User login
A pediatrician’s guide to screening for and treating depression
On Oct. 19, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association jointly declared a “national emergency in children’s mental health,” calling upon policy makers to take actions that could help address “soaring rates” of anxiety and depression.
Knowing that increasing the work force or creating new programs will come slowly if at all, they called for the integration of mental health care into primary care pediatrics and efforts to reduce the risk of suicide in children and adolescents.
Our clinical experience suggests that adolescent depression, which can lead to profoundly impaired function, impaired development, and even suicide, is a major concern in your practice. We hope to do our part by reviewing the screening, diagnosis, and management of depression that can reasonably happen in the pediatrician’s office.
Depression
Depression affects as many as 20% of adolescents, with girls experiencing major depressive disorder (MDD) twice as often as boys. The incidence of depression increases fourfold after puberty, and there is substantial evidence, but no clear cause, that it has increased by nearly 50% over the past decade, rising from a rate of 8% of U.S. adolescents in 2007 to 13% in 2017.1 In that same time period, the rate of completed suicides among U.S. youth aged 10-24 increased 57.4%, after being stable for the prior decade.2 Adolescent depression is also linked to increased substance use and high-risk behaviors such as drunk driving. In 2020, mental health–related emergency department visits by adolescents aged 12-17 increased by 31%. Visits for suicide attempts among adolescent girls in 2021 jumped by 51% from 2019.3 Clearly, MDD in adolescence is a common, potentially life-threatening problem
.
Screening and assessment
At annual checkups with patients 12 and older or at sick visits of patients with emotional, sleep, or vague somatic concerns, it should be standard practice to screen for depression. The Patient Health Questionnaire 9 modified for Adolescents (PHQ9-A) is a reliable, validated, and free screening instrument that your patients can fill out in the waiting room. (The PHQ9 can be used for your patients who are 18 and older.) It takes only 5 minutes to complete and is very easy to score. It establishes whether your patient meets DSM-5 criteria for MDD, and the degree of severity (5-9 is mild, 10-14 is moderate, 15-19 is moderately severe, and 20-27 is severe). It also screens for thoughts about suicide and past suicide attempts. You might add the more comprehensive parent-completed Pediatric Symptom Checklist, which includes a depression screen.4
These screening instruments can be completed electronically prior to or at the visit and should have a preamble explaining why depression screening is relevant. If screening is positive, interview your adolescent patients alone. This will give you the time to gather more detail about how impaired their function is at school, with friends, and in family relationships. Have they been missing school? Have their grades changed? Are they failing to hand in homework? Have they withdrawn from sports or activities? Are they less likely to hang out with friends? Do they participate in family activities? Have others noticed any changes? You should also check for associated anxiety symptoms (ruminative worries, panic attacks) and drug and alcohol use. Of course, you should ask about any suicidal thoughts (from vague morbid thoughts to specific plans, with intent and factors that have prevented them) and actual attempts. Remember, asking about suicidal thoughts and attempts will not cause or worsen them. On the contrary, your patients may feel shame, but will be relieved to not be alone with these thoughts. And this knowledge will be essential as you decide what to do next. When you meet with the parents, ask them about a family history of depression or suicide attempts, and then offer supportive interventions.
Supportive interventions
For all adolescents with depression, supportive interventions are helpful, and for those with mild symptoms, they are often adequate treatment. This begins with education for your patient and their parents about depression. It is an illness, not a problem of character or discipline. Advise your patients that adequate, restful sleep every night is critical to recovery. Regular exercise (daily is best, but at least three times weekly for 30 minutes) is often effective in mild to moderate depression. Patience and compassion for feelings of sadness, irritability, or disinterest are important at home, and maintaining connections with those people who offer support (friends, coaches, parents, etc.) is essential. They should also be told that “depression lies.” Feelings of guilt and self-reproach are a normal part of the illness, not facts. Organizations such as the National Alliance on Mental Illness (NAMI) and the American Academy of Child and Adolescent Psychiatry (AACAP) offer written materials through their websites that are very helpful educational resources. Connect them with sources of counseling support (through school, for example). For those with mild, brief, and uncomplicated depression, supportive interventions alone should offer relief within 4-6 weeks. It is hard to predict the trajectory of depression, so follow-up visits are relevant to determine if they are improving or worsening.
Psychotherapy
For your patients with moderate depression, or with hopelessness or suicidality, a referral for evidence-based psychotherapy is indicated. Both cognitive behavioral therapy and interpersonal therapy have demonstrated efficacy in treating depression in adolescents. If there is a history of trauma or high family conflict, supportive psychotherapy that will enhance communication skills within the family is very important to recovery. Identify various sources for high-quality psychotherapy services (individual, family, and group) in your community. While this may sound easier said than done, online services such as Psychology Today’s therapist locator can help. If your local university has a graduate program in social work or psychology, connect with them as they may have easier access to high-quality services through their training programs. If there is a group practice of therapists in your community, invite them to meet with your team to learn about whether they use evidence-based therapies and can support families as well as individual youth.
Pharmacologic options
For those adolescents with moderate to severe depression, psychotherapy alone is usually inadequate. Indeed, they may be so impaired that they simply cannot meaningfully engage in the work of psychotherapy. These patients require psychopharmacologic treatment first. First-line treatment is with selective serotonin reuptake inhibitors (SSRIs) (both fluoxetine and escitalopram are approved for use in adolescent depression). While many pediatricians remain reluctant about initiating SSRI treatment of depression since the Food and Drug Administration’s 2004 boxed warning was issued, the risks of untreated severe depression are more marked than are the risks of SSRI treatment. As prescription rates dipped in the following decade, rates of suicide attempts in adolescents with severe depression climbed. Subsequent research on the nature of the risk of “increased suicidality” indicated it is substantially lower than originally thought.
The AAP’s Guidelines for Adolescent Depression in Primary Care offer reassuring guidance: They recommend that pediatricians initiate treatment at a very low dose of SSRI (5 mg of fluoxetine, 12.5 mg of sertraline, or 5 mg of escitalopram) and aim to get to a therapeutic dose within 4 weeks.5 Educate the patient and parent about likely side effects (gastrointestinal upset, sleep disruption, akathisia or restlessness, and activation), which indicate the dose should be held steady until the side effects subside. Patients should be seen weekly until they get to a therapeutic dose, then biweekly to monitor for response. At these regular check-ins, the PHQ9A can follow symptom severity. You should monitor changes in function and for any change in suicidal thoughts. If your patient does not respond with at least energy improvement within 4 weeks, you should cross-taper to a different SSRI.
Managing risk
Suicidal thoughts are a common symptom of depression and an important marker of severity. Adolescents have more limited impulse control than do adults, elevating their risk for impulsively acting on these thoughts. Adolescents who are using alcohol or other substances, or who have a history of impulsivity, are at higher risk. Further compounding the degree of risk are a history of suicide attempts, impulsive aggression or psychotic symptoms, or a family history of completed suicide. In managing risk, it is critical that you assess and discuss these risk factors and discuss the need to have a safety plan.
This planning should include both patient and parent. Help the parent to identify lethal means at home (guns, rope, medications, and knives or box cutters) and make plans to secure or remove them. It includes helping your patient list those strategies that can be helpful if they are feeling more distressed (distracting with music or television, exercise, or connecting with select friends). A safety plan is not a promise or a contract to not do something, rather it is a practical set of strategies the patient and family can employ if they are feeling worse. It depends on the adolescent having a secure, trusting connection with the adults at home and with your office.
If your patient fails to improve, if the diagnosis appears complicated, or if you feel the patient is not safe, you should refer to child psychiatry or, if needed, a local emergency department. If you cannot find access to a psychiatrist, start with your state’s child psychiatric consultation hotline for access to telephone support: www.nncpap.org.
Although the suggestions outlined above are grounded in evidence and need, treating moderate to severe depression is likely a new challenge for many pediatricians. Managing the risk of suicide can be stressful, without a doubt. In our own work as child psychiatrists, we recognize that there is no single, reliable method to predict suicide and therefore no specific approach to ensuring prevention. We appreciate this burden of worry when treating a severely depressed adolescent, and follow the rule, “never worry alone” – share your concerns with parents and/or a mental health consultant (hopefully co-located in your office), or obtain a second opinion, even consult a child psychiatrist on a hotline. Offering supportive care for those with mild depression can prevent it from becoming severe, and beginning treatment for those with severe depression can make a profound difference in the course of a young person’s illness.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
References
1. Pew Research Center. National Survey on Drug Use and Health (2017).
2. Curtin SC. Natl Vital Stat Rep. 2020 Sep;69(11):1-10.
3. Yard E et al. MMWR Morb Mortal Wkly Rep. 2021 Jun 18;70(24):888-94.
4. Jellinek M et al. J Pediatr. 2021 Jun;233:220-6.e1.
5. Zuckerbrot RA et al. Pediatrics. 2018 Mar;141(3):e20174081.
On Oct. 19, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association jointly declared a “national emergency in children’s mental health,” calling upon policy makers to take actions that could help address “soaring rates” of anxiety and depression.
Knowing that increasing the work force or creating new programs will come slowly if at all, they called for the integration of mental health care into primary care pediatrics and efforts to reduce the risk of suicide in children and adolescents.
Our clinical experience suggests that adolescent depression, which can lead to profoundly impaired function, impaired development, and even suicide, is a major concern in your practice. We hope to do our part by reviewing the screening, diagnosis, and management of depression that can reasonably happen in the pediatrician’s office.
Depression
Depression affects as many as 20% of adolescents, with girls experiencing major depressive disorder (MDD) twice as often as boys. The incidence of depression increases fourfold after puberty, and there is substantial evidence, but no clear cause, that it has increased by nearly 50% over the past decade, rising from a rate of 8% of U.S. adolescents in 2007 to 13% in 2017.1 In that same time period, the rate of completed suicides among U.S. youth aged 10-24 increased 57.4%, after being stable for the prior decade.2 Adolescent depression is also linked to increased substance use and high-risk behaviors such as drunk driving. In 2020, mental health–related emergency department visits by adolescents aged 12-17 increased by 31%. Visits for suicide attempts among adolescent girls in 2021 jumped by 51% from 2019.3 Clearly, MDD in adolescence is a common, potentially life-threatening problem
.
Screening and assessment
At annual checkups with patients 12 and older or at sick visits of patients with emotional, sleep, or vague somatic concerns, it should be standard practice to screen for depression. The Patient Health Questionnaire 9 modified for Adolescents (PHQ9-A) is a reliable, validated, and free screening instrument that your patients can fill out in the waiting room. (The PHQ9 can be used for your patients who are 18 and older.) It takes only 5 minutes to complete and is very easy to score. It establishes whether your patient meets DSM-5 criteria for MDD, and the degree of severity (5-9 is mild, 10-14 is moderate, 15-19 is moderately severe, and 20-27 is severe). It also screens for thoughts about suicide and past suicide attempts. You might add the more comprehensive parent-completed Pediatric Symptom Checklist, which includes a depression screen.4
These screening instruments can be completed electronically prior to or at the visit and should have a preamble explaining why depression screening is relevant. If screening is positive, interview your adolescent patients alone. This will give you the time to gather more detail about how impaired their function is at school, with friends, and in family relationships. Have they been missing school? Have their grades changed? Are they failing to hand in homework? Have they withdrawn from sports or activities? Are they less likely to hang out with friends? Do they participate in family activities? Have others noticed any changes? You should also check for associated anxiety symptoms (ruminative worries, panic attacks) and drug and alcohol use. Of course, you should ask about any suicidal thoughts (from vague morbid thoughts to specific plans, with intent and factors that have prevented them) and actual attempts. Remember, asking about suicidal thoughts and attempts will not cause or worsen them. On the contrary, your patients may feel shame, but will be relieved to not be alone with these thoughts. And this knowledge will be essential as you decide what to do next. When you meet with the parents, ask them about a family history of depression or suicide attempts, and then offer supportive interventions.
Supportive interventions
For all adolescents with depression, supportive interventions are helpful, and for those with mild symptoms, they are often adequate treatment. This begins with education for your patient and their parents about depression. It is an illness, not a problem of character or discipline. Advise your patients that adequate, restful sleep every night is critical to recovery. Regular exercise (daily is best, but at least three times weekly for 30 minutes) is often effective in mild to moderate depression. Patience and compassion for feelings of sadness, irritability, or disinterest are important at home, and maintaining connections with those people who offer support (friends, coaches, parents, etc.) is essential. They should also be told that “depression lies.” Feelings of guilt and self-reproach are a normal part of the illness, not facts. Organizations such as the National Alliance on Mental Illness (NAMI) and the American Academy of Child and Adolescent Psychiatry (AACAP) offer written materials through their websites that are very helpful educational resources. Connect them with sources of counseling support (through school, for example). For those with mild, brief, and uncomplicated depression, supportive interventions alone should offer relief within 4-6 weeks. It is hard to predict the trajectory of depression, so follow-up visits are relevant to determine if they are improving or worsening.
Psychotherapy
For your patients with moderate depression, or with hopelessness or suicidality, a referral for evidence-based psychotherapy is indicated. Both cognitive behavioral therapy and interpersonal therapy have demonstrated efficacy in treating depression in adolescents. If there is a history of trauma or high family conflict, supportive psychotherapy that will enhance communication skills within the family is very important to recovery. Identify various sources for high-quality psychotherapy services (individual, family, and group) in your community. While this may sound easier said than done, online services such as Psychology Today’s therapist locator can help. If your local university has a graduate program in social work or psychology, connect with them as they may have easier access to high-quality services through their training programs. If there is a group practice of therapists in your community, invite them to meet with your team to learn about whether they use evidence-based therapies and can support families as well as individual youth.
Pharmacologic options
For those adolescents with moderate to severe depression, psychotherapy alone is usually inadequate. Indeed, they may be so impaired that they simply cannot meaningfully engage in the work of psychotherapy. These patients require psychopharmacologic treatment first. First-line treatment is with selective serotonin reuptake inhibitors (SSRIs) (both fluoxetine and escitalopram are approved for use in adolescent depression). While many pediatricians remain reluctant about initiating SSRI treatment of depression since the Food and Drug Administration’s 2004 boxed warning was issued, the risks of untreated severe depression are more marked than are the risks of SSRI treatment. As prescription rates dipped in the following decade, rates of suicide attempts in adolescents with severe depression climbed. Subsequent research on the nature of the risk of “increased suicidality” indicated it is substantially lower than originally thought.
The AAP’s Guidelines for Adolescent Depression in Primary Care offer reassuring guidance: They recommend that pediatricians initiate treatment at a very low dose of SSRI (5 mg of fluoxetine, 12.5 mg of sertraline, or 5 mg of escitalopram) and aim to get to a therapeutic dose within 4 weeks.5 Educate the patient and parent about likely side effects (gastrointestinal upset, sleep disruption, akathisia or restlessness, and activation), which indicate the dose should be held steady until the side effects subside. Patients should be seen weekly until they get to a therapeutic dose, then biweekly to monitor for response. At these regular check-ins, the PHQ9A can follow symptom severity. You should monitor changes in function and for any change in suicidal thoughts. If your patient does not respond with at least energy improvement within 4 weeks, you should cross-taper to a different SSRI.
Managing risk
Suicidal thoughts are a common symptom of depression and an important marker of severity. Adolescents have more limited impulse control than do adults, elevating their risk for impulsively acting on these thoughts. Adolescents who are using alcohol or other substances, or who have a history of impulsivity, are at higher risk. Further compounding the degree of risk are a history of suicide attempts, impulsive aggression or psychotic symptoms, or a family history of completed suicide. In managing risk, it is critical that you assess and discuss these risk factors and discuss the need to have a safety plan.
This planning should include both patient and parent. Help the parent to identify lethal means at home (guns, rope, medications, and knives or box cutters) and make plans to secure or remove them. It includes helping your patient list those strategies that can be helpful if they are feeling more distressed (distracting with music or television, exercise, or connecting with select friends). A safety plan is not a promise or a contract to not do something, rather it is a practical set of strategies the patient and family can employ if they are feeling worse. It depends on the adolescent having a secure, trusting connection with the adults at home and with your office.
If your patient fails to improve, if the diagnosis appears complicated, or if you feel the patient is not safe, you should refer to child psychiatry or, if needed, a local emergency department. If you cannot find access to a psychiatrist, start with your state’s child psychiatric consultation hotline for access to telephone support: www.nncpap.org.
Although the suggestions outlined above are grounded in evidence and need, treating moderate to severe depression is likely a new challenge for many pediatricians. Managing the risk of suicide can be stressful, without a doubt. In our own work as child psychiatrists, we recognize that there is no single, reliable method to predict suicide and therefore no specific approach to ensuring prevention. We appreciate this burden of worry when treating a severely depressed adolescent, and follow the rule, “never worry alone” – share your concerns with parents and/or a mental health consultant (hopefully co-located in your office), or obtain a second opinion, even consult a child psychiatrist on a hotline. Offering supportive care for those with mild depression can prevent it from becoming severe, and beginning treatment for those with severe depression can make a profound difference in the course of a young person’s illness.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
References
1. Pew Research Center. National Survey on Drug Use and Health (2017).
2. Curtin SC. Natl Vital Stat Rep. 2020 Sep;69(11):1-10.
3. Yard E et al. MMWR Morb Mortal Wkly Rep. 2021 Jun 18;70(24):888-94.
4. Jellinek M et al. J Pediatr. 2021 Jun;233:220-6.e1.
5. Zuckerbrot RA et al. Pediatrics. 2018 Mar;141(3):e20174081.
On Oct. 19, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association jointly declared a “national emergency in children’s mental health,” calling upon policy makers to take actions that could help address “soaring rates” of anxiety and depression.
Knowing that increasing the work force or creating new programs will come slowly if at all, they called for the integration of mental health care into primary care pediatrics and efforts to reduce the risk of suicide in children and adolescents.
Our clinical experience suggests that adolescent depression, which can lead to profoundly impaired function, impaired development, and even suicide, is a major concern in your practice. We hope to do our part by reviewing the screening, diagnosis, and management of depression that can reasonably happen in the pediatrician’s office.
Depression
Depression affects as many as 20% of adolescents, with girls experiencing major depressive disorder (MDD) twice as often as boys. The incidence of depression increases fourfold after puberty, and there is substantial evidence, but no clear cause, that it has increased by nearly 50% over the past decade, rising from a rate of 8% of U.S. adolescents in 2007 to 13% in 2017.1 In that same time period, the rate of completed suicides among U.S. youth aged 10-24 increased 57.4%, after being stable for the prior decade.2 Adolescent depression is also linked to increased substance use and high-risk behaviors such as drunk driving. In 2020, mental health–related emergency department visits by adolescents aged 12-17 increased by 31%. Visits for suicide attempts among adolescent girls in 2021 jumped by 51% from 2019.3 Clearly, MDD in adolescence is a common, potentially life-threatening problem
.
Screening and assessment
At annual checkups with patients 12 and older or at sick visits of patients with emotional, sleep, or vague somatic concerns, it should be standard practice to screen for depression. The Patient Health Questionnaire 9 modified for Adolescents (PHQ9-A) is a reliable, validated, and free screening instrument that your patients can fill out in the waiting room. (The PHQ9 can be used for your patients who are 18 and older.) It takes only 5 minutes to complete and is very easy to score. It establishes whether your patient meets DSM-5 criteria for MDD, and the degree of severity (5-9 is mild, 10-14 is moderate, 15-19 is moderately severe, and 20-27 is severe). It also screens for thoughts about suicide and past suicide attempts. You might add the more comprehensive parent-completed Pediatric Symptom Checklist, which includes a depression screen.4
These screening instruments can be completed electronically prior to or at the visit and should have a preamble explaining why depression screening is relevant. If screening is positive, interview your adolescent patients alone. This will give you the time to gather more detail about how impaired their function is at school, with friends, and in family relationships. Have they been missing school? Have their grades changed? Are they failing to hand in homework? Have they withdrawn from sports or activities? Are they less likely to hang out with friends? Do they participate in family activities? Have others noticed any changes? You should also check for associated anxiety symptoms (ruminative worries, panic attacks) and drug and alcohol use. Of course, you should ask about any suicidal thoughts (from vague morbid thoughts to specific plans, with intent and factors that have prevented them) and actual attempts. Remember, asking about suicidal thoughts and attempts will not cause or worsen them. On the contrary, your patients may feel shame, but will be relieved to not be alone with these thoughts. And this knowledge will be essential as you decide what to do next. When you meet with the parents, ask them about a family history of depression or suicide attempts, and then offer supportive interventions.
Supportive interventions
For all adolescents with depression, supportive interventions are helpful, and for those with mild symptoms, they are often adequate treatment. This begins with education for your patient and their parents about depression. It is an illness, not a problem of character or discipline. Advise your patients that adequate, restful sleep every night is critical to recovery. Regular exercise (daily is best, but at least three times weekly for 30 minutes) is often effective in mild to moderate depression. Patience and compassion for feelings of sadness, irritability, or disinterest are important at home, and maintaining connections with those people who offer support (friends, coaches, parents, etc.) is essential. They should also be told that “depression lies.” Feelings of guilt and self-reproach are a normal part of the illness, not facts. Organizations such as the National Alliance on Mental Illness (NAMI) and the American Academy of Child and Adolescent Psychiatry (AACAP) offer written materials through their websites that are very helpful educational resources. Connect them with sources of counseling support (through school, for example). For those with mild, brief, and uncomplicated depression, supportive interventions alone should offer relief within 4-6 weeks. It is hard to predict the trajectory of depression, so follow-up visits are relevant to determine if they are improving or worsening.
Psychotherapy
For your patients with moderate depression, or with hopelessness or suicidality, a referral for evidence-based psychotherapy is indicated. Both cognitive behavioral therapy and interpersonal therapy have demonstrated efficacy in treating depression in adolescents. If there is a history of trauma or high family conflict, supportive psychotherapy that will enhance communication skills within the family is very important to recovery. Identify various sources for high-quality psychotherapy services (individual, family, and group) in your community. While this may sound easier said than done, online services such as Psychology Today’s therapist locator can help. If your local university has a graduate program in social work or psychology, connect with them as they may have easier access to high-quality services through their training programs. If there is a group practice of therapists in your community, invite them to meet with your team to learn about whether they use evidence-based therapies and can support families as well as individual youth.
