User login
B6 a new approach for depression, anxiety?
Investigators compared supplementation with a 1-month course of vitamin B6 or B12 to supplementation with placebo in almost 500 adults. Results showed that vitamin B6 supplementation was associated with reductions in self-reported anxiety and a trend toward decreased depressive symptoms.
In addition, the vitamin B6 group showed increased levels of gamma-aminobutyric acid (GABA), as indicated by results on a visual test that was administered at the end of the trial. The test results demonstrated subtle changes in participants’ visual performance. The researchers considered this to be consistent with controlled levels of GABA-related brain activity.
However, “before practicing clinicians would recommend taking high doses of vitamin B6, a full-scale clinical trial would have to be carried out to verify the findings, assess any side effects, and find out which types of patients do or don’t benefit,” study investigator David Field, PhD, associate professor, School of Psychological and Clinical Language Sciences, University of Reading (England), told this news organization.
“My relatively small study can only be considered as an initial proof of concept,” Dr. Field said.
The findings were published online in the Journal of Human Psychopharmacology: Clinical and Experimental.
Eat Marmite?
“Recent research has connected mood disorders and some other neuropsychiatric conditions with disturbance in this balance, often in the direction of raised levels of brain activity,” Dr. Field noted.
Vitamin B6 is a coenzyme in the synthesis of GABA, an inhibitory neurotransmitter, from glutamate. Some previous research has suggested that vitamins B6 and B12 have a role in improving mood-related outcomes.
Dr. Field had reviewed a 2017 study of the effects on visual processing of eating Marmite, a type of food spread rich in vitamin B, every day for a few weeks.
“Remarkably, the results of that study suggested that eating Marmite had increased the level of the inhibitory neurotransmitter GABA in the visual part of the brain, damping down the level of neural activity slightly,” he said.
However, Marmite contains other B vitamins and other ingredients that might potentially account for this result, “plus, a lot of people don’t like the taste of Marmite,” Dr. Field noted.
Therefore, he wanted to “find out which individual ingredients were driving the effect, and B6 and B12 were the most plausible candidates.”
He decided to test these vitamins individually and to compare them to placebo. “I added the measures of anxiety and depression that were not in the Marmite study because I reasoned that if GABA levels were altered, this could improve those disorders, because we know that decreased levels of GABA in the brain occur in both of those conditions,” Dr. Field added.
Over the course of 5 years, investigators recruited 478 participants aged 18-58 years (mean age, 23 years; 381 women). Of these, 265 reported having anxiety, and 146 reported having depression.
The study participants were randomly assigned to receive either vitamin B6 (100 mg pyroxidine hydrochloride), vitamin B12 (1,000 mg methylcobalmin), or placebo tablets once daily for a month.
They also completed the Screen for Adult Anxiety Related Disorders (SCAARED) and the Mood and Feelings Questionnaire (MFQ) long version at baseline and following supplementation (“post test”), and they underwent three sensory tests that acted as assays of inhibitory function at post test.
In addition, 307 participants completed the Visual Contrast Sensitivity and Surround Suppression, which “measures the minimum percentage contrast between the lighter and darker regions of a striped pattern that can be detected (called the contrast threshold),” the investigators note.
The contrast threshold was measured with and without a suppressive surround mask that increases the threshold – an effect mediated by GABAergic connections in the visual cortex.
Participants (n = 172) also completed the Binocular Rivalry test and the Tactile Test Battery (n = 180). Both tests are designed to measure responses requiring GABAergic inhibitory activity.
‘Subtle changes’
ANOVA analyses revealed a “highly significant” reduction in anxiety at post test (F[1,173] = 10.03; P = .002; np 2 = .055), driven primarily by reduced anxiety in the B6 group (t[88] = 3.51; P < .001; d = .37). The placebo group also showed some reduction in anxiety, but it was not deemed significant, and the overall interaction itself did not reach significance.
A comparison of the B12 group with the group that received placebo revealed a significant reduction in anxiety at post test (F[1,175] = 4.08; P = .045; np 2 = .023), similarly driven by reduced anxiety in the B12 group (t[89] = 1.84; P = .069; d = .19) – but the interaction was not significant.
Among the B6 group, there was a highly significant reduction in scores on the generalized anxiety disorder and social anxiety subscales of the SCAARED, and there was a trend toward reductions on the other subscales. Among the B12 group, there was a significant reduction only on scores on the separation anxiety subscale. No significant changes were found in the placebo group.
The ANOVA test analysis of the B6 and placebo group data showed “no uniform direction of change” in depression at post test. The researchers found a “tendency” for depression scores to decrease between baseline and post test in the B6 group but to increase in the placebo group – an interaction that “approached” significance (F[1,96] = 3.08; P = .083; np 2 = .031), they report.
The ANOVA analysis of the B12 and placebo group data revealed no significant or trending effects, and the t-test comparing baseline and post-test scores in the B12 group was similarly nonsignificant.
B6 supplementation did change visual contrast thresholds, but only when a suppressive surround was present. There were “no clear effects” of B6 supplementation on other outcome measures, including binocular rivalry reversal rate and the tactile test battery, the investigators note.
“We found that supplementation with B6 produced subtle changes in tests of visual processing in a way that suggested an increase in the level of the inhibitory neurotransmitter GABA,” Dr. Field reported.
Vitamin B6 is a “cofactor for a metabolic pathway in the brain that converts the excitatory neurotransmitter glutamate into the inhibitory/calming GABA,” he said.
“By increasing the quantity of the cofactor, we slightly speed up the rate of this metabolic process, and so you end up with a bit more of the GABA neurotransmitter and a bit less glutamate. The net effect of this is to slightly reduce the amount of activity in the brain,” Dr. Field added.
Most common nutrient deficiency
Carol Johnston, PhD, professor and associate dean for faculty success, College of Health Solutions, Arizona State University, Phoenix, said vitamin B6 is “the most common nutrient deficiency in the United States;” 16% of men and 32% of women are reportedly B6 deficient.
“Young women on birth control are at higher risk for B6 deficiency due to effects of oral contraceptives on B6 metabolism,” whereas vitamin B12 deficiency is more common in older adults, said Dr. Johnston, who was not involved with the study.
The current study’s population mainly consisted of young women, and the interpretation of the data is “limited” because the researchers did not measure blood status for B6 and B12, Dr. Johnston noted. It is possible the sample was low in B6 and that the supplements “improved cognitive measures.”
Because the population was young – no one was older than 60 years – B12 status was likely “adequate in the sample, and supplementation did not have an impact,” she said.
Overall, Dr. Johnston cautioned that it is important to “alert clinicians and the general public about the concerns of overdosing B6.” For example, supplementation at high amounts can cause potentially irreversible sensory neuropathy, she noted.
“The safe upper limit defined by experts is 100 mg per day – the dosage used in this trial. Daily supplementation should not exceed this level,” Dr. Johnston said.
The vitamin tablets used in the study were supplied by Innopure. The investigators and Dr. Johnston have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared supplementation with a 1-month course of vitamin B6 or B12 to supplementation with placebo in almost 500 adults. Results showed that vitamin B6 supplementation was associated with reductions in self-reported anxiety and a trend toward decreased depressive symptoms.
In addition, the vitamin B6 group showed increased levels of gamma-aminobutyric acid (GABA), as indicated by results on a visual test that was administered at the end of the trial. The test results demonstrated subtle changes in participants’ visual performance. The researchers considered this to be consistent with controlled levels of GABA-related brain activity.
However, “before practicing clinicians would recommend taking high doses of vitamin B6, a full-scale clinical trial would have to be carried out to verify the findings, assess any side effects, and find out which types of patients do or don’t benefit,” study investigator David Field, PhD, associate professor, School of Psychological and Clinical Language Sciences, University of Reading (England), told this news organization.
“My relatively small study can only be considered as an initial proof of concept,” Dr. Field said.
The findings were published online in the Journal of Human Psychopharmacology: Clinical and Experimental.
Eat Marmite?
“Recent research has connected mood disorders and some other neuropsychiatric conditions with disturbance in this balance, often in the direction of raised levels of brain activity,” Dr. Field noted.
Vitamin B6 is a coenzyme in the synthesis of GABA, an inhibitory neurotransmitter, from glutamate. Some previous research has suggested that vitamins B6 and B12 have a role in improving mood-related outcomes.
Dr. Field had reviewed a 2017 study of the effects on visual processing of eating Marmite, a type of food spread rich in vitamin B, every day for a few weeks.
“Remarkably, the results of that study suggested that eating Marmite had increased the level of the inhibitory neurotransmitter GABA in the visual part of the brain, damping down the level of neural activity slightly,” he said.
However, Marmite contains other B vitamins and other ingredients that might potentially account for this result, “plus, a lot of people don’t like the taste of Marmite,” Dr. Field noted.
Therefore, he wanted to “find out which individual ingredients were driving the effect, and B6 and B12 were the most plausible candidates.”
He decided to test these vitamins individually and to compare them to placebo. “I added the measures of anxiety and depression that were not in the Marmite study because I reasoned that if GABA levels were altered, this could improve those disorders, because we know that decreased levels of GABA in the brain occur in both of those conditions,” Dr. Field added.
Over the course of 5 years, investigators recruited 478 participants aged 18-58 years (mean age, 23 years; 381 women). Of these, 265 reported having anxiety, and 146 reported having depression.
The study participants were randomly assigned to receive either vitamin B6 (100 mg pyroxidine hydrochloride), vitamin B12 (1,000 mg methylcobalmin), or placebo tablets once daily for a month.
They also completed the Screen for Adult Anxiety Related Disorders (SCAARED) and the Mood and Feelings Questionnaire (MFQ) long version at baseline and following supplementation (“post test”), and they underwent three sensory tests that acted as assays of inhibitory function at post test.
In addition, 307 participants completed the Visual Contrast Sensitivity and Surround Suppression, which “measures the minimum percentage contrast between the lighter and darker regions of a striped pattern that can be detected (called the contrast threshold),” the investigators note.
The contrast threshold was measured with and without a suppressive surround mask that increases the threshold – an effect mediated by GABAergic connections in the visual cortex.
Participants (n = 172) also completed the Binocular Rivalry test and the Tactile Test Battery (n = 180). Both tests are designed to measure responses requiring GABAergic inhibitory activity.
‘Subtle changes’
ANOVA analyses revealed a “highly significant” reduction in anxiety at post test (F[1,173] = 10.03; P = .002; np 2 = .055), driven primarily by reduced anxiety in the B6 group (t[88] = 3.51; P < .001; d = .37). The placebo group also showed some reduction in anxiety, but it was not deemed significant, and the overall interaction itself did not reach significance.
A comparison of the B12 group with the group that received placebo revealed a significant reduction in anxiety at post test (F[1,175] = 4.08; P = .045; np 2 = .023), similarly driven by reduced anxiety in the B12 group (t[89] = 1.84; P = .069; d = .19) – but the interaction was not significant.
Among the B6 group, there was a highly significant reduction in scores on the generalized anxiety disorder and social anxiety subscales of the SCAARED, and there was a trend toward reductions on the other subscales. Among the B12 group, there was a significant reduction only on scores on the separation anxiety subscale. No significant changes were found in the placebo group.
The ANOVA test analysis of the B6 and placebo group data showed “no uniform direction of change” in depression at post test. The researchers found a “tendency” for depression scores to decrease between baseline and post test in the B6 group but to increase in the placebo group – an interaction that “approached” significance (F[1,96] = 3.08; P = .083; np 2 = .031), they report.
The ANOVA analysis of the B12 and placebo group data revealed no significant or trending effects, and the t-test comparing baseline and post-test scores in the B12 group was similarly nonsignificant.
B6 supplementation did change visual contrast thresholds, but only when a suppressive surround was present. There were “no clear effects” of B6 supplementation on other outcome measures, including binocular rivalry reversal rate and the tactile test battery, the investigators note.
“We found that supplementation with B6 produced subtle changes in tests of visual processing in a way that suggested an increase in the level of the inhibitory neurotransmitter GABA,” Dr. Field reported.
Vitamin B6 is a “cofactor for a metabolic pathway in the brain that converts the excitatory neurotransmitter glutamate into the inhibitory/calming GABA,” he said.
“By increasing the quantity of the cofactor, we slightly speed up the rate of this metabolic process, and so you end up with a bit more of the GABA neurotransmitter and a bit less glutamate. The net effect of this is to slightly reduce the amount of activity in the brain,” Dr. Field added.
Most common nutrient deficiency
Carol Johnston, PhD, professor and associate dean for faculty success, College of Health Solutions, Arizona State University, Phoenix, said vitamin B6 is “the most common nutrient deficiency in the United States;” 16% of men and 32% of women are reportedly B6 deficient.
“Young women on birth control are at higher risk for B6 deficiency due to effects of oral contraceptives on B6 metabolism,” whereas vitamin B12 deficiency is more common in older adults, said Dr. Johnston, who was not involved with the study.
The current study’s population mainly consisted of young women, and the interpretation of the data is “limited” because the researchers did not measure blood status for B6 and B12, Dr. Johnston noted. It is possible the sample was low in B6 and that the supplements “improved cognitive measures.”
Because the population was young – no one was older than 60 years – B12 status was likely “adequate in the sample, and supplementation did not have an impact,” she said.
Overall, Dr. Johnston cautioned that it is important to “alert clinicians and the general public about the concerns of overdosing B6.” For example, supplementation at high amounts can cause potentially irreversible sensory neuropathy, she noted.
“The safe upper limit defined by experts is 100 mg per day – the dosage used in this trial. Daily supplementation should not exceed this level,” Dr. Johnston said.
The vitamin tablets used in the study were supplied by Innopure. The investigators and Dr. Johnston have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators compared supplementation with a 1-month course of vitamin B6 or B12 to supplementation with placebo in almost 500 adults. Results showed that vitamin B6 supplementation was associated with reductions in self-reported anxiety and a trend toward decreased depressive symptoms.
In addition, the vitamin B6 group showed increased levels of gamma-aminobutyric acid (GABA), as indicated by results on a visual test that was administered at the end of the trial. The test results demonstrated subtle changes in participants’ visual performance. The researchers considered this to be consistent with controlled levels of GABA-related brain activity.
However, “before practicing clinicians would recommend taking high doses of vitamin B6, a full-scale clinical trial would have to be carried out to verify the findings, assess any side effects, and find out which types of patients do or don’t benefit,” study investigator David Field, PhD, associate professor, School of Psychological and Clinical Language Sciences, University of Reading (England), told this news organization.
“My relatively small study can only be considered as an initial proof of concept,” Dr. Field said.
The findings were published online in the Journal of Human Psychopharmacology: Clinical and Experimental.
Eat Marmite?
“Recent research has connected mood disorders and some other neuropsychiatric conditions with disturbance in this balance, often in the direction of raised levels of brain activity,” Dr. Field noted.
Vitamin B6 is a coenzyme in the synthesis of GABA, an inhibitory neurotransmitter, from glutamate. Some previous research has suggested that vitamins B6 and B12 have a role in improving mood-related outcomes.
Dr. Field had reviewed a 2017 study of the effects on visual processing of eating Marmite, a type of food spread rich in vitamin B, every day for a few weeks.
“Remarkably, the results of that study suggested that eating Marmite had increased the level of the inhibitory neurotransmitter GABA in the visual part of the brain, damping down the level of neural activity slightly,” he said.
However, Marmite contains other B vitamins and other ingredients that might potentially account for this result, “plus, a lot of people don’t like the taste of Marmite,” Dr. Field noted.
Therefore, he wanted to “find out which individual ingredients were driving the effect, and B6 and B12 were the most plausible candidates.”
He decided to test these vitamins individually and to compare them to placebo. “I added the measures of anxiety and depression that were not in the Marmite study because I reasoned that if GABA levels were altered, this could improve those disorders, because we know that decreased levels of GABA in the brain occur in both of those conditions,” Dr. Field added.
