User login
Suicide Screening and Safety Plans Moved Needle on Attempts and Deaths Moving the Needle
In the winter of 2023, Cynthia Smith, MD, an internal medicine physician in Philadelphia and the chief membership and engagement officer for the American College of Physicians, treated a high-achieving, middle-aged man who said he felt completely alone and isolated.
Smith used depression and suicide screeners and found the man was actively thinking of harming himself. She and the man created a safety plan. Then, she connected her patient to a clinical social worker within her health system who helped him enter an intensive outpatient treatment program for depression.
“I am not sure if screening this patient for depression saved his life, but I do think he left the office feeling less alone and more supported than when he arrived. Screening him helped us achieve that outcome,” said Smith. “Our patient needed to know that we cared about him.”
Smith’s experience is part of a broader movement to screen patients for depression and suicide with the goal of getting people into treatment.
Prior research has shown more than 40% people who die by suicide visit a primary care clinician in the month before death, and more than 75% see a primary care physician in the year before a suicide death.
New research published in Annals of Internal Medicine showed these screening processes reduced suicide attempts and deaths by suicide by 25% in one health system.
Clinicians using screening questions to engage patients in safety planning “can know that this work is valuable, and that it will save lives,” said Julie Angerhofer, PhD, MPH, a collaborative scientist at Kaiser Permanente Washington Health Research Institute in Seattle, and a coauthor of the study. “For those who are considering investing in doing this work, it is good news because it is going to have an effect. We did not know that until we did this trial.”
Suicide is the 11th leading cause of death in the United States, accounting for 49,000 fatalities in 2022, according to the Centers for Disease Control and Prevention.
The new study findings “are significant when it comes to working with people who are at risk for suicide in primary care practice and shows that it is both feasible and effective,” said Julie Goldstein Grumet, PhD, vice president for suicide prevention strategy and director of the Zero Suicide Institute at the nonprofit Education Development Center.
Grumet said the use of standardized screening tools, like those used in the study protocol, is key.
When patients screened positive for depression with the Patient Health Questionnaire 2 (PHQ-2), they were asked to complete the additional questions of the PHQ-9. If patients reported frequent suicidal thoughts, they received a brief, self-administered version of the Columbia-Suicide Severity Rating Scale. The analysis included 333,593 patients who had 1.56 million visits for any reason to their primary care clinician.
Patients who reported some level of intent or planning for a suicide attempt in the prior month were connected to a clinical social worker for same day safety planning.
The study showed that the rate of documented fatal or nonfatal suicide attempts within 90 days of a primary care visit was 25% lower in the suicide care than in the usual care period and 24% lower in the 60 days after a visit, both statistically significant findings.
These tools help clinicians “to determine the type of care needed and to provide the right level of intervention,” Grumet said.
Both Smith and the study utilized social workers to help with safety planning. But because many clinicians do not work in integrated health systems with access to these professionals, other workflows can also support the screening and safety planning process, Angerhofer said. For instance, nurses can be trained to conduct a safety plan.
“Some systems also use centralized groups of providers trained in safety planning to support primary care teams virtually,” she said. Clinicians can also refer to free trainings on safety planning available online — including the one on the Zero Suicide website.
Smith said one of the biggest barriers to suicide care is the lack of resources needed to follow-up on a positive screen.
The study findings are “a call to action, but it can’t be the straw breaking the backs of primary care doctors; it has to be supported,” Smith said.
A safety plan includes:
- Helping patients recognize warning signs of an impending suicidal crisis
- Using social contacts as a means of distraction from suicidal thoughts
- Contacting family members or friends who may help resolve the crisis
- Contacting mental health professionals or agencies
- Making the patient’s home environment safer by reducing the potential use and availability of lethal means
The study was supported by a grant from the National Institute of Mental Health. Various study authors reported receiving consulting fees, honoraria, and grants from the University of Washington, Advocate Aurora Health, the Donaghue Medical Research Foundation’s Greater Value Portfolio program, and the Patient-Centered Outcomes Research Institute, among others.
A version of this article first appeared on Medscape.com.
In the winter of 2023, Cynthia Smith, MD, an internal medicine physician in Philadelphia and the chief membership and engagement officer for the American College of Physicians, treated a high-achieving, middle-aged man who said he felt completely alone and isolated.
Smith used depression and suicide screeners and found the man was actively thinking of harming himself. She and the man created a safety plan. Then, she connected her patient to a clinical social worker within her health system who helped him enter an intensive outpatient treatment program for depression.
“I am not sure if screening this patient for depression saved his life, but I do think he left the office feeling less alone and more supported than when he arrived. Screening him helped us achieve that outcome,” said Smith. “Our patient needed to know that we cared about him.”
Smith’s experience is part of a broader movement to screen patients for depression and suicide with the goal of getting people into treatment.
Prior research has shown more than 40% people who die by suicide visit a primary care clinician in the month before death, and more than 75% see a primary care physician in the year before a suicide death.
New research published in Annals of Internal Medicine showed these screening processes reduced suicide attempts and deaths by suicide by 25% in one health system.
Clinicians using screening questions to engage patients in safety planning “can know that this work is valuable, and that it will save lives,” said Julie Angerhofer, PhD, MPH, a collaborative scientist at Kaiser Permanente Washington Health Research Institute in Seattle, and a coauthor of the study. “For those who are considering investing in doing this work, it is good news because it is going to have an effect. We did not know that until we did this trial.”
Suicide is the 11th leading cause of death in the United States, accounting for 49,000 fatalities in 2022, according to the Centers for Disease Control and Prevention.
The new study findings “are significant when it comes to working with people who are at risk for suicide in primary care practice and shows that it is both feasible and effective,” said Julie Goldstein Grumet, PhD, vice president for suicide prevention strategy and director of the Zero Suicide Institute at the nonprofit Education Development Center.
Grumet said the use of standardized screening tools, like those used in the study protocol, is key.
When patients screened positive for depression with the Patient Health Questionnaire 2 (PHQ-2), they were asked to complete the additional questions of the PHQ-9. If patients reported frequent suicidal thoughts, they received a brief, self-administered version of the Columbia-Suicide Severity Rating Scale. The analysis included 333,593 patients who had 1.56 million visits for any reason to their primary care clinician.
Patients who reported some level of intent or planning for a suicide attempt in the prior month were connected to a clinical social worker for same day safety planning.
The study showed that the rate of documented fatal or nonfatal suicide attempts within 90 days of a primary care visit was 25% lower in the suicide care than in the usual care period and 24% lower in the 60 days after a visit, both statistically significant findings.
These tools help clinicians “to determine the type of care needed and to provide the right level of intervention,” Grumet said.
Both Smith and the study utilized social workers to help with safety planning. But because many clinicians do not work in integrated health systems with access to these professionals, other workflows can also support the screening and safety planning process, Angerhofer said. For instance, nurses can be trained to conduct a safety plan.
“Some systems also use centralized groups of providers trained in safety planning to support primary care teams virtually,” she said. Clinicians can also refer to free trainings on safety planning available online — including the one on the Zero Suicide website.
Smith said one of the biggest barriers to suicide care is the lack of resources needed to follow-up on a positive screen.
The study findings are “a call to action, but it can’t be the straw breaking the backs of primary care doctors; it has to be supported,” Smith said.
A safety plan includes:
- Helping patients recognize warning signs of an impending suicidal crisis
- Using social contacts as a means of distraction from suicidal thoughts
- Contacting family members or friends who may help resolve the crisis
- Contacting mental health professionals or agencies
- Making the patient’s home environment safer by reducing the potential use and availability of lethal means
The study was supported by a grant from the National Institute of Mental Health. Various study authors reported receiving consulting fees, honoraria, and grants from the University of Washington, Advocate Aurora Health, the Donaghue Medical Research Foundation’s Greater Value Portfolio program, and the Patient-Centered Outcomes Research Institute, among others.
A version of this article first appeared on Medscape.com.
In the winter of 2023, Cynthia Smith, MD, an internal medicine physician in Philadelphia and the chief membership and engagement officer for the American College of Physicians, treated a high-achieving, middle-aged man who said he felt completely alone and isolated.
Smith used depression and suicide screeners and found the man was actively thinking of harming himself. She and the man created a safety plan. Then, she connected her patient to a clinical social worker within her health system who helped him enter an intensive outpatient treatment program for depression.
“I am not sure if screening this patient for depression saved his life, but I do think he left the office feeling less alone and more supported than when he arrived. Screening him helped us achieve that outcome,” said Smith. “Our patient needed to know that we cared about him.”
Smith’s experience is part of a broader movement to screen patients for depression and suicide with the goal of getting people into treatment.
Prior research has shown more than 40% people who die by suicide visit a primary care clinician in the month before death, and more than 75% see a primary care physician in the year before a suicide death.
New research published in Annals of Internal Medicine showed these screening processes reduced suicide attempts and deaths by suicide by 25% in one health system.
Clinicians using screening questions to engage patients in safety planning “can know that this work is valuable, and that it will save lives,” said Julie Angerhofer, PhD, MPH, a collaborative scientist at Kaiser Permanente Washington Health Research Institute in Seattle, and a coauthor of the study. “For those who are considering investing in doing this work, it is good news because it is going to have an effect. We did not know that until we did this trial.”
Suicide is the 11th leading cause of death in the United States, accounting for 49,000 fatalities in 2022, according to the Centers for Disease Control and Prevention.
The new study findings “are significant when it comes to working with people who are at risk for suicide in primary care practice and shows that it is both feasible and effective,” said Julie Goldstein Grumet, PhD, vice president for suicide prevention strategy and director of the Zero Suicide Institute at the nonprofit Education Development Center.
Grumet said the use of standardized screening tools, like those used in the study protocol, is key.
When patients screened positive for depression with the Patient Health Questionnaire 2 (PHQ-2), they were asked to complete the additional questions of the PHQ-9. If patients reported frequent suicidal thoughts, they received a brief, self-administered version of the Columbia-Suicide Severity Rating Scale. The analysis included 333,593 patients who had 1.56 million visits for any reason to their primary care clinician.
Patients who reported some level of intent or planning for a suicide attempt in the prior month were connected to a clinical social worker for same day safety planning.
The study showed that the rate of documented fatal or nonfatal suicide attempts within 90 days of a primary care visit was 25% lower in the suicide care than in the usual care period and 24% lower in the 60 days after a visit, both statistically significant findings.
These tools help clinicians “to determine the type of care needed and to provide the right level of intervention,” Grumet said.
Both Smith and the study utilized social workers to help with safety planning. But because many clinicians do not work in integrated health systems with access to these professionals, other workflows can also support the screening and safety planning process, Angerhofer said. For instance, nurses can be trained to conduct a safety plan.
“Some systems also use centralized groups of providers trained in safety planning to support primary care teams virtually,” she said. Clinicians can also refer to free trainings on safety planning available online — including the one on the Zero Suicide website.
Smith said one of the biggest barriers to suicide care is the lack of resources needed to follow-up on a positive screen.
The study findings are “a call to action, but it can’t be the straw breaking the backs of primary care doctors; it has to be supported,” Smith said.
A safety plan includes:
- Helping patients recognize warning signs of an impending suicidal crisis
- Using social contacts as a means of distraction from suicidal thoughts
- Contacting family members or friends who may help resolve the crisis
- Contacting mental health professionals or agencies
- Making the patient’s home environment safer by reducing the potential use and availability of lethal means
The study was supported by a grant from the National Institute of Mental Health. Various study authors reported receiving consulting fees, honoraria, and grants from the University of Washington, Advocate Aurora Health, the Donaghue Medical Research Foundation’s Greater Value Portfolio program, and the Patient-Centered Outcomes Research Institute, among others.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF INTERNAL MEDICINE
Caffeine Brings Benefits and Risks
Coffee and tea are among the plants that are highest in caffeine. Their use as beverages makes caffeine the most consumed psychoactive agent in the world. Coffee is commonly used to increase alertness and work productivity. Synthetic caffeine is added to soft drinks, energy drinks, and products intended to reduce fatigue or promote weight loss.
The caffeine content varies with the type of drink: It is high in coffee, energy drinks, and caffeine tablets; intermediate in tea; and low in soft drinks. Coffee is the predominant source of the caffeine ingested by adults. The evidence for caffeine’s effects on people is ambiguous, and some risks and benefits deserve special attention because of the impact they may have on our health.
Characteristics of Caffeine
The half-life of caffeine varies according to age. In adults, it is 2.5-4.5 hours; in newborns, 80 hours; in children older than 6 months, it remains stable over time with respect to weight. Smoking accelerates caffeine metabolism by reducing the half-life by 50%. Oral contraceptives, however, double caffeine’s half-life. Caffeine metabolism is reduced during pregnancy (it is greater in the first trimester), with a half-life of more than 15 hours. Caffeine clearance can be slowed by several classes of drugs (eg, quinolones, cardiovascular drugs, bronchodilators, and antidepressants) that increase its half-life because they are metabolized by the same liver enzymes.
Caffeine passes the blood-brain barrier and, having an adenosine-like structure, inhibits adenosine’s effects by binding to adenosine receptors. In the brain, caffeine reduces fatigue, increases alertness, reduces reaction times, may reduce the risk for depression, and increases the effectiveness of nonsteroidal anti-inflammatory drugs in treating headaches and other types of pain.
Caffeine and Chronic Diseases
The evidence available on the relationship between caffeine and health has several methodological limitations. Observations of the acute effects of caffeine may not reflect long-term effects because tolerance to caffeine’s effects may develop over time. Smoking and unhealthy lifestyles are confounding factors in epidemiological studies of caffeine intake. In addition, the estimate of the amount and frequency of caffeine intake is often inaccurate because it is mainly based on self-assessment systems. Finally, prospective studies of caffeine consumption are mainly based on coffee and tea consumption, but it is unclear how much the observed outcomes can be translated to intake of other beverages such as energy drinks.
Considering the very high prevalence of arterial hypertension worldwide (31.1% of adults), many questions have been raised about the influence of coffee consumption on blood pressure (BP) and the risk for arterial hypertension. Administration of 200-300 mg caffeine is shown to induce a mean increase of 8.1 mm Hg systolic BP and 5.7 mm Hg diastolic BP. The increase is observed in the first hour after caffeine intake and lasts no longer than 3 hours.
Yet, the moderate and usual consumption of coffee does not increase, but may even reduce, the risk of developing high BP. In contrast, occasional coffee consumption can have hypertensive effects, and moderate and usual consumption in patients with high BP does not appear to increase the risk for uncontrolled BP and can reduce the risk for death from any cause. The inverse association between coffee consumption and hypertension risk was confirmed in a review and meta-analysis of cross-sectional and cohort studies.
With respect to lipid metabolism, cholesterol levels may increase after caffeine consumption because of cafestol. Concentrations of cafestol are high in unfiltered coffee, intermediate in espresso and moka pot coffee, and negligible in instant or filtered coffee. Studies on the impact of coffee on lipid levels have led to inconsistent results, however. Data have shown that people who drink more coffee have higher triglycerides, total cholesterol, and low-density lipoprotein cholesterol (LDL-C) levels. Other data have shown that caffeine promotes LDL receptor expression and clearance of LDL cholesterol.
Experimental and cohort studies have not shown an association between coffee consumption and atrial fibrillation (AF). In fact, evidence suggests that coffee consumption tends to reduce the risk for AF in a dose-response relationship. Similarly, coffee consumption is not associated with increased risk for cardiovascular events in the general population or among patients with a history of hypertension, diabetes, or cardiovascular disease.
The Coffee and Real-Time Atrial and Ventricular Ectopy study evaluated the acute effects of coffee consumption on cardiac ectopy using wearable sensors with continuous recording. It did not demonstrate any increase in daily premature atrial contractions with coffee consumption, compared with abstaining from caffeine.
In patients with type 2 diabetes, a study performed in Japan showed that coffee consumption was associated with reduced all-cause mortality. The results suggested a dose-response relationship, and drinking coffee and green tea appeared to reduce mortality risk further. The results were not generalizable, however, because of the study population’s ethnic homogeneity.
Dose and Toxicity
Caffeine at high doses (> 400 mg daily) and in susceptible patients can induce anxiety, but the effects of caffeine on sleep and anxiety can differ from patient to patient. This variation reflects differences in caffeine metabolism rate and adenosine receptor gene variants.
High caffeine intake can stimulate diuresis, but without causing damaging effects on hydration when taking moderate doses of caffeine (≤ 400 mg daily) for long periods. Stopping caffeine suddenly, in a regular consumer, can lead to withdrawal symptoms such as headache, asthenia, decreased attention, depressed mood, and flu-like symptoms.