Pharmacologic options
For those adolescents with moderate to severe depression, psychotherapy alone is usually inadequate. Indeed, they may be so impaired that they simply cannot meaningfully engage in the work of psychotherapy. These patients require psychopharmacologic treatment first. First-line treatment is with selective serotonin reuptake inhibitors (SSRIs) (both fluoxetine and escitalopram are approved for use in adolescent depression). While many pediatricians remain reluctant about initiating SSRI treatment of depression since the Food and Drug Administration’s 2004 boxed warning was issued, the risks of untreated severe depression are more marked than are the risks of SSRI treatment. As prescription rates dipped in the following decade, rates of suicide attempts in adolescents with severe depression climbed. Subsequent research on the nature of the risk of “increased suicidality” indicated it is substantially lower than originally thought.
The AAP’s Guidelines for Adolescent Depression in Primary Care offer reassuring guidance: They recommend that pediatricians initiate treatment at a very low dose of SSRI (5 mg of fluoxetine, 12.5 mg of sertraline, or 5 mg of escitalopram) and aim to get to a therapeutic dose within 4 weeks.5 Educate the patient and parent about likely side effects (gastrointestinal upset, sleep disruption, akathisia or restlessness, and activation), which indicate the dose should be held steady until the side effects subside. Patients should be seen weekly until they get to a therapeutic dose, then biweekly to monitor for response. At these regular check-ins, the PHQ9A can follow symptom severity. You should monitor changes in function and for any change in suicidal thoughts. If your patient does not respond with at least energy improvement within 4 weeks, you should cross-taper to a different SSRI.
Managing risk
Suicidal thoughts are a common symptom of depression and an important marker of severity. Adolescents have more limited impulse control than do adults, elevating their risk for impulsively acting on these thoughts. Adolescents who are using alcohol or other substances, or who have a history of impulsivity, are at higher risk. Further compounding the degree of risk are a history of suicide attempts, impulsive aggression or psychotic symptoms, or a family history of completed suicide. In managing risk, it is critical that you assess and discuss these risk factors and discuss the need to have a safety plan.
This planning should include both patient and parent. Help the parent to identify lethal means at home (guns, rope, medications, and knives or box cutters) and make plans to secure or remove them. It includes helping your patient list those strategies that can be helpful if they are feeling more distressed (distracting with music or television, exercise, or connecting with select friends). A safety plan is not a promise or a contract to not do something, rather it is a practical set of strategies the patient and family can employ if they are feeling worse. It depends on the adolescent having a secure, trusting connection with the adults at home and with your office.
If your patient fails to improve, if the diagnosis appears complicated, or if you feel the patient is not safe, you should refer to child psychiatry or, if needed, a local emergency department. If you cannot find access to a psychiatrist, start with your state’s child psychiatric consultation hotline for access to telephone support: www.nncpap.org.
Although the suggestions outlined above are grounded in evidence and need, treating moderate to severe depression is likely a new challenge for many pediatricians. Managing the risk of suicide can be stressful, without a doubt. In our own work as child psychiatrists, we recognize that there is no single, reliable method to predict suicide and therefore no specific approach to ensuring prevention. We appreciate this burden of worry when treating a severely depressed adolescent, and follow the rule, “never worry alone” – share your concerns with parents and/or a mental health consultant (hopefully co-located in your office), or obtain a second opinion, even consult a child psychiatrist on a hotline. Offering supportive care for those with mild depression can prevent it from becoming severe, and beginning treatment for those with severe depression can make a profound difference in the course of a young person’s illness.
Dr. Swick is physician in chief at Ohana, Center for Child and Adolescent Behavioral Health, Community Hospital of the Monterey (Calif.) Peninsula. Dr. Jellinek is professor emeritus of psychiatry and pediatrics, Harvard Medical School, Boston. Email them at pdnews@mdedge.com.
References
1. Pew Research Center. National Survey on Drug Use and Health (2017).
2. Curtin SC. Natl Vital Stat Rep. 2020 Sep;69(11):1-10.
3. Yard E et al. MMWR Morb Mortal Wkly Rep. 2021 Jun 18;70(24):888-94.
4. Jellinek M et al. J Pediatr. 2021 Jun;233:220-6.e1.
5. Zuckerbrot RA et al. Pediatrics. 2018 Mar;141(3):e20174081.
Aaron Beck: An appreciation
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
He always dressed the same at conferences: dark suit, white shirt, bright red bow tie.
For all his fame, he was very kind, warmly greeting those who wanted to see him and immediately turning attention toward their research rather than his own. Aaron Beck actually didn’t lecture much; he preferred to roleplay cognitive therapy with an audience member acting as the patient. He would engage in what he called Socratic questioning, or more formally, cognitive restructuring, with warmth and true curiosity:
- What might be another explanation or viewpoint?
- What are the effects of thinking this way?
- Can you think of any evidence that supports the opposite view?
The audience member/patient would benefit not only from thinking about things differently, but also from the captivating interaction with the man, Aaron Temkin Beck, MD, (who went by Tim), youngest child of Jewish immigrants from the Ukraine.
When written up in treatment manuals, cognitive restructuring can seem cold and overly logical, but in person, Dr. Beck made it come to life. This ability to nurture curiosity was a special talent; his friend and fellow cognitive psychologist Donald Meichenbaum, PhD, recalls that even over lunch, he never stopped asking questions, personal and professional, on a wide range of topics.
It is widely accepted that Dr. Beck, who died Nov. 1 at the age of 100 in suburban Philadelphia, was the most important figure in the field of cognitive-behavioral therapy (CBT).
He didn’t invent the field. Behaviorism predated him by generations, founded by figures such as John Watson and B.F. Skinner. Those psychologists set up behaviorism as an alternative to the reigning power of Freudian psychoanalysis, but they ran a distant second.
It wasn’t until Dr. Beck added a new approach, cognitive therapy, to the behavioristic movement that the new mélange, CBT, began to gain traction with clinicians and researchers. Dr. Beck, who had trained in psychiatry, developed his ideas in the 1960s while observing what he believed were limitations in the classic Freudian methods. He recognized that patients had “automatic thoughts,” not just unconscious emotions, when they engaged in Freudian free association, saying whatever came to their minds.
These thoughts often distorted reality, he observed; they were “maladaptive beliefs,” and when they changed, patients’ emotional states improved.
Dr. Beck wasn’t alone. The psychologist Albert Ellis, PhD, in New York, had come to similar conclusions a decade earlier, though with a more coldly logical and challenging style. The prominent British psychologist Hans Eysenck, PhD, had argued strongly that Freudian psychoanalysis was ineffective and that behavioral approaches were better.
Dr. Beck turned the Freudian equation around: Instead of emotion as cause and thought as effect, it was thought which affected emotion, for better or worse. Once you connected behavior as the outcome, you had the essence of CBT: thought, emotion, and behavior – each affecting the other, with thought being the strongest axis of change.
The process wasn’t bloodless. Behaviorists defended their turf against cognitivists, just as much as Freudians rejected both. At one point the behaviorists in the Association for the Advancement of Behavior Therapy tried to expel the advocates of a cognitive approach. Dr. Beck responded by leading the cognitivists in creating a new journal; he emphasized the importance of research being the main mechanism to decide what treatments worked the best.
Putting these ideas out in the 1960s and 1970s, Dr. Beck garnered support from researchers when he manualized the approach. Freudian psychoanalysis was idiosyncratic; it was almost impossible to study empirically, because the therapist would be responding to the unpredictable dreams and memories of patients engaged in free association. Each case was unique.
But CBT was systematic: The same general approach was taken to all patients; the same negative cognitions were found in depression, for instance, like all-or-nothing thinking or overgeneralization. Once manualized, CBT became the standard method of psychotherapy studied with the newly developed method of randomized controlled trials (RCTs).
By the 1980s, RCTs had proven the efficacy of CBT in depression, and the approach took off.
Dr. Beck already had developed a series of rating scales: the Beck Depression Inventory, the Beck Scale for Suicidal Ideation, the Beck Anxiety Inventory, the Beck Hopelessness Scale. Widely used, these scales extended his influence enormously. Copyrighted, they created a new industry of psychological research.
Dr. Beck’s own work was mainly in depression, but his followers extended it everywhere else: anxiety disorders and phobias, eating disorders, substance abuse, bipolar illness, even schizophrenia. Meanwhile, Freudian psychoanalysis fell into a steep decline from which it never recovered.
Some argued that it was abetted by insurance restrictions on psychotherapy, which favored shorter-term CBT; others that its research was biased in its favor because psychotherapy treatments, unlike medications, cannot be blinded; others that its efficacy could not be shown to be specific to its theory, as opposed to the interpersonal relationship between therapist and client.
Still, CBT has transformed psychotherapy and continues to expand its influence. Computer-based CBT has been proven effective, and digital CBT has become a standard approach in many smartphone applications and is central to the claims of multiple new biotechnology companies advocating for digital psychotherapy.
Aaron Beck continued publishing scientific articles to age 98. His last papers reviewed his life’s work. He characteristically gave credit to others, calmly recollected how he traveled away from psychoanalysis, described how his work started and ended in schizophrenia, and noted that the “working relationship with the therapist” remained a key factor for the success of CBT.
That parting comment reminds us that behind all the technology and research stands the kindly man in the dark suit, white shirt, and bright red bow tie, looking at you warmly, asking about your thoughts, and curiously wondering what might be another explanation or viewpoint you hadn’t considered.
Nassir Ghaemi, MD, MPH, is a professor of psychiatry at Tufts Medical Center and a lecturer in psychiatry at Harvard Medical School. He is the author of several general-interest books on psychiatry. A version of this article first appeared on Medscape.com.
Twice exceptionality: A hidden diagnosis in primary care
THE CASE
Michael T,* a 20-year-old cisgender male, visited one of our clinic’s primary care physicians (PCPs). He was reserved and quiet and spoke of his concerns about depression and social anxiety that had been present for several years. He also spoke of his inability to succeed at work and school. Following a thorough PCP review leading to diagnoses of major depressive disorder and social anxiety, the patient agreed to try medication. Over a period of 15 months, trials of medications including fluoxetine, sertraline, aripiprazole, and duloxetine did little to improve the patient’s mood. The PCP decided to consult with our clinic’s integrated health team.
The team reviewed several diagnostic possibilities (TABLE 1) and agreed with the PCP’s diagnoses of major depression and social anxiety. But these disorders alone did not explain the full picture. Team members noted the patient’s unusual communication style, characterized by remarkably long response times and slow processing speed. In particular, when discussing mood, he took several seconds to respond but would respond thoughtfully and with few words.
We administered the Wechsler Adult Intelligence Scale (WAIS-IV). Due to differences between the 4 indices within the WAIS-IV, the Full Scale Intelligence Quotient may under- or overestimate abilities across domains; this was the case for this patient. His General Ability Index (GAI) score was 130, in the very superior range and at the 98th percentile, placing him in the category of gifted intelligence. The patient’s processing speed, however, was at the 18th percentile, which explained his delayed response style and presence of developmental asynchrony, a concept occasionally reported when interpreting socio-emotional and educational maladjustment in gifted individuals.
We determined that Mr. T was twice exceptional—intellectually gifted and also having one or more areas of disability.
●
* The patient’s name has been changed to protect his identity .
In individuals with gifted intelligence, a discrepancy between cognitive and emotional development can make them vulnerable to behavioral and emotional challenges. It is not uncommon for gifted individuals to experience co-occurring distress, anxiety, depression, social withdrawal, difficulty coping with challenging tasks and experiences, low self-esteem, and excessive perfectionism.1-6 Giftedness accompanied by a delay in general abilities and processing speed (significant verbal-performance discrepancy) places an individual in the category of twice-exceptionality, or “2E”—having the potential for high achievement while displaying evidence of 1 or more disabilities including emotional or behavioral difficulties.7
2E Individuals: Prevalence, characteristics, and outcomes
Reported prevalence of twice-exceptionality varies, from approximately 180,000 to 360,000 students in the United States.7 In 2009, the National Commission on Twice Exceptional Students provided the following definition of twice exceptionality:7,8
“Twice-exceptional learners are students who demonstrate the potential for high achievement or creative productivity in one or more domains such as math, science, technology, the social arts, the visual, spatial, or performing arts or other areas of human productivity AND who manifest one or more disabilities as defined by federal or state eligibility criteria. These disabilities include specific learning disabilities; speech and language disorders; emotional/behavioral disorders; physical disabilities; Autism Spectrum Disorders (ASD); or other health impairments, such as Attention Deficit/Hyperactivity Disorder (ADHD).”
How twice-exceptionality might manifest. The literature describes 3 unique groupings of 2E children: those who excel early due to strong language abilities, but later show signs of disability, often when curricular demands rise in junior high, high school, or even college; students diagnosed with disability, but who show exceptional gifts in some areas that may be masked by their learning difficulties; and highly intelligent students who seem to be average, because their disabilities mask their giftedness or their talents mask their difficulties.9,10
Unique behavioral and emotional challenges of 2E individuals may include lower motivation and academic self-efficacy, low self-worth and feelings of failure, or disruptive behaviors.7,11,12 Anxiety and depression often result from the functional impact of twice-exceptionality as well as resultant withdrawal, social isolation, and delay or hindrance of social skills (such as difficulty interpreting social cues).13,14 The individual in our case displayed many of these challenges, including lower motivation, self-worth, and self-esteem, and comorbid anxiety and depression (TABLE 1), further clouding diagnostic clarity.
Continue to: The need for improved recognition
The need for improved recognition. Twice-exceptionality commonly manifests as children reach grade-school age, but they are underrepresented in programs for the gifted due to misunderstanding and misdiagnosis by professionals.15,16 Best practices in identifying 2E children incorporate multidimensional assessments including pre-referral and screening, preliminary intervention, evaluation procedures, and educational planning.16 Despite research asserting that 2E individuals need more support services, knowing how to best identify and support individuals across various settings can prove difficult.7,17-19
Primary care, as we will discuss in a bit, is an interdisciplinary setting in which identification and comprehensive and collaborative support can occur. Historically, though, mental and physical health care have been “siloed” and mental health professionals’ functions in medical settings have often been circumscribed.20,21
A lesson from how our case unfolded
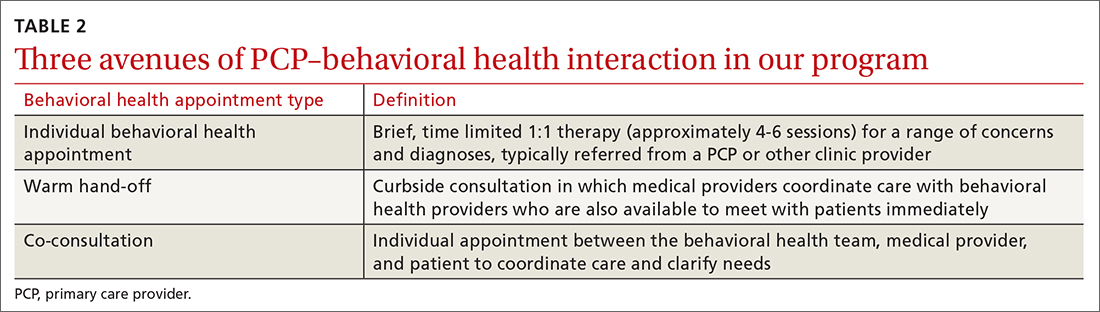
Our integrated health team, known as Integrated Behavioral Health Plus (IBH+), was developed at the University of Colorado School of Medicine, and is a system-level integration of behavioral health professionals working with medical providers to improve outcomes and satisfaction.22 Psychology supervisors and trainees, telepsychiatrists and psychiatry residents, social workers, and pharmacists work together with PCPs and residents to deliver comprehensive patient care. Our model includes a range of behavioral health access points for patients (TABLE 2) and the use of complex patient databases and care team meetings.
In the case we have described here, the nature of the patient’s presentation did not trigger any of the clinical procedures described in TABLE 2, and he fell under the radar of complex patient cases in the clinic. Instead, informal, asynchronous clinical conversations between providers were what eventually lead to diagnostic clarification. Team consultation and psychometric testing provided by IBH+ helped uncover the “hidden diagnosis” of this patient in primary care and identified him as twice-exceptional, experiencing both giftedness and significant emotional suffering (major depression and social anxiety, low self-esteem and self-worth).
Takeaways for primary care
Not all PCPs, of course, have immediate onsite access to a program such as ours. However, innovative ways to tap into available resources might include establishing a partnership with 1 or more behavioral health professionals or bridging less formal relationships with such providers in the community and schools to more easily share patient records.
Continue to: Other presentations within 2E populations
Other presentations within 2E populations. 2E individuals may have other presentations coupled with high cognitive ability7: symptoms of hyperactivity disorders; specific learning disabilities; a diagnosis of autism spectrum disorder (previously termed Asperger type); attention, organizational, social, and behavioral issues; and impulsivity or emotional volatility.
Of note, the perspective of our care team shifted from a “bugs and drugs” perspective of diagnosis and treatment—biological explanations and pharmaceutical solutions—to an approach that explored the underlying interplay between cognitive and emotional functioning for this individual. Our treatment focused on a strengths-based and patient-centered approach. Even without the resources of a full IBH+ model, primary care practices may be able to adapt our experience to their ever-growing complex populations.
Our team shifted treatment planning to the needs of the patient. The 2E identification changed the patient’s perspective about himself. After learning of his giftedness, the patient was able to reframe himself as a highly intelligent, capable individual in need of treatment for depression and social anxiety, as opposed to questioning his intelligence and experiencing confusion and hopelessness within the medical system. His PCP collaborated with the team via telecommunication to maintain an efficacious antidepressant plan and to use a strengths-based approach focused on increasing the patient’s self-view and changing the illness narrative. This narrative was changed by practicing skills, such as challenging unhelpful thought patterns, setting beneficial boundaries, and supporting assertive communication to oppose thoughts and relationships that perpetuated old, negative beliefs and assumptions.
CORRESPONDENCE
Kathryn S. Saldaña, PhD, University of Colorado, 12631 East 17th Avenue, AO1 L15, 3rd Floor, Aurora, CO 80045; kathryn. saldana@ucdenver.edu.
ACKNOWLEDGEMENTS
Our thanks to A.F. Williams Family Medicine Clinic and the University of Colorado Anschutz Medical Campus School of Medicine for their unparalleled models of resident training and multidisciplinary care.
1. Guénolé F, Louis J, Creveuil C, et al. Behavioral profiles of clinically referred children with intellectual giftedness. BioMed Res Int. 2013;2013:540153.
2. Alesi M, Rappo G, Pepi A. Emotional profile and intellectual functioning: A comparison among children with borderline intellectual functioning, average intellectual functioning, and gifted intellectual functioning. SAGE Open. 2015;5:2158244015589995.
3. Alsop G. Asynchrony: intuitively valid and theoretically reliable. Roeper Rev. 2003;25:118-127.
4. Guignard J-H, Jacquet A-Y, Lubart TI. Perfectionism and anxiety: a paradox in intellectual giftedness? PloS One. 2012;7:e41043.
5. Reis SM, McCoach DB. The underachievement of gifted students: What do we know and where do we go? Gifted Child Quarterly. 2000;44:152-170.
6. Barchmann H, Kinze W. Behaviour and achievement disorders in children with high intelligence. Acta Paedopsychiatr. 1990;53:168-172.
7. Reis SM, Baum SM, Burke E. An operational definition of twice-exceptional learners: implications and applications. Gifted Child Quarterly. 2014;58:217-230.
8. NAGC Position Statements & White Papers. Accessed September 18, 2021. http://www.nagc.org/index.aspx?id=5094
9. Neihart M. Identifying and providing services to twice exceptional children. In: Handbook of Giftedness in Children. Pfeiffer SI, ed. Springer; 2008:115-137.
10. Baum SM, Owen SV. To Be Gifted & Learning Disabled: Strategies for Helping Bright Students with Learning & Attention Difficulties. Prufrock Press Inc; 2004.
11. Reis SM. Talents in two places: case studies of high ability students with learning disabilities who have achieved. [Research Monograph 95114]. 1995.
12. Schiff MM, Kaufman AS, Kaufman NL. Scatter analysis of WISC-R profiles for learning disabled children with superior intelligence. J Learn Disabil. 1981;14:400-404.
13. King EW. Addressing the social and emotional needs of twice-exceptional students. Teaching Exceptional Child. 2005;38:16-21.
14. Stormont M, Stebbins MS, Holliday G. Characteristics and educational support needs of underrepresented gifted adolescents. Psychol Schools. 2001;38:413-423.
15. Morrison WF, Rizza MG. Creating a toolkit for identifying twice-exceptional students. J Educ Gifted. 2007;31:57-76.
16. Rizza MG, Morrison WF. Identifying twice exceptional children: a toolkit for success. Accessed September 17, 2021. https://files.eric.ed.gov/fulltext/EJ967126.pdf
17. Cohen SS, Vaughn S. Gifted students with learning disabilities: what does the research say? Learn Disabil. 1994;5:87-94.
18. National Center for Education Statistics. Students with disabilities. Accessed September 18, 2021. https://nces.ed.gov/programs/coe/indicator_cgg.asp
19. The Hechinger Report. Twice exceptional, doubly disadvantaged? How schools struggle to serve gifted students with disabilities. Accessed September 18, 2021. https://hechingerreport.org/twice-exceptional-doubly-disadvantaged-how-schools-struggle-to-serve-gifted-students-with-disabilities
20. Mendaglio S. Heightened multifaceted sensitivity of gifted students: implications for counseling. J Secondary Gifted Educ. 2002;14:72-82.
21. Pereles DA, Omdal S, Baldwin L. Response to intervention and twice-exceptional learners: a promising fit. Gifted Child Today. 2009;32:40-51.
22. Gerrity M. Evolving models of behavioral health integration: evidence update 2010-2015. Milbank Memorial Fund. 2016. Accessed September 18, 2021. www.milbank.org/wp-content/uploads/2016/05/Evolving-Models-of-BHI.pdf
THE CASE
Michael T,* a 20-year-old cisgender male, visited one of our clinic’s primary care physicians (PCPs). He was reserved and quiet and spoke of his concerns about depression and social anxiety that had been present for several years. He also spoke of his inability to succeed at work and school. Following a thorough PCP review leading to diagnoses of major depressive disorder and social anxiety, the patient agreed to try medication. Over a period of 15 months, trials of medications including fluoxetine, sertraline, aripiprazole, and duloxetine did little to improve the patient’s mood. The PCP decided to consult with our clinic’s integrated health team.
The team reviewed several diagnostic possibilities (TABLE 1) and agreed with the PCP’s diagnoses of major depression and social anxiety. But these disorders alone did not explain the full picture. Team members noted the patient’s unusual communication style, characterized by remarkably long response times and slow processing speed. In particular, when discussing mood, he took several seconds to respond but would respond thoughtfully and with few words.
We administered the Wechsler Adult Intelligence Scale (WAIS-IV). Due to differences between the 4 indices within the WAIS-IV, the Full Scale Intelligence Quotient may under- or overestimate abilities across domains; this was the case for this patient. His General Ability Index (GAI) score was 130, in the very superior range and at the 98th percentile, placing him in the category of gifted intelligence. The patient’s processing speed, however, was at the 18th percentile, which explained his delayed response style and presence of developmental asynchrony, a concept occasionally reported when interpreting socio-emotional and educational maladjustment in gifted individuals.
We determined that Mr. T was twice exceptional—intellectually gifted and also having one or more areas of disability.
●
* The patient’s name has been changed to protect his identity .
In individuals with gifted intelligence, a discrepancy between cognitive and emotional development can make them vulnerable to behavioral and emotional challenges. It is not uncommon for gifted individuals to experience co-occurring distress, anxiety, depression, social withdrawal, difficulty coping with challenging tasks and experiences, low self-esteem, and excessive perfectionism.1-6 Giftedness accompanied by a delay in general abilities and processing speed (significant verbal-performance discrepancy) places an individual in the category of twice-exceptionality, or “2E”—having the potential for high achievement while displaying evidence of 1 or more disabilities including emotional or behavioral difficulties.7
2E Individuals: Prevalence, characteristics, and outcomes
Reported prevalence of twice-exceptionality varies, from approximately 180,000 to 360,000 students in the United States.7 In 2009, the National Commission on Twice Exceptional Students provided the following definition of twice exceptionality:7,8
“Twice-exceptional learners are students who demonstrate the potential for high achievement or creative productivity in one or more domains such as math, science, technology, the social arts, the visual, spatial, or performing arts or other areas of human productivity AND who manifest one or more disabilities as defined by federal or state eligibility criteria. These disabilities include specific learning disabilities; speech and language disorders; emotional/behavioral disorders; physical disabilities; Autism Spectrum Disorders (ASD); or other health impairments, such as Attention Deficit/Hyperactivity Disorder (ADHD).”
How twice-exceptionality might manifest. The literature describes 3 unique groupings of 2E children: those who excel early due to strong language abilities, but later show signs of disability, often when curricular demands rise in junior high, high school, or even college; students diagnosed with disability, but who show exceptional gifts in some areas that may be masked by their learning difficulties; and highly intelligent students who seem to be average, because their disabilities mask their giftedness or their talents mask their difficulties.9,10
Unique behavioral and emotional challenges of 2E individuals may include lower motivation and academic self-efficacy, low self-worth and feelings of failure, or disruptive behaviors.7,11,12 Anxiety and depression often result from the functional impact of twice-exceptionality as well as resultant withdrawal, social isolation, and delay or hindrance of social skills (such as difficulty interpreting social cues).13,14 The individual in our case displayed many of these challenges, including lower motivation, self-worth, and self-esteem, and comorbid anxiety and depression (TABLE 1), further clouding diagnostic clarity.
Continue to: The need for improved recognition
The need for improved recognition. Twice-exceptionality commonly manifests as children reach grade-school age, but they are underrepresented in programs for the gifted due to misunderstanding and misdiagnosis by professionals.15,16 Best practices in identifying 2E children incorporate multidimensional assessments including pre-referral and screening, preliminary intervention, evaluation procedures, and educational planning.16 Despite research asserting that 2E individuals need more support services, knowing how to best identify and support individuals across various settings can prove difficult.7,17-19
Primary care, as we will discuss in a bit, is an interdisciplinary setting in which identification and comprehensive and collaborative support can occur. Historically, though, mental and physical health care have been “siloed” and mental health professionals’ functions in medical settings have often been circumscribed.20,21
A lesson from how our case unfolded
Our integrated health team, known as Integrated Behavioral Health Plus (IBH+), was developed at the University of Colorado School of Medicine, and is a system-level integration of behavioral health professionals working with medical providers to improve outcomes and satisfaction.22 Psychology supervisors and trainees, telepsychiatrists and psychiatry residents, social workers, and pharmacists work together with PCPs and residents to deliver comprehensive patient care. Our model includes a range of behavioral health access points for patients (TABLE 2) and the use of complex patient databases and care team meetings.
In the case we have described here, the nature of the patient’s presentation did not trigger any of the clinical procedures described in TABLE 2, and he fell under the radar of complex patient cases in the clinic. Instead, informal, asynchronous clinical conversations between providers were what eventually lead to diagnostic clarification. Team consultation and psychometric testing provided by IBH+ helped uncover the “hidden diagnosis” of this patient in primary care and identified him as twice-exceptional, experiencing both giftedness and significant emotional suffering (major depression and social anxiety, low self-esteem and self-worth).
Takeaways for primary care
Not all PCPs, of course, have immediate onsite access to a program such as ours. However, innovative ways to tap into available resources might include establishing a partnership with 1 or more behavioral health professionals or bridging less formal relationships with such providers in the community and schools to more easily share patient records.
Continue to: Other presentations within 2E populations
Other presentations within 2E populations. 2E individuals may have other presentations coupled with high cognitive ability7: symptoms of hyperactivity disorders; specific learning disabilities; a diagnosis of autism spectrum disorder (previously termed Asperger type); attention, organizational, social, and behavioral issues; and impulsivity or emotional volatility.
Of note, the perspective of our care team shifted from a “bugs and drugs” perspective of diagnosis and treatment—biological explanations and pharmaceutical solutions—to an approach that explored the underlying interplay between cognitive and emotional functioning for this individual. Our treatment focused on a strengths-based and patient-centered approach. Even without the resources of a full IBH+ model, primary care practices may be able to adapt our experience to their ever-growing complex populations.
Our team shifted treatment planning to the needs of the patient. The 2E identification changed the patient’s perspective about himself. After learning of his giftedness, the patient was able to reframe himself as a highly intelligent, capable individual in need of treatment for depression and social anxiety, as opposed to questioning his intelligence and experiencing confusion and hopelessness within the medical system. His PCP collaborated with the team via telecommunication to maintain an efficacious antidepressant plan and to use a strengths-based approach focused on increasing the patient’s self-view and changing the illness narrative. This narrative was changed by practicing skills, such as challenging unhelpful thought patterns, setting beneficial boundaries, and supporting assertive communication to oppose thoughts and relationships that perpetuated old, negative beliefs and assumptions.
CORRESPONDENCE
Kathryn S. Saldaña, PhD, University of Colorado, 12631 East 17th Avenue, AO1 L15, 3rd Floor, Aurora, CO 80045; kathryn. saldana@ucdenver.edu.
ACKNOWLEDGEMENTS
Our thanks to A.F. Williams Family Medicine Clinic and the University of Colorado Anschutz Medical Campus School of Medicine for their unparalleled models of resident training and multidisciplinary care.
THE CASE
Michael T,* a 20-year-old cisgender male, visited one of our clinic’s primary care physicians (PCPs). He was reserved and quiet and spoke of his concerns about depression and social anxiety that had been present for several years. He also spoke of his inability to succeed at work and school. Following a thorough PCP review leading to diagnoses of major depressive disorder and social anxiety, the patient agreed to try medication. Over a period of 15 months, trials of medications including fluoxetine, sertraline, aripiprazole, and duloxetine did little to improve the patient’s mood. The PCP decided to consult with our clinic’s integrated health team.
The team reviewed several diagnostic possibilities (TABLE 1) and agreed with the PCP’s diagnoses of major depression and social anxiety. But these disorders alone did not explain the full picture. Team members noted the patient’s unusual communication style, characterized by remarkably long response times and slow processing speed. In particular, when discussing mood, he took several seconds to respond but would respond thoughtfully and with few words.
We administered the Wechsler Adult Intelligence Scale (WAIS-IV). Due to differences between the 4 indices within the WAIS-IV, the Full Scale Intelligence Quotient may under- or overestimate abilities across domains; this was the case for this patient. His General Ability Index (GAI) score was 130, in the very superior range and at the 98th percentile, placing him in the category of gifted intelligence. The patient’s processing speed, however, was at the 18th percentile, which explained his delayed response style and presence of developmental asynchrony, a concept occasionally reported when interpreting socio-emotional and educational maladjustment in gifted individuals.
We determined that Mr. T was twice exceptional—intellectually gifted and also having one or more areas of disability.
●
* The patient’s name has been changed to protect his identity .
In individuals with gifted intelligence, a discrepancy between cognitive and emotional development can make them vulnerable to behavioral and emotional challenges. It is not uncommon for gifted individuals to experience co-occurring distress, anxiety, depression, social withdrawal, difficulty coping with challenging tasks and experiences, low self-esteem, and excessive perfectionism.1-6 Giftedness accompanied by a delay in general abilities and processing speed (significant verbal-performance discrepancy) places an individual in the category of twice-exceptionality, or “2E”—having the potential for high achievement while displaying evidence of 1 or more disabilities including emotional or behavioral difficulties.7
2E Individuals: Prevalence, characteristics, and outcomes
Reported prevalence of twice-exceptionality varies, from approximately 180,000 to 360,000 students in the United States.7 In 2009, the National Commission on Twice Exceptional Students provided the following definition of twice exceptionality:7,8
“Twice-exceptional learners are students who demonstrate the potential for high achievement or creative productivity in one or more domains such as math, science, technology, the social arts, the visual, spatial, or performing arts or other areas of human productivity AND who manifest one or more disabilities as defined by federal or state eligibility criteria. These disabilities include specific learning disabilities; speech and language disorders; emotional/behavioral disorders; physical disabilities; Autism Spectrum Disorders (ASD); or other health impairments, such as Attention Deficit/Hyperactivity Disorder (ADHD).”
How twice-exceptionality might manifest. The literature describes 3 unique groupings of 2E children: those who excel early due to strong language abilities, but later show signs of disability, often when curricular demands rise in junior high, high school, or even college; students diagnosed with disability, but who show exceptional gifts in some areas that may be masked by their learning difficulties; and highly intelligent students who seem to be average, because their disabilities mask their giftedness or their talents mask their difficulties.9,10
Unique behavioral and emotional challenges of 2E individuals may include lower motivation and academic self-efficacy, low self-worth and feelings of failure, or disruptive behaviors.7,11,12 Anxiety and depression often result from the functional impact of twice-exceptionality as well as resultant withdrawal, social isolation, and delay or hindrance of social skills (such as difficulty interpreting social cues).13,14 The individual in our case displayed many of these challenges, including lower motivation, self-worth, and self-esteem, and comorbid anxiety and depression (TABLE 1), further clouding diagnostic clarity.
Continue to: The need for improved recognition
The need for improved recognition. Twice-exceptionality commonly manifests as children reach grade-school age, but they are underrepresented in programs for the gifted due to misunderstanding and misdiagnosis by professionals.15,16 Best practices in identifying 2E children incorporate multidimensional assessments including pre-referral and screening, preliminary intervention, evaluation procedures, and educational planning.16 Despite research asserting that 2E individuals need more support services, knowing how to best identify and support individuals across various settings can prove difficult.7,17-19
Primary care, as we will discuss in a bit, is an interdisciplinary setting in which identification and comprehensive and collaborative support can occur. Historically, though, mental and physical health care have been “siloed” and mental health professionals’ functions in medical settings have often been circumscribed.20,21
A lesson from how our case unfolded
Our integrated health team, known as Integrated Behavioral Health Plus (IBH+), was developed at the University of Colorado School of Medicine, and is a system-level integration of behavioral health professionals working with medical providers to improve outcomes and satisfaction.22 Psychology supervisors and trainees, telepsychiatrists and psychiatry residents, social workers, and pharmacists work together with PCPs and residents to deliver comprehensive patient care. Our model includes a range of behavioral health access points for patients (TABLE 2) and the use of complex patient databases and care team meetings.
In the case we have described here, the nature of the patient’s presentation did not trigger any of the clinical procedures described in TABLE 2, and he fell under the radar of complex patient cases in the clinic. Instead, informal, asynchronous clinical conversations between providers were what eventually lead to diagnostic clarification. Team consultation and psychometric testing provided by IBH+ helped uncover the “hidden diagnosis” of this patient in primary care and identified him as twice-exceptional, experiencing both giftedness and significant emotional suffering (major depression and social anxiety, low self-esteem and self-worth).
Takeaways for primary care
Not all PCPs, of course, have immediate onsite access to a program such as ours. However, innovative ways to tap into available resources might include establishing a partnership with 1 or more behavioral health professionals or bridging less formal relationships with such providers in the community and schools to more easily share patient records.
Continue to: Other presentations within 2E populations
Other presentations within 2E populations. 2E individuals may have other presentations coupled with high cognitive ability7: symptoms of hyperactivity disorders; specific learning disabilities; a diagnosis of autism spectrum disorder (previously termed Asperger type); attention, organizational, social, and behavioral issues; and impulsivity or emotional volatility.
Of note, the perspective of our care team shifted from a “bugs and drugs” perspective of diagnosis and treatment—biological explanations and pharmaceutical solutions—to an approach that explored the underlying interplay between cognitive and emotional functioning for this individual. Our treatment focused on a strengths-based and patient-centered approach. Even without the resources of a full IBH+ model, primary care practices may be able to adapt our experience to their ever-growing complex populations.
Our team shifted treatment planning to the needs of the patient. The 2E identification changed the patient’s perspective about himself. After learning of his giftedness, the patient was able to reframe himself as a highly intelligent, capable individual in need of treatment for depression and social anxiety, as opposed to questioning his intelligence and experiencing confusion and hopelessness within the medical system. His PCP collaborated with the team via telecommunication to maintain an efficacious antidepressant plan and to use a strengths-based approach focused on increasing the patient’s self-view and changing the illness narrative. This narrative was changed by practicing skills, such as challenging unhelpful thought patterns, setting beneficial boundaries, and supporting assertive communication to oppose thoughts and relationships that perpetuated old, negative beliefs and assumptions.
CORRESPONDENCE
Kathryn S. Saldaña, PhD, University of Colorado, 12631 East 17th Avenue, AO1 L15, 3rd Floor, Aurora, CO 80045; kathryn. saldana@ucdenver.edu.
ACKNOWLEDGEMENTS
Our thanks to A.F. Williams Family Medicine Clinic and the University of Colorado Anschutz Medical Campus School of Medicine for their unparalleled models of resident training and multidisciplinary care.
1. Guénolé F, Louis J, Creveuil C, et al. Behavioral profiles of clinically referred children with intellectual giftedness. BioMed Res Int. 2013;2013:540153.
2. Alesi M, Rappo G, Pepi A. Emotional profile and intellectual functioning: A comparison among children with borderline intellectual functioning, average intellectual functioning, and gifted intellectual functioning. SAGE Open. 2015;5:2158244015589995.
3. Alsop G. Asynchrony: intuitively valid and theoretically reliable. Roeper Rev. 2003;25:118-127.
4. Guignard J-H, Jacquet A-Y, Lubart TI. Perfectionism and anxiety: a paradox in intellectual giftedness? PloS One. 2012;7:e41043.
5. Reis SM, McCoach DB. The underachievement of gifted students: What do we know and where do we go? Gifted Child Quarterly. 2000;44:152-170.
6. Barchmann H, Kinze W. Behaviour and achievement disorders in children with high intelligence. Acta Paedopsychiatr. 1990;53:168-172.
7. Reis SM, Baum SM, Burke E. An operational definition of twice-exceptional learners: implications and applications. Gifted Child Quarterly. 2014;58:217-230.
8. NAGC Position Statements & White Papers. Accessed September 18, 2021. http://www.nagc.org/index.aspx?id=5094
9. Neihart M. Identifying and providing services to twice exceptional children. In: Handbook of Giftedness in Children. Pfeiffer SI, ed. Springer; 2008:115-137.
10. Baum SM, Owen SV. To Be Gifted & Learning Disabled: Strategies for Helping Bright Students with Learning & Attention Difficulties. Prufrock Press Inc; 2004.
11. Reis SM. Talents in two places: case studies of high ability students with learning disabilities who have achieved. [Research Monograph 95114]. 1995.
12. Schiff MM, Kaufman AS, Kaufman NL. Scatter analysis of WISC-R profiles for learning disabled children with superior intelligence. J Learn Disabil. 1981;14:400-404.
13. King EW. Addressing the social and emotional needs of twice-exceptional students. Teaching Exceptional Child. 2005;38:16-21.
14. Stormont M, Stebbins MS, Holliday G. Characteristics and educational support needs of underrepresented gifted adolescents. Psychol Schools. 2001;38:413-423.
15. Morrison WF, Rizza MG. Creating a toolkit for identifying twice-exceptional students. J Educ Gifted. 2007;31:57-76.
16. Rizza MG, Morrison WF. Identifying twice exceptional children: a toolkit for success. Accessed September 17, 2021. https://files.eric.ed.gov/fulltext/EJ967126.pdf
17. Cohen SS, Vaughn S. Gifted students with learning disabilities: what does the research say? Learn Disabil. 1994;5:87-94.
18. National Center for Education Statistics. Students with disabilities. Accessed September 18, 2021. https://nces.ed.gov/programs/coe/indicator_cgg.asp
19. The Hechinger Report. Twice exceptional, doubly disadvantaged? How schools struggle to serve gifted students with disabilities. Accessed September 18, 2021. https://hechingerreport.org/twice-exceptional-doubly-disadvantaged-how-schools-struggle-to-serve-gifted-students-with-disabilities
20. Mendaglio S. Heightened multifaceted sensitivity of gifted students: implications for counseling. J Secondary Gifted Educ. 2002;14:72-82.
21. Pereles DA, Omdal S, Baldwin L. Response to intervention and twice-exceptional learners: a promising fit. Gifted Child Today. 2009;32:40-51.
22. Gerrity M. Evolving models of behavioral health integration: evidence update 2010-2015. Milbank Memorial Fund. 2016. Accessed September 18, 2021. www.milbank.org/wp-content/uploads/2016/05/Evolving-Models-of-BHI.pdf
1. Guénolé F, Louis J, Creveuil C, et al. Behavioral profiles of clinically referred children with intellectual giftedness. BioMed Res Int. 2013;2013:540153.
2. Alesi M, Rappo G, Pepi A. Emotional profile and intellectual functioning: A comparison among children with borderline intellectual functioning, average intellectual functioning, and gifted intellectual functioning. SAGE Open. 2015;5:2158244015589995.
3. Alsop G. Asynchrony: intuitively valid and theoretically reliable. Roeper Rev. 2003;25:118-127.
4. Guignard J-H, Jacquet A-Y, Lubart TI. Perfectionism and anxiety: a paradox in intellectual giftedness? PloS One. 2012;7:e41043.
5. Reis SM, McCoach DB. The underachievement of gifted students: What do we know and where do we go? Gifted Child Quarterly. 2000;44:152-170.
6. Barchmann H, Kinze W. Behaviour and achievement disorders in children with high intelligence. Acta Paedopsychiatr. 1990;53:168-172.
7. Reis SM, Baum SM, Burke E. An operational definition of twice-exceptional learners: implications and applications. Gifted Child Quarterly. 2014;58:217-230.
8. NAGC Position Statements & White Papers. Accessed September 18, 2021. http://www.nagc.org/index.aspx?id=5094
9. Neihart M. Identifying and providing services to twice exceptional children. In: Handbook of Giftedness in Children. Pfeiffer SI, ed. Springer; 2008:115-137.
10. Baum SM, Owen SV. To Be Gifted & Learning Disabled: Strategies for Helping Bright Students with Learning & Attention Difficulties. Prufrock Press Inc; 2004.
11. Reis SM. Talents in two places: case studies of high ability students with learning disabilities who have achieved. [Research Monograph 95114]. 1995.
12. Schiff MM, Kaufman AS, Kaufman NL. Scatter analysis of WISC-R profiles for learning disabled children with superior intelligence. J Learn Disabil. 1981;14:400-404.
13. King EW. Addressing the social and emotional needs of twice-exceptional students. Teaching Exceptional Child. 2005;38:16-21.
14. Stormont M, Stebbins MS, Holliday G. Characteristics and educational support needs of underrepresented gifted adolescents. Psychol Schools. 2001;38:413-423.
15. Morrison WF, Rizza MG. Creating a toolkit for identifying twice-exceptional students. J Educ Gifted. 2007;31:57-76.
16. Rizza MG, Morrison WF. Identifying twice exceptional children: a toolkit for success. Accessed September 17, 2021. https://files.eric.ed.gov/fulltext/EJ967126.pdf
17. Cohen SS, Vaughn S. Gifted students with learning disabilities: what does the research say? Learn Disabil. 1994;5:87-94.
18. National Center for Education Statistics. Students with disabilities. Accessed September 18, 2021. https://nces.ed.gov/programs/coe/indicator_cgg.asp
19. The Hechinger Report. Twice exceptional, doubly disadvantaged? How schools struggle to serve gifted students with disabilities. Accessed September 18, 2021. https://hechingerreport.org/twice-exceptional-doubly-disadvantaged-how-schools-struggle-to-serve-gifted-students-with-disabilities
20. Mendaglio S. Heightened multifaceted sensitivity of gifted students: implications for counseling. J Secondary Gifted Educ. 2002;14:72-82.
21. Pereles DA, Omdal S, Baldwin L. Response to intervention and twice-exceptional learners: a promising fit. Gifted Child Today. 2009;32:40-51.
