User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
How does SARS-CoV-2 affect other respiratory diseases?
In 2020, the rapid spread of the newly identified SARS-CoV-2 coronavirus led various global public health institutions to establish strategies to stop transmission and reduce mortality. Nonpharmacological measures – including social distancing, regular hand washing, and the use of face masks – contributed to reducing the impact of the COVID-19 pandemic on health systems in different regions of the world. However, because of the implementation of these measures, the transmission of other infectious agents also experienced a marked reduction.
Approximately 3 years after the start of the pandemic, , generating phenomena ranging from an immunity gap, which favors the increase in some diseases, to the apparent disappearance of an influenza virus lineage.
Understanding the phenomenon
In mid-2021, doctors and researchers around the world began to share their opinions about the side effect of the strict measures implemented to contain COVID-19.
In May 2021, along with some coresearchers, Emmanuel Grimprel, MD, of the Pediatric Infectious Pathology Group in Créteil, France, wrote for Infectious Disease Now, “The transmission of some pathogens is often similar to that of SARS-CoV-2, essentially large droplets, aerosols, and direct hand contact, often with lower transmissibility. The lack of immune system stimulation due to nonpharmaceutical measures induces an ‘immune debt’ that may have negative consequences when the pandemic is under control.” According to the authors, mathematical models evaluated up to that point were already suggesting that the respiratory syncytial virus (RSV) and influenza A epidemics would be more serious in subsequent years.
In July 2022, a commentary in The Lancet led by Kevin Messacar, MD, of the University of Colorado at Denver, Aurora, grew in relevance and gave prominence to the phenomenon. In the commentary, Dr. Messacar and a group of experts explained how the decrease in exposure to endemic viruses had given rise to an immunity gap.
“The immunity gap phenomenon that has been reported in articles such as The Lancet publication is mainly due to the isolation that took place to prevent SARS-CoV-2 infections. Although this distancing was a good response to combat infections, or at least delay them while coronavirus research advanced, what we are now experiencing is the increase in cases of respiratory diseases caused by other agents such as respiratory syncytial virus and influenza due to lack of exposure,” as explained to this news organization by Erandeni Martínez Jiménez, biomedicine graduate and member of the Medical Virology Laboratory of the Mexican Institute of Social Security, at the Zone No. 5 General Hospital in Metepec-Atlixco, Mexico.
“This phenomenon occurs in all age groups. However, it is more evident in children and babies, since at their age, they have been exposed to fewer pathogens and, when added to isolation, makes this immunity gap more evident. Many immunologists compare this to hygiene theory in which it is explained that a ‘sterile’ environment will cause children to avoid the everyday and common pathogens required to be able to develop an adequate immune system,” added Martínez Jimenez.
“In addition, due to the isolation, the vaccination rate in children decreased, since many parents did not risk their children going out. This causes the immunity gap to grow even further as these children are not protected against common pathogens. While a mother passes antibodies to the child through the uterus via her placenta, the mother will only pass on those antibodies to which she has been exposed and as expected due to the lockdown, exposure to other pathogens has been greatly reduced.”
On the other hand, Andreu Comas, MD, PhD, MHS, of the Center for Research in Health Sciences and Biomedicine of the Autonomous University of San Luis Potosí (Mexico), considered that there are other immunity gaps that are not limited to respiratory infections and that are related to the fall in vaccination coverage. “Children are going to experience several immunity gaps. In the middle of the previous 6-year term, we had a vaccination schedule coverage of around 70% for children. Now that vaccination coverage has fallen to 30%, today we have an immunity gap for measles, rubella, mumps, tetanus, diphtheria, whooping cough, and meningeal tuberculosis. We have a significant growth or risk for other diseases.”
Lineage extinction
Three types of influenza viruses – A, B, and C – cause infections in humans. Although influenza A virus is the main type associated with infections during seasonal periods, as of 2020, influenza B virus was considered the causative agent of about a quarter of annual influenza cases.
During the onset of the COVID-19 pandemic, cocirculation of the two distinct lineages of influenza B viruses, B/Victoria/2/1987 (B/Victoria) and B/Yamagata/16/1988 (B/Yamagata), decreased significantly. According to data from the FluNet tool, which is coordinated by the World Health Organization, since March 2020 the isolation or sequencing of viruses belonging to the Yamagata lineage was not conclusively carried out.
Specialists like John Paget, PhD, from the Netherlands Institute for Health Services Research (Nivel) in Utrecht, have indicated that determining the extinction of the B/Yamagata lineage is critical. There is the possibility of a reintroduction of the lineage, as has occurred in the past with the reemergence of influenza A (H1N1) in 1997, which could represent a risk in subsequent years.
“In the next few years, research related to viruses such as influenza B and the impact on population immunity will be important. Let’s remember that influenza changes every year due to its characteristics, so a lack of exposure will also have an impact on the development of the disease,” said Martínez Jiménez.
Vaccination is essential
According to Dr. Comas, the only way to overcome the immunity gap phenomenon is through vaccination campaigns. “There is no other way to overcome the phenomenon, and how fast it is done will depend on the effort,” he said.
“In the case of COVID-19, it is not planned to vaccinate children under 5 years of age, and if we do not vaccinate children under 5 years of age, that gap will exist. In addition, this winter season will be important to know whether we are already endemic or not. It will be the key point, and it will determine if we will have a peak or not in the summer.
“In the case of the rest of the diseases, we need to correct what has been deficient in different governments, and we are going to have the resurgence of other infectious diseases that had already been forgotten. We have the example of poliomyelitis, the increase in meningeal tuberculosis, and we will have an increase in whooping cough and pertussislike syndrome. In this sense, we are going back to the point where Mexico and the world were around the ‘60s and ‘70s, and we have to be very alert to detect, isolate, and revaccinate.”
Finally, Dr. Comas called for continuing precautionary measures before the arrival of the sixth wave. “At a national level, the sixth wave of COVID-19 has already begun, and an increase in cases is expected in January. Regarding vaccines, if you are over 18 years of age and have not had any vaccine dose, you can get Abdala, however, there are no studies on this vaccine as a booster, and it is not authorized by the Mexican government for this purpose. Therefore, it is necessary to continue with measures such as the use of face masks in crowded places or with poor ventilation, and in the event of having symptoms, avoid going out and encourage ventilation at work and schools. If we do this, at least in the case of diseases that are transmitted by the respiratory route, the impact will be minimal.”
Martínez Jiménez and Dr. Comas have disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition.
A version of this article first appeared on Medscape.com.
In 2020, the rapid spread of the newly identified SARS-CoV-2 coronavirus led various global public health institutions to establish strategies to stop transmission and reduce mortality. Nonpharmacological measures – including social distancing, regular hand washing, and the use of face masks – contributed to reducing the impact of the COVID-19 pandemic on health systems in different regions of the world. However, because of the implementation of these measures, the transmission of other infectious agents also experienced a marked reduction.
Approximately 3 years after the start of the pandemic, , generating phenomena ranging from an immunity gap, which favors the increase in some diseases, to the apparent disappearance of an influenza virus lineage.
Understanding the phenomenon
In mid-2021, doctors and researchers around the world began to share their opinions about the side effect of the strict measures implemented to contain COVID-19.
In May 2021, along with some coresearchers, Emmanuel Grimprel, MD, of the Pediatric Infectious Pathology Group in Créteil, France, wrote for Infectious Disease Now, “The transmission of some pathogens is often similar to that of SARS-CoV-2, essentially large droplets, aerosols, and direct hand contact, often with lower transmissibility. The lack of immune system stimulation due to nonpharmaceutical measures induces an ‘immune debt’ that may have negative consequences when the pandemic is under control.” According to the authors, mathematical models evaluated up to that point were already suggesting that the respiratory syncytial virus (RSV) and influenza A epidemics would be more serious in subsequent years.
In July 2022, a commentary in The Lancet led by Kevin Messacar, MD, of the University of Colorado at Denver, Aurora, grew in relevance and gave prominence to the phenomenon. In the commentary, Dr. Messacar and a group of experts explained how the decrease in exposure to endemic viruses had given rise to an immunity gap.
“The immunity gap phenomenon that has been reported in articles such as The Lancet publication is mainly due to the isolation that took place to prevent SARS-CoV-2 infections. Although this distancing was a good response to combat infections, or at least delay them while coronavirus research advanced, what we are now experiencing is the increase in cases of respiratory diseases caused by other agents such as respiratory syncytial virus and influenza due to lack of exposure,” as explained to this news organization by Erandeni Martínez Jiménez, biomedicine graduate and member of the Medical Virology Laboratory of the Mexican Institute of Social Security, at the Zone No. 5 General Hospital in Metepec-Atlixco, Mexico.
“This phenomenon occurs in all age groups. However, it is more evident in children and babies, since at their age, they have been exposed to fewer pathogens and, when added to isolation, makes this immunity gap more evident. Many immunologists compare this to hygiene theory in which it is explained that a ‘sterile’ environment will cause children to avoid the everyday and common pathogens required to be able to develop an adequate immune system,” added Martínez Jimenez.
“In addition, due to the isolation, the vaccination rate in children decreased, since many parents did not risk their children going out. This causes the immunity gap to grow even further as these children are not protected against common pathogens. While a mother passes antibodies to the child through the uterus via her placenta, the mother will only pass on those antibodies to which she has been exposed and as expected due to the lockdown, exposure to other pathogens has been greatly reduced.”
On the other hand, Andreu Comas, MD, PhD, MHS, of the Center for Research in Health Sciences and Biomedicine of the Autonomous University of San Luis Potosí (Mexico), considered that there are other immunity gaps that are not limited to respiratory infections and that are related to the fall in vaccination coverage. “Children are going to experience several immunity gaps. In the middle of the previous 6-year term, we had a vaccination schedule coverage of around 70% for children. Now that vaccination coverage has fallen to 30%, today we have an immunity gap for measles, rubella, mumps, tetanus, diphtheria, whooping cough, and meningeal tuberculosis. We have a significant growth or risk for other diseases.”
Lineage extinction
Three types of influenza viruses – A, B, and C – cause infections in humans. Although influenza A virus is the main type associated with infections during seasonal periods, as of 2020, influenza B virus was considered the causative agent of about a quarter of annual influenza cases.
During the onset of the COVID-19 pandemic, cocirculation of the two distinct lineages of influenza B viruses, B/Victoria/2/1987 (B/Victoria) and B/Yamagata/16/1988 (B/Yamagata), decreased significantly. According to data from the FluNet tool, which is coordinated by the World Health Organization, since March 2020 the isolation or sequencing of viruses belonging to the Yamagata lineage was not conclusively carried out.
Specialists like John Paget, PhD, from the Netherlands Institute for Health Services Research (Nivel) in Utrecht, have indicated that determining the extinction of the B/Yamagata lineage is critical. There is the possibility of a reintroduction of the lineage, as has occurred in the past with the reemergence of influenza A (H1N1) in 1997, which could represent a risk in subsequent years.
“In the next few years, research related to viruses such as influenza B and the impact on population immunity will be important. Let’s remember that influenza changes every year due to its characteristics, so a lack of exposure will also have an impact on the development of the disease,” said Martínez Jiménez.
Vaccination is essential
According to Dr. Comas, the only way to overcome the immunity gap phenomenon is through vaccination campaigns. “There is no other way to overcome the phenomenon, and how fast it is done will depend on the effort,” he said.
“In the case of COVID-19, it is not planned to vaccinate children under 5 years of age, and if we do not vaccinate children under 5 years of age, that gap will exist. In addition, this winter season will be important to know whether we are already endemic or not. It will be the key point, and it will determine if we will have a peak or not in the summer.
“In the case of the rest of the diseases, we need to correct what has been deficient in different governments, and we are going to have the resurgence of other infectious diseases that had already been forgotten. We have the example of poliomyelitis, the increase in meningeal tuberculosis, and we will have an increase in whooping cough and pertussislike syndrome. In this sense, we are going back to the point where Mexico and the world were around the ‘60s and ‘70s, and we have to be very alert to detect, isolate, and revaccinate.”
Finally, Dr. Comas called for continuing precautionary measures before the arrival of the sixth wave. “At a national level, the sixth wave of COVID-19 has already begun, and an increase in cases is expected in January. Regarding vaccines, if you are over 18 years of age and have not had any vaccine dose, you can get Abdala, however, there are no studies on this vaccine as a booster, and it is not authorized by the Mexican government for this purpose. Therefore, it is necessary to continue with measures such as the use of face masks in crowded places or with poor ventilation, and in the event of having symptoms, avoid going out and encourage ventilation at work and schools. If we do this, at least in the case of diseases that are transmitted by the respiratory route, the impact will be minimal.”
Martínez Jiménez and Dr. Comas have disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition.
A version of this article first appeared on Medscape.com.
In 2020, the rapid spread of the newly identified SARS-CoV-2 coronavirus led various global public health institutions to establish strategies to stop transmission and reduce mortality. Nonpharmacological measures – including social distancing, regular hand washing, and the use of face masks – contributed to reducing the impact of the COVID-19 pandemic on health systems in different regions of the world. However, because of the implementation of these measures, the transmission of other infectious agents also experienced a marked reduction.
Approximately 3 years after the start of the pandemic, , generating phenomena ranging from an immunity gap, which favors the increase in some diseases, to the apparent disappearance of an influenza virus lineage.
Understanding the phenomenon
In mid-2021, doctors and researchers around the world began to share their opinions about the side effect of the strict measures implemented to contain COVID-19.
In May 2021, along with some coresearchers, Emmanuel Grimprel, MD, of the Pediatric Infectious Pathology Group in Créteil, France, wrote for Infectious Disease Now, “The transmission of some pathogens is often similar to that of SARS-CoV-2, essentially large droplets, aerosols, and direct hand contact, often with lower transmissibility. The lack of immune system stimulation due to nonpharmaceutical measures induces an ‘immune debt’ that may have negative consequences when the pandemic is under control.” According to the authors, mathematical models evaluated up to that point were already suggesting that the respiratory syncytial virus (RSV) and influenza A epidemics would be more serious in subsequent years.
In July 2022, a commentary in The Lancet led by Kevin Messacar, MD, of the University of Colorado at Denver, Aurora, grew in relevance and gave prominence to the phenomenon. In the commentary, Dr. Messacar and a group of experts explained how the decrease in exposure to endemic viruses had given rise to an immunity gap.
