User login
Surgeon Claims Colleague Made False Board Complaints to Get Him Fired
A longtime Kaiser Permanente surgeon is suing a fellow physician for allegedly submitting false medical board complaints against him in an attempt to get him fired.
Dr. Stalfire, a board-certified ob.gyn., has worked for Kaiser Permanente in western Oregon for more than 20 years, including several years as a regional chief surgical officer.
Dr. Stalfire is accusing Dr. Hsieh of defamation and intentional emotional distress, according to the March 25 lawsuit filed in Marion County Circuit Court. Northwest Permanente P.C., a Kaiser subsidiary, is also named as a defendant.
Dr. Stalfire is asking for $1.2 million in economic damages and $300,000 in noneconomic damages. Dr. Hsieh has not yet responded to the legal complaint.
Dr. Stalfire’s attorney did not respond to a message seeking comment. Dr. Hsieh is representing himself, according to court records. A Kaiser Permanente spokeswoman told this news organization that Kaiser does not comment on pending litigation.
The conflict began in February 2023, after Dr. Stalfire underwent surgery to correct issues stemming from severe injuries when a tree fell on his leg, according to court records.
Dr. Hsieh, a Kaiser ob.gyn., senior physician, and quality assurance lead, allegedly contacted Dr. Stalfire after the surgery and demanded he return to work earlier than medically recommended. Dr. Stalfire claims Dr. Hsieh questioned his retirement plans and his ability to continue working to pressure him into quitting.
Dr. Stalfire reported Dr. Hsieh’s conduct to Kaiser’s human resources department. However, the complaint contends Dr. Hsieh’s actions only escalated after the report was made. According to the complaint, Dr. Hsieh began telling coworkers Dr. Stalfire was “lying” about his injuries. Dr. Hsieh also allegedly contacted administrators and schedulers to ask about Dr. Stalfire’s injuries and suggested that he was not “legitimately recovering from serious injuries.” The complaint claims that Dr. Hsieh told Dr. Stalfire’s colleagues that he was a “con man,” a “criminal,” and “despicable.”
According to Dr. Stalfire’s complaint, in August 2023, Dr. Hsieh submitted numerous anonymous complaints about Dr. Stalfire to the Washington Medical Commission, the Oregon Medical Board, and other governmental agencies. Dr. Stalfire defended himself against the complaints, and they were dismissed. The lawsuit does not specify the nature of the complaints.
Dr. Stalfire later made public record requests for the complaints and discovered Dr. Hsieh had used his deceased mother-in-law’s phone number as his contact information, according to the lawsuit.
Despite multiple reports about Dr. Hsieh’s conduct, Dr. Stalfire claims Kaiser retained Dr. Hsieh as an employee and took no action to prevent him from making false statements about Dr. Stalfire.
He claims Dr. Hsieh’s harassment and Kaiser’s inaction harmed his professional reputation, caused lost work time, and resulted in severe emotional distress that required mental health treatment. The harm caused continues to impact his ability to work, the suit contends.
A version of this article appeared on Medscape.com.
A longtime Kaiser Permanente surgeon is suing a fellow physician for allegedly submitting false medical board complaints against him in an attempt to get him fired.
Dr. Stalfire, a board-certified ob.gyn., has worked for Kaiser Permanente in western Oregon for more than 20 years, including several years as a regional chief surgical officer.
Dr. Stalfire is accusing Dr. Hsieh of defamation and intentional emotional distress, according to the March 25 lawsuit filed in Marion County Circuit Court. Northwest Permanente P.C., a Kaiser subsidiary, is also named as a defendant.
Dr. Stalfire is asking for $1.2 million in economic damages and $300,000 in noneconomic damages. Dr. Hsieh has not yet responded to the legal complaint.
Dr. Stalfire’s attorney did not respond to a message seeking comment. Dr. Hsieh is representing himself, according to court records. A Kaiser Permanente spokeswoman told this news organization that Kaiser does not comment on pending litigation.
The conflict began in February 2023, after Dr. Stalfire underwent surgery to correct issues stemming from severe injuries when a tree fell on his leg, according to court records.
Dr. Hsieh, a Kaiser ob.gyn., senior physician, and quality assurance lead, allegedly contacted Dr. Stalfire after the surgery and demanded he return to work earlier than medically recommended. Dr. Stalfire claims Dr. Hsieh questioned his retirement plans and his ability to continue working to pressure him into quitting.
Dr. Stalfire reported Dr. Hsieh’s conduct to Kaiser’s human resources department. However, the complaint contends Dr. Hsieh’s actions only escalated after the report was made. According to the complaint, Dr. Hsieh began telling coworkers Dr. Stalfire was “lying” about his injuries. Dr. Hsieh also allegedly contacted administrators and schedulers to ask about Dr. Stalfire’s injuries and suggested that he was not “legitimately recovering from serious injuries.” The complaint claims that Dr. Hsieh told Dr. Stalfire’s colleagues that he was a “con man,” a “criminal,” and “despicable.”
According to Dr. Stalfire’s complaint, in August 2023, Dr. Hsieh submitted numerous anonymous complaints about Dr. Stalfire to the Washington Medical Commission, the Oregon Medical Board, and other governmental agencies. Dr. Stalfire defended himself against the complaints, and they were dismissed. The lawsuit does not specify the nature of the complaints.
Dr. Stalfire later made public record requests for the complaints and discovered Dr. Hsieh had used his deceased mother-in-law’s phone number as his contact information, according to the lawsuit.
Despite multiple reports about Dr. Hsieh’s conduct, Dr. Stalfire claims Kaiser retained Dr. Hsieh as an employee and took no action to prevent him from making false statements about Dr. Stalfire.
He claims Dr. Hsieh’s harassment and Kaiser’s inaction harmed his professional reputation, caused lost work time, and resulted in severe emotional distress that required mental health treatment. The harm caused continues to impact his ability to work, the suit contends.
A version of this article appeared on Medscape.com.
A longtime Kaiser Permanente surgeon is suing a fellow physician for allegedly submitting false medical board complaints against him in an attempt to get him fired.
Dr. Stalfire, a board-certified ob.gyn., has worked for Kaiser Permanente in western Oregon for more than 20 years, including several years as a regional chief surgical officer.
Dr. Stalfire is accusing Dr. Hsieh of defamation and intentional emotional distress, according to the March 25 lawsuit filed in Marion County Circuit Court. Northwest Permanente P.C., a Kaiser subsidiary, is also named as a defendant.
Dr. Stalfire is asking for $1.2 million in economic damages and $300,000 in noneconomic damages. Dr. Hsieh has not yet responded to the legal complaint.
Dr. Stalfire’s attorney did not respond to a message seeking comment. Dr. Hsieh is representing himself, according to court records. A Kaiser Permanente spokeswoman told this news organization that Kaiser does not comment on pending litigation.
The conflict began in February 2023, after Dr. Stalfire underwent surgery to correct issues stemming from severe injuries when a tree fell on his leg, according to court records.
Dr. Hsieh, a Kaiser ob.gyn., senior physician, and quality assurance lead, allegedly contacted Dr. Stalfire after the surgery and demanded he return to work earlier than medically recommended. Dr. Stalfire claims Dr. Hsieh questioned his retirement plans and his ability to continue working to pressure him into quitting.
Dr. Stalfire reported Dr. Hsieh’s conduct to Kaiser’s human resources department. However, the complaint contends Dr. Hsieh’s actions only escalated after the report was made. According to the complaint, Dr. Hsieh began telling coworkers Dr. Stalfire was “lying” about his injuries. Dr. Hsieh also allegedly contacted administrators and schedulers to ask about Dr. Stalfire’s injuries and suggested that he was not “legitimately recovering from serious injuries.” The complaint claims that Dr. Hsieh told Dr. Stalfire’s colleagues that he was a “con man,” a “criminal,” and “despicable.”
According to Dr. Stalfire’s complaint, in August 2023, Dr. Hsieh submitted numerous anonymous complaints about Dr. Stalfire to the Washington Medical Commission, the Oregon Medical Board, and other governmental agencies. Dr. Stalfire defended himself against the complaints, and they were dismissed. The lawsuit does not specify the nature of the complaints.
Dr. Stalfire later made public record requests for the complaints and discovered Dr. Hsieh had used his deceased mother-in-law’s phone number as his contact information, according to the lawsuit.
Despite multiple reports about Dr. Hsieh’s conduct, Dr. Stalfire claims Kaiser retained Dr. Hsieh as an employee and took no action to prevent him from making false statements about Dr. Stalfire.
He claims Dr. Hsieh’s harassment and Kaiser’s inaction harmed his professional reputation, caused lost work time, and resulted in severe emotional distress that required mental health treatment. The harm caused continues to impact his ability to work, the suit contends.
A version of this article appeared on Medscape.com.
Older, Breastfeeding Mothers Face Differing Advice About Mammograms
When her obstetrician-gynecologist recommended a mammogram, Emily Legg didn’t hesitate to schedule an appointment for the screening.
Her grandmother had been diagnosed with breast cancer and her father died of prostate cancer in his mid-50s. Ms. Legg also has polycystic ovary syndrome (PCOS), which increases the risk of some cancers.
Having just turned 40, Ms. Legg said she was determined to be as proactive as possible with cancer screenings.
Before the mammogram, she arranged for childcare for her 6-month-old daughter and filled out a required questionnaire online that asked about her history and health conditions. When the appointment day arrived, Ms. Legg made the 30-minute drive to the clinic where she was prepped for the procedure and escorted to the mammography room.
But just before the screening started, Ms. Legg happened to mention to the technician that she was breastfeeding. The surprised tech immediately halted the procedure, Ms. Legg said. Because of increased breast density caused by nursing, Ms. Legg was told to wait at least 6 weeks after weaning for a mammogram.
“I didn’t even consider that breastfeeding might prevent me from getting a mammogram,” said Ms. Legg, a writing professor from Hamilton, Ohio. “I had to go home. I was frustrated, mostly because I had driven all that way. I had hyped myself up. I had childcare in line. And now I had to wait until my daughter weaned? At the time, I didn’t know if my daughter was going to breastfeed for 2 years or be done at 6 months.”
Considering her family background, Ms. Legg worried about not receiving the screening. Her sister had recently undergone a mammogram while she was breastfeeding without any problems.
When she did research, Ms. Legg found conflicting information about the subject online so she turned to Reddit, where she started a thread asking if other moms over 40 had experienced similar issues. Dozens of moms responded with questions and concerns on the subject. Some wrote about being denied a mammogram while breastfeeding, while others wrote they received the procedure without question. Guidance from health professionals on the topic appeared to vastly differ.
“That’s why I turned to [social media] because I wasn’t finding anything else,” Ms. Legg said. “There’s just a lack of clear information. As an older mom, there’s less information out there for being postpartum and being over 40.”
Confusion over screenings during breastfeeding comes at the intersection of national guidelines lowering the recommended age for first mammograms, more women having babies later in life, and women getting breast cancer earlier.
Most physician specialty associations agree that mammography is safe for breastfeeding patients and that they need not delay routine screenings. However, the safety of breast imaging during pregnancy and lactation is not well advertised, said Molly Peterson, MD, a radiologist based in St. Frances, Wisconsin, and lead author of a 2023 article about breast imaging during pregnancy and lactation in RadioGraphics, a journal of the Radiological Society of North America.
Conflicting information from nonscientific resources adds to the confusion, Dr. Peterson said. At the same time, health providers along the care spectrum may be uncertain about what imaging is safe and reasonable. Recommendations about mammography and lactation can also vary by institution, screening experts say.
“I’ve talked with pregnant and breastfeeding patients, both younger and older, who were unsure if they could have mammograms,” Dr. Peterson said. “I’ve also fielded questions from technologists, unclear what imaging we can offer these patients. ... Educating health professionals about evidence-based guidelines for screening and diagnostic imaging and reassuring patients about the safety of breast imaging during pregnancy and lactation is thus more important than ever.”
Differing Guidelines, Case-by-Case Considerations
The RadioGraphics paper emphasizes that both screening and diagnostic imaging can be safely performed using protocols based on age, breast cancer risk, and whether the patient is pregnant or lactating.
The American College of Radiology (ACR) Appropriateness Criteria also support mammography for certain patients during lactation. The guidelines state there is no contraindication to performing mammography during lactation, but note that challenges in evaluation can arise because of the unique physiological and structural breast changes that can occur.
“Hormones can change breast density and size of the breast, which could limit the clinical examination, mimic pathology, and obscure mammographic findings,” said Stamatia V. Destounis, MD, FACR, chair of the ACR Breast Imaging Commission. “It is important the patient pumps right before the mammogram or brings the baby to breastfeed prior to the imaging examination to offer the best imaging evaluation and reduce breast density as much as possible.”
In those patients who choose to prolong breastfeeding and are of the age to be screened, it is important they undergo yearly clinical breast exams, perform breast self-exams, and discuss breast cancer screening with their healthcare provider, she said. “They should not delay a routine screening mammogram. Most patients have dense breast tissue at this time, and frequently a breast ultrasound may be performed also.”
The American College of Obstetricians and Gynecologists (ACOG) does not have specific guidelines about breastfeeding mothers and mammography recommendations. Breastfeeding patients should discuss with their physicians or midwives the pros and cons of mammography, taking into account personal risk factors and how long they plan to nurse, said Joshua Copel, MD, vice chair of obstetrics, gynecology and reproductive sciences at Yale Medicine, New Haven, Connecticut, and a member of ACOG’s Committee on Obstetric Practice.
“The question for anybody to address with their physician will be, ‘Is my risk of breast cancer high enough that I should take that small risk that they’re going to over- or underread the mammogram because of my nursing status? Or should I wait until I wean the baby and have the mammogram then?’” he said.
Institutional and practice protocols meanwhile, can depend on a patient’s cancer risk.
Guidelines at the University of Wisconsin, for instance, advise that lactating patients 40 or over who are at average risk, wait 6-8 weeks after cessation of breastfeeding, said Alison Gegios, MD, a radiologist and assistant professor in breast imaging at the University of Wisconsin School of Medicine and Public Health. Average risk is defined as less than a 15% lifetime risk of breast cancer, she said.
Dr. Gegios, a coauthor on the RadioGraphics paper, said her institution recommends screening mammography if lactating patients are at intermediate or high risk, and are over 30. In such cases however, screening is generally deferred until 3-6 months after delivery, she noted.
“If patients are high risk, it’s also important to do screening breast MRIs,” Dr. Gegios said. “Studies have shown that screening breast MRIs are effective in breastfeeding patients despite their increased background parenchymal enhancement because breast cancer still stands out on our maximum intensity projections and stands out on the exam from the background.”
How to Clear Up Confusion, Promote Consistency
After her experience at the mammography practice, Ms. Legg went home and immediately sent a message to her ob.gyn. about what happened.
The doctor was similarly surprised and frustrated that Ms. Legg wasn’t able to get the mammogram, she said. To get around the difference in protocols, Ms. Legg’s ob.gyn. referred her to a high-risk clinic in Cincinnati. Ms. Legg’s history qualified her as high risk and she received genetic testing and a breast ultrasound at the clinic, she said.
“The ultrasound showed some shady spots,” Ms. Legg recalled. “They weren’t quite sure what they were. Another ultrasound later, they determined the spots were symmetrical and it ended up not being anything [serious]. Genetic-wise, I did not have any markers for cancer.”
Ms. Legg was relieved and she eventually received a mammogram when she finished breastfeeding, she said. However, she feels the overlap of older, breastfeeding moms and mammography guidelines deserves more attention.
“I would encourage all of us in the ‘geriatric mother’s club,’ to advocate for yourself, do your research, and also turn to your medical professionals and ask questions,” she said. “Make sure you know what they recommend for moms who are older and just had a baby.”
On the provider side, Dr. Destounis said physicians should revisit with patients the most updated guidelines about breastfeeding and mammography at routine appointments.
“Patients and their physicians have to have communication about screening for breast cancer if they are of screening age,” she said.
