User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
‘Forever chemicals’ up type 2 diabetes risk in midlife White women
Middle-aged White women who had higher levels of some breakdown products of phthalates – a class of endocrine disrupting chemicals (EDCs), or “forever chemicals,” that act as plasticizers – had a significantly greater risk of developing type 2 diabetes over a 6-year period compared with other similar women.
However, this association was not seen among Black or Asian middle-aged women.
These findings from the Study of Women’s Health Across the Nation – Multipollutant Study (SWAN-MPS), by Mia Q. Peng, PhD, MPH, and colleagues, have been published online in the Journal of Clinical Endocrinology & Metabolism.
“Overall, our study has added some evidence to support the potential diabetogenic effects of phthalates, but it also highlights that much is still unknown about the metabolic effects of these chemicals,” the group noted.
“The apparent racial/ethnic differences in the associations between phthalates and incident diabetes should be investigated in future studies,” they cautioned.
Recruiting younger participants and observing them longer, they suggested, “will also help us understand the effects of phthalates on different stages of the diabetogenic process, including whether body fat gain is an important mediator.”
Phthalates are all around us
Low-molecular-weight phthalates are frequently added to personal care products, such as fragrance, nail polish, and some feminine hygiene products, as solvents, plasticizers, and fixatives, the researchers explained.
And high-molecular-weight phthalates are frequently added to polyvinyl chloride plastic products, such as plastic food packaging, clothing, and vinyl flooring, as plasticizers.
Phthalates have been hypothesized to contribute to the development of diabetes, but longitudinal evidence in humans was limited.
“Given widespread exposure to phthalates and the enormous costs of diabetes to individuals and societies, ongoing investments in the research on phthalates’ metabolic effects are warranted,” the researchers concluded.
Racial differences in phthalates and incident diabetes
“A new finding is that we observed some phthalates are associated with a higher risk of diabetes development, especially in White women [that] were not seen in Black or Asian women,” senior author Sung Kyun Park, ScD, MPH, of the University of Michigan, Ann Arbor, told this news organization.
“We were surprised to see the racial/ethnic differences,” added Dr. Peng, formerly of the University of Michigan and now at Lifecourse Epidemiology of Adiposity and Diabetes Center, University of Colorado Anschutz Medical Campus.
A possible explanation is that “compared to White women, Black women develop diabetes at a younger age and are exposed to higher levels of several phthalates,” and this study excluded women who already had diabetes by midlife, she noted.
“Although our study was conducted in a cohort of women,” Dr. Park stressed, “we hope that our findings are not interpreted that only women should be concerned of phthalates. Our findings add to the current literature that phthalates may be a potential risk factor for type 2 diabetes.
“Certain phthalates are prohibited in children’s toys and child care articles,” Dr. Peng noted, as explained by the U.S. Consumer Product Safety Commission. In addition, a bill has been introduced in Congress to ban phthalates in food contact substances.
“If phthalates are removed from plastics and other consumer products,” she cautioned, “we do have to be careful in the process to avoid replacing them with some other potentially harmful chemicals.”
A well-known example of this type of “regrettable substitution,” Dr. Park added, “is ‘BPA-free’ plastics that replaced bisphenol A with other bisphenols such as bisphenol-F (BPF) or bisphenol-S (BPS). The product has a label of ‘BPA-free’, but those replaced chemicals turned out to be equally toxic. Science is slow to determine if a new chemical introduced to the market is safe and can replace a regulated chemical.”
And studies have shown that a diet rich in meat, fat, and ultraprocessed foods is associated with increased exposures to some phthalates, especially when the foods are obtained away from home, such as fast foods, Dr. Peng observed. In addition, some phthalates are added to personal care products such as fragrance.
“As a first step,” she said, “I think reducing consumption of ultraprocessed foods packaged in plastics may help reduce phthalate exposure.”
A 2020 report from the Endocrine Society and the International Pollutants Elimination Network (IPEN), titled, “Plastics, EDCs, and Health,” summarizes research on bisphenol A, per- and polyfluoroalkyl substances (PFAS), phthalates, and other EDCs that leach from plastics. The Endocrine Society website also has a link to a 2-page summary.
Levels of 12 phthalate metabolites
Previously, the researchers reported how another class of “forever chemicals,” PFAS, were associated with risk of hypertension in a 17-year follow-up of middle-aged women in the SWAN study.
In the current study, they analyzed data from 1,308 women in SWAN-MPS who had been recruited at five study sites (Oakland, Calif; Los Angeles; Detroit; Pittsburgh; and Boston).
The women were between ages 42 and 52 years in 1996-1997 and self-identified as White, Black, Chinese, or Japanese.
They did not have diabetes in 1999-2000 and had sufficient urine samples for phthalate assessment then and midway through a 6-year follow-up.
The women were a median age of 49 years in 1999-2000. About half were White, 20% were Black, 13% were Chinese, and 15% were Japanese.
Researchers analyzed levels of 12 metabolites, chosen because their parent phthalates have been widely used in industry and commerce, and exposure to these phthalates is a national biomonitoring priority.
The measured phthalates were:
Three metabolites of low-molecular-weight phthalates:
- mono-ethyl phthalate (MEP)
- mono-n-butyl phthalate (MnBP)
- mono-isobutyl phthalate (MiBP)
Four metabolites of the high-molecular-weight phthalate di(2-ethylhexyl) phthalate (DEHP), which is of particular public health interest:
- mono(2-ethylhexyl) phthalate (MEHP)
- mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP)
- mono(2-ethyl-5-oxohexyl) phthalate (MEOHP)
- mono(2-ethyl-5-carboxypentyl) phthalate (MECPP)
Five metabolites of other high-molecular-weight phthalates:
- monobenzyl phthalate (MBzP)
- monoisononyl phthalate (MiNP)
- mono-carboxyoctyl phthalate (MCOP)
- mono-carboxy-isononyl phthalate (MCNP)
- mono(3-carboxypropyl) phthalate (MCPP)
The researchers excluded MiNP from all analyses because it was detected in less than 1% of urine samples.
The different phthalate metabolites were detected in 84.8% of samples (MEHP) to 100% of samples (MnBP and MECPP).
Women who were younger, Black, current smokers, or obese generally had higher concentrations of phthalate metabolites.
Over 6 years, 61 women developed diabetes (an incidence rate of 8.1 per 1000 person-years).
Compared with other women, those with incident diabetes had significantly higher concentrations of all phthalate metabolites except DEHP metabolites and MCPP.
Phthalates were not associated with incident diabetes in Black or Asian women.
However, among White women, each doubling of the concentrations of MiBP, MBzP, MCOP, MCNP, and MCCP was associated with a 30% to 63% higher incidence of diabetes (HR 1.30 for MCNP; HR 1.63 for MiBP).
The SWAN study was supported by the National Institutes of Health, Department of Health & Human Services, National Institute on Aging, National Institute of Nursing Research, NIH Office of Research on Women’s Health, and SWAN Repository. The current study was supported by the National Center for Research Resources, National Center for Advancing Translational Sciences, NIH, National Institute of Environmental Health, and Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Dr. Peng was supported by an Interdisciplinary Research Training on Health and Aging grant from the NIA. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Middle-aged White women who had higher levels of some breakdown products of phthalates – a class of endocrine disrupting chemicals (EDCs), or “forever chemicals,” that act as plasticizers – had a significantly greater risk of developing type 2 diabetes over a 6-year period compared with other similar women.
However, this association was not seen among Black or Asian middle-aged women.
These findings from the Study of Women’s Health Across the Nation – Multipollutant Study (SWAN-MPS), by Mia Q. Peng, PhD, MPH, and colleagues, have been published online in the Journal of Clinical Endocrinology & Metabolism.
“Overall, our study has added some evidence to support the potential diabetogenic effects of phthalates, but it also highlights that much is still unknown about the metabolic effects of these chemicals,” the group noted.
“The apparent racial/ethnic differences in the associations between phthalates and incident diabetes should be investigated in future studies,” they cautioned.
Recruiting younger participants and observing them longer, they suggested, “will also help us understand the effects of phthalates on different stages of the diabetogenic process, including whether body fat gain is an important mediator.”
Phthalates are all around us
Low-molecular-weight phthalates are frequently added to personal care products, such as fragrance, nail polish, and some feminine hygiene products, as solvents, plasticizers, and fixatives, the researchers explained.
And high-molecular-weight phthalates are frequently added to polyvinyl chloride plastic products, such as plastic food packaging, clothing, and vinyl flooring, as plasticizers.
Phthalates have been hypothesized to contribute to the development of diabetes, but longitudinal evidence in humans was limited.
“Given widespread exposure to phthalates and the enormous costs of diabetes to individuals and societies, ongoing investments in the research on phthalates’ metabolic effects are warranted,” the researchers concluded.
Racial differences in phthalates and incident diabetes
“A new finding is that we observed some phthalates are associated with a higher risk of diabetes development, especially in White women [that] were not seen in Black or Asian women,” senior author Sung Kyun Park, ScD, MPH, of the University of Michigan, Ann Arbor, told this news organization.
“We were surprised to see the racial/ethnic differences,” added Dr. Peng, formerly of the University of Michigan and now at Lifecourse Epidemiology of Adiposity and Diabetes Center, University of Colorado Anschutz Medical Campus.
A possible explanation is that “compared to White women, Black women develop diabetes at a younger age and are exposed to higher levels of several phthalates,” and this study excluded women who already had diabetes by midlife, she noted.
“Although our study was conducted in a cohort of women,” Dr. Park stressed, “we hope that our findings are not interpreted that only women should be concerned of phthalates. Our findings add to the current literature that phthalates may be a potential risk factor for type 2 diabetes.
“Certain phthalates are prohibited in children’s toys and child care articles,” Dr. Peng noted, as explained by the U.S. Consumer Product Safety Commission. In addition, a bill has been introduced in Congress to ban phthalates in food contact substances.
“If phthalates are removed from plastics and other consumer products,” she cautioned, “we do have to be careful in the process to avoid replacing them with some other potentially harmful chemicals.”
A well-known example of this type of “regrettable substitution,” Dr. Park added, “is ‘BPA-free’ plastics that replaced bisphenol A with other bisphenols such as bisphenol-F (BPF) or bisphenol-S (BPS). The product has a label of ‘BPA-free’, but those replaced chemicals turned out to be equally toxic. Science is slow to determine if a new chemical introduced to the market is safe and can replace a regulated chemical.”
And studies have shown that a diet rich in meat, fat, and ultraprocessed foods is associated with increased exposures to some phthalates, especially when the foods are obtained away from home, such as fast foods, Dr. Peng observed. In addition, some phthalates are added to personal care products such as fragrance.
“As a first step,” she said, “I think reducing consumption of ultraprocessed foods packaged in plastics may help reduce phthalate exposure.”
A 2020 report from the Endocrine Society and the International Pollutants Elimination Network (IPEN), titled, “Plastics, EDCs, and Health,” summarizes research on bisphenol A, per- and polyfluoroalkyl substances (PFAS), phthalates, and other EDCs that leach from plastics. The Endocrine Society website also has a link to a 2-page summary.
Levels of 12 phthalate metabolites
Previously, the researchers reported how another class of “forever chemicals,” PFAS, were associated with risk of hypertension in a 17-year follow-up of middle-aged women in the SWAN study.
