User login
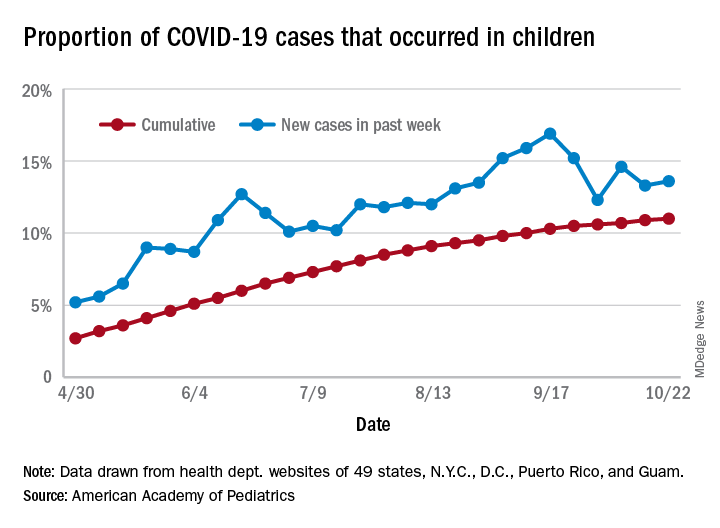
The new one-percenters: Children with COVID-19
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
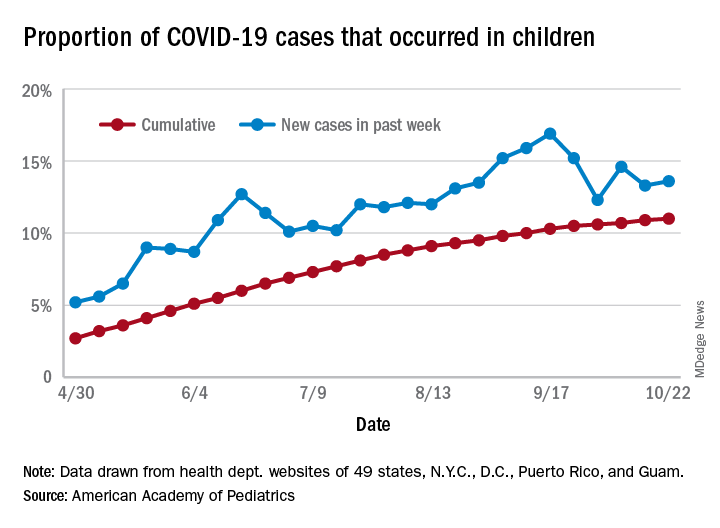
There have been 1,052 cases of COVID-19 per 100,000 children as of Oct. 22, and that works out to 1.05% of all children in the country. The cumulative number of pediatric cases is 792,188, and children now represent 11% of all COVID-19 cases, the AAP and the CHA reported Oct. 26.
There were just over 50,000 new child cases reported in the week ending Oct. 22, which was 13.6% of the national total of almost 370,000. That’s up slightly from the 13.3% the previous week but still down from the spike seen in mid-September, based on the data collected from the websites of 49 state health departments (New York does not report ages), along with the District of Columbia, New York City, Puerto Rico, and Guam.
The state-level data show that California has had more COVID-19 cases in children (92,864) than any other state, although Texas has reported ages for only 7% of its confirmed cases. Illinois is next with 46,006 cases, followed by Florida at 45,575, although Florida is using an age range of 0-14 years to define a child case, the AAP and CHA noted.
Other measures largely put small states at the extremes:
- North Dakota has the highest cumulative rate: 2,954 cases per 100,000 children.
- Vermont has the lowest cumulative rate: 190.5 per 100,000.
- Wyoming has the highest proportion of cases in children: 27.7%.
- New Jersey has the lowest proportion of child cases: 4.6%.
There were no COVID-19–related deaths in children reported the week ending Oct. 22, so the total number remains at 120, which is just 0.06% of the total for all ages, based on data from 42 states and New York City. Hospitalization figures put admissions at almost 5,600 in children, or 1.7% of all hospitalizations, although those data come from just 24 states and New York City, the AAP and CHA said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
There have been 1,052 cases of COVID-19 per 100,000 children as of Oct. 22, and that works out to 1.05% of all children in the country. The cumulative number of pediatric cases is 792,188, and children now represent 11% of all COVID-19 cases, the AAP and the CHA reported Oct. 26.
There were just over 50,000 new child cases reported in the week ending Oct. 22, which was 13.6% of the national total of almost 370,000. That’s up slightly from the 13.3% the previous week but still down from the spike seen in mid-September, based on the data collected from the websites of 49 state health departments (New York does not report ages), along with the District of Columbia, New York City, Puerto Rico, and Guam.
The state-level data show that California has had more COVID-19 cases in children (92,864) than any other state, although Texas has reported ages for only 7% of its confirmed cases. Illinois is next with 46,006 cases, followed by Florida at 45,575, although Florida is using an age range of 0-14 years to define a child case, the AAP and CHA noted.
Other measures largely put small states at the extremes:
- North Dakota has the highest cumulative rate: 2,954 cases per 100,000 children.
- Vermont has the lowest cumulative rate: 190.5 per 100,000.
- Wyoming has the highest proportion of cases in children: 27.7%.
- New Jersey has the lowest proportion of child cases: 4.6%.
There were no COVID-19–related deaths in children reported the week ending Oct. 22, so the total number remains at 120, which is just 0.06% of the total for all ages, based on data from 42 states and New York City. Hospitalization figures put admissions at almost 5,600 in children, or 1.7% of all hospitalizations, although those data come from just 24 states and New York City, the AAP and CHA said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
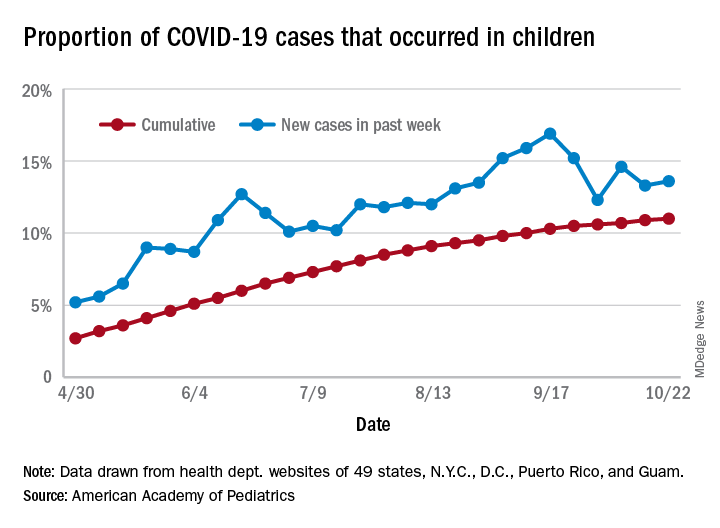
There have been 1,052 cases of COVID-19 per 100,000 children as of Oct. 22, and that works out to 1.05% of all children in the country. The cumulative number of pediatric cases is 792,188, and children now represent 11% of all COVID-19 cases, the AAP and the CHA reported Oct. 26.
There were just over 50,000 new child cases reported in the week ending Oct. 22, which was 13.6% of the national total of almost 370,000. That’s up slightly from the 13.3% the previous week but still down from the spike seen in mid-September, based on the data collected from the websites of 49 state health departments (New York does not report ages), along with the District of Columbia, New York City, Puerto Rico, and Guam.
The state-level data show that California has had more COVID-19 cases in children (92,864) than any other state, although Texas has reported ages for only 7% of its confirmed cases. Illinois is next with 46,006 cases, followed by Florida at 45,575, although Florida is using an age range of 0-14 years to define a child case, the AAP and CHA noted.
Other measures largely put small states at the extremes:
- North Dakota has the highest cumulative rate: 2,954 cases per 100,000 children.
- Vermont has the lowest cumulative rate: 190.5 per 100,000.
- Wyoming has the highest proportion of cases in children: 27.7%.
- New Jersey has the lowest proportion of child cases: 4.6%.
There were no COVID-19–related deaths in children reported the week ending Oct. 22, so the total number remains at 120, which is just 0.06% of the total for all ages, based on data from 42 states and New York City. Hospitalization figures put admissions at almost 5,600 in children, or 1.7% of all hospitalizations, although those data come from just 24 states and New York City, the AAP and CHA said.
Few women hospitalized for influenza have been vaccinated
Researchers analyzed data from 9,652 women ages 15-44 who were hospitalized with laboratory-confirmed influenza from October through April during the 2010-2019 influenza seasons. Data were pulled from the U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
Of those women, 2,697 (28%) were pregnant. Median age was 28 and median gestational age was 32 weeks. Those studied included 36% who were non-Hispanic White; 29% non-Hispanic Black; and 20% Hispanic women.
Some 89% of the women, pregnant and nonpregnant, received antivirals while in the hospital but only 31% reported they had received the flu vaccine in the current season, despite guideline recommendations citing clear evidence that vaccination is safe for mother and baby.
Rachel Holstein, MPH, an epidemiology and information science fellow at the Centers for Disease Control and Prevention, who presented her team’s work as part of IDWeek 2020, explained that the mother’s vaccination can help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
She noted that pregnant women are at high risk for influenza-associated hospitalization.
“Changes in the immune system, heart, and lungs during pregnancy make pregnant women, and women up to 2 weeks post partum, more prone to severe illness from flu, including illness resulting in hospitalization,” she said in an interview
“Vaccination has been shown to reduce the risk of flu-associated acute respiratory infection in pregnant women by up to one-half,” she said. “A 2018 study showed that getting a flu shot reduced a pregnant woman’s risk of being hospitalized with flu by an average of 40%.»
FluSurv-NET data show hospitalizations were more common in the third trimester of pregnancy compared with the first and second, Holstein said. The most common underlying conditions among these women were asthma (23%) and obesity (10%), and 12% were current tobacco smokers. Overall, 5% of pregnant women with flu required ICU admission, 2% needed mechanical ventilation, and 6% developed pneumonia.
Vaccine uptake lowest in first two trimesters
Holstein said vaccine coverage was lowest among women in their first or second trimesters for all 9 seasons, and overall vaccination coverage increased significantly over time.
Uptake also differed by age. The data showed coverage was lower among women aged 15-34 years, compared with women 35 years and older (34% vs. 50%).
“It was as low as 15% among pregnant women aged 15-34 years in the 2011-12 season,” she added.
Jeanne Sheffield, MD, director of the division of maternal-fetal medicine at Johns Hopkins Medicine, Baltimore, said in an interview the low uptake of vaccine shown in this study is both familiar and frustrating.
She said education from health care providers has improved, but women are nonetheless frequently fearful. She pointed out the widespread phenomenon of vaccine hesitancy in the general population.
Coverage was 45.3% among adults in the 2018-2019 flu season, 8.2 percentage points higher than coverage during the 2017-18 season (37.1%) according to CDC estimates.
Added to that, she said, is further hesitancy when women believe vaccination could harm the unborn baby, despite “very good data that flu vaccine is safe in pregnancy, acceptable in pregnancy in all trimesters, and is optimal standard of care.”
Holstein added, “We know from past research that a range of factors – including negative attitudes and beliefs about vaccines, less knowledge about and access to vaccines, and a lack of trust in healthcare providers and vaccines – can contribute to lower vaccination rates.”
Healthcare providers play a key role in increasing flu vaccinations among pregnant women, she said.
“A provider recommendation, combined with an offer to administer a flu vaccine at the time of visit, remains one of the best ways to accomplish this,” Holstein said.
Holstein and Sheffield have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Researchers analyzed data from 9,652 women ages 15-44 who were hospitalized with laboratory-confirmed influenza from October through April during the 2010-2019 influenza seasons. Data were pulled from the U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
Of those women, 2,697 (28%) were pregnant. Median age was 28 and median gestational age was 32 weeks. Those studied included 36% who were non-Hispanic White; 29% non-Hispanic Black; and 20% Hispanic women.
Some 89% of the women, pregnant and nonpregnant, received antivirals while in the hospital but only 31% reported they had received the flu vaccine in the current season, despite guideline recommendations citing clear evidence that vaccination is safe for mother and baby.
Rachel Holstein, MPH, an epidemiology and information science fellow at the Centers for Disease Control and Prevention, who presented her team’s work as part of IDWeek 2020, explained that the mother’s vaccination can help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
She noted that pregnant women are at high risk for influenza-associated hospitalization.
“Changes in the immune system, heart, and lungs during pregnancy make pregnant women, and women up to 2 weeks post partum, more prone to severe illness from flu, including illness resulting in hospitalization,” she said in an interview
“Vaccination has been shown to reduce the risk of flu-associated acute respiratory infection in pregnant women by up to one-half,” she said. “A 2018 study showed that getting a flu shot reduced a pregnant woman’s risk of being hospitalized with flu by an average of 40%.»
FluSurv-NET data show hospitalizations were more common in the third trimester of pregnancy compared with the first and second, Holstein said. The most common underlying conditions among these women were asthma (23%) and obesity (10%), and 12% were current tobacco smokers. Overall, 5% of pregnant women with flu required ICU admission, 2% needed mechanical ventilation, and 6% developed pneumonia.
Vaccine uptake lowest in first two trimesters
Holstein said vaccine coverage was lowest among women in their first or second trimesters for all 9 seasons, and overall vaccination coverage increased significantly over time.
Uptake also differed by age. The data showed coverage was lower among women aged 15-34 years, compared with women 35 years and older (34% vs. 50%).
“It was as low as 15% among pregnant women aged 15-34 years in the 2011-12 season,” she added.
Jeanne Sheffield, MD, director of the division of maternal-fetal medicine at Johns Hopkins Medicine, Baltimore, said in an interview the low uptake of vaccine shown in this study is both familiar and frustrating.
She said education from health care providers has improved, but women are nonetheless frequently fearful. She pointed out the widespread phenomenon of vaccine hesitancy in the general population.
Coverage was 45.3% among adults in the 2018-2019 flu season, 8.2 percentage points higher than coverage during the 2017-18 season (37.1%) according to CDC estimates.
Added to that, she said, is further hesitancy when women believe vaccination could harm the unborn baby, despite “very good data that flu vaccine is safe in pregnancy, acceptable in pregnancy in all trimesters, and is optimal standard of care.”
Holstein added, “We know from past research that a range of factors – including negative attitudes and beliefs about vaccines, less knowledge about and access to vaccines, and a lack of trust in healthcare providers and vaccines – can contribute to lower vaccination rates.”
Healthcare providers play a key role in increasing flu vaccinations among pregnant women, she said.
“A provider recommendation, combined with an offer to administer a flu vaccine at the time of visit, remains one of the best ways to accomplish this,” Holstein said.
Holstein and Sheffield have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Researchers analyzed data from 9,652 women ages 15-44 who were hospitalized with laboratory-confirmed influenza from October through April during the 2010-2019 influenza seasons. Data were pulled from the U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
Of those women, 2,697 (28%) were pregnant. Median age was 28 and median gestational age was 32 weeks. Those studied included 36% who were non-Hispanic White; 29% non-Hispanic Black; and 20% Hispanic women.
Some 89% of the women, pregnant and nonpregnant, received antivirals while in the hospital but only 31% reported they had received the flu vaccine in the current season, despite guideline recommendations citing clear evidence that vaccination is safe for mother and baby.
Rachel Holstein, MPH, an epidemiology and information science fellow at the Centers for Disease Control and Prevention, who presented her team’s work as part of IDWeek 2020, explained that the mother’s vaccination can help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
She noted that pregnant women are at high risk for influenza-associated hospitalization.
“Changes in the immune system, heart, and lungs during pregnancy make pregnant women, and women up to 2 weeks post partum, more prone to severe illness from flu, including illness resulting in hospitalization,” she said in an interview
“Vaccination has been shown to reduce the risk of flu-associated acute respiratory infection in pregnant women by up to one-half,” she said. “A 2018 study showed that getting a flu shot reduced a pregnant woman’s risk of being hospitalized with flu by an average of 40%.»
FluSurv-NET data show hospitalizations were more common in the third trimester of pregnancy compared with the first and second, Holstein said. The most common underlying conditions among these women were asthma (23%) and obesity (10%), and 12% were current tobacco smokers. Overall, 5% of pregnant women with flu required ICU admission, 2% needed mechanical ventilation, and 6% developed pneumonia.
Vaccine uptake lowest in first two trimesters
Holstein said vaccine coverage was lowest among women in their first or second trimesters for all 9 seasons, and overall vaccination coverage increased significantly over time.
Uptake also differed by age. The data showed coverage was lower among women aged 15-34 years, compared with women 35 years and older (34% vs. 50%).
“It was as low as 15% among pregnant women aged 15-34 years in the 2011-12 season,” she added.
Jeanne Sheffield, MD, director of the division of maternal-fetal medicine at Johns Hopkins Medicine, Baltimore, said in an interview the low uptake of vaccine shown in this study is both familiar and frustrating.
She said education from health care providers has improved, but women are nonetheless frequently fearful. She pointed out the widespread phenomenon of vaccine hesitancy in the general population.
Coverage was 45.3% among adults in the 2018-2019 flu season, 8.2 percentage points higher than coverage during the 2017-18 season (37.1%) according to CDC estimates.
Added to that, she said, is further hesitancy when women believe vaccination could harm the unborn baby, despite “very good data that flu vaccine is safe in pregnancy, acceptable in pregnancy in all trimesters, and is optimal standard of care.”
Holstein added, “We know from past research that a range of factors – including negative attitudes and beliefs about vaccines, less knowledge about and access to vaccines, and a lack of trust in healthcare providers and vaccines – can contribute to lower vaccination rates.”
Healthcare providers play a key role in increasing flu vaccinations among pregnant women, she said.
“A provider recommendation, combined with an offer to administer a flu vaccine at the time of visit, remains one of the best ways to accomplish this,” Holstein said.
Holstein and Sheffield have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Acute HIV cases double in ED. Is COVID-19 responsible?
David Pitrak, MD, an infectious diseases specialist at the University of Chicago Medicine, and colleagues found that the incidence ratio of acute HIV infection (AHI) jumped to 14.4 this year, compared with the 6.8 average for the previous 4 years (IR, 2.14; 95% confidence interval, 1.01-4.54; P < .05).