Dr. Copel advises physicians to run through the risks and benefits of mammograms with older, breastfeeding patients and make a shared decision. “It’s all going to vary with the individual circumstances,” he said. “If someone [has] a BRCA gene and their sister and mother had breast cancer, maybe it’s worth it. If somebody has absolutely no family history and just crossed the threshold for meeting a mammogram [recommendation], then sure, wait.”
Ms. Legg would like to see more professional literature and educational material directed toward the older, breastfeeding population about mammograms.
“At minimum, work together across departments to create an intake form, a questionnaire that is inclusive of everything,” she said. “There should be a question before you even get to the tech that asks, ‘Are you breastfeeding?’ ”
When her obstetrician-gynecologist recommended a mammogram, Emily Legg didn’t hesitate to schedule an appointment for the screening.
Her grandmother had been diagnosed with breast cancer and her father died of prostate cancer in his mid-50s. Ms. Legg also has polycystic ovary syndrome (PCOS), which increases the risk of some cancers.
Having just turned 40, Ms. Legg said she was determined to be as proactive as possible with cancer screenings.
Before the mammogram, she arranged for childcare for her 6-month-old daughter and filled out a required questionnaire online that asked about her history and health conditions. When the appointment day arrived, Ms. Legg made the 30-minute drive to the clinic where she was prepped for the procedure and escorted to the mammography room.
But just before the screening started, Ms. Legg happened to mention to the technician that she was breastfeeding. The surprised tech immediately halted the procedure, Ms. Legg said. Because of increased breast density caused by nursing, Ms. Legg was told to wait at least 6 weeks after weaning for a mammogram.
“I didn’t even consider that breastfeeding might prevent me from getting a mammogram,” said Ms. Legg, a writing professor from Hamilton, Ohio. “I had to go home. I was frustrated, mostly because I had driven all that way. I had hyped myself up. I had childcare in line. And now I had to wait until my daughter weaned? At the time, I didn’t know if my daughter was going to breastfeed for 2 years or be done at 6 months.”
Considering her family background, Ms. Legg worried about not receiving the screening. Her sister had recently undergone a mammogram while she was breastfeeding without any problems.
When she did research, Ms. Legg found conflicting information about the subject online so she turned to Reddit, where she started a thread asking if other moms over 40 had experienced similar issues. Dozens of moms responded with questions and concerns on the subject. Some wrote about being denied a mammogram while breastfeeding, while others wrote they received the procedure without question. Guidance from health professionals on the topic appeared to vastly differ.
“That’s why I turned to [social media] because I wasn’t finding anything else,” Ms. Legg said. “There’s just a lack of clear information. As an older mom, there’s less information out there for being postpartum and being over 40.”
Confusion over screenings during breastfeeding comes at the intersection of national guidelines lowering the recommended age for first mammograms, more women having babies later in life, and women getting breast cancer earlier.
Most physician specialty associations agree that mammography is safe for breastfeeding patients and that they need not delay routine screenings. However, the safety of breast imaging during pregnancy and lactation is not well advertised, said Molly Peterson, MD, a radiologist based in St. Frances, Wisconsin, and lead author of a 2023 article about breast imaging during pregnancy and lactation in RadioGraphics, a journal of the Radiological Society of North America.
Conflicting information from nonscientific resources adds to the confusion, Dr. Peterson said. At the same time, health providers along the care spectrum may be uncertain about what imaging is safe and reasonable. Recommendations about mammography and lactation can also vary by institution, screening experts say.
“I’ve talked with pregnant and breastfeeding patients, both younger and older, who were unsure if they could have mammograms,” Dr. Peterson said. “I’ve also fielded questions from technologists, unclear what imaging we can offer these patients. ... Educating health professionals about evidence-based guidelines for screening and diagnostic imaging and reassuring patients about the safety of breast imaging during pregnancy and lactation is thus more important than ever.”
Differing Guidelines, Case-by-Case Considerations
The RadioGraphics paper emphasizes that both screening and diagnostic imaging can be safely performed using protocols based on age, breast cancer risk, and whether the patient is pregnant or lactating.
The American College of Radiology (ACR) Appropriateness Criteria also support mammography for certain patients during lactation. The guidelines state there is no contraindication to performing mammography during lactation, but note that challenges in evaluation can arise because of the unique physiological and structural breast changes that can occur.
“Hormones can change breast density and size of the breast, which could limit the clinical examination, mimic pathology, and obscure mammographic findings,” said Stamatia V. Destounis, MD, FACR, chair of the ACR Breast Imaging Commission. “It is important the patient pumps right before the mammogram or brings the baby to breastfeed prior to the imaging examination to offer the best imaging evaluation and reduce breast density as much as possible.”
In those patients who choose to prolong breastfeeding and are of the age to be screened, it is important they undergo yearly clinical breast exams, perform breast self-exams, and discuss breast cancer screening with their healthcare provider, she said. “They should not delay a routine screening mammogram. Most patients have dense breast tissue at this time, and frequently a breast ultrasound may be performed also.”
The American College of Obstetricians and Gynecologists (ACOG) does not have specific guidelines about breastfeeding mothers and mammography recommendations. Breastfeeding patients should discuss with their physicians or midwives the pros and cons of mammography, taking into account personal risk factors and how long they plan to nurse, said Joshua Copel, MD, vice chair of obstetrics, gynecology and reproductive sciences at Yale Medicine, New Haven, Connecticut, and a member of ACOG’s Committee on Obstetric Practice.
“The question for anybody to address with their physician will be, ‘Is my risk of breast cancer high enough that I should take that small risk that they’re going to over- or underread the mammogram because of my nursing status? Or should I wait until I wean the baby and have the mammogram then?’” he said.
Institutional and practice protocols meanwhile, can depend on a patient’s cancer risk.
Guidelines at the University of Wisconsin, for instance, advise that lactating patients 40 or over who are at average risk, wait 6-8 weeks after cessation of breastfeeding, said Alison Gegios, MD, a radiologist and assistant professor in breast imaging at the University of Wisconsin School of Medicine and Public Health. Average risk is defined as less than a 15% lifetime risk of breast cancer, she said.
Dr. Gegios, a coauthor on the RadioGraphics paper, said her institution recommends screening mammography if lactating patients are at intermediate or high risk, and are over 30. In such cases however, screening is generally deferred until 3-6 months after delivery, she noted.
“If patients are high risk, it’s also important to do screening breast MRIs,” Dr. Gegios said. “Studies have shown that screening breast MRIs are effective in breastfeeding patients despite their increased background parenchymal enhancement because breast cancer still stands out on our maximum intensity projections and stands out on the exam from the background.”
How to Clear Up Confusion, Promote Consistency
After her experience at the mammography practice, Ms. Legg went home and immediately sent a message to her ob.gyn. about what happened.
The doctor was similarly surprised and frustrated that Ms. Legg wasn’t able to get the mammogram, she said. To get around the difference in protocols, Ms. Legg’s ob.gyn. referred her to a high-risk clinic in Cincinnati. Ms. Legg’s history qualified her as high risk and she received genetic testing and a breast ultrasound at the clinic, she said.
“The ultrasound showed some shady spots,” Ms. Legg recalled. “They weren’t quite sure what they were. Another ultrasound later, they determined the spots were symmetrical and it ended up not being anything [serious]. Genetic-wise, I did not have any markers for cancer.”
Ms. Legg was relieved and she eventually received a mammogram when she finished breastfeeding, she said. However, she feels the overlap of older, breastfeeding moms and mammography guidelines deserves more attention.
“I would encourage all of us in the ‘geriatric mother’s club,’ to advocate for yourself, do your research, and also turn to your medical professionals and ask questions,” she said. “Make sure you know what they recommend for moms who are older and just had a baby.”
On the provider side, Dr. Destounis said physicians should revisit with patients the most updated guidelines about breastfeeding and mammography at routine appointments.
“Patients and their physicians have to have communication about screening for breast cancer if they are of screening age,” she said.
Dr. Copel advises physicians to run through the risks and benefits of mammograms with older, breastfeeding patients and make a shared decision. “It’s all going to vary with the individual circumstances,” he said. “If someone [has] a BRCA gene and their sister and mother had breast cancer, maybe it’s worth it. If somebody has absolutely no family history and just crossed the threshold for meeting a mammogram [recommendation], then sure, wait.”
Ms. Legg would like to see more professional literature and educational material directed toward the older, breastfeeding population about mammograms.
“At minimum, work together across departments to create an intake form, a questionnaire that is inclusive of everything,” she said. “There should be a question before you even get to the tech that asks, ‘Are you breastfeeding?’ ”
When her obstetrician-gynecologist recommended a mammogram, Emily Legg didn’t hesitate to schedule an appointment for the screening.
Her grandmother had been diagnosed with breast cancer and her father died of prostate cancer in his mid-50s. Ms. Legg also has polycystic ovary syndrome (PCOS), which increases the risk of some cancers.
Having just turned 40, Ms. Legg said she was determined to be as proactive as possible with cancer screenings.
Before the mammogram, she arranged for childcare for her 6-month-old daughter and filled out a required questionnaire online that asked about her history and health conditions. When the appointment day arrived, Ms. Legg made the 30-minute drive to the clinic where she was prepped for the procedure and escorted to the mammography room.
But just before the screening started, Ms. Legg happened to mention to the technician that she was breastfeeding. The surprised tech immediately halted the procedure, Ms. Legg said. Because of increased breast density caused by nursing, Ms. Legg was told to wait at least 6 weeks after weaning for a mammogram.
“I didn’t even consider that breastfeeding might prevent me from getting a mammogram,” said Ms. Legg, a writing professor from Hamilton, Ohio. “I had to go home. I was frustrated, mostly because I had driven all that way. I had hyped myself up. I had childcare in line. And now I had to wait until my daughter weaned? At the time, I didn’t know if my daughter was going to breastfeed for 2 years or be done at 6 months.”
Considering her family background, Ms. Legg worried about not receiving the screening. Her sister had recently undergone a mammogram while she was breastfeeding without any problems.
When she did research, Ms. Legg found conflicting information about the subject online so she turned to Reddit, where she started a thread asking if other moms over 40 had experienced similar issues. Dozens of moms responded with questions and concerns on the subject. Some wrote about being denied a mammogram while breastfeeding, while others wrote they received the procedure without question. Guidance from health professionals on the topic appeared to vastly differ.
“That’s why I turned to [social media] because I wasn’t finding anything else,” Ms. Legg said. “There’s just a lack of clear information. As an older mom, there’s less information out there for being postpartum and being over 40.”
Confusion over screenings during breastfeeding comes at the intersection of national guidelines lowering the recommended age for first mammograms, more women having babies later in life, and women getting breast cancer earlier.
Most physician specialty associations agree that mammography is safe for breastfeeding patients and that they need not delay routine screenings. However, the safety of breast imaging during pregnancy and lactation is not well advertised, said Molly Peterson, MD, a radiologist based in St. Frances, Wisconsin, and lead author of a 2023 article about breast imaging during pregnancy and lactation in RadioGraphics, a journal of the Radiological Society of North America.
Conflicting information from nonscientific resources adds to the confusion, Dr. Peterson said. At the same time, health providers along the care spectrum may be uncertain about what imaging is safe and reasonable. Recommendations about mammography and lactation can also vary by institution, screening experts say.
“I’ve talked with pregnant and breastfeeding patients, both younger and older, who were unsure if they could have mammograms,” Dr. Peterson said. “I’ve also fielded questions from technologists, unclear what imaging we can offer these patients. ... Educating health professionals about evidence-based guidelines for screening and diagnostic imaging and reassuring patients about the safety of breast imaging during pregnancy and lactation is thus more important than ever.”
Differing Guidelines, Case-by-Case Considerations
The RadioGraphics paper emphasizes that both screening and diagnostic imaging can be safely performed using protocols based on age, breast cancer risk, and whether the patient is pregnant or lactating.
The American College of Radiology (ACR) Appropriateness Criteria also support mammography for certain patients during lactation. The guidelines state there is no contraindication to performing mammography during lactation, but note that challenges in evaluation can arise because of the unique physiological and structural breast changes that can occur.
“Hormones can change breast density and size of the breast, which could limit the clinical examination, mimic pathology, and obscure mammographic findings,” said Stamatia V. Destounis, MD, FACR, chair of the ACR Breast Imaging Commission. “It is important the patient pumps right before the mammogram or brings the baby to breastfeed prior to the imaging examination to offer the best imaging evaluation and reduce breast density as much as possible.”
In those patients who choose to prolong breastfeeding and are of the age to be screened, it is important they undergo yearly clinical breast exams, perform breast self-exams, and discuss breast cancer screening with their healthcare provider, she said. “They should not delay a routine screening mammogram. Most patients have dense breast tissue at this time, and frequently a breast ultrasound may be performed also.”
The American College of Obstetricians and Gynecologists (ACOG) does not have specific guidelines about breastfeeding mothers and mammography recommendations. Breastfeeding patients should discuss with their physicians or midwives the pros and cons of mammography, taking into account personal risk factors and how long they plan to nurse, said Joshua Copel, MD, vice chair of obstetrics, gynecology and reproductive sciences at Yale Medicine, New Haven, Connecticut, and a member of ACOG’s Committee on Obstetric Practice.
“The question for anybody to address with their physician will be, ‘Is my risk of breast cancer high enough that I should take that small risk that they’re going to over- or underread the mammogram because of my nursing status? Or should I wait until I wean the baby and have the mammogram then?’” he said.
Institutional and practice protocols meanwhile, can depend on a patient’s cancer risk.
Guidelines at the University of Wisconsin, for instance, advise that lactating patients 40 or over who are at average risk, wait 6-8 weeks after cessation of breastfeeding, said Alison Gegios, MD, a radiologist and assistant professor in breast imaging at the University of Wisconsin School of Medicine and Public Health. Average risk is defined as less than a 15% lifetime risk of breast cancer, she said.
Dr. Gegios, a coauthor on the RadioGraphics paper, said her institution recommends screening mammography if lactating patients are at intermediate or high risk, and are over 30. In such cases however, screening is generally deferred until 3-6 months after delivery, she noted.
“If patients are high risk, it’s also important to do screening breast MRIs,” Dr. Gegios said. “Studies have shown that screening breast MRIs are effective in breastfeeding patients despite their increased background parenchymal enhancement because breast cancer still stands out on our maximum intensity projections and stands out on the exam from the background.”
How to Clear Up Confusion, Promote Consistency
After her experience at the mammography practice, Ms. Legg went home and immediately sent a message to her ob.gyn. about what happened.
The doctor was similarly surprised and frustrated that Ms. Legg wasn’t able to get the mammogram, she said. To get around the difference in protocols, Ms. Legg’s ob.gyn. referred her to a high-risk clinic in Cincinnati. Ms. Legg’s history qualified her as high risk and she received genetic testing and a breast ultrasound at the clinic, she said.
“The ultrasound showed some shady spots,” Ms. Legg recalled. “They weren’t quite sure what they were. Another ultrasound later, they determined the spots were symmetrical and it ended up not being anything [serious]. Genetic-wise, I did not have any markers for cancer.”
Ms. Legg was relieved and she eventually received a mammogram when she finished breastfeeding, she said. However, she feels the overlap of older, breastfeeding moms and mammography guidelines deserves more attention.
“I would encourage all of us in the ‘geriatric mother’s club,’ to advocate for yourself, do your research, and also turn to your medical professionals and ask questions,” she said. “Make sure you know what they recommend for moms who are older and just had a baby.”
On the provider side, Dr. Destounis said physicians should revisit with patients the most updated guidelines about breastfeeding and mammography at routine appointments.
“Patients and their physicians have to have communication about screening for breast cancer if they are of screening age,” she said.
Dr. Copel advises physicians to run through the risks and benefits of mammograms with older, breastfeeding patients and make a shared decision. “It’s all going to vary with the individual circumstances,” he said. “If someone [has] a BRCA gene and their sister and mother had breast cancer, maybe it’s worth it. If somebody has absolutely no family history and just crossed the threshold for meeting a mammogram [recommendation], then sure, wait.”
Ms. Legg would like to see more professional literature and educational material directed toward the older, breastfeeding population about mammograms.
“At minimum, work together across departments to create an intake form, a questionnaire that is inclusive of everything,” she said. “There should be a question before you even get to the tech that asks, ‘Are you breastfeeding?’ ”
Maternal Lifestyle Interventions Boost Babies’ Heart Health
Infants born to women with obesity showed improved measures of cardiovascular health when their mothers adopted healthier lifestyles before and during pregnancy, based on data from a systematic review presented at the annual meeting of the Society for Reproductive Investigation.
Previous research has shown that children born to mothers with a high body mass index (BMI) are more likely to die from cardiovascular disease in later life, said presenting author Samuel J. Burden, PhD, in an interview.
“Surprisingly, early signs of these heart issues can start before birth and continue into childhood,” said Dr. Burden, a research associate in the Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom.
To examine the effect of interventions such as a healthy diet and exercise in pregnant women with obesity on the heart health of their infants, Dr. Burden and colleagues reviewed data from eight randomized, controlled trials involving diet and exercise for pregnant women with obesity. Of these, two used antenatal exercise, two used diet and physical activity, and one used preconception diet and physical activity. The studies ranged in size from 18 to 404 participants. Two studies included infants younger than 2 months of age, and four studies included children aged 3-7 years.
Overall, lifestyle interventions before conception and before birth were associated with significant changes in cardiac remodeling, specifically reduced interventricular septal wall thickness.
In addition, one of three studies of cardiac diastolic function and four of five studies of systolic function showed significant improvements. The five studies of cardiac systolic function and three studies of diastolic function also showed improvement in systolic and diastolic blood pressure in infants of mothers who took part in the interventions. The studies were limited mainly by large attrition rates, the researchers wrote in their presentation. However, more studies in larger populations that also include older children could confirm the findings and inform public health strategies to promote healthy lifestyles for pregnant women, they noted.
Encourage Healthy Lifestyle Before and During Pregnancy
The evidence supports the findings from animal studies showing that an offspring’s health is influenced by maternal lifestyle before and during pregnancy, Dr. Burden said in an interview. The data suggest that healthcare providers should encourage women with a high BMI who want to become pregnant to eat healthfully and become more active as a way to enhance the future cardiovascular health of their children, he said.
The full results of the current study are soon to be published, but more work is needed, said Dr. Burden. “While we observed a protective effect from these lifestyle programs, there is a need for more extensive studies involving a larger number of women (and their children) who were part of the initial research,” he said. “Additionally, it will be crucial to track these children into adulthood to determine whether these antenatal lifestyle interventions persist in lowering the risk of future cardiovascular disease.”
Beginning healthy lifestyle programs prior to pregnancy might yield the best results for promoting infant cardiovascular health, and more prepregnancy interventions for women with obesity are needed, Dr. Burden added.
The current study adds to the growing body of evidence that the in utero environment can have lifelong effects on offspring, Joseph R. Biggio Jr, MD, system chair of maternal fetal medicine at Ochsner Health, New Orleans, Louisiana, said in an interview.
“Several studies have previously shown that the children of mothers with diabetes, hypertension, or obesity are at increased risk for developing signs of metabolic syndrome and cardiovascular changes during childhood or adolescence,” said Dr. Biggio.
The data from this systematic review support the potential value of interventions aimed at improving maternal weight gain and cardiovascular performance before and during pregnancy that may result in reduced cardiovascular remodeling and myocardial thickening in infants, he said.
The study was supported by a British Heart Foundation Special Project Grant. The researchers had no financial conflicts to disclose. Dr. Biggio had no financial conflicts to disclose.
Infants born to women with obesity showed improved measures of cardiovascular health when their mothers adopted healthier lifestyles before and during pregnancy, based on data from a systematic review presented at the annual meeting of the Society for Reproductive Investigation.
Previous research has shown that children born to mothers with a high body mass index (BMI) are more likely to die from cardiovascular disease in later life, said presenting author Samuel J. Burden, PhD, in an interview.
“Surprisingly, early signs of these heart issues can start before birth and continue into childhood,” said Dr. Burden, a research associate in the Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom.
To examine the effect of interventions such as a healthy diet and exercise in pregnant women with obesity on the heart health of their infants, Dr. Burden and colleagues reviewed data from eight randomized, controlled trials involving diet and exercise for pregnant women with obesity. Of these, two used antenatal exercise, two used diet and physical activity, and one used preconception diet and physical activity. The studies ranged in size from 18 to 404 participants. Two studies included infants younger than 2 months of age, and four studies included children aged 3-7 years.
Overall, lifestyle interventions before conception and before birth were associated with significant changes in cardiac remodeling, specifically reduced interventricular septal wall thickness.
In addition, one of three studies of cardiac diastolic function and four of five studies of systolic function showed significant improvements. The five studies of cardiac systolic function and three studies of diastolic function also showed improvement in systolic and diastolic blood pressure in infants of mothers who took part in the interventions. The studies were limited mainly by large attrition rates, the researchers wrote in their presentation. However, more studies in larger populations that also include older children could confirm the findings and inform public health strategies to promote healthy lifestyles for pregnant women, they noted.
Encourage Healthy Lifestyle Before and During Pregnancy
The evidence supports the findings from animal studies showing that an offspring’s health is influenced by maternal lifestyle before and during pregnancy, Dr. Burden said in an interview. The data suggest that healthcare providers should encourage women with a high BMI who want to become pregnant to eat healthfully and become more active as a way to enhance the future cardiovascular health of their children, he said.
The full results of the current study are soon to be published, but more work is needed, said Dr. Burden. “While we observed a protective effect from these lifestyle programs, there is a need for more extensive studies involving a larger number of women (and their children) who were part of the initial research,” he said. “Additionally, it will be crucial to track these children into adulthood to determine whether these antenatal lifestyle interventions persist in lowering the risk of future cardiovascular disease.”
Beginning healthy lifestyle programs prior to pregnancy might yield the best results for promoting infant cardiovascular health, and more prepregnancy interventions for women with obesity are needed, Dr. Burden added.
The current study adds to the growing body of evidence that the in utero environment can have lifelong effects on offspring, Joseph R. Biggio Jr, MD, system chair of maternal fetal medicine at Ochsner Health, New Orleans, Louisiana, said in an interview.
“Several studies have previously shown that the children of mothers with diabetes, hypertension, or obesity are at increased risk for developing signs of metabolic syndrome and cardiovascular changes during childhood or adolescence,” said Dr. Biggio.
The data from this systematic review support the potential value of interventions aimed at improving maternal weight gain and cardiovascular performance before and during pregnancy that may result in reduced cardiovascular remodeling and myocardial thickening in infants, he said.
The study was supported by a British Heart Foundation Special Project Grant. The researchers had no financial conflicts to disclose. Dr. Biggio had no financial conflicts to disclose.
Infants born to women with obesity showed improved measures of cardiovascular health when their mothers adopted healthier lifestyles before and during pregnancy, based on data from a systematic review presented at the annual meeting of the Society for Reproductive Investigation.
Previous research has shown that children born to mothers with a high body mass index (BMI) are more likely to die from cardiovascular disease in later life, said presenting author Samuel J. Burden, PhD, in an interview.
“Surprisingly, early signs of these heart issues can start before birth and continue into childhood,” said Dr. Burden, a research associate in the Department of Women & Children’s Health, School of Life Course & Population Sciences, King’s College London, London, United Kingdom.
To examine the effect of interventions such as a healthy diet and exercise in pregnant women with obesity on the heart health of their infants, Dr. Burden and colleagues reviewed data from eight randomized, controlled trials involving diet and exercise for pregnant women with obesity. Of these, two used antenatal exercise, two used diet and physical activity, and one used preconception diet and physical activity. The studies ranged in size from 18 to 404 participants. Two studies included infants younger than 2 months of age, and four studies included children aged 3-7 years.
Overall, lifestyle interventions before conception and before birth were associated with significant changes in cardiac remodeling, specifically reduced interventricular septal wall thickness.
In addition, one of three studies of cardiac diastolic function and four of five studies of systolic function showed significant improvements. The five studies of cardiac systolic function and three studies of diastolic function also showed improvement in systolic and diastolic blood pressure in infants of mothers who took part in the interventions. The studies were limited mainly by large attrition rates, the researchers wrote in their presentation. However, more studies in larger populations that also include older children could confirm the findings and inform public health strategies to promote healthy lifestyles for pregnant women, they noted.
Encourage Healthy Lifestyle Before and During Pregnancy
The evidence supports the findings from animal studies showing that an offspring’s health is influenced by maternal lifestyle before and during pregnancy, Dr. Burden said in an interview. The data suggest that healthcare providers should encourage women with a high BMI who want to become pregnant to eat healthfully and become more active as a way to enhance the future cardiovascular health of their children, he said.
The full results of the current study are soon to be published, but more work is needed, said Dr. Burden. “While we observed a protective effect from these lifestyle programs, there is a need for more extensive studies involving a larger number of women (and their children) who were part of the initial research,” he said. “Additionally, it will be crucial to track these children into adulthood to determine whether these antenatal lifestyle interventions persist in lowering the risk of future cardiovascular disease.”
Beginning healthy lifestyle programs prior to pregnancy might yield the best results for promoting infant cardiovascular health, and more prepregnancy interventions for women with obesity are needed, Dr. Burden added.
The current study adds to the growing body of evidence that the in utero environment can have lifelong effects on offspring, Joseph R. Biggio Jr, MD, system chair of maternal fetal medicine at Ochsner Health, New Orleans, Louisiana, said in an interview.
“Several studies have previously shown that the children of mothers with diabetes, hypertension, or obesity are at increased risk for developing signs of metabolic syndrome and cardiovascular changes during childhood or adolescence,” said Dr. Biggio.
The data from this systematic review support the potential value of interventions aimed at improving maternal weight gain and cardiovascular performance before and during pregnancy that may result in reduced cardiovascular remodeling and myocardial thickening in infants, he said.
The study was supported by a British Heart Foundation Special Project Grant. The researchers had no financial conflicts to disclose. Dr. Biggio had no financial conflicts to disclose.
Delaying Embryo Transfers May Benefit Patients With Endometrial Polyps
A longer time between hysteroscopic polypectomy and frozen embryo transfer may improve the odds of successful pregnancy, based on data from a new analysis presented at the annual meeting of the Society for Reproductive Investigation.
Although uterine polyps have a negative effect on pregnancy rates, data supporting a specific time interval between hysteroscopic polypectomy (HP) and frozen embryo transfer (FET) are limited, according to Audrey Messelt, MD, of Baylor College of Medicine, Houston, Texas, and colleagues.
“Hysteroscopic polypectomy is a common procedure performed before embryo transfer to optimize the receptivity of the endometrium. Currently, there is no ideal recovery time lapse between surgery and an embryo transfer,” said senior author Laura Detti, MD, professor of obstetrics and gynecology at Baylor, in an interview. “This is often the last step prior to embryo transfer, and identifying a recovery time that allows the best outcome is important.”
In a retrospective analysis, the researchers examined the effect of the time between HP and FET on pregnancy outcomes. They identified 65 patients with uterine pathology based on saline-infusion sonogram who underwent hysteroscopy and FET between June 1, 2022, and September 30, 2023.
The endometrial preparation for FET included sequential administration of oral or transdermal estradiol and intramuscular progesterone.
Overall, 46 patients were diagnosed with endometrial polyps at the time of surgery; three had endometritis, one had a uterine septum that was resected, 15 had no abnormal pathology or had normal endometrium at the time of examination. No cases of hyperplasia or malignancy were identified.
A total of 58 patients underwent FET with a single euploid embryo, four with a single untested embryo, one with a low-mosaic embryo, and two with a double-embryo transfer (one euploid and one low mosaic).
After FET, 50 patients conceived and 15 did not. Patients with ongoing pregnancies who had a history of endometrial polyps had significantly more days from surgery to FET, compared to patients with a history of polyps who failed to conceive (median 70 days vs 45 days, P = .01).
By contrast, the time between hysteroscopy and FET was similar among patients with no endometrial pathology who did and did not have ongoing pregnancies (median 45 vs 52.5 days, P = .95).
The findings were limited by the relatively small sample size and exclusion of patients with pathologies other than polyps, as well as a lack of data on age group breakdowns. However, the results suggest that patients with uterine polyps may benefit from more time between HP and FET, while patients with normal surgical findings could undergo FET sooner, the researchers concluded.
Postpolypectomy Timing May Affect Pregnancy Outcomes
“We used to think that having had the first menses from surgery would be enough recovery time for the uterine cavity, even if it was just 2 weeks,” Dr. Detti said in an interview. “This still holds true when no endometrial polyps are diagnosed in the pathological specimen; however, we learned that if endometrial polyps are removed at the time of hysteroscopy, the ideal recovery time prior to an embryo transfer should be longer,” she said.
The current study is important because approximately 15% of women are diagnosed with endometrial polyps during their reproductive years, said Mark P. Trolice, MD, professor at the University of Central Florida, Orlando, and founder/medical director of the IVF Center of Central Florida in Winter Park, in an interview.
“Abnormalities of the uterine cavity have been shown to reduce embryo implantation and increase the risk of miscarriage,” said Dr. Trolice. Although the impact of small endometrial polyps on fertility and pregnancy are uncertain, most infertility specialists recommend removal of endometrial polyps via hysteroscopic polypectomy in general and prior to IVF embryo transfer in particular, he said.
Although infertility patients are anxious to undergo embryo transfer, the current study suggests a benefit in delaying the procedure following the removal of any polyps identified during the pretransfer evaluation, Dr. Trolice said in an interview. As for additional research, “it would be helpful to know the age group breakdown of patients and if the results were consistent among all categories,” he said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Trolice had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
A longer time between hysteroscopic polypectomy and frozen embryo transfer may improve the odds of successful pregnancy, based on data from a new analysis presented at the annual meeting of the Society for Reproductive Investigation.
Although uterine polyps have a negative effect on pregnancy rates, data supporting a specific time interval between hysteroscopic polypectomy (HP) and frozen embryo transfer (FET) are limited, according to Audrey Messelt, MD, of Baylor College of Medicine, Houston, Texas, and colleagues.
“Hysteroscopic polypectomy is a common procedure performed before embryo transfer to optimize the receptivity of the endometrium. Currently, there is no ideal recovery time lapse between surgery and an embryo transfer,” said senior author Laura Detti, MD, professor of obstetrics and gynecology at Baylor, in an interview. “This is often the last step prior to embryo transfer, and identifying a recovery time that allows the best outcome is important.”
In a retrospective analysis, the researchers examined the effect of the time between HP and FET on pregnancy outcomes. They identified 65 patients with uterine pathology based on saline-infusion sonogram who underwent hysteroscopy and FET between June 1, 2022, and September 30, 2023.
The endometrial preparation for FET included sequential administration of oral or transdermal estradiol and intramuscular progesterone.
Overall, 46 patients were diagnosed with endometrial polyps at the time of surgery; three had endometritis, one had a uterine septum that was resected, 15 had no abnormal pathology or had normal endometrium at the time of examination. No cases of hyperplasia or malignancy were identified.
A total of 58 patients underwent FET with a single euploid embryo, four with a single untested embryo, one with a low-mosaic embryo, and two with a double-embryo transfer (one euploid and one low mosaic).
After FET, 50 patients conceived and 15 did not. Patients with ongoing pregnancies who had a history of endometrial polyps had significantly more days from surgery to FET, compared to patients with a history of polyps who failed to conceive (median 70 days vs 45 days, P = .01).
By contrast, the time between hysteroscopy and FET was similar among patients with no endometrial pathology who did and did not have ongoing pregnancies (median 45 vs 52.5 days, P = .95).
The findings were limited by the relatively small sample size and exclusion of patients with pathologies other than polyps, as well as a lack of data on age group breakdowns. However, the results suggest that patients with uterine polyps may benefit from more time between HP and FET, while patients with normal surgical findings could undergo FET sooner, the researchers concluded.