In the current study, they analyzed data from 1,308 women in SWAN-MPS who had been recruited at five study sites (Oakland, Calif; Los Angeles; Detroit; Pittsburgh; and Boston).
The women were between ages 42 and 52 years in 1996-1997 and self-identified as White, Black, Chinese, or Japanese.
They did not have diabetes in 1999-2000 and had sufficient urine samples for phthalate assessment then and midway through a 6-year follow-up.
The women were a median age of 49 years in 1999-2000. About half were White, 20% were Black, 13% were Chinese, and 15% were Japanese.
Researchers analyzed levels of 12 metabolites, chosen because their parent phthalates have been widely used in industry and commerce, and exposure to these phthalates is a national biomonitoring priority.
The measured phthalates were:
Three metabolites of low-molecular-weight phthalates:
- mono-ethyl phthalate (MEP)
- mono-n-butyl phthalate (MnBP)
- mono-isobutyl phthalate (MiBP)
Four metabolites of the high-molecular-weight phthalate di(2-ethylhexyl) phthalate (DEHP), which is of particular public health interest:
- mono(2-ethylhexyl) phthalate (MEHP)
- mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP)
- mono(2-ethyl-5-oxohexyl) phthalate (MEOHP)
- mono(2-ethyl-5-carboxypentyl) phthalate (MECPP)
Five metabolites of other high-molecular-weight phthalates:
- monobenzyl phthalate (MBzP)
- monoisononyl phthalate (MiNP)
- mono-carboxyoctyl phthalate (MCOP)
- mono-carboxy-isononyl phthalate (MCNP)
- mono(3-carboxypropyl) phthalate (MCPP)
The researchers excluded MiNP from all analyses because it was detected in less than 1% of urine samples.
The different phthalate metabolites were detected in 84.8% of samples (MEHP) to 100% of samples (MnBP and MECPP).
Women who were younger, Black, current smokers, or obese generally had higher concentrations of phthalate metabolites.
Over 6 years, 61 women developed diabetes (an incidence rate of 8.1 per 1000 person-years).
Compared with other women, those with incident diabetes had significantly higher concentrations of all phthalate metabolites except DEHP metabolites and MCPP.
Phthalates were not associated with incident diabetes in Black or Asian women.
However, among White women, each doubling of the concentrations of MiBP, MBzP, MCOP, MCNP, and MCCP was associated with a 30% to 63% higher incidence of diabetes (HR 1.30 for MCNP; HR 1.63 for MiBP).
The SWAN study was supported by the National Institutes of Health, Department of Health & Human Services, National Institute on Aging, National Institute of Nursing Research, NIH Office of Research on Women’s Health, and SWAN Repository. The current study was supported by the National Center for Research Resources, National Center for Advancing Translational Sciences, NIH, National Institute of Environmental Health, and Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Dr. Peng was supported by an Interdisciplinary Research Training on Health and Aging grant from the NIA. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Middle-aged White women who had higher levels of some breakdown products of phthalates – a class of endocrine disrupting chemicals (EDCs), or “forever chemicals,” that act as plasticizers – had a significantly greater risk of developing type 2 diabetes over a 6-year period compared with other similar women.
However, this association was not seen among Black or Asian middle-aged women.
These findings from the Study of Women’s Health Across the Nation – Multipollutant Study (SWAN-MPS), by Mia Q. Peng, PhD, MPH, and colleagues, have been published online in the Journal of Clinical Endocrinology & Metabolism.
“Overall, our study has added some evidence to support the potential diabetogenic effects of phthalates, but it also highlights that much is still unknown about the metabolic effects of these chemicals,” the group noted.
“The apparent racial/ethnic differences in the associations between phthalates and incident diabetes should be investigated in future studies,” they cautioned.
Recruiting younger participants and observing them longer, they suggested, “will also help us understand the effects of phthalates on different stages of the diabetogenic process, including whether body fat gain is an important mediator.”
Phthalates are all around us
Low-molecular-weight phthalates are frequently added to personal care products, such as fragrance, nail polish, and some feminine hygiene products, as solvents, plasticizers, and fixatives, the researchers explained.
And high-molecular-weight phthalates are frequently added to polyvinyl chloride plastic products, such as plastic food packaging, clothing, and vinyl flooring, as plasticizers.
Phthalates have been hypothesized to contribute to the development of diabetes, but longitudinal evidence in humans was limited.
“Given widespread exposure to phthalates and the enormous costs of diabetes to individuals and societies, ongoing investments in the research on phthalates’ metabolic effects are warranted,” the researchers concluded.
Racial differences in phthalates and incident diabetes
“A new finding is that we observed some phthalates are associated with a higher risk of diabetes development, especially in White women [that] were not seen in Black or Asian women,” senior author Sung Kyun Park, ScD, MPH, of the University of Michigan, Ann Arbor, told this news organization.
“We were surprised to see the racial/ethnic differences,” added Dr. Peng, formerly of the University of Michigan and now at Lifecourse Epidemiology of Adiposity and Diabetes Center, University of Colorado Anschutz Medical Campus.
A possible explanation is that “compared to White women, Black women develop diabetes at a younger age and are exposed to higher levels of several phthalates,” and this study excluded women who already had diabetes by midlife, she noted.
“Although our study was conducted in a cohort of women,” Dr. Park stressed, “we hope that our findings are not interpreted that only women should be concerned of phthalates. Our findings add to the current literature that phthalates may be a potential risk factor for type 2 diabetes.
“Certain phthalates are prohibited in children’s toys and child care articles,” Dr. Peng noted, as explained by the U.S. Consumer Product Safety Commission. In addition, a bill has been introduced in Congress to ban phthalates in food contact substances.
“If phthalates are removed from plastics and other consumer products,” she cautioned, “we do have to be careful in the process to avoid replacing them with some other potentially harmful chemicals.”
A well-known example of this type of “regrettable substitution,” Dr. Park added, “is ‘BPA-free’ plastics that replaced bisphenol A with other bisphenols such as bisphenol-F (BPF) or bisphenol-S (BPS). The product has a label of ‘BPA-free’, but those replaced chemicals turned out to be equally toxic. Science is slow to determine if a new chemical introduced to the market is safe and can replace a regulated chemical.”
And studies have shown that a diet rich in meat, fat, and ultraprocessed foods is associated with increased exposures to some phthalates, especially when the foods are obtained away from home, such as fast foods, Dr. Peng observed. In addition, some phthalates are added to personal care products such as fragrance.
“As a first step,” she said, “I think reducing consumption of ultraprocessed foods packaged in plastics may help reduce phthalate exposure.”
A 2020 report from the Endocrine Society and the International Pollutants Elimination Network (IPEN), titled, “Plastics, EDCs, and Health,” summarizes research on bisphenol A, per- and polyfluoroalkyl substances (PFAS), phthalates, and other EDCs that leach from plastics. The Endocrine Society website also has a link to a 2-page summary.
Levels of 12 phthalate metabolites
Previously, the researchers reported how another class of “forever chemicals,” PFAS, were associated with risk of hypertension in a 17-year follow-up of middle-aged women in the SWAN study.
In the current study, they analyzed data from 1,308 women in SWAN-MPS who had been recruited at five study sites (Oakland, Calif; Los Angeles; Detroit; Pittsburgh; and Boston).
The women were between ages 42 and 52 years in 1996-1997 and self-identified as White, Black, Chinese, or Japanese.
They did not have diabetes in 1999-2000 and had sufficient urine samples for phthalate assessment then and midway through a 6-year follow-up.
The women were a median age of 49 years in 1999-2000. About half were White, 20% were Black, 13% were Chinese, and 15% were Japanese.
Researchers analyzed levels of 12 metabolites, chosen because their parent phthalates have been widely used in industry and commerce, and exposure to these phthalates is a national biomonitoring priority.
The measured phthalates were:
Three metabolites of low-molecular-weight phthalates:
- mono-ethyl phthalate (MEP)
- mono-n-butyl phthalate (MnBP)
- mono-isobutyl phthalate (MiBP)
Four metabolites of the high-molecular-weight phthalate di(2-ethylhexyl) phthalate (DEHP), which is of particular public health interest:
- mono(2-ethylhexyl) phthalate (MEHP)
- mono(2-ethyl-5-hydroxyhexyl) phthalate (MEHHP)
- mono(2-ethyl-5-oxohexyl) phthalate (MEOHP)
- mono(2-ethyl-5-carboxypentyl) phthalate (MECPP)
Five metabolites of other high-molecular-weight phthalates:
- monobenzyl phthalate (MBzP)
- monoisononyl phthalate (MiNP)
- mono-carboxyoctyl phthalate (MCOP)
- mono-carboxy-isononyl phthalate (MCNP)
- mono(3-carboxypropyl) phthalate (MCPP)
The researchers excluded MiNP from all analyses because it was detected in less than 1% of urine samples.
The different phthalate metabolites were detected in 84.8% of samples (MEHP) to 100% of samples (MnBP and MECPP).
Women who were younger, Black, current smokers, or obese generally had higher concentrations of phthalate metabolites.
Over 6 years, 61 women developed diabetes (an incidence rate of 8.1 per 1000 person-years).
Compared with other women, those with incident diabetes had significantly higher concentrations of all phthalate metabolites except DEHP metabolites and MCPP.
Phthalates were not associated with incident diabetes in Black or Asian women.
However, among White women, each doubling of the concentrations of MiBP, MBzP, MCOP, MCNP, and MCCP was associated with a 30% to 63% higher incidence of diabetes (HR 1.30 for MCNP; HR 1.63 for MiBP).
The SWAN study was supported by the National Institutes of Health, Department of Health & Human Services, National Institute on Aging, National Institute of Nursing Research, NIH Office of Research on Women’s Health, and SWAN Repository. The current study was supported by the National Center for Research Resources, National Center for Advancing Translational Sciences, NIH, National Institute of Environmental Health, and Centers for Disease Control and Prevention/National Institute for Occupational Safety and Health. Dr. Peng was supported by an Interdisciplinary Research Training on Health and Aging grant from the NIA. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FDA expands oral JAK abrocitinib to adolescents with AD
Abrocitinib, taken once daily, previously was approved only for treating adults aged 18 and older.
It joins upadacitinib (Rinvoq), previously the only oral JAK inhibitor to be approved for use by adolescents aged 12 through 17 with refractory moderate to severe AD.
The indication has been expanded for teens whose disease is not adequately controlled with other systemic drugs, including biologics, or those for whom use of those drugs is not advised.
Prescribing information was updated to reflect data from JADE TEEN, a phase 3, randomized, placebo-controlled trial that supported the indication for adolescents. That trial evaluated both the 100-mg and 200-mg doses of abrocitinib in comparison with placebo in 285 adolescents aged 12-18 who had moderate to severe AD and who were also receiving background therapy with topical medications.
The most common toxicities that were reported in at least 1% of patients treated with abrocitinib for up to 16 weeks included nasopharyngitis, nausea, and headache.
Efficacy measures included improvements in itch, skin clearance, and disease severity using the Investigator Global Assessment (IGA), the Peak Pruritus Numerical Rating Scale (PP-NRS), and the Eczema Area and Severity Index (EASI), according to the Pfizer statement announcing the expanded approval.
Select JADE TEEN findings include the following:
- IGA response rate of 0 or 1 at week 12: 39% with abrocitinib 100 mg; 46% with abrocitinib 200 mg; and 24% with placebo.
- EASI-75 response rate at week 12: 64%, 71%, and 41%, respectively.
