User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Flu, other common viruses linked to neurologic disease
People hospitalized with viral infections like the flu are more likely to have disorders that degrade the nervous system, like Alzheimer’s or Parkinson’s, later in life, a new analysis shows.
The viruses included influenza, encephalitis, herpes, hepatitis, pneumonia, meningitis, and shingles. Those viruses were linked to one or more of these conditions: Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), dementia, and multiple sclerosis.
The authors of the study, which was published this month in the journal Neuron, cautioned that their findings stopped short of saying the viruses caused the disorders.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” study author and National Institutes of Health researcher Andrew B. Singleton, PhD, said in a news release from the NIH. “Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”
For the study, two data sets were analyzed with a combined 800,000 medical records for people in Finland and the United Kingdom. People who were hospitalized with COVID-19 were excluded from the study.
Generalized dementia was the condition linked to the most viruses. People exposed to viral encephalitis, which causes brain inflammation, were 20 times more likely to be diagnosed with Alzheimer’s, compared with those who were not diagnosed with that virus.
Both influenza and pneumonia were also associated with all of the neurodegenerative disorder diagnoses studied, with the exception of multiple sclerosis. The researchers found that severe flu cases were linked to the most risks.
“Keep in mind that the individuals we studied did not have the common cold. Their infections made them so sick that they had to go to the hospital,” said study author and NIH researcher Michael Nalls, PhD. “Nevertheless, the fact that commonly used vaccines reduce the risk or severity of many of the viral illnesses observed in this study raises the possibility that the risks of neurodegenerative disorders might also be mitigated.”
The researchers examined the time from when someone was infected with a virus to the time when they were diagnosed with one of the neurodegenerative disorders. They found that most had a high risk within 1 year of infection. But in six scenarios, there were significant links that showed up after 5-15 years.
The authors wrote that vaccines that are available for some of the viruses studied may be a way to reduce the risk of getting diseases that degrade the nervous system.
A version of this article first appeared on WebMD.com.
People hospitalized with viral infections like the flu are more likely to have disorders that degrade the nervous system, like Alzheimer’s or Parkinson’s, later in life, a new analysis shows.
The viruses included influenza, encephalitis, herpes, hepatitis, pneumonia, meningitis, and shingles. Those viruses were linked to one or more of these conditions: Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), dementia, and multiple sclerosis.
The authors of the study, which was published this month in the journal Neuron, cautioned that their findings stopped short of saying the viruses caused the disorders.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” study author and National Institutes of Health researcher Andrew B. Singleton, PhD, said in a news release from the NIH. “Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”
For the study, two data sets were analyzed with a combined 800,000 medical records for people in Finland and the United Kingdom. People who were hospitalized with COVID-19 were excluded from the study.
Generalized dementia was the condition linked to the most viruses. People exposed to viral encephalitis, which causes brain inflammation, were 20 times more likely to be diagnosed with Alzheimer’s, compared with those who were not diagnosed with that virus.
Both influenza and pneumonia were also associated with all of the neurodegenerative disorder diagnoses studied, with the exception of multiple sclerosis. The researchers found that severe flu cases were linked to the most risks.
“Keep in mind that the individuals we studied did not have the common cold. Their infections made them so sick that they had to go to the hospital,” said study author and NIH researcher Michael Nalls, PhD. “Nevertheless, the fact that commonly used vaccines reduce the risk or severity of many of the viral illnesses observed in this study raises the possibility that the risks of neurodegenerative disorders might also be mitigated.”
The researchers examined the time from when someone was infected with a virus to the time when they were diagnosed with one of the neurodegenerative disorders. They found that most had a high risk within 1 year of infection. But in six scenarios, there were significant links that showed up after 5-15 years.
The authors wrote that vaccines that are available for some of the viruses studied may be a way to reduce the risk of getting diseases that degrade the nervous system.
A version of this article first appeared on WebMD.com.
People hospitalized with viral infections like the flu are more likely to have disorders that degrade the nervous system, like Alzheimer’s or Parkinson’s, later in life, a new analysis shows.
The viruses included influenza, encephalitis, herpes, hepatitis, pneumonia, meningitis, and shingles. Those viruses were linked to one or more of these conditions: Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis (ALS), dementia, and multiple sclerosis.
The authors of the study, which was published this month in the journal Neuron, cautioned that their findings stopped short of saying the viruses caused the disorders.
“Neurodegenerative disorders are a collection of diseases for which there are very few effective treatments and many risk factors,” study author and National Institutes of Health researcher Andrew B. Singleton, PhD, said in a news release from the NIH. “Our results support the idea that viral infections and related inflammation in the nervous system may be common – and possibly avoidable – risk factors for these types of disorders.”
For the study, two data sets were analyzed with a combined 800,000 medical records for people in Finland and the United Kingdom. People who were hospitalized with COVID-19 were excluded from the study.
Generalized dementia was the condition linked to the most viruses. People exposed to viral encephalitis, which causes brain inflammation, were 20 times more likely to be diagnosed with Alzheimer’s, compared with those who were not diagnosed with that virus.
Both influenza and pneumonia were also associated with all of the neurodegenerative disorder diagnoses studied, with the exception of multiple sclerosis. The researchers found that severe flu cases were linked to the most risks.
“Keep in mind that the individuals we studied did not have the common cold. Their infections made them so sick that they had to go to the hospital,” said study author and NIH researcher Michael Nalls, PhD. “Nevertheless, the fact that commonly used vaccines reduce the risk or severity of many of the viral illnesses observed in this study raises the possibility that the risks of neurodegenerative disorders might also be mitigated.”
The researchers examined the time from when someone was infected with a virus to the time when they were diagnosed with one of the neurodegenerative disorders. They found that most had a high risk within 1 year of infection. But in six scenarios, there were significant links that showed up after 5-15 years.
The authors wrote that vaccines that are available for some of the viruses studied may be a way to reduce the risk of getting diseases that degrade the nervous system.
A version of this article first appeared on WebMD.com.
FROM NEURON
High HDL-C levels linked to increased fracture risk
High levels of high-density lipoprotein cholesterol (HDL-C) in older adults are associated with a higher risk of sustaining a fracture than lower HDL-C levels, a new study suggests.
“Two animal studies showing that HDL-C reduces bone mineral density by reducing osteoblast number and function provide a plausible explanation for why high HDL-C may increase the risk of fractures,” Monira Hussain, MBBS, MPH, PhD, of Monash University in Melbourne, told this news organization. “So, it was not surprising when our analyses provided evidence that amongst those in the highest quintile of HDL-C (> 74 mg/dL), there was a [33%] increased risk of fractures.”
After adjustment, one standard deviation increment in HDL-C level was associated with a 14% higher risk of fracture during a 4-year follow-up.
Based on this and other studies, Dr. Hussain said, “I believe that the finding of a very high HDL-C [should] alert clinicians to a higher risk of mortality, fractures, and possibly other threats to their patient’s health.”
The study was published online in JAMA Cardiology.
Independent risk factor
For this report, the researchers conducted a post hoc analysis of data from the Aspirin in Reducing Events in the Elderly (ASPREE) clinical trial and the ASPREE-Fracture substudy.
ASPREE was a double-blind, randomized, placebo-controlled primary prevention trial of aspirin. Participants were 16,703 community-dwelling Australians and 2,411 individuals from the United States with a mean age of 75 and without evident cardiovascular disease, dementia, physical disability, or life-limiting chronic illness.
The ASPREE-Fracture substudy collected data on fractures reported post randomization from the Australian participants. Fractures were confirmed by imaging and adjudicated by an expert panel and included both traumatic and minimal trauma fractures.
Of the 16,262 participants who had a plasma HDL-C measurement at baseline (55% women), 1,659 (10.2%) experienced at least one fracture over a median of 4 years. This included 711 minimal trauma fractures (for example, falls from standing height) and 948 other trauma fractures, mainly falls on stairs, ladders, or stools.
Higher rates of fractures occurred in the highest quintile of HDL-C level where the mean level was 89 mg/dL. At baseline, participants in that quintile had a lower BMI, a high prevalence of current/former smoking and current alcohol use, 12 years or longer of school, more physical activity, and higher use of antiosteoporosis medication. They also had less chronic kidney disease, diabetes, prefrailty/frailty, or treatment with lipid-lowering drugs.
In a fully adjusted model, each standard deviation increment in HDL-C level was associated with a 14% higher risk of fractures (hazard ratio, 1.14). When analyzed in quintiles, compared with participants in Q1, those in Q5 had a 33% higher risk for fracture (HR, 1.33).
Prevalence rates were similar between the sexes. The increase in fracture risk appeared to be independent of traditional risk factors for fractures, including age, sex, physical activity, alcohol use, frailty, BMI, smoking status, diabetes, chronic kidney disease, use of lipid-lowering or antiosteoporosis drugs, and education, the authors note.
The results persisted in sensitivity analyses in restricted subgroups of interest and in stratified analyses – including, for example, only minimal fractures; participants not taking antiosteoporosis drugs or statins; never smokers; nondrinkers; and those engaging in minimal physical activity (walking less than 30 minutes per day).
No association was observed between non–HDL-C levels and fractures.
The authors conclude that the study “provides robust evidence that higher levels of HDL-C are associated with incident fractures in both male and female individuals, independent of conventional risk factors.”
Clinically useful?
Commenting on the study for this news organization, Marilyn Tan, MD, clinic chief of the Endocrine Clinic and clinical associate professor of medicine at Stanford (Calif.) University, said, “I certainly would not recommend anyone do anything to actively lower their HDL levels. HDL levels are largely determined by genetics, diet, and lifestyle, with some effects from certain medications/supplements. Studies have demonstrated that moderately higher HDL levels may be protective for atherosclerosis.”
In the current study, she said, “Causation has not been proven, and importantly there is no evidence that reducing HDL levels reduces fracture risk. Also, this association between raised HDL levels and fracture risk has not been demonstrated consistently in other studies.”
Furthermore, she noted, the preclinical trials on which the authors based their hypothesis – that is, an association between HDL and a reduction in the number and function of osteoblasts – “has not been demonstrated widely in human subjects.”
“We have a large armamentarium of FDA-approved treatments for osteoporosis that have been clinically proven to reduce fracture risk very significantly, and these are the tools [in addition to lifestyle changes] we should use to reduce fracture risk,” Dr. Tan concluded.
John Wilkins, MD, of Northwestern University, Chicago, and Anand Rohatgi, MD, MSCS, of UT Southwestern Medical Center, Dallas, also point out some limitations of the study in a related editorial.
They note the inclusion of predominantly healthy adults with a mean age of 75, a population that could yield different findings from middle-aged cohorts with chronic illnesses, as well as a lack of clarity regarding the possible role of alcohol intake among the study participants.
Furthermore, the editorialists write, although significant associations were shown in this study, “models were not adjusted for detailed measures of exercise/activity, triglycerides, or any other lipids, including other HDL compositional measures such as HDL-P or ApoA-I levels. There was no assessment of whether HDL-C improved discrimination, reclassification, or any other validated measures of risk prediction performance.
“Taken together,” they conclude, “this study alone leaves several unanswered questions as to whether high HDL-C could be a useful biomarker to detect fracture risk.”
No commercial funding was disclosed. The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
High levels of high-density lipoprotein cholesterol (HDL-C) in older adults are associated with a higher risk of sustaining a fracture than lower HDL-C levels, a new study suggests.
“Two animal studies showing that HDL-C reduces bone mineral density by reducing osteoblast number and function provide a plausible explanation for why high HDL-C may increase the risk of fractures,” Monira Hussain, MBBS, MPH, PhD, of Monash University in Melbourne, told this news organization. “So, it was not surprising when our analyses provided evidence that amongst those in the highest quintile of HDL-C (> 74 mg/dL), there was a [33%] increased risk of fractures.”
After adjustment, one standard deviation increment in HDL-C level was associated with a 14% higher risk of fracture during a 4-year follow-up.
Based on this and other studies, Dr. Hussain said, “I believe that the finding of a very high HDL-C [should] alert clinicians to a higher risk of mortality, fractures, and possibly other threats to their patient’s health.”
The study was published online in JAMA Cardiology.
Independent risk factor
For this report, the researchers conducted a post hoc analysis of data from the Aspirin in Reducing Events in the Elderly (ASPREE) clinical trial and the ASPREE-Fracture substudy.
ASPREE was a double-blind, randomized, placebo-controlled primary prevention trial of aspirin. Participants were 16,703 community-dwelling Australians and 2,411 individuals from the United States with a mean age of 75 and without evident cardiovascular disease, dementia, physical disability, or life-limiting chronic illness.
The ASPREE-Fracture substudy collected data on fractures reported post randomization from the Australian participants. Fractures were confirmed by imaging and adjudicated by an expert panel and included both traumatic and minimal trauma fractures.
Of the 16,262 participants who had a plasma HDL-C measurement at baseline (55% women), 1,659 (10.2%) experienced at least one fracture over a median of 4 years. This included 711 minimal trauma fractures (for example, falls from standing height) and 948 other trauma fractures, mainly falls on stairs, ladders, or stools.
Higher rates of fractures occurred in the highest quintile of HDL-C level where the mean level was 89 mg/dL. At baseline, participants in that quintile had a lower BMI, a high prevalence of current/former smoking and current alcohol use, 12 years or longer of school, more physical activity, and higher use of antiosteoporosis medication. They also had less chronic kidney disease, diabetes, prefrailty/frailty, or treatment with lipid-lowering drugs.