Postpolypectomy Timing May Affect Pregnancy Outcomes
“We used to think that having had the first menses from surgery would be enough recovery time for the uterine cavity, even if it was just 2 weeks,” Dr. Detti said in an interview. “This still holds true when no endometrial polyps are diagnosed in the pathological specimen; however, we learned that if endometrial polyps are removed at the time of hysteroscopy, the ideal recovery time prior to an embryo transfer should be longer,” she said.
The current study is important because approximately 15% of women are diagnosed with endometrial polyps during their reproductive years, said Mark P. Trolice, MD, professor at the University of Central Florida, Orlando, and founder/medical director of the IVF Center of Central Florida in Winter Park, in an interview.
“Abnormalities of the uterine cavity have been shown to reduce embryo implantation and increase the risk of miscarriage,” said Dr. Trolice. Although the impact of small endometrial polyps on fertility and pregnancy are uncertain, most infertility specialists recommend removal of endometrial polyps via hysteroscopic polypectomy in general and prior to IVF embryo transfer in particular, he said.
Although infertility patients are anxious to undergo embryo transfer, the current study suggests a benefit in delaying the procedure following the removal of any polyps identified during the pretransfer evaluation, Dr. Trolice said in an interview. As for additional research, “it would be helpful to know the age group breakdown of patients and if the results were consistent among all categories,” he said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Trolice had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
A longer time between hysteroscopic polypectomy and frozen embryo transfer may improve the odds of successful pregnancy, based on data from a new analysis presented at the annual meeting of the Society for Reproductive Investigation.
Although uterine polyps have a negative effect on pregnancy rates, data supporting a specific time interval between hysteroscopic polypectomy (HP) and frozen embryo transfer (FET) are limited, according to Audrey Messelt, MD, of Baylor College of Medicine, Houston, Texas, and colleagues.
“Hysteroscopic polypectomy is a common procedure performed before embryo transfer to optimize the receptivity of the endometrium. Currently, there is no ideal recovery time lapse between surgery and an embryo transfer,” said senior author Laura Detti, MD, professor of obstetrics and gynecology at Baylor, in an interview. “This is often the last step prior to embryo transfer, and identifying a recovery time that allows the best outcome is important.”
In a retrospective analysis, the researchers examined the effect of the time between HP and FET on pregnancy outcomes. They identified 65 patients with uterine pathology based on saline-infusion sonogram who underwent hysteroscopy and FET between June 1, 2022, and September 30, 2023.
The endometrial preparation for FET included sequential administration of oral or transdermal estradiol and intramuscular progesterone.
Overall, 46 patients were diagnosed with endometrial polyps at the time of surgery; three had endometritis, one had a uterine septum that was resected, 15 had no abnormal pathology or had normal endometrium at the time of examination. No cases of hyperplasia or malignancy were identified.
A total of 58 patients underwent FET with a single euploid embryo, four with a single untested embryo, one with a low-mosaic embryo, and two with a double-embryo transfer (one euploid and one low mosaic).
After FET, 50 patients conceived and 15 did not. Patients with ongoing pregnancies who had a history of endometrial polyps had significantly more days from surgery to FET, compared to patients with a history of polyps who failed to conceive (median 70 days vs 45 days, P = .01).
By contrast, the time between hysteroscopy and FET was similar among patients with no endometrial pathology who did and did not have ongoing pregnancies (median 45 vs 52.5 days, P = .95).
The findings were limited by the relatively small sample size and exclusion of patients with pathologies other than polyps, as well as a lack of data on age group breakdowns. However, the results suggest that patients with uterine polyps may benefit from more time between HP and FET, while patients with normal surgical findings could undergo FET sooner, the researchers concluded.
Postpolypectomy Timing May Affect Pregnancy Outcomes
“We used to think that having had the first menses from surgery would be enough recovery time for the uterine cavity, even if it was just 2 weeks,” Dr. Detti said in an interview. “This still holds true when no endometrial polyps are diagnosed in the pathological specimen; however, we learned that if endometrial polyps are removed at the time of hysteroscopy, the ideal recovery time prior to an embryo transfer should be longer,” she said.
The current study is important because approximately 15% of women are diagnosed with endometrial polyps during their reproductive years, said Mark P. Trolice, MD, professor at the University of Central Florida, Orlando, and founder/medical director of the IVF Center of Central Florida in Winter Park, in an interview.
“Abnormalities of the uterine cavity have been shown to reduce embryo implantation and increase the risk of miscarriage,” said Dr. Trolice. Although the impact of small endometrial polyps on fertility and pregnancy are uncertain, most infertility specialists recommend removal of endometrial polyps via hysteroscopic polypectomy in general and prior to IVF embryo transfer in particular, he said.
Although infertility patients are anxious to undergo embryo transfer, the current study suggests a benefit in delaying the procedure following the removal of any polyps identified during the pretransfer evaluation, Dr. Trolice said in an interview. As for additional research, “it would be helpful to know the age group breakdown of patients and if the results were consistent among all categories,” he said.
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Trolice had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
Teen Pregnancy Linked With Risk for Premature Death
Teen pregnancy is associated with a higher risk for premature mortality, both among those who carry the pregnancies to term and those who miscarry, according to a new study.
Among 2.2 million female teenagers in Ontario, Canada, the risk for premature death by age 31 years was 1.5 times higher among those who had one teen pregnancy and 2.1 times higher among those with two or more teen pregnancies.
“No person should die during childhood or early adulthood. Such deaths, unexpected and tragic, are often from preventable causes, including intentional injury,” lead author Joel Ray, MD, an obstetric medicine specialist and epidemiologist at St. Michael’s Hospital in Toronto, told this news organization.
“Women who experience teen pregnancy appear more vulnerable, often having experienced a history of adverse experiences in childhood, including abuse and economic challenges,” he said.
The study was published online in JAMA Network Open.
Analyzing Pregnancy Associations
The investigators conducted a population-based cohort study of all girls who were alive at age 12 years from April 1991 to March 2021 in Ontario. They evaluated the risk for all-cause mortality from age 12 years onward in association with the number of teen pregnancies between ages 12 and 19 years and the age at first pregnancy. The investigators adjusted the hazard ratios for year of birth, comorbidities at ages 9-11 years, area-level education, income level, and rural status.
Among more than 2.2 million teens, 163,124 (7.3%) had a pregnancy at a median age of 18 years, including 121,276 (74.3%) who had one pregnancy and 41,848 (25.6%) who had two or more. These teens were more likely to live in the lowest neighborhood income quintile and in an area with a lower rate of high school completion. They also had a higher prevalence of self-harm history between ages 12 and 19 years but not a higher prevalence of physical or mental comorbidities.
Among all teens who had a pregnancy, 60,037 (36.8%) ended in a birth, including 59,485 (99.1%) live births. A further 106,135 (65.1%) ended in induced abortion, and 17,945 (11%) ended in miscarriage or ectopic pregnancy.
Overall, there were 6030 premature deaths among those without a teen pregnancy, or 1.9 per 10,000 person-years. There were 701 deaths among those with one teen pregnancy (4.1 per 10,000 person-years) and 345 deaths among those with two or more teen pregnancies (6.1 per 10,000 person-years).
The adjusted hazard ratios (AHRs) for mortality were 1.51 for those with one pregnancy and 2.14 for those with two or more pregnancies. Compared with no teen pregnancy, the AHRs for premature death were 1.41 if the first teen pregnancy ended in an induced abortion and 2.10 if it ended in a miscarriage or birth.
Comparing those with a teen pregnancy and those without, the AHRs for premature death were 1.25 from noninjury, 2.06 from unintentional injury, and 2.02 from intentional injury. Among patients with teen pregnancy, noninjury-related premature mortality was more common, at 2.0 per 10,000 person-years, than unintentional and intentional injuries, at 1.0 per 10,000 person-years and 0.4 per 10,000 person-years, respectively.
A teen pregnancy before age 16 years entailed the highest associated risk for premature death, with an AHR of 2.00.
Next Research Steps
“We were not surprised by our findings, but it was new to us to see that the risk for premature death was higher for women who had an induced abortion in their teen years,” said Dr. Ray. “It was even higher in those whose pregnancy ended in a birth or miscarriage.”
The investigators plan to evaluate whether the future risk for premature death after teen pregnancy differs by the type of induced abortion, such as procedural or pharmaceutical, or by whether the pregnancy ended in a live birth, stillbirth, or miscarriage. Among those with a live birth, the researchers will also analyze the risk for premature death in relation to whether the newborn was taken into custody by child protection services in Canada.
Other factors associated with teen pregnancy and overall mortality, particularly adverse childhood experiences, may point to the reasons for premature mortality and should be studied further, the authors wrote. Structural and systems-related factors should be considered as well.
Stigmatization and Isolation
“Some teens choose to become pregnant, but most teen pregnancies are unintended, which exposes shortcomings in the systems that exist to educate, guide, and support young people,” said Elizabeth Cook, a research scientist at Child Trends in Rockville, Maryland.
Dr. Cook, who wasn’t involved with this study, wrote an accompanying editorial in JAMA Network Open. She conducts studies of sexual and reproductive health for Child Trends.
“Teens who become pregnant often experience stigmatization and isolation that can make it more difficult to thrive in adulthood, especially if they lack the necessary support to navigate such a significant decision,” she said. “Fortunately, the systems that youths encounter, such as healthcare, education, and child welfare, are taking on a larger role in prevention efforts than they have in the past.”
These systems are shifting the burden of unintended teen pregnancy from the teens themselves and their behaviors to the health and education systems, Dr. Cook noted, though more work is needed around local policies and lack of access to healthcare facilities.
“Teen pregnancy may offer an opportunity to intervene in the lives of people at higher risk for premature death, but knowing how best to offer support requires an understanding of the context of their lives,” she said. “As a starting point, we must celebrate and listen to all pregnant young people so they can tell us what they need to live long, fulfilled lives.”
The study was funded by grants from the PSI Foundation and the Canadian Institutes of Health Research, as well as ICES, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Ray and Dr. Cook reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Teen pregnancy is associated with a higher risk for premature mortality, both among those who carry the pregnancies to term and those who miscarry, according to a new study.
Among 2.2 million female teenagers in Ontario, Canada, the risk for premature death by age 31 years was 1.5 times higher among those who had one teen pregnancy and 2.1 times higher among those with two or more teen pregnancies.
“No person should die during childhood or early adulthood. Such deaths, unexpected and tragic, are often from preventable causes, including intentional injury,” lead author Joel Ray, MD, an obstetric medicine specialist and epidemiologist at St. Michael’s Hospital in Toronto, told this news organization.
“Women who experience teen pregnancy appear more vulnerable, often having experienced a history of adverse experiences in childhood, including abuse and economic challenges,” he said.
The study was published online in JAMA Network Open.
Analyzing Pregnancy Associations
The investigators conducted a population-based cohort study of all girls who were alive at age 12 years from April 1991 to March 2021 in Ontario. They evaluated the risk for all-cause mortality from age 12 years onward in association with the number of teen pregnancies between ages 12 and 19 years and the age at first pregnancy. The investigators adjusted the hazard ratios for year of birth, comorbidities at ages 9-11 years, area-level education, income level, and rural status.
Among more than 2.2 million teens, 163,124 (7.3%) had a pregnancy at a median age of 18 years, including 121,276 (74.3%) who had one pregnancy and 41,848 (25.6%) who had two or more. These teens were more likely to live in the lowest neighborhood income quintile and in an area with a lower rate of high school completion. They also had a higher prevalence of self-harm history between ages 12 and 19 years but not a higher prevalence of physical or mental comorbidities.
Among all teens who had a pregnancy, 60,037 (36.8%) ended in a birth, including 59,485 (99.1%) live births. A further 106,135 (65.1%) ended in induced abortion, and 17,945 (11%) ended in miscarriage or ectopic pregnancy.
Overall, there were 6030 premature deaths among those without a teen pregnancy, or 1.9 per 10,000 person-years. There were 701 deaths among those with one teen pregnancy (4.1 per 10,000 person-years) and 345 deaths among those with two or more teen pregnancies (6.1 per 10,000 person-years).
The adjusted hazard ratios (AHRs) for mortality were 1.51 for those with one pregnancy and 2.14 for those with two or more pregnancies. Compared with no teen pregnancy, the AHRs for premature death were 1.41 if the first teen pregnancy ended in an induced abortion and 2.10 if it ended in a miscarriage or birth.
Comparing those with a teen pregnancy and those without, the AHRs for premature death were 1.25 from noninjury, 2.06 from unintentional injury, and 2.02 from intentional injury. Among patients with teen pregnancy, noninjury-related premature mortality was more common, at 2.0 per 10,000 person-years, than unintentional and intentional injuries, at 1.0 per 10,000 person-years and 0.4 per 10,000 person-years, respectively.
A teen pregnancy before age 16 years entailed the highest associated risk for premature death, with an AHR of 2.00.
Next Research Steps
“We were not surprised by our findings, but it was new to us to see that the risk for premature death was higher for women who had an induced abortion in their teen years,” said Dr. Ray. “It was even higher in those whose pregnancy ended in a birth or miscarriage.”
The investigators plan to evaluate whether the future risk for premature death after teen pregnancy differs by the type of induced abortion, such as procedural or pharmaceutical, or by whether the pregnancy ended in a live birth, stillbirth, or miscarriage. Among those with a live birth, the researchers will also analyze the risk for premature death in relation to whether the newborn was taken into custody by child protection services in Canada.
Other factors associated with teen pregnancy and overall mortality, particularly adverse childhood experiences, may point to the reasons for premature mortality and should be studied further, the authors wrote. Structural and systems-related factors should be considered as well.
Stigmatization and Isolation
“Some teens choose to become pregnant, but most teen pregnancies are unintended, which exposes shortcomings in the systems that exist to educate, guide, and support young people,” said Elizabeth Cook, a research scientist at Child Trends in Rockville, Maryland.
Dr. Cook, who wasn’t involved with this study, wrote an accompanying editorial in JAMA Network Open. She conducts studies of sexual and reproductive health for Child Trends.
“Teens who become pregnant often experience stigmatization and isolation that can make it more difficult to thrive in adulthood, especially if they lack the necessary support to navigate such a significant decision,” she said. “Fortunately, the systems that youths encounter, such as healthcare, education, and child welfare, are taking on a larger role in prevention efforts than they have in the past.”
These systems are shifting the burden of unintended teen pregnancy from the teens themselves and their behaviors to the health and education systems, Dr. Cook noted, though more work is needed around local policies and lack of access to healthcare facilities.
“Teen pregnancy may offer an opportunity to intervene in the lives of people at higher risk for premature death, but knowing how best to offer support requires an understanding of the context of their lives,” she said. “As a starting point, we must celebrate and listen to all pregnant young people so they can tell us what they need to live long, fulfilled lives.”
The study was funded by grants from the PSI Foundation and the Canadian Institutes of Health Research, as well as ICES, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Ray and Dr. Cook reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Teen pregnancy is associated with a higher risk for premature mortality, both among those who carry the pregnancies to term and those who miscarry, according to a new study.
Among 2.2 million female teenagers in Ontario, Canada, the risk for premature death by age 31 years was 1.5 times higher among those who had one teen pregnancy and 2.1 times higher among those with two or more teen pregnancies.
“No person should die during childhood or early adulthood. Such deaths, unexpected and tragic, are often from preventable causes, including intentional injury,” lead author Joel Ray, MD, an obstetric medicine specialist and epidemiologist at St. Michael’s Hospital in Toronto, told this news organization.
“Women who experience teen pregnancy appear more vulnerable, often having experienced a history of adverse experiences in childhood, including abuse and economic challenges,” he said.
The study was published online in JAMA Network Open.
Analyzing Pregnancy Associations
The investigators conducted a population-based cohort study of all girls who were alive at age 12 years from April 1991 to March 2021 in Ontario. They evaluated the risk for all-cause mortality from age 12 years onward in association with the number of teen pregnancies between ages 12 and 19 years and the age at first pregnancy. The investigators adjusted the hazard ratios for year of birth, comorbidities at ages 9-11 years, area-level education, income level, and rural status.
Among more than 2.2 million teens, 163,124 (7.3%) had a pregnancy at a median age of 18 years, including 121,276 (74.3%) who had one pregnancy and 41,848 (25.6%) who had two or more. These teens were more likely to live in the lowest neighborhood income quintile and in an area with a lower rate of high school completion. They also had a higher prevalence of self-harm history between ages 12 and 19 years but not a higher prevalence of physical or mental comorbidities.
Among all teens who had a pregnancy, 60,037 (36.8%) ended in a birth, including 59,485 (99.1%) live births. A further 106,135 (65.1%) ended in induced abortion, and 17,945 (11%) ended in miscarriage or ectopic pregnancy.
Overall, there were 6030 premature deaths among those without a teen pregnancy, or 1.9 per 10,000 person-years. There were 701 deaths among those with one teen pregnancy (4.1 per 10,000 person-years) and 345 deaths among those with two or more teen pregnancies (6.1 per 10,000 person-years).
The adjusted hazard ratios (AHRs) for mortality were 1.51 for those with one pregnancy and 2.14 for those with two or more pregnancies. Compared with no teen pregnancy, the AHRs for premature death were 1.41 if the first teen pregnancy ended in an induced abortion and 2.10 if it ended in a miscarriage or birth.
Comparing those with a teen pregnancy and those without, the AHRs for premature death were 1.25 from noninjury, 2.06 from unintentional injury, and 2.02 from intentional injury. Among patients with teen pregnancy, noninjury-related premature mortality was more common, at 2.0 per 10,000 person-years, than unintentional and intentional injuries, at 1.0 per 10,000 person-years and 0.4 per 10,000 person-years, respectively.
A teen pregnancy before age 16 years entailed the highest associated risk for premature death, with an AHR of 2.00.
Next Research Steps
“We were not surprised by our findings, but it was new to us to see that the risk for premature death was higher for women who had an induced abortion in their teen years,” said Dr. Ray. “It was even higher in those whose pregnancy ended in a birth or miscarriage.”
The investigators plan to evaluate whether the future risk for premature death after teen pregnancy differs by the type of induced abortion, such as procedural or pharmaceutical, or by whether the pregnancy ended in a live birth, stillbirth, or miscarriage. Among those with a live birth, the researchers will also analyze the risk for premature death in relation to whether the newborn was taken into custody by child protection services in Canada.
Other factors associated with teen pregnancy and overall mortality, particularly adverse childhood experiences, may point to the reasons for premature mortality and should be studied further, the authors wrote. Structural and systems-related factors should be considered as well.
Stigmatization and Isolation
“Some teens choose to become pregnant, but most teen pregnancies are unintended, which exposes shortcomings in the systems that exist to educate, guide, and support young people,” said Elizabeth Cook, a research scientist at Child Trends in Rockville, Maryland.
Dr. Cook, who wasn’t involved with this study, wrote an accompanying editorial in JAMA Network Open. She conducts studies of sexual and reproductive health for Child Trends.
“Teens who become pregnant often experience stigmatization and isolation that can make it more difficult to thrive in adulthood, especially if they lack the necessary support to navigate such a significant decision,” she said. “Fortunately, the systems that youths encounter, such as healthcare, education, and child welfare, are taking on a larger role in prevention efforts than they have in the past.”
These systems are shifting the burden of unintended teen pregnancy from the teens themselves and their behaviors to the health and education systems, Dr. Cook noted, though more work is needed around local policies and lack of access to healthcare facilities.
“Teen pregnancy may offer an opportunity to intervene in the lives of people at higher risk for premature death, but knowing how best to offer support requires an understanding of the context of their lives,” she said. “As a starting point, we must celebrate and listen to all pregnant young people so they can tell us what they need to live long, fulfilled lives.”
The study was funded by grants from the PSI Foundation and the Canadian Institutes of Health Research, as well as ICES, which is funded by the Ontario Ministry of Health and the Ministry of Long-Term Care. Dr. Ray and Dr. Cook reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Infant Exposure to MS Drugs via Breastfeeding: New Data
, new research confirmed.
Registry data showed no differences in health or development in the first 3 years of life among infants exposed to natalizumab, ocrelizumab, rituximab, or ofatumumab, compared with unexposed infants.
“Most monoclonal antibody medications for multiple sclerosis are not currently approved for use while a mother is breastfeeding,” even though the disease can develop during a person’s reproductive years, study investigator Kerstin Hellwig, MD, with Ruhr University in Bochum, Germany, said in a news release.
“Our data show infants exposed to these medications through breastfeeding experienced no negative effects on health or development within the first 3 years of life,” Dr. Hellwig said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Registry Data and Analysis
Using the German MS and Pregnancy Registry, researchers identified 183 infants born to mothers taking mAbs while breastfeeding — 180 with a diagnosis of MS and three with a diagnosis of NMOSD. The infants were matched to 183 unexposed infants (control group).
Exposure to mAbs during lactation started a median of 19 days postpartum and lasted for a median of 172 days. The most commonly used mAb during lactation was natalizumab (125 women), followed by ocrelizumab (34 women), rituximab (11 women), and ofatumumab (10 women).
Among the entire infant cohort, two were first exposed to natalizumab and then ocrelizumab; one was exposed to rituximab and then ocrelizumab; three had been previously breastfed on glatiramer acetate and two on interferons.
The primary outcomes were hospitalizations, antibiotic use, developmental delay, and weight during the first 3 years of life in mAb-exposed versus unexposed infants.
In adjusted regression analyses, mAb exposure during breastfeeding was not significantly associated with annual hospitalization (rate ratio [RR], 1.23; P = .473), annual systemic antibiotic use (RR, 1.55; P = .093), developmental delay (odds ratio, 1.16; P = .716), or weight.
A limitation of the study was that only about a third of the infants were followed for the full 3 years. Therefore, Dr. Hellwig said, the results for the third year of life are less meaningful than for years 1 and 2.
‘Reassuring’ Data
Reached for comment, Edith L. Graham, MD, Department of Neurology, Multiple Sclerosis and Neuroimmunology, Northwestern University, Chicago, Illinois, noted that this is the largest group of breastfed infants exposed to mAbs used to treat MS and said the data provide “reassuring infant outcomes with no increase in hospitalization, antibiotic use, or developmental delay.”
Dr. Graham noted that recent publications have reported more on the use of anti-CD20 mAbs (ocrelizumab/rituximab/ofatumumab) while breastfeeding, “and this study adds data for patients on natalizumab.”
“It will be important to know how infusion timing after birth impacts transfer of monoclonal antibodies depending on the milk stage as it transitions from colostrum to mature milk in the first month postpartum,” Dr. Graham said.
“While infection rates of infants are reassuring, data on allergies in the exposed infants would be interesting to look at as well,” she added. “While these infusions are not orally bioavailable, we do not know the full extent of impact on the neonatal gut microbiome.”
In addition, Dr. Graham said it would be important to know whether drugs administered monthly, such as natalizumab and ofatumumab, accumulate in the breast milk at higher levels than medications such as ocrelizumab and rituximab, which are administered twice a year.
The German MS and pregnancy registry was partly supported by the Innovation Fund of the Federal Joint Committee, Almirall Hermal GmbH, Biogen GmbH Germany, Hexal AG, Merck Serono GmbH, Novartis Pharma GmbH, Roche Deutschland GmbH, Sanofi Genzyme, and Teva GmbH. Dr. Hellwig and Dr. Graham had no relevant disclosures.
A version of this article appeared on Medscape.com.
, new research confirmed.
Registry data showed no differences in health or development in the first 3 years of life among infants exposed to natalizumab, ocrelizumab, rituximab, or ofatumumab, compared with unexposed infants.
“Most monoclonal antibody medications for multiple sclerosis are not currently approved for use while a mother is breastfeeding,” even though the disease can develop during a person’s reproductive years, study investigator Kerstin Hellwig, MD, with Ruhr University in Bochum, Germany, said in a news release.
“Our data show infants exposed to these medications through breastfeeding experienced no negative effects on health or development within the first 3 years of life,” Dr. Hellwig said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Registry Data and Analysis
Using the German MS and Pregnancy Registry, researchers identified 183 infants born to mothers taking mAbs while breastfeeding — 180 with a diagnosis of MS and three with a diagnosis of NMOSD. The infants were matched to 183 unexposed infants (control group).
Exposure to mAbs during lactation started a median of 19 days postpartum and lasted for a median of 172 days. The most commonly used mAb during lactation was natalizumab (125 women), followed by ocrelizumab (34 women), rituximab (11 women), and ofatumumab (10 women).
Among the entire infant cohort, two were first exposed to natalizumab and then ocrelizumab; one was exposed to rituximab and then ocrelizumab; three had been previously breastfed on glatiramer acetate and two on interferons.
The primary outcomes were hospitalizations, antibiotic use, developmental delay, and weight during the first 3 years of life in mAb-exposed versus unexposed infants.
In adjusted regression analyses, mAb exposure during breastfeeding was not significantly associated with annual hospitalization (rate ratio [RR], 1.23; P = .473), annual systemic antibiotic use (RR, 1.55; P = .093), developmental delay (odds ratio, 1.16; P = .716), or weight.
A limitation of the study was that only about a third of the infants were followed for the full 3 years. Therefore, Dr. Hellwig said, the results for the third year of life are less meaningful than for years 1 and 2.
‘Reassuring’ Data
Reached for comment, Edith L. Graham, MD, Department of Neurology, Multiple Sclerosis and Neuroimmunology, Northwestern University, Chicago, Illinois, noted that this is the largest group of breastfed infants exposed to mAbs used to treat MS and said the data provide “reassuring infant outcomes with no increase in hospitalization, antibiotic use, or developmental delay.”
Dr. Graham noted that recent publications have reported more on the use of anti-CD20 mAbs (ocrelizumab/rituximab/ofatumumab) while breastfeeding, “and this study adds data for patients on natalizumab.”
“It will be important to know how infusion timing after birth impacts transfer of monoclonal antibodies depending on the milk stage as it transitions from colostrum to mature milk in the first month postpartum,” Dr. Graham said.
“While infection rates of infants are reassuring, data on allergies in the exposed infants would be interesting to look at as well,” she added. “While these infusions are not orally bioavailable, we do not know the full extent of impact on the neonatal gut microbiome.”
In addition, Dr. Graham said it would be important to know whether drugs administered monthly, such as natalizumab and ofatumumab, accumulate in the breast milk at higher levels than medications such as ocrelizumab and rituximab, which are administered twice a year.
The German MS and pregnancy registry was partly supported by the Innovation Fund of the Federal Joint Committee, Almirall Hermal GmbH, Biogen GmbH Germany, Hexal AG, Merck Serono GmbH, Novartis Pharma GmbH, Roche Deutschland GmbH, Sanofi Genzyme, and Teva GmbH. Dr. Hellwig and Dr. Graham had no relevant disclosures.
A version of this article appeared on Medscape.com.
, new research confirmed.
Registry data showed no differences in health or development in the first 3 years of life among infants exposed to natalizumab, ocrelizumab, rituximab, or ofatumumab, compared with unexposed infants.
“Most monoclonal antibody medications for multiple sclerosis are not currently approved for use while a mother is breastfeeding,” even though the disease can develop during a person’s reproductive years, study investigator Kerstin Hellwig, MD, with Ruhr University in Bochum, Germany, said in a news release.
“Our data show infants exposed to these medications through breastfeeding experienced no negative effects on health or development within the first 3 years of life,” Dr. Hellwig said.
The findings were released ahead of the study’s scheduled presentation at the annual meeting of the American Academy of Neurology.
Registry Data and Analysis
Using the German MS and Pregnancy Registry, researchers identified 183 infants born to mothers taking mAbs while breastfeeding — 180 with a diagnosis of MS and three with a diagnosis of NMOSD. The infants were matched to 183 unexposed infants (control group).
Exposure to mAbs during lactation started a median of 19 days postpartum and lasted for a median of 172 days. The most commonly used mAb during lactation was natalizumab (125 women), followed by ocrelizumab (34 women), rituximab (11 women), and ofatumumab (10 women).
Among the entire infant cohort, two were first exposed to natalizumab and then ocrelizumab; one was exposed to rituximab and then ocrelizumab; three had been previously breastfed on glatiramer acetate and two on interferons.
The primary outcomes were hospitalizations, antibiotic use, developmental delay, and weight during the first 3 years of life in mAb-exposed versus unexposed infants.
In adjusted regression analyses, mAb exposure during breastfeeding was not significantly associated with annual hospitalization (rate ratio [RR], 1.23; P = .473), annual systemic antibiotic use (RR, 1.55; P = .093), developmental delay (odds ratio, 1.16; P = .716), or weight.
A limitation of the study was that only about a third of the infants were followed for the full 3 years. Therefore, Dr. Hellwig said, the results for the third year of life are less meaningful than for years 1 and 2.
‘Reassuring’ Data
Reached for comment, Edith L. Graham, MD, Department of Neurology, Multiple Sclerosis and Neuroimmunology, Northwestern University, Chicago, Illinois, noted that this is the largest group of breastfed infants exposed to mAbs used to treat MS and said the data provide “reassuring infant outcomes with no increase in hospitalization, antibiotic use, or developmental delay.”
Dr. Graham noted that recent publications have reported more on the use of anti-CD20 mAbs (ocrelizumab/rituximab/ofatumumab) while breastfeeding, “and this study adds data for patients on natalizumab.”
“It will be important to know how infusion timing after birth impacts transfer of monoclonal antibodies depending on the milk stage as it transitions from colostrum to mature milk in the first month postpartum,” Dr. Graham said.
“While infection rates of infants are reassuring, data on allergies in the exposed infants would be interesting to look at as well,” she added. “While these infusions are not orally bioavailable, we do not know the full extent of impact on the neonatal gut microbiome.”
In addition, Dr. Graham said it would be important to know whether drugs administered monthly, such as natalizumab and ofatumumab, accumulate in the breast milk at higher levels than medications such as ocrelizumab and rituximab, which are administered twice a year.
The German MS and pregnancy registry was partly supported by the Innovation Fund of the Federal Joint Committee, Almirall Hermal GmbH, Biogen GmbH Germany, Hexal AG, Merck Serono GmbH, Novartis Pharma GmbH, Roche Deutschland GmbH, Sanofi Genzyme, and Teva GmbH. Dr. Hellwig and Dr. Graham had no relevant disclosures.
A version of this article appeared on Medscape.com.
Perinatal Mood and Anxiety Disorder Increasing Rapidly
The number of women with perinatal mood and anxiety disorder (PMAD) has spiked sharply in the United States. A new study explores trends by state and time period.
Between 2008 and 2020, in a national cohort of 750,004 commercially insured women with a live birth, nearly 1 in 5 (144,037 [19.2%]) were diagnosed with PMAD, according to a paper published in Health Affairs. PMAD diagnoses among privately insured women increased by 93.3% over those years, wrote lead author Kara Zivin, PhD, of the University of Michigan, Veterans Affairs Ann Arbor Healthcare System, and colleagues.
PMAD describes a spectrum of emotional complications with mild to severe symptoms that can affect women while pregnant and through the first year after giving birth.
The total number of perinatal women decreased from a high of 64,842 in 2008 to a low of 52,479 in 2020, a 19.1% decrease, but over the same time, women with diagnosed PMAD increased 56.4% from 9,520 in 2008 to 14,890 in 2020. Prevalence of PMAD doubled from 1,468 per 10,000 deliveries to 2,837 per 10,000 deliveries in 2020, according to the analysis.
Differences by State
Increases differed substantially by state. Though average annual changes across all states reached 109 additional PMAD diagnoses per 10,000 deliveries, Iowa had the greatest increase with an additional 163 PMAD diagnoses per 10,000 deliveries annually. New Mexico had the smallest annual growth, at an additional 49 per 10,000 deliveries.
The increases were accompanied by maternal health improvement efforts. The Affordable Care Act (ACA) required insurance companies to cover maternity and preventive services, which likely increased PMAD screening and detection, the researchers noted.
“Diagnosis of PMAD is rising due to increased awareness and in all likelihood, decrease in stigma, but availability of providers is so challenging,” said Lee S. Cohen, MD, who was not part of the study. Dr. Cohen is director of the Ammon-Pinizzotto Center for Women’s Mental Health and Perinatal and Reproductive Psychiatry at Massachusetts General Hospital in Boston. “The navigation to providers by women who are suffering is beyond challenging,” he said.