The toxic effects of caffeine occur with intake > 1.2 g. A dose of 10-14 g is considered fatal. Caffeine overdose is rare when considering traditional methods of intake (coffee and tea) because 70-100 cups of coffee should be sufficient for caffeine poisoning. Severe events can occur following the use of caffeine tablets or as energy drinks for the following reasons:
- The episodic consumption of caffeine does not allow for tolerance to develop.
- Young people are more vulnerable to the effects of caffeine.
- Caffeine has a synergistic effect in combination with other components in energy drinks.
- Taking caffeine in combination with alcohol or intense exertion causes serious, even fatal, outcomes.
Products Containing Caffeine
Evidence supports the relationship between high consumption (approximately 1 L) of energy drinks with a caffeine content of 320 mg and short-term cardiovascular adverse events, such as increased BP, QT-segment prolongation corrected for heart rate, and palpitations. These tests prompt the recommendation to avoid consuming these beverages in high quantities and in association with alcohol.
Weight loss products generally contain caffeine coupled with herbal extracts that are expected to improve fat metabolism, lipolysis, and oxidation. These products, because of their easy availability, presumed benefits, and high caffeine concentration, may be more susceptible to misuse because they can be taken in larger portions than recommended. The combination of multiple ingredients, concentrated amounts of caffeine, and excessive consumption increases the likelihood of adverse effects.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Coffee and tea are among the plants that are highest in caffeine. Their use as beverages makes caffeine the most consumed psychoactive agent in the world. Coffee is commonly used to increase alertness and work productivity. Synthetic caffeine is added to soft drinks, energy drinks, and products intended to reduce fatigue or promote weight loss.
The caffeine content varies with the type of drink: It is high in coffee, energy drinks, and caffeine tablets; intermediate in tea; and low in soft drinks. Coffee is the predominant source of the caffeine ingested by adults. The evidence for caffeine’s effects on people is ambiguous, and some risks and benefits deserve special attention because of the impact they may have on our health.
Characteristics of Caffeine
The half-life of caffeine varies according to age. In adults, it is 2.5-4.5 hours; in newborns, 80 hours; in children older than 6 months, it remains stable over time with respect to weight. Smoking accelerates caffeine metabolism by reducing the half-life by 50%. Oral contraceptives, however, double caffeine’s half-life. Caffeine metabolism is reduced during pregnancy (it is greater in the first trimester), with a half-life of more than 15 hours. Caffeine clearance can be slowed by several classes of drugs (eg, quinolones, cardiovascular drugs, bronchodilators, and antidepressants) that increase its half-life because they are metabolized by the same liver enzymes.
Caffeine passes the blood-brain barrier and, having an adenosine-like structure, inhibits adenosine’s effects by binding to adenosine receptors. In the brain, caffeine reduces fatigue, increases alertness, reduces reaction times, may reduce the risk for depression, and increases the effectiveness of nonsteroidal anti-inflammatory drugs in treating headaches and other types of pain.
Caffeine and Chronic Diseases
The evidence available on the relationship between caffeine and health has several methodological limitations. Observations of the acute effects of caffeine may not reflect long-term effects because tolerance to caffeine’s effects may develop over time. Smoking and unhealthy lifestyles are confounding factors in epidemiological studies of caffeine intake. In addition, the estimate of the amount and frequency of caffeine intake is often inaccurate because it is mainly based on self-assessment systems. Finally, prospective studies of caffeine consumption are mainly based on coffee and tea consumption, but it is unclear how much the observed outcomes can be translated to intake of other beverages such as energy drinks.
Considering the very high prevalence of arterial hypertension worldwide (31.1% of adults), many questions have been raised about the influence of coffee consumption on blood pressure (BP) and the risk for arterial hypertension. Administration of 200-300 mg caffeine is shown to induce a mean increase of 8.1 mm Hg systolic BP and 5.7 mm Hg diastolic BP. The increase is observed in the first hour after caffeine intake and lasts no longer than 3 hours.
Yet, the moderate and usual consumption of coffee does not increase, but may even reduce, the risk of developing high BP. In contrast, occasional coffee consumption can have hypertensive effects, and moderate and usual consumption in patients with high BP does not appear to increase the risk for uncontrolled BP and can reduce the risk for death from any cause. The inverse association between coffee consumption and hypertension risk was confirmed in a review and meta-analysis of cross-sectional and cohort studies.
With respect to lipid metabolism, cholesterol levels may increase after caffeine consumption because of cafestol. Concentrations of cafestol are high in unfiltered coffee, intermediate in espresso and moka pot coffee, and negligible in instant or filtered coffee. Studies on the impact of coffee on lipid levels have led to inconsistent results, however. Data have shown that people who drink more coffee have higher triglycerides, total cholesterol, and low-density lipoprotein cholesterol (LDL-C) levels. Other data have shown that caffeine promotes LDL receptor expression and clearance of LDL cholesterol.
Experimental and cohort studies have not shown an association between coffee consumption and atrial fibrillation (AF). In fact, evidence suggests that coffee consumption tends to reduce the risk for AF in a dose-response relationship. Similarly, coffee consumption is not associated with increased risk for cardiovascular events in the general population or among patients with a history of hypertension, diabetes, or cardiovascular disease.
The Coffee and Real-Time Atrial and Ventricular Ectopy study evaluated the acute effects of coffee consumption on cardiac ectopy using wearable sensors with continuous recording. It did not demonstrate any increase in daily premature atrial contractions with coffee consumption, compared with abstaining from caffeine.
In patients with type 2 diabetes, a study performed in Japan showed that coffee consumption was associated with reduced all-cause mortality. The results suggested a dose-response relationship, and drinking coffee and green tea appeared to reduce mortality risk further. The results were not generalizable, however, because of the study population’s ethnic homogeneity.
Dose and Toxicity
Caffeine at high doses (> 400 mg daily) and in susceptible patients can induce anxiety, but the effects of caffeine on sleep and anxiety can differ from patient to patient. This variation reflects differences in caffeine metabolism rate and adenosine receptor gene variants.
High caffeine intake can stimulate diuresis, but without causing damaging effects on hydration when taking moderate doses of caffeine (≤ 400 mg daily) for long periods. Stopping caffeine suddenly, in a regular consumer, can lead to withdrawal symptoms such as headache, asthenia, decreased attention, depressed mood, and flu-like symptoms.
The toxic effects of caffeine occur with intake > 1.2 g. A dose of 10-14 g is considered fatal. Caffeine overdose is rare when considering traditional methods of intake (coffee and tea) because 70-100 cups of coffee should be sufficient for caffeine poisoning. Severe events can occur following the use of caffeine tablets or as energy drinks for the following reasons:
- The episodic consumption of caffeine does not allow for tolerance to develop.
- Young people are more vulnerable to the effects of caffeine.
- Caffeine has a synergistic effect in combination with other components in energy drinks.
- Taking caffeine in combination with alcohol or intense exertion causes serious, even fatal, outcomes.
Products Containing Caffeine
Evidence supports the relationship between high consumption (approximately 1 L) of energy drinks with a caffeine content of 320 mg and short-term cardiovascular adverse events, such as increased BP, QT-segment prolongation corrected for heart rate, and palpitations. These tests prompt the recommendation to avoid consuming these beverages in high quantities and in association with alcohol.
Weight loss products generally contain caffeine coupled with herbal extracts that are expected to improve fat metabolism, lipolysis, and oxidation. These products, because of their easy availability, presumed benefits, and high caffeine concentration, may be more susceptible to misuse because they can be taken in larger portions than recommended. The combination of multiple ingredients, concentrated amounts of caffeine, and excessive consumption increases the likelihood of adverse effects.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Coffee and tea are among the plants that are highest in caffeine. Their use as beverages makes caffeine the most consumed psychoactive agent in the world. Coffee is commonly used to increase alertness and work productivity. Synthetic caffeine is added to soft drinks, energy drinks, and products intended to reduce fatigue or promote weight loss.
The caffeine content varies with the type of drink: It is high in coffee, energy drinks, and caffeine tablets; intermediate in tea; and low in soft drinks. Coffee is the predominant source of the caffeine ingested by adults. The evidence for caffeine’s effects on people is ambiguous, and some risks and benefits deserve special attention because of the impact they may have on our health.
Characteristics of Caffeine
The half-life of caffeine varies according to age. In adults, it is 2.5-4.5 hours; in newborns, 80 hours; in children older than 6 months, it remains stable over time with respect to weight. Smoking accelerates caffeine metabolism by reducing the half-life by 50%. Oral contraceptives, however, double caffeine’s half-life. Caffeine metabolism is reduced during pregnancy (it is greater in the first trimester), with a half-life of more than 15 hours. Caffeine clearance can be slowed by several classes of drugs (eg, quinolones, cardiovascular drugs, bronchodilators, and antidepressants) that increase its half-life because they are metabolized by the same liver enzymes.
Caffeine passes the blood-brain barrier and, having an adenosine-like structure, inhibits adenosine’s effects by binding to adenosine receptors. In the brain, caffeine reduces fatigue, increases alertness, reduces reaction times, may reduce the risk for depression, and increases the effectiveness of nonsteroidal anti-inflammatory drugs in treating headaches and other types of pain.
Caffeine and Chronic Diseases
The evidence available on the relationship between caffeine and health has several methodological limitations. Observations of the acute effects of caffeine may not reflect long-term effects because tolerance to caffeine’s effects may develop over time. Smoking and unhealthy lifestyles are confounding factors in epidemiological studies of caffeine intake. In addition, the estimate of the amount and frequency of caffeine intake is often inaccurate because it is mainly based on self-assessment systems. Finally, prospective studies of caffeine consumption are mainly based on coffee and tea consumption, but it is unclear how much the observed outcomes can be translated to intake of other beverages such as energy drinks.
Considering the very high prevalence of arterial hypertension worldwide (31.1% of adults), many questions have been raised about the influence of coffee consumption on blood pressure (BP) and the risk for arterial hypertension. Administration of 200-300 mg caffeine is shown to induce a mean increase of 8.1 mm Hg systolic BP and 5.7 mm Hg diastolic BP. The increase is observed in the first hour after caffeine intake and lasts no longer than 3 hours.
Yet, the moderate and usual consumption of coffee does not increase, but may even reduce, the risk of developing high BP. In contrast, occasional coffee consumption can have hypertensive effects, and moderate and usual consumption in patients with high BP does not appear to increase the risk for uncontrolled BP and can reduce the risk for death from any cause. The inverse association between coffee consumption and hypertension risk was confirmed in a review and meta-analysis of cross-sectional and cohort studies.
With respect to lipid metabolism, cholesterol levels may increase after caffeine consumption because of cafestol. Concentrations of cafestol are high in unfiltered coffee, intermediate in espresso and moka pot coffee, and negligible in instant or filtered coffee. Studies on the impact of coffee on lipid levels have led to inconsistent results, however. Data have shown that people who drink more coffee have higher triglycerides, total cholesterol, and low-density lipoprotein cholesterol (LDL-C) levels. Other data have shown that caffeine promotes LDL receptor expression and clearance of LDL cholesterol.
Experimental and cohort studies have not shown an association between coffee consumption and atrial fibrillation (AF). In fact, evidence suggests that coffee consumption tends to reduce the risk for AF in a dose-response relationship. Similarly, coffee consumption is not associated with increased risk for cardiovascular events in the general population or among patients with a history of hypertension, diabetes, or cardiovascular disease.
The Coffee and Real-Time Atrial and Ventricular Ectopy study evaluated the acute effects of coffee consumption on cardiac ectopy using wearable sensors with continuous recording. It did not demonstrate any increase in daily premature atrial contractions with coffee consumption, compared with abstaining from caffeine.
In patients with type 2 diabetes, a study performed in Japan showed that coffee consumption was associated with reduced all-cause mortality. The results suggested a dose-response relationship, and drinking coffee and green tea appeared to reduce mortality risk further. The results were not generalizable, however, because of the study population’s ethnic homogeneity.
Dose and Toxicity
Caffeine at high doses (> 400 mg daily) and in susceptible patients can induce anxiety, but the effects of caffeine on sleep and anxiety can differ from patient to patient. This variation reflects differences in caffeine metabolism rate and adenosine receptor gene variants.
High caffeine intake can stimulate diuresis, but without causing damaging effects on hydration when taking moderate doses of caffeine (≤ 400 mg daily) for long periods. Stopping caffeine suddenly, in a regular consumer, can lead to withdrawal symptoms such as headache, asthenia, decreased attention, depressed mood, and flu-like symptoms.
The toxic effects of caffeine occur with intake > 1.2 g. A dose of 10-14 g is considered fatal. Caffeine overdose is rare when considering traditional methods of intake (coffee and tea) because 70-100 cups of coffee should be sufficient for caffeine poisoning. Severe events can occur following the use of caffeine tablets or as energy drinks for the following reasons:
- The episodic consumption of caffeine does not allow for tolerance to develop.
- Young people are more vulnerable to the effects of caffeine.
- Caffeine has a synergistic effect in combination with other components in energy drinks.
- Taking caffeine in combination with alcohol or intense exertion causes serious, even fatal, outcomes.
Products Containing Caffeine
Evidence supports the relationship between high consumption (approximately 1 L) of energy drinks with a caffeine content of 320 mg and short-term cardiovascular adverse events, such as increased BP, QT-segment prolongation corrected for heart rate, and palpitations. These tests prompt the recommendation to avoid consuming these beverages in high quantities and in association with alcohol.
Weight loss products generally contain caffeine coupled with herbal extracts that are expected to improve fat metabolism, lipolysis, and oxidation. These products, because of their easy availability, presumed benefits, and high caffeine concentration, may be more susceptible to misuse because they can be taken in larger portions than recommended. The combination of multiple ingredients, concentrated amounts of caffeine, and excessive consumption increases the likelihood of adverse effects.
This story was translated from Univadis Italy, which is part of the Medscape professional network, using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Utilization, Cost, and Prescription Trends of Antipsychotics Prescribed by Dermatologists for Medicare Patients
To the Editor:
Patients with primary psychiatric disorders with dermatologic manifestations often seek treatment from dermatologists instead of psychiatrists.1 For example, patients with delusions of parasitosis may lack insight into the underlying etiology of their disease and instead fixate on establishing an organic cause for their symptoms. As a result, it is an increasingly common practice for dermatologists to diagnose and treat psychiatric conditions.1 The goal of this study was to evaluate trends for the top 5 antipsychotics most frequently prescribed by dermatologists in the Medicare Part D database.
In this retrospective analysis, we consulted the Medicare Provider Utilization and Payment Data for January 2013 through December 2020, which is provided to the public by the Centers for Medicare & Medicaid Services.2 Only prescribing data from dermatologists were included in this study by using the built-in filter on the website to select “dermatology” as the prescriber type. All other provider types were excluded. We chose the top 5 most prescribed antipsychotics based on the number of supply days reported. Supply days—defined by Medicare as the number of days’ worth of medication that is prescribed—were used as a metric for utilization; therefore, each drug’s total supply days prescribed by dermatologists were calculated using this combined filter of drug name and total supply days using the database.