“The immunity gap phenomenon that has been reported in articles such as The Lancet publication is mainly due to the isolation that took place to prevent SARS-CoV-2 infections. Although this distancing was a good response to combat infections, or at least delay them while coronavirus research advanced, what we are now experiencing is the increase in cases of respiratory diseases caused by other agents such as respiratory syncytial virus and influenza due to lack of exposure,” as explained to this news organization by Erandeni Martínez Jiménez, biomedicine graduate and member of the Medical Virology Laboratory of the Mexican Institute of Social Security, at the Zone No. 5 General Hospital in Metepec-Atlixco, Mexico.
“This phenomenon occurs in all age groups. However, it is more evident in children and babies, since at their age, they have been exposed to fewer pathogens and, when added to isolation, makes this immunity gap more evident. Many immunologists compare this to hygiene theory in which it is explained that a ‘sterile’ environment will cause children to avoid the everyday and common pathogens required to be able to develop an adequate immune system,” added Martínez Jimenez.
“In addition, due to the isolation, the vaccination rate in children decreased, since many parents did not risk their children going out. This causes the immunity gap to grow even further as these children are not protected against common pathogens. While a mother passes antibodies to the child through the uterus via her placenta, the mother will only pass on those antibodies to which she has been exposed and as expected due to the lockdown, exposure to other pathogens has been greatly reduced.”
On the other hand, Andreu Comas, MD, PhD, MHS, of the Center for Research in Health Sciences and Biomedicine of the Autonomous University of San Luis Potosí (Mexico), considered that there are other immunity gaps that are not limited to respiratory infections and that are related to the fall in vaccination coverage. “Children are going to experience several immunity gaps. In the middle of the previous 6-year term, we had a vaccination schedule coverage of around 70% for children. Now that vaccination coverage has fallen to 30%, today we have an immunity gap for measles, rubella, mumps, tetanus, diphtheria, whooping cough, and meningeal tuberculosis. We have a significant growth or risk for other diseases.”
Lineage extinction
Three types of influenza viruses – A, B, and C – cause infections in humans. Although influenza A virus is the main type associated with infections during seasonal periods, as of 2020, influenza B virus was considered the causative agent of about a quarter of annual influenza cases.
During the onset of the COVID-19 pandemic, cocirculation of the two distinct lineages of influenza B viruses, B/Victoria/2/1987 (B/Victoria) and B/Yamagata/16/1988 (B/Yamagata), decreased significantly. According to data from the FluNet tool, which is coordinated by the World Health Organization, since March 2020 the isolation or sequencing of viruses belonging to the Yamagata lineage was not conclusively carried out.
Specialists like John Paget, PhD, from the Netherlands Institute for Health Services Research (Nivel) in Utrecht, have indicated that determining the extinction of the B/Yamagata lineage is critical. There is the possibility of a reintroduction of the lineage, as has occurred in the past with the reemergence of influenza A (H1N1) in 1997, which could represent a risk in subsequent years.
“In the next few years, research related to viruses such as influenza B and the impact on population immunity will be important. Let’s remember that influenza changes every year due to its characteristics, so a lack of exposure will also have an impact on the development of the disease,” said Martínez Jiménez.
Vaccination is essential
According to Dr. Comas, the only way to overcome the immunity gap phenomenon is through vaccination campaigns. “There is no other way to overcome the phenomenon, and how fast it is done will depend on the effort,” he said.
“In the case of COVID-19, it is not planned to vaccinate children under 5 years of age, and if we do not vaccinate children under 5 years of age, that gap will exist. In addition, this winter season will be important to know whether we are already endemic or not. It will be the key point, and it will determine if we will have a peak or not in the summer.
“In the case of the rest of the diseases, we need to correct what has been deficient in different governments, and we are going to have the resurgence of other infectious diseases that had already been forgotten. We have the example of poliomyelitis, the increase in meningeal tuberculosis, and we will have an increase in whooping cough and pertussislike syndrome. In this sense, we are going back to the point where Mexico and the world were around the ‘60s and ‘70s, and we have to be very alert to detect, isolate, and revaccinate.”
Finally, Dr. Comas called for continuing precautionary measures before the arrival of the sixth wave. “At a national level, the sixth wave of COVID-19 has already begun, and an increase in cases is expected in January. Regarding vaccines, if you are over 18 years of age and have not had any vaccine dose, you can get Abdala, however, there are no studies on this vaccine as a booster, and it is not authorized by the Mexican government for this purpose. Therefore, it is necessary to continue with measures such as the use of face masks in crowded places or with poor ventilation, and in the event of having symptoms, avoid going out and encourage ventilation at work and schools. If we do this, at least in the case of diseases that are transmitted by the respiratory route, the impact will be minimal.”
Martínez Jiménez and Dr. Comas have disclosed no relevant financial relationships.
This article was translated from the Medscape Spanish Edition.
A version of this article first appeared on Medscape.com.
‘Very doable’ low-dose workout enough to treat knee OA
Exercise helps patients with knee osteoarthritis, but more isn’t necessarily better, new research shows.
A low-dose exercise regimen helped patients with knee OA about as much as a more intense workout plan, according to trial results published online in Annals of Internal Medicine.
Both high and low doses of exercise reduced pain and improved function and quality of life.
The improvements with the lower-dose plan and its 98% adherence rate are encouraging, said Nick Trasolini, MD, assistant professor of orthopedic surgery at Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, N.C.
“This is a very doable amount of medical exercise therapy for patients with knee osteoarthritis, and one that makes a big difference in patient-reported symptoms,” Dr. Trasolini, who was not involved in the study, said in an interview.
What’s the right dose?
Exercise is a go-to treatment for knee OA, but the precise dose to recommend has been unclear. To study this question, Tom Arild Torstensen, MSc, RPT, with Karolinska Institutet, Huddinge, Sweden, and Holten Institute, Stockholm, and colleagues conducted a trial at four centers in Sweden and Norway.
The study included 189 men and women with knee OA. Participants were randomly assigned to low- or high-dose exercise plans, which they performed three times per week for 12 weeks under the supervision of a physiotherapist.
Participants in the high-dose group performed 11 exercises during each session, which lasted 70-90 minutes.
The low-dose regimen consisted of five exercises – cycling, squats, step-ups, step-downs, and knee extensions – performed for 20–30 minutes.
The researchers measured outcomes using the Knee Injury and Osteoarthritis Outcome Score, which assesses pain, other symptoms, function in daily living, function in sports and recreation, and knee-related quality of life.
“Patients in both groups improved significantly over time, but high-dose exercise was not superior to low-dose exercise in most comparisons,” the study investigators reported
High-dose exercise was associated with better function in sports and recreational activity and knee-related quality of life at 6 months. Those differences did not persist at 1 year, however. The researchers reported no safety concerns with either intervention.
Adherence was “nearly perfect” in the low-dose group. It was slightly lower in the high-dose group, the researchers said.
“Interestingly, it seems that high-dose treatment could be preferable to low-dose treatment in the long run for people who lead active lives,” they wrote. “This should be the subject of future studies.”
All clinical practice guidelines for knee OA recommend exercise, but “we do not know the optimal dose,” Kim Bennell, PhD, a research physiotherapist at the University of Melbourne, said in an interview.
Dose has components, including number of times per week, number of exercises, sets and repetitions, intensity, and duration of exercise sessions, Dr. Bennell said.
“These results suggest that an exercise program that involves less time and fewer exercises can still offer benefits and may be easier for patients to undertake and stick at than one that involves greater time and effort,” she said.
The study was supported by the Swedish Rheumatic Fund. Dr. Trasolini and Dr. Bennell have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Exercise helps patients with knee osteoarthritis, but more isn’t necessarily better, new research shows.
A low-dose exercise regimen helped patients with knee OA about as much as a more intense workout plan, according to trial results published online in Annals of Internal Medicine.
Both high and low doses of exercise reduced pain and improved function and quality of life.
The improvements with the lower-dose plan and its 98% adherence rate are encouraging, said Nick Trasolini, MD, assistant professor of orthopedic surgery at Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, N.C.
“This is a very doable amount of medical exercise therapy for patients with knee osteoarthritis, and one that makes a big difference in patient-reported symptoms,” Dr. Trasolini, who was not involved in the study, said in an interview.
What’s the right dose?
Exercise is a go-to treatment for knee OA, but the precise dose to recommend has been unclear. To study this question, Tom Arild Torstensen, MSc, RPT, with Karolinska Institutet, Huddinge, Sweden, and Holten Institute, Stockholm, and colleagues conducted a trial at four centers in Sweden and Norway.
The study included 189 men and women with knee OA. Participants were randomly assigned to low- or high-dose exercise plans, which they performed three times per week for 12 weeks under the supervision of a physiotherapist.
Participants in the high-dose group performed 11 exercises during each session, which lasted 70-90 minutes.
The low-dose regimen consisted of five exercises – cycling, squats, step-ups, step-downs, and knee extensions – performed for 20–30 minutes.
The researchers measured outcomes using the Knee Injury and Osteoarthritis Outcome Score, which assesses pain, other symptoms, function in daily living, function in sports and recreation, and knee-related quality of life.
“Patients in both groups improved significantly over time, but high-dose exercise was not superior to low-dose exercise in most comparisons,” the study investigators reported
High-dose exercise was associated with better function in sports and recreational activity and knee-related quality of life at 6 months. Those differences did not persist at 1 year, however. The researchers reported no safety concerns with either intervention.
Adherence was “nearly perfect” in the low-dose group. It was slightly lower in the high-dose group, the researchers said.
“Interestingly, it seems that high-dose treatment could be preferable to low-dose treatment in the long run for people who lead active lives,” they wrote. “This should be the subject of future studies.”
All clinical practice guidelines for knee OA recommend exercise, but “we do not know the optimal dose,” Kim Bennell, PhD, a research physiotherapist at the University of Melbourne, said in an interview.
Dose has components, including number of times per week, number of exercises, sets and repetitions, intensity, and duration of exercise sessions, Dr. Bennell said.
“These results suggest that an exercise program that involves less time and fewer exercises can still offer benefits and may be easier for patients to undertake and stick at than one that involves greater time and effort,” she said.
The study was supported by the Swedish Rheumatic Fund. Dr. Trasolini and Dr. Bennell have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Exercise helps patients with knee osteoarthritis, but more isn’t necessarily better, new research shows.
A low-dose exercise regimen helped patients with knee OA about as much as a more intense workout plan, according to trial results published online in Annals of Internal Medicine.
Both high and low doses of exercise reduced pain and improved function and quality of life.
The improvements with the lower-dose plan and its 98% adherence rate are encouraging, said Nick Trasolini, MD, assistant professor of orthopedic surgery at Atrium Health Wake Forest Baptist Medical Center, Winston-Salem, N.C.
“This is a very doable amount of medical exercise therapy for patients with knee osteoarthritis, and one that makes a big difference in patient-reported symptoms,” Dr. Trasolini, who was not involved in the study, said in an interview.
What’s the right dose?
Exercise is a go-to treatment for knee OA, but the precise dose to recommend has been unclear. To study this question, Tom Arild Torstensen, MSc, RPT, with Karolinska Institutet, Huddinge, Sweden, and Holten Institute, Stockholm, and colleagues conducted a trial at four centers in Sweden and Norway.
The study included 189 men and women with knee OA. Participants were randomly assigned to low- or high-dose exercise plans, which they performed three times per week for 12 weeks under the supervision of a physiotherapist.
Participants in the high-dose group performed 11 exercises during each session, which lasted 70-90 minutes.
The low-dose regimen consisted of five exercises – cycling, squats, step-ups, step-downs, and knee extensions – performed for 20–30 minutes.
The researchers measured outcomes using the Knee Injury and Osteoarthritis Outcome Score, which assesses pain, other symptoms, function in daily living, function in sports and recreation, and knee-related quality of life.
“Patients in both groups improved significantly over time, but high-dose exercise was not superior to low-dose exercise in most comparisons,” the study investigators reported
High-dose exercise was associated with better function in sports and recreational activity and knee-related quality of life at 6 months. Those differences did not persist at 1 year, however. The researchers reported no safety concerns with either intervention.
Adherence was “nearly perfect” in the low-dose group. It was slightly lower in the high-dose group, the researchers said.
“Interestingly, it seems that high-dose treatment could be preferable to low-dose treatment in the long run for people who lead active lives,” they wrote. “This should be the subject of future studies.”
All clinical practice guidelines for knee OA recommend exercise, but “we do not know the optimal dose,” Kim Bennell, PhD, a research physiotherapist at the University of Melbourne, said in an interview.
Dose has components, including number of times per week, number of exercises, sets and repetitions, intensity, and duration of exercise sessions, Dr. Bennell said.
“These results suggest that an exercise program that involves less time and fewer exercises can still offer benefits and may be easier for patients to undertake and stick at than one that involves greater time and effort,” she said.
The study was supported by the Swedish Rheumatic Fund. Dr. Trasolini and Dr. Bennell have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
High-deductible health plans detrimental for those with diabetes
Individuals with diabetes who are forced to switch to high-deductible health plans have more episodes of severe hypo- and hyperglycemia compared with those on conventional insurance plans, according to a new study.
Previous studies have shown that people with diabetes who are enrolled in high-deductible health plans (HDHPs) have an increased financial burden, lower medication adherence, and more low-severity emergency department visits, and they delay care for cardiovascular conditions.
But no study has looked at the plans’ impact on acute diabetes complications and glycemic control, wrote the authors in JAMA Network Open.
They found evidence that the high-dollar plans were associated with increased odds of severe hypoglycemic and hyperglycemic events, and that the risk increased with each successive year of enrollment. Low-income individuals, Blacks, and Hispanics were disproportionately more impacted, noted senior author Rozalina G. McCoy, MD, Mayo Clinic, Rochester, Minn., and colleagues.
Overall, “enrollees may be rationing or forgoing necessary care, which is detrimental to their health and ultimately increases the morbidity, mortality, and costs associated with diabetes,” they concluded.
A systematic review of eight studies published in Endocrine Practice in 2021 backs up this latest finding. That analysis reported enrollees in HDHPs often forgo routine care and monitoring, and that they have lower medication adherence, leading to an increase in total health care expenditures for emergency department visits, hospitalizations, and preventable complications.
