User login
‘Empathy fatigue’ in clinicians rises with latest COVID-19 surge
Heidi Erickson, MD, is tired. As a pulmonary and critical care physician at Hennepin Healthcare in Minneapolis, she has been providing care for patients with COVID-19 since the start of the pandemic.
It was exhausting from the beginning, as she and her colleagues scrambled to understand how to deal with this new disease. But lately, she has noticed a different kind of exhaustion arising from the knowledge that with vaccines widely available, the latest surge was preventable.
Her intensive care unit is currently as full as it has ever been with COVID-19 patients, many of them young adults and most of them unvaccinated. After the recent death of one patient, an unvaccinated man with teenage children, she had to face his family’s questions about why ivermectin, an antiparasitic medication that was falsely promoted as a COVID-19 treatment, was not administered.
“I’m fatigued because I’m working more than ever, but more people don’t have to die,” Dr. Erickson said in an interview . “It’s been very hard physically, mentally, emotionally.”
Amid yet another surge in COVID-19 cases around the United States, clinicians are speaking out about their growing frustration with this preventable crisis.
Some are using the terms “empathy fatigue” and “compassion fatigue” – a sense that they are losing empathy for unvaccinated individuals who are fueling the pandemic.
Dr. Erickson says she is frustrated not by individual patients but by a system that has allowed disinformation to proliferate. Experts say these types of feelings fit into a widespread pattern of physician burnout that has taken a new turn at this stage of the pandemic.
Paradoxical choices
Empathy is a cornerstone of what clinicians do, and the ability to understand and share a patient’s feelings is an essential skill for providing effective care, says Kaz Nelson, MD, a psychiatrist at the University of Minnesota, Minneapolis.
Practitioners face paradoxical situations all the time, she notes. These include individuals who break bones and go skydiving again, people who have high cholesterol but continue to eat fried foods, and those with advanced lung cancer who continue to smoke.
To treat patients with compassion, practitioners learn to set aside judgment by acknowledging the complexity of human behavior. They may lament the addictive nature of nicotine and advertising that targets children, for example, while still listening and caring.
Empathy requires high-level brain function, but as stress levels rise, brain function that drives empathy tends to shut down. It’s a survival mechanism, Dr. Nelson says.
When health care workers feel overwhelmed, trapped, or threatened by patients demanding unproven treatments or by ICUs with more patients than ventilators, they may experience a fight-or-flight response that makes them defensive, frustrated, angry, or uncaring, notes Mona Masood, DO, a Philadelphia-area psychiatrist and founder of Physician Support Line, a free mental health hotline for doctors.
Some clinicians have taken to Twitter and other social media platforms to post about these types of experiences.
These feelings, which have been brewing for months, have been exacerbated by the complexity of the current situation. Clinicians see a disconnect between what is and what could be, Dr. Nelson notes.
“Prior to vaccines, there weren’t other options, and so we had toxic stress and we had fatigue, but we could still maintain little bits of empathy by saying, ‘You know, people didn’t choose to get infected, and we are in a pandemic.’ We could kind of hate the virus. Now with access to vaccines, that last connection to empathy is removed for many people,” she says.
Self-preservation vs. empathy
Compassion fatigue or empathy fatigue is just one reaction to feeling completely maxed out and overstressed, Dr. Nelson says. Anger at society, such as what Dr. Erickson experienced, is another response.
Practitioners may also feel as if they are just going through the motions of their job, or they might disassociate, ceasing to feel that their patients are human. Plenty of doctors and nurses have cried in their cars after shifts and have posted tearful videos on social media.
Early in the pandemic, Dr. Masood says, physicians who called the support hotline expressed sadness and grief. Now, she had her colleagues hear frustration and anger, along with guilt and shame for having feelings they believe they shouldn’t be having, especially toward patients. They may feel unprofessional or worse – unworthy of being physicians, she says.
One recent caller to the hotline was a long-time ICU physician who had been told so many times by patients that ivermectin was the only medicine that would cure them that he began to doubt himself, says Dr. Masood. This caller needed to be reassured by another physician that he was doing the right thing.
Another emergency department physician told Dr. Masood about a young child who had arrived at the hospital with COVID-19 symptoms. When asked whether the family had been exposed to anyone with COVID-19, the child’s parent lied so that they could be triaged faster.
The physician, who needed to step away from the situation, reached out to Dr. Masood to express her frustration so that she wouldn’t “let it out” on the patient.
“It’s hard to have empathy for people who, for all intents and purposes, are very self-centered,” Dr. Masood says. “We’re at a place where we’re having to choose between self-preservation and empathy.”
How to cope
To help practitioners cope, Dr. Masood offers words that describe what they’re experiencing. She often hears clinicians say things such as, “This is a type of burnout that I feel to my bones,” or “This makes me want to quit,” or “I feel like I’m at the end of my rope.”
She encourages them to consider the terms “empathy fatigue,” and “moral injury” in order to reconcile how their sense of responsibility to take care of people is compromised by factors outside of their control.
It is not shameful to acknowledge that they experience emotions, including difficult ones such as frustration, anger, sadness, and anxiety, Dr. Masood adds.
Being frustrated with a patient doesn’t make someone a bad doctor, and admitting those emotions is the first step toward dealing with them, she says.
before they cause a sense of callousness or other consequences that become harder to heal from as time goes on.
“We’re trained to just go, go, go and sometimes not pause and check in,” she says. Clinicians who open up are likely to find they are not the only ones feeling tired or frustrated right now, she adds.
“Connect with peers and colleagues, because chances are, they can relate,” Dr. Nelson says.
A version of this article first appeared on Medscape.com.
Heidi Erickson, MD, is tired. As a pulmonary and critical care physician at Hennepin Healthcare in Minneapolis, she has been providing care for patients with COVID-19 since the start of the pandemic.
It was exhausting from the beginning, as she and her colleagues scrambled to understand how to deal with this new disease. But lately, she has noticed a different kind of exhaustion arising from the knowledge that with vaccines widely available, the latest surge was preventable.
Her intensive care unit is currently as full as it has ever been with COVID-19 patients, many of them young adults and most of them unvaccinated. After the recent death of one patient, an unvaccinated man with teenage children, she had to face his family’s questions about why ivermectin, an antiparasitic medication that was falsely promoted as a COVID-19 treatment, was not administered.
“I’m fatigued because I’m working more than ever, but more people don’t have to die,” Dr. Erickson said in an interview . “It’s been very hard physically, mentally, emotionally.”
Amid yet another surge in COVID-19 cases around the United States, clinicians are speaking out about their growing frustration with this preventable crisis.
Some are using the terms “empathy fatigue” and “compassion fatigue” – a sense that they are losing empathy for unvaccinated individuals who are fueling the pandemic.
Dr. Erickson says she is frustrated not by individual patients but by a system that has allowed disinformation to proliferate. Experts say these types of feelings fit into a widespread pattern of physician burnout that has taken a new turn at this stage of the pandemic.
Paradoxical choices
Empathy is a cornerstone of what clinicians do, and the ability to understand and share a patient’s feelings is an essential skill for providing effective care, says Kaz Nelson, MD, a psychiatrist at the University of Minnesota, Minneapolis.
Practitioners face paradoxical situations all the time, she notes. These include individuals who break bones and go skydiving again, people who have high cholesterol but continue to eat fried foods, and those with advanced lung cancer who continue to smoke.
To treat patients with compassion, practitioners learn to set aside judgment by acknowledging the complexity of human behavior. They may lament the addictive nature of nicotine and advertising that targets children, for example, while still listening and caring.
Empathy requires high-level brain function, but as stress levels rise, brain function that drives empathy tends to shut down. It’s a survival mechanism, Dr. Nelson says.
When health care workers feel overwhelmed, trapped, or threatened by patients demanding unproven treatments or by ICUs with more patients than ventilators, they may experience a fight-or-flight response that makes them defensive, frustrated, angry, or uncaring, notes Mona Masood, DO, a Philadelphia-area psychiatrist and founder of Physician Support Line, a free mental health hotline for doctors.
Some clinicians have taken to Twitter and other social media platforms to post about these types of experiences.
These feelings, which have been brewing for months, have been exacerbated by the complexity of the current situation. Clinicians see a disconnect between what is and what could be, Dr. Nelson notes.
“Prior to vaccines, there weren’t other options, and so we had toxic stress and we had fatigue, but we could still maintain little bits of empathy by saying, ‘You know, people didn’t choose to get infected, and we are in a pandemic.’ We could kind of hate the virus. Now with access to vaccines, that last connection to empathy is removed for many people,” she says.
Self-preservation vs. empathy
Compassion fatigue or empathy fatigue is just one reaction to feeling completely maxed out and overstressed, Dr. Nelson says. Anger at society, such as what Dr. Erickson experienced, is another response.
Practitioners may also feel as if they are just going through the motions of their job, or they might disassociate, ceasing to feel that their patients are human. Plenty of doctors and nurses have cried in their cars after shifts and have posted tearful videos on social media.
Early in the pandemic, Dr. Masood says, physicians who called the support hotline expressed sadness and grief. Now, she had her colleagues hear frustration and anger, along with guilt and shame for having feelings they believe they shouldn’t be having, especially toward patients. They may feel unprofessional or worse – unworthy of being physicians, she says.
One recent caller to the hotline was a long-time ICU physician who had been told so many times by patients that ivermectin was the only medicine that would cure them that he began to doubt himself, says Dr. Masood. This caller needed to be reassured by another physician that he was doing the right thing.
Another emergency department physician told Dr. Masood about a young child who had arrived at the hospital with COVID-19 symptoms. When asked whether the family had been exposed to anyone with COVID-19, the child’s parent lied so that they could be triaged faster.
The physician, who needed to step away from the situation, reached out to Dr. Masood to express her frustration so that she wouldn’t “let it out” on the patient.
“It’s hard to have empathy for people who, for all intents and purposes, are very self-centered,” Dr. Masood says. “We’re at a place where we’re having to choose between self-preservation and empathy.”
How to cope
To help practitioners cope, Dr. Masood offers words that describe what they’re experiencing. She often hears clinicians say things such as, “This is a type of burnout that I feel to my bones,” or “This makes me want to quit,” or “I feel like I’m at the end of my rope.”
She encourages them to consider the terms “empathy fatigue,” and “moral injury” in order to reconcile how their sense of responsibility to take care of people is compromised by factors outside of their control.
It is not shameful to acknowledge that they experience emotions, including difficult ones such as frustration, anger, sadness, and anxiety, Dr. Masood adds.
Being frustrated with a patient doesn’t make someone a bad doctor, and admitting those emotions is the first step toward dealing with them, she says.
before they cause a sense of callousness or other consequences that become harder to heal from as time goes on.
“We’re trained to just go, go, go and sometimes not pause and check in,” she says. Clinicians who open up are likely to find they are not the only ones feeling tired or frustrated right now, she adds.
“Connect with peers and colleagues, because chances are, they can relate,” Dr. Nelson says.
A version of this article first appeared on Medscape.com.
Heidi Erickson, MD, is tired. As a pulmonary and critical care physician at Hennepin Healthcare in Minneapolis, she has been providing care for patients with COVID-19 since the start of the pandemic.
It was exhausting from the beginning, as she and her colleagues scrambled to understand how to deal with this new disease. But lately, she has noticed a different kind of exhaustion arising from the knowledge that with vaccines widely available, the latest surge was preventable.
Her intensive care unit is currently as full as it has ever been with COVID-19 patients, many of them young adults and most of them unvaccinated. After the recent death of one patient, an unvaccinated man with teenage children, she had to face his family’s questions about why ivermectin, an antiparasitic medication that was falsely promoted as a COVID-19 treatment, was not administered.
“I’m fatigued because I’m working more than ever, but more people don’t have to die,” Dr. Erickson said in an interview . “It’s been very hard physically, mentally, emotionally.”
Amid yet another surge in COVID-19 cases around the United States, clinicians are speaking out about their growing frustration with this preventable crisis.
Some are using the terms “empathy fatigue” and “compassion fatigue” – a sense that they are losing empathy for unvaccinated individuals who are fueling the pandemic.
Dr. Erickson says she is frustrated not by individual patients but by a system that has allowed disinformation to proliferate. Experts say these types of feelings fit into a widespread pattern of physician burnout that has taken a new turn at this stage of the pandemic.
Paradoxical choices
Empathy is a cornerstone of what clinicians do, and the ability to understand and share a patient’s feelings is an essential skill for providing effective care, says Kaz Nelson, MD, a psychiatrist at the University of Minnesota, Minneapolis.
Practitioners face paradoxical situations all the time, she notes. These include individuals who break bones and go skydiving again, people who have high cholesterol but continue to eat fried foods, and those with advanced lung cancer who continue to smoke.
To treat patients with compassion, practitioners learn to set aside judgment by acknowledging the complexity of human behavior. They may lament the addictive nature of nicotine and advertising that targets children, for example, while still listening and caring.
Empathy requires high-level brain function, but as stress levels rise, brain function that drives empathy tends to shut down. It’s a survival mechanism, Dr. Nelson says.
When health care workers feel overwhelmed, trapped, or threatened by patients demanding unproven treatments or by ICUs with more patients than ventilators, they may experience a fight-or-flight response that makes them defensive, frustrated, angry, or uncaring, notes Mona Masood, DO, a Philadelphia-area psychiatrist and founder of Physician Support Line, a free mental health hotline for doctors.
Some clinicians have taken to Twitter and other social media platforms to post about these types of experiences.
These feelings, which have been brewing for months, have been exacerbated by the complexity of the current situation. Clinicians see a disconnect between what is and what could be, Dr. Nelson notes.
“Prior to vaccines, there weren’t other options, and so we had toxic stress and we had fatigue, but we could still maintain little bits of empathy by saying, ‘You know, people didn’t choose to get infected, and we are in a pandemic.’ We could kind of hate the virus. Now with access to vaccines, that last connection to empathy is removed for many people,” she says.
