User login
What's Eating You? Cutaneous Myiasis (Wohlfahrtia magnifica)
Dust mite control measures don’t help asthma patients
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
ILLUSTRATIVE CASE
The parents of a 10-year-old patient whom you recently diagnosed with asthma want to do everything they can to reduce his asthma symptoms. They are considering buying hypoallergenic mattress covers and an expensive air filtration system to decrease the levels of dust mite allergens in their home and want to know if you think that will help their son. What do you tell them?
We want to do everything we can to help our patients control their asthma symptoms, but when it comes to household dust mite control measures, this extensive Cochrane review confirms that interventions like mattress covers and air filtration don’t work, despite recent reviews and guidelines recommending them.
Dust mites (Dermatophagoides pteronyssinus) are one of the most common allergens that provoke asthma symptoms in children and adults.2 Dust mites live in warm, humid places and feed on human skin scales. The areas with the highest levels of household infestation are carpets, mattresses, pillows, drapes, upholstered furniture, and clothing.
Guidelines still encourage mattress cover use
The National Asthma Education and Prevention Program (NAEPP) 2007 guidelines recommend using allergen-impermeable mattress and pillow covers and washing sheets and blankets in hot water. They also recommend “considering” reducing indoor humidity, removing bedroom carpets, and washing stuffed toys weekly. The NAEPP Expert Panel cites many studies to support these recommendations.3
The National Environmental Education and Training Foundation (NEETF) 2005 guidelines recommend additional measures to reduce dust mite exposure including vacuuming using a high-efficiency particulate air (HEPA) filter, removing draperies, and considering using a portable air cleaner with a HEPA filter.4
STUDY SUMMARY: 54 trials, but no support for dust mite measures
This Cochrane systematic review included 54 randomized trials that assessed the effects of physical and/or chemical interventions to reduce exposure to house dust mite antigens in the homes of patients with mite-sensitive asthma. These studies included a total of 3002 pediatric and adult asthma patients (9 - 628 patients analyzed per trial) with mite sensitization confirmed by skin testing or IgE serum assays.
Thirty-six studies tested physical interventions, including mattress covers, vacuum cleaning, heating, ventilation, freezing, washing, air filtration, and ionizers. Ten used chemical interventions to kill dust mites; 8 used a combination of physical and chemical methods. Control groups received either placebo or no treatment.
Outcomes studied. The authors extracted data for the following outcomes: subjective well-being, asthma symptom scores, use of medication, days of sick leave from school or work, number of unscheduled visits to a physician or hospital, forced expiratory volume in 1 second (FEV1), peak expiratory flow rate (PEFR), and provocative concentration that causes a 20% fall in FEV1 (PC20). Length of the intervention and follow-up ranged from 2 weeks to 2 years.
Quality of studies. According to modern standards for randomized trials, the quality of many of the 54 studies was not optimal, especially in the descriptions of randomization and the reporting of outcomes. The method of randomization and concealment of allocation was rarely described. Eleven trial reports did not contain any usable data for the meta-analysis because of the way data were reported, and there was significant potential for reporting bias in favor of a treatment effect in the studies included. Mite reduction was successful in 17 trials, unsuccessful in 24 trials, and not reported in 13 trials.
Interventions didn’t help. There were no differences between the intervention and control groups for any of the outcomes. The percentage of patients who improved after the experimental interventions was not significantly different from the percentage of patients in the control groups (relative risk [RR]=1.01; 95% confidence interval [CI], 0.80-1.27; data based on 7 trials). There was no difference in medication usage (data from 10 trials), FEV1 (data from 14 trials), morning PEFR (data from 23 trials), or PC 20 (data from 14 trials) between the intervention and control groups ( TABLE ).1
TABLE
Dust mite control measures didn’t improve these outcomes
| OUTCOME | STANDARDIZED MEAN DIFFERENCE* (95% CI) |
|---|---|
| Medication usage | -0.06 (-0.18 to 0.07) |
| FEV1 | 0.11 (-0.05 to 0.28) |
| Morning PEFR | 0.00 (-1.0 to 0.10) |
| PC 20 | 0.05 (-0.13 to 0.22) |
| CI, confidence interval; FEV1, forced expiratory volume in 1 second; PC20, provocative concentration that causes a 20% fall in FEV1; PEFR, peak expiratory flow rate. | |
| *Standardized mean difference is a common way to combine results of different studies for comparison purposes. If the 95% CI crosses 0, there is no effect of the intervention compared with the control. | |
WHAT’S NEW?: Nothing is new, yet this will be “news” to many
This Cochrane review includes 5 additional trials that have been conducted since the last Cochrane review of this topic in 2004. However, the 2004 review reported the same conclusion—that interventions to reduce house dust mite exposure in asthma patients are ineffective—as did 3 other Cochrane reviews on the same topic beginning in 1998.5-8
So why are the guidelines out of step? Schmidt and Gøtzsche (one of the authors of the Cochrane review) conducted a systematic review of narrative review articles in 2005 to answer this question. They found 70 review articles, 90% of which recommended physical methods to reduce exposure to house dust mites. They discovered that although these review articles included references to support their recommendations of dust mite control measures, the reviews showed significant bias in favor of positive studies and highlighted the results of low-quality studies, including non-randomized studies that had been excluded from the Cochrane reviews.9
CAVEATS: Duration of studies not long enough?
We know that extreme measures to reduce exposure to dust mite allergen, such as relocating to a high altitude or prolonged hospitalization, can reduce asthma symptoms,10,11 but these are clearly not practical solutions for most patients with dust mite-sensitive asthma. When it comes to this Cochrane review, some might argue that many of the interventions included were not of sufficient duration and did not sufficiently reduce the level of house mite allergen to improve asthma symptoms.
However, the subgroups of trials with long treatment duration (1-2 years) and successful mite reduction (determined by different methods, including mite counts and measured antigen levels in dust samples) also failed to show a significant difference between intervention and control groups.1
Tweak the approach? Most dust mite-sensitive asthma patients are sensitive to other allergens, so perhaps multifaceted interventions that target multiple allergens would be more effective.12 But until these potential interventions are supported by stronger evidence, we should not recommend them to our patients.
CHALLENGES TO IMPLEMENTATION: Swimming against the tide is never easy
Although the evidence to date indicates that interventions to reduce home dust mite exposure are ineffective, there are hundreds of products—including mattress and pillow covers ($10-$100), ionizers ($100-$200), and air filtration systems ($500-$800)—that are being marketed to patients with asthma. In addition, patient education handouts from sources such as the American Academy of Family Physicians, the American Academy of Pediatrics, and UpToDate recommend implementing dust mite control measures to reduce dust mite allergen exposure.13-15
We need to start educating our asthma patients properly so they can spend their time, energy, and money on interventions, such as medications, that work—and not on interventions that make no difference.
Acknowledgements
The PURLs Surveillance System is supported in part by Grant Number UL1RR024999 from the National Center for Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources or the National Institutes of Health.
This study was selected and evaluated using FPIN’s Priority Updates from the Research Literature (PURL) Surveillance System methodology. The criteria and findings leading to the selection of this study as a PURL can be accessed at www.jfponline.com/purls.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
1. Gotzsche PC, Johansen HK. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2008;(2):CD001187.-
2. German JA, Harper MB. Environmental control of allergic diseases. Am Fam Physician. 2002;66:421-426.
3. National Asthma Education and Prevention Program (NAEPP). Control of environmental factors and comorbid conditions that affect asthma. In: Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md: National Heart, Lung, and Blood Institute; 2007.
4. National Environmental Education & Training Foundation (NEETF). Environmental management of pediatric asthma. Guidelines for health care providers. Washington, DC: National Environmental Education & Training Foundation (NEETF); 2005.
5. Gøtzsche PC, Hammarquist C, Burr M. House dust mite control measures in the management of asthma: meta-analysis. BMJ. 1998;317:1105-1110.
6. Hammarquist C, Burr ML, Gotzsche PC. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2000;(2):CD001187.-
7. Gøtzsche PC, Johansen HK, Burr ML, Hammarquist C. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2001;(3):CD001187.-
8. Gøtzsche PC, Johansen HK, Schmidt LM, Burr ML. House dust mite control measures for asthma. Cochrane Database Syst Rev. 2004;(4):CD001187.-
9. Schmidt LM, Gøtzsche PC. Of mites and men: reference bias in narrative review articles: a systematic review. J Fam Pract. 2005;54:334-338.
10. Platts-Mills TA, Tovey ER, Mitchell EB, Moszoro H, Nock P, Wilkins SR. Reduction of bronchial hyperreactivity during prolonged allergen avoidance. Lancet 1982;2:675-678.
11. Grootendorst DC, Dahlen SE. Benefits of high altitude allergen avoidance in atopic adolescents with moderate to severe asthma, over and above treatment with high dose inhaled steroids. Clin Exp Allergy. 2001;31:400-408.
12. Morgan WJ, Crain EF, Gruchalla RS, et al. Results of a home-based environmental intervention among urban children with asthma. N Engl J Med. 2004;351:1068-1080.
13. American Academy of Family Physicians. Dust mites in the home [patient handout]. Available at: http://familydoctor.org/online/famdocen/home/common/asthma/triggers/683.html. Accessed October 23, 2008.
14. American Academy of Pediatrics. Non-pharmacologic approaches to asthma management [patient handout]. Available at: http://www.aap.org/sections/allergy/nonrxchild.pdf. Accessed October 23, 2008.
15. Bailey W. Patient information: Trigger avoidance in asthma. UpToDate [online database]. Version 16.2. Waltham, Mass: UpToDate; 2008.
Copyright © 2008 The Family Physicians Inquiries Network.
All rights reserved.
Unsedated colonoscopy: Time to revisit this option?
- Consider recommending unsedated colonoscopy to patients who have issues with cost, concerns about sedation, or are unable to get an escort or avoid work following the procedure.
- Explore resources in your area that offer unsedated colonoscopy.
Background Access to potentially life-saving screening colonoscopy is limited by the high cost of sedation. We explored the practicability of having supervised trainees perform unsedated colonoscopies.
Method A nursing shortage at our Veterans Administration gastroenterology training program necessitated discontinuing sedated colonoscopy. We offered the procedure without sedation to restore local access to screening colonoscopy.
Results From September 2002 to June 2005, 145 of 483 patients accepted the unsedated option. The procedure was done by second-year gastroenterology (GI) fellows who had performed about 100 sedated colonoscopies in their first year of training. Cecal intubation was achieved in 81% of 138 wellpurged patients without obstructive lesions. Implementation obviated the need for 2 registered nurses, the escort requirement, and postprocedure activity restriction. It also eliminated sedation-related complications.
Conclusion This report confirms the feasibility of unsedated colonoscopy performed by supervised trainees. The unsedated option minimizes direct and indirect costs of colonoscopy. Describing unsedated screening colonoscopy to patients as a “sedation risk–free” procedure encouraged them to consider the benefits. We recommend that future studies test primary care providers’ willingness to inform patients of the feasibility of this nonstandard option, and perhaps reshape the practice of colonoscopy for colorectal cancer screening.
Monitored sedation given for colonoscopy is a measure meant to ensure patient safety,1 but its high cost limits access to the potentially life-saving screening procedure.2,3 Unsedated colonoscopy is an option, but a controversial one, raising issues both pro4-6 and con.7-11 In the United States, gastroenterologists perform unsedated colonoscopy both for unescorted patients (~2% of all screening colonos-copies)12,13 and individuals who simply prefer to avoid sedation (~6%).7 Family physicians, too, perform unsedated colonoscopy in both rural and urban settings.14-17
Would it be feasible to make training in unsedated colonoscopy more readily available to providers, and thereby reduce costs and inconvenience for patients? We took advantage of a changing environment at our Veterans Administration program to explore this question.
Method
A nursing shortage in our VA academic GI program necessitated discontinuing sedated colonoscopy. We reviewed the literature on unsedated colonoscopy and found that it is a feasible alternative performed elsewhere.4-7,12,14,16 Our attending staff discussed the options with patients and obtained informed consent18 using the following general message:
“Sedated colonoscopy is usual practice. Even though the risks of sedation are very small, nurses are required to monitor patients continuously. Because of a nursing shortage, we must send you to another VA facility 15 miles away for sedated colonoscopy. You must have an escort, as you will not be allowed to drive after sedation. One of the medicines they administer will make you forget the discomfort you may have experienced, as well as the discussions after the examination.
“Alternatively, you may choose unsedated colonoscopy, which is practiced in the United States and many other countries. Because no medicines are used, there are no medication-induced complications. An escort is not required, and there is no activity restriction afterwards.
“You will feel air in the colon and the endoscope being pushed around inside you. The colonoscopist will talk to you throughout the examination. When you begin to experience discomfort, the colonoscopist will remove air inside the colon or straighten the loops in the colonoscope to minimize the discomfort before it becomes severe. If discomfort does become severe, you and the colonoscopist can agree to stop the advancement of the colonoscope. Complications related to taking biopsies or removing polyps are similar in sedated and unsedated procedures.”
Supervised trainees (second-year GI fellows who had performed about 100 sedated colonoscopies in their first year of training), assisted by a licensed vocational nurse, performed the procedures using appropriate techniques.5-7
The Institution Review Board of the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) approved our review of the patient data for publication.
Results
From September 2002 to June 2005, 145 of 483 patients accepted the unsedated option. The number of patients choosing this option increased in each successive academic year (31, 50, and 64), as did the wait-time in days (27±4, 46±5, 72±6) (mean±standard error of the mean [SEM]). Seven patients (4%) had poor bowel preparation or obstructing lesions limiting completion. Among the 138 well-purged patients, we achieved cecal intubation in 112 (81%). Discomfort limited completion in the remaining 19%.
Other than transient vasovagal reactions in 2 patients, no complications occurred. Patients with incomplete examinations due to discomfort underwent sedated colonoscopy or barium enema or received no further assessment, depending on the initial findings. Those who subsequently underwent sedated colonoscopy (10%) had to be purged again, escorted, and comply with activity restriction.
Colonoscopy was developed as an unsedated procedure.19,20 Discomfort experienced by some patients during sigmoid intubation led to the use of medications,20,21 which are now administered routinely.22 Interestingly, competency in unsedated colonoscopy is not required of GI fellows.23 Indeed, until recently,18 teaching GI trainees unsedated colonoscopy was deemed impractical.7 Family physicians, on the other hand, have long practiced and taught unsedated colonoscopy,14-17,24 although the actual number of family physicians performing colonoscopy is fairly small.25 One reason so few family physicians offer the service—estimated at 3.7% of the specialty—may be the intensive and costly education required.16 Even more difficult has been gaining privileges to perform the sedated procedure,26 given the training requirements set forth by GI professional societies.27
Many patients would opt for unsedated colonoscopy. The favorable reception of unsedated colonoscopy in our study is evident in the increasing number of veterans each year who opted for the procedure despite the lengthening wait-time (which was due to increased demand rather than decreased availability of endoscopists). In the course of our project, we found that the terms “unsedated,” “no sedation,” or “without sedation” tended to convey the negative connotation that relief of discomfort and induced amnesia are withheld.8,9 The term “sedation risk–free”28 emphasized the benefits of no sedation.
Cost factors favoring unsedated colonoscopy. Sedated colonoscopies performed by family physicians have offered substantial health care savings.29,30 It is intuitively obvious that the unsedated option in the hands of those with the necessary skills14-16,24 would be even less costly. Our unsedated colonoscopy project reduced direct costs, which included the cost of having 2 registered nurses on hand. Indirect costs to patients31 were also minimized by avoiding the need for an escort or activity restriction. Moreover, there were no sedation-related complications.32,33
An estimated 40 million healthy Americans are eligible for colorectal cancer screening.34 Primary care providers play a pivotal role in counseling many of these patients, who may find the indirect cost savings of unsedated colonoscopy performed by that same provider appealing.
A logical transition from flexible sigmoidoscopy. An unsedated colonoscopy is very similar to an extended flexible sigmoidoscopy.14-17,35 In patients who can tolerate a flexible sigmoidoscopy well, extended flexible sigmoidoscopy can reach the cecum >70% of the time.36 To enhance the cecal intubation rate among unsedated veterans, we developed (subsequent to the findings reported here) a novel method of water infusion in lieu of air insufflation during insertion of the colonoscope.37 This measure improved the cecal intubation rate from 76% to 97%.38 For family physicians who perform flexible sigmoidoscopy, it is worth considering performing extended flexible sigmoidoscopy or unsedated colonoscopy using this water infusion method37,38 or other methods to minimize discomfort in unsedated patients.39
Limitations of our study, and opportunities. Our report is based on uncontrolled, nonrandomized observational data. Nevertheless, it affirms the feasibility of unsedated colonoscopy performed by supervised trainees, as previously reported by a family practice training program.16 It also underscores the benefits of the unsedated option on direct and indirect costs.
Since only 3.7% of family physicians in a recent survey reported performing colonoscopy,25 it is uncertain whether primary care providers would voluntarily inform patients about the unsedated option. In select settings, gastroenterologists are willing to provide unsedated colonoscopy.6,7,12,13,18 A reasonable hypothesis to test is that primary care providers informing patients about unsedated colonoscopy could reshape the future practice of screening colonoscopy in family medicine and gastroenterology.
Funding/Support
Supported in part by vA medical research Funds and an American Society for Gastrointestinal endoscopy career Development Award (FWl 1985).
Correspondence
Felix W. Leung, MD, Division of Gastroenterology (111G), Sepulveda Ambulatory Care Center, Veterans Affairs Greater los Angeles Healthcare System, 16111 Plummer Street, North Hills, CA 91343; .
1. Comprehensive Accreditation Manual for Hospitals; The Official Handbook. Oakbrook Terrace, III: Joint Commission on Accreditation of Healthcare Organizations; 2005:160-223.
2. Lieberman DA, Weiss DG, Bond JH, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000;343:162-168.
3. El-Serag HB, Petersen L, Hampel H, et al. The use of screening colonoscopy for patients cared for by the Department of Veterans Affairs. Arch Intern Med. 2006;166:2202-2208.
4. Herman FN. Avoidance of sedation during total colonoscopy. Dis Colon Rectum. 1990;33:70-72.
5. Cataldo PA. Colonoscopy without sedation: a viable alternative. Dis Colon Rectum. 1996;39:257-261.
6. Hoffman MS, Butler TW, Shaver T. Colonoscopy without sedation. J Clin Gastroenterol. 1998;26:279-282.
7. Rex DK, Imperiale TF, Portish V. Patients willing to try colonoscopy without sedation: associated clinical factors and results of a randomized controlled trial. Gastrointest Endosc. 1999;49:554-559.
8. Levenson D. Health quality organization criticizes colonoscopies given without pain medication. Rept Med Guidelines Outcomes Res. 2001;12:9-12.
9. Leo RA. Unsedated endoscopy: you don’t get a medal for it! South Med J. 2004;97:797-798.
10. Faulx AL, Vela S, Das A, et al. The changing landscape of practice patterns regarding unsedated endoscopy and propofol use: a national Web survey. Gastrointest Endosc. 2005;62:9-15.
11. Rex DK, Khalfan HK. Sedation and the technical performance of colonoscopy. Gastrointest Endosc Clin N Am. 2005;15:661-672.
12. Nelson DB, MCQuaid KR, Bond JH, et al. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307-314.
13. Aslinia F, Uradomo L, Steele A, et al. Quality assessment of colonoscopic cecal intubation: an analysis of 6 years of continuous practice at a University Hospital. Am J Gastroenterol. 2006;101:721-731.
14. Hopper W, Kyker KA, Rodney WM. Colonoscopy by a family physician: a 9-year experience of 1048 procedures. J Fam Pract. 1996;43:561 -566.
15. Carr KW, Worthington JM, Rodney WM, et al. Advancing from flexible sigmoidoscopy to colonoscopy in rural family practice. Tenn Med. 1998;91:21-26.
16. Rodney WM, Dabov G, Orientale E, et al. Sedation associated with a more complete colonoscopy. J Fam Pract. 1993;36:394-400.
17. Knox L, Hahn RG, Lane C. A comparison of unsedated colonoscopy and flexible sigmoidoscopy in the family medicine setting: an LA Net study. J Am Board Fam Med. 2007;20:444-450.
18. Leung FW, Aharonian HS, Guth PH, et al. Involvement of trainees in routine unsedated colonoscopy—review of pilot experience. Gastrointest Endosc. 2008;67:718-722.
19. Wolff WI, Shinya H. Colonofiberoscopy. JAMA. 1971;217:1509-1512.
20. Williams C, Teague RH. Colonoscopy. Gut. 1973;14:990-1003.
21. Waye JD. Colonoscopy. Surg Clin North Am. 1972;52:1013-1024.
22. National Cancer Institute Web Site. Available at: http://www.cancer.gov/cancertopics/types/colon-and-rectal. Accessed January 23, 2008.
23. Gastroenterology required curriculum. Chicago, III: Accreditation council on Graduate medical education; 2005.
24. Edwards JK, Norris TE. Colonoscopy in rural communities: can family physicians perform the procedure with safe and efficacious results? J Am Board Fam Pract. 2004;17:353-358.
25. Wilkins T, Wagner P, Thomas A, et al. Attitudes toward performance of endoscopic colon cancer screening by family physicians. Fam Med. 2007;39:578-584.
26. Frank M. American Academy of Family Physicians response to American college of Gastroenterology’s letter and legal opinion. Sent to hospital administrators on December 12, 2005.
27. Faigel D, Baron T, Lewis B, et al. Ensuring competence in endoscopy. Prepared by the ASGe Taskforce on ensuring competence in endoscopy and American college of Gastroenterology executive and Practice management committees, 2005: 1-36.
28. Leung FW. Should minimization of cue be an option as a quality indicator in colonoscopy performed for colorectal cancer screening? Gastroin-test Endosc. 2008;67:579-580.
29. Short MW, Kelly KM, Runser lA. Colonoscopy by a family physician: a case series demonstrating health care savings. Mil Med. 2007;172:1089-1092.
30. Perry RE, Christensen JB, Christensen MA, et al. Office colonoscopy—a safe procedure in selected patients. Dis Colon Rectum. 1989;32:1031-1033.
31. Glied S. Estimating the indirect cost of illness: an assessment of the forgone earnings approach. Am J Public Health. 1996;86:1723-1728.
32. Arrowsmith JB, Gerstman BB, Fleischer DE, et al. Results from the American Society for Gastrointestinal endoscopy/uS Food and Drug Administration collaborative study on complication rates and drug use during gastrointestinal endoscopy. Gastroin-test Endosc. 1991;37:421-427.
33. Sharma VK, Nguyen CC, Crowell MD, et al. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007;66:27-34.
34. Seeff LC, Manninen DL, Dong FB, et al. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the united States? Gastroenterology. 2004;127:1661-1669.
35. Dervin JV. Feasibility of 105-cm flexible sigmoidoscopy in family practice. J Fam Pract. 1986;23:341-344.
36. Lee JG, Lum D, Urayama S, et al. Unsedated extended flexible sigmoidoscopy for colorectal cancer screening: a pilot study. Aliment Pharmacol Ther. 2006;23:945-951.
37. Leung JW, Mann S, Leung FW. Option of screening colonoscopy without sedation—a pilot study in united States veterans. Aliment Pharmacol Ther. 2007;26:627-631.
38. Leung FW, Aharonian HS, Leung JW, et al. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. In press.
39. Leung FW. Methods of reducing discomfort during colonoscopy. Dig Dis Sci. 2008;53:1462-1467.
- Consider recommending unsedated colonoscopy to patients who have issues with cost, concerns about sedation, or are unable to get an escort or avoid work following the procedure.
- Explore resources in your area that offer unsedated colonoscopy.
Background Access to potentially life-saving screening colonoscopy is limited by the high cost of sedation. We explored the practicability of having supervised trainees perform unsedated colonoscopies.
Method A nursing shortage at our Veterans Administration gastroenterology training program necessitated discontinuing sedated colonoscopy. We offered the procedure without sedation to restore local access to screening colonoscopy.
Results From September 2002 to June 2005, 145 of 483 patients accepted the unsedated option. The procedure was done by second-year gastroenterology (GI) fellows who had performed about 100 sedated colonoscopies in their first year of training. Cecal intubation was achieved in 81% of 138 wellpurged patients without obstructive lesions. Implementation obviated the need for 2 registered nurses, the escort requirement, and postprocedure activity restriction. It also eliminated sedation-related complications.
Conclusion This report confirms the feasibility of unsedated colonoscopy performed by supervised trainees. The unsedated option minimizes direct and indirect costs of colonoscopy. Describing unsedated screening colonoscopy to patients as a “sedation risk–free” procedure encouraged them to consider the benefits. We recommend that future studies test primary care providers’ willingness to inform patients of the feasibility of this nonstandard option, and perhaps reshape the practice of colonoscopy for colorectal cancer screening.
Monitored sedation given for colonoscopy is a measure meant to ensure patient safety,1 but its high cost limits access to the potentially life-saving screening procedure.2,3 Unsedated colonoscopy is an option, but a controversial one, raising issues both pro4-6 and con.7-11 In the United States, gastroenterologists perform unsedated colonoscopy both for unescorted patients (~2% of all screening colonos-copies)12,13 and individuals who simply prefer to avoid sedation (~6%).7 Family physicians, too, perform unsedated colonoscopy in both rural and urban settings.14-17
Would it be feasible to make training in unsedated colonoscopy more readily available to providers, and thereby reduce costs and inconvenience for patients? We took advantage of a changing environment at our Veterans Administration program to explore this question.
Method
A nursing shortage in our VA academic GI program necessitated discontinuing sedated colonoscopy. We reviewed the literature on unsedated colonoscopy and found that it is a feasible alternative performed elsewhere.4-7,12,14,16 Our attending staff discussed the options with patients and obtained informed consent18 using the following general message:
“Sedated colonoscopy is usual practice. Even though the risks of sedation are very small, nurses are required to monitor patients continuously. Because of a nursing shortage, we must send you to another VA facility 15 miles away for sedated colonoscopy. You must have an escort, as you will not be allowed to drive after sedation. One of the medicines they administer will make you forget the discomfort you may have experienced, as well as the discussions after the examination.
“Alternatively, you may choose unsedated colonoscopy, which is practiced in the United States and many other countries. Because no medicines are used, there are no medication-induced complications. An escort is not required, and there is no activity restriction afterwards.
“You will feel air in the colon and the endoscope being pushed around inside you. The colonoscopist will talk to you throughout the examination. When you begin to experience discomfort, the colonoscopist will remove air inside the colon or straighten the loops in the colonoscope to minimize the discomfort before it becomes severe. If discomfort does become severe, you and the colonoscopist can agree to stop the advancement of the colonoscope. Complications related to taking biopsies or removing polyps are similar in sedated and unsedated procedures.”
Supervised trainees (second-year GI fellows who had performed about 100 sedated colonoscopies in their first year of training), assisted by a licensed vocational nurse, performed the procedures using appropriate techniques.5-7
The Institution Review Board of the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) approved our review of the patient data for publication.
Results
From September 2002 to June 2005, 145 of 483 patients accepted the unsedated option. The number of patients choosing this option increased in each successive academic year (31, 50, and 64), as did the wait-time in days (27±4, 46±5, 72±6) (mean±standard error of the mean [SEM]). Seven patients (4%) had poor bowel preparation or obstructing lesions limiting completion. Among the 138 well-purged patients, we achieved cecal intubation in 112 (81%). Discomfort limited completion in the remaining 19%.
Other than transient vasovagal reactions in 2 patients, no complications occurred. Patients with incomplete examinations due to discomfort underwent sedated colonoscopy or barium enema or received no further assessment, depending on the initial findings. Those who subsequently underwent sedated colonoscopy (10%) had to be purged again, escorted, and comply with activity restriction.
Colonoscopy was developed as an unsedated procedure.19,20 Discomfort experienced by some patients during sigmoid intubation led to the use of medications,20,21 which are now administered routinely.22 Interestingly, competency in unsedated colonoscopy is not required of GI fellows.23 Indeed, until recently,18 teaching GI trainees unsedated colonoscopy was deemed impractical.7 Family physicians, on the other hand, have long practiced and taught unsedated colonoscopy,14-17,24 although the actual number of family physicians performing colonoscopy is fairly small.25 One reason so few family physicians offer the service—estimated at 3.7% of the specialty—may be the intensive and costly education required.16 Even more difficult has been gaining privileges to perform the sedated procedure,26 given the training requirements set forth by GI professional societies.27
Many patients would opt for unsedated colonoscopy. The favorable reception of unsedated colonoscopy in our study is evident in the increasing number of veterans each year who opted for the procedure despite the lengthening wait-time (which was due to increased demand rather than decreased availability of endoscopists). In the course of our project, we found that the terms “unsedated,” “no sedation,” or “without sedation” tended to convey the negative connotation that relief of discomfort and induced amnesia are withheld.8,9 The term “sedation risk–free”28 emphasized the benefits of no sedation.
Cost factors favoring unsedated colonoscopy. Sedated colonoscopies performed by family physicians have offered substantial health care savings.29,30 It is intuitively obvious that the unsedated option in the hands of those with the necessary skills14-16,24 would be even less costly. Our unsedated colonoscopy project reduced direct costs, which included the cost of having 2 registered nurses on hand. Indirect costs to patients31 were also minimized by avoiding the need for an escort or activity restriction. Moreover, there were no sedation-related complications.32,33
An estimated 40 million healthy Americans are eligible for colorectal cancer screening.34 Primary care providers play a pivotal role in counseling many of these patients, who may find the indirect cost savings of unsedated colonoscopy performed by that same provider appealing.
A logical transition from flexible sigmoidoscopy. An unsedated colonoscopy is very similar to an extended flexible sigmoidoscopy.14-17,35 In patients who can tolerate a flexible sigmoidoscopy well, extended flexible sigmoidoscopy can reach the cecum >70% of the time.36 To enhance the cecal intubation rate among unsedated veterans, we developed (subsequent to the findings reported here) a novel method of water infusion in lieu of air insufflation during insertion of the colonoscope.37 This measure improved the cecal intubation rate from 76% to 97%.38 For family physicians who perform flexible sigmoidoscopy, it is worth considering performing extended flexible sigmoidoscopy or unsedated colonoscopy using this water infusion method37,38 or other methods to minimize discomfort in unsedated patients.39
Limitations of our study, and opportunities. Our report is based on uncontrolled, nonrandomized observational data. Nevertheless, it affirms the feasibility of unsedated colonoscopy performed by supervised trainees, as previously reported by a family practice training program.16 It also underscores the benefits of the unsedated option on direct and indirect costs.
Since only 3.7% of family physicians in a recent survey reported performing colonoscopy,25 it is uncertain whether primary care providers would voluntarily inform patients about the unsedated option. In select settings, gastroenterologists are willing to provide unsedated colonoscopy.6,7,12,13,18 A reasonable hypothesis to test is that primary care providers informing patients about unsedated colonoscopy could reshape the future practice of screening colonoscopy in family medicine and gastroenterology.
Funding/Support
Supported in part by vA medical research Funds and an American Society for Gastrointestinal endoscopy career Development Award (FWl 1985).
Correspondence
Felix W. Leung, MD, Division of Gastroenterology (111G), Sepulveda Ambulatory Care Center, Veterans Affairs Greater los Angeles Healthcare System, 16111 Plummer Street, North Hills, CA 91343; .
- Consider recommending unsedated colonoscopy to patients who have issues with cost, concerns about sedation, or are unable to get an escort or avoid work following the procedure.
- Explore resources in your area that offer unsedated colonoscopy.
Background Access to potentially life-saving screening colonoscopy is limited by the high cost of sedation. We explored the practicability of having supervised trainees perform unsedated colonoscopies.
Method A nursing shortage at our Veterans Administration gastroenterology training program necessitated discontinuing sedated colonoscopy. We offered the procedure without sedation to restore local access to screening colonoscopy.
Results From September 2002 to June 2005, 145 of 483 patients accepted the unsedated option. The procedure was done by second-year gastroenterology (GI) fellows who had performed about 100 sedated colonoscopies in their first year of training. Cecal intubation was achieved in 81% of 138 wellpurged patients without obstructive lesions. Implementation obviated the need for 2 registered nurses, the escort requirement, and postprocedure activity restriction. It also eliminated sedation-related complications.
Conclusion This report confirms the feasibility of unsedated colonoscopy performed by supervised trainees. The unsedated option minimizes direct and indirect costs of colonoscopy. Describing unsedated screening colonoscopy to patients as a “sedation risk–free” procedure encouraged them to consider the benefits. We recommend that future studies test primary care providers’ willingness to inform patients of the feasibility of this nonstandard option, and perhaps reshape the practice of colonoscopy for colorectal cancer screening.
Monitored sedation given for colonoscopy is a measure meant to ensure patient safety,1 but its high cost limits access to the potentially life-saving screening procedure.2,3 Unsedated colonoscopy is an option, but a controversial one, raising issues both pro4-6 and con.7-11 In the United States, gastroenterologists perform unsedated colonoscopy both for unescorted patients (~2% of all screening colonos-copies)12,13 and individuals who simply prefer to avoid sedation (~6%).7 Family physicians, too, perform unsedated colonoscopy in both rural and urban settings.14-17
Would it be feasible to make training in unsedated colonoscopy more readily available to providers, and thereby reduce costs and inconvenience for patients? We took advantage of a changing environment at our Veterans Administration program to explore this question.
Method
A nursing shortage in our VA academic GI program necessitated discontinuing sedated colonoscopy. We reviewed the literature on unsedated colonoscopy and found that it is a feasible alternative performed elsewhere.4-7,12,14,16 Our attending staff discussed the options with patients and obtained informed consent18 using the following general message:
“Sedated colonoscopy is usual practice. Even though the risks of sedation are very small, nurses are required to monitor patients continuously. Because of a nursing shortage, we must send you to another VA facility 15 miles away for sedated colonoscopy. You must have an escort, as you will not be allowed to drive after sedation. One of the medicines they administer will make you forget the discomfort you may have experienced, as well as the discussions after the examination.
“Alternatively, you may choose unsedated colonoscopy, which is practiced in the United States and many other countries. Because no medicines are used, there are no medication-induced complications. An escort is not required, and there is no activity restriction afterwards.
“You will feel air in the colon and the endoscope being pushed around inside you. The colonoscopist will talk to you throughout the examination. When you begin to experience discomfort, the colonoscopist will remove air inside the colon or straighten the loops in the colonoscope to minimize the discomfort before it becomes severe. If discomfort does become severe, you and the colonoscopist can agree to stop the advancement of the colonoscope. Complications related to taking biopsies or removing polyps are similar in sedated and unsedated procedures.”
Supervised trainees (second-year GI fellows who had performed about 100 sedated colonoscopies in their first year of training), assisted by a licensed vocational nurse, performed the procedures using appropriate techniques.5-7
The Institution Review Board of the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) approved our review of the patient data for publication.
Results
From September 2002 to June 2005, 145 of 483 patients accepted the unsedated option. The number of patients choosing this option increased in each successive academic year (31, 50, and 64), as did the wait-time in days (27±4, 46±5, 72±6) (mean±standard error of the mean [SEM]). Seven patients (4%) had poor bowel preparation or obstructing lesions limiting completion. Among the 138 well-purged patients, we achieved cecal intubation in 112 (81%). Discomfort limited completion in the remaining 19%.
Other than transient vasovagal reactions in 2 patients, no complications occurred. Patients with incomplete examinations due to discomfort underwent sedated colonoscopy or barium enema or received no further assessment, depending on the initial findings. Those who subsequently underwent sedated colonoscopy (10%) had to be purged again, escorted, and comply with activity restriction.
Colonoscopy was developed as an unsedated procedure.19,20 Discomfort experienced by some patients during sigmoid intubation led to the use of medications,20,21 which are now administered routinely.22 Interestingly, competency in unsedated colonoscopy is not required of GI fellows.23 Indeed, until recently,18 teaching GI trainees unsedated colonoscopy was deemed impractical.7 Family physicians, on the other hand, have long practiced and taught unsedated colonoscopy,14-17,24 although the actual number of family physicians performing colonoscopy is fairly small.25 One reason so few family physicians offer the service—estimated at 3.7% of the specialty—may be the intensive and costly education required.16 Even more difficult has been gaining privileges to perform the sedated procedure,26 given the training requirements set forth by GI professional societies.27
Many patients would opt for unsedated colonoscopy. The favorable reception of unsedated colonoscopy in our study is evident in the increasing number of veterans each year who opted for the procedure despite the lengthening wait-time (which was due to increased demand rather than decreased availability of endoscopists). In the course of our project, we found that the terms “unsedated,” “no sedation,” or “without sedation” tended to convey the negative connotation that relief of discomfort and induced amnesia are withheld.8,9 The term “sedation risk–free”28 emphasized the benefits of no sedation.
Cost factors favoring unsedated colonoscopy. Sedated colonoscopies performed by family physicians have offered substantial health care savings.29,30 It is intuitively obvious that the unsedated option in the hands of those with the necessary skills14-16,24 would be even less costly. Our unsedated colonoscopy project reduced direct costs, which included the cost of having 2 registered nurses on hand. Indirect costs to patients31 were also minimized by avoiding the need for an escort or activity restriction. Moreover, there were no sedation-related complications.32,33
An estimated 40 million healthy Americans are eligible for colorectal cancer screening.34 Primary care providers play a pivotal role in counseling many of these patients, who may find the indirect cost savings of unsedated colonoscopy performed by that same provider appealing.
A logical transition from flexible sigmoidoscopy. An unsedated colonoscopy is very similar to an extended flexible sigmoidoscopy.14-17,35 In patients who can tolerate a flexible sigmoidoscopy well, extended flexible sigmoidoscopy can reach the cecum >70% of the time.36 To enhance the cecal intubation rate among unsedated veterans, we developed (subsequent to the findings reported here) a novel method of water infusion in lieu of air insufflation during insertion of the colonoscope.37 This measure improved the cecal intubation rate from 76% to 97%.38 For family physicians who perform flexible sigmoidoscopy, it is worth considering performing extended flexible sigmoidoscopy or unsedated colonoscopy using this water infusion method37,38 or other methods to minimize discomfort in unsedated patients.39
Limitations of our study, and opportunities. Our report is based on uncontrolled, nonrandomized observational data. Nevertheless, it affirms the feasibility of unsedated colonoscopy performed by supervised trainees, as previously reported by a family practice training program.16 It also underscores the benefits of the unsedated option on direct and indirect costs.