Over the course of 5 years, investigators recruited 478 participants aged 18-58 years (mean age, 23 years; 381 women). Of these, 265 reported having anxiety, and 146 reported having depression.
The study participants were randomly assigned to receive either vitamin B6 (100 mg pyroxidine hydrochloride), vitamin B12 (1,000 mg methylcobalmin), or placebo tablets once daily for a month.
They also completed the Screen for Adult Anxiety Related Disorders (SCAARED) and the Mood and Feelings Questionnaire (MFQ) long version at baseline and following supplementation (“post test”), and they underwent three sensory tests that acted as assays of inhibitory function at post test.
In addition, 307 participants completed the Visual Contrast Sensitivity and Surround Suppression, which “measures the minimum percentage contrast between the lighter and darker regions of a striped pattern that can be detected (called the contrast threshold),” the investigators note.
The contrast threshold was measured with and without a suppressive surround mask that increases the threshold – an effect mediated by GABAergic connections in the visual cortex.
Participants (n = 172) also completed the Binocular Rivalry test and the Tactile Test Battery (n = 180). Both tests are designed to measure responses requiring GABAergic inhibitory activity.
‘Subtle changes’
ANOVA analyses revealed a “highly significant” reduction in anxiety at post test (F[1,173] = 10.03; P = .002; np 2 = .055), driven primarily by reduced anxiety in the B6 group (t[88] = 3.51; P < .001; d = .37). The placebo group also showed some reduction in anxiety, but it was not deemed significant, and the overall interaction itself did not reach significance.
A comparison of the B12 group with the group that received placebo revealed a significant reduction in anxiety at post test (F[1,175] = 4.08; P = .045; np 2 = .023), similarly driven by reduced anxiety in the B12 group (t[89] = 1.84; P = .069; d = .19) – but the interaction was not significant.
Among the B6 group, there was a highly significant reduction in scores on the generalized anxiety disorder and social anxiety subscales of the SCAARED, and there was a trend toward reductions on the other subscales. Among the B12 group, there was a significant reduction only on scores on the separation anxiety subscale. No significant changes were found in the placebo group.
The ANOVA test analysis of the B6 and placebo group data showed “no uniform direction of change” in depression at post test. The researchers found a “tendency” for depression scores to decrease between baseline and post test in the B6 group but to increase in the placebo group – an interaction that “approached” significance (F[1,96] = 3.08; P = .083; np 2 = .031), they report.
The ANOVA analysis of the B12 and placebo group data revealed no significant or trending effects, and the t-test comparing baseline and post-test scores in the B12 group was similarly nonsignificant.
B6 supplementation did change visual contrast thresholds, but only when a suppressive surround was present. There were “no clear effects” of B6 supplementation on other outcome measures, including binocular rivalry reversal rate and the tactile test battery, the investigators note.
“We found that supplementation with B6 produced subtle changes in tests of visual processing in a way that suggested an increase in the level of the inhibitory neurotransmitter GABA,” Dr. Field reported.
Vitamin B6 is a “cofactor for a metabolic pathway in the brain that converts the excitatory neurotransmitter glutamate into the inhibitory/calming GABA,” he said.
“By increasing the quantity of the cofactor, we slightly speed up the rate of this metabolic process, and so you end up with a bit more of the GABA neurotransmitter and a bit less glutamate. The net effect of this is to slightly reduce the amount of activity in the brain,” Dr. Field added.
Most common nutrient deficiency
Carol Johnston, PhD, professor and associate dean for faculty success, College of Health Solutions, Arizona State University, Phoenix, said vitamin B6 is “the most common nutrient deficiency in the United States;” 16% of men and 32% of women are reportedly B6 deficient.
“Young women on birth control are at higher risk for B6 deficiency due to effects of oral contraceptives on B6 metabolism,” whereas vitamin B12 deficiency is more common in older adults, said Dr. Johnston, who was not involved with the study.
The current study’s population mainly consisted of young women, and the interpretation of the data is “limited” because the researchers did not measure blood status for B6 and B12, Dr. Johnston noted. It is possible the sample was low in B6 and that the supplements “improved cognitive measures.”
Because the population was young – no one was older than 60 years – B12 status was likely “adequate in the sample, and supplementation did not have an impact,” she said.
Overall, Dr. Johnston cautioned that it is important to “alert clinicians and the general public about the concerns of overdosing B6.” For example, supplementation at high amounts can cause potentially irreversible sensory neuropathy, she noted.
“The safe upper limit defined by experts is 100 mg per day – the dosage used in this trial. Daily supplementation should not exceed this level,” Dr. Johnston said.
The vitamin tablets used in the study were supplied by Innopure. The investigators and Dr. Johnston have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
High rate of mental health problems in transgender children
Transgender children, even those as young as 9 or 10 years old, already show increased susceptibility to mental health problems compared with their cisgender peers, new research suggests.
Investigators assessed a sample of more than 7000 children aged 9-10 years in the general population and found those who reported being transgender scored considerably higher on all six subscales of the DSM-5-oriented Child Behavior Checklist (CBCL).
Transgender children had almost sixfold higher odds of suicidality and over twice the odds of depressive and anxiety problems, compared with cisgender children. Moreover, transgender children displayed higher levels of mental health problems compared with previous studies of transgender children recruited from specialist gender clinics.
“Our findings emphasize the vulnerability of transgender children, including those who may not yet have accessed specialist support,” senior author Kenneth C. Pang, MBBS, BMedSc, PhD, associate professor, Murdoch Children’s Research Institute, University of Melbourne, Royal Children’s Hospital, Australia, told this news organization.
“Clinicians providing general health care to transgender children should keep this vulnerability in mind and proactively address any mental health problems that exist,” he said.
The findings were published online as a research letter in JAMA Network Open.
Higher levels of support?
“We felt this study was important to conduct because previous studies regarding the mental health of transgender children have been drawn from children receiving specialist gender-related care,” Dr. Pang said.
“Transgender children receiving such care are likely to enjoy higher levels of support than those unable to access such services, and this might create differences in mental health,” he added.
To investigate this issue, the researchers turned to participants (n = 7,169; mean age, 10.3 years) in the Adolescent Brain Cognitive Development (ABCD) study.
“The ABCD study is a longitudinal study of over 11,000 children who were recruited to reflect the sociodemographic variation of the U.S. population,” lead author Douglas H. Russell, MSc, a PhD candidate at the University of Melbourne, told this news organization.
To be included in the current study, children had to understand and respond to the question “Are you transgender?”
The researchers compared mental health outcomes between transgender and cisgender children (n = 58 and n = 7,111, respectively) using the CBCL, which study participants had completed at baseline.
Key protective factor
The transgender children recorded higher mean T scores for all six subscales of the CBCL, although all children scored in the references range; and the standardized mean difference was “small.”
Suicidality was measured by summing the two suicide-related items in the parent-report CBCL assessing suicidal ideation and attempts.
“For the CBCL, T scores are calculated for measures that are scored on a continuous scale,” Dr. Pang noted. “Responses to the suicidality questions on the CBCL were assessed in a categorical manner (at risk of suicide vs. not), as previously described by others. So T scores were therefore not able to be calculated.”
When the investigators determined the proportion of cisgender and transgender children who scored in the “borderline” or “clinical” range (T score, 65), they found increased odds of transgender children scoring in that range in all six subscales, as well as suicidality.
The researchers note the results for attention-deficit/hyperactivity disorder and oppositional defiant problems were not statistically significant.
Previous studies that used clinical samples of young transgender children (aged 5 -11 years) reported lower rates of depression and anxiety than what was found in the current study.
“Transgender children in the general population displayed higher levels of mental health problems compared to previous studies of transgender children recruited from specialist gender clinics,” Mr. Russell said.
One reason for that may be children in specialist clinics “are likely to have support from their families (a key protective factor for the mental health of transgender young people); in comparison, many transgender children in the general population lack parental support for their gender,” the investigators wrote.
“Our findings suggest that by 9 to 10 years of age transgender children already show increased susceptibility to mental health problems compared with their cisgender peers, which has important public health implications,” they added.
The researchers noted that whether this susceptibility “is due to stigma, minority stress, discrimination, or gender dysphoria is unclear, but providing appropriate mental health supports to this vulnerable group is paramount.”
“Pathologizing and damaging”
Commenting for this news organiztion, Jack L. Turban, MD, incoming assistant professor of child and adolescent psychiatry, University of California, San Francisco, said that “sadly” the findings are “largely in line with past studies that have shown dramatic mental health disparities” for transgender and gender diverse youth.
“The dramatically elevated odds of suicidality warrants particular public health concern,” said Dr. Turban, who was not involved with the study.
He noted these results “come at a time when transgender youth are under legislative attack in many states throughout the country, and the national rhetoric around them has been pathologizing and damaging.”
Dr. Turban said that he worries “if our national discourse around trans youth doesn’t change soon, that these disparities will worsen.”
Funding was provided to individual investigators by the Hugh Williamson Foundation, the Royal Children’s Hospital foundation, the National Health and Medical Research Council, and the Australian Government Research Training Program Scholarship. Mr. Russell and Dr. Pang reported being members of the Australian Professional Association for Trans Health. Dr. Pang is a member of the World Professional Association for Transgender Health and a member of the editorial board of the journal Transgender Health. Dr. Turban reported textbook royalties from Springer Nature, being on the scientific advisory board of Panorama Global (UpSwing Fund), and payments as an expert witness for the American Civil Liberties Union, Lambda Legal, and Cooley LLP. He has received a pilot research award from AACAP and pharmaceutical partners (Arbor and Pfizer), a research fellowship from the Sorensen Foundation, and freelance payments from the New York Times, the Washington Post, and the Los Angeles Times.
A version of this article first appeared on Medscape.com.
Transgender children, even those as young as 9 or 10 years old, already show increased susceptibility to mental health problems compared with their cisgender peers, new research suggests.
Investigators assessed a sample of more than 7000 children aged 9-10 years in the general population and found those who reported being transgender scored considerably higher on all six subscales of the DSM-5-oriented Child Behavior Checklist (CBCL).
Transgender children had almost sixfold higher odds of suicidality and over twice the odds of depressive and anxiety problems, compared with cisgender children. Moreover, transgender children displayed higher levels of mental health problems compared with previous studies of transgender children recruited from specialist gender clinics.
“Our findings emphasize the vulnerability of transgender children, including those who may not yet have accessed specialist support,” senior author Kenneth C. Pang, MBBS, BMedSc, PhD, associate professor, Murdoch Children’s Research Institute, University of Melbourne, Royal Children’s Hospital, Australia, told this news organization.
“Clinicians providing general health care to transgender children should keep this vulnerability in mind and proactively address any mental health problems that exist,” he said.
The findings were published online as a research letter in JAMA Network Open.
Higher levels of support?
“We felt this study was important to conduct because previous studies regarding the mental health of transgender children have been drawn from children receiving specialist gender-related care,” Dr. Pang said.
“Transgender children receiving such care are likely to enjoy higher levels of support than those unable to access such services, and this might create differences in mental health,” he added.
To investigate this issue, the researchers turned to participants (n = 7,169; mean age, 10.3 years) in the Adolescent Brain Cognitive Development (ABCD) study.
“The ABCD study is a longitudinal study of over 11,000 children who were recruited to reflect the sociodemographic variation of the U.S. population,” lead author Douglas H. Russell, MSc, a PhD candidate at the University of Melbourne, told this news organization.
To be included in the current study, children had to understand and respond to the question “Are you transgender?”
The researchers compared mental health outcomes between transgender and cisgender children (n = 58 and n = 7,111, respectively) using the CBCL, which study participants had completed at baseline.
Key protective factor
The transgender children recorded higher mean T scores for all six subscales of the CBCL, although all children scored in the references range; and the standardized mean difference was “small.”
Suicidality was measured by summing the two suicide-related items in the parent-report CBCL assessing suicidal ideation and attempts.
“For the CBCL, T scores are calculated for measures that are scored on a continuous scale,” Dr. Pang noted. “Responses to the suicidality questions on the CBCL were assessed in a categorical manner (at risk of suicide vs. not), as previously described by others. So T scores were therefore not able to be calculated.”
When the investigators determined the proportion of cisgender and transgender children who scored in the “borderline” or “clinical” range (T score, 65), they found increased odds of transgender children scoring in that range in all six subscales, as well as suicidality.
The researchers note the results for attention-deficit/hyperactivity disorder and oppositional defiant problems were not statistically significant.
Previous studies that used clinical samples of young transgender children (aged 5 -11 years) reported lower rates of depression and anxiety than what was found in the current study.
“Transgender children in the general population displayed higher levels of mental health problems compared to previous studies of transgender children recruited from specialist gender clinics,” Mr. Russell said.
One reason for that may be children in specialist clinics “are likely to have support from their families (a key protective factor for the mental health of transgender young people); in comparison, many transgender children in the general population lack parental support for their gender,” the investigators wrote.
“Our findings suggest that by 9 to 10 years of age transgender children already show increased susceptibility to mental health problems compared with their cisgender peers, which has important public health implications,” they added.
The researchers noted that whether this susceptibility “is due to stigma, minority stress, discrimination, or gender dysphoria is unclear, but providing appropriate mental health supports to this vulnerable group is paramount.”
“Pathologizing and damaging”
Commenting for this news organiztion, Jack L. Turban, MD, incoming assistant professor of child and adolescent psychiatry, University of California, San Francisco, said that “sadly” the findings are “largely in line with past studies that have shown dramatic mental health disparities” for transgender and gender diverse youth.
“The dramatically elevated odds of suicidality warrants particular public health concern,” said Dr. Turban, who was not involved with the study.
He noted these results “come at a time when transgender youth are under legislative attack in many states throughout the country, and the national rhetoric around them has been pathologizing and damaging.”
Dr. Turban said that he worries “if our national discourse around trans youth doesn’t change soon, that these disparities will worsen.”
Funding was provided to individual investigators by the Hugh Williamson Foundation, the Royal Children’s Hospital foundation, the National Health and Medical Research Council, and the Australian Government Research Training Program Scholarship. Mr. Russell and Dr. Pang reported being members of the Australian Professional Association for Trans Health. Dr. Pang is a member of the World Professional Association for Transgender Health and a member of the editorial board of the journal Transgender Health. Dr. Turban reported textbook royalties from Springer Nature, being on the scientific advisory board of Panorama Global (UpSwing Fund), and payments as an expert witness for the American Civil Liberties Union, Lambda Legal, and Cooley LLP. He has received a pilot research award from AACAP and pharmaceutical partners (Arbor and Pfizer), a research fellowship from the Sorensen Foundation, and freelance payments from the New York Times, the Washington Post, and the Los Angeles Times.
A version of this article first appeared on Medscape.com.
Transgender children, even those as young as 9 or 10 years old, already show increased susceptibility to mental health problems compared with their cisgender peers, new research suggests.
Investigators assessed a sample of more than 7000 children aged 9-10 years in the general population and found those who reported being transgender scored considerably higher on all six subscales of the DSM-5-oriented Child Behavior Checklist (CBCL).
Transgender children had almost sixfold higher odds of suicidality and over twice the odds of depressive and anxiety problems, compared with cisgender children. Moreover, transgender children displayed higher levels of mental health problems compared with previous studies of transgender children recruited from specialist gender clinics.
“Our findings emphasize the vulnerability of transgender children, including those who may not yet have accessed specialist support,” senior author Kenneth C. Pang, MBBS, BMedSc, PhD, associate professor, Murdoch Children’s Research Institute, University of Melbourne, Royal Children’s Hospital, Australia, told this news organization.
“Clinicians providing general health care to transgender children should keep this vulnerability in mind and proactively address any mental health problems that exist,” he said.
The findings were published online as a research letter in JAMA Network Open.
Higher levels of support?
“We felt this study was important to conduct because previous studies regarding the mental health of transgender children have been drawn from children receiving specialist gender-related care,” Dr. Pang said.
“Transgender children receiving such care are likely to enjoy higher levels of support than those unable to access such services, and this might create differences in mental health,” he added.
To investigate this issue, the researchers turned to participants (n = 7,169; mean age, 10.3 years) in the Adolescent Brain Cognitive Development (ABCD) study.
“The ABCD study is a longitudinal study of over 11,000 children who were recruited to reflect the sociodemographic variation of the U.S. population,” lead author Douglas H. Russell, MSc, a PhD candidate at the University of Melbourne, told this news organization.
To be included in the current study, children had to understand and respond to the question “Are you transgender?”
The researchers compared mental health outcomes between transgender and cisgender children (n = 58 and n = 7,111, respectively) using the CBCL, which study participants had completed at baseline.
Key protective factor
The transgender children recorded higher mean T scores for all six subscales of the CBCL, although all children scored in the references range; and the standardized mean difference was “small.”
Suicidality was measured by summing the two suicide-related items in the parent-report CBCL assessing suicidal ideation and attempts.
“For the CBCL, T scores are calculated for measures that are scored on a continuous scale,” Dr. Pang noted. “Responses to the suicidality questions on the CBCL were assessed in a categorical manner (at risk of suicide vs. not), as previously described by others. So T scores were therefore not able to be calculated.”
When the investigators determined the proportion of cisgender and transgender children who scored in the “borderline” or “clinical” range (T score, 65), they found increased odds of transgender children scoring in that range in all six subscales, as well as suicidality.
The researchers note the results for attention-deficit/hyperactivity disorder and oppositional defiant problems were not statistically significant.
Previous studies that used clinical samples of young transgender children (aged 5 -11 years) reported lower rates of depression and anxiety than what was found in the current study.
“Transgender children in the general population displayed higher levels of mental health problems compared to previous studies of transgender children recruited from specialist gender clinics,” Mr. Russell said.
One reason for that may be children in specialist clinics “are likely to have support from their families (a key protective factor for the mental health of transgender young people); in comparison, many transgender children in the general population lack parental support for their gender,” the investigators wrote.
“Our findings suggest that by 9 to 10 years of age transgender children already show increased susceptibility to mental health problems compared with their cisgender peers, which has important public health implications,” they added.
The researchers noted that whether this susceptibility “is due to stigma, minority stress, discrimination, or gender dysphoria is unclear, but providing appropriate mental health supports to this vulnerable group is paramount.”
“Pathologizing and damaging”
Commenting for this news organiztion, Jack L. Turban, MD, incoming assistant professor of child and adolescent psychiatry, University of California, San Francisco, said that “sadly” the findings are “largely in line with past studies that have shown dramatic mental health disparities” for transgender and gender diverse youth.
“The dramatically elevated odds of suicidality warrants particular public health concern,” said Dr. Turban, who was not involved with the study.
He noted these results “come at a time when transgender youth are under legislative attack in many states throughout the country, and the national rhetoric around them has been pathologizing and damaging.”
Dr. Turban said that he worries “if our national discourse around trans youth doesn’t change soon, that these disparities will worsen.”
Funding was provided to individual investigators by the Hugh Williamson Foundation, the Royal Children’s Hospital foundation, the National Health and Medical Research Council, and the Australian Government Research Training Program Scholarship. Mr. Russell and Dr. Pang reported being members of the Australian Professional Association for Trans Health. Dr. Pang is a member of the World Professional Association for Transgender Health and a member of the editorial board of the journal Transgender Health. Dr. Turban reported textbook royalties from Springer Nature, being on the scientific advisory board of Panorama Global (UpSwing Fund), and payments as an expert witness for the American Civil Liberties Union, Lambda Legal, and Cooley LLP. He has received a pilot research award from AACAP and pharmaceutical partners (Arbor and Pfizer), a research fellowship from the Sorensen Foundation, and freelance payments from the New York Times, the Washington Post, and the Los Angeles Times.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Electroacupuncture promising for depression-related insomnia
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).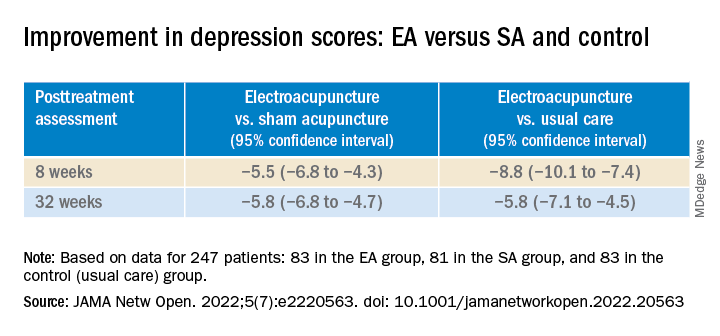
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).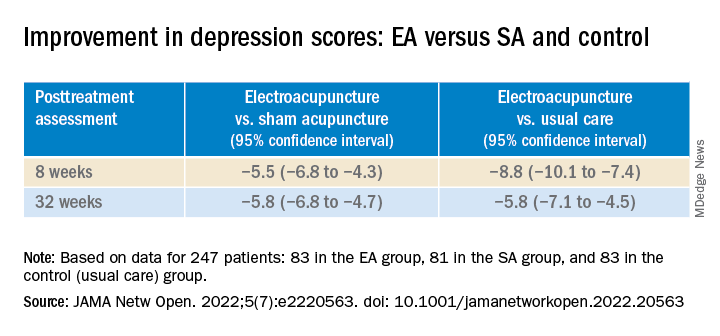
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a study of more than 200 adults with depression and comorbid insomnia, change from baseline to week 8 on the Pittsburgh Sleep Quality Index (PSQI) was 3 points greater in the group receiving EA versus a group receiving sham acupuncture (SA) plus standard care, and 5 points greater vs a control group receiving standard care only. The improvements were sustained during a 24-week postintervention follow-up.
The EA group also showed significant improvement in depression, insomnia, self-rated anxiety, and total sleep time – all of which were not found in the SA or control groups.
“Based on the results of our trial, we recommend patients with depression and insomnia seek the treatment of EA as an alternative and complementary therapy for better results,” study investigator Shifen Xu, PhD, Shanghai (China) Municipal Hospital of Traditional Chinese Medicine, Shanghai University of Traditional Chinese Medicine, told this news organization.
The findings were published online in JAMA Network Open.
Bidirectional relationship
“Sleep disturbance is the prominent symptom in patients with depression,” the investigators noted.
Depression and sleep issues have a bidirectional relationship, in that “poor sleep quality contributes to the development of depression, and having depression makes a person more likely to develop sleep issues,” they wrote.
Patients with co-occurring depression and sleep disorders are more difficult to treat and have a greater risk for relapse and recurrence of depression, they added.
Acupuncture may be an “effective drug-free approach to help treat mental illness and sleep disorders,” the researchers noted. A previous study suggested acupuncture may improve sleep efficacy and prolong total sleep in patients with primary insomnia.
“EA is the combination of traditional Chinese acupuncture with electric-impulse stimulation, and it can enhance the therapeutic effect of the acupoints throughout the needle retention time,” Dr. Xu said.
A previous pilot study of EA for depression-related insomnia showed significant improvements in sleep quality after EA treatment, but the sample size was small.
The current researchers, therefore, undertook the present study – with a larger sample size and comparison with SA and standard care. They divided 270 adults (mean age, 50.3 years; 71.9% women) at three tertiary hospitals in Shanghai into three groups, each consisting of 90 participants.
The EA plus standard care group and the SA plus standard care group received 30-minute treatments three times per week for 8 weeks. The control group received standard care only.
All participants had DSM-5–diagnosed depression; baseline PSQI scores greater than 7, with higher scores indicating worse sleep quality and a greater number or sleep disorders; and Hamilton Depression Rating Scales (HDRS-17) scores of 20-35, with higher scores indicating higher depression levels.
Patients with secondary depressive disorders caused by other conditions, medication, or psychotic disorders were excluded, as were patients with a history of alcohol abuse or drug dependence or those who had received acupuncture within the previous year.
Of the patients who completed the 8-week intervention, 83 were in the EA group, 81 in the SA group, and 83 in the control group. Almost all participants (91.5%) completed all outcome measurements by the end of the 24-week follow-up period (also known as week 32).
Calm mind, balanced mood
At the 8-week posttreatment assessment, which was the primary endpoint, the EA group had a mean reduction from baseline of 6.2 points (95% confidence interval, −6.9 to −5.6) in PSQI score.
There was a significant difference in PSQI score between the EA versus the SA group (−3.6 points; 95% CI, −4.4 to −2.8; P < .001) and vs the control group (−5.1 points; 95% CI, −6.0 to −4.2; P < .001).
The efficacy of EA in treating insomnia was sustained during the postintervention follow-up period when the EA group had a significantly greater reduction in PSQI score, compared with the SA group (−4.7; 95% CI, −5.4 to −3.9; P < .001) and the control group (−5.0; 95% CI, −5.8 to −4.1; P < .001).
Patients receiving EA also experienced significant (all P values < .001) improvement from baseline on secondary outcomes, including:
- Scores on the HDRS (−10.7; 95% CI, −11.8 to −9.7)
- Scores on the Insomnia Severity Index, (−7.6; 95% CI,−8.5 to −6.7)
- Scores on the Self-rated Anxiety Scale (−2.9; 95% CI, −4.1 to −1.7)
- Total sleep time, as recorded by sleep actigraphy (29.1 minutes; 95% CI, 21.5-36.7)
In addition, the EA group showed significant improvement in depression scores compared with the SA and control groups at both 8 and 32 weeks (all P values < .001).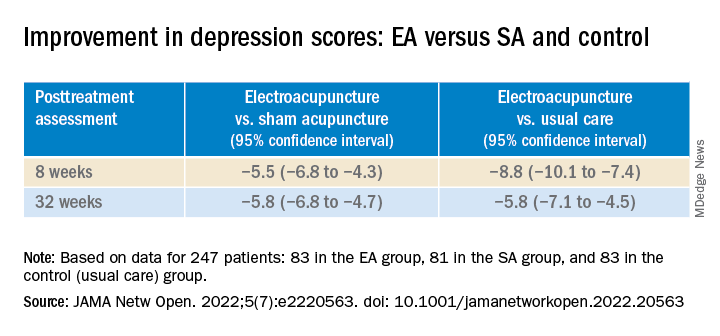
Participants in the EA group also had a 4.2% (95% CI, 2.6% - 5.8%) higher sleep efficiency score at week 8, compared with those in the SA group (P < .001).
In addition, they had lower scores on the Insomnia Severity Index and the Self-rated Anxiety Scale, and longer total sleep time, compared with the control group at week 8.
None of the participants reported any serious adverse events.
“Our findings constitute subjective and objective evidence of the efficacy and safety of EA with standard care in treating comorbid depression and insomnia compared with SA with standard care or standard care alone,” the investigators wrote.
“The acupoints we used in this trial mainly act on calming mind, relieving negative mood, and balancing the yin-yang,” Dr. Xu added.
Viable adjunctive treatment
Commenting on the study, Albert Yeung, MD, ScD, associate director of the Mass General Depression and Clinical Research Program and associate professor of psychiatry, Harvard Medical School, Boston, said that, with the evidence from this study, “acupuncture and/or electroacupuncture could be a viable adjunctive treatment for depressed patients who suffer from insomnia.”
Dr. Yeung, who was not involved with the study, is the coauthor of an accompanying editorial.
“More well-designed studies are warranted to provide evidence for integrating holistic treatment in medicine,” he said.
The study was funded by grants from the National Natural Science Foundation of China, and Shanghai Municipal Health. The investigators and Dr. Yeung reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Antidepressants may curb opioid overdose
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.
“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.
“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed insurance claims for more than 200,000 adults with a history of depression. Of these, 8,200 experienced adverse events (AEs) during the year after initiation of opioid therapy.
However, the risk for an AE such as overdose and other forms of self-harm was reduced among patients who had been treated with antidepressants for at least 6 weeks.
The take-home message is that clinicians and health systems need to be more aware that individuals in pain are more likely to be depressed and at higher risk for AEs – so the depression should be treated “more liberally,” corresponding author Bradley Stein, MD, PhD, a practicing psychiatrist in Pittsburgh and director of the Rand Corporation Opioid Policy Center, told this news organization.
“If you are treating someone with pain, particularly chronic pain, it’s critically important to better assess their depression and not to attribute depressive symptoms only to pain,” Dr. Stein said.
The findings were published online in Psychiatric Services.
Promising approach?
Opioid treatment for pain “complicates the interactions among pain, depression, and self-harm,” the investigators write. Individuals with depression receiving long-term opioid therapy are two to three times more likely to misuse opioids, compared with individuals who do not have depression.
Although comorbid depression “substantially increases overdose and suicide risk, it remains underdiagnosed and undertreated among individuals with chronic pain,” the researchers note. They add that increasing access to depression treatment may be a “potentially promising approach to preventing overdoses and suicide” in these patients.
“We know that individuals using opioids who have a history of depression are more likely to have negative outcomes, such as overdoses and self-harm events,” Dr. Stein said. “We wanted to see whether antidepressants, which would treat depression in these individuals, would help with that.”
The researchers assessed a database of commercial insurance claims of adults with a history of depression who received opioids between 2007 and 2017 (n = 283,374). The data included 336,599 opioid treatment episodes.
To be included in the study, patients had to have been diagnosed with depression before they filled their first opioid prescription.
The “outcome of interest” was time from the beginning of an opioid episode until an adverse event, such as opioid poisoning, overdose of nonopioid controlled or illicit substances, or self-harm unrelated to overdose.
Participants were followed from the onset of the opioid episode until an AE occurred, loss to follow-up, or week 52, whichever came first.
The “key independent variable” was filling an antidepressant prescription. The patient’s sex and age were considered to be independent variables as well.
Teasing out antidepressant effect
Of participants with a history of depression treatment, 8,203 experienced at least one AE during the 12 months after treatment initiation (n = 47,486 AEs). Approximately half (50.8%) filled an antidepressant prescription at least once during the 12 months after the opioid episode began.
AEs were more likely among men than among women. The highest risk was in patients aged 18-24 years.
After adjusting for age and sex, participants who had received antidepressants had a greater risk for all adverse outcomes during the first 6 weeks of antidepressant treatment. However, those who had received antidepressants for 6 weeks or longer were at reduced risk for all adverse outcomes.
“We took advantage of the fact that, for most people, antidepressants take a while to work and aren’t immediately effective, so we were able to use that difference in our research,” Dr. Stein said.
“We wouldn’t expect to see an immediate effect of antidepressants, so the difference between what we saw immediately after the person had started treatment and the time it took for the antidepressant to be effective enabled us to tease out the effect of the antidepressant,” he added.
Consider CBT?
Andrew Saxon, MD, professor, department of psychiatry and behavioral sciences, University of Washington School of Medicine, Seattle, said clinicians “tend to think categorically and give people diagnoses that are clear-cut.” But neurobiologically, “it may be hard to distinguish where chronic pain ends and depression begins, or whether there’s some commonality.”
For patients with chronic pain and those taking opioids, “we need to be very attuned to the possibility or likelihood that they have major depression and other psychiatric diagnoses, like PTSD and anxiety disorders, which are very common,” said Dr. Saxon, who is also the director of the Center of Excellence in Substance Abuse Treatment and Education at the VA Puget Sound Health Care System. He was not involved with the current research.
He noted that treating those disorders “is a very important component of managing chronic pain.” However, “patients just starting antidepressants need to be carefully monitored when they’re getting stabilized on their antidepressants because they can have side effects, particularly early on, that can destabilize them.”
Dr. Saxon added that beyond pharmacotherapy, cognitive-behavioral therapy (CBT) for pain might be an even better intervention for addressing both pain and depression.
Also commenting for this article, Brian Hurley, MD, an addiction medicine specialist and the medical director of the Division of Substance Abuse Prevention and Control for the Los Angeles County Department of Public Health, said: “In the context of the largest wave of overdose mortality in U.S. history, we know comparatively little about the impact of mental health interventions that mitigate overdose risks.”
This study “contributes important new information that treating depression with antidepressant medications reduces overdose and self-harm risks for people who are prescribed opioids,” said Dr. Hurley, who is also the president-elect of the American Society of Addiction Medicine.
It also “underscores the general importance of integrated mental health and substance use disorder treatment in both primary care and in mental health settings,” added Dr. Hurley, who was not involved with the study.
The study was funded by the National Institute on Drug Abuse. The investigators and commenters reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PSYCHIATRIC SERVICES
Surprising ethnic difference in atherosclerosis burden in Harlem, N.Y.
Non-Hispanic Black young adults in a large, ethnically diverse underserved neighborhood in New York City have about twice the prevalence of subclinical atherosclerosis as Hispanic young adults, according to a new cross-sectional study. It was noteworthy for identifying subclinical cardiovascular (CV) disease in the cohorts using 3D intravascular ultrasound (3D IVUS).
The study’s 436 Black and Hispanic adults, 82% of them women, completed questionnaires regarding nutrition, lifestyle, medical history, weight, blood pressure, cholesterol levels, and other metrics.
(24.5% vs. 9.3%). Overall Framingham scores for 10-year risk for CV events were not statistically different, at 4.6 and 3.6, respectively.
The presence of atherosclerosis in either the carotid or femoral arteries was identified with 3D IVUS in 8.7% of participants. But its prevalence was about twofold greater in Black than in Hispanic participants (12.9% vs. 6.6%), a finding that persisted after multivariable adjustment and appeared driven by a greater prevalence of carotid disease among Black participants (12.9% vs. 4.8%).
“For the same predicted CV risk, non-Hispanic Black individuals appear to be more vulnerable than people of Hispanic origin to early subclinical atherosclerosis, particularly in the carotid arteries, potentially placing them at increased risk of clinical CV disease,” concludes the report published in the Journal of the American College of Cardiology, with lead author Josep Iglesies-Grau, MD, Montreal Heart Institute.
International program
The current analysis from the FAMILIA study is part of a large international project called Science, Health, and Education (SHE), which is designed to promote early intervention in the lives of children, their caretakers, and teachers so they can develop lifelong heart-healthy habits, senior author Valentin Fuster, MD, PhD, physician-in chief, Mount Sinai Hospital, New York, said in an interview.
The SHE program has been presented to more than 50,000 children worldwide, and FAMILIA has delivered successful interventions to more than 500 preschoolers, caretakers, and educators at Head Start schools in the Harlem neighborhood of New York, where the current study was conducted.
The analysis centered on the children’s adult caregivers, of whom one-third were non-Hispanic Black and two-thirds were Hispanic. “We wanted to know if this young population of parents and caregivers [would show] development or initiation of atherosclerotic disease,” Dr. Fuster said, “thinking that when we showed them that they had disease, it would further motivate them to change their lifestyle.”
Participants were assessed for seven basic CV risk factors – hypertension, smoking, body mass index, diabetes, dyslipidemia, low physical activity levels, and poor-quality diet – as well as socioeconomic descriptors. All participants also underwent 3D IVUS to evaluate the presence and extent of atherosclerosis in the carotid and femoral arteries.
‘Expected and unexpected’ findings
Black participants were considerably more likely than their Hispanic counterparts to be hypertensive, to be active smokers, and to have higher BMIs. The Black cohort reported higher consumption of fruits and vegetables (P < .001).
There were no between-group differences in the prevalence of diabetes or in mean fasting glucose or total cholesterol levels.
The mean 10-year Framingham CV risk score across the entire study population was 4.0%, with no significant differences between the two groups. In fact, 89% of participants were classified as low risk on the basis of the score.
The overall prevalence of subclinical atherosclerosis was 8.7%, with a mean global plaque burden of 5.0 mm3. But there were dramatic differences in atherosclerotic burden. Across all 10-year Framingham risk categories, Black participants had twice the odds of having subclinical atherosclerosis as Hispanic participants (odds ratio, 2.11; 95% confidence interval, 1.09-4.08; P = .026).
Black participants also had a greater atherosclerotic disease burden (9.0 mm3 vs. 2.9 mm3), mean total plaque volume (P = .028), and a higher prevalence of disease in both the carotid and femoral arteries (8.2% vs. 3.8%; P = .026).
“Our findings were both expected and completely unexpected,” Dr. Fuster commented. “It was expected that the non-Hispanic Black population would have more hypertension, obesity, and smoking, and might therefore have more [atherosclerotic] disease. But what was unexpected was when we adjusted for the seven risk factors and socioeconomic status, the Black population had three times the amount of disease,” he said.
“We need to take better care of the risk factors already known in the Black population, which is critical.” However, “our challenge today is to identify these new risk factors, which might be genetic or socioeconomic.” Dr. Fuster said his group is “already working with artificial intelligence to identify risk factors beyond the traditional risk factors that are already established.”
Socioeconomic differences?
“The fact that we’re uncovering and demonstrating that this is an issue – especially for African American women at a young age – and we could make a significant interdiction in terms of risk reduction if we have tools and invest the necessary time and effort, that is the important part of this paper,” Keith Churchwell, MD, Yale New Haven Hospital, and Yale School of Medicine, New Haven, Conn., said in an interview.
“If you’re going to evaluate African Americans in Harlem who are socially disadvantaged, I would want to know if there is a difference between them and other African Americans who have a different socioeconomic status, in terms of atherosclerotic disease,” added Dr. Churchwell, who was not involved with the study.
The Framingham 10-year risk score is “inadequate in assessing CV disease risk in all populations and is not generalizable to non-Whites,” contend Ramdas G. Pai, MD, and Vrinda Vyas, MBBS, of the University of California, Riverside, in an accompanying editorial.
“New data are emerging in favor of imaging-based classification of CV disease risk and has been shown to improve patient adherence to and compliance with risk-modifying interventions,” they write. “Subclinical atherosclerosis may help better stratify CV disease risk so that preventive measures can be instituted to reduce cardiovascular events at a population level.”
Dr. Fuster and coauthors, Dr. Ramdas and Dr. Pai, and Dr. Churchwell report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Non-Hispanic Black young adults in a large, ethnically diverse underserved neighborhood in New York City have about twice the prevalence of subclinical atherosclerosis as Hispanic young adults, according to a new cross-sectional study. It was noteworthy for identifying subclinical cardiovascular (CV) disease in the cohorts using 3D intravascular ultrasound (3D IVUS).
The study’s 436 Black and Hispanic adults, 82% of them women, completed questionnaires regarding nutrition, lifestyle, medical history, weight, blood pressure, cholesterol levels, and other metrics.
(24.5% vs. 9.3%). Overall Framingham scores for 10-year risk for CV events were not statistically different, at 4.6 and 3.6, respectively.
The presence of atherosclerosis in either the carotid or femoral arteries was identified with 3D IVUS in 8.7% of participants. But its prevalence was about twofold greater in Black than in Hispanic participants (12.9% vs. 6.6%), a finding that persisted after multivariable adjustment and appeared driven by a greater prevalence of carotid disease among Black participants (12.9% vs. 4.8%).
“For the same predicted CV risk, non-Hispanic Black individuals appear to be more vulnerable than people of Hispanic origin to early subclinical atherosclerosis, particularly in the carotid arteries, potentially placing them at increased risk of clinical CV disease,” concludes the report published in the Journal of the American College of Cardiology, with lead author Josep Iglesies-Grau, MD, Montreal Heart Institute.
International program
The current analysis from the FAMILIA study is part of a large international project called Science, Health, and Education (SHE), which is designed to promote early intervention in the lives of children, their caretakers, and teachers so they can develop lifelong heart-healthy habits, senior author Valentin Fuster, MD, PhD, physician-in chief, Mount Sinai Hospital, New York, said in an interview.
The SHE program has been presented to more than 50,000 children worldwide, and FAMILIA has delivered successful interventions to more than 500 preschoolers, caretakers, and educators at Head Start schools in the Harlem neighborhood of New York, where the current study was conducted.
The analysis centered on the children’s adult caregivers, of whom one-third were non-Hispanic Black and two-thirds were Hispanic. “We wanted to know if this young population of parents and caregivers [would show] development or initiation of atherosclerotic disease,” Dr. Fuster said, “thinking that when we showed them that they had disease, it would further motivate them to change their lifestyle.”
Participants were assessed for seven basic CV risk factors – hypertension, smoking, body mass index, diabetes, dyslipidemia, low physical activity levels, and poor-quality diet – as well as socioeconomic descriptors. All participants also underwent 3D IVUS to evaluate the presence and extent of atherosclerosis in the carotid and femoral arteries.
‘Expected and unexpected’ findings
Black participants were considerably more likely than their Hispanic counterparts to be hypertensive, to be active smokers, and to have higher BMIs. The Black cohort reported higher consumption of fruits and vegetables (P < .001).
There were no between-group differences in the prevalence of diabetes or in mean fasting glucose or total cholesterol levels.
The mean 10-year Framingham CV risk score across the entire study population was 4.0%, with no significant differences between the two groups. In fact, 89% of participants were classified as low risk on the basis of the score.
The overall prevalence of subclinical atherosclerosis was 8.7%, with a mean global plaque burden of 5.0 mm3. But there were dramatic differences in atherosclerotic burden. Across all 10-year Framingham risk categories, Black participants had twice the odds of having subclinical atherosclerosis as Hispanic participants (odds ratio, 2.11; 95% confidence interval, 1.09-4.08; P = .026).
Black participants also had a greater atherosclerotic disease burden (9.0 mm3 vs. 2.9 mm3), mean total plaque volume (P = .028), and a higher prevalence of disease in both the carotid and femoral arteries (8.2% vs. 3.8%; P = .026).
“Our findings were both expected and completely unexpected,” Dr. Fuster commented. “It was expected that the non-Hispanic Black population would have more hypertension, obesity, and smoking, and might therefore have more [atherosclerotic] disease. But what was unexpected was when we adjusted for the seven risk factors and socioeconomic status, the Black population had three times the amount of disease,” he said.
“We need to take better care of the risk factors already known in the Black population, which is critical.” However, “our challenge today is to identify these new risk factors, which might be genetic or socioeconomic.” Dr. Fuster said his group is “already working with artificial intelligence to identify risk factors beyond the traditional risk factors that are already established.”
Socioeconomic differences?
“The fact that we’re uncovering and demonstrating that this is an issue – especially for African American women at a young age – and we could make a significant interdiction in terms of risk reduction if we have tools and invest the necessary time and effort, that is the important part of this paper,” Keith Churchwell, MD, Yale New Haven Hospital, and Yale School of Medicine, New Haven, Conn., said in an interview.
“If you’re going to evaluate African Americans in Harlem who are socially disadvantaged, I would want to know if there is a difference between them and other African Americans who have a different socioeconomic status, in terms of atherosclerotic disease,” added Dr. Churchwell, who was not involved with the study.
The Framingham 10-year risk score is “inadequate in assessing CV disease risk in all populations and is not generalizable to non-Whites,” contend Ramdas G. Pai, MD, and Vrinda Vyas, MBBS, of the University of California, Riverside, in an accompanying editorial.
“New data are emerging in favor of imaging-based classification of CV disease risk and has been shown to improve patient adherence to and compliance with risk-modifying interventions,” they write. “Subclinical atherosclerosis may help better stratify CV disease risk so that preventive measures can be instituted to reduce cardiovascular events at a population level.”
Dr. Fuster and coauthors, Dr. Ramdas and Dr. Pai, and Dr. Churchwell report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Non-Hispanic Black young adults in a large, ethnically diverse underserved neighborhood in New York City have about twice the prevalence of subclinical atherosclerosis as Hispanic young adults, according to a new cross-sectional study. It was noteworthy for identifying subclinical cardiovascular (CV) disease in the cohorts using 3D intravascular ultrasound (3D IVUS).
The study’s 436 Black and Hispanic adults, 82% of them women, completed questionnaires regarding nutrition, lifestyle, medical history, weight, blood pressure, cholesterol levels, and other metrics.
(24.5% vs. 9.3%). Overall Framingham scores for 10-year risk for CV events were not statistically different, at 4.6 and 3.6, respectively.
The presence of atherosclerosis in either the carotid or femoral arteries was identified with 3D IVUS in 8.7% of participants. But its prevalence was about twofold greater in Black than in Hispanic participants (12.9% vs. 6.6%), a finding that persisted after multivariable adjustment and appeared driven by a greater prevalence of carotid disease among Black participants (12.9% vs. 4.8%).
“For the same predicted CV risk, non-Hispanic Black individuals appear to be more vulnerable than people of Hispanic origin to early subclinical atherosclerosis, particularly in the carotid arteries, potentially placing them at increased risk of clinical CV disease,” concludes the report published in the Journal of the American College of Cardiology, with lead author Josep Iglesies-Grau, MD, Montreal Heart Institute.
International program
The current analysis from the FAMILIA study is part of a large international project called Science, Health, and Education (SHE), which is designed to promote early intervention in the lives of children, their caretakers, and teachers so they can develop lifelong heart-healthy habits, senior author Valentin Fuster, MD, PhD, physician-in chief, Mount Sinai Hospital, New York, said in an interview.
The SHE program has been presented to more than 50,000 children worldwide, and FAMILIA has delivered successful interventions to more than 500 preschoolers, caretakers, and educators at Head Start schools in the Harlem neighborhood of New York, where the current study was conducted.
The analysis centered on the children’s adult caregivers, of whom one-third were non-Hispanic Black and two-thirds were Hispanic. “We wanted to know if this young population of parents and caregivers [would show] development or initiation of atherosclerotic disease,” Dr. Fuster said, “thinking that when we showed them that they had disease, it would further motivate them to change their lifestyle.”
Participants were assessed for seven basic CV risk factors – hypertension, smoking, body mass index, diabetes, dyslipidemia, low physical activity levels, and poor-quality diet – as well as socioeconomic descriptors. All participants also underwent 3D IVUS to evaluate the presence and extent of atherosclerosis in the carotid and femoral arteries.
‘Expected and unexpected’ findings
Black participants were considerably more likely than their Hispanic counterparts to be hypertensive, to be active smokers, and to have higher BMIs. The Black cohort reported higher consumption of fruits and vegetables (P < .001).
There were no between-group differences in the prevalence of diabetes or in mean fasting glucose or total cholesterol levels.
The mean 10-year Framingham CV risk score across the entire study population was 4.0%, with no significant differences between the two groups. In fact, 89% of participants were classified as low risk on the basis of the score.
The overall prevalence of subclinical atherosclerosis was 8.7%, with a mean global plaque burden of 5.0 mm3. But there were dramatic differences in atherosclerotic burden. Across all 10-year Framingham risk categories, Black participants had twice the odds of having subclinical atherosclerosis as Hispanic participants (odds ratio, 2.11; 95% confidence interval, 1.09-4.08; P = .026).
Black participants also had a greater atherosclerotic disease burden (9.0 mm3 vs. 2.9 mm3), mean total plaque volume (P = .028), and a higher prevalence of disease in both the carotid and femoral arteries (8.2% vs. 3.8%; P = .026).
“Our findings were both expected and completely unexpected,” Dr. Fuster commented. “It was expected that the non-Hispanic Black population would have more hypertension, obesity, and smoking, and might therefore have more [atherosclerotic] disease. But what was unexpected was when we adjusted for the seven risk factors and socioeconomic status, the Black population had three times the amount of disease,” he said.
“We need to take better care of the risk factors already known in the Black population, which is critical.” However, “our challenge today is to identify these new risk factors, which might be genetic or socioeconomic.” Dr. Fuster said his group is “already working with artificial intelligence to identify risk factors beyond the traditional risk factors that are already established.”
Socioeconomic differences?
“The fact that we’re uncovering and demonstrating that this is an issue – especially for African American women at a young age – and we could make a significant interdiction in terms of risk reduction if we have tools and invest the necessary time and effort, that is the important part of this paper,” Keith Churchwell, MD, Yale New Haven Hospital, and Yale School of Medicine, New Haven, Conn., said in an interview.
“If you’re going to evaluate African Americans in Harlem who are socially disadvantaged, I would want to know if there is a difference between them and other African Americans who have a different socioeconomic status, in terms of atherosclerotic disease,” added Dr. Churchwell, who was not involved with the study.
The Framingham 10-year risk score is “inadequate in assessing CV disease risk in all populations and is not generalizable to non-Whites,” contend Ramdas G. Pai, MD, and Vrinda Vyas, MBBS, of the University of California, Riverside, in an accompanying editorial.
“New data are emerging in favor of imaging-based classification of CV disease risk and has been shown to improve patient adherence to and compliance with risk-modifying interventions,” they write. “Subclinical atherosclerosis may help better stratify CV disease risk so that preventive measures can be instituted to reduce cardiovascular events at a population level.”
Dr. Fuster and coauthors, Dr. Ramdas and Dr. Pai, and Dr. Churchwell report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Sleep-deprived physicians less empathetic to patient pain?
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
In the first of two studies, resident physicians were presented with two hypothetical scenarios involving a patient who complains of pain. They were asked about their likelihood of prescribing pain medication. The test was given to one group of residents who were just starting their day and to another group who were at the end of their night shift after being on call for 26 hours.
Results showed that the night shift residents were less likely than their daytime counterparts to say they would prescribe pain medication to the patients.
In further analysis of discharge notes from more than 13,000 electronic records of patients presenting with pain complaints at hospitals in Israel and the United States, the likelihood of an analgesic being prescribed during the night shift was 11% lower in Israel and 9% lower in the United States, compared with the day shift.
“Pain management is a major challenge, and a doctor’s perception of a patient’s subjective pain is susceptible to bias,” coinvestigator David Gozal, MD, the Marie M. and Harry L. Smith Endowed Chair of Child Health, University of Missouri–Columbia, said in a press release.
“This study demonstrated that night shift work is an important and previously unrecognized source of bias in pain management, likely stemming from impaired perception of pain,” Dr. Gozal added.
The findings were published online in the Proceedings of the National Academy of Sciences.
‘Directional’ differences
Senior investigator Alex Gileles-Hillel, MD, senior pediatric pulmonologist and sleep researcher at Hadassah University Medical Center, Jerusalem, said in an interview that physicians must make “complex assessments of patients’ subjective pain experience” – and the “subjective nature of pain management decisions can give rise to various biases.”
Dr. Gileles-Hillel has previously researched the cognitive toll of night shift work on physicians.
“It’s pretty established, for example, not to drive when sleep deprived because cognition is impaired,” he said. The current study explored whether sleep deprivation could affect areas other than cognition, including emotions and empathy.
The researchers used “two complementary approaches.” First, they administered tests to measure empathy and pain management decisions in 67 resident physicians at Hadassah Medical Centers either following a 26-hour night shift that began at 8:00 a.m. the day before (n = 36) or immediately before starting the workday (n = 31).
There were no significant differences in demographic, sleep, or burnout measures between the two groups, except that night shift physicians had slept less than those in the daytime group (2.93 vs. 5.96 hours).
Participants completed two tasks. In the empathy-for-pain task, they rated their emotional reactions to pictures of individuals in pain. In the empathy accuracy task, they were asked to assess the feelings of videotaped individuals telling emotional stories.
They were then presented with two clinical scenarios: a female patient with a headache and a male patient with a backache. Following that, they were asked to assess the magnitude of the patients’ pain and how likely they would be to prescribe pain medication.
In the empathy-for-pain task, physicians’ empathy scores were significantly lower in the night shift group than in the day group (difference, –0.83; 95% CI, –1.55 to –0.10; P = .026). There were no significant differences between the groups in the empathy accuracy task.
In both scenarios, physicians in the night shift group assessed the patient’s pain as weaker in comparison with physicians in the day group. There was a statistically significant difference in the headache scenario but not the backache scenario.
In the headache scenario, the propensity of the physicians to prescribe analgesics was “directionally lower” but did not reach statistical significance. In the backache scenario, there was no significant difference between the groups’ prescribing propensities.
In both scenarios, pain assessment was positively correlated with the propensity to prescribe analgesics.
Despite the lack of statistical significance, the findings “documented a negative effect of night shift work on physician empathy for pain and a positive association between physician assessment of patient pain and the propensity to prescribe analgesics,” the investigators wrote.
Need for naps?
The researchers then analyzed analgesic prescription patterns drawn from three datasets of discharge notes of patients presenting to the emergency department with pain complaints (n = 13,482) at two branches of Hadassah-Hebrew University Medical Center and the University of Missouri Health Center.
The researchers collected data, including discharge time, medications patients were prescribed upon discharge, and patients’ subjective pain rating on a scale of 0-10 on a visual analogue scale (VAS).
Although patients’ VAS scores did not differ with respect to time or shift, patients were discharged with significantly less prescribed analgesics during the night shift in comparison with the day shift.
No similar differences in prescriptions between night shifts and day shifts were found for nonanalgesic medications, such as for diabetes or blood pressure. This suggests “the effect was specific to pain,” Dr. Gileles-Hillel said.
The pattern remained significant after controlling for potential confounders, including patient and physician variables and emergency department characteristics.
In addition, patients seen during night shifts received fewer analgesics, particularly opioids, than recommended by the World Health Organization for pain management.
“The first study enabled us to measure empathy for pain directly and examine our hypothesis in a controlled environment, while the second enabled us to test the implications by examining real-life pain management decisions,” Dr. Gileles-Hillel said.
“Physicians need to be aware of this,” he noted. “I try to be aware when I’m taking calls [at night] that I’m less empathetic to others and I might be more brief or angry with others.”
On a “house management level, perhaps institutions should try to schedule naps either before or during overnight call. A nap might give a boost and reboot not only to cognitive but also to emotional resources,” Dr. Gileles-Hillel added.
Compromised safety
In a comment, Eti Ben Simon, PhD, a postdoctoral fellow at the Center for Human Sleep Science, University of California, Berkeley, called the study “an important contribution to a growing list of studies that reveal how long night shifts reduce overall safety” for both patients and clinicians.
“It’s time to abandon the notion that the human brain can function as normal after being deprived of sleep for 24 hours,” said Dr. Ben Simon, who was not involved with the research.
“This is especially true in medicine, where we trust others to take care of us and feel our pain. These functions are simply not possible without adequate sleep,” she added.
Also commenting, Kannan Ramar, MD, president of the American Academy of Sleep Medicine, suggested that being cognizant of these findings “may help providers to mitigate this bias” of underprescribing pain medications when treating their patients.
Dr. Ramar, who is also a critical care specialist, pulmonologist, and sleep medicine specialist at Mayo Clinic, Rochester, Minn., was not involved with the research.
He noted that “further studies that systematically evaluate this further in a prospective and blinded way will be important.”
The research was supported in part by grants from the Israel Science Foundation, Joy Ventures, the Recanati Fund at the Jerusalem School of Business at the Hebrew University, and a fellowship from the Azrieli Foundation and received grant support to various investigators from the NIH, the Leda J. Sears Foundation, and the University of Missouri. The investigators, Ramar, and Ben Simon have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE PROCEEDINGS OF THE NATIONAL ACADEMY OF SCIENCES
PTSD may accelerate cognitive decline over time
, new research suggests.
In an analysis of more than 12,000 middle-aged women who had experienced at least one trauma in their lives, those with PTSD symptoms showed an approximately twofold faster decline in cognition during follow-up compared with those who did not have PTSD symptoms.
These associations were not fully explained by other known cognition-related factors such as depression, the researchers noted.
“PTSD may increase the risk of dementia by accelerating cognitive decline at midlife,” coinvestigator Jiaxuan Liu, a doctoral candidate at Harvard TH Chan School of Public Health, Boston, said in an interview.
“Our findings may suggest the value of earlier cognitive screening among individuals with PTSD and the importance of PTSD prevention and treatment across the lifespan,” she added.
The results were published online in JAMA Network Open.
Vital public health issue
“Cognitive decline at midlife and older is of vital public health interest,” Ms. Liu said. “It is a risk factor for a variety of poor health outcomes and strongly predicts Alzheimer’s disease and other dementias.
Although PTSD has been linked to lower cognitive function and dementia incidence, it has not been known whether it is associated with decline in cognitive function, she added.
“In addition, both PTSD and dementia are more common in women than men, so it’s important to understand a possible link,” Ms. Liu said.
Because no large-scale study had examined whether PTSD is associated with cognitive decline in women, the current researchers examined PTSD symptoms and their association with repeated measures of cognitive function among a large civilian trauma-exposed cohort of women aged 50-70 years at study baseline.
Participants were drawn from the Nurses’ Health Study II, a longitudinal study of a cohort of 116,429 U.S. female nurses who were between 25 and 42 years old at enrollment in 1989. Participants completed biennial questionnaires, with follow-up on an ongoing basis.
The current analysis included 12,270 trauma-exposed women (mean age at baseline, 61.1 years) who completed assessments every 1 or 12 months for up to 24 months after baseline. The mean follow-up time was 0.9 years.
In the study population, 95.9% were non-Hispanic White, 1.3% were Hispanic, 1% were Asian, 0.6% were Black, and 1.2% were classified as “other.”
Higher depression scores
Lifetime trauma exposure and PTSD symptoms were assessed from March 1, 2008, to Feb. 28, 2010, using the Short Screening Scale for DSM-IV PTSD.
In total, 67% of the participants reported experiencing PTSD symptoms. The women were divided into four groups, on the basis of symptom number: no PTSD symptoms (n = 4,052), one to three PTSD symptoms (n = 5,058), four to five PTSD symptoms (n = 2,018), and six to seven PTSD symptoms (n = 1,052).
The Cogstate Brief Battery, a validated and self-administered online cognitive assessment, was completed by participants between Oct. 3, 2014, and July 30, 2019. The researchers measured cognitive function with two composite scores: psychomotor speed and attention, and learning and working memory.
Covariates potentially associated with cognitive decline included demographic, educational, and behavior-related health factors such as body mass index, physical activity, cigarette smoking, diet quality, and alcohol consumption.
The researchers conducted secondary analyses that adjusted for symptoms and history of depression as well as the consequences of potential practice effects of taking the test multiple times.
Behavior-related health factors “did not substantially differ by PTSD symptom level,” the investigators noted. However, compared with women who did not have PTSD symptoms, those who had such symptoms had higher depressive symptom scores and higher rates of clinician-diagnosed depression.
Both cognitive composite scores improved through the follow-up period, “likely because of practice effects,” the researchers wrote. But after adjusting for practice effects, they found a decline over time in both composite scores.
Dose-related trajectories
Results showed that having more PTSD symptoms was associated with dose-related poorer cognitive trajectories.
After adjustment for demographic characteristics, women with the highest symptom level (six to seven symptoms) had a significantly worse rate of change in both composite domains of learning and working memory (beta = −0.08 SD/y; 95% confidence interval [CI], −0.11 to −0.04 SD/y; P < .001) and of psychomotor speed and attention (beta = −0.05 SD/y; 95% CI, −0.09 to −0.01 SD/y; P = .02) compared with women with no PTSD symptoms.
Women with four to five PTSD symptoms showed a worse rate of change in learning and working memory compared with those who had no symptoms, but not in psychomotor speed and attention. Women with one to three PTSD symptoms had cognitive scores similar to those of women without PTSD symptoms.
Notably, the associations of PTSD with cognitive change remained evident after additional adjustment for behavioral factors and health conditions – and were only “partially attenuated but still evident” after further adjustment for practice effects and comorbid depression, the investigators wrote.
“We thought PTSD might be associated with worse cognitive decline through health behaviors like smoking and alcohol drinking and higher risk of other health conditions like hypertension and depression,” Ms. Liu said.
However, those factors did not account for the current study’s findings, she noted.
“We could not determine why women with PTSD had faster cognitive decline than those without PTSD,” she said.
Ms. Liu suggested that PTSD “may have effects on the brain, such as altering brain structures and affecting brain immune function.” However, more research is needed “to investigate these mechanisms that might underlie the association we found between PTSD and cognitive decline,” she said.
Neurotoxic effect
In a comment, Howard Fillit, MD, cofounder and chief science officer of the Alzheimer’s Drug Discovery Foundation, said, “It is well known that stress is neurotoxic, and PTSD is a particularly serious form of stress.”
Dr. Fillit, clinical professor of geriatric medicine and palliative care, medicine, and neuroscience at Mount Sinai Hospital, New York, was not involved with the study.
“We tend to think of PTSD in postacute settings, such as soldiers returning from war,” he said. “This study contributes to our understanding of the long-term effects of PTSD on cognitive decline, measured objectively over time”
Dr. Fillit noted that an important implication is that, by increasing the risk for cognitive decline, PTSD also increases risk for Alzheimer’s disease. This leads to the “main take-home, which is that PTSD is a risk factor not only for cognitive decline but also for Alzheimer’s and related dementias,” he said.
However, this opens a potential therapeutic approach, Dr. Fillit added.
Because cortisol and other stress hormones drive the stress response, finding ways to block the neurotoxic effects of these hormones “might be a target to prevent cognitive decline and decrease Alzheimer’s disease risk,” he said.
The study was supported by grants from the National Institute of Mental Health and the National Institutes of Health. Ms. Liu and Dr. Fillit report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In an analysis of more than 12,000 middle-aged women who had experienced at least one trauma in their lives, those with PTSD symptoms showed an approximately twofold faster decline in cognition during follow-up compared with those who did not have PTSD symptoms.
These associations were not fully explained by other known cognition-related factors such as depression, the researchers noted.
“PTSD may increase the risk of dementia by accelerating cognitive decline at midlife,” coinvestigator Jiaxuan Liu, a doctoral candidate at Harvard TH Chan School of Public Health, Boston, said in an interview.
“Our findings may suggest the value of earlier cognitive screening among individuals with PTSD and the importance of PTSD prevention and treatment across the lifespan,” she added.
The results were published online in JAMA Network Open.
Vital public health issue
“Cognitive decline at midlife and older is of vital public health interest,” Ms. Liu said. “It is a risk factor for a variety of poor health outcomes and strongly predicts Alzheimer’s disease and other dementias.
Although PTSD has been linked to lower cognitive function and dementia incidence, it has not been known whether it is associated with decline in cognitive function, she added.
“In addition, both PTSD and dementia are more common in women than men, so it’s important to understand a possible link,” Ms. Liu said.
Because no large-scale study had examined whether PTSD is associated with cognitive decline in women, the current researchers examined PTSD symptoms and their association with repeated measures of cognitive function among a large civilian trauma-exposed cohort of women aged 50-70 years at study baseline.
Participants were drawn from the Nurses’ Health Study II, a longitudinal study of a cohort of 116,429 U.S. female nurses who were between 25 and 42 years old at enrollment in 1989. Participants completed biennial questionnaires, with follow-up on an ongoing basis.
The current analysis included 12,270 trauma-exposed women (mean age at baseline, 61.1 years) who completed assessments every 1 or 12 months for up to 24 months after baseline. The mean follow-up time was 0.9 years.
In the study population, 95.9% were non-Hispanic White, 1.3% were Hispanic, 1% were Asian, 0.6% were Black, and 1.2% were classified as “other.”
Higher depression scores
Lifetime trauma exposure and PTSD symptoms were assessed from March 1, 2008, to Feb. 28, 2010, using the Short Screening Scale for DSM-IV PTSD.
In total, 67% of the participants reported experiencing PTSD symptoms. The women were divided into four groups, on the basis of symptom number: no PTSD symptoms (n = 4,052), one to three PTSD symptoms (n = 5,058), four to five PTSD symptoms (n = 2,018), and six to seven PTSD symptoms (n = 1,052).
The Cogstate Brief Battery, a validated and self-administered online cognitive assessment, was completed by participants between Oct. 3, 2014, and July 30, 2019. The researchers measured cognitive function with two composite scores: psychomotor speed and attention, and learning and working memory.
Covariates potentially associated with cognitive decline included demographic, educational, and behavior-related health factors such as body mass index, physical activity, cigarette smoking, diet quality, and alcohol consumption.
The researchers conducted secondary analyses that adjusted for symptoms and history of depression as well as the consequences of potential practice effects of taking the test multiple times.
Behavior-related health factors “did not substantially differ by PTSD symptom level,” the investigators noted. However, compared with women who did not have PTSD symptoms, those who had such symptoms had higher depressive symptom scores and higher rates of clinician-diagnosed depression.
Both cognitive composite scores improved through the follow-up period, “likely because of practice effects,” the researchers wrote. But after adjusting for practice effects, they found a decline over time in both composite scores.
Dose-related trajectories
Results showed that having more PTSD symptoms was associated with dose-related poorer cognitive trajectories.
After adjustment for demographic characteristics, women with the highest symptom level (six to seven symptoms) had a significantly worse rate of change in both composite domains of learning and working memory (beta = −0.08 SD/y; 95% confidence interval [CI], −0.11 to −0.04 SD/y; P < .001) and of psychomotor speed and attention (beta = −0.05 SD/y; 95% CI, −0.09 to −0.01 SD/y; P = .02) compared with women with no PTSD symptoms.
Women with four to five PTSD symptoms showed a worse rate of change in learning and working memory compared with those who had no symptoms, but not in psychomotor speed and attention. Women with one to three PTSD symptoms had cognitive scores similar to those of women without PTSD symptoms.
Notably, the associations of PTSD with cognitive change remained evident after additional adjustment for behavioral factors and health conditions – and were only “partially attenuated but still evident” after further adjustment for practice effects and comorbid depression, the investigators wrote.
“We thought PTSD might be associated with worse cognitive decline through health behaviors like smoking and alcohol drinking and higher risk of other health conditions like hypertension and depression,” Ms. Liu said.
However, those factors did not account for the current study’s findings, she noted.
“We could not determine why women with PTSD had faster cognitive decline than those without PTSD,” she said.
Ms. Liu suggested that PTSD “may have effects on the brain, such as altering brain structures and affecting brain immune function.” However, more research is needed “to investigate these mechanisms that might underlie the association we found between PTSD and cognitive decline,” she said.
Neurotoxic effect
In a comment, Howard Fillit, MD, cofounder and chief science officer of the Alzheimer’s Drug Discovery Foundation, said, “It is well known that stress is neurotoxic, and PTSD is a particularly serious form of stress.”
Dr. Fillit, clinical professor of geriatric medicine and palliative care, medicine, and neuroscience at Mount Sinai Hospital, New York, was not involved with the study.
“We tend to think of PTSD in postacute settings, such as soldiers returning from war,” he said. “This study contributes to our understanding of the long-term effects of PTSD on cognitive decline, measured objectively over time”
Dr. Fillit noted that an important implication is that, by increasing the risk for cognitive decline, PTSD also increases risk for Alzheimer’s disease. This leads to the “main take-home, which is that PTSD is a risk factor not only for cognitive decline but also for Alzheimer’s and related dementias,” he said.
However, this opens a potential therapeutic approach, Dr. Fillit added.
Because cortisol and other stress hormones drive the stress response, finding ways to block the neurotoxic effects of these hormones “might be a target to prevent cognitive decline and decrease Alzheimer’s disease risk,” he said.
The study was supported by grants from the National Institute of Mental Health and the National Institutes of Health. Ms. Liu and Dr. Fillit report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, new research suggests.
In an analysis of more than 12,000 middle-aged women who had experienced at least one trauma in their lives, those with PTSD symptoms showed an approximately twofold faster decline in cognition during follow-up compared with those who did not have PTSD symptoms.
These associations were not fully explained by other known cognition-related factors such as depression, the researchers noted.
“PTSD may increase the risk of dementia by accelerating cognitive decline at midlife,” coinvestigator Jiaxuan Liu, a doctoral candidate at Harvard TH Chan School of Public Health, Boston, said in an interview.
“Our findings may suggest the value of earlier cognitive screening among individuals with PTSD and the importance of PTSD prevention and treatment across the lifespan,” she added.
The results were published online in JAMA Network Open.
Vital public health issue
“Cognitive decline at midlife and older is of vital public health interest,” Ms. Liu said. “It is a risk factor for a variety of poor health outcomes and strongly predicts Alzheimer’s disease and other dementias.
Although PTSD has been linked to lower cognitive function and dementia incidence, it has not been known whether it is associated with decline in cognitive function, she added.
“In addition, both PTSD and dementia are more common in women than men, so it’s important to understand a possible link,” Ms. Liu said.
Because no large-scale study had examined whether PTSD is associated with cognitive decline in women, the current researchers examined PTSD symptoms and their association with repeated measures of cognitive function among a large civilian trauma-exposed cohort of women aged 50-70 years at study baseline.
Participants were drawn from the Nurses’ Health Study II, a longitudinal study of a cohort of 116,429 U.S. female nurses who were between 25 and 42 years old at enrollment in 1989. Participants completed biennial questionnaires, with follow-up on an ongoing basis.
The current analysis included 12,270 trauma-exposed women (mean age at baseline, 61.1 years) who completed assessments every 1 or 12 months for up to 24 months after baseline. The mean follow-up time was 0.9 years.
In the study population, 95.9% were non-Hispanic White, 1.3% were Hispanic, 1% were Asian, 0.6% were Black, and 1.2% were classified as “other.”
Higher depression scores
Lifetime trauma exposure and PTSD symptoms were assessed from March 1, 2008, to Feb. 28, 2010, using the Short Screening Scale for DSM-IV PTSD.
In total, 67% of the participants reported experiencing PTSD symptoms. The women were divided into four groups, on the basis of symptom number: no PTSD symptoms (n = 4,052), one to three PTSD symptoms (n = 5,058), four to five PTSD symptoms (n = 2,018), and six to seven PTSD symptoms (n = 1,052).
The Cogstate Brief Battery, a validated and self-administered online cognitive assessment, was completed by participants between Oct. 3, 2014, and July 30, 2019. The researchers measured cognitive function with two composite scores: psychomotor speed and attention, and learning and working memory.
Covariates potentially associated with cognitive decline included demographic, educational, and behavior-related health factors such as body mass index, physical activity, cigarette smoking, diet quality, and alcohol consumption.
The researchers conducted secondary analyses that adjusted for symptoms and history of depression as well as the consequences of potential practice effects of taking the test multiple times.
Behavior-related health factors “did not substantially differ by PTSD symptom level,” the investigators noted. However, compared with women who did not have PTSD symptoms, those who had such symptoms had higher depressive symptom scores and higher rates of clinician-diagnosed depression.
Both cognitive composite scores improved through the follow-up period, “likely because of practice effects,” the researchers wrote. But after adjusting for practice effects, they found a decline over time in both composite scores.
Dose-related trajectories
Results showed that having more PTSD symptoms was associated with dose-related poorer cognitive trajectories.
After adjustment for demographic characteristics, women with the highest symptom level (six to seven symptoms) had a significantly worse rate of change in both composite domains of learning and working memory (beta = −0.08 SD/y; 95% confidence interval [CI], −0.11 to −0.04 SD/y; P < .001) and of psychomotor speed and attention (beta = −0.05 SD/y; 95% CI, −0.09 to −0.01 SD/y; P = .02) compared with women with no PTSD symptoms.
Women with four to five PTSD symptoms showed a worse rate of change in learning and working memory compared with those who had no symptoms, but not in psychomotor speed and attention. Women with one to three PTSD symptoms had cognitive scores similar to those of women without PTSD symptoms.
Notably, the associations of PTSD with cognitive change remained evident after additional adjustment for behavioral factors and health conditions – and were only “partially attenuated but still evident” after further adjustment for practice effects and comorbid depression, the investigators wrote.
“We thought PTSD might be associated with worse cognitive decline through health behaviors like smoking and alcohol drinking and higher risk of other health conditions like hypertension and depression,” Ms. Liu said.
However, those factors did not account for the current study’s findings, she noted.
“We could not determine why women with PTSD had faster cognitive decline than those without PTSD,” she said.
Ms. Liu suggested that PTSD “may have effects on the brain, such as altering brain structures and affecting brain immune function.” However, more research is needed “to investigate these mechanisms that might underlie the association we found between PTSD and cognitive decline,” she said.
Neurotoxic effect
In a comment, Howard Fillit, MD, cofounder and chief science officer of the Alzheimer’s Drug Discovery Foundation, said, “It is well known that stress is neurotoxic, and PTSD is a particularly serious form of stress.”
Dr. Fillit, clinical professor of geriatric medicine and palliative care, medicine, and neuroscience at Mount Sinai Hospital, New York, was not involved with the study.
“We tend to think of PTSD in postacute settings, such as soldiers returning from war,” he said. “This study contributes to our understanding of the long-term effects of PTSD on cognitive decline, measured objectively over time”
Dr. Fillit noted that an important implication is that, by increasing the risk for cognitive decline, PTSD also increases risk for Alzheimer’s disease. This leads to the “main take-home, which is that PTSD is a risk factor not only for cognitive decline but also for Alzheimer’s and related dementias,” he said.
However, this opens a potential therapeutic approach, Dr. Fillit added.
Because cortisol and other stress hormones drive the stress response, finding ways to block the neurotoxic effects of these hormones “might be a target to prevent cognitive decline and decrease Alzheimer’s disease risk,” he said.
The study was supported by grants from the National Institute of Mental Health and the National Institutes of Health. Ms. Liu and Dr. Fillit report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Physicians react: Compensation isn’t worth the hassles. What’s the solution?
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
How satisfied are physicians that they are fairly compensated for their dedication, skills, and time? That’s a subject that seems to steer many physicians to heated emotions and to a variety of issues with today’s medical field – not all of which directly affect their pay.
Medscape’s Physician Compensation Report 2022: “Incomes Gain, Pay Gaps Remain” generally shows encouraging trends. Physician income rose from a year earlier, when it stagnated as COVID-19 restrictions led patients to stay home and medical practices to cut hours or close. And for the first time in Medscape’s 11 years of reporting on physician compensation, average income rose for every medical specialty surveyed.
Heartening findings, right? Yet the tone of comments to the report was anything but peppy. One physician even complained his plumber earns more than he does.
A family physician lamented that he has “made less in the past 3 years, with more hassles and work” and he “can’t wait to retire next year.” Meanwhile, he complained, the U.S. health system is “the costliest, yet wasteful, with worse outcomes; reactive, not preventative; and has the costliest drugs and social issues.”
Do NPs and PAs encroach on your income?
The conversation about fair compensation launched some commenters into a discussion about competition from nurse practitioners (NPs) and physician assistants (PAs). Some physicians expressed wariness at best, and anger at worst, about NPs and PAs evolving beyond traditional doctor support roles into certain direct patient support.
One-fourth of respondents in the compensation report said their income was negatively affected by competition from NPs, PAs, and other nonphysician providers. For example, with states like Arkansas expanding independent practice for certified registered nurse anesthetists (CRNAs), one commenter complained, “we are no longer needed.”
Added another physician, “primary care, especially internal medicine, is just going away for doctors. We wasted, by all accounts, 4 full years of our working lives because NPs are ‘just as good.’ ”
Greater independence for NPs and PAs strengthens the hands of health insurers and “will end up hastening the demise of primary care as we have known it,” another reader predicted. Other physicians’ takes: “For the institution, it’s much cheaper to hire NPs than to hire doctors” and “overall, physician negotiating power will decrease in the future.”
Medicare reimbursement rates grate
Although 7 in 10 respondents in the compensation report said they would continue to accept new Medicare or Medicaid patients, comments reveal resentment about the practical need to work with Medicare and its resentment rates.
“An open question to Medicare: Are you doing the dumbest thing possible by paying low wages and giving huge administrative burdens for internal medicine on purpose?” one physician wrote. “Or are you really that short-sighted?”
Another reader cited an analysis from the American College of Surgeons of Medicare’s 1998 surgical CPT codes. If Medicare had left those codes alone beyond annual inflation adjustments, the study found, reimbursement rates by 2019 would be half of what they became.
Another way of looking at the code reimbursement increases is a 50% pay cut over 20 years for doctors and medical practices, that reader insisted. “The rising cost of employee wages, particularly of the last two-and-a-half years of COVID-19, combined with the effective pay cuts over the last 20 years, equals time to quit!”
Another commenter concurred. “In the 1990s, most full-time docs were making almost double what you see [in the report], and everything cost almost half of what it does now. So, MD purchasing power is between half and one-quarter of what it was in the early 1990s.”
Are self-pay models better?
Do physicians have a better chance at consistently fair income under a self-pay practice that avoids dealing with insurance companies?
One commenter hypothesized that psychiatrists once trailed internists in income but today earn more because many “quit working for insurance and went to a cash business 15 years ago.” Many family physicians did something similar by switching to a direct primary care model, he said.
This physician said he has done the same “with great results” for patients as well: shorter office visits, faster booking of appointments, no deductibles owed. Best of all, “I love practicing medicine again, and my patients love the great health care they receive.”
Another commenter agreed. “Two words: cash practice.” But another objected, “I guess only the very rich can afford to cover your business costs.”
Regardless of the payment model, another physician argued for private practice over employed positions. “Save on the bureaucratic expenses. Go back to private practice and get rid of electronic records.”
A version of this article first appeared on Medscape.com.
Transdermal med may directly target hostility in schizophrenia
The results suggest that these effects are at least partially independent of general antipsychotic effects or effects on sedation or akathisia.
“It’s important not to assume that antipsychotics decrease hostility by having people feel more sedated and that the only way to treat someone hostile is by sedating them,” lead investigator Leslie Citrome, MD, MPH, clinical professor of psychiatry and behavioral sciences, New York Medical College, Valhalla, told this news organization.
“Our findings suggest that transdermal asenapine has a specific antihostility effect in patients with schizophrenia,” he added.
The study was published online in the Journal of Clinical Psychiatry.
A complex disorder
“Patients with schizophrenia are known to potentially exhibit aggressive, hostile behavior, especially during the acute phase of the illness, thus making effective management critical,” the authors write.
Dr. Citrome said schizophrenia is a complex condition that consists of five different symptom domains. These include positive (hallucinations, delusions), negative (amotivation, apathy), disorganization (cognitive symptoms), depression/anxiety, and excitability/hostility symptoms.
“These five domains are more or less independent of each other, in terms of treatment effects,” he noted.
Dr. Citrome has long been interested in the activity of antipsychotics and their impact on these various symptoms – particularly hostility – and recently published a review focusing on the impact of an array of antipsychotics on this symptom domain.
“What struck me here is that this is a transdermal system, a patch,” Dr. Citrome said. “None of the sedation that would ordinarily be associated with a sublingual asenapine would be present here.”
Dr. Citrome wanted to investigate whether the transdermal system would have an impact on hostility because, if so, “it would support the notion that hostility is an independent treatment target in schizophrenia.”
To investigate, Dr. Citrome and co-authors analyzed data from the pivotal HP-3070 phase 3 randomized, double-blind, placebo-controlled study of adults with schizophrenia who were randomly selected to receive either HP-3070 7.6 mg/24h, HP-3070 3.8 mg/24h, or placebo for 6 weeks.
The trial found that once-daily applications of HP-3070 demonstrated significant improvement in Positive and Negative Syndrome Scale (PANSS) total scores after 2-3 weeks of treatment, with the improvements sustained through week 6.
The current study was a post hoc analysis focusing specifically on 442 patients with hostility and agitation (defined as PANSS hostility item score > 1).
The outcome was the least-squares mean (LSM) changes in the PANSS hostility item. They also analyzed PANSS–Excited Component (PANSS-EC) from baseline to week 6 in all study participants. Findings were adjusted for the presence of somnolence or akathisia.
Demographic and baseline disease characteristics were “balanced” between the HP-3070–6.6-mg and the HP-3070–3.8-mg groups (n = 151 and n = 147, respectively) and the placebo group (n = 144) in the intent-to-treat analysis, with a mean (standard deviation) age of between 41.5 and 42.3 (11.6-11.9) years. Roughly three-quarters of participants were White, and most participants had a mean duration of between 15 and 16 years since diagnosis.
Independent effect
At week 6, the LSM mean change from baseline (CFB) in the PANSS hostility score was superior in both treatment groups at 6 weeks, compared with placebo (7.6 mg/24 hr: CFB, –0.4; 95% confidence interval, –0.6 to –0.2; P < .001; 3.8 mg/24 hr: CFB, –0.3; 95% CI, –0.6 to –0.1; P < .01).
The findings remained significant, even after the researchers adjusted for covariates.
For all patients, regardless of baseline PANSS hostility item score, PANSS-EC week 6 LSM CFB was greater in both treatment groups compared with placebo (7.6 mg/24 hr: CFB, –1.1; 95% CI, –1.9 to –0.4; P < .01; 3.8 mg/24 hr: CFB, –1.3; 95% CI, –2.0 to –0.6; P < .001).
Patients with a PANSS hostility score > 1 at baseline in both treatment groups also showed significant improvement in PANSS-EC score, compared with the placebo, beginning at week 2 and continuing through week 6.
“These effects of HP-3070 treatment on the PANSS hostility item score remained, even after adjustment for confounding variables, suggesting that the effect of HP-3070 on reducing symptoms of hostility may at be at least partially independent of general antipsychotic effects on hallucinations or delusions or the presence or absence of relevant medication-induced adverse effects, such as sedation or akathisia,” the authors comment.
They note that a limitation of the study is that it was conducted post hoc. In addition, the mean baseline PANSS hostility score was “low,” even among those with a score > 1, “translating to a severity level of minimal to mild,” which “limits the generalizability” of the analysis.
Important treatment target
Commenting on the study, Rifaat El-Mallakh, MD, MS, director of the Mood Disorders Research Program, department of psychiatry and behavioral sciences, University of Louisville (Ky.) School of Medicine, said, “aggression and hostility may exhibit themselves as symptoms of a psychotic illness or independent of psychosis and are an important treatment target.”
Dr. El-Mallakh, who was not involved with the study, said the “most effective anti-aggression medicine is clozapine.” He believes that it is this effect that “gives clozapine its stellar reputation,” rather than its antipsychotic effect.
“Of importance, the anti-aggression effect of clozapine is independent of its antipsychotic effect, which is an important point because if the behavior is rooted in psychosis, then successful treatment of psychosis with any agent should reduce aggression.”
The researchers “demonstrated that the effect was independent of psychosis” but because the study only recruited people with schizophrenia, the researchers “could not examine to see if the effect is independent of diagnosis,” Dr. El-Mallakh said.
“It is important to consider aggression/hostility as an independent behavior in pharmacologic studies, because it probably has its own biochemistry and neuroanatomy,” he added.
This study was funded by Hisamitsu Pharmaceutical. Dr. Citrome has received nonfinancial support from Hisamitsu Pharmaceutical and personal fees from Noven Pharmaceuticals during the conduct of the study; personal fees from numerous companies and organizations; and one-off ad hoc consulting for medical education companies such as Medscape, NACCME, NEI, Vindico, and universities and professional organizations/societies outside the submitted work. He has stocks and received royalties from numerous companies and organizations. Dr. El-Mallakh is a speaker for Noven, as well as Indivior, Intracellular, Janssen, Lundbeck, Otsuka, Sunovion, and Teva.
A version of this article first appeared on Medscape.com.
The results suggest that these effects are at least partially independent of general antipsychotic effects or effects on sedation or akathisia.
“It’s important not to assume that antipsychotics decrease hostility by having people feel more sedated and that the only way to treat someone hostile is by sedating them,” lead investigator Leslie Citrome, MD, MPH, clinical professor of psychiatry and behavioral sciences, New York Medical College, Valhalla, told this news organization.
“Our findings suggest that transdermal asenapine has a specific antihostility effect in patients with schizophrenia,” he added.
The study was published online in the Journal of Clinical Psychiatry.
A complex disorder
“Patients with schizophrenia are known to potentially exhibit aggressive, hostile behavior, especially during the acute phase of the illness, thus making effective management critical,” the authors write.
Dr. Citrome said schizophrenia is a complex condition that consists of five different symptom domains. These include positive (hallucinations, delusions), negative (amotivation, apathy), disorganization (cognitive symptoms), depression/anxiety, and excitability/hostility symptoms.
“These five domains are more or less independent of each other, in terms of treatment effects,” he noted.
Dr. Citrome has long been interested in the activity of antipsychotics and their impact on these various symptoms – particularly hostility – and recently published a review focusing on the impact of an array of antipsychotics on this symptom domain.
“What struck me here is that this is a transdermal system, a patch,” Dr. Citrome said. “None of the sedation that would ordinarily be associated with a sublingual asenapine would be present here.”
Dr. Citrome wanted to investigate whether the transdermal system would have an impact on hostility because, if so, “it would support the notion that hostility is an independent treatment target in schizophrenia.”
To investigate, Dr. Citrome and co-authors analyzed data from the pivotal HP-3070 phase 3 randomized, double-blind, placebo-controlled study of adults with schizophrenia who were randomly selected to receive either HP-3070 7.6 mg/24h, HP-3070 3.8 mg/24h, or placebo for 6 weeks.
The trial found that once-daily applications of HP-3070 demonstrated significant improvement in Positive and Negative Syndrome Scale (PANSS) total scores after 2-3 weeks of treatment, with the improvements sustained through week 6.
The current study was a post hoc analysis focusing specifically on 442 patients with hostility and agitation (defined as PANSS hostility item score > 1).
The outcome was the least-squares mean (LSM) changes in the PANSS hostility item. They also analyzed PANSS–Excited Component (PANSS-EC) from baseline to week 6 in all study participants. Findings were adjusted for the presence of somnolence or akathisia.
Demographic and baseline disease characteristics were “balanced” between the HP-3070–6.6-mg and the HP-3070–3.8-mg groups (n = 151 and n = 147, respectively) and the placebo group (n = 144) in the intent-to-treat analysis, with a mean (standard deviation) age of between 41.5 and 42.3 (11.6-11.9) years. Roughly three-quarters of participants were White, and most participants had a mean duration of between 15 and 16 years since diagnosis.
Independent effect
At week 6, the LSM mean change from baseline (CFB) in the PANSS hostility score was superior in both treatment groups at 6 weeks, compared with placebo (7.6 mg/24 hr: CFB, –0.4; 95% confidence interval, –0.6 to –0.2; P < .001; 3.8 mg/24 hr: CFB, –0.3; 95% CI, –0.6 to –0.1; P < .01).
The findings remained significant, even after the researchers adjusted for covariates.
For all patients, regardless of baseline PANSS hostility item score, PANSS-EC week 6 LSM CFB was greater in both treatment groups compared with placebo (7.6 mg/24 hr: CFB, –1.1; 95% CI, –1.9 to –0.4; P < .01; 3.8 mg/24 hr: CFB, –1.3; 95% CI, –2.0 to –0.6; P < .001).
Patients with a PANSS hostility score > 1 at baseline in both treatment groups also showed significant improvement in PANSS-EC score, compared with the placebo, beginning at week 2 and continuing through week 6.
“These effects of HP-3070 treatment on the PANSS hostility item score remained, even after adjustment for confounding variables, suggesting that the effect of HP-3070 on reducing symptoms of hostility may at be at least partially independent of general antipsychotic effects on hallucinations or delusions or the presence or absence of relevant medication-induced adverse effects, such as sedation or akathisia,” the authors comment.
They note that a limitation of the study is that it was conducted post hoc. In addition, the mean baseline PANSS hostility score was “low,” even among those with a score > 1, “translating to a severity level of minimal to mild,” which “limits the generalizability” of the analysis.
Important treatment target
Commenting on the study, Rifaat El-Mallakh, MD, MS, director of the Mood Disorders Research Program, department of psychiatry and behavioral sciences, University of Louisville (Ky.) School of Medicine, said, “aggression and hostility may exhibit themselves as symptoms of a psychotic illness or independent of psychosis and are an important treatment target.”
Dr. El-Mallakh, who was not involved with the study, said the “most effective anti-aggression medicine is clozapine.” He believes that it is this effect that “gives clozapine its stellar reputation,” rather than its antipsychotic effect.
“Of importance, the anti-aggression effect of clozapine is independent of its antipsychotic effect, which is an important point because if the behavior is rooted in psychosis, then successful treatment of psychosis with any agent should reduce aggression.”
The researchers “demonstrated that the effect was independent of psychosis” but because the study only recruited people with schizophrenia, the researchers “could not examine to see if the effect is independent of diagnosis,” Dr. El-Mallakh said.
“It is important to consider aggression/hostility as an independent behavior in pharmacologic studies, because it probably has its own biochemistry and neuroanatomy,” he added.
This study was funded by Hisamitsu Pharmaceutical. Dr. Citrome has received nonfinancial support from Hisamitsu Pharmaceutical and personal fees from Noven Pharmaceuticals during the conduct of the study; personal fees from numerous companies and organizations; and one-off ad hoc consulting for medical education companies such as Medscape, NACCME, NEI, Vindico, and universities and professional organizations/societies outside the submitted work. He has stocks and received royalties from numerous companies and organizations. Dr. El-Mallakh is a speaker for Noven, as well as Indivior, Intracellular, Janssen, Lundbeck, Otsuka, Sunovion, and Teva.
A version of this article first appeared on Medscape.com.
The results suggest that these effects are at least partially independent of general antipsychotic effects or effects on sedation or akathisia.
“It’s important not to assume that antipsychotics decrease hostility by having people feel more sedated and that the only way to treat someone hostile is by sedating them,” lead investigator Leslie Citrome, MD, MPH, clinical professor of psychiatry and behavioral sciences, New York Medical College, Valhalla, told this news organization.
“Our findings suggest that transdermal asenapine has a specific antihostility effect in patients with schizophrenia,” he added.
The study was published online in the Journal of Clinical Psychiatry.
A complex disorder
“Patients with schizophrenia are known to potentially exhibit aggressive, hostile behavior, especially during the acute phase of the illness, thus making effective management critical,” the authors write.
Dr. Citrome said schizophrenia is a complex condition that consists of five different symptom domains. These include positive (hallucinations, delusions), negative (amotivation, apathy), disorganization (cognitive symptoms), depression/anxiety, and excitability/hostility symptoms.
“These five domains are more or less independent of each other, in terms of treatment effects,” he noted.
Dr. Citrome has long been interested in the activity of antipsychotics and their impact on these various symptoms – particularly hostility – and recently published a review focusing on the impact of an array of antipsychotics on this symptom domain.
“What struck me here is that this is a transdermal system, a patch,” Dr. Citrome said. “None of the sedation that would ordinarily be associated with a sublingual asenapine would be present here.”
Dr. Citrome wanted to investigate whether the transdermal system would have an impact on hostility because, if so, “it would support the notion that hostility is an independent treatment target in schizophrenia.”
To investigate, Dr. Citrome and co-authors analyzed data from the pivotal HP-3070 phase 3 randomized, double-blind, placebo-controlled study of adults with schizophrenia who were randomly selected to receive either HP-3070 7.6 mg/24h, HP-3070 3.8 mg/24h, or placebo for 6 weeks.
The trial found that once-daily applications of HP-3070 demonstrated significant improvement in Positive and Negative Syndrome Scale (PANSS) total scores after 2-3 weeks of treatment, with the improvements sustained through week 6.
The current study was a post hoc analysis focusing specifically on 442 patients with hostility and agitation (defined as PANSS hostility item score > 1).
The outcome was the least-squares mean (LSM) changes in the PANSS hostility item. They also analyzed PANSS–Excited Component (PANSS-EC) from baseline to week 6 in all study participants. Findings were adjusted for the presence of somnolence or akathisia.
Demographic and baseline disease characteristics were “balanced” between the HP-3070–6.6-mg and the HP-3070–3.8-mg groups (n = 151 and n = 147, respectively) and the placebo group (n = 144) in the intent-to-treat analysis, with a mean (standard deviation) age of between 41.5 and 42.3 (11.6-11.9) years. Roughly three-quarters of participants were White, and most participants had a mean duration of between 15 and 16 years since diagnosis.
Independent effect
At week 6, the LSM mean change from baseline (CFB) in the PANSS hostility score was superior in both treatment groups at 6 weeks, compared with placebo (7.6 mg/24 hr: CFB, –0.4; 95% confidence interval, –0.6 to –0.2; P < .001; 3.8 mg/24 hr: CFB, –0.3; 95% CI, –0.6 to –0.1; P < .01).
The findings remained significant, even after the researchers adjusted for covariates.
For all patients, regardless of baseline PANSS hostility item score, PANSS-EC week 6 LSM CFB was greater in both treatment groups compared with placebo (7.6 mg/24 hr: CFB, –1.1; 95% CI, –1.9 to –0.4; P < .01; 3.8 mg/24 hr: CFB, –1.3; 95% CI, –2.0 to –0.6; P < .001).
Patients with a PANSS hostility score > 1 at baseline in both treatment groups also showed significant improvement in PANSS-EC score, compared with the placebo, beginning at week 2 and continuing through week 6.
“These effects of HP-3070 treatment on the PANSS hostility item score remained, even after adjustment for confounding variables, suggesting that the effect of HP-3070 on reducing symptoms of hostility may at be at least partially independent of general antipsychotic effects on hallucinations or delusions or the presence or absence of relevant medication-induced adverse effects, such as sedation or akathisia,” the authors comment.
They note that a limitation of the study is that it was conducted post hoc. In addition, the mean baseline PANSS hostility score was “low,” even among those with a score > 1, “translating to a severity level of minimal to mild,” which “limits the generalizability” of the analysis.
Important treatment target
Commenting on the study, Rifaat El-Mallakh, MD, MS, director of the Mood Disorders Research Program, department of psychiatry and behavioral sciences, University of Louisville (Ky.) School of Medicine, said, “aggression and hostility may exhibit themselves as symptoms of a psychotic illness or independent of psychosis and are an important treatment target.”
Dr. El-Mallakh, who was not involved with the study, said the “most effective anti-aggression medicine is clozapine.” He believes that it is this effect that “gives clozapine its stellar reputation,” rather than its antipsychotic effect.
“Of importance, the anti-aggression effect of clozapine is independent of its antipsychotic effect, which is an important point because if the behavior is rooted in psychosis, then successful treatment of psychosis with any agent should reduce aggression.”
The researchers “demonstrated that the effect was independent of psychosis” but because the study only recruited people with schizophrenia, the researchers “could not examine to see if the effect is independent of diagnosis,” Dr. El-Mallakh said.
“It is important to consider aggression/hostility as an independent behavior in pharmacologic studies, because it probably has its own biochemistry and neuroanatomy,” he added.
This study was funded by Hisamitsu Pharmaceutical. Dr. Citrome has received nonfinancial support from Hisamitsu Pharmaceutical and personal fees from Noven Pharmaceuticals during the conduct of the study; personal fees from numerous companies and organizations; and one-off ad hoc consulting for medical education companies such as Medscape, NACCME, NEI, Vindico, and universities and professional organizations/societies outside the submitted work. He has stocks and received royalties from numerous companies and organizations. Dr. El-Mallakh is a speaker for Noven, as well as Indivior, Intracellular, Janssen, Lundbeck, Otsuka, Sunovion, and Teva.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
New light on why some psych patients don’t respond to therapy
Although most psychiatrists have encountered patients who don’t improve with treatment, novel research sheds some light on one possible explanation for this phenomenon.
Investigators found that among
“To the best of my knowledge, this subject hasn’t been written about or explored before because we operate under the assumption that someone coming for ambulatory treatment, of course, wants to get better and thinks that they deserve to get better,” lead author Mark Zimmerman, MD, professor of psychiatry and human behavior at Brown University, Providence, R.I., said in an interview.
“This issue is not something complicated that a clinician would need to explore by administering some scale or clinical rating instrument. All you have to do is ask patients if they think they deserve to get better, particularly patients who seem to be ‘stuck,’ and explore what’s underlying that belief,” added Zimmerman, who is also the director of the Outpatient Division at the partial hospital program, Rhode Island Hospital, Providence.
The findings were published online in the Journal of Clinical Psychiatry.
Obstacle to therapy
Results from a study examining the prevalence of this belief in more than 400 patients admitted to a partial hospital program showed that 17% of the participants either did not believe they deserved to get better or weren’t sure if they deserved to get better.
When compared with their peers, patients who felt they were undeserving were significantly less likely to complete the treatment program and missed significantly more days of treatment while in the program.
Of the patients who did complete the program, those who believed they were undeserving were in treatment for significantly longer periods of time than those who believed they deserved to get better.
The average length of stay for patients in the partial hospital program is usually about 2 weeks, the investigators note. However, a minority of patients end up in treatment for more than a month and during this prolonged period, some do not seem to improve in their symptoms or functioning despite “intensive psychotherapy and ongoing pharmacotherapy.”
The researchers wanted to understand the reasons for some patients’ lack of progress and examined whether those who did not believe they were worthy of getting better actually took longer to respond to treatment.
In the current research, Dr. Zimmerman wanted to focus on these patients and assess whether they did take longer to improve and what diagnoses might be associated with feeling undeserving.
Of the 405 patients in the study, the majority (83%) reported they believed they deserved to get better, 12.8% said they were unsure, and 4.2% reported they did not believe they deserved to get better.
The researchers combined those who were unsure and those who did not believe they deserved to get better and compared them with patients who believed they did deserve to get better.
Although there were no differences between these patients in gender, race, or marital status, those who did not believe they deserved to get better were significantly younger than their counterparts who believed they deserved to get better (mean age, 32.2 years vs. 37.7 years, respectively; P < .01).
They also were diagnosed with a greater number of disorders at the time of the evaluation (mean, 3.6 vs. 2.9; P < .01).
Mirrors clinical experience
Participants who did not indicate they deserved to get better were significantly more often diagnosed with several conditions, compared with their counterparts who indicated they did deserve to get better:
- Major depressive disorder (MDD): 75.4% vs. 53.3%, respectively; P < .01.
- Panic disorder: 36.2% vs. 23.2%; P < .05.
- Agoraphobia: 27.5% vs. 11.6%; P < .01.
- Obsessive-compulsive disorder (OCD): 14.5% vs. 4.5%; P < .01.
- Posttraumatic stress disorder: 44.9% vs. 25.9%; P < .01.
- Borderline personality disorder: 29.0% vs. 17.9%; P < .05.
There were also significant differences between those who did not vs, did believe they deserved to get better in program completion (52.3% vs. 68.8%, respectively; P < .01), missed days (mean, 1.7 vs. 1.3; P < .05), and length of treatment (mean days, 14.1 vs. 11.8; P < .05).
Dr. Zimmerman called these preliminary findings “consistent” with his clinical experience.
He noted he was “surprised” that OCD had the highest odds ratio (OR, 3.5) of being associated with a sense of undeservingness. “But when I thought about it, I realized that it makes sense because people with OCD have insight and are often embarrassed by their symptoms,” he added.
Dr. Zimmerman was not surprised that MDD was associated with this sense of undeservingness. A second study currently under review is focusing specifically on MDD.
“One of the things we found, not surprisingly, was that some of the cognitive symptoms of depression, such as guilt and sense of worthlessness, are associated with it,” he said.
‘Snapshot in time’
Commenting for this news organization, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called this a “novel, important, and creative study.”
The “hypothesized role of shame squares with my experience. And the association with OCD, depression, and trauma are also consistent with what I have seen,” said Dr. Duckworth, who is also an assistant clinical professor at Harvard Medical School, Boston. He was not involved with the current research.
“The role of hopelessness, often seen as a core feature of depression and to some extent OCD and trauma, is an opportunity to see if treatments like cognitive-behavioral therapy [CBT] can make a difference. How to engage people in CBT, which works directly at changing one’s automatic negative thoughts, is important,” Dr. Duckworth said.
Describing the study as a “snapshot in time,” he noted it would be interesting to follow patients longitudinally.
“I think a whole subset would look back and say, ‘I remember feeling [undeserving] but now that I’ve gotten medication or CBT or therapy, I’m happy I got better,’” said Dr. Duckworth.
No source of study funding was listed. Dr. Zimmerman, his coauthor, and Dr. Duckworth report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although most psychiatrists have encountered patients who don’t improve with treatment, novel research sheds some light on one possible explanation for this phenomenon.
Investigators found that among
“To the best of my knowledge, this subject hasn’t been written about or explored before because we operate under the assumption that someone coming for ambulatory treatment, of course, wants to get better and thinks that they deserve to get better,” lead author Mark Zimmerman, MD, professor of psychiatry and human behavior at Brown University, Providence, R.I., said in an interview.
“This issue is not something complicated that a clinician would need to explore by administering some scale or clinical rating instrument. All you have to do is ask patients if they think they deserve to get better, particularly patients who seem to be ‘stuck,’ and explore what’s underlying that belief,” added Zimmerman, who is also the director of the Outpatient Division at the partial hospital program, Rhode Island Hospital, Providence.
The findings were published online in the Journal of Clinical Psychiatry.
Obstacle to therapy
Results from a study examining the prevalence of this belief in more than 400 patients admitted to a partial hospital program showed that 17% of the participants either did not believe they deserved to get better or weren’t sure if they deserved to get better.
When compared with their peers, patients who felt they were undeserving were significantly less likely to complete the treatment program and missed significantly more days of treatment while in the program.
Of the patients who did complete the program, those who believed they were undeserving were in treatment for significantly longer periods of time than those who believed they deserved to get better.
The average length of stay for patients in the partial hospital program is usually about 2 weeks, the investigators note. However, a minority of patients end up in treatment for more than a month and during this prolonged period, some do not seem to improve in their symptoms or functioning despite “intensive psychotherapy and ongoing pharmacotherapy.”
The researchers wanted to understand the reasons for some patients’ lack of progress and examined whether those who did not believe they were worthy of getting better actually took longer to respond to treatment.
In the current research, Dr. Zimmerman wanted to focus on these patients and assess whether they did take longer to improve and what diagnoses might be associated with feeling undeserving.
Of the 405 patients in the study, the majority (83%) reported they believed they deserved to get better, 12.8% said they were unsure, and 4.2% reported they did not believe they deserved to get better.
The researchers combined those who were unsure and those who did not believe they deserved to get better and compared them with patients who believed they did deserve to get better.
Although there were no differences between these patients in gender, race, or marital status, those who did not believe they deserved to get better were significantly younger than their counterparts who believed they deserved to get better (mean age, 32.2 years vs. 37.7 years, respectively; P < .01).
They also were diagnosed with a greater number of disorders at the time of the evaluation (mean, 3.6 vs. 2.9; P < .01).
Mirrors clinical experience
Participants who did not indicate they deserved to get better were significantly more often diagnosed with several conditions, compared with their counterparts who indicated they did deserve to get better:
- Major depressive disorder (MDD): 75.4% vs. 53.3%, respectively; P < .01.
- Panic disorder: 36.2% vs. 23.2%; P < .05.
- Agoraphobia: 27.5% vs. 11.6%; P < .01.
- Obsessive-compulsive disorder (OCD): 14.5% vs. 4.5%; P < .01.
- Posttraumatic stress disorder: 44.9% vs. 25.9%; P < .01.
- Borderline personality disorder: 29.0% vs. 17.9%; P < .05.
There were also significant differences between those who did not vs, did believe they deserved to get better in program completion (52.3% vs. 68.8%, respectively; P < .01), missed days (mean, 1.7 vs. 1.3; P < .05), and length of treatment (mean days, 14.1 vs. 11.8; P < .05).
Dr. Zimmerman called these preliminary findings “consistent” with his clinical experience.
He noted he was “surprised” that OCD had the highest odds ratio (OR, 3.5) of being associated with a sense of undeservingness. “But when I thought about it, I realized that it makes sense because people with OCD have insight and are often embarrassed by their symptoms,” he added.
Dr. Zimmerman was not surprised that MDD was associated with this sense of undeservingness. A second study currently under review is focusing specifically on MDD.
“One of the things we found, not surprisingly, was that some of the cognitive symptoms of depression, such as guilt and sense of worthlessness, are associated with it,” he said.
‘Snapshot in time’
Commenting for this news organization, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called this a “novel, important, and creative study.”
The “hypothesized role of shame squares with my experience. And the association with OCD, depression, and trauma are also consistent with what I have seen,” said Dr. Duckworth, who is also an assistant clinical professor at Harvard Medical School, Boston. He was not involved with the current research.
“The role of hopelessness, often seen as a core feature of depression and to some extent OCD and trauma, is an opportunity to see if treatments like cognitive-behavioral therapy [CBT] can make a difference. How to engage people in CBT, which works directly at changing one’s automatic negative thoughts, is important,” Dr. Duckworth said.
Describing the study as a “snapshot in time,” he noted it would be interesting to follow patients longitudinally.
“I think a whole subset would look back and say, ‘I remember feeling [undeserving] but now that I’ve gotten medication or CBT or therapy, I’m happy I got better,’” said Dr. Duckworth.
No source of study funding was listed. Dr. Zimmerman, his coauthor, and Dr. Duckworth report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although most psychiatrists have encountered patients who don’t improve with treatment, novel research sheds some light on one possible explanation for this phenomenon.
Investigators found that among
“To the best of my knowledge, this subject hasn’t been written about or explored before because we operate under the assumption that someone coming for ambulatory treatment, of course, wants to get better and thinks that they deserve to get better,” lead author Mark Zimmerman, MD, professor of psychiatry and human behavior at Brown University, Providence, R.I., said in an interview.
“This issue is not something complicated that a clinician would need to explore by administering some scale or clinical rating instrument. All you have to do is ask patients if they think they deserve to get better, particularly patients who seem to be ‘stuck,’ and explore what’s underlying that belief,” added Zimmerman, who is also the director of the Outpatient Division at the partial hospital program, Rhode Island Hospital, Providence.
The findings were published online in the Journal of Clinical Psychiatry.
Obstacle to therapy
Results from a study examining the prevalence of this belief in more than 400 patients admitted to a partial hospital program showed that 17% of the participants either did not believe they deserved to get better or weren’t sure if they deserved to get better.
When compared with their peers, patients who felt they were undeserving were significantly less likely to complete the treatment program and missed significantly more days of treatment while in the program.
Of the patients who did complete the program, those who believed they were undeserving were in treatment for significantly longer periods of time than those who believed they deserved to get better.
The average length of stay for patients in the partial hospital program is usually about 2 weeks, the investigators note. However, a minority of patients end up in treatment for more than a month and during this prolonged period, some do not seem to improve in their symptoms or functioning despite “intensive psychotherapy and ongoing pharmacotherapy.”
The researchers wanted to understand the reasons for some patients’ lack of progress and examined whether those who did not believe they were worthy of getting better actually took longer to respond to treatment.
In the current research, Dr. Zimmerman wanted to focus on these patients and assess whether they did take longer to improve and what diagnoses might be associated with feeling undeserving.
Of the 405 patients in the study, the majority (83%) reported they believed they deserved to get better, 12.8% said they were unsure, and 4.2% reported they did not believe they deserved to get better.
The researchers combined those who were unsure and those who did not believe they deserved to get better and compared them with patients who believed they did deserve to get better.
Although there were no differences between these patients in gender, race, or marital status, those who did not believe they deserved to get better were significantly younger than their counterparts who believed they deserved to get better (mean age, 32.2 years vs. 37.7 years, respectively; P < .01).
They also were diagnosed with a greater number of disorders at the time of the evaluation (mean, 3.6 vs. 2.9; P < .01).
Mirrors clinical experience
Participants who did not indicate they deserved to get better were significantly more often diagnosed with several conditions, compared with their counterparts who indicated they did deserve to get better:
- Major depressive disorder (MDD): 75.4% vs. 53.3%, respectively; P < .01.
- Panic disorder: 36.2% vs. 23.2%; P < .05.
- Agoraphobia: 27.5% vs. 11.6%; P < .01.
- Obsessive-compulsive disorder (OCD): 14.5% vs. 4.5%; P < .01.
- Posttraumatic stress disorder: 44.9% vs. 25.9%; P < .01.
- Borderline personality disorder: 29.0% vs. 17.9%; P < .05.
There were also significant differences between those who did not vs, did believe they deserved to get better in program completion (52.3% vs. 68.8%, respectively; P < .01), missed days (mean, 1.7 vs. 1.3; P < .05), and length of treatment (mean days, 14.1 vs. 11.8; P < .05).
Dr. Zimmerman called these preliminary findings “consistent” with his clinical experience.
He noted he was “surprised” that OCD had the highest odds ratio (OR, 3.5) of being associated with a sense of undeservingness. “But when I thought about it, I realized that it makes sense because people with OCD have insight and are often embarrassed by their symptoms,” he added.
Dr. Zimmerman was not surprised that MDD was associated with this sense of undeservingness. A second study currently under review is focusing specifically on MDD.
“One of the things we found, not surprisingly, was that some of the cognitive symptoms of depression, such as guilt and sense of worthlessness, are associated with it,” he said.
‘Snapshot in time’
Commenting for this news organization, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness called this a “novel, important, and creative study.”
The “hypothesized role of shame squares with my experience. And the association with OCD, depression, and trauma are also consistent with what I have seen,” said Dr. Duckworth, who is also an assistant clinical professor at Harvard Medical School, Boston. He was not involved with the current research.
“The role of hopelessness, often seen as a core feature of depression and to some extent OCD and trauma, is an opportunity to see if treatments like cognitive-behavioral therapy [CBT] can make a difference. How to engage people in CBT, which works directly at changing one’s automatic negative thoughts, is important,” Dr. Duckworth said.
Describing the study as a “snapshot in time,” he noted it would be interesting to follow patients longitudinally.
“I think a whole subset would look back and say, ‘I remember feeling [undeserving] but now that I’ve gotten medication or CBT or therapy, I’m happy I got better,’” said Dr. Duckworth.
No source of study funding was listed. Dr. Zimmerman, his coauthor, and Dr. Duckworth report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY