User login
The Rise of Positive Psychiatry (and How Pediatrics Can Join the Effort)
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Psychiatry, like all medical disciplines, changes over time. For many decades, psychiatrists were primarily psychotherapists. As medications slowly became available, these became a second tool for treatment — so much so that by the 21st century many, if not most, psychiatrists saw themselves primarily as psychopharmacologists and diagnosticians who were skilled at identifying various forms of mental illness and using medications in the hopes of inducing a clinically meaningful “response” in symptoms. While still belonging to the umbrella category of a mental health professional, more and more psychiatrists trained and practiced as mental illness professionals.
Slowly, however, there have been stirrings within the field by many who have found the identity of the psychiatrist as a “prescriber” to be too narrow, and the current “med check” model of treatment too confining. This change was partly inspired by our colleagues in clinical psychology who were challenged in the 1990s by then American Psychological Association President Martin Seligman, PhD, to develop knowledge and expertise not only in alleviating mental suffering but also in promoting true mental well-being, a construct that still was often vaguely defined. One framework of well-being that was advanced at the time was the PERMA model, representing the five well-being dimensions of Positive emotions, Engagement, Relationships, Meaning, and Accomplishment.1
While there have always been those in psychiatry who have advocated for a broad emphasis that incorporates the full spectrum of mental health, there has been a surge of interest in the past 10-15 years, urging a focus on well-being and the tools that can help a person achieve it. This trend has variably been referred to as positive psychiatry, lifestyle psychiatry, and other terms.2 As one might expect, child and adolescent psychiatry has been particularly fertile ground for such principles, and models such as the Vermont Family Based Approach have expanded the concept beyond the individual to the family and even community.3
It is important to note here that embracing the concept of well-being in treatment does not in any way require one to abandon the idea that genetic or environmental factors can lead to negative outcomes in brain development, nor does it mandate that one leaves behind important treatment modalities such as traditional psychotherapy and medication treatment. Further, this approach should not be confused with some “wellness” activities that offer quick fixes and lack scientific rigor. Positive psychiatry does, however, offer a third pathway to advance positive emotional behavioral growth, namely through health promotion activities ranging from exercise to good nutrition to positive parenting in ways that have been shown to benefit both those who are already doing fairly well as well as those who are actively struggling with significant psychiatric disorders.4
Primary care clinicians already have extensive familiarity talking about these kinds of health promoting activities with families. That said, it’s been my observation from many years of doing consultations and reviewing notes that these conversations happen almost exclusively during well-check visits and can get forgotten when a child presents with emotional behavioral challenges.
So how can the primary care clinician who is interested in more fully incorporating the burgeoning science on well-being work these principles into routine practice? Here are three suggestions.
Ask Some New Questions
It’s difficult to treat things that aren’t assessed. To best incorporate true mental health within one’s work with families, it can be very helpful to expand the regular questions one asks to include those that address some of the PERMA and health promotion areas described above. Some examples could include the following:
- Hopes. What would a perfect life look like for you when you’re older?
- Connection. Is there anything that you just love doing, so much so that time sometimes just seems to go away?
- Strengths. What are you good at? What good things would your friends say about you?
- Parenting. What are you most proud of as a parent, and where are your biggest challenges?
- Nutrition. What does a typical school day breakfast look like for you?
- Screens. Do you have any restrictions related to what you do on screens?
- Sleep. Tell me about your typical bedtime routine.
Add Some New Interventions
Counseling and medications can be powerful ways to bring improvement in a child’s life, but thinking about health promotion opens up a whole new avenue for intervention. This domain includes areas like physical activity, nutrition, sleep practices, parenting, participation in music and the arts, practicing kindness towards others, and mindfulness, among others.
For someone newly diagnosed with ADHD, for example, consider expanding your treatment plan to include not only medications but also specific guidance to exercise more, limit screen usage, practice good bedtime routines, eat a real breakfast, and reduce the helicopter parenting. Monitor these areas over time.
Another example relates to common sleep problems. Before making that melatonin recommendation, ask yourself if you understand what is happening in that child’s environment at night. Are they allowed to play video games until 2 a.m.? Are they taking naps during the day because they have nothing to do? Are they downing caffeinated drinks with dinner? Does the child get zero physical activity outside of the PE class? Maybe you still will need the melatonin, but perhaps other areas need to be addressed first.
Find Some New Colleagues
While it can be challenging sometimes to find anyone in mental health who sees new patients, there is value is finding out the approach and methodology that psychiatric clinicians and therapists apply in their practice. Working collaboratively with those who value a well-being orientation and who can work productively with the whole family to increase health promotion can yield benefits for a patient’s long-term physical and mental health.
The renewed interest and attention on well-being and health promotion activities that can optimize brain growth are a welcome and overdue development in mental health treatment. Pediatricians and other primary care clinicians can be a critical part of this growing initiative by gaining knowledge about youth well-being, applying this knowledge in day-to-day practice, and working collaboratively with those who share a similar perspective.
Dr. Rettew is a child & adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Oregon. He is on the psychiatry faculty at Oregon Health & Science University. You can follow him on Facebook and X @PediPsych. His latest book is Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.
References
1. Seligman, MEP. Flourish: a visionary new understanding of happiness and well-being. New York: Simon & Schuster; 2011.
2. Jeste DV, Palmer BW. (Eds.). Positive psychiatry: a clinical handbook. Washington DC: American Psychiatric Publishing; 2015. doi: 10.1176/appi.books.9781615370818.
3. Hudziak J, Ivanova MY. The Vermont family based approach: Family based health promotion, illness prevention, and intervention. Child Adolesc Psychiatr Clin N Am. 2016 Apr;25(2):167-78. doi: 10.1016/j.chc.2015.11.002.
4. Rettew DC. Incorporating positive psychiatry with children and adolescents. Current Psychiatry. 2022 November;21(11):12-16,45. doi: 10.12788/cp.0303.
Just gas? New study on colic suggests some longer-term implications
Pediatricians commonly are asked to see infants presenting with symptoms of colic. The frequent and intense crying associated with colic is understandably quite distressing to parents, who often worry about a serious underlying medical cause. There also is the stress of trying to soothe an irritable infant who often does not seem to respond to the typical interventions.
Conventional wisdom about colic has been that the behaviors are the result of some gastrointestinal problem that, while not perfectly understood, tends to be mercifully self-limited and not predictive of future medical or mental health problems. This perspective then leads to pediatricians typically offering mainly sympathy and reassurance at these visits.
A new study,1 however, challenges some of this traditional thinking. The data come from a remarkable longitudinal study called the Generation R Study (R being Rotterdam in the Netherlands) that has prospectively studied a group of nearly 5,000 children from before birth into adolescence. Colic symptoms were briefly assessed when infants were about 3 months old and emotional-behavioral problems have been prospectively measured at multiple time points subsequently using well-validated rating scales.
The main finding of the study was and, to a lesser extent, in adolescence. This held for both internalizing problems (like anxiety and depressive symptoms) and externalizing problems (like defiance and aggressive behavior). At age 10, participants also underwent an MRI scan and those who were excessive criers as infants were found to have a smaller amygdala, a region known for being important in regulating emotions.
The authors concluded that colicky behavior in infancy may reflect some underlying temperamental vulnerabilities and may have more predictive value than previously thought. The connection between excessive crying and a measurable brain region difference later in life is also interesting, although these kinds of brain imaging findings have been notoriously difficult to interpret clinically.
Overall, this is a solid study that deserves to be considered. Colic may reflect a bit more than most of us have been taught and shouldn’t necessarily be “shrugged off,” as the authors state in their discussion.
At the same time, however, it is important not to overinterpret the findings. The magnitude of the effects were on the small side (about 0.2 of a standard deviation) and most children with excessive crying in early infancy did not manifest high levels of mental health problems later in life. The mothers of high crying infants also had slightly higher levels of mental health problems themselves so there could be other mechanisms at work here, such as genetic differences between the two groups.
So how could a pediatrician best use this new information without taking things too far? Regardless of the question of whether the excessive crying infancy is a true risk factor for later behavior problems (in the causal sense) or whether it represents more of a marker for something else, its presence so early in life offers an opportunity. Primary care clinicians would still likely want to provide the reassurance that has typically been given in these visits but perhaps with the caveat that some of these kids go on to struggle a bit more with mental health and that they might benefit from some additional support. We are not talking about prophylactic medications here, but something like additional parenting skills. Especially if you, as the pediatrician, suspect that the parents might benefit from expanding their parenting toolkit already, here is a nice opportunity to invite them to learn some new approaches and skills — framed in a way that focuses on the temperament of the child rather than any “deficits” you perceive in the parents. Some parents may be more receptive and less defensive to the idea of participating in parent training under the framework that they are doing this because they have a temperamentally more challenging child (rather than feeling that they are deficient in basic parenting skills).
It’s always a good idea to know about what resources are available in the community when it comes to teaching parenting skills. In addition to scientifically supported books and podcasts, there has been a steady increase in reliable websites, apps, and other digital platforms related to parenting, as well as standard in-person groups and classes. This could also be a great use of an integrated behavioral health professional for practices fortunate enough to have one.
In summary, there is some new evidence that colic can represent a little more than “just gas,” and while we shouldn’t take this one study to the extreme, there may be some good opportunities here to discuss and support good parenting practices in general.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
1. Sammallahti S et al. Excessive crying, behavior problems, and amygdala volume: A study from infancy to adolescence. J Am Acad Child Adolesc Psychiatry. 2023 Jun;62(6):675-83. doi: 10.1016/j.jaac.2023.01.014.
Pediatricians commonly are asked to see infants presenting with symptoms of colic. The frequent and intense crying associated with colic is understandably quite distressing to parents, who often worry about a serious underlying medical cause. There also is the stress of trying to soothe an irritable infant who often does not seem to respond to the typical interventions.
Conventional wisdom about colic has been that the behaviors are the result of some gastrointestinal problem that, while not perfectly understood, tends to be mercifully self-limited and not predictive of future medical or mental health problems. This perspective then leads to pediatricians typically offering mainly sympathy and reassurance at these visits.
A new study,1 however, challenges some of this traditional thinking. The data come from a remarkable longitudinal study called the Generation R Study (R being Rotterdam in the Netherlands) that has prospectively studied a group of nearly 5,000 children from before birth into adolescence. Colic symptoms were briefly assessed when infants were about 3 months old and emotional-behavioral problems have been prospectively measured at multiple time points subsequently using well-validated rating scales.
The main finding of the study was and, to a lesser extent, in adolescence. This held for both internalizing problems (like anxiety and depressive symptoms) and externalizing problems (like defiance and aggressive behavior). At age 10, participants also underwent an MRI scan and those who were excessive criers as infants were found to have a smaller amygdala, a region known for being important in regulating emotions.
The authors concluded that colicky behavior in infancy may reflect some underlying temperamental vulnerabilities and may have more predictive value than previously thought. The connection between excessive crying and a measurable brain region difference later in life is also interesting, although these kinds of brain imaging findings have been notoriously difficult to interpret clinically.
Overall, this is a solid study that deserves to be considered. Colic may reflect a bit more than most of us have been taught and shouldn’t necessarily be “shrugged off,” as the authors state in their discussion.
At the same time, however, it is important not to overinterpret the findings. The magnitude of the effects were on the small side (about 0.2 of a standard deviation) and most children with excessive crying in early infancy did not manifest high levels of mental health problems later in life. The mothers of high crying infants also had slightly higher levels of mental health problems themselves so there could be other mechanisms at work here, such as genetic differences between the two groups.
So how could a pediatrician best use this new information without taking things too far? Regardless of the question of whether the excessive crying infancy is a true risk factor for later behavior problems (in the causal sense) or whether it represents more of a marker for something else, its presence so early in life offers an opportunity. Primary care clinicians would still likely want to provide the reassurance that has typically been given in these visits but perhaps with the caveat that some of these kids go on to struggle a bit more with mental health and that they might benefit from some additional support. We are not talking about prophylactic medications here, but something like additional parenting skills. Especially if you, as the pediatrician, suspect that the parents might benefit from expanding their parenting toolkit already, here is a nice opportunity to invite them to learn some new approaches and skills — framed in a way that focuses on the temperament of the child rather than any “deficits” you perceive in the parents. Some parents may be more receptive and less defensive to the idea of participating in parent training under the framework that they are doing this because they have a temperamentally more challenging child (rather than feeling that they are deficient in basic parenting skills).
It’s always a good idea to know about what resources are available in the community when it comes to teaching parenting skills. In addition to scientifically supported books and podcasts, there has been a steady increase in reliable websites, apps, and other digital platforms related to parenting, as well as standard in-person groups and classes. This could also be a great use of an integrated behavioral health professional for practices fortunate enough to have one.
In summary, there is some new evidence that colic can represent a little more than “just gas,” and while we shouldn’t take this one study to the extreme, there may be some good opportunities here to discuss and support good parenting practices in general.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
1. Sammallahti S et al. Excessive crying, behavior problems, and amygdala volume: A study from infancy to adolescence. J Am Acad Child Adolesc Psychiatry. 2023 Jun;62(6):675-83. doi: 10.1016/j.jaac.2023.01.014.
Pediatricians commonly are asked to see infants presenting with symptoms of colic. The frequent and intense crying associated with colic is understandably quite distressing to parents, who often worry about a serious underlying medical cause. There also is the stress of trying to soothe an irritable infant who often does not seem to respond to the typical interventions.
Conventional wisdom about colic has been that the behaviors are the result of some gastrointestinal problem that, while not perfectly understood, tends to be mercifully self-limited and not predictive of future medical or mental health problems. This perspective then leads to pediatricians typically offering mainly sympathy and reassurance at these visits.
A new study,1 however, challenges some of this traditional thinking. The data come from a remarkable longitudinal study called the Generation R Study (R being Rotterdam in the Netherlands) that has prospectively studied a group of nearly 5,000 children from before birth into adolescence. Colic symptoms were briefly assessed when infants were about 3 months old and emotional-behavioral problems have been prospectively measured at multiple time points subsequently using well-validated rating scales.
The main finding of the study was and, to a lesser extent, in adolescence. This held for both internalizing problems (like anxiety and depressive symptoms) and externalizing problems (like defiance and aggressive behavior). At age 10, participants also underwent an MRI scan and those who were excessive criers as infants were found to have a smaller amygdala, a region known for being important in regulating emotions.
The authors concluded that colicky behavior in infancy may reflect some underlying temperamental vulnerabilities and may have more predictive value than previously thought. The connection between excessive crying and a measurable brain region difference later in life is also interesting, although these kinds of brain imaging findings have been notoriously difficult to interpret clinically.
Overall, this is a solid study that deserves to be considered. Colic may reflect a bit more than most of us have been taught and shouldn’t necessarily be “shrugged off,” as the authors state in their discussion.
At the same time, however, it is important not to overinterpret the findings. The magnitude of the effects were on the small side (about 0.2 of a standard deviation) and most children with excessive crying in early infancy did not manifest high levels of mental health problems later in life. The mothers of high crying infants also had slightly higher levels of mental health problems themselves so there could be other mechanisms at work here, such as genetic differences between the two groups.
So how could a pediatrician best use this new information without taking things too far? Regardless of the question of whether the excessive crying infancy is a true risk factor for later behavior problems (in the causal sense) or whether it represents more of a marker for something else, its presence so early in life offers an opportunity. Primary care clinicians would still likely want to provide the reassurance that has typically been given in these visits but perhaps with the caveat that some of these kids go on to struggle a bit more with mental health and that they might benefit from some additional support. We are not talking about prophylactic medications here, but something like additional parenting skills. Especially if you, as the pediatrician, suspect that the parents might benefit from expanding their parenting toolkit already, here is a nice opportunity to invite them to learn some new approaches and skills — framed in a way that focuses on the temperament of the child rather than any “deficits” you perceive in the parents. Some parents may be more receptive and less defensive to the idea of participating in parent training under the framework that they are doing this because they have a temperamentally more challenging child (rather than feeling that they are deficient in basic parenting skills).
It’s always a good idea to know about what resources are available in the community when it comes to teaching parenting skills. In addition to scientifically supported books and podcasts, there has been a steady increase in reliable websites, apps, and other digital platforms related to parenting, as well as standard in-person groups and classes. This could also be a great use of an integrated behavioral health professional for practices fortunate enough to have one.
In summary, there is some new evidence that colic can represent a little more than “just gas,” and while we shouldn’t take this one study to the extreme, there may be some good opportunities here to discuss and support good parenting practices in general.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
1. Sammallahti S et al. Excessive crying, behavior problems, and amygdala volume: A study from infancy to adolescence. J Am Acad Child Adolesc Psychiatry. 2023 Jun;62(6):675-83. doi: 10.1016/j.jaac.2023.01.014.
Integrating mental health and primary care: From dipping a toe to taking a plunge
In case anybody hasn’t noticed, the good ole days are long gone in which pediatric patients with mental health challenges could be simply referred out to be promptly assessed and treated by specialists. Due to a shortage of psychiatrists coupled with large increases in the number of youth presenting with emotional-behavioral difficulties, primary care clinicians are now called upon to fill in much of this gap, with professional organizations like the AAP articulating that .1
To meet this need, new models of integrated or collaborative care between primary care and mental health clinicians have been attempted and tested. While these initiatives have certainly been a welcome advance to many pediatricians, the large numbers of different models and initiatives out there have made for a rather confusing landscape that many busy primary care clinicians have found difficult to navigate.
In an attempt to offer some guidance on the subject, the American Academy of Child and Adolescent Psychiatry recently published a clinical update on pediatric collaborative care.2 The report is rich with resources and ideas. One of the main points of the document is that there are different levels of integration that exist. Kind of like the situation with recycling and household waste reduction, it is possible to make valuable improvements at any level of participation, although evidence suggests that more extensive efforts offer the most benefits. At one end of the spectrum, psychiatrists and primary care clinicians maintain separate practices and medical records and occasionally discuss mutual patients. Middle levels may include “colocation” with mental health and primary care professionals sharing a building and/or being part of the same overall system but continuing to work mainly independently. At the highest levels of integration, there is a coordinated and collaborative team that supports an intentional system of care with consistent communication about individual patients and general workflows. These approaches vary in the amount that the following four core areas of integrated care are incorporated.
- Direct service. Many integrated care initiatives heavily rely on the services of an on-site mental health care manager or behavioral health consultant who can provide a number of important functions such as overseeing of the integrated care program, conducting brief therapy with youth and parents, overseeing mental health screenings at the clinic, and providing general mental health promotion guidance.
- Care coordination. Helping patients and families find needed mental health, social services, and educational resources is a key component of integrated care. This task can fall to the practice’s behavioral health consultant, if there is one, but more general care coordinators can also be trained for this important role. The University of Washington’s Center for Advancing Integrated Mental Health Solutions has some published guidelines in this area.3
- Consultation. More advanced integrated care models often have established relationships to specific child psychiatric clinicians who are able to meet with the primary care team to discuss cases and general approaches to various problems. Alternatively, a number of states have implemented what are called Child Psychiatry Access Programs that give primary care clinicians a phone number to an organization (often affiliated with an academic medical center) that can provide quick and even immediate access to a child psychiatry provider for specific questions. Recent federal grants have led to many if not most states now having one of these programs in place, and a website listing these programs and their contact information is available.4
- Education. As mental health training was traditionally not part of a typical pediatrics residency, there have been a number of strategies introduced to help primary care clinicians increase their proficiency and comfort level when it comes to assessing and treating emotional-behavioral problems. These include specific conferences, online programs, and case-based training through mechanisms like the ECHO program.5,6 The AAP itself has released a number of toolkits and training materials related to mental health care that are available.7
The report also outlines some obstacles that continue to get in the way of more extensive integrative care efforts. Chief among them are financial concerns, including how to pay for what often are traditionally nonbillable efforts, particularly those that involve the communication of two expensive health care professionals. Some improvements have been made, however, such as the creation of some relatively new codes (such as 99451 and 99452) that can be submitted by both a primary care and mental health professional when there is a consultation that occurs that does not involve an actual face-to-face encounter.
One area that, in my view, has not received the level of attention it deserves when it comes to integrated care is the degree to which these programs have the potential not only to improve the care of children and adolescents already struggling with mental health challenges but also to serve as a powerful prevention tool to lower the risk of being diagnosed with a psychiatric disorder in the future and generally to improve levels of well-being. Thus far, however, research on various integrated programs has shown promising results that indicate that overall care for patients with mental health challenges improves.8 Further, when it comes to costs, there is some evidence to suggest that some of the biggest financial gains associated with integrated care has to do with reduced nonpsychiatric medical expenses of patients.9 This, then, suggests that practices that participate in capitated or accountable care organization structures could particularly benefit both clinically and financially from these collaborations.
If your practice has been challenged with the level of mental health care you are now expected to provide and has been contemplating even some small moves toward integrated care, now may the time to put those thoughts into action.
References
1. Foy JM et al. American Academy of Pediatrics policy statement. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757.
2. AACAP Committee on Collaborative and Integrated Care and AACAP Committee on Quality Issues. Clinical update: Collaborative mental health care for children and adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. 2023;62(2):91-119.
3. Behavioral health care managers. AIMS Center, University of Washington. Accessed May 5, 2023. Available at https://aims.uw.edu/online-bhcm-modules.
4. National Network of Child Psychiatry Access Programs. Accessed May 5, 2023. Available at https://www.nncpap.org/.
5. Project Echo Programs. Accessed May 5, 2023. https://hsc.unm.edu/echo.
6. Project TEACH. Accessed May 5, 2023. https://projectteachny.org.
7. Earls MF et al. Addressing mental health concerns in pediatrics: A practical resource toolkit for clinicians, 2nd edition. Itasca, Ill.: American Academy of Pediatrics, 2021.
8. Asarnow JR et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta analysis. JAMA Pediatr. 2015;169(10):929-37.
9. Unutzer J et al. Long-term costs effects of collaborative care for late-life depression. Am J Manag Care. 2008.14(2):95-100.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
In case anybody hasn’t noticed, the good ole days are long gone in which pediatric patients with mental health challenges could be simply referred out to be promptly assessed and treated by specialists. Due to a shortage of psychiatrists coupled with large increases in the number of youth presenting with emotional-behavioral difficulties, primary care clinicians are now called upon to fill in much of this gap, with professional organizations like the AAP articulating that .1
To meet this need, new models of integrated or collaborative care between primary care and mental health clinicians have been attempted and tested. While these initiatives have certainly been a welcome advance to many pediatricians, the large numbers of different models and initiatives out there have made for a rather confusing landscape that many busy primary care clinicians have found difficult to navigate.
In an attempt to offer some guidance on the subject, the American Academy of Child and Adolescent Psychiatry recently published a clinical update on pediatric collaborative care.2 The report is rich with resources and ideas. One of the main points of the document is that there are different levels of integration that exist. Kind of like the situation with recycling and household waste reduction, it is possible to make valuable improvements at any level of participation, although evidence suggests that more extensive efforts offer the most benefits. At one end of the spectrum, psychiatrists and primary care clinicians maintain separate practices and medical records and occasionally discuss mutual patients. Middle levels may include “colocation” with mental health and primary care professionals sharing a building and/or being part of the same overall system but continuing to work mainly independently. At the highest levels of integration, there is a coordinated and collaborative team that supports an intentional system of care with consistent communication about individual patients and general workflows. These approaches vary in the amount that the following four core areas of integrated care are incorporated.
- Direct service. Many integrated care initiatives heavily rely on the services of an on-site mental health care manager or behavioral health consultant who can provide a number of important functions such as overseeing of the integrated care program, conducting brief therapy with youth and parents, overseeing mental health screenings at the clinic, and providing general mental health promotion guidance.
- Care coordination. Helping patients and families find needed mental health, social services, and educational resources is a key component of integrated care. This task can fall to the practice’s behavioral health consultant, if there is one, but more general care coordinators can also be trained for this important role. The University of Washington’s Center for Advancing Integrated Mental Health Solutions has some published guidelines in this area.3
- Consultation. More advanced integrated care models often have established relationships to specific child psychiatric clinicians who are able to meet with the primary care team to discuss cases and general approaches to various problems. Alternatively, a number of states have implemented what are called Child Psychiatry Access Programs that give primary care clinicians a phone number to an organization (often affiliated with an academic medical center) that can provide quick and even immediate access to a child psychiatry provider for specific questions. Recent federal grants have led to many if not most states now having one of these programs in place, and a website listing these programs and their contact information is available.4
- Education. As mental health training was traditionally not part of a typical pediatrics residency, there have been a number of strategies introduced to help primary care clinicians increase their proficiency and comfort level when it comes to assessing and treating emotional-behavioral problems. These include specific conferences, online programs, and case-based training through mechanisms like the ECHO program.5,6 The AAP itself has released a number of toolkits and training materials related to mental health care that are available.7
The report also outlines some obstacles that continue to get in the way of more extensive integrative care efforts. Chief among them are financial concerns, including how to pay for what often are traditionally nonbillable efforts, particularly those that involve the communication of two expensive health care professionals. Some improvements have been made, however, such as the creation of some relatively new codes (such as 99451 and 99452) that can be submitted by both a primary care and mental health professional when there is a consultation that occurs that does not involve an actual face-to-face encounter.
One area that, in my view, has not received the level of attention it deserves when it comes to integrated care is the degree to which these programs have the potential not only to improve the care of children and adolescents already struggling with mental health challenges but also to serve as a powerful prevention tool to lower the risk of being diagnosed with a psychiatric disorder in the future and generally to improve levels of well-being. Thus far, however, research on various integrated programs has shown promising results that indicate that overall care for patients with mental health challenges improves.8 Further, when it comes to costs, there is some evidence to suggest that some of the biggest financial gains associated with integrated care has to do with reduced nonpsychiatric medical expenses of patients.9 This, then, suggests that practices that participate in capitated or accountable care organization structures could particularly benefit both clinically and financially from these collaborations.
If your practice has been challenged with the level of mental health care you are now expected to provide and has been contemplating even some small moves toward integrated care, now may the time to put those thoughts into action.
References
1. Foy JM et al. American Academy of Pediatrics policy statement. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757.
2. AACAP Committee on Collaborative and Integrated Care and AACAP Committee on Quality Issues. Clinical update: Collaborative mental health care for children and adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. 2023;62(2):91-119.
3. Behavioral health care managers. AIMS Center, University of Washington. Accessed May 5, 2023. Available at https://aims.uw.edu/online-bhcm-modules.
4. National Network of Child Psychiatry Access Programs. Accessed May 5, 2023. Available at https://www.nncpap.org/.
5. Project Echo Programs. Accessed May 5, 2023. https://hsc.unm.edu/echo.
6. Project TEACH. Accessed May 5, 2023. https://projectteachny.org.
7. Earls MF et al. Addressing mental health concerns in pediatrics: A practical resource toolkit for clinicians, 2nd edition. Itasca, Ill.: American Academy of Pediatrics, 2021.
8. Asarnow JR et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta analysis. JAMA Pediatr. 2015;169(10):929-37.
9. Unutzer J et al. Long-term costs effects of collaborative care for late-life depression. Am J Manag Care. 2008.14(2):95-100.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
In case anybody hasn’t noticed, the good ole days are long gone in which pediatric patients with mental health challenges could be simply referred out to be promptly assessed and treated by specialists. Due to a shortage of psychiatrists coupled with large increases in the number of youth presenting with emotional-behavioral difficulties, primary care clinicians are now called upon to fill in much of this gap, with professional organizations like the AAP articulating that .1
To meet this need, new models of integrated or collaborative care between primary care and mental health clinicians have been attempted and tested. While these initiatives have certainly been a welcome advance to many pediatricians, the large numbers of different models and initiatives out there have made for a rather confusing landscape that many busy primary care clinicians have found difficult to navigate.
In an attempt to offer some guidance on the subject, the American Academy of Child and Adolescent Psychiatry recently published a clinical update on pediatric collaborative care.2 The report is rich with resources and ideas. One of the main points of the document is that there are different levels of integration that exist. Kind of like the situation with recycling and household waste reduction, it is possible to make valuable improvements at any level of participation, although evidence suggests that more extensive efforts offer the most benefits. At one end of the spectrum, psychiatrists and primary care clinicians maintain separate practices and medical records and occasionally discuss mutual patients. Middle levels may include “colocation” with mental health and primary care professionals sharing a building and/or being part of the same overall system but continuing to work mainly independently. At the highest levels of integration, there is a coordinated and collaborative team that supports an intentional system of care with consistent communication about individual patients and general workflows. These approaches vary in the amount that the following four core areas of integrated care are incorporated.
- Direct service. Many integrated care initiatives heavily rely on the services of an on-site mental health care manager or behavioral health consultant who can provide a number of important functions such as overseeing of the integrated care program, conducting brief therapy with youth and parents, overseeing mental health screenings at the clinic, and providing general mental health promotion guidance.
- Care coordination. Helping patients and families find needed mental health, social services, and educational resources is a key component of integrated care. This task can fall to the practice’s behavioral health consultant, if there is one, but more general care coordinators can also be trained for this important role. The University of Washington’s Center for Advancing Integrated Mental Health Solutions has some published guidelines in this area.3
- Consultation. More advanced integrated care models often have established relationships to specific child psychiatric clinicians who are able to meet with the primary care team to discuss cases and general approaches to various problems. Alternatively, a number of states have implemented what are called Child Psychiatry Access Programs that give primary care clinicians a phone number to an organization (often affiliated with an academic medical center) that can provide quick and even immediate access to a child psychiatry provider for specific questions. Recent federal grants have led to many if not most states now having one of these programs in place, and a website listing these programs and their contact information is available.4
- Education. As mental health training was traditionally not part of a typical pediatrics residency, there have been a number of strategies introduced to help primary care clinicians increase their proficiency and comfort level when it comes to assessing and treating emotional-behavioral problems. These include specific conferences, online programs, and case-based training through mechanisms like the ECHO program.5,6 The AAP itself has released a number of toolkits and training materials related to mental health care that are available.7
The report also outlines some obstacles that continue to get in the way of more extensive integrative care efforts. Chief among them are financial concerns, including how to pay for what often are traditionally nonbillable efforts, particularly those that involve the communication of two expensive health care professionals. Some improvements have been made, however, such as the creation of some relatively new codes (such as 99451 and 99452) that can be submitted by both a primary care and mental health professional when there is a consultation that occurs that does not involve an actual face-to-face encounter.
One area that, in my view, has not received the level of attention it deserves when it comes to integrated care is the degree to which these programs have the potential not only to improve the care of children and adolescents already struggling with mental health challenges but also to serve as a powerful prevention tool to lower the risk of being diagnosed with a psychiatric disorder in the future and generally to improve levels of well-being. Thus far, however, research on various integrated programs has shown promising results that indicate that overall care for patients with mental health challenges improves.8 Further, when it comes to costs, there is some evidence to suggest that some of the biggest financial gains associated with integrated care has to do with reduced nonpsychiatric medical expenses of patients.9 This, then, suggests that practices that participate in capitated or accountable care organization structures could particularly benefit both clinically and financially from these collaborations.
If your practice has been challenged with the level of mental health care you are now expected to provide and has been contemplating even some small moves toward integrated care, now may the time to put those thoughts into action.
References
1. Foy JM et al. American Academy of Pediatrics policy statement. Mental health competencies for pediatric practice. Pediatrics. 2019;144(5):e20192757.
2. AACAP Committee on Collaborative and Integrated Care and AACAP Committee on Quality Issues. Clinical update: Collaborative mental health care for children and adolescents in pediatric primary care. J Am Acad Child Adolesc Psychiatry. 2023;62(2):91-119.
3. Behavioral health care managers. AIMS Center, University of Washington. Accessed May 5, 2023. Available at https://aims.uw.edu/online-bhcm-modules.
4. National Network of Child Psychiatry Access Programs. Accessed May 5, 2023. Available at https://www.nncpap.org/.
5. Project Echo Programs. Accessed May 5, 2023. https://hsc.unm.edu/echo.
6. Project TEACH. Accessed May 5, 2023. https://projectteachny.org.
7. Earls MF et al. Addressing mental health concerns in pediatrics: A practical resource toolkit for clinicians, 2nd edition. Itasca, Ill.: American Academy of Pediatrics, 2021.
8. Asarnow JR et al. Integrated medical-behavioral care compared with usual primary care for child and adolescent behavioral health: A meta analysis. JAMA Pediatr. 2015;169(10):929-37.
9. Unutzer J et al. Long-term costs effects of collaborative care for late-life depression. Am J Manag Care. 2008.14(2):95-100.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows about the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
AAP vs. AED on obesity treatment: Is there a middle ground?
While there is little controversy that both obesity and eating disorders represent important public health concerns, each deserving of clinical attention, how best to address one without worsening the other has been the crux of the discussion.
Sparking the dispute was a recent publication from the American Academy of Pediatrics that outlines the scope of the obesity problem and makes specific recommendations for assessment and treatment.1 The ambitious 100-page document, with 801 citations, puts new emphasis on the medical and psychological costs associated with obesity and advocates that pediatric primary care clinicians be more assertive in its treatment. While the guidelines certainly don’t urge the use of medications or surgery options as first-line treatment, the new recommendations do put them on the table as options.
In response, the Academy of Eating Disorders issued a public statement outlining several concerns regarding these guidelines that centered around a lack of a detailed plan to screen and address eating disorders; concerns that pediatricians don’t have the level of training and “skills” to conduct these conversations with patients and families with enough sensitivity; and worries about the premature use of antiobesity medications and surgeries in this population.2
It is fair to say that the critique was sharply worded, invoking physicians’ Hippocratic oath, criticizing their training, and suggesting that the guidelines could be biased by pharmaceutical industry influence (of note, the authors of the guidelines reported no ties to any pharmaceutical company). The AED urged that the guidelines be “revised” after consultation with other groups, including them.
Not unexpectedly, this response, especially coming from a group whose leadership and members are primarily nonphysicians, triggered its own sharp rebukes, including a recent commentary that counter-accused some of the eating disorder clinicians of being more concerned with their pet diets than actual health improvements.3
After everyone takes some deep breaths, it’s worth looking to see if there is some middle ground to explore here. The AAP document, to my reading, shows some important acknowledgments of the stigma associated with being overweight, even coming from pediatricians themselves. One passage reads, “Pediatricians and other PHCPs [primary health care providers] have been – and remain – a source of weight bias. They first need to uncover and address their own attitudes regarding children with obesity. Understanding weight stigma and bias, and learning how to reduce it in the clinical setting, sets the stage for productive discussions and improved relationships between families and pediatricians or other PHCPs.”
The guidelines also include some suggestions for how to talk to youth and families about obesity in less stigmatizing ways and offer a fairly lengthy summary of motivational interviewing techniques as they might apply to obesity discussions and lifestyle change. There is also a section on the interface between obesity and eating disorders with suggestions for further reading on their assessment and management.4
Indeed, research has looked specifically at how to minimize the triggering of eating disorders when addressing weight problems, a concern that has been raised by pediatricians themselves as documented in a qualitative study that also invoked the “do no harm” principle.5 One study asked more than 2,000 teens about how various conversations about weight affected their behavior.6 A main finding from that study was that conversations that focused on healthy eating rather than weight per se were less likely to be associated with unhealthy weight control behaviors. This message was emphasized in a publication that came from the AAP itself; it addresses the interaction between eating disorders and obesity.7 Strangely, however, the suggestion to try to minimize the focus on weight in discussions with patients isn’t well emphasized in the publication.
Overall, though, the AAP guidelines offer a well-informed and balanced approach to helping overweight youth. Pediatricians and other pediatric primary care clinicians are frequently called upon to engage in extremely sensitive and difficult discussions with patients and families on a wide variety of topics and most do so quite skillfully, especially when given the proper time and tools. While it is an area in which many of us, including mental health professionals, could do better, it’s no surprise that the AED’s disparaging of pediatricians’ communication competence came off as insulting. Similarly, productive dialogue would be likely enhanced if both sides avoided unfounded speculation about bias and motive and worked from a good faith perspective that all of us are engaged in this important discussion because of a desire to improve the lives of kids.
From my reading, it is quite a stretch to conclude that this document is urging a hasty and financially driven descent into GLP-1 analogues and bariatric surgery. That said, this wouldn’t be the first time a professional organization issues detailed, thoughtful, and nuanced care guidelines only to have them “condensed” within the practical confines of a busy office practice. Leaders would do well to remember that there remains much work to do to empower clinicians to be able to follow these guidelines as intended.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Hampl SE et al. Pediatrics. 2023;151(2):e2022060640.
2. Academy of Eating Disorders. Jan. 26, 2023. Accessed February 2, 2023. Available at The Academy for Eating Disorders Releases a Statement on the Recent American Academy of Pediatrics Clinical Practice Guideline for Weight-Related Care: First, Do No Harm (newswise.com).
3. Freedhoff Y. MDedge Pediatrics 2023. Available at https://www.mdedge.com/pediatrics/article/260894/obesity/weight-bias-affects-views-kids-obesity-recommendations?channel=52.
4. Hornberger LL, Lane MA et al. Pediatrics. 2021;147(1):e202004027989.
5. Loth KA, Lebow J et al. Global Pediatric Health. 2021;8:1-9.
6. Berge JM et al. JAMA Pediatrics. 2013;167(8):746-53.
7. Golden NH et al. Pediatrics. 2016;138(3):e20161649.
While there is little controversy that both obesity and eating disorders represent important public health concerns, each deserving of clinical attention, how best to address one without worsening the other has been the crux of the discussion.
