User login
The five biggest changes in the 2023 adult vaccine schedules
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Hello. I’m Dr Sandra Fryhofer. Welcome to Medicine Matters.
It’s a new year, which means a new ACIP adult immunization schedule – a valuable resource collating ACIP’s most up-to-date vaccination recommendations.
Here are this year’s five most important changes:
- COVID vaccines now front and center
- New emphasis on polio vaccination
- Inclusion of some nonvaccine products (such as monoclonal antibody products)
- Pharmacists group has approved the schedule for the first time
- New shared clinical decision-making option for pneumococcal vaccines
The schedule’s organization remains the same. It still has four sections:
- Table 1: vaccinations by age
- Table 2: vaccinations by medical condition and other indications
- The Notes section (alphabetically ordered by vaccine type)
- Appendix listing of vaccine-specific contraindications and precautions
But what’s unique this year is that some of the abbreviations have historical implications. The first change is no big surprise in light of what we’ve gone through in the past few years. COVID vaccines are listed first on the cover page by brand name for those authorized and by company name for those still under US emergency use authorization. They’re also listed first on the graphics and in the notes.
COVID and mRNA and protein-based vaccines have now been assigned official abbreviations based on vaccine platform and valency.
- 1vCOV-mRNA: Comirnaty/Pfizer-BioNTech and Spikevax Moderna COVID-19 vaccines
- 2vCOV-mRNA: Pfizer-BioNTech and Moderna bivalent COVID-19 vaccines
- 1vCOV-aPS: Novavax COVID-19 vaccine
Also remarkable is the absence of COVID viral vector vaccines on the list. However, the viral vector COVID vaccine (which has been available but is not preferred) does have a CDC website link in the Notes section.
A sad but necessary inclusion was triggered by recent polio cases in New York. Polio was believed to be eradicated, and we thought adults no longer needed to be vaccinated against polio. In the new schedule, the polio vaccine is listed on the cover page but is not included in the tables. Current polio vaccination recommendations are now in the Notes section.
Also of historical significance and something that may set a precedent is the inclusion of nonvaccine products. The value of COVID preexposure prophylaxis with products including monoclonal antibodies (such as Evusheld) for people who are moderately or severely immunocompromised is mentioned in the Notes section.
For the first time ever, the schedule has been approved by the American Pharmacists Association, which validates pharmacists as established partners in vaccine administration.
Color-code key
One aspect of the schedule that has not changed is the color-code key:
- Yellow: Recommended if the patient meets the age requirement
- Purple: Indicated for those with additional risk factors or another indication
- Blue: Recommended based on shared clinical decision-making
- Orange: Precaution
- Red: Contraindicated or not recommended; the vaccine should not be administered. Overlays on the red more precisely clarify whether a vaccine is really contraindicated or just not recommended. An asterisk on red means vaccinate after pregnancy if indicated.
- Gray: No recommendation or not applicable
Vaccinations by age
Table 1 lists recommended vaccinations by age. There is one major change. COVID vaccines are on the first row of the graphic, with the need for both a primary series and boosters emphasized on the overlay. The notes have hyperlinks to the most up-to-date COVID vaccination recommendations.
Pneumococcal vaccination. Pneumococcal vaccination is routinely recommended starting at age 65. Current recommendations for those not previously vaccinated have not changed since last year. But on Table 1, the bottom half of the row for those 65 or older is now blue (and that’s new). This new color blue means shared clinical decision-making and applies to people who were previously considered fully vaccinated with the now extinct combination of PCV13 and PPSV23. These patients now have the option of getting a dose of PCV20 five years after completing their PCV13-PPSV23 combo series. This option is blue because the decision is up to you and your patient.
Check the notes for more pneumococcal vaccination details. For example, for those partially vaccinated using lower valency vaccines, there’s an option of substituting PCV20 for PPSV23 to broaden and increase durability of protection.
The pneumococcal vaccination recommendation options are complicated. A new pneumococcal vaccination app can help.
Hepatitis B. For adults under age 60, the color code for the hepatitis B vaccine is yellow, meaning it’s indicated for all. For older patients, the color code is purple. If a patient who is age 60 or older wants the hepatitis B vaccine, they can have it even in the absence of additional risk indications.
Vaccinations by medical condition or other indications
Other than a few minor word changes on the overlay, the only thing that’s new is the COVID vaccine row.
This table is helpful for matching vaccine recommendations with specific medical conditions, including pregnancy, immunocompromise, HIV (with specifics according to CD4 count), asplenia, complement deficiencies, heart disease, lung disease, alcoholism, chronic liver disease, diabetes, health care personnel, and men who have sex with men.
Use this table to dot the i’s and cross the t’s when it comes to vaccination recommendations. For example, take a look at the pregnancy column. Live virus vaccines, including LAIV, MMR, and varicella, are contraindicated and color-coded red. MMR and varicella also have an asterisk, meaning vaccinate after pregnancy if indicated. HPV vaccines are not live virus vaccines, but the overlay says they are not recommended during pregnancy. The asterisk indicates that you can vaccinate after pregnancy.
Vaccine notes
The notes are in alphabetical order, and their organization (routine, special situations, and shared clinical decision-making when indicated) has not changed. They are concise and succinct, but sometimes they’re not enough. That’s why vaccine-specific links to more complete recommendations are so convenient.
Notes for hepatitis B contain nuances on specific dosing for vaccinating patients on dialysis, as well as a reminder that newer hepatitis C vaccines such as Heplisav and PreHevbrio are not recommended during pregnancy due to lack of safety data.
For influenza, everyone 6 months or older still needs yearly flu vaccination with an age- and health-appropriate flu vaccine. But for those aged 65 or older, the notes specify the three vaccine versions now preferred: high-dose, recombinant, or adjuvanted versions. However, if these aren’t available, it’s better to get any flu vaccine than to go without.
Under meningococcal vaccines, the notes for MenACWY and MenB are combined. For MenB, trade names Bexsero and Trumenba are specified because the products are not interchangeable. Booster intervals for those still at risk are different for each vaccine type: every 5 years for MenACWY boosters, and every 2-3 years for boosts of MenB.
The recent polio cases in New York have put polio vaccination in the spotlight. ACIP has now reinstated its Polio Vaccine Work Group. The new schedule lists polio vaccines on the cover page. Current recommendations have been added to the notes section. Routine vaccination for adults is not necessary, at least for now. However, those at increased risk for exposure to polio fall in the special-situation category. For those at increased risk who have completed a polio vaccine series, a single lifetime IPV booster can be given. For those at increased risk who have not completed their polio vaccine series, now would be the time to finish the series.
Appendix
The final step in using the new schedule is checking the appendix and its list of vaccine-specific contraindications and precautions.
I hope this review of the new ACIP adult immunization schedule has been helpful. For Medicine Matters, I’m Dr. Sandra Fryhofer.
Dr. Fryhofer is clinical associate professor of medicine, Emory University, Atlanta. She reported numerous conflicts of interest.
A version of this article first appeared on Medscape.com.
Weaponizing Education: The Rise, Fall, and Return of the GI Bill
Growing up I can remember my father telling stories of service members in the medical battalion he commanded in World War II (WWII) who after the war with his encouragement and their GI Bill educational benefits went to school to become doctors, nurses, and dentists. They were among the 2,300,000 veterans who attended US colleges and universities through the Servicemen’s Readjustment Act passed in 1944. The American Legion navigated the bill through the twists and turns of congressional support, and it was one of their leaders who invented the catchy GI Bill shorthand.2
As with most political legislation, there were mixed motives driving passage of the act, and like many policies in America, the primary impetus was economic. While the war was raging overseas, at home the US Department of Labor predicted that by the war’s end, 16 million service members would be jobless. Apprehensive about the prospect of yet another financial depression, in 1943 a White House agency recommended that the federal government fund education and training for the individuals who had served during the war.2
While troops stormed the beaches of Normandy, wartime President Franklin D. Roosevelt (FDR) signed the bill that delivered not only educational and training opportunities for service members and veterans, but also funded home loans and US Department of Veterans Affairs (VA) hospitals. The bill was practical in that it provided not only tuition, but also books, supplies, a living stipend, and counseling for the students. The bill technically expired in 1956, but a series of extensions and expansions has been true to the original intention to offer those who served their nation in the military a better life as citizens.
Articles describing the impact of the GI Bill use terms like life changing and transformative.3,4 Our contemporary culture makes it difficult to imagine how out of reach a college education was for the generation that fought WWII. Universities were primarily for the rich and connected, the powerful and privileged. Were it not for the upward social mobility the GI Bill propelled, the American dream would not have become a reality for many farmers, small town merchants, and factory workers. The GI Bill though could not by itself ensure equity. The systemic racism endemic in the United States and among the elected representatives who debated the bill resulted in many Black service members especially in the South being denied entrance to institutions of higher learning.5 Despite this invidious discrimination, the bill was a profound effort to help many other service members to successfully reintegrate into the society they had preserved and defended.4
“With the signing of this bill, a well-rounded program of special veterans’ benefits is nearly completed,” FDR said, capturing its noble intent: “It gives emphatic notice to the men and women in our armed forces that the American people do not intend to let them down.”6
Regrettably, we have not kept FDR’s pledge. Now unscrupulous businesses are preying on the aspirations of military personnel and veterans for an education and thwarting their ability to seek gainful employment. For more than a decade, respected news media have reported that for-profit universities were exploiting service members trying to improve their lives through obtaining a college education via the GI Bill.7 The sad irony is that what enabled the exploitation to occur was a major expansion of the benefits under the Post-9/11 GI Bill. This version granted educational funding to any individual who had served on active duty for 90 days or more after September 10, 2001.8 Federal law prohibits for-profit educational institutions from receiving more than 90% of their total revenue from federal student aid. A loophole in the law enabled these institutions to categorize GI Bill funding as private not government dollars. Bad old American greed drove these for-profit colleges and universities to aggressively recruit veterans who trusted in the good faith of the academic institutions. Once the GI Bill monies were exhausted, veterans had already invested so much time and energy in a degree or certificate, the schools could persuade them to take out student loans with the promise of job placement assistance that never materialized. They took advantage of the veterans’ hopes to fatten their own bottom line in the face of declining enrolments.9 Journalists, government, think tank reports, and even a documentary described the tragic stories of service members left unemployed with immense debt and degrees that to many of them were now worthless.10
After years of reporters exposing the scam and politically thwarted efforts to stop it, Congress and President Biden closed what was known as the 90/10 loophole. This ended the weaponization of education it had promoted. In October 2022, the US Department of Education announced its final rule to prohibit the widespread educational fraud that had betrayed so many veterans and service members, which Secretary Dennis McDonough described as “abuse.”11Some readers may wonder why I have devoted an editorial to a topic that seems somewhat distant from the health care that is the primary domain of Federal Practitioner. It happens that education is in closer proximity to health for our patients than many of us might have realized. A 2018 Military Medicine study found that veterans who took advantage of the educational opportunities of the GI Bill had better health and reduced smoking, among other benefits.12 This connection between health and education should serve as a source of pride for all of us in federal practice as we are part of organizations that affirm the holistic concept of health that embraces not just medicine but education, housing, and other services essential for comprehensive well-being.
1. Mandela NR. Lighting your way to a better future: speech delivered by Mr. N R Mandela at the launch of Mindset Network. July 16, 2003. Accessed January 23, 2023. http://db.nelsonmandela.org/speeches/pub_view.asp?pg=item&ItemID=NMS909&txtstr=Lighting%20your%20way%20to%20a%20better%20future
2. US National Archives and Records Administration. Milestones Documents: Servicemen’s Readjustment Act (1944). Updated May 3, 2022. Accessed January 23, 2023. https://www.archives.gov/milestone-documents/servicemens-readjustment-act
3. O’Brien C. A brief history of the GI Bill. Army Times. March 10, 2021. Accessed January 23, 2023. https://www.armytimes.com/education-transition/2021/03/10/a-brief-history-of-the-gi-bill
4. US Department of Defense. 75 years of the GI Bill: how transformative it’s been. June 9, 2019. Accessed January 23, 2023. https://www.defense.gov/News/Feature-Stories/story/Article/1727086/75-years-of-the-gi-bill-how-transformative-its-been
5. Thompson J. The GI Bill should’ve been race neutral, politicos made sure it wasn’t. Army Times. November 9, 2019. Accessed January 23, 2023. https://www.armytimes.com/military-honor/salute-veterans/2019/11/10/the-gi-bill-shouldve-been-race-neutral-politicos-made-sure-it-wasnt
6. US Department of Veterans Affairs. Born of controversy: the GI Bill of Rights. Accessed January 23, 2023. https://www.va.gov/opa/publications/celebrate/gi-bill.pdf
7. Lipton E. Profit and scrutiny for colleges courting veterans. New York Times. December 8, 2010. Accessed January 23, 2023. https://www.nytimes.com/2010/12/09/education/09colleges.html
8. Post-9/11 GI Bill. Accessed January 23, 2023. https://www.military.com/education/gi-bill/post-9-11
9. Veterans Education Success. Large for-profit schools remain dependent on recruiting GI Bill students despite overall enrollment declines. Veterans Perspective Brief 2018;4. Accessed January 23, 2023. https://static1.squarespace.com/static/556718b2e4b02e470eb1b186/t/5ae241e588251be6319e24a5/1524777445871/VES+Issue+Brief+%234+Enrollment.FINAL.v2.pdf
10. Hernandez K. Why these veterans regret their for-profit degrees—and debt. PBS Newshour. October 23, 2018. Accessed January 23, 2023. https://www.pbs.org/newshour/education/why-these-veterans-regret-their-for-profit-college-degrees-and-debt
11. US Department of Education. Education Department unveils final rules to protect veterans and service members, improve college access for incarcerated individuals and improve oversight when colleges change owners. Press release. Published October 27, 2022. Accessed January 23, 2023. https://www.ed.gov/news/press-releases/education-department-unveils-final-rules-protect-veterans-and-service-members-improve-college-access-incarcerated-individuals-and-improve-oversight-when-colleges-change-owners
12. Rumery ZR, Patel N, Richard P. The association between the use of the education benefits from the G.I. Bill and veterans’ health. Mil Med. 2018;183(5-6):e241-e248. doi:10.1093/milmed/usx102
Growing up I can remember my father telling stories of service members in the medical battalion he commanded in World War II (WWII) who after the war with his encouragement and their GI Bill educational benefits went to school to become doctors, nurses, and dentists. They were among the 2,300,000 veterans who attended US colleges and universities through the Servicemen’s Readjustment Act passed in 1944. The American Legion navigated the bill through the twists and turns of congressional support, and it was one of their leaders who invented the catchy GI Bill shorthand.2
As with most political legislation, there were mixed motives driving passage of the act, and like many policies in America, the primary impetus was economic. While the war was raging overseas, at home the US Department of Labor predicted that by the war’s end, 16 million service members would be jobless. Apprehensive about the prospect of yet another financial depression, in 1943 a White House agency recommended that the federal government fund education and training for the individuals who had served during the war.2
While troops stormed the beaches of Normandy, wartime President Franklin D. Roosevelt (FDR) signed the bill that delivered not only educational and training opportunities for service members and veterans, but also funded home loans and US Department of Veterans Affairs (VA) hospitals. The bill was practical in that it provided not only tuition, but also books, supplies, a living stipend, and counseling for the students. The bill technically expired in 1956, but a series of extensions and expansions has been true to the original intention to offer those who served their nation in the military a better life as citizens.
Articles describing the impact of the GI Bill use terms like life changing and transformative.3,4 Our contemporary culture makes it difficult to imagine how out of reach a college education was for the generation that fought WWII. Universities were primarily for the rich and connected, the powerful and privileged. Were it not for the upward social mobility the GI Bill propelled, the American dream would not have become a reality for many farmers, small town merchants, and factory workers. The GI Bill though could not by itself ensure equity. The systemic racism endemic in the United States and among the elected representatives who debated the bill resulted in many Black service members especially in the South being denied entrance to institutions of higher learning.5 Despite this invidious discrimination, the bill was a profound effort to help many other service members to successfully reintegrate into the society they had preserved and defended.4
“With the signing of this bill, a well-rounded program of special veterans’ benefits is nearly completed,” FDR said, capturing its noble intent: “It gives emphatic notice to the men and women in our armed forces that the American people do not intend to let them down.”6
Regrettably, we have not kept FDR’s pledge. Now unscrupulous businesses are preying on the aspirations of military personnel and veterans for an education and thwarting their ability to seek gainful employment. For more than a decade, respected news media have reported that for-profit universities were exploiting service members trying to improve their lives through obtaining a college education via the GI Bill.7 The sad irony is that what enabled the exploitation to occur was a major expansion of the benefits under the Post-9/11 GI Bill. This version granted educational funding to any individual who had served on active duty for 90 days or more after September 10, 2001.8 Federal law prohibits for-profit educational institutions from receiving more than 90% of their total revenue from federal student aid. A loophole in the law enabled these institutions to categorize GI Bill funding as private not government dollars. Bad old American greed drove these for-profit colleges and universities to aggressively recruit veterans who trusted in the good faith of the academic institutions. Once the GI Bill monies were exhausted, veterans had already invested so much time and energy in a degree or certificate, the schools could persuade them to take out student loans with the promise of job placement assistance that never materialized. They took advantage of the veterans’ hopes to fatten their own bottom line in the face of declining enrolments.9 Journalists, government, think tank reports, and even a documentary described the tragic stories of service members left unemployed with immense debt and degrees that to many of them were now worthless.10
After years of reporters exposing the scam and politically thwarted efforts to stop it, Congress and President Biden closed what was known as the 90/10 loophole. This ended the weaponization of education it had promoted. In October 2022, the US Department of Education announced its final rule to prohibit the widespread educational fraud that had betrayed so many veterans and service members, which Secretary Dennis McDonough described as “abuse.”11Some readers may wonder why I have devoted an editorial to a topic that seems somewhat distant from the health care that is the primary domain of Federal Practitioner. It happens that education is in closer proximity to health for our patients than many of us might have realized. A 2018 Military Medicine study found that veterans who took advantage of the educational opportunities of the GI Bill had better health and reduced smoking, among other benefits.12 This connection between health and education should serve as a source of pride for all of us in federal practice as we are part of organizations that affirm the holistic concept of health that embraces not just medicine but education, housing, and other services essential for comprehensive well-being.
Growing up I can remember my father telling stories of service members in the medical battalion he commanded in World War II (WWII) who after the war with his encouragement and their GI Bill educational benefits went to school to become doctors, nurses, and dentists. They were among the 2,300,000 veterans who attended US colleges and universities through the Servicemen’s Readjustment Act passed in 1944. The American Legion navigated the bill through the twists and turns of congressional support, and it was one of their leaders who invented the catchy GI Bill shorthand.2
As with most political legislation, there were mixed motives driving passage of the act, and like many policies in America, the primary impetus was economic. While the war was raging overseas, at home the US Department of Labor predicted that by the war’s end, 16 million service members would be jobless. Apprehensive about the prospect of yet another financial depression, in 1943 a White House agency recommended that the federal government fund education and training for the individuals who had served during the war.2
While troops stormed the beaches of Normandy, wartime President Franklin D. Roosevelt (FDR) signed the bill that delivered not only educational and training opportunities for service members and veterans, but also funded home loans and US Department of Veterans Affairs (VA) hospitals. The bill was practical in that it provided not only tuition, but also books, supplies, a living stipend, and counseling for the students. The bill technically expired in 1956, but a series of extensions and expansions has been true to the original intention to offer those who served their nation in the military a better life as citizens.
