User login
Tackle TB
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Report Critical Care
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
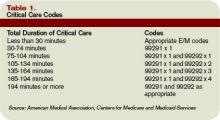
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
The OIG Aftermath
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
Your First Chair Job
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
Teamwork Triumphs
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Combat Adverse Effects
A serious adverse drug event (ADE) is defined as one that causes death, disability, or permanent damage, hospitalization (initial or prolonged), or birth defects.
According to Moore, et al., the number of serious ADEs has increased significantly since 1998 through 2005, according to reports in the Food and Drug Administration (FDA) adverse event reporting system, also known as MedWatch.1 During that time, 467,809 serious ADEs were reported, and the annual number of reports had increased from 34,966 to 89,842.
The number of fatal ADEs increased in that period as well, from 4,419 to 15,109. Further, ADEs related to biotech drugs increased 15.8-fold. The most commonly reported classes with serious ADEs included anti-tumor necrosis factor drugs, interferons, and insulins. Drugs associated with ADEs included some that had been withdrawn from the U.S. market over safety concerns, as well as products that remained on the market.
On Sept. 27, the FDA Amendments Act of 2007 was passed. The measure includes the Prescription Drug User Fee Act (PDUFA), which authorizes the FDA to collect fees from drug makers to supplement funding for the drug-review process.2 A key revision now lets the agency require—not just request—that drug companies perform phase four clinical studies. The PDUFA also includes additional staff for reviewing medical devices. Additional stipulations are that the FDA will:
- Assess signals of serious risk related to drug use as they arise;
- Identify unexpected serious risks;
- Identify when post-marketing studies are needed; and
- Quickly submit a supplement proposing changes to the approved labeling of a drug to reflect new safety information, including changes to boxed warnings, contraindications, warnings, precautions, or adverse reactions within 30 days of identification.
This legislation has brought a number of new warnings on FDA-approved products.
The Warnings
A study in the May 2007 issue of Lancet Infectious Diseases noted higher all-cause mortality in patients treated with cefepime (Maxipime) compared with other beta-lactam antibiotics.3 Cefepime is FDA approved for the treatment of infections caused by susceptible gram-positive and gram-negative micro-organisms. The risk ratio (RR) was 1.26 (95% confidence interval [CI] 1.08–1.49) for cefepime and for the subgroup of patients with febrile neutropenia (RR 1.42 [95% CI 1.09–1.84]). The FDA is reviewing safety data and has requested additional data from Bristol-Myers Squibb to further evaluate the risk of death in cefepime-treated patients. The FDA asks healthcare professionals to report adverse events from cefepime and other agents to MedWatch at www.fda.gov/medwatch/report.htm.
A new warning regarding the pregnancy category and teratogenic effects has been added to the label of mycophenolic acid (MPA) delayed-release tablets (Myfortic). The FDA notes that use of MPA during pregnancy is associated with increased risks of pregnancy loss and congenital malformations, thereby changing the pregnancy category to D (positive evidence of fetal risk) from C (risk of fetal harm cannot be ruled out).
The MPA warnings and precautions sections also have changed. Results from postmarketing data from the U.S. National Transplantation Pregnancy Registry and additional postmarketing data collected in women exposed to systemic mycophenolate mofetil (MMF) during pregnancy brought these revisions. MMF is converted to the active ingredient in MPA following intravenous or oral administration. A patient planning to get pregnant should not use MMF/MPA unless she cannot be treated with other immunosuppressant drugs. Additionally, female patients of childbearing potential must receive contraceptive counseling and use contraception while on this agent. Remember, not only transplant patients receive MMF/MPA; patients with lupus nephritis also use it.
On Nov. 27, the Pediatric Advisory Committee of the FDA recommended changing the label of the two neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), to reflect the potential for neuropsychiatric effects (mostly in children). Last year, Roche revised the oseltamivir label to add warnings of potential confusion and self-injury with the product. According to the FDA, about five patients died as a result of these neuropsychiatric effects, and nearly 600 cases of psychiatric problems were reported.
On Nov. 14, the FDA added to the black box label of rosiglitazone (Avandia) regarding an increased risk of myocardial infarction. The warning states that a recent meta-analysis of 42 clinical studies (mean duration six months, n=14,237) mostly comparing rosiglitazone with placebo, showed it to be associated with an increased risk of myocardial ischemic events. Further, three other studies (mean duration 41 months; n=14,067), comparing rosiglitazone with other oral antidiabetic agents or placebo, have not confirmed or excluded this risk. The available data on the risk of myocardial ischemia are currently inconclusive.
The FDA has asked that GlaxoSmithKline conduct extensive long-term, post-marketing trials to determine rosiglitazone’s cardiovascular safety. A study of this type, is a direct result of the new PDUFA legislation. The trial is expected to begin after July and end by 2014. Updates to the warnings, precautions, and indications sections were also added to the label. For example, rosiglitazone is not recommended for heart disease patients who are taking nitrates, nor is it recommended in combination with insulin.
Finally, the FDA is evaluating postmarketing adverse event reports for varenicline (Chantix) describing suicidal ideation, suicide, and aggressive and erratic behavior in patients taking it for smoking cessation. While the review proceeds, physicians are advised to evaluate patients for behavior and mood disorders, as well as drowsiness. In patients taking varenicline, caution is advised while driving or operating machinery until the patient’s response to it is known. TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Moore TJ, Cohen MJ, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Wechsler J. No shortage of recommendations for PDUFA IV as Congress and professional organizations weigh in on drug safety. Formulary 2007;42:264-265.
- Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007 May;7(5):338-348.
A serious adverse drug event (ADE) is defined as one that causes death, disability, or permanent damage, hospitalization (initial or prolonged), or birth defects.
According to Moore, et al., the number of serious ADEs has increased significantly since 1998 through 2005, according to reports in the Food and Drug Administration (FDA) adverse event reporting system, also known as MedWatch.1 During that time, 467,809 serious ADEs were reported, and the annual number of reports had increased from 34,966 to 89,842.
The number of fatal ADEs increased in that period as well, from 4,419 to 15,109. Further, ADEs related to biotech drugs increased 15.8-fold. The most commonly reported classes with serious ADEs included anti-tumor necrosis factor drugs, interferons, and insulins. Drugs associated with ADEs included some that had been withdrawn from the U.S. market over safety concerns, as well as products that remained on the market.
On Sept. 27, the FDA Amendments Act of 2007 was passed. The measure includes the Prescription Drug User Fee Act (PDUFA), which authorizes the FDA to collect fees from drug makers to supplement funding for the drug-review process.2 A key revision now lets the agency require—not just request—that drug companies perform phase four clinical studies. The PDUFA also includes additional staff for reviewing medical devices. Additional stipulations are that the FDA will:
- Assess signals of serious risk related to drug use as they arise;
- Identify unexpected serious risks;
- Identify when post-marketing studies are needed; and
- Quickly submit a supplement proposing changes to the approved labeling of a drug to reflect new safety information, including changes to boxed warnings, contraindications, warnings, precautions, or adverse reactions within 30 days of identification.
This legislation has brought a number of new warnings on FDA-approved products.
The Warnings
A study in the May 2007 issue of Lancet Infectious Diseases noted higher all-cause mortality in patients treated with cefepime (Maxipime) compared with other beta-lactam antibiotics.3 Cefepime is FDA approved for the treatment of infections caused by susceptible gram-positive and gram-negative micro-organisms. The risk ratio (RR) was 1.26 (95% confidence interval [CI] 1.08–1.49) for cefepime and for the subgroup of patients with febrile neutropenia (RR 1.42 [95% CI 1.09–1.84]). The FDA is reviewing safety data and has requested additional data from Bristol-Myers Squibb to further evaluate the risk of death in cefepime-treated patients. The FDA asks healthcare professionals to report adverse events from cefepime and other agents to MedWatch at www.fda.gov/medwatch/report.htm.
A new warning regarding the pregnancy category and teratogenic effects has been added to the label of mycophenolic acid (MPA) delayed-release tablets (Myfortic). The FDA notes that use of MPA during pregnancy is associated with increased risks of pregnancy loss and congenital malformations, thereby changing the pregnancy category to D (positive evidence of fetal risk) from C (risk of fetal harm cannot be ruled out).
The MPA warnings and precautions sections also have changed. Results from postmarketing data from the U.S. National Transplantation Pregnancy Registry and additional postmarketing data collected in women exposed to systemic mycophenolate mofetil (MMF) during pregnancy brought these revisions. MMF is converted to the active ingredient in MPA following intravenous or oral administration. A patient planning to get pregnant should not use MMF/MPA unless she cannot be treated with other immunosuppressant drugs. Additionally, female patients of childbearing potential must receive contraceptive counseling and use contraception while on this agent. Remember, not only transplant patients receive MMF/MPA; patients with lupus nephritis also use it.
On Nov. 27, the Pediatric Advisory Committee of the FDA recommended changing the label of the two neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), to reflect the potential for neuropsychiatric effects (mostly in children). Last year, Roche revised the oseltamivir label to add warnings of potential confusion and self-injury with the product. According to the FDA, about five patients died as a result of these neuropsychiatric effects, and nearly 600 cases of psychiatric problems were reported.
On Nov. 14, the FDA added to the black box label of rosiglitazone (Avandia) regarding an increased risk of myocardial infarction. The warning states that a recent meta-analysis of 42 clinical studies (mean duration six months, n=14,237) mostly comparing rosiglitazone with placebo, showed it to be associated with an increased risk of myocardial ischemic events. Further, three other studies (mean duration 41 months; n=14,067), comparing rosiglitazone with other oral antidiabetic agents or placebo, have not confirmed or excluded this risk. The available data on the risk of myocardial ischemia are currently inconclusive.
The FDA has asked that GlaxoSmithKline conduct extensive long-term, post-marketing trials to determine rosiglitazone’s cardiovascular safety. A study of this type, is a direct result of the new PDUFA legislation. The trial is expected to begin after July and end by 2014. Updates to the warnings, precautions, and indications sections were also added to the label. For example, rosiglitazone is not recommended for heart disease patients who are taking nitrates, nor is it recommended in combination with insulin.
Finally, the FDA is evaluating postmarketing adverse event reports for varenicline (Chantix) describing suicidal ideation, suicide, and aggressive and erratic behavior in patients taking it for smoking cessation. While the review proceeds, physicians are advised to evaluate patients for behavior and mood disorders, as well as drowsiness. In patients taking varenicline, caution is advised while driving or operating machinery until the patient’s response to it is known. TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Moore TJ, Cohen MJ, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Wechsler J. No shortage of recommendations for PDUFA IV as Congress and professional organizations weigh in on drug safety. Formulary 2007;42:264-265.
- Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007 May;7(5):338-348.
A serious adverse drug event (ADE) is defined as one that causes death, disability, or permanent damage, hospitalization (initial or prolonged), or birth defects.
According to Moore, et al., the number of serious ADEs has increased significantly since 1998 through 2005, according to reports in the Food and Drug Administration (FDA) adverse event reporting system, also known as MedWatch.1 During that time, 467,809 serious ADEs were reported, and the annual number of reports had increased from 34,966 to 89,842.
The number of fatal ADEs increased in that period as well, from 4,419 to 15,109. Further, ADEs related to biotech drugs increased 15.8-fold. The most commonly reported classes with serious ADEs included anti-tumor necrosis factor drugs, interferons, and insulins. Drugs associated with ADEs included some that had been withdrawn from the U.S. market over safety concerns, as well as products that remained on the market.
On Sept. 27, the FDA Amendments Act of 2007 was passed. The measure includes the Prescription Drug User Fee Act (PDUFA), which authorizes the FDA to collect fees from drug makers to supplement funding for the drug-review process.2 A key revision now lets the agency require—not just request—that drug companies perform phase four clinical studies. The PDUFA also includes additional staff for reviewing medical devices. Additional stipulations are that the FDA will:
- Assess signals of serious risk related to drug use as they arise;
- Identify unexpected serious risks;
- Identify when post-marketing studies are needed; and
- Quickly submit a supplement proposing changes to the approved labeling of a drug to reflect new safety information, including changes to boxed warnings, contraindications, warnings, precautions, or adverse reactions within 30 days of identification.
This legislation has brought a number of new warnings on FDA-approved products.
The Warnings
A study in the May 2007 issue of Lancet Infectious Diseases noted higher all-cause mortality in patients treated with cefepime (Maxipime) compared with other beta-lactam antibiotics.3 Cefepime is FDA approved for the treatment of infections caused by susceptible gram-positive and gram-negative micro-organisms. The risk ratio (RR) was 1.26 (95% confidence interval [CI] 1.08–1.49) for cefepime and for the subgroup of patients with febrile neutropenia (RR 1.42 [95% CI 1.09–1.84]). The FDA is reviewing safety data and has requested additional data from Bristol-Myers Squibb to further evaluate the risk of death in cefepime-treated patients. The FDA asks healthcare professionals to report adverse events from cefepime and other agents to MedWatch at www.fda.gov/medwatch/report.htm.
A new warning regarding the pregnancy category and teratogenic effects has been added to the label of mycophenolic acid (MPA) delayed-release tablets (Myfortic). The FDA notes that use of MPA during pregnancy is associated with increased risks of pregnancy loss and congenital malformations, thereby changing the pregnancy category to D (positive evidence of fetal risk) from C (risk of fetal harm cannot be ruled out).
The MPA warnings and precautions sections also have changed. Results from postmarketing data from the U.S. National Transplantation Pregnancy Registry and additional postmarketing data collected in women exposed to systemic mycophenolate mofetil (MMF) during pregnancy brought these revisions. MMF is converted to the active ingredient in MPA following intravenous or oral administration. A patient planning to get pregnant should not use MMF/MPA unless she cannot be treated with other immunosuppressant drugs. Additionally, female patients of childbearing potential must receive contraceptive counseling and use contraception while on this agent. Remember, not only transplant patients receive MMF/MPA; patients with lupus nephritis also use it.
On Nov. 27, the Pediatric Advisory Committee of the FDA recommended changing the label of the two neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza), to reflect the potential for neuropsychiatric effects (mostly in children). Last year, Roche revised the oseltamivir label to add warnings of potential confusion and self-injury with the product. According to the FDA, about five patients died as a result of these neuropsychiatric effects, and nearly 600 cases of psychiatric problems were reported.
On Nov. 14, the FDA added to the black box label of rosiglitazone (Avandia) regarding an increased risk of myocardial infarction. The warning states that a recent meta-analysis of 42 clinical studies (mean duration six months, n=14,237) mostly comparing rosiglitazone with placebo, showed it to be associated with an increased risk of myocardial ischemic events. Further, three other studies (mean duration 41 months; n=14,067), comparing rosiglitazone with other oral antidiabetic agents or placebo, have not confirmed or excluded this risk. The available data on the risk of myocardial ischemia are currently inconclusive.
