categorized as well differentiated that were reclassified as moderate to poorly differentiated on analysis of debulk specimens obtained via shave removal.
An 80-year-old man (patient 1) presented with a tender 2-cm erythematous plaque with dried hemorrhagic crusting on the frontal scalp. He had a history of nonmelanoma skin cancers. A biopsy revealed a well-differentiated cSCC, which was upgraded from a T2a tumor to T2b during MMS due to galea involvement. Debulk analysis revealed moderate to poorly differentiated cSCC, with the least-differentiated cells at the deep margin (Figure 1A). Given T2b staging, baseline imaging and radiation therapy were recommended.
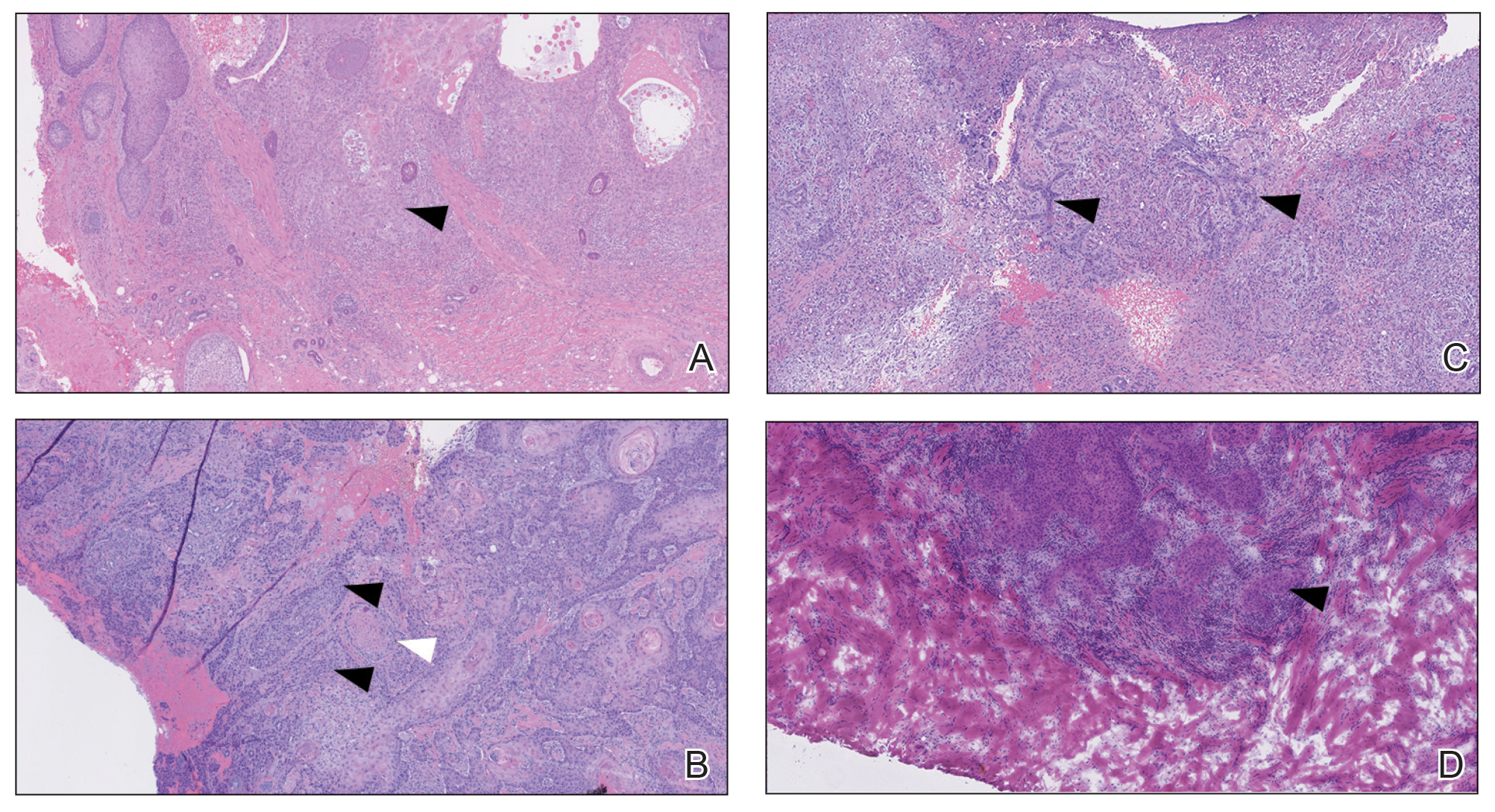
A 75-year-old man (patient 2) presented with a 2-cm erythematous plaque on the left vertex scalp with hemorrhagic crusting, yellow scale, and purulent drainage. He had a history of cSCCs. A biopsy revealed well-differentiated invasive cSCC, which was upgraded from a T2a tumor to T2b during MMS due to tumor extension beyond the subcutaneous fat. Examination of the second Mohs stage revealed moderately differentiated cSCC, with the least-differentiated cells at the deep margin, infiltration beyond the subcutaneous fat, and perineural invasion (Figure 1B). Given T2b staging, baseline imaging and radiation therapy were recommended.
An 86-year-old woman (patient 3) presented with a tender 2.4-cm plum-colored nodule on the right lower leg. She had a history of basal cell carcinoma. A biopsy revealed a well-differentiated invasive cSCC staged at T2a. Debulk analysis revealed moderately differentiated cSCC, with the least-differentiated cells at the deep margin, though the staging remained the same (Figure 1C).
An 82-year-old man (patient 4) presented with a 2.7-cm ulcerated nodule with adjacent scaling on the vertex scalp. He had no history of skin cancer. A biopsy revealed a well-differentiated cSCC (Figure 2) that was upgraded from a T2a tumor to T2b during MMS due to tumor extension beyond the subcutaneous fat. Debulk analysis revealed moderate to poorly differentiated cSCC, with the least-differentiated cells with single-cell extension at the deep margin in the galea (Figure 1D). Given T2b staging, baseline imaging and radiation therapy were recommended.
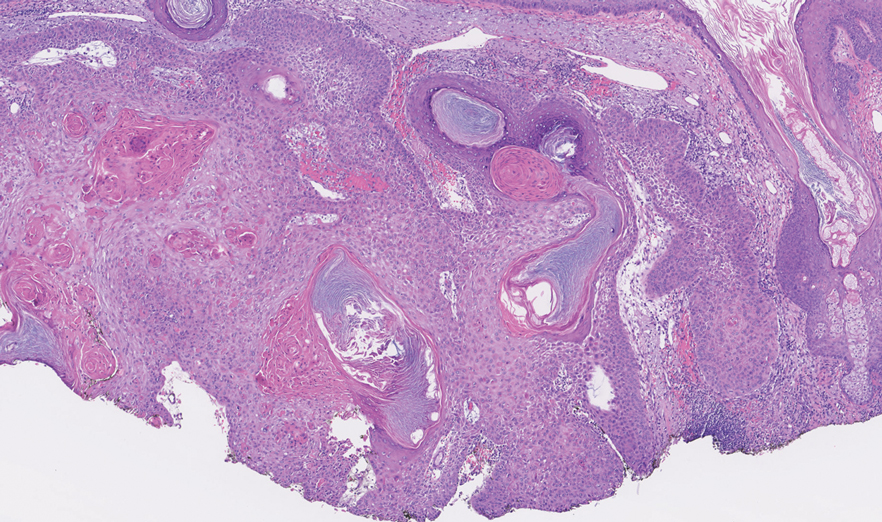
Tumor differentiation is a factor included in the Brigham and Women’s Hospital staging system, and intratumor variability can be clinically relevant for tumor staging.1 Specifically, cSCCs may exhibit intratumor heterogeneity in which predominantly well-differentiated tumors contain focal areas of poorer differentiation.2 This intratumor heterogeneity complicates estimation of tumor risk, as a well-differentiated tumor on biopsy may exhibit poor differentiation at a deeper margin. Our cases highlight that the cells at the deeper margin indeed can show poorer differentiation or other higher-risk tumor features. Thus, the most clinically relevant cells for tumor staging and prognostication may not be visible on initial biopsy, underscoring the utility of close examination of the deep layer of the debulk specimen and Mohs layer for comprehensive staging.
Genetic studies have attempted to identify gene expression patterns in cSCCs that predispose to invasion.3 Three of the top 6 genes in this “invasion signature gene set” were matrix metalloproteases; additionally, IL-24 messenger RNA was upregulated in both the cSCC invasion front and in situ cSCCs. IL-24 has been shown to upregulate the expression of matrix metalloprotease 7 in vitro, suggesting that it may influence tumor progression.3 Although gene expression was not included in this series, the identification of genetic variability in the most poorly differentiated cells residing in the deep margins is of great interest and may reveal mutations contributing to irregular cell morphology and cSCC invasiveness.
Prior studies have indicated that a proportion of cSCCs are histopathologically upgraded from the initial biopsy during MMS due to evidence of perineural invasion, bony invasion, or lesser differentiation noted during MMS stages or debulk analysis.1,4 However, the majority of Mohs surgeons report immediately discarding debulk specimens without further evaluation.5 Herein, we highlight 4 cSCC cases in which the deep margins of the debulk specimen contained the most dedifferentiated cells. Our findings emphasize the importance of thoroughly examining deep tumor margins for complete staging yet also highlight that identifying cells at these margins may not change patient management when high-risk criteria are already met.
- McIlwee BE, Abidi NY, Ravi M, et al. Utility of debulk specimens during Mohs micrographic surgery for cutaneous squamous cell carcinoma. Dermatol Surg. 2021;47:599-604.
- Ramón y Cajal S, Sesé M, Capdevila C, et al. Clinical implications of intratumor heterogeneity: challenges and opportunities. J Mol Med. 2020;98:161-177.
- Mitsui H, Suárez-Fariñas M, Gulati N, et al. Gene expression profiling of the leading edge of cutaneous squamous cell carcinoma: IL-24-driven MMP-7. J Invest Dermatol. 2014;134:1418-1427.
- Chung E, Hoang S, McEvoy AM, et al. Histopathologic upgrading of cutaneous squamous cell carcinomas during Mohs micrographic surgery: a retrospective cohort study. J Am Acad Dermatol. 2021;85:923-930.
- Alniemi DT, Swanson AM, Lasarev M, et al. Tumor debulking trends for keratinocyte carcinomas among Mohs surgeons. Dermatol Surg. 2021;47:1660-1661.
To the Editor:
Histopathologic analysis of debulk specimens in Mohs micrographic surgery (MMS) may augment identification of high-risk factors in cutaneous squamous cell carcinoma (cSCC), which may warrant tumor upstaging.1 Intratumor location has not been studied when looking at these high-risk factors. Herein, we report 4 cSCCs initially categorized as well differentiated that were reclassified as moderate to poorly differentiated on analysis of debulk specimens obtained via shave removal.
An 80-year-old man (patient 1) presented with a tender 2-cm erythematous plaque with dried hemorrhagic crusting on the frontal scalp. He had a history of nonmelanoma skin cancers. A biopsy revealed a well-differentiated cSCC, which was upgraded from a T2a tumor to T2b during MMS due to galea involvement. Debulk analysis revealed moderate to poorly differentiated cSCC, with the least-differentiated cells at the deep margin (Figure 1A). Given T2b staging, baseline imaging and radiation therapy were recommended.
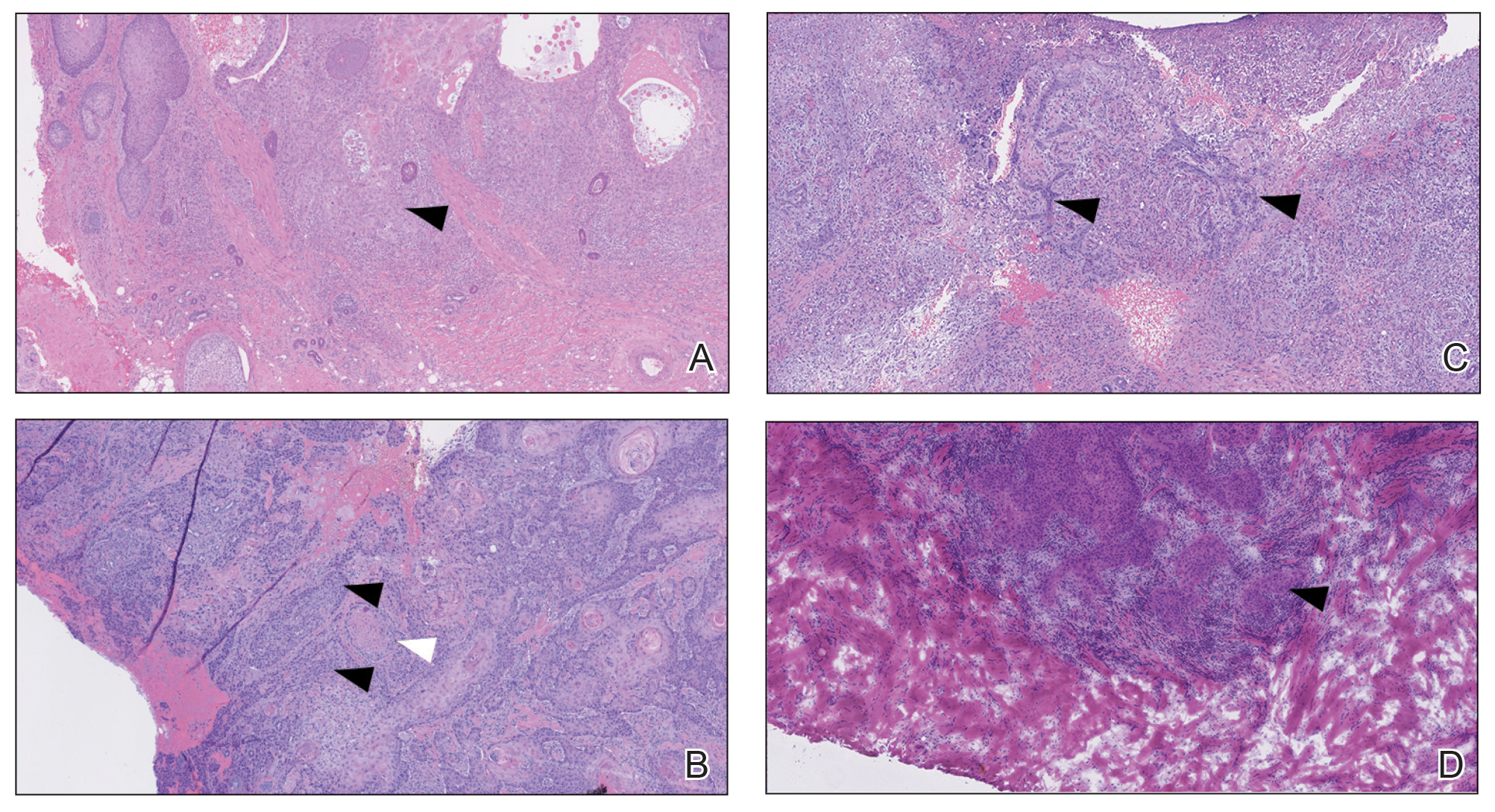
A 75-year-old man (patient 2) presented with a 2-cm erythematous plaque on the left vertex scalp with hemorrhagic crusting, yellow scale, and purulent drainage. He had a history of cSCCs. A biopsy revealed well-differentiated invasive cSCC, which was upgraded from a T2a tumor to T2b during MMS due to tumor extension beyond the subcutaneous fat. Examination of the second Mohs stage revealed moderately differentiated cSCC, with the least-differentiated cells at the deep margin, infiltration beyond the subcutaneous fat, and perineural invasion (Figure 1B). Given T2b staging, baseline imaging and radiation therapy were recommended.
An 86-year-old woman (patient 3) presented with a tender 2.4-cm plum-colored nodule on the right lower leg. She had a history of basal cell carcinoma. A biopsy revealed a well-differentiated invasive cSCC staged at T2a. Debulk analysis revealed moderately differentiated cSCC, with the least-differentiated cells at the deep margin, though the staging remained the same (Figure 1C).
An 82-year-old man (patient 4) presented with a 2.7-cm ulcerated nodule with adjacent scaling on the vertex scalp. He had no history of skin cancer. A biopsy revealed a well-differentiated cSCC (Figure 2) that was upgraded from a T2a tumor to T2b during MMS due to tumor extension beyond the subcutaneous fat. Debulk analysis revealed moderate to poorly differentiated cSCC, with the least-differentiated cells with single-cell extension at the deep margin in the galea (Figure 1D). Given T2b staging, baseline imaging and radiation therapy were recommended.
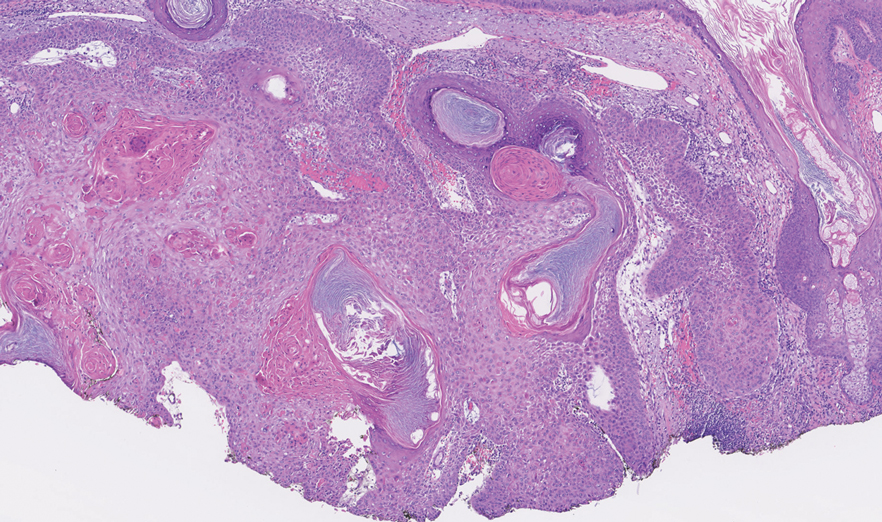
Tumor differentiation is a factor included in the Brigham and Women’s Hospital staging system, and intratumor variability can be clinically relevant for tumor staging.1 Specifically, cSCCs may exhibit intratumor heterogeneity in which predominantly well-differentiated tumors contain focal areas of poorer differentiation.2 This intratumor heterogeneity complicates estimation of tumor risk, as a well-differentiated tumor on biopsy may exhibit poor differentiation at a deeper margin. Our cases highlight that the cells at the deeper margin indeed can show poorer differentiation or other higher-risk tumor features. Thus, the most clinically relevant cells for tumor staging and prognostication may not be visible on initial biopsy, underscoring the utility of close examination of the deep layer of the debulk specimen and Mohs layer for comprehensive staging.
Genetic studies have attempted to identify gene expression patterns in cSCCs that predispose to invasion.3 Three of the top 6 genes in this “invasion signature gene set” were matrix metalloproteases; additionally, IL-24 messenger RNA was upregulated in both the cSCC invasion front and in situ cSCCs. IL-24 has been shown to upregulate the expression of matrix metalloprotease 7 in vitro, suggesting that it may influence tumor progression.3 Although gene expression was not included in this series, the identification of genetic variability in the most poorly differentiated cells residing in the deep margins is of great interest and may reveal mutations contributing to irregular cell morphology and cSCC invasiveness.
Prior studies have indicated that a proportion of cSCCs are histopathologically upgraded from the initial biopsy during MMS due to evidence of perineural invasion, bony invasion, or lesser differentiation noted during MMS stages or debulk analysis.1,4 However, the majority of Mohs surgeons report immediately discarding debulk specimens without further evaluation.5 Herein, we highlight 4 cSCC cases in which the deep margins of the debulk specimen contained the most dedifferentiated cells. Our findings emphasize the importance of thoroughly examining deep tumor margins for complete staging yet also highlight that identifying cells at these margins may not change patient management when high-risk criteria are already met.
To the Editor:
Histopathologic analysis of debulk specimens in Mohs micrographic surgery (MMS) may augment identification of high-risk factors in cutaneous squamous cell carcinoma (cSCC), which may warrant tumor upstaging.1 Intratumor location has not been studied when looking at these high-risk factors. Herein, we report 4 cSCCs initially categorized as well differentiated that were reclassified as moderate to poorly differentiated on analysis of debulk specimens obtained via shave removal.
An 80-year-old man (patient 1) presented with a tender 2-cm erythematous plaque with dried hemorrhagic crusting on the frontal scalp. He had a history of nonmelanoma skin cancers. A biopsy revealed a well-differentiated cSCC, which was upgraded from a T2a tumor to T2b during MMS due to galea involvement. Debulk analysis revealed moderate to poorly differentiated cSCC, with the least-differentiated cells at the deep margin (Figure 1A). Given T2b staging, baseline imaging and radiation therapy were recommended.
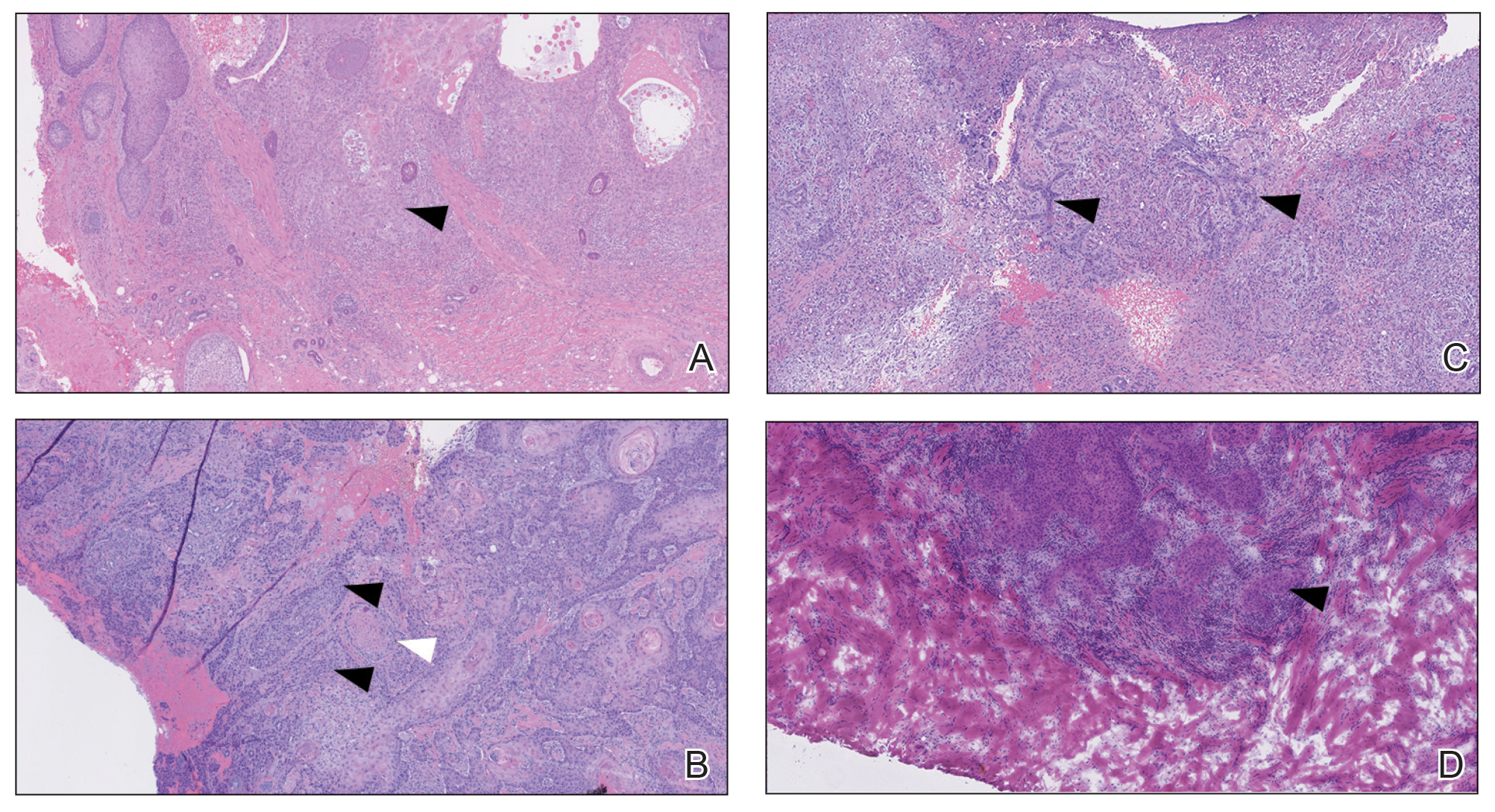
A 75-year-old man (patient 2) presented with a 2-cm erythematous plaque on the left vertex scalp with hemorrhagic crusting, yellow scale, and purulent drainage. He had a history of cSCCs. A biopsy revealed well-differentiated invasive cSCC, which was upgraded from a T2a tumor to T2b during MMS due to tumor extension beyond the subcutaneous fat. Examination of the second Mohs stage revealed moderately differentiated cSCC, with the least-differentiated cells at the deep margin, infiltration beyond the subcutaneous fat, and perineural invasion (Figure 1B). Given T2b staging, baseline imaging and radiation therapy were recommended.
An 86-year-old woman (patient 3) presented with a tender 2.4-cm plum-colored nodule on the right lower leg. She had a history of basal cell carcinoma. A biopsy revealed a well-differentiated invasive cSCC staged at T2a. Debulk analysis revealed moderately differentiated cSCC, with the least-differentiated cells at the deep margin, though the staging remained the same (Figure 1C).
An 82-year-old man (patient 4) presented with a 2.7-cm ulcerated nodule with adjacent scaling on the vertex scalp. He had no history of skin cancer. A biopsy revealed a well-differentiated cSCC (Figure 2) that was upgraded from a T2a tumor to T2b during MMS due to tumor extension beyond the subcutaneous fat. Debulk analysis revealed moderate to poorly differentiated cSCC, with the least-differentiated cells with single-cell extension at the deep margin in the galea (Figure 1D). Given T2b staging, baseline imaging and radiation therapy were recommended.
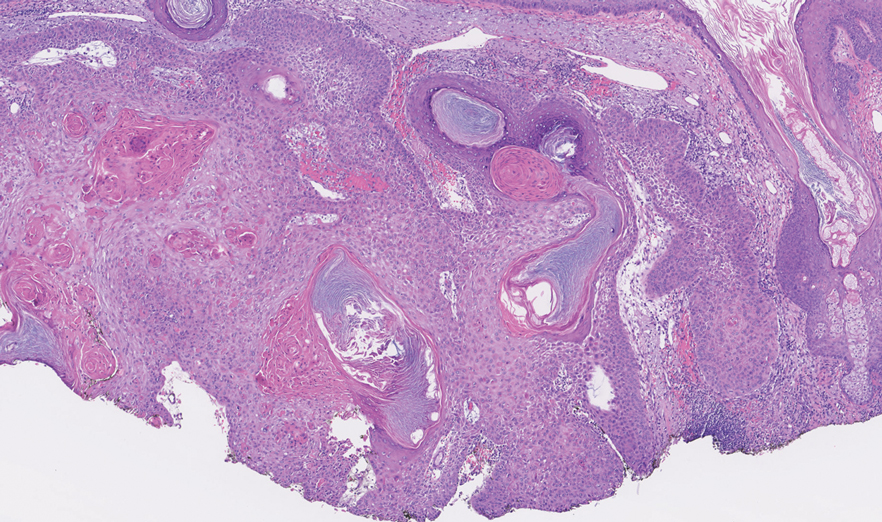
Tumor differentiation is a factor included in the Brigham and Women’s Hospital staging system, and intratumor variability can be clinically relevant for tumor staging.1 Specifically, cSCCs may exhibit intratumor heterogeneity in which predominantly well-differentiated tumors contain focal areas of poorer differentiation.2 This intratumor heterogeneity complicates estimation of tumor risk, as a well-differentiated tumor on biopsy may exhibit poor differentiation at a deeper margin. Our cases highlight that the cells at the deeper margin indeed can show poorer differentiation or other higher-risk tumor features. Thus, the most clinically relevant cells for tumor staging and prognostication may not be visible on initial biopsy, underscoring the utility of close examination of the deep layer of the debulk specimen and Mohs layer for comprehensive staging.
Genetic studies have attempted to identify gene expression patterns in cSCCs that predispose to invasion.3 Three of the top 6 genes in this “invasion signature gene set” were matrix metalloproteases; additionally, IL-24 messenger RNA was upregulated in both the cSCC invasion front and in situ cSCCs. IL-24 has been shown to upregulate the expression of matrix metalloprotease 7 in vitro, suggesting that it may influence tumor progression.3 Although gene expression was not included in this series, the identification of genetic variability in the most poorly differentiated cells residing in the deep margins is of great interest and may reveal mutations contributing to irregular cell morphology and cSCC invasiveness.
Prior studies have indicated that a proportion of cSCCs are histopathologically upgraded from the initial biopsy during MMS due to evidence of perineural invasion, bony invasion, or lesser differentiation noted during MMS stages or debulk analysis.1,4 However, the majority of Mohs surgeons report immediately discarding debulk specimens without further evaluation.5 Herein, we highlight 4 cSCC cases in which the deep margins of the debulk specimen contained the most dedifferentiated cells. Our findings emphasize the importance of thoroughly examining deep tumor margins for complete staging yet also highlight that identifying cells at these margins may not change patient management when high-risk criteria are already met.
- McIlwee BE, Abidi NY, Ravi M, et al. Utility of debulk specimens during Mohs micrographic surgery for cutaneous squamous cell carcinoma. Dermatol Surg. 2021;47:599-604.
- Ramón y Cajal S, Sesé M, Capdevila C, et al. Clinical implications of intratumor heterogeneity: challenges and opportunities. J Mol Med. 2020;98:161-177.
- Mitsui H, Suárez-Fariñas M, Gulati N, et al. Gene expression profiling of the leading edge of cutaneous squamous cell carcinoma: IL-24-driven MMP-7. J Invest Dermatol. 2014;134:1418-1427.
- Chung E, Hoang S, McEvoy AM, et al. Histopathologic upgrading of cutaneous squamous cell carcinomas during Mohs micrographic surgery: a retrospective cohort study. J Am Acad Dermatol. 2021;85:923-930.
- Alniemi DT, Swanson AM, Lasarev M, et al. Tumor debulking trends for keratinocyte carcinomas among Mohs surgeons. Dermatol Surg. 2021;47:1660-1661.
- McIlwee BE, Abidi NY, Ravi M, et al. Utility of debulk specimens during Mohs micrographic surgery for cutaneous squamous cell carcinoma. Dermatol Surg. 2021;47:599-604.
- Ramón y Cajal S, Sesé M, Capdevila C, et al. Clinical implications of intratumor heterogeneity: challenges and opportunities. J Mol Med. 2020;98:161-177.
- Mitsui H, Suárez-Fariñas M, Gulati N, et al. Gene expression profiling of the leading edge of cutaneous squamous cell carcinoma: IL-24-driven MMP-7. J Invest Dermatol. 2014;134:1418-1427.
- Chung E, Hoang S, McEvoy AM, et al. Histopathologic upgrading of cutaneous squamous cell carcinomas during Mohs micrographic surgery: a retrospective cohort study. J Am Acad Dermatol. 2021;85:923-930.
- Alniemi DT, Swanson AM, Lasarev M, et al. Tumor debulking trends for keratinocyte carcinomas among Mohs surgeons. Dermatol Surg. 2021;47:1660-1661.
Practice Points
- A proportion of cutaneous squamous cell carcinomas are upgraded from the initial biopsy during Mohs micrographic surgery due to evidence of perineural invasion, bony invasion, or lesser differentiation noted on Mohs stages or debulk analysis.
- Thorough inspection of the deep tumor margins may be required for accurate tumor staging and evaluation of metastatic risk. Cells at the deep margin of the tumor may demonstrate poorer differentiation and/or other higher-risk tumor features than those closer to the surface.
- Tumor staging may be incomplete until the deep margins are assessed to find the most dysplastic and likely clinically relevant cells, which may be missed without evaluation of the debulked tumor.
New Options for Treating Atopic Dermatitis Available, and in Development
HUNTINGTON BEACH, CALIFORNIA — If the number of recent drug approvals for atopic dermatitis (AD) is overwhelming, the future is unlikely to be any less challenging: According to the National Eczema Association, the current pipeline for AD includes 39 injectable medications, 21 oral agents, and 49 topicals, some with novel targets, like human umbilical cord blood derived stem cells.
“It’s amazing how many drugs are coming out for AD,” Robert Sidbury, MD, MPH, said at the annual meeting of the Pacific Dermatologic Association (PDA). and is approved in Europe for the treatment of moderate to severe AD in patients aged ≥ 12 years. (On September 13, after the PDA meeting, lebrikizumab was approved by the Food and Drug Administration [FDA] for treatment of moderate to severe AD in adults and adolescents aged ≥ 12 years.)
In two identical phase 3 trials known as ADvocate 1 and ADvocate 2, researchers randomly assigned 851 patients with moderate to severe AD in a 2:1 ratio to receive either lebrikizumab at a dose of 250 mg (loading dose of 500 mg at baseline and week 2) or placebo, administered subcutaneously every 2 weeks, through week 16. The primary outcome was an Investigator’s Global Assessment (IGA) score of 0 or 1, indicating clear or almost clear skin. The researchers reported that an IGA score of 0 or 1 was achieved by 43.1% of patients in the lebrikizumab arm compared with 12.7% of those in the placebo arm.
“Those are good numbers,” said Dr. Sidbury, who was not involved with the study. Conjunctivitis occurred more often in those who received lebrikizumab compared with those who received placebo (7.4% vs 2.8%, respectively), “which is not surprising because it is an IL-13 agent,” he said.
In a subsequent study presented during the Revolutionizing Atopic Dermatitis meeting in the fall of 2023, researchers presented data on Eczema Severity and Area Index (EASI)-90 responses in the ADvocate trial participants, showing EASI-90 responses were sustained up to 38 weeks after lebrikizumab withdrawal, while serum concentrations were negligible. They found that between week 14 and week 32, approximately five serum concentration half-lives of the medication had elapsed since patients randomized to the withdrawal arm received their last dose of lebrikizumab, extending to approximately 11 half-lives by week 52. “That durability of response with next to no blood levels of drug in many of the study participants is interesting,” said Dr. Sidbury, who cochairs the current iteration of the American Academy of Dermatology Atopic Dermatitis Guidelines.
Nemolizumab is a neuroimmune response modulator that inhibits the IL-31 receptor and is approved in Japan for the treatment of itch associated with AD in patients aged ≥ 13 years. Results from two identical phase 3, randomized, controlled trials known as ARCADIA 1 and ARCADIA 2 found that 36% of patients in ARCADIA 1 and 38% in ARCADIA 2 achieved clear skin, compared with 25% and 26% of patients in the placebo group, respectively. (Nemolizumab was recently approved by the FDA for treating prurigo nodularis and is under FDA review for AD.)
In terms of safety, Dr. Sidbury, who is a member of the steering committee for the ARCADIA trials, said that nemolizumab has been “generally well tolerated;” with 1%-3% of study participants experiencing at least one serious treatment-emergent adverse event that included asthma exacerbation, facial edema, and peripheral edema. “The latest data are reassuring but we are watching these safety concerns carefully,” he said.
Dr. Sidbury disclosed that he is an investigator for Regeneron, Pfizer, Galderma, UCB, and Castle; a consultant for Lilly, Leo, Arcutis, and Dermavant; and a member of the speaker’s bureau for Beiersdorf.
A version of this article appeared on Medscape.com.
HUNTINGTON BEACH, CALIFORNIA — If the number of recent drug approvals for atopic dermatitis (AD) is overwhelming, the future is unlikely to be any less challenging: According to the National Eczema Association, the current pipeline for AD includes 39 injectable medications, 21 oral agents, and 49 topicals, some with novel targets, like human umbilical cord blood derived stem cells.
“It’s amazing how many drugs are coming out for AD,” Robert Sidbury, MD, MPH, said at the annual meeting of the Pacific Dermatologic Association (PDA). and is approved in Europe for the treatment of moderate to severe AD in patients aged ≥ 12 years. (On September 13, after the PDA meeting, lebrikizumab was approved by the Food and Drug Administration [FDA] for treatment of moderate to severe AD in adults and adolescents aged ≥ 12 years.)
In two identical phase 3 trials known as ADvocate 1 and ADvocate 2, researchers randomly assigned 851 patients with moderate to severe AD in a 2:1 ratio to receive either lebrikizumab at a dose of 250 mg (loading dose of 500 mg at baseline and week 2) or placebo, administered subcutaneously every 2 weeks, through week 16. The primary outcome was an Investigator’s Global Assessment (IGA) score of 0 or 1, indicating clear or almost clear skin. The researchers reported that an IGA score of 0 or 1 was achieved by 43.1% of patients in the lebrikizumab arm compared with 12.7% of those in the placebo arm.
“Those are good numbers,” said Dr. Sidbury, who was not involved with the study. Conjunctivitis occurred more often in those who received lebrikizumab compared with those who received placebo (7.4% vs 2.8%, respectively), “which is not surprising because it is an IL-13 agent,” he said.
In a subsequent study presented during the Revolutionizing Atopic Dermatitis meeting in the fall of 2023, researchers presented data on Eczema Severity and Area Index (EASI)-90 responses in the ADvocate trial participants, showing EASI-90 responses were sustained up to 38 weeks after lebrikizumab withdrawal, while serum concentrations were negligible. They found that between week 14 and week 32, approximately five serum concentration half-lives of the medication had elapsed since patients randomized to the withdrawal arm received their last dose of lebrikizumab, extending to approximately 11 half-lives by week 52. “That durability of response with next to no blood levels of drug in many of the study participants is interesting,” said Dr. Sidbury, who cochairs the current iteration of the American Academy of Dermatology Atopic Dermatitis Guidelines.
Nemolizumab is a neuroimmune response modulator that inhibits the IL-31 receptor and is approved in Japan for the treatment of itch associated with AD in patients aged ≥ 13 years. Results from two identical phase 3, randomized, controlled trials known as ARCADIA 1 and ARCADIA 2 found that 36% of patients in ARCADIA 1 and 38% in ARCADIA 2 achieved clear skin, compared with 25% and 26% of patients in the placebo group, respectively. (Nemolizumab was recently approved by the FDA for treating prurigo nodularis and is under FDA review for AD.)
In terms of safety, Dr. Sidbury, who is a member of the steering committee for the ARCADIA trials, said that nemolizumab has been “generally well tolerated;” with 1%-3% of study participants experiencing at least one serious treatment-emergent adverse event that included asthma exacerbation, facial edema, and peripheral edema. “The latest data are reassuring but we are watching these safety concerns carefully,” he said.
Dr. Sidbury disclosed that he is an investigator for Regeneron, Pfizer, Galderma, UCB, and Castle; a consultant for Lilly, Leo, Arcutis, and Dermavant; and a member of the speaker’s bureau for Beiersdorf.
A version of this article appeared on Medscape.com.
HUNTINGTON BEACH, CALIFORNIA — If the number of recent drug approvals for atopic dermatitis (AD) is overwhelming, the future is unlikely to be any less challenging: According to the National Eczema Association, the current pipeline for AD includes 39 injectable medications, 21 oral agents, and 49 topicals, some with novel targets, like human umbilical cord blood derived stem cells.
“It’s amazing how many drugs are coming out for AD,” Robert Sidbury, MD, MPH, said at the annual meeting of the Pacific Dermatologic Association (PDA). and is approved in Europe for the treatment of moderate to severe AD in patients aged ≥ 12 years. (On September 13, after the PDA meeting, lebrikizumab was approved by the Food and Drug Administration [FDA] for treatment of moderate to severe AD in adults and adolescents aged ≥ 12 years.)
In two identical phase 3 trials known as ADvocate 1 and ADvocate 2, researchers randomly assigned 851 patients with moderate to severe AD in a 2:1 ratio to receive either lebrikizumab at a dose of 250 mg (loading dose of 500 mg at baseline and week 2) or placebo, administered subcutaneously every 2 weeks, through week 16. The primary outcome was an Investigator’s Global Assessment (IGA) score of 0 or 1, indicating clear or almost clear skin. The researchers reported that an IGA score of 0 or 1 was achieved by 43.1% of patients in the lebrikizumab arm compared with 12.7% of those in the placebo arm.
“Those are good numbers,” said Dr. Sidbury, who was not involved with the study. Conjunctivitis occurred more often in those who received lebrikizumab compared with those who received placebo (7.4% vs 2.8%, respectively), “which is not surprising because it is an IL-13 agent,” he said.
In a subsequent study presented during the Revolutionizing Atopic Dermatitis meeting in the fall of 2023, researchers presented data on Eczema Severity and Area Index (EASI)-90 responses in the ADvocate trial participants, showing EASI-90 responses were sustained up to 38 weeks after lebrikizumab withdrawal, while serum concentrations were negligible. They found that between week 14 and week 32, approximately five serum concentration half-lives of the medication had elapsed since patients randomized to the withdrawal arm received their last dose of lebrikizumab, extending to approximately 11 half-lives by week 52. “That durability of response with next to no blood levels of drug in many of the study participants is interesting,” said Dr. Sidbury, who cochairs the current iteration of the American Academy of Dermatology Atopic Dermatitis Guidelines.
Nemolizumab is a neuroimmune response modulator that inhibits the IL-31 receptor and is approved in Japan for the treatment of itch associated with AD in patients aged ≥ 13 years. Results from two identical phase 3, randomized, controlled trials known as ARCADIA 1 and ARCADIA 2 found that 36% of patients in ARCADIA 1 and 38% in ARCADIA 2 achieved clear skin, compared with 25% and 26% of patients in the placebo group, respectively. (Nemolizumab was recently approved by the FDA for treating prurigo nodularis and is under FDA review for AD.)
In terms of safety, Dr. Sidbury, who is a member of the steering committee for the ARCADIA trials, said that nemolizumab has been “generally well tolerated;” with 1%-3% of study participants experiencing at least one serious treatment-emergent adverse event that included asthma exacerbation, facial edema, and peripheral edema. “The latest data are reassuring but we are watching these safety concerns carefully,” he said.
Dr. Sidbury disclosed that he is an investigator for Regeneron, Pfizer, Galderma, UCB, and Castle; a consultant for Lilly, Leo, Arcutis, and Dermavant; and a member of the speaker’s bureau for Beiersdorf.
A version of this article appeared on Medscape.com.
FROM PDA 2024
Hypnosis May Offer Relief During Sharp Debridement of Skin Ulcers
TOPLINE:
Hypnosis reduces pain during sharp debridement of skin ulcers in patients with immune-mediated inflammatory diseases, with most patients reporting decreased pain awareness and lasting pain relief for 2-3 days after the procedure.
METHODOLOGY:
- Researchers reported their experience with the anecdotal use of hypnosis for pain management in debridement of skin ulcers in immune-mediated inflammatory diseases.
- They studied 16 participants (14 women; mean age, 56 years; 14 with systemic sclerosis or morphea) with recurrent skin ulcerations requiring sharp debridement, who presented to a wound care clinic at the Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom. The participants had negative experiences with pharmacologic pain management.
- Participants consented to hypnosis during debridement as the only mode of analgesia, conducted by the same hypnosis-trained, experienced healthcare professional in charge of their ulcer care.
- Ulcer pain scores were recorded using a numerical rating pain scale before and immediately after debridement, with a score of 0 indicating no pain and 10 indicating worst pain.
TAKEAWAY:
- Hypnosis reduced the median pre-debridement ulcer pain score from 8 (interquartile range [IQR], 7-10) to 0.5 (IQR, 0-2) immediately after the procedure.
- Of 16 participants, 14 reported being aware of the procedure but not feeling the pain, with only two participants experiencing a brief spike in pain.
- The other two participants reported experiencing reduced awareness and being pain-free during the procedure.
- Five participants reported a lasting decrease in pain perception for 2-3 days after the procedure.
IN PRACTICE:
“These preliminary data underscore the potential for the integration of hypnosis into the management of intervention-related pain in clinical care,” the authors wrote.
SOURCE:
The study was led by Begonya Alcacer-Pitarch, PhD, Leeds Institute of Rheumatic and Musculoskeletal Medicine, the University of Leeds, and Chapel Allerton Hospital in Leeds, United Kingdom. It was published as a correspondence on September 10, 2024, in The Lancet Rheumatology.
LIMITATIONS:
The small sample size may limit the generalizability of the findings. The methods used for data collection were not standardized, and the individuals included in the study may have introduced selection bias.
DISCLOSURES:
The study did not have a funding source. The authors declared no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Hypnosis reduces pain during sharp debridement of skin ulcers in patients with immune-mediated inflammatory diseases, with most patients reporting decreased pain awareness and lasting pain relief for 2-3 days after the procedure.
METHODOLOGY:
- Researchers reported their experience with the anecdotal use of hypnosis for pain management in debridement of skin ulcers in immune-mediated inflammatory diseases.
- They studied 16 participants (14 women; mean age, 56 years; 14 with systemic sclerosis or morphea) with recurrent skin ulcerations requiring sharp debridement, who presented to a wound care clinic at the Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom. The participants had negative experiences with pharmacologic pain management.
- Participants consented to hypnosis during debridement as the only mode of analgesia, conducted by the same hypnosis-trained, experienced healthcare professional in charge of their ulcer care.
- Ulcer pain scores were recorded using a numerical rating pain scale before and immediately after debridement, with a score of 0 indicating no pain and 10 indicating worst pain.
TAKEAWAY:
- Hypnosis reduced the median pre-debridement ulcer pain score from 8 (interquartile range [IQR], 7-10) to 0.5 (IQR, 0-2) immediately after the procedure.
- Of 16 participants, 14 reported being aware of the procedure but not feeling the pain, with only two participants experiencing a brief spike in pain.
- The other two participants reported experiencing reduced awareness and being pain-free during the procedure.
- Five participants reported a lasting decrease in pain perception for 2-3 days after the procedure.
IN PRACTICE:
“These preliminary data underscore the potential for the integration of hypnosis into the management of intervention-related pain in clinical care,” the authors wrote.
SOURCE:
The study was led by Begonya Alcacer-Pitarch, PhD, Leeds Institute of Rheumatic and Musculoskeletal Medicine, the University of Leeds, and Chapel Allerton Hospital in Leeds, United Kingdom. It was published as a correspondence on September 10, 2024, in The Lancet Rheumatology.
LIMITATIONS:
The small sample size may limit the generalizability of the findings. The methods used for data collection were not standardized, and the individuals included in the study may have introduced selection bias.
DISCLOSURES:
The study did not have a funding source. The authors declared no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
TOPLINE:
Hypnosis reduces pain during sharp debridement of skin ulcers in patients with immune-mediated inflammatory diseases, with most patients reporting decreased pain awareness and lasting pain relief for 2-3 days after the procedure.
METHODOLOGY:
- Researchers reported their experience with the anecdotal use of hypnosis for pain management in debridement of skin ulcers in immune-mediated inflammatory diseases.
- They studied 16 participants (14 women; mean age, 56 years; 14 with systemic sclerosis or morphea) with recurrent skin ulcerations requiring sharp debridement, who presented to a wound care clinic at the Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom. The participants had negative experiences with pharmacologic pain management.
- Participants consented to hypnosis during debridement as the only mode of analgesia, conducted by the same hypnosis-trained, experienced healthcare professional in charge of their ulcer care.
- Ulcer pain scores were recorded using a numerical rating pain scale before and immediately after debridement, with a score of 0 indicating no pain and 10 indicating worst pain.
TAKEAWAY:
- Hypnosis reduced the median pre-debridement ulcer pain score from 8 (interquartile range [IQR], 7-10) to 0.5 (IQR, 0-2) immediately after the procedure.
- Of 16 participants, 14 reported being aware of the procedure but not feeling the pain, with only two participants experiencing a brief spike in pain.
- The other two participants reported experiencing reduced awareness and being pain-free during the procedure.
- Five participants reported a lasting decrease in pain perception for 2-3 days after the procedure.
IN PRACTICE:
“These preliminary data underscore the potential for the integration of hypnosis into the management of intervention-related pain in clinical care,” the authors wrote.
SOURCE:
The study was led by Begonya Alcacer-Pitarch, PhD, Leeds Institute of Rheumatic and Musculoskeletal Medicine, the University of Leeds, and Chapel Allerton Hospital in Leeds, United Kingdom. It was published as a correspondence on September 10, 2024, in The Lancet Rheumatology.
LIMITATIONS:
The small sample size may limit the generalizability of the findings. The methods used for data collection were not standardized, and the individuals included in the study may have introduced selection bias.
DISCLOSURES:
The study did not have a funding source. The authors declared no relevant conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Treating Family: Ethicist Discusses Whether It’s Appropriate
This transcript has been edited for clarity.
There’s a very interesting story in the medical press. A few years ago, a plastic surgeon named Edmond Cabbabe was preparing to do a follow-up cosmetic procedure on his wife at Mercy Hospital South, which is a big hospital in the St. Louis, Missouri, area.
He put her on the operating schedule, and he had done that when he had performed the original operation on her. On the day of the surgery, he got a call from the hospital saying the procedure was canceled. They said that the hospital’s policy, maybe a new one, would not allow doctors to operate on family members.
This physician was a past president of the Missouri State Medical Association. I think he was also on the board or president of the American Medical Association (AMA) Foundation. This was a physician not only in a skilled area where he felt confident he could take care of his wife, but also someone who was prominent in medical politics and medical policy.
The AMA forever has had a policy that says don’t treat relatives. This physician basically said, I think that policy is too restrictive, too cautious, and it doesn’t make much sense to continue to say that you can’t treat family and friends.
By implication, he was saying, I know exactly what I’m doing in my field and I know exactly what I’m doing with her procedure. I should have a right to perform it. I think I do a great job and I’d be best for her.
If you look at medical boards, every once in a while in some state, someone is brought up on a charge of doing different things with family members and saying that they’re going to get censured. They don’t usually lose their license, but they get a reprimand or get told that is just not ethical to do.
I think, in the long run, the policy about not treating your family and friends makes sense. The problem is, as is well known from the social sciences and psychology, people get biased when they deal with those they care about, love, and hold close to them.
It’s hard for the doctor to be objective when dealing with people that they really like or love. It’s also difficult for patients because they may not want to bring up something or they are uncomfortable talking with a doctor who’s a family member or close friend. They may not want to complain. They may be a little bit embarrassed about things. It just adds an emotional edge, I think, that’s difficult.
All that said, do I know doctors who regularly prescribe, say, an ointment for something that’s itchy or some kind of a pill when allergy season breaks out? I do. Do I think they’re acting in a horribly unethical manner? I don’t.
You need some judgment here. There are absolutely minor things where objectivity, fear, and anxiety are not in play. You’re going to be able to prescribe the routine thing for the routine itch without worrying too much about whether it’s a stranger, a friend, or your daughter.
What sorts of things am I really talking about when I say that minor variability ought to be allowed? It’s one thing when someone has poison ivy and they’re going to need some kind of standard medicine to treat it. A very different area that’s much more dangerous, and one I would avoid, is in the mental health field, and for that matter, the pain field.
It’s tempting to say: “Oh, my relative is just having a bad time. I’ll give her a little bit of antidepressant medicine,” or “They seem to be having pain after an operation or something, and I’m going to give them a little bit of pain meds just to get them through.”
Those areas are flying red flags. It’s easy to abuse and easy for someone to become a user and manipulate a friend or a doctor who’s a relative into getting things that another doctor wouldn’t be giving. I think that’s the space where you’ve got to exercise extreme caution.
Time and again, when those people get called up in front of the boards for treating relatives, it’s in those spaces of mental health, anxiety, and pain control. Again, when you know that there’s a likelihood of abuse, I think that’s the place where the line has to hold. Don’t treat the relative. Don’t treat the friend.
At the end of the day, I wouldn’t change the AMA policy. I think we should keep it in place and morally try to discourage doctors from caring for those they’re close to or they have emotional ties to.
At the same time, as with all ethical situations, there has to be a little bit of wiggle room for those super-minor cases where it just makes sense to say: “You don’t have to go find somebody else to do this. I can prescribe this ointment or this minor thing for you. No one’s objectivity is going to be soured, and you’re not going to feel in any way at risk because I’m going to prescribe this for you.”
Common sense ought to prevail. The default position is don’t do it; however, maybe with a tiny bit of space for what’s minor, what’s routine, and what really does just save people some inconvenience, there I might just give a little.
Dr. Caplan, Director, Division of Medical Ethics, New York University Langone Medical Center, New York City, has disclosed relationships with Johnson & Johnson’s Panel for Compassionate Drug Use and Medscape.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
There’s a very interesting story in the medical press. A few years ago, a plastic surgeon named Edmond Cabbabe was preparing to do a follow-up cosmetic procedure on his wife at Mercy Hospital South, which is a big hospital in the St. Louis, Missouri, area.
He put her on the operating schedule, and he had done that when he had performed the original operation on her. On the day of the surgery, he got a call from the hospital saying the procedure was canceled. They said that the hospital’s policy, maybe a new one, would not allow doctors to operate on family members.
This physician was a past president of the Missouri State Medical Association. I think he was also on the board or president of the American Medical Association (AMA) Foundation. This was a physician not only in a skilled area where he felt confident he could take care of his wife, but also someone who was prominent in medical politics and medical policy.
The AMA forever has had a policy that says don’t treat relatives. This physician basically said, I think that policy is too restrictive, too cautious, and it doesn’t make much sense to continue to say that you can’t treat family and friends.
By implication, he was saying, I know exactly what I’m doing in my field and I know exactly what I’m doing with her procedure. I should have a right to perform it. I think I do a great job and I’d be best for her.
If you look at medical boards, every once in a while in some state, someone is brought up on a charge of doing different things with family members and saying that they’re going to get censured. They don’t usually lose their license, but they get a reprimand or get told that is just not ethical to do.
I think, in the long run, the policy about not treating your family and friends makes sense. The problem is, as is well known from the social sciences and psychology, people get biased when they deal with those they care about, love, and hold close to them.
It’s hard for the doctor to be objective when dealing with people that they really like or love. It’s also difficult for patients because they may not want to bring up something or they are uncomfortable talking with a doctor who’s a family member or close friend. They may not want to complain. They may be a little bit embarrassed about things. It just adds an emotional edge, I think, that’s difficult.
All that said, do I know doctors who regularly prescribe, say, an ointment for something that’s itchy or some kind of a pill when allergy season breaks out? I do. Do I think they’re acting in a horribly unethical manner? I don’t.
You need some judgment here. There are absolutely minor things where objectivity, fear, and anxiety are not in play. You’re going to be able to prescribe the routine thing for the routine itch without worrying too much about whether it’s a stranger, a friend, or your daughter.
What sorts of things am I really talking about when I say that minor variability ought to be allowed? It’s one thing when someone has poison ivy and they’re going to need some kind of standard medicine to treat it. A very different area that’s much more dangerous, and one I would avoid, is in the mental health field, and for that matter, the pain field.
It’s tempting to say: “Oh, my relative is just having a bad time. I’ll give her a little bit of antidepressant medicine,” or “They seem to be having pain after an operation or something, and I’m going to give them a little bit of pain meds just to get them through.”
Those areas are flying red flags. It’s easy to abuse and easy for someone to become a user and manipulate a friend or a doctor who’s a relative into getting things that another doctor wouldn’t be giving. I think that’s the space where you’ve got to exercise extreme caution.
Time and again, when those people get called up in front of the boards for treating relatives, it’s in those spaces of mental health, anxiety, and pain control. Again, when you know that there’s a likelihood of abuse, I think that’s the place where the line has to hold. Don’t treat the relative. Don’t treat the friend.
At the end of the day, I wouldn’t change the AMA policy. I think we should keep it in place and morally try to discourage doctors from caring for those they’re close to or they have emotional ties to.
At the same time, as with all ethical situations, there has to be a little bit of wiggle room for those super-minor cases where it just makes sense to say: “You don’t have to go find somebody else to do this. I can prescribe this ointment or this minor thing for you. No one’s objectivity is going to be soured, and you’re not going to feel in any way at risk because I’m going to prescribe this for you.”
Common sense ought to prevail. The default position is don’t do it; however, maybe with a tiny bit of space for what’s minor, what’s routine, and what really does just save people some inconvenience, there I might just give a little.
Dr. Caplan, Director, Division of Medical Ethics, New York University Langone Medical Center, New York City, has disclosed relationships with Johnson & Johnson’s Panel for Compassionate Drug Use and Medscape.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
There’s a very interesting story in the medical press. A few years ago, a plastic surgeon named Edmond Cabbabe was preparing to do a follow-up cosmetic procedure on his wife at Mercy Hospital South, which is a big hospital in the St. Louis, Missouri, area.
He put her on the operating schedule, and he had done that when he had performed the original operation on her. On the day of the surgery, he got a call from the hospital saying the procedure was canceled. They said that the hospital’s policy, maybe a new one, would not allow doctors to operate on family members.
This physician was a past president of the Missouri State Medical Association. I think he was also on the board or president of the American Medical Association (AMA) Foundation. This was a physician not only in a skilled area where he felt confident he could take care of his wife, but also someone who was prominent in medical politics and medical policy.
The AMA forever has had a policy that says don’t treat relatives. This physician basically said, I think that policy is too restrictive, too cautious, and it doesn’t make much sense to continue to say that you can’t treat family and friends.
By implication, he was saying, I know exactly what I’m doing in my field and I know exactly what I’m doing with her procedure. I should have a right to perform it. I think I do a great job and I’d be best for her.
If you look at medical boards, every once in a while in some state, someone is brought up on a charge of doing different things with family members and saying that they’re going to get censured. They don’t usually lose their license, but they get a reprimand or get told that is just not ethical to do.
I think, in the long run, the policy about not treating your family and friends makes sense. The problem is, as is well known from the social sciences and psychology, people get biased when they deal with those they care about, love, and hold close to them.
It’s hard for the doctor to be objective when dealing with people that they really like or love. It’s also difficult for patients because they may not want to bring up something or they are uncomfortable talking with a doctor who’s a family member or close friend. They may not want to complain. They may be a little bit embarrassed about things. It just adds an emotional edge, I think, that’s difficult.
All that said, do I know doctors who regularly prescribe, say, an ointment for something that’s itchy or some kind of a pill when allergy season breaks out? I do. Do I think they’re acting in a horribly unethical manner? I don’t.
You need some judgment here. There are absolutely minor things where objectivity, fear, and anxiety are not in play. You’re going to be able to prescribe the routine thing for the routine itch without worrying too much about whether it’s a stranger, a friend, or your daughter.
What sorts of things am I really talking about when I say that minor variability ought to be allowed? It’s one thing when someone has poison ivy and they’re going to need some kind of standard medicine to treat it. A very different area that’s much more dangerous, and one I would avoid, is in the mental health field, and for that matter, the pain field.
It’s tempting to say: “Oh, my relative is just having a bad time. I’ll give her a little bit of antidepressant medicine,” or “They seem to be having pain after an operation or something, and I’m going to give them a little bit of pain meds just to get them through.”
Those areas are flying red flags. It’s easy to abuse and easy for someone to become a user and manipulate a friend or a doctor who’s a relative into getting things that another doctor wouldn’t be giving. I think that’s the space where you’ve got to exercise extreme caution.
Time and again, when those people get called up in front of the boards for treating relatives, it’s in those spaces of mental health, anxiety, and pain control. Again, when you know that there’s a likelihood of abuse, I think that’s the place where the line has to hold. Don’t treat the relative. Don’t treat the friend.
At the end of the day, I wouldn’t change the AMA policy. I think we should keep it in place and morally try to discourage doctors from caring for those they’re close to or they have emotional ties to.
At the same time, as with all ethical situations, there has to be a little bit of wiggle room for those super-minor cases where it just makes sense to say: “You don’t have to go find somebody else to do this. I can prescribe this ointment or this minor thing for you. No one’s objectivity is going to be soured, and you’re not going to feel in any way at risk because I’m going to prescribe this for you.”
Common sense ought to prevail. The default position is don’t do it; however, maybe with a tiny bit of space for what’s minor, what’s routine, and what really does just save people some inconvenience, there I might just give a little.
Dr. Caplan, Director, Division of Medical Ethics, New York University Langone Medical Center, New York City, has disclosed relationships with Johnson & Johnson’s Panel for Compassionate Drug Use and Medscape.
A version of this article first appeared on Medscape.com.