The authors reported that all states except Vermont saw increasing rates of PMAD diagnoses post-ACA vs. pre-ACA. The researchers also found that relative to the period from 2008 to 2014, psychotherapy rates continued rising from 2015 to 2020 and suicidality (suicidal ideation or self-harm diagnoses) rates declined.
States’ Suicidality Rates Vary Widely
“Overall, access to psychotherapy may have stemmed suicidality despite increasing PMAD diagnoses. But although more PMAD diagnoses may have led to increased psychotherapy, therapy access depends on provider availability, which varies by geographic region and insurance coverage network,” the authors wrote.
Suicidality rates differed greatly by state. Louisiana’s annual rate of increase was greatest, at 22 per 10,000 while Maryland had the greatest negative annual rate of change, at −15 per 10,000 deliveries, the authors explained.
“Observed trends in PMAD diagnoses among privately insured people during 2008-2020 and in associated suicidality and psychotherapy use suggest an increasingly rapid worsening of US maternal mental health,” the authors wrote.
The authors noted that this study did not include those on public insurance, a group that may experience disproportionate maternal morbidity and mortality burden, and urged that future studies include them.
Strengths of Study
Kimberly McKee, PhD, MPH, assistant professor in the department of family medicine at University of Michigan in Ann Arbor, who was not part of this research, said this paper gives a broader look than prior work because it includes the year before and after birth, rather than delivery and hospitalization.
“It’s really important to look out at least 12 months postpartum,” she noted.
Another strength is that the study was able to look at use of services such as psychotherapy before and post ACA. She noted the increased use of psychotherapy and the decrease in suicidal ideation was an association, but said, “I think it’s reasonable to assume that there was a benefit.”
She noted that these data go through 2020 and the COVID-19 pandemic has even further stressed the healthcare system, which could affect these numbers.
Primary Care’s Role
“The opportunity for primary care to really be the medical home for reproductive-age women is key here,” Dr. McKee said, adding that primary care can provide the continuity if women go off and on insurance around pregnancy and make sure the women get follow-up care and referrals to specialty care.
Models that integrate behavioral health and primary care are particularly promising, she said. Inclusion of social workers at the point of care can also help meet needs regarding social determinants of health.
Telehealth is another avenue for expansion extending the reach for following perinatal women, she said. “Using every tool we have to reach individuals where they are can allow for more frequent check-ins, which is really important here.”
Dr. McKee said the paper highlights an important reality: Mental health is a leading cause and contributor to maternal mortality, which “is 100% preventable.” Yet, current literature continues to show increases.
“This is a fairly common problem that affects not just women, but the fetus, their children, their families,” she noted.
The authors and Dr. Cohen and Dr. McKee reported no relevant financial relationships.
The number of women with perinatal mood and anxiety disorder (PMAD) has spiked sharply in the United States. A new study explores trends by state and time period.
Between 2008 and 2020, in a national cohort of 750,004 commercially insured women with a live birth, nearly 1 in 5 (144,037 [19.2%]) were diagnosed with PMAD, according to a paper published in Health Affairs. PMAD diagnoses among privately insured women increased by 93.3% over those years, wrote lead author Kara Zivin, PhD, of the University of Michigan, Veterans Affairs Ann Arbor Healthcare System, and colleagues.
PMAD describes a spectrum of emotional complications with mild to severe symptoms that can affect women while pregnant and through the first year after giving birth.
The total number of perinatal women decreased from a high of 64,842 in 2008 to a low of 52,479 in 2020, a 19.1% decrease, but over the same time, women with diagnosed PMAD increased 56.4% from 9,520 in 2008 to 14,890 in 2020. Prevalence of PMAD doubled from 1,468 per 10,000 deliveries to 2,837 per 10,000 deliveries in 2020, according to the analysis.
Differences by State
Increases differed substantially by state. Though average annual changes across all states reached 109 additional PMAD diagnoses per 10,000 deliveries, Iowa had the greatest increase with an additional 163 PMAD diagnoses per 10,000 deliveries annually. New Mexico had the smallest annual growth, at an additional 49 per 10,000 deliveries.
The increases were accompanied by maternal health improvement efforts. The Affordable Care Act (ACA) required insurance companies to cover maternity and preventive services, which likely increased PMAD screening and detection, the researchers noted.
“Diagnosis of PMAD is rising due to increased awareness and in all likelihood, decrease in stigma, but availability of providers is so challenging,” said Lee S. Cohen, MD, who was not part of the study. Dr. Cohen is director of the Ammon-Pinizzotto Center for Women’s Mental Health and Perinatal and Reproductive Psychiatry at Massachusetts General Hospital in Boston. “The navigation to providers by women who are suffering is beyond challenging,” he said.
The authors reported that all states except Vermont saw increasing rates of PMAD diagnoses post-ACA vs. pre-ACA. The researchers also found that relative to the period from 2008 to 2014, psychotherapy rates continued rising from 2015 to 2020 and suicidality (suicidal ideation or self-harm diagnoses) rates declined.
States’ Suicidality Rates Vary Widely
“Overall, access to psychotherapy may have stemmed suicidality despite increasing PMAD diagnoses. But although more PMAD diagnoses may have led to increased psychotherapy, therapy access depends on provider availability, which varies by geographic region and insurance coverage network,” the authors wrote.
Suicidality rates differed greatly by state. Louisiana’s annual rate of increase was greatest, at 22 per 10,000 while Maryland had the greatest negative annual rate of change, at −15 per 10,000 deliveries, the authors explained.
“Observed trends in PMAD diagnoses among privately insured people during 2008-2020 and in associated suicidality and psychotherapy use suggest an increasingly rapid worsening of US maternal mental health,” the authors wrote.
The authors noted that this study did not include those on public insurance, a group that may experience disproportionate maternal morbidity and mortality burden, and urged that future studies include them.
Strengths of Study
Kimberly McKee, PhD, MPH, assistant professor in the department of family medicine at University of Michigan in Ann Arbor, who was not part of this research, said this paper gives a broader look than prior work because it includes the year before and after birth, rather than delivery and hospitalization.
“It’s really important to look out at least 12 months postpartum,” she noted.
Another strength is that the study was able to look at use of services such as psychotherapy before and post ACA. She noted the increased use of psychotherapy and the decrease in suicidal ideation was an association, but said, “I think it’s reasonable to assume that there was a benefit.”
She noted that these data go through 2020 and the COVID-19 pandemic has even further stressed the healthcare system, which could affect these numbers.
Primary Care’s Role
“The opportunity for primary care to really be the medical home for reproductive-age women is key here,” Dr. McKee said, adding that primary care can provide the continuity if women go off and on insurance around pregnancy and make sure the women get follow-up care and referrals to specialty care.
Models that integrate behavioral health and primary care are particularly promising, she said. Inclusion of social workers at the point of care can also help meet needs regarding social determinants of health.
Telehealth is another avenue for expansion extending the reach for following perinatal women, she said. “Using every tool we have to reach individuals where they are can allow for more frequent check-ins, which is really important here.”
Dr. McKee said the paper highlights an important reality: Mental health is a leading cause and contributor to maternal mortality, which “is 100% preventable.” Yet, current literature continues to show increases.
“This is a fairly common problem that affects not just women, but the fetus, their children, their families,” she noted.
The authors and Dr. Cohen and Dr. McKee reported no relevant financial relationships.
The number of women with perinatal mood and anxiety disorder (PMAD) has spiked sharply in the United States. A new study explores trends by state and time period.
Between 2008 and 2020, in a national cohort of 750,004 commercially insured women with a live birth, nearly 1 in 5 (144,037 [19.2%]) were diagnosed with PMAD, according to a paper published in Health Affairs. PMAD diagnoses among privately insured women increased by 93.3% over those years, wrote lead author Kara Zivin, PhD, of the University of Michigan, Veterans Affairs Ann Arbor Healthcare System, and colleagues.
PMAD describes a spectrum of emotional complications with mild to severe symptoms that can affect women while pregnant and through the first year after giving birth.
The total number of perinatal women decreased from a high of 64,842 in 2008 to a low of 52,479 in 2020, a 19.1% decrease, but over the same time, women with diagnosed PMAD increased 56.4% from 9,520 in 2008 to 14,890 in 2020. Prevalence of PMAD doubled from 1,468 per 10,000 deliveries to 2,837 per 10,000 deliveries in 2020, according to the analysis.
Differences by State
Increases differed substantially by state. Though average annual changes across all states reached 109 additional PMAD diagnoses per 10,000 deliveries, Iowa had the greatest increase with an additional 163 PMAD diagnoses per 10,000 deliveries annually. New Mexico had the smallest annual growth, at an additional 49 per 10,000 deliveries.
The increases were accompanied by maternal health improvement efforts. The Affordable Care Act (ACA) required insurance companies to cover maternity and preventive services, which likely increased PMAD screening and detection, the researchers noted.
“Diagnosis of PMAD is rising due to increased awareness and in all likelihood, decrease in stigma, but availability of providers is so challenging,” said Lee S. Cohen, MD, who was not part of the study. Dr. Cohen is director of the Ammon-Pinizzotto Center for Women’s Mental Health and Perinatal and Reproductive Psychiatry at Massachusetts General Hospital in Boston. “The navigation to providers by women who are suffering is beyond challenging,” he said.
The authors reported that all states except Vermont saw increasing rates of PMAD diagnoses post-ACA vs. pre-ACA. The researchers also found that relative to the period from 2008 to 2014, psychotherapy rates continued rising from 2015 to 2020 and suicidality (suicidal ideation or self-harm diagnoses) rates declined.
States’ Suicidality Rates Vary Widely
“Overall, access to psychotherapy may have stemmed suicidality despite increasing PMAD diagnoses. But although more PMAD diagnoses may have led to increased psychotherapy, therapy access depends on provider availability, which varies by geographic region and insurance coverage network,” the authors wrote.
Suicidality rates differed greatly by state. Louisiana’s annual rate of increase was greatest, at 22 per 10,000 while Maryland had the greatest negative annual rate of change, at −15 per 10,000 deliveries, the authors explained.
“Observed trends in PMAD diagnoses among privately insured people during 2008-2020 and in associated suicidality and psychotherapy use suggest an increasingly rapid worsening of US maternal mental health,” the authors wrote.
The authors noted that this study did not include those on public insurance, a group that may experience disproportionate maternal morbidity and mortality burden, and urged that future studies include them.
Strengths of Study
Kimberly McKee, PhD, MPH, assistant professor in the department of family medicine at University of Michigan in Ann Arbor, who was not part of this research, said this paper gives a broader look than prior work because it includes the year before and after birth, rather than delivery and hospitalization.
“It’s really important to look out at least 12 months postpartum,” she noted.
Another strength is that the study was able to look at use of services such as psychotherapy before and post ACA. She noted the increased use of psychotherapy and the decrease in suicidal ideation was an association, but said, “I think it’s reasonable to assume that there was a benefit.”
She noted that these data go through 2020 and the COVID-19 pandemic has even further stressed the healthcare system, which could affect these numbers.
Primary Care’s Role
“The opportunity for primary care to really be the medical home for reproductive-age women is key here,” Dr. McKee said, adding that primary care can provide the continuity if women go off and on insurance around pregnancy and make sure the women get follow-up care and referrals to specialty care.
Models that integrate behavioral health and primary care are particularly promising, she said. Inclusion of social workers at the point of care can also help meet needs regarding social determinants of health.
Telehealth is another avenue for expansion extending the reach for following perinatal women, she said. “Using every tool we have to reach individuals where they are can allow for more frequent check-ins, which is really important here.”
Dr. McKee said the paper highlights an important reality: Mental health is a leading cause and contributor to maternal mortality, which “is 100% preventable.” Yet, current literature continues to show increases.
“This is a fairly common problem that affects not just women, but the fetus, their children, their families,” she noted.
The authors and Dr. Cohen and Dr. McKee reported no relevant financial relationships.
FROM HEALTH AFFAIRS
Study Links Maternal Hidradenitis Suppurativa to Risk for Childhood Morbidity
SAN DIEGO — , and other conditions.
Those are key findings from a longitudinal cohort study that was presented during a poster session at the annual meeting of the American Academy of Dermatology.
“HS is associated with morbidity in women of reproductive age and adverse pregnancy outcomes, [but] its effect on offspring outcomes remains unclear,” corresponding author Kaiyang Li, a third-year medical student at McGill University, Quebec, Canada, and coauthors wrote in their abstract.
To investigate the association between maternal HS and offspring outcomes at birth and with up to 16 years of follow-up, the researchers drew from a longitudinal cohort of 1,275,593 children born in Quebec between April 1, 2006 and March 31, 2022. They matched children with their mothers and used identification numbers to follow the children to note morbidities that led to hospital admissions before age 16 years. The exposure of interest was HS, and the main outcome measure was childhood hospitalizations for respiratory, cardiovascular, metabolic, and other morbidities prior to age 16 years.
Next, they estimated hazard ratios (HR) and 95% CIs for the association of maternal HS with childhood morbidity in adjusted Cox proportional hazards regression models. “As prenatal exposure to hyperandrogenism may influence boys and girls differently, we carried out subgroup analyses stratified by child sex,” they wrote.
The study population included 1283 children whose mothers had HS and 1,274,310 unexposed children. As for infant outcomes, compared with no exposure, maternal HS was associated with an increased risk for preterm birth (relative risk [RR], 1.29; 95% CI, 1,08-1.55), neonatal death (RR, 2.07; 95% CI, 1.03-14.13), birth defects (RR, 1.29; 95% CI, 1.07-1.56), congenital heart defects (RR, 1.57; 95% CI, 1.02-2.44), and orofacial defects (RR 4.29; 95% CI, 1.85-9.97).
As for long-term outcomes in the children, compared with those whose mothers did not have HS, maternal HS was associated with an increased risk for any childhood hospitalization (HR, 1.31; 95% CI, 1.19-1.44), respiratory hospitalization (HR, 1.21; 95% CI, 1.05-1.40), metabolic hospitalization (HR, 2.64; 95% CI, 1.67-4.20), gastrointestinal hospitalization (HR, 1.34; 95% CI, 1.03-1.74), and developmental hospitalization (HR, 1.92; 95% CI, 1.43-2.58).
Commenting on the results after the meeting, Ms. Li said that the findings support the need for timely management of HS in expectant mothers and people planning to conceive, and for “interdisciplinary care and follow up for both the mother and the baby, involving the dermatologist, the obstetrician, and the neonatologist or pediatrician if needed.”
“HS is a multidisciplinary disease, plain and simple,” Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington, who was asked to comment on the study, said in an interview. “This study highlights the importance of collaboration between dermatology and obstetrician-gynecologist given the potential negative pregnancy outcomes, but to me raising alarm bells given the known gaps and delays in diagnosis matched to disease onset,” said Dr. Friedman, who was not involved with the study. “We need to do better to ensure the safety of both patient and patient-to-be.”
The researchers reported having no financial disclosures. The abstract was selected as the second-place winner in the AAD’s poster competition. Dr. Friedman has no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — , and other conditions.
Those are key findings from a longitudinal cohort study that was presented during a poster session at the annual meeting of the American Academy of Dermatology.
“HS is associated with morbidity in women of reproductive age and adverse pregnancy outcomes, [but] its effect on offspring outcomes remains unclear,” corresponding author Kaiyang Li, a third-year medical student at McGill University, Quebec, Canada, and coauthors wrote in their abstract.
To investigate the association between maternal HS and offspring outcomes at birth and with up to 16 years of follow-up, the researchers drew from a longitudinal cohort of 1,275,593 children born in Quebec between April 1, 2006 and March 31, 2022. They matched children with their mothers and used identification numbers to follow the children to note morbidities that led to hospital admissions before age 16 years. The exposure of interest was HS, and the main outcome measure was childhood hospitalizations for respiratory, cardiovascular, metabolic, and other morbidities prior to age 16 years.