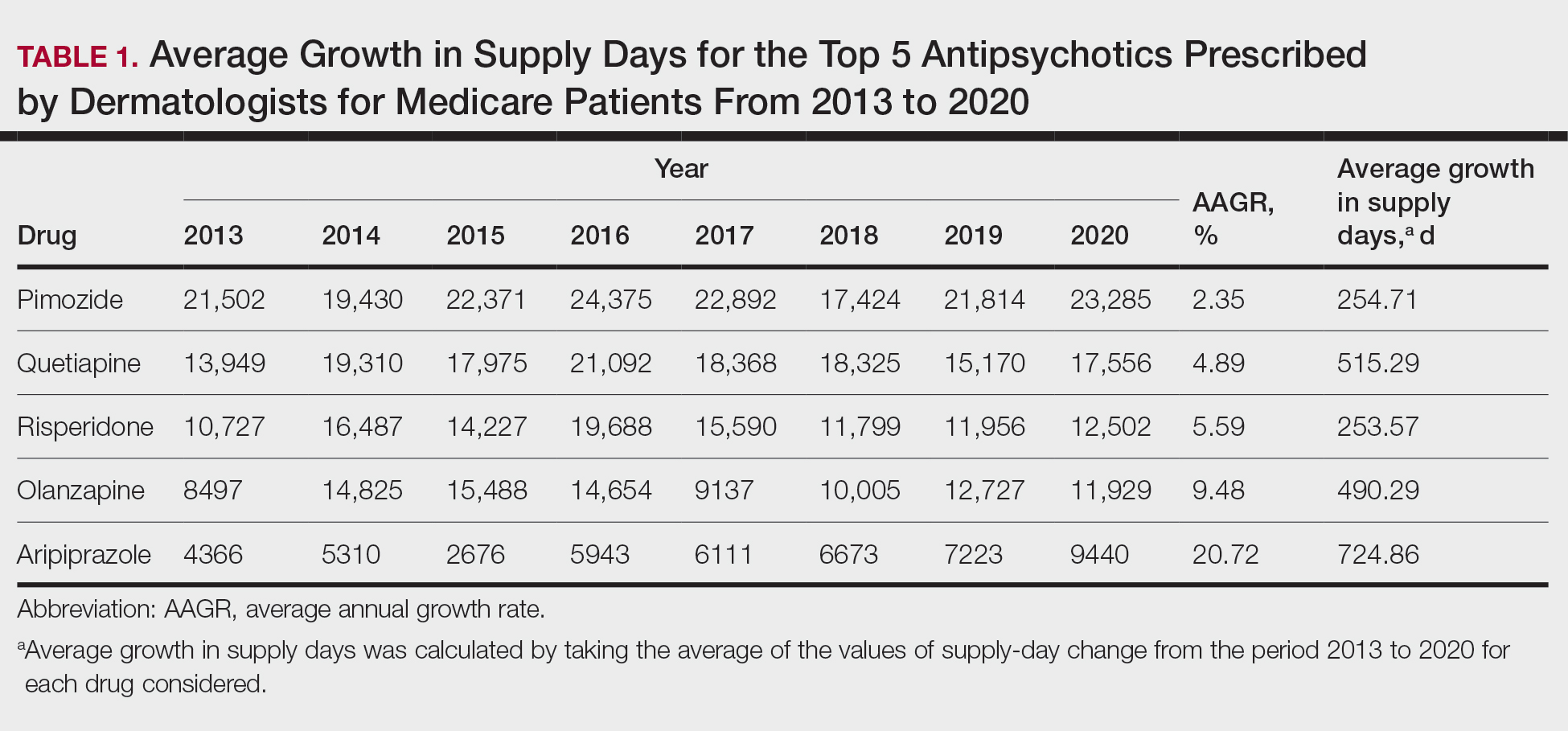
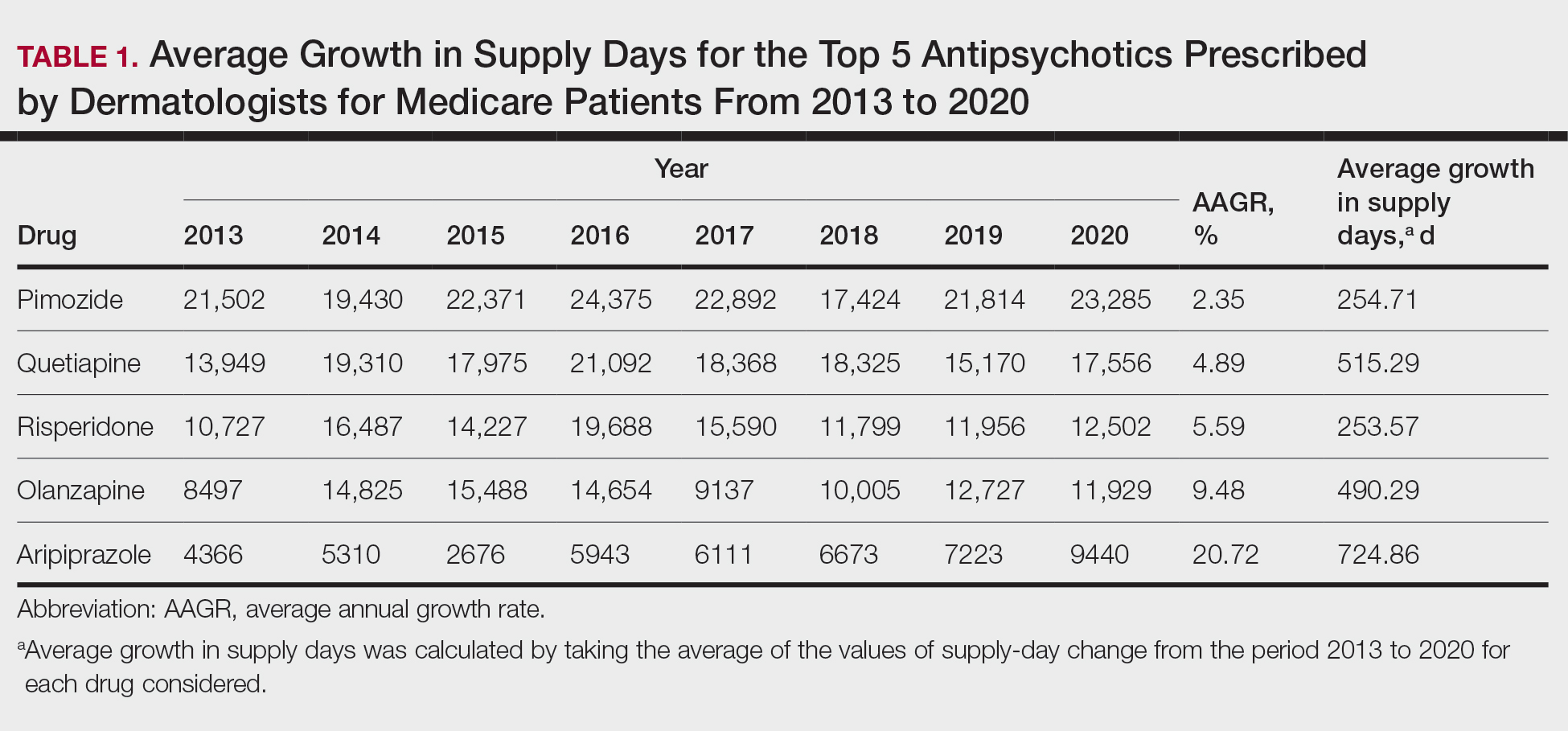
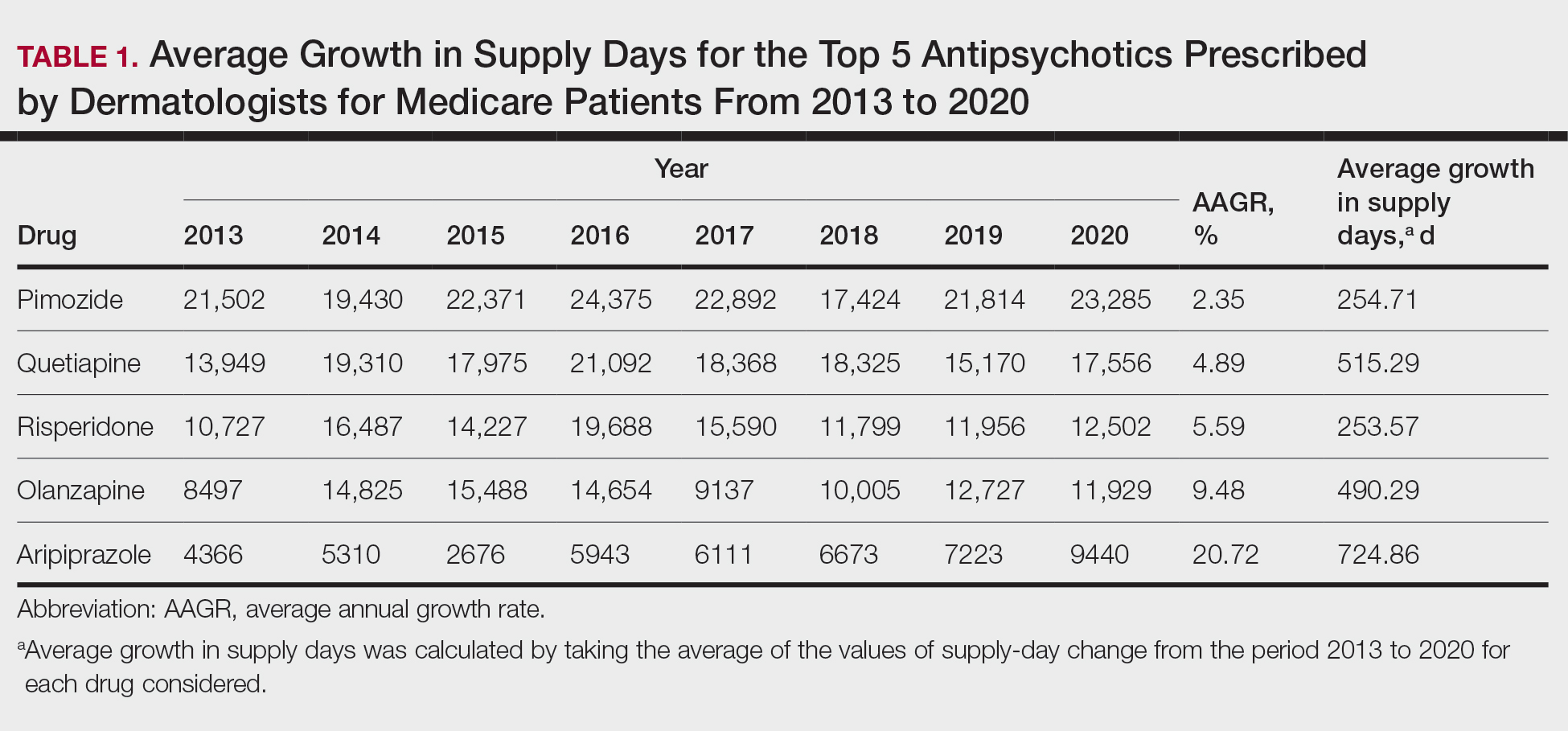
To analyze utilization over time, the annual average growth rate (AAGR) was calculated by determining the growth rate in total supply days annually from 2013 to 2020 and then averaging those rates to determine the overall AAGR. For greater clinical relevance, we calculated the average growth in supply days for the entire study period by determining the difference in the number of supply days for each year and then averaging these values. This was done to consider overall trends across dermatology rather than individual dermatologist prescribing patterns.
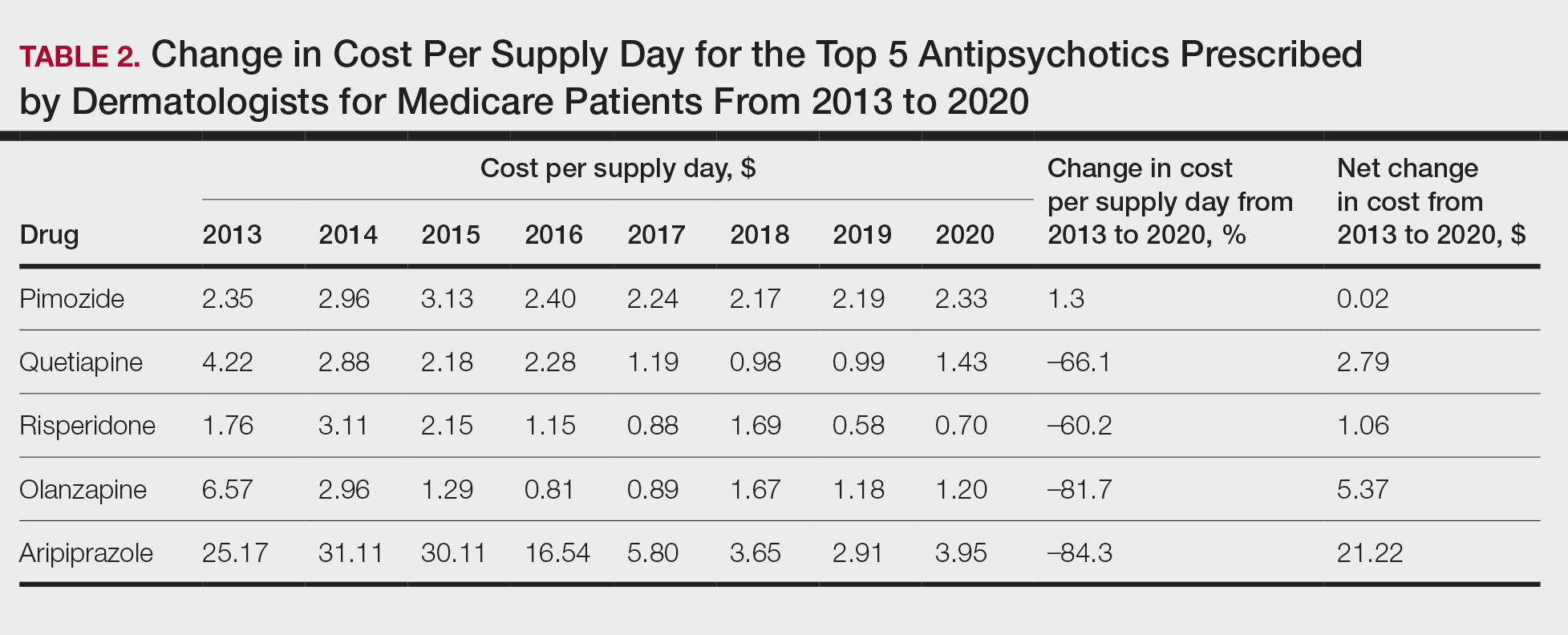
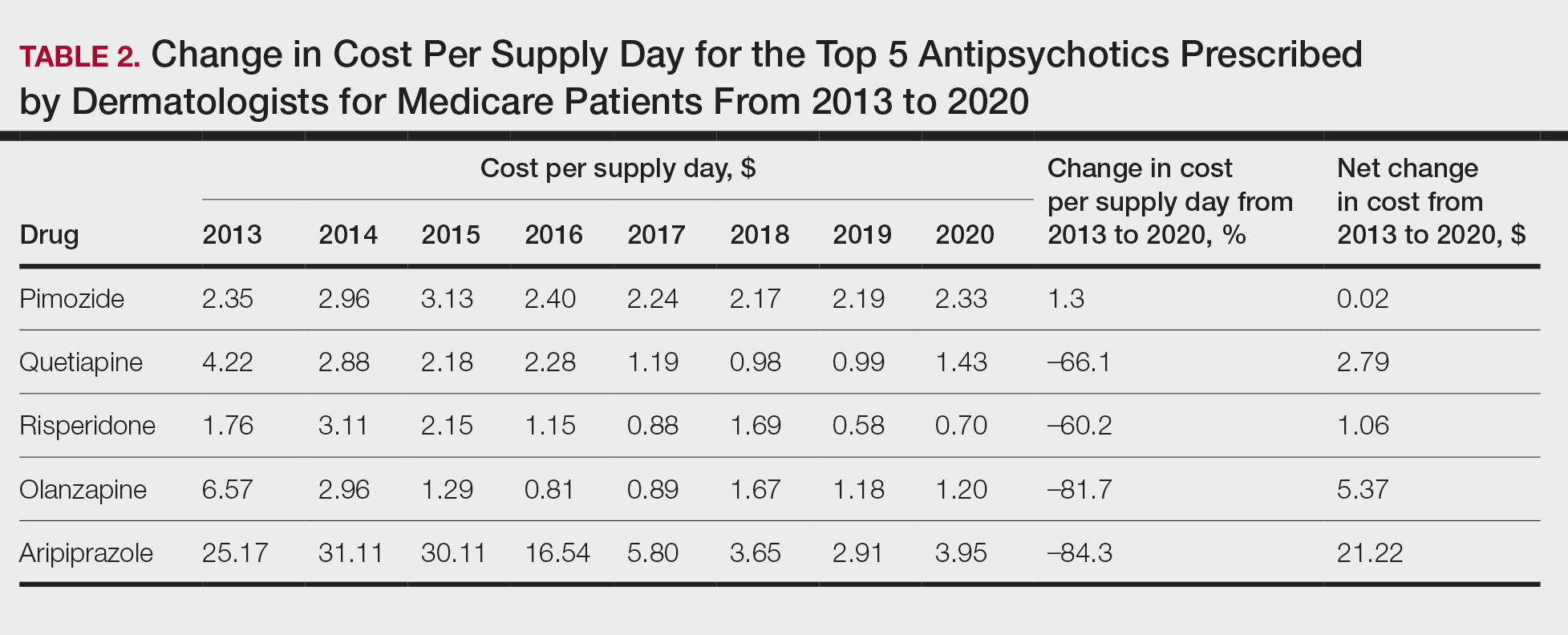
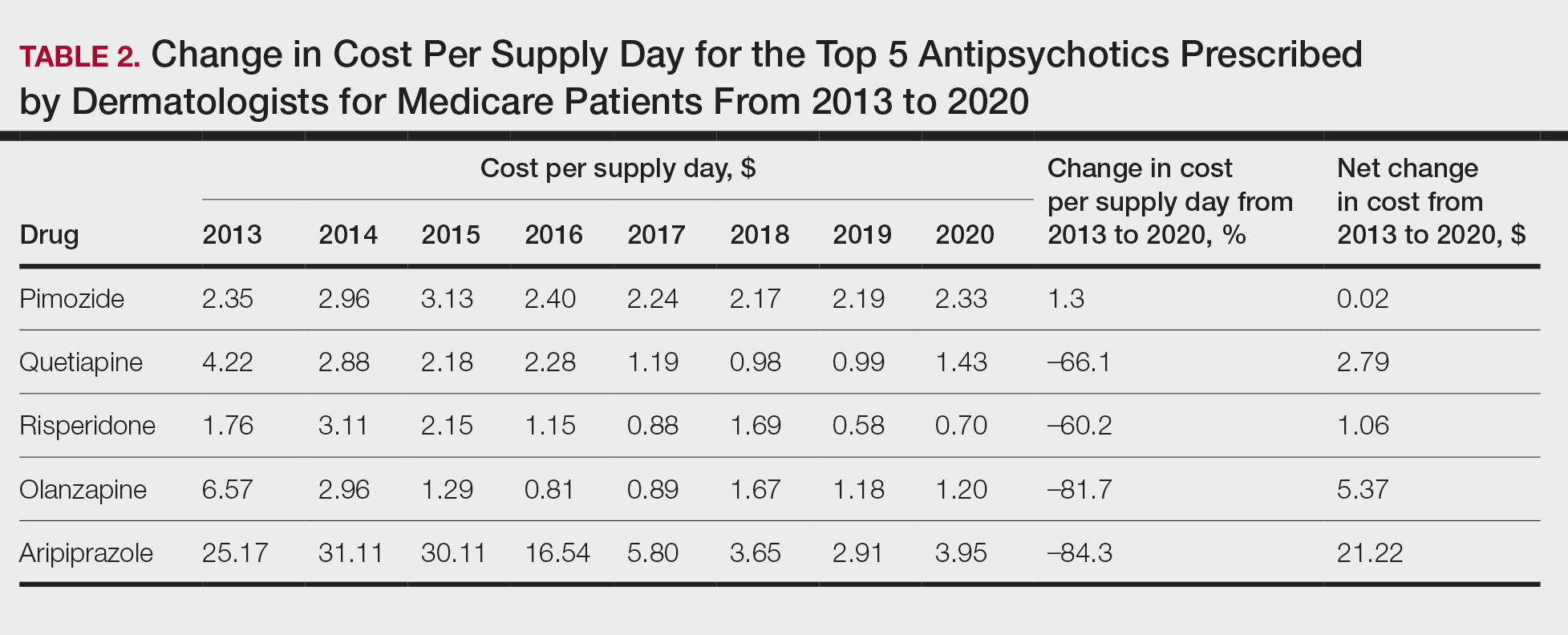
Based on our analysis, the antipsychotics most frequently prescribed by dermatologists for Medicare patients from January 2013 to December 2020 were pimozide, quetiapine, risperidone, olanzapine, and aripiprazole. The AAGR for each drug was 2.35%, 4.89%, 5.59%, 9.48%, and 20.72%, respectively, which is consistent with increased utilization over the study period for all 5 drugs (Table 1). The change in cost per supply day for the same period was 1.3%, –66.1%, –60.2%, –81.7%, and –84.3%, respectively. The net difference in cost per supply day over this entire period was $0.02, –$2.79, –$1.06, –$5.37, and –$21.22, respectively (Table 2).
