User login
Neurology Reviews covers innovative and emerging news in neurology and neuroscience every month, with a focus on practical approaches to treating Parkinson's disease, epilepsy, headache, stroke, multiple sclerosis, Alzheimer's disease, and other neurologic disorders.
PML
Progressive multifocal leukoencephalopathy
Rituxan
The leading independent newspaper covering neurology news and commentary.
Children with ASD less likely to get vision screening
Children with autism spectrum disorder (ASD) are significantly less likely to have vision screening at well visits for 3- to 5-year-olds than are typically developing children, researchers have found.
The report, by Kimberly Hoover, MD, of Thomas Jefferson University in Philadelphia, and colleagues, was published online in Pediatrics.
While 59.9% of children without ASD got vision screening in these visits, only 36.5% of children with ASD got the screening. Both screening rates miss the mark set by American Academy of Pediatrics guidelines.
The AAP recommends “annual instrument-based vision screening, if available, at well visits for children starting at age 12 months to 3 years, and direct visual acuity testing beginning at 4 years of age. However, in children with developmental delays, the AAP recommends instrument-based screening, such as photoscreening, as a useful alternative at any age.”
Racial, age disparities as well
Racial disparities were evident in the data as well. Of the children who had ASD, Black children had the lowest rates of screening (27.6%), while the rate for White children was 39.7%. The rate for other/multiracial children with ASD was 39.8%.
The lowest rates of screening occurred in the youngest children, at the 3-year visit.
The researchers analyzed data from 63,829 well-child visits between January 2016 and December 2019, collected from the large primary care database PEDSnet.
Photoscreening vs. acuity screening
The authors pointed out that children with ASD are less likely to complete a vision test, which can be problematic in a busy primary care office.
“Children with ASD were significantly less likely to have at least one completed vision screening (43.2%) compared with children without ASD (72.1%; P <. 01),” the authors wrote, “with only 6.9% of children with ASD having had two or more vision screenings compared with 22.3% of children without ASD.”
The researchers saw higher vision test completion rates with photoscreening, using a sophisticated camera, compared with acuity screening, which uses a wall chart and requires responses.
Less patient participation is required for photoscreening and it can be done in less than 2 minutes.
If ability to complete the vision tests is a concern, the authors wrote, photoscreening may be a better solution.
Photoscreening takes 90 seconds
“Photoscreening has high sensitivity in detecting ocular conditions in children with ASD and has an average screening time of 90 seconds, and [it has] been validated in both children with ASD and developmental delays,” the authors wrote.
Andrew Adesman, MD, chief of developmental and behavioral pediatrics at Cohen Children’s Medical Center in New Hyde Park, N.Y., said the authors of this study quantify the gap between need and reality for vision tests for those with ASD.
“Other studies have shown that children on the autism spectrum have more than three times greater risk of having eye disease or vision problems,” he said in an interview. “You’ve got a high-risk population in need of assessment and the likelihood of them getting an assessment is much reduced.”
He said in addition to attention problems in taking the test, vision screening may get lost in the plethora of concerns parents want to talk about in well-child visits.
“If you’re the parent of a child with developmental delays, language delays, poor social engagement, there are a multitude of things the visit could be focused on and it may be that vision screening possibly gets compromised or not done,” Dr. Adesman said.
That, he said, may be a focus area for improving the screening numbers.
Neither parents nor providers should forget that vision screening is important, despite the myriad other issues to address, he said. “They don’t have to take a long time.”
When it comes to vision problems and children, “the earlier they’re identified the better,” Dr. Adesman says, particularly to identify the need for eye muscle surgery or corrective lenses, the two major interventions for strabismus or refractive error.
“If those problems are significant and go untreated, there’s a risk of loss of vision in the affected eye,” he said.
Reimbursement concerns for photoscreening
This study strongly supports the use of routine photoscreening to help eliminate the vision screening gap in children with ASD, the authors wrote.
They noted, however, that would require insurance reimbursement for primary care practices to effectively use that screening.
The researchers advised, “Providers treating patients with race, ethnicity, region, or age categories that reduce the adjusted odds of photoscreening can take steps in their practices to address these disparities, particularly in children with ASD.”
The study authors and Dr. Adesman reported no relevant financial relationships.
Children with autism spectrum disorder (ASD) are significantly less likely to have vision screening at well visits for 3- to 5-year-olds than are typically developing children, researchers have found.
The report, by Kimberly Hoover, MD, of Thomas Jefferson University in Philadelphia, and colleagues, was published online in Pediatrics.
While 59.9% of children without ASD got vision screening in these visits, only 36.5% of children with ASD got the screening. Both screening rates miss the mark set by American Academy of Pediatrics guidelines.
The AAP recommends “annual instrument-based vision screening, if available, at well visits for children starting at age 12 months to 3 years, and direct visual acuity testing beginning at 4 years of age. However, in children with developmental delays, the AAP recommends instrument-based screening, such as photoscreening, as a useful alternative at any age.”
Racial, age disparities as well
Racial disparities were evident in the data as well. Of the children who had ASD, Black children had the lowest rates of screening (27.6%), while the rate for White children was 39.7%. The rate for other/multiracial children with ASD was 39.8%.
The lowest rates of screening occurred in the youngest children, at the 3-year visit.
The researchers analyzed data from 63,829 well-child visits between January 2016 and December 2019, collected from the large primary care database PEDSnet.
Photoscreening vs. acuity screening
The authors pointed out that children with ASD are less likely to complete a vision test, which can be problematic in a busy primary care office.
“Children with ASD were significantly less likely to have at least one completed vision screening (43.2%) compared with children without ASD (72.1%; P <. 01),” the authors wrote, “with only 6.9% of children with ASD having had two or more vision screenings compared with 22.3% of children without ASD.”
The researchers saw higher vision test completion rates with photoscreening, using a sophisticated camera, compared with acuity screening, which uses a wall chart and requires responses.
Less patient participation is required for photoscreening and it can be done in less than 2 minutes.
If ability to complete the vision tests is a concern, the authors wrote, photoscreening may be a better solution.
Photoscreening takes 90 seconds
“Photoscreening has high sensitivity in detecting ocular conditions in children with ASD and has an average screening time of 90 seconds, and [it has] been validated in both children with ASD and developmental delays,” the authors wrote.
Andrew Adesman, MD, chief of developmental and behavioral pediatrics at Cohen Children’s Medical Center in New Hyde Park, N.Y., said the authors of this study quantify the gap between need and reality for vision tests for those with ASD.
“Other studies have shown that children on the autism spectrum have more than three times greater risk of having eye disease or vision problems,” he said in an interview. “You’ve got a high-risk population in need of assessment and the likelihood of them getting an assessment is much reduced.”
He said in addition to attention problems in taking the test, vision screening may get lost in the plethora of concerns parents want to talk about in well-child visits.
“If you’re the parent of a child with developmental delays, language delays, poor social engagement, there are a multitude of things the visit could be focused on and it may be that vision screening possibly gets compromised or not done,” Dr. Adesman said.
That, he said, may be a focus area for improving the screening numbers.
Neither parents nor providers should forget that vision screening is important, despite the myriad other issues to address, he said. “They don’t have to take a long time.”
When it comes to vision problems and children, “the earlier they’re identified the better,” Dr. Adesman says, particularly to identify the need for eye muscle surgery or corrective lenses, the two major interventions for strabismus or refractive error.
“If those problems are significant and go untreated, there’s a risk of loss of vision in the affected eye,” he said.
Reimbursement concerns for photoscreening
This study strongly supports the use of routine photoscreening to help eliminate the vision screening gap in children with ASD, the authors wrote.
They noted, however, that would require insurance reimbursement for primary care practices to effectively use that screening.
The researchers advised, “Providers treating patients with race, ethnicity, region, or age categories that reduce the adjusted odds of photoscreening can take steps in their practices to address these disparities, particularly in children with ASD.”
The study authors and Dr. Adesman reported no relevant financial relationships.
Children with autism spectrum disorder (ASD) are significantly less likely to have vision screening at well visits for 3- to 5-year-olds than are typically developing children, researchers have found.
The report, by Kimberly Hoover, MD, of Thomas Jefferson University in Philadelphia, and colleagues, was published online in Pediatrics.
While 59.9% of children without ASD got vision screening in these visits, only 36.5% of children with ASD got the screening. Both screening rates miss the mark set by American Academy of Pediatrics guidelines.
The AAP recommends “annual instrument-based vision screening, if available, at well visits for children starting at age 12 months to 3 years, and direct visual acuity testing beginning at 4 years of age. However, in children with developmental delays, the AAP recommends instrument-based screening, such as photoscreening, as a useful alternative at any age.”
Racial, age disparities as well
Racial disparities were evident in the data as well. Of the children who had ASD, Black children had the lowest rates of screening (27.6%), while the rate for White children was 39.7%. The rate for other/multiracial children with ASD was 39.8%.
The lowest rates of screening occurred in the youngest children, at the 3-year visit.
The researchers analyzed data from 63,829 well-child visits between January 2016 and December 2019, collected from the large primary care database PEDSnet.
Photoscreening vs. acuity screening
The authors pointed out that children with ASD are less likely to complete a vision test, which can be problematic in a busy primary care office.
“Children with ASD were significantly less likely to have at least one completed vision screening (43.2%) compared with children without ASD (72.1%; P <. 01),” the authors wrote, “with only 6.9% of children with ASD having had two or more vision screenings compared with 22.3% of children without ASD.”
The researchers saw higher vision test completion rates with photoscreening, using a sophisticated camera, compared with acuity screening, which uses a wall chart and requires responses.
Less patient participation is required for photoscreening and it can be done in less than 2 minutes.
If ability to complete the vision tests is a concern, the authors wrote, photoscreening may be a better solution.
Photoscreening takes 90 seconds
“Photoscreening has high sensitivity in detecting ocular conditions in children with ASD and has an average screening time of 90 seconds, and [it has] been validated in both children with ASD and developmental delays,” the authors wrote.
Andrew Adesman, MD, chief of developmental and behavioral pediatrics at Cohen Children’s Medical Center in New Hyde Park, N.Y., said the authors of this study quantify the gap between need and reality for vision tests for those with ASD.
“Other studies have shown that children on the autism spectrum have more than three times greater risk of having eye disease or vision problems,” he said in an interview. “You’ve got a high-risk population in need of assessment and the likelihood of them getting an assessment is much reduced.”
He said in addition to attention problems in taking the test, vision screening may get lost in the plethora of concerns parents want to talk about in well-child visits.
“If you’re the parent of a child with developmental delays, language delays, poor social engagement, there are a multitude of things the visit could be focused on and it may be that vision screening possibly gets compromised or not done,” Dr. Adesman said.
That, he said, may be a focus area for improving the screening numbers.
Neither parents nor providers should forget that vision screening is important, despite the myriad other issues to address, he said. “They don’t have to take a long time.”
When it comes to vision problems and children, “the earlier they’re identified the better,” Dr. Adesman says, particularly to identify the need for eye muscle surgery or corrective lenses, the two major interventions for strabismus or refractive error.
“If those problems are significant and go untreated, there’s a risk of loss of vision in the affected eye,” he said.
Reimbursement concerns for photoscreening
This study strongly supports the use of routine photoscreening to help eliminate the vision screening gap in children with ASD, the authors wrote.
They noted, however, that would require insurance reimbursement for primary care practices to effectively use that screening.
The researchers advised, “Providers treating patients with race, ethnicity, region, or age categories that reduce the adjusted odds of photoscreening can take steps in their practices to address these disparities, particularly in children with ASD.”
The study authors and Dr. Adesman reported no relevant financial relationships.
FROM PEDIATRICS
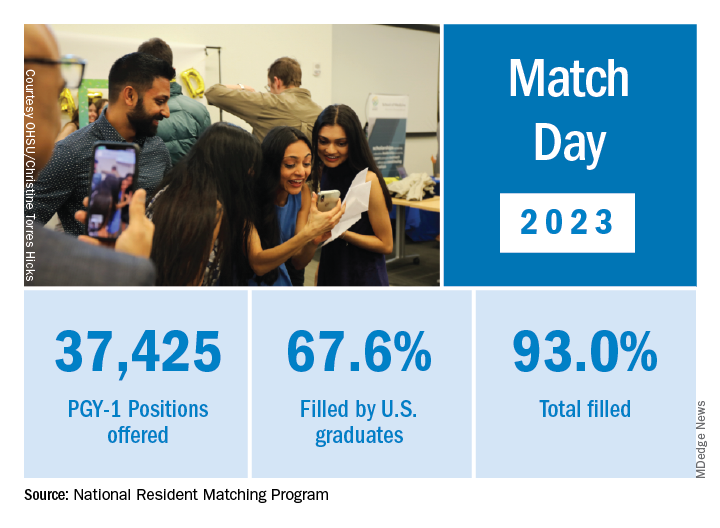
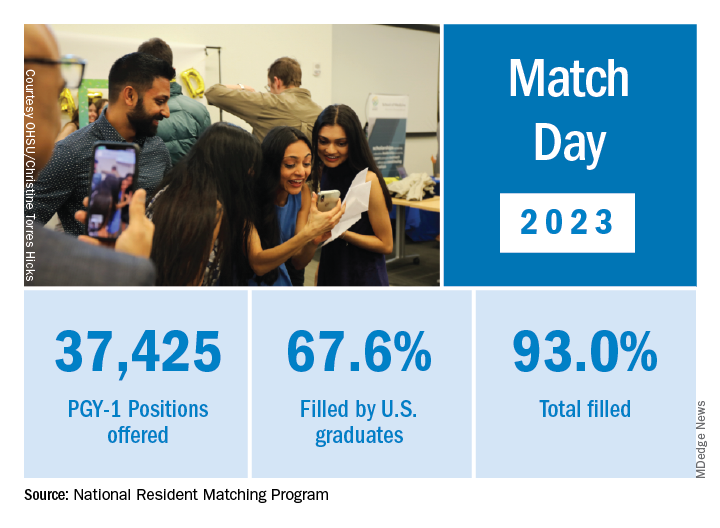
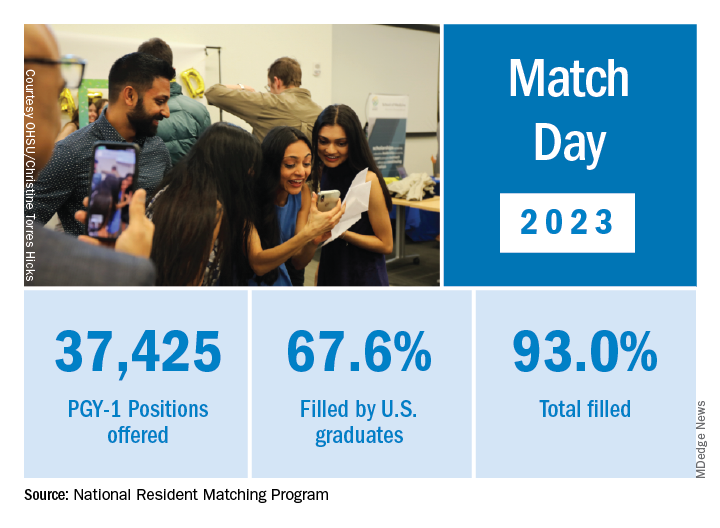
Match Day: Record number of residencies offered
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Baily Nagle, vice president of her graduating class at Harvard Medical School, Boston, celebrated “the luck of the Irish” on St. Patrick’s Day that allowed her to match into her chosen specialty and top choice of residency programs: anesthesia at Brigham and Women’s Hospital.
“I am feeling very excited and relieved – I matched,” she said in an interview upon hearing her good fortune on Match Monday, March 13. She had a similar reaction on Match Day, March 17. “After a lot of long nights and hard work, happy to have it pay off.”
Ms. Nagle was so determined to match into her specialty that she didn’t have any other specialties in mind as a backup.
The annual process of matching medical school graduates with compatible residency programs is an emotional roller coaster for all applicants, their personal March Madness, so to speak. But Ms. Nagle was one of the more fortunate applicants. She didn’t have to confront the heartbreak other applicants felt when the National Resident Matching Program (NRMP) announced results of the main residency match and the Supplemental Offer and Acceptance Program (SOAP), which offers alternate programs for unfilled positions or unmatched applicants.
During the 2023 Match process, this news organization has been following a handful of students, checking in with them periodically for updates on their progress. Most of them matched successfully, but at least one international medical graduate (IMG) did not. What the others have in common is that their hearts were set on a chosen specialty. Like Ms. Nagle, another student banked on landing his chosen specialty without a backup plan, whereas another said that she’d continue through the SOAP if she didn’t match successfully.
Overall, Match Day resulted in a record number of residency positions offered, most notably in primary care, which “hit an all-time high,” according to NRMP President and CEO Donna L. Lamb, DHSc, MBA, BSN. The number of positions has “consistently increased over the past 5 years, and most importantly the fill rate for primary care has remained steady,” Dr.. Lamb noted in the NRMP release of Match Day results. The release coincided with students learning through emails at noon Eastern Time to which residency or supplemental programs they were matched.