Since only 3.7% of family physicians in a recent survey reported performing colonoscopy,25 it is uncertain whether primary care providers would voluntarily inform patients about the unsedated option. In select settings, gastroenterologists are willing to provide unsedated colonoscopy.6,7,12,13,18 A reasonable hypothesis to test is that primary care providers informing patients about unsedated colonoscopy could reshape the future practice of screening colonoscopy in family medicine and gastroenterology.
Funding/Support
Supported in part by vA medical research Funds and an American Society for Gastrointestinal endoscopy career Development Award (FWl 1985).
Correspondence
Felix W. Leung, MD, Division of Gastroenterology (111G), Sepulveda Ambulatory Care Center, Veterans Affairs Greater los Angeles Healthcare System, 16111 Plummer Street, North Hills, CA 91343; .
1. Comprehensive Accreditation Manual for Hospitals; The Official Handbook. Oakbrook Terrace, III: Joint Commission on Accreditation of Healthcare Organizations; 2005:160-223.
2. Lieberman DA, Weiss DG, Bond JH, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000;343:162-168.
3. El-Serag HB, Petersen L, Hampel H, et al. The use of screening colonoscopy for patients cared for by the Department of Veterans Affairs. Arch Intern Med. 2006;166:2202-2208.
4. Herman FN. Avoidance of sedation during total colonoscopy. Dis Colon Rectum. 1990;33:70-72.
5. Cataldo PA. Colonoscopy without sedation: a viable alternative. Dis Colon Rectum. 1996;39:257-261.
6. Hoffman MS, Butler TW, Shaver T. Colonoscopy without sedation. J Clin Gastroenterol. 1998;26:279-282.
7. Rex DK, Imperiale TF, Portish V. Patients willing to try colonoscopy without sedation: associated clinical factors and results of a randomized controlled trial. Gastrointest Endosc. 1999;49:554-559.
8. Levenson D. Health quality organization criticizes colonoscopies given without pain medication. Rept Med Guidelines Outcomes Res. 2001;12:9-12.
9. Leo RA. Unsedated endoscopy: you don’t get a medal for it! South Med J. 2004;97:797-798.
10. Faulx AL, Vela S, Das A, et al. The changing landscape of practice patterns regarding unsedated endoscopy and propofol use: a national Web survey. Gastrointest Endosc. 2005;62:9-15.
11. Rex DK, Khalfan HK. Sedation and the technical performance of colonoscopy. Gastrointest Endosc Clin N Am. 2005;15:661-672.
12. Nelson DB, MCQuaid KR, Bond JH, et al. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307-314.
13. Aslinia F, Uradomo L, Steele A, et al. Quality assessment of colonoscopic cecal intubation: an analysis of 6 years of continuous practice at a University Hospital. Am J Gastroenterol. 2006;101:721-731.
14. Hopper W, Kyker KA, Rodney WM. Colonoscopy by a family physician: a 9-year experience of 1048 procedures. J Fam Pract. 1996;43:561 -566.
15. Carr KW, Worthington JM, Rodney WM, et al. Advancing from flexible sigmoidoscopy to colonoscopy in rural family practice. Tenn Med. 1998;91:21-26.
16. Rodney WM, Dabov G, Orientale E, et al. Sedation associated with a more complete colonoscopy. J Fam Pract. 1993;36:394-400.
17. Knox L, Hahn RG, Lane C. A comparison of unsedated colonoscopy and flexible sigmoidoscopy in the family medicine setting: an LA Net study. J Am Board Fam Med. 2007;20:444-450.
18. Leung FW, Aharonian HS, Guth PH, et al. Involvement of trainees in routine unsedated colonoscopy—review of pilot experience. Gastrointest Endosc. 2008;67:718-722.
19. Wolff WI, Shinya H. Colonofiberoscopy. JAMA. 1971;217:1509-1512.
20. Williams C, Teague RH. Colonoscopy. Gut. 1973;14:990-1003.
21. Waye JD. Colonoscopy. Surg Clin North Am. 1972;52:1013-1024.
22. National Cancer Institute Web Site. Available at: http://www.cancer.gov/cancertopics/types/colon-and-rectal. Accessed January 23, 2008.
23. Gastroenterology required curriculum. Chicago, III: Accreditation council on Graduate medical education; 2005.
24. Edwards JK, Norris TE. Colonoscopy in rural communities: can family physicians perform the procedure with safe and efficacious results? J Am Board Fam Pract. 2004;17:353-358.
25. Wilkins T, Wagner P, Thomas A, et al. Attitudes toward performance of endoscopic colon cancer screening by family physicians. Fam Med. 2007;39:578-584.
26. Frank M. American Academy of Family Physicians response to American college of Gastroenterology’s letter and legal opinion. Sent to hospital administrators on December 12, 2005.
27. Faigel D, Baron T, Lewis B, et al. Ensuring competence in endoscopy. Prepared by the ASGe Taskforce on ensuring competence in endoscopy and American college of Gastroenterology executive and Practice management committees, 2005: 1-36.
28. Leung FW. Should minimization of cue be an option as a quality indicator in colonoscopy performed for colorectal cancer screening? Gastroin-test Endosc. 2008;67:579-580.
29. Short MW, Kelly KM, Runser lA. Colonoscopy by a family physician: a case series demonstrating health care savings. Mil Med. 2007;172:1089-1092.
30. Perry RE, Christensen JB, Christensen MA, et al. Office colonoscopy—a safe procedure in selected patients. Dis Colon Rectum. 1989;32:1031-1033.
31. Glied S. Estimating the indirect cost of illness: an assessment of the forgone earnings approach. Am J Public Health. 1996;86:1723-1728.
32. Arrowsmith JB, Gerstman BB, Fleischer DE, et al. Results from the American Society for Gastrointestinal endoscopy/uS Food and Drug Administration collaborative study on complication rates and drug use during gastrointestinal endoscopy. Gastroin-test Endosc. 1991;37:421-427.
33. Sharma VK, Nguyen CC, Crowell MD, et al. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007;66:27-34.
34. Seeff LC, Manninen DL, Dong FB, et al. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the united States? Gastroenterology. 2004;127:1661-1669.
35. Dervin JV. Feasibility of 105-cm flexible sigmoidoscopy in family practice. J Fam Pract. 1986;23:341-344.
36. Lee JG, Lum D, Urayama S, et al. Unsedated extended flexible sigmoidoscopy for colorectal cancer screening: a pilot study. Aliment Pharmacol Ther. 2006;23:945-951.
37. Leung JW, Mann S, Leung FW. Option of screening colonoscopy without sedation—a pilot study in united States veterans. Aliment Pharmacol Ther. 2007;26:627-631.
38. Leung FW, Aharonian HS, Leung JW, et al. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. In press.
39. Leung FW. Methods of reducing discomfort during colonoscopy. Dig Dis Sci. 2008;53:1462-1467.
1. Comprehensive Accreditation Manual for Hospitals; The Official Handbook. Oakbrook Terrace, III: Joint Commission on Accreditation of Healthcare Organizations; 2005:160-223.
2. Lieberman DA, Weiss DG, Bond JH, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000;343:162-168.
3. El-Serag HB, Petersen L, Hampel H, et al. The use of screening colonoscopy for patients cared for by the Department of Veterans Affairs. Arch Intern Med. 2006;166:2202-2208.
4. Herman FN. Avoidance of sedation during total colonoscopy. Dis Colon Rectum. 1990;33:70-72.
5. Cataldo PA. Colonoscopy without sedation: a viable alternative. Dis Colon Rectum. 1996;39:257-261.
6. Hoffman MS, Butler TW, Shaver T. Colonoscopy without sedation. J Clin Gastroenterol. 1998;26:279-282.
7. Rex DK, Imperiale TF, Portish V. Patients willing to try colonoscopy without sedation: associated clinical factors and results of a randomized controlled trial. Gastrointest Endosc. 1999;49:554-559.
8. Levenson D. Health quality organization criticizes colonoscopies given without pain medication. Rept Med Guidelines Outcomes Res. 2001;12:9-12.
9. Leo RA. Unsedated endoscopy: you don’t get a medal for it! South Med J. 2004;97:797-798.
10. Faulx AL, Vela S, Das A, et al. The changing landscape of practice patterns regarding unsedated endoscopy and propofol use: a national Web survey. Gastrointest Endosc. 2005;62:9-15.
11. Rex DK, Khalfan HK. Sedation and the technical performance of colonoscopy. Gastrointest Endosc Clin N Am. 2005;15:661-672.
12. Nelson DB, MCQuaid KR, Bond JH, et al. Procedural success and complications of large-scale screening colonoscopy. Gastrointest Endosc. 2002;55:307-314.
13. Aslinia F, Uradomo L, Steele A, et al. Quality assessment of colonoscopic cecal intubation: an analysis of 6 years of continuous practice at a University Hospital. Am J Gastroenterol. 2006;101:721-731.
14. Hopper W, Kyker KA, Rodney WM. Colonoscopy by a family physician: a 9-year experience of 1048 procedures. J Fam Pract. 1996;43:561 -566.
15. Carr KW, Worthington JM, Rodney WM, et al. Advancing from flexible sigmoidoscopy to colonoscopy in rural family practice. Tenn Med. 1998;91:21-26.
16. Rodney WM, Dabov G, Orientale E, et al. Sedation associated with a more complete colonoscopy. J Fam Pract. 1993;36:394-400.
17. Knox L, Hahn RG, Lane C. A comparison of unsedated colonoscopy and flexible sigmoidoscopy in the family medicine setting: an LA Net study. J Am Board Fam Med. 2007;20:444-450.
18. Leung FW, Aharonian HS, Guth PH, et al. Involvement of trainees in routine unsedated colonoscopy—review of pilot experience. Gastrointest Endosc. 2008;67:718-722.
19. Wolff WI, Shinya H. Colonofiberoscopy. JAMA. 1971;217:1509-1512.
20. Williams C, Teague RH. Colonoscopy. Gut. 1973;14:990-1003.
21. Waye JD. Colonoscopy. Surg Clin North Am. 1972;52:1013-1024.
22. National Cancer Institute Web Site. Available at: http://www.cancer.gov/cancertopics/types/colon-and-rectal. Accessed January 23, 2008.
23. Gastroenterology required curriculum. Chicago, III: Accreditation council on Graduate medical education; 2005.
24. Edwards JK, Norris TE. Colonoscopy in rural communities: can family physicians perform the procedure with safe and efficacious results? J Am Board Fam Pract. 2004;17:353-358.
25. Wilkins T, Wagner P, Thomas A, et al. Attitudes toward performance of endoscopic colon cancer screening by family physicians. Fam Med. 2007;39:578-584.
26. Frank M. American Academy of Family Physicians response to American college of Gastroenterology’s letter and legal opinion. Sent to hospital administrators on December 12, 2005.
27. Faigel D, Baron T, Lewis B, et al. Ensuring competence in endoscopy. Prepared by the ASGe Taskforce on ensuring competence in endoscopy and American college of Gastroenterology executive and Practice management committees, 2005: 1-36.
28. Leung FW. Should minimization of cue be an option as a quality indicator in colonoscopy performed for colorectal cancer screening? Gastroin-test Endosc. 2008;67:579-580.
29. Short MW, Kelly KM, Runser lA. Colonoscopy by a family physician: a case series demonstrating health care savings. Mil Med. 2007;172:1089-1092.
30. Perry RE, Christensen JB, Christensen MA, et al. Office colonoscopy—a safe procedure in selected patients. Dis Colon Rectum. 1989;32:1031-1033.
31. Glied S. Estimating the indirect cost of illness: an assessment of the forgone earnings approach. Am J Public Health. 1996;86:1723-1728.
32. Arrowsmith JB, Gerstman BB, Fleischer DE, et al. Results from the American Society for Gastrointestinal endoscopy/uS Food and Drug Administration collaborative study on complication rates and drug use during gastrointestinal endoscopy. Gastroin-test Endosc. 1991;37:421-427.
33. Sharma VK, Nguyen CC, Crowell MD, et al. A national study of cardiopulmonary unplanned events after GI endoscopy. Gastrointest Endosc. 2007;66:27-34.
34. Seeff LC, Manninen DL, Dong FB, et al. Is there endoscopic capacity to provide colorectal cancer screening to the unscreened population in the united States? Gastroenterology. 2004;127:1661-1669.
35. Dervin JV. Feasibility of 105-cm flexible sigmoidoscopy in family practice. J Fam Pract. 1986;23:341-344.
36. Lee JG, Lum D, Urayama S, et al. Unsedated extended flexible sigmoidoscopy for colorectal cancer screening: a pilot study. Aliment Pharmacol Ther. 2006;23:945-951.
37. Leung JW, Mann S, Leung FW. Option of screening colonoscopy without sedation—a pilot study in united States veterans. Aliment Pharmacol Ther. 2007;26:627-631.
38. Leung FW, Aharonian HS, Leung JW, et al. Impact of a novel water method on scheduled unsedated colonoscopy in U.S. veterans. Gastrointest Endosc. In press.
39. Leung FW. Methods of reducing discomfort during colonoscopy. Dig Dis Sci. 2008;53:1462-1467.
Driving with dementia: How to assess safety behind the wheel
Mr. D, age 75, presents to your office with a 5-year history of gradually declining memory. His wife reports he is having difficulty with word finding, managing his finances, and shopping, and he needs supervision when using the stove. Nonetheless, he enjoys playing golf and drives himself to the golf course 3 times a week. He is compliant with his chronic medical therapy for hypertension, hypercholesterolemia, and asthma.
Patients with dementia who continue to drive pose a potential danger on the road, worry their families, and present challenges to clinicians. Most people would agree that patients with moderate or severe dementia should not drive, but a careful evaluation is required to assess whether a patient such as Mr. D with mild dementia remains fit to drive.
This article explores how dementia exacerbates age-related changes in driving ability and discusses how to assess driving in patients with dementia. Our goal is to help clinicians sort through data from in-office physical and cognitive assessments, family caregivers/informants’ reports, and (when available) on-road testing. We also discuss:
- guidelines for assessing older drivers that can help balance patients’ need for autonomy with public safety
- strategies for discussing driving cessation with patients and their families.
Driving: A privilege, not a right
Driving is central to older adults’ autonomy, and >75% of persons age ≥75 rely on driving as their primary mode of transportation.1 Driving cessation in this population has been associated with a 3-fold decrease in out-of-home activity2 and a 2.5-fold increase in depressive symptoms.3 Nonetheless, some 4.5 million Americans have Alzheimer’s disease (AD),4 and dementia poses a substantial risk to safe driving.
Although driving must be sacrificed when personal and public safety is at risk, most physicians perceive an uncomfortable conflict of interest between patient confidentiality and public safety.5 Assessing driving safety of patients with dementia can undermine the doctor-patient relationship and pose hardships for patients.
Mr. D has a 5-year history of memory problems that affect his daily functioning, yet he continues to drive. A longitudinal study of persons with dementia found that among the 29% who were driving at baseline, more than one-half were still behind the wheel 2 years later.6
Age and driving safety. Even in the absence of dementia, driving ability declines with aging (Tables 1 and 2).7,8 Older persons may self-regulate and restrict their driving to shorter distances, with fewer trips at night, on high-speed roads, or in unfamiliar situations. Their driving is rarely aggressive and they are unlikely to speed, but they may drive more slowly than other traffic.7,8 Although the overall rate of motor vehicle collisions declines with age:
- the rate of collisions per mile driven increases after age 659
- drivers age >65 have the highest fatality rate per mile driven among adults age ≥25.10
A dementia diagnosis is not sufficient to withdraw driving privileges, according to American Medical Association (AMA)/National Highway Traffic Safety Administration (NHTSA) guidelines. These recommend that you base decisions on the individual’s driving ability, and—when you have concerns—factor in a focused medical assessment and formal assessment of driving skills.10
Table 1
Age-related changes that may affect driving fitness
| Decreased physical capabilities, including declining muscle tone, flexibility, and reaction time |
| Decreased hearing and visual acuity |
| Increased fragility, resulting in longer time to heal should injuries occur |
| Increased medication use with possible side effect of drowsiness |
| Source: References 7,8 |
Table 2
Older drivers’ common traffic violations leading to crashes*
| Failure to obey traffic signals, including stop signs and red lights |
| Unsafe left turns (driver may inaccurately judge speed of oncoming vehicle) |
| Inappropriate turns (such as difficulty judging distance from oncoming cars, wide or narrow turns, or not timing the turn correctly with traffic lights) |
| Unsafe passing |
| Failure to yield |
| * These errors often lead to multivehicle accidents Source: References 7,8 |
CASE CONTINUED: Cognitive deficits quantified
You perform a Mini-Mental State Examination (MMSE). Mr. D scores 24/30, losing 1 point for orientation, 2 points for attention, 2 points for recall, and 1 point for copying. This score, along with his history, indicates mild dementia, although he claims he is a safe driver. On further cognitive testing, Mr. D completes the Trails A test in 90 seconds and Trails B test in 250 seconds (well below 1.5 standard deviations of the norm for his age and education).11 On the clock-drawing task, he drew a poorly organized clock, with unequal spaces between numbers and hands pointing to “10” and “11” instead of properly indicating “10 after 11.”
Mr. D and his wife live in a rural area, 5 miles from the nearest grocery store. His wife never drove, and she relies on him for weekly shopping trips and to drive her to her bridge club. She denies any problems with his driving but states, “Other drivers have become so aggressive; they’re always honking at him.” Their daughter denies that Mr. D has driving problems but admits that for the last 2 years she has refused to allow her child to ride in his car.
Focused in-office assessment
Information to assess driving ability can come from the patient, family caregiver/informant, and clinical judgment. Patients with dementia are notoriously inaccurate in self-reported driving ability, either for lack of insight or as a testament to the importance of driving to their autonomy. Caregivers often are more accurate in describing a patient’s driving, but other agendas may color their responses.
In a study of patients with very mild or mild AD, 94% reported themselves as safe drivers, whereas on-road driving instructors rated <50% of drivers in these groups as safe. Caregivers were better able to classify driving performance, but 36% of their ratings were incorrect.12
Cognitive assessment. To assess older drivers’ cognition, AMA/NHTSA’s Guide to Assessing and Counseling Older Drivers recommends the Trail-Making Test, Part B and the clock-drawing test.10 The Canadian Medical Association suggests the MMSE.13 Both guides say that abnormalities in these tests indicate a need for more detailed testing, including referral to specialized driving assessment and retesting at regular intervals (Algorithm). Retest patients with mild dementia at least every 6 months or sooner when dementia severity increases noticeably14 (Box 1).6,15
The MMSE is widely used to screen for cognitive impairment and identify dementia or delirium, but it is not a diagnostic tool or proxy driving test. A patient with dementia may produce a high MMSE score and yet be an unsafe driver. For example, well-educated patients or those with vascular or frontotemporal dementia may retain cognitive abilities as measured by the MMSE until later in the disease.
Considerable effort has been put into developing tools to help clinicians quickly and accurately differentiate safe from unsafe drivers by assessing cognition. Unfortunately, no consistent link has been found between cognitive test results and driving outcome measures. A systematic review of office-based predictors of fitness to drive in dementia found 5 studies showing an association between MMSE scores and driving and 5 studies showing no such association.16 Thus, although the AMA/NHTSA guide recommends the MMSE, Trails B, and clock-drawing tests, cognitive tests—including these—are not sufficient to assess driving ability.
Severity of dementia. International consensus groups have attempted to create guidelines for patients with dementia who drive. American, Canadian, and Australian groups suggest that a diagnosis of moderate to severe dementia precludes driving, and the driver’s licenses of persons with these conditions should be revoked.17
In general, AD is considered severe when the MMSE score is <10 or the patient becomes dependent on a caregiver for survival.18 AD of moderate severity is more difficult to define, but a Canadian consensus conference suggested a practical approach: Patients with AD would be considered to have moderate to severe dementia and should not drive when they cannot independently perform multiple instrumental activities of daily living or any of the basic activities of daily living.19
Some dementias may impair driving more quickly than AD does. For example, hallucinations may occur early in Lewy body dementia, as may impulsivity in frontotemporal dementia and motor impairment in vascular dementia.
Mrs. Y visits your office for a follow-up regarding mild Alzheimer’s disease (AD), which was diagnosed 2 years ago. She passed an on-road test 3 months ago and has an Mini-Mental State Examination score of 24/30. Over the last month she has become depressed, with insomnia and mild psychomotor retardation. She occasionally has hallucinations.
Behavioral and psychological symptoms such as agitation, aggression, hallucinations, apathy, depression, and anxiety are common neuropsychiatric sequelae of AD. Little is known about the risks these symptoms pose to road safety, but we recommend that clinicians strongly consider the potential for impaired driving.
In a longitudinal study, cognitive impairment and behavioral disturbances—especially agitation, apathy, and hallucinations—were strong predictors of driving cessation among patients with dementia.6 Furthermore, a case crossover study of patients with dementia found a 54% increase in risk of motor vehicle collisions associated with the use of psychotropic medications.15
Consider all aspects of the patient’s clinical status, including neuropsychiatric symptoms, psychotropic medications, comorbid medical conditions (including hearing and vision impairment), and concomitant therapy for medical conditions. Any could change a safe driver with mild dementia into an unsafe driver.
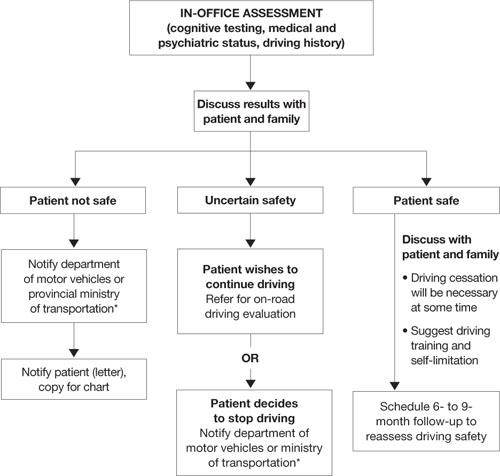
Algorithm: 3 options for drivers with dementia, based on in-office assessment
* Observe legislation or statutes that address reporting unsafe drivers to the department of motor vehicles or ministry of transportation
On-road driving tests
Because some individuals with mild dementia can drive safely for extended periods, international recommendations for assessing the driver with dementia emphasize on-road driving tests.10,13,20–22 American10 and Canadian guidelines13 suggest that a dementia diagnosis is not sufficient to withdraw licensure.
A formal driving assessment is necessary to establish road safety for patients with mild dementia except when the need for license withdrawal is evident, such as when the patient has:
- a history of major driving problems (such as crashes or driving the wrong way on a highway)
- significant contraindications to driving on the history or physical examination (such as severe inattention or psychosis).
Challenges of on-road testing. On-road tests may be the gold standard, but they are not without clinical problems.
Need to retest. Because almost all dementias are progressive and driving skills deteriorate over time, most guidelines recommend periodic retesting. For patients with dementia who pass on-road evaluations, limited evidence supports retesting every 6 months.14 Take an individual approach, however, because of the various rates at which the dementias progress.
Testing vs real world conditions. Structured on-road testing is not equivalent to unstructured real-world driving, in which the patient often must navigate without instruction or assistance.
Rural vs urban driving. Road tests conducted in urban areas assess skills associated with complex conditions and the need to respond quickly to crises. They might not assess as well rural driving, which requires sustained attention on monotonous roads.
Inaccessibility. Cost and lack of availability of on-road tests, particularly in rural areas, limit the number of patients whose performance can be evaluated.
CASE CONTINUED: Distressing results
Mr. D has a history of decline in cognition and function, objective cognitive difficulties, and a subtle history of driving problems. You refer him for a specialized on-road test, and the report indicates that he failed. Errors included wide turns, driving too slowly, getting caught in an intersection twice during red lights while attempting to turn left, driving on the shoulder, and failing to signal lane changes. You review the results with Mr. D and his wife and recommend that he cease driving immediately.
Mr. D is furious, and his wife is dismayed. He demands to know how he can continue to play golf, which is his only form of exercise and recreation. Will she have to give up her bridge club? How will they shop for food? They request permission to at least to drive to the grocery store during the daytime.
You explain that no system allows individuals to drive only at certain times, and for the sake of safety you cannot grant them special permission. You discuss alternatives, such as asking their daughter for assistance with grocery shopping and taking taxis or ride-sharing with friends who play golf and bridge.
Remain firm, but ease the blow
Driving cessation orders distress patients, families, and clinicians. A failed road test clearly indicates unsafe driving, and driving cessation is critical to public safety.
A review by Man-Son-Hing et al23 found that drivers with dementia performed worse than nondemented controls in all studies that examined driving performance (on-road, simulator, or caregiver report). Simulators showed problems such as off-road driving, deviation from posted speed, and more time to negotiate left turns.24
By comparison, only 1 of 3 studies using state crash records showed an increased risk of collisions in persons with dementia compared with controls.23 From a research perspective, however, studies that use state-reported collisions to assess driving risk are confounded by driving restrictions on persons with dementia.
Mr. D wants to continue driving with restrictions. No studies have shown reduced crash rates when drivers with dementia used compensatory strategies such as restrictions, retraining/education, having a passenger “co-pilot,” on-board navigation, or cognitive enhancers.23
If Mr. D had passed the road test, the situation would have been more ambiguous. Two studies have examined on-road driving performance over time in patients with early-stage dementia.25,26 Both studies followed drivers prospectively for 2 years, and those with mild dementia (vs very mild or no dementia) were most likely to show a decline in driving skills:
- All participants with mild dementia were rated as “not safe” by the end of 2 years by Duchek et al.25
- Median time to “failure” (or a rating of unsafe) was 324 days for drivers with mild dementia vs 605 days for those with very mild dementia, as reported by Ott et al.26
Mr. D’s passionate plea for reconsideration highlights the need for communities to develop alternate transportation for seniors whose driving becomes unsafe (Box 2).
Legal liability? Physicians often are concerned about legal responsibilities and risks involved in reporting unsafe drivers. Be aware of local statutes or legislations regarding mandatory reporting of patients you deem unsafe to drive.17 These laws usually protect physicians from lawsuits related to violating patient confidentiality. Civil lawsuits remain possible, however, if clinicians fail to report an unsafe driver who subsequently is involved in a motor vehicle collision.27
1. Meet with family first. Help them assume a positive and supportive role. Explain concretely and empathically your concern for the safety of the patient and others. Clearly outline your findings that the patient is not fit to drive, and explain that the law requires you to report the patient to the authorities.
Remind family members that the goal of driving assessment is to prevent a collision, and they carry some responsibility because they are aware of the potential risk of letting their family member continue to drive. If necessary, have family members witness a repeat performance by the patient on the most revealing test. Discuss the importance of finding alternate transportation to reduce the risk of isolation and depression that can follow driving cessation.
2. Meet with patient. Having the family present can be helpful, but ask them to assume a supportive role. Give the patient a positive role by recognizing that he or she has been a responsible driver, and part of this responsibility is to stop driving before an accident occurs. Acknowledge that it is normal to be unhappy upon learning that one’s driving privileges are being revoked.
Sometimes it helps to give the patient a prescription in their name that says, “Do not drive.” Families who receive a copy may find this very helpful, too, for reminding the patient later about what you said.
If your patient argues with your position, remain firm and do not argue. Indicate that you have made notes on the meeting and are notifying the authorities about the patient’s unsafe driving. You can add that your chart could be subpoenaed and the patient may be legally liable and financially responsible should he or she continue to drive and have a collision.
3. Talk about transportation options. Family members could share driving responsibilities. Taxi rides can cost less than maintaining a car if the patient drives <4,000 km (2,500 miles) per year. Suggest that patients or families find volunteer drivers or contact helpful taxi drivers a day before an outing is planned.
4. If patient refuses to comply, meet with the family again and encourage them to remove the patient’s opportunity to drive (confiscate the keys, disable the car, or remove the car altogether).
Provide a written statement to the patient and family outlining why the patient can no longer drive. Indicate that it is your legal responsibility to report unsafe drivers, and you intend to notify the authorities regarding the patient’s driving status. If the patient remains noncompliant, continue to encourage family to remove the opportunity to drive.
Related resources
- Physician’s guide to assessing and counseling older drivers. American Medical Association and the National Highway Traffic Safety Administration, 2003. www.nhtsa.dot.gov/people/injury/olddrive/OlderDriversBook.
- Determining medical fitness to operate motor vehicles. Canadian Medical Association. 2006. www.cma.ca/index.cfm/ci_id/18223/la_id/1.htm.
- Canadian Driving Research Initiative for Vehicular Safety in the Elderly (CanDRIVE). www.candrive.ca.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rapoport receives grant/research support from the Canadian Institute of Health Research and the Ontario Neurotrauma Foundation.
1. Stowell-Ritter A, Straight A, Evans EL. Understanding senior transportation: report and analysis of a survey of consumers age 50+. Washington, DC: American Association of Retired Persons; 2002.
2. Marottoli RA, de Leon CFM, Glass TA, et al. Consequences of driving cessation: decreased out-of-home activity levels. J Gerontol B Psychol Sci Soc Sci 2000;55(6):S334-40.
3. Marottoli RA, Mendes de Leon CF, Glass TA, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J Am Geriatr Soc 1997;45(2):202-6.
4. Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003;60(8):1119-22.
5. Jang RW, Man-Son-Hing M, Molnar FJ, et al. Family physicians’ attitudes and practices regarding assessments of medical fitness to drive in older persons. J Gen Intern Med 2007;22(4):531-43.
6. Herrmann N, Rapoport MJ, Sambrook R, et al. Predictors of driving cessation in mild-to-moderate dementia. CMAJ 2006;175(6):591-5.
7. Hedlund J. Countermeasures that work: a highway safety countermeasure guide for state highway safety offices. Washington, DC: National Highway Traffic Safety Administration; 2006.
8. Dobbs B. Medical conditions and driving: a review of the literature (1960-2000). Washington, DC: National Highway Traffic Safety Administration; 2005. Available at: http://www.nhtsa.dot.gov/people/injury/research/Medical_Condition_Driving/pages/TRD.html. Accessed September 29, 2008.
9. Li G, Braver ER, Chen LH. Fragility versus excessive crash involvement as determinants of high death rates per vehicle-mile of travel among older drivers. Accid Anal Prev 2003;35(2):227-35.
10. Physician’s guide to assessing and counseling older drivers. Washington, DC: National Highway Traffic Safety Administration; 2003. Available at: http://www.nhtsa.dot.gov/people/injury/olddrive/OlderDriversBook. Accessed September 29, 2008.
11. Yeudall LT, Reddon JR, Gill DM, et al. Normative data for the Halstead-Reitan neuropsychological tests stratified by age and sex. J Clin Psychol 1987;43(3):346-67.
12. Brown LB, Ott BR, Papandonatos GD, et al. Prediction of on-road driving performance in patients with early Alzheimer’s disease. J Am Geriatr Soc 2005;53(1):94-8.
13. Determining medical fitness to operate motor vehicles. CMA driver’s guide. 7th ed. Ottawa, Ontario, Canada: Canadian Medical Association; 2006.
14. Molnar FJ, Patel A, Marshall SC, et al. Systematic review of the optimal frequency of follow-up in persons with mild dementia who continue to drive. Alzheimer Dis Assoc Disord 2006;20(4):295-7.
15. Rapoport MJ, Herrmann N, Molnar FJ, et al. Psychotropic medications and motor vehicle collisions in patients with dementia (letter). J Am Geriatr Soc 2008;56(10):1968-70.
16. Molnar FJ, Patel A, Marshall SC, et al. Clinical utility of office-based cognitive predictors of fitness to drive in persons with dementia: a systematic review. J Am Geriatr Soc 2006;54(12):1809-24.
17. Rapoport MJ, Herrmann N, Molnar FJ, et al. Sharing the responsibility for assessing the risk of the driver with dementia. CMAJ. 2007;177(6):599-601.
18. Herrmann N, Gauthier S, Lysy PG. Clinical practice guidelines for severe Alzheimer’s disease. Alzheimers Dement 2007;3(4):385-97.
19. Hogan DB, Bailey P, Carswell A, et al. Management of mild to moderate Alzheimer’s disease and dementia. Alzheimers Dement 2007;3(4):355-84.
19. Assessing fitness to drive for commercial and private vehicle drivers. Sydney, Australia: National Library of Australia; 2006. Available at: http://www.austroads.com.au/aftd/index.html. Accessed November 4, 2008.
21. Medical aspects of fitness to drive. A guide for medical practitioners. Wellington, New Zealand: Land Transport Safety Authority; 2002. Available at: http://www.transfund.govt.nz/licensing/docs/ltsa-medical-aspects.pdf. Accessed September 29, 2008.
22. At a glance guide to the current medical standards of fitness to drive. Swansea, UK: Drivers Medical Group, Driver and Vehicle Licensing Agency; 2008. Available at: http://www.dvla.gov.uk/medical/ataglance.aspx. Accessed September 29, 2008.
23. Man-Son-Hing M, Marshall SC, Molnar FJ, Wilson KG. Systematic review of driving risk and the efficacy of compensatory strategies in persons with dementia. J Am Geriatr Soc 2007;55(6):878-84.
24. Cox DJ, Quillian WC, Thorndike FP, et al. Evaluating driving performance of outpatients with Alzheimer disease. J Am Board Fam Pract 1998;11(4):264-71.
25. Duchek JM, Carr DB, Hunt L, et al. Longitudinal driving performance in early-stage dementia of the Alzheimer type. J Am Geriatr Soc 2003;51(10):1342-7.
26. Ott BR, Heindel WC, Papandonatos GD, et al. A longitudinal study of drivers with Alzheimer disease. Neurology 2008;70(14):1171-8.
27. Molnar FJ, Byszewski AM, Marshall SC, Man-Son-Hing M. In-office evaluation of medical fitness to drive: practical approaches for assessing older people. Can Fam Physician 2005;51:372-9.
Mr. D, age 75, presents to your office with a 5-year history of gradually declining memory. His wife reports he is having difficulty with word finding, managing his finances, and shopping, and he needs supervision when using the stove. Nonetheless, he enjoys playing golf and drives himself to the golf course 3 times a week. He is compliant with his chronic medical therapy for hypertension, hypercholesterolemia, and asthma.
Patients with dementia who continue to drive pose a potential danger on the road, worry their families, and present challenges to clinicians. Most people would agree that patients with moderate or severe dementia should not drive, but a careful evaluation is required to assess whether a patient such as Mr. D with mild dementia remains fit to drive.
This article explores how dementia exacerbates age-related changes in driving ability and discusses how to assess driving in patients with dementia. Our goal is to help clinicians sort through data from in-office physical and cognitive assessments, family caregivers/informants’ reports, and (when available) on-road testing. We also discuss:
- guidelines for assessing older drivers that can help balance patients’ need for autonomy with public safety
- strategies for discussing driving cessation with patients and their families.
Driving: A privilege, not a right
Driving is central to older adults’ autonomy, and >75% of persons age ≥75 rely on driving as their primary mode of transportation.1 Driving cessation in this population has been associated with a 3-fold decrease in out-of-home activity2 and a 2.5-fold increase in depressive symptoms.3 Nonetheless, some 4.5 million Americans have Alzheimer’s disease (AD),4 and dementia poses a substantial risk to safe driving.
Although driving must be sacrificed when personal and public safety is at risk, most physicians perceive an uncomfortable conflict of interest between patient confidentiality and public safety.5 Assessing driving safety of patients with dementia can undermine the doctor-patient relationship and pose hardships for patients.
Mr. D has a 5-year history of memory problems that affect his daily functioning, yet he continues to drive. A longitudinal study of persons with dementia found that among the 29% who were driving at baseline, more than one-half were still behind the wheel 2 years later.6
Age and driving safety. Even in the absence of dementia, driving ability declines with aging (Tables 1 and 2).7,8 Older persons may self-regulate and restrict their driving to shorter distances, with fewer trips at night, on high-speed roads, or in unfamiliar situations. Their driving is rarely aggressive and they are unlikely to speed, but they may drive more slowly than other traffic.7,8 Although the overall rate of motor vehicle collisions declines with age:
- the rate of collisions per mile driven increases after age 659
- drivers age >65 have the highest fatality rate per mile driven among adults age ≥25.10
A dementia diagnosis is not sufficient to withdraw driving privileges, according to American Medical Association (AMA)/National Highway Traffic Safety Administration (NHTSA) guidelines. These recommend that you base decisions on the individual’s driving ability, and—when you have concerns—factor in a focused medical assessment and formal assessment of driving skills.10
Table 1
Age-related changes that may affect driving fitness
| Decreased physical capabilities, including declining muscle tone, flexibility, and reaction time |
| Decreased hearing and visual acuity |
| Increased fragility, resulting in longer time to heal should injuries occur |
| Increased medication use with possible side effect of drowsiness |
| Source: References 7,8 |
Table 2
Older drivers’ common traffic violations leading to crashes*
| Failure to obey traffic signals, including stop signs and red lights |
| Unsafe left turns (driver may inaccurately judge speed of oncoming vehicle) |
| Inappropriate turns (such as difficulty judging distance from oncoming cars, wide or narrow turns, or not timing the turn correctly with traffic lights) |
| Unsafe passing |
| Failure to yield |
| * These errors often lead to multivehicle accidents Source: References 7,8 |
CASE CONTINUED: Cognitive deficits quantified
You perform a Mini-Mental State Examination (MMSE). Mr. D scores 24/30, losing 1 point for orientation, 2 points for attention, 2 points for recall, and 1 point for copying. This score, along with his history, indicates mild dementia, although he claims he is a safe driver. On further cognitive testing, Mr. D completes the Trails A test in 90 seconds and Trails B test in 250 seconds (well below 1.5 standard deviations of the norm for his age and education).11 On the clock-drawing task, he drew a poorly organized clock, with unequal spaces between numbers and hands pointing to “10” and “11” instead of properly indicating “10 after 11.”
Mr. D and his wife live in a rural area, 5 miles from the nearest grocery store. His wife never drove, and she relies on him for weekly shopping trips and to drive her to her bridge club. She denies any problems with his driving but states, “Other drivers have become so aggressive; they’re always honking at him.” Their daughter denies that Mr. D has driving problems but admits that for the last 2 years she has refused to allow her child to ride in his car.
Focused in-office assessment
Information to assess driving ability can come from the patient, family caregiver/informant, and clinical judgment. Patients with dementia are notoriously inaccurate in self-reported driving ability, either for lack of insight or as a testament to the importance of driving to their autonomy. Caregivers often are more accurate in describing a patient’s driving, but other agendas may color their responses.
In a study of patients with very mild or mild AD, 94% reported themselves as safe drivers, whereas on-road driving instructors rated <50% of drivers in these groups as safe. Caregivers were better able to classify driving performance, but 36% of their ratings were incorrect.12
Cognitive assessment. To assess older drivers’ cognition, AMA/NHTSA’s Guide to Assessing and Counseling Older Drivers recommends the Trail-Making Test, Part B and the clock-drawing test.10 The Canadian Medical Association suggests the MMSE.13 Both guides say that abnormalities in these tests indicate a need for more detailed testing, including referral to specialized driving assessment and retesting at regular intervals (Algorithm). Retest patients with mild dementia at least every 6 months or sooner when dementia severity increases noticeably14 (Box 1).6,15
The MMSE is widely used to screen for cognitive impairment and identify dementia or delirium, but it is not a diagnostic tool or proxy driving test. A patient with dementia may produce a high MMSE score and yet be an unsafe driver. For example, well-educated patients or those with vascular or frontotemporal dementia may retain cognitive abilities as measured by the MMSE until later in the disease.
Considerable effort has been put into developing tools to help clinicians quickly and accurately differentiate safe from unsafe drivers by assessing cognition. Unfortunately, no consistent link has been found between cognitive test results and driving outcome measures. A systematic review of office-based predictors of fitness to drive in dementia found 5 studies showing an association between MMSE scores and driving and 5 studies showing no such association.16 Thus, although the AMA/NHTSA guide recommends the MMSE, Trails B, and clock-drawing tests, cognitive tests—including these—are not sufficient to assess driving ability.
Severity of dementia. International consensus groups have attempted to create guidelines for patients with dementia who drive. American, Canadian, and Australian groups suggest that a diagnosis of moderate to severe dementia precludes driving, and the driver’s licenses of persons with these conditions should be revoked.17
In general, AD is considered severe when the MMSE score is <10 or the patient becomes dependent on a caregiver for survival.18 AD of moderate severity is more difficult to define, but a Canadian consensus conference suggested a practical approach: Patients with AD would be considered to have moderate to severe dementia and should not drive when they cannot independently perform multiple instrumental activities of daily living or any of the basic activities of daily living.19
Some dementias may impair driving more quickly than AD does. For example, hallucinations may occur early in Lewy body dementia, as may impulsivity in frontotemporal dementia and motor impairment in vascular dementia.
Mrs. Y visits your office for a follow-up regarding mild Alzheimer’s disease (AD), which was diagnosed 2 years ago. She passed an on-road test 3 months ago and has an Mini-Mental State Examination score of 24/30. Over the last month she has become depressed, with insomnia and mild psychomotor retardation. She occasionally has hallucinations.
Behavioral and psychological symptoms such as agitation, aggression, hallucinations, apathy, depression, and anxiety are common neuropsychiatric sequelae of AD. Little is known about the risks these symptoms pose to road safety, but we recommend that clinicians strongly consider the potential for impaired driving.
In a longitudinal study, cognitive impairment and behavioral disturbances—especially agitation, apathy, and hallucinations—were strong predictors of driving cessation among patients with dementia.6 Furthermore, a case crossover study of patients with dementia found a 54% increase in risk of motor vehicle collisions associated with the use of psychotropic medications.15
Consider all aspects of the patient’s clinical status, including neuropsychiatric symptoms, psychotropic medications, comorbid medical conditions (including hearing and vision impairment), and concomitant therapy for medical conditions. Any could change a safe driver with mild dementia into an unsafe driver.
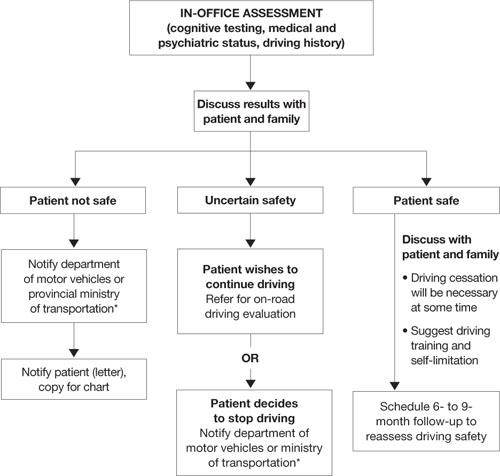
Algorithm: 3 options for drivers with dementia, based on in-office assessment
* Observe legislation or statutes that address reporting unsafe drivers to the department of motor vehicles or ministry of transportation
On-road driving tests
Because some individuals with mild dementia can drive safely for extended periods, international recommendations for assessing the driver with dementia emphasize on-road driving tests.10,13,20–22 American10 and Canadian guidelines13 suggest that a dementia diagnosis is not sufficient to withdraw licensure.
A formal driving assessment is necessary to establish road safety for patients with mild dementia except when the need for license withdrawal is evident, such as when the patient has:
- a history of major driving problems (such as crashes or driving the wrong way on a highway)
- significant contraindications to driving on the history or physical examination (such as severe inattention or psychosis).
Challenges of on-road testing. On-road tests may be the gold standard, but they are not without clinical problems.
Need to retest. Because almost all dementias are progressive and driving skills deteriorate over time, most guidelines recommend periodic retesting. For patients with dementia who pass on-road evaluations, limited evidence supports retesting every 6 months.14 Take an individual approach, however, because of the various rates at which the dementias progress.
Testing vs real world conditions. Structured on-road testing is not equivalent to unstructured real-world driving, in which the patient often must navigate without instruction or assistance.
Rural vs urban driving. Road tests conducted in urban areas assess skills associated with complex conditions and the need to respond quickly to crises. They might not assess as well rural driving, which requires sustained attention on monotonous roads.
Inaccessibility. Cost and lack of availability of on-road tests, particularly in rural areas, limit the number of patients whose performance can be evaluated.
CASE CONTINUED: Distressing results
Mr. D has a history of decline in cognition and function, objective cognitive difficulties, and a subtle history of driving problems. You refer him for a specialized on-road test, and the report indicates that he failed. Errors included wide turns, driving too slowly, getting caught in an intersection twice during red lights while attempting to turn left, driving on the shoulder, and failing to signal lane changes. You review the results with Mr. D and his wife and recommend that he cease driving immediately.
Mr. D is furious, and his wife is dismayed. He demands to know how he can continue to play golf, which is his only form of exercise and recreation. Will she have to give up her bridge club? How will they shop for food? They request permission to at least to drive to the grocery store during the daytime.
You explain that no system allows individuals to drive only at certain times, and for the sake of safety you cannot grant them special permission. You discuss alternatives, such as asking their daughter for assistance with grocery shopping and taking taxis or ride-sharing with friends who play golf and bridge.
Remain firm, but ease the blow
Driving cessation orders distress patients, families, and clinicians. A failed road test clearly indicates unsafe driving, and driving cessation is critical to public safety.
A review by Man-Son-Hing et al23 found that drivers with dementia performed worse than nondemented controls in all studies that examined driving performance (on-road, simulator, or caregiver report). Simulators showed problems such as off-road driving, deviation from posted speed, and more time to negotiate left turns.24
By comparison, only 1 of 3 studies using state crash records showed an increased risk of collisions in persons with dementia compared with controls.23 From a research perspective, however, studies that use state-reported collisions to assess driving risk are confounded by driving restrictions on persons with dementia.
Mr. D wants to continue driving with restrictions. No studies have shown reduced crash rates when drivers with dementia used compensatory strategies such as restrictions, retraining/education, having a passenger “co-pilot,” on-board navigation, or cognitive enhancers.23
If Mr. D had passed the road test, the situation would have been more ambiguous. Two studies have examined on-road driving performance over time in patients with early-stage dementia.25,26 Both studies followed drivers prospectively for 2 years, and those with mild dementia (vs very mild or no dementia) were most likely to show a decline in driving skills:
- All participants with mild dementia were rated as “not safe” by the end of 2 years by Duchek et al.25
- Median time to “failure” (or a rating of unsafe) was 324 days for drivers with mild dementia vs 605 days for those with very mild dementia, as reported by Ott et al.26
Mr. D’s passionate plea for reconsideration highlights the need for communities to develop alternate transportation for seniors whose driving becomes unsafe (Box 2).
Legal liability? Physicians often are concerned about legal responsibilities and risks involved in reporting unsafe drivers. Be aware of local statutes or legislations regarding mandatory reporting of patients you deem unsafe to drive.17 These laws usually protect physicians from lawsuits related to violating patient confidentiality. Civil lawsuits remain possible, however, if clinicians fail to report an unsafe driver who subsequently is involved in a motor vehicle collision.27
1. Meet with family first. Help them assume a positive and supportive role. Explain concretely and empathically your concern for the safety of the patient and others. Clearly outline your findings that the patient is not fit to drive, and explain that the law requires you to report the patient to the authorities.
Remind family members that the goal of driving assessment is to prevent a collision, and they carry some responsibility because they are aware of the potential risk of letting their family member continue to drive. If necessary, have family members witness a repeat performance by the patient on the most revealing test. Discuss the importance of finding alternate transportation to reduce the risk of isolation and depression that can follow driving cessation.
2. Meet with patient. Having the family present can be helpful, but ask them to assume a supportive role. Give the patient a positive role by recognizing that he or she has been a responsible driver, and part of this responsibility is to stop driving before an accident occurs. Acknowledge that it is normal to be unhappy upon learning that one’s driving privileges are being revoked.
Sometimes it helps to give the patient a prescription in their name that says, “Do not drive.” Families who receive a copy may find this very helpful, too, for reminding the patient later about what you said.
If your patient argues with your position, remain firm and do not argue. Indicate that you have made notes on the meeting and are notifying the authorities about the patient’s unsafe driving. You can add that your chart could be subpoenaed and the patient may be legally liable and financially responsible should he or she continue to drive and have a collision.
3. Talk about transportation options. Family members could share driving responsibilities. Taxi rides can cost less than maintaining a car if the patient drives <4,000 km (2,500 miles) per year. Suggest that patients or families find volunteer drivers or contact helpful taxi drivers a day before an outing is planned.
4. If patient refuses to comply, meet with the family again and encourage them to remove the patient’s opportunity to drive (confiscate the keys, disable the car, or remove the car altogether).
Provide a written statement to the patient and family outlining why the patient can no longer drive. Indicate that it is your legal responsibility to report unsafe drivers, and you intend to notify the authorities regarding the patient’s driving status. If the patient remains noncompliant, continue to encourage family to remove the opportunity to drive.
Related resources
- Physician’s guide to assessing and counseling older drivers. American Medical Association and the National Highway Traffic Safety Administration, 2003. www.nhtsa.dot.gov/people/injury/olddrive/OlderDriversBook.
- Determining medical fitness to operate motor vehicles. Canadian Medical Association. 2006. www.cma.ca/index.cfm/ci_id/18223/la_id/1.htm.
- Canadian Driving Research Initiative for Vehicular Safety in the Elderly (CanDRIVE). www.candrive.ca.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rapoport receives grant/research support from the Canadian Institute of Health Research and the Ontario Neurotrauma Foundation.
Mr. D, age 75, presents to your office with a 5-year history of gradually declining memory. His wife reports he is having difficulty with word finding, managing his finances, and shopping, and he needs supervision when using the stove. Nonetheless, he enjoys playing golf and drives himself to the golf course 3 times a week. He is compliant with his chronic medical therapy for hypertension, hypercholesterolemia, and asthma.
Patients with dementia who continue to drive pose a potential danger on the road, worry their families, and present challenges to clinicians. Most people would agree that patients with moderate or severe dementia should not drive, but a careful evaluation is required to assess whether a patient such as Mr. D with mild dementia remains fit to drive.
This article explores how dementia exacerbates age-related changes in driving ability and discusses how to assess driving in patients with dementia. Our goal is to help clinicians sort through data from in-office physical and cognitive assessments, family caregivers/informants’ reports, and (when available) on-road testing. We also discuss:
- guidelines for assessing older drivers that can help balance patients’ need for autonomy with public safety
- strategies for discussing driving cessation with patients and their families.
Driving: A privilege, not a right
Driving is central to older adults’ autonomy, and >75% of persons age ≥75 rely on driving as their primary mode of transportation.1 Driving cessation in this population has been associated with a 3-fold decrease in out-of-home activity2 and a 2.5-fold increase in depressive symptoms.3 Nonetheless, some 4.5 million Americans have Alzheimer’s disease (AD),4 and dementia poses a substantial risk to safe driving.
Although driving must be sacrificed when personal and public safety is at risk, most physicians perceive an uncomfortable conflict of interest between patient confidentiality and public safety.5 Assessing driving safety of patients with dementia can undermine the doctor-patient relationship and pose hardships for patients.
Mr. D has a 5-year history of memory problems that affect his daily functioning, yet he continues to drive. A longitudinal study of persons with dementia found that among the 29% who were driving at baseline, more than one-half were still behind the wheel 2 years later.6
Age and driving safety. Even in the absence of dementia, driving ability declines with aging (Tables 1 and 2).7,8 Older persons may self-regulate and restrict their driving to shorter distances, with fewer trips at night, on high-speed roads, or in unfamiliar situations. Their driving is rarely aggressive and they are unlikely to speed, but they may drive more slowly than other traffic.7,8 Although the overall rate of motor vehicle collisions declines with age:
- the rate of collisions per mile driven increases after age 659
- drivers age >65 have the highest fatality rate per mile driven among adults age ≥25.10
A dementia diagnosis is not sufficient to withdraw driving privileges, according to American Medical Association (AMA)/National Highway Traffic Safety Administration (NHTSA) guidelines. These recommend that you base decisions on the individual’s driving ability, and—when you have concerns—factor in a focused medical assessment and formal assessment of driving skills.10
Table 1
Age-related changes that may affect driving fitness
| Decreased physical capabilities, including declining muscle tone, flexibility, and reaction time |
| Decreased hearing and visual acuity |
| Increased fragility, resulting in longer time to heal should injuries occur |
| Increased medication use with possible side effect of drowsiness |
| Source: References 7,8 |
Table 2
Older drivers’ common traffic violations leading to crashes*
| Failure to obey traffic signals, including stop signs and red lights |
| Unsafe left turns (driver may inaccurately judge speed of oncoming vehicle) |
| Inappropriate turns (such as difficulty judging distance from oncoming cars, wide or narrow turns, or not timing the turn correctly with traffic lights) |
| Unsafe passing |
| Failure to yield |
| * These errors often lead to multivehicle accidents Source: References 7,8 |
CASE CONTINUED: Cognitive deficits quantified
You perform a Mini-Mental State Examination (MMSE). Mr. D scores 24/30, losing 1 point for orientation, 2 points for attention, 2 points for recall, and 1 point for copying. This score, along with his history, indicates mild dementia, although he claims he is a safe driver. On further cognitive testing, Mr. D completes the Trails A test in 90 seconds and Trails B test in 250 seconds (well below 1.5 standard deviations of the norm for his age and education).11 On the clock-drawing task, he drew a poorly organized clock, with unequal spaces between numbers and hands pointing to “10” and “11” instead of properly indicating “10 after 11.”
Mr. D and his wife live in a rural area, 5 miles from the nearest grocery store. His wife never drove, and she relies on him for weekly shopping trips and to drive her to her bridge club. She denies any problems with his driving but states, “Other drivers have become so aggressive; they’re always honking at him.” Their daughter denies that Mr. D has driving problems but admits that for the last 2 years she has refused to allow her child to ride in his car.
Focused in-office assessment
Information to assess driving ability can come from the patient, family caregiver/informant, and clinical judgment. Patients with dementia are notoriously inaccurate in self-reported driving ability, either for lack of insight or as a testament to the importance of driving to their autonomy. Caregivers often are more accurate in describing a patient’s driving, but other agendas may color their responses.
In a study of patients with very mild or mild AD, 94% reported themselves as safe drivers, whereas on-road driving instructors rated <50% of drivers in these groups as safe. Caregivers were better able to classify driving performance, but 36% of their ratings were incorrect.12
Cognitive assessment. To assess older drivers’ cognition, AMA/NHTSA’s Guide to Assessing and Counseling Older Drivers recommends the Trail-Making Test, Part B and the clock-drawing test.10 The Canadian Medical Association suggests the MMSE.13 Both guides say that abnormalities in these tests indicate a need for more detailed testing, including referral to specialized driving assessment and retesting at regular intervals (Algorithm). Retest patients with mild dementia at least every 6 months or sooner when dementia severity increases noticeably14 (Box 1).6,15
The MMSE is widely used to screen for cognitive impairment and identify dementia or delirium, but it is not a diagnostic tool or proxy driving test. A patient with dementia may produce a high MMSE score and yet be an unsafe driver. For example, well-educated patients or those with vascular or frontotemporal dementia may retain cognitive abilities as measured by the MMSE until later in the disease.
Considerable effort has been put into developing tools to help clinicians quickly and accurately differentiate safe from unsafe drivers by assessing cognition. Unfortunately, no consistent link has been found between cognitive test results and driving outcome measures. A systematic review of office-based predictors of fitness to drive in dementia found 5 studies showing an association between MMSE scores and driving and 5 studies showing no such association.16 Thus, although the AMA/NHTSA guide recommends the MMSE, Trails B, and clock-drawing tests, cognitive tests—including these—are not sufficient to assess driving ability.
Severity of dementia. International consensus groups have attempted to create guidelines for patients with dementia who drive. American, Canadian, and Australian groups suggest that a diagnosis of moderate to severe dementia precludes driving, and the driver’s licenses of persons with these conditions should be revoked.17
In general, AD is considered severe when the MMSE score is <10 or the patient becomes dependent on a caregiver for survival.18 AD of moderate severity is more difficult to define, but a Canadian consensus conference suggested a practical approach: Patients with AD would be considered to have moderate to severe dementia and should not drive when they cannot independently perform multiple instrumental activities of daily living or any of the basic activities of daily living.19
Some dementias may impair driving more quickly than AD does. For example, hallucinations may occur early in Lewy body dementia, as may impulsivity in frontotemporal dementia and motor impairment in vascular dementia.
Mrs. Y visits your office for a follow-up regarding mild Alzheimer’s disease (AD), which was diagnosed 2 years ago. She passed an on-road test 3 months ago and has an Mini-Mental State Examination score of 24/30. Over the last month she has become depressed, with insomnia and mild psychomotor retardation. She occasionally has hallucinations.
Behavioral and psychological symptoms such as agitation, aggression, hallucinations, apathy, depression, and anxiety are common neuropsychiatric sequelae of AD. Little is known about the risks these symptoms pose to road safety, but we recommend that clinicians strongly consider the potential for impaired driving.
In a longitudinal study, cognitive impairment and behavioral disturbances—especially agitation, apathy, and hallucinations—were strong predictors of driving cessation among patients with dementia.6 Furthermore, a case crossover study of patients with dementia found a 54% increase in risk of motor vehicle collisions associated with the use of psychotropic medications.15
Consider all aspects of the patient’s clinical status, including neuropsychiatric symptoms, psychotropic medications, comorbid medical conditions (including hearing and vision impairment), and concomitant therapy for medical conditions. Any could change a safe driver with mild dementia into an unsafe driver.
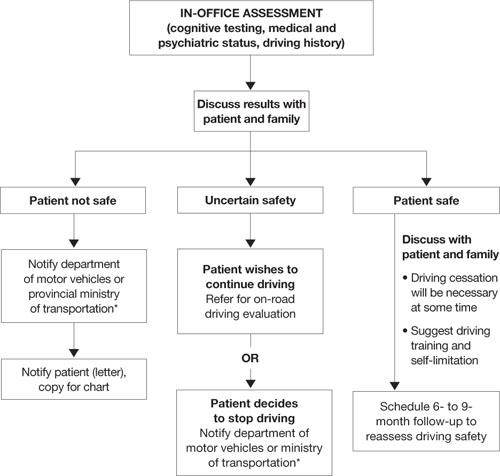
Algorithm: 3 options for drivers with dementia, based on in-office assessment
* Observe legislation or statutes that address reporting unsafe drivers to the department of motor vehicles or ministry of transportation
On-road driving tests
Because some individuals with mild dementia can drive safely for extended periods, international recommendations for assessing the driver with dementia emphasize on-road driving tests.10,13,20–22 American10 and Canadian guidelines13 suggest that a dementia diagnosis is not sufficient to withdraw licensure.
A formal driving assessment is necessary to establish road safety for patients with mild dementia except when the need for license withdrawal is evident, such as when the patient has:
- a history of major driving problems (such as crashes or driving the wrong way on a highway)
- significant contraindications to driving on the history or physical examination (such as severe inattention or psychosis).
Challenges of on-road testing. On-road tests may be the gold standard, but they are not without clinical problems.
Need to retest. Because almost all dementias are progressive and driving skills deteriorate over time, most guidelines recommend periodic retesting. For patients with dementia who pass on-road evaluations, limited evidence supports retesting every 6 months.14 Take an individual approach, however, because of the various rates at which the dementias progress.
Testing vs real world conditions. Structured on-road testing is not equivalent to unstructured real-world driving, in which the patient often must navigate without instruction or assistance.
Rural vs urban driving. Road tests conducted in urban areas assess skills associated with complex conditions and the need to respond quickly to crises. They might not assess as well rural driving, which requires sustained attention on monotonous roads.
Inaccessibility. Cost and lack of availability of on-road tests, particularly in rural areas, limit the number of patients whose performance can be evaluated.
CASE CONTINUED: Distressing results
Mr. D has a history of decline in cognition and function, objective cognitive difficulties, and a subtle history of driving problems. You refer him for a specialized on-road test, and the report indicates that he failed. Errors included wide turns, driving too slowly, getting caught in an intersection twice during red lights while attempting to turn left, driving on the shoulder, and failing to signal lane changes. You review the results with Mr. D and his wife and recommend that he cease driving immediately.
Mr. D is furious, and his wife is dismayed. He demands to know how he can continue to play golf, which is his only form of exercise and recreation. Will she have to give up her bridge club? How will they shop for food? They request permission to at least to drive to the grocery store during the daytime.
You explain that no system allows individuals to drive only at certain times, and for the sake of safety you cannot grant them special permission. You discuss alternatives, such as asking their daughter for assistance with grocery shopping and taking taxis or ride-sharing with friends who play golf and bridge.
Remain firm, but ease the blow
Driving cessation orders distress patients, families, and clinicians. A failed road test clearly indicates unsafe driving, and driving cessation is critical to public safety.
A review by Man-Son-Hing et al23 found that drivers with dementia performed worse than nondemented controls in all studies that examined driving performance (on-road, simulator, or caregiver report). Simulators showed problems such as off-road driving, deviation from posted speed, and more time to negotiate left turns.24
By comparison, only 1 of 3 studies using state crash records showed an increased risk of collisions in persons with dementia compared with controls.23 From a research perspective, however, studies that use state-reported collisions to assess driving risk are confounded by driving restrictions on persons with dementia.
Mr. D wants to continue driving with restrictions. No studies have shown reduced crash rates when drivers with dementia used compensatory strategies such as restrictions, retraining/education, having a passenger “co-pilot,” on-board navigation, or cognitive enhancers.23
If Mr. D had passed the road test, the situation would have been more ambiguous. Two studies have examined on-road driving performance over time in patients with early-stage dementia.25,26 Both studies followed drivers prospectively for 2 years, and those with mild dementia (vs very mild or no dementia) were most likely to show a decline in driving skills:
- All participants with mild dementia were rated as “not safe” by the end of 2 years by Duchek et al.25
- Median time to “failure” (or a rating of unsafe) was 324 days for drivers with mild dementia vs 605 days for those with very mild dementia, as reported by Ott et al.26
Mr. D’s passionate plea for reconsideration highlights the need for communities to develop alternate transportation for seniors whose driving becomes unsafe (Box 2).
Legal liability? Physicians often are concerned about legal responsibilities and risks involved in reporting unsafe drivers. Be aware of local statutes or legislations regarding mandatory reporting of patients you deem unsafe to drive.17 These laws usually protect physicians from lawsuits related to violating patient confidentiality. Civil lawsuits remain possible, however, if clinicians fail to report an unsafe driver who subsequently is involved in a motor vehicle collision.27
1. Meet with family first. Help them assume a positive and supportive role. Explain concretely and empathically your concern for the safety of the patient and others. Clearly outline your findings that the patient is not fit to drive, and explain that the law requires you to report the patient to the authorities.
Remind family members that the goal of driving assessment is to prevent a collision, and they carry some responsibility because they are aware of the potential risk of letting their family member continue to drive. If necessary, have family members witness a repeat performance by the patient on the most revealing test. Discuss the importance of finding alternate transportation to reduce the risk of isolation and depression that can follow driving cessation.
2. Meet with patient. Having the family present can be helpful, but ask them to assume a supportive role. Give the patient a positive role by recognizing that he or she has been a responsible driver, and part of this responsibility is to stop driving before an accident occurs. Acknowledge that it is normal to be unhappy upon learning that one’s driving privileges are being revoked.
Sometimes it helps to give the patient a prescription in their name that says, “Do not drive.” Families who receive a copy may find this very helpful, too, for reminding the patient later about what you said.
If your patient argues with your position, remain firm and do not argue. Indicate that you have made notes on the meeting and are notifying the authorities about the patient’s unsafe driving. You can add that your chart could be subpoenaed and the patient may be legally liable and financially responsible should he or she continue to drive and have a collision.
3. Talk about transportation options. Family members could share driving responsibilities. Taxi rides can cost less than maintaining a car if the patient drives <4,000 km (2,500 miles) per year. Suggest that patients or families find volunteer drivers or contact helpful taxi drivers a day before an outing is planned.
4. If patient refuses to comply, meet with the family again and encourage them to remove the patient’s opportunity to drive (confiscate the keys, disable the car, or remove the car altogether).
Provide a written statement to the patient and family outlining why the patient can no longer drive. Indicate that it is your legal responsibility to report unsafe drivers, and you intend to notify the authorities regarding the patient’s driving status. If the patient remains noncompliant, continue to encourage family to remove the opportunity to drive.
Related resources
- Physician’s guide to assessing and counseling older drivers. American Medical Association and the National Highway Traffic Safety Administration, 2003. www.nhtsa.dot.gov/people/injury/olddrive/OlderDriversBook.
- Determining medical fitness to operate motor vehicles. Canadian Medical Association. 2006. www.cma.ca/index.cfm/ci_id/18223/la_id/1.htm.
- Canadian Driving Research Initiative for Vehicular Safety in the Elderly (CanDRIVE). www.candrive.ca.
Disclosures
The authors report no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dr. Rapoport receives grant/research support from the Canadian Institute of Health Research and the Ontario Neurotrauma Foundation.
1. Stowell-Ritter A, Straight A, Evans EL. Understanding senior transportation: report and analysis of a survey of consumers age 50+. Washington, DC: American Association of Retired Persons; 2002.
2. Marottoli RA, de Leon CFM, Glass TA, et al. Consequences of driving cessation: decreased out-of-home activity levels. J Gerontol B Psychol Sci Soc Sci 2000;55(6):S334-40.
3. Marottoli RA, Mendes de Leon CF, Glass TA, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J Am Geriatr Soc 1997;45(2):202-6.
4. Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003;60(8):1119-22.
5. Jang RW, Man-Son-Hing M, Molnar FJ, et al. Family physicians’ attitudes and practices regarding assessments of medical fitness to drive in older persons. J Gen Intern Med 2007;22(4):531-43.
6. Herrmann N, Rapoport MJ, Sambrook R, et al. Predictors of driving cessation in mild-to-moderate dementia. CMAJ 2006;175(6):591-5.
7. Hedlund J. Countermeasures that work: a highway safety countermeasure guide for state highway safety offices. Washington, DC: National Highway Traffic Safety Administration; 2006.
8. Dobbs B. Medical conditions and driving: a review of the literature (1960-2000). Washington, DC: National Highway Traffic Safety Administration; 2005. Available at: http://www.nhtsa.dot.gov/people/injury/research/Medical_Condition_Driving/pages/TRD.html. Accessed September 29, 2008.
9. Li G, Braver ER, Chen LH. Fragility versus excessive crash involvement as determinants of high death rates per vehicle-mile of travel among older drivers. Accid Anal Prev 2003;35(2):227-35.
10. Physician’s guide to assessing and counseling older drivers. Washington, DC: National Highway Traffic Safety Administration; 2003. Available at: http://www.nhtsa.dot.gov/people/injury/olddrive/OlderDriversBook. Accessed September 29, 2008.
11. Yeudall LT, Reddon JR, Gill DM, et al. Normative data for the Halstead-Reitan neuropsychological tests stratified by age and sex. J Clin Psychol 1987;43(3):346-67.
12. Brown LB, Ott BR, Papandonatos GD, et al. Prediction of on-road driving performance in patients with early Alzheimer’s disease. J Am Geriatr Soc 2005;53(1):94-8.
13. Determining medical fitness to operate motor vehicles. CMA driver’s guide. 7th ed. Ottawa, Ontario, Canada: Canadian Medical Association; 2006.
14. Molnar FJ, Patel A, Marshall SC, et al. Systematic review of the optimal frequency of follow-up in persons with mild dementia who continue to drive. Alzheimer Dis Assoc Disord 2006;20(4):295-7.
15. Rapoport MJ, Herrmann N, Molnar FJ, et al. Psychotropic medications and motor vehicle collisions in patients with dementia (letter). J Am Geriatr Soc 2008;56(10):1968-70.
16. Molnar FJ, Patel A, Marshall SC, et al. Clinical utility of office-based cognitive predictors of fitness to drive in persons with dementia: a systematic review. J Am Geriatr Soc 2006;54(12):1809-24.
17. Rapoport MJ, Herrmann N, Molnar FJ, et al. Sharing the responsibility for assessing the risk of the driver with dementia. CMAJ. 2007;177(6):599-601.
18. Herrmann N, Gauthier S, Lysy PG. Clinical practice guidelines for severe Alzheimer’s disease. Alzheimers Dement 2007;3(4):385-97.
19. Hogan DB, Bailey P, Carswell A, et al. Management of mild to moderate Alzheimer’s disease and dementia. Alzheimers Dement 2007;3(4):355-84.
19. Assessing fitness to drive for commercial and private vehicle drivers. Sydney, Australia: National Library of Australia; 2006. Available at: http://www.austroads.com.au/aftd/index.html. Accessed November 4, 2008.
21. Medical aspects of fitness to drive. A guide for medical practitioners. Wellington, New Zealand: Land Transport Safety Authority; 2002. Available at: http://www.transfund.govt.nz/licensing/docs/ltsa-medical-aspects.pdf. Accessed September 29, 2008.
22. At a glance guide to the current medical standards of fitness to drive. Swansea, UK: Drivers Medical Group, Driver and Vehicle Licensing Agency; 2008. Available at: http://www.dvla.gov.uk/medical/ataglance.aspx. Accessed September 29, 2008.
23. Man-Son-Hing M, Marshall SC, Molnar FJ, Wilson KG. Systematic review of driving risk and the efficacy of compensatory strategies in persons with dementia. J Am Geriatr Soc 2007;55(6):878-84.
24. Cox DJ, Quillian WC, Thorndike FP, et al. Evaluating driving performance of outpatients with Alzheimer disease. J Am Board Fam Pract 1998;11(4):264-71.
25. Duchek JM, Carr DB, Hunt L, et al. Longitudinal driving performance in early-stage dementia of the Alzheimer type. J Am Geriatr Soc 2003;51(10):1342-7.
26. Ott BR, Heindel WC, Papandonatos GD, et al. A longitudinal study of drivers with Alzheimer disease. Neurology 2008;70(14):1171-8.
27. Molnar FJ, Byszewski AM, Marshall SC, Man-Son-Hing M. In-office evaluation of medical fitness to drive: practical approaches for assessing older people. Can Fam Physician 2005;51:372-9.
1. Stowell-Ritter A, Straight A, Evans EL. Understanding senior transportation: report and analysis of a survey of consumers age 50+. Washington, DC: American Association of Retired Persons; 2002.
2. Marottoli RA, de Leon CFM, Glass TA, et al. Consequences of driving cessation: decreased out-of-home activity levels. J Gerontol B Psychol Sci Soc Sci 2000;55(6):S334-40.
3. Marottoli RA, Mendes de Leon CF, Glass TA, et al. Driving cessation and increased depressive symptoms: prospective evidence from the New Haven EPESE. Established Populations for Epidemiologic Studies of the Elderly. J Am Geriatr Soc 1997;45(2):202-6.
4. Hebert LE, Scherr PA, Bienias JL, et al. Alzheimer disease in the US population: prevalence estimates using the 2000 census. Arch Neurol 2003;60(8):1119-22.
5. Jang RW, Man-Son-Hing M, Molnar FJ, et al. Family physicians’ attitudes and practices regarding assessments of medical fitness to drive in older persons. J Gen Intern Med 2007;22(4):531-43.
6. Herrmann N, Rapoport MJ, Sambrook R, et al. Predictors of driving cessation in mild-to-moderate dementia. CMAJ 2006;175(6):591-5.
7. Hedlund J. Countermeasures that work: a highway safety countermeasure guide for state highway safety offices. Washington, DC: National Highway Traffic Safety Administration; 2006.
8. Dobbs B. Medical conditions and driving: a review of the literature (1960-2000). Washington, DC: National Highway Traffic Safety Administration; 2005. Available at: http://www.nhtsa.dot.gov/people/injury/research/Medical_Condition_Driving/pages/TRD.html. Accessed September 29, 2008.
9. Li G, Braver ER, Chen LH. Fragility versus excessive crash involvement as determinants of high death rates per vehicle-mile of travel among older drivers. Accid Anal Prev 2003;35(2):227-35.
10. Physician’s guide to assessing and counseling older drivers. Washington, DC: National Highway Traffic Safety Administration; 2003. Available at: http://www.nhtsa.dot.gov/people/injury/olddrive/OlderDriversBook. Accessed September 29, 2008.
11. Yeudall LT, Reddon JR, Gill DM, et al. Normative data for the Halstead-Reitan neuropsychological tests stratified by age and sex. J Clin Psychol 1987;43(3):346-67.
12. Brown LB, Ott BR, Papandonatos GD, et al. Prediction of on-road driving performance in patients with early Alzheimer’s disease. J Am Geriatr Soc 2005;53(1):94-8.
13. Determining medical fitness to operate motor vehicles. CMA driver’s guide. 7th ed. Ottawa, Ontario, Canada: Canadian Medical Association; 2006.
14. Molnar FJ, Patel A, Marshall SC, et al. Systematic review of the optimal frequency of follow-up in persons with mild dementia who continue to drive. Alzheimer Dis Assoc Disord 2006;20(4):295-7.
15. Rapoport MJ, Herrmann N, Molnar FJ, et al. Psychotropic medications and motor vehicle collisions in patients with dementia (letter). J Am Geriatr Soc 2008;56(10):1968-70.
16. Molnar FJ, Patel A, Marshall SC, et al. Clinical utility of office-based cognitive predictors of fitness to drive in persons with dementia: a systematic review. J Am Geriatr Soc 2006;54(12):1809-24.
17. Rapoport MJ, Herrmann N, Molnar FJ, et al. Sharing the responsibility for assessing the risk of the driver with dementia. CMAJ. 2007;177(6):599-601.
18. Herrmann N, Gauthier S, Lysy PG. Clinical practice guidelines for severe Alzheimer’s disease. Alzheimers Dement 2007;3(4):385-97.
19. Hogan DB, Bailey P, Carswell A, et al. Management of mild to moderate Alzheimer’s disease and dementia. Alzheimers Dement 2007;3(4):355-84.
19. Assessing fitness to drive for commercial and private vehicle drivers. Sydney, Australia: National Library of Australia; 2006. Available at: http://www.austroads.com.au/aftd/index.html. Accessed November 4, 2008.
21. Medical aspects of fitness to drive. A guide for medical practitioners. Wellington, New Zealand: Land Transport Safety Authority; 2002. Available at: http://www.transfund.govt.nz/licensing/docs/ltsa-medical-aspects.pdf. Accessed September 29, 2008.
22. At a glance guide to the current medical standards of fitness to drive. Swansea, UK: Drivers Medical Group, Driver and Vehicle Licensing Agency; 2008. Available at: http://www.dvla.gov.uk/medical/ataglance.aspx. Accessed September 29, 2008.
23. Man-Son-Hing M, Marshall SC, Molnar FJ, Wilson KG. Systematic review of driving risk and the efficacy of compensatory strategies in persons with dementia. J Am Geriatr Soc 2007;55(6):878-84.
24. Cox DJ, Quillian WC, Thorndike FP, et al. Evaluating driving performance of outpatients with Alzheimer disease. J Am Board Fam Pract 1998;11(4):264-71.
25. Duchek JM, Carr DB, Hunt L, et al. Longitudinal driving performance in early-stage dementia of the Alzheimer type. J Am Geriatr Soc 2003;51(10):1342-7.
26. Ott BR, Heindel WC, Papandonatos GD, et al. A longitudinal study of drivers with Alzheimer disease. Neurology 2008;70(14):1171-8.
27. Molnar FJ, Byszewski AM, Marshall SC, Man-Son-Hing M. In-office evaluation of medical fitness to drive: practical approaches for assessing older people. Can Fam Physician 2005;51:372-9.
Novel agent more effective than standard therapy in NHL
Preliminary results of a phase 3 study indicate that pixantrone is more effective than standard chemotherapy in patients with advanced, relapsed, aggressive non-Hodgkin lymphoma (NHL).
The phase 3 EXTEND PIX301 trial enrolled 140 NHL patients from 130 sites in 17 countries. Patients had received 2 or more prior therapies and were sensitive to anthracycline treatment.
They were randomized to receive either pixantrone or another single-agent drug currently used in this patient population and selected by a physician. The trial assessed patients’ complete remission or unconfirmed complete remission rate, overall survival, and progression-free survival.
Twenty percent of patients who received pixantrone achieved either a confirmed or unconfirmed complete remission, compared to 5.7% of patients on standard chemotherapy. Eleven percent of pixantrone patients’ remissions were confirmed, whereas none of the standard chemotherapy remissions were.
The overall response rate was 37.1% with pixantrone and 14.3% for patients on standard chemotherapy. Response rates were determined by an independent assessment panel that was blinded to treatment assignments.
Complete safety information for this study is not yet available. However, the study was monitored on an ongoing basis by an independent Data Safety Monitoring Committee, and no serious concerns were raised. The most common serious toxicities (> 5%) observed in previous trials of pixantrone include grade 3 and 4 neutropenia and febrile neutropenia.
Seventy-four percent of patients enrolled in this study discontinued therapy due to disease progression or death, the majority of which were in the standard chemotherapy control arm.
This study was funded by Cell Therapeutics, Inc., the company developing pixantrone.
Cell Therapeutics says it plans to submit complete study data for presentation at a major scientific conference. The organization also plans to request a pre-New Drug Application meeting with the FDA and expects to begin submission of a rolling New Drug Application to the FDA in early 2009.
Pixantrone is an antitumor agent that contains an aza-anthracenedione molecular structure, which differentiates it from anthracycline chemotherapy agents. ![]()
Preliminary results of a phase 3 study indicate that pixantrone is more effective than standard chemotherapy in patients with advanced, relapsed, aggressive non-Hodgkin lymphoma (NHL).
The phase 3 EXTEND PIX301 trial enrolled 140 NHL patients from 130 sites in 17 countries. Patients had received 2 or more prior therapies and were sensitive to anthracycline treatment.
They were randomized to receive either pixantrone or another single-agent drug currently used in this patient population and selected by a physician. The trial assessed patients’ complete remission or unconfirmed complete remission rate, overall survival, and progression-free survival.
Twenty percent of patients who received pixantrone achieved either a confirmed or unconfirmed complete remission, compared to 5.7% of patients on standard chemotherapy. Eleven percent of pixantrone patients’ remissions were confirmed, whereas none of the standard chemotherapy remissions were.
The overall response rate was 37.1% with pixantrone and 14.3% for patients on standard chemotherapy. Response rates were determined by an independent assessment panel that was blinded to treatment assignments.
Complete safety information for this study is not yet available. However, the study was monitored on an ongoing basis by an independent Data Safety Monitoring Committee, and no serious concerns were raised. The most common serious toxicities (> 5%) observed in previous trials of pixantrone include grade 3 and 4 neutropenia and febrile neutropenia.
Seventy-four percent of patients enrolled in this study discontinued therapy due to disease progression or death, the majority of which were in the standard chemotherapy control arm.
This study was funded by Cell Therapeutics, Inc., the company developing pixantrone.
Cell Therapeutics says it plans to submit complete study data for presentation at a major scientific conference. The organization also plans to request a pre-New Drug Application meeting with the FDA and expects to begin submission of a rolling New Drug Application to the FDA in early 2009.
Pixantrone is an antitumor agent that contains an aza-anthracenedione molecular structure, which differentiates it from anthracycline chemotherapy agents. ![]()
Preliminary results of a phase 3 study indicate that pixantrone is more effective than standard chemotherapy in patients with advanced, relapsed, aggressive non-Hodgkin lymphoma (NHL).
The phase 3 EXTEND PIX301 trial enrolled 140 NHL patients from 130 sites in 17 countries. Patients had received 2 or more prior therapies and were sensitive to anthracycline treatment.
They were randomized to receive either pixantrone or another single-agent drug currently used in this patient population and selected by a physician. The trial assessed patients’ complete remission or unconfirmed complete remission rate, overall survival, and progression-free survival.
Twenty percent of patients who received pixantrone achieved either a confirmed or unconfirmed complete remission, compared to 5.7% of patients on standard chemotherapy. Eleven percent of pixantrone patients’ remissions were confirmed, whereas none of the standard chemotherapy remissions were.
The overall response rate was 37.1% with pixantrone and 14.3% for patients on standard chemotherapy. Response rates were determined by an independent assessment panel that was blinded to treatment assignments.
Complete safety information for this study is not yet available. However, the study was monitored on an ongoing basis by an independent Data Safety Monitoring Committee, and no serious concerns were raised. The most common serious toxicities (> 5%) observed in previous trials of pixantrone include grade 3 and 4 neutropenia and febrile neutropenia.
Seventy-four percent of patients enrolled in this study discontinued therapy due to disease progression or death, the majority of which were in the standard chemotherapy control arm.
This study was funded by Cell Therapeutics, Inc., the company developing pixantrone.
Cell Therapeutics says it plans to submit complete study data for presentation at a major scientific conference. The organization also plans to request a pre-New Drug Application meeting with the FDA and expects to begin submission of a rolling New Drug Application to the FDA in early 2009.
Pixantrone is an antitumor agent that contains an aza-anthracenedione molecular structure, which differentiates it from anthracycline chemotherapy agents. ![]()
Proceedings of the Ethical Challenges in Surgical Innovation Summit
Supplement Editors:
Allen Bashour, MD, and Eric Kodish, MD
Contents
Most of the articles in this supplement were developed from audio transcripts of the summit’s presentations and panel discussions. The transcripts were edited by the Cleveland Clinic Journal of Medicine staff for clarity and conciseness, and were then review and revised/approved by the respective speaker or panelists. Exceptions are the articles followed by an asterisk (*) below, which were submitted as manuscripts by their authors.
From the summit directors*
Eric Kodish, MD, and Allen Bashour, MD
Editors and contributors
Welcome—Ethics in surgical innovation: Vigorous discussion will foster future progress
Delos M. Cosgrove, MD
Panel 1: Surgical Innovation and Ethical Dilemmas
Surgical innovation and ethical dilemmas: Precautions and proximity*
Joseph J. Fins, MD
Surgical innovation and ethical dilemmas: A panel discussion
Isador Lieberman, MD; James Herndon, MD; Joseph Hahn, MD; Joseph J. Fins, MD; and Ali Rezai, MD
Panel 2: Transplant Innovation and Ethical Challenges
Pushing the envelope in transplantation: Three lives at stake*
Pauline W. Chen, MD
Transplant innovation and ethical challenges: What have we learned? A collection of perspectives and panel discussion
Denton A. Cooley, MD; John J. Fung, MD, PhD; James B. Young, MD; Thomas E. Starzl, MD, PhD; Mark Siegler, MD; and Pauline W. Chen, MD
We have come far, but selecting organ recipients remains an ethical minefield—Denton A. Cooley, MD
Despite the odds, the transplant field has progressed rapidly—John J. Fung, MD, PhD
A continued need for evidence-based guidance—James B. Young, MD
What does—and does not—spur innovation?—Thomas E. Starzl, MD, PhD
Panel discussion—Moderated by Mark Siegler, MD
Keynote Address
Medical professionalism in a commercialized health care market*
Arnold S. Relman, MD
Panel 3: Inside the Operating Room
Inside the operating room—balancing the risks and benefi ts of new surgical procedures: A collection of perspectives and panel discussion
Joel D. Cooper, MD; Ralph V. Clayman, MD; Thomas M. Krummel, MD; Philip R. Schauer, MD; Christopher Thompson, MD, MHES; and Jonathan D. Moreno, PhD
How should we introduce and evaluate new procedures?—Joel D. Cooper, MD
Idea to implementation: A personal perspective on the development of laparoscopic nephrectomy—Ralph V. Clayman, MD
Special perspectives in infants and children—Thomas M. Krummel, MD
Bariatric surgery: What role for ethics as established procedures approach new frontiers?—Philip R. Schauer, MD
Natural orifice transluminal endoscopic surgery: Too much too soon?—Christopher Thompson, MD, MHES
Panel discussion—Moderated by Jonathan D. Moreno, PhD
Keynote Address
Will the United States maintain its position as a world leader in medical technology?
Thomas J. Fogarty, MD
Panel 4: Outside the Operating Room
Outside the operating room—economic, regulatory, and legal challenges: A collection of perspectives and panel discussion
Lawrence K. Altman, MD; Michael A. Mussallem; Rebecca Dresser, JD; Paul A. Lombardo, PhD, JD; Peter A. Ubel, MD; and Christopher L. White, Esq
Preface—Lawrence K. Altman, MD (Moderator)
A device company perspective: Serving patients is the key to sustainable success—Michael A. Mussallem
A regulatory and legal perspective: Issues in off-label device use—Rebecca Dresser, JD
A historical perspective: The more things change, the more they remain the same—Paul A. Lombardo, PhD, JD
An economic value perspective: Setting limits on health care can be ethical—Peter A. Ubel, MD
An industry perspective: Proactive self-regulation through an industry code of ethics—Christopher L. White, Esq
Panel discussion—Moderated by Lawrence K. Altman, MD
Panel 5: New Surgical Devices and Ethical Challenges
New surgical devices and ethical challenges: A collection of perspectives and panel discussion
Daniel Schultz, MD; Mary H. McGrath, MD, MPH; Thomas H. Murray, PhD; Roy K. Greenberg, MD; and Thomas J. Fogarty, MD
An FDA perspective on device regulation—Daniel Schultz, MD
Responsibilities of the media, FDA, and professional societies—Mary H. McGrath, MD, MPH
Promoting swift, safe, and smart innovation—Thomas H. Murray, PhD
Panel discussion—Moderated by Roy K. Greenberg, MD
Supplement Editors:
Allen Bashour, MD, and Eric Kodish, MD
Contents
Most of the articles in this supplement were developed from audio transcripts of the summit’s presentations and panel discussions. The transcripts were edited by the Cleveland Clinic Journal of Medicine staff for clarity and conciseness, and were then review and revised/approved by the respective speaker or panelists. Exceptions are the articles followed by an asterisk (*) below, which were submitted as manuscripts by their authors.
From the summit directors*
Eric Kodish, MD, and Allen Bashour, MD
Editors and contributors
Welcome—Ethics in surgical innovation: Vigorous discussion will foster future progress
Delos M. Cosgrove, MD
Panel 1: Surgical Innovation and Ethical Dilemmas
Surgical innovation and ethical dilemmas: Precautions and proximity*
Joseph J. Fins, MD
Surgical innovation and ethical dilemmas: A panel discussion
Isador Lieberman, MD; James Herndon, MD; Joseph Hahn, MD; Joseph J. Fins, MD; and Ali Rezai, MD
Panel 2: Transplant Innovation and Ethical Challenges
Pushing the envelope in transplantation: Three lives at stake*
Pauline W. Chen, MD
Transplant innovation and ethical challenges: What have we learned? A collection of perspectives and panel discussion
Denton A. Cooley, MD; John J. Fung, MD, PhD; James B. Young, MD; Thomas E. Starzl, MD, PhD; Mark Siegler, MD; and Pauline W. Chen, MD
We have come far, but selecting organ recipients remains an ethical minefield—Denton A. Cooley, MD
Despite the odds, the transplant field has progressed rapidly—John J. Fung, MD, PhD
A continued need for evidence-based guidance—James B. Young, MD
What does—and does not—spur innovation?—Thomas E. Starzl, MD, PhD
Panel discussion—Moderated by Mark Siegler, MD
Keynote Address
Medical professionalism in a commercialized health care market*
Arnold S. Relman, MD
Panel 3: Inside the Operating Room
Inside the operating room—balancing the risks and benefi ts of new surgical procedures: A collection of perspectives and panel discussion
Joel D. Cooper, MD; Ralph V. Clayman, MD; Thomas M. Krummel, MD; Philip R. Schauer, MD; Christopher Thompson, MD, MHES; and Jonathan D. Moreno, PhD
How should we introduce and evaluate new procedures?—Joel D. Cooper, MD
Idea to implementation: A personal perspective on the development of laparoscopic nephrectomy—Ralph V. Clayman, MD
Special perspectives in infants and children—Thomas M. Krummel, MD
Bariatric surgery: What role for ethics as established procedures approach new frontiers?—Philip R. Schauer, MD
Natural orifice transluminal endoscopic surgery: Too much too soon?—Christopher Thompson, MD, MHES
Panel discussion—Moderated by Jonathan D. Moreno, PhD
Keynote Address
Will the United States maintain its position as a world leader in medical technology?
Thomas J. Fogarty, MD
Panel 4: Outside the Operating Room
Outside the operating room—economic, regulatory, and legal challenges: A collection of perspectives and panel discussion
Lawrence K. Altman, MD; Michael A. Mussallem; Rebecca Dresser, JD; Paul A. Lombardo, PhD, JD; Peter A. Ubel, MD; and Christopher L. White, Esq
Preface—Lawrence K. Altman, MD (Moderator)
A device company perspective: Serving patients is the key to sustainable success—Michael A. Mussallem
A regulatory and legal perspective: Issues in off-label device use—Rebecca Dresser, JD
A historical perspective: The more things change, the more they remain the same—Paul A. Lombardo, PhD, JD
An economic value perspective: Setting limits on health care can be ethical—Peter A. Ubel, MD
An industry perspective: Proactive self-regulation through an industry code of ethics—Christopher L. White, Esq
Panel discussion—Moderated by Lawrence K. Altman, MD
Panel 5: New Surgical Devices and Ethical Challenges
New surgical devices and ethical challenges: A collection of perspectives and panel discussion
Daniel Schultz, MD; Mary H. McGrath, MD, MPH; Thomas H. Murray, PhD; Roy K. Greenberg, MD; and Thomas J. Fogarty, MD
An FDA perspective on device regulation—Daniel Schultz, MD
Responsibilities of the media, FDA, and professional societies—Mary H. McGrath, MD, MPH
Promoting swift, safe, and smart innovation—Thomas H. Murray, PhD
Panel discussion—Moderated by Roy K. Greenberg, MD
Supplement Editors:
Allen Bashour, MD, and Eric Kodish, MD
Contents
Most of the articles in this supplement were developed from audio transcripts of the summit’s presentations and panel discussions. The transcripts were edited by the Cleveland Clinic Journal of Medicine staff for clarity and conciseness, and were then review and revised/approved by the respective speaker or panelists. Exceptions are the articles followed by an asterisk (*) below, which were submitted as manuscripts by their authors.
From the summit directors*
Eric Kodish, MD, and Allen Bashour, MD
Editors and contributors
Welcome—Ethics in surgical innovation: Vigorous discussion will foster future progress
Delos M. Cosgrove, MD
Panel 1: Surgical Innovation and Ethical Dilemmas
Surgical innovation and ethical dilemmas: Precautions and proximity*
Joseph J. Fins, MD
Surgical innovation and ethical dilemmas: A panel discussion
Isador Lieberman, MD; James Herndon, MD; Joseph Hahn, MD; Joseph J. Fins, MD; and Ali Rezai, MD
Panel 2: Transplant Innovation and Ethical Challenges
Pushing the envelope in transplantation: Three lives at stake*
Pauline W. Chen, MD
Transplant innovation and ethical challenges: What have we learned? A collection of perspectives and panel discussion
Denton A. Cooley, MD; John J. Fung, MD, PhD; James B. Young, MD; Thomas E. Starzl, MD, PhD; Mark Siegler, MD; and Pauline W. Chen, MD
We have come far, but selecting organ recipients remains an ethical minefield—Denton A. Cooley, MD
Despite the odds, the transplant field has progressed rapidly—John J. Fung, MD, PhD
A continued need for evidence-based guidance—James B. Young, MD
What does—and does not—spur innovation?—Thomas E. Starzl, MD, PhD
Panel discussion—Moderated by Mark Siegler, MD
Keynote Address
Medical professionalism in a commercialized health care market*
Arnold S. Relman, MD
Panel 3: Inside the Operating Room
Inside the operating room—balancing the risks and benefi ts of new surgical procedures: A collection of perspectives and panel discussion
Joel D. Cooper, MD; Ralph V. Clayman, MD; Thomas M. Krummel, MD; Philip R. Schauer, MD; Christopher Thompson, MD, MHES; and Jonathan D. Moreno, PhD
How should we introduce and evaluate new procedures?—Joel D. Cooper, MD
Idea to implementation: A personal perspective on the development of laparoscopic nephrectomy—Ralph V. Clayman, MD
Special perspectives in infants and children—Thomas M. Krummel, MD
Bariatric surgery: What role for ethics as established procedures approach new frontiers?—Philip R. Schauer, MD
Natural orifice transluminal endoscopic surgery: Too much too soon?—Christopher Thompson, MD, MHES
Panel discussion—Moderated by Jonathan D. Moreno, PhD
Keynote Address
Will the United States maintain its position as a world leader in medical technology?
Thomas J. Fogarty, MD
Panel 4: Outside the Operating Room
Outside the operating room—economic, regulatory, and legal challenges: A collection of perspectives and panel discussion
Lawrence K. Altman, MD; Michael A. Mussallem; Rebecca Dresser, JD; Paul A. Lombardo, PhD, JD; Peter A. Ubel, MD; and Christopher L. White, Esq
Preface—Lawrence K. Altman, MD (Moderator)
A device company perspective: Serving patients is the key to sustainable success—Michael A. Mussallem
A regulatory and legal perspective: Issues in off-label device use—Rebecca Dresser, JD
A historical perspective: The more things change, the more they remain the same—Paul A. Lombardo, PhD, JD
An economic value perspective: Setting limits on health care can be ethical—Peter A. Ubel, MD
An industry perspective: Proactive self-regulation through an industry code of ethics—Christopher L. White, Esq
Panel discussion—Moderated by Lawrence K. Altman, MD
Panel 5: New Surgical Devices and Ethical Challenges
New surgical devices and ethical challenges: A collection of perspectives and panel discussion
Daniel Schultz, MD; Mary H. McGrath, MD, MPH; Thomas H. Murray, PhD; Roy K. Greenberg, MD; and Thomas J. Fogarty, MD
An FDA perspective on device regulation—Daniel Schultz, MD
Responsibilities of the media, FDA, and professional societies—Mary H. McGrath, MD, MPH
Promoting swift, safe, and smart innovation—Thomas H. Murray, PhD
Panel discussion—Moderated by Roy K. Greenberg, MD
From the summit directors
Surgical innovation lives on the border between tradition and regulation in a vaguely defined frontier. Over the course of many centuries, a framework for clinical medical ethics has developed with broad consensus regarding fiduciary obligations between patient and doctor, the principles of beneficence and nonmaleficence, and, more recently, respect for persons and autonomy. During the past century, a parallel set of ethical and regulatory norms has developed surrounding the ethics of research involving human subjects. While both sets of frameworks—those governing clinical ethics and those governing research ethics—contribute to understanding the ethical challenges that arise in the course of surgical innovation, neither is alone sufficient to provide clear guidance.
We decided that further discourse would help resolve some of the ambiguity that exists between the frameworks of clinical ethics and research ethics, and we set out to convene a summit meeting to provide a forum for this discourse. It was our hope that bringing together some of the nation’s foremost surgical innovators with leading bioethicists would catalyze a series of presentations and discussions to create a meaningful ethical framework for thinking about surgical innovation. The summit took place May 8–9, 2008, at Cleveland Clinic, and we were not disappointed. We now have the pleasure of presenting the proceedings in text form.
The summit’s five panel presentations and discussions and two keynote addresses shared the objective of educating participants about moral dilemmas that often arise in the conduct of device development and other innovations in surgery. Panelists suggested potential solutions to the challenges of protecting patients from risk without hindering creativity and progress.
The ethical challenges faced by surgical innovators will not go away. As we develop and refine technology, including new devices, procedures, and transplants, new problems will arise. Two examples of complicated issues on the horizon are robotic surgery and natural orifice transluminal endoscopic surgery (NOTES). While the specific developments will change, the ethical basis of our actions should remain constant. We need to always ask the same questions:
- Is this in the best interests of the patient?
- Have we been thoughtful and effective in the process of informed consent?
- Will our actions be consistent with our own professional integrity?
Our hope is that these proceedings will prompt the necessary next steps: further development of these ideas, writing of papers and convening of more meetings, and, most importantly, further innovation to continue helping patients.
Surgical innovation lives on the border between tradition and regulation in a vaguely defined frontier. Over the course of many centuries, a framework for clinical medical ethics has developed with broad consensus regarding fiduciary obligations between patient and doctor, the principles of beneficence and nonmaleficence, and, more recently, respect for persons and autonomy. During the past century, a parallel set of ethical and regulatory norms has developed surrounding the ethics of research involving human subjects. While both sets of frameworks—those governing clinical ethics and those governing research ethics—contribute to understanding the ethical challenges that arise in the course of surgical innovation, neither is alone sufficient to provide clear guidance.
We decided that further discourse would help resolve some of the ambiguity that exists between the frameworks of clinical ethics and research ethics, and we set out to convene a summit meeting to provide a forum for this discourse. It was our hope that bringing together some of the nation’s foremost surgical innovators with leading bioethicists would catalyze a series of presentations and discussions to create a meaningful ethical framework for thinking about surgical innovation. The summit took place May 8–9, 2008, at Cleveland Clinic, and we were not disappointed. We now have the pleasure of presenting the proceedings in text form.
The summit’s five panel presentations and discussions and two keynote addresses shared the objective of educating participants about moral dilemmas that often arise in the conduct of device development and other innovations in surgery. Panelists suggested potential solutions to the challenges of protecting patients from risk without hindering creativity and progress.
The ethical challenges faced by surgical innovators will not go away. As we develop and refine technology, including new devices, procedures, and transplants, new problems will arise. Two examples of complicated issues on the horizon are robotic surgery and natural orifice transluminal endoscopic surgery (NOTES). While the specific developments will change, the ethical basis of our actions should remain constant. We need to always ask the same questions:
- Is this in the best interests of the patient?
- Have we been thoughtful and effective in the process of informed consent?
- Will our actions be consistent with our own professional integrity?
Our hope is that these proceedings will prompt the necessary next steps: further development of these ideas, writing of papers and convening of more meetings, and, most importantly, further innovation to continue helping patients.
Surgical innovation lives on the border between tradition and regulation in a vaguely defined frontier. Over the course of many centuries, a framework for clinical medical ethics has developed with broad consensus regarding fiduciary obligations between patient and doctor, the principles of beneficence and nonmaleficence, and, more recently, respect for persons and autonomy. During the past century, a parallel set of ethical and regulatory norms has developed surrounding the ethics of research involving human subjects. While both sets of frameworks—those governing clinical ethics and those governing research ethics—contribute to understanding the ethical challenges that arise in the course of surgical innovation, neither is alone sufficient to provide clear guidance.
We decided that further discourse would help resolve some of the ambiguity that exists between the frameworks of clinical ethics and research ethics, and we set out to convene a summit meeting to provide a forum for this discourse. It was our hope that bringing together some of the nation’s foremost surgical innovators with leading bioethicists would catalyze a series of presentations and discussions to create a meaningful ethical framework for thinking about surgical innovation. The summit took place May 8–9, 2008, at Cleveland Clinic, and we were not disappointed. We now have the pleasure of presenting the proceedings in text form.
The summit’s five panel presentations and discussions and two keynote addresses shared the objective of educating participants about moral dilemmas that often arise in the conduct of device development and other innovations in surgery. Panelists suggested potential solutions to the challenges of protecting patients from risk without hindering creativity and progress.
The ethical challenges faced by surgical innovators will not go away. As we develop and refine technology, including new devices, procedures, and transplants, new problems will arise. Two examples of complicated issues on the horizon are robotic surgery and natural orifice transluminal endoscopic surgery (NOTES). While the specific developments will change, the ethical basis of our actions should remain constant. We need to always ask the same questions:
- Is this in the best interests of the patient?
- Have we been thoughtful and effective in the process of informed consent?
- Will our actions be consistent with our own professional integrity?
Our hope is that these proceedings will prompt the necessary next steps: further development of these ideas, writing of papers and convening of more meetings, and, most importantly, further innovation to continue helping patients.
Ethics in surgical innovation: Vigorous discussion will foster future progress
Welcome to Cleveland Clinic. We are delighted to have you here, and I am sure this is going to be a very interesting and provocative meeting.
In 1873 Sir John Eric Erichsen, surgeon to Queen Victoria, wrote that “although methods of practice may be modified and varied, and even improved to some extent,” “the knife cannot always have fresh fields for conquest.” How wrong he was.
Surgical innovation has continued without a break from Erichsen’s day to ours. In 1873 only 2.5% of the population survived to age 65. Over the past 100 years, surgical innovation has helped to extend the average life expectancy to 76 years.
AN UNRULY TRADITION
Surgical innovation has happened largely without rules and by its own unruly tradition. In some ways, it is the last frontier in medicine. Today surgical innovation is arguably defined and barely regulated. Technical variation is the norm, and every patient is different. The boundary between taking an alternative approach and embarking on a novel human experimentation may be finely shaded. No surgical equivalent to the Food and Drug Administration monitors the operating room. Professional ethics and common sense guide routine intraoperative intervention.
Formal research projects are carried out in compliance with the institutional review board (IRB) and the usual ethical and regulatory standards for human subjects research. Between these two posts lies a large, vaguely defined field. That is where this symposium will be spending the majority of its time.
Surgical progress is problem-driven and rarely planned. It has often taken place under stress or in response to contingent need or opportunity.
In our own lifetimes we have seen the development of cardiac surgery in a virtually rule-free environment. Surgery for coronary artery disease did not develop out of a surgical protocol but arose out of new knowledge of the disease mechanism and improvements in imaging, anesthesia, extracorporeal oxygenation, and a combination of gifted surgeons and experienced surgical teams. It was immediately accepted as therapy. There are similar examples in every surgical field.
Over the past 40 years only 10% to 20% of surgical techniques have undergone clinical trials. Transplant is a classic example. Cardiac transplant moved forward without clinical trials, and it is unlikely that clinical trials will ever be done. The laparoscopic revolution came about in the same way.
A REGULATORY BALANCING ACT
Regulation is necessary, but where and how much? In a recent speech here at Cleveland Clinic, Anne Mulcahy, chief executive officer of Xerox, said, “Most great things happen by accident and experimentation. The moment you try to streamline and keep everything captive to very focused and disciplined outcomes, you lose your ability to really invent.”
On the other hand, we cannot let surgery devolve into what a past president of the Canadian Medical Association called “a chaos of techniques devoid of moral purpose.”
Finding the right balance will be difficult. All of this makes this symposium on ethics in surgical innovation relevant, necessary, and likely to be of interest well beyond these rooms. The profession of surgery has everything to gain from a frank discussion of the issues surrounding innovation. A solid grasp of ethics will improve our practice, protect our patients, and foster progress and innovation as we go forward.
You have a wonderful opportunity to discuss with some of the finest innovators in surgery—who are here in this room—the ethical and moral dilemmas of innovation. We cannot, on the one hand, proceed completely without plan; on the other hand, we cannot regulate innovation out of existence. In the end, it is about our patients, and their interest has to be placed first.
Thank you for joining us. I am sure you are going to have an excellent symposium.
Welcome to Cleveland Clinic. We are delighted to have you here, and I am sure this is going to be a very interesting and provocative meeting.
In 1873 Sir John Eric Erichsen, surgeon to Queen Victoria, wrote that “although methods of practice may be modified and varied, and even improved to some extent,” “the knife cannot always have fresh fields for conquest.” How wrong he was.
Surgical innovation has continued without a break from Erichsen’s day to ours. In 1873 only 2.5% of the population survived to age 65. Over the past 100 years, surgical innovation has helped to extend the average life expectancy to 76 years.
AN UNRULY TRADITION
Surgical innovation has happened largely without rules and by its own unruly tradition. In some ways, it is the last frontier in medicine. Today surgical innovation is arguably defined and barely regulated. Technical variation is the norm, and every patient is different. The boundary between taking an alternative approach and embarking on a novel human experimentation may be finely shaded. No surgical equivalent to the Food and Drug Administration monitors the operating room. Professional ethics and common sense guide routine intraoperative intervention.
Formal research projects are carried out in compliance with the institutional review board (IRB) and the usual ethical and regulatory standards for human subjects research. Between these two posts lies a large, vaguely defined field. That is where this symposium will be spending the majority of its time.
Surgical progress is problem-driven and rarely planned. It has often taken place under stress or in response to contingent need or opportunity.
In our own lifetimes we have seen the development of cardiac surgery in a virtually rule-free environment. Surgery for coronary artery disease did not develop out of a surgical protocol but arose out of new knowledge of the disease mechanism and improvements in imaging, anesthesia, extracorporeal oxygenation, and a combination of gifted surgeons and experienced surgical teams. It was immediately accepted as therapy. There are similar examples in every surgical field.
Over the past 40 years only 10% to 20% of surgical techniques have undergone clinical trials. Transplant is a classic example. Cardiac transplant moved forward without clinical trials, and it is unlikely that clinical trials will ever be done. The laparoscopic revolution came about in the same way.
A REGULATORY BALANCING ACT
Regulation is necessary, but where and how much? In a recent speech here at Cleveland Clinic, Anne Mulcahy, chief executive officer of Xerox, said, “Most great things happen by accident and experimentation. The moment you try to streamline and keep everything captive to very focused and disciplined outcomes, you lose your ability to really invent.”
On the other hand, we cannot let surgery devolve into what a past president of the Canadian Medical Association called “a chaos of techniques devoid of moral purpose.”
Finding the right balance will be difficult. All of this makes this symposium on ethics in surgical innovation relevant, necessary, and likely to be of interest well beyond these rooms. The profession of surgery has everything to gain from a frank discussion of the issues surrounding innovation. A solid grasp of ethics will improve our practice, protect our patients, and foster progress and innovation as we go forward.
You have a wonderful opportunity to discuss with some of the finest innovators in surgery—who are here in this room—the ethical and moral dilemmas of innovation. We cannot, on the one hand, proceed completely without plan; on the other hand, we cannot regulate innovation out of existence. In the end, it is about our patients, and their interest has to be placed first.
Thank you for joining us. I am sure you are going to have an excellent symposium.
Welcome to Cleveland Clinic. We are delighted to have you here, and I am sure this is going to be a very interesting and provocative meeting.
In 1873 Sir John Eric Erichsen, surgeon to Queen Victoria, wrote that “although methods of practice may be modified and varied, and even improved to some extent,” “the knife cannot always have fresh fields for conquest.” How wrong he was.
Surgical innovation has continued without a break from Erichsen’s day to ours. In 1873 only 2.5% of the population survived to age 65. Over the past 100 years, surgical innovation has helped to extend the average life expectancy to 76 years.
AN UNRULY TRADITION
Surgical innovation has happened largely without rules and by its own unruly tradition. In some ways, it is the last frontier in medicine. Today surgical innovation is arguably defined and barely regulated. Technical variation is the norm, and every patient is different. The boundary between taking an alternative approach and embarking on a novel human experimentation may be finely shaded. No surgical equivalent to the Food and Drug Administration monitors the operating room. Professional ethics and common sense guide routine intraoperative intervention.
Formal research projects are carried out in compliance with the institutional review board (IRB) and the usual ethical and regulatory standards for human subjects research. Between these two posts lies a large, vaguely defined field. That is where this symposium will be spending the majority of its time.
Surgical progress is problem-driven and rarely planned. It has often taken place under stress or in response to contingent need or opportunity.
In our own lifetimes we have seen the development of cardiac surgery in a virtually rule-free environment. Surgery for coronary artery disease did not develop out of a surgical protocol but arose out of new knowledge of the disease mechanism and improvements in imaging, anesthesia, extracorporeal oxygenation, and a combination of gifted surgeons and experienced surgical teams. It was immediately accepted as therapy. There are similar examples in every surgical field.
Over the past 40 years only 10% to 20% of surgical techniques have undergone clinical trials. Transplant is a classic example. Cardiac transplant moved forward without clinical trials, and it is unlikely that clinical trials will ever be done. The laparoscopic revolution came about in the same way.
A REGULATORY BALANCING ACT
Regulation is necessary, but where and how much? In a recent speech here at Cleveland Clinic, Anne Mulcahy, chief executive officer of Xerox, said, “Most great things happen by accident and experimentation. The moment you try to streamline and keep everything captive to very focused and disciplined outcomes, you lose your ability to really invent.”
On the other hand, we cannot let surgery devolve into what a past president of the Canadian Medical Association called “a chaos of techniques devoid of moral purpose.”
Finding the right balance will be difficult. All of this makes this symposium on ethics in surgical innovation relevant, necessary, and likely to be of interest well beyond these rooms. The profession of surgery has everything to gain from a frank discussion of the issues surrounding innovation. A solid grasp of ethics will improve our practice, protect our patients, and foster progress and innovation as we go forward.
You have a wonderful opportunity to discuss with some of the finest innovators in surgery—who are here in this room—the ethical and moral dilemmas of innovation. We cannot, on the one hand, proceed completely without plan; on the other hand, we cannot regulate innovation out of existence. In the end, it is about our patients, and their interest has to be placed first.
Thank you for joining us. I am sure you are going to have an excellent symposium.
Surgical innovation and ethical dilemmas: Precautions and proximity
No! I am not Prince Hamlet, nor was meant to be;
Am an attendant lord, one that will do
To swell a progress, start a scene or two…
—T.S. Eliot, The Love Song of J. Alfred Prufrock
Let me start by thanking the organizers for their invitation to be here and to start this off. I am not sure if that invitation was an act of kindness or of throwing a fellow bioethicist to the lions, as we will be addressing a complicated set of issues upon which well-intentioned folks disagree and sometimes disagree with a passion.
What I would like to do is to lay out some of the inherent ethical problems related to surgical innovation. I will argue that some of these problems are unique to surgery and that others relate to how we have chosen to define categories like research and practice. Other problems involve how we view the proportionality of risks and benefits in surgical research. I will argue that we have falsely analogized surgical progress to progress made in other areas of biomedical research and misunderstood the highly personal, or proximate, nature of surgical inquiry. Without appreciating the import of what I will call “surgical proximity,” we will be unable to adequately address ethical issues in surgical innovation.
PROBLEMS OR DILEMMAS?
So let me begin with the title of our session, “Surgical Innovation and Ethical Dilemmas,” and why this juxta position is counterproductive. A colleague long ago taught me to distinguish problems from dilemmas—the former being resolvable, the latter intractable, often involving a choice between two equally unfavorable choices.
Although I may be making too much of the semantics, I do think the title betrays a presumption that surgical innovation invariably forces adversarial choices. It tends to dichotomize ethical reflection, pitting those who favor prudence against those who endorse progress, or it creates too stark a difference between ethical issues in surgical practice and those encountered in the conduct of surgical research.
Even therapeutic, validated surgery in many ways has the potential to become innovative, if not outright experimental. Patients may have anatomical differences that require surgical improvisation, or complications may arise during “routine” surgery, creating the need for an imaginative response.1 At what point do these departures from expected care become novel interventions, innovative or even experimental? A routine case with an unexpected turn can even become a case report opening up a new field of endeavor.
For instance, the field of stereotactic functional neurosurgery was born out of a “routine” case of ablative surgery for Parkinson’s disease in the 1980s, when the French neurosurgeon Alim Benabid was using electrodes to determine which areas of the brain should be destroyed. As he was mapping the thalamus, he noted that the tremor of his patient abated. This led him to wonder if one could treat drug-resistant Parkinson’s with electrical stimulation instead of destructive lesioning.2 Benabid’s translational insight during an ordinary case led to the development of the rather extraordinary field of stereotactic functional neurosurgery and neuromodulation.3,4
Another example from an earlier era comes from the life work of neurosurgeon Wilder Penfield, who did pioneering work in the surgical treatment of epilepsy. Here, the accumulation of experience from “routine care” led to generalizable knowledge, much like hypotheses are validated in experimental work. In Penfield’s case, his clinical use of electrical stimulation to plan resections of scar tissue causing epilepsy led him to map the human homunculus, a magnificent achievement of profound importance.5,6
So let us avoid simplistic and confounding demarcations. Instead of dichotomizing innovation and prudence—or surgical research and surgical practice—let us try to start our deliberations with an eye toward a more synthetic approach. Like most things in nature and in biology, ethics too is on a continuum with gradations that can fit into an Aristotelian taxonomy. Let us emulate what Aristotle called phronesis, or practical wisdom, these next 2 days so that we achieve constructive outcomes, or what the pragmatists would call instrumental goods.7
If we are successful in laying out the ethical issues in this clinically pragmatic fashion, we can turn intractable “dilemmas” into problems amenable to resolution through the particularistic invocation of ethical principles as they relate to the surgical context.8 If we follow this inductive method of moral problem solving, we will avoid sweeping ethical generalizations, or categoricals, that can misrepresent the complexity of innovative research and deprive society of its benefits.9
INNOVATION VS PRUDENCE: A FALSE DICHOTOMY
So let us start by understanding the presuppositions that led to the expectation that dilemmas will descend upon those who engage in surgical innovation. In my view, this expectation begins with what is called the precautionary principle, a concept with some currency in the realm of environmental ethics.10
The precautionary principle urges caution and prudence when facing unknowns and is an antecedent sort of utilitarianism. One makes judgments about the advisability of actions based on a prior assessment of foreseeable risks and benefits. If the risks are excessive or exceed benefits, the precautionary principle urges care, caution, and even avoidance of a given course of action.
When the precautionary principle is implicitly invoked in making judgments about research, the objective is to pursue a degree of safety that is comparable to that of established therapy. But interventions that have progressed to being deemed “therapeutic” have of course achieved a requisite degree of both safety and efficacy—that is what makes them therapeutic, as opposed to investigational, interventions. One cannot know before one has conducted a clinical trial, and completed statistical analysis, whether a new surgical advance or device meets these expectations. Because of this lack of knowledge, there is an inherent degree of risk in any novel intervention.
The challenge posed by innovation or novelty creates the possibility of untoward events. It leads to invocation of the precautionary principle, which, echoing the admonitions of the philosopher Hans Jonas, urges us to “give greater weight to the prognosis of doom than to that of bliss.”11,12
This is not a bad way to go through life, assuming one wants to emulate T.S. Eliot’s J. Alfred Prufrock, who lamentably “measured out my life with coffee spoons.”13 Unlike the surgeon, who must make decisions in real time, Eliot’s protagonist could not move forward. Despite his desire to avoid the indecision of Prince Hamlet, alluded to in this paper’s epigraph, Prufrock was paralyzed by doubts and fears, with “time yet for a hundred indecisions, and for a hundred visions and revisions.”13
Despite Eliot’s invocation of “a patient etherised upon a table,”13 the poem shares little with the surgical life. It has much more in common with the precautionary principle. Like Prufrock, the precautionary principle favors what is known— the status quo—as what is unknown is invariably more risky than the familiar. Needless to say, this is antithetical to innovation because discovery invariably requires scenarios that involve novelty and unknown risks. When faced with the certain security of stasis or the potential dangers of innovation, the precautionary principle will invariably choose stasis, leading us, as the legal scholar Cass Sunstein notes, “in no direction at all.”14
Seen through the prism of the precautionary principle, then, surgical innovation invariably presents a dilemma. Discovery and innovation are fundamentally at odds with the precautionary principle, because of their potential for risk.15
The challenge posed by the precautionary principle—which, to be fair, is seen in all areas of clinical research—becomes even more pronounced in surgical research because of the size and scope of clinical trials. As is well appreciated here, compared with drug trials, surgical trials are small. Sometimes they can involve a single subject, whereas drug trials may include thousands of participants. Because of drug trials’ large volume of subjects, therapeutic effects can be small to justify ongoing research. In a surgical trial or a device trial, the number of subjects is smaller, so the therapeutic impact has to be larger to warrant further development and ongoing study. This burden of scale increases the probability of reciprocally large adverse effects. This potential for disaster magnifies the impact of the precautionary principle and may lead to a distortion in ethical judgment along the lines of Hans Jonas’ admonition.12
By all of this I am not suggesting that we abandon precautions and prudence. Instead, my point is to explicate the additional challenges faced by surgical research and the sway of the precautionary principle over this area of inquiry and innovation. By being explicit about the impact of this principle, we can be cognizant of its potential to distort judgments about risks and benefits. Only then can we hope to balance the pursuit of progress with that of safety.
SURGICAL RESPONSIBILITY
These distortions also need to be recognized, and made explicit, because surgical research, more so than pharmacologic research, is much more personal and intimate. This point becomes clear if we consider a surgical trial that does not succeed.
In the surgical arena, such failures are taken to heart and personalized. Unlike trials that involve drugs, surgical research is more proximate. It is not just the failure of a drug or of pharmacology; it is also possibly the failure of the operator, the surgeon who did not achieve the desired goal because of poor execution of surgical technique.
This crucial difference in medical versus surgical cultures is captured by Charles Bosk in his magisterial sociological study of surgery, Forgive and Remember: Managing Medical Failure. In a discussion of morbidity and mortality rounds, Bosk writes:
The specific nature of surgical treatment links the action of the physician and the response of the patient more intimately than in other areas of medicine....When the patient of an internist dies, the natural question his colleagues ask is, “What happened?” When the patient of a surgeon dies, his colleagues ask, “What did you do?”16
As in clinical surgical practice, in surgical research, it is the personal and individualized mediation of the surgeon that is central to the intervention. Here the intermediary is neither a drug nor its bioavailability; rather, it is the operator’s technique plus or minus the operative design and the reliability of an instrument or a device. In either case, the contribution is more proximate and personal, stemming from the actions of individual surgeons and the work of their hands.
History is instructive on this theme of surgical causality and personal culpability if we consider the life of Harvey Cushing, a Cleveland native whose ashes are buried nearby in Lake View Cemetery.17 Cushing was a gifted and innovative surgeon whose technique handling tissues changed how the brain was approached operatively. He is acknowledged as the father of neurosurgery, having created a professional nexus to institutionalize and carry on his innovative work.18
Cushing’s greatest innovation was probably in his individual efforts as a working surgeon. Over the course of his lifetime, he made the resection of brain tumors a safe and sometimes effective treatment for an otherwise dread disease. Michael Bliss, Cushing’s most recent biographer, reports mortality data from more than 2,400 surgeries done by Cushing during his operative lifetime.17 Early in his career (from 1896 to 1911), while he was at Johns Hopkins, Cushing’s case mortality rate was 24.7%. During his later years at the Brigham Hospital, it was 16.2%. By 1930–1931 it was down to 8.8%.
These were extraordinary statistics: no one matched Cushing’s numbers, or his ability to do what he did. Bliss cites mortality data from his surgical contemporaries in the late 1920s as ranging from approximately 35% to 45%. By the numbers Bliss compares Cushing’s talent—his truly brilliant outlier performance—to that of his Jazz Age contemporary, Babe Ruth, who also had outsized talent compared with his peers.17
Cushing himself, a collegiate second baseman at Yale, linked sport and statistics in a most telling way. Documenting his ongoing surgical progress was a hedge against failure and lightened the emotional burdens of the surgical suite. Cushing observed: “A neurosurgeon’s responsibilities would be insufferable if he did not feel that his knowledge of an intricate subject was constantly growing—that his game was improving.”17
This quote and Cushing’s operative statistics point to his nascent effort to engage in evidence-based research and speaks to the spectacular difference that a surgical innovator can make. The extraordinary results achieved by Cushing in his day also suggest that surgeons are not fungible at the vanguard of discovery. History tells us, as contemporary assessments of current research cannot, that only Harvey Cushing could achieve Cushingoid results.
A second point that stems from Cushing’s comment about the burdens of operative work and surgical research is how personally taxing that responsibility can be. Without making progress, he said, the “responsibilities would be insufferable”17 (my italics).
Even the great Harvey Cushing perceived the weight of these burdens, suggesting that any effort to depersonalize the ethics of surgical innovation would be naïve. The singularity of Cushing’s surgical accomplishments (his operative excellence as compared with his peer group) and the felt weight of these achievements suggest that surgical innovation is highly personal and proximate to the surgical researcher in a way that is distinct for surgical innovation. This relationship of operative causality and personal culpability can be subsumed under what I will call surgical proximity.
SURGICAL PROXIMITY
Surgical proximity has several implications for the conduct of research. In this section I will address two issues: conflicts of interest and clinical equipoise.
Surgical proximity and conflicts of interest
As the Cushing example illustrates, at least at the outset of a clinical trial the surgeon himself is part of the actual design of the trial. The same surgical method in the hands of one of his contemporaries would have led to a dramatically different result. The surgeon who is at the forefront of innovation becomes an experimental variable until the methods can be generalized.
The importance of the operator as an essential ingredient in early surgical research points to a key difference with pharmaceutical trials, where the purity of the drug-based intervention can be maintained. This difference has implications for the “rebuttable presumption” stance promulgated by the Association of American Medical Colleges (AAMC), which looks askance at innovators conducting clinical trials if they have a conflict of interest, such as intellectual property rights for their discoveries.19,20
In many cases, the work that surgical innovators do, as in the case of device development, could not be done without collaborations with industry. Taking the surgical talent of the potentially conflicted—but highly talented—innovator out of the equation may be counterproductive.
Time does not allow me to fully address the conflict-of-interest issue in this forum; suffice it to say that the differential knowledge, skill, and talent of early surgical innovators may be the difference between a trial’s early success or failure. The role of such innovators should neither be truncated or precluded nor be viewed a priori in a prejudicial fashion. Instead, their talents and vision should be welcomed as instrumental to the potential success of the work, managed of course with the proper degree of transparency and disclosure.
As I have noted previously,4,21 if the rationale for a conflict of interest is to allow laudable work to continue that otherwise could not occur without the personal intervention, and talents, of a surgical innovator, it seems prejudicial to view the conflict of interest as disqualifying until proven otherwise. This view is consistent with the legal framework of the US Constitution, which explicitly authorizes Congress “to promote the Progress of Science and the useful Arts, by securing for limited Times to Authors and Inventors the exclusive Right to their respective Writings and Discoveries.”22 It is also embedded in the Patent Act of 1790,23 which balances the patent’s period of exclusivity against the inventor’s obligation to share and disseminate expertise. This role for the innovator is also consistent with the intent and incentives within the framework of the Bayh-Dole Act of 1980,24 which was passed with the expectation that industrial partnerships would move ideas from the bench to the bedside.
I hope that others at this conference will be able to return to the issue of conflicts of interest and how the question of surgical proximity may, or may not, alter our ethical judgments about the surgeon’s role in research where there may be a conflict of interest.
Surgical proximity and equipoise
Surgical proximity also has an impact on clinical equipoise, the ethical neutrality about outcomes felt necessary for the conduct of clinical trials.25 The surgeon’s sense of causality and proximity to the operative act makes surgical research different because the equipoise, which exists objectively about the research questions at hand, may not exist in the mind of the surgical researcher. Let me explain.
Taking a patient to surgery is highly consequential. As we have seen from Bosk’s work,16 surgeons feel a sense of responsibility for their operative acts and surgical work. This felt responsibility, inculcated in surgical training and surgical culture, obligates the surgeon to make a proportionality judgment about bringing a patient to the operating room, be it for research or for clinical practice. In this way, surgical investigators have determined, at least in their own minds, that net benefits outweigh net risks, thus breaching clinical equipoise.
It is hard for a surgeon to commit to an operative procedure—be it for clinical care or for research— with all its attendant risks if he or she does not believe that the intervention is safe and effective. We can appreciate the importance of the surgeon’s perspective on the utility of any proposed operation if we consider the opposing question of futility in clinical practice.26 Whereas internists or intensivists might be compelled by families to continue aggressive intensive care, surgeons cannot be compelled to take a patient to the operating room when they deem that the risks outweigh the benefits. Because the surgeon is such a proximate moral agent, he or she will be held culpable for the actions that occur in theater. This degree of responsibility is accompanied by a retained degree of discretion—an almost old-world paternalistic discretion27—to counter the demands for disproportionate care.
This same sense of culpability and responsibility informs the surgeon’s willingness to take any patient to the operating room. In the case of research, this willingness becomes an issue of concern because it means that in the surgeon’s mind, favorable operative proportionality has been achieved.
This process of self-regulation28 can have implications for the informed-consent process because surgeons believe in their work and can exert a strong dynamic transference on subjects who may be desperate for cure.29 Because of this potential bias, surgical research may become especially prone to a therapeutic misconception. That is, if the surgeon is willing to take the risks of doing an innovative procedure in the operating room, then it has crossed some sort of internal threshold of proportionality in which the risks, whatever they are, have become acceptable given the putative benefits. Given what Bosk has written about surgical failure,16 a high bar is crossed when a surgeon takes a patient to the operating room for a novel procedure, even though motivations at that bar may occasionally be mixed.* (*Lest I be misconstrued as too idealistic, this burdens-vs-benefits equation may be fueled by a complex mosaic of motivations and may not always be informed fully by patient-centered benefits. If the surgeon is the innovator and the inventor, these benefits may be for the pursuit of a hypothesis and associated with potential fame or fortune. But even in these cases, judgments about proportionality are informed by surgical proximity. [For more on the ethics of conflicts of interest, see references 4 and 21.])
FROM SURGICAL RESEARCH TO EDUCATION
This leads to my closing observations about transitions in surgical research, when the work of the pioneering surgeon is bequeathed to the broader surgical community to pick up the torch—or scalpel—and expand the work.
This takes me away from research and, fittingly here at a medical school dedicated to research training, brings me to medical education. To transcend the personal dimensions of surgical innovation—and the courage and vision of the founders—and sustain it more broadly, innovators also have to become educators of future surgeons, organizers of talent, and moral exemplars for the next generation. They have to appreciate that the work that they started, if it is important, will not be completed during their tenure but that future generations will carry it forward and expand upon it. They also have to prepare the next generation with the tools and orientation to appreciate their vision and to embrace what Thomas Kuhn might call new scientific paradigms.30
On several occasions Wilder Penfield, who founded the Montreal Neurological Institute, wrote with regret about Victor Horsley, the neurosurgeon at Queens Square in London. Penfield viewed Horsley as the founder of his field, but Horsley left no disciples. In his autobiography, fittingly entitled No Man Alone, Penfield noted that Horsley, “the most distinguished pioneer neurosurgeon, had died in 1916 without having established a school of neurosurgery.”5 This is in contrast to the discipline-building work of Cushing.
It is not an accident that Dr. Cushing founded a field full of trainees and protégés, of which my co-panelists are descendants. It was intentional and part of his ethos of being truly innovative. And it is not an accident that the distinguished surgical innovators at this symposium have also created institutional structures to continue their work for decades to come. Their achievements have transcended the individual innovator and have become systematic. It is said that Dr. Thomas Starzl launched a field.31 Dr. Denton Cooley founded the Texas Heart Institute.32 Dr. Thomas Fogarty started the Fogarty Institute for Innovation, whose mission statement explicitly notes that it is “an educational non-profit that mentors, trains and inspires the next generation of medical innovators.”33 Each of these pioneers, I believe, appreciates the need for continuity and dissemination.
But even here there is something that we nonsurgeons need to understand: although the work transcends the individual surgeon, the ties remain personal and linked to the impact and legacy of founders. Take, for example, highly prized membership in the Denton A. Cooley Cardiovascular Surgical Society.34 This too is about the importance of individuals and surgical proximity, but here it is transgenerational.
CONCLUSION
If we truly want to continue the dialogue begun here today, we need to understand these social and professional networks and the importance of surgical proximity in transmitting both methods and values. The proximate nature of surgical research—and the causality and responsibility that accrues to the surgeon—makes surgical research different than other areas of biomedical inquiry. This difference has implications for risk-benefit analysis, conflicts of interest, and clinical equipoise. I hope that my colleagues return to these themes in the coming days so that the regulation of this important area of research can be informed by a deeper understanding of the ethics of surgical discovery and innovation.35
Acknowledgments
Dr. Fins gratefully acknowledges the invitation to participate in this symposium, the helpful suggestions of Dr. Eric Kodish, and partial grant support of the Weill Cornell Medical College Research Ethics Core, NIH Clinical & Translational Science Center UL1-RR024966.
- Frader JE, Caniano DA. Research and innovation in surgery. In: McCullough LB, Jones JW, Brody BA, eds. Surgical Ethics. New York, NY: Oxford University Press; 1998:216–241.
- Speelman JD, Bosch DA. Resurgence of functional neurosurgery for Parkinson’s disease: a historical perspective. Mov Disord 1998; 13:582–588.
- Holstein WJ. Rewiring the brain: how a bright idea became an innovative medical device. US News & World Report. March 1, 1999:52–53.
- Fins JJ, Schachter M. Investigators, industry, and the heuristic device: ethics, patent law, and clinical innovation. Account Res 2001; 8:219–233.
- Penfield W. No Man Alone: A Neurosurgeon’s Life. Boston, MA: Little Brown; 1977.
- Feindel W. The contributions of Wilder Penfield to the functional anatomy of the human brain. Hum Neurobiol 1982; 1:231–234.
- Aristotle. The Nicomachean Ethics. Weldon JEC, trans. Amherst, NY: Prometheus Books; 1987.
- Fins JJ, Bacchetta MD, Miller FG. Clinical pragmatism: a method of moral problem solving. Kennedy Inst Ethics J 1997; 7:129–145.
- Miller FG, Fins JJ. Protecting human subjects in brain research: a pragmatic perspective. In: Illes J, ed. Neuroethics: Defining the Issues in Theory, Practice and Policy. New York, NY: Oxford University Press; 2005.
- Pollan M. The year in ideas: A to Z.; precautionary principle. New York Times. December 9, 2001.
- van den Belt H. Debating the precautionary principle: “guilty until proven innocent” or “innocent until proven guilty”? Plant Physiol 2003; 132:1122–1126.
- Jonas H. The Imperative of Responsibility: In Search of an Ethics for the Technological Age. Chicago, IL: University of Chicago Press; 1985:34.
- Eliot TS. The Love Song of J. Alfred Prufrock. In: Abrams MH, ed. The Norton Anthology of English Literature. Vol 2. 4th ed. New York, NY: W.W. Norton & Co; 1979:2259–2264.
- Sunstein CR. The paralyzing principle. Regulation. Winter 2002– 2003; 25(4):32–37.
- Holm S, Harris J. Precautionary principle stifles discovery. Nature 1999; 400:398.
- Bosk C. Forgive and Remember: Managing Medical Failure. Chicago, IL: University of Chicago Press; 1979:29–30.
- Bliss M. Harvey Cushing: A Life in Surgery. Oxford, UK: Oxford University Press; 2005.
- Pinkus RL. Mistakes as a social construct: an historical approach. Kennedy Inst Ethics J 2001; 11:117–133.
- AAMC Task Force on Financial Conflicts of Interest in Clinical Research. Protecting subjects, preserving trust, promoting progress I: policy and guidelines for the oversight of individual financial interests in human subjects research. Acad Med 2003; 78:225–236.
- AAMC Task Force on Financial Conflicts of Interest in Clinical Research. Protecting subjects, preserving trust, promoting progress II: principles and recommendations for oversight of an institution’s financial interests in human subjects research. Acad Med 2003; 78:237– 245.
- Fins JJ. Disclose and justify: intellectual property, conflicts of interest, and neurosurgery. Congress Quarterly (Official Newsmagazine of the Congress of Neurological Surgeons) 2007; 8(3):34–36.
- U.S. Constitution, art. I, §8, cl. 8; see also id. at art. I, §8, cl. 18.
- Patent Act of 1790, ch. 7, 1 Stat. 109–111 (1790).
- Patent and Trademark Act Amendments of 1980 (Bayh-Dole Act); Pub L No. 96-517. Codified as 35 USC §§200–212 (1994).
- Freedman B. Equipoise and the ethics of clinical research. N Engl J Med 1987; 317:141–145.
- Callahan D. Necessity, futility, and the good society. J Am Geriatr Soc 1994; 42:866–867.
- Katz J. The Silent World of Doctor and Patient. New York, NY: Free Press; 1984.
- Jones RS, Fletcher JC. Self-regulation of surgical practice and research. In: McCullough LB, Jones JW, Brody BA, eds. Surgical Ethics. New York, NY: Oxford University Press; 1998:255–279.
- Kim SY. Assessing and communicating the risks and benefits of gene transfer clinical trials. Curr Opin Mol Ther 2006; 8:384– 389.
- Kuhn TS. The Structure of Scientific Revolutions. 2nd ed. Chicago, IL: University of Chicago Press; 1970.
- Starzl TE. The Puzzle People: Memoirs of a Transplant Surgeon. Pittsburgh, PA: University of Pittsburgh Press; 2003.
- Twenty Five Years of Excellence: A History of the Texas Heart Institute. Houston, TX: Texas Heart Institute Foundation; 1989.
- Fogarty Institute for Innovation Web site. Available at: http://01659a8. netsolhost.com/aboutus.html. Accessed June 6, 2008.
- Denton A. Cooley Cardiovascular Surgical Society Web site. Available at: http://www.cooleysociety.com/about.html. Accessed June 6, 2008.
- de Melo-Martín I, Palmer LI, Fins JJ. Viewpoint: developing a research ethics consultation service to foster responsive and responsible clinical research. Acad Med 2007; 82:900–904.
No! I am not Prince Hamlet, nor was meant to be;
Am an attendant lord, one that will do
To swell a progress, start a scene or two…
—T.S. Eliot, The Love Song of J. Alfred Prufrock
Let me start by thanking the organizers for their invitation to be here and to start this off. I am not sure if that invitation was an act of kindness or of throwing a fellow bioethicist to the lions, as we will be addressing a complicated set of issues upon which well-intentioned folks disagree and sometimes disagree with a passion.
What I would like to do is to lay out some of the inherent ethical problems related to surgical innovation. I will argue that some of these problems are unique to surgery and that others relate to how we have chosen to define categories like research and practice. Other problems involve how we view the proportionality of risks and benefits in surgical research. I will argue that we have falsely analogized surgical progress to progress made in other areas of biomedical research and misunderstood the highly personal, or proximate, nature of surgical inquiry. Without appreciating the import of what I will call “surgical proximity,” we will be unable to adequately address ethical issues in surgical innovation.
PROBLEMS OR DILEMMAS?
So let me begin with the title of our session, “Surgical Innovation and Ethical Dilemmas,” and why this juxta position is counterproductive. A colleague long ago taught me to distinguish problems from dilemmas—the former being resolvable, the latter intractable, often involving a choice between two equally unfavorable choices.
Although I may be making too much of the semantics, I do think the title betrays a presumption that surgical innovation invariably forces adversarial choices. It tends to dichotomize ethical reflection, pitting those who favor prudence against those who endorse progress, or it creates too stark a difference between ethical issues in surgical practice and those encountered in the conduct of surgical research.
Even therapeutic, validated surgery in many ways has the potential to become innovative, if not outright experimental. Patients may have anatomical differences that require surgical improvisation, or complications may arise during “routine” surgery, creating the need for an imaginative response.1 At what point do these departures from expected care become novel interventions, innovative or even experimental? A routine case with an unexpected turn can even become a case report opening up a new field of endeavor.
For instance, the field of stereotactic functional neurosurgery was born out of a “routine” case of ablative surgery for Parkinson’s disease in the 1980s, when the French neurosurgeon Alim Benabid was using electrodes to determine which areas of the brain should be destroyed. As he was mapping the thalamus, he noted that the tremor of his patient abated. This led him to wonder if one could treat drug-resistant Parkinson’s with electrical stimulation instead of destructive lesioning.2 Benabid’s translational insight during an ordinary case led to the development of the rather extraordinary field of stereotactic functional neurosurgery and neuromodulation.3,4
Another example from an earlier era comes from the life work of neurosurgeon Wilder Penfield, who did pioneering work in the surgical treatment of epilepsy. Here, the accumulation of experience from “routine care” led to generalizable knowledge, much like hypotheses are validated in experimental work. In Penfield’s case, his clinical use of electrical stimulation to plan resections of scar tissue causing epilepsy led him to map the human homunculus, a magnificent achievement of profound importance.5,6
So let us avoid simplistic and confounding demarcations. Instead of dichotomizing innovation and prudence—or surgical research and surgical practice—let us try to start our deliberations with an eye toward a more synthetic approach. Like most things in nature and in biology, ethics too is on a continuum with gradations that can fit into an Aristotelian taxonomy. Let us emulate what Aristotle called phronesis, or practical wisdom, these next 2 days so that we achieve constructive outcomes, or what the pragmatists would call instrumental goods.7
If we are successful in laying out the ethical issues in this clinically pragmatic fashion, we can turn intractable “dilemmas” into problems amenable to resolution through the particularistic invocation of ethical principles as they relate to the surgical context.8 If we follow this inductive method of moral problem solving, we will avoid sweeping ethical generalizations, or categoricals, that can misrepresent the complexity of innovative research and deprive society of its benefits.9
INNOVATION VS PRUDENCE: A FALSE DICHOTOMY
So let us start by understanding the presuppositions that led to the expectation that dilemmas will descend upon those who engage in surgical innovation. In my view, this expectation begins with what is called the precautionary principle, a concept with some currency in the realm of environmental ethics.10
The precautionary principle urges caution and prudence when facing unknowns and is an antecedent sort of utilitarianism. One makes judgments about the advisability of actions based on a prior assessment of foreseeable risks and benefits. If the risks are excessive or exceed benefits, the precautionary principle urges care, caution, and even avoidance of a given course of action.
When the precautionary principle is implicitly invoked in making judgments about research, the objective is to pursue a degree of safety that is comparable to that of established therapy. But interventions that have progressed to being deemed “therapeutic” have of course achieved a requisite degree of both safety and efficacy—that is what makes them therapeutic, as opposed to investigational, interventions. One cannot know before one has conducted a clinical trial, and completed statistical analysis, whether a new surgical advance or device meets these expectations. Because of this lack of knowledge, there is an inherent degree of risk in any novel intervention.
The challenge posed by innovation or novelty creates the possibility of untoward events. It leads to invocation of the precautionary principle, which, echoing the admonitions of the philosopher Hans Jonas, urges us to “give greater weight to the prognosis of doom than to that of bliss.”11,12
This is not a bad way to go through life, assuming one wants to emulate T.S. Eliot’s J. Alfred Prufrock, who lamentably “measured out my life with coffee spoons.”13 Unlike the surgeon, who must make decisions in real time, Eliot’s protagonist could not move forward. Despite his desire to avoid the indecision of Prince Hamlet, alluded to in this paper’s epigraph, Prufrock was paralyzed by doubts and fears, with “time yet for a hundred indecisions, and for a hundred visions and revisions.”13
Despite Eliot’s invocation of “a patient etherised upon a table,”13 the poem shares little with the surgical life. It has much more in common with the precautionary principle. Like Prufrock, the precautionary principle favors what is known— the status quo—as what is unknown is invariably more risky than the familiar. Needless to say, this is antithetical to innovation because discovery invariably requires scenarios that involve novelty and unknown risks. When faced with the certain security of stasis or the potential dangers of innovation, the precautionary principle will invariably choose stasis, leading us, as the legal scholar Cass Sunstein notes, “in no direction at all.”14
Seen through the prism of the precautionary principle, then, surgical innovation invariably presents a dilemma. Discovery and innovation are fundamentally at odds with the precautionary principle, because of their potential for risk.15
The challenge posed by the precautionary principle—which, to be fair, is seen in all areas of clinical research—becomes even more pronounced in surgical research because of the size and scope of clinical trials. As is well appreciated here, compared with drug trials, surgical trials are small. Sometimes they can involve a single subject, whereas drug trials may include thousands of participants. Because of drug trials’ large volume of subjects, therapeutic effects can be small to justify ongoing research. In a surgical trial or a device trial, the number of subjects is smaller, so the therapeutic impact has to be larger to warrant further development and ongoing study. This burden of scale increases the probability of reciprocally large adverse effects. This potential for disaster magnifies the impact of the precautionary principle and may lead to a distortion in ethical judgment along the lines of Hans Jonas’ admonition.12
By all of this I am not suggesting that we abandon precautions and prudence. Instead, my point is to explicate the additional challenges faced by surgical research and the sway of the precautionary principle over this area of inquiry and innovation. By being explicit about the impact of this principle, we can be cognizant of its potential to distort judgments about risks and benefits. Only then can we hope to balance the pursuit of progress with that of safety.
SURGICAL RESPONSIBILITY
These distortions also need to be recognized, and made explicit, because surgical research, more so than pharmacologic research, is much more personal and intimate. This point becomes clear if we consider a surgical trial that does not succeed.
In the surgical arena, such failures are taken to heart and personalized. Unlike trials that involve drugs, surgical research is more proximate. It is not just the failure of a drug or of pharmacology; it is also possibly the failure of the operator, the surgeon who did not achieve the desired goal because of poor execution of surgical technique.
This crucial difference in medical versus surgical cultures is captured by Charles Bosk in his magisterial sociological study of surgery, Forgive and Remember: Managing Medical Failure. In a discussion of morbidity and mortality rounds, Bosk writes:
The specific nature of surgical treatment links the action of the physician and the response of the patient more intimately than in other areas of medicine....When the patient of an internist dies, the natural question his colleagues ask is, “What happened?” When the patient of a surgeon dies, his colleagues ask, “What did you do?”16
As in clinical surgical practice, in surgical research, it is the personal and individualized mediation of the surgeon that is central to the intervention. Here the intermediary is neither a drug nor its bioavailability; rather, it is the operator’s technique plus or minus the operative design and the reliability of an instrument or a device. In either case, the contribution is more proximate and personal, stemming from the actions of individual surgeons and the work of their hands.
History is instructive on this theme of surgical causality and personal culpability if we consider the life of Harvey Cushing, a Cleveland native whose ashes are buried nearby in Lake View Cemetery.17 Cushing was a gifted and innovative surgeon whose technique handling tissues changed how the brain was approached operatively. He is acknowledged as the father of neurosurgery, having created a professional nexus to institutionalize and carry on his innovative work.18
Cushing’s greatest innovation was probably in his individual efforts as a working surgeon. Over the course of his lifetime, he made the resection of brain tumors a safe and sometimes effective treatment for an otherwise dread disease. Michael Bliss, Cushing’s most recent biographer, reports mortality data from more than 2,400 surgeries done by Cushing during his operative lifetime.17 Early in his career (from 1896 to 1911), while he was at Johns Hopkins, Cushing’s case mortality rate was 24.7%. During his later years at the Brigham Hospital, it was 16.2%. By 1930–1931 it was down to 8.8%.
These were extraordinary statistics: no one matched Cushing’s numbers, or his ability to do what he did. Bliss cites mortality data from his surgical contemporaries in the late 1920s as ranging from approximately 35% to 45%. By the numbers Bliss compares Cushing’s talent—his truly brilliant outlier performance—to that of his Jazz Age contemporary, Babe Ruth, who also had outsized talent compared with his peers.17
Cushing himself, a collegiate second baseman at Yale, linked sport and statistics in a most telling way. Documenting his ongoing surgical progress was a hedge against failure and lightened the emotional burdens of the surgical suite. Cushing observed: “A neurosurgeon’s responsibilities would be insufferable if he did not feel that his knowledge of an intricate subject was constantly growing—that his game was improving.”17
This quote and Cushing’s operative statistics point to his nascent effort to engage in evidence-based research and speaks to the spectacular difference that a surgical innovator can make. The extraordinary results achieved by Cushing in his day also suggest that surgeons are not fungible at the vanguard of discovery. History tells us, as contemporary assessments of current research cannot, that only Harvey Cushing could achieve Cushingoid results.
A second point that stems from Cushing’s comment about the burdens of operative work and surgical research is how personally taxing that responsibility can be. Without making progress, he said, the “responsibilities would be insufferable”17 (my italics).
Even the great Harvey Cushing perceived the weight of these burdens, suggesting that any effort to depersonalize the ethics of surgical innovation would be naïve. The singularity of Cushing’s surgical accomplishments (his operative excellence as compared with his peer group) and the felt weight of these achievements suggest that surgical innovation is highly personal and proximate to the surgical researcher in a way that is distinct for surgical innovation. This relationship of operative causality and personal culpability can be subsumed under what I will call surgical proximity.
SURGICAL PROXIMITY
Surgical proximity has several implications for the conduct of research. In this section I will address two issues: conflicts of interest and clinical equipoise.
Surgical proximity and conflicts of interest
As the Cushing example illustrates, at least at the outset of a clinical trial the surgeon himself is part of the actual design of the trial. The same surgical method in the hands of one of his contemporaries would have led to a dramatically different result. The surgeon who is at the forefront of innovation becomes an experimental variable until the methods can be generalized.
The importance of the operator as an essential ingredient in early surgical research points to a key difference with pharmaceutical trials, where the purity of the drug-based intervention can be maintained. This difference has implications for the “rebuttable presumption” stance promulgated by the Association of American Medical Colleges (AAMC), which looks askance at innovators conducting clinical trials if they have a conflict of interest, such as intellectual property rights for their discoveries.19,20
In many cases, the work that surgical innovators do, as in the case of device development, could not be done without collaborations with industry. Taking the surgical talent of the potentially conflicted—but highly talented—innovator out of the equation may be counterproductive.
Time does not allow me to fully address the conflict-of-interest issue in this forum; suffice it to say that the differential knowledge, skill, and talent of early surgical innovators may be the difference between a trial’s early success or failure. The role of such innovators should neither be truncated or precluded nor be viewed a priori in a prejudicial fashion. Instead, their talents and vision should be welcomed as instrumental to the potential success of the work, managed of course with the proper degree of transparency and disclosure.
As I have noted previously,4,21 if the rationale for a conflict of interest is to allow laudable work to continue that otherwise could not occur without the personal intervention, and talents, of a surgical innovator, it seems prejudicial to view the conflict of interest as disqualifying until proven otherwise. This view is consistent with the legal framework of the US Constitution, which explicitly authorizes Congress “to promote the Progress of Science and the useful Arts, by securing for limited Times to Authors and Inventors the exclusive Right to their respective Writings and Discoveries.”22 It is also embedded in the Patent Act of 1790,23 which balances the patent’s period of exclusivity against the inventor’s obligation to share and disseminate expertise. This role for the innovator is also consistent with the intent and incentives within the framework of the Bayh-Dole Act of 1980,24 which was passed with the expectation that industrial partnerships would move ideas from the bench to the bedside.
I hope that others at this conference will be able to return to the issue of conflicts of interest and how the question of surgical proximity may, or may not, alter our ethical judgments about the surgeon’s role in research where there may be a conflict of interest.
Surgical proximity and equipoise
Surgical proximity also has an impact on clinical equipoise, the ethical neutrality about outcomes felt necessary for the conduct of clinical trials.25 The surgeon’s sense of causality and proximity to the operative act makes surgical research different because the equipoise, which exists objectively about the research questions at hand, may not exist in the mind of the surgical researcher. Let me explain.
Taking a patient to surgery is highly consequential. As we have seen from Bosk’s work,16 surgeons feel a sense of responsibility for their operative acts and surgical work. This felt responsibility, inculcated in surgical training and surgical culture, obligates the surgeon to make a proportionality judgment about bringing a patient to the operating room, be it for research or for clinical practice. In this way, surgical investigators have determined, at least in their own minds, that net benefits outweigh net risks, thus breaching clinical equipoise.
It is hard for a surgeon to commit to an operative procedure—be it for clinical care or for research— with all its attendant risks if he or she does not believe that the intervention is safe and effective. We can appreciate the importance of the surgeon’s perspective on the utility of any proposed operation if we consider the opposing question of futility in clinical practice.26 Whereas internists or intensivists might be compelled by families to continue aggressive intensive care, surgeons cannot be compelled to take a patient to the operating room when they deem that the risks outweigh the benefits. Because the surgeon is such a proximate moral agent, he or she will be held culpable for the actions that occur in theater. This degree of responsibility is accompanied by a retained degree of discretion—an almost old-world paternalistic discretion27—to counter the demands for disproportionate care.
This same sense of culpability and responsibility informs the surgeon’s willingness to take any patient to the operating room. In the case of research, this willingness becomes an issue of concern because it means that in the surgeon’s mind, favorable operative proportionality has been achieved.
This process of self-regulation28 can have implications for the informed-consent process because surgeons believe in their work and can exert a strong dynamic transference on subjects who may be desperate for cure.29 Because of this potential bias, surgical research may become especially prone to a therapeutic misconception. That is, if the surgeon is willing to take the risks of doing an innovative procedure in the operating room, then it has crossed some sort of internal threshold of proportionality in which the risks, whatever they are, have become acceptable given the putative benefits. Given what Bosk has written about surgical failure,16 a high bar is crossed when a surgeon takes a patient to the operating room for a novel procedure, even though motivations at that bar may occasionally be mixed.* (*Lest I be misconstrued as too idealistic, this burdens-vs-benefits equation may be fueled by a complex mosaic of motivations and may not always be informed fully by patient-centered benefits. If the surgeon is the innovator and the inventor, these benefits may be for the pursuit of a hypothesis and associated with potential fame or fortune. But even in these cases, judgments about proportionality are informed by surgical proximity. [For more on the ethics of conflicts of interest, see references 4 and 21.])
FROM SURGICAL RESEARCH TO EDUCATION
This leads to my closing observations about transitions in surgical research, when the work of the pioneering surgeon is bequeathed to the broader surgical community to pick up the torch—or scalpel—and expand the work.
This takes me away from research and, fittingly here at a medical school dedicated to research training, brings me to medical education. To transcend the personal dimensions of surgical innovation—and the courage and vision of the founders—and sustain it more broadly, innovators also have to become educators of future surgeons, organizers of talent, and moral exemplars for the next generation. They have to appreciate that the work that they started, if it is important, will not be completed during their tenure but that future generations will carry it forward and expand upon it. They also have to prepare the next generation with the tools and orientation to appreciate their vision and to embrace what Thomas Kuhn might call new scientific paradigms.30
On several occasions Wilder Penfield, who founded the Montreal Neurological Institute, wrote with regret about Victor Horsley, the neurosurgeon at Queens Square in London. Penfield viewed Horsley as the founder of his field, but Horsley left no disciples. In his autobiography, fittingly entitled No Man Alone, Penfield noted that Horsley, “the most distinguished pioneer neurosurgeon, had died in 1916 without having established a school of neurosurgery.”5 This is in contrast to the discipline-building work of Cushing.
It is not an accident that Dr. Cushing founded a field full of trainees and protégés, of which my co-panelists are descendants. It was intentional and part of his ethos of being truly innovative. And it is not an accident that the distinguished surgical innovators at this symposium have also created institutional structures to continue their work for decades to come. Their achievements have transcended the individual innovator and have become systematic. It is said that Dr. Thomas Starzl launched a field.31 Dr. Denton Cooley founded the Texas Heart Institute.32 Dr. Thomas Fogarty started the Fogarty Institute for Innovation, whose mission statement explicitly notes that it is “an educational non-profit that mentors, trains and inspires the next generation of medical innovators.”33 Each of these pioneers, I believe, appreciates the need for continuity and dissemination.
But even here there is something that we nonsurgeons need to understand: although the work transcends the individual surgeon, the ties remain personal and linked to the impact and legacy of founders. Take, for example, highly prized membership in the Denton A. Cooley Cardiovascular Surgical Society.34 This too is about the importance of individuals and surgical proximity, but here it is transgenerational.
CONCLUSION
If we truly want to continue the dialogue begun here today, we need to understand these social and professional networks and the importance of surgical proximity in transmitting both methods and values. The proximate nature of surgical research—and the causality and responsibility that accrues to the surgeon—makes surgical research different than other areas of biomedical inquiry. This difference has implications for risk-benefit analysis, conflicts of interest, and clinical equipoise. I hope that my colleagues return to these themes in the coming days so that the regulation of this important area of research can be informed by a deeper understanding of the ethics of surgical discovery and innovation.35
Acknowledgments
Dr. Fins gratefully acknowledges the invitation to participate in this symposium, the helpful suggestions of Dr. Eric Kodish, and partial grant support of the Weill Cornell Medical College Research Ethics Core, NIH Clinical & Translational Science Center UL1-RR024966.
No! I am not Prince Hamlet, nor was meant to be;
Am an attendant lord, one that will do
To swell a progress, start a scene or two…
—T.S. Eliot, The Love Song of J. Alfred Prufrock
Let me start by thanking the organizers for their invitation to be here and to start this off. I am not sure if that invitation was an act of kindness or of throwing a fellow bioethicist to the lions, as we will be addressing a complicated set of issues upon which well-intentioned folks disagree and sometimes disagree with a passion.
What I would like to do is to lay out some of the inherent ethical problems related to surgical innovation. I will argue that some of these problems are unique to surgery and that others relate to how we have chosen to define categories like research and practice. Other problems involve how we view the proportionality of risks and benefits in surgical research. I will argue that we have falsely analogized surgical progress to progress made in other areas of biomedical research and misunderstood the highly personal, or proximate, nature of surgical inquiry. Without appreciating the import of what I will call “surgical proximity,” we will be unable to adequately address ethical issues in surgical innovation.
PROBLEMS OR DILEMMAS?
So let me begin with the title of our session, “Surgical Innovation and Ethical Dilemmas,” and why this juxta position is counterproductive. A colleague long ago taught me to distinguish problems from dilemmas—the former being resolvable, the latter intractable, often involving a choice between two equally unfavorable choices.
Although I may be making too much of the semantics, I do think the title betrays a presumption that surgical innovation invariably forces adversarial choices. It tends to dichotomize ethical reflection, pitting those who favor prudence against those who endorse progress, or it creates too stark a difference between ethical issues in surgical practice and those encountered in the conduct of surgical research.
Even therapeutic, validated surgery in many ways has the potential to become innovative, if not outright experimental. Patients may have anatomical differences that require surgical improvisation, or complications may arise during “routine” surgery, creating the need for an imaginative response.1 At what point do these departures from expected care become novel interventions, innovative or even experimental? A routine case with an unexpected turn can even become a case report opening up a new field of endeavor.
For instance, the field of stereotactic functional neurosurgery was born out of a “routine” case of ablative surgery for Parkinson’s disease in the 1980s, when the French neurosurgeon Alim Benabid was using electrodes to determine which areas of the brain should be destroyed. As he was mapping the thalamus, he noted that the tremor of his patient abated. This led him to wonder if one could treat drug-resistant Parkinson’s with electrical stimulation instead of destructive lesioning.2 Benabid’s translational insight during an ordinary case led to the development of the rather extraordinary field of stereotactic functional neurosurgery and neuromodulation.3,4
Another example from an earlier era comes from the life work of neurosurgeon Wilder Penfield, who did pioneering work in the surgical treatment of epilepsy. Here, the accumulation of experience from “routine care” led to generalizable knowledge, much like hypotheses are validated in experimental work. In Penfield’s case, his clinical use of electrical stimulation to plan resections of scar tissue causing epilepsy led him to map the human homunculus, a magnificent achievement of profound importance.5,6
So let us avoid simplistic and confounding demarcations. Instead of dichotomizing innovation and prudence—or surgical research and surgical practice—let us try to start our deliberations with an eye toward a more synthetic approach. Like most things in nature and in biology, ethics too is on a continuum with gradations that can fit into an Aristotelian taxonomy. Let us emulate what Aristotle called phronesis, or practical wisdom, these next 2 days so that we achieve constructive outcomes, or what the pragmatists would call instrumental goods.7
If we are successful in laying out the ethical issues in this clinically pragmatic fashion, we can turn intractable “dilemmas” into problems amenable to resolution through the particularistic invocation of ethical principles as they relate to the surgical context.8 If we follow this inductive method of moral problem solving, we will avoid sweeping ethical generalizations, or categoricals, that can misrepresent the complexity of innovative research and deprive society of its benefits.9
INNOVATION VS PRUDENCE: A FALSE DICHOTOMY
So let us start by understanding the presuppositions that led to the expectation that dilemmas will descend upon those who engage in surgical innovation. In my view, this expectation begins with what is called the precautionary principle, a concept with some currency in the realm of environmental ethics.10
The precautionary principle urges caution and prudence when facing unknowns and is an antecedent sort of utilitarianism. One makes judgments about the advisability of actions based on a prior assessment of foreseeable risks and benefits. If the risks are excessive or exceed benefits, the precautionary principle urges care, caution, and even avoidance of a given course of action.
When the precautionary principle is implicitly invoked in making judgments about research, the objective is to pursue a degree of safety that is comparable to that of established therapy. But interventions that have progressed to being deemed “therapeutic” have of course achieved a requisite degree of both safety and efficacy—that is what makes them therapeutic, as opposed to investigational, interventions. One cannot know before one has conducted a clinical trial, and completed statistical analysis, whether a new surgical advance or device meets these expectations. Because of this lack of knowledge, there is an inherent degree of risk in any novel intervention.
The challenge posed by innovation or novelty creates the possibility of untoward events. It leads to invocation of the precautionary principle, which, echoing the admonitions of the philosopher Hans Jonas, urges us to “give greater weight to the prognosis of doom than to that of bliss.”11,12
This is not a bad way to go through life, assuming one wants to emulate T.S. Eliot’s J. Alfred Prufrock, who lamentably “measured out my life with coffee spoons.”13 Unlike the surgeon, who must make decisions in real time, Eliot’s protagonist could not move forward. Despite his desire to avoid the indecision of Prince Hamlet, alluded to in this paper’s epigraph, Prufrock was paralyzed by doubts and fears, with “time yet for a hundred indecisions, and for a hundred visions and revisions.”13
Despite Eliot’s invocation of “a patient etherised upon a table,”13 the poem shares little with the surgical life. It has much more in common with the precautionary principle. Like Prufrock, the precautionary principle favors what is known— the status quo—as what is unknown is invariably more risky than the familiar. Needless to say, this is antithetical to innovation because discovery invariably requires scenarios that involve novelty and unknown risks. When faced with the certain security of stasis or the potential dangers of innovation, the precautionary principle will invariably choose stasis, leading us, as the legal scholar Cass Sunstein notes, “in no direction at all.”14
Seen through the prism of the precautionary principle, then, surgical innovation invariably presents a dilemma. Discovery and innovation are fundamentally at odds with the precautionary principle, because of their potential for risk.15
The challenge posed by the precautionary principle—which, to be fair, is seen in all areas of clinical research—becomes even more pronounced in surgical research because of the size and scope of clinical trials. As is well appreciated here, compared with drug trials, surgical trials are small. Sometimes they can involve a single subject, whereas drug trials may include thousands of participants. Because of drug trials’ large volume of subjects, therapeutic effects can be small to justify ongoing research. In a surgical trial or a device trial, the number of subjects is smaller, so the therapeutic impact has to be larger to warrant further development and ongoing study. This burden of scale increases the probability of reciprocally large adverse effects. This potential for disaster magnifies the impact of the precautionary principle and may lead to a distortion in ethical judgment along the lines of Hans Jonas’ admonition.12
By all of this I am not suggesting that we abandon precautions and prudence. Instead, my point is to explicate the additional challenges faced by surgical research and the sway of the precautionary principle over this area of inquiry and innovation. By being explicit about the impact of this principle, we can be cognizant of its potential to distort judgments about risks and benefits. Only then can we hope to balance the pursuit of progress with that of safety.
SURGICAL RESPONSIBILITY
These distortions also need to be recognized, and made explicit, because surgical research, more so than pharmacologic research, is much more personal and intimate. This point becomes clear if we consider a surgical trial that does not succeed.
In the surgical arena, such failures are taken to heart and personalized. Unlike trials that involve drugs, surgical research is more proximate. It is not just the failure of a drug or of pharmacology; it is also possibly the failure of the operator, the surgeon who did not achieve the desired goal because of poor execution of surgical technique.
This crucial difference in medical versus surgical cultures is captured by Charles Bosk in his magisterial sociological study of surgery, Forgive and Remember: Managing Medical Failure. In a discussion of morbidity and mortality rounds, Bosk writes:
The specific nature of surgical treatment links the action of the physician and the response of the patient more intimately than in other areas of medicine....When the patient of an internist dies, the natural question his colleagues ask is, “What happened?” When the patient of a surgeon dies, his colleagues ask, “What did you do?”16
As in clinical surgical practice, in surgical research, it is the personal and individualized mediation of the surgeon that is central to the intervention. Here the intermediary is neither a drug nor its bioavailability; rather, it is the operator’s technique plus or minus the operative design and the reliability of an instrument or a device. In either case, the contribution is more proximate and personal, stemming from the actions of individual surgeons and the work of their hands.
History is instructive on this theme of surgical causality and personal culpability if we consider the life of Harvey Cushing, a Cleveland native whose ashes are buried nearby in Lake View Cemetery.17 Cushing was a gifted and innovative surgeon whose technique handling tissues changed how the brain was approached operatively. He is acknowledged as the father of neurosurgery, having created a professional nexus to institutionalize and carry on his innovative work.18
Cushing’s greatest innovation was probably in his individual efforts as a working surgeon. Over the course of his lifetime, he made the resection of brain tumors a safe and sometimes effective treatment for an otherwise dread disease. Michael Bliss, Cushing’s most recent biographer, reports mortality data from more than 2,400 surgeries done by Cushing during his operative lifetime.17 Early in his career (from 1896 to 1911), while he was at Johns Hopkins, Cushing’s case mortality rate was 24.7%. During his later years at the Brigham Hospital, it was 16.2%. By 1930–1931 it was down to 8.8%.
These were extraordinary statistics: no one matched Cushing’s numbers, or his ability to do what he did. Bliss cites mortality data from his surgical contemporaries in the late 1920s as ranging from approximately 35% to 45%. By the numbers Bliss compares Cushing’s talent—his truly brilliant outlier performance—to that of his Jazz Age contemporary, Babe Ruth, who also had outsized talent compared with his peers.17
Cushing himself, a collegiate second baseman at Yale, linked sport and statistics in a most telling way. Documenting his ongoing surgical progress was a hedge against failure and lightened the emotional burdens of the surgical suite. Cushing observed: “A neurosurgeon’s responsibilities would be insufferable if he did not feel that his knowledge of an intricate subject was constantly growing—that his game was improving.”17
This quote and Cushing’s operative statistics point to his nascent effort to engage in evidence-based research and speaks to the spectacular difference that a surgical innovator can make. The extraordinary results achieved by Cushing in his day also suggest that surgeons are not fungible at the vanguard of discovery. History tells us, as contemporary assessments of current research cannot, that only Harvey Cushing could achieve Cushingoid results.
A second point that stems from Cushing’s comment about the burdens of operative work and surgical research is how personally taxing that responsibility can be. Without making progress, he said, the “responsibilities would be insufferable”17 (my italics).
Even the great Harvey Cushing perceived the weight of these burdens, suggesting that any effort to depersonalize the ethics of surgical innovation would be naïve. The singularity of Cushing’s surgical accomplishments (his operative excellence as compared with his peer group) and the felt weight of these achievements suggest that surgical innovation is highly personal and proximate to the surgical researcher in a way that is distinct for surgical innovation. This relationship of operative causality and personal culpability can be subsumed under what I will call surgical proximity.
SURGICAL PROXIMITY
Surgical proximity has several implications for the conduct of research. In this section I will address two issues: conflicts of interest and clinical equipoise.
Surgical proximity and conflicts of interest
As the Cushing example illustrates, at least at the outset of a clinical trial the surgeon himself is part of the actual design of the trial. The same surgical method in the hands of one of his contemporaries would have led to a dramatically different result. The surgeon who is at the forefront of innovation becomes an experimental variable until the methods can be generalized.
The importance of the operator as an essential ingredient in early surgical research points to a key difference with pharmaceutical trials, where the purity of the drug-based intervention can be maintained. This difference has implications for the “rebuttable presumption” stance promulgated by the Association of American Medical Colleges (AAMC), which looks askance at innovators conducting clinical trials if they have a conflict of interest, such as intellectual property rights for their discoveries.19,20
In many cases, the work that surgical innovators do, as in the case of device development, could not be done without collaborations with industry. Taking the surgical talent of the potentially conflicted—but highly talented—innovator out of the equation may be counterproductive.
Time does not allow me to fully address the conflict-of-interest issue in this forum; suffice it to say that the differential knowledge, skill, and talent of early surgical innovators may be the difference between a trial’s early success or failure. The role of such innovators should neither be truncated or precluded nor be viewed a priori in a prejudicial fashion. Instead, their talents and vision should be welcomed as instrumental to the potential success of the work, managed of course with the proper degree of transparency and disclosure.
As I have noted previously,4,21 if the rationale for a conflict of interest is to allow laudable work to continue that otherwise could not occur without the personal intervention, and talents, of a surgical innovator, it seems prejudicial to view the conflict of interest as disqualifying until proven otherwise. This view is consistent with the legal framework of the US Constitution, which explicitly authorizes Congress “to promote the Progress of Science and the useful Arts, by securing for limited Times to Authors and Inventors the exclusive Right to their respective Writings and Discoveries.”22 It is also embedded in the Patent Act of 1790,23 which balances the patent’s period of exclusivity against the inventor’s obligation to share and disseminate expertise. This role for the innovator is also consistent with the intent and incentives within the framework of the Bayh-Dole Act of 1980,24 which was passed with the expectation that industrial partnerships would move ideas from the bench to the bedside.
I hope that others at this conference will be able to return to the issue of conflicts of interest and how the question of surgical proximity may, or may not, alter our ethical judgments about the surgeon’s role in research where there may be a conflict of interest.
Surgical proximity and equipoise
Surgical proximity also has an impact on clinical equipoise, the ethical neutrality about outcomes felt necessary for the conduct of clinical trials.25 The surgeon’s sense of causality and proximity to the operative act makes surgical research different because the equipoise, which exists objectively about the research questions at hand, may not exist in the mind of the surgical researcher. Let me explain.
Taking a patient to surgery is highly consequential. As we have seen from Bosk’s work,16 surgeons feel a sense of responsibility for their operative acts and surgical work. This felt responsibility, inculcated in surgical training and surgical culture, obligates the surgeon to make a proportionality judgment about bringing a patient to the operating room, be it for research or for clinical practice. In this way, surgical investigators have determined, at least in their own minds, that net benefits outweigh net risks, thus breaching clinical equipoise.
It is hard for a surgeon to commit to an operative procedure—be it for clinical care or for research— with all its attendant risks if he or she does not believe that the intervention is safe and effective. We can appreciate the importance of the surgeon’s perspective on the utility of any proposed operation if we consider the opposing question of futility in clinical practice.26 Whereas internists or intensivists might be compelled by families to continue aggressive intensive care, surgeons cannot be compelled to take a patient to the operating room when they deem that the risks outweigh the benefits. Because the surgeon is such a proximate moral agent, he or she will be held culpable for the actions that occur in theater. This degree of responsibility is accompanied by a retained degree of discretion—an almost old-world paternalistic discretion27—to counter the demands for disproportionate care.
This same sense of culpability and responsibility informs the surgeon’s willingness to take any patient to the operating room. In the case of research, this willingness becomes an issue of concern because it means that in the surgeon’s mind, favorable operative proportionality has been achieved.
This process of self-regulation28 can have implications for the informed-consent process because surgeons believe in their work and can exert a strong dynamic transference on subjects who may be desperate for cure.29 Because of this potential bias, surgical research may become especially prone to a therapeutic misconception. That is, if the surgeon is willing to take the risks of doing an innovative procedure in the operating room, then it has crossed some sort of internal threshold of proportionality in which the risks, whatever they are, have become acceptable given the putative benefits. Given what Bosk has written about surgical failure,16 a high bar is crossed when a surgeon takes a patient to the operating room for a novel procedure, even though motivations at that bar may occasionally be mixed.* (*Lest I be misconstrued as too idealistic, this burdens-vs-benefits equation may be fueled by a complex mosaic of motivations and may not always be informed fully by patient-centered benefits. If the surgeon is the innovator and the inventor, these benefits may be for the pursuit of a hypothesis and associated with potential fame or fortune. But even in these cases, judgments about proportionality are informed by surgical proximity. [For more on the ethics of conflicts of interest, see references 4 and 21.])
FROM SURGICAL RESEARCH TO EDUCATION
This leads to my closing observations about transitions in surgical research, when the work of the pioneering surgeon is bequeathed to the broader surgical community to pick up the torch—or scalpel—and expand the work.
This takes me away from research and, fittingly here at a medical school dedicated to research training, brings me to medical education. To transcend the personal dimensions of surgical innovation—and the courage and vision of the founders—and sustain it more broadly, innovators also have to become educators of future surgeons, organizers of talent, and moral exemplars for the next generation. They have to appreciate that the work that they started, if it is important, will not be completed during their tenure but that future generations will carry it forward and expand upon it. They also have to prepare the next generation with the tools and orientation to appreciate their vision and to embrace what Thomas Kuhn might call new scientific paradigms.30
On several occasions Wilder Penfield, who founded the Montreal Neurological Institute, wrote with regret about Victor Horsley, the neurosurgeon at Queens Square in London. Penfield viewed Horsley as the founder of his field, but Horsley left no disciples. In his autobiography, fittingly entitled No Man Alone, Penfield noted that Horsley, “the most distinguished pioneer neurosurgeon, had died in 1916 without having established a school of neurosurgery.”5 This is in contrast to the discipline-building work of Cushing.
It is not an accident that Dr. Cushing founded a field full of trainees and protégés, of which my co-panelists are descendants. It was intentional and part of his ethos of being truly innovative. And it is not an accident that the distinguished surgical innovators at this symposium have also created institutional structures to continue their work for decades to come. Their achievements have transcended the individual innovator and have become systematic. It is said that Dr. Thomas Starzl launched a field.31 Dr. Denton Cooley founded the Texas Heart Institute.32 Dr. Thomas Fogarty started the Fogarty Institute for Innovation, whose mission statement explicitly notes that it is “an educational non-profit that mentors, trains and inspires the next generation of medical innovators.”33 Each of these pioneers, I believe, appreciates the need for continuity and dissemination.
But even here there is something that we nonsurgeons need to understand: although the work transcends the individual surgeon, the ties remain personal and linked to the impact and legacy of founders. Take, for example, highly prized membership in the Denton A. Cooley Cardiovascular Surgical Society.34 This too is about the importance of individuals and surgical proximity, but here it is transgenerational.
CONCLUSION
If we truly want to continue the dialogue begun here today, we need to understand these social and professional networks and the importance of surgical proximity in transmitting both methods and values. The proximate nature of surgical research—and the causality and responsibility that accrues to the surgeon—makes surgical research different than other areas of biomedical inquiry. This difference has implications for risk-benefit analysis, conflicts of interest, and clinical equipoise. I hope that my colleagues return to these themes in the coming days so that the regulation of this important area of research can be informed by a deeper understanding of the ethics of surgical discovery and innovation.35
Acknowledgments
Dr. Fins gratefully acknowledges the invitation to participate in this symposium, the helpful suggestions of Dr. Eric Kodish, and partial grant support of the Weill Cornell Medical College Research Ethics Core, NIH Clinical & Translational Science Center UL1-RR024966.
- Frader JE, Caniano DA. Research and innovation in surgery. In: McCullough LB, Jones JW, Brody BA, eds. Surgical Ethics. New York, NY: Oxford University Press; 1998:216–241.
- Speelman JD, Bosch DA. Resurgence of functional neurosurgery for Parkinson’s disease: a historical perspective. Mov Disord 1998; 13:582–588.
- Holstein WJ. Rewiring the brain: how a bright idea became an innovative medical device. US News & World Report. March 1, 1999:52–53.
- Fins JJ, Schachter M. Investigators, industry, and the heuristic device: ethics, patent law, and clinical innovation. Account Res 2001; 8:219–233.
- Penfield W. No Man Alone: A Neurosurgeon’s Life. Boston, MA: Little Brown; 1977.
- Feindel W. The contributions of Wilder Penfield to the functional anatomy of the human brain. Hum Neurobiol 1982; 1:231–234.
- Aristotle. The Nicomachean Ethics. Weldon JEC, trans. Amherst, NY: Prometheus Books; 1987.
- Fins JJ, Bacchetta MD, Miller FG. Clinical pragmatism: a method of moral problem solving. Kennedy Inst Ethics J 1997; 7:129–145.
- Miller FG, Fins JJ. Protecting human subjects in brain research: a pragmatic perspective. In: Illes J, ed. Neuroethics: Defining the Issues in Theory, Practice and Policy. New York, NY: Oxford University Press; 2005.
- Pollan M. The year in ideas: A to Z.; precautionary principle. New York Times. December 9, 2001.
- van den Belt H. Debating the precautionary principle: “guilty until proven innocent” or “innocent until proven guilty”? Plant Physiol 2003; 132:1122–1126.
- Jonas H. The Imperative of Responsibility: In Search of an Ethics for the Technological Age. Chicago, IL: University of Chicago Press; 1985:34.
- Eliot TS. The Love Song of J. Alfred Prufrock. In: Abrams MH, ed. The Norton Anthology of English Literature. Vol 2. 4th ed. New York, NY: W.W. Norton & Co; 1979:2259–2264.
- Sunstein CR. The paralyzing principle. Regulation. Winter 2002– 2003; 25(4):32–37.
- Holm S, Harris J. Precautionary principle stifles discovery. Nature 1999; 400:398.
- Bosk C. Forgive and Remember: Managing Medical Failure. Chicago, IL: University of Chicago Press; 1979:29–30.
- Bliss M. Harvey Cushing: A Life in Surgery. Oxford, UK: Oxford University Press; 2005.
- Pinkus RL. Mistakes as a social construct: an historical approach. Kennedy Inst Ethics J 2001; 11:117–133.
- AAMC Task Force on Financial Conflicts of Interest in Clinical Research. Protecting subjects, preserving trust, promoting progress I: policy and guidelines for the oversight of individual financial interests in human subjects research. Acad Med 2003; 78:225–236.
- AAMC Task Force on Financial Conflicts of Interest in Clinical Research. Protecting subjects, preserving trust, promoting progress II: principles and recommendations for oversight of an institution’s financial interests in human subjects research. Acad Med 2003; 78:237– 245.
- Fins JJ. Disclose and justify: intellectual property, conflicts of interest, and neurosurgery. Congress Quarterly (Official Newsmagazine of the Congress of Neurological Surgeons) 2007; 8(3):34–36.
- U.S. Constitution, art. I, §8, cl. 8; see also id. at art. I, §8, cl. 18.
- Patent Act of 1790, ch. 7, 1 Stat. 109–111 (1790).
- Patent and Trademark Act Amendments of 1980 (Bayh-Dole Act); Pub L No. 96-517. Codified as 35 USC §§200–212 (1994).
- Freedman B. Equipoise and the ethics of clinical research. N Engl J Med 1987; 317:141–145.
- Callahan D. Necessity, futility, and the good society. J Am Geriatr Soc 1994; 42:866–867.
- Katz J. The Silent World of Doctor and Patient. New York, NY: Free Press; 1984.
- Jones RS, Fletcher JC. Self-regulation of surgical practice and research. In: McCullough LB, Jones JW, Brody BA, eds. Surgical Ethics. New York, NY: Oxford University Press; 1998:255–279.
- Kim SY. Assessing and communicating the risks and benefits of gene transfer clinical trials. Curr Opin Mol Ther 2006; 8:384– 389.
- Kuhn TS. The Structure of Scientific Revolutions. 2nd ed. Chicago, IL: University of Chicago Press; 1970.
- Starzl TE. The Puzzle People: Memoirs of a Transplant Surgeon. Pittsburgh, PA: University of Pittsburgh Press; 2003.
- Twenty Five Years of Excellence: A History of the Texas Heart Institute. Houston, TX: Texas Heart Institute Foundation; 1989.
- Fogarty Institute for Innovation Web site. Available at: http://01659a8. netsolhost.com/aboutus.html. Accessed June 6, 2008.
- Denton A. Cooley Cardiovascular Surgical Society Web site. Available at: http://www.cooleysociety.com/about.html. Accessed June 6, 2008.
- de Melo-Martín I, Palmer LI, Fins JJ. Viewpoint: developing a research ethics consultation service to foster responsive and responsible clinical research. Acad Med 2007; 82:900–904.
- Frader JE, Caniano DA. Research and innovation in surgery. In: McCullough LB, Jones JW, Brody BA, eds. Surgical Ethics. New York, NY: Oxford University Press; 1998:216–241.
- Speelman JD, Bosch DA. Resurgence of functional neurosurgery for Parkinson’s disease: a historical perspective. Mov Disord 1998; 13:582–588.
- Holstein WJ. Rewiring the brain: how a bright idea became an innovative medical device. US News & World Report. March 1, 1999:52–53.
- Fins JJ, Schachter M. Investigators, industry, and the heuristic device: ethics, patent law, and clinical innovation. Account Res 2001; 8:219–233.
- Penfield W. No Man Alone: A Neurosurgeon’s Life. Boston, MA: Little Brown; 1977.
- Feindel W. The contributions of Wilder Penfield to the functional anatomy of the human brain. Hum Neurobiol 1982; 1:231–234.
- Aristotle. The Nicomachean Ethics. Weldon JEC, trans. Amherst, NY: Prometheus Books; 1987.
- Fins JJ, Bacchetta MD, Miller FG. Clinical pragmatism: a method of moral problem solving. Kennedy Inst Ethics J 1997; 7:129–145.
- Miller FG, Fins JJ. Protecting human subjects in brain research: a pragmatic perspective. In: Illes J, ed. Neuroethics: Defining the Issues in Theory, Practice and Policy. New York, NY: Oxford University Press; 2005.
- Pollan M. The year in ideas: A to Z.; precautionary principle. New York Times. December 9, 2001.
- van den Belt H. Debating the precautionary principle: “guilty until proven innocent” or “innocent until proven guilty”? Plant Physiol 2003; 132:1122–1126.
- Jonas H. The Imperative of Responsibility: In Search of an Ethics for the Technological Age. Chicago, IL: University of Chicago Press; 1985:34.
- Eliot TS. The Love Song of J. Alfred Prufrock. In: Abrams MH, ed. The Norton Anthology of English Literature. Vol 2. 4th ed. New York, NY: W.W. Norton & Co; 1979:2259–2264.
- Sunstein CR. The paralyzing principle. Regulation. Winter 2002– 2003; 25(4):32–37.
- Holm S, Harris J. Precautionary principle stifles discovery. Nature 1999; 400:398.
- Bosk C. Forgive and Remember: Managing Medical Failure. Chicago, IL: University of Chicago Press; 1979:29–30.
- Bliss M. Harvey Cushing: A Life in Surgery. Oxford, UK: Oxford University Press; 2005.
- Pinkus RL. Mistakes as a social construct: an historical approach. Kennedy Inst Ethics J 2001; 11:117–133.
- AAMC Task Force on Financial Conflicts of Interest in Clinical Research. Protecting subjects, preserving trust, promoting progress I: policy and guidelines for the oversight of individual financial interests in human subjects research. Acad Med 2003; 78:225–236.
- AAMC Task Force on Financial Conflicts of Interest in Clinical Research. Protecting subjects, preserving trust, promoting progress II: principles and recommendations for oversight of an institution’s financial interests in human subjects research. Acad Med 2003; 78:237– 245.
- Fins JJ. Disclose and justify: intellectual property, conflicts of interest, and neurosurgery. Congress Quarterly (Official Newsmagazine of the Congress of Neurological Surgeons) 2007; 8(3):34–36.
- U.S. Constitution, art. I, §8, cl. 8; see also id. at art. I, §8, cl. 18.
- Patent Act of 1790, ch. 7, 1 Stat. 109–111 (1790).
- Patent and Trademark Act Amendments of 1980 (Bayh-Dole Act); Pub L No. 96-517. Codified as 35 USC §§200–212 (1994).
- Freedman B. Equipoise and the ethics of clinical research. N Engl J Med 1987; 317:141–145.
- Callahan D. Necessity, futility, and the good society. J Am Geriatr Soc 1994; 42:866–867.
- Katz J. The Silent World of Doctor and Patient. New York, NY: Free Press; 1984.
- Jones RS, Fletcher JC. Self-regulation of surgical practice and research. In: McCullough LB, Jones JW, Brody BA, eds. Surgical Ethics. New York, NY: Oxford University Press; 1998:255–279.
- Kim SY. Assessing and communicating the risks and benefits of gene transfer clinical trials. Curr Opin Mol Ther 2006; 8:384– 389.
- Kuhn TS. The Structure of Scientific Revolutions. 2nd ed. Chicago, IL: University of Chicago Press; 1970.
- Starzl TE. The Puzzle People: Memoirs of a Transplant Surgeon. Pittsburgh, PA: University of Pittsburgh Press; 2003.
- Twenty Five Years of Excellence: A History of the Texas Heart Institute. Houston, TX: Texas Heart Institute Foundation; 1989.
- Fogarty Institute for Innovation Web site. Available at: http://01659a8. netsolhost.com/aboutus.html. Accessed June 6, 2008.
- Denton A. Cooley Cardiovascular Surgical Society Web site. Available at: http://www.cooleysociety.com/about.html. Accessed June 6, 2008.
- de Melo-Martín I, Palmer LI, Fins JJ. Viewpoint: developing a research ethics consultation service to foster responsive and responsible clinical research. Acad Med 2007; 82:900–904.
Surgical innovation and ethical dilemmas: A panel discussion
END RESULTS: WHY SO ELUSIVE STILL?
Dr. Isador Lieberman, Moderator: Let me begin this discussion with a 1910 quote from Ernest Codman, a general surgeon at Massachusetts General Hospital, who stated:
In 1900 I became interested in what I called the “end result” idea, which was merely the commonsense notion that every hospital should follow every patient it treats long enough to determine whether or not the treatment has been successful, and then should inquire, “If not, why not?” with a view to preventing similar failure in the future.
My questions to the panel are: What has changed in the last 100 years? Are we documenting our end results? Have we gone wrong and, if so, where have we gone wrong?
Dr. James Herndon: Although Codman’s ideas in this area were not well received at the time, today we do have some “end result” ideas. We have outcomes data, but I would argue that they are far too limited and not to the level required in the 21st century. I have asked myself many times why the surgical profession has not focused on this issue more than it has. I agree with Dr. [Joseph] Fins’ comments in his presentation [see previous article in this supplement] that it would be nice to have a bottom-up approach rather than a top-down approach, but I do not see a change until we as physicians step up to the plate and make a change.
Why haven’t we? There are a number of reasons. The malpractice climate in the United States has been one major factor. Surgeons fear disclosure. The relationship between a surgeon and the patient is professional and private, and physicians do not want transparency—they do not want their patient or anyone to know that an adverse event or bad outcome has occurred.
Also, doctors, especially surgeons, are reluctant to use guidelines or follow protocols. I participated a number of years ago in an American Academy of Orthopaedic Surgeons project called MODEMS; it was an attempt to set up guidelines for orthopedic surgeons to manage back pain, shoulder pain, and other orthopedic conditions. By the time we finished we had accomplished nothing, because the protocols and guidelines were so extensive that almost any type of management for any patient would be compliant.
Additionally, hospitals in the United States have become more like for-profit businesses, with a focus on short-term profits and with short tenures for their chief executive officers (CEOs)—4 or 5 years, on average. With nearly 50% of US hospitals bordering on bankruptcy, they are not able or willing to invest in major patient safety protocols and guidelines because the CEOs do not see a short-term benefit to them. Witness the fact that only 15% of US hospitals have computerized physician order entry systems and electronic medical records. From what I have read, it takes about 5 years before a hospital recoups such investments from the resulting safety improvements and efficiencies.
These are some, but by no means all, of the reasons we do not have appropriate outcomes in all specialty fields. My plea is that physicians lead the effort to measure and report outcomes down the road.
Dr. Lieberman: Dr. Hahn, why do you think we have not kept up with Dr. Codman’s premise from 100 years ago?
Dr. Joseph Hahn: We hold a yearly Medical Innovation Summit at the Cleveland Clinic, and what has emerged from many of those meetings is a lack of interest in paying for outcomes analyses. The providers, the government, and industry all say that they do not have the money for these analyses. So the first reason that Codman’s premise has not been lived up to is that the source of funding remains undetermined. Second, most surgical innovations have been geared toward inventing devices to overcome very specific problems that arise during or following surgery rather than toward substantiating the worth of a procedure through collection of evidence. A third reason involves the pressure that investors place on industry to make money, which tends to lead to investments in getting products to market rather than outcomes research. With all of these factors and the pressures from so many directions, the surgical profession hasn’t stepped back to thoroughly consider what we are doing to our patients and just how worthwhile it is.
Dr. Lieberman: Who do you think should be paying for outcomes analyses?
Dr. Hahn: I think the government should. The role of government is to take care of its citizens. The Centers for Medicare and Medicaid Services (CMS) does its best with the information it has, but it admits that it pays for some procedures without knowing whether or not they are truly worthwhile. An example is the use of artificial discs in the cervical spine. I am sure that the artificial disc manufacturers made a case for their product to CMS by claiming it was associated with less pain and resulted in a superior outcome compared to fusion using bone from the hip, regardless of whether they had the scientific evidence to prove it.
Dr. Lieberman: Dr. Fins, would you like to weigh in on Codman’s “end result” premise?
Dr. Joseph Fins: I would just point out that the history is not homogeneous. I have been involved in deep brain stimulation work, and the legacy of psychosurgery has been an egregious lack of outcomes studies, but now we do have outcomes studies and scales. For example, there is now the Yale-Brown Obsessive Compulsive Scale to rate the severity of symptoms in obsessive-compulsive disorder. In our deep brain stimulation study,1 we are using a coma recovery scale, and the Food and Drug Administration’s (FDA’s) investigational device exemption (IDE) process requires us to produce outcomes data to protect potential subjects. It may be an example of neuropsychiatric exceptionalism that neurology and psychiatry are areas of increased focus while somatic therapies are somehow presumed to be okay.
Dr. Hahn: FDA may be requiring the outcomes data, but I have not heard that they are willing to pay for it.
Dr. Fins: You are correct.
Dr. Ali Rezai: Part of the problem is the translation of rapid scientific discoveries and technological advances into the field, and education has a role here. Surgeons’ reluctance to integrate guidelines and outcomes measures into practice must be addressed very early in their training—in medical school—and then continued throughout residency and fellowship programs. The same early and continuing approach should be taken with respect to how to conduct and properly interpret a clinical trial.
Dr. Herndon: That is a good point. Surgical education programs have slipped a bit in the past 5 to 10 years, at least in orthopedics. With the reductions in residents’ work hours and the fast pace of residency programs, our residents spend most of their time in the operating room, struggling to master the multitude of procedures in orthopedics. As a result, they are not discussing outcomes or adequately following patients long-term after surgery. I have a hard time getting our faculty to bring residents into their offices so that the residents can examine patients and see why they are operating on certain kinds of patients, as well as the types of follow-up information that can and should be obtained from patients. Training today is so oriented to operative techniques that residencies have difficulty dealing with these other important issues.
WHO DEFINES THE INDICATIONS?
Dr. Lieberman: As new devices and new techniques emerge, who defines their indications? The inventor of the device, a government authority that may or may not have the medical background, patient advocacy groups, or the device manufacturer? And how should we regulate those indications?
Dr. Fins: I would echo Dr. Wilder Penfield’s words, “No man alone.” The orthopedic surgeon or neurosurgeon does not have to do this alone; it is really about teams. And those teams can and should include biostatisticians, recognizing that the biostatistician needs to fully understand what the surgeon is doing. There also has to be attention given to patients’ individualistic outcomes. I recently met with some FDA staff and learned that the FDA is very interested in novel methodologies to better understand what counts as an outcome for individual patients. So I think indications should be guided by individualistic outcomes coupled with the surgical possibilities and with the rigorous biostatistical methods that are now evolving. A conference like this represents an opportunity to generalize the conversation and support more collaboration on indications going forward.
Dr. Rezai: Indications should be defined using a team-oriented approach. Part of the problem of psychosurgery in the past was that the surgeon was defining indications without collaborating with the psychiatrist. In my field of deep brain stimulation and brain pacemakers, everything we have done for the past 20 years—surgery for Parkinson’s disease, depression, obsessive-compulsive disorder, traumatic brain injury, epilepsy—has involved working closely with neurologists, epileptologists, brain injury specialists, psychiatrists, and psychologists to agree on indications. These teams also need to have close partnerships with ethicists. Teamwork is a vital aspect of proper development of an indication.
Dr. Hahn: It has to be the clinicians who set forth the indications. Of course, that may be done by a team of clinicians, but as a surgeon I certainly do not want the manufacturers of an artificial disc telling me what they think the indications for an artificial disc are.
As for the role of patients, some of them are very well informed about their problem. I cannot tell you how many have shown up in my office with reprints of articles I have written. This is a trend that has really mushroomed over the past 10 years. But even though patients are catching up, they are still at a disadvantage. Patients are going to have a say, but it is still the clinicians whose role is to decide the indications and then provide patients with a risk-benefit analysis.
Dr. Herndon: I agree. Although patients are becoming more involved in the process, real shared decision-making has not yet happened in my field.
More broadly, I feel that our professional organizations have to become more actively involved in the process of defining indications. Otherwise, after the innovators develop a device or procedure that will significantly change the approach to a particular problem, it will enter the market at large without any critical assessment of the technology involved and without accounting for the learning curve for each individual surgeon.
Take the example of minimally invasive total hip replacement, which involves a 1-inch incision in the front of the hip and a 1-inch incision in the back of the hip. The learning curve for this procedure appears to be about 40 cases, based on the opinion of experts around the country. Yet when this minimally invasive approach emerged, every surgeon who had been performing total hip replacements wanted this new operation at his or her fingertips because patients were demanding it. Some surgeons adopted it too quickly, without adequate training. I know one distraught surgeon who abandoned the procedure because of numerous failures during his first 100 cases. He returned to the standard hip replacement approach.
Our profession cannot let this experience continue or proliferate. Yet the professional organizations in orthopedics have walked away from technology assessment because industry does not want it; technology assessment is not in industry’s best interest. We have had a number of conflicts in our professional organizations when attempting to move technology assessment forward. It is also very expensive to do.
Finally, indications can sometimes be governed more by economics than by science. I was asked to write a letter to the editor about two technologies for managing intertrochanteric fractures of the hip that were recently featured in the Journal of Bone and Joint Surgery.2,3 One technology involves a compression screw that has been shown to be effective in outcomes studies. The other is an intramedullary nail that has not been well studied and has no proven benefit over the compression screw. In doing research for my letter,4 I found that Medicare assigns more relative value units (RVUs) for the intramedullary nail than for the compression screw. In Boston, the total dollar difference in RVUs between the two is $300: the surgeon makes $1,500 for the procedure that involves the intramedullary nail versus $1,200 for using the compression screw. Not surprisingly, use of the intramedullary nail has been climbing rapidly in the United States without any evidence to justify its use over the other, less expensive technique.
CREDENTIALING: CAN IT KEEP PACE WITH INNOVATION?
Dr. Fins: I agree that surgical competence and regulation—self-regulation or professional regulation—are big issues. One of my greatest fears is that surgeons will do procedures they are not trained to do, and cause great harm as a result. We are hearing about this now with the resurgence of psychosurgery in China.
It strikes me as interesting that the field of neurosurgery is as yet undifferentiated and that there is no subspecialty certification in stereotactic neurosurgery. This is in contrast to invasive cardiology on the medical side, where physicians who do catheterizations and electrophysiologic studies have special additional training.
As innovations develop, we have to track qualifications and credentialing along the way. There should be provisions to grandfather surgeons in if they are in a post-training point in their career, but we have to ensure that the new technology is matched by the operator’s skill. This is particularly pertinent in light of the concept of “surgical proximity”5 and the importance of the individual operator; this is not comparable to just disseminating a new drug.
Dr. Lieberman: Who should do the credentialing? Should it be the government or our profession?
Dr. Fins: Recertification or credentialing should be by peers—the American College of Surgeons and the surgical boards. Of course, funders or payors may request an additional level of certification to do certain procedures, which I would endorse as a safety measure and to help ensure a minimal standard of care for innovative interventions.
Dr. Hahn: But it is not so simple. There is a blurring of surgical expertise once surgeons complete their training. Spine surgery used to be done by either neurosurgeons or orthopedic surgeons; now we have spine surgeons. What we neurosurgeons started to see with that change was that our neurosurgery trainees were being told they could not get on hospital staffs because they did not have credentials in spine surgery or, to take another example, in pediatric surgery. Well, the neurosurgery board made a conscious decision to not offer certificates of added qualification (CAQs). We challenged the hospitals in court and won. But the overriding message is that it is all about economics.
Dr. Herndon: In orthopedics we now have two CAQs—one in hand surgery and one (starting in 2009) in sports medicine. The hand surgeons have not noticed any adverse effect because they do not generate as much revenue as the spine surgeons do. Most orthopedic surgeons start as general orthopedists and then change their practice characteristics as their practices mature. Over time they may focus on one particular area, such as arthroscopic knee surgery or total hip or knee replacement, which makes it difficult for them to pass a general orthopedic examination. Our board recognized this trend and developed oral and written board exams with case reviews concentrating on the surgeon’s self-chosen specialty. We do not need the CAQs because they have been misused, and we as a profession have been letting others misuse them. Again, I think we need to get back to controlling the process ourselves.
Dr. Hahn: What do you do when a surgeon has finished training and then becomes interested in performing a new procedure developed since the time of his or her training? This can really be a challenge when the surgeon hears of a new procedure, goes and takes a 3-day training seminar on it, and comes back believing that he or she is ready to perform the procedure. I have had creative surgeons on staff who want to try a new procedure but have never done any cases, believing that the new technology alone will suffice. What we finally decided to do in these instances was to put in place other staff to proctor these cases to ensure that no harm was coming to patients.
Dr. Herndon: I admire that approach, because we as a profession have to educate our colleagues about whatever new procedures they are about to use in their practice. There is a learning curve for every operation, and learning on one’s own, at the expense of patients, is not appropriate. Should we have experienced colleagues work with surgeons on new procedures until they have performed the 40 or so cases necessary to be proficient? Should we send surgeons to other institutions to do their 40 cases under experienced supervision? I am not sure what the best approach is, but this is a question that a forum like this should begin to address.
HOW MUCH RISK IS ACCEPTABLE?
Dr. Lieberman: Let’s build on this issue of credentialing by turning to the concept of risk. What is an acceptable level of risk with a new device? Is a 50% risk of an adverse outcome appropriate? What about 10%? And who determines the acceptable risk? The profession? The regulatory bodies? Patients?
Dr. Fins: Our expectation about risks in clinical practice should evolve from what was anticipated and actually observed in the clinical trial of an intervention. Adverse events should be envisioned prospectively in the design of a trial, with the magnitude of risks delineated in the protocol. Any unexpected risks that occur, even if small, could be a major reporting issue. Beyond that, it is difficult to say what an acceptable level of risk is without a particularistic clinical trial. Whatever the risk of an intervention, the assessment of the risk must account for regional variation, variation among surgeons, and also systems issues.
The Institute of Medicine report, To Err is Human, attributed medical errors to faulty systems, processes, and conditions. So when we think about errors and risk, we have to consider more than just the individual operator. Just as To Err is Human analogized medical errors to airplane crashes, we might think of surgical retraining in the context of how pilots get retrained using flight simulators. If pilots have not flown a particular aircraft in a long time, they lose their flight certification for that type of craft and then must be retrained to operate it.
As surgical technology gets more advanced, specific, and nuanced, the discordance between one’s training and the potential things one can do becomes greater. Paradoxically, innovation can at least potentially make situations more dangerous in that the operator may not be able to perform the task with the improved technology. For example, pilots who know how to fly a Cessna can fly another simply constructed plane, but if they attempt to fly a higher-technology aircraft, like an F-16, they have a greater risk of having a catastrophic event even though the F-16 flies better, faster, and higher.
Dr. Lieberman: But are you willing to identify a level of acceptable risk?
Dr. Fins: It is based on the patient’s preference, after informed consent. An acceptable level of risk is the level that people are willing to accept. What I am concerned about is the variance around a known risk, whatever it may be, that is attributable to human errors that may be preventable through training or by solving systems problems.
Dr. Lieberman: Dr. Rezai, you place needles into the brain. Who should decide the risk of that action? You? The patient? And what do you feel is an acceptable risk level?
Dr. Rezai: It is a complex question, of course, and a number of variables come into play. Whether or not the patient’s condition is life-threatening or disabling is a very important factor in the risk-benefit ratio. Regulatory guidance from the FDA is strong with respect to defining device-related adverse effects as serious or nonserious, and our peers, both surgeons and nonsurgeons, help to further dictate the risk and tolerability of a procedure and its alternatives. For example, in considering a surgical procedure, one must weigh its risk against the risks of medications to treat the disorder, such as side effects, the ease of medication adherence, and the number of emergency room visits that may result from adverse effects of the medications.
Determining acceptable risk rests fundamentally and first with the patient and then with the surgeon and his or her peers (surgeons and nonsurgeons) in conjunction with regulatory components and oversight. All of these factors contribute.
In my field of deep brain stimulation, the threshold for acceptable risk can be high since we see patients with chronic conditions in whom all previous medication attempts have failed, many of whom are disabled, intractable to current therapies, and with a significant compromise of quality of life. Examples include wheelchair-dependent patients with severe Parkinson’s disease, severely depressed patients who will not leave the house and have attempted suicide, and obsessive-compulsive disorder patients who need 10 hours just to take a shower. This type of intractability to current therapies and the suffering of patients and families with limited options and little hope infl uence assessments of procedural risk.
Dr. Hahn: Performing a controlled clinical trial of a surgical procedure is difficult at best. I recall a clinical trial in which patients with parkinsonism were to be randomized either to have stem cells implanted in their brain or to undergo a sham operation with no stem cells. Well, very few patients signed up for the trial because everyone wanted the stem cells. So, obtaining a large enough denominator to define the risk of, for example, hemorrhage from sticking a needle into a vessel is almost impossible.
Dr. Herndon: Except when there are risks of serious life-threatening events, I believe the patient is the one who makes the decision after having the risks fully explained to him or her. Surgeons are educated in a system in which we learn to accept complications. It is the risk of doing business. We have not learned very well how to differentiate a complication from an adverse event or an error. We must learn to do that. We live with complications every day. Those complications must be conveyed to patients so that they understand what they are about to undergo, what can happen, and what cannot happen. The patient is the ultimate decider, in my opinion.
Dr. Lieberman: That reminds me of something one of my mentors often said: “If you are going to run with the big dogs, expect to get bitten in the butt once in a while.”
ETHICAL DILEMMAS ARISING FROM NEW OPTIONS
Question from audience: In my specialty, we have a non-life-threatening condition with a well-established 25% recurrence rate after traditional surgery with sutures, and a 25% rate of reoperation. A device comes along and it improves the outcomes so that the recurrence rate declines to 10%, but along with the extra costs of doing the procedure with the device, there is also a complication rate of about 10% that requires reoperation with the device, and a few of those patients actually end up worse. Ethically, how should the clinician proceed in this situation? The old way, or the new way that improves outcomes but at a higher cost and risk?
Dr. Fins: Based on the size of the populations, is the difference in the combined rates of recurrence and complications between the traditional and new methods (25% vs 20%) statistically significant?
Response from questioner: The difference is probably not statistically significant.
Dr. Fins: Okay, so you are saying that the numbers are basically equal. That is the first consideration, but there is a nuance to one of the variables, and that is an improvement in quality of life with one of the treatments. Measuring its significance is subjective. A patient may place greater emphasis on quality of life than would somebody who is not a beneficiary of the operation. That is why I said before that biostatistical input that goes beyond crude measures of mortality or reoperation rates can be very helpful. The risk of reoperation may be one that the patient is willing to take for a chance at an improvement in quality of life.
There is a wonderful book by Howard Brody called The Healer’s Power6 in which he writes about the physician’s power to frame a question so as to engineer outcomes. While that is not something that Brody endorses, he does endorse the use of the physician’s power to guide patients using good informed consent, providing direction without being so determinative that patients feel compelled to choose the physician’s recommendation. Patients should be able to decline your recommendation while still having the benefit of your counsel. And in a case like this, your counsel should include variables that may seem “softer” or more difficult to quantify than crude measures such as mortality or reoperation rates.
Dr. Rezai: You have to compare multiple outcomes between the two approaches—surgical time, recovery time, patient quality of life (as assessed by scales), family quality of life, time to return to work, etc. I think it is important to try new technologies because the failure rate or the complication rate may be reduced over time, but only if you evaluate the failures and then restrategize. Only in doing so can you reduce risk, and if the benefit profile and the risk profile prove to be good, then the new technology should be pushed forward.
Dr. Herndon: If the volume of procedures performed by the surgeon is important with respect to outcomes with either one of these two procedures, that should be taken into account. Also, if a new procedure carries a higher complication rate than the traditional procedure, I think that more cohort studies from large centers are needed to gauge the true complication rate before the new technology enters the general market. Continued surveillance, such as with a postmarket registry of outcomes with these procedures, would also be helpful to make adjustments in the future if necessary.
Dr. Hahn: If you looked at the early experience of Med tronic with pacers, you would be amazed at the number of deaths and complications that occurred during the first 3 years. But we do not even think about that now.
CAN INNOVATION HAPPEN WITHOUT INCENTIVES?
Question from audience: Dr. Hahn alluded earlier to the infl uence of money. All of you on the panel are institutionally based, and you are used to practicing with colleagues. I would suggest that surgery today is really not an individual sport, but that is the way it is practiced in much of the nation. Would we be better off if we developed a system that removed us from direct financial influence? Can we get the money out of the equation so that people have motives other than direct personal gain?
Dr. Hahn: I went to an institutional review board (IRB) retreat that included, of course, some IRB members who were not clinicians. They asked the same question that you just did: Why would you even expect to get anything for what you invent? I think that is naïve. People who work hard and invent things deserve to reap a reward. The challenge lies in working with industry, which may try to convince us to use its innovations without our input, as opposed to working with us to identify a clinical problem and trying to solve it together. In that way, the end product and the logic behind its use will be better.
I will give you an example from when I was head of surgery here. A company made a voice-activated table that would obey the surgeon’s commands, such as “left,” “right,” “up,” or “down.” I asked the representative why such a product was needed, and he responded that the surgeon wants to be in total control of the operating room. I told him we do not change the position of the table very often. After a 2-week trial, the table was a dud. He fired the entire group that was working on the project. It was a case of a company simply trying to come up with a product it could sell.
The opposite scenario is if I invent the latest and greatest stent for the carotids and I want to use it. The question becomes how to strike a balance: how to protect the patients while at the same time rewarding the inventor. Another challenge is that device companies want you to stay on their scientific advisory board and they will pay you for it.
These questions are a big concern, and we have spent a lot of time on these issues at Cleveland Clinic. In fact, we held our own conference on biomedical confl icts of interest in September 2006 with attendees from around the country to discuss the necessary firewalls for ensuring that data are not contaminated, that the surgeon-inventor does not fudge data so that his innovation will make it to the marketplace, etc. At that conference, a number of people spoke about Vioxx. I am a surgeon, and my take on the COX-2 inhibitors is that a lot of my patients take these drugs and think they are wonderful, but there are some problems and risks. What is wrong with explaining to patients the risks and complications of these drugs, making your own recommendation about their use (unless you are receiving money from their manufacturers, which you would need to disclose to patients), and then letting patients make their own informed decisions? Personally, I was on Bextra for 3 years and was furious when it was pulled from the market because nobody gave me a choice whether or not to continue using it.
Dr. Lieberman: Let’s explore this concept a little deeper. We know that innovation is so important, but how do we encourage clinicians to innovate in this environment? Dr. Hahn, you served as chairman of CC Innovations, which is Cleveland Clinic’s technology commercialization arm. What were some of the strategies you came across in that role?
Dr. Hahn: We look for creative staff. We tell them up front that we want them to come to Cleveland Clinic and invent things. Our mission is literally to work on problems and take solutions to our patients. The culture here is meant to be creative. As a part of that culture, we welcome working with industry, as opposed to industry thrusting its innovations on us.
We are averaging more than 200 invention disclosures per year. More than 500 of our staff are involved with various industrial partners, and we are not going to hide that. In fact, we are going to make it public. The thought is that we owe it to our patients to work on their problems. At the same time, we owe it to our patients to say when we are working with industry on a particular product and explain to them why we think it would work in their case, if we think it would. While doing so, we need to make it clear that we will be happy to refer them for a second opinion if they would like. If I have a patient who wants a second opinion, I will offer to make the phone call for them and get them in. I think that is an advantage of the model we have here.
The reality is that there are some procedures that can only be done by one surgeon here, a surgeon who may have helped develop the procedure or some technology involved in it. Are we going to tell that surgeon that he or she cannot perform the procedure on anyone? That does not make sense. So you need to have a management plan that puts in place firewalls to protect the data on that procedure from any possible contamination.
So yes, we do reward staff who are doing innovation, and we do work with industry, and we do tell our patients we are doing it, and we do build firewalls to protect the data.
Dr. Lieberman: How about the rest of the panel? What are your thoughts on providing incentives for innovation?
Dr. Fins: Money is a key issue. The way the landscape is now structured, collaborations with industry are part of the mix. Under the Bayh-Dole Act of 1980, institutions are granted intellectual property rights to ideas or inventions developed by their researchers, and then the institutions can enter into contracts with industry to move the innovations forward. If industry support of research were removed, we would have to double the budget of the National Institutes of Health to compensate.
On the other hand, industry support can sometimes prove to be a disincentive to innovation in that it may engineer certain kinds of research or deprive investigators of tools they may need to do more basic science types of research. It is an academic freedom issue. At a translational level, industry may be helpful and catalytic. But sometimes it pushes an investigator to work for a short-term innovative application at the expense of a more speculative, riskier innovation.
We need to acknowledge that industry collaborations are part and parcel of the universe and focus on working with industry to moderate its influences. At the same time, we must use our leverage on the investigative side of the equation to pursue academic freedom and to leverage industry resources to perhaps pay for some of the care that innovative devices make possible. For example, contracting agreements could be drawn up so that money came back to the populations that participated in a clinical trial, or to a community that otherwise may need the device but cannot afford it. I think we have to create some type of charitable impulse to moderate the excesses of the profits and use them for the common good.
Dr. Herndon: I would like to touch on disclosure. The orthopedic implant industry has been required by law to disclose its relationships with orthopedic surgeons, including the amount of money that surgeons may be getting from industry. This requirement has had unintended consequences that underscore the importance of disclosure. First, some of the monetary awards, whether market-driven or not, are quite excessive. Second, reviewing the contracts for royalties has led to the discovery that many are not supported by patents or intellectual property rights. Third, these disclosures have revealed that certain surgeons who work at major US institutions, and who thus have an obligation to pay the institution some of the monies from their research, have not disclosed their relationships for years and have kept those monies solely for themselves. So this disclosure requirement has brought many things to light.
Dr. Rezai: As long as there is human disease and suffering, innovation will continue. It has in the past and it will in the future. Most innovators have it in their genes and in their blood. They can be taught to innovate, but they have to have the intrinsic curiosity and the creative mind to be an innovator. Institutional support of innovation is important, as is respect for the process that must be followed, including transparency and disclosure. If you put all these together, then innovation can be facilitated.
IF TESTING MOVES OFFSHORE, CAN ETHICS FOLLOW?
Dr. Lieberman: I am going to paint a scenario on which I would like each panelist to briefly comment. New Device X is backed by a big vendor. It is a great device, but because of all the regulatory issues in the United States, it is taken to China or South America and is being implanted there, where the regulatory environment is much more lenient. Can we rationalize this practice? How is it possibly ethical?
Dr. Fins: I can answer in 5 seconds: we shouldn’t do it.
Dr. Rezai: This is a reality we are facing with increasing rules and regulations in the United States. You have to engage the process, and it takes time. If you have colleagues who can follow clinical trials outside the United States, you can have the device tested outside and then bring it back to the United States. Unfortunately, the reality is that the regulatory process can be slow, so more testing will be done abroad, in my opinion.
Dr. Hahn: I disagree with Dr. Fins. This may be the only way to get the trials started, and we then are able to use some of the offshore data to approach the FDA for approval. I do not think that it is taking advantage of anybody; it is a way of getting things through the system.
Dr. Herndon: The door has been opened, and it is only going to increase. My only request would be that the investigators who do this function as they would here in the United States, under IRB controls and the other kinds of oversight that they would expect and demand of themselves in their own institutions.
- Schiff ND, Giacino JT, Kalmar K, et al. Behavioral improvements with thalamic stimulation after severe traumatic brain injury. Nature 2007; 448:600–603.
- Forte ML, Virnig BA, Kane RL, et al. Geographic variation in device use for intertrochanteric hip fractures. J Bone Joint Surg Am 2008; 90:691–699.
- Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery database. J Bone Joint Surg Am 2008; 90:700–707.
- Herndon JH. Technology assessment and adoption in orthopaedics [letter]. J Bone Joint Surg Am 2008; 90e. http://www.ejbjs.org/cgi/eletters/90/4/689. Published April 1, 2008. Accessed August 25, 2008.
- Fins JJ. Surgical innovation and ethical dilemmas: precautions and proximity. Cleve Clin J Med 2008; 75(suppl 6):S7–S12.
- Brody H. The Healer’s Power. New Haven, CT: Yale University Press; 1992.
END RESULTS: WHY SO ELUSIVE STILL?
Dr. Isador Lieberman, Moderator: Let me begin this discussion with a 1910 quote from Ernest Codman, a general surgeon at Massachusetts General Hospital, who stated:
In 1900 I became interested in what I called the “end result” idea, which was merely the commonsense notion that every hospital should follow every patient it treats long enough to determine whether or not the treatment has been successful, and then should inquire, “If not, why not?” with a view to preventing similar failure in the future.
My questions to the panel are: What has changed in the last 100 years? Are we documenting our end results? Have we gone wrong and, if so, where have we gone wrong?
Dr. James Herndon: Although Codman’s ideas in this area were not well received at the time, today we do have some “end result” ideas. We have outcomes data, but I would argue that they are far too limited and not to the level required in the 21st century. I have asked myself many times why the surgical profession has not focused on this issue more than it has. I agree with Dr. [Joseph] Fins’ comments in his presentation [see previous article in this supplement] that it would be nice to have a bottom-up approach rather than a top-down approach, but I do not see a change until we as physicians step up to the plate and make a change.
Why haven’t we? There are a number of reasons. The malpractice climate in the United States has been one major factor. Surgeons fear disclosure. The relationship between a surgeon and the patient is professional and private, and physicians do not want transparency—they do not want their patient or anyone to know that an adverse event or bad outcome has occurred.
Also, doctors, especially surgeons, are reluctant to use guidelines or follow protocols. I participated a number of years ago in an American Academy of Orthopaedic Surgeons project called MODEMS; it was an attempt to set up guidelines for orthopedic surgeons to manage back pain, shoulder pain, and other orthopedic conditions. By the time we finished we had accomplished nothing, because the protocols and guidelines were so extensive that almost any type of management for any patient would be compliant.
Additionally, hospitals in the United States have become more like for-profit businesses, with a focus on short-term profits and with short tenures for their chief executive officers (CEOs)—4 or 5 years, on average. With nearly 50% of US hospitals bordering on bankruptcy, they are not able or willing to invest in major patient safety protocols and guidelines because the CEOs do not see a short-term benefit to them. Witness the fact that only 15% of US hospitals have computerized physician order entry systems and electronic medical records. From what I have read, it takes about 5 years before a hospital recoups such investments from the resulting safety improvements and efficiencies.
These are some, but by no means all, of the reasons we do not have appropriate outcomes in all specialty fields. My plea is that physicians lead the effort to measure and report outcomes down the road.
Dr. Lieberman: Dr. Hahn, why do you think we have not kept up with Dr. Codman’s premise from 100 years ago?
Dr. Joseph Hahn: We hold a yearly Medical Innovation Summit at the Cleveland Clinic, and what has emerged from many of those meetings is a lack of interest in paying for outcomes analyses. The providers, the government, and industry all say that they do not have the money for these analyses. So the first reason that Codman’s premise has not been lived up to is that the source of funding remains undetermined. Second, most surgical innovations have been geared toward inventing devices to overcome very specific problems that arise during or following surgery rather than toward substantiating the worth of a procedure through collection of evidence. A third reason involves the pressure that investors place on industry to make money, which tends to lead to investments in getting products to market rather than outcomes research. With all of these factors and the pressures from so many directions, the surgical profession hasn’t stepped back to thoroughly consider what we are doing to our patients and just how worthwhile it is.
Dr. Lieberman: Who do you think should be paying for outcomes analyses?
Dr. Hahn: I think the government should. The role of government is to take care of its citizens. The Centers for Medicare and Medicaid Services (CMS) does its best with the information it has, but it admits that it pays for some procedures without knowing whether or not they are truly worthwhile. An example is the use of artificial discs in the cervical spine. I am sure that the artificial disc manufacturers made a case for their product to CMS by claiming it was associated with less pain and resulted in a superior outcome compared to fusion using bone from the hip, regardless of whether they had the scientific evidence to prove it.
Dr. Lieberman: Dr. Fins, would you like to weigh in on Codman’s “end result” premise?
Dr. Joseph Fins: I would just point out that the history is not homogeneous. I have been involved in deep brain stimulation work, and the legacy of psychosurgery has been an egregious lack of outcomes studies, but now we do have outcomes studies and scales. For example, there is now the Yale-Brown Obsessive Compulsive Scale to rate the severity of symptoms in obsessive-compulsive disorder. In our deep brain stimulation study,1 we are using a coma recovery scale, and the Food and Drug Administration’s (FDA’s) investigational device exemption (IDE) process requires us to produce outcomes data to protect potential subjects. It may be an example of neuropsychiatric exceptionalism that neurology and psychiatry are areas of increased focus while somatic therapies are somehow presumed to be okay.
Dr. Hahn: FDA may be requiring the outcomes data, but I have not heard that they are willing to pay for it.
Dr. Fins: You are correct.
Dr. Ali Rezai: Part of the problem is the translation of rapid scientific discoveries and technological advances into the field, and education has a role here. Surgeons’ reluctance to integrate guidelines and outcomes measures into practice must be addressed very early in their training—in medical school—and then continued throughout residency and fellowship programs. The same early and continuing approach should be taken with respect to how to conduct and properly interpret a clinical trial.
Dr. Herndon: That is a good point. Surgical education programs have slipped a bit in the past 5 to 10 years, at least in orthopedics. With the reductions in residents’ work hours and the fast pace of residency programs, our residents spend most of their time in the operating room, struggling to master the multitude of procedures in orthopedics. As a result, they are not discussing outcomes or adequately following patients long-term after surgery. I have a hard time getting our faculty to bring residents into their offices so that the residents can examine patients and see why they are operating on certain kinds of patients, as well as the types of follow-up information that can and should be obtained from patients. Training today is so oriented to operative techniques that residencies have difficulty dealing with these other important issues.
WHO DEFINES THE INDICATIONS?
Dr. Lieberman: As new devices and new techniques emerge, who defines their indications? The inventor of the device, a government authority that may or may not have the medical background, patient advocacy groups, or the device manufacturer? And how should we regulate those indications?
Dr. Fins: I would echo Dr. Wilder Penfield’s words, “No man alone.” The orthopedic surgeon or neurosurgeon does not have to do this alone; it is really about teams. And those teams can and should include biostatisticians, recognizing that the biostatistician needs to fully understand what the surgeon is doing. There also has to be attention given to patients’ individualistic outcomes. I recently met with some FDA staff and learned that the FDA is very interested in novel methodologies to better understand what counts as an outcome for individual patients. So I think indications should be guided by individualistic outcomes coupled with the surgical possibilities and with the rigorous biostatistical methods that are now evolving. A conference like this represents an opportunity to generalize the conversation and support more collaboration on indications going forward.
Dr. Rezai: Indications should be defined using a team-oriented approach. Part of the problem of psychosurgery in the past was that the surgeon was defining indications without collaborating with the psychiatrist. In my field of deep brain stimulation and brain pacemakers, everything we have done for the past 20 years—surgery for Parkinson’s disease, depression, obsessive-compulsive disorder, traumatic brain injury, epilepsy—has involved working closely with neurologists, epileptologists, brain injury specialists, psychiatrists, and psychologists to agree on indications. These teams also need to have close partnerships with ethicists. Teamwork is a vital aspect of proper development of an indication.
Dr. Hahn: It has to be the clinicians who set forth the indications. Of course, that may be done by a team of clinicians, but as a surgeon I certainly do not want the manufacturers of an artificial disc telling me what they think the indications for an artificial disc are.
As for the role of patients, some of them are very well informed about their problem. I cannot tell you how many have shown up in my office with reprints of articles I have written. This is a trend that has really mushroomed over the past 10 years. But even though patients are catching up, they are still at a disadvantage. Patients are going to have a say, but it is still the clinicians whose role is to decide the indications and then provide patients with a risk-benefit analysis.
Dr. Herndon: I agree. Although patients are becoming more involved in the process, real shared decision-making has not yet happened in my field.
More broadly, I feel that our professional organizations have to become more actively involved in the process of defining indications. Otherwise, after the innovators develop a device or procedure that will significantly change the approach to a particular problem, it will enter the market at large without any critical assessment of the technology involved and without accounting for the learning curve for each individual surgeon.
Take the example of minimally invasive total hip replacement, which involves a 1-inch incision in the front of the hip and a 1-inch incision in the back of the hip. The learning curve for this procedure appears to be about 40 cases, based on the opinion of experts around the country. Yet when this minimally invasive approach emerged, every surgeon who had been performing total hip replacements wanted this new operation at his or her fingertips because patients were demanding it. Some surgeons adopted it too quickly, without adequate training. I know one distraught surgeon who abandoned the procedure because of numerous failures during his first 100 cases. He returned to the standard hip replacement approach.
Our profession cannot let this experience continue or proliferate. Yet the professional organizations in orthopedics have walked away from technology assessment because industry does not want it; technology assessment is not in industry’s best interest. We have had a number of conflicts in our professional organizations when attempting to move technology assessment forward. It is also very expensive to do.
Finally, indications can sometimes be governed more by economics than by science. I was asked to write a letter to the editor about two technologies for managing intertrochanteric fractures of the hip that were recently featured in the Journal of Bone and Joint Surgery.2,3 One technology involves a compression screw that has been shown to be effective in outcomes studies. The other is an intramedullary nail that has not been well studied and has no proven benefit over the compression screw. In doing research for my letter,4 I found that Medicare assigns more relative value units (RVUs) for the intramedullary nail than for the compression screw. In Boston, the total dollar difference in RVUs between the two is $300: the surgeon makes $1,500 for the procedure that involves the intramedullary nail versus $1,200 for using the compression screw. Not surprisingly, use of the intramedullary nail has been climbing rapidly in the United States without any evidence to justify its use over the other, less expensive technique.
CREDENTIALING: CAN IT KEEP PACE WITH INNOVATION?
Dr. Fins: I agree that surgical competence and regulation—self-regulation or professional regulation—are big issues. One of my greatest fears is that surgeons will do procedures they are not trained to do, and cause great harm as a result. We are hearing about this now with the resurgence of psychosurgery in China.
It strikes me as interesting that the field of neurosurgery is as yet undifferentiated and that there is no subspecialty certification in stereotactic neurosurgery. This is in contrast to invasive cardiology on the medical side, where physicians who do catheterizations and electrophysiologic studies have special additional training.
As innovations develop, we have to track qualifications and credentialing along the way. There should be provisions to grandfather surgeons in if they are in a post-training point in their career, but we have to ensure that the new technology is matched by the operator’s skill. This is particularly pertinent in light of the concept of “surgical proximity”5 and the importance of the individual operator; this is not comparable to just disseminating a new drug.
Dr. Lieberman: Who should do the credentialing? Should it be the government or our profession?
Dr. Fins: Recertification or credentialing should be by peers—the American College of Surgeons and the surgical boards. Of course, funders or payors may request an additional level of certification to do certain procedures, which I would endorse as a safety measure and to help ensure a minimal standard of care for innovative interventions.
Dr. Hahn: But it is not so simple. There is a blurring of surgical expertise once surgeons complete their training. Spine surgery used to be done by either neurosurgeons or orthopedic surgeons; now we have spine surgeons. What we neurosurgeons started to see with that change was that our neurosurgery trainees were being told they could not get on hospital staffs because they did not have credentials in spine surgery or, to take another example, in pediatric surgery. Well, the neurosurgery board made a conscious decision to not offer certificates of added qualification (CAQs). We challenged the hospitals in court and won. But the overriding message is that it is all about economics.
Dr. Herndon: In orthopedics we now have two CAQs—one in hand surgery and one (starting in 2009) in sports medicine. The hand surgeons have not noticed any adverse effect because they do not generate as much revenue as the spine surgeons do. Most orthopedic surgeons start as general orthopedists and then change their practice characteristics as their practices mature. Over time they may focus on one particular area, such as arthroscopic knee surgery or total hip or knee replacement, which makes it difficult for them to pass a general orthopedic examination. Our board recognized this trend and developed oral and written board exams with case reviews concentrating on the surgeon’s self-chosen specialty. We do not need the CAQs because they have been misused, and we as a profession have been letting others misuse them. Again, I think we need to get back to controlling the process ourselves.
Dr. Hahn: What do you do when a surgeon has finished training and then becomes interested in performing a new procedure developed since the time of his or her training? This can really be a challenge when the surgeon hears of a new procedure, goes and takes a 3-day training seminar on it, and comes back believing that he or she is ready to perform the procedure. I have had creative surgeons on staff who want to try a new procedure but have never done any cases, believing that the new technology alone will suffice. What we finally decided to do in these instances was to put in place other staff to proctor these cases to ensure that no harm was coming to patients.
Dr. Herndon: I admire that approach, because we as a profession have to educate our colleagues about whatever new procedures they are about to use in their practice. There is a learning curve for every operation, and learning on one’s own, at the expense of patients, is not appropriate. Should we have experienced colleagues work with surgeons on new procedures until they have performed the 40 or so cases necessary to be proficient? Should we send surgeons to other institutions to do their 40 cases under experienced supervision? I am not sure what the best approach is, but this is a question that a forum like this should begin to address.
HOW MUCH RISK IS ACCEPTABLE?
Dr. Lieberman: Let’s build on this issue of credentialing by turning to the concept of risk. What is an acceptable level of risk with a new device? Is a 50% risk of an adverse outcome appropriate? What about 10%? And who determines the acceptable risk? The profession? The regulatory bodies? Patients?
Dr. Fins: Our expectation about risks in clinical practice should evolve from what was anticipated and actually observed in the clinical trial of an intervention. Adverse events should be envisioned prospectively in the design of a trial, with the magnitude of risks delineated in the protocol. Any unexpected risks that occur, even if small, could be a major reporting issue. Beyond that, it is difficult to say what an acceptable level of risk is without a particularistic clinical trial. Whatever the risk of an intervention, the assessment of the risk must account for regional variation, variation among surgeons, and also systems issues.
The Institute of Medicine report, To Err is Human, attributed medical errors to faulty systems, processes, and conditions. So when we think about errors and risk, we have to consider more than just the individual operator. Just as To Err is Human analogized medical errors to airplane crashes, we might think of surgical retraining in the context of how pilots get retrained using flight simulators. If pilots have not flown a particular aircraft in a long time, they lose their flight certification for that type of craft and then must be retrained to operate it.
As surgical technology gets more advanced, specific, and nuanced, the discordance between one’s training and the potential things one can do becomes greater. Paradoxically, innovation can at least potentially make situations more dangerous in that the operator may not be able to perform the task with the improved technology. For example, pilots who know how to fly a Cessna can fly another simply constructed plane, but if they attempt to fly a higher-technology aircraft, like an F-16, they have a greater risk of having a catastrophic event even though the F-16 flies better, faster, and higher.
Dr. Lieberman: But are you willing to identify a level of acceptable risk?
Dr. Fins: It is based on the patient’s preference, after informed consent. An acceptable level of risk is the level that people are willing to accept. What I am concerned about is the variance around a known risk, whatever it may be, that is attributable to human errors that may be preventable through training or by solving systems problems.
Dr. Lieberman: Dr. Rezai, you place needles into the brain. Who should decide the risk of that action? You? The patient? And what do you feel is an acceptable risk level?
Dr. Rezai: It is a complex question, of course, and a number of variables come into play. Whether or not the patient’s condition is life-threatening or disabling is a very important factor in the risk-benefit ratio. Regulatory guidance from the FDA is strong with respect to defining device-related adverse effects as serious or nonserious, and our peers, both surgeons and nonsurgeons, help to further dictate the risk and tolerability of a procedure and its alternatives. For example, in considering a surgical procedure, one must weigh its risk against the risks of medications to treat the disorder, such as side effects, the ease of medication adherence, and the number of emergency room visits that may result from adverse effects of the medications.
Determining acceptable risk rests fundamentally and first with the patient and then with the surgeon and his or her peers (surgeons and nonsurgeons) in conjunction with regulatory components and oversight. All of these factors contribute.
In my field of deep brain stimulation, the threshold for acceptable risk can be high since we see patients with chronic conditions in whom all previous medication attempts have failed, many of whom are disabled, intractable to current therapies, and with a significant compromise of quality of life. Examples include wheelchair-dependent patients with severe Parkinson’s disease, severely depressed patients who will not leave the house and have attempted suicide, and obsessive-compulsive disorder patients who need 10 hours just to take a shower. This type of intractability to current therapies and the suffering of patients and families with limited options and little hope infl uence assessments of procedural risk.
Dr. Hahn: Performing a controlled clinical trial of a surgical procedure is difficult at best. I recall a clinical trial in which patients with parkinsonism were to be randomized either to have stem cells implanted in their brain or to undergo a sham operation with no stem cells. Well, very few patients signed up for the trial because everyone wanted the stem cells. So, obtaining a large enough denominator to define the risk of, for example, hemorrhage from sticking a needle into a vessel is almost impossible.
Dr. Herndon: Except when there are risks of serious life-threatening events, I believe the patient is the one who makes the decision after having the risks fully explained to him or her. Surgeons are educated in a system in which we learn to accept complications. It is the risk of doing business. We have not learned very well how to differentiate a complication from an adverse event or an error. We must learn to do that. We live with complications every day. Those complications must be conveyed to patients so that they understand what they are about to undergo, what can happen, and what cannot happen. The patient is the ultimate decider, in my opinion.
Dr. Lieberman: That reminds me of something one of my mentors often said: “If you are going to run with the big dogs, expect to get bitten in the butt once in a while.”
ETHICAL DILEMMAS ARISING FROM NEW OPTIONS
Question from audience: In my specialty, we have a non-life-threatening condition with a well-established 25% recurrence rate after traditional surgery with sutures, and a 25% rate of reoperation. A device comes along and it improves the outcomes so that the recurrence rate declines to 10%, but along with the extra costs of doing the procedure with the device, there is also a complication rate of about 10% that requires reoperation with the device, and a few of those patients actually end up worse. Ethically, how should the clinician proceed in this situation? The old way, or the new way that improves outcomes but at a higher cost and risk?
Dr. Fins: Based on the size of the populations, is the difference in the combined rates of recurrence and complications between the traditional and new methods (25% vs 20%) statistically significant?
Response from questioner: The difference is probably not statistically significant.
Dr. Fins: Okay, so you are saying that the numbers are basically equal. That is the first consideration, but there is a nuance to one of the variables, and that is an improvement in quality of life with one of the treatments. Measuring its significance is subjective. A patient may place greater emphasis on quality of life than would somebody who is not a beneficiary of the operation. That is why I said before that biostatistical input that goes beyond crude measures of mortality or reoperation rates can be very helpful. The risk of reoperation may be one that the patient is willing to take for a chance at an improvement in quality of life.
There is a wonderful book by Howard Brody called The Healer’s Power6 in which he writes about the physician’s power to frame a question so as to engineer outcomes. While that is not something that Brody endorses, he does endorse the use of the physician’s power to guide patients using good informed consent, providing direction without being so determinative that patients feel compelled to choose the physician’s recommendation. Patients should be able to decline your recommendation while still having the benefit of your counsel. And in a case like this, your counsel should include variables that may seem “softer” or more difficult to quantify than crude measures such as mortality or reoperation rates.
Dr. Rezai: You have to compare multiple outcomes between the two approaches—surgical time, recovery time, patient quality of life (as assessed by scales), family quality of life, time to return to work, etc. I think it is important to try new technologies because the failure rate or the complication rate may be reduced over time, but only if you evaluate the failures and then restrategize. Only in doing so can you reduce risk, and if the benefit profile and the risk profile prove to be good, then the new technology should be pushed forward.
Dr. Herndon: If the volume of procedures performed by the surgeon is important with respect to outcomes with either one of these two procedures, that should be taken into account. Also, if a new procedure carries a higher complication rate than the traditional procedure, I think that more cohort studies from large centers are needed to gauge the true complication rate before the new technology enters the general market. Continued surveillance, such as with a postmarket registry of outcomes with these procedures, would also be helpful to make adjustments in the future if necessary.
Dr. Hahn: If you looked at the early experience of Med tronic with pacers, you would be amazed at the number of deaths and complications that occurred during the first 3 years. But we do not even think about that now.
CAN INNOVATION HAPPEN WITHOUT INCENTIVES?
Question from audience: Dr. Hahn alluded earlier to the infl uence of money. All of you on the panel are institutionally based, and you are used to practicing with colleagues. I would suggest that surgery today is really not an individual sport, but that is the way it is practiced in much of the nation. Would we be better off if we developed a system that removed us from direct financial influence? Can we get the money out of the equation so that people have motives other than direct personal gain?
Dr. Hahn: I went to an institutional review board (IRB) retreat that included, of course, some IRB members who were not clinicians. They asked the same question that you just did: Why would you even expect to get anything for what you invent? I think that is naïve. People who work hard and invent things deserve to reap a reward. The challenge lies in working with industry, which may try to convince us to use its innovations without our input, as opposed to working with us to identify a clinical problem and trying to solve it together. In that way, the end product and the logic behind its use will be better.
I will give you an example from when I was head of surgery here. A company made a voice-activated table that would obey the surgeon’s commands, such as “left,” “right,” “up,” or “down.” I asked the representative why such a product was needed, and he responded that the surgeon wants to be in total control of the operating room. I told him we do not change the position of the table very often. After a 2-week trial, the table was a dud. He fired the entire group that was working on the project. It was a case of a company simply trying to come up with a product it could sell.
The opposite scenario is if I invent the latest and greatest stent for the carotids and I want to use it. The question becomes how to strike a balance: how to protect the patients while at the same time rewarding the inventor. Another challenge is that device companies want you to stay on their scientific advisory board and they will pay you for it.
These questions are a big concern, and we have spent a lot of time on these issues at Cleveland Clinic. In fact, we held our own conference on biomedical confl icts of interest in September 2006 with attendees from around the country to discuss the necessary firewalls for ensuring that data are not contaminated, that the surgeon-inventor does not fudge data so that his innovation will make it to the marketplace, etc. At that conference, a number of people spoke about Vioxx. I am a surgeon, and my take on the COX-2 inhibitors is that a lot of my patients take these drugs and think they are wonderful, but there are some problems and risks. What is wrong with explaining to patients the risks and complications of these drugs, making your own recommendation about their use (unless you are receiving money from their manufacturers, which you would need to disclose to patients), and then letting patients make their own informed decisions? Personally, I was on Bextra for 3 years and was furious when it was pulled from the market because nobody gave me a choice whether or not to continue using it.
Dr. Lieberman: Let’s explore this concept a little deeper. We know that innovation is so important, but how do we encourage clinicians to innovate in this environment? Dr. Hahn, you served as chairman of CC Innovations, which is Cleveland Clinic’s technology commercialization arm. What were some of the strategies you came across in that role?
Dr. Hahn: We look for creative staff. We tell them up front that we want them to come to Cleveland Clinic and invent things. Our mission is literally to work on problems and take solutions to our patients. The culture here is meant to be creative. As a part of that culture, we welcome working with industry, as opposed to industry thrusting its innovations on us.
We are averaging more than 200 invention disclosures per year. More than 500 of our staff are involved with various industrial partners, and we are not going to hide that. In fact, we are going to make it public. The thought is that we owe it to our patients to work on their problems. At the same time, we owe it to our patients to say when we are working with industry on a particular product and explain to them why we think it would work in their case, if we think it would. While doing so, we need to make it clear that we will be happy to refer them for a second opinion if they would like. If I have a patient who wants a second opinion, I will offer to make the phone call for them and get them in. I think that is an advantage of the model we have here.
The reality is that there are some procedures that can only be done by one surgeon here, a surgeon who may have helped develop the procedure or some technology involved in it. Are we going to tell that surgeon that he or she cannot perform the procedure on anyone? That does not make sense. So you need to have a management plan that puts in place firewalls to protect the data on that procedure from any possible contamination.
So yes, we do reward staff who are doing innovation, and we do work with industry, and we do tell our patients we are doing it, and we do build firewalls to protect the data.
Dr. Lieberman: How about the rest of the panel? What are your thoughts on providing incentives for innovation?
Dr. Fins: Money is a key issue. The way the landscape is now structured, collaborations with industry are part of the mix. Under the Bayh-Dole Act of 1980, institutions are granted intellectual property rights to ideas or inventions developed by their researchers, and then the institutions can enter into contracts with industry to move the innovations forward. If industry support of research were removed, we would have to double the budget of the National Institutes of Health to compensate.
On the other hand, industry support can sometimes prove to be a disincentive to innovation in that it may engineer certain kinds of research or deprive investigators of tools they may need to do more basic science types of research. It is an academic freedom issue. At a translational level, industry may be helpful and catalytic. But sometimes it pushes an investigator to work for a short-term innovative application at the expense of a more speculative, riskier innovation.
We need to acknowledge that industry collaborations are part and parcel of the universe and focus on working with industry to moderate its influences. At the same time, we must use our leverage on the investigative side of the equation to pursue academic freedom and to leverage industry resources to perhaps pay for some of the care that innovative devices make possible. For example, contracting agreements could be drawn up so that money came back to the populations that participated in a clinical trial, or to a community that otherwise may need the device but cannot afford it. I think we have to create some type of charitable impulse to moderate the excesses of the profits and use them for the common good.
Dr. Herndon: I would like to touch on disclosure. The orthopedic implant industry has been required by law to disclose its relationships with orthopedic surgeons, including the amount of money that surgeons may be getting from industry. This requirement has had unintended consequences that underscore the importance of disclosure. First, some of the monetary awards, whether market-driven or not, are quite excessive. Second, reviewing the contracts for royalties has led to the discovery that many are not supported by patents or intellectual property rights. Third, these disclosures have revealed that certain surgeons who work at major US institutions, and who thus have an obligation to pay the institution some of the monies from their research, have not disclosed their relationships for years and have kept those monies solely for themselves. So this disclosure requirement has brought many things to light.
Dr. Rezai: As long as there is human disease and suffering, innovation will continue. It has in the past and it will in the future. Most innovators have it in their genes and in their blood. They can be taught to innovate, but they have to have the intrinsic curiosity and the creative mind to be an innovator. Institutional support of innovation is important, as is respect for the process that must be followed, including transparency and disclosure. If you put all these together, then innovation can be facilitated.
IF TESTING MOVES OFFSHORE, CAN ETHICS FOLLOW?
Dr. Lieberman: I am going to paint a scenario on which I would like each panelist to briefly comment. New Device X is backed by a big vendor. It is a great device, but because of all the regulatory issues in the United States, it is taken to China or South America and is being implanted there, where the regulatory environment is much more lenient. Can we rationalize this practice? How is it possibly ethical?
Dr. Fins: I can answer in 5 seconds: we shouldn’t do it.
Dr. Rezai: This is a reality we are facing with increasing rules and regulations in the United States. You have to engage the process, and it takes time. If you have colleagues who can follow clinical trials outside the United States, you can have the device tested outside and then bring it back to the United States. Unfortunately, the reality is that the regulatory process can be slow, so more testing will be done abroad, in my opinion.
Dr. Hahn: I disagree with Dr. Fins. This may be the only way to get the trials started, and we then are able to use some of the offshore data to approach the FDA for approval. I do not think that it is taking advantage of anybody; it is a way of getting things through the system.
Dr. Herndon: The door has been opened, and it is only going to increase. My only request would be that the investigators who do this function as they would here in the United States, under IRB controls and the other kinds of oversight that they would expect and demand of themselves in their own institutions.
END RESULTS: WHY SO ELUSIVE STILL?
Dr. Isador Lieberman, Moderator: Let me begin this discussion with a 1910 quote from Ernest Codman, a general surgeon at Massachusetts General Hospital, who stated:
In 1900 I became interested in what I called the “end result” idea, which was merely the commonsense notion that every hospital should follow every patient it treats long enough to determine whether or not the treatment has been successful, and then should inquire, “If not, why not?” with a view to preventing similar failure in the future.
My questions to the panel are: What has changed in the last 100 years? Are we documenting our end results? Have we gone wrong and, if so, where have we gone wrong?
Dr. James Herndon: Although Codman’s ideas in this area were not well received at the time, today we do have some “end result” ideas. We have outcomes data, but I would argue that they are far too limited and not to the level required in the 21st century. I have asked myself many times why the surgical profession has not focused on this issue more than it has. I agree with Dr. [Joseph] Fins’ comments in his presentation [see previous article in this supplement] that it would be nice to have a bottom-up approach rather than a top-down approach, but I do not see a change until we as physicians step up to the plate and make a change.
Why haven’t we? There are a number of reasons. The malpractice climate in the United States has been one major factor. Surgeons fear disclosure. The relationship between a surgeon and the patient is professional and private, and physicians do not want transparency—they do not want their patient or anyone to know that an adverse event or bad outcome has occurred.
Also, doctors, especially surgeons, are reluctant to use guidelines or follow protocols. I participated a number of years ago in an American Academy of Orthopaedic Surgeons project called MODEMS; it was an attempt to set up guidelines for orthopedic surgeons to manage back pain, shoulder pain, and other orthopedic conditions. By the time we finished we had accomplished nothing, because the protocols and guidelines were so extensive that almost any type of management for any patient would be compliant.
Additionally, hospitals in the United States have become more like for-profit businesses, with a focus on short-term profits and with short tenures for their chief executive officers (CEOs)—4 or 5 years, on average. With nearly 50% of US hospitals bordering on bankruptcy, they are not able or willing to invest in major patient safety protocols and guidelines because the CEOs do not see a short-term benefit to them. Witness the fact that only 15% of US hospitals have computerized physician order entry systems and electronic medical records. From what I have read, it takes about 5 years before a hospital recoups such investments from the resulting safety improvements and efficiencies.
These are some, but by no means all, of the reasons we do not have appropriate outcomes in all specialty fields. My plea is that physicians lead the effort to measure and report outcomes down the road.
Dr. Lieberman: Dr. Hahn, why do you think we have not kept up with Dr. Codman’s premise from 100 years ago?
Dr. Joseph Hahn: We hold a yearly Medical Innovation Summit at the Cleveland Clinic, and what has emerged from many of those meetings is a lack of interest in paying for outcomes analyses. The providers, the government, and industry all say that they do not have the money for these analyses. So the first reason that Codman’s premise has not been lived up to is that the source of funding remains undetermined. Second, most surgical innovations have been geared toward inventing devices to overcome very specific problems that arise during or following surgery rather than toward substantiating the worth of a procedure through collection of evidence. A third reason involves the pressure that investors place on industry to make money, which tends to lead to investments in getting products to market rather than outcomes research. With all of these factors and the pressures from so many directions, the surgical profession hasn’t stepped back to thoroughly consider what we are doing to our patients and just how worthwhile it is.
Dr. Lieberman: Who do you think should be paying for outcomes analyses?
Dr. Hahn: I think the government should. The role of government is to take care of its citizens. The Centers for Medicare and Medicaid Services (CMS) does its best with the information it has, but it admits that it pays for some procedures without knowing whether or not they are truly worthwhile. An example is the use of artificial discs in the cervical spine. I am sure that the artificial disc manufacturers made a case for their product to CMS by claiming it was associated with less pain and resulted in a superior outcome compared to fusion using bone from the hip, regardless of whether they had the scientific evidence to prove it.
Dr. Lieberman: Dr. Fins, would you like to weigh in on Codman’s “end result” premise?
Dr. Joseph Fins: I would just point out that the history is not homogeneous. I have been involved in deep brain stimulation work, and the legacy of psychosurgery has been an egregious lack of outcomes studies, but now we do have outcomes studies and scales. For example, there is now the Yale-Brown Obsessive Compulsive Scale to rate the severity of symptoms in obsessive-compulsive disorder. In our deep brain stimulation study,1 we are using a coma recovery scale, and the Food and Drug Administration’s (FDA’s) investigational device exemption (IDE) process requires us to produce outcomes data to protect potential subjects. It may be an example of neuropsychiatric exceptionalism that neurology and psychiatry are areas of increased focus while somatic therapies are somehow presumed to be okay.
Dr. Hahn: FDA may be requiring the outcomes data, but I have not heard that they are willing to pay for it.
Dr. Fins: You are correct.
Dr. Ali Rezai: Part of the problem is the translation of rapid scientific discoveries and technological advances into the field, and education has a role here. Surgeons’ reluctance to integrate guidelines and outcomes measures into practice must be addressed very early in their training—in medical school—and then continued throughout residency and fellowship programs. The same early and continuing approach should be taken with respect to how to conduct and properly interpret a clinical trial.
Dr. Herndon: That is a good point. Surgical education programs have slipped a bit in the past 5 to 10 years, at least in orthopedics. With the reductions in residents’ work hours and the fast pace of residency programs, our residents spend most of their time in the operating room, struggling to master the multitude of procedures in orthopedics. As a result, they are not discussing outcomes or adequately following patients long-term after surgery. I have a hard time getting our faculty to bring residents into their offices so that the residents can examine patients and see why they are operating on certain kinds of patients, as well as the types of follow-up information that can and should be obtained from patients. Training today is so oriented to operative techniques that residencies have difficulty dealing with these other important issues.
WHO DEFINES THE INDICATIONS?
Dr. Lieberman: As new devices and new techniques emerge, who defines their indications? The inventor of the device, a government authority that may or may not have the medical background, patient advocacy groups, or the device manufacturer? And how should we regulate those indications?
Dr. Fins: I would echo Dr. Wilder Penfield’s words, “No man alone.” The orthopedic surgeon or neurosurgeon does not have to do this alone; it is really about teams. And those teams can and should include biostatisticians, recognizing that the biostatistician needs to fully understand what the surgeon is doing. There also has to be attention given to patients’ individualistic outcomes. I recently met with some FDA staff and learned that the FDA is very interested in novel methodologies to better understand what counts as an outcome for individual patients. So I think indications should be guided by individualistic outcomes coupled with the surgical possibilities and with the rigorous biostatistical methods that are now evolving. A conference like this represents an opportunity to generalize the conversation and support more collaboration on indications going forward.
Dr. Rezai: Indications should be defined using a team-oriented approach. Part of the problem of psychosurgery in the past was that the surgeon was defining indications without collaborating with the psychiatrist. In my field of deep brain stimulation and brain pacemakers, everything we have done for the past 20 years—surgery for Parkinson’s disease, depression, obsessive-compulsive disorder, traumatic brain injury, epilepsy—has involved working closely with neurologists, epileptologists, brain injury specialists, psychiatrists, and psychologists to agree on indications. These teams also need to have close partnerships with ethicists. Teamwork is a vital aspect of proper development of an indication.
Dr. Hahn: It has to be the clinicians who set forth the indications. Of course, that may be done by a team of clinicians, but as a surgeon I certainly do not want the manufacturers of an artificial disc telling me what they think the indications for an artificial disc are.
As for the role of patients, some of them are very well informed about their problem. I cannot tell you how many have shown up in my office with reprints of articles I have written. This is a trend that has really mushroomed over the past 10 years. But even though patients are catching up, they are still at a disadvantage. Patients are going to have a say, but it is still the clinicians whose role is to decide the indications and then provide patients with a risk-benefit analysis.
Dr. Herndon: I agree. Although patients are becoming more involved in the process, real shared decision-making has not yet happened in my field.
More broadly, I feel that our professional organizations have to become more actively involved in the process of defining indications. Otherwise, after the innovators develop a device or procedure that will significantly change the approach to a particular problem, it will enter the market at large without any critical assessment of the technology involved and without accounting for the learning curve for each individual surgeon.
Take the example of minimally invasive total hip replacement, which involves a 1-inch incision in the front of the hip and a 1-inch incision in the back of the hip. The learning curve for this procedure appears to be about 40 cases, based on the opinion of experts around the country. Yet when this minimally invasive approach emerged, every surgeon who had been performing total hip replacements wanted this new operation at his or her fingertips because patients were demanding it. Some surgeons adopted it too quickly, without adequate training. I know one distraught surgeon who abandoned the procedure because of numerous failures during his first 100 cases. He returned to the standard hip replacement approach.
Our profession cannot let this experience continue or proliferate. Yet the professional organizations in orthopedics have walked away from technology assessment because industry does not want it; technology assessment is not in industry’s best interest. We have had a number of conflicts in our professional organizations when attempting to move technology assessment forward. It is also very expensive to do.
Finally, indications can sometimes be governed more by economics than by science. I was asked to write a letter to the editor about two technologies for managing intertrochanteric fractures of the hip that were recently featured in the Journal of Bone and Joint Surgery.2,3 One technology involves a compression screw that has been shown to be effective in outcomes studies. The other is an intramedullary nail that has not been well studied and has no proven benefit over the compression screw. In doing research for my letter,4 I found that Medicare assigns more relative value units (RVUs) for the intramedullary nail than for the compression screw. In Boston, the total dollar difference in RVUs between the two is $300: the surgeon makes $1,500 for the procedure that involves the intramedullary nail versus $1,200 for using the compression screw. Not surprisingly, use of the intramedullary nail has been climbing rapidly in the United States without any evidence to justify its use over the other, less expensive technique.
CREDENTIALING: CAN IT KEEP PACE WITH INNOVATION?
Dr. Fins: I agree that surgical competence and regulation—self-regulation or professional regulation—are big issues. One of my greatest fears is that surgeons will do procedures they are not trained to do, and cause great harm as a result. We are hearing about this now with the resurgence of psychosurgery in China.
It strikes me as interesting that the field of neurosurgery is as yet undifferentiated and that there is no subspecialty certification in stereotactic neurosurgery. This is in contrast to invasive cardiology on the medical side, where physicians who do catheterizations and electrophysiologic studies have special additional training.
As innovations develop, we have to track qualifications and credentialing along the way. There should be provisions to grandfather surgeons in if they are in a post-training point in their career, but we have to ensure that the new technology is matched by the operator’s skill. This is particularly pertinent in light of the concept of “surgical proximity”5 and the importance of the individual operator; this is not comparable to just disseminating a new drug.
Dr. Lieberman: Who should do the credentialing? Should it be the government or our profession?
Dr. Fins: Recertification or credentialing should be by peers—the American College of Surgeons and the surgical boards. Of course, funders or payors may request an additional level of certification to do certain procedures, which I would endorse as a safety measure and to help ensure a minimal standard of care for innovative interventions.
Dr. Hahn: But it is not so simple. There is a blurring of surgical expertise once surgeons complete their training. Spine surgery used to be done by either neurosurgeons or orthopedic surgeons; now we have spine surgeons. What we neurosurgeons started to see with that change was that our neurosurgery trainees were being told they could not get on hospital staffs because they did not have credentials in spine surgery or, to take another example, in pediatric surgery. Well, the neurosurgery board made a conscious decision to not offer certificates of added qualification (CAQs). We challenged the hospitals in court and won. But the overriding message is that it is all about economics.
Dr. Herndon: In orthopedics we now have two CAQs—one in hand surgery and one (starting in 2009) in sports medicine. The hand surgeons have not noticed any adverse effect because they do not generate as much revenue as the spine surgeons do. Most orthopedic surgeons start as general orthopedists and then change their practice characteristics as their practices mature. Over time they may focus on one particular area, such as arthroscopic knee surgery or total hip or knee replacement, which makes it difficult for them to pass a general orthopedic examination. Our board recognized this trend and developed oral and written board exams with case reviews concentrating on the surgeon’s self-chosen specialty. We do not need the CAQs because they have been misused, and we as a profession have been letting others misuse them. Again, I think we need to get back to controlling the process ourselves.
Dr. Hahn: What do you do when a surgeon has finished training and then becomes interested in performing a new procedure developed since the time of his or her training? This can really be a challenge when the surgeon hears of a new procedure, goes and takes a 3-day training seminar on it, and comes back believing that he or she is ready to perform the procedure. I have had creative surgeons on staff who want to try a new procedure but have never done any cases, believing that the new technology alone will suffice. What we finally decided to do in these instances was to put in place other staff to proctor these cases to ensure that no harm was coming to patients.
Dr. Herndon: I admire that approach, because we as a profession have to educate our colleagues about whatever new procedures they are about to use in their practice. There is a learning curve for every operation, and learning on one’s own, at the expense of patients, is not appropriate. Should we have experienced colleagues work with surgeons on new procedures until they have performed the 40 or so cases necessary to be proficient? Should we send surgeons to other institutions to do their 40 cases under experienced supervision? I am not sure what the best approach is, but this is a question that a forum like this should begin to address.
HOW MUCH RISK IS ACCEPTABLE?
Dr. Lieberman: Let’s build on this issue of credentialing by turning to the concept of risk. What is an acceptable level of risk with a new device? Is a 50% risk of an adverse outcome appropriate? What about 10%? And who determines the acceptable risk? The profession? The regulatory bodies? Patients?
Dr. Fins: Our expectation about risks in clinical practice should evolve from what was anticipated and actually observed in the clinical trial of an intervention. Adverse events should be envisioned prospectively in the design of a trial, with the magnitude of risks delineated in the protocol. Any unexpected risks that occur, even if small, could be a major reporting issue. Beyond that, it is difficult to say what an acceptable level of risk is without a particularistic clinical trial. Whatever the risk of an intervention, the assessment of the risk must account for regional variation, variation among surgeons, and also systems issues.
The Institute of Medicine report, To Err is Human, attributed medical errors to faulty systems, processes, and conditions. So when we think about errors and risk, we have to consider more than just the individual operator. Just as To Err is Human analogized medical errors to airplane crashes, we might think of surgical retraining in the context of how pilots get retrained using flight simulators. If pilots have not flown a particular aircraft in a long time, they lose their flight certification for that type of craft and then must be retrained to operate it.
As surgical technology gets more advanced, specific, and nuanced, the discordance between one’s training and the potential things one can do becomes greater. Paradoxically, innovation can at least potentially make situations more dangerous in that the operator may not be able to perform the task with the improved technology. For example, pilots who know how to fly a Cessna can fly another simply constructed plane, but if they attempt to fly a higher-technology aircraft, like an F-16, they have a greater risk of having a catastrophic event even though the F-16 flies better, faster, and higher.
Dr. Lieberman: But are you willing to identify a level of acceptable risk?
Dr. Fins: It is based on the patient’s preference, after informed consent. An acceptable level of risk is the level that people are willing to accept. What I am concerned about is the variance around a known risk, whatever it may be, that is attributable to human errors that may be preventable through training or by solving systems problems.
Dr. Lieberman: Dr. Rezai, you place needles into the brain. Who should decide the risk of that action? You? The patient? And what do you feel is an acceptable risk level?
Dr. Rezai: It is a complex question, of course, and a number of variables come into play. Whether or not the patient’s condition is life-threatening or disabling is a very important factor in the risk-benefit ratio. Regulatory guidance from the FDA is strong with respect to defining device-related adverse effects as serious or nonserious, and our peers, both surgeons and nonsurgeons, help to further dictate the risk and tolerability of a procedure and its alternatives. For example, in considering a surgical procedure, one must weigh its risk against the risks of medications to treat the disorder, such as side effects, the ease of medication adherence, and the number of emergency room visits that may result from adverse effects of the medications.
Determining acceptable risk rests fundamentally and first with the patient and then with the surgeon and his or her peers (surgeons and nonsurgeons) in conjunction with regulatory components and oversight. All of these factors contribute.
In my field of deep brain stimulation, the threshold for acceptable risk can be high since we see patients with chronic conditions in whom all previous medication attempts have failed, many of whom are disabled, intractable to current therapies, and with a significant compromise of quality of life. Examples include wheelchair-dependent patients with severe Parkinson’s disease, severely depressed patients who will not leave the house and have attempted suicide, and obsessive-compulsive disorder patients who need 10 hours just to take a shower. This type of intractability to current therapies and the suffering of patients and families with limited options and little hope infl uence assessments of procedural risk.
Dr. Hahn: Performing a controlled clinical trial of a surgical procedure is difficult at best. I recall a clinical trial in which patients with parkinsonism were to be randomized either to have stem cells implanted in their brain or to undergo a sham operation with no stem cells. Well, very few patients signed up for the trial because everyone wanted the stem cells. So, obtaining a large enough denominator to define the risk of, for example, hemorrhage from sticking a needle into a vessel is almost impossible.
Dr. Herndon: Except when there are risks of serious life-threatening events, I believe the patient is the one who makes the decision after having the risks fully explained to him or her. Surgeons are educated in a system in which we learn to accept complications. It is the risk of doing business. We have not learned very well how to differentiate a complication from an adverse event or an error. We must learn to do that. We live with complications every day. Those complications must be conveyed to patients so that they understand what they are about to undergo, what can happen, and what cannot happen. The patient is the ultimate decider, in my opinion.
Dr. Lieberman: That reminds me of something one of my mentors often said: “If you are going to run with the big dogs, expect to get bitten in the butt once in a while.”
ETHICAL DILEMMAS ARISING FROM NEW OPTIONS
Question from audience: In my specialty, we have a non-life-threatening condition with a well-established 25% recurrence rate after traditional surgery with sutures, and a 25% rate of reoperation. A device comes along and it improves the outcomes so that the recurrence rate declines to 10%, but along with the extra costs of doing the procedure with the device, there is also a complication rate of about 10% that requires reoperation with the device, and a few of those patients actually end up worse. Ethically, how should the clinician proceed in this situation? The old way, or the new way that improves outcomes but at a higher cost and risk?
Dr. Fins: Based on the size of the populations, is the difference in the combined rates of recurrence and complications between the traditional and new methods (25% vs 20%) statistically significant?
Response from questioner: The difference is probably not statistically significant.
Dr. Fins: Okay, so you are saying that the numbers are basically equal. That is the first consideration, but there is a nuance to one of the variables, and that is an improvement in quality of life with one of the treatments. Measuring its significance is subjective. A patient may place greater emphasis on quality of life than would somebody who is not a beneficiary of the operation. That is why I said before that biostatistical input that goes beyond crude measures of mortality or reoperation rates can be very helpful. The risk of reoperation may be one that the patient is willing to take for a chance at an improvement in quality of life.
There is a wonderful book by Howard Brody called The Healer’s Power6 in which he writes about the physician’s power to frame a question so as to engineer outcomes. While that is not something that Brody endorses, he does endorse the use of the physician’s power to guide patients using good informed consent, providing direction without being so determinative that patients feel compelled to choose the physician’s recommendation. Patients should be able to decline your recommendation while still having the benefit of your counsel. And in a case like this, your counsel should include variables that may seem “softer” or more difficult to quantify than crude measures such as mortality or reoperation rates.
Dr. Rezai: You have to compare multiple outcomes between the two approaches—surgical time, recovery time, patient quality of life (as assessed by scales), family quality of life, time to return to work, etc. I think it is important to try new technologies because the failure rate or the complication rate may be reduced over time, but only if you evaluate the failures and then restrategize. Only in doing so can you reduce risk, and if the benefit profile and the risk profile prove to be good, then the new technology should be pushed forward.
Dr. Herndon: If the volume of procedures performed by the surgeon is important with respect to outcomes with either one of these two procedures, that should be taken into account. Also, if a new procedure carries a higher complication rate than the traditional procedure, I think that more cohort studies from large centers are needed to gauge the true complication rate before the new technology enters the general market. Continued surveillance, such as with a postmarket registry of outcomes with these procedures, would also be helpful to make adjustments in the future if necessary.
Dr. Hahn: If you looked at the early experience of Med tronic with pacers, you would be amazed at the number of deaths and complications that occurred during the first 3 years. But we do not even think about that now.
CAN INNOVATION HAPPEN WITHOUT INCENTIVES?
Question from audience: Dr. Hahn alluded earlier to the infl uence of money. All of you on the panel are institutionally based, and you are used to practicing with colleagues. I would suggest that surgery today is really not an individual sport, but that is the way it is practiced in much of the nation. Would we be better off if we developed a system that removed us from direct financial influence? Can we get the money out of the equation so that people have motives other than direct personal gain?
Dr. Hahn: I went to an institutional review board (IRB) retreat that included, of course, some IRB members who were not clinicians. They asked the same question that you just did: Why would you even expect to get anything for what you invent? I think that is naïve. People who work hard and invent things deserve to reap a reward. The challenge lies in working with industry, which may try to convince us to use its innovations without our input, as opposed to working with us to identify a clinical problem and trying to solve it together. In that way, the end product and the logic behind its use will be better.
I will give you an example from when I was head of surgery here. A company made a voice-activated table that would obey the surgeon’s commands, such as “left,” “right,” “up,” or “down.” I asked the representative why such a product was needed, and he responded that the surgeon wants to be in total control of the operating room. I told him we do not change the position of the table very often. After a 2-week trial, the table was a dud. He fired the entire group that was working on the project. It was a case of a company simply trying to come up with a product it could sell.
The opposite scenario is if I invent the latest and greatest stent for the carotids and I want to use it. The question becomes how to strike a balance: how to protect the patients while at the same time rewarding the inventor. Another challenge is that device companies want you to stay on their scientific advisory board and they will pay you for it.
These questions are a big concern, and we have spent a lot of time on these issues at Cleveland Clinic. In fact, we held our own conference on biomedical confl icts of interest in September 2006 with attendees from around the country to discuss the necessary firewalls for ensuring that data are not contaminated, that the surgeon-inventor does not fudge data so that his innovation will make it to the marketplace, etc. At that conference, a number of people spoke about Vioxx. I am a surgeon, and my take on the COX-2 inhibitors is that a lot of my patients take these drugs and think they are wonderful, but there are some problems and risks. What is wrong with explaining to patients the risks and complications of these drugs, making your own recommendation about their use (unless you are receiving money from their manufacturers, which you would need to disclose to patients), and then letting patients make their own informed decisions? Personally, I was on Bextra for 3 years and was furious when it was pulled from the market because nobody gave me a choice whether or not to continue using it.
Dr. Lieberman: Let’s explore this concept a little deeper. We know that innovation is so important, but how do we encourage clinicians to innovate in this environment? Dr. Hahn, you served as chairman of CC Innovations, which is Cleveland Clinic’s technology commercialization arm. What were some of the strategies you came across in that role?
Dr. Hahn: We look for creative staff. We tell them up front that we want them to come to Cleveland Clinic and invent things. Our mission is literally to work on problems and take solutions to our patients. The culture here is meant to be creative. As a part of that culture, we welcome working with industry, as opposed to industry thrusting its innovations on us.
We are averaging more than 200 invention disclosures per year. More than 500 of our staff are involved with various industrial partners, and we are not going to hide that. In fact, we are going to make it public. The thought is that we owe it to our patients to work on their problems. At the same time, we owe it to our patients to say when we are working with industry on a particular product and explain to them why we think it would work in their case, if we think it would. While doing so, we need to make it clear that we will be happy to refer them for a second opinion if they would like. If I have a patient who wants a second opinion, I will offer to make the phone call for them and get them in. I think that is an advantage of the model we have here.
The reality is that there are some procedures that can only be done by one surgeon here, a surgeon who may have helped develop the procedure or some technology involved in it. Are we going to tell that surgeon that he or she cannot perform the procedure on anyone? That does not make sense. So you need to have a management plan that puts in place firewalls to protect the data on that procedure from any possible contamination.
So yes, we do reward staff who are doing innovation, and we do work with industry, and we do tell our patients we are doing it, and we do build firewalls to protect the data.
Dr. Lieberman: How about the rest of the panel? What are your thoughts on providing incentives for innovation?
Dr. Fins: Money is a key issue. The way the landscape is now structured, collaborations with industry are part of the mix. Under the Bayh-Dole Act of 1980, institutions are granted intellectual property rights to ideas or inventions developed by their researchers, and then the institutions can enter into contracts with industry to move the innovations forward. If industry support of research were removed, we would have to double the budget of the National Institutes of Health to compensate.
On the other hand, industry support can sometimes prove to be a disincentive to innovation in that it may engineer certain kinds of research or deprive investigators of tools they may need to do more basic science types of research. It is an academic freedom issue. At a translational level, industry may be helpful and catalytic. But sometimes it pushes an investigator to work for a short-term innovative application at the expense of a more speculative, riskier innovation.
We need to acknowledge that industry collaborations are part and parcel of the universe and focus on working with industry to moderate its influences. At the same time, we must use our leverage on the investigative side of the equation to pursue academic freedom and to leverage industry resources to perhaps pay for some of the care that innovative devices make possible. For example, contracting agreements could be drawn up so that money came back to the populations that participated in a clinical trial, or to a community that otherwise may need the device but cannot afford it. I think we have to create some type of charitable impulse to moderate the excesses of the profits and use them for the common good.
Dr. Herndon: I would like to touch on disclosure. The orthopedic implant industry has been required by law to disclose its relationships with orthopedic surgeons, including the amount of money that surgeons may be getting from industry. This requirement has had unintended consequences that underscore the importance of disclosure. First, some of the monetary awards, whether market-driven or not, are quite excessive. Second, reviewing the contracts for royalties has led to the discovery that many are not supported by patents or intellectual property rights. Third, these disclosures have revealed that certain surgeons who work at major US institutions, and who thus have an obligation to pay the institution some of the monies from their research, have not disclosed their relationships for years and have kept those monies solely for themselves. So this disclosure requirement has brought many things to light.
Dr. Rezai: As long as there is human disease and suffering, innovation will continue. It has in the past and it will in the future. Most innovators have it in their genes and in their blood. They can be taught to innovate, but they have to have the intrinsic curiosity and the creative mind to be an innovator. Institutional support of innovation is important, as is respect for the process that must be followed, including transparency and disclosure. If you put all these together, then innovation can be facilitated.
IF TESTING MOVES OFFSHORE, CAN ETHICS FOLLOW?
Dr. Lieberman: I am going to paint a scenario on which I would like each panelist to briefly comment. New Device X is backed by a big vendor. It is a great device, but because of all the regulatory issues in the United States, it is taken to China or South America and is being implanted there, where the regulatory environment is much more lenient. Can we rationalize this practice? How is it possibly ethical?
Dr. Fins: I can answer in 5 seconds: we shouldn’t do it.
Dr. Rezai: This is a reality we are facing with increasing rules and regulations in the United States. You have to engage the process, and it takes time. If you have colleagues who can follow clinical trials outside the United States, you can have the device tested outside and then bring it back to the United States. Unfortunately, the reality is that the regulatory process can be slow, so more testing will be done abroad, in my opinion.
Dr. Hahn: I disagree with Dr. Fins. This may be the only way to get the trials started, and we then are able to use some of the offshore data to approach the FDA for approval. I do not think that it is taking advantage of anybody; it is a way of getting things through the system.
Dr. Herndon: The door has been opened, and it is only going to increase. My only request would be that the investigators who do this function as they would here in the United States, under IRB controls and the other kinds of oversight that they would expect and demand of themselves in their own institutions.
- Schiff ND, Giacino JT, Kalmar K, et al. Behavioral improvements with thalamic stimulation after severe traumatic brain injury. Nature 2007; 448:600–603.
- Forte ML, Virnig BA, Kane RL, et al. Geographic variation in device use for intertrochanteric hip fractures. J Bone Joint Surg Am 2008; 90:691–699.
- Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery database. J Bone Joint Surg Am 2008; 90:700–707.
- Herndon JH. Technology assessment and adoption in orthopaedics [letter]. J Bone Joint Surg Am 2008; 90e. http://www.ejbjs.org/cgi/eletters/90/4/689. Published April 1, 2008. Accessed August 25, 2008.
- Fins JJ. Surgical innovation and ethical dilemmas: precautions and proximity. Cleve Clin J Med 2008; 75(suppl 6):S7–S12.
- Brody H. The Healer’s Power. New Haven, CT: Yale University Press; 1992.
- Schiff ND, Giacino JT, Kalmar K, et al. Behavioral improvements with thalamic stimulation after severe traumatic brain injury. Nature 2007; 448:600–603.
- Forte ML, Virnig BA, Kane RL, et al. Geographic variation in device use for intertrochanteric hip fractures. J Bone Joint Surg Am 2008; 90:691–699.
- Anglen JO, Weinstein JN. Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery database. J Bone Joint Surg Am 2008; 90:700–707.
- Herndon JH. Technology assessment and adoption in orthopaedics [letter]. J Bone Joint Surg Am 2008; 90e. http://www.ejbjs.org/cgi/eletters/90/4/689. Published April 1, 2008. Accessed August 25, 2008.
- Fins JJ. Surgical innovation and ethical dilemmas: precautions and proximity. Cleve Clin J Med 2008; 75(suppl 6):S7–S12.
- Brody H. The Healer’s Power. New Haven, CT: Yale University Press; 1992.