In a fully adjusted model, each standard deviation increment in HDL-C level was associated with a 14% higher risk of fractures (hazard ratio, 1.14). When analyzed in quintiles, compared with participants in Q1, those in Q5 had a 33% higher risk for fracture (HR, 1.33).
Prevalence rates were similar between the sexes. The increase in fracture risk appeared to be independent of traditional risk factors for fractures, including age, sex, physical activity, alcohol use, frailty, BMI, smoking status, diabetes, chronic kidney disease, use of lipid-lowering or antiosteoporosis drugs, and education, the authors note.
The results persisted in sensitivity analyses in restricted subgroups of interest and in stratified analyses – including, for example, only minimal fractures; participants not taking antiosteoporosis drugs or statins; never smokers; nondrinkers; and those engaging in minimal physical activity (walking less than 30 minutes per day).
No association was observed between non–HDL-C levels and fractures.
The authors conclude that the study “provides robust evidence that higher levels of HDL-C are associated with incident fractures in both male and female individuals, independent of conventional risk factors.”
Clinically useful?
Commenting on the study for this news organization, Marilyn Tan, MD, clinic chief of the Endocrine Clinic and clinical associate professor of medicine at Stanford (Calif.) University, said, “I certainly would not recommend anyone do anything to actively lower their HDL levels. HDL levels are largely determined by genetics, diet, and lifestyle, with some effects from certain medications/supplements. Studies have demonstrated that moderately higher HDL levels may be protective for atherosclerosis.”
In the current study, she said, “Causation has not been proven, and importantly there is no evidence that reducing HDL levels reduces fracture risk. Also, this association between raised HDL levels and fracture risk has not been demonstrated consistently in other studies.”
Furthermore, she noted, the preclinical trials on which the authors based their hypothesis – that is, an association between HDL and a reduction in the number and function of osteoblasts – “has not been demonstrated widely in human subjects.”
“We have a large armamentarium of FDA-approved treatments for osteoporosis that have been clinically proven to reduce fracture risk very significantly, and these are the tools [in addition to lifestyle changes] we should use to reduce fracture risk,” Dr. Tan concluded.
John Wilkins, MD, of Northwestern University, Chicago, and Anand Rohatgi, MD, MSCS, of UT Southwestern Medical Center, Dallas, also point out some limitations of the study in a related editorial.
They note the inclusion of predominantly healthy adults with a mean age of 75, a population that could yield different findings from middle-aged cohorts with chronic illnesses, as well as a lack of clarity regarding the possible role of alcohol intake among the study participants.
Furthermore, the editorialists write, although significant associations were shown in this study, “models were not adjusted for detailed measures of exercise/activity, triglycerides, or any other lipids, including other HDL compositional measures such as HDL-P or ApoA-I levels. There was no assessment of whether HDL-C improved discrimination, reclassification, or any other validated measures of risk prediction performance.
“Taken together,” they conclude, “this study alone leaves several unanswered questions as to whether high HDL-C could be a useful biomarker to detect fracture risk.”
No commercial funding was disclosed. The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
High levels of high-density lipoprotein cholesterol (HDL-C) in older adults are associated with a higher risk of sustaining a fracture than lower HDL-C levels, a new study suggests.
“Two animal studies showing that HDL-C reduces bone mineral density by reducing osteoblast number and function provide a plausible explanation for why high HDL-C may increase the risk of fractures,” Monira Hussain, MBBS, MPH, PhD, of Monash University in Melbourne, told this news organization. “So, it was not surprising when our analyses provided evidence that amongst those in the highest quintile of HDL-C (> 74 mg/dL), there was a [33%] increased risk of fractures.”
After adjustment, one standard deviation increment in HDL-C level was associated with a 14% higher risk of fracture during a 4-year follow-up.
Based on this and other studies, Dr. Hussain said, “I believe that the finding of a very high HDL-C [should] alert clinicians to a higher risk of mortality, fractures, and possibly other threats to their patient’s health.”
The study was published online in JAMA Cardiology.
Independent risk factor
For this report, the researchers conducted a post hoc analysis of data from the Aspirin in Reducing Events in the Elderly (ASPREE) clinical trial and the ASPREE-Fracture substudy.
ASPREE was a double-blind, randomized, placebo-controlled primary prevention trial of aspirin. Participants were 16,703 community-dwelling Australians and 2,411 individuals from the United States with a mean age of 75 and without evident cardiovascular disease, dementia, physical disability, or life-limiting chronic illness.
The ASPREE-Fracture substudy collected data on fractures reported post randomization from the Australian participants. Fractures were confirmed by imaging and adjudicated by an expert panel and included both traumatic and minimal trauma fractures.
Of the 16,262 participants who had a plasma HDL-C measurement at baseline (55% women), 1,659 (10.2%) experienced at least one fracture over a median of 4 years. This included 711 minimal trauma fractures (for example, falls from standing height) and 948 other trauma fractures, mainly falls on stairs, ladders, or stools.
Higher rates of fractures occurred in the highest quintile of HDL-C level where the mean level was 89 mg/dL. At baseline, participants in that quintile had a lower BMI, a high prevalence of current/former smoking and current alcohol use, 12 years or longer of school, more physical activity, and higher use of antiosteoporosis medication. They also had less chronic kidney disease, diabetes, prefrailty/frailty, or treatment with lipid-lowering drugs.
In a fully adjusted model, each standard deviation increment in HDL-C level was associated with a 14% higher risk of fractures (hazard ratio, 1.14). When analyzed in quintiles, compared with participants in Q1, those in Q5 had a 33% higher risk for fracture (HR, 1.33).
Prevalence rates were similar between the sexes. The increase in fracture risk appeared to be independent of traditional risk factors for fractures, including age, sex, physical activity, alcohol use, frailty, BMI, smoking status, diabetes, chronic kidney disease, use of lipid-lowering or antiosteoporosis drugs, and education, the authors note.
The results persisted in sensitivity analyses in restricted subgroups of interest and in stratified analyses – including, for example, only minimal fractures; participants not taking antiosteoporosis drugs or statins; never smokers; nondrinkers; and those engaging in minimal physical activity (walking less than 30 minutes per day).
No association was observed between non–HDL-C levels and fractures.
The authors conclude that the study “provides robust evidence that higher levels of HDL-C are associated with incident fractures in both male and female individuals, independent of conventional risk factors.”
Clinically useful?
Commenting on the study for this news organization, Marilyn Tan, MD, clinic chief of the Endocrine Clinic and clinical associate professor of medicine at Stanford (Calif.) University, said, “I certainly would not recommend anyone do anything to actively lower their HDL levels. HDL levels are largely determined by genetics, diet, and lifestyle, with some effects from certain medications/supplements. Studies have demonstrated that moderately higher HDL levels may be protective for atherosclerosis.”
In the current study, she said, “Causation has not been proven, and importantly there is no evidence that reducing HDL levels reduces fracture risk. Also, this association between raised HDL levels and fracture risk has not been demonstrated consistently in other studies.”
Furthermore, she noted, the preclinical trials on which the authors based their hypothesis – that is, an association between HDL and a reduction in the number and function of osteoblasts – “has not been demonstrated widely in human subjects.”
“We have a large armamentarium of FDA-approved treatments for osteoporosis that have been clinically proven to reduce fracture risk very significantly, and these are the tools [in addition to lifestyle changes] we should use to reduce fracture risk,” Dr. Tan concluded.
John Wilkins, MD, of Northwestern University, Chicago, and Anand Rohatgi, MD, MSCS, of UT Southwestern Medical Center, Dallas, also point out some limitations of the study in a related editorial.
They note the inclusion of predominantly healthy adults with a mean age of 75, a population that could yield different findings from middle-aged cohorts with chronic illnesses, as well as a lack of clarity regarding the possible role of alcohol intake among the study participants.
Furthermore, the editorialists write, although significant associations were shown in this study, “models were not adjusted for detailed measures of exercise/activity, triglycerides, or any other lipids, including other HDL compositional measures such as HDL-P or ApoA-I levels. There was no assessment of whether HDL-C improved discrimination, reclassification, or any other validated measures of risk prediction performance.
“Taken together,” they conclude, “this study alone leaves several unanswered questions as to whether high HDL-C could be a useful biomarker to detect fracture risk.”
No commercial funding was disclosed. The authors report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Medicare policy tweak on LVADs may reduce access to transplant
A recent change in Medicare policy designed to increase access to left ventricular assist devices (LVADs) may have had the unintended consequence of increasing inequalities in access to heart transplant for patients with advanced heart failure.
In December 2020, the Centers for Medicare & Medicaid Services relaxed restrictions on centers that implant LVADs but don’t perform heart transplants. Specifically, they dropped the requirement that LVAD-only centers obtain permission from a Medicare-approved heart transplant center authorizing LVAD implantation with “bridge-to-transplant” (BTT) intent, meaning the patient is a transplant candidate.
While the relaxed requirement has the potential to increase access to LVADs for appropriate patients, a look back at 22,221 LVAD recipients found that patients who received LVADs at transplant-capable centers had a 79% higher likelihood of receiving a BTT LVAD designation.
The 2-year heart transplant rate following LVAD implant was 25.6% for patients who received an LVAD at a heart transplant center, compared with 11.9% at LVAD-only centers.
Thomas Cascino, MD, with University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, and colleagues reported their findings in JAMA Network Open.
Differential assessment?
Nontransplant LVAD centers are increasing in number in the United States now that the CMS has made establishing an LVAD-only center easier.
“Although there should be enthusiasm for the potential of LVAD-only centers to increase access to LVAD, it appears that receiving an LVAD at a center that does not perform transplants results in differential assessment of transplant eligibility at the time of LVAD implant and inequities in receipt of transplant,” Dr. Cascino and colleagues said.
“Being cared for at a center that does not perform heart transplant should not result in a lesser chance to receive a heart transplant,” Dr. Cascino added in a university news release. “Our study shows that this disparity existed before the policy change, and we think it will likely grow larger now that there is less collaboration.”
The CMS policy will likely “further challenge equity in access to transplant for patients seeking care at nontransplant centers and may have the unintended consequence of contributing to increasing inequities in access to transplants, as has been feared,” the researchers wrote.
They also note that recent changes in the adult heart allocation system under the United Network for Organ Sharing have significantly reduced the likelihood of transplant after durable LVAD implant unless candidates are listed as being at higher urgency status owing to an LVAD complication or clinical deterioration.
“The reality is that durable LVADs are much less likely to be a bridge to the best therapy (that is, transplant) in the current allocation system. As a result, there is a critical need to select appropriate durable LVAD and transplant candidates at the initial evaluation,” the authors said.
“This puts the onus on the transplant community to select appropriate LVAD and transplant candidates during the initial evaluation. We need a system in which any patient can walk into the same hospital and get the right therapy for them,” Dr. Cascino added in the news release.
The research was supported in part through funding from the University of Michigan Health department of cardiac surgery and the National Institutes of Health, National Heart, Lung, and Blood Institute. Dr. Cascino has received grants from Johnson & Johnson.
A version of this article first appeared on Medscape.com.
A recent change in Medicare policy designed to increase access to left ventricular assist devices (LVADs) may have had the unintended consequence of increasing inequalities in access to heart transplant for patients with advanced heart failure.
In December 2020, the Centers for Medicare & Medicaid Services relaxed restrictions on centers that implant LVADs but don’t perform heart transplants. Specifically, they dropped the requirement that LVAD-only centers obtain permission from a Medicare-approved heart transplant center authorizing LVAD implantation with “bridge-to-transplant” (BTT) intent, meaning the patient is a transplant candidate.
While the relaxed requirement has the potential to increase access to LVADs for appropriate patients, a look back at 22,221 LVAD recipients found that patients who received LVADs at transplant-capable centers had a 79% higher likelihood of receiving a BTT LVAD designation.
The 2-year heart transplant rate following LVAD implant was 25.6% for patients who received an LVAD at a heart transplant center, compared with 11.9% at LVAD-only centers.
Thomas Cascino, MD, with University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, and colleagues reported their findings in JAMA Network Open.
Differential assessment?
Nontransplant LVAD centers are increasing in number in the United States now that the CMS has made establishing an LVAD-only center easier.
“Although there should be enthusiasm for the potential of LVAD-only centers to increase access to LVAD, it appears that receiving an LVAD at a center that does not perform transplants results in differential assessment of transplant eligibility at the time of LVAD implant and inequities in receipt of transplant,” Dr. Cascino and colleagues said.
“Being cared for at a center that does not perform heart transplant should not result in a lesser chance to receive a heart transplant,” Dr. Cascino added in a university news release. “Our study shows that this disparity existed before the policy change, and we think it will likely grow larger now that there is less collaboration.”
The CMS policy will likely “further challenge equity in access to transplant for patients seeking care at nontransplant centers and may have the unintended consequence of contributing to increasing inequities in access to transplants, as has been feared,” the researchers wrote.
They also note that recent changes in the adult heart allocation system under the United Network for Organ Sharing have significantly reduced the likelihood of transplant after durable LVAD implant unless candidates are listed as being at higher urgency status owing to an LVAD complication or clinical deterioration.
“The reality is that durable LVADs are much less likely to be a bridge to the best therapy (that is, transplant) in the current allocation system. As a result, there is a critical need to select appropriate durable LVAD and transplant candidates at the initial evaluation,” the authors said.
“This puts the onus on the transplant community to select appropriate LVAD and transplant candidates during the initial evaluation. We need a system in which any patient can walk into the same hospital and get the right therapy for them,” Dr. Cascino added in the news release.
The research was supported in part through funding from the University of Michigan Health department of cardiac surgery and the National Institutes of Health, National Heart, Lung, and Blood Institute. Dr. Cascino has received grants from Johnson & Johnson.
A version of this article first appeared on Medscape.com.
A recent change in Medicare policy designed to increase access to left ventricular assist devices (LVADs) may have had the unintended consequence of increasing inequalities in access to heart transplant for patients with advanced heart failure.
In December 2020, the Centers for Medicare & Medicaid Services relaxed restrictions on centers that implant LVADs but don’t perform heart transplants. Specifically, they dropped the requirement that LVAD-only centers obtain permission from a Medicare-approved heart transplant center authorizing LVAD implantation with “bridge-to-transplant” (BTT) intent, meaning the patient is a transplant candidate.
While the relaxed requirement has the potential to increase access to LVADs for appropriate patients, a look back at 22,221 LVAD recipients found that patients who received LVADs at transplant-capable centers had a 79% higher likelihood of receiving a BTT LVAD designation.
The 2-year heart transplant rate following LVAD implant was 25.6% for patients who received an LVAD at a heart transplant center, compared with 11.9% at LVAD-only centers.
Thomas Cascino, MD, with University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, and colleagues reported their findings in JAMA Network Open.
Differential assessment?
Nontransplant LVAD centers are increasing in number in the United States now that the CMS has made establishing an LVAD-only center easier.
“Although there should be enthusiasm for the potential of LVAD-only centers to increase access to LVAD, it appears that receiving an LVAD at a center that does not perform transplants results in differential assessment of transplant eligibility at the time of LVAD implant and inequities in receipt of transplant,” Dr. Cascino and colleagues said.
“Being cared for at a center that does not perform heart transplant should not result in a lesser chance to receive a heart transplant,” Dr. Cascino added in a university news release. “Our study shows that this disparity existed before the policy change, and we think it will likely grow larger now that there is less collaboration.”
The CMS policy will likely “further challenge equity in access to transplant for patients seeking care at nontransplant centers and may have the unintended consequence of contributing to increasing inequities in access to transplants, as has been feared,” the researchers wrote.
They also note that recent changes in the adult heart allocation system under the United Network for Organ Sharing have significantly reduced the likelihood of transplant after durable LVAD implant unless candidates are listed as being at higher urgency status owing to an LVAD complication or clinical deterioration.
“The reality is that durable LVADs are much less likely to be a bridge to the best therapy (that is, transplant) in the current allocation system. As a result, there is a critical need to select appropriate durable LVAD and transplant candidates at the initial evaluation,” the authors said.
“This puts the onus on the transplant community to select appropriate LVAD and transplant candidates during the initial evaluation. We need a system in which any patient can walk into the same hospital and get the right therapy for them,” Dr. Cascino added in the news release.
The research was supported in part through funding from the University of Michigan Health department of cardiac surgery and the National Institutes of Health, National Heart, Lung, and Blood Institute. Dr. Cascino has received grants from Johnson & Johnson.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Eye check important before starting semaglutide for diabetes
A small potential increased risk of retinopathy worsening at 1 year with injected semaglutide (Ozempic, Novo Nordisk), a glucagon-like peptide 1 (GLP-1) agonist approved for type 2 diabetes, doesn’t outweigh the drug’s cardiovascular benefits but does highlight the need for baseline ophthalmologic evaluation before initiating treatment and ongoing retinal monitoring, researchers say.
That conclusion was based on data from a meta-analysis of the seven major cardiovascular outcomes trials of GLP-1 agonists currently on the market.
The findings were recently published in Diabetes & Metabolic Syndrome: Clinical Research & Reviews, by Stewart G. Albert, MD, and colleagues.
Concerns about retinopathy worsening with the GLP-1 agonist drug class first arose from the SUSTAIN-6 cardiovascular outcomes trial for injectable semaglutide, although a subsequent analysis of data from that trial appeared to suggest the problem is likely due to rapid glucose-lowering in already vulnerable patients rather than a drug-specific effect. This effect had been previously reported, most notably in the landmark Diabetes Control and Complications Trial.
In this new meta-analysis, “we showed that with improvements in A1c there were correlations with decreases in the rate of cardiovascular events but increases in the rate of retinopathy,” Dr. Albert, of St. Louis University, told this news organization.
“As a class of drugs, we did not find an increased rate of retinopathy. The effect of GLP-1 agonists on retinopathy did not appear to be due to an immediate direct toxic effect of the drug. The worsening of the rate of retinopathy was seen with semaglutide after 1 year of therapy and when there was a decrease in A1c of 1%,” he explained.
He noted that because the increased risk was seen primarily among those who already had retinopathy at baseline, “it would seem prudent to know the level of retinopathy either before or plan for close ophthalmologic monitoring around the time of drug initiation ... We routinely evaluate patients with known type 2 diabetes mellitus at yearly intervals for retinopathy. From our data, we saw worsening at 1 year of drug exposure, but we do not know the exact time when the changes occurred during that year.”
The Ozempic label advises that “patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy” but doesn’t specifically mention baseline assessment at the time of drug initiation.
No increase in retinopathy risk for GLP-1 agonist class overall
The seven trials in the meta-analysis comprised 56,004 participants, with baseline retinopathy prevalence ranging from 9% to 31%.
For the GLP-1 agonist class overall, there was no significant increase in the relative rate (RR) of retinopathy (RR, 1.09; P = .36), while there were significant reductions in relative rates of major adverse cardiac events, overall deaths, and cardiovascular deaths (all P < .001 or P = .001).
The increased retinopathy risk was seen only in the subcutaneous semaglutide group (RR, 1.73; P = .02).
The overall number needed to harm was 1,000 and the number to treat was 77. For semaglutide, those values were 77 and 43, respectively.
There was a significant correlation between a decrease in major adverse cardiac events and a decrease in A1c (P = .014), while for retinopathy, the risk increased with improved A1c (P = .076).
Semaglutide subanalysis finds increased retinopathy worsening
Dr. Albert and colleagues conducted a separate subanalysis of 11 studies of semaglutide that enrolled 11,894 patients, of which 6 studies (n = 5,610) were of oral semaglutide (Rybelsus) and 5 studies were of subcutaneous semaglutide (Ozempic; n = 6,284).
In the subanalysis, there was an overall increase in relative rates of new or worsening retinopathy (RR, 1.218; P = .049).
The change in relative rate of retinopathy was predominantly found for subcutaneous semaglutide given for longer than 1 year (RR, 1.559; P = .022) and decreases in A1c of more than 1.0% (RR, 1.590; P = .016). No such differences were seen with oral semaglutide.
A further evaluation of the data without the SUSTAIN 6 trial showed no effect on retinopathy but the analysis lacked power.
Dr. Albert told this news organization: “We did not find an immediate toxic effect of any drug. However, we cannot rule out that there was a cumulative effect of the dose over longer times.”
No disclosures were given.
A version of this article first appeared on Medscape.com.
A small potential increased risk of retinopathy worsening at 1 year with injected semaglutide (Ozempic, Novo Nordisk), a glucagon-like peptide 1 (GLP-1) agonist approved for type 2 diabetes, doesn’t outweigh the drug’s cardiovascular benefits but does highlight the need for baseline ophthalmologic evaluation before initiating treatment and ongoing retinal monitoring, researchers say.
That conclusion was based on data from a meta-analysis of the seven major cardiovascular outcomes trials of GLP-1 agonists currently on the market.
The findings were recently published in Diabetes & Metabolic Syndrome: Clinical Research & Reviews, by Stewart G. Albert, MD, and colleagues.
Concerns about retinopathy worsening with the GLP-1 agonist drug class first arose from the SUSTAIN-6 cardiovascular outcomes trial for injectable semaglutide, although a subsequent analysis of data from that trial appeared to suggest the problem is likely due to rapid glucose-lowering in already vulnerable patients rather than a drug-specific effect. This effect had been previously reported, most notably in the landmark Diabetes Control and Complications Trial.
In this new meta-analysis, “we showed that with improvements in A1c there were correlations with decreases in the rate of cardiovascular events but increases in the rate of retinopathy,” Dr. Albert, of St. Louis University, told this news organization.
“As a class of drugs, we did not find an increased rate of retinopathy. The effect of GLP-1 agonists on retinopathy did not appear to be due to an immediate direct toxic effect of the drug. The worsening of the rate of retinopathy was seen with semaglutide after 1 year of therapy and when there was a decrease in A1c of 1%,” he explained.
He noted that because the increased risk was seen primarily among those who already had retinopathy at baseline, “it would seem prudent to know the level of retinopathy either before or plan for close ophthalmologic monitoring around the time of drug initiation ... We routinely evaluate patients with known type 2 diabetes mellitus at yearly intervals for retinopathy. From our data, we saw worsening at 1 year of drug exposure, but we do not know the exact time when the changes occurred during that year.”
The Ozempic label advises that “patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy” but doesn’t specifically mention baseline assessment at the time of drug initiation.
No increase in retinopathy risk for GLP-1 agonist class overall
The seven trials in the meta-analysis comprised 56,004 participants, with baseline retinopathy prevalence ranging from 9% to 31%.
For the GLP-1 agonist class overall, there was no significant increase in the relative rate (RR) of retinopathy (RR, 1.09; P = .36), while there were significant reductions in relative rates of major adverse cardiac events, overall deaths, and cardiovascular deaths (all P < .001 or P = .001).
The increased retinopathy risk was seen only in the subcutaneous semaglutide group (RR, 1.73; P = .02).
The overall number needed to harm was 1,000 and the number to treat was 77. For semaglutide, those values were 77 and 43, respectively.
There was a significant correlation between a decrease in major adverse cardiac events and a decrease in A1c (P = .014), while for retinopathy, the risk increased with improved A1c (P = .076).
Semaglutide subanalysis finds increased retinopathy worsening
Dr. Albert and colleagues conducted a separate subanalysis of 11 studies of semaglutide that enrolled 11,894 patients, of which 6 studies (n = 5,610) were of oral semaglutide (Rybelsus) and 5 studies were of subcutaneous semaglutide (Ozempic; n = 6,284).
In the subanalysis, there was an overall increase in relative rates of new or worsening retinopathy (RR, 1.218; P = .049).
The change in relative rate of retinopathy was predominantly found for subcutaneous semaglutide given for longer than 1 year (RR, 1.559; P = .022) and decreases in A1c of more than 1.0% (RR, 1.590; P = .016). No such differences were seen with oral semaglutide.
A further evaluation of the data without the SUSTAIN 6 trial showed no effect on retinopathy but the analysis lacked power.
Dr. Albert told this news organization: “We did not find an immediate toxic effect of any drug. However, we cannot rule out that there was a cumulative effect of the dose over longer times.”
No disclosures were given.
A version of this article first appeared on Medscape.com.
A small potential increased risk of retinopathy worsening at 1 year with injected semaglutide (Ozempic, Novo Nordisk), a glucagon-like peptide 1 (GLP-1) agonist approved for type 2 diabetes, doesn’t outweigh the drug’s cardiovascular benefits but does highlight the need for baseline ophthalmologic evaluation before initiating treatment and ongoing retinal monitoring, researchers say.
That conclusion was based on data from a meta-analysis of the seven major cardiovascular outcomes trials of GLP-1 agonists currently on the market.
The findings were recently published in Diabetes & Metabolic Syndrome: Clinical Research & Reviews, by Stewart G. Albert, MD, and colleagues.
Concerns about retinopathy worsening with the GLP-1 agonist drug class first arose from the SUSTAIN-6 cardiovascular outcomes trial for injectable semaglutide, although a subsequent analysis of data from that trial appeared to suggest the problem is likely due to rapid glucose-lowering in already vulnerable patients rather than a drug-specific effect. This effect had been previously reported, most notably in the landmark Diabetes Control and Complications Trial.
In this new meta-analysis, “we showed that with improvements in A1c there were correlations with decreases in the rate of cardiovascular events but increases in the rate of retinopathy,” Dr. Albert, of St. Louis University, told this news organization.
“As a class of drugs, we did not find an increased rate of retinopathy. The effect of GLP-1 agonists on retinopathy did not appear to be due to an immediate direct toxic effect of the drug. The worsening of the rate of retinopathy was seen with semaglutide after 1 year of therapy and when there was a decrease in A1c of 1%,” he explained.
He noted that because the increased risk was seen primarily among those who already had retinopathy at baseline, “it would seem prudent to know the level of retinopathy either before or plan for close ophthalmologic monitoring around the time of drug initiation ... We routinely evaluate patients with known type 2 diabetes mellitus at yearly intervals for retinopathy. From our data, we saw worsening at 1 year of drug exposure, but we do not know the exact time when the changes occurred during that year.”
The Ozempic label advises that “patients with a history of diabetic retinopathy should be monitored for progression of diabetic retinopathy” but doesn’t specifically mention baseline assessment at the time of drug initiation.
No increase in retinopathy risk for GLP-1 agonist class overall
The seven trials in the meta-analysis comprised 56,004 participants, with baseline retinopathy prevalence ranging from 9% to 31%.
For the GLP-1 agonist class overall, there was no significant increase in the relative rate (RR) of retinopathy (RR, 1.09; P = .36), while there were significant reductions in relative rates of major adverse cardiac events, overall deaths, and cardiovascular deaths (all P < .001 or P = .001).
The increased retinopathy risk was seen only in the subcutaneous semaglutide group (RR, 1.73; P = .02).
The overall number needed to harm was 1,000 and the number to treat was 77. For semaglutide, those values were 77 and 43, respectively.
There was a significant correlation between a decrease in major adverse cardiac events and a decrease in A1c (P = .014), while for retinopathy, the risk increased with improved A1c (P = .076).
Semaglutide subanalysis finds increased retinopathy worsening
Dr. Albert and colleagues conducted a separate subanalysis of 11 studies of semaglutide that enrolled 11,894 patients, of which 6 studies (n = 5,610) were of oral semaglutide (Rybelsus) and 5 studies were of subcutaneous semaglutide (Ozempic; n = 6,284).
In the subanalysis, there was an overall increase in relative rates of new or worsening retinopathy (RR, 1.218; P = .049).
The change in relative rate of retinopathy was predominantly found for subcutaneous semaglutide given for longer than 1 year (RR, 1.559; P = .022) and decreases in A1c of more than 1.0% (RR, 1.590; P = .016). No such differences were seen with oral semaglutide.
A further evaluation of the data without the SUSTAIN 6 trial showed no effect on retinopathy but the analysis lacked power.
Dr. Albert told this news organization: “We did not find an immediate toxic effect of any drug. However, we cannot rule out that there was a cumulative effect of the dose over longer times.”
No disclosures were given.
A version of this article first appeared on Medscape.com.
FROM DIABETES & METABOLIC SYNDROME: CLINICAL RESEARCH & REVIEWS
FDA okays Tidepool Loop app to help guide insulin delivery
The Food and Drug Administration has cleared the Tidepool Loop, a mobile application for use with compatible continuous glucose monitors (CGMs) and insulin pumps to enable automated insulin delivery.
Indicated for people with type 1 diabetes ages 6 years and up, the app algorithm was developed by the diabetes startup Tidepool, which already hosts a cloud-based platform for users to download and review data from different glucose meters, insulin pumps, and CGM systems. The Tidepool Loop project arose from patient-led, open-source initiatives to enable interoperability between the devices.
“The [FDA] authorization of the Tidepool Loop is a huge win for the type 1 diabetes (T1D) community and is a vital step towards a world where people with T1D can choose the pump, CGM, and algorithm that are best for them – and have all three work together seamlessly,” Aaron Kowalski, PhD, CEO of the advocacy organization JDRF, said in a statement.
JDRF helped support preclinical and clinical research in the development of the Loop algorithm, along with The Leona M. and Harry B. Helmsley Charitable Trust, the Tullman Foundation, and partnerships with device makers and donations from the T1D community.
Available by prescription only, the Tidepool app is for single patient use. It works with designated “integrated CGMs” and “alternate controller enabled pumps” to automatically increase, decrease, or suspend insulin delivery, based on the glucose readings and predicted values. The app can also recommend correction doses, which the user can confirm.
According to an FDA statement:“Tidepool Loop’s algorithm technology is designed to be compatible with other individual interoperable devices that meet prespecified acceptance criteria set forth in a validation and integration plan provided by the sponsor and cleared by the FDA as part of the premarket submission.”
Tidepool is finalizing agreements with the various device manufacturers “to create a seamless experience for both physicians prescribing Tidepool Loop and the patients using it,” according to a company statement.
Tidepool’s initial launch device partners have not yet been announced, but the company “has a development partnership with Dexcom and other yet-to-be-named medical device companies for future inclusion of their components with the Tidepool Loop platform,” the statement says.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has cleared the Tidepool Loop, a mobile application for use with compatible continuous glucose monitors (CGMs) and insulin pumps to enable automated insulin delivery.
Indicated for people with type 1 diabetes ages 6 years and up, the app algorithm was developed by the diabetes startup Tidepool, which already hosts a cloud-based platform for users to download and review data from different glucose meters, insulin pumps, and CGM systems. The Tidepool Loop project arose from patient-led, open-source initiatives to enable interoperability between the devices.
“The [FDA] authorization of the Tidepool Loop is a huge win for the type 1 diabetes (T1D) community and is a vital step towards a world where people with T1D can choose the pump, CGM, and algorithm that are best for them – and have all three work together seamlessly,” Aaron Kowalski, PhD, CEO of the advocacy organization JDRF, said in a statement.
JDRF helped support preclinical and clinical research in the development of the Loop algorithm, along with The Leona M. and Harry B. Helmsley Charitable Trust, the Tullman Foundation, and partnerships with device makers and donations from the T1D community.
Available by prescription only, the Tidepool app is for single patient use. It works with designated “integrated CGMs” and “alternate controller enabled pumps” to automatically increase, decrease, or suspend insulin delivery, based on the glucose readings and predicted values. The app can also recommend correction doses, which the user can confirm.
According to an FDA statement:“Tidepool Loop’s algorithm technology is designed to be compatible with other individual interoperable devices that meet prespecified acceptance criteria set forth in a validation and integration plan provided by the sponsor and cleared by the FDA as part of the premarket submission.”
Tidepool is finalizing agreements with the various device manufacturers “to create a seamless experience for both physicians prescribing Tidepool Loop and the patients using it,” according to a company statement.
Tidepool’s initial launch device partners have not yet been announced, but the company “has a development partnership with Dexcom and other yet-to-be-named medical device companies for future inclusion of their components with the Tidepool Loop platform,” the statement says.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has cleared the Tidepool Loop, a mobile application for use with compatible continuous glucose monitors (CGMs) and insulin pumps to enable automated insulin delivery.
Indicated for people with type 1 diabetes ages 6 years and up, the app algorithm was developed by the diabetes startup Tidepool, which already hosts a cloud-based platform for users to download and review data from different glucose meters, insulin pumps, and CGM systems. The Tidepool Loop project arose from patient-led, open-source initiatives to enable interoperability between the devices.
“The [FDA] authorization of the Tidepool Loop is a huge win for the type 1 diabetes (T1D) community and is a vital step towards a world where people with T1D can choose the pump, CGM, and algorithm that are best for them – and have all three work together seamlessly,” Aaron Kowalski, PhD, CEO of the advocacy organization JDRF, said in a statement.
JDRF helped support preclinical and clinical research in the development of the Loop algorithm, along with The Leona M. and Harry B. Helmsley Charitable Trust, the Tullman Foundation, and partnerships with device makers and donations from the T1D community.
Available by prescription only, the Tidepool app is for single patient use. It works with designated “integrated CGMs” and “alternate controller enabled pumps” to automatically increase, decrease, or suspend insulin delivery, based on the glucose readings and predicted values. The app can also recommend correction doses, which the user can confirm.
According to an FDA statement:“Tidepool Loop’s algorithm technology is designed to be compatible with other individual interoperable devices that meet prespecified acceptance criteria set forth in a validation and integration plan provided by the sponsor and cleared by the FDA as part of the premarket submission.”
Tidepool is finalizing agreements with the various device manufacturers “to create a seamless experience for both physicians prescribing Tidepool Loop and the patients using it,” according to a company statement.
Tidepool’s initial launch device partners have not yet been announced, but the company “has a development partnership with Dexcom and other yet-to-be-named medical device companies for future inclusion of their components with the Tidepool Loop platform,” the statement says.
A version of this article first appeared on Medscape.com.
Food additives may exacerbate IBD
AURORA, COLO. – Dietary additives lurking in processed foods may contribute to the development or exacerbation of inflammatory bowel disease (IBD), a leading gastroenterologist contends.
At the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association, James D. Lewis, MD, MSCE, AGAF, of the University of Pennsylvania in Philadelphia, highlighted research from both animal and human studies pointing to certain widely used food additives such as carboxymethycellulose (CMC), polysorbate 80, and carrageenan as potential instigators in gastrointestinal inflammation.
he said.
Some additives appear to have deleterious effects on intestinal microbiota, while others may exert their baleful influence through mechanisms such as endoplasmic stress.
“It looks like some people might be a little more sensitive to additives than others, and if you were going to use any of this [research] to try and give some advice, maybe we would say that patients or first-degree relatives of people with IBD may want to avoid foods that contain high levels of additives, and if for no other reason, mothers or people with a family history of IBD might be encouraged to breastfeed to avoid early exposure to additives that are in infant formulas,” he advised.
Processed foods defined
The typical American diet may include a large proportion of processed foods, defined as “foods that have undergone biological, chemical, or physical process to improve texture, taste, or shelf life.”
Processed foods tend to be higher in fats, added sugars, and salts, and lower in fiber and intrinsic vitamins than minimally processed foods.
There is also a category of “ultraprocessed” foods, which contain little or no whole foods but are high in energy density. Many of these super(bad) foods are staples of the American diet, such as chips, hot dogs, chicken nuggets, breakfast cereal, soda, candy, and margarine. These and similar foods contribute from 25% to 50% of daily energy intake in the United States and Canada, Dr. Lewis said.
And North America is not alone, he added, pointing to a 2015 study showing that the consumption of ultraprocessed foods in Sweden increased “dramatically” from 1960 through 2010, and that this increase mirrored an increase in obesity prevalence in that nation.
Emulsifiers and thickeners
Dr. Lewis focused on emulsifiers and thickeners that are commonly added to processed foods and are, according to the Food and Drug Administration, “generally recognized as safe.”
Emulsifiers are “detergent-like molecules that stabilize mixtures of immiscible [nonhomegenous] liquids.”
Thickeners are additives that increase the viscosity of liquids without otherwise substantially changing their other properties.
In addition to the aforementioned products, other common additives include xanthan gum (a polysaccharide used as an emulsifier in salad dressings, baked goods, ice cream, and gluten-free products), maltodextrin (a sugar substitute marketed as “Splenda”), and soy lecithin (a soy derivative used as an emulsifier, stabilizer, and wetting agent).
Evidence of harm
Dr. Lewis noted that in 2013, investigators at the University of Liverpool, England, published a hypothesis suggesting that consumption of emulsifiers in processed foods may promote Crohn’s disease by increasing bacterial translocation. Their hypothesis was based in part on evidence that “very small concentrations of the emulsifier polysorbate 80 enhance bacterial translocation across intestinal epithelia. Undigested emulsifiers may increase bacterial translocation, particularly in the small intestine where the mucus layer is discontinuous. “
The authors also suggested that their hypothesis could be tested in clinical trials comparing enteral feeding with and without emulsifiers.
Other suggestive if not definitive evidence of a potential link between additives and IBD are data showing that IBD is very rare in young children.
“In your early stages of your life, you’re not consuming a lot of ultraprocessed foods. Indeed, the rate of intake of at least fast foods, which you can think of almost as a surrogate for ultraprocessed foods, goes up dramatically when people get to their teens, and this is the same time as we see, really, the big uptick in the incidence of IBD,” Dr. Lewis said.
A link between ultraprocessed food consumption and later development of IBD, primarily Crohn’s disease, is also suggested by data from the Nurses Health Study I and II and Health Professionals Follow-Up study. Among 245,112 participants with about 5.5 million person-years of follow-up, the highest vs. lowest quartile of consumption of ultraprocessed foods was associated with a 70% increase in risk for developing Crohn’s (hazard ratio 1.70, P = .0008).
Animal studies
Evidence for a possible mechanism whereby emulsifiers and thickeners cause intestinal changes comes from a study published in Nature in 2015 showing that adding CMC and PS80 to the drinking water of mice resulted in major shifts in the gut microbiota in both wild-type and interleukin 10 knockout mice, a model for IBD.
When the additives were put into the water the mice had a thinning of the mucus layer, allowing bacteria in closer proximity to the epithelium.
“When you put these into the drinking water of IL-10 knockout mice that are already predisposed to developing colitis, they were far more likely to go on to develop colitis over the course of 3 months,” Dr. Lewis said.
From mouse to man
Dr. Lewis briefly summarized results of the FRESH study that he and colleagues recently published in Gastronterology. In this trial, 16 healthy adult volunteers who agreed to stay and eat all meals at the research center were randomized to receive either an emulsifier-free diet or the identical diet enriched with 15 g of CMC daily for 11 days.
“I will comment that that’s a lot of carboxymethycellulose,” Dr. Lewis said.
The volunteers fed the CMC-enriched diet had a slight increase in abdominal discomfort after eating and a reduction in species diversity in the gut microbiota. In addition, these participants had reductions in levels of short-chain fatty acids and free amino acids, both of which are signs of a health gut environment.
“Furthermore, we identified 2 subjects consuming CMC who exhibited increased microbiota encroachment into the normally sterile inner mucus layer, a central feature of gut inflammation, as well as stark alterations in microbiota composition,” the investigators wrote.
Dr. Lewis cited a separate small study by investigators at the University of Illinois at Chicago and the University of Chicago. These investigators randomized patients with UC in remission to take supplements containing carrageenan – a seaweed-derived food additive that has been shown to cause inflammation in both in vitro and animal models – or placebo . The amount of carrageenan in the capsules was less than that found in an average daily Western diet, the authors noted.
The participants were followed with telephone calls every 2 weeks or until relapse, which was defined as an increase of 2 or more points on the Simple Clinical Colitis Activity Index (SCCAI) and intensification of treatment for UC.
Of the 12 patients who completed the study, 3 in the carrageenan group experienced relapses, compared with none of the patients in the placebo group (P = .046). The relapse occurred at 5, 32, and 42 weeks of follow-up.