At a press conference at IDWeek 2020, he said that this year, acute patients made up one quarter of all new diagnoses (9 of 35), “the highest percentage we have ever seen.
“Patients with acute infection, especially those with symptoms, have extremely high viral loads and progress more rapidly. Because of those high viral loads, there’s risk of transmission to others, so rapid linkage to care and ART [antiretroviral treatment] is really important,” he said.
After the IDWeek abstract was submitted in September, Dr. Pitrak said, three additional AHI cases were diagnosed in the ED, bringing the IR of AHI during the pandemic to 2.57 (95% CI, 1.29-5.11).
Should all EDs link HIV screening to COVID-19 testing?
The ED at UCM incorporated blood draws for HIV screening as part of COVID-19 evaluations early on during the pandemic, and they recommend that practice for EDs across the nation.
After a positive test result, the ID team was able to quickly link the HIV patients to care and initiation of antiretroviral treatment without adding staff or resources, Dr. Pitrak said in an interview.
Dr. Pitrak and colleagues reviewed data from 13 health care centers on the south and west sides of Chicago. At most of the centers, fourth- and fifth-generation antibody tests were available. The investigators found that the number of HIV screens that were conducted dropped significantly during the COVID-19 pandemic.
At the height of the pandemic, HIV screening at the sites decreased an average of 58%, the researchers found. As of the end of June, the number was decreased by 32%.
“This is a global problem,” he said. “HIV services have been severely impacted worldwide, with the greatest impact on the LGBTQ community.”
UCM performed 19,111 HIV screens (11,133 in the ED) between Jan. 1 and Aug. 17 this year. It performed 14,754 COVID polymerase chain reaction tests in the ED between March 17 and Aug. 17. All of the acute cases were identified in the ED.
Dr. Pitrak mentioned some possible causes of an increase in the number of patients with acute cases who present in the ED. People who do not suspect they have AHI may be coming to the ED because they think they have COVID-19, inasmuch as many of the symptoms overlap. One of the AHI patients actually did have a coinfection, Dr. Pitrak noted.
“There is also the possibility that this could be bad news,” Dr. Pitrak said in an interview. “It could be that there are more acute cases presenting because there are more community transmissions.”
He noted that follow-up visits have been canceled or converted to telehealth visits during the pandemic, and the number of patients who are initiating pre-exposure prophylaxis has declined significantly.
“I hope we’re not seeing an increase in new transmissions after so much work has been done to decrease transmissions over the past few years,” he said.
Partnership with emergency physicians
Critical to screening these patients is building a solid partnership between ID and ED physicians.
Coauthor Kimberly Stanford, MD, MPH, an assistant professor in emergency medicine at UCM, said, “You need a champion within the emergency department who can help make sure that the work flow is not disrupted, that however you implement your screening program, you’re not putting extra work on the staff.
“We can feel extremely confident that if I send a test and it comes back positive, I know someone is going to call that patient and make sure they get into care.”
Although the testing is performed in the ED at UCM, the follow-up, linkage to care, and initiation of treatment are conducted by the ID specialists.
Beverly E. Sha, MD, professor in the division of infectious diseases, department of internal medicine, Rush Medical College, Chicago, said in an interview that although she agrees that HIV screening programs in EDs “make absolute sense,” there are different ways to conduct such programs. Dr. Sha was not involved in Dr. Pitrak’s study.
At Rush’s ED, she says, HIV testing is linked with a complete blood count.
“If someone presents with fever, we would often be doing that test as well,” she said. “I think just globally increasing screening [in the ED] is what makes the most sense.”
Dr. Sha said they have not seen a similar surge in acute cases in the ED at Rush during the pandemic.
She noted, however, that UCM tested more than 11,000 people for HIV in the ED this year, whereas “we probably only did about 3500.
“The reason testing is so important, whether for HIV or COVID, is the more you test, the more you’re going to find,” she said, “especially in cities like Chicago.”
Dr. Pitrak received grant support from Gilead Sciences. His coauthors and Dr. Sha reported no relevant financial relationships.
This article first appeared on Medscape.com.
David Pitrak, MD, an infectious diseases specialist at the University of Chicago Medicine, and colleagues found that the incidence ratio of acute HIV infection (AHI) jumped to 14.4 this year, compared with the 6.8 average for the previous 4 years (IR, 2.14; 95% confidence interval, 1.01-4.54; P < .05).
At a press conference at IDWeek 2020, he said that this year, acute patients made up one quarter of all new diagnoses (9 of 35), “the highest percentage we have ever seen.
“Patients with acute infection, especially those with symptoms, have extremely high viral loads and progress more rapidly. Because of those high viral loads, there’s risk of transmission to others, so rapid linkage to care and ART [antiretroviral treatment] is really important,” he said.
After the IDWeek abstract was submitted in September, Dr. Pitrak said, three additional AHI cases were diagnosed in the ED, bringing the IR of AHI during the pandemic to 2.57 (95% CI, 1.29-5.11).
Should all EDs link HIV screening to COVID-19 testing?
The ED at UCM incorporated blood draws for HIV screening as part of COVID-19 evaluations early on during the pandemic, and they recommend that practice for EDs across the nation.
After a positive test result, the ID team was able to quickly link the HIV patients to care and initiation of antiretroviral treatment without adding staff or resources, Dr. Pitrak said in an interview.
Dr. Pitrak and colleagues reviewed data from 13 health care centers on the south and west sides of Chicago. At most of the centers, fourth- and fifth-generation antibody tests were available. The investigators found that the number of HIV screens that were conducted dropped significantly during the COVID-19 pandemic.
At the height of the pandemic, HIV screening at the sites decreased an average of 58%, the researchers found. As of the end of June, the number was decreased by 32%.
“This is a global problem,” he said. “HIV services have been severely impacted worldwide, with the greatest impact on the LGBTQ community.”
UCM performed 19,111 HIV screens (11,133 in the ED) between Jan. 1 and Aug. 17 this year. It performed 14,754 COVID polymerase chain reaction tests in the ED between March 17 and Aug. 17. All of the acute cases were identified in the ED.
Dr. Pitrak mentioned some possible causes of an increase in the number of patients with acute cases who present in the ED. People who do not suspect they have AHI may be coming to the ED because they think they have COVID-19, inasmuch as many of the symptoms overlap. One of the AHI patients actually did have a coinfection, Dr. Pitrak noted.
“There is also the possibility that this could be bad news,” Dr. Pitrak said in an interview. “It could be that there are more acute cases presenting because there are more community transmissions.”
He noted that follow-up visits have been canceled or converted to telehealth visits during the pandemic, and the number of patients who are initiating pre-exposure prophylaxis has declined significantly.
“I hope we’re not seeing an increase in new transmissions after so much work has been done to decrease transmissions over the past few years,” he said.
Partnership with emergency physicians
Critical to screening these patients is building a solid partnership between ID and ED physicians.
Coauthor Kimberly Stanford, MD, MPH, an assistant professor in emergency medicine at UCM, said, “You need a champion within the emergency department who can help make sure that the work flow is not disrupted, that however you implement your screening program, you’re not putting extra work on the staff.
“We can feel extremely confident that if I send a test and it comes back positive, I know someone is going to call that patient and make sure they get into care.”
Although the testing is performed in the ED at UCM, the follow-up, linkage to care, and initiation of treatment are conducted by the ID specialists.
Beverly E. Sha, MD, professor in the division of infectious diseases, department of internal medicine, Rush Medical College, Chicago, said in an interview that although she agrees that HIV screening programs in EDs “make absolute sense,” there are different ways to conduct such programs. Dr. Sha was not involved in Dr. Pitrak’s study.
At Rush’s ED, she says, HIV testing is linked with a complete blood count.
“If someone presents with fever, we would often be doing that test as well,” she said. “I think just globally increasing screening [in the ED] is what makes the most sense.”
Dr. Sha said they have not seen a similar surge in acute cases in the ED at Rush during the pandemic.
She noted, however, that UCM tested more than 11,000 people for HIV in the ED this year, whereas “we probably only did about 3500.
“The reason testing is so important, whether for HIV or COVID, is the more you test, the more you’re going to find,” she said, “especially in cities like Chicago.”
Dr. Pitrak received grant support from Gilead Sciences. His coauthors and Dr. Sha reported no relevant financial relationships.
This article first appeared on Medscape.com.
David Pitrak, MD, an infectious diseases specialist at the University of Chicago Medicine, and colleagues found that the incidence ratio of acute HIV infection (AHI) jumped to 14.4 this year, compared with the 6.8 average for the previous 4 years (IR, 2.14; 95% confidence interval, 1.01-4.54; P < .05).
At a press conference at IDWeek 2020, he said that this year, acute patients made up one quarter of all new diagnoses (9 of 35), “the highest percentage we have ever seen.
“Patients with acute infection, especially those with symptoms, have extremely high viral loads and progress more rapidly. Because of those high viral loads, there’s risk of transmission to others, so rapid linkage to care and ART [antiretroviral treatment] is really important,” he said.
After the IDWeek abstract was submitted in September, Dr. Pitrak said, three additional AHI cases were diagnosed in the ED, bringing the IR of AHI during the pandemic to 2.57 (95% CI, 1.29-5.11).
Should all EDs link HIV screening to COVID-19 testing?
The ED at UCM incorporated blood draws for HIV screening as part of COVID-19 evaluations early on during the pandemic, and they recommend that practice for EDs across the nation.
After a positive test result, the ID team was able to quickly link the HIV patients to care and initiation of antiretroviral treatment without adding staff or resources, Dr. Pitrak said in an interview.
Dr. Pitrak and colleagues reviewed data from 13 health care centers on the south and west sides of Chicago. At most of the centers, fourth- and fifth-generation antibody tests were available. The investigators found that the number of HIV screens that were conducted dropped significantly during the COVID-19 pandemic.
At the height of the pandemic, HIV screening at the sites decreased an average of 58%, the researchers found. As of the end of June, the number was decreased by 32%.
“This is a global problem,” he said. “HIV services have been severely impacted worldwide, with the greatest impact on the LGBTQ community.”
UCM performed 19,111 HIV screens (11,133 in the ED) between Jan. 1 and Aug. 17 this year. It performed 14,754 COVID polymerase chain reaction tests in the ED between March 17 and Aug. 17. All of the acute cases were identified in the ED.
Dr. Pitrak mentioned some possible causes of an increase in the number of patients with acute cases who present in the ED. People who do not suspect they have AHI may be coming to the ED because they think they have COVID-19, inasmuch as many of the symptoms overlap. One of the AHI patients actually did have a coinfection, Dr. Pitrak noted.
“There is also the possibility that this could be bad news,” Dr. Pitrak said in an interview. “It could be that there are more acute cases presenting because there are more community transmissions.”
He noted that follow-up visits have been canceled or converted to telehealth visits during the pandemic, and the number of patients who are initiating pre-exposure prophylaxis has declined significantly.
“I hope we’re not seeing an increase in new transmissions after so much work has been done to decrease transmissions over the past few years,” he said.
Partnership with emergency physicians
Critical to screening these patients is building a solid partnership between ID and ED physicians.
Coauthor Kimberly Stanford, MD, MPH, an assistant professor in emergency medicine at UCM, said, “You need a champion within the emergency department who can help make sure that the work flow is not disrupted, that however you implement your screening program, you’re not putting extra work on the staff.
“We can feel extremely confident that if I send a test and it comes back positive, I know someone is going to call that patient and make sure they get into care.”
Although the testing is performed in the ED at UCM, the follow-up, linkage to care, and initiation of treatment are conducted by the ID specialists.
Beverly E. Sha, MD, professor in the division of infectious diseases, department of internal medicine, Rush Medical College, Chicago, said in an interview that although she agrees that HIV screening programs in EDs “make absolute sense,” there are different ways to conduct such programs. Dr. Sha was not involved in Dr. Pitrak’s study.
At Rush’s ED, she says, HIV testing is linked with a complete blood count.
“If someone presents with fever, we would often be doing that test as well,” she said. “I think just globally increasing screening [in the ED] is what makes the most sense.”
Dr. Sha said they have not seen a similar surge in acute cases in the ED at Rush during the pandemic.
She noted, however, that UCM tested more than 11,000 people for HIV in the ED this year, whereas “we probably only did about 3500.
“The reason testing is so important, whether for HIV or COVID, is the more you test, the more you’re going to find,” she said, “especially in cities like Chicago.”
Dr. Pitrak received grant support from Gilead Sciences. His coauthors and Dr. Sha reported no relevant financial relationships.
This article first appeared on Medscape.com.
COVID-19: Thromboembolic events high despite prophylaxis
in a new large observational U.S. study.
“Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis,” lead author Gregory Piazza, MD, Brigham and Women’s Hospital, Boston, said in an interview.
“Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses,” he added.
However, Dr. Piazza cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The current study was published online ahead of print in the Nov. 3 issue of the Journal of the American College of Cardiology.
Rates similar to other very sick patients
The study showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, Dr. Piazza noted.
“The numbers we were seeing in early reports were so high we couldn’t figure out how that was possible,” he said. “Our study suggests that, in a U.S. population receiving thromboprophylaxis, the rate of thromboembolic complications [are] more in line with what we would expect to see in other very sick patients who end up in ICU.”
He suggested that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there. “Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the U.S. population.”
Dr. Piazza attributed the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
“We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients,” he said.
“We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven’t had enough critically ill patients at any one time to raise the flag about thromboprophylaxis,” he commented.
The study also found a high rate of cardiovascular complications. They are seeing an increase in the risk of MI, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don’t always have underlying cardiovascular disease, he said.
“So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick,” Dr. Piazza said. “If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates.”
For the current report, the researchers analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latino and 44% were non-White.
Cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non–intensive care setting.
Results showed that major arterial or venous thromboembolism (VTE) occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
Major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Symptomatic VTE occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
“We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU,” Dr. Piazza said.
“These results suggest that we don’t need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it – those with risk factors for thromboembolism.”
Catheter- and device-associated deep vein thrombosis accounted for 76.9% of the DVTs observed in the study.
“Our finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring,” the researchers wrote.
ARDS biggest risk factor
Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or VTE, major adverse cardiovascular events, symptomatic VTE, and death.
“The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis,” the researchers wrote. “They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation.”
They point out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large health care network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
“The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations,” the authors noted.
“The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts,” they concluded.
The study is continuing, and the researchers expect to have data on 10,000 patients by the end of winter.
Wait for randomized trials
In an accompanying editorial, Robert McBane, MD, Mayo Clinic, Rochester, Minn., said that these data provide important real-world arterial and venous thrombotic event rates across a large, integrated health care network and an experienced roster of clinician-scientists devoted to thrombosis research.
Noting that whether to interpret these results as alarming or reassuring requires a comparison of expected thromboembolic event rates separate from the pandemic, he pointed out that, while the overall VTE rate among ICU patients was high, the vast majority of these events were attributable to central venous lines, and apart from these, the event rates do not appear inflated relative to prior published incidence rates from the pre–COVID-19 era.
“It is therefore important to resist the urge to overprevent or overtreat patients and expose them to the serious risks of major bleeding,” Dr. McBane wrote, adding that “the systematized approach to delivery of guideline-driven VTE prophylaxis across this large, integrated health network likely contributed to the relatively low rates of serious thrombotic outcomes reported.”
He further noted that, as the majority of VTE events were related to central venous lines in ICU patients, “this underscores the importance of a bundled care approach to central venous line management with daily assessment of the continued necessity of central access.
“A number of important clinical trials aimed at optimizing thromboprophylaxis during hospitalization, following hospital dismissal, and in ambulatory settings are underway. Until available, the lessons of thoughtful anticoagulant prophylaxis and treatment guidelines harvested from years of clinical research appear to apply,” he concluded.
This study was funded, in part, by a research grant from Janssen Pharmaceuticals. Dr. Piazza has received research grant support from EKOS Corporation, Bayer, Bristol-Myers Squibb/Pfizer, Portola Pharmaceuticals, and Janssen Pharmaceuticals; and has received consulting fees from Amgen, Pfizer, Boston Scientific, Agile, and Thrombolex. Dr. McBane reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
in a new large observational U.S. study.
“Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis,” lead author Gregory Piazza, MD, Brigham and Women’s Hospital, Boston, said in an interview.
“Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses,” he added.
However, Dr. Piazza cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The current study was published online ahead of print in the Nov. 3 issue of the Journal of the American College of Cardiology.
Rates similar to other very sick patients
The study showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, Dr. Piazza noted.
“The numbers we were seeing in early reports were so high we couldn’t figure out how that was possible,” he said. “Our study suggests that, in a U.S. population receiving thromboprophylaxis, the rate of thromboembolic complications [are] more in line with what we would expect to see in other very sick patients who end up in ICU.”
He suggested that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there. “Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the U.S. population.”
Dr. Piazza attributed the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
“We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients,” he said.
“We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven’t had enough critically ill patients at any one time to raise the flag about thromboprophylaxis,” he commented.
The study also found a high rate of cardiovascular complications. They are seeing an increase in the risk of MI, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don’t always have underlying cardiovascular disease, he said.
“So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick,” Dr. Piazza said. “If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates.”
For the current report, the researchers analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latino and 44% were non-White.
Cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non–intensive care setting.
Results showed that major arterial or venous thromboembolism (VTE) occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
Major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Symptomatic VTE occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
“We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU,” Dr. Piazza said.
“These results suggest that we don’t need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it – those with risk factors for thromboembolism.”
Catheter- and device-associated deep vein thrombosis accounted for 76.9% of the DVTs observed in the study.
“Our finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring,” the researchers wrote.
ARDS biggest risk factor
Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or VTE, major adverse cardiovascular events, symptomatic VTE, and death.
“The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis,” the researchers wrote. “They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation.”
They point out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large health care network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
“The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations,” the authors noted.
“The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts,” they concluded.
The study is continuing, and the researchers expect to have data on 10,000 patients by the end of winter.
Wait for randomized trials
In an accompanying editorial, Robert McBane, MD, Mayo Clinic, Rochester, Minn., said that these data provide important real-world arterial and venous thrombotic event rates across a large, integrated health care network and an experienced roster of clinician-scientists devoted to thrombosis research.