22. Gerrity M. Evolving models of behavioral health integration: evidence update 2010-2015. Milbank Memorial Fund. 2016. Accessed September 18, 2021. www.milbank.org/wp-content/uploads/2016/05/Evolving-Models-of-BHI.pdf
Unmasking Our Grief
Since the start of the pandemic, health care systems have requested many in-services for staff on self-care and stress management to help health care workers (HCWs) cope with the heavy toll of COVID-19. The pandemic has set off a global mental health crisis, with unprecedented numbers of individuals meeting criteria for anxiety, depression, and other mental health disorders in response to the intense stressors of living through a pandemic. These calls to assist staff with self-care and burnout prevention have been especially salient for psychologists working in palliative care and geriatrics, where fears of COVID-19 infection and numbers of patient deaths have been high.
Throughout these painful times, we have been grateful for an online community of palliative care psychologists within the US Department of Veterans Affairs (VA) from across the continuum of care and across the country. This community brought together many of us who were both struggling ourselves and striving to support the teams and HCWs around us. We are psychologists who provide home-care services in North Carolina, inpatient hospice and long-term care services in California, and long-term care and outpatient palliative care services in Massachusetts. Through our shared struggles and challenges navigating the pandemic, we realized that our respective teams requested similar services, all focused on staff support.
The psychological impact of COVID-19 on HCWs was clear from the beginning. Early in the pandemic our respective teams requested us to provide staff support and education about coping to our local HCWs. Soon national groups for long-term care staff requested education programs. Through this work, we realized that the emotional needs of HCWs ran much deeper than simple self-care. At the onset of the pandemic, before realizing its chronicity, the trainings we offered focused on stress and coping strategies. We cited several frameworks for staff support and eagerly shared anything that might help us, and our colleagues, survive the immediate anxiety and tumult surrounding us.1-3 In this paper, we briefly discuss the distress affecting the geriatric care workforce, reflect on our efforts to cope as HCWs, and offer recommendations at individual and organization levels to help address our collective grief.
Impact of COVID-19
As the death toll mounted and hospitals were pushed to the brink, we saw the suffering of our fellow HCWs. The lack of personal protective equipment (PPE) and testing supplies led to evolving and increasing anxiety for HCWs about contracting COVID-19, potentially spreading it to one’s social circle or family, fears of becoming sick and dying, and fears of inadvertently spreading the virus to medically-vulnerable patients. Increasing demands on staff required many to work outside their areas of expertise. Clinical practice guidelines changed frequently as information emerged about the virus. Staff members struggled to keep pace with the increasing number of patients, many of whom died despite heroic efforts to save them.
As the medical crisis grew, so too did social uprisings as the general public gained a strengthened awareness of the legacy and ongoing effects of systemic oppression, racism, and social inequities in the United States. Individuals grappled with their own privileges, which often hid such disparities from view. Many HCWs and clinicians of color had to navigate unsolicited questions and discussions about racial injustices while also trying to survive. As psychologists, we strove to support the HCWs around us while also struggling with our own stressors. As the magnitude of the pandemic and ongoing social injustices came into view, we realized that presentations on self-care and burnout prevention did not suffice. We needed discussions on unmasking our grief, acknowledging our traumas, and working toward collective healing.
Geriatric Care Workers
Experiences of grief and trauma hit the geriatric care workforce and especially long-term care facilities particularly hard given the high morbidity and mortality rates of COVID-19.4 The geriatric care workforce itself suffers from institutional vulnerabilities. Individuals are often underpaid, undertrained, and work within a system that continually experiences staffing shortages, high burnout, and consequently high levels of turnover.5,6 Recent immigrants and racial/ethnic minorities disproportionately make up this workforce, who often live in multigenerational households and work in multiple facilities to get by.7,8 Amid the pandemic these HCWs continued to work despite demoralizing negative media coverage of nursing homes.9 Notably, facilities with unionized staff were less likely to need second or third jobs to survive, thus reducing spread across facilities. This along with better access to PPE may have contributed to their lower COVID-19 infection and mortality rates relative to non-unionized staff.10
Similar to long-term care workers, home-care staff had related fears and anxieties, magnified by the need to enter multiple homes. This often overlooked but growing sector of the geriatric care workforce faced the added anxiety of the unknown as they entered multiple homes to provide care to their patients. These staff have little control over who may be in the home when they arrive, the sanitation/PPE practices of the patient/family, and therefore little control over their potential exposure to COVID-19. This also applies to home health aides who, although not providing medical services, are a critical part of home-care services and allow older adults to remain living independently in their home.
Reflection on Grief
As we witnessed the interactive effects of the pandemic and social inequities in geriatrics and palliative care, we frequently sought solace in online communities of psychologists working in similar settings. Over time, our regular community meetings developed a different tone: discussions about caring for others shifted to caring for ourselves. It seemed that in holding others’ pain, many of us neglected to address our own. We needed emotional support. We needed to acknowledge that we were not all okay; that the masks we wear for protection also reveal our vulnerabilities; and that protective equipment in hospitals do not protect us from the hate and bias targeting many of us face everywhere we go.
As we let ourselves be vulnerable with each other, we saw the true face of our pain: it was not stress, it was grief. We were sad, broken, mourning innumerable losses, and grieving, mostly alone. It felt overwhelming. Our minds and hearts often grew numb to find respite from pain. At times we found ourselves seeking haven in our offices, convincing ourselves that paperwork needed to be done when in reality we had no space to hold anyone else’s pain; we could barely contain our own. We could only take so much.
Without space to process, grief festers and eats away at our remaining compassion. How do we hold grace for ourselves, dare to be vulnerable, and allow ourselves to feel, when doing so opens the door to our own grief? How do we allow room for emotional processing when we learned to numb-out in order to function? And as women with diverse intersectional identities, how do we honor our humanity when we live in a society that reflects its indifference? We needed to process our pain in order to heal in the slow and uneven way that grief heals.
Caring During Tough Times
The pain we feel is real and it tears at us over time. Pushing it away disenfranchises ourselves of the opportunity to heal and grow. Our collective grief and trauma demand collective healing and acknowledgment of our individual suffering. We must honor our shared humanity and find commonality amid our differences. Typical self-care (healthy eating, sleep, basic hygiene) may not be enough to mitigate the enormity of these stressors. A glass of wine or a virtual dinner with friends may distract but does not heal our wounds.
Self-care, by definition, centers the self and ignores the larger systemic factors that maintain our struggles. It keeps the focus on the individual and in so doing, risks inducing self-blame should we continue feeling burnout. We must do more. We can advocate that systems acknowledge our grief and suffering as well as our strengths and resiliencies. We can demand that organizations recognize human limits and provide support, rather than promote environments that encourage silent perseverance. And we can deconstruct the cultural narrative that vulnerability is weakness or that we are the “heroes.” Heroism suggests superhuman qualities or extreme courage and often negates the fear and trepidation in its midst.11,12 We can also recognize how intersectional aspects of our identities make navigating the pandemic and systemic racism harder and more dangerous for some than for others.
As noted by President Biden in a speech honoring those lost to COVID-19, “We have to resist becoming numb to the sorrow.”13 The nature of our work (and that of most clinicians) is that it is expected and sometimes necessary to compartmentalize and turn off the emotions so that we can function in a professional manner. But this way of being also serves to hold us back. It does not make space for the very real emotions of trauma and grief that have pervaded HCWs during this pandemic. We must learn a different way of functioning—one where grief is acknowledged and even actively processed while still going about our work. Grief therapist Megan Devine proposes to “tend to pain and grief by bearing witness” and notes that “when we allow the reality of grief to exist, we can focus on helping ourselves—and one another—survive inside pain.”14 She advocates for self-compassion and directs us to “find ways to show our grief to others, in ways that honor the truth of our experience” saying, “we have to be willing to stop diminishing our own pain so that others can be comfortable around us.” But what does this look like among health care teams who are traumatized and grieving?
In our experience, caring for ourselves and our teams in times of prolonged stress, trauma, and grief is essential to maintain functioning over time. We strongly believe that it must occur at both the organizational and individual levels. In the throes of a crisis, teams need support immediately. To offer a timely response, we gathered knowledge of team-based care and collaboration to develop practical strategies that can be implemented swiftly to provide support across the team.15-19
The strategies we developed offer steps for creating and maintaining a supportive, compassionate, and psychologically safe work environment. First, the CARES Strategies for Practical Team Intervention highlights the importance of clear communication, assessing team needs regularly, recognizing the stress that is occurring, engaging staff in discussions, and ensuring psychological safety and comfort (Figure 1). Next, the SHARE approach is laid out to allow for interpersonal support among team members (Figure 2). Showing each other empathy, hoping for better days, acknowledging each other’s pain, reaching out for assistance, and expressing our needs allow HCWs to open up about their grief, stress, and trauma. Of note, we found these sets of strategies interdependent: a team that does not believe the leader/organization CARES is not likely to SHARE. Therefore, we also feel that it is especially important that team leaders work to create or enhance the sense of psychological safety for the team. If team members do not feel safe, they will not disclose their grief and remain stuck in the old mode of suffering in silence.
Conclusions
This pandemic and the collective efforts toward social justice advocacy have revealed our vulnerabilities as well as our strengths. These experiences have forced us to reckon with our past and consider possible futures. It has revealed the inequities in our health care system, including our failure to protect those on the ground who keep our systems running, and prompted us to consider new ways of operating in low-resourced and high-demand environments. These experiences also present us with opportunities to be better and do better as both professionals and people; to reflect on our past and consider what we want different in our lives. As we yearn for better days and brace ourselves for what is to come, we hope that teams and organizations will take advantage of these opportunities for self-reflection and continue unmasking our grief, healing our wounds, and honoring our shared humanity.
1. Blake H, Bermingham F. Psychological wellbeing for health care workers: mitigating the impact of covid-19. Version 2.0. Updated June 18, 2020. Accessed October 12, 2021. https://www.nottingham.ac.uk/toolkits/play_22794
2. Harris R. FACE COVID: how to respond effectively to the corona crisis. Published 2020. Accessed October 12, 2021. http://louisville.edu/counseling/coping-with-covid-19/face-covid-by-dr-russ-harris/view
3. Norcross JC, Phillips CM. Psychologist self-care during the pandemic: now more than ever [published online ahead of print, 2020 May 2]. J Health Serv Psychol. 2020;1-5. doi:10.1007/s42843-020-00010-5
4. Kaiser Family Foundation. State reports of long-term care facility cases and deaths related to COVID-19. 2020. Published April 23, 2020. Accessed October 12, 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities
5. Sterling MR, Tseng E, Poon A, et al. Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA Intern Med. 2020;180(11):1453-1459. doi:10.1001/jamainternmed.2020.3930
6. Stone R, Wilhelm J, Bishop CE, Bryant NS, Hermer L, Squillace MR. Predictors of intent to leave the job among home health workers: analysis of the National Home Health Aide Survey. Gerontologist. 2017;57(5):890-899. doi:10.1093/geront/gnw075
7. Scales K. It’s time to care: a detailed profile of America’s direct care workforce. PHI. 2020. Published January 21, 2020. Accessed October 12, 2021. https://phinational.org/wp-content/uploads/2020/01/Its-Time-to-Care-2020-PHI.pdf
8. Wolfe R, Harknett K, Schneider D. Inequities at work and the toll of COVID-19. Health Aff Health Policy Brief. Published June 4, 2021. doi: 10.1377/hpb20210428.863621
9. White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic [published correction appears in J Am Med Dir Assoc. 2021 May;22(5):1123]. J Am Med Dir Assoc. 2021;22(1):199-203. doi:10.1016/j.jamda.2020.11.022
10. Dean A, Venkataramani A, Kimmel S. Mortality rates from COVID-19 are lower In unionized nursing homes. Health Aff (Millwood). 2020;39(11):1993-2001.doi:10.1377/hlthaff.2020.01011
11. Cox CL. ‘Healthcare Heroes’: problems with media focus on heroism from healthcare workers during the COVID-19 pandemic. J Med Ethics. 2020;46(8):510-513. doi:10.1136/medethics-2020-106398
12. Stokes-Parish J, Elliott R, Rolls K, Massey D. Angels and heroes: the unintended consequence of the hero narrative. J Nurs Scholarsh. 2020;52(5):462-466. doi:10.1111/jnu.12591
13. Biden J. Remarks by President Biden on the more than 500,000 American lives lost to COVID-19. Published February 22, 2021. Accessed October 12, 2021. https://www.whitehouse.gov/briefing-room/speeches-remarks/2021/02/22/remarks-by-president-biden-on-the-more-than-500000-american-lives-lost-to-covid-19
14. Devine M. It’s Okay That You’re Not Okay: Meeting Grief and Loss in a Culture That Doesn’t Understand. Sounds True; 2017.
15. Center for the Study of Traumatic Stress. Grief leadership during COVID-19. Accessed October 12, 2021. https://www.cstsonline.org/assets/media/documents/CSTS_FS_Grief_Leadership_During_COVID19.pdf
16. Center for the Study of Traumatic Stress. Sustaining the well-being of healthcare personnel during coronavirus and other infectious disease outbreaks. Accessed October 12, 2021. https://www.cstsonline.org/assets/media/documents/CSTS_FS_Sustaining_Well_Being_Health care_Personnel_during.pdf
17. Fessell D, Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: micropractices for burnout prevention and emotional wellness. J Am Coll Radiol. 2020;17(6):746-748. doi:10.1016/j.jacr.2020.03.013
18. US Department of Veterans Affairs, National Center for PTSD. Managing healthcare workers’ stress associated with the COVID-19 virus outbreak. Updated March 25, 2020, Accessed October 12, 2021. https://www.ptsd.va.gov/covid/COVID_healthcare_workers.asp
19. US Department of Veterans Affairs, Veterans Health Administration, National Center for Organization Development (NCOD). Team Development Guide. 2017. https://vaww.va.gov/NCOD/docs/Team_Development_Guide.docx [Nonpublic source, not verified.]
Since the start of the pandemic, health care systems have requested many in-services for staff on self-care and stress management to help health care workers (HCWs) cope with the heavy toll of COVID-19. The pandemic has set off a global mental health crisis, with unprecedented numbers of individuals meeting criteria for anxiety, depression, and other mental health disorders in response to the intense stressors of living through a pandemic. These calls to assist staff with self-care and burnout prevention have been especially salient for psychologists working in palliative care and geriatrics, where fears of COVID-19 infection and numbers of patient deaths have been high.
Throughout these painful times, we have been grateful for an online community of palliative care psychologists within the US Department of Veterans Affairs (VA) from across the continuum of care and across the country. This community brought together many of us who were both struggling ourselves and striving to support the teams and HCWs around us. We are psychologists who provide home-care services in North Carolina, inpatient hospice and long-term care services in California, and long-term care and outpatient palliative care services in Massachusetts. Through our shared struggles and challenges navigating the pandemic, we realized that our respective teams requested similar services, all focused on staff support.
The psychological impact of COVID-19 on HCWs was clear from the beginning. Early in the pandemic our respective teams requested us to provide staff support and education about coping to our local HCWs. Soon national groups for long-term care staff requested education programs. Through this work, we realized that the emotional needs of HCWs ran much deeper than simple self-care. At the onset of the pandemic, before realizing its chronicity, the trainings we offered focused on stress and coping strategies. We cited several frameworks for staff support and eagerly shared anything that might help us, and our colleagues, survive the immediate anxiety and tumult surrounding us.1-3 In this paper, we briefly discuss the distress affecting the geriatric care workforce, reflect on our efforts to cope as HCWs, and offer recommendations at individual and organization levels to help address our collective grief.
Impact of COVID-19
As the death toll mounted and hospitals were pushed to the brink, we saw the suffering of our fellow HCWs. The lack of personal protective equipment (PPE) and testing supplies led to evolving and increasing anxiety for HCWs about contracting COVID-19, potentially spreading it to one’s social circle or family, fears of becoming sick and dying, and fears of inadvertently spreading the virus to medically-vulnerable patients. Increasing demands on staff required many to work outside their areas of expertise. Clinical practice guidelines changed frequently as information emerged about the virus. Staff members struggled to keep pace with the increasing number of patients, many of whom died despite heroic efforts to save them.
As the medical crisis grew, so too did social uprisings as the general public gained a strengthened awareness of the legacy and ongoing effects of systemic oppression, racism, and social inequities in the United States. Individuals grappled with their own privileges, which often hid such disparities from view. Many HCWs and clinicians of color had to navigate unsolicited questions and discussions about racial injustices while also trying to survive. As psychologists, we strove to support the HCWs around us while also struggling with our own stressors. As the magnitude of the pandemic and ongoing social injustices came into view, we realized that presentations on self-care and burnout prevention did not suffice. We needed discussions on unmasking our grief, acknowledging our traumas, and working toward collective healing.
Geriatric Care Workers
Experiences of grief and trauma hit the geriatric care workforce and especially long-term care facilities particularly hard given the high morbidity and mortality rates of COVID-19.4 The geriatric care workforce itself suffers from institutional vulnerabilities. Individuals are often underpaid, undertrained, and work within a system that continually experiences staffing shortages, high burnout, and consequently high levels of turnover.5,6 Recent immigrants and racial/ethnic minorities disproportionately make up this workforce, who often live in multigenerational households and work in multiple facilities to get by.7,8 Amid the pandemic these HCWs continued to work despite demoralizing negative media coverage of nursing homes.9 Notably, facilities with unionized staff were less likely to need second or third jobs to survive, thus reducing spread across facilities. This along with better access to PPE may have contributed to their lower COVID-19 infection and mortality rates relative to non-unionized staff.10
Similar to long-term care workers, home-care staff had related fears and anxieties, magnified by the need to enter multiple homes. This often overlooked but growing sector of the geriatric care workforce faced the added anxiety of the unknown as they entered multiple homes to provide care to their patients. These staff have little control over who may be in the home when they arrive, the sanitation/PPE practices of the patient/family, and therefore little control over their potential exposure to COVID-19. This also applies to home health aides who, although not providing medical services, are a critical part of home-care services and allow older adults to remain living independently in their home.
Reflection on Grief
As we witnessed the interactive effects of the pandemic and social inequities in geriatrics and palliative care, we frequently sought solace in online communities of psychologists working in similar settings. Over time, our regular community meetings developed a different tone: discussions about caring for others shifted to caring for ourselves. It seemed that in holding others’ pain, many of us neglected to address our own. We needed emotional support. We needed to acknowledge that we were not all okay; that the masks we wear for protection also reveal our vulnerabilities; and that protective equipment in hospitals do not protect us from the hate and bias targeting many of us face everywhere we go.
As we let ourselves be vulnerable with each other, we saw the true face of our pain: it was not stress, it was grief. We were sad, broken, mourning innumerable losses, and grieving, mostly alone. It felt overwhelming. Our minds and hearts often grew numb to find respite from pain. At times we found ourselves seeking haven in our offices, convincing ourselves that paperwork needed to be done when in reality we had no space to hold anyone else’s pain; we could barely contain our own. We could only take so much.
Without space to process, grief festers and eats away at our remaining compassion. How do we hold grace for ourselves, dare to be vulnerable, and allow ourselves to feel, when doing so opens the door to our own grief? How do we allow room for emotional processing when we learned to numb-out in order to function? And as women with diverse intersectional identities, how do we honor our humanity when we live in a society that reflects its indifference? We needed to process our pain in order to heal in the slow and uneven way that grief heals.
Caring During Tough Times
The pain we feel is real and it tears at us over time. Pushing it away disenfranchises ourselves of the opportunity to heal and grow. Our collective grief and trauma demand collective healing and acknowledgment of our individual suffering. We must honor our shared humanity and find commonality amid our differences. Typical self-care (healthy eating, sleep, basic hygiene) may not be enough to mitigate the enormity of these stressors. A glass of wine or a virtual dinner with friends may distract but does not heal our wounds.
Self-care, by definition, centers the self and ignores the larger systemic factors that maintain our struggles. It keeps the focus on the individual and in so doing, risks inducing self-blame should we continue feeling burnout. We must do more. We can advocate that systems acknowledge our grief and suffering as well as our strengths and resiliencies. We can demand that organizations recognize human limits and provide support, rather than promote environments that encourage silent perseverance. And we can deconstruct the cultural narrative that vulnerability is weakness or that we are the “heroes.” Heroism suggests superhuman qualities or extreme courage and often negates the fear and trepidation in its midst.11,12 We can also recognize how intersectional aspects of our identities make navigating the pandemic and systemic racism harder and more dangerous for some than for others.
As noted by President Biden in a speech honoring those lost to COVID-19, “We have to resist becoming numb to the sorrow.”13 The nature of our work (and that of most clinicians) is that it is expected and sometimes necessary to compartmentalize and turn off the emotions so that we can function in a professional manner. But this way of being also serves to hold us back. It does not make space for the very real emotions of trauma and grief that have pervaded HCWs during this pandemic. We must learn a different way of functioning—one where grief is acknowledged and even actively processed while still going about our work. Grief therapist Megan Devine proposes to “tend to pain and grief by bearing witness” and notes that “when we allow the reality of grief to exist, we can focus on helping ourselves—and one another—survive inside pain.”14 She advocates for self-compassion and directs us to “find ways to show our grief to others, in ways that honor the truth of our experience” saying, “we have to be willing to stop diminishing our own pain so that others can be comfortable around us.” But what does this look like among health care teams who are traumatized and grieving?
In our experience, caring for ourselves and our teams in times of prolonged stress, trauma, and grief is essential to maintain functioning over time. We strongly believe that it must occur at both the organizational and individual levels. In the throes of a crisis, teams need support immediately. To offer a timely response, we gathered knowledge of team-based care and collaboration to develop practical strategies that can be implemented swiftly to provide support across the team.15-19
The strategies we developed offer steps for creating and maintaining a supportive, compassionate, and psychologically safe work environment. First, the CARES Strategies for Practical Team Intervention highlights the importance of clear communication, assessing team needs regularly, recognizing the stress that is occurring, engaging staff in discussions, and ensuring psychological safety and comfort (Figure 1). Next, the SHARE approach is laid out to allow for interpersonal support among team members (Figure 2). Showing each other empathy, hoping for better days, acknowledging each other’s pain, reaching out for assistance, and expressing our needs allow HCWs to open up about their grief, stress, and trauma. Of note, we found these sets of strategies interdependent: a team that does not believe the leader/organization CARES is not likely to SHARE. Therefore, we also feel that it is especially important that team leaders work to create or enhance the sense of psychological safety for the team. If team members do not feel safe, they will not disclose their grief and remain stuck in the old mode of suffering in silence.