Though more applicants registered for the Match in 2023 than in 2022 – driven primarily by non-U.S. IMGs – the NRMP stated that it was surprised by the decrease in U.S. MD senior applicants.
U.S. MD seniors had a nearly 94% Match rate, a small increase over 2022. U.S. citizen IMGs saw a nearly 68% Match rate, which NRMP reported as an “all-time high” and about six percentage points over in 2022, whereas non-U.S. IMGs had a nearly 60% Match rate, a 1.3 percentage point increase over 2022.
Among the specialties that filled all available positions in 2023 were orthopedic surgery, plastic surgery (integrated), and radiology – diagnostic and thoracic surgery.
Not everyone matches
On March 13, the American College of Emergency Physicians issued a joint statement with other emergency medicine (EM) organizations about a high rate of unfilled EM positions expected in 2023.
NRMP acknowledged March 17 that 554 positions remained unfilled, an increase of 335 more unfilled positions than 2022. NRMP attributed the increase in unfilled positions in part to a decrease in the number of U.S. MD and U.S. DO seniors who submitted ranks for the specialty, which “could reflect changing applicant interests or projections about workforce opportunities post residency.”
Applicants who didn’t match usually try to obtain an unfilled position through SOAP. In 2023, 2,685 positions were unfilled after the matching algorithm was processed, an increase of nearly 19% over 2022. The vast majority of those positions were placed in SOAP, an increase of 17.5% over 2022.
Asim Ansari was one of the unlucky ones. Mr. Ansari was trying to match for the fifth time. He was unsuccessful in doing so again in 2023 in the Match and SOAP. Still, he was offered and accepted a child and adolescent psychiatry fellowship at Kansas University Medical Center in Kansas City. Psychiatry was his chosen specialty, so he was “feeling good. It’s a nice place to go to do the next 2 years.”
Mr. Ansari, who started the #MatchMadness support group for unmatched doctors on Twitter Spaces, was quick to cheer on his fellow matching peers on March 13 while revealing his own fate: “Congratulations to everyone who matched!!! Y’all are amazing. So proud of each one of you!!! I didn’t.”
Soon after the results, #MatchMadness held a #Soap2023 support session, and Mr. Ansari sought advice for those willing to review SOAP applications. Elsewhere on Twitter Match Day threads, a few doctors offered their support to those who planned to SOAP, students announced their matches, and others either congratulated or encouraged those still trying to match.
Couples match
Not everyone who matched considered the alternative. Before March 13, William Boyer said that he hadn’t given much thought to what would happen if he didn’t match because he was “optimistically confident” he would match into his chosen EM specialty. But he did and got his top choice of programs: Yale New Haven (Conn.) Hospital.
“I feel great,” he said in an interview. “I was definitely nervous opening the envelope” that revealed his residency program, “but there was a rush of relief” when he saw he landed Yale.
Earlier in the match cycle, he said in an interview that he “interviewed at a few ‘reach’ programs, so I hope I don’t match lower than expected on my rank list.”
Mr. Boyer considers himself “a mature applicant,” entering the University of South Carolina, Columbia, after 4 years as an insurance broker.
“I am celebrating today by playing pickleball with a few close medical friends who also matched this morning,” Mr. Boyer said on March 13. “I definitely had periods of nervousness leading up to this morning though that quickly turned into joy and relief” after learning he matched.
Mr. Boyer believes that his professional experience in the insurance industry and health care lobbying efforts with the National Association of Health Underwriters set him apart from other applicants.
“I changed careers to pursue this aspiration, which demonstrates my full dedication to the medical profession.”
He applied to 48 programs and was offered interviews to nearly half. Mr. Boyer visited the majority of those virtually. He said he targeted programs close to where his and his partner’s families are located: Massachusetts, North Carolina, and Texas. “My partner, who I met in medical school, matched into ortho as well so the whole household is very happy,” Mr. Boyer said.
She matched into her top choice as well on March 17, though a distance away at UT Health in San Antonio, he said. “We are both ecstatic. We both got our no. 1 choice. That was the plan going into it. We will make it work. I have 4 weeks of vacation.”
In his program choices, Mr. Boyer prioritized access to nature, minimal leadership turnover, a mix of clinical training sites, and adequate elective rotations and fellowship opportunities, such as in wilderness medicine and health policy.
NRMP reported that there were 1,239 couples participating in the Match; 1,095 had both partners match, and 114 had one partner match to residency training programs for a match rate of 93%.
Like Mr. Boyer, Hannah Hedriana matched into EM, one of the more popular despite the reported unfilled positions. In the past few years, it has consistently been one of the fastest-growing specialties, according to the NRMP.
Still Ms. Hedriana had a fall-back plan. “If I don’t match, then I do plan on going through SOAP. With the number of EM spots that were unfilled in 2022, there’s a chance I could still be an EM physician, but if not, then that’s okay with me.”
Her reaction on March 13, after learning she matched? “Super excited, celebrating with my friends right now.” On Match Day, she said she was “ecstatic” to be matched into Lakeland (Fla.) Regional Health. “This was my first choice so now I can stay close to family and friends,” she said in an interview soon after the results were released.
A first-generation, Filipino American student from the University of South Florida, Tampa, Ms. Hedriana comes from a family of health care professionals. Her father is a respiratory therapist turned physical therapist; her mother a registered nurse. Her sister is a patient care technician applying to nursing school.
Ms. Hedriana applied to 70 programs and interviewed mostly online with 24. Her goal was to stay on the East Coast.
“My partner is a licensed dentist in the state of Florida, and so for his career it would be more practical to stay in state, rather than get relicensed in another state, which could take months,” she said earlier in the matching cycle. “However, when we discussed choosing a residency program, he ultimately left it up to me and wanted me to pick where I thought I’d flourish best,” Ms. Hedriana said, adding that her family lives in Florida, too.
She said she sought a residency program that values family and teamwork.
“A program gets more points in my book if they have sites at nonprofit hospitals or has residents that regularly volunteer throughout their communities or participate in DEI [diversity, equity, and inclusion] initiatives.”
Ms. Hedriana noted that some specialties exclusively offered virtual interviews in 2023, whereas other specialties favored in-person interviews. “This year, many of my classmates were able to do multiple away rotations, which they saw as a positive regarding their chances of matching.” During COVID, in-person visits were limited.
“However, I’ve noticed that many of my classmates are not fond of the signaling aspect that was present for this year’s cycle,” she said. Signaling is a relatively new process that allows applicants to indicate interest in a limited number of residency programs. Not all residencies participate, but it’s growing in popularity among specialties, according to the American Medical Association.
‘Extremely competitive’
Ms. Nagle, a second lieutenant in the U.S. Air Force, applied to 12 programs and interviewed with half of them online. She said that she wasn’t targeting any specific type of program through the match.
“I believe you can get phenomenal training anywhere where you mesh with the residents and leadership. My ultimate priority is to (1) be near good people, (2) be near good food (Indian and Thai are a must), and (3) be near an international airport so I can flee the country during breaks.”
Meanwhile, she said that she found the application process, in which students have to articulate their entire medical school experience, extremely competitive. “I think this process is so easy to get wound up in and the anxiety can be palpable,” Ms. Nagle said. “People around you match your energy. So if you are a ball of anxiety then so are your attendings and residents – and that doesn’t bode well for passing the ‘do I want to be on call with them’ test.”
Looking back at medical school, Ms. Nagle recalled having a baby named after her during her first anesthesia rotation and being featured on The Kelly Clarkson Show. Ms. Nagle said that she had walked into the delivery room where new parents had been debating names of babies beginning with the letter B. “And when I introduced myself, they looked at each other and said, ‘Yep, that’s the one.’”
Mr. Boyer recounted how the majority of his medical school experience involved online education. “Roughly two-thirds of my first year was in-person prior to the pandemic. However, from spring break first year to in-person clinical rotations at the beginning of third year, we were all virtual. While I missed interacting with my classmates, I benefited from the virtual learning environment as I learn more efficiently from reading and visual aids than auditory lectures.”
Ms. Hedriana cited the friends and memories she made while learning to be a doctor. “Medical school was hard, but I wouldn’t have changed a thing.”
A version of this article first appeared on Medscape.com.
Older men more at risk as dangerous falls rise for all seniors
When Senate Minority Leader Mitch McConnell (R-Ky.) fell recently at a dinner event in Washington, he unfortunately joined a large group of his senior citizen peers.
This wasn’t the first tumble the 81-year-old has taken. In 2019, he fell in his home, fracturing his shoulder. This time, he got a concussion and was recently released to an in-patient rehabilitation facility. While Sen. McConnell didn’t fracture his skull, in falling and hitting his head, he became part of an emerging statistic: One that reveals falls are more dangerous for senior men than senior women.
This new research, which appeared in the American Journal of Emergency Medicine, came as a surprise to lead researcher Scott Alter, MD, associate professor of emergency medicine at the Florida Atlantic University, Boca Raton.
“We always hear about lower bone density rates among females, so we didn’t expect to see males with more skull fractures,” he said.
Dr. Alter said that as a clinician in a southern Florida facility, his emergency department was the perfect study grounds to evaluate incoming geriatric patients due to falls. Older “patients are at higher risk of skull fractures and intercranial bleeding, and we wanted to look at any patient presenting with a head injury. Some 80% were fall related, however.”
The statistics bear out the fact that falls of all types are common among the elderly: Some 800,000 seniors wind up in the hospital each year because of falls.
The numbers show death rates from falls are on the rise in the senior citizen age group, too, up 30% from 2007 to 2016. Falls account for 70% of accidental deaths in people 75 and older. They are the leading cause of injury-related visits to emergency departments in the country, too.
Jennifer Stevens, MD, a gerontologist and executive director at Florida-based Abbey Delray South, is aware of the dire numbers and sees their consequences regularly. “The reasons seniors are at a high fall risk are many,” she said. “They include balance issues, declining strength, diseases like Parkinson’s and Alzheimer’s, side effects of their medications, and more.”
In addition, many seniors live in spaces that are not necessarily equipped for their limitations, and hazards exist all over their homes. Put together, and the risks for falls are everywhere. But there are steps seniors, their families, and even middle-aged people can take to mitigate and hopefully prevent dangerous falls.
Starting early
While in many cases the journey to lessen fall risks begins after a fall, the time to begin addressing the issue is long before you hit your senior years. Mary Therese Cole, a physical therapist and certified dementia practitioner at Manual Edge Physical Therapy in Colorado Springs, Colo., says that age 50 is a good time to start paying attention and addressing physical declines.
“This is an age where your vision might begin deteriorating,” she said. “It’s a big reason why elderly people trip and fall.”
As our brains begin to age in our middle years, the neural pathways from brain to extremities start to decline, too. The result is that many people stop picking up their feet as well as they used to do, making them more likely to trip.
“You’re not elderly yet, but you’re not a spring chicken, either,” Ms. Cole said. “Any issues you have now will only get worse if you’re not working on them.”
A good starting point in middle age, then, is to work on both strength training and balance exercises. A certified personal trainer or physical therapist can help get you on a program to ward off many of these declines.
If you’ve reached your later years, however, and are experiencing physical declines, it’s smart to check in with your primary care doctor for an assessment. “He or she can get your started on regular PT to evaluate any shortcomings and then address them,” Ms. Cole said.
She noted that when she’s working with senior patients, she’ll test their strength getting into and out of a chair, do a manual strength test to check on lower extremities, check their walking stride, and ask about conditions such as diabetes, former surgeries, and other conditions.
From there, Ms. Cole said she can write up a plan for the patient. Likewise, Dr. Stevens uses a program called Be Active that allows her to test seniors on a variety of measurements, including flexibility, balance, hand strength, and more.
“Then we match them with classes to address their shortcomings,” she said. “It’s critical that seniors have the ability to recover and not fall if they get knocked off balance.”
Beyond working on your physical limitations, taking a good look at your home is essential, too. “You can have an occupational therapist come to your home and do an evaluation,” Dr. Stevens said. “They can help you rearrange and reorganize for a safer environment.”
Big, common household fall hazards include throw rugs, lack of nightlights for middle-of-the-night visits to the bathroom, a lack of grab bars in the shower/bathtub, and furniture that blocks pathways.
For his part, Dr. Alter likes to point seniors and their doctors to the CDC’s STEADI program, which is aimed at stopping elderly accidents, deaths, and injuries.
“It includes screening for fall risk, assessing factors you can modify or improve, and more tools,” he said.
Dr. Alter also recommended seniors talk to their doctors about medications, particularly blood thinners.
“At a certain point, you need to weigh the benefits of disease prevention with the risk of injury if you fall,” he said. “The bleeding risk might be too high if the patient is at a high risk of falls.”
A version of this article originally appeared on WebMD.com.
When Senate Minority Leader Mitch McConnell (R-Ky.) fell recently at a dinner event in Washington, he unfortunately joined a large group of his senior citizen peers.
This wasn’t the first tumble the 81-year-old has taken. In 2019, he fell in his home, fracturing his shoulder. This time, he got a concussion and was recently released to an in-patient rehabilitation facility. While Sen. McConnell didn’t fracture his skull, in falling and hitting his head, he became part of an emerging statistic: One that reveals falls are more dangerous for senior men than senior women.
This new research, which appeared in the American Journal of Emergency Medicine, came as a surprise to lead researcher Scott Alter, MD, associate professor of emergency medicine at the Florida Atlantic University, Boca Raton.
“We always hear about lower bone density rates among females, so we didn’t expect to see males with more skull fractures,” he said.
Dr. Alter said that as a clinician in a southern Florida facility, his emergency department was the perfect study grounds to evaluate incoming geriatric patients due to falls. Older “patients are at higher risk of skull fractures and intercranial bleeding, and we wanted to look at any patient presenting with a head injury. Some 80% were fall related, however.”
The statistics bear out the fact that falls of all types are common among the elderly: Some 800,000 seniors wind up in the hospital each year because of falls.
The numbers show death rates from falls are on the rise in the senior citizen age group, too, up 30% from 2007 to 2016. Falls account for 70% of accidental deaths in people 75 and older. They are the leading cause of injury-related visits to emergency departments in the country, too.
Jennifer Stevens, MD, a gerontologist and executive director at Florida-based Abbey Delray South, is aware of the dire numbers and sees their consequences regularly. “The reasons seniors are at a high fall risk are many,” she said. “They include balance issues, declining strength, diseases like Parkinson’s and Alzheimer’s, side effects of their medications, and more.”
In addition, many seniors live in spaces that are not necessarily equipped for their limitations, and hazards exist all over their homes. Put together, and the risks for falls are everywhere. But there are steps seniors, their families, and even middle-aged people can take to mitigate and hopefully prevent dangerous falls.
Starting early
While in many cases the journey to lessen fall risks begins after a fall, the time to begin addressing the issue is long before you hit your senior years. Mary Therese Cole, a physical therapist and certified dementia practitioner at Manual Edge Physical Therapy in Colorado Springs, Colo., says that age 50 is a good time to start paying attention and addressing physical declines.
“This is an age where your vision might begin deteriorating,” she said. “It’s a big reason why elderly people trip and fall.”
As our brains begin to age in our middle years, the neural pathways from brain to extremities start to decline, too. The result is that many people stop picking up their feet as well as they used to do, making them more likely to trip.
“You’re not elderly yet, but you’re not a spring chicken, either,” Ms. Cole said. “Any issues you have now will only get worse if you’re not working on them.”
A good starting point in middle age, then, is to work on both strength training and balance exercises. A certified personal trainer or physical therapist can help get you on a program to ward off many of these declines.
If you’ve reached your later years, however, and are experiencing physical declines, it’s smart to check in with your primary care doctor for an assessment. “He or she can get your started on regular PT to evaluate any shortcomings and then address them,” Ms. Cole said.
She noted that when she’s working with senior patients, she’ll test their strength getting into and out of a chair, do a manual strength test to check on lower extremities, check their walking stride, and ask about conditions such as diabetes, former surgeries, and other conditions.
From there, Ms. Cole said she can write up a plan for the patient. Likewise, Dr. Stevens uses a program called Be Active that allows her to test seniors on a variety of measurements, including flexibility, balance, hand strength, and more.
“Then we match them with classes to address their shortcomings,” she said. “It’s critical that seniors have the ability to recover and not fall if they get knocked off balance.”
Beyond working on your physical limitations, taking a good look at your home is essential, too. “You can have an occupational therapist come to your home and do an evaluation,” Dr. Stevens said. “They can help you rearrange and reorganize for a safer environment.”
Big, common household fall hazards include throw rugs, lack of nightlights for middle-of-the-night visits to the bathroom, a lack of grab bars in the shower/bathtub, and furniture that blocks pathways.