- Proportion of participants achieving PP-NRS with at least a 4-point decrease from baseline at week 2: 13%, 25%, and 8%, respectively.
Data included in the prescribing information now encompass five randomized, placebo-controlled clinical trials and a long-term extension study with more than 1,600 patients treated with abrocitinib, according to the statement from Pfizer.
In a 2021 story, when JADE TEEN trial results were presented, Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and Rady Children’s Hospital, San Diego, told this news organization that he welcomed oral JAKs as a weapon against atopic dermatitis.
He noted that moderate to severe AD can have a tremendous impact on adolescents. “Traditionally, we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control,” he said.
Abrocitinib is not recommended for use with other JAK inhibitors, biologic immunomodulators, or other immunosuppressants.
AD, one of the most common inflammatory skin diseases, affects approximately 5%-10% of adults in the United States and approximately 11% of children. About one in three adults and one in three children and adolescents aged 17 and younger with AD have moderate to severe disease.
JAK inhibition is thought to modulate multiple cytokines involved in AD, including interleukin (IL)–4, IL-13, IL-31, IL-22, and thymic stromal lymphopoietin.
Prescribing information includes a warning that use of abrocitinib should be avoided by patients with an active, serious infection, including localized infections. A boxed warning is included in the labels of JAK inhibitors regarding the risk of serious infections, mortality, major cardiovascular events, and thrombosis.
Treatment risks and benefits should be carefully considered for patients with chronic or recurrent infections or those who have lived in or traveled in areas of endemic tuberculosis or endemic mycoses, the information states.
A version of this article first appeared on Medscape.com.
Abrocitinib, taken once daily, previously was approved only for treating adults aged 18 and older.
It joins upadacitinib (Rinvoq), previously the only oral JAK inhibitor to be approved for use by adolescents aged 12 through 17 with refractory moderate to severe AD.
The indication has been expanded for teens whose disease is not adequately controlled with other systemic drugs, including biologics, or those for whom use of those drugs is not advised.
Prescribing information was updated to reflect data from JADE TEEN, a phase 3, randomized, placebo-controlled trial that supported the indication for adolescents. That trial evaluated both the 100-mg and 200-mg doses of abrocitinib in comparison with placebo in 285 adolescents aged 12-18 who had moderate to severe AD and who were also receiving background therapy with topical medications.
The most common toxicities that were reported in at least 1% of patients treated with abrocitinib for up to 16 weeks included nasopharyngitis, nausea, and headache.
Efficacy measures included improvements in itch, skin clearance, and disease severity using the Investigator Global Assessment (IGA), the Peak Pruritus Numerical Rating Scale (PP-NRS), and the Eczema Area and Severity Index (EASI), according to the Pfizer statement announcing the expanded approval.
Select JADE TEEN findings include the following:
- IGA response rate of 0 or 1 at week 12: 39% with abrocitinib 100 mg; 46% with abrocitinib 200 mg; and 24% with placebo.
- EASI-75 response rate at week 12: 64%, 71%, and 41%, respectively.
- Proportion of participants achieving PP-NRS with at least a 4-point decrease from baseline at week 2: 13%, 25%, and 8%, respectively.
Data included in the prescribing information now encompass five randomized, placebo-controlled clinical trials and a long-term extension study with more than 1,600 patients treated with abrocitinib, according to the statement from Pfizer.
In a 2021 story, when JADE TEEN trial results were presented, Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and Rady Children’s Hospital, San Diego, told this news organization that he welcomed oral JAKs as a weapon against atopic dermatitis.
He noted that moderate to severe AD can have a tremendous impact on adolescents. “Traditionally, we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control,” he said.
Abrocitinib is not recommended for use with other JAK inhibitors, biologic immunomodulators, or other immunosuppressants.
AD, one of the most common inflammatory skin diseases, affects approximately 5%-10% of adults in the United States and approximately 11% of children. About one in three adults and one in three children and adolescents aged 17 and younger with AD have moderate to severe disease.
JAK inhibition is thought to modulate multiple cytokines involved in AD, including interleukin (IL)–4, IL-13, IL-31, IL-22, and thymic stromal lymphopoietin.
Prescribing information includes a warning that use of abrocitinib should be avoided by patients with an active, serious infection, including localized infections. A boxed warning is included in the labels of JAK inhibitors regarding the risk of serious infections, mortality, major cardiovascular events, and thrombosis.
Treatment risks and benefits should be carefully considered for patients with chronic or recurrent infections or those who have lived in or traveled in areas of endemic tuberculosis or endemic mycoses, the information states.
A version of this article first appeared on Medscape.com.
Abrocitinib, taken once daily, previously was approved only for treating adults aged 18 and older.
It joins upadacitinib (Rinvoq), previously the only oral JAK inhibitor to be approved for use by adolescents aged 12 through 17 with refractory moderate to severe AD.
The indication has been expanded for teens whose disease is not adequately controlled with other systemic drugs, including biologics, or those for whom use of those drugs is not advised.
Prescribing information was updated to reflect data from JADE TEEN, a phase 3, randomized, placebo-controlled trial that supported the indication for adolescents. That trial evaluated both the 100-mg and 200-mg doses of abrocitinib in comparison with placebo in 285 adolescents aged 12-18 who had moderate to severe AD and who were also receiving background therapy with topical medications.
The most common toxicities that were reported in at least 1% of patients treated with abrocitinib for up to 16 weeks included nasopharyngitis, nausea, and headache.
Efficacy measures included improvements in itch, skin clearance, and disease severity using the Investigator Global Assessment (IGA), the Peak Pruritus Numerical Rating Scale (PP-NRS), and the Eczema Area and Severity Index (EASI), according to the Pfizer statement announcing the expanded approval.
Select JADE TEEN findings include the following:
- IGA response rate of 0 or 1 at week 12: 39% with abrocitinib 100 mg; 46% with abrocitinib 200 mg; and 24% with placebo.
- EASI-75 response rate at week 12: 64%, 71%, and 41%, respectively.
- Proportion of participants achieving PP-NRS with at least a 4-point decrease from baseline at week 2: 13%, 25%, and 8%, respectively.
Data included in the prescribing information now encompass five randomized, placebo-controlled clinical trials and a long-term extension study with more than 1,600 patients treated with abrocitinib, according to the statement from Pfizer.
In a 2021 story, when JADE TEEN trial results were presented, Lawrence Eichenfield, MD, professor of dermatology and pediatrics, University of California, San Diego, and Rady Children’s Hospital, San Diego, told this news organization that he welcomed oral JAKs as a weapon against atopic dermatitis.
He noted that moderate to severe AD can have a tremendous impact on adolescents. “Traditionally, we have treated it with intermittent topical corticosteroids, but this has left a significant percentage of patients without long-term disease control,” he said.
Abrocitinib is not recommended for use with other JAK inhibitors, biologic immunomodulators, or other immunosuppressants.
AD, one of the most common inflammatory skin diseases, affects approximately 5%-10% of adults in the United States and approximately 11% of children. About one in three adults and one in three children and adolescents aged 17 and younger with AD have moderate to severe disease.
JAK inhibition is thought to modulate multiple cytokines involved in AD, including interleukin (IL)–4, IL-13, IL-31, IL-22, and thymic stromal lymphopoietin.
Prescribing information includes a warning that use of abrocitinib should be avoided by patients with an active, serious infection, including localized infections. A boxed warning is included in the labels of JAK inhibitors regarding the risk of serious infections, mortality, major cardiovascular events, and thrombosis.
Treatment risks and benefits should be carefully considered for patients with chronic or recurrent infections or those who have lived in or traveled in areas of endemic tuberculosis or endemic mycoses, the information states.
A version of this article first appeared on Medscape.com.
Scientists create ‘vagina on a chip’: What to know
For years, women’s health advocates have argued that far more research is needed on women’s bodies and health. The world’s first-ever “vagina on a chip,” recently developed at Harvard’s Wyss Institute for Biologically Inspired Engineering in Boston, could go a long way to making that happen.
“Women’s health has not received the attention it deserves,” says Don Ingber, MD, PhD, who led the team that created the vagina chip. The advance quickly drew media attention after it was reported in the journal Microbiome. But researchers hope for more than headlines. They see the chip as a way to facilitate vaginal health research and open the door to vital new treatments.
By now, you may have heard of “organs on chips”: tiny devices about the size of a flash drive that are designed to mimic the biological activity of human organs. These glass chips contain living human cells within grooves that allow the passage of fluid, to either maintain or disrupt the cells’ function. So far, Dr. Ingber and his team at the Wyss Institute have developed more than 15 organ chip models, including chips that mimic the lung, intestine, kidney, and bone marrow.
The idea to develop a vagina chip grew out of research, funded by the Gates Foundation, on a childhood disease called environmental enteric dysfunction, an intestinal disease most commonly found in low-resource nations that is the second leading cause of death in children under 5. That’s when Dr. Ingber discovered just how much the child’s microbiome influences this disease.
Stemming from that work, the Gates Foundation turned its attention to newborn health – in particular, the impact of bacterial vaginosis, an imbalance in the vagina’s bacterial makeup. Bacterial vaginosis occurs in one out of four women worldwide and has been linked to premature birth as well as HIV, HPV persistence, and cervical cancer.
The goal was to test “live biotherapeutic products,” or living microbes like probiotics, that might restore the vagina’s microbiome to health.
No other preclinical model exists to perform tests like that, says Dr. Ingber.
“The vagina chip is a way to help make some advances,” he says.
The Gates Foundation recognized that women’s reproductive health is a major issue, not only in low-income nations, but everywhere around the world. As the project evolved, Dr. Ingber began to hear from female colleagues about how neglected women’s reproductive health is in medical science.
“It is something I became sensitive to and realized this is just the starting point,” Dr. Ingber says.
Take bacterial vaginosis, for example. Since 1982, treatment has revolved around the same two antibiotics. That’s partly because there is no animal model to study. No other species has the same vaginal bacterial community as humans do.
That makes developing any new therapy “incredibly challenging,” explains Caroline Mitchell, MD, MPH, an ob.gyn. at Massachusetts General Hospital, Boston, and a member of the consortium.
It turns out, replicating the vagina in a lab dish is, to use the technical term, very hard.
“That’s where a vagina chip offers an opportunity,” Dr. Mitchell says. “It’s not super-high throughput, but it’s way more high throughput than a [human] clinical trial.”
As such, the vagina chip could help scientists find new treatments much faster.
Like Dr. Ingber, Dr. Mitchell also sees the chip as a way to bring more attention to the largely unmet needs in female reproductive medicine.
“Women’s reproductive health has been under-resourced, under-prioritized, and largely disregarded for decades,” she says. And the time may be ripe for change: Dr. Mitchell says she was encouraged by the National Institutes of Health’s Advancing NIH Research on the Health of Women conference, held in 2021 in response to a congressional request to address women’s health research efforts.
Beyond bacterial vaginosis, Dr. Mitchell imagines the chip could help scientists find new treatments for vaginal yeast infection (candidiasis), chlamydia, and endometriosis. As with bacterial vaginosis, medicines for vaginal yeast infections have not advanced in decades, Dr. Mitchell says. Efforts to develop a vaccine for chlamydia – which can cause permanent damage to a woman’s reproductive system – have dragged on for many years. And endometriosis, an often painful condition in which the tissue that makes up the uterine lining grows outside the uterus, remains under-researched despite affecting 10% of childbearing-age women.