Self-preservation vs. empathy
Compassion fatigue or empathy fatigue is just one reaction to feeling completely maxed out and overstressed, Dr. Nelson says. Anger at society, such as what Dr. Erickson experienced, is another response.
Practitioners may also feel as if they are just going through the motions of their job, or they might disassociate, ceasing to feel that their patients are human. Plenty of doctors and nurses have cried in their cars after shifts and have posted tearful videos on social media.
Early in the pandemic, Dr. Masood says, physicians who called the support hotline expressed sadness and grief. Now, she had her colleagues hear frustration and anger, along with guilt and shame for having feelings they believe they shouldn’t be having, especially toward patients. They may feel unprofessional or worse – unworthy of being physicians, she says.
One recent caller to the hotline was a long-time ICU physician who had been told so many times by patients that ivermectin was the only medicine that would cure them that he began to doubt himself, says Dr. Masood. This caller needed to be reassured by another physician that he was doing the right thing.
Another emergency department physician told Dr. Masood about a young child who had arrived at the hospital with COVID-19 symptoms. When asked whether the family had been exposed to anyone with COVID-19, the child’s parent lied so that they could be triaged faster.
The physician, who needed to step away from the situation, reached out to Dr. Masood to express her frustration so that she wouldn’t “let it out” on the patient.
“It’s hard to have empathy for people who, for all intents and purposes, are very self-centered,” Dr. Masood says. “We’re at a place where we’re having to choose between self-preservation and empathy.”
How to cope
To help practitioners cope, Dr. Masood offers words that describe what they’re experiencing. She often hears clinicians say things such as, “This is a type of burnout that I feel to my bones,” or “This makes me want to quit,” or “I feel like I’m at the end of my rope.”
She encourages them to consider the terms “empathy fatigue,” and “moral injury” in order to reconcile how their sense of responsibility to take care of people is compromised by factors outside of their control.
It is not shameful to acknowledge that they experience emotions, including difficult ones such as frustration, anger, sadness, and anxiety, Dr. Masood adds.
Being frustrated with a patient doesn’t make someone a bad doctor, and admitting those emotions is the first step toward dealing with them, she says.
before they cause a sense of callousness or other consequences that become harder to heal from as time goes on.
“We’re trained to just go, go, go and sometimes not pause and check in,” she says. Clinicians who open up are likely to find they are not the only ones feeling tired or frustrated right now, she adds.
“Connect with peers and colleagues, because chances are, they can relate,” Dr. Nelson says.
A version of this article first appeared on Medscape.com.
Online mental health treatment: Is this the answer we’ve been waiting for?
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
If you haven’t noticed yet, there has been an explosion of new online companies specializing in slicing off some little sliver of health care and leaving traditional medicine to take care of the rest of the patient. Lately, many of these startups involve mental health care, traditionally a difficult area to make profitable unless one caters just to the wealthy. Many pediatricians have been unsure exactly what to make of these new efforts. Are these the rescuers we’ve been waiting for to fill what seems like an enormous and growing unmet need? Are they just another means to extract money from desperate people and leave the real work to someone else? Something in-between? This article outlines some points to consider when evaluating this new frontier.
Case vignette
A 12-year-old girl presents with her parents for an annual exam. She has been struggling with her mood and anxiety over the past 2 years along with occasional superficial cutting. You have started treatment with a selective serotonin reuptake inhibitor and have recommended that she see a mental health professional but the parents report that one attempt with a therapist was a poor fit and nobody in the area seems to be accepting new patients. The parents state that they saw an advertisement on TV for a company that offers online psychotherapy by video appointments or text. They think this might be an option to pursue but are a little skeptical of the whole idea. They look for your opinion on this topic.
Most of these companies operate by having subscribers pay a monthly fee for different levels of services such as videoconference therapy sessions, supportive text messages, or even some psychopharmacological care. Many also offer the ability to switch rapidly between clinicians if you don’t like the one you have.
These arrangements sound great as the world grows increasingly comfortable with online communication and the mental health needs of children and adolescents increase with the seemingly endless COVID pandemic. Further, research generally finds that online mental health treatment is just as effective as services delivered in person, although the data on therapy by text are less robust.
Nevertheless, a lot of skepticism remains about online mental health treatment, particularly among those involved in more traditionally delivered mental health care. Some of the concerns that often get brought up include the following:
- Cost. Most of these online groups, especially the big national companies, don’t interact directly with insurance companies, leaving a lot of out-of-pocket expenses or the need for families to work things out directly with their insurance provider.
- Care fragmentation. In many ways, the online mental health care surge seems at odds with the growing “integrated care” movement that is trying to embed more behavioral care within primary care practices. From this lens, outsourcing someone’s mental health treatment to a therapist across the country that the patient has never actually met seems like a step in the wrong direction. Further, concerns arise about how much these folks will know about local resources in the community.
- The corporate model in mental health care. While being able to shop for a therapist like you would for a pillow sounds great on the surface, there are many times where a patient may need to be supportively confronted by their therapist or told no when asking about things like certain medications. The “customer is always right” principle often falls short when it comes to good mental health treatment.
- Depth and type of treatment. It is probably fair to say that most online therapy could be described as supportive psychotherapy. This type of therapy can be quite helpful for many but may lack the depth or specific techniques that some people need. For youth, some of the most effective types of psychotherapy, like cognitive-behavioral therapy (CBT), can be harder to find, and implement, online.
- Emergencies. While many online companies claim to offer round-the-clock support for paying customers, they can quickly punt to “call your doctor” or even “call 911” if there is any real mental health crisis.
Balancing these potential benefits and pitfalls of online therapy, here are a few questions your patients may want to consider before signing onto a long-term contract with an online therapy company.
- Would the online clinician have any knowledge of my community? In some cases, this may not matter that much, while for others it could be quite important.
- What happens in an emergency? Would the regular online therapist be available to help through a crisis or would things revert back to local resources?
- What about privacy and collaboration? Effective communication between a patient’s primary care clinician and their therapist can be crucial to good care, and asking the patient always to be the intermediary can be fraught with difficulty.
- How long is the contract? Just like those gym memberships, these companies bank on individuals who sign up but then don’t really use the service.
- What kind of training do the therapists at the site have? Is it possible to receive specific types of therapy, like CBT or parent training? Otherwise, pediatricians might be quite likely to hear back from the family wondering about medications after therapy “isn’t helping.”
Overall, mental health treatment delivered by telehealth is here to stay whether we like it or not. For some families, it is likely to provide new access to services not easily obtainable locally, while for others it could end up being a costly and ineffective enterprise. For families who use these services, a key challenge for pediatricians that may be important to overcome is finding a way for these clinicians to integrate into the overall medical team rather than being a detached island unto themselves.
Dr. Rettew is a child and adolescent psychiatrist and associate professor of psychiatry and pediatrics at the University of Vermont Larner College of Medicine, Burlington. Follow him on Twitter @PediPsych. His book, “Parenting Made Complicated: What Science Really Knows About the Greatest Debates of Early Childhood” (New York: Oxford University Press, 2021). Email him at pdnews@mdedge.com.
Opioid overdoses tied to lasting cognitive impairment
Opioid overdoses usually aren’t fatal, but a new review of numerous studies, mostly case reports and case series, suggests that they can have long-lasting effects on cognition, possibly because of hypoxia resulting from respiratory depression.
Erin L. Winstanley, PhD, MA, and associates noted in the review that opioids cause about 80% of worldwide deaths from illicit drug use, and the Centers for Disease Control and Prevention’s provisional August 2021 number of more than 88,000 opioid-caused deaths in the United States is the highest ever recorded – a 27% increase over what was reported last December. That number suggests that the opioid epidemic continues to rage, but the study results also show that the neurological consequences of nonfatal overdoses are an important public health problem.
And that’s something that may be overlooked, according to Mark S. Gold, MD, who was not involved with the study and was asked to comment on the review, which was published in the Journal of Addiction Science.
“Assuming that an overdose has no effect on the brain, mood, and behavior is not supported by experience or the literature. He is a University of Florida, Gainesville, Emeritus Eminent Scholar, adjunct professor of psychiatry at Washington University in St. Louis, and a member of the clinical council of Washington University’s Public Health Institute.
A common pattern among patients with opioid use disorder (OUD) is that they undergo treatment with medication-assisted therapy (MAT), only to drop out of treatment and then repeat the treatment at a later date. That suggests that physicians should take a harder look at the limitations of MAT and other treatments, Dr. Gold said.
Although the review found some associations between neurocognitive deficits and opioid overdose, the authors point out that it is difficult to make direct comparisons because of biases and differences in methodology among the included studies. They were not able to reach conclusions about the prevalence of brain injuries following nonfatal opioid overdoses. Few included studies controlled for confounding factors that might contribute to or explain neurocognitive impairments, reported Dr. Winstanley, associate professor in the department of behavioral medicine and psychiatry at the University of West Virginia, Morgantown, and associates.
Still, distinct patterns emerged from the analysis of almost 3,500 subjects in 79 studies in 21 countries. Twenty-nine studies reported diagnoses of leukoencephalopathy, which affects white matter. Spongiform leukoencephalopathy is known to occur secondarily after exposure to a variety of toxic agents, including carbon monoxide poisoning and drugs of abuse. The damage can lead to erosion of higher cerebral function. The condition can occur from 2 to 180 days after a hypoxic brain injury, potentially complicating efforts to attribute it specifically to an opioid overdose. Amnestic syndrome was also reported in some studies. One study found that about 39% of people seeking buprenorphine treatment suffered from neurocognitive impairment.
Dr. Gold called the study’s findings novel and of public health importance. “Each overdose takes a toll on the body, and especially the brain,” he said.
Better documentation needed
The variability in symptoms, as well as their timing, present challenges to initial treatment, which often occur before a patient reaches the hospital. This is a vital window because the length of time of inadequate respiration because of opioid overdose is likely to predict the extent of brain injury. The duration of inadequate respiration may not be captured in electronic medical records, and emergency departments don’t typically collect toxicology information, which may lead health care providers to attribute neurocognitive impairments to ongoing drug use rather than an acute anoxic or hypoxic episode. Further neurocognitive damage may have a delayed onset, and better documentation of these events could help physicians determine whether those symptoms stem from the acute event.
Dr. Winstanley and associates called for more research, including prospective case-control studies to identify brain changes following opioid-related overdose.
The authors also suggested that physicians might want to consider screening patients who experience prolonged anoxia or hypoxia for neurocognitive impairments and brain injuries. Dr. Gold agreed.
“Clinicians working with OUD patients should take these data to heart and take a comprehensive history of previous overdoses, loss of consciousness, head trauma, and following up on the history with neuropsychological and other tests of brain function,” Dr. Gold said. “After an assessment, rehabilitation and treatment might then be more personalized and effective.”
Dr. Gold had no relevant financial disclosures.
Opioid overdoses usually aren’t fatal, but a new review of numerous studies, mostly case reports and case series, suggests that they can have long-lasting effects on cognition, possibly because of hypoxia resulting from respiratory depression.
Erin L. Winstanley, PhD, MA, and associates noted in the review that opioids cause about 80% of worldwide deaths from illicit drug use, and the Centers for Disease Control and Prevention’s provisional August 2021 number of more than 88,000 opioid-caused deaths in the United States is the highest ever recorded – a 27% increase over what was reported last December. That number suggests that the opioid epidemic continues to rage, but the study results also show that the neurological consequences of nonfatal overdoses are an important public health problem.
And that’s something that may be overlooked, according to Mark S. Gold, MD, who was not involved with the study and was asked to comment on the review, which was published in the Journal of Addiction Science.
“Assuming that an overdose has no effect on the brain, mood, and behavior is not supported by experience or the literature. He is a University of Florida, Gainesville, Emeritus Eminent Scholar, adjunct professor of psychiatry at Washington University in St. Louis, and a member of the clinical council of Washington University’s Public Health Institute.
A common pattern among patients with opioid use disorder (OUD) is that they undergo treatment with medication-assisted therapy (MAT), only to drop out of treatment and then repeat the treatment at a later date. That suggests that physicians should take a harder look at the limitations of MAT and other treatments, Dr. Gold said.
Although the review found some associations between neurocognitive deficits and opioid overdose, the authors point out that it is difficult to make direct comparisons because of biases and differences in methodology among the included studies. They were not able to reach conclusions about the prevalence of brain injuries following nonfatal opioid overdoses. Few included studies controlled for confounding factors that might contribute to or explain neurocognitive impairments, reported Dr. Winstanley, associate professor in the department of behavioral medicine and psychiatry at the University of West Virginia, Morgantown, and associates.
Still, distinct patterns emerged from the analysis of almost 3,500 subjects in 79 studies in 21 countries. Twenty-nine studies reported diagnoses of leukoencephalopathy, which affects white matter. Spongiform leukoencephalopathy is known to occur secondarily after exposure to a variety of toxic agents, including carbon monoxide poisoning and drugs of abuse. The damage can lead to erosion of higher cerebral function. The condition can occur from 2 to 180 days after a hypoxic brain injury, potentially complicating efforts to attribute it specifically to an opioid overdose. Amnestic syndrome was also reported in some studies. One study found that about 39% of people seeking buprenorphine treatment suffered from neurocognitive impairment.
Dr. Gold called the study’s findings novel and of public health importance. “Each overdose takes a toll on the body, and especially the brain,” he said.
Better documentation needed
The variability in symptoms, as well as their timing, present challenges to initial treatment, which often occur before a patient reaches the hospital. This is a vital window because the length of time of inadequate respiration because of opioid overdose is likely to predict the extent of brain injury. The duration of inadequate respiration may not be captured in electronic medical records, and emergency departments don’t typically collect toxicology information, which may lead health care providers to attribute neurocognitive impairments to ongoing drug use rather than an acute anoxic or hypoxic episode. Further neurocognitive damage may have a delayed onset, and better documentation of these events could help physicians determine whether those symptoms stem from the acute event.
Dr. Winstanley and associates called for more research, including prospective case-control studies to identify brain changes following opioid-related overdose.
The authors also suggested that physicians might want to consider screening patients who experience prolonged anoxia or hypoxia for neurocognitive impairments and brain injuries. Dr. Gold agreed.
“Clinicians working with OUD patients should take these data to heart and take a comprehensive history of previous overdoses, loss of consciousness, head trauma, and following up on the history with neuropsychological and other tests of brain function,” Dr. Gold said. “After an assessment, rehabilitation and treatment might then be more personalized and effective.”
Dr. Gold had no relevant financial disclosures.
Opioid overdoses usually aren’t fatal, but a new review of numerous studies, mostly case reports and case series, suggests that they can have long-lasting effects on cognition, possibly because of hypoxia resulting from respiratory depression.
Erin L. Winstanley, PhD, MA, and associates noted in the review that opioids cause about 80% of worldwide deaths from illicit drug use, and the Centers for Disease Control and Prevention’s provisional August 2021 number of more than 88,000 opioid-caused deaths in the United States is the highest ever recorded – a 27% increase over what was reported last December. That number suggests that the opioid epidemic continues to rage, but the study results also show that the neurological consequences of nonfatal overdoses are an important public health problem.
And that’s something that may be overlooked, according to Mark S. Gold, MD, who was not involved with the study and was asked to comment on the review, which was published in the Journal of Addiction Science.
“Assuming that an overdose has no effect on the brain, mood, and behavior is not supported by experience or the literature. He is a University of Florida, Gainesville, Emeritus Eminent Scholar, adjunct professor of psychiatry at Washington University in St. Louis, and a member of the clinical council of Washington University’s Public Health Institute.
A common pattern among patients with opioid use disorder (OUD) is that they undergo treatment with medication-assisted therapy (MAT), only to drop out of treatment and then repeat the treatment at a later date. That suggests that physicians should take a harder look at the limitations of MAT and other treatments, Dr. Gold said.
Although the review found some associations between neurocognitive deficits and opioid overdose, the authors point out that it is difficult to make direct comparisons because of biases and differences in methodology among the included studies. They were not able to reach conclusions about the prevalence of brain injuries following nonfatal opioid overdoses. Few included studies controlled for confounding factors that might contribute to or explain neurocognitive impairments, reported Dr. Winstanley, associate professor in the department of behavioral medicine and psychiatry at the University of West Virginia, Morgantown, and associates.
Still, distinct patterns emerged from the analysis of almost 3,500 subjects in 79 studies in 21 countries. Twenty-nine studies reported diagnoses of leukoencephalopathy, which affects white matter. Spongiform leukoencephalopathy is known to occur secondarily after exposure to a variety of toxic agents, including carbon monoxide poisoning and drugs of abuse. The damage can lead to erosion of higher cerebral function. The condition can occur from 2 to 180 days after a hypoxic brain injury, potentially complicating efforts to attribute it specifically to an opioid overdose. Amnestic syndrome was also reported in some studies. One study found that about 39% of people seeking buprenorphine treatment suffered from neurocognitive impairment.
Dr. Gold called the study’s findings novel and of public health importance. “Each overdose takes a toll on the body, and especially the brain,” he said.
Better documentation needed
The variability in symptoms, as well as their timing, present challenges to initial treatment, which often occur before a patient reaches the hospital. This is a vital window because the length of time of inadequate respiration because of opioid overdose is likely to predict the extent of brain injury. The duration of inadequate respiration may not be captured in electronic medical records, and emergency departments don’t typically collect toxicology information, which may lead health care providers to attribute neurocognitive impairments to ongoing drug use rather than an acute anoxic or hypoxic episode. Further neurocognitive damage may have a delayed onset, and better documentation of these events could help physicians determine whether those symptoms stem from the acute event.
Dr. Winstanley and associates called for more research, including prospective case-control studies to identify brain changes following opioid-related overdose.
The authors also suggested that physicians might want to consider screening patients who experience prolonged anoxia or hypoxia for neurocognitive impairments and brain injuries. Dr. Gold agreed.
“Clinicians working with OUD patients should take these data to heart and take a comprehensive history of previous overdoses, loss of consciousness, head trauma, and following up on the history with neuropsychological and other tests of brain function,” Dr. Gold said. “After an assessment, rehabilitation and treatment might then be more personalized and effective.”
Dr. Gold had no relevant financial disclosures.
FROM THE JOURNAL OF ADDICTION SCIENCE
The role of probiotics in mental health
In 1950, at Staten Island’s Sea View Hospital, a group of patients with terminal tuberculosis were given a new antibiotic called isoniazid, which caused some unexpected side effects. The patients reported euphoria, mental stimulation, and improved sleep, and even began socializing with more vigor. The press was all over the case, writing about the sick “dancing in the halls tho’ they had holes in their lungs.” Soon doctors started prescribing isoniazid as the first-ever antidepressant.
The Sea View Hospital experiment was an early hint that changing the composition of the gut microbiome – in this case, via antibiotics – might affect our mental health. Yet only in the last 2 decades has research into connections between what we ingest and psychiatric disorders really taken off. In 2004, a landmark study showed that germ-free mice (born in such sterile conditions that they lacked a microbiome) had an exaggerated stress response. The effects were reversed, however, if the mice were fed a bacterial strain, Bifidobacterium infantis, a probiotic. This sparked academic interest, and thousands of research papers followed.
According to Stephen Ilardi, PhD, a clinical psychologist at the University of Kansas, Lawrence, focusing on the etiology and treatment of depression, now is the “time of exciting discovery” in the field of probiotics and psychiatric disorders, although, admittedly, a lot still remains unknown.
Gut microbiome profiles in mental health disorders
We humans have about 100 trillion microbes residing in our guts. Some of these are archaea, some fungi, some protozoans and even viruses, but most are bacteria. Things like diet, sleep, and stress can all impact the composition of our gut microbiome. When the microbiome differs considerably from the typical, doctors and researchers describe it as dysbiosis, or imbalance. Studies have uncovered dysbiosis in patients with depression, anxiety, schizophrenia, and bipolar disorder.
“I think there is now pretty good evidence that the gut microbiome is actually an important factor in a number of psychiatric disorders,” says Allan Young, MBChB, clinical psychiatrist at King’s College London. The gut microbiome composition does seem to differ between psychiatric patients and the healthy. In depression, for example, a recent review of nine studies found an increase on the genus level in Streptococcus and Oscillibacter and low abundance of Lactobacillus and Coprococcus, among others. In generalized anxiety disorder, meanwhile, there appears to be an increase in Fusobacteria and Escherichia/Shigella .
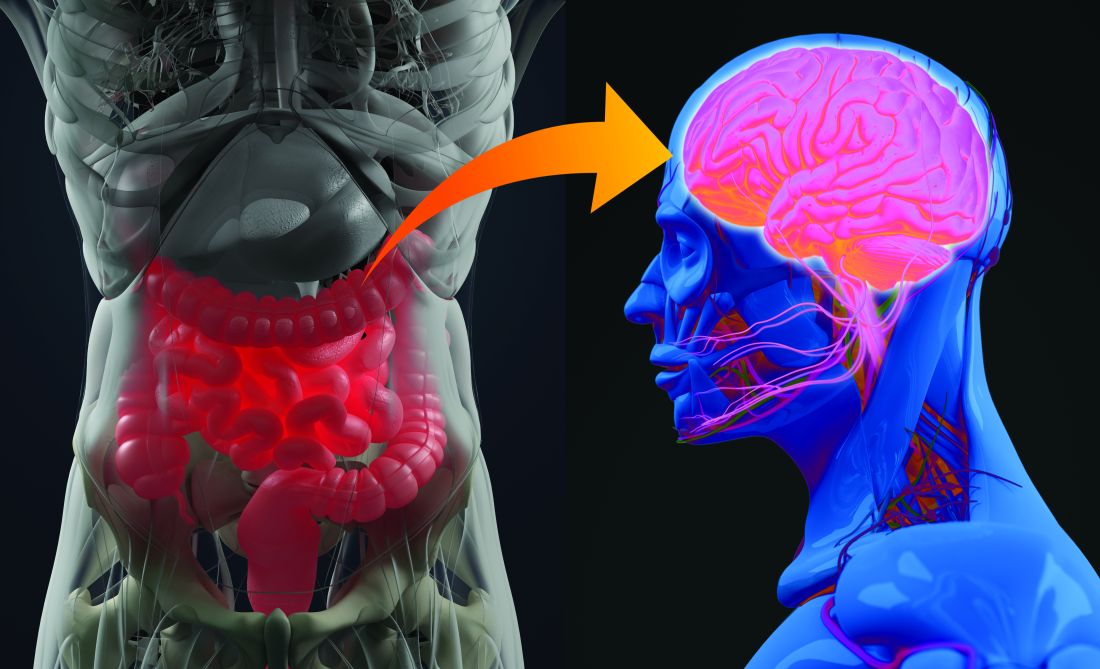
For Dr. Ilardi, the next important question is whether there are plausible mechanisms that could explain how gut microbiota may influence brain function. And, it appears there are.
“The microbes in the gut can release neurotransmitters into blood that cross into the brain and influence brain function. They can release hormones into the blood that again cross into the brain. They’ve got a lot of tricks up their sleeve,” he says.
One particularly important pathway runs through the vagus nerve – the longest nerve that emerges directly from the brain, connecting it to the gut. Another is the immune pathway. Gut bacteria can interact with immune cells and reduce cytokine production, which in turn can reduce systemic inflammation. Inflammatory processes have been implicated in both depression and bipolar disorder. What’s more, gut microbes can upregulate the expression of a protein called BDNF – brain-derived neurotrophic factor – which helps the development and survival of nerve cells in the brain.
Probiotics’ promise varies for different conditions
As the pathways by which gut dysbiosis may influence psychiatric disorders become clearer, the next logical step is to try to influence the composition of the microbiome to prevent and treat depression, anxiety, or schizophrenia. That’s where probiotics come in.
The evidence for the effects of probiotics – live microorganisms which, when ingested in adequate amounts, confer a health benefit – so far is the strongest for depression, says Viktoriya Nikolova, MRes, MSc, a PhD student and researcher at King’s College London. In their 2021 meta-analysis of seven trials, Mr. Nikolova and colleagues revealed that probiotics can significantly reduce depressive symptoms after just 8 weeks. There was a caveat, however – the probiotics only worked when used in addition to an approved antidepressant. Another meta-analysis, published in 2018, also showed that probiotics, when compared with placebo, improve mood in people with depressive symptoms (here, no antidepressant treatment was necessary).
Roumen Milev, MD, PhD, a neuroscientist at Queen’s University, Kingston, Ont., and coauthor of a review on probiotics and depression published in the Annals of General Psychiatry, warns, however, that the research is still in its infancy. “,” he says.
When it comes to using probiotics to relieve anxiety, “the evidence in the animal literature is really compelling,” says Dr. Ilardi. Human studies are less convincing, however, which Dr. Dr. Ilardi showed in his 2018 review and meta-analysis involving 743 animals and 1,527 humans. “Studies are small for the most part, and some of them aren’t terribly well conducted, and they often use very low doses of probiotics,” he says. One of the larger double-blind and placebo-controlled trials showed that supplementation with Lactobacillus plantarum helps reduce stress and anxiety, while the levels of proinflammatory cytokines go down. Another meta-analysis, published in June, revealed that, when it comes to reducing stress and anxiety in youth, the results are mixed.
Evidence of probiotics’ efficiency in schizophrenia is emerging, yet also limited. A 2019 review concluded that currently available results only “hint” at a possibility that probiotics could make a difference in schizophrenia. Similarly, a 2020 review summed up that the role of probiotics in bipolar disorder “remains unclear and underexplored.”
Better studies, remaining questions
Apart from small samples, one issue with research on probiotics is that they generally tend to use varied doses of different strains of bacteria, or even multistrain mixtures, making it tough to compare results. Although there are hundreds of species of bacteria in the human gut, only a few have been evaluated for their antidepressant or antianxiety effects.
“To make it even worse, it’s almost certainly the case that depending on a person’s actual genetics or maybe their epigenetics, a strain that is helpful for one person may not be helpful for another. There is almost certainly no one-size-fits-all probiotic formulation,” says Dr. Ilardi.
Another critical question that remains to be answered is that of potential side effects.
“Probiotics are often seen as food supplements, so they don’t follow under the same regulations as drugs would,” says Mr. Nikolova. “They don’t necessarily have to follow the pattern of drug trials in many countries, which means that the monitoring of side effects is not the requirement.”
That’s something that worries King’s College psychiatrist Young too. “If you are giving it to modulate how the brain works, you could potentially induce psychiatric symptoms or a psychiatric disorder. There could be allergic reactions. There could be lots of different things,” he says.
When you search the web for “probiotics,” chances are you will come across sites boasting amazing effects that such products can have on cardiovascular heath, the immune system, and yes, mental well-being. Many also sell various probiotic supplements “formulated” for your gut health or improved moods. However, many such commercially available strains have never been actually tested in clinical trials. What’s more, according to Kathrin Cohen Kadosh, PhD, a neuroscientist at University of Surrey (England), “it is not always clear whether the different strains actually reach the gut intact.”
For now, considering the limited research evidence, a safer bet is to try to improve gut health through consumption of fermented foods that naturally contain probiotics, such as miso, kefir, or sauerkraut. Alternatively, you could reach for prebiotics, such as foods containing fiber (prebiotics enhance the growth of beneficial gut microbes). This, Dr. Kadosh says, could be “a gentler way of improving gut health” than popping a pill. Whether an improved mental well-being might follow still remains to be seen.
A version of this article first appeared on Medscape.com.
In 1950, at Staten Island’s Sea View Hospital, a group of patients with terminal tuberculosis were given a new antibiotic called isoniazid, which caused some unexpected side effects. The patients reported euphoria, mental stimulation, and improved sleep, and even began socializing with more vigor. The press was all over the case, writing about the sick “dancing in the halls tho’ they had holes in their lungs.” Soon doctors started prescribing isoniazid as the first-ever antidepressant.