Conclusions
This pandemic and the collective efforts toward social justice advocacy have revealed our vulnerabilities as well as our strengths. These experiences have forced us to reckon with our past and consider possible futures. It has revealed the inequities in our health care system, including our failure to protect those on the ground who keep our systems running, and prompted us to consider new ways of operating in low-resourced and high-demand environments. These experiences also present us with opportunities to be better and do better as both professionals and people; to reflect on our past and consider what we want different in our lives. As we yearn for better days and brace ourselves for what is to come, we hope that teams and organizations will take advantage of these opportunities for self-reflection and continue unmasking our grief, healing our wounds, and honoring our shared humanity.
Since the start of the pandemic, health care systems have requested many in-services for staff on self-care and stress management to help health care workers (HCWs) cope with the heavy toll of COVID-19. The pandemic has set off a global mental health crisis, with unprecedented numbers of individuals meeting criteria for anxiety, depression, and other mental health disorders in response to the intense stressors of living through a pandemic. These calls to assist staff with self-care and burnout prevention have been especially salient for psychologists working in palliative care and geriatrics, where fears of COVID-19 infection and numbers of patient deaths have been high.
Throughout these painful times, we have been grateful for an online community of palliative care psychologists within the US Department of Veterans Affairs (VA) from across the continuum of care and across the country. This community brought together many of us who were both struggling ourselves and striving to support the teams and HCWs around us. We are psychologists who provide home-care services in North Carolina, inpatient hospice and long-term care services in California, and long-term care and outpatient palliative care services in Massachusetts. Through our shared struggles and challenges navigating the pandemic, we realized that our respective teams requested similar services, all focused on staff support.
The psychological impact of COVID-19 on HCWs was clear from the beginning. Early in the pandemic our respective teams requested us to provide staff support and education about coping to our local HCWs. Soon national groups for long-term care staff requested education programs. Through this work, we realized that the emotional needs of HCWs ran much deeper than simple self-care. At the onset of the pandemic, before realizing its chronicity, the trainings we offered focused on stress and coping strategies. We cited several frameworks for staff support and eagerly shared anything that might help us, and our colleagues, survive the immediate anxiety and tumult surrounding us.1-3 In this paper, we briefly discuss the distress affecting the geriatric care workforce, reflect on our efforts to cope as HCWs, and offer recommendations at individual and organization levels to help address our collective grief.
Impact of COVID-19
As the death toll mounted and hospitals were pushed to the brink, we saw the suffering of our fellow HCWs. The lack of personal protective equipment (PPE) and testing supplies led to evolving and increasing anxiety for HCWs about contracting COVID-19, potentially spreading it to one’s social circle or family, fears of becoming sick and dying, and fears of inadvertently spreading the virus to medically-vulnerable patients. Increasing demands on staff required many to work outside their areas of expertise. Clinical practice guidelines changed frequently as information emerged about the virus. Staff members struggled to keep pace with the increasing number of patients, many of whom died despite heroic efforts to save them.
As the medical crisis grew, so too did social uprisings as the general public gained a strengthened awareness of the legacy and ongoing effects of systemic oppression, racism, and social inequities in the United States. Individuals grappled with their own privileges, which often hid such disparities from view. Many HCWs and clinicians of color had to navigate unsolicited questions and discussions about racial injustices while also trying to survive. As psychologists, we strove to support the HCWs around us while also struggling with our own stressors. As the magnitude of the pandemic and ongoing social injustices came into view, we realized that presentations on self-care and burnout prevention did not suffice. We needed discussions on unmasking our grief, acknowledging our traumas, and working toward collective healing.
Geriatric Care Workers
Experiences of grief and trauma hit the geriatric care workforce and especially long-term care facilities particularly hard given the high morbidity and mortality rates of COVID-19.4 The geriatric care workforce itself suffers from institutional vulnerabilities. Individuals are often underpaid, undertrained, and work within a system that continually experiences staffing shortages, high burnout, and consequently high levels of turnover.5,6 Recent immigrants and racial/ethnic minorities disproportionately make up this workforce, who often live in multigenerational households and work in multiple facilities to get by.7,8 Amid the pandemic these HCWs continued to work despite demoralizing negative media coverage of nursing homes.9 Notably, facilities with unionized staff were less likely to need second or third jobs to survive, thus reducing spread across facilities. This along with better access to PPE may have contributed to their lower COVID-19 infection and mortality rates relative to non-unionized staff.10
Similar to long-term care workers, home-care staff had related fears and anxieties, magnified by the need to enter multiple homes. This often overlooked but growing sector of the geriatric care workforce faced the added anxiety of the unknown as they entered multiple homes to provide care to their patients. These staff have little control over who may be in the home when they arrive, the sanitation/PPE practices of the patient/family, and therefore little control over their potential exposure to COVID-19. This also applies to home health aides who, although not providing medical services, are a critical part of home-care services and allow older adults to remain living independently in their home.
Reflection on Grief
As we witnessed the interactive effects of the pandemic and social inequities in geriatrics and palliative care, we frequently sought solace in online communities of psychologists working in similar settings. Over time, our regular community meetings developed a different tone: discussions about caring for others shifted to caring for ourselves. It seemed that in holding others’ pain, many of us neglected to address our own. We needed emotional support. We needed to acknowledge that we were not all okay; that the masks we wear for protection also reveal our vulnerabilities; and that protective equipment in hospitals do not protect us from the hate and bias targeting many of us face everywhere we go.
As we let ourselves be vulnerable with each other, we saw the true face of our pain: it was not stress, it was grief. We were sad, broken, mourning innumerable losses, and grieving, mostly alone. It felt overwhelming. Our minds and hearts often grew numb to find respite from pain. At times we found ourselves seeking haven in our offices, convincing ourselves that paperwork needed to be done when in reality we had no space to hold anyone else’s pain; we could barely contain our own. We could only take so much.
Without space to process, grief festers and eats away at our remaining compassion. How do we hold grace for ourselves, dare to be vulnerable, and allow ourselves to feel, when doing so opens the door to our own grief? How do we allow room for emotional processing when we learned to numb-out in order to function? And as women with diverse intersectional identities, how do we honor our humanity when we live in a society that reflects its indifference? We needed to process our pain in order to heal in the slow and uneven way that grief heals.
Caring During Tough Times
The pain we feel is real and it tears at us over time. Pushing it away disenfranchises ourselves of the opportunity to heal and grow. Our collective grief and trauma demand collective healing and acknowledgment of our individual suffering. We must honor our shared humanity and find commonality amid our differences. Typical self-care (healthy eating, sleep, basic hygiene) may not be enough to mitigate the enormity of these stressors. A glass of wine or a virtual dinner with friends may distract but does not heal our wounds.
Self-care, by definition, centers the self and ignores the larger systemic factors that maintain our struggles. It keeps the focus on the individual and in so doing, risks inducing self-blame should we continue feeling burnout. We must do more. We can advocate that systems acknowledge our grief and suffering as well as our strengths and resiliencies. We can demand that organizations recognize human limits and provide support, rather than promote environments that encourage silent perseverance. And we can deconstruct the cultural narrative that vulnerability is weakness or that we are the “heroes.” Heroism suggests superhuman qualities or extreme courage and often negates the fear and trepidation in its midst.11,12 We can also recognize how intersectional aspects of our identities make navigating the pandemic and systemic racism harder and more dangerous for some than for others.
As noted by President Biden in a speech honoring those lost to COVID-19, “We have to resist becoming numb to the sorrow.”13 The nature of our work (and that of most clinicians) is that it is expected and sometimes necessary to compartmentalize and turn off the emotions so that we can function in a professional manner. But this way of being also serves to hold us back. It does not make space for the very real emotions of trauma and grief that have pervaded HCWs during this pandemic. We must learn a different way of functioning—one where grief is acknowledged and even actively processed while still going about our work. Grief therapist Megan Devine proposes to “tend to pain and grief by bearing witness” and notes that “when we allow the reality of grief to exist, we can focus on helping ourselves—and one another—survive inside pain.”14 She advocates for self-compassion and directs us to “find ways to show our grief to others, in ways that honor the truth of our experience” saying, “we have to be willing to stop diminishing our own pain so that others can be comfortable around us.” But what does this look like among health care teams who are traumatized and grieving?
In our experience, caring for ourselves and our teams in times of prolonged stress, trauma, and grief is essential to maintain functioning over time. We strongly believe that it must occur at both the organizational and individual levels. In the throes of a crisis, teams need support immediately. To offer a timely response, we gathered knowledge of team-based care and collaboration to develop practical strategies that can be implemented swiftly to provide support across the team.15-19
The strategies we developed offer steps for creating and maintaining a supportive, compassionate, and psychologically safe work environment. First, the CARES Strategies for Practical Team Intervention highlights the importance of clear communication, assessing team needs regularly, recognizing the stress that is occurring, engaging staff in discussions, and ensuring psychological safety and comfort (Figure 1). Next, the SHARE approach is laid out to allow for interpersonal support among team members (Figure 2). Showing each other empathy, hoping for better days, acknowledging each other’s pain, reaching out for assistance, and expressing our needs allow HCWs to open up about their grief, stress, and trauma. Of note, we found these sets of strategies interdependent: a team that does not believe the leader/organization CARES is not likely to SHARE. Therefore, we also feel that it is especially important that team leaders work to create or enhance the sense of psychological safety for the team. If team members do not feel safe, they will not disclose their grief and remain stuck in the old mode of suffering in silence.
Conclusions
This pandemic and the collective efforts toward social justice advocacy have revealed our vulnerabilities as well as our strengths. These experiences have forced us to reckon with our past and consider possible futures. It has revealed the inequities in our health care system, including our failure to protect those on the ground who keep our systems running, and prompted us to consider new ways of operating in low-resourced and high-demand environments. These experiences also present us with opportunities to be better and do better as both professionals and people; to reflect on our past and consider what we want different in our lives. As we yearn for better days and brace ourselves for what is to come, we hope that teams and organizations will take advantage of these opportunities for self-reflection and continue unmasking our grief, healing our wounds, and honoring our shared humanity.
1. Blake H, Bermingham F. Psychological wellbeing for health care workers: mitigating the impact of covid-19. Version 2.0. Updated June 18, 2020. Accessed October 12, 2021. https://www.nottingham.ac.uk/toolkits/play_22794
2. Harris R. FACE COVID: how to respond effectively to the corona crisis. Published 2020. Accessed October 12, 2021. http://louisville.edu/counseling/coping-with-covid-19/face-covid-by-dr-russ-harris/view
3. Norcross JC, Phillips CM. Psychologist self-care during the pandemic: now more than ever [published online ahead of print, 2020 May 2]. J Health Serv Psychol. 2020;1-5. doi:10.1007/s42843-020-00010-5
4. Kaiser Family Foundation. State reports of long-term care facility cases and deaths related to COVID-19. 2020. Published April 23, 2020. Accessed October 12, 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities
5. Sterling MR, Tseng E, Poon A, et al. Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA Intern Med. 2020;180(11):1453-1459. doi:10.1001/jamainternmed.2020.3930
6. Stone R, Wilhelm J, Bishop CE, Bryant NS, Hermer L, Squillace MR. Predictors of intent to leave the job among home health workers: analysis of the National Home Health Aide Survey. Gerontologist. 2017;57(5):890-899. doi:10.1093/geront/gnw075
7. Scales K. It’s time to care: a detailed profile of America’s direct care workforce. PHI. 2020. Published January 21, 2020. Accessed October 12, 2021. https://phinational.org/wp-content/uploads/2020/01/Its-Time-to-Care-2020-PHI.pdf
8. Wolfe R, Harknett K, Schneider D. Inequities at work and the toll of COVID-19. Health Aff Health Policy Brief. Published June 4, 2021. doi: 10.1377/hpb20210428.863621
9. White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic [published correction appears in J Am Med Dir Assoc. 2021 May;22(5):1123]. J Am Med Dir Assoc. 2021;22(1):199-203. doi:10.1016/j.jamda.2020.11.022
10. Dean A, Venkataramani A, Kimmel S. Mortality rates from COVID-19 are lower In unionized nursing homes. Health Aff (Millwood). 2020;39(11):1993-2001.doi:10.1377/hlthaff.2020.01011
11. Cox CL. ‘Healthcare Heroes’: problems with media focus on heroism from healthcare workers during the COVID-19 pandemic. J Med Ethics. 2020;46(8):510-513. doi:10.1136/medethics-2020-106398
12. Stokes-Parish J, Elliott R, Rolls K, Massey D. Angels and heroes: the unintended consequence of the hero narrative. J Nurs Scholarsh. 2020;52(5):462-466. doi:10.1111/jnu.12591
13. Biden J. Remarks by President Biden on the more than 500,000 American lives lost to COVID-19. Published February 22, 2021. Accessed October 12, 2021. https://www.whitehouse.gov/briefing-room/speeches-remarks/2021/02/22/remarks-by-president-biden-on-the-more-than-500000-american-lives-lost-to-covid-19
14. Devine M. It’s Okay That You’re Not Okay: Meeting Grief and Loss in a Culture That Doesn’t Understand. Sounds True; 2017.
15. Center for the Study of Traumatic Stress. Grief leadership during COVID-19. Accessed October 12, 2021. https://www.cstsonline.org/assets/media/documents/CSTS_FS_Grief_Leadership_During_COVID19.pdf
16. Center for the Study of Traumatic Stress. Sustaining the well-being of healthcare personnel during coronavirus and other infectious disease outbreaks. Accessed October 12, 2021. https://www.cstsonline.org/assets/media/documents/CSTS_FS_Sustaining_Well_Being_Health care_Personnel_during.pdf
17. Fessell D, Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: micropractices for burnout prevention and emotional wellness. J Am Coll Radiol. 2020;17(6):746-748. doi:10.1016/j.jacr.2020.03.013
18. US Department of Veterans Affairs, National Center for PTSD. Managing healthcare workers’ stress associated with the COVID-19 virus outbreak. Updated March 25, 2020, Accessed October 12, 2021. https://www.ptsd.va.gov/covid/COVID_healthcare_workers.asp
19. US Department of Veterans Affairs, Veterans Health Administration, National Center for Organization Development (NCOD). Team Development Guide. 2017. https://vaww.va.gov/NCOD/docs/Team_Development_Guide.docx [Nonpublic source, not verified.]
1. Blake H, Bermingham F. Psychological wellbeing for health care workers: mitigating the impact of covid-19. Version 2.0. Updated June 18, 2020. Accessed October 12, 2021. https://www.nottingham.ac.uk/toolkits/play_22794
2. Harris R. FACE COVID: how to respond effectively to the corona crisis. Published 2020. Accessed October 12, 2021. http://louisville.edu/counseling/coping-with-covid-19/face-covid-by-dr-russ-harris/view
3. Norcross JC, Phillips CM. Psychologist self-care during the pandemic: now more than ever [published online ahead of print, 2020 May 2]. J Health Serv Psychol. 2020;1-5. doi:10.1007/s42843-020-00010-5
4. Kaiser Family Foundation. State reports of long-term care facility cases and deaths related to COVID-19. 2020. Published April 23, 2020. Accessed October 12, 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/state-reporting-of-cases-and-deaths-due-to-covid-19-in-long-term-care-facilities
5. Sterling MR, Tseng E, Poon A, et al. Experiences of home health care workers in New York City during the coronavirus disease 2019 pandemic: a qualitative analysis. JAMA Intern Med. 2020;180(11):1453-1459. doi:10.1001/jamainternmed.2020.3930
6. Stone R, Wilhelm J, Bishop CE, Bryant NS, Hermer L, Squillace MR. Predictors of intent to leave the job among home health workers: analysis of the National Home Health Aide Survey. Gerontologist. 2017;57(5):890-899. doi:10.1093/geront/gnw075
7. Scales K. It’s time to care: a detailed profile of America’s direct care workforce. PHI. 2020. Published January 21, 2020. Accessed October 12, 2021. https://phinational.org/wp-content/uploads/2020/01/Its-Time-to-Care-2020-PHI.pdf
8. Wolfe R, Harknett K, Schneider D. Inequities at work and the toll of COVID-19. Health Aff Health Policy Brief. Published June 4, 2021. doi: 10.1377/hpb20210428.863621
9. White EM, Wetle TF, Reddy A, Baier RR. Front-line nursing home staff experiences during the COVID-19 pandemic [published correction appears in J Am Med Dir Assoc. 2021 May;22(5):1123]. J Am Med Dir Assoc. 2021;22(1):199-203. doi:10.1016/j.jamda.2020.11.022
10. Dean A, Venkataramani A, Kimmel S. Mortality rates from COVID-19 are lower In unionized nursing homes. Health Aff (Millwood). 2020;39(11):1993-2001.doi:10.1377/hlthaff.2020.01011
11. Cox CL. ‘Healthcare Heroes’: problems with media focus on heroism from healthcare workers during the COVID-19 pandemic. J Med Ethics. 2020;46(8):510-513. doi:10.1136/medethics-2020-106398
12. Stokes-Parish J, Elliott R, Rolls K, Massey D. Angels and heroes: the unintended consequence of the hero narrative. J Nurs Scholarsh. 2020;52(5):462-466. doi:10.1111/jnu.12591
13. Biden J. Remarks by President Biden on the more than 500,000 American lives lost to COVID-19. Published February 22, 2021. Accessed October 12, 2021. https://www.whitehouse.gov/briefing-room/speeches-remarks/2021/02/22/remarks-by-president-biden-on-the-more-than-500000-american-lives-lost-to-covid-19
14. Devine M. It’s Okay That You’re Not Okay: Meeting Grief and Loss in a Culture That Doesn’t Understand. Sounds True; 2017.
15. Center for the Study of Traumatic Stress. Grief leadership during COVID-19. Accessed October 12, 2021. https://www.cstsonline.org/assets/media/documents/CSTS_FS_Grief_Leadership_During_COVID19.pdf
16. Center for the Study of Traumatic Stress. Sustaining the well-being of healthcare personnel during coronavirus and other infectious disease outbreaks. Accessed October 12, 2021. https://www.cstsonline.org/assets/media/documents/CSTS_FS_Sustaining_Well_Being_Health care_Personnel_during.pdf
17. Fessell D, Cherniss C. Coronavirus disease 2019 (COVID-19) and beyond: micropractices for burnout prevention and emotional wellness. J Am Coll Radiol. 2020;17(6):746-748. doi:10.1016/j.jacr.2020.03.013
18. US Department of Veterans Affairs, National Center for PTSD. Managing healthcare workers’ stress associated with the COVID-19 virus outbreak. Updated March 25, 2020, Accessed October 12, 2021. https://www.ptsd.va.gov/covid/COVID_healthcare_workers.asp
19. US Department of Veterans Affairs, Veterans Health Administration, National Center for Organization Development (NCOD). Team Development Guide. 2017. https://vaww.va.gov/NCOD/docs/Team_Development_Guide.docx [Nonpublic source, not verified.]
Universal depression screening in schools doubles odds for teen treatment
Universal screening for adolescent depression in schools, compared with the usual process of targeting students for referral after observing behaviors, resulted in significantly higher odds of identifying major depressive disorder (MDD) and of starting treatment for it, a study of more than 12,000 students suggests. Findings were published online in JAMA Network Open.
Deepa L. Sekhar, MD, MSc, with the department of pediatrics at Pennsylvania State College of Medicine in Hershey, Pa., and colleagues conducted a randomized clinical trial comparing the two screening methods from November 2018 to November 2020.
The trial included students in grades 9 through 12 enrolled at any of the 14 participating Pennsylvania public high schools. Researchers compared the two groups using mixed-effects logistic regression.
They found that adolescents in the universal screening intervention group had 5.92 times higher odds (95% confidence interval [CI], 5.07-6.93) of being identified with MDD symptoms, 3.30 times higher odds (95% CI, 2.49-4.38) of the Student Assistance Program (SAP) confirming follow-up needs, and 2.07 times higher odds (95% CI, 1.39-3.10) of starting MDD treatment.
The study comprised 12,909 students, with an average age of 16 years. Of those students, 2,687 (20.8%) were Hispanic; 2,891 (22.4%) were non-Hispanic Black, 5,842 (45.3%) were non-Hispanic White; and 1,489 (11.5%) were multiracial or of other race or ethnicity.
In the universal screening intervention (n = 6,473) all students completed the Patient Health Questionnaire–9 (PHQ-9). Students who screened positive proceeded to the Student Assistance Program. Students could receive a targeted referral to SAP if they had concerning behavior beyond the PHQ-9.
In the targeted screening group (n = 6,436), students with behaviors prompting concern for MDD were referred to the Student Assistance Program (SAP), mandated in all Pennsylvania schools. The SAP determined follow-up.
The U.S. Preventive Services Task Force (USPSTF) endorsed primary care screening in 2009 and again in 2016 for all adolescents 12-18 years old.
However, the study authors wrote, most U.S. adolescents (more than 60%) don’t have routine access to preventive health care, which limits primary care offices’ ability to properly address the growing numbers.
“[S]creening is inconsistent, with inequalities by race and ethnicity and region, and potential worsening with the COVID-19 pandemic,” they noted.
Depression rates see sharp increase
Meanwhile, the prevalence of adolescents reporting MDD symptoms has “nearly doubled in the last decade, increasing from 8.3% in 2008 to 14.4% in 2018.”
The American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association recently declared a national emergency in children’s mental health, citing COVID-19’s toll on top of existing challenges.
This study provides further evidence that universal screening is the better approach to identify and treat adolescent depression to save lives, Andres Pumariega, MD, a child and adolescent psychiatrist at University of Florida in Gainesville, told this news organization.
“If you catch these kids early, you can prevent suicide attempts and suicide. You can also prevent complicating costs of care,” he said.
He noted the universal screening removes the potential for bias.
“Relying purely on referral and clinical identification means a lot of kids in minority groups will not be identified and will not be treated accurately. Many clinicians have a problem identifying depression in diverse kids,” he said.
Pushback for universal screening likely
However, he said he has been part of such efforts to implement such programs in Mexico and the United States and said in the Unites States, the political climate will guarantee pushback from having schools more involved in health care and prevention. Recent controversy around COVID-19 vaccines for children illustrates the potential backlash, he said.