Increased frequency of hypoglycemia is detrimental
The new study published in JAMA Network Open was based on data for adults enrolled in private insurance programs from 2010 to 2018. Researchers analyzed medical and pharmacy claims data contained in a large health insurance claims database, comparing adults with diabetes who had been in an HDHP for at least 1 year (and after a year of being in a conventional plan), with those who were in a conventional plan.
They identified 42,326 individuals who had been switched from a conventional plan to an HDHP. Of those, 7,375 (17.4%) were Black, 5,740 (13.6%) were Hispanic, 26,572 (62.8%) were non-Hispanic White, and 6,880 (16.3%) had a household income below $40,000 a year.
Baseline characteristics of the 202,729 people in conventional plans were similar to those in the HDHP group.
The median deductible for individuals in the HDHP group was $1,500 and for families it was $3,000, compared with $350 and $800, respectively, for those in conventional plans.
The odds of having any severe hypoglycemic event were significantly higher in the HDHP group (odds ratio [OR], 1.11; P < .001). Each year of HDHP enrollment increased the odds of a hypoglycemia-related ED or hospital visit by 2% (OR, 1.02; P = .04).
Aware that only a small number of severe hypoglycemic events, as well as an unknown number of such events, result in an emergency department visit or hospitalization, and that “the decision to seek ED or hospital care may be influenced by health plan assignment,” the authors also looked at office visits where severe, or any, hypoglycemia or hyperglycemia was coded or documented.
The proportion of HDHP enrollees where hypoglycemia was coded was 14% higher than for conventional plan enrollees (OR, 1.14; P < .001), with each year of the high-dollar plan enrollment increasing these odds by 6% (OR, 1.06; P < .001).
The tally of hypoglycemic events is an underestimate because HDHP enrollees might forgo ambulatory care for cost-related reasons, wrote the authors. Hypoglycemia might also be treated at home. But that is not necessarily a positive, they noted.
“The increased frequency of severe hypoglycemia – no matter where managed and discussed – is a sign of detrimental effects of HDHP enrollment for people living with diabetes.”
They found that individuals of racial and ethnic minorities were less likely than were White patients to have an increase in hypoglycemia-related office visits, which suggests that those patients were deferring care, wrote Dr. McCoy and colleagues.
Switching to an HDHP was associated with a significant increase in the odds of having at least one hyperglycemia-related ED or hospital visit per year (OR, 1.25; P < .001). Each successive year in the plan increased these odds by 5% (OR, 1.05; P = .02). However, the authors found no increase in hyperglycemia-related office visits.
“Because severe dysglycemic events may be prevented with optimal glycemic management, the increase in the frequency of their occurrence suggests important gaps in access to and implementation of diabetes therapy,” wrote the authors.
They noted that people with diabetes already face high out-of-pocket expenses. A high-deductible plan might make care even less affordable, they wrote.
“Individuals may be forced to ration medications, glucose-monitoring supplies, diabetes self-management education, food, and other essential cares to the detriment of their health,” they noted.
The authors added that because the study was observational, they could not delve into the root causes of the glycemic events or whether, for instance, any HDHP enrollees also had health savings accounts (HSAs) that might help defray costs.
They suggested that employers offer a wide variety of health plans, or if they are offering only a high-deductible plan that they be more transparent about potential costs. “Previous studies have shown that enrollees are not fully aware of the details within their health plans and may be focusing on reducing the cost of monthly premiums – not overall care – when choosing health plans.”
The authors said employers should find ways to fund HSAs for people with low incomes – those who appear to be most vulnerable to the effects of HDHPs.
A study published in JAMA Internal Medicine in 2017 found that low-income and HSA-eligible individuals with diabetes switched to an HDHP had major increases in emergency department visits for preventable acute diabetes complications.
The study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Mayo Clinic K2R Research Award, and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. McCoy has reported receiving grants from the NIDDK, AARP, and the Patient-Centered Outcomes Research Institute, and personal fees from Emmi for the development of patient education materials about diabetes outside the submitted work.
A version of this article first appeared on Medscape.com.
Individuals with diabetes who are forced to switch to high-deductible health plans have more episodes of severe hypo- and hyperglycemia compared with those on conventional insurance plans, according to a new study.
Previous studies have shown that people with diabetes who are enrolled in high-deductible health plans (HDHPs) have an increased financial burden, lower medication adherence, and more low-severity emergency department visits, and they delay care for cardiovascular conditions.
But no study has looked at the plans’ impact on acute diabetes complications and glycemic control, wrote the authors in JAMA Network Open.
They found evidence that the high-dollar plans were associated with increased odds of severe hypoglycemic and hyperglycemic events, and that the risk increased with each successive year of enrollment. Low-income individuals, Blacks, and Hispanics were disproportionately more impacted, noted senior author Rozalina G. McCoy, MD, Mayo Clinic, Rochester, Minn., and colleagues.
Overall, “enrollees may be rationing or forgoing necessary care, which is detrimental to their health and ultimately increases the morbidity, mortality, and costs associated with diabetes,” they concluded.
A systematic review of eight studies published in Endocrine Practice in 2021 backs up this latest finding. That analysis reported enrollees in HDHPs often forgo routine care and monitoring, and that they have lower medication adherence, leading to an increase in total health care expenditures for emergency department visits, hospitalizations, and preventable complications.
Increased frequency of hypoglycemia is detrimental
The new study published in JAMA Network Open was based on data for adults enrolled in private insurance programs from 2010 to 2018. Researchers analyzed medical and pharmacy claims data contained in a large health insurance claims database, comparing adults with diabetes who had been in an HDHP for at least 1 year (and after a year of being in a conventional plan), with those who were in a conventional plan.
They identified 42,326 individuals who had been switched from a conventional plan to an HDHP. Of those, 7,375 (17.4%) were Black, 5,740 (13.6%) were Hispanic, 26,572 (62.8%) were non-Hispanic White, and 6,880 (16.3%) had a household income below $40,000 a year.
Baseline characteristics of the 202,729 people in conventional plans were similar to those in the HDHP group.
The median deductible for individuals in the HDHP group was $1,500 and for families it was $3,000, compared with $350 and $800, respectively, for those in conventional plans.
The odds of having any severe hypoglycemic event were significantly higher in the HDHP group (odds ratio [OR], 1.11; P < .001). Each year of HDHP enrollment increased the odds of a hypoglycemia-related ED or hospital visit by 2% (OR, 1.02; P = .04).
Aware that only a small number of severe hypoglycemic events, as well as an unknown number of such events, result in an emergency department visit or hospitalization, and that “the decision to seek ED or hospital care may be influenced by health plan assignment,” the authors also looked at office visits where severe, or any, hypoglycemia or hyperglycemia was coded or documented.
The proportion of HDHP enrollees where hypoglycemia was coded was 14% higher than for conventional plan enrollees (OR, 1.14; P < .001), with each year of the high-dollar plan enrollment increasing these odds by 6% (OR, 1.06; P < .001).
The tally of hypoglycemic events is an underestimate because HDHP enrollees might forgo ambulatory care for cost-related reasons, wrote the authors. Hypoglycemia might also be treated at home. But that is not necessarily a positive, they noted.
“The increased frequency of severe hypoglycemia – no matter where managed and discussed – is a sign of detrimental effects of HDHP enrollment for people living with diabetes.”
They found that individuals of racial and ethnic minorities were less likely than were White patients to have an increase in hypoglycemia-related office visits, which suggests that those patients were deferring care, wrote Dr. McCoy and colleagues.
Switching to an HDHP was associated with a significant increase in the odds of having at least one hyperglycemia-related ED or hospital visit per year (OR, 1.25; P < .001). Each successive year in the plan increased these odds by 5% (OR, 1.05; P = .02). However, the authors found no increase in hyperglycemia-related office visits.
“Because severe dysglycemic events may be prevented with optimal glycemic management, the increase in the frequency of their occurrence suggests important gaps in access to and implementation of diabetes therapy,” wrote the authors.
They noted that people with diabetes already face high out-of-pocket expenses. A high-deductible plan might make care even less affordable, they wrote.
“Individuals may be forced to ration medications, glucose-monitoring supplies, diabetes self-management education, food, and other essential cares to the detriment of their health,” they noted.
The authors added that because the study was observational, they could not delve into the root causes of the glycemic events or whether, for instance, any HDHP enrollees also had health savings accounts (HSAs) that might help defray costs.
They suggested that employers offer a wide variety of health plans, or if they are offering only a high-deductible plan that they be more transparent about potential costs. “Previous studies have shown that enrollees are not fully aware of the details within their health plans and may be focusing on reducing the cost of monthly premiums – not overall care – when choosing health plans.”
The authors said employers should find ways to fund HSAs for people with low incomes – those who appear to be most vulnerable to the effects of HDHPs.
A study published in JAMA Internal Medicine in 2017 found that low-income and HSA-eligible individuals with diabetes switched to an HDHP had major increases in emergency department visits for preventable acute diabetes complications.
The study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Mayo Clinic K2R Research Award, and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. McCoy has reported receiving grants from the NIDDK, AARP, and the Patient-Centered Outcomes Research Institute, and personal fees from Emmi for the development of patient education materials about diabetes outside the submitted work.
A version of this article first appeared on Medscape.com.
Individuals with diabetes who are forced to switch to high-deductible health plans have more episodes of severe hypo- and hyperglycemia compared with those on conventional insurance plans, according to a new study.
Previous studies have shown that people with diabetes who are enrolled in high-deductible health plans (HDHPs) have an increased financial burden, lower medication adherence, and more low-severity emergency department visits, and they delay care for cardiovascular conditions.
But no study has looked at the plans’ impact on acute diabetes complications and glycemic control, wrote the authors in JAMA Network Open.
They found evidence that the high-dollar plans were associated with increased odds of severe hypoglycemic and hyperglycemic events, and that the risk increased with each successive year of enrollment. Low-income individuals, Blacks, and Hispanics were disproportionately more impacted, noted senior author Rozalina G. McCoy, MD, Mayo Clinic, Rochester, Minn., and colleagues.
Overall, “enrollees may be rationing or forgoing necessary care, which is detrimental to their health and ultimately increases the morbidity, mortality, and costs associated with diabetes,” they concluded.
A systematic review of eight studies published in Endocrine Practice in 2021 backs up this latest finding. That analysis reported enrollees in HDHPs often forgo routine care and monitoring, and that they have lower medication adherence, leading to an increase in total health care expenditures for emergency department visits, hospitalizations, and preventable complications.
Increased frequency of hypoglycemia is detrimental
The new study published in JAMA Network Open was based on data for adults enrolled in private insurance programs from 2010 to 2018. Researchers analyzed medical and pharmacy claims data contained in a large health insurance claims database, comparing adults with diabetes who had been in an HDHP for at least 1 year (and after a year of being in a conventional plan), with those who were in a conventional plan.
They identified 42,326 individuals who had been switched from a conventional plan to an HDHP. Of those, 7,375 (17.4%) were Black, 5,740 (13.6%) were Hispanic, 26,572 (62.8%) were non-Hispanic White, and 6,880 (16.3%) had a household income below $40,000 a year.
Baseline characteristics of the 202,729 people in conventional plans were similar to those in the HDHP group.
The median deductible for individuals in the HDHP group was $1,500 and for families it was $3,000, compared with $350 and $800, respectively, for those in conventional plans.
The odds of having any severe hypoglycemic event were significantly higher in the HDHP group (odds ratio [OR], 1.11; P < .001). Each year of HDHP enrollment increased the odds of a hypoglycemia-related ED or hospital visit by 2% (OR, 1.02; P = .04).
Aware that only a small number of severe hypoglycemic events, as well as an unknown number of such events, result in an emergency department visit or hospitalization, and that “the decision to seek ED or hospital care may be influenced by health plan assignment,” the authors also looked at office visits where severe, or any, hypoglycemia or hyperglycemia was coded or documented.
The proportion of HDHP enrollees where hypoglycemia was coded was 14% higher than for conventional plan enrollees (OR, 1.14; P < .001), with each year of the high-dollar plan enrollment increasing these odds by 6% (OR, 1.06; P < .001).
The tally of hypoglycemic events is an underestimate because HDHP enrollees might forgo ambulatory care for cost-related reasons, wrote the authors. Hypoglycemia might also be treated at home. But that is not necessarily a positive, they noted.
“The increased frequency of severe hypoglycemia – no matter where managed and discussed – is a sign of detrimental effects of HDHP enrollment for people living with diabetes.”
They found that individuals of racial and ethnic minorities were less likely than were White patients to have an increase in hypoglycemia-related office visits, which suggests that those patients were deferring care, wrote Dr. McCoy and colleagues.
Switching to an HDHP was associated with a significant increase in the odds of having at least one hyperglycemia-related ED or hospital visit per year (OR, 1.25; P < .001). Each successive year in the plan increased these odds by 5% (OR, 1.05; P = .02). However, the authors found no increase in hyperglycemia-related office visits.
“Because severe dysglycemic events may be prevented with optimal glycemic management, the increase in the frequency of their occurrence suggests important gaps in access to and implementation of diabetes therapy,” wrote the authors.
They noted that people with diabetes already face high out-of-pocket expenses. A high-deductible plan might make care even less affordable, they wrote.
“Individuals may be forced to ration medications, glucose-monitoring supplies, diabetes self-management education, food, and other essential cares to the detriment of their health,” they noted.
The authors added that because the study was observational, they could not delve into the root causes of the glycemic events or whether, for instance, any HDHP enrollees also had health savings accounts (HSAs) that might help defray costs.
They suggested that employers offer a wide variety of health plans, or if they are offering only a high-deductible plan that they be more transparent about potential costs. “Previous studies have shown that enrollees are not fully aware of the details within their health plans and may be focusing on reducing the cost of monthly premiums – not overall care – when choosing health plans.”
The authors said employers should find ways to fund HSAs for people with low incomes – those who appear to be most vulnerable to the effects of HDHPs.
A study published in JAMA Internal Medicine in 2017 found that low-income and HSA-eligible individuals with diabetes switched to an HDHP had major increases in emergency department visits for preventable acute diabetes complications.
