User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Fair access crucial for new diabetes/kidney disease drugs, say guidelines
The 2022 guideline update released by the KDIGO organization for managing people with diabetes and chronic kidney disease (CKD) highlighted the safety and expanded, evidence-based role for agents from three drug classes: the SGLT2 inhibitors, the GLP-1 receptor agonists, and the nonsteroidal mineralocorticoid receptor antagonists.
But this key take-away from the guideline also underscored the challenges for ensuring fair and affordable access among US patients to these practice-changing medications.
The impact of widespread adoption of these three drug classes into routine US management of people with diabetes and CKD “will be determined by how effective the health care system and its patients and clinicians are at overcoming individual and structural barriers,” write Milda Saunders, MD, and Neda Laiteerapong, MD, in an editorial that accompanied the publication of a synopsis of the 2022 guideline update in Annals of Internal Medicine.
The synopsis is an 11-page distillation of the full 128-page guideline released by the Kidney Disease: Improving Global Outcomes (KDIGO) organization in 2022.
The recommendations in the 2022 guideline update “are exciting for their potential to change the natural history of CKD and diabetes, but their effect could be highly limited by barriers at multiple levels,” write Dr. Saunders and Dr. Laiteerapong, two internal medicine physicians at the University of Chicago.
“Without equitable implementation of the KDIGO 2022 guidelines there is a potential that clinical practice variation will increase and widen health inequities for minoritized people with CKD and diabetes,” they warn.
Generics to the rescue
One potentially effective, and likely imminent, way to level the prescribing field for patients with CKD and diabetes is for agents from the sodium-glucose cotransporter 2 (SGLT2) inhibitor, glucagonlike peptide-1 (GLP-1) receptor agonist, and nonsteroidal mineralocorticoid receptor antagonist classes to become available in generic formulations.
That should lower prices and thereby boost wider access and will likely occur fairly soon for at least two of the three drug classes, Dr. Laiteerapong predicts.
Some GLP-1 receptor agonists have already escaped patent exclusivity or will do so in 2023, she notes, including the anticipated ability of one drugmaker to start U.S. marketing of generic liraglutide by the end of 2023.
However, whether that manufacturer, Teva, proceeds with generic liraglutide “is a big question,” Dr. Laiteerapong said in an interview. She cited Teva’s history of failing to introduce a generic formulation of exenatide onto the U.S. market even though it has had a green light to do so since 2017.
The only nonsteroidal mineralocorticoid receptor antagonist now on the market is finerenone (Kerendia), which will not go off patent for several more years, but for some branded SGLT2 inhibitors, U.S. patents will expire in 2025. In addition, remogliflozin is an SGLT2 inhibitor that “may have already lost patent exclusivity,” noted Dr. Laiteerapong, although it has also never received U.S. marketing approval.
Dr. Laiteerapong expressed optimism that the overall trajectory of access is on the rise. “Many people have type 2 diabetes, and these drugs are in demand,” she noted. She also pointed to progress recently made on insulin affordability. “Things will get better as long as people advocate and argue for equity,” she maintained.
Incentivize formulary listings
Dr. Laiteerapong cited other approaches that could boost access to these medications, such as “creating incentives for pharmaceutical companies to ensure that [these drugs] are on formularies” of large, government-affiliated U.S. health insurance programs, such as Medicare Advantage plans, Medicare Part D, state Medicaid plans, and coverage through U.S. Veterans Affairs and the Tricare health insurance plans available to active members of the US military.
The editorial she coauthored with Dr. Saunders also calls for future collaborations among various medical societies to create “a more unified and streamlined set of recommendations” that benefits patients with diabetes, CKD, and multiple other chronic conditions.
“Over the last decade, we have seen more societies willing to present cooperative guidelines, as well as a surge in research on patients who live with multiple chronic conditions. There is momentum that will allow these different societies to work together,” Dr. Laiteerapong said.
Dr. Laiteerapong and Dr. Saunders have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The 2022 guideline update released by the KDIGO organization for managing people with diabetes and chronic kidney disease (CKD) highlighted the safety and expanded, evidence-based role for agents from three drug classes: the SGLT2 inhibitors, the GLP-1 receptor agonists, and the nonsteroidal mineralocorticoid receptor antagonists.
But this key take-away from the guideline also underscored the challenges for ensuring fair and affordable access among US patients to these practice-changing medications.
The impact of widespread adoption of these three drug classes into routine US management of people with diabetes and CKD “will be determined by how effective the health care system and its patients and clinicians are at overcoming individual and structural barriers,” write Milda Saunders, MD, and Neda Laiteerapong, MD, in an editorial that accompanied the publication of a synopsis of the 2022 guideline update in Annals of Internal Medicine.
The synopsis is an 11-page distillation of the full 128-page guideline released by the Kidney Disease: Improving Global Outcomes (KDIGO) organization in 2022.
The recommendations in the 2022 guideline update “are exciting for their potential to change the natural history of CKD and diabetes, but their effect could be highly limited by barriers at multiple levels,” write Dr. Saunders and Dr. Laiteerapong, two internal medicine physicians at the University of Chicago.
“Without equitable implementation of the KDIGO 2022 guidelines there is a potential that clinical practice variation will increase and widen health inequities for minoritized people with CKD and diabetes,” they warn.
Generics to the rescue
One potentially effective, and likely imminent, way to level the prescribing field for patients with CKD and diabetes is for agents from the sodium-glucose cotransporter 2 (SGLT2) inhibitor, glucagonlike peptide-1 (GLP-1) receptor agonist, and nonsteroidal mineralocorticoid receptor antagonist classes to become available in generic formulations.
That should lower prices and thereby boost wider access and will likely occur fairly soon for at least two of the three drug classes, Dr. Laiteerapong predicts.
Some GLP-1 receptor agonists have already escaped patent exclusivity or will do so in 2023, she notes, including the anticipated ability of one drugmaker to start U.S. marketing of generic liraglutide by the end of 2023.
However, whether that manufacturer, Teva, proceeds with generic liraglutide “is a big question,” Dr. Laiteerapong said in an interview. She cited Teva’s history of failing to introduce a generic formulation of exenatide onto the U.S. market even though it has had a green light to do so since 2017.
The only nonsteroidal mineralocorticoid receptor antagonist now on the market is finerenone (Kerendia), which will not go off patent for several more years, but for some branded SGLT2 inhibitors, U.S. patents will expire in 2025. In addition, remogliflozin is an SGLT2 inhibitor that “may have already lost patent exclusivity,” noted Dr. Laiteerapong, although it has also never received U.S. marketing approval.
Dr. Laiteerapong expressed optimism that the overall trajectory of access is on the rise. “Many people have type 2 diabetes, and these drugs are in demand,” she noted. She also pointed to progress recently made on insulin affordability. “Things will get better as long as people advocate and argue for equity,” she maintained.
Incentivize formulary listings
Dr. Laiteerapong cited other approaches that could boost access to these medications, such as “creating incentives for pharmaceutical companies to ensure that [these drugs] are on formularies” of large, government-affiliated U.S. health insurance programs, such as Medicare Advantage plans, Medicare Part D, state Medicaid plans, and coverage through U.S. Veterans Affairs and the Tricare health insurance plans available to active members of the US military.
The editorial she coauthored with Dr. Saunders also calls for future collaborations among various medical societies to create “a more unified and streamlined set of recommendations” that benefits patients with diabetes, CKD, and multiple other chronic conditions.
“Over the last decade, we have seen more societies willing to present cooperative guidelines, as well as a surge in research on patients who live with multiple chronic conditions. There is momentum that will allow these different societies to work together,” Dr. Laiteerapong said.
Dr. Laiteerapong and Dr. Saunders have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The 2022 guideline update released by the KDIGO organization for managing people with diabetes and chronic kidney disease (CKD) highlighted the safety and expanded, evidence-based role for agents from three drug classes: the SGLT2 inhibitors, the GLP-1 receptor agonists, and the nonsteroidal mineralocorticoid receptor antagonists.
But this key take-away from the guideline also underscored the challenges for ensuring fair and affordable access among US patients to these practice-changing medications.
The impact of widespread adoption of these three drug classes into routine US management of people with diabetes and CKD “will be determined by how effective the health care system and its patients and clinicians are at overcoming individual and structural barriers,” write Milda Saunders, MD, and Neda Laiteerapong, MD, in an editorial that accompanied the publication of a synopsis of the 2022 guideline update in Annals of Internal Medicine.
The synopsis is an 11-page distillation of the full 128-page guideline released by the Kidney Disease: Improving Global Outcomes (KDIGO) organization in 2022.
The recommendations in the 2022 guideline update “are exciting for their potential to change the natural history of CKD and diabetes, but their effect could be highly limited by barriers at multiple levels,” write Dr. Saunders and Dr. Laiteerapong, two internal medicine physicians at the University of Chicago.
“Without equitable implementation of the KDIGO 2022 guidelines there is a potential that clinical practice variation will increase and widen health inequities for minoritized people with CKD and diabetes,” they warn.
Generics to the rescue
One potentially effective, and likely imminent, way to level the prescribing field for patients with CKD and diabetes is for agents from the sodium-glucose cotransporter 2 (SGLT2) inhibitor, glucagonlike peptide-1 (GLP-1) receptor agonist, and nonsteroidal mineralocorticoid receptor antagonist classes to become available in generic formulations.
That should lower prices and thereby boost wider access and will likely occur fairly soon for at least two of the three drug classes, Dr. Laiteerapong predicts.
Some GLP-1 receptor agonists have already escaped patent exclusivity or will do so in 2023, she notes, including the anticipated ability of one drugmaker to start U.S. marketing of generic liraglutide by the end of 2023.
However, whether that manufacturer, Teva, proceeds with generic liraglutide “is a big question,” Dr. Laiteerapong said in an interview. She cited Teva’s history of failing to introduce a generic formulation of exenatide onto the U.S. market even though it has had a green light to do so since 2017.
The only nonsteroidal mineralocorticoid receptor antagonist now on the market is finerenone (Kerendia), which will not go off patent for several more years, but for some branded SGLT2 inhibitors, U.S. patents will expire in 2025. In addition, remogliflozin is an SGLT2 inhibitor that “may have already lost patent exclusivity,” noted Dr. Laiteerapong, although it has also never received U.S. marketing approval.
Dr. Laiteerapong expressed optimism that the overall trajectory of access is on the rise. “Many people have type 2 diabetes, and these drugs are in demand,” she noted. She also pointed to progress recently made on insulin affordability. “Things will get better as long as people advocate and argue for equity,” she maintained.
Incentivize formulary listings
Dr. Laiteerapong cited other approaches that could boost access to these medications, such as “creating incentives for pharmaceutical companies to ensure that [these drugs] are on formularies” of large, government-affiliated U.S. health insurance programs, such as Medicare Advantage plans, Medicare Part D, state Medicaid plans, and coverage through U.S. Veterans Affairs and the Tricare health insurance plans available to active members of the US military.
The editorial she coauthored with Dr. Saunders also calls for future collaborations among various medical societies to create “a more unified and streamlined set of recommendations” that benefits patients with diabetes, CKD, and multiple other chronic conditions.
“Over the last decade, we have seen more societies willing to present cooperative guidelines, as well as a surge in research on patients who live with multiple chronic conditions. There is momentum that will allow these different societies to work together,” Dr. Laiteerapong said.
Dr. Laiteerapong and Dr. Saunders have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
PPI use in type 2 diabetes links with cardiovascular events
Among people with type 2 diabetes who self-reported regularly using a proton pump inhibitor (PPI), the incidence of cardiovascular disease (CVD) events as well as all-cause death was significantly increased in a study of more than 19,000 people with type 2 diabetes in a prospective U.K. database.
During median follow-up of about 11 years, regular use of a PPI by people with type 2 diabetes was significantly linked with a 27% relative increase in the incidence of coronary artery disease, compared with nonuse of a PPI, after full adjustment for potential confounding variables.
The results also show PPI use was significantly linked after full adjustment with a 34% relative increase in MI, a 35% relative increase in heart failure, and a 30% relative increase in all-cause death, say a team of Chinese researchers in a recent report in the Journal of Clinical Endocrinology and Metabolism.
PPIs are a medication class widely used in both over-the-counter and prescription formulations to reduce acid production in the stomach and to treat gastroesophageal reflux disease and other acid-related disorders. The PPI class includes such widely used agents as esomeprazole (Nexium), lansoprazole (Prevacid), and omeprazole (Prilosec).
The analyses in this report, which used data collected in the UK Biobank, are “rigorous,” and the findings of “a modest elevation of CVD risk are consistent with a growing number of observational studies in populations with and without diabetes,” commented Mary R. Rooney, PhD, an epidemiologist at Johns Hopkins University, Baltimore, who focuses on diabetes and cardiovascular diseases.
Prior observational reports
For example, a report from a prospective, observational study of more than 4300 U.S. residents published in 2021 that Dr. Rooney coauthored documented that cumulative PPI exposure for more than 5 years was significantly linked with a twofold increase in the rate of CVD events, compared with people who did not use a PPI. (This analysis did not examine a possible effect of diabetes status.)
And in a separate prospective, observational study of more than 1,000 Australians with type 2 diabetes, initiation of PPI treatment was significantly linked with a 3.6-fold increased incidence of CVD events, compared with PPI nonuse.
However, Dr. Rooney cautioned that the role of PPI use in raising CVD events “is still an unresolved question. It is too soon to tell if PPI use in people with diabetes should trigger additional caution.” Findings are needed from prospective, randomized trials to determine more definitively whether PPIs play a causal role in the incidence of CVD events, she said in an interview.
U.S. practice often results in unwarranted prolongation of PPI treatment, said the authors of an editorial that accompanied the 2021 report by Dr. Rooney and coauthors.
Long-term PPI use threatens harm
“The practice of initiating stress ulcer prophylaxis [by administering a PPI] in critical care is common,” wrote the authors of the 2021 editorial, Nitin Malik, MD, and William S. Weintraub, MD. “Although it is data driven and well intentioned, the possibility of causing harm – if it is continued on a long-term basis after resolution of the acute illness – is palpable.”