Sparking the dispute was a recent publication from the American Academy of Pediatrics that outlines the scope of the obesity problem and makes specific recommendations for assessment and treatment.1 The ambitious 100-page document, with 801 citations, puts new emphasis on the medical and psychological costs associated with obesity and advocates that pediatric primary care clinicians be more assertive in its treatment. While the guidelines certainly don’t urge the use of medications or surgery options as first-line treatment, the new recommendations do put them on the table as options.
In response, the Academy of Eating Disorders issued a public statement outlining several concerns regarding these guidelines that centered around a lack of a detailed plan to screen and address eating disorders; concerns that pediatricians don’t have the level of training and “skills” to conduct these conversations with patients and families with enough sensitivity; and worries about the premature use of antiobesity medications and surgeries in this population.2
It is fair to say that the critique was sharply worded, invoking physicians’ Hippocratic oath, criticizing their training, and suggesting that the guidelines could be biased by pharmaceutical industry influence (of note, the authors of the guidelines reported no ties to any pharmaceutical company). The AED urged that the guidelines be “revised” after consultation with other groups, including them.
Not unexpectedly, this response, especially coming from a group whose leadership and members are primarily nonphysicians, triggered its own sharp rebukes, including a recent commentary that counter-accused some of the eating disorder clinicians of being more concerned with their pet diets than actual health improvements.3
After everyone takes some deep breaths, it’s worth looking to see if there is some middle ground to explore here. The AAP document, to my reading, shows some important acknowledgments of the stigma associated with being overweight, even coming from pediatricians themselves. One passage reads, “Pediatricians and other PHCPs [primary health care providers] have been – and remain – a source of weight bias. They first need to uncover and address their own attitudes regarding children with obesity. Understanding weight stigma and bias, and learning how to reduce it in the clinical setting, sets the stage for productive discussions and improved relationships between families and pediatricians or other PHCPs.”
The guidelines also include some suggestions for how to talk to youth and families about obesity in less stigmatizing ways and offer a fairly lengthy summary of motivational interviewing techniques as they might apply to obesity discussions and lifestyle change. There is also a section on the interface between obesity and eating disorders with suggestions for further reading on their assessment and management.4
Indeed, research has looked specifically at how to minimize the triggering of eating disorders when addressing weight problems, a concern that has been raised by pediatricians themselves as documented in a qualitative study that also invoked the “do no harm” principle.5 One study asked more than 2,000 teens about how various conversations about weight affected their behavior.6 A main finding from that study was that conversations that focused on healthy eating rather than weight per se were less likely to be associated with unhealthy weight control behaviors. This message was emphasized in a publication that came from the AAP itself; it addresses the interaction between eating disorders and obesity.7 Strangely, however, the suggestion to try to minimize the focus on weight in discussions with patients isn’t well emphasized in the publication.
Overall, though, the AAP guidelines offer a well-informed and balanced approach to helping overweight youth. Pediatricians and other pediatric primary care clinicians are frequently called upon to engage in extremely sensitive and difficult discussions with patients and families on a wide variety of topics and most do so quite skillfully, especially when given the proper time and tools. While it is an area in which many of us, including mental health professionals, could do better, it’s no surprise that the AED’s disparaging of pediatricians’ communication competence came off as insulting. Similarly, productive dialogue would be likely enhanced if both sides avoided unfounded speculation about bias and motive and worked from a good faith perspective that all of us are engaged in this important discussion because of a desire to improve the lives of kids.
From my reading, it is quite a stretch to conclude that this document is urging a hasty and financially driven descent into GLP-1 analogues and bariatric surgery. That said, this wouldn’t be the first time a professional organization issues detailed, thoughtful, and nuanced care guidelines only to have them “condensed” within the practical confines of a busy office practice. Leaders would do well to remember that there remains much work to do to empower clinicians to be able to follow these guidelines as intended.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Hampl SE et al. Pediatrics. 2023;151(2):e2022060640.
2. Academy of Eating Disorders. Jan. 26, 2023. Accessed February 2, 2023. Available at The Academy for Eating Disorders Releases a Statement on the Recent American Academy of Pediatrics Clinical Practice Guideline for Weight-Related Care: First, Do No Harm (newswise.com).
3. Freedhoff Y. MDedge Pediatrics 2023. Available at https://www.mdedge.com/pediatrics/article/260894/obesity/weight-bias-affects-views-kids-obesity-recommendations?channel=52.
4. Hornberger LL, Lane MA et al. Pediatrics. 2021;147(1):e202004027989.
5. Loth KA, Lebow J et al. Global Pediatric Health. 2021;8:1-9.
6. Berge JM et al. JAMA Pediatrics. 2013;167(8):746-53.
7. Golden NH et al. Pediatrics. 2016;138(3):e20161649.
While there is little controversy that both obesity and eating disorders represent important public health concerns, each deserving of clinical attention, how best to address one without worsening the other has been the crux of the discussion.
Sparking the dispute was a recent publication from the American Academy of Pediatrics that outlines the scope of the obesity problem and makes specific recommendations for assessment and treatment.1 The ambitious 100-page document, with 801 citations, puts new emphasis on the medical and psychological costs associated with obesity and advocates that pediatric primary care clinicians be more assertive in its treatment. While the guidelines certainly don’t urge the use of medications or surgery options as first-line treatment, the new recommendations do put them on the table as options.
In response, the Academy of Eating Disorders issued a public statement outlining several concerns regarding these guidelines that centered around a lack of a detailed plan to screen and address eating disorders; concerns that pediatricians don’t have the level of training and “skills” to conduct these conversations with patients and families with enough sensitivity; and worries about the premature use of antiobesity medications and surgeries in this population.2
It is fair to say that the critique was sharply worded, invoking physicians’ Hippocratic oath, criticizing their training, and suggesting that the guidelines could be biased by pharmaceutical industry influence (of note, the authors of the guidelines reported no ties to any pharmaceutical company). The AED urged that the guidelines be “revised” after consultation with other groups, including them.
Not unexpectedly, this response, especially coming from a group whose leadership and members are primarily nonphysicians, triggered its own sharp rebukes, including a recent commentary that counter-accused some of the eating disorder clinicians of being more concerned with their pet diets than actual health improvements.3
After everyone takes some deep breaths, it’s worth looking to see if there is some middle ground to explore here. The AAP document, to my reading, shows some important acknowledgments of the stigma associated with being overweight, even coming from pediatricians themselves. One passage reads, “Pediatricians and other PHCPs [primary health care providers] have been – and remain – a source of weight bias. They first need to uncover and address their own attitudes regarding children with obesity. Understanding weight stigma and bias, and learning how to reduce it in the clinical setting, sets the stage for productive discussions and improved relationships between families and pediatricians or other PHCPs.”
The guidelines also include some suggestions for how to talk to youth and families about obesity in less stigmatizing ways and offer a fairly lengthy summary of motivational interviewing techniques as they might apply to obesity discussions and lifestyle change. There is also a section on the interface between obesity and eating disorders with suggestions for further reading on their assessment and management.4
Indeed, research has looked specifically at how to minimize the triggering of eating disorders when addressing weight problems, a concern that has been raised by pediatricians themselves as documented in a qualitative study that also invoked the “do no harm” principle.5 One study asked more than 2,000 teens about how various conversations about weight affected their behavior.6 A main finding from that study was that conversations that focused on healthy eating rather than weight per se were less likely to be associated with unhealthy weight control behaviors. This message was emphasized in a publication that came from the AAP itself; it addresses the interaction between eating disorders and obesity.7 Strangely, however, the suggestion to try to minimize the focus on weight in discussions with patients isn’t well emphasized in the publication.
Overall, though, the AAP guidelines offer a well-informed and balanced approach to helping overweight youth. Pediatricians and other pediatric primary care clinicians are frequently called upon to engage in extremely sensitive and difficult discussions with patients and families on a wide variety of topics and most do so quite skillfully, especially when given the proper time and tools. While it is an area in which many of us, including mental health professionals, could do better, it’s no surprise that the AED’s disparaging of pediatricians’ communication competence came off as insulting. Similarly, productive dialogue would be likely enhanced if both sides avoided unfounded speculation about bias and motive and worked from a good faith perspective that all of us are engaged in this important discussion because of a desire to improve the lives of kids.
From my reading, it is quite a stretch to conclude that this document is urging a hasty and financially driven descent into GLP-1 analogues and bariatric surgery. That said, this wouldn’t be the first time a professional organization issues detailed, thoughtful, and nuanced care guidelines only to have them “condensed” within the practical confines of a busy office practice. Leaders would do well to remember that there remains much work to do to empower clinicians to be able to follow these guidelines as intended.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Hampl SE et al. Pediatrics. 2023;151(2):e2022060640.
2. Academy of Eating Disorders. Jan. 26, 2023. Accessed February 2, 2023. Available at The Academy for Eating Disorders Releases a Statement on the Recent American Academy of Pediatrics Clinical Practice Guideline for Weight-Related Care: First, Do No Harm (newswise.com).
3. Freedhoff Y. MDedge Pediatrics 2023. Available at https://www.mdedge.com/pediatrics/article/260894/obesity/weight-bias-affects-views-kids-obesity-recommendations?channel=52.
4. Hornberger LL, Lane MA et al. Pediatrics. 2021;147(1):e202004027989.
5. Loth KA, Lebow J et al. Global Pediatric Health. 2021;8:1-9.
6. Berge JM et al. JAMA Pediatrics. 2013;167(8):746-53.
7. Golden NH et al. Pediatrics. 2016;138(3):e20161649.
New guidelines say pediatricians should screen for anxiety: Now what?
Recently the U.S. Preventive Services Task Force issued a formal recommendation that adolescents and children as young as 8 should be screened for anxiety.1 The advice was based on a review of the research that concluded that anxiety disorders were common in youth (prevalence around 8%), screening was not overly burdensome or dangerous, and treatments were available and effective.
While pediatricians fully appreciate how common clinically significant anxiety is and its impact on the lives of youth, the reception for the recommendations have been mixed. Some are concerned that it could lead to the overprescribing of medications. Arguably, the biggest pushback, however, relates to the question of what to do when a child screens positive in a time when finding an available child and adolescent psychiatrist or other type of pediatric mental health professional can feel next to impossible. The hope of this article is to fill in some of those gaps.
Screening for anxiety disorders
The recommendations suggest using a rating scale as part of the screen but doesn’t dictate which one. A common instrument that has been employed is the Screen for Child Anxiety and Related Disorders, which is a freely available 41-item instrument that has versions for youth self-report and parent-report. A shorter 7-item rating scale, the General Anxiety Disorder–7, and the even shorter GAD-2 (the first two questions of the GAD-7), are also popular but focus, as the name applies, on general anxiety disorder and not related conditions such as social or separation anxiety that can have some different symptoms. These instruments can be given to patients and families in the waiting room or administered with the help of a nurse, physician, or embedded mental health professional. The recommendations do not include specific guidance on how often the screening should be done but repeated screenings are likely important at some interval.
Confirming the diagnosis
Of course, a screening isn’t a formal diagnosis. The American Academy of Pediatrics has expressed the view that the initial diagnosis and treatment for anxiety disorders is well within a pediatrician’s scope of practice, which means further steps are likely required beyond a referral. Fortunately, going from a positive screen to an initial diagnosis does not have to overly laborious and can focus on reviewing the DSM-5 criteria for key anxiety disorders while also ensuring that there isn’t a nonpsychiatric cause driving the symptoms, such as the often cited but rarely seen pheochromocytoma. More common rule-outs include medication-induced anxiety or substance use, excessive caffeine intake, and cardiac arrhythmias. Assessing for current and past trauma or specific causes of the anxiety such as bullying are also important.
It is important to note that it is the rule rather than the exception that youth with clinical levels of anxiety will frequently endorse a number of criteria that span multiple diagnoses including generalized anxiety disorder, social anxiety disorder, and separation anxiety disorder.2 Spending a lot of effort to narrow things down to a single anxiety diagnosis often is unnecessary, as both pharmacologic and nonpharmacologic treatments don’t change all that much between individual diagnoses.
Explaining the diagnosis
In general, I’m a strong proponent of trying to explain any behavioral diagnoses that you make to kids in a way that is accurate but nonstigmatizing. When it comes to anxiety, one parallel I often draw is to our immune system, which most youth understand at least in basic terms. Both our immune system and our anxiety networks are natural and important; as a species, we wouldn’t have lasted long without them. Both are built to assess and respond to threats. Problems can arise, however, if the response is too strong relative to the threat or the response is activated when it doesn’t need to be. Treatment is directed not at ridding ourselves of anxiety but at helping regulate it so it works for us and not against us. Spending a few minutes going through a discussion like this can be very helpful, and perhaps more so than some dry summary of DSM-5 criteria.
Starting treatment
It is important to note that best practice recommendations when it comes to the treatment of anxiety disorder in youth do not suggest medications as the only type of treatment and often urge clinicians to try nonpharmacological interventions first.3 A specific type of psychotherapy called cognitive-behavioral therapy has the strongest scientific support as an effective treatment for anxiety but other modalities, including parenting guidance, can be helpful as well. Consequently, a referral to a good psychotherapist is paramount. For many kids, the key to overcoming anxiety is exposure: which means confronting anxiety slowly, with support, and with specific skills.
If there is a traumatic source of the anxiety, addressing that as much as possible is obviously critical and could involve working with the family or school. For some kids, this may involve frightening things they are seeing online or through other media. Finally, some health promotion activities such as exercise or mindfulness can also be quite useful.
Despite the fact that SSRIs are referred to as antidepressants, there is increasing appreciation that these medications are useful for anxiety, perhaps even more so than for mood. While only one medication, duloxetine, has Food and Drug Administration approval to treat anxiety in children as young as 7, there is good evidence to support the use of many of the most common SSRIs in treating clinical anxiety. Buspirone, beta-blockers, and antihistamine medications like hydroxyzine also can have their place in treatment, while benzodiazepines and antipsychotic medications are generally best avoided for anxious youth, especially in the primary care setting. A short but helpful medication guide with regard to pediatric anxiety has been published by the American Academy of Child and Adolescent Psychiatry.4
Conclusions
Clinical levels of anxiety in children and adolescents are both common and quite treatable, which has prompted new recommendations that primary care clinicians screen for them starting at age 8. While this recommendation may at first seem like yet one more task to fit in, following the guidance can be accomplished with the help of short screening tools and a managed multimodal approach to treatment.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. You can follow him on Twitter and Facebook @PediPsych.
References
1. U.S. Preventive Services Task Force. JAMA. 2022;328(14):1438-44.
2. Strawn JR. Curr Psychiatry. 2012;11(9):16-21.
3. Walter HJ et al. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1107-24.
4. Anxiety Disorders: Parents’ Medication Guide Workgroup. “Anxiety disorders: Parents’ medication guide.” Washington D.C.: American Academy of Child & Adolescent Psychiatry, 2020.
Recently the U.S. Preventive Services Task Force issued a formal recommendation that adolescents and children as young as 8 should be screened for anxiety.1 The advice was based on a review of the research that concluded that anxiety disorders were common in youth (prevalence around 8%), screening was not overly burdensome or dangerous, and treatments were available and effective.
While pediatricians fully appreciate how common clinically significant anxiety is and its impact on the lives of youth, the reception for the recommendations have been mixed. Some are concerned that it could lead to the overprescribing of medications. Arguably, the biggest pushback, however, relates to the question of what to do when a child screens positive in a time when finding an available child and adolescent psychiatrist or other type of pediatric mental health professional can feel next to impossible. The hope of this article is to fill in some of those gaps.
Screening for anxiety disorders
The recommendations suggest using a rating scale as part of the screen but doesn’t dictate which one. A common instrument that has been employed is the Screen for Child Anxiety and Related Disorders, which is a freely available 41-item instrument that has versions for youth self-report and parent-report. A shorter 7-item rating scale, the General Anxiety Disorder–7, and the even shorter GAD-2 (the first two questions of the GAD-7), are also popular but focus, as the name applies, on general anxiety disorder and not related conditions such as social or separation anxiety that can have some different symptoms. These instruments can be given to patients and families in the waiting room or administered with the help of a nurse, physician, or embedded mental health professional. The recommendations do not include specific guidance on how often the screening should be done but repeated screenings are likely important at some interval.
Confirming the diagnosis
Of course, a screening isn’t a formal diagnosis. The American Academy of Pediatrics has expressed the view that the initial diagnosis and treatment for anxiety disorders is well within a pediatrician’s scope of practice, which means further steps are likely required beyond a referral. Fortunately, going from a positive screen to an initial diagnosis does not have to overly laborious and can focus on reviewing the DSM-5 criteria for key anxiety disorders while also ensuring that there isn’t a nonpsychiatric cause driving the symptoms, such as the often cited but rarely seen pheochromocytoma. More common rule-outs include medication-induced anxiety or substance use, excessive caffeine intake, and cardiac arrhythmias. Assessing for current and past trauma or specific causes of the anxiety such as bullying are also important.
It is important to note that it is the rule rather than the exception that youth with clinical levels of anxiety will frequently endorse a number of criteria that span multiple diagnoses including generalized anxiety disorder, social anxiety disorder, and separation anxiety disorder.2 Spending a lot of effort to narrow things down to a single anxiety diagnosis often is unnecessary, as both pharmacologic and nonpharmacologic treatments don’t change all that much between individual diagnoses.
Explaining the diagnosis
In general, I’m a strong proponent of trying to explain any behavioral diagnoses that you make to kids in a way that is accurate but nonstigmatizing. When it comes to anxiety, one parallel I often draw is to our immune system, which most youth understand at least in basic terms. Both our immune system and our anxiety networks are natural and important; as a species, we wouldn’t have lasted long without them. Both are built to assess and respond to threats. Problems can arise, however, if the response is too strong relative to the threat or the response is activated when it doesn’t need to be. Treatment is directed not at ridding ourselves of anxiety but at helping regulate it so it works for us and not against us. Spending a few minutes going through a discussion like this can be very helpful, and perhaps more so than some dry summary of DSM-5 criteria.
Starting treatment
It is important to note that best practice recommendations when it comes to the treatment of anxiety disorder in youth do not suggest medications as the only type of treatment and often urge clinicians to try nonpharmacological interventions first.3 A specific type of psychotherapy called cognitive-behavioral therapy has the strongest scientific support as an effective treatment for anxiety but other modalities, including parenting guidance, can be helpful as well. Consequently, a referral to a good psychotherapist is paramount. For many kids, the key to overcoming anxiety is exposure: which means confronting anxiety slowly, with support, and with specific skills.
If there is a traumatic source of the anxiety, addressing that as much as possible is obviously critical and could involve working with the family or school. For some kids, this may involve frightening things they are seeing online or through other media. Finally, some health promotion activities such as exercise or mindfulness can also be quite useful.