The study was funded by a grant from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), the Mayo Clinic K2R Research Award, and the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery. Dr. McCoy has reported receiving grants from the NIDDK, AARP, and the Patient-Centered Outcomes Research Institute, and personal fees from Emmi for the development of patient education materials about diabetes outside the submitted work.
A version of this article first appeared on Medscape.com.
FDA approves new type 2 diabetes drug bexagliflozin
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
AHA scientific statement on rapid evaluation for suspected TIA
TIAs are “warning shots” of a future stroke and require emergency evaluation, Hardik Amin, MD, chair of the writing committee and medical stroke director, Yale New Haven (Conn.) Hospital, said in an AHA podcast.
A key aim of the scientific statement is to help clinicians properly risk-stratify patients with suspected TIA and determine which patients need to be admitted to the hospital and which patients might be safely discharged as long as proper and prompt follow-up has been arranged, Dr. Amin explained.
The statement, published online in the journal Stroke, addresses “how we can identify and be confident in diagnosing a TIA patient and what might suggest an alternative diagnosis,” he added.
Diagnostic challenge
It’s estimated that nearly one in five people who suffer a TIA will have a full-blown stroke within 3 months; close to half of these strokes will happen within 2 days.
The challenge with TIAs is that they can be tough to diagnose because many patients no longer have symptoms when they arrive at the emergency department. There is also no confirmatory test. Limited resources and access to stroke specialists in rural centers may exacerbate these challenges, the authors noted.
The statement pointed out that the F.A.S.T. acronym for stroke symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call 911) can also be used to identify a TIA – even if the symptoms resolve.
The statement also provided guidance on how to tell the difference between a TIA and a TIA mimic.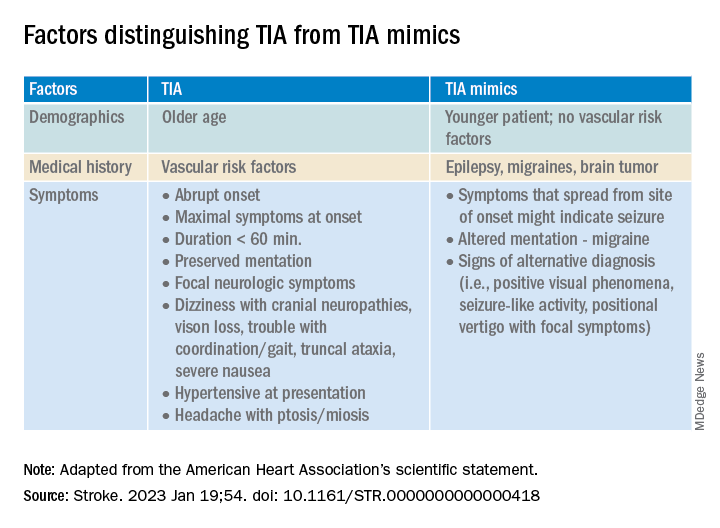
If available, a noncontrast head CT (NCCT) scan should be done initially in the emergency department to evaluate for subacute ischemia, hemorrhage, or mass lesion. Although the sensitivity of NCCT to detect an acute infarct is low, NCCT is useful for ruling out TIA mimics, the writing group said.
Multimodal brain MRI is the “preferred” method to evaluate for acute ischemic infarct and ideally should be obtained within 24 hours of symptom onset, and in most centers will follow an NCCT.
“When MRI cannot be obtained acutely to definitively distinguish TIA from stroke, it remains reasonable to make a clinical diagnosis of TIA in the ED on the basis of a negative NCCT and symptom resolution within 24 hours,” the authors said.
“A potential next step would be hospital admission for MRI, comprehensive workup, and neurology consultation. Other options might include transferring patients to a facility with advanced imaging and vascular neurology expertise or arranging a timely (ideally < 24 hours) outpatient MRI,” they advised.
The statement also provides guidance on the advantages, limitations, and considerations of Doppler ultrasonography, CT angiography, and magnetic resonance angiography for TIA assessment.
Once TIA is diagnosed, a cardiac work-up is advised because of the potential for heart-related factors to cause a TIA.
An individual’s risk of future stroke after TIA can be rapidly assessed using the ABCD2 score, which stratifies patients into low, medium, and high risk based on age, blood pressure, clinical features, duration of symptoms, and diabetes.
“It is up to each center to use the resources available and create a pathway to ensure successful management and disposition of patients with TIA, with the ultimate goal of reducing the risk of future stroke,” the authors concluded.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Emergency Neurovascular Care Committee of the Stroke Council and the Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, and it is endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons.
A version of this article first appeared on Medscape.com.
TIAs are “warning shots” of a future stroke and require emergency evaluation, Hardik Amin, MD, chair of the writing committee and medical stroke director, Yale New Haven (Conn.) Hospital, said in an AHA podcast.
A key aim of the scientific statement is to help clinicians properly risk-stratify patients with suspected TIA and determine which patients need to be admitted to the hospital and which patients might be safely discharged as long as proper and prompt follow-up has been arranged, Dr. Amin explained.
The statement, published online in the journal Stroke, addresses “how we can identify and be confident in diagnosing a TIA patient and what might suggest an alternative diagnosis,” he added.
Diagnostic challenge
It’s estimated that nearly one in five people who suffer a TIA will have a full-blown stroke within 3 months; close to half of these strokes will happen within 2 days.
The challenge with TIAs is that they can be tough to diagnose because many patients no longer have symptoms when they arrive at the emergency department. There is also no confirmatory test. Limited resources and access to stroke specialists in rural centers may exacerbate these challenges, the authors noted.
The statement pointed out that the F.A.S.T. acronym for stroke symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call 911) can also be used to identify a TIA – even if the symptoms resolve.
The statement also provided guidance on how to tell the difference between a TIA and a TIA mimic.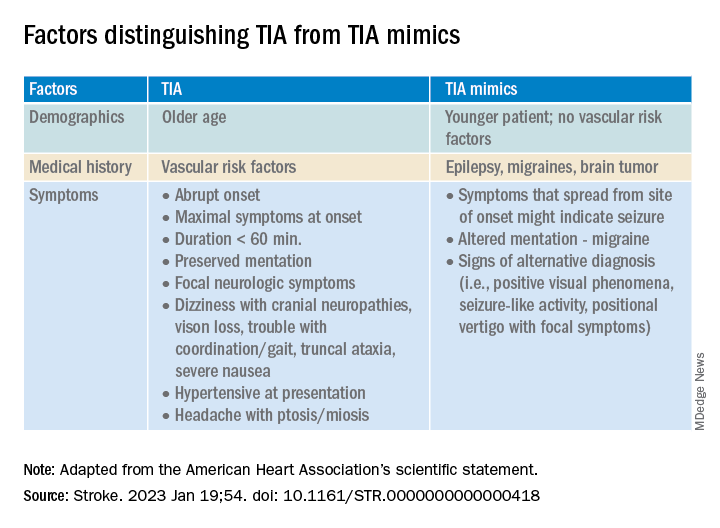
If available, a noncontrast head CT (NCCT) scan should be done initially in the emergency department to evaluate for subacute ischemia, hemorrhage, or mass lesion. Although the sensitivity of NCCT to detect an acute infarct is low, NCCT is useful for ruling out TIA mimics, the writing group said.
Multimodal brain MRI is the “preferred” method to evaluate for acute ischemic infarct and ideally should be obtained within 24 hours of symptom onset, and in most centers will follow an NCCT.
“When MRI cannot be obtained acutely to definitively distinguish TIA from stroke, it remains reasonable to make a clinical diagnosis of TIA in the ED on the basis of a negative NCCT and symptom resolution within 24 hours,” the authors said.
“A potential next step would be hospital admission for MRI, comprehensive workup, and neurology consultation. Other options might include transferring patients to a facility with advanced imaging and vascular neurology expertise or arranging a timely (ideally < 24 hours) outpatient MRI,” they advised.
The statement also provides guidance on the advantages, limitations, and considerations of Doppler ultrasonography, CT angiography, and magnetic resonance angiography for TIA assessment.
Once TIA is diagnosed, a cardiac work-up is advised because of the potential for heart-related factors to cause a TIA.
An individual’s risk of future stroke after TIA can be rapidly assessed using the ABCD2 score, which stratifies patients into low, medium, and high risk based on age, blood pressure, clinical features, duration of symptoms, and diabetes.
“It is up to each center to use the resources available and create a pathway to ensure successful management and disposition of patients with TIA, with the ultimate goal of reducing the risk of future stroke,” the authors concluded.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Emergency Neurovascular Care Committee of the Stroke Council and the Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, and it is endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons.
A version of this article first appeared on Medscape.com.
TIAs are “warning shots” of a future stroke and require emergency evaluation, Hardik Amin, MD, chair of the writing committee and medical stroke director, Yale New Haven (Conn.) Hospital, said in an AHA podcast.
A key aim of the scientific statement is to help clinicians properly risk-stratify patients with suspected TIA and determine which patients need to be admitted to the hospital and which patients might be safely discharged as long as proper and prompt follow-up has been arranged, Dr. Amin explained.
The statement, published online in the journal Stroke, addresses “how we can identify and be confident in diagnosing a TIA patient and what might suggest an alternative diagnosis,” he added.
Diagnostic challenge
It’s estimated that nearly one in five people who suffer a TIA will have a full-blown stroke within 3 months; close to half of these strokes will happen within 2 days.
The challenge with TIAs is that they can be tough to diagnose because many patients no longer have symptoms when they arrive at the emergency department. There is also no confirmatory test. Limited resources and access to stroke specialists in rural centers may exacerbate these challenges, the authors noted.
The statement pointed out that the F.A.S.T. acronym for stroke symptoms (Face drooping, Arm weakness, Speech difficulty, Time to call 911) can also be used to identify a TIA – even if the symptoms resolve.
The statement also provided guidance on how to tell the difference between a TIA and a TIA mimic.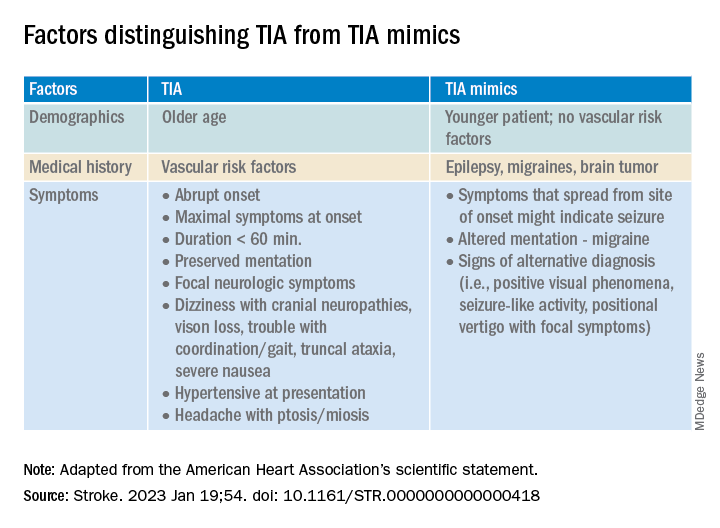
If available, a noncontrast head CT (NCCT) scan should be done initially in the emergency department to evaluate for subacute ischemia, hemorrhage, or mass lesion. Although the sensitivity of NCCT to detect an acute infarct is low, NCCT is useful for ruling out TIA mimics, the writing group said.
Multimodal brain MRI is the “preferred” method to evaluate for acute ischemic infarct and ideally should be obtained within 24 hours of symptom onset, and in most centers will follow an NCCT.
“When MRI cannot be obtained acutely to definitively distinguish TIA from stroke, it remains reasonable to make a clinical diagnosis of TIA in the ED on the basis of a negative NCCT and symptom resolution within 24 hours,” the authors said.
“A potential next step would be hospital admission for MRI, comprehensive workup, and neurology consultation. Other options might include transferring patients to a facility with advanced imaging and vascular neurology expertise or arranging a timely (ideally < 24 hours) outpatient MRI,” they advised.
The statement also provides guidance on the advantages, limitations, and considerations of Doppler ultrasonography, CT angiography, and magnetic resonance angiography for TIA assessment.
Once TIA is diagnosed, a cardiac work-up is advised because of the potential for heart-related factors to cause a TIA.
An individual’s risk of future stroke after TIA can be rapidly assessed using the ABCD2 score, which stratifies patients into low, medium, and high risk based on age, blood pressure, clinical features, duration of symptoms, and diabetes.
“It is up to each center to use the resources available and create a pathway to ensure successful management and disposition of patients with TIA, with the ultimate goal of reducing the risk of future stroke,” the authors concluded.
This scientific statement was prepared by the volunteer writing group on behalf of the American Heart Association’s Emergency Neurovascular Care Committee of the Stroke Council and the Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists, and it is endorsed by the American Association of Neurological Surgeons/Congress of Neurological Surgeons.
A version of this article first appeared on Medscape.com.
FROM STROKE
Doctors’ happiness has not rebounded as pandemic drags on
Physicians reported similar levels of unhappiness in 2022 too.
Fewer than half of physicians said they were currently somewhat or very happy at work, compared with 75% of physicians who said they were somewhat or very happy at work in a previous survey conducted before the pandemic, the new Medscape Physician Lifestyle & Happiness Report 2023 shows.*
“I am not surprised that we’re less happy now,” said Amaryllis Sánchez, MD, a board-certified family medicine physician and a certified physician coach.
“I speak to physicians around the country and I hear that their workplaces are understaffed, they’re overworked and they don’t feel safe. Although we’re in a different phase of the pandemic, doctors feel that the ground beneath them is still shaky,” said Dr. Sánchez, the author of “Recapturing Joy in Medicine.”
Most doctors are seeing more patients than they can handle and are expected to do that consistently. “When you no longer have the capacity to give of yourself, that becomes a nearly impossible task,” said Dr. Sánchez.
Also, physicians in understaffed workplaces often must take on additional work such as administrative or nursing duties, said Katie Cole, DO, a board-certified psychiatrist and a physician coach.
While health systems are aware that physicians need time to rest and recharge, staffing shortages prevent doctors from taking time off because they can’t find coverage, said Dr. Cole.
“While we know that it’s important for physicians to take vacations, more than one-third of doctors still take 2 weeks or less of vacation annually,” said Dr. Cole.