The Sea View Hospital experiment was an early hint that changing the composition of the gut microbiome – in this case, via antibiotics – might affect our mental health. Yet only in the last 2 decades has research into connections between what we ingest and psychiatric disorders really taken off. In 2004, a landmark study showed that germ-free mice (born in such sterile conditions that they lacked a microbiome) had an exaggerated stress response. The effects were reversed, however, if the mice were fed a bacterial strain, Bifidobacterium infantis, a probiotic. This sparked academic interest, and thousands of research papers followed.
According to Stephen Ilardi, PhD, a clinical psychologist at the University of Kansas, Lawrence, focusing on the etiology and treatment of depression, now is the “time of exciting discovery” in the field of probiotics and psychiatric disorders, although, admittedly, a lot still remains unknown.
Gut microbiome profiles in mental health disorders
We humans have about 100 trillion microbes residing in our guts. Some of these are archaea, some fungi, some protozoans and even viruses, but most are bacteria. Things like diet, sleep, and stress can all impact the composition of our gut microbiome. When the microbiome differs considerably from the typical, doctors and researchers describe it as dysbiosis, or imbalance. Studies have uncovered dysbiosis in patients with depression, anxiety, schizophrenia, and bipolar disorder.
“I think there is now pretty good evidence that the gut microbiome is actually an important factor in a number of psychiatric disorders,” says Allan Young, MBChB, clinical psychiatrist at King’s College London. The gut microbiome composition does seem to differ between psychiatric patients and the healthy. In depression, for example, a recent review of nine studies found an increase on the genus level in Streptococcus and Oscillibacter and low abundance of Lactobacillus and Coprococcus, among others. In generalized anxiety disorder, meanwhile, there appears to be an increase in Fusobacteria and Escherichia/Shigella .
For Dr. Ilardi, the next important question is whether there are plausible mechanisms that could explain how gut microbiota may influence brain function. And, it appears there are.
“The microbes in the gut can release neurotransmitters into blood that cross into the brain and influence brain function. They can release hormones into the blood that again cross into the brain. They’ve got a lot of tricks up their sleeve,” he says.
One particularly important pathway runs through the vagus nerve – the longest nerve that emerges directly from the brain, connecting it to the gut. Another is the immune pathway. Gut bacteria can interact with immune cells and reduce cytokine production, which in turn can reduce systemic inflammation. Inflammatory processes have been implicated in both depression and bipolar disorder. What’s more, gut microbes can upregulate the expression of a protein called BDNF – brain-derived neurotrophic factor – which helps the development and survival of nerve cells in the brain.
Probiotics’ promise varies for different conditions
As the pathways by which gut dysbiosis may influence psychiatric disorders become clearer, the next logical step is to try to influence the composition of the microbiome to prevent and treat depression, anxiety, or schizophrenia. That’s where probiotics come in.
The evidence for the effects of probiotics – live microorganisms which, when ingested in adequate amounts, confer a health benefit – so far is the strongest for depression, says Viktoriya Nikolova, MRes, MSc, a PhD student and researcher at King’s College London. In their 2021 meta-analysis of seven trials, Mr. Nikolova and colleagues revealed that probiotics can significantly reduce depressive symptoms after just 8 weeks. There was a caveat, however – the probiotics only worked when used in addition to an approved antidepressant. Another meta-analysis, published in 2018, also showed that probiotics, when compared with placebo, improve mood in people with depressive symptoms (here, no antidepressant treatment was necessary).
Roumen Milev, MD, PhD, a neuroscientist at Queen’s University, Kingston, Ont., and coauthor of a review on probiotics and depression published in the Annals of General Psychiatry, warns, however, that the research is still in its infancy. “,” he says.
When it comes to using probiotics to relieve anxiety, “the evidence in the animal literature is really compelling,” says Dr. Ilardi. Human studies are less convincing, however, which Dr. Dr. Ilardi showed in his 2018 review and meta-analysis involving 743 animals and 1,527 humans. “Studies are small for the most part, and some of them aren’t terribly well conducted, and they often use very low doses of probiotics,” he says. One of the larger double-blind and placebo-controlled trials showed that supplementation with Lactobacillus plantarum helps reduce stress and anxiety, while the levels of proinflammatory cytokines go down. Another meta-analysis, published in June, revealed that, when it comes to reducing stress and anxiety in youth, the results are mixed.
Evidence of probiotics’ efficiency in schizophrenia is emerging, yet also limited. A 2019 review concluded that currently available results only “hint” at a possibility that probiotics could make a difference in schizophrenia. Similarly, a 2020 review summed up that the role of probiotics in bipolar disorder “remains unclear and underexplored.”
Better studies, remaining questions
Apart from small samples, one issue with research on probiotics is that they generally tend to use varied doses of different strains of bacteria, or even multistrain mixtures, making it tough to compare results. Although there are hundreds of species of bacteria in the human gut, only a few have been evaluated for their antidepressant or antianxiety effects.
“To make it even worse, it’s almost certainly the case that depending on a person’s actual genetics or maybe their epigenetics, a strain that is helpful for one person may not be helpful for another. There is almost certainly no one-size-fits-all probiotic formulation,” says Dr. Ilardi.
Another critical question that remains to be answered is that of potential side effects.
“Probiotics are often seen as food supplements, so they don’t follow under the same regulations as drugs would,” says Mr. Nikolova. “They don’t necessarily have to follow the pattern of drug trials in many countries, which means that the monitoring of side effects is not the requirement.”
That’s something that worries King’s College psychiatrist Young too. “If you are giving it to modulate how the brain works, you could potentially induce psychiatric symptoms or a psychiatric disorder. There could be allergic reactions. There could be lots of different things,” he says.
When you search the web for “probiotics,” chances are you will come across sites boasting amazing effects that such products can have on cardiovascular heath, the immune system, and yes, mental well-being. Many also sell various probiotic supplements “formulated” for your gut health or improved moods. However, many such commercially available strains have never been actually tested in clinical trials. What’s more, according to Kathrin Cohen Kadosh, PhD, a neuroscientist at University of Surrey (England), “it is not always clear whether the different strains actually reach the gut intact.”
For now, considering the limited research evidence, a safer bet is to try to improve gut health through consumption of fermented foods that naturally contain probiotics, such as miso, kefir, or sauerkraut. Alternatively, you could reach for prebiotics, such as foods containing fiber (prebiotics enhance the growth of beneficial gut microbes). This, Dr. Kadosh says, could be “a gentler way of improving gut health” than popping a pill. Whether an improved mental well-being might follow still remains to be seen.
A version of this article first appeared on Medscape.com.
In 1950, at Staten Island’s Sea View Hospital, a group of patients with terminal tuberculosis were given a new antibiotic called isoniazid, which caused some unexpected side effects. The patients reported euphoria, mental stimulation, and improved sleep, and even began socializing with more vigor. The press was all over the case, writing about the sick “dancing in the halls tho’ they had holes in their lungs.” Soon doctors started prescribing isoniazid as the first-ever antidepressant.
The Sea View Hospital experiment was an early hint that changing the composition of the gut microbiome – in this case, via antibiotics – might affect our mental health. Yet only in the last 2 decades has research into connections between what we ingest and psychiatric disorders really taken off. In 2004, a landmark study showed that germ-free mice (born in such sterile conditions that they lacked a microbiome) had an exaggerated stress response. The effects were reversed, however, if the mice were fed a bacterial strain, Bifidobacterium infantis, a probiotic. This sparked academic interest, and thousands of research papers followed.
According to Stephen Ilardi, PhD, a clinical psychologist at the University of Kansas, Lawrence, focusing on the etiology and treatment of depression, now is the “time of exciting discovery” in the field of probiotics and psychiatric disorders, although, admittedly, a lot still remains unknown.
Gut microbiome profiles in mental health disorders
We humans have about 100 trillion microbes residing in our guts. Some of these are archaea, some fungi, some protozoans and even viruses, but most are bacteria. Things like diet, sleep, and stress can all impact the composition of our gut microbiome. When the microbiome differs considerably from the typical, doctors and researchers describe it as dysbiosis, or imbalance. Studies have uncovered dysbiosis in patients with depression, anxiety, schizophrenia, and bipolar disorder.
“I think there is now pretty good evidence that the gut microbiome is actually an important factor in a number of psychiatric disorders,” says Allan Young, MBChB, clinical psychiatrist at King’s College London. The gut microbiome composition does seem to differ between psychiatric patients and the healthy. In depression, for example, a recent review of nine studies found an increase on the genus level in Streptococcus and Oscillibacter and low abundance of Lactobacillus and Coprococcus, among others. In generalized anxiety disorder, meanwhile, there appears to be an increase in Fusobacteria and Escherichia/Shigella .
For Dr. Ilardi, the next important question is whether there are plausible mechanisms that could explain how gut microbiota may influence brain function. And, it appears there are.
“The microbes in the gut can release neurotransmitters into blood that cross into the brain and influence brain function. They can release hormones into the blood that again cross into the brain. They’ve got a lot of tricks up their sleeve,” he says.
One particularly important pathway runs through the vagus nerve – the longest nerve that emerges directly from the brain, connecting it to the gut. Another is the immune pathway. Gut bacteria can interact with immune cells and reduce cytokine production, which in turn can reduce systemic inflammation. Inflammatory processes have been implicated in both depression and bipolar disorder. What’s more, gut microbes can upregulate the expression of a protein called BDNF – brain-derived neurotrophic factor – which helps the development and survival of nerve cells in the brain.
Probiotics’ promise varies for different conditions
As the pathways by which gut dysbiosis may influence psychiatric disorders become clearer, the next logical step is to try to influence the composition of the microbiome to prevent and treat depression, anxiety, or schizophrenia. That’s where probiotics come in.
The evidence for the effects of probiotics – live microorganisms which, when ingested in adequate amounts, confer a health benefit – so far is the strongest for depression, says Viktoriya Nikolova, MRes, MSc, a PhD student and researcher at King’s College London. In their 2021 meta-analysis of seven trials, Mr. Nikolova and colleagues revealed that probiotics can significantly reduce depressive symptoms after just 8 weeks. There was a caveat, however – the probiotics only worked when used in addition to an approved antidepressant. Another meta-analysis, published in 2018, also showed that probiotics, when compared with placebo, improve mood in people with depressive symptoms (here, no antidepressant treatment was necessary).
Roumen Milev, MD, PhD, a neuroscientist at Queen’s University, Kingston, Ont., and coauthor of a review on probiotics and depression published in the Annals of General Psychiatry, warns, however, that the research is still in its infancy. “,” he says.
When it comes to using probiotics to relieve anxiety, “the evidence in the animal literature is really compelling,” says Dr. Ilardi. Human studies are less convincing, however, which Dr. Dr. Ilardi showed in his 2018 review and meta-analysis involving 743 animals and 1,527 humans. “Studies are small for the most part, and some of them aren’t terribly well conducted, and they often use very low doses of probiotics,” he says. One of the larger double-blind and placebo-controlled trials showed that supplementation with Lactobacillus plantarum helps reduce stress and anxiety, while the levels of proinflammatory cytokines go down. Another meta-analysis, published in June, revealed that, when it comes to reducing stress and anxiety in youth, the results are mixed.
Evidence of probiotics’ efficiency in schizophrenia is emerging, yet also limited. A 2019 review concluded that currently available results only “hint” at a possibility that probiotics could make a difference in schizophrenia. Similarly, a 2020 review summed up that the role of probiotics in bipolar disorder “remains unclear and underexplored.”
Better studies, remaining questions
Apart from small samples, one issue with research on probiotics is that they generally tend to use varied doses of different strains of bacteria, or even multistrain mixtures, making it tough to compare results. Although there are hundreds of species of bacteria in the human gut, only a few have been evaluated for their antidepressant or antianxiety effects.
“To make it even worse, it’s almost certainly the case that depending on a person’s actual genetics or maybe their epigenetics, a strain that is helpful for one person may not be helpful for another. There is almost certainly no one-size-fits-all probiotic formulation,” says Dr. Ilardi.
Another critical question that remains to be answered is that of potential side effects.
“Probiotics are often seen as food supplements, so they don’t follow under the same regulations as drugs would,” says Mr. Nikolova. “They don’t necessarily have to follow the pattern of drug trials in many countries, which means that the monitoring of side effects is not the requirement.”
That’s something that worries King’s College psychiatrist Young too. “If you are giving it to modulate how the brain works, you could potentially induce psychiatric symptoms or a psychiatric disorder. There could be allergic reactions. There could be lots of different things,” he says.
When you search the web for “probiotics,” chances are you will come across sites boasting amazing effects that such products can have on cardiovascular heath, the immune system, and yes, mental well-being. Many also sell various probiotic supplements “formulated” for your gut health or improved moods. However, many such commercially available strains have never been actually tested in clinical trials. What’s more, according to Kathrin Cohen Kadosh, PhD, a neuroscientist at University of Surrey (England), “it is not always clear whether the different strains actually reach the gut intact.”
For now, considering the limited research evidence, a safer bet is to try to improve gut health through consumption of fermented foods that naturally contain probiotics, such as miso, kefir, or sauerkraut. Alternatively, you could reach for prebiotics, such as foods containing fiber (prebiotics enhance the growth of beneficial gut microbes). This, Dr. Kadosh says, could be “a gentler way of improving gut health” than popping a pill. Whether an improved mental well-being might follow still remains to be seen.
A version of this article first appeared on Medscape.com.
Nature versus nurture: Seasonal affective disorder
With summer coming to an end, and pumpkin spice lattes trending again, we might also expect to say hello to an old friend ... seasonal affective disorder (SAD).
Have you ever woken up one morning during the fall or winter and felt out of it for a prolonged period, not your regular self? I’m not referring to a day here and there, but consistently experiencing this “down mood” around the same time each year? At some point in their life, it is estimated that 2-3% of Canadians will experience SAD. To add to that, 15% of individuals will experience milder (and less impairing) SAD.