Noting that whether to interpret these results as alarming or reassuring requires a comparison of expected thromboembolic event rates separate from the pandemic, he pointed out that, while the overall VTE rate among ICU patients was high, the vast majority of these events were attributable to central venous lines, and apart from these, the event rates do not appear inflated relative to prior published incidence rates from the pre–COVID-19 era.
“It is therefore important to resist the urge to overprevent or overtreat patients and expose them to the serious risks of major bleeding,” Dr. McBane wrote, adding that “the systematized approach to delivery of guideline-driven VTE prophylaxis across this large, integrated health network likely contributed to the relatively low rates of serious thrombotic outcomes reported.”
He further noted that, as the majority of VTE events were related to central venous lines in ICU patients, “this underscores the importance of a bundled care approach to central venous line management with daily assessment of the continued necessity of central access.
“A number of important clinical trials aimed at optimizing thromboprophylaxis during hospitalization, following hospital dismissal, and in ambulatory settings are underway. Until available, the lessons of thoughtful anticoagulant prophylaxis and treatment guidelines harvested from years of clinical research appear to apply,” he concluded.
This study was funded, in part, by a research grant from Janssen Pharmaceuticals. Dr. Piazza has received research grant support from EKOS Corporation, Bayer, Bristol-Myers Squibb/Pfizer, Portola Pharmaceuticals, and Janssen Pharmaceuticals; and has received consulting fees from Amgen, Pfizer, Boston Scientific, Agile, and Thrombolex. Dr. McBane reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
in a new large observational U.S. study.
“Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis,” lead author Gregory Piazza, MD, Brigham and Women’s Hospital, Boston, said in an interview.
“Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses,” he added.
However, Dr. Piazza cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The current study was published online ahead of print in the Nov. 3 issue of the Journal of the American College of Cardiology.
Rates similar to other very sick patients
The study showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, Dr. Piazza noted.
“The numbers we were seeing in early reports were so high we couldn’t figure out how that was possible,” he said. “Our study suggests that, in a U.S. population receiving thromboprophylaxis, the rate of thromboembolic complications [are] more in line with what we would expect to see in other very sick patients who end up in ICU.”
He suggested that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there. “Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the U.S. population.”
Dr. Piazza attributed the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
“We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients,” he said.
“We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven’t had enough critically ill patients at any one time to raise the flag about thromboprophylaxis,” he commented.
The study also found a high rate of cardiovascular complications. They are seeing an increase in the risk of MI, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don’t always have underlying cardiovascular disease, he said.
“So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick,” Dr. Piazza said. “If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates.”
For the current report, the researchers analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latino and 44% were non-White.
Cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non–intensive care setting.
Results showed that major arterial or venous thromboembolism (VTE) occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
Major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Symptomatic VTE occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
“We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU,” Dr. Piazza said.
“These results suggest that we don’t need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it – those with risk factors for thromboembolism.”
Catheter- and device-associated deep vein thrombosis accounted for 76.9% of the DVTs observed in the study.
“Our finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring,” the researchers wrote.
ARDS biggest risk factor
Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or VTE, major adverse cardiovascular events, symptomatic VTE, and death.
“The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis,” the researchers wrote. “They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation.”
They point out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large health care network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
“The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations,” the authors noted.
“The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts,” they concluded.
The study is continuing, and the researchers expect to have data on 10,000 patients by the end of winter.
Wait for randomized trials
In an accompanying editorial, Robert McBane, MD, Mayo Clinic, Rochester, Minn., said that these data provide important real-world arterial and venous thrombotic event rates across a large, integrated health care network and an experienced roster of clinician-scientists devoted to thrombosis research.
Noting that whether to interpret these results as alarming or reassuring requires a comparison of expected thromboembolic event rates separate from the pandemic, he pointed out that, while the overall VTE rate among ICU patients was high, the vast majority of these events were attributable to central venous lines, and apart from these, the event rates do not appear inflated relative to prior published incidence rates from the pre–COVID-19 era.
“It is therefore important to resist the urge to overprevent or overtreat patients and expose them to the serious risks of major bleeding,” Dr. McBane wrote, adding that “the systematized approach to delivery of guideline-driven VTE prophylaxis across this large, integrated health network likely contributed to the relatively low rates of serious thrombotic outcomes reported.”
He further noted that, as the majority of VTE events were related to central venous lines in ICU patients, “this underscores the importance of a bundled care approach to central venous line management with daily assessment of the continued necessity of central access.
“A number of important clinical trials aimed at optimizing thromboprophylaxis during hospitalization, following hospital dismissal, and in ambulatory settings are underway. Until available, the lessons of thoughtful anticoagulant prophylaxis and treatment guidelines harvested from years of clinical research appear to apply,” he concluded.
This study was funded, in part, by a research grant from Janssen Pharmaceuticals. Dr. Piazza has received research grant support from EKOS Corporation, Bayer, Bristol-Myers Squibb/Pfizer, Portola Pharmaceuticals, and Janssen Pharmaceuticals; and has received consulting fees from Amgen, Pfizer, Boston Scientific, Agile, and Thrombolex. Dr. McBane reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
COVID spikes exacerbate health worker shortages in Rocky Mountains, Great Plains
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
TDF preferred in PrEP for Blacks and women, studies indicate
Although the efficacy of two pre-exposure prophylaxis (PrEP) regimens containing differing prodrug formulations of tenofovir are virtually identical, the balance between benefit and risk tips in favor of the combination using the older formulation, tenofovir disoproxil fumarate (TDF), a pharmacology researcher said.
An analysis of the pharmacologic profiles of TDF plus emtricitabine (FTC; Truvada and generic) with tenofovir alafenamide (TAF) plus FTC (Descovy) shows that the risk of decreased bone mineral density and renal toxicity with TDF are significantly lower than those of weight gain and related metabolic and cardiovascular problems associated with the newer tenofovir formulation TAF, according to pharmacology research fellow Andrew Hill, MD, PhD, from the University of Liverpool (England).
“I think when we’re comparing these two drugs overall, we have a clear benefit/risk, and we need to take both of these potential toxicities seriously, “ he said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases held virtually this year.
“But in my view, treating women – Black women – with TAF/FTC is a bad thing,” he continued. “I think it’s going lead to more harm, more myocardial infarctions, more cases of diabetes, and potentially more adverse birth outcomes, and I think that is a risk that is not worth taking, given that the apparent benefit in terms of bone mineral density and renal markers is a hypothesis at best, and is not translated into hard clinical endpoints.”
Adverse event profiles
Dr. Hill compared the side effect profiles of the two agents when used both in antiretroviral therapy (ART) in combination the integrase inhibitor dolutegravir (DTG; Tivicay), and in PrEP.
World Health Organization guidelines for first-line ART recommend the use of TDF/FTC/DTG, reserving TAF plus lamivudine (3TC) and DTG for use in special circumstances only, Dr. Hill noted.
He pointed to a pooled analysis of data from eight randomized, controlled trials of treatment-naive people living with HIV who started on ART from 2003 to 2015. The authors found that demographic factors associated with weight gain included lower CD4 cell counter, higher levels of HIV type 1 RNA, no injection drug use, female sex, and Black race.
They also found that, among nucleoside/nucleotide reverse transcriptase inhibitors, TAF was associated with more weight gain than TDF, abacavir, or zidovudine.
“This pattern is seen consistently across studies both of pre-exposure prophylaxis or treatment comparing tenofovir with either TAF or other nucleoside analogs,” he said.
The greater weight gain with TAF versus TDF was seen in both treatment trials and in the DISCOVER PrEP trial.
In addition, in a crossover trial conducted in Germany, patients who switched from TDF to TAF had an approximately 2 kg increase in body weight.
TAF has also been associated with higher grade 3 or 4 glucose and LDL cholesterol than TDF in clinical trials for the treatment of hepatitis B infections, and with higher LDL cholesterol and total cholesterol levels as well as diabetes in patients treated with the drugs in combination in the EMERALD HIV trial.
Clinical trials also tend to underestimate the real-world population of persons at highest risk for adverse events from TAF, Dr. Hill said, noting that the percentage of Black women in phase 3 trials for dolutegravir was 9%, compared with 42% among persons infected with HIV worldwide. The respective percentages for Black men are 16% versus 30%. These differences are similar across clinical trial programs for other ART agents.
“Generally, it’s women and Black people who seem to be at greatest risk for safety issues,” he said.
In the ADVANCE trial comparing TAF/FTC/DTG with TDF/FTC/DTG and a control arm of TDF, FTC and efavirenz, the mean change in weight among men after 3 years on the TAF-based regimen was a gain of 7.2 kg (15.9 lbs), compared with 5.5 kg (12 lbs) with TDF, and 2.6 kg (5.7 lbs) with the efavirenz-containing regimen.
In women enrolled in the same trial, the respective mean weight gains were 12.3 kg (27 lbs), 7.4 kg (16.3 lbs), and 5.5 kg (12 lbs).
“All of our analyses so far have shown that the weight continues to go up. We’re actually seeing people doubling in their body weight. We’ve seen some women come into clinic and their doctors don’t even recognize them because they’ve put on so much weight,” he said.
In women, most of the gain in weight occurs as limb or trunk fat, with a predominance of visceral fat.
People taking TAF in the trial were also at significantly greater risk for developing the metabolic syndrome, and at week 96, 27% of women on TAF/FTC/DTG had treatment-emergent obesity, compared with 17% for those on TDF/FTC/DTG and 11% for those on TDF/FTC/EFV. In men, the respective 96-week rates of treatment-emergent obesity were 7%, 3%, and 2%.
Clinical obesity itself is a risk factor for obstetric complications and birth outcomes, Alzheimer’s disease, type 2 diabetes, cardiovascular disease, hypertension and cancer, and an average 4-year reduction in life expectancy, Dr. Hill said. “I think it’s actually very unlikely that the [World Health Organization] guidelines will now change and allow the widespread use of TAF/FTC in combination with integrase inhibitors worldwide given these potential implications.”
Modern times
The bad rap that TDF gets for its alleged effects on bone mineral density and kidneys comes from studies where the drug was given in a boosted regimen that can amplify tenofovir toxicities, Dr. Hill said.
He noted that data from Gilead Sciences shows through 7 years of therapy in previously ART-naive patients, the combination of TDF/3TC/EFV showed sustained durable efficacy, no discontinuations to renal adverse effects, and no evidence of clinically relevant bone effects.
“I think we need to be very careful when we look at tenofovir and TAF. We need to look at the more modern way that these drugs are used, which is not with pharmacokinetic boosters anymore, and in that situation the toxicity profile of tenofovir/3TC – the original TDF – is very favorable,” he said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Hill presented his data, said that his clinical experience mirrors the pharmacokinetic findings.
“I certainly have strong feelings about the use of TDF in pre-exposure prophylaxis,” he said in an interview. “TDF is an effective and safe formulation of tenofovir to be used in pre-exposure prophylaxis, and one that we have more experience with. It’s the formulation of tenofovir that I use for all of my patients who are on pre-exposure prophylaxis, and I think it is the most cost-effective.’
No funding source was reported. Andrew Hill consults for Tibotec on clinical trial programs for darunavir, etravirine, and rilpivirine. Dr. Goldstein reported having no relevant disclosures.
Although the efficacy of two pre-exposure prophylaxis (PrEP) regimens containing differing prodrug formulations of tenofovir are virtually identical, the balance between benefit and risk tips in favor of the combination using the older formulation, tenofovir disoproxil fumarate (TDF), a pharmacology researcher said.
An analysis of the pharmacologic profiles of TDF plus emtricitabine (FTC; Truvada and generic) with tenofovir alafenamide (TAF) plus FTC (Descovy) shows that the risk of decreased bone mineral density and renal toxicity with TDF are significantly lower than those of weight gain and related metabolic and cardiovascular problems associated with the newer tenofovir formulation TAF, according to pharmacology research fellow Andrew Hill, MD, PhD, from the University of Liverpool (England).
“I think when we’re comparing these two drugs overall, we have a clear benefit/risk, and we need to take both of these potential toxicities seriously, “ he said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases held virtually this year.
“But in my view, treating women – Black women – with TAF/FTC is a bad thing,” he continued. “I think it’s going lead to more harm, more myocardial infarctions, more cases of diabetes, and potentially more adverse birth outcomes, and I think that is a risk that is not worth taking, given that the apparent benefit in terms of bone mineral density and renal markers is a hypothesis at best, and is not translated into hard clinical endpoints.”
Adverse event profiles
Dr. Hill compared the side effect profiles of the two agents when used both in antiretroviral therapy (ART) in combination the integrase inhibitor dolutegravir (DTG; Tivicay), and in PrEP.
World Health Organization guidelines for first-line ART recommend the use of TDF/FTC/DTG, reserving TAF plus lamivudine (3TC) and DTG for use in special circumstances only, Dr. Hill noted.
He pointed to a pooled analysis of data from eight randomized, controlled trials of treatment-naive people living with HIV who started on ART from 2003 to 2015. The authors found that demographic factors associated with weight gain included lower CD4 cell counter, higher levels of HIV type 1 RNA, no injection drug use, female sex, and Black race.
They also found that, among nucleoside/nucleotide reverse transcriptase inhibitors, TAF was associated with more weight gain than TDF, abacavir, or zidovudine.
“This pattern is seen consistently across studies both of pre-exposure prophylaxis or treatment comparing tenofovir with either TAF or other nucleoside analogs,” he said.
The greater weight gain with TAF versus TDF was seen in both treatment trials and in the DISCOVER PrEP trial.
In addition, in a crossover trial conducted in Germany, patients who switched from TDF to TAF had an approximately 2 kg increase in body weight.
TAF has also been associated with higher grade 3 or 4 glucose and LDL cholesterol than TDF in clinical trials for the treatment of hepatitis B infections, and with higher LDL cholesterol and total cholesterol levels as well as diabetes in patients treated with the drugs in combination in the EMERALD HIV trial.
Clinical trials also tend to underestimate the real-world population of persons at highest risk for adverse events from TAF, Dr. Hill said, noting that the percentage of Black women in phase 3 trials for dolutegravir was 9%, compared with 42% among persons infected with HIV worldwide. The respective percentages for Black men are 16% versus 30%. These differences are similar across clinical trial programs for other ART agents.
“Generally, it’s women and Black people who seem to be at greatest risk for safety issues,” he said.
In the ADVANCE trial comparing TAF/FTC/DTG with TDF/FTC/DTG and a control arm of TDF, FTC and efavirenz, the mean change in weight among men after 3 years on the TAF-based regimen was a gain of 7.2 kg (15.9 lbs), compared with 5.5 kg (12 lbs) with TDF, and 2.6 kg (5.7 lbs) with the efavirenz-containing regimen.
In women enrolled in the same trial, the respective mean weight gains were 12.3 kg (27 lbs), 7.4 kg (16.3 lbs), and 5.5 kg (12 lbs).
“All of our analyses so far have shown that the weight continues to go up. We’re actually seeing people doubling in their body weight. We’ve seen some women come into clinic and their doctors don’t even recognize them because they’ve put on so much weight,” he said.
In women, most of the gain in weight occurs as limb or trunk fat, with a predominance of visceral fat.
People taking TAF in the trial were also at significantly greater risk for developing the metabolic syndrome, and at week 96, 27% of women on TAF/FTC/DTG had treatment-emergent obesity, compared with 17% for those on TDF/FTC/DTG and 11% for those on TDF/FTC/EFV. In men, the respective 96-week rates of treatment-emergent obesity were 7%, 3%, and 2%.
Clinical obesity itself is a risk factor for obstetric complications and birth outcomes, Alzheimer’s disease, type 2 diabetes, cardiovascular disease, hypertension and cancer, and an average 4-year reduction in life expectancy, Dr. Hill said. “I think it’s actually very unlikely that the [World Health Organization] guidelines will now change and allow the widespread use of TAF/FTC in combination with integrase inhibitors worldwide given these potential implications.”
Modern times
The bad rap that TDF gets for its alleged effects on bone mineral density and kidneys comes from studies where the drug was given in a boosted regimen that can amplify tenofovir toxicities, Dr. Hill said.
He noted that data from Gilead Sciences shows through 7 years of therapy in previously ART-naive patients, the combination of TDF/3TC/EFV showed sustained durable efficacy, no discontinuations to renal adverse effects, and no evidence of clinically relevant bone effects.
“I think we need to be very careful when we look at tenofovir and TAF. We need to look at the more modern way that these drugs are used, which is not with pharmacokinetic boosters anymore, and in that situation the toxicity profile of tenofovir/3TC – the original TDF – is very favorable,” he said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Hill presented his data, said that his clinical experience mirrors the pharmacokinetic findings.
“I certainly have strong feelings about the use of TDF in pre-exposure prophylaxis,” he said in an interview. “TDF is an effective and safe formulation of tenofovir to be used in pre-exposure prophylaxis, and one that we have more experience with. It’s the formulation of tenofovir that I use for all of my patients who are on pre-exposure prophylaxis, and I think it is the most cost-effective.’
No funding source was reported. Andrew Hill consults for Tibotec on clinical trial programs for darunavir, etravirine, and rilpivirine. Dr. Goldstein reported having no relevant disclosures.
Although the efficacy of two pre-exposure prophylaxis (PrEP) regimens containing differing prodrug formulations of tenofovir are virtually identical, the balance between benefit and risk tips in favor of the combination using the older formulation, tenofovir disoproxil fumarate (TDF), a pharmacology researcher said.
An analysis of the pharmacologic profiles of TDF plus emtricitabine (FTC; Truvada and generic) with tenofovir alafenamide (TAF) plus FTC (Descovy) shows that the risk of decreased bone mineral density and renal toxicity with TDF are significantly lower than those of weight gain and related metabolic and cardiovascular problems associated with the newer tenofovir formulation TAF, according to pharmacology research fellow Andrew Hill, MD, PhD, from the University of Liverpool (England).
“I think when we’re comparing these two drugs overall, we have a clear benefit/risk, and we need to take both of these potential toxicities seriously, “ he said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases held virtually this year.