Physicians also tend to have less compassion for themselves and sacrifice self-care compared to other health care workers. “When a patient dies, nurses get together, debrief, and hug each other, whereas doctors have another patient to see. The culture of medicine doesn’t support self-compassion for physicians,” said Dr. Cole.
Physicians also felt less safe at work during the pandemic because of to shortages of personal protective equipment, said Dr. Sánchez. They have also witnessed or experienced an increase in abusive behavior, violence and threats of violence.
Physicians’ personal life suffers
Doctors maintain their mental health primarily by spending time with family members and friends, according to 2022’s Medscape Physician Lifestyle & Happiness Report. Yet half of doctors reported in a survey by the Physicians Foundation that they withdrew from family, friends or coworkers in 2022, said Dr. Sánchez.
“When you exceed your mental, emotional, and physical capacity at work, you have no reserve left for your personal life,” said Dr. Cole.
That may explain why only 58% of doctors reported feeling somewhat or very happy outside of work, compared with 84% who felt that way before the pandemic.
More women doctors said they deal with stronger feelings of conflict in trying to balance parenting responsibilities with a highly demanding job. Nearly one in two women physician-parents reported feeling very conflicted at work, compared with about one in four male physician-parents.
When physicians go home, they may be emotionally drained and tired mentally from making a lot of decisions at work, said Dr. Cole.
“As a woman, if you have children and a husband and you’re responsible for dinner, picking up the kids at daycare or helping them with homework, and making all these decisions when you get home, it’s overwhelming,” said Dr. Cole.
Prioritize your well-being
Doctors need to prioritize their own well-being, said Dr. Sánchez. “That’s not being selfish, that’s doing what’s necessary to stay well and be able to take care of patients. If doctors don’t take care of themselves, no one else will.”
Dr. Sánchez recommended that doctors regularly interact with relatives, friends, trusted colleagues, or clergy to help maintain their well-being, rather than waiting until a crisis to reach out.
A good coach, mentor, or counselor can help physicians gain enough self-awareness to handle their emotions and gain more clarity about what changes need to be made, she said.
Dr. Cole suggested that doctors figure out what makes them happy and fulfilled at work and try to spend more time on that activity. “Knowing what makes you happy and your strengths are foundational for creating a life you love.”
She urged doctors to “start thinking now about what you love about medicine and what is going right at home, and what areas you want to change. Then, start advocating for your needs.”
A version of this article originally appeared on Medscape.com.
Correction, 1/26/23: An earlier version of this article misstated the findings of the survey.
Physicians reported similar levels of unhappiness in 2022 too.
Fewer than half of physicians said they were currently somewhat or very happy at work, compared with 75% of physicians who said they were somewhat or very happy at work in a previous survey conducted before the pandemic, the new Medscape Physician Lifestyle & Happiness Report 2023 shows.*
“I am not surprised that we’re less happy now,” said Amaryllis Sánchez, MD, a board-certified family medicine physician and a certified physician coach.
“I speak to physicians around the country and I hear that their workplaces are understaffed, they’re overworked and they don’t feel safe. Although we’re in a different phase of the pandemic, doctors feel that the ground beneath them is still shaky,” said Dr. Sánchez, the author of “Recapturing Joy in Medicine.”
Most doctors are seeing more patients than they can handle and are expected to do that consistently. “When you no longer have the capacity to give of yourself, that becomes a nearly impossible task,” said Dr. Sánchez.
Also, physicians in understaffed workplaces often must take on additional work such as administrative or nursing duties, said Katie Cole, DO, a board-certified psychiatrist and a physician coach.
While health systems are aware that physicians need time to rest and recharge, staffing shortages prevent doctors from taking time off because they can’t find coverage, said Dr. Cole.
“While we know that it’s important for physicians to take vacations, more than one-third of doctors still take 2 weeks or less of vacation annually,” said Dr. Cole.
Physicians also tend to have less compassion for themselves and sacrifice self-care compared to other health care workers. “When a patient dies, nurses get together, debrief, and hug each other, whereas doctors have another patient to see. The culture of medicine doesn’t support self-compassion for physicians,” said Dr. Cole.
Physicians also felt less safe at work during the pandemic because of to shortages of personal protective equipment, said Dr. Sánchez. They have also witnessed or experienced an increase in abusive behavior, violence and threats of violence.
Physicians’ personal life suffers
Doctors maintain their mental health primarily by spending time with family members and friends, according to 2022’s Medscape Physician Lifestyle & Happiness Report. Yet half of doctors reported in a survey by the Physicians Foundation that they withdrew from family, friends or coworkers in 2022, said Dr. Sánchez.
“When you exceed your mental, emotional, and physical capacity at work, you have no reserve left for your personal life,” said Dr. Cole.
That may explain why only 58% of doctors reported feeling somewhat or very happy outside of work, compared with 84% who felt that way before the pandemic.
More women doctors said they deal with stronger feelings of conflict in trying to balance parenting responsibilities with a highly demanding job. Nearly one in two women physician-parents reported feeling very conflicted at work, compared with about one in four male physician-parents.
When physicians go home, they may be emotionally drained and tired mentally from making a lot of decisions at work, said Dr. Cole.
“As a woman, if you have children and a husband and you’re responsible for dinner, picking up the kids at daycare or helping them with homework, and making all these decisions when you get home, it’s overwhelming,” said Dr. Cole.
Prioritize your well-being
Doctors need to prioritize their own well-being, said Dr. Sánchez. “That’s not being selfish, that’s doing what’s necessary to stay well and be able to take care of patients. If doctors don’t take care of themselves, no one else will.”
Dr. Sánchez recommended that doctors regularly interact with relatives, friends, trusted colleagues, or clergy to help maintain their well-being, rather than waiting until a crisis to reach out.
A good coach, mentor, or counselor can help physicians gain enough self-awareness to handle their emotions and gain more clarity about what changes need to be made, she said.
Dr. Cole suggested that doctors figure out what makes them happy and fulfilled at work and try to spend more time on that activity. “Knowing what makes you happy and your strengths are foundational for creating a life you love.”
She urged doctors to “start thinking now about what you love about medicine and what is going right at home, and what areas you want to change. Then, start advocating for your needs.”
A version of this article originally appeared on Medscape.com.
Correction, 1/26/23: An earlier version of this article misstated the findings of the survey.
Physicians reported similar levels of unhappiness in 2022 too.
Fewer than half of physicians said they were currently somewhat or very happy at work, compared with 75% of physicians who said they were somewhat or very happy at work in a previous survey conducted before the pandemic, the new Medscape Physician Lifestyle & Happiness Report 2023 shows.*
“I am not surprised that we’re less happy now,” said Amaryllis Sánchez, MD, a board-certified family medicine physician and a certified physician coach.
“I speak to physicians around the country and I hear that their workplaces are understaffed, they’re overworked and they don’t feel safe. Although we’re in a different phase of the pandemic, doctors feel that the ground beneath them is still shaky,” said Dr. Sánchez, the author of “Recapturing Joy in Medicine.”
Most doctors are seeing more patients than they can handle and are expected to do that consistently. “When you no longer have the capacity to give of yourself, that becomes a nearly impossible task,” said Dr. Sánchez.
Also, physicians in understaffed workplaces often must take on additional work such as administrative or nursing duties, said Katie Cole, DO, a board-certified psychiatrist and a physician coach.
While health systems are aware that physicians need time to rest and recharge, staffing shortages prevent doctors from taking time off because they can’t find coverage, said Dr. Cole.
“While we know that it’s important for physicians to take vacations, more than one-third of doctors still take 2 weeks or less of vacation annually,” said Dr. Cole.
Physicians also tend to have less compassion for themselves and sacrifice self-care compared to other health care workers. “When a patient dies, nurses get together, debrief, and hug each other, whereas doctors have another patient to see. The culture of medicine doesn’t support self-compassion for physicians,” said Dr. Cole.
Physicians also felt less safe at work during the pandemic because of to shortages of personal protective equipment, said Dr. Sánchez. They have also witnessed or experienced an increase in abusive behavior, violence and threats of violence.
Physicians’ personal life suffers
Doctors maintain their mental health primarily by spending time with family members and friends, according to 2022’s Medscape Physician Lifestyle & Happiness Report. Yet half of doctors reported in a survey by the Physicians Foundation that they withdrew from family, friends or coworkers in 2022, said Dr. Sánchez.
“When you exceed your mental, emotional, and physical capacity at work, you have no reserve left for your personal life,” said Dr. Cole.
That may explain why only 58% of doctors reported feeling somewhat or very happy outside of work, compared with 84% who felt that way before the pandemic.
More women doctors said they deal with stronger feelings of conflict in trying to balance parenting responsibilities with a highly demanding job. Nearly one in two women physician-parents reported feeling very conflicted at work, compared with about one in four male physician-parents.
When physicians go home, they may be emotionally drained and tired mentally from making a lot of decisions at work, said Dr. Cole.
“As a woman, if you have children and a husband and you’re responsible for dinner, picking up the kids at daycare or helping them with homework, and making all these decisions when you get home, it’s overwhelming,” said Dr. Cole.
Prioritize your well-being
Doctors need to prioritize their own well-being, said Dr. Sánchez. “That’s not being selfish, that’s doing what’s necessary to stay well and be able to take care of patients. If doctors don’t take care of themselves, no one else will.”
Dr. Sánchez recommended that doctors regularly interact with relatives, friends, trusted colleagues, or clergy to help maintain their well-being, rather than waiting until a crisis to reach out.
A good coach, mentor, or counselor can help physicians gain enough self-awareness to handle their emotions and gain more clarity about what changes need to be made, she said.
Dr. Cole suggested that doctors figure out what makes them happy and fulfilled at work and try to spend more time on that activity. “Knowing what makes you happy and your strengths are foundational for creating a life you love.”
She urged doctors to “start thinking now about what you love about medicine and what is going right at home, and what areas you want to change. Then, start advocating for your needs.”
A version of this article originally appeared on Medscape.com.
Correction, 1/26/23: An earlier version of this article misstated the findings of the survey.
A patient named ‘Settle’ decides to sue instead
On Nov. 1, 2020, Dallas Settle went to Plateau Medical Center, Oak Hill, W.Va., complaining of pain that was later described in court documents as being “in his right mid-abdomen migrating to his right lower abdomen.” Following a CT scan, Mr. Settle was diagnosed with diverticulitis resulting in pneumoperitoneum, which is the presence of air or other gas in the abdominal cavity. The patient, it was decided, required surgery to correct the problem, but Plateau Medical Center didn’t have the staff to perform the procedure.
Mr. Settle was then transferred to another West Virginia hospital, Charleston Area Medical Center (CAMC). Here, he was evaluated by doctors in the facility’s General Division, who initiated treatment with IV fluids and opiate analgesics. He was then placed under the care of a trauma surgeon, who initially decided to treat the patient nonoperatively. If that approach failed, the surgeon believed, Mr. Settle would probably require a laparotomy, bowel resection, and ostomy.
Another surgical team performed an exploratory laparotomy the following day. The team determined that Mr. Settle was suffering from a ruptured appendicitis and allegedly performed an appendectomy. But Mr. Settle’s condition continued to deteriorate the following day.
Another CT scan followed. It revealed various problems – multiple fluid collections, an ileus, distended loops of the patient’s small bowel, a left renal cyst, subcentimeter mesenteric, and retroperitoneal adenopathy. Additional CT scans conducted 4 days later indicated other problems, including fluid collections in the patient’s right- and left-lower quadrants.
Over the next few days, doctors performed further exploratory laparotomies. Finally, on Nov. 22, Mr. Settle was transferred out of the intensive care unit in preparation for his discharge the following day.
His pain continued to worsen, however, and he was readmitted to CAMC a day later. At this point, an examination revealed that his surgical incisions had become infected.
Worse news was on the horizon. On Nov. 28, the trauma surgeon who had first agreed to treat Mr. Settle informed him that, despite claims to the contrary, his appendix hadn’t been removed.
Eventually, Mr. Settle was referred to the Cleveland Clinic, where at press time he was still being treated.
Mr. Settle has hired the firm Calwell Luce diTrapano to sue CAMC, accusing it of medical malpractice, medical negligence, and other lapses in the standard of care. In his complaint, he accused the hospital and its staff of breaching their duty of care “by negligently and improperly treating him” and by failing “to exercise the degree of care, skill, and learning required and expected of reasonable health care providers.”
His suit seeks not only compensatory damages and other relief but also punitive damages.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article originally appeared on Medscape.com.
On Nov. 1, 2020, Dallas Settle went to Plateau Medical Center, Oak Hill, W.Va., complaining of pain that was later described in court documents as being “in his right mid-abdomen migrating to his right lower abdomen.” Following a CT scan, Mr. Settle was diagnosed with diverticulitis resulting in pneumoperitoneum, which is the presence of air or other gas in the abdominal cavity. The patient, it was decided, required surgery to correct the problem, but Plateau Medical Center didn’t have the staff to perform the procedure.
Mr. Settle was then transferred to another West Virginia hospital, Charleston Area Medical Center (CAMC). Here, he was evaluated by doctors in the facility’s General Division, who initiated treatment with IV fluids and opiate analgesics. He was then placed under the care of a trauma surgeon, who initially decided to treat the patient nonoperatively. If that approach failed, the surgeon believed, Mr. Settle would probably require a laparotomy, bowel resection, and ostomy.
Another surgical team performed an exploratory laparotomy the following day. The team determined that Mr. Settle was suffering from a ruptured appendicitis and allegedly performed an appendectomy. But Mr. Settle’s condition continued to deteriorate the following day.
Another CT scan followed. It revealed various problems – multiple fluid collections, an ileus, distended loops of the patient’s small bowel, a left renal cyst, subcentimeter mesenteric, and retroperitoneal adenopathy. Additional CT scans conducted 4 days later indicated other problems, including fluid collections in the patient’s right- and left-lower quadrants.
Over the next few days, doctors performed further exploratory laparotomies. Finally, on Nov. 22, Mr. Settle was transferred out of the intensive care unit in preparation for his discharge the following day.
His pain continued to worsen, however, and he was readmitted to CAMC a day later. At this point, an examination revealed that his surgical incisions had become infected.