For his part, Dr. Alter likes to point seniors and their doctors to the CDC’s STEADI program, which is aimed at stopping elderly accidents, deaths, and injuries.
“It includes screening for fall risk, assessing factors you can modify or improve, and more tools,” he said.
Dr. Alter also recommended seniors talk to their doctors about medications, particularly blood thinners.
“At a certain point, you need to weigh the benefits of disease prevention with the risk of injury if you fall,” he said. “The bleeding risk might be too high if the patient is at a high risk of falls.”
A version of this article originally appeared on WebMD.com.
When Senate Minority Leader Mitch McConnell (R-Ky.) fell recently at a dinner event in Washington, he unfortunately joined a large group of his senior citizen peers.
This wasn’t the first tumble the 81-year-old has taken. In 2019, he fell in his home, fracturing his shoulder. This time, he got a concussion and was recently released to an in-patient rehabilitation facility. While Sen. McConnell didn’t fracture his skull, in falling and hitting his head, he became part of an emerging statistic: One that reveals falls are more dangerous for senior men than senior women.
This new research, which appeared in the American Journal of Emergency Medicine, came as a surprise to lead researcher Scott Alter, MD, associate professor of emergency medicine at the Florida Atlantic University, Boca Raton.
“We always hear about lower bone density rates among females, so we didn’t expect to see males with more skull fractures,” he said.
Dr. Alter said that as a clinician in a southern Florida facility, his emergency department was the perfect study grounds to evaluate incoming geriatric patients due to falls. Older “patients are at higher risk of skull fractures and intercranial bleeding, and we wanted to look at any patient presenting with a head injury. Some 80% were fall related, however.”
The statistics bear out the fact that falls of all types are common among the elderly: Some 800,000 seniors wind up in the hospital each year because of falls.
The numbers show death rates from falls are on the rise in the senior citizen age group, too, up 30% from 2007 to 2016. Falls account for 70% of accidental deaths in people 75 and older. They are the leading cause of injury-related visits to emergency departments in the country, too.
Jennifer Stevens, MD, a gerontologist and executive director at Florida-based Abbey Delray South, is aware of the dire numbers and sees their consequences regularly. “The reasons seniors are at a high fall risk are many,” she said. “They include balance issues, declining strength, diseases like Parkinson’s and Alzheimer’s, side effects of their medications, and more.”
In addition, many seniors live in spaces that are not necessarily equipped for their limitations, and hazards exist all over their homes. Put together, and the risks for falls are everywhere. But there are steps seniors, their families, and even middle-aged people can take to mitigate and hopefully prevent dangerous falls.
Starting early
While in many cases the journey to lessen fall risks begins after a fall, the time to begin addressing the issue is long before you hit your senior years. Mary Therese Cole, a physical therapist and certified dementia practitioner at Manual Edge Physical Therapy in Colorado Springs, Colo., says that age 50 is a good time to start paying attention and addressing physical declines.
“This is an age where your vision might begin deteriorating,” she said. “It’s a big reason why elderly people trip and fall.”
As our brains begin to age in our middle years, the neural pathways from brain to extremities start to decline, too. The result is that many people stop picking up their feet as well as they used to do, making them more likely to trip.
“You’re not elderly yet, but you’re not a spring chicken, either,” Ms. Cole said. “Any issues you have now will only get worse if you’re not working on them.”
A good starting point in middle age, then, is to work on both strength training and balance exercises. A certified personal trainer or physical therapist can help get you on a program to ward off many of these declines.
If you’ve reached your later years, however, and are experiencing physical declines, it’s smart to check in with your primary care doctor for an assessment. “He or she can get your started on regular PT to evaluate any shortcomings and then address them,” Ms. Cole said.
She noted that when she’s working with senior patients, she’ll test their strength getting into and out of a chair, do a manual strength test to check on lower extremities, check their walking stride, and ask about conditions such as diabetes, former surgeries, and other conditions.
From there, Ms. Cole said she can write up a plan for the patient. Likewise, Dr. Stevens uses a program called Be Active that allows her to test seniors on a variety of measurements, including flexibility, balance, hand strength, and more.
“Then we match them with classes to address their shortcomings,” she said. “It’s critical that seniors have the ability to recover and not fall if they get knocked off balance.”
Beyond working on your physical limitations, taking a good look at your home is essential, too. “You can have an occupational therapist come to your home and do an evaluation,” Dr. Stevens said. “They can help you rearrange and reorganize for a safer environment.”
Big, common household fall hazards include throw rugs, lack of nightlights for middle-of-the-night visits to the bathroom, a lack of grab bars in the shower/bathtub, and furniture that blocks pathways.
For his part, Dr. Alter likes to point seniors and their doctors to the CDC’s STEADI program, which is aimed at stopping elderly accidents, deaths, and injuries.
“It includes screening for fall risk, assessing factors you can modify or improve, and more tools,” he said.
Dr. Alter also recommended seniors talk to their doctors about medications, particularly blood thinners.
“At a certain point, you need to weigh the benefits of disease prevention with the risk of injury if you fall,” he said. “The bleeding risk might be too high if the patient is at a high risk of falls.”
A version of this article originally appeared on WebMD.com.
What’s driving the "world’s fastest-growing brain disease"?
An international team of researchers reviewed previous research and cited data that suggest the chemical trichloroethylene (TCE) is associated with as much as a 500% increased risk for Parkinson’s disease (PD).
Lead investigator Ray Dorsey, MD, professor of neurology, University of Rochester, N.Y., called PD “the world’s fastest-growing brain disease,” and told this news organization that it “may be largely preventable.”
“Countless people have died over generations from cancer and other disease linked to TCE [and] Parkinson’s may be the latest,” he said. “Banning these chemicals, containing contaminated sites, and protecting homes, schools, and buildings at risk may all create a world where Parkinson’s is increasingly rare, not common.”
The paper was published online in the Journal of Parkinson’s Disease.
Invisible, ubiquitous
TCE was first synthesized in a lab in 1864, with commercial production beginning in 1920, the researchers noted.
“Because of its unique properties, TCE has had countless industrial, commercial, military, and medical applications,” including producing refrigerants, cleaning electronics, and degreasing engine parts.
In addition, it’s been used in dry cleaning, although a similar chemical (perchloroethylene [PCE]) is currently more widely used for that purpose. Nevertheless, the authors noted, in anaerobic conditions, perchloroethylene often transforms into TCE “and their toxicity may be similar.”
Consumer products in which TCE is found include typewriter correction fluid, paint removers, gun cleaners, and aerosol cleaning products. Up until the 1970s, it was used to decaffeinate coffee.
TCE exposure isn’t confined to those who work with it. It also pollutes outdoor air, taints groundwater, and contaminates indoor air. It’s present in a substantial amount of groundwater in the United States and it “evaporates from underlying soil and groundwater and enters homes, workplaces, or schools, often undetected,” the researchers noted.
“Exposure can come via occupation or the environment and is often largely unknown at the time it occurs,” Dr. Dorsey said.
He noted that the rapid increase in PD incidence cannot be explained by genetic factors alone, which affect only about 15% of patients with PD, nor can it be explained by aging alone. “Certain pesticides ... are likely causes but would not explain the high prevalence of PD in urban areas, as is the case in the U.S.” Rather, “other factors” are involved, and “TCE is likely one such factor.”
Yet, “despite widespread contamination and increasing industrial, commercial, and military use, clinical investigations of TCE and PD have been limited.”
To fill this knowledge gap, Dr. Dorsey and his coauthors of the book, “Ending Parkinson’s Disease: A Prescription for Action,” took a deep dive into studies focusing on the potential association of TCE and PD and presented seven cases to illustrate the association.
“Like many genetic mutations (e.g., Parkin) and other environmental toxicants ... TCE damages the energy-producing parts of cells, i.e., the mitochondria,” said Dr. Dorsey.
TCE and PCE “likely mediate their toxicity through a common metabolite.” Because both are lipophilic, they “readily distribute in the brain and body tissues and appear to cause mitochondrial dysfunction at high doses,” the researchers hypothesized.
Dopaminergic neurons are particularly sensitive to mitochondrial neurotoxicants, so this might “partially explain the link to PD.”
Animal studies have shown that TCE “caused selective loss of dopaminergic neurons.” Moreover, PD-related neuropathology was found in the substantia nigra of rodents exposed to TCE over time. In addition, studies as early as 1960 were showing an association between TCE and parkinsonism.
The authors describe TCE as “ubiquitous” in the 1970s, with 10 million Americans working with the chemical or other organic solvents daily. The review details an extensive list of industries and occupations in which TCE exposure continues to occur.
People working with TCE might inhale it or touch it; but “millions more encounter the chemical unknowingly through outdoor air, contaminated groundwater, and indoor air pollution.”
They noted that TCE contaminates up to one-third of U.S. drinking water, has polluted the groundwater in more than 20 different countries on five continents, and is found in half of the 1,300 most toxic “Superfund” sites that are “part of a federal clean-up program, including 15 in California’s Silicon Valley, where TCE was used to clean electronics.”
Although the U.S. military stopped using TCE, numerous sites have been contaminated, including Marine Corps Base Camp Lejeune in North Carolina, where TCE and PCE were found in drinking water at 280 times the recommended safety standards.
The researchers highlighted seven cases of individuals who developed PD after likely exposure to TCE, including NBA basketball player Brian Grant, who developed symptoms of PD in 2006 at the age of 34.
Mr. Grant and his family had lived in Camp Lejeune when he was a child, during which time he drank, bathed, and swam in contaminated water, “unaware of its toxicity.” His father also died of esophageal cancer, “which is linked to TCE,” the authors of the study wrote. Mr. Grant has created a foundation to inspire and support patients with PD.
All of the individuals either grew up in or spent time in an area where they were extensively exposed to TCE, PCE, or other chemicals, or experienced occupational exposure.
The authors acknowledged that the role of TCE in PD, as illustrated by the cases, is “far from definitive.” For example, exposure to TCE is often combined with exposure to other toxins, or with unmeasured genetic risk factors.
They highlighted the need for more research and called for cleaning and containing contaminated sites, monitoring TCE levels, and publicly communicating risk and a ban on TCE.
Recall bias?
Commenting for this news organization, Rebecca Gilbert, MD, PhD, chief scientific officer, American Parkinson Disease Association (APDA), noted that the authors “are very frank about the limitations of this approach [illustrative cases] as proof of causation between PD and TCE exposure.”
Another limitation is that TCE exposure is very common, “as argued in the paper.” But “most people with exposure do not develop PD,” Dr. Gilbert pointed out. “By probing the TCE exposure of those who already have PD, there is a danger of recall bias.”
Dr. Gilbert, associate professor of neurology at NYU Langone Health, who was not involved with the study, acknowledged that the authors “present their work as hypothesis and clearly state that more work is needed to understand the connection between TCE and PD.”
In the meantime, however, there are “well-established health risks of TCE exposure, including development of various cancers,” she said. Therefore, the authors’ goals appear to be educating the public about known health risks, working to clean up known sites of contamination, and advocating to ban future use of TCE.
These goals “do not need to wait for [proof of] firm causation between TCE and PD,” she stated.
Dr. Dorsey reported he has received honoraria for speaking at the American Academy of Neurology and at multiple other societies and foundations and has received compensation for consulting services from pharmaceutical companies, foundations, medical education companies, and medical publications; he owns stock in several companies. The other authors’ disclosures can be found in the original paper. Dr. Gilbert is employed by the American Parkinson Disease Association and Bellevue Hospital Center in New York City.
A version of this article first appeared on Medscape.com.
An international team of researchers reviewed previous research and cited data that suggest the chemical trichloroethylene (TCE) is associated with as much as a 500% increased risk for Parkinson’s disease (PD).
Lead investigator Ray Dorsey, MD, professor of neurology, University of Rochester, N.Y., called PD “the world’s fastest-growing brain disease,” and told this news organization that it “may be largely preventable.”
“Countless people have died over generations from cancer and other disease linked to TCE [and] Parkinson’s may be the latest,” he said. “Banning these chemicals, containing contaminated sites, and protecting homes, schools, and buildings at risk may all create a world where Parkinson’s is increasingly rare, not common.”
The paper was published online in the Journal of Parkinson’s Disease.
Invisible, ubiquitous
TCE was first synthesized in a lab in 1864, with commercial production beginning in 1920, the researchers noted.
“Because of its unique properties, TCE has had countless industrial, commercial, military, and medical applications,” including producing refrigerants, cleaning electronics, and degreasing engine parts.
In addition, it’s been used in dry cleaning, although a similar chemical (perchloroethylene [PCE]) is currently more widely used for that purpose. Nevertheless, the authors noted, in anaerobic conditions, perchloroethylene often transforms into TCE “and their toxicity may be similar.”
Consumer products in which TCE is found include typewriter correction fluid, paint removers, gun cleaners, and aerosol cleaning products. Up until the 1970s, it was used to decaffeinate coffee.
TCE exposure isn’t confined to those who work with it. It also pollutes outdoor air, taints groundwater, and contaminates indoor air. It’s present in a substantial amount of groundwater in the United States and it “evaporates from underlying soil and groundwater and enters homes, workplaces, or schools, often undetected,” the researchers noted.
“Exposure can come via occupation or the environment and is often largely unknown at the time it occurs,” Dr. Dorsey said.
He noted that the rapid increase in PD incidence cannot be explained by genetic factors alone, which affect only about 15% of patients with PD, nor can it be explained by aging alone. “Certain pesticides ... are likely causes but would not explain the high prevalence of PD in urban areas, as is the case in the U.S.” Rather, “other factors” are involved, and “TCE is likely one such factor.”
Yet, “despite widespread contamination and increasing industrial, commercial, and military use, clinical investigations of TCE and PD have been limited.”
To fill this knowledge gap, Dr. Dorsey and his coauthors of the book, “Ending Parkinson’s Disease: A Prescription for Action,” took a deep dive into studies focusing on the potential association of TCE and PD and presented seven cases to illustrate the association.
“Like many genetic mutations (e.g., Parkin) and other environmental toxicants ... TCE damages the energy-producing parts of cells, i.e., the mitochondria,” said Dr. Dorsey.
TCE and PCE “likely mediate their toxicity through a common metabolite.” Because both are lipophilic, they “readily distribute in the brain and body tissues and appear to cause mitochondrial dysfunction at high doses,” the researchers hypothesized.
Dopaminergic neurons are particularly sensitive to mitochondrial neurotoxicants, so this might “partially explain the link to PD.”
Animal studies have shown that TCE “caused selective loss of dopaminergic neurons.” Moreover, PD-related neuropathology was found in the substantia nigra of rodents exposed to TCE over time. In addition, studies as early as 1960 were showing an association between TCE and parkinsonism.
The authors describe TCE as “ubiquitous” in the 1970s, with 10 million Americans working with the chemical or other organic solvents daily. The review details an extensive list of industries and occupations in which TCE exposure continues to occur.
People working with TCE might inhale it or touch it; but “millions more encounter the chemical unknowingly through outdoor air, contaminated groundwater, and indoor air pollution.”
They noted that TCE contaminates up to one-third of U.S. drinking water, has polluted the groundwater in more than 20 different countries on five continents, and is found in half of the 1,300 most toxic “Superfund” sites that are “part of a federal clean-up program, including 15 in California’s Silicon Valley, where TCE was used to clean electronics.”
Although the U.S. military stopped using TCE, numerous sites have been contaminated, including Marine Corps Base Camp Lejeune in North Carolina, where TCE and PCE were found in drinking water at 280 times the recommended safety standards.
The researchers highlighted seven cases of individuals who developed PD after likely exposure to TCE, including NBA basketball player Brian Grant, who developed symptoms of PD in 2006 at the age of 34.
Mr. Grant and his family had lived in Camp Lejeune when he was a child, during which time he drank, bathed, and swam in contaminated water, “unaware of its toxicity.” His father also died of esophageal cancer, “which is linked to TCE,” the authors of the study wrote. Mr. Grant has created a foundation to inspire and support patients with PD.
All of the individuals either grew up in or spent time in an area where they were extensively exposed to TCE, PCE, or other chemicals, or experienced occupational exposure.
The authors acknowledged that the role of TCE in PD, as illustrated by the cases, is “far from definitive.” For example, exposure to TCE is often combined with exposure to other toxins, or with unmeasured genetic risk factors.
They highlighted the need for more research and called for cleaning and containing contaminated sites, monitoring TCE levels, and publicly communicating risk and a ban on TCE.
Recall bias?
Commenting for this news organization, Rebecca Gilbert, MD, PhD, chief scientific officer, American Parkinson Disease Association (APDA), noted that the authors “are very frank about the limitations of this approach [illustrative cases] as proof of causation between PD and TCE exposure.”
Another limitation is that TCE exposure is very common, “as argued in the paper.” But “most people with exposure do not develop PD,” Dr. Gilbert pointed out. “By probing the TCE exposure of those who already have PD, there is a danger of recall bias.”