Exceptions to the rule
“It’s not clear that all additives are harmful,” Dr. Lewis said, pointing to a placebo-controlled study suggesting a beneficial effect of soy lecithin in patients with UC. The additive is composed of at least 30% of phosphatidycholine, a component of intestinal mucus.
He also noted that there is an ongoing randomized, placebo-controlled trial comparing a low-additive diet to a habitual diet in 154 patients with mildly active, stable Crohn’s disease.
Session moderator Michael J. Rosen, MD, MSCI, a pediatric gastroenterologist at Stanford University Medical Center in Palo Alto, Calif., told this news organization that dietary components do appear to have an influence on the disease course in patients with IBD.
“I do think there are patients with IBD who are maybe genetically predisposed to being sensitive to certain components of diet,” he said in an interview seeking objective commentary.
“Particularly in pediatrics there are lines of evidence of diets maybe having some efficacy in treatment. It needs further study, but one commonality about those diets is that they tend to eliminate processed foods and focus on whole foods,” he said.
Dr. Lewis’ work is supported by grants from the National Institutes of Health, and from AbbVie, Takeda, Janssen, and Nestlé Health Science. He has served as a consultant to and data safety monitoring board member for several entitities. Dr. Rosen reported no conflicts of interest to disclose.
AURORA, COLO. – Dietary additives lurking in processed foods may contribute to the development or exacerbation of inflammatory bowel disease (IBD), a leading gastroenterologist contends.
At the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association, James D. Lewis, MD, MSCE, AGAF, of the University of Pennsylvania in Philadelphia, highlighted research from both animal and human studies pointing to certain widely used food additives such as carboxymethycellulose (CMC), polysorbate 80, and carrageenan as potential instigators in gastrointestinal inflammation.
he said.
Some additives appear to have deleterious effects on intestinal microbiota, while others may exert their baleful influence through mechanisms such as endoplasmic stress.
“It looks like some people might be a little more sensitive to additives than others, and if you were going to use any of this [research] to try and give some advice, maybe we would say that patients or first-degree relatives of people with IBD may want to avoid foods that contain high levels of additives, and if for no other reason, mothers or people with a family history of IBD might be encouraged to breastfeed to avoid early exposure to additives that are in infant formulas,” he advised.
Processed foods defined
The typical American diet may include a large proportion of processed foods, defined as “foods that have undergone biological, chemical, or physical process to improve texture, taste, or shelf life.”
Processed foods tend to be higher in fats, added sugars, and salts, and lower in fiber and intrinsic vitamins than minimally processed foods.
There is also a category of “ultraprocessed” foods, which contain little or no whole foods but are high in energy density. Many of these super(bad) foods are staples of the American diet, such as chips, hot dogs, chicken nuggets, breakfast cereal, soda, candy, and margarine. These and similar foods contribute from 25% to 50% of daily energy intake in the United States and Canada, Dr. Lewis said.
And North America is not alone, he added, pointing to a 2015 study showing that the consumption of ultraprocessed foods in Sweden increased “dramatically” from 1960 through 2010, and that this increase mirrored an increase in obesity prevalence in that nation.
Emulsifiers and thickeners
Dr. Lewis focused on emulsifiers and thickeners that are commonly added to processed foods and are, according to the Food and Drug Administration, “generally recognized as safe.”
Emulsifiers are “detergent-like molecules that stabilize mixtures of immiscible [nonhomegenous] liquids.”
Thickeners are additives that increase the viscosity of liquids without otherwise substantially changing their other properties.
In addition to the aforementioned products, other common additives include xanthan gum (a polysaccharide used as an emulsifier in salad dressings, baked goods, ice cream, and gluten-free products), maltodextrin (a sugar substitute marketed as “Splenda”), and soy lecithin (a soy derivative used as an emulsifier, stabilizer, and wetting agent).
Evidence of harm
Dr. Lewis noted that in 2013, investigators at the University of Liverpool, England, published a hypothesis suggesting that consumption of emulsifiers in processed foods may promote Crohn’s disease by increasing bacterial translocation. Their hypothesis was based in part on evidence that “very small concentrations of the emulsifier polysorbate 80 enhance bacterial translocation across intestinal epithelia. Undigested emulsifiers may increase bacterial translocation, particularly in the small intestine where the mucus layer is discontinuous. “
The authors also suggested that their hypothesis could be tested in clinical trials comparing enteral feeding with and without emulsifiers.
Other suggestive if not definitive evidence of a potential link between additives and IBD are data showing that IBD is very rare in young children.
“In your early stages of your life, you’re not consuming a lot of ultraprocessed foods. Indeed, the rate of intake of at least fast foods, which you can think of almost as a surrogate for ultraprocessed foods, goes up dramatically when people get to their teens, and this is the same time as we see, really, the big uptick in the incidence of IBD,” Dr. Lewis said.
A link between ultraprocessed food consumption and later development of IBD, primarily Crohn’s disease, is also suggested by data from the Nurses Health Study I and II and Health Professionals Follow-Up study. Among 245,112 participants with about 5.5 million person-years of follow-up, the highest vs. lowest quartile of consumption of ultraprocessed foods was associated with a 70% increase in risk for developing Crohn’s (hazard ratio 1.70, P = .0008).
Animal studies
Evidence for a possible mechanism whereby emulsifiers and thickeners cause intestinal changes comes from a study published in Nature in 2015 showing that adding CMC and PS80 to the drinking water of mice resulted in major shifts in the gut microbiota in both wild-type and interleukin 10 knockout mice, a model for IBD.
When the additives were put into the water the mice had a thinning of the mucus layer, allowing bacteria in closer proximity to the epithelium.
“When you put these into the drinking water of IL-10 knockout mice that are already predisposed to developing colitis, they were far more likely to go on to develop colitis over the course of 3 months,” Dr. Lewis said.
From mouse to man
Dr. Lewis briefly summarized results of the FRESH study that he and colleagues recently published in Gastronterology. In this trial, 16 healthy adult volunteers who agreed to stay and eat all meals at the research center were randomized to receive either an emulsifier-free diet or the identical diet enriched with 15 g of CMC daily for 11 days.
“I will comment that that’s a lot of carboxymethycellulose,” Dr. Lewis said.
The volunteers fed the CMC-enriched diet had a slight increase in abdominal discomfort after eating and a reduction in species diversity in the gut microbiota. In addition, these participants had reductions in levels of short-chain fatty acids and free amino acids, both of which are signs of a health gut environment.
“Furthermore, we identified 2 subjects consuming CMC who exhibited increased microbiota encroachment into the normally sterile inner mucus layer, a central feature of gut inflammation, as well as stark alterations in microbiota composition,” the investigators wrote.
Dr. Lewis cited a separate small study by investigators at the University of Illinois at Chicago and the University of Chicago. These investigators randomized patients with UC in remission to take supplements containing carrageenan – a seaweed-derived food additive that has been shown to cause inflammation in both in vitro and animal models – or placebo . The amount of carrageenan in the capsules was less than that found in an average daily Western diet, the authors noted.
The participants were followed with telephone calls every 2 weeks or until relapse, which was defined as an increase of 2 or more points on the Simple Clinical Colitis Activity Index (SCCAI) and intensification of treatment for UC.
Of the 12 patients who completed the study, 3 in the carrageenan group experienced relapses, compared with none of the patients in the placebo group (P = .046). The relapse occurred at 5, 32, and 42 weeks of follow-up.
Exceptions to the rule
“It’s not clear that all additives are harmful,” Dr. Lewis said, pointing to a placebo-controlled study suggesting a beneficial effect of soy lecithin in patients with UC. The additive is composed of at least 30% of phosphatidycholine, a component of intestinal mucus.
He also noted that there is an ongoing randomized, placebo-controlled trial comparing a low-additive diet to a habitual diet in 154 patients with mildly active, stable Crohn’s disease.
Session moderator Michael J. Rosen, MD, MSCI, a pediatric gastroenterologist at Stanford University Medical Center in Palo Alto, Calif., told this news organization that dietary components do appear to have an influence on the disease course in patients with IBD.
“I do think there are patients with IBD who are maybe genetically predisposed to being sensitive to certain components of diet,” he said in an interview seeking objective commentary.
“Particularly in pediatrics there are lines of evidence of diets maybe having some efficacy in treatment. It needs further study, but one commonality about those diets is that they tend to eliminate processed foods and focus on whole foods,” he said.
Dr. Lewis’ work is supported by grants from the National Institutes of Health, and from AbbVie, Takeda, Janssen, and Nestlé Health Science. He has served as a consultant to and data safety monitoring board member for several entitities. Dr. Rosen reported no conflicts of interest to disclose.
AURORA, COLO. – Dietary additives lurking in processed foods may contribute to the development or exacerbation of inflammatory bowel disease (IBD), a leading gastroenterologist contends.
At the annual Crohn’s & Colitis Congress®, a partnership of the Crohn’s & Colitis Foundation and the American Gastroenterological Association, James D. Lewis, MD, MSCE, AGAF, of the University of Pennsylvania in Philadelphia, highlighted research from both animal and human studies pointing to certain widely used food additives such as carboxymethycellulose (CMC), polysorbate 80, and carrageenan as potential instigators in gastrointestinal inflammation.
he said.
Some additives appear to have deleterious effects on intestinal microbiota, while others may exert their baleful influence through mechanisms such as endoplasmic stress.
“It looks like some people might be a little more sensitive to additives than others, and if you were going to use any of this [research] to try and give some advice, maybe we would say that patients or first-degree relatives of people with IBD may want to avoid foods that contain high levels of additives, and if for no other reason, mothers or people with a family history of IBD might be encouraged to breastfeed to avoid early exposure to additives that are in infant formulas,” he advised.
Processed foods defined
The typical American diet may include a large proportion of processed foods, defined as “foods that have undergone biological, chemical, or physical process to improve texture, taste, or shelf life.”
Processed foods tend to be higher in fats, added sugars, and salts, and lower in fiber and intrinsic vitamins than minimally processed foods.
There is also a category of “ultraprocessed” foods, which contain little or no whole foods but are high in energy density. Many of these super(bad) foods are staples of the American diet, such as chips, hot dogs, chicken nuggets, breakfast cereal, soda, candy, and margarine. These and similar foods contribute from 25% to 50% of daily energy intake in the United States and Canada, Dr. Lewis said.
And North America is not alone, he added, pointing to a 2015 study showing that the consumption of ultraprocessed foods in Sweden increased “dramatically” from 1960 through 2010, and that this increase mirrored an increase in obesity prevalence in that nation.
Emulsifiers and thickeners
Dr. Lewis focused on emulsifiers and thickeners that are commonly added to processed foods and are, according to the Food and Drug Administration, “generally recognized as safe.”
Emulsifiers are “detergent-like molecules that stabilize mixtures of immiscible [nonhomegenous] liquids.”
Thickeners are additives that increase the viscosity of liquids without otherwise substantially changing their other properties.
In addition to the aforementioned products, other common additives include xanthan gum (a polysaccharide used as an emulsifier in salad dressings, baked goods, ice cream, and gluten-free products), maltodextrin (a sugar substitute marketed as “Splenda”), and soy lecithin (a soy derivative used as an emulsifier, stabilizer, and wetting agent).
Evidence of harm
Dr. Lewis noted that in 2013, investigators at the University of Liverpool, England, published a hypothesis suggesting that consumption of emulsifiers in processed foods may promote Crohn’s disease by increasing bacterial translocation. Their hypothesis was based in part on evidence that “very small concentrations of the emulsifier polysorbate 80 enhance bacterial translocation across intestinal epithelia. Undigested emulsifiers may increase bacterial translocation, particularly in the small intestine where the mucus layer is discontinuous. “
The authors also suggested that their hypothesis could be tested in clinical trials comparing enteral feeding with and without emulsifiers.
Other suggestive if not definitive evidence of a potential link between additives and IBD are data showing that IBD is very rare in young children.
“In your early stages of your life, you’re not consuming a lot of ultraprocessed foods. Indeed, the rate of intake of at least fast foods, which you can think of almost as a surrogate for ultraprocessed foods, goes up dramatically when people get to their teens, and this is the same time as we see, really, the big uptick in the incidence of IBD,” Dr. Lewis said.
A link between ultraprocessed food consumption and later development of IBD, primarily Crohn’s disease, is also suggested by data from the Nurses Health Study I and II and Health Professionals Follow-Up study. Among 245,112 participants with about 5.5 million person-years of follow-up, the highest vs. lowest quartile of consumption of ultraprocessed foods was associated with a 70% increase in risk for developing Crohn’s (hazard ratio 1.70, P = .0008).
Animal studies
Evidence for a possible mechanism whereby emulsifiers and thickeners cause intestinal changes comes from a study published in Nature in 2015 showing that adding CMC and PS80 to the drinking water of mice resulted in major shifts in the gut microbiota in both wild-type and interleukin 10 knockout mice, a model for IBD.
When the additives were put into the water the mice had a thinning of the mucus layer, allowing bacteria in closer proximity to the epithelium.
“When you put these into the drinking water of IL-10 knockout mice that are already predisposed to developing colitis, they were far more likely to go on to develop colitis over the course of 3 months,” Dr. Lewis said.
From mouse to man
Dr. Lewis briefly summarized results of the FRESH study that he and colleagues recently published in Gastronterology. In this trial, 16 healthy adult volunteers who agreed to stay and eat all meals at the research center were randomized to receive either an emulsifier-free diet or the identical diet enriched with 15 g of CMC daily for 11 days.
“I will comment that that’s a lot of carboxymethycellulose,” Dr. Lewis said.