Articles describing the impact of the GI Bill use terms like life changing and transformative.3,4 Our contemporary culture makes it difficult to imagine how out of reach a college education was for the generation that fought WWII. Universities were primarily for the rich and connected, the powerful and privileged. Were it not for the upward social mobility the GI Bill propelled, the American dream would not have become a reality for many farmers, small town merchants, and factory workers. The GI Bill though could not by itself ensure equity. The systemic racism endemic in the United States and among the elected representatives who debated the bill resulted in many Black service members especially in the South being denied entrance to institutions of higher learning.5 Despite this invidious discrimination, the bill was a profound effort to help many other service members to successfully reintegrate into the society they had preserved and defended.4
“With the signing of this bill, a well-rounded program of special veterans’ benefits is nearly completed,” FDR said, capturing its noble intent: “It gives emphatic notice to the men and women in our armed forces that the American people do not intend to let them down.”6
Regrettably, we have not kept FDR’s pledge. Now unscrupulous businesses are preying on the aspirations of military personnel and veterans for an education and thwarting their ability to seek gainful employment. For more than a decade, respected news media have reported that for-profit universities were exploiting service members trying to improve their lives through obtaining a college education via the GI Bill.7 The sad irony is that what enabled the exploitation to occur was a major expansion of the benefits under the Post-9/11 GI Bill. This version granted educational funding to any individual who had served on active duty for 90 days or more after September 10, 2001.8 Federal law prohibits for-profit educational institutions from receiving more than 90% of their total revenue from federal student aid. A loophole in the law enabled these institutions to categorize GI Bill funding as private not government dollars. Bad old American greed drove these for-profit colleges and universities to aggressively recruit veterans who trusted in the good faith of the academic institutions. Once the GI Bill monies were exhausted, veterans had already invested so much time and energy in a degree or certificate, the schools could persuade them to take out student loans with the promise of job placement assistance that never materialized. They took advantage of the veterans’ hopes to fatten their own bottom line in the face of declining enrolments.9 Journalists, government, think tank reports, and even a documentary described the tragic stories of service members left unemployed with immense debt and degrees that to many of them were now worthless.10
After years of reporters exposing the scam and politically thwarted efforts to stop it, Congress and President Biden closed what was known as the 90/10 loophole. This ended the weaponization of education it had promoted. In October 2022, the US Department of Education announced its final rule to prohibit the widespread educational fraud that had betrayed so many veterans and service members, which Secretary Dennis McDonough described as “abuse.”11Some readers may wonder why I have devoted an editorial to a topic that seems somewhat distant from the health care that is the primary domain of Federal Practitioner. It happens that education is in closer proximity to health for our patients than many of us might have realized. A 2018 Military Medicine study found that veterans who took advantage of the educational opportunities of the GI Bill had better health and reduced smoking, among other benefits.12 This connection between health and education should serve as a source of pride for all of us in federal practice as we are part of organizations that affirm the holistic concept of health that embraces not just medicine but education, housing, and other services essential for comprehensive well-being.
1. Mandela NR. Lighting your way to a better future: speech delivered by Mr. N R Mandela at the launch of Mindset Network. July 16, 2003. Accessed January 23, 2023. http://db.nelsonmandela.org/speeches/pub_view.asp?pg=item&ItemID=NMS909&txtstr=Lighting%20your%20way%20to%20a%20better%20future
2. US National Archives and Records Administration. Milestones Documents: Servicemen’s Readjustment Act (1944). Updated May 3, 2022. Accessed January 23, 2023. https://www.archives.gov/milestone-documents/servicemens-readjustment-act
3. O’Brien C. A brief history of the GI Bill. Army Times. March 10, 2021. Accessed January 23, 2023. https://www.armytimes.com/education-transition/2021/03/10/a-brief-history-of-the-gi-bill
4. US Department of Defense. 75 years of the GI Bill: how transformative it’s been. June 9, 2019. Accessed January 23, 2023. https://www.defense.gov/News/Feature-Stories/story/Article/1727086/75-years-of-the-gi-bill-how-transformative-its-been
5. Thompson J. The GI Bill should’ve been race neutral, politicos made sure it wasn’t. Army Times. November 9, 2019. Accessed January 23, 2023. https://www.armytimes.com/military-honor/salute-veterans/2019/11/10/the-gi-bill-shouldve-been-race-neutral-politicos-made-sure-it-wasnt
6. US Department of Veterans Affairs. Born of controversy: the GI Bill of Rights. Accessed January 23, 2023. https://www.va.gov/opa/publications/celebrate/gi-bill.pdf
7. Lipton E. Profit and scrutiny for colleges courting veterans. New York Times. December 8, 2010. Accessed January 23, 2023. https://www.nytimes.com/2010/12/09/education/09colleges.html
8. Post-9/11 GI Bill. Accessed January 23, 2023. https://www.military.com/education/gi-bill/post-9-11
9. Veterans Education Success. Large for-profit schools remain dependent on recruiting GI Bill students despite overall enrollment declines. Veterans Perspective Brief 2018;4. Accessed January 23, 2023. https://static1.squarespace.com/static/556718b2e4b02e470eb1b186/t/5ae241e588251be6319e24a5/1524777445871/VES+Issue+Brief+%234+Enrollment.FINAL.v2.pdf
10. Hernandez K. Why these veterans regret their for-profit degrees—and debt. PBS Newshour. October 23, 2018. Accessed January 23, 2023. https://www.pbs.org/newshour/education/why-these-veterans-regret-their-for-profit-college-degrees-and-debt
11. US Department of Education. Education Department unveils final rules to protect veterans and service members, improve college access for incarcerated individuals and improve oversight when colleges change owners. Press release. Published October 27, 2022. Accessed January 23, 2023. https://www.ed.gov/news/press-releases/education-department-unveils-final-rules-protect-veterans-and-service-members-improve-college-access-incarcerated-individuals-and-improve-oversight-when-colleges-change-owners
12. Rumery ZR, Patel N, Richard P. The association between the use of the education benefits from the G.I. Bill and veterans’ health. Mil Med. 2018;183(5-6):e241-e248. doi:10.1093/milmed/usx102
1. Mandela NR. Lighting your way to a better future: speech delivered by Mr. N R Mandela at the launch of Mindset Network. July 16, 2003. Accessed January 23, 2023. http://db.nelsonmandela.org/speeches/pub_view.asp?pg=item&ItemID=NMS909&txtstr=Lighting%20your%20way%20to%20a%20better%20future
2. US National Archives and Records Administration. Milestones Documents: Servicemen’s Readjustment Act (1944). Updated May 3, 2022. Accessed January 23, 2023. https://www.archives.gov/milestone-documents/servicemens-readjustment-act
3. O’Brien C. A brief history of the GI Bill. Army Times. March 10, 2021. Accessed January 23, 2023. https://www.armytimes.com/education-transition/2021/03/10/a-brief-history-of-the-gi-bill
4. US Department of Defense. 75 years of the GI Bill: how transformative it’s been. June 9, 2019. Accessed January 23, 2023. https://www.defense.gov/News/Feature-Stories/story/Article/1727086/75-years-of-the-gi-bill-how-transformative-its-been
5. Thompson J. The GI Bill should’ve been race neutral, politicos made sure it wasn’t. Army Times. November 9, 2019. Accessed January 23, 2023. https://www.armytimes.com/military-honor/salute-veterans/2019/11/10/the-gi-bill-shouldve-been-race-neutral-politicos-made-sure-it-wasnt
6. US Department of Veterans Affairs. Born of controversy: the GI Bill of Rights. Accessed January 23, 2023. https://www.va.gov/opa/publications/celebrate/gi-bill.pdf
7. Lipton E. Profit and scrutiny for colleges courting veterans. New York Times. December 8, 2010. Accessed January 23, 2023. https://www.nytimes.com/2010/12/09/education/09colleges.html
8. Post-9/11 GI Bill. Accessed January 23, 2023. https://www.military.com/education/gi-bill/post-9-11
9. Veterans Education Success. Large for-profit schools remain dependent on recruiting GI Bill students despite overall enrollment declines. Veterans Perspective Brief 2018;4. Accessed January 23, 2023. https://static1.squarespace.com/static/556718b2e4b02e470eb1b186/t/5ae241e588251be6319e24a5/1524777445871/VES+Issue+Brief+%234+Enrollment.FINAL.v2.pdf
10. Hernandez K. Why these veterans regret their for-profit degrees—and debt. PBS Newshour. October 23, 2018. Accessed January 23, 2023. https://www.pbs.org/newshour/education/why-these-veterans-regret-their-for-profit-college-degrees-and-debt
11. US Department of Education. Education Department unveils final rules to protect veterans and service members, improve college access for incarcerated individuals and improve oversight when colleges change owners. Press release. Published October 27, 2022. Accessed January 23, 2023. https://www.ed.gov/news/press-releases/education-department-unveils-final-rules-protect-veterans-and-service-members-improve-college-access-incarcerated-individuals-and-improve-oversight-when-colleges-change-owners
12. Rumery ZR, Patel N, Richard P. The association between the use of the education benefits from the G.I. Bill and veterans’ health. Mil Med. 2018;183(5-6):e241-e248. doi:10.1093/milmed/usx102
Trauma-Informed Training for Veterans Treatment Court Professionals: Program Development and Initial Feedback
Veterans who interact with the criminal justice system (ie, justice-involved veterans) have heightened rates of mental health and psychosocial needs, including posttraumatic stress disorder (PTSD), substance use disorder, depression, suicidal ideation and attempt, and homelessness.1,2 Alongside these criminogenic risk factors, recidivism is common among justice-involved veterans: About 70% of incarcerated veterans disclosed at least one prior incarceration.3
To address the complex interplay of psychosocial factors, mental health concerns, and justice involvement among veterans, veterans treatment courts (VTCs) emerged as an alternative to incarceration.4 VTC participation often consists of integrated treatment and rehabilitative services (eg, vocational training, health care), ongoing monitoring for substance use, graduated responses to address treatment adherence, and ongoing communication with the judge and legal counsel.4
A primary aim of these courts is to address psychosocial needs believed to underlie criminal behavior, thus reducing risk of recidivism and promoting successful recovery and community integration for eligible veterans. To do so, VTCs collaborate with community-based and/or US Department of Veterans Affairs services, such as the Veterans Justice Outreach program (VJO). VJO specialists identify and refer justice-involved veterans to Veterans Health Administration (VHA) and community care and serve as a liaison between VTC staff and VHA health care professionals (HCPs).5
VTC outcome studies highlight the importance of not only diverting veterans to problem-solving courts, but also ensuring their optimal participation. Successful graduates of VTC programs demonstrate significant improvements in mental health symptoms, life satisfaction, and social support, as well as lower rates of law enforcement interactions.6,7 However, less is known about supporting those veterans who have difficulty engaging in VTCs and either discontinue participation or require lengthier periods of participation to meet court graduation requirements.8 One possibility to improve engagement among these veterans is to enhance court practices to best meet their needs.
In addition to delivering treatment, VHA mental health professionals may serve a critical interdisciplinary role by lending expertise to support VTC practices. For example, equipping court professionals with clinical knowledge and skills related to motivation may strengthen the staff’s interactions with participants, enabling them to address barriers as they arise and to facilitate veterans’ treatment adherence. Additionally, responsiveness to the impact of trauma exposure, which is common among this population, may prove important as related symptoms can affect veterans’ engagement, receptivity, and behavior in court settings. Indeed, prior examinations of justice-involved veterans have found trauma exposure rates ranging from 60% to 90% and PTSD rates ranging from 27% to 40%.1,2 Notably, involvement with the justice system (eg, incarceration) may itself further increase risk of trauma exposure (eg, experiencing a physical or sexual assault in prison) or exacerbate existing PTSD.9 Nonetheless, whereas many drug courts and domestic violence courts have been established, problem-solving courts with a specialized focus on trauma exposure remain rare, suggesting a potential gap in court training.
VHA HCPs have the potential to facilitate justice-involved veterans’ successful court and treatment participation by coordinating with VJO specialists to provide training and consultation to the courts. Supporting efforts to effectively and responsively address criminogenic risk (eg, mental health) in VTC settings may in turn reduce the likelihood of recidivism.10 Given the elevated rates of trauma exposure among justice-involved veterans and the relative lack of trauma-focused VTCs, we developed a trauma-informed training for VTC professionals that centered on related clinical presentations of justice-involved veterans and frequently occurring challenges in the context of court participation.
Program Development
This educational program aimed to (1) provide psychoeducation on trauma exposure, PTSD, and existing evidence-based treatments; (2) present clinical considerations for justice-involved veterans related to trauma exposure and/or PTSD; and (3) introduce skills to facilitate effective communication and trauma-informed care practices among professionals working with veterans in a treatment court.
Prior to piloting the program, we conducted a needs assessment with VTC professionals and identified relevant theoretical constructs and brief interventions for inclusion in the training. Additionally, given the dearth of prior research on mental health education for VTCs, the team consulted with the developers of PTSD 101, a VHA workshop for veterans’ families that promotes psychoeducation, support, and effective communication.11 Doing so informed approaches to delivering education to nonclinical audiences that interact with veterans with histories of trauma exposure. As this was a program development project, it was determined to be exempt from institutional review board review.
Needs Assessment
In the initial stages of development, local VJO specialists identified regional VTCs and facilitated introductions to these courts. Two of the 3 Rocky Mountain region VTCs that were contacted expressed interest in receiving trauma-informed training. Based on preliminary interest, the facilitators conducted a needs assessment with VJO and VTC staff from these 2 courts to capture requests for specific content and past experiences with other mental health trainings.
Guided by the focus group model, the needs assessments took place during three 1-hour meetings with VJO specialists and a 1-hour meeting with VJO specialists, VTC professionals, and community-based clinical partners.12 Additionally, attending a VTC graduation and court session allowed for observations of court practices and interactions with veterans. A total of 13 professionals (judges, court coordinators, case managers, peer mentors, VJO specialists, and clinicians who specialize in substance use disorder and intimate partner violence) participated in the needs assessments.
The most critical need identified by court professionals was a focus on how to apply knowledge about trauma and PTSD to interactions with justice-involved veterans. This was reportedly absent from prior training sessions the courts had received. Both Rocky Mountain region VTCs expressed a strong interest in and openness to adapting practices based on research and practice recommendations. Additional requests that emerged included a refresher on psychoeducation related to trauma and how to address the personal impact of working with this population (eg, compassion fatigue).
Training Components
Based on the needs identified by VTC professionals and informed by consultation with the developers of PTSD 101,
Psychoeducation. The initial portion of the training consisted of psychoeducation to increase VTC staff familiarity with the distinctions between trauma exposure and a formal diagnosis of PTSD, mechanisms underlying PTSD, and evidence-based treatment. To deepen conceptual understanding of trauma and PTSD beyond an overview of criteria set forth in The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), psychoeducation centered on the drivers of avoidance (eg, short-term benefit vs long-term consequences), behaviors that often facilitate avoidance (eg, substance use), functions underlying these behaviors (eg, distress reduction), and structure and mechanisms of change in evidence-based treatments for PTSD, including cognitive processing therapy and prolonged exposure.13,14
Fostering court familiarity with cognitive processing therapy and prolonged exposure may bolster veteran engagement in treatment through regular reinforcement of skills and concepts introduced in therapy. This may prove particularly salient given the limited engagement with mental health treatment and elevated dropout rates from PTSD treatment among the general veteran population.15,16
Exercises and metaphors were used to illustrate concepts in multiple ways. For example, training attendees engaged in a “stop, drop, and roll” thought exercise in which they were asked to brainstorm behavioral reactions to catching on fire. This exercise illustrated the tendency for individuals to revert to common yet unhelpful attempts at problem solving (eg, running due to panic, which would exacerbate the fire), particularly in crisis and without prior education regarding adaptive ways to respond. Attendee-generated examples, such as running, were used to demonstrate the importance of practicing and reinforcing skill development prior to a crisis, to ensure proficiency and optimal response. Additionally, in prompting consideration of one’s response tendencies, this exercise may engender empathy and understanding for veterans.
Skills training. Efforts to promote veteran engagement in court, facilitate motivation and readiness for change, and address barriers that arise (eg, distress associated with court appearances) may support successful and timely graduation. As such, skills training constituted the largest component of the training and drew from observations of court practices and the VTCs’ identified challenges. Consistent with the project’s aims and reported needs of the court, skills that target common presentations following trauma exposure (eg, avoidance, hypervigilance) were prioritized for this pilot training. Strategies included brief interventions from dialectical behavior therapy, acceptance and commitment therapy, and motivational interviewing to strengthen the support provided by staff to veterans and address their needs (Table 2).
Training attendees also participated in exercises to reiterate skills. For example, attendees completed an ambivalence matrix using an audience-identified common behavior that is difficult to change (eg, heavy alcohol use as a coping mechanism for distress).
Attendees engaged in an exercise that involved identifying unhelpful thoughts and behaviors, targets for validation, and veteran strengths from a hypothetical case vignette. This vignette involved a VTC participant who initially engaged effectively but began to demonstrate difficulty appropriately engaging in court and mental health treatment as well as challenging interactions with VTC staff (eg, raised voice during court sessions, not respecting communication boundaries).
Pilot Test
Based on scheduling parameters communicated by court coordinators, the pilot training was designed as a presentation during times reserved for court staffing meetings. To accommodate court preferences due to the COVID-19 pandemic, one 90-minute training was conducted virtually in March 2022, and the other training was conducted in person in April 2022 for 2 hours. The trainings were facilitated by 2 VHA clinical psychologists and included the judge, court coordinator, VJO specialist, peer mentors, case managers, probation/parole officers, and community-based HCPs who partner with the court (eg, social workers, psychologists). About 12 to 15 professionals attended each training session.
Feedback
Feedback was solicited from attendees via an anonymous online survey. Seven participants completed the survey; the response rate of about 20% was consistent with those observed for other surveys of court professionals.20 Many attendees also provided feedback directly to the facilitators. Feedback highlighted that the skills-based components not only were perceived as most helpful but also notably distinguished this training. “What set this training apart from other training events was the practical applications,” one attendee noted. “It was not just information or education, both instructors did an incredible job of explaining exactly how we could apply the knowledge they were sharing. They did this in such a way that it was easy to understand and apply.”
Specific skills were consistently identified as helpful, including managing intense emotions, addressing ambivalence, and approaching sanctions and rewards. Additionally, employing a less formal approach to the training, with relatable overviews of concepts and immediate responsiveness to requests for expansion on a topic, was perceived as a unique benefit: Another attendee appreciated that “It was beneficial to sit around a table with a less formal presentation and be able to ask questions.” This approach seemed particularly well suited for the program’s cross-disciplinary audience. Attendees reported that they valued the relatively limited focus on DSM-5 criteria. Attendees emphasized that education specific to veterans on evidence-based PTSD treatments, psychoeducation, and avoidance was very helpful. Respondents also recommended that the training be lengthened to a daylong workshop to accommodate greater opportunity to practice skills and consultation.
The consultation portion of the training provided insight into additional areas of importance to incorporate into future iterations. Identified needs included appropriate and realistic boundary setting (eg, addressing disruptions in the courtroom), suggestions for improving and expanding homework assigned by the court, and ways to address concerns about PTSD treatment shared by veterans in court (eg, attributing substance use relapses to the intensiveness of trauma-focused treatment vs lack of familiarity with alternate coping skills). Additionally, the VTC professionals’ desire to support mental health professionals’ work with veterans was clearly evident, highlighting the bidirectional value of interdisciplinary collaboration between VHA mental health professionals and VTC professionals.
Discussion
A trauma-informed training was developed and delivered to 2 VTCs in the Rocky Mountain region with the goal of providing relevant psychoeducation and introducing skills to bolster court practices that address veteran needs. Psychoeducational components of the training that were particularly well received and prompted significant participant engagement included discussions and examples of avoidance, levels of validation, language to facilitate motivation and address barriers, mechanisms underlying treatment, and potential functions underlying limited veteran treatment engagement. Distress tolerance, approaches to sanctions and rewards, and use of ambivalence matrices to guide motivation were identified as particularly helpful skills.
The pilot phase of this trauma-informed training provided valuable insights into developing mental health trainings for VTCs. Specifically, VTCs may benefit from the expertise of VHA HCPs and are particularly interested in learning brief skills to improve their practices. The usefulness of such trainings may be bolstered by efforts to form relationships with the court to identify their perceived needs and employing an iterative process that is responsive to feedback both during and after the training. Last, each stage of this project was strengthened by collaboration with VJO specialists, highlighting the importance of future collaboration between VJO and VHA mental health clinics to further support justice-involved veterans. For example, VJO specialists were instrumental in identifying training needs related to veterans’ clinical presentations in court, facilitating introductions to local VTCs, and helping to address barriers to piloting, like scheduling.
Modifications and Future Directions
The insights gained through the process of training design, delivery, and feedback inform future development of this training. Based on the feedback received, subsequent versions of the training may be expanded into a half- or full-day workshop to allow for adequate time for skills training and feedback, as well as consultation. Doing so will enable facilitators to further foster attendees’ familiarity with and confidence in their ability to use these skills. Furthermore, the consultation portion of this training revealed areas that may benefit from greater attention, including how to address challenging interactions in court (eg, addressing gender dynamics between court professionals and participants) and better support veterans who are having difficulty engaging in mental health treatment (eg, courts’ observation of high rates of dropout around the third or fourth session of evidence-based treatment for PTSD). Last, all attendees who responded to the survey expressed interest in a brief resource guide based on the training, emphasizing the need for ready access to key skills and concepts to support the use of strategies learned.