While some mouse models are used in chlamydia research, it’s hard to say if they’ll translate to humans, given the vaginal and cervical bacterial differences.
“Our understanding of the basic physiology of the environment of the vagina and cervix is another area where we’re woefully ignorant,” Dr. Mitchell says.
To that end, Dr. Ingber’s team is developing more complex chips mimicking the vagina and the cervix. One of his team members wants to use the chips to study infertility. The researchers have already used the chips to see how bacterial vaginosis and mucous changes impact the way sperm migrates up the reproductive tract.
The lab is now linking vagina and cervix chips together to study viral infections of the cervix, like HPV, and all types of bacterial diseases of the vaginal tract. By applying cervical mucus to the vagina chip, they hope to learn more about how female reproductive tissues respond to infection and inflammation.
“I always say that organ chips are like synthetic biology at the cell tissue and organ level,” says Dr. Ingber. “You start simple and see if you [can] mimic a clinical situation.”
As they make the chips more complex – perhaps by adding blood vessel cells and female hormones – Dr. Ingber foresees being able to study the response to hormonal changes during the menstrual cycle.
“We can begin to explore the effects of cycling over time as well as other types of hormonal effects,” he says.
Dr. Ingber also envisions linking the vagina chip to other organ chips – he’s already succeeded in linking eight different organ types together. But for now, the team hopes the vagina chip will enhance our understanding of basic female reproductive biology and speed up the process of developing new treatments for women’s health.
A version of this article first appeared on WebMD.com.
For years, women’s health advocates have argued that far more research is needed on women’s bodies and health. The world’s first-ever “vagina on a chip,” recently developed at Harvard’s Wyss Institute for Biologically Inspired Engineering in Boston, could go a long way to making that happen.
“Women’s health has not received the attention it deserves,” says Don Ingber, MD, PhD, who led the team that created the vagina chip. The advance quickly drew media attention after it was reported in the journal Microbiome. But researchers hope for more than headlines. They see the chip as a way to facilitate vaginal health research and open the door to vital new treatments.
By now, you may have heard of “organs on chips”: tiny devices about the size of a flash drive that are designed to mimic the biological activity of human organs. These glass chips contain living human cells within grooves that allow the passage of fluid, to either maintain or disrupt the cells’ function. So far, Dr. Ingber and his team at the Wyss Institute have developed more than 15 organ chip models, including chips that mimic the lung, intestine, kidney, and bone marrow.
The idea to develop a vagina chip grew out of research, funded by the Gates Foundation, on a childhood disease called environmental enteric dysfunction, an intestinal disease most commonly found in low-resource nations that is the second leading cause of death in children under 5. That’s when Dr. Ingber discovered just how much the child’s microbiome influences this disease.
Stemming from that work, the Gates Foundation turned its attention to newborn health – in particular, the impact of bacterial vaginosis, an imbalance in the vagina’s bacterial makeup. Bacterial vaginosis occurs in one out of four women worldwide and has been linked to premature birth as well as HIV, HPV persistence, and cervical cancer.
The goal was to test “live biotherapeutic products,” or living microbes like probiotics, that might restore the vagina’s microbiome to health.
No other preclinical model exists to perform tests like that, says Dr. Ingber.
“The vagina chip is a way to help make some advances,” he says.
The Gates Foundation recognized that women’s reproductive health is a major issue, not only in low-income nations, but everywhere around the world. As the project evolved, Dr. Ingber began to hear from female colleagues about how neglected women’s reproductive health is in medical science.
“It is something I became sensitive to and realized this is just the starting point,” Dr. Ingber says.
Take bacterial vaginosis, for example. Since 1982, treatment has revolved around the same two antibiotics. That’s partly because there is no animal model to study. No other species has the same vaginal bacterial community as humans do.
That makes developing any new therapy “incredibly challenging,” explains Caroline Mitchell, MD, MPH, an ob.gyn. at Massachusetts General Hospital, Boston, and a member of the consortium.
It turns out, replicating the vagina in a lab dish is, to use the technical term, very hard.
“That’s where a vagina chip offers an opportunity,” Dr. Mitchell says. “It’s not super-high throughput, but it’s way more high throughput than a [human] clinical trial.”
As such, the vagina chip could help scientists find new treatments much faster.
Like Dr. Ingber, Dr. Mitchell also sees the chip as a way to bring more attention to the largely unmet needs in female reproductive medicine.
“Women’s reproductive health has been under-resourced, under-prioritized, and largely disregarded for decades,” she says. And the time may be ripe for change: Dr. Mitchell says she was encouraged by the National Institutes of Health’s Advancing NIH Research on the Health of Women conference, held in 2021 in response to a congressional request to address women’s health research efforts.
Beyond bacterial vaginosis, Dr. Mitchell imagines the chip could help scientists find new treatments for vaginal yeast infection (candidiasis), chlamydia, and endometriosis. As with bacterial vaginosis, medicines for vaginal yeast infections have not advanced in decades, Dr. Mitchell says. Efforts to develop a vaccine for chlamydia – which can cause permanent damage to a woman’s reproductive system – have dragged on for many years. And endometriosis, an often painful condition in which the tissue that makes up the uterine lining grows outside the uterus, remains under-researched despite affecting 10% of childbearing-age women.
While some mouse models are used in chlamydia research, it’s hard to say if they’ll translate to humans, given the vaginal and cervical bacterial differences.
“Our understanding of the basic physiology of the environment of the vagina and cervix is another area where we’re woefully ignorant,” Dr. Mitchell says.
To that end, Dr. Ingber’s team is developing more complex chips mimicking the vagina and the cervix. One of his team members wants to use the chips to study infertility. The researchers have already used the chips to see how bacterial vaginosis and mucous changes impact the way sperm migrates up the reproductive tract.
The lab is now linking vagina and cervix chips together to study viral infections of the cervix, like HPV, and all types of bacterial diseases of the vaginal tract. By applying cervical mucus to the vagina chip, they hope to learn more about how female reproductive tissues respond to infection and inflammation.
“I always say that organ chips are like synthetic biology at the cell tissue and organ level,” says Dr. Ingber. “You start simple and see if you [can] mimic a clinical situation.”
As they make the chips more complex – perhaps by adding blood vessel cells and female hormones – Dr. Ingber foresees being able to study the response to hormonal changes during the menstrual cycle.
“We can begin to explore the effects of cycling over time as well as other types of hormonal effects,” he says.
Dr. Ingber also envisions linking the vagina chip to other organ chips – he’s already succeeded in linking eight different organ types together. But for now, the team hopes the vagina chip will enhance our understanding of basic female reproductive biology and speed up the process of developing new treatments for women’s health.
A version of this article first appeared on WebMD.com.
For years, women’s health advocates have argued that far more research is needed on women’s bodies and health. The world’s first-ever “vagina on a chip,” recently developed at Harvard’s Wyss Institute for Biologically Inspired Engineering in Boston, could go a long way to making that happen.
“Women’s health has not received the attention it deserves,” says Don Ingber, MD, PhD, who led the team that created the vagina chip. The advance quickly drew media attention after it was reported in the journal Microbiome. But researchers hope for more than headlines. They see the chip as a way to facilitate vaginal health research and open the door to vital new treatments.
By now, you may have heard of “organs on chips”: tiny devices about the size of a flash drive that are designed to mimic the biological activity of human organs. These glass chips contain living human cells within grooves that allow the passage of fluid, to either maintain or disrupt the cells’ function. So far, Dr. Ingber and his team at the Wyss Institute have developed more than 15 organ chip models, including chips that mimic the lung, intestine, kidney, and bone marrow.
The idea to develop a vagina chip grew out of research, funded by the Gates Foundation, on a childhood disease called environmental enteric dysfunction, an intestinal disease most commonly found in low-resource nations that is the second leading cause of death in children under 5. That’s when Dr. Ingber discovered just how much the child’s microbiome influences this disease.
Stemming from that work, the Gates Foundation turned its attention to newborn health – in particular, the impact of bacterial vaginosis, an imbalance in the vagina’s bacterial makeup. Bacterial vaginosis occurs in one out of four women worldwide and has been linked to premature birth as well as HIV, HPV persistence, and cervical cancer.
The goal was to test “live biotherapeutic products,” or living microbes like probiotics, that might restore the vagina’s microbiome to health.
No other preclinical model exists to perform tests like that, says Dr. Ingber.
“The vagina chip is a way to help make some advances,” he says.
The Gates Foundation recognized that women’s reproductive health is a major issue, not only in low-income nations, but everywhere around the world. As the project evolved, Dr. Ingber began to hear from female colleagues about how neglected women’s reproductive health is in medical science.
“It is something I became sensitive to and realized this is just the starting point,” Dr. Ingber says.
Take bacterial vaginosis, for example. Since 1982, treatment has revolved around the same two antibiotics. That’s partly because there is no animal model to study. No other species has the same vaginal bacterial community as humans do.
That makes developing any new therapy “incredibly challenging,” explains Caroline Mitchell, MD, MPH, an ob.gyn. at Massachusetts General Hospital, Boston, and a member of the consortium.
It turns out, replicating the vagina in a lab dish is, to use the technical term, very hard.
“That’s where a vagina chip offers an opportunity,” Dr. Mitchell says. “It’s not super-high throughput, but it’s way more high throughput than a [human] clinical trial.”
As such, the vagina chip could help scientists find new treatments much faster.
Like Dr. Ingber, Dr. Mitchell also sees the chip as a way to bring more attention to the largely unmet needs in female reproductive medicine.
“Women’s reproductive health has been under-resourced, under-prioritized, and largely disregarded for decades,” she says. And the time may be ripe for change: Dr. Mitchell says she was encouraged by the National Institutes of Health’s Advancing NIH Research on the Health of Women conference, held in 2021 in response to a congressional request to address women’s health research efforts.
Beyond bacterial vaginosis, Dr. Mitchell imagines the chip could help scientists find new treatments for vaginal yeast infection (candidiasis), chlamydia, and endometriosis. As with bacterial vaginosis, medicines for vaginal yeast infections have not advanced in decades, Dr. Mitchell says. Efforts to develop a vaccine for chlamydia – which can cause permanent damage to a woman’s reproductive system – have dragged on for many years. And endometriosis, an often painful condition in which the tissue that makes up the uterine lining grows outside the uterus, remains under-researched despite affecting 10% of childbearing-age women.
While some mouse models are used in chlamydia research, it’s hard to say if they’ll translate to humans, given the vaginal and cervical bacterial differences.
“Our understanding of the basic physiology of the environment of the vagina and cervix is another area where we’re woefully ignorant,” Dr. Mitchell says.
To that end, Dr. Ingber’s team is developing more complex chips mimicking the vagina and the cervix. One of his team members wants to use the chips to study infertility. The researchers have already used the chips to see how bacterial vaginosis and mucous changes impact the way sperm migrates up the reproductive tract.
The lab is now linking vagina and cervix chips together to study viral infections of the cervix, like HPV, and all types of bacterial diseases of the vaginal tract. By applying cervical mucus to the vagina chip, they hope to learn more about how female reproductive tissues respond to infection and inflammation.
“I always say that organ chips are like synthetic biology at the cell tissue and organ level,” says Dr. Ingber. “You start simple and see if you [can] mimic a clinical situation.”
As they make the chips more complex – perhaps by adding blood vessel cells and female hormones – Dr. Ingber foresees being able to study the response to hormonal changes during the menstrual cycle.