The FDA has asked that GlaxoSmithKline conduct extensive long-term, post-marketing trials to determine rosiglitazone’s cardiovascular safety. A study of this type, is a direct result of the new PDUFA legislation. The trial is expected to begin after July and end by 2014. Updates to the warnings, precautions, and indications sections were also added to the label. For example, rosiglitazone is not recommended for heart disease patients who are taking nitrates, nor is it recommended in combination with insulin.
Finally, the FDA is evaluating postmarketing adverse event reports for varenicline (Chantix) describing suicidal ideation, suicide, and aggressive and erratic behavior in patients taking it for smoking cessation. While the review proceeds, physicians are advised to evaluate patients for behavior and mood disorders, as well as drowsiness. In patients taking varenicline, caution is advised while driving or operating machinery until the patient’s response to it is known. TH
Michele B. Kaufman is a freelance medical writer based in New York City.
References
- Moore TJ, Cohen MJ, Furberg CD. Serious adverse drug events reported to the Food and Drug Administration, 1998-2005. Arch Intern Med. 2007;167:1752-1759.
- Wechsler J. No shortage of recommendations for PDUFA IV as Congress and professional organizations weigh in on drug safety. Formulary 2007;42:264-265.
- Yahav D, Paul M, Fraser A, Sarid N, Leibovici L. Efficacy and safety of cefepime: a systematic review and meta-analysis. Lancet Infect Dis. 2007 May;7(5):338-348.
In the Literature
LITERATURE AT A GLANCE
Use this guide to find the abstracts below that correspond to these recent clinical findings
- 24-hour TIA clinic improves outcomes.
- More rapid treatment after TIA and minor stroke reduce risk for recurrent stroke.
- Prasugrel more efficacious than clopidogrel in acute coronary syndrome, but with higher bleeding rates.
- Zoledronic acid use after hip fracture repair reduces probability of new fractures.
- No benefit in quality measures and resource use for surgical patients receiving medical consultation.
- Pediatric RRTs reduce mortality rate.
- Influenza vaccinations prevent hospitalization, death among elderly.
- Chlorhexidine bathing reduces catheter-associated bloodstream infections.
- Chlorhexidine-based antiseptic solution reduces rates of catheter-associated infections
Would 24-hour Hospital Clinic Reduce LOS, Stroke Risk?
Background: Transient ischemic attacks (TIA) precede up to 25% of completed strokes and can provide opportunity for critical intervention if identified early. A specialty clinic with immediate access to imaging facilities could provide early identification and intervention.
Study design: Cohort study statistical analysis of data.
Setting: SOS-TIA hospital clinic in Paris.
Synopsis: A leaflet about TIA with a toll-free telephone number for SOS-TIA was sent to 15,000 family doctors, cardiologists, neurologists, and ophthalmologists in Paris. Between January 2003 and December 2005, 1,085 patients with suspected TIA were admitted to the clinic. The median duration of symptoms was 15 minutes. All patients were started on a stroke-prevention program, 5% had urgent carotid revascularization, and 5% were treated for atrial fibrillation with anticoagulants. Further, 74% of all patients seen were sent home the same day. The 90-day stroke rate was 1.24%; the rate predicted was 5.96%. Limitations of the study included selective patient recruitment from family doctors and office-based specialists. Also, the study lacked a randomized control group.
Bottom line: Prompt evaluation and treatment of patients in a dedicated TIA clinic is associated with a lower stroke risk. The TIA clinic also may lower costs via decreased length of hospital stay.
Citation: Lavallee P, Meseguer E, Abboud H, et al. A transient ischemic attack clinic with round the clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960.
Can Early Treatment after TIA or Minor Stroke Reduce Risk of Early Recurrent Stroke?
Background: In the week following a TIA or a minor stroke, the risk of recurrent stroke grows to 10%. These warning events provide a limited window of opportunity for prevention. Several treatments are effective in stroke prevention following TIA or minor ischemic stroke if identified early. These include aspirin, other antiplatelet agents, blood-pressure (BP) medications, statins, anticoagulation for atrial fibrillation, and endarterectomy.
Study design: Prospective before-versus-after study (Oxford Vascular Study, or OXVASC) within population-based incidence study.
Setting:: The study population was located in primary care practices in the United Kingdom.
Synopsis: The OXVASC study looked at 1,278 patients who presented with TIA or stroke: 607 were referred directly to the hospital, 620 were referred for outpatient assessment, and 51 were not referred to secondary care. In phase 1, a daily TIA and minor stroke clinic was introduced. Collaborating primary care physicians were asked to refer all patients suspected of having TIA and minor stroke. Phase 1 took place between April 1, 2002, and Sept. 30, 2004. The treatment protocol recommended aspirin in patients not already on anti-platelet therapy (75 mg daily) or clopidogrel if aspirin was contraindicated; simvastatin (40 mg daily); BP lowering agents unless systolic BP less than 130 mm Hg; and anticoagulation as required.
In phase 2, from Oct. 1, 2004, to March 31, 2007, a clinic was established at which no appointments were necessary, treatment was initiated immediately, and diagnosis was confirmed. Patients were assessed in the same way as in phase 1, but all those considered to have had a TIA or stroke were given aspirin 300 mg together with a prescription of any other study medication to start the same day. A loading dose of clopidogrel 300 mg was also prescribed. The 90-day risk if recurrent stroke in the patients referred to the study clinic was 10.3% in phase 1 and 2.1% in phase 2.
Bottom line: Early treatment after TIA or minor stroke was associated with an 80% reduction in the risk of recurrent stroke.
Citation: Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischemic attack (TIA) and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-1442.
How Does Prasugrel Compare With Clopidogrel in Acute Coronary Syndrome?
Background: Short-term and long-term benefits of a dual anti-platelet therapy for patients with acute coronary syndromes and/or PTCA has been well established but limited by recurrent atherothrombatic events and safety issues.
Study design: Double-blind, randomized study.
Setting: Triton-TIMI 38 Study Group.
Synopsis: This study randomly assigned 13,608 patients with acute coronary syndromes from 30 countries to a treatment group between November 2004 and January 2007. The study protocol used a loading dose of prasugrel (60 mg) within 72 hours before randomization and one hour after cardiac catheterization.
After percutaneous coronary intervention (PCI) patients received maintenance doses of either prasugrel (10 mg) or clopidogrel (75 mg) daily. Daily aspirin (75-162 mg) was required. The outcome of this study showed a significant reduction in the rate of ischemic end points (nonfatal myocardial infarction, stroke, and death) and stent re-thrombosis with prasugrel over clopidogrel. This was theorized to be due to the more rapid onset of antiplatelet effect with prasugrel and improved inhibition of platelet aggregation. Bleeding episodes were more frequent in the prasugrel group. Limitations of the study included the choice of vessels treated, devices used, and adjunctive medication administered to support PCI. All were left to the discretion of the treating physician.
Bottom line: Prasugrel therapy was significantly better than clopidogrel but with an increased risk of major bleeding.
Citation: Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
Can the Rate of New Hip Fracture Be Reduced with Zoledronic Acid?
Background: Mortality is markedly increased following hip fractures, and medical interventions exist to improve clinical outcomes.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: International, multicenter trial involving patients with recent hip fracture.
Synopsis: This study, know as the HORIZON trial, involved 2,127 patients. Of those, 1,065 (mean age of 74.5) were assigned to receive yearly infusions of 5 mg IV zoledronic acid within 90 days after surgical hip fracture repair. Meantime, 1,062 were assigned to receive placebo.
All patients received supplemental vitamin D and calcium. The median follow-up was 1.9 years, and the primary end point was a new clinical fracture. The rate of any new clinical fracture was 8.6% in the zoledronic acid group and 13.9% in the placebo group. This represents a 35% relative risk reduction with zoledronic acid.
Limitations of the study included a slightly younger and healthier patient population with hip fracture than the general population.
Bottom line: An annual infusion of zoledronic acid within 90 days after repair of hip fracture was associated with reduced new fractures and improved survival.
Citation: Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799-1809.
Does Peri-operative Consultation Improve Post-operative Outcome, Reduce Hospital Cost?
Background: Hospitalist-surgical co-management of the surgical inpatient is a model of care enjoying increasing interest. However, there is little published evidence of the effectiveness of this model.
Study design: Retrospective chart review.
Setting: Surgical service of academic teaching hospital.
Synopsis: Of 1,282 surgical patients, 9.1% underwent perioperative medical consultation in a retrospective review. Based on a number of measurement variables (post-operative serum glucose, venous thromboembolism [VTE] prophylaxis, use of perioperative beta-blockers), consulted patients had the same outcome, length of stay and cost as did non-consulted patients. This was, however, a retrospective observational study, using chart abstraction and administrative techniques. This introduces considerable weakness to the validity of the findings.
Bottom line:: In a retrospective study, no value was found to the use of peri-operative medical consultation of surgical patients in a large academic teaching hospital. Because of the weakness in study design, no conclusion can be drawn regarding the true effectiveness of perioperative medical consultation of the surgical patient.
Citation: Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007 Nov 26;167(21):2338-2344.
Does an RRT Save Children Outside the ICU?
Background: The Institute for Healthcare Improvement initiative known as the 100,000 lives campaign recommended six strategies to decrease preventable inpatient deaths. Implementation of a rapid response team (RRT) was one such strategy.
Study design: Cohort study design.
Setting: A 264-bed academic children’s hospital, between Jan. 1, 2001, and March 31, 2007.
Synopsis:
A total of 22,037 patient admissions and 102,537 patient days were evaluated pre-intervention, and 7,257 admissions and 34,420 patient days were evaluated post-intervention. Once the RRT was implemented, the mean morality rate decreased by 18% and the mean monthly code rate per 1,000 patient days were decreased by 71.2%. Study limitations included small differences in gender and race between pre-intervention and post-intervention populations.
This study is the first published study of pediatric inpatients to show significant reductions in both hospital wide mortality rate and code rate outside the intensive-care unit (ICU) setting after implementation of an RRT.
Bottom line: In an era of widely publicized hospital-related patient deaths the use of a pediatric RRT appears associated with reductions in inpatient codes and mortality.
Citation: Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298(19):2267-2274.
Does Influenza Vaccine Reduce Hospitalization, Death among Community Elderly?
Background: Most studies assessing the overall effectiveness of the influenza vaccine cover only a few influenza seasons. The need for long-term assessment was determined. Data were extracted retrospectively from HMO databases.
Study design: Retrospective (regression) analysis of pooled data.
Setting: One U.S. health maintenance organization. Data were pooled from 18 cohorts of community-dwelling elderly members of the HMO from 1990-2000.Synopsis: This study reviewed the effectiveness of influenza vaccine among patients 65 and older in community dwelling HMO members.
The study analyzed 713,872 person seasons over a 10-year period. The regression analysis revealed that influenza vaccination was associated with a 27% reduction in hospitalization for pneumonia/influenza and a 48% reduction in risk of death. The study was limited by inclusion of HMO enrollees only and may not have evaluated the vaccine effectiveness among the frailest elderly (e.g., nursing home dwellers). The study may have also been limited by misclassification of vaccination status.
Bottom line: Hospitalizations and deaths are prevented by influenza vaccination.
Citation: Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community dwelling elderly. N Engl J Med. 2007, 357; 1373-1381.
Is There a Simple, Effective Strategy to Reduce Primary Blood Stream Infections?
Background: An estimated 80,000 patients in U.S. ICUs incur catheter-associated bloodstream infections (BSIs). Reduction in BSI risk is the focus of several recent patient safety initiatives.
Study design: Two-arm, crossover clinical trial.
Setting: 22-bed medical ICU in Chicago.
Synopsis: This study took place over 52 weeks and involved 836 MICU patients. The patients were located in two ICUs at Cook County Hospital. One hospital unit was selected to serve as the intervention unit during which patients were bathed daily with 2% chlorhexidine gluconate (CHG)-impregnated washcloths. Patients in the concurrent control unit were bathed daily with soap and water. Outcome measures included incidences of primary BSIs and clinical sepsis (primary outcomes) and incidences of other infections (secondary outcomes). There were 4.1 vs. 10.4 primary infections per 1,000 patient days in the CHG intervention patients. Limitations in the CHG arm of the study were that patients had a slightly longer length of stay.
Bottom line: Daily cleansing of MICU patients with CHG-impregnated cloths is a simple and effective strategy to reduce primary BSIs.
Citation: Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med. 2007;167:2073-2079.
Is There a Better Way to Prevent Central Venous Catheter-related Infections?
Background: The Centers for Disease Control and Prevention (CDC) has identified catheter-associated adverse events, including bloodstream infections, as one of its seven safety challenges. The CDC has set a goal to reduce these events by 50% in five years. This is the first study comparing chlorhexidine-based solutions and alcohol-based povidone-iodine solutions for skin disinfection at central venous catheter-insertion sites.
Study design: Randomized comparison study.
Setting: Surgical ICU of University Hospital of Poitiers, France.
Synopsis: This study randomized 538 catheters inserted in the ICU to the two antiseptic groups. The trial was conducted from May 14, 2004, through June 29, 2006. Before catheter insertion, the skin was disinfected twice with the assigned solution. Catheters were removed aseptically, and the distal 5 cm was placed in a sterile tube for subsequent culture in the microbiology lab.
The microbiologists were unaware of the type of antiseptic solution used. In all, 481 catheters produced culture results. The chlorhexidine-based solution was associated with a 50% decrease in catheter colonization. The study couldn’t be conducted in a blinded manner because the two solutions are different colors.
Bottom line: Chlorhexidine-based solutions should be used as a replacement for povidone-iodine formulations to prevent central venous catheter-related infections.
Citation: Mimoz O, Villeminey S, Ragot S, et al. Chlorhexidine-based antiseptic solution vs. alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med. 2007;167:2066-2072. TH
LITERATURE AT A GLANCE
Use this guide to find the abstracts below that correspond to these recent clinical findings
- 24-hour TIA clinic improves outcomes.
- More rapid treatment after TIA and minor stroke reduce risk for recurrent stroke.
- Prasugrel more efficacious than clopidogrel in acute coronary syndrome, but with higher bleeding rates.
- Zoledronic acid use after hip fracture repair reduces probability of new fractures.
- No benefit in quality measures and resource use for surgical patients receiving medical consultation.
- Pediatric RRTs reduce mortality rate.
- Influenza vaccinations prevent hospitalization, death among elderly.
- Chlorhexidine bathing reduces catheter-associated bloodstream infections.
- Chlorhexidine-based antiseptic solution reduces rates of catheter-associated infections
Would 24-hour Hospital Clinic Reduce LOS, Stroke Risk?
Background: Transient ischemic attacks (TIA) precede up to 25% of completed strokes and can provide opportunity for critical intervention if identified early. A specialty clinic with immediate access to imaging facilities could provide early identification and intervention.
Study design: Cohort study statistical analysis of data.
Setting: SOS-TIA hospital clinic in Paris.