The volunteers fed the CMC-enriched diet had a slight increase in abdominal discomfort after eating and a reduction in species diversity in the gut microbiota. In addition, these participants had reductions in levels of short-chain fatty acids and free amino acids, both of which are signs of a health gut environment.
“Furthermore, we identified 2 subjects consuming CMC who exhibited increased microbiota encroachment into the normally sterile inner mucus layer, a central feature of gut inflammation, as well as stark alterations in microbiota composition,” the investigators wrote.
Dr. Lewis cited a separate small study by investigators at the University of Illinois at Chicago and the University of Chicago. These investigators randomized patients with UC in remission to take supplements containing carrageenan – a seaweed-derived food additive that has been shown to cause inflammation in both in vitro and animal models – or placebo . The amount of carrageenan in the capsules was less than that found in an average daily Western diet, the authors noted.
The participants were followed with telephone calls every 2 weeks or until relapse, which was defined as an increase of 2 or more points on the Simple Clinical Colitis Activity Index (SCCAI) and intensification of treatment for UC.
Of the 12 patients who completed the study, 3 in the carrageenan group experienced relapses, compared with none of the patients in the placebo group (P = .046). The relapse occurred at 5, 32, and 42 weeks of follow-up.
Exceptions to the rule
“It’s not clear that all additives are harmful,” Dr. Lewis said, pointing to a placebo-controlled study suggesting a beneficial effect of soy lecithin in patients with UC. The additive is composed of at least 30% of phosphatidycholine, a component of intestinal mucus.
He also noted that there is an ongoing randomized, placebo-controlled trial comparing a low-additive diet to a habitual diet in 154 patients with mildly active, stable Crohn’s disease.
Session moderator Michael J. Rosen, MD, MSCI, a pediatric gastroenterologist at Stanford University Medical Center in Palo Alto, Calif., told this news organization that dietary components do appear to have an influence on the disease course in patients with IBD.
“I do think there are patients with IBD who are maybe genetically predisposed to being sensitive to certain components of diet,” he said in an interview seeking objective commentary.
“Particularly in pediatrics there are lines of evidence of diets maybe having some efficacy in treatment. It needs further study, but one commonality about those diets is that they tend to eliminate processed foods and focus on whole foods,” he said.
Dr. Lewis’ work is supported by grants from the National Institutes of Health, and from AbbVie, Takeda, Janssen, and Nestlé Health Science. He has served as a consultant to and data safety monitoring board member for several entitities. Dr. Rosen reported no conflicts of interest to disclose.
AT THE CROHN’S & COLITIS CONGRESS
EMR screening in emergency department tags undiagnosed diabetes
A diabetes screening program built into an electronic medical records system identified diabetes or prediabetes in 52% of individuals flagged for abnormal hemoglobin A1c, based on data from more than 2,000 adults.
“Despite the best efforts of clinicians, researchers, and educators, the number of patients living with undiagnosed diabetes is still rising and is currently at approximately 8.5 million, and the number of people unaware of their prediabetes is approximately 77 million,” lead investigator Kristie K. Danielson, PhD, said in an interview. Screening for diabetes is critical to start treatment early, to potentially reverse prediabetes, and to prevent the long-term complications of diabetes and reduced life expectancy.
In a pilot study published in JAMA Network Open, Dr. Danielson and colleagues reviewed data from 8,441 adults who visited a single emergency department in Chicago during February–April 2021.
The EMR at the hospital contained a built-in best practice alert (BPA) that flagged patients as being at risk for type 2 diabetes based the American Diabetes Association recommendations; the identification algorithm included age 45 years and older, or those aged 18-44 years with a body mass index of 25 kg/m2 or higher, no previous history of diabetes, and no A1c measure in the last 3 years, according to the EMR.
A total of 8,441 adult patients visited the ED during the study period; 2,576 triggered BPA tests, and 2,074 had A1c results for review. Among the patients with A1c results, 52% had elevated values of 5.7% or higher. Of these, a total of 758 individuals were identified with prediabetes (A1c, 5.7%-6.4%), 265 with diabetes (A1c, 6.5%-9.9%), and 62 with severe diabetes (A1c, 10% or higher).
After testing, 352 patients with elevated A1c were contacted by the researchers. The mean age of this group was 52.2 years, 54.5% were women, and nearly two-thirds (64.8%) were non-Hispanic Black. The median income of those contacted was in the 44th percentile, and 50% had public insurance.
Most of those contacted (264 patients) were not aware of a previous diagnosis of prediabetes or diabetes; the remaining 88 had a previous diagnosis, but only 51 self-reported receiving treatment, the researchers noted.
Although the screening program successfully identified a significant number of previously undiagnosed individuals with diabetes, prediabetes, or poorly controlled diabetes, its feasibility in routine practice requires further study, the researchers wrote.
The findings were limited by several factors including the identification of patients previously diagnosed with diabetes but who were not being treated, and the potential bias toward individuals of higher socioeconomic status, the researchers noted. However, the results support further exploration of the program as a way to identify undiagnosed diabetes, especially in underserved populations.
Diabetes in underserved groups goes undetected
“We were surprised by the sheer number of people newly diagnosed with diabetes or prediabetes,” which was far greater than expected, commented Dr. Danielson of the University of Illinois at Chicago. “Clearly, we tapped into a new population that has not often been seen by primary care providers or endocrinologists, as is often the case for underserved and vulnerable individuals who visit the emergency department as a first line for health care.”
The screening alert system is straightforward to build into an existing EMR, with technical support, Dr. Danielson said. “In theory, it should be able to be incorporated into other clinical centers and emergency departments. One of the current limitations that we are seeing is that the EMR is still flagging some people already diagnosed with diabetes to be screened for diabetes.” However, “because of this, we also see this as an opportunity to identify and reach out to those with diabetes who are still underserved and not receiving the appropriate diabetes care they need.”
The study results have broader public health implications, Dr. Danielson added. “We have identified a new, large population of people with diabetes who need medical care and diabetes education. This will further add to the burden of health care and costs, and it raises the ethical question of screening and not having full resources readily available to help.
“In my opinion, the study sheds light on a significant issue that will hopefully help drive change at both a health systems and public health level locally and nationally,” she added.
“One of the significant research gaps that has emerged now is how to link these new patients to health care and diabetes education at our institution after they leave the emergency department,” said Dr. Danielson. Diabetes screening in the ED setting is “a very novel area for health system scientists, social workers, and others to now come to the table and collaborate on next steps to help our patients.”
The study was initiated by the investigators, but was supported by a grant from Novo Nordisk to two coauthors. Dr. Danielson also disclosed grant funding from Novo Nordisk during the conduct of the study.
A diabetes screening program built into an electronic medical records system identified diabetes or prediabetes in 52% of individuals flagged for abnormal hemoglobin A1c, based on data from more than 2,000 adults.
“Despite the best efforts of clinicians, researchers, and educators, the number of patients living with undiagnosed diabetes is still rising and is currently at approximately 8.5 million, and the number of people unaware of their prediabetes is approximately 77 million,” lead investigator Kristie K. Danielson, PhD, said in an interview. Screening for diabetes is critical to start treatment early, to potentially reverse prediabetes, and to prevent the long-term complications of diabetes and reduced life expectancy.
In a pilot study published in JAMA Network Open, Dr. Danielson and colleagues reviewed data from 8,441 adults who visited a single emergency department in Chicago during February–April 2021.
The EMR at the hospital contained a built-in best practice alert (BPA) that flagged patients as being at risk for type 2 diabetes based the American Diabetes Association recommendations; the identification algorithm included age 45 years and older, or those aged 18-44 years with a body mass index of 25 kg/m2 or higher, no previous history of diabetes, and no A1c measure in the last 3 years, according to the EMR.
A total of 8,441 adult patients visited the ED during the study period; 2,576 triggered BPA tests, and 2,074 had A1c results for review. Among the patients with A1c results, 52% had elevated values of 5.7% or higher. Of these, a total of 758 individuals were identified with prediabetes (A1c, 5.7%-6.4%), 265 with diabetes (A1c, 6.5%-9.9%), and 62 with severe diabetes (A1c, 10% or higher).
After testing, 352 patients with elevated A1c were contacted by the researchers. The mean age of this group was 52.2 years, 54.5% were women, and nearly two-thirds (64.8%) were non-Hispanic Black. The median income of those contacted was in the 44th percentile, and 50% had public insurance.
Most of those contacted (264 patients) were not aware of a previous diagnosis of prediabetes or diabetes; the remaining 88 had a previous diagnosis, but only 51 self-reported receiving treatment, the researchers noted.
Although the screening program successfully identified a significant number of previously undiagnosed individuals with diabetes, prediabetes, or poorly controlled diabetes, its feasibility in routine practice requires further study, the researchers wrote.
The findings were limited by several factors including the identification of patients previously diagnosed with diabetes but who were not being treated, and the potential bias toward individuals of higher socioeconomic status, the researchers noted. However, the results support further exploration of the program as a way to identify undiagnosed diabetes, especially in underserved populations.
Diabetes in underserved groups goes undetected
“We were surprised by the sheer number of people newly diagnosed with diabetes or prediabetes,” which was far greater than expected, commented Dr. Danielson of the University of Illinois at Chicago. “Clearly, we tapped into a new population that has not often been seen by primary care providers or endocrinologists, as is often the case for underserved and vulnerable individuals who visit the emergency department as a first line for health care.”
The screening alert system is straightforward to build into an existing EMR, with technical support, Dr. Danielson said. “In theory, it should be able to be incorporated into other clinical centers and emergency departments. One of the current limitations that we are seeing is that the EMR is still flagging some people already diagnosed with diabetes to be screened for diabetes.” However, “because of this, we also see this as an opportunity to identify and reach out to those with diabetes who are still underserved and not receiving the appropriate diabetes care they need.”
The study results have broader public health implications, Dr. Danielson added. “We have identified a new, large population of people with diabetes who need medical care and diabetes education. This will further add to the burden of health care and costs, and it raises the ethical question of screening and not having full resources readily available to help.
“In my opinion, the study sheds light on a significant issue that will hopefully help drive change at both a health systems and public health level locally and nationally,” she added.
“One of the significant research gaps that has emerged now is how to link these new patients to health care and diabetes education at our institution after they leave the emergency department,” said Dr. Danielson. Diabetes screening in the ED setting is “a very novel area for health system scientists, social workers, and others to now come to the table and collaborate on next steps to help our patients.”
The study was initiated by the investigators, but was supported by a grant from Novo Nordisk to two coauthors. Dr. Danielson also disclosed grant funding from Novo Nordisk during the conduct of the study.
A diabetes screening program built into an electronic medical records system identified diabetes or prediabetes in 52% of individuals flagged for abnormal hemoglobin A1c, based on data from more than 2,000 adults.
“Despite the best efforts of clinicians, researchers, and educators, the number of patients living with undiagnosed diabetes is still rising and is currently at approximately 8.5 million, and the number of people unaware of their prediabetes is approximately 77 million,” lead investigator Kristie K. Danielson, PhD, said in an interview. Screening for diabetes is critical to start treatment early, to potentially reverse prediabetes, and to prevent the long-term complications of diabetes and reduced life expectancy.
In a pilot study published in JAMA Network Open, Dr. Danielson and colleagues reviewed data from 8,441 adults who visited a single emergency department in Chicago during February–April 2021.
The EMR at the hospital contained a built-in best practice alert (BPA) that flagged patients as being at risk for type 2 diabetes based the American Diabetes Association recommendations; the identification algorithm included age 45 years and older, or those aged 18-44 years with a body mass index of 25 kg/m2 or higher, no previous history of diabetes, and no A1c measure in the last 3 years, according to the EMR.
A total of 8,441 adult patients visited the ED during the study period; 2,576 triggered BPA tests, and 2,074 had A1c results for review. Among the patients with A1c results, 52% had elevated values of 5.7% or higher. Of these, a total of 758 individuals were identified with prediabetes (A1c, 5.7%-6.4%), 265 with diabetes (A1c, 6.5%-9.9%), and 62 with severe diabetes (A1c, 10% or higher).
After testing, 352 patients with elevated A1c were contacted by the researchers. The mean age of this group was 52.2 years, 54.5% were women, and nearly two-thirds (64.8%) were non-Hispanic Black. The median income of those contacted was in the 44th percentile, and 50% had public insurance.
Most of those contacted (264 patients) were not aware of a previous diagnosis of prediabetes or diabetes; the remaining 88 had a previous diagnosis, but only 51 self-reported receiving treatment, the researchers noted.
Although the screening program successfully identified a significant number of previously undiagnosed individuals with diabetes, prediabetes, or poorly controlled diabetes, its feasibility in routine practice requires further study, the researchers wrote.
The findings were limited by several factors including the identification of patients previously diagnosed with diabetes but who were not being treated, and the potential bias toward individuals of higher socioeconomic status, the researchers noted. However, the results support further exploration of the program as a way to identify undiagnosed diabetes, especially in underserved populations.
Diabetes in underserved groups goes undetected
“We were surprised by the sheer number of people newly diagnosed with diabetes or prediabetes,” which was far greater than expected, commented Dr. Danielson of the University of Illinois at Chicago. “Clearly, we tapped into a new population that has not often been seen by primary care providers or endocrinologists, as is often the case for underserved and vulnerable individuals who visit the emergency department as a first line for health care.”
