User login
Conflicting blood pressure targets: Déjà vu all over again
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
New ESH hypertension guidelines aim for simplified message
The guidelines, which are endorsed by the European Renal Association and the International Society of Hypertension, were presented during the annual European Meeting on Hypertension and Cardiovascular Protection Meeting in Milan, Italy.
The guidelines consensus document was also published online in the Journal of Hypertension. Giuseppe Mancia, MD, professor emeritus of medicine, University Milano-Bicocca, Italy, and Reinhold Kreutz, MD, PhD, Charité–University Medicine Berlin, were cochairs of the task force that created the document.
“We have tried to provide a simplified message to key topics with these new guidelines,” Dr. Kreutz said in an interview.
“We have confirmed the definition of hypertension and provide clear guidance for blood pressure monitoring and a simplified general strategy targeting similar blood pressure goals for most patients, although the treatment algorithms of how you get there may be different for different patient groups.”
Dr. Kreutz added: “Because hypertension is so prevalent and many patients have comorbidities, it is not easy to have one approach for all, but we have tried to simplify the key messages as much as possible, with a target that is more general to the whole population.”
While there are no major surprises in the guidelines, there are multiple advances and added-value changes, including clear advice on how to measure blood pressure, an upgrade for beta-blockers in the treatment algorithms, and a new definition and treatment recommendations for “true resistant hypertension.”
Definition remains unchanged
The definition of hypertension remains unchanged from the previous guidelines – repeated office systolic blood pressure values of ≥ 140 mm Hg and/or diastolic blood pressure values of ≥ 90 mm Hg.
“The definition and classification of hypertension has not changed in these new guidelines,” Dr. Kreutz said. “While there have been suggestions that the definition/target should be changed again, particularly about blood pressure lowering being beneficial at the very low pressure range, after reviewing all the evidence we do not agree with this, and we are standing with the definition of hypertension when intervention is beneficial rather than doing nothing or causing harm.”
Clear guidance on measurement
Dr. Kreutz points out that the correct measurement of blood pressure is of key importance, and the new guidelines include a detailed algorithm on how to measure blood pressure. The preferred method is automated cuff-based blood pressure measurement.
“There are still many variations in blood pressure measurement in clinical practice, so we now have clear guidance on how to measure blood pressure in the office but also at home,” he commented.
They have upgraded the use of out-of-office blood pressure measurement, particularly home measurement, as useful in long-term management. “In future, there should be more emphasis on follow-up using technology with remote control and virtual care.”
Thresholds for starting treatment
On thresholds for initiating antihypertensive therapy, the guidelines recommend that treatment be initiated for most patients when systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg.
The same recommendation is given for patients with grade 1 hypertension (systolic, 140-159 mm Hg; and/or diastolic, 90-99 mm Hg) irrespective of cardiovascular risk, although they add that for patients in the lower blood pressure range who have no hypertension-mediated organ damage and who are at low cardiovascular risk, consideration may be given to starting treatment with lifestyle changes only. If, however, blood pressure control is not achieved within a few months of a lifestyle-based approach alone, drug treatment is necessary.
For older patients (aged 80 or older), the task force recommends initiation of drug treatment at 160 mm Hg systolic, although a lower systolic threshold of 140-160 mm Hg may be considered. The authors note that thresholds for the initiation of drug treatment for very frail patients should be individualized.
Blood pressure targets
In the new guidelines, the blood pressure target is the same as in the previous guidelines for the general population of patients with hypertension. The goal is < 140/80 mm Hg for most patients. This accounts for the major portion of the protective effect of blood pressure lowering.
However, the consensus document notes that despite the smaller incremental benefit, an effort should be made to reach a range of 120-129/70-79 mm Hg, but only if treatment is well tolerated to avoid the risk of treatment discontinuation because of adverse events, which might offset, in part or completely, the incremental reduction in cardiovascular outcomes.
Elaborating on this, Dr. Kreutz said, “We should aim for the systolic blood pressure to be within the range of below 140 mm Hg down to 120 mm Hg, with a specific target of around 130 mm Hg for most patients and lower in patients in whom drug treatments are well tolerated and who are at high risk.
“The problem is, if we go for a target of lower that 130 mm Hg, the evidence gets weaker, the benefits diminish, and we risk losing patients because of adverse effects from using so many drugs,” he added. “But in younger and fitter patients, we would recommend the lower the better, but not below 120 mm Hg.”
Dr. Kreutz noted that the new guidelines have tried to simplify recommendations on target pressures. “We have tried to simplify guidance to focus on a target of around 130 for almost all patients. Before, it wasn’t so clear. There were different targets for different groups of patients with various comorbidities or older patients. But now we are saying the range of 120 to 139 is suitable for the vast majority of patients.”
The guidelines do allow slightly higher targets for older and very frail patients.
Drug treatments
The guidelines advise that blood pressure lowering be prioritized over the selection of specific antihypertensive drug classes. The use of any of the five major drug classes – angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium blockers, and thiazide/thiazidelike diuretics – and their combinations are recommended as the basis of antihypertensive treatment strategies.
They advise starting with a two-drug combination for most patients. The preferred combinations including a renin-angiotensin blocker (either an ACE inhibitor or an ARB) with a calcium blocker or a thiazide/thiazidelike diuretic, preferably in a single-pill combination to reduce pill burden and improve adherence and outcome.
If blood pressure is not controlled with the initial two-drug combination at the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination.
“We can control 60% of patients in the general hypertensive population with dual therapy, and up to 90% with triple therapy,” Dr. Kreutz said. “Only a small percentage need a fourth drug.”
A new feature of the guidelines is the upgrading of beta-blockers in the treatment algorithms.
“Beta-blockers may not have previously been considered as a first choice of antihypertensive medication, but we see that in clinical practice, many patients are actually treated with these drugs because there are so many conditions in which beta-blockers have a compelling evidence-based indication or are believed to be favorable,” he said. “So, we are now positioning beta-blockers as drugs that can be used at any step of the treatment algorithm if there is a guideline directed indication or other conditions for which they are thought to be beneficial.”
The guidelines also recommend that all drugs be given as once-daily preparations and that they be taken preferably in the morning.
“The new TIME study has established that there is no difference in outcome with morning or evening dosing, but we know that adherence is often better when drugs are taken in the morning, and it is not advisable to take diuretics in the evening,” Dr. Kreutz said.
‘True resistant hypertension’
The guidelines have introduced a new term, “true resistant hypertension,” defined as systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mm Hg in the presence of the following conditions: the maximum recommended and tolerated doses of a three-drug combination comprising a renin-angiotensin system blocker (either an ACE inhibitor or an ARB), a calcium blocker, and a thiazide/thiazidelike diuretic were used; inadequate blood pressure control has been confirmed by ambulatory (preferable) or home blood pressure measurement; and various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
“There are many patients who may appear to have resistant hypertension, but we need to screen them carefully to ensure they are adherent to treatment, and then most of these patients are found not to be truly resistant,” Dr. Kreutz explained. “We estimate that only about 5% of patients have true resistant hypertension.”
For these patients with true resistant hypertension, two treatment approaches are recommended.
For those who do not have advanced kidney disease (glomerular filtration rate > 40 mL/min), renal denervation can be considered. This is a new II B recommendation.
Dr. Kreutz noted that studies of renal denervation excluded patients with advanced kidney disease, so there are no data for this group. For these patients, the guidelines suggest that a combination diuretic approach (chlorthalidone with a loop diuretic) could be considered in light of the results of the recent CLICK study.
Differences from U.S. guidelines?
Commenting on the new European guidelines for this news organization, Paul Whelton, MD, chair of the most recent American College of Cardiology/American Heart Association hypertension guidelines committee, said: “Publication of these guidelines is important. I congratulate the European task force. It is an enormous amount of time and effort.”
Dr. Whelton, who is Show Chwan Chair in Global Public Health at Tulane University, New Orleans, and president of the World Hypertension League, added: “I would say the changes are incremental rather than major, but that is probably appropriate.”
He welcomed the greater emphasis on out-of-office blood pressure measurement, saying, “That’s where we should be headed.”
Asked how the European guidelines differ from the U.S. guidelines, Dr. Whelton commented: “There are differences, but they are not huge. The major hypertension guidelines across the world are much more alike than they are different.”
He pointed out that both the U.S. and European guidelines aim for a target blood pressure of 130/80 mm Hg for most patients but have different ways of issuing that advice.
“The Europeans recommend a minimum goal of 140/90 mm Hg, and if there are no issues, then press on to get to under 130/80 mm Hg. That’s kind of a two-step process,” he said. “In the U.S., we’ve gone for a more direct approach of just recommending less than 130/80 mm Hg.
“My fear with the European approach is that by saying, get to 140/90 mm Hg first, then move on to 130/80 mm Hg, is that you’re likely to lose people. And doctors could feel that 140/90 is fine.”
More effort needed on implementation
Dr. Whelton says that where all hypertension guidelines are lacking is in the implementation of the recommendations.
“We are all falling down on implementation,” he said. “We have a huge burden of illness, and it is a very cost-effective area for management, but still, rates of blood pressure control are very bad. Generally speaking, even with a very conservative target of 140/90, the best countries only have control rates of around 30%, and this can be as low as 8% in some low/middle-income countries.”
Dr. Whelton believes the approach to blood pressure management needs to change.
“We know that the current traditional model of care, where blood pressure is managed by your local doctor, is not working. It is hopeless,” he said. “That is not an indictment of these doctors. It’s just that they have more pressing issues to deal with, so we need to look at other models.”
He suggests that the way forward is through convenient, community-based care delivered by a team in which nonphysicians assist in much of the management and in which reliable, affordable medications are given at the point of care, with patients tracked with electronic health records so as to identify those who are not adhering to their medication regimens.
“We know that using simple protocols will work for the vast majority of people. We don’t need to individualize or complicate this too much. That tends to lose people in the process.”
Dr. Whelton makes the point that it is well known how to diagnose and treat hypertension, yet this is not being done well.
“We are doing these things really badly. In routine care, blood pressure is measured horribly. Nobody would accept a pilot of a plane saying he should be doing all these procedures but he’s too busy and it’s probably okay, but that’s the way blood pressure is often measured in clinical practice,” he added. “And we can’t really do a good job if were not measuring the key variable properly that the diagnosis is based on.”
Dr. Whelton also points out that the medical profession is not making enough effort to have patients reach target levels.
“If you’re in a country where very few people are being treated and very high pressures are common, then of course you have to focus on that group first. But in most of the Western world, we are long past that, so we can move on down the chain. We then get to a lot more people with moderately high blood pressure getting exposed to increases in risk, and while this is not quite as dramatic as those with very high pressures at the individual risk level, because there are so many of them, that’s where a lot of events are occurring,” he says.
“If we get everyone to 140/90 mm Hg, we can probably prevent 60% of blood pressure–related events. But if we can get them all down to 130 mm Hg systolic, then we can prevent 75%-80% of events. It’s often quite easy to get to that target, but patients need help and encouragement.”
Going forward, he concluded, guidelines should pivot to focus more on implementation.
“We all try to make the guidelines as approachable as possible, but they are encyclopedic, and many doctors just continue doing what they are doing. That is our big challenge.”
A version of this article first appeared on Medscape.com.
The guidelines, which are endorsed by the European Renal Association and the International Society of Hypertension, were presented during the annual European Meeting on Hypertension and Cardiovascular Protection Meeting in Milan, Italy.
The guidelines consensus document was also published online in the Journal of Hypertension. Giuseppe Mancia, MD, professor emeritus of medicine, University Milano-Bicocca, Italy, and Reinhold Kreutz, MD, PhD, Charité–University Medicine Berlin, were cochairs of the task force that created the document.
“We have tried to provide a simplified message to key topics with these new guidelines,” Dr. Kreutz said in an interview.
“We have confirmed the definition of hypertension and provide clear guidance for blood pressure monitoring and a simplified general strategy targeting similar blood pressure goals for most patients, although the treatment algorithms of how you get there may be different for different patient groups.”
Dr. Kreutz added: “Because hypertension is so prevalent and many patients have comorbidities, it is not easy to have one approach for all, but we have tried to simplify the key messages as much as possible, with a target that is more general to the whole population.”
While there are no major surprises in the guidelines, there are multiple advances and added-value changes, including clear advice on how to measure blood pressure, an upgrade for beta-blockers in the treatment algorithms, and a new definition and treatment recommendations for “true resistant hypertension.”
Definition remains unchanged
The definition of hypertension remains unchanged from the previous guidelines – repeated office systolic blood pressure values of ≥ 140 mm Hg and/or diastolic blood pressure values of ≥ 90 mm Hg.
“The definition and classification of hypertension has not changed in these new guidelines,” Dr. Kreutz said. “While there have been suggestions that the definition/target should be changed again, particularly about blood pressure lowering being beneficial at the very low pressure range, after reviewing all the evidence we do not agree with this, and we are standing with the definition of hypertension when intervention is beneficial rather than doing nothing or causing harm.”
Clear guidance on measurement
Dr. Kreutz points out that the correct measurement of blood pressure is of key importance, and the new guidelines include a detailed algorithm on how to measure blood pressure. The preferred method is automated cuff-based blood pressure measurement.
“There are still many variations in blood pressure measurement in clinical practice, so we now have clear guidance on how to measure blood pressure in the office but also at home,” he commented.
They have upgraded the use of out-of-office blood pressure measurement, particularly home measurement, as useful in long-term management. “In future, there should be more emphasis on follow-up using technology with remote control and virtual care.”
Thresholds for starting treatment
On thresholds for initiating antihypertensive therapy, the guidelines recommend that treatment be initiated for most patients when systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg.
The same recommendation is given for patients with grade 1 hypertension (systolic, 140-159 mm Hg; and/or diastolic, 90-99 mm Hg) irrespective of cardiovascular risk, although they add that for patients in the lower blood pressure range who have no hypertension-mediated organ damage and who are at low cardiovascular risk, consideration may be given to starting treatment with lifestyle changes only. If, however, blood pressure control is not achieved within a few months of a lifestyle-based approach alone, drug treatment is necessary.
For older patients (aged 80 or older), the task force recommends initiation of drug treatment at 160 mm Hg systolic, although a lower systolic threshold of 140-160 mm Hg may be considered. The authors note that thresholds for the initiation of drug treatment for very frail patients should be individualized.
Blood pressure targets
In the new guidelines, the blood pressure target is the same as in the previous guidelines for the general population of patients with hypertension. The goal is < 140/80 mm Hg for most patients. This accounts for the major portion of the protective effect of blood pressure lowering.
However, the consensus document notes that despite the smaller incremental benefit, an effort should be made to reach a range of 120-129/70-79 mm Hg, but only if treatment is well tolerated to avoid the risk of treatment discontinuation because of adverse events, which might offset, in part or completely, the incremental reduction in cardiovascular outcomes.
Elaborating on this, Dr. Kreutz said, “We should aim for the systolic blood pressure to be within the range of below 140 mm Hg down to 120 mm Hg, with a specific target of around 130 mm Hg for most patients and lower in patients in whom drug treatments are well tolerated and who are at high risk.
“The problem is, if we go for a target of lower that 130 mm Hg, the evidence gets weaker, the benefits diminish, and we risk losing patients because of adverse effects from using so many drugs,” he added. “But in younger and fitter patients, we would recommend the lower the better, but not below 120 mm Hg.”
Dr. Kreutz noted that the new guidelines have tried to simplify recommendations on target pressures. “We have tried to simplify guidance to focus on a target of around 130 for almost all patients. Before, it wasn’t so clear. There were different targets for different groups of patients with various comorbidities or older patients. But now we are saying the range of 120 to 139 is suitable for the vast majority of patients.”
The guidelines do allow slightly higher targets for older and very frail patients.
Drug treatments
The guidelines advise that blood pressure lowering be prioritized over the selection of specific antihypertensive drug classes. The use of any of the five major drug classes – angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium blockers, and thiazide/thiazidelike diuretics – and their combinations are recommended as the basis of antihypertensive treatment strategies.
They advise starting with a two-drug combination for most patients. The preferred combinations including a renin-angiotensin blocker (either an ACE inhibitor or an ARB) with a calcium blocker or a thiazide/thiazidelike diuretic, preferably in a single-pill combination to reduce pill burden and improve adherence and outcome.
If blood pressure is not controlled with the initial two-drug combination at the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination.
“We can control 60% of patients in the general hypertensive population with dual therapy, and up to 90% with triple therapy,” Dr. Kreutz said. “Only a small percentage need a fourth drug.”
A new feature of the guidelines is the upgrading of beta-blockers in the treatment algorithms.
“Beta-blockers may not have previously been considered as a first choice of antihypertensive medication, but we see that in clinical practice, many patients are actually treated with these drugs because there are so many conditions in which beta-blockers have a compelling evidence-based indication or are believed to be favorable,” he said. “So, we are now positioning beta-blockers as drugs that can be used at any step of the treatment algorithm if there is a guideline directed indication or other conditions for which they are thought to be beneficial.”
The guidelines also recommend that all drugs be given as once-daily preparations and that they be taken preferably in the morning.
“The new TIME study has established that there is no difference in outcome with morning or evening dosing, but we know that adherence is often better when drugs are taken in the morning, and it is not advisable to take diuretics in the evening,” Dr. Kreutz said.
‘True resistant hypertension’
The guidelines have introduced a new term, “true resistant hypertension,” defined as systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mm Hg in the presence of the following conditions: the maximum recommended and tolerated doses of a three-drug combination comprising a renin-angiotensin system blocker (either an ACE inhibitor or an ARB), a calcium blocker, and a thiazide/thiazidelike diuretic were used; inadequate blood pressure control has been confirmed by ambulatory (preferable) or home blood pressure measurement; and various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
“There are many patients who may appear to have resistant hypertension, but we need to screen them carefully to ensure they are adherent to treatment, and then most of these patients are found not to be truly resistant,” Dr. Kreutz explained. “We estimate that only about 5% of patients have true resistant hypertension.”
For these patients with true resistant hypertension, two treatment approaches are recommended.
For those who do not have advanced kidney disease (glomerular filtration rate > 40 mL/min), renal denervation can be considered. This is a new II B recommendation.
Dr. Kreutz noted that studies of renal denervation excluded patients with advanced kidney disease, so there are no data for this group. For these patients, the guidelines suggest that a combination diuretic approach (chlorthalidone with a loop diuretic) could be considered in light of the results of the recent CLICK study.
Differences from U.S. guidelines?
Commenting on the new European guidelines for this news organization, Paul Whelton, MD, chair of the most recent American College of Cardiology/American Heart Association hypertension guidelines committee, said: “Publication of these guidelines is important. I congratulate the European task force. It is an enormous amount of time and effort.”
Dr. Whelton, who is Show Chwan Chair in Global Public Health at Tulane University, New Orleans, and president of the World Hypertension League, added: “I would say the changes are incremental rather than major, but that is probably appropriate.”
He welcomed the greater emphasis on out-of-office blood pressure measurement, saying, “That’s where we should be headed.”
Asked how the European guidelines differ from the U.S. guidelines, Dr. Whelton commented: “There are differences, but they are not huge. The major hypertension guidelines across the world are much more alike than they are different.”
He pointed out that both the U.S. and European guidelines aim for a target blood pressure of 130/80 mm Hg for most patients but have different ways of issuing that advice.
“The Europeans recommend a minimum goal of 140/90 mm Hg, and if there are no issues, then press on to get to under 130/80 mm Hg. That’s kind of a two-step process,” he said. “In the U.S., we’ve gone for a more direct approach of just recommending less than 130/80 mm Hg.
“My fear with the European approach is that by saying, get to 140/90 mm Hg first, then move on to 130/80 mm Hg, is that you’re likely to lose people. And doctors could feel that 140/90 is fine.”
More effort needed on implementation
Dr. Whelton says that where all hypertension guidelines are lacking is in the implementation of the recommendations.
“We are all falling down on implementation,” he said. “We have a huge burden of illness, and it is a very cost-effective area for management, but still, rates of blood pressure control are very bad. Generally speaking, even with a very conservative target of 140/90, the best countries only have control rates of around 30%, and this can be as low as 8% in some low/middle-income countries.”
Dr. Whelton believes the approach to blood pressure management needs to change.
“We know that the current traditional model of care, where blood pressure is managed by your local doctor, is not working. It is hopeless,” he said. “That is not an indictment of these doctors. It’s just that they have more pressing issues to deal with, so we need to look at other models.”
He suggests that the way forward is through convenient, community-based care delivered by a team in which nonphysicians assist in much of the management and in which reliable, affordable medications are given at the point of care, with patients tracked with electronic health records so as to identify those who are not adhering to their medication regimens.
“We know that using simple protocols will work for the vast majority of people. We don’t need to individualize or complicate this too much. That tends to lose people in the process.”
Dr. Whelton makes the point that it is well known how to diagnose and treat hypertension, yet this is not being done well.
“We are doing these things really badly. In routine care, blood pressure is measured horribly. Nobody would accept a pilot of a plane saying he should be doing all these procedures but he’s too busy and it’s probably okay, but that’s the way blood pressure is often measured in clinical practice,” he added. “And we can’t really do a good job if were not measuring the key variable properly that the diagnosis is based on.”
Dr. Whelton also points out that the medical profession is not making enough effort to have patients reach target levels.
“If you’re in a country where very few people are being treated and very high pressures are common, then of course you have to focus on that group first. But in most of the Western world, we are long past that, so we can move on down the chain. We then get to a lot more people with moderately high blood pressure getting exposed to increases in risk, and while this is not quite as dramatic as those with very high pressures at the individual risk level, because there are so many of them, that’s where a lot of events are occurring,” he says.
“If we get everyone to 140/90 mm Hg, we can probably prevent 60% of blood pressure–related events. But if we can get them all down to 130 mm Hg systolic, then we can prevent 75%-80% of events. It’s often quite easy to get to that target, but patients need help and encouragement.”
Going forward, he concluded, guidelines should pivot to focus more on implementation.
“We all try to make the guidelines as approachable as possible, but they are encyclopedic, and many doctors just continue doing what they are doing. That is our big challenge.”
A version of this article first appeared on Medscape.com.
The guidelines, which are endorsed by the European Renal Association and the International Society of Hypertension, were presented during the annual European Meeting on Hypertension and Cardiovascular Protection Meeting in Milan, Italy.
The guidelines consensus document was also published online in the Journal of Hypertension. Giuseppe Mancia, MD, professor emeritus of medicine, University Milano-Bicocca, Italy, and Reinhold Kreutz, MD, PhD, Charité–University Medicine Berlin, were cochairs of the task force that created the document.
“We have tried to provide a simplified message to key topics with these new guidelines,” Dr. Kreutz said in an interview.
“We have confirmed the definition of hypertension and provide clear guidance for blood pressure monitoring and a simplified general strategy targeting similar blood pressure goals for most patients, although the treatment algorithms of how you get there may be different for different patient groups.”
Dr. Kreutz added: “Because hypertension is so prevalent and many patients have comorbidities, it is not easy to have one approach for all, but we have tried to simplify the key messages as much as possible, with a target that is more general to the whole population.”
While there are no major surprises in the guidelines, there are multiple advances and added-value changes, including clear advice on how to measure blood pressure, an upgrade for beta-blockers in the treatment algorithms, and a new definition and treatment recommendations for “true resistant hypertension.”
Definition remains unchanged
The definition of hypertension remains unchanged from the previous guidelines – repeated office systolic blood pressure values of ≥ 140 mm Hg and/or diastolic blood pressure values of ≥ 90 mm Hg.
“The definition and classification of hypertension has not changed in these new guidelines,” Dr. Kreutz said. “While there have been suggestions that the definition/target should be changed again, particularly about blood pressure lowering being beneficial at the very low pressure range, after reviewing all the evidence we do not agree with this, and we are standing with the definition of hypertension when intervention is beneficial rather than doing nothing or causing harm.”
Clear guidance on measurement
Dr. Kreutz points out that the correct measurement of blood pressure is of key importance, and the new guidelines include a detailed algorithm on how to measure blood pressure. The preferred method is automated cuff-based blood pressure measurement.
“There are still many variations in blood pressure measurement in clinical practice, so we now have clear guidance on how to measure blood pressure in the office but also at home,” he commented.
They have upgraded the use of out-of-office blood pressure measurement, particularly home measurement, as useful in long-term management. “In future, there should be more emphasis on follow-up using technology with remote control and virtual care.”
Thresholds for starting treatment
On thresholds for initiating antihypertensive therapy, the guidelines recommend that treatment be initiated for most patients when systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg.
The same recommendation is given for patients with grade 1 hypertension (systolic, 140-159 mm Hg; and/or diastolic, 90-99 mm Hg) irrespective of cardiovascular risk, although they add that for patients in the lower blood pressure range who have no hypertension-mediated organ damage and who are at low cardiovascular risk, consideration may be given to starting treatment with lifestyle changes only. If, however, blood pressure control is not achieved within a few months of a lifestyle-based approach alone, drug treatment is necessary.
For older patients (aged 80 or older), the task force recommends initiation of drug treatment at 160 mm Hg systolic, although a lower systolic threshold of 140-160 mm Hg may be considered. The authors note that thresholds for the initiation of drug treatment for very frail patients should be individualized.
Blood pressure targets
In the new guidelines, the blood pressure target is the same as in the previous guidelines for the general population of patients with hypertension. The goal is < 140/80 mm Hg for most patients. This accounts for the major portion of the protective effect of blood pressure lowering.
However, the consensus document notes that despite the smaller incremental benefit, an effort should be made to reach a range of 120-129/70-79 mm Hg, but only if treatment is well tolerated to avoid the risk of treatment discontinuation because of adverse events, which might offset, in part or completely, the incremental reduction in cardiovascular outcomes.
Elaborating on this, Dr. Kreutz said, “We should aim for the systolic blood pressure to be within the range of below 140 mm Hg down to 120 mm Hg, with a specific target of around 130 mm Hg for most patients and lower in patients in whom drug treatments are well tolerated and who are at high risk.
“The problem is, if we go for a target of lower that 130 mm Hg, the evidence gets weaker, the benefits diminish, and we risk losing patients because of adverse effects from using so many drugs,” he added. “But in younger and fitter patients, we would recommend the lower the better, but not below 120 mm Hg.”
Dr. Kreutz noted that the new guidelines have tried to simplify recommendations on target pressures. “We have tried to simplify guidance to focus on a target of around 130 for almost all patients. Before, it wasn’t so clear. There were different targets for different groups of patients with various comorbidities or older patients. But now we are saying the range of 120 to 139 is suitable for the vast majority of patients.”
The guidelines do allow slightly higher targets for older and very frail patients.
Drug treatments
The guidelines advise that blood pressure lowering be prioritized over the selection of specific antihypertensive drug classes. The use of any of the five major drug classes – angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium blockers, and thiazide/thiazidelike diuretics – and their combinations are recommended as the basis of antihypertensive treatment strategies.
They advise starting with a two-drug combination for most patients. The preferred combinations including a renin-angiotensin blocker (either an ACE inhibitor or an ARB) with a calcium blocker or a thiazide/thiazidelike diuretic, preferably in a single-pill combination to reduce pill burden and improve adherence and outcome.
If blood pressure is not controlled with the initial two-drug combination at the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination.
“We can control 60% of patients in the general hypertensive population with dual therapy, and up to 90% with triple therapy,” Dr. Kreutz said. “Only a small percentage need a fourth drug.”
A new feature of the guidelines is the upgrading of beta-blockers in the treatment algorithms.
“Beta-blockers may not have previously been considered as a first choice of antihypertensive medication, but we see that in clinical practice, many patients are actually treated with these drugs because there are so many conditions in which beta-blockers have a compelling evidence-based indication or are believed to be favorable,” he said. “So, we are now positioning beta-blockers as drugs that can be used at any step of the treatment algorithm if there is a guideline directed indication or other conditions for which they are thought to be beneficial.”
The guidelines also recommend that all drugs be given as once-daily preparations and that they be taken preferably in the morning.
“The new TIME study has established that there is no difference in outcome with morning or evening dosing, but we know that adherence is often better when drugs are taken in the morning, and it is not advisable to take diuretics in the evening,” Dr. Kreutz said.
‘True resistant hypertension’
The guidelines have introduced a new term, “true resistant hypertension,” defined as systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mm Hg in the presence of the following conditions: the maximum recommended and tolerated doses of a three-drug combination comprising a renin-angiotensin system blocker (either an ACE inhibitor or an ARB), a calcium blocker, and a thiazide/thiazidelike diuretic were used; inadequate blood pressure control has been confirmed by ambulatory (preferable) or home blood pressure measurement; and various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
“There are many patients who may appear to have resistant hypertension, but we need to screen them carefully to ensure they are adherent to treatment, and then most of these patients are found not to be truly resistant,” Dr. Kreutz explained. “We estimate that only about 5% of patients have true resistant hypertension.”
For these patients with true resistant hypertension, two treatment approaches are recommended.
For those who do not have advanced kidney disease (glomerular filtration rate > 40 mL/min), renal denervation can be considered. This is a new II B recommendation.
Dr. Kreutz noted that studies of renal denervation excluded patients with advanced kidney disease, so there are no data for this group. For these patients, the guidelines suggest that a combination diuretic approach (chlorthalidone with a loop diuretic) could be considered in light of the results of the recent CLICK study.
Differences from U.S. guidelines?
Commenting on the new European guidelines for this news organization, Paul Whelton, MD, chair of the most recent American College of Cardiology/American Heart Association hypertension guidelines committee, said: “Publication of these guidelines is important. I congratulate the European task force. It is an enormous amount of time and effort.”
Dr. Whelton, who is Show Chwan Chair in Global Public Health at Tulane University, New Orleans, and president of the World Hypertension League, added: “I would say the changes are incremental rather than major, but that is probably appropriate.”
He welcomed the greater emphasis on out-of-office blood pressure measurement, saying, “That’s where we should be headed.”
Asked how the European guidelines differ from the U.S. guidelines, Dr. Whelton commented: “There are differences, but they are not huge. The major hypertension guidelines across the world are much more alike than they are different.”
He pointed out that both the U.S. and European guidelines aim for a target blood pressure of 130/80 mm Hg for most patients but have different ways of issuing that advice.
“The Europeans recommend a minimum goal of 140/90 mm Hg, and if there are no issues, then press on to get to under 130/80 mm Hg. That’s kind of a two-step process,” he said. “In the U.S., we’ve gone for a more direct approach of just recommending less than 130/80 mm Hg.
“My fear with the European approach is that by saying, get to 140/90 mm Hg first, then move on to 130/80 mm Hg, is that you’re likely to lose people. And doctors could feel that 140/90 is fine.”
More effort needed on implementation
Dr. Whelton says that where all hypertension guidelines are lacking is in the implementation of the recommendations.
“We are all falling down on implementation,” he said. “We have a huge burden of illness, and it is a very cost-effective area for management, but still, rates of blood pressure control are very bad. Generally speaking, even with a very conservative target of 140/90, the best countries only have control rates of around 30%, and this can be as low as 8% in some low/middle-income countries.”
Dr. Whelton believes the approach to blood pressure management needs to change.
“We know that the current traditional model of care, where blood pressure is managed by your local doctor, is not working. It is hopeless,” he said. “That is not an indictment of these doctors. It’s just that they have more pressing issues to deal with, so we need to look at other models.”
He suggests that the way forward is through convenient, community-based care delivered by a team in which nonphysicians assist in much of the management and in which reliable, affordable medications are given at the point of care, with patients tracked with electronic health records so as to identify those who are not adhering to their medication regimens.
“We know that using simple protocols will work for the vast majority of people. We don’t need to individualize or complicate this too much. That tends to lose people in the process.”
Dr. Whelton makes the point that it is well known how to diagnose and treat hypertension, yet this is not being done well.
“We are doing these things really badly. In routine care, blood pressure is measured horribly. Nobody would accept a pilot of a plane saying he should be doing all these procedures but he’s too busy and it’s probably okay, but that’s the way blood pressure is often measured in clinical practice,” he added. “And we can’t really do a good job if were not measuring the key variable properly that the diagnosis is based on.”
Dr. Whelton also points out that the medical profession is not making enough effort to have patients reach target levels.
“If you’re in a country where very few people are being treated and very high pressures are common, then of course you have to focus on that group first. But in most of the Western world, we are long past that, so we can move on down the chain. We then get to a lot more people with moderately high blood pressure getting exposed to increases in risk, and while this is not quite as dramatic as those with very high pressures at the individual risk level, because there are so many of them, that’s where a lot of events are occurring,” he says.
“If we get everyone to 140/90 mm Hg, we can probably prevent 60% of blood pressure–related events. But if we can get them all down to 130 mm Hg systolic, then we can prevent 75%-80% of events. It’s often quite easy to get to that target, but patients need help and encouragement.”
Going forward, he concluded, guidelines should pivot to focus more on implementation.
“We all try to make the guidelines as approachable as possible, but they are encyclopedic, and many doctors just continue doing what they are doing. That is our big challenge.”
A version of this article first appeared on Medscape.com.
New definition for iron deficiency in CV disease proposed
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.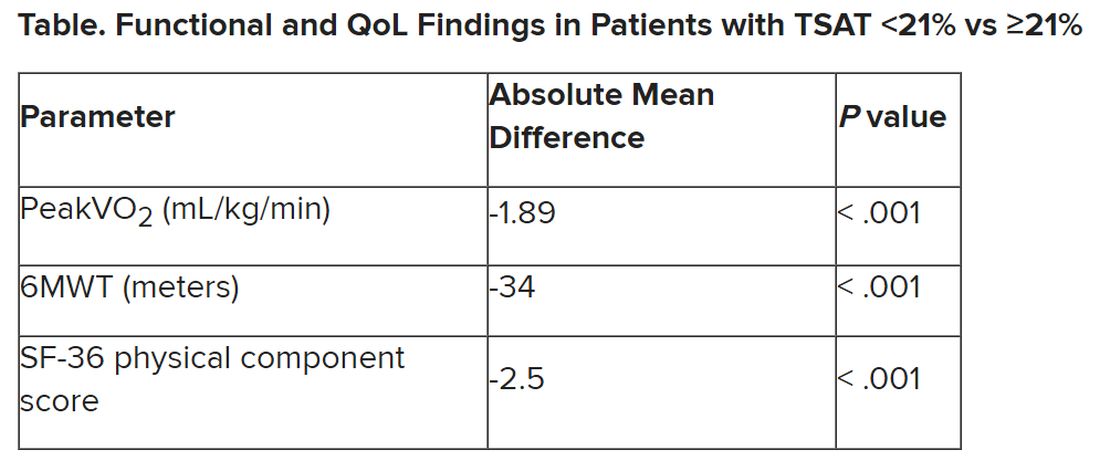
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.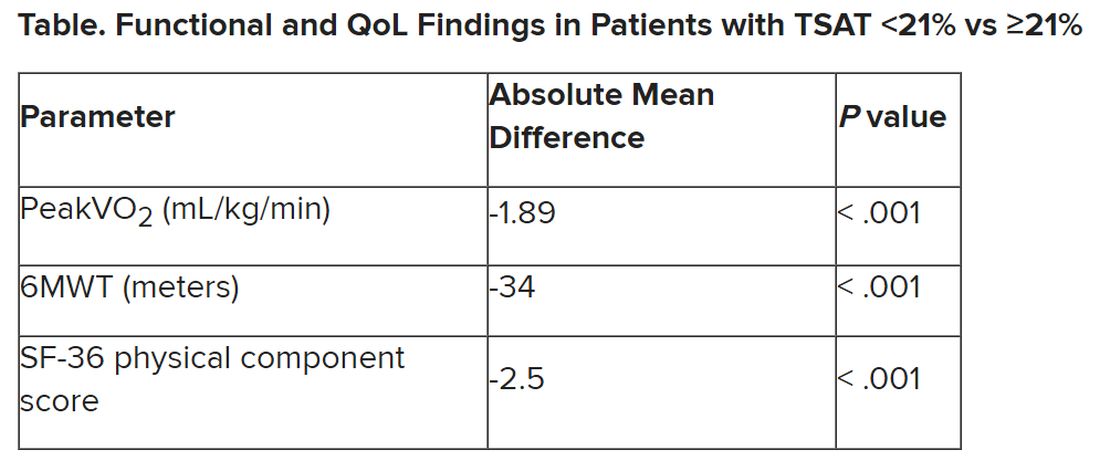
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.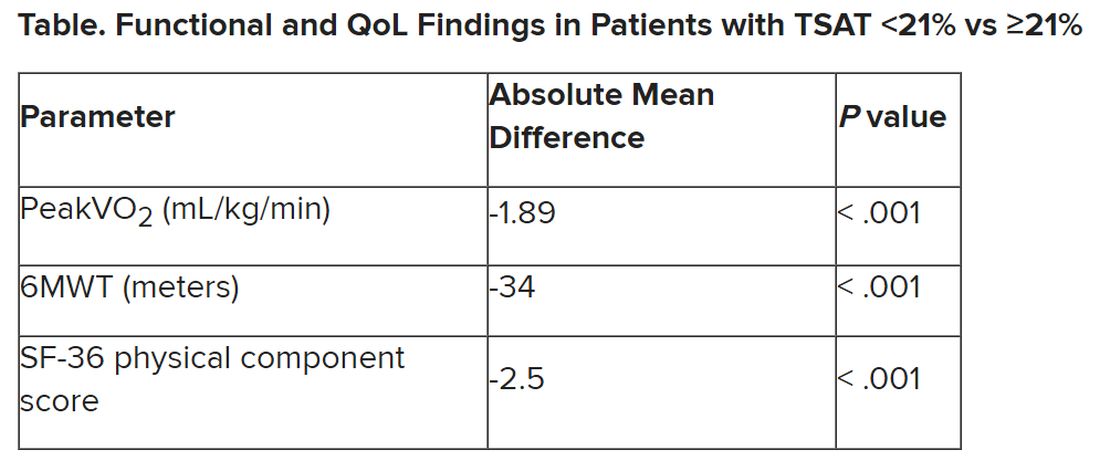
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
FROM EUROPEAN HEART JOURNAL
Low-dose oral minoxidil for hair loss soars after NYT article
.
The weekly rate of first-time low-dose oral minoxidil (LDOM) prescriptions per 10,000 outpatient encounters was “significantly higher 8 weeks after vs. 8 weeks before article publication,” at 0.9 prescriptions, compared with 0.5 per 10,000, wrote the authors of the research letter, published in JAMA Network Open. There was no similar bump for first-time finasteride or hypertension prescriptions, wrote the authors, from Harvard Medical School and Massachusetts General Hospital, Boston, and Truveta, a company that provides EHR data from U.S. health care systems.
The New York Times article noted that LDOM was relatively unknown to patients and doctors – and not approved by the Food and Drug Administration for treating hair loss – but that it was inexpensive, safe, and very effective for many individuals. “The article did not report new research findings or large-scale randomized evidence,” wrote the authors of the JAMA study.
Rodney Sinclair, MD, professor of dermatology at the University of Melbourne, who conducted the original research on LDOM and hair loss and was quoted in the Times story, told this news organization that “the sharp uplift after the New York Times article was on the back of a gradual increase.” He added that “the momentum for minoxidil prescriptions is increasing,” so much so that it has led to a global shortage of LDOM. The drug appears to still be widely available in the United States, however. It is not on the ASHP shortages list.
“There has been growing momentum for minoxidil use since I first presented our data about 6 years ago,” Dr. Sinclair said. He noted that 2022 International Society of Hair Restoration Surgery survey data found that 26% of treating physicians always or often prescribed off-label oral minoxidil, up from 10% in 2019 and 0% in 2017, while another 20% said they prescribed it sometimes.
The authors of the new study looked at prescriptions for patients at eight health care systems before and after the Times article was published in August 2022. They calculated the rate of first-time oral minoxidil prescriptions for 2.5 mg and 5 mg tablets, excluding 10 mg tablets, which are prescribed for hypertension.
Among those receiving first-time prescriptions, 2,846 received them in the 7 months before the article and 3,695 in the 5 months after publication. Men (43.6% after vs. 37.7% before publication) and White individuals (68.6% after vs. 60.8% before publication) accounted for a higher proportion of prescriptions after the article was published. There was a 2.4-fold increase in first-time prescriptions among men, and a 1.7-fold increase among females, while people with comorbidities accounted for a smaller proportion after the publication.
“Socioeconomic factors, such as access to health care and education and income levels, may be associated with individuals seeking low-dose oral minoxidil after article publication,” wrote the authors.
In an interview, Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said that he was not surprised to see an uptick in prescriptions after the Times article.
He and his colleagues were curious as to whether the article might have prompted newfound interest in LDOM. They experienced an uptick at George Washington, which Dr. Friedman thought could have been because he was quoted in the Times story. He and colleagues conducted a national survey of dermatologists asking if more patients had called, emailed, or come in to the office asking about LDOM after the article’s publication. “Over 85% said yes,” Dr. Friedman said in the interview. He and his coauthors also found a huge increase in Google searches for terms such as hair loss, alopecia, and minoxidil in the weeks after the article, he said.
The results are expected to published soon in the Journal of Drugs in Dermatology.
“I think a lot of people know about [LDOM] and it’s certainly has gained a lot more attention and acceptance in recent years,” said Dr. Friedman, but he added that “there’s no question” that the Times article increased interest.
That is not necessarily a bad thing, he said. “With one article, education on a common disease was disseminated worldwide in a way that no one doctor can do,” he said. The article was truthful, evidence-based, and included expert dermatologists, he noted.
“It probably got people who never thought twice about their hair thinning to actually think that there’s hope,” he said, adding that it also likely prompted them to seek care, and, more importantly, “to seek care from the person who should be taking care of this, which is the dermatologist.”
However, the article might also inspire some people to think LDOM can help when it can’t, or they might insist on a prescription when another medication is more appropriate, said Dr. Friedman.
Both he and Dr. Sinclair expect demand for LDOM to continue increasing.
“Word of mouth will drive the next wave of prescriptions,” said Dr. Sinclair. “We are continuing to do work to improve safety, to understand its mechanism of action, and identify ways to improve equity of access to treatment for men and women who are concerned about their hair loss and motivated to treat it,” he said.
Dr. Sinclair and Dr. Friedman report no relevant financial relationships.
.
The weekly rate of first-time low-dose oral minoxidil (LDOM) prescriptions per 10,000 outpatient encounters was “significantly higher 8 weeks after vs. 8 weeks before article publication,” at 0.9 prescriptions, compared with 0.5 per 10,000, wrote the authors of the research letter, published in JAMA Network Open. There was no similar bump for first-time finasteride or hypertension prescriptions, wrote the authors, from Harvard Medical School and Massachusetts General Hospital, Boston, and Truveta, a company that provides EHR data from U.S. health care systems.
The New York Times article noted that LDOM was relatively unknown to patients and doctors – and not approved by the Food and Drug Administration for treating hair loss – but that it was inexpensive, safe, and very effective for many individuals. “The article did not report new research findings or large-scale randomized evidence,” wrote the authors of the JAMA study.
Rodney Sinclair, MD, professor of dermatology at the University of Melbourne, who conducted the original research on LDOM and hair loss and was quoted in the Times story, told this news organization that “the sharp uplift after the New York Times article was on the back of a gradual increase.” He added that “the momentum for minoxidil prescriptions is increasing,” so much so that it has led to a global shortage of LDOM. The drug appears to still be widely available in the United States, however. It is not on the ASHP shortages list.
“There has been growing momentum for minoxidil use since I first presented our data about 6 years ago,” Dr. Sinclair said. He noted that 2022 International Society of Hair Restoration Surgery survey data found that 26% of treating physicians always or often prescribed off-label oral minoxidil, up from 10% in 2019 and 0% in 2017, while another 20% said they prescribed it sometimes.
The authors of the new study looked at prescriptions for patients at eight health care systems before and after the Times article was published in August 2022. They calculated the rate of first-time oral minoxidil prescriptions for 2.5 mg and 5 mg tablets, excluding 10 mg tablets, which are prescribed for hypertension.
Among those receiving first-time prescriptions, 2,846 received them in the 7 months before the article and 3,695 in the 5 months after publication. Men (43.6% after vs. 37.7% before publication) and White individuals (68.6% after vs. 60.8% before publication) accounted for a higher proportion of prescriptions after the article was published. There was a 2.4-fold increase in first-time prescriptions among men, and a 1.7-fold increase among females, while people with comorbidities accounted for a smaller proportion after the publication.
“Socioeconomic factors, such as access to health care and education and income levels, may be associated with individuals seeking low-dose oral minoxidil after article publication,” wrote the authors.
In an interview, Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said that he was not surprised to see an uptick in prescriptions after the Times article.
He and his colleagues were curious as to whether the article might have prompted newfound interest in LDOM. They experienced an uptick at George Washington, which Dr. Friedman thought could have been because he was quoted in the Times story. He and colleagues conducted a national survey of dermatologists asking if more patients had called, emailed, or come in to the office asking about LDOM after the article’s publication. “Over 85% said yes,” Dr. Friedman said in the interview. He and his coauthors also found a huge increase in Google searches for terms such as hair loss, alopecia, and minoxidil in the weeks after the article, he said.
The results are expected to published soon in the Journal of Drugs in Dermatology.
“I think a lot of people know about [LDOM] and it’s certainly has gained a lot more attention and acceptance in recent years,” said Dr. Friedman, but he added that “there’s no question” that the Times article increased interest.
That is not necessarily a bad thing, he said. “With one article, education on a common disease was disseminated worldwide in a way that no one doctor can do,” he said. The article was truthful, evidence-based, and included expert dermatologists, he noted.
“It probably got people who never thought twice about their hair thinning to actually think that there’s hope,” he said, adding that it also likely prompted them to seek care, and, more importantly, “to seek care from the person who should be taking care of this, which is the dermatologist.”
However, the article might also inspire some people to think LDOM can help when it can’t, or they might insist on a prescription when another medication is more appropriate, said Dr. Friedman.
Both he and Dr. Sinclair expect demand for LDOM to continue increasing.
“Word of mouth will drive the next wave of prescriptions,” said Dr. Sinclair. “We are continuing to do work to improve safety, to understand its mechanism of action, and identify ways to improve equity of access to treatment for men and women who are concerned about their hair loss and motivated to treat it,” he said.
Dr. Sinclair and Dr. Friedman report no relevant financial relationships.
.
The weekly rate of first-time low-dose oral minoxidil (LDOM) prescriptions per 10,000 outpatient encounters was “significantly higher 8 weeks after vs. 8 weeks before article publication,” at 0.9 prescriptions, compared with 0.5 per 10,000, wrote the authors of the research letter, published in JAMA Network Open. There was no similar bump for first-time finasteride or hypertension prescriptions, wrote the authors, from Harvard Medical School and Massachusetts General Hospital, Boston, and Truveta, a company that provides EHR data from U.S. health care systems.
The New York Times article noted that LDOM was relatively unknown to patients and doctors – and not approved by the Food and Drug Administration for treating hair loss – but that it was inexpensive, safe, and very effective for many individuals. “The article did not report new research findings or large-scale randomized evidence,” wrote the authors of the JAMA study.
Rodney Sinclair, MD, professor of dermatology at the University of Melbourne, who conducted the original research on LDOM and hair loss and was quoted in the Times story, told this news organization that “the sharp uplift after the New York Times article was on the back of a gradual increase.” He added that “the momentum for minoxidil prescriptions is increasing,” so much so that it has led to a global shortage of LDOM. The drug appears to still be widely available in the United States, however. It is not on the ASHP shortages list.
“There has been growing momentum for minoxidil use since I first presented our data about 6 years ago,” Dr. Sinclair said. He noted that 2022 International Society of Hair Restoration Surgery survey data found that 26% of treating physicians always or often prescribed off-label oral minoxidil, up from 10% in 2019 and 0% in 2017, while another 20% said they prescribed it sometimes.
The authors of the new study looked at prescriptions for patients at eight health care systems before and after the Times article was published in August 2022. They calculated the rate of first-time oral minoxidil prescriptions for 2.5 mg and 5 mg tablets, excluding 10 mg tablets, which are prescribed for hypertension.
Among those receiving first-time prescriptions, 2,846 received them in the 7 months before the article and 3,695 in the 5 months after publication. Men (43.6% after vs. 37.7% before publication) and White individuals (68.6% after vs. 60.8% before publication) accounted for a higher proportion of prescriptions after the article was published. There was a 2.4-fold increase in first-time prescriptions among men, and a 1.7-fold increase among females, while people with comorbidities accounted for a smaller proportion after the publication.
“Socioeconomic factors, such as access to health care and education and income levels, may be associated with individuals seeking low-dose oral minoxidil after article publication,” wrote the authors.
In an interview, Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said that he was not surprised to see an uptick in prescriptions after the Times article.
He and his colleagues were curious as to whether the article might have prompted newfound interest in LDOM. They experienced an uptick at George Washington, which Dr. Friedman thought could have been because he was quoted in the Times story. He and colleagues conducted a national survey of dermatologists asking if more patients had called, emailed, or come in to the office asking about LDOM after the article’s publication. “Over 85% said yes,” Dr. Friedman said in the interview. He and his coauthors also found a huge increase in Google searches for terms such as hair loss, alopecia, and minoxidil in the weeks after the article, he said.
The results are expected to published soon in the Journal of Drugs in Dermatology.
“I think a lot of people know about [LDOM] and it’s certainly has gained a lot more attention and acceptance in recent years,” said Dr. Friedman, but he added that “there’s no question” that the Times article increased interest.
That is not necessarily a bad thing, he said. “With one article, education on a common disease was disseminated worldwide in a way that no one doctor can do,” he said. The article was truthful, evidence-based, and included expert dermatologists, he noted.
“It probably got people who never thought twice about their hair thinning to actually think that there’s hope,” he said, adding that it also likely prompted them to seek care, and, more importantly, “to seek care from the person who should be taking care of this, which is the dermatologist.”
However, the article might also inspire some people to think LDOM can help when it can’t, or they might insist on a prescription when another medication is more appropriate, said Dr. Friedman.
Both he and Dr. Sinclair expect demand for LDOM to continue increasing.
“Word of mouth will drive the next wave of prescriptions,” said Dr. Sinclair. “We are continuing to do work to improve safety, to understand its mechanism of action, and identify ways to improve equity of access to treatment for men and women who are concerned about their hair loss and motivated to treat it,” he said.
Dr. Sinclair and Dr. Friedman report no relevant financial relationships.
FROM JAMA NETWORK OPEN
Cuffless blood pressure monitors: Still a numbers game
Medscape’s Editor-in-Chief Eric Topol, MD, referred to continual noninvasive, cuffless, accurate blood pressure devices as “a holy grail in sensor technology.”
He personally tested a cuff-calibrated, over-the-counter device available in Europe that claims to monitor daily blood pressure changes and produce data that can help physicians titrate medications.
Dr. Topol does not believe that it is ready for prime time. Yes, cuffless devices are easy to use, and generate lots of data. But are those data accurate?
Many experts say not yet, even as the market continues to grow and more devices are introduced and highlighted at high-profile consumer events.
Burned before
Limitations of cuffed devices are well known, including errors related to cuff size, patient positioning, patient habits or behaviors (for example, caffeine/nicotine use, acute meal digestion, full bladder, very recent physical activity) and clinicians’ failure to take accurate measurements.
Like many clinicians, Timothy B. Plante, MD, MHS, assistant professor at the University of Vermont Medical Center thrombosis & hemostasis program in Burlington, is very excited about cuffless technology. However, “we’ve been burned by it before,” he said in an interview.
Dr. Plante’s 2016 validation study of an instant blood pressure smartphone app found that its measurements were “highly inaccurate,” with such low sensitivity that more than three-quarters of individuals with hypertensive blood levels would be falsely reassured that their blood pressure was in the normal range.
His team’s 2023 review of the current landscape, which includes more sophisticated devices, concluded that accuracy remains an issue: “Unfortunately, the pace of regulation of these devices has failed to match the speed of innovation and direct availability to patient consumers. There is an urgent need to develop a consensus on standards by which cuffless BP devices can be tested for accuracy.”
Devices, indications differ
Cuffless devices estimate blood pressure indirectly. Most operate based on pulse wave analysis and pulse arrival time (PWA-PAT), explained Ramakrishna Mukkamala, PhD, in a commentary. Dr. Mukkamala is a professor in the departments of bioengineering and anesthesiology and perioperative medicine at the University of Pittsburgh.
PWA involves measuring a peripheral arterial waveform using an optical sensor such as the green lights on the back of a wrist-worn device, or a ‘force sensor’ such as a finger cuff or pressing on a smartphone. Certain features are extracted from the waveform using machine learning and calibrated to blood pressure values.
PAT techniques work together with PWA; they record the ECG and extract features from that signal as well as the arterial waveform for calibration to blood pressure values.
The algorithm used to generate the BP numbers comprises a proprietary baseline model that may include demographics and other patient characteristics. A cuff measurement is often part of the baseline model because most cuffless devices require periodic (typically weekly or monthly) calibration using a cuffed device.
Cuffless devices that require cuff calibration compare the estimate they get to the cuff-calibrated number. In this scenario, the cuffless device may come up with the same blood pressure numbers simply because the baseline model – which is made up of thousands of data points relevant to the patient – has not changed.
This has led some experts to question whether PWA-PAT cuffless device readings actually add anything to the baseline model.
They don’t, according to Microsoft Research in what Dr. Mukkamala and coauthors referred to (in a review published in Hypertension) as “a complex article describing perhaps the most important and highest resource project to date (Aurora Project) on assessing the accuracy of PWA and PWA devices.”
The Microsoft article was written for bioengineers. The review in Hypertension explains the project for clinicians, and concludes that, “Cuffless BP devices based on PWA and PWA-PAT, which are similar to some regulatory-cleared devices, were of no additional value in measuring auscultatory or 24-hour ambulatory cuff BP when compared with a baseline model in which BP was predicted without an actual measurement.”
IEEE and FDA validation
Despite these concerns, several cuffless devices using PWA and PAT have been cleared by the Food and Drug Administration.
Validating cuffless devices is no simple matter. The Institute of Electrical and Electronics Engineers published a validation protocol for cuffless blood pressure devices in 2014 that was amended in 2019 to include a requirement to evaluate performance in different positions and in the presence of motion with varying degrees of noise artifact.
However, Daichi Shimbo, MD, codirector of the Columbia Hypertension Center in New York and vice chair of the American Heart Association Statement on blood pressure monitoring, and colleagues point out limitations, even in the updated standard. These include not requiring evaluation for drift over time; lack of specific dynamic testing protocols for stressors such as exercise or environmental temperatures; and an unsuitable reference standard (oscillometric cuff-based devices) during movement.
Dr. Shimbo said in an interview that, although he is excited about them, “these cuffless devices are not aligned with regulatory bodies. If a device gives someone a wrong blood pressure, they might be diagnosed with hypertension when they don’t have it or might miss the fact that they’re hypertensive because they get a normal blood pressure reading. If there’s no yardstick by which you say these devices are good, what are we really doing – helping, or causing a problem?”
“The specifics of how a device estimates blood pressure can determine what testing is needed to ensure that it is providing accurate performance in the intended conditions of use,” Jeremy Kahn, an FDA press officer, said in an interview. “For example, for cuffless devices that are calibrated initially with a cuff-based blood pressure device, the cuffless device needs to specify the period over which it can provide accurate readings and have testing to demonstrate that it provides accurate results over that period of use.”
The FDA said its testing is different from what the Microsoft Aurora Project used in their study.
“The intent of that testing, as the agency understands it, is to evaluate whether the device is providing useful input based on the current physiology of the patient rather than relying on predetermined values based on calibration or patient attributes. We evaluate this clinically in two separate tests: an induced change in blood pressure test and tracking of natural blood pressure changes with longer term device use,” Mr. Kahn explained.
Analyzing a device’s performance on individuals who have had natural changes in blood pressure as compared to a calibration value or initial reading “can also help discern if the device is using physiological data from the patient to determine their blood pressure accurately,” he said.
Experts interviewed for this article who remain skeptical about cuffless BP monitoring question whether the numbers that appear during the induced blood pressure change, and with the natural blood pressure changes that may occur over time, accurately reflect a patient’s blood pressure.
“The FDA doesn’t approve these devices; they clear them,” Dr. Shimbo pointed out. “Clearing them means they can be sold to the general public in the U.S. It’s not a strong statement that they’re accurate.”
Moving toward validation, standards
Ultimately, cuffless BP monitors may require more than one validation protocol and standard, depending on their technology, how and where they will be used, and by whom.
And as Dr. Plante and colleagues write, “Importantly, validation should be performed in diverse and special populations, including pregnant women and individuals across a range of heart rates, skin tones, wrist sizes, common arrhythmias, and beta-blocker use.”
Organizations that might be expected to help move validation and standards forward have mostly remained silent. The American Medical Association’s US Blood Pressure Validated Device Listing website includes only cuffed devices, as does the website of the international scientific nonprofit STRIDE BP.
The European Society of Hypertension 2022 consensus statement on cuffless devices concluded that, until there is an internationally accepted accuracy standard and the devices have been tested in healthy people and those with suspected or diagnosed hypertension, “cuffless BP devices should not be used for the evaluation or management of hypertension in clinical practice.”
This month, ESH published recommendations for “specific, clinically meaningful, and pragmatic validation procedures for different types of intermittent cuffless devices” that will be presented at their upcoming annual meeting June 26.
Updated protocols from IEEE “are coming out soon,” according to Dr. Shimbo. The FDA says currently cleared devices won’t need to revalidate according to new standards unless the sponsor makes significant modifications in software algorithms, device hardware, or targeted patient populations.
Device makers take the initiative
In the face of conflicting reports on accuracy and lack of a robust standard, some device makers are publishing their own tests or encouraging validation by potential customers.
For example, institutions that are considering using the Biobeat cuffless blood pressure monitor watch “usually start with small pilots with our devices to do internal validation,” Lior Ben Shettrit, the company’s vice president of business development, said in an interview. “Only after they complete the internal validation are they willing to move forward to full implementation.”
Cardiologist Dean Nachman, MD, is leading validation studies of the Biobeat device at the Hadassah Ein Kerem Medical Center in Jerusalem. For the first validation, the team recruited 1,057 volunteers who did a single blood pressure measurement with the cuffless device and with a cuffed device.
“We found 96.3% agreement in identifying hypertension and an interclass correlation coefficient of 0.99 and 0.97 for systolic and diastolic measurements, respectively,” he said. “Then we took it to the next level and compared the device to ambulatory 24-hour blood pressure monitoring and found comparable measurements.”
The investigators are not done yet. “We need data from thousands of patients, with subgroups, to not have any concerns,” he says. “Right now, we are using the device as a general monitor – as an EKG plus heart rate plus oxygen saturation level monitor – and as a blood pressure monitor for 24-hour blood pressure monitoring.”
The developers of the Aktiia device, which is the one Dr. Topol tested, take a different perspective. “When somebody introduces a new technology that is disrupting something that has been in place for over 100 years, there will always be some grumblings, ruffling of feathers, people saying it’s not ready, it’s not ready, it’s not ready,” Aktiia’s chief medical officer Jay Shah, MD, noted.
“But a lot of those comments are coming from the isolation of an ivory tower,” he said.
Aktiia cofounder and chief technology officer Josep Solà said that “no device is probably as accurate as if you have an invasive catheter,” adding that “we engage patients to look at their blood pressure day by day. … If each individual measurement of each of those patient is slightly less accurate than a cuff, who cares? We have 40 measurements per day on each patient. The accuracy and precision of each of those is good.”
Researchers from the George Institute for Global Health recently compared the Aktiia device to conventional ambulatory monitoring in 41 patients and found that “it did not accurately track night-time BP decline and results suggested it was unable to track medication-induced BP changes.”
“In the context of 24/7 monitoring of hypertensive patients,” Mr. Solà said, “whatever you do, if it’s better than a sham device or a baseline model and you track the blood pressure changes, it’s a hundred times much better than doing nothing.”
Dr. Nachman and Dr. Plante reported no relevant financial relationships. Dr. Shimbo reported that he received funding from NIH and has consulted for Abbott Vascular, Edward Lifesciences, Medtronic, and Tryton Medical.
A version of this article first appeared on Medscape.com.
Medscape’s Editor-in-Chief Eric Topol, MD, referred to continual noninvasive, cuffless, accurate blood pressure devices as “a holy grail in sensor technology.”
He personally tested a cuff-calibrated, over-the-counter device available in Europe that claims to monitor daily blood pressure changes and produce data that can help physicians titrate medications.
Dr. Topol does not believe that it is ready for prime time. Yes, cuffless devices are easy to use, and generate lots of data. But are those data accurate?
Many experts say not yet, even as the market continues to grow and more devices are introduced and highlighted at high-profile consumer events.
Burned before
Limitations of cuffed devices are well known, including errors related to cuff size, patient positioning, patient habits or behaviors (for example, caffeine/nicotine use, acute meal digestion, full bladder, very recent physical activity) and clinicians’ failure to take accurate measurements.
Like many clinicians, Timothy B. Plante, MD, MHS, assistant professor at the University of Vermont Medical Center thrombosis & hemostasis program in Burlington, is very excited about cuffless technology. However, “we’ve been burned by it before,” he said in an interview.
Dr. Plante’s 2016 validation study of an instant blood pressure smartphone app found that its measurements were “highly inaccurate,” with such low sensitivity that more than three-quarters of individuals with hypertensive blood levels would be falsely reassured that their blood pressure was in the normal range.
His team’s 2023 review of the current landscape, which includes more sophisticated devices, concluded that accuracy remains an issue: “Unfortunately, the pace of regulation of these devices has failed to match the speed of innovation and direct availability to patient consumers. There is an urgent need to develop a consensus on standards by which cuffless BP devices can be tested for accuracy.”
Devices, indications differ
Cuffless devices estimate blood pressure indirectly. Most operate based on pulse wave analysis and pulse arrival time (PWA-PAT), explained Ramakrishna Mukkamala, PhD, in a commentary. Dr. Mukkamala is a professor in the departments of bioengineering and anesthesiology and perioperative medicine at the University of Pittsburgh.
PWA involves measuring a peripheral arterial waveform using an optical sensor such as the green lights on the back of a wrist-worn device, or a ‘force sensor’ such as a finger cuff or pressing on a smartphone. Certain features are extracted from the waveform using machine learning and calibrated to blood pressure values.
PAT techniques work together with PWA; they record the ECG and extract features from that signal as well as the arterial waveform for calibration to blood pressure values.
The algorithm used to generate the BP numbers comprises a proprietary baseline model that may include demographics and other patient characteristics. A cuff measurement is often part of the baseline model because most cuffless devices require periodic (typically weekly or monthly) calibration using a cuffed device.
Cuffless devices that require cuff calibration compare the estimate they get to the cuff-calibrated number. In this scenario, the cuffless device may come up with the same blood pressure numbers simply because the baseline model – which is made up of thousands of data points relevant to the patient – has not changed.
This has led some experts to question whether PWA-PAT cuffless device readings actually add anything to the baseline model.
They don’t, according to Microsoft Research in what Dr. Mukkamala and coauthors referred to (in a review published in Hypertension) as “a complex article describing perhaps the most important and highest resource project to date (Aurora Project) on assessing the accuracy of PWA and PWA devices.”
The Microsoft article was written for bioengineers. The review in Hypertension explains the project for clinicians, and concludes that, “Cuffless BP devices based on PWA and PWA-PAT, which are similar to some regulatory-cleared devices, were of no additional value in measuring auscultatory or 24-hour ambulatory cuff BP when compared with a baseline model in which BP was predicted without an actual measurement.”
IEEE and FDA validation
Despite these concerns, several cuffless devices using PWA and PAT have been cleared by the Food and Drug Administration.
Validating cuffless devices is no simple matter. The Institute of Electrical and Electronics Engineers published a validation protocol for cuffless blood pressure devices in 2014 that was amended in 2019 to include a requirement to evaluate performance in different positions and in the presence of motion with varying degrees of noise artifact.
However, Daichi Shimbo, MD, codirector of the Columbia Hypertension Center in New York and vice chair of the American Heart Association Statement on blood pressure monitoring, and colleagues point out limitations, even in the updated standard. These include not requiring evaluation for drift over time; lack of specific dynamic testing protocols for stressors such as exercise or environmental temperatures; and an unsuitable reference standard (oscillometric cuff-based devices) during movement.
Dr. Shimbo said in an interview that, although he is excited about them, “these cuffless devices are not aligned with regulatory bodies. If a device gives someone a wrong blood pressure, they might be diagnosed with hypertension when they don’t have it or might miss the fact that they’re hypertensive because they get a normal blood pressure reading. If there’s no yardstick by which you say these devices are good, what are we really doing – helping, or causing a problem?”
“The specifics of how a device estimates blood pressure can determine what testing is needed to ensure that it is providing accurate performance in the intended conditions of use,” Jeremy Kahn, an FDA press officer, said in an interview. “For example, for cuffless devices that are calibrated initially with a cuff-based blood pressure device, the cuffless device needs to specify the period over which it can provide accurate readings and have testing to demonstrate that it provides accurate results over that period of use.”
The FDA said its testing is different from what the Microsoft Aurora Project used in their study.
“The intent of that testing, as the agency understands it, is to evaluate whether the device is providing useful input based on the current physiology of the patient rather than relying on predetermined values based on calibration or patient attributes. We evaluate this clinically in two separate tests: an induced change in blood pressure test and tracking of natural blood pressure changes with longer term device use,” Mr. Kahn explained.
Analyzing a device’s performance on individuals who have had natural changes in blood pressure as compared to a calibration value or initial reading “can also help discern if the device is using physiological data from the patient to determine their blood pressure accurately,” he said.
Experts interviewed for this article who remain skeptical about cuffless BP monitoring question whether the numbers that appear during the induced blood pressure change, and with the natural blood pressure changes that may occur over time, accurately reflect a patient’s blood pressure.
“The FDA doesn’t approve these devices; they clear them,” Dr. Shimbo pointed out. “Clearing them means they can be sold to the general public in the U.S. It’s not a strong statement that they’re accurate.”
Moving toward validation, standards
Ultimately, cuffless BP monitors may require more than one validation protocol and standard, depending on their technology, how and where they will be used, and by whom.
And as Dr. Plante and colleagues write, “Importantly, validation should be performed in diverse and special populations, including pregnant women and individuals across a range of heart rates, skin tones, wrist sizes, common arrhythmias, and beta-blocker use.”
Organizations that might be expected to help move validation and standards forward have mostly remained silent. The American Medical Association’s US Blood Pressure Validated Device Listing website includes only cuffed devices, as does the website of the international scientific nonprofit STRIDE BP.
The European Society of Hypertension 2022 consensus statement on cuffless devices concluded that, until there is an internationally accepted accuracy standard and the devices have been tested in healthy people and those with suspected or diagnosed hypertension, “cuffless BP devices should not be used for the evaluation or management of hypertension in clinical practice.”
This month, ESH published recommendations for “specific, clinically meaningful, and pragmatic validation procedures for different types of intermittent cuffless devices” that will be presented at their upcoming annual meeting June 26.
Updated protocols from IEEE “are coming out soon,” according to Dr. Shimbo. The FDA says currently cleared devices won’t need to revalidate according to new standards unless the sponsor makes significant modifications in software algorithms, device hardware, or targeted patient populations.
Device makers take the initiative
In the face of conflicting reports on accuracy and lack of a robust standard, some device makers are publishing their own tests or encouraging validation by potential customers.
For example, institutions that are considering using the Biobeat cuffless blood pressure monitor watch “usually start with small pilots with our devices to do internal validation,” Lior Ben Shettrit, the company’s vice president of business development, said in an interview. “Only after they complete the internal validation are they willing to move forward to full implementation.”
Cardiologist Dean Nachman, MD, is leading validation studies of the Biobeat device at the Hadassah Ein Kerem Medical Center in Jerusalem. For the first validation, the team recruited 1,057 volunteers who did a single blood pressure measurement with the cuffless device and with a cuffed device.
“We found 96.3% agreement in identifying hypertension and an interclass correlation coefficient of 0.99 and 0.97 for systolic and diastolic measurements, respectively,” he said. “Then we took it to the next level and compared the device to ambulatory 24-hour blood pressure monitoring and found comparable measurements.”
The investigators are not done yet. “We need data from thousands of patients, with subgroups, to not have any concerns,” he says. “Right now, we are using the device as a general monitor – as an EKG plus heart rate plus oxygen saturation level monitor – and as a blood pressure monitor for 24-hour blood pressure monitoring.”
The developers of the Aktiia device, which is the one Dr. Topol tested, take a different perspective. “When somebody introduces a new technology that is disrupting something that has been in place for over 100 years, there will always be some grumblings, ruffling of feathers, people saying it’s not ready, it’s not ready, it’s not ready,” Aktiia’s chief medical officer Jay Shah, MD, noted.
“But a lot of those comments are coming from the isolation of an ivory tower,” he said.
Aktiia cofounder and chief technology officer Josep Solà said that “no device is probably as accurate as if you have an invasive catheter,” adding that “we engage patients to look at their blood pressure day by day. … If each individual measurement of each of those patient is slightly less accurate than a cuff, who cares? We have 40 measurements per day on each patient. The accuracy and precision of each of those is good.”
Researchers from the George Institute for Global Health recently compared the Aktiia device to conventional ambulatory monitoring in 41 patients and found that “it did not accurately track night-time BP decline and results suggested it was unable to track medication-induced BP changes.”
“In the context of 24/7 monitoring of hypertensive patients,” Mr. Solà said, “whatever you do, if it’s better than a sham device or a baseline model and you track the blood pressure changes, it’s a hundred times much better than doing nothing.”
Dr. Nachman and Dr. Plante reported no relevant financial relationships. Dr. Shimbo reported that he received funding from NIH and has consulted for Abbott Vascular, Edward Lifesciences, Medtronic, and Tryton Medical.
A version of this article first appeared on Medscape.com.
Medscape’s Editor-in-Chief Eric Topol, MD, referred to continual noninvasive, cuffless, accurate blood pressure devices as “a holy grail in sensor technology.”
He personally tested a cuff-calibrated, over-the-counter device available in Europe that claims to monitor daily blood pressure changes and produce data that can help physicians titrate medications.
Dr. Topol does not believe that it is ready for prime time. Yes, cuffless devices are easy to use, and generate lots of data. But are those data accurate?
Many experts say not yet, even as the market continues to grow and more devices are introduced and highlighted at high-profile consumer events.
Burned before
Limitations of cuffed devices are well known, including errors related to cuff size, patient positioning, patient habits or behaviors (for example, caffeine/nicotine use, acute meal digestion, full bladder, very recent physical activity) and clinicians’ failure to take accurate measurements.
Like many clinicians, Timothy B. Plante, MD, MHS, assistant professor at the University of Vermont Medical Center thrombosis & hemostasis program in Burlington, is very excited about cuffless technology. However, “we’ve been burned by it before,” he said in an interview.
Dr. Plante’s 2016 validation study of an instant blood pressure smartphone app found that its measurements were “highly inaccurate,” with such low sensitivity that more than three-quarters of individuals with hypertensive blood levels would be falsely reassured that their blood pressure was in the normal range.
His team’s 2023 review of the current landscape, which includes more sophisticated devices, concluded that accuracy remains an issue: “Unfortunately, the pace of regulation of these devices has failed to match the speed of innovation and direct availability to patient consumers. There is an urgent need to develop a consensus on standards by which cuffless BP devices can be tested for accuracy.”
Devices, indications differ
Cuffless devices estimate blood pressure indirectly. Most operate based on pulse wave analysis and pulse arrival time (PWA-PAT), explained Ramakrishna Mukkamala, PhD, in a commentary. Dr. Mukkamala is a professor in the departments of bioengineering and anesthesiology and perioperative medicine at the University of Pittsburgh.
PWA involves measuring a peripheral arterial waveform using an optical sensor such as the green lights on the back of a wrist-worn device, or a ‘force sensor’ such as a finger cuff or pressing on a smartphone. Certain features are extracted from the waveform using machine learning and calibrated to blood pressure values.
PAT techniques work together with PWA; they record the ECG and extract features from that signal as well as the arterial waveform for calibration to blood pressure values.
The algorithm used to generate the BP numbers comprises a proprietary baseline model that may include demographics and other patient characteristics. A cuff measurement is often part of the baseline model because most cuffless devices require periodic (typically weekly or monthly) calibration using a cuffed device.
Cuffless devices that require cuff calibration compare the estimate they get to the cuff-calibrated number. In this scenario, the cuffless device may come up with the same blood pressure numbers simply because the baseline model – which is made up of thousands of data points relevant to the patient – has not changed.
This has led some experts to question whether PWA-PAT cuffless device readings actually add anything to the baseline model.
They don’t, according to Microsoft Research in what Dr. Mukkamala and coauthors referred to (in a review published in Hypertension) as “a complex article describing perhaps the most important and highest resource project to date (Aurora Project) on assessing the accuracy of PWA and PWA devices.”
The Microsoft article was written for bioengineers. The review in Hypertension explains the project for clinicians, and concludes that, “Cuffless BP devices based on PWA and PWA-PAT, which are similar to some regulatory-cleared devices, were of no additional value in measuring auscultatory or 24-hour ambulatory cuff BP when compared with a baseline model in which BP was predicted without an actual measurement.”
IEEE and FDA validation
Despite these concerns, several cuffless devices using PWA and PAT have been cleared by the Food and Drug Administration.
Validating cuffless devices is no simple matter. The Institute of Electrical and Electronics Engineers published a validation protocol for cuffless blood pressure devices in 2014 that was amended in 2019 to include a requirement to evaluate performance in different positions and in the presence of motion with varying degrees of noise artifact.
However, Daichi Shimbo, MD, codirector of the Columbia Hypertension Center in New York and vice chair of the American Heart Association Statement on blood pressure monitoring, and colleagues point out limitations, even in the updated standard. These include not requiring evaluation for drift over time; lack of specific dynamic testing protocols for stressors such as exercise or environmental temperatures; and an unsuitable reference standard (oscillometric cuff-based devices) during movement.
Dr. Shimbo said in an interview that, although he is excited about them, “these cuffless devices are not aligned with regulatory bodies. If a device gives someone a wrong blood pressure, they might be diagnosed with hypertension when they don’t have it or might miss the fact that they’re hypertensive because they get a normal blood pressure reading. If there’s no yardstick by which you say these devices are good, what are we really doing – helping, or causing a problem?”
“The specifics of how a device estimates blood pressure can determine what testing is needed to ensure that it is providing accurate performance in the intended conditions of use,” Jeremy Kahn, an FDA press officer, said in an interview. “For example, for cuffless devices that are calibrated initially with a cuff-based blood pressure device, the cuffless device needs to specify the period over which it can provide accurate readings and have testing to demonstrate that it provides accurate results over that period of use.”
The FDA said its testing is different from what the Microsoft Aurora Project used in their study.
“The intent of that testing, as the agency understands it, is to evaluate whether the device is providing useful input based on the current physiology of the patient rather than relying on predetermined values based on calibration or patient attributes. We evaluate this clinically in two separate tests: an induced change in blood pressure test and tracking of natural blood pressure changes with longer term device use,” Mr. Kahn explained.
Analyzing a device’s performance on individuals who have had natural changes in blood pressure as compared to a calibration value or initial reading “can also help discern if the device is using physiological data from the patient to determine their blood pressure accurately,” he said.
Experts interviewed for this article who remain skeptical about cuffless BP monitoring question whether the numbers that appear during the induced blood pressure change, and with the natural blood pressure changes that may occur over time, accurately reflect a patient’s blood pressure.
“The FDA doesn’t approve these devices; they clear them,” Dr. Shimbo pointed out. “Clearing them means they can be sold to the general public in the U.S. It’s not a strong statement that they’re accurate.”
Moving toward validation, standards
Ultimately, cuffless BP monitors may require more than one validation protocol and standard, depending on their technology, how and where they will be used, and by whom.
And as Dr. Plante and colleagues write, “Importantly, validation should be performed in diverse and special populations, including pregnant women and individuals across a range of heart rates, skin tones, wrist sizes, common arrhythmias, and beta-blocker use.”
Organizations that might be expected to help move validation and standards forward have mostly remained silent. The American Medical Association’s US Blood Pressure Validated Device Listing website includes only cuffed devices, as does the website of the international scientific nonprofit STRIDE BP.
The European Society of Hypertension 2022 consensus statement on cuffless devices concluded that, until there is an internationally accepted accuracy standard and the devices have been tested in healthy people and those with suspected or diagnosed hypertension, “cuffless BP devices should not be used for the evaluation or management of hypertension in clinical practice.”
This month, ESH published recommendations for “specific, clinically meaningful, and pragmatic validation procedures for different types of intermittent cuffless devices” that will be presented at their upcoming annual meeting June 26.
Updated protocols from IEEE “are coming out soon,” according to Dr. Shimbo. The FDA says currently cleared devices won’t need to revalidate according to new standards unless the sponsor makes significant modifications in software algorithms, device hardware, or targeted patient populations.
Device makers take the initiative
In the face of conflicting reports on accuracy and lack of a robust standard, some device makers are publishing their own tests or encouraging validation by potential customers.
For example, institutions that are considering using the Biobeat cuffless blood pressure monitor watch “usually start with small pilots with our devices to do internal validation,” Lior Ben Shettrit, the company’s vice president of business development, said in an interview. “Only after they complete the internal validation are they willing to move forward to full implementation.”
Cardiologist Dean Nachman, MD, is leading validation studies of the Biobeat device at the Hadassah Ein Kerem Medical Center in Jerusalem. For the first validation, the team recruited 1,057 volunteers who did a single blood pressure measurement with the cuffless device and with a cuffed device.
“We found 96.3% agreement in identifying hypertension and an interclass correlation coefficient of 0.99 and 0.97 for systolic and diastolic measurements, respectively,” he said. “Then we took it to the next level and compared the device to ambulatory 24-hour blood pressure monitoring and found comparable measurements.”
The investigators are not done yet. “We need data from thousands of patients, with subgroups, to not have any concerns,” he says. “Right now, we are using the device as a general monitor – as an EKG plus heart rate plus oxygen saturation level monitor – and as a blood pressure monitor for 24-hour blood pressure monitoring.”
The developers of the Aktiia device, which is the one Dr. Topol tested, take a different perspective. “When somebody introduces a new technology that is disrupting something that has been in place for over 100 years, there will always be some grumblings, ruffling of feathers, people saying it’s not ready, it’s not ready, it’s not ready,” Aktiia’s chief medical officer Jay Shah, MD, noted.
“But a lot of those comments are coming from the isolation of an ivory tower,” he said.
Aktiia cofounder and chief technology officer Josep Solà said that “no device is probably as accurate as if you have an invasive catheter,” adding that “we engage patients to look at their blood pressure day by day. … If each individual measurement of each of those patient is slightly less accurate than a cuff, who cares? We have 40 measurements per day on each patient. The accuracy and precision of each of those is good.”
Researchers from the George Institute for Global Health recently compared the Aktiia device to conventional ambulatory monitoring in 41 patients and found that “it did not accurately track night-time BP decline and results suggested it was unable to track medication-induced BP changes.”
“In the context of 24/7 monitoring of hypertensive patients,” Mr. Solà said, “whatever you do, if it’s better than a sham device or a baseline model and you track the blood pressure changes, it’s a hundred times much better than doing nothing.”
Dr. Nachman and Dr. Plante reported no relevant financial relationships. Dr. Shimbo reported that he received funding from NIH and has consulted for Abbott Vascular, Edward Lifesciences, Medtronic, and Tryton Medical.
A version of this article first appeared on Medscape.com.
Overweight in heterozygous FH tied to even higher CAD risk
MANNHEIM, GERMANY – – rates that appear to have a substantial impact on these patients’ already increased risk of coronary artery disease, a registry analysis suggests.
Data on almost 36,000 individuals with FH were collated from an international registry, revealing that 55% of adults and 25% of children and adolescents with the homozygous form of FH had overweight or obesity. The figures for heterozygous FH were 52% and 27%, respectively.
Crucially, overweight or obesity was associated with substantially increased rates of coronary artery disease, particularly in persons with heterozygous FH, among whom adults with obesity faced a twofold increased risk, rising to more than sixfold in children and adolescents.
Moreover, “obesity is associated with a worse lipid profile, even from childhood, regardless of whether a patient is on medication,” said study presenter Amany Elshorbagy, DPhil, Cardiovascular Epidemiologist, department of primary care and public health, Imperial College London.
She added that, with the increased risk of coronary artery disease associated with heterozygous FH, the results showed that “together with lipid-lowering medication, weight management is needed.”
The research was presented at the annual meeting of the European Atherosclerosis Society.
Tended to be thin
Alberico L. Catapano, MD, PhD, director of cardiovascular research and of the Lipoproteins and Atherosclerosis Laboratory of IRCCS Multimedica, Milan, and past president of the EAS, said in an interview that, historically, few FH patients were overweight or obese; rather, they tended to be thin.
However, there is now “a trend for people with FH to show more diabetes and obesity,” with the “bottom line” being that, as they are already at increased risk of coronary artery disease, it pushes their risk up even further.
In other words, if a risk factor such as obesity is added “on top of the strongest risk factor, that is LDL cholesterol, it is not one plus one makes two, it is one plus one makes three,” he said.
As such, Dr. Catapano believes that the study is “very interesting,” because it further underlines the importance of weight management for individuals with increased LDL cholesterol, “especially when you have genetic forms, like FH.”
Dr. Catapano’s comments were echoed by session co-chair Ulrike Schatz, MD, leader of the lipidology specialty department at the University Hospital Carl Gustav Carus, Technical University of Dresden (Germany).
Indeed, she told Dr. Elshorbagy before her presentation that she finds “a lot of my FH patients have a tendency towards anorexia.”
In an interview, Dr. Elshorbagy said that that reaction was typical of “most of the clinicians” she had spoken to. Upon seeing her data, especially for homozygous FH patients, they say, “They are on the lean side.”
Consequently, the research team went into the study “with the expectation that they might have a lower prevalence of obesity and overweight than the general population,” but “that’s not what we’re seeing.”
Dr. Elshorbagy noted that it would be helpful to have longitudinal data to determine whether, 50 years ago, patients with HF “were leaner, along with the rest of the population.”
The registry data are cross-sectional, and the team is now reaching out to the respective national lead investigators to submit follow-up data on their patients, with the aim of looking at changes in body weight and the impact on outcomes over time.
Another key question for the researchers is in regard to fat distribution, as body mass index “is not the best predictor of heart disease,” Dr. Elshorbagy said, but is rather central obesity.
Although they have also asked investigators to share waist circumference data, she conceded that it is a measurement that “is a lot harder to standardize across centers and countries; it’s not like putting patients on a scale.”
Overall, Dr. Elshorbagy believes that her findings indicate that clinicians should take a broader, more holistic approach toward their patients – in other words, an approach in which lipid lowering medication is “key but is just one of several things we need to do to make sure the coronary event rate goes down.”
More with than without
Dr. Elshorbagy began her presentation by highlighting that the prevalence of overweight and obesity ranges from 50% to 70% and that it is “the only health condition where you’ve got more people worldwide with the condition than without.”
Crucially, overweight increases the risk of coronary artery disease by approximately 20%. Among patients with obesity, the risk rises to 50%.
Given that FH patients “already have a very high risk of cardiovascular disease from their high cholesterol levels,” the team set out to determine rates of obesity and overweight in this population and their impact on coronary artery disease risk.
They used cross-sectional data from the EAS FH Studies Collaboration Global Registry, which involves 29,262 adults aged greater than or equal to 18 years and 6,275 children and adolescents aged 5 to 17 years with heterozygous FH, and 325 adults and 57 children with homozygous FH.
Dividing the adults into standard BMI categories, they found that 16% of heterozygous and 23% of homozygous FH patients had obesity, while 52% and 55%, respectively, had overweight or obesity.
For children, the team used World Health Organization z score cutoffs, which indicated that 9% of patients with heterozygous FH and 7% of patients with homozygous FH had obesity. Rates of overweight or obesity were 27% and 25%, respectively.
Among patients with heterozygous FH, rates of overweight or obesity among adults were 50% in high-income countries and 63% in other countries; among children, the rates were and 27% and 29%, respectively.
Stratified by region, the team found that the lowest rate of overweight or obesity among adult patients with heterozygous FH was in Eastern Asia, at 27%, while the highest was in Northern Africa/Western Asia (the Middle East), at 82%.
In North America, 56% of adult patients had overweight or obesity. The prevalence of coronary artery disease rose with increasing BMI.
Among adult patients with heterozygous FH, 11.3% of those with normal weight had coronary artery disease; the percentage rose to 22.9% among those with overweight, and 30.9% among those with obesity. Among children, the corresponding figures were 0.1%, 0.2%, and 0.7%.
Putting adults and children with homozygous FH together, the researchers found that 29.0% of patients with normal weight had coronary artery disease, compared with 31.3% of those with overweight and 49.3% of those with obesity.
Moreover, the results showed that levels of LDL and remnant cholesterol were significantly associated with BMI in adults and children with heterozygous FH, even after adjusting for age, sex, and lipid-lowering medication (P < .001 for all).
Multivariate analysis that took into account age, sex, lipid-lowering medication, and LDL cholesterol revealed that having obesity, compared with not having obesity, was associated with a substantial increase in the risk of coronary artery disease among patients with heterozygous FH.
Among adults with the condition, the odds ratio was 2.16 (95% confidence interval, 1.97-2.36), while among children and adolescents, it was 6.87 (95% CI, 1.55-30.46).
The results remained similar after further adjustment for the presence of diabetes and when considering peripheral artery disease and stroke.
No funding for the study was declared. Dr. Elshorbagy has relationships with Amgen, Daiichi Sankyo, and Regeneron.
A version of this article first appeared on Medscape.com.
MANNHEIM, GERMANY – – rates that appear to have a substantial impact on these patients’ already increased risk of coronary artery disease, a registry analysis suggests.
Data on almost 36,000 individuals with FH were collated from an international registry, revealing that 55% of adults and 25% of children and adolescents with the homozygous form of FH had overweight or obesity. The figures for heterozygous FH were 52% and 27%, respectively.
Crucially, overweight or obesity was associated with substantially increased rates of coronary artery disease, particularly in persons with heterozygous FH, among whom adults with obesity faced a twofold increased risk, rising to more than sixfold in children and adolescents.
Moreover, “obesity is associated with a worse lipid profile, even from childhood, regardless of whether a patient is on medication,” said study presenter Amany Elshorbagy, DPhil, Cardiovascular Epidemiologist, department of primary care and public health, Imperial College London.
She added that, with the increased risk of coronary artery disease associated with heterozygous FH, the results showed that “together with lipid-lowering medication, weight management is needed.”
The research was presented at the annual meeting of the European Atherosclerosis Society.
Tended to be thin
Alberico L. Catapano, MD, PhD, director of cardiovascular research and of the Lipoproteins and Atherosclerosis Laboratory of IRCCS Multimedica, Milan, and past president of the EAS, said in an interview that, historically, few FH patients were overweight or obese; rather, they tended to be thin.
However, there is now “a trend for people with FH to show more diabetes and obesity,” with the “bottom line” being that, as they are already at increased risk of coronary artery disease, it pushes their risk up even further.
In other words, if a risk factor such as obesity is added “on top of the strongest risk factor, that is LDL cholesterol, it is not one plus one makes two, it is one plus one makes three,” he said.
As such, Dr. Catapano believes that the study is “very interesting,” because it further underlines the importance of weight management for individuals with increased LDL cholesterol, “especially when you have genetic forms, like FH.”
Dr. Catapano’s comments were echoed by session co-chair Ulrike Schatz, MD, leader of the lipidology specialty department at the University Hospital Carl Gustav Carus, Technical University of Dresden (Germany).
Indeed, she told Dr. Elshorbagy before her presentation that she finds “a lot of my FH patients have a tendency towards anorexia.”
In an interview, Dr. Elshorbagy said that that reaction was typical of “most of the clinicians” she had spoken to. Upon seeing her data, especially for homozygous FH patients, they say, “They are on the lean side.”
Consequently, the research team went into the study “with the expectation that they might have a lower prevalence of obesity and overweight than the general population,” but “that’s not what we’re seeing.”
Dr. Elshorbagy noted that it would be helpful to have longitudinal data to determine whether, 50 years ago, patients with HF “were leaner, along with the rest of the population.”
The registry data are cross-sectional, and the team is now reaching out to the respective national lead investigators to submit follow-up data on their patients, with the aim of looking at changes in body weight and the impact on outcomes over time.
Another key question for the researchers is in regard to fat distribution, as body mass index “is not the best predictor of heart disease,” Dr. Elshorbagy said, but is rather central obesity.
Although they have also asked investigators to share waist circumference data, she conceded that it is a measurement that “is a lot harder to standardize across centers and countries; it’s not like putting patients on a scale.”
Overall, Dr. Elshorbagy believes that her findings indicate that clinicians should take a broader, more holistic approach toward their patients – in other words, an approach in which lipid lowering medication is “key but is just one of several things we need to do to make sure the coronary event rate goes down.”
More with than without
Dr. Elshorbagy began her presentation by highlighting that the prevalence of overweight and obesity ranges from 50% to 70% and that it is “the only health condition where you’ve got more people worldwide with the condition than without.”
Crucially, overweight increases the risk of coronary artery disease by approximately 20%. Among patients with obesity, the risk rises to 50%.
Given that FH patients “already have a very high risk of cardiovascular disease from their high cholesterol levels,” the team set out to determine rates of obesity and overweight in this population and their impact on coronary artery disease risk.
They used cross-sectional data from the EAS FH Studies Collaboration Global Registry, which involves 29,262 adults aged greater than or equal to 18 years and 6,275 children and adolescents aged 5 to 17 years with heterozygous FH, and 325 adults and 57 children with homozygous FH.
Dividing the adults into standard BMI categories, they found that 16% of heterozygous and 23% of homozygous FH patients had obesity, while 52% and 55%, respectively, had overweight or obesity.
For children, the team used World Health Organization z score cutoffs, which indicated that 9% of patients with heterozygous FH and 7% of patients with homozygous FH had obesity. Rates of overweight or obesity were 27% and 25%, respectively.
Among patients with heterozygous FH, rates of overweight or obesity among adults were 50% in high-income countries and 63% in other countries; among children, the rates were and 27% and 29%, respectively.
Stratified by region, the team found that the lowest rate of overweight or obesity among adult patients with heterozygous FH was in Eastern Asia, at 27%, while the highest was in Northern Africa/Western Asia (the Middle East), at 82%.
In North America, 56% of adult patients had overweight or obesity. The prevalence of coronary artery disease rose with increasing BMI.
Among adult patients with heterozygous FH, 11.3% of those with normal weight had coronary artery disease; the percentage rose to 22.9% among those with overweight, and 30.9% among those with obesity. Among children, the corresponding figures were 0.1%, 0.2%, and 0.7%.
Putting adults and children with homozygous FH together, the researchers found that 29.0% of patients with normal weight had coronary artery disease, compared with 31.3% of those with overweight and 49.3% of those with obesity.
Moreover, the results showed that levels of LDL and remnant cholesterol were significantly associated with BMI in adults and children with heterozygous FH, even after adjusting for age, sex, and lipid-lowering medication (P < .001 for all).
Multivariate analysis that took into account age, sex, lipid-lowering medication, and LDL cholesterol revealed that having obesity, compared with not having obesity, was associated with a substantial increase in the risk of coronary artery disease among patients with heterozygous FH.
Among adults with the condition, the odds ratio was 2.16 (95% confidence interval, 1.97-2.36), while among children and adolescents, it was 6.87 (95% CI, 1.55-30.46).
The results remained similar after further adjustment for the presence of diabetes and when considering peripheral artery disease and stroke.
No funding for the study was declared. Dr. Elshorbagy has relationships with Amgen, Daiichi Sankyo, and Regeneron.
A version of this article first appeared on Medscape.com.
MANNHEIM, GERMANY – – rates that appear to have a substantial impact on these patients’ already increased risk of coronary artery disease, a registry analysis suggests.
Data on almost 36,000 individuals with FH were collated from an international registry, revealing that 55% of adults and 25% of children and adolescents with the homozygous form of FH had overweight or obesity. The figures for heterozygous FH were 52% and 27%, respectively.
Crucially, overweight or obesity was associated with substantially increased rates of coronary artery disease, particularly in persons with heterozygous FH, among whom adults with obesity faced a twofold increased risk, rising to more than sixfold in children and adolescents.
Moreover, “obesity is associated with a worse lipid profile, even from childhood, regardless of whether a patient is on medication,” said study presenter Amany Elshorbagy, DPhil, Cardiovascular Epidemiologist, department of primary care and public health, Imperial College London.
She added that, with the increased risk of coronary artery disease associated with heterozygous FH, the results showed that “together with lipid-lowering medication, weight management is needed.”
The research was presented at the annual meeting of the European Atherosclerosis Society.
Tended to be thin
Alberico L. Catapano, MD, PhD, director of cardiovascular research and of the Lipoproteins and Atherosclerosis Laboratory of IRCCS Multimedica, Milan, and past president of the EAS, said in an interview that, historically, few FH patients were overweight or obese; rather, they tended to be thin.
However, there is now “a trend for people with FH to show more diabetes and obesity,” with the “bottom line” being that, as they are already at increased risk of coronary artery disease, it pushes their risk up even further.
In other words, if a risk factor such as obesity is added “on top of the strongest risk factor, that is LDL cholesterol, it is not one plus one makes two, it is one plus one makes three,” he said.
As such, Dr. Catapano believes that the study is “very interesting,” because it further underlines the importance of weight management for individuals with increased LDL cholesterol, “especially when you have genetic forms, like FH.”
Dr. Catapano’s comments were echoed by session co-chair Ulrike Schatz, MD, leader of the lipidology specialty department at the University Hospital Carl Gustav Carus, Technical University of Dresden (Germany).
Indeed, she told Dr. Elshorbagy before her presentation that she finds “a lot of my FH patients have a tendency towards anorexia.”
In an interview, Dr. Elshorbagy said that that reaction was typical of “most of the clinicians” she had spoken to. Upon seeing her data, especially for homozygous FH patients, they say, “They are on the lean side.”
Consequently, the research team went into the study “with the expectation that they might have a lower prevalence of obesity and overweight than the general population,” but “that’s not what we’re seeing.”
Dr. Elshorbagy noted that it would be helpful to have longitudinal data to determine whether, 50 years ago, patients with HF “were leaner, along with the rest of the population.”
The registry data are cross-sectional, and the team is now reaching out to the respective national lead investigators to submit follow-up data on their patients, with the aim of looking at changes in body weight and the impact on outcomes over time.
Another key question for the researchers is in regard to fat distribution, as body mass index “is not the best predictor of heart disease,” Dr. Elshorbagy said, but is rather central obesity.
Although they have also asked investigators to share waist circumference data, she conceded that it is a measurement that “is a lot harder to standardize across centers and countries; it’s not like putting patients on a scale.”
Overall, Dr. Elshorbagy believes that her findings indicate that clinicians should take a broader, more holistic approach toward their patients – in other words, an approach in which lipid lowering medication is “key but is just one of several things we need to do to make sure the coronary event rate goes down.”
More with than without
Dr. Elshorbagy began her presentation by highlighting that the prevalence of overweight and obesity ranges from 50% to 70% and that it is “the only health condition where you’ve got more people worldwide with the condition than without.”
Crucially, overweight increases the risk of coronary artery disease by approximately 20%. Among patients with obesity, the risk rises to 50%.
Given that FH patients “already have a very high risk of cardiovascular disease from their high cholesterol levels,” the team set out to determine rates of obesity and overweight in this population and their impact on coronary artery disease risk.
They used cross-sectional data from the EAS FH Studies Collaboration Global Registry, which involves 29,262 adults aged greater than or equal to 18 years and 6,275 children and adolescents aged 5 to 17 years with heterozygous FH, and 325 adults and 57 children with homozygous FH.
Dividing the adults into standard BMI categories, they found that 16% of heterozygous and 23% of homozygous FH patients had obesity, while 52% and 55%, respectively, had overweight or obesity.
For children, the team used World Health Organization z score cutoffs, which indicated that 9% of patients with heterozygous FH and 7% of patients with homozygous FH had obesity. Rates of overweight or obesity were 27% and 25%, respectively.
Among patients with heterozygous FH, rates of overweight or obesity among adults were 50% in high-income countries and 63% in other countries; among children, the rates were and 27% and 29%, respectively.
Stratified by region, the team found that the lowest rate of overweight or obesity among adult patients with heterozygous FH was in Eastern Asia, at 27%, while the highest was in Northern Africa/Western Asia (the Middle East), at 82%.
In North America, 56% of adult patients had overweight or obesity. The prevalence of coronary artery disease rose with increasing BMI.
Among adult patients with heterozygous FH, 11.3% of those with normal weight had coronary artery disease; the percentage rose to 22.9% among those with overweight, and 30.9% among those with obesity. Among children, the corresponding figures were 0.1%, 0.2%, and 0.7%.
Putting adults and children with homozygous FH together, the researchers found that 29.0% of patients with normal weight had coronary artery disease, compared with 31.3% of those with overweight and 49.3% of those with obesity.
Moreover, the results showed that levels of LDL and remnant cholesterol were significantly associated with BMI in adults and children with heterozygous FH, even after adjusting for age, sex, and lipid-lowering medication (P < .001 for all).
Multivariate analysis that took into account age, sex, lipid-lowering medication, and LDL cholesterol revealed that having obesity, compared with not having obesity, was associated with a substantial increase in the risk of coronary artery disease among patients with heterozygous FH.
Among adults with the condition, the odds ratio was 2.16 (95% confidence interval, 1.97-2.36), while among children and adolescents, it was 6.87 (95% CI, 1.55-30.46).
The results remained similar after further adjustment for the presence of diabetes and when considering peripheral artery disease and stroke.
No funding for the study was declared. Dr. Elshorbagy has relationships with Amgen, Daiichi Sankyo, and Regeneron.
A version of this article first appeared on Medscape.com.
AT EAS 2023
CKD Screening in all U.S. adults found cost effective
(UACR) followed by confirmatory tests and treatment of confirmed cases with current standard-care medications, according to an analysis published in the Annals of Internal Medicine.
This new evidence may prove important as the U.S. Preventive Services Task Force has begun revisiting its 2012 conclusion that “evidence is insufficient to assess the balance of benefits and harms of routine screening for chronic kidney disease in asymptomatic adults.”
A big difference between 2012 and today has been that sodium-glucose cotransporter 2 (SGLT2) inhibitors arrived on the scene as an important complement to well-established treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker. SGLT2 inhibitors have been documented as safe and effective for slowing CKD progression regardless of a person’s diabetes status, and have “dramatically altered” first-line treatment of adults with CKD, wrote the authors of the new study.
‘Large population health gains’ from CKD screening
“Given the high prevalence of CKD, even among those without risk factors, low-cost screening combined with effective treatment using SGLT2 inhibitors represent value,” explained Marika M. Cusick, lead author of the report, a PhD student, and a health policy researcher at Stanford (Calif.) University. “Our results show large population health gains can be achieved through CKD screening,” she said in an interview.
“This is a well-designed cost-effectiveness analysis that, importantly, considers newer treatments shown to be effective for slowing progression of CKD. The overall findings are convincing,” commented Deidra C. Crews, MD, a nephrologist and professor at Johns Hopkins University in Baltimore who was not involved in the research.
Dr. Crews, who is also president-elect of the American Society of Nephrology noted that the findings “may be a conservative estimate of the cost-effectiveness of CKD screening in certain subgroups, particularly when considering profound racial, ethnic and socioeconomic disparities in survival and CKD progression.”
The USPSTF starts a relook
The new evidence of cost-effectiveness of routine CKD screening follows the USPSTF’s release in January 2023 of a draft research plan to reassess the potential role for CKD screening of asymptomatic adults in the United States, the first step on a potential path to a revised set of recommendations. Public comment on the draft plan closed in February, and based on the standard USPSTF development steps and time frames, a final recommendation statement could appear by early 2026.
Revisiting the prior USPSTF decision from 2012 received endorsement earlier in 2023 from the ASN. The organization issued a statement last January that cited “more than a decade of advocacy in support of more kidney health screening by ASN and other stakeholders dedicated to intervening earlier to slow or stop the progression of kidney diseases.”
A more detailed letter of support for CKD screening sent to top USPSTF officials followed in February 2023 from ASN president Michelle A. Josephson, MD, who said in part that “ASN believes that kidney care is at an inflection point. There are now far more novel therapeutics to slow the progression of CKD, evidence to support the impact of nonpharmacologic interventions on CKD, and an increased commitment in public health to confront disparities and their causes.”
USPSTF recommendation could make a difference
Dr. Josephson also cited the modest effect that CKD screening recommendations from other groups have had up to now.
“Although guidance from Kidney Disease Improving Global Outcomes and the National Kidney Foundation recommends CKD screening among patients with hypertension, only approximately 10% of individuals with hypertension receive yearly screening. Furthermore, American Diabetes Association guidelines recommend yearly CKD screening in patients with diabetes, but only 40%-50% of patients receive this.”
“USPSTF recommendations tend to reach clinicians in primary care settings, where screening for diseases most commonly occurs, much more than recommendations from professional or patient organizations,” Dr. Crews said in an interview. “USPSTF recommendations also often influence health policies that might financially incentivize clinicians and health systems to screen their patients.”
“We hope [the USPSTF] will be interested in including our results within the totality of evidence assessed in their review of CKD screening,” said Ms. Cusick.
Preventing hundreds of thousands dialysis cases
The Stanford researchers developed a decision analytic Markov cohort model of CKD progression in U.S. adults aged 35 years or older and fit their model to data from the National Health and Nutrition Examination Survey (NHANES). They found that implementing one-time screening and adding SGLT2 inhibitors to treatment of the 158 million U.S. adults 35-75 years old would prevent the need for kidney replacement therapy (dialysis or transplant) in approximately 398,000 people over their lifetimes, representing a 10% decrease in such cases, compared with the status quo. Screening every 10 or 5 years combined with SGLT2 inhibitors would prevent approximately 598,000 or 658,000 people, respectively, from requiring kidney replacement therapy, compared with not screening.
Analysis showed that one-time screening produced an incremental cost-effectiveness ratio of $86,300 per quality-adjusted life-year (QALY) gained when one-time screening occurred in adults when they reached 55 years old. Screening every 10 years until people became 75 years old cost $98,400 per QALY gained for this group when adults were 35 years old, and $89,800 per QALY gained when screening occurred at 65 years old. These QALY costs are less than “commonly used” U.S. thresholds for acceptable cost-effectiveness of $100,000-$150,000 per QALY gained, the authors said.
Ms. Cusick highlighted the advantages of population-level screening for all U.S. adults, including those who are asymptomatic, compared with focusing on adults with risk factors, such as hypertension or diabetes.
“While risk-based screening can be more cost effective in some settings, risk factors are not always known, especially in marginalized and disadvantaged populations. This may lead to disparities in the use of screening and downstream health outcomes that could be avoided through universal screening policies,” she explained.
The study received no commercial funding. Ms. Cusick had no disclosures. Dr. Crews has received research grants from Somatus. Dr. Josephson has been a consultant to Exosome Diagnostics, IMMUCOR, Labcorp, Otsuka, UBC, and Vera Therapeutics, and has an ownership interest in Seagen.
(UACR) followed by confirmatory tests and treatment of confirmed cases with current standard-care medications, according to an analysis published in the Annals of Internal Medicine.
This new evidence may prove important as the U.S. Preventive Services Task Force has begun revisiting its 2012 conclusion that “evidence is insufficient to assess the balance of benefits and harms of routine screening for chronic kidney disease in asymptomatic adults.”
A big difference between 2012 and today has been that sodium-glucose cotransporter 2 (SGLT2) inhibitors arrived on the scene as an important complement to well-established treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker. SGLT2 inhibitors have been documented as safe and effective for slowing CKD progression regardless of a person’s diabetes status, and have “dramatically altered” first-line treatment of adults with CKD, wrote the authors of the new study.
‘Large population health gains’ from CKD screening
“Given the high prevalence of CKD, even among those without risk factors, low-cost screening combined with effective treatment using SGLT2 inhibitors represent value,” explained Marika M. Cusick, lead author of the report, a PhD student, and a health policy researcher at Stanford (Calif.) University. “Our results show large population health gains can be achieved through CKD screening,” she said in an interview.
“This is a well-designed cost-effectiveness analysis that, importantly, considers newer treatments shown to be effective for slowing progression of CKD. The overall findings are convincing,” commented Deidra C. Crews, MD, a nephrologist and professor at Johns Hopkins University in Baltimore who was not involved in the research.
Dr. Crews, who is also president-elect of the American Society of Nephrology noted that the findings “may be a conservative estimate of the cost-effectiveness of CKD screening in certain subgroups, particularly when considering profound racial, ethnic and socioeconomic disparities in survival and CKD progression.”
The USPSTF starts a relook
The new evidence of cost-effectiveness of routine CKD screening follows the USPSTF’s release in January 2023 of a draft research plan to reassess the potential role for CKD screening of asymptomatic adults in the United States, the first step on a potential path to a revised set of recommendations. Public comment on the draft plan closed in February, and based on the standard USPSTF development steps and time frames, a final recommendation statement could appear by early 2026.
Revisiting the prior USPSTF decision from 2012 received endorsement earlier in 2023 from the ASN. The organization issued a statement last January that cited “more than a decade of advocacy in support of more kidney health screening by ASN and other stakeholders dedicated to intervening earlier to slow or stop the progression of kidney diseases.”
A more detailed letter of support for CKD screening sent to top USPSTF officials followed in February 2023 from ASN president Michelle A. Josephson, MD, who said in part that “ASN believes that kidney care is at an inflection point. There are now far more novel therapeutics to slow the progression of CKD, evidence to support the impact of nonpharmacologic interventions on CKD, and an increased commitment in public health to confront disparities and their causes.”
USPSTF recommendation could make a difference
Dr. Josephson also cited the modest effect that CKD screening recommendations from other groups have had up to now.
“Although guidance from Kidney Disease Improving Global Outcomes and the National Kidney Foundation recommends CKD screening among patients with hypertension, only approximately 10% of individuals with hypertension receive yearly screening. Furthermore, American Diabetes Association guidelines recommend yearly CKD screening in patients with diabetes, but only 40%-50% of patients receive this.”
“USPSTF recommendations tend to reach clinicians in primary care settings, where screening for diseases most commonly occurs, much more than recommendations from professional or patient organizations,” Dr. Crews said in an interview. “USPSTF recommendations also often influence health policies that might financially incentivize clinicians and health systems to screen their patients.”
“We hope [the USPSTF] will be interested in including our results within the totality of evidence assessed in their review of CKD screening,” said Ms. Cusick.
Preventing hundreds of thousands dialysis cases
The Stanford researchers developed a decision analytic Markov cohort model of CKD progression in U.S. adults aged 35 years or older and fit their model to data from the National Health and Nutrition Examination Survey (NHANES). They found that implementing one-time screening and adding SGLT2 inhibitors to treatment of the 158 million U.S. adults 35-75 years old would prevent the need for kidney replacement therapy (dialysis or transplant) in approximately 398,000 people over their lifetimes, representing a 10% decrease in such cases, compared with the status quo. Screening every 10 or 5 years combined with SGLT2 inhibitors would prevent approximately 598,000 or 658,000 people, respectively, from requiring kidney replacement therapy, compared with not screening.
Analysis showed that one-time screening produced an incremental cost-effectiveness ratio of $86,300 per quality-adjusted life-year (QALY) gained when one-time screening occurred in adults when they reached 55 years old. Screening every 10 years until people became 75 years old cost $98,400 per QALY gained for this group when adults were 35 years old, and $89,800 per QALY gained when screening occurred at 65 years old. These QALY costs are less than “commonly used” U.S. thresholds for acceptable cost-effectiveness of $100,000-$150,000 per QALY gained, the authors said.
Ms. Cusick highlighted the advantages of population-level screening for all U.S. adults, including those who are asymptomatic, compared with focusing on adults with risk factors, such as hypertension or diabetes.
“While risk-based screening can be more cost effective in some settings, risk factors are not always known, especially in marginalized and disadvantaged populations. This may lead to disparities in the use of screening and downstream health outcomes that could be avoided through universal screening policies,” she explained.
The study received no commercial funding. Ms. Cusick had no disclosures. Dr. Crews has received research grants from Somatus. Dr. Josephson has been a consultant to Exosome Diagnostics, IMMUCOR, Labcorp, Otsuka, UBC, and Vera Therapeutics, and has an ownership interest in Seagen.
(UACR) followed by confirmatory tests and treatment of confirmed cases with current standard-care medications, according to an analysis published in the Annals of Internal Medicine.
This new evidence may prove important as the U.S. Preventive Services Task Force has begun revisiting its 2012 conclusion that “evidence is insufficient to assess the balance of benefits and harms of routine screening for chronic kidney disease in asymptomatic adults.”
A big difference between 2012 and today has been that sodium-glucose cotransporter 2 (SGLT2) inhibitors arrived on the scene as an important complement to well-established treatment with an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker. SGLT2 inhibitors have been documented as safe and effective for slowing CKD progression regardless of a person’s diabetes status, and have “dramatically altered” first-line treatment of adults with CKD, wrote the authors of the new study.
‘Large population health gains’ from CKD screening
“Given the high prevalence of CKD, even among those without risk factors, low-cost screening combined with effective treatment using SGLT2 inhibitors represent value,” explained Marika M. Cusick, lead author of the report, a PhD student, and a health policy researcher at Stanford (Calif.) University. “Our results show large population health gains can be achieved through CKD screening,” she said in an interview.
“This is a well-designed cost-effectiveness analysis that, importantly, considers newer treatments shown to be effective for slowing progression of CKD. The overall findings are convincing,” commented Deidra C. Crews, MD, a nephrologist and professor at Johns Hopkins University in Baltimore who was not involved in the research.
Dr. Crews, who is also president-elect of the American Society of Nephrology noted that the findings “may be a conservative estimate of the cost-effectiveness of CKD screening in certain subgroups, particularly when considering profound racial, ethnic and socioeconomic disparities in survival and CKD progression.”
The USPSTF starts a relook
The new evidence of cost-effectiveness of routine CKD screening follows the USPSTF’s release in January 2023 of a draft research plan to reassess the potential role for CKD screening of asymptomatic adults in the United States, the first step on a potential path to a revised set of recommendations. Public comment on the draft plan closed in February, and based on the standard USPSTF development steps and time frames, a final recommendation statement could appear by early 2026.
Revisiting the prior USPSTF decision from 2012 received endorsement earlier in 2023 from the ASN. The organization issued a statement last January that cited “more than a decade of advocacy in support of more kidney health screening by ASN and other stakeholders dedicated to intervening earlier to slow or stop the progression of kidney diseases.”
A more detailed letter of support for CKD screening sent to top USPSTF officials followed in February 2023 from ASN president Michelle A. Josephson, MD, who said in part that “ASN believes that kidney care is at an inflection point. There are now far more novel therapeutics to slow the progression of CKD, evidence to support the impact of nonpharmacologic interventions on CKD, and an increased commitment in public health to confront disparities and their causes.”
USPSTF recommendation could make a difference
Dr. Josephson also cited the modest effect that CKD screening recommendations from other groups have had up to now.
“Although guidance from Kidney Disease Improving Global Outcomes and the National Kidney Foundation recommends CKD screening among patients with hypertension, only approximately 10% of individuals with hypertension receive yearly screening. Furthermore, American Diabetes Association guidelines recommend yearly CKD screening in patients with diabetes, but only 40%-50% of patients receive this.”
“USPSTF recommendations tend to reach clinicians in primary care settings, where screening for diseases most commonly occurs, much more than recommendations from professional or patient organizations,” Dr. Crews said in an interview. “USPSTF recommendations also often influence health policies that might financially incentivize clinicians and health systems to screen their patients.”
“We hope [the USPSTF] will be interested in including our results within the totality of evidence assessed in their review of CKD screening,” said Ms. Cusick.
Preventing hundreds of thousands dialysis cases
The Stanford researchers developed a decision analytic Markov cohort model of CKD progression in U.S. adults aged 35 years or older and fit their model to data from the National Health and Nutrition Examination Survey (NHANES). They found that implementing one-time screening and adding SGLT2 inhibitors to treatment of the 158 million U.S. adults 35-75 years old would prevent the need for kidney replacement therapy (dialysis or transplant) in approximately 398,000 people over their lifetimes, representing a 10% decrease in such cases, compared with the status quo. Screening every 10 or 5 years combined with SGLT2 inhibitors would prevent approximately 598,000 or 658,000 people, respectively, from requiring kidney replacement therapy, compared with not screening.
Analysis showed that one-time screening produced an incremental cost-effectiveness ratio of $86,300 per quality-adjusted life-year (QALY) gained when one-time screening occurred in adults when they reached 55 years old. Screening every 10 years until people became 75 years old cost $98,400 per QALY gained for this group when adults were 35 years old, and $89,800 per QALY gained when screening occurred at 65 years old. These QALY costs are less than “commonly used” U.S. thresholds for acceptable cost-effectiveness of $100,000-$150,000 per QALY gained, the authors said.
Ms. Cusick highlighted the advantages of population-level screening for all U.S. adults, including those who are asymptomatic, compared with focusing on adults with risk factors, such as hypertension or diabetes.
“While risk-based screening can be more cost effective in some settings, risk factors are not always known, especially in marginalized and disadvantaged populations. This may lead to disparities in the use of screening and downstream health outcomes that could be avoided through universal screening policies,” she explained.
The study received no commercial funding. Ms. Cusick had no disclosures. Dr. Crews has received research grants from Somatus. Dr. Josephson has been a consultant to Exosome Diagnostics, IMMUCOR, Labcorp, Otsuka, UBC, and Vera Therapeutics, and has an ownership interest in Seagen.
FROM ANNALS OF INTERNAL MEDICINE
Early gestational diabetes treatment may improve neonatal outcomes
Screening and treatment for gestational diabetes are currently recommended at 24-28 weeks’ gestation, with earlier testing recommended for women at increased risk, but the potential benefits of earlier intervention remain debatable, wrote David Simmons, MD, of Western Sydney University, Campbelltown, Australia, and colleagues.
“Until now, there has been complete equipoise over whether to treat hyperglycemia below that of overt diabetes early in pregnancy,” Dr. Simmons said in an interview. The conflicting questions: “Would early treatment reduce the excess deposition of fat on the baby with all of its sequelae; but would early treatment reduce fuel supply to some babies at a critical time and lead to SGA [small for gestational age]?” Dr. Simmons noted.
In a study published in the New England Journal of Medicine, Dr. Simmons and colleagues randomized 406 women aged 18 years and older with singleton pregnancies to immediate treatment for gestational diabetes. Another 396 women were randomized to a control group for deferred treatment or no treatment, based on results of an oral glucose tolerance test at 24-28 weeks’ gestation. All participants had at least one risk factor for hyperglycemia, and met the World Health Organization criteria for gestational diabetes. Women with preexisting diabetes or contraindicating comorbid medical conditions were excluded.
The study had three primary outcomes. The first was a composite of neonatal outcomes including birth before 37 weeks’ gestation, birth weight of 4,500 g or higher, birth trauma, neonatal respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia.
The final sample included 748 women for adverse neonatal outcomes, 750 for pregnancy-related hypertension, and 492 for neonatal lean body mass. The mean age of the participants was 32 years; approximately one-third were white European and another third were South Asian. Overall baseline demographics were similar between the groups, and the initial oral glucose tolerance tests were performed at a mean of 15.6 weeks’ gestation.
Overall, 24.9% of women in the early treatment group experienced an adverse neonatal event vs. 30.5% of controls, for an adjusted risk difference of –5.6% and adjusted relative risk of 0.82.
Notably, in an exploratory subgroup analysis, respiratory distress occurred in 9.8% of infants born to women in the immediate treatment group vs. 17.0% of infants in the control group. “Neonatal respiratory distress was the main driver of the between-group difference observed for the first primary outcome,” the researchers wrote. A prespecified subgroup analysis suggested that the impact of an earlier intervention on adverse neonatal outcomes might be greater among women with a higher glycemic value and those whose oral glucose tolerance tests occurred at less than 14 weeks’ gestation, they noted. Stillbirths or neonatal deaths were similar and infrequent in both groups.
Pregnancy-related hypertension occurred in 10.6% of the immediate-treatment group and 9.9% of the controls group (adjusted risk difference, 0.7%). For the third outcome, the mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g for the controls (adjusted mean difference, −0.04 g).
No differences in serious adverse events related to either screening or treatment were noted between the groups.
Impact on neonatal outcomes merits further study
Dr. Simmons said that he was surprised by the study findings. “We thought if there was an effect, it would be small, but it isn’t,” he told this publication.
“If you combine the severe adverse outcomes, the perineal trauma and the reduction in days in NICU/special care unit, this is a significant impact on morbidity and likely on cost,” and researchers are currently examining data for cost-effectiveness, he said.
“We did not expect the likely large impact on reducing respiratory distress and perineal trauma,” he noted. “These findings have not been previously reported, perhaps because they were not looked for.” By contrast, “we thought here might be reductions in lower gestational age and cesarean delivery, but there was not,” he added.
The findings were limited by several factors including the nonstandardized approach to gestational diabetes treatment and the use of third-trimester treatment targets that had not been tested in earlier trimesters, the researchers noted. Other limitations included the focus on women already at high risk for hyperglycemia; therefore, the results might not generalize to women not at risk, they wrote.
The current study represents a beginning of answers, with data suggesting that early treatment for gestational diabetes reduces severe adverse pregnancy outcomes, days in NICU/special care unit, and perineal trauma, likely from the first trimester, said Dr. Simmons. However, the findings must be interpreted with caution, as criteria that are too low “might lead to more small babies,” he said. “We look forward to working with others to translate these findings into practice,” he added.
Much more research is needed to answer the many questions prompted by the current study, including who did and did not have complications, Dr. Simmons told this publication. Other studies are needed to collect data on cost-effectiveness, as well as consumer views, especially “different perspectives from different parts of the globe,” he said. Although there is not enough evidence yet to draw conclusions about the role of continuous glucose monitoring (CGM) in managing gestational diabetes, many studies are underway; “we look forward to the results,” of these studies, Dr. Simmons added.
Findings support early screening
Gestational diabetes is one of the most common medical complications of pregnancy, and accounts for more than 80% of diabetes-related diagnoses in pregnancy, said Emily Fay, MD, a maternal-fetal medicine specialist at the University of Washington, Seattle, in an interview.
“Previous studies have found that women with gestational diabetes are at higher risk in their pregnancy, including higher chance of developing preeclampsia, higher chance of cesarean delivery, and higher risks for their baby, including risk of shoulder dystocia, birth trauma, and jaundice, and higher birth weights,” she said. “Fortunately, studies have also shown that treatment of gestational diabetes helps lower these risks,” she noted. Currently, patients undergo routine screening for gestational diabetes between 24 and 28 weeks of pregnancy, but some who have risk factors for gestational diabetes may have screening in the early part of pregnancy, said Dr. Fay.
The current findings were not surprising overall, said Dr. Fay, who was not involved in the study. “The study authors looked at a variety of outcomes including neonatal adverse outcomes, neonatal body weight, and pregnancy-related hypertension,” she said.
The researchers found that patients treated early had a lower rate of adverse neonatal outcomes, which was to be expected, Dr. Fay said. “They did not find a difference in neonatal body weight; this also was not surprising, as the women who were not in the early treatment group still received treatment at the time of diagnosis later in pregnancy, which likely helped normalize the weights,” she explained.
“My takeaway from this study is that we should continue to screen patients with risk factors for gestational diabetes early in pregnancy and treat them at the time of diagnosis,” Dr. Fay told this publication. However, barriers that may exist to early treatment involve access to care, including being able to see a provider early in pregnancy, she said. “The treatment for gestational diabetes includes dietary education with diet changes and checking blood sugars frequently. Access to nutrition education can be limited and access to healthy foods can be expensive and difficult to obtain,” she noted. “Checking blood sugars throughout the day can also be difficult for those who are busy or working and who may not have the ability to take time to do this,” she said. However, “these barriers may be overcome by health care reform that improves patient access to and coverage of pregnancy care, improved access and affordability of healthy foods, and employer flexibility to allow the time and space to check blood sugars if needed,” she added.
Looking ahead, the use of continuous glucose monitors in pregnancy is an expanding area of research, said Dr. Fay. “Patients can quickly view their blood sugar without the use of finger sticks, which may help overcome some of the barriers patients may have with using finger sticks,” she noted. “Continuous glucose monitors have been used for those with type 1 and type 2 diabetes with success, and we need to better understand if these can also be helpful in gestational diabetes,” she said. Dr. Fay and colleagues at the University of Washington are currently conducting an ongoing study to explore the use of CGM in gestational diabetes.
The study was supported by the National Health and Medical Research Council, the Region Örebro Research Committee, the Medical Scientific Fund of the Mayor of Vienna, the South Western Sydney Local Health District Academic Unit, and a Western Sydney University Ainsworth Trust Grant. The researchers had no financial conflicts to disclose. Dr. Fay had no relevant financial conflicts to disclose.
Screening and treatment for gestational diabetes are currently recommended at 24-28 weeks’ gestation, with earlier testing recommended for women at increased risk, but the potential benefits of earlier intervention remain debatable, wrote David Simmons, MD, of Western Sydney University, Campbelltown, Australia, and colleagues.
“Until now, there has been complete equipoise over whether to treat hyperglycemia below that of overt diabetes early in pregnancy,” Dr. Simmons said in an interview. The conflicting questions: “Would early treatment reduce the excess deposition of fat on the baby with all of its sequelae; but would early treatment reduce fuel supply to some babies at a critical time and lead to SGA [small for gestational age]?” Dr. Simmons noted.
In a study published in the New England Journal of Medicine, Dr. Simmons and colleagues randomized 406 women aged 18 years and older with singleton pregnancies to immediate treatment for gestational diabetes. Another 396 women were randomized to a control group for deferred treatment or no treatment, based on results of an oral glucose tolerance test at 24-28 weeks’ gestation. All participants had at least one risk factor for hyperglycemia, and met the World Health Organization criteria for gestational diabetes. Women with preexisting diabetes or contraindicating comorbid medical conditions were excluded.
The study had three primary outcomes. The first was a composite of neonatal outcomes including birth before 37 weeks’ gestation, birth weight of 4,500 g or higher, birth trauma, neonatal respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia.
The final sample included 748 women for adverse neonatal outcomes, 750 for pregnancy-related hypertension, and 492 for neonatal lean body mass. The mean age of the participants was 32 years; approximately one-third were white European and another third were South Asian. Overall baseline demographics were similar between the groups, and the initial oral glucose tolerance tests were performed at a mean of 15.6 weeks’ gestation.
Overall, 24.9% of women in the early treatment group experienced an adverse neonatal event vs. 30.5% of controls, for an adjusted risk difference of –5.6% and adjusted relative risk of 0.82.
Notably, in an exploratory subgroup analysis, respiratory distress occurred in 9.8% of infants born to women in the immediate treatment group vs. 17.0% of infants in the control group. “Neonatal respiratory distress was the main driver of the between-group difference observed for the first primary outcome,” the researchers wrote. A prespecified subgroup analysis suggested that the impact of an earlier intervention on adverse neonatal outcomes might be greater among women with a higher glycemic value and those whose oral glucose tolerance tests occurred at less than 14 weeks’ gestation, they noted. Stillbirths or neonatal deaths were similar and infrequent in both groups.
Pregnancy-related hypertension occurred in 10.6% of the immediate-treatment group and 9.9% of the controls group (adjusted risk difference, 0.7%). For the third outcome, the mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g for the controls (adjusted mean difference, −0.04 g).
No differences in serious adverse events related to either screening or treatment were noted between the groups.
Impact on neonatal outcomes merits further study
Dr. Simmons said that he was surprised by the study findings. “We thought if there was an effect, it would be small, but it isn’t,” he told this publication.
“If you combine the severe adverse outcomes, the perineal trauma and the reduction in days in NICU/special care unit, this is a significant impact on morbidity and likely on cost,” and researchers are currently examining data for cost-effectiveness, he said.
“We did not expect the likely large impact on reducing respiratory distress and perineal trauma,” he noted. “These findings have not been previously reported, perhaps because they were not looked for.” By contrast, “we thought here might be reductions in lower gestational age and cesarean delivery, but there was not,” he added.
The findings were limited by several factors including the nonstandardized approach to gestational diabetes treatment and the use of third-trimester treatment targets that had not been tested in earlier trimesters, the researchers noted. Other limitations included the focus on women already at high risk for hyperglycemia; therefore, the results might not generalize to women not at risk, they wrote.
The current study represents a beginning of answers, with data suggesting that early treatment for gestational diabetes reduces severe adverse pregnancy outcomes, days in NICU/special care unit, and perineal trauma, likely from the first trimester, said Dr. Simmons. However, the findings must be interpreted with caution, as criteria that are too low “might lead to more small babies,” he said. “We look forward to working with others to translate these findings into practice,” he added.
Much more research is needed to answer the many questions prompted by the current study, including who did and did not have complications, Dr. Simmons told this publication. Other studies are needed to collect data on cost-effectiveness, as well as consumer views, especially “different perspectives from different parts of the globe,” he said. Although there is not enough evidence yet to draw conclusions about the role of continuous glucose monitoring (CGM) in managing gestational diabetes, many studies are underway; “we look forward to the results,” of these studies, Dr. Simmons added.
Findings support early screening
Gestational diabetes is one of the most common medical complications of pregnancy, and accounts for more than 80% of diabetes-related diagnoses in pregnancy, said Emily Fay, MD, a maternal-fetal medicine specialist at the University of Washington, Seattle, in an interview.
“Previous studies have found that women with gestational diabetes are at higher risk in their pregnancy, including higher chance of developing preeclampsia, higher chance of cesarean delivery, and higher risks for their baby, including risk of shoulder dystocia, birth trauma, and jaundice, and higher birth weights,” she said. “Fortunately, studies have also shown that treatment of gestational diabetes helps lower these risks,” she noted. Currently, patients undergo routine screening for gestational diabetes between 24 and 28 weeks of pregnancy, but some who have risk factors for gestational diabetes may have screening in the early part of pregnancy, said Dr. Fay.
The current findings were not surprising overall, said Dr. Fay, who was not involved in the study. “The study authors looked at a variety of outcomes including neonatal adverse outcomes, neonatal body weight, and pregnancy-related hypertension,” she said.
The researchers found that patients treated early had a lower rate of adverse neonatal outcomes, which was to be expected, Dr. Fay said. “They did not find a difference in neonatal body weight; this also was not surprising, as the women who were not in the early treatment group still received treatment at the time of diagnosis later in pregnancy, which likely helped normalize the weights,” she explained.
“My takeaway from this study is that we should continue to screen patients with risk factors for gestational diabetes early in pregnancy and treat them at the time of diagnosis,” Dr. Fay told this publication. However, barriers that may exist to early treatment involve access to care, including being able to see a provider early in pregnancy, she said. “The treatment for gestational diabetes includes dietary education with diet changes and checking blood sugars frequently. Access to nutrition education can be limited and access to healthy foods can be expensive and difficult to obtain,” she noted. “Checking blood sugars throughout the day can also be difficult for those who are busy or working and who may not have the ability to take time to do this,” she said. However, “these barriers may be overcome by health care reform that improves patient access to and coverage of pregnancy care, improved access and affordability of healthy foods, and employer flexibility to allow the time and space to check blood sugars if needed,” she added.
Looking ahead, the use of continuous glucose monitors in pregnancy is an expanding area of research, said Dr. Fay. “Patients can quickly view their blood sugar without the use of finger sticks, which may help overcome some of the barriers patients may have with using finger sticks,” she noted. “Continuous glucose monitors have been used for those with type 1 and type 2 diabetes with success, and we need to better understand if these can also be helpful in gestational diabetes,” she said. Dr. Fay and colleagues at the University of Washington are currently conducting an ongoing study to explore the use of CGM in gestational diabetes.
The study was supported by the National Health and Medical Research Council, the Region Örebro Research Committee, the Medical Scientific Fund of the Mayor of Vienna, the South Western Sydney Local Health District Academic Unit, and a Western Sydney University Ainsworth Trust Grant. The researchers had no financial conflicts to disclose. Dr. Fay had no relevant financial conflicts to disclose.
Screening and treatment for gestational diabetes are currently recommended at 24-28 weeks’ gestation, with earlier testing recommended for women at increased risk, but the potential benefits of earlier intervention remain debatable, wrote David Simmons, MD, of Western Sydney University, Campbelltown, Australia, and colleagues.
“Until now, there has been complete equipoise over whether to treat hyperglycemia below that of overt diabetes early in pregnancy,” Dr. Simmons said in an interview. The conflicting questions: “Would early treatment reduce the excess deposition of fat on the baby with all of its sequelae; but would early treatment reduce fuel supply to some babies at a critical time and lead to SGA [small for gestational age]?” Dr. Simmons noted.
In a study published in the New England Journal of Medicine, Dr. Simmons and colleagues randomized 406 women aged 18 years and older with singleton pregnancies to immediate treatment for gestational diabetes. Another 396 women were randomized to a control group for deferred treatment or no treatment, based on results of an oral glucose tolerance test at 24-28 weeks’ gestation. All participants had at least one risk factor for hyperglycemia, and met the World Health Organization criteria for gestational diabetes. Women with preexisting diabetes or contraindicating comorbid medical conditions were excluded.
The study had three primary outcomes. The first was a composite of neonatal outcomes including birth before 37 weeks’ gestation, birth weight of 4,500 g or higher, birth trauma, neonatal respiratory distress, phototherapy, stillbirth or neonatal death, or shoulder dystocia.
The final sample included 748 women for adverse neonatal outcomes, 750 for pregnancy-related hypertension, and 492 for neonatal lean body mass. The mean age of the participants was 32 years; approximately one-third were white European and another third were South Asian. Overall baseline demographics were similar between the groups, and the initial oral glucose tolerance tests were performed at a mean of 15.6 weeks’ gestation.
Overall, 24.9% of women in the early treatment group experienced an adverse neonatal event vs. 30.5% of controls, for an adjusted risk difference of –5.6% and adjusted relative risk of 0.82.
Notably, in an exploratory subgroup analysis, respiratory distress occurred in 9.8% of infants born to women in the immediate treatment group vs. 17.0% of infants in the control group. “Neonatal respiratory distress was the main driver of the between-group difference observed for the first primary outcome,” the researchers wrote. A prespecified subgroup analysis suggested that the impact of an earlier intervention on adverse neonatal outcomes might be greater among women with a higher glycemic value and those whose oral glucose tolerance tests occurred at less than 14 weeks’ gestation, they noted. Stillbirths or neonatal deaths were similar and infrequent in both groups.
Pregnancy-related hypertension occurred in 10.6% of the immediate-treatment group and 9.9% of the controls group (adjusted risk difference, 0.7%). For the third outcome, the mean neonatal lean body mass was 2.86 g in the immediate-treatment group and 2.91 g for the controls (adjusted mean difference, −0.04 g).
No differences in serious adverse events related to either screening or treatment were noted between the groups.
Impact on neonatal outcomes merits further study
Dr. Simmons said that he was surprised by the study findings. “We thought if there was an effect, it would be small, but it isn’t,” he told this publication.
“If you combine the severe adverse outcomes, the perineal trauma and the reduction in days in NICU/special care unit, this is a significant impact on morbidity and likely on cost,” and researchers are currently examining data for cost-effectiveness, he said.
“We did not expect the likely large impact on reducing respiratory distress and perineal trauma,” he noted. “These findings have not been previously reported, perhaps because they were not looked for.” By contrast, “we thought here might be reductions in lower gestational age and cesarean delivery, but there was not,” he added.
The findings were limited by several factors including the nonstandardized approach to gestational diabetes treatment and the use of third-trimester treatment targets that had not been tested in earlier trimesters, the researchers noted. Other limitations included the focus on women already at high risk for hyperglycemia; therefore, the results might not generalize to women not at risk, they wrote.
The current study represents a beginning of answers, with data suggesting that early treatment for gestational diabetes reduces severe adverse pregnancy outcomes, days in NICU/special care unit, and perineal trauma, likely from the first trimester, said Dr. Simmons. However, the findings must be interpreted with caution, as criteria that are too low “might lead to more small babies,” he said. “We look forward to working with others to translate these findings into practice,” he added.
Much more research is needed to answer the many questions prompted by the current study, including who did and did not have complications, Dr. Simmons told this publication. Other studies are needed to collect data on cost-effectiveness, as well as consumer views, especially “different perspectives from different parts of the globe,” he said. Although there is not enough evidence yet to draw conclusions about the role of continuous glucose monitoring (CGM) in managing gestational diabetes, many studies are underway; “we look forward to the results,” of these studies, Dr. Simmons added.
Findings support early screening
Gestational diabetes is one of the most common medical complications of pregnancy, and accounts for more than 80% of diabetes-related diagnoses in pregnancy, said Emily Fay, MD, a maternal-fetal medicine specialist at the University of Washington, Seattle, in an interview.
“Previous studies have found that women with gestational diabetes are at higher risk in their pregnancy, including higher chance of developing preeclampsia, higher chance of cesarean delivery, and higher risks for their baby, including risk of shoulder dystocia, birth trauma, and jaundice, and higher birth weights,” she said. “Fortunately, studies have also shown that treatment of gestational diabetes helps lower these risks,” she noted. Currently, patients undergo routine screening for gestational diabetes between 24 and 28 weeks of pregnancy, but some who have risk factors for gestational diabetes may have screening in the early part of pregnancy, said Dr. Fay.
The current findings were not surprising overall, said Dr. Fay, who was not involved in the study. “The study authors looked at a variety of outcomes including neonatal adverse outcomes, neonatal body weight, and pregnancy-related hypertension,” she said.
The researchers found that patients treated early had a lower rate of adverse neonatal outcomes, which was to be expected, Dr. Fay said. “They did not find a difference in neonatal body weight; this also was not surprising, as the women who were not in the early treatment group still received treatment at the time of diagnosis later in pregnancy, which likely helped normalize the weights,” she explained.
“My takeaway from this study is that we should continue to screen patients with risk factors for gestational diabetes early in pregnancy and treat them at the time of diagnosis,” Dr. Fay told this publication. However, barriers that may exist to early treatment involve access to care, including being able to see a provider early in pregnancy, she said. “The treatment for gestational diabetes includes dietary education with diet changes and checking blood sugars frequently. Access to nutrition education can be limited and access to healthy foods can be expensive and difficult to obtain,” she noted. “Checking blood sugars throughout the day can also be difficult for those who are busy or working and who may not have the ability to take time to do this,” she said. However, “these barriers may be overcome by health care reform that improves patient access to and coverage of pregnancy care, improved access and affordability of healthy foods, and employer flexibility to allow the time and space to check blood sugars if needed,” she added.
Looking ahead, the use of continuous glucose monitors in pregnancy is an expanding area of research, said Dr. Fay. “Patients can quickly view their blood sugar without the use of finger sticks, which may help overcome some of the barriers patients may have with using finger sticks,” she noted. “Continuous glucose monitors have been used for those with type 1 and type 2 diabetes with success, and we need to better understand if these can also be helpful in gestational diabetes,” she said. Dr. Fay and colleagues at the University of Washington are currently conducting an ongoing study to explore the use of CGM in gestational diabetes.
The study was supported by the National Health and Medical Research Council, the Region Örebro Research Committee, the Medical Scientific Fund of the Mayor of Vienna, the South Western Sydney Local Health District Academic Unit, and a Western Sydney University Ainsworth Trust Grant. The researchers had no financial conflicts to disclose. Dr. Fay had no relevant financial conflicts to disclose.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Expert discusses which diets are best, based on the evidence
according to a speaker at the annual meeting of the American College of Physicians.
“Evidence from studies can help clinicians and their patients develop a successful dietary management plan and achieve optimal health,” said internist Michelle Hauser, MD, clinical associate professor at Stanford (Calif.) University. She also discussed evidence-based techniques to support patients in maintaining dietary modifications.
Predominantly plant‐based diets
Popular predominantly plant‐based diets include a Mediterranean diet, healthy vegetarian diet, predominantly whole-food plant‐based (WFPB) diet, and a dietary approach to stop hypertension (DASH).
The DASH diet was originally designed to help patients manage their blood pressure, but evidence suggests that it also can help adults with obesity lose weight. In contrast to the DASH diet, the Mediterranean diet is not low-fat and not very restrictive. Yet the evidence suggests that the Mediterranean diet is not only helpful for losing weight but also can reduce the risk of various chronic diseases, including obesity, type 2 diabetes, cardiovascular disease (CVD), and cancer, Dr. Hauser said. In addition, data suggest that the Mediterranean diet may reduce the risk of all-cause mortality and lower the levels of cholesterol.
“I like to highlight all these protective effects to my patients, because even if their goal is to lose weight, knowing that hard work pays off in additional ways can keep them motivated,” Dr. Hauser stated.
A healthy vegetarian diet and a WFPB diet are similar, and both are helpful in weight loss and management of total cholesterol and LDL‐C levels. Furthermore, healthy vegetarian and WFPB diets may reduce the risk of type 2 diabetes, CVD, and some cancers. Cohort study data suggest that progressively more vegetarian diets are associated with lower BMIs.
“My interpretation of these data is that predominantly plant-based diets rich in whole foods are healthful and can be done in a way that is sustainable for most,” said Dr. Hauser. However, this generally requires a lot of support at the outset to address gaps in knowledge, skills, and other potential barriers.
For example, she referred one obese patient at risk of diabetes and cardiovascular disease to a registered dietitian to develop a dietary plan. The patient also attended a behavioral medicine weight management program to learn strategies such as using smaller plates, and his family attended a healthy cooking class together to improve meal planning and cooking skills.
Time‐restricted feeding
There are numerous variations of time-restricted feeding, commonly referred to as intermittent fasting, but the principles are similar – limiting food intake to a specific window of time each day or week.
Although some studies have shown that time-restricted feeding may help patients reduce adiposity and improve lipid markers, most studies comparing time-restricted feeding to a calorie-restricted diet have shown little to no difference in weight-related outcomes, Dr. Hauser said.
These data suggest that time-restricted feeding may help patients with weight loss only if time restriction helps them reduce calorie intake. She also warned that time-restrictive feeding might cause late-night cravings and might not be helpful in individuals prone to food cravings.
Low‐carbohydrate and ketogenic diets
Losing muscle mass can prevent some people from dieting, but evidence suggests that a high-fat, very low-carbohydrate diet – also called a ketogenic diet – may help patients reduce weight and fat mass while preserving fat‐free mass, Dr. Hauser said.
The evidence regarding the usefulness of a low-carbohydrate (non-keto) diet is less clear because most studies compared it to a low-fat diet, and these two diets might lead to a similar extent of weight loss.
Rating the level of scientific evidence behind different diet options
Nutrition studies do no provide the same level of evidence as drug studies, said Dr. Hauser, because it is easier to conduct a randomized controlled trial of a drug versus placebo. Diets have many more variables, and it also takes much longer to observe most outcomes of a dietary change.
In addition, clinical trials of dietary interventions are typically short and focus on disease markers such as serum lipids and hemoglobin A1c levels. To obtain reliable information on the usefulness of a diet, researchers need to collect detailed health and lifestyle information from hundreds of thousands of people over several decades, which is not always feasible. “This is why meta-analyses of pooled dietary study data are more likely to yield dependable findings,” she noted.
Getting to know patients is essential to help them maintain diet modifications
When developing a diet plan for a patient, it is important to consider the sustainability of a dietary pattern. “The benefits of any healthy dietary change will only last as long as they can be maintained,” said Dr. Hauser. “Counseling someone on choosing an appropriate long-term dietary pattern requires getting to know them – taste preferences, food traditions, barriers, facilitators, food access, and time and cost restrictions.”
In an interview after the session, David Bittleman, MD, an internist at Veterans Affairs San Diego Health Care System, agreed that getting to know patients is essential for successfully advising them on diet.
“I always start developing a diet plan by trying to find out what [a patient’s] diet is like and what their goals are. I need to know what they are already doing in order to make suggestions about what they can do to make their diet healthier,” he said.
When asked about her approach to supporting patients in the long term, Dr. Hauser said that she recommends sequential, gradual changes. Dr. Hauser added that she suggests her patients prioritize implementing dietary changes that they are confident they can maintain.
Dr. Hauser and Dr. Bittleman report no relevant financial relationships.
according to a speaker at the annual meeting of the American College of Physicians.
“Evidence from studies can help clinicians and their patients develop a successful dietary management plan and achieve optimal health,” said internist Michelle Hauser, MD, clinical associate professor at Stanford (Calif.) University. She also discussed evidence-based techniques to support patients in maintaining dietary modifications.
Predominantly plant‐based diets
Popular predominantly plant‐based diets include a Mediterranean diet, healthy vegetarian diet, predominantly whole-food plant‐based (WFPB) diet, and a dietary approach to stop hypertension (DASH).
The DASH diet was originally designed to help patients manage their blood pressure, but evidence suggests that it also can help adults with obesity lose weight. In contrast to the DASH diet, the Mediterranean diet is not low-fat and not very restrictive. Yet the evidence suggests that the Mediterranean diet is not only helpful for losing weight but also can reduce the risk of various chronic diseases, including obesity, type 2 diabetes, cardiovascular disease (CVD), and cancer, Dr. Hauser said. In addition, data suggest that the Mediterranean diet may reduce the risk of all-cause mortality and lower the levels of cholesterol.
“I like to highlight all these protective effects to my patients, because even if their goal is to lose weight, knowing that hard work pays off in additional ways can keep them motivated,” Dr. Hauser stated.
A healthy vegetarian diet and a WFPB diet are similar, and both are helpful in weight loss and management of total cholesterol and LDL‐C levels. Furthermore, healthy vegetarian and WFPB diets may reduce the risk of type 2 diabetes, CVD, and some cancers. Cohort study data suggest that progressively more vegetarian diets are associated with lower BMIs.
“My interpretation of these data is that predominantly plant-based diets rich in whole foods are healthful and can be done in a way that is sustainable for most,” said Dr. Hauser. However, this generally requires a lot of support at the outset to address gaps in knowledge, skills, and other potential barriers.
For example, she referred one obese patient at risk of diabetes and cardiovascular disease to a registered dietitian to develop a dietary plan. The patient also attended a behavioral medicine weight management program to learn strategies such as using smaller plates, and his family attended a healthy cooking class together to improve meal planning and cooking skills.
Time‐restricted feeding
There are numerous variations of time-restricted feeding, commonly referred to as intermittent fasting, but the principles are similar – limiting food intake to a specific window of time each day or week.
Although some studies have shown that time-restricted feeding may help patients reduce adiposity and improve lipid markers, most studies comparing time-restricted feeding to a calorie-restricted diet have shown little to no difference in weight-related outcomes, Dr. Hauser said.
These data suggest that time-restricted feeding may help patients with weight loss only if time restriction helps them reduce calorie intake. She also warned that time-restrictive feeding might cause late-night cravings and might not be helpful in individuals prone to food cravings.
Low‐carbohydrate and ketogenic diets
Losing muscle mass can prevent some people from dieting, but evidence suggests that a high-fat, very low-carbohydrate diet – also called a ketogenic diet – may help patients reduce weight and fat mass while preserving fat‐free mass, Dr. Hauser said.
The evidence regarding the usefulness of a low-carbohydrate (non-keto) diet is less clear because most studies compared it to a low-fat diet, and these two diets might lead to a similar extent of weight loss.
Rating the level of scientific evidence behind different diet options
Nutrition studies do no provide the same level of evidence as drug studies, said Dr. Hauser, because it is easier to conduct a randomized controlled trial of a drug versus placebo. Diets have many more variables, and it also takes much longer to observe most outcomes of a dietary change.
In addition, clinical trials of dietary interventions are typically short and focus on disease markers such as serum lipids and hemoglobin A1c levels. To obtain reliable information on the usefulness of a diet, researchers need to collect detailed health and lifestyle information from hundreds of thousands of people over several decades, which is not always feasible. “This is why meta-analyses of pooled dietary study data are more likely to yield dependable findings,” she noted.
Getting to know patients is essential to help them maintain diet modifications
When developing a diet plan for a patient, it is important to consider the sustainability of a dietary pattern. “The benefits of any healthy dietary change will only last as long as they can be maintained,” said Dr. Hauser. “Counseling someone on choosing an appropriate long-term dietary pattern requires getting to know them – taste preferences, food traditions, barriers, facilitators, food access, and time and cost restrictions.”
In an interview after the session, David Bittleman, MD, an internist at Veterans Affairs San Diego Health Care System, agreed that getting to know patients is essential for successfully advising them on diet.
“I always start developing a diet plan by trying to find out what [a patient’s] diet is like and what their goals are. I need to know what they are already doing in order to make suggestions about what they can do to make their diet healthier,” he said.
When asked about her approach to supporting patients in the long term, Dr. Hauser said that she recommends sequential, gradual changes. Dr. Hauser added that she suggests her patients prioritize implementing dietary changes that they are confident they can maintain.
Dr. Hauser and Dr. Bittleman report no relevant financial relationships.
according to a speaker at the annual meeting of the American College of Physicians.
“Evidence from studies can help clinicians and their patients develop a successful dietary management plan and achieve optimal health,” said internist Michelle Hauser, MD, clinical associate professor at Stanford (Calif.) University. She also discussed evidence-based techniques to support patients in maintaining dietary modifications.
Predominantly plant‐based diets
Popular predominantly plant‐based diets include a Mediterranean diet, healthy vegetarian diet, predominantly whole-food plant‐based (WFPB) diet, and a dietary approach to stop hypertension (DASH).
The DASH diet was originally designed to help patients manage their blood pressure, but evidence suggests that it also can help adults with obesity lose weight. In contrast to the DASH diet, the Mediterranean diet is not low-fat and not very restrictive. Yet the evidence suggests that the Mediterranean diet is not only helpful for losing weight but also can reduce the risk of various chronic diseases, including obesity, type 2 diabetes, cardiovascular disease (CVD), and cancer, Dr. Hauser said. In addition, data suggest that the Mediterranean diet may reduce the risk of all-cause mortality and lower the levels of cholesterol.
“I like to highlight all these protective effects to my patients, because even if their goal is to lose weight, knowing that hard work pays off in additional ways can keep them motivated,” Dr. Hauser stated.
A healthy vegetarian diet and a WFPB diet are similar, and both are helpful in weight loss and management of total cholesterol and LDL‐C levels. Furthermore, healthy vegetarian and WFPB diets may reduce the risk of type 2 diabetes, CVD, and some cancers. Cohort study data suggest that progressively more vegetarian diets are associated with lower BMIs.
“My interpretation of these data is that predominantly plant-based diets rich in whole foods are healthful and can be done in a way that is sustainable for most,” said Dr. Hauser. However, this generally requires a lot of support at the outset to address gaps in knowledge, skills, and other potential barriers.
For example, she referred one obese patient at risk of diabetes and cardiovascular disease to a registered dietitian to develop a dietary plan. The patient also attended a behavioral medicine weight management program to learn strategies such as using smaller plates, and his family attended a healthy cooking class together to improve meal planning and cooking skills.
Time‐restricted feeding
There are numerous variations of time-restricted feeding, commonly referred to as intermittent fasting, but the principles are similar – limiting food intake to a specific window of time each day or week.
Although some studies have shown that time-restricted feeding may help patients reduce adiposity and improve lipid markers, most studies comparing time-restricted feeding to a calorie-restricted diet have shown little to no difference in weight-related outcomes, Dr. Hauser said.
These data suggest that time-restricted feeding may help patients with weight loss only if time restriction helps them reduce calorie intake. She also warned that time-restrictive feeding might cause late-night cravings and might not be helpful in individuals prone to food cravings.
Low‐carbohydrate and ketogenic diets
Losing muscle mass can prevent some people from dieting, but evidence suggests that a high-fat, very low-carbohydrate diet – also called a ketogenic diet – may help patients reduce weight and fat mass while preserving fat‐free mass, Dr. Hauser said.
The evidence regarding the usefulness of a low-carbohydrate (non-keto) diet is less clear because most studies compared it to a low-fat diet, and these two diets might lead to a similar extent of weight loss.
Rating the level of scientific evidence behind different diet options
Nutrition studies do no provide the same level of evidence as drug studies, said Dr. Hauser, because it is easier to conduct a randomized controlled trial of a drug versus placebo. Diets have many more variables, and it also takes much longer to observe most outcomes of a dietary change.
In addition, clinical trials of dietary interventions are typically short and focus on disease markers such as serum lipids and hemoglobin A1c levels. To obtain reliable information on the usefulness of a diet, researchers need to collect detailed health and lifestyle information from hundreds of thousands of people over several decades, which is not always feasible. “This is why meta-analyses of pooled dietary study data are more likely to yield dependable findings,” she noted.
Getting to know patients is essential to help them maintain diet modifications
When developing a diet plan for a patient, it is important to consider the sustainability of a dietary pattern. “The benefits of any healthy dietary change will only last as long as they can be maintained,” said Dr. Hauser. “Counseling someone on choosing an appropriate long-term dietary pattern requires getting to know them – taste preferences, food traditions, barriers, facilitators, food access, and time and cost restrictions.”
In an interview after the session, David Bittleman, MD, an internist at Veterans Affairs San Diego Health Care System, agreed that getting to know patients is essential for successfully advising them on diet.
“I always start developing a diet plan by trying to find out what [a patient’s] diet is like and what their goals are. I need to know what they are already doing in order to make suggestions about what they can do to make their diet healthier,” he said.
When asked about her approach to supporting patients in the long term, Dr. Hauser said that she recommends sequential, gradual changes. Dr. Hauser added that she suggests her patients prioritize implementing dietary changes that they are confident they can maintain.
Dr. Hauser and Dr. Bittleman report no relevant financial relationships.
AT INTERNAL MEDICINE 2023
10 popular diets for heart health ranked
An evidence-based analysis of 10 popular dietary patterns shows that some promote heart health better than others.
A new American Heart Association scientific statement concludes that the Mediterranean, Dietary Approach to Stop Hypertension (DASH), pescatarian, and vegetarian eating patterns most strongly align with heart-healthy eating guidelines issued by the AHA in 2021, whereas the popular paleolithic (paleo) and ketogenic (keto) diets fall short.
“The good news for the public and their clinicians is that there are several dietary patterns that allow for substantial flexibility for following a heart healthy diet – DASH, Mediterranean, vegetarian,” writing-group chair Christopher Gardner, PhD, with Stanford (Calif.) University, told this news organization.
“However, some of the popular diets – particularly paleo and keto – are so strictly restrictive of specific food groups that when these diets are followed as intended by their proponents, they are not aligned with the scientific evidence for a heart-healthy diet,” Dr. Gardner said.
The statement was published online in Circulation.
A tool for clinicians
“The number of different, popular dietary patterns has proliferated in recent years, and the amount of misinformation about them on social media has reached critical levels,” Dr. Gardner said in a news release.
“The public – and even many health care professionals – may rightfully be confused about heart-healthy eating, and they may feel that they don’t have the time or the training to evaluate the different diets. We hope this statement serves as a tool for clinicians and the public to understand which diets promote good cardiometabolic health,” he noted.
The writing group rated on a scale of 1-100 how well 10 popular diets or eating patterns align with AHA dietary advice for heart-healthy eating.
That advice includes consuming a wide variety of fruits and vegetables; choosing mostly whole grains instead of refined grains; using liquid plant oils rather than tropical oils; eating healthy sources of protein, such as from plants, seafood, or lean meats; minimizing added sugars and salt; limiting alcohol; choosing minimally processed foods instead of ultraprocessed foods; and following this guidance wherever food is prepared or consumed.
The 10 diets/dietary patterns were DASH, Mediterranean-style, pescatarian, ovo-lacto vegetarian, vegan, low-fat, very low–fat, low-carbohydrate, paleo, and very low–carbohydrate/keto patterns.
The diets were divided into four tiers on the basis of their scores, which ranged from a low of 31 to a high of 100.
Only the DASH eating plan got a perfect score of 100. This eating pattern is low in salt, added sugar, tropical oil, alcohol, and processed foods and high in nonstarchy vegetables, fruits, whole grains, and legumes. Proteins are mostly plant-based, such as legumes, beans, or nuts, along with fish or seafood, lean poultry and meats, and low-fat or fat-free dairy products.
The Mediterranean eating pattern achieved a slightly lower score of 89 because unlike DASH, it allows for moderate alcohol consumption and does not address added salt.
The other two top tier eating patterns were pescatarian, with a score of 92, and vegetarian, with a score of 86.
“If implemented as intended, the top-tier dietary patterns align best with the American Heart Association’s guidance and may be adapted to respect cultural practices, food preferences and budgets to enable people to always eat this way, for the long term,” Dr. Gardner said in the release.
Vegan and low-fat diets (each with a score of 78) fell into the second tier.
Though these diets emphasize fruits, vegetables, whole grains, legumes, and nuts while limiting alcohol and added sugars, the vegan diet is so restrictive that it could be challenging to follow long-term or when eating out and may increase the risk for vitamin B12 deficiency, which can lead to anemia, the writing group notes.
There also are concerns that low-fat diets treat all fats equally, whereas the AHA guidance calls for replacing saturated fats with healthier fats, they point out.
The third tier includes the very low–fat diet (score 72) and low-carb diet (score 64), whereas the paleo and very low–carb/keto diets fall into the fourth tier, with the lowest scores of 53 and 31, respectively.
Dr. Gardner said that it’s important to note that all 10 diet patterns “share four positive characteristics: more veggies, more whole foods, less added sugars, less refined grains.”
“These are all areas for which Americans have substantial room for improvement, and these are all things that we could work on together. Progress across these aspects would make a large difference in the heart-healthiness of the U.S. diet,” he told this news organization.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Lifestyle and Cardiometabolic Health, the Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, and the Council on Peripheral Vascular Disease.
A version of this article first appeared on Medscape.com.
An evidence-based analysis of 10 popular dietary patterns shows that some promote heart health better than others.
A new American Heart Association scientific statement concludes that the Mediterranean, Dietary Approach to Stop Hypertension (DASH), pescatarian, and vegetarian eating patterns most strongly align with heart-healthy eating guidelines issued by the AHA in 2021, whereas the popular paleolithic (paleo) and ketogenic (keto) diets fall short.
“The good news for the public and their clinicians is that there are several dietary patterns that allow for substantial flexibility for following a heart healthy diet – DASH, Mediterranean, vegetarian,” writing-group chair Christopher Gardner, PhD, with Stanford (Calif.) University, told this news organization.
“However, some of the popular diets – particularly paleo and keto – are so strictly restrictive of specific food groups that when these diets are followed as intended by their proponents, they are not aligned with the scientific evidence for a heart-healthy diet,” Dr. Gardner said.
The statement was published online in Circulation.
A tool for clinicians
“The number of different, popular dietary patterns has proliferated in recent years, and the amount of misinformation about them on social media has reached critical levels,” Dr. Gardner said in a news release.
“The public – and even many health care professionals – may rightfully be confused about heart-healthy eating, and they may feel that they don’t have the time or the training to evaluate the different diets. We hope this statement serves as a tool for clinicians and the public to understand which diets promote good cardiometabolic health,” he noted.
The writing group rated on a scale of 1-100 how well 10 popular diets or eating patterns align with AHA dietary advice for heart-healthy eating.
That advice includes consuming a wide variety of fruits and vegetables; choosing mostly whole grains instead of refined grains; using liquid plant oils rather than tropical oils; eating healthy sources of protein, such as from plants, seafood, or lean meats; minimizing added sugars and salt; limiting alcohol; choosing minimally processed foods instead of ultraprocessed foods; and following this guidance wherever food is prepared or consumed.
The 10 diets/dietary patterns were DASH, Mediterranean-style, pescatarian, ovo-lacto vegetarian, vegan, low-fat, very low–fat, low-carbohydrate, paleo, and very low–carbohydrate/keto patterns.
The diets were divided into four tiers on the basis of their scores, which ranged from a low of 31 to a high of 100.
Only the DASH eating plan got a perfect score of 100. This eating pattern is low in salt, added sugar, tropical oil, alcohol, and processed foods and high in nonstarchy vegetables, fruits, whole grains, and legumes. Proteins are mostly plant-based, such as legumes, beans, or nuts, along with fish or seafood, lean poultry and meats, and low-fat or fat-free dairy products.
The Mediterranean eating pattern achieved a slightly lower score of 89 because unlike DASH, it allows for moderate alcohol consumption and does not address added salt.
The other two top tier eating patterns were pescatarian, with a score of 92, and vegetarian, with a score of 86.
“If implemented as intended, the top-tier dietary patterns align best with the American Heart Association’s guidance and may be adapted to respect cultural practices, food preferences and budgets to enable people to always eat this way, for the long term,” Dr. Gardner said in the release.
Vegan and low-fat diets (each with a score of 78) fell into the second tier.
Though these diets emphasize fruits, vegetables, whole grains, legumes, and nuts while limiting alcohol and added sugars, the vegan diet is so restrictive that it could be challenging to follow long-term or when eating out and may increase the risk for vitamin B12 deficiency, which can lead to anemia, the writing group notes.
There also are concerns that low-fat diets treat all fats equally, whereas the AHA guidance calls for replacing saturated fats with healthier fats, they point out.
The third tier includes the very low–fat diet (score 72) and low-carb diet (score 64), whereas the paleo and very low–carb/keto diets fall into the fourth tier, with the lowest scores of 53 and 31, respectively.
Dr. Gardner said that it’s important to note that all 10 diet patterns “share four positive characteristics: more veggies, more whole foods, less added sugars, less refined grains.”
“These are all areas for which Americans have substantial room for improvement, and these are all things that we could work on together. Progress across these aspects would make a large difference in the heart-healthiness of the U.S. diet,” he told this news organization.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Lifestyle and Cardiometabolic Health, the Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, and the Council on Peripheral Vascular Disease.
A version of this article first appeared on Medscape.com.
An evidence-based analysis of 10 popular dietary patterns shows that some promote heart health better than others.
A new American Heart Association scientific statement concludes that the Mediterranean, Dietary Approach to Stop Hypertension (DASH), pescatarian, and vegetarian eating patterns most strongly align with heart-healthy eating guidelines issued by the AHA in 2021, whereas the popular paleolithic (paleo) and ketogenic (keto) diets fall short.
“The good news for the public and their clinicians is that there are several dietary patterns that allow for substantial flexibility for following a heart healthy diet – DASH, Mediterranean, vegetarian,” writing-group chair Christopher Gardner, PhD, with Stanford (Calif.) University, told this news organization.
“However, some of the popular diets – particularly paleo and keto – are so strictly restrictive of specific food groups that when these diets are followed as intended by their proponents, they are not aligned with the scientific evidence for a heart-healthy diet,” Dr. Gardner said.
The statement was published online in Circulation.
A tool for clinicians
“The number of different, popular dietary patterns has proliferated in recent years, and the amount of misinformation about them on social media has reached critical levels,” Dr. Gardner said in a news release.
“The public – and even many health care professionals – may rightfully be confused about heart-healthy eating, and they may feel that they don’t have the time or the training to evaluate the different diets. We hope this statement serves as a tool for clinicians and the public to understand which diets promote good cardiometabolic health,” he noted.
The writing group rated on a scale of 1-100 how well 10 popular diets or eating patterns align with AHA dietary advice for heart-healthy eating.
That advice includes consuming a wide variety of fruits and vegetables; choosing mostly whole grains instead of refined grains; using liquid plant oils rather than tropical oils; eating healthy sources of protein, such as from plants, seafood, or lean meats; minimizing added sugars and salt; limiting alcohol; choosing minimally processed foods instead of ultraprocessed foods; and following this guidance wherever food is prepared or consumed.
The 10 diets/dietary patterns were DASH, Mediterranean-style, pescatarian, ovo-lacto vegetarian, vegan, low-fat, very low–fat, low-carbohydrate, paleo, and very low–carbohydrate/keto patterns.
The diets were divided into four tiers on the basis of their scores, which ranged from a low of 31 to a high of 100.
Only the DASH eating plan got a perfect score of 100. This eating pattern is low in salt, added sugar, tropical oil, alcohol, and processed foods and high in nonstarchy vegetables, fruits, whole grains, and legumes. Proteins are mostly plant-based, such as legumes, beans, or nuts, along with fish or seafood, lean poultry and meats, and low-fat or fat-free dairy products.
The Mediterranean eating pattern achieved a slightly lower score of 89 because unlike DASH, it allows for moderate alcohol consumption and does not address added salt.
The other two top tier eating patterns were pescatarian, with a score of 92, and vegetarian, with a score of 86.
“If implemented as intended, the top-tier dietary patterns align best with the American Heart Association’s guidance and may be adapted to respect cultural practices, food preferences and budgets to enable people to always eat this way, for the long term,” Dr. Gardner said in the release.
Vegan and low-fat diets (each with a score of 78) fell into the second tier.
Though these diets emphasize fruits, vegetables, whole grains, legumes, and nuts while limiting alcohol and added sugars, the vegan diet is so restrictive that it could be challenging to follow long-term or when eating out and may increase the risk for vitamin B12 deficiency, which can lead to anemia, the writing group notes.
There also are concerns that low-fat diets treat all fats equally, whereas the AHA guidance calls for replacing saturated fats with healthier fats, they point out.
The third tier includes the very low–fat diet (score 72) and low-carb diet (score 64), whereas the paleo and very low–carb/keto diets fall into the fourth tier, with the lowest scores of 53 and 31, respectively.
Dr. Gardner said that it’s important to note that all 10 diet patterns “share four positive characteristics: more veggies, more whole foods, less added sugars, less refined grains.”
“These are all areas for which Americans have substantial room for improvement, and these are all things that we could work on together. Progress across these aspects would make a large difference in the heart-healthiness of the U.S. diet,” he told this news organization.
This scientific statement was prepared by the volunteer writing group on behalf of the AHA Council on Lifestyle and Cardiometabolic Health, the Council on Cardiovascular and Stroke Nursing, the Council on Hypertension, and the Council on Peripheral Vascular Disease.
A version of this article first appeared on Medscape.com.