There were several limitations to our study. Our analysis was limited to the Medicare population. Uninsured patients and those with Medicare Advantage or private health insurance plans were not included. In the Medicare database, only prescribers who prescribed a medication 10 times or more were recorded; therefore, some prescribers were not captured.
Although there was an increase in the dermatologic use of all 5 drugs in this study, perhaps the most marked growth was exhibited by aripiprazole, which had an AAGR of 20.72% (Table 1). Affordability may have been a factor, as the most marked reduction in price per supply day was noted for aripiprazole during the study period. Pimozide, which traditionally has been the first-line therapy for delusions of parasitosis, is the only first-generation antipsychotic drug among the 5 most frequently prescribed antipsychotics.3 Interestingly, pimozide had the lowest AAGR compared with the 4 second-generation antipsychotics. This finding also is corroborated by the average growth in supply days. While pimozide is a first-generation antipsychotic and had the lowest AAGR, pimozide still was the most prescribed antipsychotic in this study. Considering the average growth in Medicare beneficiaries during the study period was 2.70% per year,2 the AAGR of the 4 other drugs excluding pimozide shows that this growth was larger than what can be attributed to an increase in population size.
The most common conditions for which dermatologists prescribe antipsychotics are primary delusional infestation disorders as well as a range of self-inflicted dermatologic manifestations of dermatitis artefacta.4 Particularly, dermatologist-prescribed antipsychotics are first-line for these conditions in which perception of a persistent disease state is present.4 Importantly, dermatologists must differentiate between other dermatology-related psychiatric conditions such as trichotillomania and body dysmorphic disorder, which tend to respond better to selective serotonin reuptake inhibitors.4 Our data suggest that dermatologists are increasing their utilization of second-generation antipsychotics at a higher rate than first-generation antipsychotics, likely due to the lower risk of extrapyramidal symptoms. Patients are more willing to initiate a trial of psychiatric medication when it is prescribed by a dermatologist vs a psychiatrist due to lack of perceived stigma, which can lead to greater treatment compliance rates.5 As mentioned previously, as part of the differential, dermatologists also can effectively prescribe medications such as selective serotonin reuptake inhibitors for symptoms including anxiety, trichotillomania, body dysmorphic disorder, or secondary psychiatric disorders as a result of the burden of skin disease.5
In many cases, a dermatologist may be the first and only specialist to evaluate patients with conditions that overlap within the jurisdiction of dermatology and psychiatry. It is imperative that dermatologists feel comfortable treating this vulnerable patient population. As demonstrated by Medicare prescription data, the increasing utilization of antipsychotics in our specialty demands that dermatologists possess an adequate working knowledge of psychopharmacology, which may be accomplished during residency training through several directives, including focused didactic sessions, elective rotations in psychiatry, increased exposure to psychocutaneous lectures at national conferences, and finally through the establishment of joint dermatology-psychiatry clinics with interdepartmental collaboration.
- Weber MB, Recuero JK, Almeida CS. Use of psychiatric drugs in dermatology. An Bras Dermatol. 2020;95:133-143. doi:10.1016/j.abd.2019.12.002
- Centers for Medicare & Medicaid Services. Medicare provider utilization and payment data: part D prescriber. Updated September 10, 2024. Accessed October 7, 2024. https://www.cms.gov/data -research/statistics-trends-and-reports/medicare-provider-utilization-payment-data/part-d-prescriber
- Bolognia J, Schaffe JV, Lorenzo C. Dermatology. In: Duncan KO, Koo JYM, eds. Psychocutaneous Diseases. Elsevier; 2017:128-136.
- Gupta MA, Vujcic B, Pur DR, et al. Use of antipsychotic drugs in dermatology. Clin Dermatol. 2018;36:765-773. doi:10.1016/j.clindermatol.2018.08.006
- Jafferany M, Stamu-O’Brien C, Mkhoyan R, et al. Psychotropic drugs in dermatology: a dermatologist’s approach and choice of medications. Dermatol Ther. 2020;33:E13385. doi:10.1111/dth.13385
To the Editor:
Patients with primary psychiatric disorders with dermatologic manifestations often seek treatment from dermatologists instead of psychiatrists.1 For example, patients with delusions of parasitosis may lack insight into the underlying etiology of their disease and instead fixate on establishing an organic cause for their symptoms. As a result, it is an increasingly common practice for dermatologists to diagnose and treat psychiatric conditions.1 The goal of this study was to evaluate trends for the top 5 antipsychotics most frequently prescribed by dermatologists in the Medicare Part D database.
In this retrospective analysis, we consulted the Medicare Provider Utilization and Payment Data for January 2013 through December 2020, which is provided to the public by the Centers for Medicare & Medicaid Services.2 Only prescribing data from dermatologists were included in this study by using the built-in filter on the website to select “dermatology” as the prescriber type. All other provider types were excluded. We chose the top 5 most prescribed antipsychotics based on the number of supply days reported. Supply days—defined by Medicare as the number of days’ worth of medication that is prescribed—were used as a metric for utilization; therefore, each drug’s total supply days prescribed by dermatologists were calculated using this combined filter of drug name and total supply days using the database.
To analyze utilization over time, the annual average growth rate (AAGR) was calculated by determining the growth rate in total supply days annually from 2013 to 2020 and then averaging those rates to determine the overall AAGR. For greater clinical relevance, we calculated the average growth in supply days for the entire study period by determining the difference in the number of supply days for each year and then averaging these values. This was done to consider overall trends across dermatology rather than individual dermatologist prescribing patterns.
Based on our analysis, the antipsychotics most frequently prescribed by dermatologists for Medicare patients from January 2013 to December 2020 were pimozide, quetiapine, risperidone, olanzapine, and aripiprazole. The AAGR for each drug was 2.35%, 4.89%, 5.59%, 9.48%, and 20.72%, respectively, which is consistent with increased utilization over the study period for all 5 drugs (Table 1). The change in cost per supply day for the same period was 1.3%, –66.1%, –60.2%, –81.7%, and –84.3%, respectively. The net difference in cost per supply day over this entire period was $0.02, –$2.79, –$1.06, –$5.37, and –$21.22, respectively (Table 2).
There were several limitations to our study. Our analysis was limited to the Medicare population. Uninsured patients and those with Medicare Advantage or private health insurance plans were not included. In the Medicare database, only prescribers who prescribed a medication 10 times or more were recorded; therefore, some prescribers were not captured.
Although there was an increase in the dermatologic use of all 5 drugs in this study, perhaps the most marked growth was exhibited by aripiprazole, which had an AAGR of 20.72% (Table 1). Affordability may have been a factor, as the most marked reduction in price per supply day was noted for aripiprazole during the study period. Pimozide, which traditionally has been the first-line therapy for delusions of parasitosis, is the only first-generation antipsychotic drug among the 5 most frequently prescribed antipsychotics.3 Interestingly, pimozide had the lowest AAGR compared with the 4 second-generation antipsychotics. This finding also is corroborated by the average growth in supply days. While pimozide is a first-generation antipsychotic and had the lowest AAGR, pimozide still was the most prescribed antipsychotic in this study. Considering the average growth in Medicare beneficiaries during the study period was 2.70% per year,2 the AAGR of the 4 other drugs excluding pimozide shows that this growth was larger than what can be attributed to an increase in population size.
The most common conditions for which dermatologists prescribe antipsychotics are primary delusional infestation disorders as well as a range of self-inflicted dermatologic manifestations of dermatitis artefacta.4 Particularly, dermatologist-prescribed antipsychotics are first-line for these conditions in which perception of a persistent disease state is present.4 Importantly, dermatologists must differentiate between other dermatology-related psychiatric conditions such as trichotillomania and body dysmorphic disorder, which tend to respond better to selective serotonin reuptake inhibitors.4 Our data suggest that dermatologists are increasing their utilization of second-generation antipsychotics at a higher rate than first-generation antipsychotics, likely due to the lower risk of extrapyramidal symptoms. Patients are more willing to initiate a trial of psychiatric medication when it is prescribed by a dermatologist vs a psychiatrist due to lack of perceived stigma, which can lead to greater treatment compliance rates.5 As mentioned previously, as part of the differential, dermatologists also can effectively prescribe medications such as selective serotonin reuptake inhibitors for symptoms including anxiety, trichotillomania, body dysmorphic disorder, or secondary psychiatric disorders as a result of the burden of skin disease.5
In many cases, a dermatologist may be the first and only specialist to evaluate patients with conditions that overlap within the jurisdiction of dermatology and psychiatry. It is imperative that dermatologists feel comfortable treating this vulnerable patient population. As demonstrated by Medicare prescription data, the increasing utilization of antipsychotics in our specialty demands that dermatologists possess an adequate working knowledge of psychopharmacology, which may be accomplished during residency training through several directives, including focused didactic sessions, elective rotations in psychiatry, increased exposure to psychocutaneous lectures at national conferences, and finally through the establishment of joint dermatology-psychiatry clinics with interdepartmental collaboration.
To the Editor:
Patients with primary psychiatric disorders with dermatologic manifestations often seek treatment from dermatologists instead of psychiatrists.1 For example, patients with delusions of parasitosis may lack insight into the underlying etiology of their disease and instead fixate on establishing an organic cause for their symptoms. As a result, it is an increasingly common practice for dermatologists to diagnose and treat psychiatric conditions.1 The goal of this study was to evaluate trends for the top 5 antipsychotics most frequently prescribed by dermatologists in the Medicare Part D database.
In this retrospective analysis, we consulted the Medicare Provider Utilization and Payment Data for January 2013 through December 2020, which is provided to the public by the Centers for Medicare & Medicaid Services.2 Only prescribing data from dermatologists were included in this study by using the built-in filter on the website to select “dermatology” as the prescriber type. All other provider types were excluded. We chose the top 5 most prescribed antipsychotics based on the number of supply days reported. Supply days—defined by Medicare as the number of days’ worth of medication that is prescribed—were used as a metric for utilization; therefore, each drug’s total supply days prescribed by dermatologists were calculated using this combined filter of drug name and total supply days using the database.
To analyze utilization over time, the annual average growth rate (AAGR) was calculated by determining the growth rate in total supply days annually from 2013 to 2020 and then averaging those rates to determine the overall AAGR. For greater clinical relevance, we calculated the average growth in supply days for the entire study period by determining the difference in the number of supply days for each year and then averaging these values. This was done to consider overall trends across dermatology rather than individual dermatologist prescribing patterns.
Based on our analysis, the antipsychotics most frequently prescribed by dermatologists for Medicare patients from January 2013 to December 2020 were pimozide, quetiapine, risperidone, olanzapine, and aripiprazole. The AAGR for each drug was 2.35%, 4.89%, 5.59%, 9.48%, and 20.72%, respectively, which is consistent with increased utilization over the study period for all 5 drugs (Table 1). The change in cost per supply day for the same period was 1.3%, –66.1%, –60.2%, –81.7%, and –84.3%, respectively. The net difference in cost per supply day over this entire period was $0.02, –$2.79, –$1.06, –$5.37, and –$21.22, respectively (Table 2).
There were several limitations to our study. Our analysis was limited to the Medicare population. Uninsured patients and those with Medicare Advantage or private health insurance plans were not included. In the Medicare database, only prescribers who prescribed a medication 10 times or more were recorded; therefore, some prescribers were not captured.
Although there was an increase in the dermatologic use of all 5 drugs in this study, perhaps the most marked growth was exhibited by aripiprazole, which had an AAGR of 20.72% (Table 1). Affordability may have been a factor, as the most marked reduction in price per supply day was noted for aripiprazole during the study period. Pimozide, which traditionally has been the first-line therapy for delusions of parasitosis, is the only first-generation antipsychotic drug among the 5 most frequently prescribed antipsychotics.3 Interestingly, pimozide had the lowest AAGR compared with the 4 second-generation antipsychotics. This finding also is corroborated by the average growth in supply days. While pimozide is a first-generation antipsychotic and had the lowest AAGR, pimozide still was the most prescribed antipsychotic in this study. Considering the average growth in Medicare beneficiaries during the study period was 2.70% per year,2 the AAGR of the 4 other drugs excluding pimozide shows that this growth was larger than what can be attributed to an increase in population size.
The most common conditions for which dermatologists prescribe antipsychotics are primary delusional infestation disorders as well as a range of self-inflicted dermatologic manifestations of dermatitis artefacta.4 Particularly, dermatologist-prescribed antipsychotics are first-line for these conditions in which perception of a persistent disease state is present.4 Importantly, dermatologists must differentiate between other dermatology-related psychiatric conditions such as trichotillomania and body dysmorphic disorder, which tend to respond better to selective serotonin reuptake inhibitors.4 Our data suggest that dermatologists are increasing their utilization of second-generation antipsychotics at a higher rate than first-generation antipsychotics, likely due to the lower risk of extrapyramidal symptoms. Patients are more willing to initiate a trial of psychiatric medication when it is prescribed by a dermatologist vs a psychiatrist due to lack of perceived stigma, which can lead to greater treatment compliance rates.5 As mentioned previously, as part of the differential, dermatologists also can effectively prescribe medications such as selective serotonin reuptake inhibitors for symptoms including anxiety, trichotillomania, body dysmorphic disorder, or secondary psychiatric disorders as a result of the burden of skin disease.5
In many cases, a dermatologist may be the first and only specialist to evaluate patients with conditions that overlap within the jurisdiction of dermatology and psychiatry. It is imperative that dermatologists feel comfortable treating this vulnerable patient population. As demonstrated by Medicare prescription data, the increasing utilization of antipsychotics in our specialty demands that dermatologists possess an adequate working knowledge of psychopharmacology, which may be accomplished during residency training through several directives, including focused didactic sessions, elective rotations in psychiatry, increased exposure to psychocutaneous lectures at national conferences, and finally through the establishment of joint dermatology-psychiatry clinics with interdepartmental collaboration.
- Weber MB, Recuero JK, Almeida CS. Use of psychiatric drugs in dermatology. An Bras Dermatol. 2020;95:133-143. doi:10.1016/j.abd.2019.12.002
- Centers for Medicare & Medicaid Services. Medicare provider utilization and payment data: part D prescriber. Updated September 10, 2024. Accessed October 7, 2024. https://www.cms.gov/data -research/statistics-trends-and-reports/medicare-provider-utilization-payment-data/part-d-prescriber
- Bolognia J, Schaffe JV, Lorenzo C. Dermatology. In: Duncan KO, Koo JYM, eds. Psychocutaneous Diseases. Elsevier; 2017:128-136.
- Gupta MA, Vujcic B, Pur DR, et al. Use of antipsychotic drugs in dermatology. Clin Dermatol. 2018;36:765-773. doi:10.1016/j.clindermatol.2018.08.006
- Jafferany M, Stamu-O’Brien C, Mkhoyan R, et al. Psychotropic drugs in dermatology: a dermatologist’s approach and choice of medications. Dermatol Ther. 2020;33:E13385. doi:10.1111/dth.13385
- Weber MB, Recuero JK, Almeida CS. Use of psychiatric drugs in dermatology. An Bras Dermatol. 2020;95:133-143. doi:10.1016/j.abd.2019.12.002
- Centers for Medicare & Medicaid Services. Medicare provider utilization and payment data: part D prescriber. Updated September 10, 2024. Accessed October 7, 2024. https://www.cms.gov/data -research/statistics-trends-and-reports/medicare-provider-utilization-payment-data/part-d-prescriber
- Bolognia J, Schaffe JV, Lorenzo C. Dermatology. In: Duncan KO, Koo JYM, eds. Psychocutaneous Diseases. Elsevier; 2017:128-136.
- Gupta MA, Vujcic B, Pur DR, et al. Use of antipsychotic drugs in dermatology. Clin Dermatol. 2018;36:765-773. doi:10.1016/j.clindermatol.2018.08.006
- Jafferany M, Stamu-O’Brien C, Mkhoyan R, et al. Psychotropic drugs in dermatology: a dermatologist’s approach and choice of medications. Dermatol Ther. 2020;33:E13385. doi:10.1111/dth.13385
Practice Points
- Dermatologists are frontline medical providers who can be useful in screening for primary psychiatric disorders in patients with dermatologic manifestations.
- Second-generation antipsychotics are effective for treating many psychiatric disorders.
New Scanner Creates Highly Detailed, 3D Images of Blood Vessels in Seconds
A new scanner can provide three-dimensional (3D) photoacoustic images of millimeter-scale veins and arteries in seconds.
The scanner, developed by researchers at University College London (UCL) in England, could help clinicians better visualize and track microvascular changes for a wide range of diseases, including cancer, rheumatoid arthritis (RA), and peripheral vascular disease (PVD).
The case studies “illustrate potential areas of application that warrant future, more comprehensive clinical studies,” the authors wrote. “Moreover, they demonstrate the feasibility of using the scanner on a real-world patient cohort where imaging is more challenging due to frailty, comorbidity, or pain that may limit their ability to tolerate prolonged scan times.”
The work was published online in Nature Biomedical Engineering.
Improving Photoacoustic Imaging
PAT works using the photoacoustic effect, a phenomenon where sound waves are generated when light is absorbed by a material. When pulsed light from a laser is directed at tissue, some of that light is absorbed and causes an increase in heat in the targeted area. This localized heat also increases pressure, which generates ultrasound waves that can be detected by specialized sensors.
While previous PAT scanners translated these sound waves to electric signals directly to generate imaging, UCL engineers developed a sensor in the early 2000s that can detect these ultrasound waves using light. The result was much clearer, 3D images.
“That was great, but the problem was it was very slow, and it would take 5 minutes to get an image,” explained Paul Beard, PhD, professor of biomedical photoacoustics at UCL and senior author of the study. “That’s fine if you’re imaging a dead mouse or an anesthetized mouse, but not so useful for human imaging,” he continued, where motion would blur the image.
In this new paper, Beard and colleagues outlined how they cut scanning times to an order of seconds (or fraction of a second) rather than minutes. While previous iterations could detect only acoustic waves from one point at a time, this new scanner can detect waves from multiple points simultaneously. The scanner can visualize veins and arteries up to 15 mm deep in human tissue and can also provide dynamic, 3D images of “time-varying tissue perfusion and other hemodynamic events,” the authors wrote.
With these types of scanners, there is always a trade-off between imaging quality and imaging speed, explained Srivalleesha Mallidi, PhD, an assistant professor of biomedical engineering at Tufts University in Medford, Massachusetts. She was not involved with the work.
“With the resolution that [the authors] are providing and the depth at which they are seeing the signals, it is one of the fastest systems,” she said.
Clinical Utility
Beard and colleagues also tested the scanner to visualize blood vessels in participants with RA, suspected PVD, and skin inflammation. The scanning images “illustrated how vascular abnormalities such as increased vessel tortuosity, which has previously been linked to PVD, and the neovascularization associated with inflammation can be visualized and quantified,” the authors wrote.
The next step, Beard noted, is testing whether these characteristics can be used as a marker for the progression of disease.
Nehal Mehta, MD, a cardiologist and professor of medicine at the George Washington University, Washington, DC, agreed that more longitudinal research is needed to understand how the abnormalities captured in these images can inform detection and diagnosis of various diseases.
“You don’t know whether these images look bad because of reverse causation — the disease is doing this — or true causation — that this is actually detecting the root cause of the disease,” he explained. “Until we have a bank of normal and abnormal scans, we don’t know what any of these things mean.”
Though still some time away from entering the clinic, Mehta likened the technology to the introduction of optical coherence tomography in the 1980s. Before being adapted for clinical use, researchers first needed to visualize differences between normal coronary vasculature and myocardial infarction.
“I think this is an amazingly strong first proof of concept,” Mehta said. “This technology is showing a true promise in the field imaging.”
The work was funded by grants from Cancer Research UK, the Engineering & Physical Sciences Research Council, Wellcome Trust, the European Research Council, and the National Institute for Health and Care Research University College London Hospitals Biomedical Research Centre. Beard and two coauthors are shareholders of DeepColor Imaging to which the intellectual property associated with the new scanner has been licensed, but the company was not involved in any of this research. Mallidi and Mehta had no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new scanner can provide three-dimensional (3D) photoacoustic images of millimeter-scale veins and arteries in seconds.
The scanner, developed by researchers at University College London (UCL) in England, could help clinicians better visualize and track microvascular changes for a wide range of diseases, including cancer, rheumatoid arthritis (RA), and peripheral vascular disease (PVD).
The case studies “illustrate potential areas of application that warrant future, more comprehensive clinical studies,” the authors wrote. “Moreover, they demonstrate the feasibility of using the scanner on a real-world patient cohort where imaging is more challenging due to frailty, comorbidity, or pain that may limit their ability to tolerate prolonged scan times.”
The work was published online in Nature Biomedical Engineering.
Improving Photoacoustic Imaging
PAT works using the photoacoustic effect, a phenomenon where sound waves are generated when light is absorbed by a material. When pulsed light from a laser is directed at tissue, some of that light is absorbed and causes an increase in heat in the targeted area. This localized heat also increases pressure, which generates ultrasound waves that can be detected by specialized sensors.
While previous PAT scanners translated these sound waves to electric signals directly to generate imaging, UCL engineers developed a sensor in the early 2000s that can detect these ultrasound waves using light. The result was much clearer, 3D images.
“That was great, but the problem was it was very slow, and it would take 5 minutes to get an image,” explained Paul Beard, PhD, professor of biomedical photoacoustics at UCL and senior author of the study. “That’s fine if you’re imaging a dead mouse or an anesthetized mouse, but not so useful for human imaging,” he continued, where motion would blur the image.
In this new paper, Beard and colleagues outlined how they cut scanning times to an order of seconds (or fraction of a second) rather than minutes. While previous iterations could detect only acoustic waves from one point at a time, this new scanner can detect waves from multiple points simultaneously. The scanner can visualize veins and arteries up to 15 mm deep in human tissue and can also provide dynamic, 3D images of “time-varying tissue perfusion and other hemodynamic events,” the authors wrote.
With these types of scanners, there is always a trade-off between imaging quality and imaging speed, explained Srivalleesha Mallidi, PhD, an assistant professor of biomedical engineering at Tufts University in Medford, Massachusetts. She was not involved with the work.
“With the resolution that [the authors] are providing and the depth at which they are seeing the signals, it is one of the fastest systems,” she said.
Clinical Utility
Beard and colleagues also tested the scanner to visualize blood vessels in participants with RA, suspected PVD, and skin inflammation. The scanning images “illustrated how vascular abnormalities such as increased vessel tortuosity, which has previously been linked to PVD, and the neovascularization associated with inflammation can be visualized and quantified,” the authors wrote.
The next step, Beard noted, is testing whether these characteristics can be used as a marker for the progression of disease.
Nehal Mehta, MD, a cardiologist and professor of medicine at the George Washington University, Washington, DC, agreed that more longitudinal research is needed to understand how the abnormalities captured in these images can inform detection and diagnosis of various diseases.
“You don’t know whether these images look bad because of reverse causation — the disease is doing this — or true causation — that this is actually detecting the root cause of the disease,” he explained. “Until we have a bank of normal and abnormal scans, we don’t know what any of these things mean.”
Though still some time away from entering the clinic, Mehta likened the technology to the introduction of optical coherence tomography in the 1980s. Before being adapted for clinical use, researchers first needed to visualize differences between normal coronary vasculature and myocardial infarction.
“I think this is an amazingly strong first proof of concept,” Mehta said. “This technology is showing a true promise in the field imaging.”
The work was funded by grants from Cancer Research UK, the Engineering & Physical Sciences Research Council, Wellcome Trust, the European Research Council, and the National Institute for Health and Care Research University College London Hospitals Biomedical Research Centre. Beard and two coauthors are shareholders of DeepColor Imaging to which the intellectual property associated with the new scanner has been licensed, but the company was not involved in any of this research. Mallidi and Mehta had no relevant disclosures.
A version of this article first appeared on Medscape.com.
A new scanner can provide three-dimensional (3D) photoacoustic images of millimeter-scale veins and arteries in seconds.
The scanner, developed by researchers at University College London (UCL) in England, could help clinicians better visualize and track microvascular changes for a wide range of diseases, including cancer, rheumatoid arthritis (RA), and peripheral vascular disease (PVD).
The case studies “illustrate potential areas of application that warrant future, more comprehensive clinical studies,” the authors wrote. “Moreover, they demonstrate the feasibility of using the scanner on a real-world patient cohort where imaging is more challenging due to frailty, comorbidity, or pain that may limit their ability to tolerate prolonged scan times.”
The work was published online in Nature Biomedical Engineering.
Improving Photoacoustic Imaging
PAT works using the photoacoustic effect, a phenomenon where sound waves are generated when light is absorbed by a material. When pulsed light from a laser is directed at tissue, some of that light is absorbed and causes an increase in heat in the targeted area. This localized heat also increases pressure, which generates ultrasound waves that can be detected by specialized sensors.
While previous PAT scanners translated these sound waves to electric signals directly to generate imaging, UCL engineers developed a sensor in the early 2000s that can detect these ultrasound waves using light. The result was much clearer, 3D images.
“That was great, but the problem was it was very slow, and it would take 5 minutes to get an image,” explained Paul Beard, PhD, professor of biomedical photoacoustics at UCL and senior author of the study. “That’s fine if you’re imaging a dead mouse or an anesthetized mouse, but not so useful for human imaging,” he continued, where motion would blur the image.
In this new paper, Beard and colleagues outlined how they cut scanning times to an order of seconds (or fraction of a second) rather than minutes. While previous iterations could detect only acoustic waves from one point at a time, this new scanner can detect waves from multiple points simultaneously. The scanner can visualize veins and arteries up to 15 mm deep in human tissue and can also provide dynamic, 3D images of “time-varying tissue perfusion and other hemodynamic events,” the authors wrote.
With these types of scanners, there is always a trade-off between imaging quality and imaging speed, explained Srivalleesha Mallidi, PhD, an assistant professor of biomedical engineering at Tufts University in Medford, Massachusetts. She was not involved with the work.
“With the resolution that [the authors] are providing and the depth at which they are seeing the signals, it is one of the fastest systems,” she said.
Clinical Utility
Beard and colleagues also tested the scanner to visualize blood vessels in participants with RA, suspected PVD, and skin inflammation. The scanning images “illustrated how vascular abnormalities such as increased vessel tortuosity, which has previously been linked to PVD, and the neovascularization associated with inflammation can be visualized and quantified,” the authors wrote.
The next step, Beard noted, is testing whether these characteristics can be used as a marker for the progression of disease.
Nehal Mehta, MD, a cardiologist and professor of medicine at the George Washington University, Washington, DC, agreed that more longitudinal research is needed to understand how the abnormalities captured in these images can inform detection and diagnosis of various diseases.
“You don’t know whether these images look bad because of reverse causation — the disease is doing this — or true causation — that this is actually detecting the root cause of the disease,” he explained. “Until we have a bank of normal and abnormal scans, we don’t know what any of these things mean.”
Though still some time away from entering the clinic, Mehta likened the technology to the introduction of optical coherence tomography in the 1980s. Before being adapted for clinical use, researchers first needed to visualize differences between normal coronary vasculature and myocardial infarction.
“I think this is an amazingly strong first proof of concept,” Mehta said. “This technology is showing a true promise in the field imaging.”
The work was funded by grants from Cancer Research UK, the Engineering & Physical Sciences Research Council, Wellcome Trust, the European Research Council, and the National Institute for Health and Care Research University College London Hospitals Biomedical Research Centre. Beard and two coauthors are shareholders of DeepColor Imaging to which the intellectual property associated with the new scanner has been licensed, but the company was not involved in any of this research. Mallidi and Mehta had no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM NATURE BIOMEDICAL ENGINEERING
Excess Body Weight Tied to Increased Risk for Second Cancers
TOPLINE:
Cancer survivors who had overweight or obesity at the time of their initial cancer diagnosis have a higher risk for a second primary cancer, particularly an obesity-related cancer, a new analysis found.
METHODOLOGY:
- Cancer survivors have an increased risk for another primary cancer. Studies suggest that lifestyle factors, such as excess body weight, may contribute to the risk for a second cancer; however, prospective long-term data on this association remain limited.
- Researchers evaluated 26,894 participants (mean age at first cancer diagnosis, 72.2 years; 97.6% White) from the Cancer Prevention Study II Nutrition cohort, who were diagnosed with a first nonmetastatic primary cancer between 1992 and 2015.
- Body mass index (BMI) was calculated from self-reported data at the time of the first primary cancer diagnosis; 10,713 participants had a normal BMI (18.5 to < 25.0), 11,497 had overweight (25.0 to < 30.0), and 4684 had obesity (≥ 30.0). Participants were followed through 2017.
- The study outcomes were the incidences of any second primary cancer and obesity-related second cancers.
- The most common first primary cancers were prostate (35.0%), breast (19.1%), and colorectal (9.5%) cancers; almost 40% of all first primary cancers were related to obesity.
TAKEAWAY:
- Overall, 13.9% participants (3749 of 26,894) were diagnosed with a second cancer over a median of 7.9 years; 33.2% of these cancers were related to obesity.
- Compared with participants with a normal BMI, those who had overweight had a 15% higher risk for any second cancer (adjusted hazard ratio [aHR], 1.15) and a 40% higher risk for an obesity-related second cancer (aHR, 1.40). Additionally, those with obesity had a 34% higher risk for any second cancer and a 78% higher risk for an obesity-related second cancer.
- For every 5-unit increase in BMI, the risk for an obesity-related cancer (aHR, 1.28) was considerably higher than the risk for any second cancer (aHR, 1.13).
- Among all survivors, every 5-unit increase in BMI was associated with a 42% increased risk for colorectal cancer as a second cancer (aHR, 1.42) and a 70% higher risk for kidney cancer as a second cancer (aHR, 1.70).
IN PRACTICE:
“In this cohort study of older survivors of nonmetastatic cancer, those who had overweight or obesity at the time of their first cancer diagnosis were at higher risk of developing a second cancer, especially obesity-related cancers,” the authors wrote. “These findings have important public health implications and may inform evidence-based survivorship guidelines to reduce the risk of second primary cancers among cancer survivors.”
SOURCE:
This study, led by Clara Bodelon, PhD, MS, American Cancer Society, Atlanta, was published online in JAMA Network Open.
LIMITATIONS:
The exclusion of multiple primary cancers in the same site could have underestimated the magnitude of the association of excess body weight with the risk for second primary cancers. BMI was used as a measure of excess body fat in this study, which does not differentiate between fat and lean mass. Unmeasured or residual confounding factors might be present.
DISCLOSURES:
The study was supported by grants from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Cancer survivors who had overweight or obesity at the time of their initial cancer diagnosis have a higher risk for a second primary cancer, particularly an obesity-related cancer, a new analysis found.
METHODOLOGY:
- Cancer survivors have an increased risk for another primary cancer. Studies suggest that lifestyle factors, such as excess body weight, may contribute to the risk for a second cancer; however, prospective long-term data on this association remain limited.
- Researchers evaluated 26,894 participants (mean age at first cancer diagnosis, 72.2 years; 97.6% White) from the Cancer Prevention Study II Nutrition cohort, who were diagnosed with a first nonmetastatic primary cancer between 1992 and 2015.
- Body mass index (BMI) was calculated from self-reported data at the time of the first primary cancer diagnosis; 10,713 participants had a normal BMI (18.5 to < 25.0), 11,497 had overweight (25.0 to < 30.0), and 4684 had obesity (≥ 30.0). Participants were followed through 2017.
- The study outcomes were the incidences of any second primary cancer and obesity-related second cancers.
- The most common first primary cancers were prostate (35.0%), breast (19.1%), and colorectal (9.5%) cancers; almost 40% of all first primary cancers were related to obesity.
TAKEAWAY:
- Overall, 13.9% participants (3749 of 26,894) were diagnosed with a second cancer over a median of 7.9 years; 33.2% of these cancers were related to obesity.
- Compared with participants with a normal BMI, those who had overweight had a 15% higher risk for any second cancer (adjusted hazard ratio [aHR], 1.15) and a 40% higher risk for an obesity-related second cancer (aHR, 1.40). Additionally, those with obesity had a 34% higher risk for any second cancer and a 78% higher risk for an obesity-related second cancer.
- For every 5-unit increase in BMI, the risk for an obesity-related cancer (aHR, 1.28) was considerably higher than the risk for any second cancer (aHR, 1.13).
- Among all survivors, every 5-unit increase in BMI was associated with a 42% increased risk for colorectal cancer as a second cancer (aHR, 1.42) and a 70% higher risk for kidney cancer as a second cancer (aHR, 1.70).
IN PRACTICE:
“In this cohort study of older survivors of nonmetastatic cancer, those who had overweight or obesity at the time of their first cancer diagnosis were at higher risk of developing a second cancer, especially obesity-related cancers,” the authors wrote. “These findings have important public health implications and may inform evidence-based survivorship guidelines to reduce the risk of second primary cancers among cancer survivors.”
SOURCE:
This study, led by Clara Bodelon, PhD, MS, American Cancer Society, Atlanta, was published online in JAMA Network Open.
LIMITATIONS:
The exclusion of multiple primary cancers in the same site could have underestimated the magnitude of the association of excess body weight with the risk for second primary cancers. BMI was used as a measure of excess body fat in this study, which does not differentiate between fat and lean mass. Unmeasured or residual confounding factors might be present.
DISCLOSURES:
The study was supported by grants from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Cancer survivors who had overweight or obesity at the time of their initial cancer diagnosis have a higher risk for a second primary cancer, particularly an obesity-related cancer, a new analysis found.
METHODOLOGY:
- Cancer survivors have an increased risk for another primary cancer. Studies suggest that lifestyle factors, such as excess body weight, may contribute to the risk for a second cancer; however, prospective long-term data on this association remain limited.
- Researchers evaluated 26,894 participants (mean age at first cancer diagnosis, 72.2 years; 97.6% White) from the Cancer Prevention Study II Nutrition cohort, who were diagnosed with a first nonmetastatic primary cancer between 1992 and 2015.
- Body mass index (BMI) was calculated from self-reported data at the time of the first primary cancer diagnosis; 10,713 participants had a normal BMI (18.5 to < 25.0), 11,497 had overweight (25.0 to < 30.0), and 4684 had obesity (≥ 30.0). Participants were followed through 2017.
- The study outcomes were the incidences of any second primary cancer and obesity-related second cancers.
- The most common first primary cancers were prostate (35.0%), breast (19.1%), and colorectal (9.5%) cancers; almost 40% of all first primary cancers were related to obesity.
TAKEAWAY:
- Overall, 13.9% participants (3749 of 26,894) were diagnosed with a second cancer over a median of 7.9 years; 33.2% of these cancers were related to obesity.
- Compared with participants with a normal BMI, those who had overweight had a 15% higher risk for any second cancer (adjusted hazard ratio [aHR], 1.15) and a 40% higher risk for an obesity-related second cancer (aHR, 1.40). Additionally, those with obesity had a 34% higher risk for any second cancer and a 78% higher risk for an obesity-related second cancer.
- For every 5-unit increase in BMI, the risk for an obesity-related cancer (aHR, 1.28) was considerably higher than the risk for any second cancer (aHR, 1.13).
- Among all survivors, every 5-unit increase in BMI was associated with a 42% increased risk for colorectal cancer as a second cancer (aHR, 1.42) and a 70% higher risk for kidney cancer as a second cancer (aHR, 1.70).
IN PRACTICE:
“In this cohort study of older survivors of nonmetastatic cancer, those who had overweight or obesity at the time of their first cancer diagnosis were at higher risk of developing a second cancer, especially obesity-related cancers,” the authors wrote. “These findings have important public health implications and may inform evidence-based survivorship guidelines to reduce the risk of second primary cancers among cancer survivors.”
SOURCE:
This study, led by Clara Bodelon, PhD, MS, American Cancer Society, Atlanta, was published online in JAMA Network Open.
LIMITATIONS:
The exclusion of multiple primary cancers in the same site could have underestimated the magnitude of the association of excess body weight with the risk for second primary cancers. BMI was used as a measure of excess body fat in this study, which does not differentiate between fat and lean mass. Unmeasured or residual confounding factors might be present.
DISCLOSURES:
The study was supported by grants from the Centers for Disease Control and Prevention’s National Program of Cancer Registries and cancer registries supported by the National Cancer Institute’s Surveillance, Epidemiology, and End Results Program. No relevant conflicts of interest were disclosed by the authors.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Long-Term Cognitive Monitoring Warranted After First Stroke
A first stroke in older adults is associated with substantial immediate and accelerated long-term cognitive decline, suggested a new study that underscores the need for continuous cognitive monitoring in this patient population.
Results from the study, which included 14 international cohorts of older adults, showed that stroke was associated with a significant acute decline in global cognition and a small, but significant, acceleration in the rate of cognitive decline over time.
Cognitive assessments in primary care are “crucial, especially since cognitive impairment is frequently missed or undiagnosed in hospitals,” lead author Jessica Lo, MSc, biostatistician and research associate with the Center for Healthy Brain Aging, University of New South Wales, Sydney, Australia, told this news organization.
She suggested clinicians incorporate long-term cognitive assessments into care plans, using more sensitive neuropsychological tests in primary care to detect early signs of cognitive impairment. “Early detection would enable timely interventions to improve outcomes,” Lo said.
She also noted that poststroke care typically includes physical rehabilitation but not cognitive rehabilitation, which many rehabilitation centers aren’t equipped to provide.
The study was published online in JAMA Network Open.
Mapping Cognitive Decline Trajectory
Cognitive impairment after stroke is common, but the trajectory of cognitive decline following a first stroke, relative to prestroke cognitive function, remains unclear.
The investigators leveraged data from 14 population-based cohort studies of 20,860 adults (mean age, 73 years; 59% women) to map the trajectory of cognitive function before and after a first stroke.
The primary outcome was global cognition, defined as the standardized average of four cognitive domains (language, memory, processing speed, and executive function).
During a mean follow-up of 7.5 years, 1041 (5%) adults (mean age, 79 years) experienced a first stroke, a mean of 4.5 years after study entry.
In adjusted analyses, stroke was associated with a significant acute decline of 0.25 SD in global cognition and a “small but significant” acceleration in the rate of decline of −0.038 SD per year, the authors reported.
Stroke was also associated with acute decline in all individual cognitive domains except for memory, with effect sizes ranging from −0.17 to −0.22 SD. Poststroke declines in Mini-Mental State Examination scores (−0.36 SD) were also noted.
In terms of cognitive trajectory, the rate of decline before stroke in survivors was similar to that seen in peers who didn’t have a stroke (−0.048 and −0.049 SD per year in global cognition, respectively).
The researchers did not identify any vascular risk factors moderating cognitive decline following a stroke, consistent with prior research. However, cognitive decline was significantly more rapid in individuals without stroke, regardless of any future stroke, who had a history of diabetes, hypertension, high cholesterol, cardiovascular disease, depression, smoking, or were APOE4 carriers.
“Targeting modifiable vascular risk factors at an early stage may reduce the risk of stroke but also subsequent risk of stroke-related cognitive decline and cognitive impairment,” the researchers noted.
A ‘Major Step’ in the Right Direction
As previously reported by this news organization, in 2023 the American Heart Association (AHA) issued a statement noting that screening for cognitive impairment should be part of multidisciplinary care for stroke survivors.
Commenting for this news organization, Mitchell Elkind, MD, MS, AHA chief clinical science officer, said these new data are consistent with current AHA guidelines and statements that “support screening for cognitive and functional decline in patients both acutely and over the long term after stroke.”
Elkind noted that the 2022 guideline for intracerebral hemorrhage states that cognitive screening should occur “across the continuum of inpatient care and at intervals in the outpatient setting” and provides recommendations for cognitive therapy.
“Our 2021 scientific statement on the primary care of patients after stroke also recommends screening for both depression and cognitive impairment over both the short- and long-term,” said Elkind, professor of neurology and epidemiology at Columbia University Irving Medical Center in New York City.
“These documents recognize the fact that function and cognition can continue to decline years after stroke and that patients’ rehabilitation and support needs may therefore change over time after stroke,” Elkind added.
The authors of an accompanying commentary called it a “major step” in the right direction for the future of long-term stroke outcome assessment.
“As we develop new devices, indications, and time windows for stroke treatment, it may perhaps be wise to ensure trials steer away from simpler outcomes to more complex, granular ones,” wrote Yasmin Sadigh, MSc, and Victor Volovici, MD, PhD, with Erasmus University Medical Center, Rotterdam, the Netherlands.
The study had no commercial funding. The authors and commentary writers and Elkind have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
A first stroke in older adults is associated with substantial immediate and accelerated long-term cognitive decline, suggested a new study that underscores the need for continuous cognitive monitoring in this patient population.
Results from the study, which included 14 international cohorts of older adults, showed that stroke was associated with a significant acute decline in global cognition and a small, but significant, acceleration in the rate of cognitive decline over time.
Cognitive assessments in primary care are “crucial, especially since cognitive impairment is frequently missed or undiagnosed in hospitals,” lead author Jessica Lo, MSc, biostatistician and research associate with the Center for Healthy Brain Aging, University of New South Wales, Sydney, Australia, told this news organization.
She suggested clinicians incorporate long-term cognitive assessments into care plans, using more sensitive neuropsychological tests in primary care to detect early signs of cognitive impairment. “Early detection would enable timely interventions to improve outcomes,” Lo said.
She also noted that poststroke care typically includes physical rehabilitation but not cognitive rehabilitation, which many rehabilitation centers aren’t equipped to provide.
The study was published online in JAMA Network Open.
Mapping Cognitive Decline Trajectory
Cognitive impairment after stroke is common, but the trajectory of cognitive decline following a first stroke, relative to prestroke cognitive function, remains unclear.
The investigators leveraged data from 14 population-based cohort studies of 20,860 adults (mean age, 73 years; 59% women) to map the trajectory of cognitive function before and after a first stroke.
The primary outcome was global cognition, defined as the standardized average of four cognitive domains (language, memory, processing speed, and executive function).
During a mean follow-up of 7.5 years, 1041 (5%) adults (mean age, 79 years) experienced a first stroke, a mean of 4.5 years after study entry.
In adjusted analyses, stroke was associated with a significant acute decline of 0.25 SD in global cognition and a “small but significant” acceleration in the rate of decline of −0.038 SD per year, the authors reported.
Stroke was also associated with acute decline in all individual cognitive domains except for memory, with effect sizes ranging from −0.17 to −0.22 SD. Poststroke declines in Mini-Mental State Examination scores (−0.36 SD) were also noted.
In terms of cognitive trajectory, the rate of decline before stroke in survivors was similar to that seen in peers who didn’t have a stroke (−0.048 and −0.049 SD per year in global cognition, respectively).
The researchers did not identify any vascular risk factors moderating cognitive decline following a stroke, consistent with prior research. However, cognitive decline was significantly more rapid in individuals without stroke, regardless of any future stroke, who had a history of diabetes, hypertension, high cholesterol, cardiovascular disease, depression, smoking, or were APOE4 carriers.
“Targeting modifiable vascular risk factors at an early stage may reduce the risk of stroke but also subsequent risk of stroke-related cognitive decline and cognitive impairment,” the researchers noted.
A ‘Major Step’ in the Right Direction
As previously reported by this news organization, in 2023 the American Heart Association (AHA) issued a statement noting that screening for cognitive impairment should be part of multidisciplinary care for stroke survivors.
Commenting for this news organization, Mitchell Elkind, MD, MS, AHA chief clinical science officer, said these new data are consistent with current AHA guidelines and statements that “support screening for cognitive and functional decline in patients both acutely and over the long term after stroke.”
Elkind noted that the 2022 guideline for intracerebral hemorrhage states that cognitive screening should occur “across the continuum of inpatient care and at intervals in the outpatient setting” and provides recommendations for cognitive therapy.
“Our 2021 scientific statement on the primary care of patients after stroke also recommends screening for both depression and cognitive impairment over both the short- and long-term,” said Elkind, professor of neurology and epidemiology at Columbia University Irving Medical Center in New York City.
“These documents recognize the fact that function and cognition can continue to decline years after stroke and that patients’ rehabilitation and support needs may therefore change over time after stroke,” Elkind added.
The authors of an accompanying commentary called it a “major step” in the right direction for the future of long-term stroke outcome assessment.
“As we develop new devices, indications, and time windows for stroke treatment, it may perhaps be wise to ensure trials steer away from simpler outcomes to more complex, granular ones,” wrote Yasmin Sadigh, MSc, and Victor Volovici, MD, PhD, with Erasmus University Medical Center, Rotterdam, the Netherlands.
The study had no commercial funding. The authors and commentary writers and Elkind have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
A first stroke in older adults is associated with substantial immediate and accelerated long-term cognitive decline, suggested a new study that underscores the need for continuous cognitive monitoring in this patient population.
Results from the study, which included 14 international cohorts of older adults, showed that stroke was associated with a significant acute decline in global cognition and a small, but significant, acceleration in the rate of cognitive decline over time.
Cognitive assessments in primary care are “crucial, especially since cognitive impairment is frequently missed or undiagnosed in hospitals,” lead author Jessica Lo, MSc, biostatistician and research associate with the Center for Healthy Brain Aging, University of New South Wales, Sydney, Australia, told this news organization.
She suggested clinicians incorporate long-term cognitive assessments into care plans, using more sensitive neuropsychological tests in primary care to detect early signs of cognitive impairment. “Early detection would enable timely interventions to improve outcomes,” Lo said.
She also noted that poststroke care typically includes physical rehabilitation but not cognitive rehabilitation, which many rehabilitation centers aren’t equipped to provide.
The study was published online in JAMA Network Open.
Mapping Cognitive Decline Trajectory
Cognitive impairment after stroke is common, but the trajectory of cognitive decline following a first stroke, relative to prestroke cognitive function, remains unclear.
The investigators leveraged data from 14 population-based cohort studies of 20,860 adults (mean age, 73 years; 59% women) to map the trajectory of cognitive function before and after a first stroke.
The primary outcome was global cognition, defined as the standardized average of four cognitive domains (language, memory, processing speed, and executive function).
During a mean follow-up of 7.5 years, 1041 (5%) adults (mean age, 79 years) experienced a first stroke, a mean of 4.5 years after study entry.
In adjusted analyses, stroke was associated with a significant acute decline of 0.25 SD in global cognition and a “small but significant” acceleration in the rate of decline of −0.038 SD per year, the authors reported.
Stroke was also associated with acute decline in all individual cognitive domains except for memory, with effect sizes ranging from −0.17 to −0.22 SD. Poststroke declines in Mini-Mental State Examination scores (−0.36 SD) were also noted.
In terms of cognitive trajectory, the rate of decline before stroke in survivors was similar to that seen in peers who didn’t have a stroke (−0.048 and −0.049 SD per year in global cognition, respectively).
The researchers did not identify any vascular risk factors moderating cognitive decline following a stroke, consistent with prior research. However, cognitive decline was significantly more rapid in individuals without stroke, regardless of any future stroke, who had a history of diabetes, hypertension, high cholesterol, cardiovascular disease, depression, smoking, or were APOE4 carriers.
“Targeting modifiable vascular risk factors at an early stage may reduce the risk of stroke but also subsequent risk of stroke-related cognitive decline and cognitive impairment,” the researchers noted.
A ‘Major Step’ in the Right Direction
As previously reported by this news organization, in 2023 the American Heart Association (AHA) issued a statement noting that screening for cognitive impairment should be part of multidisciplinary care for stroke survivors.
Commenting for this news organization, Mitchell Elkind, MD, MS, AHA chief clinical science officer, said these new data are consistent with current AHA guidelines and statements that “support screening for cognitive and functional decline in patients both acutely and over the long term after stroke.”
Elkind noted that the 2022 guideline for intracerebral hemorrhage states that cognitive screening should occur “across the continuum of inpatient care and at intervals in the outpatient setting” and provides recommendations for cognitive therapy.
“Our 2021 scientific statement on the primary care of patients after stroke also recommends screening for both depression and cognitive impairment over both the short- and long-term,” said Elkind, professor of neurology and epidemiology at Columbia University Irving Medical Center in New York City.
“These documents recognize the fact that function and cognition can continue to decline years after stroke and that patients’ rehabilitation and support needs may therefore change over time after stroke,” Elkind added.
The authors of an accompanying commentary called it a “major step” in the right direction for the future of long-term stroke outcome assessment.
“As we develop new devices, indications, and time windows for stroke treatment, it may perhaps be wise to ensure trials steer away from simpler outcomes to more complex, granular ones,” wrote Yasmin Sadigh, MSc, and Victor Volovici, MD, PhD, with Erasmus University Medical Center, Rotterdam, the Netherlands.
The study had no commercial funding. The authors and commentary writers and Elkind have declared no conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Maternal Serum Folate Levels During Pregnancy Linked to Congenital Heart Disease Risk
TOPLINE:
Maternal serum folate levels during early to midpregnancy show a U-shaped association with congenital heart disease (CHD) risk in offspring. Both low and high folate levels are linked to an increased risk, with vitamin B12 deficiency and elevated homocysteine levels further exacerbating this risk.
METHODOLOGY:
- Researchers conducted a case-control study with 129 participants with CHD and 516 matched control participants from Guangdong Provincial People’s Hospital in China between 2015 and 2018.
- Maternal serum levels of folate, vitamin B12, and homocysteine were measured at around 16 weeks of gestation using a chemiluminescence microparticle immunoassay.
- CHD was confirmed using echocardiography, and the participants were matched by maternal age at a ratio of 1:4.
- Covariates included periconceptional folic acid supplementation, maternal education, occupation, parity, abortion history, pregnancy complications, and genetic polymorphisms related to folate metabolism.
- Conditional logistic regression was used to assess the associations, with adjustments for various covariates and sensitivity analyses excluding participants with missing genetic data.
TAKEAWAY:
- A U-shaped association was found between maternal serum folate levels and CHD risk in offspring, with both low and high levels linked to increased risk (P < .001).
- Low maternal folate levels were associated with an adjusted odds ratio (aOR) of 3.09 (95% CI, 1.88-5.08) for CHD risk, whereas high levels had an aOR of 1.81 (95% CI, 1.07-3.06).
- Using World Health Organization criteria, folate deficiency (< 5.9 ng/mL) had an aOR of 18.97 (95% CI, 3.87-93.11) and elevated levels (> 20 ng/mL) had an aOR of 5.71 (95% CI, 2.72-11.98) for CHD risk.
- Vitamin B12 deficiency and elevated homocysteine levels further increased the risk associated with both low and high maternal folate levels.
IN PRACTICE:
“Insufficient folate and vitamin B12 can lead to increased homocysteine levels, which is harmful to the cardiovascular system. Thus, homocysteine might act as a central mediator in the relationships between deficiencies in folate and vitamin B12 and the risk of CHD. Additionally, the role of folate extends beyond homocysteine mediation, contributing independently to placental implantation and vascular remodeling, irrespective of vitamin B12 and homocysteine levels,” the authors wrote.
SOURCE:
The study was led by Yanji Qu, PhD, and Jie Li, PhD, Global Health Research Center, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Southern Medical University, Guangzhou, China. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations included the measurement of maternal serum folate levels at a single time point, which may not reflect preconception and early postconception periods. The study’s findings may not be generalizable to other populations as participants were recruited from a single cardiac referral center in Southern China. Additionally, the lack of dietary intake data limited the ability to account for related biases. The sample size, while relatively large for CHD research, may lack sufficient power for stratified analyses.
DISCLOSURES:
One coauthor reported receiving personal fees from Guangdong Cardiovascular Institute outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Maternal serum folate levels during early to midpregnancy show a U-shaped association with congenital heart disease (CHD) risk in offspring. Both low and high folate levels are linked to an increased risk, with vitamin B12 deficiency and elevated homocysteine levels further exacerbating this risk.
METHODOLOGY:
- Researchers conducted a case-control study with 129 participants with CHD and 516 matched control participants from Guangdong Provincial People’s Hospital in China between 2015 and 2018.
- Maternal serum levels of folate, vitamin B12, and homocysteine were measured at around 16 weeks of gestation using a chemiluminescence microparticle immunoassay.
- CHD was confirmed using echocardiography, and the participants were matched by maternal age at a ratio of 1:4.
- Covariates included periconceptional folic acid supplementation, maternal education, occupation, parity, abortion history, pregnancy complications, and genetic polymorphisms related to folate metabolism.
- Conditional logistic regression was used to assess the associations, with adjustments for various covariates and sensitivity analyses excluding participants with missing genetic data.
TAKEAWAY:
- A U-shaped association was found between maternal serum folate levels and CHD risk in offspring, with both low and high levels linked to increased risk (P < .001).
- Low maternal folate levels were associated with an adjusted odds ratio (aOR) of 3.09 (95% CI, 1.88-5.08) for CHD risk, whereas high levels had an aOR of 1.81 (95% CI, 1.07-3.06).
- Using World Health Organization criteria, folate deficiency (< 5.9 ng/mL) had an aOR of 18.97 (95% CI, 3.87-93.11) and elevated levels (> 20 ng/mL) had an aOR of 5.71 (95% CI, 2.72-11.98) for CHD risk.
- Vitamin B12 deficiency and elevated homocysteine levels further increased the risk associated with both low and high maternal folate levels.
IN PRACTICE:
“Insufficient folate and vitamin B12 can lead to increased homocysteine levels, which is harmful to the cardiovascular system. Thus, homocysteine might act as a central mediator in the relationships between deficiencies in folate and vitamin B12 and the risk of CHD. Additionally, the role of folate extends beyond homocysteine mediation, contributing independently to placental implantation and vascular remodeling, irrespective of vitamin B12 and homocysteine levels,” the authors wrote.
SOURCE:
The study was led by Yanji Qu, PhD, and Jie Li, PhD, Global Health Research Center, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Southern Medical University, Guangzhou, China. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations included the measurement of maternal serum folate levels at a single time point, which may not reflect preconception and early postconception periods. The study’s findings may not be generalizable to other populations as participants were recruited from a single cardiac referral center in Southern China. Additionally, the lack of dietary intake data limited the ability to account for related biases. The sample size, while relatively large for CHD research, may lack sufficient power for stratified analyses.
DISCLOSURES:
One coauthor reported receiving personal fees from Guangdong Cardiovascular Institute outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Maternal serum folate levels during early to midpregnancy show a U-shaped association with congenital heart disease (CHD) risk in offspring. Both low and high folate levels are linked to an increased risk, with vitamin B12 deficiency and elevated homocysteine levels further exacerbating this risk.
METHODOLOGY:
- Researchers conducted a case-control study with 129 participants with CHD and 516 matched control participants from Guangdong Provincial People’s Hospital in China between 2015 and 2018.
- Maternal serum levels of folate, vitamin B12, and homocysteine were measured at around 16 weeks of gestation using a chemiluminescence microparticle immunoassay.
- CHD was confirmed using echocardiography, and the participants were matched by maternal age at a ratio of 1:4.
- Covariates included periconceptional folic acid supplementation, maternal education, occupation, parity, abortion history, pregnancy complications, and genetic polymorphisms related to folate metabolism.
- Conditional logistic regression was used to assess the associations, with adjustments for various covariates and sensitivity analyses excluding participants with missing genetic data.
TAKEAWAY:
- A U-shaped association was found between maternal serum folate levels and CHD risk in offspring, with both low and high levels linked to increased risk (P < .001).
- Low maternal folate levels were associated with an adjusted odds ratio (aOR) of 3.09 (95% CI, 1.88-5.08) for CHD risk, whereas high levels had an aOR of 1.81 (95% CI, 1.07-3.06).
- Using World Health Organization criteria, folate deficiency (< 5.9 ng/mL) had an aOR of 18.97 (95% CI, 3.87-93.11) and elevated levels (> 20 ng/mL) had an aOR of 5.71 (95% CI, 2.72-11.98) for CHD risk.
- Vitamin B12 deficiency and elevated homocysteine levels further increased the risk associated with both low and high maternal folate levels.
IN PRACTICE:
“Insufficient folate and vitamin B12 can lead to increased homocysteine levels, which is harmful to the cardiovascular system. Thus, homocysteine might act as a central mediator in the relationships between deficiencies in folate and vitamin B12 and the risk of CHD. Additionally, the role of folate extends beyond homocysteine mediation, contributing independently to placental implantation and vascular remodeling, irrespective of vitamin B12 and homocysteine levels,” the authors wrote.
SOURCE:
The study was led by Yanji Qu, PhD, and Jie Li, PhD, Global Health Research Center, Guangdong Provincial People’s Hospital, Guangdong Academy of Medical Sciences, Southern Medical University, Guangzhou, China. It was published online in JAMA Network Open.
LIMITATIONS:
The study’s limitations included the measurement of maternal serum folate levels at a single time point, which may not reflect preconception and early postconception periods. The study’s findings may not be generalizable to other populations as participants were recruited from a single cardiac referral center in Southern China. Additionally, the lack of dietary intake data limited the ability to account for related biases. The sample size, while relatively large for CHD research, may lack sufficient power for stratified analyses.
DISCLOSURES:
One coauthor reported receiving personal fees from Guangdong Cardiovascular Institute outside the submitted work. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Increasing Non–Candida albicans Yeasts in Vulvovaginal Candidiasis and Fluconazole Resistance in Leeds
TOPLINE:
Fluconazole resistance in yeast isolates from women with recurrent vulvovaginal candidiasis in Leeds, England, increased from 3.5% to 9.6% over 3 years. Non–Candida albicans yeasts also rose from 6.0% to 12.6% during the same period.
METHODOLOGY:
- Researchers conducted a retrospective data search of vaginal cultures from adult women in Leeds, England, between April 2018 and March 2021.
- A total of 5461 vaginal samples from women with clinical information indicating complicated/recurrent vulvovaginal candidiasis were included.
- Samples were processed on the WASPLAB automated platform, and species identification and antifungal susceptibility testing were performed in the Mycology Reference Centre by Matrix-assisted laser desorption ionization–time-of-flight mass spectrometry.
- Susceptibility to fluconazole was determined using disc diffusion and the Sensititre YeastOne microbroth dilution assay.
TAKEAWAY:
According to the authors, the prevalence of non–C albicans yeasts increased from 6.0% in 2018-2019 to 12.6% in 2020-2021 (P = .0003).
Fluconazole-sensitive (dose-dependent) and fluconazole-resistant isolates increased from 3.5% in 2018-2019 to 9.6% in 2020-2021 (P = .0001).
Most fluconazole resistance was observed in C albicans, with other species such as Nakaseomyces glabrata and Pichia kudriavzevii also showing resistance.
The authors state that the increase in fluconazole resistance and non–C albicans yeasts may be linked to a policy change encouraging empirical treatment of vulvovaginal candidiasis in primary care.
IN PRACTICE:
“This study shows that the rates of non–Candida albicans and fluconazole-resistant C albicans have increased year on year in the 3 years studied. The exact reasons for this increase remain unclear, but it follows the introduction of restricted access to fungal cultures for the diagnosis of vulvovaginal candidiasis by those working in primary care. A clinical diagnosis, followed by empirical treatment, has been recommended instead. Consequently, we believe this policy of encouraging empirical vaginitis treatment based on nonspecific symptoms and signs needs revisiting,” the authors wrote.
SOURCE:
The study was led by Jennifer C. Ratner, Leeds Teaching Hospitals NHS Trust, England. It was published online in Sexually Transmitted Infections.
LIMITATIONS:
The study’s limitations included a potential bias introduced by the reduced number of samples received from specialist sexual health clinics during the COVID-19 pandemic. Additionally, the study could not distinguish between cases of recurrent vulvovaginal candidiasis with complete resolution of symptoms and those with persistent symptoms despite treatment.
DISCLOSURES:
One coauthor disclosed receiving fees from Pfizer for contributing to webinar presentations in 2023. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Fluconazole resistance in yeast isolates from women with recurrent vulvovaginal candidiasis in Leeds, England, increased from 3.5% to 9.6% over 3 years. Non–Candida albicans yeasts also rose from 6.0% to 12.6% during the same period.
METHODOLOGY:
- Researchers conducted a retrospective data search of vaginal cultures from adult women in Leeds, England, between April 2018 and March 2021.
- A total of 5461 vaginal samples from women with clinical information indicating complicated/recurrent vulvovaginal candidiasis were included.
- Samples were processed on the WASPLAB automated platform, and species identification and antifungal susceptibility testing were performed in the Mycology Reference Centre by Matrix-assisted laser desorption ionization–time-of-flight mass spectrometry.
- Susceptibility to fluconazole was determined using disc diffusion and the Sensititre YeastOne microbroth dilution assay.
TAKEAWAY:
According to the authors, the prevalence of non–C albicans yeasts increased from 6.0% in 2018-2019 to 12.6% in 2020-2021 (P = .0003).
Fluconazole-sensitive (dose-dependent) and fluconazole-resistant isolates increased from 3.5% in 2018-2019 to 9.6% in 2020-2021 (P = .0001).
Most fluconazole resistance was observed in C albicans, with other species such as Nakaseomyces glabrata and Pichia kudriavzevii also showing resistance.
The authors state that the increase in fluconazole resistance and non–C albicans yeasts may be linked to a policy change encouraging empirical treatment of vulvovaginal candidiasis in primary care.
IN PRACTICE:
“This study shows that the rates of non–Candida albicans and fluconazole-resistant C albicans have increased year on year in the 3 years studied. The exact reasons for this increase remain unclear, but it follows the introduction of restricted access to fungal cultures for the diagnosis of vulvovaginal candidiasis by those working in primary care. A clinical diagnosis, followed by empirical treatment, has been recommended instead. Consequently, we believe this policy of encouraging empirical vaginitis treatment based on nonspecific symptoms and signs needs revisiting,” the authors wrote.
SOURCE:
The study was led by Jennifer C. Ratner, Leeds Teaching Hospitals NHS Trust, England. It was published online in Sexually Transmitted Infections.
LIMITATIONS:
The study’s limitations included a potential bias introduced by the reduced number of samples received from specialist sexual health clinics during the COVID-19 pandemic. Additionally, the study could not distinguish between cases of recurrent vulvovaginal candidiasis with complete resolution of symptoms and those with persistent symptoms despite treatment.
DISCLOSURES:
One coauthor disclosed receiving fees from Pfizer for contributing to webinar presentations in 2023. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Fluconazole resistance in yeast isolates from women with recurrent vulvovaginal candidiasis in Leeds, England, increased from 3.5% to 9.6% over 3 years. Non–Candida albicans yeasts also rose from 6.0% to 12.6% during the same period.
METHODOLOGY:
- Researchers conducted a retrospective data search of vaginal cultures from adult women in Leeds, England, between April 2018 and March 2021.
- A total of 5461 vaginal samples from women with clinical information indicating complicated/recurrent vulvovaginal candidiasis were included.
- Samples were processed on the WASPLAB automated platform, and species identification and antifungal susceptibility testing were performed in the Mycology Reference Centre by Matrix-assisted laser desorption ionization–time-of-flight mass spectrometry.
- Susceptibility to fluconazole was determined using disc diffusion and the Sensititre YeastOne microbroth dilution assay.
TAKEAWAY:
According to the authors, the prevalence of non–C albicans yeasts increased from 6.0% in 2018-2019 to 12.6% in 2020-2021 (P = .0003).
Fluconazole-sensitive (dose-dependent) and fluconazole-resistant isolates increased from 3.5% in 2018-2019 to 9.6% in 2020-2021 (P = .0001).