“But in my view, treating women – Black women – with TAF/FTC is a bad thing,” he continued. “I think it’s going lead to more harm, more myocardial infarctions, more cases of diabetes, and potentially more adverse birth outcomes, and I think that is a risk that is not worth taking, given that the apparent benefit in terms of bone mineral density and renal markers is a hypothesis at best, and is not translated into hard clinical endpoints.”
Adverse event profiles
Dr. Hill compared the side effect profiles of the two agents when used both in antiretroviral therapy (ART) in combination the integrase inhibitor dolutegravir (DTG; Tivicay), and in PrEP.
World Health Organization guidelines for first-line ART recommend the use of TDF/FTC/DTG, reserving TAF plus lamivudine (3TC) and DTG for use in special circumstances only, Dr. Hill noted.
He pointed to a pooled analysis of data from eight randomized, controlled trials of treatment-naive people living with HIV who started on ART from 2003 to 2015. The authors found that demographic factors associated with weight gain included lower CD4 cell counter, higher levels of HIV type 1 RNA, no injection drug use, female sex, and Black race.
They also found that, among nucleoside/nucleotide reverse transcriptase inhibitors, TAF was associated with more weight gain than TDF, abacavir, or zidovudine.
“This pattern is seen consistently across studies both of pre-exposure prophylaxis or treatment comparing tenofovir with either TAF or other nucleoside analogs,” he said.
The greater weight gain with TAF versus TDF was seen in both treatment trials and in the DISCOVER PrEP trial.
In addition, in a crossover trial conducted in Germany, patients who switched from TDF to TAF had an approximately 2 kg increase in body weight.
TAF has also been associated with higher grade 3 or 4 glucose and LDL cholesterol than TDF in clinical trials for the treatment of hepatitis B infections, and with higher LDL cholesterol and total cholesterol levels as well as diabetes in patients treated with the drugs in combination in the EMERALD HIV trial.
Clinical trials also tend to underestimate the real-world population of persons at highest risk for adverse events from TAF, Dr. Hill said, noting that the percentage of Black women in phase 3 trials for dolutegravir was 9%, compared with 42% among persons infected with HIV worldwide. The respective percentages for Black men are 16% versus 30%. These differences are similar across clinical trial programs for other ART agents.
“Generally, it’s women and Black people who seem to be at greatest risk for safety issues,” he said.
In the ADVANCE trial comparing TAF/FTC/DTG with TDF/FTC/DTG and a control arm of TDF, FTC and efavirenz, the mean change in weight among men after 3 years on the TAF-based regimen was a gain of 7.2 kg (15.9 lbs), compared with 5.5 kg (12 lbs) with TDF, and 2.6 kg (5.7 lbs) with the efavirenz-containing regimen.
In women enrolled in the same trial, the respective mean weight gains were 12.3 kg (27 lbs), 7.4 kg (16.3 lbs), and 5.5 kg (12 lbs).
“All of our analyses so far have shown that the weight continues to go up. We’re actually seeing people doubling in their body weight. We’ve seen some women come into clinic and their doctors don’t even recognize them because they’ve put on so much weight,” he said.
In women, most of the gain in weight occurs as limb or trunk fat, with a predominance of visceral fat.
People taking TAF in the trial were also at significantly greater risk for developing the metabolic syndrome, and at week 96, 27% of women on TAF/FTC/DTG had treatment-emergent obesity, compared with 17% for those on TDF/FTC/DTG and 11% for those on TDF/FTC/EFV. In men, the respective 96-week rates of treatment-emergent obesity were 7%, 3%, and 2%.
Clinical obesity itself is a risk factor for obstetric complications and birth outcomes, Alzheimer’s disease, type 2 diabetes, cardiovascular disease, hypertension and cancer, and an average 4-year reduction in life expectancy, Dr. Hill said. “I think it’s actually very unlikely that the [World Health Organization] guidelines will now change and allow the widespread use of TAF/FTC in combination with integrase inhibitors worldwide given these potential implications.”
Modern times
The bad rap that TDF gets for its alleged effects on bone mineral density and kidneys comes from studies where the drug was given in a boosted regimen that can amplify tenofovir toxicities, Dr. Hill said.
He noted that data from Gilead Sciences shows through 7 years of therapy in previously ART-naive patients, the combination of TDF/3TC/EFV showed sustained durable efficacy, no discontinuations to renal adverse effects, and no evidence of clinically relevant bone effects.
“I think we need to be very careful when we look at tenofovir and TAF. We need to look at the more modern way that these drugs are used, which is not with pharmacokinetic boosters anymore, and in that situation the toxicity profile of tenofovir/3TC – the original TDF – is very favorable,” he said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Hill presented his data, said that his clinical experience mirrors the pharmacokinetic findings.
“I certainly have strong feelings about the use of TDF in pre-exposure prophylaxis,” he said in an interview. “TDF is an effective and safe formulation of tenofovir to be used in pre-exposure prophylaxis, and one that we have more experience with. It’s the formulation of tenofovir that I use for all of my patients who are on pre-exposure prophylaxis, and I think it is the most cost-effective.’
No funding source was reported. Andrew Hill consults for Tibotec on clinical trial programs for darunavir, etravirine, and rilpivirine. Dr. Goldstein reported having no relevant disclosures.
FROM IDWEEK 2020
Cutaneous Filariasis in an American Traveler
To the Editor:
Cutaneous filariasis is a group of infectious diseases caused by more than 60 different nematode species and endemic to approximately 83 countries.1,2 These infections are transmitted to humans by vectors such as mosquitoes, blackflies, biting midges, or Tabanid flies.1 The blood meal taken by vectors allow microfilariae to enter the skin and develop into adult worms.1-3 It is postulated that filarial infections were first described in 2000
Filarial parasites have been categorized into groups based on the site of adult worm stage habitat. The cutaneous group includes Loa loa, Onchocerca volvulus, Mansonella perstans, and Dipetalonema streptocerca. The lymphatic group includes Wuchereria bancrofti, Brugia malayi, and Brugia timori. Lastly, the body cavity group includes Mansonella ozzardi. Because humidity is required for survival of the infective larval stage, individuals from tropical countries in Africa, Central America, and South America most commonly are affected.1 These diseases also are related to poor housing quality and inadequate sanitation.1,3,4 Travel for business, medical missions, pleasure, or emigration has caused increased filarial infections globally. In fact, dermatologic disorders with infectious etiologies cause approximately 17% of travelers to seek medical attention.3
Dermatologic manifestations indicative of a potential cutaneous filarial infection include papules, nodules, excoriations with secondary xerosis, lichenification, skin pigment changes, and/or severe pruritus. However, individuals from filarial endemic regions may not demonstrate any clinical signs or symptoms, despite having microfilariae in their blood,1 which enables the disease to propagate and poses a major public health concern. In fact, patients with chronic filarial infections are at increased risk for developing lymphedema, elephantiasis, or blindness, which are hypothesized to be the second largest cause of permanent disability worldwide.1 Although rarely seen in US citizens, cutaneous filariasis should always be a diagnostic consideration in patients who present with a pruritic eruption and have a travel history to tropical countries. We report a case of cutaneous onchocerciasis in a US citizen who developed a pruritic eczematous eruption on the right upper arm following an arthropod assault while working in an Onchocerca endemic region approximately 1.5 years prior.
A 33-year-old woman presented to our outpatient dermatology clinic with the chief concern of a pruritic rash on the right arm (Figure 1). She revealed a history of travel to Peru, associated symptoms, prior diagnoses, and attempted treatment regimens. Over a 1.5-year period, the patient traveled for work-related reasons to Madre de Dios, Peru. During that time, the patient experienced 2 bouts of severe abdominal pain, nausea, and vomiting that she attributed to poor food and water quality. She did not immediately seek medical attention. She also developed skin manifestations that began as a pruritic and irritating pinpoint-sized red papule on the right eyelid, possibly a site of an arthropod assault. She then experienced episodic eyelash loss (Figure 2) and subsequent vision changes, including blurry vision, halos around lights, and dimming around the periphery. When the patient developed circular, pink, pruritic plaques on the right upper extremity, she sought medical attention in Lima, Peru. She was diagnosed with tinea corporis and prescribed an oral antibiotic and topical antifungal.
This treatment regimen did not result in improvement. In the following months, the patient noticed worsening of the ocular symptoms, and she developed a dry cough with occasional dyspnea. She again sought medical attention in Peru and was referred to an ophthalmologist who suspected Demodex mite or fungal infection; however, workup for those pathologies was negative. The respiratory symptoms continued to worsen, particularly at night, and she began to experience palpitations.
Upon returning to the United States, the patient was evaluated by her primary care physician who ordered the following laboratory tests: a complete blood cell count with differential, comprehensive metabolic panel, vitamin D level, blood culture, lipid panel, ferritin level, and thyroid function. An electrocardiogram, throat culture, and stool culture for ova and parasites also were obtained. The electrocardiogram showed sinus tachycardia, and the stool culture revealed blastocystis, for which she was prescribed oral metronidazole and tinidazole. The other results were within reference range, and the throat culture showed normal oropharyngeal microbes.
A few days after the treatment for the blastocystis, the gastrointestinal tract symptoms improved, but dermatologic, ocular, pulmonary, and cardiac symptoms persisted. She also began experiencing night sweats and hot flashes. In between visits to the primary care physician, she sought medical attention at an urgent care clinic for worsening pulmonary and cardiac symptoms. At that time, results of a chest radiograph were normal.
The primary care physician referred her to infectious disease and dermatology for further evaluation within a few weeks of returning to the United States. Upon presentation to dermatology, the patient described a waxing and waning nature to the rash on the arm with associated intermittent pain. Physical examination revealed several erythematous patches on the triceps and a 1-cm subcutaneous nodule on the right elbow with overlying skin discoloration. The patient stated that she first noticed the inflamed painful nodule when she returned to the United States. Since its discovery, the nodule increased in size and became firm. The patient also described occasional limited range of motion of the right arm due to the discomfort of the rash and inflamed nodule. Interestingly, the patient’s partner who accompanied her to Peru also developed a similar pruritic rash on the chest. He was evaluated by dermatology and infectious disease; however, biopsies of his rash performed at a different practice revealed nonspecific results. Due to her partner’s inconclusive results, our patient initially refused a biopsy; however, she returned to the office after 1 week with worsening symptoms, and a 4-mm punch biopsy of the right arm was obtained in addition to rapid plasma reagin and QuantiFERON-TB Gold test.
Based on the patient’s travel history, clinical course, and physical examination, the clinical differential diagnosis included nummular dermatitis, panniculitis/nodular vasculitis, tinea corporis, secondary syphilis, pinta, tuberculosis, or cutaneous filariasis. Rapid plasma reagin and QuantiFERON-TB Gold test results were negative, and a periodic acid–Schiff stain of the biopsy was negative for fungal elements. Dermatopathology revealed intradermal filarial nematodes of 120 to 150 µm in diameter and 1-to 2-mm cuticles eliciting a predominantly superficial and deep lymphohistiocytic reaction (Figure 3). The histopathologic differential diagnosis based on the diameter of the nematode included M perstans, W bancrofti, and O volvulus. Clinical correlation was highly recommended to obtain a final diagnosis and management plan. A portion of the biopsy was sent to the Centers for Disease Control and Prevention, which confirmed the presence of a filarial nematode consistent with a zoonotic Brugia but also with zoonotic Onchocerca as a possible differential. Therefore, considering the history, clinical course, and histopathologic analysis, the final diagnosis of cutaneous onchocerciasis was made.
The patient was referred back to infectious disease and started on combination therapy of ivermectin (25.5 mg) plus albendazole (800 mg) taken at once followed by doxycycline (200 mg) for 6 weeks. The symptoms initially worsened, then she experienced near-complete resolution of dermatologic, pulmonary, and ocular symptoms after approximately 2 weeks of treatment. She continued to report fatigue and palpitations, for she continued to see a cardiologist. We highly encouraged her to continue following up with infectious disease to ensure complete eradication of the infection.
Onchocerciasis is common in individuals who live or work in equatorial Africa, Central America, and South America. The disease process has dermatologic, ocular, and other systemic manifestations if the infection continues long-term without treatment.2,5 Although rare, this infection has been observed in US citizens who have traveled to filarial endemic regions for a period of time ranging from 2 weeks to 39 years.2,6,7
Blackflies (genus Simulium), the intermediate host of O volvulus, breed in areas close to freely flowing water. The blackfly bites a human host, and within 7 days the microfilariae undergo 2 molts to reach the infective stage. The larvae remain in the dermis and subcutaneous tissue for 2 additional molts until they develop into adult worms. Then, adult worms may become encapsulated, eliciting and forming subcutaneous nodules, also known as onchocercomas.2,3
A fertilized female in the subcutaneous tissue releases microfilariae that may remain in the skin or travel to the eyes of the host.3 The host may demonstrate signs of infection within 3 to 15 months.2 Most commonly, patients report localized or generalized pruritus, and one extremity develops swelling, papules, lymphadenopathy, and alterations of skin pigment (hypopigmentation or hyperpigmentation).5-8 Our patient developed a pruritic eczematous eruption that only affected her right arm with an inflamed firm nodule overlying the elbow, a suspected onchocercoma. Onchocercomas are the direct result of adult worms coiled in the dermis, subcutaneous tissue, and deep fascia. These commonly are found in close proximity to bony prominences with the specific location pending the geographic area of infection.8 For example, onchocercomas more commonly are found over bony prominences in the head and upper body region in patients who acquired the disease from Central or South America, whereas individuals infected in Africa more commonly develop onchocercomas near the femoral, coccyx, or sacral regions.2
The immune response mounted by the infected host is responsible for the ocular signs and symptoms.2 Specifically, the inflammatory reaction may impact the patient’s cornea, anterior uveal tract, chorioretinal zone, or optic nerve. In fact, onchocerciasis, or river blindness, is the leading cause of blindness in the world.2 The host immune response also is responsible for the dermatologic manifestations of this disease. In addition to the dermatologic manifestations already mentioned, others include epidermal atrophy, ulcerations, femoral or inguinal lymphadenitis, lymphedema, and/or general wasting in more severe long-standing infections. Additionally, patients may experience systemic signs resulting from an underlying O volvulus infection.8 Our patient demonstrated a subjectively remarkable systemic response manifested by shortness of breath, dyspnea, cough, and palpitations, likely the result of her existing filarial infection.
Diagnosis of onchocerciasis is made by identification of microfilariae or adult worms in skin snips or punch biopsies. Histopathologic analysis of onchocerciasis has been described as several adult worms in the subcutaneous tissue surrounded by a granulomatous, fibrotic, calcified, or sometimes ossified inflammatory reaction.8 Microfilariae may migrate to the upper dermis and typically are surrounded by lymphocytes, histiocytes, plasma cells, and eosinophils with an absence of neutrophils,5,8 which directly causes the overlying epidermis to undergo reactive changes. Measurement of filarial nematodes often helps differentiate species. For example, O volvulus typically measures 230 to 500 mm in length for females and 16 to 42 mm in length for males.8 The thickness of cuticles typically measures 4 to 8 µm for females and 3 to 5 µm for males. Microfilariae of O volvulus also have been identified in patient’s sputum, urine, blood, and spinal fluid.8 An alternative diagnostic method described by Stingl et al9 is a diethylcarbamazine (DEC) patch test that was 92% accurate in onchocerciasis cases diagnosed by skin snip analysis.9 Therefore, this test may be a practical alternative when skin specimens are inconclusive.
Management of onchocerciasis should include excision of subcutaneous nodules to remove adult worms. In the past, DEC with suramin was prescribed and kills both microfilariae and adult worms.8 However, DEC may induce pruritus, chorioretinal damage, and optic neuritis and suramin is nephrotoxic.2 Therefore, oral ivermectin (0.15–0.20 mg/kg one-time dose, may be repeated in 3–12 months) is supported to be a less harmful option. Patients treated with ivermectin have a decreased risk for transmitting infection to the blackfly vector for up to 6 months after treatment, and it is a more effective microfilaricidal agent than DEC.2,3 Oral doxycycline (100 mg/d for 6 weeks) commonly is added as adjuvant therapy because it kills Wolbachia species, a bacterium that is needed for O volvulus reproduction.3
Although rare in the United States, cutaneous filariasis has become a prevalent public health concern, especially in tropical countries. Individuals with chronic cutaneous filarial infections are at increased risk for debilitating complications that negatively affect their quality of life and productivity. Although the World Health Organization has attempted to eradicate cutaneous filarial infections by mass drug administration, transmission of these diseases remains a challenge. Further research on treatment and methods to prevent transmission by controlling arthropod vectors is required to avoid short-term and long-term health consequences caused by cutaneous filariasis.
Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel to foreign countries located in Africa, Central America, and South America. Dermatologists in the United States should increase familiarity with these infections because of increased travel, economic globalization, and the impact of global climate change on the geographic distribution of vector arthropods. To control these infections, research efforts should focus on improved sanitation; drug treatment; transmission prevention; and improved education of their clinical manifestations, especially mucocutaneous signs.
- Mendoza N, Li A, Gill A, et al. Filariasis: diagnosis and treatment. Dermatol Ther. 2009;22:475-490.
- Maso MJ, Kapila R, Schwartz RA, et al. Cutaneous onchocerciasis. Int J Dermatol. 1987;26:593-596.
- Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections. J Am Acad Dermatol. 2015;73:929-944.
- Bolivar-Meija A, Alarcon-Olave C, Rodriguez-Morales AJ. Skin manifestations of arthropod-borne infection in Latin America. Curr Opin. 2014;27:288-294.
- Okulicz JF, Stibich AS, Elston DM, et al. Cutaneous onchocercoma. Int J Dermatol. 2004;43:170-172.
- Nguyen JC, Murphy ME, Nutman TB, et al. Cutaneous onchocerciasis in an American traveler. Int Soc Dermatol. 2005;44:125-128.
- Toovey S, Moerman F, van Gompel A. Special infectious disease risks of expatriates and long-term travelers in tropical countries part II: infections other than malaria. J Travel Med. 2007;14:50-60.
- Meyers WM, Neafie RC, Connor DH. Bancroftian and malayan filariasis. In Binford CH, ed. Pathology of Tropical and Extraordinary Diseases. Vol 2. Fort Sam Houston, TX: Armed Forces Institute of Pathology; 1976:340-355.
- Stingl P, Ross M, Gibson DW, et al. A diagnostic “patch-test” for onchocerciasis using topical diethylcarbamazine. Trans R Soc Trop Med Hyg.
To the Editor:
Cutaneous filariasis is a group of infectious diseases caused by more than 60 different nematode species and endemic to approximately 83 countries.1,2 These infections are transmitted to humans by vectors such as mosquitoes, blackflies, biting midges, or Tabanid flies.1 The blood meal taken by vectors allow microfilariae to enter the skin and develop into adult worms.1-3 It is postulated that filarial infections were first described in 2000
Filarial parasites have been categorized into groups based on the site of adult worm stage habitat. The cutaneous group includes Loa loa, Onchocerca volvulus, Mansonella perstans, and Dipetalonema streptocerca. The lymphatic group includes Wuchereria bancrofti, Brugia malayi, and Brugia timori. Lastly, the body cavity group includes Mansonella ozzardi. Because humidity is required for survival of the infective larval stage, individuals from tropical countries in Africa, Central America, and South America most commonly are affected.1 These diseases also are related to poor housing quality and inadequate sanitation.1,3,4 Travel for business, medical missions, pleasure, or emigration has caused increased filarial infections globally. In fact, dermatologic disorders with infectious etiologies cause approximately 17% of travelers to seek medical attention.3
Dermatologic manifestations indicative of a potential cutaneous filarial infection include papules, nodules, excoriations with secondary xerosis, lichenification, skin pigment changes, and/or severe pruritus. However, individuals from filarial endemic regions may not demonstrate any clinical signs or symptoms, despite having microfilariae in their blood,1 which enables the disease to propagate and poses a major public health concern. In fact, patients with chronic filarial infections are at increased risk for developing lymphedema, elephantiasis, or blindness, which are hypothesized to be the second largest cause of permanent disability worldwide.1 Although rarely seen in US citizens, cutaneous filariasis should always be a diagnostic consideration in patients who present with a pruritic eruption and have a travel history to tropical countries. We report a case of cutaneous onchocerciasis in a US citizen who developed a pruritic eczematous eruption on the right upper arm following an arthropod assault while working in an Onchocerca endemic region approximately 1.5 years prior.
A 33-year-old woman presented to our outpatient dermatology clinic with the chief concern of a pruritic rash on the right arm (Figure 1). She revealed a history of travel to Peru, associated symptoms, prior diagnoses, and attempted treatment regimens. Over a 1.5-year period, the patient traveled for work-related reasons to Madre de Dios, Peru. During that time, the patient experienced 2 bouts of severe abdominal pain, nausea, and vomiting that she attributed to poor food and water quality. She did not immediately seek medical attention. She also developed skin manifestations that began as a pruritic and irritating pinpoint-sized red papule on the right eyelid, possibly a site of an arthropod assault. She then experienced episodic eyelash loss (Figure 2) and subsequent vision changes, including blurry vision, halos around lights, and dimming around the periphery. When the patient developed circular, pink, pruritic plaques on the right upper extremity, she sought medical attention in Lima, Peru. She was diagnosed with tinea corporis and prescribed an oral antibiotic and topical antifungal.
This treatment regimen did not result in improvement. In the following months, the patient noticed worsening of the ocular symptoms, and she developed a dry cough with occasional dyspnea. She again sought medical attention in Peru and was referred to an ophthalmologist who suspected Demodex mite or fungal infection; however, workup for those pathologies was negative. The respiratory symptoms continued to worsen, particularly at night, and she began to experience palpitations.
Upon returning to the United States, the patient was evaluated by her primary care physician who ordered the following laboratory tests: a complete blood cell count with differential, comprehensive metabolic panel, vitamin D level, blood culture, lipid panel, ferritin level, and thyroid function. An electrocardiogram, throat culture, and stool culture for ova and parasites also were obtained. The electrocardiogram showed sinus tachycardia, and the stool culture revealed blastocystis, for which she was prescribed oral metronidazole and tinidazole. The other results were within reference range, and the throat culture showed normal oropharyngeal microbes.
A few days after the treatment for the blastocystis, the gastrointestinal tract symptoms improved, but dermatologic, ocular, pulmonary, and cardiac symptoms persisted. She also began experiencing night sweats and hot flashes. In between visits to the primary care physician, she sought medical attention at an urgent care clinic for worsening pulmonary and cardiac symptoms. At that time, results of a chest radiograph were normal.
The primary care physician referred her to infectious disease and dermatology for further evaluation within a few weeks of returning to the United States. Upon presentation to dermatology, the patient described a waxing and waning nature to the rash on the arm with associated intermittent pain. Physical examination revealed several erythematous patches on the triceps and a 1-cm subcutaneous nodule on the right elbow with overlying skin discoloration. The patient stated that she first noticed the inflamed painful nodule when she returned to the United States. Since its discovery, the nodule increased in size and became firm. The patient also described occasional limited range of motion of the right arm due to the discomfort of the rash and inflamed nodule. Interestingly, the patient’s partner who accompanied her to Peru also developed a similar pruritic rash on the chest. He was evaluated by dermatology and infectious disease; however, biopsies of his rash performed at a different practice revealed nonspecific results. Due to her partner’s inconclusive results, our patient initially refused a biopsy; however, she returned to the office after 1 week with worsening symptoms, and a 4-mm punch biopsy of the right arm was obtained in addition to rapid plasma reagin and QuantiFERON-TB Gold test.
Based on the patient’s travel history, clinical course, and physical examination, the clinical differential diagnosis included nummular dermatitis, panniculitis/nodular vasculitis, tinea corporis, secondary syphilis, pinta, tuberculosis, or cutaneous filariasis. Rapid plasma reagin and QuantiFERON-TB Gold test results were negative, and a periodic acid–Schiff stain of the biopsy was negative for fungal elements. Dermatopathology revealed intradermal filarial nematodes of 120 to 150 µm in diameter and 1-to 2-mm cuticles eliciting a predominantly superficial and deep lymphohistiocytic reaction (Figure 3). The histopathologic differential diagnosis based on the diameter of the nematode included M perstans, W bancrofti, and O volvulus. Clinical correlation was highly recommended to obtain a final diagnosis and management plan. A portion of the biopsy was sent to the Centers for Disease Control and Prevention, which confirmed the presence of a filarial nematode consistent with a zoonotic Brugia but also with zoonotic Onchocerca as a possible differential. Therefore, considering the history, clinical course, and histopathologic analysis, the final diagnosis of cutaneous onchocerciasis was made.
The patient was referred back to infectious disease and started on combination therapy of ivermectin (25.5 mg) plus albendazole (800 mg) taken at once followed by doxycycline (200 mg) for 6 weeks. The symptoms initially worsened, then she experienced near-complete resolution of dermatologic, pulmonary, and ocular symptoms after approximately 2 weeks of treatment. She continued to report fatigue and palpitations, for she continued to see a cardiologist. We highly encouraged her to continue following up with infectious disease to ensure complete eradication of the infection.
Onchocerciasis is common in individuals who live or work in equatorial Africa, Central America, and South America. The disease process has dermatologic, ocular, and other systemic manifestations if the infection continues long-term without treatment.2,5 Although rare, this infection has been observed in US citizens who have traveled to filarial endemic regions for a period of time ranging from 2 weeks to 39 years.2,6,7
Blackflies (genus Simulium), the intermediate host of O volvulus, breed in areas close to freely flowing water. The blackfly bites a human host, and within 7 days the microfilariae undergo 2 molts to reach the infective stage. The larvae remain in the dermis and subcutaneous tissue for 2 additional molts until they develop into adult worms. Then, adult worms may become encapsulated, eliciting and forming subcutaneous nodules, also known as onchocercomas.2,3
A fertilized female in the subcutaneous tissue releases microfilariae that may remain in the skin or travel to the eyes of the host.3 The host may demonstrate signs of infection within 3 to 15 months.2 Most commonly, patients report localized or generalized pruritus, and one extremity develops swelling, papules, lymphadenopathy, and alterations of skin pigment (hypopigmentation or hyperpigmentation).5-8 Our patient developed a pruritic eczematous eruption that only affected her right arm with an inflamed firm nodule overlying the elbow, a suspected onchocercoma. Onchocercomas are the direct result of adult worms coiled in the dermis, subcutaneous tissue, and deep fascia. These commonly are found in close proximity to bony prominences with the specific location pending the geographic area of infection.8 For example, onchocercomas more commonly are found over bony prominences in the head and upper body region in patients who acquired the disease from Central or South America, whereas individuals infected in Africa more commonly develop onchocercomas near the femoral, coccyx, or sacral regions.2
The immune response mounted by the infected host is responsible for the ocular signs and symptoms.2 Specifically, the inflammatory reaction may impact the patient’s cornea, anterior uveal tract, chorioretinal zone, or optic nerve. In fact, onchocerciasis, or river blindness, is the leading cause of blindness in the world.2 The host immune response also is responsible for the dermatologic manifestations of this disease. In addition to the dermatologic manifestations already mentioned, others include epidermal atrophy, ulcerations, femoral or inguinal lymphadenitis, lymphedema, and/or general wasting in more severe long-standing infections. Additionally, patients may experience systemic signs resulting from an underlying O volvulus infection.8 Our patient demonstrated a subjectively remarkable systemic response manifested by shortness of breath, dyspnea, cough, and palpitations, likely the result of her existing filarial infection.
Diagnosis of onchocerciasis is made by identification of microfilariae or adult worms in skin snips or punch biopsies. Histopathologic analysis of onchocerciasis has been described as several adult worms in the subcutaneous tissue surrounded by a granulomatous, fibrotic, calcified, or sometimes ossified inflammatory reaction.8 Microfilariae may migrate to the upper dermis and typically are surrounded by lymphocytes, histiocytes, plasma cells, and eosinophils with an absence of neutrophils,5,8 which directly causes the overlying epidermis to undergo reactive changes. Measurement of filarial nematodes often helps differentiate species. For example, O volvulus typically measures 230 to 500 mm in length for females and 16 to 42 mm in length for males.8 The thickness of cuticles typically measures 4 to 8 µm for females and 3 to 5 µm for males. Microfilariae of O volvulus also have been identified in patient’s sputum, urine, blood, and spinal fluid.8 An alternative diagnostic method described by Stingl et al9 is a diethylcarbamazine (DEC) patch test that was 92% accurate in onchocerciasis cases diagnosed by skin snip analysis.9 Therefore, this test may be a practical alternative when skin specimens are inconclusive.
Management of onchocerciasis should include excision of subcutaneous nodules to remove adult worms. In the past, DEC with suramin was prescribed and kills both microfilariae and adult worms.8 However, DEC may induce pruritus, chorioretinal damage, and optic neuritis and suramin is nephrotoxic.2 Therefore, oral ivermectin (0.15–0.20 mg/kg one-time dose, may be repeated in 3–12 months) is supported to be a less harmful option. Patients treated with ivermectin have a decreased risk for transmitting infection to the blackfly vector for up to 6 months after treatment, and it is a more effective microfilaricidal agent than DEC.2,3 Oral doxycycline (100 mg/d for 6 weeks) commonly is added as adjuvant therapy because it kills Wolbachia species, a bacterium that is needed for O volvulus reproduction.3
Although rare in the United States, cutaneous filariasis has become a prevalent public health concern, especially in tropical countries. Individuals with chronic cutaneous filarial infections are at increased risk for debilitating complications that negatively affect their quality of life and productivity. Although the World Health Organization has attempted to eradicate cutaneous filarial infections by mass drug administration, transmission of these diseases remains a challenge. Further research on treatment and methods to prevent transmission by controlling arthropod vectors is required to avoid short-term and long-term health consequences caused by cutaneous filariasis.
Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel to foreign countries located in Africa, Central America, and South America. Dermatologists in the United States should increase familiarity with these infections because of increased travel, economic globalization, and the impact of global climate change on the geographic distribution of vector arthropods. To control these infections, research efforts should focus on improved sanitation; drug treatment; transmission prevention; and improved education of their clinical manifestations, especially mucocutaneous signs.
To the Editor:
Cutaneous filariasis is a group of infectious diseases caused by more than 60 different nematode species and endemic to approximately 83 countries.1,2 These infections are transmitted to humans by vectors such as mosquitoes, blackflies, biting midges, or Tabanid flies.1 The blood meal taken by vectors allow microfilariae to enter the skin and develop into adult worms.1-3 It is postulated that filarial infections were first described in 2000
Filarial parasites have been categorized into groups based on the site of adult worm stage habitat. The cutaneous group includes Loa loa, Onchocerca volvulus, Mansonella perstans, and Dipetalonema streptocerca. The lymphatic group includes Wuchereria bancrofti, Brugia malayi, and Brugia timori. Lastly, the body cavity group includes Mansonella ozzardi. Because humidity is required for survival of the infective larval stage, individuals from tropical countries in Africa, Central America, and South America most commonly are affected.1 These diseases also are related to poor housing quality and inadequate sanitation.1,3,4 Travel for business, medical missions, pleasure, or emigration has caused increased filarial infections globally. In fact, dermatologic disorders with infectious etiologies cause approximately 17% of travelers to seek medical attention.3
Dermatologic manifestations indicative of a potential cutaneous filarial infection include papules, nodules, excoriations with secondary xerosis, lichenification, skin pigment changes, and/or severe pruritus. However, individuals from filarial endemic regions may not demonstrate any clinical signs or symptoms, despite having microfilariae in their blood,1 which enables the disease to propagate and poses a major public health concern. In fact, patients with chronic filarial infections are at increased risk for developing lymphedema, elephantiasis, or blindness, which are hypothesized to be the second largest cause of permanent disability worldwide.1 Although rarely seen in US citizens, cutaneous filariasis should always be a diagnostic consideration in patients who present with a pruritic eruption and have a travel history to tropical countries. We report a case of cutaneous onchocerciasis in a US citizen who developed a pruritic eczematous eruption on the right upper arm following an arthropod assault while working in an Onchocerca endemic region approximately 1.5 years prior.
A 33-year-old woman presented to our outpatient dermatology clinic with the chief concern of a pruritic rash on the right arm (Figure 1). She revealed a history of travel to Peru, associated symptoms, prior diagnoses, and attempted treatment regimens. Over a 1.5-year period, the patient traveled for work-related reasons to Madre de Dios, Peru. During that time, the patient experienced 2 bouts of severe abdominal pain, nausea, and vomiting that she attributed to poor food and water quality. She did not immediately seek medical attention. She also developed skin manifestations that began as a pruritic and irritating pinpoint-sized red papule on the right eyelid, possibly a site of an arthropod assault. She then experienced episodic eyelash loss (Figure 2) and subsequent vision changes, including blurry vision, halos around lights, and dimming around the periphery. When the patient developed circular, pink, pruritic plaques on the right upper extremity, she sought medical attention in Lima, Peru. She was diagnosed with tinea corporis and prescribed an oral antibiotic and topical antifungal.
This treatment regimen did not result in improvement. In the following months, the patient noticed worsening of the ocular symptoms, and she developed a dry cough with occasional dyspnea. She again sought medical attention in Peru and was referred to an ophthalmologist who suspected Demodex mite or fungal infection; however, workup for those pathologies was negative. The respiratory symptoms continued to worsen, particularly at night, and she began to experience palpitations.
Upon returning to the United States, the patient was evaluated by her primary care physician who ordered the following laboratory tests: a complete blood cell count with differential, comprehensive metabolic panel, vitamin D level, blood culture, lipid panel, ferritin level, and thyroid function. An electrocardiogram, throat culture, and stool culture for ova and parasites also were obtained. The electrocardiogram showed sinus tachycardia, and the stool culture revealed blastocystis, for which she was prescribed oral metronidazole and tinidazole. The other results were within reference range, and the throat culture showed normal oropharyngeal microbes.
A few days after the treatment for the blastocystis, the gastrointestinal tract symptoms improved, but dermatologic, ocular, pulmonary, and cardiac symptoms persisted. She also began experiencing night sweats and hot flashes. In between visits to the primary care physician, she sought medical attention at an urgent care clinic for worsening pulmonary and cardiac symptoms. At that time, results of a chest radiograph were normal.
The primary care physician referred her to infectious disease and dermatology for further evaluation within a few weeks of returning to the United States. Upon presentation to dermatology, the patient described a waxing and waning nature to the rash on the arm with associated intermittent pain. Physical examination revealed several erythematous patches on the triceps and a 1-cm subcutaneous nodule on the right elbow with overlying skin discoloration. The patient stated that she first noticed the inflamed painful nodule when she returned to the United States. Since its discovery, the nodule increased in size and became firm. The patient also described occasional limited range of motion of the right arm due to the discomfort of the rash and inflamed nodule. Interestingly, the patient’s partner who accompanied her to Peru also developed a similar pruritic rash on the chest. He was evaluated by dermatology and infectious disease; however, biopsies of his rash performed at a different practice revealed nonspecific results. Due to her partner’s inconclusive results, our patient initially refused a biopsy; however, she returned to the office after 1 week with worsening symptoms, and a 4-mm punch biopsy of the right arm was obtained in addition to rapid plasma reagin and QuantiFERON-TB Gold test.
Based on the patient’s travel history, clinical course, and physical examination, the clinical differential diagnosis included nummular dermatitis, panniculitis/nodular vasculitis, tinea corporis, secondary syphilis, pinta, tuberculosis, or cutaneous filariasis. Rapid plasma reagin and QuantiFERON-TB Gold test results were negative, and a periodic acid–Schiff stain of the biopsy was negative for fungal elements. Dermatopathology revealed intradermal filarial nematodes of 120 to 150 µm in diameter and 1-to 2-mm cuticles eliciting a predominantly superficial and deep lymphohistiocytic reaction (Figure 3). The histopathologic differential diagnosis based on the diameter of the nematode included M perstans, W bancrofti, and O volvulus. Clinical correlation was highly recommended to obtain a final diagnosis and management plan. A portion of the biopsy was sent to the Centers for Disease Control and Prevention, which confirmed the presence of a filarial nematode consistent with a zoonotic Brugia but also with zoonotic Onchocerca as a possible differential. Therefore, considering the history, clinical course, and histopathologic analysis, the final diagnosis of cutaneous onchocerciasis was made.
The patient was referred back to infectious disease and started on combination therapy of ivermectin (25.5 mg) plus albendazole (800 mg) taken at once followed by doxycycline (200 mg) for 6 weeks. The symptoms initially worsened, then she experienced near-complete resolution of dermatologic, pulmonary, and ocular symptoms after approximately 2 weeks of treatment. She continued to report fatigue and palpitations, for she continued to see a cardiologist. We highly encouraged her to continue following up with infectious disease to ensure complete eradication of the infection.
Onchocerciasis is common in individuals who live or work in equatorial Africa, Central America, and South America. The disease process has dermatologic, ocular, and other systemic manifestations if the infection continues long-term without treatment.2,5 Although rare, this infection has been observed in US citizens who have traveled to filarial endemic regions for a period of time ranging from 2 weeks to 39 years.2,6,7
Blackflies (genus Simulium), the intermediate host of O volvulus, breed in areas close to freely flowing water. The blackfly bites a human host, and within 7 days the microfilariae undergo 2 molts to reach the infective stage. The larvae remain in the dermis and subcutaneous tissue for 2 additional molts until they develop into adult worms. Then, adult worms may become encapsulated, eliciting and forming subcutaneous nodules, also known as onchocercomas.2,3
A fertilized female in the subcutaneous tissue releases microfilariae that may remain in the skin or travel to the eyes of the host.3 The host may demonstrate signs of infection within 3 to 15 months.2 Most commonly, patients report localized or generalized pruritus, and one extremity develops swelling, papules, lymphadenopathy, and alterations of skin pigment (hypopigmentation or hyperpigmentation).5-8 Our patient developed a pruritic eczematous eruption that only affected her right arm with an inflamed firm nodule overlying the elbow, a suspected onchocercoma. Onchocercomas are the direct result of adult worms coiled in the dermis, subcutaneous tissue, and deep fascia. These commonly are found in close proximity to bony prominences with the specific location pending the geographic area of infection.8 For example, onchocercomas more commonly are found over bony prominences in the head and upper body region in patients who acquired the disease from Central or South America, whereas individuals infected in Africa more commonly develop onchocercomas near the femoral, coccyx, or sacral regions.2
The immune response mounted by the infected host is responsible for the ocular signs and symptoms.2 Specifically, the inflammatory reaction may impact the patient’s cornea, anterior uveal tract, chorioretinal zone, or optic nerve. In fact, onchocerciasis, or river blindness, is the leading cause of blindness in the world.2 The host immune response also is responsible for the dermatologic manifestations of this disease. In addition to the dermatologic manifestations already mentioned, others include epidermal atrophy, ulcerations, femoral or inguinal lymphadenitis, lymphedema, and/or general wasting in more severe long-standing infections. Additionally, patients may experience systemic signs resulting from an underlying O volvulus infection.8 Our patient demonstrated a subjectively remarkable systemic response manifested by shortness of breath, dyspnea, cough, and palpitations, likely the result of her existing filarial infection.
Diagnosis of onchocerciasis is made by identification of microfilariae or adult worms in skin snips or punch biopsies. Histopathologic analysis of onchocerciasis has been described as several adult worms in the subcutaneous tissue surrounded by a granulomatous, fibrotic, calcified, or sometimes ossified inflammatory reaction.8 Microfilariae may migrate to the upper dermis and typically are surrounded by lymphocytes, histiocytes, plasma cells, and eosinophils with an absence of neutrophils,5,8 which directly causes the overlying epidermis to undergo reactive changes. Measurement of filarial nematodes often helps differentiate species. For example, O volvulus typically measures 230 to 500 mm in length for females and 16 to 42 mm in length for males.8 The thickness of cuticles typically measures 4 to 8 µm for females and 3 to 5 µm for males. Microfilariae of O volvulus also have been identified in patient’s sputum, urine, blood, and spinal fluid.8 An alternative diagnostic method described by Stingl et al9 is a diethylcarbamazine (DEC) patch test that was 92% accurate in onchocerciasis cases diagnosed by skin snip analysis.9 Therefore, this test may be a practical alternative when skin specimens are inconclusive.
Management of onchocerciasis should include excision of subcutaneous nodules to remove adult worms. In the past, DEC with suramin was prescribed and kills both microfilariae and adult worms.8 However, DEC may induce pruritus, chorioretinal damage, and optic neuritis and suramin is nephrotoxic.2 Therefore, oral ivermectin (0.15–0.20 mg/kg one-time dose, may be repeated in 3–12 months) is supported to be a less harmful option. Patients treated with ivermectin have a decreased risk for transmitting infection to the blackfly vector for up to 6 months after treatment, and it is a more effective microfilaricidal agent than DEC.2,3 Oral doxycycline (100 mg/d for 6 weeks) commonly is added as adjuvant therapy because it kills Wolbachia species, a bacterium that is needed for O volvulus reproduction.3
Although rare in the United States, cutaneous filariasis has become a prevalent public health concern, especially in tropical countries. Individuals with chronic cutaneous filarial infections are at increased risk for debilitating complications that negatively affect their quality of life and productivity. Although the World Health Organization has attempted to eradicate cutaneous filarial infections by mass drug administration, transmission of these diseases remains a challenge. Further research on treatment and methods to prevent transmission by controlling arthropod vectors is required to avoid short-term and long-term health consequences caused by cutaneous filariasis.
Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel to foreign countries located in Africa, Central America, and South America. Dermatologists in the United States should increase familiarity with these infections because of increased travel, economic globalization, and the impact of global climate change on the geographic distribution of vector arthropods. To control these infections, research efforts should focus on improved sanitation; drug treatment; transmission prevention; and improved education of their clinical manifestations, especially mucocutaneous signs.
- Mendoza N, Li A, Gill A, et al. Filariasis: diagnosis and treatment. Dermatol Ther. 2009;22:475-490.
- Maso MJ, Kapila R, Schwartz RA, et al. Cutaneous onchocerciasis. Int J Dermatol. 1987;26:593-596.
- Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections. J Am Acad Dermatol. 2015;73:929-944.
- Bolivar-Meija A, Alarcon-Olave C, Rodriguez-Morales AJ. Skin manifestations of arthropod-borne infection in Latin America. Curr Opin. 2014;27:288-294.
- Okulicz JF, Stibich AS, Elston DM, et al. Cutaneous onchocercoma. Int J Dermatol. 2004;43:170-172.
- Nguyen JC, Murphy ME, Nutman TB, et al. Cutaneous onchocerciasis in an American traveler. Int Soc Dermatol. 2005;44:125-128.
- Toovey S, Moerman F, van Gompel A. Special infectious disease risks of expatriates and long-term travelers in tropical countries part II: infections other than malaria. J Travel Med. 2007;14:50-60.
- Meyers WM, Neafie RC, Connor DH. Bancroftian and malayan filariasis. In Binford CH, ed. Pathology of Tropical and Extraordinary Diseases. Vol 2. Fort Sam Houston, TX: Armed Forces Institute of Pathology; 1976:340-355.
- Stingl P, Ross M, Gibson DW, et al. A diagnostic “patch-test” for onchocerciasis using topical diethylcarbamazine. Trans R Soc Trop Med Hyg.
- Mendoza N, Li A, Gill A, et al. Filariasis: diagnosis and treatment. Dermatol Ther. 2009;22:475-490.
- Maso MJ, Kapila R, Schwartz RA, et al. Cutaneous onchocerciasis. Int J Dermatol. 1987;26:593-596.
- Lupi O, Downing C, Lee M, et al. Mucocutaneous manifestations of helminth infections. J Am Acad Dermatol. 2015;73:929-944.
- Bolivar-Meija A, Alarcon-Olave C, Rodriguez-Morales AJ. Skin manifestations of arthropod-borne infection in Latin America. Curr Opin. 2014;27:288-294.
- Okulicz JF, Stibich AS, Elston DM, et al. Cutaneous onchocercoma. Int J Dermatol. 2004;43:170-172.
- Nguyen JC, Murphy ME, Nutman TB, et al. Cutaneous onchocerciasis in an American traveler. Int Soc Dermatol. 2005;44:125-128.
- Toovey S, Moerman F, van Gompel A. Special infectious disease risks of expatriates and long-term travelers in tropical countries part II: infections other than malaria. J Travel Med. 2007;14:50-60.
- Meyers WM, Neafie RC, Connor DH. Bancroftian and malayan filariasis. In Binford CH, ed. Pathology of Tropical and Extraordinary Diseases. Vol 2. Fort Sam Houston, TX: Armed Forces Institute of Pathology; 1976:340-355.
- Stingl P, Ross M, Gibson DW, et al. A diagnostic “patch-test” for onchocerciasis using topical diethylcarbamazine. Trans R Soc Trop Med Hyg.
Practice Points
- Parasitic infections should always be a diagnostic consideration in individuals who present with a pruritic eruption and a history of travel.
- To control parasitic infections, research efforts should focus on improved sanitation, drug treatment, transmission prevention, and improved education of clinical manifestations to increase early detection.
The Dermatologist Nose Best: Correlation of Nose-Picking Habits and <i>Staphylococcus aureus</i>–Related Dermatologic Disease
Primitive human habits have withstood the test of time but can pose health risks. Exploring a nasal cavity with a finger might have first occurred shortly after whichever species first developed a nasal opening and a digit able to reach it. Humans have been keen on continuing the long-standing yet taboo habit of nose-picking (rhinotillexis).
Even though nose-picking is stigmatized, anonymous surveys show that almost all adolescents and adults do it.1 People are typically unaware of the risks of regular rhinotillexis. Studies exploring the intranasal human microbiome have elicited asymptomatic yet potential disease-causing microbes, including the notorious bacterium Staphylococcus aureus. As many as 30% of humans are asymptomatically permanently colonized with S aureus in their anterior nares.2 These natural reservoirs can be the source of opportunistic infection that increases morbidity, mortality, and overall health care costs.
With the rise of antimicrobial resistance, especially methicillin-resistant S aureus (MRSA), a more direct approach might be necessary to curb nasally sourced cutaneous infection. Since dermatology patients deal with a wide array of skin barrier defects that put them at risk for S aureus–related infection, a medical provider’s understanding about the role of nasal colonization and transmission is important. Addressing the awkward question of “Do you pick your nose?” and providing education on the topic might be uncomfortable, but it might be necessary for dermatology patients at risk for S aureus–related cutaneous disease.
Staphylococcus aureus colonizes the anterior nares of 20% to 80% of humans; nasal colonization can begin during the first days of life.2 The anterior nares are noted as the main reservoir of chronic carriage of S aureus, but carriage can occur at various body sites, including the rectum, vagina, gastrointestinal tract, and axilla, as well as other cutaneous sites. Hands are noted as the main vector of S aureus transmission from source to nose; a positive correlation between nose-picking habits and nasal carriage of S aureus has been noted.2
The percentage of S aureus–colonized humans who harbor MRSA is unknown, but it is a topic of concern with the rise of MRSA-related infection. Multisite MRSA carriage increases the risk for nasal MRSA colonization, and nasal MRSA has been noted to be more difficult to decolonize than nonresistant strains. Health care workers carrying S aureus can trigger a potential hospital outbreak of MRSA. Studies have shown that bacterial transmission is increased 40-fold when the nasal host is co-infected by rhinovirus.2 Health care workers can be a source of MRSA during outbreaks, but they have not been shown to be more likely to carry MRSA than the general population.2 Understanding which patients might be at risk for S aureus–associated disease in dermatology can lead clinicians to consider decolonization strategies.
Nasal colonization has been noted more frequently in patients with predisposing risk factors, including human immunodeficiency virus infection, obesity, diabetes mellitus, granulomatosis with polyangiitis, HLA-DR3 phenotype, skin and soft-tissue infections, atopic dermatitis, impetigo, and recurrent furunculosis.2Staphylococcus aureus is the most frequently noted pathogen in diabetic foot infection. A study found that 36% of sampled diabetic foot-infection patients also had S aureus isolated from both nares and the foot wound, with 65% of isolated strains being identical.2 Although there are clear data on decolonization of patients prior to heart and orthopedic surgery, more data are needed to determine the benefit of screening and treating nasal carriers in populations with diabetic foot ulcers.
Staphylococcus aureus nasal colonization also has been shown in approximately 60% of patients with recurrent furunculosis and impetigo.2 Although it is clear that there is a correlation between S aureus–related skin infection and nasal colonization, it is unclear what role nose-picking might have in perpetuating these complications.
There are multiple approaches to S aureus decolonization, including intranasal mupirocin, chlorhexidine body wipes, bleach baths, and even oral antibiotics (eg, trimethoprim-sulfamethoxazole, clindamycin). The Infectious Diseases Society of America has published guidelines for treating recurrent MRSA infection, including 5 to 10 days of intranasal mupirocin plus either body decolonization with a daily chlorhexidine wash for 5 to 14 days or a 15-minute dilute bleach bath twice weekly for 3 months.3,4
There are ample meta-analyses and systematic reviews regarding S aureus decolonization and management in patients undergoing dialysis or surgery but limited data when it comes to this topic in dermatology. Those limited studies do show a benefit to decolonization in several diseases, including atopic dermatitis, hand dermatitis, recurrent skin and soft-tissue infections, cutaneous T-cell lymphoma, and surgical infection following Mohs micrographic surgery.4 Typically, it also is necessary to treat those who might come in contact with the patient or caregiver; in theory, treating contacts helps reduce the chance that the patient will become recolonized shortly afterward, but the data are limited regarding long-term colonization status following treatment. Contact surfaces, especially cell phones, are noted to be a contributing factor to nares colonization; therefore, it also may be necessary to educate patients on surface-cleaning techniques.5 Because there are multiple sources of S aureus that patients can come in contact with after decolonization attempts, a nose-picking habit might play a vital role in recolonization.
Due to rising bacterial resistance to mupirocin and chlorhexidine decolonization strategies, there is a growing need for more effective, long-term decolonization strategies.4 These strategies must address patients’ environmental exposure and nasal-touching habits. Overcoming the habit of nose-picking might aid S aureus decolonization strategies and thus aid in preventing future antimicrobial resistance.
But are at-risk patients receiving sufficient screening and education on the dangers of a nose-picking habit? Effective strategies to assess these practices and recommend the discontinuation of the habit could have positive effects in maintaining long-term decolonization. Potential euphemistic ways to approach this somewhat taboo topic include questions that elicit information on whether the patient ever touches the inside of his/her nose, washes his/her hands before and after touching the inside of the nose, knows about transfer of bacteria from hand to nose, or understands what decolonization is doing for them. The patient might be inclined to deny such activity, but education on nasal hygiene should be provided regardless, especially in pediatric patients.
Staphylococcus aureus might be a normal human nasal inhabitant, but it can cause a range of problems for dermatologic disease. Although pharmacotherapeutic decolonization strategies can have a positive effect on dermatologic disease, growing antibiotic resistance calls for health care providers to assess patients’ nose picking-habits and educate them on effective ways to prevent finger-to-nose practices.
- Andrade C, Srihari BS. A preliminary survey of rhinotillexomania in an adolescent sample. J Clin Psychiatry. 2001;62:426-431.
- Sakr A, Brégeon F, Mège J-L, et al. Staphylococcus aureus nasal colonization: an update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285-292.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in healthcare: a dermatology perspective. J Healthc Eng. 2018;2018:2382050.
- Creech CB, Al-Zubeidi DN, Fritz SA. Prevention of recurrent staphylococcal kin infections. Infect Dis Clin North Am. 2015;29:429-464.
Primitive human habits have withstood the test of time but can pose health risks. Exploring a nasal cavity with a finger might have first occurred shortly after whichever species first developed a nasal opening and a digit able to reach it. Humans have been keen on continuing the long-standing yet taboo habit of nose-picking (rhinotillexis).
Even though nose-picking is stigmatized, anonymous surveys show that almost all adolescents and adults do it.1 People are typically unaware of the risks of regular rhinotillexis. Studies exploring the intranasal human microbiome have elicited asymptomatic yet potential disease-causing microbes, including the notorious bacterium Staphylococcus aureus. As many as 30% of humans are asymptomatically permanently colonized with S aureus in their anterior nares.2 These natural reservoirs can be the source of opportunistic infection that increases morbidity, mortality, and overall health care costs.
With the rise of antimicrobial resistance, especially methicillin-resistant S aureus (MRSA), a more direct approach might be necessary to curb nasally sourced cutaneous infection. Since dermatology patients deal with a wide array of skin barrier defects that put them at risk for S aureus–related infection, a medical provider’s understanding about the role of nasal colonization and transmission is important. Addressing the awkward question of “Do you pick your nose?” and providing education on the topic might be uncomfortable, but it might be necessary for dermatology patients at risk for S aureus–related cutaneous disease.
Staphylococcus aureus colonizes the anterior nares of 20% to 80% of humans; nasal colonization can begin during the first days of life.2 The anterior nares are noted as the main reservoir of chronic carriage of S aureus, but carriage can occur at various body sites, including the rectum, vagina, gastrointestinal tract, and axilla, as well as other cutaneous sites. Hands are noted as the main vector of S aureus transmission from source to nose; a positive correlation between nose-picking habits and nasal carriage of S aureus has been noted.2
The percentage of S aureus–colonized humans who harbor MRSA is unknown, but it is a topic of concern with the rise of MRSA-related infection. Multisite MRSA carriage increases the risk for nasal MRSA colonization, and nasal MRSA has been noted to be more difficult to decolonize than nonresistant strains. Health care workers carrying S aureus can trigger a potential hospital outbreak of MRSA. Studies have shown that bacterial transmission is increased 40-fold when the nasal host is co-infected by rhinovirus.2 Health care workers can be a source of MRSA during outbreaks, but they have not been shown to be more likely to carry MRSA than the general population.2 Understanding which patients might be at risk for S aureus–associated disease in dermatology can lead clinicians to consider decolonization strategies.