Next, they estimated hazard ratios (HR) and 95% CIs for the association of maternal HS with childhood morbidity in adjusted Cox proportional hazards regression models. “As prenatal exposure to hyperandrogenism may influence boys and girls differently, we carried out subgroup analyses stratified by child sex,” they wrote.
The study population included 1283 children whose mothers had HS and 1,274,310 unexposed children. As for infant outcomes, compared with no exposure, maternal HS was associated with an increased risk for preterm birth (relative risk [RR], 1.29; 95% CI, 1,08-1.55), neonatal death (RR, 2.07; 95% CI, 1.03-14.13), birth defects (RR, 1.29; 95% CI, 1.07-1.56), congenital heart defects (RR, 1.57; 95% CI, 1.02-2.44), and orofacial defects (RR 4.29; 95% CI, 1.85-9.97).
As for long-term outcomes in the children, compared with those whose mothers did not have HS, maternal HS was associated with an increased risk for any childhood hospitalization (HR, 1.31; 95% CI, 1.19-1.44), respiratory hospitalization (HR, 1.21; 95% CI, 1.05-1.40), metabolic hospitalization (HR, 2.64; 95% CI, 1.67-4.20), gastrointestinal hospitalization (HR, 1.34; 95% CI, 1.03-1.74), and developmental hospitalization (HR, 1.92; 95% CI, 1.43-2.58).
Commenting on the results after the meeting, Ms. Li said that the findings support the need for timely management of HS in expectant mothers and people planning to conceive, and for “interdisciplinary care and follow up for both the mother and the baby, involving the dermatologist, the obstetrician, and the neonatologist or pediatrician if needed.”
“HS is a multidisciplinary disease, plain and simple,” Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington, who was asked to comment on the study, said in an interview. “This study highlights the importance of collaboration between dermatology and obstetrician-gynecologist given the potential negative pregnancy outcomes, but to me raising alarm bells given the known gaps and delays in diagnosis matched to disease onset,” said Dr. Friedman, who was not involved with the study. “We need to do better to ensure the safety of both patient and patient-to-be.”
The researchers reported having no financial disclosures. The abstract was selected as the second-place winner in the AAD’s poster competition. Dr. Friedman has no relevant disclosures.
A version of this article appeared on Medscape.com.
SAN DIEGO — , and other conditions.
Those are key findings from a longitudinal cohort study that was presented during a poster session at the annual meeting of the American Academy of Dermatology.
“HS is associated with morbidity in women of reproductive age and adverse pregnancy outcomes, [but] its effect on offspring outcomes remains unclear,” corresponding author Kaiyang Li, a third-year medical student at McGill University, Quebec, Canada, and coauthors wrote in their abstract.
To investigate the association between maternal HS and offspring outcomes at birth and with up to 16 years of follow-up, the researchers drew from a longitudinal cohort of 1,275,593 children born in Quebec between April 1, 2006 and March 31, 2022. They matched children with their mothers and used identification numbers to follow the children to note morbidities that led to hospital admissions before age 16 years. The exposure of interest was HS, and the main outcome measure was childhood hospitalizations for respiratory, cardiovascular, metabolic, and other morbidities prior to age 16 years.
Next, they estimated hazard ratios (HR) and 95% CIs for the association of maternal HS with childhood morbidity in adjusted Cox proportional hazards regression models. “As prenatal exposure to hyperandrogenism may influence boys and girls differently, we carried out subgroup analyses stratified by child sex,” they wrote.
The study population included 1283 children whose mothers had HS and 1,274,310 unexposed children. As for infant outcomes, compared with no exposure, maternal HS was associated with an increased risk for preterm birth (relative risk [RR], 1.29; 95% CI, 1,08-1.55), neonatal death (RR, 2.07; 95% CI, 1.03-14.13), birth defects (RR, 1.29; 95% CI, 1.07-1.56), congenital heart defects (RR, 1.57; 95% CI, 1.02-2.44), and orofacial defects (RR 4.29; 95% CI, 1.85-9.97).
As for long-term outcomes in the children, compared with those whose mothers did not have HS, maternal HS was associated with an increased risk for any childhood hospitalization (HR, 1.31; 95% CI, 1.19-1.44), respiratory hospitalization (HR, 1.21; 95% CI, 1.05-1.40), metabolic hospitalization (HR, 2.64; 95% CI, 1.67-4.20), gastrointestinal hospitalization (HR, 1.34; 95% CI, 1.03-1.74), and developmental hospitalization (HR, 1.92; 95% CI, 1.43-2.58).
Commenting on the results after the meeting, Ms. Li said that the findings support the need for timely management of HS in expectant mothers and people planning to conceive, and for “interdisciplinary care and follow up for both the mother and the baby, involving the dermatologist, the obstetrician, and the neonatologist or pediatrician if needed.”
“HS is a multidisciplinary disease, plain and simple,” Adam Friedman, MD, professor and chair of dermatology, George Washington University, Washington, who was asked to comment on the study, said in an interview. “This study highlights the importance of collaboration between dermatology and obstetrician-gynecologist given the potential negative pregnancy outcomes, but to me raising alarm bells given the known gaps and delays in diagnosis matched to disease onset,” said Dr. Friedman, who was not involved with the study. “We need to do better to ensure the safety of both patient and patient-to-be.”
The researchers reported having no financial disclosures. The abstract was selected as the second-place winner in the AAD’s poster competition. Dr. Friedman has no relevant disclosures.
A version of this article appeared on Medscape.com.
FROM AAD 2024
Paid Parental Leave: Impact on Maternal Mental Health and Child Wellbeing
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
Maternal mental health has a profound impact on the health and wellbeing of the child. Since the onset of the pandemic, rates of postpartum depression have increased, affecting an estimated 1 in 5 women.1 Numerous studies show the impact of postpartum depression on the newborn child across multiple domains, from bonding to healthy weight gain to meeting developmental milestones.
While new medications are being studied and approved to specifically target postpartum depression, these treatments are inaccessible to many because of high costs and long wait lists. Beyond medication, structural changes such as paid parental leave have been shown to have a substantial impact on maternal mental health, thus impacting the health of children as well.
Implications for Mothers and Children
Psychiatric diagnoses such as postpartum depression are on the rise.1,2 This is likely attributable to a combination of factors, including increased isolation since the start of the pandemic, worsening health inequities across race and socioeconomic status, and difficulty accessing mental health care.3-5 The effect that postpartum depression has on the family is significant for the newborn as well as other children in the home.
Data suggest that postpartum depression impacts both the physical and mental health of the child. Infants of mothers with postpartum depression may experience challenges with weight gain, decreased breastfeeding, sleep disruptions, and delays in achieving developmental milestones.6-9 They may also show decreased maternal infant bonding, challenges with cognitive development including language and IQ, and increased risk of behavioral disturbances.10,11 These effects are likely attributable to a combination of factors, including decreased maternal responsiveness to infant cues.7,12 Many of these effects are mediated by the chronicity and severity of depressive symptoms, suggesting the importance of screening and treatment of postpartum depression.10,11 However, treatment for postpartum depression can be difficult to access, particularly given the increased level of need.
It is therefore critical to consider what structural interventions and policy changes can decrease the risk of developing postpartum depression. Data consistently show that access to paid parental leave improves maternal mental health outcomes. Among patients with access to parental leave, research shows that paid leave of longer duration, at least 2-3 months, is the most protective.13 Studies have identified decreased depressive symptoms, decreased stress, decreased use of mental health services, and decreased hospital admissions among women with longer parental leave.13 The positive effects of paid parental leave on maternal mental health can extend beyond the postpartum period, solidifying its impact on the long-term health outcomes of both mother and child.13
Advocacy Is Imperative
In 2024, the United States is the only high-income country, and one of only seven countries in the world, that does not guarantee access to paid parental leave. The Family Medical Leave Act is a 31-year-old federal law that requires some employers to provide unpaid leave to eligible employees. It is narrow in scope, and it excludes many low-wage workers and LGBTQ+ families. Thirteen states — California, Colorado, Connecticut, Delaware, Maine, Massachusetts, Maryland, Minnesota, New Jersey, New York, Oregon, Rhode Island, and Washington — as well as the District of Columbia, have enacted their own paid leave policies. However, there are no federal laws requiring access to paid parental leave. As of 2023, fewer than 30% of workers in the United States have access to paid parental leave, and only 16% of employees in the service industry have access to paid parental leave.14 This disproportionately affects families from lower income backgrounds, and further exacerbates socioeconomic, racial, and gender inequities. From a health systems lens, this increases risk of adverse maternal mental health outcomes among those who already have decreased access to mental health services, worsening health disparities.
Paid parental leave has strong public support across party lines, with polls showing the majority of Americans support comprehensive paid family and medical leave.15 Despite this, the United States has failed to enact legislation on this issue since 1993. Multiple attempts at expanding leave have not come to fruition. In the past year, both the house and the senate have announced bipartisan efforts to expand access to paid parental leave. However, legislative frameworks are still in early stages.
As physicians, it is crucial that we advocate for expanded access to paid parental leave. We must use our expertise to speak to the impact that paid parental leave can have on the mental and physical health of parents, children, and families. By advocating for paid parental leave, we can help create a more just and equitable healthcare system.
Dr. Shannon is a second-year psychiatry resident at University of California, Los Angeles. She attended Stanford University for her undergraduate degree and Dartmouth Geisel School of Medicine for medical school. Her interests include perinatal psychiatry, health systems research, and mental health policy advocacy. Dr. Richards is assistant clinical professor in the department of psychiatry and biobehavioral sciences; program director of the child and adolescent psychiatry fellowship; and associate medical director of the perinatal program at the UCLA Semel Institute for Neuroscience and Human Behavior, Los Angeles.
References
1. Wang Z et al. Mapping Global Prevalence of Depression Among Postpartum Women. Transl Psychiatry. 2021 Oct 20. doi: 10.1038/s41398-021-01663-6.
2. Iyengar U et al. One Year Into the Pandemic: A Systematic Review of Perinatal Mental Health Outcomes During COVID-19. Front Psychiatry. 2021 Jun 24. doi: 10.3389/fpsyt.2021.674194.
3. World Health Organization. Mental Health and COVID-19: Early Evidence of the Pandemic’s Impact: Scientific Brief. 2022 Mar 2. www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
4. Masters GA et al. Impact of the COVID-19 Pandemic on Mental Health, Access to Care, and Health Disparities in the Perinatal Period. J Psychiatr Res. 2021 May. doi: 10.1016/j.jpsychires.2021.02.056.
5. Shuffrey LC et al. Improving Perinatal Maternal Mental Health Starts With Addressing Structural Inequities. JAMA Psychiatry. 2022 May 1. doi: 10.1001/jamapsychiatry.2022.0097.
6. Lubotzky-Gete S et al. Postpartum Depression and Infant Development Up to 24 months: A Nationwide Population-Based Study. J Affect Disord. 2021 Apr 15. doi: 10.1016/j.jad.2021.02.042.
7. Saharoy R et al. Postpartum Depression and Maternal Care: Exploring the Complex Effects on Mothers and Infants. Cureus. 2023 Jul 4. doi: 10.7759/cureus.41381..
8. Gress-Smith JL et al. Postpartum Depression Prevalence and Impact on Infant Health, Weight, and Sleep in Low-Income and Ethnic Minority Women and Infants. Matern Child Health J. 2012 May. doi: 10.1007/s10995-011-0812-y.
9. Kim S et al. The Impact of Antepartum Depression and Postpartum Depression on Exclusive Breastfeeding: A Systematic Review and Meta-Analysis. Clin Nurs Res. 2022 Jun. doi: 10.1177/10547738211053507.
10. Mirhosseini H et al. Cognitive Behavioral Development in Children Following Maternal Postpartum Depression: A Review Article. Electron Physician. 2015 Dec 20. doi: 10.19082/1673.
11. Grace SL et al. The Effect of Postpartum Depression on Child Cognitive Development and Behavior: A Review and Critical Analysis of the Literature. Arch Womens Ment Health. 2003 Nov. doi: 10.1007/s00737-003-0024-6.
12. Milgrom J et al. The Mediating Role of Maternal Responsiveness in Some Longer Term Effects of Postnatal Depression on Infant Development. Infant Behavior and Development. 2004 Sep 11. doi.org/10.1016/j.infbeh.2004.03.003.
13. Heshmati A et al. The Effect of Parental Leave on Parents’ Mental Health: A Systematic Review. Lancet Public Health. 2023 Jan. doi: 10.1016/S2468-2667(22)00311-5.
14. U.S. Bureau of Labor Statistics, What Data Does the BLS Publish on Family Leave? 2023 Sept 21. www.bls.gov/ebs/factsheets/family-leave-benefits-fact-sheet.htm.
15. Horowitz JM et al. Americans Widely Support Paid Family and Medical Leave, But Differ Over Specific Policies. Pew Research Center’s Social & Demographic Trends Project, Pew Research Center. 2017 Mar 23. www.pewresearch.org/social-trends/2017/03/23/americans-widely-support-paid-family-and-medical-leave-but-differ-over-specific-policies/.
New Research Dissects Transgenerational Obesity and Diabetes
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1). 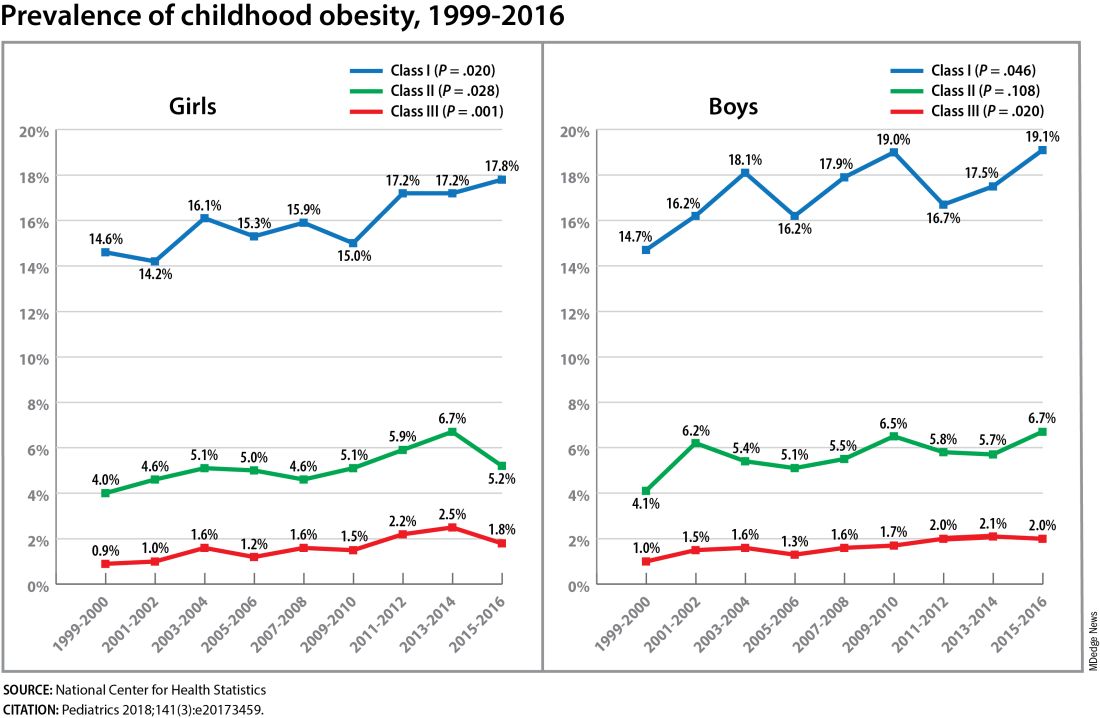
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1). 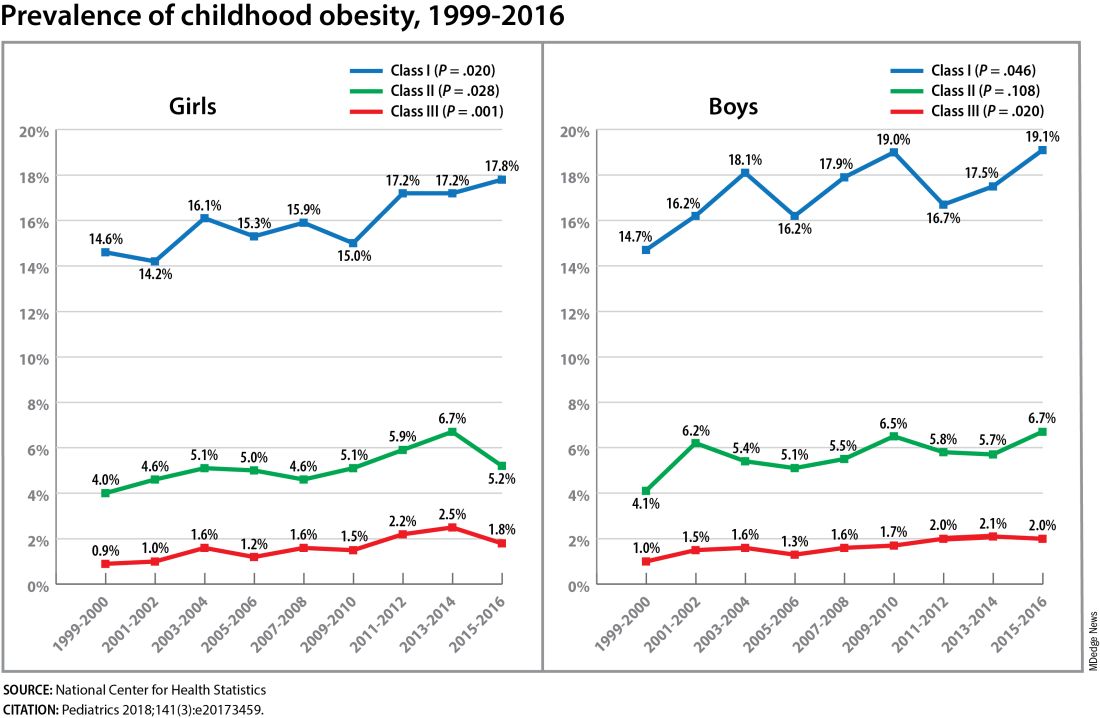
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FAIRFAX, VIRGINIA — Nearly 30 years ago, in a 1995 paper, the British physician-epidemiologist David Barker, MD, PhD, wrote about his fetal origins hypothesis — the idea that programs to address fetal undernutrition and low birth weight produced later coronary heart disease (BMJ 1995;311:171-4).