Seasonal affective disorder can be thought of as a type of depression that occurs during a specific time of the year, usually the winter or fall (with remission outside this period). It is typically characterized by symptoms of clinical depression such as low energy, difficulty with concentration, sleep problems, extreme fatigue, and agitation. While the evidence related to the risk factors for SAD are limited, it is suggested that a family history of SAD, female sex, location farther from the equator (that is, fewer days of sunlight), and being between the ages of 18-30 increase your risk for SAD.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) does not provide a separate and distinct categorization for SAD. Rather, SAD is categorized as a subtype of depression. However,
Nature versus nurture: An evolutionary perspective
The pathophysiology of SAD is not yet well understood. However, it is hypothesized that SAD is an adaptive response related to physiologic and behavioral patterns of reproduction and childrearing.
Historically, reproduction was closely linked to food and natural resource availability (for example, water, sunlight). Males primarily handled the hunting, while females were primarily responsible for agricultural work, a job closely tied to the seasons. With this in mind, it would logically follow that natural selection favored reproduction during times of food abundance and did not favor reproduction during times of food scarcity (that is, low energy).
Consequently, conception would occur when the growing season began (around the summer), giving females the chance to rest when heavily pregnant in the winter, and give birth in the spring. Accordingly, from an evolutionary perspective, greater seasonal variation in mood and behavior is a function of historic patterns of reproduction and food gathering.
An alternative hypothesis of SAD is the dual vulnerability hypothesis. This hypothesis posits that SAD is the result of seasonality and depression (or “vulnerability traits”). Seasonality refers to external environmental factors such as light availability.
It’s quite well known, and perhaps your personal experience can speak to this topic as well, that shorter days may trigger SAD because reduced light exposure is associated with phase-delayed circadian rhythms. As a result, less dopamine is produced, and relatively higher levels of melatonin are produced, compared to individuals without SAD. “Vulnerability traits” refer to a genetic predisposition, or external effects (for example, stress).
A disorder of the past?
By nature of natural selection, SAD is likely not to be considered an advantageous adaptive trait that would help with survival and reproduction. In fact, it could be considered a maladaptive trait. In that case, will SAD eventually fall to natural selection?
Leanna M.W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
With summer coming to an end, and pumpkin spice lattes trending again, we might also expect to say hello to an old friend ... seasonal affective disorder (SAD).
Have you ever woken up one morning during the fall or winter and felt out of it for a prolonged period, not your regular self? I’m not referring to a day here and there, but consistently experiencing this “down mood” around the same time each year? At some point in their life, it is estimated that 2-3% of Canadians will experience SAD. To add to that, 15% of individuals will experience milder (and less impairing) SAD.
Seasonal affective disorder can be thought of as a type of depression that occurs during a specific time of the year, usually the winter or fall (with remission outside this period). It is typically characterized by symptoms of clinical depression such as low energy, difficulty with concentration, sleep problems, extreme fatigue, and agitation. While the evidence related to the risk factors for SAD are limited, it is suggested that a family history of SAD, female sex, location farther from the equator (that is, fewer days of sunlight), and being between the ages of 18-30 increase your risk for SAD.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) does not provide a separate and distinct categorization for SAD. Rather, SAD is categorized as a subtype of depression. However,
Nature versus nurture: An evolutionary perspective
The pathophysiology of SAD is not yet well understood. However, it is hypothesized that SAD is an adaptive response related to physiologic and behavioral patterns of reproduction and childrearing.
Historically, reproduction was closely linked to food and natural resource availability (for example, water, sunlight). Males primarily handled the hunting, while females were primarily responsible for agricultural work, a job closely tied to the seasons. With this in mind, it would logically follow that natural selection favored reproduction during times of food abundance and did not favor reproduction during times of food scarcity (that is, low energy).
Consequently, conception would occur when the growing season began (around the summer), giving females the chance to rest when heavily pregnant in the winter, and give birth in the spring. Accordingly, from an evolutionary perspective, greater seasonal variation in mood and behavior is a function of historic patterns of reproduction and food gathering.
An alternative hypothesis of SAD is the dual vulnerability hypothesis. This hypothesis posits that SAD is the result of seasonality and depression (or “vulnerability traits”). Seasonality refers to external environmental factors such as light availability.
It’s quite well known, and perhaps your personal experience can speak to this topic as well, that shorter days may trigger SAD because reduced light exposure is associated with phase-delayed circadian rhythms. As a result, less dopamine is produced, and relatively higher levels of melatonin are produced, compared to individuals without SAD. “Vulnerability traits” refer to a genetic predisposition, or external effects (for example, stress).
A disorder of the past?
By nature of natural selection, SAD is likely not to be considered an advantageous adaptive trait that would help with survival and reproduction. In fact, it could be considered a maladaptive trait. In that case, will SAD eventually fall to natural selection?
Leanna M.W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
With summer coming to an end, and pumpkin spice lattes trending again, we might also expect to say hello to an old friend ... seasonal affective disorder (SAD).
Have you ever woken up one morning during the fall or winter and felt out of it for a prolonged period, not your regular self? I’m not referring to a day here and there, but consistently experiencing this “down mood” around the same time each year? At some point in their life, it is estimated that 2-3% of Canadians will experience SAD. To add to that, 15% of individuals will experience milder (and less impairing) SAD.
Seasonal affective disorder can be thought of as a type of depression that occurs during a specific time of the year, usually the winter or fall (with remission outside this period). It is typically characterized by symptoms of clinical depression such as low energy, difficulty with concentration, sleep problems, extreme fatigue, and agitation. While the evidence related to the risk factors for SAD are limited, it is suggested that a family history of SAD, female sex, location farther from the equator (that is, fewer days of sunlight), and being between the ages of 18-30 increase your risk for SAD.
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5) does not provide a separate and distinct categorization for SAD. Rather, SAD is categorized as a subtype of depression. However,
Nature versus nurture: An evolutionary perspective
The pathophysiology of SAD is not yet well understood. However, it is hypothesized that SAD is an adaptive response related to physiologic and behavioral patterns of reproduction and childrearing.
Historically, reproduction was closely linked to food and natural resource availability (for example, water, sunlight). Males primarily handled the hunting, while females were primarily responsible for agricultural work, a job closely tied to the seasons. With this in mind, it would logically follow that natural selection favored reproduction during times of food abundance and did not favor reproduction during times of food scarcity (that is, low energy).
Consequently, conception would occur when the growing season began (around the summer), giving females the chance to rest when heavily pregnant in the winter, and give birth in the spring. Accordingly, from an evolutionary perspective, greater seasonal variation in mood and behavior is a function of historic patterns of reproduction and food gathering.
An alternative hypothesis of SAD is the dual vulnerability hypothesis. This hypothesis posits that SAD is the result of seasonality and depression (or “vulnerability traits”). Seasonality refers to external environmental factors such as light availability.
It’s quite well known, and perhaps your personal experience can speak to this topic as well, that shorter days may trigger SAD because reduced light exposure is associated with phase-delayed circadian rhythms. As a result, less dopamine is produced, and relatively higher levels of melatonin are produced, compared to individuals without SAD. “Vulnerability traits” refer to a genetic predisposition, or external effects (for example, stress).
A disorder of the past?
By nature of natural selection, SAD is likely not to be considered an advantageous adaptive trait that would help with survival and reproduction. In fact, it could be considered a maladaptive trait. In that case, will SAD eventually fall to natural selection?
Leanna M.W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
Is social media worsening our social fears?
Ping. Here’s a picture of your friends on a trip without you.
Ding. In your inbox, you find an email from your attending dismissing you from a very important project or patient.
Ring. There’s that call from your colleague telling you all about the incredible dinner with some other residents, which you weren’t invited to.
FoMO. Fear of missing out.
FoMO refers to a social anxiety phenomenon fueled by the need or desire to participate in an experience, event, interaction, or investment. It can be conceptualized in two parts: (1) social ostracism and (2) the need to maintain social connectedness through a sense of belonging and/or strong relationships. It is generally characterized by episodic feelings of regret, discontent, social inferiority, and/or loneliness.
Social networking sites and FoMO
Social networking sites (SNS) are a great way for people to connect instantaneously and without borders. However, they may also decrease the quality of intimate connections and relationships. In the current COVID-19 era of Zoom, most of us could agree that face-to-face and in-person communication triumphs over Internet-based interactions. I can attest that Zoom university, endless FaceTime calls, and late-night Netflix parties are not fulfilling my desire for in-person interactions. That is to say, SNS cannot fully compensate for our unmet social needs.
In fact, achieving social compensation through SNS may exacerbate social fears and anxiety disorders, and encourage rumination. For example, a recent systematic review investigating social media use among individuals who are socially anxious and lonely found that both of the foregoing factors may lead to greater negative and inhibitory behavior as a result of social media use. Feelings of inadequacy can lead to a distorted sense of oneself.
Ping. Ding. Ring. In 2021, almost half of people in the United States spend 5-6 hours on their phones daily.
Most of us are one click away from what essentially is a “live stream” of continuous updates on peoples’ lives. With these constant updates, we often start to imagine what we’re missing out on: trips, dinners, parties, and everything under the sun. However, in reality, what we see on social media is only a fraction of true reality. For example, that 10-second video of your friend going hiking cannot begin to sum up the entire day. The 24/7 nature of SNS can often lead to a perversion of the truth and unhealthy self-comparisons.
In this vicious cycle of notifications and constant entertainment, unreasonable expectations are created that adversely impact self-confidence and self-esteem, and may even lead to the emergence of depressive symptoms.
FoMO and negative associations of SNS go hand in hand. While SNS are a powerful tool for connection and information, they have also been reported to negatively impact quality of interactions.
Next time you see a picture, video, or post of a missed event, perhaps it’s best to stop thinking of the “what ifs” and start crafting your own narrative.
Ms Lui completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate. She has received income from Braxia Scientific Corp. A version of this article first appeared on Medscape.com.
Ping. Here’s a picture of your friends on a trip without you.
Ding. In your inbox, you find an email from your attending dismissing you from a very important project or patient.
Ring. There’s that call from your colleague telling you all about the incredible dinner with some other residents, which you weren’t invited to.
FoMO. Fear of missing out.
FoMO refers to a social anxiety phenomenon fueled by the need or desire to participate in an experience, event, interaction, or investment. It can be conceptualized in two parts: (1) social ostracism and (2) the need to maintain social connectedness through a sense of belonging and/or strong relationships. It is generally characterized by episodic feelings of regret, discontent, social inferiority, and/or loneliness.
Social networking sites and FoMO
Social networking sites (SNS) are a great way for people to connect instantaneously and without borders. However, they may also decrease the quality of intimate connections and relationships. In the current COVID-19 era of Zoom, most of us could agree that face-to-face and in-person communication triumphs over Internet-based interactions. I can attest that Zoom university, endless FaceTime calls, and late-night Netflix parties are not fulfilling my desire for in-person interactions. That is to say, SNS cannot fully compensate for our unmet social needs.
In fact, achieving social compensation through SNS may exacerbate social fears and anxiety disorders, and encourage rumination. For example, a recent systematic review investigating social media use among individuals who are socially anxious and lonely found that both of the foregoing factors may lead to greater negative and inhibitory behavior as a result of social media use. Feelings of inadequacy can lead to a distorted sense of oneself.
Ping. Ding. Ring. In 2021, almost half of people in the United States spend 5-6 hours on their phones daily.
Most of us are one click away from what essentially is a “live stream” of continuous updates on peoples’ lives. With these constant updates, we often start to imagine what we’re missing out on: trips, dinners, parties, and everything under the sun. However, in reality, what we see on social media is only a fraction of true reality. For example, that 10-second video of your friend going hiking cannot begin to sum up the entire day. The 24/7 nature of SNS can often lead to a perversion of the truth and unhealthy self-comparisons.
In this vicious cycle of notifications and constant entertainment, unreasonable expectations are created that adversely impact self-confidence and self-esteem, and may even lead to the emergence of depressive symptoms.
FoMO and negative associations of SNS go hand in hand. While SNS are a powerful tool for connection and information, they have also been reported to negatively impact quality of interactions.
Next time you see a picture, video, or post of a missed event, perhaps it’s best to stop thinking of the “what ifs” and start crafting your own narrative.
Ms Lui completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate. She has received income from Braxia Scientific Corp. A version of this article first appeared on Medscape.com.
Ping. Here’s a picture of your friends on a trip without you.
Ding. In your inbox, you find an email from your attending dismissing you from a very important project or patient.
Ring. There’s that call from your colleague telling you all about the incredible dinner with some other residents, which you weren’t invited to.
FoMO. Fear of missing out.
FoMO refers to a social anxiety phenomenon fueled by the need or desire to participate in an experience, event, interaction, or investment. It can be conceptualized in two parts: (1) social ostracism and (2) the need to maintain social connectedness through a sense of belonging and/or strong relationships. It is generally characterized by episodic feelings of regret, discontent, social inferiority, and/or loneliness.
Social networking sites and FoMO
Social networking sites (SNS) are a great way for people to connect instantaneously and without borders. However, they may also decrease the quality of intimate connections and relationships. In the current COVID-19 era of Zoom, most of us could agree that face-to-face and in-person communication triumphs over Internet-based interactions. I can attest that Zoom university, endless FaceTime calls, and late-night Netflix parties are not fulfilling my desire for in-person interactions. That is to say, SNS cannot fully compensate for our unmet social needs.
In fact, achieving social compensation through SNS may exacerbate social fears and anxiety disorders, and encourage rumination. For example, a recent systematic review investigating social media use among individuals who are socially anxious and lonely found that both of the foregoing factors may lead to greater negative and inhibitory behavior as a result of social media use. Feelings of inadequacy can lead to a distorted sense of oneself.
Ping. Ding. Ring. In 2021, almost half of people in the United States spend 5-6 hours on their phones daily.
Most of us are one click away from what essentially is a “live stream” of continuous updates on peoples’ lives. With these constant updates, we often start to imagine what we’re missing out on: trips, dinners, parties, and everything under the sun. However, in reality, what we see on social media is only a fraction of true reality. For example, that 10-second video of your friend going hiking cannot begin to sum up the entire day. The 24/7 nature of SNS can often lead to a perversion of the truth and unhealthy self-comparisons.
In this vicious cycle of notifications and constant entertainment, unreasonable expectations are created that adversely impact self-confidence and self-esteem, and may even lead to the emergence of depressive symptoms.
FoMO and negative associations of SNS go hand in hand. While SNS are a powerful tool for connection and information, they have also been reported to negatively impact quality of interactions.
Next time you see a picture, video, or post of a missed event, perhaps it’s best to stop thinking of the “what ifs” and start crafting your own narrative.
Ms Lui completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate. She has received income from Braxia Scientific Corp. A version of this article first appeared on Medscape.com.
Why misinformation spreads
Over the past 16 months, the COVID-19 pandemic has highlighted not only our vulnerability to disease outbreaks but also our susceptibility to misinformation and the dangers of “fake news.”
In fact, COVID-19 is not a pandemic but rather a syndemic of viral disease and misinformation. In the current digital age, there is an abundance of information at our fingertips. This has resulted in a surplus of accurate as well as inaccurate information – information that is subject to the various biases we humans are subject to.
Our decision making and cognition are colored by our internal and external environmental biases, whether through our emotions, societal influences, or cues from the “machines” that are now such an omnipresent part of our lives.
Let’s break them down:
- Emotional bias: We’re only human, and our emotions often overwhelm objective judgment. Even when the evidence is of low quality, emotional attachments can deter us from rational thinking. This kind of bias can be rooted in personal experiences.
- Societal bias: Thoughts, opinions, or perspectives of peers are powerful forces that may influence our decisions and viewpoints. We can conceptualize our social networks as partisan circles and “echo chambers.” This bias is perhaps most evident in various online social media platforms.
- Machine bias: Our online platforms are laced with algorithms that tailor the content we see. Accordingly, the curated content we see (and, by extension, the less diverse content we view) may reinforce existing biases, such as confirmation bias.
- Although bias plays a significant role in decision making, we should also consider intuition versus deliberation – and whether the “gut” is a reliable source of information.
Intuition versus deliberation: The power of reasoning
The dual process theory suggests that thought may be categorized in two ways: System 1, referred to as rapid, intuitive, or automatic thinking (which may be a result of personal experience); and system 2, referred to as deliberate or controlled thinking (for example, reasoned thinking). System 1 versus system 2 may be conceptualized as fast versus slow thinking.
Let’s use the Cognitive Reflection Test to illustrate the dual process theory. This test measures the ability to reflect and deliberate on a question and to forgo an intuitive, rapid response. One of the questions asks: “A bat and a ball cost $1.10 in total. The bat costs $1.00 more than the ball. How much does the ball cost?” A common answer is that the ball costs $0.10. However, the ball actually costs $0.05. The common response is a “gut” response, rather than an analytic or deliberate response.
This example can be extrapolated to social media behavior, such as when individuals endorse beliefs and behaviors that may be far from the truth (for example, conspiracy ideation). It is not uncommon for individuals to rely on intuition, which may be incorrect, as a driving source of truth. Although one’s intuition can be correct, it’s important to be careful and to deliberate.
But would deliberate engagement lead to more politically valenced perspectives? One hypothesis posits that system 2 can lead to false claims and worsening discernment of truth. Another, and more popular, account of classical reasoning says that more thoughtful engagement (regardless of one’s political beliefs) is less susceptible to false news (for example, hyperpartisan news).
Additionally, having good literacy (political, scientific, or general) is important for discerning the truth, especially regarding events in which the information and/or claims of knowledge have been heavily manipulated.
Are believing and sharing the same?
Interestingly, believing in a headline and sharing it are not the same. A study that investigated the difference between the two found that although individuals were able to discern the validity of headlines, the veracity of those headlines was not a determining factor in sharing the story on social media.
It has been suggested that social media context may distract individuals from engaging in deliberate thinking that would enhance their ability to determine the accuracy of the content. The dissociation between truthfulness and sharing may be a result of the “attention economy,” which refers to user engagement of likes, comments, shares, and so forth. As such, social media behavior and content consumption may not necessarily reflect one’s beliefs and may be influenced by what others value.
To combat the spread of misinformation, it has been suggested that proactive interventions – “prebunking” or “inoculation” – are necessary. This idea is in accordance with the inoculation theory, which suggests that pre-exposure can confer resistance to challenge. This line of thinking is aligned with the use of vaccines to counter medical illnesses. Increasing awareness of individual vulnerability to manipulation and misinformation has also been proposed as a strategy to resist persuasion.
The age old tale of what others think of us versus what we believe to be true has existed long before the viral overtake of social media. The main difference today is that social media acts as a catalyst for pockets of misinformation. Although social media outlets are cracking down on “false news,” we must consider what criteria should be employed to identify false information. Should external bodies regulate our content consumption? We are certainly entering a gray zone of “wrong” versus “right.” With the overabundance of information available online, it may be the case of “them” versus “us” – that is, those who do not believe in the existence of misinformation versus those who do.
Leanna M. W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
Over the past 16 months, the COVID-19 pandemic has highlighted not only our vulnerability to disease outbreaks but also our susceptibility to misinformation and the dangers of “fake news.”
In fact, COVID-19 is not a pandemic but rather a syndemic of viral disease and misinformation. In the current digital age, there is an abundance of information at our fingertips. This has resulted in a surplus of accurate as well as inaccurate information – information that is subject to the various biases we humans are subject to.
Our decision making and cognition are colored by our internal and external environmental biases, whether through our emotions, societal influences, or cues from the “machines” that are now such an omnipresent part of our lives.
Let’s break them down:
- Emotional bias: We’re only human, and our emotions often overwhelm objective judgment. Even when the evidence is of low quality, emotional attachments can deter us from rational thinking. This kind of bias can be rooted in personal experiences.
- Societal bias: Thoughts, opinions, or perspectives of peers are powerful forces that may influence our decisions and viewpoints. We can conceptualize our social networks as partisan circles and “echo chambers.” This bias is perhaps most evident in various online social media platforms.
- Machine bias: Our online platforms are laced with algorithms that tailor the content we see. Accordingly, the curated content we see (and, by extension, the less diverse content we view) may reinforce existing biases, such as confirmation bias.
- Although bias plays a significant role in decision making, we should also consider intuition versus deliberation – and whether the “gut” is a reliable source of information.
Intuition versus deliberation: The power of reasoning
The dual process theory suggests that thought may be categorized in two ways: System 1, referred to as rapid, intuitive, or automatic thinking (which may be a result of personal experience); and system 2, referred to as deliberate or controlled thinking (for example, reasoned thinking). System 1 versus system 2 may be conceptualized as fast versus slow thinking.
Let’s use the Cognitive Reflection Test to illustrate the dual process theory. This test measures the ability to reflect and deliberate on a question and to forgo an intuitive, rapid response. One of the questions asks: “A bat and a ball cost $1.10 in total. The bat costs $1.00 more than the ball. How much does the ball cost?” A common answer is that the ball costs $0.10. However, the ball actually costs $0.05. The common response is a “gut” response, rather than an analytic or deliberate response.
This example can be extrapolated to social media behavior, such as when individuals endorse beliefs and behaviors that may be far from the truth (for example, conspiracy ideation). It is not uncommon for individuals to rely on intuition, which may be incorrect, as a driving source of truth. Although one’s intuition can be correct, it’s important to be careful and to deliberate.
But would deliberate engagement lead to more politically valenced perspectives? One hypothesis posits that system 2 can lead to false claims and worsening discernment of truth. Another, and more popular, account of classical reasoning says that more thoughtful engagement (regardless of one’s political beliefs) is less susceptible to false news (for example, hyperpartisan news).
Additionally, having good literacy (political, scientific, or general) is important for discerning the truth, especially regarding events in which the information and/or claims of knowledge have been heavily manipulated.
Are believing and sharing the same?
Interestingly, believing in a headline and sharing it are not the same. A study that investigated the difference between the two found that although individuals were able to discern the validity of headlines, the veracity of those headlines was not a determining factor in sharing the story on social media.
It has been suggested that social media context may distract individuals from engaging in deliberate thinking that would enhance their ability to determine the accuracy of the content. The dissociation between truthfulness and sharing may be a result of the “attention economy,” which refers to user engagement of likes, comments, shares, and so forth. As such, social media behavior and content consumption may not necessarily reflect one’s beliefs and may be influenced by what others value.
To combat the spread of misinformation, it has been suggested that proactive interventions – “prebunking” or “inoculation” – are necessary. This idea is in accordance with the inoculation theory, which suggests that pre-exposure can confer resistance to challenge. This line of thinking is aligned with the use of vaccines to counter medical illnesses. Increasing awareness of individual vulnerability to manipulation and misinformation has also been proposed as a strategy to resist persuasion.
The age old tale of what others think of us versus what we believe to be true has existed long before the viral overtake of social media. The main difference today is that social media acts as a catalyst for pockets of misinformation. Although social media outlets are cracking down on “false news,” we must consider what criteria should be employed to identify false information. Should external bodies regulate our content consumption? We are certainly entering a gray zone of “wrong” versus “right.” With the overabundance of information available online, it may be the case of “them” versus “us” – that is, those who do not believe in the existence of misinformation versus those who do.
Leanna M. W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
Over the past 16 months, the COVID-19 pandemic has highlighted not only our vulnerability to disease outbreaks but also our susceptibility to misinformation and the dangers of “fake news.”
In fact, COVID-19 is not a pandemic but rather a syndemic of viral disease and misinformation. In the current digital age, there is an abundance of information at our fingertips. This has resulted in a surplus of accurate as well as inaccurate information – information that is subject to the various biases we humans are subject to.
Our decision making and cognition are colored by our internal and external environmental biases, whether through our emotions, societal influences, or cues from the “machines” that are now such an omnipresent part of our lives.
Let’s break them down:
- Emotional bias: We’re only human, and our emotions often overwhelm objective judgment. Even when the evidence is of low quality, emotional attachments can deter us from rational thinking. This kind of bias can be rooted in personal experiences.
- Societal bias: Thoughts, opinions, or perspectives of peers are powerful forces that may influence our decisions and viewpoints. We can conceptualize our social networks as partisan circles and “echo chambers.” This bias is perhaps most evident in various online social media platforms.
- Machine bias: Our online platforms are laced with algorithms that tailor the content we see. Accordingly, the curated content we see (and, by extension, the less diverse content we view) may reinforce existing biases, such as confirmation bias.
- Although bias plays a significant role in decision making, we should also consider intuition versus deliberation – and whether the “gut” is a reliable source of information.
Intuition versus deliberation: The power of reasoning
The dual process theory suggests that thought may be categorized in two ways: System 1, referred to as rapid, intuitive, or automatic thinking (which may be a result of personal experience); and system 2, referred to as deliberate or controlled thinking (for example, reasoned thinking). System 1 versus system 2 may be conceptualized as fast versus slow thinking.
Let’s use the Cognitive Reflection Test to illustrate the dual process theory. This test measures the ability to reflect and deliberate on a question and to forgo an intuitive, rapid response. One of the questions asks: “A bat and a ball cost $1.10 in total. The bat costs $1.00 more than the ball. How much does the ball cost?” A common answer is that the ball costs $0.10. However, the ball actually costs $0.05. The common response is a “gut” response, rather than an analytic or deliberate response.
This example can be extrapolated to social media behavior, such as when individuals endorse beliefs and behaviors that may be far from the truth (for example, conspiracy ideation). It is not uncommon for individuals to rely on intuition, which may be incorrect, as a driving source of truth. Although one’s intuition can be correct, it’s important to be careful and to deliberate.
But would deliberate engagement lead to more politically valenced perspectives? One hypothesis posits that system 2 can lead to false claims and worsening discernment of truth. Another, and more popular, account of classical reasoning says that more thoughtful engagement (regardless of one’s political beliefs) is less susceptible to false news (for example, hyperpartisan news).
Additionally, having good literacy (political, scientific, or general) is important for discerning the truth, especially regarding events in which the information and/or claims of knowledge have been heavily manipulated.
Are believing and sharing the same?
Interestingly, believing in a headline and sharing it are not the same. A study that investigated the difference between the two found that although individuals were able to discern the validity of headlines, the veracity of those headlines was not a determining factor in sharing the story on social media.
It has been suggested that social media context may distract individuals from engaging in deliberate thinking that would enhance their ability to determine the accuracy of the content. The dissociation between truthfulness and sharing may be a result of the “attention economy,” which refers to user engagement of likes, comments, shares, and so forth. As such, social media behavior and content consumption may not necessarily reflect one’s beliefs and may be influenced by what others value.
To combat the spread of misinformation, it has been suggested that proactive interventions – “prebunking” or “inoculation” – are necessary. This idea is in accordance with the inoculation theory, which suggests that pre-exposure can confer resistance to challenge. This line of thinking is aligned with the use of vaccines to counter medical illnesses. Increasing awareness of individual vulnerability to manipulation and misinformation has also been proposed as a strategy to resist persuasion.
The age old tale of what others think of us versus what we believe to be true has existed long before the viral overtake of social media. The main difference today is that social media acts as a catalyst for pockets of misinformation. Although social media outlets are cracking down on “false news,” we must consider what criteria should be employed to identify false information. Should external bodies regulate our content consumption? We are certainly entering a gray zone of “wrong” versus “right.” With the overabundance of information available online, it may be the case of “them” versus “us” – that is, those who do not believe in the existence of misinformation versus those who do.
Leanna M. W. Lui, HBSc, completed an HBSc global health specialist degree at the University of Toronto, where she is now an MSc candidate.
A version of this article first appeared on Medscape.com.
Office clutter linked to work, life burnout
As people begin to return to offices after working remotely, a new study suggests that clutter on the job is more than just an annoyance to neatniks. It might also be an indicator that employees are unhappy at work, especially if they have upper-level positions.