The new analyses using UK Biobank data included 19,229 adults with type 2 diabetes and no preexisting coronary artery disease, MI, heart failure, or stroke. The cohort included 15,954 people (83%) who did not report using a PPI and 3,275 who currently used PPIs regularly. Study limitations include self-report as the only verification of PPI use and lack of information on type of PPI, dose size, or use duration.
The findings remained consistent in several sensitivity analyses, including a propensity score–matched analysis and after further adjustment for use of histamine2 receptor antagonists, a drug class with indications similar to those for PPIs.
The authors of the report speculated that mechanisms that might link PPI use and increased CVD and mortality risk could include changes to the gut microbiota and possible interactions between PPIs and antiplatelet agents.
The study received no commercial funding. The authors and Dr. Rooney disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among people with type 2 diabetes who self-reported regularly using a proton pump inhibitor (PPI), the incidence of cardiovascular disease (CVD) events as well as all-cause death was significantly increased in a study of more than 19,000 people with type 2 diabetes in a prospective U.K. database.
During median follow-up of about 11 years, regular use of a PPI by people with type 2 diabetes was significantly linked with a 27% relative increase in the incidence of coronary artery disease, compared with nonuse of a PPI, after full adjustment for potential confounding variables.
The results also show PPI use was significantly linked after full adjustment with a 34% relative increase in MI, a 35% relative increase in heart failure, and a 30% relative increase in all-cause death, say a team of Chinese researchers in a recent report in the Journal of Clinical Endocrinology and Metabolism.
PPIs are a medication class widely used in both over-the-counter and prescription formulations to reduce acid production in the stomach and to treat gastroesophageal reflux disease and other acid-related disorders. The PPI class includes such widely used agents as esomeprazole (Nexium), lansoprazole (Prevacid), and omeprazole (Prilosec).
The analyses in this report, which used data collected in the UK Biobank, are “rigorous,” and the findings of “a modest elevation of CVD risk are consistent with a growing number of observational studies in populations with and without diabetes,” commented Mary R. Rooney, PhD, an epidemiologist at Johns Hopkins University, Baltimore, who focuses on diabetes and cardiovascular diseases.
Prior observational reports
For example, a report from a prospective, observational study of more than 4300 U.S. residents published in 2021 that Dr. Rooney coauthored documented that cumulative PPI exposure for more than 5 years was significantly linked with a twofold increase in the rate of CVD events, compared with people who did not use a PPI. (This analysis did not examine a possible effect of diabetes status.)
And in a separate prospective, observational study of more than 1,000 Australians with type 2 diabetes, initiation of PPI treatment was significantly linked with a 3.6-fold increased incidence of CVD events, compared with PPI nonuse.
However, Dr. Rooney cautioned that the role of PPI use in raising CVD events “is still an unresolved question. It is too soon to tell if PPI use in people with diabetes should trigger additional caution.” Findings are needed from prospective, randomized trials to determine more definitively whether PPIs play a causal role in the incidence of CVD events, she said in an interview.
U.S. practice often results in unwarranted prolongation of PPI treatment, said the authors of an editorial that accompanied the 2021 report by Dr. Rooney and coauthors.
Long-term PPI use threatens harm
“The practice of initiating stress ulcer prophylaxis [by administering a PPI] in critical care is common,” wrote the authors of the 2021 editorial, Nitin Malik, MD, and William S. Weintraub, MD. “Although it is data driven and well intentioned, the possibility of causing harm – if it is continued on a long-term basis after resolution of the acute illness – is palpable.”
The new analyses using UK Biobank data included 19,229 adults with type 2 diabetes and no preexisting coronary artery disease, MI, heart failure, or stroke. The cohort included 15,954 people (83%) who did not report using a PPI and 3,275 who currently used PPIs regularly. Study limitations include self-report as the only verification of PPI use and lack of information on type of PPI, dose size, or use duration.
The findings remained consistent in several sensitivity analyses, including a propensity score–matched analysis and after further adjustment for use of histamine2 receptor antagonists, a drug class with indications similar to those for PPIs.
The authors of the report speculated that mechanisms that might link PPI use and increased CVD and mortality risk could include changes to the gut microbiota and possible interactions between PPIs and antiplatelet agents.
The study received no commercial funding. The authors and Dr. Rooney disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among people with type 2 diabetes who self-reported regularly using a proton pump inhibitor (PPI), the incidence of cardiovascular disease (CVD) events as well as all-cause death was significantly increased in a study of more than 19,000 people with type 2 diabetes in a prospective U.K. database.
During median follow-up of about 11 years, regular use of a PPI by people with type 2 diabetes was significantly linked with a 27% relative increase in the incidence of coronary artery disease, compared with nonuse of a PPI, after full adjustment for potential confounding variables.
The results also show PPI use was significantly linked after full adjustment with a 34% relative increase in MI, a 35% relative increase in heart failure, and a 30% relative increase in all-cause death, say a team of Chinese researchers in a recent report in the Journal of Clinical Endocrinology and Metabolism.
PPIs are a medication class widely used in both over-the-counter and prescription formulations to reduce acid production in the stomach and to treat gastroesophageal reflux disease and other acid-related disorders. The PPI class includes such widely used agents as esomeprazole (Nexium), lansoprazole (Prevacid), and omeprazole (Prilosec).
The analyses in this report, which used data collected in the UK Biobank, are “rigorous,” and the findings of “a modest elevation of CVD risk are consistent with a growing number of observational studies in populations with and without diabetes,” commented Mary R. Rooney, PhD, an epidemiologist at Johns Hopkins University, Baltimore, who focuses on diabetes and cardiovascular diseases.
Prior observational reports
For example, a report from a prospective, observational study of more than 4300 U.S. residents published in 2021 that Dr. Rooney coauthored documented that cumulative PPI exposure for more than 5 years was significantly linked with a twofold increase in the rate of CVD events, compared with people who did not use a PPI. (This analysis did not examine a possible effect of diabetes status.)
And in a separate prospective, observational study of more than 1,000 Australians with type 2 diabetes, initiation of PPI treatment was significantly linked with a 3.6-fold increased incidence of CVD events, compared with PPI nonuse.
However, Dr. Rooney cautioned that the role of PPI use in raising CVD events “is still an unresolved question. It is too soon to tell if PPI use in people with diabetes should trigger additional caution.” Findings are needed from prospective, randomized trials to determine more definitively whether PPIs play a causal role in the incidence of CVD events, she said in an interview.
U.S. practice often results in unwarranted prolongation of PPI treatment, said the authors of an editorial that accompanied the 2021 report by Dr. Rooney and coauthors.
Long-term PPI use threatens harm
“The practice of initiating stress ulcer prophylaxis [by administering a PPI] in critical care is common,” wrote the authors of the 2021 editorial, Nitin Malik, MD, and William S. Weintraub, MD. “Although it is data driven and well intentioned, the possibility of causing harm – if it is continued on a long-term basis after resolution of the acute illness – is palpable.”
The new analyses using UK Biobank data included 19,229 adults with type 2 diabetes and no preexisting coronary artery disease, MI, heart failure, or stroke. The cohort included 15,954 people (83%) who did not report using a PPI and 3,275 who currently used PPIs regularly. Study limitations include self-report as the only verification of PPI use and lack of information on type of PPI, dose size, or use duration.
The findings remained consistent in several sensitivity analyses, including a propensity score–matched analysis and after further adjustment for use of histamine2 receptor antagonists, a drug class with indications similar to those for PPIs.
The authors of the report speculated that mechanisms that might link PPI use and increased CVD and mortality risk could include changes to the gut microbiota and possible interactions between PPIs and antiplatelet agents.
The study received no commercial funding. The authors and Dr. Rooney disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY AND METABOLISM
Some BP meds tied to significantly lower risk for dementia, Alzheimer’s
Antihypertensive medications that stimulate rather than inhibit type 2 and 4 angiotensin II receptors can lower the rate of dementia among new users of these medications, new research suggests.
Results from a cohort study of more than 57,000 older Medicare beneficiaries showed that the initiation of antihypertensives that stimulate the receptors was linked to a 16% lower risk for incident Alzheimer’s disease and related dementia (ADRD) and an 18% lower risk for vascular dementia compared with those that inhibit the receptors.
“Achieving appropriate blood pressure control is essential for maximizing brain health, and this promising research suggests certain antihypertensives could yield brain benefit compared to others,” lead study author Zachary A. Marcum, PharmD, PhD, associate professor, University of Washington School of Pharmacy, Seattle, told this news organization.
The findings were published online in JAMA Network Open.
Medicare beneficiaries
Previous observational studies showed that antihypertensive medications that stimulate type 2 and 4 angiotensin II receptors, in comparison with those that don’t, were associated with lower rates of dementia. However, those studies included individuals with prevalent hypertension and were relatively small.
The new retrospective cohort study included a random sample of 57,773 Medicare beneficiaries aged at least 65 years with new-onset hypertension. The mean age of participants was 73.8 years, 62.9% were women, and 86.9% were White.
Over the course of the study, some participants filled at least one prescription for a stimulating angiotensin II receptor type 2 and 4, such as angiotensin II receptor type 1 blockers, dihydropyridine calcium channel blockers, and thiazide diuretics.
Others participants filled a prescription for an inhibiting type 2 and 4 angiotensin II receptors, including angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and nondihydropyridine calcium channel blockers.
“All these medications lower blood pressure, but they do it in different ways,” said Dr. Marcum.
The researchers were interested in the varying activity of these drugs at the type 2 and 4 angiotensin II receptors.
For each 30-day interval, they categorized beneficiaries into four groups: a stimulating medication group (n = 4,879) consisting of individuals mostly taking stimulating antihypertensives; an inhibiting medication group (n = 10,303) that mostly included individuals prescribed this type of antihypertensive; a mixed group (n = 2,179) that included a combination of the first two classifications; and a nonuser group (n = 40,413) of individuals who were not using either type of drug.
The primary outcome was time to first occurrence of ADRD. The secondary outcome was time to first occurrence of vascular dementia.
Researchers controlled for cardiovascular risk factors and sociodemographic characteristics, such as age, sex, race/ethnicity, and receipt of low-income subsidy.
Unanswered questions
After adjustments, results showed that initiation of an antihypertensive medication regimen that exclusively stimulates, rather than inhibits, type 2 and 4 angiotensin II receptors was associated with a 16% lower risk for incident ADRD over a follow-up of just under 7 years (hazard ratio, 0.84; 95% confidence interval, 0.79-0.90; P < .001).
The mixed regimen was also associated with statistically significant (P = .001) reduced odds of ADRD compared with the inhibiting medications.
As for vascular dementia, use of stimulating vs. inhibiting medications was associated with an 18% lower risk (HR, 0.82; 95% CI, 0.69-0.96; P = .02).
Again, use of the mixed regimen was associated with reduced risk of vascular dementia compared with the inhibiting medications (P = .03).
A variety of potential mechanisms might explain the superiority of stimulating agents when it comes to dementia risk, said Dr. Marcum. These could include, for example, increased blood flow to the brain and reduced amyloid.
“But more mechanistic work is needed as well as evaluation of dose responses, because that’s not something we looked at in this study,” Dr. Marcum said. “There are still a lot of unanswered questions.”
Stimulators instead of inhibitors?
The results of the current analysis come on the heels of some previous work showing the benefits of lowering blood pressure. For example, the Systolic Blood Pressure Intervention Trial (SPRINT) showed that targeting a systolic blood pressure below 120 mm Hg significantly reduces risk for heart disease, stroke, and death from these diseases.
But in contrast to previous research, the current study included only beneficiaries with incident hypertension and new use of antihypertensive medications, and it adjusted for time-varying confounding.
Prescribing stimulating instead of inhibiting treatments could make a difference at the population level, Dr. Marcum noted.
“If we could shift the prescribing a little bit from inhibiting to stimulating, that could possibly reduce dementia risk,” he said.
However, “we’re not suggesting [that all patients] have their regimen switched,” he added.
That’s because inhibiting medications still have an important place in the antihypertensive treatment armamentarium, Dr. Marcum noted. As an example, beta-blockers are used post heart attack.
As well, factors such as cost and side effects should be taken into consideration when prescribing an antihypertensive drug.
The new results could be used to set up a comparison in a future randomized controlled trial that would provide the strongest evidence for estimating causal effects of treatments, said Dr. Marcum.
‘More convincing’
Carlos G. Santos-Gallego, MD, Icahn School of Medicine at Mount Sinai, New York, said the study is “more convincing” than previous related research, as it has a larger sample size and a longer follow-up.
“And the exquisite statistical analysis gives more robustness, more solidity, to the hypothesis that drugs that stimulate type 2 and 4 angiotensin II receptors might be protective for dementia,” said Dr. Santos-Gallego, who was not involved with the research.
However, he noted that the retrospective study had some limitations, including the underdiagnosis of dementia. “The diagnosis of dementia is, honestly, very poorly done in the clinical setting,” he said.
As well, the study could be subject to “confounding by indication,” Dr. Santos-Gallego said. “There could be a third variable, another confounding factor, that’s responsible both for the dementia and for the prescription of these drugs,” he added.
For example, he noted that comorbidities such as atrial fibrillation, myocardial infarction, and heart failure might increase the risk of dementia.
He agreed with the investigators that a randomized clinical trial would address these limitations. “All comorbidities would be equally shared” in the randomized groups, and all participants would be given “a specific test for dementia at the same time,” Dr. Santos-Gallego said.
Still, he noted that the new results are in keeping with hypertension guidelines that recommend stimulating drugs.
“This trial definitely shows that the current hypertension guidelines are good treatment for our patients, not only to control blood pressure and not only to prevent infarction to prevent stroke but also to prevent dementia,” said Dr. Santos-Gallego.
Also commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations at the Alzheimer’s Association, said the new data provide “clarity” on why previous research had differing results on the effect of antihypertensives on cognition.
Among the caveats of this new analysis is that “it’s unclear if the demographics in this study are fully representative of Medicare beneficiaries,” said Dr. Snyder.
She, too, said a clinical trial is important “to understand if there is a preventative and/or treatment potential in the medications that stimulate type 2 and 4 angiotensin II receptors.”
The study received funding from the National Institute on Aging. Dr. Marcum and Dr. Santos-Gallego have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Antihypertensive medications that stimulate rather than inhibit type 2 and 4 angiotensin II receptors can lower the rate of dementia among new users of these medications, new research suggests.
Results from a cohort study of more than 57,000 older Medicare beneficiaries showed that the initiation of antihypertensives that stimulate the receptors was linked to a 16% lower risk for incident Alzheimer’s disease and related dementia (ADRD) and an 18% lower risk for vascular dementia compared with those that inhibit the receptors.
“Achieving appropriate blood pressure control is essential for maximizing brain health, and this promising research suggests certain antihypertensives could yield brain benefit compared to others,” lead study author Zachary A. Marcum, PharmD, PhD, associate professor, University of Washington School of Pharmacy, Seattle, told this news organization.
The findings were published online in JAMA Network Open.
Medicare beneficiaries
Previous observational studies showed that antihypertensive medications that stimulate type 2 and 4 angiotensin II receptors, in comparison with those that don’t, were associated with lower rates of dementia. However, those studies included individuals with prevalent hypertension and were relatively small.
The new retrospective cohort study included a random sample of 57,773 Medicare beneficiaries aged at least 65 years with new-onset hypertension. The mean age of participants was 73.8 years, 62.9% were women, and 86.9% were White.
Over the course of the study, some participants filled at least one prescription for a stimulating angiotensin II receptor type 2 and 4, such as angiotensin II receptor type 1 blockers, dihydropyridine calcium channel blockers, and thiazide diuretics.
Others participants filled a prescription for an inhibiting type 2 and 4 angiotensin II receptors, including angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and nondihydropyridine calcium channel blockers.
“All these medications lower blood pressure, but they do it in different ways,” said Dr. Marcum.
The researchers were interested in the varying activity of these drugs at the type 2 and 4 angiotensin II receptors.
For each 30-day interval, they categorized beneficiaries into four groups: a stimulating medication group (n = 4,879) consisting of individuals mostly taking stimulating antihypertensives; an inhibiting medication group (n = 10,303) that mostly included individuals prescribed this type of antihypertensive; a mixed group (n = 2,179) that included a combination of the first two classifications; and a nonuser group (n = 40,413) of individuals who were not using either type of drug.
The primary outcome was time to first occurrence of ADRD. The secondary outcome was time to first occurrence of vascular dementia.
Researchers controlled for cardiovascular risk factors and sociodemographic characteristics, such as age, sex, race/ethnicity, and receipt of low-income subsidy.
Unanswered questions
After adjustments, results showed that initiation of an antihypertensive medication regimen that exclusively stimulates, rather than inhibits, type 2 and 4 angiotensin II receptors was associated with a 16% lower risk for incident ADRD over a follow-up of just under 7 years (hazard ratio, 0.84; 95% confidence interval, 0.79-0.90; P < .001).
The mixed regimen was also associated with statistically significant (P = .001) reduced odds of ADRD compared with the inhibiting medications.
As for vascular dementia, use of stimulating vs. inhibiting medications was associated with an 18% lower risk (HR, 0.82; 95% CI, 0.69-0.96; P = .02).
Again, use of the mixed regimen was associated with reduced risk of vascular dementia compared with the inhibiting medications (P = .03).
A variety of potential mechanisms might explain the superiority of stimulating agents when it comes to dementia risk, said Dr. Marcum. These could include, for example, increased blood flow to the brain and reduced amyloid.
“But more mechanistic work is needed as well as evaluation of dose responses, because that’s not something we looked at in this study,” Dr. Marcum said. “There are still a lot of unanswered questions.”
Stimulators instead of inhibitors?
The results of the current analysis come on the heels of some previous work showing the benefits of lowering blood pressure. For example, the Systolic Blood Pressure Intervention Trial (SPRINT) showed that targeting a systolic blood pressure below 120 mm Hg significantly reduces risk for heart disease, stroke, and death from these diseases.
But in contrast to previous research, the current study included only beneficiaries with incident hypertension and new use of antihypertensive medications, and it adjusted for time-varying confounding.
Prescribing stimulating instead of inhibiting treatments could make a difference at the population level, Dr. Marcum noted.
“If we could shift the prescribing a little bit from inhibiting to stimulating, that could possibly reduce dementia risk,” he said.
However, “we’re not suggesting [that all patients] have their regimen switched,” he added.
That’s because inhibiting medications still have an important place in the antihypertensive treatment armamentarium, Dr. Marcum noted. As an example, beta-blockers are used post heart attack.
As well, factors such as cost and side effects should be taken into consideration when prescribing an antihypertensive drug.
The new results could be used to set up a comparison in a future randomized controlled trial that would provide the strongest evidence for estimating causal effects of treatments, said Dr. Marcum.
‘More convincing’
Carlos G. Santos-Gallego, MD, Icahn School of Medicine at Mount Sinai, New York, said the study is “more convincing” than previous related research, as it has a larger sample size and a longer follow-up.
“And the exquisite statistical analysis gives more robustness, more solidity, to the hypothesis that drugs that stimulate type 2 and 4 angiotensin II receptors might be protective for dementia,” said Dr. Santos-Gallego, who was not involved with the research.
However, he noted that the retrospective study had some limitations, including the underdiagnosis of dementia. “The diagnosis of dementia is, honestly, very poorly done in the clinical setting,” he said.
As well, the study could be subject to “confounding by indication,” Dr. Santos-Gallego said. “There could be a third variable, another confounding factor, that’s responsible both for the dementia and for the prescription of these drugs,” he added.
For example, he noted that comorbidities such as atrial fibrillation, myocardial infarction, and heart failure might increase the risk of dementia.
He agreed with the investigators that a randomized clinical trial would address these limitations. “All comorbidities would be equally shared” in the randomized groups, and all participants would be given “a specific test for dementia at the same time,” Dr. Santos-Gallego said.
Still, he noted that the new results are in keeping with hypertension guidelines that recommend stimulating drugs.
“This trial definitely shows that the current hypertension guidelines are good treatment for our patients, not only to control blood pressure and not only to prevent infarction to prevent stroke but also to prevent dementia,” said Dr. Santos-Gallego.
Also commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations at the Alzheimer’s Association, said the new data provide “clarity” on why previous research had differing results on the effect of antihypertensives on cognition.
Among the caveats of this new analysis is that “it’s unclear if the demographics in this study are fully representative of Medicare beneficiaries,” said Dr. Snyder.
She, too, said a clinical trial is important “to understand if there is a preventative and/or treatment potential in the medications that stimulate type 2 and 4 angiotensin II receptors.”
The study received funding from the National Institute on Aging. Dr. Marcum and Dr. Santos-Gallego have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Antihypertensive medications that stimulate rather than inhibit type 2 and 4 angiotensin II receptors can lower the rate of dementia among new users of these medications, new research suggests.
Results from a cohort study of more than 57,000 older Medicare beneficiaries showed that the initiation of antihypertensives that stimulate the receptors was linked to a 16% lower risk for incident Alzheimer’s disease and related dementia (ADRD) and an 18% lower risk for vascular dementia compared with those that inhibit the receptors.
“Achieving appropriate blood pressure control is essential for maximizing brain health, and this promising research suggests certain antihypertensives could yield brain benefit compared to others,” lead study author Zachary A. Marcum, PharmD, PhD, associate professor, University of Washington School of Pharmacy, Seattle, told this news organization.
The findings were published online in JAMA Network Open.
Medicare beneficiaries
Previous observational studies showed that antihypertensive medications that stimulate type 2 and 4 angiotensin II receptors, in comparison with those that don’t, were associated with lower rates of dementia. However, those studies included individuals with prevalent hypertension and were relatively small.
The new retrospective cohort study included a random sample of 57,773 Medicare beneficiaries aged at least 65 years with new-onset hypertension. The mean age of participants was 73.8 years, 62.9% were women, and 86.9% were White.
Over the course of the study, some participants filled at least one prescription for a stimulating angiotensin II receptor type 2 and 4, such as angiotensin II receptor type 1 blockers, dihydropyridine calcium channel blockers, and thiazide diuretics.
Others participants filled a prescription for an inhibiting type 2 and 4 angiotensin II receptors, including angiotensin-converting enzyme (ACE) inhibitors, beta-blockers, and nondihydropyridine calcium channel blockers.
“All these medications lower blood pressure, but they do it in different ways,” said Dr. Marcum.
The researchers were interested in the varying activity of these drugs at the type 2 and 4 angiotensin II receptors.
For each 30-day interval, they categorized beneficiaries into four groups: a stimulating medication group (n = 4,879) consisting of individuals mostly taking stimulating antihypertensives; an inhibiting medication group (n = 10,303) that mostly included individuals prescribed this type of antihypertensive; a mixed group (n = 2,179) that included a combination of the first two classifications; and a nonuser group (n = 40,413) of individuals who were not using either type of drug.
The primary outcome was time to first occurrence of ADRD. The secondary outcome was time to first occurrence of vascular dementia.
Researchers controlled for cardiovascular risk factors and sociodemographic characteristics, such as age, sex, race/ethnicity, and receipt of low-income subsidy.
Unanswered questions
After adjustments, results showed that initiation of an antihypertensive medication regimen that exclusively stimulates, rather than inhibits, type 2 and 4 angiotensin II receptors was associated with a 16% lower risk for incident ADRD over a follow-up of just under 7 years (hazard ratio, 0.84; 95% confidence interval, 0.79-0.90; P < .001).
The mixed regimen was also associated with statistically significant (P = .001) reduced odds of ADRD compared with the inhibiting medications.
As for vascular dementia, use of stimulating vs. inhibiting medications was associated with an 18% lower risk (HR, 0.82; 95% CI, 0.69-0.96; P = .02).
Again, use of the mixed regimen was associated with reduced risk of vascular dementia compared with the inhibiting medications (P = .03).
A variety of potential mechanisms might explain the superiority of stimulating agents when it comes to dementia risk, said Dr. Marcum. These could include, for example, increased blood flow to the brain and reduced amyloid.
“But more mechanistic work is needed as well as evaluation of dose responses, because that’s not something we looked at in this study,” Dr. Marcum said. “There are still a lot of unanswered questions.”
Stimulators instead of inhibitors?
The results of the current analysis come on the heels of some previous work showing the benefits of lowering blood pressure. For example, the Systolic Blood Pressure Intervention Trial (SPRINT) showed that targeting a systolic blood pressure below 120 mm Hg significantly reduces risk for heart disease, stroke, and death from these diseases.
But in contrast to previous research, the current study included only beneficiaries with incident hypertension and new use of antihypertensive medications, and it adjusted for time-varying confounding.
Prescribing stimulating instead of inhibiting treatments could make a difference at the population level, Dr. Marcum noted.
“If we could shift the prescribing a little bit from inhibiting to stimulating, that could possibly reduce dementia risk,” he said.
However, “we’re not suggesting [that all patients] have their regimen switched,” he added.
That’s because inhibiting medications still have an important place in the antihypertensive treatment armamentarium, Dr. Marcum noted. As an example, beta-blockers are used post heart attack.
As well, factors such as cost and side effects should be taken into consideration when prescribing an antihypertensive drug.
The new results could be used to set up a comparison in a future randomized controlled trial that would provide the strongest evidence for estimating causal effects of treatments, said Dr. Marcum.
‘More convincing’
Carlos G. Santos-Gallego, MD, Icahn School of Medicine at Mount Sinai, New York, said the study is “more convincing” than previous related research, as it has a larger sample size and a longer follow-up.
“And the exquisite statistical analysis gives more robustness, more solidity, to the hypothesis that drugs that stimulate type 2 and 4 angiotensin II receptors might be protective for dementia,” said Dr. Santos-Gallego, who was not involved with the research.
However, he noted that the retrospective study had some limitations, including the underdiagnosis of dementia. “The diagnosis of dementia is, honestly, very poorly done in the clinical setting,” he said.
As well, the study could be subject to “confounding by indication,” Dr. Santos-Gallego said. “There could be a third variable, another confounding factor, that’s responsible both for the dementia and for the prescription of these drugs,” he added.
For example, he noted that comorbidities such as atrial fibrillation, myocardial infarction, and heart failure might increase the risk of dementia.
He agreed with the investigators that a randomized clinical trial would address these limitations. “All comorbidities would be equally shared” in the randomized groups, and all participants would be given “a specific test for dementia at the same time,” Dr. Santos-Gallego said.
Still, he noted that the new results are in keeping with hypertension guidelines that recommend stimulating drugs.
“This trial definitely shows that the current hypertension guidelines are good treatment for our patients, not only to control blood pressure and not only to prevent infarction to prevent stroke but also to prevent dementia,” said Dr. Santos-Gallego.
Also commenting for this news organization, Heather Snyder, PhD, vice president of medical and scientific relations at the Alzheimer’s Association, said the new data provide “clarity” on why previous research had differing results on the effect of antihypertensives on cognition.
Among the caveats of this new analysis is that “it’s unclear if the demographics in this study are fully representative of Medicare beneficiaries,” said Dr. Snyder.
She, too, said a clinical trial is important “to understand if there is a preventative and/or treatment potential in the medications that stimulate type 2 and 4 angiotensin II receptors.”
The study received funding from the National Institute on Aging. Dr. Marcum and Dr. Santos-Gallego have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Spikes out: A COVID mystery
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
To date, it has been a mystery, like “Glass Onion.” And in the spirit of all the great mysteries, to get to the bottom of this, we’ll need to round up the usual suspects.
Appearing in Circulation, a new study does a great job of systematically evaluating multiple hypotheses linking vaccination to myocarditis, and eliminating them, Poirot-style, one by one until only one remains. We’ll get there.
But first, let’s review the suspects. Why do the mRNA vaccines cause myocarditis in a small subset of people?
There are a few leading candidates.
Number one: antibody responses. There are two flavors here. The quantitative hypothesis suggests that some people simply generate too many antibodies to the vaccine, leading to increased inflammation and heart damage.
The qualitative hypothesis suggests that maybe it’s the nature of the antibodies generated rather than the amount; they might cross-react with some protein on the surface of heart cells for instance.
Or maybe it is driven by T-cell responses, which, of course, are independent of antibody levels.
There’s the idea that myocarditis is due to excessive cytokine release – sort of like what we see in the multisystem inflammatory syndrome in children.
Or it could be due to the viral antigens themselves – the spike protein the mRNA codes for that is generated after vaccination.
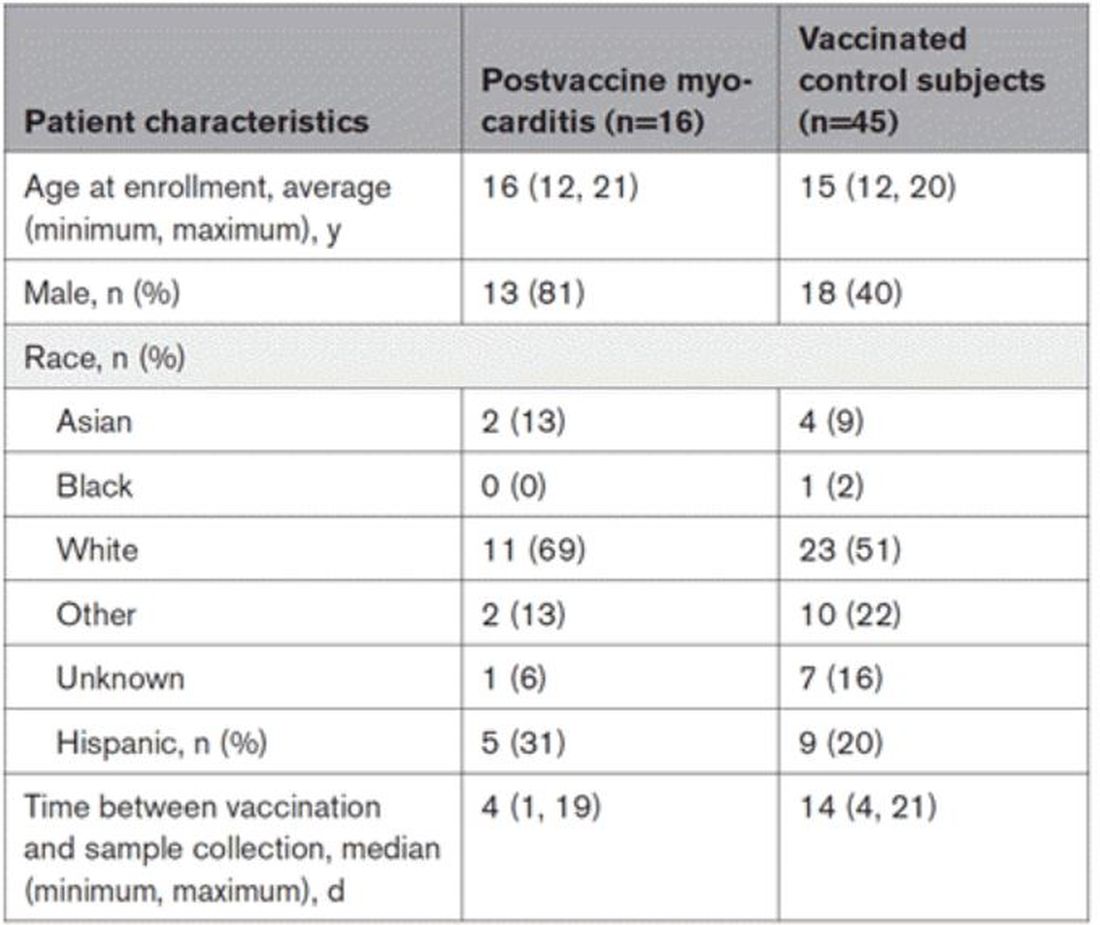
To tease all these possibilities apart, researchers led by Lael Yonker at Mass General performed a case-control study. Sixteen children with postvaccine myocarditis were matched by age to 45 control children who had been vaccinated without complications.
The matching was OK, but as you can see here, there were more boys in the myocarditis group, and the time from vaccination was a bit shorter in that group as well. We’ll keep that in mind as we go through the results.
OK, let’s start eliminating suspects.
First, quantitative antibodies. Seems unlikely. Absolute antibody titers were really no different in the myocarditis vs. the control group.
What about the quality of the antibodies? Would the kids with myocarditis have more self-recognizing antibodies present? It doesn’t appear so. Autoantibody levels were similar in the two groups.
Take antibodies off the list.
T-cell responses come next, and, again, no major differences here, save for one specific T-cell subtype that was moderately elevated in the myocarditis group. Not what I would call a smoking gun, frankly.
Cytokines give us a bit more to chew on. Levels of interleukin (IL)-8, IL-6, tumor necrosis factor (TNF)-alpha, and IL-10 were all substantially higher in the kids with myocarditis.
But the thing about cytokines is that they are not particularly specific. OK, kids with myocarditis have more systemic inflammation than kids without; that’s not really surprising. It still leaves us with the question of what is causing all this inflammation? Who is the arch-villain? The kingpin? The don?
It’s the analyses of antigens – the protein products of vaccination – that may hold the key here.
In 12 out of 16 kids with myocarditis, the researchers were able to measure free spike protein in the blood – that is to say spike protein, not bound by antispike antibodies.
These free spikes were present in – wait for it – zero of the 45 control patients. That makes spike protein itself our prime suspect. J’accuse free spike protein!
Of course, all good detectives need to wrap up the case with a good story: How was it all done?
And here’s where we could use Agatha Christie’s help. How could this all work? The vaccine gets injected; mRNA is taken up into cells, where spike protein is generated and released, generating antibody and T-cell responses all the while. Those responses rapidly clear that spike protein from the system – this has been demonstrated in multiple studies – in adults, at least. But in some small number of people, apparently, spike protein is not cleared. Why? It makes no damn sense. Compels me, though. Some have suggested that inadvertent intravenous injection of vaccine, compared with the appropriate intramuscular route, might distribute the vaccine to sites with less immune surveillance. But that is definitely not proven yet.
We are on the path for sure, but this is, as Benoit Blanc would say, a twisted web – and we are not finished untangling it. Not yet.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t,” is available for preorder now. He reports no conflicts of interest.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
To date, it has been a mystery, like “Glass Onion.” And in the spirit of all the great mysteries, to get to the bottom of this, we’ll need to round up the usual suspects.
Appearing in Circulation, a new study does a great job of systematically evaluating multiple hypotheses linking vaccination to myocarditis, and eliminating them, Poirot-style, one by one until only one remains. We’ll get there.
But first, let’s review the suspects. Why do the mRNA vaccines cause myocarditis in a small subset of people?
There are a few leading candidates.
Number one: antibody responses. There are two flavors here. The quantitative hypothesis suggests that some people simply generate too many antibodies to the vaccine, leading to increased inflammation and heart damage.
The qualitative hypothesis suggests that maybe it’s the nature of the antibodies generated rather than the amount; they might cross-react with some protein on the surface of heart cells for instance.
Or maybe it is driven by T-cell responses, which, of course, are independent of antibody levels.
There’s the idea that myocarditis is due to excessive cytokine release – sort of like what we see in the multisystem inflammatory syndrome in children.
Or it could be due to the viral antigens themselves – the spike protein the mRNA codes for that is generated after vaccination.
To tease all these possibilities apart, researchers led by Lael Yonker at Mass General performed a case-control study. Sixteen children with postvaccine myocarditis were matched by age to 45 control children who had been vaccinated without complications.
The matching was OK, but as you can see here, there were more boys in the myocarditis group, and the time from vaccination was a bit shorter in that group as well. We’ll keep that in mind as we go through the results.
OK, let’s start eliminating suspects.
First, quantitative antibodies. Seems unlikely. Absolute antibody titers were really no different in the myocarditis vs. the control group.
What about the quality of the antibodies? Would the kids with myocarditis have more self-recognizing antibodies present? It doesn’t appear so. Autoantibody levels were similar in the two groups.
Take antibodies off the list.
T-cell responses come next, and, again, no major differences here, save for one specific T-cell subtype that was moderately elevated in the myocarditis group. Not what I would call a smoking gun, frankly.
Cytokines give us a bit more to chew on. Levels of interleukin (IL)-8, IL-6, tumor necrosis factor (TNF)-alpha, and IL-10 were all substantially higher in the kids with myocarditis.
But the thing about cytokines is that they are not particularly specific. OK, kids with myocarditis have more systemic inflammation than kids without; that’s not really surprising. It still leaves us with the question of what is causing all this inflammation? Who is the arch-villain? The kingpin? The don?
It’s the analyses of antigens – the protein products of vaccination – that may hold the key here.
In 12 out of 16 kids with myocarditis, the researchers were able to measure free spike protein in the blood – that is to say spike protein, not bound by antispike antibodies.
These free spikes were present in – wait for it – zero of the 45 control patients. That makes spike protein itself our prime suspect. J’accuse free spike protein!
Of course, all good detectives need to wrap up the case with a good story: How was it all done?
And here’s where we could use Agatha Christie’s help. How could this all work? The vaccine gets injected; mRNA is taken up into cells, where spike protein is generated and released, generating antibody and T-cell responses all the while. Those responses rapidly clear that spike protein from the system – this has been demonstrated in multiple studies – in adults, at least. But in some small number of people, apparently, spike protein is not cleared. Why? It makes no damn sense. Compels me, though. Some have suggested that inadvertent intravenous injection of vaccine, compared with the appropriate intramuscular route, might distribute the vaccine to sites with less immune surveillance. But that is definitely not proven yet.
We are on the path for sure, but this is, as Benoit Blanc would say, a twisted web – and we are not finished untangling it. Not yet.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t,” is available for preorder now. He reports no conflicts of interest.
A version of this article first appeared on Medscape.com.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
To date, it has been a mystery, like “Glass Onion.” And in the spirit of all the great mysteries, to get to the bottom of this, we’ll need to round up the usual suspects.
Appearing in Circulation, a new study does a great job of systematically evaluating multiple hypotheses linking vaccination to myocarditis, and eliminating them, Poirot-style, one by one until only one remains. We’ll get there.
But first, let’s review the suspects. Why do the mRNA vaccines cause myocarditis in a small subset of people?
There are a few leading candidates.
Number one: antibody responses. There are two flavors here. The quantitative hypothesis suggests that some people simply generate too many antibodies to the vaccine, leading to increased inflammation and heart damage.
The qualitative hypothesis suggests that maybe it’s the nature of the antibodies generated rather than the amount; they might cross-react with some protein on the surface of heart cells for instance.
Or maybe it is driven by T-cell responses, which, of course, are independent of antibody levels.
There’s the idea that myocarditis is due to excessive cytokine release – sort of like what we see in the multisystem inflammatory syndrome in children.
Or it could be due to the viral antigens themselves – the spike protein the mRNA codes for that is generated after vaccination.
To tease all these possibilities apart, researchers led by Lael Yonker at Mass General performed a case-control study. Sixteen children with postvaccine myocarditis were matched by age to 45 control children who had been vaccinated without complications.
The matching was OK, but as you can see here, there were more boys in the myocarditis group, and the time from vaccination was a bit shorter in that group as well. We’ll keep that in mind as we go through the results.
OK, let’s start eliminating suspects.
First, quantitative antibodies. Seems unlikely. Absolute antibody titers were really no different in the myocarditis vs. the control group.
What about the quality of the antibodies? Would the kids with myocarditis have more self-recognizing antibodies present? It doesn’t appear so. Autoantibody levels were similar in the two groups.
Take antibodies off the list.
T-cell responses come next, and, again, no major differences here, save for one specific T-cell subtype that was moderately elevated in the myocarditis group. Not what I would call a smoking gun, frankly.
Cytokines give us a bit more to chew on. Levels of interleukin (IL)-8, IL-6, tumor necrosis factor (TNF)-alpha, and IL-10 were all substantially higher in the kids with myocarditis.
But the thing about cytokines is that they are not particularly specific. OK, kids with myocarditis have more systemic inflammation than kids without; that’s not really surprising. It still leaves us with the question of what is causing all this inflammation? Who is the arch-villain? The kingpin? The don?
It’s the analyses of antigens – the protein products of vaccination – that may hold the key here.
In 12 out of 16 kids with myocarditis, the researchers were able to measure free spike protein in the blood – that is to say spike protein, not bound by antispike antibodies.
These free spikes were present in – wait for it – zero of the 45 control patients. That makes spike protein itself our prime suspect. J’accuse free spike protein!
Of course, all good detectives need to wrap up the case with a good story: How was it all done?
And here’s where we could use Agatha Christie’s help. How could this all work? The vaccine gets injected; mRNA is taken up into cells, where spike protein is generated and released, generating antibody and T-cell responses all the while. Those responses rapidly clear that spike protein from the system – this has been demonstrated in multiple studies – in adults, at least. But in some small number of people, apparently, spike protein is not cleared. Why? It makes no damn sense. Compels me, though. Some have suggested that inadvertent intravenous injection of vaccine, compared with the appropriate intramuscular route, might distribute the vaccine to sites with less immune surveillance. But that is definitely not proven yet.
We are on the path for sure, but this is, as Benoit Blanc would say, a twisted web – and we are not finished untangling it. Not yet.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and director of Yale’s Clinical and Translational Research Accelerator. His science communication work can be found in the Huffington Post, on NPR, and here. He tweets @fperrywilson and his new book, “How Medicine Works and When It Doesn’t,” is available for preorder now. He reports no conflicts of interest.
A version of this article first appeared on Medscape.com.
Study spotlights clinicopathologic features, survival outcomes of pediatric melanoma
.
“Cutaneous melanomas are rare in children and much less common in adolescents than in later life,” researchers led by Mary-Ann El Sharouni, PhD, wrote in the study, which was published online in the Journal of the American Academy of Dermatology. “Management of these young patients currently follows guidelines developed for adults. Better understanding of melanoma occurring in the first 2 decades of life is, therefore, warranted.”
