User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
EHR alerts to both doc and patient may boost statin prescribing
Automated alerts to aid clinical decision-making are designed with the best of intentions but can be easy to ignore or overlook. But a randomized trial testing such electronic alerts or “nudges” for promoting statin prescribing may have identified a few design features that help their success, researchers say.
In the trial’s primary finding, for example, reminders displayed to primary care physicians in the electronic health record worked best when the system also reached out to the patient.
Reminders sent only to the clinician also boosted statin prescribing, but not as well, and nudging only the patient didn’t work at all, compared to a nudge-free usual care approach. The patient-only nudges consisted of text messages explaining why a statin prescription may figure in their upcoming appointment.
Nudge trustworthiness
Importantly, the clinician nudges were more than simply reminders to consider a statin prescription, Mitesh S. Patel, MD, MBA, Ascension Health, St. Louis, told this news organization. They also displayed the patient’s atherosclerotic cardiovascular disease (ASCVD) 10-year risk score and explained why a statin may be appropriate. He thinks that information, often left out of such clinical decision support alerts, increases physician trust in them.
In another key feature, Dr. Patel said, the EHR nudges themselves were actionable – that is, they were functional in ways that streamlined the prescribing process. In particular, they include checkbox shortcuts to prescribing statins at appropriate patient-specific dosages, making the entire process “faster and easier,” said Dr. Patel, who is senior author on the study published in JAMA Cardiology with lead author Srinath Adusumalli, MD, University of Pennsylvania, Philadelphia.
The timing may matter as well, he observed. In previous iterations of the study’s EHR nudge system, the nudge would appear “when you open the chart,” he said. “Now, it’s when you go to the orders section, which is when you’re going to be in the mindset of ordering prescriptions and tests.”
Prescription rates were higher with the doctor-patient nudges than with the doctor-only approach, Dr. Patel speculates, largely because the decision process for initiating statins is shared. “The most effective intervention is going to recognize that and try to bring the two groups together.”
Two text messages
The trial, with 158 participating physicians in 28 primary care practices, randomly assigned 4,131 patients to three intervention groups and one control group. Nudges were sent only to the physician, only to the patient, or to both physician and patient; and there was a no-nudge usual-care group.
Patient nudges consisted of two text messages, one 4 days and another 15 minutes before the appointment, announcing that prescription of a statin “to reduce the chance of a heart attack” would be discussed with the physician, the report states.
Statins are grossly underprescribed nationally, it notes, and that was reflected in prescription rates seen during the study’s initial 12-month, no-intervention period of observation. Rates ranged from only 4.7% up to 6% of patients across the four assignment groups.
During the subsequent 6-month intervention period, however, the rates climbed in the doctor-only and doctor-plus-patient nudge groups compared with usual care, by 5.5 (P = .01) and 7.2 (P = .001) absolute percentage points, respectively.
The overall cohort’s mean age was 65.5. About half were male, 29% were Black, 66% were White, and 22.6% already had a cardiovascular disease diagnosis. The analysis was adjusted for calendar month and preintervention statin prescribing rates. Further adjustment for demographics, insurance type, household income, and comorbidities yielded results similar to the primary analysis, the report states.
The results in context
“Although the differences in the combined clinician and patient and clinician-only arms were small, this outcome needs to be interpreted in the context of the population in which the study was performed,” an editorial accompanying the published report states.
For example, “the majority of untreated patients were candidates for primary, not secondary, prevention, making this group of patients particularly challenging for seeing large effect sizes of interventions.”
Moreover, “There was a high baseline prescription rate of statins in the statin-eligible population (approximately 70%) and a high rate of already established patients,” write Faraz S. Ahmad, MD, and Stephen D. Persell, MD, of Northwestern University, Chicago.
Among the approximately 30% of patients who had not previously been prescribed statins, the true target of the nudge interventions, the published trial report states, about 98% were not seeing the physician for the first time.
So “this may not have been the first opportunity to discuss statins,” they write. “It is possible that many of these patients were resistant to statins in the past, which could have created a ceiling effect for prescribing rates.”
Dr. Patel reports owning and receiving personal fees from Catalyst Health and serving on an advisory board for and receiving personal fees from Humana. Dr. Adusumalli reports having been employed by CVS Health. Dr. Ahmad reports receiving consulting fees from Teladoc Livongo and Pfizer. Dr. Persell discloses receiving grants from Omron Healthcare.
A version of this article first appeared on Medscape.com.
Automated alerts to aid clinical decision-making are designed with the best of intentions but can be easy to ignore or overlook. But a randomized trial testing such electronic alerts or “nudges” for promoting statin prescribing may have identified a few design features that help their success, researchers say.
In the trial’s primary finding, for example, reminders displayed to primary care physicians in the electronic health record worked best when the system also reached out to the patient.
Reminders sent only to the clinician also boosted statin prescribing, but not as well, and nudging only the patient didn’t work at all, compared to a nudge-free usual care approach. The patient-only nudges consisted of text messages explaining why a statin prescription may figure in their upcoming appointment.
Nudge trustworthiness
Importantly, the clinician nudges were more than simply reminders to consider a statin prescription, Mitesh S. Patel, MD, MBA, Ascension Health, St. Louis, told this news organization. They also displayed the patient’s atherosclerotic cardiovascular disease (ASCVD) 10-year risk score and explained why a statin may be appropriate. He thinks that information, often left out of such clinical decision support alerts, increases physician trust in them.
In another key feature, Dr. Patel said, the EHR nudges themselves were actionable – that is, they were functional in ways that streamlined the prescribing process. In particular, they include checkbox shortcuts to prescribing statins at appropriate patient-specific dosages, making the entire process “faster and easier,” said Dr. Patel, who is senior author on the study published in JAMA Cardiology with lead author Srinath Adusumalli, MD, University of Pennsylvania, Philadelphia.
The timing may matter as well, he observed. In previous iterations of the study’s EHR nudge system, the nudge would appear “when you open the chart,” he said. “Now, it’s when you go to the orders section, which is when you’re going to be in the mindset of ordering prescriptions and tests.”
Prescription rates were higher with the doctor-patient nudges than with the doctor-only approach, Dr. Patel speculates, largely because the decision process for initiating statins is shared. “The most effective intervention is going to recognize that and try to bring the two groups together.”
Two text messages
The trial, with 158 participating physicians in 28 primary care practices, randomly assigned 4,131 patients to three intervention groups and one control group. Nudges were sent only to the physician, only to the patient, or to both physician and patient; and there was a no-nudge usual-care group.
Patient nudges consisted of two text messages, one 4 days and another 15 minutes before the appointment, announcing that prescription of a statin “to reduce the chance of a heart attack” would be discussed with the physician, the report states.
Statins are grossly underprescribed nationally, it notes, and that was reflected in prescription rates seen during the study’s initial 12-month, no-intervention period of observation. Rates ranged from only 4.7% up to 6% of patients across the four assignment groups.
During the subsequent 6-month intervention period, however, the rates climbed in the doctor-only and doctor-plus-patient nudge groups compared with usual care, by 5.5 (P = .01) and 7.2 (P = .001) absolute percentage points, respectively.
The overall cohort’s mean age was 65.5. About half were male, 29% were Black, 66% were White, and 22.6% already had a cardiovascular disease diagnosis. The analysis was adjusted for calendar month and preintervention statin prescribing rates. Further adjustment for demographics, insurance type, household income, and comorbidities yielded results similar to the primary analysis, the report states.
The results in context
“Although the differences in the combined clinician and patient and clinician-only arms were small, this outcome needs to be interpreted in the context of the population in which the study was performed,” an editorial accompanying the published report states.
For example, “the majority of untreated patients were candidates for primary, not secondary, prevention, making this group of patients particularly challenging for seeing large effect sizes of interventions.”
Moreover, “There was a high baseline prescription rate of statins in the statin-eligible population (approximately 70%) and a high rate of already established patients,” write Faraz S. Ahmad, MD, and Stephen D. Persell, MD, of Northwestern University, Chicago.
Among the approximately 30% of patients who had not previously been prescribed statins, the true target of the nudge interventions, the published trial report states, about 98% were not seeing the physician for the first time.
So “this may not have been the first opportunity to discuss statins,” they write. “It is possible that many of these patients were resistant to statins in the past, which could have created a ceiling effect for prescribing rates.”
Dr. Patel reports owning and receiving personal fees from Catalyst Health and serving on an advisory board for and receiving personal fees from Humana. Dr. Adusumalli reports having been employed by CVS Health. Dr. Ahmad reports receiving consulting fees from Teladoc Livongo and Pfizer. Dr. Persell discloses receiving grants from Omron Healthcare.
A version of this article first appeared on Medscape.com.
Automated alerts to aid clinical decision-making are designed with the best of intentions but can be easy to ignore or overlook. But a randomized trial testing such electronic alerts or “nudges” for promoting statin prescribing may have identified a few design features that help their success, researchers say.
In the trial’s primary finding, for example, reminders displayed to primary care physicians in the electronic health record worked best when the system also reached out to the patient.
Reminders sent only to the clinician also boosted statin prescribing, but not as well, and nudging only the patient didn’t work at all, compared to a nudge-free usual care approach. The patient-only nudges consisted of text messages explaining why a statin prescription may figure in their upcoming appointment.
Nudge trustworthiness
Importantly, the clinician nudges were more than simply reminders to consider a statin prescription, Mitesh S. Patel, MD, MBA, Ascension Health, St. Louis, told this news organization. They also displayed the patient’s atherosclerotic cardiovascular disease (ASCVD) 10-year risk score and explained why a statin may be appropriate. He thinks that information, often left out of such clinical decision support alerts, increases physician trust in them.
In another key feature, Dr. Patel said, the EHR nudges themselves were actionable – that is, they were functional in ways that streamlined the prescribing process. In particular, they include checkbox shortcuts to prescribing statins at appropriate patient-specific dosages, making the entire process “faster and easier,” said Dr. Patel, who is senior author on the study published in JAMA Cardiology with lead author Srinath Adusumalli, MD, University of Pennsylvania, Philadelphia.
The timing may matter as well, he observed. In previous iterations of the study’s EHR nudge system, the nudge would appear “when you open the chart,” he said. “Now, it’s when you go to the orders section, which is when you’re going to be in the mindset of ordering prescriptions and tests.”
Prescription rates were higher with the doctor-patient nudges than with the doctor-only approach, Dr. Patel speculates, largely because the decision process for initiating statins is shared. “The most effective intervention is going to recognize that and try to bring the two groups together.”
Two text messages
The trial, with 158 participating physicians in 28 primary care practices, randomly assigned 4,131 patients to three intervention groups and one control group. Nudges were sent only to the physician, only to the patient, or to both physician and patient; and there was a no-nudge usual-care group.
Patient nudges consisted of two text messages, one 4 days and another 15 minutes before the appointment, announcing that prescription of a statin “to reduce the chance of a heart attack” would be discussed with the physician, the report states.
Statins are grossly underprescribed nationally, it notes, and that was reflected in prescription rates seen during the study’s initial 12-month, no-intervention period of observation. Rates ranged from only 4.7% up to 6% of patients across the four assignment groups.
During the subsequent 6-month intervention period, however, the rates climbed in the doctor-only and doctor-plus-patient nudge groups compared with usual care, by 5.5 (P = .01) and 7.2 (P = .001) absolute percentage points, respectively.
The overall cohort’s mean age was 65.5. About half were male, 29% were Black, 66% were White, and 22.6% already had a cardiovascular disease diagnosis. The analysis was adjusted for calendar month and preintervention statin prescribing rates. Further adjustment for demographics, insurance type, household income, and comorbidities yielded results similar to the primary analysis, the report states.
The results in context
“Although the differences in the combined clinician and patient and clinician-only arms were small, this outcome needs to be interpreted in the context of the population in which the study was performed,” an editorial accompanying the published report states.
For example, “the majority of untreated patients were candidates for primary, not secondary, prevention, making this group of patients particularly challenging for seeing large effect sizes of interventions.”
Moreover, “There was a high baseline prescription rate of statins in the statin-eligible population (approximately 70%) and a high rate of already established patients,” write Faraz S. Ahmad, MD, and Stephen D. Persell, MD, of Northwestern University, Chicago.
Among the approximately 30% of patients who had not previously been prescribed statins, the true target of the nudge interventions, the published trial report states, about 98% were not seeing the physician for the first time.
So “this may not have been the first opportunity to discuss statins,” they write. “It is possible that many of these patients were resistant to statins in the past, which could have created a ceiling effect for prescribing rates.”
Dr. Patel reports owning and receiving personal fees from Catalyst Health and serving on an advisory board for and receiving personal fees from Humana. Dr. Adusumalli reports having been employed by CVS Health. Dr. Ahmad reports receiving consulting fees from Teladoc Livongo and Pfizer. Dr. Persell discloses receiving grants from Omron Healthcare.
A version of this article first appeared on Medscape.com.
Review gives weight to supplements for hair loss
because of small sample sizes, heterogeneity of hair loss types in study subjects, or other limitations.
The review, published online in JAMA Dermatology, notes that “Twelve of the 20 nutritional interventions had high-quality studies suggesting objectively evaluated effectiveness.”
It is “ground breaking,” in part because of its breadth and depth, said Eva Simmons-O’Brien, MD, a dermatologist in Towson, Md., who often recommends supplements for her patients with hair loss. “It basically kind of vindicates what some of us have been doing for a number of years in terms of treating hair loss,” she told this news organization. “It should hopefully make it more commonplace for dermatologists to consider using nutritional supplements as an adjuvant to treating hair loss,” added Dr. Simmons-O’Brien.
The review “is very helpful,” agreed Lynne J. Goldberg, MD, professor of dermatology and pathology and laboratory medicine at Boston University. Dr. Goldberg noted that many patients are already taking supplements and want to know whether they are safe and effective. The review “points out what the problems are; it talks about what the individual ingredients are and what they do, what the problems are; and it concluded that some people may find these helpful. Which is exactly what I tell my patients,” said Dr. Goldberg, who is also director of the Hair Clinic at Boston Medical Center.
“For patients who are highly motivated and eager to try this, we’re hoping that this systematic review serves as a foundation to have a conversation,” study coauthor Arash Mostaghimi, MD, MPA, MPH, of the department of dermatology at Harvard Medical School, told this news organization. “When there’s medical uncertainty and the question is how much risk is one willing to take, the most important thing to do is to present the data and engage in shared decision-making with the patient,” noted Dr. Mostaghimi, who is also director of the inpatient dermatology consult service at Brigham and Women’s Hospital, Boston.
Surprising effectiveness
Going into the study, “we felt it would be likely that majority of nutritional supplements would either not be effective or not studied,” he said.
Dr. Mostaghimi and his coauthors conducted the study because so many patients take nutritional supplements to address hair loss, he said. An initial literature survey yielded more than 6,300 citations, but after screening and reviews, the authors included 30 articles for evaluation.
The review begins with a look at studies of saw palmetto (Serenoa repens), a botanical compound thought to inhibit the enzyme 5-alpha reductase (5AR), which converts testosterone to dihydroxytestosterone (DHT). DHT is a mediator of androgenic alopecia (AGA). The studies suggest that the compound might stabilize hair loss, “although its effect is likely less than that of finasteride,” write the authors. They also note that side effects associated with finasteride, such as sexual dysfunction, were also observed with saw palmetto “but to a lesser extent.”
For AGA, pumpkin seed oil may also be effective and a “potential alternative” to finasteride for AGA, and Forti5, a nutritional supplement that includes botanical 5AR inhibitors and other ingredients, had favorable effects in one study, the authors write. But neither has been compared to finasteride, and the Forti5 study lacked a control group.
The review also examines the micronutrients vitamin D, zinc, B vitamins, and antioxidants. Low levels of vitamin D have been associated with alopecia areata (AA), AGA, and telogen effluvium (TE) in some studies, and zinc deficiencies have been associated with TE, hair breakage, and thinning, according to the review. A single-arm vitamin D study showed improved results at 6 months for women with TE, but there was no control group and TE is self-resolving, the authors add. Studies in patients with normal zinc levels at baseline who had AA or hair loss showed significant hair regrowth and increased hair thickness and density, but the trials were a mishmash of controls and no controls and relied on self-perceived hair-loss data.
Larger more rigorous studies should be done to evaluate zinc’s effectiveness with AA, the authors comment.
Many patients take vitamin B7 (biotin) for hair loss. It has not been studied on its own but was an ingredient in some supplements in the review. Dr. Simmons-O’Brien said that biotin won’t result in new hair growth but that it can help strengthen the new hairs that grow as a result of other therapies. Both she and the study authors note that the Food and Drug Administration has warned against biotin supplementation because it can interfere with troponin and other test results.
The review also finds that immunomodulators –such as Chinese herbal extracts from paeony and glycyrrhizin – were effective in severe AA. Growth hormone modulators targeting deficiencies in insulin growth factor 1 or growth hormone are also promising. Studies of the modulators capsaicin and isoflavones – used topically – spurred hair growth, the authors write.
Products containing marine protein supplements, including Viviscal and Nourkrin, appeared effective in increasing hair counts in men and women, but the studies were funded by the manufacturer and were not well controlled. Side effects with Viviscal included bloating, according to the review.
The multi-ingredient supplements Nutrafol, Omni-Three, Apple Nutraceutical, and Lambdapil were also included in the review. Only Omni-Three showed no effectiveness, but studies of the other supplements had various limitations, including lack of controls and small sample sizes.
Complicated problem, multiple solutions
Given the many reasons for hair loss, multiple solutions are needed, the dermatologists note.
Dr. Mostaghimi said that he’s still a bit skeptical that supplements work as consistently as described or as well as described, given that he and his coauthors were unable to find any negative studies. In talking with patients who are taking supplements, he said that his first aim is to make sure they are safe. At least the supplements in the review have been studied for safety, he added.
He will encourage replacement of vitamin D or zinc or other vitamins or minerals if patients are deficient but said that he does not “actively encourage supplementation.”
Dr. Simmons-O’Brien said that, when evaluating patients with hair loss, she orders lab tests to determine whether the patient has anemia or a thyroid issue or deficiencies in vitamins or minerals or other nutritional deficiencies, asks about diet and styling practices, and takes a scalp biopsy. It is not uncommon to recommend supplementation on the basis of those findings, she added.
“As a hair-loss specialist, my job is to treat the patient at their level, in their framework, in their comfort zone,” said Dr. Goldberg. Some patients don’t want to take medications for hair loss, so she might recommend supplements in those cases but tells patients that they aren’t well studied.
She added that it can be hard to tell whether a supplement is working, particularly if it has multiple ingredients.
Dr. Mostaghimi reported consulting fees from Pfizer, Concert, Lilly, Hims and Hers, Equillium, AbbVie, Digital Diagnostics, and Bioniz and grants from Pfizer, all outside the submitted work. In addition, Dr. Mostaghimi disclosed that he is an associate editor of JAMA Dermatology but was not involved in any of the decisions regarding the review of the manuscript or its acceptance. No other disclosures were reported by the other study authors. Dr. Goldberg reported no disclosures. Dr. Simmons-O›Brien is a medical consultant for Isdin, but not for hair products.
A version of this article first appeared on Medscape.com.
because of small sample sizes, heterogeneity of hair loss types in study subjects, or other limitations.
The review, published online in JAMA Dermatology, notes that “Twelve of the 20 nutritional interventions had high-quality studies suggesting objectively evaluated effectiveness.”
It is “ground breaking,” in part because of its breadth and depth, said Eva Simmons-O’Brien, MD, a dermatologist in Towson, Md., who often recommends supplements for her patients with hair loss. “It basically kind of vindicates what some of us have been doing for a number of years in terms of treating hair loss,” she told this news organization. “It should hopefully make it more commonplace for dermatologists to consider using nutritional supplements as an adjuvant to treating hair loss,” added Dr. Simmons-O’Brien.
The review “is very helpful,” agreed Lynne J. Goldberg, MD, professor of dermatology and pathology and laboratory medicine at Boston University. Dr. Goldberg noted that many patients are already taking supplements and want to know whether they are safe and effective. The review “points out what the problems are; it talks about what the individual ingredients are and what they do, what the problems are; and it concluded that some people may find these helpful. Which is exactly what I tell my patients,” said Dr. Goldberg, who is also director of the Hair Clinic at Boston Medical Center.
“For patients who are highly motivated and eager to try this, we’re hoping that this systematic review serves as a foundation to have a conversation,” study coauthor Arash Mostaghimi, MD, MPA, MPH, of the department of dermatology at Harvard Medical School, told this news organization. “When there’s medical uncertainty and the question is how much risk is one willing to take, the most important thing to do is to present the data and engage in shared decision-making with the patient,” noted Dr. Mostaghimi, who is also director of the inpatient dermatology consult service at Brigham and Women’s Hospital, Boston.
Surprising effectiveness
Going into the study, “we felt it would be likely that majority of nutritional supplements would either not be effective or not studied,” he said.
Dr. Mostaghimi and his coauthors conducted the study because so many patients take nutritional supplements to address hair loss, he said. An initial literature survey yielded more than 6,300 citations, but after screening and reviews, the authors included 30 articles for evaluation.
The review begins with a look at studies of saw palmetto (Serenoa repens), a botanical compound thought to inhibit the enzyme 5-alpha reductase (5AR), which converts testosterone to dihydroxytestosterone (DHT). DHT is a mediator of androgenic alopecia (AGA). The studies suggest that the compound might stabilize hair loss, “although its effect is likely less than that of finasteride,” write the authors. They also note that side effects associated with finasteride, such as sexual dysfunction, were also observed with saw palmetto “but to a lesser extent.”
For AGA, pumpkin seed oil may also be effective and a “potential alternative” to finasteride for AGA, and Forti5, a nutritional supplement that includes botanical 5AR inhibitors and other ingredients, had favorable effects in one study, the authors write. But neither has been compared to finasteride, and the Forti5 study lacked a control group.
The review also examines the micronutrients vitamin D, zinc, B vitamins, and antioxidants. Low levels of vitamin D have been associated with alopecia areata (AA), AGA, and telogen effluvium (TE) in some studies, and zinc deficiencies have been associated with TE, hair breakage, and thinning, according to the review. A single-arm vitamin D study showed improved results at 6 months for women with TE, but there was no control group and TE is self-resolving, the authors add. Studies in patients with normal zinc levels at baseline who had AA or hair loss showed significant hair regrowth and increased hair thickness and density, but the trials were a mishmash of controls and no controls and relied on self-perceived hair-loss data.
Larger more rigorous studies should be done to evaluate zinc’s effectiveness with AA, the authors comment.
Many patients take vitamin B7 (biotin) for hair loss. It has not been studied on its own but was an ingredient in some supplements in the review. Dr. Simmons-O’Brien said that biotin won’t result in new hair growth but that it can help strengthen the new hairs that grow as a result of other therapies. Both she and the study authors note that the Food and Drug Administration has warned against biotin supplementation because it can interfere with troponin and other test results.
The review also finds that immunomodulators –such as Chinese herbal extracts from paeony and glycyrrhizin – were effective in severe AA. Growth hormone modulators targeting deficiencies in insulin growth factor 1 or growth hormone are also promising. Studies of the modulators capsaicin and isoflavones – used topically – spurred hair growth, the authors write.
Products containing marine protein supplements, including Viviscal and Nourkrin, appeared effective in increasing hair counts in men and women, but the studies were funded by the manufacturer and were not well controlled. Side effects with Viviscal included bloating, according to the review.
The multi-ingredient supplements Nutrafol, Omni-Three, Apple Nutraceutical, and Lambdapil were also included in the review. Only Omni-Three showed no effectiveness, but studies of the other supplements had various limitations, including lack of controls and small sample sizes.
Complicated problem, multiple solutions
Given the many reasons for hair loss, multiple solutions are needed, the dermatologists note.
Dr. Mostaghimi said that he’s still a bit skeptical that supplements work as consistently as described or as well as described, given that he and his coauthors were unable to find any negative studies. In talking with patients who are taking supplements, he said that his first aim is to make sure they are safe. At least the supplements in the review have been studied for safety, he added.
He will encourage replacement of vitamin D or zinc or other vitamins or minerals if patients are deficient but said that he does not “actively encourage supplementation.”
Dr. Simmons-O’Brien said that, when evaluating patients with hair loss, she orders lab tests to determine whether the patient has anemia or a thyroid issue or deficiencies in vitamins or minerals or other nutritional deficiencies, asks about diet and styling practices, and takes a scalp biopsy. It is not uncommon to recommend supplementation on the basis of those findings, she added.
“As a hair-loss specialist, my job is to treat the patient at their level, in their framework, in their comfort zone,” said Dr. Goldberg. Some patients don’t want to take medications for hair loss, so she might recommend supplements in those cases but tells patients that they aren’t well studied.
She added that it can be hard to tell whether a supplement is working, particularly if it has multiple ingredients.
Dr. Mostaghimi reported consulting fees from Pfizer, Concert, Lilly, Hims and Hers, Equillium, AbbVie, Digital Diagnostics, and Bioniz and grants from Pfizer, all outside the submitted work. In addition, Dr. Mostaghimi disclosed that he is an associate editor of JAMA Dermatology but was not involved in any of the decisions regarding the review of the manuscript or its acceptance. No other disclosures were reported by the other study authors. Dr. Goldberg reported no disclosures. Dr. Simmons-O›Brien is a medical consultant for Isdin, but not for hair products.
A version of this article first appeared on Medscape.com.
because of small sample sizes, heterogeneity of hair loss types in study subjects, or other limitations.
The review, published online in JAMA Dermatology, notes that “Twelve of the 20 nutritional interventions had high-quality studies suggesting objectively evaluated effectiveness.”
It is “ground breaking,” in part because of its breadth and depth, said Eva Simmons-O’Brien, MD, a dermatologist in Towson, Md., who often recommends supplements for her patients with hair loss. “It basically kind of vindicates what some of us have been doing for a number of years in terms of treating hair loss,” she told this news organization. “It should hopefully make it more commonplace for dermatologists to consider using nutritional supplements as an adjuvant to treating hair loss,” added Dr. Simmons-O’Brien.
The review “is very helpful,” agreed Lynne J. Goldberg, MD, professor of dermatology and pathology and laboratory medicine at Boston University. Dr. Goldberg noted that many patients are already taking supplements and want to know whether they are safe and effective. The review “points out what the problems are; it talks about what the individual ingredients are and what they do, what the problems are; and it concluded that some people may find these helpful. Which is exactly what I tell my patients,” said Dr. Goldberg, who is also director of the Hair Clinic at Boston Medical Center.
“For patients who are highly motivated and eager to try this, we’re hoping that this systematic review serves as a foundation to have a conversation,” study coauthor Arash Mostaghimi, MD, MPA, MPH, of the department of dermatology at Harvard Medical School, told this news organization. “When there’s medical uncertainty and the question is how much risk is one willing to take, the most important thing to do is to present the data and engage in shared decision-making with the patient,” noted Dr. Mostaghimi, who is also director of the inpatient dermatology consult service at Brigham and Women’s Hospital, Boston.
Surprising effectiveness
Going into the study, “we felt it would be likely that majority of nutritional supplements would either not be effective or not studied,” he said.
Dr. Mostaghimi and his coauthors conducted the study because so many patients take nutritional supplements to address hair loss, he said. An initial literature survey yielded more than 6,300 citations, but after screening and reviews, the authors included 30 articles for evaluation.
The review begins with a look at studies of saw palmetto (Serenoa repens), a botanical compound thought to inhibit the enzyme 5-alpha reductase (5AR), which converts testosterone to dihydroxytestosterone (DHT). DHT is a mediator of androgenic alopecia (AGA). The studies suggest that the compound might stabilize hair loss, “although its effect is likely less than that of finasteride,” write the authors. They also note that side effects associated with finasteride, such as sexual dysfunction, were also observed with saw palmetto “but to a lesser extent.”
For AGA, pumpkin seed oil may also be effective and a “potential alternative” to finasteride for AGA, and Forti5, a nutritional supplement that includes botanical 5AR inhibitors and other ingredients, had favorable effects in one study, the authors write. But neither has been compared to finasteride, and the Forti5 study lacked a control group.
The review also examines the micronutrients vitamin D, zinc, B vitamins, and antioxidants. Low levels of vitamin D have been associated with alopecia areata (AA), AGA, and telogen effluvium (TE) in some studies, and zinc deficiencies have been associated with TE, hair breakage, and thinning, according to the review. A single-arm vitamin D study showed improved results at 6 months for women with TE, but there was no control group and TE is self-resolving, the authors add. Studies in patients with normal zinc levels at baseline who had AA or hair loss showed significant hair regrowth and increased hair thickness and density, but the trials were a mishmash of controls and no controls and relied on self-perceived hair-loss data.
Larger more rigorous studies should be done to evaluate zinc’s effectiveness with AA, the authors comment.
Many patients take vitamin B7 (biotin) for hair loss. It has not been studied on its own but was an ingredient in some supplements in the review. Dr. Simmons-O’Brien said that biotin won’t result in new hair growth but that it can help strengthen the new hairs that grow as a result of other therapies. Both she and the study authors note that the Food and Drug Administration has warned against biotin supplementation because it can interfere with troponin and other test results.
The review also finds that immunomodulators –such as Chinese herbal extracts from paeony and glycyrrhizin – were effective in severe AA. Growth hormone modulators targeting deficiencies in insulin growth factor 1 or growth hormone are also promising. Studies of the modulators capsaicin and isoflavones – used topically – spurred hair growth, the authors write.
Products containing marine protein supplements, including Viviscal and Nourkrin, appeared effective in increasing hair counts in men and women, but the studies were funded by the manufacturer and were not well controlled. Side effects with Viviscal included bloating, according to the review.
The multi-ingredient supplements Nutrafol, Omni-Three, Apple Nutraceutical, and Lambdapil were also included in the review. Only Omni-Three showed no effectiveness, but studies of the other supplements had various limitations, including lack of controls and small sample sizes.
Complicated problem, multiple solutions
Given the many reasons for hair loss, multiple solutions are needed, the dermatologists note.
Dr. Mostaghimi said that he’s still a bit skeptical that supplements work as consistently as described or as well as described, given that he and his coauthors were unable to find any negative studies. In talking with patients who are taking supplements, he said that his first aim is to make sure they are safe. At least the supplements in the review have been studied for safety, he added.
He will encourage replacement of vitamin D or zinc or other vitamins or minerals if patients are deficient but said that he does not “actively encourage supplementation.”
Dr. Simmons-O’Brien said that, when evaluating patients with hair loss, she orders lab tests to determine whether the patient has anemia or a thyroid issue or deficiencies in vitamins or minerals or other nutritional deficiencies, asks about diet and styling practices, and takes a scalp biopsy. It is not uncommon to recommend supplementation on the basis of those findings, she added.
“As a hair-loss specialist, my job is to treat the patient at their level, in their framework, in their comfort zone,” said Dr. Goldberg. Some patients don’t want to take medications for hair loss, so she might recommend supplements in those cases but tells patients that they aren’t well studied.
She added that it can be hard to tell whether a supplement is working, particularly if it has multiple ingredients.
Dr. Mostaghimi reported consulting fees from Pfizer, Concert, Lilly, Hims and Hers, Equillium, AbbVie, Digital Diagnostics, and Bioniz and grants from Pfizer, all outside the submitted work. In addition, Dr. Mostaghimi disclosed that he is an associate editor of JAMA Dermatology but was not involved in any of the decisions regarding the review of the manuscript or its acceptance. No other disclosures were reported by the other study authors. Dr. Goldberg reported no disclosures. Dr. Simmons-O›Brien is a medical consultant for Isdin, but not for hair products.
A version of this article first appeared on Medscape.com.
Ultraprocessed foods tied to faster rate of cognitive decline
Results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil), which included more than 10,000 people aged 35 and older, showed that higher intake of UPF was significantly associated with a faster rate of decline in executive and global cognitive function.
“These findings show that lifestyle choices, particularly high intake of ultraprocessed foods, can influence our cognitive health many years later,” coinvestigator Natalia Goncalves, PhD, University of São Paulo, Brazil, said in an interview.
The study was published online in JAMA Neurology.
The study’s findings were presented in August at the Alzheimer’s Association International Conference (AAIC) 2022 and were reported by this news organization at that time.
High sugar, salt, fat
The new results align with another recent study linking a diet high in UPFs to an increased risk for dementia.
UPFs are highly manipulated, are packed with added ingredients, including sugar, fat, and salt, and are low in protein and fiber. Examples of UPFs are soft drinks, chips, chocolate, candy, ice cream, sweetened breakfast cereals, packaged soups, chicken nuggets, hot dogs, and fries.
The ELSA-Brasil study comprised 10,775 adults (mean age, 50.6 years at baseline; 55% women; 53% White) who were evaluated in three waves approximately 4 years apart from 2008 to 2017.
Information on diet was obtained via food frequency questionnaires and included details regarding consumption of unprocessed foods, minimally processed foods, and UPFs.
Participants were grouped according to UPF consumption quartiles (lowest to highest). Cognitive performance was evaluated by use of a standardized battery of tests.
During median follow-up of 8 years, people who consumed more than 20% of daily calories from UPFs (quartiles 2-4) experienced a 28% faster rate of decline in global cognition (beta = –0.004; 95% confidence interval [CI], –0.006 to –0.001; P = .003) and a 25% faster rate of decline in executive function (beta = –0.003, 95% CI, –0.005 to 0.000; P = .01) compared to peers in quartile 1 who consumed less than 20% of daily calories from UPFs.
The researchers did not investigate individual groups of UPFs.
However, Dr. Goncalves noted that some studies have linked the consumption of sugar-sweetened beverages with lower cognitive performance, lower brain volume, and poorer memory performance. Another group of ultraprocessed foods, processed meats, has been associated with increased all-cause dementia and Alzheimer’s disease.
Other limitations include the fact that self-reported diet habits were assessed only at baseline using a food frequency questionnaire that was not designed to assess the degree of processing.
While analyses were adjusted for several sociodemographic and clinical confounders, the researchers said they could not exclude the possibility of residual confounding.
Also, since neuroimaging is not available in the ELSA-Brasil study, they were not able to investigate potential mechanisms that could explain the association between higher UPF consumption and cognitive decline.
Despite these limitations, the researchers said their findings suggest that “limiting UPF consumption, particularly in middle-aged adults, may be an efficient form to prevent cognitive decline.”
Weighing the evidence
Several experts weighed in on the results in a statement from the UK nonprofit organization, Science Media Centre.
Kevin McConway, PhD, with Open University, Milton Keynes, England, said it’s important to note that the study suggests “an association, a correlation, and that doesn’t necessarily mean that the cognitive decline was caused by eating more ultra-processed foods.”
He also noted that some types of cognitive decline that are associated with aging occurred in participants in all four quartiles, which were defined by the percentage of their daily energy that came from consuming UPFs.
“That’s hardly surprising – it’s a sad fact of life that pretty well all of us gradually lose some of our cognitive functions as we go through middle and older age,” Dr. McConway said.
“The study doesn’t establish that differences in speed of cognitive decline are caused by ultra-processed food consumption anyway. That’s because it’s an observational study. If the consumption of ultra-processed food causes the differences in rate of cognitive decline, then eating less of it might slow cognitive decline, but if the cause is something else, then that won’t happen,” Dr. McConway added.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading, England, noted that UPFs have become a “fashionable term to explain associations between diet and ill health, and many studies have attempted to show associations.
“Most studies have been observational and had a key limitation: It is very difficult to determine ultra-processed food intake using methods that are not designed to do so, and so authors need to make a lot of assumptions. Bread and meat products are often classed as ‘ultra-processed,’ even though this is often wrong,” Dr. Kuhnle noted.
“The same applies to this study – the method used to measure ultra-processed food intake was not designed for that task and relied on assumptions. This makes it virtually impossible to draw any conclusions,” Dr. Kuhnle said.
Duane Mellor, PhD, RD, RNutr, registered dietitian and senior teaching fellow, Aston University, Birmingham, England, said the study does not change how we should try to eat to maintain good brain function and cognition.
“We should try to eat less foods which are high in added sugar, salt, and fat, which would include many of the foods classified as being ultra-processed, while eating more in terms of both quantity and variety of vegetables, fruit, nuts, seeds, and pulses, which are known to be beneficial for both our cognitive and overall health,” Dr. Mellor said.
The ELSA-Brasil study was supported by the Brazilian Ministry of Health, the Ministry of Science, Technology and Innovation, and the National Council for Scientific and Technological Development. The authors as well as Dr. McConway, Dr. Mellor, and Dr. Kuhnle have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil), which included more than 10,000 people aged 35 and older, showed that higher intake of UPF was significantly associated with a faster rate of decline in executive and global cognitive function.
“These findings show that lifestyle choices, particularly high intake of ultraprocessed foods, can influence our cognitive health many years later,” coinvestigator Natalia Goncalves, PhD, University of São Paulo, Brazil, said in an interview.
The study was published online in JAMA Neurology.
The study’s findings were presented in August at the Alzheimer’s Association International Conference (AAIC) 2022 and were reported by this news organization at that time.
High sugar, salt, fat
The new results align with another recent study linking a diet high in UPFs to an increased risk for dementia.
UPFs are highly manipulated, are packed with added ingredients, including sugar, fat, and salt, and are low in protein and fiber. Examples of UPFs are soft drinks, chips, chocolate, candy, ice cream, sweetened breakfast cereals, packaged soups, chicken nuggets, hot dogs, and fries.
The ELSA-Brasil study comprised 10,775 adults (mean age, 50.6 years at baseline; 55% women; 53% White) who were evaluated in three waves approximately 4 years apart from 2008 to 2017.
Information on diet was obtained via food frequency questionnaires and included details regarding consumption of unprocessed foods, minimally processed foods, and UPFs.
Participants were grouped according to UPF consumption quartiles (lowest to highest). Cognitive performance was evaluated by use of a standardized battery of tests.
During median follow-up of 8 years, people who consumed more than 20% of daily calories from UPFs (quartiles 2-4) experienced a 28% faster rate of decline in global cognition (beta = –0.004; 95% confidence interval [CI], –0.006 to –0.001; P = .003) and a 25% faster rate of decline in executive function (beta = –0.003, 95% CI, –0.005 to 0.000; P = .01) compared to peers in quartile 1 who consumed less than 20% of daily calories from UPFs.
The researchers did not investigate individual groups of UPFs.
However, Dr. Goncalves noted that some studies have linked the consumption of sugar-sweetened beverages with lower cognitive performance, lower brain volume, and poorer memory performance. Another group of ultraprocessed foods, processed meats, has been associated with increased all-cause dementia and Alzheimer’s disease.
Other limitations include the fact that self-reported diet habits were assessed only at baseline using a food frequency questionnaire that was not designed to assess the degree of processing.
While analyses were adjusted for several sociodemographic and clinical confounders, the researchers said they could not exclude the possibility of residual confounding.
Also, since neuroimaging is not available in the ELSA-Brasil study, they were not able to investigate potential mechanisms that could explain the association between higher UPF consumption and cognitive decline.
Despite these limitations, the researchers said their findings suggest that “limiting UPF consumption, particularly in middle-aged adults, may be an efficient form to prevent cognitive decline.”
Weighing the evidence
Several experts weighed in on the results in a statement from the UK nonprofit organization, Science Media Centre.
Kevin McConway, PhD, with Open University, Milton Keynes, England, said it’s important to note that the study suggests “an association, a correlation, and that doesn’t necessarily mean that the cognitive decline was caused by eating more ultra-processed foods.”
He also noted that some types of cognitive decline that are associated with aging occurred in participants in all four quartiles, which were defined by the percentage of their daily energy that came from consuming UPFs.
“That’s hardly surprising – it’s a sad fact of life that pretty well all of us gradually lose some of our cognitive functions as we go through middle and older age,” Dr. McConway said.
“The study doesn’t establish that differences in speed of cognitive decline are caused by ultra-processed food consumption anyway. That’s because it’s an observational study. If the consumption of ultra-processed food causes the differences in rate of cognitive decline, then eating less of it might slow cognitive decline, but if the cause is something else, then that won’t happen,” Dr. McConway added.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading, England, noted that UPFs have become a “fashionable term to explain associations between diet and ill health, and many studies have attempted to show associations.
“Most studies have been observational and had a key limitation: It is very difficult to determine ultra-processed food intake using methods that are not designed to do so, and so authors need to make a lot of assumptions. Bread and meat products are often classed as ‘ultra-processed,’ even though this is often wrong,” Dr. Kuhnle noted.
“The same applies to this study – the method used to measure ultra-processed food intake was not designed for that task and relied on assumptions. This makes it virtually impossible to draw any conclusions,” Dr. Kuhnle said.
Duane Mellor, PhD, RD, RNutr, registered dietitian and senior teaching fellow, Aston University, Birmingham, England, said the study does not change how we should try to eat to maintain good brain function and cognition.
“We should try to eat less foods which are high in added sugar, salt, and fat, which would include many of the foods classified as being ultra-processed, while eating more in terms of both quantity and variety of vegetables, fruit, nuts, seeds, and pulses, which are known to be beneficial for both our cognitive and overall health,” Dr. Mellor said.
The ELSA-Brasil study was supported by the Brazilian Ministry of Health, the Ministry of Science, Technology and Innovation, and the National Council for Scientific and Technological Development. The authors as well as Dr. McConway, Dr. Mellor, and Dr. Kuhnle have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results from the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil), which included more than 10,000 people aged 35 and older, showed that higher intake of UPF was significantly associated with a faster rate of decline in executive and global cognitive function.
“These findings show that lifestyle choices, particularly high intake of ultraprocessed foods, can influence our cognitive health many years later,” coinvestigator Natalia Goncalves, PhD, University of São Paulo, Brazil, said in an interview.
The study was published online in JAMA Neurology.
The study’s findings were presented in August at the Alzheimer’s Association International Conference (AAIC) 2022 and were reported by this news organization at that time.
High sugar, salt, fat
The new results align with another recent study linking a diet high in UPFs to an increased risk for dementia.
UPFs are highly manipulated, are packed with added ingredients, including sugar, fat, and salt, and are low in protein and fiber. Examples of UPFs are soft drinks, chips, chocolate, candy, ice cream, sweetened breakfast cereals, packaged soups, chicken nuggets, hot dogs, and fries.
The ELSA-Brasil study comprised 10,775 adults (mean age, 50.6 years at baseline; 55% women; 53% White) who were evaluated in three waves approximately 4 years apart from 2008 to 2017.
Information on diet was obtained via food frequency questionnaires and included details regarding consumption of unprocessed foods, minimally processed foods, and UPFs.
Participants were grouped according to UPF consumption quartiles (lowest to highest). Cognitive performance was evaluated by use of a standardized battery of tests.
During median follow-up of 8 years, people who consumed more than 20% of daily calories from UPFs (quartiles 2-4) experienced a 28% faster rate of decline in global cognition (beta = –0.004; 95% confidence interval [CI], –0.006 to –0.001; P = .003) and a 25% faster rate of decline in executive function (beta = –0.003, 95% CI, –0.005 to 0.000; P = .01) compared to peers in quartile 1 who consumed less than 20% of daily calories from UPFs.
The researchers did not investigate individual groups of UPFs.
However, Dr. Goncalves noted that some studies have linked the consumption of sugar-sweetened beverages with lower cognitive performance, lower brain volume, and poorer memory performance. Another group of ultraprocessed foods, processed meats, has been associated with increased all-cause dementia and Alzheimer’s disease.
Other limitations include the fact that self-reported diet habits were assessed only at baseline using a food frequency questionnaire that was not designed to assess the degree of processing.
While analyses were adjusted for several sociodemographic and clinical confounders, the researchers said they could not exclude the possibility of residual confounding.
Also, since neuroimaging is not available in the ELSA-Brasil study, they were not able to investigate potential mechanisms that could explain the association between higher UPF consumption and cognitive decline.
Despite these limitations, the researchers said their findings suggest that “limiting UPF consumption, particularly in middle-aged adults, may be an efficient form to prevent cognitive decline.”
Weighing the evidence
Several experts weighed in on the results in a statement from the UK nonprofit organization, Science Media Centre.
Kevin McConway, PhD, with Open University, Milton Keynes, England, said it’s important to note that the study suggests “an association, a correlation, and that doesn’t necessarily mean that the cognitive decline was caused by eating more ultra-processed foods.”
He also noted that some types of cognitive decline that are associated with aging occurred in participants in all four quartiles, which were defined by the percentage of their daily energy that came from consuming UPFs.
“That’s hardly surprising – it’s a sad fact of life that pretty well all of us gradually lose some of our cognitive functions as we go through middle and older age,” Dr. McConway said.
“The study doesn’t establish that differences in speed of cognitive decline are caused by ultra-processed food consumption anyway. That’s because it’s an observational study. If the consumption of ultra-processed food causes the differences in rate of cognitive decline, then eating less of it might slow cognitive decline, but if the cause is something else, then that won’t happen,” Dr. McConway added.
Gunter Kuhnle, PhD, professor of nutrition and food science, University of Reading, England, noted that UPFs have become a “fashionable term to explain associations between diet and ill health, and many studies have attempted to show associations.
“Most studies have been observational and had a key limitation: It is very difficult to determine ultra-processed food intake using methods that are not designed to do so, and so authors need to make a lot of assumptions. Bread and meat products are often classed as ‘ultra-processed,’ even though this is often wrong,” Dr. Kuhnle noted.
“The same applies to this study – the method used to measure ultra-processed food intake was not designed for that task and relied on assumptions. This makes it virtually impossible to draw any conclusions,” Dr. Kuhnle said.
Duane Mellor, PhD, RD, RNutr, registered dietitian and senior teaching fellow, Aston University, Birmingham, England, said the study does not change how we should try to eat to maintain good brain function and cognition.
“We should try to eat less foods which are high in added sugar, salt, and fat, which would include many of the foods classified as being ultra-processed, while eating more in terms of both quantity and variety of vegetables, fruit, nuts, seeds, and pulses, which are known to be beneficial for both our cognitive and overall health,” Dr. Mellor said.
The ELSA-Brasil study was supported by the Brazilian Ministry of Health, the Ministry of Science, Technology and Innovation, and the National Council for Scientific and Technological Development. The authors as well as Dr. McConway, Dr. Mellor, and Dr. Kuhnle have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
‘Meth’ heart failure on the rise, often more severe
a literature review indicates.
MethHF is associated with increased severity for HF, longer inpatient stay, and more readmissions, compared with non-MethHF, the data show.
Clinicians “need to consider methamphetamine as a potential etiology for heart failure and include a substance use history when evaluating patients. Treating methamphetamine use disorder improves heart failure outcomes,” first author Veena Manja, MD, PhD, with Stanford (Calif.) University, said in an interview.
The study was published online in the journal Heart.
Poor outcomes, ‘staggering’ costs
This “thoughtful” review is “important and necessary,” Jonathan Davis, MD, director of the heart failure program, Zuckerberg San Francisco General Hospital, wrote in an editorial in the journal.
Dr. Davis noted that patients with Meth HF are at increased risk for poor outcomes and death and the health care costs related to MethHF are “staggering.”
As an example, inpatient data for California show annual charges related to MethHF rose by 840% from 2008 to 2018, from $41.5 million to $390.2 million, compared with 82% for all HF, which rose from $3.5 billion to $6.8 billion.
Illicit use of methamphetamine – also known as “crystal meth,” “ice,” and “speed” – has been linked to hypertension, MI, stroke, aortic dissection, and sudden death. But until now, there was no comprehensive systematic review of published studies on MethHF.
“Our goal was to compile current knowledge on the topic, increase awareness of this condition and identify areas for future research,” Dr. Manja said.
The researchers reviewed 21 observational studies, mostly from the United States (14 from California), between 1997 and 2020. The mean age of adults with MethHF ranged in age from 35 to 60 and more than half were male (57%).
Illicit methamphetamine was inhaled, injected, swallowed, smoked, and snorted. The reported frequency ranged from daily to every other week, and the total monthly dose ranged from 0.35 g to 24.5 g.
The average duration of meth use before HF diagnosis was 5 years. However, 18% of users developed HF within 1 year of starting to use illicit methamphetamine. In some cases, HF was diagnosed after a single use.
The researchers also note that MethHF with preserved left ventricular ejection fraction, seen in up to 44% of cases, is a distinct entity that may progress to reduced LVEF with continued use.
MethHF is also associated with a greater likelihood of other substance abuse, PTSD, depression, and other heart and kidney disease.
Factors associated with improved MethHF outcomes include female sex, meth abstinence, and adherence to guideline-directed HF therapy.
Improvement in MethHF outcomes is possible even if abstinence is not consistent, a finding that lends support to harm reduction principles of “meeting patients where they are instead of insisting on complete abstinence,” the researchers said.
Large gaps in knowledge
They were unable to combine the results into a meta-analysis because of heterogeneity in study design, population, comparator, and outcome assessment. Also, the overall risk of bias is moderate because of the presence of confounders, selection bias and poor matching, and the overall certainty in the evidence is very low,.
No study evaluated the incidence or prevalence of HF among methamphetamine users and inconsistent history taking and testing in patients with HF impeded accurate MethHF prevalence assessment.
Several studies, however, document an increasing incidence of MethHF, particularly over the past decade.
One study from California reported a 585% increase in MethHF hospital admissions between 2008 and 2018. An analysis of the National Inpatient Survey found a 12-fold increase in annual MethHF hospitalizations between 2002 and 2014.
“The results of this systematic review highlight large gaps in our knowledge” of MethHF, Dr. Manja said in an interview.
“We need to understand the epidemiology, prevalence, factors that confer susceptibility to cardiovascular outcomes, and need research into treatment targeted toward this disease,” Dr. Manja added. “We should consider options to integrate substance use treatment in HF/cardiology/primary care clinics and design a multidisciplinary patient-centered approach.”
Dr. Davis agreed. This work “highlights that the standard of care academically and clinically must be a broad team across the care spectrum to simultaneously address methamphetamine use, heart failure, and social determinants of health.”
This research had no specific funding. Dr. Manja and Dr. Davis reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
a literature review indicates.
MethHF is associated with increased severity for HF, longer inpatient stay, and more readmissions, compared with non-MethHF, the data show.
Clinicians “need to consider methamphetamine as a potential etiology for heart failure and include a substance use history when evaluating patients. Treating methamphetamine use disorder improves heart failure outcomes,” first author Veena Manja, MD, PhD, with Stanford (Calif.) University, said in an interview.
The study was published online in the journal Heart.
Poor outcomes, ‘staggering’ costs
This “thoughtful” review is “important and necessary,” Jonathan Davis, MD, director of the heart failure program, Zuckerberg San Francisco General Hospital, wrote in an editorial in the journal.
Dr. Davis noted that patients with Meth HF are at increased risk for poor outcomes and death and the health care costs related to MethHF are “staggering.”
As an example, inpatient data for California show annual charges related to MethHF rose by 840% from 2008 to 2018, from $41.5 million to $390.2 million, compared with 82% for all HF, which rose from $3.5 billion to $6.8 billion.
Illicit use of methamphetamine – also known as “crystal meth,” “ice,” and “speed” – has been linked to hypertension, MI, stroke, aortic dissection, and sudden death. But until now, there was no comprehensive systematic review of published studies on MethHF.
“Our goal was to compile current knowledge on the topic, increase awareness of this condition and identify areas for future research,” Dr. Manja said.
The researchers reviewed 21 observational studies, mostly from the United States (14 from California), between 1997 and 2020. The mean age of adults with MethHF ranged in age from 35 to 60 and more than half were male (57%).
Illicit methamphetamine was inhaled, injected, swallowed, smoked, and snorted. The reported frequency ranged from daily to every other week, and the total monthly dose ranged from 0.35 g to 24.5 g.
The average duration of meth use before HF diagnosis was 5 years. However, 18% of users developed HF within 1 year of starting to use illicit methamphetamine. In some cases, HF was diagnosed after a single use.
The researchers also note that MethHF with preserved left ventricular ejection fraction, seen in up to 44% of cases, is a distinct entity that may progress to reduced LVEF with continued use.
MethHF is also associated with a greater likelihood of other substance abuse, PTSD, depression, and other heart and kidney disease.
Factors associated with improved MethHF outcomes include female sex, meth abstinence, and adherence to guideline-directed HF therapy.
Improvement in MethHF outcomes is possible even if abstinence is not consistent, a finding that lends support to harm reduction principles of “meeting patients where they are instead of insisting on complete abstinence,” the researchers said.
Large gaps in knowledge
They were unable to combine the results into a meta-analysis because of heterogeneity in study design, population, comparator, and outcome assessment. Also, the overall risk of bias is moderate because of the presence of confounders, selection bias and poor matching, and the overall certainty in the evidence is very low,.
No study evaluated the incidence or prevalence of HF among methamphetamine users and inconsistent history taking and testing in patients with HF impeded accurate MethHF prevalence assessment.
Several studies, however, document an increasing incidence of MethHF, particularly over the past decade.
One study from California reported a 585% increase in MethHF hospital admissions between 2008 and 2018. An analysis of the National Inpatient Survey found a 12-fold increase in annual MethHF hospitalizations between 2002 and 2014.
“The results of this systematic review highlight large gaps in our knowledge” of MethHF, Dr. Manja said in an interview.
“We need to understand the epidemiology, prevalence, factors that confer susceptibility to cardiovascular outcomes, and need research into treatment targeted toward this disease,” Dr. Manja added. “We should consider options to integrate substance use treatment in HF/cardiology/primary care clinics and design a multidisciplinary patient-centered approach.”
Dr. Davis agreed. This work “highlights that the standard of care academically and clinically must be a broad team across the care spectrum to simultaneously address methamphetamine use, heart failure, and social determinants of health.”
This research had no specific funding. Dr. Manja and Dr. Davis reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
a literature review indicates.
MethHF is associated with increased severity for HF, longer inpatient stay, and more readmissions, compared with non-MethHF, the data show.
Clinicians “need to consider methamphetamine as a potential etiology for heart failure and include a substance use history when evaluating patients. Treating methamphetamine use disorder improves heart failure outcomes,” first author Veena Manja, MD, PhD, with Stanford (Calif.) University, said in an interview.
The study was published online in the journal Heart.
Poor outcomes, ‘staggering’ costs
This “thoughtful” review is “important and necessary,” Jonathan Davis, MD, director of the heart failure program, Zuckerberg San Francisco General Hospital, wrote in an editorial in the journal.
Dr. Davis noted that patients with Meth HF are at increased risk for poor outcomes and death and the health care costs related to MethHF are “staggering.”
As an example, inpatient data for California show annual charges related to MethHF rose by 840% from 2008 to 2018, from $41.5 million to $390.2 million, compared with 82% for all HF, which rose from $3.5 billion to $6.8 billion.
Illicit use of methamphetamine – also known as “crystal meth,” “ice,” and “speed” – has been linked to hypertension, MI, stroke, aortic dissection, and sudden death. But until now, there was no comprehensive systematic review of published studies on MethHF.
“Our goal was to compile current knowledge on the topic, increase awareness of this condition and identify areas for future research,” Dr. Manja said.
The researchers reviewed 21 observational studies, mostly from the United States (14 from California), between 1997 and 2020. The mean age of adults with MethHF ranged in age from 35 to 60 and more than half were male (57%).
Illicit methamphetamine was inhaled, injected, swallowed, smoked, and snorted. The reported frequency ranged from daily to every other week, and the total monthly dose ranged from 0.35 g to 24.5 g.
The average duration of meth use before HF diagnosis was 5 years. However, 18% of users developed HF within 1 year of starting to use illicit methamphetamine. In some cases, HF was diagnosed after a single use.
The researchers also note that MethHF with preserved left ventricular ejection fraction, seen in up to 44% of cases, is a distinct entity that may progress to reduced LVEF with continued use.
MethHF is also associated with a greater likelihood of other substance abuse, PTSD, depression, and other heart and kidney disease.
Factors associated with improved MethHF outcomes include female sex, meth abstinence, and adherence to guideline-directed HF therapy.
Improvement in MethHF outcomes is possible even if abstinence is not consistent, a finding that lends support to harm reduction principles of “meeting patients where they are instead of insisting on complete abstinence,” the researchers said.
Large gaps in knowledge
They were unable to combine the results into a meta-analysis because of heterogeneity in study design, population, comparator, and outcome assessment. Also, the overall risk of bias is moderate because of the presence of confounders, selection bias and poor matching, and the overall certainty in the evidence is very low,.
No study evaluated the incidence or prevalence of HF among methamphetamine users and inconsistent history taking and testing in patients with HF impeded accurate MethHF prevalence assessment.
Several studies, however, document an increasing incidence of MethHF, particularly over the past decade.
One study from California reported a 585% increase in MethHF hospital admissions between 2008 and 2018. An analysis of the National Inpatient Survey found a 12-fold increase in annual MethHF hospitalizations between 2002 and 2014.
“The results of this systematic review highlight large gaps in our knowledge” of MethHF, Dr. Manja said in an interview.
“We need to understand the epidemiology, prevalence, factors that confer susceptibility to cardiovascular outcomes, and need research into treatment targeted toward this disease,” Dr. Manja added. “We should consider options to integrate substance use treatment in HF/cardiology/primary care clinics and design a multidisciplinary patient-centered approach.”
Dr. Davis agreed. This work “highlights that the standard of care academically and clinically must be a broad team across the care spectrum to simultaneously address methamphetamine use, heart failure, and social determinants of health.”
This research had no specific funding. Dr. Manja and Dr. Davis reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM HEART
High rates of inappropriate PPI use in hospitalized patients
The research was published online in the journal Digestive and Liver Disease.
First author Orly Sneh-Arbib, MD, division of gastroenterology and liver disease, Clalit Health Services, Talpiot, Jerusalem, said in an interview that she and her co-authors were “very surprised” that the rates of inappropriate prescribing remained so high, especially as they had discussed the adverse effects of the drugs numerous times during departmental meetings.
She believes that, for many clinicians, handing out a prescription for PPIs has become a habit, with the thought being: “Just take this; it’s like a vitamin.”
In the paper, the researchers write, “Undoubtedly, more action is needed to raise physicians’ knowledge and attention to the subject while providing automated and standardized technology-based tools to reduce inappropriate PPI use using an acceptable algorithm.”
For the study, Dr. Sneh-Arbib and her colleagues developed an algorithm to assess inappropriate PPI prescribing in almost 4,000 internal medicine patients. To try to limit future overprescribing, their algorithm is now included in the clinical records system.
Consequently, every time a clinician tries to prescribe a PPI, they have to confirm that there is a valid indication for doing so, with the aim of adding an “extra step in the process,” Dr. Sneh-Arbib said.
Clear but complex PPI indications
There are a small, well-defined number of indications for long-term PPI use, the authors write. The indications include prior upper gastrointestinal bleeding, maintenance treatment after healing of erosive esophagitis, Barrett’s esophagus, the use of nonsteroidal anti-inflammatory drugs or antiplatelet agents in patients with increased bleeding risk, and maintenance therapy for symptom control in patients with gastroesophageal reflux disease.
The authors also note that the “appropriateness of PPIs is complex,” with multiple factors to consider for long-term PPI use, including complex drug combinations and medical history.
But having seen patients in their 30s prescribed PPIs “just because of taking steroids or aspirin,” Dr. Sneh-Arbib said she wanted to investigate further.
To examine the rate of inappropriate long-term PPI prescription on discharge from internal medicine departments, the team conducted a retrospective analysis of adults admitted to their institution for the first 6 months of 2014 and the first 6 months of 2017.
They included all patients prescribed PPIs on discharge with a recommendation for long-term use and excluded those who were transferred between departments or who had a hospital stay longer than 3 months.
Information on age, gender, ethnicity, socioeconomic status, current and past diagnoses including all relevant gastrointestinal diagnoses, Charlson comorbidity index, and medications on admission and discharge were recorded.
Guidelines for use of PPIs
To assess inappropriate PPI prescribing, the team searched for published recommendations on long-term use, Dr. Sneh-Arbib said. They developed an algorithm based on the U.K. National Institute for Health and Care Excellence (NICE) clinical guideline, “Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management.”
The guideline is “not perfect,” Dr. Sneh-Arbib said, but it was suitable. The team then randomly chose 100 patients from their records to validate the resulting algorithm, finding an accuracy of 96%.
The full analysis included 3,982 patients, of whom 74% were aged 65 years or older, and 50.8% were women. PPIs were first prescribed before hospital admission in 92.4% of cases.
The researchers found that the overall rate of inappropriate PPI prescriptions was 44.3%, a figure that was stable between the two the study periods. In 2014, the rate of inappropriate use was 43.2%, and it was 45.6% in 2017, a nonsignificant difference.
Inappropriate PPIs were higher (68.1%) in patients younger than 65 years, compared with those aged 65 years and older (36%).
The researchers analyzed factors associated with inappropriate PPIs, first excluding 448 patients with clear gastrointestinal indications.
In the majority of cases, the inappropriate PPI prescriptions occurred in patients who were not taking dual antiplatelet treatment (89.4%), in younger patients who were taking aspirin only (8.6%), and in patients receiving a single antiplatelet agent other than aspirin (1.9%), according to multivariate analysis.
Overall, 42.4% of patients classified as inappropriate PPI use were not using aspirin, nonsteroidal anti-inflammatory drugs, antiplatelets, antiaggregants, anticoagulants, or steroids, the researchers found.
They also note that most patients in the study (92.3%) had received PPIs before admission, prescribed by their general practitioner or during a previous hospitalization. This raises concerns about unneeded continuation of the drugs and lack of review by clinicians, they write.
PPI deprescribing
Approached for comment, Adrienna Jirik, MD, a gastroenterologist at the Cleveland Clinic, told this news organization that “PPI overprescription is a common problem worldwide, with the United States being no exception.”
They are “one of the most prescribed medications in the world, with several formulations readily available as an over-the-counter medication,” she added.
Dr. Jirik, who was not involved with the study, said that the algorithm used is “on par with the United States clinical practice guidelines for PPI use” and a “great start to initiate an encounter with a patient on PPIs in the outpatient setting to review the indications and to de-escalate and deprescribe therapy.”
Indeed, the American Gastroenterological Association recently published a clinical practice update on deprescribing PPIs.
“It may be useful to incorporate a version of this algorithm as a ‘hard stop’ on some outpatient EMR [electronic medical record] templates to remind providers to address this issue prior to closing an encounter,” Dr. Jirik added.
She noted, however, that tackling any medication reconciliation is a very important but difficult and time-consuming task.
“Education is definitely key for both primary and subspecialty providers,” Dr. Jirik said. “If patients have been on a long-term PPI, the inpatient provider can suggest a plan for de-escalation based on practice guidelines and arrange proper outpatient follow-up for eventual deprescribing.”
No funding was declared. The authors and Dr. Jirik report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The research was published online in the journal Digestive and Liver Disease.
First author Orly Sneh-Arbib, MD, division of gastroenterology and liver disease, Clalit Health Services, Talpiot, Jerusalem, said in an interview that she and her co-authors were “very surprised” that the rates of inappropriate prescribing remained so high, especially as they had discussed the adverse effects of the drugs numerous times during departmental meetings.
She believes that, for many clinicians, handing out a prescription for PPIs has become a habit, with the thought being: “Just take this; it’s like a vitamin.”
In the paper, the researchers write, “Undoubtedly, more action is needed to raise physicians’ knowledge and attention to the subject while providing automated and standardized technology-based tools to reduce inappropriate PPI use using an acceptable algorithm.”
For the study, Dr. Sneh-Arbib and her colleagues developed an algorithm to assess inappropriate PPI prescribing in almost 4,000 internal medicine patients. To try to limit future overprescribing, their algorithm is now included in the clinical records system.
Consequently, every time a clinician tries to prescribe a PPI, they have to confirm that there is a valid indication for doing so, with the aim of adding an “extra step in the process,” Dr. Sneh-Arbib said.
Clear but complex PPI indications
There are a small, well-defined number of indications for long-term PPI use, the authors write. The indications include prior upper gastrointestinal bleeding, maintenance treatment after healing of erosive esophagitis, Barrett’s esophagus, the use of nonsteroidal anti-inflammatory drugs or antiplatelet agents in patients with increased bleeding risk, and maintenance therapy for symptom control in patients with gastroesophageal reflux disease.
The authors also note that the “appropriateness of PPIs is complex,” with multiple factors to consider for long-term PPI use, including complex drug combinations and medical history.
But having seen patients in their 30s prescribed PPIs “just because of taking steroids or aspirin,” Dr. Sneh-Arbib said she wanted to investigate further.
To examine the rate of inappropriate long-term PPI prescription on discharge from internal medicine departments, the team conducted a retrospective analysis of adults admitted to their institution for the first 6 months of 2014 and the first 6 months of 2017.
They included all patients prescribed PPIs on discharge with a recommendation for long-term use and excluded those who were transferred between departments or who had a hospital stay longer than 3 months.
Information on age, gender, ethnicity, socioeconomic status, current and past diagnoses including all relevant gastrointestinal diagnoses, Charlson comorbidity index, and medications on admission and discharge were recorded.
Guidelines for use of PPIs
To assess inappropriate PPI prescribing, the team searched for published recommendations on long-term use, Dr. Sneh-Arbib said. They developed an algorithm based on the U.K. National Institute for Health and Care Excellence (NICE) clinical guideline, “Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management.”
The guideline is “not perfect,” Dr. Sneh-Arbib said, but it was suitable. The team then randomly chose 100 patients from their records to validate the resulting algorithm, finding an accuracy of 96%.
The full analysis included 3,982 patients, of whom 74% were aged 65 years or older, and 50.8% were women. PPIs were first prescribed before hospital admission in 92.4% of cases.
The researchers found that the overall rate of inappropriate PPI prescriptions was 44.3%, a figure that was stable between the two the study periods. In 2014, the rate of inappropriate use was 43.2%, and it was 45.6% in 2017, a nonsignificant difference.
Inappropriate PPIs were higher (68.1%) in patients younger than 65 years, compared with those aged 65 years and older (36%).
The researchers analyzed factors associated with inappropriate PPIs, first excluding 448 patients with clear gastrointestinal indications.
In the majority of cases, the inappropriate PPI prescriptions occurred in patients who were not taking dual antiplatelet treatment (89.4%), in younger patients who were taking aspirin only (8.6%), and in patients receiving a single antiplatelet agent other than aspirin (1.9%), according to multivariate analysis.
Overall, 42.4% of patients classified as inappropriate PPI use were not using aspirin, nonsteroidal anti-inflammatory drugs, antiplatelets, antiaggregants, anticoagulants, or steroids, the researchers found.
They also note that most patients in the study (92.3%) had received PPIs before admission, prescribed by their general practitioner or during a previous hospitalization. This raises concerns about unneeded continuation of the drugs and lack of review by clinicians, they write.
PPI deprescribing
Approached for comment, Adrienna Jirik, MD, a gastroenterologist at the Cleveland Clinic, told this news organization that “PPI overprescription is a common problem worldwide, with the United States being no exception.”
They are “one of the most prescribed medications in the world, with several formulations readily available as an over-the-counter medication,” she added.
Dr. Jirik, who was not involved with the study, said that the algorithm used is “on par with the United States clinical practice guidelines for PPI use” and a “great start to initiate an encounter with a patient on PPIs in the outpatient setting to review the indications and to de-escalate and deprescribe therapy.”
Indeed, the American Gastroenterological Association recently published a clinical practice update on deprescribing PPIs.
“It may be useful to incorporate a version of this algorithm as a ‘hard stop’ on some outpatient EMR [electronic medical record] templates to remind providers to address this issue prior to closing an encounter,” Dr. Jirik added.
She noted, however, that tackling any medication reconciliation is a very important but difficult and time-consuming task.
“Education is definitely key for both primary and subspecialty providers,” Dr. Jirik said. “If patients have been on a long-term PPI, the inpatient provider can suggest a plan for de-escalation based on practice guidelines and arrange proper outpatient follow-up for eventual deprescribing.”
No funding was declared. The authors and Dr. Jirik report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The research was published online in the journal Digestive and Liver Disease.
First author Orly Sneh-Arbib, MD, division of gastroenterology and liver disease, Clalit Health Services, Talpiot, Jerusalem, said in an interview that she and her co-authors were “very surprised” that the rates of inappropriate prescribing remained so high, especially as they had discussed the adverse effects of the drugs numerous times during departmental meetings.
She believes that, for many clinicians, handing out a prescription for PPIs has become a habit, with the thought being: “Just take this; it’s like a vitamin.”
In the paper, the researchers write, “Undoubtedly, more action is needed to raise physicians’ knowledge and attention to the subject while providing automated and standardized technology-based tools to reduce inappropriate PPI use using an acceptable algorithm.”
For the study, Dr. Sneh-Arbib and her colleagues developed an algorithm to assess inappropriate PPI prescribing in almost 4,000 internal medicine patients. To try to limit future overprescribing, their algorithm is now included in the clinical records system.
Consequently, every time a clinician tries to prescribe a PPI, they have to confirm that there is a valid indication for doing so, with the aim of adding an “extra step in the process,” Dr. Sneh-Arbib said.
Clear but complex PPI indications
There are a small, well-defined number of indications for long-term PPI use, the authors write. The indications include prior upper gastrointestinal bleeding, maintenance treatment after healing of erosive esophagitis, Barrett’s esophagus, the use of nonsteroidal anti-inflammatory drugs or antiplatelet agents in patients with increased bleeding risk, and maintenance therapy for symptom control in patients with gastroesophageal reflux disease.
The authors also note that the “appropriateness of PPIs is complex,” with multiple factors to consider for long-term PPI use, including complex drug combinations and medical history.
But having seen patients in their 30s prescribed PPIs “just because of taking steroids or aspirin,” Dr. Sneh-Arbib said she wanted to investigate further.
To examine the rate of inappropriate long-term PPI prescription on discharge from internal medicine departments, the team conducted a retrospective analysis of adults admitted to their institution for the first 6 months of 2014 and the first 6 months of 2017.
They included all patients prescribed PPIs on discharge with a recommendation for long-term use and excluded those who were transferred between departments or who had a hospital stay longer than 3 months.
Information on age, gender, ethnicity, socioeconomic status, current and past diagnoses including all relevant gastrointestinal diagnoses, Charlson comorbidity index, and medications on admission and discharge were recorded.
Guidelines for use of PPIs
To assess inappropriate PPI prescribing, the team searched for published recommendations on long-term use, Dr. Sneh-Arbib said. They developed an algorithm based on the U.K. National Institute for Health and Care Excellence (NICE) clinical guideline, “Gastro-oesophageal reflux disease and dyspepsia in adults: investigation and management.”
The guideline is “not perfect,” Dr. Sneh-Arbib said, but it was suitable. The team then randomly chose 100 patients from their records to validate the resulting algorithm, finding an accuracy of 96%.
The full analysis included 3,982 patients, of whom 74% were aged 65 years or older, and 50.8% were women. PPIs were first prescribed before hospital admission in 92.4% of cases.
The researchers found that the overall rate of inappropriate PPI prescriptions was 44.3%, a figure that was stable between the two the study periods. In 2014, the rate of inappropriate use was 43.2%, and it was 45.6% in 2017, a nonsignificant difference.
Inappropriate PPIs were higher (68.1%) in patients younger than 65 years, compared with those aged 65 years and older (36%).
The researchers analyzed factors associated with inappropriate PPIs, first excluding 448 patients with clear gastrointestinal indications.
In the majority of cases, the inappropriate PPI prescriptions occurred in patients who were not taking dual antiplatelet treatment (89.4%), in younger patients who were taking aspirin only (8.6%), and in patients receiving a single antiplatelet agent other than aspirin (1.9%), according to multivariate analysis.
Overall, 42.4% of patients classified as inappropriate PPI use were not using aspirin, nonsteroidal anti-inflammatory drugs, antiplatelets, antiaggregants, anticoagulants, or steroids, the researchers found.
They also note that most patients in the study (92.3%) had received PPIs before admission, prescribed by their general practitioner or during a previous hospitalization. This raises concerns about unneeded continuation of the drugs and lack of review by clinicians, they write.
PPI deprescribing
Approached for comment, Adrienna Jirik, MD, a gastroenterologist at the Cleveland Clinic, told this news organization that “PPI overprescription is a common problem worldwide, with the United States being no exception.”
They are “one of the most prescribed medications in the world, with several formulations readily available as an over-the-counter medication,” she added.
Dr. Jirik, who was not involved with the study, said that the algorithm used is “on par with the United States clinical practice guidelines for PPI use” and a “great start to initiate an encounter with a patient on PPIs in the outpatient setting to review the indications and to de-escalate and deprescribe therapy.”
Indeed, the American Gastroenterological Association recently published a clinical practice update on deprescribing PPIs.
“It may be useful to incorporate a version of this algorithm as a ‘hard stop’ on some outpatient EMR [electronic medical record] templates to remind providers to address this issue prior to closing an encounter,” Dr. Jirik added.
She noted, however, that tackling any medication reconciliation is a very important but difficult and time-consuming task.
“Education is definitely key for both primary and subspecialty providers,” Dr. Jirik said. “If patients have been on a long-term PPI, the inpatient provider can suggest a plan for de-escalation based on practice guidelines and arrange proper outpatient follow-up for eventual deprescribing.”
No funding was declared. The authors and Dr. Jirik report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Vaccination cuts long COVID risk for rheumatic disease patients
Patients with rheumatic disease are at least half as likely to develop long COVID after a SARS-CoV-2 infection if they have been fully vaccinated against COVID-19, according to research published in Annals of the Rheumatic Diseases (2022 Nov 28. doi: 10.1136/ard-2022-223439).
“Moreover, those who were vaccinated prior to getting COVID-19 had less pain and fatigue after their infection,” Zachary S. Wallace, MD, MSc, an assistant professor of medicine at Harvard Medical School, Boston, and a study author, said in an interview. “These findings reinforce the importance of vaccination in this population.”
Messaging around the value of COVID vaccination has been confusing for some with rheumatic disease “because our concern regarding a blunted response to vaccination has led many patients to think that they do not provide much benefit if they are on immunosuppression,” Dr. Wallace said. “In our cohort, which included many patients on immunosuppression of varying degrees, being vaccinated was quite beneficial.”
Leonard H. Calabrese, DO, director of the R.J. Fasenmyer Center for Clinical Immunology and a professor of medicine at the Cleveland Clinic, said in an interview that the study is an “extremely important contribution to our understanding of COVID-19 and its pattern of recovery in patients with immune-mediated inflammatory diseases [IMIDs].” Remaining unanswered questions are “whether patients with IMIDs develop more frequent PASC [post–acute sequelae of COVID-19] from COVID-19 and, if so, is it milder or more severe, and does it differ in its clinical phenotype?”
Long COVID risk assessed at 4 weeks and 3 months after infection
The researchers prospectively tracked 280 adult patients in the Mass General Brigham health care system in the greater Boston area who had systemic autoimmune rheumatic diseases and had an acute COVID-19 infection between March 2020 and July 2022. Patients were an average 53 years old, and most were White (82%) and female (80%). More than half (59%) had inflammatory arthritis, a quarter (24%) had connective tissue disease, and most others had a vasculitis condition or multiple conditions.
A total of 11% of patients were unvaccinated, 28% were partially vaccinated with one mRNA COVID-19 vaccine dose, and 41% were fully vaccinated with two mRNA vaccine doses or one Johnson & Johnson dose. The 116 fully vaccinated patients were considered to have a breakthrough infection while the other 164 were considered to have a nonbreakthrough infection. The breakthrough and nonbreakthrough groups were similar in terms of age, sex, race, ethnicity, smoking status, and type of rheumatic disease. Comorbidities were also similar, except obesity, which was more common in the non–breakthrough infection group (25%) than the breakthrough infection group (10%).
The researchers queried patients on their COVID-19 symptoms, how long symptoms lasted, treatments they received, and hospitalization details. COVID-19 symptoms assessed included fever, sore throat, new cough, nasal congestion/rhinorrhea, dyspnea, chest pain, rash, myalgia, fatigue/malaise, headache, nausea/vomiting, diarrhea, anosmia, dysgeusia, and joint pain.
Patients completed surveys about symptoms at 4 weeks and 3 months after infection. Long COVID, or PASC, was defined as any persistent symptom at the times assessed.
Vaccinated patients fared better across outcomes
At 4 weeks after infection, 41% of fully vaccinated patients had at least one persistent symptom, compared with 54% of unvaccinated or partially vaccinated patients (P = .04). At 3 months after infection, 21% of fully vaccinated patients had at least one persistent symptom, compared with 41% of unvaccinated or partially vaccinated patients (P < .0001).
Vaccinated patients were half as likely to have long COVID at 4 weeks after infection (adjusted odds ratio, 0.49) and 90% less likely to have long COVID 3 months after infection (aOR, 0.1), after adjustment for age, sex, race, comorbidities, and use of any of four immune-suppressing medications (anti-CD20 monoclonal antibodies, methotrexate, mycophenolate, or glucocorticoids).
Fully vaccinated patients with breakthrough infections had an average 21 additional days without symptoms during follow-up, compared with unvaccinated and partially vaccinated patients (P = .04).
Reduced risk of long COVID did not change for vaccinated patients after sensitivity analyses for those who did not receive nirmatrelvir/ritonavir (Paxlovid) or monoclonal antibodies, those who didn’t receive any COVID-19-related treatment, those who completed their questionnaires within 6 months after infection, and those who were not hospitalized.
“One important message is that among those who did get PASC, the severity appears similar among those with and without a breakthrough infection,” Dr. Wallace said. “This highlights the need for ongoing research to improve recognition, diagnosis, and treatment of PASC.”
Many more breakthrough infections (72%) than nonbreakthrough infections (2%) occurred during Omicron. The authors acknowledged that different variants might play a role in different long COVID risks but said such potential confounding is unlikely to fully explain the results.
“Even with data suggesting that the Omicron variants may be intrinsically less severe, vaccination still has an impact on severity of infection, rates of hospitalization, and other outcomes and thus may play a role in the risk of PASC,” lead author Naomi Patel, MD, an instructor at Harvard Medical School and a rheumatologist at Massachusetts General Hospital, said in an interview. “A study evaluating the proportions with PASC by vaccination status during the time in which a single variant is predominant, such as the early Omicron era, could help to better assess the more isolated impact of vaccination on PASC.”
Dr. Calabrese said he is convinced that Omicron infections are less likely to result in more severe forms of acute COVID than pre-Omicron infections, and he suspects Omicron infections are also less likely to result in long COVID, although less evidence currently supports this hypothesis.
Hospitalization was more common in unvaccinated/partly vaccinated patients than in vaccinated patients (27% vs. 5%; P = .001). Although pain and fatigue were lower in those with breakthrough infections, functional scores and health-related quality of life were similar in both groups.
Some symptoms significantly differed between vaccinated and unvaccinated/partly vaccinated groups, possibly caused partly by different variants. Nasal congestion was more common (73%) in those with breakthrough infections than in those with nonbreakthrough infections (46%; P < .0001). Those who were unvaccinated/partly vaccinated were significantly more likely to have loss of smell (46% vs. 22%) or taste (45% vs. 28%) or to have joint pain (11% vs. 4%).
Treatment with nirmatrelvir/ritonavir was also more common in vaccinated patients (12%) than in unvaccinated/partly vaccinated patients (1%; P < .0001), as was treatment with monoclonal antibodies (34% vs. 8%; P < .0001).
The study was limited by its low diversity and being at a single health care system, the authors said. Study coauthor Jeffrey A. Sparks, MD, MMSc, an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, said in an interview that the group is planning additional studies as their cohort grows, including “investigating the relationships between COVID-19 and specific rheumatic diseases and immunomodulating medications, expansion of autoimmunity and systemic inflammation, and lung damage among specific patient populations.”
Dr. Calabrese said it will be important for follow-up study of the symptomatic patients to “determine how many of these patients will fit the clinical picture of long COVID or long-haul phenotypes over the months and years ahead, including documenting exertional malaise and quality of life.
This study only assessed patients who received zero, one, or two doses of a vaccine, but many patients with rheumatic disease today will likely have received booster doses. However, Dr. Calabrese said it would be difficult to quantify whether a third, fourth, or fifth dose offers additional protection from long-term COVID complications after full vaccination or hybrid vaccination.
The research was funded by the Rheumatology Research Foundation, the National Institutes of Health, the R. Bruce and Joan M. Mickey Research Scholar Fund, and the Llura Gund Award for Rheumatoid Arthritis Research and Care. Dr. Wallace has received research support from Bristol-Myers Squibb and Principia/Sanofi and consulting fees from Zenas BioPharma, Horizon, Sanofi, Shionogi, Viela Bio, and Medpace. Dr. Sparks has received research support from Bristol-Myers Squibb and consulting fees from AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer. Dr. Patel has received consulting fees from FVC Health. Calabrese has consulted for Genentech, Sanofi-Regeneron, AstraZeneca, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
Patients with rheumatic disease are at least half as likely to develop long COVID after a SARS-CoV-2 infection if they have been fully vaccinated against COVID-19, according to research published in Annals of the Rheumatic Diseases (2022 Nov 28. doi: 10.1136/ard-2022-223439).
“Moreover, those who were vaccinated prior to getting COVID-19 had less pain and fatigue after their infection,” Zachary S. Wallace, MD, MSc, an assistant professor of medicine at Harvard Medical School, Boston, and a study author, said in an interview. “These findings reinforce the importance of vaccination in this population.”
Messaging around the value of COVID vaccination has been confusing for some with rheumatic disease “because our concern regarding a blunted response to vaccination has led many patients to think that they do not provide much benefit if they are on immunosuppression,” Dr. Wallace said. “In our cohort, which included many patients on immunosuppression of varying degrees, being vaccinated was quite beneficial.”
Leonard H. Calabrese, DO, director of the R.J. Fasenmyer Center for Clinical Immunology and a professor of medicine at the Cleveland Clinic, said in an interview that the study is an “extremely important contribution to our understanding of COVID-19 and its pattern of recovery in patients with immune-mediated inflammatory diseases [IMIDs].” Remaining unanswered questions are “whether patients with IMIDs develop more frequent PASC [post–acute sequelae of COVID-19] from COVID-19 and, if so, is it milder or more severe, and does it differ in its clinical phenotype?”
Long COVID risk assessed at 4 weeks and 3 months after infection
The researchers prospectively tracked 280 adult patients in the Mass General Brigham health care system in the greater Boston area who had systemic autoimmune rheumatic diseases and had an acute COVID-19 infection between March 2020 and July 2022. Patients were an average 53 years old, and most were White (82%) and female (80%). More than half (59%) had inflammatory arthritis, a quarter (24%) had connective tissue disease, and most others had a vasculitis condition or multiple conditions.
A total of 11% of patients were unvaccinated, 28% were partially vaccinated with one mRNA COVID-19 vaccine dose, and 41% were fully vaccinated with two mRNA vaccine doses or one Johnson & Johnson dose. The 116 fully vaccinated patients were considered to have a breakthrough infection while the other 164 were considered to have a nonbreakthrough infection. The breakthrough and nonbreakthrough groups were similar in terms of age, sex, race, ethnicity, smoking status, and type of rheumatic disease. Comorbidities were also similar, except obesity, which was more common in the non–breakthrough infection group (25%) than the breakthrough infection group (10%).
The researchers queried patients on their COVID-19 symptoms, how long symptoms lasted, treatments they received, and hospitalization details. COVID-19 symptoms assessed included fever, sore throat, new cough, nasal congestion/rhinorrhea, dyspnea, chest pain, rash, myalgia, fatigue/malaise, headache, nausea/vomiting, diarrhea, anosmia, dysgeusia, and joint pain.
Patients completed surveys about symptoms at 4 weeks and 3 months after infection. Long COVID, or PASC, was defined as any persistent symptom at the times assessed.
Vaccinated patients fared better across outcomes
At 4 weeks after infection, 41% of fully vaccinated patients had at least one persistent symptom, compared with 54% of unvaccinated or partially vaccinated patients (P = .04). At 3 months after infection, 21% of fully vaccinated patients had at least one persistent symptom, compared with 41% of unvaccinated or partially vaccinated patients (P < .0001).
Vaccinated patients were half as likely to have long COVID at 4 weeks after infection (adjusted odds ratio, 0.49) and 90% less likely to have long COVID 3 months after infection (aOR, 0.1), after adjustment for age, sex, race, comorbidities, and use of any of four immune-suppressing medications (anti-CD20 monoclonal antibodies, methotrexate, mycophenolate, or glucocorticoids).
Fully vaccinated patients with breakthrough infections had an average 21 additional days without symptoms during follow-up, compared with unvaccinated and partially vaccinated patients (P = .04).
Reduced risk of long COVID did not change for vaccinated patients after sensitivity analyses for those who did not receive nirmatrelvir/ritonavir (Paxlovid) or monoclonal antibodies, those who didn’t receive any COVID-19-related treatment, those who completed their questionnaires within 6 months after infection, and those who were not hospitalized.
“One important message is that among those who did get PASC, the severity appears similar among those with and without a breakthrough infection,” Dr. Wallace said. “This highlights the need for ongoing research to improve recognition, diagnosis, and treatment of PASC.”
Many more breakthrough infections (72%) than nonbreakthrough infections (2%) occurred during Omicron. The authors acknowledged that different variants might play a role in different long COVID risks but said such potential confounding is unlikely to fully explain the results.
“Even with data suggesting that the Omicron variants may be intrinsically less severe, vaccination still has an impact on severity of infection, rates of hospitalization, and other outcomes and thus may play a role in the risk of PASC,” lead author Naomi Patel, MD, an instructor at Harvard Medical School and a rheumatologist at Massachusetts General Hospital, said in an interview. “A study evaluating the proportions with PASC by vaccination status during the time in which a single variant is predominant, such as the early Omicron era, could help to better assess the more isolated impact of vaccination on PASC.”
Dr. Calabrese said he is convinced that Omicron infections are less likely to result in more severe forms of acute COVID than pre-Omicron infections, and he suspects Omicron infections are also less likely to result in long COVID, although less evidence currently supports this hypothesis.
Hospitalization was more common in unvaccinated/partly vaccinated patients than in vaccinated patients (27% vs. 5%; P = .001). Although pain and fatigue were lower in those with breakthrough infections, functional scores and health-related quality of life were similar in both groups.
Some symptoms significantly differed between vaccinated and unvaccinated/partly vaccinated groups, possibly caused partly by different variants. Nasal congestion was more common (73%) in those with breakthrough infections than in those with nonbreakthrough infections (46%; P < .0001). Those who were unvaccinated/partly vaccinated were significantly more likely to have loss of smell (46% vs. 22%) or taste (45% vs. 28%) or to have joint pain (11% vs. 4%).
Treatment with nirmatrelvir/ritonavir was also more common in vaccinated patients (12%) than in unvaccinated/partly vaccinated patients (1%; P < .0001), as was treatment with monoclonal antibodies (34% vs. 8%; P < .0001).
The study was limited by its low diversity and being at a single health care system, the authors said. Study coauthor Jeffrey A. Sparks, MD, MMSc, an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, said in an interview that the group is planning additional studies as their cohort grows, including “investigating the relationships between COVID-19 and specific rheumatic diseases and immunomodulating medications, expansion of autoimmunity and systemic inflammation, and lung damage among specific patient populations.”
Dr. Calabrese said it will be important for follow-up study of the symptomatic patients to “determine how many of these patients will fit the clinical picture of long COVID or long-haul phenotypes over the months and years ahead, including documenting exertional malaise and quality of life.
This study only assessed patients who received zero, one, or two doses of a vaccine, but many patients with rheumatic disease today will likely have received booster doses. However, Dr. Calabrese said it would be difficult to quantify whether a third, fourth, or fifth dose offers additional protection from long-term COVID complications after full vaccination or hybrid vaccination.
The research was funded by the Rheumatology Research Foundation, the National Institutes of Health, the R. Bruce and Joan M. Mickey Research Scholar Fund, and the Llura Gund Award for Rheumatoid Arthritis Research and Care. Dr. Wallace has received research support from Bristol-Myers Squibb and Principia/Sanofi and consulting fees from Zenas BioPharma, Horizon, Sanofi, Shionogi, Viela Bio, and Medpace. Dr. Sparks has received research support from Bristol-Myers Squibb and consulting fees from AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer. Dr. Patel has received consulting fees from FVC Health. Calabrese has consulted for Genentech, Sanofi-Regeneron, AstraZeneca, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
Patients with rheumatic disease are at least half as likely to develop long COVID after a SARS-CoV-2 infection if they have been fully vaccinated against COVID-19, according to research published in Annals of the Rheumatic Diseases (2022 Nov 28. doi: 10.1136/ard-2022-223439).
“Moreover, those who were vaccinated prior to getting COVID-19 had less pain and fatigue after their infection,” Zachary S. Wallace, MD, MSc, an assistant professor of medicine at Harvard Medical School, Boston, and a study author, said in an interview. “These findings reinforce the importance of vaccination in this population.”
Messaging around the value of COVID vaccination has been confusing for some with rheumatic disease “because our concern regarding a blunted response to vaccination has led many patients to think that they do not provide much benefit if they are on immunosuppression,” Dr. Wallace said. “In our cohort, which included many patients on immunosuppression of varying degrees, being vaccinated was quite beneficial.”
Leonard H. Calabrese, DO, director of the R.J. Fasenmyer Center for Clinical Immunology and a professor of medicine at the Cleveland Clinic, said in an interview that the study is an “extremely important contribution to our understanding of COVID-19 and its pattern of recovery in patients with immune-mediated inflammatory diseases [IMIDs].” Remaining unanswered questions are “whether patients with IMIDs develop more frequent PASC [post–acute sequelae of COVID-19] from COVID-19 and, if so, is it milder or more severe, and does it differ in its clinical phenotype?”
Long COVID risk assessed at 4 weeks and 3 months after infection
The researchers prospectively tracked 280 adult patients in the Mass General Brigham health care system in the greater Boston area who had systemic autoimmune rheumatic diseases and had an acute COVID-19 infection between March 2020 and July 2022. Patients were an average 53 years old, and most were White (82%) and female (80%). More than half (59%) had inflammatory arthritis, a quarter (24%) had connective tissue disease, and most others had a vasculitis condition or multiple conditions.
A total of 11% of patients were unvaccinated, 28% were partially vaccinated with one mRNA COVID-19 vaccine dose, and 41% were fully vaccinated with two mRNA vaccine doses or one Johnson & Johnson dose. The 116 fully vaccinated patients were considered to have a breakthrough infection while the other 164 were considered to have a nonbreakthrough infection. The breakthrough and nonbreakthrough groups were similar in terms of age, sex, race, ethnicity, smoking status, and type of rheumatic disease. Comorbidities were also similar, except obesity, which was more common in the non–breakthrough infection group (25%) than the breakthrough infection group (10%).
The researchers queried patients on their COVID-19 symptoms, how long symptoms lasted, treatments they received, and hospitalization details. COVID-19 symptoms assessed included fever, sore throat, new cough, nasal congestion/rhinorrhea, dyspnea, chest pain, rash, myalgia, fatigue/malaise, headache, nausea/vomiting, diarrhea, anosmia, dysgeusia, and joint pain.
Patients completed surveys about symptoms at 4 weeks and 3 months after infection. Long COVID, or PASC, was defined as any persistent symptom at the times assessed.
Vaccinated patients fared better across outcomes
At 4 weeks after infection, 41% of fully vaccinated patients had at least one persistent symptom, compared with 54% of unvaccinated or partially vaccinated patients (P = .04). At 3 months after infection, 21% of fully vaccinated patients had at least one persistent symptom, compared with 41% of unvaccinated or partially vaccinated patients (P < .0001).
Vaccinated patients were half as likely to have long COVID at 4 weeks after infection (adjusted odds ratio, 0.49) and 90% less likely to have long COVID 3 months after infection (aOR, 0.1), after adjustment for age, sex, race, comorbidities, and use of any of four immune-suppressing medications (anti-CD20 monoclonal antibodies, methotrexate, mycophenolate, or glucocorticoids).
Fully vaccinated patients with breakthrough infections had an average 21 additional days without symptoms during follow-up, compared with unvaccinated and partially vaccinated patients (P = .04).
Reduced risk of long COVID did not change for vaccinated patients after sensitivity analyses for those who did not receive nirmatrelvir/ritonavir (Paxlovid) or monoclonal antibodies, those who didn’t receive any COVID-19-related treatment, those who completed their questionnaires within 6 months after infection, and those who were not hospitalized.
“One important message is that among those who did get PASC, the severity appears similar among those with and without a breakthrough infection,” Dr. Wallace said. “This highlights the need for ongoing research to improve recognition, diagnosis, and treatment of PASC.”
Many more breakthrough infections (72%) than nonbreakthrough infections (2%) occurred during Omicron. The authors acknowledged that different variants might play a role in different long COVID risks but said such potential confounding is unlikely to fully explain the results.
“Even with data suggesting that the Omicron variants may be intrinsically less severe, vaccination still has an impact on severity of infection, rates of hospitalization, and other outcomes and thus may play a role in the risk of PASC,” lead author Naomi Patel, MD, an instructor at Harvard Medical School and a rheumatologist at Massachusetts General Hospital, said in an interview. “A study evaluating the proportions with PASC by vaccination status during the time in which a single variant is predominant, such as the early Omicron era, could help to better assess the more isolated impact of vaccination on PASC.”
Dr. Calabrese said he is convinced that Omicron infections are less likely to result in more severe forms of acute COVID than pre-Omicron infections, and he suspects Omicron infections are also less likely to result in long COVID, although less evidence currently supports this hypothesis.
Hospitalization was more common in unvaccinated/partly vaccinated patients than in vaccinated patients (27% vs. 5%; P = .001). Although pain and fatigue were lower in those with breakthrough infections, functional scores and health-related quality of life were similar in both groups.
Some symptoms significantly differed between vaccinated and unvaccinated/partly vaccinated groups, possibly caused partly by different variants. Nasal congestion was more common (73%) in those with breakthrough infections than in those with nonbreakthrough infections (46%; P < .0001). Those who were unvaccinated/partly vaccinated were significantly more likely to have loss of smell (46% vs. 22%) or taste (45% vs. 28%) or to have joint pain (11% vs. 4%).
Treatment with nirmatrelvir/ritonavir was also more common in vaccinated patients (12%) than in unvaccinated/partly vaccinated patients (1%; P < .0001), as was treatment with monoclonal antibodies (34% vs. 8%; P < .0001).
The study was limited by its low diversity and being at a single health care system, the authors said. Study coauthor Jeffrey A. Sparks, MD, MMSc, an assistant professor of medicine at Brigham and Women’s Hospital and Harvard Medical School, said in an interview that the group is planning additional studies as their cohort grows, including “investigating the relationships between COVID-19 and specific rheumatic diseases and immunomodulating medications, expansion of autoimmunity and systemic inflammation, and lung damage among specific patient populations.”
Dr. Calabrese said it will be important for follow-up study of the symptomatic patients to “determine how many of these patients will fit the clinical picture of long COVID or long-haul phenotypes over the months and years ahead, including documenting exertional malaise and quality of life.
This study only assessed patients who received zero, one, or two doses of a vaccine, but many patients with rheumatic disease today will likely have received booster doses. However, Dr. Calabrese said it would be difficult to quantify whether a third, fourth, or fifth dose offers additional protection from long-term COVID complications after full vaccination or hybrid vaccination.
The research was funded by the Rheumatology Research Foundation, the National Institutes of Health, the R. Bruce and Joan M. Mickey Research Scholar Fund, and the Llura Gund Award for Rheumatoid Arthritis Research and Care. Dr. Wallace has received research support from Bristol-Myers Squibb and Principia/Sanofi and consulting fees from Zenas BioPharma, Horizon, Sanofi, Shionogi, Viela Bio, and Medpace. Dr. Sparks has received research support from Bristol-Myers Squibb and consulting fees from AbbVie, Amgen, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, Inova Diagnostics, Janssen, Optum, and Pfizer. Dr. Patel has received consulting fees from FVC Health. Calabrese has consulted for Genentech, Sanofi-Regeneron, AstraZeneca, and GlaxoSmithKline.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF THE RHEUMATIC DISEASES
Children and COVID: Hospitalizations provide a tale of two sources
New cases of COVID-19 in children largely held steady over the Thanksgiving holiday, but hospital admissions are telling a somewhat different story.
New pediatric COVID cases for the week ending on Thanksgiving (11/18-11/24) were up by 5.3% over the previous week, but in the most recent week (11/25-12/1) new cases dropped by 2.6%, according to state data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
In both weeks, though, the total case count stayed below 30,000 – a streak that has now lasted 8 weeks – so the actual number of weekly cases remained fairly low, the AAP/CHA weekly report indicates.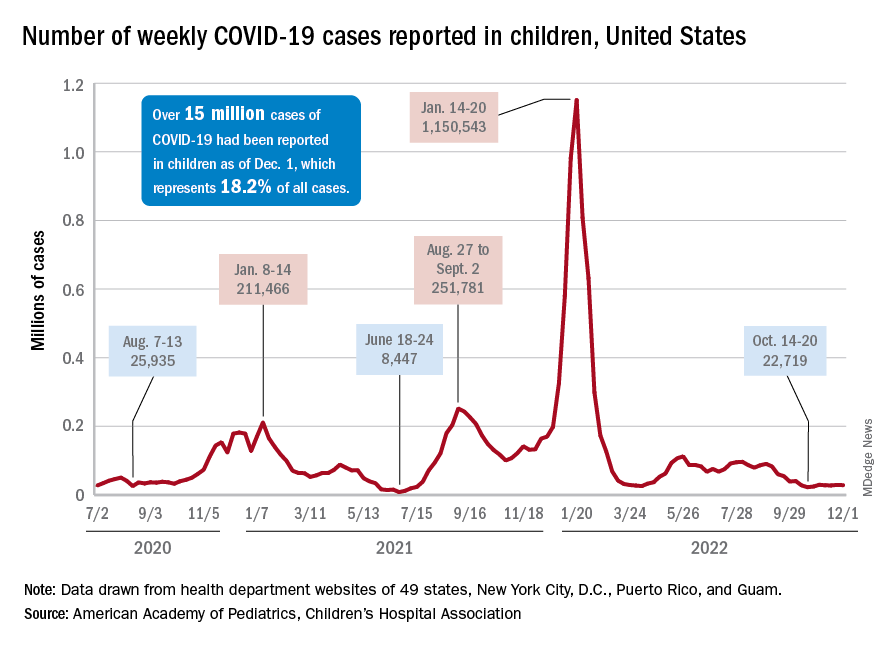
The nation’s emergency departments also experienced a small Thanksgiving bump, as the proportion of visits with diagnosed COVID went from 1.0% of all ED visits for children aged 0-11 years on Nov. 14 to 2.0% on Nov. 27, just 3 days after the official holiday, based on data from the Centers for Disease Control and Prevention. The rate was down to 1.5% on Dec. 1, and similar patterns can be seen for children aged 12-15 and 16-17 years.
New hospital admissions, on the other hand, seem to be following a different path, at least according to the CDC. The hospitalization rate for children aged 0-17 years bottomed out at 0.16 new admissions per 100,000 population back on Oct. 21 and has climbed fairly steadily since then. It was up to 0.20 per 100,000 by Nov. 14, had reached 0.22 per 100,000 on Thanksgiving day (11/24), and then continued to 0.26 per 100,000 by Dec. 2, the latest date for which CDC data are available.
The hospitalization story, however, offers yet another twist. The New York Times, using data from the U.S. Department of Health & Human Services, reports that new COVID-related admissions have held steady at 1.0 per 100,000 since Nov. 18. The rate is much higher than has been reported by the CDC, but no increase can be seen in recent weeks among children, which is not the case for Americans overall, Medscape recently reported.
New cases of COVID-19 in children largely held steady over the Thanksgiving holiday, but hospital admissions are telling a somewhat different story.
New pediatric COVID cases for the week ending on Thanksgiving (11/18-11/24) were up by 5.3% over the previous week, but in the most recent week (11/25-12/1) new cases dropped by 2.6%, according to state data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
In both weeks, though, the total case count stayed below 30,000 – a streak that has now lasted 8 weeks – so the actual number of weekly cases remained fairly low, the AAP/CHA weekly report indicates.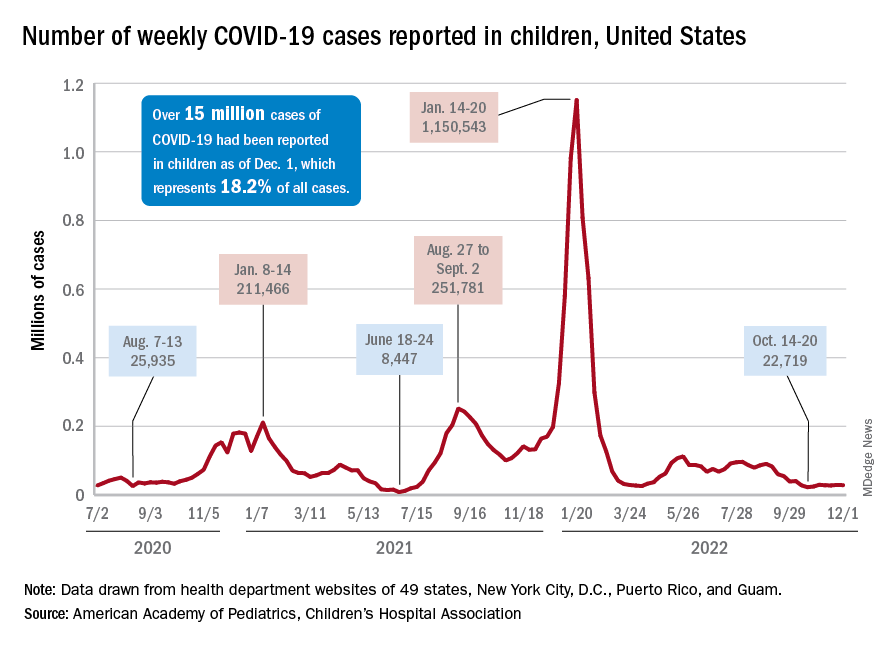
The nation’s emergency departments also experienced a small Thanksgiving bump, as the proportion of visits with diagnosed COVID went from 1.0% of all ED visits for children aged 0-11 years on Nov. 14 to 2.0% on Nov. 27, just 3 days after the official holiday, based on data from the Centers for Disease Control and Prevention. The rate was down to 1.5% on Dec. 1, and similar patterns can be seen for children aged 12-15 and 16-17 years.
New hospital admissions, on the other hand, seem to be following a different path, at least according to the CDC. The hospitalization rate for children aged 0-17 years bottomed out at 0.16 new admissions per 100,000 population back on Oct. 21 and has climbed fairly steadily since then. It was up to 0.20 per 100,000 by Nov. 14, had reached 0.22 per 100,000 on Thanksgiving day (11/24), and then continued to 0.26 per 100,000 by Dec. 2, the latest date for which CDC data are available.
The hospitalization story, however, offers yet another twist. The New York Times, using data from the U.S. Department of Health & Human Services, reports that new COVID-related admissions have held steady at 1.0 per 100,000 since Nov. 18. The rate is much higher than has been reported by the CDC, but no increase can be seen in recent weeks among children, which is not the case for Americans overall, Medscape recently reported.
New cases of COVID-19 in children largely held steady over the Thanksgiving holiday, but hospital admissions are telling a somewhat different story.
New pediatric COVID cases for the week ending on Thanksgiving (11/18-11/24) were up by 5.3% over the previous week, but in the most recent week (11/25-12/1) new cases dropped by 2.6%, according to state data collected by the American Academy of Pediatrics and the Children’s Hospital Association.
In both weeks, though, the total case count stayed below 30,000 – a streak that has now lasted 8 weeks – so the actual number of weekly cases remained fairly low, the AAP/CHA weekly report indicates.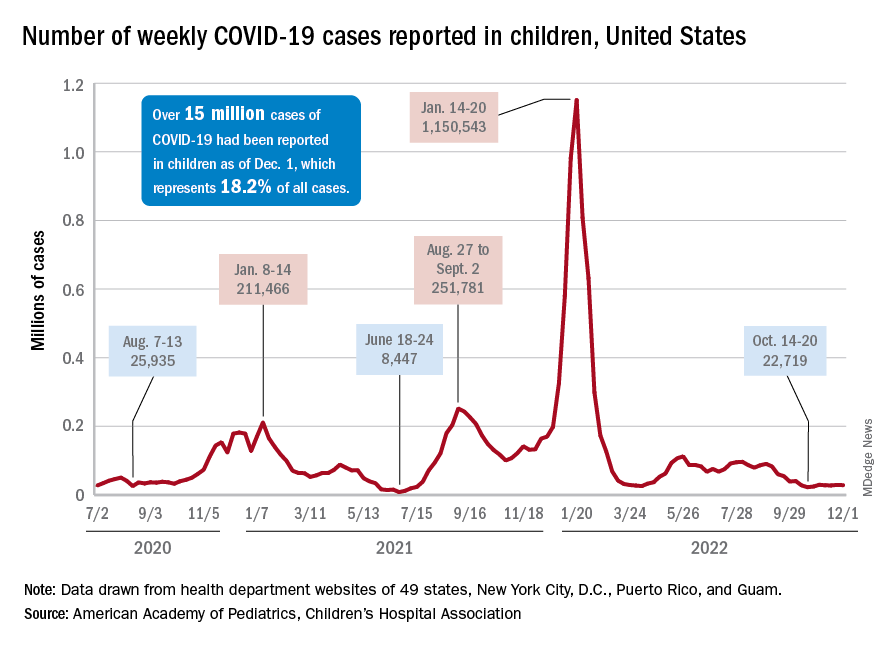
The nation’s emergency departments also experienced a small Thanksgiving bump, as the proportion of visits with diagnosed COVID went from 1.0% of all ED visits for children aged 0-11 years on Nov. 14 to 2.0% on Nov. 27, just 3 days after the official holiday, based on data from the Centers for Disease Control and Prevention. The rate was down to 1.5% on Dec. 1, and similar patterns can be seen for children aged 12-15 and 16-17 years.
New hospital admissions, on the other hand, seem to be following a different path, at least according to the CDC. The hospitalization rate for children aged 0-17 years bottomed out at 0.16 new admissions per 100,000 population back on Oct. 21 and has climbed fairly steadily since then. It was up to 0.20 per 100,000 by Nov. 14, had reached 0.22 per 100,000 on Thanksgiving day (11/24), and then continued to 0.26 per 100,000 by Dec. 2, the latest date for which CDC data are available.
The hospitalization story, however, offers yet another twist. The New York Times, using data from the U.S. Department of Health & Human Services, reports that new COVID-related admissions have held steady at 1.0 per 100,000 since Nov. 18. The rate is much higher than has been reported by the CDC, but no increase can be seen in recent weeks among children, which is not the case for Americans overall, Medscape recently reported.
Less than a third of Americans aware of cancer risk from alcohol
The new findings, from a nationally representative survey that included responses from 3,865 adults, show a low awareness of the cancer risk from alcohol, and also that the risk varies by type of drink. Just under a third (31.2%) of respondents thought that consuming liquor/spirits was associated with a risk of cancer, but this fell to 24.9% for drinking beer and even further, to 20.3%, for drinking wine.
In fact, some respondents though the opposite – that drinking alcohol has health benefits; 10.3% of respondents thought that drinking wine was associated with a decreased cancer risk, while 2.25% thought the same for drinking beer, and 1.7% thought that for drinking liquor.
Most U.S. adults (> 50%) reported not knowing how these beverages affected cancer risk, the authors report.
“This study’s findings underscore the need to develop interventions for educating the public about the cancer risks of alcohol use, particularly in the prevailing context of national dialogue about the purported heart health benefits of wine,” commented senior author William M. P. Klein, PhD, associate director of the National Cancer Institute’s Behavioral Research Program, in a statement.
“All types of alcoholic beverages, including wine, increase cancer risk,” Dr. Klein said.
The findings were published online in Cancer Epidemiology, Biomarkers & Prevention.
The results echo the findings of a previous national survey that also found that the majority of Americans are not aware that alcohol consumption is associated with an increased risk of developing a variety of cancers.
In contrast, within the scientific community, there is long-standing and increasing awareness of alcohol consumption as a leading modifiable risk factor for cancer, and there is a growing movement calling for more public health awareness of the link.
Recently, there has been some public support for adding written warnings about the cancer risk from alcohol. A Citizen Petition was filed in 2021, and in August 2022, The New England Journal of Medicine issued a call for new labeling.
Several cancer organizations are petitioning for warnings to be added to alcoholic beverages. The petition is supported by the American Society of Clinical Oncology, the American Institute for Cancer Research, and Breast Cancer Prevention Partners, all in collaboration with several public health organizations. Proposed labeling would read: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
Dr. Klein and colleagues suggest that public health interventions, including mass media campaigns, cancer warning labels, and patient-provider communications, could help disseminate information about cancer and alcohol. “Educating the public about how alcohol increases cancer risk will not only empower consumers to make more informed decisions but may also prevent and reduce excessive alcohol use, as well as cancer morbidity and mortality,” Dr. Klein said.
The study was supported by the Division of Cancer Control and Population Sciences at the National Cancer Institute. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The new findings, from a nationally representative survey that included responses from 3,865 adults, show a low awareness of the cancer risk from alcohol, and also that the risk varies by type of drink. Just under a third (31.2%) of respondents thought that consuming liquor/spirits was associated with a risk of cancer, but this fell to 24.9% for drinking beer and even further, to 20.3%, for drinking wine.
In fact, some respondents though the opposite – that drinking alcohol has health benefits; 10.3% of respondents thought that drinking wine was associated with a decreased cancer risk, while 2.25% thought the same for drinking beer, and 1.7% thought that for drinking liquor.
Most U.S. adults (> 50%) reported not knowing how these beverages affected cancer risk, the authors report.
“This study’s findings underscore the need to develop interventions for educating the public about the cancer risks of alcohol use, particularly in the prevailing context of national dialogue about the purported heart health benefits of wine,” commented senior author William M. P. Klein, PhD, associate director of the National Cancer Institute’s Behavioral Research Program, in a statement.
“All types of alcoholic beverages, including wine, increase cancer risk,” Dr. Klein said.
The findings were published online in Cancer Epidemiology, Biomarkers & Prevention.
The results echo the findings of a previous national survey that also found that the majority of Americans are not aware that alcohol consumption is associated with an increased risk of developing a variety of cancers.
In contrast, within the scientific community, there is long-standing and increasing awareness of alcohol consumption as a leading modifiable risk factor for cancer, and there is a growing movement calling for more public health awareness of the link.
Recently, there has been some public support for adding written warnings about the cancer risk from alcohol. A Citizen Petition was filed in 2021, and in August 2022, The New England Journal of Medicine issued a call for new labeling.
Several cancer organizations are petitioning for warnings to be added to alcoholic beverages. The petition is supported by the American Society of Clinical Oncology, the American Institute for Cancer Research, and Breast Cancer Prevention Partners, all in collaboration with several public health organizations. Proposed labeling would read: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
Dr. Klein and colleagues suggest that public health interventions, including mass media campaigns, cancer warning labels, and patient-provider communications, could help disseminate information about cancer and alcohol. “Educating the public about how alcohol increases cancer risk will not only empower consumers to make more informed decisions but may also prevent and reduce excessive alcohol use, as well as cancer morbidity and mortality,” Dr. Klein said.
The study was supported by the Division of Cancer Control and Population Sciences at the National Cancer Institute. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The new findings, from a nationally representative survey that included responses from 3,865 adults, show a low awareness of the cancer risk from alcohol, and also that the risk varies by type of drink. Just under a third (31.2%) of respondents thought that consuming liquor/spirits was associated with a risk of cancer, but this fell to 24.9% for drinking beer and even further, to 20.3%, for drinking wine.
In fact, some respondents though the opposite – that drinking alcohol has health benefits; 10.3% of respondents thought that drinking wine was associated with a decreased cancer risk, while 2.25% thought the same for drinking beer, and 1.7% thought that for drinking liquor.
Most U.S. adults (> 50%) reported not knowing how these beverages affected cancer risk, the authors report.
“This study’s findings underscore the need to develop interventions for educating the public about the cancer risks of alcohol use, particularly in the prevailing context of national dialogue about the purported heart health benefits of wine,” commented senior author William M. P. Klein, PhD, associate director of the National Cancer Institute’s Behavioral Research Program, in a statement.
“All types of alcoholic beverages, including wine, increase cancer risk,” Dr. Klein said.
The findings were published online in Cancer Epidemiology, Biomarkers & Prevention.
The results echo the findings of a previous national survey that also found that the majority of Americans are not aware that alcohol consumption is associated with an increased risk of developing a variety of cancers.
In contrast, within the scientific community, there is long-standing and increasing awareness of alcohol consumption as a leading modifiable risk factor for cancer, and there is a growing movement calling for more public health awareness of the link.
Recently, there has been some public support for adding written warnings about the cancer risk from alcohol. A Citizen Petition was filed in 2021, and in August 2022, The New England Journal of Medicine issued a call for new labeling.
Several cancer organizations are petitioning for warnings to be added to alcoholic beverages. The petition is supported by the American Society of Clinical Oncology, the American Institute for Cancer Research, and Breast Cancer Prevention Partners, all in collaboration with several public health organizations. Proposed labeling would read: “WARNING: According to the Surgeon General, consumption of alcoholic beverages can cause cancer, including breast and colon cancers.”
Dr. Klein and colleagues suggest that public health interventions, including mass media campaigns, cancer warning labels, and patient-provider communications, could help disseminate information about cancer and alcohol. “Educating the public about how alcohol increases cancer risk will not only empower consumers to make more informed decisions but may also prevent and reduce excessive alcohol use, as well as cancer morbidity and mortality,” Dr. Klein said.
The study was supported by the Division of Cancer Control and Population Sciences at the National Cancer Institute. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS & PREVENTION
Study comparing surgical and N95 masks sparks concern
The study’s senior author is John Conly, MD, an infectious disease specialist and professor at the University of Calgary (Alta.), and Alberta Health Services. The findings are not consistent with those of many other studies on this topic.
Commenting about Dr. Conly’s study, Eric Topol, MD, editor-in-chief of Medscape, wrote: “It’s woefully underpowered but ruled out a doubling of hazard for use of medical masks.”
The study, which was partially funded by the World Health Organization, was published online in Annals of Internal Medicine.
This is not the first time that Dr. Conly, who also advises the WHO, has been the subject of controversy. He previously denied that COVID-19 is airborne – a position that is contradicted by strong evidence. In 2021, Dr. Conly made headlines with his controversial claim that N95 respirators can cause harms, including oxygen depletion and carbon dioxide retention.
A detailed examination by the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota, Minneapolis, pointed out numerous scientific flaws in the study, including inconsistent use of both types of masks. The study also examined health care workers in four very different countries (Canada, Israel, Egypt, and Pakistan) during different periods of the pandemic, which may have affected the results. Furthermore, the study did not account for vaccination status and lacked a control group. CIDRAP receives funding from 3M, which makes N95 respirators.
In a commentary published alongside the study, Roger Chou, MD, professor of medicine at Oregon Health & Science University, Portland, said that the results were “not definitive,” with “a generous noninferiority threshold” that is actually “consistent with up to a relative 70% increased risk ... which may be unacceptable to many health workers.”
Lead study author Mark Loeb, MD, professor of infectious diseases at McMaster University, Hamilton, Ont., defended the findings. “The confidence intervals around this, that is, what the possible results could be if the trial was repeated many times, range from −2.5% to 4.9%,” he told this news organization. “This means that the risk of a COVID-19 infection in those using the medical masks could have ranged from anywhere from 2.5% reduction in risk to a 4.9% increase in risk. Readers and policy makers can decide for themselves about this.”
“There is no point continuing to run underpowered, poorly designed studies that are designed to confirm existing biases,” Raina MacIntyre, PhD, professor of global biosecurity and head of the Biosecurity Program at the Kirby Institute, Sydney, said in an interview. “The new study in Annals of Internal Medicine is entirely consistent with our finding that to prevent infection, you need an N95, and it needs to be worn throughout the whole shift. A surgical mask and intermittent use of N95 are equally ineffective. This should not surprise anyone, given a surgical mask is not designed as respiratory protection but is designed to prevent splash or spray of liquid on the face. Only a respirator is designed as respiratory protection through both the seal around the face and the filter of the face piece to prevent inhalation of virus laden aerosols, but you need to wear it continually in a high-risk environment like a hospital.”
“It makes zero sense to do a randomized trial on something you can measure directly,” said Kimberly Prather, PhD, an atmospheric chemist, professor, and director of the NSF Center for Aerosol Impacts on Chemistry of the Environment at the University of California, San Diego. “In fact, many studies have shown aerosols leaking out of surgical masks. Surgical masks are designed to block large spray droplets. Aerosols (0.5-3 mcm), which have been shown to contain infectious SARS-CoV-2 virus, travel with the air flow, and escape.”
“This study ... will be used to justify policies of supplying health care workers, and perhaps patients and visitors, too, with inadequate protection,” Trish Greenhalgh, MD, professor of primary care health sciences at the University of Oxford (England), told this news organization.
“These authors have been pushing back against treating COVID as airborne for 3 years,” David Fisman, MD, an epidemiologist and infectious disease specialist at the University of Toronto, said in an interview. “So, you’ll see these folks brandishing this very flawed trial to justify continuing the infection control practices that have been so disastrous throughout the pandemic.”
The study was funded by the World Health Organization, the Canadian Institutes of Health Research, and the Juravinski Research Institute. Dr. Conly reported receiving grants from the Canadian Institutes for Health Research, Pfizer, and the WHO. Dr. Chou disclosed being a methodologist for WHO guidelines on infection prevention and control measures for COVID-19. Dr. Loeb disclosed payment for expert testimony on personal protective equipment from the government of Manitoba and the Peel District School Board. Dr. MacIntyre has led a large body of research on masks and respirators in health workers, including four randomized clinical trials. She is the author of a book, “Dark Winter: An insider’s guide to pandemics and biosecurity” (Syndey: NewSouth Publishing, 2022), which covers the history and politics of the controversies around N95 and masks. Dr. Prather reported no disclosures. Dr. Greenhalgh is a member of Independent SAGE and an unpaid adviser to the philanthropic fund Balvi. Dr. Fisman has served as a paid legal expert for the Ontario Nurses’ Association in their challenge to Directive 5, which restricted access to N95 masks in health care. He also served as a paid legal expert for the Elementary Teachers’ Federation of Ontario in its efforts to make schools safer in Ontario.
A version of this article first appeared on Medscape.com.
The study’s senior author is John Conly, MD, an infectious disease specialist and professor at the University of Calgary (Alta.), and Alberta Health Services. The findings are not consistent with those of many other studies on this topic.
Commenting about Dr. Conly’s study, Eric Topol, MD, editor-in-chief of Medscape, wrote: “It’s woefully underpowered but ruled out a doubling of hazard for use of medical masks.”
The study, which was partially funded by the World Health Organization, was published online in Annals of Internal Medicine.
This is not the first time that Dr. Conly, who also advises the WHO, has been the subject of controversy. He previously denied that COVID-19 is airborne – a position that is contradicted by strong evidence. In 2021, Dr. Conly made headlines with his controversial claim that N95 respirators can cause harms, including oxygen depletion and carbon dioxide retention.
A detailed examination by the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota, Minneapolis, pointed out numerous scientific flaws in the study, including inconsistent use of both types of masks. The study also examined health care workers in four very different countries (Canada, Israel, Egypt, and Pakistan) during different periods of the pandemic, which may have affected the results. Furthermore, the study did not account for vaccination status and lacked a control group. CIDRAP receives funding from 3M, which makes N95 respirators.
In a commentary published alongside the study, Roger Chou, MD, professor of medicine at Oregon Health & Science University, Portland, said that the results were “not definitive,” with “a generous noninferiority threshold” that is actually “consistent with up to a relative 70% increased risk ... which may be unacceptable to many health workers.”
Lead study author Mark Loeb, MD, professor of infectious diseases at McMaster University, Hamilton, Ont., defended the findings. “The confidence intervals around this, that is, what the possible results could be if the trial was repeated many times, range from −2.5% to 4.9%,” he told this news organization. “This means that the risk of a COVID-19 infection in those using the medical masks could have ranged from anywhere from 2.5% reduction in risk to a 4.9% increase in risk. Readers and policy makers can decide for themselves about this.”
“There is no point continuing to run underpowered, poorly designed studies that are designed to confirm existing biases,” Raina MacIntyre, PhD, professor of global biosecurity and head of the Biosecurity Program at the Kirby Institute, Sydney, said in an interview. “The new study in Annals of Internal Medicine is entirely consistent with our finding that to prevent infection, you need an N95, and it needs to be worn throughout the whole shift. A surgical mask and intermittent use of N95 are equally ineffective. This should not surprise anyone, given a surgical mask is not designed as respiratory protection but is designed to prevent splash or spray of liquid on the face. Only a respirator is designed as respiratory protection through both the seal around the face and the filter of the face piece to prevent inhalation of virus laden aerosols, but you need to wear it continually in a high-risk environment like a hospital.”
“It makes zero sense to do a randomized trial on something you can measure directly,” said Kimberly Prather, PhD, an atmospheric chemist, professor, and director of the NSF Center for Aerosol Impacts on Chemistry of the Environment at the University of California, San Diego. “In fact, many studies have shown aerosols leaking out of surgical masks. Surgical masks are designed to block large spray droplets. Aerosols (0.5-3 mcm), which have been shown to contain infectious SARS-CoV-2 virus, travel with the air flow, and escape.”
“This study ... will be used to justify policies of supplying health care workers, and perhaps patients and visitors, too, with inadequate protection,” Trish Greenhalgh, MD, professor of primary care health sciences at the University of Oxford (England), told this news organization.
“These authors have been pushing back against treating COVID as airborne for 3 years,” David Fisman, MD, an epidemiologist and infectious disease specialist at the University of Toronto, said in an interview. “So, you’ll see these folks brandishing this very flawed trial to justify continuing the infection control practices that have been so disastrous throughout the pandemic.”
The study was funded by the World Health Organization, the Canadian Institutes of Health Research, and the Juravinski Research Institute. Dr. Conly reported receiving grants from the Canadian Institutes for Health Research, Pfizer, and the WHO. Dr. Chou disclosed being a methodologist for WHO guidelines on infection prevention and control measures for COVID-19. Dr. Loeb disclosed payment for expert testimony on personal protective equipment from the government of Manitoba and the Peel District School Board. Dr. MacIntyre has led a large body of research on masks and respirators in health workers, including four randomized clinical trials. She is the author of a book, “Dark Winter: An insider’s guide to pandemics and biosecurity” (Syndey: NewSouth Publishing, 2022), which covers the history and politics of the controversies around N95 and masks. Dr. Prather reported no disclosures. Dr. Greenhalgh is a member of Independent SAGE and an unpaid adviser to the philanthropic fund Balvi. Dr. Fisman has served as a paid legal expert for the Ontario Nurses’ Association in their challenge to Directive 5, which restricted access to N95 masks in health care. He also served as a paid legal expert for the Elementary Teachers’ Federation of Ontario in its efforts to make schools safer in Ontario.
A version of this article first appeared on Medscape.com.
The study’s senior author is John Conly, MD, an infectious disease specialist and professor at the University of Calgary (Alta.), and Alberta Health Services. The findings are not consistent with those of many other studies on this topic.
Commenting about Dr. Conly’s study, Eric Topol, MD, editor-in-chief of Medscape, wrote: “It’s woefully underpowered but ruled out a doubling of hazard for use of medical masks.”
The study, which was partially funded by the World Health Organization, was published online in Annals of Internal Medicine.
This is not the first time that Dr. Conly, who also advises the WHO, has been the subject of controversy. He previously denied that COVID-19 is airborne – a position that is contradicted by strong evidence. In 2021, Dr. Conly made headlines with his controversial claim that N95 respirators can cause harms, including oxygen depletion and carbon dioxide retention.
A detailed examination by the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota, Minneapolis, pointed out numerous scientific flaws in the study, including inconsistent use of both types of masks. The study also examined health care workers in four very different countries (Canada, Israel, Egypt, and Pakistan) during different periods of the pandemic, which may have affected the results. Furthermore, the study did not account for vaccination status and lacked a control group. CIDRAP receives funding from 3M, which makes N95 respirators.
In a commentary published alongside the study, Roger Chou, MD, professor of medicine at Oregon Health & Science University, Portland, said that the results were “not definitive,” with “a generous noninferiority threshold” that is actually “consistent with up to a relative 70% increased risk ... which may be unacceptable to many health workers.”
Lead study author Mark Loeb, MD, professor of infectious diseases at McMaster University, Hamilton, Ont., defended the findings. “The confidence intervals around this, that is, what the possible results could be if the trial was repeated many times, range from −2.5% to 4.9%,” he told this news organization. “This means that the risk of a COVID-19 infection in those using the medical masks could have ranged from anywhere from 2.5% reduction in risk to a 4.9% increase in risk. Readers and policy makers can decide for themselves about this.”
“There is no point continuing to run underpowered, poorly designed studies that are designed to confirm existing biases,” Raina MacIntyre, PhD, professor of global biosecurity and head of the Biosecurity Program at the Kirby Institute, Sydney, said in an interview. “The new study in Annals of Internal Medicine is entirely consistent with our finding that to prevent infection, you need an N95, and it needs to be worn throughout the whole shift. A surgical mask and intermittent use of N95 are equally ineffective. This should not surprise anyone, given a surgical mask is not designed as respiratory protection but is designed to prevent splash or spray of liquid on the face. Only a respirator is designed as respiratory protection through both the seal around the face and the filter of the face piece to prevent inhalation of virus laden aerosols, but you need to wear it continually in a high-risk environment like a hospital.”
“It makes zero sense to do a randomized trial on something you can measure directly,” said Kimberly Prather, PhD, an atmospheric chemist, professor, and director of the NSF Center for Aerosol Impacts on Chemistry of the Environment at the University of California, San Diego. “In fact, many studies have shown aerosols leaking out of surgical masks. Surgical masks are designed to block large spray droplets. Aerosols (0.5-3 mcm), which have been shown to contain infectious SARS-CoV-2 virus, travel with the air flow, and escape.”
“This study ... will be used to justify policies of supplying health care workers, and perhaps patients and visitors, too, with inadequate protection,” Trish Greenhalgh, MD, professor of primary care health sciences at the University of Oxford (England), told this news organization.
“These authors have been pushing back against treating COVID as airborne for 3 years,” David Fisman, MD, an epidemiologist and infectious disease specialist at the University of Toronto, said in an interview. “So, you’ll see these folks brandishing this very flawed trial to justify continuing the infection control practices that have been so disastrous throughout the pandemic.”
The study was funded by the World Health Organization, the Canadian Institutes of Health Research, and the Juravinski Research Institute. Dr. Conly reported receiving grants from the Canadian Institutes for Health Research, Pfizer, and the WHO. Dr. Chou disclosed being a methodologist for WHO guidelines on infection prevention and control measures for COVID-19. Dr. Loeb disclosed payment for expert testimony on personal protective equipment from the government of Manitoba and the Peel District School Board. Dr. MacIntyre has led a large body of research on masks and respirators in health workers, including four randomized clinical trials. She is the author of a book, “Dark Winter: An insider’s guide to pandemics and biosecurity” (Syndey: NewSouth Publishing, 2022), which covers the history and politics of the controversies around N95 and masks. Dr. Prather reported no disclosures. Dr. Greenhalgh is a member of Independent SAGE and an unpaid adviser to the philanthropic fund Balvi. Dr. Fisman has served as a paid legal expert for the Ontario Nurses’ Association in their challenge to Directive 5, which restricted access to N95 masks in health care. He also served as a paid legal expert for the Elementary Teachers’ Federation of Ontario in its efforts to make schools safer in Ontario.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Florida doc dies by suicide after allegedly drugging and raping patients
according to a police statement.
A week later, a Collier County Sheriff’s deputy found Dr. Salata’s body near his Naples home with a gunshot wound to the head, according to police. The medical examiner later ruled it a suicide.
Dr. Salata co-owned Pura Vida Medical Spa in Naples with his wife Jill Salata, a certified family nurse practitioner. They specialized in cosmetic treatment and surgery.
Naples police said that they arrested Dr. Salata after two female patients accused the doctor of allegedly drugging and raping them while they were still unconscious.
Both victims described being given nitrous oxide, also called laughing gas, for sedation and pain from the cosmetic procedure. The first victim, age 51, said Dr. Salata prescribed alprazolam (Xanax) to take before the procedure and then also gave her nitrous oxide and tequila, causing her to black out, according to NBC2 News.
The second victim, age 72, told police that as the nitrous oxide was wearing off, she found Dr. Salata performing sexual intercourse. The victim felt shocked after the sedation subsided about what had taken place, contacted police, and submitted to a sexual assault examination, according to the police statement.
At Dr. Salata’s November 22 hearing before Judge Michael Provost, a prosecutor asked the judge whether Dr. Salata should surrender his firearms; Provost reportedly dismissed the idea.
“It is disappointing and frustrating that Dr. Salata has escaped justice,” said one victim’s attorney, Adam Horowitz, in a blog post. “Yet, we are relieved that no other women will be assaulted by Dr. Salata again. It took tremendous courage for my client to tell her truth. She was ready to hold him accountable in court.”
Horowitz says he plans to file a civil lawsuit on behalf of his client against Dr. Salata’s estate. The Naples police are continuing their investigation into the victims’ cases, which now includes a third woman, said spokesman Lt. Bryan McGinn.
Meanwhile, the Pura Vida Medical Spa has closed permanently and its website has been deleted. One reviewer named Soul F. wrote on the spa’s Yelp page: “And now may God have mercy on this rapist’s soul. Amen.”
A version of this article first appeared on Medscape.com.
according to a police statement.
A week later, a Collier County Sheriff’s deputy found Dr. Salata’s body near his Naples home with a gunshot wound to the head, according to police. The medical examiner later ruled it a suicide.
Dr. Salata co-owned Pura Vida Medical Spa in Naples with his wife Jill Salata, a certified family nurse practitioner. They specialized in cosmetic treatment and surgery.
Naples police said that they arrested Dr. Salata after two female patients accused the doctor of allegedly drugging and raping them while they were still unconscious.
Both victims described being given nitrous oxide, also called laughing gas, for sedation and pain from the cosmetic procedure. The first victim, age 51, said Dr. Salata prescribed alprazolam (Xanax) to take before the procedure and then also gave her nitrous oxide and tequila, causing her to black out, according to NBC2 News.
The second victim, age 72, told police that as the nitrous oxide was wearing off, she found Dr. Salata performing sexual intercourse. The victim felt shocked after the sedation subsided about what had taken place, contacted police, and submitted to a sexual assault examination, according to the police statement.
At Dr. Salata’s November 22 hearing before Judge Michael Provost, a prosecutor asked the judge whether Dr. Salata should surrender his firearms; Provost reportedly dismissed the idea.
“It is disappointing and frustrating that Dr. Salata has escaped justice,” said one victim’s attorney, Adam Horowitz, in a blog post. “Yet, we are relieved that no other women will be assaulted by Dr. Salata again. It took tremendous courage for my client to tell her truth. She was ready to hold him accountable in court.”
Horowitz says he plans to file a civil lawsuit on behalf of his client against Dr. Salata’s estate. The Naples police are continuing their investigation into the victims’ cases, which now includes a third woman, said spokesman Lt. Bryan McGinn.
Meanwhile, the Pura Vida Medical Spa has closed permanently and its website has been deleted. One reviewer named Soul F. wrote on the spa’s Yelp page: “And now may God have mercy on this rapist’s soul. Amen.”
A version of this article first appeared on Medscape.com.
according to a police statement.
A week later, a Collier County Sheriff’s deputy found Dr. Salata’s body near his Naples home with a gunshot wound to the head, according to police. The medical examiner later ruled it a suicide.
Dr. Salata co-owned Pura Vida Medical Spa in Naples with his wife Jill Salata, a certified family nurse practitioner. They specialized in cosmetic treatment and surgery.
Naples police said that they arrested Dr. Salata after two female patients accused the doctor of allegedly drugging and raping them while they were still unconscious.
Both victims described being given nitrous oxide, also called laughing gas, for sedation and pain from the cosmetic procedure. The first victim, age 51, said Dr. Salata prescribed alprazolam (Xanax) to take before the procedure and then also gave her nitrous oxide and tequila, causing her to black out, according to NBC2 News.
The second victim, age 72, told police that as the nitrous oxide was wearing off, she found Dr. Salata performing sexual intercourse. The victim felt shocked after the sedation subsided about what had taken place, contacted police, and submitted to a sexual assault examination, according to the police statement.
At Dr. Salata’s November 22 hearing before Judge Michael Provost, a prosecutor asked the judge whether Dr. Salata should surrender his firearms; Provost reportedly dismissed the idea.
“It is disappointing and frustrating that Dr. Salata has escaped justice,” said one victim’s attorney, Adam Horowitz, in a blog post. “Yet, we are relieved that no other women will be assaulted by Dr. Salata again. It took tremendous courage for my client to tell her truth. She was ready to hold him accountable in court.”
Horowitz says he plans to file a civil lawsuit on behalf of his client against Dr. Salata’s estate. The Naples police are continuing their investigation into the victims’ cases, which now includes a third woman, said spokesman Lt. Bryan McGinn.
Meanwhile, the Pura Vida Medical Spa has closed permanently and its website has been deleted. One reviewer named Soul F. wrote on the spa’s Yelp page: “And now may God have mercy on this rapist’s soul. Amen.”
A version of this article first appeared on Medscape.com.