Worse news was on the horizon. On Nov. 28, the trauma surgeon who had first agreed to treat Mr. Settle informed him that, despite claims to the contrary, his appendix hadn’t been removed.
Eventually, Mr. Settle was referred to the Cleveland Clinic, where at press time he was still being treated.
Mr. Settle has hired the firm Calwell Luce diTrapano to sue CAMC, accusing it of medical malpractice, medical negligence, and other lapses in the standard of care. In his complaint, he accused the hospital and its staff of breaching their duty of care “by negligently and improperly treating him” and by failing “to exercise the degree of care, skill, and learning required and expected of reasonable health care providers.”
His suit seeks not only compensatory damages and other relief but also punitive damages.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article originally appeared on Medscape.com.
On Nov. 1, 2020, Dallas Settle went to Plateau Medical Center, Oak Hill, W.Va., complaining of pain that was later described in court documents as being “in his right mid-abdomen migrating to his right lower abdomen.” Following a CT scan, Mr. Settle was diagnosed with diverticulitis resulting in pneumoperitoneum, which is the presence of air or other gas in the abdominal cavity. The patient, it was decided, required surgery to correct the problem, but Plateau Medical Center didn’t have the staff to perform the procedure.
Mr. Settle was then transferred to another West Virginia hospital, Charleston Area Medical Center (CAMC). Here, he was evaluated by doctors in the facility’s General Division, who initiated treatment with IV fluids and opiate analgesics. He was then placed under the care of a trauma surgeon, who initially decided to treat the patient nonoperatively. If that approach failed, the surgeon believed, Mr. Settle would probably require a laparotomy, bowel resection, and ostomy.
Another surgical team performed an exploratory laparotomy the following day. The team determined that Mr. Settle was suffering from a ruptured appendicitis and allegedly performed an appendectomy. But Mr. Settle’s condition continued to deteriorate the following day.
Another CT scan followed. It revealed various problems – multiple fluid collections, an ileus, distended loops of the patient’s small bowel, a left renal cyst, subcentimeter mesenteric, and retroperitoneal adenopathy. Additional CT scans conducted 4 days later indicated other problems, including fluid collections in the patient’s right- and left-lower quadrants.
Over the next few days, doctors performed further exploratory laparotomies. Finally, on Nov. 22, Mr. Settle was transferred out of the intensive care unit in preparation for his discharge the following day.
His pain continued to worsen, however, and he was readmitted to CAMC a day later. At this point, an examination revealed that his surgical incisions had become infected.
Worse news was on the horizon. On Nov. 28, the trauma surgeon who had first agreed to treat Mr. Settle informed him that, despite claims to the contrary, his appendix hadn’t been removed.
Eventually, Mr. Settle was referred to the Cleveland Clinic, where at press time he was still being treated.
Mr. Settle has hired the firm Calwell Luce diTrapano to sue CAMC, accusing it of medical malpractice, medical negligence, and other lapses in the standard of care. In his complaint, he accused the hospital and its staff of breaching their duty of care “by negligently and improperly treating him” and by failing “to exercise the degree of care, skill, and learning required and expected of reasonable health care providers.”
His suit seeks not only compensatory damages and other relief but also punitive damages.
The content contained in this article is for informational purposes only and does not constitute legal advice. Reliance on any information provided in this article is solely at your own risk.
A version of this article originally appeared on Medscape.com.
Long-pulsed 1,064 nm Nd:YAG for nonaggressive BCC ‘effective and easy’
SAN DIEGO – After Arisa E. Ortiz, MD, and colleagues published results of a multicenter study reporting that one treatment with the long-pulsed 1,064-nm Nd:YAG laser cleared nonaggressive basal cell carcinoma (BCC) on the trunk and extremities in 90% of patients, she heard from colleagues who were skeptical of the approach.
Maybe it’s just the biopsy alone that’s clearing these tumors, some told her. Others postulated that since the energy was delivered with a 5- to 6-mm spot size at a fluence of 125-140 J/cm2 and a 7- to 10-ms pulse duration, bulk heating likely disrupted the tumors. However, treatments were generally well tolerated, required no anesthesia, and caused no significant adverse events.
“It’s almost scarless,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said at the annual Masters of Aesthetics Symposium. “Sometimes the treatment does leave a mark, but I think the scars are always acceptable. We do have good histologic evidence that we can penetrate 2.15 mm, which is a lot deeper than what the pulsed-dye laser or other superficial wavelengths are able to penetrate.”
Data is well powered to reject the null hypothesis that laser treatment does not have an effect on nodular and superficial BCC lesions, she continued, noting that it is at least comparable if not superior with clearance rates reported for methyl aminolevulinate–PDT (73%), imiquimod cream (83%), and fluorouracil cream (80%). “Maybe we’re not specifically targeting the vasculature [with this approach], but we did some optical coherence tomography imaging and saw that the blood vessels in the tumor were coagulated while the vasculature in the surrounding normal skin were spared,” said Dr. Ortiz, who is also vice president of the American Society for Laser Medicine and Surgery.
In a more recent analysis, she and her colleagues retrospectively analyzed long-term outcomes in 11 patients with BCC who had 16 lesions treated with the 1,064-nm Nd:YAG laser. At a mean of 9 months, 100% of lesions remained clear as determined by clinical observation.
In a subsequent, as yet unpublished study, she and her collaborators followed 34 patients with BCC one year following laser treatment. “Of these, 33 had no recurrence at 1-year follow-up,” Dr. Ortiz said, noting that the one patient with a recurrence was on a biologic agent for Crohn’s disease.
One key advantage of using the long-pulsed 1,064-nm Nd:YAG laser for nonaggressive BCC is the potential for one treatment visit. “They don’t have to come back for suture removal,” she said. “It’s a quick procedure, takes only about 5 minutes. There’s no limitation on activity and there’s minimal wound care, light ointment, and a band-aid; that’s it.”
In addition, she said, there is a lower risk of complications, infections, and bleeding, and there is minimal scarring. It is “also an alternative for treating patients with multiple tumors or those who are poor surgical candidates, such as the elderly and those with Gorlin syndrome.”
Dr. Ortiz avoids treating aggressive subtypes “because we don’t know what margin to treat,” she added. “Avoid the face. I do make some exceptions for patients if they’re elderly or if they’ve had multiple tumors. Monitor for recurrence like you would using any other modality.”
She uses lidocaine without epinephrine to avoid vasoconstriction and treats with the 1,064-nm Nd:YAG laser as follows: a 5-mm spot size, a fluence of 140 J/cm2, and a pulse duration of 8 ms, with no cooling, which are the settings for the Excel V Laser System, she noted. “If you’re using a different Nd:YAG laser, your pulse duration may vary. I do let the device cool in between pulses to avoid bulk heating.”
The immediate endpoint to strive for is slight greying and slight contraction, and the procedure is covered by insurance, billed as malignant destruction/EDC (CPT codes 17260-17266 trunk and 17280-17283 face). “I do biopsy prior to treatment,” she said. “I like the biopsy to be healed when I’m using the laser, so I’ll treat them about a month later.”
As for future directions, Dr. Ortiz and colleagues plan to evaluate the use of gold nanoparticles to more selectively target BCC during treatment with the 1,064-nm Nd:YAG laser. For now, she sees no downside of the procedure for proper candidates. “I do think that patients really like it,” she said. “It’s effective and easy.”
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
SAN DIEGO – After Arisa E. Ortiz, MD, and colleagues published results of a multicenter study reporting that one treatment with the long-pulsed 1,064-nm Nd:YAG laser cleared nonaggressive basal cell carcinoma (BCC) on the trunk and extremities in 90% of patients, she heard from colleagues who were skeptical of the approach.
Maybe it’s just the biopsy alone that’s clearing these tumors, some told her. Others postulated that since the energy was delivered with a 5- to 6-mm spot size at a fluence of 125-140 J/cm2 and a 7- to 10-ms pulse duration, bulk heating likely disrupted the tumors. However, treatments were generally well tolerated, required no anesthesia, and caused no significant adverse events.
“It’s almost scarless,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said at the annual Masters of Aesthetics Symposium. “Sometimes the treatment does leave a mark, but I think the scars are always acceptable. We do have good histologic evidence that we can penetrate 2.15 mm, which is a lot deeper than what the pulsed-dye laser or other superficial wavelengths are able to penetrate.”
Data is well powered to reject the null hypothesis that laser treatment does not have an effect on nodular and superficial BCC lesions, she continued, noting that it is at least comparable if not superior with clearance rates reported for methyl aminolevulinate–PDT (73%), imiquimod cream (83%), and fluorouracil cream (80%). “Maybe we’re not specifically targeting the vasculature [with this approach], but we did some optical coherence tomography imaging and saw that the blood vessels in the tumor were coagulated while the vasculature in the surrounding normal skin were spared,” said Dr. Ortiz, who is also vice president of the American Society for Laser Medicine and Surgery.
In a more recent analysis, she and her colleagues retrospectively analyzed long-term outcomes in 11 patients with BCC who had 16 lesions treated with the 1,064-nm Nd:YAG laser. At a mean of 9 months, 100% of lesions remained clear as determined by clinical observation.
In a subsequent, as yet unpublished study, she and her collaborators followed 34 patients with BCC one year following laser treatment. “Of these, 33 had no recurrence at 1-year follow-up,” Dr. Ortiz said, noting that the one patient with a recurrence was on a biologic agent for Crohn’s disease.
One key advantage of using the long-pulsed 1,064-nm Nd:YAG laser for nonaggressive BCC is the potential for one treatment visit. “They don’t have to come back for suture removal,” she said. “It’s a quick procedure, takes only about 5 minutes. There’s no limitation on activity and there’s minimal wound care, light ointment, and a band-aid; that’s it.”
In addition, she said, there is a lower risk of complications, infections, and bleeding, and there is minimal scarring. It is “also an alternative for treating patients with multiple tumors or those who are poor surgical candidates, such as the elderly and those with Gorlin syndrome.”
Dr. Ortiz avoids treating aggressive subtypes “because we don’t know what margin to treat,” she added. “Avoid the face. I do make some exceptions for patients if they’re elderly or if they’ve had multiple tumors. Monitor for recurrence like you would using any other modality.”
She uses lidocaine without epinephrine to avoid vasoconstriction and treats with the 1,064-nm Nd:YAG laser as follows: a 5-mm spot size, a fluence of 140 J/cm2, and a pulse duration of 8 ms, with no cooling, which are the settings for the Excel V Laser System, she noted. “If you’re using a different Nd:YAG laser, your pulse duration may vary. I do let the device cool in between pulses to avoid bulk heating.”
The immediate endpoint to strive for is slight greying and slight contraction, and the procedure is covered by insurance, billed as malignant destruction/EDC (CPT codes 17260-17266 trunk and 17280-17283 face). “I do biopsy prior to treatment,” she said. “I like the biopsy to be healed when I’m using the laser, so I’ll treat them about a month later.”
As for future directions, Dr. Ortiz and colleagues plan to evaluate the use of gold nanoparticles to more selectively target BCC during treatment with the 1,064-nm Nd:YAG laser. For now, she sees no downside of the procedure for proper candidates. “I do think that patients really like it,” she said. “It’s effective and easy.”
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
SAN DIEGO – After Arisa E. Ortiz, MD, and colleagues published results of a multicenter study reporting that one treatment with the long-pulsed 1,064-nm Nd:YAG laser cleared nonaggressive basal cell carcinoma (BCC) on the trunk and extremities in 90% of patients, she heard from colleagues who were skeptical of the approach.
Maybe it’s just the biopsy alone that’s clearing these tumors, some told her. Others postulated that since the energy was delivered with a 5- to 6-mm spot size at a fluence of 125-140 J/cm2 and a 7- to 10-ms pulse duration, bulk heating likely disrupted the tumors. However, treatments were generally well tolerated, required no anesthesia, and caused no significant adverse events.
“It’s almost scarless,” Dr. Ortiz, director of laser and cosmetic dermatology at the University of California, San Diego, said at the annual Masters of Aesthetics Symposium. “Sometimes the treatment does leave a mark, but I think the scars are always acceptable. We do have good histologic evidence that we can penetrate 2.15 mm, which is a lot deeper than what the pulsed-dye laser or other superficial wavelengths are able to penetrate.”
Data is well powered to reject the null hypothesis that laser treatment does not have an effect on nodular and superficial BCC lesions, she continued, noting that it is at least comparable if not superior with clearance rates reported for methyl aminolevulinate–PDT (73%), imiquimod cream (83%), and fluorouracil cream (80%). “Maybe we’re not specifically targeting the vasculature [with this approach], but we did some optical coherence tomography imaging and saw that the blood vessels in the tumor were coagulated while the vasculature in the surrounding normal skin were spared,” said Dr. Ortiz, who is also vice president of the American Society for Laser Medicine and Surgery.
In a more recent analysis, she and her colleagues retrospectively analyzed long-term outcomes in 11 patients with BCC who had 16 lesions treated with the 1,064-nm Nd:YAG laser. At a mean of 9 months, 100% of lesions remained clear as determined by clinical observation.
In a subsequent, as yet unpublished study, she and her collaborators followed 34 patients with BCC one year following laser treatment. “Of these, 33 had no recurrence at 1-year follow-up,” Dr. Ortiz said, noting that the one patient with a recurrence was on a biologic agent for Crohn’s disease.
One key advantage of using the long-pulsed 1,064-nm Nd:YAG laser for nonaggressive BCC is the potential for one treatment visit. “They don’t have to come back for suture removal,” she said. “It’s a quick procedure, takes only about 5 minutes. There’s no limitation on activity and there’s minimal wound care, light ointment, and a band-aid; that’s it.”
In addition, she said, there is a lower risk of complications, infections, and bleeding, and there is minimal scarring. It is “also an alternative for treating patients with multiple tumors or those who are poor surgical candidates, such as the elderly and those with Gorlin syndrome.”
Dr. Ortiz avoids treating aggressive subtypes “because we don’t know what margin to treat,” she added. “Avoid the face. I do make some exceptions for patients if they’re elderly or if they’ve had multiple tumors. Monitor for recurrence like you would using any other modality.”