Despite the fact that SSRIs are referred to as antidepressants, there is increasing appreciation that these medications are useful for anxiety, perhaps even more so than for mood. While only one medication, duloxetine, has Food and Drug Administration approval to treat anxiety in children as young as 7, there is good evidence to support the use of many of the most common SSRIs in treating clinical anxiety. Buspirone, beta-blockers, and antihistamine medications like hydroxyzine also can have their place in treatment, while benzodiazepines and antipsychotic medications are generally best avoided for anxious youth, especially in the primary care setting. A short but helpful medication guide with regard to pediatric anxiety has been published by the American Academy of Child and Adolescent Psychiatry.4
Conclusions
Clinical levels of anxiety in children and adolescents are both common and quite treatable, which has prompted new recommendations that primary care clinicians screen for them starting at age 8. While this recommendation may at first seem like yet one more task to fit in, following the guidance can be accomplished with the help of short screening tools and a managed multimodal approach to treatment.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. You can follow him on Twitter and Facebook @PediPsych.
References
1. U.S. Preventive Services Task Force. JAMA. 2022;328(14):1438-44.
2. Strawn JR. Curr Psychiatry. 2012;11(9):16-21.
3. Walter HJ et al. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1107-24.
4. Anxiety Disorders: Parents’ Medication Guide Workgroup. “Anxiety disorders: Parents’ medication guide.” Washington D.C.: American Academy of Child & Adolescent Psychiatry, 2020.
Recently the U.S. Preventive Services Task Force issued a formal recommendation that adolescents and children as young as 8 should be screened for anxiety.1 The advice was based on a review of the research that concluded that anxiety disorders were common in youth (prevalence around 8%), screening was not overly burdensome or dangerous, and treatments were available and effective.
While pediatricians fully appreciate how common clinically significant anxiety is and its impact on the lives of youth, the reception for the recommendations have been mixed. Some are concerned that it could lead to the overprescribing of medications. Arguably, the biggest pushback, however, relates to the question of what to do when a child screens positive in a time when finding an available child and adolescent psychiatrist or other type of pediatric mental health professional can feel next to impossible. The hope of this article is to fill in some of those gaps.
Screening for anxiety disorders
The recommendations suggest using a rating scale as part of the screen but doesn’t dictate which one. A common instrument that has been employed is the Screen for Child Anxiety and Related Disorders, which is a freely available 41-item instrument that has versions for youth self-report and parent-report. A shorter 7-item rating scale, the General Anxiety Disorder–7, and the even shorter GAD-2 (the first two questions of the GAD-7), are also popular but focus, as the name applies, on general anxiety disorder and not related conditions such as social or separation anxiety that can have some different symptoms. These instruments can be given to patients and families in the waiting room or administered with the help of a nurse, physician, or embedded mental health professional. The recommendations do not include specific guidance on how often the screening should be done but repeated screenings are likely important at some interval.
Confirming the diagnosis
Of course, a screening isn’t a formal diagnosis. The American Academy of Pediatrics has expressed the view that the initial diagnosis and treatment for anxiety disorders is well within a pediatrician’s scope of practice, which means further steps are likely required beyond a referral. Fortunately, going from a positive screen to an initial diagnosis does not have to overly laborious and can focus on reviewing the DSM-5 criteria for key anxiety disorders while also ensuring that there isn’t a nonpsychiatric cause driving the symptoms, such as the often cited but rarely seen pheochromocytoma. More common rule-outs include medication-induced anxiety or substance use, excessive caffeine intake, and cardiac arrhythmias. Assessing for current and past trauma or specific causes of the anxiety such as bullying are also important.
It is important to note that it is the rule rather than the exception that youth with clinical levels of anxiety will frequently endorse a number of criteria that span multiple diagnoses including generalized anxiety disorder, social anxiety disorder, and separation anxiety disorder.2 Spending a lot of effort to narrow things down to a single anxiety diagnosis often is unnecessary, as both pharmacologic and nonpharmacologic treatments don’t change all that much between individual diagnoses.
Explaining the diagnosis
In general, I’m a strong proponent of trying to explain any behavioral diagnoses that you make to kids in a way that is accurate but nonstigmatizing. When it comes to anxiety, one parallel I often draw is to our immune system, which most youth understand at least in basic terms. Both our immune system and our anxiety networks are natural and important; as a species, we wouldn’t have lasted long without them. Both are built to assess and respond to threats. Problems can arise, however, if the response is too strong relative to the threat or the response is activated when it doesn’t need to be. Treatment is directed not at ridding ourselves of anxiety but at helping regulate it so it works for us and not against us. Spending a few minutes going through a discussion like this can be very helpful, and perhaps more so than some dry summary of DSM-5 criteria.
Starting treatment
It is important to note that best practice recommendations when it comes to the treatment of anxiety disorder in youth do not suggest medications as the only type of treatment and often urge clinicians to try nonpharmacological interventions first.3 A specific type of psychotherapy called cognitive-behavioral therapy has the strongest scientific support as an effective treatment for anxiety but other modalities, including parenting guidance, can be helpful as well. Consequently, a referral to a good psychotherapist is paramount. For many kids, the key to overcoming anxiety is exposure: which means confronting anxiety slowly, with support, and with specific skills.
If there is a traumatic source of the anxiety, addressing that as much as possible is obviously critical and could involve working with the family or school. For some kids, this may involve frightening things they are seeing online or through other media. Finally, some health promotion activities such as exercise or mindfulness can also be quite useful.
Despite the fact that SSRIs are referred to as antidepressants, there is increasing appreciation that these medications are useful for anxiety, perhaps even more so than for mood. While only one medication, duloxetine, has Food and Drug Administration approval to treat anxiety in children as young as 7, there is good evidence to support the use of many of the most common SSRIs in treating clinical anxiety. Buspirone, beta-blockers, and antihistamine medications like hydroxyzine also can have their place in treatment, while benzodiazepines and antipsychotic medications are generally best avoided for anxious youth, especially in the primary care setting. A short but helpful medication guide with regard to pediatric anxiety has been published by the American Academy of Child and Adolescent Psychiatry.4
Conclusions
Clinical levels of anxiety in children and adolescents are both common and quite treatable, which has prompted new recommendations that primary care clinicians screen for them starting at age 8. While this recommendation may at first seem like yet one more task to fit in, following the guidance can be accomplished with the help of short screening tools and a managed multimodal approach to treatment.
Dr. Rettew is a child and adolescent psychiatrist with Lane County Behavioral Health in Eugene, Ore., and Oregon Health & Science University, Portland. You can follow him on Twitter and Facebook @PediPsych.
References
1. U.S. Preventive Services Task Force. JAMA. 2022;328(14):1438-44.
2. Strawn JR. Curr Psychiatry. 2012;11(9):16-21.
3. Walter HJ et al. J Am Acad Child Adolesc Psychiatry. 2020;59(10):1107-24.
4. Anxiety Disorders: Parents’ Medication Guide Workgroup. “Anxiety disorders: Parents’ medication guide.” Washington D.C.: American Academy of Child & Adolescent Psychiatry, 2020.
Incorporating positive psychiatry with children and adolescents
The principles and practices of positive psychiatry are especially well-suited for work with children, adolescents, and families. Positive psychiatry is “the science and practice of psychiatry that seeks to understand and promote well-being through assessments and interventions aimed at enhancing positive psychosocial factors among people who have or are at risk for developing mental or physical illnesses.”1 The concept sprung from the momentum of positive psychology, which originated from Seligman et al.2 Importantly, the standards and techniques of positive psychiatry are designed as an enhancement, perhaps even as a completion, of more traditional psychiatry, rather than an alternative.3 They come from an acknowledgment that to be most effective as a mental health professional, it is important for clinicians to be experts in the full range of mental functioning.4,5
For most clinicians currently practicing “traditional” child and adolescent psychiatry, adapting at least some of the principles of positive psychiatry within one’s routine practice will not necessarily involve a radical transformation of thought or effort. Indeed, upon hearing about positive psychiatry principles, many nonprofessionals express surprise that this is not already considered routine practice. This article briefly outlines some of the basic tenets of positive child psychiatry and describes practical initial steps that can be readily incorporated into one’s day-to-day approach.
Defining pediatric positive psychiatry
There remains a fair amount of discussion and debate regarding what positive psychiatry is and isn’t, and how it fits into routine practice. While there is no official doctrine as to what “counts” as the practice of positive psychiatry, one can arguably divide most of its interventions into 2 main areas. The first is paying additional clinical attention to behaviors commonly associated with wellness or health promotion in youth. These include domains such as exercise, sleep habits, an authoritative parenting style, screen limits, and nutrition. The second area relates to specific techniques or procedures designed to cultivate positive emotions and mindsets; these often are referred to as positive psychology interventions (PPIs).6 Examples include gratitude exercises, practicing forgiveness, and activities that build optimism and hope. Many of the latter procedures share poorly defined boundaries with “tried and true” cognitive-behavioral therapy techniques, while others are more distinct to positive psychology and psychiatry. For both health promotion and PPIs, the goal of these interventions is to go beyond response and even remission for a patient to actual mental well-being, which is a construct that has also proven to be somewhat elusive and difficult to define. One well-described model by Seligman7 that has been gaining traction is the PERMA model, which breaks down well-being into 5 main components: positive emotions, engagement, relationships, meaning, and accomplishment.
Positive psychiatry: The evidence base
One myth about positive psychiatry is that it involves the pursuit of fringe and scientifically suspect techniques that have fallen under the expanding umbrella of “wellness.” Sadly, numerous unscientific and ineffective remedies have been widely promoted under the guise of wellness, leaving many families and clinicians uncertain about which areas have a solid evidence base and which are scientifically on shakier ground. While the lines delineating what are often referred to as PPI and more traditional psychotherapeutic techniques are blurry, there is increasing evidence supporting the use of PPI.8 A recent meta-analysis indicated that these techniques have larger effect sizes for children and young adults compared to older adults.9 More research, however, is needed, particularly for youth with diagnosable mental health conditions and for younger children.10
The evidence supporting the role of wellness and health promotion in preventing and treating pediatric mental health conditions has a quite robust research base. For example, a recent randomized controlled trial found greater reductions in multiple areas of emotional-behavior problems in children treated in a primary care setting with a wellness and health promotion model (the Vermont Family Based Approach) compared to those in a control condition.11 Another study examining the course of attention-deficit/hyperactivity disorder (ADHD) showed a 62% reduction of diagnosis among children who met 7 of 9 health promotion recommendations in areas such as nutrition, physical activity, and screen time, compared to those who met just 1 to 3 of these recommendations.12 Techniques such as mindfulness also have been found to be useful for adolescents with anxiety disorders.13 While a full review of the evidence is beyond the scope of this article, it is fair to say that many health promotion areas (such as exercise, nutrition, sleep habits, positive parenting skills, and some types of mindfulness) have strong scientific support—arguably at a level that is comparable to or even exceeds that of the off-label use of many psychiatric medications. The American Academy of Child and Adolescent Psychiatry has published a brief document that summarizes many age-related health promotion recommendations.14 The studies that underlie many of these recommendations contradict the misperception that wellness activities are only for already healthy individuals who want to become healthier, and show their utility for patients with more significant and chronic mental health conditions.
Incorporating core principles of positive psychiatry
Table 1 summarizes the core principles of positive child and adolescent psychiatry. There is no official procedure or certification one must complete to be considered a “positive psychiatrist,” and the term itself is somewhat debatable. Incorporating many of the principles of positive psychiatry into one’s daily routine does not necessitate a practice overhaul, and clinicians can integrate as many of these ideas as they deem clinically appropriate. That said, some adjustments to one’s perspective, approach, and workflow are likely needed, and the practice of positive psychiatry is arguably difficult to accomplish within the common “med check” model that emphasizes high volumes of short appointments that focus primarily on symptoms and adverse effects of medications.

Contrary to another misconception about positive psychiatry, working within a positive psychiatry framework does not involve encouraging patients to “put on a happy face” and ignore the very real suffering and trauma that many of them have experienced. Further, adhering to positive psychiatry does not entail abandoning the use of psychopharmacology (although careful prescribing is generally recommended) or applying gimmicks to superficially cover a person’s emotional pain.
Continue to: Rather, incorporating positive psychiatry...
Rather, incorporating positive psychiatry is best viewed as the creation of a supplementary toolbox that allows clinicians an expanded set of focus areas that can be used along with traditional psychotherapy and pharmacotherapy to help patients achieve a more robust and sustained response to treatment.4,5,15 The positive psychiatrist looks beyond the individual to examine a youth’s entire environment, and beyond areas of challenge to assess strengths, hopes, and aspirations.16 While many of these values are already in the formal description of a child psychiatrist, these priorities can take a back seat when trying to get through a busy day. For some, being a positive child psychiatrist means prescribing exercise rather than a sleep medication, assessing a child’s character strengths in addition to their behavioral challenges, or discussing the concept of parental warmth and how a struggling mother or father can replenish their tank when it feels like there is little left to give. It can mean reading literature on subjects such as happiness and optimal parenting practices in addition to depression and child maltreatment, and seeing oneself as an expert in mental health rather than just mental illness.
I have published a previous case example of positive psychiatry.17 Here I provide a brief vignette to further illustrate these concepts, and to compare traditional vs positive child psychiatry (Table 2).
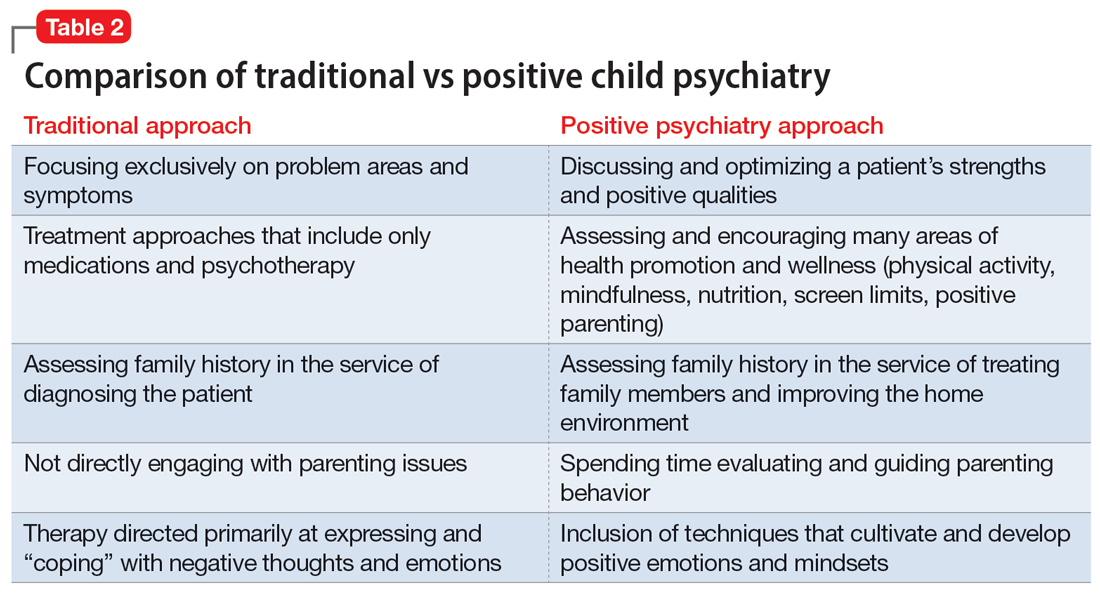
CASE REPORT
Tyler, age 7, presents to a child and adolescent psychiatrist for refractory ADHD problems, continued defiance, and aggressive outbursts. Approximately 1 year ago, Tyler’s pediatrician had diagnosed him with fairly classic ADHD symptoms and prescribed long-acting methylphenidate. Tyler’s attention has improved somewhat at school, but there remains a significant degree of conflict and dysregulation at home. Tyler remains easily frustrated and is often very negative. The pediatrician is looking for additional treatment recommendations.
Traditional approach
The child psychiatrist assesses Tyler and gathers data from the patient, his parents, and his school. She confirms the diagnosis of ADHD, but in reviewing other potential conditions also discovers that Tyler meets DSM-5 criteria for oppositional defiant disorder. The clinician suspects there may also be a co-occurring learning disability and notices that Tyler has chronic difficulties getting to sleep. She also hypothesizes the stimulant medication is wearing off at about the time Tyler gets home from school. The psychiatrist recommends adding an immediate-release formulation of methylphenidate upon return from school, melatonin at night, a school psychoeducational assessment, and behavioral therapy for Tyler and his parents to focus on his disrespectful and oppositional behavior.
Three months later, there has been incremental improvement with the additional medication and a school individualized education plan. Tyler is also working with a therapist, who does some play therapy with Tyler and works on helping his parents create incentives for prosocial behavior, but progress has been slow and the amount of improvement in this area is minimal. Further, the initial positive effect of the melatonin on sleep has waned lately, and the parents now ask about “something stronger.”
Continue to: Positive psychiatry approach
Positive psychiatry approach
In addition to assessing problem areas and DSM-5 criteria, the psychiatrist assesses a number of other domains. She finds that most of the interaction between Tyler and his parents are negative to the point that his parents often just stay out of his way. She also discovers that Tyler does little in the way of structured activities and spends most of his time at home playing video games, sometimes well into the evening. He gets little to no physical activity outside of school. He also is a very selective eater and often skips breakfast entirely due to the usually chaotic home scene in the morning. A brief mental health screen of the parents further reveals that the mother would also likely meet criteria for ADHD, and the father may be experiencing depression.
The psychiatrist prescribes an additional immediate-release formulation stimulant for the afternoon but holds off on prescribing sleep medication. Instead, she discusses a plan in which Tyler can earn his screen time by reading or exercising, and urges the parents to do some regular physical activity together. She discusses the findings of her screenings of the parents and helps them get a more thorough assessment. She also encourages more family time and introduces them to the “rose, thorn, bud” exercise where each family member discusses a success, challenge, and opportunity of the day.
Three months later, Tyler’s attention and negativity have decreased. His increased physical activity has helped his sleep, and ADHD treatment for the mother has made the mornings much smoother, allowing Tyler to eat a regular breakfast. Both improvements contribute further to Tyler’s improved attention during the day. Challenges remain, but the increased positive family experiences are helping the parents feel less depleted. As a result, they engage with Tyler more productively, and he has responded with more confidence and enthusiasm.
A natural extension of traditional work
The principles and practices associated with positive psychiatry represent a natural and highly needed extension of traditional work within child and adolescent psychiatry. Its emphasis on health promotion activities, family functioning, parental mental health, and utilization of strengths align closely with the growing scientific knowledge base that supports the complex interplay between the many genetic and environmental factors that underlie mental and physical health across the lifespan. For most psychiatrists, incorporating these important concepts and approaches will not require a radical transformation of one’s outlook or methodology, although some adjustments to practice and knowledge base augmentations are often needed. Clinicians interested in supplementing their skill set and working toward becoming an expert in the full range of mental functioning are encouraged to begin taking some of the steps outlined in this article to further their proficiency in the emerging discipline of positive psychiatry.