Drawing from two datasets – one from the Netherlands and the other from Melanoma Institute Australia (MIA) at the University of Sydney – Dr. El Sharouni of the MIA and of the department of dermatology at University Medical Center Utrecht in the Netherlands, and colleagues, evaluated all patients younger than 20 years of age who were diagnosed with invasive melanoma between January 2000 and December 2014. The pooled cohort included 397 Dutch and 117 Australian individuals. Of these, 62 were children and 452 were adolescents. To determine melanoma subtypes, the researchers reevaluated pathology reports and used multivariate Cox models to calculate recurrence-free survival (RFS) and overall survival (OS).
The median Breslow thickness was 2.7 mm in children and 1.0 mm in adolescents. Most patients (83%) had conventional melanoma, which consisted of superficial spreading, nodular, desmoplastic, and acral lentiginous forms, while 78 had spitzoid melanoma and 8 had melanoma associated with a congenital nevus. The 10-year RFS was 91.5% in children and 86.4% in adolescents (P =.32), while the 10-year OS was 100% in children and 92.7% in adolescents (P = .09).
On multivariable analysis, which was possible only for the adolescent cohort because of the small number of children, ulceration status and anatomic site were associated with RFS and OS, whereas age, sex, mitotic index, sentinel node status, and melanoma subtype were not. Breslow thickness > 4 mm was associated with worse RFS. As for affected anatomic site, those with melanomas located on the upper and lower limbs had a better overall RFS and OS compared with those who had head or neck melanomas.
The authors acknowledged certain limitation of the analysis, including its retrospective design and the small number of children. “Our data suggest that adolescent melanomas are often similar to adult-type melanomas, whilst those which occur in young children frequently occur via different molecular mechanisms,” they concluded. “In the future it is likely that further understanding of these molecular mechanisms and ability to classify melanomas based on their molecular characteristics will assist in further refining prognostic estimates and possible guiding treatment for young patients with melanoma.”
Rebecca M. Thiede, MD, assistant program director of the division of dermatology at the University of Arizona, Tucson, who was asked to comment on the study, said that the analysis “greatly contributes to dermatology, as we are still learning the differences between melanoma in children and adolescents versus adults.
This study found that adolescents with melanoma had worse survival if mitosis were present and/or located on head/neck, which could aid in aggressiveness of treatment.”
A key strength of analysis, she continued, is the large sample size of 514 patients, “given that melanoma in this population is very rare. A limitation which [the researchers] brought up is the discrepancy of diagnosis via histopathology of melanoma in children versus adults. The study relied on the pathology report given the retrospective nature of this [analysis, and it] was based on Australian and Dutch populations, which may limit its scope in other countries.”
Dr. El Sharouni was supported by a research fellowship grant from the European Academy of Dermatology and Venereology (EADV), while two of her coauthors, Richard A. Scolyer, MD, and John F. Thompson, MD, were recipients of an Australian National Health and Medical Research Council Program Grant. The study was also supported by a research program grant from Cancer Institute New South Wales. Dr. Thiede reported having no financial disclosures.
.
“Cutaneous melanomas are rare in children and much less common in adolescents than in later life,” researchers led by Mary-Ann El Sharouni, PhD, wrote in the study, which was published online in the Journal of the American Academy of Dermatology. “Management of these young patients currently follows guidelines developed for adults. Better understanding of melanoma occurring in the first 2 decades of life is, therefore, warranted.”
Drawing from two datasets – one from the Netherlands and the other from Melanoma Institute Australia (MIA) at the University of Sydney – Dr. El Sharouni of the MIA and of the department of dermatology at University Medical Center Utrecht in the Netherlands, and colleagues, evaluated all patients younger than 20 years of age who were diagnosed with invasive melanoma between January 2000 and December 2014. The pooled cohort included 397 Dutch and 117 Australian individuals. Of these, 62 were children and 452 were adolescents. To determine melanoma subtypes, the researchers reevaluated pathology reports and used multivariate Cox models to calculate recurrence-free survival (RFS) and overall survival (OS).
The median Breslow thickness was 2.7 mm in children and 1.0 mm in adolescents. Most patients (83%) had conventional melanoma, which consisted of superficial spreading, nodular, desmoplastic, and acral lentiginous forms, while 78 had spitzoid melanoma and 8 had melanoma associated with a congenital nevus. The 10-year RFS was 91.5% in children and 86.4% in adolescents (P =.32), while the 10-year OS was 100% in children and 92.7% in adolescents (P = .09).
On multivariable analysis, which was possible only for the adolescent cohort because of the small number of children, ulceration status and anatomic site were associated with RFS and OS, whereas age, sex, mitotic index, sentinel node status, and melanoma subtype were not. Breslow thickness > 4 mm was associated with worse RFS. As for affected anatomic site, those with melanomas located on the upper and lower limbs had a better overall RFS and OS compared with those who had head or neck melanomas.
The authors acknowledged certain limitation of the analysis, including its retrospective design and the small number of children. “Our data suggest that adolescent melanomas are often similar to adult-type melanomas, whilst those which occur in young children frequently occur via different molecular mechanisms,” they concluded. “In the future it is likely that further understanding of these molecular mechanisms and ability to classify melanomas based on their molecular characteristics will assist in further refining prognostic estimates and possible guiding treatment for young patients with melanoma.”
Rebecca M. Thiede, MD, assistant program director of the division of dermatology at the University of Arizona, Tucson, who was asked to comment on the study, said that the analysis “greatly contributes to dermatology, as we are still learning the differences between melanoma in children and adolescents versus adults.
This study found that adolescents with melanoma had worse survival if mitosis were present and/or located on head/neck, which could aid in aggressiveness of treatment.”
A key strength of analysis, she continued, is the large sample size of 514 patients, “given that melanoma in this population is very rare. A limitation which [the researchers] brought up is the discrepancy of diagnosis via histopathology of melanoma in children versus adults. The study relied on the pathology report given the retrospective nature of this [analysis, and it] was based on Australian and Dutch populations, which may limit its scope in other countries.”
Dr. El Sharouni was supported by a research fellowship grant from the European Academy of Dermatology and Venereology (EADV), while two of her coauthors, Richard A. Scolyer, MD, and John F. Thompson, MD, were recipients of an Australian National Health and Medical Research Council Program Grant. The study was also supported by a research program grant from Cancer Institute New South Wales. Dr. Thiede reported having no financial disclosures.
.
“Cutaneous melanomas are rare in children and much less common in adolescents than in later life,” researchers led by Mary-Ann El Sharouni, PhD, wrote in the study, which was published online in the Journal of the American Academy of Dermatology. “Management of these young patients currently follows guidelines developed for adults. Better understanding of melanoma occurring in the first 2 decades of life is, therefore, warranted.”
Drawing from two datasets – one from the Netherlands and the other from Melanoma Institute Australia (MIA) at the University of Sydney – Dr. El Sharouni of the MIA and of the department of dermatology at University Medical Center Utrecht in the Netherlands, and colleagues, evaluated all patients younger than 20 years of age who were diagnosed with invasive melanoma between January 2000 and December 2014. The pooled cohort included 397 Dutch and 117 Australian individuals. Of these, 62 were children and 452 were adolescents. To determine melanoma subtypes, the researchers reevaluated pathology reports and used multivariate Cox models to calculate recurrence-free survival (RFS) and overall survival (OS).
The median Breslow thickness was 2.7 mm in children and 1.0 mm in adolescents. Most patients (83%) had conventional melanoma, which consisted of superficial spreading, nodular, desmoplastic, and acral lentiginous forms, while 78 had spitzoid melanoma and 8 had melanoma associated with a congenital nevus. The 10-year RFS was 91.5% in children and 86.4% in adolescents (P =.32), while the 10-year OS was 100% in children and 92.7% in adolescents (P = .09).
On multivariable analysis, which was possible only for the adolescent cohort because of the small number of children, ulceration status and anatomic site were associated with RFS and OS, whereas age, sex, mitotic index, sentinel node status, and melanoma subtype were not. Breslow thickness > 4 mm was associated with worse RFS. As for affected anatomic site, those with melanomas located on the upper and lower limbs had a better overall RFS and OS compared with those who had head or neck melanomas.
The authors acknowledged certain limitation of the analysis, including its retrospective design and the small number of children. “Our data suggest that adolescent melanomas are often similar to adult-type melanomas, whilst those which occur in young children frequently occur via different molecular mechanisms,” they concluded. “In the future it is likely that further understanding of these molecular mechanisms and ability to classify melanomas based on their molecular characteristics will assist in further refining prognostic estimates and possible guiding treatment for young patients with melanoma.”
Rebecca M. Thiede, MD, assistant program director of the division of dermatology at the University of Arizona, Tucson, who was asked to comment on the study, said that the analysis “greatly contributes to dermatology, as we are still learning the differences between melanoma in children and adolescents versus adults.
This study found that adolescents with melanoma had worse survival if mitosis were present and/or located on head/neck, which could aid in aggressiveness of treatment.”
A key strength of analysis, she continued, is the large sample size of 514 patients, “given that melanoma in this population is very rare. A limitation which [the researchers] brought up is the discrepancy of diagnosis via histopathology of melanoma in children versus adults. The study relied on the pathology report given the retrospective nature of this [analysis, and it] was based on Australian and Dutch populations, which may limit its scope in other countries.”
Dr. El Sharouni was supported by a research fellowship grant from the European Academy of Dermatology and Venereology (EADV), while two of her coauthors, Richard A. Scolyer, MD, and John F. Thompson, MD, were recipients of an Australian National Health and Medical Research Council Program Grant. The study was also supported by a research program grant from Cancer Institute New South Wales. Dr. Thiede reported having no financial disclosures.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
New Omicron subvariant is ‘crazy infectious,’ COVID expert warns
“It’s crazy infectious,” said Paula Cannon, PhD, a virologist at the University of Southern California, Los Angeles. “All the things that have protected you for the past couple of years, I don’t think are going to protect you against this new crop of variants.”
XBB.1.5 is spreading quickly in the United States. It accounted for 27.6% of cases in the country in the week ending on Jan. 7, up from about 1% of cases at one point in December, according to the Centers for Disease Control and Prevention. It’s especially prevalent in the Northeast, now accounting for more than 70% of the cases in that region.
It’s spreading across the globe, too. Maria Van Kerkhove, PhD, technical lead of the World Health Organization, has called XBB.1.5 is “the most transmissible subvariant that has been detected yet.”
Ashish Jha, MD, the White House COVID-19 response coordinator, tweeted a few days ago that the spread of XBB.1.5 is “stunning” but cautioned that it’s unclear if the symptoms of infection will be more severe than for previous variants.
“Whether we’ll have an XBB.1.5 wave (and if yes, how big) will depend on many factors including immunity of the population, people’s actions, etc.,” he tweeted.
He urged people to get up to date on their boosters, wear a snug-fitting mask, and avoid crowded indoor spaces. He noted that people who haven’t been infected recently or haven’t gotten the bivalent booster likely have little protection against infection.
The symptoms for XBB.1.5 appear to be the same as for other versions of COVID-19. However, it’s less common for people infected with XBB.1.5 to report losing their sense of taste and smell, USA Today reported.
A version of this article first appeared on WebMD.com.
“It’s crazy infectious,” said Paula Cannon, PhD, a virologist at the University of Southern California, Los Angeles. “All the things that have protected you for the past couple of years, I don’t think are going to protect you against this new crop of variants.”
XBB.1.5 is spreading quickly in the United States. It accounted for 27.6% of cases in the country in the week ending on Jan. 7, up from about 1% of cases at one point in December, according to the Centers for Disease Control and Prevention. It’s especially prevalent in the Northeast, now accounting for more than 70% of the cases in that region.
It’s spreading across the globe, too. Maria Van Kerkhove, PhD, technical lead of the World Health Organization, has called XBB.1.5 is “the most transmissible subvariant that has been detected yet.”
Ashish Jha, MD, the White House COVID-19 response coordinator, tweeted a few days ago that the spread of XBB.1.5 is “stunning” but cautioned that it’s unclear if the symptoms of infection will be more severe than for previous variants.
“Whether we’ll have an XBB.1.5 wave (and if yes, how big) will depend on many factors including immunity of the population, people’s actions, etc.,” he tweeted.
He urged people to get up to date on their boosters, wear a snug-fitting mask, and avoid crowded indoor spaces. He noted that people who haven’t been infected recently or haven’t gotten the bivalent booster likely have little protection against infection.
The symptoms for XBB.1.5 appear to be the same as for other versions of COVID-19. However, it’s less common for people infected with XBB.1.5 to report losing their sense of taste and smell, USA Today reported.
A version of this article first appeared on WebMD.com.
“It’s crazy infectious,” said Paula Cannon, PhD, a virologist at the University of Southern California, Los Angeles. “All the things that have protected you for the past couple of years, I don’t think are going to protect you against this new crop of variants.”
XBB.1.5 is spreading quickly in the United States. It accounted for 27.6% of cases in the country in the week ending on Jan. 7, up from about 1% of cases at one point in December, according to the Centers for Disease Control and Prevention. It’s especially prevalent in the Northeast, now accounting for more than 70% of the cases in that region.
It’s spreading across the globe, too. Maria Van Kerkhove, PhD, technical lead of the World Health Organization, has called XBB.1.5 is “the most transmissible subvariant that has been detected yet.”
Ashish Jha, MD, the White House COVID-19 response coordinator, tweeted a few days ago that the spread of XBB.1.5 is “stunning” but cautioned that it’s unclear if the symptoms of infection will be more severe than for previous variants.
“Whether we’ll have an XBB.1.5 wave (and if yes, how big) will depend on many factors including immunity of the population, people’s actions, etc.,” he tweeted.
He urged people to get up to date on their boosters, wear a snug-fitting mask, and avoid crowded indoor spaces. He noted that people who haven’t been infected recently or haven’t gotten the bivalent booster likely have little protection against infection.
The symptoms for XBB.1.5 appear to be the same as for other versions of COVID-19. However, it’s less common for people infected with XBB.1.5 to report losing their sense of taste and smell, USA Today reported.
A version of this article first appeared on WebMD.com.
Autopsies show COVID virus invades entire body
A study on the subject was published in the journal Nature. The researchers completed autopsies from April 2020 to March 2021 of 44 unvaccinated people who had severe COVID-19. The median age was 62.5 years old, and 30% were female. Extensive brain sampling was done for 11 cases.
Because of its nature as a respiratory illness, SARS-CoV-2 was most widespread in the respiratory system such as in the lungs. But it was also found in 79 other body locations, including the heart, kidneys, liver, muscles, nerves, reproductive tract, and eyes.
The researchers said their work shows the SARS-CoV-2 “is capable of infecting and replicating within the human brain.” They also said their results indicate the virus spreads via the blood early during infection, which “seeds the virus throughout the body following infection of the respiratory tract.”
The authors noted that, while the virus was found outside the respiratory tract, they did not find signs of inflammation beyond the respiratory system.
The results will help narrow down treatments for long COVID, and particularly support the idea of using the antiviral drug Paxlovid to treat long COVID, according to a blog post from the National Institute of Allergy and Infectious Diseases. A clinical trial is already underway examining the treatment, and results are expected in January 2024.
A version of this article first appeared on WebMD.com.
A study on the subject was published in the journal Nature. The researchers completed autopsies from April 2020 to March 2021 of 44 unvaccinated people who had severe COVID-19. The median age was 62.5 years old, and 30% were female. Extensive brain sampling was done for 11 cases.
Because of its nature as a respiratory illness, SARS-CoV-2 was most widespread in the respiratory system such as in the lungs. But it was also found in 79 other body locations, including the heart, kidneys, liver, muscles, nerves, reproductive tract, and eyes.
The researchers said their work shows the SARS-CoV-2 “is capable of infecting and replicating within the human brain.” They also said their results indicate the virus spreads via the blood early during infection, which “seeds the virus throughout the body following infection of the respiratory tract.”
The authors noted that, while the virus was found outside the respiratory tract, they did not find signs of inflammation beyond the respiratory system.
The results will help narrow down treatments for long COVID, and particularly support the idea of using the antiviral drug Paxlovid to treat long COVID, according to a blog post from the National Institute of Allergy and Infectious Diseases. A clinical trial is already underway examining the treatment, and results are expected in January 2024.
A version of this article first appeared on WebMD.com.
A study on the subject was published in the journal Nature. The researchers completed autopsies from April 2020 to March 2021 of 44 unvaccinated people who had severe COVID-19. The median age was 62.5 years old, and 30% were female. Extensive brain sampling was done for 11 cases.
Because of its nature as a respiratory illness, SARS-CoV-2 was most widespread in the respiratory system such as in the lungs. But it was also found in 79 other body locations, including the heart, kidneys, liver, muscles, nerves, reproductive tract, and eyes.
The researchers said their work shows the SARS-CoV-2 “is capable of infecting and replicating within the human brain.” They also said their results indicate the virus spreads via the blood early during infection, which “seeds the virus throughout the body following infection of the respiratory tract.”
The authors noted that, while the virus was found outside the respiratory tract, they did not find signs of inflammation beyond the respiratory system.
The results will help narrow down treatments for long COVID, and particularly support the idea of using the antiviral drug Paxlovid to treat long COVID, according to a blog post from the National Institute of Allergy and Infectious Diseases. A clinical trial is already underway examining the treatment, and results are expected in January 2024.
A version of this article first appeared on WebMD.com.
FROM NATURE
Atrial fibrillation: Sex differences and modifiable risk factors
This transcript has been edited for clarity.
Hello. This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital.
We looked at these questions in our vitamin D and omega-3 trial VITAL in an ancillary study called VITAL Rhythm, led by Dr. Christine Albert at Cedars-Sinai. And this particular project was led by Dr. Hasan Siddiqi at Vanderbilt.
As you know, AF is the most common arrhythmia in the world, and it’s burgeoning in numbers, primarily because of the aging of the population. It’s also a major cause of stroke, heart failure, and cardiovascular mortality. Although women are known to have lower rates of AF than men, they’re also known to have a higher risk for cardiovascular complications and sequelae, such as higher risk for stroke and CVD mortality. Therefore, we thought that understanding sex differences in risk and modifiable risk factors for AF that could reduce the burden of disease would be important.
It’s known that greater height is a risk factor for AF, but the extent to which it explains the differences in AF risk between men and women isn’t really known. So we looked at these questions in the VITAL cohort. VITAL has more than 25,000 participants. It’s a large, diverse, nationwide cohort. About 51% are women, and all are aged 50 years or older, with a mean age of 67. All were free of known clinical cardiovascular disease at the start of the study.
AF reports were confirmed by medical records and also supplemented by Medicare CMS linkage for fuller ascertainment of outcomes. We had 900 incident cases of AF in the study, and we did see that women were less likely to be diagnosed with AF. They had a 32% lower risk – strongly statistically significant compared with men, with a P < .001. Women were also more likely to be symptomatic: About 77% of women vs. 63% of men had symptoms prior to or at diagnosis.
It was very interesting that adjustment for height eliminated the lower risk for AF in women compared with men. After accounting for height, there was not only no reduction in risk for AF among the women, there was actually a reversal of the association so that there was a slightly higher risk for AF in the women. Other risk factors for AF in the cohort included older age, higher body mass index, hypertension, and higher consumption of alcohol. We did not see an association between diabetes and higher risk for AF. We also saw no clear association with physical activity, although very strenuous physical activity has been linked to AF in some other studies.
We looked at the interventions of vitamin D (2,000 IU/day) and omega-3 fatty acids (460 mg/day of EPA and 380 mg/day of DHA) and found no association with AF, although some other studies have seen increased risk for AF with higher doses of the marine omega-3s > 1 g/day and certainly at doses of 4 g/day. So overall, the findings highlight the fact that many of the risk factors for AF do seem to be modifiable, and it is really important to identify and try to reduce these risk factors in order to reduce the burden of AF. This may be particularly important in women because women are more likely to have stroke and cardiovascular mortality in these adverse cardiovascular outcomes.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital.
We looked at these questions in our vitamin D and omega-3 trial VITAL in an ancillary study called VITAL Rhythm, led by Dr. Christine Albert at Cedars-Sinai. And this particular project was led by Dr. Hasan Siddiqi at Vanderbilt.
As you know, AF is the most common arrhythmia in the world, and it’s burgeoning in numbers, primarily because of the aging of the population. It’s also a major cause of stroke, heart failure, and cardiovascular mortality. Although women are known to have lower rates of AF than men, they’re also known to have a higher risk for cardiovascular complications and sequelae, such as higher risk for stroke and CVD mortality. Therefore, we thought that understanding sex differences in risk and modifiable risk factors for AF that could reduce the burden of disease would be important.
It’s known that greater height is a risk factor for AF, but the extent to which it explains the differences in AF risk between men and women isn’t really known. So we looked at these questions in the VITAL cohort. VITAL has more than 25,000 participants. It’s a large, diverse, nationwide cohort. About 51% are women, and all are aged 50 years or older, with a mean age of 67. All were free of known clinical cardiovascular disease at the start of the study.
AF reports were confirmed by medical records and also supplemented by Medicare CMS linkage for fuller ascertainment of outcomes. We had 900 incident cases of AF in the study, and we did see that women were less likely to be diagnosed with AF. They had a 32% lower risk – strongly statistically significant compared with men, with a P < .001. Women were also more likely to be symptomatic: About 77% of women vs. 63% of men had symptoms prior to or at diagnosis.
It was very interesting that adjustment for height eliminated the lower risk for AF in women compared with men. After accounting for height, there was not only no reduction in risk for AF among the women, there was actually a reversal of the association so that there was a slightly higher risk for AF in the women. Other risk factors for AF in the cohort included older age, higher body mass index, hypertension, and higher consumption of alcohol. We did not see an association between diabetes and higher risk for AF. We also saw no clear association with physical activity, although very strenuous physical activity has been linked to AF in some other studies.
We looked at the interventions of vitamin D (2,000 IU/day) and omega-3 fatty acids (460 mg/day of EPA and 380 mg/day of DHA) and found no association with AF, although some other studies have seen increased risk for AF with higher doses of the marine omega-3s > 1 g/day and certainly at doses of 4 g/day. So overall, the findings highlight the fact that many of the risk factors for AF do seem to be modifiable, and it is really important to identify and try to reduce these risk factors in order to reduce the burden of AF. This may be particularly important in women because women are more likely to have stroke and cardiovascular mortality in these adverse cardiovascular outcomes.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. This is Dr. JoAnn Manson, professor of medicine at Harvard Medical School and Brigham and Women’s Hospital.
We looked at these questions in our vitamin D and omega-3 trial VITAL in an ancillary study called VITAL Rhythm, led by Dr. Christine Albert at Cedars-Sinai. And this particular project was led by Dr. Hasan Siddiqi at Vanderbilt.
As you know, AF is the most common arrhythmia in the world, and it’s burgeoning in numbers, primarily because of the aging of the population. It’s also a major cause of stroke, heart failure, and cardiovascular mortality. Although women are known to have lower rates of AF than men, they’re also known to have a higher risk for cardiovascular complications and sequelae, such as higher risk for stroke and CVD mortality. Therefore, we thought that understanding sex differences in risk and modifiable risk factors for AF that could reduce the burden of disease would be important.
It’s known that greater height is a risk factor for AF, but the extent to which it explains the differences in AF risk between men and women isn’t really known. So we looked at these questions in the VITAL cohort. VITAL has more than 25,000 participants. It’s a large, diverse, nationwide cohort. About 51% are women, and all are aged 50 years or older, with a mean age of 67. All were free of known clinical cardiovascular disease at the start of the study.
AF reports were confirmed by medical records and also supplemented by Medicare CMS linkage for fuller ascertainment of outcomes. We had 900 incident cases of AF in the study, and we did see that women were less likely to be diagnosed with AF. They had a 32% lower risk – strongly statistically significant compared with men, with a P < .001. Women were also more likely to be symptomatic: About 77% of women vs. 63% of men had symptoms prior to or at diagnosis.
It was very interesting that adjustment for height eliminated the lower risk for AF in women compared with men. After accounting for height, there was not only no reduction in risk for AF among the women, there was actually a reversal of the association so that there was a slightly higher risk for AF in the women. Other risk factors for AF in the cohort included older age, higher body mass index, hypertension, and higher consumption of alcohol. We did not see an association between diabetes and higher risk for AF. We also saw no clear association with physical activity, although very strenuous physical activity has been linked to AF in some other studies.
We looked at the interventions of vitamin D (2,000 IU/day) and omega-3 fatty acids (460 mg/day of EPA and 380 mg/day of DHA) and found no association with AF, although some other studies have seen increased risk for AF with higher doses of the marine omega-3s > 1 g/day and certainly at doses of 4 g/day. So overall, the findings highlight the fact that many of the risk factors for AF do seem to be modifiable, and it is really important to identify and try to reduce these risk factors in order to reduce the burden of AF. This may be particularly important in women because women are more likely to have stroke and cardiovascular mortality in these adverse cardiovascular outcomes.
A version of this article first appeared on Medscape.com.
New guidelines on peds obesity call for aggressive treatment
and hope the problem solves itself. That’s the upshot of new guidelines from the American Academy of Pediatrics.
The authors of the guidelines also encourage primary care doctors to collaborate with other medical professionals to treat the comorbidities often linked to obesity, rather than take on the entire challenge themselves.
“It’s impossible to treat obesity within the four walls of the clinic. That’s one thing I have learned,” Ihuoma Eneli, MD, associate director of the AAP Institute for Healthy Childhood Weight, told this news organization. For example, a primary care doctor could partner with a gastroenterologist when treating a child who has nonalcoholic fatty liver disease, added Dr. Eneli, a professor of pediatrics at the Ohio State University, Columbus, who helped write the recommendations.
The new document updates 2007 recommendations from AAP about treating children and adolescents who are overweight or obese. The earlier statement focused on behavioral modification and healthy eating behaviors and paid less attention to weight-lowering medications or bariatric surgery for young people. That document did not offer specific advice to health care providers about how to address childhood overweight or obesity.
The 2023 guidelines recommend that pediatricians offer anyone aged 12 years and older with obesity – defined as a body mass index (BMI) at the 95th percentile or higher – the option of receiving weight-loss medications in addition to ongoing support for lifestyle modifications, such as exercising more and eating healthier foods.
The same approach holds for bariatric surgery once children reach age 13, and AAP stressed that no physician should ever stigmatize children or imply that they are to blame for their weight.
AAP did not receive any industry funding to develop the guidelines.
As children reach the threshold BMI levels, physicians should conduct complete physicals and order blood tests to get a fuller picture of the patients’ health.
These are the first guidelines from AAP aimed at giving pediatricians and other primary care providers concrete guidance for managing overweight and obesity in younger patients.
“Obesity is a complex, chronic disease, and that’s a frame shift here,” said Sandra S. Hassink, MD, leader of the guideline group and director of the AAP Institute for Healthy Childhood Weight.
Dr. Hassink compared obesity to asthma, another chronic disease that merits prompt attention and ongoing treatment. A physician would never let a child with asthma go untreated until their breathing problems are so severe that they turn blue, Dr. Hassink said; similarly, physicians should treat obesity in young people promptly and over time.
While some aspects of treating overweight and obesity are the same for children and adults, Dr. Hassink noted distinct differences. “Every child is embedded in a family and extended support structure,” Dr. Hassink said, which means that any obesity management technique needs the buy-in and support of the child’s family too.
AAP’s new advice reflects current understanding that excess weight or obesity in children is a result of biological and social factors, such as living in a food desert or experiencing the effects of structural racism.
The guidelines synthesize the results of hundreds of studies about the best way to treat excess weight in young people. If multiple studies were of high quality and all reached similar conclusions, they received an “A.” Less robust but still informative studies rated a “B.” In aggregate, the guideline about weight-lowering medication is based on “B” evidence that could shift with further research.
The authors recommend that clinicians calculate a child’s BMI beginning at age 2 years, with particular attention to those at the 85th percentile or higher for their age and sex (which would be defined as overweight), at the 95th percentile or higher (obesity), or at the 120th percentile and higher (severe obesity). Clinicians also should monitor blood pressure and cholesterol in their patients with overweight or obesity, particularly once they reach age 10.