She uses lidocaine without epinephrine to avoid vasoconstriction and treats with the 1,064-nm Nd:YAG laser as follows: a 5-mm spot size, a fluence of 140 J/cm2, and a pulse duration of 8 ms, with no cooling, which are the settings for the Excel V Laser System, she noted. “If you’re using a different Nd:YAG laser, your pulse duration may vary. I do let the device cool in between pulses to avoid bulk heating.”
The immediate endpoint to strive for is slight greying and slight contraction, and the procedure is covered by insurance, billed as malignant destruction/EDC (CPT codes 17260-17266 trunk and 17280-17283 face). “I do biopsy prior to treatment,” she said. “I like the biopsy to be healed when I’m using the laser, so I’ll treat them about a month later.”
As for future directions, Dr. Ortiz and colleagues plan to evaluate the use of gold nanoparticles to more selectively target BCC during treatment with the 1,064-nm Nd:YAG laser. For now, she sees no downside of the procedure for proper candidates. “I do think that patients really like it,” she said. “It’s effective and easy.”
Dr. Ortiz disclosed having financial relationships with several pharmaceutical and device companies. She is also cochair of the MOAS.
AT MOAS 2022
Do biologics protect against cancer progression in IBD?
in an observational study conducted in Japan.
IBD-associated intestinal cancer is thought to be caused by chronic inflammation of the intestinal mucosa, and controlling inflammation is thought to be effective in reducing cancer risk.
It’s generally considered that biologics do not change the risk of cancer, and whether they lower the risk remains unclear, write Ryo Seishima, MD, PhD, with Keio University in Tokyo, and colleagues. However, few studies have focused on cancer progression, namely, the risk of advanced-stage cancer.
To investigate, researchers reviewed the medical records of 828 patients with UC and 214 with CD who were diagnosed with IBD-associated intestinal neoplasia (dysplasia or cancer) from 1983 to 2020.
Therapeutic agents taken within 1 year before neoplasia diagnosis were classified into three types: biologics (infliximab, vedolizumab, golimumab, and adalimumab), 5-aminosalicylic acid (5-ASA), and immunomodulators.
The primary endpoint was the pathologic cancer stage at the time of diagnosis. Early-stage cancer was defined as either dysplasia or pathologic stage 0/I cancer, and advanced-stage cancer was defined as pathologic stage II/III/IV cancer.
Advanced-stage cancer was found in 297 patients (35.9%) with UC and 159 patients (74.3%) with CD.
The researchers say the higher percentage of advanced cancer in patients with CD rather than in patients with UC may suggest that regular surveillance was not effective for patients with CD or that physicians were less adherent to surveillance intervals. This question merits further study, they suggest.
None of the drug types were significantly associated with cancer stage in the CD cohort, they report.
Benefits seen in UC
In the UC cohort, advanced-stage cancer (vs. early-stage) was significantly associated with less use of biologics (2% vs. 7.7%; P < .001), 5-ASA (75.4% vs. 87.6%; P < .001), and immunomodulators (11.8% vs. 22.4%; P < .001). Steroid use was also significantly lower in the advanced-stage cancer group (26.3% vs. 33.3%; P = .035).
In multivariate analysis that was adjusted for age, diagnosis year, regular surveillance, and histologic type in UC, biologics (odds ratio, 0.11; P < .001) and 5-ASA (OR, 0.63; P = .041) were significantly associated with a lower risk of advanced-stage cancer.
The study was published online in The American Journal of Gastroenterology.
“These results indicate that biologics and 5-ASA are drugs that are potentially associated with a lower risk of advanced cancer in patients with UC but not with CD,” Dr. Seishima and colleagues say.
They also suggest that the mechanism of cancer progression in UC and CD may differ and needs to be investigated further.
Reassuring data with caveats
The study is “interesting and reassuring, but there are a lot of limitations with the study design,” said Ashwin Ananthakrishnan, MD, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in the research.
“By focusing only on those who have been diagnosed with cancer, one cannot actually conclude what the risk of cancer is and if these medications reduce the risk of colon cancer, which is a far more important and interesting question,” he said.
Patients undergoing treatment with biologics likely receive closer follow-up, so in these patients, cancers are less likely to be diagnosed at an advanced stage, said Dr. Ananthakrishnan. For that reason, the study can’t clearly establish the degree to which the effect was from medication or surveillance, he added.
As for whether biologics affect the overall risk of cancer development, the study doesn’t change “current thinking that biologics are safe in this setting,” he added.
Erin Forster, MD, MPH, with the Medical University of South Carolina, Charleston, also weighed in on medication safety.
“Prior research has shown that the risk of uncontrolled inflammation outweighs the risk of our current medications,” Dr. Forster, who was not involved in the research, said in an interview.
The study had no specific funding. Dr. Seishima, Dr. Ananthakrishnan, and Dr. Forster have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in an observational study conducted in Japan.
IBD-associated intestinal cancer is thought to be caused by chronic inflammation of the intestinal mucosa, and controlling inflammation is thought to be effective in reducing cancer risk.
It’s generally considered that biologics do not change the risk of cancer, and whether they lower the risk remains unclear, write Ryo Seishima, MD, PhD, with Keio University in Tokyo, and colleagues. However, few studies have focused on cancer progression, namely, the risk of advanced-stage cancer.
To investigate, researchers reviewed the medical records of 828 patients with UC and 214 with CD who were diagnosed with IBD-associated intestinal neoplasia (dysplasia or cancer) from 1983 to 2020.
Therapeutic agents taken within 1 year before neoplasia diagnosis were classified into three types: biologics (infliximab, vedolizumab, golimumab, and adalimumab), 5-aminosalicylic acid (5-ASA), and immunomodulators.
The primary endpoint was the pathologic cancer stage at the time of diagnosis. Early-stage cancer was defined as either dysplasia or pathologic stage 0/I cancer, and advanced-stage cancer was defined as pathologic stage II/III/IV cancer.
Advanced-stage cancer was found in 297 patients (35.9%) with UC and 159 patients (74.3%) with CD.
The researchers say the higher percentage of advanced cancer in patients with CD rather than in patients with UC may suggest that regular surveillance was not effective for patients with CD or that physicians were less adherent to surveillance intervals. This question merits further study, they suggest.
None of the drug types were significantly associated with cancer stage in the CD cohort, they report.
Benefits seen in UC
In the UC cohort, advanced-stage cancer (vs. early-stage) was significantly associated with less use of biologics (2% vs. 7.7%; P < .001), 5-ASA (75.4% vs. 87.6%; P < .001), and immunomodulators (11.8% vs. 22.4%; P < .001). Steroid use was also significantly lower in the advanced-stage cancer group (26.3% vs. 33.3%; P = .035).
In multivariate analysis that was adjusted for age, diagnosis year, regular surveillance, and histologic type in UC, biologics (odds ratio, 0.11; P < .001) and 5-ASA (OR, 0.63; P = .041) were significantly associated with a lower risk of advanced-stage cancer.
The study was published online in The American Journal of Gastroenterology.
“These results indicate that biologics and 5-ASA are drugs that are potentially associated with a lower risk of advanced cancer in patients with UC but not with CD,” Dr. Seishima and colleagues say.
They also suggest that the mechanism of cancer progression in UC and CD may differ and needs to be investigated further.
Reassuring data with caveats
The study is “interesting and reassuring, but there are a lot of limitations with the study design,” said Ashwin Ananthakrishnan, MD, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in the research.
“By focusing only on those who have been diagnosed with cancer, one cannot actually conclude what the risk of cancer is and if these medications reduce the risk of colon cancer, which is a far more important and interesting question,” he said.
Patients undergoing treatment with biologics likely receive closer follow-up, so in these patients, cancers are less likely to be diagnosed at an advanced stage, said Dr. Ananthakrishnan. For that reason, the study can’t clearly establish the degree to which the effect was from medication or surveillance, he added.
As for whether biologics affect the overall risk of cancer development, the study doesn’t change “current thinking that biologics are safe in this setting,” he added.
Erin Forster, MD, MPH, with the Medical University of South Carolina, Charleston, also weighed in on medication safety.
“Prior research has shown that the risk of uncontrolled inflammation outweighs the risk of our current medications,” Dr. Forster, who was not involved in the research, said in an interview.
The study had no specific funding. Dr. Seishima, Dr. Ananthakrishnan, and Dr. Forster have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in an observational study conducted in Japan.
IBD-associated intestinal cancer is thought to be caused by chronic inflammation of the intestinal mucosa, and controlling inflammation is thought to be effective in reducing cancer risk.
It’s generally considered that biologics do not change the risk of cancer, and whether they lower the risk remains unclear, write Ryo Seishima, MD, PhD, with Keio University in Tokyo, and colleagues. However, few studies have focused on cancer progression, namely, the risk of advanced-stage cancer.
To investigate, researchers reviewed the medical records of 828 patients with UC and 214 with CD who were diagnosed with IBD-associated intestinal neoplasia (dysplasia or cancer) from 1983 to 2020.
Therapeutic agents taken within 1 year before neoplasia diagnosis were classified into three types: biologics (infliximab, vedolizumab, golimumab, and adalimumab), 5-aminosalicylic acid (5-ASA), and immunomodulators.
The primary endpoint was the pathologic cancer stage at the time of diagnosis. Early-stage cancer was defined as either dysplasia or pathologic stage 0/I cancer, and advanced-stage cancer was defined as pathologic stage II/III/IV cancer.
Advanced-stage cancer was found in 297 patients (35.9%) with UC and 159 patients (74.3%) with CD.
The researchers say the higher percentage of advanced cancer in patients with CD rather than in patients with UC may suggest that regular surveillance was not effective for patients with CD or that physicians were less adherent to surveillance intervals. This question merits further study, they suggest.
None of the drug types were significantly associated with cancer stage in the CD cohort, they report.
Benefits seen in UC
In the UC cohort, advanced-stage cancer (vs. early-stage) was significantly associated with less use of biologics (2% vs. 7.7%; P < .001), 5-ASA (75.4% vs. 87.6%; P < .001), and immunomodulators (11.8% vs. 22.4%; P < .001). Steroid use was also significantly lower in the advanced-stage cancer group (26.3% vs. 33.3%; P = .035).
In multivariate analysis that was adjusted for age, diagnosis year, regular surveillance, and histologic type in UC, biologics (odds ratio, 0.11; P < .001) and 5-ASA (OR, 0.63; P = .041) were significantly associated with a lower risk of advanced-stage cancer.
The study was published online in The American Journal of Gastroenterology.
“These results indicate that biologics and 5-ASA are drugs that are potentially associated with a lower risk of advanced cancer in patients with UC but not with CD,” Dr. Seishima and colleagues say.
They also suggest that the mechanism of cancer progression in UC and CD may differ and needs to be investigated further.
Reassuring data with caveats
The study is “interesting and reassuring, but there are a lot of limitations with the study design,” said Ashwin Ananthakrishnan, MD, MPH, with Massachusetts General Hospital and Harvard Medical School in Boston, who was not involved in the research.
“By focusing only on those who have been diagnosed with cancer, one cannot actually conclude what the risk of cancer is and if these medications reduce the risk of colon cancer, which is a far more important and interesting question,” he said.
Patients undergoing treatment with biologics likely receive closer follow-up, so in these patients, cancers are less likely to be diagnosed at an advanced stage, said Dr. Ananthakrishnan. For that reason, the study can’t clearly establish the degree to which the effect was from medication or surveillance, he added.
As for whether biologics affect the overall risk of cancer development, the study doesn’t change “current thinking that biologics are safe in this setting,” he added.
Erin Forster, MD, MPH, with the Medical University of South Carolina, Charleston, also weighed in on medication safety.
“Prior research has shown that the risk of uncontrolled inflammation outweighs the risk of our current medications,” Dr. Forster, who was not involved in the research, said in an interview.
The study had no specific funding. Dr. Seishima, Dr. Ananthakrishnan, and Dr. Forster have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Age-related atopic dermatitis phenotypes evaluated in study
, while older adults tend to present with less flexural eczema and the fewest associated signs.
Those are key findings from a study conducted at a single academic medical center, which aimed to identify the age-related clinical phenotypes of AD.
“Previous studies have found differences in the clinical characteristics of AD depending on age of AD onset, ethnic background, and AD severity,” senior author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the department of dermatology at George Washington University, Washington, and his coauthor wrote in the study, which was published online in JAAD International. “However, none have prospectively compared the clinical characteristics and associated signs by age group. Improved understanding of the clinical phenotypes of AD may help guide choice of treatment and improve health outcomes,” they added.
Along with coauthor Sheena Chatrath, a dermatology research fellow in the department, Dr. Silverberg prospectively reviewed self-reported questionnaires that were completed by 380 patients prior to their visit at GWU’s eczema clinic between 2013 and 2019. Questions included age of AD onset, sociodemographics, Visual Analog Scale (VAS) itch and sleep for Scoring AD, and Numeric Rating Scale (NRS) for skin pain and itch. The researchers used the Eczema Area Severity Index to assess AD severity and a dermatologist conducted full body skin exams, noting the distribution of AD involvement as well as associated signs.
Of the 380 patients, 6.1% were younger than aged 18 years, 46.3% were young adults aged 18-39 years, and 47.6% were older adults 40 years of age and older.
Compared with pediatric patients, both young and older adults were less likely to experience AD on the ankles (adjusted odds ratio [aOR], 0.41 and 0.43, respectively), moderate to severe AD lesions on flexures (aOR, 0.47 and 0.30), pityriasis alba (aOR, 0.24 and 0.07), oozing lesions (aOR, 0.44 and 0.35), and moderate to severe excoriations (aOR, 0.49 and 0.44).
In children, severe itch was more common, reported in 47.1%, compared with 43.4% of the young adults and 38.6% of the older adults, and itch was less severe among the young and older adults. “Interestingly, despite increased itch in pediatric patients, we found no difference in the severity of skin pain across all age groups,” the researchers wrote. “Moreover, pediatric patients reported skin pain less often than adult patients. This may be due to age-related differences of pain perception.”
In other findings, compared with pediatric patients, young adults were more likely to experience AD around the eyes (aOR, 2.92), while older adults were less likely to experience AD on elbows (aOR, 0.34), nipples (aOR, 0.40), knees (aOR, 0.27), and less likely to have keratosis pilaris (aOR, 0.38), and lichenification (aOR, 0.47).
Dr. Silverberg and Ms. Chatrath used latent class analysis to identify four classes for distribution of AD lesions. In this model, class 1 had low probabilities of AD involvement at all sites examined and class 2 had low probabilities of scalp, face, and foot involvement, and intermediate probability of all other AD sites. Class 3 had low probabilities of hand and foot involvement, high probability of facial erythema, and intermediate probability of all other AD signs, while class 4 had intermediate probability of postauricular and foot involvement, and high probability of all other AD sites examined.
“Pediatric patients were most commonly in class 4 (33.3%), followed by class 1 and 2 (26.7%), and least commonly in class 3 (13.3%),” the authors wrote. “In young adults, class 4 and 1 were most common (32.4% and 29.4%), followed by class 2 (27.9%), and least commonly class 3 (10.3%). In older adults, class 1 was most common (40.3%), followed by class 4 (23.6%), and least commonly classes 2 and 3 (18.1%).”
The researchers also used latent class analysis to identify four classes for the signs and symptoms of AD. In this model, class 1 had zero-low probability of all AD signs and class 2 had low probability of all AD signs. Class 3 had high probability of oozing lesions and low probability of all other signs, while class 4 had high probability of xerosis, intermediate probability of ichthyosis and palmar hyperlinearity, and low probability of all other AD signs.
In all three groups, the most common class was class 1 (85.6% of older adults, 81.8% of younger adults, and 82.6% of pediatric patients). Among the pediatric patients, they wrote, “class 3 was the second most common (8.7%), followed by class 2 and 4 (4.4%).” Among the young adults, 9.7% were in class 2, 5.7% were in class 4, and 2.8% were in class 3; and among the older adults, 8.3% were in class 4, 4.4% were in class 2, and 1.67% were in class 3.
Zelma Chiesa Fuxench, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, who was asked to comment on the study, said that while AD is traditionally largely thought of as a disease of children primarily involving the flexural areas, “this study provides additional evidence to support that AD is more than just a disease of childhood with a fixed clinical presentation, but is a heterogeneous disease whose clinical presentation varies across different population groups.”
While the study provides insight into the clinical differences that may be observed across AD groups, “care must be taken when interpreting these results as the study was done in a single center with observations collected during one single visit,” she added. “AD is not a ‘static’ disease; its presentation can stay the same in one patient but can vary even in another patient throughout their lifetime. Therefore, studies of a more prospective nature that evaluate the change in clinical presentation using multiple measures throughout time in these individuals would be a step forward to better understand if these phenotypic differences truly exist and, as such, what implications could they have for treatment selection.”
This study was supported by grants from the Agency for Healthcare Research and Quality and the Dermatology Foundation. The researchers reported having no disclosures. Dr. Chiesa Fuxench disclosed serving as a consultant for the Asthma and Allergy Foundation of America, National Eczema Association, Pfizer, AbbVie, and Incyte, for which she has received honoraria for AD-related work. She is the recipient of research grants through Regeneron, Sanofi, Tioga, Vanda, Menlo Therapeutics, Leo Pharma, and Eli Lilly for work related to AD as well as honoraria for continuing medical education work related to AD sponsored through educational grants from Regeneron/Sanofi and Pfizer.
, while older adults tend to present with less flexural eczema and the fewest associated signs.
Those are key findings from a study conducted at a single academic medical center, which aimed to identify the age-related clinical phenotypes of AD.
“Previous studies have found differences in the clinical characteristics of AD depending on age of AD onset, ethnic background, and AD severity,” senior author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the department of dermatology at George Washington University, Washington, and his coauthor wrote in the study, which was published online in JAAD International. “However, none have prospectively compared the clinical characteristics and associated signs by age group. Improved understanding of the clinical phenotypes of AD may help guide choice of treatment and improve health outcomes,” they added.
Along with coauthor Sheena Chatrath, a dermatology research fellow in the department, Dr. Silverberg prospectively reviewed self-reported questionnaires that were completed by 380 patients prior to their visit at GWU’s eczema clinic between 2013 and 2019. Questions included age of AD onset, sociodemographics, Visual Analog Scale (VAS) itch and sleep for Scoring AD, and Numeric Rating Scale (NRS) for skin pain and itch. The researchers used the Eczema Area Severity Index to assess AD severity and a dermatologist conducted full body skin exams, noting the distribution of AD involvement as well as associated signs.
Of the 380 patients, 6.1% were younger than aged 18 years, 46.3% were young adults aged 18-39 years, and 47.6% were older adults 40 years of age and older.
Compared with pediatric patients, both young and older adults were less likely to experience AD on the ankles (adjusted odds ratio [aOR], 0.41 and 0.43, respectively), moderate to severe AD lesions on flexures (aOR, 0.47 and 0.30), pityriasis alba (aOR, 0.24 and 0.07), oozing lesions (aOR, 0.44 and 0.35), and moderate to severe excoriations (aOR, 0.49 and 0.44).
In children, severe itch was more common, reported in 47.1%, compared with 43.4% of the young adults and 38.6% of the older adults, and itch was less severe among the young and older adults. “Interestingly, despite increased itch in pediatric patients, we found no difference in the severity of skin pain across all age groups,” the researchers wrote. “Moreover, pediatric patients reported skin pain less often than adult patients. This may be due to age-related differences of pain perception.”
In other findings, compared with pediatric patients, young adults were more likely to experience AD around the eyes (aOR, 2.92), while older adults were less likely to experience AD on elbows (aOR, 0.34), nipples (aOR, 0.40), knees (aOR, 0.27), and less likely to have keratosis pilaris (aOR, 0.38), and lichenification (aOR, 0.47).
Dr. Silverberg and Ms. Chatrath used latent class analysis to identify four classes for distribution of AD lesions. In this model, class 1 had low probabilities of AD involvement at all sites examined and class 2 had low probabilities of scalp, face, and foot involvement, and intermediate probability of all other AD sites. Class 3 had low probabilities of hand and foot involvement, high probability of facial erythema, and intermediate probability of all other AD signs, while class 4 had intermediate probability of postauricular and foot involvement, and high probability of all other AD sites examined.
“Pediatric patients were most commonly in class 4 (33.3%), followed by class 1 and 2 (26.7%), and least commonly in class 3 (13.3%),” the authors wrote. “In young adults, class 4 and 1 were most common (32.4% and 29.4%), followed by class 2 (27.9%), and least commonly class 3 (10.3%). In older adults, class 1 was most common (40.3%), followed by class 4 (23.6%), and least commonly classes 2 and 3 (18.1%).”
The researchers also used latent class analysis to identify four classes for the signs and symptoms of AD. In this model, class 1 had zero-low probability of all AD signs and class 2 had low probability of all AD signs. Class 3 had high probability of oozing lesions and low probability of all other signs, while class 4 had high probability of xerosis, intermediate probability of ichthyosis and palmar hyperlinearity, and low probability of all other AD signs.
In all three groups, the most common class was class 1 (85.6% of older adults, 81.8% of younger adults, and 82.6% of pediatric patients). Among the pediatric patients, they wrote, “class 3 was the second most common (8.7%), followed by class 2 and 4 (4.4%).” Among the young adults, 9.7% were in class 2, 5.7% were in class 4, and 2.8% were in class 3; and among the older adults, 8.3% were in class 4, 4.4% were in class 2, and 1.67% were in class 3.
Zelma Chiesa Fuxench, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, who was asked to comment on the study, said that while AD is traditionally largely thought of as a disease of children primarily involving the flexural areas, “this study provides additional evidence to support that AD is more than just a disease of childhood with a fixed clinical presentation, but is a heterogeneous disease whose clinical presentation varies across different population groups.”
While the study provides insight into the clinical differences that may be observed across AD groups, “care must be taken when interpreting these results as the study was done in a single center with observations collected during one single visit,” she added. “AD is not a ‘static’ disease; its presentation can stay the same in one patient but can vary even in another patient throughout their lifetime. Therefore, studies of a more prospective nature that evaluate the change in clinical presentation using multiple measures throughout time in these individuals would be a step forward to better understand if these phenotypic differences truly exist and, as such, what implications could they have for treatment selection.”
This study was supported by grants from the Agency for Healthcare Research and Quality and the Dermatology Foundation. The researchers reported having no disclosures. Dr. Chiesa Fuxench disclosed serving as a consultant for the Asthma and Allergy Foundation of America, National Eczema Association, Pfizer, AbbVie, and Incyte, for which she has received honoraria for AD-related work. She is the recipient of research grants through Regeneron, Sanofi, Tioga, Vanda, Menlo Therapeutics, Leo Pharma, and Eli Lilly for work related to AD as well as honoraria for continuing medical education work related to AD sponsored through educational grants from Regeneron/Sanofi and Pfizer.
, while older adults tend to present with less flexural eczema and the fewest associated signs.
Those are key findings from a study conducted at a single academic medical center, which aimed to identify the age-related clinical phenotypes of AD.
“Previous studies have found differences in the clinical characteristics of AD depending on age of AD onset, ethnic background, and AD severity,” senior author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the department of dermatology at George Washington University, Washington, and his coauthor wrote in the study, which was published online in JAAD International. “However, none have prospectively compared the clinical characteristics and associated signs by age group. Improved understanding of the clinical phenotypes of AD may help guide choice of treatment and improve health outcomes,” they added.
Along with coauthor Sheena Chatrath, a dermatology research fellow in the department, Dr. Silverberg prospectively reviewed self-reported questionnaires that were completed by 380 patients prior to their visit at GWU’s eczema clinic between 2013 and 2019. Questions included age of AD onset, sociodemographics, Visual Analog Scale (VAS) itch and sleep for Scoring AD, and Numeric Rating Scale (NRS) for skin pain and itch. The researchers used the Eczema Area Severity Index to assess AD severity and a dermatologist conducted full body skin exams, noting the distribution of AD involvement as well as associated signs.
Of the 380 patients, 6.1% were younger than aged 18 years, 46.3% were young adults aged 18-39 years, and 47.6% were older adults 40 years of age and older.
Compared with pediatric patients, both young and older adults were less likely to experience AD on the ankles (adjusted odds ratio [aOR], 0.41 and 0.43, respectively), moderate to severe AD lesions on flexures (aOR, 0.47 and 0.30), pityriasis alba (aOR, 0.24 and 0.07), oozing lesions (aOR, 0.44 and 0.35), and moderate to severe excoriations (aOR, 0.49 and 0.44).
In children, severe itch was more common, reported in 47.1%, compared with 43.4% of the young adults and 38.6% of the older adults, and itch was less severe among the young and older adults. “Interestingly, despite increased itch in pediatric patients, we found no difference in the severity of skin pain across all age groups,” the researchers wrote. “Moreover, pediatric patients reported skin pain less often than adult patients. This may be due to age-related differences of pain perception.”
In other findings, compared with pediatric patients, young adults were more likely to experience AD around the eyes (aOR, 2.92), while older adults were less likely to experience AD on elbows (aOR, 0.34), nipples (aOR, 0.40), knees (aOR, 0.27), and less likely to have keratosis pilaris (aOR, 0.38), and lichenification (aOR, 0.47).
Dr. Silverberg and Ms. Chatrath used latent class analysis to identify four classes for distribution of AD lesions. In this model, class 1 had low probabilities of AD involvement at all sites examined and class 2 had low probabilities of scalp, face, and foot involvement, and intermediate probability of all other AD sites. Class 3 had low probabilities of hand and foot involvement, high probability of facial erythema, and intermediate probability of all other AD signs, while class 4 had intermediate probability of postauricular and foot involvement, and high probability of all other AD sites examined.
“Pediatric patients were most commonly in class 4 (33.3%), followed by class 1 and 2 (26.7%), and least commonly in class 3 (13.3%),” the authors wrote. “In young adults, class 4 and 1 were most common (32.4% and 29.4%), followed by class 2 (27.9%), and least commonly class 3 (10.3%). In older adults, class 1 was most common (40.3%), followed by class 4 (23.6%), and least commonly classes 2 and 3 (18.1%).”
The researchers also used latent class analysis to identify four classes for the signs and symptoms of AD. In this model, class 1 had zero-low probability of all AD signs and class 2 had low probability of all AD signs. Class 3 had high probability of oozing lesions and low probability of all other signs, while class 4 had high probability of xerosis, intermediate probability of ichthyosis and palmar hyperlinearity, and low probability of all other AD signs.
In all three groups, the most common class was class 1 (85.6% of older adults, 81.8% of younger adults, and 82.6% of pediatric patients). Among the pediatric patients, they wrote, “class 3 was the second most common (8.7%), followed by class 2 and 4 (4.4%).” Among the young adults, 9.7% were in class 2, 5.7% were in class 4, and 2.8% were in class 3; and among the older adults, 8.3% were in class 4, 4.4% were in class 2, and 1.67% were in class 3.
Zelma Chiesa Fuxench, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, who was asked to comment on the study, said that while AD is traditionally largely thought of as a disease of children primarily involving the flexural areas, “this study provides additional evidence to support that AD is more than just a disease of childhood with a fixed clinical presentation, but is a heterogeneous disease whose clinical presentation varies across different population groups.”
While the study provides insight into the clinical differences that may be observed across AD groups, “care must be taken when interpreting these results as the study was done in a single center with observations collected during one single visit,” she added. “AD is not a ‘static’ disease; its presentation can stay the same in one patient but can vary even in another patient throughout their lifetime. Therefore, studies of a more prospective nature that evaluate the change in clinical presentation using multiple measures throughout time in these individuals would be a step forward to better understand if these phenotypic differences truly exist and, as such, what implications could they have for treatment selection.”
This study was supported by grants from the Agency for Healthcare Research and Quality and the Dermatology Foundation. The researchers reported having no disclosures. Dr. Chiesa Fuxench disclosed serving as a consultant for the Asthma and Allergy Foundation of America, National Eczema Association, Pfizer, AbbVie, and Incyte, for which she has received honoraria for AD-related work. She is the recipient of research grants through Regeneron, Sanofi, Tioga, Vanda, Menlo Therapeutics, Leo Pharma, and Eli Lilly for work related to AD as well as honoraria for continuing medical education work related to AD sponsored through educational grants from Regeneron/Sanofi and Pfizer.
FROM JAAD INTERNATIONAL