Researchers surveyed 202 office workers and linked higher perceived levels of clutter to less satisfaction/pleasure from work and more work-related burnout/tension. While the findings don’t confirm which came first – clutter or unhappiness on the job – they do suggest that the office work environment is more than an matter of appearances.
Study lead author Joseph R. Ferrari, PhD, a professor of psychology at DePaul University, Chicago, goes even further and suggests that clutter might undermine well-being. “If someone comes into [a therapist’s office] with lots of clutter, they probably have it at home and work, and it’s hindering their life,” Dr. Ferrari said in an interview. “Having a lot of clutter piles is really not a good thing. It makes you less effective.”
Dr. Ferrari has conducted several studies into clutter. He and colleagues launched the new study, published in the International Journal of Psychological Research and Reviews, to explore the impact of clutter at the office.
“The impact of clutter on employee well-being may affect profit, staff motivation, the buildup of slack/extraneous resources, interpersonal conflict, attitudes about work, and employee behavior,” Dr. Ferrari and colleagues wrote.
The researchers surveyed participants in 290 workers in 2019 and focused on 209 who worked in offices (60% were men, 87% were 45 years old or younger, 65% held a college or advanced degree, and 79% were White). Most were lower-level employees rather than higher-level employees with management responsibilities.
Both upper-and lower-level employees mentioned the same types of clutter most often – paper, office equipment, and trash, such as used coffee cups. The upper-level workers reported more problems with clutter, although this might be because they are more sensitive to it than lower-level workers, Dr. Ferrari said.
The researchers found that “office clutter was significantly negatively related to ... satisfaction/pleasure from work and significantly positively related to a risk for burnout/tension from work.” They also reported that “upper-level workers were significantly more likely to report clutter and being at risk for burnout/tension than lower-level workers.”
Specifically, a technique known as exploratory factor analysis determined that “63% of office clutter behavior can be explained by either satisfaction/pleasure with one’s work or risk for burnout,” Dr. Ferrari said. The findings suggest that clutter leads to negative feelings about work, not the other way around, he said.
The new study does not address whether clutter has positive attributes, as suggested by a 2013 report published in Psychological Science.
Darby Saxbe, PhD, an associate professor of psychology at the University of Southern California, Los Angeles, who studies work stress, said in an interview that it can be difficult to figure out the direction of causality in a study like this. “Someone who’s overwhelmed might generate more clutter and not have the bandwidth to put things away. If the space is really cluttered, you won’t be able to find things as effectively, or keep track of projects as well, and that will feed more feelings of stress and burnout.”
David Spiegel, MD, Willson Professor of psychiatry and behavioral sciences at Stanford (Calif.) University, agreed.
“The idea of clutter in the environment having a negative effect on mood is interesting, but it is equally likely that clutter reflects burnout, inability to complete tasks and dispose of their remnants,” he said in an interview. “There may be a relationship, and they may interact, but the direction is not clear,” said Dr. Spiegel, who is also director of Stanford’s Center on Stress and Health.
Still, he said, “in these days of Zoom therapy, observing clutter in a patient’s room or office may provide a hint about potential burnout and depression.”
No funding is reported. Dr. Ferrari, Dr. Saxbe, and Dr. Spiegel reported no disclosures.
As people begin to return to offices after working remotely, a new study suggests that clutter on the job is more than just an annoyance to neatniks. It might also be an indicator that employees are unhappy at work, especially if they have upper-level positions.
Researchers surveyed 202 office workers and linked higher perceived levels of clutter to less satisfaction/pleasure from work and more work-related burnout/tension. While the findings don’t confirm which came first – clutter or unhappiness on the job – they do suggest that the office work environment is more than an matter of appearances.
Study lead author Joseph R. Ferrari, PhD, a professor of psychology at DePaul University, Chicago, goes even further and suggests that clutter might undermine well-being. “If someone comes into [a therapist’s office] with lots of clutter, they probably have it at home and work, and it’s hindering their life,” Dr. Ferrari said in an interview. “Having a lot of clutter piles is really not a good thing. It makes you less effective.”
Dr. Ferrari has conducted several studies into clutter. He and colleagues launched the new study, published in the International Journal of Psychological Research and Reviews, to explore the impact of clutter at the office.
“The impact of clutter on employee well-being may affect profit, staff motivation, the buildup of slack/extraneous resources, interpersonal conflict, attitudes about work, and employee behavior,” Dr. Ferrari and colleagues wrote.
The researchers surveyed participants in 290 workers in 2019 and focused on 209 who worked in offices (60% were men, 87% were 45 years old or younger, 65% held a college or advanced degree, and 79% were White). Most were lower-level employees rather than higher-level employees with management responsibilities.
Both upper-and lower-level employees mentioned the same types of clutter most often – paper, office equipment, and trash, such as used coffee cups. The upper-level workers reported more problems with clutter, although this might be because they are more sensitive to it than lower-level workers, Dr. Ferrari said.
The researchers found that “office clutter was significantly negatively related to ... satisfaction/pleasure from work and significantly positively related to a risk for burnout/tension from work.” They also reported that “upper-level workers were significantly more likely to report clutter and being at risk for burnout/tension than lower-level workers.”
Specifically, a technique known as exploratory factor analysis determined that “63% of office clutter behavior can be explained by either satisfaction/pleasure with one’s work or risk for burnout,” Dr. Ferrari said. The findings suggest that clutter leads to negative feelings about work, not the other way around, he said.
The new study does not address whether clutter has positive attributes, as suggested by a 2013 report published in Psychological Science.
Darby Saxbe, PhD, an associate professor of psychology at the University of Southern California, Los Angeles, who studies work stress, said in an interview that it can be difficult to figure out the direction of causality in a study like this. “Someone who’s overwhelmed might generate more clutter and not have the bandwidth to put things away. If the space is really cluttered, you won’t be able to find things as effectively, or keep track of projects as well, and that will feed more feelings of stress and burnout.”
David Spiegel, MD, Willson Professor of psychiatry and behavioral sciences at Stanford (Calif.) University, agreed.
“The idea of clutter in the environment having a negative effect on mood is interesting, but it is equally likely that clutter reflects burnout, inability to complete tasks and dispose of their remnants,” he said in an interview. “There may be a relationship, and they may interact, but the direction is not clear,” said Dr. Spiegel, who is also director of Stanford’s Center on Stress and Health.
Still, he said, “in these days of Zoom therapy, observing clutter in a patient’s room or office may provide a hint about potential burnout and depression.”
No funding is reported. Dr. Ferrari, Dr. Saxbe, and Dr. Spiegel reported no disclosures.
As people begin to return to offices after working remotely, a new study suggests that clutter on the job is more than just an annoyance to neatniks. It might also be an indicator that employees are unhappy at work, especially if they have upper-level positions.
Researchers surveyed 202 office workers and linked higher perceived levels of clutter to less satisfaction/pleasure from work and more work-related burnout/tension. While the findings don’t confirm which came first – clutter or unhappiness on the job – they do suggest that the office work environment is more than an matter of appearances.
Study lead author Joseph R. Ferrari, PhD, a professor of psychology at DePaul University, Chicago, goes even further and suggests that clutter might undermine well-being. “If someone comes into [a therapist’s office] with lots of clutter, they probably have it at home and work, and it’s hindering their life,” Dr. Ferrari said in an interview. “Having a lot of clutter piles is really not a good thing. It makes you less effective.”
Dr. Ferrari has conducted several studies into clutter. He and colleagues launched the new study, published in the International Journal of Psychological Research and Reviews, to explore the impact of clutter at the office.
“The impact of clutter on employee well-being may affect profit, staff motivation, the buildup of slack/extraneous resources, interpersonal conflict, attitudes about work, and employee behavior,” Dr. Ferrari and colleagues wrote.
The researchers surveyed participants in 290 workers in 2019 and focused on 209 who worked in offices (60% were men, 87% were 45 years old or younger, 65% held a college or advanced degree, and 79% were White). Most were lower-level employees rather than higher-level employees with management responsibilities.
Both upper-and lower-level employees mentioned the same types of clutter most often – paper, office equipment, and trash, such as used coffee cups. The upper-level workers reported more problems with clutter, although this might be because they are more sensitive to it than lower-level workers, Dr. Ferrari said.
The researchers found that “office clutter was significantly negatively related to ... satisfaction/pleasure from work and significantly positively related to a risk for burnout/tension from work.” They also reported that “upper-level workers were significantly more likely to report clutter and being at risk for burnout/tension than lower-level workers.”
Specifically, a technique known as exploratory factor analysis determined that “63% of office clutter behavior can be explained by either satisfaction/pleasure with one’s work or risk for burnout,” Dr. Ferrari said. The findings suggest that clutter leads to negative feelings about work, not the other way around, he said.
The new study does not address whether clutter has positive attributes, as suggested by a 2013 report published in Psychological Science.
Darby Saxbe, PhD, an associate professor of psychology at the University of Southern California, Los Angeles, who studies work stress, said in an interview that it can be difficult to figure out the direction of causality in a study like this. “Someone who’s overwhelmed might generate more clutter and not have the bandwidth to put things away. If the space is really cluttered, you won’t be able to find things as effectively, or keep track of projects as well, and that will feed more feelings of stress and burnout.”
David Spiegel, MD, Willson Professor of psychiatry and behavioral sciences at Stanford (Calif.) University, agreed.
“The idea of clutter in the environment having a negative effect on mood is interesting, but it is equally likely that clutter reflects burnout, inability to complete tasks and dispose of their remnants,” he said in an interview. “There may be a relationship, and they may interact, but the direction is not clear,” said Dr. Spiegel, who is also director of Stanford’s Center on Stress and Health.
Still, he said, “in these days of Zoom therapy, observing clutter in a patient’s room or office may provide a hint about potential burnout and depression.”
No funding is reported. Dr. Ferrari, Dr. Saxbe, and Dr. Spiegel reported no disclosures.
FROM THE INTERNATIONAL JOURNAL OF PSYCHOLOGICAL RESEARCH AND REVIEWS
CBT via telehealth or in-person: Which is best for insomnia?
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Optimal antipsychotic dose for schizophrenia relapse identified
A middle-of-the-road dose of an antipsychotic appears to be optimal for relapse prevention in stable schizophrenia, new research suggests.
Results of a meta-analysis show a 5-mg/day equivalent risperidone dose worked best. Higher doses were associated with more adverse events without showing substantial gains in relapse prevention, and lower doses were associated with greater relapse risk.
“The safest approach is to just to carry on with 5 mg,” which in many cases represents a full dose, lead author Stefan Leucht, MD, professor, department of psychiatry and psychotherapy, Technical University of Munich School of Medicine, Germany, told this news organization.
However, he added, patient preferences and other factors should be considered in dosage decision-making.
The findings were published online August 18 in JAMA Psychiatry.
Unique meta-analysis
Antipsychotic drugs are effective for short-term treatment of schizophrenia and prevention of relapse but are associated with movement disorders, weight gain, and other metabolic changes. They are also associated with even more severe adverse events, including tardive dyskinesia and increased cardiovascular risk.
For years, researchers have tried to find the optimal dose of antipsychotic drugs to prevent relapse in patients with stable schizophrenia while mitigating adverse event risk.
For the meta-analysis, researchers searched for fixed-dose, randomized, blinded, or open trials that lasted longer than 3 months and compared two first-generation antipsychotics – haloperidol or fluphenazine – or a second-generation antipsychotic with placebo or a different dose of the same drug.
The analysis included 26 studies with 72 individual dose arms and 4,776 participants with stable schizophrenia.
Researchers used a dose-response meta-analysis. Unlike a simple meta-analysis that provides an “arbitrary” cut-off of superiority of one drug over placebo or another drug, a dose-response meta-analysis gives a plot or curve “that shows how this evolves with different doses,” Dr. Leucht noted.
The investigators estimated dose-response curves for each antipsychotic drug compared with placebo separately and as a group.
They did not have enough data for most of the single antipsychotics, so they converted doses to risperidone equivalents for a pooled analysis across drugs. They chose risperidone because its equivalents “are pretty well-defined,” said Dr. Leucht.
Go slow to go low
For the primary outcome of relapse, the dose-response curve showed a hyperbolic shape with a clear plateau. Initially, the plot decreased sharply but then flattened at about 5-mg/day risperidone equivalent (odds ratio, 0.20; 95% confidence interval, 0.13-0.31; relative risk, 0.43; 95% CI, 0.31-0.57).
“We were a little disappointed because we hoped that a dose lower than 5 mg would be most efficacious in terms of relapse rate because this would have reduced the side-effect burden,” Dr. Leucht said.
Nevertheless, he emphasized that doses lower than 5 mg/day risperidone equivalent are not completely ineffective. For example, the 2.5-mg dose reduced risk to relapse in relative terms by about 40% (RR, 0.63).
Dr. Leucht also pointed out there is “huge interindividual variability.” Therefore, “It just means for the average patient it’s safest, let’s say, to keep her or him on 5 mg,” he said.
When lowering the dose, Dr. Leucht noted clinicians should “be very careful and to do it very slowly. It should be very small reductions every 3 to 6 months.”
For the secondary endpoint of rehospitalizations, the shape of the curve was similar to the one for relapse but with lower rates.
“If patients need to be rehospitalized, it usually means that the relapse was major and not only a minor increase in symptoms,” said Dr. Leucht.
The curves for all-cause discontinuation and reduction in overall symptoms were also similar to that of relapse.
However, the curve for dropouts because of adverse events showed that higher doses led to more adverse events. For example, with 5-mg/day dose, the OR was 1.4 (95% CI, 0.87-2.25) and the RR was 1.38 (95% CI, 0.87-2.15), but for the 15-mg/day dose, the OR was 2.88 (95% CI, 1.52-5.45) and the RR was 2.68 (95% CI, 1.49-4.62).
Patient preference key
The data were insufficient to assess differences between men and women or between older and younger patients, Dr. Leucht noted.
However, post-hoc subgroup analyses turned up some interesting findings, he added. For example, patients who take high-potency first-generation antipsychotics such as haloperidol might do well on a lower dose, said Dr. Leucht.