Nasal colonization has been noted more frequently in patients with predisposing risk factors, including human immunodeficiency virus infection, obesity, diabetes mellitus, granulomatosis with polyangiitis, HLA-DR3 phenotype, skin and soft-tissue infections, atopic dermatitis, impetigo, and recurrent furunculosis.2Staphylococcus aureus is the most frequently noted pathogen in diabetic foot infection. A study found that 36% of sampled diabetic foot-infection patients also had S aureus isolated from both nares and the foot wound, with 65% of isolated strains being identical.2 Although there are clear data on decolonization of patients prior to heart and orthopedic surgery, more data are needed to determine the benefit of screening and treating nasal carriers in populations with diabetic foot ulcers.
Staphylococcus aureus nasal colonization also has been shown in approximately 60% of patients with recurrent furunculosis and impetigo.2 Although it is clear that there is a correlation between S aureus–related skin infection and nasal colonization, it is unclear what role nose-picking might have in perpetuating these complications.
There are multiple approaches to S aureus decolonization, including intranasal mupirocin, chlorhexidine body wipes, bleach baths, and even oral antibiotics (eg, trimethoprim-sulfamethoxazole, clindamycin). The Infectious Diseases Society of America has published guidelines for treating recurrent MRSA infection, including 5 to 10 days of intranasal mupirocin plus either body decolonization with a daily chlorhexidine wash for 5 to 14 days or a 15-minute dilute bleach bath twice weekly for 3 months.3,4
There are ample meta-analyses and systematic reviews regarding S aureus decolonization and management in patients undergoing dialysis or surgery but limited data when it comes to this topic in dermatology. Those limited studies do show a benefit to decolonization in several diseases, including atopic dermatitis, hand dermatitis, recurrent skin and soft-tissue infections, cutaneous T-cell lymphoma, and surgical infection following Mohs micrographic surgery.4 Typically, it also is necessary to treat those who might come in contact with the patient or caregiver; in theory, treating contacts helps reduce the chance that the patient will become recolonized shortly afterward, but the data are limited regarding long-term colonization status following treatment. Contact surfaces, especially cell phones, are noted to be a contributing factor to nares colonization; therefore, it also may be necessary to educate patients on surface-cleaning techniques.5 Because there are multiple sources of S aureus that patients can come in contact with after decolonization attempts, a nose-picking habit might play a vital role in recolonization.
Due to rising bacterial resistance to mupirocin and chlorhexidine decolonization strategies, there is a growing need for more effective, long-term decolonization strategies.4 These strategies must address patients’ environmental exposure and nasal-touching habits. Overcoming the habit of nose-picking might aid S aureus decolonization strategies and thus aid in preventing future antimicrobial resistance.
But are at-risk patients receiving sufficient screening and education on the dangers of a nose-picking habit? Effective strategies to assess these practices and recommend the discontinuation of the habit could have positive effects in maintaining long-term decolonization. Potential euphemistic ways to approach this somewhat taboo topic include questions that elicit information on whether the patient ever touches the inside of his/her nose, washes his/her hands before and after touching the inside of the nose, knows about transfer of bacteria from hand to nose, or understands what decolonization is doing for them. The patient might be inclined to deny such activity, but education on nasal hygiene should be provided regardless, especially in pediatric patients.
Staphylococcus aureus might be a normal human nasal inhabitant, but it can cause a range of problems for dermatologic disease. Although pharmacotherapeutic decolonization strategies can have a positive effect on dermatologic disease, growing antibiotic resistance calls for health care providers to assess patients’ nose picking-habits and educate them on effective ways to prevent finger-to-nose practices.
Primitive human habits have withstood the test of time but can pose health risks. Exploring a nasal cavity with a finger might have first occurred shortly after whichever species first developed a nasal opening and a digit able to reach it. Humans have been keen on continuing the long-standing yet taboo habit of nose-picking (rhinotillexis).
Even though nose-picking is stigmatized, anonymous surveys show that almost all adolescents and adults do it.1 People are typically unaware of the risks of regular rhinotillexis. Studies exploring the intranasal human microbiome have elicited asymptomatic yet potential disease-causing microbes, including the notorious bacterium Staphylococcus aureus. As many as 30% of humans are asymptomatically permanently colonized with S aureus in their anterior nares.2 These natural reservoirs can be the source of opportunistic infection that increases morbidity, mortality, and overall health care costs.
With the rise of antimicrobial resistance, especially methicillin-resistant S aureus (MRSA), a more direct approach might be necessary to curb nasally sourced cutaneous infection. Since dermatology patients deal with a wide array of skin barrier defects that put them at risk for S aureus–related infection, a medical provider’s understanding about the role of nasal colonization and transmission is important. Addressing the awkward question of “Do you pick your nose?” and providing education on the topic might be uncomfortable, but it might be necessary for dermatology patients at risk for S aureus–related cutaneous disease.
Staphylococcus aureus colonizes the anterior nares of 20% to 80% of humans; nasal colonization can begin during the first days of life.2 The anterior nares are noted as the main reservoir of chronic carriage of S aureus, but carriage can occur at various body sites, including the rectum, vagina, gastrointestinal tract, and axilla, as well as other cutaneous sites. Hands are noted as the main vector of S aureus transmission from source to nose; a positive correlation between nose-picking habits and nasal carriage of S aureus has been noted.2
The percentage of S aureus–colonized humans who harbor MRSA is unknown, but it is a topic of concern with the rise of MRSA-related infection. Multisite MRSA carriage increases the risk for nasal MRSA colonization, and nasal MRSA has been noted to be more difficult to decolonize than nonresistant strains. Health care workers carrying S aureus can trigger a potential hospital outbreak of MRSA. Studies have shown that bacterial transmission is increased 40-fold when the nasal host is co-infected by rhinovirus.2 Health care workers can be a source of MRSA during outbreaks, but they have not been shown to be more likely to carry MRSA than the general population.2 Understanding which patients might be at risk for S aureus–associated disease in dermatology can lead clinicians to consider decolonization strategies.
Nasal colonization has been noted more frequently in patients with predisposing risk factors, including human immunodeficiency virus infection, obesity, diabetes mellitus, granulomatosis with polyangiitis, HLA-DR3 phenotype, skin and soft-tissue infections, atopic dermatitis, impetigo, and recurrent furunculosis.2Staphylococcus aureus is the most frequently noted pathogen in diabetic foot infection. A study found that 36% of sampled diabetic foot-infection patients also had S aureus isolated from both nares and the foot wound, with 65% of isolated strains being identical.2 Although there are clear data on decolonization of patients prior to heart and orthopedic surgery, more data are needed to determine the benefit of screening and treating nasal carriers in populations with diabetic foot ulcers.
Staphylococcus aureus nasal colonization also has been shown in approximately 60% of patients with recurrent furunculosis and impetigo.2 Although it is clear that there is a correlation between S aureus–related skin infection and nasal colonization, it is unclear what role nose-picking might have in perpetuating these complications.
There are multiple approaches to S aureus decolonization, including intranasal mupirocin, chlorhexidine body wipes, bleach baths, and even oral antibiotics (eg, trimethoprim-sulfamethoxazole, clindamycin). The Infectious Diseases Society of America has published guidelines for treating recurrent MRSA infection, including 5 to 10 days of intranasal mupirocin plus either body decolonization with a daily chlorhexidine wash for 5 to 14 days or a 15-minute dilute bleach bath twice weekly for 3 months.3,4
There are ample meta-analyses and systematic reviews regarding S aureus decolonization and management in patients undergoing dialysis or surgery but limited data when it comes to this topic in dermatology. Those limited studies do show a benefit to decolonization in several diseases, including atopic dermatitis, hand dermatitis, recurrent skin and soft-tissue infections, cutaneous T-cell lymphoma, and surgical infection following Mohs micrographic surgery.4 Typically, it also is necessary to treat those who might come in contact with the patient or caregiver; in theory, treating contacts helps reduce the chance that the patient will become recolonized shortly afterward, but the data are limited regarding long-term colonization status following treatment. Contact surfaces, especially cell phones, are noted to be a contributing factor to nares colonization; therefore, it also may be necessary to educate patients on surface-cleaning techniques.5 Because there are multiple sources of S aureus that patients can come in contact with after decolonization attempts, a nose-picking habit might play a vital role in recolonization.
Due to rising bacterial resistance to mupirocin and chlorhexidine decolonization strategies, there is a growing need for more effective, long-term decolonization strategies.4 These strategies must address patients’ environmental exposure and nasal-touching habits. Overcoming the habit of nose-picking might aid S aureus decolonization strategies and thus aid in preventing future antimicrobial resistance.
But are at-risk patients receiving sufficient screening and education on the dangers of a nose-picking habit? Effective strategies to assess these practices and recommend the discontinuation of the habit could have positive effects in maintaining long-term decolonization. Potential euphemistic ways to approach this somewhat taboo topic include questions that elicit information on whether the patient ever touches the inside of his/her nose, washes his/her hands before and after touching the inside of the nose, knows about transfer of bacteria from hand to nose, or understands what decolonization is doing for them. The patient might be inclined to deny such activity, but education on nasal hygiene should be provided regardless, especially in pediatric patients.
Staphylococcus aureus might be a normal human nasal inhabitant, but it can cause a range of problems for dermatologic disease. Although pharmacotherapeutic decolonization strategies can have a positive effect on dermatologic disease, growing antibiotic resistance calls for health care providers to assess patients’ nose picking-habits and educate them on effective ways to prevent finger-to-nose practices.
- Andrade C, Srihari BS. A preliminary survey of rhinotillexomania in an adolescent sample. J Clin Psychiatry. 2001;62:426-431.
- Sakr A, Brégeon F, Mège J-L, et al. Staphylococcus aureus nasal colonization: an update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285-292.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in healthcare: a dermatology perspective. J Healthc Eng. 2018;2018:2382050.
- Creech CB, Al-Zubeidi DN, Fritz SA. Prevention of recurrent staphylococcal kin infections. Infect Dis Clin North Am. 2015;29:429-464.
- Andrade C, Srihari BS. A preliminary survey of rhinotillexomania in an adolescent sample. J Clin Psychiatry. 2001;62:426-431.
- Sakr A, Brégeon F, Mège J-L, et al. Staphylococcus aureus nasal colonization: an update on mechanisms, epidemiology, risk factors, and subsequent infections. Front Microbiol. 2018;9:2419.
- Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin Infect Dis. 2011;52:285-292.
- Kuraitis D, Williams L. Decolonization of Staphylococcus aureus in healthcare: a dermatology perspective. J Healthc Eng. 2018;2018:2382050.
- Creech CB, Al-Zubeidi DN, Fritz SA. Prevention of recurrent staphylococcal kin infections. Infect Dis Clin North Am. 2015;29:429-464.
Practice Points
- Staphylococcus aureus colonizes the anterior nares of approximately 20% to 80% of humans and can play a large factor in dermatologic disease.
- Staphylococcus aureus decolonization practices for at-risk dermatology patients may overlook the role that nose-picking plays.
Shared decision-making aids choice of PrEP
A patient-centered approach can help guide persons at risk for HIV exposure to decide on the best choice of pre-exposure prophylaxis (PrEP) regimens for them, stifling the noise generated by direct-to-consumer advertising, an infectious disease specialist recommends.
The decision for patients whether to start or remain on the PrEP combination of tenofovir disoproxil fumarate (TDF) plus emtricitabine (FTC; Truvada and generic) or on tenofovir alafenamide (TAF) plus FTC (Descovy) is made more fraught by confusion regarding the use of the newer and allegedly safer TAF prodrug of tenofovir in HIV treatment regimens, said Oni Blackstock, MD, founder and executive director of Health Justice and an attending physician in the division of infectious diseases at Harlem Hospital, New York.
“There have been commercials on TV as well as on social media around class-action lawsuits against [Truvada maker] Gilead,” she said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases, held virtually this year.
“These lawsuits focus on TDF for HIV treatment, but they have sown a great deal of confusion about TDF versus TAF for PrEP among potential and actual PrEP users,” she added.
Dr. Blackstock described her approach to shared decision-making regarding TDF/FTC versus TAF/FTC, and to helping patients understand the relative benefits and risks of each formulation.
In January of 2020, Dr. Blackstock, who was then assistant commissioner of the HIV bureau of the New York City Department of Health and Mental Hygiene, issued with other Bureau members a “Dear colleague” letter stating why they believed that TDF/FTC should remain the first-line regimen for PrEP.
That opinion, she said, was bolstered by an editorial published in February 2020 by Douglas E. Krakower, MD, from Beth Israel Deaconess Medical Center in Boston, and colleagues, which questioned the rush to shift from TDF to TAF in HIV treatment, and cautioned against the same approach to PrEP.
“Despite evidence that TAF/FTC would not be cost-effective, compared with generic TDF/FTC , the newer regimen quickly and irrevocably displaced TDF/FTC for HIV treatment in the U.S. A similar shift for PrEP – especially for populations in which TAF/FTC is untested – would be premature, costly, and counterproductive for population impact,” Krakower et al. wrote.
Shared decision-making
Clinicians can help patients who may be a candidate for either PrEP regimen by engaging them in shared decision-making.
“The clinician provides information in this case about a prevention strategy, options, benefits and risks, alternatives, and the patient provides their preferences and values, and together the clinician and patient make a decision,” Dr. Blackstock said.
The process differs from the model of informed decision-making, where the clinician gives the patient the information and the patient comes to a decision, or the old, “paternalistic” model in which the clinician gives information and makes recommendations to the patient.
“Shared decision-making has been studied extensively and has been shown to improve patient satisfaction, patient communication, and also potentially reducing health inequities that we see,” she said.
The model for shared decision-making for clinical practice includes three distinct portions: a choice talk, option talk, and decision talk.
Choice
To begin the discussion, the physician informs the patients of the availability of choices and justifies them, saying, for example, “there is good information about how these two PrEP options differ that I’d like to discuss with you,” and “the two PrEP options have different side effects … some will matter more to you than other people.”
At this stage the clinician should defer closure by offering a more detailed discussion of the choices.
Option
Here the clinician solicits information about what the patient has heard or read about PrEP, describes each option in practical terms, and points out where the two regimens differ, being specific about the pros and cons of each (for example, potential bone mineral density loss or renal complications with TDF, and potential weight gain with subsequent metabolic and cardiovascular consequences with TAF).
The TDF versus TAF-based PrEP discussion could also focus on what’s known about the comparative effectiveness of each regimen.
For example, TDF/FTC has been shown to be about 99% effective at preventing infection in men who have sex with men and in transgender women, also about 99% effective in heterosexual women and men, and 74%-84% effective in persons who inject drugs.
In contrast, TAF/FTC has been shown to be about 99% effective in men who have sex with men and transgender women, but it’s efficacy in the other two categories is unknown, Dr. Blackstock said.
The option discussion should include a comparison of the evidence base for each regimen, including the real-world experience with TDF/FTC since 2012, and much more limited experience with TAF/FTC.
Discussing relative costs, although the wholesale costs of the regimens are similar, there is now a generic version of TDF/FTC made by Teva Pharmaceuticals that sells for about $400 less per month than the brand name, which might make the option more acceptable to health insurers.
Decision
The decision talk is about considering the patients preferences and deciding with them what is best.
The clinician could say, for example: “What, from your point of view, matters most to you?”
The clinician should also be willing to allow the patient to defer a decision or to guide them depending on their stated wish, asking something like: “Are you ready to decide, or do you want more time? Do you have more questions? Are there more things we should discuss?
Offering the patient a chance to review the decision can also be a good way to arrive at closure, Dr. Blackstock said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Blackstock presented her talk, said that he also uses a similar approach to the PrEP discussion.
“I use a very patient-centered approach of providing information and talking through the data that are available,” he said.
“I will say that, as patients come to me talking about the transition from TDF to TAF for pre-exposure prophylaxis, I am very clear with them about the limited benefit or no benefit that I see with TAF for pre-exposure prophylaxis, and all of my patients have remained on TDF for pre-exposure prophylaxis,” he added.
No funding source for the presentation was reported. Dr. Blackstock and Dr. Goldstein reported having no conflicts of interest to disclose.
A patient-centered approach can help guide persons at risk for HIV exposure to decide on the best choice of pre-exposure prophylaxis (PrEP) regimens for them, stifling the noise generated by direct-to-consumer advertising, an infectious disease specialist recommends.
The decision for patients whether to start or remain on the PrEP combination of tenofovir disoproxil fumarate (TDF) plus emtricitabine (FTC; Truvada and generic) or on tenofovir alafenamide (TAF) plus FTC (Descovy) is made more fraught by confusion regarding the use of the newer and allegedly safer TAF prodrug of tenofovir in HIV treatment regimens, said Oni Blackstock, MD, founder and executive director of Health Justice and an attending physician in the division of infectious diseases at Harlem Hospital, New York.
“There have been commercials on TV as well as on social media around class-action lawsuits against [Truvada maker] Gilead,” she said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases, held virtually this year.
“These lawsuits focus on TDF for HIV treatment, but they have sown a great deal of confusion about TDF versus TAF for PrEP among potential and actual PrEP users,” she added.
Dr. Blackstock described her approach to shared decision-making regarding TDF/FTC versus TAF/FTC, and to helping patients understand the relative benefits and risks of each formulation.
In January of 2020, Dr. Blackstock, who was then assistant commissioner of the HIV bureau of the New York City Department of Health and Mental Hygiene, issued with other Bureau members a “Dear colleague” letter stating why they believed that TDF/FTC should remain the first-line regimen for PrEP.
That opinion, she said, was bolstered by an editorial published in February 2020 by Douglas E. Krakower, MD, from Beth Israel Deaconess Medical Center in Boston, and colleagues, which questioned the rush to shift from TDF to TAF in HIV treatment, and cautioned against the same approach to PrEP.
“Despite evidence that TAF/FTC would not be cost-effective, compared with generic TDF/FTC , the newer regimen quickly and irrevocably displaced TDF/FTC for HIV treatment in the U.S. A similar shift for PrEP – especially for populations in which TAF/FTC is untested – would be premature, costly, and counterproductive for population impact,” Krakower et al. wrote.
Shared decision-making
Clinicians can help patients who may be a candidate for either PrEP regimen by engaging them in shared decision-making.
“The clinician provides information in this case about a prevention strategy, options, benefits and risks, alternatives, and the patient provides their preferences and values, and together the clinician and patient make a decision,” Dr. Blackstock said.
The process differs from the model of informed decision-making, where the clinician gives the patient the information and the patient comes to a decision, or the old, “paternalistic” model in which the clinician gives information and makes recommendations to the patient.
“Shared decision-making has been studied extensively and has been shown to improve patient satisfaction, patient communication, and also potentially reducing health inequities that we see,” she said.
The model for shared decision-making for clinical practice includes three distinct portions: a choice talk, option talk, and decision talk.
Choice
To begin the discussion, the physician informs the patients of the availability of choices and justifies them, saying, for example, “there is good information about how these two PrEP options differ that I’d like to discuss with you,” and “the two PrEP options have different side effects … some will matter more to you than other people.”
At this stage the clinician should defer closure by offering a more detailed discussion of the choices.
Option
Here the clinician solicits information about what the patient has heard or read about PrEP, describes each option in practical terms, and points out where the two regimens differ, being specific about the pros and cons of each (for example, potential bone mineral density loss or renal complications with TDF, and potential weight gain with subsequent metabolic and cardiovascular consequences with TAF).
The TDF versus TAF-based PrEP discussion could also focus on what’s known about the comparative effectiveness of each regimen.
For example, TDF/FTC has been shown to be about 99% effective at preventing infection in men who have sex with men and in transgender women, also about 99% effective in heterosexual women and men, and 74%-84% effective in persons who inject drugs.
In contrast, TAF/FTC has been shown to be about 99% effective in men who have sex with men and transgender women, but it’s efficacy in the other two categories is unknown, Dr. Blackstock said.
The option discussion should include a comparison of the evidence base for each regimen, including the real-world experience with TDF/FTC since 2012, and much more limited experience with TAF/FTC.
Discussing relative costs, although the wholesale costs of the regimens are similar, there is now a generic version of TDF/FTC made by Teva Pharmaceuticals that sells for about $400 less per month than the brand name, which might make the option more acceptable to health insurers.
Decision
The decision talk is about considering the patients preferences and deciding with them what is best.
The clinician could say, for example: “What, from your point of view, matters most to you?”
The clinician should also be willing to allow the patient to defer a decision or to guide them depending on their stated wish, asking something like: “Are you ready to decide, or do you want more time? Do you have more questions? Are there more things we should discuss?
Offering the patient a chance to review the decision can also be a good way to arrive at closure, Dr. Blackstock said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Blackstock presented her talk, said that he also uses a similar approach to the PrEP discussion.
“I use a very patient-centered approach of providing information and talking through the data that are available,” he said.
“I will say that, as patients come to me talking about the transition from TDF to TAF for pre-exposure prophylaxis, I am very clear with them about the limited benefit or no benefit that I see with TAF for pre-exposure prophylaxis, and all of my patients have remained on TDF for pre-exposure prophylaxis,” he added.
No funding source for the presentation was reported. Dr. Blackstock and Dr. Goldstein reported having no conflicts of interest to disclose.
A patient-centered approach can help guide persons at risk for HIV exposure to decide on the best choice of pre-exposure prophylaxis (PrEP) regimens for them, stifling the noise generated by direct-to-consumer advertising, an infectious disease specialist recommends.
The decision for patients whether to start or remain on the PrEP combination of tenofovir disoproxil fumarate (TDF) plus emtricitabine (FTC; Truvada and generic) or on tenofovir alafenamide (TAF) plus FTC (Descovy) is made more fraught by confusion regarding the use of the newer and allegedly safer TAF prodrug of tenofovir in HIV treatment regimens, said Oni Blackstock, MD, founder and executive director of Health Justice and an attending physician in the division of infectious diseases at Harlem Hospital, New York.
“There have been commercials on TV as well as on social media around class-action lawsuits against [Truvada maker] Gilead,” she said in an online presentation during IDWeek 2020, an annual scientific meeting on infectious diseases, held virtually this year.
“These lawsuits focus on TDF for HIV treatment, but they have sown a great deal of confusion about TDF versus TAF for PrEP among potential and actual PrEP users,” she added.
Dr. Blackstock described her approach to shared decision-making regarding TDF/FTC versus TAF/FTC, and to helping patients understand the relative benefits and risks of each formulation.
In January of 2020, Dr. Blackstock, who was then assistant commissioner of the HIV bureau of the New York City Department of Health and Mental Hygiene, issued with other Bureau members a “Dear colleague” letter stating why they believed that TDF/FTC should remain the first-line regimen for PrEP.
That opinion, she said, was bolstered by an editorial published in February 2020 by Douglas E. Krakower, MD, from Beth Israel Deaconess Medical Center in Boston, and colleagues, which questioned the rush to shift from TDF to TAF in HIV treatment, and cautioned against the same approach to PrEP.
“Despite evidence that TAF/FTC would not be cost-effective, compared with generic TDF/FTC , the newer regimen quickly and irrevocably displaced TDF/FTC for HIV treatment in the U.S. A similar shift for PrEP – especially for populations in which TAF/FTC is untested – would be premature, costly, and counterproductive for population impact,” Krakower et al. wrote.
Shared decision-making
Clinicians can help patients who may be a candidate for either PrEP regimen by engaging them in shared decision-making.
“The clinician provides information in this case about a prevention strategy, options, benefits and risks, alternatives, and the patient provides their preferences and values, and together the clinician and patient make a decision,” Dr. Blackstock said.
The process differs from the model of informed decision-making, where the clinician gives the patient the information and the patient comes to a decision, or the old, “paternalistic” model in which the clinician gives information and makes recommendations to the patient.
“Shared decision-making has been studied extensively and has been shown to improve patient satisfaction, patient communication, and also potentially reducing health inequities that we see,” she said.
The model for shared decision-making for clinical practice includes three distinct portions: a choice talk, option talk, and decision talk.
Choice
To begin the discussion, the physician informs the patients of the availability of choices and justifies them, saying, for example, “there is good information about how these two PrEP options differ that I’d like to discuss with you,” and “the two PrEP options have different side effects … some will matter more to you than other people.”
At this stage the clinician should defer closure by offering a more detailed discussion of the choices.
Option
Here the clinician solicits information about what the patient has heard or read about PrEP, describes each option in practical terms, and points out where the two regimens differ, being specific about the pros and cons of each (for example, potential bone mineral density loss or renal complications with TDF, and potential weight gain with subsequent metabolic and cardiovascular consequences with TAF).
The TDF versus TAF-based PrEP discussion could also focus on what’s known about the comparative effectiveness of each regimen.
For example, TDF/FTC has been shown to be about 99% effective at preventing infection in men who have sex with men and in transgender women, also about 99% effective in heterosexual women and men, and 74%-84% effective in persons who inject drugs.
In contrast, TAF/FTC has been shown to be about 99% effective in men who have sex with men and transgender women, but it’s efficacy in the other two categories is unknown, Dr. Blackstock said.
The option discussion should include a comparison of the evidence base for each regimen, including the real-world experience with TDF/FTC since 2012, and much more limited experience with TAF/FTC.
Discussing relative costs, although the wholesale costs of the regimens are similar, there is now a generic version of TDF/FTC made by Teva Pharmaceuticals that sells for about $400 less per month than the brand name, which might make the option more acceptable to health insurers.
Decision
The decision talk is about considering the patients preferences and deciding with them what is best.
The clinician could say, for example: “What, from your point of view, matters most to you?”
The clinician should also be willing to allow the patient to defer a decision or to guide them depending on their stated wish, asking something like: “Are you ready to decide, or do you want more time? Do you have more questions? Are there more things we should discuss?
Offering the patient a chance to review the decision can also be a good way to arrive at closure, Dr. Blackstock said.
Robert Goldstein, MD, PhD, an infectious disease specialist and medical director of the transgender health program at Massachusetts General Hospital in Boston, who comoderated the session where Dr. Blackstock presented her talk, said that he also uses a similar approach to the PrEP discussion.
“I use a very patient-centered approach of providing information and talking through the data that are available,” he said.
“I will say that, as patients come to me talking about the transition from TDF to TAF for pre-exposure prophylaxis, I am very clear with them about the limited benefit or no benefit that I see with TAF for pre-exposure prophylaxis, and all of my patients have remained on TDF for pre-exposure prophylaxis,” he added.
No funding source for the presentation was reported. Dr. Blackstock and Dr. Goldstein reported having no conflicts of interest to disclose.
FROM IDWEEK 2020
COVID-19 vaccine standards questioned at FDA advisory meeting
The FDA’s Vaccines and Related Biological Products Advisory Committee met for a wide-ranging discussion beginning around 10 am. The FDA did not ask the panel to weigh in on any particular vaccine. Instead, the FDA asked for the panel’s feedback on a series of questions, including considerations for continuing phase 3 trials if a product were to get an interim clearance known as an emergency use authorization (EUA).
Speakers at the hearing made a variety of requests, including asking for data showing COVID-19 vaccines can prevent serious illness and urging transparency about the agency’s deliberations for each product to be considered.
FDA staff are closely tracking the crop of experimental vaccines that have made it into advanced stages of testing, including products from Pfizer Inc, AstraZeneca, Johnson & Johnson, and Moderna.
‘Time for a reset’
Among the speakers at the public hearing was Peter Lurie, MD, who served as an FDA associate commissioner from 2014 to 2017. Now the president of the Center for Science in the Public Interest, Lurie was among the speakers who asked the agency to make its independence clear.
President Donald Trump has for months been making predictions about COVID-19 vaccine approvals that have been overly optimistic. In one example, the president, who is seeking re-election on November 3, last month spoke about being able to begin distributing a vaccine in October.
“Until now the process of developing candidate vaccines has been inappropriately politicized with an eye on the election calendar, rather than the deliberate timeframe science requires,” Lurie told the FDA advisory panel. “Now is the time for a reset. This committee has a unique opportunity to set a new tone for vaccine deliberations going forward.”
Lurie asked the panel to press the FDA to commit to hold an advisory committee meeting on requests by drugmakers for EUAs. He also asked the panel to demand that informed consent forms and minutes from institutional review board (IRB) discussions of COVID-19 vaccines trials be made public.
Also among the speakers at the public hearing was Peter Doshi, PhD, an associate professor at the University of Maryland School of Pharmacy, who argued that the current trials won’t answer the right questions about the COVID-19 vaccines.
“We could end up with approved vaccines that reduce the risk of mild infection, but do not decrease the risk of hospitalization, ICU use, or death — either at all or by a clinically relevant amount,” Doshi told the panel.
In his presentation, he reiterated points he had made previously, including in an October 21 article in the BMJ, for which he is an associate editor. Doshi also raised these concerns in a September opinion article in The New York Times, co-authored with Eric Topol, MD, director of the Scripps Research Translational Institute and editor-in-chief of Medscape.
Risks of a ‘rushed vaccine’
Other complaints about the FDA’s approach included criticism of a 2-month follow-up time after vaccination, which was seen as too short. ECRI, a nonprofit organization that seeks to improve the safety, quality, and cost-effectiveness of medicines, has argued that approving a weak COVID-19 vaccine might worsen the pandemic.
In an October 21 statement, ECRI noted the risk of a partially effective vaccine, which could be welcomed as a means of slowing transmission of the virus. But public response and attitudes over the past 9 months in the United States suggest that people would relax their precautions as soon as a vaccine is available.
“Resulting infections may offset the vaccine’s impact and end up increasing the mortality and morbidity burden,” ECRI said in the brief.
“The risks and consequences of a rushed vaccine could be very severe if the review is anything shy of thorough,” ECRI Chief Executive Officer Marcus Schabacker, MD, PhD, said in a statement prepared for the hearing.
This article first appeared on Medscape.com.
The FDA’s Vaccines and Related Biological Products Advisory Committee met for a wide-ranging discussion beginning around 10 am. The FDA did not ask the panel to weigh in on any particular vaccine. Instead, the FDA asked for the panel’s feedback on a series of questions, including considerations for continuing phase 3 trials if a product were to get an interim clearance known as an emergency use authorization (EUA).
Speakers at the hearing made a variety of requests, including asking for data showing COVID-19 vaccines can prevent serious illness and urging transparency about the agency’s deliberations for each product to be considered.
FDA staff are closely tracking the crop of experimental vaccines that have made it into advanced stages of testing, including products from Pfizer Inc, AstraZeneca, Johnson & Johnson, and Moderna.
‘Time for a reset’
Among the speakers at the public hearing was Peter Lurie, MD, who served as an FDA associate commissioner from 2014 to 2017. Now the president of the Center for Science in the Public Interest, Lurie was among the speakers who asked the agency to make its independence clear.
President Donald Trump has for months been making predictions about COVID-19 vaccine approvals that have been overly optimistic. In one example, the president, who is seeking re-election on November 3, last month spoke about being able to begin distributing a vaccine in October.
“Until now the process of developing candidate vaccines has been inappropriately politicized with an eye on the election calendar, rather than the deliberate timeframe science requires,” Lurie told the FDA advisory panel. “Now is the time for a reset. This committee has a unique opportunity to set a new tone for vaccine deliberations going forward.”
Lurie asked the panel to press the FDA to commit to hold an advisory committee meeting on requests by drugmakers for EUAs. He also asked the panel to demand that informed consent forms and minutes from institutional review board (IRB) discussions of COVID-19 vaccines trials be made public.
Also among the speakers at the public hearing was Peter Doshi, PhD, an associate professor at the University of Maryland School of Pharmacy, who argued that the current trials won’t answer the right questions about the COVID-19 vaccines.
“We could end up with approved vaccines that reduce the risk of mild infection, but do not decrease the risk of hospitalization, ICU use, or death — either at all or by a clinically relevant amount,” Doshi told the panel.
In his presentation, he reiterated points he had made previously, including in an October 21 article in the BMJ, for which he is an associate editor. Doshi also raised these concerns in a September opinion article in The New York Times, co-authored with Eric Topol, MD, director of the Scripps Research Translational Institute and editor-in-chief of Medscape.
Risks of a ‘rushed vaccine’
Other complaints about the FDA’s approach included criticism of a 2-month follow-up time after vaccination, which was seen as too short. ECRI, a nonprofit organization that seeks to improve the safety, quality, and cost-effectiveness of medicines, has argued that approving a weak COVID-19 vaccine might worsen the pandemic.
In an October 21 statement, ECRI noted the risk of a partially effective vaccine, which could be welcomed as a means of slowing transmission of the virus. But public response and attitudes over the past 9 months in the United States suggest that people would relax their precautions as soon as a vaccine is available.
“Resulting infections may offset the vaccine’s impact and end up increasing the mortality and morbidity burden,” ECRI said in the brief.
“The risks and consequences of a rushed vaccine could be very severe if the review is anything shy of thorough,” ECRI Chief Executive Officer Marcus Schabacker, MD, PhD, said in a statement prepared for the hearing.
This article first appeared on Medscape.com.
The FDA’s Vaccines and Related Biological Products Advisory Committee met for a wide-ranging discussion beginning around 10 am. The FDA did not ask the panel to weigh in on any particular vaccine. Instead, the FDA asked for the panel’s feedback on a series of questions, including considerations for continuing phase 3 trials if a product were to get an interim clearance known as an emergency use authorization (EUA).
Speakers at the hearing made a variety of requests, including asking for data showing COVID-19 vaccines can prevent serious illness and urging transparency about the agency’s deliberations for each product to be considered.
FDA staff are closely tracking the crop of experimental vaccines that have made it into advanced stages of testing, including products from Pfizer Inc, AstraZeneca, Johnson & Johnson, and Moderna.
‘Time for a reset’
Among the speakers at the public hearing was Peter Lurie, MD, who served as an FDA associate commissioner from 2014 to 2017. Now the president of the Center for Science in the Public Interest, Lurie was among the speakers who asked the agency to make its independence clear.
President Donald Trump has for months been making predictions about COVID-19 vaccine approvals that have been overly optimistic. In one example, the president, who is seeking re-election on November 3, last month spoke about being able to begin distributing a vaccine in October.
“Until now the process of developing candidate vaccines has been inappropriately politicized with an eye on the election calendar, rather than the deliberate timeframe science requires,” Lurie told the FDA advisory panel. “Now is the time for a reset. This committee has a unique opportunity to set a new tone for vaccine deliberations going forward.”
Lurie asked the panel to press the FDA to commit to hold an advisory committee meeting on requests by drugmakers for EUAs. He also asked the panel to demand that informed consent forms and minutes from institutional review board (IRB) discussions of COVID-19 vaccines trials be made public.
Also among the speakers at the public hearing was Peter Doshi, PhD, an associate professor at the University of Maryland School of Pharmacy, who argued that the current trials won’t answer the right questions about the COVID-19 vaccines.
“We could end up with approved vaccines that reduce the risk of mild infection, but do not decrease the risk of hospitalization, ICU use, or death — either at all or by a clinically relevant amount,” Doshi told the panel.
In his presentation, he reiterated points he had made previously, including in an October 21 article in the BMJ, for which he is an associate editor. Doshi also raised these concerns in a September opinion article in The New York Times, co-authored with Eric Topol, MD, director of the Scripps Research Translational Institute and editor-in-chief of Medscape.
Risks of a ‘rushed vaccine’
Other complaints about the FDA’s approach included criticism of a 2-month follow-up time after vaccination, which was seen as too short. ECRI, a nonprofit organization that seeks to improve the safety, quality, and cost-effectiveness of medicines, has argued that approving a weak COVID-19 vaccine might worsen the pandemic.
In an October 21 statement, ECRI noted the risk of a partially effective vaccine, which could be welcomed as a means of slowing transmission of the virus. But public response and attitudes over the past 9 months in the United States suggest that people would relax their precautions as soon as a vaccine is available.
“Resulting infections may offset the vaccine’s impact and end up increasing the mortality and morbidity burden,” ECRI said in the brief.
“The risks and consequences of a rushed vaccine could be very severe if the review is anything shy of thorough,” ECRI Chief Executive Officer Marcus Schabacker, MD, PhD, said in a statement prepared for the hearing.
This article first appeared on Medscape.com.