Starting at age 6, providers should interview patients and their families about what would motivate them to lose weight, then tailor interventions to those factors rather than just make a blanket declaration that weight loss is necessary. This step should be coupled with intensive support – ideally, at least 26 hours of face-to-face support over the course of a year, although more is better – about effective exercise and dietary habits that result in weight loss.
The intensive support model should remain in place throughout childhood and adolescence and should be coupled with referrals for weight-loss medications or bariatric surgeries as needed once children reach age 12 or 13. Those age cutoffs are based on current evidence as to when weight-loss medications or surgery becomes effective, Dr. Hassink said, and could be shifted to lower ages if that’s what new evidence shows.
“Intensive health behavioral and lifestyle treatment is the base of all other treatment extensions,” Dr. Eneli said.
Young patients who needed weight-lowering medication used to have fewer options, according to Aaron S. Kelly, PhD, the Minnesota American Legion and Auxiliary Chair in Children’s Health at the University of Minnesota, Minneapolis.
.No longer.
Dr. Kelly was not involved in drafting the guidelines but was the lead investigator for trials of liraglutide (Saxenda), which in 2020 received U.S. Food and Drug Administration approval for treating obesity in adolescents. In 2022, the agency approved phentermine and topiramate extended-release capsules (Qsymia) for long-term weight management for patients aged 12 years and older, along with a once-weekly injection of semaglutide (Wegovy) patients in this age group. There are no weight-lowering medications for children younger than 12, Dr. Kelly said.
“Obesity is not a lifestyle problem. A lot of it is driven by the underlying biology,” Dr. Kelly said. “Really, what these medicines do is make it easier for people to make the right lifestyle choices by pushing back against the biology.”
For example, a drug can make people feel full for longer or disrupt chemical pathways that result in craving certain foods. Dr. Kelly emphasized that these drugs do not give license for people to eat as much as they want.
As for bariatric surgery, the new guidelines adhere closely to those in a 2019 AAP statement that bariatric surgery is safe and effective in pediatric settings. This is gratifying to Kirk W. Reichard, MD, MBA, a lead author of the 2019 article and director of the bariatric surgery program at Nemours Children’s Health.
Even if the information isn’t new as of 2023, Dr. Reichard said, AAP’s imprimatur could cause some eligible families to consider bariatric surgery when they may not have done so before.
Dr. Eneli, Dr. Hassink, and Dr. Reichard reported no relevant financial conflicts of interest. Dr. Kelly has relationships with Boehringer Ingelheim, Eli Lilly, Novo Nordisk, and Vivus.
A version of this article first appeared on Medscape.com.
and hope the problem solves itself. That’s the upshot of new guidelines from the American Academy of Pediatrics.
The authors of the guidelines also encourage primary care doctors to collaborate with other medical professionals to treat the comorbidities often linked to obesity, rather than take on the entire challenge themselves.
“It’s impossible to treat obesity within the four walls of the clinic. That’s one thing I have learned,” Ihuoma Eneli, MD, associate director of the AAP Institute for Healthy Childhood Weight, told this news organization. For example, a primary care doctor could partner with a gastroenterologist when treating a child who has nonalcoholic fatty liver disease, added Dr. Eneli, a professor of pediatrics at the Ohio State University, Columbus, who helped write the recommendations.
The new document updates 2007 recommendations from AAP about treating children and adolescents who are overweight or obese. The earlier statement focused on behavioral modification and healthy eating behaviors and paid less attention to weight-lowering medications or bariatric surgery for young people. That document did not offer specific advice to health care providers about how to address childhood overweight or obesity.
The 2023 guidelines recommend that pediatricians offer anyone aged 12 years and older with obesity – defined as a body mass index (BMI) at the 95th percentile or higher – the option of receiving weight-loss medications in addition to ongoing support for lifestyle modifications, such as exercising more and eating healthier foods.
The same approach holds for bariatric surgery once children reach age 13, and AAP stressed that no physician should ever stigmatize children or imply that they are to blame for their weight.
AAP did not receive any industry funding to develop the guidelines.
As children reach the threshold BMI levels, physicians should conduct complete physicals and order blood tests to get a fuller picture of the patients’ health.
These are the first guidelines from AAP aimed at giving pediatricians and other primary care providers concrete guidance for managing overweight and obesity in younger patients.
“Obesity is a complex, chronic disease, and that’s a frame shift here,” said Sandra S. Hassink, MD, leader of the guideline group and director of the AAP Institute for Healthy Childhood Weight.
Dr. Hassink compared obesity to asthma, another chronic disease that merits prompt attention and ongoing treatment. A physician would never let a child with asthma go untreated until their breathing problems are so severe that they turn blue, Dr. Hassink said; similarly, physicians should treat obesity in young people promptly and over time.
While some aspects of treating overweight and obesity are the same for children and adults, Dr. Hassink noted distinct differences. “Every child is embedded in a family and extended support structure,” Dr. Hassink said, which means that any obesity management technique needs the buy-in and support of the child’s family too.
AAP’s new advice reflects current understanding that excess weight or obesity in children is a result of biological and social factors, such as living in a food desert or experiencing the effects of structural racism.
The guidelines synthesize the results of hundreds of studies about the best way to treat excess weight in young people. If multiple studies were of high quality and all reached similar conclusions, they received an “A.” Less robust but still informative studies rated a “B.” In aggregate, the guideline about weight-lowering medication is based on “B” evidence that could shift with further research.
The authors recommend that clinicians calculate a child’s BMI beginning at age 2 years, with particular attention to those at the 85th percentile or higher for their age and sex (which would be defined as overweight), at the 95th percentile or higher (obesity), or at the 120th percentile and higher (severe obesity). Clinicians also should monitor blood pressure and cholesterol in their patients with overweight or obesity, particularly once they reach age 10.
Starting at age 6, providers should interview patients and their families about what would motivate them to lose weight, then tailor interventions to those factors rather than just make a blanket declaration that weight loss is necessary. This step should be coupled with intensive support – ideally, at least 26 hours of face-to-face support over the course of a year, although more is better – about effective exercise and dietary habits that result in weight loss.
The intensive support model should remain in place throughout childhood and adolescence and should be coupled with referrals for weight-loss medications or bariatric surgeries as needed once children reach age 12 or 13. Those age cutoffs are based on current evidence as to when weight-loss medications or surgery becomes effective, Dr. Hassink said, and could be shifted to lower ages if that’s what new evidence shows.
“Intensive health behavioral and lifestyle treatment is the base of all other treatment extensions,” Dr. Eneli said.
Young patients who needed weight-lowering medication used to have fewer options, according to Aaron S. Kelly, PhD, the Minnesota American Legion and Auxiliary Chair in Children’s Health at the University of Minnesota, Minneapolis.
.No longer.
Dr. Kelly was not involved in drafting the guidelines but was the lead investigator for trials of liraglutide (Saxenda), which in 2020 received U.S. Food and Drug Administration approval for treating obesity in adolescents. In 2022, the agency approved phentermine and topiramate extended-release capsules (Qsymia) for long-term weight management for patients aged 12 years and older, along with a once-weekly injection of semaglutide (Wegovy) patients in this age group. There are no weight-lowering medications for children younger than 12, Dr. Kelly said.
“Obesity is not a lifestyle problem. A lot of it is driven by the underlying biology,” Dr. Kelly said. “Really, what these medicines do is make it easier for people to make the right lifestyle choices by pushing back against the biology.”
For example, a drug can make people feel full for longer or disrupt chemical pathways that result in craving certain foods. Dr. Kelly emphasized that these drugs do not give license for people to eat as much as they want.
As for bariatric surgery, the new guidelines adhere closely to those in a 2019 AAP statement that bariatric surgery is safe and effective in pediatric settings. This is gratifying to Kirk W. Reichard, MD, MBA, a lead author of the 2019 article and director of the bariatric surgery program at Nemours Children’s Health.
Even if the information isn’t new as of 2023, Dr. Reichard said, AAP’s imprimatur could cause some eligible families to consider bariatric surgery when they may not have done so before.
Dr. Eneli, Dr. Hassink, and Dr. Reichard reported no relevant financial conflicts of interest. Dr. Kelly has relationships with Boehringer Ingelheim, Eli Lilly, Novo Nordisk, and Vivus.
A version of this article first appeared on Medscape.com.
and hope the problem solves itself. That’s the upshot of new guidelines from the American Academy of Pediatrics.
The authors of the guidelines also encourage primary care doctors to collaborate with other medical professionals to treat the comorbidities often linked to obesity, rather than take on the entire challenge themselves.
“It’s impossible to treat obesity within the four walls of the clinic. That’s one thing I have learned,” Ihuoma Eneli, MD, associate director of the AAP Institute for Healthy Childhood Weight, told this news organization. For example, a primary care doctor could partner with a gastroenterologist when treating a child who has nonalcoholic fatty liver disease, added Dr. Eneli, a professor of pediatrics at the Ohio State University, Columbus, who helped write the recommendations.
The new document updates 2007 recommendations from AAP about treating children and adolescents who are overweight or obese. The earlier statement focused on behavioral modification and healthy eating behaviors and paid less attention to weight-lowering medications or bariatric surgery for young people. That document did not offer specific advice to health care providers about how to address childhood overweight or obesity.
The 2023 guidelines recommend that pediatricians offer anyone aged 12 years and older with obesity – defined as a body mass index (BMI) at the 95th percentile or higher – the option of receiving weight-loss medications in addition to ongoing support for lifestyle modifications, such as exercising more and eating healthier foods.
The same approach holds for bariatric surgery once children reach age 13, and AAP stressed that no physician should ever stigmatize children or imply that they are to blame for their weight.
AAP did not receive any industry funding to develop the guidelines.
As children reach the threshold BMI levels, physicians should conduct complete physicals and order blood tests to get a fuller picture of the patients’ health.
These are the first guidelines from AAP aimed at giving pediatricians and other primary care providers concrete guidance for managing overweight and obesity in younger patients.
“Obesity is a complex, chronic disease, and that’s a frame shift here,” said Sandra S. Hassink, MD, leader of the guideline group and director of the AAP Institute for Healthy Childhood Weight.
Dr. Hassink compared obesity to asthma, another chronic disease that merits prompt attention and ongoing treatment. A physician would never let a child with asthma go untreated until their breathing problems are so severe that they turn blue, Dr. Hassink said; similarly, physicians should treat obesity in young people promptly and over time.
While some aspects of treating overweight and obesity are the same for children and adults, Dr. Hassink noted distinct differences. “Every child is embedded in a family and extended support structure,” Dr. Hassink said, which means that any obesity management technique needs the buy-in and support of the child’s family too.
AAP’s new advice reflects current understanding that excess weight or obesity in children is a result of biological and social factors, such as living in a food desert or experiencing the effects of structural racism.
The guidelines synthesize the results of hundreds of studies about the best way to treat excess weight in young people. If multiple studies were of high quality and all reached similar conclusions, they received an “A.” Less robust but still informative studies rated a “B.” In aggregate, the guideline about weight-lowering medication is based on “B” evidence that could shift with further research.
The authors recommend that clinicians calculate a child’s BMI beginning at age 2 years, with particular attention to those at the 85th percentile or higher for their age and sex (which would be defined as overweight), at the 95th percentile or higher (obesity), or at the 120th percentile and higher (severe obesity). Clinicians also should monitor blood pressure and cholesterol in their patients with overweight or obesity, particularly once they reach age 10.
Starting at age 6, providers should interview patients and their families about what would motivate them to lose weight, then tailor interventions to those factors rather than just make a blanket declaration that weight loss is necessary. This step should be coupled with intensive support – ideally, at least 26 hours of face-to-face support over the course of a year, although more is better – about effective exercise and dietary habits that result in weight loss.
The intensive support model should remain in place throughout childhood and adolescence and should be coupled with referrals for weight-loss medications or bariatric surgeries as needed once children reach age 12 or 13. Those age cutoffs are based on current evidence as to when weight-loss medications or surgery becomes effective, Dr. Hassink said, and could be shifted to lower ages if that’s what new evidence shows.
“Intensive health behavioral and lifestyle treatment is the base of all other treatment extensions,” Dr. Eneli said.
Young patients who needed weight-lowering medication used to have fewer options, according to Aaron S. Kelly, PhD, the Minnesota American Legion and Auxiliary Chair in Children’s Health at the University of Minnesota, Minneapolis.
.No longer.
Dr. Kelly was not involved in drafting the guidelines but was the lead investigator for trials of liraglutide (Saxenda), which in 2020 received U.S. Food and Drug Administration approval for treating obesity in adolescents. In 2022, the agency approved phentermine and topiramate extended-release capsules (Qsymia) for long-term weight management for patients aged 12 years and older, along with a once-weekly injection of semaglutide (Wegovy) patients in this age group. There are no weight-lowering medications for children younger than 12, Dr. Kelly said.
“Obesity is not a lifestyle problem. A lot of it is driven by the underlying biology,” Dr. Kelly said. “Really, what these medicines do is make it easier for people to make the right lifestyle choices by pushing back against the biology.”
For example, a drug can make people feel full for longer or disrupt chemical pathways that result in craving certain foods. Dr. Kelly emphasized that these drugs do not give license for people to eat as much as they want.
As for bariatric surgery, the new guidelines adhere closely to those in a 2019 AAP statement that bariatric surgery is safe and effective in pediatric settings. This is gratifying to Kirk W. Reichard, MD, MBA, a lead author of the 2019 article and director of the bariatric surgery program at Nemours Children’s Health.
Even if the information isn’t new as of 2023, Dr. Reichard said, AAP’s imprimatur could cause some eligible families to consider bariatric surgery when they may not have done so before.
Dr. Eneli, Dr. Hassink, and Dr. Reichard reported no relevant financial conflicts of interest. Dr. Kelly has relationships with Boehringer Ingelheim, Eli Lilly, Novo Nordisk, and Vivus.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Little-used fitness measure could be key to exercise results
A new study out of Brigham Young University, Provo, Utah, suggests doctors could take that initiative to the next level, prescribing exercise plans that result in a specific health outcome; say, lowering your blood pressure or losing weight.
“The findings of this study, and others, suggest that we should be able to more consistently and accurately prescribe exercise like medicine,” says senior study author Jayson Gifford, PhD, an exercise sciences professor at BYU.
These exercise prescriptions would be tailored to patients based on a largely ignored fitness measure called critical power, or maximum steady state – the fastest you can go while maintaining a pace you can sustain for a long time.
By crafting workouts around critical power instead of the more frequently used VO2 max (maximum effort), we could more accurately predict health outcomes, just as we can with medicine, the researchers wrote in the Journal of Applied Physiology.
“We’ve known for centuries that exercise is part of the way to develop a healthy and long life,” says Jordan Metzl, MD, a sports medicine doctor at the Hospital for Special Surgery in New York and author of The Exercise Cure. “But it’s only in the past 70 years that we’ve recognized the medicinal value of exercise.”
Dr. Metzl, who was not involved in the study, helped develop an annual seminar at Cornell Medical School teaching medical students ways to prescribe exercise that go beyond the “30 minutes per day” cookie-cutter advice. Still, doctors and other health care professionals often struggle to prescribe exercise to prevent or treat disease. And a recent study from Oxford found that when doctors do give weight loss advice, it’s often vague and hard for patients to use.
“The drug of movement is one of the safest and most effective forms of preventive health,” says Dr. Metzl. “We need to get the medical community fully engaged in prescribing exercise for their patients.”
This study suggests that a focus on critical power could be key in making that happen.
What the research found
In the study, 22 adults completed 8 weeks of either moderate-intensity training or high-intensity interval training (HIIT). The intensity levels specified in both plans were based on VO2 max. So, the people in the study trained at given percentages of their VO2 max.
Both groups saw improvements in endurance, but results varied greatly from person to person. Those mixed results could be explained by individual differences in critical power.
“Improvement was much more correlated with the percentage of critical powers the individuals worked at rather than the percentage of their VO2max, like exercise physiologists have thought for years,” says lead study author Jessica Collins, a researcher at Brigham Young University.
Not only that but several subjects who did not improve their VO2 max did see an increase in critical power and endurance.
“People tend to only focus on VO2 max,” Dr. Gifford says. “Many might see the lack of increase in VO2 max for some people and conclude that the training was ineffective. I personally believe that a lot of potentially useful therapies have been ruled out because of an almost exclusive focus on VO2 max.”
Turns out, critical power varies a lot from person to person, even among those with similar VO2 maxes.
“Let’s say you and Jessica had the same VO2 max,” explains Dr. Gifford. “If we had you both going at 70% of [your VO2 max], it could be above your maximum steady state, which would make it really hard for you. And it could be below her maximum steady state, which would make it easy for her.”
This means you are each stressing your body differently, and that stress is what triggers improvements in fitness and endurance.
“Below critical power, the metabolic stressors are well-managed and maintained at elevated-but-steady levels,” Dr. Gifford says. “Above critical power, the metabolic stressors are produced so fast that they cannot be controlled, and consistently accrue until reaching very high levels that cause failure.”
Knowing your critical power means you can predict how those stressors will build up, and you can tailor an exercise program that provides just the right stressor “dose” for you, Dr. Gifford says.
Such programs could be used for rehab patients recovering from a heart attack or from lung disease, Dr. Gifford suggests. Or they could help older adults improve endurance and physical function, Ms. Collins notes.
But first, researchers must confirm these results by programming workouts based on people’s critical power and seeing how much different measures improve.
How to find your critical power
Critical power is not new, but exercise physiologists and medical professionals have largely ignored it because it’s not easy to measure.
“People generally train off VO2 max or maximum heart rate, which is even less precise,” Dr. Gifford says.
Finding people’s critical power in the study involved multiple timed trials and calculating the relationship between speed/power and time, Dr. Gifford explains.
But for a rough measure of your critical power, you could use an app that measures functional threshold power (FTP), something Dr. Gifford refers to as the “Walmart version” of critical power. “It’s not exactly the same, but it’s close,” he says. (The app Strava features FTP as well as a pretty sophisticated power analysis.)
Or skip the tech and go by feel. If you’re below your critical power, “it’s going to be challenging, but you’ll feel under control,” Dr. Gifford says. Above your critical power, “your breathing and heart rate will continuously climb until you fail in about 2 to 15 minutes, depending on how far above you are.” Still, you don’t need to know your critical power to start exercising, Ms. Collins notes.
“The beauty of exercise is that it is such a powerful drug that you can see benefits without fine-tuning the workout this way,” Dr. Gifford explains. “I would hate for this to become a barrier to exercising. The important thing is to do something.”
A version of this article first appeared on WebMD.com.
A new study out of Brigham Young University, Provo, Utah, suggests doctors could take that initiative to the next level, prescribing exercise plans that result in a specific health outcome; say, lowering your blood pressure or losing weight.
“The findings of this study, and others, suggest that we should be able to more consistently and accurately prescribe exercise like medicine,” says senior study author Jayson Gifford, PhD, an exercise sciences professor at BYU.
These exercise prescriptions would be tailored to patients based on a largely ignored fitness measure called critical power, or maximum steady state – the fastest you can go while maintaining a pace you can sustain for a long time.
By crafting workouts around critical power instead of the more frequently used VO2 max (maximum effort), we could more accurately predict health outcomes, just as we can with medicine, the researchers wrote in the Journal of Applied Physiology.
“We’ve known for centuries that exercise is part of the way to develop a healthy and long life,” says Jordan Metzl, MD, a sports medicine doctor at the Hospital for Special Surgery in New York and author of The Exercise Cure. “But it’s only in the past 70 years that we’ve recognized the medicinal value of exercise.”
Dr. Metzl, who was not involved in the study, helped develop an annual seminar at Cornell Medical School teaching medical students ways to prescribe exercise that go beyond the “30 minutes per day” cookie-cutter advice. Still, doctors and other health care professionals often struggle to prescribe exercise to prevent or treat disease. And a recent study from Oxford found that when doctors do give weight loss advice, it’s often vague and hard for patients to use.
“The drug of movement is one of the safest and most effective forms of preventive health,” says Dr. Metzl. “We need to get the medical community fully engaged in prescribing exercise for their patients.”
This study suggests that a focus on critical power could be key in making that happen.
What the research found
In the study, 22 adults completed 8 weeks of either moderate-intensity training or high-intensity interval training (HIIT). The intensity levels specified in both plans were based on VO2 max. So, the people in the study trained at given percentages of their VO2 max.
Both groups saw improvements in endurance, but results varied greatly from person to person. Those mixed results could be explained by individual differences in critical power.
“Improvement was much more correlated with the percentage of critical powers the individuals worked at rather than the percentage of their VO2max, like exercise physiologists have thought for years,” says lead study author Jessica Collins, a researcher at Brigham Young University.
Not only that but several subjects who did not improve their VO2 max did see an increase in critical power and endurance.
“People tend to only focus on VO2 max,” Dr. Gifford says. “Many might see the lack of increase in VO2 max for some people and conclude that the training was ineffective. I personally believe that a lot of potentially useful therapies have been ruled out because of an almost exclusive focus on VO2 max.”
Turns out, critical power varies a lot from person to person, even among those with similar VO2 maxes.
“Let’s say you and Jessica had the same VO2 max,” explains Dr. Gifford. “If we had you both going at 70% of [your VO2 max], it could be above your maximum steady state, which would make it really hard for you. And it could be below her maximum steady state, which would make it easy for her.”
This means you are each stressing your body differently, and that stress is what triggers improvements in fitness and endurance.
“Below critical power, the metabolic stressors are well-managed and maintained at elevated-but-steady levels,” Dr. Gifford says. “Above critical power, the metabolic stressors are produced so fast that they cannot be controlled, and consistently accrue until reaching very high levels that cause failure.”
Knowing your critical power means you can predict how those stressors will build up, and you can tailor an exercise program that provides just the right stressor “dose” for you, Dr. Gifford says.
Such programs could be used for rehab patients recovering from a heart attack or from lung disease, Dr. Gifford suggests. Or they could help older adults improve endurance and physical function, Ms. Collins notes.
But first, researchers must confirm these results by programming workouts based on people’s critical power and seeing how much different measures improve.
How to find your critical power
Critical power is not new, but exercise physiologists and medical professionals have largely ignored it because it’s not easy to measure.
“People generally train off VO2 max or maximum heart rate, which is even less precise,” Dr. Gifford says.
Finding people’s critical power in the study involved multiple timed trials and calculating the relationship between speed/power and time, Dr. Gifford explains.
But for a rough measure of your critical power, you could use an app that measures functional threshold power (FTP), something Dr. Gifford refers to as the “Walmart version” of critical power. “It’s not exactly the same, but it’s close,” he says. (The app Strava features FTP as well as a pretty sophisticated power analysis.)
Or skip the tech and go by feel. If you’re below your critical power, “it’s going to be challenging, but you’ll feel under control,” Dr. Gifford says. Above your critical power, “your breathing and heart rate will continuously climb until you fail in about 2 to 15 minutes, depending on how far above you are.” Still, you don’t need to know your critical power to start exercising, Ms. Collins notes.
“The beauty of exercise is that it is such a powerful drug that you can see benefits without fine-tuning the workout this way,” Dr. Gifford explains. “I would hate for this to become a barrier to exercising. The important thing is to do something.”
A version of this article first appeared on WebMD.com.
A new study out of Brigham Young University, Provo, Utah, suggests doctors could take that initiative to the next level, prescribing exercise plans that result in a specific health outcome; say, lowering your blood pressure or losing weight.
“The findings of this study, and others, suggest that we should be able to more consistently and accurately prescribe exercise like medicine,” says senior study author Jayson Gifford, PhD, an exercise sciences professor at BYU.
These exercise prescriptions would be tailored to patients based on a largely ignored fitness measure called critical power, or maximum steady state – the fastest you can go while maintaining a pace you can sustain for a long time.
By crafting workouts around critical power instead of the more frequently used VO2 max (maximum effort), we could more accurately predict health outcomes, just as we can with medicine, the researchers wrote in the Journal of Applied Physiology.
“We’ve known for centuries that exercise is part of the way to develop a healthy and long life,” says Jordan Metzl, MD, a sports medicine doctor at the Hospital for Special Surgery in New York and author of The Exercise Cure. “But it’s only in the past 70 years that we’ve recognized the medicinal value of exercise.”
Dr. Metzl, who was not involved in the study, helped develop an annual seminar at Cornell Medical School teaching medical students ways to prescribe exercise that go beyond the “30 minutes per day” cookie-cutter advice. Still, doctors and other health care professionals often struggle to prescribe exercise to prevent or treat disease. And a recent study from Oxford found that when doctors do give weight loss advice, it’s often vague and hard for patients to use.
“The drug of movement is one of the safest and most effective forms of preventive health,” says Dr. Metzl. “We need to get the medical community fully engaged in prescribing exercise for their patients.”
This study suggests that a focus on critical power could be key in making that happen.
What the research found
In the study, 22 adults completed 8 weeks of either moderate-intensity training or high-intensity interval training (HIIT). The intensity levels specified in both plans were based on VO2 max. So, the people in the study trained at given percentages of their VO2 max.
Both groups saw improvements in endurance, but results varied greatly from person to person. Those mixed results could be explained by individual differences in critical power.
“Improvement was much more correlated with the percentage of critical powers the individuals worked at rather than the percentage of their VO2max, like exercise physiologists have thought for years,” says lead study author Jessica Collins, a researcher at Brigham Young University.
Not only that but several subjects who did not improve their VO2 max did see an increase in critical power and endurance.
“People tend to only focus on VO2 max,” Dr. Gifford says. “Many might see the lack of increase in VO2 max for some people and conclude that the training was ineffective. I personally believe that a lot of potentially useful therapies have been ruled out because of an almost exclusive focus on VO2 max.”
Turns out, critical power varies a lot from person to person, even among those with similar VO2 maxes.
“Let’s say you and Jessica had the same VO2 max,” explains Dr. Gifford. “If we had you both going at 70% of [your VO2 max], it could be above your maximum steady state, which would make it really hard for you. And it could be below her maximum steady state, which would make it easy for her.”
This means you are each stressing your body differently, and that stress is what triggers improvements in fitness and endurance.
“Below critical power, the metabolic stressors are well-managed and maintained at elevated-but-steady levels,” Dr. Gifford says. “Above critical power, the metabolic stressors are produced so fast that they cannot be controlled, and consistently accrue until reaching very high levels that cause failure.”
Knowing your critical power means you can predict how those stressors will build up, and you can tailor an exercise program that provides just the right stressor “dose” for you, Dr. Gifford says.
Such programs could be used for rehab patients recovering from a heart attack or from lung disease, Dr. Gifford suggests. Or they could help older adults improve endurance and physical function, Ms. Collins notes.
But first, researchers must confirm these results by programming workouts based on people’s critical power and seeing how much different measures improve.
How to find your critical power
Critical power is not new, but exercise physiologists and medical professionals have largely ignored it because it’s not easy to measure.
“People generally train off VO2 max or maximum heart rate, which is even less precise,” Dr. Gifford says.
Finding people’s critical power in the study involved multiple timed trials and calculating the relationship between speed/power and time, Dr. Gifford explains.
But for a rough measure of your critical power, you could use an app that measures functional threshold power (FTP), something Dr. Gifford refers to as the “Walmart version” of critical power. “It’s not exactly the same, but it’s close,” he says. (The app Strava features FTP as well as a pretty sophisticated power analysis.)
Or skip the tech and go by feel. If you’re below your critical power, “it’s going to be challenging, but you’ll feel under control,” Dr. Gifford says. Above your critical power, “your breathing and heart rate will continuously climb until you fail in about 2 to 15 minutes, depending on how far above you are.” Still, you don’t need to know your critical power to start exercising, Ms. Collins notes.
“The beauty of exercise is that it is such a powerful drug that you can see benefits without fine-tuning the workout this way,” Dr. Gifford explains. “I would hate for this to become a barrier to exercising. The important thing is to do something.”
A version of this article first appeared on WebMD.com.
FROM THE JOURNAL OF APPLIED PHYSIOLOGY