“They may need a dose even lower than 5 mg, perhaps something like 2.5 mg, because these drugs bind so strongly to dopamine receptors,” he said.
He reiterated that patient preferences should always be considered when deciding on antipsychotic dosage.
“Many patients will say they don’t want to relapse anymore, but others will say these drugs have horrible side effects, and they want to go on a lower dose,” said Dr. Leucht.
Clinicians should also factor in patient characteristics, such as comorbidities or substance abuse, as well as severity of past relapses and properties of individual drugs, he added.
Reflects real-world experience
Commenting on the findings, Thomas Sedlak, MD, PhD, director, Schizophrenia and Psychosis Consult Clinic and assistant professor of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, said the research “is a fine addition” to a previous analysis that explored dose-response relationships of antipsychotic drugs in the acute phase.
Crunching all the data from studies that have different types of patients and extracting a single dosage that provides maximum benefit is “a great challenge,” said Dr. Sedlak, who was not involved with the research.
The fact that most patients won’t get additional benefit above 5 mg, at which point they start getting more adverse events, and that 2.5 mg is sufficient for certain subgroups “agrees well with the experience of many who use these medications regularly,” Dr. Sedlak said.
However, he cautioned that psychiatrists “don’t always intuitively know which patients fall into which dose category or who might require clozapine.”
“Clinicians need to be mindful that it’s easy to overshoot an optimal dose and elicit side effects,” said Dr. Sedlak.
He also noted that severely ill patients are often underrepresented in clinical trials because they are too impaired to participate, “so they may have a different optimal dosage,” he concluded.
Dr. Leucht has reported receiving personal fees for consulting, advising, and/or speaking outside the submitted work from Angelini, Boehringer Ingelheim, Geodon & Richter, Janssen, Johnson & Johnson, Lundbeck, LTS Lohmann, MSD, Otsuka, Recordati, Sanofi Aventis, Sandoz, Sunovion, Teva, Eisai, Rovi, and Amiabel. Dr. Sedlak has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A middle-of-the-road dose of an antipsychotic appears to be optimal for relapse prevention in stable schizophrenia, new research suggests.
Results of a meta-analysis show a 5-mg/day equivalent risperidone dose worked best. Higher doses were associated with more adverse events without showing substantial gains in relapse prevention, and lower doses were associated with greater relapse risk.
“The safest approach is to just to carry on with 5 mg,” which in many cases represents a full dose, lead author Stefan Leucht, MD, professor, department of psychiatry and psychotherapy, Technical University of Munich School of Medicine, Germany, told this news organization.
However, he added, patient preferences and other factors should be considered in dosage decision-making.
The findings were published online August 18 in JAMA Psychiatry.
Unique meta-analysis
Antipsychotic drugs are effective for short-term treatment of schizophrenia and prevention of relapse but are associated with movement disorders, weight gain, and other metabolic changes. They are also associated with even more severe adverse events, including tardive dyskinesia and increased cardiovascular risk.
For years, researchers have tried to find the optimal dose of antipsychotic drugs to prevent relapse in patients with stable schizophrenia while mitigating adverse event risk.
For the meta-analysis, researchers searched for fixed-dose, randomized, blinded, or open trials that lasted longer than 3 months and compared two first-generation antipsychotics – haloperidol or fluphenazine – or a second-generation antipsychotic with placebo or a different dose of the same drug.
The analysis included 26 studies with 72 individual dose arms and 4,776 participants with stable schizophrenia.
Researchers used a dose-response meta-analysis. Unlike a simple meta-analysis that provides an “arbitrary” cut-off of superiority of one drug over placebo or another drug, a dose-response meta-analysis gives a plot or curve “that shows how this evolves with different doses,” Dr. Leucht noted.
The investigators estimated dose-response curves for each antipsychotic drug compared with placebo separately and as a group.
They did not have enough data for most of the single antipsychotics, so they converted doses to risperidone equivalents for a pooled analysis across drugs. They chose risperidone because its equivalents “are pretty well-defined,” said Dr. Leucht.
Go slow to go low
For the primary outcome of relapse, the dose-response curve showed a hyperbolic shape with a clear plateau. Initially, the plot decreased sharply but then flattened at about 5-mg/day risperidone equivalent (odds ratio, 0.20; 95% confidence interval, 0.13-0.31; relative risk, 0.43; 95% CI, 0.31-0.57).
“We were a little disappointed because we hoped that a dose lower than 5 mg would be most efficacious in terms of relapse rate because this would have reduced the side-effect burden,” Dr. Leucht said.
Nevertheless, he emphasized that doses lower than 5 mg/day risperidone equivalent are not completely ineffective. For example, the 2.5-mg dose reduced risk to relapse in relative terms by about 40% (RR, 0.63).
Dr. Leucht also pointed out there is “huge interindividual variability.” Therefore, “It just means for the average patient it’s safest, let’s say, to keep her or him on 5 mg,” he said.
When lowering the dose, Dr. Leucht noted clinicians should “be very careful and to do it very slowly. It should be very small reductions every 3 to 6 months.”
For the secondary endpoint of rehospitalizations, the shape of the curve was similar to the one for relapse but with lower rates.
“If patients need to be rehospitalized, it usually means that the relapse was major and not only a minor increase in symptoms,” said Dr. Leucht.
The curves for all-cause discontinuation and reduction in overall symptoms were also similar to that of relapse.
However, the curve for dropouts because of adverse events showed that higher doses led to more adverse events. For example, with 5-mg/day dose, the OR was 1.4 (95% CI, 0.87-2.25) and the RR was 1.38 (95% CI, 0.87-2.15), but for the 15-mg/day dose, the OR was 2.88 (95% CI, 1.52-5.45) and the RR was 2.68 (95% CI, 1.49-4.62).
Patient preference key
The data were insufficient to assess differences between men and women or between older and younger patients, Dr. Leucht noted.
However, post-hoc subgroup analyses turned up some interesting findings, he added. For example, patients who take high-potency first-generation antipsychotics such as haloperidol might do well on a lower dose, said Dr. Leucht.
“They may need a dose even lower than 5 mg, perhaps something like 2.5 mg, because these drugs bind so strongly to dopamine receptors,” he said.
He reiterated that patient preferences should always be considered when deciding on antipsychotic dosage.
“Many patients will say they don’t want to relapse anymore, but others will say these drugs have horrible side effects, and they want to go on a lower dose,” said Dr. Leucht.
Clinicians should also factor in patient characteristics, such as comorbidities or substance abuse, as well as severity of past relapses and properties of individual drugs, he added.
Reflects real-world experience
Commenting on the findings, Thomas Sedlak, MD, PhD, director, Schizophrenia and Psychosis Consult Clinic and assistant professor of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, said the research “is a fine addition” to a previous analysis that explored dose-response relationships of antipsychotic drugs in the acute phase.
Crunching all the data from studies that have different types of patients and extracting a single dosage that provides maximum benefit is “a great challenge,” said Dr. Sedlak, who was not involved with the research.
The fact that most patients won’t get additional benefit above 5 mg, at which point they start getting more adverse events, and that 2.5 mg is sufficient for certain subgroups “agrees well with the experience of many who use these medications regularly,” Dr. Sedlak said.
However, he cautioned that psychiatrists “don’t always intuitively know which patients fall into which dose category or who might require clozapine.”
“Clinicians need to be mindful that it’s easy to overshoot an optimal dose and elicit side effects,” said Dr. Sedlak.
He also noted that severely ill patients are often underrepresented in clinical trials because they are too impaired to participate, “so they may have a different optimal dosage,” he concluded.
Dr. Leucht has reported receiving personal fees for consulting, advising, and/or speaking outside the submitted work from Angelini, Boehringer Ingelheim, Geodon & Richter, Janssen, Johnson & Johnson, Lundbeck, LTS Lohmann, MSD, Otsuka, Recordati, Sanofi Aventis, Sandoz, Sunovion, Teva, Eisai, Rovi, and Amiabel. Dr. Sedlak has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A middle-of-the-road dose of an antipsychotic appears to be optimal for relapse prevention in stable schizophrenia, new research suggests.
Results of a meta-analysis show a 5-mg/day equivalent risperidone dose worked best. Higher doses were associated with more adverse events without showing substantial gains in relapse prevention, and lower doses were associated with greater relapse risk.
“The safest approach is to just to carry on with 5 mg,” which in many cases represents a full dose, lead author Stefan Leucht, MD, professor, department of psychiatry and psychotherapy, Technical University of Munich School of Medicine, Germany, told this news organization.
However, he added, patient preferences and other factors should be considered in dosage decision-making.
The findings were published online August 18 in JAMA Psychiatry.
Unique meta-analysis
Antipsychotic drugs are effective for short-term treatment of schizophrenia and prevention of relapse but are associated with movement disorders, weight gain, and other metabolic changes. They are also associated with even more severe adverse events, including tardive dyskinesia and increased cardiovascular risk.
For years, researchers have tried to find the optimal dose of antipsychotic drugs to prevent relapse in patients with stable schizophrenia while mitigating adverse event risk.
For the meta-analysis, researchers searched for fixed-dose, randomized, blinded, or open trials that lasted longer than 3 months and compared two first-generation antipsychotics – haloperidol or fluphenazine – or a second-generation antipsychotic with placebo or a different dose of the same drug.
The analysis included 26 studies with 72 individual dose arms and 4,776 participants with stable schizophrenia.
Researchers used a dose-response meta-analysis. Unlike a simple meta-analysis that provides an “arbitrary” cut-off of superiority of one drug over placebo or another drug, a dose-response meta-analysis gives a plot or curve “that shows how this evolves with different doses,” Dr. Leucht noted.
The investigators estimated dose-response curves for each antipsychotic drug compared with placebo separately and as a group.
They did not have enough data for most of the single antipsychotics, so they converted doses to risperidone equivalents for a pooled analysis across drugs. They chose risperidone because its equivalents “are pretty well-defined,” said Dr. Leucht.
Go slow to go low
For the primary outcome of relapse, the dose-response curve showed a hyperbolic shape with a clear plateau. Initially, the plot decreased sharply but then flattened at about 5-mg/day risperidone equivalent (odds ratio, 0.20; 95% confidence interval, 0.13-0.31; relative risk, 0.43; 95% CI, 0.31-0.57).
“We were a little disappointed because we hoped that a dose lower than 5 mg would be most efficacious in terms of relapse rate because this would have reduced the side-effect burden,” Dr. Leucht said.
Nevertheless, he emphasized that doses lower than 5 mg/day risperidone equivalent are not completely ineffective. For example, the 2.5-mg dose reduced risk to relapse in relative terms by about 40% (RR, 0.63).
Dr. Leucht also pointed out there is “huge interindividual variability.” Therefore, “It just means for the average patient it’s safest, let’s say, to keep her or him on 5 mg,” he said.
When lowering the dose, Dr. Leucht noted clinicians should “be very careful and to do it very slowly. It should be very small reductions every 3 to 6 months.”
For the secondary endpoint of rehospitalizations, the shape of the curve was similar to the one for relapse but with lower rates.
“If patients need to be rehospitalized, it usually means that the relapse was major and not only a minor increase in symptoms,” said Dr. Leucht.
The curves for all-cause discontinuation and reduction in overall symptoms were also similar to that of relapse.
However, the curve for dropouts because of adverse events showed that higher doses led to more adverse events. For example, with 5-mg/day dose, the OR was 1.4 (95% CI, 0.87-2.25) and the RR was 1.38 (95% CI, 0.87-2.15), but for the 15-mg/day dose, the OR was 2.88 (95% CI, 1.52-5.45) and the RR was 2.68 (95% CI, 1.49-4.62).
Patient preference key
The data were insufficient to assess differences between men and women or between older and younger patients, Dr. Leucht noted.
However, post-hoc subgroup analyses turned up some interesting findings, he added. For example, patients who take high-potency first-generation antipsychotics such as haloperidol might do well on a lower dose, said Dr. Leucht.
“They may need a dose even lower than 5 mg, perhaps something like 2.5 mg, because these drugs bind so strongly to dopamine receptors,” he said.
He reiterated that patient preferences should always be considered when deciding on antipsychotic dosage.
“Many patients will say they don’t want to relapse anymore, but others will say these drugs have horrible side effects, and they want to go on a lower dose,” said Dr. Leucht.
Clinicians should also factor in patient characteristics, such as comorbidities or substance abuse, as well as severity of past relapses and properties of individual drugs, he added.
Reflects real-world experience
Commenting on the findings, Thomas Sedlak, MD, PhD, director, Schizophrenia and Psychosis Consult Clinic and assistant professor of psychiatry and behavioral sciences, Johns Hopkins School of Medicine, Baltimore, said the research “is a fine addition” to a previous analysis that explored dose-response relationships of antipsychotic drugs in the acute phase.
Crunching all the data from studies that have different types of patients and extracting a single dosage that provides maximum benefit is “a great challenge,” said Dr. Sedlak, who was not involved with the research.
The fact that most patients won’t get additional benefit above 5 mg, at which point they start getting more adverse events, and that 2.5 mg is sufficient for certain subgroups “agrees well with the experience of many who use these medications regularly,” Dr. Sedlak said.
However, he cautioned that psychiatrists “don’t always intuitively know which patients fall into which dose category or who might require clozapine.”
“Clinicians need to be mindful that it’s easy to overshoot an optimal dose and elicit side effects,” said Dr. Sedlak.
He also noted that severely ill patients are often underrepresented in clinical trials because they are too impaired to participate, “so they may have a different optimal dosage,” he concluded.
Dr. Leucht has reported receiving personal fees for consulting, advising, and/or speaking outside the submitted work from Angelini, Boehringer Ingelheim, Geodon & Richter, Janssen, Johnson & Johnson, Lundbeck, LTS Lohmann, MSD, Otsuka, Recordati, Sanofi Aventis, Sandoz, Sunovion, Teva, Eisai, Rovi, and Amiabel. Dr. Sedlak has reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.