“We can begin to explore the effects of cycling over time as well as other types of hormonal effects,” he says.
Dr. Ingber also envisions linking the vagina chip to other organ chips – he’s already succeeded in linking eight different organ types together. But for now, the team hopes the vagina chip will enhance our understanding of basic female reproductive biology and speed up the process of developing new treatments for women’s health.
A version of this article first appeared on WebMD.com.
FROM MICROBIOME
Unexpected link between light drinking and dementia risk
new research suggests.
Investigators assessed dementia risk using changes in alcohol consumption over a 2-year period in nearly 4 million people in South Korea. After about 7 years, dementia was 21% less likely in mild drinkers and 17% less likely in moderate drinkers. Heavy drinking was linked to an 8% increased risk.
Other studies of the relationship between alcohol and dementia have yielded mixed results, and this study does little to clear those murky waters. Nor do the results mean that drinking is recommended, the investigators note.
But the study does offer new information on how risk changes over time as people change their drinking habits, lead investigator Keun Hye Jeon, MD, assistant professor of family medicine at Cha Gumi Medical Center at Cha University, Gumi, South Korea, told this news organization.
“Although numerous studies have shown a relationship between alcohol consumption and dementia, there is a paucity of understanding as to how the incidence of dementia changes with changes in drinking habits,” Dr. Jeon said.
“By measuring alcohol consumption at two time points, we were able to study the relationship between reducing, ceasing, maintaining, and increasing alcohol consumption and incident dementia,” he added.
The findings were published online in JAMA Network Open.
Tracking drinking habits
Researchers analyzed data from nearly 4 million individuals aged 40 years and older in the Korean National Health Insurance Service who completed questionnaires and underwent physical exams in 2009 and 2011.
Study participants completed questionnaires on their drinking habits and were assigned to one of five groups according to change in alcohol consumption during the study period. These groups consisted of sustained nondrinkers; those who stopped drinking (quitters); those who reduced their consumption of alcohol but did not stop drinking (reducers); those who maintained the same level of consumption (sustainers); and those who increased their level of consumption (increasers).
A standard drink in the United States contains 14 g of alcohol. For this study, mild drinking was defined as less than 15 g/day, or one drink; moderate consumption as 15-29.9 g/day, or one to two drinks; and heavy drinking as 30 g/day or more, or three or more drinks.
At baseline, 54.8% of participants were nondrinkers, 26.7% were mild drinkers, 11.0% were moderate drinkers, and 7.5% were heavy drinkers.
From 2009 to 2011, 24.2% of mild drinkers, 8.4% of moderate drinkers, and 7.6% of heavy drinkers became quitters. In the same period, 13.9% of nondrinkers, 16.1% of mild drinkers, and 17.4% of moderate drinkers increased their drinking level.
After a mean follow-up of 6.3 years, 2.5% of participants were diagnosed with dementia, 2.0% with Alzheimer’s disease, and 0.3% with vascular dementia.
Unexpected finding
Compared with consistently not drinking, mild and moderate alcohol consumption was associated with a 21% (adjust hazard ratio, 0.79; 95% confidence interval, 0.77-0.81) and 17% (aHR, 0.83; 95% CI, 0.79-0.88) decreased risk for dementia, respectively.
Heavy drinking was linked to an 8% increased risk (aHR, 1.08; 95% CI, 1.03-1.12).
Similar associations were found between alcohol consumption and risk for Alzheimer’s disease and vascular dementia.
Reducing drinking habits from heavy to moderate led to a reduction in risk for dementia and Alzheimer’s, and increasing drinking levels led to an increase in risk for both conditions.
But when the researchers analyzed dementia risk for nondrinkers who began drinking at mild levels during the study period, they found something unexpected – the risk in this group decreased by 7% for dementia (aHR, 0.93; 95% CI, 0.90-0.96) and by 8% for Alzheimer’s (aHR, 0.92; 95% CI, 0.89-0.95), compared with sustained mild drinkers.
“Our study showed that initiation of mild alcohol consumption leads to a reduced risk of all-cause dementia and Alzheimer’s disease, which has never been reported in previous studies,” Dr. Jeon said.
However, Dr. Jeon was quick to point out that this doesn’t mean that people who don’t drink should start.
Previous studies have shown that heavy alcohol use can triple an individual’s dementia risk, while other studies have shown that no amount of alcohol consumption is good for the brain.
“None of the existing health guidelines recommend starting alcohol drinking,” Dr. Jeon said. “Our findings regarding an initiation of mild alcohol consumption cannot be directly translated into clinical recommendations,” but the findings do warrant additional study, he added.
Risks persist
Commenting on the findings, Percy Griffin, PhD, director of scientific engagement for the Alzheimer’s Association in Chicago, agrees.
“While this study is interesting, and this topic deserves further study, no one should drink alcohol as a method of reducing risk of Alzheimer’s disease or other dementia based on this study,” said Dr. Griffin, who was not part of the study.
The exact tipping point in alcohol consumption that can lead to problems with cognition or increased dementia risk is unknown, Dr. Griffin said. Nor do researchers understand why mild drinking may have a protective effect.
“We do know, however, that excessive alcohol consumption has negative effects on heart health and general health, which can lead to problems with brain function,” he said. “Clinicians should have discussions with their patients around their alcohol consumption patterns and the risks associated with drinking in excess, including potential damage to their cognition.”
Funding for the study was not disclosed. Dr. Jeon and Dr. Griffin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators assessed dementia risk using changes in alcohol consumption over a 2-year period in nearly 4 million people in South Korea. After about 7 years, dementia was 21% less likely in mild drinkers and 17% less likely in moderate drinkers. Heavy drinking was linked to an 8% increased risk.
Other studies of the relationship between alcohol and dementia have yielded mixed results, and this study does little to clear those murky waters. Nor do the results mean that drinking is recommended, the investigators note.
But the study does offer new information on how risk changes over time as people change their drinking habits, lead investigator Keun Hye Jeon, MD, assistant professor of family medicine at Cha Gumi Medical Center at Cha University, Gumi, South Korea, told this news organization.
“Although numerous studies have shown a relationship between alcohol consumption and dementia, there is a paucity of understanding as to how the incidence of dementia changes with changes in drinking habits,” Dr. Jeon said.
“By measuring alcohol consumption at two time points, we were able to study the relationship between reducing, ceasing, maintaining, and increasing alcohol consumption and incident dementia,” he added.
The findings were published online in JAMA Network Open.
Tracking drinking habits
Researchers analyzed data from nearly 4 million individuals aged 40 years and older in the Korean National Health Insurance Service who completed questionnaires and underwent physical exams in 2009 and 2011.
Study participants completed questionnaires on their drinking habits and were assigned to one of five groups according to change in alcohol consumption during the study period. These groups consisted of sustained nondrinkers; those who stopped drinking (quitters); those who reduced their consumption of alcohol but did not stop drinking (reducers); those who maintained the same level of consumption (sustainers); and those who increased their level of consumption (increasers).
A standard drink in the United States contains 14 g of alcohol. For this study, mild drinking was defined as less than 15 g/day, or one drink; moderate consumption as 15-29.9 g/day, or one to two drinks; and heavy drinking as 30 g/day or more, or three or more drinks.
At baseline, 54.8% of participants were nondrinkers, 26.7% were mild drinkers, 11.0% were moderate drinkers, and 7.5% were heavy drinkers.
From 2009 to 2011, 24.2% of mild drinkers, 8.4% of moderate drinkers, and 7.6% of heavy drinkers became quitters. In the same period, 13.9% of nondrinkers, 16.1% of mild drinkers, and 17.4% of moderate drinkers increased their drinking level.
After a mean follow-up of 6.3 years, 2.5% of participants were diagnosed with dementia, 2.0% with Alzheimer’s disease, and 0.3% with vascular dementia.
Unexpected finding
Compared with consistently not drinking, mild and moderate alcohol consumption was associated with a 21% (adjust hazard ratio, 0.79; 95% confidence interval, 0.77-0.81) and 17% (aHR, 0.83; 95% CI, 0.79-0.88) decreased risk for dementia, respectively.
Heavy drinking was linked to an 8% increased risk (aHR, 1.08; 95% CI, 1.03-1.12).
Similar associations were found between alcohol consumption and risk for Alzheimer’s disease and vascular dementia.
Reducing drinking habits from heavy to moderate led to a reduction in risk for dementia and Alzheimer’s, and increasing drinking levels led to an increase in risk for both conditions.
But when the researchers analyzed dementia risk for nondrinkers who began drinking at mild levels during the study period, they found something unexpected – the risk in this group decreased by 7% for dementia (aHR, 0.93; 95% CI, 0.90-0.96) and by 8% for Alzheimer’s (aHR, 0.92; 95% CI, 0.89-0.95), compared with sustained mild drinkers.
“Our study showed that initiation of mild alcohol consumption leads to a reduced risk of all-cause dementia and Alzheimer’s disease, which has never been reported in previous studies,” Dr. Jeon said.
However, Dr. Jeon was quick to point out that this doesn’t mean that people who don’t drink should start.
Previous studies have shown that heavy alcohol use can triple an individual’s dementia risk, while other studies have shown that no amount of alcohol consumption is good for the brain.
“None of the existing health guidelines recommend starting alcohol drinking,” Dr. Jeon said. “Our findings regarding an initiation of mild alcohol consumption cannot be directly translated into clinical recommendations,” but the findings do warrant additional study, he added.
Risks persist
Commenting on the findings, Percy Griffin, PhD, director of scientific engagement for the Alzheimer’s Association in Chicago, agrees.
“While this study is interesting, and this topic deserves further study, no one should drink alcohol as a method of reducing risk of Alzheimer’s disease or other dementia based on this study,” said Dr. Griffin, who was not part of the study.
The exact tipping point in alcohol consumption that can lead to problems with cognition or increased dementia risk is unknown, Dr. Griffin said. Nor do researchers understand why mild drinking may have a protective effect.
“We do know, however, that excessive alcohol consumption has negative effects on heart health and general health, which can lead to problems with brain function,” he said. “Clinicians should have discussions with their patients around their alcohol consumption patterns and the risks associated with drinking in excess, including potential damage to their cognition.”
Funding for the study was not disclosed. Dr. Jeon and Dr. Griffin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
Investigators assessed dementia risk using changes in alcohol consumption over a 2-year period in nearly 4 million people in South Korea. After about 7 years, dementia was 21% less likely in mild drinkers and 17% less likely in moderate drinkers. Heavy drinking was linked to an 8% increased risk.
Other studies of the relationship between alcohol and dementia have yielded mixed results, and this study does little to clear those murky waters. Nor do the results mean that drinking is recommended, the investigators note.
But the study does offer new information on how risk changes over time as people change their drinking habits, lead investigator Keun Hye Jeon, MD, assistant professor of family medicine at Cha Gumi Medical Center at Cha University, Gumi, South Korea, told this news organization.
“Although numerous studies have shown a relationship between alcohol consumption and dementia, there is a paucity of understanding as to how the incidence of dementia changes with changes in drinking habits,” Dr. Jeon said.
“By measuring alcohol consumption at two time points, we were able to study the relationship between reducing, ceasing, maintaining, and increasing alcohol consumption and incident dementia,” he added.
The findings were published online in JAMA Network Open.
Tracking drinking habits
Researchers analyzed data from nearly 4 million individuals aged 40 years and older in the Korean National Health Insurance Service who completed questionnaires and underwent physical exams in 2009 and 2011.
Study participants completed questionnaires on their drinking habits and were assigned to one of five groups according to change in alcohol consumption during the study period. These groups consisted of sustained nondrinkers; those who stopped drinking (quitters); those who reduced their consumption of alcohol but did not stop drinking (reducers); those who maintained the same level of consumption (sustainers); and those who increased their level of consumption (increasers).
A standard drink in the United States contains 14 g of alcohol. For this study, mild drinking was defined as less than 15 g/day, or one drink; moderate consumption as 15-29.9 g/day, or one to two drinks; and heavy drinking as 30 g/day or more, or three or more drinks.
At baseline, 54.8% of participants were nondrinkers, 26.7% were mild drinkers, 11.0% were moderate drinkers, and 7.5% were heavy drinkers.
From 2009 to 2011, 24.2% of mild drinkers, 8.4% of moderate drinkers, and 7.6% of heavy drinkers became quitters. In the same period, 13.9% of nondrinkers, 16.1% of mild drinkers, and 17.4% of moderate drinkers increased their drinking level.
After a mean follow-up of 6.3 years, 2.5% of participants were diagnosed with dementia, 2.0% with Alzheimer’s disease, and 0.3% with vascular dementia.
Unexpected finding
Compared with consistently not drinking, mild and moderate alcohol consumption was associated with a 21% (adjust hazard ratio, 0.79; 95% confidence interval, 0.77-0.81) and 17% (aHR, 0.83; 95% CI, 0.79-0.88) decreased risk for dementia, respectively.
Heavy drinking was linked to an 8% increased risk (aHR, 1.08; 95% CI, 1.03-1.12).
Similar associations were found between alcohol consumption and risk for Alzheimer’s disease and vascular dementia.
Reducing drinking habits from heavy to moderate led to a reduction in risk for dementia and Alzheimer’s, and increasing drinking levels led to an increase in risk for both conditions.
But when the researchers analyzed dementia risk for nondrinkers who began drinking at mild levels during the study period, they found something unexpected – the risk in this group decreased by 7% for dementia (aHR, 0.93; 95% CI, 0.90-0.96) and by 8% for Alzheimer’s (aHR, 0.92; 95% CI, 0.89-0.95), compared with sustained mild drinkers.
“Our study showed that initiation of mild alcohol consumption leads to a reduced risk of all-cause dementia and Alzheimer’s disease, which has never been reported in previous studies,” Dr. Jeon said.
However, Dr. Jeon was quick to point out that this doesn’t mean that people who don’t drink should start.
Previous studies have shown that heavy alcohol use can triple an individual’s dementia risk, while other studies have shown that no amount of alcohol consumption is good for the brain.
“None of the existing health guidelines recommend starting alcohol drinking,” Dr. Jeon said. “Our findings regarding an initiation of mild alcohol consumption cannot be directly translated into clinical recommendations,” but the findings do warrant additional study, he added.
Risks persist
Commenting on the findings, Percy Griffin, PhD, director of scientific engagement for the Alzheimer’s Association in Chicago, agrees.
“While this study is interesting, and this topic deserves further study, no one should drink alcohol as a method of reducing risk of Alzheimer’s disease or other dementia based on this study,” said Dr. Griffin, who was not part of the study.
The exact tipping point in alcohol consumption that can lead to problems with cognition or increased dementia risk is unknown, Dr. Griffin said. Nor do researchers understand why mild drinking may have a protective effect.
“We do know, however, that excessive alcohol consumption has negative effects on heart health and general health, which can lead to problems with brain function,” he said. “Clinicians should have discussions with their patients around their alcohol consumption patterns and the risks associated with drinking in excess, including potential damage to their cognition.”
Funding for the study was not disclosed. Dr. Jeon and Dr. Griffin report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
The five biggest changes in the 2023 adult vaccine schedules
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
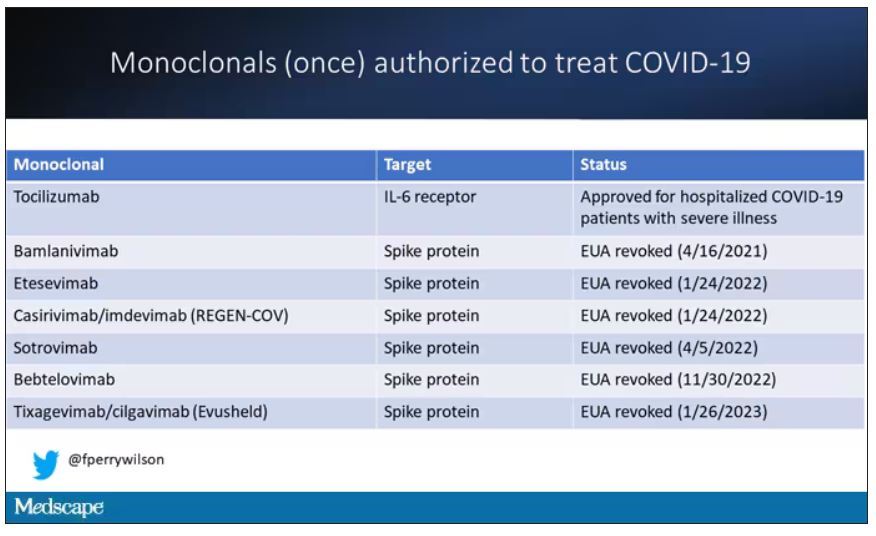
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
AAP approves 2023 child and adolescent immunization schedule
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
The American Academy of Pediatrics said it supports the Recommended Childhood and Adolescent Immunization Schedule: United States, 2023.
In a policy statement published online in the journal Pediatrics, the AAP said the updated recommendations do not include major changes from those released in 2022 by the Advisory Committee on Immunization Practices of the Centers for Disease Control and Prevention.
In one small shift, COVID-19 is now addressed in the main text instead of being relegated to the notes section.
“And a new vaccine – Priorix [GlaxoSmithKline] – has been added for MMR [measles, mumps, rubella], so now there are two available,” Sean T. O’Leary, MD, MPH, chair of the AAP’s Committee on Infectious Diseases, told this news organization. “There’s also a second pneumococcal conjugate vaccine listed, PCV15, and this and PCV13 can essentially be used interchangeably.”
Minor updates to the schedule, reflected on the cover page, relate to vaccines for COVID-19, dengue fever, and pneumococcal disease, added Dr. O’Leary, a professor of pediatrics at the University of Colorado Anschutz Medical Campus and Children’s Hospital Colorado, Aurora.
The committee also changed layouts to improve the usability of the schedule. Updated annually, the guidance provides a table on recommended pediatric immunizations from birth to age 18 years, and catch-up recommendations for children aged 4 months to 18 years who start their vaccinations late or are more than 1 month behind the recommended age for vaccine administration.
“We hope this annual update will encourage clinicians to make sure all their patients are up to date on their routine vaccinations,” Dr. O’Leary said. “It’s an opportunity to develop strategies to improve vaccination rates.”
The 2023 schedule follows news from the CDC that kindergarten vaccination rates declined during the 2021-2022 school year. Only 93% of kindergarteners obtained full vaccinations, representing a drop of 1 percentage point from the year before and 2 percentage points from the 2019-2020 school year.
The dip in coverage has been attributed to disruptions caused by the COVID-19 pandemic. AAP advises health care professionals to urge families to make sure their child’s vaccines are current.
Among other additions:
In Table 1
- MMR: Second vaccine added (Priorix, GlaxoSmithKline Biologicals)
- Pneumococcal disease: second conjugate vaccine, PCV15, added (Vaxneuvance, Merck Sharp & Dohme).
- COVID-19: New row added.
- Dengue: Text changed from “Seropositive in endemic areas only” to “Seropositive in endemic dengue areas.”
- Inactivated polio vaccine: “See Notes” added to the column for children aged 18 years.
In Table 2
- PCV: Dose 3 to dose 4 interval revised to align with ACIP’s recommendation for dose 4. This dose is necessary only for children ages 12-59 months regardless of risk, or age 60-71 months with any risk who received three doses before age 12 months.
A parent-friendly vaccine schedule for children and adolescents is available on the CDC’s website.
“Vaccines are essential for the health of our whole society, including children and adolescents,” Dr. O’Leary said in a press release from AAP. “These schedules provide a road map [that] parents and pediatricians can follow to help children get the vaccines they need so their immune systems will be ready to recognize and resist diseases.”
As previously, the 2023 schedule was adjusted to ensure consistency between the formats of the childhood/adolescent and adult immunization guidance. A meeting of stakeholder organizations in October 2022 harmonized the two formats.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
AAP vs. AED on obesity treatment: Is there a middle ground?
While there is little controversy that both obesity and eating disorders represent important public health concerns, each deserving of clinical attention, how best to address one without worsening the other has been the crux of the discussion.
Sparking the dispute was a recent publication from the American Academy of Pediatrics that outlines the scope of the obesity problem and makes specific recommendations for assessment and treatment.1 The ambitious 100-page document, with 801 citations, puts new emphasis on the medical and psychological costs associated with obesity and advocates that pediatric primary care clinicians be more assertive in its treatment. While the guidelines certainly don’t urge the use of medications or surgery options as first-line treatment, the new recommendations do put them on the table as options.
In response, the Academy of Eating Disorders issued a public statement outlining several concerns regarding these guidelines that centered around a lack of a detailed plan to screen and address eating disorders; concerns that pediatricians don’t have the level of training and “skills” to conduct these conversations with patients and families with enough sensitivity; and worries about the premature use of antiobesity medications and surgeries in this population.2
It is fair to say that the critique was sharply worded, invoking physicians’ Hippocratic oath, criticizing their training, and suggesting that the guidelines could be biased by pharmaceutical industry influence (of note, the authors of the guidelines reported no ties to any pharmaceutical company). The AED urged that the guidelines be “revised” after consultation with other groups, including them.
Not unexpectedly, this response, especially coming from a group whose leadership and members are primarily nonphysicians, triggered its own sharp rebukes, including a recent commentary that counter-accused some of the eating disorder clinicians of being more concerned with their pet diets than actual health improvements.3
After everyone takes some deep breaths, it’s worth looking to see if there is some middle ground to explore here. The AAP document, to my reading, shows some important acknowledgments of the stigma associated with being overweight, even coming from pediatricians themselves. One passage reads, “Pediatricians and other PHCPs [primary health care providers] have been – and remain – a source of weight bias. They first need to uncover and address their own attitudes regarding children with obesity. Understanding weight stigma and bias, and learning how to reduce it in the clinical setting, sets the stage for productive discussions and improved relationships between families and pediatricians or other PHCPs.”
The guidelines also include some suggestions for how to talk to youth and families about obesity in less stigmatizing ways and offer a fairly lengthy summary of motivational interviewing techniques as they might apply to obesity discussions and lifestyle change. There is also a section on the interface between obesity and eating disorders with suggestions for further reading on their assessment and management.4
Indeed, research has looked specifically at how to minimize the triggering of eating disorders when addressing weight problems, a concern that has been raised by pediatricians themselves as documented in a qualitative study that also invoked the “do no harm” principle.5 One study asked more than 2,000 teens about how various conversations about weight affected their behavior.6 A main finding from that study was that conversations that focused on healthy eating rather than weight per se were less likely to be associated with unhealthy weight control behaviors. This message was emphasized in a publication that came from the AAP itself; it addresses the interaction between eating disorders and obesity.7 Strangely, however, the suggestion to try to minimize the focus on weight in discussions with patients isn’t well emphasized in the publication.
Overall, though, the AAP guidelines offer a well-informed and balanced approach to helping overweight youth. Pediatricians and other pediatric primary care clinicians are frequently called upon to engage in extremely sensitive and difficult discussions with patients and families on a wide variety of topics and most do so quite skillfully, especially when given the proper time and tools. While it is an area in which many of us, including mental health professionals, could do better, it’s no surprise that the AED’s disparaging of pediatricians’ communication competence came off as insulting. Similarly, productive dialogue would be likely enhanced if both sides avoided unfounded speculation about bias and motive and worked from a good faith perspective that all of us are engaged in this important discussion because of a desire to improve the lives of kids.
From my reading, it is quite a stretch to conclude that this document is urging a hasty and financially driven descent into GLP-1 analogues and bariatric surgery. That said, this wouldn’t be the first time a professional organization issues detailed, thoughtful, and nuanced care guidelines only to have them “condensed” within the practical confines of a busy office practice. Leaders would do well to remember that there remains much work to do to empower clinicians to be able to follow these guidelines as intended.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Hampl SE et al. Pediatrics. 2023;151(2):e2022060640.
2. Academy of Eating Disorders. Jan. 26, 2023. Accessed February 2, 2023. Available at The Academy for Eating Disorders Releases a Statement on the Recent American Academy of Pediatrics Clinical Practice Guideline for Weight-Related Care: First, Do No Harm (newswise.com).
3. Freedhoff Y. MDedge Pediatrics 2023. Available at https://www.mdedge.com/pediatrics/article/260894/obesity/weight-bias-affects-views-kids-obesity-recommendations?channel=52.
4. Hornberger LL, Lane MA et al. Pediatrics. 2021;147(1):e202004027989.
5. Loth KA, Lebow J et al. Global Pediatric Health. 2021;8:1-9.
6. Berge JM et al. JAMA Pediatrics. 2013;167(8):746-53.
7. Golden NH et al. Pediatrics. 2016;138(3):e20161649.
While there is little controversy that both obesity and eating disorders represent important public health concerns, each deserving of clinical attention, how best to address one without worsening the other has been the crux of the discussion.
Sparking the dispute was a recent publication from the American Academy of Pediatrics that outlines the scope of the obesity problem and makes specific recommendations for assessment and treatment.1 The ambitious 100-page document, with 801 citations, puts new emphasis on the medical and psychological costs associated with obesity and advocates that pediatric primary care clinicians be more assertive in its treatment. While the guidelines certainly don’t urge the use of medications or surgery options as first-line treatment, the new recommendations do put them on the table as options.
In response, the Academy of Eating Disorders issued a public statement outlining several concerns regarding these guidelines that centered around a lack of a detailed plan to screen and address eating disorders; concerns that pediatricians don’t have the level of training and “skills” to conduct these conversations with patients and families with enough sensitivity; and worries about the premature use of antiobesity medications and surgeries in this population.2
It is fair to say that the critique was sharply worded, invoking physicians’ Hippocratic oath, criticizing their training, and suggesting that the guidelines could be biased by pharmaceutical industry influence (of note, the authors of the guidelines reported no ties to any pharmaceutical company). The AED urged that the guidelines be “revised” after consultation with other groups, including them.
Not unexpectedly, this response, especially coming from a group whose leadership and members are primarily nonphysicians, triggered its own sharp rebukes, including a recent commentary that counter-accused some of the eating disorder clinicians of being more concerned with their pet diets than actual health improvements.3
After everyone takes some deep breaths, it’s worth looking to see if there is some middle ground to explore here. The AAP document, to my reading, shows some important acknowledgments of the stigma associated with being overweight, even coming from pediatricians themselves. One passage reads, “Pediatricians and other PHCPs [primary health care providers] have been – and remain – a source of weight bias. They first need to uncover and address their own attitudes regarding children with obesity. Understanding weight stigma and bias, and learning how to reduce it in the clinical setting, sets the stage for productive discussions and improved relationships between families and pediatricians or other PHCPs.”
The guidelines also include some suggestions for how to talk to youth and families about obesity in less stigmatizing ways and offer a fairly lengthy summary of motivational interviewing techniques as they might apply to obesity discussions and lifestyle change. There is also a section on the interface between obesity and eating disorders with suggestions for further reading on their assessment and management.4
Indeed, research has looked specifically at how to minimize the triggering of eating disorders when addressing weight problems, a concern that has been raised by pediatricians themselves as documented in a qualitative study that also invoked the “do no harm” principle.5 One study asked more than 2,000 teens about how various conversations about weight affected their behavior.6 A main finding from that study was that conversations that focused on healthy eating rather than weight per se were less likely to be associated with unhealthy weight control behaviors. This message was emphasized in a publication that came from the AAP itself; it addresses the interaction between eating disorders and obesity.7 Strangely, however, the suggestion to try to minimize the focus on weight in discussions with patients isn’t well emphasized in the publication.
Overall, though, the AAP guidelines offer a well-informed and balanced approach to helping overweight youth. Pediatricians and other pediatric primary care clinicians are frequently called upon to engage in extremely sensitive and difficult discussions with patients and families on a wide variety of topics and most do so quite skillfully, especially when given the proper time and tools. While it is an area in which many of us, including mental health professionals, could do better, it’s no surprise that the AED’s disparaging of pediatricians’ communication competence came off as insulting. Similarly, productive dialogue would be likely enhanced if both sides avoided unfounded speculation about bias and motive and worked from a good faith perspective that all of us are engaged in this important discussion because of a desire to improve the lives of kids.
From my reading, it is quite a stretch to conclude that this document is urging a hasty and financially driven descent into GLP-1 analogues and bariatric surgery. That said, this wouldn’t be the first time a professional organization issues detailed, thoughtful, and nuanced care guidelines only to have them “condensed” within the practical confines of a busy office practice. Leaders would do well to remember that there remains much work to do to empower clinicians to be able to follow these guidelines as intended.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Hampl SE et al. Pediatrics. 2023;151(2):e2022060640.
2. Academy of Eating Disorders. Jan. 26, 2023. Accessed February 2, 2023. Available at The Academy for Eating Disorders Releases a Statement on the Recent American Academy of Pediatrics Clinical Practice Guideline for Weight-Related Care: First, Do No Harm (newswise.com).
3. Freedhoff Y. MDedge Pediatrics 2023. Available at https://www.mdedge.com/pediatrics/article/260894/obesity/weight-bias-affects-views-kids-obesity-recommendations?channel=52.
4. Hornberger LL, Lane MA et al. Pediatrics. 2021;147(1):e202004027989.
5. Loth KA, Lebow J et al. Global Pediatric Health. 2021;8:1-9.
6. Berge JM et al. JAMA Pediatrics. 2013;167(8):746-53.
7. Golden NH et al. Pediatrics. 2016;138(3):e20161649.
While there is little controversy that both obesity and eating disorders represent important public health concerns, each deserving of clinical attention, how best to address one without worsening the other has been the crux of the discussion.
Sparking the dispute was a recent publication from the American Academy of Pediatrics that outlines the scope of the obesity problem and makes specific recommendations for assessment and treatment.1 The ambitious 100-page document, with 801 citations, puts new emphasis on the medical and psychological costs associated with obesity and advocates that pediatric primary care clinicians be more assertive in its treatment. While the guidelines certainly don’t urge the use of medications or surgery options as first-line treatment, the new recommendations do put them on the table as options.
In response, the Academy of Eating Disorders issued a public statement outlining several concerns regarding these guidelines that centered around a lack of a detailed plan to screen and address eating disorders; concerns that pediatricians don’t have the level of training and “skills” to conduct these conversations with patients and families with enough sensitivity; and worries about the premature use of antiobesity medications and surgeries in this population.2
It is fair to say that the critique was sharply worded, invoking physicians’ Hippocratic oath, criticizing their training, and suggesting that the guidelines could be biased by pharmaceutical industry influence (of note, the authors of the guidelines reported no ties to any pharmaceutical company). The AED urged that the guidelines be “revised” after consultation with other groups, including them.
Not unexpectedly, this response, especially coming from a group whose leadership and members are primarily nonphysicians, triggered its own sharp rebukes, including a recent commentary that counter-accused some of the eating disorder clinicians of being more concerned with their pet diets than actual health improvements.3
After everyone takes some deep breaths, it’s worth looking to see if there is some middle ground to explore here. The AAP document, to my reading, shows some important acknowledgments of the stigma associated with being overweight, even coming from pediatricians themselves. One passage reads, “Pediatricians and other PHCPs [primary health care providers] have been – and remain – a source of weight bias. They first need to uncover and address their own attitudes regarding children with obesity. Understanding weight stigma and bias, and learning how to reduce it in the clinical setting, sets the stage for productive discussions and improved relationships between families and pediatricians or other PHCPs.”
The guidelines also include some suggestions for how to talk to youth and families about obesity in less stigmatizing ways and offer a fairly lengthy summary of motivational interviewing techniques as they might apply to obesity discussions and lifestyle change. There is also a section on the interface between obesity and eating disorders with suggestions for further reading on their assessment and management.4
Indeed, research has looked specifically at how to minimize the triggering of eating disorders when addressing weight problems, a concern that has been raised by pediatricians themselves as documented in a qualitative study that also invoked the “do no harm” principle.5 One study asked more than 2,000 teens about how various conversations about weight affected their behavior.6 A main finding from that study was that conversations that focused on healthy eating rather than weight per se were less likely to be associated with unhealthy weight control behaviors. This message was emphasized in a publication that came from the AAP itself; it addresses the interaction between eating disorders and obesity.7 Strangely, however, the suggestion to try to minimize the focus on weight in discussions with patients isn’t well emphasized in the publication.
Overall, though, the AAP guidelines offer a well-informed and balanced approach to helping overweight youth. Pediatricians and other pediatric primary care clinicians are frequently called upon to engage in extremely sensitive and difficult discussions with patients and families on a wide variety of topics and most do so quite skillfully, especially when given the proper time and tools. While it is an area in which many of us, including mental health professionals, could do better, it’s no surprise that the AED’s disparaging of pediatricians’ communication competence came off as insulting. Similarly, productive dialogue would be likely enhanced if both sides avoided unfounded speculation about bias and motive and worked from a good faith perspective that all of us are engaged in this important discussion because of a desire to improve the lives of kids.
From my reading, it is quite a stretch to conclude that this document is urging a hasty and financially driven descent into GLP-1 analogues and bariatric surgery. That said, this wouldn’t be the first time a professional organization issues detailed, thoughtful, and nuanced care guidelines only to have them “condensed” within the practical confines of a busy office practice. Leaders would do well to remember that there remains much work to do to empower clinicians to be able to follow these guidelines as intended.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Hampl SE et al. Pediatrics. 2023;151(2):e2022060640.
2. Academy of Eating Disorders. Jan. 26, 2023. Accessed February 2, 2023. Available at The Academy for Eating Disorders Releases a Statement on the Recent American Academy of Pediatrics Clinical Practice Guideline for Weight-Related Care: First, Do No Harm (newswise.com).
3. Freedhoff Y. MDedge Pediatrics 2023. Available at https://www.mdedge.com/pediatrics/article/260894/obesity/weight-bias-affects-views-kids-obesity-recommendations?channel=52.
4. Hornberger LL, Lane MA et al. Pediatrics. 2021;147(1):e202004027989.
5. Loth KA, Lebow J et al. Global Pediatric Health. 2021;8:1-9.
6. Berge JM et al. JAMA Pediatrics. 2013;167(8):746-53.
7. Golden NH et al. Pediatrics. 2016;138(3):e20161649.
A new (old) drug joins the COVID fray, and guess what? It works
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
At this point, with the monoclonals found to be essentially useless, we are left with remdesivir with its modest efficacy and Paxlovid, which, for some reason, people don’t seem to be taking.
Part of the reason the monoclonals have failed lately is because of their specificity; they are homogeneous antibodies targeted toward a very specific epitope that may change from variant to variant. We need a broader therapeutic, one that has activity across all variants — maybe even one that has activity against all viruses? We’ve got one. Interferon.
The first mention of interferon as a potential COVID therapy was at the very start of the pandemic, so I’m sort of surprised that the first large, randomized trial is only being reported now in the New England Journal of Medicine.
Before we dig into the results, let’s talk mechanism. This is a trial of interferon-lambda, also known as interleukin-29.
The lambda interferons were only discovered in 2003. They differ from the more familiar interferons only in their cellular receptors; the downstream effects seem quite similar. As opposed to the cellular receptors for interferon alfa, which are widely expressed, the receptors for lambda are restricted to epithelial tissues. This makes it a good choice as a COVID treatment, since the virus also preferentially targets those epithelial cells.
In this study, 1,951 participants from Brazil and Canada, but mostly Brazil, with new COVID infections who were not yet hospitalized were randomized to receive 180 mcg of interferon lambda or placebo.
This was a relatively current COVID trial, as you can see from the participant characteristics. The majority had been vaccinated, and nearly half of the infections were during the Omicron phase of the pandemic.
If you just want to cut to the chase, interferon worked.
The primary outcome – hospitalization or a prolonged emergency room visit for COVID – was 50% lower in the interferon group.
Key secondary outcomes, including death from COVID, were lower in the interferon group as well. These effects persisted across most of the subgroups I was looking out for.
Interferon seemed to help those who were already vaccinated and those who were unvaccinated. There’s a hint that it works better within the first few days of symptoms, which isn’t surprising; we’ve seen this for many of the therapeutics, including Paxlovid. Time is of the essence. Encouragingly, the effect was a bit more pronounced among those infected with Omicron.
Of course, if you have any experience with interferon, you know that the side effects can be pretty rough. In the bad old days when we treated hepatitis C infection with interferon, patients would get their injections on Friday in anticipation of being essentially out of commission with flu-like symptoms through the weekend. But we don’t see much evidence of adverse events in this trial, maybe due to the greater specificity of interferon lambda.
Putting it all together, the state of play for interferons in COVID may be changing. To date, the FDA has not recommended the use of interferon alfa or -beta for COVID-19, citing some data that they are ineffective or even harmful in hospitalized patients with COVID. Interferon lambda is not FDA approved and thus not even available in the United States. But the reason it has not been approved is that there has not been a large, well-conducted interferon lambda trial. Now there is. Will this study be enough to prompt an emergency use authorization? The elephant in the room, of course, is Paxlovid, which at this point has a longer safety track record and, importantly, is oral. I’d love to see a head-to-head trial. Short of that, I tend to be in favor of having more options on the table.
Dr. Perry Wilson is associate professor, department of medicine, and director, Clinical and Translational Research Accelerator, at Yale University, New Haven, Conn. He disclosed no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Can a hormone shot rescue low libido?
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
according to results from two small randomized controlled trials.
The data suggest that injections of kisspeptin can boost sexual desire in men and women and can increase penile rigidity in men.
Together, these two studies provide proof of concept for the development of kisspeptin-based therapeutics for men and women with distressing hypoactive sexual desire disorder (HSDD), study investigator Alexander Comninos, MD, PhD, Imperial College London, said in a news release.
One study was published online Feb. 3, 2022, in JAMA Network Open. The other was published in October 2022.
Unmet need
HSDD affects up to 10% of women and 8% of men worldwide and leads to psychological and social harm, the news release noted.
“There is a real unmet need to find new, safer, and more effective therapies for this distressing condition for both women and men seeking treatment,” Dr. Comninos said.
Kisspeptin is a naturally occurring reproductive hormone that serves as a crucial activator of the reproductive system. Emerging evidence from animal models shows that kisspeptin signaling has key roles in modulating reproductive behavior, including sexual motivation and erections.
In a double-blind, placebo-controlled, crossover study, the researchers enrolled 32 healthy heterosexual men (mean age, 37.9 years) who had HSDD.
At the first study visit, the men were given an infusion of kisspeptin-54 (1 nmol/kg per hour) or placebo (saline) over 75 minutes. The participants then crossed over to the other treatment at a second study visit at least 7 days later.
The active treatment significantly increased circulating kisspeptin levels. A steady state was reached after 30-75 minutes of infusion, the researchers reported.
Similar data in men, women
While the men viewed sexual videos, kisspeptin significantly modulated brain activity on fMRI in key structures of the sexual-processing network, compared with placebo (P = .003).
In addition, the treatment led to significant increases in penile tumescence in response to sexual stimuli (by up to 56% more than placebo; P = .02) and behavioral measures of sexual desire – most notably increased happiness about sex (P = .02).
Given the significant stimulatory effect of kisspeptin administration on penile rigidity, coupled with its demonstrated proerectile effect in rodents, future studies should examine the use of kisspeptin for patients with erectile dysfunction, the researchers wrote.
The second study included 32 women with HSDD and had the same design. Its results also showed that kisspeptin restored sexual and attraction brain processing without adverse effects.
“It is highly encouraging to see the same boosting effect in both women and men, although the precise brain pathways were slightly different, as might be expected,” coinvestigator Waljit Dhillo, PhD, Imperial College London, said in the news release.
“Collectively, the results suggest that kisspeptin may offer a safe and much-needed treatment for HSDD that affects millions of people around the world; and we look forward to taking this forward in future larger studies and in other patient groups,” Dr. Dhillo added.
The study was funded by the National Institute for Health and Care Research Imperial Biomedical Research Centre and the Medical Research Council, part of UK Research and Innovation. Dr. Comninos reported no relevant financial relationships. Dr. Dhillo reported receiving consulting fees from Myovant Sciences and KaNDy Therapeutics outside the submitted work.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Pound of flesh buys less prison time
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.
Pound of flesh buys less prison time
We should all have more Shakespeare in our lives. Yeah, yeah, Shakespeare is meant to be played, not read, and it can be a struggle to herd teenagers through the Bard’s interesting and bloody tragedies, but even a perfunctory reading of “The Merchant of Venice” would hopefully have prevented the dystopian nightmare Massachusetts has presented us with today.
The United States has a massive shortage of donor organs. This is an unfortunate truth. So, to combat this issue, a pair of Massachusetts congresspeople have proposed HD 3822, which would allow prisoners to donate organs and/or bone marrow (a pound of flesh, so to speak) in exchange for up to a year in reduced prison time. Yes, that’s right. Give up pieces of yourself and the state of Massachusetts will deign to reduce your long prison sentence.
Oh, and before you dismiss this as typical Republican antics, the bill was sponsored by two Democrats, and in a statement one of them hoped to address racial disparities in organ donation, as people of color are much less likely to receive organs. Never mind that Black people are imprisoned at a much higher rate than Whites.
Yeah, this whole thing is what people in the business like to call an ethical disaster.
Fortunately, the bill will likely never be passed and it’s probably illegal anyway. A federal law from 1984 (how’s that for a coincidence) prevents people from donating organs for use in human transplantation in exchange for “valuable consideration.” In other words, you can’t sell your organs for profit, and in this case, reducing prison time would probably count as valuable consideration in the eyes of the courts.
Oh, and in case you’ve never read Merchant of Venice, Shylock, the character looking for the pound of flesh as payment for a debt? He’s the villain. In fact, it’s pretty safe to say that anyone looking to extract payment from human dismemberment is probably the bad guy of the story. Apparently that wasn’t clear.
How do you stop a fungi? With a deadly guy
Thanks to the new HBO series “The Last of Us,” there’s been a lot of talk about the upcoming fungi-pocalypse, as the show depicts the real-life “zombie fungus” Cordyceps turning humans into, you know, zombies.
No need to worry, ladies and gentleman, because science has discovered a way to turn back the fungal horde. A heroic, and environmentally friendly, alternative to chemical pesticides “in the fight against resistant fungi [that] are now resistant to antimycotics – partly because they are used in large quantities in agricultural fields,” investigators at the Leibniz Institute for Natural Product Research and Infection Biology in Jena, Germany, said in a written statement.
We are, of course, talking about Keanu Reeves. Wait a second. He’s not even in “The Last of Us.” Sorry folks, we are being told that it really is Keanu Reeves. Our champion in the inevitable fungal pandemic is movie star Keanu Reeves. Sort of. It’s actually keanumycin, a substance produced by bacteria of the genus Pseudomonas.
Really? Keanumycin? “The lipopeptides kill so efficiently that we named them after Keanu Reeves because he, too, is extremely deadly in his roles,” lead author Sebastian Götze, PhD, explained.
Dr. Götze and his associates had been working with pseudomonads for quite a while before they were able to isolate the toxins responsible for their ability to kill amoebae, which resemble fungi in some characteristics. When then finally tried the keanumycin against gray mold rot on hydrangea leaves, the intensely contemplative star of “The Matrix” and “John Wick” – sorry, wrong Keanu – the bacterial derivative significantly inhibited growth of the fungus, they said.
Additional testing has shown that keanumycin is not highly toxic to human cells and is effective against fungi such as Candida albicans in very low concentrations, which makes it a good candidate for future pharmaceutical development.
To that news there can be only one response from the substance’s namesake.
High fat, bye parasites
Fat. Fat. Fat. Seems like everyone is trying to avoid it these days, but fat may be good thing when it comes to weaseling out a parasite.
The parasite in this case is the whipworm, aka Trichuris trichiura. You can find this guy in the intestines of millions of people, where it causes long-lasting infections. Yikes … Researchers have found that the plan of attack to get rid of this invasive species is to boost the immune system, but instead of vitamin C and zinc it’s fat they’re pumping in. Yes, fat.
The developing countries with poor sewage that are at the highest risk for contracting parasites such as this also are among those where people ingest cheaper diets that are generally higher in fat. The investigators were interested to see how a high-fat diet would affect immune responses to the whipworms.
And, as with almost everything else, the researchers turned to mice, which were introduced to a closely related species, Trichuris muris.
A high-fat diet, rather than obesity itself, increases a molecule on T-helper cells called ST2, and this allows an increased T-helper 2 response, effectively giving eviction notices to the parasites in the intestinal lining.
To say the least, the researchers were surprised since “high-fat diets are mostly associated with increased pathology during disease,” said senior author Richard Grencis, PhD, of the University of Manchester (England), who noted that ST2 is not normally triggered with a standard diet in mice but the high-fat diet gave it a boost and an “alternate pathway” out.
Now before you start ordering extra-large fries at the drive-through to keep the whipworms away, the researchers added that they “have previously published that weight loss can aid the expulsion of a different gut parasite worm.” Figures.
Once again, though, signs are pointing to the gut for improved health.