Dr. Gilbert, associate professor of neurology at NYU Langone Health, who was not involved with the study, acknowledged that the authors “present their work as hypothesis and clearly state that more work is needed to understand the connection between TCE and PD.”
In the meantime, however, there are “well-established health risks of TCE exposure, including development of various cancers,” she said. Therefore, the authors’ goals appear to be educating the public about known health risks, working to clean up known sites of contamination, and advocating to ban future use of TCE.
These goals “do not need to wait for [proof of] firm causation between TCE and PD,” she stated.
Dr. Dorsey reported he has received honoraria for speaking at the American Academy of Neurology and at multiple other societies and foundations and has received compensation for consulting services from pharmaceutical companies, foundations, medical education companies, and medical publications; he owns stock in several companies. The other authors’ disclosures can be found in the original paper. Dr. Gilbert is employed by the American Parkinson Disease Association and Bellevue Hospital Center in New York City.
A version of this article first appeared on Medscape.com.
An international team of researchers reviewed previous research and cited data that suggest the chemical trichloroethylene (TCE) is associated with as much as a 500% increased risk for Parkinson’s disease (PD).
Lead investigator Ray Dorsey, MD, professor of neurology, University of Rochester, N.Y., called PD “the world’s fastest-growing brain disease,” and told this news organization that it “may be largely preventable.”
“Countless people have died over generations from cancer and other disease linked to TCE [and] Parkinson’s may be the latest,” he said. “Banning these chemicals, containing contaminated sites, and protecting homes, schools, and buildings at risk may all create a world where Parkinson’s is increasingly rare, not common.”
The paper was published online in the Journal of Parkinson’s Disease.
Invisible, ubiquitous
TCE was first synthesized in a lab in 1864, with commercial production beginning in 1920, the researchers noted.
“Because of its unique properties, TCE has had countless industrial, commercial, military, and medical applications,” including producing refrigerants, cleaning electronics, and degreasing engine parts.
In addition, it’s been used in dry cleaning, although a similar chemical (perchloroethylene [PCE]) is currently more widely used for that purpose. Nevertheless, the authors noted, in anaerobic conditions, perchloroethylene often transforms into TCE “and their toxicity may be similar.”
Consumer products in which TCE is found include typewriter correction fluid, paint removers, gun cleaners, and aerosol cleaning products. Up until the 1970s, it was used to decaffeinate coffee.
TCE exposure isn’t confined to those who work with it. It also pollutes outdoor air, taints groundwater, and contaminates indoor air. It’s present in a substantial amount of groundwater in the United States and it “evaporates from underlying soil and groundwater and enters homes, workplaces, or schools, often undetected,” the researchers noted.
“Exposure can come via occupation or the environment and is often largely unknown at the time it occurs,” Dr. Dorsey said.
He noted that the rapid increase in PD incidence cannot be explained by genetic factors alone, which affect only about 15% of patients with PD, nor can it be explained by aging alone. “Certain pesticides ... are likely causes but would not explain the high prevalence of PD in urban areas, as is the case in the U.S.” Rather, “other factors” are involved, and “TCE is likely one such factor.”
Yet, “despite widespread contamination and increasing industrial, commercial, and military use, clinical investigations of TCE and PD have been limited.”
To fill this knowledge gap, Dr. Dorsey and his coauthors of the book, “Ending Parkinson’s Disease: A Prescription for Action,” took a deep dive into studies focusing on the potential association of TCE and PD and presented seven cases to illustrate the association.
“Like many genetic mutations (e.g., Parkin) and other environmental toxicants ... TCE damages the energy-producing parts of cells, i.e., the mitochondria,” said Dr. Dorsey.
TCE and PCE “likely mediate their toxicity through a common metabolite.” Because both are lipophilic, they “readily distribute in the brain and body tissues and appear to cause mitochondrial dysfunction at high doses,” the researchers hypothesized.
Dopaminergic neurons are particularly sensitive to mitochondrial neurotoxicants, so this might “partially explain the link to PD.”
Animal studies have shown that TCE “caused selective loss of dopaminergic neurons.” Moreover, PD-related neuropathology was found in the substantia nigra of rodents exposed to TCE over time. In addition, studies as early as 1960 were showing an association between TCE and parkinsonism.
The authors describe TCE as “ubiquitous” in the 1970s, with 10 million Americans working with the chemical or other organic solvents daily. The review details an extensive list of industries and occupations in which TCE exposure continues to occur.
People working with TCE might inhale it or touch it; but “millions more encounter the chemical unknowingly through outdoor air, contaminated groundwater, and indoor air pollution.”
They noted that TCE contaminates up to one-third of U.S. drinking water, has polluted the groundwater in more than 20 different countries on five continents, and is found in half of the 1,300 most toxic “Superfund” sites that are “part of a federal clean-up program, including 15 in California’s Silicon Valley, where TCE was used to clean electronics.”
Although the U.S. military stopped using TCE, numerous sites have been contaminated, including Marine Corps Base Camp Lejeune in North Carolina, where TCE and PCE were found in drinking water at 280 times the recommended safety standards.
The researchers highlighted seven cases of individuals who developed PD after likely exposure to TCE, including NBA basketball player Brian Grant, who developed symptoms of PD in 2006 at the age of 34.
Mr. Grant and his family had lived in Camp Lejeune when he was a child, during which time he drank, bathed, and swam in contaminated water, “unaware of its toxicity.” His father also died of esophageal cancer, “which is linked to TCE,” the authors of the study wrote. Mr. Grant has created a foundation to inspire and support patients with PD.
All of the individuals either grew up in or spent time in an area where they were extensively exposed to TCE, PCE, or other chemicals, or experienced occupational exposure.
The authors acknowledged that the role of TCE in PD, as illustrated by the cases, is “far from definitive.” For example, exposure to TCE is often combined with exposure to other toxins, or with unmeasured genetic risk factors.
They highlighted the need for more research and called for cleaning and containing contaminated sites, monitoring TCE levels, and publicly communicating risk and a ban on TCE.
Recall bias?
Commenting for this news organization, Rebecca Gilbert, MD, PhD, chief scientific officer, American Parkinson Disease Association (APDA), noted that the authors “are very frank about the limitations of this approach [illustrative cases] as proof of causation between PD and TCE exposure.”
Another limitation is that TCE exposure is very common, “as argued in the paper.” But “most people with exposure do not develop PD,” Dr. Gilbert pointed out. “By probing the TCE exposure of those who already have PD, there is a danger of recall bias.”
Dr. Gilbert, associate professor of neurology at NYU Langone Health, who was not involved with the study, acknowledged that the authors “present their work as hypothesis and clearly state that more work is needed to understand the connection between TCE and PD.”
In the meantime, however, there are “well-established health risks of TCE exposure, including development of various cancers,” she said. Therefore, the authors’ goals appear to be educating the public about known health risks, working to clean up known sites of contamination, and advocating to ban future use of TCE.
These goals “do not need to wait for [proof of] firm causation between TCE and PD,” she stated.
Dr. Dorsey reported he has received honoraria for speaking at the American Academy of Neurology and at multiple other societies and foundations and has received compensation for consulting services from pharmaceutical companies, foundations, medical education companies, and medical publications; he owns stock in several companies. The other authors’ disclosures can be found in the original paper. Dr. Gilbert is employed by the American Parkinson Disease Association and Bellevue Hospital Center in New York City.
A version of this article first appeared on Medscape.com.
FROM JOURNAL OF PARKINSON’S DISEASE
Physician suicide: Investigating its prevalence and cause
Physicians are admired for their sacrifice and dedication. Yet beneath the surface lies a painful, quiet reality:
The Physicians Foundation says that 55% of physicians know a doctor who considered, attempted, or died by suicide. Doctor’s Burden: Medscape Physician Suicide Report 2023 asked more than 9,000 doctors if they had suicidal thoughts. Nine percent of male physicians and 11% of female physicians said yes.
Why do so many doctors take their own lives?
“It’s not a new phenomenon,” says Rajnish Jaiswal, MD, associate chief of emergency medicine at NYC H+H Metropolitan Hospital and assistant professor of emergency medicine at New York Medical College. “There was a paper 150 years ago, published in England, which commented on the high rates of physician suicides compared to other professionals, and that trend has continued.”
Dr. Jaiswal says that the feeling in the physician community is that the numbers are even higher than what’s reported, unfortunately, which is an opinion echoed by other doctors this news organization spoke with for this story.
A perfect storm
Jodie Eckleberry-Hunt, PhD, a board-certified health psychologist, executive coach, and author, says the most significant culprit historically may be a rigid mindset that many physicians have. “There’s black and white, there’s a right answer and a wrong answer, there’s good and bad, and some physicians have a really hard time flexing,” she says.
Psychological flexibility underlies resilience. Dr. Eckleberry-Hunt says, “Think about your bounce factor and how that resilience is protective. Life isn’t always going to go well. You have to be able to flex and bounce, and some physicians (not all of them, of course) tend to be lower on cognitive flexibility.”
Brad Fern, coach and psychotherapist at Fern Executive and Physician Consulting, Minneapolis, says he uses two analogies that help when he works with physicians. One is the evil twins, and the other is the pressure cooker.
Mr. Fern says that the evil twins are silence and isolation and that several professions, including physicians, fall prey to these. To put any dent in suicidal ideations and suicide, Mr. Fern says, these must be addressed.
“Physicians tend not to talk about what’s bothering them, and that’s for many different reasons. They disproportionally tend to be great at helping other people but not great at receiving help themselves.”
On top of that, there’s a pressure cooker where they work. Mr. Fern doesn’t think anyone would argue that the health care system in the United States is not dysfunctional, at least to some degree. He says that this dysfunction acts like the physicians’ pressure cooker.
Add in circumstances, cultures, and day-to-day issues everyone has, like relational issues, parenting issues, and mental health problems. Then, toss in an individual’s lower resiliency, the inability to receive help, and a predicament for good measure – a loss, a divorce, or financial woes, for instance, which can overwhelm. Mr. Fern says it can be a mathematical equation for suicidal ideation.
Is there a why?
“Some people think there’s a reason for suicide, but often, there’s a spectrum of reasons,” says Mr. Fern. He says that some physicians are trying to escape emotional pain. For others, it can be fear or a revenge thing, like, “the hell with you, I’m going to kill myself.” It can be getting attention the way teens do, as professionals have seen. Then there’s the organic component, like brain trauma, brain imbalance, depression, anxiety, or bipolar disorder. And finally, a drug or alcohol issue.
“But the reason why physician suicide is elevated, I think, is because there’s this ethos around being silent and, ‘I’m going to listen to and solve everyone else’s problems, but I’m not going to reach out and get help for my own,’ ” says Mr. Fern. “If you take advantage of mental health services, you’re implying that you’re mentally ill. And most physicians aren’t going to do that.”
On the positive side, Dr. Eckleberry-Hunt says that she sees many younger physicians discussing trauma. As a result, they’re more open to receiving help than previous generations. She speculates whether physicians have always had trauma from their past and whether current-day issues are now triggering it or whether they have more trauma these days. “Are they talking about it more, or is it experienced more?”
The failure of the system
The building blocks for physician suicide may have been there from the beginning. “From your first day of medical school and throughout your career, there was a very rigid system in place that is quite unforgiving, is quite stressful, and demands a lot,” says Dr. Jaiswal. And it’s within this system that physicians must operate.
“You have all the corporations, entities, organizations, [and] medical societies talking about physician wellness, burnout, and suicide, but the reality is it’s not making that much of a difference,” he says.
In her report, “What I’ve Learned From 1,710 Doctor Suicides,” Pamelia Wible, MD, who runs a physician suicide helpline that physicians can email and get an immediate callback, likens the current system to assembly line medicine.
Dr. Eckleberry-Hunt thinks the message has been bungled in health care. Everyone discusses burnout, meditation, self-care, and other essential constructs. “But we don’t deal with the root cause [of suicide]. Instead, we teach you soothing strategies.”
Further, Dr. Jaiswal says that not all physicians who commit suicide experience burnout or are experiencing burnout and that the vast majority of physicians who experience burnout don’t have suicidal ideation. “In the sense, that ‘let’s address physician burnout and that will hopefully translate to a reduced number of physician suicides’ – there is a very tenuous argument to be made for that because that is just one aspect in this complex system,” he says.
We need more than just lip service on suicide
Overall, the experts interviewed for this article acknowledged that the system is at least talking about physician suicide, which is a big first step. However, most agree that where big health entities go wrong is that they set up wellness or mental health programs, they implement a wellness officer, they write up talking points for physicians who need mental health care to get that care, and they think they’ve done their job, that they’ve done what’s required to address the problem.
But Dr. Jaiswal thinks these are often mostly public-relations rebuttals. Mr. Fern suggests, “It’s a show that’s not effective.” And Dr. Eckleberry-Hunt says that “even if you had a legit, well-funded well-being program for health care providers, you would still have a baseline rate of physician suicide, and that gets down to having drug and alcohol education and talking about having a system for physicians to access that doesn’t come along with insurance billing” – one that doesn’t create a paper trail and follow physician licensure and job applications for the rest of their career; one that doesn’t associate their mental health care with their work institution; one that offers confidentiality.
“For most folks, there is still a big distrust in the system. As physicians, very few of them feel that the system that they’re operating in has their best interest at heart. And that is why very few physicians will self-report any mental health issues, depression, or even ideation to colleagues, superiors, or managers,” says Dr. Jaiswal. Many more feel skeptical about the confidentiality of the programs in place.
The experts acknowledge that many people are trying to work on this and bring about change on multiple levels – grassroots, department levels, state, and federal. “But I think the biggest thing that the system has to do is earn back the trust of the physician,” Dr. Jaiswal adds.
“Physician suicide is a very visible problem in a very broken system. So, it’ll be very difficult in isolation to treat it without making any systemic changes, because that’s happening right now, and it’s not working,” says Dr. Jaiswal.
“The thing that I am most hopeful about is that I am seeing an influx of younger physicians who seek me out, and granted, their training programs tell them to come and see me, but they are ready and willing to talk about their mental health separate from work. They’re not coming in saying, ‘Here are all the people who I blame.’ They’re saying, ‘These are my struggles, and I want to be a better, happier physician,’ ” says Dr. Eckleberry-Hunt.
A version of this article originally appeared on Medscape.com.
Physicians are admired for their sacrifice and dedication. Yet beneath the surface lies a painful, quiet reality:
The Physicians Foundation says that 55% of physicians know a doctor who considered, attempted, or died by suicide. Doctor’s Burden: Medscape Physician Suicide Report 2023 asked more than 9,000 doctors if they had suicidal thoughts. Nine percent of male physicians and 11% of female physicians said yes.
Why do so many doctors take their own lives?
“It’s not a new phenomenon,” says Rajnish Jaiswal, MD, associate chief of emergency medicine at NYC H+H Metropolitan Hospital and assistant professor of emergency medicine at New York Medical College. “There was a paper 150 years ago, published in England, which commented on the high rates of physician suicides compared to other professionals, and that trend has continued.”
Dr. Jaiswal says that the feeling in the physician community is that the numbers are even higher than what’s reported, unfortunately, which is an opinion echoed by other doctors this news organization spoke with for this story.
A perfect storm
Jodie Eckleberry-Hunt, PhD, a board-certified health psychologist, executive coach, and author, says the most significant culprit historically may be a rigid mindset that many physicians have. “There’s black and white, there’s a right answer and a wrong answer, there’s good and bad, and some physicians have a really hard time flexing,” she says.
Psychological flexibility underlies resilience. Dr. Eckleberry-Hunt says, “Think about your bounce factor and how that resilience is protective. Life isn’t always going to go well. You have to be able to flex and bounce, and some physicians (not all of them, of course) tend to be lower on cognitive flexibility.”
Brad Fern, coach and psychotherapist at Fern Executive and Physician Consulting, Minneapolis, says he uses two analogies that help when he works with physicians. One is the evil twins, and the other is the pressure cooker.
Mr. Fern says that the evil twins are silence and isolation and that several professions, including physicians, fall prey to these. To put any dent in suicidal ideations and suicide, Mr. Fern says, these must be addressed.
“Physicians tend not to talk about what’s bothering them, and that’s for many different reasons. They disproportionally tend to be great at helping other people but not great at receiving help themselves.”
On top of that, there’s a pressure cooker where they work. Mr. Fern doesn’t think anyone would argue that the health care system in the United States is not dysfunctional, at least to some degree. He says that this dysfunction acts like the physicians’ pressure cooker.
Add in circumstances, cultures, and day-to-day issues everyone has, like relational issues, parenting issues, and mental health problems. Then, toss in an individual’s lower resiliency, the inability to receive help, and a predicament for good measure – a loss, a divorce, or financial woes, for instance, which can overwhelm. Mr. Fern says it can be a mathematical equation for suicidal ideation.
Is there a why?