Parents often fight such programs as attempts to “label” their children, he said.
“If I have cancer, I sure want to be labeled. A label is used to get them help. We need to find ways to educate parents and support them in facing these issues,” he added.
One concern he has with this intervention is having the SAPs, composed largely of nonclinicians, be the triage point “instead of doing that objectively through objective criteria and by clinicians,” he said. “If we are to have a comprehensive health system where we can serve all kids and manage costs, schools need to be a major part of it.”
School settings offer the chance to see more children, collaborate with teachers and counselors, and integrate results with educational outcomes, he added.
In the study by Sekhar and colleagues, 7 of the 14 schools were classified as urban, with a median size of 370 students.
Researchers noted that the benefit of the universal screening is likely understated because of COVID-19–related school closures during the study period. The closures meant screening wasn’t completed for 7% of students.
The authors concluded that universal screening finds teens living with depression who otherwise would not be found. They said such a program likely works best in schools with strong SAP.
“Adolescents’ consistent contact with schools has been used to support physical health screenings that affect academic success,” the authors wrote. “Major depressive disorder similarly affects academic success, suggesting school-based screening may be especially beneficial.”
In the past 3 years, Dr. Sekhar reported receiving funding from Pfizer through the American Academy of Pediatrics, the Penn State Clinical and Translational Science Awards Program, and a Eugene Washington Patient-Centered Outcomes Research Institute Engagement Award. Full disclosures for coauthors are available in the journal article.
This work was supported in part by the Patient-Centered Outcomes Research Institute. The use of REDCap (Research Electronic Data Capture) in this project was supported by the National Institutes of Health.
Universal screening for adolescent depression in schools, compared with the usual process of targeting students for referral after observing behaviors, resulted in significantly higher odds of identifying major depressive disorder (MDD) and of starting treatment for it, a study of more than 12,000 students suggests. Findings were published online in JAMA Network Open.
Deepa L. Sekhar, MD, MSc, with the department of pediatrics at Pennsylvania State College of Medicine in Hershey, Pa., and colleagues conducted a randomized clinical trial comparing the two screening methods from November 2018 to November 2020.
The trial included students in grades 9 through 12 enrolled at any of the 14 participating Pennsylvania public high schools. Researchers compared the two groups using mixed-effects logistic regression.
They found that adolescents in the universal screening intervention group had 5.92 times higher odds (95% confidence interval [CI], 5.07-6.93) of being identified with MDD symptoms, 3.30 times higher odds (95% CI, 2.49-4.38) of the Student Assistance Program (SAP) confirming follow-up needs, and 2.07 times higher odds (95% CI, 1.39-3.10) of starting MDD treatment.
The study comprised 12,909 students, with an average age of 16 years. Of those students, 2,687 (20.8%) were Hispanic; 2,891 (22.4%) were non-Hispanic Black, 5,842 (45.3%) were non-Hispanic White; and 1,489 (11.5%) were multiracial or of other race or ethnicity.
In the universal screening intervention (n = 6,473) all students completed the Patient Health Questionnaire–9 (PHQ-9). Students who screened positive proceeded to the Student Assistance Program. Students could receive a targeted referral to SAP if they had concerning behavior beyond the PHQ-9.
In the targeted screening group (n = 6,436), students with behaviors prompting concern for MDD were referred to the Student Assistance Program (SAP), mandated in all Pennsylvania schools. The SAP determined follow-up.
The U.S. Preventive Services Task Force (USPSTF) endorsed primary care screening in 2009 and again in 2016 for all adolescents 12-18 years old.
However, the study authors wrote, most U.S. adolescents (more than 60%) don’t have routine access to preventive health care, which limits primary care offices’ ability to properly address the growing numbers.
“[S]creening is inconsistent, with inequalities by race and ethnicity and region, and potential worsening with the COVID-19 pandemic,” they noted.
Depression rates see sharp increase
Meanwhile, the prevalence of adolescents reporting MDD symptoms has “nearly doubled in the last decade, increasing from 8.3% in 2008 to 14.4% in 2018.”
The American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association recently declared a national emergency in children’s mental health, citing COVID-19’s toll on top of existing challenges.
This study provides further evidence that universal screening is the better approach to identify and treat adolescent depression to save lives, Andres Pumariega, MD, a child and adolescent psychiatrist at University of Florida in Gainesville, told this news organization.
“If you catch these kids early, you can prevent suicide attempts and suicide. You can also prevent complicating costs of care,” he said.
He noted the universal screening removes the potential for bias.
“Relying purely on referral and clinical identification means a lot of kids in minority groups will not be identified and will not be treated accurately. Many clinicians have a problem identifying depression in diverse kids,” he said.
Pushback for universal screening likely
However, he said he has been part of such efforts to implement such programs in Mexico and the United States and said in the Unites States, the political climate will guarantee pushback from having schools more involved in health care and prevention. Recent controversy around COVID-19 vaccines for children illustrates the potential backlash, he said.
Parents often fight such programs as attempts to “label” their children, he said.
“If I have cancer, I sure want to be labeled. A label is used to get them help. We need to find ways to educate parents and support them in facing these issues,” he added.
One concern he has with this intervention is having the SAPs, composed largely of nonclinicians, be the triage point “instead of doing that objectively through objective criteria and by clinicians,” he said. “If we are to have a comprehensive health system where we can serve all kids and manage costs, schools need to be a major part of it.”
School settings offer the chance to see more children, collaborate with teachers and counselors, and integrate results with educational outcomes, he added.
In the study by Sekhar and colleagues, 7 of the 14 schools were classified as urban, with a median size of 370 students.
Researchers noted that the benefit of the universal screening is likely understated because of COVID-19–related school closures during the study period. The closures meant screening wasn’t completed for 7% of students.
The authors concluded that universal screening finds teens living with depression who otherwise would not be found. They said such a program likely works best in schools with strong SAP.
“Adolescents’ consistent contact with schools has been used to support physical health screenings that affect academic success,” the authors wrote. “Major depressive disorder similarly affects academic success, suggesting school-based screening may be especially beneficial.”
In the past 3 years, Dr. Sekhar reported receiving funding from Pfizer through the American Academy of Pediatrics, the Penn State Clinical and Translational Science Awards Program, and a Eugene Washington Patient-Centered Outcomes Research Institute Engagement Award. Full disclosures for coauthors are available in the journal article.
This work was supported in part by the Patient-Centered Outcomes Research Institute. The use of REDCap (Research Electronic Data Capture) in this project was supported by the National Institutes of Health.
Universal screening for adolescent depression in schools, compared with the usual process of targeting students for referral after observing behaviors, resulted in significantly higher odds of identifying major depressive disorder (MDD) and of starting treatment for it, a study of more than 12,000 students suggests. Findings were published online in JAMA Network Open.
Deepa L. Sekhar, MD, MSc, with the department of pediatrics at Pennsylvania State College of Medicine in Hershey, Pa., and colleagues conducted a randomized clinical trial comparing the two screening methods from November 2018 to November 2020.
The trial included students in grades 9 through 12 enrolled at any of the 14 participating Pennsylvania public high schools. Researchers compared the two groups using mixed-effects logistic regression.
They found that adolescents in the universal screening intervention group had 5.92 times higher odds (95% confidence interval [CI], 5.07-6.93) of being identified with MDD symptoms, 3.30 times higher odds (95% CI, 2.49-4.38) of the Student Assistance Program (SAP) confirming follow-up needs, and 2.07 times higher odds (95% CI, 1.39-3.10) of starting MDD treatment.
The study comprised 12,909 students, with an average age of 16 years. Of those students, 2,687 (20.8%) were Hispanic; 2,891 (22.4%) were non-Hispanic Black, 5,842 (45.3%) were non-Hispanic White; and 1,489 (11.5%) were multiracial or of other race or ethnicity.
In the universal screening intervention (n = 6,473) all students completed the Patient Health Questionnaire–9 (PHQ-9). Students who screened positive proceeded to the Student Assistance Program. Students could receive a targeted referral to SAP if they had concerning behavior beyond the PHQ-9.
In the targeted screening group (n = 6,436), students with behaviors prompting concern for MDD were referred to the Student Assistance Program (SAP), mandated in all Pennsylvania schools. The SAP determined follow-up.
The U.S. Preventive Services Task Force (USPSTF) endorsed primary care screening in 2009 and again in 2016 for all adolescents 12-18 years old.
However, the study authors wrote, most U.S. adolescents (more than 60%) don’t have routine access to preventive health care, which limits primary care offices’ ability to properly address the growing numbers.
“[S]creening is inconsistent, with inequalities by race and ethnicity and region, and potential worsening with the COVID-19 pandemic,” they noted.
Depression rates see sharp increase
Meanwhile, the prevalence of adolescents reporting MDD symptoms has “nearly doubled in the last decade, increasing from 8.3% in 2008 to 14.4% in 2018.”
The American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and Children’s Hospital Association recently declared a national emergency in children’s mental health, citing COVID-19’s toll on top of existing challenges.
This study provides further evidence that universal screening is the better approach to identify and treat adolescent depression to save lives, Andres Pumariega, MD, a child and adolescent psychiatrist at University of Florida in Gainesville, told this news organization.
“If you catch these kids early, you can prevent suicide attempts and suicide. You can also prevent complicating costs of care,” he said.
He noted the universal screening removes the potential for bias.
“Relying purely on referral and clinical identification means a lot of kids in minority groups will not be identified and will not be treated accurately. Many clinicians have a problem identifying depression in diverse kids,” he said.
Pushback for universal screening likely
However, he said he has been part of such efforts to implement such programs in Mexico and the United States and said in the Unites States, the political climate will guarantee pushback from having schools more involved in health care and prevention. Recent controversy around COVID-19 vaccines for children illustrates the potential backlash, he said.
Parents often fight such programs as attempts to “label” their children, he said.
“If I have cancer, I sure want to be labeled. A label is used to get them help. We need to find ways to educate parents and support them in facing these issues,” he added.
One concern he has with this intervention is having the SAPs, composed largely of nonclinicians, be the triage point “instead of doing that objectively through objective criteria and by clinicians,” he said. “If we are to have a comprehensive health system where we can serve all kids and manage costs, schools need to be a major part of it.”
School settings offer the chance to see more children, collaborate with teachers and counselors, and integrate results with educational outcomes, he added.
In the study by Sekhar and colleagues, 7 of the 14 schools were classified as urban, with a median size of 370 students.
Researchers noted that the benefit of the universal screening is likely understated because of COVID-19–related school closures during the study period. The closures meant screening wasn’t completed for 7% of students.
The authors concluded that universal screening finds teens living with depression who otherwise would not be found. They said such a program likely works best in schools with strong SAP.
“Adolescents’ consistent contact with schools has been used to support physical health screenings that affect academic success,” the authors wrote. “Major depressive disorder similarly affects academic success, suggesting school-based screening may be especially beneficial.”
In the past 3 years, Dr. Sekhar reported receiving funding from Pfizer through the American Academy of Pediatrics, the Penn State Clinical and Translational Science Awards Program, and a Eugene Washington Patient-Centered Outcomes Research Institute Engagement Award. Full disclosures for coauthors are available in the journal article.
This work was supported in part by the Patient-Centered Outcomes Research Institute. The use of REDCap (Research Electronic Data Capture) in this project was supported by the National Institutes of Health.
JAMA NETWORK OPEN
COVID-19 has brought more complex, longer office visits
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
Evidence of this came from the latest Primary Care Collaborative (PCC) survey, which found that primary care clinicians are seeing more complex patients requiring longer appointments in the wake of COVID-19.
The PCC with the Larry A. Green Center regularly surveys primary care clinicians. This round of questions came August 14-17 and included 1,263 respondents from 49 states, the District of Columbia, and two territories.
More than 7 in 10 (71%) respondents said their patients are more complex and nearly the same percentage said appointments are taking more time.
Ann Greiner, president and CEO of the PCC, said in an interview that 55% of respondents reported that clinicians are struggling to keep up with pent-up demand after patients have delayed or canceled care. Sixty-five percent in the survey said they had seen a rise in children’s mental health issues, and 58% said they were unsure how to help their patients with long COVID.
In addition, primary care clinicians are having repeated conversations with patients on why they should get a vaccine and which one.
“I think that’s adding to the complexity. There is a lot going on here with patient trust,” Ms. Greiner said.
‘We’re going to be playing catch-up’
Jacqueline Fincher, MD, an internist in Thompson, Ga., said in an interview that appointments have gotten longer and more complex in the wake of the pandemic – “no question.”
The immediate past president of the American College of Physicians is seeing patients with chronic disease that has gone untreated for sometimes a year or more, she said.
“Their blood pressure was not under good control, they were under more stress, their sugars were up and weren’t being followed as closely for conditions such as congestive heart failure,” she said.
Dr. Fincher, who works in a rural practice 40 miles from Augusta, Ga., with her physician husband and two other physicians, said patients are ready to come back in, “but I don’t have enough slots for them.”
She said she prioritizes what to help patients with first and schedules the next tier for the next appointment, but added, “honestly, over the next 2 years we’re going to be playing catch-up.”
At the same time, the CDC has estimated that 45% of U.S. adults are at increased risk for complications from COVID-19 because of cardiovascular disease, diabetes, respiratory disease, hypertension, or cancer. Rates ranged from 19.8% for people 18-29 years old to 80.7% for people over 80 years of age.
Long COVID could overwhelm existing health care capacity
Primary care physicians are also having to diagnose sometimes “invisible” symptoms after people have recovered from acute COVID-19 infection. Diagnosing takes intent listening to patients who describe symptoms that tests can’t confirm.
As this news organization has previously reported, half of COVID-19 survivors report postacute sequelae of COVID-19 (PASC) lasting longer than 6 months.
“These long-term PASC effects occur on a scale that could overwhelm existing health care capacity, particularly in low- and middle-income countries,” the authors wrote.
Anxiety, depression ‘have gone off the charts’
Danielle Loeb, MD, MPH, associate professor of internal medicine at the University of Colorado in Denver, who studies complexity in primary care, said in the wake of COVID-19, more patients have developed “new, serious anxiety.”
“That got extremely exacerbated during the pandemic. Anxiety and depression have gone off the charts,” said Dr. Loeb, who prefers the pronoun “they.”
Dr. Loeb cares for a large number of transgender patients. As offices reopen, some patients are having trouble reintegrating into the workplace and resuming social contacts. The primary care doctor says appointments can get longer because of the need to complete tasks, such as filling out forms for Family Medical Leave Act for those not yet ready to return to work.
COVID-19–related fears are keeping many patients from coming into the office, Dr. Loeb said, either from fear of exposure or because they have mental health issues that keep them from feeling safe leaving the house.
“That really affects my ability to care for them,” they said.
Loss of employment in the pandemic or fear of job loss and subsequent changing of insurance has complicated primary care in terms of treatment and administrative tasks, according to Dr. Loeb.
To help treat patients with acute mental health issues and manage other patients, Dr. Loeb’s practice has brought in a social worker and a therapist.
Team-based care is key in the survival of primary care practices, though providing that is difficult in the smaller clinics because of the critical mass of patients needed to make it viable, they said.
“It’s the only answer. It’s the only way you don’t drown,” Dr. Loeb added. “I’m not drowning, and I credit that to my clinic having the help to support the mental health piece of things.”
Rethinking workflow
Tricia McGinnis, MPP, MPH, executive vice president of the nonprofit Center for Health Care Strategies (CHCS) says complexity has forced rethinking workflow.
“A lot of the trends we’re seeing in primary care were there pre-COVID, but COVID has exacerbated those trends,” she said in an interview.
“The good news ... is that it was already becoming clear that primary care needed to provide basic mental health services and integrate with behavioral health. It had also become clear that effective primary care needed to address social issues that keep patients from accessing health care,” she said.
Expanding care teams, as Dr. Loeb mentioned, is a key strategy, according to Ms. McGinnis. Potential teams would include the clinical staff, but also social workers and community health workers – people who come from the community primary care is serving who can help build trust with patients and connect the patient to the primary care team.
“There’s a lot that needs to happen that the clinician doesn’t need to do,” she said.
Telehealth can be a big factor in coordinating the team, Ms. McGinnis added.
“It’s thinking less about who’s doing the work, but more about the work that needs to be done to keep people healthy. Then let’s think about the type of workers best suited to perform those tasks,” she said.
As for reimbursing more complex care, population-based, up-front capitated payments linked to high-quality care and better outcomes will need to replace fee-for-service models, according to Ms. McGinnis.
That will provide reliable incomes for primary care offices, but also flexibility in how each patient with different levels of complexity is managed, she said.
Ms. Greiner, Dr. Fincher, Dr. Loeb, and Ms. McGinnis have no relevant financial relationships.
City or country life? Genetic risk for mental illness may decide
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a genetic predisposition to schizophrenia, bipolar disorder (BD), autism spectrum disorder (ASD), or anorexia nervosa (AN) are significantly more likely to move from a rural to an urban setting, whereas those at high genetic risk for attention-deficit/hyperactivity disorder were more likely to do the opposite.
The findings held even in those at high genetic risk who had never been diagnosed with a psychiatric disorder, highlighting a genetic factor that previous research linking urban living to mental illness has not explored.
“It’s not as simple as saying that urban environment is responsible for schizophrenia and everyone should move out of urban environments and they will be safe,” study investigator Evangelos Vassos, MD, PhD, senior clinical research fellow at King’s College London, and a consulting psychiatrist, said in an interview. “If you are genetically predisposed to schizophrenia, you will still be predisposed to schizophrenia even if you move.”
The study was published online in JAMA Psychiatry.
Genetic influence
The study results don’t rule out environmental influence, but offer evidence that the migration pattern researchers have tracked for years may have a multifactorial explanation.
“Our research shows that, at some level, an individual’s genes select their environment and that the relationship between environmental and genetic influences on mental health is interrelated,” Jessye Maxwell, MSc, lead author and a PhD candidate in psychiatry at King’s College, said in a statement. “This overlap needs to be considered when developing models to predict the risk of people developing mental health conditions in the future.”
For the study, the investigators calculated polygenic risk scores (PRS) of different psychiatric illnesses for 385,793 U.K. Biobank participants aged 37-73. PRS analyzes genetic information across a person’s entire genome, rather than by individual genes.
They used address history and U.K. census records from 1931 to 2011 to map population density over time.
PRS analyses showed significant associations with higher population density throughout adulthood, reaching highest significance between age 45 and 55 years for schizophrenia (88 people/km2; 95% confidence interval, 65-98 people/km2), BD (44 people/km2; 95%CI, 34-54 people/km2), AN (36 people/km2; 95%CI, 22-50 people/km2), and ASD (35 people/km2; 95%CI, 25-45 people/km2).
When they compared those who were born and stayed in rural or suburban areas to their counterparts who moved from those areas to cities, they found the odds of moving to urban areas ranged from 5% among people at high genetic risk for schizophrenia to 13% of those with a high risk for BD. Only people at high risk for ADHD were more likely to move to rural areas.
However, the study is not without its limitations. Only people of European descent were included, family medical history was unavailable for some participants, and only about 50,000 people had a lifetime diagnosis of mental illness, which is not representative of the general population.
‘Convincing evidence’
Still, the research adds another piece of the puzzle scientists seek to solve about where people live and mental illness risk, said Jordan DeVylder, PhD, associate professor of social work at Fordham University, New York, who commented on the study for this news organization.
Dr. DeVylder, who has also published research on the topic but was not part of the current study, noted that urban living has long been thought to be among the most consistent environmental risk factors for psychosis. However, he noted, “this association can also be explained by genetic selection, in which the same genes that predispose one to schizophrenia also predispose one to choose urban living.”
“This study presents the most convincing evidence to date that genetics have a major role in this association, at least in the countries where this association between urban living and psychosis exists,” he said.
The study was funded by National Institute for Health Research, Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. The authors and Dr. DeVylder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Resident doctor who attempted suicide three times fights for change
In early 2020, Justin Bullock, MD, MPH, did what few, if any, resident physicians have done: He published an honest account in the New England Journal of Medicine of a would-be suicide attempt during medical training.
In the article, Dr. Bullock matter-of-factly laid out how, in 2019, intern-year night shifts contributed to a depressive episode. For Dr. Bullock, who has a bipolar disorder, sleep dysregulation can be deadly. He had a plan for completing suicide, and this wouldn’t have been his first attempt. Thanks to his history and openness about his condition, Dr. Bullock had an experienced care team that helped him get to a psychiatric hospital before anything happened. While there for around 5 days, he wrote the bulk of the NEJM article.
The article took Dr. Bullock’s impact nationwide. On Twitter and in interviews, Dr. Bullock is an unapologetic advocate for accommodations for people in medicine with mental illness. “One of the things that inspired me to speak out early on is that I feel I stand in a place of so much privilege,” Dr. Bullock told this news organization. “I often feel this sense of ... ‘you have to speak up, Justin; no one else can.’ ”
Dr. Bullock’s activism is especially noteworthy, given that he is still establishing his career. In August, while an internal medicine resident at the University of California, San Francisco, he received a lifetime teaching award from UCSF because he had received three prior teaching awards; a recognition like this is considered rare someone so early in their career. Now in his final year of residency, he actively researches medical education, advocates for mental health support, and is working to become a leading voice on related issues.
“It seems to be working,” his older sister, Jacquis Mahoney, RN, said during a visit to the UCSF campus. Instead of any awkwardness, everyone is thrilled to learn that she is Justin’s sister. “There’s a lot of pride and excitement.”
Suicide attempts during medical training
Now 28, Dr. Bullock grew up in Detroit, with his mom and two older sisters. His father was incarcerated for much of Dr. Bullock’s childhood, in part because of his own bipolar disorder not being well controlled, Dr. Bullock said.
When he was younger, Dr. Bullock was the peacekeeper in the house between his two sisters, said Ms. Mahoney: “Justin was always very delicate and kind.”
He played soccer and ran track but also loved math and science. While outwardly accumulating an impressive resume, Dr. Bullock was internally struggling. In high school, he made what he now calls an “immature” attempt at suicide after coming out as gay to his family. While Dr. Bullock said he doesn’t necessarily dwell on the discrimination he has faced as a gay, Black man, his awareness of how others perceive and treat him because of his identity increases the background stress present in his daily life.