Bottom Line
Positive psychiatry is an important development that complements traditional approaches to child and adolescent mental health treatment through health promotion and cultivation of positive emotions and qualities. Incorporating it into routine practice is well within reach.
Related Resources
- Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015.
- Positive Psychology Center. University of Pennsylvania School of Arts and Sciences. https://ppc.sas.upenn.edu/
- Rettew DC. Building healthy brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
Drug Brand Names
Methylphenidate extended-release • Concerta, Ritalin LA
1. Jeste DV, Palmer BW. Introduction: What is positive psychiatry? In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:1-16.
2. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5-14.
3. Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76:675-683.
4. Rettew DC. Better than better: the new focus on well-being in child psychiatry. Child Adolesc Psychiatr Clin N Am. 2019;28:127-135.
5. Rettew DC. Positive child psychiatry. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:285-304.
6. Parks AC, Kleiman EM, Kashdan TB, et al. Positive psychotherapeutic and behavioral interventions. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:147-165.
7. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon & Shuster; 2012.
8. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042-1054.
9. Carr A, Cullen K, Keeney C, et al. Effectiveness of positive psychology interventions: a systematic review and meta-analysis. J Pos Psychol. 2021:16:749-769.
10. Benoit V, Gabola P. Effects of positive psychology interventions on the well-being of young children: a systematic literature review. Int J Environ Res Public Health. 2021;18:12065.
11. Ivanova MY, Hall A, Weinberger S, et al. The Vermont family based approach in primary care pediatrics: effects on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. Child Psychiatry Hum Dev. Published online March 4, 2022. doi: 10.1007/s10578-022-01329-4
12. Lowen OK, Maximova K, Ekwaru JP, et al. Adherence to life-style recommendations and attention-deficit/hyperactivity disorder. Psychosom Med. 2020;82:305-315.
13. Zhou X, Guo J, et al. Effects of mindfulness-based stress reduction on anxiety symptoms in young people: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113002.
14. Rettew DC. Building health brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. Accessed May 11, 2022. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
15. Pustilnik S. Adapting well-being into outpatient child psychiatry. Child Adolesc Psychiatry Clin N Am. 2019;28:221-235.
16. Schlechter AD, O’Brien KH, Stewart C. The positive assessment: a model for integrating well-being and strengths-based approaches into the child and adolescent psychiatry clinical evaluation. Child Adolesc Psychiatry Clin N Am. 2019;28:157-169.
17. Rettew DC. A family- and wellness-based approach to child emotional-behavioral problems. In: RF Summers, Jeste DV, eds. Positive Psychiatry: A Casebook. American Psychiatric Association Publishing; 2019:29-44.
The principles and practices of positive psychiatry are especially well-suited for work with children, adolescents, and families. Positive psychiatry is “the science and practice of psychiatry that seeks to understand and promote well-being through assessments and interventions aimed at enhancing positive psychosocial factors among people who have or are at risk for developing mental or physical illnesses.”1 The concept sprung from the momentum of positive psychology, which originated from Seligman et al.2 Importantly, the standards and techniques of positive psychiatry are designed as an enhancement, perhaps even as a completion, of more traditional psychiatry, rather than an alternative.3 They come from an acknowledgment that to be most effective as a mental health professional, it is important for clinicians to be experts in the full range of mental functioning.4,5
For most clinicians currently practicing “traditional” child and adolescent psychiatry, adapting at least some of the principles of positive psychiatry within one’s routine practice will not necessarily involve a radical transformation of thought or effort. Indeed, upon hearing about positive psychiatry principles, many nonprofessionals express surprise that this is not already considered routine practice. This article briefly outlines some of the basic tenets of positive child psychiatry and describes practical initial steps that can be readily incorporated into one’s day-to-day approach.
Defining pediatric positive psychiatry
There remains a fair amount of discussion and debate regarding what positive psychiatry is and isn’t, and how it fits into routine practice. While there is no official doctrine as to what “counts” as the practice of positive psychiatry, one can arguably divide most of its interventions into 2 main areas. The first is paying additional clinical attention to behaviors commonly associated with wellness or health promotion in youth. These include domains such as exercise, sleep habits, an authoritative parenting style, screen limits, and nutrition. The second area relates to specific techniques or procedures designed to cultivate positive emotions and mindsets; these often are referred to as positive psychology interventions (PPIs).6 Examples include gratitude exercises, practicing forgiveness, and activities that build optimism and hope. Many of the latter procedures share poorly defined boundaries with “tried and true” cognitive-behavioral therapy techniques, while others are more distinct to positive psychology and psychiatry. For both health promotion and PPIs, the goal of these interventions is to go beyond response and even remission for a patient to actual mental well-being, which is a construct that has also proven to be somewhat elusive and difficult to define. One well-described model by Seligman7 that has been gaining traction is the PERMA model, which breaks down well-being into 5 main components: positive emotions, engagement, relationships, meaning, and accomplishment.
Positive psychiatry: The evidence base
One myth about positive psychiatry is that it involves the pursuit of fringe and scientifically suspect techniques that have fallen under the expanding umbrella of “wellness.” Sadly, numerous unscientific and ineffective remedies have been widely promoted under the guise of wellness, leaving many families and clinicians uncertain about which areas have a solid evidence base and which are scientifically on shakier ground. While the lines delineating what are often referred to as PPI and more traditional psychotherapeutic techniques are blurry, there is increasing evidence supporting the use of PPI.8 A recent meta-analysis indicated that these techniques have larger effect sizes for children and young adults compared to older adults.9 More research, however, is needed, particularly for youth with diagnosable mental health conditions and for younger children.10
The evidence supporting the role of wellness and health promotion in preventing and treating pediatric mental health conditions has a quite robust research base. For example, a recent randomized controlled trial found greater reductions in multiple areas of emotional-behavior problems in children treated in a primary care setting with a wellness and health promotion model (the Vermont Family Based Approach) compared to those in a control condition.11 Another study examining the course of attention-deficit/hyperactivity disorder (ADHD) showed a 62% reduction of diagnosis among children who met 7 of 9 health promotion recommendations in areas such as nutrition, physical activity, and screen time, compared to those who met just 1 to 3 of these recommendations.12 Techniques such as mindfulness also have been found to be useful for adolescents with anxiety disorders.13 While a full review of the evidence is beyond the scope of this article, it is fair to say that many health promotion areas (such as exercise, nutrition, sleep habits, positive parenting skills, and some types of mindfulness) have strong scientific support—arguably at a level that is comparable to or even exceeds that of the off-label use of many psychiatric medications. The American Academy of Child and Adolescent Psychiatry has published a brief document that summarizes many age-related health promotion recommendations.14 The studies that underlie many of these recommendations contradict the misperception that wellness activities are only for already healthy individuals who want to become healthier, and show their utility for patients with more significant and chronic mental health conditions.
Incorporating core principles of positive psychiatry
Table 1 summarizes the core principles of positive child and adolescent psychiatry. There is no official procedure or certification one must complete to be considered a “positive psychiatrist,” and the term itself is somewhat debatable. Incorporating many of the principles of positive psychiatry into one’s daily routine does not necessitate a practice overhaul, and clinicians can integrate as many of these ideas as they deem clinically appropriate. That said, some adjustments to one’s perspective, approach, and workflow are likely needed, and the practice of positive psychiatry is arguably difficult to accomplish within the common “med check” model that emphasizes high volumes of short appointments that focus primarily on symptoms and adverse effects of medications.

Contrary to another misconception about positive psychiatry, working within a positive psychiatry framework does not involve encouraging patients to “put on a happy face” and ignore the very real suffering and trauma that many of them have experienced. Further, adhering to positive psychiatry does not entail abandoning the use of psychopharmacology (although careful prescribing is generally recommended) or applying gimmicks to superficially cover a person’s emotional pain.
Continue to: Rather, incorporating positive psychiatry...
Rather, incorporating positive psychiatry is best viewed as the creation of a supplementary toolbox that allows clinicians an expanded set of focus areas that can be used along with traditional psychotherapy and pharmacotherapy to help patients achieve a more robust and sustained response to treatment.4,5,15 The positive psychiatrist looks beyond the individual to examine a youth’s entire environment, and beyond areas of challenge to assess strengths, hopes, and aspirations.16 While many of these values are already in the formal description of a child psychiatrist, these priorities can take a back seat when trying to get through a busy day. For some, being a positive child psychiatrist means prescribing exercise rather than a sleep medication, assessing a child’s character strengths in addition to their behavioral challenges, or discussing the concept of parental warmth and how a struggling mother or father can replenish their tank when it feels like there is little left to give. It can mean reading literature on subjects such as happiness and optimal parenting practices in addition to depression and child maltreatment, and seeing oneself as an expert in mental health rather than just mental illness.
I have published a previous case example of positive psychiatry.17 Here I provide a brief vignette to further illustrate these concepts, and to compare traditional vs positive child psychiatry (Table 2).
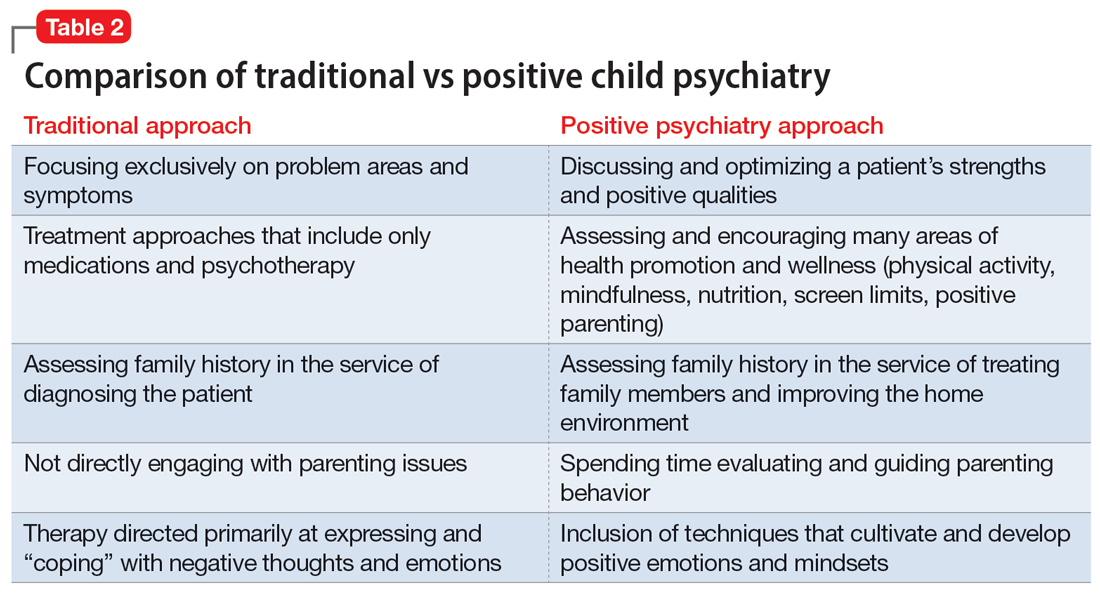
CASE REPORT
Tyler, age 7, presents to a child and adolescent psychiatrist for refractory ADHD problems, continued defiance, and aggressive outbursts. Approximately 1 year ago, Tyler’s pediatrician had diagnosed him with fairly classic ADHD symptoms and prescribed long-acting methylphenidate. Tyler’s attention has improved somewhat at school, but there remains a significant degree of conflict and dysregulation at home. Tyler remains easily frustrated and is often very negative. The pediatrician is looking for additional treatment recommendations.
Traditional approach
The child psychiatrist assesses Tyler and gathers data from the patient, his parents, and his school. She confirms the diagnosis of ADHD, but in reviewing other potential conditions also discovers that Tyler meets DSM-5 criteria for oppositional defiant disorder. The clinician suspects there may also be a co-occurring learning disability and notices that Tyler has chronic difficulties getting to sleep. She also hypothesizes the stimulant medication is wearing off at about the time Tyler gets home from school. The psychiatrist recommends adding an immediate-release formulation of methylphenidate upon return from school, melatonin at night, a school psychoeducational assessment, and behavioral therapy for Tyler and his parents to focus on his disrespectful and oppositional behavior.
Three months later, there has been incremental improvement with the additional medication and a school individualized education plan. Tyler is also working with a therapist, who does some play therapy with Tyler and works on helping his parents create incentives for prosocial behavior, but progress has been slow and the amount of improvement in this area is minimal. Further, the initial positive effect of the melatonin on sleep has waned lately, and the parents now ask about “something stronger.”
Continue to: Positive psychiatry approach
Positive psychiatry approach
In addition to assessing problem areas and DSM-5 criteria, the psychiatrist assesses a number of other domains. She finds that most of the interaction between Tyler and his parents are negative to the point that his parents often just stay out of his way. She also discovers that Tyler does little in the way of structured activities and spends most of his time at home playing video games, sometimes well into the evening. He gets little to no physical activity outside of school. He also is a very selective eater and often skips breakfast entirely due to the usually chaotic home scene in the morning. A brief mental health screen of the parents further reveals that the mother would also likely meet criteria for ADHD, and the father may be experiencing depression.
The psychiatrist prescribes an additional immediate-release formulation stimulant for the afternoon but holds off on prescribing sleep medication. Instead, she discusses a plan in which Tyler can earn his screen time by reading or exercising, and urges the parents to do some regular physical activity together. She discusses the findings of her screenings of the parents and helps them get a more thorough assessment. She also encourages more family time and introduces them to the “rose, thorn, bud” exercise where each family member discusses a success, challenge, and opportunity of the day.
Three months later, Tyler’s attention and negativity have decreased. His increased physical activity has helped his sleep, and ADHD treatment for the mother has made the mornings much smoother, allowing Tyler to eat a regular breakfast. Both improvements contribute further to Tyler’s improved attention during the day. Challenges remain, but the increased positive family experiences are helping the parents feel less depleted. As a result, they engage with Tyler more productively, and he has responded with more confidence and enthusiasm.
A natural extension of traditional work
The principles and practices associated with positive psychiatry represent a natural and highly needed extension of traditional work within child and adolescent psychiatry. Its emphasis on health promotion activities, family functioning, parental mental health, and utilization of strengths align closely with the growing scientific knowledge base that supports the complex interplay between the many genetic and environmental factors that underlie mental and physical health across the lifespan. For most psychiatrists, incorporating these important concepts and approaches will not require a radical transformation of one’s outlook or methodology, although some adjustments to practice and knowledge base augmentations are often needed. Clinicians interested in supplementing their skill set and working toward becoming an expert in the full range of mental functioning are encouraged to begin taking some of the steps outlined in this article to further their proficiency in the emerging discipline of positive psychiatry.
Bottom Line
Positive psychiatry is an important development that complements traditional approaches to child and adolescent mental health treatment through health promotion and cultivation of positive emotions and qualities. Incorporating it into routine practice is well within reach.
Related Resources
- Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015.
- Positive Psychology Center. University of Pennsylvania School of Arts and Sciences. https://ppc.sas.upenn.edu/
- Rettew DC. Building healthy brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
Drug Brand Names
Methylphenidate extended-release • Concerta, Ritalin LA
The principles and practices of positive psychiatry are especially well-suited for work with children, adolescents, and families. Positive psychiatry is “the science and practice of psychiatry that seeks to understand and promote well-being through assessments and interventions aimed at enhancing positive psychosocial factors among people who have or are at risk for developing mental or physical illnesses.”1 The concept sprung from the momentum of positive psychology, which originated from Seligman et al.2 Importantly, the standards and techniques of positive psychiatry are designed as an enhancement, perhaps even as a completion, of more traditional psychiatry, rather than an alternative.3 They come from an acknowledgment that to be most effective as a mental health professional, it is important for clinicians to be experts in the full range of mental functioning.4,5
For most clinicians currently practicing “traditional” child and adolescent psychiatry, adapting at least some of the principles of positive psychiatry within one’s routine practice will not necessarily involve a radical transformation of thought or effort. Indeed, upon hearing about positive psychiatry principles, many nonprofessionals express surprise that this is not already considered routine practice. This article briefly outlines some of the basic tenets of positive child psychiatry and describes practical initial steps that can be readily incorporated into one’s day-to-day approach.
Defining pediatric positive psychiatry
There remains a fair amount of discussion and debate regarding what positive psychiatry is and isn’t, and how it fits into routine practice. While there is no official doctrine as to what “counts” as the practice of positive psychiatry, one can arguably divide most of its interventions into 2 main areas. The first is paying additional clinical attention to behaviors commonly associated with wellness or health promotion in youth. These include domains such as exercise, sleep habits, an authoritative parenting style, screen limits, and nutrition. The second area relates to specific techniques or procedures designed to cultivate positive emotions and mindsets; these often are referred to as positive psychology interventions (PPIs).6 Examples include gratitude exercises, practicing forgiveness, and activities that build optimism and hope. Many of the latter procedures share poorly defined boundaries with “tried and true” cognitive-behavioral therapy techniques, while others are more distinct to positive psychology and psychiatry. For both health promotion and PPIs, the goal of these interventions is to go beyond response and even remission for a patient to actual mental well-being, which is a construct that has also proven to be somewhat elusive and difficult to define. One well-described model by Seligman7 that has been gaining traction is the PERMA model, which breaks down well-being into 5 main components: positive emotions, engagement, relationships, meaning, and accomplishment.
Positive psychiatry: The evidence base
One myth about positive psychiatry is that it involves the pursuit of fringe and scientifically suspect techniques that have fallen under the expanding umbrella of “wellness.” Sadly, numerous unscientific and ineffective remedies have been widely promoted under the guise of wellness, leaving many families and clinicians uncertain about which areas have a solid evidence base and which are scientifically on shakier ground. While the lines delineating what are often referred to as PPI and more traditional psychotherapeutic techniques are blurry, there is increasing evidence supporting the use of PPI.8 A recent meta-analysis indicated that these techniques have larger effect sizes for children and young adults compared to older adults.9 More research, however, is needed, particularly for youth with diagnosable mental health conditions and for younger children.10
The evidence supporting the role of wellness and health promotion in preventing and treating pediatric mental health conditions has a quite robust research base. For example, a recent randomized controlled trial found greater reductions in multiple areas of emotional-behavior problems in children treated in a primary care setting with a wellness and health promotion model (the Vermont Family Based Approach) compared to those in a control condition.11 Another study examining the course of attention-deficit/hyperactivity disorder (ADHD) showed a 62% reduction of diagnosis among children who met 7 of 9 health promotion recommendations in areas such as nutrition, physical activity, and screen time, compared to those who met just 1 to 3 of these recommendations.12 Techniques such as mindfulness also have been found to be useful for adolescents with anxiety disorders.13 While a full review of the evidence is beyond the scope of this article, it is fair to say that many health promotion areas (such as exercise, nutrition, sleep habits, positive parenting skills, and some types of mindfulness) have strong scientific support—arguably at a level that is comparable to or even exceeds that of the off-label use of many psychiatric medications. The American Academy of Child and Adolescent Psychiatry has published a brief document that summarizes many age-related health promotion recommendations.14 The studies that underlie many of these recommendations contradict the misperception that wellness activities are only for already healthy individuals who want to become healthier, and show their utility for patients with more significant and chronic mental health conditions.
Incorporating core principles of positive psychiatry
Table 1 summarizes the core principles of positive child and adolescent psychiatry. There is no official procedure or certification one must complete to be considered a “positive psychiatrist,” and the term itself is somewhat debatable. Incorporating many of the principles of positive psychiatry into one’s daily routine does not necessitate a practice overhaul, and clinicians can integrate as many of these ideas as they deem clinically appropriate. That said, some adjustments to one’s perspective, approach, and workflow are likely needed, and the practice of positive psychiatry is arguably difficult to accomplish within the common “med check” model that emphasizes high volumes of short appointments that focus primarily on symptoms and adverse effects of medications.

Contrary to another misconception about positive psychiatry, working within a positive psychiatry framework does not involve encouraging patients to “put on a happy face” and ignore the very real suffering and trauma that many of them have experienced. Further, adhering to positive psychiatry does not entail abandoning the use of psychopharmacology (although careful prescribing is generally recommended) or applying gimmicks to superficially cover a person’s emotional pain.
Continue to: Rather, incorporating positive psychiatry...
Rather, incorporating positive psychiatry is best viewed as the creation of a supplementary toolbox that allows clinicians an expanded set of focus areas that can be used along with traditional psychotherapy and pharmacotherapy to help patients achieve a more robust and sustained response to treatment.4,5,15 The positive psychiatrist looks beyond the individual to examine a youth’s entire environment, and beyond areas of challenge to assess strengths, hopes, and aspirations.16 While many of these values are already in the formal description of a child psychiatrist, these priorities can take a back seat when trying to get through a busy day. For some, being a positive child psychiatrist means prescribing exercise rather than a sleep medication, assessing a child’s character strengths in addition to their behavioral challenges, or discussing the concept of parental warmth and how a struggling mother or father can replenish their tank when it feels like there is little left to give. It can mean reading literature on subjects such as happiness and optimal parenting practices in addition to depression and child maltreatment, and seeing oneself as an expert in mental health rather than just mental illness.
I have published a previous case example of positive psychiatry.17 Here I provide a brief vignette to further illustrate these concepts, and to compare traditional vs positive child psychiatry (Table 2).
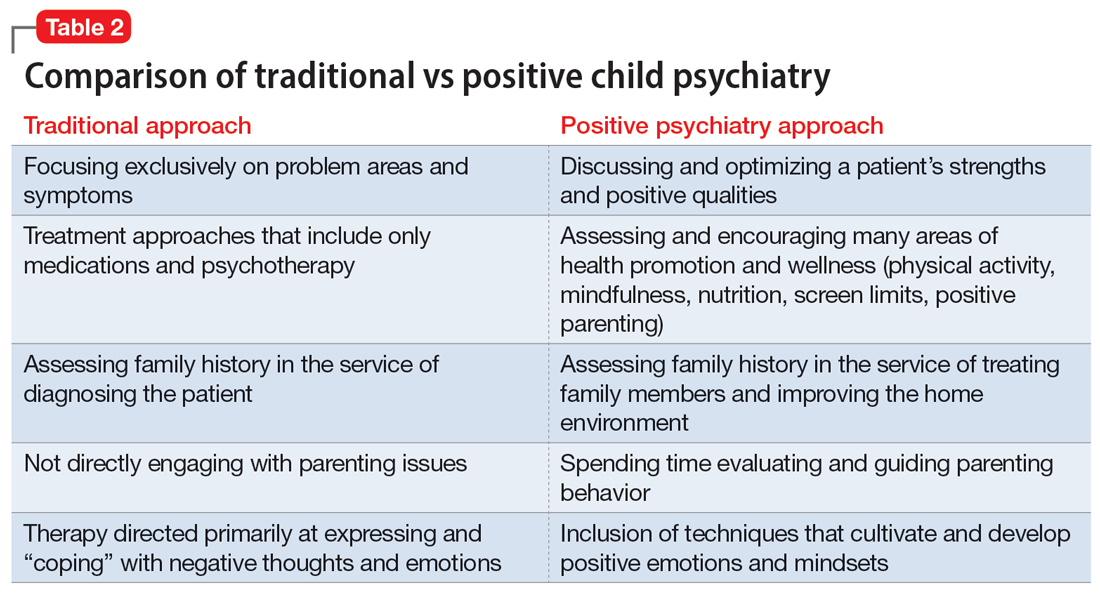
CASE REPORT
Tyler, age 7, presents to a child and adolescent psychiatrist for refractory ADHD problems, continued defiance, and aggressive outbursts. Approximately 1 year ago, Tyler’s pediatrician had diagnosed him with fairly classic ADHD symptoms and prescribed long-acting methylphenidate. Tyler’s attention has improved somewhat at school, but there remains a significant degree of conflict and dysregulation at home. Tyler remains easily frustrated and is often very negative. The pediatrician is looking for additional treatment recommendations.
Traditional approach
The child psychiatrist assesses Tyler and gathers data from the patient, his parents, and his school. She confirms the diagnosis of ADHD, but in reviewing other potential conditions also discovers that Tyler meets DSM-5 criteria for oppositional defiant disorder. The clinician suspects there may also be a co-occurring learning disability and notices that Tyler has chronic difficulties getting to sleep. She also hypothesizes the stimulant medication is wearing off at about the time Tyler gets home from school. The psychiatrist recommends adding an immediate-release formulation of methylphenidate upon return from school, melatonin at night, a school psychoeducational assessment, and behavioral therapy for Tyler and his parents to focus on his disrespectful and oppositional behavior.
Three months later, there has been incremental improvement with the additional medication and a school individualized education plan. Tyler is also working with a therapist, who does some play therapy with Tyler and works on helping his parents create incentives for prosocial behavior, but progress has been slow and the amount of improvement in this area is minimal. Further, the initial positive effect of the melatonin on sleep has waned lately, and the parents now ask about “something stronger.”
Continue to: Positive psychiatry approach
Positive psychiatry approach
In addition to assessing problem areas and DSM-5 criteria, the psychiatrist assesses a number of other domains. She finds that most of the interaction between Tyler and his parents are negative to the point that his parents often just stay out of his way. She also discovers that Tyler does little in the way of structured activities and spends most of his time at home playing video games, sometimes well into the evening. He gets little to no physical activity outside of school. He also is a very selective eater and often skips breakfast entirely due to the usually chaotic home scene in the morning. A brief mental health screen of the parents further reveals that the mother would also likely meet criteria for ADHD, and the father may be experiencing depression.
The psychiatrist prescribes an additional immediate-release formulation stimulant for the afternoon but holds off on prescribing sleep medication. Instead, she discusses a plan in which Tyler can earn his screen time by reading or exercising, and urges the parents to do some regular physical activity together. She discusses the findings of her screenings of the parents and helps them get a more thorough assessment. She also encourages more family time and introduces them to the “rose, thorn, bud” exercise where each family member discusses a success, challenge, and opportunity of the day.
Three months later, Tyler’s attention and negativity have decreased. His increased physical activity has helped his sleep, and ADHD treatment for the mother has made the mornings much smoother, allowing Tyler to eat a regular breakfast. Both improvements contribute further to Tyler’s improved attention during the day. Challenges remain, but the increased positive family experiences are helping the parents feel less depleted. As a result, they engage with Tyler more productively, and he has responded with more confidence and enthusiasm.
A natural extension of traditional work
The principles and practices associated with positive psychiatry represent a natural and highly needed extension of traditional work within child and adolescent psychiatry. Its emphasis on health promotion activities, family functioning, parental mental health, and utilization of strengths align closely with the growing scientific knowledge base that supports the complex interplay between the many genetic and environmental factors that underlie mental and physical health across the lifespan. For most psychiatrists, incorporating these important concepts and approaches will not require a radical transformation of one’s outlook or methodology, although some adjustments to practice and knowledge base augmentations are often needed. Clinicians interested in supplementing their skill set and working toward becoming an expert in the full range of mental functioning are encouraged to begin taking some of the steps outlined in this article to further their proficiency in the emerging discipline of positive psychiatry.
Bottom Line
Positive psychiatry is an important development that complements traditional approaches to child and adolescent mental health treatment through health promotion and cultivation of positive emotions and qualities. Incorporating it into routine practice is well within reach.
Related Resources
- Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015.
- Positive Psychology Center. University of Pennsylvania School of Arts and Sciences. https://ppc.sas.upenn.edu/
- Rettew DC. Building healthy brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
Drug Brand Names
Methylphenidate extended-release • Concerta, Ritalin LA
1. Jeste DV, Palmer BW. Introduction: What is positive psychiatry? In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:1-16.
2. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5-14.
3. Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76:675-683.
4. Rettew DC. Better than better: the new focus on well-being in child psychiatry. Child Adolesc Psychiatr Clin N Am. 2019;28:127-135.
5. Rettew DC. Positive child psychiatry. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:285-304.
6. Parks AC, Kleiman EM, Kashdan TB, et al. Positive psychotherapeutic and behavioral interventions. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:147-165.
7. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon & Shuster; 2012.
8. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042-1054.
9. Carr A, Cullen K, Keeney C, et al. Effectiveness of positive psychology interventions: a systematic review and meta-analysis. J Pos Psychol. 2021:16:749-769.
10. Benoit V, Gabola P. Effects of positive psychology interventions on the well-being of young children: a systematic literature review. Int J Environ Res Public Health. 2021;18:12065.
11. Ivanova MY, Hall A, Weinberger S, et al. The Vermont family based approach in primary care pediatrics: effects on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. Child Psychiatry Hum Dev. Published online March 4, 2022. doi: 10.1007/s10578-022-01329-4
12. Lowen OK, Maximova K, Ekwaru JP, et al. Adherence to life-style recommendations and attention-deficit/hyperactivity disorder. Psychosom Med. 2020;82:305-315.
13. Zhou X, Guo J, et al. Effects of mindfulness-based stress reduction on anxiety symptoms in young people: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113002.
14. Rettew DC. Building health brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. Accessed May 11, 2022. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
15. Pustilnik S. Adapting well-being into outpatient child psychiatry. Child Adolesc Psychiatry Clin N Am. 2019;28:221-235.
16. Schlechter AD, O’Brien KH, Stewart C. The positive assessment: a model for integrating well-being and strengths-based approaches into the child and adolescent psychiatry clinical evaluation. Child Adolesc Psychiatry Clin N Am. 2019;28:157-169.
17. Rettew DC. A family- and wellness-based approach to child emotional-behavioral problems. In: RF Summers, Jeste DV, eds. Positive Psychiatry: A Casebook. American Psychiatric Association Publishing; 2019:29-44.
1. Jeste DV, Palmer BW. Introduction: What is positive psychiatry? In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:1-16.
2. Seligman MEP, Csikszentmihalyi M. Positive psychology: an introduction. Am Psychol. 2000;55:5-14.
3. Jeste DV, Palmer BW, Rettew DC, et al. Positive psychiatry: its time has come. J Clin Psychiatry. 2015;76:675-683.
4. Rettew DC. Better than better: the new focus on well-being in child psychiatry. Child Adolesc Psychiatr Clin N Am. 2019;28:127-135.
5. Rettew DC. Positive child psychiatry. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:285-304.
6. Parks AC, Kleiman EM, Kashdan TB, et al. Positive psychotherapeutic and behavioral interventions. In: Jeste DV, Palmer BW, eds. Positive Psychiatry: A Clinical Handbook. American Psychiatric Publishing; 2015:147-165.
7. Seligman MEP. Flourish: A Visionary New Understanding of Happiness and Well-Being. Simon & Shuster; 2012.
8. Brunwasser SM, Gillham JE, Kim ES. A meta-analytic review of the Penn Resiliency Program’s effect on depressive symptoms. J Consult Clin Psychol. 2009;77:1042-1054.
9. Carr A, Cullen K, Keeney C, et al. Effectiveness of positive psychology interventions: a systematic review and meta-analysis. J Pos Psychol. 2021:16:749-769.
10. Benoit V, Gabola P. Effects of positive psychology interventions on the well-being of young children: a systematic literature review. Int J Environ Res Public Health. 2021;18:12065.
11. Ivanova MY, Hall A, Weinberger S, et al. The Vermont family based approach in primary care pediatrics: effects on children’s and parents’ emotional and behavioral problems and parents’ health-related quality of life. Child Psychiatry Hum Dev. Published online March 4, 2022. doi: 10.1007/s10578-022-01329-4
12. Lowen OK, Maximova K, Ekwaru JP, et al. Adherence to life-style recommendations and attention-deficit/hyperactivity disorder. Psychosom Med. 2020;82:305-315.
13. Zhou X, Guo J, et al. Effects of mindfulness-based stress reduction on anxiety symptoms in young people: a systematic review and meta-analysis. Psychiatry Res. 2020;289:113002.
14. Rettew DC. Building health brains: a brief tip sheet for parents and schools. American Academy of Child & Adolescent Psychiatry. Accessed May 11, 2022. https://www.aacap.org/App_Themes/AACAP/Docs/resource_centers/schools/Wellness_Dev_Tips.pdf
15. Pustilnik S. Adapting well-being into outpatient child psychiatry. Child Adolesc Psychiatry Clin N Am. 2019;28:221-235.
16. Schlechter AD, O’Brien KH, Stewart C. The positive assessment: a model for integrating well-being and strengths-based approaches into the child and adolescent psychiatry clinical evaluation. Child Adolesc Psychiatry Clin N Am. 2019;28:157-169.
17. Rettew DC. A family- and wellness-based approach to child emotional-behavioral problems. In: RF Summers, Jeste DV, eds. Positive Psychiatry: A Casebook. American Psychiatric Association Publishing; 2019:29-44.
Surgeon General releases child mental health call to action
The nation’s Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, recently released an advisory report on the current state of youth mental health and recommendations to improve well-being. This action follows a number of emergency declarations that have been made by professional organizations such as the American Academy of Child and Adolescent Psychiatry (AACAP), the American Academy of Pediatrics (AAP), and other health care groups to raise awareness about the alarming increase of depression, suicide, anxiety, and other mental health problems in youth.
These reports can be helpful in focusing attention and resources for important public health problems. Many still reference the 1999 report from former Surgeon General David Satcher, MD, PhD, which offered a number of eye-opening statistics regarding the prevalence of mental health conditions and the amount of disability associated with them.
Sadly, the present report indicates that many of these indices have grown worse in the past 20 years. For example, the advisory notes that, even before COVID-19, fully half of female high school students reported persistent feelings of sadness or hopelessness (up 40% from 2009). The report then goes on to cite a number of studies documenting even further rises in youth mental health problems associated with the pandemic.
Most of the advisory, however, is devoted to actions that can be taken by different groups, including young people themselves, parents, educators, the government, and even social media and video game companies, to support mental health and well-being. Multiple online resources are provided at the end of each of these sections.
One of the segments is aimed at health care organizations and professionals. While first making a fairly sweeping statement that “our health care system today is not set up optimally to support the mental health and well-being of children and youth,” this part then outlines five broad recommendations that might help improve the fit. These include the following.
- Increase prevention efforts, such as coordination to enrichment programs and referrals for economic and legal supports for families in need.
- Screen routinely for mental health conditions and link those who screen in with appropriate care.
- Identify mental health needs in parents and caregivers such as depression and substance use that can have negative effects on children.
- Increase partnerships between health care groups and community organizations.
- Build multidisciplinary teams that are culturally appropriate and maximally engage children and caretakers in the decision-making process.
The current report is downloadable for free (see reference below) and it is certainly worthwhile for pediatricians to take a look. Dr. Murthy writes, regarding the current state of mental health, that “it would be a tragedy if we beat back one public health crisis only to allow another to grow in its place.”
The report also outlines specific areas where additional research is needed, such as data on racial and sexual minorities and research on innovative and scalable therapies. In addition to the online resources that are provided, the report is backed by over 250 references.
Since its release, the report has generally been well received, and, indeed, there is much to support. The well-known Child Mind Institute in New York tweeted that “this document is a wake-up call for the country and a long-overdue statement of leadership from the federal government.”
Many of the recommendations are admittedly somewhat commons sense, but there are some that are much less so. For example, one recommendation to youth themselves is to serve others – something that may first come across as counterintuitive but can indeed help children and adolescents develop a sense of purpose and self-worth. The call for pediatric health care professionals to screen parents in addition to the patients themselves will likely result in some debate as well. The recommendation to reduce access to lethal means, including the specific naming of firearms, is also a welcome addition. This report also rightly puts a spotlight on the role of societal factors such as racism and poverty in the development of mental health problems and in getting access to quality treatment.
Also worth noting is how much of the advisory examined the role of media in both the problem and the solution. While recognizing that technology, smartphones, and social media are here to stay, a number of suggestions were given to parents, media organizations, journalists, and entertainment companies to reduce the negative impacts these mediums can have. Explicitly recognized in the report is that “there can be tension between what’s best for the technology company and what’s best for the individual user or society.” Also acknowledged was that the link between media of various types and mental health is complex and inconsistent with there being a strong need for additional work in this area when it comes to academic research as well as product development within these companies themselves.
Yet while there is much to like about the advisory, there remain some areas that seem lacking. For example, the text about what causes mental health conditions gets a little dualistic in mentioning biological and environmental factors without much appreciation that these are hardly independent domains. Perhaps more substantially, there was surprisingly little airtime devoted to an enormous issue that underlies so many other challenges related to mental health care – namely an inadequate workforce that gets smaller by the minute. The topic was treated much too superficially with lots of vague calls to “expand” the workforce that lacked substance or detail.
Overall, however, the new Surgeon General’s Advisory is a welcome document that offers updated knowledge of our current challenges and provides practical responses that truly could make a difference. Now all we have to do is put these recommendations into action.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
“Protecting Youth Mental Health – The U.S. Surgeon General’s Advisory,” U.S. Department of Health & Human Services (2021).
The nation’s Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, recently released an advisory report on the current state of youth mental health and recommendations to improve well-being. This action follows a number of emergency declarations that have been made by professional organizations such as the American Academy of Child and Adolescent Psychiatry (AACAP), the American Academy of Pediatrics (AAP), and other health care groups to raise awareness about the alarming increase of depression, suicide, anxiety, and other mental health problems in youth.
These reports can be helpful in focusing attention and resources for important public health problems. Many still reference the 1999 report from former Surgeon General David Satcher, MD, PhD, which offered a number of eye-opening statistics regarding the prevalence of mental health conditions and the amount of disability associated with them.
Sadly, the present report indicates that many of these indices have grown worse in the past 20 years. For example, the advisory notes that, even before COVID-19, fully half of female high school students reported persistent feelings of sadness or hopelessness (up 40% from 2009). The report then goes on to cite a number of studies documenting even further rises in youth mental health problems associated with the pandemic.
Most of the advisory, however, is devoted to actions that can be taken by different groups, including young people themselves, parents, educators, the government, and even social media and video game companies, to support mental health and well-being. Multiple online resources are provided at the end of each of these sections.
One of the segments is aimed at health care organizations and professionals. While first making a fairly sweeping statement that “our health care system today is not set up optimally to support the mental health and well-being of children and youth,” this part then outlines five broad recommendations that might help improve the fit. These include the following.
- Increase prevention efforts, such as coordination to enrichment programs and referrals for economic and legal supports for families in need.
- Screen routinely for mental health conditions and link those who screen in with appropriate care.
- Identify mental health needs in parents and caregivers such as depression and substance use that can have negative effects on children.
- Increase partnerships between health care groups and community organizations.
- Build multidisciplinary teams that are culturally appropriate and maximally engage children and caretakers in the decision-making process.
The current report is downloadable for free (see reference below) and it is certainly worthwhile for pediatricians to take a look. Dr. Murthy writes, regarding the current state of mental health, that “it would be a tragedy if we beat back one public health crisis only to allow another to grow in its place.”
The report also outlines specific areas where additional research is needed, such as data on racial and sexual minorities and research on innovative and scalable therapies. In addition to the online resources that are provided, the report is backed by over 250 references.
Since its release, the report has generally been well received, and, indeed, there is much to support. The well-known Child Mind Institute in New York tweeted that “this document is a wake-up call for the country and a long-overdue statement of leadership from the federal government.”
Many of the recommendations are admittedly somewhat commons sense, but there are some that are much less so. For example, one recommendation to youth themselves is to serve others – something that may first come across as counterintuitive but can indeed help children and adolescents develop a sense of purpose and self-worth. The call for pediatric health care professionals to screen parents in addition to the patients themselves will likely result in some debate as well. The recommendation to reduce access to lethal means, including the specific naming of firearms, is also a welcome addition. This report also rightly puts a spotlight on the role of societal factors such as racism and poverty in the development of mental health problems and in getting access to quality treatment.
Also worth noting is how much of the advisory examined the role of media in both the problem and the solution. While recognizing that technology, smartphones, and social media are here to stay, a number of suggestions were given to parents, media organizations, journalists, and entertainment companies to reduce the negative impacts these mediums can have. Explicitly recognized in the report is that “there can be tension between what’s best for the technology company and what’s best for the individual user or society.” Also acknowledged was that the link between media of various types and mental health is complex and inconsistent with there being a strong need for additional work in this area when it comes to academic research as well as product development within these companies themselves.
Yet while there is much to like about the advisory, there remain some areas that seem lacking. For example, the text about what causes mental health conditions gets a little dualistic in mentioning biological and environmental factors without much appreciation that these are hardly independent domains. Perhaps more substantially, there was surprisingly little airtime devoted to an enormous issue that underlies so many other challenges related to mental health care – namely an inadequate workforce that gets smaller by the minute. The topic was treated much too superficially with lots of vague calls to “expand” the workforce that lacked substance or detail.
Overall, however, the new Surgeon General’s Advisory is a welcome document that offers updated knowledge of our current challenges and provides practical responses that truly could make a difference. Now all we have to do is put these recommendations into action.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
“Protecting Youth Mental Health – The U.S. Surgeon General’s Advisory,” U.S. Department of Health & Human Services (2021).
The nation’s Surgeon General, Vice Admiral Vivek H. Murthy, MD, MBA, recently released an advisory report on the current state of youth mental health and recommendations to improve well-being. This action follows a number of emergency declarations that have been made by professional organizations such as the American Academy of Child and Adolescent Psychiatry (AACAP), the American Academy of Pediatrics (AAP), and other health care groups to raise awareness about the alarming increase of depression, suicide, anxiety, and other mental health problems in youth.
These reports can be helpful in focusing attention and resources for important public health problems. Many still reference the 1999 report from former Surgeon General David Satcher, MD, PhD, which offered a number of eye-opening statistics regarding the prevalence of mental health conditions and the amount of disability associated with them.
Sadly, the present report indicates that many of these indices have grown worse in the past 20 years. For example, the advisory notes that, even before COVID-19, fully half of female high school students reported persistent feelings of sadness or hopelessness (up 40% from 2009). The report then goes on to cite a number of studies documenting even further rises in youth mental health problems associated with the pandemic.
Most of the advisory, however, is devoted to actions that can be taken by different groups, including young people themselves, parents, educators, the government, and even social media and video game companies, to support mental health and well-being. Multiple online resources are provided at the end of each of these sections.
One of the segments is aimed at health care organizations and professionals. While first making a fairly sweeping statement that “our health care system today is not set up optimally to support the mental health and well-being of children and youth,” this part then outlines five broad recommendations that might help improve the fit. These include the following.
- Increase prevention efforts, such as coordination to enrichment programs and referrals for economic and legal supports for families in need.
- Screen routinely for mental health conditions and link those who screen in with appropriate care.
- Identify mental health needs in parents and caregivers such as depression and substance use that can have negative effects on children.
- Increase partnerships between health care groups and community organizations.
- Build multidisciplinary teams that are culturally appropriate and maximally engage children and caretakers in the decision-making process.
The current report is downloadable for free (see reference below) and it is certainly worthwhile for pediatricians to take a look. Dr. Murthy writes, regarding the current state of mental health, that “it would be a tragedy if we beat back one public health crisis only to allow another to grow in its place.”
The report also outlines specific areas where additional research is needed, such as data on racial and sexual minorities and research on innovative and scalable therapies. In addition to the online resources that are provided, the report is backed by over 250 references.
Since its release, the report has generally been well received, and, indeed, there is much to support. The well-known Child Mind Institute in New York tweeted that “this document is a wake-up call for the country and a long-overdue statement of leadership from the federal government.”
Many of the recommendations are admittedly somewhat commons sense, but there are some that are much less so. For example, one recommendation to youth themselves is to serve others – something that may first come across as counterintuitive but can indeed help children and adolescents develop a sense of purpose and self-worth. The call for pediatric health care professionals to screen parents in addition to the patients themselves will likely result in some debate as well. The recommendation to reduce access to lethal means, including the specific naming of firearms, is also a welcome addition. This report also rightly puts a spotlight on the role of societal factors such as racism and poverty in the development of mental health problems and in getting access to quality treatment.
Also worth noting is how much of the advisory examined the role of media in both the problem and the solution. While recognizing that technology, smartphones, and social media are here to stay, a number of suggestions were given to parents, media organizations, journalists, and entertainment companies to reduce the negative impacts these mediums can have. Explicitly recognized in the report is that “there can be tension between what’s best for the technology company and what’s best for the individual user or society.” Also acknowledged was that the link between media of various types and mental health is complex and inconsistent with there being a strong need for additional work in this area when it comes to academic research as well as product development within these companies themselves.
Yet while there is much to like about the advisory, there remain some areas that seem lacking. For example, the text about what causes mental health conditions gets a little dualistic in mentioning biological and environmental factors without much appreciation that these are hardly independent domains. Perhaps more substantially, there was surprisingly little airtime devoted to an enormous issue that underlies so many other challenges related to mental health care – namely an inadequate workforce that gets smaller by the minute. The topic was treated much too superficially with lots of vague calls to “expand” the workforce that lacked substance or detail.
Overall, however, the new Surgeon General’s Advisory is a welcome document that offers updated knowledge of our current challenges and provides practical responses that truly could make a difference. Now all we have to do is put these recommendations into action.
Dr. Rettew is a child and adolescent psychiatrist and medical director of Lane County Behavioral Health in Eugene, Ore. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.” You can follow him on Twitter and Facebook @PediPsych.
Reference
“Protecting Youth Mental Health – The U.S. Surgeon General’s Advisory,” U.S. Department of Health & Human Services (2021).
Online mental health treatment: Is this the answer we’ve been waiting for?
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
Ending the ED ‘boarding’ of youth with mental health needs
All over the country, high numbers of youth experiencing a mental health crisis are presenting to emergency departments, where they are assessed to need an inpatient psychiatric hospitalization but then wait for days and sometimes weeks with nowhere to go. In Colorado, one of the largest children’s hospitals in the state declared their own state of emergency to call attention to the problem after facing a 72% increase in volume for mental health emergency visits.1 This problem is hardly new, but the COVID pandemic has appeared to take the problem to new heights. In Massachusetts, the “boarding” of youth awaiting psychiatric hospitalization has more than doubled since the pandemic, according to a recent report from National Public Radio.2 Like many public health problems, there is evidence that the burden falls disproportionately on groups that have faced health inequities in the past.3
What is causing this? The proximal cause is fairly simple: Acute mental health problems in youth are rising while the supply of intensive services is dropping. The number of available inpatient psychiatric beds has steadily been falling over the years even prior to the COVID pandemic, which then took more capacity offline because of staffing shortages and requirements for additional distance between patients (such as eliminating double-occupancy rooms). Meanwhile, levels of anxiety, depression, and suicidality have been rising in youth for reasons still not adequately understood.
The stories of these youth and their families waiting for stabilization and treatment are heartbreaking, and nobody disagrees with the idea that a child being confined to a small ED room for days is not good care. What is debated, however, is how best to fix this problem both in the short and long term. In the eyes of many, the ultimate solution is clear: more inpatient beds. This may indeed be required for some areas, but a closer look at how an entire mental health system operates often reveals both more complex problems and some alternative potential solutions. For example, hospital staff will often acknowledge that they have patients ready for discharge but who need more intensive step-down services like a residential treatment or partial hospital program to be able to do so safely. You can’t have hospital admissions if you don’t have hospital discharges, so without good step-down options patients back up and the regular flow is disrupted. Upstream of the crisis that sends many youth to EDs is another opportunity area, as these tipping points are often seen coming by others, including their pediatricians, but referrals to clinicians or programs that might bring improvement and prevent the need for an ED evaluation are also in short supply.
In the short term, efforts are being directed by some EDs to make the physical space more therapeutic for individuals experiencing mental health problems and to offer more actual treatment when people are there. This can take the form of having a secure space in which to move around, or being offered some supportive psychotherapy sessions and possible medication changes while in the ED. It can also involve simple things like the availability of books, video games, and toys to help pass the time. Such efforts are greatly needed, and many feel that the notion of mental health emergencies somehow being outside the “lane” of emergency medicine training and practice should have been retired long ago.
Medium-term solutions can involve the standing up of more intensive mental health programs that are below the level of inpatient hospitalizations, such as intensive outpatient or partial hospitalization programs, or improved mobile response services that go beyond triage and actually bring supports and techniques directly to families in need. As mentioned, these levels of services can provide both a step-down option that facilitates a hospital discharge and a measure that can prevent the need for some hospitalizations in the first place.
Looking over the long term, health care systems and governments need to evaluate the degree to which more hospital or residential beds may still be needed, despite our best efforts to improve flow and prevent mental health crises from originating. This can often be a contentious topic, however, and securing public dollars to support more beds is often quite difficult even where there seems to be a clear need.
Hovering over nearly all potential solutions, of course, is the challenge of finding the mental health workforce to implement any new programs and initiatives without stealing from services already in place. This dilemma speaks to ongoing issues of parity between resources devoted to mental health versus physical health care. Some mental health care organizations are currently trying to recruit new workers with bonuses or new incentives, but longer-term fixes are likely to require a hard look at the degree to which our actual commitment to mental health care matches the political rhetoric.
Discussions of how to solve the problem of ED boarding can easily deteriorate into a lot of finger pointing of what somebody else should be doing. The truth is, however, that there are many actions that can be taken by those in very different roles.
While many of these steps require efforts from mental health organizations, emergency departments, government agencies, and hospitals, there are things that can be done within the purview of the primary care clinician. First, look for opportunities to increase your collaboration with mental health professionals through initiatives such as integrated care programs. The Health Resources and Services Administration is now using funds from the American Rescue Plan Act to strengthen integrated care programs across the country and new opportunities may well be available soon to get additional mental health supports to primary care offices. Second, get involved and advocate for the mental health of your patients by communicating with other groups to make other potential solutions a reality.
Children and adolescents waiting for days to get the mental health care they need and deserve is an unacceptable situation that we can and must overcome. Quick fixes will be hard to find, but with some collaborative effort, forward thinking, and, yes, financial investments, we can find solutions that reflect the principle of mental health being a foundation for all health.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Tabachnik S. Colorado health leaders declare youth mental health state of emergency: “Our kids have run out of resilience.” Denver Post. 2021 May 25.
2. Bebinger M. Kids in mental health crisis can languish for days inside ERs. National Public Radio. 2021 Jun 23.
3. Nash KA et al. Pediatrics. 2021:147:5. e2020030692.
All over the country, high numbers of youth experiencing a mental health crisis are presenting to emergency departments, where they are assessed to need an inpatient psychiatric hospitalization but then wait for days and sometimes weeks with nowhere to go. In Colorado, one of the largest children’s hospitals in the state declared their own state of emergency to call attention to the problem after facing a 72% increase in volume for mental health emergency visits.1 This problem is hardly new, but the COVID pandemic has appeared to take the problem to new heights. In Massachusetts, the “boarding” of youth awaiting psychiatric hospitalization has more than doubled since the pandemic, according to a recent report from National Public Radio.2 Like many public health problems, there is evidence that the burden falls disproportionately on groups that have faced health inequities in the past.3
What is causing this? The proximal cause is fairly simple: Acute mental health problems in youth are rising while the supply of intensive services is dropping. The number of available inpatient psychiatric beds has steadily been falling over the years even prior to the COVID pandemic, which then took more capacity offline because of staffing shortages and requirements for additional distance between patients (such as eliminating double-occupancy rooms). Meanwhile, levels of anxiety, depression, and suicidality have been rising in youth for reasons still not adequately understood.
The stories of these youth and their families waiting for stabilization and treatment are heartbreaking, and nobody disagrees with the idea that a child being confined to a small ED room for days is not good care. What is debated, however, is how best to fix this problem both in the short and long term. In the eyes of many, the ultimate solution is clear: more inpatient beds. This may indeed be required for some areas, but a closer look at how an entire mental health system operates often reveals both more complex problems and some alternative potential solutions. For example, hospital staff will often acknowledge that they have patients ready for discharge but who need more intensive step-down services like a residential treatment or partial hospital program to be able to do so safely. You can’t have hospital admissions if you don’t have hospital discharges, so without good step-down options patients back up and the regular flow is disrupted. Upstream of the crisis that sends many youth to EDs is another opportunity area, as these tipping points are often seen coming by others, including their pediatricians, but referrals to clinicians or programs that might bring improvement and prevent the need for an ED evaluation are also in short supply.
In the short term, efforts are being directed by some EDs to make the physical space more therapeutic for individuals experiencing mental health problems and to offer more actual treatment when people are there. This can take the form of having a secure space in which to move around, or being offered some supportive psychotherapy sessions and possible medication changes while in the ED. It can also involve simple things like the availability of books, video games, and toys to help pass the time. Such efforts are greatly needed, and many feel that the notion of mental health emergencies somehow being outside the “lane” of emergency medicine training and practice should have been retired long ago.
Medium-term solutions can involve the standing up of more intensive mental health programs that are below the level of inpatient hospitalizations, such as intensive outpatient or partial hospitalization programs, or improved mobile response services that go beyond triage and actually bring supports and techniques directly to families in need. As mentioned, these levels of services can provide both a step-down option that facilitates a hospital discharge and a measure that can prevent the need for some hospitalizations in the first place.
Looking over the long term, health care systems and governments need to evaluate the degree to which more hospital or residential beds may still be needed, despite our best efforts to improve flow and prevent mental health crises from originating. This can often be a contentious topic, however, and securing public dollars to support more beds is often quite difficult even where there seems to be a clear need.
Hovering over nearly all potential solutions, of course, is the challenge of finding the mental health workforce to implement any new programs and initiatives without stealing from services already in place. This dilemma speaks to ongoing issues of parity between resources devoted to mental health versus physical health care. Some mental health care organizations are currently trying to recruit new workers with bonuses or new incentives, but longer-term fixes are likely to require a hard look at the degree to which our actual commitment to mental health care matches the political rhetoric.
Discussions of how to solve the problem of ED boarding can easily deteriorate into a lot of finger pointing of what somebody else should be doing. The truth is, however, that there are many actions that can be taken by those in very different roles.
While many of these steps require efforts from mental health organizations, emergency departments, government agencies, and hospitals, there are things that can be done within the purview of the primary care clinician. First, look for opportunities to increase your collaboration with mental health professionals through initiatives such as integrated care programs. The Health Resources and Services Administration is now using funds from the American Rescue Plan Act to strengthen integrated care programs across the country and new opportunities may well be available soon to get additional mental health supports to primary care offices. Second, get involved and advocate for the mental health of your patients by communicating with other groups to make other potential solutions a reality.
Children and adolescents waiting for days to get the mental health care they need and deserve is an unacceptable situation that we can and must overcome. Quick fixes will be hard to find, but with some collaborative effort, forward thinking, and, yes, financial investments, we can find solutions that reflect the principle of mental health being a foundation for all health.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Tabachnik S. Colorado health leaders declare youth mental health state of emergency: “Our kids have run out of resilience.” Denver Post. 2021 May 25.
2. Bebinger M. Kids in mental health crisis can languish for days inside ERs. National Public Radio. 2021 Jun 23.
3. Nash KA et al. Pediatrics. 2021:147:5. e2020030692.
All over the country, high numbers of youth experiencing a mental health crisis are presenting to emergency departments, where they are assessed to need an inpatient psychiatric hospitalization but then wait for days and sometimes weeks with nowhere to go. In Colorado, one of the largest children’s hospitals in the state declared their own state of emergency to call attention to the problem after facing a 72% increase in volume for mental health emergency visits.1 This problem is hardly new, but the COVID pandemic has appeared to take the problem to new heights. In Massachusetts, the “boarding” of youth awaiting psychiatric hospitalization has more than doubled since the pandemic, according to a recent report from National Public Radio.2 Like many public health problems, there is evidence that the burden falls disproportionately on groups that have faced health inequities in the past.3
What is causing this? The proximal cause is fairly simple: Acute mental health problems in youth are rising while the supply of intensive services is dropping. The number of available inpatient psychiatric beds has steadily been falling over the years even prior to the COVID pandemic, which then took more capacity offline because of staffing shortages and requirements for additional distance between patients (such as eliminating double-occupancy rooms). Meanwhile, levels of anxiety, depression, and suicidality have been rising in youth for reasons still not adequately understood.
The stories of these youth and their families waiting for stabilization and treatment are heartbreaking, and nobody disagrees with the idea that a child being confined to a small ED room for days is not good care. What is debated, however, is how best to fix this problem both in the short and long term. In the eyes of many, the ultimate solution is clear: more inpatient beds. This may indeed be required for some areas, but a closer look at how an entire mental health system operates often reveals both more complex problems and some alternative potential solutions. For example, hospital staff will often acknowledge that they have patients ready for discharge but who need more intensive step-down services like a residential treatment or partial hospital program to be able to do so safely. You can’t have hospital admissions if you don’t have hospital discharges, so without good step-down options patients back up and the regular flow is disrupted. Upstream of the crisis that sends many youth to EDs is another opportunity area, as these tipping points are often seen coming by others, including their pediatricians, but referrals to clinicians or programs that might bring improvement and prevent the need for an ED evaluation are also in short supply.
In the short term, efforts are being directed by some EDs to make the physical space more therapeutic for individuals experiencing mental health problems and to offer more actual treatment when people are there. This can take the form of having a secure space in which to move around, or being offered some supportive psychotherapy sessions and possible medication changes while in the ED. It can also involve simple things like the availability of books, video games, and toys to help pass the time. Such efforts are greatly needed, and many feel that the notion of mental health emergencies somehow being outside the “lane” of emergency medicine training and practice should have been retired long ago.
Medium-term solutions can involve the standing up of more intensive mental health programs that are below the level of inpatient hospitalizations, such as intensive outpatient or partial hospitalization programs, or improved mobile response services that go beyond triage and actually bring supports and techniques directly to families in need. As mentioned, these levels of services can provide both a step-down option that facilitates a hospital discharge and a measure that can prevent the need for some hospitalizations in the first place.
Looking over the long term, health care systems and governments need to evaluate the degree to which more hospital or residential beds may still be needed, despite our best efforts to improve flow and prevent mental health crises from originating. This can often be a contentious topic, however, and securing public dollars to support more beds is often quite difficult even where there seems to be a clear need.
Hovering over nearly all potential solutions, of course, is the challenge of finding the mental health workforce to implement any new programs and initiatives without stealing from services already in place. This dilemma speaks to ongoing issues of parity between resources devoted to mental health versus physical health care. Some mental health care organizations are currently trying to recruit new workers with bonuses or new incentives, but longer-term fixes are likely to require a hard look at the degree to which our actual commitment to mental health care matches the political rhetoric.
Discussions of how to solve the problem of ED boarding can easily deteriorate into a lot of finger pointing of what somebody else should be doing. The truth is, however, that there are many actions that can be taken by those in very different roles.
While many of these steps require efforts from mental health organizations, emergency departments, government agencies, and hospitals, there are things that can be done within the purview of the primary care clinician. First, look for opportunities to increase your collaboration with mental health professionals through initiatives such as integrated care programs. The Health Resources and Services Administration is now using funds from the American Rescue Plan Act to strengthen integrated care programs across the country and new opportunities may well be available soon to get additional mental health supports to primary care offices. Second, get involved and advocate for the mental health of your patients by communicating with other groups to make other potential solutions a reality.
Children and adolescents waiting for days to get the mental health care they need and deserve is an unacceptable situation that we can and must overcome. Quick fixes will be hard to find, but with some collaborative effort, forward thinking, and, yes, financial investments, we can find solutions that reflect the principle of mental health being a foundation for all health.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont, Burlington. Follow him on Twitter @PediPsych. His latest book is “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood.”
References
1. Tabachnik S. Colorado health leaders declare youth mental health state of emergency: “Our kids have run out of resilience.” Denver Post. 2021 May 25.
2. Bebinger M. Kids in mental health crisis can languish for days inside ERs. National Public Radio. 2021 Jun 23.
3. Nash KA et al. Pediatrics. 2021:147:5. e2020030692.
COVID-19 and youth suicide: Do the numbers match the headlines?
There’s little doubt that the COVID-19 pandemic has been hard on many children and adolescents just as it has been difficult for adults. The disruption of routines, reduced contact with friends, concern over getting ill, and financial turmoil suffered by many families is exacting a toll on our mental health, as has been documented by a number of recent surveys and studies.1,2
Quite understandably, concern about rising levels of anxiety and depression in youth prompts additional worries about suicide, the second leading cause of death in adolescents and young adults. In response, many organizations have rallied to provide additional resources to help prevent suicidal thinking and actions. Online mental health tips, support phone and text lines, and the availability of telemedicine have all been mobilized to help people cope and stay safe both physically and psychologically.
But what are the actual numbers when it comes to youth suicide during COVID-19? According to many headlines in the press, the statistics are grim and support many of distressing predictions that have been made. A December story in an Arizona newspaper, “With Teen Suicides on the Rise, Tucson Educators Struggle to Prioritize Mental Health,” described a 67% increase in teen suicides in 2020 compared with 2019 in one county.3 Another post from Psychology Today, “America is Facing a Teen Suicide Pandemic,” raised similar alarms.4 Concern over suicide has even been used politically to argue against restrictions that could reduce the spread of COVID-19 infections.
But despite this common perception shared by both health care professionals and the public, there actually is not evidence at this point that the COVID-19 pandemic has led to a broad spike in youth suicide deaths or attempts. A recent study published in the journal Pediatrics compared suicide screening results on youth presenting to emergency departments for any reason in 2020 to the same month in 2019.5 The authors found no consistent increases in reported suicidal ideation or suicide attempts with scattered elevations found in some months during 2020 compared with the previous year (including February 2020 before the pandemic really began) but not others. Internationally, newly analyzed data from 2020 with regard to suicide deaths have suggested “either no rise in suicide rates ... or a fall in the early months of the pandemic.” In my home and, admittedly small, state of Vermont, data from the Department of Health have shown 93 suicide deaths across all ages as of mid-November 2020 compared with a 5-year average of 96.
Why don’t the data match the headlines? There are a number of possibilities.
1. Suicide rates in youth were going up before the pandemic. As it takes time to verify and analyze data from large populations, many of the reports on suicide that have been published and released in 2020 summarize data from prior years. Without looking closely, a news organization can easily slap on a headline that implies that the data were obtained during the pandemic.
2. Fluctuations tend to occur from year to year. Thankfully, youth suicide remains rare (although not rare enough). With small numbers, regular variations from year to year can look huge in terms of percentages, especially if one doesn’t pull back and look at longer trends over time.
3. People are reaching out for mental health services. The public health message to access support and treatment for COVID 19–related mental health struggles appears to be having an effect, but this increased demand should not necessarily be viewed as a proxy for suicidal ideation and attempts.
While the understanding that we are not actually in the midst of a surge in COVID 19–related youth suicide is reassuring, it is important not to get complacent. Much of the data remains preliminary, and, even if these numbers hold up, there is no guarantee that things will continue this way, especially if the pandemic and it restrictions continue to drag on for many more months. And of course, whether or not the pandemic is making things significantly worse, youth suicide remains an enormous public health imperative with every one being a human tragedy.
It is also quite possible that more detailed analyses will eventually reveal a more complex association between youth suicide and COVID-19, with effects of the pandemic being realized regionally or more for some groups than others. Data from before the pandemic indicated, for example, that suicide rates are increasing more rapidly among African American youth compared with white children and adolescents.6 With the COVID-19 pandemic itself affecting disadvantaged communities more strongly, one could readily expect variable impacts in mental health related to race or socioeconomic status. A recent article voices these concerns for indigenous youth in Montana: a state with one of the highest per capita suicide rates in the country.7 The article notes, however, that the rate of suicide overall in Montana in 2020 is comparable to those of previous years.
Overall, pediatricians should not be needlessly panicked that the COVID-19 pandemic has sparked a surge in youth suicide. The data at this point simply don’t support that assertion despite many headlines to the contrary. At the same time, many children and adolescents are certainly struggling with the stresses the pandemic has created and continue to need our close monitoring and support.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine. Follow him on Twitter @PediPsych. His new book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood,” launches Feb. 1, 2021.
References
1. Copeland WE et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2020;60(1):134-41. doi: 10.1016/j.jaac.2020.08.466.
2. Qiu J et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatry. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213.
3. Dhmara K. With teen suicides on the rise, Tucson educators struggle to prioritize mental health. Tuscon.com. Dec. 27, 2020.
4. Chafouleas, SM. America is facing a suicide epidemic: New data confirm the urgency of confronting it now. Psychology Today blog. Sept. 4, 2020.
5. Hill RM et al. Suicide ideation and attempts in a pediatric emergency department before and after COVID-19. Pediatrics. 2020. doi: 10.1542/peds.2020-029280.
6. John A et al. Trends in suicide during the covid-19 pandemic. BMJ 2020;371:m4352. doi: 10.1136/bmj.m4352.
7. Reardon S. Health officials fear COVID-19 pandemic-related suicide spike among indigenous youth. Time Magazine. December 2020.
There’s little doubt that the COVID-19 pandemic has been hard on many children and adolescents just as it has been difficult for adults. The disruption of routines, reduced contact with friends, concern over getting ill, and financial turmoil suffered by many families is exacting a toll on our mental health, as has been documented by a number of recent surveys and studies.1,2
Quite understandably, concern about rising levels of anxiety and depression in youth prompts additional worries about suicide, the second leading cause of death in adolescents and young adults. In response, many organizations have rallied to provide additional resources to help prevent suicidal thinking and actions. Online mental health tips, support phone and text lines, and the availability of telemedicine have all been mobilized to help people cope and stay safe both physically and psychologically.
But what are the actual numbers when it comes to youth suicide during COVID-19? According to many headlines in the press, the statistics are grim and support many of distressing predictions that have been made. A December story in an Arizona newspaper, “With Teen Suicides on the Rise, Tucson Educators Struggle to Prioritize Mental Health,” described a 67% increase in teen suicides in 2020 compared with 2019 in one county.3 Another post from Psychology Today, “America is Facing a Teen Suicide Pandemic,” raised similar alarms.4 Concern over suicide has even been used politically to argue against restrictions that could reduce the spread of COVID-19 infections.
But despite this common perception shared by both health care professionals and the public, there actually is not evidence at this point that the COVID-19 pandemic has led to a broad spike in youth suicide deaths or attempts. A recent study published in the journal Pediatrics compared suicide screening results on youth presenting to emergency departments for any reason in 2020 to the same month in 2019.5 The authors found no consistent increases in reported suicidal ideation or suicide attempts with scattered elevations found in some months during 2020 compared with the previous year (including February 2020 before the pandemic really began) but not others. Internationally, newly analyzed data from 2020 with regard to suicide deaths have suggested “either no rise in suicide rates ... or a fall in the early months of the pandemic.” In my home and, admittedly small, state of Vermont, data from the Department of Health have shown 93 suicide deaths across all ages as of mid-November 2020 compared with a 5-year average of 96.
Why don’t the data match the headlines? There are a number of possibilities.
1. Suicide rates in youth were going up before the pandemic. As it takes time to verify and analyze data from large populations, many of the reports on suicide that have been published and released in 2020 summarize data from prior years. Without looking closely, a news organization can easily slap on a headline that implies that the data were obtained during the pandemic.
2. Fluctuations tend to occur from year to year. Thankfully, youth suicide remains rare (although not rare enough). With small numbers, regular variations from year to year can look huge in terms of percentages, especially if one doesn’t pull back and look at longer trends over time.
3. People are reaching out for mental health services. The public health message to access support and treatment for COVID 19–related mental health struggles appears to be having an effect, but this increased demand should not necessarily be viewed as a proxy for suicidal ideation and attempts.
While the understanding that we are not actually in the midst of a surge in COVID 19–related youth suicide is reassuring, it is important not to get complacent. Much of the data remains preliminary, and, even if these numbers hold up, there is no guarantee that things will continue this way, especially if the pandemic and it restrictions continue to drag on for many more months. And of course, whether or not the pandemic is making things significantly worse, youth suicide remains an enormous public health imperative with every one being a human tragedy.
It is also quite possible that more detailed analyses will eventually reveal a more complex association between youth suicide and COVID-19, with effects of the pandemic being realized regionally or more for some groups than others. Data from before the pandemic indicated, for example, that suicide rates are increasing more rapidly among African American youth compared with white children and adolescents.6 With the COVID-19 pandemic itself affecting disadvantaged communities more strongly, one could readily expect variable impacts in mental health related to race or socioeconomic status. A recent article voices these concerns for indigenous youth in Montana: a state with one of the highest per capita suicide rates in the country.7 The article notes, however, that the rate of suicide overall in Montana in 2020 is comparable to those of previous years.
Overall, pediatricians should not be needlessly panicked that the COVID-19 pandemic has sparked a surge in youth suicide. The data at this point simply don’t support that assertion despite many headlines to the contrary. At the same time, many children and adolescents are certainly struggling with the stresses the pandemic has created and continue to need our close monitoring and support.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine. Follow him on Twitter @PediPsych. His new book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood,” launches Feb. 1, 2021.
References
1. Copeland WE et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2020;60(1):134-41. doi: 10.1016/j.jaac.2020.08.466.
2. Qiu J et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatry. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213.
3. Dhmara K. With teen suicides on the rise, Tucson educators struggle to prioritize mental health. Tuscon.com. Dec. 27, 2020.
4. Chafouleas, SM. America is facing a suicide epidemic: New data confirm the urgency of confronting it now. Psychology Today blog. Sept. 4, 2020.
5. Hill RM et al. Suicide ideation and attempts in a pediatric emergency department before and after COVID-19. Pediatrics. 2020. doi: 10.1542/peds.2020-029280.
6. John A et al. Trends in suicide during the covid-19 pandemic. BMJ 2020;371:m4352. doi: 10.1136/bmj.m4352.
7. Reardon S. Health officials fear COVID-19 pandemic-related suicide spike among indigenous youth. Time Magazine. December 2020.
There’s little doubt that the COVID-19 pandemic has been hard on many children and adolescents just as it has been difficult for adults. The disruption of routines, reduced contact with friends, concern over getting ill, and financial turmoil suffered by many families is exacting a toll on our mental health, as has been documented by a number of recent surveys and studies.1,2
Quite understandably, concern about rising levels of anxiety and depression in youth prompts additional worries about suicide, the second leading cause of death in adolescents and young adults. In response, many organizations have rallied to provide additional resources to help prevent suicidal thinking and actions. Online mental health tips, support phone and text lines, and the availability of telemedicine have all been mobilized to help people cope and stay safe both physically and psychologically.
But what are the actual numbers when it comes to youth suicide during COVID-19? According to many headlines in the press, the statistics are grim and support many of distressing predictions that have been made. A December story in an Arizona newspaper, “With Teen Suicides on the Rise, Tucson Educators Struggle to Prioritize Mental Health,” described a 67% increase in teen suicides in 2020 compared with 2019 in one county.3 Another post from Psychology Today, “America is Facing a Teen Suicide Pandemic,” raised similar alarms.4 Concern over suicide has even been used politically to argue against restrictions that could reduce the spread of COVID-19 infections.
But despite this common perception shared by both health care professionals and the public, there actually is not evidence at this point that the COVID-19 pandemic has led to a broad spike in youth suicide deaths or attempts. A recent study published in the journal Pediatrics compared suicide screening results on youth presenting to emergency departments for any reason in 2020 to the same month in 2019.5 The authors found no consistent increases in reported suicidal ideation or suicide attempts with scattered elevations found in some months during 2020 compared with the previous year (including February 2020 before the pandemic really began) but not others. Internationally, newly analyzed data from 2020 with regard to suicide deaths have suggested “either no rise in suicide rates ... or a fall in the early months of the pandemic.” In my home and, admittedly small, state of Vermont, data from the Department of Health have shown 93 suicide deaths across all ages as of mid-November 2020 compared with a 5-year average of 96.
Why don’t the data match the headlines? There are a number of possibilities.
1. Suicide rates in youth were going up before the pandemic. As it takes time to verify and analyze data from large populations, many of the reports on suicide that have been published and released in 2020 summarize data from prior years. Without looking closely, a news organization can easily slap on a headline that implies that the data were obtained during the pandemic.
2. Fluctuations tend to occur from year to year. Thankfully, youth suicide remains rare (although not rare enough). With small numbers, regular variations from year to year can look huge in terms of percentages, especially if one doesn’t pull back and look at longer trends over time.
3. People are reaching out for mental health services. The public health message to access support and treatment for COVID 19–related mental health struggles appears to be having an effect, but this increased demand should not necessarily be viewed as a proxy for suicidal ideation and attempts.
While the understanding that we are not actually in the midst of a surge in COVID 19–related youth suicide is reassuring, it is important not to get complacent. Much of the data remains preliminary, and, even if these numbers hold up, there is no guarantee that things will continue this way, especially if the pandemic and it restrictions continue to drag on for many more months. And of course, whether or not the pandemic is making things significantly worse, youth suicide remains an enormous public health imperative with every one being a human tragedy.
It is also quite possible that more detailed analyses will eventually reveal a more complex association between youth suicide and COVID-19, with effects of the pandemic being realized regionally or more for some groups than others. Data from before the pandemic indicated, for example, that suicide rates are increasing more rapidly among African American youth compared with white children and adolescents.6 With the COVID-19 pandemic itself affecting disadvantaged communities more strongly, one could readily expect variable impacts in mental health related to race or socioeconomic status. A recent article voices these concerns for indigenous youth in Montana: a state with one of the highest per capita suicide rates in the country.7 The article notes, however, that the rate of suicide overall in Montana in 2020 is comparable to those of previous years.
Overall, pediatricians should not be needlessly panicked that the COVID-19 pandemic has sparked a surge in youth suicide. The data at this point simply don’t support that assertion despite many headlines to the contrary. At the same time, many children and adolescents are certainly struggling with the stresses the pandemic has created and continue to need our close monitoring and support.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine. Follow him on Twitter @PediPsych. His new book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood,” launches Feb. 1, 2021.
References
1. Copeland WE et al. Impact of COVID-19 pandemic on college student mental health and wellness. J Am Acad Child Adolesc Psychiatry. 2020;60(1):134-41. doi: 10.1016/j.jaac.2020.08.466.
2. Qiu J et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatry. 2020;33:e100213. doi: 10.1136/gpsych-2020-100213.
3. Dhmara K. With teen suicides on the rise, Tucson educators struggle to prioritize mental health. Tuscon.com. Dec. 27, 2020.
4. Chafouleas, SM. America is facing a suicide epidemic: New data confirm the urgency of confronting it now. Psychology Today blog. Sept. 4, 2020.
5. Hill RM et al. Suicide ideation and attempts in a pediatric emergency department before and after COVID-19. Pediatrics. 2020. doi: 10.1542/peds.2020-029280.
6. John A et al. Trends in suicide during the covid-19 pandemic. BMJ 2020;371:m4352. doi: 10.1136/bmj.m4352.
7. Reardon S. Health officials fear COVID-19 pandemic-related suicide spike among indigenous youth. Time Magazine. December 2020.