An additional future aim of this project is to conduct a more thorough evaluation of the needs and outcomes related to this trauma-informed training for VTC professionals. With the rapid growth of VTCs nationwide, relatively little examination of court processes and practices has occurred, and there is a lack of research on the development or effectiveness of mental health trainings provided to VTCs.21 Therefore, we intend to conduct larger scale qualitative interviews with court personnel and VJO specialists to obtain a clearer understanding of the needs related to skills-based training and gaps in psychoeducation. These comprehensive needs assessments may also capture common comorbidities that were not incorporated into the pilot training (eg, substance use disorders) but may be important training targets for court professionals. This information will be used to inform subsequent expansion and adaptation of the training into a longer workshop. Program evaluation will be conducted via survey-based feedback on perceived usefulness of the workshop and self-report of confidence in and use of strategies to improve court practices. Furthermore, efforts to obtain veteran outcome data, such as treatment engagement and successful participation in VTC, may be pursued.
Limitations
This training development and pilot project provided valuable foundational information regarding a largely unexamined component of treatment courts—the benefit of skills-based trainings to facilitate court practices related to justice-involved veterans. However, it is worth noting that survey responses were limited; thus, the feedback received may not reflect all attendees’ perceptions. Additionally, because both training sessions were conducted solely with 2 courts in the Rocky Mountain area, feedback may be limited to the needs of this geographic region.
Conclusions
A trauma-informed training was developed for VTCs to facilitate relevant understanding of justice-involved veterans’ needs and presentations in court, introduce skills to address challenges that arise (eg, motivation, emotional dysregulation), and provide interdisciplinary support to court professionals. This training was an important step toward fostering strong collaborations between VHA HCPs and community-based veterans courts, and feedback received during development and following implementation highlighted the perceived need for a skills-based approach to such trainings. Further program development and evaluation can strengthen this training and provide a foundation for dissemination to a broader scope of VTCs, with the goal of reducing recidivism risk among justice-involved veterans by promoting effective engagement in problem-solving court.
1. Blodgett JC, Avoundjian T, Finlay AK, et al. Prevalence of mental health disorders among justice-involved veterans. Epidemiol Rev. 2015;37(1):163-176. doi:10.1093/epirev/mxu003
2. Saxon AJ, Davis TM, Sloan KL, McKnight KM, McFall ME, Kivlahan DR. Trauma, symptoms of posttraumatic stress disorder, and associated problems among incarcerated veterans. Psychiatr Serv. 2001;52(7):959-964. doi:10.1176/appi.ps.52.7.959
3. Bronson J, Carson AC, Noonan M. Veterans in prison and jail, 2011-12. December 2015. Accessed January 11, 2023. https://bjs.ojp.gov/content/pub/pdf/vpj1112.pdf
4. Cartwright T. “To care for him who shall have borne the battle”: the recent development of veterans treatment courts in America. Stanford Law Rev. 2011;22(1):295-316.
5. Finlay AK, Smelson D, Sawh L, et al. U.S. Department of Veterans Affairs Veterans Justice Outreach Program: connecting justice-involved veterans with mental health and substance use disorder Treatment. Crim Justice Policy Rev. 2016;27(2):10.1177/0887403414562601. doi:10.1177/0887403414562601
6. Knudsen KJ, Wingenfeld S. A specialized treatment court for veterans with trauma exposure: implications for the field. Community Ment Health J. 2016;52(2):127-135. doi:10.1007/s10597-015-9845-9
7. Montgomery LM, Olson JN. Veterans treatment court impact on veteran mental health and life satisfaction. J Psychol Behav Sci. 2018;6(1):1-4. doi:10.15640/jpbs.v6n1a1
8. Tsai J, Finlay A, Flatley B, Kasprow WJ, Clark S. A national study of veterans treatment court participants: who benefits and who recidivates. Adm Policy Ment Health. 2018;45(2):236-244. doi:10.1007/s10488-017-0816-z
9. Wolff NL, Shi J. Trauma and incarcerated persons. In: Scott CL, ed. Handbook of Correctional Mental Health. American Psychiatric Publishing, Inc.; 2010:277-320.
10. Bonta J, Andrews DA. Risk-need-responsivity model for offender assessment and rehabilitation. Rehabilitation. 2007;6:1-22. https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/rsk-nd-rspnsvty/index-en.aspx
11. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention, Family Services Section; Caska-Wallace CM, Campbell SB, Glynn SM. PTSD 101 for family and friends: a support and education workshop. 2020.
12. Tipping J. Focus groups: a method of needs assessment. J Contin Educ Health Prof. 1998;18(3):150-154. doi:10.1002/chp.1340180304
13. Resick PA, Monson CM, Chard KM. Cognitive Processing Therapy for PTSD: A Comprehensive Manual. The Guilford Press; 2017.
14. Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide. Oxford University Press; 2007. doi:10.1093/med:psych/9780195308501.001.0001
15. Seal KH, Maguen S, Cohen B, et al. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23(1):5-16. doi:10.1002/jts.20493
16. Edwards-Stewart A, Smolenski DJ, Bush NE, et al. Posttraumatic stress disorder treatment dropout among military and veteran populations: a systematic review and meta-analysis. J Trauma Stress. 2021;34(4):808-818. doi:10.1002/jts.22653
17. Linehan MM. Dialectical Behavior Therapy Skills Training Manual. 2nd ed. Guildford Press; 2015.
18. Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. 2nd ed. Guildford Press; 2016.
19. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. The Guildford Press; 2002.
20. National Center for State Courts. A survey of members of major national court organizations. October 2010. Accessed January 11, 2023. https://www.ncsc.org/__data/assets/pdf_file/0015/16350/survey-summary-10-26.pdf
21. Baldwin JM, Brooke EJ. Pausing in the wake of rapid adoption: a call to critically examine the veterans treatment court concept. J Offender Rehabil. 2019;58(1):1-29. doi:10.1080/10509674.2018.1549181
Veterans who interact with the criminal justice system (ie, justice-involved veterans) have heightened rates of mental health and psychosocial needs, including posttraumatic stress disorder (PTSD), substance use disorder, depression, suicidal ideation and attempt, and homelessness.1,2 Alongside these criminogenic risk factors, recidivism is common among justice-involved veterans: About 70% of incarcerated veterans disclosed at least one prior incarceration.3
To address the complex interplay of psychosocial factors, mental health concerns, and justice involvement among veterans, veterans treatment courts (VTCs) emerged as an alternative to incarceration.4 VTC participation often consists of integrated treatment and rehabilitative services (eg, vocational training, health care), ongoing monitoring for substance use, graduated responses to address treatment adherence, and ongoing communication with the judge and legal counsel.4
A primary aim of these courts is to address psychosocial needs believed to underlie criminal behavior, thus reducing risk of recidivism and promoting successful recovery and community integration for eligible veterans. To do so, VTCs collaborate with community-based and/or US Department of Veterans Affairs services, such as the Veterans Justice Outreach program (VJO). VJO specialists identify and refer justice-involved veterans to Veterans Health Administration (VHA) and community care and serve as a liaison between VTC staff and VHA health care professionals (HCPs).5
VTC outcome studies highlight the importance of not only diverting veterans to problem-solving courts, but also ensuring their optimal participation. Successful graduates of VTC programs demonstrate significant improvements in mental health symptoms, life satisfaction, and social support, as well as lower rates of law enforcement interactions.6,7 However, less is known about supporting those veterans who have difficulty engaging in VTCs and either discontinue participation or require lengthier periods of participation to meet court graduation requirements.8 One possibility to improve engagement among these veterans is to enhance court practices to best meet their needs.
In addition to delivering treatment, VHA mental health professionals may serve a critical interdisciplinary role by lending expertise to support VTC practices. For example, equipping court professionals with clinical knowledge and skills related to motivation may strengthen the staff’s interactions with participants, enabling them to address barriers as they arise and to facilitate veterans’ treatment adherence. Additionally, responsiveness to the impact of trauma exposure, which is common among this population, may prove important as related symptoms can affect veterans’ engagement, receptivity, and behavior in court settings. Indeed, prior examinations of justice-involved veterans have found trauma exposure rates ranging from 60% to 90% and PTSD rates ranging from 27% to 40%.1,2 Notably, involvement with the justice system (eg, incarceration) may itself further increase risk of trauma exposure (eg, experiencing a physical or sexual assault in prison) or exacerbate existing PTSD.9 Nonetheless, whereas many drug courts and domestic violence courts have been established, problem-solving courts with a specialized focus on trauma exposure remain rare, suggesting a potential gap in court training.
VHA HCPs have the potential to facilitate justice-involved veterans’ successful court and treatment participation by coordinating with VJO specialists to provide training and consultation to the courts. Supporting efforts to effectively and responsively address criminogenic risk (eg, mental health) in VTC settings may in turn reduce the likelihood of recidivism.10 Given the elevated rates of trauma exposure among justice-involved veterans and the relative lack of trauma-focused VTCs, we developed a trauma-informed training for VTC professionals that centered on related clinical presentations of justice-involved veterans and frequently occurring challenges in the context of court participation.
Program Development
This educational program aimed to (1) provide psychoeducation on trauma exposure, PTSD, and existing evidence-based treatments; (2) present clinical considerations for justice-involved veterans related to trauma exposure and/or PTSD; and (3) introduce skills to facilitate effective communication and trauma-informed care practices among professionals working with veterans in a treatment court.
Prior to piloting the program, we conducted a needs assessment with VTC professionals and identified relevant theoretical constructs and brief interventions for inclusion in the training. Additionally, given the dearth of prior research on mental health education for VTCs, the team consulted with the developers of PTSD 101, a VHA workshop for veterans’ families that promotes psychoeducation, support, and effective communication.11 Doing so informed approaches to delivering education to nonclinical audiences that interact with veterans with histories of trauma exposure. As this was a program development project, it was determined to be exempt from institutional review board review.
Needs Assessment
In the initial stages of development, local VJO specialists identified regional VTCs and facilitated introductions to these courts. Two of the 3 Rocky Mountain region VTCs that were contacted expressed interest in receiving trauma-informed training. Based on preliminary interest, the facilitators conducted a needs assessment with VJO and VTC staff from these 2 courts to capture requests for specific content and past experiences with other mental health trainings.
Guided by the focus group model, the needs assessments took place during three 1-hour meetings with VJO specialists and a 1-hour meeting with VJO specialists, VTC professionals, and community-based clinical partners.12 Additionally, attending a VTC graduation and court session allowed for observations of court practices and interactions with veterans. A total of 13 professionals (judges, court coordinators, case managers, peer mentors, VJO specialists, and clinicians who specialize in substance use disorder and intimate partner violence) participated in the needs assessments.
The most critical need identified by court professionals was a focus on how to apply knowledge about trauma and PTSD to interactions with justice-involved veterans. This was reportedly absent from prior training sessions the courts had received. Both Rocky Mountain region VTCs expressed a strong interest in and openness to adapting practices based on research and practice recommendations. Additional requests that emerged included a refresher on psychoeducation related to trauma and how to address the personal impact of working with this population (eg, compassion fatigue).
Training Components
Based on the needs identified by VTC professionals and informed by consultation with the developers of PTSD 101,
Psychoeducation. The initial portion of the training consisted of psychoeducation to increase VTC staff familiarity with the distinctions between trauma exposure and a formal diagnosis of PTSD, mechanisms underlying PTSD, and evidence-based treatment. To deepen conceptual understanding of trauma and PTSD beyond an overview of criteria set forth in The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), psychoeducation centered on the drivers of avoidance (eg, short-term benefit vs long-term consequences), behaviors that often facilitate avoidance (eg, substance use), functions underlying these behaviors (eg, distress reduction), and structure and mechanisms of change in evidence-based treatments for PTSD, including cognitive processing therapy and prolonged exposure.13,14
Fostering court familiarity with cognitive processing therapy and prolonged exposure may bolster veteran engagement in treatment through regular reinforcement of skills and concepts introduced in therapy. This may prove particularly salient given the limited engagement with mental health treatment and elevated dropout rates from PTSD treatment among the general veteran population.15,16
Exercises and metaphors were used to illustrate concepts in multiple ways. For example, training attendees engaged in a “stop, drop, and roll” thought exercise in which they were asked to brainstorm behavioral reactions to catching on fire. This exercise illustrated the tendency for individuals to revert to common yet unhelpful attempts at problem solving (eg, running due to panic, which would exacerbate the fire), particularly in crisis and without prior education regarding adaptive ways to respond. Attendee-generated examples, such as running, were used to demonstrate the importance of practicing and reinforcing skill development prior to a crisis, to ensure proficiency and optimal response. Additionally, in prompting consideration of one’s response tendencies, this exercise may engender empathy and understanding for veterans.
Skills training. Efforts to promote veteran engagement in court, facilitate motivation and readiness for change, and address barriers that arise (eg, distress associated with court appearances) may support successful and timely graduation. As such, skills training constituted the largest component of the training and drew from observations of court practices and the VTCs’ identified challenges. Consistent with the project’s aims and reported needs of the court, skills that target common presentations following trauma exposure (eg, avoidance, hypervigilance) were prioritized for this pilot training. Strategies included brief interventions from dialectical behavior therapy, acceptance and commitment therapy, and motivational interviewing to strengthen the support provided by staff to veterans and address their needs (Table 2).
Training attendees also participated in exercises to reiterate skills. For example, attendees completed an ambivalence matrix using an audience-identified common behavior that is difficult to change (eg, heavy alcohol use as a coping mechanism for distress).
Attendees engaged in an exercise that involved identifying unhelpful thoughts and behaviors, targets for validation, and veteran strengths from a hypothetical case vignette. This vignette involved a VTC participant who initially engaged effectively but began to demonstrate difficulty appropriately engaging in court and mental health treatment as well as challenging interactions with VTC staff (eg, raised voice during court sessions, not respecting communication boundaries).
Pilot Test
Based on scheduling parameters communicated by court coordinators, the pilot training was designed as a presentation during times reserved for court staffing meetings. To accommodate court preferences due to the COVID-19 pandemic, one 90-minute training was conducted virtually in March 2022, and the other training was conducted in person in April 2022 for 2 hours. The trainings were facilitated by 2 VHA clinical psychologists and included the judge, court coordinator, VJO specialist, peer mentors, case managers, probation/parole officers, and community-based HCPs who partner with the court (eg, social workers, psychologists). About 12 to 15 professionals attended each training session.
Feedback
Feedback was solicited from attendees via an anonymous online survey. Seven participants completed the survey; the response rate of about 20% was consistent with those observed for other surveys of court professionals.20 Many attendees also provided feedback directly to the facilitators. Feedback highlighted that the skills-based components not only were perceived as most helpful but also notably distinguished this training. “What set this training apart from other training events was the practical applications,” one attendee noted. “It was not just information or education, both instructors did an incredible job of explaining exactly how we could apply the knowledge they were sharing. They did this in such a way that it was easy to understand and apply.”
Specific skills were consistently identified as helpful, including managing intense emotions, addressing ambivalence, and approaching sanctions and rewards. Additionally, employing a less formal approach to the training, with relatable overviews of concepts and immediate responsiveness to requests for expansion on a topic, was perceived as a unique benefit: Another attendee appreciated that “It was beneficial to sit around a table with a less formal presentation and be able to ask questions.” This approach seemed particularly well suited for the program’s cross-disciplinary audience. Attendees reported that they valued the relatively limited focus on DSM-5 criteria. Attendees emphasized that education specific to veterans on evidence-based PTSD treatments, psychoeducation, and avoidance was very helpful. Respondents also recommended that the training be lengthened to a daylong workshop to accommodate greater opportunity to practice skills and consultation.
The consultation portion of the training provided insight into additional areas of importance to incorporate into future iterations. Identified needs included appropriate and realistic boundary setting (eg, addressing disruptions in the courtroom), suggestions for improving and expanding homework assigned by the court, and ways to address concerns about PTSD treatment shared by veterans in court (eg, attributing substance use relapses to the intensiveness of trauma-focused treatment vs lack of familiarity with alternate coping skills). Additionally, the VTC professionals’ desire to support mental health professionals’ work with veterans was clearly evident, highlighting the bidirectional value of interdisciplinary collaboration between VHA mental health professionals and VTC professionals.
Discussion
A trauma-informed training was developed and delivered to 2 VTCs in the Rocky Mountain region with the goal of providing relevant psychoeducation and introducing skills to bolster court practices that address veteran needs. Psychoeducational components of the training that were particularly well received and prompted significant participant engagement included discussions and examples of avoidance, levels of validation, language to facilitate motivation and address barriers, mechanisms underlying treatment, and potential functions underlying limited veteran treatment engagement. Distress tolerance, approaches to sanctions and rewards, and use of ambivalence matrices to guide motivation were identified as particularly helpful skills.
The pilot phase of this trauma-informed training provided valuable insights into developing mental health trainings for VTCs. Specifically, VTCs may benefit from the expertise of VHA HCPs and are particularly interested in learning brief skills to improve their practices. The usefulness of such trainings may be bolstered by efforts to form relationships with the court to identify their perceived needs and employing an iterative process that is responsive to feedback both during and after the training. Last, each stage of this project was strengthened by collaboration with VJO specialists, highlighting the importance of future collaboration between VJO and VHA mental health clinics to further support justice-involved veterans. For example, VJO specialists were instrumental in identifying training needs related to veterans’ clinical presentations in court, facilitating introductions to local VTCs, and helping to address barriers to piloting, like scheduling.
Modifications and Future Directions
The insights gained through the process of training design, delivery, and feedback inform future development of this training. Based on the feedback received, subsequent versions of the training may be expanded into a half- or full-day workshop to allow for adequate time for skills training and feedback, as well as consultation. Doing so will enable facilitators to further foster attendees’ familiarity with and confidence in their ability to use these skills. Furthermore, the consultation portion of this training revealed areas that may benefit from greater attention, including how to address challenging interactions in court (eg, addressing gender dynamics between court professionals and participants) and better support veterans who are having difficulty engaging in mental health treatment (eg, courts’ observation of high rates of dropout around the third or fourth session of evidence-based treatment for PTSD). Last, all attendees who responded to the survey expressed interest in a brief resource guide based on the training, emphasizing the need for ready access to key skills and concepts to support the use of strategies learned.
An additional future aim of this project is to conduct a more thorough evaluation of the needs and outcomes related to this trauma-informed training for VTC professionals. With the rapid growth of VTCs nationwide, relatively little examination of court processes and practices has occurred, and there is a lack of research on the development or effectiveness of mental health trainings provided to VTCs.21 Therefore, we intend to conduct larger scale qualitative interviews with court personnel and VJO specialists to obtain a clearer understanding of the needs related to skills-based training and gaps in psychoeducation. These comprehensive needs assessments may also capture common comorbidities that were not incorporated into the pilot training (eg, substance use disorders) but may be important training targets for court professionals. This information will be used to inform subsequent expansion and adaptation of the training into a longer workshop. Program evaluation will be conducted via survey-based feedback on perceived usefulness of the workshop and self-report of confidence in and use of strategies to improve court practices. Furthermore, efforts to obtain veteran outcome data, such as treatment engagement and successful participation in VTC, may be pursued.
Limitations
This training development and pilot project provided valuable foundational information regarding a largely unexamined component of treatment courts—the benefit of skills-based trainings to facilitate court practices related to justice-involved veterans. However, it is worth noting that survey responses were limited; thus, the feedback received may not reflect all attendees’ perceptions. Additionally, because both training sessions were conducted solely with 2 courts in the Rocky Mountain area, feedback may be limited to the needs of this geographic region.
Conclusions
A trauma-informed training was developed for VTCs to facilitate relevant understanding of justice-involved veterans’ needs and presentations in court, introduce skills to address challenges that arise (eg, motivation, emotional dysregulation), and provide interdisciplinary support to court professionals. This training was an important step toward fostering strong collaborations between VHA HCPs and community-based veterans courts, and feedback received during development and following implementation highlighted the perceived need for a skills-based approach to such trainings. Further program development and evaluation can strengthen this training and provide a foundation for dissemination to a broader scope of VTCs, with the goal of reducing recidivism risk among justice-involved veterans by promoting effective engagement in problem-solving court.
Veterans who interact with the criminal justice system (ie, justice-involved veterans) have heightened rates of mental health and psychosocial needs, including posttraumatic stress disorder (PTSD), substance use disorder, depression, suicidal ideation and attempt, and homelessness.1,2 Alongside these criminogenic risk factors, recidivism is common among justice-involved veterans: About 70% of incarcerated veterans disclosed at least one prior incarceration.3
To address the complex interplay of psychosocial factors, mental health concerns, and justice involvement among veterans, veterans treatment courts (VTCs) emerged as an alternative to incarceration.4 VTC participation often consists of integrated treatment and rehabilitative services (eg, vocational training, health care), ongoing monitoring for substance use, graduated responses to address treatment adherence, and ongoing communication with the judge and legal counsel.4
A primary aim of these courts is to address psychosocial needs believed to underlie criminal behavior, thus reducing risk of recidivism and promoting successful recovery and community integration for eligible veterans. To do so, VTCs collaborate with community-based and/or US Department of Veterans Affairs services, such as the Veterans Justice Outreach program (VJO). VJO specialists identify and refer justice-involved veterans to Veterans Health Administration (VHA) and community care and serve as a liaison between VTC staff and VHA health care professionals (HCPs).5
VTC outcome studies highlight the importance of not only diverting veterans to problem-solving courts, but also ensuring their optimal participation. Successful graduates of VTC programs demonstrate significant improvements in mental health symptoms, life satisfaction, and social support, as well as lower rates of law enforcement interactions.6,7 However, less is known about supporting those veterans who have difficulty engaging in VTCs and either discontinue participation or require lengthier periods of participation to meet court graduation requirements.8 One possibility to improve engagement among these veterans is to enhance court practices to best meet their needs.
In addition to delivering treatment, VHA mental health professionals may serve a critical interdisciplinary role by lending expertise to support VTC practices. For example, equipping court professionals with clinical knowledge and skills related to motivation may strengthen the staff’s interactions with participants, enabling them to address barriers as they arise and to facilitate veterans’ treatment adherence. Additionally, responsiveness to the impact of trauma exposure, which is common among this population, may prove important as related symptoms can affect veterans’ engagement, receptivity, and behavior in court settings. Indeed, prior examinations of justice-involved veterans have found trauma exposure rates ranging from 60% to 90% and PTSD rates ranging from 27% to 40%.1,2 Notably, involvement with the justice system (eg, incarceration) may itself further increase risk of trauma exposure (eg, experiencing a physical or sexual assault in prison) or exacerbate existing PTSD.9 Nonetheless, whereas many drug courts and domestic violence courts have been established, problem-solving courts with a specialized focus on trauma exposure remain rare, suggesting a potential gap in court training.
VHA HCPs have the potential to facilitate justice-involved veterans’ successful court and treatment participation by coordinating with VJO specialists to provide training and consultation to the courts. Supporting efforts to effectively and responsively address criminogenic risk (eg, mental health) in VTC settings may in turn reduce the likelihood of recidivism.10 Given the elevated rates of trauma exposure among justice-involved veterans and the relative lack of trauma-focused VTCs, we developed a trauma-informed training for VTC professionals that centered on related clinical presentations of justice-involved veterans and frequently occurring challenges in the context of court participation.
Program Development
This educational program aimed to (1) provide psychoeducation on trauma exposure, PTSD, and existing evidence-based treatments; (2) present clinical considerations for justice-involved veterans related to trauma exposure and/or PTSD; and (3) introduce skills to facilitate effective communication and trauma-informed care practices among professionals working with veterans in a treatment court.
Prior to piloting the program, we conducted a needs assessment with VTC professionals and identified relevant theoretical constructs and brief interventions for inclusion in the training. Additionally, given the dearth of prior research on mental health education for VTCs, the team consulted with the developers of PTSD 101, a VHA workshop for veterans’ families that promotes psychoeducation, support, and effective communication.11 Doing so informed approaches to delivering education to nonclinical audiences that interact with veterans with histories of trauma exposure. As this was a program development project, it was determined to be exempt from institutional review board review.
Needs Assessment
In the initial stages of development, local VJO specialists identified regional VTCs and facilitated introductions to these courts. Two of the 3 Rocky Mountain region VTCs that were contacted expressed interest in receiving trauma-informed training. Based on preliminary interest, the facilitators conducted a needs assessment with VJO and VTC staff from these 2 courts to capture requests for specific content and past experiences with other mental health trainings.
Guided by the focus group model, the needs assessments took place during three 1-hour meetings with VJO specialists and a 1-hour meeting with VJO specialists, VTC professionals, and community-based clinical partners.12 Additionally, attending a VTC graduation and court session allowed for observations of court practices and interactions with veterans. A total of 13 professionals (judges, court coordinators, case managers, peer mentors, VJO specialists, and clinicians who specialize in substance use disorder and intimate partner violence) participated in the needs assessments.
The most critical need identified by court professionals was a focus on how to apply knowledge about trauma and PTSD to interactions with justice-involved veterans. This was reportedly absent from prior training sessions the courts had received. Both Rocky Mountain region VTCs expressed a strong interest in and openness to adapting practices based on research and practice recommendations. Additional requests that emerged included a refresher on psychoeducation related to trauma and how to address the personal impact of working with this population (eg, compassion fatigue).
Training Components
Based on the needs identified by VTC professionals and informed by consultation with the developers of PTSD 101,
Psychoeducation. The initial portion of the training consisted of psychoeducation to increase VTC staff familiarity with the distinctions between trauma exposure and a formal diagnosis of PTSD, mechanisms underlying PTSD, and evidence-based treatment. To deepen conceptual understanding of trauma and PTSD beyond an overview of criteria set forth in The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), psychoeducation centered on the drivers of avoidance (eg, short-term benefit vs long-term consequences), behaviors that often facilitate avoidance (eg, substance use), functions underlying these behaviors (eg, distress reduction), and structure and mechanisms of change in evidence-based treatments for PTSD, including cognitive processing therapy and prolonged exposure.13,14
Fostering court familiarity with cognitive processing therapy and prolonged exposure may bolster veteran engagement in treatment through regular reinforcement of skills and concepts introduced in therapy. This may prove particularly salient given the limited engagement with mental health treatment and elevated dropout rates from PTSD treatment among the general veteran population.15,16
Exercises and metaphors were used to illustrate concepts in multiple ways. For example, training attendees engaged in a “stop, drop, and roll” thought exercise in which they were asked to brainstorm behavioral reactions to catching on fire. This exercise illustrated the tendency for individuals to revert to common yet unhelpful attempts at problem solving (eg, running due to panic, which would exacerbate the fire), particularly in crisis and without prior education regarding adaptive ways to respond. Attendee-generated examples, such as running, were used to demonstrate the importance of practicing and reinforcing skill development prior to a crisis, to ensure proficiency and optimal response. Additionally, in prompting consideration of one’s response tendencies, this exercise may engender empathy and understanding for veterans.
Skills training. Efforts to promote veteran engagement in court, facilitate motivation and readiness for change, and address barriers that arise (eg, distress associated with court appearances) may support successful and timely graduation. As such, skills training constituted the largest component of the training and drew from observations of court practices and the VTCs’ identified challenges. Consistent with the project’s aims and reported needs of the court, skills that target common presentations following trauma exposure (eg, avoidance, hypervigilance) were prioritized for this pilot training. Strategies included brief interventions from dialectical behavior therapy, acceptance and commitment therapy, and motivational interviewing to strengthen the support provided by staff to veterans and address their needs (Table 2).
Training attendees also participated in exercises to reiterate skills. For example, attendees completed an ambivalence matrix using an audience-identified common behavior that is difficult to change (eg, heavy alcohol use as a coping mechanism for distress).
Attendees engaged in an exercise that involved identifying unhelpful thoughts and behaviors, targets for validation, and veteran strengths from a hypothetical case vignette. This vignette involved a VTC participant who initially engaged effectively but began to demonstrate difficulty appropriately engaging in court and mental health treatment as well as challenging interactions with VTC staff (eg, raised voice during court sessions, not respecting communication boundaries).
Pilot Test
Based on scheduling parameters communicated by court coordinators, the pilot training was designed as a presentation during times reserved for court staffing meetings. To accommodate court preferences due to the COVID-19 pandemic, one 90-minute training was conducted virtually in March 2022, and the other training was conducted in person in April 2022 for 2 hours. The trainings were facilitated by 2 VHA clinical psychologists and included the judge, court coordinator, VJO specialist, peer mentors, case managers, probation/parole officers, and community-based HCPs who partner with the court (eg, social workers, psychologists). About 12 to 15 professionals attended each training session.
Feedback
Feedback was solicited from attendees via an anonymous online survey. Seven participants completed the survey; the response rate of about 20% was consistent with those observed for other surveys of court professionals.20 Many attendees also provided feedback directly to the facilitators. Feedback highlighted that the skills-based components not only were perceived as most helpful but also notably distinguished this training. “What set this training apart from other training events was the practical applications,” one attendee noted. “It was not just information or education, both instructors did an incredible job of explaining exactly how we could apply the knowledge they were sharing. They did this in such a way that it was easy to understand and apply.”
Specific skills were consistently identified as helpful, including managing intense emotions, addressing ambivalence, and approaching sanctions and rewards. Additionally, employing a less formal approach to the training, with relatable overviews of concepts and immediate responsiveness to requests for expansion on a topic, was perceived as a unique benefit: Another attendee appreciated that “It was beneficial to sit around a table with a less formal presentation and be able to ask questions.” This approach seemed particularly well suited for the program’s cross-disciplinary audience. Attendees reported that they valued the relatively limited focus on DSM-5 criteria. Attendees emphasized that education specific to veterans on evidence-based PTSD treatments, psychoeducation, and avoidance was very helpful. Respondents also recommended that the training be lengthened to a daylong workshop to accommodate greater opportunity to practice skills and consultation.
The consultation portion of the training provided insight into additional areas of importance to incorporate into future iterations. Identified needs included appropriate and realistic boundary setting (eg, addressing disruptions in the courtroom), suggestions for improving and expanding homework assigned by the court, and ways to address concerns about PTSD treatment shared by veterans in court (eg, attributing substance use relapses to the intensiveness of trauma-focused treatment vs lack of familiarity with alternate coping skills). Additionally, the VTC professionals’ desire to support mental health professionals’ work with veterans was clearly evident, highlighting the bidirectional value of interdisciplinary collaboration between VHA mental health professionals and VTC professionals.
Discussion
A trauma-informed training was developed and delivered to 2 VTCs in the Rocky Mountain region with the goal of providing relevant psychoeducation and introducing skills to bolster court practices that address veteran needs. Psychoeducational components of the training that were particularly well received and prompted significant participant engagement included discussions and examples of avoidance, levels of validation, language to facilitate motivation and address barriers, mechanisms underlying treatment, and potential functions underlying limited veteran treatment engagement. Distress tolerance, approaches to sanctions and rewards, and use of ambivalence matrices to guide motivation were identified as particularly helpful skills.
The pilot phase of this trauma-informed training provided valuable insights into developing mental health trainings for VTCs. Specifically, VTCs may benefit from the expertise of VHA HCPs and are particularly interested in learning brief skills to improve their practices. The usefulness of such trainings may be bolstered by efforts to form relationships with the court to identify their perceived needs and employing an iterative process that is responsive to feedback both during and after the training. Last, each stage of this project was strengthened by collaboration with VJO specialists, highlighting the importance of future collaboration between VJO and VHA mental health clinics to further support justice-involved veterans. For example, VJO specialists were instrumental in identifying training needs related to veterans’ clinical presentations in court, facilitating introductions to local VTCs, and helping to address barriers to piloting, like scheduling.
Modifications and Future Directions
The insights gained through the process of training design, delivery, and feedback inform future development of this training. Based on the feedback received, subsequent versions of the training may be expanded into a half- or full-day workshop to allow for adequate time for skills training and feedback, as well as consultation. Doing so will enable facilitators to further foster attendees’ familiarity with and confidence in their ability to use these skills. Furthermore, the consultation portion of this training revealed areas that may benefit from greater attention, including how to address challenging interactions in court (eg, addressing gender dynamics between court professionals and participants) and better support veterans who are having difficulty engaging in mental health treatment (eg, courts’ observation of high rates of dropout around the third or fourth session of evidence-based treatment for PTSD). Last, all attendees who responded to the survey expressed interest in a brief resource guide based on the training, emphasizing the need for ready access to key skills and concepts to support the use of strategies learned.
An additional future aim of this project is to conduct a more thorough evaluation of the needs and outcomes related to this trauma-informed training for VTC professionals. With the rapid growth of VTCs nationwide, relatively little examination of court processes and practices has occurred, and there is a lack of research on the development or effectiveness of mental health trainings provided to VTCs.21 Therefore, we intend to conduct larger scale qualitative interviews with court personnel and VJO specialists to obtain a clearer understanding of the needs related to skills-based training and gaps in psychoeducation. These comprehensive needs assessments may also capture common comorbidities that were not incorporated into the pilot training (eg, substance use disorders) but may be important training targets for court professionals. This information will be used to inform subsequent expansion and adaptation of the training into a longer workshop. Program evaluation will be conducted via survey-based feedback on perceived usefulness of the workshop and self-report of confidence in and use of strategies to improve court practices. Furthermore, efforts to obtain veteran outcome data, such as treatment engagement and successful participation in VTC, may be pursued.
Limitations
This training development and pilot project provided valuable foundational information regarding a largely unexamined component of treatment courts—the benefit of skills-based trainings to facilitate court practices related to justice-involved veterans. However, it is worth noting that survey responses were limited; thus, the feedback received may not reflect all attendees’ perceptions. Additionally, because both training sessions were conducted solely with 2 courts in the Rocky Mountain area, feedback may be limited to the needs of this geographic region.
Conclusions
A trauma-informed training was developed for VTCs to facilitate relevant understanding of justice-involved veterans’ needs and presentations in court, introduce skills to address challenges that arise (eg, motivation, emotional dysregulation), and provide interdisciplinary support to court professionals. This training was an important step toward fostering strong collaborations between VHA HCPs and community-based veterans courts, and feedback received during development and following implementation highlighted the perceived need for a skills-based approach to such trainings. Further program development and evaluation can strengthen this training and provide a foundation for dissemination to a broader scope of VTCs, with the goal of reducing recidivism risk among justice-involved veterans by promoting effective engagement in problem-solving court.
1. Blodgett JC, Avoundjian T, Finlay AK, et al. Prevalence of mental health disorders among justice-involved veterans. Epidemiol Rev. 2015;37(1):163-176. doi:10.1093/epirev/mxu003
2. Saxon AJ, Davis TM, Sloan KL, McKnight KM, McFall ME, Kivlahan DR. Trauma, symptoms of posttraumatic stress disorder, and associated problems among incarcerated veterans. Psychiatr Serv. 2001;52(7):959-964. doi:10.1176/appi.ps.52.7.959
3. Bronson J, Carson AC, Noonan M. Veterans in prison and jail, 2011-12. December 2015. Accessed January 11, 2023. https://bjs.ojp.gov/content/pub/pdf/vpj1112.pdf
4. Cartwright T. “To care for him who shall have borne the battle”: the recent development of veterans treatment courts in America. Stanford Law Rev. 2011;22(1):295-316.
5. Finlay AK, Smelson D, Sawh L, et al. U.S. Department of Veterans Affairs Veterans Justice Outreach Program: connecting justice-involved veterans with mental health and substance use disorder Treatment. Crim Justice Policy Rev. 2016;27(2):10.1177/0887403414562601. doi:10.1177/0887403414562601
6. Knudsen KJ, Wingenfeld S. A specialized treatment court for veterans with trauma exposure: implications for the field. Community Ment Health J. 2016;52(2):127-135. doi:10.1007/s10597-015-9845-9
7. Montgomery LM, Olson JN. Veterans treatment court impact on veteran mental health and life satisfaction. J Psychol Behav Sci. 2018;6(1):1-4. doi:10.15640/jpbs.v6n1a1
8. Tsai J, Finlay A, Flatley B, Kasprow WJ, Clark S. A national study of veterans treatment court participants: who benefits and who recidivates. Adm Policy Ment Health. 2018;45(2):236-244. doi:10.1007/s10488-017-0816-z
9. Wolff NL, Shi J. Trauma and incarcerated persons. In: Scott CL, ed. Handbook of Correctional Mental Health. American Psychiatric Publishing, Inc.; 2010:277-320.
10. Bonta J, Andrews DA. Risk-need-responsivity model for offender assessment and rehabilitation. Rehabilitation. 2007;6:1-22. https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/rsk-nd-rspnsvty/index-en.aspx
11. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention, Family Services Section; Caska-Wallace CM, Campbell SB, Glynn SM. PTSD 101 for family and friends: a support and education workshop. 2020.
12. Tipping J. Focus groups: a method of needs assessment. J Contin Educ Health Prof. 1998;18(3):150-154. doi:10.1002/chp.1340180304
13. Resick PA, Monson CM, Chard KM. Cognitive Processing Therapy for PTSD: A Comprehensive Manual. The Guilford Press; 2017.
14. Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide. Oxford University Press; 2007. doi:10.1093/med:psych/9780195308501.001.0001
15. Seal KH, Maguen S, Cohen B, et al. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23(1):5-16. doi:10.1002/jts.20493
16. Edwards-Stewart A, Smolenski DJ, Bush NE, et al. Posttraumatic stress disorder treatment dropout among military and veteran populations: a systematic review and meta-analysis. J Trauma Stress. 2021;34(4):808-818. doi:10.1002/jts.22653
17. Linehan MM. Dialectical Behavior Therapy Skills Training Manual. 2nd ed. Guildford Press; 2015.
18. Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. 2nd ed. Guildford Press; 2016.
19. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. The Guildford Press; 2002.
20. National Center for State Courts. A survey of members of major national court organizations. October 2010. Accessed January 11, 2023. https://www.ncsc.org/__data/assets/pdf_file/0015/16350/survey-summary-10-26.pdf
21. Baldwin JM, Brooke EJ. Pausing in the wake of rapid adoption: a call to critically examine the veterans treatment court concept. J Offender Rehabil. 2019;58(1):1-29. doi:10.1080/10509674.2018.1549181
1. Blodgett JC, Avoundjian T, Finlay AK, et al. Prevalence of mental health disorders among justice-involved veterans. Epidemiol Rev. 2015;37(1):163-176. doi:10.1093/epirev/mxu003
2. Saxon AJ, Davis TM, Sloan KL, McKnight KM, McFall ME, Kivlahan DR. Trauma, symptoms of posttraumatic stress disorder, and associated problems among incarcerated veterans. Psychiatr Serv. 2001;52(7):959-964. doi:10.1176/appi.ps.52.7.959
3. Bronson J, Carson AC, Noonan M. Veterans in prison and jail, 2011-12. December 2015. Accessed January 11, 2023. https://bjs.ojp.gov/content/pub/pdf/vpj1112.pdf
4. Cartwright T. “To care for him who shall have borne the battle”: the recent development of veterans treatment courts in America. Stanford Law Rev. 2011;22(1):295-316.
5. Finlay AK, Smelson D, Sawh L, et al. U.S. Department of Veterans Affairs Veterans Justice Outreach Program: connecting justice-involved veterans with mental health and substance use disorder Treatment. Crim Justice Policy Rev. 2016;27(2):10.1177/0887403414562601. doi:10.1177/0887403414562601
6. Knudsen KJ, Wingenfeld S. A specialized treatment court for veterans with trauma exposure: implications for the field. Community Ment Health J. 2016;52(2):127-135. doi:10.1007/s10597-015-9845-9
7. Montgomery LM, Olson JN. Veterans treatment court impact on veteran mental health and life satisfaction. J Psychol Behav Sci. 2018;6(1):1-4. doi:10.15640/jpbs.v6n1a1
8. Tsai J, Finlay A, Flatley B, Kasprow WJ, Clark S. A national study of veterans treatment court participants: who benefits and who recidivates. Adm Policy Ment Health. 2018;45(2):236-244. doi:10.1007/s10488-017-0816-z
9. Wolff NL, Shi J. Trauma and incarcerated persons. In: Scott CL, ed. Handbook of Correctional Mental Health. American Psychiatric Publishing, Inc.; 2010:277-320.
10. Bonta J, Andrews DA. Risk-need-responsivity model for offender assessment and rehabilitation. Rehabilitation. 2007;6:1-22. https://www.publicsafety.gc.ca/cnt/rsrcs/pblctns/rsk-nd-rspnsvty/index-en.aspx
11. US Department of Veterans Affairs, Office of Mental Health and Suicide Prevention, Family Services Section; Caska-Wallace CM, Campbell SB, Glynn SM. PTSD 101 for family and friends: a support and education workshop. 2020.
12. Tipping J. Focus groups: a method of needs assessment. J Contin Educ Health Prof. 1998;18(3):150-154. doi:10.1002/chp.1340180304
13. Resick PA, Monson CM, Chard KM. Cognitive Processing Therapy for PTSD: A Comprehensive Manual. The Guilford Press; 2017.
14. Foa EB, Hembree EA, Rothbaum BO. Prolonged Exposure Therapy for PTSD: Emotional Processing of Traumatic Experiences: Therapist Guide. Oxford University Press; 2007. doi:10.1093/med:psych/9780195308501.001.0001
15. Seal KH, Maguen S, Cohen B, et al. VA mental health services utilization in Iraq and Afghanistan veterans in the first year of receiving new mental health diagnoses. J Trauma Stress. 2010;23(1):5-16. doi:10.1002/jts.20493
16. Edwards-Stewart A, Smolenski DJ, Bush NE, et al. Posttraumatic stress disorder treatment dropout among military and veteran populations: a systematic review and meta-analysis. J Trauma Stress. 2021;34(4):808-818. doi:10.1002/jts.22653
17. Linehan MM. Dialectical Behavior Therapy Skills Training Manual. 2nd ed. Guildford Press; 2015.
18. Hayes SC, Strosahl KD, Wilson KG. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. 2nd ed. Guildford Press; 2016.
19. Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2nd ed. The Guildford Press; 2002.
20. National Center for State Courts. A survey of members of major national court organizations. October 2010. Accessed January 11, 2023. https://www.ncsc.org/__data/assets/pdf_file/0015/16350/survey-summary-10-26.pdf
21. Baldwin JM, Brooke EJ. Pausing in the wake of rapid adoption: a call to critically examine the veterans treatment court concept. J Offender Rehabil. 2019;58(1):1-29. doi:10.1080/10509674.2018.1549181
Biden to end COVID emergencies in May
Doing so will have many effects, including the end of free vaccines and health services to fight the pandemic. The public health emergency has been renewed every 90 days since it was declared by the Trump administration in January 2020.
The declaration allowed major changes throughout the health care system to deal with the pandemic, including the free distribution of vaccines, testing, and treatments. In addition, telehealth services were expanded, and Medicaid and the Children’s Health Insurance Program were extended to millions more Americans.
Biden said the COVID-19 national emergency is set to expire March 1 while the declared public health emergency would currently expire on April 11. The president said both will be extended to end May 11.
There were nearly 300,000 newly reported COVID-19 cases in the United States for the week ending Jan. 25, according to CDC data, as well as more than 3,750 deaths.
A version of this article first appeared on WebMD.com.
Doing so will have many effects, including the end of free vaccines and health services to fight the pandemic. The public health emergency has been renewed every 90 days since it was declared by the Trump administration in January 2020.
The declaration allowed major changes throughout the health care system to deal with the pandemic, including the free distribution of vaccines, testing, and treatments. In addition, telehealth services were expanded, and Medicaid and the Children’s Health Insurance Program were extended to millions more Americans.
Biden said the COVID-19 national emergency is set to expire March 1 while the declared public health emergency would currently expire on April 11. The president said both will be extended to end May 11.
There were nearly 300,000 newly reported COVID-19 cases in the United States for the week ending Jan. 25, according to CDC data, as well as more than 3,750 deaths.
A version of this article first appeared on WebMD.com.
Doing so will have many effects, including the end of free vaccines and health services to fight the pandemic. The public health emergency has been renewed every 90 days since it was declared by the Trump administration in January 2020.
The declaration allowed major changes throughout the health care system to deal with the pandemic, including the free distribution of vaccines, testing, and treatments. In addition, telehealth services were expanded, and Medicaid and the Children’s Health Insurance Program were extended to millions more Americans.
Biden said the COVID-19 national emergency is set to expire March 1 while the declared public health emergency would currently expire on April 11. The president said both will be extended to end May 11.
There were nearly 300,000 newly reported COVID-19 cases in the United States for the week ending Jan. 25, according to CDC data, as well as more than 3,750 deaths.
A version of this article first appeared on WebMD.com.
Surgeon General says 13-year-olds shouldn’t be on social media
The U.S. Surgeon General says 13 years old is too young to begin using social media.
Most social media platforms including TikTok, Snapchat, Instagram, and Facebook allow users to create accounts if they say they are at least 13 years old.
“I, personally, based on the data I’ve seen, believe that 13 is too early. ... It’s a time where it’s really important for us to be thoughtful about what’s going into how they think about their own self-worth and their relationships, and the skewed and often distorted environment of social media often does a disservice to many of those children,” U.S. Surgeon General Vivek Murthy, MD, told CNN.
Research has shown that teens are susceptible to cyberbullying and serious mental health impacts from social media usage and online activity during an era when the influence of the Internet has become everywhere for young people.
According to the Pew Research Center, 95% of teens age 13 and up have a smartphone, and 97% of teens say they use the Internet daily. Among 13- and 14-year-olds, 61% say they use TikTok and 51% say they use Snapchat. Older teens ages 15-17 use those social media platforms at higher rates, with 71% saying they use TikTok and 65% using Snapchat.
“If parents can band together and say you know, as a group, we’re not going to allow our kids to use social media until 16 or 17 or 18 or whatever age they choose, that’s a much more effective strategy in making sure your kids don’t get exposed to harm early,” Dr. Murthy said.
A version of this article originally appeared on WebMD.com.
The U.S. Surgeon General says 13 years old is too young to begin using social media.
Most social media platforms including TikTok, Snapchat, Instagram, and Facebook allow users to create accounts if they say they are at least 13 years old.
“I, personally, based on the data I’ve seen, believe that 13 is too early. ... It’s a time where it’s really important for us to be thoughtful about what’s going into how they think about their own self-worth and their relationships, and the skewed and often distorted environment of social media often does a disservice to many of those children,” U.S. Surgeon General Vivek Murthy, MD, told CNN.
Research has shown that teens are susceptible to cyberbullying and serious mental health impacts from social media usage and online activity during an era when the influence of the Internet has become everywhere for young people.
According to the Pew Research Center, 95% of teens age 13 and up have a smartphone, and 97% of teens say they use the Internet daily. Among 13- and 14-year-olds, 61% say they use TikTok and 51% say they use Snapchat. Older teens ages 15-17 use those social media platforms at higher rates, with 71% saying they use TikTok and 65% using Snapchat.
“If parents can band together and say you know, as a group, we’re not going to allow our kids to use social media until 16 or 17 or 18 or whatever age they choose, that’s a much more effective strategy in making sure your kids don’t get exposed to harm early,” Dr. Murthy said.
A version of this article originally appeared on WebMD.com.
The U.S. Surgeon General says 13 years old is too young to begin using social media.
Most social media platforms including TikTok, Snapchat, Instagram, and Facebook allow users to create accounts if they say they are at least 13 years old.
“I, personally, based on the data I’ve seen, believe that 13 is too early. ... It’s a time where it’s really important for us to be thoughtful about what’s going into how they think about their own self-worth and their relationships, and the skewed and often distorted environment of social media often does a disservice to many of those children,” U.S. Surgeon General Vivek Murthy, MD, told CNN.
Research has shown that teens are susceptible to cyberbullying and serious mental health impacts from social media usage and online activity during an era when the influence of the Internet has become everywhere for young people.
According to the Pew Research Center, 95% of teens age 13 and up have a smartphone, and 97% of teens say they use the Internet daily. Among 13- and 14-year-olds, 61% say they use TikTok and 51% say they use Snapchat. Older teens ages 15-17 use those social media platforms at higher rates, with 71% saying they use TikTok and 65% using Snapchat.
“If parents can band together and say you know, as a group, we’re not going to allow our kids to use social media until 16 or 17 or 18 or whatever age they choose, that’s a much more effective strategy in making sure your kids don’t get exposed to harm early,” Dr. Murthy said.
A version of this article originally appeared on WebMD.com.
Meet the JCOM Author with Dr. Barkoudah: Diagnostic Errors in Hospitalized Patients
Meet the JCOM Author with Dr. Barkoudah: Development of a Safety Awards Program at a VA Health Care System



Meet the JCOM Author with Dr. Barkoudah: Teaching Quality Improvement to Internal Medicine Residents



FDA wants annual COVID boosters, just like annual flu shots
The U.S. Food and Drug Administration is suggesting a single annual shot. The formulation would be selected in June targeting the most threatening COVID-19 strains, and then people could get a shot in the fall when people begin spending more time indoors and exposure increases.
Some people, such as those who are older or immunocompromised, may need more than one dose.
A national advisory committee is expected to vote on the proposal at a meeting Jan. 26.
People in the United States have been much less likely to get an updated COVID-19 booster shot, compared with widespread uptake of the primary vaccine series. In its proposal, the FDA indicated it hoped a single annual shot would overcome challenges created by the complexity of the process – both in messaging and administration – attributed to that low booster rate. Nine in 10 people age 12 or older got the primary vaccine series in the United States, but only 15% got the latest booster shot for COVID-19.
About half of children and adults in the U.S. get an annual flu shot, according to Centers for Disease Control and Prevention data.
The FDA also wants to move to a single COVID-19 vaccine formulation that would be used for primary vaccine series and for booster shots.
COVID-19 cases, hospitalizations, and deaths are trending downward, according to the data tracker from the New York Times. Cases are down 28%, with 47,290 tallied daily. Hospitalizations are down 22%, with 37,474 daily. Deaths are down 4%, with an average of 489 per day as of Jan. 22.
A version of this article originally appeared on WebMD.com.
The U.S. Food and Drug Administration is suggesting a single annual shot. The formulation would be selected in June targeting the most threatening COVID-19 strains, and then people could get a shot in the fall when people begin spending more time indoors and exposure increases.
Some people, such as those who are older or immunocompromised, may need more than one dose.
A national advisory committee is expected to vote on the proposal at a meeting Jan. 26.
People in the United States have been much less likely to get an updated COVID-19 booster shot, compared with widespread uptake of the primary vaccine series. In its proposal, the FDA indicated it hoped a single annual shot would overcome challenges created by the complexity of the process – both in messaging and administration – attributed to that low booster rate. Nine in 10 people age 12 or older got the primary vaccine series in the United States, but only 15% got the latest booster shot for COVID-19.
About half of children and adults in the U.S. get an annual flu shot, according to Centers for Disease Control and Prevention data.
The FDA also wants to move to a single COVID-19 vaccine formulation that would be used for primary vaccine series and for booster shots.
COVID-19 cases, hospitalizations, and deaths are trending downward, according to the data tracker from the New York Times. Cases are down 28%, with 47,290 tallied daily. Hospitalizations are down 22%, with 37,474 daily. Deaths are down 4%, with an average of 489 per day as of Jan. 22.
A version of this article originally appeared on WebMD.com.
The U.S. Food and Drug Administration is suggesting a single annual shot. The formulation would be selected in June targeting the most threatening COVID-19 strains, and then people could get a shot in the fall when people begin spending more time indoors and exposure increases.
Some people, such as those who are older or immunocompromised, may need more than one dose.
A national advisory committee is expected to vote on the proposal at a meeting Jan. 26.
People in the United States have been much less likely to get an updated COVID-19 booster shot, compared with widespread uptake of the primary vaccine series. In its proposal, the FDA indicated it hoped a single annual shot would overcome challenges created by the complexity of the process – both in messaging and administration – attributed to that low booster rate. Nine in 10 people age 12 or older got the primary vaccine series in the United States, but only 15% got the latest booster shot for COVID-19.
About half of children and adults in the U.S. get an annual flu shot, according to Centers for Disease Control and Prevention data.
The FDA also wants to move to a single COVID-19 vaccine formulation that would be used for primary vaccine series and for booster shots.
COVID-19 cases, hospitalizations, and deaths are trending downward, according to the data tracker from the New York Times. Cases are down 28%, with 47,290 tallied daily. Hospitalizations are down 22%, with 37,474 daily. Deaths are down 4%, with an average of 489 per day as of Jan. 22.
A version of this article originally appeared on WebMD.com.
Development of a Safety Awards Program at a Veterans Affairs Health Care System: A Quality Improvement Initiative
ABSTRACT
Objective: Promoting a culture of safety is a critical component of improving health care quality. Recognizing staff who stop the line for safety can positively impact the growth of a culture of safety. The purpose of this initiative was to demonstrate to staff the importance of speaking up for safety and being acknowledged for doing so.
Methods: Following a review of the literature on safety awards programs and their role in promoting a culture of safety in health care covering the period 2017 to 2020, a formal process was developed and implemented to disseminate safety awards to employees.
Results: During the initial 18 months of the initiative, a total of 59 awards were presented. The awards were well received by the recipients and other staff members. Within this period, adjustments were made to enhance the scope and reach of the program.
Conclusion: Recognizing staff behaviors that support a culture of safety is important for improving health care quality and employee engagement. Future research should focus on a formal evaluation of the impact of safety awards programs on patient safety outcomes.
Keywords: patient safety, culture of safety, incident reporting, near miss.
A key aspect of improving health care quality is promoting and sustaining a culture of safety in the workplace. Improving the quality of health care services and systems involves making informed choices regarding the types of strategies to implement.1 An essential aspect of supporting a safety culture is safety-event reporting. To approach the goal of zero harm, all safety events, whether they result in actual harm or are considered near misses, need to be reported. Near-miss events are errors that occur while care is being provided but are detected and corrected before harm reaches the patient.1-3 Near-miss reporting plays a critical role in helping to identify and correct weaknesses in health care delivery systems and processes.4 However, evidence shows that there are a multitude of barriers to the reporting of near-miss events, such as fear of punitive actions, additional workload, unsupportive work environments, a culture with poor psychological safety, knowledge deficit, and lack of recognition of staff who do report near misses.4-11
According to The Joint Commission (TJC), acknowledging health care team members who recognize and report unsafe conditions that provide insight for improving patient safety is a key method for promoting the reporting of near-miss events.6 As a result, some health care organizations and patient safety agencies have started to institute some form of recognition for their employees in the realm of safety.8-10 The Pennsylvania Patient Safety Authority offers exceptional guidance for creating a safety awards program to promote a culture of safety.12 Furthermore, TJC supports recognizing individuals and health care teams who identify and report near misses, or who have suggestions for initiatives to promote patient safety, with “good catch” awards. Individuals or teams working to promote and sustain a culture of safety should be recognized for their efforts. Acknowledging “good catches” to reward the identification, communication, and resolution of safety issues is an effective strategy for improving patient safety and health care quality.6,8
This quality improvement (QI) initiative was undertaken to demonstrate to staff that, in building an organizational culture of safety, it is important that staff be encouraged to speak up for safety and be acknowledged for doing so. If health care organizations want staff to be motivated to report near misses and improve safety and health care quality, the culture needs to shift from focusing on blame to incentivizing individuals and teams to speak up when they have concerns.8-10 Although deciding which safety actions are worthy of recognition can be challenging, recognizing all safe acts, regardless of how big or small they are perceived to be, is important. This QI initiative aimed to establish a tiered approach to recognize staff members for various categories of safety acts.
METHODS
A review of the literature from January 2017 to May 2020 for peer-reviewed publications regarding how other organizations implemented safety award programs to promote a culture of safety resulted in a dearth of evidence. This prompted us at the Veterans Affairs Connecticut Healthcare System to develop and implement a formal program to disseminate safety awards to employees.
Program Launch and Promotion
In 2020, our institution embarked on a journey to high reliability with the goal of approaching zero harm. As part of efforts to promote a culture of safety, the hospital’s High Reliability Organization (HRO) team worked to develop a safety awards recognition program. Prior to the launch, the hospital’s patient safety committee recognized staff members through the medical center safety event reporting system (the Joint Patient Safety Reporting system [JPSR]) or through direct communication with staff members on safety actions they were engaged in. JPSR is the Veterans Health Administration National Center for Patient Safety incident reporting system for reporting, tracking, and trending of patient incidents in a national database. The award consisted of a certificate presented by the patient safety committee chairpersons to the employee in front of their peers in their respective work area. Hospital leadership was not involved in the safety awards recognition program at that time. No nomination process existed prior to our QI launch.
Once the QI initiative was launched and marketed heavily at staff meetings, we started to receive nominations for actions that were truly exceptional, while many others were submitted for behaviors that were within the day-to-day scope of practice of the staff member. For those early nominations that did not meet criteria for an award, we thanked staff for their submissions with a gentle statement that their nomination did not meet the criteria for an award. After following this practice for a few weeks, we became concerned that if we did not acknowledge the staff who came forward to request recognition for their routine work that supported safety, we could risk losing their engagement in a culture of safety. As such, we decided to create 3 levels of awards to recognize behaviors that went above and beyond while also acknowledging staff for actions within their scope of practice. Additionally, hospital leadership wanted to ensure that all staff recognize that their safety efforts are valued by leadership and that that sense of value will hopefully contribute to a culture of safety over time.
Initially, the single award system was called the “Good Catch Award” to acknowledge staff who go above and beyond to speak up and take action when they have safety concerns. This particular recognition includes a certificate, an encased baseball card that has been personalized by including the staff member’s picture and safety event identified, a stress-release baseball, and a stick of Bazooka gum (similar to what used to come in baseball cards packs). The award is presented to employees in their work area by the HRO and patient safety teams and includes representatives from the executive leadership team (ELT). The safety event identified is described by an ELT member, and all items are presented to the employee. Participation by the leadership team communicates how much the work being done to promote a culture of safety and advance quality health care is appreciated. This action also encourages others in the organization to identify and report safety concerns.13
With the rollout of the QI initiative, the volume of nominations submitted quickly increased (eg, approximately 1 every 2 months before to 3 per month following implementation). Frequently, nominations were for actions believed to be within the scope of the employee’s responsibilities. Our institution’s leadership team quickly recognized that, as an organization, not diminishing the importance of the “Good Catch Award” was important. However, the
The original Good Catch Award was labelled as a Level 1 award. The Level 2 safety recognition award, named the HRO Safety Champion Award, is given to employees who stop the line for a safety concern within their scope of practice and also participate as part of a team to investigate and improve processes to avoid recurring safety concerns in the future. For the Level Two award, a certificate is presented to an employee by the hospital’s HRO lead, HRO physician champion, patient safety manager, immediate supervisor, and peers. With the Level 3 award, the Culture of Safety Appreciation Award, individuals are recognized for addressing safety concerns within their assigned scope of responsibilities. Recognition is bestowed by an email of appreciation sent to the employee, acknowledging their commitment to promoting a culture of safety and quality health care. The recipient’s direct supervisor and other hospital leaders are copied on the message.14 See Table 1 for a
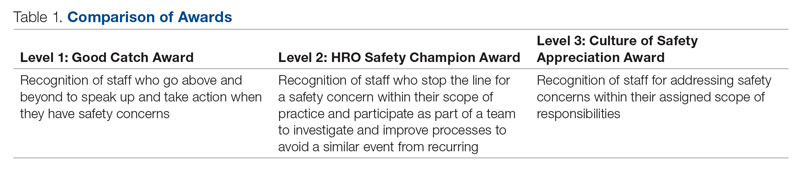
Our institution’s HRO and patient safety teams utilized many additional venues to disseminate information regarding awardees and their actions. These included our monthly HRO newsletter, monthly safety forums, and biweekly Team Connecticut Healthcare system-wide huddles.
Nomination Process
Awards nominations are submitted via the hospital intranet homepage, where there is an “HRO Safety Award Nomination” icon. Once a staff member clicks the icon, a template opens asking for information, such as the reason for the nomination submission, and then walks them through the template using the CAR (C-context, A-actions, and R-results)15 format for describing the situation, identifying actions taken, and specifying the outcome of the action. Emails with award nominations can also be sent to the HRO lead, HRO champion, or Patient Safety Committee co-chairs. Calls for nominations are made at several venues attended by employees as well as supervisors. These include monthly safety forums, biweekly Team Connecticut Healthcare system-wide huddles, supervisory staff meetings, department and unit-based staff meetings, and many other formal and informal settings. This QI initiative has allowed us to capture potential awardees through several avenues, including self-nominations. All nominations are reviewed by a safety awards committee. Each committee member ranks the nomination as a Level 1, 2, or 3 award. For nominations where conflicting scores are obtained, the committee discusses the nomination together to resolve discrepancies.
Needed Resources
Material resources required for this QI initiative include certificate paper, plastic baseball card sleeves, stress-release baseballs, and Bazooka gum. The largest resource investment was the time needed to support the initiative. This included the time spent scheduling the Level 1 and 2 award presentations with staff and leadership. Time was also required to put the individual award packages together, which included printing the paper certificates, obtaining awardee pictures, placing them with their safety stories in a plastic baseball card sleeve, and arranging for the hospital photographer to take pictures of the awardees with their peers and leaders.
RESULTS
Prior to this QI initiative launch, 14 awards were given out over the preceding 2-year period. During the initial 18 months of the initiative (December 2020 to June 2022), 59 awards were presented (Level 1, n = 26; Level 2, n = 22; and Level 3, n = 11). Looking further into the Level 1 awards presented, 25 awardees worked in clinical roles and 1 in a nonclinical position (Table 2). The awardees represented multidisciplinary areas, including medical/surgical (med/surg) inpatient units, anesthesia, operating room, pharmacy, mental health clinics, surgical intensive care, specialty care clinics, and nutrition and food services. With the Level 2 awards, 18 clinical staff and 4 nonclinical staff received awards from the areas of med/surg inpatient, outpatient surgical suites, the medical center director’s office, radiology, pharmacy, primary care, facilities management, environmental management, infection prevention, and emergency services. All Level 3 awardees were from clinical areas, including primary care, hospital education, sterile processing, pharmacies, operating rooms, and med/surg inpatient units.
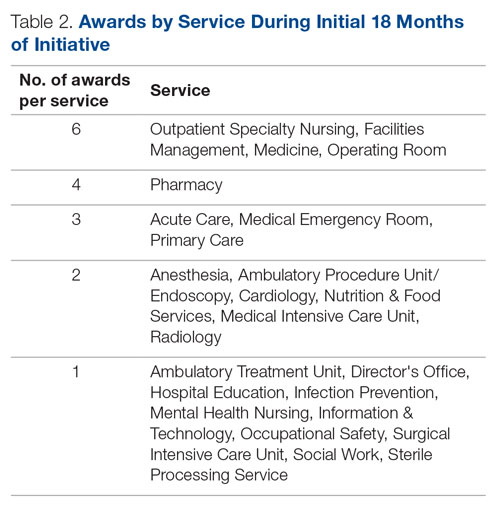
With the inception of this QI initiative, our organization has begun to see trends reflecting increased reporting of both actual and close-call events in JPSR (Figure 1). 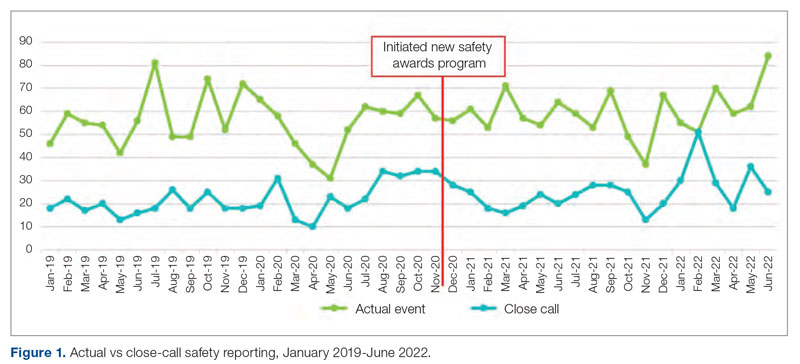
With the inclusion of information regarding awardees and their actions in monthly safety forums, attendance at these forums has increased from an average of 64 attendees per month in 2021 to an average of 131 attendees per month in 2022 (Figure 2).
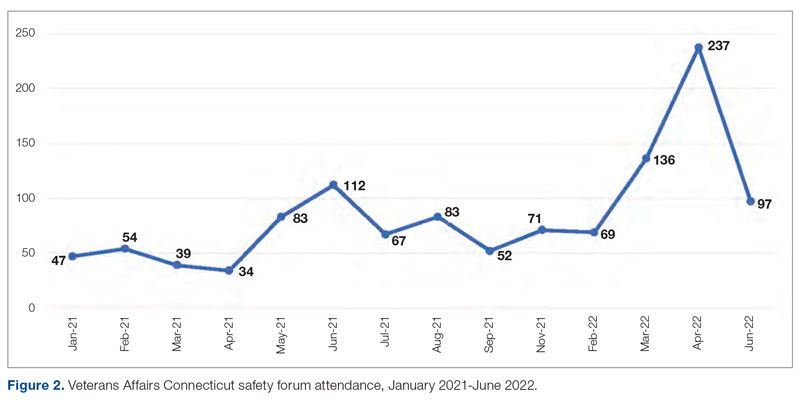
Finally, our organization’s annual All-Employee Survey results have shown incremental increases in staff reporting feeling psychologically safe and not fearing reprisal (Figure 3). It is important to note that there may be other contributing factors to these incremental changes.
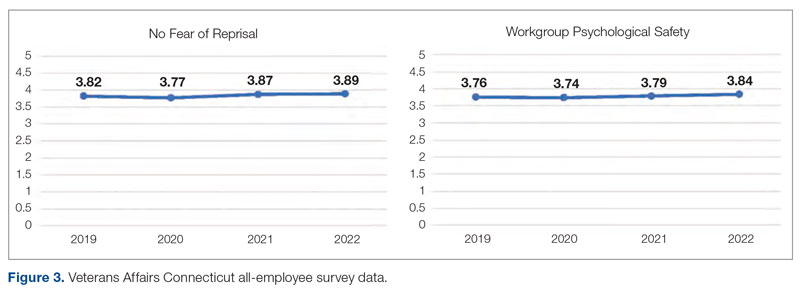
Level 1 – Good Catch Award. M.S. was assigned as a continuous safety monitor, or “sitter,” on one of the med/surg inpatient units. M.S. arrived at the bedside and asked for a report on the patient at a change in shift. The report stated that the patient was sleeping and had not moved in a while. M.S. set about to perform the functions of a sitter and did her usual tasks in cleaning and tidying the room for the patient for breakfast and taking care of all items in the room, in general. M.S. introduced herself to the patient, who she thought might wake up because of her speaking to him. She thought the patient was in an odd position, and knowing that a patient should be a little further up in the bed, she tried with touch to awaken him to adjust his position. M.S. found that the patient was rather chilly to the touch and immediately became concerned. She continued to attempt to rouse the patient. M.S. called for the nurse and began to adjust the patient’s position. M.S. insisted that the patient was cold and “something was wrong.” A set of vitals was taken and a rapid response team code was called. The patient was immediately transferred to the intensive care unit to receive a higher level of care. If not for the diligence and caring attitude of M.S., this patient may have had a very poor outcome.
Reason for criteria being met: The scope of practice of a sitter is to be present in a patient’s room to monitor for falls and overall safety. This employee noticed that the patient was not responsive to verbal or tactile stimuli. Her immediate reporting of her concern to the nurse resulted in prompt intervention. If she had let the patient be, the patient could have died. The staff member went above and beyond by speaking up and taking action when she had a patient safety concern.
Level 2 – HRO Safety Champion Award. A patient presented to an outpatient clinic for monoclonal antibody (mAb) therapy for a COVID-19 infection; the treatment has been scheduled by the patient’s primary care provider. At that time, outpatient mAb therapy was the recommended care option for patients stable enough to receive treatment in this setting, but it is contraindicated in patients who are too unstable to receive mAb therapy in an outpatient setting, such as those with increased oxygen demands. R.L., a staff nurse, assessed the patient on arrival and found that his vital signs were stable, except for a slightly elevated respiratory rate. Upon questioning, the patient reported that he had increased his oxygen use at home from 2 to 4 L via a nasal cannula. R.L. assessed that the patient was too high-risk for outpatient mAb therapy and had the patient checked into the emergency department (ED) to receive a full diagnostic workup and evaluation by Dr. W., an ED provider. The patient required admission to the hospital for a higher level of care in an inpatient unit because of severe COVID-19 infection. Within 48 hours of admission, the patient’s condition further declined, requiring an upgrade to the medical intensive care unit with progressive interventions. Owing to the clinical assessment skills and prompt action of R.L., the patient was admitted to the hospital instead of receiving treatment in a suboptimal care setting and returning home. Had the patient gone home, his rapid decline could have had serious consequences.
Reason for criteria being met: On a cursory look, the patient may have passed as someone sufficiently stable to undergo outpatient treatment. However, the nurse stopped the line, paid close attention, and picked up on an abnormal vital sign and the projected consequences. The nurse brought the patient to a higher level of care in the ED so that he could get the attention he needed. If this patient was given mAb therapy in the outpatient setting, he would have been discharged and become sicker with the COVID-19 illness. As a result of this incident, R.L. is working with the outpatient clinic and ED staff to enahance triage and evaluation of patients referred for outpatient therapy for COVID-19 infections to prevent a similar event from recurring.
Level 3 – Culture of Safety Appreciation Award. While C.C. was reviewing the hazardous item
Reason for criteria being met: The employee works in the hospital education department. It is within her scope of responsibilities to provide ongoing education to staff in order to address potential safety concerns.
DISCUSSION
This QI initiative was undertaken to demonstrate to staff that, in building an organizational culture of safety and advancing quality health care, it is important that staff be encouraged to speak up for safety and be acknowledged for doing so. As part of efforts to continuously build on a safety-first culture, transparency and celebration of successes were demonstrated. This QI initiative demonstrated that a diverse and wide range of employees were reached, from clinical to nonclinical staff, and frontline to supervisory staff, as all were included in the recognition process. While many award nominations were received through the submission of safety concerns to the high-reliability team and patient safety office, several came directly from staff who wanted to recognize their peers for their work, supporting a culture of safety. This showed that staff felt that taking the time to submit a write-up to recognize a peer was an important task. Achieving zero harm for patients and staff alike is a top priority for our institution and guides all decisions, which reinforces that everyone has a responsibility to ensure that safety is always the first consideration. A culture of safety is enhanced by staff recognition. This QI initiative also showed that staff felt valued when they were acknowledged, regardless of the level of recognition they received. The theme of feeling valued came from unsolicited feedback. For example, some direct comments from awardees are presented in the Box.
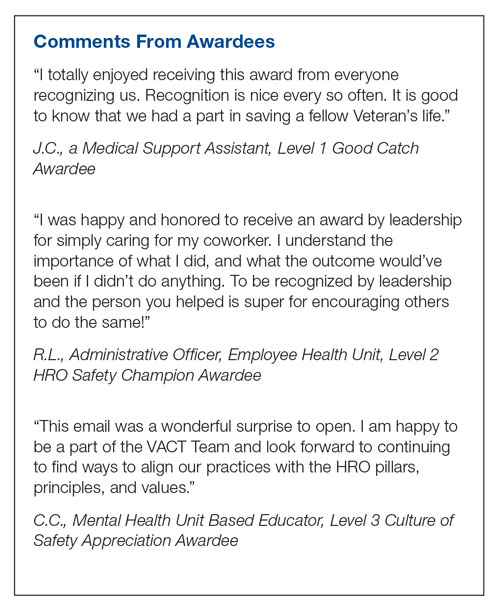
In addition to endorsing the importance of safe practices to staff, safety award programs can identify gaps in existing standard procedures that can be updated quickly and shared broadly across a health care organization. The authors observed that the existence of the award program gives staff permission to use their voice to speak up when they have questions or concerns related to safety and to proactively engage in safety practices; a cultural shift of this kind informs safety practices and procedures and contributes to a more inspiring workplace. Staff at our organization who have received any of the safety awards, and those who are aware of these awards, have embraced the program readily. At the time of submission of this manuscript, there was a relative paucity of published literature on the details, performance, and impact of such programs. This initiative aims to share a road map highlighting the various dimensions of staff recognition and how the program supports our health care system in fostering a strong, sustainable culture of safety and health care quality. A next step is to formally assess the impact of the awards program on our culture of safety and quality using a psychometrically sound measurement tool, as recommended by TJC,16 such as the
CONCLUSION
A health care organization safety awards program is a strategy for building and sustaining a culture of safety. This QI initiative may be valuable to other organizations in the process of establishing a safety awards program of their own. Future research should focus on a formal evaluation of the impact of safety awards programs on patient safety outcomes.
Corresponding author: John S. Murray, PhD, MPH, MSGH, RN, FAAN, 20 Chapel Street, Unit A502, Brookline, MA 02446; JMurray325@aol.com
Disclosures: None reported.
1. National Center for Biotechnology Information. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies. National Library of Medicine; 2019.
2.
3. Agency for Healthcare Research and Quality. Implementing near-miss reporting and improvement tracking in primary care practices: lessons learned. Agency for Healthcare Research and Quality; 2017.
4. Hamed M, Konstantinidis S. Barriers to incident reporting among nurses: a qualitative systematic review. West J Nurs Res. 2022;44(5):506-523. doi:10.1177/0193945921999449
5. Mohamed M, Abubeker IY, Al-Mohanadi D, et al. Perceived barriers of incident reporting among internists: results from Hamad medical corporation in Qatar. Avicenna J Med. 2021;11(3):139-144. doi:10.1055/s-0041-1734386
6. The Joint Commission. The essential role of leadership in developing a safety culture. The Joint Commission; 2017.
7. Yali G, Nzala S. Healthcare providers’ perspective on barriers to patient safety incident reporting in Lusaka District. J Prev Rehabil Med. 2022;4:44-52. doi:10.21617/jprm2022.417
8. Herzer KR, Mirrer M, Xie Y, et al. Patient safety reporting systems: sustained quality improvement using a multidisciplinary team and “good catch” awards. Jt Comm J Qual Patient Saf. 2012;38(8):339-347. doi:10.1016/s1553-7250(12)38044-6
9. Rogers E, Griffin E, Carnie W, et al. A just culture approach to managing medication errors. Hosp Pharm. 2017;52(4):308-315. doi:10.1310/hpj5204-308
10. Murray JS, Clifford J, Larson S, et al. Implementing just culture to improve patient safety. Mil Med. 2022;0: 1. doi:10.1093/milmed/usac115
11. Paradiso L, Sweeney N. Just culture: it’s more than policy. Nurs Manag. 2019;50(6):38–45. doi:10.1097/01.NUMA.0000558482.07815.ae
12. Wallace S, Mamrol M, Finley E; Pennsylvania Patient Safety Authority. Promote a culture of safety with good catch reports. PA Patient Saf Advis. 2017;14(3).
13. Tan KH, Pang NL, Siau C, et al: Building an organizational culture of patient safety. J Patient Saf Risk Manag. 2019;24:253-261. doi.10.1177/251604351987897
14. Merchant N, O’Neal J, Dealino-Perez C, et al: A high reliability mindset. Am J Med Qual. 2022;37(6):504-510. doi:10.1097/JMQ.0000000000000086
15. Behavioral interview questions and answers. Hudson. Accessed December 23, 2022. https://au.hudson.com/insights/career-advice/job-interviews/behavioural-interview-questions-and-answers/
16. The Joint Commission. Safety culture assessment: Improving the survey process. Accessed December 26, 2022. https://www.jointcommission.org/-/media/tjc/documents/accred-and-cert/safety_culture_assessment_improving_the_survey_process.pdf
17. Reis CT, Paiva SG, Sousa P. The patient safety culture: a systematic review by characteristics of hospital survey on patient safety culture dimensions. Int J Qual Heal Care. 2018;30(9):660-677. doi:10.1093/intqhc/mzy080
18. Fourar YO, Benhassine W, Boughaba A, et al. Contribution to the assessment of patient safety culture in Algerian healthcare settings: the ASCO project. Int J Healthc Manag. 2022;15:52-61. doi.org/10.1080/20479700.2020.1836736
ABSTRACT
Objective: Promoting a culture of safety is a critical component of improving health care quality. Recognizing staff who stop the line for safety can positively impact the growth of a culture of safety. The purpose of this initiative was to demonstrate to staff the importance of speaking up for safety and being acknowledged for doing so.
Methods: Following a review of the literature on safety awards programs and their role in promoting a culture of safety in health care covering the period 2017 to 2020, a formal process was developed and implemented to disseminate safety awards to employees.
Results: During the initial 18 months of the initiative, a total of 59 awards were presented. The awards were well received by the recipients and other staff members. Within this period, adjustments were made to enhance the scope and reach of the program.
Conclusion: Recognizing staff behaviors that support a culture of safety is important for improving health care quality and employee engagement. Future research should focus on a formal evaluation of the impact of safety awards programs on patient safety outcomes.
Keywords: patient safety, culture of safety, incident reporting, near miss.
A key aspect of improving health care quality is promoting and sustaining a culture of safety in the workplace. Improving the quality of health care services and systems involves making informed choices regarding the types of strategies to implement.1 An essential aspect of supporting a safety culture is safety-event reporting. To approach the goal of zero harm, all safety events, whether they result in actual harm or are considered near misses, need to be reported. Near-miss events are errors that occur while care is being provided but are detected and corrected before harm reaches the patient.1-3 Near-miss reporting plays a critical role in helping to identify and correct weaknesses in health care delivery systems and processes.4 However, evidence shows that there are a multitude of barriers to the reporting of near-miss events, such as fear of punitive actions, additional workload, unsupportive work environments, a culture with poor psychological safety, knowledge deficit, and lack of recognition of staff who do report near misses.4-11
According to The Joint Commission (TJC), acknowledging health care team members who recognize and report unsafe conditions that provide insight for improving patient safety is a key method for promoting the reporting of near-miss events.6 As a result, some health care organizations and patient safety agencies have started to institute some form of recognition for their employees in the realm of safety.8-10 The Pennsylvania Patient Safety Authority offers exceptional guidance for creating a safety awards program to promote a culture of safety.12 Furthermore, TJC supports recognizing individuals and health care teams who identify and report near misses, or who have suggestions for initiatives to promote patient safety, with “good catch” awards. Individuals or teams working to promote and sustain a culture of safety should be recognized for their efforts. Acknowledging “good catches” to reward the identification, communication, and resolution of safety issues is an effective strategy for improving patient safety and health care quality.6,8
This quality improvement (QI) initiative was undertaken to demonstrate to staff that, in building an organizational culture of safety, it is important that staff be encouraged to speak up for safety and be acknowledged for doing so. If health care organizations want staff to be motivated to report near misses and improve safety and health care quality, the culture needs to shift from focusing on blame to incentivizing individuals and teams to speak up when they have concerns.8-10 Although deciding which safety actions are worthy of recognition can be challenging, recognizing all safe acts, regardless of how big or small they are perceived to be, is important. This QI initiative aimed to establish a tiered approach to recognize staff members for various categories of safety acts.
METHODS
A review of the literature from January 2017 to May 2020 for peer-reviewed publications regarding how other organizations implemented safety award programs to promote a culture of safety resulted in a dearth of evidence. This prompted us at the Veterans Affairs Connecticut Healthcare System to develop and implement a formal program to disseminate safety awards to employees.
Program Launch and Promotion
In 2020, our institution embarked on a journey to high reliability with the goal of approaching zero harm. As part of efforts to promote a culture of safety, the hospital’s High Reliability Organization (HRO) team worked to develop a safety awards recognition program. Prior to the launch, the hospital’s patient safety committee recognized staff members through the medical center safety event reporting system (the Joint Patient Safety Reporting system [JPSR]) or through direct communication with staff members on safety actions they were engaged in. JPSR is the Veterans Health Administration National Center for Patient Safety incident reporting system for reporting, tracking, and trending of patient incidents in a national database. The award consisted of a certificate presented by the patient safety committee chairpersons to the employee in front of their peers in their respective work area. Hospital leadership was not involved in the safety awards recognition program at that time. No nomination process existed prior to our QI launch.
Once the QI initiative was launched and marketed heavily at staff meetings, we started to receive nominations for actions that were truly exceptional, while many others were submitted for behaviors that were within the day-to-day scope of practice of the staff member. For those early nominations that did not meet criteria for an award, we thanked staff for their submissions with a gentle statement that their nomination did not meet the criteria for an award. After following this practice for a few weeks, we became concerned that if we did not acknowledge the staff who came forward to request recognition for their routine work that supported safety, we could risk losing their engagement in a culture of safety. As such, we decided to create 3 levels of awards to recognize behaviors that went above and beyond while also acknowledging staff for actions within their scope of practice. Additionally, hospital leadership wanted to ensure that all staff recognize that their safety efforts are valued by leadership and that that sense of value will hopefully contribute to a culture of safety over time.
Initially, the single award system was called the “Good Catch Award” to acknowledge staff who go above and beyond to speak up and take action when they have safety concerns. This particular recognition includes a certificate, an encased baseball card that has been personalized by including the staff member’s picture and safety event identified, a stress-release baseball, and a stick of Bazooka gum (similar to what used to come in baseball cards packs). The award is presented to employees in their work area by the HRO and patient safety teams and includes representatives from the executive leadership team (ELT). The safety event identified is described by an ELT member, and all items are presented to the employee. Participation by the leadership team communicates how much the work being done to promote a culture of safety and advance quality health care is appreciated. This action also encourages others in the organization to identify and report safety concerns.13
With the rollout of the QI initiative, the volume of nominations submitted quickly increased (eg, approximately 1 every 2 months before to 3 per month following implementation). Frequently, nominations were for actions believed to be within the scope of the employee’s responsibilities. Our institution’s leadership team quickly recognized that, as an organization, not diminishing the importance of the “Good Catch Award” was important. However, the
The original Good Catch Award was labelled as a Level 1 award. The Level 2 safety recognition award, named the HRO Safety Champion Award, is given to employees who stop the line for a safety concern within their scope of practice and also participate as part of a team to investigate and improve processes to avoid recurring safety concerns in the future. For the Level Two award, a certificate is presented to an employee by the hospital’s HRO lead, HRO physician champion, patient safety manager, immediate supervisor, and peers. With the Level 3 award, the Culture of Safety Appreciation Award, individuals are recognized for addressing safety concerns within their assigned scope of responsibilities. Recognition is bestowed by an email of appreciation sent to the employee, acknowledging their commitment to promoting a culture of safety and quality health care. The recipient’s direct supervisor and other hospital leaders are copied on the message.14 See Table 1 for a
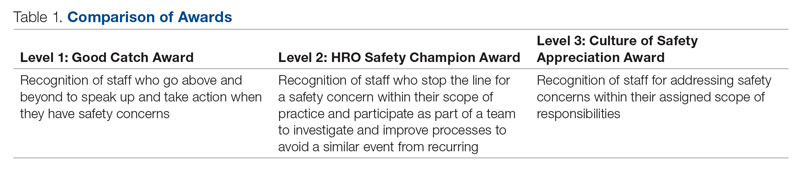
Our institution’s HRO and patient safety teams utilized many additional venues to disseminate information regarding awardees and their actions. These included our monthly HRO newsletter, monthly safety forums, and biweekly Team Connecticut Healthcare system-wide huddles.
Nomination Process
Awards nominations are submitted via the hospital intranet homepage, where there is an “HRO Safety Award Nomination” icon. Once a staff member clicks the icon, a template opens asking for information, such as the reason for the nomination submission, and then walks them through the template using the CAR (C-context, A-actions, and R-results)15 format for describing the situation, identifying actions taken, and specifying the outcome of the action. Emails with award nominations can also be sent to the HRO lead, HRO champion, or Patient Safety Committee co-chairs. Calls for nominations are made at several venues attended by employees as well as supervisors. These include monthly safety forums, biweekly Team Connecticut Healthcare system-wide huddles, supervisory staff meetings, department and unit-based staff meetings, and many other formal and informal settings. This QI initiative has allowed us to capture potential awardees through several avenues, including self-nominations. All nominations are reviewed by a safety awards committee. Each committee member ranks the nomination as a Level 1, 2, or 3 award. For nominations where conflicting scores are obtained, the committee discusses the nomination together to resolve discrepancies.
Needed Resources
Material resources required for this QI initiative include certificate paper, plastic baseball card sleeves, stress-release baseballs, and Bazooka gum. The largest resource investment was the time needed to support the initiative. This included the time spent scheduling the Level 1 and 2 award presentations with staff and leadership. Time was also required to put the individual award packages together, which included printing the paper certificates, obtaining awardee pictures, placing them with their safety stories in a plastic baseball card sleeve, and arranging for the hospital photographer to take pictures of the awardees with their peers and leaders.
RESULTS
Prior to this QI initiative launch, 14 awards were given out over the preceding 2-year period. During the initial 18 months of the initiative (December 2020 to June 2022), 59 awards were presented (Level 1, n = 26; Level 2, n = 22; and Level 3, n = 11). Looking further into the Level 1 awards presented, 25 awardees worked in clinical roles and 1 in a nonclinical position (Table 2). The awardees represented multidisciplinary areas, including medical/surgical (med/surg) inpatient units, anesthesia, operating room, pharmacy, mental health clinics, surgical intensive care, specialty care clinics, and nutrition and food services. With the Level 2 awards, 18 clinical staff and 4 nonclinical staff received awards from the areas of med/surg inpatient, outpatient surgical suites, the medical center director’s office, radiology, pharmacy, primary care, facilities management, environmental management, infection prevention, and emergency services. All Level 3 awardees were from clinical areas, including primary care, hospital education, sterile processing, pharmacies, operating rooms, and med/surg inpatient units.
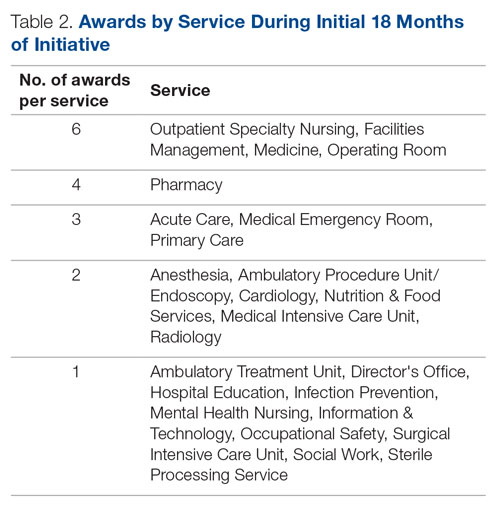
With the inception of this QI initiative, our organization has begun to see trends reflecting increased reporting of both actual and close-call events in JPSR (Figure 1). 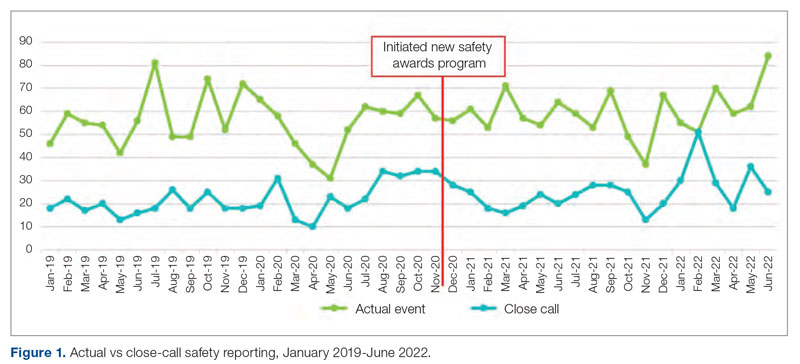
With the inclusion of information regarding awardees and their actions in monthly safety forums, attendance at these forums has increased from an average of 64 attendees per month in 2021 to an average of 131 attendees per month in 2022 (Figure 2).
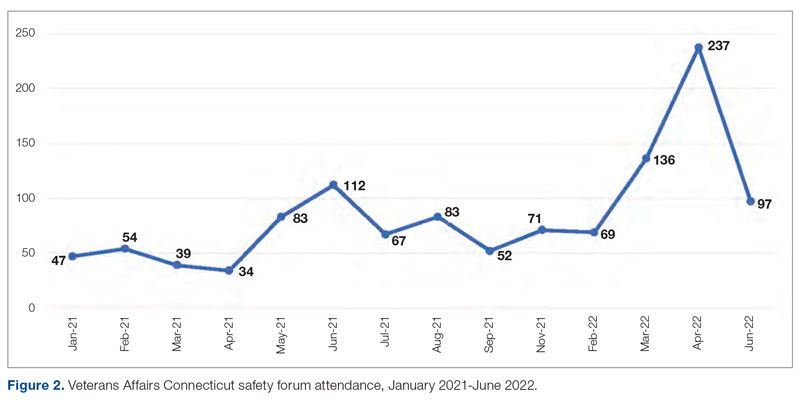
Finally, our organization’s annual All-Employee Survey results have shown incremental increases in staff reporting feeling psychologically safe and not fearing reprisal (Figure 3). It is important to note that there may be other contributing factors to these incremental changes.
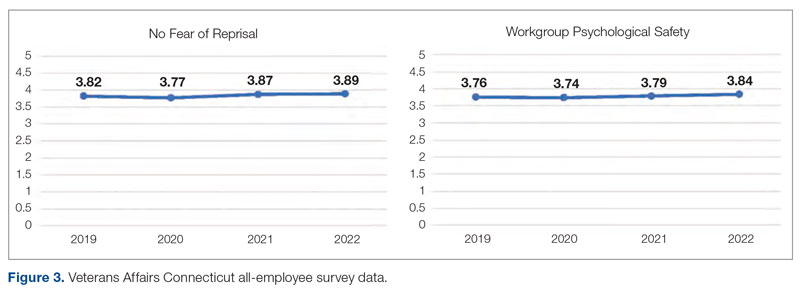
Level 1 – Good Catch Award. M.S. was assigned as a continuous safety monitor, or “sitter,” on one of the med/surg inpatient units. M.S. arrived at the bedside and asked for a report on the patient at a change in shift. The report stated that the patient was sleeping and had not moved in a while. M.S. set about to perform the functions of a sitter and did her usual tasks in cleaning and tidying the room for the patient for breakfast and taking care of all items in the room, in general. M.S. introduced herself to the patient, who she thought might wake up because of her speaking to him. She thought the patient was in an odd position, and knowing that a patient should be a little further up in the bed, she tried with touch to awaken him to adjust his position. M.S. found that the patient was rather chilly to the touch and immediately became concerned. She continued to attempt to rouse the patient. M.S. called for the nurse and began to adjust the patient’s position. M.S. insisted that the patient was cold and “something was wrong.” A set of vitals was taken and a rapid response team code was called. The patient was immediately transferred to the intensive care unit to receive a higher level of care. If not for the diligence and caring attitude of M.S., this patient may have had a very poor outcome.
Reason for criteria being met: The scope of practice of a sitter is to be present in a patient’s room to monitor for falls and overall safety. This employee noticed that the patient was not responsive to verbal or tactile stimuli. Her immediate reporting of her concern to the nurse resulted in prompt intervention. If she had let the patient be, the patient could have died. The staff member went above and beyond by speaking up and taking action when she had a patient safety concern.
Level 2 – HRO Safety Champion Award. A patient presented to an outpatient clinic for monoclonal antibody (mAb) therapy for a COVID-19 infection; the treatment has been scheduled by the patient’s primary care provider. At that time, outpatient mAb therapy was the recommended care option for patients stable enough to receive treatment in this setting, but it is contraindicated in patients who are too unstable to receive mAb therapy in an outpatient setting, such as those with increased oxygen demands. R.L., a staff nurse, assessed the patient on arrival and found that his vital signs were stable, except for a slightly elevated respiratory rate. Upon questioning, the patient reported that he had increased his oxygen use at home from 2 to 4 L via a nasal cannula. R.L. assessed that the patient was too high-risk for outpatient mAb therapy and had the patient checked into the emergency department (ED) to receive a full diagnostic workup and evaluation by Dr. W., an ED provider. The patient required admission to the hospital for a higher level of care in an inpatient unit because of severe COVID-19 infection. Within 48 hours of admission, the patient’s condition further declined, requiring an upgrade to the medical intensive care unit with progressive interventions. Owing to the clinical assessment skills and prompt action of R.L., the patient was admitted to the hospital instead of receiving treatment in a suboptimal care setting and returning home. Had the patient gone home, his rapid decline could have had serious consequences.
Reason for criteria being met: On a cursory look, the patient may have passed as someone sufficiently stable to undergo outpatient treatment. However, the nurse stopped the line, paid close attention, and picked up on an abnormal vital sign and the projected consequences. The nurse brought the patient to a higher level of care in the ED so that he could get the attention he needed. If this patient was given mAb therapy in the outpatient setting, he would have been discharged and become sicker with the COVID-19 illness. As a result of this incident, R.L. is working with the outpatient clinic and ED staff to enahance triage and evaluation of patients referred for outpatient therapy for COVID-19 infections to prevent a similar event from recurring.
Level 3 – Culture of Safety Appreciation Award. While C.C. was reviewing the hazardous item
Reason for criteria being met: The employee works in the hospital education department. It is within her scope of responsibilities to provide ongoing education to staff in order to address potential safety concerns.
DISCUSSION
This QI initiative was undertaken to demonstrate to staff that, in building an organizational culture of safety and advancing quality health care, it is important that staff be encouraged to speak up for safety and be acknowledged for doing so. As part of efforts to continuously build on a safety-first culture, transparency and celebration of successes were demonstrated. This QI initiative demonstrated that a diverse and wide range of employees were reached, from clinical to nonclinical staff, and frontline to supervisory staff, as all were included in the recognition process. While many award nominations were received through the submission of safety concerns to the high-reliability team and patient safety office, several came directly from staff who wanted to recognize their peers for their work, supporting a culture of safety. This showed that staff felt that taking the time to submit a write-up to recognize a peer was an important task. Achieving zero harm for patients and staff alike is a top priority for our institution and guides all decisions, which reinforces that everyone has a responsibility to ensure that safety is always the first consideration. A culture of safety is enhanced by staff recognition. This QI initiative also showed that staff felt valued when they were acknowledged, regardless of the level of recognition they received. The theme of feeling valued came from unsolicited feedback. For example, some direct comments from awardees are presented in the Box.
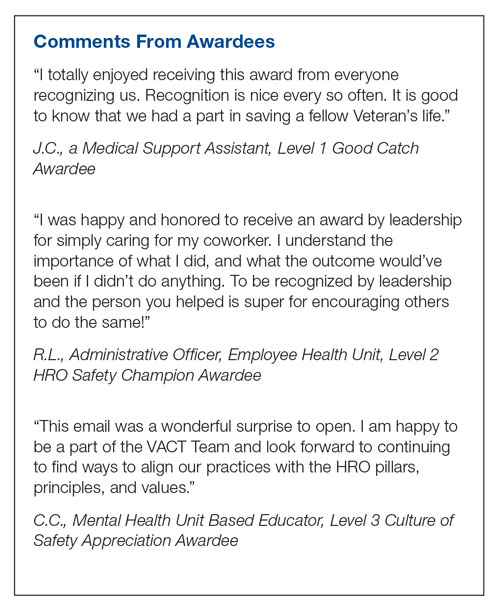
In addition to endorsing the importance of safe practices to staff, safety award programs can identify gaps in existing standard procedures that can be updated quickly and shared broadly across a health care organization. The authors observed that the existence of the award program gives staff permission to use their voice to speak up when they have questions or concerns related to safety and to proactively engage in safety practices; a cultural shift of this kind informs safety practices and procedures and contributes to a more inspiring workplace. Staff at our organization who have received any of the safety awards, and those who are aware of these awards, have embraced the program readily. At the time of submission of this manuscript, there was a relative paucity of published literature on the details, performance, and impact of such programs. This initiative aims to share a road map highlighting the various dimensions of staff recognition and how the program supports our health care system in fostering a strong, sustainable culture of safety and health care quality. A next step is to formally assess the impact of the awards program on our culture of safety and quality using a psychometrically sound measurement tool, as recommended by TJC,16 such as the
CONCLUSION
A health care organization safety awards program is a strategy for building and sustaining a culture of safety. This QI initiative may be valuable to other organizations in the process of establishing a safety awards program of their own. Future research should focus on a formal evaluation of the impact of safety awards programs on patient safety outcomes.
Corresponding author: John S. Murray, PhD, MPH, MSGH, RN, FAAN, 20 Chapel Street, Unit A502, Brookline, MA 02446; JMurray325@aol.com
Disclosures: None reported.
ABSTRACT
Objective: Promoting a culture of safety is a critical component of improving health care quality. Recognizing staff who stop the line for safety can positively impact the growth of a culture of safety. The purpose of this initiative was to demonstrate to staff the importance of speaking up for safety and being acknowledged for doing so.
Methods: Following a review of the literature on safety awards programs and their role in promoting a culture of safety in health care covering the period 2017 to 2020, a formal process was developed and implemented to disseminate safety awards to employees.
Results: During the initial 18 months of the initiative, a total of 59 awards were presented. The awards were well received by the recipients and other staff members. Within this period, adjustments were made to enhance the scope and reach of the program.
Conclusion: Recognizing staff behaviors that support a culture of safety is important for improving health care quality and employee engagement. Future research should focus on a formal evaluation of the impact of safety awards programs on patient safety outcomes.
Keywords: patient safety, culture of safety, incident reporting, near miss.
A key aspect of improving health care quality is promoting and sustaining a culture of safety in the workplace. Improving the quality of health care services and systems involves making informed choices regarding the types of strategies to implement.1 An essential aspect of supporting a safety culture is safety-event reporting. To approach the goal of zero harm, all safety events, whether they result in actual harm or are considered near misses, need to be reported. Near-miss events are errors that occur while care is being provided but are detected and corrected before harm reaches the patient.1-3 Near-miss reporting plays a critical role in helping to identify and correct weaknesses in health care delivery systems and processes.4 However, evidence shows that there are a multitude of barriers to the reporting of near-miss events, such as fear of punitive actions, additional workload, unsupportive work environments, a culture with poor psychological safety, knowledge deficit, and lack of recognition of staff who do report near misses.4-11
According to The Joint Commission (TJC), acknowledging health care team members who recognize and report unsafe conditions that provide insight for improving patient safety is a key method for promoting the reporting of near-miss events.6 As a result, some health care organizations and patient safety agencies have started to institute some form of recognition for their employees in the realm of safety.8-10 The Pennsylvania Patient Safety Authority offers exceptional guidance for creating a safety awards program to promote a culture of safety.12 Furthermore, TJC supports recognizing individuals and health care teams who identify and report near misses, or who have suggestions for initiatives to promote patient safety, with “good catch” awards. Individuals or teams working to promote and sustain a culture of safety should be recognized for their efforts. Acknowledging “good catches” to reward the identification, communication, and resolution of safety issues is an effective strategy for improving patient safety and health care quality.6,8
This quality improvement (QI) initiative was undertaken to demonstrate to staff that, in building an organizational culture of safety, it is important that staff be encouraged to speak up for safety and be acknowledged for doing so. If health care organizations want staff to be motivated to report near misses and improve safety and health care quality, the culture needs to shift from focusing on blame to incentivizing individuals and teams to speak up when they have concerns.8-10 Although deciding which safety actions are worthy of recognition can be challenging, recognizing all safe acts, regardless of how big or small they are perceived to be, is important. This QI initiative aimed to establish a tiered approach to recognize staff members for various categories of safety acts.
METHODS
A review of the literature from January 2017 to May 2020 for peer-reviewed publications regarding how other organizations implemented safety award programs to promote a culture of safety resulted in a dearth of evidence. This prompted us at the Veterans Affairs Connecticut Healthcare System to develop and implement a formal program to disseminate safety awards to employees.
Program Launch and Promotion
In 2020, our institution embarked on a journey to high reliability with the goal of approaching zero harm. As part of efforts to promote a culture of safety, the hospital’s High Reliability Organization (HRO) team worked to develop a safety awards recognition program. Prior to the launch, the hospital’s patient safety committee recognized staff members through the medical center safety event reporting system (the Joint Patient Safety Reporting system [JPSR]) or through direct communication with staff members on safety actions they were engaged in. JPSR is the Veterans Health Administration National Center for Patient Safety incident reporting system for reporting, tracking, and trending of patient incidents in a national database. The award consisted of a certificate presented by the patient safety committee chairpersons to the employee in front of their peers in their respective work area. Hospital leadership was not involved in the safety awards recognition program at that time. No nomination process existed prior to our QI launch.
Once the QI initiative was launched and marketed heavily at staff meetings, we started to receive nominations for actions that were truly exceptional, while many others were submitted for behaviors that were within the day-to-day scope of practice of the staff member. For those early nominations that did not meet criteria for an award, we thanked staff for their submissions with a gentle statement that their nomination did not meet the criteria for an award. After following this practice for a few weeks, we became concerned that if we did not acknowledge the staff who came forward to request recognition for their routine work that supported safety, we could risk losing their engagement in a culture of safety. As such, we decided to create 3 levels of awards to recognize behaviors that went above and beyond while also acknowledging staff for actions within their scope of practice. Additionally, hospital leadership wanted to ensure that all staff recognize that their safety efforts are valued by leadership and that that sense of value will hopefully contribute to a culture of safety over time.
Initially, the single award system was called the “Good Catch Award” to acknowledge staff who go above and beyond to speak up and take action when they have safety concerns. This particular recognition includes a certificate, an encased baseball card that has been personalized by including the staff member’s picture and safety event identified, a stress-release baseball, and a stick of Bazooka gum (similar to what used to come in baseball cards packs). The award is presented to employees in their work area by the HRO and patient safety teams and includes representatives from the executive leadership team (ELT). The safety event identified is described by an ELT member, and all items are presented to the employee. Participation by the leadership team communicates how much the work being done to promote a culture of safety and advance quality health care is appreciated. This action also encourages others in the organization to identify and report safety concerns.13
With the rollout of the QI initiative, the volume of nominations submitted quickly increased (eg, approximately 1 every 2 months before to 3 per month following implementation). Frequently, nominations were for actions believed to be within the scope of the employee’s responsibilities. Our institution’s leadership team quickly recognized that, as an organization, not diminishing the importance of the “Good Catch Award” was important. However, the
The original Good Catch Award was labelled as a Level 1 award. The Level 2 safety recognition award, named the HRO Safety Champion Award, is given to employees who stop the line for a safety concern within their scope of practice and also participate as part of a team to investigate and improve processes to avoid recurring safety concerns in the future. For the Level Two award, a certificate is presented to an employee by the hospital’s HRO lead, HRO physician champion, patient safety manager, immediate supervisor, and peers. With the Level 3 award, the Culture of Safety Appreciation Award, individuals are recognized for addressing safety concerns within their assigned scope of responsibilities. Recognition is bestowed by an email of appreciation sent to the employee, acknowledging their commitment to promoting a culture of safety and quality health care. The recipient’s direct supervisor and other hospital leaders are copied on the message.14 See Table 1 for a
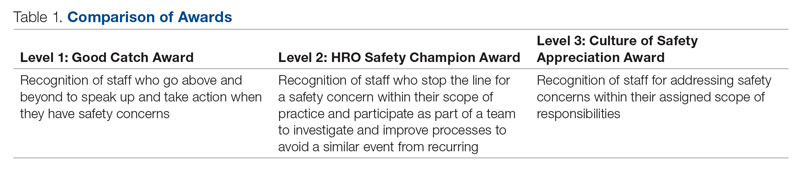
Our institution’s HRO and patient safety teams utilized many additional venues to disseminate information regarding awardees and their actions. These included our monthly HRO newsletter, monthly safety forums, and biweekly Team Connecticut Healthcare system-wide huddles.
Nomination Process
Awards nominations are submitted via the hospital intranet homepage, where there is an “HRO Safety Award Nomination” icon. Once a staff member clicks the icon, a template opens asking for information, such as the reason for the nomination submission, and then walks them through the template using the CAR (C-context, A-actions, and R-results)15 format for describing the situation, identifying actions taken, and specifying the outcome of the action. Emails with award nominations can also be sent to the HRO lead, HRO champion, or Patient Safety Committee co-chairs. Calls for nominations are made at several venues attended by employees as well as supervisors. These include monthly safety forums, biweekly Team Connecticut Healthcare system-wide huddles, supervisory staff meetings, department and unit-based staff meetings, and many other formal and informal settings. This QI initiative has allowed us to capture potential awardees through several avenues, including self-nominations. All nominations are reviewed by a safety awards committee. Each committee member ranks the nomination as a Level 1, 2, or 3 award. For nominations where conflicting scores are obtained, the committee discusses the nomination together to resolve discrepancies.
Needed Resources
Material resources required for this QI initiative include certificate paper, plastic baseball card sleeves, stress-release baseballs, and Bazooka gum. The largest resource investment was the time needed to support the initiative. This included the time spent scheduling the Level 1 and 2 award presentations with staff and leadership. Time was also required to put the individual award packages together, which included printing the paper certificates, obtaining awardee pictures, placing them with their safety stories in a plastic baseball card sleeve, and arranging for the hospital photographer to take pictures of the awardees with their peers and leaders.
RESULTS
Prior to this QI initiative launch, 14 awards were given out over the preceding 2-year period. During the initial 18 months of the initiative (December 2020 to June 2022), 59 awards were presented (Level 1, n = 26; Level 2, n = 22; and Level 3, n = 11). Looking further into the Level 1 awards presented, 25 awardees worked in clinical roles and 1 in a nonclinical position (Table 2). The awardees represented multidisciplinary areas, including medical/surgical (med/surg) inpatient units, anesthesia, operating room, pharmacy, mental health clinics, surgical intensive care, specialty care clinics, and nutrition and food services. With the Level 2 awards, 18 clinical staff and 4 nonclinical staff received awards from the areas of med/surg inpatient, outpatient surgical suites, the medical center director’s office, radiology, pharmacy, primary care, facilities management, environmental management, infection prevention, and emergency services. All Level 3 awardees were from clinical areas, including primary care, hospital education, sterile processing, pharmacies, operating rooms, and med/surg inpatient units.
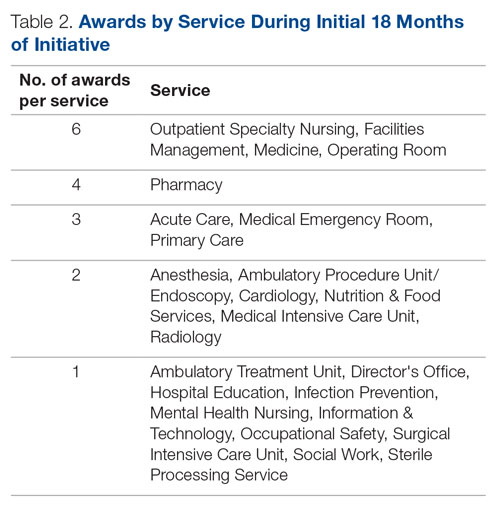
With the inception of this QI initiative, our organization has begun to see trends reflecting increased reporting of both actual and close-call events in JPSR (Figure 1). 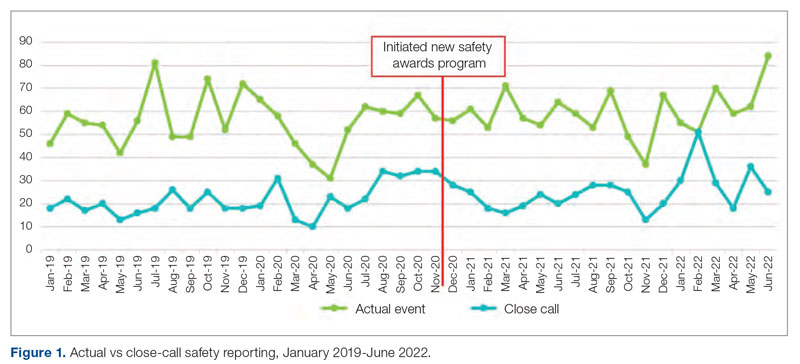
With the inclusion of information regarding awardees and their actions in monthly safety forums, attendance at these forums has increased from an average of 64 attendees per month in 2021 to an average of 131 attendees per month in 2022 (Figure 2).
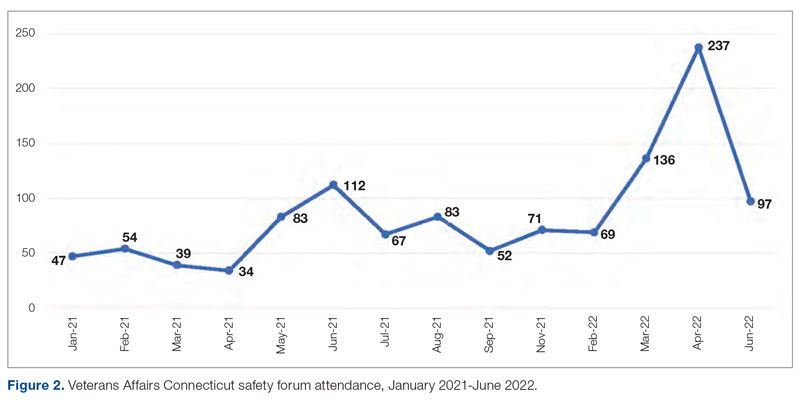
Finally, our organization’s annual All-Employee Survey results have shown incremental increases in staff reporting feeling psychologically safe and not fearing reprisal (Figure 3). It is important to note that there may be other contributing factors to these incremental changes.
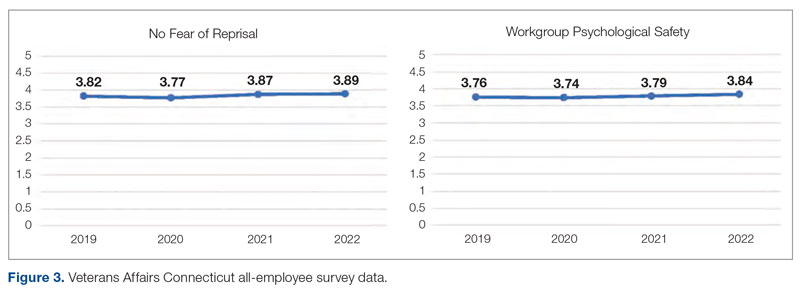
Level 1 – Good Catch Award. M.S. was assigned as a continuous safety monitor, or “sitter,” on one of the med/surg inpatient units. M.S. arrived at the bedside and asked for a report on the patient at a change in shift. The report stated that the patient was sleeping and had not moved in a while. M.S. set about to perform the functions of a sitter and did her usual tasks in cleaning and tidying the room for the patient for breakfast and taking care of all items in the room, in general. M.S. introduced herself to the patient, who she thought might wake up because of her speaking to him. She thought the patient was in an odd position, and knowing that a patient should be a little further up in the bed, she tried with touch to awaken him to adjust his position. M.S. found that the patient was rather chilly to the touch and immediately became concerned. She continued to attempt to rouse the patient. M.S. called for the nurse and began to adjust the patient’s position. M.S. insisted that the patient was cold and “something was wrong.” A set of vitals was taken and a rapid response team code was called. The patient was immediately transferred to the intensive care unit to receive a higher level of care. If not for the diligence and caring attitude of M.S., this patient may have had a very poor outcome.
Reason for criteria being met: The scope of practice of a sitter is to be present in a patient’s room to monitor for falls and overall safety. This employee noticed that the patient was not responsive to verbal or tactile stimuli. Her immediate reporting of her concern to the nurse resulted in prompt intervention. If she had let the patient be, the patient could have died. The staff member went above and beyond by speaking up and taking action when she had a patient safety concern.
Level 2 – HRO Safety Champion Award. A patient presented to an outpatient clinic for monoclonal antibody (mAb) therapy for a COVID-19 infection; the treatment has been scheduled by the patient’s primary care provider. At that time, outpatient mAb therapy was the recommended care option for patients stable enough to receive treatment in this setting, but it is contraindicated in patients who are too unstable to receive mAb therapy in an outpatient setting, such as those with increased oxygen demands. R.L., a staff nurse, assessed the patient on arrival and found that his vital signs were stable, except for a slightly elevated respiratory rate. Upon questioning, the patient reported that he had increased his oxygen use at home from 2 to 4 L via a nasal cannula. R.L. assessed that the patient was too high-risk for outpatient mAb therapy and had the patient checked into the emergency department (ED) to receive a full diagnostic workup and evaluation by Dr. W., an ED provider. The patient required admission to the hospital for a higher level of care in an inpatient unit because of severe COVID-19 infection. Within 48 hours of admission, the patient’s condition further declined, requiring an upgrade to the medical intensive care unit with progressive interventions. Owing to the clinical assessment skills and prompt action of R.L., the patient was admitted to the hospital instead of receiving treatment in a suboptimal care setting and returning home. Had the patient gone home, his rapid decline could have had serious consequences.
Reason for criteria being met: On a cursory look, the patient may have passed as someone sufficiently stable to undergo outpatient treatment. However, the nurse stopped the line, paid close attention, and picked up on an abnormal vital sign and the projected consequences. The nurse brought the patient to a higher level of care in the ED so that he could get the attention he needed. If this patient was given mAb therapy in the outpatient setting, he would have been discharged and become sicker with the COVID-19 illness. As a result of this incident, R.L. is working with the outpatient clinic and ED staff to enahance triage and evaluation of patients referred for outpatient therapy for COVID-19 infections to prevent a similar event from recurring.
Level 3 – Culture of Safety Appreciation Award. While C.C. was reviewing the hazardous item
Reason for criteria being met: The employee works in the hospital education department. It is within her scope of responsibilities to provide ongoing education to staff in order to address potential safety concerns.
DISCUSSION
This QI initiative was undertaken to demonstrate to staff that, in building an organizational culture of safety and advancing quality health care, it is important that staff be encouraged to speak up for safety and be acknowledged for doing so. As part of efforts to continuously build on a safety-first culture, transparency and celebration of successes were demonstrated. This QI initiative demonstrated that a diverse and wide range of employees were reached, from clinical to nonclinical staff, and frontline to supervisory staff, as all were included in the recognition process. While many award nominations were received through the submission of safety concerns to the high-reliability team and patient safety office, several came directly from staff who wanted to recognize their peers for their work, supporting a culture of safety. This showed that staff felt that taking the time to submit a write-up to recognize a peer was an important task. Achieving zero harm for patients and staff alike is a top priority for our institution and guides all decisions, which reinforces that everyone has a responsibility to ensure that safety is always the first consideration. A culture of safety is enhanced by staff recognition. This QI initiative also showed that staff felt valued when they were acknowledged, regardless of the level of recognition they received. The theme of feeling valued came from unsolicited feedback. For example, some direct comments from awardees are presented in the Box.
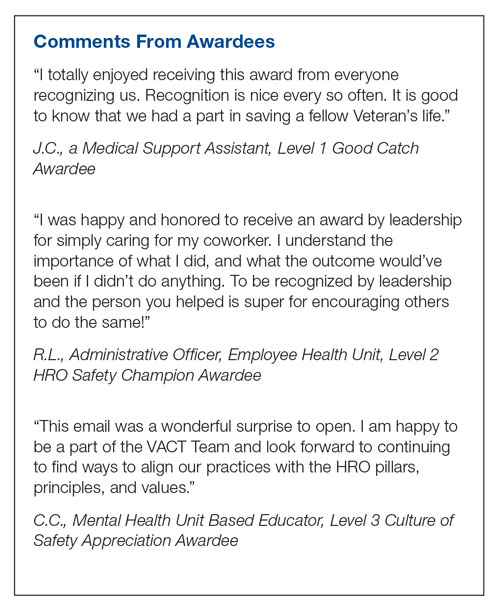
In addition to endorsing the importance of safe practices to staff, safety award programs can identify gaps in existing standard procedures that can be updated quickly and shared broadly across a health care organization. The authors observed that the existence of the award program gives staff permission to use their voice to speak up when they have questions or concerns related to safety and to proactively engage in safety practices; a cultural shift of this kind informs safety practices and procedures and contributes to a more inspiring workplace. Staff at our organization who have received any of the safety awards, and those who are aware of these awards, have embraced the program readily. At the time of submission of this manuscript, there was a relative paucity of published literature on the details, performance, and impact of such programs. This initiative aims to share a road map highlighting the various dimensions of staff recognition and how the program supports our health care system in fostering a strong, sustainable culture of safety and health care quality. A next step is to formally assess the impact of the awards program on our culture of safety and quality using a psychometrically sound measurement tool, as recommended by TJC,16 such as the
CONCLUSION
A health care organization safety awards program is a strategy for building and sustaining a culture of safety. This QI initiative may be valuable to other organizations in the process of establishing a safety awards program of their own. Future research should focus on a formal evaluation of the impact of safety awards programs on patient safety outcomes.
Corresponding author: John S. Murray, PhD, MPH, MSGH, RN, FAAN, 20 Chapel Street, Unit A502, Brookline, MA 02446; JMurray325@aol.com
Disclosures: None reported.
1. National Center for Biotechnology Information. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies. National Library of Medicine; 2019.
2.
3. Agency for Healthcare Research and Quality. Implementing near-miss reporting and improvement tracking in primary care practices: lessons learned. Agency for Healthcare Research and Quality; 2017.
4. Hamed M, Konstantinidis S. Barriers to incident reporting among nurses: a qualitative systematic review. West J Nurs Res. 2022;44(5):506-523. doi:10.1177/0193945921999449
5. Mohamed M, Abubeker IY, Al-Mohanadi D, et al. Perceived barriers of incident reporting among internists: results from Hamad medical corporation in Qatar. Avicenna J Med. 2021;11(3):139-144. doi:10.1055/s-0041-1734386
6. The Joint Commission. The essential role of leadership in developing a safety culture. The Joint Commission; 2017.
7. Yali G, Nzala S. Healthcare providers’ perspective on barriers to patient safety incident reporting in Lusaka District. J Prev Rehabil Med. 2022;4:44-52. doi:10.21617/jprm2022.417
8. Herzer KR, Mirrer M, Xie Y, et al. Patient safety reporting systems: sustained quality improvement using a multidisciplinary team and “good catch” awards. Jt Comm J Qual Patient Saf. 2012;38(8):339-347. doi:10.1016/s1553-7250(12)38044-6
9. Rogers E, Griffin E, Carnie W, et al. A just culture approach to managing medication errors. Hosp Pharm. 2017;52(4):308-315. doi:10.1310/hpj5204-308
10. Murray JS, Clifford J, Larson S, et al. Implementing just culture to improve patient safety. Mil Med. 2022;0: 1. doi:10.1093/milmed/usac115
11. Paradiso L, Sweeney N. Just culture: it’s more than policy. Nurs Manag. 2019;50(6):38–45. doi:10.1097/01.NUMA.0000558482.07815.ae
12. Wallace S, Mamrol M, Finley E; Pennsylvania Patient Safety Authority. Promote a culture of safety with good catch reports. PA Patient Saf Advis. 2017;14(3).
13. Tan KH, Pang NL, Siau C, et al: Building an organizational culture of patient safety. J Patient Saf Risk Manag. 2019;24:253-261. doi.10.1177/251604351987897
14. Merchant N, O’Neal J, Dealino-Perez C, et al: A high reliability mindset. Am J Med Qual. 2022;37(6):504-510. doi:10.1097/JMQ.0000000000000086
15. Behavioral interview questions and answers. Hudson. Accessed December 23, 2022. https://au.hudson.com/insights/career-advice/job-interviews/behavioural-interview-questions-and-answers/
16. The Joint Commission. Safety culture assessment: Improving the survey process. Accessed December 26, 2022. https://www.jointcommission.org/-/media/tjc/documents/accred-and-cert/safety_culture_assessment_improving_the_survey_process.pdf
17. Reis CT, Paiva SG, Sousa P. The patient safety culture: a systematic review by characteristics of hospital survey on patient safety culture dimensions. Int J Qual Heal Care. 2018;30(9):660-677. doi:10.1093/intqhc/mzy080
18. Fourar YO, Benhassine W, Boughaba A, et al. Contribution to the assessment of patient safety culture in Algerian healthcare settings: the ASCO project. Int J Healthc Manag. 2022;15:52-61. doi.org/10.1080/20479700.2020.1836736
1. National Center for Biotechnology Information. Improving healthcare quality in Europe: Characteristics, effectiveness and implementation of different strategies. National Library of Medicine; 2019.
2.
3. Agency for Healthcare Research and Quality. Implementing near-miss reporting and improvement tracking in primary care practices: lessons learned. Agency for Healthcare Research and Quality; 2017.
4. Hamed M, Konstantinidis S. Barriers to incident reporting among nurses: a qualitative systematic review. West J Nurs Res. 2022;44(5):506-523. doi:10.1177/0193945921999449
5. Mohamed M, Abubeker IY, Al-Mohanadi D, et al. Perceived barriers of incident reporting among internists: results from Hamad medical corporation in Qatar. Avicenna J Med. 2021;11(3):139-144. doi:10.1055/s-0041-1734386
6. The Joint Commission. The essential role of leadership in developing a safety culture. The Joint Commission; 2017.
7. Yali G, Nzala S. Healthcare providers’ perspective on barriers to patient safety incident reporting in Lusaka District. J Prev Rehabil Med. 2022;4:44-52. doi:10.21617/jprm2022.417
8. Herzer KR, Mirrer M, Xie Y, et al. Patient safety reporting systems: sustained quality improvement using a multidisciplinary team and “good catch” awards. Jt Comm J Qual Patient Saf. 2012;38(8):339-347. doi:10.1016/s1553-7250(12)38044-6
9. Rogers E, Griffin E, Carnie W, et al. A just culture approach to managing medication errors. Hosp Pharm. 2017;52(4):308-315. doi:10.1310/hpj5204-308
10. Murray JS, Clifford J, Larson S, et al. Implementing just culture to improve patient safety. Mil Med. 2022;0: 1. doi:10.1093/milmed/usac115
11. Paradiso L, Sweeney N. Just culture: it’s more than policy. Nurs Manag. 2019;50(6):38–45. doi:10.1097/01.NUMA.0000558482.07815.ae
12. Wallace S, Mamrol M, Finley E; Pennsylvania Patient Safety Authority. Promote a culture of safety with good catch reports. PA Patient Saf Advis. 2017;14(3).
13. Tan KH, Pang NL, Siau C, et al: Building an organizational culture of patient safety. J Patient Saf Risk Manag. 2019;24:253-261. doi.10.1177/251604351987897
14. Merchant N, O’Neal J, Dealino-Perez C, et al: A high reliability mindset. Am J Med Qual. 2022;37(6):504-510. doi:10.1097/JMQ.0000000000000086
15. Behavioral interview questions and answers. Hudson. Accessed December 23, 2022. https://au.hudson.com/insights/career-advice/job-interviews/behavioural-interview-questions-and-answers/
16. The Joint Commission. Safety culture assessment: Improving the survey process. Accessed December 26, 2022. https://www.jointcommission.org/-/media/tjc/documents/accred-and-cert/safety_culture_assessment_improving_the_survey_process.pdf
17. Reis CT, Paiva SG, Sousa P. The patient safety culture: a systematic review by characteristics of hospital survey on patient safety culture dimensions. Int J Qual Heal Care. 2018;30(9):660-677. doi:10.1093/intqhc/mzy080
18. Fourar YO, Benhassine W, Boughaba A, et al. Contribution to the assessment of patient safety culture in Algerian healthcare settings: the ASCO project. Int J Healthc Manag. 2022;15:52-61. doi.org/10.1080/20479700.2020.1836736