After high school, Dr. Bullock went to MIT in Boston, where he continued running and studied chemical-biological engineering. During college, Dr. Bullock thought he was going to have to withdraw from MIT because of his depression. Thankfully, he received counseling from student services and advice from a track coach who sat him down and talked about pragmatic solutions, like medication. “That was life-changing,” said Dr. Bullock.
When trying to decide between engineering and medicine, Dr. Bullock realized he preferred contemplating medical problems to engineering ones. So he applied to medical school. Dr. Bullock eventually ended up at UCSF, where he was selected to participate in the Program in Medical Education for the Urban Underserved, a 5-year track at the college for students committed to working with underserved communities.
By the time Dr. Bullock got to medical school, he was feeling good. In consultation with his psychiatrist, he thought it worthwhile to take a break from his medications. At that time, his diagnosis was major depressive disorder and he had only had one serious depressive episode, which didn’t necessarily indicate that he would need medication long-term, he said.
Dr. Bullock loved everything about medical school. “One day when I was in my first year of med school, I called my mom and said: ‘It’s like science summer camp but every day!’” he recalled.
Despite his enthusiasm, though, he began feeling something troubling. Recognizing the symptoms of early depression, Dr. Bullock restarted his medication. But this time, the same SSRI only made things worse. He went from sleeping 8 hours to 90 minutes a night. He felt angry. One day, he went on a furious 22-mile run. Plus, within the first 6 months of moving to San Francisco, Dr. Bullock was stopped by the police three different times while riding his bike. He attributes this to his race, which has only further added to his stress. In September 2015, during his second year of medical school, Dr. Bullock attempted suicide again. This time, he was intubated in the ED and rushed to the ICU.
He was given a new diagnosis: bipolar disorder. He changed medications and lived for a time with Ms. Mahoney and his other sister, who moved from Chicago to California to be with him. “My family has helped me a lot,” he said.
Dr. Bullock was initially not sure whether he would be able to return to school after his attempted suicide. Overall, UCSF was extremely supportive, he said. That came as a relief. Medical school was a grounding force in his life, not a destabilizing one: “If I had been pushed out, it would have been really harmful to me.”
Then Dr. Bullock started residency. The sleep disruption that comes with the night shift – the resident rite of passage – triggered another episode. At first, Dr. Bullock was overly productive; his mind was active and alert after staying up all night. He worked on new research during the day instead of sleeping.
Sleep disturbance is a hallmark symptom of bipolar disorder. “Justin should never be on a 24-hour call,” said Lisa Meeks, PhD, associate professor of psychiatry and family medicine at the University of Colorado at Denver, Aurora, and a leading scholar on disability advocacy for medical trainees. When he started residency, Dr. Bullock was open with his program director about his diagnosis and sought accommodations to go to therapy each week. But he didn’t try to get out of night shifts or 24-hour calls, despite his care team urging him to do so. “I have this sense of wanting to tough it out,” he said. He also felt guilty making his peers take on his share of those challenging shifts.
In December 2019, Dr. Bullock was voluntarily hospitalized for a few days and started writing the article that would later appear in NEJM. In January, a friend and UCSF medical student completed suicide. In March, the same month his NEJM article came out, Dr. Bullock attempted suicide again. This time, he quickly recognized that he was making a mistake and called an ambulance. “For me, as far as suicide attempts go, it’s the most positive one.”
Advocating for changes in medical training
Throughout his medical training, Dr. Bullock was always open about his struggles with his peers and with the administration. He shared his suicidal thoughts at a Mental Illness Among Us event during medical school. His story resonated with peers who were surprised that Dr. Bullock, who was thriving academically, could be struggling emotionally.
During residency, he led small group discussions and gave lectures at the medical school, including a talk about his attempts to create institutional change at UCSF, such as his public fight against the college’s Fitness for Duty (FFD) assessment process. That discussion earned him an Outstanding Lecturer award. Because it was the third award he had received from the medical school, Dr. Bullock also automatically earned a lifetime teaching award. When he told his mom, a teacher herself, about the award, she joked: “Are you old enough for ‘lifetime’ anything?”
Dr. Bullock has also spoken out and actively fought against the processes within the medical community that prevent people from coming forward until it is too late. Physicians and trainees often fear that if they seek mental health treatment, they will have to disclose that treatment to a potential employer or licensing board and then be barred from practicing medicine. Because he has been open about his mental health for so long, Dr. Bullock feels that he is in a position to push back against these norms. For example, in June he coauthored another article, this time for the Journal of Hospital Medicine, describing the traumatizing FFD assessment that followed his March 2020 suicide attempt.
In that article, Dr. Bullock wrote how no mental health professional served on the UCSF Physician Well Being Committee – comprising physicians and lawyers who evaluate physician impairment or potential physician impairment – that evaluated him. Dr. Bullock was referred to an outside psychiatrist. He also describes how he was forced to release all of his psychiatric records and undergo extensive drug testing, despite having no history of substance abuse. To return to work, he had to sign a contract, agreeing to be monitored and to attend a specific kind of therapy.
While steps like these can, in the right circumstances, protect both the public and doctors-in-training in important ways, they can also “be very punitive and isolating for someone going through a mental health crisis,” said Dr. Meeks. There were also no Black physicians or lawyers on the committee evaluating Dr. Bullock. “That was really egregious, when you look back.” Dr. Meeks is a coauthor on Dr. Bullock’s JHM article and a mentor and previous student disability officer at UCSF.
Dr. Bullock raised objections to UCSF administrators about how he felt that the committee was discriminating against him because of his mental illness despite assurances from the director of his program that there have never been any performance or professionalism concerns with him. He said the administrators told him he was the first person to question the FFD process. This isn’t surprising, given that all the power in such situations usually lies with the hospital and the administrators, whereas the resident or physician is worried about losing their job and their license, said Dr. Meeks.
Dr. Bullock contends that he’s in a unique position to speak out, considering his stellar academic and work records, openness about his mental illness before a crisis, access to quality mental health care, and extensive personal network among the UCSF administration. “I know that I hold power within my institution; I spoke out because I could,” Dr. Bullock said. In addition to writing an article about his experience, Dr. Bullock shared his story with a task force appointed by the medical staff president to review the Physician Well-Being Committee and the overall FFD process. Even before Dr. Bullock shared his story with the public, the task force had already been appointed as a result of the increased concern about physician mental health during the ongoing COVID-19 pandemic, Michelle Guy, MD, clinical professor of medicine at UCSF, told this news organization.
Elizabeth Fernandez, a UCSF senior public information representative, declined to comment on Dr. Bullock’s specific experience as reported in the JHM. “As with every hospital accredited by the Joint Commission, UCSF Medical Center has a Physician Well Being Committee that provides resources for physicians who may need help with chemical dependency or mental illness,” Ms. Fernandez said.
“Our goal through this program is always, first, to provide the compassion and assistance our physicians need to address the issues they face and continue to pursue their careers. This program is entirely voluntary and is bound by federal and state laws and regulations to protect the confidentiality of its participants, while ensuring that – first and foremost – no one is harmed by the situation, including the participant.”
Overcoming stigma to change the system
All of the attention – from national media outlets such as Vox to struggling peers and others – is fulfilling, Dr. Bullock said. But it can also be overwhelming. “I have definitely been praised as ‘Black excellence,’ and that definitely has added to the pressure to keep going ... to keep pushing at times,” he said.
Ms. Mahoney added: “He’s willing to sacrifice himself in order to make a difference. He would be a sacrificial lamb” for the Black community, the gay community, or any minority community.
Despite these concerns and his past suicide attempts, colleagues feel that Dr. Bullock is in a strong place to make decisions. “I trust Justin to put the boundaries up when they are needed and to engage in a way that feels comfortable for him,” said Ms. Meeks. “He is someone who has incredible self-awareness.”
Dr. Bullock’s history isn’t just something he overcame: It’s something that makes him a better, more empathetic doctor, said Ms. Mahoney. He knows what it’s like to be hospitalized, to deal with the frustration of insurance, to navigate the complexity of the health care system as a patient, or to be facing a deep internal darkness. He “can genuinely hold that person’s hand and say: ‘I know what you’re going through and we’re going to work through this day by day,’ ” she said. “That is something he can bring that no other physician can bring.”
In his advocacy on Twitter, in lectures, and in conversations with UCSF administrators, Dr. Bullock is pushing for board licensing questions to be reformed so physicians are no longer penalized for seeking mental health treatment. He would also like residency programs to make it easier and less stigmatizing for trainees to receive accommodations for a disability or mental illness.
“They say one person can’t change a system,” said Dr. Meeks, “but I do think Justin is calling an awful lot of attention to the system and I do think there will be changes because of his advocacy.”
A version of this article first appeared on Medscape.com.
In early 2020, Justin Bullock, MD, MPH, did what few, if any, resident physicians have done: He published an honest account in the New England Journal of Medicine of a would-be suicide attempt during medical training.
In the article, Dr. Bullock matter-of-factly laid out how, in 2019, intern-year night shifts contributed to a depressive episode. For Dr. Bullock, who has a bipolar disorder, sleep dysregulation can be deadly. He had a plan for completing suicide, and this wouldn’t have been his first attempt. Thanks to his history and openness about his condition, Dr. Bullock had an experienced care team that helped him get to a psychiatric hospital before anything happened. While there for around 5 days, he wrote the bulk of the NEJM article.
The article took Dr. Bullock’s impact nationwide. On Twitter and in interviews, Dr. Bullock is an unapologetic advocate for accommodations for people in medicine with mental illness. “One of the things that inspired me to speak out early on is that I feel I stand in a place of so much privilege,” Dr. Bullock told this news organization. “I often feel this sense of ... ‘you have to speak up, Justin; no one else can.’ ”
Dr. Bullock’s activism is especially noteworthy, given that he is still establishing his career. In August, while an internal medicine resident at the University of California, San Francisco, he received a lifetime teaching award from UCSF because he had received three prior teaching awards; a recognition like this is considered rare someone so early in their career. Now in his final year of residency, he actively researches medical education, advocates for mental health support, and is working to become a leading voice on related issues.
“It seems to be working,” his older sister, Jacquis Mahoney, RN, said during a visit to the UCSF campus. Instead of any awkwardness, everyone is thrilled to learn that she is Justin’s sister. “There’s a lot of pride and excitement.”
Suicide attempts during medical training
Now 28, Dr. Bullock grew up in Detroit, with his mom and two older sisters. His father was incarcerated for much of Dr. Bullock’s childhood, in part because of his own bipolar disorder not being well controlled, Dr. Bullock said.
When he was younger, Dr. Bullock was the peacekeeper in the house between his two sisters, said Ms. Mahoney: “Justin was always very delicate and kind.”
He played soccer and ran track but also loved math and science. While outwardly accumulating an impressive resume, Dr. Bullock was internally struggling. In high school, he made what he now calls an “immature” attempt at suicide after coming out as gay to his family. While Dr. Bullock said he doesn’t necessarily dwell on the discrimination he has faced as a gay, Black man, his awareness of how others perceive and treat him because of his identity increases the background stress present in his daily life.
After high school, Dr. Bullock went to MIT in Boston, where he continued running and studied chemical-biological engineering. During college, Dr. Bullock thought he was going to have to withdraw from MIT because of his depression. Thankfully, he received counseling from student services and advice from a track coach who sat him down and talked about pragmatic solutions, like medication. “That was life-changing,” said Dr. Bullock.
When trying to decide between engineering and medicine, Dr. Bullock realized he preferred contemplating medical problems to engineering ones. So he applied to medical school. Dr. Bullock eventually ended up at UCSF, where he was selected to participate in the Program in Medical Education for the Urban Underserved, a 5-year track at the college for students committed to working with underserved communities.
By the time Dr. Bullock got to medical school, he was feeling good. In consultation with his psychiatrist, he thought it worthwhile to take a break from his medications. At that time, his diagnosis was major depressive disorder and he had only had one serious depressive episode, which didn’t necessarily indicate that he would need medication long-term, he said.
Dr. Bullock loved everything about medical school. “One day when I was in my first year of med school, I called my mom and said: ‘It’s like science summer camp but every day!’” he recalled.
Despite his enthusiasm, though, he began feeling something troubling. Recognizing the symptoms of early depression, Dr. Bullock restarted his medication. But this time, the same SSRI only made things worse. He went from sleeping 8 hours to 90 minutes a night. He felt angry. One day, he went on a furious 22-mile run. Plus, within the first 6 months of moving to San Francisco, Dr. Bullock was stopped by the police three different times while riding his bike. He attributes this to his race, which has only further added to his stress. In September 2015, during his second year of medical school, Dr. Bullock attempted suicide again. This time, he was intubated in the ED and rushed to the ICU.
He was given a new diagnosis: bipolar disorder. He changed medications and lived for a time with Ms. Mahoney and his other sister, who moved from Chicago to California to be with him. “My family has helped me a lot,” he said.
Dr. Bullock was initially not sure whether he would be able to return to school after his attempted suicide. Overall, UCSF was extremely supportive, he said. That came as a relief. Medical school was a grounding force in his life, not a destabilizing one: “If I had been pushed out, it would have been really harmful to me.”
Then Dr. Bullock started residency. The sleep disruption that comes with the night shift – the resident rite of passage – triggered another episode. At first, Dr. Bullock was overly productive; his mind was active and alert after staying up all night. He worked on new research during the day instead of sleeping.
Sleep disturbance is a hallmark symptom of bipolar disorder. “Justin should never be on a 24-hour call,” said Lisa Meeks, PhD, associate professor of psychiatry and family medicine at the University of Colorado at Denver, Aurora, and a leading scholar on disability advocacy for medical trainees. When he started residency, Dr. Bullock was open with his program director about his diagnosis and sought accommodations to go to therapy each week. But he didn’t try to get out of night shifts or 24-hour calls, despite his care team urging him to do so. “I have this sense of wanting to tough it out,” he said. He also felt guilty making his peers take on his share of those challenging shifts.
In December 2019, Dr. Bullock was voluntarily hospitalized for a few days and started writing the article that would later appear in NEJM. In January, a friend and UCSF medical student completed suicide. In March, the same month his NEJM article came out, Dr. Bullock attempted suicide again. This time, he quickly recognized that he was making a mistake and called an ambulance. “For me, as far as suicide attempts go, it’s the most positive one.”
Advocating for changes in medical training
Throughout his medical training, Dr. Bullock was always open about his struggles with his peers and with the administration. He shared his suicidal thoughts at a Mental Illness Among Us event during medical school. His story resonated with peers who were surprised that Dr. Bullock, who was thriving academically, could be struggling emotionally.
During residency, he led small group discussions and gave lectures at the medical school, including a talk about his attempts to create institutional change at UCSF, such as his public fight against the college’s Fitness for Duty (FFD) assessment process. That discussion earned him an Outstanding Lecturer award. Because it was the third award he had received from the medical school, Dr. Bullock also automatically earned a lifetime teaching award. When he told his mom, a teacher herself, about the award, she joked: “Are you old enough for ‘lifetime’ anything?”
Dr. Bullock has also spoken out and actively fought against the processes within the medical community that prevent people from coming forward until it is too late. Physicians and trainees often fear that if they seek mental health treatment, they will have to disclose that treatment to a potential employer or licensing board and then be barred from practicing medicine. Because he has been open about his mental health for so long, Dr. Bullock feels that he is in a position to push back against these norms. For example, in June he coauthored another article, this time for the Journal of Hospital Medicine, describing the traumatizing FFD assessment that followed his March 2020 suicide attempt.
In that article, Dr. Bullock wrote how no mental health professional served on the UCSF Physician Well Being Committee – comprising physicians and lawyers who evaluate physician impairment or potential physician impairment – that evaluated him. Dr. Bullock was referred to an outside psychiatrist. He also describes how he was forced to release all of his psychiatric records and undergo extensive drug testing, despite having no history of substance abuse. To return to work, he had to sign a contract, agreeing to be monitored and to attend a specific kind of therapy.
While steps like these can, in the right circumstances, protect both the public and doctors-in-training in important ways, they can also “be very punitive and isolating for someone going through a mental health crisis,” said Dr. Meeks. There were also no Black physicians or lawyers on the committee evaluating Dr. Bullock. “That was really egregious, when you look back.” Dr. Meeks is a coauthor on Dr. Bullock’s JHM article and a mentor and previous student disability officer at UCSF.
Dr. Bullock raised objections to UCSF administrators about how he felt that the committee was discriminating against him because of his mental illness despite assurances from the director of his program that there have never been any performance or professionalism concerns with him. He said the administrators told him he was the first person to question the FFD process. This isn’t surprising, given that all the power in such situations usually lies with the hospital and the administrators, whereas the resident or physician is worried about losing their job and their license, said Dr. Meeks.
Dr. Bullock contends that he’s in a unique position to speak out, considering his stellar academic and work records, openness about his mental illness before a crisis, access to quality mental health care, and extensive personal network among the UCSF administration. “I know that I hold power within my institution; I spoke out because I could,” Dr. Bullock said. In addition to writing an article about his experience, Dr. Bullock shared his story with a task force appointed by the medical staff president to review the Physician Well-Being Committee and the overall FFD process. Even before Dr. Bullock shared his story with the public, the task force had already been appointed as a result of the increased concern about physician mental health during the ongoing COVID-19 pandemic, Michelle Guy, MD, clinical professor of medicine at UCSF, told this news organization.
Elizabeth Fernandez, a UCSF senior public information representative, declined to comment on Dr. Bullock’s specific experience as reported in the JHM. “As with every hospital accredited by the Joint Commission, UCSF Medical Center has a Physician Well Being Committee that provides resources for physicians who may need help with chemical dependency or mental illness,” Ms. Fernandez said.
“Our goal through this program is always, first, to provide the compassion and assistance our physicians need to address the issues they face and continue to pursue their careers. This program is entirely voluntary and is bound by federal and state laws and regulations to protect the confidentiality of its participants, while ensuring that – first and foremost – no one is harmed by the situation, including the participant.”
Overcoming stigma to change the system
All of the attention – from national media outlets such as Vox to struggling peers and others – is fulfilling, Dr. Bullock said. But it can also be overwhelming. “I have definitely been praised as ‘Black excellence,’ and that definitely has added to the pressure to keep going ... to keep pushing at times,” he said.
Ms. Mahoney added: “He’s willing to sacrifice himself in order to make a difference. He would be a sacrificial lamb” for the Black community, the gay community, or any minority community.
Despite these concerns and his past suicide attempts, colleagues feel that Dr. Bullock is in a strong place to make decisions. “I trust Justin to put the boundaries up when they are needed and to engage in a way that feels comfortable for him,” said Ms. Meeks. “He is someone who has incredible self-awareness.”
Dr. Bullock’s history isn’t just something he overcame: It’s something that makes him a better, more empathetic doctor, said Ms. Mahoney. He knows what it’s like to be hospitalized, to deal with the frustration of insurance, to navigate the complexity of the health care system as a patient, or to be facing a deep internal darkness. He “can genuinely hold that person’s hand and say: ‘I know what you’re going through and we’re going to work through this day by day,’ ” she said. “That is something he can bring that no other physician can bring.”
In his advocacy on Twitter, in lectures, and in conversations with UCSF administrators, Dr. Bullock is pushing for board licensing questions to be reformed so physicians are no longer penalized for seeking mental health treatment. He would also like residency programs to make it easier and less stigmatizing for trainees to receive accommodations for a disability or mental illness.
“They say one person can’t change a system,” said Dr. Meeks, “but I do think Justin is calling an awful lot of attention to the system and I do think there will be changes because of his advocacy.”
A version of this article first appeared on Medscape.com.
In early 2020, Justin Bullock, MD, MPH, did what few, if any, resident physicians have done: He published an honest account in the New England Journal of Medicine of a would-be suicide attempt during medical training.
In the article, Dr. Bullock matter-of-factly laid out how, in 2019, intern-year night shifts contributed to a depressive episode. For Dr. Bullock, who has a bipolar disorder, sleep dysregulation can be deadly. He had a plan for completing suicide, and this wouldn’t have been his first attempt. Thanks to his history and openness about his condition, Dr. Bullock had an experienced care team that helped him get to a psychiatric hospital before anything happened. While there for around 5 days, he wrote the bulk of the NEJM article.
The article took Dr. Bullock’s impact nationwide. On Twitter and in interviews, Dr. Bullock is an unapologetic advocate for accommodations for people in medicine with mental illness. “One of the things that inspired me to speak out early on is that I feel I stand in a place of so much privilege,” Dr. Bullock told this news organization. “I often feel this sense of ... ‘you have to speak up, Justin; no one else can.’ ”
Dr. Bullock’s activism is especially noteworthy, given that he is still establishing his career. In August, while an internal medicine resident at the University of California, San Francisco, he received a lifetime teaching award from UCSF because he had received three prior teaching awards; a recognition like this is considered rare someone so early in their career. Now in his final year of residency, he actively researches medical education, advocates for mental health support, and is working to become a leading voice on related issues.
“It seems to be working,” his older sister, Jacquis Mahoney, RN, said during a visit to the UCSF campus. Instead of any awkwardness, everyone is thrilled to learn that she is Justin’s sister. “There’s a lot of pride and excitement.”
Suicide attempts during medical training
Now 28, Dr. Bullock grew up in Detroit, with his mom and two older sisters. His father was incarcerated for much of Dr. Bullock’s childhood, in part because of his own bipolar disorder not being well controlled, Dr. Bullock said.
When he was younger, Dr. Bullock was the peacekeeper in the house between his two sisters, said Ms. Mahoney: “Justin was always very delicate and kind.”
He played soccer and ran track but also loved math and science. While outwardly accumulating an impressive resume, Dr. Bullock was internally struggling. In high school, he made what he now calls an “immature” attempt at suicide after coming out as gay to his family. While Dr. Bullock said he doesn’t necessarily dwell on the discrimination he has faced as a gay, Black man, his awareness of how others perceive and treat him because of his identity increases the background stress present in his daily life.
After high school, Dr. Bullock went to MIT in Boston, where he continued running and studied chemical-biological engineering. During college, Dr. Bullock thought he was going to have to withdraw from MIT because of his depression. Thankfully, he received counseling from student services and advice from a track coach who sat him down and talked about pragmatic solutions, like medication. “That was life-changing,” said Dr. Bullock.
When trying to decide between engineering and medicine, Dr. Bullock realized he preferred contemplating medical problems to engineering ones. So he applied to medical school. Dr. Bullock eventually ended up at UCSF, where he was selected to participate in the Program in Medical Education for the Urban Underserved, a 5-year track at the college for students committed to working with underserved communities.
By the time Dr. Bullock got to medical school, he was feeling good. In consultation with his psychiatrist, he thought it worthwhile to take a break from his medications. At that time, his diagnosis was major depressive disorder and he had only had one serious depressive episode, which didn’t necessarily indicate that he would need medication long-term, he said.
Dr. Bullock loved everything about medical school. “One day when I was in my first year of med school, I called my mom and said: ‘It’s like science summer camp but every day!’” he recalled.
Despite his enthusiasm, though, he began feeling something troubling. Recognizing the symptoms of early depression, Dr. Bullock restarted his medication. But this time, the same SSRI only made things worse. He went from sleeping 8 hours to 90 minutes a night. He felt angry. One day, he went on a furious 22-mile run. Plus, within the first 6 months of moving to San Francisco, Dr. Bullock was stopped by the police three different times while riding his bike. He attributes this to his race, which has only further added to his stress. In September 2015, during his second year of medical school, Dr. Bullock attempted suicide again. This time, he was intubated in the ED and rushed to the ICU.
He was given a new diagnosis: bipolar disorder. He changed medications and lived for a time with Ms. Mahoney and his other sister, who moved from Chicago to California to be with him. “My family has helped me a lot,” he said.
Dr. Bullock was initially not sure whether he would be able to return to school after his attempted suicide. Overall, UCSF was extremely supportive, he said. That came as a relief. Medical school was a grounding force in his life, not a destabilizing one: “If I had been pushed out, it would have been really harmful to me.”
Then Dr. Bullock started residency. The sleep disruption that comes with the night shift – the resident rite of passage – triggered another episode. At first, Dr. Bullock was overly productive; his mind was active and alert after staying up all night. He worked on new research during the day instead of sleeping.
Sleep disturbance is a hallmark symptom of bipolar disorder. “Justin should never be on a 24-hour call,” said Lisa Meeks, PhD, associate professor of psychiatry and family medicine at the University of Colorado at Denver, Aurora, and a leading scholar on disability advocacy for medical trainees. When he started residency, Dr. Bullock was open with his program director about his diagnosis and sought accommodations to go to therapy each week. But he didn’t try to get out of night shifts or 24-hour calls, despite his care team urging him to do so. “I have this sense of wanting to tough it out,” he said. He also felt guilty making his peers take on his share of those challenging shifts.
In December 2019, Dr. Bullock was voluntarily hospitalized for a few days and started writing the article that would later appear in NEJM. In January, a friend and UCSF medical student completed suicide. In March, the same month his NEJM article came out, Dr. Bullock attempted suicide again. This time, he quickly recognized that he was making a mistake and called an ambulance. “For me, as far as suicide attempts go, it’s the most positive one.”
Advocating for changes in medical training
Throughout his medical training, Dr. Bullock was always open about his struggles with his peers and with the administration. He shared his suicidal thoughts at a Mental Illness Among Us event during medical school. His story resonated with peers who were surprised that Dr. Bullock, who was thriving academically, could be struggling emotionally.
During residency, he led small group discussions and gave lectures at the medical school, including a talk about his attempts to create institutional change at UCSF, such as his public fight against the college’s Fitness for Duty (FFD) assessment process. That discussion earned him an Outstanding Lecturer award. Because it was the third award he had received from the medical school, Dr. Bullock also automatically earned a lifetime teaching award. When he told his mom, a teacher herself, about the award, she joked: “Are you old enough for ‘lifetime’ anything?”
Dr. Bullock has also spoken out and actively fought against the processes within the medical community that prevent people from coming forward until it is too late. Physicians and trainees often fear that if they seek mental health treatment, they will have to disclose that treatment to a potential employer or licensing board and then be barred from practicing medicine. Because he has been open about his mental health for so long, Dr. Bullock feels that he is in a position to push back against these norms. For example, in June he coauthored another article, this time for the Journal of Hospital Medicine, describing the traumatizing FFD assessment that followed his March 2020 suicide attempt.
In that article, Dr. Bullock wrote how no mental health professional served on the UCSF Physician Well Being Committee – comprising physicians and lawyers who evaluate physician impairment or potential physician impairment – that evaluated him. Dr. Bullock was referred to an outside psychiatrist. He also describes how he was forced to release all of his psychiatric records and undergo extensive drug testing, despite having no history of substance abuse. To return to work, he had to sign a contract, agreeing to be monitored and to attend a specific kind of therapy.
While steps like these can, in the right circumstances, protect both the public and doctors-in-training in important ways, they can also “be very punitive and isolating for someone going through a mental health crisis,” said Dr. Meeks. There were also no Black physicians or lawyers on the committee evaluating Dr. Bullock. “That was really egregious, when you look back.” Dr. Meeks is a coauthor on Dr. Bullock’s JHM article and a mentor and previous student disability officer at UCSF.
Dr. Bullock raised objections to UCSF administrators about how he felt that the committee was discriminating against him because of his mental illness despite assurances from the director of his program that there have never been any performance or professionalism concerns with him. He said the administrators told him he was the first person to question the FFD process. This isn’t surprising, given that all the power in such situations usually lies with the hospital and the administrators, whereas the resident or physician is worried about losing their job and their license, said Dr. Meeks.
Dr. Bullock contends that he’s in a unique position to speak out, considering his stellar academic and work records, openness about his mental illness before a crisis, access to quality mental health care, and extensive personal network among the UCSF administration. “I know that I hold power within my institution; I spoke out because I could,” Dr. Bullock said. In addition to writing an article about his experience, Dr. Bullock shared his story with a task force appointed by the medical staff president to review the Physician Well-Being Committee and the overall FFD process. Even before Dr. Bullock shared his story with the public, the task force had already been appointed as a result of the increased concern about physician mental health during the ongoing COVID-19 pandemic, Michelle Guy, MD, clinical professor of medicine at UCSF, told this news organization.
Elizabeth Fernandez, a UCSF senior public information representative, declined to comment on Dr. Bullock’s specific experience as reported in the JHM. “As with every hospital accredited by the Joint Commission, UCSF Medical Center has a Physician Well Being Committee that provides resources for physicians who may need help with chemical dependency or mental illness,” Ms. Fernandez said.
“Our goal through this program is always, first, to provide the compassion and assistance our physicians need to address the issues they face and continue to pursue their careers. This program is entirely voluntary and is bound by federal and state laws and regulations to protect the confidentiality of its participants, while ensuring that – first and foremost – no one is harmed by the situation, including the participant.”
Overcoming stigma to change the system
All of the attention – from national media outlets such as Vox to struggling peers and others – is fulfilling, Dr. Bullock said. But it can also be overwhelming. “I have definitely been praised as ‘Black excellence,’ and that definitely has added to the pressure to keep going ... to keep pushing at times,” he said.
Ms. Mahoney added: “He’s willing to sacrifice himself in order to make a difference. He would be a sacrificial lamb” for the Black community, the gay community, or any minority community.
Despite these concerns and his past suicide attempts, colleagues feel that Dr. Bullock is in a strong place to make decisions. “I trust Justin to put the boundaries up when they are needed and to engage in a way that feels comfortable for him,” said Ms. Meeks. “He is someone who has incredible self-awareness.”
Dr. Bullock’s history isn’t just something he overcame: It’s something that makes him a better, more empathetic doctor, said Ms. Mahoney. He knows what it’s like to be hospitalized, to deal with the frustration of insurance, to navigate the complexity of the health care system as a patient, or to be facing a deep internal darkness. He “can genuinely hold that person’s hand and say: ‘I know what you’re going through and we’re going to work through this day by day,’ ” she said. “That is something he can bring that no other physician can bring.”
In his advocacy on Twitter, in lectures, and in conversations with UCSF administrators, Dr. Bullock is pushing for board licensing questions to be reformed so physicians are no longer penalized for seeking mental health treatment. He would also like residency programs to make it easier and less stigmatizing for trainees to receive accommodations for a disability or mental illness.
“They say one person can’t change a system,” said Dr. Meeks, “but I do think Justin is calling an awful lot of attention to the system and I do think there will be changes because of his advocacy.”
A version of this article first appeared on Medscape.com.
Time to attack hypoactivity in our children
My 50th medical school reunion has come and gone. This milestone offered me another opportunity to look back over the last 5 decades of pediatrics that I have watched pass under the bridge. Triggered by the discovery of two recently published studies, this particular view back over my shoulder induced a wave of sadness, anger, and frustration that I have had trouble shaking.
The first study demonstrated a strong positive effect of exercise on academic achievement, the other found that children who were more physically active have weathered the pandemic with fewer mental health problems.
These studies are just two pieces of a growing body of evidence that our sedentary lifestyles are shortening our lives and launching our children into adulthood burdened with a raft of health risks they could possibly have avoided by being more physically active. Encountering these two papers just as the alumni office was inviting me to engage in an orgy of retrospection and introspection made me consider how little I and others in my profession have done to substantially address this scourge on our young people.
Yes, I have tried to encourage my patients to be less sedentary and more active. Yes, I have tried to set a very visible example by bicycling and walking around town. Yes, I have coached youth sports teams. All of my children and grandchildren are leading active lives and appear to be reaping the benefits. But in the grander scheme of things I feel that neither I nor the American Academy of Pediatrics has made a difference.
In March of 2020 the AAP published a clinical report that lists the numerous positive associations between activity and health that includes a comprehensive collection of suggestions for providers on how we might assess the problem of inactivity and then play a role in addressing it with our patients and our communities. Unfortunately, the message’s importance was lost in the glut of pandemic news.
While the AAP’s report should have been published many decades ago, I doubt the delay lessened its impact significantly because the report is primarily a compendium of recommendations that in the long run will be seen as just another example of us believers preaching to the choir.
Making lifestyle changes on the order of magnitude necessary to convert an increasingly sedentary population into one that unconsciously becomes physically active requires more than recommendations. It is only natural that folks have trouble saying “No.”
No to the entertainment of electronic devices. No to the comforts of all-weather enclosed transportation. No to hours on the couch. Overcoming the inertia built into our society is going to require more than encouragement, recommendations, and professional sports–sponsored presidential initiatives.
Mandate has become a politically charged dirty word. But our current experience with the COVID-19 vaccines should help us realize that there is a significant segment of the population that doesn’t like being told what to do even if the outcome is in their best interest. Education and rewards have fallen short, but the evidence is mounting that mandates can work.
There was a time when physical activity was built into every child’s school day. For a variety of bad reasons, vigorous physical education classes and once- or twice-daily outdoor recesses have disappeared from the educational landscape. It is time to return to them in a robust form. Unfortunately, because activity isn’t happening at home it will take a government mandate.
There will be pushback. Even from some educators whose observations should have shown them the critical role of physical activity in health and academic success. We must move the distraction of the phenomenon once known simply as hyperactivity to the back burner and tackle the real epidemic of hypoactivity that is destroying our children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
My 50th medical school reunion has come and gone. This milestone offered me another opportunity to look back over the last 5 decades of pediatrics that I have watched pass under the bridge. Triggered by the discovery of two recently published studies, this particular view back over my shoulder induced a wave of sadness, anger, and frustration that I have had trouble shaking.
The first study demonstrated a strong positive effect of exercise on academic achievement, the other found that children who were more physically active have weathered the pandemic with fewer mental health problems.
These studies are just two pieces of a growing body of evidence that our sedentary lifestyles are shortening our lives and launching our children into adulthood burdened with a raft of health risks they could possibly have avoided by being more physically active. Encountering these two papers just as the alumni office was inviting me to engage in an orgy of retrospection and introspection made me consider how little I and others in my profession have done to substantially address this scourge on our young people.
Yes, I have tried to encourage my patients to be less sedentary and more active. Yes, I have tried to set a very visible example by bicycling and walking around town. Yes, I have coached youth sports teams. All of my children and grandchildren are leading active lives and appear to be reaping the benefits. But in the grander scheme of things I feel that neither I nor the American Academy of Pediatrics has made a difference.
In March of 2020 the AAP published a clinical report that lists the numerous positive associations between activity and health that includes a comprehensive collection of suggestions for providers on how we might assess the problem of inactivity and then play a role in addressing it with our patients and our communities. Unfortunately, the message’s importance was lost in the glut of pandemic news.
While the AAP’s report should have been published many decades ago, I doubt the delay lessened its impact significantly because the report is primarily a compendium of recommendations that in the long run will be seen as just another example of us believers preaching to the choir.
Making lifestyle changes on the order of magnitude necessary to convert an increasingly sedentary population into one that unconsciously becomes physically active requires more than recommendations. It is only natural that folks have trouble saying “No.”
No to the entertainment of electronic devices. No to the comforts of all-weather enclosed transportation. No to hours on the couch. Overcoming the inertia built into our society is going to require more than encouragement, recommendations, and professional sports–sponsored presidential initiatives.
Mandate has become a politically charged dirty word. But our current experience with the COVID-19 vaccines should help us realize that there is a significant segment of the population that doesn’t like being told what to do even if the outcome is in their best interest. Education and rewards have fallen short, but the evidence is mounting that mandates can work.
There was a time when physical activity was built into every child’s school day. For a variety of bad reasons, vigorous physical education classes and once- or twice-daily outdoor recesses have disappeared from the educational landscape. It is time to return to them in a robust form. Unfortunately, because activity isn’t happening at home it will take a government mandate.
There will be pushback. Even from some educators whose observations should have shown them the critical role of physical activity in health and academic success. We must move the distraction of the phenomenon once known simply as hyperactivity to the back burner and tackle the real epidemic of hypoactivity that is destroying our children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
My 50th medical school reunion has come and gone. This milestone offered me another opportunity to look back over the last 5 decades of pediatrics that I have watched pass under the bridge. Triggered by the discovery of two recently published studies, this particular view back over my shoulder induced a wave of sadness, anger, and frustration that I have had trouble shaking.
The first study demonstrated a strong positive effect of exercise on academic achievement, the other found that children who were more physically active have weathered the pandemic with fewer mental health problems.
These studies are just two pieces of a growing body of evidence that our sedentary lifestyles are shortening our lives and launching our children into adulthood burdened with a raft of health risks they could possibly have avoided by being more physically active. Encountering these two papers just as the alumni office was inviting me to engage in an orgy of retrospection and introspection made me consider how little I and others in my profession have done to substantially address this scourge on our young people.
Yes, I have tried to encourage my patients to be less sedentary and more active. Yes, I have tried to set a very visible example by bicycling and walking around town. Yes, I have coached youth sports teams. All of my children and grandchildren are leading active lives and appear to be reaping the benefits. But in the grander scheme of things I feel that neither I nor the American Academy of Pediatrics has made a difference.
In March of 2020 the AAP published a clinical report that lists the numerous positive associations between activity and health that includes a comprehensive collection of suggestions for providers on how we might assess the problem of inactivity and then play a role in addressing it with our patients and our communities. Unfortunately, the message’s importance was lost in the glut of pandemic news.
While the AAP’s report should have been published many decades ago, I doubt the delay lessened its impact significantly because the report is primarily a compendium of recommendations that in the long run will be seen as just another example of us believers preaching to the choir.
Making lifestyle changes on the order of magnitude necessary to convert an increasingly sedentary population into one that unconsciously becomes physically active requires more than recommendations. It is only natural that folks have trouble saying “No.”
No to the entertainment of electronic devices. No to the comforts of all-weather enclosed transportation. No to hours on the couch. Overcoming the inertia built into our society is going to require more than encouragement, recommendations, and professional sports–sponsored presidential initiatives.
Mandate has become a politically charged dirty word. But our current experience with the COVID-19 vaccines should help us realize that there is a significant segment of the population that doesn’t like being told what to do even if the outcome is in their best interest. Education and rewards have fallen short, but the evidence is mounting that mandates can work.
There was a time when physical activity was built into every child’s school day. For a variety of bad reasons, vigorous physical education classes and once- or twice-daily outdoor recesses have disappeared from the educational landscape. It is time to return to them in a robust form. Unfortunately, because activity isn’t happening at home it will take a government mandate.
There will be pushback. Even from some educators whose observations should have shown them the critical role of physical activity in health and academic success. We must move the distraction of the phenomenon once known simply as hyperactivity to the back burner and tackle the real epidemic of hypoactivity that is destroying our children.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at pdnews@mdedge.com.
FDA not recognizing efficacy of psychopharmacologic therapies
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
Many years ago, drug development in psychiatry turned to control of specific symptoms across disorders rather than within disorders, but regulatory agencies are still not yet on board, according to an expert psychopharmacologist outlining the ongoing evolution at the virtual Psychopharmacology Update presented by Current Psychiatry and the American Academy of Clinical Psychiatrists, sponsored by Medscape Live.
If this reorientation is going to lead to the broad indications the newer drugs likely deserve, which is control of specific types of symptoms regardless of the diagnosis, “we have to move the [Food and Drug Administration] along,” said Stephen M. Stahl, MD, PhD, chairman of the Neuroscience Institute and an adjunct professor of psychiatry at the University of California, San Diego.
On the side of drug development and clinical practice, the reorientation has already taken place. Dr. Stahl described numerous brain circuits known to produce symptoms when function is altered that are now treatment targets. This includes the ventral medial prefrontal cortex where deficient information processing leads to depression and the orbital frontal cortex where altered function leads to impulsivity.
“It is not like each part of the brain does a little bit of everything. Rather, each part of the brain has an assignment and duty and function,” Dr. Stahl explained. By addressing the disturbed signaling in brain circuits that lead to depression, impulsivity, agitation, or other symptoms, there is an opportunity for control, regardless of the psychiatric diagnosis with which the symptom is associated.
For example, Dr. Stahl predicted that pimavanserin, a highly selective 5-HT2A inverse agonist that is already approved for psychosis in Parkinson’s disease, is now likely to be approved for psychosis associated with other conditions on the basis of recent positive clinical studies in these other disorders.
Brexpiprazole, a serotonin-dopamine activity modulator already known to be useful for control of the agitation characteristic of schizophrenia, is now showing the same type of activity against agitation when it is associated with Alzheimer’s disease. Again, Dr. Stahl thinks this drug is on course for an indication across diseases once studies are conducted in each disease individually.
Another drug being evaluated for agitation, the N-methyl-D-aspartate receptor antagonist dextromethorphan bupropion, is also being tested for treatment of symptoms across multiple disorders, he reported.
However, the FDA has so far taken the position that each drug must be tested separately for a given symptom in each disorder for which it is being considered despite the underlying premise that it is the symptom, not the disease, that is important.
Unlike physiological diseases where symptoms, like a fever or abdominal cramps, are the product of a disease, psychiatric symptoms are the disease and a fundamental target – regardless of the DSM-based diagnosis.
To some degree, the symptoms of psychiatric disorders have always been the focus of treatment, but a pivot toward developing therapies that will control a symptom regardless of the underlying diagnosis is an important conceptual change. It is being made possible by advances in the detail with which the neuropathology of these symptoms is understood .
“By my count, 79 symptoms are described in DSM-5, but they are spread across hundreds of syndromes because they are grouped together in different ways,” Dr. Stahl observed.
He noted that clinicians make a diagnosis on the basis symptom groupings, but their interventions are selected to address the manifestations of the disease, not the disease itself.
“If you are a real psychopharmacologist treating real patients, you are treating the specific symptoms of the specific patient,” according to Dr. Stahl.
So far, the FDA has not made this leap, insisting on trials in these categorical disorders rather than permitting trial designs that allow benefit to be demonstrated against a symptom regardless of the syndrome with which it is associated.
Of egregious examples, Dr. Stahl recounted a recent trial of a 5-HT2 antagonist that looked so promising against psychosis in Alzheimer’s disease that the trialists enrolled patients with psychosis regardless of type of dementia, such as vascular dementia and Lewy body disease. The efficacy was impressive.
“It worked so well that they stopped the trial, but the FDA declined to approve it,” Dr. Stahl recounted. Despite clear evidence of benefit, the regulators insisted that the investigators needed to show a significant benefit in each condition individually.
While the trial investigators acknowledged that there was not enough power in the trial to show a statistically significant benefit in each category, they argued that the overall benefit and the consistent response across categories required them to stop the trial for ethical reasons.
“That’s your problem, the FDA said to the investigators,” according to Dr. Stahl.
The failure of the FDA to recognize the efficacy of psychopharmacologic therapies across symptoms regardless of the associated disease is a failure to stay current with an important evolution in medicine, Dr. Stahl indicated.
“What we have come to understand is the neurobiology of any given symptom is likely to be the same across disorders,” he said.
Agency’s arbitrary decisions cited
“I completely agree with Dr. Stahl,” said Henry A. Nasrallah, MD, professor of psychiatry, neurology, and neuroscience, University of Cincinnati.
In addition to the fact that symptoms are present across multiple categories, many patients manifest multiple symptoms at one time, Dr. Nasrallah pointed out. For neurodegenerative disorders associated with psychosis, depression, anxiety, aggression, and other symptoms, it is already well known that the heterogeneous symptoms “cannot be treated with a single drug,” he said. Rather different drugs targeting each symptom individually is essential for effective management.
Dr. Nasrallah, who chaired the Psychopharmacology Update meeting, has made this point many times in the past, including in his role as the editor of Current Psychiatry. In one editorial 10 years ago, he wrote that “it makes little sense for the FDA to mandate that a drug must work for a DSM diagnosis instead of specific symptoms.”
“The FDA must update its old policy, which has led to the widespread off-label use of psychiatric drugs, an artificial concept, simply because the FDA arbitrarily decided a long time ago that new drugs must be approved for a specific DSM diagnosis,” Dr. Nasrallah said.
Dr. Stahl reported financial relationships with more than 20 pharmaceutical companies, including those that are involved in the development of drugs included in his talk. Medscape Live and this news organization are owned by the same parent company.
FROM PSYCHOPHARMACOLOGY UPDATE