The screening alert system is straightforward to build into an existing EMR, with technical support, Dr. Danielson said. “In theory, it should be able to be incorporated into other clinical centers and emergency departments. One of the current limitations that we are seeing is that the EMR is still flagging some people already diagnosed with diabetes to be screened for diabetes.” However, “because of this, we also see this as an opportunity to identify and reach out to those with diabetes who are still underserved and not receiving the appropriate diabetes care they need.”
The study results have broader public health implications, Dr. Danielson added. “We have identified a new, large population of people with diabetes who need medical care and diabetes education. This will further add to the burden of health care and costs, and it raises the ethical question of screening and not having full resources readily available to help.
“In my opinion, the study sheds light on a significant issue that will hopefully help drive change at both a health systems and public health level locally and nationally,” she added.
“One of the significant research gaps that has emerged now is how to link these new patients to health care and diabetes education at our institution after they leave the emergency department,” said Dr. Danielson. Diabetes screening in the ED setting is “a very novel area for health system scientists, social workers, and others to now come to the table and collaborate on next steps to help our patients.”
The study was initiated by the investigators, but was supported by a grant from Novo Nordisk to two coauthors. Dr. Danielson also disclosed grant funding from Novo Nordisk during the conduct of the study.
FROM JAMA NETWORK OPEN
Circular patch on chest
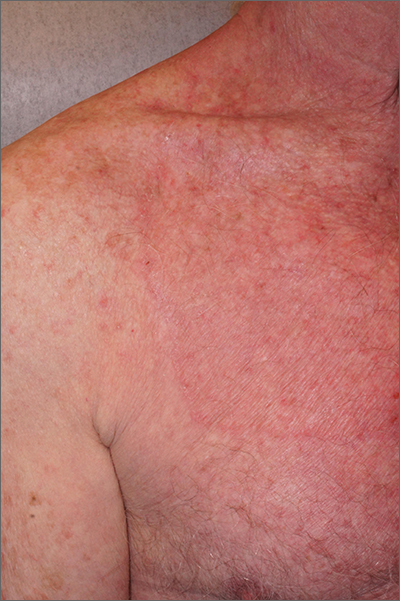
A skin scraping and potassium hydroxide (KOH) prep confirmed the presence of branching hyphae, consistent with tinea corporis. The large size of this plaque could have easily made this diagnosis more difficult. When tinea corporis is suspected, look at the edge of the plaque; there is often thin scale and sometimes small pustules corresponding to follicular involvement.
Commonly called by the misnomer “ringworm,” tinea corporis is a skin infection caused by a wide variety of dermatophytes and affects all ages, sexes, and skin types. Trichophyton, Microsporum, and Epidermophyton species are frequently isolated.1 Patients with atopic dermatitis or weakened immunity may be more susceptible to more frequent or long-lasting episodes. Diabetes may have contributed to the extent of the disease in this case.
Patients with tinea corporis present with one or several annular patches to plaques that grow in size. When the source of contagion is an animal, inflammation can be dramatic. In the case above, there was minimal to no itching and the patient didn’t notice the rash; thus, it was able to enlarge for months.
Treatment options include systemic and topical antifungal therapy. Consideration should be given to the severity of the disease and causal organism. Azoles, terbinafine, and ciclopirox are common treatment options. Topical therapy with an appropriately selected antifungal for 1 to 6 weeks, based on clinical response, is safe and effective. It is important to consider other foci of infection, including the feet and hands. More extensive disease may be treated with oral therapy such as terbinafine, fluconazole, or itraconazole.
Because of the extent of the disease and the challenge of effective coverage with topical therapy, this patient was treated with oral terbinafine 250 mg daily for 3 weeks. The plaque cleared completely.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Leung AK, Lam JM, Leong KF, et al. Tinea corporis: an updated review. Drugs Context. 2020;9:2020-5-6. doi: 10.7573/dic.2020-5-6
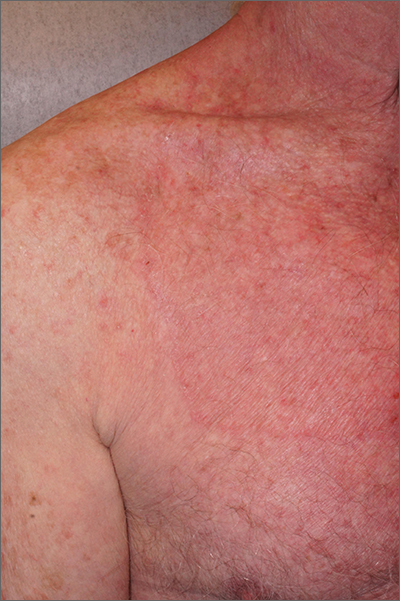
A skin scraping and potassium hydroxide (KOH) prep confirmed the presence of branching hyphae, consistent with tinea corporis. The large size of this plaque could have easily made this diagnosis more difficult. When tinea corporis is suspected, look at the edge of the plaque; there is often thin scale and sometimes small pustules corresponding to follicular involvement.
Commonly called by the misnomer “ringworm,” tinea corporis is a skin infection caused by a wide variety of dermatophytes and affects all ages, sexes, and skin types. Trichophyton, Microsporum, and Epidermophyton species are frequently isolated.1 Patients with atopic dermatitis or weakened immunity may be more susceptible to more frequent or long-lasting episodes. Diabetes may have contributed to the extent of the disease in this case.
Patients with tinea corporis present with one or several annular patches to plaques that grow in size. When the source of contagion is an animal, inflammation can be dramatic. In the case above, there was minimal to no itching and the patient didn’t notice the rash; thus, it was able to enlarge for months.
Treatment options include systemic and topical antifungal therapy. Consideration should be given to the severity of the disease and causal organism. Azoles, terbinafine, and ciclopirox are common treatment options. Topical therapy with an appropriately selected antifungal for 1 to 6 weeks, based on clinical response, is safe and effective. It is important to consider other foci of infection, including the feet and hands. More extensive disease may be treated with oral therapy such as terbinafine, fluconazole, or itraconazole.
Because of the extent of the disease and the challenge of effective coverage with topical therapy, this patient was treated with oral terbinafine 250 mg daily for 3 weeks. The plaque cleared completely.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
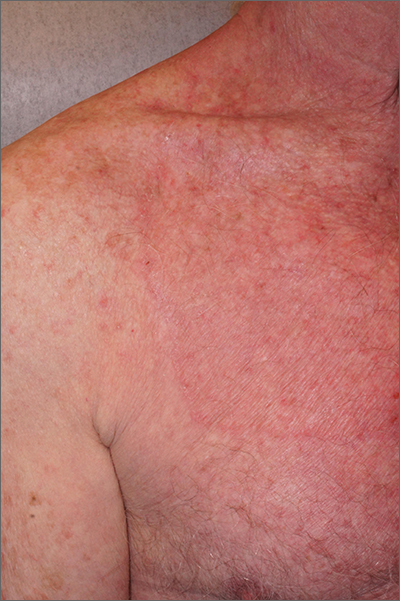
A skin scraping and potassium hydroxide (KOH) prep confirmed the presence of branching hyphae, consistent with tinea corporis. The large size of this plaque could have easily made this diagnosis more difficult. When tinea corporis is suspected, look at the edge of the plaque; there is often thin scale and sometimes small pustules corresponding to follicular involvement.
Commonly called by the misnomer “ringworm,” tinea corporis is a skin infection caused by a wide variety of dermatophytes and affects all ages, sexes, and skin types. Trichophyton, Microsporum, and Epidermophyton species are frequently isolated.1 Patients with atopic dermatitis or weakened immunity may be more susceptible to more frequent or long-lasting episodes. Diabetes may have contributed to the extent of the disease in this case.
Patients with tinea corporis present with one or several annular patches to plaques that grow in size. When the source of contagion is an animal, inflammation can be dramatic. In the case above, there was minimal to no itching and the patient didn’t notice the rash; thus, it was able to enlarge for months.
Treatment options include systemic and topical antifungal therapy. Consideration should be given to the severity of the disease and causal organism. Azoles, terbinafine, and ciclopirox are common treatment options. Topical therapy with an appropriately selected antifungal for 1 to 6 weeks, based on clinical response, is safe and effective. It is important to consider other foci of infection, including the feet and hands. More extensive disease may be treated with oral therapy such as terbinafine, fluconazole, or itraconazole.
Because of the extent of the disease and the challenge of effective coverage with topical therapy, this patient was treated with oral terbinafine 250 mg daily for 3 weeks. The plaque cleared completely.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME.
1. Leung AK, Lam JM, Leong KF, et al. Tinea corporis: an updated review. Drugs Context. 2020;9:2020-5-6. doi: 10.7573/dic.2020-5-6
1. Leung AK, Lam JM, Leong KF, et al. Tinea corporis: an updated review. Drugs Context. 2020;9:2020-5-6. doi: 10.7573/dic.2020-5-6
FDA wants annual COVID boosters, just like annual flu shots
The U.S. Food and Drug Administration is suggesting a single annual shot. The formulation would be selected in June targeting the most threatening COVID-19 strains, and then people could get a shot in the fall when people begin spending more time indoors and exposure increases.
Some people, such as those who are older or immunocompromised, may need more than one dose.
A national advisory committee is expected to vote on the proposal at a meeting Jan. 26.
People in the United States have been much less likely to get an updated COVID-19 booster shot, compared with widespread uptake of the primary vaccine series. In its proposal, the FDA indicated it hoped a single annual shot would overcome challenges created by the complexity of the process – both in messaging and administration – attributed to that low booster rate. Nine in 10 people age 12 or older got the primary vaccine series in the United States, but only 15% got the latest booster shot for COVID-19.
About half of children and adults in the U.S. get an annual flu shot, according to Centers for Disease Control and Prevention data.
The FDA also wants to move to a single COVID-19 vaccine formulation that would be used for primary vaccine series and for booster shots.
COVID-19 cases, hospitalizations, and deaths are trending downward, according to the data tracker from the New York Times. Cases are down 28%, with 47,290 tallied daily. Hospitalizations are down 22%, with 37,474 daily. Deaths are down 4%, with an average of 489 per day as of Jan. 22.
A version of this article originally appeared on WebMD.com.
The U.S. Food and Drug Administration is suggesting a single annual shot. The formulation would be selected in June targeting the most threatening COVID-19 strains, and then people could get a shot in the fall when people begin spending more time indoors and exposure increases.
Some people, such as those who are older or immunocompromised, may need more than one dose.
A national advisory committee is expected to vote on the proposal at a meeting Jan. 26.
People in the United States have been much less likely to get an updated COVID-19 booster shot, compared with widespread uptake of the primary vaccine series. In its proposal, the FDA indicated it hoped a single annual shot would overcome challenges created by the complexity of the process – both in messaging and administration – attributed to that low booster rate. Nine in 10 people age 12 or older got the primary vaccine series in the United States, but only 15% got the latest booster shot for COVID-19.
About half of children and adults in the U.S. get an annual flu shot, according to Centers for Disease Control and Prevention data.
The FDA also wants to move to a single COVID-19 vaccine formulation that would be used for primary vaccine series and for booster shots.
COVID-19 cases, hospitalizations, and deaths are trending downward, according to the data tracker from the New York Times. Cases are down 28%, with 47,290 tallied daily. Hospitalizations are down 22%, with 37,474 daily. Deaths are down 4%, with an average of 489 per day as of Jan. 22.
A version of this article originally appeared on WebMD.com.
The U.S. Food and Drug Administration is suggesting a single annual shot. The formulation would be selected in June targeting the most threatening COVID-19 strains, and then people could get a shot in the fall when people begin spending more time indoors and exposure increases.
Some people, such as those who are older or immunocompromised, may need more than one dose.
A national advisory committee is expected to vote on the proposal at a meeting Jan. 26.
People in the United States have been much less likely to get an updated COVID-19 booster shot, compared with widespread uptake of the primary vaccine series. In its proposal, the FDA indicated it hoped a single annual shot would overcome challenges created by the complexity of the process – both in messaging and administration – attributed to that low booster rate. Nine in 10 people age 12 or older got the primary vaccine series in the United States, but only 15% got the latest booster shot for COVID-19.
About half of children and adults in the U.S. get an annual flu shot, according to Centers for Disease Control and Prevention data.
The FDA also wants to move to a single COVID-19 vaccine formulation that would be used for primary vaccine series and for booster shots.
COVID-19 cases, hospitalizations, and deaths are trending downward, according to the data tracker from the New York Times. Cases are down 28%, with 47,290 tallied daily. Hospitalizations are down 22%, with 37,474 daily. Deaths are down 4%, with an average of 489 per day as of Jan. 22.
A version of this article originally appeared on WebMD.com.
VEXAS syndrome: More common, variable, and severe than expected
A recently discovered inflammatory disease known as VEXAS syndrome is more common, variable, and dangerous than previously understood, according to results of a retrospective observational study of a large health care system database. The findings, published in JAMA, found that it struck 1 in 4,269 men over the age of 50 in a largely White population and caused a wide variety of symptoms.
“The disease is quite severe,” study lead author David Beck, MD, PhD, of the department of medicine at NYU Langone Health, said in an interview. Patients with the condition “have a variety of clinical symptoms affecting different parts of the body and are being managed by different medical specialties.”
Dr. Beck and colleagues first described VEXAS (vacuoles, E1-ubiquitin-activating enzyme, X-linked, autoinflammatory, somatic) syndrome in 2020. They linked it to mutations in the UBA1 (ubiquitin-like modifier activating enzyme 1) gene. The enzyme initiates a process that identifies misfolded proteins as targets for degradation.
“VEXAS syndrome is characterized by anemia and inflammation in the skin, lungs, cartilage, and joints,” Dr. Beck said. “These symptoms are frequently mistaken for other rheumatic or hematologic diseases. However, this syndrome has a different cause, is treated differently, requires additional monitoring, and can be far more severe.”
According to him, hundreds of people have been diagnosed with the disease in the short time since it was defined. The disease is believed to be fatal in some cases. A previous report found that the median survival was 9 years among patients with a certain variant; that was significantly less than patients with two other variants.
For the new study, researchers searched for UBA1 variants in genetic data from 163,096 subjects (mean age, 52.8 years; 94% White, 61% women) who took part in the Geisinger MyCode Community Health Initiative. The 1996-2022 data comes from patients at 10 Pennsylvania hospitals.
Eleven people (9 males, 2 females) had likely UBA1 variants, and all had anemia. The cases accounted for 1 in 13,591 unrelated people (95% confidence interval, 1:7,775-1:23,758), 1 in 4,269 men older than 50 years (95% CI, 1:2,319-1:7,859), and 1 in 26,238 women older than 50 years (95% CI, 1:7,196-1:147,669).
Other common findings included macrocytosis (91%), skin problems (73%), and pulmonary disease (91%). Ten patients (91%) required transfusions.
Five of the 11 subjects didn’t meet the previously defined criteria for VEXAS syndrome. None had been diagnosed with the condition, which is not surprising considering that it hadn’t been discovered and described until recently.
Just over half of the patients – 55% – had a clinical diagnosis that was previously linked to VEXAS syndrome. “This means that slightly less than half of the patients with VEXAS syndrome had no clear associated clinical diagnosis,” Dr. Beck said. “The lack of associated clinical diagnoses may be due to the variety of nonspecific clinical characteristics that span different subspecialities in VEXAS syndrome. VEXAS syndrome represents an example of a multisystem disease where patients and their symptoms may get lost in the shuffle.”
In the future, “professionals should look out for patients with unexplained inflammation – and some combination of hematologic, rheumatologic, pulmonary, and dermatologic clinical manifestations – that either don’t carry a clinical diagnosis or don’t respond to first-line therapies,” Dr. Beck said. “These patients will also frequently be anemic, have low platelet counts, elevated markers of inflammation in the blood, and be dependent on corticosteroids.”
Diagnosis can be made via genetic testing, but the study authors note that it “is not routinely offered on standard workup for myeloid neoplasms or immune dysregulation diagnostic panels.”
As for treatment, Dr. Beck said the disease “can be partially controlled by multiple different anticytokine therapies or biologics. However, in most cases, patients still need additional steroids and/or disease-modifying antirheumatic agents [DMARDs]. In addition, bone marrow transplantation has shown signs of being a highly effective therapy.”
The study authors say more research is needed to understand the disease’s prevalence in more diverse populations.
In an interview, Matthew J. Koster, MD, a rheumatologist at Mayo Clinic in Rochester, Minn., who’s studied the disease but didn’t take part in this research project, said the findings are valid and “highly important.
“The findings of this study highlight what many academic and quaternary referral centers were wondering: Is VEXAS really more common than we think, with patients hiding in plain sight? The answer is yes,” he said. “Currently, there are less than 400 cases reported in the literature of VEXAS, but large centers are diagnosing this condition with some frequency. For example, at Mayo Clinic in Rochester, we diagnose on average one new patient with VEXAS every 7-14 days and have diagnosed 60 in the past 18 months. A national collaborative group in France has diagnosed approximately 250 patients over that same time frame when pooling patients nationwide.”
The prevalence is high enough, he said, that “clinicians should consider that some of the patients with diseases that are not responding to treatment may in fact have VEXAS rather than ‘refractory’ relapsing polychondritis or ‘recalcitrant’ rheumatoid arthritis, etc.”
The National Institute of Health funded the study. Dr. Beck, the other authors, and Dr. Koster report no disclosures.
A recently discovered inflammatory disease known as VEXAS syndrome is more common, variable, and dangerous than previously understood, according to results of a retrospective observational study of a large health care system database. The findings, published in JAMA, found that it struck 1 in 4,269 men over the age of 50 in a largely White population and caused a wide variety of symptoms.
“The disease is quite severe,” study lead author David Beck, MD, PhD, of the department of medicine at NYU Langone Health, said in an interview. Patients with the condition “have a variety of clinical symptoms affecting different parts of the body and are being managed by different medical specialties.”
Dr. Beck and colleagues first described VEXAS (vacuoles, E1-ubiquitin-activating enzyme, X-linked, autoinflammatory, somatic) syndrome in 2020. They linked it to mutations in the UBA1 (ubiquitin-like modifier activating enzyme 1) gene. The enzyme initiates a process that identifies misfolded proteins as targets for degradation.
“VEXAS syndrome is characterized by anemia and inflammation in the skin, lungs, cartilage, and joints,” Dr. Beck said. “These symptoms are frequently mistaken for other rheumatic or hematologic diseases. However, this syndrome has a different cause, is treated differently, requires additional monitoring, and can be far more severe.”
According to him, hundreds of people have been diagnosed with the disease in the short time since it was defined. The disease is believed to be fatal in some cases. A previous report found that the median survival was 9 years among patients with a certain variant; that was significantly less than patients with two other variants.
For the new study, researchers searched for UBA1 variants in genetic data from 163,096 subjects (mean age, 52.8 years; 94% White, 61% women) who took part in the Geisinger MyCode Community Health Initiative. The 1996-2022 data comes from patients at 10 Pennsylvania hospitals.
Eleven people (9 males, 2 females) had likely UBA1 variants, and all had anemia. The cases accounted for 1 in 13,591 unrelated people (95% confidence interval, 1:7,775-1:23,758), 1 in 4,269 men older than 50 years (95% CI, 1:2,319-1:7,859), and 1 in 26,238 women older than 50 years (95% CI, 1:7,196-1:147,669).
Other common findings included macrocytosis (91%), skin problems (73%), and pulmonary disease (91%). Ten patients (91%) required transfusions.
Five of the 11 subjects didn’t meet the previously defined criteria for VEXAS syndrome. None had been diagnosed with the condition, which is not surprising considering that it hadn’t been discovered and described until recently.
Just over half of the patients – 55% – had a clinical diagnosis that was previously linked to VEXAS syndrome. “This means that slightly less than half of the patients with VEXAS syndrome had no clear associated clinical diagnosis,” Dr. Beck said. “The lack of associated clinical diagnoses may be due to the variety of nonspecific clinical characteristics that span different subspecialities in VEXAS syndrome. VEXAS syndrome represents an example of a multisystem disease where patients and their symptoms may get lost in the shuffle.”
In the future, “professionals should look out for patients with unexplained inflammation – and some combination of hematologic, rheumatologic, pulmonary, and dermatologic clinical manifestations – that either don’t carry a clinical diagnosis or don’t respond to first-line therapies,” Dr. Beck said. “These patients will also frequently be anemic, have low platelet counts, elevated markers of inflammation in the blood, and be dependent on corticosteroids.”
Diagnosis can be made via genetic testing, but the study authors note that it “is not routinely offered on standard workup for myeloid neoplasms or immune dysregulation diagnostic panels.”
As for treatment, Dr. Beck said the disease “can be partially controlled by multiple different anticytokine therapies or biologics. However, in most cases, patients still need additional steroids and/or disease-modifying antirheumatic agents [DMARDs]. In addition, bone marrow transplantation has shown signs of being a highly effective therapy.”
The study authors say more research is needed to understand the disease’s prevalence in more diverse populations.
In an interview, Matthew J. Koster, MD, a rheumatologist at Mayo Clinic in Rochester, Minn., who’s studied the disease but didn’t take part in this research project, said the findings are valid and “highly important.
“The findings of this study highlight what many academic and quaternary referral centers were wondering: Is VEXAS really more common than we think, with patients hiding in plain sight? The answer is yes,” he said. “Currently, there are less than 400 cases reported in the literature of VEXAS, but large centers are diagnosing this condition with some frequency. For example, at Mayo Clinic in Rochester, we diagnose on average one new patient with VEXAS every 7-14 days and have diagnosed 60 in the past 18 months. A national collaborative group in France has diagnosed approximately 250 patients over that same time frame when pooling patients nationwide.”
The prevalence is high enough, he said, that “clinicians should consider that some of the patients with diseases that are not responding to treatment may in fact have VEXAS rather than ‘refractory’ relapsing polychondritis or ‘recalcitrant’ rheumatoid arthritis, etc.”
The National Institute of Health funded the study. Dr. Beck, the other authors, and Dr. Koster report no disclosures.
A recently discovered inflammatory disease known as VEXAS syndrome is more common, variable, and dangerous than previously understood, according to results of a retrospective observational study of a large health care system database. The findings, published in JAMA, found that it struck 1 in 4,269 men over the age of 50 in a largely White population and caused a wide variety of symptoms.
“The disease is quite severe,” study lead author David Beck, MD, PhD, of the department of medicine at NYU Langone Health, said in an interview. Patients with the condition “have a variety of clinical symptoms affecting different parts of the body and are being managed by different medical specialties.”
Dr. Beck and colleagues first described VEXAS (vacuoles, E1-ubiquitin-activating enzyme, X-linked, autoinflammatory, somatic) syndrome in 2020. They linked it to mutations in the UBA1 (ubiquitin-like modifier activating enzyme 1) gene. The enzyme initiates a process that identifies misfolded proteins as targets for degradation.
“VEXAS syndrome is characterized by anemia and inflammation in the skin, lungs, cartilage, and joints,” Dr. Beck said. “These symptoms are frequently mistaken for other rheumatic or hematologic diseases. However, this syndrome has a different cause, is treated differently, requires additional monitoring, and can be far more severe.”
According to him, hundreds of people have been diagnosed with the disease in the short time since it was defined. The disease is believed to be fatal in some cases. A previous report found that the median survival was 9 years among patients with a certain variant; that was significantly less than patients with two other variants.
For the new study, researchers searched for UBA1 variants in genetic data from 163,096 subjects (mean age, 52.8 years; 94% White, 61% women) who took part in the Geisinger MyCode Community Health Initiative. The 1996-2022 data comes from patients at 10 Pennsylvania hospitals.
Eleven people (9 males, 2 females) had likely UBA1 variants, and all had anemia. The cases accounted for 1 in 13,591 unrelated people (95% confidence interval, 1:7,775-1:23,758), 1 in 4,269 men older than 50 years (95% CI, 1:2,319-1:7,859), and 1 in 26,238 women older than 50 years (95% CI, 1:7,196-1:147,669).
Other common findings included macrocytosis (91%), skin problems (73%), and pulmonary disease (91%). Ten patients (91%) required transfusions.
Five of the 11 subjects didn’t meet the previously defined criteria for VEXAS syndrome. None had been diagnosed with the condition, which is not surprising considering that it hadn’t been discovered and described until recently.
Just over half of the patients – 55% – had a clinical diagnosis that was previously linked to VEXAS syndrome. “This means that slightly less than half of the patients with VEXAS syndrome had no clear associated clinical diagnosis,” Dr. Beck said. “The lack of associated clinical diagnoses may be due to the variety of nonspecific clinical characteristics that span different subspecialities in VEXAS syndrome. VEXAS syndrome represents an example of a multisystem disease where patients and their symptoms may get lost in the shuffle.”
In the future, “professionals should look out for patients with unexplained inflammation – and some combination of hematologic, rheumatologic, pulmonary, and dermatologic clinical manifestations – that either don’t carry a clinical diagnosis or don’t respond to first-line therapies,” Dr. Beck said. “These patients will also frequently be anemic, have low platelet counts, elevated markers of inflammation in the blood, and be dependent on corticosteroids.”
Diagnosis can be made via genetic testing, but the study authors note that it “is not routinely offered on standard workup for myeloid neoplasms or immune dysregulation diagnostic panels.”
As for treatment, Dr. Beck said the disease “can be partially controlled by multiple different anticytokine therapies or biologics. However, in most cases, patients still need additional steroids and/or disease-modifying antirheumatic agents [DMARDs]. In addition, bone marrow transplantation has shown signs of being a highly effective therapy.”
The study authors say more research is needed to understand the disease’s prevalence in more diverse populations.
In an interview, Matthew J. Koster, MD, a rheumatologist at Mayo Clinic in Rochester, Minn., who’s studied the disease but didn’t take part in this research project, said the findings are valid and “highly important.
“The findings of this study highlight what many academic and quaternary referral centers were wondering: Is VEXAS really more common than we think, with patients hiding in plain sight? The answer is yes,” he said. “Currently, there are less than 400 cases reported in the literature of VEXAS, but large centers are diagnosing this condition with some frequency. For example, at Mayo Clinic in Rochester, we diagnose on average one new patient with VEXAS every 7-14 days and have diagnosed 60 in the past 18 months. A national collaborative group in France has diagnosed approximately 250 patients over that same time frame when pooling patients nationwide.”
The prevalence is high enough, he said, that “clinicians should consider that some of the patients with diseases that are not responding to treatment may in fact have VEXAS rather than ‘refractory’ relapsing polychondritis or ‘recalcitrant’ rheumatoid arthritis, etc.”
The National Institute of Health funded the study. Dr. Beck, the other authors, and Dr. Koster report no disclosures.
FROM JAMA