Synopsis: A leaflet about TIA with a toll-free telephone number for SOS-TIA was sent to 15,000 family doctors, cardiologists, neurologists, and ophthalmologists in Paris. Between January 2003 and December 2005, 1,085 patients with suspected TIA were admitted to the clinic. The median duration of symptoms was 15 minutes. All patients were started on a stroke-prevention program, 5% had urgent carotid revascularization, and 5% were treated for atrial fibrillation with anticoagulants. Further, 74% of all patients seen were sent home the same day. The 90-day stroke rate was 1.24%; the rate predicted was 5.96%. Limitations of the study included selective patient recruitment from family doctors and office-based specialists. Also, the study lacked a randomized control group.
Bottom line: Prompt evaluation and treatment of patients in a dedicated TIA clinic is associated with a lower stroke risk. The TIA clinic also may lower costs via decreased length of hospital stay.
Citation: Lavallee P, Meseguer E, Abboud H, et al. A transient ischemic attack clinic with round the clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960.
Can Early Treatment after TIA or Minor Stroke Reduce Risk of Early Recurrent Stroke?
Background: In the week following a TIA or a minor stroke, the risk of recurrent stroke grows to 10%. These warning events provide a limited window of opportunity for prevention. Several treatments are effective in stroke prevention following TIA or minor ischemic stroke if identified early. These include aspirin, other antiplatelet agents, blood-pressure (BP) medications, statins, anticoagulation for atrial fibrillation, and endarterectomy.
Study design: Prospective before-versus-after study (Oxford Vascular Study, or OXVASC) within population-based incidence study.
Setting:: The study population was located in primary care practices in the United Kingdom.
Synopsis: The OXVASC study looked at 1,278 patients who presented with TIA or stroke: 607 were referred directly to the hospital, 620 were referred for outpatient assessment, and 51 were not referred to secondary care. In phase 1, a daily TIA and minor stroke clinic was introduced. Collaborating primary care physicians were asked to refer all patients suspected of having TIA and minor stroke. Phase 1 took place between April 1, 2002, and Sept. 30, 2004. The treatment protocol recommended aspirin in patients not already on anti-platelet therapy (75 mg daily) or clopidogrel if aspirin was contraindicated; simvastatin (40 mg daily); BP lowering agents unless systolic BP less than 130 mm Hg; and anticoagulation as required.
In phase 2, from Oct. 1, 2004, to March 31, 2007, a clinic was established at which no appointments were necessary, treatment was initiated immediately, and diagnosis was confirmed. Patients were assessed in the same way as in phase 1, but all those considered to have had a TIA or stroke were given aspirin 300 mg together with a prescription of any other study medication to start the same day. A loading dose of clopidogrel 300 mg was also prescribed. The 90-day risk if recurrent stroke in the patients referred to the study clinic was 10.3% in phase 1 and 2.1% in phase 2.
Bottom line: Early treatment after TIA or minor stroke was associated with an 80% reduction in the risk of recurrent stroke.
Citation: Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischemic attack (TIA) and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-1442.
How Does Prasugrel Compare With Clopidogrel in Acute Coronary Syndrome?
Background: Short-term and long-term benefits of a dual anti-platelet therapy for patients with acute coronary syndromes and/or PTCA has been well established but limited by recurrent atherothrombatic events and safety issues.
Study design: Double-blind, randomized study.
Setting: Triton-TIMI 38 Study Group.
Synopsis: This study randomly assigned 13,608 patients with acute coronary syndromes from 30 countries to a treatment group between November 2004 and January 2007. The study protocol used a loading dose of prasugrel (60 mg) within 72 hours before randomization and one hour after cardiac catheterization.
After percutaneous coronary intervention (PCI) patients received maintenance doses of either prasugrel (10 mg) or clopidogrel (75 mg) daily. Daily aspirin (75-162 mg) was required. The outcome of this study showed a significant reduction in the rate of ischemic end points (nonfatal myocardial infarction, stroke, and death) and stent re-thrombosis with prasugrel over clopidogrel. This was theorized to be due to the more rapid onset of antiplatelet effect with prasugrel and improved inhibition of platelet aggregation. Bleeding episodes were more frequent in the prasugrel group. Limitations of the study included the choice of vessels treated, devices used, and adjunctive medication administered to support PCI. All were left to the discretion of the treating physician.
Bottom line: Prasugrel therapy was significantly better than clopidogrel but with an increased risk of major bleeding.
Citation: Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
Can the Rate of New Hip Fracture Be Reduced with Zoledronic Acid?
Background: Mortality is markedly increased following hip fractures, and medical interventions exist to improve clinical outcomes.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: International, multicenter trial involving patients with recent hip fracture.
Synopsis: This study, know as the HORIZON trial, involved 2,127 patients. Of those, 1,065 (mean age of 74.5) were assigned to receive yearly infusions of 5 mg IV zoledronic acid within 90 days after surgical hip fracture repair. Meantime, 1,062 were assigned to receive placebo.
All patients received supplemental vitamin D and calcium. The median follow-up was 1.9 years, and the primary end point was a new clinical fracture. The rate of any new clinical fracture was 8.6% in the zoledronic acid group and 13.9% in the placebo group. This represents a 35% relative risk reduction with zoledronic acid.
Limitations of the study included a slightly younger and healthier patient population with hip fracture than the general population.
Bottom line: An annual infusion of zoledronic acid within 90 days after repair of hip fracture was associated with reduced new fractures and improved survival.
Citation: Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799-1809.
Does Peri-operative Consultation Improve Post-operative Outcome, Reduce Hospital Cost?
Background: Hospitalist-surgical co-management of the surgical inpatient is a model of care enjoying increasing interest. However, there is little published evidence of the effectiveness of this model.
Study design: Retrospective chart review.
Setting: Surgical service of academic teaching hospital.
Synopsis: Of 1,282 surgical patients, 9.1% underwent perioperative medical consultation in a retrospective review. Based on a number of measurement variables (post-operative serum glucose, venous thromboembolism [VTE] prophylaxis, use of perioperative beta-blockers), consulted patients had the same outcome, length of stay and cost as did non-consulted patients. This was, however, a retrospective observational study, using chart abstraction and administrative techniques. This introduces considerable weakness to the validity of the findings.
Bottom line:: In a retrospective study, no value was found to the use of peri-operative medical consultation of surgical patients in a large academic teaching hospital. Because of the weakness in study design, no conclusion can be drawn regarding the true effectiveness of perioperative medical consultation of the surgical patient.
Citation: Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007 Nov 26;167(21):2338-2344.
Does an RRT Save Children Outside the ICU?
Background: The Institute for Healthcare Improvement initiative known as the 100,000 lives campaign recommended six strategies to decrease preventable inpatient deaths. Implementation of a rapid response team (RRT) was one such strategy.
Study design: Cohort study design.
Setting: A 264-bed academic children’s hospital, between Jan. 1, 2001, and March 31, 2007.
Synopsis:
A total of 22,037 patient admissions and 102,537 patient days were evaluated pre-intervention, and 7,257 admissions and 34,420 patient days were evaluated post-intervention. Once the RRT was implemented, the mean morality rate decreased by 18% and the mean monthly code rate per 1,000 patient days were decreased by 71.2%. Study limitations included small differences in gender and race between pre-intervention and post-intervention populations.
This study is the first published study of pediatric inpatients to show significant reductions in both hospital wide mortality rate and code rate outside the intensive-care unit (ICU) setting after implementation of an RRT.
Bottom line: In an era of widely publicized hospital-related patient deaths the use of a pediatric RRT appears associated with reductions in inpatient codes and mortality.
Citation: Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298(19):2267-2274.
Does Influenza Vaccine Reduce Hospitalization, Death among Community Elderly?
Background: Most studies assessing the overall effectiveness of the influenza vaccine cover only a few influenza seasons. The need for long-term assessment was determined. Data were extracted retrospectively from HMO databases.
Study design: Retrospective (regression) analysis of pooled data.
Setting: One U.S. health maintenance organization. Data were pooled from 18 cohorts of community-dwelling elderly members of the HMO from 1990-2000.Synopsis: This study reviewed the effectiveness of influenza vaccine among patients 65 and older in community dwelling HMO members.
The study analyzed 713,872 person seasons over a 10-year period. The regression analysis revealed that influenza vaccination was associated with a 27% reduction in hospitalization for pneumonia/influenza and a 48% reduction in risk of death. The study was limited by inclusion of HMO enrollees only and may not have evaluated the vaccine effectiveness among the frailest elderly (e.g., nursing home dwellers). The study may have also been limited by misclassification of vaccination status.
Bottom line: Hospitalizations and deaths are prevented by influenza vaccination.
Citation: Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community dwelling elderly. N Engl J Med. 2007, 357; 1373-1381.
Is There a Simple, Effective Strategy to Reduce Primary Blood Stream Infections?
Background: An estimated 80,000 patients in U.S. ICUs incur catheter-associated bloodstream infections (BSIs). Reduction in BSI risk is the focus of several recent patient safety initiatives.
Study design: Two-arm, crossover clinical trial.
Setting: 22-bed medical ICU in Chicago.
Synopsis: This study took place over 52 weeks and involved 836 MICU patients. The patients were located in two ICUs at Cook County Hospital. One hospital unit was selected to serve as the intervention unit during which patients were bathed daily with 2% chlorhexidine gluconate (CHG)-impregnated washcloths. Patients in the concurrent control unit were bathed daily with soap and water. Outcome measures included incidences of primary BSIs and clinical sepsis (primary outcomes) and incidences of other infections (secondary outcomes). There were 4.1 vs. 10.4 primary infections per 1,000 patient days in the CHG intervention patients. Limitations in the CHG arm of the study were that patients had a slightly longer length of stay.
Bottom line: Daily cleansing of MICU patients with CHG-impregnated cloths is a simple and effective strategy to reduce primary BSIs.
Citation: Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med. 2007;167:2073-2079.
Is There a Better Way to Prevent Central Venous Catheter-related Infections?
Background: The Centers for Disease Control and Prevention (CDC) has identified catheter-associated adverse events, including bloodstream infections, as one of its seven safety challenges. The CDC has set a goal to reduce these events by 50% in five years. This is the first study comparing chlorhexidine-based solutions and alcohol-based povidone-iodine solutions for skin disinfection at central venous catheter-insertion sites.
Study design: Randomized comparison study.
Setting: Surgical ICU of University Hospital of Poitiers, France.
Synopsis: This study randomized 538 catheters inserted in the ICU to the two antiseptic groups. The trial was conducted from May 14, 2004, through June 29, 2006. Before catheter insertion, the skin was disinfected twice with the assigned solution. Catheters were removed aseptically, and the distal 5 cm was placed in a sterile tube for subsequent culture in the microbiology lab.
The microbiologists were unaware of the type of antiseptic solution used. In all, 481 catheters produced culture results. The chlorhexidine-based solution was associated with a 50% decrease in catheter colonization. The study couldn’t be conducted in a blinded manner because the two solutions are different colors.
Bottom line: Chlorhexidine-based solutions should be used as a replacement for povidone-iodine formulations to prevent central venous catheter-related infections.
Citation: Mimoz O, Villeminey S, Ragot S, et al. Chlorhexidine-based antiseptic solution vs. alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med. 2007;167:2066-2072. TH
LITERATURE AT A GLANCE
Use this guide to find the abstracts below that correspond to these recent clinical findings
- 24-hour TIA clinic improves outcomes.
- More rapid treatment after TIA and minor stroke reduce risk for recurrent stroke.
- Prasugrel more efficacious than clopidogrel in acute coronary syndrome, but with higher bleeding rates.
- Zoledronic acid use after hip fracture repair reduces probability of new fractures.
- No benefit in quality measures and resource use for surgical patients receiving medical consultation.
- Pediatric RRTs reduce mortality rate.
- Influenza vaccinations prevent hospitalization, death among elderly.
- Chlorhexidine bathing reduces catheter-associated bloodstream infections.
- Chlorhexidine-based antiseptic solution reduces rates of catheter-associated infections
Would 24-hour Hospital Clinic Reduce LOS, Stroke Risk?
Background: Transient ischemic attacks (TIA) precede up to 25% of completed strokes and can provide opportunity for critical intervention if identified early. A specialty clinic with immediate access to imaging facilities could provide early identification and intervention.
Study design: Cohort study statistical analysis of data.
Setting: SOS-TIA hospital clinic in Paris.
Synopsis: A leaflet about TIA with a toll-free telephone number for SOS-TIA was sent to 15,000 family doctors, cardiologists, neurologists, and ophthalmologists in Paris. Between January 2003 and December 2005, 1,085 patients with suspected TIA were admitted to the clinic. The median duration of symptoms was 15 minutes. All patients were started on a stroke-prevention program, 5% had urgent carotid revascularization, and 5% were treated for atrial fibrillation with anticoagulants. Further, 74% of all patients seen were sent home the same day. The 90-day stroke rate was 1.24%; the rate predicted was 5.96%. Limitations of the study included selective patient recruitment from family doctors and office-based specialists. Also, the study lacked a randomized control group.
Bottom line: Prompt evaluation and treatment of patients in a dedicated TIA clinic is associated with a lower stroke risk. The TIA clinic also may lower costs via decreased length of hospital stay.
Citation: Lavallee P, Meseguer E, Abboud H, et al. A transient ischemic attack clinic with round the clock access (SOS-TIA): feasibility and effects. Lancet Neurol. 2007;6(11):953-960.
Can Early Treatment after TIA or Minor Stroke Reduce Risk of Early Recurrent Stroke?
Background: In the week following a TIA or a minor stroke, the risk of recurrent stroke grows to 10%. These warning events provide a limited window of opportunity for prevention. Several treatments are effective in stroke prevention following TIA or minor ischemic stroke if identified early. These include aspirin, other antiplatelet agents, blood-pressure (BP) medications, statins, anticoagulation for atrial fibrillation, and endarterectomy.
Study design: Prospective before-versus-after study (Oxford Vascular Study, or OXVASC) within population-based incidence study.
Setting:: The study population was located in primary care practices in the United Kingdom.
Synopsis: The OXVASC study looked at 1,278 patients who presented with TIA or stroke: 607 were referred directly to the hospital, 620 were referred for outpatient assessment, and 51 were not referred to secondary care. In phase 1, a daily TIA and minor stroke clinic was introduced. Collaborating primary care physicians were asked to refer all patients suspected of having TIA and minor stroke. Phase 1 took place between April 1, 2002, and Sept. 30, 2004. The treatment protocol recommended aspirin in patients not already on anti-platelet therapy (75 mg daily) or clopidogrel if aspirin was contraindicated; simvastatin (40 mg daily); BP lowering agents unless systolic BP less than 130 mm Hg; and anticoagulation as required.
In phase 2, from Oct. 1, 2004, to March 31, 2007, a clinic was established at which no appointments were necessary, treatment was initiated immediately, and diagnosis was confirmed. Patients were assessed in the same way as in phase 1, but all those considered to have had a TIA or stroke were given aspirin 300 mg together with a prescription of any other study medication to start the same day. A loading dose of clopidogrel 300 mg was also prescribed. The 90-day risk if recurrent stroke in the patients referred to the study clinic was 10.3% in phase 1 and 2.1% in phase 2.
Bottom line: Early treatment after TIA or minor stroke was associated with an 80% reduction in the risk of recurrent stroke.
Citation: Rothwell PM, Giles MF, Chandratheva A, et al. Effect of urgent treatment of transient ischemic attack (TIA) and minor stroke on early recurrent stroke (EXPRESS study): a prospective population-based sequential comparison. Lancet 2007;370:1432-1442.
How Does Prasugrel Compare With Clopidogrel in Acute Coronary Syndrome?
Background: Short-term and long-term benefits of a dual anti-platelet therapy for patients with acute coronary syndromes and/or PTCA has been well established but limited by recurrent atherothrombatic events and safety issues.
Study design: Double-blind, randomized study.
Setting: Triton-TIMI 38 Study Group.
Synopsis: This study randomly assigned 13,608 patients with acute coronary syndromes from 30 countries to a treatment group between November 2004 and January 2007. The study protocol used a loading dose of prasugrel (60 mg) within 72 hours before randomization and one hour after cardiac catheterization.
After percutaneous coronary intervention (PCI) patients received maintenance doses of either prasugrel (10 mg) or clopidogrel (75 mg) daily. Daily aspirin (75-162 mg) was required. The outcome of this study showed a significant reduction in the rate of ischemic end points (nonfatal myocardial infarction, stroke, and death) and stent re-thrombosis with prasugrel over clopidogrel. This was theorized to be due to the more rapid onset of antiplatelet effect with prasugrel and improved inhibition of platelet aggregation. Bleeding episodes were more frequent in the prasugrel group. Limitations of the study included the choice of vessels treated, devices used, and adjunctive medication administered to support PCI. All were left to the discretion of the treating physician.
Bottom line: Prasugrel therapy was significantly better than clopidogrel but with an increased risk of major bleeding.
Citation: Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007;357:2001-2015.
Can the Rate of New Hip Fracture Be Reduced with Zoledronic Acid?
Background: Mortality is markedly increased following hip fractures, and medical interventions exist to improve clinical outcomes.
Study design: Randomized, double-blind, placebo-controlled trial.
Setting: International, multicenter trial involving patients with recent hip fracture.
Synopsis: This study, know as the HORIZON trial, involved 2,127 patients. Of those, 1,065 (mean age of 74.5) were assigned to receive yearly infusions of 5 mg IV zoledronic acid within 90 days after surgical hip fracture repair. Meantime, 1,062 were assigned to receive placebo.
All patients received supplemental vitamin D and calcium. The median follow-up was 1.9 years, and the primary end point was a new clinical fracture. The rate of any new clinical fracture was 8.6% in the zoledronic acid group and 13.9% in the placebo group. This represents a 35% relative risk reduction with zoledronic acid.
Limitations of the study included a slightly younger and healthier patient population with hip fracture than the general population.
Bottom line: An annual infusion of zoledronic acid within 90 days after repair of hip fracture was associated with reduced new fractures and improved survival.
Citation: Lyles KW, Colon-Emeric CS, Magaziner JS, et al. Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med. 2007;357:1799-1809.
Does Peri-operative Consultation Improve Post-operative Outcome, Reduce Hospital Cost?
Background: Hospitalist-surgical co-management of the surgical inpatient is a model of care enjoying increasing interest. However, there is little published evidence of the effectiveness of this model.
Study design: Retrospective chart review.
Setting: Surgical service of academic teaching hospital.
Synopsis: Of 1,282 surgical patients, 9.1% underwent perioperative medical consultation in a retrospective review. Based on a number of measurement variables (post-operative serum glucose, venous thromboembolism [VTE] prophylaxis, use of perioperative beta-blockers), consulted patients had the same outcome, length of stay and cost as did non-consulted patients. This was, however, a retrospective observational study, using chart abstraction and administrative techniques. This introduces considerable weakness to the validity of the findings.
Bottom line:: In a retrospective study, no value was found to the use of peri-operative medical consultation of surgical patients in a large academic teaching hospital. Because of the weakness in study design, no conclusion can be drawn regarding the true effectiveness of perioperative medical consultation of the surgical patient.
Citation: Auerbach AD, Rasic MA, Sehgal N, Ide B, Stone B, Maselli J. Opportunity missed: medical consultation, resource use, and quality of care of patients undergoing major surgery. Arch Intern Med. 2007 Nov 26;167(21):2338-2344.
Does an RRT Save Children Outside the ICU?
Background: The Institute for Healthcare Improvement initiative known as the 100,000 lives campaign recommended six strategies to decrease preventable inpatient deaths. Implementation of a rapid response team (RRT) was one such strategy.
Study design: Cohort study design.
Setting: A 264-bed academic children’s hospital, between Jan. 1, 2001, and March 31, 2007.
Synopsis:
A total of 22,037 patient admissions and 102,537 patient days were evaluated pre-intervention, and 7,257 admissions and 34,420 patient days were evaluated post-intervention. Once the RRT was implemented, the mean morality rate decreased by 18% and the mean monthly code rate per 1,000 patient days were decreased by 71.2%. Study limitations included small differences in gender and race between pre-intervention and post-intervention populations.
This study is the first published study of pediatric inpatients to show significant reductions in both hospital wide mortality rate and code rate outside the intensive-care unit (ICU) setting after implementation of an RRT.
Bottom line: In an era of widely publicized hospital-related patient deaths the use of a pediatric RRT appears associated with reductions in inpatient codes and mortality.
Citation: Sharek PJ, Parast LM, Leong K, et al. Effect of a rapid response team on hospital-wide mortality and code rates outside the ICU in a children’s hospital. JAMA. 2007;298(19):2267-2274.
Does Influenza Vaccine Reduce Hospitalization, Death among Community Elderly?
Background: Most studies assessing the overall effectiveness of the influenza vaccine cover only a few influenza seasons. The need for long-term assessment was determined. Data were extracted retrospectively from HMO databases.
Study design: Retrospective (regression) analysis of pooled data.
Setting: One U.S. health maintenance organization. Data were pooled from 18 cohorts of community-dwelling elderly members of the HMO from 1990-2000.Synopsis: This study reviewed the effectiveness of influenza vaccine among patients 65 and older in community dwelling HMO members.
The study analyzed 713,872 person seasons over a 10-year period. The regression analysis revealed that influenza vaccination was associated with a 27% reduction in hospitalization for pneumonia/influenza and a 48% reduction in risk of death. The study was limited by inclusion of HMO enrollees only and may not have evaluated the vaccine effectiveness among the frailest elderly (e.g., nursing home dwellers). The study may have also been limited by misclassification of vaccination status.
Bottom line: Hospitalizations and deaths are prevented by influenza vaccination.
Citation: Nichol KL, Nordin JD, Nelson DB, Mullooly JP, Hak E. Effectiveness of influenza vaccine in the community dwelling elderly. N Engl J Med. 2007, 357; 1373-1381.
Is There a Simple, Effective Strategy to Reduce Primary Blood Stream Infections?
Background: An estimated 80,000 patients in U.S. ICUs incur catheter-associated bloodstream infections (BSIs). Reduction in BSI risk is the focus of several recent patient safety initiatives.
Study design: Two-arm, crossover clinical trial.
Setting: 22-bed medical ICU in Chicago.
Synopsis: This study took place over 52 weeks and involved 836 MICU patients. The patients were located in two ICUs at Cook County Hospital. One hospital unit was selected to serve as the intervention unit during which patients were bathed daily with 2% chlorhexidine gluconate (CHG)-impregnated washcloths. Patients in the concurrent control unit were bathed daily with soap and water. Outcome measures included incidences of primary BSIs and clinical sepsis (primary outcomes) and incidences of other infections (secondary outcomes). There were 4.1 vs. 10.4 primary infections per 1,000 patient days in the CHG intervention patients. Limitations in the CHG arm of the study were that patients had a slightly longer length of stay.
Bottom line: Daily cleansing of MICU patients with CHG-impregnated cloths is a simple and effective strategy to reduce primary BSIs.
Citation: Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med. 2007;167:2073-2079.
Is There a Better Way to Prevent Central Venous Catheter-related Infections?
Background: The Centers for Disease Control and Prevention (CDC) has identified catheter-associated adverse events, including bloodstream infections, as one of its seven safety challenges. The CDC has set a goal to reduce these events by 50% in five years. This is the first study comparing chlorhexidine-based solutions and alcohol-based povidone-iodine solutions for skin disinfection at central venous catheter-insertion sites.
Study design: Randomized comparison study.
Setting: Surgical ICU of University Hospital of Poitiers, France.
Synopsis: This study randomized 538 catheters inserted in the ICU to the two antiseptic groups. The trial was conducted from May 14, 2004, through June 29, 2006. Before catheter insertion, the skin was disinfected twice with the assigned solution. Catheters were removed aseptically, and the distal 5 cm was placed in a sterile tube for subsequent culture in the microbiology lab.
The microbiologists were unaware of the type of antiseptic solution used. In all, 481 catheters produced culture results. The chlorhexidine-based solution was associated with a 50% decrease in catheter colonization. The study couldn’t be conducted in a blinded manner because the two solutions are different colors.
Bottom line: Chlorhexidine-based solutions should be used as a replacement for povidone-iodine formulations to prevent central venous catheter-related infections.
Citation: Mimoz O, Villeminey S, Ragot S, et al. Chlorhexidine-based antiseptic solution vs. alcohol-based povidone-iodine for central venous catheter care. Arch Intern Med. 2007;167:2066-2072. TH
SHM Takes on VTE
Venous thromboembolic (VTE) disease, ranging from asymptomatic deep-vein thrombosis (DVT) to massive pulmonary embolism (PE), is a significant cause of morbidity and mortality in hospitalized patients. Almost all hospitalized patients are at risk for VTE, and the literature suggests approximately half of all VTEs are hospital-acquired.
Hospitalists are ideally positioned to reduce the incidence of preventable VTEs, both by using known best practices to improve care delivered to their own patients, and, more importantly, by leading hospitalwide efforts that improve care for all patients at their home institutions.
In recognition of this important clinical issue and the role hospitalists can play in addressing it, SHM launched the VTE Prevention Collaborative (VTEPC) in January 2007. The program offers individualized assistance to hospitalists wishing to take the lead in this area.
The VTEPC offers two technical assistance options. Individuals interested in securing ongoing support for their planned or active VTE prevention projects can enroll in the mentoring program. This allows a full year of access to and support from SHM mentors with VTE and quality-improvement (QI) expertise. Mentoring occurs in eight telephone calls, during which mentors offer individualized assistance on any topics, tasks, or barriers commonly encountered in designing, implementing, and evaluating a VTE prevention project.
An on-site consultation program is designed for individuals interested in securing expert evaluation and input on a VTE prevention program but who don’t feel they need ongoing, longitudinal support. In this program, SHM consultants with VTE and QI expertise visit applicants’ hospitals to evaluate active or planned VTE prevention programs. The consultation visits feature a structured evaluation of the site’s strengths and resources, barriers to improvement, and the design and function of active or proposed VTE prevention interventions.
For both programs, support and instruction are organized around the VTE QI workbook, “Preventing Hospital-Acquired Venous Thromboembolism: A Guide for Effective Quality Improvement,” SHM’s step-by-step guide for developing a VTE prevention program. SHM secured the services of Greg Maynard, MD, and Jason Stein, MD, to provide mentoring and conduct consultation visits. Drs. Maynard and Stein have led successful local VTE prevention QI projects, hold QI leadership positions, and have taught QI and VTE prevention principals to local and national audiences. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California, San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of medicine at Emory University School of Medicine, and director of quality improvement for the Emory Hospital Medicine Unit.
Both were also instrumental in developing SHM’s online VTE Resource Room and the VTE QI workbook.
Strong Responses
Twenty-seven hospitalists enrolled in the VTEPC in its first year of operation, 24 in the mentoring program and three in the consultation program.
Enrollees have broad experience in VTE prevention and QI. Some enrollees have been in practice for two years, others more than 25 years. Some fill QI leadership roles in their hospitals or hospital medicine groups. For others the VTE prevention project is their first experience leading a QI effort. Regional representation (19 states), hospital system representation (18 systems), hospital size (135 to 700 staffed beds), and hospital type (academic centers, community teaching hospitals, and community hospitals) are also broad. One enrollee works at a long-term acute care hospital, all others work at acute-care hospitals.
What They Said
Participants in the mentoring and consultation programs have reported that the support they’ve received has been enormously helpful.
According to feedback from one participant, support from the mentoring program made the potentially overwhelming prospect of launching a hospitalwide improvement effort much more manageable: “The prospect of launching a multihospital VTE Prevention Protocol was extremely daunting; however, with the help of my SHM mentor, we stand ready to pilot the program within the week. Our mentor carefully constructed a step-by-step process that allowed me to investigate the scope of the problem at the local level and develop a protocol that was embraced by our administration and physicians. He supplied me with resources and knowledge that allowed me to successfully handle multiple obstacles that arose along the way. What we have accomplished will have an enormous impact on the quality of care that we provide for our patients.”
Other participants have reported that having access to objective input from an external expert can help transform a slow-developing or ineffective prevention program. As one participant put it: “Mentoring through SHM’s VTE Prevention Collaborative has been an invaluable experience. Through monthly phone calls and frequent e-mails, our mentor focused our previously ineffective efforts and guided us to develop a streamlined tool that was custom-fit to the workflow at our hospital. He has saved us tremendous frustrations by directing us to the appropriate resources in our institution to accomplish tasks we would have attempted ourselves. Since our first phone call, he has been both our coach and cheerleader. The processes and techniques that he has taught us are applicable to every quality endeavor we engage in.”
What Impressed Experts
Drs. Maynard and Stein have been enormously impressed by what VTEPC members have achieved. “What is most impressive to me is how all these hospitalist project leaders in different settings are overcoming a wide variety of intuitional barriers, medical staff barriers, infrastructure barriers—all the obstacles that can challenge the typical big QI project,” says Dr. Maynard. He notes that not only are participants utilizing all the basic QI principles in all the ways that were outlined in the QI workbook, but they also are coming up with innovations and approaches beyond what the workbook authors envisioned.
“We learn from them as they come up with innovations to meet their own challenges,” Dr. Stein says. “It shows the resilience and flexibility of the QI framework. If you really work in your local setting on these things with the improvement framework in mind you can get by almost any barrier.” Drs. Maynard and Stein have noted that participants have been able to design and implement VTE prevention programs at a pace that far outstrips what the two mentors achieved at their home institutions.
Many participants have found real-time ways to identify patients who are not on prophylaxis but should be. At many sites, identification begins with a report generated by the hospital’s inpatient pharmacy service, which typically shows the anti-coagulation regimen for each patient in a given hospital ward. The floor pharmacist or nurse can identify who is not on prophylaxis, assess risk factors and contraindications, and act to mitigate the situation—for example, by placing a call to the patient’s attending physician. Other sites have developed more sophisticated reports that capture information about relative risk for DVT and the absence or presence of contraindications to pharmacologic prophylaxis; these features reduce the effort required to investigate each case.
How to Learn More
The Quality Track at the 2008 Annual Meeting (April 3-5 at the Manchester Hyatt, San Diego, Calif.) includes a session on the “VTE Collaborative Experience” (1-2:25 p.m. April 4). Drs. Maynard and Stein will discuss the initiative, as will collaborative members, who will describe key successes and innovations that furthered their efforts to establish effective VTE prevention programs. Questions about the VTEPC and the Annual Meeting session can be directed to vtepc@hospitalmedicine.org.
Update on Hand-Offs
SHM task force continues to refine transitions-of-care checklist
by Shannon Roach
Among hospitalists and other organizations, there has been an increasing interest surrounding the improvement of the quality of patient care, especially within transitions of care and patient discharge. As the leader in the hospital medicine field, SHM continues to support and lead initiatives for the improvement of care as related to patient discharge and transitions. Last year’s creation of the Hand-Offs Communication Task Force (HCTF) has upheld SHM’s position of being dedicated to the promotion of the highest quality care for all hospitalized patients.
Derived from members of the Hospital Quality and Patient Safety Committee and the Education Committee, this task force was led by Vineet Arora, MD, MA, assistant professor of medicine, University of Chicago. Collaborating with her were Preetha Basaviah, MD, clinical instructor, Stanford University Medical Center in Calif.; Dan Dressler, MD, instructor of medicine, Emory University School of Medicine in Atlanta; Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.; Sunil Kripalani, MD, MSc, an instructor at Emory University in Atlanta; and Efren Manjarrez, MD, assistant clinical professor of medicine at the Miller School of Medicine, University of Miami.
This team set out to create a formally recognized set of recommendations for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service.
The task force’s first step was to determine what information was available as a basis for these recommendations. Though data were limited, the group decided that recommendations for effective hand-offs would be broken into three categories: program policy, verbal exchange, and content exchange.
As the need for more evidence-based data for the improvement of in-hospital hand-offs became clear, the group decided a valuable follow-up approach for these recommendations would be to incorporate a research agenda into the findings. This proposal suggests a need for a rigorous evaluation of these recommendations, with an emphasis on controlled interventions. It also encourages the development of patient-based outcomes sensitive to hand-off quality.
As a test run for these recommendations, the HCTF presented its findings at Hospital Medicine 2007 in Dallas. Their session “Developing Communications and Hand-Off Standards for Hospitalists” drew a passionate response. During this session they unveiled a checklist outlining the important elements of an in-hospital physician hand-off. Attendees were encouraged to offer feedback and vote on proposed hand-off elements. They also were encouraged to submit suggestions if they believed something was missing.
Using that feedback, the group produced a final draft of recommendations and distributed it to a multidisciplinary team of experts for a final review. On the panel were Linda Bell, RN, MSN; Emily Patterson, PhD; Erik Van Eaton, MD; and Arpana Vidyarthi, MD. These experts reflect the perspective of nonphysician members of the hospital community, representing the interests of technology, nursing, human factors research, and hospital medicine. They reviewed the paper and hand-off recommendations by participating in conference calls in which they were asked to comment on questions regarding the working paper. These discussions gave the task force invaluable, candid feedback adopted into the working paper to create a more robust set of recommendations.
The final product was reviewed by SHM’s Board of Directors in January; a dissemination plan is in progress. If these recommendations are endorsed by an institution or a hospitalist group, they will act as a guide to ensure the coordination of hand-offs and the mangement of important clinical care issues.
Through their research and interactions with a large number of individuals concerned with this issue, the HCTF discovered that the quality improvement of patient transitions is a complex, global issue. They believe this checklist of hand-off elements is essential to these efforts.
Venous thromboembolic (VTE) disease, ranging from asymptomatic deep-vein thrombosis (DVT) to massive pulmonary embolism (PE), is a significant cause of morbidity and mortality in hospitalized patients. Almost all hospitalized patients are at risk for VTE, and the literature suggests approximately half of all VTEs are hospital-acquired.
Hospitalists are ideally positioned to reduce the incidence of preventable VTEs, both by using known best practices to improve care delivered to their own patients, and, more importantly, by leading hospitalwide efforts that improve care for all patients at their home institutions.
In recognition of this important clinical issue and the role hospitalists can play in addressing it, SHM launched the VTE Prevention Collaborative (VTEPC) in January 2007. The program offers individualized assistance to hospitalists wishing to take the lead in this area.
The VTEPC offers two technical assistance options. Individuals interested in securing ongoing support for their planned or active VTE prevention projects can enroll in the mentoring program. This allows a full year of access to and support from SHM mentors with VTE and quality-improvement (QI) expertise. Mentoring occurs in eight telephone calls, during which mentors offer individualized assistance on any topics, tasks, or barriers commonly encountered in designing, implementing, and evaluating a VTE prevention project.
An on-site consultation program is designed for individuals interested in securing expert evaluation and input on a VTE prevention program but who don’t feel they need ongoing, longitudinal support. In this program, SHM consultants with VTE and QI expertise visit applicants’ hospitals to evaluate active or planned VTE prevention programs. The consultation visits feature a structured evaluation of the site’s strengths and resources, barriers to improvement, and the design and function of active or proposed VTE prevention interventions.
For both programs, support and instruction are organized around the VTE QI workbook, “Preventing Hospital-Acquired Venous Thromboembolism: A Guide for Effective Quality Improvement,” SHM’s step-by-step guide for developing a VTE prevention program. SHM secured the services of Greg Maynard, MD, and Jason Stein, MD, to provide mentoring and conduct consultation visits. Drs. Maynard and Stein have led successful local VTE prevention QI projects, hold QI leadership positions, and have taught QI and VTE prevention principals to local and national audiences. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California, San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of medicine at Emory University School of Medicine, and director of quality improvement for the Emory Hospital Medicine Unit.
Both were also instrumental in developing SHM’s online VTE Resource Room and the VTE QI workbook.
Strong Responses
Twenty-seven hospitalists enrolled in the VTEPC in its first year of operation, 24 in the mentoring program and three in the consultation program.
Enrollees have broad experience in VTE prevention and QI. Some enrollees have been in practice for two years, others more than 25 years. Some fill QI leadership roles in their hospitals or hospital medicine groups. For others the VTE prevention project is their first experience leading a QI effort. Regional representation (19 states), hospital system representation (18 systems), hospital size (135 to 700 staffed beds), and hospital type (academic centers, community teaching hospitals, and community hospitals) are also broad. One enrollee works at a long-term acute care hospital, all others work at acute-care hospitals.
What They Said
Participants in the mentoring and consultation programs have reported that the support they’ve received has been enormously helpful.
According to feedback from one participant, support from the mentoring program made the potentially overwhelming prospect of launching a hospitalwide improvement effort much more manageable: “The prospect of launching a multihospital VTE Prevention Protocol was extremely daunting; however, with the help of my SHM mentor, we stand ready to pilot the program within the week. Our mentor carefully constructed a step-by-step process that allowed me to investigate the scope of the problem at the local level and develop a protocol that was embraced by our administration and physicians. He supplied me with resources and knowledge that allowed me to successfully handle multiple obstacles that arose along the way. What we have accomplished will have an enormous impact on the quality of care that we provide for our patients.”
Other participants have reported that having access to objective input from an external expert can help transform a slow-developing or ineffective prevention program. As one participant put it: “Mentoring through SHM’s VTE Prevention Collaborative has been an invaluable experience. Through monthly phone calls and frequent e-mails, our mentor focused our previously ineffective efforts and guided us to develop a streamlined tool that was custom-fit to the workflow at our hospital. He has saved us tremendous frustrations by directing us to the appropriate resources in our institution to accomplish tasks we would have attempted ourselves. Since our first phone call, he has been both our coach and cheerleader. The processes and techniques that he has taught us are applicable to every quality endeavor we engage in.”
What Impressed Experts
Drs. Maynard and Stein have been enormously impressed by what VTEPC members have achieved. “What is most impressive to me is how all these hospitalist project leaders in different settings are overcoming a wide variety of intuitional barriers, medical staff barriers, infrastructure barriers—all the obstacles that can challenge the typical big QI project,” says Dr. Maynard. He notes that not only are participants utilizing all the basic QI principles in all the ways that were outlined in the QI workbook, but they also are coming up with innovations and approaches beyond what the workbook authors envisioned.
“We learn from them as they come up with innovations to meet their own challenges,” Dr. Stein says. “It shows the resilience and flexibility of the QI framework. If you really work in your local setting on these things with the improvement framework in mind you can get by almost any barrier.” Drs. Maynard and Stein have noted that participants have been able to design and implement VTE prevention programs at a pace that far outstrips what the two mentors achieved at their home institutions.
Many participants have found real-time ways to identify patients who are not on prophylaxis but should be. At many sites, identification begins with a report generated by the hospital’s inpatient pharmacy service, which typically shows the anti-coagulation regimen for each patient in a given hospital ward. The floor pharmacist or nurse can identify who is not on prophylaxis, assess risk factors and contraindications, and act to mitigate the situation—for example, by placing a call to the patient’s attending physician. Other sites have developed more sophisticated reports that capture information about relative risk for DVT and the absence or presence of contraindications to pharmacologic prophylaxis; these features reduce the effort required to investigate each case.
How to Learn More
The Quality Track at the 2008 Annual Meeting (April 3-5 at the Manchester Hyatt, San Diego, Calif.) includes a session on the “VTE Collaborative Experience” (1-2:25 p.m. April 4). Drs. Maynard and Stein will discuss the initiative, as will collaborative members, who will describe key successes and innovations that furthered their efforts to establish effective VTE prevention programs. Questions about the VTEPC and the Annual Meeting session can be directed to vtepc@hospitalmedicine.org.
Update on Hand-Offs
SHM task force continues to refine transitions-of-care checklist
by Shannon Roach
Among hospitalists and other organizations, there has been an increasing interest surrounding the improvement of the quality of patient care, especially within transitions of care and patient discharge. As the leader in the hospital medicine field, SHM continues to support and lead initiatives for the improvement of care as related to patient discharge and transitions. Last year’s creation of the Hand-Offs Communication Task Force (HCTF) has upheld SHM’s position of being dedicated to the promotion of the highest quality care for all hospitalized patients.
Derived from members of the Hospital Quality and Patient Safety Committee and the Education Committee, this task force was led by Vineet Arora, MD, MA, assistant professor of medicine, University of Chicago. Collaborating with her were Preetha Basaviah, MD, clinical instructor, Stanford University Medical Center in Calif.; Dan Dressler, MD, instructor of medicine, Emory University School of Medicine in Atlanta; Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.; Sunil Kripalani, MD, MSc, an instructor at Emory University in Atlanta; and Efren Manjarrez, MD, assistant clinical professor of medicine at the Miller School of Medicine, University of Miami.
This team set out to create a formally recognized set of recommendations for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service.
The task force’s first step was to determine what information was available as a basis for these recommendations. Though data were limited, the group decided that recommendations for effective hand-offs would be broken into three categories: program policy, verbal exchange, and content exchange.
As the need for more evidence-based data for the improvement of in-hospital hand-offs became clear, the group decided a valuable follow-up approach for these recommendations would be to incorporate a research agenda into the findings. This proposal suggests a need for a rigorous evaluation of these recommendations, with an emphasis on controlled interventions. It also encourages the development of patient-based outcomes sensitive to hand-off quality.
As a test run for these recommendations, the HCTF presented its findings at Hospital Medicine 2007 in Dallas. Their session “Developing Communications and Hand-Off Standards for Hospitalists” drew a passionate response. During this session they unveiled a checklist outlining the important elements of an in-hospital physician hand-off. Attendees were encouraged to offer feedback and vote on proposed hand-off elements. They also were encouraged to submit suggestions if they believed something was missing.
Using that feedback, the group produced a final draft of recommendations and distributed it to a multidisciplinary team of experts for a final review. On the panel were Linda Bell, RN, MSN; Emily Patterson, PhD; Erik Van Eaton, MD; and Arpana Vidyarthi, MD. These experts reflect the perspective of nonphysician members of the hospital community, representing the interests of technology, nursing, human factors research, and hospital medicine. They reviewed the paper and hand-off recommendations by participating in conference calls in which they were asked to comment on questions regarding the working paper. These discussions gave the task force invaluable, candid feedback adopted into the working paper to create a more robust set of recommendations.
The final product was reviewed by SHM’s Board of Directors in January; a dissemination plan is in progress. If these recommendations are endorsed by an institution or a hospitalist group, they will act as a guide to ensure the coordination of hand-offs and the mangement of important clinical care issues.
Through their research and interactions with a large number of individuals concerned with this issue, the HCTF discovered that the quality improvement of patient transitions is a complex, global issue. They believe this checklist of hand-off elements is essential to these efforts.
Venous thromboembolic (VTE) disease, ranging from asymptomatic deep-vein thrombosis (DVT) to massive pulmonary embolism (PE), is a significant cause of morbidity and mortality in hospitalized patients. Almost all hospitalized patients are at risk for VTE, and the literature suggests approximately half of all VTEs are hospital-acquired.
Hospitalists are ideally positioned to reduce the incidence of preventable VTEs, both by using known best practices to improve care delivered to their own patients, and, more importantly, by leading hospitalwide efforts that improve care for all patients at their home institutions.
In recognition of this important clinical issue and the role hospitalists can play in addressing it, SHM launched the VTE Prevention Collaborative (VTEPC) in January 2007. The program offers individualized assistance to hospitalists wishing to take the lead in this area.
The VTEPC offers two technical assistance options. Individuals interested in securing ongoing support for their planned or active VTE prevention projects can enroll in the mentoring program. This allows a full year of access to and support from SHM mentors with VTE and quality-improvement (QI) expertise. Mentoring occurs in eight telephone calls, during which mentors offer individualized assistance on any topics, tasks, or barriers commonly encountered in designing, implementing, and evaluating a VTE prevention project.
An on-site consultation program is designed for individuals interested in securing expert evaluation and input on a VTE prevention program but who don’t feel they need ongoing, longitudinal support. In this program, SHM consultants with VTE and QI expertise visit applicants’ hospitals to evaluate active or planned VTE prevention programs. The consultation visits feature a structured evaluation of the site’s strengths and resources, barriers to improvement, and the design and function of active or proposed VTE prevention interventions.
For both programs, support and instruction are organized around the VTE QI workbook, “Preventing Hospital-Acquired Venous Thromboembolism: A Guide for Effective Quality Improvement,” SHM’s step-by-step guide for developing a VTE prevention program. SHM secured the services of Greg Maynard, MD, and Jason Stein, MD, to provide mentoring and conduct consultation visits. Drs. Maynard and Stein have led successful local VTE prevention QI projects, hold QI leadership positions, and have taught QI and VTE prevention principals to local and national audiences. Dr. Maynard is head of the Division of Hospital Medicine and associate clinical professor of medicine at the University of California, San Diego. Dr. Stein is a hospitalist at Atlanta’s Emory University Hospital, assistant professor of medicine at Emory University School of Medicine, and director of quality improvement for the Emory Hospital Medicine Unit.
Both were also instrumental in developing SHM’s online VTE Resource Room and the VTE QI workbook.
Strong Responses
Twenty-seven hospitalists enrolled in the VTEPC in its first year of operation, 24 in the mentoring program and three in the consultation program.
Enrollees have broad experience in VTE prevention and QI. Some enrollees have been in practice for two years, others more than 25 years. Some fill QI leadership roles in their hospitals or hospital medicine groups. For others the VTE prevention project is their first experience leading a QI effort. Regional representation (19 states), hospital system representation (18 systems), hospital size (135 to 700 staffed beds), and hospital type (academic centers, community teaching hospitals, and community hospitals) are also broad. One enrollee works at a long-term acute care hospital, all others work at acute-care hospitals.
What They Said
Participants in the mentoring and consultation programs have reported that the support they’ve received has been enormously helpful.
According to feedback from one participant, support from the mentoring program made the potentially overwhelming prospect of launching a hospitalwide improvement effort much more manageable: “The prospect of launching a multihospital VTE Prevention Protocol was extremely daunting; however, with the help of my SHM mentor, we stand ready to pilot the program within the week. Our mentor carefully constructed a step-by-step process that allowed me to investigate the scope of the problem at the local level and develop a protocol that was embraced by our administration and physicians. He supplied me with resources and knowledge that allowed me to successfully handle multiple obstacles that arose along the way. What we have accomplished will have an enormous impact on the quality of care that we provide for our patients.”
Other participants have reported that having access to objective input from an external expert can help transform a slow-developing or ineffective prevention program. As one participant put it: “Mentoring through SHM’s VTE Prevention Collaborative has been an invaluable experience. Through monthly phone calls and frequent e-mails, our mentor focused our previously ineffective efforts and guided us to develop a streamlined tool that was custom-fit to the workflow at our hospital. He has saved us tremendous frustrations by directing us to the appropriate resources in our institution to accomplish tasks we would have attempted ourselves. Since our first phone call, he has been both our coach and cheerleader. The processes and techniques that he has taught us are applicable to every quality endeavor we engage in.”
What Impressed Experts
Drs. Maynard and Stein have been enormously impressed by what VTEPC members have achieved. “What is most impressive to me is how all these hospitalist project leaders in different settings are overcoming a wide variety of intuitional barriers, medical staff barriers, infrastructure barriers—all the obstacles that can challenge the typical big QI project,” says Dr. Maynard. He notes that not only are participants utilizing all the basic QI principles in all the ways that were outlined in the QI workbook, but they also are coming up with innovations and approaches beyond what the workbook authors envisioned.
“We learn from them as they come up with innovations to meet their own challenges,” Dr. Stein says. “It shows the resilience and flexibility of the QI framework. If you really work in your local setting on these things with the improvement framework in mind you can get by almost any barrier.” Drs. Maynard and Stein have noted that participants have been able to design and implement VTE prevention programs at a pace that far outstrips what the two mentors achieved at their home institutions.
Many participants have found real-time ways to identify patients who are not on prophylaxis but should be. At many sites, identification begins with a report generated by the hospital’s inpatient pharmacy service, which typically shows the anti-coagulation regimen for each patient in a given hospital ward. The floor pharmacist or nurse can identify who is not on prophylaxis, assess risk factors and contraindications, and act to mitigate the situation—for example, by placing a call to the patient’s attending physician. Other sites have developed more sophisticated reports that capture information about relative risk for DVT and the absence or presence of contraindications to pharmacologic prophylaxis; these features reduce the effort required to investigate each case.
How to Learn More
The Quality Track at the 2008 Annual Meeting (April 3-5 at the Manchester Hyatt, San Diego, Calif.) includes a session on the “VTE Collaborative Experience” (1-2:25 p.m. April 4). Drs. Maynard and Stein will discuss the initiative, as will collaborative members, who will describe key successes and innovations that furthered their efforts to establish effective VTE prevention programs. Questions about the VTEPC and the Annual Meeting session can be directed to vtepc@hospitalmedicine.org.
Update on Hand-Offs
SHM task force continues to refine transitions-of-care checklist
by Shannon Roach
Among hospitalists and other organizations, there has been an increasing interest surrounding the improvement of the quality of patient care, especially within transitions of care and patient discharge. As the leader in the hospital medicine field, SHM continues to support and lead initiatives for the improvement of care as related to patient discharge and transitions. Last year’s creation of the Hand-Offs Communication Task Force (HCTF) has upheld SHM’s position of being dedicated to the promotion of the highest quality care for all hospitalized patients.
Derived from members of the Hospital Quality and Patient Safety Committee and the Education Committee, this task force was led by Vineet Arora, MD, MA, assistant professor of medicine, University of Chicago. Collaborating with her were Preetha Basaviah, MD, clinical instructor, Stanford University Medical Center in Calif.; Dan Dressler, MD, instructor of medicine, Emory University School of Medicine in Atlanta; Lakshmi Halasyamani, MD, associate chairperson of the Department of Internal Medicine at St. Joseph Mercy Hospital in Ann Arbor, Mich.; Sunil Kripalani, MD, MSc, an instructor at Emory University in Atlanta; and Efren Manjarrez, MD, assistant clinical professor of medicine at the Miller School of Medicine, University of Miami.
This team set out to create a formally recognized set of recommendations for ensuring optimum communication and continuity of care at the end of a medical professional’s shift or a patient’s change in service.
The task force’s first step was to determine what information was available as a basis for these recommendations. Though data were limited, the group decided that recommendations for effective hand-offs would be broken into three categories: program policy, verbal exchange, and content exchange.
As the need for more evidence-based data for the improvement of in-hospital hand-offs became clear, the group decided a valuable follow-up approach for these recommendations would be to incorporate a research agenda into the findings. This proposal suggests a need for a rigorous evaluation of these recommendations, with an emphasis on controlled interventions. It also encourages the development of patient-based outcomes sensitive to hand-off quality.
As a test run for these recommendations, the HCTF presented its findings at Hospital Medicine 2007 in Dallas. Their session “Developing Communications and Hand-Off Standards for Hospitalists” drew a passionate response. During this session they unveiled a checklist outlining the important elements of an in-hospital physician hand-off. Attendees were encouraged to offer feedback and vote on proposed hand-off elements. They also were encouraged to submit suggestions if they believed something was missing.
Using that feedback, the group produced a final draft of recommendations and distributed it to a multidisciplinary team of experts for a final review. On the panel were Linda Bell, RN, MSN; Emily Patterson, PhD; Erik Van Eaton, MD; and Arpana Vidyarthi, MD. These experts reflect the perspective of nonphysician members of the hospital community, representing the interests of technology, nursing, human factors research, and hospital medicine. They reviewed the paper and hand-off recommendations by participating in conference calls in which they were asked to comment on questions regarding the working paper. These discussions gave the task force invaluable, candid feedback adopted into the working paper to create a more robust set of recommendations.
The final product was reviewed by SHM’s Board of Directors in January; a dissemination plan is in progress. If these recommendations are endorsed by an institution or a hospitalist group, they will act as a guide to ensure the coordination of hand-offs and the mangement of important clinical care issues.
Through their research and interactions with a large number of individuals concerned with this issue, the HCTF discovered that the quality improvement of patient transitions is a complex, global issue. They believe this checklist of hand-off elements is essential to these efforts.
Patient-activated RRTs Catch On Around the U.S.
A growing trend in U.S. hospitals that allows patients and their relatives or loved ones to activate a rapid response team (RRT) under certain conditions is winning acceptance from hospitalists nationwide.
The practice was started in May 2005 at the University of Pittsburgh Medical Center (UPMC) after an 18-month-old girl died from narcotic misuse, dehydration, and a breakdown in communication.
The child’s mother told hospital officials that if they had a patient-family initiated RRT, she believed her daughter would be alive today. An official with the hospital’s Center for Quality Improvement and Innovation (CQII) agreed, and a study of the practice was under way.
Within months, the UPMC decided to put the plan—called Condition H (for Help)—into practice. Sue Martin, RN, with the center’s CQII, calls Condition H “a corporate function that supports all of the [19] hospitals in our health system.”
Today there are some 20 hospitals in the U.S., besides those in the UPMC system, that have instituted a version of the plan. More will soon, having read or heard about the success UPMC says it’s having.
“When we first started doing it, people wondered why we would let the patient or visiting relatives activate the rapid response team, since they were nonprofessionals,” Martin says. “But after it was explained to them and they were told of its success, they accepted the concept.”
She says UPMC began getting inquiries—and still does—every month from hospitals and others in the medical community asking how the plan works. They ask if UPMC would teach them about Condition H, Martin says.
“We’ve been doing that ever since,” she says. “Look, things are not perfect in the health system, but we’re fixing them. And as we do, we need a community to help keep our patients safe.”
Just about the time UPMC began its patient-activated RRT in May 2005, the Greater Baltimore Medical Center (GBMC) followed suit.
“Our RRT covers both inpatients and outpatients, and includes a hospitalist,” says Michael Schwartzberg, media relations manager at GBMC.
“Our patient-activated RRT Code Help initiative was a natural outgrowth of the rapid response team,” he says. “While our RRT averages about 40 calls a month, to date there have been only several Code Help calls—but the initiative is still young.”
Schwartzberg says the purpose of Code Help is to reduce the number of “codes” outside intensive care units by initiating rapid diagnosis and interventions for patients with changing medical conditions.
“Code Help serves as a resource for patients as well as their families 24/7 in the event that they feel additional help is needed,” he says.
Schwartzberg says as GBMC continues to focus on ways to improve patient safety, “implementing Code Help is an integral component of our mission to provide medical care and service of the highest quality to each patient. Offering the Code Help program is a way to support that mission.”
Four months after UPMC implemented its Condition H program, St. Joseph Medical Center (SJMC) in Towson, Md., did likewise.
“During the past three months, our mortality (rate) is lower than it had been,” says Richard Boehler, MD, vice president of medical affairs and chief medical officer for SJMC. He spearheaded the RRT initiative. “Three months isn’t a trend or a pattern yet, but there aren’t that many things in my career that I have seen have such a profound impact. We’ve had a nice curve in terms of declining mortality.”
Dr. Boehler says the launch of an RRT at SJMC, comprising a critical care physician, an intensive care nurse, and a respiratory therapist, “is helping to prevent codes and mortality by intervening at the patient bedside or anywhere in the hospital where a patient’s condition is declining.”
Johns Hopkins Hospital (JHH) in Baltimore, Md., was planning to test a patient-activated system in its neuroscience unit this past fall but ran into a snag, according to Brad Winters, MD, assistant professor of anesthesiology and critical medicine at JHH.
“It got political when it was first proposed,” says Dr. Winters. “Some people had issues with it that had to be ironed out. It was modeled after (UPMC’s) program from which we created a brochure describing it in detail. But some of the feedback we got was negative.”
After much discussion and some revisions, “we ironed out the issues, and everyone is now on board with what we ended up with,” says Dr. Winters. “When the brochures come back from the printers now, they will tell families how the program works, why we have it, and how to use it. We intend to implement it not only in our neuroscience unit, but pediatrics.”
Dr. Winters says to a large degree the decision to implement the patient-activated RRT program “came from our attending conferences over the past couple of years. We considered the topic an important issue as we discussed it from a patient-care point of view.”
As far as he’s concerned, Dr. Winters says all hospitals “should consider such a policy since the families and loved ones of patients recognize subtle changes in the patient’s condition, while nurses, especially in pediatrics where moms and dads recognize those subtle changes quickly, may not.”
He says one of the initial concerns was that the program might be abused. “My take on it is that UPMC had it for a while and it was successful,” he says. “Nurses are very good, of course. But once in awhile the family picks up on something they miss, so it’s best to have as many eyes as possible involved. The more people we have observing a patient, the more likely that patient is to get good care.”
Back at UPMC, Martin says they’ve had no complaints about the program and Condition H is “spreading to every acute care hospital.” In the first nine months of 2005, Condition H was used 21 times “successfully,” she says. That’s about average use annually, she says.
But some hospitalists remain skeptical.
“In my opinion, having a patient or family call a code is the medical equivalent of having a patient tell the surgeon where to make an incision,” says Dr. Michael Rudolph, MD, a hospitalist for the past three years at Milford Hospital in Milford, Conn. “This ‘solution’ practiced [by UPMC] demonstrates a complete failure in communication between all the hospital staff and physicians and the patient and family.”
He suggests a more restrained, collaborative approach.
“A policy of the patient or family always having the ‘right’ to a face-to-face physician evaluation would do much more for patient care,” says Dr. Rudolph. “A family or patient demanding urgent evaluation is often appropriately concerned, anxious, or angry. This is an excellent time for the physician to review the case to make sure all is being done appropriately and to address the patient and family's medical and emotional needs.”
Dr. Rudolph also says allowing patients and families to call a code “will frequently result in the staff feeling that the patient cried wolf, which will invalidate the patient’s and family's concerns.” He asserts that while patient and family involvement in care “is critical to the healing process ... the physician has to set limits on how much of the care the patient and family can dictate.”
A hospitalist working in a hospital with a policy like UPMC’s “would lose significant ability to prioritize his/her work,” Dr. Rudolph continues. “There are so many unplanned interruptions that a hospitalist needs to learn to deal with on a routine basis that increasing the number of interruptions where dropping everything is necessary would lead to a sense of loss of control and an increased burn-out rate.”
He says it would also force hospitalists to second-guess their colleagues, “which will adversely affect team medicine in rapid fashion and may further increase wasteful, defensive medicine practices.”
But Joseph Li, MD, director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and a member of SHM’s board of directors, counters that patient-activated RRTs are a useful part of a team approach to care.
“I’m a strong believer in terms of ‘the patient knows best’,” says Dr. Li. “Ultimately, it’s a very good thing to allow patients to participate in their care. I would say the potential advantages (of a Condition H RRT policy) far outweigh any drawbacks.”
Dr. Li sees a potential upside not only for patients and their families, but for hospitalists.
“More than anybody, hospitalists oftentimes are leaders in rapid response teams, and if the policy becomes widespread, hospitals would require more resources for the hospitalist,” he says. That, he says, could lead to hiring more hospitalists.
There are those who theorize that while a Condition H policy might benefit patients, it may also be another source of confusion for families. These critics fear alienating some who believe it is the hospital’s job to be sure their family member is doing well, not theirs.
Dr. Li strongly disagrees. “We have a situation in this country where often the patient’s voice is not heard,” he says. “Anytime we can improve the opportunity for a patient to be heard, that’s good for the patient and good for our healthcare system.
Martin puts it another way.
“It’s the right thing to do,” she asserts. “Think about it: relatives and friends call 911 from home or wherever when there‘s an emergency. Condition H is similar to that. Why wouldn’t we let patients and family do that in the hospital?” TH
Tom Giordano is a journalist based in Connecticut.
A growing trend in U.S. hospitals that allows patients and their relatives or loved ones to activate a rapid response team (RRT) under certain conditions is winning acceptance from hospitalists nationwide.
The practice was started in May 2005 at the University of Pittsburgh Medical Center (UPMC) after an 18-month-old girl died from narcotic misuse, dehydration, and a breakdown in communication.
The child’s mother told hospital officials that if they had a patient-family initiated RRT, she believed her daughter would be alive today. An official with the hospital’s Center for Quality Improvement and Innovation (CQII) agreed, and a study of the practice was under way.
Within months, the UPMC decided to put the plan—called Condition H (for Help)—into practice. Sue Martin, RN, with the center’s CQII, calls Condition H “a corporate function that supports all of the [19] hospitals in our health system.”
Today there are some 20 hospitals in the U.S., besides those in the UPMC system, that have instituted a version of the plan. More will soon, having read or heard about the success UPMC says it’s having.
“When we first started doing it, people wondered why we would let the patient or visiting relatives activate the rapid response team, since they were nonprofessionals,” Martin says. “But after it was explained to them and they were told of its success, they accepted the concept.”
She says UPMC began getting inquiries—and still does—every month from hospitals and others in the medical community asking how the plan works. They ask if UPMC would teach them about Condition H, Martin says.
“We’ve been doing that ever since,” she says. “Look, things are not perfect in the health system, but we’re fixing them. And as we do, we need a community to help keep our patients safe.”
Just about the time UPMC began its patient-activated RRT in May 2005, the Greater Baltimore Medical Center (GBMC) followed suit.
“Our RRT covers both inpatients and outpatients, and includes a hospitalist,” says Michael Schwartzberg, media relations manager at GBMC.
“Our patient-activated RRT Code Help initiative was a natural outgrowth of the rapid response team,” he says. “While our RRT averages about 40 calls a month, to date there have been only several Code Help calls—but the initiative is still young.”
Schwartzberg says the purpose of Code Help is to reduce the number of “codes” outside intensive care units by initiating rapid diagnosis and interventions for patients with changing medical conditions.
“Code Help serves as a resource for patients as well as their families 24/7 in the event that they feel additional help is needed,” he says.
Schwartzberg says as GBMC continues to focus on ways to improve patient safety, “implementing Code Help is an integral component of our mission to provide medical care and service of the highest quality to each patient. Offering the Code Help program is a way to support that mission.”
Four months after UPMC implemented its Condition H program, St. Joseph Medical Center (SJMC) in Towson, Md., did likewise.
“During the past three months, our mortality (rate) is lower than it had been,” says Richard Boehler, MD, vice president of medical affairs and chief medical officer for SJMC. He spearheaded the RRT initiative. “Three months isn’t a trend or a pattern yet, but there aren’t that many things in my career that I have seen have such a profound impact. We’ve had a nice curve in terms of declining mortality.”
Dr. Boehler says the launch of an RRT at SJMC, comprising a critical care physician, an intensive care nurse, and a respiratory therapist, “is helping to prevent codes and mortality by intervening at the patient bedside or anywhere in the hospital where a patient’s condition is declining.”
Johns Hopkins Hospital (JHH) in Baltimore, Md., was planning to test a patient-activated system in its neuroscience unit this past fall but ran into a snag, according to Brad Winters, MD, assistant professor of anesthesiology and critical medicine at JHH.
“It got political when it was first proposed,” says Dr. Winters. “Some people had issues with it that had to be ironed out. It was modeled after (UPMC’s) program from which we created a brochure describing it in detail. But some of the feedback we got was negative.”
After much discussion and some revisions, “we ironed out the issues, and everyone is now on board with what we ended up with,” says Dr. Winters. “When the brochures come back from the printers now, they will tell families how the program works, why we have it, and how to use it. We intend to implement it not only in our neuroscience unit, but pediatrics.”
Dr. Winters says to a large degree the decision to implement the patient-activated RRT program “came from our attending conferences over the past couple of years. We considered the topic an important issue as we discussed it from a patient-care point of view.”
As far as he’s concerned, Dr. Winters says all hospitals “should consider such a policy since the families and loved ones of patients recognize subtle changes in the patient’s condition, while nurses, especially in pediatrics where moms and dads recognize those subtle changes quickly, may not.”
He says one of the initial concerns was that the program might be abused. “My take on it is that UPMC had it for a while and it was successful,” he says. “Nurses are very good, of course. But once in awhile the family picks up on something they miss, so it’s best to have as many eyes as possible involved. The more people we have observing a patient, the more likely that patient is to get good care.”
Back at UPMC, Martin says they’ve had no complaints about the program and Condition H is “spreading to every acute care hospital.” In the first nine months of 2005, Condition H was used 21 times “successfully,” she says. That’s about average use annually, she says.
But some hospitalists remain skeptical.
“In my opinion, having a patient or family call a code is the medical equivalent of having a patient tell the surgeon where to make an incision,” says Dr. Michael Rudolph, MD, a hospitalist for the past three years at Milford Hospital in Milford, Conn. “This ‘solution’ practiced [by UPMC] demonstrates a complete failure in communication between all the hospital staff and physicians and the patient and family.”
He suggests a more restrained, collaborative approach.
“A policy of the patient or family always having the ‘right’ to a face-to-face physician evaluation would do much more for patient care,” says Dr. Rudolph. “A family or patient demanding urgent evaluation is often appropriately concerned, anxious, or angry. This is an excellent time for the physician to review the case to make sure all is being done appropriately and to address the patient and family's medical and emotional needs.”
Dr. Rudolph also says allowing patients and families to call a code “will frequently result in the staff feeling that the patient cried wolf, which will invalidate the patient’s and family's concerns.” He asserts that while patient and family involvement in care “is critical to the healing process ... the physician has to set limits on how much of the care the patient and family can dictate.”
A hospitalist working in a hospital with a policy like UPMC’s “would lose significant ability to prioritize his/her work,” Dr. Rudolph continues. “There are so many unplanned interruptions that a hospitalist needs to learn to deal with on a routine basis that increasing the number of interruptions where dropping everything is necessary would lead to a sense of loss of control and an increased burn-out rate.”
He says it would also force hospitalists to second-guess their colleagues, “which will adversely affect team medicine in rapid fashion and may further increase wasteful, defensive medicine practices.”
But Joseph Li, MD, director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and a member of SHM’s board of directors, counters that patient-activated RRTs are a useful part of a team approach to care.
“I’m a strong believer in terms of ‘the patient knows best’,” says Dr. Li. “Ultimately, it’s a very good thing to allow patients to participate in their care. I would say the potential advantages (of a Condition H RRT policy) far outweigh any drawbacks.”
Dr. Li sees a potential upside not only for patients and their families, but for hospitalists.
“More than anybody, hospitalists oftentimes are leaders in rapid response teams, and if the policy becomes widespread, hospitals would require more resources for the hospitalist,” he says. That, he says, could lead to hiring more hospitalists.
There are those who theorize that while a Condition H policy might benefit patients, it may also be another source of confusion for families. These critics fear alienating some who believe it is the hospital’s job to be sure their family member is doing well, not theirs.
Dr. Li strongly disagrees. “We have a situation in this country where often the patient’s voice is not heard,” he says. “Anytime we can improve the opportunity for a patient to be heard, that’s good for the patient and good for our healthcare system.
Martin puts it another way.
“It’s the right thing to do,” she asserts. “Think about it: relatives and friends call 911 from home or wherever when there‘s an emergency. Condition H is similar to that. Why wouldn’t we let patients and family do that in the hospital?” TH
Tom Giordano is a journalist based in Connecticut.
A growing trend in U.S. hospitals that allows patients and their relatives or loved ones to activate a rapid response team (RRT) under certain conditions is winning acceptance from hospitalists nationwide.
The practice was started in May 2005 at the University of Pittsburgh Medical Center (UPMC) after an 18-month-old girl died from narcotic misuse, dehydration, and a breakdown in communication.
The child’s mother told hospital officials that if they had a patient-family initiated RRT, she believed her daughter would be alive today. An official with the hospital’s Center for Quality Improvement and Innovation (CQII) agreed, and a study of the practice was under way.
Within months, the UPMC decided to put the plan—called Condition H (for Help)—into practice. Sue Martin, RN, with the center’s CQII, calls Condition H “a corporate function that supports all of the [19] hospitals in our health system.”
Today there are some 20 hospitals in the U.S., besides those in the UPMC system, that have instituted a version of the plan. More will soon, having read or heard about the success UPMC says it’s having.
“When we first started doing it, people wondered why we would let the patient or visiting relatives activate the rapid response team, since they were nonprofessionals,” Martin says. “But after it was explained to them and they were told of its success, they accepted the concept.”
She says UPMC began getting inquiries—and still does—every month from hospitals and others in the medical community asking how the plan works. They ask if UPMC would teach them about Condition H, Martin says.
“We’ve been doing that ever since,” she says. “Look, things are not perfect in the health system, but we’re fixing them. And as we do, we need a community to help keep our patients safe.”
Just about the time UPMC began its patient-activated RRT in May 2005, the Greater Baltimore Medical Center (GBMC) followed suit.
“Our RRT covers both inpatients and outpatients, and includes a hospitalist,” says Michael Schwartzberg, media relations manager at GBMC.
“Our patient-activated RRT Code Help initiative was a natural outgrowth of the rapid response team,” he says. “While our RRT averages about 40 calls a month, to date there have been only several Code Help calls—but the initiative is still young.”
Schwartzberg says the purpose of Code Help is to reduce the number of “codes” outside intensive care units by initiating rapid diagnosis and interventions for patients with changing medical conditions.
“Code Help serves as a resource for patients as well as their families 24/7 in the event that they feel additional help is needed,” he says.
Schwartzberg says as GBMC continues to focus on ways to improve patient safety, “implementing Code Help is an integral component of our mission to provide medical care and service of the highest quality to each patient. Offering the Code Help program is a way to support that mission.”
Four months after UPMC implemented its Condition H program, St. Joseph Medical Center (SJMC) in Towson, Md., did likewise.
“During the past three months, our mortality (rate) is lower than it had been,” says Richard Boehler, MD, vice president of medical affairs and chief medical officer for SJMC. He spearheaded the RRT initiative. “Three months isn’t a trend or a pattern yet, but there aren’t that many things in my career that I have seen have such a profound impact. We’ve had a nice curve in terms of declining mortality.”
Dr. Boehler says the launch of an RRT at SJMC, comprising a critical care physician, an intensive care nurse, and a respiratory therapist, “is helping to prevent codes and mortality by intervening at the patient bedside or anywhere in the hospital where a patient’s condition is declining.”
Johns Hopkins Hospital (JHH) in Baltimore, Md., was planning to test a patient-activated system in its neuroscience unit this past fall but ran into a snag, according to Brad Winters, MD, assistant professor of anesthesiology and critical medicine at JHH.
“It got political when it was first proposed,” says Dr. Winters. “Some people had issues with it that had to be ironed out. It was modeled after (UPMC’s) program from which we created a brochure describing it in detail. But some of the feedback we got was negative.”
After much discussion and some revisions, “we ironed out the issues, and everyone is now on board with what we ended up with,” says Dr. Winters. “When the brochures come back from the printers now, they will tell families how the program works, why we have it, and how to use it. We intend to implement it not only in our neuroscience unit, but pediatrics.”
Dr. Winters says to a large degree the decision to implement the patient-activated RRT program “came from our attending conferences over the past couple of years. We considered the topic an important issue as we discussed it from a patient-care point of view.”
As far as he’s concerned, Dr. Winters says all hospitals “should consider such a policy since the families and loved ones of patients recognize subtle changes in the patient’s condition, while nurses, especially in pediatrics where moms and dads recognize those subtle changes quickly, may not.”
He says one of the initial concerns was that the program might be abused. “My take on it is that UPMC had it for a while and it was successful,” he says. “Nurses are very good, of course. But once in awhile the family picks up on something they miss, so it’s best to have as many eyes as possible involved. The more people we have observing a patient, the more likely that patient is to get good care.”
Back at UPMC, Martin says they’ve had no complaints about the program and Condition H is “spreading to every acute care hospital.” In the first nine months of 2005, Condition H was used 21 times “successfully,” she says. That’s about average use annually, she says.
But some hospitalists remain skeptical.
“In my opinion, having a patient or family call a code is the medical equivalent of having a patient tell the surgeon where to make an incision,” says Dr. Michael Rudolph, MD, a hospitalist for the past three years at Milford Hospital in Milford, Conn. “This ‘solution’ practiced [by UPMC] demonstrates a complete failure in communication between all the hospital staff and physicians and the patient and family.”
He suggests a more restrained, collaborative approach.
“A policy of the patient or family always having the ‘right’ to a face-to-face physician evaluation would do much more for patient care,” says Dr. Rudolph. “A family or patient demanding urgent evaluation is often appropriately concerned, anxious, or angry. This is an excellent time for the physician to review the case to make sure all is being done appropriately and to address the patient and family's medical and emotional needs.”
Dr. Rudolph also says allowing patients and families to call a code “will frequently result in the staff feeling that the patient cried wolf, which will invalidate the patient’s and family's concerns.” He asserts that while patient and family involvement in care “is critical to the healing process ... the physician has to set limits on how much of the care the patient and family can dictate.”
A hospitalist working in a hospital with a policy like UPMC’s “would lose significant ability to prioritize his/her work,” Dr. Rudolph continues. “There are so many unplanned interruptions that a hospitalist needs to learn to deal with on a routine basis that increasing the number of interruptions where dropping everything is necessary would lead to a sense of loss of control and an increased burn-out rate.”
He says it would also force hospitalists to second-guess their colleagues, “which will adversely affect team medicine in rapid fashion and may further increase wasteful, defensive medicine practices.”
But Joseph Li, MD, director of the hospital medicine program at Beth Israel Deaconess Medical Center in Boston and a member of SHM’s board of directors, counters that patient-activated RRTs are a useful part of a team approach to care.
“I’m a strong believer in terms of ‘the patient knows best’,” says Dr. Li. “Ultimately, it’s a very good thing to allow patients to participate in their care. I would say the potential advantages (of a Condition H RRT policy) far outweigh any drawbacks.”
Dr. Li sees a potential upside not only for patients and their families, but for hospitalists.
“More than anybody, hospitalists oftentimes are leaders in rapid response teams, and if the policy becomes widespread, hospitals would require more resources for the hospitalist,” he says. That, he says, could lead to hiring more hospitalists.
There are those who theorize that while a Condition H policy might benefit patients, it may also be another source of confusion for families. These critics fear alienating some who believe it is the hospital’s job to be sure their family member is doing well, not theirs.
Dr. Li strongly disagrees. “We have a situation in this country where often the patient’s voice is not heard,” he says. “Anytime we can improve the opportunity for a patient to be heard, that’s good for the patient and good for our healthcare system.
Martin puts it another way.
“It’s the right thing to do,” she asserts. “Think about it: relatives and friends call 911 from home or wherever when there‘s an emergency. Condition H is similar to that. Why wouldn’t we let patients and family do that in the hospital?” TH
Tom Giordano is a journalist based in Connecticut.
Safety in Numbers
Patient safety organizations, commonly referred to as PSOs, are about to take off. And when they do, PSOs should provide hospitalists with invaluable data on improving patient safety.
“PSOs are a great concept, but even though it’s been around since 2005, I haven’t seen it clinically,” says Janet Nagamine, RN, MD, hospitalist at Kaiser Permanente in Santa Clara, Calif., and chair of SHM’s Hospital Quality and Patient Safety Committee.
This calendar year, Nagamine and the rest of hospital medicine should start to see some movement—“PSO 1.0,” if you will.
Background
PSOs are public and private organizations approved by the Agency for Healthcare Research and Quality (AHRQ); they include such groups as Health Watch Inc., Human Performance Technology Group, and the Institute for Safe Medication Practices, which will collect, aggregate, and analyze data on patient safety events. Hospitals and other healthcare providers will voluntarily and confidentially report data. The ultimate goal is to advance changes in culture, processes, and systems to enhance patient safety.
PSOs grew out of the Patient Safety and Quality Improvement Act of 2005, which was a response to the Institute of Medicine’s landmark report “To Err Is Human: Building a Safer Health System.” But it wasn’t until last year that the U.S. Department of Health and Human Services issued a final rule outlining PSO requirements and procedures. The rule became effective Jan. 19, 2009.
AHRQ is responsible for coordinating the development of a set of common definitions and reporting formats, called common formats, for collecting the data. Eventually, AHRQ will create a network of patient safety databases to which PSOs, providers, and others can voluntarily contribute non-identifiable patient safety information. This network will serve as an interactive evidence-based management resource for providers, PSOs, and other entities. AHRQ will use data from the network to analyze national and regional statistics regarding patient safety events. Findings will be made public and will be included in AHRQ’s annual National Healthcare Quality Report.
IT Example
To date, the only comparable data-collection system is MedMarx, which compiles information on medication errors. The Joint Commission requires providers to supply a root-cause analysis on every Level 1 incident, “but that’s just scratching the surface of what occurs,” Dr. Nagamine says. “There are far many more Level 2 and Level 3 events with the same precursors, and that information would be very valuable.”
By collecting nationwide data on patient safety events, PSOs will be able to bridge the gaps in the reporting system and provide crucial patient safety information to the healthcare industry. “In general, the concept of aggregate information that allows us to compare events is incredibly important,” Dr. Nagamine says. “A hospitalist working in one hospital has only the information about events in that hospital, but 5,000 hospitals can provide more specific and actionable information. We just haven’t seen this operationalized yet.”
Dr. Nagamine uses a technology example to show the value PSOs could have in identifying patterns or problems that threaten patient safety: “Every hospital has a horror story of implementing a new information technology (IT) system, and we’re getting some very interesting feedback from hospitals about unintended consequences,” she says. “We’re hearing that patients are being hurt because of mistakes in systems—the use of dropdown menus (on computer screens) that don’t drop down far enough to reveal all options, or a screen where it’s easy to click the wrong item.”
Current systems might not allow problems like these to be highlighted. Even if staff knows of a problem, their hospital’s coding system might not allow them to detail it. “It may fall under ‘communications’ or ‘physician computerized order entry’ or something vague, so the data won’t show the specifics of what happened,” Dr. Nagamine points out. “If we had aggregate data on issues like this, we could address it. Right now, we just have word of mouth.”
An isolated event at a hospital is one thing, but similar data from around the nation is significant. “Drug companies or IT vendors confronted with (patterns) might make some changes,” she says. “That kind of data is powerful.”
Hospital Medicine on Board
When hospitals start reporting data to PSOs, where will hospitalists fit into the process? Hospitalists likely will be interviewed to answer some of the PSO’s questions, but they will not be the ones filling out the forms, Dr. Nagamine says. Hospitalists also will be among the ranks of healthcare professionals eagerly awaiting the release of the data. “The way that PSOs approach patient safety and quality—what’s near and dear to our hearts—is it gives us more data,” Dr. Nagamine says. This is crucial for hospitalists leading quality-improvement projects and similar tasks. “Without that data, it’s hard to get traction and movement. That data will help convince someone to invest more time and money in a particular problem area.”
Phase One: Participation
AHRQ has established a comprehensive Web site (www.pso.ahrq.gov) that includes information on the first draft of common formats for use with hospital inpatients. These are found on downloadable paper forms, available at the PSO Privacy Protection Center (PPC) Web site at www.psoppc.org/ web/patientsafety/paperforms.
“The forms are a first step,” Dr. Nagamine explains. “If we had these data points on every incident at every hospital, we’d know a lot more than we do now. We’d be able to harness that information.”
It will be a while before healthcare providers can search the data for patterns and possible solutions in patient safety, but the wait should be worth it. “You’ve got to start somewhere, and it’s not going to happen in one sweep,” Dr. Nagamine says. “This is simply a start. Hopefully, in a decade, we’ll have a lot more actionable information.” TH
Jane Jerrard is a medical writer based in Chicago.
Patient safety organizations, commonly referred to as PSOs, are about to take off. And when they do, PSOs should provide hospitalists with invaluable data on improving patient safety.
“PSOs are a great concept, but even though it’s been around since 2005, I haven’t seen it clinically,” says Janet Nagamine, RN, MD, hospitalist at Kaiser Permanente in Santa Clara, Calif., and chair of SHM’s Hospital Quality and Patient Safety Committee.
This calendar year, Nagamine and the rest of hospital medicine should start to see some movement—“PSO 1.0,” if you will.
Background
PSOs are public and private organizations approved by the Agency for Healthcare Research and Quality (AHRQ); they include such groups as Health Watch Inc., Human Performance Technology Group, and the Institute for Safe Medication Practices, which will collect, aggregate, and analyze data on patient safety events. Hospitals and other healthcare providers will voluntarily and confidentially report data. The ultimate goal is to advance changes in culture, processes, and systems to enhance patient safety.
PSOs grew out of the Patient Safety and Quality Improvement Act of 2005, which was a response to the Institute of Medicine’s landmark report “To Err Is Human: Building a Safer Health System.” But it wasn’t until last year that the U.S. Department of Health and Human Services issued a final rule outlining PSO requirements and procedures. The rule became effective Jan. 19, 2009.
AHRQ is responsible for coordinating the development of a set of common definitions and reporting formats, called common formats, for collecting the data. Eventually, AHRQ will create a network of patient safety databases to which PSOs, providers, and others can voluntarily contribute non-identifiable patient safety information. This network will serve as an interactive evidence-based management resource for providers, PSOs, and other entities. AHRQ will use data from the network to analyze national and regional statistics regarding patient safety events. Findings will be made public and will be included in AHRQ’s annual National Healthcare Quality Report.
IT Example
To date, the only comparable data-collection system is MedMarx, which compiles information on medication errors. The Joint Commission requires providers to supply a root-cause analysis on every Level 1 incident, “but that’s just scratching the surface of what occurs,” Dr. Nagamine says. “There are far many more Level 2 and Level 3 events with the same precursors, and that information would be very valuable.”
By collecting nationwide data on patient safety events, PSOs will be able to bridge the gaps in the reporting system and provide crucial patient safety information to the healthcare industry. “In general, the concept of aggregate information that allows us to compare events is incredibly important,” Dr. Nagamine says. “A hospitalist working in one hospital has only the information about events in that hospital, but 5,000 hospitals can provide more specific and actionable information. We just haven’t seen this operationalized yet.”
Dr. Nagamine uses a technology example to show the value PSOs could have in identifying patterns or problems that threaten patient safety: “Every hospital has a horror story of implementing a new information technology (IT) system, and we’re getting some very interesting feedback from hospitals about unintended consequences,” she says. “We’re hearing that patients are being hurt because of mistakes in systems—the use of dropdown menus (on computer screens) that don’t drop down far enough to reveal all options, or a screen where it’s easy to click the wrong item.”
Current systems might not allow problems like these to be highlighted. Even if staff knows of a problem, their hospital’s coding system might not allow them to detail it. “It may fall under ‘communications’ or ‘physician computerized order entry’ or something vague, so the data won’t show the specifics of what happened,” Dr. Nagamine points out. “If we had aggregate data on issues like this, we could address it. Right now, we just have word of mouth.”
An isolated event at a hospital is one thing, but similar data from around the nation is significant. “Drug companies or IT vendors confronted with (patterns) might make some changes,” she says. “That kind of data is powerful.”
Hospital Medicine on Board
When hospitals start reporting data to PSOs, where will hospitalists fit into the process? Hospitalists likely will be interviewed to answer some of the PSO’s questions, but they will not be the ones filling out the forms, Dr. Nagamine says. Hospitalists also will be among the ranks of healthcare professionals eagerly awaiting the release of the data. “The way that PSOs approach patient safety and quality—what’s near and dear to our hearts—is it gives us more data,” Dr. Nagamine says. This is crucial for hospitalists leading quality-improvement projects and similar tasks. “Without that data, it’s hard to get traction and movement. That data will help convince someone to invest more time and money in a particular problem area.”
Phase One: Participation
AHRQ has established a comprehensive Web site (www.pso.ahrq.gov) that includes information on the first draft of common formats for use with hospital inpatients. These are found on downloadable paper forms, available at the PSO Privacy Protection Center (PPC) Web site at www.psoppc.org/ web/patientsafety/paperforms.
“The forms are a first step,” Dr. Nagamine explains. “If we had these data points on every incident at every hospital, we’d know a lot more than we do now. We’d be able to harness that information.”
It will be a while before healthcare providers can search the data for patterns and possible solutions in patient safety, but the wait should be worth it. “You’ve got to start somewhere, and it’s not going to happen in one sweep,” Dr. Nagamine says. “This is simply a start. Hopefully, in a decade, we’ll have a lot more actionable information.” TH
Jane Jerrard is a medical writer based in Chicago.
Patient safety organizations, commonly referred to as PSOs, are about to take off. And when they do, PSOs should provide hospitalists with invaluable data on improving patient safety.
“PSOs are a great concept, but even though it’s been around since 2005, I haven’t seen it clinically,” says Janet Nagamine, RN, MD, hospitalist at Kaiser Permanente in Santa Clara, Calif., and chair of SHM’s Hospital Quality and Patient Safety Committee.
This calendar year, Nagamine and the rest of hospital medicine should start to see some movement—“PSO 1.0,” if you will.
Background
PSOs are public and private organizations approved by the Agency for Healthcare Research and Quality (AHRQ); they include such groups as Health Watch Inc., Human Performance Technology Group, and the Institute for Safe Medication Practices, which will collect, aggregate, and analyze data on patient safety events. Hospitals and other healthcare providers will voluntarily and confidentially report data. The ultimate goal is to advance changes in culture, processes, and systems to enhance patient safety.
PSOs grew out of the Patient Safety and Quality Improvement Act of 2005, which was a response to the Institute of Medicine’s landmark report “To Err Is Human: Building a Safer Health System.” But it wasn’t until last year that the U.S. Department of Health and Human Services issued a final rule outlining PSO requirements and procedures. The rule became effective Jan. 19, 2009.
AHRQ is responsible for coordinating the development of a set of common definitions and reporting formats, called common formats, for collecting the data. Eventually, AHRQ will create a network of patient safety databases to which PSOs, providers, and others can voluntarily contribute non-identifiable patient safety information. This network will serve as an interactive evidence-based management resource for providers, PSOs, and other entities. AHRQ will use data from the network to analyze national and regional statistics regarding patient safety events. Findings will be made public and will be included in AHRQ’s annual National Healthcare Quality Report.
IT Example
To date, the only comparable data-collection system is MedMarx, which compiles information on medication errors. The Joint Commission requires providers to supply a root-cause analysis on every Level 1 incident, “but that’s just scratching the surface of what occurs,” Dr. Nagamine says. “There are far many more Level 2 and Level 3 events with the same precursors, and that information would be very valuable.”
By collecting nationwide data on patient safety events, PSOs will be able to bridge the gaps in the reporting system and provide crucial patient safety information to the healthcare industry. “In general, the concept of aggregate information that allows us to compare events is incredibly important,” Dr. Nagamine says. “A hospitalist working in one hospital has only the information about events in that hospital, but 5,000 hospitals can provide more specific and actionable information. We just haven’t seen this operationalized yet.”
Dr. Nagamine uses a technology example to show the value PSOs could have in identifying patterns or problems that threaten patient safety: “Every hospital has a horror story of implementing a new information technology (IT) system, and we’re getting some very interesting feedback from hospitals about unintended consequences,” she says. “We’re hearing that patients are being hurt because of mistakes in systems—the use of dropdown menus (on computer screens) that don’t drop down far enough to reveal all options, or a screen where it’s easy to click the wrong item.”
Current systems might not allow problems like these to be highlighted. Even if staff knows of a problem, their hospital’s coding system might not allow them to detail it. “It may fall under ‘communications’ or ‘physician computerized order entry’ or something vague, so the data won’t show the specifics of what happened,” Dr. Nagamine points out. “If we had aggregate data on issues like this, we could address it. Right now, we just have word of mouth.”
An isolated event at a hospital is one thing, but similar data from around the nation is significant. “Drug companies or IT vendors confronted with (patterns) might make some changes,” she says. “That kind of data is powerful.”
Hospital Medicine on Board
When hospitals start reporting data to PSOs, where will hospitalists fit into the process? Hospitalists likely will be interviewed to answer some of the PSO’s questions, but they will not be the ones filling out the forms, Dr. Nagamine says. Hospitalists also will be among the ranks of healthcare professionals eagerly awaiting the release of the data. “The way that PSOs approach patient safety and quality—what’s near and dear to our hearts—is it gives us more data,” Dr. Nagamine says. This is crucial for hospitalists leading quality-improvement projects and similar tasks. “Without that data, it’s hard to get traction and movement. That data will help convince someone to invest more time and money in a particular problem area.”
Phase One: Participation
AHRQ has established a comprehensive Web site (www.pso.ahrq.gov) that includes information on the first draft of common formats for use with hospital inpatients. These are found on downloadable paper forms, available at the PSO Privacy Protection Center (PPC) Web site at www.psoppc.org/ web/patientsafety/paperforms.
“The forms are a first step,” Dr. Nagamine explains. “If we had these data points on every incident at every hospital, we’d know a lot more than we do now. We’d be able to harness that information.”
It will be a while before healthcare providers can search the data for patterns and possible solutions in patient safety, but the wait should be worth it. “You’ve got to start somewhere, and it’s not going to happen in one sweep,” Dr. Nagamine says. “This is simply a start. Hopefully, in a decade, we’ll have a lot more actionable information.” TH
Jane Jerrard is a medical writer based in Chicago.