User login
Study Finds No Significant Effect of Low-Dose Oral Minoxidil on BP
TOPLINE:
but is associated with a slight increase in heart rate and a 5% incidence of hypotensive symptoms.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis of 16 studies, which involved 2387 patients with alopecia (60.7% women) who received minoxidil, a vasodilator originally developed as an antihypertensive, at doses of 5 mg or less per day.
- Outcomes included changes in mean arterial pressure, systolic BP, diastolic BP, and heart rate.
- Mean differences were calculated between pretreatment and posttreatment values.
TAKEAWAY:
- Hypotensive symptoms were reported in 5% patients, with no significant hypotensive episodes. About 1.8% patients experienced lightheadedness or syncope, 1.2% experienced dizziness, 0.9% had tachycardia, and 0.8% had palpitations.
- LDOM did not significantly alter systolic BP (mean difference, –0.13; 95% CI, –2.67 to 2.41), diastolic BP (mean difference, –1.25; 95% CI, –3.21 to 0.71), and mean arterial pressure (mean difference, –1.92; 95% CI, –4.00 to 0.17).
- LDOM led to a significant increase in heart rate (mean difference, 2.67 beats/min; 95% CI, 0.34-5.01), a difference the authors wrote would “likely not be clinically significant for most patients.”
- Hypertrichosis was the most common side effect (59.6%) and reason for stopping treatment (accounting for nearly 35% of discontinuations).
IN PRACTICE:
“LDOM appears to be a safe treatment for alopecia with no significant impact on blood pressure,” the authors wrote, noting that the study “addresses gaps in clinical knowledge involving LDOM.” Based on their results, they recommended that BP and heart rate “do not need to be closely monitored in patients without prior cardiovascular risk history.”
SOURCE:
The study was led by Matthew Chen, BS, Stony Brook Dermatology in New York. It was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The studies included had small sample sizes and retrospective designs, which may limit the reliability of the findings. Additional limitations include the absence of control groups, a potential recall bias in adverse effect reporting, and variability in dosing regimens and BP monitoring.
DISCLOSURES:
The authors reported no external funding or conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
but is associated with a slight increase in heart rate and a 5% incidence of hypotensive symptoms.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis of 16 studies, which involved 2387 patients with alopecia (60.7% women) who received minoxidil, a vasodilator originally developed as an antihypertensive, at doses of 5 mg or less per day.
- Outcomes included changes in mean arterial pressure, systolic BP, diastolic BP, and heart rate.
- Mean differences were calculated between pretreatment and posttreatment values.
TAKEAWAY:
- Hypotensive symptoms were reported in 5% patients, with no significant hypotensive episodes. About 1.8% patients experienced lightheadedness or syncope, 1.2% experienced dizziness, 0.9% had tachycardia, and 0.8% had palpitations.
- LDOM did not significantly alter systolic BP (mean difference, –0.13; 95% CI, –2.67 to 2.41), diastolic BP (mean difference, –1.25; 95% CI, –3.21 to 0.71), and mean arterial pressure (mean difference, –1.92; 95% CI, –4.00 to 0.17).
- LDOM led to a significant increase in heart rate (mean difference, 2.67 beats/min; 95% CI, 0.34-5.01), a difference the authors wrote would “likely not be clinically significant for most patients.”
- Hypertrichosis was the most common side effect (59.6%) and reason for stopping treatment (accounting for nearly 35% of discontinuations).
IN PRACTICE:
“LDOM appears to be a safe treatment for alopecia with no significant impact on blood pressure,” the authors wrote, noting that the study “addresses gaps in clinical knowledge involving LDOM.” Based on their results, they recommended that BP and heart rate “do not need to be closely monitored in patients without prior cardiovascular risk history.”
SOURCE:
The study was led by Matthew Chen, BS, Stony Brook Dermatology in New York. It was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The studies included had small sample sizes and retrospective designs, which may limit the reliability of the findings. Additional limitations include the absence of control groups, a potential recall bias in adverse effect reporting, and variability in dosing regimens and BP monitoring.
DISCLOSURES:
The authors reported no external funding or conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
but is associated with a slight increase in heart rate and a 5% incidence of hypotensive symptoms.
METHODOLOGY:
- Researchers conducted a systematic review and meta-analysis of 16 studies, which involved 2387 patients with alopecia (60.7% women) who received minoxidil, a vasodilator originally developed as an antihypertensive, at doses of 5 mg or less per day.
- Outcomes included changes in mean arterial pressure, systolic BP, diastolic BP, and heart rate.
- Mean differences were calculated between pretreatment and posttreatment values.
TAKEAWAY:
- Hypotensive symptoms were reported in 5% patients, with no significant hypotensive episodes. About 1.8% patients experienced lightheadedness or syncope, 1.2% experienced dizziness, 0.9% had tachycardia, and 0.8% had palpitations.
- LDOM did not significantly alter systolic BP (mean difference, –0.13; 95% CI, –2.67 to 2.41), diastolic BP (mean difference, –1.25; 95% CI, –3.21 to 0.71), and mean arterial pressure (mean difference, –1.92; 95% CI, –4.00 to 0.17).
- LDOM led to a significant increase in heart rate (mean difference, 2.67 beats/min; 95% CI, 0.34-5.01), a difference the authors wrote would “likely not be clinically significant for most patients.”
- Hypertrichosis was the most common side effect (59.6%) and reason for stopping treatment (accounting for nearly 35% of discontinuations).
IN PRACTICE:
“LDOM appears to be a safe treatment for alopecia with no significant impact on blood pressure,” the authors wrote, noting that the study “addresses gaps in clinical knowledge involving LDOM.” Based on their results, they recommended that BP and heart rate “do not need to be closely monitored in patients without prior cardiovascular risk history.”
SOURCE:
The study was led by Matthew Chen, BS, Stony Brook Dermatology in New York. It was published online in The Journal of the American Academy of Dermatology.
LIMITATIONS:
The studies included had small sample sizes and retrospective designs, which may limit the reliability of the findings. Additional limitations include the absence of control groups, a potential recall bias in adverse effect reporting, and variability in dosing regimens and BP monitoring.
DISCLOSURES:
The authors reported no external funding or conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Is Acute Kidney Injury Really a Single Disease?
The search for a better biomarker than creatine for acute kidney injury (AKI) has been “long and elusive.” However, could researchers be on the right path now?
“The thinking is moving away from trying to find one biomarker that can be used for different types of kidney injury to a recognition that AKI is not just a single disease that a patient has or doesn’t have,” Rob D. Nerenz, PhD, an associate professor in the Department of Pathology and Laboratory Medicine at the Medical College of Wisconsin, Milwaukee, told this news organization. “It’s lots of different diseases that all affect the kidney in different ways.”
AKI is actually a “loose collection” of hepatorenal, cardiorenal, nephrotoxic, and sepsis-associated syndromes, as well as acute interstitial nephritis (AIN), he said. “So the question is not: ‘Is AKI present — yes or no?’ It’s: ‘What kind of AKI is present, and how do I treat it?’ ”
‘Mediocre Markers’
AKI affects about 10%-30% of hospitalized patients, according to Nerenz. It’s associated with an increased risk for adverse outcomes, including post-AKI chronic kidney disease and a mortality rate of approximately 24%.
Currently, AKI is defined by a rapid increase in serum creatinine, a decrease in urine output, or both.
“Those are mediocre markers,” Nerenz said, as serum creatinine is not very sensitive to acute change, and the increase is often detected after the therapeutic window of intervention has passed. In addition, “it only tells us that the kidneys are unhappy; it doesn’t say anything about the cause.”
Urine output is limited as a marker because many conditions affect it. “If you’re dehydrated, urine output is going to decrease,” he said. “And in some forms of AKI, urine output actually goes up.”
What’s needed, he said, is a more sensitive biomarker that’s detectable within a shorter timeframe of 2-6 hours following injury.
“Right now, we’re looking at 48 hours before a change becomes apparent, and that’s just too long. Plus, it should be kidney specific. One of the major limitations of the biomarkers that have been evaluated to this point is that, yes, they’re released by the kidney, but they’re also released by other tissue types within the body, and that hinders their effectiveness as a marker.”
Neutrophil Gelatinase-Associated Lipocalin (NGAL)
Although research on better biomarkers is ongoing, “there’s also a recognition that some of the protein markers that have been around for a while, if used appropriately, can provide value,” Nerenz said. These include, among others, NGAL.
NGAL works well in pediatric patients without other comorbidities, but it has been less useful in adult patients because it is also released by other cell types. However, recent research suggests it shows promise in patients with both cirrhosis and AKI.
There are three main causes of AKI in cirrhosis, Nerenz explained. The first is prerenal and can be primarily addressed through rehydration.
“When these patients come in, clinicians won’t do anything right away other than provide fluids. If creatinine improves over the 48-hour period of fluid replenishment, then the patient is sent home because there really isn’t extensive damage to the kidneys.”
If improvement isn’t seen after those 48 hours, then it could be one of two things: Hepatorenal syndrome or acute tubular necrosis. Patients with hepatorenal syndrome are candidates for terlipressin, which the Food and Drug Administration (FDA) approved for this indication in 2022 after it displayed notable efficacy in a double-blind study.
“You don’t want to give terlipressin to just anybody because if the issue is not a diminished blood supply to the kidney, it’s not going to help, and comes with some serious side effects, such as respiratory failure,” Nerenz explained. “Having a biomarker that can distinguish between hepatorenal syndrome and acute tubular necrosis really helps clinicians confidently identify which patients are good candidates for this drug. Right now, we’re flying blind to a certain extent, basically using clinical intuition.”
Currently, the determination of NGAL is FDA cleared only for pediatric use. One way hospitals have dealt with that is by making the test in their own labs, using appropriate reagents, validation, and so forth. These tests are then safe for use in adults but haven’t gone through the FDA approval process.
However, the FDA’s recent announcement stating that the agency should oversee lab-developed tests has made this situation unclear, Nerenz said.
“At this point, we don’t know if there’s still an opportunity to take the NGAL test (or any other cleared biomarker) and validate it for use in a different patient population. Many hospital labs simply don’t have the resources to take these tests through the whole FDA approval process.”
A New Biomarker for AIN?
Meanwhile, research is also moving forward on a better biomarker for AIN, which is also under the AKI umbrella.
“It’s important to diagnose AIN because it has a very specific treatment,” Dennis G. Moledina, MD, PhD, Yale School of Medicine in New Haven, Connecticut, told this news organization.
“AIN is caused by a bunch of different medications, such as proton pump inhibitors, cancer drugs, nonsteroidal anti-inflammatory drugs, and antibiotics, so when someone has this condition, you have to stop potentially life-saving medications and give unnecessary and potentially toxic immunosuppressive drugs, like prednisone,” he said. “If you get the diagnosis wrong, you’re stopping vital drugs and giving immunosuppression for no reason. And if you miss the diagnosis, AIN can lead to permanent chronic kidney disease.”
“Right now, the only way to diagnose AIN is to do a kidney biopsy, which is risky because it can often lead to significant bleeding,” he said. “Some people can’t undergo a biopsy because they’re on medications that increase the risk of bleeding, and they can’t be stopped.”
Furthermore, he noted, “the longer a patient takes a drug that’s causing AIN without getting a diagnosis, the less the chances of recovery because the longer you let this kidney inflammation go on, the more fibrosis and permanent damage develops. So it is important to diagnose it as early as possible, and that’s again why we have a real need for a noninvasive biomarker that can be tested rapidly.”
Moledina and colleagues have been working on identifying a suitable biomarker for close to 10 years, the latest example of which is their 2023 study validating urinary CXCL9 as just such a marker.
“We’re most excited about CXCL9 because it’s already used to diagnose some other diseases in plasma,” Moledina said. “We think that we can convince labs to test it in urine.”
In an accompanying editorial, Mark Canney, PhD, and colleagues at the University of Ottawa and The Ottawa Hospital in Ontario, Canada, wrote that the CXCL9 study findings “are exciting because they provide a road map of where diagnostics can get to for this common, yet poorly identified and treated, cause of kidney damage. The need for a different approach can be readily identified from the fact that clinicians’ gestalt for diagnosing AIN was almost tantamount to tossing a coin (AUC, 0.57). CXCL9 alone outperformed not only the clinician’s prebiopsy suspicion but also an existing diagnostic model and other candidate biomarkers both in the discovery and external validation cohorts.”
Like NGAL, CXCL9 will have to go through the FDA approval process before it can be used for AIN. Therefore, it may be a few years before it can become routinely available, Moledina said.
Nevertheless, Nerenz added, “I think the next steps for AKI are probably continuing on this path of context-dependent, selective biomarker use. I anticipate that we’ll see ongoing development in this space, just expanding to a wider variety of clinical scenarios.”
Nerenz declared receiving research funding from Abbott Labs for evaluation of an AKI biomarker. Moledina is a co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis”; a cofounder of the diagnostics company Predict AIN; and a consultant for Biohaven.
A version of this article first appeared on Medscape.com.
The search for a better biomarker than creatine for acute kidney injury (AKI) has been “long and elusive.” However, could researchers be on the right path now?
“The thinking is moving away from trying to find one biomarker that can be used for different types of kidney injury to a recognition that AKI is not just a single disease that a patient has or doesn’t have,” Rob D. Nerenz, PhD, an associate professor in the Department of Pathology and Laboratory Medicine at the Medical College of Wisconsin, Milwaukee, told this news organization. “It’s lots of different diseases that all affect the kidney in different ways.”
AKI is actually a “loose collection” of hepatorenal, cardiorenal, nephrotoxic, and sepsis-associated syndromes, as well as acute interstitial nephritis (AIN), he said. “So the question is not: ‘Is AKI present — yes or no?’ It’s: ‘What kind of AKI is present, and how do I treat it?’ ”
‘Mediocre Markers’
AKI affects about 10%-30% of hospitalized patients, according to Nerenz. It’s associated with an increased risk for adverse outcomes, including post-AKI chronic kidney disease and a mortality rate of approximately 24%.
Currently, AKI is defined by a rapid increase in serum creatinine, a decrease in urine output, or both.
“Those are mediocre markers,” Nerenz said, as serum creatinine is not very sensitive to acute change, and the increase is often detected after the therapeutic window of intervention has passed. In addition, “it only tells us that the kidneys are unhappy; it doesn’t say anything about the cause.”
Urine output is limited as a marker because many conditions affect it. “If you’re dehydrated, urine output is going to decrease,” he said. “And in some forms of AKI, urine output actually goes up.”
What’s needed, he said, is a more sensitive biomarker that’s detectable within a shorter timeframe of 2-6 hours following injury.
“Right now, we’re looking at 48 hours before a change becomes apparent, and that’s just too long. Plus, it should be kidney specific. One of the major limitations of the biomarkers that have been evaluated to this point is that, yes, they’re released by the kidney, but they’re also released by other tissue types within the body, and that hinders their effectiveness as a marker.”
Neutrophil Gelatinase-Associated Lipocalin (NGAL)
Although research on better biomarkers is ongoing, “there’s also a recognition that some of the protein markers that have been around for a while, if used appropriately, can provide value,” Nerenz said. These include, among others, NGAL.
NGAL works well in pediatric patients without other comorbidities, but it has been less useful in adult patients because it is also released by other cell types. However, recent research suggests it shows promise in patients with both cirrhosis and AKI.
There are three main causes of AKI in cirrhosis, Nerenz explained. The first is prerenal and can be primarily addressed through rehydration.
“When these patients come in, clinicians won’t do anything right away other than provide fluids. If creatinine improves over the 48-hour period of fluid replenishment, then the patient is sent home because there really isn’t extensive damage to the kidneys.”
If improvement isn’t seen after those 48 hours, then it could be one of two things: Hepatorenal syndrome or acute tubular necrosis. Patients with hepatorenal syndrome are candidates for terlipressin, which the Food and Drug Administration (FDA) approved for this indication in 2022 after it displayed notable efficacy in a double-blind study.
“You don’t want to give terlipressin to just anybody because if the issue is not a diminished blood supply to the kidney, it’s not going to help, and comes with some serious side effects, such as respiratory failure,” Nerenz explained. “Having a biomarker that can distinguish between hepatorenal syndrome and acute tubular necrosis really helps clinicians confidently identify which patients are good candidates for this drug. Right now, we’re flying blind to a certain extent, basically using clinical intuition.”
Currently, the determination of NGAL is FDA cleared only for pediatric use. One way hospitals have dealt with that is by making the test in their own labs, using appropriate reagents, validation, and so forth. These tests are then safe for use in adults but haven’t gone through the FDA approval process.
However, the FDA’s recent announcement stating that the agency should oversee lab-developed tests has made this situation unclear, Nerenz said.
“At this point, we don’t know if there’s still an opportunity to take the NGAL test (or any other cleared biomarker) and validate it for use in a different patient population. Many hospital labs simply don’t have the resources to take these tests through the whole FDA approval process.”
A New Biomarker for AIN?
Meanwhile, research is also moving forward on a better biomarker for AIN, which is also under the AKI umbrella.
“It’s important to diagnose AIN because it has a very specific treatment,” Dennis G. Moledina, MD, PhD, Yale School of Medicine in New Haven, Connecticut, told this news organization.
“AIN is caused by a bunch of different medications, such as proton pump inhibitors, cancer drugs, nonsteroidal anti-inflammatory drugs, and antibiotics, so when someone has this condition, you have to stop potentially life-saving medications and give unnecessary and potentially toxic immunosuppressive drugs, like prednisone,” he said. “If you get the diagnosis wrong, you’re stopping vital drugs and giving immunosuppression for no reason. And if you miss the diagnosis, AIN can lead to permanent chronic kidney disease.”
“Right now, the only way to diagnose AIN is to do a kidney biopsy, which is risky because it can often lead to significant bleeding,” he said. “Some people can’t undergo a biopsy because they’re on medications that increase the risk of bleeding, and they can’t be stopped.”
Furthermore, he noted, “the longer a patient takes a drug that’s causing AIN without getting a diagnosis, the less the chances of recovery because the longer you let this kidney inflammation go on, the more fibrosis and permanent damage develops. So it is important to diagnose it as early as possible, and that’s again why we have a real need for a noninvasive biomarker that can be tested rapidly.”
Moledina and colleagues have been working on identifying a suitable biomarker for close to 10 years, the latest example of which is their 2023 study validating urinary CXCL9 as just such a marker.
“We’re most excited about CXCL9 because it’s already used to diagnose some other diseases in plasma,” Moledina said. “We think that we can convince labs to test it in urine.”
In an accompanying editorial, Mark Canney, PhD, and colleagues at the University of Ottawa and The Ottawa Hospital in Ontario, Canada, wrote that the CXCL9 study findings “are exciting because they provide a road map of where diagnostics can get to for this common, yet poorly identified and treated, cause of kidney damage. The need for a different approach can be readily identified from the fact that clinicians’ gestalt for diagnosing AIN was almost tantamount to tossing a coin (AUC, 0.57). CXCL9 alone outperformed not only the clinician’s prebiopsy suspicion but also an existing diagnostic model and other candidate biomarkers both in the discovery and external validation cohorts.”
Like NGAL, CXCL9 will have to go through the FDA approval process before it can be used for AIN. Therefore, it may be a few years before it can become routinely available, Moledina said.
Nevertheless, Nerenz added, “I think the next steps for AKI are probably continuing on this path of context-dependent, selective biomarker use. I anticipate that we’ll see ongoing development in this space, just expanding to a wider variety of clinical scenarios.”
Nerenz declared receiving research funding from Abbott Labs for evaluation of an AKI biomarker. Moledina is a co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis”; a cofounder of the diagnostics company Predict AIN; and a consultant for Biohaven.
A version of this article first appeared on Medscape.com.
The search for a better biomarker than creatine for acute kidney injury (AKI) has been “long and elusive.” However, could researchers be on the right path now?
“The thinking is moving away from trying to find one biomarker that can be used for different types of kidney injury to a recognition that AKI is not just a single disease that a patient has or doesn’t have,” Rob D. Nerenz, PhD, an associate professor in the Department of Pathology and Laboratory Medicine at the Medical College of Wisconsin, Milwaukee, told this news organization. “It’s lots of different diseases that all affect the kidney in different ways.”
AKI is actually a “loose collection” of hepatorenal, cardiorenal, nephrotoxic, and sepsis-associated syndromes, as well as acute interstitial nephritis (AIN), he said. “So the question is not: ‘Is AKI present — yes or no?’ It’s: ‘What kind of AKI is present, and how do I treat it?’ ”
‘Mediocre Markers’
AKI affects about 10%-30% of hospitalized patients, according to Nerenz. It’s associated with an increased risk for adverse outcomes, including post-AKI chronic kidney disease and a mortality rate of approximately 24%.
Currently, AKI is defined by a rapid increase in serum creatinine, a decrease in urine output, or both.
“Those are mediocre markers,” Nerenz said, as serum creatinine is not very sensitive to acute change, and the increase is often detected after the therapeutic window of intervention has passed. In addition, “it only tells us that the kidneys are unhappy; it doesn’t say anything about the cause.”
Urine output is limited as a marker because many conditions affect it. “If you’re dehydrated, urine output is going to decrease,” he said. “And in some forms of AKI, urine output actually goes up.”
What’s needed, he said, is a more sensitive biomarker that’s detectable within a shorter timeframe of 2-6 hours following injury.
“Right now, we’re looking at 48 hours before a change becomes apparent, and that’s just too long. Plus, it should be kidney specific. One of the major limitations of the biomarkers that have been evaluated to this point is that, yes, they’re released by the kidney, but they’re also released by other tissue types within the body, and that hinders their effectiveness as a marker.”
Neutrophil Gelatinase-Associated Lipocalin (NGAL)
Although research on better biomarkers is ongoing, “there’s also a recognition that some of the protein markers that have been around for a while, if used appropriately, can provide value,” Nerenz said. These include, among others, NGAL.
NGAL works well in pediatric patients without other comorbidities, but it has been less useful in adult patients because it is also released by other cell types. However, recent research suggests it shows promise in patients with both cirrhosis and AKI.
There are three main causes of AKI in cirrhosis, Nerenz explained. The first is prerenal and can be primarily addressed through rehydration.
“When these patients come in, clinicians won’t do anything right away other than provide fluids. If creatinine improves over the 48-hour period of fluid replenishment, then the patient is sent home because there really isn’t extensive damage to the kidneys.”
If improvement isn’t seen after those 48 hours, then it could be one of two things: Hepatorenal syndrome or acute tubular necrosis. Patients with hepatorenal syndrome are candidates for terlipressin, which the Food and Drug Administration (FDA) approved for this indication in 2022 after it displayed notable efficacy in a double-blind study.
“You don’t want to give terlipressin to just anybody because if the issue is not a diminished blood supply to the kidney, it’s not going to help, and comes with some serious side effects, such as respiratory failure,” Nerenz explained. “Having a biomarker that can distinguish between hepatorenal syndrome and acute tubular necrosis really helps clinicians confidently identify which patients are good candidates for this drug. Right now, we’re flying blind to a certain extent, basically using clinical intuition.”
Currently, the determination of NGAL is FDA cleared only for pediatric use. One way hospitals have dealt with that is by making the test in their own labs, using appropriate reagents, validation, and so forth. These tests are then safe for use in adults but haven’t gone through the FDA approval process.
However, the FDA’s recent announcement stating that the agency should oversee lab-developed tests has made this situation unclear, Nerenz said.
“At this point, we don’t know if there’s still an opportunity to take the NGAL test (or any other cleared biomarker) and validate it for use in a different patient population. Many hospital labs simply don’t have the resources to take these tests through the whole FDA approval process.”
A New Biomarker for AIN?
Meanwhile, research is also moving forward on a better biomarker for AIN, which is also under the AKI umbrella.
“It’s important to diagnose AIN because it has a very specific treatment,” Dennis G. Moledina, MD, PhD, Yale School of Medicine in New Haven, Connecticut, told this news organization.
“AIN is caused by a bunch of different medications, such as proton pump inhibitors, cancer drugs, nonsteroidal anti-inflammatory drugs, and antibiotics, so when someone has this condition, you have to stop potentially life-saving medications and give unnecessary and potentially toxic immunosuppressive drugs, like prednisone,” he said. “If you get the diagnosis wrong, you’re stopping vital drugs and giving immunosuppression for no reason. And if you miss the diagnosis, AIN can lead to permanent chronic kidney disease.”
“Right now, the only way to diagnose AIN is to do a kidney biopsy, which is risky because it can often lead to significant bleeding,” he said. “Some people can’t undergo a biopsy because they’re on medications that increase the risk of bleeding, and they can’t be stopped.”
Furthermore, he noted, “the longer a patient takes a drug that’s causing AIN without getting a diagnosis, the less the chances of recovery because the longer you let this kidney inflammation go on, the more fibrosis and permanent damage develops. So it is important to diagnose it as early as possible, and that’s again why we have a real need for a noninvasive biomarker that can be tested rapidly.”
Moledina and colleagues have been working on identifying a suitable biomarker for close to 10 years, the latest example of which is their 2023 study validating urinary CXCL9 as just such a marker.
“We’re most excited about CXCL9 because it’s already used to diagnose some other diseases in plasma,” Moledina said. “We think that we can convince labs to test it in urine.”
In an accompanying editorial, Mark Canney, PhD, and colleagues at the University of Ottawa and The Ottawa Hospital in Ontario, Canada, wrote that the CXCL9 study findings “are exciting because they provide a road map of where diagnostics can get to for this common, yet poorly identified and treated, cause of kidney damage. The need for a different approach can be readily identified from the fact that clinicians’ gestalt for diagnosing AIN was almost tantamount to tossing a coin (AUC, 0.57). CXCL9 alone outperformed not only the clinician’s prebiopsy suspicion but also an existing diagnostic model and other candidate biomarkers both in the discovery and external validation cohorts.”
Like NGAL, CXCL9 will have to go through the FDA approval process before it can be used for AIN. Therefore, it may be a few years before it can become routinely available, Moledina said.
Nevertheless, Nerenz added, “I think the next steps for AKI are probably continuing on this path of context-dependent, selective biomarker use. I anticipate that we’ll see ongoing development in this space, just expanding to a wider variety of clinical scenarios.”
Nerenz declared receiving research funding from Abbott Labs for evaluation of an AKI biomarker. Moledina is a co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis”; a cofounder of the diagnostics company Predict AIN; and a consultant for Biohaven.
A version of this article first appeared on Medscape.com.
Endometriosis Raises Rates of Postpartum Depression, Other Disorders
Women with endometriosis have a much higher risk of being diagnosed with several psychiatric disorders during the postpartum period according to an oral abstract presented at the American Society for Reproductive Medicine’s 2024 Scientific Congress and Expo in Denver, Colorado.
Researchers compared rates of postpartum depression, anxiety, mood disturbance (temporary low or anxious mood requiring no treatment), and obsessive-compulsive disorder (OCD) diagnoses among over 200 million adult women from 67 healthcare organizations who had a child between 2005 and 2023.
Within a year after giving birth, women with prepregnancy endometriosis were 25% more likely to be diagnosed with postpartum depression, 85% more likely to be diagnosed with postpartum mood disturbance, 44% more likely to be diagnosed with anxiety, and 1.26 times more likely to be diagnosed with OCD.
About 75% of women studied had no preexisting depression. This population had a 17% higher risk of receiving a postpartum depression diagnosis, a 95% higher risk of receiving an OCD diagnosis, a 72% higher risk of receiving a postpartum mood disturbance diagnosis, and a 38% risk of receiving an anxiety diagnosis.
Among women without preexisting depression, the risk increased by 64% for OCD, 42% for postpartum mood disturbance, and 25% for anxiety, while the risk for postpartum depression was negligible, indicating that women already experiencing depression likely have a higher baseline risk for worsening symptoms postpartum, said the study’s lead author Tina Yi-Jin Hsieh, MD, MPH, biomedical researcher at Harvard Medical School in Boston, Massachusetts.
“We think that because preexisting depression is the more dominant risk factor, it doesn’t really matter if you have another additional risk factor like endometriosis to really change the risk of postpartum depression,” said Hsieh.
Endometriosis is a debilitating condition in which tissue similar to uterine lining grows on the outside of the uterus, causing chronic pain and infertility. It affects between 6% and 10% of women worldwide and takes an average of between 4 and 11 years to be diagnosed. It has been linked to depression and anxiety disorders, yet the study authors say there’s little research examining its impact on women in the year after giving birth.
“Endometriosis is a complex condition that can affect both physical and mental health over much of a person’s life,” said Anna Modest, PhD, assistant professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School and a study author. “Perinatal and maternal mental health can have a huge impact on children and their family — we need to better understand who is at risk for challenges in the postpartum period.”
“Most chronic medical illnesses, particularly those causing pain, have been shown to increase the risk of mood disorders,” said Ripal Shah, MD, MPH, clinical associate professor of Psychiatry and Behavioral Sciences at Stanford Medicine in California. Shah specializes in reproductive psychiatry and was not associated with the study.
“What’s interesting about endometriosis though is that genome-wide association studies have shown that there may be a genetic predisposition for some women to develop both endometriosis and a mood disorder,” said Shah.
A 2023 study suggested that endometriosis, anxiety, and depression may be connected through a shared genetic basis.
But the experience patients with endometriosis go through also lends itself to the development of mood disorders, said Daniel Ginn, DO, assistant clinical professor of Obstetrics and Gynecology at the David Geffen School of Medicine at the University of California, Los Angeles. Ginn specializes in the treatment of endometriosis and was not a part of the study.
Beyond postpartum depression, Ginn wasn’t surprised by the association of endometriosis with anxiety or OCD because what he hears from patients “on a daily basis is the telling of a history that has been hallmarked by not being listened to, not being believed, and not having symptoms managed well.”
As a result, he said many patients focus heavily on learning about their condition, coming into office visits with binders full of test results and information in an effort to understand and manage it themselves. This “does lead to a certain sense of a need to grasp for control because no one else is helping them [treat their condition effectively].”
He added: “I find it hard to believe that anxiety and OCD were preexisting of the conditions rather than the consequence of a long-term suboptimally managed disease.”
The authors reported no disclosures or sources of funding.
A version of this article first appeared on Medscape.com.
Women with endometriosis have a much higher risk of being diagnosed with several psychiatric disorders during the postpartum period according to an oral abstract presented at the American Society for Reproductive Medicine’s 2024 Scientific Congress and Expo in Denver, Colorado.
Researchers compared rates of postpartum depression, anxiety, mood disturbance (temporary low or anxious mood requiring no treatment), and obsessive-compulsive disorder (OCD) diagnoses among over 200 million adult women from 67 healthcare organizations who had a child between 2005 and 2023.
Within a year after giving birth, women with prepregnancy endometriosis were 25% more likely to be diagnosed with postpartum depression, 85% more likely to be diagnosed with postpartum mood disturbance, 44% more likely to be diagnosed with anxiety, and 1.26 times more likely to be diagnosed with OCD.
About 75% of women studied had no preexisting depression. This population had a 17% higher risk of receiving a postpartum depression diagnosis, a 95% higher risk of receiving an OCD diagnosis, a 72% higher risk of receiving a postpartum mood disturbance diagnosis, and a 38% risk of receiving an anxiety diagnosis.
Among women without preexisting depression, the risk increased by 64% for OCD, 42% for postpartum mood disturbance, and 25% for anxiety, while the risk for postpartum depression was negligible, indicating that women already experiencing depression likely have a higher baseline risk for worsening symptoms postpartum, said the study’s lead author Tina Yi-Jin Hsieh, MD, MPH, biomedical researcher at Harvard Medical School in Boston, Massachusetts.
“We think that because preexisting depression is the more dominant risk factor, it doesn’t really matter if you have another additional risk factor like endometriosis to really change the risk of postpartum depression,” said Hsieh.
Endometriosis is a debilitating condition in which tissue similar to uterine lining grows on the outside of the uterus, causing chronic pain and infertility. It affects between 6% and 10% of women worldwide and takes an average of between 4 and 11 years to be diagnosed. It has been linked to depression and anxiety disorders, yet the study authors say there’s little research examining its impact on women in the year after giving birth.
“Endometriosis is a complex condition that can affect both physical and mental health over much of a person’s life,” said Anna Modest, PhD, assistant professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School and a study author. “Perinatal and maternal mental health can have a huge impact on children and their family — we need to better understand who is at risk for challenges in the postpartum period.”
“Most chronic medical illnesses, particularly those causing pain, have been shown to increase the risk of mood disorders,” said Ripal Shah, MD, MPH, clinical associate professor of Psychiatry and Behavioral Sciences at Stanford Medicine in California. Shah specializes in reproductive psychiatry and was not associated with the study.
“What’s interesting about endometriosis though is that genome-wide association studies have shown that there may be a genetic predisposition for some women to develop both endometriosis and a mood disorder,” said Shah.
A 2023 study suggested that endometriosis, anxiety, and depression may be connected through a shared genetic basis.
But the experience patients with endometriosis go through also lends itself to the development of mood disorders, said Daniel Ginn, DO, assistant clinical professor of Obstetrics and Gynecology at the David Geffen School of Medicine at the University of California, Los Angeles. Ginn specializes in the treatment of endometriosis and was not a part of the study.
Beyond postpartum depression, Ginn wasn’t surprised by the association of endometriosis with anxiety or OCD because what he hears from patients “on a daily basis is the telling of a history that has been hallmarked by not being listened to, not being believed, and not having symptoms managed well.”
As a result, he said many patients focus heavily on learning about their condition, coming into office visits with binders full of test results and information in an effort to understand and manage it themselves. This “does lead to a certain sense of a need to grasp for control because no one else is helping them [treat their condition effectively].”
He added: “I find it hard to believe that anxiety and OCD were preexisting of the conditions rather than the consequence of a long-term suboptimally managed disease.”
The authors reported no disclosures or sources of funding.
A version of this article first appeared on Medscape.com.
Women with endometriosis have a much higher risk of being diagnosed with several psychiatric disorders during the postpartum period according to an oral abstract presented at the American Society for Reproductive Medicine’s 2024 Scientific Congress and Expo in Denver, Colorado.
Researchers compared rates of postpartum depression, anxiety, mood disturbance (temporary low or anxious mood requiring no treatment), and obsessive-compulsive disorder (OCD) diagnoses among over 200 million adult women from 67 healthcare organizations who had a child between 2005 and 2023.
Within a year after giving birth, women with prepregnancy endometriosis were 25% more likely to be diagnosed with postpartum depression, 85% more likely to be diagnosed with postpartum mood disturbance, 44% more likely to be diagnosed with anxiety, and 1.26 times more likely to be diagnosed with OCD.
About 75% of women studied had no preexisting depression. This population had a 17% higher risk of receiving a postpartum depression diagnosis, a 95% higher risk of receiving an OCD diagnosis, a 72% higher risk of receiving a postpartum mood disturbance diagnosis, and a 38% risk of receiving an anxiety diagnosis.
Among women without preexisting depression, the risk increased by 64% for OCD, 42% for postpartum mood disturbance, and 25% for anxiety, while the risk for postpartum depression was negligible, indicating that women already experiencing depression likely have a higher baseline risk for worsening symptoms postpartum, said the study’s lead author Tina Yi-Jin Hsieh, MD, MPH, biomedical researcher at Harvard Medical School in Boston, Massachusetts.
“We think that because preexisting depression is the more dominant risk factor, it doesn’t really matter if you have another additional risk factor like endometriosis to really change the risk of postpartum depression,” said Hsieh.
Endometriosis is a debilitating condition in which tissue similar to uterine lining grows on the outside of the uterus, causing chronic pain and infertility. It affects between 6% and 10% of women worldwide and takes an average of between 4 and 11 years to be diagnosed. It has been linked to depression and anxiety disorders, yet the study authors say there’s little research examining its impact on women in the year after giving birth.
“Endometriosis is a complex condition that can affect both physical and mental health over much of a person’s life,” said Anna Modest, PhD, assistant professor of Obstetrics, Gynecology, and Reproductive Biology at Harvard Medical School and a study author. “Perinatal and maternal mental health can have a huge impact on children and their family — we need to better understand who is at risk for challenges in the postpartum period.”
“Most chronic medical illnesses, particularly those causing pain, have been shown to increase the risk of mood disorders,” said Ripal Shah, MD, MPH, clinical associate professor of Psychiatry and Behavioral Sciences at Stanford Medicine in California. Shah specializes in reproductive psychiatry and was not associated with the study.
“What’s interesting about endometriosis though is that genome-wide association studies have shown that there may be a genetic predisposition for some women to develop both endometriosis and a mood disorder,” said Shah.
A 2023 study suggested that endometriosis, anxiety, and depression may be connected through a shared genetic basis.
But the experience patients with endometriosis go through also lends itself to the development of mood disorders, said Daniel Ginn, DO, assistant clinical professor of Obstetrics and Gynecology at the David Geffen School of Medicine at the University of California, Los Angeles. Ginn specializes in the treatment of endometriosis and was not a part of the study.
Beyond postpartum depression, Ginn wasn’t surprised by the association of endometriosis with anxiety or OCD because what he hears from patients “on a daily basis is the telling of a history that has been hallmarked by not being listened to, not being believed, and not having symptoms managed well.”
As a result, he said many patients focus heavily on learning about their condition, coming into office visits with binders full of test results and information in an effort to understand and manage it themselves. This “does lead to a certain sense of a need to grasp for control because no one else is helping them [treat their condition effectively].”
He added: “I find it hard to believe that anxiety and OCD were preexisting of the conditions rather than the consequence of a long-term suboptimally managed disease.”
The authors reported no disclosures or sources of funding.
A version of this article first appeared on Medscape.com.
FROM ASRM 2024
Fibroids: Medical Therapy Not Hysterectomy Should Be First Treatment Choice Interventional Options Case Study
Although hysterectomy remains the most common procedure for treating fibroids and fibroids are the leading indication for hysterectomy, its long-term sequelae make less invasive alternatives the better choice for managing most of these myometrial masses, an invited clinical practice paper in the New England Journal of Medicine (NEJM) asserts.
The practice summary also calls for earlier identification and treatment of fibroid disease and may raise awareness among general gynecologists and primary care physicians less familiar with newer treatments.
Based on a review of evidence and existing formal guidelines, the paper urges wider use of uterus-sparing approaches such as hormone therapy, uterine-artery embolization, focused ultrasound ablation, and radiofrequency ablation. Authored by ob.gyns. Elizabeth A. Stewart, MD, and Shannon K. Laughlin-Tommaso, MD, MPH, of the Mayo Clinic in Rochester, Minnesota, the document also features textbook-style diagrams illustrating procedures.
“To clarify, this is not a new guidance but an invited clinical practice paper,” Laughlin-Tommaso told this news organization. “I believe NEJM recognized the gap in knowledge among all providers, for early diagnosis of uterine fibroids, especially in young patients and those presenting with anemia.”
The less invasive treatments highlighted in the paper can help women recover faster and resume their normal activities more quickly, said Laughlin-Tommaso. “Additionally, many studies have now shown that there are health benefits to keeping the uterus and the ovaries.”
Despite multiple uterine-sparing options, however, a recent study in a commercially insured population found nearly 60% of fibroid patients undergoing hysterectomy had never received a prior conservative treatment.
Why hysterectomy for a benign condition? Hysterectomy, which is universally available in ob.gyn. practices, makes decision-making easier for medical providers and patients, Laughlin-Tommaso explained. “It’s the only treatment that is definitive in that patients will not have bleeding or fibroids in the future and providers don’t have to determine which fibroids to treat or remove.”
More common in Black women, fibroids affect up to 80% of persons with a uterus during their lifetime and up to 50% have symptoms such as heavy and prolonged menstrual bleeding, anemia-associated fatigue, pelvic pressure, and menstrual and nonmenstrual pain, the authors noted. These lesions can also compress nearby structures causing painful intercourse, constipation, and urinary frequency, urgency, or retention.
In 2021 the American College of Obstetricians and Gynecologists issued a practice bulletin on the management of symptomatic uterine leiomyomas, similarly endorsing individualized care that accounts for the desire to preserve fertility or the uterus, increase quality of life, and reduce symptoms. It, too, recommended medical management as first-line treatment for symptomatic fibroids.
“This paper will be helpful for clinicians by covering some of the newer options such as gonadotropin-releasing hormone antagonists introduced in the past 5 years and tailoring treatment to patients depending on whether they still want to conceive,” Sandra M. Hurtado, MD, an ob.gyn. and an assistant professor at UTHealth Houston Medical Center and McGovern Medical School in Houston, Texas, said in an interview. “And the illustrations will be useful to doctors who are not gynecologists and will help to explain the interventional options to patients,” added Hurtado, who was not involved in the paper.
Offering another outside perspective on the paper, Charles J. Ascher-Walsh, MD, senior system vice chair for gynecology and division director of urogynecology in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology and Reproductive Science at Mount Sinai in New York City, called it a useful though not new summary. Reaching the wider audience of NEJM may raise awareness of newer fibroid therapies among general, nonspecialist ob.gyns., whose practices may concentrate largely on obstetrics, he added, “and the excellent illustrations clarify the treatment options.” In his view, broader awareness may increase much-needed funding for this neglected area of research.
Among the paper’s recommendations:
Diagnosis
Pelvic ultrasonography is the most cost-effective imaging method, providing information on size, location, and number of fibroids and ruling out adnexal masses. It is limited, however, by less-accurate resolution if the uterine volume is greater than 375 mL or if fibroids number more than four.
Medical Alternatives to Hysterectomy
Early diagnosis and first-line medical therapies are recommended.
Contraceptive hormones to control heavy menstrual bleeding are the first step in most algorithms for treating fibroid-related bleeding, despite low-quality evidence.
Nonsteroidal anti-inflammatory agents and tranexamic acid during menstruation also limit heavy menses but have more evidence of efficacy for idiopathic heavy menses.
Gonadotropin-releasing hormone (GnRH) agonists in depot form are approved for short-term preoperative therapy. While they cause amenorrhea in nearly 90% of patients and reduce uterine volume by 30%-60%, they have a high incidence of hypogonadal symptoms, including bone loss and hot flushes. They also cause a “steroidal flare” when the stored gonadotropins are released and cause subsequent heavy menstrual bleeding with the rapid decrease in estrogen levels.
Oral GnRH antagonist combinations are a major therapeutic advance, pairing a GnRH antagonist (such as elagolix or relugolix, which rapidly inhibit ovarian steroidogenesis) with estradiol and progestin at doses equivalent to systemic levels in the early follicular phase of the menstrual cycle.
In clinical trials these combinations decreased heavy menstrual bleeding by 50%-75%, pain by 40%-50%, and bulk-related symptoms through a 10% decrease in uterine volume. Side effects are few, with hot flushes, headaches, and nausea occurring in fewer than 20% of participants.
Smaller fibroids in the submucosal to intramural spaces can be treated transcervically, while larger lesions of any type or smaller subserosa fibroids are treated abdominally.
Uterine-artery embolization uses minimally invasive radiologically guided catheterization to release embolic particles directly into both uterine arteries. This process causes ischemic infarction of the fibroids and decreases bleeding, pain, and bulk-related symptoms.
Other procedures shrink individual fibroids with energy that creates coagulative necrosis. These include focused ultrasound ablation (with MRI or ultrasound guidance) and radiofrequency ablation (with laparoscopic or transcervical ultrasound guidance).
Unlike uterine-artery embolization, which treats all fibroids concurrently, these therapies require individual targeting of fibroids.
Radiofrequency ablation can be done concurrently with other surgical therapies, such as laparoscopic excision of endometriosis or hysteroscopic myomectomy.
Myomectomy, or the surgical removal of fibroids, is most often used in persons actively seeking pregnancy or having very large fibroids in whom shrinkage would be inadequate. Most guidelines recommend surgical excision rather than shrinking procedures to optimize fertility. However, myomectomy often commits patients to future cesarean section, which increases pregnancy-related morbidity.
Although myomectomy is seen as superior to uterine-artery embolization for improving quality of life, both approaches provide substantial symptom relief.
Recurrence
Incidence of recurring fibroids is high, with, for example, new fibroids developing in approximately 50% of persons within 5 years of myomectomy.
Earlier this year, a large cohort study reported that myomectomy was best for avoiding reintervention after surgical leiomyoma management.
Reintervention rates vary according to procedure, patient age, disease extent, and symptoms and can be as high as 33% up to 5 years after treatment, with lower percentages seen among persons older than 45 years of age.
Hysterectomy
Minimally invasive hysterectomy is recommended. Drawbacks to hysterectomy include perioperative risk and concomitant oophorectomy, which was common until the early 2000s when large cohort studies showed elevated risks of death, cardiovascular disease, dementia, and other illnesses compared with hysterectomy plus ovarian conservation. Oophorectomy but not hysterectomy rates have since decreased.
Still needing study, according to Laughlin-Tommaso are the underlying reasons for health disparities in fibroids, especially among Black and Latina individuals. “Some studies have found associations with vitamin D deficiency and with stress and racism,” she said.
Looking ahead, the authors stressed the need for a fibroid risk-prediction model, a staging system, and large randomized trials of treatment effectiveness. Also needed are methods for primary and secondary prevention. “Earlier screening and medical treatment in primary care settings could potentially minimize morbidity and the incidence of unnecessary hysterectomies, and primary care–based screening trials are warranted,” they wrote.
In addition to procedural illustrations the practice document includes a vignette of a 33-year-old never-pregnant Black woman (but desiring motherhood) with heavy menstrual bleeding, abdominal bloating, and non–iron deficiency anemia. Evaluation for thalassemia and sickle cell anemia is negative, but ultrasonography reveals an enlarged uterus with multiple fibroids and normal ovaries.
In line with the clinical review, the authors prescribe oral GnRH agonist combination therapy, plus iron and multivitamin supplementation, and recommend annual reassessment — earlier if pregnancy is desired or if symptoms escalate. Since the patient prioritizes fertility, hysterectomy would be appropriate only if she had biopsy-proven cancer.
The authors received no external funding for this practice paper, but both have funding from the National Institutes of Health for fibroid research. Laughlin-Tommaso reported royalties from UpToDate. Stewart reported research support from the Agency for Healthcare Research and Quality, and speaking, data-monitoring, and consulting fees for various private companies, including AbbVie, Anylam Pharmaceuticals, ASKA Pharma, and Myovant Sciences. She holds a patent on treatment for abnormal uterine bleeding and has been involved in CME for various medical educational agencies. Hurtado and Ascher-Walsh had no relevant conflicts of interest to declare.
A version of this article first appeared on Medscape.com.
Although hysterectomy remains the most common procedure for treating fibroids and fibroids are the leading indication for hysterectomy, its long-term sequelae make less invasive alternatives the better choice for managing most of these myometrial masses, an invited clinical practice paper in the New England Journal of Medicine (NEJM) asserts.
The practice summary also calls for earlier identification and treatment of fibroid disease and may raise awareness among general gynecologists and primary care physicians less familiar with newer treatments.
Based on a review of evidence and existing formal guidelines, the paper urges wider use of uterus-sparing approaches such as hormone therapy, uterine-artery embolization, focused ultrasound ablation, and radiofrequency ablation. Authored by ob.gyns. Elizabeth A. Stewart, MD, and Shannon K. Laughlin-Tommaso, MD, MPH, of the Mayo Clinic in Rochester, Minnesota, the document also features textbook-style diagrams illustrating procedures.
“To clarify, this is not a new guidance but an invited clinical practice paper,” Laughlin-Tommaso told this news organization. “I believe NEJM recognized the gap in knowledge among all providers, for early diagnosis of uterine fibroids, especially in young patients and those presenting with anemia.”
The less invasive treatments highlighted in the paper can help women recover faster and resume their normal activities more quickly, said Laughlin-Tommaso. “Additionally, many studies have now shown that there are health benefits to keeping the uterus and the ovaries.”
Despite multiple uterine-sparing options, however, a recent study in a commercially insured population found nearly 60% of fibroid patients undergoing hysterectomy had never received a prior conservative treatment.
Why hysterectomy for a benign condition? Hysterectomy, which is universally available in ob.gyn. practices, makes decision-making easier for medical providers and patients, Laughlin-Tommaso explained. “It’s the only treatment that is definitive in that patients will not have bleeding or fibroids in the future and providers don’t have to determine which fibroids to treat or remove.”
More common in Black women, fibroids affect up to 80% of persons with a uterus during their lifetime and up to 50% have symptoms such as heavy and prolonged menstrual bleeding, anemia-associated fatigue, pelvic pressure, and menstrual and nonmenstrual pain, the authors noted. These lesions can also compress nearby structures causing painful intercourse, constipation, and urinary frequency, urgency, or retention.
In 2021 the American College of Obstetricians and Gynecologists issued a practice bulletin on the management of symptomatic uterine leiomyomas, similarly endorsing individualized care that accounts for the desire to preserve fertility or the uterus, increase quality of life, and reduce symptoms. It, too, recommended medical management as first-line treatment for symptomatic fibroids.
“This paper will be helpful for clinicians by covering some of the newer options such as gonadotropin-releasing hormone antagonists introduced in the past 5 years and tailoring treatment to patients depending on whether they still want to conceive,” Sandra M. Hurtado, MD, an ob.gyn. and an assistant professor at UTHealth Houston Medical Center and McGovern Medical School in Houston, Texas, said in an interview. “And the illustrations will be useful to doctors who are not gynecologists and will help to explain the interventional options to patients,” added Hurtado, who was not involved in the paper.
Offering another outside perspective on the paper, Charles J. Ascher-Walsh, MD, senior system vice chair for gynecology and division director of urogynecology in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology and Reproductive Science at Mount Sinai in New York City, called it a useful though not new summary. Reaching the wider audience of NEJM may raise awareness of newer fibroid therapies among general, nonspecialist ob.gyns., whose practices may concentrate largely on obstetrics, he added, “and the excellent illustrations clarify the treatment options.” In his view, broader awareness may increase much-needed funding for this neglected area of research.
Among the paper’s recommendations:
Diagnosis
Pelvic ultrasonography is the most cost-effective imaging method, providing information on size, location, and number of fibroids and ruling out adnexal masses. It is limited, however, by less-accurate resolution if the uterine volume is greater than 375 mL or if fibroids number more than four.
Medical Alternatives to Hysterectomy
Early diagnosis and first-line medical therapies are recommended.
Contraceptive hormones to control heavy menstrual bleeding are the first step in most algorithms for treating fibroid-related bleeding, despite low-quality evidence.
Nonsteroidal anti-inflammatory agents and tranexamic acid during menstruation also limit heavy menses but have more evidence of efficacy for idiopathic heavy menses.
Gonadotropin-releasing hormone (GnRH) agonists in depot form are approved for short-term preoperative therapy. While they cause amenorrhea in nearly 90% of patients and reduce uterine volume by 30%-60%, they have a high incidence of hypogonadal symptoms, including bone loss and hot flushes. They also cause a “steroidal flare” when the stored gonadotropins are released and cause subsequent heavy menstrual bleeding with the rapid decrease in estrogen levels.
Oral GnRH antagonist combinations are a major therapeutic advance, pairing a GnRH antagonist (such as elagolix or relugolix, which rapidly inhibit ovarian steroidogenesis) with estradiol and progestin at doses equivalent to systemic levels in the early follicular phase of the menstrual cycle.
In clinical trials these combinations decreased heavy menstrual bleeding by 50%-75%, pain by 40%-50%, and bulk-related symptoms through a 10% decrease in uterine volume. Side effects are few, with hot flushes, headaches, and nausea occurring in fewer than 20% of participants.
Smaller fibroids in the submucosal to intramural spaces can be treated transcervically, while larger lesions of any type or smaller subserosa fibroids are treated abdominally.
Uterine-artery embolization uses minimally invasive radiologically guided catheterization to release embolic particles directly into both uterine arteries. This process causes ischemic infarction of the fibroids and decreases bleeding, pain, and bulk-related symptoms.
Other procedures shrink individual fibroids with energy that creates coagulative necrosis. These include focused ultrasound ablation (with MRI or ultrasound guidance) and radiofrequency ablation (with laparoscopic or transcervical ultrasound guidance).
Unlike uterine-artery embolization, which treats all fibroids concurrently, these therapies require individual targeting of fibroids.
Radiofrequency ablation can be done concurrently with other surgical therapies, such as laparoscopic excision of endometriosis or hysteroscopic myomectomy.
Myomectomy, or the surgical removal of fibroids, is most often used in persons actively seeking pregnancy or having very large fibroids in whom shrinkage would be inadequate. Most guidelines recommend surgical excision rather than shrinking procedures to optimize fertility. However, myomectomy often commits patients to future cesarean section, which increases pregnancy-related morbidity.
Although myomectomy is seen as superior to uterine-artery embolization for improving quality of life, both approaches provide substantial symptom relief.
Recurrence
Incidence of recurring fibroids is high, with, for example, new fibroids developing in approximately 50% of persons within 5 years of myomectomy.
Earlier this year, a large cohort study reported that myomectomy was best for avoiding reintervention after surgical leiomyoma management.
Reintervention rates vary according to procedure, patient age, disease extent, and symptoms and can be as high as 33% up to 5 years after treatment, with lower percentages seen among persons older than 45 years of age.
Hysterectomy
Minimally invasive hysterectomy is recommended. Drawbacks to hysterectomy include perioperative risk and concomitant oophorectomy, which was common until the early 2000s when large cohort studies showed elevated risks of death, cardiovascular disease, dementia, and other illnesses compared with hysterectomy plus ovarian conservation. Oophorectomy but not hysterectomy rates have since decreased.
Still needing study, according to Laughlin-Tommaso are the underlying reasons for health disparities in fibroids, especially among Black and Latina individuals. “Some studies have found associations with vitamin D deficiency and with stress and racism,” she said.
Looking ahead, the authors stressed the need for a fibroid risk-prediction model, a staging system, and large randomized trials of treatment effectiveness. Also needed are methods for primary and secondary prevention. “Earlier screening and medical treatment in primary care settings could potentially minimize morbidity and the incidence of unnecessary hysterectomies, and primary care–based screening trials are warranted,” they wrote.
In addition to procedural illustrations the practice document includes a vignette of a 33-year-old never-pregnant Black woman (but desiring motherhood) with heavy menstrual bleeding, abdominal bloating, and non–iron deficiency anemia. Evaluation for thalassemia and sickle cell anemia is negative, but ultrasonography reveals an enlarged uterus with multiple fibroids and normal ovaries.
In line with the clinical review, the authors prescribe oral GnRH agonist combination therapy, plus iron and multivitamin supplementation, and recommend annual reassessment — earlier if pregnancy is desired or if symptoms escalate. Since the patient prioritizes fertility, hysterectomy would be appropriate only if she had biopsy-proven cancer.
The authors received no external funding for this practice paper, but both have funding from the National Institutes of Health for fibroid research. Laughlin-Tommaso reported royalties from UpToDate. Stewart reported research support from the Agency for Healthcare Research and Quality, and speaking, data-monitoring, and consulting fees for various private companies, including AbbVie, Anylam Pharmaceuticals, ASKA Pharma, and Myovant Sciences. She holds a patent on treatment for abnormal uterine bleeding and has been involved in CME for various medical educational agencies. Hurtado and Ascher-Walsh had no relevant conflicts of interest to declare.
A version of this article first appeared on Medscape.com.
Although hysterectomy remains the most common procedure for treating fibroids and fibroids are the leading indication for hysterectomy, its long-term sequelae make less invasive alternatives the better choice for managing most of these myometrial masses, an invited clinical practice paper in the New England Journal of Medicine (NEJM) asserts.
The practice summary also calls for earlier identification and treatment of fibroid disease and may raise awareness among general gynecologists and primary care physicians less familiar with newer treatments.
Based on a review of evidence and existing formal guidelines, the paper urges wider use of uterus-sparing approaches such as hormone therapy, uterine-artery embolization, focused ultrasound ablation, and radiofrequency ablation. Authored by ob.gyns. Elizabeth A. Stewart, MD, and Shannon K. Laughlin-Tommaso, MD, MPH, of the Mayo Clinic in Rochester, Minnesota, the document also features textbook-style diagrams illustrating procedures.
“To clarify, this is not a new guidance but an invited clinical practice paper,” Laughlin-Tommaso told this news organization. “I believe NEJM recognized the gap in knowledge among all providers, for early diagnosis of uterine fibroids, especially in young patients and those presenting with anemia.”
The less invasive treatments highlighted in the paper can help women recover faster and resume their normal activities more quickly, said Laughlin-Tommaso. “Additionally, many studies have now shown that there are health benefits to keeping the uterus and the ovaries.”
Despite multiple uterine-sparing options, however, a recent study in a commercially insured population found nearly 60% of fibroid patients undergoing hysterectomy had never received a prior conservative treatment.
Why hysterectomy for a benign condition? Hysterectomy, which is universally available in ob.gyn. practices, makes decision-making easier for medical providers and patients, Laughlin-Tommaso explained. “It’s the only treatment that is definitive in that patients will not have bleeding or fibroids in the future and providers don’t have to determine which fibroids to treat or remove.”
More common in Black women, fibroids affect up to 80% of persons with a uterus during their lifetime and up to 50% have symptoms such as heavy and prolonged menstrual bleeding, anemia-associated fatigue, pelvic pressure, and menstrual and nonmenstrual pain, the authors noted. These lesions can also compress nearby structures causing painful intercourse, constipation, and urinary frequency, urgency, or retention.
In 2021 the American College of Obstetricians and Gynecologists issued a practice bulletin on the management of symptomatic uterine leiomyomas, similarly endorsing individualized care that accounts for the desire to preserve fertility or the uterus, increase quality of life, and reduce symptoms. It, too, recommended medical management as first-line treatment for symptomatic fibroids.
“This paper will be helpful for clinicians by covering some of the newer options such as gonadotropin-releasing hormone antagonists introduced in the past 5 years and tailoring treatment to patients depending on whether they still want to conceive,” Sandra M. Hurtado, MD, an ob.gyn. and an assistant professor at UTHealth Houston Medical Center and McGovern Medical School in Houston, Texas, said in an interview. “And the illustrations will be useful to doctors who are not gynecologists and will help to explain the interventional options to patients,” added Hurtado, who was not involved in the paper.
Offering another outside perspective on the paper, Charles J. Ascher-Walsh, MD, senior system vice chair for gynecology and division director of urogynecology in the Raquel and Jaime Gilinski Department of Obstetrics, Gynecology and Reproductive Science at Mount Sinai in New York City, called it a useful though not new summary. Reaching the wider audience of NEJM may raise awareness of newer fibroid therapies among general, nonspecialist ob.gyns., whose practices may concentrate largely on obstetrics, he added, “and the excellent illustrations clarify the treatment options.” In his view, broader awareness may increase much-needed funding for this neglected area of research.
Among the paper’s recommendations:
Diagnosis
Pelvic ultrasonography is the most cost-effective imaging method, providing information on size, location, and number of fibroids and ruling out adnexal masses. It is limited, however, by less-accurate resolution if the uterine volume is greater than 375 mL or if fibroids number more than four.
Medical Alternatives to Hysterectomy
Early diagnosis and first-line medical therapies are recommended.
Contraceptive hormones to control heavy menstrual bleeding are the first step in most algorithms for treating fibroid-related bleeding, despite low-quality evidence.
Nonsteroidal anti-inflammatory agents and tranexamic acid during menstruation also limit heavy menses but have more evidence of efficacy for idiopathic heavy menses.
Gonadotropin-releasing hormone (GnRH) agonists in depot form are approved for short-term preoperative therapy. While they cause amenorrhea in nearly 90% of patients and reduce uterine volume by 30%-60%, they have a high incidence of hypogonadal symptoms, including bone loss and hot flushes. They also cause a “steroidal flare” when the stored gonadotropins are released and cause subsequent heavy menstrual bleeding with the rapid decrease in estrogen levels.
Oral GnRH antagonist combinations are a major therapeutic advance, pairing a GnRH antagonist (such as elagolix or relugolix, which rapidly inhibit ovarian steroidogenesis) with estradiol and progestin at doses equivalent to systemic levels in the early follicular phase of the menstrual cycle.
In clinical trials these combinations decreased heavy menstrual bleeding by 50%-75%, pain by 40%-50%, and bulk-related symptoms through a 10% decrease in uterine volume. Side effects are few, with hot flushes, headaches, and nausea occurring in fewer than 20% of participants.
Smaller fibroids in the submucosal to intramural spaces can be treated transcervically, while larger lesions of any type or smaller subserosa fibroids are treated abdominally.
Uterine-artery embolization uses minimally invasive radiologically guided catheterization to release embolic particles directly into both uterine arteries. This process causes ischemic infarction of the fibroids and decreases bleeding, pain, and bulk-related symptoms.
Other procedures shrink individual fibroids with energy that creates coagulative necrosis. These include focused ultrasound ablation (with MRI or ultrasound guidance) and radiofrequency ablation (with laparoscopic or transcervical ultrasound guidance).
Unlike uterine-artery embolization, which treats all fibroids concurrently, these therapies require individual targeting of fibroids.
Radiofrequency ablation can be done concurrently with other surgical therapies, such as laparoscopic excision of endometriosis or hysteroscopic myomectomy.
Myomectomy, or the surgical removal of fibroids, is most often used in persons actively seeking pregnancy or having very large fibroids in whom shrinkage would be inadequate. Most guidelines recommend surgical excision rather than shrinking procedures to optimize fertility. However, myomectomy often commits patients to future cesarean section, which increases pregnancy-related morbidity.
Although myomectomy is seen as superior to uterine-artery embolization for improving quality of life, both approaches provide substantial symptom relief.
Recurrence
Incidence of recurring fibroids is high, with, for example, new fibroids developing in approximately 50% of persons within 5 years of myomectomy.
Earlier this year, a large cohort study reported that myomectomy was best for avoiding reintervention after surgical leiomyoma management.
Reintervention rates vary according to procedure, patient age, disease extent, and symptoms and can be as high as 33% up to 5 years after treatment, with lower percentages seen among persons older than 45 years of age.
Hysterectomy
Minimally invasive hysterectomy is recommended. Drawbacks to hysterectomy include perioperative risk and concomitant oophorectomy, which was common until the early 2000s when large cohort studies showed elevated risks of death, cardiovascular disease, dementia, and other illnesses compared with hysterectomy plus ovarian conservation. Oophorectomy but not hysterectomy rates have since decreased.
Still needing study, according to Laughlin-Tommaso are the underlying reasons for health disparities in fibroids, especially among Black and Latina individuals. “Some studies have found associations with vitamin D deficiency and with stress and racism,” she said.
Looking ahead, the authors stressed the need for a fibroid risk-prediction model, a staging system, and large randomized trials of treatment effectiveness. Also needed are methods for primary and secondary prevention. “Earlier screening and medical treatment in primary care settings could potentially minimize morbidity and the incidence of unnecessary hysterectomies, and primary care–based screening trials are warranted,” they wrote.
In addition to procedural illustrations the practice document includes a vignette of a 33-year-old never-pregnant Black woman (but desiring motherhood) with heavy menstrual bleeding, abdominal bloating, and non–iron deficiency anemia. Evaluation for thalassemia and sickle cell anemia is negative, but ultrasonography reveals an enlarged uterus with multiple fibroids and normal ovaries.
In line with the clinical review, the authors prescribe oral GnRH agonist combination therapy, plus iron and multivitamin supplementation, and recommend annual reassessment — earlier if pregnancy is desired or if symptoms escalate. Since the patient prioritizes fertility, hysterectomy would be appropriate only if she had biopsy-proven cancer.
The authors received no external funding for this practice paper, but both have funding from the National Institutes of Health for fibroid research. Laughlin-Tommaso reported royalties from UpToDate. Stewart reported research support from the Agency for Healthcare Research and Quality, and speaking, data-monitoring, and consulting fees for various private companies, including AbbVie, Anylam Pharmaceuticals, ASKA Pharma, and Myovant Sciences. She holds a patent on treatment for abnormal uterine bleeding and has been involved in CME for various medical educational agencies. Hurtado and Ascher-Walsh had no relevant conflicts of interest to declare.
A version of this article first appeared on Medscape.com.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Heat Waves Pose Significant Health Risks for Dually Eligible Older Individuals
TOPLINE:
Heat waves are associated with an increase in heat-related emergency department visits, hospitalizations, and deaths among dually eligible individuals older than 65 years.
METHODOLOGY:
- The researchers conducted a retrospective time-series study using national Medicare and Medicaid data from 2016 to 2019 to assess the link between heat waves during warm months and adverse health events.
- A total of 5,448,499 dually eligible individuals (66% women; 20% aged ≥ 85 years) were included from 28,404 zip code areas across 50 states and Washington, DC.
- Heat waves were defined as three or more consecutive days of extreme heat with a maximum temperature of at least 90 °F and within the 97th percentile of daily maximum temperatures for each zip code.
- Primary outcomes were daily counts of heat-related emergency department visits and hospitalizations.
- Secondary outcomes were all-cause and heat-specific emergency department visits, all-cause and heat-specific hospitalizations, deaths, and long-term nursing facility placements within 3 months after a heat wave.
TAKEAWAY:
- Heat waves were associated with a 10% increase in heat-related emergency department visits (incidence rate ratio [IRR], 1.10; 95% CI, 1.08-1.12) and a 7% increase in heat-related hospitalizations (IRR, 1.07; 95% CI, 1.04-1.09).
- Mortality rates were 4% higher during heat wave days than during non–heat wave days (IRR, 1.04; 95% CI, 1.01-1.07).
- No significant difference was found in rates of long-term nursing facility placements or heat-related emergency department visits for nursing facility residents.
- All racial and ethnic groups showed higher incidence rates of heat-related emergency department visits during heat waves, especially among beneficiaries identified as Asian (IRR, 1.21; 95% CI, 1.12-1.29). Rates were higher among individuals residing in the Northwest, Ohio Valley, and the West.
IN PRACTICE:
“In healthcare settings, clinicians should incorporate routine heat wave risk assessments into clinical practice, especially in regions more susceptible to extreme heat, for all dual-eligible beneficiaries and other at-risk patients,” wrote Jose F. Figueroa, MD, MPH, of the Harvard T.H. Chan School of Public Health in Boston, in an invited commentary. “Beyond offering preventive advice, clinicians can adjust medications that may increase their patients’ susceptibility during heat waves, or they can refer patients to social workers and social service organizations to ensure that they are protected at home.”
SOURCE:
This study was led by Hyunjee Kim, PhD, of the Center for Health Systems Effectiveness at Oregon Health & Science University, Portland. It was published online in JAMA Health Forum.
LIMITATIONS:
This study relied on a claims database to identify adverse events, which may have led to omissions in coding, particularly for heat-related conditions if the diagnostic codes for heat-related symptoms had not been adopted. This study did not adjust for variations in air quality or green space, which could have confounded the association of interest. Indoor heat exposures or adaptive behaviors, such as air conditioning use, were not considered. The analysis could not compare the association of heat waves with adverse events between those with dual eligibility and those without dual eligibility.
DISCLOSURES:
This study was supported by the National Institute on Aging. One author reported receiving grants from the National Institutes of Health outside the submitted work. No other disclosures were reported.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Heat waves are associated with an increase in heat-related emergency department visits, hospitalizations, and deaths among dually eligible individuals older than 65 years.
METHODOLOGY:
- The researchers conducted a retrospective time-series study using national Medicare and Medicaid data from 2016 to 2019 to assess the link between heat waves during warm months and adverse health events.
- A total of 5,448,499 dually eligible individuals (66% women; 20% aged ≥ 85 years) were included from 28,404 zip code areas across 50 states and Washington, DC.
- Heat waves were defined as three or more consecutive days of extreme heat with a maximum temperature of at least 90 °F and within the 97th percentile of daily maximum temperatures for each zip code.
- Primary outcomes were daily counts of heat-related emergency department visits and hospitalizations.
- Secondary outcomes were all-cause and heat-specific emergency department visits, all-cause and heat-specific hospitalizations, deaths, and long-term nursing facility placements within 3 months after a heat wave.
TAKEAWAY:
- Heat waves were associated with a 10% increase in heat-related emergency department visits (incidence rate ratio [IRR], 1.10; 95% CI, 1.08-1.12) and a 7% increase in heat-related hospitalizations (IRR, 1.07; 95% CI, 1.04-1.09).
- Mortality rates were 4% higher during heat wave days than during non–heat wave days (IRR, 1.04; 95% CI, 1.01-1.07).
- No significant difference was found in rates of long-term nursing facility placements or heat-related emergency department visits for nursing facility residents.
- All racial and ethnic groups showed higher incidence rates of heat-related emergency department visits during heat waves, especially among beneficiaries identified as Asian (IRR, 1.21; 95% CI, 1.12-1.29). Rates were higher among individuals residing in the Northwest, Ohio Valley, and the West.
IN PRACTICE:
“In healthcare settings, clinicians should incorporate routine heat wave risk assessments into clinical practice, especially in regions more susceptible to extreme heat, for all dual-eligible beneficiaries and other at-risk patients,” wrote Jose F. Figueroa, MD, MPH, of the Harvard T.H. Chan School of Public Health in Boston, in an invited commentary. “Beyond offering preventive advice, clinicians can adjust medications that may increase their patients’ susceptibility during heat waves, or they can refer patients to social workers and social service organizations to ensure that they are protected at home.”
SOURCE:
This study was led by Hyunjee Kim, PhD, of the Center for Health Systems Effectiveness at Oregon Health & Science University, Portland. It was published online in JAMA Health Forum.
LIMITATIONS:
This study relied on a claims database to identify adverse events, which may have led to omissions in coding, particularly for heat-related conditions if the diagnostic codes for heat-related symptoms had not been adopted. This study did not adjust for variations in air quality or green space, which could have confounded the association of interest. Indoor heat exposures or adaptive behaviors, such as air conditioning use, were not considered. The analysis could not compare the association of heat waves with adverse events between those with dual eligibility and those without dual eligibility.
DISCLOSURES:
This study was supported by the National Institute on Aging. One author reported receiving grants from the National Institutes of Health outside the submitted work. No other disclosures were reported.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Heat waves are associated with an increase in heat-related emergency department visits, hospitalizations, and deaths among dually eligible individuals older than 65 years.
METHODOLOGY:
- The researchers conducted a retrospective time-series study using national Medicare and Medicaid data from 2016 to 2019 to assess the link between heat waves during warm months and adverse health events.
- A total of 5,448,499 dually eligible individuals (66% women; 20% aged ≥ 85 years) were included from 28,404 zip code areas across 50 states and Washington, DC.
- Heat waves were defined as three or more consecutive days of extreme heat with a maximum temperature of at least 90 °F and within the 97th percentile of daily maximum temperatures for each zip code.
- Primary outcomes were daily counts of heat-related emergency department visits and hospitalizations.
- Secondary outcomes were all-cause and heat-specific emergency department visits, all-cause and heat-specific hospitalizations, deaths, and long-term nursing facility placements within 3 months after a heat wave.
TAKEAWAY:
- Heat waves were associated with a 10% increase in heat-related emergency department visits (incidence rate ratio [IRR], 1.10; 95% CI, 1.08-1.12) and a 7% increase in heat-related hospitalizations (IRR, 1.07; 95% CI, 1.04-1.09).
- Mortality rates were 4% higher during heat wave days than during non–heat wave days (IRR, 1.04; 95% CI, 1.01-1.07).
- No significant difference was found in rates of long-term nursing facility placements or heat-related emergency department visits for nursing facility residents.
- All racial and ethnic groups showed higher incidence rates of heat-related emergency department visits during heat waves, especially among beneficiaries identified as Asian (IRR, 1.21; 95% CI, 1.12-1.29). Rates were higher among individuals residing in the Northwest, Ohio Valley, and the West.
IN PRACTICE:
“In healthcare settings, clinicians should incorporate routine heat wave risk assessments into clinical practice, especially in regions more susceptible to extreme heat, for all dual-eligible beneficiaries and other at-risk patients,” wrote Jose F. Figueroa, MD, MPH, of the Harvard T.H. Chan School of Public Health in Boston, in an invited commentary. “Beyond offering preventive advice, clinicians can adjust medications that may increase their patients’ susceptibility during heat waves, or they can refer patients to social workers and social service organizations to ensure that they are protected at home.”
SOURCE:
This study was led by Hyunjee Kim, PhD, of the Center for Health Systems Effectiveness at Oregon Health & Science University, Portland. It was published online in JAMA Health Forum.
LIMITATIONS:
This study relied on a claims database to identify adverse events, which may have led to omissions in coding, particularly for heat-related conditions if the diagnostic codes for heat-related symptoms had not been adopted. This study did not adjust for variations in air quality or green space, which could have confounded the association of interest. Indoor heat exposures or adaptive behaviors, such as air conditioning use, were not considered. The analysis could not compare the association of heat waves with adverse events between those with dual eligibility and those without dual eligibility.
DISCLOSURES:
This study was supported by the National Institute on Aging. One author reported receiving grants from the National Institutes of Health outside the submitted work. No other disclosures were reported.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
‘Round Face’: A Viral Term’s Real Diagnostic Implications
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
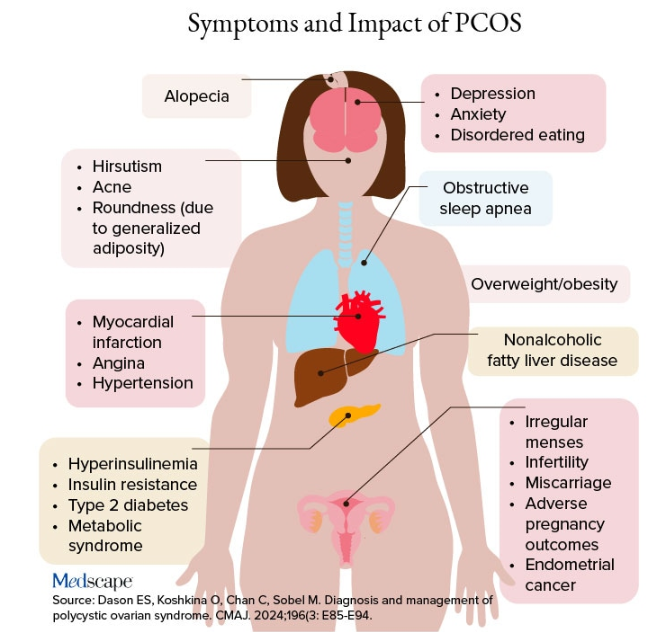
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
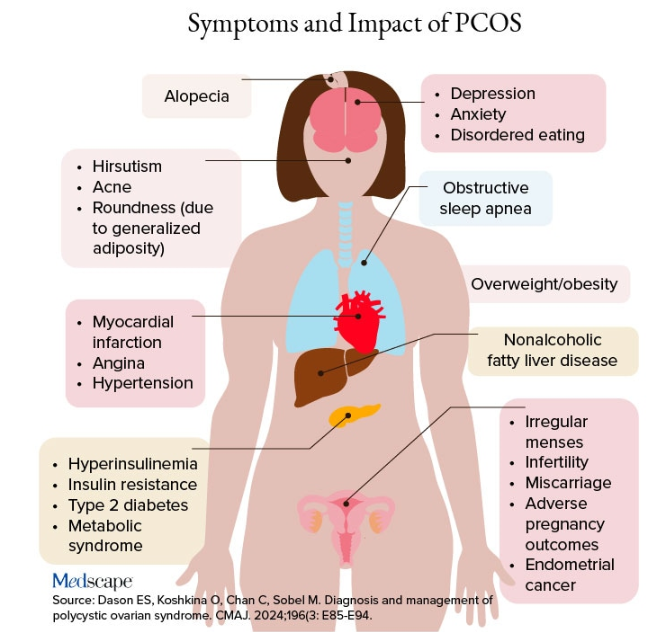
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
“Cortisol” has become a household word, popularized by social media and tagged in videos that garnered nearly 800 million views in 2023. This is linked to the also-trending term “moon face,” which TikTok influencers and others have suggested is caused by high cortisol levels and, conversely, can be reduced through stress reduction.
“When we hear the term ‘moon face,’ we’re typically referring to Cushing syndrome [CS] or treatment with prolonged high-dose glucocorticoids,” said Anat Ben-Shlomo, MD, co-director of the Multidisciplinary Adrenal Program, Pituitary Center, Division of Endocrinology, Diabetes and Metabolism at Cedars-Sinai Medical Center, Los Angeles. Medscape Medical News previously discussed moon face in an article detailing how to diagnose CS.
Ben-Shlomo noted that the labels “moon face” and “moon facies” should be avoided for their potentially derogatory, unprofessional-sounding connotations, and that the preferred terms are “rounded face” or “round plethoric face.”
There are several disorders that can be associated with facial roundness, not all of which relate to elevated cortisol.
“It’s important for clinicians to be able distinguish between presentations due to other pathophysiologies, identify the unique constellation of Cushing-associated signs and symptoms, engage in a differential diagnosis, and treat whatever the condition is appropriately,” Katherine Sherif, MD, professor and vice chair of academic affairs, Department of Medicine, Thomas Jefferson University, Philadelphia, said in an interview.
The Unique Presentation of CS
CS results from “prolonged elevation” in plasma cortisol levels caused by either exogenous steroid use or excess endogenous steroid production.
“The shape of the face isn’t the only feature associated with CS,” Ben-Shlomo said. “There’s central obesity, particularly in the neck, supraclavicular area, chest, and abdomen. You sometimes see a posterior cervical thoracic fat pad, colloquially — but unprofessionally — called a ‘cervical hump.’ Simultaneously, the arms and legs are getting thinner.” The development of a round, plethoric face is common in long-standing significant CS, and a reddening of the skin can appear.
Additional symptoms include hirsutism and acne. “These can also be seen in other conditions, such as PCOS [polycystic ovary syndrome] but, combined with the other facial features, are more suggestive of CS,” Ben-Shlomo said.
Deep, wide purple striae appear in the trunk, breast, upper arms, and thighs, but not in the face, Ben-Shlomo advised. These appear as the fragile, thinning under-skin breaks when the patient gains weight.
Additional metabolic issues that can occur comorbidly include insulin resistance and diabetes, hypertension, osteoporosis, dyslipidemia, ecchymoses, increased susceptibility to infections, mood changes, cognitive dysfunction, low libido, infertility, weakness of muscles in the shoulders and thighs, episodes of bleeding and/or clotting, and an increased risk for heart attacks and strokes, Ben-Shlomo said.
“Not everyone presents with full-blown disease, but if you see any of these symptoms, be suspicious of CS and conduct a biochemical evaluation.” Three screening tests to use as a starting point are recommended by the Pituitary Society’s updated Consensus on Diagnosis and Management of Cushing’s Disease. The tests should be repeated to account for intra-patient variability. If two or all three tests are positive, clinicians should be suspicious of CS and move to additional testing to identify the underlying cause, Ben-Shlomo said.
‘Subclinical’ CS
Ben-Shlomo highlighted a condition called minimal autonomous cortisol secretion (formerly “subclinical CS”). “This condition is found when a person has an adrenal nodule that produces cortisol in excess, however not to levels observed in CS. An abnormal finding on the overnight 1-mg low-dose dexamethasone suppression test (LDDST) will identify this disorder, showing mildly unsuppressed morning cortisol level, while all other tests will be within normal range.”
She described minimal autonomous cortisol secretion as a form of “smoldering CS,” which has become more commonly diagnosed. “The condition needs to be treated because the patient can develop insulin resistance, metabolic syndrome, and osteoporosis over time.”
Once a cause has been determined, the optimal course of action is to take a multidisciplinary approach because CS affects multiple systems.
‘Pseudo-Cushing Syndrome’
A variety of abnormalities of the hypothalamus-pituitary adrenal (HPA) axis can be associated with hypercortisolemia and a rounder facial appearance but aren’t actually CS, Ben-Shlomo said.
Often called “pseudo-Cushing syndrome,” these conditions have recently been renamed “non-neoplastic hypercortisolism” or “physiologic non-neoplastic endogenous hypercortisolism.” They share some clinical and biochemical features of CS, but the hypercortisolemia is usually secondary to other factors. They increase the secretion of hypothalamic corticotropin-releasing hormone, which stimulates adrenocorticotropic hormone (ACTH) and adrenal cortisol secretion.
Identifying PCOS
PCOS is often associated with central obesity, Sherif noted, but not all women with PCOS have overweight or a central distribution of fat.
“Ask about menstrual periods and whether they come monthly,” Sherif advised. “If women using hormonal contraception say they have a regular cycle, ask if their cycle was regular prior to starting contraception. So many women with PCOS are undiagnosed because they started contraception in their teens to ‘regulate their periods’ and never realized they had PCOS.”
Additional symptoms of PCOS and its impact are found in the figure below.
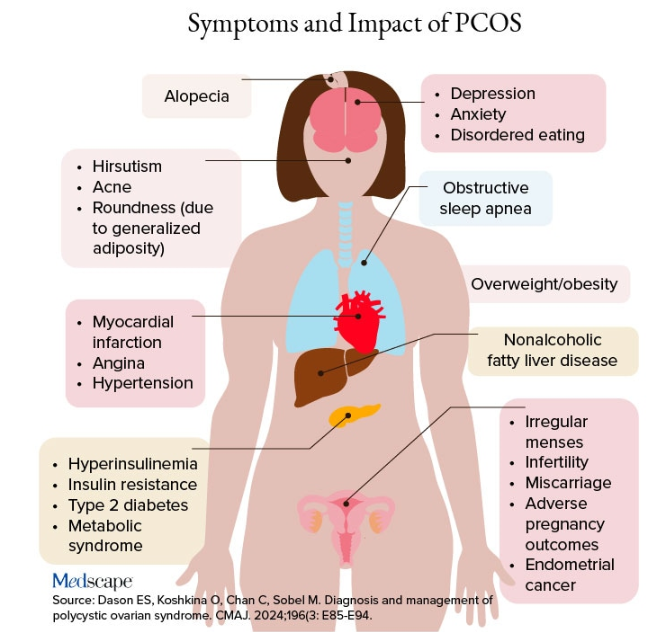
PCOS is diagnosed when two of the following three Rotterdam criteria are met, and other diagnoses are excluded:
- Irregular menstrual cycles
- Clinical hyperandrogenism or biochemical hyperandrogenism
- Polycystic ovarian morphology on transvaginal ultrasonography or high anti-mullerian hormone (applicable only if patient is ≥ 8 years from menarche)
If PCOS is suspected, further tests can be conducted to confirm or rule out the diagnosis.
Alcohol Abuse: Alcohol abuse stimulates hypothalamic corticotropin-releasing hormone, leading to increased ACTH levels. It’s associated with a higher fasting cortisol level, particularly at 8:30 AM or so, and attributable to impaired cortisol clearance due to alcohol-related hepatic dysfunction. The LDDST will show abnormal cortisol suppression.
Sherif advised asking patients about alcohol use, recommending treatment for alcohol use disorder, and repeating clinical and biochemical workup after patients have discontinued alcohol consumption for ≥ 1 month.
Eating Disorders Mimicking CS: Eating disorders, particularly anorexia nervosa, are associated with endocrine abnormalities, amenorrhea, impaired body temperature regulation, and hypercortisolism, likely due to chronic fasting-related stress. Dysregulation of the HPA axis may linger, even after weight recovery.
It’s unlikely that patients with anorexia will display the “rounded face” associated with hypercortisolism, but some research suggests that anorexia can result in a disproportionate accumulation of central adiposity after recovery from the illness.
Neuropsychiatric Disorders: Major depressive disorder (MDD) is associated with HPA axis hyperactivity, with 20%-30% of patients with MDD showing hypercortisolemia. The post-awakening cortisol surge is more pronounced in those with MDD, and about half of patients with MDD also have high evening cortisol levels, suggesting disrupted diurnal cortisol rhythms.
Some patients with MDD have greater resistance to the feedback action of glucocorticoids on HPA axis activity, with weaker sensitivity often restored by effective pharmacotherapy of the depressive condition. Neuropsychiatric disorders are also associated with reduced activity of cortisol-deactivating enzymes. Posttraumatic stress disorder and anxiety are similarly associated with hypercortisolemia.
Addressing neuropsychiatric conditions with appropriate pharmacotherapy and psychotherapy can restore cortisol levels to normal proportions.
Diabetes, Obesity, and Metabolic Syndrome: Diabetes, obesity, and metabolic syndrome can occur comorbidly with CS, and many patients with these conditions may display both a rounder face, some central adiposity, and hypercortisolemia. For example, obesity is often related to a hyperresponsive HPA axis, with elevated cortisol secretion but normal-to-low circulatory concentrations.
Obesity is associated with increased cortisol reactivity after acute physical and/or psychosocial stressors but preserved pituitary sensitivity to feedback inhibition by the LDDST. When these conditions are appropriately managed with pharmacotherapy and lifestyle changes, cortisol levels should normalize, according to the experts.
Hypothyroidism: Hypothyroidism— Hashimoto disease as well as the subclinical variety — can be associated with weight gain, which may take the form of central obesity. Some research suggests a bidirectional relationship between hypothyroidism and obesity.
“Years ago, we didn’t conduct thyroid tests very often but now they’re easy to do, so we usually catch people with hypothyroidism at the beginning of the condition,” Sherif said. “If the patient’s thyroid hasn’t been checked in a year or so, thyroid hormone testing should be conducted.”
Thyroid disease can easily be managed with the administration of thyroid hormones.
Obstructive Sleep Apnea (OSA): OSA has an impact on HPA axis activation, especially when accompanied by obesity and hypertension. A meta-analysis of 22 studies, encompassing over 600 participants, found that continuous positive airway pressure treatment in patients with OSA reduced cortisol levels as well as blood pressure.
Treatment With Exogenous Corticosteroids: Oral corticosteroid treatment is a cornerstone of therapy in transplant, rheumatic, and autoimmune diseases. The impact of chronic exposure to exogenous glucocorticoids is similar to that with endogenous glucocorticoids.
Sherif said corticosteroid treatment can cause facial roundness in as little as 2 weeks and is characteristic in people taking these agents for longer periods. Although the effects are most pronounced with oral agents, systemic effects can be associated with inhaled corticosteroids as well.
Finding alternative anti-inflammatory treatments is advisable, if possible. The co-administration of metformin might lead to improvements in both the metabolic profile and the clinical outcomes of patients receiving glucocorticoids for inflammatory conditions.
Educating Patients: “There’s much we still don’t know about hypercortisolemia and CS, including the reasons for its impact on metabolic derangement and for the accumulation of fat in particular adipose patterns,” Ben-Shlomo said. “But experienced endocrinologists do know relatively well how to diagnose the condition, distinguish it from other conditions presenting with central obesity or a rounder face, and treat it.”
Given the casual use of the terms “moon face” and “extra cortisol” on social media, it’s important for physicians to educate patients about what elevated cortisol does and doesn’t do, and design treatment strategies accordingly.
Neither Ben-Shlomo nor Sherif reported having any disclosures.
A version of this article appeared on Medscape.com.
Barzolvolimab Effective for CSU in Phase 2 Study
of an ongoing phase 2 study.
Moreover, in the study, barzolvolimab, an anti-KIT monoclonal antibody that inhibits the activation of and depletes mast cells, induced comparable responses in a subset of patients who had taken omalizumab, an anti–immunoglobulin E monoclonal antibody approved by the Food and Drug Administration for treating CSU.
The findings were presented at the annual European Academy of Dermatology and Venereology (EADV) 2024 Congress. Barzolvolimab is being developed by Celldex Therapeutics.
“Barzolvolimab treatment resulted in rapid, profound, and durable improvement in UAS7 [weekly Urticaria Activity Score 7],” said presenter Martin Metz, MD, professor of dermatology, Institute of Allergology, Charité – Universitätsmedizin Berlin in Germany, “with a deepening of response over 52 weeks in patients with antihistamine-refractory CSU.”
“Similar robust improvement was seen in patients previously treated with omalizumab, including refractory patients,” he added.
Because barzolvolimab was well tolerated over the course of the follow-up period, Metz said, it “has the potential to be an important new treatment option,” noting that patients are now being enrolled in global phase 3 studies of barzolvolimab.
Sustained Symptom Relief
Ana M. Giménez-Arnau, MD, PhD, associate professor of dermatology, Autonomous University and Pompeu Fabra University, Barcelona, Spain, told Medscape Medical News that the results are important, as they showed people who switched from placebo to the active drug also saw a long-term benefit.
What is “remarkable” about barzolvolimab, continued Giménez-Arnau, who was not involved in the study, is that it is the first drug to target the KIT receptor on mast cells and interfere with stimulating growth factors, thus making the cells that drive the development of CSU “disappear.”
The study included three different barzolvolimab regimens, with the 150-mg dose every 4 weeks and the 300-mg dose every 8 weeks achieving similar results, noted Giménez-Arnau.
For her, there are important questions to answer around the pharmacokinetic and pharmacodynamic profiles of the two regimens that remain, but she underlined that for the patient, the choice of regimen could have an impact on their quality of life.
“If we give 300 mg every 8 weeks,” she said, it appears “you can achieve disease control” while halving the frequency of subcutaneous injections.
She said that it would be “interesting to know” if 300 mg every 8 weeks is given as two 150-mg injections every 2 months or one 300-mg injection. If it is the former, Giménez Arnau said, “This is potentially an important benefit for the patient.”
Sustained Benefits at 1 Year
The study enrolled 208 patients with antihistamine-refractory CSU at sites in 10 countries, randomizing them to one of four arms: Subcutaneous injections of barzolvolimab 75 mg or 150 mg every 4 weeks, 300 mg every 8 weeks, or placebo every 4 weeks.
The mean age in each arm was between 42 and 47 years, and around 75% were women. Across the arms, 64%-76% had severe disease, as measured on the UAS7, at a mean score of 30.0-31.3. Around 20% had previously been treated with omalizumab.
Patients were treated for 16 weeks, during which time they completed daily and weekly diaries and attended six clinic visits at weeks 0, 2, 4, 8, 12, and 16. Results from the trial published earlier this year demonstrated that both the regimens (150 mg every 4 weeks and 300 mg every 8 weeks) achieved clinically meaningful and statistically significant improvement in UAS7, the primary endpoint, vs placebo at 12 weeks.
Participants in the barzolvolimab 75 mg and placebo arms were then randomized to receive barzolvolimab 150 mg every 4 weeks or 300 mg every 8 weeks, and those who had been in the 150-mg and 300-mg treatment arms continued with that treatment for a further 36 weeks. (The remaining patients have been continued on a further 24-week follow-up, but the data are not yet available.)
By the 52-week follow-up, 25% of patients who started in each of the barzolvolimab arms had discontinued treatment, as well as 16% first randomized to the placebo arm.
Metz reported that the improvements in UAS7 scores, observed as early as week 1, were sustained through week 52 in patients in both the ongoing 150-mg and 300-mg arms. Patients who initially started in the placebo and the barzolvolimab 75-mg groups caught up with those who had started on the higher doses, so that by week 52, there were no significant differences in urticaria activity, hives, or itch scores between the arms.
By week 52, the proportion of patients achieving well-controlled disease, defined as a UAS7 score ≤ 6, was 73.7% in the barzolvolimab 150 mg every 4-week arm and 68.2% in the 300 mg barzolvolimab every 8-week arm.
Notably, just 12.8% of patients in the placebo arm had achieved well-controlled CSU by week 16, but after switching to barzolvolimab 150 mg every 4 weeks or 300 mg every 8 weeks, 63% reached that target at week 52.
“Maybe even more striking and very interesting to look at,” said Metz, was the complete control of symptoms, meaning “not one single wheal and no itch.” By week 52, 52% of those on 300 mg every 8 weeks and 71.1% of those on 150 mg every 4 weeks had a complete response, with no itch/hives (UAS7 of 0).
Importantly, complete responses with barzolvolimab were observed early and were sustained or improved to week 52, Metz said, with, again, placebo and former barzolvolimab 75 mg patients catching up with those who started on 150 mg every 4 weeks and 300 mg every 8 weeks once they switched at week 16.
“This is the best data for chronic spontaneous urticaria that we have so far seen,” he said, adding that the responses were seen regardless of prior experience with omalizumab.
Changes in Hair Color, Skin Pigmentation
As for safety, during the first 16 weeks, 66% of those on active treatment and 39% on placebo experienced at least one adverse event. There were no treatment-related serious adverse events, compared with two among those who received treatment for the full 52 weeks.
The most common adverse events with active treatment were hair color changes (14% in the first 16 weeks and 26% among those treated for the full 52 weeks), neutropenia/reduced neutrophil count (9% in the first 16 weeks and 17% among those treated for the full 52 weeks), and skin hypopigmentation (1% in the first 16 weeks, 13% among those treated for the full 52 weeks, and 19% among those who switched from placebo to active treatment at 36 weeks). Urticaria was reported by 10% among patients on active treatment and 10% among those on placebo in the first 16 weeks, and by 15% of those treated for the full 52 weeks.
In the post-presentation discussion, Metz explained that the hypopigmentation appears to start around the hair follicle and is diffuse, so tends to look like vitiligo.
He suggested that the melanocytes around the hair follicle “seem to be the ones that are more stressed, maybe because of the hair follicle cycling,” adding that the effect is reversible and does not appear to be dose dependent.
The study was funded by Celldex Therapeutics. Metz declared relationships with AbbVie, ALK-Abelló, Almirall, Amgen, argenx, AstraZeneca, Astria, Attovia Therapeutics, Celldex, Celltrion, Escient Pharmaceuticals, Galen, Galderma, GSK, Incyte, Jasper, Lilly, Novartis, Pfizer, Pharvaris, Regeneron, Sanofi, Teva, Third Harmonic Bio, and Vifor.
A version of this article first appeared on Medscape.com.
of an ongoing phase 2 study.
Moreover, in the study, barzolvolimab, an anti-KIT monoclonal antibody that inhibits the activation of and depletes mast cells, induced comparable responses in a subset of patients who had taken omalizumab, an anti–immunoglobulin E monoclonal antibody approved by the Food and Drug Administration for treating CSU.
The findings were presented at the annual European Academy of Dermatology and Venereology (EADV) 2024 Congress. Barzolvolimab is being developed by Celldex Therapeutics.
“Barzolvolimab treatment resulted in rapid, profound, and durable improvement in UAS7 [weekly Urticaria Activity Score 7],” said presenter Martin Metz, MD, professor of dermatology, Institute of Allergology, Charité – Universitätsmedizin Berlin in Germany, “with a deepening of response over 52 weeks in patients with antihistamine-refractory CSU.”
“Similar robust improvement was seen in patients previously treated with omalizumab, including refractory patients,” he added.
Because barzolvolimab was well tolerated over the course of the follow-up period, Metz said, it “has the potential to be an important new treatment option,” noting that patients are now being enrolled in global phase 3 studies of barzolvolimab.
Sustained Symptom Relief
Ana M. Giménez-Arnau, MD, PhD, associate professor of dermatology, Autonomous University and Pompeu Fabra University, Barcelona, Spain, told Medscape Medical News that the results are important, as they showed people who switched from placebo to the active drug also saw a long-term benefit.
What is “remarkable” about barzolvolimab, continued Giménez-Arnau, who was not involved in the study, is that it is the first drug to target the KIT receptor on mast cells and interfere with stimulating growth factors, thus making the cells that drive the development of CSU “disappear.”
The study included three different barzolvolimab regimens, with the 150-mg dose every 4 weeks and the 300-mg dose every 8 weeks achieving similar results, noted Giménez-Arnau.
For her, there are important questions to answer around the pharmacokinetic and pharmacodynamic profiles of the two regimens that remain, but she underlined that for the patient, the choice of regimen could have an impact on their quality of life.
“If we give 300 mg every 8 weeks,” she said, it appears “you can achieve disease control” while halving the frequency of subcutaneous injections.
She said that it would be “interesting to know” if 300 mg every 8 weeks is given as two 150-mg injections every 2 months or one 300-mg injection. If it is the former, Giménez Arnau said, “This is potentially an important benefit for the patient.”
Sustained Benefits at 1 Year
The study enrolled 208 patients with antihistamine-refractory CSU at sites in 10 countries, randomizing them to one of four arms: Subcutaneous injections of barzolvolimab 75 mg or 150 mg every 4 weeks, 300 mg every 8 weeks, or placebo every 4 weeks.
The mean age in each arm was between 42 and 47 years, and around 75% were women. Across the arms, 64%-76% had severe disease, as measured on the UAS7, at a mean score of 30.0-31.3. Around 20% had previously been treated with omalizumab.
Patients were treated for 16 weeks, during which time they completed daily and weekly diaries and attended six clinic visits at weeks 0, 2, 4, 8, 12, and 16. Results from the trial published earlier this year demonstrated that both the regimens (150 mg every 4 weeks and 300 mg every 8 weeks) achieved clinically meaningful and statistically significant improvement in UAS7, the primary endpoint, vs placebo at 12 weeks.
Participants in the barzolvolimab 75 mg and placebo arms were then randomized to receive barzolvolimab 150 mg every 4 weeks or 300 mg every 8 weeks, and those who had been in the 150-mg and 300-mg treatment arms continued with that treatment for a further 36 weeks. (The remaining patients have been continued on a further 24-week follow-up, but the data are not yet available.)
By the 52-week follow-up, 25% of patients who started in each of the barzolvolimab arms had discontinued treatment, as well as 16% first randomized to the placebo arm.
Metz reported that the improvements in UAS7 scores, observed as early as week 1, were sustained through week 52 in patients in both the ongoing 150-mg and 300-mg arms. Patients who initially started in the placebo and the barzolvolimab 75-mg groups caught up with those who had started on the higher doses, so that by week 52, there were no significant differences in urticaria activity, hives, or itch scores between the arms.
By week 52, the proportion of patients achieving well-controlled disease, defined as a UAS7 score ≤ 6, was 73.7% in the barzolvolimab 150 mg every 4-week arm and 68.2% in the 300 mg barzolvolimab every 8-week arm.
Notably, just 12.8% of patients in the placebo arm had achieved well-controlled CSU by week 16, but after switching to barzolvolimab 150 mg every 4 weeks or 300 mg every 8 weeks, 63% reached that target at week 52.
“Maybe even more striking and very interesting to look at,” said Metz, was the complete control of symptoms, meaning “not one single wheal and no itch.” By week 52, 52% of those on 300 mg every 8 weeks and 71.1% of those on 150 mg every 4 weeks had a complete response, with no itch/hives (UAS7 of 0).
Importantly, complete responses with barzolvolimab were observed early and were sustained or improved to week 52, Metz said, with, again, placebo and former barzolvolimab 75 mg patients catching up with those who started on 150 mg every 4 weeks and 300 mg every 8 weeks once they switched at week 16.
“This is the best data for chronic spontaneous urticaria that we have so far seen,” he said, adding that the responses were seen regardless of prior experience with omalizumab.
Changes in Hair Color, Skin Pigmentation
As for safety, during the first 16 weeks, 66% of those on active treatment and 39% on placebo experienced at least one adverse event. There were no treatment-related serious adverse events, compared with two among those who received treatment for the full 52 weeks.
The most common adverse events with active treatment were hair color changes (14% in the first 16 weeks and 26% among those treated for the full 52 weeks), neutropenia/reduced neutrophil count (9% in the first 16 weeks and 17% among those treated for the full 52 weeks), and skin hypopigmentation (1% in the first 16 weeks, 13% among those treated for the full 52 weeks, and 19% among those who switched from placebo to active treatment at 36 weeks). Urticaria was reported by 10% among patients on active treatment and 10% among those on placebo in the first 16 weeks, and by 15% of those treated for the full 52 weeks.
In the post-presentation discussion, Metz explained that the hypopigmentation appears to start around the hair follicle and is diffuse, so tends to look like vitiligo.
He suggested that the melanocytes around the hair follicle “seem to be the ones that are more stressed, maybe because of the hair follicle cycling,” adding that the effect is reversible and does not appear to be dose dependent.
The study was funded by Celldex Therapeutics. Metz declared relationships with AbbVie, ALK-Abelló, Almirall, Amgen, argenx, AstraZeneca, Astria, Attovia Therapeutics, Celldex, Celltrion, Escient Pharmaceuticals, Galen, Galderma, GSK, Incyte, Jasper, Lilly, Novartis, Pfizer, Pharvaris, Regeneron, Sanofi, Teva, Third Harmonic Bio, and Vifor.
A version of this article first appeared on Medscape.com.
of an ongoing phase 2 study.
Moreover, in the study, barzolvolimab, an anti-KIT monoclonal antibody that inhibits the activation of and depletes mast cells, induced comparable responses in a subset of patients who had taken omalizumab, an anti–immunoglobulin E monoclonal antibody approved by the Food and Drug Administration for treating CSU.
The findings were presented at the annual European Academy of Dermatology and Venereology (EADV) 2024 Congress. Barzolvolimab is being developed by Celldex Therapeutics.
“Barzolvolimab treatment resulted in rapid, profound, and durable improvement in UAS7 [weekly Urticaria Activity Score 7],” said presenter Martin Metz, MD, professor of dermatology, Institute of Allergology, Charité – Universitätsmedizin Berlin in Germany, “with a deepening of response over 52 weeks in patients with antihistamine-refractory CSU.”
“Similar robust improvement was seen in patients previously treated with omalizumab, including refractory patients,” he added.
Because barzolvolimab was well tolerated over the course of the follow-up period, Metz said, it “has the potential to be an important new treatment option,” noting that patients are now being enrolled in global phase 3 studies of barzolvolimab.
Sustained Symptom Relief
Ana M. Giménez-Arnau, MD, PhD, associate professor of dermatology, Autonomous University and Pompeu Fabra University, Barcelona, Spain, told Medscape Medical News that the results are important, as they showed people who switched from placebo to the active drug also saw a long-term benefit.
What is “remarkable” about barzolvolimab, continued Giménez-Arnau, who was not involved in the study, is that it is the first drug to target the KIT receptor on mast cells and interfere with stimulating growth factors, thus making the cells that drive the development of CSU “disappear.”
The study included three different barzolvolimab regimens, with the 150-mg dose every 4 weeks and the 300-mg dose every 8 weeks achieving similar results, noted Giménez-Arnau.
For her, there are important questions to answer around the pharmacokinetic and pharmacodynamic profiles of the two regimens that remain, but she underlined that for the patient, the choice of regimen could have an impact on their quality of life.
“If we give 300 mg every 8 weeks,” she said, it appears “you can achieve disease control” while halving the frequency of subcutaneous injections.
She said that it would be “interesting to know” if 300 mg every 8 weeks is given as two 150-mg injections every 2 months or one 300-mg injection. If it is the former, Giménez Arnau said, “This is potentially an important benefit for the patient.”
Sustained Benefits at 1 Year
The study enrolled 208 patients with antihistamine-refractory CSU at sites in 10 countries, randomizing them to one of four arms: Subcutaneous injections of barzolvolimab 75 mg or 150 mg every 4 weeks, 300 mg every 8 weeks, or placebo every 4 weeks.
The mean age in each arm was between 42 and 47 years, and around 75% were women. Across the arms, 64%-76% had severe disease, as measured on the UAS7, at a mean score of 30.0-31.3. Around 20% had previously been treated with omalizumab.
Patients were treated for 16 weeks, during which time they completed daily and weekly diaries and attended six clinic visits at weeks 0, 2, 4, 8, 12, and 16. Results from the trial published earlier this year demonstrated that both the regimens (150 mg every 4 weeks and 300 mg every 8 weeks) achieved clinically meaningful and statistically significant improvement in UAS7, the primary endpoint, vs placebo at 12 weeks.
Participants in the barzolvolimab 75 mg and placebo arms were then randomized to receive barzolvolimab 150 mg every 4 weeks or 300 mg every 8 weeks, and those who had been in the 150-mg and 300-mg treatment arms continued with that treatment for a further 36 weeks. (The remaining patients have been continued on a further 24-week follow-up, but the data are not yet available.)
By the 52-week follow-up, 25% of patients who started in each of the barzolvolimab arms had discontinued treatment, as well as 16% first randomized to the placebo arm.
Metz reported that the improvements in UAS7 scores, observed as early as week 1, were sustained through week 52 in patients in both the ongoing 150-mg and 300-mg arms. Patients who initially started in the placebo and the barzolvolimab 75-mg groups caught up with those who had started on the higher doses, so that by week 52, there were no significant differences in urticaria activity, hives, or itch scores between the arms.
By week 52, the proportion of patients achieving well-controlled disease, defined as a UAS7 score ≤ 6, was 73.7% in the barzolvolimab 150 mg every 4-week arm and 68.2% in the 300 mg barzolvolimab every 8-week arm.
Notably, just 12.8% of patients in the placebo arm had achieved well-controlled CSU by week 16, but after switching to barzolvolimab 150 mg every 4 weeks or 300 mg every 8 weeks, 63% reached that target at week 52.
“Maybe even more striking and very interesting to look at,” said Metz, was the complete control of symptoms, meaning “not one single wheal and no itch.” By week 52, 52% of those on 300 mg every 8 weeks and 71.1% of those on 150 mg every 4 weeks had a complete response, with no itch/hives (UAS7 of 0).
Importantly, complete responses with barzolvolimab were observed early and were sustained or improved to week 52, Metz said, with, again, placebo and former barzolvolimab 75 mg patients catching up with those who started on 150 mg every 4 weeks and 300 mg every 8 weeks once they switched at week 16.
“This is the best data for chronic spontaneous urticaria that we have so far seen,” he said, adding that the responses were seen regardless of prior experience with omalizumab.
Changes in Hair Color, Skin Pigmentation
As for safety, during the first 16 weeks, 66% of those on active treatment and 39% on placebo experienced at least one adverse event. There were no treatment-related serious adverse events, compared with two among those who received treatment for the full 52 weeks.
The most common adverse events with active treatment were hair color changes (14% in the first 16 weeks and 26% among those treated for the full 52 weeks), neutropenia/reduced neutrophil count (9% in the first 16 weeks and 17% among those treated for the full 52 weeks), and skin hypopigmentation (1% in the first 16 weeks, 13% among those treated for the full 52 weeks, and 19% among those who switched from placebo to active treatment at 36 weeks). Urticaria was reported by 10% among patients on active treatment and 10% among those on placebo in the first 16 weeks, and by 15% of those treated for the full 52 weeks.
In the post-presentation discussion, Metz explained that the hypopigmentation appears to start around the hair follicle and is diffuse, so tends to look like vitiligo.
He suggested that the melanocytes around the hair follicle “seem to be the ones that are more stressed, maybe because of the hair follicle cycling,” adding that the effect is reversible and does not appear to be dose dependent.
The study was funded by Celldex Therapeutics. Metz declared relationships with AbbVie, ALK-Abelló, Almirall, Amgen, argenx, AstraZeneca, Astria, Attovia Therapeutics, Celldex, Celltrion, Escient Pharmaceuticals, Galen, Galderma, GSK, Incyte, Jasper, Lilly, Novartis, Pfizer, Pharvaris, Regeneron, Sanofi, Teva, Third Harmonic Bio, and Vifor.
A version of this article first appeared on Medscape.com.
FROM EADV 2024
Children With Severe Atopic Dermatitis Catch Up on Growth With Dupilumab
AMSTERDAM — , revealed a post hoc trial analysis.
The research was presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
The trial included a “rigorously selected … well-characterized, well-studied” population of children aged 6-11 years, said presenter Alan D. Irvine, MD, DSc, professor of dermatology, Trinity College Dublin, Ireland.
It showed that “severe atopic dermatitis does cause restriction of growth, as well as a higher weight, and therefore obviously a higher BMI [body mass index].”
He continued, however, that children at the lower percentiles of height receiving prompt treatment with dupilumab (Dupixent) “were able to rapidly move through the centiles over the 16 weeks of the study, and that may be the window for catch-up growth … when children are growing rapidly.”
Anna Yasmine Kirkorian, MD, chief of dermatology, Children’s National Hospital, Washington, DC, who was not involved in the study, said that she was “surprised” at the degree of growth achieved over the study period, as height is not something that jumps up “overnight.”
“On the other hand, it fits with my experience with children who’ve had the brakes on all of their life due to inflammation, whether it be height, going to school, sleeping — everything is sort of put on pause by this terrible inflammatory process,” she said.
“When you take the brakes off, they get to be who they are going to be,” Kirkorian added. “So I was surprised by the speed of it, but not by the fact that height was acquired.”
Her belief is that in the pre-dupilumab era, severe atopic dermatitis was often insufficiently controlled, so children were “smaller than you would predict from parental height,” and the treatment is “allowing them to reach their genetic potential.”
Post Hoc Analysis
In his presentation, Irvine emphasized that it has been clearly demonstrated that adolescents with moderate and severe atopic dermatitis have a significantly higher likelihood of being below the 25th percentile of height on growth reference charts.
Such children are also at a higher risk of having low bone mineral density and low serum alkaline phosphatase (ALP) levels . While data presented at the EADV 2023 Congress showed that dupilumab significantly increased serum levels of bone ALP compared with placebo, the underlying mechanism remains unclear.
For the current analysis, Irvine and colleagues determined that the proportion of children aged 6-11 years with severe atopic dermatitis and lower stature reach a ≥ 5 centile improvement in height following 16 weeks of dupilumab treatment.
They examined data from the LIBERTY AD PEDS trial, in which patients aged 6-11 years with severe atopic dermatitis were randomized to 300 mg dupilumab every 4 weeks or placebo along with a mild or moderately potent topical corticosteroid. The study found that, overall, dupilumab was associated with significant improvements in signs, symptoms, and quality of life compared with placebo.
Height measures at baseline revealed that “more boys and more girls were below the 50th centile than you would predict for a healthy, normal control population,” Irvine said. “If we look at weight, we see the opposite,” he continued, “with a disproportionate number of boys and girls who are above the 50th centile for weight at baseline.”
Consequently, “we’re seeing these children who are shorter and heavier than the predicted healthy weight range and, as a result, obviously have higher BMI,” Irvine noted, with 67% girls and 62% boys found to have a higher BMI than normal for their age.
After 16 weeks of treatment with dupilumab, there was a much greater gain in height than that seen among those on placebo, with the most pronounced effect seen in children who had the lowest height at baseline. Indeed, among children in the lowest 25% height percentile at baseline, 30.6% on dupilumab vs 11.9% on placebo experienced an increase in height of 5 centiles or more(P < .05).
“This reflects what we see in clinical practice,” Irvine said. “Children often grow dramatically on treatment for atopic dermatitis.”
Among patients with a baseline height below the 30th percentile, 31.9% treated with dupilumab vs 11.1% treated with placebo gained at least 5 centiles in height. The figures for children below the 40th height percentile at baseline were 31.3% vs 15.5% (P < .05 for both).
Although there remained a marked difference in the proportion of children below the 50th height percentile at baseline gaining 5 centiles or more in height, at 29.0% with dupilumab versus 15.7% with placebo, it was no longer significant.
“So the effect of catch-up growth, or growth through the centiles, is most marked in those who are in the 40th centile or below,” Irvine said, indicating that the “more growth restricted kids have much more potential to catch up.”
‘Convincing’ Data
Overall, Kirkorian said in the interview, the data are “convincing” and support her view that severe atopic dermatitis is a “terrible chronic disease that we really underappreciate.” Atopic dermatitis, she added, “should get the respect that any severe chronic illness would have, whether that be arthritis, diabetes, or cardiac disease, because it is a systemic disorder that … profoundly affects quality of life, every minute of every day.”
However, “we don’t get all the referrals we should, until the child has suffered for years and years, and the family has suffered,” as there is a bias that it can be outgrown — although not everybody does — and it “doesn’t look as conspicuous as other chronic skin disorders,” such as psoriasis.
“Now with this study,” Kirkorian said, “it gives us a really compelling point to make to parents, to the community, and to insurers that not only are we affecting the quality of life from the itch standpoint [with dupilumab] but we may have long profound effects on growth and bone health.”
The research was sponsored by Sanofi and Regeneron Pharmaceuticals. Irvine declared relationships with AbbVie, Arena Pharmaceuticals, BenevolentAI, Chugai Pharmaceutical, Dermavant, Eli Lily, Genentech, LEO Pharma, Menlo Therapeutics, Novartis, Pfizer, Regeneron, Sanofi, UCB, DS Biopharma, and Inflazome. Kirkorian declared relationships with Dermavant, Verrica Pharmaceuticals, Pfizer, and Incyte.
A version of this article first appeared on Medscape.com.
AMSTERDAM — , revealed a post hoc trial analysis.
The research was presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
The trial included a “rigorously selected … well-characterized, well-studied” population of children aged 6-11 years, said presenter Alan D. Irvine, MD, DSc, professor of dermatology, Trinity College Dublin, Ireland.
It showed that “severe atopic dermatitis does cause restriction of growth, as well as a higher weight, and therefore obviously a higher BMI [body mass index].”
He continued, however, that children at the lower percentiles of height receiving prompt treatment with dupilumab (Dupixent) “were able to rapidly move through the centiles over the 16 weeks of the study, and that may be the window for catch-up growth … when children are growing rapidly.”
Anna Yasmine Kirkorian, MD, chief of dermatology, Children’s National Hospital, Washington, DC, who was not involved in the study, said that she was “surprised” at the degree of growth achieved over the study period, as height is not something that jumps up “overnight.”
“On the other hand, it fits with my experience with children who’ve had the brakes on all of their life due to inflammation, whether it be height, going to school, sleeping — everything is sort of put on pause by this terrible inflammatory process,” she said.
“When you take the brakes off, they get to be who they are going to be,” Kirkorian added. “So I was surprised by the speed of it, but not by the fact that height was acquired.”
Her belief is that in the pre-dupilumab era, severe atopic dermatitis was often insufficiently controlled, so children were “smaller than you would predict from parental height,” and the treatment is “allowing them to reach their genetic potential.”
Post Hoc Analysis
In his presentation, Irvine emphasized that it has been clearly demonstrated that adolescents with moderate and severe atopic dermatitis have a significantly higher likelihood of being below the 25th percentile of height on growth reference charts.
Such children are also at a higher risk of having low bone mineral density and low serum alkaline phosphatase (ALP) levels . While data presented at the EADV 2023 Congress showed that dupilumab significantly increased serum levels of bone ALP compared with placebo, the underlying mechanism remains unclear.
For the current analysis, Irvine and colleagues determined that the proportion of children aged 6-11 years with severe atopic dermatitis and lower stature reach a ≥ 5 centile improvement in height following 16 weeks of dupilumab treatment.
They examined data from the LIBERTY AD PEDS trial, in which patients aged 6-11 years with severe atopic dermatitis were randomized to 300 mg dupilumab every 4 weeks or placebo along with a mild or moderately potent topical corticosteroid. The study found that, overall, dupilumab was associated with significant improvements in signs, symptoms, and quality of life compared with placebo.
Height measures at baseline revealed that “more boys and more girls were below the 50th centile than you would predict for a healthy, normal control population,” Irvine said. “If we look at weight, we see the opposite,” he continued, “with a disproportionate number of boys and girls who are above the 50th centile for weight at baseline.”
Consequently, “we’re seeing these children who are shorter and heavier than the predicted healthy weight range and, as a result, obviously have higher BMI,” Irvine noted, with 67% girls and 62% boys found to have a higher BMI than normal for their age.
After 16 weeks of treatment with dupilumab, there was a much greater gain in height than that seen among those on placebo, with the most pronounced effect seen in children who had the lowest height at baseline. Indeed, among children in the lowest 25% height percentile at baseline, 30.6% on dupilumab vs 11.9% on placebo experienced an increase in height of 5 centiles or more(P < .05).
“This reflects what we see in clinical practice,” Irvine said. “Children often grow dramatically on treatment for atopic dermatitis.”
Among patients with a baseline height below the 30th percentile, 31.9% treated with dupilumab vs 11.1% treated with placebo gained at least 5 centiles in height. The figures for children below the 40th height percentile at baseline were 31.3% vs 15.5% (P < .05 for both).
Although there remained a marked difference in the proportion of children below the 50th height percentile at baseline gaining 5 centiles or more in height, at 29.0% with dupilumab versus 15.7% with placebo, it was no longer significant.
“So the effect of catch-up growth, or growth through the centiles, is most marked in those who are in the 40th centile or below,” Irvine said, indicating that the “more growth restricted kids have much more potential to catch up.”
‘Convincing’ Data
Overall, Kirkorian said in the interview, the data are “convincing” and support her view that severe atopic dermatitis is a “terrible chronic disease that we really underappreciate.” Atopic dermatitis, she added, “should get the respect that any severe chronic illness would have, whether that be arthritis, diabetes, or cardiac disease, because it is a systemic disorder that … profoundly affects quality of life, every minute of every day.”
However, “we don’t get all the referrals we should, until the child has suffered for years and years, and the family has suffered,” as there is a bias that it can be outgrown — although not everybody does — and it “doesn’t look as conspicuous as other chronic skin disorders,” such as psoriasis.
“Now with this study,” Kirkorian said, “it gives us a really compelling point to make to parents, to the community, and to insurers that not only are we affecting the quality of life from the itch standpoint [with dupilumab] but we may have long profound effects on growth and bone health.”
The research was sponsored by Sanofi and Regeneron Pharmaceuticals. Irvine declared relationships with AbbVie, Arena Pharmaceuticals, BenevolentAI, Chugai Pharmaceutical, Dermavant, Eli Lily, Genentech, LEO Pharma, Menlo Therapeutics, Novartis, Pfizer, Regeneron, Sanofi, UCB, DS Biopharma, and Inflazome. Kirkorian declared relationships with Dermavant, Verrica Pharmaceuticals, Pfizer, and Incyte.
A version of this article first appeared on Medscape.com.
AMSTERDAM — , revealed a post hoc trial analysis.
The research was presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
The trial included a “rigorously selected … well-characterized, well-studied” population of children aged 6-11 years, said presenter Alan D. Irvine, MD, DSc, professor of dermatology, Trinity College Dublin, Ireland.
It showed that “severe atopic dermatitis does cause restriction of growth, as well as a higher weight, and therefore obviously a higher BMI [body mass index].”
He continued, however, that children at the lower percentiles of height receiving prompt treatment with dupilumab (Dupixent) “were able to rapidly move through the centiles over the 16 weeks of the study, and that may be the window for catch-up growth … when children are growing rapidly.”
Anna Yasmine Kirkorian, MD, chief of dermatology, Children’s National Hospital, Washington, DC, who was not involved in the study, said that she was “surprised” at the degree of growth achieved over the study period, as height is not something that jumps up “overnight.”
“On the other hand, it fits with my experience with children who’ve had the brakes on all of their life due to inflammation, whether it be height, going to school, sleeping — everything is sort of put on pause by this terrible inflammatory process,” she said.
“When you take the brakes off, they get to be who they are going to be,” Kirkorian added. “So I was surprised by the speed of it, but not by the fact that height was acquired.”
Her belief is that in the pre-dupilumab era, severe atopic dermatitis was often insufficiently controlled, so children were “smaller than you would predict from parental height,” and the treatment is “allowing them to reach their genetic potential.”
Post Hoc Analysis
In his presentation, Irvine emphasized that it has been clearly demonstrated that adolescents with moderate and severe atopic dermatitis have a significantly higher likelihood of being below the 25th percentile of height on growth reference charts.
Such children are also at a higher risk of having low bone mineral density and low serum alkaline phosphatase (ALP) levels . While data presented at the EADV 2023 Congress showed that dupilumab significantly increased serum levels of bone ALP compared with placebo, the underlying mechanism remains unclear.
For the current analysis, Irvine and colleagues determined that the proportion of children aged 6-11 years with severe atopic dermatitis and lower stature reach a ≥ 5 centile improvement in height following 16 weeks of dupilumab treatment.
They examined data from the LIBERTY AD PEDS trial, in which patients aged 6-11 years with severe atopic dermatitis were randomized to 300 mg dupilumab every 4 weeks or placebo along with a mild or moderately potent topical corticosteroid. The study found that, overall, dupilumab was associated with significant improvements in signs, symptoms, and quality of life compared with placebo.
Height measures at baseline revealed that “more boys and more girls were below the 50th centile than you would predict for a healthy, normal control population,” Irvine said. “If we look at weight, we see the opposite,” he continued, “with a disproportionate number of boys and girls who are above the 50th centile for weight at baseline.”
Consequently, “we’re seeing these children who are shorter and heavier than the predicted healthy weight range and, as a result, obviously have higher BMI,” Irvine noted, with 67% girls and 62% boys found to have a higher BMI than normal for their age.
After 16 weeks of treatment with dupilumab, there was a much greater gain in height than that seen among those on placebo, with the most pronounced effect seen in children who had the lowest height at baseline. Indeed, among children in the lowest 25% height percentile at baseline, 30.6% on dupilumab vs 11.9% on placebo experienced an increase in height of 5 centiles or more(P < .05).
“This reflects what we see in clinical practice,” Irvine said. “Children often grow dramatically on treatment for atopic dermatitis.”
Among patients with a baseline height below the 30th percentile, 31.9% treated with dupilumab vs 11.1% treated with placebo gained at least 5 centiles in height. The figures for children below the 40th height percentile at baseline were 31.3% vs 15.5% (P < .05 for both).
Although there remained a marked difference in the proportion of children below the 50th height percentile at baseline gaining 5 centiles or more in height, at 29.0% with dupilumab versus 15.7% with placebo, it was no longer significant.
“So the effect of catch-up growth, or growth through the centiles, is most marked in those who are in the 40th centile or below,” Irvine said, indicating that the “more growth restricted kids have much more potential to catch up.”
‘Convincing’ Data
Overall, Kirkorian said in the interview, the data are “convincing” and support her view that severe atopic dermatitis is a “terrible chronic disease that we really underappreciate.” Atopic dermatitis, she added, “should get the respect that any severe chronic illness would have, whether that be arthritis, diabetes, or cardiac disease, because it is a systemic disorder that … profoundly affects quality of life, every minute of every day.”
However, “we don’t get all the referrals we should, until the child has suffered for years and years, and the family has suffered,” as there is a bias that it can be outgrown — although not everybody does — and it “doesn’t look as conspicuous as other chronic skin disorders,” such as psoriasis.
“Now with this study,” Kirkorian said, “it gives us a really compelling point to make to parents, to the community, and to insurers that not only are we affecting the quality of life from the itch standpoint [with dupilumab] but we may have long profound effects on growth and bone health.”
The research was sponsored by Sanofi and Regeneron Pharmaceuticals. Irvine declared relationships with AbbVie, Arena Pharmaceuticals, BenevolentAI, Chugai Pharmaceutical, Dermavant, Eli Lily, Genentech, LEO Pharma, Menlo Therapeutics, Novartis, Pfizer, Regeneron, Sanofi, UCB, DS Biopharma, and Inflazome. Kirkorian declared relationships with Dermavant, Verrica Pharmaceuticals, Pfizer, and Incyte.
A version of this article first appeared on Medscape.com.
FROM EADV 2024
Nemolizumab Benefits for Atopic Dermatitis Maintained in Long-Term Follow-Up Study
(AD), revealed an interim analysis of the ARCADIA open-label extension study.
The research was presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
The results showed nemolizumab was associated with “ongoing clinically meaningful improvements in itch, skin lesions, and sleep disturbance,” said study presenter Diamant Thaçi, MD, PhD, of the Comprehensive Center for Inflammation Medicine, University of Lü̈beck in Germany.
Moreover, “patient-reported outcomes, including quality of life ... continued to improve over 56 weeks of treatment.” In addition, Thaçi added, the “safety data support the long-term use of nemolizumab for the treatment of adolescent and adult patients with moderate to severe atopic dermatitis.”
He explained that interleukin (IL) 31 is a key neuroimmune cytokine in AD, triggering itch, skin barrier disruption, and exacerbation of inflammation via its receptor. Nemolizumab inhibits IL-31 receptor binding and was shown in the ARCADIA 1 and ARCADIA 2 trials to provide, along with background topical corticosteroids, clinically meaningful improvements in itch, skin lesions, and sleep for up to weeks 48 of follow-up in adolescents and adults with moderate to severe AD.
The current open-label long-term extension study involved patients who were enrolled in both ARCADIA 1 and 2 trials, as well as those from four phase 2 and 2b studies, a phase 3b study, and adolescents who had not been included in a trial but who met the criteria for the extension study. All patients, whether they started on placebo plus background topical corticosteroids in a prior study, were treated with nemolizumab 30 mg subcutaneously every 4 weeks along with topical corticosteroids.
The interim analysis included all efficacy and safety data up to the cutoff of September 30, 2022, on 723 patients who had completed 56 weeks of treatment among the 1751 patients initially enrolled in the extension study.
The results showed that, regardless of whether patients were nemolizumab naive at enrollment or had previously taken the drug, there were increases in the proportion of patients with an Investigator Global Assessment (IGA) score of 0/1 and an Eczema Area and Severity Index (EASI) score of at least 75 (EASI-75) over the 56 weeks of the study.
In those naive to nemolizumab, the increase in the proportion with an IGA score of 0/1 increased from 17.7% at baseline to 49.0% at 56 weeks, while the proportion with an EASI-75 increased from 24.0% to 78.7%.
The increase in the proportion of patients with an IGA score 0/1 among those who had previously received nemolizumab increased from 28.5% at baseline to 47.1% at 56 weeks. The proportion with an EASI-75 was 38.1% at baseline, rising to 73.0% at 56 weeks.
Increases in the proportion of patients with an EASI score of at least 50 and at least 90 were also seen with nemolizumab, as were increases in the proportion of patients with an improvement of at least four points on the SCORing Atopic Dermatitis Pruritus visual analogue scale and Sleep loss scores.
Similarly, the proportion of patients with a reduction in Dermatology Life Quality Index of at least four points increased over the study period.
Regarding safety, Thaçi said, there appeared to be fewer adverse events than had been previously reported with nemolizumab. “We don’t see any signs of conjunctivitis,” he continued, or significant risk of infection apart from for COVID-19, but he pointed out that the study was conducted during the pandemic, which was “a very difficult time.”
The most common treatment-related adverse events were, aside from COVID-19, nasopharyngitis in about 10%-11% of patients, upper respiratory tract infection in about 6% to almost 7%, and headache in about 5%.
Among the adverse events of special interest, newly diagnosed asthma or worsening of asthma occurred in 4.7%-4.8% of patients, while peripheral edema was seen in 0.8%-1.7%.
“Besides this, the study results are really looking very good,” he said, adding: “It means, in a long-term study, we can say today that nemolizumab has revealed the [same] safety profile that was shown in the ARCADIA 1 and 2 trials.”
Alan D. Irvine, MD, DSc, professor of dermatology, Trinity College Dublin in Ireland, who was not involved in the study, underlined that the current interim assessment does not represent the complete dataset and is based on observed cases rather than a more rigorous methodology, such as net reclassification improvement analysis.
“So it makes it a little harder to interpret when you don’t know how many people are dropping out and why they’re dropping out,” he told this news organization. “That said, those who remain on drug out to 56 weeks do experience ongoing improvement in disease control.”
Consequently, “the most reliable message you can take from this interim analysis of long-term data is that there were no new safety signals,” and nemolizumab looks “safe and well-tolerated.”
Where nemolizumab would fit into the treatment pathway for moderate to severe AD remains an open question, Irvine said, although he believes that IL-13 pathway inhibitors such as dupilumab, tralokinumab, and lebrikizumab “will remain the treatment of choice for the immediate future due to prescriber familiarity and good efficacy data.”
However, for patients who are unsuitable for IL-13 inhibitors and/or Janus kinase inhibitors such as abrocitinib and upadacitinib, nemolizumab “could be an interesting alternative.”
“That’s probably where it is going to start,” Irvine said, “and then obviously that will change over time and as the data mature and prescribers become more familiar with the drug in the real world.”
Nemolizumab (Nemluvio) is approved for treating prurigo nodularis (PN) in the United States and in Japan and is under Food and Drug Administration review for treating AD. It is also under review for PN and AD in Europe, Canada, the United Kingdom, and several other countries, according to Galderma. It is also approved for treating pruritus associated with AD in pediatric, adolescent, and adult patients in Japan.
The study was funded by Galderma. Thaçi declared relationships with AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celltrion, Galderma, Janssen-Cilag, Kyowa Kirin, LEO Pharma, L’Oréal, Eli Lilly, Novartis, Pfizer, Regeneron, Sanofi, Target RWE, and UCB. Irvine declared relationships with AbbVie, Arena Pharmaceuticals, BenevolentAl, Chugai Pharmaceutical, Dermavant, Eli Lily, Genentech, LEO Pharma, Menlo Therapeutics, Novartis, Pfizer, Regeneron, Sanofi, UCB, DS Biopharma, and Inflazome.
A version of this article first appeared on Medscape.com.
(AD), revealed an interim analysis of the ARCADIA open-label extension study.
The research was presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
The results showed nemolizumab was associated with “ongoing clinically meaningful improvements in itch, skin lesions, and sleep disturbance,” said study presenter Diamant Thaçi, MD, PhD, of the Comprehensive Center for Inflammation Medicine, University of Lü̈beck in Germany.
Moreover, “patient-reported outcomes, including quality of life ... continued to improve over 56 weeks of treatment.” In addition, Thaçi added, the “safety data support the long-term use of nemolizumab for the treatment of adolescent and adult patients with moderate to severe atopic dermatitis.”
He explained that interleukin (IL) 31 is a key neuroimmune cytokine in AD, triggering itch, skin barrier disruption, and exacerbation of inflammation via its receptor. Nemolizumab inhibits IL-31 receptor binding and was shown in the ARCADIA 1 and ARCADIA 2 trials to provide, along with background topical corticosteroids, clinically meaningful improvements in itch, skin lesions, and sleep for up to weeks 48 of follow-up in adolescents and adults with moderate to severe AD.
The current open-label long-term extension study involved patients who were enrolled in both ARCADIA 1 and 2 trials, as well as those from four phase 2 and 2b studies, a phase 3b study, and adolescents who had not been included in a trial but who met the criteria for the extension study. All patients, whether they started on placebo plus background topical corticosteroids in a prior study, were treated with nemolizumab 30 mg subcutaneously every 4 weeks along with topical corticosteroids.
The interim analysis included all efficacy and safety data up to the cutoff of September 30, 2022, on 723 patients who had completed 56 weeks of treatment among the 1751 patients initially enrolled in the extension study.
The results showed that, regardless of whether patients were nemolizumab naive at enrollment or had previously taken the drug, there were increases in the proportion of patients with an Investigator Global Assessment (IGA) score of 0/1 and an Eczema Area and Severity Index (EASI) score of at least 75 (EASI-75) over the 56 weeks of the study.
In those naive to nemolizumab, the increase in the proportion with an IGA score of 0/1 increased from 17.7% at baseline to 49.0% at 56 weeks, while the proportion with an EASI-75 increased from 24.0% to 78.7%.
The increase in the proportion of patients with an IGA score 0/1 among those who had previously received nemolizumab increased from 28.5% at baseline to 47.1% at 56 weeks. The proportion with an EASI-75 was 38.1% at baseline, rising to 73.0% at 56 weeks.
Increases in the proportion of patients with an EASI score of at least 50 and at least 90 were also seen with nemolizumab, as were increases in the proportion of patients with an improvement of at least four points on the SCORing Atopic Dermatitis Pruritus visual analogue scale and Sleep loss scores.
Similarly, the proportion of patients with a reduction in Dermatology Life Quality Index of at least four points increased over the study period.
Regarding safety, Thaçi said, there appeared to be fewer adverse events than had been previously reported with nemolizumab. “We don’t see any signs of conjunctivitis,” he continued, or significant risk of infection apart from for COVID-19, but he pointed out that the study was conducted during the pandemic, which was “a very difficult time.”
The most common treatment-related adverse events were, aside from COVID-19, nasopharyngitis in about 10%-11% of patients, upper respiratory tract infection in about 6% to almost 7%, and headache in about 5%.
Among the adverse events of special interest, newly diagnosed asthma or worsening of asthma occurred in 4.7%-4.8% of patients, while peripheral edema was seen in 0.8%-1.7%.
“Besides this, the study results are really looking very good,” he said, adding: “It means, in a long-term study, we can say today that nemolizumab has revealed the [same] safety profile that was shown in the ARCADIA 1 and 2 trials.”
Alan D. Irvine, MD, DSc, professor of dermatology, Trinity College Dublin in Ireland, who was not involved in the study, underlined that the current interim assessment does not represent the complete dataset and is based on observed cases rather than a more rigorous methodology, such as net reclassification improvement analysis.
“So it makes it a little harder to interpret when you don’t know how many people are dropping out and why they’re dropping out,” he told this news organization. “That said, those who remain on drug out to 56 weeks do experience ongoing improvement in disease control.”
Consequently, “the most reliable message you can take from this interim analysis of long-term data is that there were no new safety signals,” and nemolizumab looks “safe and well-tolerated.”
Where nemolizumab would fit into the treatment pathway for moderate to severe AD remains an open question, Irvine said, although he believes that IL-13 pathway inhibitors such as dupilumab, tralokinumab, and lebrikizumab “will remain the treatment of choice for the immediate future due to prescriber familiarity and good efficacy data.”
However, for patients who are unsuitable for IL-13 inhibitors and/or Janus kinase inhibitors such as abrocitinib and upadacitinib, nemolizumab “could be an interesting alternative.”
“That’s probably where it is going to start,” Irvine said, “and then obviously that will change over time and as the data mature and prescribers become more familiar with the drug in the real world.”
Nemolizumab (Nemluvio) is approved for treating prurigo nodularis (PN) in the United States and in Japan and is under Food and Drug Administration review for treating AD. It is also under review for PN and AD in Europe, Canada, the United Kingdom, and several other countries, according to Galderma. It is also approved for treating pruritus associated with AD in pediatric, adolescent, and adult patients in Japan.
The study was funded by Galderma. Thaçi declared relationships with AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celltrion, Galderma, Janssen-Cilag, Kyowa Kirin, LEO Pharma, L’Oréal, Eli Lilly, Novartis, Pfizer, Regeneron, Sanofi, Target RWE, and UCB. Irvine declared relationships with AbbVie, Arena Pharmaceuticals, BenevolentAl, Chugai Pharmaceutical, Dermavant, Eli Lily, Genentech, LEO Pharma, Menlo Therapeutics, Novartis, Pfizer, Regeneron, Sanofi, UCB, DS Biopharma, and Inflazome.
A version of this article first appeared on Medscape.com.
(AD), revealed an interim analysis of the ARCADIA open-label extension study.
The research was presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress.
The results showed nemolizumab was associated with “ongoing clinically meaningful improvements in itch, skin lesions, and sleep disturbance,” said study presenter Diamant Thaçi, MD, PhD, of the Comprehensive Center for Inflammation Medicine, University of Lü̈beck in Germany.
Moreover, “patient-reported outcomes, including quality of life ... continued to improve over 56 weeks of treatment.” In addition, Thaçi added, the “safety data support the long-term use of nemolizumab for the treatment of adolescent and adult patients with moderate to severe atopic dermatitis.”
He explained that interleukin (IL) 31 is a key neuroimmune cytokine in AD, triggering itch, skin barrier disruption, and exacerbation of inflammation via its receptor. Nemolizumab inhibits IL-31 receptor binding and was shown in the ARCADIA 1 and ARCADIA 2 trials to provide, along with background topical corticosteroids, clinically meaningful improvements in itch, skin lesions, and sleep for up to weeks 48 of follow-up in adolescents and adults with moderate to severe AD.
The current open-label long-term extension study involved patients who were enrolled in both ARCADIA 1 and 2 trials, as well as those from four phase 2 and 2b studies, a phase 3b study, and adolescents who had not been included in a trial but who met the criteria for the extension study. All patients, whether they started on placebo plus background topical corticosteroids in a prior study, were treated with nemolizumab 30 mg subcutaneously every 4 weeks along with topical corticosteroids.
The interim analysis included all efficacy and safety data up to the cutoff of September 30, 2022, on 723 patients who had completed 56 weeks of treatment among the 1751 patients initially enrolled in the extension study.
The results showed that, regardless of whether patients were nemolizumab naive at enrollment or had previously taken the drug, there were increases in the proportion of patients with an Investigator Global Assessment (IGA) score of 0/1 and an Eczema Area and Severity Index (EASI) score of at least 75 (EASI-75) over the 56 weeks of the study.
In those naive to nemolizumab, the increase in the proportion with an IGA score of 0/1 increased from 17.7% at baseline to 49.0% at 56 weeks, while the proportion with an EASI-75 increased from 24.0% to 78.7%.
The increase in the proportion of patients with an IGA score 0/1 among those who had previously received nemolizumab increased from 28.5% at baseline to 47.1% at 56 weeks. The proportion with an EASI-75 was 38.1% at baseline, rising to 73.0% at 56 weeks.
Increases in the proportion of patients with an EASI score of at least 50 and at least 90 were also seen with nemolizumab, as were increases in the proportion of patients with an improvement of at least four points on the SCORing Atopic Dermatitis Pruritus visual analogue scale and Sleep loss scores.
Similarly, the proportion of patients with a reduction in Dermatology Life Quality Index of at least four points increased over the study period.
Regarding safety, Thaçi said, there appeared to be fewer adverse events than had been previously reported with nemolizumab. “We don’t see any signs of conjunctivitis,” he continued, or significant risk of infection apart from for COVID-19, but he pointed out that the study was conducted during the pandemic, which was “a very difficult time.”
The most common treatment-related adverse events were, aside from COVID-19, nasopharyngitis in about 10%-11% of patients, upper respiratory tract infection in about 6% to almost 7%, and headache in about 5%.
Among the adverse events of special interest, newly diagnosed asthma or worsening of asthma occurred in 4.7%-4.8% of patients, while peripheral edema was seen in 0.8%-1.7%.
“Besides this, the study results are really looking very good,” he said, adding: “It means, in a long-term study, we can say today that nemolizumab has revealed the [same] safety profile that was shown in the ARCADIA 1 and 2 trials.”
Alan D. Irvine, MD, DSc, professor of dermatology, Trinity College Dublin in Ireland, who was not involved in the study, underlined that the current interim assessment does not represent the complete dataset and is based on observed cases rather than a more rigorous methodology, such as net reclassification improvement analysis.
“So it makes it a little harder to interpret when you don’t know how many people are dropping out and why they’re dropping out,” he told this news organization. “That said, those who remain on drug out to 56 weeks do experience ongoing improvement in disease control.”
Consequently, “the most reliable message you can take from this interim analysis of long-term data is that there were no new safety signals,” and nemolizumab looks “safe and well-tolerated.”
Where nemolizumab would fit into the treatment pathway for moderate to severe AD remains an open question, Irvine said, although he believes that IL-13 pathway inhibitors such as dupilumab, tralokinumab, and lebrikizumab “will remain the treatment of choice for the immediate future due to prescriber familiarity and good efficacy data.”
However, for patients who are unsuitable for IL-13 inhibitors and/or Janus kinase inhibitors such as abrocitinib and upadacitinib, nemolizumab “could be an interesting alternative.”
“That’s probably where it is going to start,” Irvine said, “and then obviously that will change over time and as the data mature and prescribers become more familiar with the drug in the real world.”
Nemolizumab (Nemluvio) is approved for treating prurigo nodularis (PN) in the United States and in Japan and is under Food and Drug Administration review for treating AD. It is also under review for PN and AD in Europe, Canada, the United Kingdom, and several other countries, according to Galderma. It is also approved for treating pruritus associated with AD in pediatric, adolescent, and adult patients in Japan.
The study was funded by Galderma. Thaçi declared relationships with AbbVie, Almirall, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Celltrion, Galderma, Janssen-Cilag, Kyowa Kirin, LEO Pharma, L’Oréal, Eli Lilly, Novartis, Pfizer, Regeneron, Sanofi, Target RWE, and UCB. Irvine declared relationships with AbbVie, Arena Pharmaceuticals, BenevolentAl, Chugai Pharmaceutical, Dermavant, Eli Lily, Genentech, LEO Pharma, Menlo Therapeutics, Novartis, Pfizer, Regeneron, Sanofi, UCB, DS Biopharma, and Inflazome.
A version of this article first appeared on Medscape.com.
FROM EADV 2024
Lichen Planus Responds to Treatment with Topical Ruxolitinib in Phase 2 Study
both when given twice daily and as needed, according to data from a phase 2 trial.
The research, presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress, involved 64 patients older than 18 years. Ruxolitinib cream (Opzelura) is a topical formulation of a Janus kinase (JAK)1/JAK2 inhibitor, approved by the Food and Drug Administration (FDA) for treating mild to moderate atopic dermatitis and for nonsegmental vitiligo in adults and children aged 12 years or older.
Ruxolitinib cream twice daily resulted in “significant improvements in cutaneous lichen planus disease severity vs vehicle” after 16 weeks of treatment, said the study presenter, Aaron R. Mangold, MD, a dermatologist at Mayo Clinic, Scottsdale, Arizona.
Further improvements were seen during another 16 weeks of additional open-label, as-needed application, he added, and the topical treatment was “generally well tolerated.”
Consequently, “ruxolitinib cream represents a promising potential treatment for cutaneous lichen planus,” Mangold concluded.
Asked to comment on the results, Adam Friedman, MD, Professor and Chair of Dermatology, George Washington University, Washington, DC, who was not involved with the study, said that in keeping with the characterization of lichen planus using the four Ps — purple, polygonal, pruritic, papules — it is “Pretty common, Predictably disabling and disfiguring, and Passed over again and again in the drug development world.”
He said in an interview that this chronic inflammatory skin condition, which affects roughly 2% of the population, also “lacks consensus on work-up and management, likely in part owing to the absence of sizable clinical trial data.”
A recent survey conducted at a meeting indicated that dermatologists “heavily lean on topical therapies for the management of all severity levels,” noted Friedman, one of the survey authors. “Therefore, the phase 2 data presented at EADV is a welcome addition to the mix.”
Phase 2 Study Results
At the meeting, Mangold said that a previous proof-of-concept single-arm study in 12 patients suggested that topical ruxolitinib was highly effective in treating cutaneous lichen planus.
The current phase 2 trial enrolled 64 patients with predominantly cutaneous disease who had an Investigator’s Global Assessment (IGA) score of 3 or 4 and an Itch Numeric Rating Scale (NRS) score of ≥ 4. Their median age was 57 years, and 71.9% were women. Nearly 63% were White, 28.1% were Black, and 6.3% were Asian. The median duration of disease was 4.9 years, and 90.6% had received prior treatment for their lichen planus.
They were randomized to receive 1.5% ruxolitinib cream or a vehicle cream twice daily for 16 weeks, and following a primary endpoint assessment, they were transferred to an open-label extension period, during which they used ruxolitinib cream as needed for another 16 weeks. There was an additional 30-day safety follow-up period.
At week 16, significantly more patients treated with the ruxolitinib cream (50.0%) vs vehicle cream (21.9%) achieved IGA treatment success (the primary endpoint), defined as an IGA score of 0 or 1 with ≥ 2-grade improvement from baseline (odds ratio, 4.04; P = .0129).
In the open-label extension, when all patients used the active cream as needed, the proportion achieving IGA treatment success increased to 60% among the patients originally treated with ruxolitinib cream and 60.9% among those who switched from the vehicle cream.
A similar pattern was seen with Itch NRS scores. At 16 weeks, 57.7% of those treated with the ruxolitinib cream and 19.2% of those given the vehicle cream achieved an Itch NRS score of ≥ 4 (P < .01), rising to 84.2% and 73.3%, respectively, during the open-label extension.
The time to achievement of an Itch NRS of ≥ 4 was also significantly shorter with the ruxolitinib cream than with the vehicle cream (median days, 17 vs 97; hazard ratio, 2.85; P = .0008).
In both treatment groups, Skin Pain NRS scores decreased by a mean of 3.0 with ruxolitinib cream and 1.3 with the vehicle cream at week 16. By the end of the open-label extension, scores dropped by 4.3 among those who continued on active treatment and by 3.5 among those who switched from vehicle to topical ruxolitinib.
There were few treatment-emergent adverse events, with just three ruxolitinib patients affected during the randomized phase of the trial. There was one grade ≥ 3 event considered unrelated to the study drug, and no serious treatment-emergent adverse events were reported.
The most common adverse events during the randomized period were nasopharyngitis, hypertension, and contusion, all experienced by fewer than 10% of patients, whereas sinusitis, increased blood cholesterol levels, and increased blood creatine phosphokinase were most common in the open-label extension, experienced by no more than 5% of patients.
In the interview, Friedman commented that “these data provide hope that one day soon, there will be an FDA-approved, effective, and well-tolerated approach for this condition, validating the patient and supporting the dermatologist with an evidence-based option.”
The study was funded by Incyte. Mangold declared relationships with Argenx, Boehringer Ingelheim, Bristol-Myers Squibb, Clarivate, Incyte Corporation, Janssen, Nuvig Therapeutics, Pfizer, Regeneron Pharmaceuticals, Soligenix, Tourmaline Bio, AbbVie, Corbus, Eli Lilly, Kyowa, Merck, miRagen Therapeutics, Palvella Therapeutics, Priovant Therapeutics, and Adelphi Values. Friedman declared a relationship with Incyte, but it is not related to this topic.
A version of this article first appeared on Medscape.com.
both when given twice daily and as needed, according to data from a phase 2 trial.
The research, presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress, involved 64 patients older than 18 years. Ruxolitinib cream (Opzelura) is a topical formulation of a Janus kinase (JAK)1/JAK2 inhibitor, approved by the Food and Drug Administration (FDA) for treating mild to moderate atopic dermatitis and for nonsegmental vitiligo in adults and children aged 12 years or older.
Ruxolitinib cream twice daily resulted in “significant improvements in cutaneous lichen planus disease severity vs vehicle” after 16 weeks of treatment, said the study presenter, Aaron R. Mangold, MD, a dermatologist at Mayo Clinic, Scottsdale, Arizona.
Further improvements were seen during another 16 weeks of additional open-label, as-needed application, he added, and the topical treatment was “generally well tolerated.”
Consequently, “ruxolitinib cream represents a promising potential treatment for cutaneous lichen planus,” Mangold concluded.
Asked to comment on the results, Adam Friedman, MD, Professor and Chair of Dermatology, George Washington University, Washington, DC, who was not involved with the study, said that in keeping with the characterization of lichen planus using the four Ps — purple, polygonal, pruritic, papules — it is “Pretty common, Predictably disabling and disfiguring, and Passed over again and again in the drug development world.”
He said in an interview that this chronic inflammatory skin condition, which affects roughly 2% of the population, also “lacks consensus on work-up and management, likely in part owing to the absence of sizable clinical trial data.”
A recent survey conducted at a meeting indicated that dermatologists “heavily lean on topical therapies for the management of all severity levels,” noted Friedman, one of the survey authors. “Therefore, the phase 2 data presented at EADV is a welcome addition to the mix.”
Phase 2 Study Results
At the meeting, Mangold said that a previous proof-of-concept single-arm study in 12 patients suggested that topical ruxolitinib was highly effective in treating cutaneous lichen planus.
The current phase 2 trial enrolled 64 patients with predominantly cutaneous disease who had an Investigator’s Global Assessment (IGA) score of 3 or 4 and an Itch Numeric Rating Scale (NRS) score of ≥ 4. Their median age was 57 years, and 71.9% were women. Nearly 63% were White, 28.1% were Black, and 6.3% were Asian. The median duration of disease was 4.9 years, and 90.6% had received prior treatment for their lichen planus.
They were randomized to receive 1.5% ruxolitinib cream or a vehicle cream twice daily for 16 weeks, and following a primary endpoint assessment, they were transferred to an open-label extension period, during which they used ruxolitinib cream as needed for another 16 weeks. There was an additional 30-day safety follow-up period.
At week 16, significantly more patients treated with the ruxolitinib cream (50.0%) vs vehicle cream (21.9%) achieved IGA treatment success (the primary endpoint), defined as an IGA score of 0 or 1 with ≥ 2-grade improvement from baseline (odds ratio, 4.04; P = .0129).
In the open-label extension, when all patients used the active cream as needed, the proportion achieving IGA treatment success increased to 60% among the patients originally treated with ruxolitinib cream and 60.9% among those who switched from the vehicle cream.
A similar pattern was seen with Itch NRS scores. At 16 weeks, 57.7% of those treated with the ruxolitinib cream and 19.2% of those given the vehicle cream achieved an Itch NRS score of ≥ 4 (P < .01), rising to 84.2% and 73.3%, respectively, during the open-label extension.
The time to achievement of an Itch NRS of ≥ 4 was also significantly shorter with the ruxolitinib cream than with the vehicle cream (median days, 17 vs 97; hazard ratio, 2.85; P = .0008).
In both treatment groups, Skin Pain NRS scores decreased by a mean of 3.0 with ruxolitinib cream and 1.3 with the vehicle cream at week 16. By the end of the open-label extension, scores dropped by 4.3 among those who continued on active treatment and by 3.5 among those who switched from vehicle to topical ruxolitinib.
There were few treatment-emergent adverse events, with just three ruxolitinib patients affected during the randomized phase of the trial. There was one grade ≥ 3 event considered unrelated to the study drug, and no serious treatment-emergent adverse events were reported.
The most common adverse events during the randomized period were nasopharyngitis, hypertension, and contusion, all experienced by fewer than 10% of patients, whereas sinusitis, increased blood cholesterol levels, and increased blood creatine phosphokinase were most common in the open-label extension, experienced by no more than 5% of patients.
In the interview, Friedman commented that “these data provide hope that one day soon, there will be an FDA-approved, effective, and well-tolerated approach for this condition, validating the patient and supporting the dermatologist with an evidence-based option.”
The study was funded by Incyte. Mangold declared relationships with Argenx, Boehringer Ingelheim, Bristol-Myers Squibb, Clarivate, Incyte Corporation, Janssen, Nuvig Therapeutics, Pfizer, Regeneron Pharmaceuticals, Soligenix, Tourmaline Bio, AbbVie, Corbus, Eli Lilly, Kyowa, Merck, miRagen Therapeutics, Palvella Therapeutics, Priovant Therapeutics, and Adelphi Values. Friedman declared a relationship with Incyte, but it is not related to this topic.
A version of this article first appeared on Medscape.com.
both when given twice daily and as needed, according to data from a phase 2 trial.
The research, presented at the European Academy of Dermatology and Venereology (EADV) 2024 Congress, involved 64 patients older than 18 years. Ruxolitinib cream (Opzelura) is a topical formulation of a Janus kinase (JAK)1/JAK2 inhibitor, approved by the Food and Drug Administration (FDA) for treating mild to moderate atopic dermatitis and for nonsegmental vitiligo in adults and children aged 12 years or older.
Ruxolitinib cream twice daily resulted in “significant improvements in cutaneous lichen planus disease severity vs vehicle” after 16 weeks of treatment, said the study presenter, Aaron R. Mangold, MD, a dermatologist at Mayo Clinic, Scottsdale, Arizona.
Further improvements were seen during another 16 weeks of additional open-label, as-needed application, he added, and the topical treatment was “generally well tolerated.”
Consequently, “ruxolitinib cream represents a promising potential treatment for cutaneous lichen planus,” Mangold concluded.
Asked to comment on the results, Adam Friedman, MD, Professor and Chair of Dermatology, George Washington University, Washington, DC, who was not involved with the study, said that in keeping with the characterization of lichen planus using the four Ps — purple, polygonal, pruritic, papules — it is “Pretty common, Predictably disabling and disfiguring, and Passed over again and again in the drug development world.”
He said in an interview that this chronic inflammatory skin condition, which affects roughly 2% of the population, also “lacks consensus on work-up and management, likely in part owing to the absence of sizable clinical trial data.”
A recent survey conducted at a meeting indicated that dermatologists “heavily lean on topical therapies for the management of all severity levels,” noted Friedman, one of the survey authors. “Therefore, the phase 2 data presented at EADV is a welcome addition to the mix.”
Phase 2 Study Results
At the meeting, Mangold said that a previous proof-of-concept single-arm study in 12 patients suggested that topical ruxolitinib was highly effective in treating cutaneous lichen planus.
The current phase 2 trial enrolled 64 patients with predominantly cutaneous disease who had an Investigator’s Global Assessment (IGA) score of 3 or 4 and an Itch Numeric Rating Scale (NRS) score of ≥ 4. Their median age was 57 years, and 71.9% were women. Nearly 63% were White, 28.1% were Black, and 6.3% were Asian. The median duration of disease was 4.9 years, and 90.6% had received prior treatment for their lichen planus.
They were randomized to receive 1.5% ruxolitinib cream or a vehicle cream twice daily for 16 weeks, and following a primary endpoint assessment, they were transferred to an open-label extension period, during which they used ruxolitinib cream as needed for another 16 weeks. There was an additional 30-day safety follow-up period.
At week 16, significantly more patients treated with the ruxolitinib cream (50.0%) vs vehicle cream (21.9%) achieved IGA treatment success (the primary endpoint), defined as an IGA score of 0 or 1 with ≥ 2-grade improvement from baseline (odds ratio, 4.04; P = .0129).
In the open-label extension, when all patients used the active cream as needed, the proportion achieving IGA treatment success increased to 60% among the patients originally treated with ruxolitinib cream and 60.9% among those who switched from the vehicle cream.
A similar pattern was seen with Itch NRS scores. At 16 weeks, 57.7% of those treated with the ruxolitinib cream and 19.2% of those given the vehicle cream achieved an Itch NRS score of ≥ 4 (P < .01), rising to 84.2% and 73.3%, respectively, during the open-label extension.
The time to achievement of an Itch NRS of ≥ 4 was also significantly shorter with the ruxolitinib cream than with the vehicle cream (median days, 17 vs 97; hazard ratio, 2.85; P = .0008).
In both treatment groups, Skin Pain NRS scores decreased by a mean of 3.0 with ruxolitinib cream and 1.3 with the vehicle cream at week 16. By the end of the open-label extension, scores dropped by 4.3 among those who continued on active treatment and by 3.5 among those who switched from vehicle to topical ruxolitinib.
There were few treatment-emergent adverse events, with just three ruxolitinib patients affected during the randomized phase of the trial. There was one grade ≥ 3 event considered unrelated to the study drug, and no serious treatment-emergent adverse events were reported.
The most common adverse events during the randomized period were nasopharyngitis, hypertension, and contusion, all experienced by fewer than 10% of patients, whereas sinusitis, increased blood cholesterol levels, and increased blood creatine phosphokinase were most common in the open-label extension, experienced by no more than 5% of patients.
In the interview, Friedman commented that “these data provide hope that one day soon, there will be an FDA-approved, effective, and well-tolerated approach for this condition, validating the patient and supporting the dermatologist with an evidence-based option.”
The study was funded by Incyte. Mangold declared relationships with Argenx, Boehringer Ingelheim, Bristol-Myers Squibb, Clarivate, Incyte Corporation, Janssen, Nuvig Therapeutics, Pfizer, Regeneron Pharmaceuticals, Soligenix, Tourmaline Bio, AbbVie, Corbus, Eli Lilly, Kyowa, Merck, miRagen Therapeutics, Palvella Therapeutics, Priovant Therapeutics, and Adelphi Values. Friedman declared a relationship with Incyte, but it is not related to this topic.
A version of this article first appeared on Medscape.com.
FROM EADV 2024