Most fluconazole resistance was observed in C albicans, with other species such as Nakaseomyces glabrata and Pichia kudriavzevii also showing resistance.
The authors state that the increase in fluconazole resistance and non–C albicans yeasts may be linked to a policy change encouraging empirical treatment of vulvovaginal candidiasis in primary care.
IN PRACTICE:
“This study shows that the rates of non–Candida albicans and fluconazole-resistant C albicans have increased year on year in the 3 years studied. The exact reasons for this increase remain unclear, but it follows the introduction of restricted access to fungal cultures for the diagnosis of vulvovaginal candidiasis by those working in primary care. A clinical diagnosis, followed by empirical treatment, has been recommended instead. Consequently, we believe this policy of encouraging empirical vaginitis treatment based on nonspecific symptoms and signs needs revisiting,” the authors wrote.
SOURCE:
The study was led by Jennifer C. Ratner, Leeds Teaching Hospitals NHS Trust, England. It was published online in Sexually Transmitted Infections.
LIMITATIONS:
The study’s limitations included a potential bias introduced by the reduced number of samples received from specialist sexual health clinics during the COVID-19 pandemic. Additionally, the study could not distinguish between cases of recurrent vulvovaginal candidiasis with complete resolution of symptoms and those with persistent symptoms despite treatment.
DISCLOSURES:
One coauthor disclosed receiving fees from Pfizer for contributing to webinar presentations in 2023. Additional disclosures are noted in the original article.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
Underutilized Mifepristone Shows Promise in Care of Early Pregnancy Loss
TOPLINE:
Mifepristone plus misoprostol reduces the need for subsequent uterine aspiration and emergency department visits in the management of early pregnancy loss. Despite its effectiveness, mifepristone remains underutilized, with 8.6% of patients receiving it in 2022.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using national insurance claims data of US patients with commercial insurance.
- More than 31,000 pregnant women (mean age, 32.7 years) with a diagnosis of early pregnancy loss between 2015 and 2022 were included.
- The diagnosis of patients included having a missed abortion (72.3%), spontaneous abortion (26.9%), or both (0.8%).
- Researchers compared the outcomes of individuals who received a combination of mifepristone and misoprostol vs those who received misoprostol alone. The outcome measures included the need for subsequent procedural management (uterine aspiration), return visits to the emergency department or an outpatient clinic, hospitalizations, and complications within 6 weeks of initial diagnosis.
TAKEAWAY:
- The use of mifepristone was more common in outpatient clinics than in emergency departments (3.4% vs 0.9%; P < .001).
- The use of mifepristone plus misoprostol vs misoprostol alone was linked to a lower incidence of subsequent procedural management (10.5% vs 14.0%; P = .002) and fewer emergency department visits (3.5% vs 7.9%; P < .001).
- The multivariable analysis showed that the use of mifepristone was linked to decreased odds of subsequent procedural management (adjusted odds ratio, 0.71; 95% CI, 0.57-0.87).
- Despite its effectiveness, mifepristone was used in only 8.6% of those receiving medication management for early pregnancy loss in 2022.
IN PRACTICE:
“Continued efforts are needed to reduce barriers to mifepristone use for medication management of EPL,” the authors wrote.
“Any practitioner who cares for patients experiencing early pregnancy loss should consider mifepristone pretreatment to misoprostol to be the standard of care for medication management. Provision of the evidence-based standard of care with the use of mifepristone for early pregnancy loss is an opportunity to advocate for an essential strategy in improving sexual and reproductive health in the US,” wrote Sarita Sonalkar, MD, MPH, and Rachel McKean, MD, MPH, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, in an invited commentary.
SOURCE:
The study was led by Lyndsey S. Benson, MD, MS, of the University of Washington School of Medicine, Seattle, and was published online in JAMA Network Open.
LIMITATIONS:
The study was limited by the accuracy of the diagnosis of early pregnancy loss and procedure codes because claims data are intended for billing purposes and may be incomplete or inaccurate. The use of de-identified data meant that specific gestational durations, exact dosing, or routes of misoprostol administration could not be determined. The findings may not be generalizable to those with public insurance or no insurance.
DISCLOSURES:
The study was supported in part by a grant from a Women’s Reproductive Health Research grant from the National Institutes of Health Eunice Kennedy Shriver National Institute for Child Health and Human Development. One author reported serving as an adviser and investigator, while another reported receiving personal fees and serving as an expert witness, contributing editor, and course instructor outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Mifepristone plus misoprostol reduces the need for subsequent uterine aspiration and emergency department visits in the management of early pregnancy loss. Despite its effectiveness, mifepristone remains underutilized, with 8.6% of patients receiving it in 2022.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using national insurance claims data of US patients with commercial insurance.
- More than 31,000 pregnant women (mean age, 32.7 years) with a diagnosis of early pregnancy loss between 2015 and 2022 were included.
- The diagnosis of patients included having a missed abortion (72.3%), spontaneous abortion (26.9%), or both (0.8%).
- Researchers compared the outcomes of individuals who received a combination of mifepristone and misoprostol vs those who received misoprostol alone. The outcome measures included the need for subsequent procedural management (uterine aspiration), return visits to the emergency department or an outpatient clinic, hospitalizations, and complications within 6 weeks of initial diagnosis.
TAKEAWAY:
- The use of mifepristone was more common in outpatient clinics than in emergency departments (3.4% vs 0.9%; P < .001).
- The use of mifepristone plus misoprostol vs misoprostol alone was linked to a lower incidence of subsequent procedural management (10.5% vs 14.0%; P = .002) and fewer emergency department visits (3.5% vs 7.9%; P < .001).
- The multivariable analysis showed that the use of mifepristone was linked to decreased odds of subsequent procedural management (adjusted odds ratio, 0.71; 95% CI, 0.57-0.87).
- Despite its effectiveness, mifepristone was used in only 8.6% of those receiving medication management for early pregnancy loss in 2022.
IN PRACTICE:
“Continued efforts are needed to reduce barriers to mifepristone use for medication management of EPL,” the authors wrote.
“Any practitioner who cares for patients experiencing early pregnancy loss should consider mifepristone pretreatment to misoprostol to be the standard of care for medication management. Provision of the evidence-based standard of care with the use of mifepristone for early pregnancy loss is an opportunity to advocate for an essential strategy in improving sexual and reproductive health in the US,” wrote Sarita Sonalkar, MD, MPH, and Rachel McKean, MD, MPH, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, in an invited commentary.
SOURCE:
The study was led by Lyndsey S. Benson, MD, MS, of the University of Washington School of Medicine, Seattle, and was published online in JAMA Network Open.
LIMITATIONS:
The study was limited by the accuracy of the diagnosis of early pregnancy loss and procedure codes because claims data are intended for billing purposes and may be incomplete or inaccurate. The use of de-identified data meant that specific gestational durations, exact dosing, or routes of misoprostol administration could not be determined. The findings may not be generalizable to those with public insurance or no insurance.
DISCLOSURES:
The study was supported in part by a grant from a Women’s Reproductive Health Research grant from the National Institutes of Health Eunice Kennedy Shriver National Institute for Child Health and Human Development. One author reported serving as an adviser and investigator, while another reported receiving personal fees and serving as an expert witness, contributing editor, and course instructor outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
TOPLINE:
Mifepristone plus misoprostol reduces the need for subsequent uterine aspiration and emergency department visits in the management of early pregnancy loss. Despite its effectiveness, mifepristone remains underutilized, with 8.6% of patients receiving it in 2022.
METHODOLOGY:
- Researchers conducted a retrospective cohort study using national insurance claims data of US patients with commercial insurance.
- More than 31,000 pregnant women (mean age, 32.7 years) with a diagnosis of early pregnancy loss between 2015 and 2022 were included.
- The diagnosis of patients included having a missed abortion (72.3%), spontaneous abortion (26.9%), or both (0.8%).
- Researchers compared the outcomes of individuals who received a combination of mifepristone and misoprostol vs those who received misoprostol alone. The outcome measures included the need for subsequent procedural management (uterine aspiration), return visits to the emergency department or an outpatient clinic, hospitalizations, and complications within 6 weeks of initial diagnosis.
TAKEAWAY:
- The use of mifepristone was more common in outpatient clinics than in emergency departments (3.4% vs 0.9%; P < .001).
- The use of mifepristone plus misoprostol vs misoprostol alone was linked to a lower incidence of subsequent procedural management (10.5% vs 14.0%; P = .002) and fewer emergency department visits (3.5% vs 7.9%; P < .001).
- The multivariable analysis showed that the use of mifepristone was linked to decreased odds of subsequent procedural management (adjusted odds ratio, 0.71; 95% CI, 0.57-0.87).
- Despite its effectiveness, mifepristone was used in only 8.6% of those receiving medication management for early pregnancy loss in 2022.
IN PRACTICE:
“Continued efforts are needed to reduce barriers to mifepristone use for medication management of EPL,” the authors wrote.
“Any practitioner who cares for patients experiencing early pregnancy loss should consider mifepristone pretreatment to misoprostol to be the standard of care for medication management. Provision of the evidence-based standard of care with the use of mifepristone for early pregnancy loss is an opportunity to advocate for an essential strategy in improving sexual and reproductive health in the US,” wrote Sarita Sonalkar, MD, MPH, and Rachel McKean, MD, MPH, of the Perelman School of Medicine at the University of Pennsylvania, Philadelphia, in an invited commentary.
SOURCE:
The study was led by Lyndsey S. Benson, MD, MS, of the University of Washington School of Medicine, Seattle, and was published online in JAMA Network Open.
LIMITATIONS:
The study was limited by the accuracy of the diagnosis of early pregnancy loss and procedure codes because claims data are intended for billing purposes and may be incomplete or inaccurate. The use of de-identified data meant that specific gestational durations, exact dosing, or routes of misoprostol administration could not be determined. The findings may not be generalizable to those with public insurance or no insurance.
DISCLOSURES:
The study was supported in part by a grant from a Women’s Reproductive Health Research grant from the National Institutes of Health Eunice Kennedy Shriver National Institute for Child Health and Human Development. One author reported serving as an adviser and investigator, while another reported receiving personal fees and serving as an expert witness, contributing editor, and course instructor outside the submitted work.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article first appeared on Medscape.com.
What Should You Do When a Patient Asks for a PSA Test?
Many patients ask us to request a prostate-specific antigen (PSA) test. According to the Brazilian Ministry of Health, prostate cancer is the second most common type of cancer in the male population in all regions of our country. It is the second-leading cause of cancer death in the male population, reaffirming its epidemiologic importance in Brazil. On the other hand, a Ministry of Health technical paper recommends against population-based screening for prostate cancer. So, what should we do?
First, it is important to distinguish early diagnosis from screening. Early diagnosis is the identification of cancer in early stages in people with signs and symptoms. Screening is characterized by the systematic application of exams — digital rectal exam and PSA test — in asymptomatic people, with the aim of identifying cancer in an early stage.
A recent European epidemiologic study reinforced this thesis and helps guide us.
The study included men aged 35-84 years from 26 European countries. Data on cancer incidence and mortality were collected between 1980 and 2017. The data suggested overdiagnosis of prostate cancer, which varied over time and among populations. The findings supported previous recommendations that any implementation of prostate cancer screening should be carefully designed, with an emphasis on minimizing the harms of overdiagnosis.
The clinical evolution of prostate cancer is still not well understood. Increasing age is associated with increased mortality. Many men with less aggressive disease tend to die with cancer rather than die of cancer. However, it is not always possible at the time of diagnosis to determine which tumors will be aggressive and which will grow slowly.
On the other hand, with screening, many of these indolent cancers are unnecessarily detected, generating excessive exams and treatments with negative repercussions (eg, pain, bleeding, infections, stress, and urinary and sexual dysfunction).
So, how should we as clinicians proceed regarding screening?
We should request the PSA test and emphasize the importance of digital rectal exam by a urologist for those at high risk for prostatic neoplasia (ie, those with family history) or those with urinary symptoms that may be associated with prostate cancer.
In general, we should draw attention to the possible risks and benefits of testing and adopt a shared decision-making approach with asymptomatic men or those at low risk who wish to have the screening exam. But achieving a shared decision is not a simple task.
I always have a thorough conversation with patients, but I confess that I request the exam in most cases.
Dr. Wajngarten is a professor of cardiology, Faculty of Medicine, at the University of São Paulo in Brazil. Dr. Wajngarten reported no conflicts of interest.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Many patients ask us to request a prostate-specific antigen (PSA) test. According to the Brazilian Ministry of Health, prostate cancer is the second most common type of cancer in the male population in all regions of our country. It is the second-leading cause of cancer death in the male population, reaffirming its epidemiologic importance in Brazil. On the other hand, a Ministry of Health technical paper recommends against population-based screening for prostate cancer. So, what should we do?
First, it is important to distinguish early diagnosis from screening. Early diagnosis is the identification of cancer in early stages in people with signs and symptoms. Screening is characterized by the systematic application of exams — digital rectal exam and PSA test — in asymptomatic people, with the aim of identifying cancer in an early stage.
A recent European epidemiologic study reinforced this thesis and helps guide us.
The study included men aged 35-84 years from 26 European countries. Data on cancer incidence and mortality were collected between 1980 and 2017. The data suggested overdiagnosis of prostate cancer, which varied over time and among populations. The findings supported previous recommendations that any implementation of prostate cancer screening should be carefully designed, with an emphasis on minimizing the harms of overdiagnosis.
The clinical evolution of prostate cancer is still not well understood. Increasing age is associated with increased mortality. Many men with less aggressive disease tend to die with cancer rather than die of cancer. However, it is not always possible at the time of diagnosis to determine which tumors will be aggressive and which will grow slowly.
On the other hand, with screening, many of these indolent cancers are unnecessarily detected, generating excessive exams and treatments with negative repercussions (eg, pain, bleeding, infections, stress, and urinary and sexual dysfunction).
So, how should we as clinicians proceed regarding screening?
We should request the PSA test and emphasize the importance of digital rectal exam by a urologist for those at high risk for prostatic neoplasia (ie, those with family history) or those with urinary symptoms that may be associated with prostate cancer.
In general, we should draw attention to the possible risks and benefits of testing and adopt a shared decision-making approach with asymptomatic men or those at low risk who wish to have the screening exam. But achieving a shared decision is not a simple task.
I always have a thorough conversation with patients, but I confess that I request the exam in most cases.
Dr. Wajngarten is a professor of cardiology, Faculty of Medicine, at the University of São Paulo in Brazil. Dr. Wajngarten reported no conflicts of interest.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
Many patients ask us to request a prostate-specific antigen (PSA) test. According to the Brazilian Ministry of Health, prostate cancer is the second most common type of cancer in the male population in all regions of our country. It is the second-leading cause of cancer death in the male population, reaffirming its epidemiologic importance in Brazil. On the other hand, a Ministry of Health technical paper recommends against population-based screening for prostate cancer. So, what should we do?
First, it is important to distinguish early diagnosis from screening. Early diagnosis is the identification of cancer in early stages in people with signs and symptoms. Screening is characterized by the systematic application of exams — digital rectal exam and PSA test — in asymptomatic people, with the aim of identifying cancer in an early stage.
A recent European epidemiologic study reinforced this thesis and helps guide us.
The study included men aged 35-84 years from 26 European countries. Data on cancer incidence and mortality were collected between 1980 and 2017. The data suggested overdiagnosis of prostate cancer, which varied over time and among populations. The findings supported previous recommendations that any implementation of prostate cancer screening should be carefully designed, with an emphasis on minimizing the harms of overdiagnosis.
The clinical evolution of prostate cancer is still not well understood. Increasing age is associated with increased mortality. Many men with less aggressive disease tend to die with cancer rather than die of cancer. However, it is not always possible at the time of diagnosis to determine which tumors will be aggressive and which will grow slowly.
On the other hand, with screening, many of these indolent cancers are unnecessarily detected, generating excessive exams and treatments with negative repercussions (eg, pain, bleeding, infections, stress, and urinary and sexual dysfunction).
So, how should we as clinicians proceed regarding screening?
We should request the PSA test and emphasize the importance of digital rectal exam by a urologist for those at high risk for prostatic neoplasia (ie, those with family history) or those with urinary symptoms that may be associated with prostate cancer.
In general, we should draw attention to the possible risks and benefits of testing and adopt a shared decision-making approach with asymptomatic men or those at low risk who wish to have the screening exam. But achieving a shared decision is not a simple task.
I always have a thorough conversation with patients, but I confess that I request the exam in most cases.
Dr. Wajngarten is a professor of cardiology, Faculty of Medicine, at the University of São Paulo in Brazil. Dr. Wajngarten reported no conflicts of interest.
This story was translated from the Medscape Portuguese edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.