“Some people think there’s a reason for suicide, but often, there’s a spectrum of reasons,” says Mr. Fern. He says that some physicians are trying to escape emotional pain. For others, it can be fear or a revenge thing, like, “the hell with you, I’m going to kill myself.” It can be getting attention the way teens do, as professionals have seen. Then there’s the organic component, like brain trauma, brain imbalance, depression, anxiety, or bipolar disorder. And finally, a drug or alcohol issue.
“But the reason why physician suicide is elevated, I think, is because there’s this ethos around being silent and, ‘I’m going to listen to and solve everyone else’s problems, but I’m not going to reach out and get help for my own,’ ” says Mr. Fern. “If you take advantage of mental health services, you’re implying that you’re mentally ill. And most physicians aren’t going to do that.”
On the positive side, Dr. Eckleberry-Hunt says that she sees many younger physicians discussing trauma. As a result, they’re more open to receiving help than previous generations. She speculates whether physicians have always had trauma from their past and whether current-day issues are now triggering it or whether they have more trauma these days. “Are they talking about it more, or is it experienced more?”
The failure of the system
The building blocks for physician suicide may have been there from the beginning. “From your first day of medical school and throughout your career, there was a very rigid system in place that is quite unforgiving, is quite stressful, and demands a lot,” says Dr. Jaiswal. And it’s within this system that physicians must operate.
“You have all the corporations, entities, organizations, [and] medical societies talking about physician wellness, burnout, and suicide, but the reality is it’s not making that much of a difference,” he says.
In her report, “What I’ve Learned From 1,710 Doctor Suicides,” Pamelia Wible, MD, who runs a physician suicide helpline that physicians can email and get an immediate callback, likens the current system to assembly line medicine.
Dr. Eckleberry-Hunt thinks the message has been bungled in health care. Everyone discusses burnout, meditation, self-care, and other essential constructs. “But we don’t deal with the root cause [of suicide]. Instead, we teach you soothing strategies.”
Further, Dr. Jaiswal says that not all physicians who commit suicide experience burnout or are experiencing burnout and that the vast majority of physicians who experience burnout don’t have suicidal ideation. “In the sense, that ‘let’s address physician burnout and that will hopefully translate to a reduced number of physician suicides’ – there is a very tenuous argument to be made for that because that is just one aspect in this complex system,” he says.
We need more than just lip service on suicide
Overall, the experts interviewed for this article acknowledged that the system is at least talking about physician suicide, which is a big first step. However, most agree that where big health entities go wrong is that they set up wellness or mental health programs, they implement a wellness officer, they write up talking points for physicians who need mental health care to get that care, and they think they’ve done their job, that they’ve done what’s required to address the problem.
But Dr. Jaiswal thinks these are often mostly public-relations rebuttals. Mr. Fern suggests, “It’s a show that’s not effective.” And Dr. Eckleberry-Hunt says that “even if you had a legit, well-funded well-being program for health care providers, you would still have a baseline rate of physician suicide, and that gets down to having drug and alcohol education and talking about having a system for physicians to access that doesn’t come along with insurance billing” – one that doesn’t create a paper trail and follow physician licensure and job applications for the rest of their career; one that doesn’t associate their mental health care with their work institution; one that offers confidentiality.
“For most folks, there is still a big distrust in the system. As physicians, very few of them feel that the system that they’re operating in has their best interest at heart. And that is why very few physicians will self-report any mental health issues, depression, or even ideation to colleagues, superiors, or managers,” says Dr. Jaiswal. Many more feel skeptical about the confidentiality of the programs in place.
The experts acknowledge that many people are trying to work on this and bring about change on multiple levels – grassroots, department levels, state, and federal. “But I think the biggest thing that the system has to do is earn back the trust of the physician,” Dr. Jaiswal adds.
“Physician suicide is a very visible problem in a very broken system. So, it’ll be very difficult in isolation to treat it without making any systemic changes, because that’s happening right now, and it’s not working,” says Dr. Jaiswal.
“The thing that I am most hopeful about is that I am seeing an influx of younger physicians who seek me out, and granted, their training programs tell them to come and see me, but they are ready and willing to talk about their mental health separate from work. They’re not coming in saying, ‘Here are all the people who I blame.’ They’re saying, ‘These are my struggles, and I want to be a better, happier physician,’ ” says Dr. Eckleberry-Hunt.
A version of this article originally appeared on Medscape.com.
Physicians are admired for their sacrifice and dedication. Yet beneath the surface lies a painful, quiet reality:
The Physicians Foundation says that 55% of physicians know a doctor who considered, attempted, or died by suicide. Doctor’s Burden: Medscape Physician Suicide Report 2023 asked more than 9,000 doctors if they had suicidal thoughts. Nine percent of male physicians and 11% of female physicians said yes.
Why do so many doctors take their own lives?
“It’s not a new phenomenon,” says Rajnish Jaiswal, MD, associate chief of emergency medicine at NYC H+H Metropolitan Hospital and assistant professor of emergency medicine at New York Medical College. “There was a paper 150 years ago, published in England, which commented on the high rates of physician suicides compared to other professionals, and that trend has continued.”
Dr. Jaiswal says that the feeling in the physician community is that the numbers are even higher than what’s reported, unfortunately, which is an opinion echoed by other doctors this news organization spoke with for this story.
A perfect storm
Jodie Eckleberry-Hunt, PhD, a board-certified health psychologist, executive coach, and author, says the most significant culprit historically may be a rigid mindset that many physicians have. “There’s black and white, there’s a right answer and a wrong answer, there’s good and bad, and some physicians have a really hard time flexing,” she says.
Psychological flexibility underlies resilience. Dr. Eckleberry-Hunt says, “Think about your bounce factor and how that resilience is protective. Life isn’t always going to go well. You have to be able to flex and bounce, and some physicians (not all of them, of course) tend to be lower on cognitive flexibility.”
Brad Fern, coach and psychotherapist at Fern Executive and Physician Consulting, Minneapolis, says he uses two analogies that help when he works with physicians. One is the evil twins, and the other is the pressure cooker.
Mr. Fern says that the evil twins are silence and isolation and that several professions, including physicians, fall prey to these. To put any dent in suicidal ideations and suicide, Mr. Fern says, these must be addressed.
“Physicians tend not to talk about what’s bothering them, and that’s for many different reasons. They disproportionally tend to be great at helping other people but not great at receiving help themselves.”
On top of that, there’s a pressure cooker where they work. Mr. Fern doesn’t think anyone would argue that the health care system in the United States is not dysfunctional, at least to some degree. He says that this dysfunction acts like the physicians’ pressure cooker.
Add in circumstances, cultures, and day-to-day issues everyone has, like relational issues, parenting issues, and mental health problems. Then, toss in an individual’s lower resiliency, the inability to receive help, and a predicament for good measure – a loss, a divorce, or financial woes, for instance, which can overwhelm. Mr. Fern says it can be a mathematical equation for suicidal ideation.
Is there a why?
“Some people think there’s a reason for suicide, but often, there’s a spectrum of reasons,” says Mr. Fern. He says that some physicians are trying to escape emotional pain. For others, it can be fear or a revenge thing, like, “the hell with you, I’m going to kill myself.” It can be getting attention the way teens do, as professionals have seen. Then there’s the organic component, like brain trauma, brain imbalance, depression, anxiety, or bipolar disorder. And finally, a drug or alcohol issue.
“But the reason why physician suicide is elevated, I think, is because there’s this ethos around being silent and, ‘I’m going to listen to and solve everyone else’s problems, but I’m not going to reach out and get help for my own,’ ” says Mr. Fern. “If you take advantage of mental health services, you’re implying that you’re mentally ill. And most physicians aren’t going to do that.”
On the positive side, Dr. Eckleberry-Hunt says that she sees many younger physicians discussing trauma. As a result, they’re more open to receiving help than previous generations. She speculates whether physicians have always had trauma from their past and whether current-day issues are now triggering it or whether they have more trauma these days. “Are they talking about it more, or is it experienced more?”
The failure of the system
The building blocks for physician suicide may have been there from the beginning. “From your first day of medical school and throughout your career, there was a very rigid system in place that is quite unforgiving, is quite stressful, and demands a lot,” says Dr. Jaiswal. And it’s within this system that physicians must operate.
“You have all the corporations, entities, organizations, [and] medical societies talking about physician wellness, burnout, and suicide, but the reality is it’s not making that much of a difference,” he says.
In her report, “What I’ve Learned From 1,710 Doctor Suicides,” Pamelia Wible, MD, who runs a physician suicide helpline that physicians can email and get an immediate callback, likens the current system to assembly line medicine.
Dr. Eckleberry-Hunt thinks the message has been bungled in health care. Everyone discusses burnout, meditation, self-care, and other essential constructs. “But we don’t deal with the root cause [of suicide]. Instead, we teach you soothing strategies.”
Further, Dr. Jaiswal says that not all physicians who commit suicide experience burnout or are experiencing burnout and that the vast majority of physicians who experience burnout don’t have suicidal ideation. “In the sense, that ‘let’s address physician burnout and that will hopefully translate to a reduced number of physician suicides’ – there is a very tenuous argument to be made for that because that is just one aspect in this complex system,” he says.
We need more than just lip service on suicide
Overall, the experts interviewed for this article acknowledged that the system is at least talking about physician suicide, which is a big first step. However, most agree that where big health entities go wrong is that they set up wellness or mental health programs, they implement a wellness officer, they write up talking points for physicians who need mental health care to get that care, and they think they’ve done their job, that they’ve done what’s required to address the problem.
But Dr. Jaiswal thinks these are often mostly public-relations rebuttals. Mr. Fern suggests, “It’s a show that’s not effective.” And Dr. Eckleberry-Hunt says that “even if you had a legit, well-funded well-being program for health care providers, you would still have a baseline rate of physician suicide, and that gets down to having drug and alcohol education and talking about having a system for physicians to access that doesn’t come along with insurance billing” – one that doesn’t create a paper trail and follow physician licensure and job applications for the rest of their career; one that doesn’t associate their mental health care with their work institution; one that offers confidentiality.
“For most folks, there is still a big distrust in the system. As physicians, very few of them feel that the system that they’re operating in has their best interest at heart. And that is why very few physicians will self-report any mental health issues, depression, or even ideation to colleagues, superiors, or managers,” says Dr. Jaiswal. Many more feel skeptical about the confidentiality of the programs in place.
The experts acknowledge that many people are trying to work on this and bring about change on multiple levels – grassroots, department levels, state, and federal. “But I think the biggest thing that the system has to do is earn back the trust of the physician,” Dr. Jaiswal adds.
“Physician suicide is a very visible problem in a very broken system. So, it’ll be very difficult in isolation to treat it without making any systemic changes, because that’s happening right now, and it’s not working,” says Dr. Jaiswal.
“The thing that I am most hopeful about is that I am seeing an influx of younger physicians who seek me out, and granted, their training programs tell them to come and see me, but they are ready and willing to talk about their mental health separate from work. They’re not coming in saying, ‘Here are all the people who I blame.’ They’re saying, ‘These are my struggles, and I want to be a better, happier physician,’ ” says Dr. Eckleberry-Hunt.
A version of this article originally appeared on Medscape.com.
The human-looking robot therapist will coach your well-being now
Do android therapists dream of electric employees?
Robots. It can be tough to remember that, when they’re not dooming humanity to apocalypse or just telling you that you’re doomed, robots have real-world uses. There are actual robots in the world, and they can do things beyond bend girders, sing about science, or run the navy.
Look, we’ll stop with the pop-culture references when pop culture runs out of robots to reference. It may take a while.
Robots are indelibly rooted in the public consciousness, and that plays into our expectations when we encounter a real-life robot. This leads us into a recent study conducted by researchers at the University of Cambridge, who developed a robot-led mental well-being program that a tech company utilized for 4 weeks. Why choose a robot? Well, why spring for a qualified therapist who requires a salary when you could simply get a robot to do the job for free? Get with the capitalist agenda here. Surely it won’t backfire.
The 26 people enrolled in the study received coaching from one of two robots, both programmed identically to act like mental health coaches, based on interviews with human therapists. Both acted identically and had identical expressions. The only difference between the two was their appearance. QTRobot was nearly a meter tall and looked like a human child; Misty II was much smaller and looked like a toy.
People who received coaching from Misty II were better able to connect and had a better experience than those who received coaching from QTRobot. According to those in the QTRobot group, their expectations didn’t match reality. The robots are good coaches, but they don’t act human. This wasn’t a problem for Misty II, since it doesn’t look human, but for QTRobot, the participants were expecting “to hell with our orders,” but received “Daisy, Daisy, give me your answer do.” When you’ve been programmed to think of robots as metal humans, it can be off-putting to see them act as, well, robots.
That said, all participants found the exercises helpful and were open to receiving more robot-led therapy in the future. And while we’re sure the technology will advance to make robot therapists more empathetic and more human, hopefully scientists won’t go too far. We don’t need depressed robots.
Birthing experience is all in the mindset
Alexa, play Peer Gynt Suite No. 1, Op. 46 - I. Morning Mood.
Birth.
Giving birth is a common experience for many, if not most, female mammals, but wanting it to be a pleasurable one seems distinctly human. There are many methods and practices that may make giving birth an easier and enjoyable experience for the mother, but a new study suggests that the key could be in her mind.
The mindset of the expectant mother during pregnancy, it seems, has some effect on how smooth or intervention-filled delivery is. If the mothers saw their experience as a natural process, they were less likely to need pain medication or a C-section, but mothers who viewed the experience as more of a “medical procedure” were more likely to require more medical supervision and intervention, according to investigators from the University of Bonn (Germany).
Now, the researchers wanted to be super clear in saying that there’s no right or wrong mindset to have. They just focused on the outcomes of those mindsets and whether they actually do have some effect on occurrences.
Apparently, yes.
“Mindsets can be understood as a kind of mental lense that guide our perception of the world around us and can influence our behavior,” Dr. Lisa Hoffmann said in a statement from the university. “The study highlights the importance of psychological factors in childbirth.”
The researchers surveyed 300 women with an online tool before and after delivery and found the effects of the natural process mindset lingered even after giving birth. They had lower rates of depression and posttraumatic stress, which may have a snowballing effect on mother-child bonding after childbirth.
Preparation for the big day, then, should be about more than gathering diapers and shopping for car seats. Women should prepare their minds as well. If it’s going to make giving birth better, why not?
Becoming a parent is going to create a psychological shift, no matter how you slice it.
Giant inflatable colon reported in Utah
Do not be alarmed! Yes, there is a giant inflatable colon currently at large in the Beehive State, but it will not harm you. The giant inflatable colon is in Utah as part of Intermountain Health’s “Let’s get to the bottom of colon cancer tour” and he only wants to help you.
The giant inflatable colon, whose name happens to be Collin, is 12 feet long and weighs 113 pounds. March is Colon Cancer Awareness Month, so Collin is traveling around Utah and Idaho to raise awareness about colon cancer and the various screening options. He is not going to change local weather patterns, eat small children, or take over local governments and raise your taxes.
Instead, Collin is planning to display “portions of a healthy colon, polyps or bumps on the colon, malignant polyps which look more vascular and have more redness, cancerous cells, advanced cancer cells, and Crohn’s disease,” KSL.com said.
Collin the colon is on loan to Intermountain Health from medical device manufacturer Boston Scientific and will be traveling to Spanish Fork, Provo, and Ogden, among other locations in Utah, as well as Burley and Meridian, Idaho, in the coming days.
Collin the colon’s participation in the tour has created some serious buzz in the Colin/Collin community:
- Colin Powell (four-star general and Secretary of State): “Back then, the second-most important topic among the Joint Chiefs of Staff was colon cancer screening. And the Navy guy – I can’t remember his name – was a huge fan of giant inflatable organs.”
- Colin Jost (comedian and Saturday Night Live “Weekend Update” cohost): “He’s funnier than Tucker Carlson and Pete Davidson combined.”
Do android therapists dream of electric employees?
Robots. It can be tough to remember that, when they’re not dooming humanity to apocalypse or just telling you that you’re doomed, robots have real-world uses. There are actual robots in the world, and they can do things beyond bend girders, sing about science, or run the navy.
Look, we’ll stop with the pop-culture references when pop culture runs out of robots to reference. It may take a while.
Robots are indelibly rooted in the public consciousness, and that plays into our expectations when we encounter a real-life robot. This leads us into a recent study conducted by researchers at the University of Cambridge, who developed a robot-led mental well-being program that a tech company utilized for 4 weeks. Why choose a robot? Well, why spring for a qualified therapist who requires a salary when you could simply get a robot to do the job for free? Get with the capitalist agenda here. Surely it won’t backfire.
The 26 people enrolled in the study received coaching from one of two robots, both programmed identically to act like mental health coaches, based on interviews with human therapists. Both acted identically and had identical expressions. The only difference between the two was their appearance. QTRobot was nearly a meter tall and looked like a human child; Misty II was much smaller and looked like a toy.
People who received coaching from Misty II were better able to connect and had a better experience than those who received coaching from QTRobot. According to those in the QTRobot group, their expectations didn’t match reality. The robots are good coaches, but they don’t act human. This wasn’t a problem for Misty II, since it doesn’t look human, but for QTRobot, the participants were expecting “to hell with our orders,” but received “Daisy, Daisy, give me your answer do.” When you’ve been programmed to think of robots as metal humans, it can be off-putting to see them act as, well, robots.
That said, all participants found the exercises helpful and were open to receiving more robot-led therapy in the future. And while we’re sure the technology will advance to make robot therapists more empathetic and more human, hopefully scientists won’t go too far. We don’t need depressed robots.
Birthing experience is all in the mindset
Alexa, play Peer Gynt Suite No. 1, Op. 46 - I. Morning Mood.
Birth.
Giving birth is a common experience for many, if not most, female mammals, but wanting it to be a pleasurable one seems distinctly human. There are many methods and practices that may make giving birth an easier and enjoyable experience for the mother, but a new study suggests that the key could be in her mind.
The mindset of the expectant mother during pregnancy, it seems, has some effect on how smooth or intervention-filled delivery is. If the mothers saw their experience as a natural process, they were less likely to need pain medication or a C-section, but mothers who viewed the experience as more of a “medical procedure” were more likely to require more medical supervision and intervention, according to investigators from the University of Bonn (Germany).
Now, the researchers wanted to be super clear in saying that there’s no right or wrong mindset to have. They just focused on the outcomes of those mindsets and whether they actually do have some effect on occurrences.
Apparently, yes.
“Mindsets can be understood as a kind of mental lense that guide our perception of the world around us and can influence our behavior,” Dr. Lisa Hoffmann said in a statement from the university. “The study highlights the importance of psychological factors in childbirth.”
The researchers surveyed 300 women with an online tool before and after delivery and found the effects of the natural process mindset lingered even after giving birth. They had lower rates of depression and posttraumatic stress, which may have a snowballing effect on mother-child bonding after childbirth.
Preparation for the big day, then, should be about more than gathering diapers and shopping for car seats. Women should prepare their minds as well. If it’s going to make giving birth better, why not?
Becoming a parent is going to create a psychological shift, no matter how you slice it.
Giant inflatable colon reported in Utah
Do not be alarmed! Yes, there is a giant inflatable colon currently at large in the Beehive State, but it will not harm you. The giant inflatable colon is in Utah as part of Intermountain Health’s “Let’s get to the bottom of colon cancer tour” and he only wants to help you.
The giant inflatable colon, whose name happens to be Collin, is 12 feet long and weighs 113 pounds. March is Colon Cancer Awareness Month, so Collin is traveling around Utah and Idaho to raise awareness about colon cancer and the various screening options. He is not going to change local weather patterns, eat small children, or take over local governments and raise your taxes.
Instead, Collin is planning to display “portions of a healthy colon, polyps or bumps on the colon, malignant polyps which look more vascular and have more redness, cancerous cells, advanced cancer cells, and Crohn’s disease,” KSL.com said.
Collin the colon is on loan to Intermountain Health from medical device manufacturer Boston Scientific and will be traveling to Spanish Fork, Provo, and Ogden, among other locations in Utah, as well as Burley and Meridian, Idaho, in the coming days.
Collin the colon’s participation in the tour has created some serious buzz in the Colin/Collin community:
- Colin Powell (four-star general and Secretary of State): “Back then, the second-most important topic among the Joint Chiefs of Staff was colon cancer screening. And the Navy guy – I can’t remember his name – was a huge fan of giant inflatable organs.”
- Colin Jost (comedian and Saturday Night Live “Weekend Update” cohost): “He’s funnier than Tucker Carlson and Pete Davidson combined.”
Do android therapists dream of electric employees?
Robots. It can be tough to remember that, when they’re not dooming humanity to apocalypse or just telling you that you’re doomed, robots have real-world uses. There are actual robots in the world, and they can do things beyond bend girders, sing about science, or run the navy.
Look, we’ll stop with the pop-culture references when pop culture runs out of robots to reference. It may take a while.
Robots are indelibly rooted in the public consciousness, and that plays into our expectations when we encounter a real-life robot. This leads us into a recent study conducted by researchers at the University of Cambridge, who developed a robot-led mental well-being program that a tech company utilized for 4 weeks. Why choose a robot? Well, why spring for a qualified therapist who requires a salary when you could simply get a robot to do the job for free? Get with the capitalist agenda here. Surely it won’t backfire.
The 26 people enrolled in the study received coaching from one of two robots, both programmed identically to act like mental health coaches, based on interviews with human therapists. Both acted identically and had identical expressions. The only difference between the two was their appearance. QTRobot was nearly a meter tall and looked like a human child; Misty II was much smaller and looked like a toy.
People who received coaching from Misty II were better able to connect and had a better experience than those who received coaching from QTRobot. According to those in the QTRobot group, their expectations didn’t match reality. The robots are good coaches, but they don’t act human. This wasn’t a problem for Misty II, since it doesn’t look human, but for QTRobot, the participants were expecting “to hell with our orders,” but received “Daisy, Daisy, give me your answer do.” When you’ve been programmed to think of robots as metal humans, it can be off-putting to see them act as, well, robots.
That said, all participants found the exercises helpful and were open to receiving more robot-led therapy in the future. And while we’re sure the technology will advance to make robot therapists more empathetic and more human, hopefully scientists won’t go too far. We don’t need depressed robots.
Birthing experience is all in the mindset
Alexa, play Peer Gynt Suite No. 1, Op. 46 - I. Morning Mood.
Birth.
Giving birth is a common experience for many, if not most, female mammals, but wanting it to be a pleasurable one seems distinctly human. There are many methods and practices that may make giving birth an easier and enjoyable experience for the mother, but a new study suggests that the key could be in her mind.
The mindset of the expectant mother during pregnancy, it seems, has some effect on how smooth or intervention-filled delivery is. If the mothers saw their experience as a natural process, they were less likely to need pain medication or a C-section, but mothers who viewed the experience as more of a “medical procedure” were more likely to require more medical supervision and intervention, according to investigators from the University of Bonn (Germany).
Now, the researchers wanted to be super clear in saying that there’s no right or wrong mindset to have. They just focused on the outcomes of those mindsets and whether they actually do have some effect on occurrences.
Apparently, yes.
“Mindsets can be understood as a kind of mental lense that guide our perception of the world around us and can influence our behavior,” Dr. Lisa Hoffmann said in a statement from the university. “The study highlights the importance of psychological factors in childbirth.”
The researchers surveyed 300 women with an online tool before and after delivery and found the effects of the natural process mindset lingered even after giving birth. They had lower rates of depression and posttraumatic stress, which may have a snowballing effect on mother-child bonding after childbirth.
Preparation for the big day, then, should be about more than gathering diapers and shopping for car seats. Women should prepare their minds as well. If it’s going to make giving birth better, why not?
Becoming a parent is going to create a psychological shift, no matter how you slice it.
Giant inflatable colon reported in Utah
Do not be alarmed! Yes, there is a giant inflatable colon currently at large in the Beehive State, but it will not harm you. The giant inflatable colon is in Utah as part of Intermountain Health’s “Let’s get to the bottom of colon cancer tour” and he only wants to help you.
The giant inflatable colon, whose name happens to be Collin, is 12 feet long and weighs 113 pounds. March is Colon Cancer Awareness Month, so Collin is traveling around Utah and Idaho to raise awareness about colon cancer and the various screening options. He is not going to change local weather patterns, eat small children, or take over local governments and raise your taxes.
Instead, Collin is planning to display “portions of a healthy colon, polyps or bumps on the colon, malignant polyps which look more vascular and have more redness, cancerous cells, advanced cancer cells, and Crohn’s disease,” KSL.com said.
Collin the colon is on loan to Intermountain Health from medical device manufacturer Boston Scientific and will be traveling to Spanish Fork, Provo, and Ogden, among other locations in Utah, as well as Burley and Meridian, Idaho, in the coming days.
Collin the colon’s participation in the tour has created some serious buzz in the Colin/Collin community:
- Colin Powell (four-star general and Secretary of State): “Back then, the second-most important topic among the Joint Chiefs of Staff was colon cancer screening. And the Navy guy – I can’t remember his name – was a huge fan of giant inflatable organs.”
- Colin Jost (comedian and Saturday Night Live “Weekend Update” cohost): “He’s funnier than Tucker Carlson and Pete Davidson combined.”
FDA OKs first drug for Rett syndrome
Rett syndrome is a rare, genetic neurodevelopmental disorder that affects about 6,000-9,000 people in the United States, mostly females.
Symptoms typically present between 6 and 18 months of age, with patients experiencing a rapid decline with loss of fine motor and communication skills.
Trofinetide is a synthetic analogue of the amino-terminal tripeptide of insulinlike growth factor-1 (IGF-1), which occurs naturally in the brain. The drug is designed to treat the core symptoms of Rett syndrome by potentially reducing neuroinflammation and supporting synaptic function.
The approval of trofinetide was supported by results from the pivotal phase 3 LAVENDER study that tested the efficacy and safety of trofinetide vs. placebo in 187 female patients with Rett syndrome, aged 5-20 years.
A total of 93 participants were randomly assigned to twice-daily oral trofinetide, and 94 received placebo for 12 weeks.
After 12 weeks, trofinetide showed a statistically significant improvement from baseline, compared with placebo, on both the caregiver-assessed Rett Syndrome Behavior Questionnaire (RSBQ) and 7-point Clinical Global Impression-Improvement (CGI-I) scale.
The drug also outperformed placebo at 12 weeks in a key secondary endpoint: the composite score on the Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist-Social (CSBS-DP-IT Social), a scale on which caregivers assess nonverbal communication.
The most common adverse events with trofinetide treatment were diarrhea and vomiting. Almost all these events were considered mild or moderate.
‘Historic day’
“This is a historic day for the Rett syndrome community and a meaningful moment for the patients and caregivers who have eagerly awaited the arrival of an approved treatment for this condition,” Melissa Kennedy, MHA, chief executive officer of the International Rett Syndrome Foundation, said in a news release issued by Acadia.
“Rett syndrome is a complicated, devastating disease that affects not only the individual patient, but whole families. With today’s FDA decision, those impacted by Rett have a promising new treatment option that has demonstrated benefit across a variety of Rett symptoms, including those that impact the daily lives of those living with Rett and their loved ones,” Ms. Kennedy said.
Trofinetide is expected to be available in the United States by the end of April.
A version of this article first appeared on Medscape.com.
Rett syndrome is a rare, genetic neurodevelopmental disorder that affects about 6,000-9,000 people in the United States, mostly females.
Symptoms typically present between 6 and 18 months of age, with patients experiencing a rapid decline with loss of fine motor and communication skills.
Trofinetide is a synthetic analogue of the amino-terminal tripeptide of insulinlike growth factor-1 (IGF-1), which occurs naturally in the brain. The drug is designed to treat the core symptoms of Rett syndrome by potentially reducing neuroinflammation and supporting synaptic function.
The approval of trofinetide was supported by results from the pivotal phase 3 LAVENDER study that tested the efficacy and safety of trofinetide vs. placebo in 187 female patients with Rett syndrome, aged 5-20 years.
A total of 93 participants were randomly assigned to twice-daily oral trofinetide, and 94 received placebo for 12 weeks.
After 12 weeks, trofinetide showed a statistically significant improvement from baseline, compared with placebo, on both the caregiver-assessed Rett Syndrome Behavior Questionnaire (RSBQ) and 7-point Clinical Global Impression-Improvement (CGI-I) scale.
The drug also outperformed placebo at 12 weeks in a key secondary endpoint: the composite score on the Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist-Social (CSBS-DP-IT Social), a scale on which caregivers assess nonverbal communication.
The most common adverse events with trofinetide treatment were diarrhea and vomiting. Almost all these events were considered mild or moderate.
‘Historic day’
“This is a historic day for the Rett syndrome community and a meaningful moment for the patients and caregivers who have eagerly awaited the arrival of an approved treatment for this condition,” Melissa Kennedy, MHA, chief executive officer of the International Rett Syndrome Foundation, said in a news release issued by Acadia.
“Rett syndrome is a complicated, devastating disease that affects not only the individual patient, but whole families. With today’s FDA decision, those impacted by Rett have a promising new treatment option that has demonstrated benefit across a variety of Rett symptoms, including those that impact the daily lives of those living with Rett and their loved ones,” Ms. Kennedy said.
Trofinetide is expected to be available in the United States by the end of April.
A version of this article first appeared on Medscape.com.
Rett syndrome is a rare, genetic neurodevelopmental disorder that affects about 6,000-9,000 people in the United States, mostly females.
Symptoms typically present between 6 and 18 months of age, with patients experiencing a rapid decline with loss of fine motor and communication skills.
Trofinetide is a synthetic analogue of the amino-terminal tripeptide of insulinlike growth factor-1 (IGF-1), which occurs naturally in the brain. The drug is designed to treat the core symptoms of Rett syndrome by potentially reducing neuroinflammation and supporting synaptic function.
The approval of trofinetide was supported by results from the pivotal phase 3 LAVENDER study that tested the efficacy and safety of trofinetide vs. placebo in 187 female patients with Rett syndrome, aged 5-20 years.
A total of 93 participants were randomly assigned to twice-daily oral trofinetide, and 94 received placebo for 12 weeks.
After 12 weeks, trofinetide showed a statistically significant improvement from baseline, compared with placebo, on both the caregiver-assessed Rett Syndrome Behavior Questionnaire (RSBQ) and 7-point Clinical Global Impression-Improvement (CGI-I) scale.
The drug also outperformed placebo at 12 weeks in a key secondary endpoint: the composite score on the Communication and Symbolic Behavior Scales Developmental Profile Infant-Toddler Checklist-Social (CSBS-DP-IT Social), a scale on which caregivers assess nonverbal communication.
The most common adverse events with trofinetide treatment were diarrhea and vomiting. Almost all these events were considered mild or moderate.
‘Historic day’
“This is a historic day for the Rett syndrome community and a meaningful moment for the patients and caregivers who have eagerly awaited the arrival of an approved treatment for this condition,” Melissa Kennedy, MHA, chief executive officer of the International Rett Syndrome Foundation, said in a news release issued by Acadia.
“Rett syndrome is a complicated, devastating disease that affects not only the individual patient, but whole families. With today’s FDA decision, those impacted by Rett have a promising new treatment option that has demonstrated benefit across a variety of Rett symptoms, including those that impact the daily lives of those living with Rett and their loved ones,” Ms. Kennedy said.
Trofinetide is expected to be available in the United States by the end of April.
A version of this article first appeared on Medscape.com.
Can particles in dairy and beef cause cancer and MS?
In Western diets, dairy and beef are ubiquitous: Milk goes with coffee, melted cheese with pizza, and chili with rice. But what if dairy products and beef contained a new kind of pathogen that could infect you as a child and trigger cancer or multiple sclerosis (MS) 40-70 years later?
However, in two joint statements, the German Federal Institute for Risk Assessment (BfR) and the Max Rubner Institute (MRI) have rejected such theories.
In 2008, Harald zur Hausen, MD, DSc, received the Nobel Prize in Medicine for his discovery that human papillomaviruses cause cervical cancer. His starting point was the observation that sexually abstinent women, such as nuns, rarely develop this cancer. So it was possible to draw the conclusion that pathogens are transmitted during sexual intercourse, explain Dr. zur Hausen and his wife Ethel-Michele de Villiers, PhD, both of DKFZ Heidelberg.
Papillomaviruses, as well as human herpes and Epstein-Barr viruses (EBV), polyomaviruses, and retroviruses, cause cancer in a direct way: by inserting their genes into the DNA of human cells. With a latency of a few years to a few decades, the proteins formed through expression stimulate malignant growth by altering the regulating host gene.
Acid radicals
However, viruses – just like bacteria and parasites – can also indirectly trigger cancer. One mechanism for this triggering is the disruption of immune defenses, as shown by the sometimes drastically increased tumor incidence with AIDS or with immunosuppressants after transplants. Chronic inflammation is a second mechanism that generates acid radicals and thereby causes random mutations in replicating cells. Examples include stomach cancer caused by Helicobacter pylori and liver cancer caused by Schistosoma, liver fluke, and hepatitis B and C viruses.
According to Dr. de Villiers and Dr. zur Hausen, there are good reasons to believe that other pathogens could cause chronic inflammation and thereby lead to cancer. Epidemiologic data suggest that dairy and meat products from European cows (Bos taurus) are a potential source. This is because colon cancer and breast cancer commonly occur in places where these foods are heavily consumed (that is, in North America, Argentina, Europe, and Australia). In contrast, the rate is low in India, where cows are revered as holy animals. Also noteworthy is that women with a lactose intolerance rarely develop breast cancer.
Viral progeny
In fact, the researchers found single-stranded DNA rings that originated in viruses, which they named bovine meat and milk factors (BMMF), in the intestines of patients with colon cancer. They reported, “This new class of pathogen deserves, in our opinion at least, to become the focus of cancer development and further chronic diseases.” They also detected elevated levels of acid radicals in these areas (that is, oxidative stress), which is typical for chronic inflammation.
The researchers assume that infants, whose immune system is not yet fully matured, ingest the BMMF as soon as they have dairy. Therefore, there is no need for adults to avoid dairy or beef because everyone is infected anyway, said Dr. zur Hausen.
‘Breast milk is healthy’
Dr. De Villiers and Dr. zur Hausen outlined more evidence of cancer-triggering pathogens. Mothers who have breastfed are less likely, especially after multiple pregnancies, to develop tumors in various organs or to have MS and type 2 diabetes. The authors attribute the protective effect to oligosaccharides in breast milk, which begin to be formed midway through the pregnancy. They bind to lectin receptors and, in so doing, mask the terminal molecule onto which the viruses need to dock. As a result, their port of entry into the cells is blocked.
The oligosaccharides also protect the baby against life-threatening infections by blocking access by rotaviruses and noroviruses. In this way, especially if breastfeeding lasts a long time – around 1 year – the period of incomplete immunocompetence is bridged.
Colon cancer
To date, it has been assumed that around 20% of all cancerous diseases globally are caused by infections, said the researchers. But if the suspected BMMF cases are included, this figure rises to 50%, even to around 80%, for colon cancer. If the suspicion is confirmed, the consequences for prevention and therapy would be significant.
The voice of a Nobel prize winner undoubtedly carries weight, but at the time, Dr. zur Hausen still had to convince a host of skeptics with his discovery that a viral infection is a major cause of cervical cancer. Nonetheless, some indicators suggest that he and his wife have found a dead end this time.
Institutional skepticism
When his working group made the results public in February 2019, the DKFZ felt the need to give an all-clear signal in response to alarmed press reports. There is no reason to see dairy and meat consumption as something negative. Similarly, in their first joint statement, the BfR and the MRI judged the data to be insufficient and called for further studies. Multiple research teams began to focus on BMMF as a result. In what foods can they be found? Are they more common in patients with cancer than in healthy people? Are they infectious? Do they cause inflammation and cancer?
The findings presented in a second statement by the BfR and MRI at the end of November 2022 contradicted the claims made by the DKFZ scientists across the board. In no way do BMMF represent new pathogens. They are variants of already known DNA sequences. In addition, they are present in numerous animal-based and plant-based foods, including pork, fish, fruit, vegetables, and nuts.
BMMF do not possess the ability to infect human cells, the institutes said. The proof that they are damaging to one’s health was also absent. It is true that the incidence of intestinal tumors correlates positively with the consumption of red and processed meat – which in no way signifies causality – but dairy products are linked to a reduced risk. On the other hand, breast cancer cannot be associated with the consumption of beef or dairy.
Therefore, both institutes recommend continuing to use these products as supplementary diet for infants because of their micronutrients. They further stated that the products are safe for people of all ages.
Association with MS?
Unperturbed, Dr. de Villiers and Dr. zur Hausen went one step further in their current article. They posited that MS is also associated with the consumption of dairy products and beef. Here too geographic distribution prompted the idea to look for BMMF in the brain lesions of patients with MS. The researchers isolated ring-shaped DNA molecules that proved to be closely related to BMMF from dairy and cattle blood. “The result was electrifying for us.”
However, there are several other factors to consider, such as vitamin D3 deficiency. This is because the incidence of MS decreases the further you travel from the poles toward the equator (that is, as solar radiation increases). Also, EBV clearly plays a role because patients with MS display increased titers of EBV antibodies. One study also showed that people in Antarctica excreted reactivated EBV in their saliva during winter and that vitamin D3 stopped the viral secretion.
Under these conditions, the researchers hypothesized that MS is caused by a double infection of brain cells by EBV and BMMF. EBV is reactivated by a lack of vitamin D3, and the BMMF multiply and are eventually converted into proteins. A focal immunoreaction causes the Schwann cells and oligodendrocytes to malfunction, which leads to the destruction of the myelin sheaths around the nerve fibers.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
In Western diets, dairy and beef are ubiquitous: Milk goes with coffee, melted cheese with pizza, and chili with rice. But what if dairy products and beef contained a new kind of pathogen that could infect you as a child and trigger cancer or multiple sclerosis (MS) 40-70 years later?
However, in two joint statements, the German Federal Institute for Risk Assessment (BfR) and the Max Rubner Institute (MRI) have rejected such theories.
In 2008, Harald zur Hausen, MD, DSc, received the Nobel Prize in Medicine for his discovery that human papillomaviruses cause cervical cancer. His starting point was the observation that sexually abstinent women, such as nuns, rarely develop this cancer. So it was possible to draw the conclusion that pathogens are transmitted during sexual intercourse, explain Dr. zur Hausen and his wife Ethel-Michele de Villiers, PhD, both of DKFZ Heidelberg.
Papillomaviruses, as well as human herpes and Epstein-Barr viruses (EBV), polyomaviruses, and retroviruses, cause cancer in a direct way: by inserting their genes into the DNA of human cells. With a latency of a few years to a few decades, the proteins formed through expression stimulate malignant growth by altering the regulating host gene.
Acid radicals
However, viruses – just like bacteria and parasites – can also indirectly trigger cancer. One mechanism for this triggering is the disruption of immune defenses, as shown by the sometimes drastically increased tumor incidence with AIDS or with immunosuppressants after transplants. Chronic inflammation is a second mechanism that generates acid radicals and thereby causes random mutations in replicating cells. Examples include stomach cancer caused by Helicobacter pylori and liver cancer caused by Schistosoma, liver fluke, and hepatitis B and C viruses.
According to Dr. de Villiers and Dr. zur Hausen, there are good reasons to believe that other pathogens could cause chronic inflammation and thereby lead to cancer. Epidemiologic data suggest that dairy and meat products from European cows (Bos taurus) are a potential source. This is because colon cancer and breast cancer commonly occur in places where these foods are heavily consumed (that is, in North America, Argentina, Europe, and Australia). In contrast, the rate is low in India, where cows are revered as holy animals. Also noteworthy is that women with a lactose intolerance rarely develop breast cancer.
Viral progeny
In fact, the researchers found single-stranded DNA rings that originated in viruses, which they named bovine meat and milk factors (BMMF), in the intestines of patients with colon cancer. They reported, “This new class of pathogen deserves, in our opinion at least, to become the focus of cancer development and further chronic diseases.” They also detected elevated levels of acid radicals in these areas (that is, oxidative stress), which is typical for chronic inflammation.
The researchers assume that infants, whose immune system is not yet fully matured, ingest the BMMF as soon as they have dairy. Therefore, there is no need for adults to avoid dairy or beef because everyone is infected anyway, said Dr. zur Hausen.
‘Breast milk is healthy’
Dr. De Villiers and Dr. zur Hausen outlined more evidence of cancer-triggering pathogens. Mothers who have breastfed are less likely, especially after multiple pregnancies, to develop tumors in various organs or to have MS and type 2 diabetes. The authors attribute the protective effect to oligosaccharides in breast milk, which begin to be formed midway through the pregnancy. They bind to lectin receptors and, in so doing, mask the terminal molecule onto which the viruses need to dock. As a result, their port of entry into the cells is blocked.
The oligosaccharides also protect the baby against life-threatening infections by blocking access by rotaviruses and noroviruses. In this way, especially if breastfeeding lasts a long time – around 1 year – the period of incomplete immunocompetence is bridged.
Colon cancer
To date, it has been assumed that around 20% of all cancerous diseases globally are caused by infections, said the researchers. But if the suspected BMMF cases are included, this figure rises to 50%, even to around 80%, for colon cancer. If the suspicion is confirmed, the consequences for prevention and therapy would be significant.
The voice of a Nobel prize winner undoubtedly carries weight, but at the time, Dr. zur Hausen still had to convince a host of skeptics with his discovery that a viral infection is a major cause of cervical cancer. Nonetheless, some indicators suggest that he and his wife have found a dead end this time.
Institutional skepticism
When his working group made the results public in February 2019, the DKFZ felt the need to give an all-clear signal in response to alarmed press reports. There is no reason to see dairy and meat consumption as something negative. Similarly, in their first joint statement, the BfR and the MRI judged the data to be insufficient and called for further studies. Multiple research teams began to focus on BMMF as a result. In what foods can they be found? Are they more common in patients with cancer than in healthy people? Are they infectious? Do they cause inflammation and cancer?
The findings presented in a second statement by the BfR and MRI at the end of November 2022 contradicted the claims made by the DKFZ scientists across the board. In no way do BMMF represent new pathogens. They are variants of already known DNA sequences. In addition, they are present in numerous animal-based and plant-based foods, including pork, fish, fruit, vegetables, and nuts.
BMMF do not possess the ability to infect human cells, the institutes said. The proof that they are damaging to one’s health was also absent. It is true that the incidence of intestinal tumors correlates positively with the consumption of red and processed meat – which in no way signifies causality – but dairy products are linked to a reduced risk. On the other hand, breast cancer cannot be associated with the consumption of beef or dairy.
Therefore, both institutes recommend continuing to use these products as supplementary diet for infants because of their micronutrients. They further stated that the products are safe for people of all ages.
Association with MS?
Unperturbed, Dr. de Villiers and Dr. zur Hausen went one step further in their current article. They posited that MS is also associated with the consumption of dairy products and beef. Here too geographic distribution prompted the idea to look for BMMF in the brain lesions of patients with MS. The researchers isolated ring-shaped DNA molecules that proved to be closely related to BMMF from dairy and cattle blood. “The result was electrifying for us.”
However, there are several other factors to consider, such as vitamin D3 deficiency. This is because the incidence of MS decreases the further you travel from the poles toward the equator (that is, as solar radiation increases). Also, EBV clearly plays a role because patients with MS display increased titers of EBV antibodies. One study also showed that people in Antarctica excreted reactivated EBV in their saliva during winter and that vitamin D3 stopped the viral secretion.
Under these conditions, the researchers hypothesized that MS is caused by a double infection of brain cells by EBV and BMMF. EBV is reactivated by a lack of vitamin D3, and the BMMF multiply and are eventually converted into proteins. A focal immunoreaction causes the Schwann cells and oligodendrocytes to malfunction, which leads to the destruction of the myelin sheaths around the nerve fibers.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
In Western diets, dairy and beef are ubiquitous: Milk goes with coffee, melted cheese with pizza, and chili with rice. But what if dairy products and beef contained a new kind of pathogen that could infect you as a child and trigger cancer or multiple sclerosis (MS) 40-70 years later?
However, in two joint statements, the German Federal Institute for Risk Assessment (BfR) and the Max Rubner Institute (MRI) have rejected such theories.
In 2008, Harald zur Hausen, MD, DSc, received the Nobel Prize in Medicine for his discovery that human papillomaviruses cause cervical cancer. His starting point was the observation that sexually abstinent women, such as nuns, rarely develop this cancer. So it was possible to draw the conclusion that pathogens are transmitted during sexual intercourse, explain Dr. zur Hausen and his wife Ethel-Michele de Villiers, PhD, both of DKFZ Heidelberg.
Papillomaviruses, as well as human herpes and Epstein-Barr viruses (EBV), polyomaviruses, and retroviruses, cause cancer in a direct way: by inserting their genes into the DNA of human cells. With a latency of a few years to a few decades, the proteins formed through expression stimulate malignant growth by altering the regulating host gene.
Acid radicals
However, viruses – just like bacteria and parasites – can also indirectly trigger cancer. One mechanism for this triggering is the disruption of immune defenses, as shown by the sometimes drastically increased tumor incidence with AIDS or with immunosuppressants after transplants. Chronic inflammation is a second mechanism that generates acid radicals and thereby causes random mutations in replicating cells. Examples include stomach cancer caused by Helicobacter pylori and liver cancer caused by Schistosoma, liver fluke, and hepatitis B and C viruses.
According to Dr. de Villiers and Dr. zur Hausen, there are good reasons to believe that other pathogens could cause chronic inflammation and thereby lead to cancer. Epidemiologic data suggest that dairy and meat products from European cows (Bos taurus) are a potential source. This is because colon cancer and breast cancer commonly occur in places where these foods are heavily consumed (that is, in North America, Argentina, Europe, and Australia). In contrast, the rate is low in India, where cows are revered as holy animals. Also noteworthy is that women with a lactose intolerance rarely develop breast cancer.
Viral progeny
In fact, the researchers found single-stranded DNA rings that originated in viruses, which they named bovine meat and milk factors (BMMF), in the intestines of patients with colon cancer. They reported, “This new class of pathogen deserves, in our opinion at least, to become the focus of cancer development and further chronic diseases.” They also detected elevated levels of acid radicals in these areas (that is, oxidative stress), which is typical for chronic inflammation.
The researchers assume that infants, whose immune system is not yet fully matured, ingest the BMMF as soon as they have dairy. Therefore, there is no need for adults to avoid dairy or beef because everyone is infected anyway, said Dr. zur Hausen.
‘Breast milk is healthy’
Dr. De Villiers and Dr. zur Hausen outlined more evidence of cancer-triggering pathogens. Mothers who have breastfed are less likely, especially after multiple pregnancies, to develop tumors in various organs or to have MS and type 2 diabetes. The authors attribute the protective effect to oligosaccharides in breast milk, which begin to be formed midway through the pregnancy. They bind to lectin receptors and, in so doing, mask the terminal molecule onto which the viruses need to dock. As a result, their port of entry into the cells is blocked.
The oligosaccharides also protect the baby against life-threatening infections by blocking access by rotaviruses and noroviruses. In this way, especially if breastfeeding lasts a long time – around 1 year – the period of incomplete immunocompetence is bridged.
Colon cancer
To date, it has been assumed that around 20% of all cancerous diseases globally are caused by infections, said the researchers. But if the suspected BMMF cases are included, this figure rises to 50%, even to around 80%, for colon cancer. If the suspicion is confirmed, the consequences for prevention and therapy would be significant.
The voice of a Nobel prize winner undoubtedly carries weight, but at the time, Dr. zur Hausen still had to convince a host of skeptics with his discovery that a viral infection is a major cause of cervical cancer. Nonetheless, some indicators suggest that he and his wife have found a dead end this time.
Institutional skepticism
When his working group made the results public in February 2019, the DKFZ felt the need to give an all-clear signal in response to alarmed press reports. There is no reason to see dairy and meat consumption as something negative. Similarly, in their first joint statement, the BfR and the MRI judged the data to be insufficient and called for further studies. Multiple research teams began to focus on BMMF as a result. In what foods can they be found? Are they more common in patients with cancer than in healthy people? Are they infectious? Do they cause inflammation and cancer?
The findings presented in a second statement by the BfR and MRI at the end of November 2022 contradicted the claims made by the DKFZ scientists across the board. In no way do BMMF represent new pathogens. They are variants of already known DNA sequences. In addition, they are present in numerous animal-based and plant-based foods, including pork, fish, fruit, vegetables, and nuts.
BMMF do not possess the ability to infect human cells, the institutes said. The proof that they are damaging to one’s health was also absent. It is true that the incidence of intestinal tumors correlates positively with the consumption of red and processed meat – which in no way signifies causality – but dairy products are linked to a reduced risk. On the other hand, breast cancer cannot be associated with the consumption of beef or dairy.
Therefore, both institutes recommend continuing to use these products as supplementary diet for infants because of their micronutrients. They further stated that the products are safe for people of all ages.
Association with MS?
Unperturbed, Dr. de Villiers and Dr. zur Hausen went one step further in their current article. They posited that MS is also associated with the consumption of dairy products and beef. Here too geographic distribution prompted the idea to look for BMMF in the brain lesions of patients with MS. The researchers isolated ring-shaped DNA molecules that proved to be closely related to BMMF from dairy and cattle blood. “The result was electrifying for us.”
However, there are several other factors to consider, such as vitamin D3 deficiency. This is because the incidence of MS decreases the further you travel from the poles toward the equator (that is, as solar radiation increases). Also, EBV clearly plays a role because patients with MS display increased titers of EBV antibodies. One study also showed that people in Antarctica excreted reactivated EBV in their saliva during winter and that vitamin D3 stopped the viral secretion.
Under these conditions, the researchers hypothesized that MS is caused by a double infection of brain cells by EBV and BMMF. EBV is reactivated by a lack of vitamin D3, and the BMMF multiply and are eventually converted into proteins. A focal immunoreaction causes the Schwann cells and oligodendrocytes to malfunction, which leads to the destruction of the myelin sheaths around the nerve fibers.
This article was translated from the Medscape German Edition. A version appeared on Medscape.com.
Two diets tied to lower Alzheimer’s pathology at autopsy
In a cohort of deceased older adults, those who had adhered to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) and Mediterranean diets for nearly a decade before death had less global Alzheimer’s disease–related pathology, primarily less beta-amyloid, at autopsy.
Those who most closely followed these diets had almost 40% lower odds of having an Alzheimer’s disease diagnosis at death. The findings offer one mechanism by which healthy diets protect cognition.
“While our research doesn’t prove that a healthy diet resulted in fewer brain deposits of amyloid plaques ... we know there is a relationship, and following the MIND and Mediterranean diets may be one way that people can improve their brain health and protect cognition as they age,” study investigator Puja Agarwal, PhD, of RUSH University Medical Center in Chicago, said in a statement.
The study was published online in Neurology.
Green leafy veggies key
The MIND diet was pioneered by the late Martha Clare Morris, ScD, a Rush nutritional epidemiologist, who died of cancer in 2020 at age 64.
Although similar, the Mediterranean diet recommends vegetables, fruit, and three or more servings of fish per week, whereas the MIND diet prioritizes green leafy vegetables, such as spinach, kale, and collard greens, along with other vegetables. The MIND diet also prioritizes berries over other fruit and recommends one or more servings of fish per week. Both diets recommend small amounts of wine.
The current study focused on 581 older adults who died while participating in the Rush Memory and Aging Project (MAP). All participants agreed to undergo annual clinical evaluations and brain autopsy after death.
Participants completed annual food frequency questionnaires beginning at a mean age of 84. The mean age at death was 91. Mean follow-up was 6.8 years.
Around the time of death, 224 participants (39%) had a diagnosis of clinical dementia, and 383 participants (66%) had a pathologic Alzheimer’s disease diagnosis at time of death.
The researchers used a series of regression analyses to investigate the MIND and Mediterranean diets and dietary components associated with Alzheimer’s disease pathology. They controlled for age at death, sex, education, APO-epsilon 4 status, and total calories.
Overall, both diets were significantly associated with lower global Alzheimer’s disease pathology (MIND: beta = –0.022, P = .034; and Mediterranean: beta = –0.007, P = .039) – specifically, with less beta-amyloid (MIND: beta = –0.068, P = .050; and Mediterranean: beta = –0.040, P = .004).
The findings persisted when the analysis was further adjusted for physical activity, smoking, and vascular disease burden and when participants with mild cognitive impairment or dementia at the baseline dietary assessment were excluded.
Individuals who most closely followed the Mediterranean diet had average beta-amyloid load similar to being 18 years younger than peers with the lowest adherence. And those who most closely followed the MIND diet had average beta-amyloid amounts similar to being 12 years younger than those with the lowest adherence.
A MIND diet score 1 point higher corresponded to typical plaque deposition of participants who are 4.25 years younger in age.
Regarding individual dietary components, those who ate seven or more servings of green leafy vegetables weekly had less global Alzheimer’s disease pathology than peers who ate one or fewer (beta = –0.115, P = .0038). Those who ate seven or more servings per week had plaque amounts in their brains corresponding to being almost 19 years younger in comparison with those who ate the fewest servings per week.
“Our finding that eating more green leafy vegetables is in itself associated with fewer signs of Alzheimer’s disease in the brain is intriguing enough for people to consider adding more of these vegetables to their diet,” Dr. Agarwal said in the news release.
Previous data from the MAP cohort showed that adherence to the MIND diet can improve memory and thinking skills of older adults, even in the presence of Alzheimer’s disease pathology.
Novel study, intriguing results
Heather Snyder, PhD, vice president of medical and scientific relations with the Alzheimer’s Association, noted that a number of studies have linked overall nutrition – especially a balanced diet low in saturated fats and sugar and high in vegetables – with brain health, including cognition, as one ages.
This new study “takes what we know about the link between nutrition and risk for cognitive decline a step further by looking at the specific brain changes that occur in Alzheimer’s disease. The study found an association of certain nutrition behaviors with less of these Alzheimer’s brain changes,” said Dr. Snyder, who was not involved in the study.
“This is intriguing, and more research is needed to test via an intervention if healthy dietary behaviors can modify the presence of Alzheimer’s brain changes and reduce risk of cognitive decline.”
The Alzheimer’s Association is leading a 2-year clinical trial known as US POINTER to study how targeting known dementia risk factors in combination may reduce risk of cognitive decline in older adults. The MIND diet is being used in US POINTER.
“But while we work to find an exact ‘recipe’ for risk reduction, it’s important to eat a heart-healthy diet that incorporates nutrients that our bodies and brains need to be at their best,” Dr. Snyder said.
The study was funded by the National Institutes of Health. Dr. Agarwal and Dr. Snyder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a cohort of deceased older adults, those who had adhered to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) and Mediterranean diets for nearly a decade before death had less global Alzheimer’s disease–related pathology, primarily less beta-amyloid, at autopsy.
Those who most closely followed these diets had almost 40% lower odds of having an Alzheimer’s disease diagnosis at death. The findings offer one mechanism by which healthy diets protect cognition.
“While our research doesn’t prove that a healthy diet resulted in fewer brain deposits of amyloid plaques ... we know there is a relationship, and following the MIND and Mediterranean diets may be one way that people can improve their brain health and protect cognition as they age,” study investigator Puja Agarwal, PhD, of RUSH University Medical Center in Chicago, said in a statement.
The study was published online in Neurology.
Green leafy veggies key
The MIND diet was pioneered by the late Martha Clare Morris, ScD, a Rush nutritional epidemiologist, who died of cancer in 2020 at age 64.
Although similar, the Mediterranean diet recommends vegetables, fruit, and three or more servings of fish per week, whereas the MIND diet prioritizes green leafy vegetables, such as spinach, kale, and collard greens, along with other vegetables. The MIND diet also prioritizes berries over other fruit and recommends one or more servings of fish per week. Both diets recommend small amounts of wine.
The current study focused on 581 older adults who died while participating in the Rush Memory and Aging Project (MAP). All participants agreed to undergo annual clinical evaluations and brain autopsy after death.
Participants completed annual food frequency questionnaires beginning at a mean age of 84. The mean age at death was 91. Mean follow-up was 6.8 years.
Around the time of death, 224 participants (39%) had a diagnosis of clinical dementia, and 383 participants (66%) had a pathologic Alzheimer’s disease diagnosis at time of death.
The researchers used a series of regression analyses to investigate the MIND and Mediterranean diets and dietary components associated with Alzheimer’s disease pathology. They controlled for age at death, sex, education, APO-epsilon 4 status, and total calories.
Overall, both diets were significantly associated with lower global Alzheimer’s disease pathology (MIND: beta = –0.022, P = .034; and Mediterranean: beta = –0.007, P = .039) – specifically, with less beta-amyloid (MIND: beta = –0.068, P = .050; and Mediterranean: beta = –0.040, P = .004).
The findings persisted when the analysis was further adjusted for physical activity, smoking, and vascular disease burden and when participants with mild cognitive impairment or dementia at the baseline dietary assessment were excluded.
Individuals who most closely followed the Mediterranean diet had average beta-amyloid load similar to being 18 years younger than peers with the lowest adherence. And those who most closely followed the MIND diet had average beta-amyloid amounts similar to being 12 years younger than those with the lowest adherence.
A MIND diet score 1 point higher corresponded to typical plaque deposition of participants who are 4.25 years younger in age.
Regarding individual dietary components, those who ate seven or more servings of green leafy vegetables weekly had less global Alzheimer’s disease pathology than peers who ate one or fewer (beta = –0.115, P = .0038). Those who ate seven or more servings per week had plaque amounts in their brains corresponding to being almost 19 years younger in comparison with those who ate the fewest servings per week.
“Our finding that eating more green leafy vegetables is in itself associated with fewer signs of Alzheimer’s disease in the brain is intriguing enough for people to consider adding more of these vegetables to their diet,” Dr. Agarwal said in the news release.
Previous data from the MAP cohort showed that adherence to the MIND diet can improve memory and thinking skills of older adults, even in the presence of Alzheimer’s disease pathology.
Novel study, intriguing results
Heather Snyder, PhD, vice president of medical and scientific relations with the Alzheimer’s Association, noted that a number of studies have linked overall nutrition – especially a balanced diet low in saturated fats and sugar and high in vegetables – with brain health, including cognition, as one ages.
This new study “takes what we know about the link between nutrition and risk for cognitive decline a step further by looking at the specific brain changes that occur in Alzheimer’s disease. The study found an association of certain nutrition behaviors with less of these Alzheimer’s brain changes,” said Dr. Snyder, who was not involved in the study.
“This is intriguing, and more research is needed to test via an intervention if healthy dietary behaviors can modify the presence of Alzheimer’s brain changes and reduce risk of cognitive decline.”
The Alzheimer’s Association is leading a 2-year clinical trial known as US POINTER to study how targeting known dementia risk factors in combination may reduce risk of cognitive decline in older adults. The MIND diet is being used in US POINTER.
“But while we work to find an exact ‘recipe’ for risk reduction, it’s important to eat a heart-healthy diet that incorporates nutrients that our bodies and brains need to be at their best,” Dr. Snyder said.
The study was funded by the National Institutes of Health. Dr. Agarwal and Dr. Snyder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a cohort of deceased older adults, those who had adhered to the Mediterranean-DASH Intervention for Neurodegenerative Delay (MIND) and Mediterranean diets for nearly a decade before death had less global Alzheimer’s disease–related pathology, primarily less beta-amyloid, at autopsy.
Those who most closely followed these diets had almost 40% lower odds of having an Alzheimer’s disease diagnosis at death. The findings offer one mechanism by which healthy diets protect cognition.
“While our research doesn’t prove that a healthy diet resulted in fewer brain deposits of amyloid plaques ... we know there is a relationship, and following the MIND and Mediterranean diets may be one way that people can improve their brain health and protect cognition as they age,” study investigator Puja Agarwal, PhD, of RUSH University Medical Center in Chicago, said in a statement.
The study was published online in Neurology.
Green leafy veggies key
The MIND diet was pioneered by the late Martha Clare Morris, ScD, a Rush nutritional epidemiologist, who died of cancer in 2020 at age 64.
Although similar, the Mediterranean diet recommends vegetables, fruit, and three or more servings of fish per week, whereas the MIND diet prioritizes green leafy vegetables, such as spinach, kale, and collard greens, along with other vegetables. The MIND diet also prioritizes berries over other fruit and recommends one or more servings of fish per week. Both diets recommend small amounts of wine.
The current study focused on 581 older adults who died while participating in the Rush Memory and Aging Project (MAP). All participants agreed to undergo annual clinical evaluations and brain autopsy after death.
Participants completed annual food frequency questionnaires beginning at a mean age of 84. The mean age at death was 91. Mean follow-up was 6.8 years.
Around the time of death, 224 participants (39%) had a diagnosis of clinical dementia, and 383 participants (66%) had a pathologic Alzheimer’s disease diagnosis at time of death.
The researchers used a series of regression analyses to investigate the MIND and Mediterranean diets and dietary components associated with Alzheimer’s disease pathology. They controlled for age at death, sex, education, APO-epsilon 4 status, and total calories.
Overall, both diets were significantly associated with lower global Alzheimer’s disease pathology (MIND: beta = –0.022, P = .034; and Mediterranean: beta = –0.007, P = .039) – specifically, with less beta-amyloid (MIND: beta = –0.068, P = .050; and Mediterranean: beta = –0.040, P = .004).
The findings persisted when the analysis was further adjusted for physical activity, smoking, and vascular disease burden and when participants with mild cognitive impairment or dementia at the baseline dietary assessment were excluded.
Individuals who most closely followed the Mediterranean diet had average beta-amyloid load similar to being 18 years younger than peers with the lowest adherence. And those who most closely followed the MIND diet had average beta-amyloid amounts similar to being 12 years younger than those with the lowest adherence.
A MIND diet score 1 point higher corresponded to typical plaque deposition of participants who are 4.25 years younger in age.
Regarding individual dietary components, those who ate seven or more servings of green leafy vegetables weekly had less global Alzheimer’s disease pathology than peers who ate one or fewer (beta = –0.115, P = .0038). Those who ate seven or more servings per week had plaque amounts in their brains corresponding to being almost 19 years younger in comparison with those who ate the fewest servings per week.
“Our finding that eating more green leafy vegetables is in itself associated with fewer signs of Alzheimer’s disease in the brain is intriguing enough for people to consider adding more of these vegetables to their diet,” Dr. Agarwal said in the news release.
Previous data from the MAP cohort showed that adherence to the MIND diet can improve memory and thinking skills of older adults, even in the presence of Alzheimer’s disease pathology.
Novel study, intriguing results
Heather Snyder, PhD, vice president of medical and scientific relations with the Alzheimer’s Association, noted that a number of studies have linked overall nutrition – especially a balanced diet low in saturated fats and sugar and high in vegetables – with brain health, including cognition, as one ages.
This new study “takes what we know about the link between nutrition and risk for cognitive decline a step further by looking at the specific brain changes that occur in Alzheimer’s disease. The study found an association of certain nutrition behaviors with less of these Alzheimer’s brain changes,” said Dr. Snyder, who was not involved in the study.
“This is intriguing, and more research is needed to test via an intervention if healthy dietary behaviors can modify the presence of Alzheimer’s brain changes and reduce risk of cognitive decline.”
The Alzheimer’s Association is leading a 2-year clinical trial known as US POINTER to study how targeting known dementia risk factors in combination may reduce risk of cognitive decline in older adults. The MIND diet is being used in US POINTER.
“But while we work to find an exact ‘recipe’ for risk reduction, it’s important to eat a heart-healthy diet that incorporates nutrients that our bodies and brains need to be at their best,” Dr. Snyder said.
The study was funded by the National Institutes of Health. Dr. Agarwal and Dr. Snyder have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
High stress levels linked to cognitive decline
, a new study shows.
Individuals with elevated stress levels also had higher rates of diabetes, hypertension, and other cardiovascular disease (CVD) risk factors. But even after controlling for those risk factors, stress remained an independent predictor of cognitive decline.
The national cohort study showed that the association between stress and cognition was similar between Black and White individuals and that those with controlled stress were less likely to have cognitive impairment than those with uncontrolled or new stress.
“We have known for a while that excess levels of stress can be harmful for the human body and the heart, but we are now adding more evidence that excess levels of stress can be harmful for cognition,” said lead investigator Ambar Kulshreshtha, MD, PhD, associate professor of family and preventive medicine and epidemiology at Emory University, Atlanta. “We were able to see that regardless of race or gender, stress is bad.”
The findings were published online in JAMA Network Open.
Independent risk factor
For the study, investigators analyzed data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a national population-based cohort of Black and White participants aged 45 years or older, sampled from the U.S. population.
Participants completed a questionnaire designed to evaluate stress levels when they were enrolled in the study between 2003 and 2007 and again about 11 years after enrollment.
Of the 24,448 participants (41.6% Black) in the study, 22.9% reported elevated stress levels.
Those with high stress were more likely to be younger, female, Black, smokers, and have a higher body mass index and less likely to have a college degree and to be physically active. They also had a lower family income and were more likely to have cardiovascular disease risk factors, such as hypertension, diabetes, and dyslipidemia.
Participants with elevated levels of perceived stress were 37% more likely to have poor cognition after adjustment for sociodemographic variables, cardiovascular risk factors, and depression (adjusted odds ratio, 1.37; 95% confidence interval, 1.22-1.53).
There was no significant difference between Black and White participants.
Damaging consequences
Researchers also found a dose-response relationship, with the greatest cognitive decline found in people who reported high stress at both time points and those who had new stress at follow up (aOR, 1.16; 95% CI, 0.92-1.45), compared with those with resolved stress (aOR, 1.03; 95% CI, 0.81-1.32) or no stress (aOR, 0.81; 95% CI, 0.68-0.97).
A change in perceived stress by 1 unit was associated with 4% increased risk of cognitive impairment after adjusting for sociodemographic variables, CVD risk factors, lifestyle factors, and depressive symptoms (aOR, 1.04; 95% CI, 1.02-1.06).
Although the study didn’t reveal the mechanisms that might link stress and cognition, it does point to stress as a potentially modifiable risk factor for cognitive decline, Dr. Kulshreshtha said.
“One in three of my patients have had to deal with extra levels of stress and anxiety over the past few years,” said Dr. Kulshreshtha. “We as clinicians are aware that stress can have damaging consequences to the heart and other organs, and when we see patients who have these complaints, especially elderly patients, we should spend some time asking people about their stress and how they are managing it.”
Additional screening
Gregory Day, MD, a neurologist at the Mayo Clinic, Jacksonville, Fla., said that the findings help fill a void in the research about stress and cognition.
“It’s a potentially important association that’s easy for us to miss in clinical practice,” said Dr. Day, who was not a part of the study. “It’s one of those things that we can all recognize impacts health, but we have very few large, well thought out studies that give us the data we need to inform its place in clinical decision-making.”
In addition to its large sample size, the overrepresentation of diverse populations is a strength of the study and a contribution to the field, Dr. