User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Strong two-way link between epilepsy and depression
, with implications for diagnosis and patient care. The findings “strongly support previous observations of a bidirectional association between these two brain disorders,” said Eva Bølling-Ladegaard, MD, a PhD student, department of clinical medicine (Neurology), Aarhus (Denmark) University.
“We add to the existing evidence in temporal range, showing that the increased risks of depression following epilepsy, and vice versa, are sustained over a much more extended time period than previously shown; that is, 20 years on both sides of receiving a diagnosis of the index disorder,” Ms. Bølling-Ladegaard said.
The study was published online in Neurology.
Epilepsy then depression
The researchers examined the magnitude and long-term temporal association between epilepsy and depression. They compared the risk of the two brain disorders following another chronic disorder (asthma) in a nationwide, register-based, matched cohort study.
In a population of more than 8.7 million people, they identified 139,014 persons with epilepsy (54% males; median age at diagnosis, 43 years), 219,990 with depression (37% males; median age at diagnosis, 43 years), and 358,821 with asthma (49% males; median age at diagnosis, 29 years).
The rate of developing depression was increased nearly twofold among people with epilepsy compared with the matched population who did not have epilepsy (adjusted hazard ratio, 1.88; 95% confidence interval, 1.82-1.95).
The rate of depression was highest during the first months and years after epilepsy diagnosis. It declined over time, yet remained significantly elevated throughout the 20+ years of observation.
The cumulative incidence of depression at 5 and 35 years’ follow-up in the epilepsy cohort was 1.37% and 6.05%, respectively, compared with 0.59% and 3.92% in the reference population.
The highest rate of depression after epilepsy was among individuals aged 40-59 years, and the lowest was among those aged 0-19 years at first epilepsy diagnosis.
Depression then epilepsy
The rate of developing epilepsy was increased more than twofold among patients with incident depression compared with the matched population who were without depression (aHR, 2.35; 95% CI, 2.25-2.44).
As in the opposite analysis, the rate of epilepsy was highest during the first months and years after depression diagnosis and declined over time.
The cumulative incidence of epilepsy at 5 and 35 years after depression diagnosis was 1.10% and 4.19%, respectively, compared with 0.32% and 2.06% in the reference population.
The rate of epilepsy was highest among those aged 0-19 years at time of first depression diagnosis and was lowest among those aged 80+ at first depression diagnosis.
For comparison, after asthma diagnosis, rates of depression and epilepsy were increased 1.63-fold (95% CI, 1.59-1.67) and 1.48-fold (95% CI, 1.44-1.53), respectively, compared with matched individuals without asthma.
Using admission with seizures as a proxy for treatment failure, the researchers observed an increased risk of treatment failure among people with epilepsy who were diagnosed with depression.
“Our results support previous findings indicating worse seizure outcomes in people with epilepsy and coexisting depression,” said Ms. Bølling-Ladegaard.
“Increased clinical awareness of the association between epilepsy and depression is therefore needed in order to increase the proportion of patients that receive appropriate treatment and improve outcomes for these patient groups,” she said.
Clinical implications
Reached for comment, Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, noted that the link between epilepsy and depression is “well-known.”
“However, typically one thinks of epilepsy as leading to depression, not vice versa. Here they show the risk of epilepsy following depression to be high (highest of the risks given), which is thought provoking. However, association does not imply causation,” Dr. Haneef said.
“Prima facie, there is no biological rationale for depression to lead to epilepsy,” he said. He noted that some antidepressants can reduce the seizure threshold.
The findings do have implications for care, he said.
“For neurologists, this is another study that exhorts them to screen for depression and treat adequately in all patients with epilepsy,” Dr. Haneef said.
“For psychiatrists, this study may give guidance to watch more carefully for seizures in patients with depression, especially when using antidepressant medications that induce seizures.
“For the general public with either epilepsy or depression, it would help them be aware about this bidirectional association,” Dr. Haneef said.
The study was funded by the Lundbeck Foundation, the Danish Epilepsy Association, and the Novo Nordisk Foundation. Ms. Bølling-Ladegaard and Dr. Haneef have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with implications for diagnosis and patient care. The findings “strongly support previous observations of a bidirectional association between these two brain disorders,” said Eva Bølling-Ladegaard, MD, a PhD student, department of clinical medicine (Neurology), Aarhus (Denmark) University.
“We add to the existing evidence in temporal range, showing that the increased risks of depression following epilepsy, and vice versa, are sustained over a much more extended time period than previously shown; that is, 20 years on both sides of receiving a diagnosis of the index disorder,” Ms. Bølling-Ladegaard said.
The study was published online in Neurology.
Epilepsy then depression
The researchers examined the magnitude and long-term temporal association between epilepsy and depression. They compared the risk of the two brain disorders following another chronic disorder (asthma) in a nationwide, register-based, matched cohort study.
In a population of more than 8.7 million people, they identified 139,014 persons with epilepsy (54% males; median age at diagnosis, 43 years), 219,990 with depression (37% males; median age at diagnosis, 43 years), and 358,821 with asthma (49% males; median age at diagnosis, 29 years).
The rate of developing depression was increased nearly twofold among people with epilepsy compared with the matched population who did not have epilepsy (adjusted hazard ratio, 1.88; 95% confidence interval, 1.82-1.95).
The rate of depression was highest during the first months and years after epilepsy diagnosis. It declined over time, yet remained significantly elevated throughout the 20+ years of observation.
The cumulative incidence of depression at 5 and 35 years’ follow-up in the epilepsy cohort was 1.37% and 6.05%, respectively, compared with 0.59% and 3.92% in the reference population.
The highest rate of depression after epilepsy was among individuals aged 40-59 years, and the lowest was among those aged 0-19 years at first epilepsy diagnosis.
Depression then epilepsy
The rate of developing epilepsy was increased more than twofold among patients with incident depression compared with the matched population who were without depression (aHR, 2.35; 95% CI, 2.25-2.44).
As in the opposite analysis, the rate of epilepsy was highest during the first months and years after depression diagnosis and declined over time.
The cumulative incidence of epilepsy at 5 and 35 years after depression diagnosis was 1.10% and 4.19%, respectively, compared with 0.32% and 2.06% in the reference population.
The rate of epilepsy was highest among those aged 0-19 years at time of first depression diagnosis and was lowest among those aged 80+ at first depression diagnosis.
For comparison, after asthma diagnosis, rates of depression and epilepsy were increased 1.63-fold (95% CI, 1.59-1.67) and 1.48-fold (95% CI, 1.44-1.53), respectively, compared with matched individuals without asthma.
Using admission with seizures as a proxy for treatment failure, the researchers observed an increased risk of treatment failure among people with epilepsy who were diagnosed with depression.
“Our results support previous findings indicating worse seizure outcomes in people with epilepsy and coexisting depression,” said Ms. Bølling-Ladegaard.
“Increased clinical awareness of the association between epilepsy and depression is therefore needed in order to increase the proportion of patients that receive appropriate treatment and improve outcomes for these patient groups,” she said.
Clinical implications
Reached for comment, Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, noted that the link between epilepsy and depression is “well-known.”
“However, typically one thinks of epilepsy as leading to depression, not vice versa. Here they show the risk of epilepsy following depression to be high (highest of the risks given), which is thought provoking. However, association does not imply causation,” Dr. Haneef said.
“Prima facie, there is no biological rationale for depression to lead to epilepsy,” he said. He noted that some antidepressants can reduce the seizure threshold.
The findings do have implications for care, he said.
“For neurologists, this is another study that exhorts them to screen for depression and treat adequately in all patients with epilepsy,” Dr. Haneef said.
“For psychiatrists, this study may give guidance to watch more carefully for seizures in patients with depression, especially when using antidepressant medications that induce seizures.
“For the general public with either epilepsy or depression, it would help them be aware about this bidirectional association,” Dr. Haneef said.
The study was funded by the Lundbeck Foundation, the Danish Epilepsy Association, and the Novo Nordisk Foundation. Ms. Bølling-Ladegaard and Dr. Haneef have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with implications for diagnosis and patient care. The findings “strongly support previous observations of a bidirectional association between these two brain disorders,” said Eva Bølling-Ladegaard, MD, a PhD student, department of clinical medicine (Neurology), Aarhus (Denmark) University.
“We add to the existing evidence in temporal range, showing that the increased risks of depression following epilepsy, and vice versa, are sustained over a much more extended time period than previously shown; that is, 20 years on both sides of receiving a diagnosis of the index disorder,” Ms. Bølling-Ladegaard said.
The study was published online in Neurology.
Epilepsy then depression
The researchers examined the magnitude and long-term temporal association between epilepsy and depression. They compared the risk of the two brain disorders following another chronic disorder (asthma) in a nationwide, register-based, matched cohort study.
In a population of more than 8.7 million people, they identified 139,014 persons with epilepsy (54% males; median age at diagnosis, 43 years), 219,990 with depression (37% males; median age at diagnosis, 43 years), and 358,821 with asthma (49% males; median age at diagnosis, 29 years).
The rate of developing depression was increased nearly twofold among people with epilepsy compared with the matched population who did not have epilepsy (adjusted hazard ratio, 1.88; 95% confidence interval, 1.82-1.95).
The rate of depression was highest during the first months and years after epilepsy diagnosis. It declined over time, yet remained significantly elevated throughout the 20+ years of observation.
The cumulative incidence of depression at 5 and 35 years’ follow-up in the epilepsy cohort was 1.37% and 6.05%, respectively, compared with 0.59% and 3.92% in the reference population.
The highest rate of depression after epilepsy was among individuals aged 40-59 years, and the lowest was among those aged 0-19 years at first epilepsy diagnosis.
Depression then epilepsy
The rate of developing epilepsy was increased more than twofold among patients with incident depression compared with the matched population who were without depression (aHR, 2.35; 95% CI, 2.25-2.44).
As in the opposite analysis, the rate of epilepsy was highest during the first months and years after depression diagnosis and declined over time.
The cumulative incidence of epilepsy at 5 and 35 years after depression diagnosis was 1.10% and 4.19%, respectively, compared with 0.32% and 2.06% in the reference population.
The rate of epilepsy was highest among those aged 0-19 years at time of first depression diagnosis and was lowest among those aged 80+ at first depression diagnosis.
For comparison, after asthma diagnosis, rates of depression and epilepsy were increased 1.63-fold (95% CI, 1.59-1.67) and 1.48-fold (95% CI, 1.44-1.53), respectively, compared with matched individuals without asthma.
Using admission with seizures as a proxy for treatment failure, the researchers observed an increased risk of treatment failure among people with epilepsy who were diagnosed with depression.
“Our results support previous findings indicating worse seizure outcomes in people with epilepsy and coexisting depression,” said Ms. Bølling-Ladegaard.
“Increased clinical awareness of the association between epilepsy and depression is therefore needed in order to increase the proportion of patients that receive appropriate treatment and improve outcomes for these patient groups,” she said.
Clinical implications
Reached for comment, Zulfi Haneef, MBBS, MD, associate professor of neurology, Baylor College of Medicine, Houston, noted that the link between epilepsy and depression is “well-known.”
“However, typically one thinks of epilepsy as leading to depression, not vice versa. Here they show the risk of epilepsy following depression to be high (highest of the risks given), which is thought provoking. However, association does not imply causation,” Dr. Haneef said.
“Prima facie, there is no biological rationale for depression to lead to epilepsy,” he said. He noted that some antidepressants can reduce the seizure threshold.
The findings do have implications for care, he said.
“For neurologists, this is another study that exhorts them to screen for depression and treat adequately in all patients with epilepsy,” Dr. Haneef said.
“For psychiatrists, this study may give guidance to watch more carefully for seizures in patients with depression, especially when using antidepressant medications that induce seizures.
“For the general public with either epilepsy or depression, it would help them be aware about this bidirectional association,” Dr. Haneef said.
The study was funded by the Lundbeck Foundation, the Danish Epilepsy Association, and the Novo Nordisk Foundation. Ms. Bølling-Ladegaard and Dr. Haneef have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
High drug costs exclude most neurology patients from cutting-edge treatment
, new research shows.
“Our study of people with neurologic conditions found that fewer than 20% were being treated with new medications,” study author Brian C. Callaghan, MD, with University of Michigan Health in Ann Arbor, said in a statement.
“For new, high-cost medications that have similar effectiveness to older drugs, limited use is likely appropriate. However, future studies are needed to look into whether the high costs are barriers to those new medications that can really make a difference for people living with neurologic disease,” Dr. Callaghan said.
The study was published online in Neurology.
Most expensive drugs
Using insurance claims data, the investigators compared the utilization and costs of new-to-market drugs from 2014 to 2018 with those for existing guideline-supported medications for treating 11 neurologic conditions.
The new drugs included:
- erenumab, fremanezumab, and galcanezumab for migraine.
- ocrelizumab and peginterferon beta-1a for multiple sclerosis (MS).
- pimavanserin and safinamide for Parkinson’s disease.
- droxidopa for orthostatic hypertension.
- eculizumab for myasthenia gravis (MG).
- edaravone for amyotrophic lateral sclerosis (ALS).
- deutetrabenazine and valbenazine for Huntington’s disease and tardive dyskinesia.
- patisiran and inotersen for transthyretin amyloidosis (ATTR).
- eteplirsen and deflazacort for Duchenne disease.
- nusinersen for spinal muscular atrophy (SMA).
Utilization of new drugs was modest – they accounted for one in five prescriptions for every condition except tardive dyskinesia (32% for valbenazine), the researchers noted.
Mean out-of-pocket costs were significantly higher for the new medications, although there was large variability among individual drugs.
The two most expensive drugs were edaravone, for ALS, with a mean out-of-pocket cost of $713 for a 30-day supply, and eculizumab, for MG, which costs $91 per month.
“For new-to-market medications, the distribution of out-of-pocket costs were highly variable and the trends over time were unpredictable compared with existing guideline-supported medications,” the authors reported.
They noted that potential reasons for low utilization of newer agents include delay in provider uptake and prescriber and/or patient avoidance because of high cost.
Given that most of the new neurologic agents offer little advantage compared with existing treatments – exceptions being new drugs for SMA and ATTR – drug costs should be a key consideration in prescribing decisions, Dr. Callaghan and colleagues concluded.
One limitation of the study is that follow-up time was short for some of the recently approved medications. Another limitation is that the number of people in the study who had rare diseases was small.
Revolution in neurotherapeutics
“We are living in a time when new treatments bring hope to people with neurologic diseases and disorders,” Orly Avitzur, MD, president of the American Academy of Neurology, said in a statement.
“However, even existing prescription medication can be expensive and drug prices continue to rise. In order for neurologists to provide people with the highest quality care, it is imperative that new drugs are accessible and affordable to the people who need them,” Dr. Avitzur added.
Writing in a linked editorial, A. Gordon Smith, MD, professor and chair, department of neurology, Virginia Commonwealth University, Richmond, said there is a revolution in neurotherapeutics, with particularly robust growth in new drug approvals for orphan diseases (those affecting < 200,000 Americans).
“This study adds to a growing literature indicating rising drug prices are a threat to the health care system. No matter how effective a disease-modifying therapy may be, if a patient cannot afford the cost, it doesn’t work,” Dr. Smith wrote.
He added that neurologists must be “diligent in assessing for financial toxicity and appropriately tailor individual treatment recommendations. We must insist on development of point-of-care tools to accurately estimate each patient’s potential financial toxicity including RTBT [real-time benefit tools].
“Neurologists’ primary obligation is to the individual patient, but we are also compelled to support access to high-quality care for all people, which requires advocacy for appropriate policy reforms to ensure value based and fair drug pricing and treatment success,” Dr. Smith added.
The study was funded by the American Academy of Neurology Health Services Research Subcommittee. Dr. Callaghan consults for a PCORI grant, DynaMed, receives research support from the American Academy of Neurology, and performs medical/legal consultations, including consultations for the Vaccine Injury Compensation Program. Dr. Smith has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
“Our study of people with neurologic conditions found that fewer than 20% were being treated with new medications,” study author Brian C. Callaghan, MD, with University of Michigan Health in Ann Arbor, said in a statement.
“For new, high-cost medications that have similar effectiveness to older drugs, limited use is likely appropriate. However, future studies are needed to look into whether the high costs are barriers to those new medications that can really make a difference for people living with neurologic disease,” Dr. Callaghan said.
The study was published online in Neurology.
Most expensive drugs
Using insurance claims data, the investigators compared the utilization and costs of new-to-market drugs from 2014 to 2018 with those for existing guideline-supported medications for treating 11 neurologic conditions.
The new drugs included:
- erenumab, fremanezumab, and galcanezumab for migraine.
- ocrelizumab and peginterferon beta-1a for multiple sclerosis (MS).
- pimavanserin and safinamide for Parkinson’s disease.
- droxidopa for orthostatic hypertension.
- eculizumab for myasthenia gravis (MG).
- edaravone for amyotrophic lateral sclerosis (ALS).
- deutetrabenazine and valbenazine for Huntington’s disease and tardive dyskinesia.
- patisiran and inotersen for transthyretin amyloidosis (ATTR).
- eteplirsen and deflazacort for Duchenne disease.
- nusinersen for spinal muscular atrophy (SMA).
Utilization of new drugs was modest – they accounted for one in five prescriptions for every condition except tardive dyskinesia (32% for valbenazine), the researchers noted.
Mean out-of-pocket costs were significantly higher for the new medications, although there was large variability among individual drugs.
The two most expensive drugs were edaravone, for ALS, with a mean out-of-pocket cost of $713 for a 30-day supply, and eculizumab, for MG, which costs $91 per month.
“For new-to-market medications, the distribution of out-of-pocket costs were highly variable and the trends over time were unpredictable compared with existing guideline-supported medications,” the authors reported.
They noted that potential reasons for low utilization of newer agents include delay in provider uptake and prescriber and/or patient avoidance because of high cost.
Given that most of the new neurologic agents offer little advantage compared with existing treatments – exceptions being new drugs for SMA and ATTR – drug costs should be a key consideration in prescribing decisions, Dr. Callaghan and colleagues concluded.
One limitation of the study is that follow-up time was short for some of the recently approved medications. Another limitation is that the number of people in the study who had rare diseases was small.
Revolution in neurotherapeutics
“We are living in a time when new treatments bring hope to people with neurologic diseases and disorders,” Orly Avitzur, MD, president of the American Academy of Neurology, said in a statement.
“However, even existing prescription medication can be expensive and drug prices continue to rise. In order for neurologists to provide people with the highest quality care, it is imperative that new drugs are accessible and affordable to the people who need them,” Dr. Avitzur added.
Writing in a linked editorial, A. Gordon Smith, MD, professor and chair, department of neurology, Virginia Commonwealth University, Richmond, said there is a revolution in neurotherapeutics, with particularly robust growth in new drug approvals for orphan diseases (those affecting < 200,000 Americans).
“This study adds to a growing literature indicating rising drug prices are a threat to the health care system. No matter how effective a disease-modifying therapy may be, if a patient cannot afford the cost, it doesn’t work,” Dr. Smith wrote.
He added that neurologists must be “diligent in assessing for financial toxicity and appropriately tailor individual treatment recommendations. We must insist on development of point-of-care tools to accurately estimate each patient’s potential financial toxicity including RTBT [real-time benefit tools].
“Neurologists’ primary obligation is to the individual patient, but we are also compelled to support access to high-quality care for all people, which requires advocacy for appropriate policy reforms to ensure value based and fair drug pricing and treatment success,” Dr. Smith added.
The study was funded by the American Academy of Neurology Health Services Research Subcommittee. Dr. Callaghan consults for a PCORI grant, DynaMed, receives research support from the American Academy of Neurology, and performs medical/legal consultations, including consultations for the Vaccine Injury Compensation Program. Dr. Smith has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research shows.
“Our study of people with neurologic conditions found that fewer than 20% were being treated with new medications,” study author Brian C. Callaghan, MD, with University of Michigan Health in Ann Arbor, said in a statement.
“For new, high-cost medications that have similar effectiveness to older drugs, limited use is likely appropriate. However, future studies are needed to look into whether the high costs are barriers to those new medications that can really make a difference for people living with neurologic disease,” Dr. Callaghan said.
The study was published online in Neurology.
Most expensive drugs
Using insurance claims data, the investigators compared the utilization and costs of new-to-market drugs from 2014 to 2018 with those for existing guideline-supported medications for treating 11 neurologic conditions.
The new drugs included:
- erenumab, fremanezumab, and galcanezumab for migraine.
- ocrelizumab and peginterferon beta-1a for multiple sclerosis (MS).
- pimavanserin and safinamide for Parkinson’s disease.
- droxidopa for orthostatic hypertension.
- eculizumab for myasthenia gravis (MG).
- edaravone for amyotrophic lateral sclerosis (ALS).
- deutetrabenazine and valbenazine for Huntington’s disease and tardive dyskinesia.
- patisiran and inotersen for transthyretin amyloidosis (ATTR).
- eteplirsen and deflazacort for Duchenne disease.
- nusinersen for spinal muscular atrophy (SMA).
Utilization of new drugs was modest – they accounted for one in five prescriptions for every condition except tardive dyskinesia (32% for valbenazine), the researchers noted.
Mean out-of-pocket costs were significantly higher for the new medications, although there was large variability among individual drugs.
The two most expensive drugs were edaravone, for ALS, with a mean out-of-pocket cost of $713 for a 30-day supply, and eculizumab, for MG, which costs $91 per month.
“For new-to-market medications, the distribution of out-of-pocket costs were highly variable and the trends over time were unpredictable compared with existing guideline-supported medications,” the authors reported.
They noted that potential reasons for low utilization of newer agents include delay in provider uptake and prescriber and/or patient avoidance because of high cost.
Given that most of the new neurologic agents offer little advantage compared with existing treatments – exceptions being new drugs for SMA and ATTR – drug costs should be a key consideration in prescribing decisions, Dr. Callaghan and colleagues concluded.
One limitation of the study is that follow-up time was short for some of the recently approved medications. Another limitation is that the number of people in the study who had rare diseases was small.
Revolution in neurotherapeutics
“We are living in a time when new treatments bring hope to people with neurologic diseases and disorders,” Orly Avitzur, MD, president of the American Academy of Neurology, said in a statement.
“However, even existing prescription medication can be expensive and drug prices continue to rise. In order for neurologists to provide people with the highest quality care, it is imperative that new drugs are accessible and affordable to the people who need them,” Dr. Avitzur added.
Writing in a linked editorial, A. Gordon Smith, MD, professor and chair, department of neurology, Virginia Commonwealth University, Richmond, said there is a revolution in neurotherapeutics, with particularly robust growth in new drug approvals for orphan diseases (those affecting < 200,000 Americans).
“This study adds to a growing literature indicating rising drug prices are a threat to the health care system. No matter how effective a disease-modifying therapy may be, if a patient cannot afford the cost, it doesn’t work,” Dr. Smith wrote.
He added that neurologists must be “diligent in assessing for financial toxicity and appropriately tailor individual treatment recommendations. We must insist on development of point-of-care tools to accurately estimate each patient’s potential financial toxicity including RTBT [real-time benefit tools].
“Neurologists’ primary obligation is to the individual patient, but we are also compelled to support access to high-quality care for all people, which requires advocacy for appropriate policy reforms to ensure value based and fair drug pricing and treatment success,” Dr. Smith added.
The study was funded by the American Academy of Neurology Health Services Research Subcommittee. Dr. Callaghan consults for a PCORI grant, DynaMed, receives research support from the American Academy of Neurology, and performs medical/legal consultations, including consultations for the Vaccine Injury Compensation Program. Dr. Smith has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Green Mediterranean diet lowers visceral adipose tissue
according to a new analysis of the 18-month Dietary Intervention Randomized Controlled Trial Polyphenols Unprocessed (DIRECT-PLUS) trial.
The new results indicate that the green Mediterranean diet lowered visceral fat by twice as much as the standard Mediterranean diet (14% vs. 7%), reported Iris Shai, PhD, of Ben-Gurion University of the Negev in Be’er Sheva, Israel, and colleagues.
“This study may suggest an improved dietary protocol for treating visceral adiposity,” the authors wrote in their article, published recently in BMC Medicine.
“A healthy lifestyle is a strong basis for any weight-loss program. We learned from the results of our experiment that the quality of food is no less important than the number of calories consumed and the goal today is to understand the mechanisms of various nutrients, for example, positive ones such as the polyphenols, and negative ones such as empty carbohydrates and processed red meat, on the pace of fat cell differentiation and their aggregation in the viscera,” Dr. Shai said in a press release from Ben‐Gurion University.
“A 14% reduction in visceral fat is a dramatic achievement for making simple changes to your diet and lifestyle. Weight loss is an important goal only if it is accompanied by impressive results in reducing adipose tissue,” added coauthor Hila Zelicha, RD, PhD, also of Ben‐Gurion University of the Negev.
Previous randomized controlled trials have shown that dietary changes with a higher polyphenol content tend to produce better cardiometabolic outcomes and appear to mobilize particular ectopic fat depots, the researchers noted.
The main results of the DIRECT-PLUS trial were published in 2020 in Heart. Almost 300 participants with abdominal obesity/dyslipidemia were randomized to one of three diet groups (all accompanied by physical activity): standard healthy dietary guidelines (HDG), standard Mediterranean diet, and the so-called green Mediterranean diet. The mean age of participants was 51 years, and men comprised 88% of the study cohort.
Participants in both Mediterranean diet groups ate 28 grams/day of walnuts, which accounted for about 440 mg/day of polyphenols. Participants in the green Mediterranean group also ate 100 grams/day of frozen cubes of a Wolffia globosa (duckweed strain) plant green shake, and three to four cups/day of green tea, which contributed to consumption of 800 mg/day of polyphenols, and decreased red meat consumption.
Both the green and standard Mediterranean diet groups achieved similar weight loss (–6.2 kg and –5.4 kg) compared with the HDG group (–1.5 kg; P < .001). However, the green Mediterranean diet group had a greater reduction in waist circumference (–8.6 cm) than the standard Mediterranean diet group (–6.8 cm; P = .033) and HDG group (–4.3 cm; P < .001). Stratification by gender showed these differences were significant only among men.
Explaining the rationale for the study, the researchers noted that visceral adipose tissue accumulation is a key factor that differentiates metabolic healthy and unhealthy obese individuals, is closely related to the development of multiple cardiovascular risk factors, including hypertension, dyslipidemia, and type 2 diabetes, and is an independent marker of mortality.
Now, their latest data show the green Mediterranean diet group lost approximately twice as much visceral adipose tissue compared with the standard Mediterranean diet and HDG groups (−14.1%, −6.0%, and − 4.2%; P < .05 independent of weight loss, sex, waist circumference, or age).
Lower red meat consumption, greater dietary consumption of walnuts, Wolffia globosa, and green tea, increased urine urolithin A polyphenol, and elevated total plasma polyphenols were significantly associated with greater visceral adipose tissue loss (P < .05, multivariate models).
“A green Mediterranean diet enriched with polyphenols and decreased red meat consumption might serve as an improved version of the Mediterranean diet for targeted VAT reduction. Future studies are needed to explore the exact mechanisms of specific polyphenol-rich foods on visceral adiposity,” the study authors concluded.
A version of this article first appeared on Medscape.com.
according to a new analysis of the 18-month Dietary Intervention Randomized Controlled Trial Polyphenols Unprocessed (DIRECT-PLUS) trial.
The new results indicate that the green Mediterranean diet lowered visceral fat by twice as much as the standard Mediterranean diet (14% vs. 7%), reported Iris Shai, PhD, of Ben-Gurion University of the Negev in Be’er Sheva, Israel, and colleagues.
“This study may suggest an improved dietary protocol for treating visceral adiposity,” the authors wrote in their article, published recently in BMC Medicine.
“A healthy lifestyle is a strong basis for any weight-loss program. We learned from the results of our experiment that the quality of food is no less important than the number of calories consumed and the goal today is to understand the mechanisms of various nutrients, for example, positive ones such as the polyphenols, and negative ones such as empty carbohydrates and processed red meat, on the pace of fat cell differentiation and their aggregation in the viscera,” Dr. Shai said in a press release from Ben‐Gurion University.
“A 14% reduction in visceral fat is a dramatic achievement for making simple changes to your diet and lifestyle. Weight loss is an important goal only if it is accompanied by impressive results in reducing adipose tissue,” added coauthor Hila Zelicha, RD, PhD, also of Ben‐Gurion University of the Negev.
Previous randomized controlled trials have shown that dietary changes with a higher polyphenol content tend to produce better cardiometabolic outcomes and appear to mobilize particular ectopic fat depots, the researchers noted.
The main results of the DIRECT-PLUS trial were published in 2020 in Heart. Almost 300 participants with abdominal obesity/dyslipidemia were randomized to one of three diet groups (all accompanied by physical activity): standard healthy dietary guidelines (HDG), standard Mediterranean diet, and the so-called green Mediterranean diet. The mean age of participants was 51 years, and men comprised 88% of the study cohort.
Participants in both Mediterranean diet groups ate 28 grams/day of walnuts, which accounted for about 440 mg/day of polyphenols. Participants in the green Mediterranean group also ate 100 grams/day of frozen cubes of a Wolffia globosa (duckweed strain) plant green shake, and three to four cups/day of green tea, which contributed to consumption of 800 mg/day of polyphenols, and decreased red meat consumption.
Both the green and standard Mediterranean diet groups achieved similar weight loss (–6.2 kg and –5.4 kg) compared with the HDG group (–1.5 kg; P < .001). However, the green Mediterranean diet group had a greater reduction in waist circumference (–8.6 cm) than the standard Mediterranean diet group (–6.8 cm; P = .033) and HDG group (–4.3 cm; P < .001). Stratification by gender showed these differences were significant only among men.
Explaining the rationale for the study, the researchers noted that visceral adipose tissue accumulation is a key factor that differentiates metabolic healthy and unhealthy obese individuals, is closely related to the development of multiple cardiovascular risk factors, including hypertension, dyslipidemia, and type 2 diabetes, and is an independent marker of mortality.
Now, their latest data show the green Mediterranean diet group lost approximately twice as much visceral adipose tissue compared with the standard Mediterranean diet and HDG groups (−14.1%, −6.0%, and − 4.2%; P < .05 independent of weight loss, sex, waist circumference, or age).
Lower red meat consumption, greater dietary consumption of walnuts, Wolffia globosa, and green tea, increased urine urolithin A polyphenol, and elevated total plasma polyphenols were significantly associated with greater visceral adipose tissue loss (P < .05, multivariate models).
“A green Mediterranean diet enriched with polyphenols and decreased red meat consumption might serve as an improved version of the Mediterranean diet for targeted VAT reduction. Future studies are needed to explore the exact mechanisms of specific polyphenol-rich foods on visceral adiposity,” the study authors concluded.
A version of this article first appeared on Medscape.com.
according to a new analysis of the 18-month Dietary Intervention Randomized Controlled Trial Polyphenols Unprocessed (DIRECT-PLUS) trial.
The new results indicate that the green Mediterranean diet lowered visceral fat by twice as much as the standard Mediterranean diet (14% vs. 7%), reported Iris Shai, PhD, of Ben-Gurion University of the Negev in Be’er Sheva, Israel, and colleagues.
“This study may suggest an improved dietary protocol for treating visceral adiposity,” the authors wrote in their article, published recently in BMC Medicine.
“A healthy lifestyle is a strong basis for any weight-loss program. We learned from the results of our experiment that the quality of food is no less important than the number of calories consumed and the goal today is to understand the mechanisms of various nutrients, for example, positive ones such as the polyphenols, and negative ones such as empty carbohydrates and processed red meat, on the pace of fat cell differentiation and their aggregation in the viscera,” Dr. Shai said in a press release from Ben‐Gurion University.
“A 14% reduction in visceral fat is a dramatic achievement for making simple changes to your diet and lifestyle. Weight loss is an important goal only if it is accompanied by impressive results in reducing adipose tissue,” added coauthor Hila Zelicha, RD, PhD, also of Ben‐Gurion University of the Negev.
Previous randomized controlled trials have shown that dietary changes with a higher polyphenol content tend to produce better cardiometabolic outcomes and appear to mobilize particular ectopic fat depots, the researchers noted.
The main results of the DIRECT-PLUS trial were published in 2020 in Heart. Almost 300 participants with abdominal obesity/dyslipidemia were randomized to one of three diet groups (all accompanied by physical activity): standard healthy dietary guidelines (HDG), standard Mediterranean diet, and the so-called green Mediterranean diet. The mean age of participants was 51 years, and men comprised 88% of the study cohort.
Participants in both Mediterranean diet groups ate 28 grams/day of walnuts, which accounted for about 440 mg/day of polyphenols. Participants in the green Mediterranean group also ate 100 grams/day of frozen cubes of a Wolffia globosa (duckweed strain) plant green shake, and three to four cups/day of green tea, which contributed to consumption of 800 mg/day of polyphenols, and decreased red meat consumption.
Both the green and standard Mediterranean diet groups achieved similar weight loss (–6.2 kg and –5.4 kg) compared with the HDG group (–1.5 kg; P < .001). However, the green Mediterranean diet group had a greater reduction in waist circumference (–8.6 cm) than the standard Mediterranean diet group (–6.8 cm; P = .033) and HDG group (–4.3 cm; P < .001). Stratification by gender showed these differences were significant only among men.
Explaining the rationale for the study, the researchers noted that visceral adipose tissue accumulation is a key factor that differentiates metabolic healthy and unhealthy obese individuals, is closely related to the development of multiple cardiovascular risk factors, including hypertension, dyslipidemia, and type 2 diabetes, and is an independent marker of mortality.
Now, their latest data show the green Mediterranean diet group lost approximately twice as much visceral adipose tissue compared with the standard Mediterranean diet and HDG groups (−14.1%, −6.0%, and − 4.2%; P < .05 independent of weight loss, sex, waist circumference, or age).
Lower red meat consumption, greater dietary consumption of walnuts, Wolffia globosa, and green tea, increased urine urolithin A polyphenol, and elevated total plasma polyphenols were significantly associated with greater visceral adipose tissue loss (P < .05, multivariate models).
“A green Mediterranean diet enriched with polyphenols and decreased red meat consumption might serve as an improved version of the Mediterranean diet for targeted VAT reduction. Future studies are needed to explore the exact mechanisms of specific polyphenol-rich foods on visceral adiposity,” the study authors concluded.
A version of this article first appeared on Medscape.com.
FROM BMC MEDICINE
FDA pulls U.S. authorization for Eli Lilly’s COVID drug bebtelovimab
the Food and Drug Administration said, citing it is not expected to neutralize the dominant BQ.1 and BQ.1.1 subvariants of Omicron.
The announcement on Nov. 30 takes away authorization from the last COVID-19 monoclonal antibody treatment, leaving Pfizer’s antiviral drug Paxlovid, Merck’s Lagevrio, and Gilead Sciences’ Veklury as treatments for the disease, besides convalescent plasma for some patients.
AstraZeneca’s monoclonal antibody Evusheld is also authorized for protection against COVID-19 infection in some people.
Eli Lilly and its authorized distributors have paused commercial distribution of the monoclonal antibody until further notice from the agency, while the U.S. government has also paused fulfillment of any pending requests under its scheme to help uninsured and underinsured Americans access the drug.
The drug, which was discovered by Abcellera and commercialized by Eli Lilly, received an authorization from the FDA in February.
BQ.1 and BQ.1.1 have become the dominant strains in the United States after a steady increase in prevalence over the last 2 months, surpassing Omicron’s BA.5 subvariant, which had driven cases earlier in the year.
The subvariants accounted for around 57% of the cases nationally, as per government data last week.
Reuters Health Information © 2022
the Food and Drug Administration said, citing it is not expected to neutralize the dominant BQ.1 and BQ.1.1 subvariants of Omicron.
The announcement on Nov. 30 takes away authorization from the last COVID-19 monoclonal antibody treatment, leaving Pfizer’s antiviral drug Paxlovid, Merck’s Lagevrio, and Gilead Sciences’ Veklury as treatments for the disease, besides convalescent plasma for some patients.
AstraZeneca’s monoclonal antibody Evusheld is also authorized for protection against COVID-19 infection in some people.
Eli Lilly and its authorized distributors have paused commercial distribution of the monoclonal antibody until further notice from the agency, while the U.S. government has also paused fulfillment of any pending requests under its scheme to help uninsured and underinsured Americans access the drug.
The drug, which was discovered by Abcellera and commercialized by Eli Lilly, received an authorization from the FDA in February.
BQ.1 and BQ.1.1 have become the dominant strains in the United States after a steady increase in prevalence over the last 2 months, surpassing Omicron’s BA.5 subvariant, which had driven cases earlier in the year.
The subvariants accounted for around 57% of the cases nationally, as per government data last week.
Reuters Health Information © 2022
the Food and Drug Administration said, citing it is not expected to neutralize the dominant BQ.1 and BQ.1.1 subvariants of Omicron.
The announcement on Nov. 30 takes away authorization from the last COVID-19 monoclonal antibody treatment, leaving Pfizer’s antiviral drug Paxlovid, Merck’s Lagevrio, and Gilead Sciences’ Veklury as treatments for the disease, besides convalescent plasma for some patients.
AstraZeneca’s monoclonal antibody Evusheld is also authorized for protection against COVID-19 infection in some people.
Eli Lilly and its authorized distributors have paused commercial distribution of the monoclonal antibody until further notice from the agency, while the U.S. government has also paused fulfillment of any pending requests under its scheme to help uninsured and underinsured Americans access the drug.
The drug, which was discovered by Abcellera and commercialized by Eli Lilly, received an authorization from the FDA in February.
BQ.1 and BQ.1.1 have become the dominant strains in the United States after a steady increase in prevalence over the last 2 months, surpassing Omicron’s BA.5 subvariant, which had driven cases earlier in the year.
The subvariants accounted for around 57% of the cases nationally, as per government data last week.
Reuters Health Information © 2022
Confirmed: Amyloid, tau levels rise years before Alzheimer’s onset
“Our results confirm accelerated biomarker changes during preclinical AD and highlight the important role of amyloid levels in tau accelerations,” the investigators note.
“These data may suggest that there is a short therapeutic window for slowing AD pathogenesis prior to the emergence of clinical symptoms – and that this window may occur after amyloid accumulation begins but before amyloid has substantial impacts on tau accumulation,” study investigator Corinne Pettigrew, PhD, department of neurology, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
The study was published online in Alzheimer’s and Dementia.
Novel long-term CSF data
The study builds on previous research by examining changes in cerebrospinal fluid (CSF) biomarkers over longer periods than had been done previously, particularly among largely middle-aged and cognitively normal at baseline individuals.
The researchers examined changes in amyloid beta (Aβ) 42/Aβ40, phosphorylated tau181 (p-tau181), and total tau (t-tau) in CSF over an average of 10.7 years (and up to 23 years) among 278 individuals who were largely middle-aged persons who were cognitively normal at baseline.
“To our knowledge, no prior study among initially cognitively normal, primarily middle-aged individuals has described CSF AD biomarker changes over this duration of follow-up,” the researchers write.
During follow-up, 94 individuals who initially had normal cognition developed mild cognitive impairment (MCI).
Lower baseline levels of amyloid were associated with greater increases in tau (more strongly in men than women), while accelerations in tau were more closely linked to onset of MCI, the researchers report.
Among individuals who developed MCI, biomarker levels were more abnormal and tau increased to a greater extent prior to the onset of MCI symptoms, they found.
Clear impact of APOE4
The findings also suggest that among APOE4 carriers, amyloid onset occurs at an earlier age and rates of amyloid positivity are higher, but there are no differences in rates of change in amyloid over time.
“APOE4 genetic status was not related to changes in CSF beta-amyloid after accounting for the fact that APOE4 carriers have higher rates of amyloid positivity,” said Dr. Pettigrew.
“These findings suggest that APOE4 genetic status shifts the age of onset of amyloid accumulation (with APOE4 carriers having an earlier age of onset compared to non-carriers), but that APOE4 is not related to rates of change in CSF beta-amyloid over time,” she added.
“Thus, cognitively normal APOE4 carriers may be in more advanced preclinical AD stages at younger ages than individuals who are not APOE4 carriers, which is likely relevant for optimizing clinical trial recruitment strategies,” she said.
Funding for the study was provided by the National Institutes of Health. Dr. Pettigrew has disclosed no relevant financial relationships. The original article contains a complete list of author disclosures.
A version of this article first appeared on Medscape.com.
“Our results confirm accelerated biomarker changes during preclinical AD and highlight the important role of amyloid levels in tau accelerations,” the investigators note.
“These data may suggest that there is a short therapeutic window for slowing AD pathogenesis prior to the emergence of clinical symptoms – and that this window may occur after amyloid accumulation begins but before amyloid has substantial impacts on tau accumulation,” study investigator Corinne Pettigrew, PhD, department of neurology, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
The study was published online in Alzheimer’s and Dementia.
Novel long-term CSF data
The study builds on previous research by examining changes in cerebrospinal fluid (CSF) biomarkers over longer periods than had been done previously, particularly among largely middle-aged and cognitively normal at baseline individuals.
The researchers examined changes in amyloid beta (Aβ) 42/Aβ40, phosphorylated tau181 (p-tau181), and total tau (t-tau) in CSF over an average of 10.7 years (and up to 23 years) among 278 individuals who were largely middle-aged persons who were cognitively normal at baseline.
“To our knowledge, no prior study among initially cognitively normal, primarily middle-aged individuals has described CSF AD biomarker changes over this duration of follow-up,” the researchers write.
During follow-up, 94 individuals who initially had normal cognition developed mild cognitive impairment (MCI).
Lower baseline levels of amyloid were associated with greater increases in tau (more strongly in men than women), while accelerations in tau were more closely linked to onset of MCI, the researchers report.
Among individuals who developed MCI, biomarker levels were more abnormal and tau increased to a greater extent prior to the onset of MCI symptoms, they found.
Clear impact of APOE4
The findings also suggest that among APOE4 carriers, amyloid onset occurs at an earlier age and rates of amyloid positivity are higher, but there are no differences in rates of change in amyloid over time.
“APOE4 genetic status was not related to changes in CSF beta-amyloid after accounting for the fact that APOE4 carriers have higher rates of amyloid positivity,” said Dr. Pettigrew.
“These findings suggest that APOE4 genetic status shifts the age of onset of amyloid accumulation (with APOE4 carriers having an earlier age of onset compared to non-carriers), but that APOE4 is not related to rates of change in CSF beta-amyloid over time,” she added.
“Thus, cognitively normal APOE4 carriers may be in more advanced preclinical AD stages at younger ages than individuals who are not APOE4 carriers, which is likely relevant for optimizing clinical trial recruitment strategies,” she said.
Funding for the study was provided by the National Institutes of Health. Dr. Pettigrew has disclosed no relevant financial relationships. The original article contains a complete list of author disclosures.
A version of this article first appeared on Medscape.com.
“Our results confirm accelerated biomarker changes during preclinical AD and highlight the important role of amyloid levels in tau accelerations,” the investigators note.
“These data may suggest that there is a short therapeutic window for slowing AD pathogenesis prior to the emergence of clinical symptoms – and that this window may occur after amyloid accumulation begins but before amyloid has substantial impacts on tau accumulation,” study investigator Corinne Pettigrew, PhD, department of neurology, Johns Hopkins University School of Medicine, Baltimore, told this news organization.
The study was published online in Alzheimer’s and Dementia.
Novel long-term CSF data
The study builds on previous research by examining changes in cerebrospinal fluid (CSF) biomarkers over longer periods than had been done previously, particularly among largely middle-aged and cognitively normal at baseline individuals.
The researchers examined changes in amyloid beta (Aβ) 42/Aβ40, phosphorylated tau181 (p-tau181), and total tau (t-tau) in CSF over an average of 10.7 years (and up to 23 years) among 278 individuals who were largely middle-aged persons who were cognitively normal at baseline.
“To our knowledge, no prior study among initially cognitively normal, primarily middle-aged individuals has described CSF AD biomarker changes over this duration of follow-up,” the researchers write.
During follow-up, 94 individuals who initially had normal cognition developed mild cognitive impairment (MCI).
Lower baseline levels of amyloid were associated with greater increases in tau (more strongly in men than women), while accelerations in tau were more closely linked to onset of MCI, the researchers report.
Among individuals who developed MCI, biomarker levels were more abnormal and tau increased to a greater extent prior to the onset of MCI symptoms, they found.
Clear impact of APOE4
The findings also suggest that among APOE4 carriers, amyloid onset occurs at an earlier age and rates of amyloid positivity are higher, but there are no differences in rates of change in amyloid over time.
“APOE4 genetic status was not related to changes in CSF beta-amyloid after accounting for the fact that APOE4 carriers have higher rates of amyloid positivity,” said Dr. Pettigrew.
“These findings suggest that APOE4 genetic status shifts the age of onset of amyloid accumulation (with APOE4 carriers having an earlier age of onset compared to non-carriers), but that APOE4 is not related to rates of change in CSF beta-amyloid over time,” she added.
“Thus, cognitively normal APOE4 carriers may be in more advanced preclinical AD stages at younger ages than individuals who are not APOE4 carriers, which is likely relevant for optimizing clinical trial recruitment strategies,” she said.
Funding for the study was provided by the National Institutes of Health. Dr. Pettigrew has disclosed no relevant financial relationships. The original article contains a complete list of author disclosures.
A version of this article first appeared on Medscape.com.
FROM ALZHEIMER’S AND DEMENTIA
Multiple Annular Erythematous Plaques
The Diagnosis: Mid-Borderline Multibacillary Leprosy
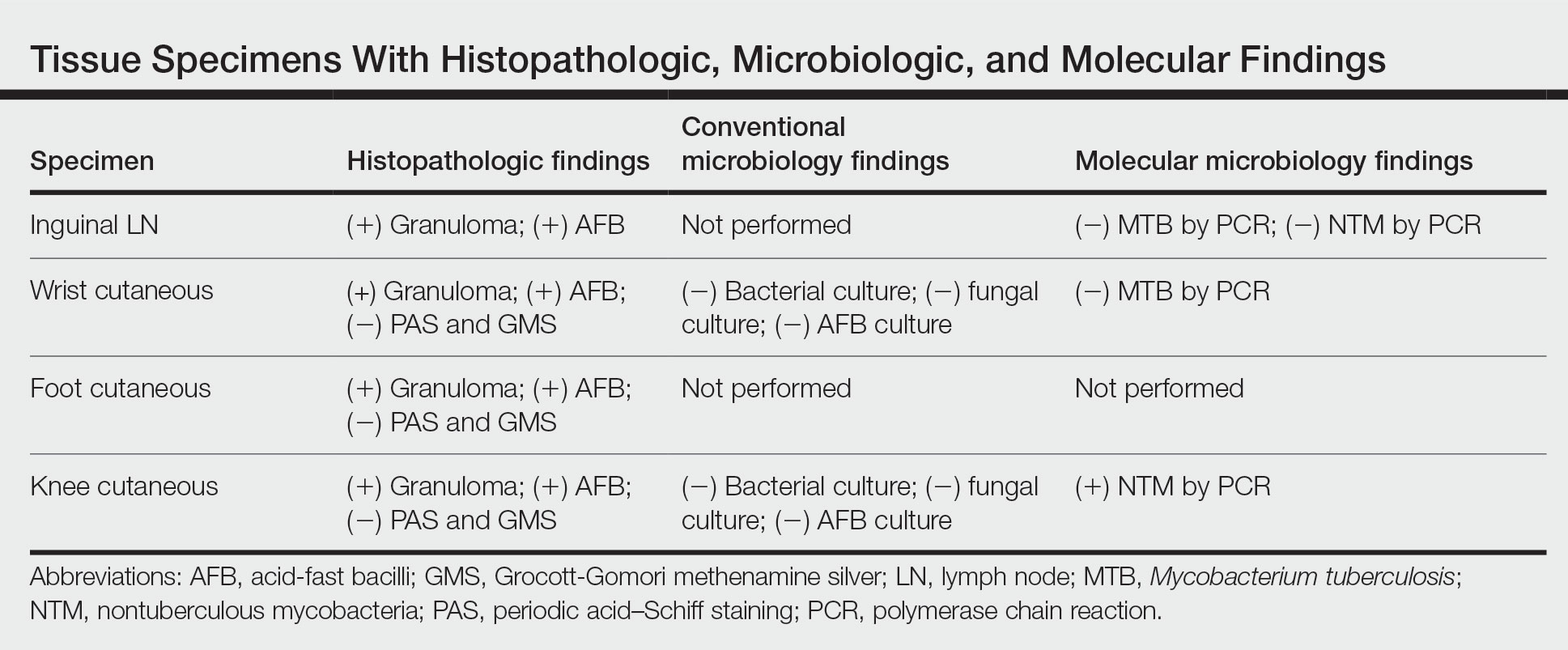
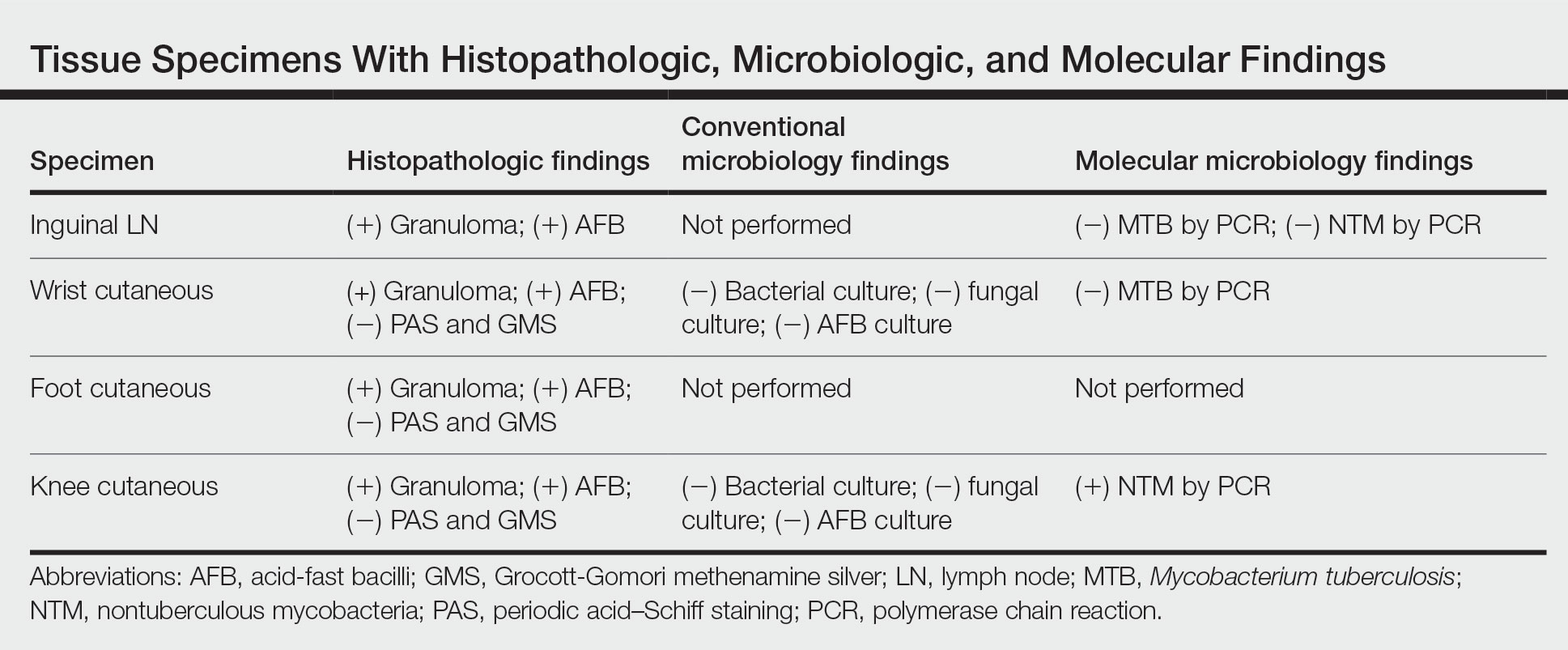
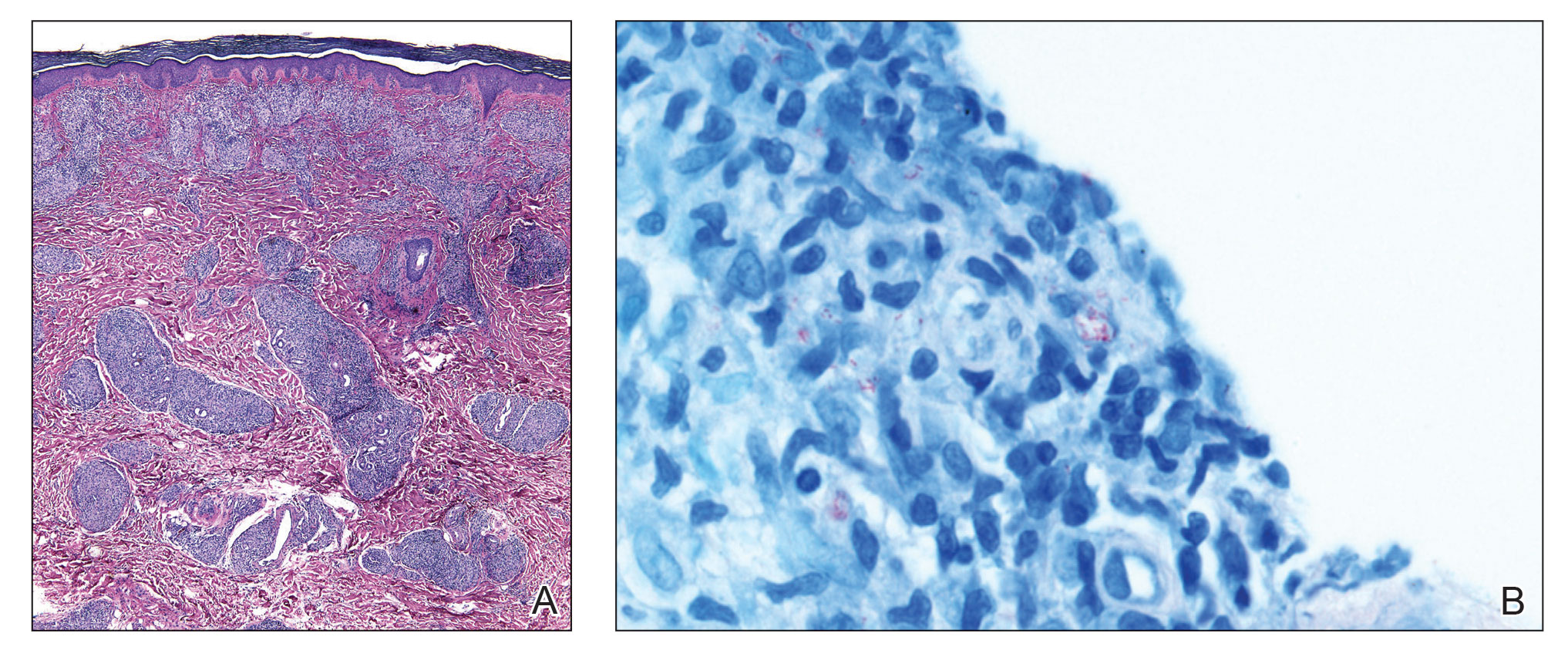
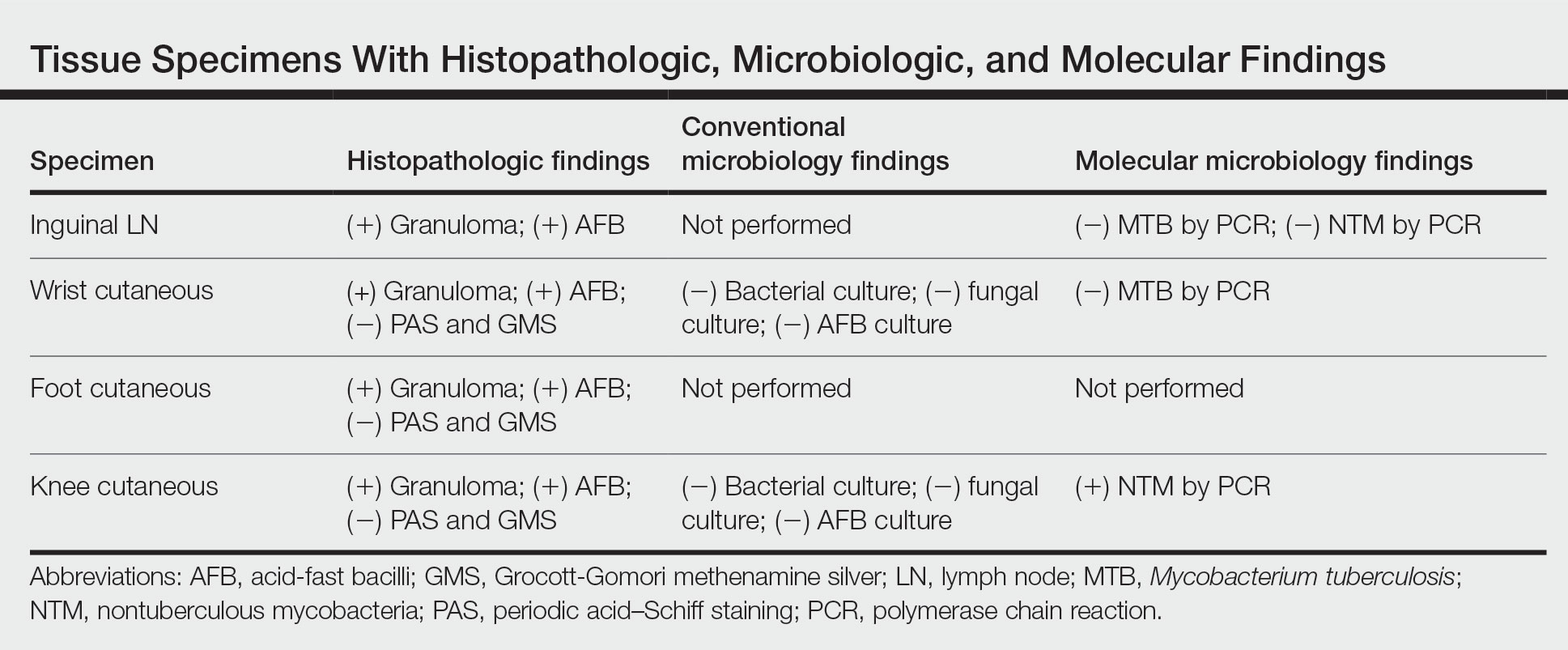
The biopsies showed a granulomatous dermatitis involving the dermis and subcutaneous adipose tissue (Figure, A). Fite staining also revealed numerous acid-fast bacilli (AFB) throughout the dermis (Figure, B); however, polymerase chain reaction (PCR) for Mycobacterium tuberculosis was negative, and concomitant AFB tissue culture showed no growth after 8 weeks of incubation from the left wrist biopsy (Table). Interestingly, a left inguinal lymph node biopsy performed 6 months prior to presentation that helped to establish the diagnosis of follicular lymphoma also revealed nonnecrotizing granulomas and the presence of rare AFB; this formalin-fixed specimen subsequently tested negative for M tuberculosis and nontuberculous mycobacteria (NTM) by broad-range PCR. Due to a high index of suspicion, another unpreserved skin biopsy of the right knee was sent for NTM testing with PCR. Primers to 16S ribosomal RNA and the beta subunit of RNA polymerase, rpoB, gene detected Mycobacterium leprae DNA, leading to the diagnosis of mid-borderline (or borderline-borderline) multibacillary leprosy. Our patient subsequently reported subtle hypoesthesia of the plaques on the knees. He recalled eating undercooked armadillo meat in the southern United States more than 30 years prior to admission. In addition, he had a history of being incarcerated in the northeastern United States. This case was reported to the National Hansen’s Disease Program, and our patient was started on a 2-year course of daily clarithromycin, daily minocycline, and once-monthly moxifloxacin. His family also was evaluated and did not have any skin lesions concerning for leprosy.
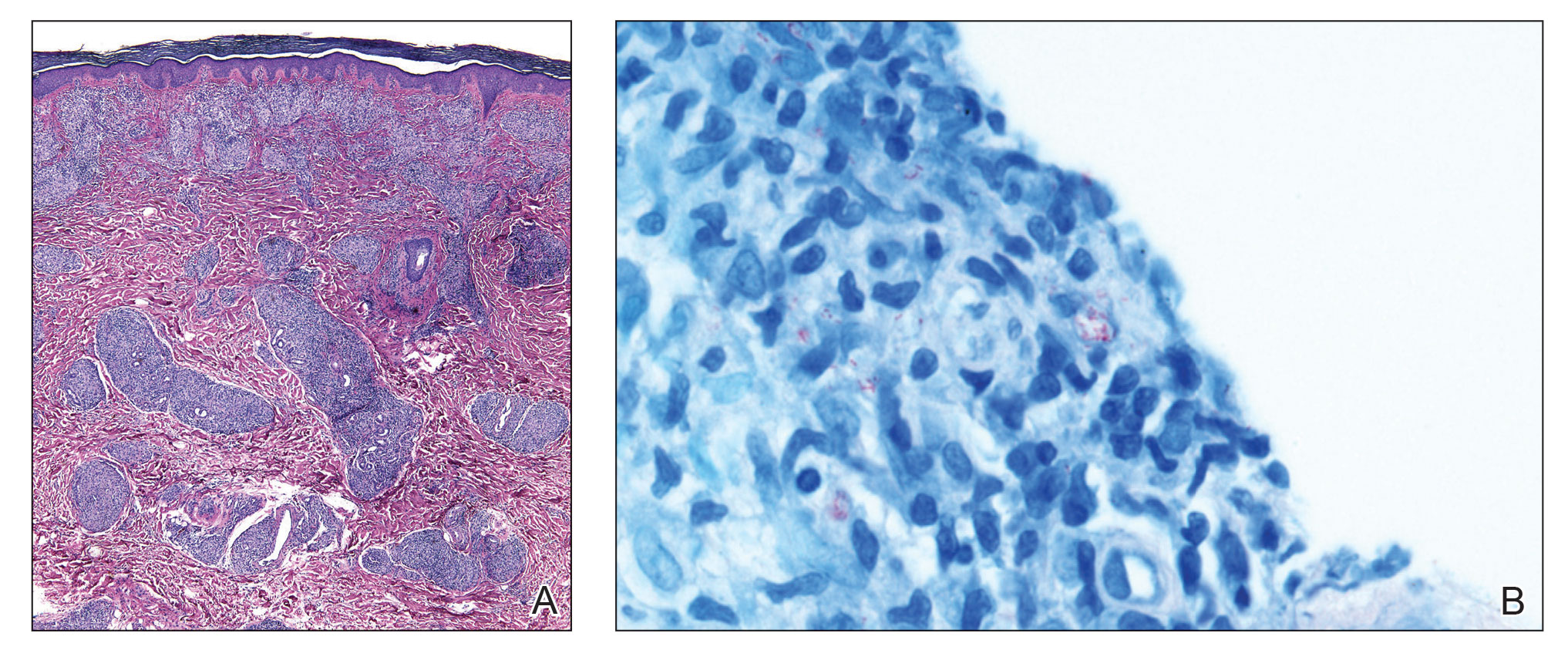
Leprosy is a major global health concern, transmitted via breaks in the skin, respiratory secretions, and contact with armadillos. It continues to be endemic in India, Brazil, and Indonesia.1 In the United States where leprosy is nonendemic, 159 new cases were detected in 2020; the most notable risk factors in the United States are armadillo exposure and travel history.2,3Mycobacterium leprae are intracellular bacilli that preferentially infect macrophages and Schwann cells, resulting in erythematous or hypopigmented skin lesions that often are anesthetic. Mycobacterium leprae has the longest doubling time of all bacteria with unknown in vitro growth requirements and a typical in vivo incubation period of 2 to 10 years.4 Therefore, in vitro cultures will yield no growth, as seen in our case. In our patient, Fite stain showed acid-fast organisms in multiple tissue specimens, but AFB cultures demonstrated no growth after 8 weeks of incubation. Although clinicopathologic correlation is most important, PCR analysis can help to assist in the diagnosis of leprosy. Unpreserved tissue should be used when possible, as the fixation process may adversely affect the analytic sensitivity of subsequent PCR-based assays.5 In our case, NTM were not detected by PCR in the inguinal lymph node specimen despite demonstrating rare AFB staining. This result likely was multifactorial, including the effect of formalin fixation and paraffin embedding as well as concomitant low biomass.
Leprosy is known as a great imitator, and clinical manifestations (both neurologic and cutaneous) depend on host immune response to the mycobacteria. Although tuberculoid leprosy (associated with T helper type 1 immune response) is distinguished by few asymmetric, well-demarcated, and often hypopigmented plaques, lepromatous leprosy (associated with T helper type 2 response) is characterized by numerous symmetric and poorly defined lesions. Borderline leprosy, as seen in our patient, is the most common type of leprosy and shows features of both tuberculoid and lepromatous leprosy.4 It also may be particularly difficult to diagnose.6,7 Borderline-borderline leprosy involves lesions that mostly are of the lepromatous type and symmetric but also may include raised plaques, as in tuberculoid leprosy.4 Plaques in an annular configuration with central clearing, as seen in our patient, are considered suggestive.8 Histopathology of borderline-borderline leprosy lesions shows subepidermal clear zones, and granulomas are more diffuse than in tuberculoid leprosy.4
Given the noncaseating granulomatous dermatitis seen on histopathology and the relatively higher incidence of sarcoidosis in our region of practice, our initial differential included sarcoidosis and other granulomatous disorders such as granuloma annulare. Interestingly, sarcoidosis has been misdiagnosed as leprosy on multiple occasions in countries where leprosy is endemic.9,10 Localized cutaneous leishmaniasis typically presents with infiltrated plaques and nodules that may ulcerate; diffuse and disseminated as well as mucocutaneous presentations may occur depending on the species and severity of infection. Parasitized macrophages containing amastigotes may be seen in the dermis highlighted by CD1a immunostaining. Mycosis fungoides presents as papulosquamous patches or plaques, often favoring sunprotected sites; the hypopigmented variant may mimic the central clearing seen in leprosy.
The diagnosis of leprosy can be challenging due to varying clinical presentation; indolent growth of the causative organism; and indeterminate nature of stains, including the Fite stain. Although leprosy is an uncommon diagnosis, this case underscores the need to keep it in the differential of granulomatous dermatoses in the appropriate clinical setting, particularly in patients with risk factors for exposure.8
- Blok DJ, De Vlas SJ, Richardus JH. Global elimination of leprosy by 2020: are we on track? Parasit Vectors. 2015;8:548. doi:10.1186/s13071-015-1143-4
- National Hansen’s disease (leprosy) program caring and curing since 1894. Health Resources and Services Administration website. Published April 13, 2017. Accessed November 17, 2022. https://www.hrsa.gov/hansens-disease/index.html
- Aslam S, Peraza J, Mekaiel A, et al. Major risk factors for leprosy in a non-endemic area of the United States: a case series. IDCases. 2019;17:E00557. doi:10.1016/j.idcr.2019.e00557
- Kundakci N, Erdem C. Leprosy: a great imitator. Clin Dermatol. 2019;37:200-212. doi:10.1016/j.clindermatol.2019.01.002
- Marchetti G, Gori A, Catozzi L, et al. Evaluation of PCR in detection of Mycobacterium tuberculosis from formalin-fixed, paraffin-embedded tissues: comparison of four amplification assays. J Clin Microbiol. 1998;36:1512-1517.
- Pawar M, Zawar V. Mid-borderline leprosy masquerading as an overlap syndrome. Rheumatology (Oxford). 2018;57:1686-1688. doi:10.1093 /rheumatology/key125
- Day W, Prodanovic E. Borderline lepromatous leprosy masking as tinea versicolor. Int J Dermatol. 2019;58:E125-E126. doi:10.1111/ijd.14439
- Lastória JC, de Abreu MAMM. Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects: part 1. An Bras Dermatol. 2014;89:205-218. doi:10.1590/abd1806-4841.20142450
- Kaushik A, Vinay K, Narang T, et al. Ichthyosiform sarcoidosis: a mimic of leprosy? Clin Exp Dermatol. 2019;44:677-680. doi:10.1111/ced.13863
- Chowdhary KN, Rao R, Priya P, et al. Cutaneous sarcoidosis misdiagnosed as leprosy. report of two cases and review of literature. Indian J Lepr. 2016;88:177-183.
The Diagnosis: Mid-Borderline Multibacillary Leprosy
The biopsies showed a granulomatous dermatitis involving the dermis and subcutaneous adipose tissue (Figure, A). Fite staining also revealed numerous acid-fast bacilli (AFB) throughout the dermis (Figure, B); however, polymerase chain reaction (PCR) for Mycobacterium tuberculosis was negative, and concomitant AFB tissue culture showed no growth after 8 weeks of incubation from the left wrist biopsy (Table). Interestingly, a left inguinal lymph node biopsy performed 6 months prior to presentation that helped to establish the diagnosis of follicular lymphoma also revealed nonnecrotizing granulomas and the presence of rare AFB; this formalin-fixed specimen subsequently tested negative for M tuberculosis and nontuberculous mycobacteria (NTM) by broad-range PCR. Due to a high index of suspicion, another unpreserved skin biopsy of the right knee was sent for NTM testing with PCR. Primers to 16S ribosomal RNA and the beta subunit of RNA polymerase, rpoB, gene detected Mycobacterium leprae DNA, leading to the diagnosis of mid-borderline (or borderline-borderline) multibacillary leprosy. Our patient subsequently reported subtle hypoesthesia of the plaques on the knees. He recalled eating undercooked armadillo meat in the southern United States more than 30 years prior to admission. In addition, he had a history of being incarcerated in the northeastern United States. This case was reported to the National Hansen’s Disease Program, and our patient was started on a 2-year course of daily clarithromycin, daily minocycline, and once-monthly moxifloxacin. His family also was evaluated and did not have any skin lesions concerning for leprosy.
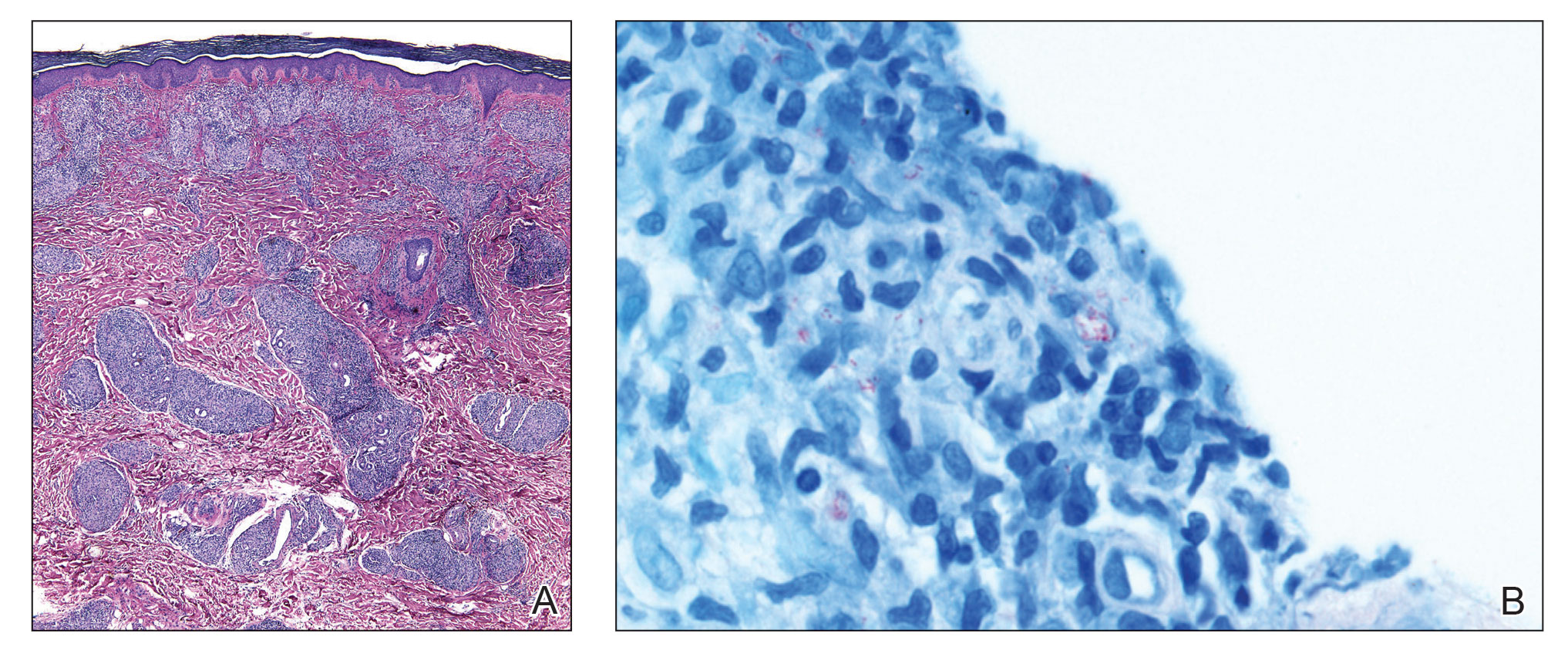
Leprosy is a major global health concern, transmitted via breaks in the skin, respiratory secretions, and contact with armadillos. It continues to be endemic in India, Brazil, and Indonesia.1 In the United States where leprosy is nonendemic, 159 new cases were detected in 2020; the most notable risk factors in the United States are armadillo exposure and travel history.2,3Mycobacterium leprae are intracellular bacilli that preferentially infect macrophages and Schwann cells, resulting in erythematous or hypopigmented skin lesions that often are anesthetic. Mycobacterium leprae has the longest doubling time of all bacteria with unknown in vitro growth requirements and a typical in vivo incubation period of 2 to 10 years.4 Therefore, in vitro cultures will yield no growth, as seen in our case. In our patient, Fite stain showed acid-fast organisms in multiple tissue specimens, but AFB cultures demonstrated no growth after 8 weeks of incubation. Although clinicopathologic correlation is most important, PCR analysis can help to assist in the diagnosis of leprosy. Unpreserved tissue should be used when possible, as the fixation process may adversely affect the analytic sensitivity of subsequent PCR-based assays.5 In our case, NTM were not detected by PCR in the inguinal lymph node specimen despite demonstrating rare AFB staining. This result likely was multifactorial, including the effect of formalin fixation and paraffin embedding as well as concomitant low biomass.
Leprosy is known as a great imitator, and clinical manifestations (both neurologic and cutaneous) depend on host immune response to the mycobacteria. Although tuberculoid leprosy (associated with T helper type 1 immune response) is distinguished by few asymmetric, well-demarcated, and often hypopigmented plaques, lepromatous leprosy (associated with T helper type 2 response) is characterized by numerous symmetric and poorly defined lesions. Borderline leprosy, as seen in our patient, is the most common type of leprosy and shows features of both tuberculoid and lepromatous leprosy.4 It also may be particularly difficult to diagnose.6,7 Borderline-borderline leprosy involves lesions that mostly are of the lepromatous type and symmetric but also may include raised plaques, as in tuberculoid leprosy.4 Plaques in an annular configuration with central clearing, as seen in our patient, are considered suggestive.8 Histopathology of borderline-borderline leprosy lesions shows subepidermal clear zones, and granulomas are more diffuse than in tuberculoid leprosy.4
Given the noncaseating granulomatous dermatitis seen on histopathology and the relatively higher incidence of sarcoidosis in our region of practice, our initial differential included sarcoidosis and other granulomatous disorders such as granuloma annulare. Interestingly, sarcoidosis has been misdiagnosed as leprosy on multiple occasions in countries where leprosy is endemic.9,10 Localized cutaneous leishmaniasis typically presents with infiltrated plaques and nodules that may ulcerate; diffuse and disseminated as well as mucocutaneous presentations may occur depending on the species and severity of infection. Parasitized macrophages containing amastigotes may be seen in the dermis highlighted by CD1a immunostaining. Mycosis fungoides presents as papulosquamous patches or plaques, often favoring sunprotected sites; the hypopigmented variant may mimic the central clearing seen in leprosy.
The diagnosis of leprosy can be challenging due to varying clinical presentation; indolent growth of the causative organism; and indeterminate nature of stains, including the Fite stain. Although leprosy is an uncommon diagnosis, this case underscores the need to keep it in the differential of granulomatous dermatoses in the appropriate clinical setting, particularly in patients with risk factors for exposure.8
The Diagnosis: Mid-Borderline Multibacillary Leprosy
The biopsies showed a granulomatous dermatitis involving the dermis and subcutaneous adipose tissue (Figure, A). Fite staining also revealed numerous acid-fast bacilli (AFB) throughout the dermis (Figure, B); however, polymerase chain reaction (PCR) for Mycobacterium tuberculosis was negative, and concomitant AFB tissue culture showed no growth after 8 weeks of incubation from the left wrist biopsy (Table). Interestingly, a left inguinal lymph node biopsy performed 6 months prior to presentation that helped to establish the diagnosis of follicular lymphoma also revealed nonnecrotizing granulomas and the presence of rare AFB; this formalin-fixed specimen subsequently tested negative for M tuberculosis and nontuberculous mycobacteria (NTM) by broad-range PCR. Due to a high index of suspicion, another unpreserved skin biopsy of the right knee was sent for NTM testing with PCR. Primers to 16S ribosomal RNA and the beta subunit of RNA polymerase, rpoB, gene detected Mycobacterium leprae DNA, leading to the diagnosis of mid-borderline (or borderline-borderline) multibacillary leprosy. Our patient subsequently reported subtle hypoesthesia of the plaques on the knees. He recalled eating undercooked armadillo meat in the southern United States more than 30 years prior to admission. In addition, he had a history of being incarcerated in the northeastern United States. This case was reported to the National Hansen’s Disease Program, and our patient was started on a 2-year course of daily clarithromycin, daily minocycline, and once-monthly moxifloxacin. His family also was evaluated and did not have any skin lesions concerning for leprosy.
Leprosy is a major global health concern, transmitted via breaks in the skin, respiratory secretions, and contact with armadillos. It continues to be endemic in India, Brazil, and Indonesia.1 In the United States where leprosy is nonendemic, 159 new cases were detected in 2020; the most notable risk factors in the United States are armadillo exposure and travel history.2,3Mycobacterium leprae are intracellular bacilli that preferentially infect macrophages and Schwann cells, resulting in erythematous or hypopigmented skin lesions that often are anesthetic. Mycobacterium leprae has the longest doubling time of all bacteria with unknown in vitro growth requirements and a typical in vivo incubation period of 2 to 10 years.4 Therefore, in vitro cultures will yield no growth, as seen in our case. In our patient, Fite stain showed acid-fast organisms in multiple tissue specimens, but AFB cultures demonstrated no growth after 8 weeks of incubation. Although clinicopathologic correlation is most important, PCR analysis can help to assist in the diagnosis of leprosy. Unpreserved tissue should be used when possible, as the fixation process may adversely affect the analytic sensitivity of subsequent PCR-based assays.5 In our case, NTM were not detected by PCR in the inguinal lymph node specimen despite demonstrating rare AFB staining. This result likely was multifactorial, including the effect of formalin fixation and paraffin embedding as well as concomitant low biomass.
Leprosy is known as a great imitator, and clinical manifestations (both neurologic and cutaneous) depend on host immune response to the mycobacteria. Although tuberculoid leprosy (associated with T helper type 1 immune response) is distinguished by few asymmetric, well-demarcated, and often hypopigmented plaques, lepromatous leprosy (associated with T helper type 2 response) is characterized by numerous symmetric and poorly defined lesions. Borderline leprosy, as seen in our patient, is the most common type of leprosy and shows features of both tuberculoid and lepromatous leprosy.4 It also may be particularly difficult to diagnose.6,7 Borderline-borderline leprosy involves lesions that mostly are of the lepromatous type and symmetric but also may include raised plaques, as in tuberculoid leprosy.4 Plaques in an annular configuration with central clearing, as seen in our patient, are considered suggestive.8 Histopathology of borderline-borderline leprosy lesions shows subepidermal clear zones, and granulomas are more diffuse than in tuberculoid leprosy.4
Given the noncaseating granulomatous dermatitis seen on histopathology and the relatively higher incidence of sarcoidosis in our region of practice, our initial differential included sarcoidosis and other granulomatous disorders such as granuloma annulare. Interestingly, sarcoidosis has been misdiagnosed as leprosy on multiple occasions in countries where leprosy is endemic.9,10 Localized cutaneous leishmaniasis typically presents with infiltrated plaques and nodules that may ulcerate; diffuse and disseminated as well as mucocutaneous presentations may occur depending on the species and severity of infection. Parasitized macrophages containing amastigotes may be seen in the dermis highlighted by CD1a immunostaining. Mycosis fungoides presents as papulosquamous patches or plaques, often favoring sunprotected sites; the hypopigmented variant may mimic the central clearing seen in leprosy.
The diagnosis of leprosy can be challenging due to varying clinical presentation; indolent growth of the causative organism; and indeterminate nature of stains, including the Fite stain. Although leprosy is an uncommon diagnosis, this case underscores the need to keep it in the differential of granulomatous dermatoses in the appropriate clinical setting, particularly in patients with risk factors for exposure.8
- Blok DJ, De Vlas SJ, Richardus JH. Global elimination of leprosy by 2020: are we on track? Parasit Vectors. 2015;8:548. doi:10.1186/s13071-015-1143-4
- National Hansen’s disease (leprosy) program caring and curing since 1894. Health Resources and Services Administration website. Published April 13, 2017. Accessed November 17, 2022. https://www.hrsa.gov/hansens-disease/index.html
- Aslam S, Peraza J, Mekaiel A, et al. Major risk factors for leprosy in a non-endemic area of the United States: a case series. IDCases. 2019;17:E00557. doi:10.1016/j.idcr.2019.e00557
- Kundakci N, Erdem C. Leprosy: a great imitator. Clin Dermatol. 2019;37:200-212. doi:10.1016/j.clindermatol.2019.01.002
- Marchetti G, Gori A, Catozzi L, et al. Evaluation of PCR in detection of Mycobacterium tuberculosis from formalin-fixed, paraffin-embedded tissues: comparison of four amplification assays. J Clin Microbiol. 1998;36:1512-1517.
- Pawar M, Zawar V. Mid-borderline leprosy masquerading as an overlap syndrome. Rheumatology (Oxford). 2018;57:1686-1688. doi:10.1093 /rheumatology/key125
- Day W, Prodanovic E. Borderline lepromatous leprosy masking as tinea versicolor. Int J Dermatol. 2019;58:E125-E126. doi:10.1111/ijd.14439
- Lastória JC, de Abreu MAMM. Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects: part 1. An Bras Dermatol. 2014;89:205-218. doi:10.1590/abd1806-4841.20142450
- Kaushik A, Vinay K, Narang T, et al. Ichthyosiform sarcoidosis: a mimic of leprosy? Clin Exp Dermatol. 2019;44:677-680. doi:10.1111/ced.13863
- Chowdhary KN, Rao R, Priya P, et al. Cutaneous sarcoidosis misdiagnosed as leprosy. report of two cases and review of literature. Indian J Lepr. 2016;88:177-183.
- Blok DJ, De Vlas SJ, Richardus JH. Global elimination of leprosy by 2020: are we on track? Parasit Vectors. 2015;8:548. doi:10.1186/s13071-015-1143-4
- National Hansen’s disease (leprosy) program caring and curing since 1894. Health Resources and Services Administration website. Published April 13, 2017. Accessed November 17, 2022. https://www.hrsa.gov/hansens-disease/index.html
- Aslam S, Peraza J, Mekaiel A, et al. Major risk factors for leprosy in a non-endemic area of the United States: a case series. IDCases. 2019;17:E00557. doi:10.1016/j.idcr.2019.e00557
- Kundakci N, Erdem C. Leprosy: a great imitator. Clin Dermatol. 2019;37:200-212. doi:10.1016/j.clindermatol.2019.01.002
- Marchetti G, Gori A, Catozzi L, et al. Evaluation of PCR in detection of Mycobacterium tuberculosis from formalin-fixed, paraffin-embedded tissues: comparison of four amplification assays. J Clin Microbiol. 1998;36:1512-1517.
- Pawar M, Zawar V. Mid-borderline leprosy masquerading as an overlap syndrome. Rheumatology (Oxford). 2018;57:1686-1688. doi:10.1093 /rheumatology/key125
- Day W, Prodanovic E. Borderline lepromatous leprosy masking as tinea versicolor. Int J Dermatol. 2019;58:E125-E126. doi:10.1111/ijd.14439
- Lastória JC, de Abreu MAMM. Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects: part 1. An Bras Dermatol. 2014;89:205-218. doi:10.1590/abd1806-4841.20142450
- Kaushik A, Vinay K, Narang T, et al. Ichthyosiform sarcoidosis: a mimic of leprosy? Clin Exp Dermatol. 2019;44:677-680. doi:10.1111/ced.13863
- Chowdhary KN, Rao R, Priya P, et al. Cutaneous sarcoidosis misdiagnosed as leprosy. report of two cases and review of literature. Indian J Lepr. 2016;88:177-183.
A 59-year-old man was admitted to the medical ward with multiple annular erythematous plaques and polyarthralgia of several months’ duration. His medical history included low-grade stage IIA follicular lymphoma diagnosed 6 months prior to presentation, substance abuse with opiates and cocaine, coronary artery disease, ascending aortic aneurysm, and chronic lower back pain. Physical examination revealed multiple red to red-brown papules and plaques, some in an annular configuration, that were distributed on the cheeks, left wrist, knees, dorsal feet, and soles. Bilateral inguinal lymphadenopathy also was noted. Serological testing for HIV, hepatitis B and C viruses, Treponema pallidum, Borrelia burgdorferi, and tuberculosis assay were negative. Arthrocentesis of the left wrist 1 week prior to admission noted 5333 nucleated cells/μL (reference range, <3000 cells/μL) and no crystals; culture of the fluid was sterile. Skin biopsies of plaques on the left wrist, left dorsal foot, and right knee were obtained for histopathologic analysis.

RSV surge stuns parents and strains providers, but doctors offer help
RSV cases peaked in mid-November, according to the latest Centers for Disease Control and Prevention data, with RSV-associated hospitalizations in the United States among patients 0-4 years having maxed out five times higher than they were at the same time in 2021. These surges strained providers and left parents scrambling for care. Fortunately, pediatric hospitalizations appear to be subsiding.
In interviews, the parents of the child who had a severe case of RSV reflected on their son’s bout with the illness, and doctors described challenges to dealing with the surge in RSV cases this season. The physicians also offered advice on how recognize and respond to future cases of the virus.
Sebastian Witt’s story
“I didn’t even know what RSV was,” said Malte Witt, whose son, Sebastian, 2, was recently hospitalized for RSV in Denver.
Mr. Witt and his wife, Emily Witt, both 32, thought they were dealing with a typical cold until Sebastian’s condition dramatically deteriorated about 36 hours after symptom onset.
“He basically just slumped over and collapsed, coughing uncontrollably,” Mr. Witt said in an interview. “He couldn’t catch his breath.”
The Witts rushed Sebastian to the ED at Children’s Hospital Colorado, expecting to see a doctor immediately. Instead, they spent the night in an overcrowded waiting room alongside many other families in the same situation.
“There was no room for anyone to sit anywhere,” Mr. Witt said. “There were people sitting on the floor. I counted maybe six children hooked up to oxygen when we walked in.”
After waiting approximately 45 minutes, a nurse checked Sebastian’s oxygen saturation. The readings were 79%-83%. This range is significantly below thresholds for supplemental oxygen described by most pediatric guidelines, which range from 90 to 94%.
The nurse connected Sebastian to bottled oxygen in the waiting room, and a recheck 4 hours later showed that his oxygen saturation had improved.
But the improvement didn’t last.
“At roughly hour 10 in the waiting room – it was 4 in the morning – you could tell that Seb was exhausted, really not acting like himself,” Mr. Witt said. “We thought maybe it’s just late at night, he hasn’t really slept. But then Emily noticed that his oxygen tank had run out.”
Mr. Witt told a nurse, and after another check revealed low oxygen saturation, Sebastian was finally admitted.
Early RSV surge strains pediatric providers
With RSV-associated hospitalizations peaking at 48 per 100,000 children, Colorado has been among the states hardest hit by the virus. New Mexico – where hospitalizations peaked at 56.4 per 100,000 children – comes in second. Even in states like California, where hospitalization rates have been almost 10-fold lower than New Mexico, pediatric providers have been stretched to their limits.
“Many hospitals are really being overwhelmed with admissions for RSV, both routine RSV – relatively mild hospitalizations with bronchiolitis – as well as kids in the ICU with more severe cases,” said Dean Blumberg, MD, chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, said in an interview.
Dr. Blumberg believes the severity of the 2022-2023 RSV season is likely COVID related.
“All community-associated respiratory viral infections are out of whack because of the pandemic, and all the masking and social distancing that was occurring,” he said.
This may also explain why older kids are coming down with more severe cases of RSV.
“Some children are getting RSV for the first time as older children,” Dr. Blumberg said, noting that, historically, most children were infected in the first 2 years of life. “There are reports of children 3 or 4 years of age being admitted with their first episode of RSV because of the [COVID] pandemic.”
This year’s RSV season is also notable for arriving early, potentially catching the community off guard, according to Jennifer D. Kusma, MD, a primary care pediatrician at Ann & Robert H. Lurie Children’s Hospital of Chicago.
“People who should have been protected often weren’t protected yet,” Dr. Kusma said in an interview.
Treatments new, old, and unproven
On Nov. 17, in the midst of the RSV surge, the American Academy of Pediatrics issued updated guidance for palivizumab, an RSV-targeting monoclonal antibody labeled for children at risk of severe RSV, including those with pre-existing lung or heart conditions, and infants with a history of premature birth (less than or equal to 35 weeks’ gestational age).
“If RSV disease activity persists at high levels in a given region through the fall and winter, the AAP supports providing more than five consecutive doses of palivizumab to eligible children,” the update stated.
Insurance companies appear to be responding in kind, covering additional doses for children in need.
“[Payers] have agreed that, if [palivizumab] needs to be given for an additional month or 2 or 3, then they’re making a commitment that they’ll reimburse hospitals for providing that,” Dr. Blumberg said.
For ineligible patients, such as Sebastian, who was born prematurely at 36 weeks – 1 week shy of the label requirement – treatment relies upon supportive care with oxygen and IV fluids.
At home, parents are left with simpler options.
Dr. Blumberg and Dr. Kusma recommended keeping children hydrated, maintaining humidified air, and using saline nose drops with bulb suction to clear mucus.
In the Witts’ experience, that last step may be easier said than done.
“Every time a nurse would walk into the room, Sebastian would yell: ‘Go away, doctor! I don’t want snot sucker!’” Mr. Witt said.
“If you over snot-suck, that’s really uncomfortable for the kid, and really hard for you,” Ms. Witt said. “And it doesn’t make much of a difference. It’s just very hard to find a middle ground, where you’re helping and keeping them comfortable.”
Some parents are turning to novel strategies, such as nebulized hypertonic saline, currently marketed on Amazon for children with RSV.
Although the AAP offers a weak recommendation for nebulized hypertonic saline in children hospitalized more than 72 hours, they advise against it in the emergency setting, citing inconsistent findings in clinical trials.
To any parents tempted by thousands of positive Amazon reviews, Dr. Blumberg said, “I wouldn’t waste my money on that.”
Dr. Kusma agreed.
“[Nebulized hypertonic saline] can be irritating,” she said. “It’s saltwater, essentially. If a parent is in the position where they’re worried about their child’s breathing to the point that they think they need to use it, I would err on the side of calling your pediatrician and being seen.”
Going in, coming home
Dr. Kusma said parents should seek medical attention if a child is breathing faster and working harder to get air. Increased work of breathing is characterized by pulling of the skin at the notch where the throat meets the chest bone (tracheal tugging), and flattening of the belly that makes the ribcage more prominent.
Mr. Witt saw these signs in Sebastian. He knew they were significant, because a friend who is a nurse had previously shown him some examples of children who exhibited these symptoms online.
“That’s how I knew that things were actually really dangerous,” Mr. Witt said. “Had she not shown me those videos a month and a half before this happened, I don’t know that we would have hit the alarm bell as quickly as we did.”
After spending their second night and the following day in a cramped preoperative room converted to manage overflow from the emergency department, Sebastian’s condition improved, and he was discharged. The Witts are relieved to be home, but frustrations from their ordeal remain, especially considering the estimated $5,000 in out-of-pocket costs they expect to pay.
“How is this our health care system?” Ms. Witt asked. “This is unbelievable.”
An optimistic outlook
RSV seasons typically demonstrate a clear peak, followed by a decline through the rest of the season, suggesting better times lie ahead; however, this season has been anything but typical.
“I’m hopeful that it will just go away and stay away,” Dr. Kusma said, citing this trend. “But I can’t know for sure.”
To anxious parents, Dr. Blumberg offered an optimistic view of RSV seasons to come.
“There’s hope,” he said. “There are vaccines that are being developed that are very close to FDA approval. So, it’s possible that this time next year, we might have widespread RSV vaccination available for children so that we don’t have to go through this nightmare again.”
Dr. Blumberg and Dr. Kusma disclosed no relevant conflicts of interest.
RSV cases peaked in mid-November, according to the latest Centers for Disease Control and Prevention data, with RSV-associated hospitalizations in the United States among patients 0-4 years having maxed out five times higher than they were at the same time in 2021. These surges strained providers and left parents scrambling for care. Fortunately, pediatric hospitalizations appear to be subsiding.
In interviews, the parents of the child who had a severe case of RSV reflected on their son’s bout with the illness, and doctors described challenges to dealing with the surge in RSV cases this season. The physicians also offered advice on how recognize and respond to future cases of the virus.
Sebastian Witt’s story
“I didn’t even know what RSV was,” said Malte Witt, whose son, Sebastian, 2, was recently hospitalized for RSV in Denver.
Mr. Witt and his wife, Emily Witt, both 32, thought they were dealing with a typical cold until Sebastian’s condition dramatically deteriorated about 36 hours after symptom onset.
“He basically just slumped over and collapsed, coughing uncontrollably,” Mr. Witt said in an interview. “He couldn’t catch his breath.”
The Witts rushed Sebastian to the ED at Children’s Hospital Colorado, expecting to see a doctor immediately. Instead, they spent the night in an overcrowded waiting room alongside many other families in the same situation.
“There was no room for anyone to sit anywhere,” Mr. Witt said. “There were people sitting on the floor. I counted maybe six children hooked up to oxygen when we walked in.”
After waiting approximately 45 minutes, a nurse checked Sebastian’s oxygen saturation. The readings were 79%-83%. This range is significantly below thresholds for supplemental oxygen described by most pediatric guidelines, which range from 90 to 94%.
The nurse connected Sebastian to bottled oxygen in the waiting room, and a recheck 4 hours later showed that his oxygen saturation had improved.
But the improvement didn’t last.
“At roughly hour 10 in the waiting room – it was 4 in the morning – you could tell that Seb was exhausted, really not acting like himself,” Mr. Witt said. “We thought maybe it’s just late at night, he hasn’t really slept. But then Emily noticed that his oxygen tank had run out.”
Mr. Witt told a nurse, and after another check revealed low oxygen saturation, Sebastian was finally admitted.
Early RSV surge strains pediatric providers
With RSV-associated hospitalizations peaking at 48 per 100,000 children, Colorado has been among the states hardest hit by the virus. New Mexico – where hospitalizations peaked at 56.4 per 100,000 children – comes in second. Even in states like California, where hospitalization rates have been almost 10-fold lower than New Mexico, pediatric providers have been stretched to their limits.
“Many hospitals are really being overwhelmed with admissions for RSV, both routine RSV – relatively mild hospitalizations with bronchiolitis – as well as kids in the ICU with more severe cases,” said Dean Blumberg, MD, chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, said in an interview.
Dr. Blumberg believes the severity of the 2022-2023 RSV season is likely COVID related.
“All community-associated respiratory viral infections are out of whack because of the pandemic, and all the masking and social distancing that was occurring,” he said.
This may also explain why older kids are coming down with more severe cases of RSV.
“Some children are getting RSV for the first time as older children,” Dr. Blumberg said, noting that, historically, most children were infected in the first 2 years of life. “There are reports of children 3 or 4 years of age being admitted with their first episode of RSV because of the [COVID] pandemic.”
This year’s RSV season is also notable for arriving early, potentially catching the community off guard, according to Jennifer D. Kusma, MD, a primary care pediatrician at Ann & Robert H. Lurie Children’s Hospital of Chicago.
“People who should have been protected often weren’t protected yet,” Dr. Kusma said in an interview.
Treatments new, old, and unproven
On Nov. 17, in the midst of the RSV surge, the American Academy of Pediatrics issued updated guidance for palivizumab, an RSV-targeting monoclonal antibody labeled for children at risk of severe RSV, including those with pre-existing lung or heart conditions, and infants with a history of premature birth (less than or equal to 35 weeks’ gestational age).
“If RSV disease activity persists at high levels in a given region through the fall and winter, the AAP supports providing more than five consecutive doses of palivizumab to eligible children,” the update stated.
Insurance companies appear to be responding in kind, covering additional doses for children in need.
“[Payers] have agreed that, if [palivizumab] needs to be given for an additional month or 2 or 3, then they’re making a commitment that they’ll reimburse hospitals for providing that,” Dr. Blumberg said.
For ineligible patients, such as Sebastian, who was born prematurely at 36 weeks – 1 week shy of the label requirement – treatment relies upon supportive care with oxygen and IV fluids.
At home, parents are left with simpler options.
Dr. Blumberg and Dr. Kusma recommended keeping children hydrated, maintaining humidified air, and using saline nose drops with bulb suction to clear mucus.
In the Witts’ experience, that last step may be easier said than done.
“Every time a nurse would walk into the room, Sebastian would yell: ‘Go away, doctor! I don’t want snot sucker!’” Mr. Witt said.
“If you over snot-suck, that’s really uncomfortable for the kid, and really hard for you,” Ms. Witt said. “And it doesn’t make much of a difference. It’s just very hard to find a middle ground, where you’re helping and keeping them comfortable.”
Some parents are turning to novel strategies, such as nebulized hypertonic saline, currently marketed on Amazon for children with RSV.
Although the AAP offers a weak recommendation for nebulized hypertonic saline in children hospitalized more than 72 hours, they advise against it in the emergency setting, citing inconsistent findings in clinical trials.
To any parents tempted by thousands of positive Amazon reviews, Dr. Blumberg said, “I wouldn’t waste my money on that.”
Dr. Kusma agreed.
“[Nebulized hypertonic saline] can be irritating,” she said. “It’s saltwater, essentially. If a parent is in the position where they’re worried about their child’s breathing to the point that they think they need to use it, I would err on the side of calling your pediatrician and being seen.”
Going in, coming home
Dr. Kusma said parents should seek medical attention if a child is breathing faster and working harder to get air. Increased work of breathing is characterized by pulling of the skin at the notch where the throat meets the chest bone (tracheal tugging), and flattening of the belly that makes the ribcage more prominent.
Mr. Witt saw these signs in Sebastian. He knew they were significant, because a friend who is a nurse had previously shown him some examples of children who exhibited these symptoms online.
“That’s how I knew that things were actually really dangerous,” Mr. Witt said. “Had she not shown me those videos a month and a half before this happened, I don’t know that we would have hit the alarm bell as quickly as we did.”
After spending their second night and the following day in a cramped preoperative room converted to manage overflow from the emergency department, Sebastian’s condition improved, and he was discharged. The Witts are relieved to be home, but frustrations from their ordeal remain, especially considering the estimated $5,000 in out-of-pocket costs they expect to pay.
“How is this our health care system?” Ms. Witt asked. “This is unbelievable.”
An optimistic outlook
RSV seasons typically demonstrate a clear peak, followed by a decline through the rest of the season, suggesting better times lie ahead; however, this season has been anything but typical.
“I’m hopeful that it will just go away and stay away,” Dr. Kusma said, citing this trend. “But I can’t know for sure.”
To anxious parents, Dr. Blumberg offered an optimistic view of RSV seasons to come.
“There’s hope,” he said. “There are vaccines that are being developed that are very close to FDA approval. So, it’s possible that this time next year, we might have widespread RSV vaccination available for children so that we don’t have to go through this nightmare again.”
Dr. Blumberg and Dr. Kusma disclosed no relevant conflicts of interest.
RSV cases peaked in mid-November, according to the latest Centers for Disease Control and Prevention data, with RSV-associated hospitalizations in the United States among patients 0-4 years having maxed out five times higher than they were at the same time in 2021. These surges strained providers and left parents scrambling for care. Fortunately, pediatric hospitalizations appear to be subsiding.
In interviews, the parents of the child who had a severe case of RSV reflected on their son’s bout with the illness, and doctors described challenges to dealing with the surge in RSV cases this season. The physicians also offered advice on how recognize and respond to future cases of the virus.
Sebastian Witt’s story
“I didn’t even know what RSV was,” said Malte Witt, whose son, Sebastian, 2, was recently hospitalized for RSV in Denver.
Mr. Witt and his wife, Emily Witt, both 32, thought they were dealing with a typical cold until Sebastian’s condition dramatically deteriorated about 36 hours after symptom onset.
“He basically just slumped over and collapsed, coughing uncontrollably,” Mr. Witt said in an interview. “He couldn’t catch his breath.”
The Witts rushed Sebastian to the ED at Children’s Hospital Colorado, expecting to see a doctor immediately. Instead, they spent the night in an overcrowded waiting room alongside many other families in the same situation.
“There was no room for anyone to sit anywhere,” Mr. Witt said. “There were people sitting on the floor. I counted maybe six children hooked up to oxygen when we walked in.”
After waiting approximately 45 minutes, a nurse checked Sebastian’s oxygen saturation. The readings were 79%-83%. This range is significantly below thresholds for supplemental oxygen described by most pediatric guidelines, which range from 90 to 94%.
The nurse connected Sebastian to bottled oxygen in the waiting room, and a recheck 4 hours later showed that his oxygen saturation had improved.
But the improvement didn’t last.
“At roughly hour 10 in the waiting room – it was 4 in the morning – you could tell that Seb was exhausted, really not acting like himself,” Mr. Witt said. “We thought maybe it’s just late at night, he hasn’t really slept. But then Emily noticed that his oxygen tank had run out.”
Mr. Witt told a nurse, and after another check revealed low oxygen saturation, Sebastian was finally admitted.
Early RSV surge strains pediatric providers
With RSV-associated hospitalizations peaking at 48 per 100,000 children, Colorado has been among the states hardest hit by the virus. New Mexico – where hospitalizations peaked at 56.4 per 100,000 children – comes in second. Even in states like California, where hospitalization rates have been almost 10-fold lower than New Mexico, pediatric providers have been stretched to their limits.
“Many hospitals are really being overwhelmed with admissions for RSV, both routine RSV – relatively mild hospitalizations with bronchiolitis – as well as kids in the ICU with more severe cases,” said Dean Blumberg, MD, chief of the division of pediatric infectious diseases at UC Davis Health, Sacramento, said in an interview.
Dr. Blumberg believes the severity of the 2022-2023 RSV season is likely COVID related.
“All community-associated respiratory viral infections are out of whack because of the pandemic, and all the masking and social distancing that was occurring,” he said.
This may also explain why older kids are coming down with more severe cases of RSV.
“Some children are getting RSV for the first time as older children,” Dr. Blumberg said, noting that, historically, most children were infected in the first 2 years of life. “There are reports of children 3 or 4 years of age being admitted with their first episode of RSV because of the [COVID] pandemic.”
This year’s RSV season is also notable for arriving early, potentially catching the community off guard, according to Jennifer D. Kusma, MD, a primary care pediatrician at Ann & Robert H. Lurie Children’s Hospital of Chicago.
“People who should have been protected often weren’t protected yet,” Dr. Kusma said in an interview.
Treatments new, old, and unproven
On Nov. 17, in the midst of the RSV surge, the American Academy of Pediatrics issued updated guidance for palivizumab, an RSV-targeting monoclonal antibody labeled for children at risk of severe RSV, including those with pre-existing lung or heart conditions, and infants with a history of premature birth (less than or equal to 35 weeks’ gestational age).
“If RSV disease activity persists at high levels in a given region through the fall and winter, the AAP supports providing more than five consecutive doses of palivizumab to eligible children,” the update stated.
Insurance companies appear to be responding in kind, covering additional doses for children in need.
“[Payers] have agreed that, if [palivizumab] needs to be given for an additional month or 2 or 3, then they’re making a commitment that they’ll reimburse hospitals for providing that,” Dr. Blumberg said.
For ineligible patients, such as Sebastian, who was born prematurely at 36 weeks – 1 week shy of the label requirement – treatment relies upon supportive care with oxygen and IV fluids.
At home, parents are left with simpler options.
Dr. Blumberg and Dr. Kusma recommended keeping children hydrated, maintaining humidified air, and using saline nose drops with bulb suction to clear mucus.
In the Witts’ experience, that last step may be easier said than done.
“Every time a nurse would walk into the room, Sebastian would yell: ‘Go away, doctor! I don’t want snot sucker!’” Mr. Witt said.
“If you over snot-suck, that’s really uncomfortable for the kid, and really hard for you,” Ms. Witt said. “And it doesn’t make much of a difference. It’s just very hard to find a middle ground, where you’re helping and keeping them comfortable.”
Some parents are turning to novel strategies, such as nebulized hypertonic saline, currently marketed on Amazon for children with RSV.
Although the AAP offers a weak recommendation for nebulized hypertonic saline in children hospitalized more than 72 hours, they advise against it in the emergency setting, citing inconsistent findings in clinical trials.
To any parents tempted by thousands of positive Amazon reviews, Dr. Blumberg said, “I wouldn’t waste my money on that.”
Dr. Kusma agreed.
“[Nebulized hypertonic saline] can be irritating,” she said. “It’s saltwater, essentially. If a parent is in the position where they’re worried about their child’s breathing to the point that they think they need to use it, I would err on the side of calling your pediatrician and being seen.”
Going in, coming home
Dr. Kusma said parents should seek medical attention if a child is breathing faster and working harder to get air. Increased work of breathing is characterized by pulling of the skin at the notch where the throat meets the chest bone (tracheal tugging), and flattening of the belly that makes the ribcage more prominent.
Mr. Witt saw these signs in Sebastian. He knew they were significant, because a friend who is a nurse had previously shown him some examples of children who exhibited these symptoms online.
“That’s how I knew that things were actually really dangerous,” Mr. Witt said. “Had she not shown me those videos a month and a half before this happened, I don’t know that we would have hit the alarm bell as quickly as we did.”
After spending their second night and the following day in a cramped preoperative room converted to manage overflow from the emergency department, Sebastian’s condition improved, and he was discharged. The Witts are relieved to be home, but frustrations from their ordeal remain, especially considering the estimated $5,000 in out-of-pocket costs they expect to pay.
“How is this our health care system?” Ms. Witt asked. “This is unbelievable.”
An optimistic outlook
RSV seasons typically demonstrate a clear peak, followed by a decline through the rest of the season, suggesting better times lie ahead; however, this season has been anything but typical.
“I’m hopeful that it will just go away and stay away,” Dr. Kusma said, citing this trend. “But I can’t know for sure.”
To anxious parents, Dr. Blumberg offered an optimistic view of RSV seasons to come.
“There’s hope,” he said. “There are vaccines that are being developed that are very close to FDA approval. So, it’s possible that this time next year, we might have widespread RSV vaccination available for children so that we don’t have to go through this nightmare again.”
Dr. Blumberg and Dr. Kusma disclosed no relevant conflicts of interest.
Flu, RSV infecting children at staggering rates
There has been no ebb in the flurry of respiratory illnesses infecting America’s youngest children. More pediatric wards across the country are announcing crises as beds reach capacity, the pediatric death toll jumped significantly in the past week, and sometimes children are being infected with more than one virus at a time.
In Oregon, for example, the governor announced an official state of emergency to help hospitals deal with the surge of respiratory viruses. Doernbecher Children’s Hospital in Portland, which houses half of all pediatric ICU beds statewide, moved to “crisis mode” and said every pediatric ICU bed was full, Oregon Public Broadcasting reported.
Last month, pediatricians nationwide called for a similar emergency declaration from the federal government to help them respond to the wave of illnesses, which include influenza and respiratory syncytial virus (RSV).
“What’s concerning to us are not only the number of infections, but the severity of these infections, leading to a high number of emergency room visits and hospitalizations,” pediatric infectious disease expert Oscar G. Gómez-Duarte, MD, PhD, said in a news release.
Five more pediatric deaths due to the flu were logged by the CDC in the past week, bringing the total for pediatric flu deaths this season to 12. Nearly 21 per 100,000 children ages 4 and under are being hospitalized for the flu, which is double the rate for children ages 5-17. Last year at this time, fewer than 1 child under age 4 per 100,000 were being hospitalized for the flu.
RSV rates are also stunningly high.
“If we look at CDC data, the RSV hospitalization rate is 10 times higher than usual for this point in the season,” American Medical Association Vice President Andrea Garcia, JD, said in this week’s AMA podcast. “And 171 out of every 100,000 infants younger than 6 months were hospitalized with RSV for the week ending Nov. 12. That is more than double the RSV hospitalization rate for newborns last year and seven times the rate in 2018, which is the last complete season we saw before the pandemic.”
Dr. Gómez-Duarte said hospitals are admitting children with respiratory illnesses who had otherwise been healthy, and sometimes they are even seeing patients with more than one illness.
“Yes, some children are getting what we call coinfections, where they become infected with more than one virus at a time. In some instances, a child becomes initially infected with flu, begins to recover, and subsequently comes down with rhinovirus (a common cold virus), RSV, or any other respiratory virus,” he said. “These coinfections tend to be more severe than when the child just has one infection.”
A version of this article first appeared on Medscape.com.
There has been no ebb in the flurry of respiratory illnesses infecting America’s youngest children. More pediatric wards across the country are announcing crises as beds reach capacity, the pediatric death toll jumped significantly in the past week, and sometimes children are being infected with more than one virus at a time.
In Oregon, for example, the governor announced an official state of emergency to help hospitals deal with the surge of respiratory viruses. Doernbecher Children’s Hospital in Portland, which houses half of all pediatric ICU beds statewide, moved to “crisis mode” and said every pediatric ICU bed was full, Oregon Public Broadcasting reported.
Last month, pediatricians nationwide called for a similar emergency declaration from the federal government to help them respond to the wave of illnesses, which include influenza and respiratory syncytial virus (RSV).
“What’s concerning to us are not only the number of infections, but the severity of these infections, leading to a high number of emergency room visits and hospitalizations,” pediatric infectious disease expert Oscar G. Gómez-Duarte, MD, PhD, said in a news release.
Five more pediatric deaths due to the flu were logged by the CDC in the past week, bringing the total for pediatric flu deaths this season to 12. Nearly 21 per 100,000 children ages 4 and under are being hospitalized for the flu, which is double the rate for children ages 5-17. Last year at this time, fewer than 1 child under age 4 per 100,000 were being hospitalized for the flu.
RSV rates are also stunningly high.
“If we look at CDC data, the RSV hospitalization rate is 10 times higher than usual for this point in the season,” American Medical Association Vice President Andrea Garcia, JD, said in this week’s AMA podcast. “And 171 out of every 100,000 infants younger than 6 months were hospitalized with RSV for the week ending Nov. 12. That is more than double the RSV hospitalization rate for newborns last year and seven times the rate in 2018, which is the last complete season we saw before the pandemic.”
Dr. Gómez-Duarte said hospitals are admitting children with respiratory illnesses who had otherwise been healthy, and sometimes they are even seeing patients with more than one illness.
“Yes, some children are getting what we call coinfections, where they become infected with more than one virus at a time. In some instances, a child becomes initially infected with flu, begins to recover, and subsequently comes down with rhinovirus (a common cold virus), RSV, or any other respiratory virus,” he said. “These coinfections tend to be more severe than when the child just has one infection.”
A version of this article first appeared on Medscape.com.
There has been no ebb in the flurry of respiratory illnesses infecting America’s youngest children. More pediatric wards across the country are announcing crises as beds reach capacity, the pediatric death toll jumped significantly in the past week, and sometimes children are being infected with more than one virus at a time.
In Oregon, for example, the governor announced an official state of emergency to help hospitals deal with the surge of respiratory viruses. Doernbecher Children’s Hospital in Portland, which houses half of all pediatric ICU beds statewide, moved to “crisis mode” and said every pediatric ICU bed was full, Oregon Public Broadcasting reported.
Last month, pediatricians nationwide called for a similar emergency declaration from the federal government to help them respond to the wave of illnesses, which include influenza and respiratory syncytial virus (RSV).
“What’s concerning to us are not only the number of infections, but the severity of these infections, leading to a high number of emergency room visits and hospitalizations,” pediatric infectious disease expert Oscar G. Gómez-Duarte, MD, PhD, said in a news release.
Five more pediatric deaths due to the flu were logged by the CDC in the past week, bringing the total for pediatric flu deaths this season to 12. Nearly 21 per 100,000 children ages 4 and under are being hospitalized for the flu, which is double the rate for children ages 5-17. Last year at this time, fewer than 1 child under age 4 per 100,000 were being hospitalized for the flu.
RSV rates are also stunningly high.
“If we look at CDC data, the RSV hospitalization rate is 10 times higher than usual for this point in the season,” American Medical Association Vice President Andrea Garcia, JD, said in this week’s AMA podcast. “And 171 out of every 100,000 infants younger than 6 months were hospitalized with RSV for the week ending Nov. 12. That is more than double the RSV hospitalization rate for newborns last year and seven times the rate in 2018, which is the last complete season we saw before the pandemic.”
Dr. Gómez-Duarte said hospitals are admitting children with respiratory illnesses who had otherwise been healthy, and sometimes they are even seeing patients with more than one illness.
“Yes, some children are getting what we call coinfections, where they become infected with more than one virus at a time. In some instances, a child becomes initially infected with flu, begins to recover, and subsequently comes down with rhinovirus (a common cold virus), RSV, or any other respiratory virus,” he said. “These coinfections tend to be more severe than when the child just has one infection.”
A version of this article first appeared on Medscape.com.
Women docs: How your next job contract can reflect your real goals
Rebecca Chester, MD, an Arizona-based interventional cardiologist, recently left her position in a private practice and started employment at a hospital system.
“When I was negotiating my previous contract with the private practice, I found that navigating contracts from the standpoint of a woman still in childbearing years was a little disappointing and challenging,” Dr. Chester told this news organization.
“I wanted to have more children and hired a lawyer recommended by a male colleague to help me not only understand the contract but also negotiate time off and maternity leave, but the lawyer discouraged me from advocating for maternity leave, feeling that it might stigmatize me and prevent me from getting a job,” she says.
He also didn’t explain very much. “He just said it falls under ‘disability leave’ and left it at that.”
Fortunately, Dr. Chester had a good experience with the group. “As things turned out, I did have a child later that year, and they treated me well – I actually got time off – and they didn’t make me take extra call. But it might have turned out very differently because I didn’t know what I was getting into. If I hadn’t worked for such a conscientious group, I might have been in a much tougher situation.”
Since then, Dr. Chester has spoken to female colleagues who received “more support from their legal advisors regarding maternity leave.” She suggests turning to female physicians for recommendations to a lawyer.
Although the central components of a contract (for example, noncompete covenants, malpractice “tail” coverage, bonus structure, vacation time, disability, and call) are relevant to physicians of all genders, the needs of women and men are often different.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, told this news organization that women physicians have “several issues that need special attention when negotiating their physician employment agreements.”
It starts with the interview
“Women have to be sensitive to the interviewer’s casual ‘let’s-get-to-know-each-other’ types of questions that may seem natural but really are unlawful to bring into an employment interview,” said Mr. Hursh.
He warned women to beware of questions such as “Are you married? Do you have kids? Are you planning to start a family?” These may be friendly chit-chat for male interviewees but there may be other agendas when asked to a prospective female employee.
Many of Mr. Hursh’s female clients have been asked this type of question, which “should be regarded as a ‘red flag.’ Yes, it may be an innocent, well-intentioned ice-breaker, but it’s actually unlawful to bring that up in an employment setting and, according to the Equal Opportunity Commission, can be seen as a form of discrimination.” He advises female physicians not to engage with the question and simply to refocus the discussion.
Know your worth and go for it
Medscape’s Physician Compensation surveys have consistently found discrepancies in earnings between male and female physicians, both in primary care and in specialties. In 2022, male primary care physicians earned 23% more than their female counterparts, whereas male specialists earned 31% more.
One reason may be that women tend to be more timid about negotiating for better compensation packages. Amanda Hill of Hill Health Law, a health care practice based in Austin, Tex., told this news organization that in her experience one of the most “overarching” features of female physicians is “that they either don’t know what they’re worth or they undersell themselves.”
In contrast to men, “many women are afraid of coming across as greedy or crass, or even demanding or bossy. But it’s a misperception that if you ask for more money, your future employer will hate you or won’t hire you,” said Ms. Hill.
Ms. Hill and Mr. Hursh encourage physicians to find out what they’re worth, which varies by region and specialty, by consulting benchmarks provided by companies such as Medical Group Management Association.
Jon Appino, MBA, principal and founder of Contract Diagnostics, a Kansas City–based consulting company that specializes in physician employment contract reviews, told this news organization that it’s important to look beyond the salary at other aspects of the position. For example, some figures “don’t take into account how much call a physician is taking. You may know what the average ob.gyn. is making, but an ob.gyn. may be working 3 days a week, while another one is working 6 days a week, one may be on call 15 times per month and another may be on call 15 times a quarter.” Other components of compensation include relative value unit (RVU) thresholds and bonuses.
Once you have that information, “don’t be intimidated, even if you’re sitting in front of several executives who are savvy about negotiations, and don’t worry about coming across as ‘high-maintenance’ or ‘all about money,’ ” Mr. Appino says. Proceed with confidence, knowing your worth and pursuing it.
Part-time vs. full-time
Mr. Appino has seen “more female than male physicians who want to work less than full-time. So it’s important to clarify whether that’s a possibility now or in the future and to understand the implications of working part-time.”
He explained that a full-time employee typically puts in a 40-hour work week, which translates into 1.0 Full-Time Equivalent (FTE), or one unit of work. “For example, if a person wants to work 0.8 FTEs – 4 days a week – is vacation time pro-rated? At what point is there a medical insurance fall-off or a higher monthly premium?”
In medical settings, FTEs may be tied to different metrics rather than the number of weekly hours – for example, for a hospitalist, it might be a certain number of shifts and might also vary by specialty. And it affects the call schedule too. “Call is hard to pro-rate. Many hospital bylaws mandate that call be divided equally, but if one surgeon is working 1.0 FTEs and another is working 0.8 FTEs, how does that call schedule get divided?”
Maternity leave: A tricky question
Many attorneys counsel against raising the question out of fear of scaring away potential employers.
“On the one hand, it is and should be absolutely reasonable to ask about the maternity leave policy or even negotiate for paid leave or additional leave, but it also highlights that you’re planning to have a baby and be out for months,” said Ms. Hill.
“And as much as we want people to be fair and reasonable, on the side of the employer, bias still very much exists, especially in a situation where revenue is based on group numbers. So suddenly, the employer thinks up some ‘nondiscriminatory’ reason why that person isn’t a great fit for the organization.”
Andrew Knoll, MD, JD, a former hospitalist who is now a partner with Cohen Compagni Beckman Appler & Knoll PLLC in Syracuse, N.Y., said that maternity leave is “rare” in an employment agreement, except sometimes in small private practice groups, because it often falls under the purview of “disability leave,” and “from a legal perspective, it’s no different than any other type of disability leave.”
The Family and Medical Leave Act (FMLA), which applies if a group is large enough, allows employees 12 weeks of unpaid leave, during which time their job is protected and their benefits maintained. And some states require employers to offer paid family leave.
“During this time, the woman can take time off – albeit without pay sometimes – to bond with the baby,” Dr. Knoll says. “Since there are statutory laws that protect the employee’s job, offering specific paid maternity leave is very unlikely.”
Ms. Hill advises carefully examining the employer’s comprehensive benefits plan to ascertain if paid maternity leave is included in the benefits. “But unless you’re currently pregnant and want to start off the relationship with true transparency – ‘I’m due in April and curious how we can handle that if you hire me now’ – I would keep the family planning questions to yourself before you get the job.”
Mr. Hursh, author of “The Final Hurdle: A Physician’s Guide to Negotiating a Fair Employment Agreement” (Charleston, S.C.: Advantage, 2012), has a different perspective. “I think all women, no matter how old they are, should ask about maternity leave, whether or not they’re planning a family,” he said.
“The employer may say, ‘We treat maternity leave like any other disability; our policy is such-and-such.’ If they cite an unacceptable policy, it’s a red flag about how they treat women, and should give a woman pause before accepting a position at that organization. Even if your rights are protected under the law and the organization’s policy is violating the law, no one wants to go to battle with HR or to have to go to court.”
Do you want partnership?
Not all female physicians entering a private practice want to advance to becoming partners. Many who are balancing family and work commitments “would prefer to just go into the office, perform their clinical responsibilities, go home, and be done” without the extra headaches, tasks, and time involved with business leadership, says Mr. Appino.
Some private practices have different contracts for those on partnership vs. nonpartnership tracks, so “you should ascertain this information and make sure it’s not automatically assumed that you would like to be on a partnership track,” says Mr. Appino.
On the other hand, you may want to become a partner. “I always suggest asking about the possibility of obtaining a leadership position in an organization or becoming an owner in a private practice,” says Mr. Hursh. “You may be told, ‘We’ve never had a woman in leadership before.’ This might be innocent if you’re the first woman hired, but it might be a red flag as to how women are regarded.” Either way, it’s important to have the information and know what your options are.
The impact of shift schedule
Mr. Hursh advises drilling down into the specifics of the schedule if you’re considering becoming a hospitalist. “Does a ‘week-on/week-off’ shift schedule assume you’ll be taking your vacation time or completing your CME requirements during the week off? This is important for all physicians, but especially for women who might want to use their weeks off to attend to children and family.”
Moreover, “there should be limits on shifts. You shouldn’t have a full day shift followed by a night shift. And there should be a limit on the number of shifts you work without time off. Twelve would be a brutal schedule. Seven is a reasonable amount. Make sure this is in writing and that the contract protects you. Don’t allow the employer to say, ‘We expect you to do the work we assign’ and leave it vague.”
Often, hospitalists will receive an annual salary under the assumption that a certain minimum number of shifts will be completed, but there is no maximum. “It’s important that the salary includes the minimum number of shifts, but that a compensation structure is created so that additional shifts receive additional compensation,” Mr. Hursh said.
Removing the ‘golden handcuffs’
Ms. Hill observes that there are some “really terrible contracts out there, which physicians – especially women – often feel pressured into signing.” They’re told, “This is our standard contract. You won’t find anything better.” Or, “Don’t worry about the small print and legalese.” The physician “gets scared or is artificially reassured, signs an overwhelmingly unfair contract, and then feels stuck.”
Being stuck in a bad contract “is debilitating and adds to burnout, feeling of depression, and the sense that there is no recourse and nowhere to go, especially if your family depends on you,” Ms. Hill said.
“More women than men feel hamstrung or are resigned to being harassed – which is not uncommon in the medical setting, especially in surgical specialties – or just accept poor treatment,” Ms. Hill added. Yes, you can “fight the system and go to HR, but fighting the system is very hard.”
She urges women “not to feel stuck or imprisoned by the ‘golden handcuffs’ but to consult a good lawyer, even if you have to break the contract.” Be aware of the reasons for your unhappiness and bring them to your lawyer – perhaps the system has engaged in fraud, perhaps there has been sexual or racial harassment, perhaps the organization hasn’t followed its own compliance policies.
Dr. Chester consulted Ms. Hill before signing the contract for her current position. “I wanted someone who could give me personalized advice, not only generic advice, and who understood my needs as a woman.”
Ms. Hill helped her to understand “what was and wasn’t fair and reasonable, what changes I could request based on my goals and whether they were realistic, and how to pick my battles. For example, I tried to negotiate tail coverage up front in my previous job but was unsuccessful. The new employer paid tail for me, both from my previous employment and for my current employment.”
Dr. Chester advises other female physicians “never to sign anything without having a lawyer review it and to make sure that the lawyer is sensitive to their specific needs.”
It can be hard to be a female physician. Having the right knowledge and ammunition and knowing how to negotiate well paves the way for success and thriving in an often male-dominated market.
A version of this article first appeared on Medscape.com.
Rebecca Chester, MD, an Arizona-based interventional cardiologist, recently left her position in a private practice and started employment at a hospital system.
“When I was negotiating my previous contract with the private practice, I found that navigating contracts from the standpoint of a woman still in childbearing years was a little disappointing and challenging,” Dr. Chester told this news organization.
“I wanted to have more children and hired a lawyer recommended by a male colleague to help me not only understand the contract but also negotiate time off and maternity leave, but the lawyer discouraged me from advocating for maternity leave, feeling that it might stigmatize me and prevent me from getting a job,” she says.
He also didn’t explain very much. “He just said it falls under ‘disability leave’ and left it at that.”
Fortunately, Dr. Chester had a good experience with the group. “As things turned out, I did have a child later that year, and they treated me well – I actually got time off – and they didn’t make me take extra call. But it might have turned out very differently because I didn’t know what I was getting into. If I hadn’t worked for such a conscientious group, I might have been in a much tougher situation.”
Since then, Dr. Chester has spoken to female colleagues who received “more support from their legal advisors regarding maternity leave.” She suggests turning to female physicians for recommendations to a lawyer.
Although the central components of a contract (for example, noncompete covenants, malpractice “tail” coverage, bonus structure, vacation time, disability, and call) are relevant to physicians of all genders, the needs of women and men are often different.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, told this news organization that women physicians have “several issues that need special attention when negotiating their physician employment agreements.”
It starts with the interview
“Women have to be sensitive to the interviewer’s casual ‘let’s-get-to-know-each-other’ types of questions that may seem natural but really are unlawful to bring into an employment interview,” said Mr. Hursh.
He warned women to beware of questions such as “Are you married? Do you have kids? Are you planning to start a family?” These may be friendly chit-chat for male interviewees but there may be other agendas when asked to a prospective female employee.
Many of Mr. Hursh’s female clients have been asked this type of question, which “should be regarded as a ‘red flag.’ Yes, it may be an innocent, well-intentioned ice-breaker, but it’s actually unlawful to bring that up in an employment setting and, according to the Equal Opportunity Commission, can be seen as a form of discrimination.” He advises female physicians not to engage with the question and simply to refocus the discussion.
Know your worth and go for it
Medscape’s Physician Compensation surveys have consistently found discrepancies in earnings between male and female physicians, both in primary care and in specialties. In 2022, male primary care physicians earned 23% more than their female counterparts, whereas male specialists earned 31% more.
One reason may be that women tend to be more timid about negotiating for better compensation packages. Amanda Hill of Hill Health Law, a health care practice based in Austin, Tex., told this news organization that in her experience one of the most “overarching” features of female physicians is “that they either don’t know what they’re worth or they undersell themselves.”
In contrast to men, “many women are afraid of coming across as greedy or crass, or even demanding or bossy. But it’s a misperception that if you ask for more money, your future employer will hate you or won’t hire you,” said Ms. Hill.
Ms. Hill and Mr. Hursh encourage physicians to find out what they’re worth, which varies by region and specialty, by consulting benchmarks provided by companies such as Medical Group Management Association.
Jon Appino, MBA, principal and founder of Contract Diagnostics, a Kansas City–based consulting company that specializes in physician employment contract reviews, told this news organization that it’s important to look beyond the salary at other aspects of the position. For example, some figures “don’t take into account how much call a physician is taking. You may know what the average ob.gyn. is making, but an ob.gyn. may be working 3 days a week, while another one is working 6 days a week, one may be on call 15 times per month and another may be on call 15 times a quarter.” Other components of compensation include relative value unit (RVU) thresholds and bonuses.
Once you have that information, “don’t be intimidated, even if you’re sitting in front of several executives who are savvy about negotiations, and don’t worry about coming across as ‘high-maintenance’ or ‘all about money,’ ” Mr. Appino says. Proceed with confidence, knowing your worth and pursuing it.
Part-time vs. full-time
Mr. Appino has seen “more female than male physicians who want to work less than full-time. So it’s important to clarify whether that’s a possibility now or in the future and to understand the implications of working part-time.”
He explained that a full-time employee typically puts in a 40-hour work week, which translates into 1.0 Full-Time Equivalent (FTE), or one unit of work. “For example, if a person wants to work 0.8 FTEs – 4 days a week – is vacation time pro-rated? At what point is there a medical insurance fall-off or a higher monthly premium?”
In medical settings, FTEs may be tied to different metrics rather than the number of weekly hours – for example, for a hospitalist, it might be a certain number of shifts and might also vary by specialty. And it affects the call schedule too. “Call is hard to pro-rate. Many hospital bylaws mandate that call be divided equally, but if one surgeon is working 1.0 FTEs and another is working 0.8 FTEs, how does that call schedule get divided?”
Maternity leave: A tricky question
Many attorneys counsel against raising the question out of fear of scaring away potential employers.
“On the one hand, it is and should be absolutely reasonable to ask about the maternity leave policy or even negotiate for paid leave or additional leave, but it also highlights that you’re planning to have a baby and be out for months,” said Ms. Hill.
“And as much as we want people to be fair and reasonable, on the side of the employer, bias still very much exists, especially in a situation where revenue is based on group numbers. So suddenly, the employer thinks up some ‘nondiscriminatory’ reason why that person isn’t a great fit for the organization.”
Andrew Knoll, MD, JD, a former hospitalist who is now a partner with Cohen Compagni Beckman Appler & Knoll PLLC in Syracuse, N.Y., said that maternity leave is “rare” in an employment agreement, except sometimes in small private practice groups, because it often falls under the purview of “disability leave,” and “from a legal perspective, it’s no different than any other type of disability leave.”
The Family and Medical Leave Act (FMLA), which applies if a group is large enough, allows employees 12 weeks of unpaid leave, during which time their job is protected and their benefits maintained. And some states require employers to offer paid family leave.
“During this time, the woman can take time off – albeit without pay sometimes – to bond with the baby,” Dr. Knoll says. “Since there are statutory laws that protect the employee’s job, offering specific paid maternity leave is very unlikely.”
Ms. Hill advises carefully examining the employer’s comprehensive benefits plan to ascertain if paid maternity leave is included in the benefits. “But unless you’re currently pregnant and want to start off the relationship with true transparency – ‘I’m due in April and curious how we can handle that if you hire me now’ – I would keep the family planning questions to yourself before you get the job.”
Mr. Hursh, author of “The Final Hurdle: A Physician’s Guide to Negotiating a Fair Employment Agreement” (Charleston, S.C.: Advantage, 2012), has a different perspective. “I think all women, no matter how old they are, should ask about maternity leave, whether or not they’re planning a family,” he said.
“The employer may say, ‘We treat maternity leave like any other disability; our policy is such-and-such.’ If they cite an unacceptable policy, it’s a red flag about how they treat women, and should give a woman pause before accepting a position at that organization. Even if your rights are protected under the law and the organization’s policy is violating the law, no one wants to go to battle with HR or to have to go to court.”
Do you want partnership?
Not all female physicians entering a private practice want to advance to becoming partners. Many who are balancing family and work commitments “would prefer to just go into the office, perform their clinical responsibilities, go home, and be done” without the extra headaches, tasks, and time involved with business leadership, says Mr. Appino.
Some private practices have different contracts for those on partnership vs. nonpartnership tracks, so “you should ascertain this information and make sure it’s not automatically assumed that you would like to be on a partnership track,” says Mr. Appino.
On the other hand, you may want to become a partner. “I always suggest asking about the possibility of obtaining a leadership position in an organization or becoming an owner in a private practice,” says Mr. Hursh. “You may be told, ‘We’ve never had a woman in leadership before.’ This might be innocent if you’re the first woman hired, but it might be a red flag as to how women are regarded.” Either way, it’s important to have the information and know what your options are.
The impact of shift schedule
Mr. Hursh advises drilling down into the specifics of the schedule if you’re considering becoming a hospitalist. “Does a ‘week-on/week-off’ shift schedule assume you’ll be taking your vacation time or completing your CME requirements during the week off? This is important for all physicians, but especially for women who might want to use their weeks off to attend to children and family.”
Moreover, “there should be limits on shifts. You shouldn’t have a full day shift followed by a night shift. And there should be a limit on the number of shifts you work without time off. Twelve would be a brutal schedule. Seven is a reasonable amount. Make sure this is in writing and that the contract protects you. Don’t allow the employer to say, ‘We expect you to do the work we assign’ and leave it vague.”
Often, hospitalists will receive an annual salary under the assumption that a certain minimum number of shifts will be completed, but there is no maximum. “It’s important that the salary includes the minimum number of shifts, but that a compensation structure is created so that additional shifts receive additional compensation,” Mr. Hursh said.
Removing the ‘golden handcuffs’
Ms. Hill observes that there are some “really terrible contracts out there, which physicians – especially women – often feel pressured into signing.” They’re told, “This is our standard contract. You won’t find anything better.” Or, “Don’t worry about the small print and legalese.” The physician “gets scared or is artificially reassured, signs an overwhelmingly unfair contract, and then feels stuck.”
Being stuck in a bad contract “is debilitating and adds to burnout, feeling of depression, and the sense that there is no recourse and nowhere to go, especially if your family depends on you,” Ms. Hill said.
“More women than men feel hamstrung or are resigned to being harassed – which is not uncommon in the medical setting, especially in surgical specialties – or just accept poor treatment,” Ms. Hill added. Yes, you can “fight the system and go to HR, but fighting the system is very hard.”
She urges women “not to feel stuck or imprisoned by the ‘golden handcuffs’ but to consult a good lawyer, even if you have to break the contract.” Be aware of the reasons for your unhappiness and bring them to your lawyer – perhaps the system has engaged in fraud, perhaps there has been sexual or racial harassment, perhaps the organization hasn’t followed its own compliance policies.
Dr. Chester consulted Ms. Hill before signing the contract for her current position. “I wanted someone who could give me personalized advice, not only generic advice, and who understood my needs as a woman.”
Ms. Hill helped her to understand “what was and wasn’t fair and reasonable, what changes I could request based on my goals and whether they were realistic, and how to pick my battles. For example, I tried to negotiate tail coverage up front in my previous job but was unsuccessful. The new employer paid tail for me, both from my previous employment and for my current employment.”
Dr. Chester advises other female physicians “never to sign anything without having a lawyer review it and to make sure that the lawyer is sensitive to their specific needs.”
It can be hard to be a female physician. Having the right knowledge and ammunition and knowing how to negotiate well paves the way for success and thriving in an often male-dominated market.
A version of this article first appeared on Medscape.com.
Rebecca Chester, MD, an Arizona-based interventional cardiologist, recently left her position in a private practice and started employment at a hospital system.
“When I was negotiating my previous contract with the private practice, I found that navigating contracts from the standpoint of a woman still in childbearing years was a little disappointing and challenging,” Dr. Chester told this news organization.
“I wanted to have more children and hired a lawyer recommended by a male colleague to help me not only understand the contract but also negotiate time off and maternity leave, but the lawyer discouraged me from advocating for maternity leave, feeling that it might stigmatize me and prevent me from getting a job,” she says.
He also didn’t explain very much. “He just said it falls under ‘disability leave’ and left it at that.”
Fortunately, Dr. Chester had a good experience with the group. “As things turned out, I did have a child later that year, and they treated me well – I actually got time off – and they didn’t make me take extra call. But it might have turned out very differently because I didn’t know what I was getting into. If I hadn’t worked for such a conscientious group, I might have been in a much tougher situation.”
Since then, Dr. Chester has spoken to female colleagues who received “more support from their legal advisors regarding maternity leave.” She suggests turning to female physicians for recommendations to a lawyer.
Although the central components of a contract (for example, noncompete covenants, malpractice “tail” coverage, bonus structure, vacation time, disability, and call) are relevant to physicians of all genders, the needs of women and men are often different.
Dennis Hursh, managing partner of Physician Agreements Health Law, a Pennsylvania-based law firm that represents physicians, told this news organization that women physicians have “several issues that need special attention when negotiating their physician employment agreements.”
It starts with the interview
“Women have to be sensitive to the interviewer’s casual ‘let’s-get-to-know-each-other’ types of questions that may seem natural but really are unlawful to bring into an employment interview,” said Mr. Hursh.
He warned women to beware of questions such as “Are you married? Do you have kids? Are you planning to start a family?” These may be friendly chit-chat for male interviewees but there may be other agendas when asked to a prospective female employee.
Many of Mr. Hursh’s female clients have been asked this type of question, which “should be regarded as a ‘red flag.’ Yes, it may be an innocent, well-intentioned ice-breaker, but it’s actually unlawful to bring that up in an employment setting and, according to the Equal Opportunity Commission, can be seen as a form of discrimination.” He advises female physicians not to engage with the question and simply to refocus the discussion.
Know your worth and go for it
Medscape’s Physician Compensation surveys have consistently found discrepancies in earnings between male and female physicians, both in primary care and in specialties. In 2022, male primary care physicians earned 23% more than their female counterparts, whereas male specialists earned 31% more.
One reason may be that women tend to be more timid about negotiating for better compensation packages. Amanda Hill of Hill Health Law, a health care practice based in Austin, Tex., told this news organization that in her experience one of the most “overarching” features of female physicians is “that they either don’t know what they’re worth or they undersell themselves.”
In contrast to men, “many women are afraid of coming across as greedy or crass, or even demanding or bossy. But it’s a misperception that if you ask for more money, your future employer will hate you or won’t hire you,” said Ms. Hill.
Ms. Hill and Mr. Hursh encourage physicians to find out what they’re worth, which varies by region and specialty, by consulting benchmarks provided by companies such as Medical Group Management Association.
Jon Appino, MBA, principal and founder of Contract Diagnostics, a Kansas City–based consulting company that specializes in physician employment contract reviews, told this news organization that it’s important to look beyond the salary at other aspects of the position. For example, some figures “don’t take into account how much call a physician is taking. You may know what the average ob.gyn. is making, but an ob.gyn. may be working 3 days a week, while another one is working 6 days a week, one may be on call 15 times per month and another may be on call 15 times a quarter.” Other components of compensation include relative value unit (RVU) thresholds and bonuses.
Once you have that information, “don’t be intimidated, even if you’re sitting in front of several executives who are savvy about negotiations, and don’t worry about coming across as ‘high-maintenance’ or ‘all about money,’ ” Mr. Appino says. Proceed with confidence, knowing your worth and pursuing it.
Part-time vs. full-time
Mr. Appino has seen “more female than male physicians who want to work less than full-time. So it’s important to clarify whether that’s a possibility now or in the future and to understand the implications of working part-time.”
He explained that a full-time employee typically puts in a 40-hour work week, which translates into 1.0 Full-Time Equivalent (FTE), or one unit of work. “For example, if a person wants to work 0.8 FTEs – 4 days a week – is vacation time pro-rated? At what point is there a medical insurance fall-off or a higher monthly premium?”
In medical settings, FTEs may be tied to different metrics rather than the number of weekly hours – for example, for a hospitalist, it might be a certain number of shifts and might also vary by specialty. And it affects the call schedule too. “Call is hard to pro-rate. Many hospital bylaws mandate that call be divided equally, but if one surgeon is working 1.0 FTEs and another is working 0.8 FTEs, how does that call schedule get divided?”
Maternity leave: A tricky question
Many attorneys counsel against raising the question out of fear of scaring away potential employers.
“On the one hand, it is and should be absolutely reasonable to ask about the maternity leave policy or even negotiate for paid leave or additional leave, but it also highlights that you’re planning to have a baby and be out for months,” said Ms. Hill.
“And as much as we want people to be fair and reasonable, on the side of the employer, bias still very much exists, especially in a situation where revenue is based on group numbers. So suddenly, the employer thinks up some ‘nondiscriminatory’ reason why that person isn’t a great fit for the organization.”
Andrew Knoll, MD, JD, a former hospitalist who is now a partner with Cohen Compagni Beckman Appler & Knoll PLLC in Syracuse, N.Y., said that maternity leave is “rare” in an employment agreement, except sometimes in small private practice groups, because it often falls under the purview of “disability leave,” and “from a legal perspective, it’s no different than any other type of disability leave.”
The Family and Medical Leave Act (FMLA), which applies if a group is large enough, allows employees 12 weeks of unpaid leave, during which time their job is protected and their benefits maintained. And some states require employers to offer paid family leave.
“During this time, the woman can take time off – albeit without pay sometimes – to bond with the baby,” Dr. Knoll says. “Since there are statutory laws that protect the employee’s job, offering specific paid maternity leave is very unlikely.”
Ms. Hill advises carefully examining the employer’s comprehensive benefits plan to ascertain if paid maternity leave is included in the benefits. “But unless you’re currently pregnant and want to start off the relationship with true transparency – ‘I’m due in April and curious how we can handle that if you hire me now’ – I would keep the family planning questions to yourself before you get the job.”
Mr. Hursh, author of “The Final Hurdle: A Physician’s Guide to Negotiating a Fair Employment Agreement” (Charleston, S.C.: Advantage, 2012), has a different perspective. “I think all women, no matter how old they are, should ask about maternity leave, whether or not they’re planning a family,” he said.
“The employer may say, ‘We treat maternity leave like any other disability; our policy is such-and-such.’ If they cite an unacceptable policy, it’s a red flag about how they treat women, and should give a woman pause before accepting a position at that organization. Even if your rights are protected under the law and the organization’s policy is violating the law, no one wants to go to battle with HR or to have to go to court.”
Do you want partnership?
Not all female physicians entering a private practice want to advance to becoming partners. Many who are balancing family and work commitments “would prefer to just go into the office, perform their clinical responsibilities, go home, and be done” without the extra headaches, tasks, and time involved with business leadership, says Mr. Appino.
Some private practices have different contracts for those on partnership vs. nonpartnership tracks, so “you should ascertain this information and make sure it’s not automatically assumed that you would like to be on a partnership track,” says Mr. Appino.
On the other hand, you may want to become a partner. “I always suggest asking about the possibility of obtaining a leadership position in an organization or becoming an owner in a private practice,” says Mr. Hursh. “You may be told, ‘We’ve never had a woman in leadership before.’ This might be innocent if you’re the first woman hired, but it might be a red flag as to how women are regarded.” Either way, it’s important to have the information and know what your options are.
The impact of shift schedule
Mr. Hursh advises drilling down into the specifics of the schedule if you’re considering becoming a hospitalist. “Does a ‘week-on/week-off’ shift schedule assume you’ll be taking your vacation time or completing your CME requirements during the week off? This is important for all physicians, but especially for women who might want to use their weeks off to attend to children and family.”
Moreover, “there should be limits on shifts. You shouldn’t have a full day shift followed by a night shift. And there should be a limit on the number of shifts you work without time off. Twelve would be a brutal schedule. Seven is a reasonable amount. Make sure this is in writing and that the contract protects you. Don’t allow the employer to say, ‘We expect you to do the work we assign’ and leave it vague.”
Often, hospitalists will receive an annual salary under the assumption that a certain minimum number of shifts will be completed, but there is no maximum. “It’s important that the salary includes the minimum number of shifts, but that a compensation structure is created so that additional shifts receive additional compensation,” Mr. Hursh said.
Removing the ‘golden handcuffs’
Ms. Hill observes that there are some “really terrible contracts out there, which physicians – especially women – often feel pressured into signing.” They’re told, “This is our standard contract. You won’t find anything better.” Or, “Don’t worry about the small print and legalese.” The physician “gets scared or is artificially reassured, signs an overwhelmingly unfair contract, and then feels stuck.”
Being stuck in a bad contract “is debilitating and adds to burnout, feeling of depression, and the sense that there is no recourse and nowhere to go, especially if your family depends on you,” Ms. Hill said.
“More women than men feel hamstrung or are resigned to being harassed – which is not uncommon in the medical setting, especially in surgical specialties – or just accept poor treatment,” Ms. Hill added. Yes, you can “fight the system and go to HR, but fighting the system is very hard.”
She urges women “not to feel stuck or imprisoned by the ‘golden handcuffs’ but to consult a good lawyer, even if you have to break the contract.” Be aware of the reasons for your unhappiness and bring them to your lawyer – perhaps the system has engaged in fraud, perhaps there has been sexual or racial harassment, perhaps the organization hasn’t followed its own compliance policies.
Dr. Chester consulted Ms. Hill before signing the contract for her current position. “I wanted someone who could give me personalized advice, not only generic advice, and who understood my needs as a woman.”
Ms. Hill helped her to understand “what was and wasn’t fair and reasonable, what changes I could request based on my goals and whether they were realistic, and how to pick my battles. For example, I tried to negotiate tail coverage up front in my previous job but was unsuccessful. The new employer paid tail for me, both from my previous employment and for my current employment.”
Dr. Chester advises other female physicians “never to sign anything without having a lawyer review it and to make sure that the lawyer is sensitive to their specific needs.”
It can be hard to be a female physician. Having the right knowledge and ammunition and knowing how to negotiate well paves the way for success and thriving in an often male-dominated market.
A version of this article first appeared on Medscape.com.
Buzzy Lancet long COVID paper under investigation for ‘data errors’
An editorial that accompanied the paper when it was published in January of last year described it as “the first large cohort study with 6-months’ follow-up” of people hospitalized with COVID-19. The article has received plenty of attention since then.
Titled “6-month consequences of COVID-19 in patients discharged from hospital: a cohort study,” the paper has been cited nearly 1,600 times, according to Clarivate’s Web of Science. Altmetric finds references to it in multiple documents from the World Health Organization.
According to the expression of concern, dated November 24, a reader found inconsistencies between the data in the article and a later paper describing the same cohort of patients after a year of follow-up. That discovery sparked an investigation that is still ongoing:
- On Jan 8, 2021, The Lancet published an Article, 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, by Chaolin Huang and colleagues. 1 On Aug 28, 2021, The Lancet published an Article, 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study, by Lixue Huang and colleagues. 2 We received an inquiry from a researcher on data inconsistencies between these two Articles, and we sought an explanation from the corresponding author of the two papers. On Nov 7, 2022, Lancet editors were informed that inconsistencies between the 6-month and the 1-year data were due to “some variables in the dataset used for the 6-month paper were mistakenly disrupted in order”. In view of the extent of these data errors, we now issue an Expression of Concern about the 6-month paper 1 while we investigate further, including further statistical and clinical review of the corrected data. We will update this notice as soon as we have further information.
The corresponding author of both papers, Bin Cao of China’s National Center for Respiratory Medicine and the China-Japan Friendship Hospital in Beijing, has not responded to our request for comment.
A profile of Cao published in Lancet Infectious Diseases last March described him as “a leading researcher in pneumonia and influenza” who “has been instrumental in increasing knowledge about COVID-19.” In addition to the follow-up study of hospitalized COVID patients:
- Cao’s seminal papers during the COVID-19 pandemic include the first report of the clinical characteristics of COVID-19 patients in Wuhan, the description of the risk factors for mortality for adult inpatients, and the results of trials testing the use of antiviral drugs, including lopinavir-ritonavir, to treat COVID-19 in China.
We reached out to The Lancet’s press office and Richard Horton, the journal’s editor-in-chief, and received this statement:
- The Lancet Group treats all communications between editors and authors or readers as confidential. Investigations are continuing, and the Expression of Concern will be updated as soon as we have further information to share. More information about our policies is available here:
This year, The Lancet overtook the New England Journal of Medicine as the medical journal with the highest impact factor, in large part due to the papers it published about COVID-19.
We’ve counted retractions for three of those papers, most notably a paper about the use of the drug hydroxychloroquine that claimed to use medical data from a company called Surgisphere. As Retraction Watch readers may remember, the article was retracted after sleuths questioned if the data were real, and the company would not produce it for review.
This article first appeared on Retraction Watch.
An editorial that accompanied the paper when it was published in January of last year described it as “the first large cohort study with 6-months’ follow-up” of people hospitalized with COVID-19. The article has received plenty of attention since then.
Titled “6-month consequences of COVID-19 in patients discharged from hospital: a cohort study,” the paper has been cited nearly 1,600 times, according to Clarivate’s Web of Science. Altmetric finds references to it in multiple documents from the World Health Organization.
According to the expression of concern, dated November 24, a reader found inconsistencies between the data in the article and a later paper describing the same cohort of patients after a year of follow-up. That discovery sparked an investigation that is still ongoing:
- On Jan 8, 2021, The Lancet published an Article, 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, by Chaolin Huang and colleagues. 1 On Aug 28, 2021, The Lancet published an Article, 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study, by Lixue Huang and colleagues. 2 We received an inquiry from a researcher on data inconsistencies between these two Articles, and we sought an explanation from the corresponding author of the two papers. On Nov 7, 2022, Lancet editors were informed that inconsistencies between the 6-month and the 1-year data were due to “some variables in the dataset used for the 6-month paper were mistakenly disrupted in order”. In view of the extent of these data errors, we now issue an Expression of Concern about the 6-month paper 1 while we investigate further, including further statistical and clinical review of the corrected data. We will update this notice as soon as we have further information.
The corresponding author of both papers, Bin Cao of China’s National Center for Respiratory Medicine and the China-Japan Friendship Hospital in Beijing, has not responded to our request for comment.
A profile of Cao published in Lancet Infectious Diseases last March described him as “a leading researcher in pneumonia and influenza” who “has been instrumental in increasing knowledge about COVID-19.” In addition to the follow-up study of hospitalized COVID patients:
- Cao’s seminal papers during the COVID-19 pandemic include the first report of the clinical characteristics of COVID-19 patients in Wuhan, the description of the risk factors for mortality for adult inpatients, and the results of trials testing the use of antiviral drugs, including lopinavir-ritonavir, to treat COVID-19 in China.
We reached out to The Lancet’s press office and Richard Horton, the journal’s editor-in-chief, and received this statement:
- The Lancet Group treats all communications between editors and authors or readers as confidential. Investigations are continuing, and the Expression of Concern will be updated as soon as we have further information to share. More information about our policies is available here:
This year, The Lancet overtook the New England Journal of Medicine as the medical journal with the highest impact factor, in large part due to the papers it published about COVID-19.
We’ve counted retractions for three of those papers, most notably a paper about the use of the drug hydroxychloroquine that claimed to use medical data from a company called Surgisphere. As Retraction Watch readers may remember, the article was retracted after sleuths questioned if the data were real, and the company would not produce it for review.
This article first appeared on Retraction Watch.
An editorial that accompanied the paper when it was published in January of last year described it as “the first large cohort study with 6-months’ follow-up” of people hospitalized with COVID-19. The article has received plenty of attention since then.
Titled “6-month consequences of COVID-19 in patients discharged from hospital: a cohort study,” the paper has been cited nearly 1,600 times, according to Clarivate’s Web of Science. Altmetric finds references to it in multiple documents from the World Health Organization.
According to the expression of concern, dated November 24, a reader found inconsistencies between the data in the article and a later paper describing the same cohort of patients after a year of follow-up. That discovery sparked an investigation that is still ongoing:
- On Jan 8, 2021, The Lancet published an Article, 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study, by Chaolin Huang and colleagues. 1 On Aug 28, 2021, The Lancet published an Article, 1-year outcomes in hospital survivors with COVID-19: a longitudinal cohort study, by Lixue Huang and colleagues. 2 We received an inquiry from a researcher on data inconsistencies between these two Articles, and we sought an explanation from the corresponding author of the two papers. On Nov 7, 2022, Lancet editors were informed that inconsistencies between the 6-month and the 1-year data were due to “some variables in the dataset used for the 6-month paper were mistakenly disrupted in order”. In view of the extent of these data errors, we now issue an Expression of Concern about the 6-month paper 1 while we investigate further, including further statistical and clinical review of the corrected data. We will update this notice as soon as we have further information.
The corresponding author of both papers, Bin Cao of China’s National Center for Respiratory Medicine and the China-Japan Friendship Hospital in Beijing, has not responded to our request for comment.
A profile of Cao published in Lancet Infectious Diseases last March described him as “a leading researcher in pneumonia and influenza” who “has been instrumental in increasing knowledge about COVID-19.” In addition to the follow-up study of hospitalized COVID patients:
- Cao’s seminal papers during the COVID-19 pandemic include the first report of the clinical characteristics of COVID-19 patients in Wuhan, the description of the risk factors for mortality for adult inpatients, and the results of trials testing the use of antiviral drugs, including lopinavir-ritonavir, to treat COVID-19 in China.
We reached out to The Lancet’s press office and Richard Horton, the journal’s editor-in-chief, and received this statement:
- The Lancet Group treats all communications between editors and authors or readers as confidential. Investigations are continuing, and the Expression of Concern will be updated as soon as we have further information to share. More information about our policies is available here:
This year, The Lancet overtook the New England Journal of Medicine as the medical journal with the highest impact factor, in large part due to the papers it published about COVID-19.
We’ve counted retractions for three of those papers, most notably a paper about the use of the drug hydroxychloroquine that claimed to use medical data from a company called Surgisphere. As Retraction Watch readers may remember, the article was retracted after sleuths questioned if the data were real, and the company would not produce it for review.
This article first appeared on Retraction Watch.