User login
What is the target blood glucose for noncritical care patients?
Case
A 65-year-old obese (100 kg) man with type 2 diabetes, hypertension, and a pack-a-day smoking habit is admitted with moderately severe bilobar pneumonia. His condition is manifest by fever, cough, chills, leukocytosis, and a modest oxygen requirement. You order oxygen, intravenous (IV) fluids, diet, and appropriate antibiotics while continuing the history and chart review. The patient uses metformin and glyburide, and his home glucose readings are generally in the 160 to 180 mg/dL range. An HbA1c level performed three months ago was 9.8, leading to an increased dose of glyburide. As you finish the history, the nurse reports a glucose reading of 198 mg/dL. What is the target blood glucose for noncritical care adult inpatients?
Overview
Diabetes mellitus is an epidemic in the United States. At least 9.3% of adults older than 20 (more than 20 million people) have diabetes. Approximately 30% are unaware they have diabetes.1 Concurrent with the increasing prevalence of diabetes in the U.S. from 1980 through 2003, the number of hospital discharges with diabetes as any listed diagnosis more than doubled between 1980 and 2003. These trends are expected to accelerate.2 Studies suggest 26% of inpatients have diabetes and 12% have pre-diabetes, previously undiagnosed diabetes, or stress hyperglycemia.3
Review of the Data
A full review of the evidence is beyond the scope of this article. What follows is a sampling of the most representative or influential critical care studies.
Physiology
Fluid and electrolyte balance, left ventricular (LV) function, leukocyte action, wound healing, endothelial function, and immunoglobulin function are all impaired with hyperglycemia.
A prothrombotic state and enhanced platelet aggregation have been demonstrated with even mild elevations of blood glucose.
The mechanisms are multifactorial and complex and involve metabolic derangements leading to oxidative stress, release of free fatty acids, and counter-regulatory hormones.4-6
Observational Studies
A strong and consistent association with hyperglycemia and adverse outcomes is seen in a wide variety of critical care and peri-operative settings. Trauma survival, stroke survival and function, and the incidence of post-operative infections are all adversely affected by hyperglycemia.7-10 Acute myocardial infarction (MI) mortality, acute MI infarct size, and LV dysfunction are also consistently adversely affected in these studies.11-13
This association is typically present in hyperglycemic patients whether they have a diagnosis of diabetes or not, and the association is often even stronger in those lacking a pre-existing diagnosis. Dysfunction typically is detectable at only modest elevations of blood glucose and becomes more marked in a dose response relationship.
Uncontrolled Interventional Studies
The Portland Diabetic Project is a prospective, non-randomized, observational study of 5,510 consecutive diabetic cardiac surgery patients.14-15 The three-day blood glucose average (3-BG) has been progressively reduced for the population through the use of continuous insulin infusion (CII).
The last reported glycemic target is less than 130 mg/dL, and the current glycemic target is less than 110 mg/dL. Both CII for three days and a favorable 3-BG were independently associated with improved mortality, deep sternal-wound infection rates, and length of stay. Mortality and deep sternal-wound infection rates for diabetic patients with well-controlled glucose levels are equal to patients without diabetes.
Another study compared 800 mixed medical-surgical ICU patients with tight glycemic control (mean BG 130.7 mg/dL) to historical controls with a mean glucose of 152.3 mg/dL. The insulin infusion group had associated significant reductions in mortality and median length of ICU stay.16
Randomized Controlled Trials and Meta-Analyses
In the first Diabetes and Insulin-Glucose study (DIGAMI 1), patients with acute MI received IV insulin therapy for 24 hours, followed by multiple daily injections for three months or longer. The insulin group had lower glucose values and a 29% reduction in mortality at one year and 28% reduction at 3.4 years compared with the control group.17-18
In the most influential study to date, van den Berghe, et al., randomized 1,548 surgical intensive-care unit (ICU) patients to either intensive (IT) or conventional (CT) insulin therapy.19 The glycemic target in the IT arm was 80 to 110 mg/dL (mean glucose attained was 103 mg/dL), while the CT arm had a mean glucose level of 153 mg/dL. The IT group enjoyed substantial reductions in both ICU and total in-hospital mortality, as well as reductions in blood stream infections, acute renal failure, transfusions and the duration of mechanical ventilation (p<0.01 for all).
While a similar study in a medical ICU did not achieve statistical significance in the overall intention-to-treat analysis for mortality, it did demonstrate reductions in mortality in patients with at least three days of ICU treatment and significant reductions in morbidity.20
A meta-analysis of these two studies demonstrated a relative risk reduction in mortality (23.6 to 20.4%) and morbidity in all patients treated with intensive insulin therapy.21
A separate meta-analysis of 35 clinical trials evaluating the effect of intensive insulin infusion therapy on mortality in critically ill inpatients revealed a 15% reduction in short-term mortality.22
Noncritical Care Settings
There are no randomized controlled trials establishing the optimal glycemic target for noncritical care inpatients. There are a number of observational and pilot studies that reinforce the studies performed in critical care settings.
In a retrospective review of almost 1,900 general medical-surgical admissions, Umpierrez, et al., reported an 18-fold increase in mortality in hyperglycemic patients without prior history of diabetes and a 2.5-fold increase in mortality in patients with known diabetes compared to controls. These associations persisted with adjustment for severity of illness.23
A variety of observational and pilot studies associate hyperglycemia with poor outcomes in community acquired pneumonia, renal transplant, and the durability of remission in acute lymphocytic leukemia.24-25
Guidelines and Recommendations
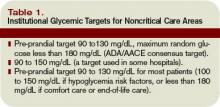
Spurred by the emerging controlled trial evidence, the American Association of Clinical Endocrinologists (AACE) convened a consensus conference involving nine organizations, including SHM. Recommendations for the management of inpatient hyperglycemia included stringent glycemic targets for critical care and noncritical care areas.26 The American Diabetes Association (ADA) produced an excellent technical review on inpatient diabetes that provided the basis for ADA Clinical Practice Guideline glycemic targets.27 The glycemic targets recommended are shown in Table 1 (above).
Caveats
Before accepting these recommended glycemic targets, review the shortcomings of the literature supporting them and consider institutional and individual patient factors that might modify the glycemic target.
Insulin has beneficial vascular and anti-inflammatory effects in its own right, making it difficult in some studies to distinguish the benefit of glucose lowering from the benefit of the insulin used to attain improved control.
The majority of studies supporting inpatient glycemic targets are observational or non-randomized. Some use admission blood glucose concentrations as the sole measure of glucose control.
While most of these studies used valid methods to control for severity of illness and co-morbidities, these methods are not perfect. In some cases, hyperglycemia may have been a marker of a more stressed and sick patient rather than an independent source of adverse outcome.
The dramatic results from the first van den Berghe study have proved difficult to replicate, in part because other investigators have had difficulty achieving stringent glycemic targets safely. Two international multicenter studies recently stopped enrollment due to excess rates of hypoglycemia, but the studies have not yet been published in final form.28-29
Finally, it bears repeating that the proposed glucose targets for noncritically ill patients are based on essentially no clinical trial data in that population. In part, the glycemic targets reflect the evidence derived from landmark outpatient randomized trials.30-31 In the outpatient setting, insulin requirements and nutritional intake are far more reliable than the inpatient setting, where the iatrogenic induction of excessive hypoglycemia is a valid concern.
Safe Glycemic Control
Rapidly fluctuating nutritional status, changing insulin requirements, varied levels of expertise, and hand-offs between geographic locations and providers are all common in the inpatient setting.
Aggressively pursuing glycemic targets without having systems and safeguards in place could lead to net harm.
The AACE recently identified these barriers and recommended a multidisciplinary team approach, reliable metrics, and a standardized method for insulin protocols, orders, and hypoglycemia prevention and treatment techniques.32
Both the AACE and SHM have produced toolkits to assist institutions to safely achieve improved glycemic control and care.33-34 The SHM Glycemic Control Task Force recently summarized key concepts to emphasize in formulating protocols and order sets in the noncritical care setting (see Table 2, left).
Stringent glycemic targets recommended by the ADA and the AACE may be appropriately moderated in centers that do not yet have the systems in place to achieve those goals safely.
Your glycemic target need not be identical to the ADA and AACE glycemic targets but should be similar to them. Examples of glycemic targets for noncritically ill inpatients are shown in Table 3 (see p. 48).
The glycemic target should be actionable, in that some institutionally endorsed action should result when a patient’s glycemic target is consistently not met.
Back to the Case
Your patient has an active infection, a glucose of 198 mg/dL and an elevated HbA1c. You hold the oral agents and start a basal bolus insulin regimen.
You generate an estimate for a safe insulin total daily dose of 60 units (100 kg x 0.6 units per kg for an obese, type 2 diabetes patient), and administer half as basal insulin, with the remaining 30 units distributed as rapid acting insulin in three divided doses. Your orders include routine glucose monitoring, and you plan to adjust the insulin daily as needed to adhere to the institutional glycemic target for noncritically ill patients of 90 to 150 mg/dL. TH
Dr. Maynard is the division chief for hospital medicine at the University of California, San Diego. He is the leader of SHM’s Glycemic Control Task Force and a leader of the VTE Prevention Collaborative.
References
- Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263-1268.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/diabetes/pubs/factsheet05.htm. Last accessed September 18, 2007.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, the Diabetes In Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals (Technical Review). Diabetes Care. 2004;27:553–591.
- Zarich SW. Mechanism by which hyperglycemia plays a role in the setting of acute cardiovascular illness. Rev Cardiovasc Med. 2006;7 (Suppl 2):S35-43.
- Hansen T, Thiel S, Wouters P, Christiansen J, VandenBerghe B. Intensive insulin therapy exerts anti-inflammatory effects in critically ill patients and counteracts the adverse effect of low mannose-gind lectin levels. J Clin Endocrinol Metab. 2003;88:1082-1088.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein H. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–
- 2432.
- Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist 2004;10(4):195-200.
- Pomposelli JJ, Baxter JK, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr.1998;22(2):77-81.
- Ainla T, Baburin A, Teesalu R, Rahu M. The association between hyperglycaemia on admission and 180-day mortality in acute myocardial infarction patients with and without diabetes. Diabet Med. 2005;22(10):1321-1325.
- Timmer JR, van der Horst IC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399-404.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778.
- Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006:12 (Suppl 3): 22-26.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007–1021.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478.
- Malmberg K. Prospective randomised study of intensive insulin treatment on long-term survival after acute myocardial infarction inpatients with diabetes mellitus. BMJ. 1997;314:1512–1515.
- Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626–2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367.
- Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-461.
- Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55(11):3151-3159.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(18):2005-2011.
- McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810-815.
- Thomas M, Mathew T, Russ G, Rao M, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321-1324.
- Weiser MA, Cabanillas ME, Konopleva M, et al. Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer. 2004;100(6):1179-1185.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al., American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77–82.
- Standards of medical care in diabetes-2006. Diabetes Care. 2006;29 (Suppl. 1):S4-S42.
- Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132(1):268-278.
- Devos P, Preiser JC. Current controversies around tight glucose control in critically ill patients. Curr Opin Clin Nutr Metab Care. 2007;10(2):206-209.
- The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care. 2006;29(8):1955-1962.
- American Association of Clinical Endocrinologists Inpatient Glycemic Control Resource Center 2007. Available at http://resources.aace.com/index.asp. Last accessed December 18, 2007.
- Society of Hospital Medicine Glycemic Control Resource Room. Available at www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Last accessed Nov. 25, 2007.
Case
A 65-year-old obese (100 kg) man with type 2 diabetes, hypertension, and a pack-a-day smoking habit is admitted with moderately severe bilobar pneumonia. His condition is manifest by fever, cough, chills, leukocytosis, and a modest oxygen requirement. You order oxygen, intravenous (IV) fluids, diet, and appropriate antibiotics while continuing the history and chart review. The patient uses metformin and glyburide, and his home glucose readings are generally in the 160 to 180 mg/dL range. An HbA1c level performed three months ago was 9.8, leading to an increased dose of glyburide. As you finish the history, the nurse reports a glucose reading of 198 mg/dL. What is the target blood glucose for noncritical care adult inpatients?
Overview
Diabetes mellitus is an epidemic in the United States. At least 9.3% of adults older than 20 (more than 20 million people) have diabetes. Approximately 30% are unaware they have diabetes.1 Concurrent with the increasing prevalence of diabetes in the U.S. from 1980 through 2003, the number of hospital discharges with diabetes as any listed diagnosis more than doubled between 1980 and 2003. These trends are expected to accelerate.2 Studies suggest 26% of inpatients have diabetes and 12% have pre-diabetes, previously undiagnosed diabetes, or stress hyperglycemia.3
Review of the Data
A full review of the evidence is beyond the scope of this article. What follows is a sampling of the most representative or influential critical care studies.
Physiology
Fluid and electrolyte balance, left ventricular (LV) function, leukocyte action, wound healing, endothelial function, and immunoglobulin function are all impaired with hyperglycemia.
A prothrombotic state and enhanced platelet aggregation have been demonstrated with even mild elevations of blood glucose.
The mechanisms are multifactorial and complex and involve metabolic derangements leading to oxidative stress, release of free fatty acids, and counter-regulatory hormones.4-6
Observational Studies
A strong and consistent association with hyperglycemia and adverse outcomes is seen in a wide variety of critical care and peri-operative settings. Trauma survival, stroke survival and function, and the incidence of post-operative infections are all adversely affected by hyperglycemia.7-10 Acute myocardial infarction (MI) mortality, acute MI infarct size, and LV dysfunction are also consistently adversely affected in these studies.11-13
This association is typically present in hyperglycemic patients whether they have a diagnosis of diabetes or not, and the association is often even stronger in those lacking a pre-existing diagnosis. Dysfunction typically is detectable at only modest elevations of blood glucose and becomes more marked in a dose response relationship.
Uncontrolled Interventional Studies
The Portland Diabetic Project is a prospective, non-randomized, observational study of 5,510 consecutive diabetic cardiac surgery patients.14-15 The three-day blood glucose average (3-BG) has been progressively reduced for the population through the use of continuous insulin infusion (CII).
The last reported glycemic target is less than 130 mg/dL, and the current glycemic target is less than 110 mg/dL. Both CII for three days and a favorable 3-BG were independently associated with improved mortality, deep sternal-wound infection rates, and length of stay. Mortality and deep sternal-wound infection rates for diabetic patients with well-controlled glucose levels are equal to patients without diabetes.
Another study compared 800 mixed medical-surgical ICU patients with tight glycemic control (mean BG 130.7 mg/dL) to historical controls with a mean glucose of 152.3 mg/dL. The insulin infusion group had associated significant reductions in mortality and median length of ICU stay.16
Randomized Controlled Trials and Meta-Analyses
In the first Diabetes and Insulin-Glucose study (DIGAMI 1), patients with acute MI received IV insulin therapy for 24 hours, followed by multiple daily injections for three months or longer. The insulin group had lower glucose values and a 29% reduction in mortality at one year and 28% reduction at 3.4 years compared with the control group.17-18
In the most influential study to date, van den Berghe, et al., randomized 1,548 surgical intensive-care unit (ICU) patients to either intensive (IT) or conventional (CT) insulin therapy.19 The glycemic target in the IT arm was 80 to 110 mg/dL (mean glucose attained was 103 mg/dL), while the CT arm had a mean glucose level of 153 mg/dL. The IT group enjoyed substantial reductions in both ICU and total in-hospital mortality, as well as reductions in blood stream infections, acute renal failure, transfusions and the duration of mechanical ventilation (p<0.01 for all).
While a similar study in a medical ICU did not achieve statistical significance in the overall intention-to-treat analysis for mortality, it did demonstrate reductions in mortality in patients with at least three days of ICU treatment and significant reductions in morbidity.20
A meta-analysis of these two studies demonstrated a relative risk reduction in mortality (23.6 to 20.4%) and morbidity in all patients treated with intensive insulin therapy.21
A separate meta-analysis of 35 clinical trials evaluating the effect of intensive insulin infusion therapy on mortality in critically ill inpatients revealed a 15% reduction in short-term mortality.22
Noncritical Care Settings
There are no randomized controlled trials establishing the optimal glycemic target for noncritical care inpatients. There are a number of observational and pilot studies that reinforce the studies performed in critical care settings.
In a retrospective review of almost 1,900 general medical-surgical admissions, Umpierrez, et al., reported an 18-fold increase in mortality in hyperglycemic patients without prior history of diabetes and a 2.5-fold increase in mortality in patients with known diabetes compared to controls. These associations persisted with adjustment for severity of illness.23
A variety of observational and pilot studies associate hyperglycemia with poor outcomes in community acquired pneumonia, renal transplant, and the durability of remission in acute lymphocytic leukemia.24-25
Guidelines and Recommendations
Spurred by the emerging controlled trial evidence, the American Association of Clinical Endocrinologists (AACE) convened a consensus conference involving nine organizations, including SHM. Recommendations for the management of inpatient hyperglycemia included stringent glycemic targets for critical care and noncritical care areas.26 The American Diabetes Association (ADA) produced an excellent technical review on inpatient diabetes that provided the basis for ADA Clinical Practice Guideline glycemic targets.27 The glycemic targets recommended are shown in Table 1 (above).
Caveats
Before accepting these recommended glycemic targets, review the shortcomings of the literature supporting them and consider institutional and individual patient factors that might modify the glycemic target.
Insulin has beneficial vascular and anti-inflammatory effects in its own right, making it difficult in some studies to distinguish the benefit of glucose lowering from the benefit of the insulin used to attain improved control.
The majority of studies supporting inpatient glycemic targets are observational or non-randomized. Some use admission blood glucose concentrations as the sole measure of glucose control.
While most of these studies used valid methods to control for severity of illness and co-morbidities, these methods are not perfect. In some cases, hyperglycemia may have been a marker of a more stressed and sick patient rather than an independent source of adverse outcome.
The dramatic results from the first van den Berghe study have proved difficult to replicate, in part because other investigators have had difficulty achieving stringent glycemic targets safely. Two international multicenter studies recently stopped enrollment due to excess rates of hypoglycemia, but the studies have not yet been published in final form.28-29
Finally, it bears repeating that the proposed glucose targets for noncritically ill patients are based on essentially no clinical trial data in that population. In part, the glycemic targets reflect the evidence derived from landmark outpatient randomized trials.30-31 In the outpatient setting, insulin requirements and nutritional intake are far more reliable than the inpatient setting, where the iatrogenic induction of excessive hypoglycemia is a valid concern.
Safe Glycemic Control
Rapidly fluctuating nutritional status, changing insulin requirements, varied levels of expertise, and hand-offs between geographic locations and providers are all common in the inpatient setting.
Aggressively pursuing glycemic targets without having systems and safeguards in place could lead to net harm.
The AACE recently identified these barriers and recommended a multidisciplinary team approach, reliable metrics, and a standardized method for insulin protocols, orders, and hypoglycemia prevention and treatment techniques.32
Both the AACE and SHM have produced toolkits to assist institutions to safely achieve improved glycemic control and care.33-34 The SHM Glycemic Control Task Force recently summarized key concepts to emphasize in formulating protocols and order sets in the noncritical care setting (see Table 2, left).
Stringent glycemic targets recommended by the ADA and the AACE may be appropriately moderated in centers that do not yet have the systems in place to achieve those goals safely.
Your glycemic target need not be identical to the ADA and AACE glycemic targets but should be similar to them. Examples of glycemic targets for noncritically ill inpatients are shown in Table 3 (see p. 48).
The glycemic target should be actionable, in that some institutionally endorsed action should result when a patient’s glycemic target is consistently not met.
Back to the Case
Your patient has an active infection, a glucose of 198 mg/dL and an elevated HbA1c. You hold the oral agents and start a basal bolus insulin regimen.
You generate an estimate for a safe insulin total daily dose of 60 units (100 kg x 0.6 units per kg for an obese, type 2 diabetes patient), and administer half as basal insulin, with the remaining 30 units distributed as rapid acting insulin in three divided doses. Your orders include routine glucose monitoring, and you plan to adjust the insulin daily as needed to adhere to the institutional glycemic target for noncritically ill patients of 90 to 150 mg/dL. TH
Dr. Maynard is the division chief for hospital medicine at the University of California, San Diego. He is the leader of SHM’s Glycemic Control Task Force and a leader of the VTE Prevention Collaborative.
References
- Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263-1268.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/diabetes/pubs/factsheet05.htm. Last accessed September 18, 2007.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, the Diabetes In Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals (Technical Review). Diabetes Care. 2004;27:553–591.
- Zarich SW. Mechanism by which hyperglycemia plays a role in the setting of acute cardiovascular illness. Rev Cardiovasc Med. 2006;7 (Suppl 2):S35-43.
- Hansen T, Thiel S, Wouters P, Christiansen J, VandenBerghe B. Intensive insulin therapy exerts anti-inflammatory effects in critically ill patients and counteracts the adverse effect of low mannose-gind lectin levels. J Clin Endocrinol Metab. 2003;88:1082-1088.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein H. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–
- 2432.
- Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist 2004;10(4):195-200.
- Pomposelli JJ, Baxter JK, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr.1998;22(2):77-81.
- Ainla T, Baburin A, Teesalu R, Rahu M. The association between hyperglycaemia on admission and 180-day mortality in acute myocardial infarction patients with and without diabetes. Diabet Med. 2005;22(10):1321-1325.
- Timmer JR, van der Horst IC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399-404.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778.
- Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006:12 (Suppl 3): 22-26.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007–1021.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478.
- Malmberg K. Prospective randomised study of intensive insulin treatment on long-term survival after acute myocardial infarction inpatients with diabetes mellitus. BMJ. 1997;314:1512–1515.
- Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626–2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367.
- Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-461.
- Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55(11):3151-3159.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(18):2005-2011.
- McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810-815.
- Thomas M, Mathew T, Russ G, Rao M, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321-1324.
- Weiser MA, Cabanillas ME, Konopleva M, et al. Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer. 2004;100(6):1179-1185.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al., American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77–82.
- Standards of medical care in diabetes-2006. Diabetes Care. 2006;29 (Suppl. 1):S4-S42.
- Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132(1):268-278.
- Devos P, Preiser JC. Current controversies around tight glucose control in critically ill patients. Curr Opin Clin Nutr Metab Care. 2007;10(2):206-209.
- The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care. 2006;29(8):1955-1962.
- American Association of Clinical Endocrinologists Inpatient Glycemic Control Resource Center 2007. Available at http://resources.aace.com/index.asp. Last accessed December 18, 2007.
- Society of Hospital Medicine Glycemic Control Resource Room. Available at www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Last accessed Nov. 25, 2007.
Case
A 65-year-old obese (100 kg) man with type 2 diabetes, hypertension, and a pack-a-day smoking habit is admitted with moderately severe bilobar pneumonia. His condition is manifest by fever, cough, chills, leukocytosis, and a modest oxygen requirement. You order oxygen, intravenous (IV) fluids, diet, and appropriate antibiotics while continuing the history and chart review. The patient uses metformin and glyburide, and his home glucose readings are generally in the 160 to 180 mg/dL range. An HbA1c level performed three months ago was 9.8, leading to an increased dose of glyburide. As you finish the history, the nurse reports a glucose reading of 198 mg/dL. What is the target blood glucose for noncritical care adult inpatients?
Overview
Diabetes mellitus is an epidemic in the United States. At least 9.3% of adults older than 20 (more than 20 million people) have diabetes. Approximately 30% are unaware they have diabetes.1 Concurrent with the increasing prevalence of diabetes in the U.S. from 1980 through 2003, the number of hospital discharges with diabetes as any listed diagnosis more than doubled between 1980 and 2003. These trends are expected to accelerate.2 Studies suggest 26% of inpatients have diabetes and 12% have pre-diabetes, previously undiagnosed diabetes, or stress hyperglycemia.3
Review of the Data
A full review of the evidence is beyond the scope of this article. What follows is a sampling of the most representative or influential critical care studies.
Physiology
Fluid and electrolyte balance, left ventricular (LV) function, leukocyte action, wound healing, endothelial function, and immunoglobulin function are all impaired with hyperglycemia.
A prothrombotic state and enhanced platelet aggregation have been demonstrated with even mild elevations of blood glucose.
The mechanisms are multifactorial and complex and involve metabolic derangements leading to oxidative stress, release of free fatty acids, and counter-regulatory hormones.4-6
Observational Studies
A strong and consistent association with hyperglycemia and adverse outcomes is seen in a wide variety of critical care and peri-operative settings. Trauma survival, stroke survival and function, and the incidence of post-operative infections are all adversely affected by hyperglycemia.7-10 Acute myocardial infarction (MI) mortality, acute MI infarct size, and LV dysfunction are also consistently adversely affected in these studies.11-13
This association is typically present in hyperglycemic patients whether they have a diagnosis of diabetes or not, and the association is often even stronger in those lacking a pre-existing diagnosis. Dysfunction typically is detectable at only modest elevations of blood glucose and becomes more marked in a dose response relationship.
Uncontrolled Interventional Studies
The Portland Diabetic Project is a prospective, non-randomized, observational study of 5,510 consecutive diabetic cardiac surgery patients.14-15 The three-day blood glucose average (3-BG) has been progressively reduced for the population through the use of continuous insulin infusion (CII).
The last reported glycemic target is less than 130 mg/dL, and the current glycemic target is less than 110 mg/dL. Both CII for three days and a favorable 3-BG were independently associated with improved mortality, deep sternal-wound infection rates, and length of stay. Mortality and deep sternal-wound infection rates for diabetic patients with well-controlled glucose levels are equal to patients without diabetes.
Another study compared 800 mixed medical-surgical ICU patients with tight glycemic control (mean BG 130.7 mg/dL) to historical controls with a mean glucose of 152.3 mg/dL. The insulin infusion group had associated significant reductions in mortality and median length of ICU stay.16
Randomized Controlled Trials and Meta-Analyses
In the first Diabetes and Insulin-Glucose study (DIGAMI 1), patients with acute MI received IV insulin therapy for 24 hours, followed by multiple daily injections for three months or longer. The insulin group had lower glucose values and a 29% reduction in mortality at one year and 28% reduction at 3.4 years compared with the control group.17-18
In the most influential study to date, van den Berghe, et al., randomized 1,548 surgical intensive-care unit (ICU) patients to either intensive (IT) or conventional (CT) insulin therapy.19 The glycemic target in the IT arm was 80 to 110 mg/dL (mean glucose attained was 103 mg/dL), while the CT arm had a mean glucose level of 153 mg/dL. The IT group enjoyed substantial reductions in both ICU and total in-hospital mortality, as well as reductions in blood stream infections, acute renal failure, transfusions and the duration of mechanical ventilation (p<0.01 for all).
While a similar study in a medical ICU did not achieve statistical significance in the overall intention-to-treat analysis for mortality, it did demonstrate reductions in mortality in patients with at least three days of ICU treatment and significant reductions in morbidity.20
A meta-analysis of these two studies demonstrated a relative risk reduction in mortality (23.6 to 20.4%) and morbidity in all patients treated with intensive insulin therapy.21
A separate meta-analysis of 35 clinical trials evaluating the effect of intensive insulin infusion therapy on mortality in critically ill inpatients revealed a 15% reduction in short-term mortality.22
Noncritical Care Settings
There are no randomized controlled trials establishing the optimal glycemic target for noncritical care inpatients. There are a number of observational and pilot studies that reinforce the studies performed in critical care settings.
In a retrospective review of almost 1,900 general medical-surgical admissions, Umpierrez, et al., reported an 18-fold increase in mortality in hyperglycemic patients without prior history of diabetes and a 2.5-fold increase in mortality in patients with known diabetes compared to controls. These associations persisted with adjustment for severity of illness.23
A variety of observational and pilot studies associate hyperglycemia with poor outcomes in community acquired pneumonia, renal transplant, and the durability of remission in acute lymphocytic leukemia.24-25
Guidelines and Recommendations
Spurred by the emerging controlled trial evidence, the American Association of Clinical Endocrinologists (AACE) convened a consensus conference involving nine organizations, including SHM. Recommendations for the management of inpatient hyperglycemia included stringent glycemic targets for critical care and noncritical care areas.26 The American Diabetes Association (ADA) produced an excellent technical review on inpatient diabetes that provided the basis for ADA Clinical Practice Guideline glycemic targets.27 The glycemic targets recommended are shown in Table 1 (above).
Caveats
Before accepting these recommended glycemic targets, review the shortcomings of the literature supporting them and consider institutional and individual patient factors that might modify the glycemic target.
Insulin has beneficial vascular and anti-inflammatory effects in its own right, making it difficult in some studies to distinguish the benefit of glucose lowering from the benefit of the insulin used to attain improved control.
The majority of studies supporting inpatient glycemic targets are observational or non-randomized. Some use admission blood glucose concentrations as the sole measure of glucose control.
While most of these studies used valid methods to control for severity of illness and co-morbidities, these methods are not perfect. In some cases, hyperglycemia may have been a marker of a more stressed and sick patient rather than an independent source of adverse outcome.
The dramatic results from the first van den Berghe study have proved difficult to replicate, in part because other investigators have had difficulty achieving stringent glycemic targets safely. Two international multicenter studies recently stopped enrollment due to excess rates of hypoglycemia, but the studies have not yet been published in final form.28-29
Finally, it bears repeating that the proposed glucose targets for noncritically ill patients are based on essentially no clinical trial data in that population. In part, the glycemic targets reflect the evidence derived from landmark outpatient randomized trials.30-31 In the outpatient setting, insulin requirements and nutritional intake are far more reliable than the inpatient setting, where the iatrogenic induction of excessive hypoglycemia is a valid concern.
Safe Glycemic Control
Rapidly fluctuating nutritional status, changing insulin requirements, varied levels of expertise, and hand-offs between geographic locations and providers are all common in the inpatient setting.
Aggressively pursuing glycemic targets without having systems and safeguards in place could lead to net harm.
The AACE recently identified these barriers and recommended a multidisciplinary team approach, reliable metrics, and a standardized method for insulin protocols, orders, and hypoglycemia prevention and treatment techniques.32
Both the AACE and SHM have produced toolkits to assist institutions to safely achieve improved glycemic control and care.33-34 The SHM Glycemic Control Task Force recently summarized key concepts to emphasize in formulating protocols and order sets in the noncritical care setting (see Table 2, left).
Stringent glycemic targets recommended by the ADA and the AACE may be appropriately moderated in centers that do not yet have the systems in place to achieve those goals safely.
Your glycemic target need not be identical to the ADA and AACE glycemic targets but should be similar to them. Examples of glycemic targets for noncritically ill inpatients are shown in Table 3 (see p. 48).
The glycemic target should be actionable, in that some institutionally endorsed action should result when a patient’s glycemic target is consistently not met.
Back to the Case
Your patient has an active infection, a glucose of 198 mg/dL and an elevated HbA1c. You hold the oral agents and start a basal bolus insulin regimen.
You generate an estimate for a safe insulin total daily dose of 60 units (100 kg x 0.6 units per kg for an obese, type 2 diabetes patient), and administer half as basal insulin, with the remaining 30 units distributed as rapid acting insulin in three divided doses. Your orders include routine glucose monitoring, and you plan to adjust the insulin daily as needed to adhere to the institutional glycemic target for noncritically ill patients of 90 to 150 mg/dL. TH
Dr. Maynard is the division chief for hospital medicine at the University of California, San Diego. He is the leader of SHM’s Glycemic Control Task Force and a leader of the VTE Prevention Collaborative.
References
- Cowie CC, Rust KF, Byrd-Holt DD, et al. Prevalence of diabetes and impaired fasting glucose in adults in the U.S. population: National Health And Nutrition Examination Survey 1999-2002. Diabetes Care. 2006;29(6):1263-1268.
- Centers for Disease Control and Prevention. National diabetes fact sheet: general information and national estimates on diabetes in the United States, 2005. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/diabetes/pubs/factsheet05.htm. Last accessed September 18, 2007.
- Umpierrez GE, Isaacs SD, Bazargan N, You X, Thaler LM, Kitabchi AE. Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. J Clin Endocrinol Metab. 2002;87(3):978-982.
- Clement S, Braithwaite SS, Magee MF, Ahmann A, Smith EP, Schafer RG, Hirsch IB, the Diabetes In Hospitals Writing Committee. Management of diabetes and hyperglycemia in hospitals (Technical Review). Diabetes Care. 2004;27:553–591.
- Zarich SW. Mechanism by which hyperglycemia plays a role in the setting of acute cardiovascular illness. Rev Cardiovasc Med. 2006;7 (Suppl 2):S35-43.
- Hansen T, Thiel S, Wouters P, Christiansen J, VandenBerghe B. Intensive insulin therapy exerts anti-inflammatory effects in critically ill patients and counteracts the adverse effect of low mannose-gind lectin levels. J Clin Endocrinol Metab. 2003;88:1082-1088.
- Yendamuri S, Fulda GJ, Tinkoff GH. Admission hyperglycemia as a prognostic indicator in trauma. J Trauma. 2003;55:33-38.
- Capes SE, Hunt D, Malmberg K, Pathak P, Gerstein H. Stress hyperglycemia and prognosis of stroke in nondiabetic and diabetic patients: a systematic overview. Stroke. 2001;32:2426–
- 2432.
- Bruno A, Williams LS, Kent TA. How important is hyperglycemia during acute brain infarction? Neurologist 2004;10(4):195-200.
- Pomposelli JJ, Baxter JK, Babineau TJ, et al. Early postoperative glucose control predicts nosocomial infection rate in diabetic patients. J Parenter Enteral Nutr.1998;22(2):77-81.
- Ainla T, Baburin A, Teesalu R, Rahu M. The association between hyperglycaemia on admission and 180-day mortality in acute myocardial infarction patients with and without diabetes. Diabet Med. 2005;22(10):1321-1325.
- Timmer JR, van der Horst IC, Ottervanger JP, et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004;148:399-404.
- Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet. 2000;355:773–778.
- Furnary AP, Wu Y. Clinical effects of hyperglycemia in the cardiac surgery population: the Portland Diabetic Project. Endocr Pract. 2006:12 (Suppl 3): 22-26.
- Furnary AP, Gao G, Grunkemeier GL, et al. Continuous insulin infusion reduces mortality in patients with diabetes undergoing coronary artery bypass grafting. J Thorac Cardiovasc Surg. 2003;125:1007–1021.
- Krinsley JS. Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clin Proc. 2003;78:1471–1478.
- Malmberg K. Prospective randomised study of intensive insulin treatment on long-term survival after acute myocardial infarction inpatients with diabetes mellitus. BMJ. 1997;314:1512–1515.
- Malmberg K, Norhammar A, Wedel H, Ryden L. Glycometabolic state at admission: important risk marker of mortality in conventionally treated patients with diabetes mellitus and acute myocardial infarction: long-term results from the Diabetes and Insulin-Glucose Infusion in Acute Myocardial Infarction (DIGAMI) study. Circulation. 1999;99:2626–2632.
- Van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–1367.
- Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354(5):449-461.
- Van den Berghe G, Wilmer A, Milants I, et al. Intensive insulin therapy in mixed medical/surgical intensive care units: benefit versus harm. Diabetes. 2006;55(11):3151-3159.
- Pittas AG, Siegel RD, Lau J. Insulin therapy for critically ill hospitalized patients: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(18):2005-2011.
- McAlister FA, Majumdar SR, Blitz S, Rowe BH, Romney J, Marrie TJ. The relation between hyperglycemia and outcomes in 2,471 patients admitted to the hospital with community-acquired pneumonia. Diabetes Care. 2005;28(4):810-815.
- Thomas M, Mathew T, Russ G, Rao M, Moran J. Early peri-operative glycaemic control and allograft rejection in patients with diabetes mellitus: a pilot study. Transplantation. 2001;72(7):1321-1324.
- Weiser MA, Cabanillas ME, Konopleva M, et al. Relation between the duration of remission and hyperglycemia during induction chemotherapy for acute lymphocytic leukemia with a hyperfractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone/methotrexate-cytarabine regimen. Cancer. 2004;100(6):1179-1185.
- Garber AJ, Moghissi ES, Bransome ED Jr, et al., American College of Endocrinology Task Force on Inpatient Diabetes Metabolic Control. American College of Endocrinology position statement on inpatient diabetes and metabolic control. Endocr Pract. 2004;10:77–82.
- Standards of medical care in diabetes-2006. Diabetes Care. 2006;29 (Suppl. 1):S4-S42.
- Vanhorebeek I, Langouche L, Van den Berghe G. Tight blood glucose control with insulin in the ICU: facts and controversies. Chest. 2007;132(1):268-278.
- Devos P, Preiser JC. Current controversies around tight glucose control in critically ill patients. Curr Opin Clin Nutr Metab Care. 2007;10(2):206-209.
- The Diabetes Control and Complications Trial Research Group (DCCT). The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977-986.
- UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
- American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control: a call to action. Diabetes Care. 2006;29(8):1955-1962.
- American Association of Clinical Endocrinologists Inpatient Glycemic Control Resource Center 2007. Available at http://resources.aace.com/index.asp. Last accessed December 18, 2007.
- Society of Hospital Medicine Glycemic Control Resource Room. Available at www.hospitalmedicine.org/ResourceRoomRedesign/GlycemicControl.cfm. Last accessed Nov. 25, 2007.
Make a Move
As elderly patients suffering functional decline and immobility face prolonged hospital stays, placement in nursing homes, and increased risk of mortality, hospitalists must focus on one mission: Keep them moving.#1
With today’s emphasis on cost containment and quality assurance, keeping patients moving is one small step toward improving the quality of a patient’s hospitalization.
At the core of elders’ quality of life is independent mobility. When mobility is lost, a patient’s ability to socialize with peers and family, perform activities of daily living (ADLs), and participate in decisions regarding their well-being is severely compromised.
Most hospital admissions begin with the assignment of a patient to a bed. Although acute illness, medications, and a new environment all take their toll on patient functionality, simply putting a patient in recline has a significant impact.
If a young healthy person is ordered to rest for more than 72 hours, muscle mass and strength decrease, gait speed slows, and coordination becomes impaired.#2 If that patient is put to bed for more than 72 hours, organs other than the musculoskeletal system become compromised. Cardiovascular deconditioning with resting tachycardia and orthostatic hypotension, glucose intolerance, venous thromboembolism, hypercalcemia and osteoporosis, constipation and fecal impaction, pressure ulcers, and even depression can occur.3# Imagine then how elderly patients would fare.
Unfortunately, the independence of elderly patients is continually undermined by the same environment that offers treatment and care—the inpatient ward. And staff and patient family members are at fault.#4
Establish a Baseline
Teaching patients to move autonomously requires extra nursing time. Most on the nursing staff find it easier to provide a bedpan rather than assist a patient to the bathroom. When assisted ambulation is offered, patients may resist.
Families may hinder the resumption of mobility by performing tasks for patients instead of encouraging them to do them themselves. Further, changes in mobility are difficult to quantify and communicate due to limited mobility terminology in nursing practice and limited physician time. When a pre-admission functional status is not clearly documented, hospital staff often assumes that the patient’s compromised state is little changed from its baseline.
With so many barriers to patient mobility, obtaining an accurate assessment of a patient’s functional status two weeks prior to admission is key in establishing a plan for helping elderly patients regain mobility.
Ideally, one should speak to the patient as well as someone closely involved with the patient’s care who can verify or clarify the patient’s description of his or her prior activities. Significant information to obtain includes which ADLs the patient can independently perform, how far the patient can ambulate and with what assistive devices, and whether glasses, hearing aids, specially fitted shoes and orthotics, and knee braces are normally required for ambulation.#5
Though no screening tool has been validated as an absolute predictor of inpatient functional decline, lower functional status before admission, cognitive impairment, depression, advanced age, and prolonged length of hospital stay have been associated with loss of independence. Their presence may warrant a more aggressive regimen for regaining mobility.
Set the Stage
Before calling in a transfer to inpatient rehab, there are several steps one can take to maximize the return of function. By optimizing a patient’s functional capabilities during the admission, you enable them to integrate necessary skills into a daily routine—something they’re unlikely to learn at a rehabilitation center. Take these steps:6
- Control pain. Adequate analgesia is imperative for regaining mobility. Opiates and opiate agonists may be necessary for optimal control. Constipation should be expected and treated, and patients should be closely monitored for orthostasis, confusion, and urinary retention;
- Get the patient to a chair with assistive devices nearby. This includes canes, braces, walkers, orthopedic shoes, glasses, and hearing aids;
- Minimize IVs, catheters, and drains. Those that cannot be removed can be taped to minimize their interference with ambulation. Regular clothes, particularly jogging suits, promote ambulation and comfort;
- Coordinate with nursing department so the patient has periods of activity and rest. A walk down the corridor should be followed by a commensurate period of minimal activity, not a two-hour nap;
- Encourage sleep hygiene. Daytime activities can be maximized only when preceded by a restful night’s sleep. Limiting caffeinated beverages, restricting television time, and encouraging relaxing evening activities like reading may be necessary to ensure adequate sleep. Well-rested patients are better equipped to challenge themselves physically during the day and are less at risk for the side effects associated with sleeping medications;
- Give early referral to physical and occupational therapies. Even if the patient can barely tolerate sitting in a chair, a passive range of motion exercises for all joints should be undertaken daily. Additionally, active resistance exercises may be feasible for even debilitated patients if they receive daily assistance and continual encouragement. With persistence, skeletal muscles and the cardiovascular and pulmonary systems will show more endurance.#
Follow Progress
Accurately following a patient’s progress in regaining mobility requires the use of an assessment tool. The Elderly Mobility Scale (EMS) is useful for assessing improvements in mobility of elderly patients receiving physical therapy.
Balance, range of motion, and ambulation are scored initially, and the scores are updated during daily physical therapy. A review of this assessment tool was published in the Journal of Ageing this year, with the authors concluding that the EMS is a valid, reliable scale that can be readily applied during daily clinical work.7# Further, a review in Clinical Rehabilitation found the EMS to be a reliable test of motor function in elderly patients with a range of functional levels.#8 This assessment falls short in its lack of predictive validity in terms of falls or discharge destination.
Elderly patients suffer more hospital-associated falls than those younger than 65. According to a 2000 article from the British Medical Journal, patients older than 65 were seven times as likely to experience a preventable fall while in the hospital compared with younger age groups.#9
Patient factors that contribute to falls include age-related changes in postural control, impaired gait, decreased visual acuity, medications, the presence of acute and chronic diseases that affect sensory input, the central nervous system, and coordination. Osteoporosis is also an important factor—pathologic fractures often precede a fall. Environmental factors include poor lighting, obtrusive furniture, slippery floors, loose floor coverings, and bathrooms without handrails or grab bars.
The items most commonly included in fall risk-assessment tools include:10
- Comorbid patient characteristics or conditions associated with falling, such as cognitive impairment;
- History of a fall;
- Mobility impairment;
- Incontinence;
- Medications affecting balance/cognition and polypharmacy;
- Sensory deficits; and
- Advanced age.
The presence of more than three of these items identifies a patient at high risk for falling. But calculating a fall assessment includes not only identifying relevant risk factors, but also performing a focused physical exam. In ambulatory patients, the timed “get up and go” test is a useful predictor of falls. The patient is observed as she rises from a chair, walks 10 feet, then returns to the chair. If the patient requires more than 16 seconds to complete the task, he or she is at greater risk for a fall.
Early Intervention
While management depends on the underlying etiology of the fall, some generally acceptable practices are effective:
- Maintain a safe physical environment. Making sure spills are cleaned up quickly and walkways are kept free of obstruction is as important as maintaining adequate lighting in all areas where older adults will walk;
- Avoid use of restraints. Though restraints are often employed to prevent falls, they have not proved effective in medical trials. It has been demonstrated that their use increases the injury associated with falls, and several restraint-reduction projects have demonstrated that restraints can be removed without a significant increase in falls or injuries;
- Deal with medication side effects. The side effects of CNS altering drugs, and drugs affecting postural blood pressure, balance, and gait should be expected and addressed. Polypharmacy should be minimized;
- Watch patients closely. High risk patients should be positioned by the nursing station so that their visibility to the staff is maximized; and
- Promote mobility. There has been considerable research demonstrating the positive effect of exercise on reducing fall risk among community-residing older adults. While no study to date has addressed the impact of exercise in the hospital-based community, improved balance, mobility, and flexibility have been documented in nursing home residents receiving aggressive physical therapy. TH
Dr. Landis is a frequent contributor to The Hospitalist.
References
- Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, et al. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs. 2007 Jan;16(1):46-57.
- Callen BL, Mahoney JE, Wells TJ, et al. Admission and discharge mobility of frail hospitalized older adults. MedSurg Nursing 2004:13(3):156-163.
- Resnick NM, Marcantonio ER. How should clinical care of the aged differ? Lancet 2002; 350:1157-1167.
- Watters JM, McClaran JC, Man-Son-Hing M. The elderly surgical patient. ACS surgery: principles and practice. Medscape 2005.
- Miller KE, Zylstra RG, Standridge JB. The geriatric patient: a systematic approach to maintaining health. Am Fam Physician. 2000;61(4):1080-1098.
- Rydwik E, Frändin K, Akner G. Effects of physical training on physical performance in institutionalized elderly patients with multiple diagnoses. Age Ageing. 2004 Jan;33(1):13-23.
- Kuys SS , Brauer SG. Validation and reliability of the Modified Elderly Mobility Scale. Australas J Ageing 2006; 25(3):140-144.
- Spilg EG, Martin BJ, Mitchell SL, et al. A comparison of mobility assessments in a geriatric day hospital. Clin Rehabil. 2001 Jun;15(3):296-300.
- Thomas EJ, Brennan TA. Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ 2000;320(7237):741-744
- Gray-Miceli DL, Capezuti E. A nursing guide to the prevention and management of falls in geriatric patients in long-term care settings. Medscape; May 19, 2005.
As elderly patients suffering functional decline and immobility face prolonged hospital stays, placement in nursing homes, and increased risk of mortality, hospitalists must focus on one mission: Keep them moving.#1
With today’s emphasis on cost containment and quality assurance, keeping patients moving is one small step toward improving the quality of a patient’s hospitalization.
At the core of elders’ quality of life is independent mobility. When mobility is lost, a patient’s ability to socialize with peers and family, perform activities of daily living (ADLs), and participate in decisions regarding their well-being is severely compromised.
Most hospital admissions begin with the assignment of a patient to a bed. Although acute illness, medications, and a new environment all take their toll on patient functionality, simply putting a patient in recline has a significant impact.
If a young healthy person is ordered to rest for more than 72 hours, muscle mass and strength decrease, gait speed slows, and coordination becomes impaired.#2 If that patient is put to bed for more than 72 hours, organs other than the musculoskeletal system become compromised. Cardiovascular deconditioning with resting tachycardia and orthostatic hypotension, glucose intolerance, venous thromboembolism, hypercalcemia and osteoporosis, constipation and fecal impaction, pressure ulcers, and even depression can occur.3# Imagine then how elderly patients would fare.
Unfortunately, the independence of elderly patients is continually undermined by the same environment that offers treatment and care—the inpatient ward. And staff and patient family members are at fault.#4
Establish a Baseline
Teaching patients to move autonomously requires extra nursing time. Most on the nursing staff find it easier to provide a bedpan rather than assist a patient to the bathroom. When assisted ambulation is offered, patients may resist.
Families may hinder the resumption of mobility by performing tasks for patients instead of encouraging them to do them themselves. Further, changes in mobility are difficult to quantify and communicate due to limited mobility terminology in nursing practice and limited physician time. When a pre-admission functional status is not clearly documented, hospital staff often assumes that the patient’s compromised state is little changed from its baseline.
With so many barriers to patient mobility, obtaining an accurate assessment of a patient’s functional status two weeks prior to admission is key in establishing a plan for helping elderly patients regain mobility.
Ideally, one should speak to the patient as well as someone closely involved with the patient’s care who can verify or clarify the patient’s description of his or her prior activities. Significant information to obtain includes which ADLs the patient can independently perform, how far the patient can ambulate and with what assistive devices, and whether glasses, hearing aids, specially fitted shoes and orthotics, and knee braces are normally required for ambulation.#5
Though no screening tool has been validated as an absolute predictor of inpatient functional decline, lower functional status before admission, cognitive impairment, depression, advanced age, and prolonged length of hospital stay have been associated with loss of independence. Their presence may warrant a more aggressive regimen for regaining mobility.
Set the Stage
Before calling in a transfer to inpatient rehab, there are several steps one can take to maximize the return of function. By optimizing a patient’s functional capabilities during the admission, you enable them to integrate necessary skills into a daily routine—something they’re unlikely to learn at a rehabilitation center. Take these steps:6
- Control pain. Adequate analgesia is imperative for regaining mobility. Opiates and opiate agonists may be necessary for optimal control. Constipation should be expected and treated, and patients should be closely monitored for orthostasis, confusion, and urinary retention;
- Get the patient to a chair with assistive devices nearby. This includes canes, braces, walkers, orthopedic shoes, glasses, and hearing aids;
- Minimize IVs, catheters, and drains. Those that cannot be removed can be taped to minimize their interference with ambulation. Regular clothes, particularly jogging suits, promote ambulation and comfort;
- Coordinate with nursing department so the patient has periods of activity and rest. A walk down the corridor should be followed by a commensurate period of minimal activity, not a two-hour nap;
- Encourage sleep hygiene. Daytime activities can be maximized only when preceded by a restful night’s sleep. Limiting caffeinated beverages, restricting television time, and encouraging relaxing evening activities like reading may be necessary to ensure adequate sleep. Well-rested patients are better equipped to challenge themselves physically during the day and are less at risk for the side effects associated with sleeping medications;
- Give early referral to physical and occupational therapies. Even if the patient can barely tolerate sitting in a chair, a passive range of motion exercises for all joints should be undertaken daily. Additionally, active resistance exercises may be feasible for even debilitated patients if they receive daily assistance and continual encouragement. With persistence, skeletal muscles and the cardiovascular and pulmonary systems will show more endurance.#
Follow Progress
Accurately following a patient’s progress in regaining mobility requires the use of an assessment tool. The Elderly Mobility Scale (EMS) is useful for assessing improvements in mobility of elderly patients receiving physical therapy.
Balance, range of motion, and ambulation are scored initially, and the scores are updated during daily physical therapy. A review of this assessment tool was published in the Journal of Ageing this year, with the authors concluding that the EMS is a valid, reliable scale that can be readily applied during daily clinical work.7# Further, a review in Clinical Rehabilitation found the EMS to be a reliable test of motor function in elderly patients with a range of functional levels.#8 This assessment falls short in its lack of predictive validity in terms of falls or discharge destination.
Elderly patients suffer more hospital-associated falls than those younger than 65. According to a 2000 article from the British Medical Journal, patients older than 65 were seven times as likely to experience a preventable fall while in the hospital compared with younger age groups.#9
Patient factors that contribute to falls include age-related changes in postural control, impaired gait, decreased visual acuity, medications, the presence of acute and chronic diseases that affect sensory input, the central nervous system, and coordination. Osteoporosis is also an important factor—pathologic fractures often precede a fall. Environmental factors include poor lighting, obtrusive furniture, slippery floors, loose floor coverings, and bathrooms without handrails or grab bars.
The items most commonly included in fall risk-assessment tools include:10
- Comorbid patient characteristics or conditions associated with falling, such as cognitive impairment;
- History of a fall;
- Mobility impairment;
- Incontinence;
- Medications affecting balance/cognition and polypharmacy;
- Sensory deficits; and
- Advanced age.
The presence of more than three of these items identifies a patient at high risk for falling. But calculating a fall assessment includes not only identifying relevant risk factors, but also performing a focused physical exam. In ambulatory patients, the timed “get up and go” test is a useful predictor of falls. The patient is observed as she rises from a chair, walks 10 feet, then returns to the chair. If the patient requires more than 16 seconds to complete the task, he or she is at greater risk for a fall.
Early Intervention
While management depends on the underlying etiology of the fall, some generally acceptable practices are effective:
- Maintain a safe physical environment. Making sure spills are cleaned up quickly and walkways are kept free of obstruction is as important as maintaining adequate lighting in all areas where older adults will walk;
- Avoid use of restraints. Though restraints are often employed to prevent falls, they have not proved effective in medical trials. It has been demonstrated that their use increases the injury associated with falls, and several restraint-reduction projects have demonstrated that restraints can be removed without a significant increase in falls or injuries;
- Deal with medication side effects. The side effects of CNS altering drugs, and drugs affecting postural blood pressure, balance, and gait should be expected and addressed. Polypharmacy should be minimized;
- Watch patients closely. High risk patients should be positioned by the nursing station so that their visibility to the staff is maximized; and
- Promote mobility. There has been considerable research demonstrating the positive effect of exercise on reducing fall risk among community-residing older adults. While no study to date has addressed the impact of exercise in the hospital-based community, improved balance, mobility, and flexibility have been documented in nursing home residents receiving aggressive physical therapy. TH
Dr. Landis is a frequent contributor to The Hospitalist.
References
- Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, et al. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs. 2007 Jan;16(1):46-57.
- Callen BL, Mahoney JE, Wells TJ, et al. Admission and discharge mobility of frail hospitalized older adults. MedSurg Nursing 2004:13(3):156-163.
- Resnick NM, Marcantonio ER. How should clinical care of the aged differ? Lancet 2002; 350:1157-1167.
- Watters JM, McClaran JC, Man-Son-Hing M. The elderly surgical patient. ACS surgery: principles and practice. Medscape 2005.
- Miller KE, Zylstra RG, Standridge JB. The geriatric patient: a systematic approach to maintaining health. Am Fam Physician. 2000;61(4):1080-1098.
- Rydwik E, Frändin K, Akner G. Effects of physical training on physical performance in institutionalized elderly patients with multiple diagnoses. Age Ageing. 2004 Jan;33(1):13-23.
- Kuys SS , Brauer SG. Validation and reliability of the Modified Elderly Mobility Scale. Australas J Ageing 2006; 25(3):140-144.
- Spilg EG, Martin BJ, Mitchell SL, et al. A comparison of mobility assessments in a geriatric day hospital. Clin Rehabil. 2001 Jun;15(3):296-300.
- Thomas EJ, Brennan TA. Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ 2000;320(7237):741-744
- Gray-Miceli DL, Capezuti E. A nursing guide to the prevention and management of falls in geriatric patients in long-term care settings. Medscape; May 19, 2005.
As elderly patients suffering functional decline and immobility face prolonged hospital stays, placement in nursing homes, and increased risk of mortality, hospitalists must focus on one mission: Keep them moving.#1
With today’s emphasis on cost containment and quality assurance, keeping patients moving is one small step toward improving the quality of a patient’s hospitalization.
At the core of elders’ quality of life is independent mobility. When mobility is lost, a patient’s ability to socialize with peers and family, perform activities of daily living (ADLs), and participate in decisions regarding their well-being is severely compromised.
Most hospital admissions begin with the assignment of a patient to a bed. Although acute illness, medications, and a new environment all take their toll on patient functionality, simply putting a patient in recline has a significant impact.
If a young healthy person is ordered to rest for more than 72 hours, muscle mass and strength decrease, gait speed slows, and coordination becomes impaired.#2 If that patient is put to bed for more than 72 hours, organs other than the musculoskeletal system become compromised. Cardiovascular deconditioning with resting tachycardia and orthostatic hypotension, glucose intolerance, venous thromboembolism, hypercalcemia and osteoporosis, constipation and fecal impaction, pressure ulcers, and even depression can occur.3# Imagine then how elderly patients would fare.
Unfortunately, the independence of elderly patients is continually undermined by the same environment that offers treatment and care—the inpatient ward. And staff and patient family members are at fault.#4
Establish a Baseline
Teaching patients to move autonomously requires extra nursing time. Most on the nursing staff find it easier to provide a bedpan rather than assist a patient to the bathroom. When assisted ambulation is offered, patients may resist.
Families may hinder the resumption of mobility by performing tasks for patients instead of encouraging them to do them themselves. Further, changes in mobility are difficult to quantify and communicate due to limited mobility terminology in nursing practice and limited physician time. When a pre-admission functional status is not clearly documented, hospital staff often assumes that the patient’s compromised state is little changed from its baseline.
With so many barriers to patient mobility, obtaining an accurate assessment of a patient’s functional status two weeks prior to admission is key in establishing a plan for helping elderly patients regain mobility.
Ideally, one should speak to the patient as well as someone closely involved with the patient’s care who can verify or clarify the patient’s description of his or her prior activities. Significant information to obtain includes which ADLs the patient can independently perform, how far the patient can ambulate and with what assistive devices, and whether glasses, hearing aids, specially fitted shoes and orthotics, and knee braces are normally required for ambulation.#5
Though no screening tool has been validated as an absolute predictor of inpatient functional decline, lower functional status before admission, cognitive impairment, depression, advanced age, and prolonged length of hospital stay have been associated with loss of independence. Their presence may warrant a more aggressive regimen for regaining mobility.
Set the Stage
Before calling in a transfer to inpatient rehab, there are several steps one can take to maximize the return of function. By optimizing a patient’s functional capabilities during the admission, you enable them to integrate necessary skills into a daily routine—something they’re unlikely to learn at a rehabilitation center. Take these steps:6
- Control pain. Adequate analgesia is imperative for regaining mobility. Opiates and opiate agonists may be necessary for optimal control. Constipation should be expected and treated, and patients should be closely monitored for orthostasis, confusion, and urinary retention;
- Get the patient to a chair with assistive devices nearby. This includes canes, braces, walkers, orthopedic shoes, glasses, and hearing aids;
- Minimize IVs, catheters, and drains. Those that cannot be removed can be taped to minimize their interference with ambulation. Regular clothes, particularly jogging suits, promote ambulation and comfort;
- Coordinate with nursing department so the patient has periods of activity and rest. A walk down the corridor should be followed by a commensurate period of minimal activity, not a two-hour nap;
- Encourage sleep hygiene. Daytime activities can be maximized only when preceded by a restful night’s sleep. Limiting caffeinated beverages, restricting television time, and encouraging relaxing evening activities like reading may be necessary to ensure adequate sleep. Well-rested patients are better equipped to challenge themselves physically during the day and are less at risk for the side effects associated with sleeping medications;
- Give early referral to physical and occupational therapies. Even if the patient can barely tolerate sitting in a chair, a passive range of motion exercises for all joints should be undertaken daily. Additionally, active resistance exercises may be feasible for even debilitated patients if they receive daily assistance and continual encouragement. With persistence, skeletal muscles and the cardiovascular and pulmonary systems will show more endurance.#
Follow Progress
Accurately following a patient’s progress in regaining mobility requires the use of an assessment tool. The Elderly Mobility Scale (EMS) is useful for assessing improvements in mobility of elderly patients receiving physical therapy.
Balance, range of motion, and ambulation are scored initially, and the scores are updated during daily physical therapy. A review of this assessment tool was published in the Journal of Ageing this year, with the authors concluding that the EMS is a valid, reliable scale that can be readily applied during daily clinical work.7# Further, a review in Clinical Rehabilitation found the EMS to be a reliable test of motor function in elderly patients with a range of functional levels.#8 This assessment falls short in its lack of predictive validity in terms of falls or discharge destination.
Elderly patients suffer more hospital-associated falls than those younger than 65. According to a 2000 article from the British Medical Journal, patients older than 65 were seven times as likely to experience a preventable fall while in the hospital compared with younger age groups.#9
Patient factors that contribute to falls include age-related changes in postural control, impaired gait, decreased visual acuity, medications, the presence of acute and chronic diseases that affect sensory input, the central nervous system, and coordination. Osteoporosis is also an important factor—pathologic fractures often precede a fall. Environmental factors include poor lighting, obtrusive furniture, slippery floors, loose floor coverings, and bathrooms without handrails or grab bars.
The items most commonly included in fall risk-assessment tools include:10
- Comorbid patient characteristics or conditions associated with falling, such as cognitive impairment;
- History of a fall;
- Mobility impairment;
- Incontinence;
- Medications affecting balance/cognition and polypharmacy;
- Sensory deficits; and
- Advanced age.
The presence of more than three of these items identifies a patient at high risk for falling. But calculating a fall assessment includes not only identifying relevant risk factors, but also performing a focused physical exam. In ambulatory patients, the timed “get up and go” test is a useful predictor of falls. The patient is observed as she rises from a chair, walks 10 feet, then returns to the chair. If the patient requires more than 16 seconds to complete the task, he or she is at greater risk for a fall.
Early Intervention
While management depends on the underlying etiology of the fall, some generally acceptable practices are effective:
- Maintain a safe physical environment. Making sure spills are cleaned up quickly and walkways are kept free of obstruction is as important as maintaining adequate lighting in all areas where older adults will walk;
- Avoid use of restraints. Though restraints are often employed to prevent falls, they have not proved effective in medical trials. It has been demonstrated that their use increases the injury associated with falls, and several restraint-reduction projects have demonstrated that restraints can be removed without a significant increase in falls or injuries;
- Deal with medication side effects. The side effects of CNS altering drugs, and drugs affecting postural blood pressure, balance, and gait should be expected and addressed. Polypharmacy should be minimized;
- Watch patients closely. High risk patients should be positioned by the nursing station so that their visibility to the staff is maximized; and
- Promote mobility. There has been considerable research demonstrating the positive effect of exercise on reducing fall risk among community-residing older adults. While no study to date has addressed the impact of exercise in the hospital-based community, improved balance, mobility, and flexibility have been documented in nursing home residents receiving aggressive physical therapy. TH
Dr. Landis is a frequent contributor to The Hospitalist.
References
- Hoogerduijn JG, Schuurmans MJ, Duijnstee MS, et al. A systematic review of predictors and screening instruments to identify older hospitalized patients at risk for functional decline. J Clin Nurs. 2007 Jan;16(1):46-57.
- Callen BL, Mahoney JE, Wells TJ, et al. Admission and discharge mobility of frail hospitalized older adults. MedSurg Nursing 2004:13(3):156-163.
- Resnick NM, Marcantonio ER. How should clinical care of the aged differ? Lancet 2002; 350:1157-1167.
- Watters JM, McClaran JC, Man-Son-Hing M. The elderly surgical patient. ACS surgery: principles and practice. Medscape 2005.
- Miller KE, Zylstra RG, Standridge JB. The geriatric patient: a systematic approach to maintaining health. Am Fam Physician. 2000;61(4):1080-1098.
- Rydwik E, Frändin K, Akner G. Effects of physical training on physical performance in institutionalized elderly patients with multiple diagnoses. Age Ageing. 2004 Jan;33(1):13-23.
- Kuys SS , Brauer SG. Validation and reliability of the Modified Elderly Mobility Scale. Australas J Ageing 2006; 25(3):140-144.
- Spilg EG, Martin BJ, Mitchell SL, et al. A comparison of mobility assessments in a geriatric day hospital. Clin Rehabil. 2001 Jun;15(3):296-300.
- Thomas EJ, Brennan TA. Incidence and types of preventable adverse events in elderly patients: population based review of medical records. BMJ 2000;320(7237):741-744
- Gray-Miceli DL, Capezuti E. A nursing guide to the prevention and management of falls in geriatric patients in long-term care settings. Medscape; May 19, 2005.
Subtle Skills
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists with a hunger for taking on administrative roles often pursue an advanced degree. But whether it’s to assume a leadership role or just do a better job, it’s the not-altogether-obvious skills that can help hospitalists improve their careers and job satisfaction.
By refining communication styles, being receptive to mentoring, or learning how to influence decision-makers, hospitalists can convey competence to their peers and superiors. Intangible strengths such as these will help the hospitalist who wishes to carve a niche as a quality-improvement researcher, director of a medical education clerkship, patient safety officer, or medical director.
Who Needs What
The administrative skills hospitalists need depend on their career goals. Those who reflect on their career goals, identify their core values, and consider what is feasible at different stages in their lives can more quickly build the abilities they’ll need. This self-awareness is perhaps the first skill to develop.
The setting and practice model hospitalists work in also influences which skills they may need.
“Although the skills needed in different settings may be fundamentally the same, the politics differ between a community hospital and a teaching hospital,” says Sayeed Khan, MD, director of the hospitalist program of Lakeside Medical Group. “Communication skills may be even more crucial in a community hospital, where it’s less understood what a hospitalist is.” Such ability to educate people in Hospitalist 101 is yet another skill a savvy administrator or administrator-to-be should hone.
Hospitalists also need to understand quality control and other measures—and what the numbers mean.
For example, says Dr. Khan, it’s valuable to know:
- What it means to have good bed days at the end of the month and an average length of stay of 3.3 days;
- How that compares with other groups in other hospitals; and
- The implications of those measures in terms of outcomes, dollar costs, and savings to the hospital as well as the group—and how that translates for the patient.
“Those are the types of figures that many hospitalists don’t really understand,” says Dr. Khan.
But hospitalists can learn by observing and studying. “I’m a good example of that in that I do not have a formal business background,” Dr. Khan says. “Along with the literature, networking with other people, particularly at the SHM annual meeting, can help hospitalists gain a better understanding of what these numbers mean and what the benchmarks are.”
He believes administrative skills can be divided into two categories: those related to metrics (the math behind what hospitalists do) and those related to patient care.
In regard to patient care, effective committee participation is an administrative ability that can influence the standard of care. For example, Dr. Khan is participating in committee work in the area of maintaining patients’ glycemic control.
“Historically, that issue was not well addressed,” he says. It is now recognized that patients who have tight glycemic control do much better while hospitalized, irrespective of whether they have diabetes. “But it’s difficult to get other clinicians to change their practice styles,” says Dr. Khan. “You can implement change in your own practice, and others can learn by example. But if you are on a committee that designs new protocols and those get implemented, then you’ve directly changed how medicine is practiced at that hospital.”
Being able to win buy-in for your ideas makes that possible. “Purely speaking, committee participation is not an administrative role,” says Dr. Khan. “But it is an administrative skill in that it is outside the scope of what’s normally required for a hospitalist.”
Get Help
Honing one’s receptivity to mentorship is another vital ability for the upwardly mobile hospitalist. Mentors can direct inexperienced physicians to resources that may help them develop proficiency. A mentor who has grappled with the same issues can help open doors to opportunities hospitalists may not know about.
As she reflects on her early career, when she had no mentors and no administrative experience, Sylvia C.W. McKean, MD, realizes she could have used guidance and advocacy. Effective mentorship helps hospitalists reach their goals faster with fewer impediments, she says.
“Mentorship is critical,” says Dr. McKean, medical director, Brigham and Women’s Hospital/Faulkner Hospitalist Service of Brigham and Women’s Hospital in Boston. “But knowing how to receive the information you’re getting and how to apply it to your own specific professional goals can really help you develop the skills that will help you move your career forward. Informal mentorship is one area where there has been less opportunity for women in the past, resulting in more promotions for men.”
Other skills women may especially need are learning the written and unwritten rules of promotion, being more assertive in finding out what they are, and developing diplomacy—including learning to say no with finesse.
“The reality is that if you are in an environment that has predominantly male leadership, it is important for [a woman] to have male advocates to support whatever it is that you are trying to do,” says Dr. McKean. “In some instances they may have to speak for you.”
Efficiency and setting priorities are also important skills.
“I learned very early on that efficiency was critical to managing several roles—administrative, patient care, and raising three boys,” says Dr. McKean. “There were some things, however, that in retrospect I did not need to do. For example, I did my own home-improvement tasks instead of hiring someone else to do them. For women in particular, you don’t have to be a super everything. At different phases in your life your priorities will vary. Get help so that you’re not spending time doing tasks that don’t further your goals.”
Communication
Facility with communication, of course, is paramount in every aspect of medicine. Being poised, articulate, concise, and persuasive to get your message across, says Dr. McKean, goes a long way toward advancing one’s career.
“It took me a long time to realize this,” says Dr. McKean. “For example, whenever I generated reports I tried to have as much information in there as possible because I thought it would look like I was very knowledgeable. A one-page document that summarizes the key points is often more effective in getting people’s attention.”
Another subset of communication is skill at public speaking, which may lead to being invited to give lectures.
Dr. Khan believes shy, less-articulate clinicians can begin to improve their public speaking by serving on committees. “Unless the committee is a committee of two, that is the appropriate forum to begin voicing your opinions and expertise on a particular matter,” he says. “There’s a certain comfort level built into that because you’re not necessarily speaking on a topic you are unfamiliar with.”
Another intangible administrative skill, he says, is the ability to deal with people from different walks of life. Some highly placed hospital administrators don’t have clinical backgrounds and will require explanations of clinical situations that mesh with their business understanding.
Time Management
Organization is a critical administrative skill no matter what career path a hospitalist follows.
“As hospitalists we are typically juggling more than one thing at one time,” Dr. Khan says. “As a hospitalist who is involved in administrative tasks, if you’re not organized, that is a path to failure.”
Strive to hire the right people for clerical and administrative staff positions. They will fill in the weak spots to keep you on track and present a good image as your front person. But having a good clerical or administrative assistant doesn’t let you off the hook; you, too, must demonstrate solid time management. Make sure you take good notes at committees, quickly access data or documentation, and research and report back well.
The Interpersonal
Robert L. Benak, MD, a hospitalist and medical director of Champlain Valley Physicians Hospital (CVPH) Medical Center, a 341-bed acute care hospital and 54-bed skilled nursing facility in Plattsburgh, N.Y., thinks the most important intangible skills involve managing relationships.
Again, self-reflection helps. “Understand what your personality is like on a calm day and what it is like on a stressful day,” he says.
He says it’s critical to be able to negotiate with others. “Understanding what lies underneath, what common and different interests the two negotiating partners have helps you focus on getting the best compromise of conflicting interests to resolve a disagreement in an amicable and effective way,” he says.
Dr. Benak, who joined SHM around the time his group started in October 2006, thanks the SHM Leadership Academy for strengthening his interpersonal skills. He has tried to bring home what he learned to his group of five hospitalists.
Recently, he had to determine whether to designate a patient with abdominal pain as a surgical or medical patient. Dr. Benak invoked his “ability to sit down with the orthopedic surgeon and general surgeon, recognizing that they’ve got legitimate interests and concerns, as do I, and figuring out what works well for us, and more importantly, what works best for the patient.”
That ability to compromise is indispensable to growth as a hospitalist, he says.
“I was a chemistry major in college and loved working with concrete, though sometimes complicated, problems where you’re either right or you’re wrong,” he says. “I’ve come to see that giving up being right, and giving up any sense of entitlement I may feel in having the principal position, are skills. Even if you think the other person is being unreasonable, you have to accept that as a fact and figure out how to cope with that in a way that is a credit to yourself and your program.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Hospitalists on Top
Many technically skilled professionals—including computer programmers, stockbrokers, or hospitalists—aspire to the executive suite.
The burgeoning field of hospital medicine offers especially enticing rewards for business-minded doctors, inducing frontline leaders to trade the white coat for wing tips and a shot at the top.
The pinnacle can be stratospheric. Adam Singer, MD, CEO of California-based IPC-The Hospitalist Company, traded his white coat for the so-called C suite. He has since filed an initial public offering that should produce $105 million for IPC’s stakeholders.
There’s also lots of room for hospitalists with more modest executive aspirations. The skills acquired by good hospitalists—thoroughness, the ability to solve complex problems, critical thinking, strong motivation, sound work ethic, and teamwork—serve physician executives well. Some physicians back into the executive suite once they realize they’re attracted to the business end of medicine. Those are the clinicians who volunteer to do the group’s scheduling or find that they enjoy negotiating contracts with new hires and payers. Others pursue a personal road map to the C suite.
Balancing Act
The biggest decision facing a hospitalist with managerial aspirations is whether to relinquish patient care.
“For most of your career you must remain active clinically, even though your time is disjointed because you’re intensely needed in both clinical and administrative areas,” says Andrew Urbach, MD, medical director of clinical excellence and service at Children’s Hospital of Pittsburgh. He manages both by constantly adapting. His time had been evenly split between clinical and administrative duties until July, when he cut back on his clinical duties. He now spends one week every quarter as a hospitalist and a half-day a week at the clinic. “It’s difficult balancing both, and reaching the highest level of excellence in two areas is demanding,” he says. “But the best hospitalist managers continue to see patients to maintain credibility with their peers.”
Stacy Goldsholl, MD, president of Knoxville, Tenn.-based Team Health, Hospital Medicine Division, was a staff hospitalist who ceded clinical work for a managerial career. After a three-year stint as a hospitalist with Covenant HealthCare’s hospital medicine program at Covenant Medical Center in Saginaw, Mich., her mentors recruited her to “jump around the country starting hospitalist programs during 2004 and 2005,” she says. “I was in the right place at the right time, and I had the confidence to move my agenda in a diplomatic way and with humor.”
Dr. Goldsholl reluctantly gave up clinical responsibilities three years ago. “It’s all about balance in my life,” she says. “It was a conscious decision to give up patient care. I miss it, but I wanted to take my career to a national level. I travel a great deal, which isn’t compatible with patient care.”
Business School
Hospitalists attracted to management often realize they need more business schooling, says Kevin Shulman, MD, MBA, professor of medicine and management at Duke University Medical Center and the Fuqua School of Business in Durham, N.C.
“The issues in medical training are clinical, not organizational,” he says. “As you move up in administration you don’t have business skills you need. When doctors feel frustrated about not being effective organizationally, that’s when they think about business school.”
Edward Ogata, MD, MBA, chief medical officer of Children’s Memorial Hospital in Chicago, and a pediatric neonatologist, realized how useful an MBA would be as he moved from clinical work to management. “I went back to school for an MBA at Northwestern University Kellogg School of Management 27 years after graduating from medical school,” he says. Pushed by the healthcare market into negotiating managed-care contracts in the 1980s, Dr. Ogata realized he knew little about accounting and finance. The always-precarious financial situations of children’s hospitals encouraged him to get the business skills to cope.
At Kellogg, in Chicago, Dr. Ogata was assigned homework and teamwork with executives from Motorola, Lucent, and GE. The first year was difficult because he was still covering call and juggling administrative tasks. He got up at 4 a.m. every day to study. Armed with business skills, Dr. Ogata feels better equipped to meet the financial and administrative needs of his inner-city hospital. “We’re not in a nice suburb with a favorable payer mix, and a hospital isn’t really a business in the conventional sense,’’ he notes. “But we are committed to doing the best.”
For Joy Drass, MD, MBA, a critical care trauma surgeon for 13 years and president of Georgetown University Hospital in Washington, D.C., methodically performing clinical tasks prepared her for top management. She assumed the presidency of the troubled hospital in 2001, one year after MedStar Health in Columbia, Md., acquired it. The hospital had recorded losses in excess of $200 million before MedStar stepped in.
“Many skills I developed as a critical care physician had an absolute application in this stressed organization,” she says. “In medicine, it’s called triage. In business, it’s prioritizing. You look at a situation and quickly set goals to get from point A to point B, encourage team work, and develop structures to support people when they are struggling through uncertainty.” Skills she learned as a graduate of the Wharton business school in Philadelphia helped her stabilize hospital operations, improve customer service and revenue collection, and develop a long-term strategic plan to improve the hospital’s chances of survival.
Varied Paths
Some hospitalists acquire business smarts from instinct and experience. When he was 13 years old, Dr. Urbach ran his family’s retail business for weeks at a time when his parents were away.
“I’ve had no formal [business] school training, but my entrepreneurial instincts and management skills were honed early in life,” he says.
Team Health’s Dr. Goldsholl intended to get a formal MBA, but was too busy. “SHM’s Leadership Academy and other programs gave me management skills, and I chose CME credits in business and management areas,” she says. “I’m also more of an experiential than a classroom learner. Mentoring and other informal settings work for me.”
Michael Ruhlen, MD, MHM, Toledo (Ohio) Children’s Hospital corporate vice president of medical informatics and vice president of medical affairs, made a successful if not easy move from clinician to manager. Acting as a hospitalist seven years before the discipline was named in 1996, he developed systematic, data-driven clinical pathways and trained other would-be pediatric hospitalists in acute care pediatrics. In 2001 he was the first recipient of the National Association of Inpatient Physician’s Award for Outstanding Service in Hospital Medicine. The award recognized his managerial skill in building a hospitalist program from scratch.
Unlike hospitalists who are moving from well-defined clinical tracks to managerial roles, Dr. Ruhlen operated in uncharted territory in his first decade as a hospitalist. From the beginning of his hospitalist career, Dr. Ruhlen’s business head identified volume-dependent competency as critical to clinical and financial success. “I saw how to create time and quality efficiencies,” he explains. “If you do one or two lumbar punctures a year, you might stick a child five or six times. Doing a higher volume of procedures led to smoother operations.”
Recognizing the complexities of hospital management, Dr. Ruhlen returned to school to sharpen his management skills. He chose the Harvard School of Public Health’s master’s in healthcare management over an MBA because, as he puts it, “I’m interested in managing a hospital, not running Campbell’s Soup.” As a hospitalist executive, he works on improving the hospital’s IT systems, developing new physician leaders, and taking the lead on change management and patient safety issues. He also has been tapped twice to serve as acting hospital president.
Medicine as Business
Hospitalists enjoy an array of career choices. Those who savor the pure joy of clinical work can continue on that path, while others can choose a career in management; some can blend both. No matter what their career paths, healthcare’s increasing complexity will keep them fully occupied.
“As medicine grows more complex, students spend their time mastering clinical issues,” Dr. Shulman notes. “Many third-year med students don’t even know the difference between Medicaid and Medicare. As they practice as hospitalists and want to move up the administrative ranks, they will acquire the general business skills that will help them be effective and reshape healthcare policy.” TH
Marlene Piturro is a medical writer based in New York.
Many technically skilled professionals—including computer programmers, stockbrokers, or hospitalists—aspire to the executive suite.
The burgeoning field of hospital medicine offers especially enticing rewards for business-minded doctors, inducing frontline leaders to trade the white coat for wing tips and a shot at the top.
The pinnacle can be stratospheric. Adam Singer, MD, CEO of California-based IPC-The Hospitalist Company, traded his white coat for the so-called C suite. He has since filed an initial public offering that should produce $105 million for IPC’s stakeholders.
There’s also lots of room for hospitalists with more modest executive aspirations. The skills acquired by good hospitalists—thoroughness, the ability to solve complex problems, critical thinking, strong motivation, sound work ethic, and teamwork—serve physician executives well. Some physicians back into the executive suite once they realize they’re attracted to the business end of medicine. Those are the clinicians who volunteer to do the group’s scheduling or find that they enjoy negotiating contracts with new hires and payers. Others pursue a personal road map to the C suite.
Balancing Act
The biggest decision facing a hospitalist with managerial aspirations is whether to relinquish patient care.
“For most of your career you must remain active clinically, even though your time is disjointed because you’re intensely needed in both clinical and administrative areas,” says Andrew Urbach, MD, medical director of clinical excellence and service at Children’s Hospital of Pittsburgh. He manages both by constantly adapting. His time had been evenly split between clinical and administrative duties until July, when he cut back on his clinical duties. He now spends one week every quarter as a hospitalist and a half-day a week at the clinic. “It’s difficult balancing both, and reaching the highest level of excellence in two areas is demanding,” he says. “But the best hospitalist managers continue to see patients to maintain credibility with their peers.”
Stacy Goldsholl, MD, president of Knoxville, Tenn.-based Team Health, Hospital Medicine Division, was a staff hospitalist who ceded clinical work for a managerial career. After a three-year stint as a hospitalist with Covenant HealthCare’s hospital medicine program at Covenant Medical Center in Saginaw, Mich., her mentors recruited her to “jump around the country starting hospitalist programs during 2004 and 2005,” she says. “I was in the right place at the right time, and I had the confidence to move my agenda in a diplomatic way and with humor.”
Dr. Goldsholl reluctantly gave up clinical responsibilities three years ago. “It’s all about balance in my life,” she says. “It was a conscious decision to give up patient care. I miss it, but I wanted to take my career to a national level. I travel a great deal, which isn’t compatible with patient care.”
Business School
Hospitalists attracted to management often realize they need more business schooling, says Kevin Shulman, MD, MBA, professor of medicine and management at Duke University Medical Center and the Fuqua School of Business in Durham, N.C.
“The issues in medical training are clinical, not organizational,” he says. “As you move up in administration you don’t have business skills you need. When doctors feel frustrated about not being effective organizationally, that’s when they think about business school.”
Edward Ogata, MD, MBA, chief medical officer of Children’s Memorial Hospital in Chicago, and a pediatric neonatologist, realized how useful an MBA would be as he moved from clinical work to management. “I went back to school for an MBA at Northwestern University Kellogg School of Management 27 years after graduating from medical school,” he says. Pushed by the healthcare market into negotiating managed-care contracts in the 1980s, Dr. Ogata realized he knew little about accounting and finance. The always-precarious financial situations of children’s hospitals encouraged him to get the business skills to cope.
At Kellogg, in Chicago, Dr. Ogata was assigned homework and teamwork with executives from Motorola, Lucent, and GE. The first year was difficult because he was still covering call and juggling administrative tasks. He got up at 4 a.m. every day to study. Armed with business skills, Dr. Ogata feels better equipped to meet the financial and administrative needs of his inner-city hospital. “We’re not in a nice suburb with a favorable payer mix, and a hospital isn’t really a business in the conventional sense,’’ he notes. “But we are committed to doing the best.”
For Joy Drass, MD, MBA, a critical care trauma surgeon for 13 years and president of Georgetown University Hospital in Washington, D.C., methodically performing clinical tasks prepared her for top management. She assumed the presidency of the troubled hospital in 2001, one year after MedStar Health in Columbia, Md., acquired it. The hospital had recorded losses in excess of $200 million before MedStar stepped in.
“Many skills I developed as a critical care physician had an absolute application in this stressed organization,” she says. “In medicine, it’s called triage. In business, it’s prioritizing. You look at a situation and quickly set goals to get from point A to point B, encourage team work, and develop structures to support people when they are struggling through uncertainty.” Skills she learned as a graduate of the Wharton business school in Philadelphia helped her stabilize hospital operations, improve customer service and revenue collection, and develop a long-term strategic plan to improve the hospital’s chances of survival.
Varied Paths
Some hospitalists acquire business smarts from instinct and experience. When he was 13 years old, Dr. Urbach ran his family’s retail business for weeks at a time when his parents were away.
“I’ve had no formal [business] school training, but my entrepreneurial instincts and management skills were honed early in life,” he says.
Team Health’s Dr. Goldsholl intended to get a formal MBA, but was too busy. “SHM’s Leadership Academy and other programs gave me management skills, and I chose CME credits in business and management areas,” she says. “I’m also more of an experiential than a classroom learner. Mentoring and other informal settings work for me.”
Michael Ruhlen, MD, MHM, Toledo (Ohio) Children’s Hospital corporate vice president of medical informatics and vice president of medical affairs, made a successful if not easy move from clinician to manager. Acting as a hospitalist seven years before the discipline was named in 1996, he developed systematic, data-driven clinical pathways and trained other would-be pediatric hospitalists in acute care pediatrics. In 2001 he was the first recipient of the National Association of Inpatient Physician’s Award for Outstanding Service in Hospital Medicine. The award recognized his managerial skill in building a hospitalist program from scratch.
Unlike hospitalists who are moving from well-defined clinical tracks to managerial roles, Dr. Ruhlen operated in uncharted territory in his first decade as a hospitalist. From the beginning of his hospitalist career, Dr. Ruhlen’s business head identified volume-dependent competency as critical to clinical and financial success. “I saw how to create time and quality efficiencies,” he explains. “If you do one or two lumbar punctures a year, you might stick a child five or six times. Doing a higher volume of procedures led to smoother operations.”
Recognizing the complexities of hospital management, Dr. Ruhlen returned to school to sharpen his management skills. He chose the Harvard School of Public Health’s master’s in healthcare management over an MBA because, as he puts it, “I’m interested in managing a hospital, not running Campbell’s Soup.” As a hospitalist executive, he works on improving the hospital’s IT systems, developing new physician leaders, and taking the lead on change management and patient safety issues. He also has been tapped twice to serve as acting hospital president.
Medicine as Business
Hospitalists enjoy an array of career choices. Those who savor the pure joy of clinical work can continue on that path, while others can choose a career in management; some can blend both. No matter what their career paths, healthcare’s increasing complexity will keep them fully occupied.
“As medicine grows more complex, students spend their time mastering clinical issues,” Dr. Shulman notes. “Many third-year med students don’t even know the difference between Medicaid and Medicare. As they practice as hospitalists and want to move up the administrative ranks, they will acquire the general business skills that will help them be effective and reshape healthcare policy.” TH
Marlene Piturro is a medical writer based in New York.
Many technically skilled professionals—including computer programmers, stockbrokers, or hospitalists—aspire to the executive suite.
The burgeoning field of hospital medicine offers especially enticing rewards for business-minded doctors, inducing frontline leaders to trade the white coat for wing tips and a shot at the top.
The pinnacle can be stratospheric. Adam Singer, MD, CEO of California-based IPC-The Hospitalist Company, traded his white coat for the so-called C suite. He has since filed an initial public offering that should produce $105 million for IPC’s stakeholders.
There’s also lots of room for hospitalists with more modest executive aspirations. The skills acquired by good hospitalists—thoroughness, the ability to solve complex problems, critical thinking, strong motivation, sound work ethic, and teamwork—serve physician executives well. Some physicians back into the executive suite once they realize they’re attracted to the business end of medicine. Those are the clinicians who volunteer to do the group’s scheduling or find that they enjoy negotiating contracts with new hires and payers. Others pursue a personal road map to the C suite.
Balancing Act
The biggest decision facing a hospitalist with managerial aspirations is whether to relinquish patient care.
“For most of your career you must remain active clinically, even though your time is disjointed because you’re intensely needed in both clinical and administrative areas,” says Andrew Urbach, MD, medical director of clinical excellence and service at Children’s Hospital of Pittsburgh. He manages both by constantly adapting. His time had been evenly split between clinical and administrative duties until July, when he cut back on his clinical duties. He now spends one week every quarter as a hospitalist and a half-day a week at the clinic. “It’s difficult balancing both, and reaching the highest level of excellence in two areas is demanding,” he says. “But the best hospitalist managers continue to see patients to maintain credibility with their peers.”
Stacy Goldsholl, MD, president of Knoxville, Tenn.-based Team Health, Hospital Medicine Division, was a staff hospitalist who ceded clinical work for a managerial career. After a three-year stint as a hospitalist with Covenant HealthCare’s hospital medicine program at Covenant Medical Center in Saginaw, Mich., her mentors recruited her to “jump around the country starting hospitalist programs during 2004 and 2005,” she says. “I was in the right place at the right time, and I had the confidence to move my agenda in a diplomatic way and with humor.”
Dr. Goldsholl reluctantly gave up clinical responsibilities three years ago. “It’s all about balance in my life,” she says. “It was a conscious decision to give up patient care. I miss it, but I wanted to take my career to a national level. I travel a great deal, which isn’t compatible with patient care.”
Business School
Hospitalists attracted to management often realize they need more business schooling, says Kevin Shulman, MD, MBA, professor of medicine and management at Duke University Medical Center and the Fuqua School of Business in Durham, N.C.
“The issues in medical training are clinical, not organizational,” he says. “As you move up in administration you don’t have business skills you need. When doctors feel frustrated about not being effective organizationally, that’s when they think about business school.”
Edward Ogata, MD, MBA, chief medical officer of Children’s Memorial Hospital in Chicago, and a pediatric neonatologist, realized how useful an MBA would be as he moved from clinical work to management. “I went back to school for an MBA at Northwestern University Kellogg School of Management 27 years after graduating from medical school,” he says. Pushed by the healthcare market into negotiating managed-care contracts in the 1980s, Dr. Ogata realized he knew little about accounting and finance. The always-precarious financial situations of children’s hospitals encouraged him to get the business skills to cope.
At Kellogg, in Chicago, Dr. Ogata was assigned homework and teamwork with executives from Motorola, Lucent, and GE. The first year was difficult because he was still covering call and juggling administrative tasks. He got up at 4 a.m. every day to study. Armed with business skills, Dr. Ogata feels better equipped to meet the financial and administrative needs of his inner-city hospital. “We’re not in a nice suburb with a favorable payer mix, and a hospital isn’t really a business in the conventional sense,’’ he notes. “But we are committed to doing the best.”
For Joy Drass, MD, MBA, a critical care trauma surgeon for 13 years and president of Georgetown University Hospital in Washington, D.C., methodically performing clinical tasks prepared her for top management. She assumed the presidency of the troubled hospital in 2001, one year after MedStar Health in Columbia, Md., acquired it. The hospital had recorded losses in excess of $200 million before MedStar stepped in.
“Many skills I developed as a critical care physician had an absolute application in this stressed organization,” she says. “In medicine, it’s called triage. In business, it’s prioritizing. You look at a situation and quickly set goals to get from point A to point B, encourage team work, and develop structures to support people when they are struggling through uncertainty.” Skills she learned as a graduate of the Wharton business school in Philadelphia helped her stabilize hospital operations, improve customer service and revenue collection, and develop a long-term strategic plan to improve the hospital’s chances of survival.
Varied Paths
Some hospitalists acquire business smarts from instinct and experience. When he was 13 years old, Dr. Urbach ran his family’s retail business for weeks at a time when his parents were away.
“I’ve had no formal [business] school training, but my entrepreneurial instincts and management skills were honed early in life,” he says.
Team Health’s Dr. Goldsholl intended to get a formal MBA, but was too busy. “SHM’s Leadership Academy and other programs gave me management skills, and I chose CME credits in business and management areas,” she says. “I’m also more of an experiential than a classroom learner. Mentoring and other informal settings work for me.”
Michael Ruhlen, MD, MHM, Toledo (Ohio) Children’s Hospital corporate vice president of medical informatics and vice president of medical affairs, made a successful if not easy move from clinician to manager. Acting as a hospitalist seven years before the discipline was named in 1996, he developed systematic, data-driven clinical pathways and trained other would-be pediatric hospitalists in acute care pediatrics. In 2001 he was the first recipient of the National Association of Inpatient Physician’s Award for Outstanding Service in Hospital Medicine. The award recognized his managerial skill in building a hospitalist program from scratch.
Unlike hospitalists who are moving from well-defined clinical tracks to managerial roles, Dr. Ruhlen operated in uncharted territory in his first decade as a hospitalist. From the beginning of his hospitalist career, Dr. Ruhlen’s business head identified volume-dependent competency as critical to clinical and financial success. “I saw how to create time and quality efficiencies,” he explains. “If you do one or two lumbar punctures a year, you might stick a child five or six times. Doing a higher volume of procedures led to smoother operations.”
Recognizing the complexities of hospital management, Dr. Ruhlen returned to school to sharpen his management skills. He chose the Harvard School of Public Health’s master’s in healthcare management over an MBA because, as he puts it, “I’m interested in managing a hospital, not running Campbell’s Soup.” As a hospitalist executive, he works on improving the hospital’s IT systems, developing new physician leaders, and taking the lead on change management and patient safety issues. He also has been tapped twice to serve as acting hospital president.
Medicine as Business
Hospitalists enjoy an array of career choices. Those who savor the pure joy of clinical work can continue on that path, while others can choose a career in management; some can blend both. No matter what their career paths, healthcare’s increasing complexity will keep them fully occupied.
“As medicine grows more complex, students spend their time mastering clinical issues,” Dr. Shulman notes. “Many third-year med students don’t even know the difference between Medicaid and Medicare. As they practice as hospitalists and want to move up the administrative ranks, they will acquire the general business skills that will help them be effective and reshape healthcare policy.” TH
Marlene Piturro is a medical writer based in New York.
Safety Sentries
At Mercy Hospital in Iowa City, Iowa, the implementation of safety and quality systems is “stirring up the pot,” says Mercy hospitalist and medical director Martin Izakovic, MD.
He has been recruited to supervise Mercy’s latest safety initiatives, including electronic medical records, pay-for-performance measures, development of treatment protocols, standardization of care, and deep-vein thrombosis prophylaxis.
Hospitalists at Mercy face the challenges their peers around the country face in their quest to improve quality and safeguard patients. The leader in these areas needs to be a role model and respected peer for the physicians he or she must lead day after day, says Dr. Izakovic.
How do hospitalists, who are so well-positioned to become leaders in patient safety, develop in that direction?
“The biggest challenge I see is the spectrum of polarization between clinicians and administrators,” he says. “One of the most important qualities that a patient safety officer needs is the ability to overbridge the doctors on one hand and the administrators on the other.”
What They Need
A patient safety officer (PSO) requires a critical mix of clinical and administrative skills, says Peter B. Angood, MD, vice president and chief patient safety officer for The Joint Commission, in Oakbrook, Ill.
On the clinical side, the hospitalist who wishes to be a PSO needs more than awareness of safety and quality improvement processes. He or she must be knowledgeable about and conversant in safety science in industries beyond healthcare. That expertise needs to encompass leadership, behaviors and cultures, human factors, and process redesign or systems engineering. Important, too, is training in how to corral the pieces of an organization and ensure they operate well together.
An understanding of organizational behavior is of great value. The potential PSO should understand how the key players interact: the board of directors with chief executives, chief executives with senior management, senior management with all staff (including the allied professionals), and medical staff with the organization as a whole.
“Because safety is a systemwide process, the patient safety [person] is pivotal in forming a hub from which much of the quality, safety, and process improvement occurs,” says Dr. Angood.
Jason Adelman, MD, MS, former hospitalist and current PSO at Montefiore Medical Center in New York City, says developing patient safety leaders should embrace technology. “Pay attention to the latest and greatest ideas, products, and services,” he urges. “Come up with strategic plans to implement in healthcare, get the information quickly into the hands of physicians, have physicians report, and include forcing functions [whereby computers will not process to completion when key data are missing].”
Above all, the patient safety officer must train to be a change agent. “Influencing patient safety means you have to be there in the capital-allocation process,” says David Shulkin, MD, chief executive officer at Beth Israel Medical Center in New York City. “You have to be there when they’re designing facilities. You have to understand your human resource policies and the skill sets and aptitudes of the people that the hospital is hiring. To be a good patient safety officer, the training needs to involve broad exposure with a slant toward operations.”
Build a Bridge
As a young physician who wanted to develop as a leader in the field of quality and safety, Dr. Shulkin had to forge his own path. In 1992, after he became chief medical officer (CMO) at the Hospital of the University of Pennsylvania in Philadelphia, he fielded several inquiries a month from young physicians who wanted to pursue a similar career. In response to that need, he designed a quality improvement/patient safety fellowship at his school.
David Bernard, MD, now chief medical officer at Beth Israel, had been practicing medicine for 30 years when at age 50 he took a year’s leave of absence from Boston University and enrolled as Dr. Shulkin’s first fellow in 1994. Dr. Bernard, a nephrologist, was a vice dean in the school of medicine at Boston University Medical Center, a hospital vice president for clinical affairs, and a senior clinician in his specialty group.
Drs. Shulkin and Bernard left the University of Pennsylvania in 1999 to take the concepts of quality transparency to a higher level and formed DoctorQuality Inc. in Conshohocken, Pa. To continue their work, DoctorQuality funded the fellowship. In 2005 when Dr. Shulkin went to Beth Israel in New York, the fellowship was restarted as the Don Hoskins Quality Improvement/Patient Safety program and funded for five years with private philanthropy.
Modeled after graduate medical education, the fellowship is predominantly hands-on. Fellows work on real projects alongside professionals in management, quality, and safety.
Under the Hood
Giving trainees the inside view into the intricacies of how to change physician behavior and cultural issues in hospitals is the backbone of Beth Israel’s program. Fellows see what clinicians rarely see: the real-world complexity of hospitals, why there is so much inertia, and the reasons changing systems can be so difficult. Fellows learn how almost every hospital issue involves financial, personnel, facility, policy and political considerations. By allowing entrée into the executive offices, the fellow gets to hear the many different perspectives when people react to an issue.
“After a quality-improvement meeting, for instance, where people are positioning and requesting different things rather than taking action,” says Dr. Shulkin, “the fellow gets to hear the behind-the-scenes analysis—how executives sometimes label people and develop strategies to overcome some of these barriers.”
Understanding how administrators, directors of social work, or nurses, for instance, view situations and understand their culture helps the leader be more effective.
“To get both leadership and clinician buy-in, and to get leadership to motivate clinicians to participate in system changes, you also need to be politically savvy,” says Dr. Adelman. “Plenty of people resist change. The PSO needs to come off as sincere, passionate, and smart, and has to be able to answer people’s tough questions.”
It can take an ambassador’s touch to make headway in the traditional physician culture.
“The patient safety officers, the chief medical officers, often have to function as diplomats,” says Dr. Angood. “This physician engagement piece is one of the most complicated issues out there, and it arises because physicians historically are trained to be autonomous, to be independent, and to expect that institutions are there to serve them.”
—Latha Sivaprasad, MD, Don Hoskins Quality Improvement/Patient Safety fellow, Beth Israel Medical Center, New York City
One Hospitalist’s View
When Latha Sivaprasad, MD, current Don Hoskins fellow at Beth Israel, started her fellowship six months ago, she was astonished how little she knew about patient safety and quality. Although she felt she knew the day-to-day deficiencies in the hospital and on the front line—and despite having practiced in three other hospitals—she wasn’t prepared to learn what she hadn’t known she didn’t know.
“In my five years as a hospitalist, I knew very little about patient safety and quality—to my shock now,” she says. “Since I’ve been a fellow here, I realize how much I had been underutilized and how much more I could have contributed to making my respective hospitals run more safely.”
Understanding people’s motivations and meeting their needs to make a hospital safer is an intricate process.
“I think it is important for hospitalists to understand how complicated and time-consuming system changes are,” she says. “You do not have that perspective as a clinician. You think that change can occur from a memo or from good intentions to do the right thing.”
She has learned to think about the bigger world outside the clinical portion of running a hospital.
“To be a change agent you really need to appreciate the hospital from the penthouse view, which is what this fellowship provides,” she says. “You need to have access to every meeting, every record, every clinician, and every senior executive to put the pieces of the puzzle together to understand how things change.”
The hospital is working to apply the Toyota method of employee involvement to the issue of how an obstetric patient progresses from triage in the emergency department (ED) to labor and delivery, and how much time passes before the triage the patient is discharged or admitted. Their focus first targeted convening the right group to discuss the issue and identify the details of the problem, then put a plan in place to track ED triage. They looked for ways to make that process more efficient, met again to determine how to implement a new version of that process, then tracked the difference. “All of this was a multihour ordeal,” she says.
It’s exhilarating, frustrating, and intriguing—and sometimes discouraging. “It’s very tedious making change, and I didn’t appreciate that before the fellowship,” she says.
Dr. Sivaprasad advises hospitalists that to be effective in patient safety efforts means being a problem solver, highly empathetic, sensitive to others, and above all, extremely patient. But results often emerge slowly.
“You must have several things brewing at once because if certain programs’ changes are taking time, you need to complete the loop on something else,” she advises.
The Ideal Candidate
Of the 20 fellows Dr. Shulkin has mentored, about half were older and more experienced than he was. Reflecting on the successful fellows and those who benefited less makes him think the distinction of experience and age is less important than the individual’s personality.
“What is important is the personality and motivation and self-directedness of the fellow,” says Dr. Shulkin. “This is a very autonomous fellowship. One of the pluses and minuses of working with senior executives is that they are very busy; they don’t have time the way traditional academic program directors or residency directors do to think, ‘Where are my fellows and what are they doing?’”
Those who will get the most out of this type of experience know how to be delicately assertive yet drive their own agendas.
To Drs. Shulkin and Bernard, a good patient safety leader is naturally curious about what makes healthcare organizations tick. The ideal candidate has an appreciation for hospital financing and the science behind physician behavior change, and the capacity to be a good listener. The trainee also needs to put aside his or her ego while transitioning from a physician in charge to stepping back into the student role to learn the new language and environment.
—David Shulkin, MD, chief executive officer, Beth Israel Medical Center, New York City
Where to Begin
The institution sponsoring the development of the patient safety officer is just as important as who that candidate is.
“The administration has to have a visionary leadership that recognizes that healthcare quality and safety is the way you do business,” says Dr. Bernard. “You have to be in an institution that is not just paying lip service to moving quality and safety. It has to be part of the fabric of the institution.”
The institution also has to be able to offer a variety of experiences, making this kind of training difficult in a nonacademic setting.
For those interested in pursuing this area of leadership, the natural first step is to meet with the CMO or CEO to explore whether the individual’s and hospital’s interests can be aligned.
“But you can’t force it,” warns Dr. Shulkin. “If that is not a natural fit, if the CMO or CEO doesn’t see their role as, or have an interest in, training faculty people; or if they don’t have the expertise to do it, it’s not going to be a good experience. In those cases, the hospitalist should look elsewhere. An increasing number of centers can offer this kind of experience for a year,” he says. “Then the hospitalist might return to their institution to take on a leadership role there.”
Creating a costly infrastructure to train a patient safety officer is not required. What is necessary is chemistry in the mentor-trainee relationship.
“This is the first time in my postgraduate career that I actually have consistently committed mentors who care about how I am molded as a physician and what my ultimate contribution to the medical field will be,” says Dr. Sivaprasad. TH
Andrea Sattinger is a medical writer based in North Carolina.
At Mercy Hospital in Iowa City, Iowa, the implementation of safety and quality systems is “stirring up the pot,” says Mercy hospitalist and medical director Martin Izakovic, MD.
He has been recruited to supervise Mercy’s latest safety initiatives, including electronic medical records, pay-for-performance measures, development of treatment protocols, standardization of care, and deep-vein thrombosis prophylaxis.
Hospitalists at Mercy face the challenges their peers around the country face in their quest to improve quality and safeguard patients. The leader in these areas needs to be a role model and respected peer for the physicians he or she must lead day after day, says Dr. Izakovic.
How do hospitalists, who are so well-positioned to become leaders in patient safety, develop in that direction?
“The biggest challenge I see is the spectrum of polarization between clinicians and administrators,” he says. “One of the most important qualities that a patient safety officer needs is the ability to overbridge the doctors on one hand and the administrators on the other.”
What They Need
A patient safety officer (PSO) requires a critical mix of clinical and administrative skills, says Peter B. Angood, MD, vice president and chief patient safety officer for The Joint Commission, in Oakbrook, Ill.
On the clinical side, the hospitalist who wishes to be a PSO needs more than awareness of safety and quality improvement processes. He or she must be knowledgeable about and conversant in safety science in industries beyond healthcare. That expertise needs to encompass leadership, behaviors and cultures, human factors, and process redesign or systems engineering. Important, too, is training in how to corral the pieces of an organization and ensure they operate well together.
An understanding of organizational behavior is of great value. The potential PSO should understand how the key players interact: the board of directors with chief executives, chief executives with senior management, senior management with all staff (including the allied professionals), and medical staff with the organization as a whole.
“Because safety is a systemwide process, the patient safety [person] is pivotal in forming a hub from which much of the quality, safety, and process improvement occurs,” says Dr. Angood.
Jason Adelman, MD, MS, former hospitalist and current PSO at Montefiore Medical Center in New York City, says developing patient safety leaders should embrace technology. “Pay attention to the latest and greatest ideas, products, and services,” he urges. “Come up with strategic plans to implement in healthcare, get the information quickly into the hands of physicians, have physicians report, and include forcing functions [whereby computers will not process to completion when key data are missing].”
Above all, the patient safety officer must train to be a change agent. “Influencing patient safety means you have to be there in the capital-allocation process,” says David Shulkin, MD, chief executive officer at Beth Israel Medical Center in New York City. “You have to be there when they’re designing facilities. You have to understand your human resource policies and the skill sets and aptitudes of the people that the hospital is hiring. To be a good patient safety officer, the training needs to involve broad exposure with a slant toward operations.”
Build a Bridge
As a young physician who wanted to develop as a leader in the field of quality and safety, Dr. Shulkin had to forge his own path. In 1992, after he became chief medical officer (CMO) at the Hospital of the University of Pennsylvania in Philadelphia, he fielded several inquiries a month from young physicians who wanted to pursue a similar career. In response to that need, he designed a quality improvement/patient safety fellowship at his school.
David Bernard, MD, now chief medical officer at Beth Israel, had been practicing medicine for 30 years when at age 50 he took a year’s leave of absence from Boston University and enrolled as Dr. Shulkin’s first fellow in 1994. Dr. Bernard, a nephrologist, was a vice dean in the school of medicine at Boston University Medical Center, a hospital vice president for clinical affairs, and a senior clinician in his specialty group.
Drs. Shulkin and Bernard left the University of Pennsylvania in 1999 to take the concepts of quality transparency to a higher level and formed DoctorQuality Inc. in Conshohocken, Pa. To continue their work, DoctorQuality funded the fellowship. In 2005 when Dr. Shulkin went to Beth Israel in New York, the fellowship was restarted as the Don Hoskins Quality Improvement/Patient Safety program and funded for five years with private philanthropy.
Modeled after graduate medical education, the fellowship is predominantly hands-on. Fellows work on real projects alongside professionals in management, quality, and safety.
Under the Hood
Giving trainees the inside view into the intricacies of how to change physician behavior and cultural issues in hospitals is the backbone of Beth Israel’s program. Fellows see what clinicians rarely see: the real-world complexity of hospitals, why there is so much inertia, and the reasons changing systems can be so difficult. Fellows learn how almost every hospital issue involves financial, personnel, facility, policy and political considerations. By allowing entrée into the executive offices, the fellow gets to hear the many different perspectives when people react to an issue.
“After a quality-improvement meeting, for instance, where people are positioning and requesting different things rather than taking action,” says Dr. Shulkin, “the fellow gets to hear the behind-the-scenes analysis—how executives sometimes label people and develop strategies to overcome some of these barriers.”
Understanding how administrators, directors of social work, or nurses, for instance, view situations and understand their culture helps the leader be more effective.
“To get both leadership and clinician buy-in, and to get leadership to motivate clinicians to participate in system changes, you also need to be politically savvy,” says Dr. Adelman. “Plenty of people resist change. The PSO needs to come off as sincere, passionate, and smart, and has to be able to answer people’s tough questions.”
It can take an ambassador’s touch to make headway in the traditional physician culture.
“The patient safety officers, the chief medical officers, often have to function as diplomats,” says Dr. Angood. “This physician engagement piece is one of the most complicated issues out there, and it arises because physicians historically are trained to be autonomous, to be independent, and to expect that institutions are there to serve them.”
—Latha Sivaprasad, MD, Don Hoskins Quality Improvement/Patient Safety fellow, Beth Israel Medical Center, New York City
One Hospitalist’s View
When Latha Sivaprasad, MD, current Don Hoskins fellow at Beth Israel, started her fellowship six months ago, she was astonished how little she knew about patient safety and quality. Although she felt she knew the day-to-day deficiencies in the hospital and on the front line—and despite having practiced in three other hospitals—she wasn’t prepared to learn what she hadn’t known she didn’t know.
“In my five years as a hospitalist, I knew very little about patient safety and quality—to my shock now,” she says. “Since I’ve been a fellow here, I realize how much I had been underutilized and how much more I could have contributed to making my respective hospitals run more safely.”
Understanding people’s motivations and meeting their needs to make a hospital safer is an intricate process.
“I think it is important for hospitalists to understand how complicated and time-consuming system changes are,” she says. “You do not have that perspective as a clinician. You think that change can occur from a memo or from good intentions to do the right thing.”
She has learned to think about the bigger world outside the clinical portion of running a hospital.
“To be a change agent you really need to appreciate the hospital from the penthouse view, which is what this fellowship provides,” she says. “You need to have access to every meeting, every record, every clinician, and every senior executive to put the pieces of the puzzle together to understand how things change.”
The hospital is working to apply the Toyota method of employee involvement to the issue of how an obstetric patient progresses from triage in the emergency department (ED) to labor and delivery, and how much time passes before the triage the patient is discharged or admitted. Their focus first targeted convening the right group to discuss the issue and identify the details of the problem, then put a plan in place to track ED triage. They looked for ways to make that process more efficient, met again to determine how to implement a new version of that process, then tracked the difference. “All of this was a multihour ordeal,” she says.
It’s exhilarating, frustrating, and intriguing—and sometimes discouraging. “It’s very tedious making change, and I didn’t appreciate that before the fellowship,” she says.
Dr. Sivaprasad advises hospitalists that to be effective in patient safety efforts means being a problem solver, highly empathetic, sensitive to others, and above all, extremely patient. But results often emerge slowly.
“You must have several things brewing at once because if certain programs’ changes are taking time, you need to complete the loop on something else,” she advises.
The Ideal Candidate
Of the 20 fellows Dr. Shulkin has mentored, about half were older and more experienced than he was. Reflecting on the successful fellows and those who benefited less makes him think the distinction of experience and age is less important than the individual’s personality.
“What is important is the personality and motivation and self-directedness of the fellow,” says Dr. Shulkin. “This is a very autonomous fellowship. One of the pluses and minuses of working with senior executives is that they are very busy; they don’t have time the way traditional academic program directors or residency directors do to think, ‘Where are my fellows and what are they doing?’”
Those who will get the most out of this type of experience know how to be delicately assertive yet drive their own agendas.
To Drs. Shulkin and Bernard, a good patient safety leader is naturally curious about what makes healthcare organizations tick. The ideal candidate has an appreciation for hospital financing and the science behind physician behavior change, and the capacity to be a good listener. The trainee also needs to put aside his or her ego while transitioning from a physician in charge to stepping back into the student role to learn the new language and environment.
—David Shulkin, MD, chief executive officer, Beth Israel Medical Center, New York City
Where to Begin
The institution sponsoring the development of the patient safety officer is just as important as who that candidate is.
“The administration has to have a visionary leadership that recognizes that healthcare quality and safety is the way you do business,” says Dr. Bernard. “You have to be in an institution that is not just paying lip service to moving quality and safety. It has to be part of the fabric of the institution.”
The institution also has to be able to offer a variety of experiences, making this kind of training difficult in a nonacademic setting.
For those interested in pursuing this area of leadership, the natural first step is to meet with the CMO or CEO to explore whether the individual’s and hospital’s interests can be aligned.
“But you can’t force it,” warns Dr. Shulkin. “If that is not a natural fit, if the CMO or CEO doesn’t see their role as, or have an interest in, training faculty people; or if they don’t have the expertise to do it, it’s not going to be a good experience. In those cases, the hospitalist should look elsewhere. An increasing number of centers can offer this kind of experience for a year,” he says. “Then the hospitalist might return to their institution to take on a leadership role there.”
Creating a costly infrastructure to train a patient safety officer is not required. What is necessary is chemistry in the mentor-trainee relationship.
“This is the first time in my postgraduate career that I actually have consistently committed mentors who care about how I am molded as a physician and what my ultimate contribution to the medical field will be,” says Dr. Sivaprasad. TH
Andrea Sattinger is a medical writer based in North Carolina.
At Mercy Hospital in Iowa City, Iowa, the implementation of safety and quality systems is “stirring up the pot,” says Mercy hospitalist and medical director Martin Izakovic, MD.
He has been recruited to supervise Mercy’s latest safety initiatives, including electronic medical records, pay-for-performance measures, development of treatment protocols, standardization of care, and deep-vein thrombosis prophylaxis.
Hospitalists at Mercy face the challenges their peers around the country face in their quest to improve quality and safeguard patients. The leader in these areas needs to be a role model and respected peer for the physicians he or she must lead day after day, says Dr. Izakovic.
How do hospitalists, who are so well-positioned to become leaders in patient safety, develop in that direction?
“The biggest challenge I see is the spectrum of polarization between clinicians and administrators,” he says. “One of the most important qualities that a patient safety officer needs is the ability to overbridge the doctors on one hand and the administrators on the other.”
What They Need
A patient safety officer (PSO) requires a critical mix of clinical and administrative skills, says Peter B. Angood, MD, vice president and chief patient safety officer for The Joint Commission, in Oakbrook, Ill.
On the clinical side, the hospitalist who wishes to be a PSO needs more than awareness of safety and quality improvement processes. He or she must be knowledgeable about and conversant in safety science in industries beyond healthcare. That expertise needs to encompass leadership, behaviors and cultures, human factors, and process redesign or systems engineering. Important, too, is training in how to corral the pieces of an organization and ensure they operate well together.
An understanding of organizational behavior is of great value. The potential PSO should understand how the key players interact: the board of directors with chief executives, chief executives with senior management, senior management with all staff (including the allied professionals), and medical staff with the organization as a whole.
“Because safety is a systemwide process, the patient safety [person] is pivotal in forming a hub from which much of the quality, safety, and process improvement occurs,” says Dr. Angood.
Jason Adelman, MD, MS, former hospitalist and current PSO at Montefiore Medical Center in New York City, says developing patient safety leaders should embrace technology. “Pay attention to the latest and greatest ideas, products, and services,” he urges. “Come up with strategic plans to implement in healthcare, get the information quickly into the hands of physicians, have physicians report, and include forcing functions [whereby computers will not process to completion when key data are missing].”
Above all, the patient safety officer must train to be a change agent. “Influencing patient safety means you have to be there in the capital-allocation process,” says David Shulkin, MD, chief executive officer at Beth Israel Medical Center in New York City. “You have to be there when they’re designing facilities. You have to understand your human resource policies and the skill sets and aptitudes of the people that the hospital is hiring. To be a good patient safety officer, the training needs to involve broad exposure with a slant toward operations.”
Build a Bridge
As a young physician who wanted to develop as a leader in the field of quality and safety, Dr. Shulkin had to forge his own path. In 1992, after he became chief medical officer (CMO) at the Hospital of the University of Pennsylvania in Philadelphia, he fielded several inquiries a month from young physicians who wanted to pursue a similar career. In response to that need, he designed a quality improvement/patient safety fellowship at his school.
David Bernard, MD, now chief medical officer at Beth Israel, had been practicing medicine for 30 years when at age 50 he took a year’s leave of absence from Boston University and enrolled as Dr. Shulkin’s first fellow in 1994. Dr. Bernard, a nephrologist, was a vice dean in the school of medicine at Boston University Medical Center, a hospital vice president for clinical affairs, and a senior clinician in his specialty group.
Drs. Shulkin and Bernard left the University of Pennsylvania in 1999 to take the concepts of quality transparency to a higher level and formed DoctorQuality Inc. in Conshohocken, Pa. To continue their work, DoctorQuality funded the fellowship. In 2005 when Dr. Shulkin went to Beth Israel in New York, the fellowship was restarted as the Don Hoskins Quality Improvement/Patient Safety program and funded for five years with private philanthropy.
Modeled after graduate medical education, the fellowship is predominantly hands-on. Fellows work on real projects alongside professionals in management, quality, and safety.
Under the Hood
Giving trainees the inside view into the intricacies of how to change physician behavior and cultural issues in hospitals is the backbone of Beth Israel’s program. Fellows see what clinicians rarely see: the real-world complexity of hospitals, why there is so much inertia, and the reasons changing systems can be so difficult. Fellows learn how almost every hospital issue involves financial, personnel, facility, policy and political considerations. By allowing entrée into the executive offices, the fellow gets to hear the many different perspectives when people react to an issue.
“After a quality-improvement meeting, for instance, where people are positioning and requesting different things rather than taking action,” says Dr. Shulkin, “the fellow gets to hear the behind-the-scenes analysis—how executives sometimes label people and develop strategies to overcome some of these barriers.”
Understanding how administrators, directors of social work, or nurses, for instance, view situations and understand their culture helps the leader be more effective.
“To get both leadership and clinician buy-in, and to get leadership to motivate clinicians to participate in system changes, you also need to be politically savvy,” says Dr. Adelman. “Plenty of people resist change. The PSO needs to come off as sincere, passionate, and smart, and has to be able to answer people’s tough questions.”
It can take an ambassador’s touch to make headway in the traditional physician culture.
“The patient safety officers, the chief medical officers, often have to function as diplomats,” says Dr. Angood. “This physician engagement piece is one of the most complicated issues out there, and it arises because physicians historically are trained to be autonomous, to be independent, and to expect that institutions are there to serve them.”
—Latha Sivaprasad, MD, Don Hoskins Quality Improvement/Patient Safety fellow, Beth Israel Medical Center, New York City
One Hospitalist’s View
When Latha Sivaprasad, MD, current Don Hoskins fellow at Beth Israel, started her fellowship six months ago, she was astonished how little she knew about patient safety and quality. Although she felt she knew the day-to-day deficiencies in the hospital and on the front line—and despite having practiced in three other hospitals—she wasn’t prepared to learn what she hadn’t known she didn’t know.
“In my five years as a hospitalist, I knew very little about patient safety and quality—to my shock now,” she says. “Since I’ve been a fellow here, I realize how much I had been underutilized and how much more I could have contributed to making my respective hospitals run more safely.”
Understanding people’s motivations and meeting their needs to make a hospital safer is an intricate process.
“I think it is important for hospitalists to understand how complicated and time-consuming system changes are,” she says. “You do not have that perspective as a clinician. You think that change can occur from a memo or from good intentions to do the right thing.”
She has learned to think about the bigger world outside the clinical portion of running a hospital.
“To be a change agent you really need to appreciate the hospital from the penthouse view, which is what this fellowship provides,” she says. “You need to have access to every meeting, every record, every clinician, and every senior executive to put the pieces of the puzzle together to understand how things change.”
The hospital is working to apply the Toyota method of employee involvement to the issue of how an obstetric patient progresses from triage in the emergency department (ED) to labor and delivery, and how much time passes before the triage the patient is discharged or admitted. Their focus first targeted convening the right group to discuss the issue and identify the details of the problem, then put a plan in place to track ED triage. They looked for ways to make that process more efficient, met again to determine how to implement a new version of that process, then tracked the difference. “All of this was a multihour ordeal,” she says.
It’s exhilarating, frustrating, and intriguing—and sometimes discouraging. “It’s very tedious making change, and I didn’t appreciate that before the fellowship,” she says.
Dr. Sivaprasad advises hospitalists that to be effective in patient safety efforts means being a problem solver, highly empathetic, sensitive to others, and above all, extremely patient. But results often emerge slowly.
“You must have several things brewing at once because if certain programs’ changes are taking time, you need to complete the loop on something else,” she advises.
The Ideal Candidate
Of the 20 fellows Dr. Shulkin has mentored, about half were older and more experienced than he was. Reflecting on the successful fellows and those who benefited less makes him think the distinction of experience and age is less important than the individual’s personality.
“What is important is the personality and motivation and self-directedness of the fellow,” says Dr. Shulkin. “This is a very autonomous fellowship. One of the pluses and minuses of working with senior executives is that they are very busy; they don’t have time the way traditional academic program directors or residency directors do to think, ‘Where are my fellows and what are they doing?’”
Those who will get the most out of this type of experience know how to be delicately assertive yet drive their own agendas.
To Drs. Shulkin and Bernard, a good patient safety leader is naturally curious about what makes healthcare organizations tick. The ideal candidate has an appreciation for hospital financing and the science behind physician behavior change, and the capacity to be a good listener. The trainee also needs to put aside his or her ego while transitioning from a physician in charge to stepping back into the student role to learn the new language and environment.
—David Shulkin, MD, chief executive officer, Beth Israel Medical Center, New York City
Where to Begin
The institution sponsoring the development of the patient safety officer is just as important as who that candidate is.
“The administration has to have a visionary leadership that recognizes that healthcare quality and safety is the way you do business,” says Dr. Bernard. “You have to be in an institution that is not just paying lip service to moving quality and safety. It has to be part of the fabric of the institution.”
The institution also has to be able to offer a variety of experiences, making this kind of training difficult in a nonacademic setting.
For those interested in pursuing this area of leadership, the natural first step is to meet with the CMO or CEO to explore whether the individual’s and hospital’s interests can be aligned.
“But you can’t force it,” warns Dr. Shulkin. “If that is not a natural fit, if the CMO or CEO doesn’t see their role as, or have an interest in, training faculty people; or if they don’t have the expertise to do it, it’s not going to be a good experience. In those cases, the hospitalist should look elsewhere. An increasing number of centers can offer this kind of experience for a year,” he says. “Then the hospitalist might return to their institution to take on a leadership role there.”
Creating a costly infrastructure to train a patient safety officer is not required. What is necessary is chemistry in the mentor-trainee relationship.
“This is the first time in my postgraduate career that I actually have consistently committed mentors who care about how I am molded as a physician and what my ultimate contribution to the medical field will be,” says Dr. Sivaprasad. TH
Andrea Sattinger is a medical writer based in North Carolina.
Tackle TB
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Atlanta lawyer Andrew Speaker sparked a media frenzy and public outrage, when—despite having been told he had active and extensively drug-resistant (XDR) tuberculosis (TB)—he flew to Europe for his 2007 wedding and honeymoon and put his fellow air travelers at risk.
When a federal order—the first of its kind in more than 40 years—quarantined him, further testing revealed he had less-severe multidrug resistant (MDR) TB. The subsequent furor over the case served as a wake-up call to the medical community.
“The Andrew Speaker story reminded hospitalists that Mycobacterium tuberculosis infects up to one-third of the world’s population, about 2 billion people,” says Stephen J. Swanson, MD, a staff physician with Hennepin County Medical Center in Minneapolis.
Dr. Swanson, who works as a pediatric hospitalist and completed a two-year fellowship with the Epidemic Intelligence Service (EIS) for the Centers for Disease Control and Prevention from 2004-2006, would like to see tuberculosis more on hospitalists’ radar screens.
Jay Routson, MD, a teaching hospitalist and clinical assistant professor of medicine in the Idaho State University Department of Family Medicine in Pocatello, says he does not feel entirely up to date on TB testing and MDR TB. “I rely on [infectious disease] and pulmonary specialists if I need the assistance,” he says. The last time he treated a case of suspected TB, the protocol called for four-drug therapy while awaiting sensitivities. He presumes this is unchanged. “I am comfortable with the [purified protein derivative (PPD) test], [polymerase chain reaction (PCR) test], and a bronchoscopic approach, but I’m ready for a review of newer testing modalities.”
Epidemiology
New cases of tuberculosis in the United States have declined since 1993. As of 2006, almost 14,000 cases of active tuberculosis disease were reported—about 4.6 cases per 100,000 population. Foreign-born patients represent a greater proportion of these cases—50% of cases of tuberculosis in all age groups.
“In Minnesota, one-quarter of our foreign-born tuberculosis patients have been in the U.S. for less than a year before they were diagnosed,” Dr. Swanson says. “Most are not arriving with active tuberculosis; they are developing tuberculosis disease and being diagnosed years after their arrival in the U.S.”
In the United States, active tuberculosis often develops in people who acquired latent TB infection in their country of birth and then came to the U.S. Or, they have been exposed to infected people who have recently arrived in the U.S. About 1 million international travelers arrive in the U.S. each day.
But active TB also occurs in U.S.-born individuals (see Fig. 1, above). Risk factors include immunosuppression (e.g., HIV) and being older than 50, reflecting probable exposure to someone with active TB when it was more prevalent in the U.S.
—Stephen J. Swanson, MD, staff physician, Hennepin County Medical Center, Minneapolis.
Misconceptions
Hospitalists should remain aware of the following erroneous beliefs about TB:
Active tuberculosis is primarily being seen with immunocompromised individuals, particularly those with HIV/AIDS. “Not true,” says Dr. Swanson, who is also a pediatric tropical medicine and infectious disease specialist. While the risk of TB disease is greatly increased in the immunocompromised, it occurs most commonly among the immunocompetent.
Tuberculosis is predominantly a pulmonary disease. Also not true. “At least in Minnesota, we know that more than 50% of our reported cases of tuberculosis disease are extrapulmonary,” says Dr. Swanson. “The rate of extrapulmonary tuberculosis is, in fact, much more common in the foreign-born than in the U.S.-born patients.”
Infants and young children with TB frequently have extrapulmonary manifestations such as meningitis, says Samir S. Shah, MD, MSCE, pediatric hospitalist and pediatric infectious disease specialist at the Children’s Hospital of Philadelphia.
Extrapulmonary tuberculosis is more likely among foreign-born individuals, even if they have been in the U.S. for five years or longer. This phenomenon also occurs among the elderly and immunocompromised patients, including those receiving corticosteroid therapy.
A negative PPD skin test rules out tuberculosis. A PPD can easily be falsely negative, says Dr. Swanson. “In fact, among normal adults, probably 25% of all cases of active pulmonary tuberculosis will have a negative PPD, even when their sputum demonstrates acid-fast bacilli,” he says. “The incidence of a false-negative PPD is even higher in children, and also higher if it is extrapulmonary tuberculosis. In half of these children with extrapulmonary tuberculosis you may easily have a falsely negative PPD.”
With that said, hospitalists should approach TB treatment while being mindful of these caveats:
Because tuberculosis may be extrapulmonary, it may not be identified with a chest X-ray. Almost every organ structure and body site can be a site of infection for tuberculosis, including the central nervous system, pericardium, bone, joints, skin, lymph nodes, and gastrointestinal tract.
Whether tuberculosis bacilli can be detected in sputum is a key determinant of transmissibility. “The reality is that Andrew Speaker, as it turns out, was smear negative, so they didn’t see any organisms with acid-fast stains,” says Dr. Shah. “[But] if individuals are smear-negative, they are they are still capable of transmitting disease.”
If you encounter a pediatric case of tuberculosis, transmission most likely has occurred from a household contact. Up to 17% of new cases of tuberculosis came from contact with someone with a negative acid-fast bacilli smear. If a sputum sample contains fewer than 1,000 bacteria/mL, the organism may not be detected on acid-fast staining, but still hold enough tuberculous bacilli to infect a person, especially with close and prolonged exposure. It takes only one to five bacilli arriving at the terminal pulmonary alveolus to infect an individual.
“We believe that roughly one-third to two-thirds of people exposed to a smear-positive individual with pulmonary tuberculosis will become infected,” says Dr. Swanson. “Although most will develop only latent tuberculosis infection, some will progress to active disease, particularly infected infants and young children.”
Detection
Because young children do not produce sputum, TB diagnosis in children is problematic. Infected children will present with malaise, fever, failure to thrive, and possibly erythema nodosum. Presentation is atypical: cough is infrequent except with endobronchial disease.
“One has to have a low index of suspicion and actively look for tuberculosis in children,” says Dr. Swanson.
Using gastric aspirates is one method, but is probably not more than 50% sensitive. The test is not ideal because it is time consuming, uncomfortable for young children, and aspirate samples must be collected on three consecutive early mornings.
Other approaches include ultrasound-guided transesophageal biopsies or computed tomography (CT)-guided biopsies of primarily hilar or paratracheal lymph nodes evident on CT.
There are also molecular diagnostic methods. In older children and adolescents, hospitalists can collect sputum induced with hypertonic saline. Even when acid-fast stains are negative, PCRs can be used to rapidly detect the presence of M. tuberculosis complex in sputum samples, tissue samples, and gastric aspirates, and stool samples when looking for intestinal tuberculosis.
The QuantiFERON TB Gold test (Cellestis International) is used to measure the interferon gamma released when blood samples are mixed with TB antigens and incubated. Although it has been around a number of years, it has just been incorporated into practice in the past two. The test is highly sensitive and specific but does not distinguish active from latent infection.
“It’s a pretty good test, although certainly not 100%,” says Dr. Shah, who is also an assistant professor of pediatrics and epidemiology at the University of Pennsylvania School of Medicine. “It can be used as an adjunct to skin testing to help exclude or confirm tuberculosis disease, but it should not replace clinical judgment.” Further, it is not clear how reliable the test is in children.
PPD tests are valuable when positive. False positive PPDs are rare; they generally develop from exposure to environmental non-tuberculosis mycobacterial species. A false-positive PPD can result from prior vaccination with the Bacillus Calmette-Guérin (BCG) vaccine used overseas. “Generally speaking, I do not let a patient’s BCG status influence how I interpret their PPD, especially when I am suspecting tuberculosis in the patient,” says Dr. Swanson. “Furthermore, a positive PPD is useful in confirming infection with tuberculosis, but a negative PPD will not definitively exclude TB infection.”
Susceptibility
Although molecular diagnostics can verify the presence or absence of the tubercular bacillus, drug susceptibility testing is crucial to determine whether and how the organism should be treated. MDR TB is resistant to at least the first-line drugs rifampin and isoniazid. XDR TB is also resistant to any fluoroquinolone and at least one of three injectable second-line drugs: amikacin, kanamycin, and capreomycin.
Between 1993 and 2006, 49 cases (3% of evaluable MDR TB cases) met the revised case definition for XDR TB from the World Health Organization’s Emergency Global Task Force on XDR TB. Roughly 3% of TB cases in the U.S. are multidrug resistant, says Dr. Shah.
Emergence of drug resistance is more likely in cases of incomplete or intermittent therapy, or when an adequate treatment regimen was not begun after learning the initial two-month treatment phase has been done incompletely, inadequately, or with the incorrect medications.
“I will delay initiation of therapy on a patient so that I can get adequate samples from sputum, gastric aspirates, or tissue for mycobacterial isolation and susceptibility testing. This is because of the recognition that our hospital treats a large population of foreign-born individuals with a higher prevalence of drug resistance,” says Dr. Swanson. “You need to know your susceptibilities before blindly embarking on a treatment regimen.”
In the end, for all the renewed focus on the disease, “[drug resistance with tuberculosis] is not a new phenomenon … it has been flying under the radar,” says Dr. Shah.
Dr. Swanson serves up this analogy: “XDR tuberculosis is like Britney Spears. It gets a lot of attention. But there’s a lot more dysfunction and psychopathology in Hollywood than just Britney Spears, and a lot more disease and debilitation produced by non-XDR tuberculosis.” TH
Andrea Sattinger is a medical writer based in North Carolina.
Report Critical Care
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
Hospitalists often encounter patients who are or could become critically ill. The increased efforts while caring for these patients are best captured through critical-care service codes 99291 and 99292.
Although these codes yield higher reimbursement ($204.15 and $102.45, respectively, per national Medicare average payment), they are reported only under certain circumstances. The physician’s documentation must include enough detail to support critical-care claims: the patient’s condition, the nature of the physician’s care, and the time spent rendering care. Documentation of any other pertinent information is strongly encouraged because these services often come under payer scrutiny.
Condition and Care
A patient’s condition must meet the established criteria before the service qualifies as critical care. More specifically, the patient must have a critical illness or injury that acutely impairs one or more vital organ systems such that there is a high probability of imminent or life-threatening deterioration in the patient’s condition.
The physician’s personal attention (i.e., care involving one critically ill patient at a time) is essential for rendering the highly complex decisions necessary to prevent the patient’s decline if left untreated. Given the seriousness of the patient’s condition, the physician is expected to focus only on the patient for whom critical-care time is reported.
Duration
Critical care is a time-based service. It constitutes the physician’s time spent providing direct care at the bedside and gathering and reviewing data on the patient’s unit or floor.
If the physician is not immediately available to the patient, the time associated with indirect care (e.g., reviewing data, calling the family from the office) is not counted in the overall critical-care service.
The physician keeps tracks of his/her total critical-care time throughout the day. A new period of critical-care time begins each calendar day. There is no prohibition against reporting multiple hours or days of critical care, as long as the patient’s condition prompts the service and documentation supports it.
Code 99291 represents the first “hour” of critical care, which physicians may report after accumulating the first 30 minutes of care. Alternately, physician management of the patient involving less than 30 minutes of critical-care time on a given day must be reported with the appropriate evaluation and management (E/M) code:
- Initial inpatient service (99221-99223);
- Subsequent hospital care (99231-99233); or
- Inpatient consultation (99251-99255).
Once the physician achieves 75 minutes of critical-care time, he/she reports 99292 for the additional “30 minutes” of care beyond the first hour. Never report 99292 alone on the claim form. Code 99292 is considered an “add-on” code, which means it must be reported in addition to a primary code. Code 99291 is always the primary code (reported once per physician/group per day) for critical-care services. Code 99292 can be reported in multiple units per physician/group per day according to the number of minutes spent after the initial hour (see Table 1, p. 30).
Service Inclusions
Critical care involves highly complex decision making to manage the patient’s condition. This includes the physician’s performance and/or interpretation of labs, diagnostic studies, and procedures inherent in critical care.
Therefore, do not report the following services when billing 99291-99292:
- Cardiac output measurements (93561, 93562);
- Chest X-rays (71010, 71015, 71020);
- Pulse oximetry (94760, 94761, 94762); and
- Blood gases (multiple codes).
Further, don’t report interpretation of data stored in computers:
- Electrocardiograms, blood pressures, hematologic data (99090);
- Gastric intubation (43752, 91105);
- Temporary transcutaneous pacing (92953);
- Ventilation management (94002-94004, 94660, 94662); and
- Vascular access procedures (36000, 36410, 36415, 36591, 36600).
Any other service or procedure provided by the physician can be billed in addition to 99291-99292.
Be sure not to add separately billable procedure time into the physician’s total critical-care time. A notation in the medical record should reflect this (e.g., time spent inserting a central line is not included in today’s critical-care time).
Location
Because a patient can become seriously ill in any setting, physicians often provide critical-care services in emergency departments (EDs) and on standard medical-surgical floors before the patient is transferred to the intensive care unit (ICU).
Bed location alone does not determine critical-care reporting. Patients assigned to an ICU might be critically ill or injured and meet the “condition” requirements for 99291-99292.
However, the care provided may not meet the remaining requirements. According to the American Medical Association’s Current Procedural Terminology 2008 (Professional Edition) and the Medicare Claims Processing Manual, payment can be made for critical-care services provided in any location as long as the care provided meets the definition of critical care. Services for a patient who is not critically ill and unstable but who happens to be receiving care in a critical-care, intensive-care, or other specialized-care unit are reported using subsequent hospital care codes 99231-99233 or hospital consultation codes 99251-99255. TH
Carol Pohlig is a billing and coding expert with the University of Pennsylvania Medical Center, Philadelphia. She is also on the faculty of SHM’s inpatient coding course.
The OIG Aftermath
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
Your First Chair Job
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
An increase in uninsured patients who show up in emergency departments (EDs), physician specialty shortages, and a physician population unwilling to take call all have led to a now-common practice: hospitals pay physician-specialists for on-call coverage of their EDs.
Though essential for providing adequate emergency care, this hospital-physician arrangement can violate anti-kickback laws. But recently, one hospital’s payments to on-call physicians was given an official federal stamp of approval. What does this official statement mean for hospital medicine groups and the hospitalists they employ?
Origins of the Opinion
In September 2007, the Office of the Inspector General (OIG) issued an advisory opinion that a hospital that pays physicians for providing on-call and indigent care services in the ED does not violate the federal anti-kickback statute.
An unnamed medical center requested the opinion and submitted details on the comprehensive, detailed program it had created to ensure coverage of the ED.
The hospital’s program includes varied payment structures for staff physicians based on their participation in an on-call schedule for the ED and provision of inpatient follow-up care to patients seen while on call, among other actions.
The program applies to 18 specialties including hospitalists, and all participating physicians receive a per-diem payment for each on-call day.
Lou Glaser, partner at law firm of Sonnenschein Nath & Rosenthal, LLP, in Chicago, wrote the request.
“In this particular case, the hospital extended the program to nearly every specialty on the staff,” he explains. “Few hospitals have gone that far. But my client wanted to ensure that this program was appropriate and, if questioned, wanted to be able to say that they did everything possible to set up an appropriate program. They also, to the extent that if the OIG said no, wanted to be able to tell their physicians that they tried everything possible” to set up a fair payment system.
Ron Greeno, MD, FCCP, chief medical officer at Cogent Healthcare in Irvine, Calif., and a member of SHM’s Public Policy Committee, is surprised the opinion was requested.
“It came out of the blue,” he says. “We weren’t worrying about it.” He believes the shortage of physicians willing to provide on-call care in the ED—particularly to uninsured patients—forces hospitals to create similar payment structures.
“The opinion basically says the OIG doesn’t frown on the current practice,” Dr. Greeno says. “There’s no reason they would—and if they did, it would mean a staffing crisis for all hospitals.” Part of this potential crisis includes care for uninsured patients, for which the hospital isn’t compensated.
Uninsured Patients
A pivotal point in the OIG opinion and in the problems hospitals have with ED on-call staffing is payment for care of uninsured patients—especially those who require an on-call physician at the ED in the middle of the night.
“My client wanted a solution to this, a solution that ensured their indigent patients would receive care from all necessary specialties,” says Glaser.
The payment program created by Glaser’s client hospitals was structured to include care for indigent patients. “The OIG latched on to that for a number of reasons,” says Glaser. “But basically it shows that physicians are being paid for something that they would not otherwise be paid for.”
Effect on Hospitalists
Though the OIG opinion doesn’t change status quo for most, it provides valuable guidance on what the government considers an acceptable plan for covering on-call shortages. Criteria outlined in the opinion include:
- There must be a clear, demonstrated need for the on-call service;
- Participating physicians would otherwise be un- or under-compensated for a meaningful portion of their work, such as caring for uninsured admissions;
- Participating physicians deliver defined added value such as better outcomes, or participation in quality initiatives; and
- Reimbursement reflects market value.
Because most hospitalists are employed by or supported by the hospital for which they are on call, they are entirely exempt from anti-kickback issues. Therefore, the OIG opinion won’t affect their on-call payments.
“The opinion obviously isn’t geared toward any specialty,” Glaser points out. “In fact, the OIG noted that the hospital could not select specific groups and try to steer money toward those. That said, hospitalists are in a slightly different position than other medical staff. They maintain their practice at the hospital, and depend on that for their volume and income.”
If your hospital medicine group is not supported primarily by the hospital, how can you ensure your on-call payments are legally acceptable?
First, have a lawyer review your arrangements. While the onus for staying within the bounds of the law is on hospitals, it’s important for every hospital medicine group to have local legal experts examine their current or proposed payment structure for on-call and indigent care.
“Any time a hospital gives money to a doctor, [he or she] is subject to scrutiny,” says Dr. Greeno. “This has to be legally vetted.”
Second, document your own payment system. “There was a great deal of discussion in the request for opinion on how the hospital established its payment structure,” says Glaser. “The opinion shows the importance of having a well-documented process for establishing the rates to be paid, and showing that that’s fair.”
You can start your review of your own payment program by downloading a comprehensive overview of the OIG advisory opinion at SHM’s Web site, www.hospitalmedicine.org.
“For most of us who have been minding their p’s and q’s, [the opinion] doesn’t require any changes,” Dr. Greeno stresses. However, hospital medicine directors should stay on the safe side and check any on-call payment programs you might be participating in. TH
Jane Jerrard has written for The Hospitalist since 2005.
Teamwork Triumphs
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.
Hospitalists regularly list daily workload and long working hours among their top concerns—but some of their tasks can be delegated to another member of the healthcare team.
“There is a perception that a lot of the activities hospitalists spend their time on don’t need to be done by a hospitalist,” said Kevin O’Leary, MD, assistant professor of medicine and associate division chief, Division of Hospital Medicine, Northwestern University Feinberg School of Medicine in Chicago.
For example, at Northwestern, hospitalists engage in discharge activities, case management, and communication with families. All this can be performed by someone else with clinical training, Dr. O’Leary says. The hospital has unit-based care coordinators (UCCs), but they follow all patients on a 30-bed unit and do not go on rounds with the hospitalists. “Their duties were more aligned with the hospital’s interests than the hospitalists’,” Dr. O’Leary explains. He and his colleagues decided to study the effect of assigning hospitalist care coordinators (HCCs) to work with hospitalists exclusively. Their findings are featured in this month’s Journal of Hospital Medicine.
The study covered the 12 weeks from September 2006, through November 2006. During that time, half the hospitalists on duty each week were randomly assigned to work with an HCC, while the other hospitalists continued working in their usual fashion. The HCCs performed the same duties as the UCCs, plus additional ones such as obtaining outside medical records and attending to more discharge details (see Table 1, below). All the HCCs were registered nurses who performed only team-related duties for the duration of the study.
The hospitalists and HCCs rounded together each morning as a team. They collaborated on the daily plan of care and decided on specific duties for each team member to accomplish. Essentially, the HCCs “allowed the physicians to focus more on clinical rather than ancillary issues,” Dr. O’Leary notes.
Activities related to the discharge process were a key feature of the HCC role. Among other things, they started discharge, arranged for home care, and wrote instructions. “We think that if this program is adopted long-term, HCCs could be key in planning the discharge process to improve patient safety,” Dr. O’Leary says. “For example, they could call patients at home to make sure they’re taking their medication.”
At the end of each week, the hospitalists completed an on-line survey measuring their satisfaction with the program and its effects on their efficiency. Patients also were contacted seven to 14 days after discharge and asked about their satisfaction with the discharge process.
Five hospitalists were on duty on any given week, for a total 60 hospitalist weeks. Of those, hospitalist-HCC teams accounted for 31 weeks (52%), and control hospitalists the remaining 29 (48%). Of the 31 hospitalists who completed a team week, 28 (90%) reported that the team approach improved their efficiency and job satisfaction. They singled out activities relating to communication with nurses and those associated with discharge planning and execution as particularly benefiting from the presence of an HCC.
“One of the advantages that hospitalists told us about working with the HCC was that it allowed them to be in two places at once,” Dr. O’Leary says. “[For example,] if a new admission came in before they were done with morning rounds, the hospitalist could begin the admission while the HCC looked in on their old patients. Or, if two admissions came at once, the hospitalist could begin to admit one of the patients while the HCC gathered background information on the second.
“Also, having an extra pair of hands was incredibly helpful on rounds for patients who had wounds that needed to be undressed and examined, or for helping to turn or move patients who were otherwise difficult to examine.”
The HCCs were not formally surveyed, but all said they would rather continue as team members than return to their old duties.
Of 71 patients who completed the discharge satisfaction interview, 44 (62%) were cared for by a hospitalist-HCC team, but their satisfaction levels were no different from those reported by patients cared for by control hospitalists.
There was also a suggestion that the addition of the HCC lowered costs and shortened length of stay. Patients cared for by a team incurred an unadjusted mean cost of $10,052.96 +/-$11,708.73, compared with an unadjusted mean cost of $11,703.19 +/-$20,455.78 incurred by the control patients (p=0.008). Unadjusted mean length of stay was 4.70 +/-4.15 days for patients cared for by a team, compared with 5.07 +/- 3.99 for patients seen by control hospitalists (p=0.005). Both findings lost significance on multivariate regression analysis, but the hospital is planning a longer study with a larger sample size to see if truly significant differences emerge.
The HCCs helped in two basic ways, Dr. O’Leary concludes. They lightened the physicians’ workload, and they were able to add a nurse’s perspective to patient care. For example, if the hospitalist wrote an order for a diuretic, the HCC could alert the unit nurse to check the computer for the order. “They had a unique ability to see what the nurses needed to know, because they were nurses themselves,” he says.
Hospitalists aren’t the only physicians who could benefit from this arrangement, he adds. “For physicians in a lot of specialties, there are lots of activities that don’t necessarily need to be done by the doctor. The right support would make them happier and more efficient.”TH
Norra MacReady is a medical writer based in California.