His hypothesis and subsequent research led to the concept of adult diseases of fetal origins, which today extends beyond low birth weight and implicates the in utero environment as a significant determinant of risk for adverse childhood and adult metabolic outcomes and for major chronic diseases, including diabetes and obesity. Studies have shown that the offspring of pregnant mothers with diabetes have a higher risk of developing obesity and diabetes themselves.
“It’s a whole discipline [of research],” E. Albert Reece, MD, PhD, MBA, of the University of Maryland School of Medicine (UMSOM), said in an interview. “But what we’ve never quite understood is the ‘how’ and ‘why’? What are the mechanisms driving the fetal origins of such adverse outcomes in offspring?
At the biennial meeting of the Diabetes in Pregnancy Study Group of North America (DPSG), investigators described studies underway that are digging deeper into the associations between the intrauterine milieu and longer-term offspring health — and that are searching for biological and molecular processes that may be involved.
The studies are like “branches of the Barker hypothesis,” said Dr. Reece, former dean of UMSOM and current director of the UMSOM Center for Advanced Research Training and Innovation, who co-organized the DPSG meeting. “They’re taking the hypothesis and dissecting it by asking, for instance, it is possible that transgenerational obesity may align with the Barker hypothesis? Is it possible that it involves epigenetics regulation? Could we find biomarkers?”
The need for a better understanding of the fetal origins framework — and its subsequent transgenerational impact — is urgent. From 2000 to 2018, the prevalence of childhood obesity increased from 14.7% to 19.2% (a 31% increase) and the prevalence of severe childhood obesity rose from 3.9% to 6.1% (a 56% increase), according to data from the U.S. National Health and Nutrition Examination Survey (Obes Facts. 2022;15[4]:560-9).
Children aged 2-5 years have had an especially sharp increase in obesity (Pediatrics 2018;141[3]:e20173459), Christine Wey Hockett, PhD, of the University of South Dakota School of Medicine, said at the DPSG meeting (Figure 1). 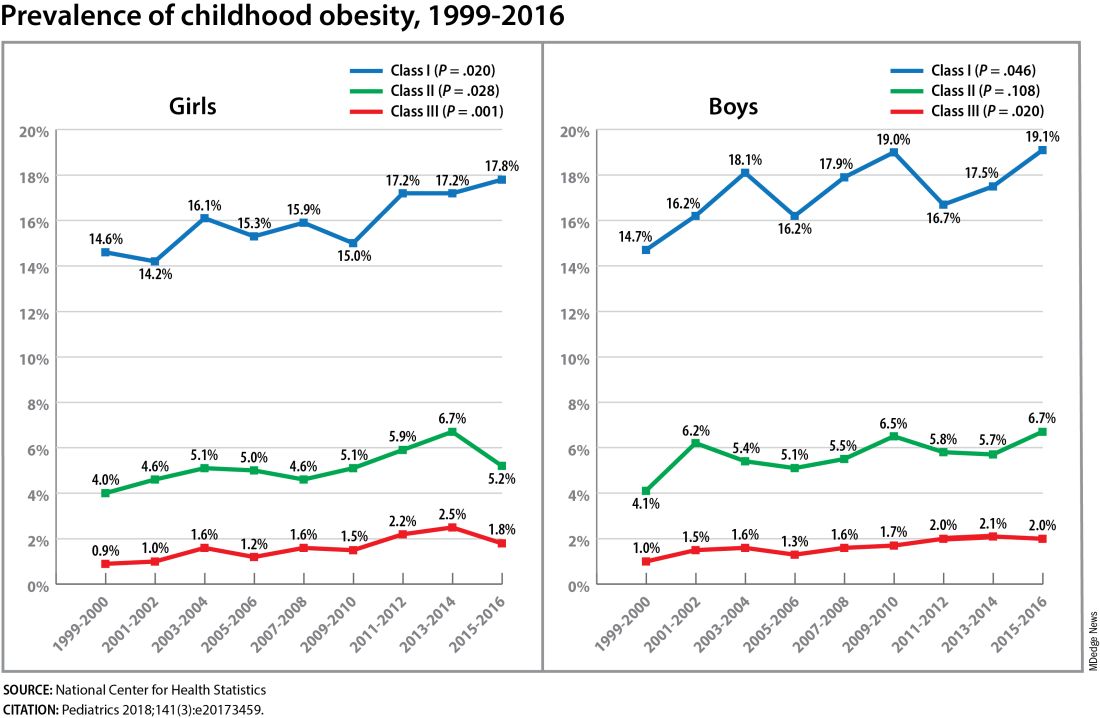
Also notable, she said, is that one-quarter of today’s pediatric diabetes cases are type 2 diabetes, which “is significant as there is a higher prevalence of early complications and comorbidities in youth with type 2 diabetes compared to type 1 diabetes.”
Moreover, recent projections estimate that 57% of today’s children will be obese at 35 years of age (N Engl J Med. 2017;377[22]:2145-53) and that 45% will have diabetes or prediabetes by 2030 (Popul Health Manag. 2017;20[1]:6-12), said Dr. Hockett, assistant professor in the university’s department of pediatrics. An investigator of the Exploring Perinatal Outcomes Among Children (EPOCH) study, which looked at gestational diabetes (GDM) and offspring cardiometabolic risks, she said more chronic disease “at increasingly younger ages [points toward] prebirth influences.”
She noted that there are critical periods postnatally — such as infancy and puberty — that can “impact or further shift the trajectory of chronic disease.” The developmental origins theory posits that life events and biological and environmental processes during the lifespan can modify the effects of intrauterine exposures.
The transgenerational implications “are clear,” she said. “As the number of reproductive-aged individuals with chronic diseases rises, the number of exposed offspring also rises ... It leads to a vicious cycle.”
Deeper Dives Into Associations, Potential Mechanisms
The EPOCH prospective cohort study with which Dr. Hockett was involved gave her a front-seat view of the transgenerational adverse effects of in utero exposure to hyperglycemia. The study recruited ethnically diverse maternal/child dyads from the Kaiser Permanente of Colorado perinatal database from 1992 to 2002 and assessed 418 offspring at two points — a mean age of 10.5 years and 16.5 years — for fasting blood glucose, adiposity, and diet and physical activity. The second visit also involved an oral glucose tolerance test.
The 77 offspring who had been exposed in utero to GDM had a homeostatic model assessment of insulin resistance (HOMA-IR) that was 18% higher, a 19% lower Matsuda index, and a 9% greater HOMA of β-cell function (HOMA-β) than the 341 offspring whose mothers did not have diabetes. Each 5-kg/m2 increase in prepregnancy body mass index predicted increased insulin resistance, but there was no combined effect of both maternal obesity and diabetes in utero.
Exposed offspring had a higher BMI and increased adiposity, but when BMI was controlled for in the analysis of metabolic outcomes, maternal diabetes was still associated with 12% higher HOMA-IR and a 17% lower Matsuda index. “So [the metabolic outcomes] are a direct effect of maternal diabetes,” Dr. Hockett said at the DPSG meeting, noting the fetal overnutrition hypothesis in which maternal glucose, but not maternal insulin, freely passes through the placenta, promoting growth and adiposity in the fetus.
[The EPOCH results on metabolic outcomes and offspring adiposity were published in 2017 and 2019, respectively (Diabet Med. 2017;34:1392-9; Diabetologia. 2019;62:2017-24). In 2020, EPOCH researchers reported sex-specific effects on cardiovascular outcomes, with GDM exposure associated with higher total and LDL cholesterol in girls and higher systolic blood pressure in boys (Pediatr Obes. 2020;15[5]:e12611).]
Now, a new longitudinal cohort study underway in Phoenix, is taking a deeper dive, trying to pinpoint what exactly influences childhood obesity and metabolic risk by following Hispanic and American Indian maternal/child dyads from pregnancy until 18 years postpartum. Researchers are looking not only at associations between maternal risk factors (pregnancy BMI, gestational weight gain, and diabetes in pregnancy) and offspring BMI, adiposity, and growth patterns, but also how various factors during pregnancy — clinical, genetic, lifestyle, biochemical — ”may mediate the associations,” said lead investigator Madhumita Sinha, MD.
“We need a better understanding at the molecular level of the biological processes that lead to obesity in children and that cause metabolic dysfunction,” said Dr. Sinha, who heads the Diabetes Epidemiology and Clinical Research Section of the of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) branch in Phoenix.
The populations being enrolled in the ETCHED study (for Early Tracking of Childhood Health Determinants) are at especially high risk of childhood obesity and metabolic dysfunction. Research conducted decades ago by the NIDDK in Phoenix showed that approximately 50% of Pima Indian children from diabetic pregnancies develop type 2 diabetes by age 25 (N Engl J Med. 1983;308:242-5). Years later, to tease out possible genetic factors, researchers compared siblings born before and after their mother was found to have type 2 diabetes, and found significantly higher rates of diabetes in those born after the mother’s diagnosis, affirming the role of in utero toxicity (Diabetes 2000;49:2208-11).
In the new study, the researchers will look at adipokines and inflammatory biomarkers in the mothers and offspring in addition to traditional anthropometric and glycemic measures. They’ll analyze placental tissue, breast milk, and the gut microbiome longitudinally, and they’ll lean heavily on genomics/epigenomics, proteomics, and metabolomics. “There’s potential,” Dr. Sinha said, “to develop a more accurate predictive and prognostic model of childhood obesity.”
The researchers also will study the role of family, socioeconomics, and environmental factors in influencing child growth patterns and they’ll look at neurodevelopment in infancy and childhood. As of October 2023, almost 80 pregnant women, most with obesity and almost one-third with type 2 diabetes, had enrolled in the study. Over the next several years, the study aims to enroll 750 dyads.
The Timing of In Utero Exposure
Shelley Ehrlich, MD, ScD, MPH, of the University of Cincinnati and Cincinnati Children’s Hospital Medical Center, is aiming, meanwhile, to learn how the timing of in utero exposure to hyperglycemia predicts specific metabolic and cardiovascular morbidities in the adult offspring of diabetic mothers.
“While we know that exposure to maternal diabetes, regardless of type, increases the risk of obesity, insulin resistance, diabetes, renal compromise, and cardiovascular disease in the offspring, there is little known about the level and timing of hyperglycemic exposure during fetal development that triggers these adverse outcomes,” said Dr. Ehrlich. A goal, she said, is to identify gestational profiles that predict phenotypes of offspring at risk for morbidity in later life.
She and other investigators with the TEAM (Transgenerational Effect on Adult Morbidity) study have recruited over 170 offspring of mothers who participated in the Diabetes in Pregnancy Program Project Grant (PPG) at the University of Cincinnati Medical Center from 1978 to 1995 — a landmark study that demonstrated the effect of strict glucose control in reducing major congenital malformations.
The women in the PPG study had frequent glucose monitoring (up to 6-8 times a day) throughout their pregnancies, and now, their recruited offspring, who are up to 43 years of age, are being assessed for obesity, diabetes/metabolic health, cardiovascular disease/cardiac and peripheral vascular structure and function, and other outcomes including those that may be amenable to secondary prevention (J Diabetes Res. Nov 1;2021:6590431).
Preliminary findings from over 170 offspring recruited between 2017 and 2022 suggest that in utero exposure to dysglycemia (as measured by standard deviations of glycohemoglobin) in the third trimester appears to increase the risk of morbid obesity in adulthood, while exposure to dysglycemia in the first trimester increases the risk of impaired glucose tolerance. The risk of B-cell dysfunction, meanwhile, appears to be linked to dysglycemia in the first and third trimesters — particularly the first — Dr. Ehrlich reported.
Cognitive outcomes in offspring have also been assessed and here it appears that dysglycemia in the third trimester is linked to worse scores on the Wechsler Abbreviated Scale of Intelligence (WASI-II), said Katherine Bowers, PhD, MPH, a TEAM study coinvestigator, also of Cincinnati Children’s Hospital Medical Center.
“We’ve already observed [an association between] diabetes in pregnancy and cognition in early childhood and through adolescence, but [the question has been] does this association persist into adulthood?” she said.
Preliminary analyses of 104 offspring show no statistically significant associations between maternal dysglycemia in the first or second trimesters and offspring cognition, but “consistent inverse associations between maternal glycohemoglobin in the third trimester across two [WASI-II] subscales and composite measures of cognition,” Dr. Bowers said.
Their analysis adjusted for a variety of factors, including maternal age, prepregnancy and first trimester BMI, race, family history of diabetes, and diabetes severity/macrovascular complications.
Back In The Laboratory
At the other end of the research spectrum, basic research scientists are also investigating the mechanisms and sequelae of in utero hyperglycemia and other injuries, including congenital malformations, placental adaptive responses and fetal programming. Researchers are asking, for instance, what does placental metabolic reprogramming entail? What role do placental extracellular vesicles play in GDM? Can we alter the in utero environment and thus improve the short and long-term fetal/infant outcomes?
Animal research done at the UMSOM Center for Birth Defects Research, led by Dr. Reece and Peixin Yang, PhD, suggests that “a good portion of in utero injury is due to epigenetics,” Dr. Reece said in the interview. “We’ve shown that under conditions of hyperglycemia, for example, genetic regulation and genetic function can be altered.”
Through in vivo research, they have also shown that antioxidants or membrane stabilizers such as arachidonic acid or myo-inositol, or experimental inhibitors to certain pro-apoptotic intermediates, can individually or collectively result in reduced malformations. “It is highly likely that understanding the biological impact of various altered in utero environments, and then modifying or reversing those environments, will result in short and long-term outcome improvements similar to those shown with congenital malformations,” Dr. Reece said.
FROM DPSG-NA 2023




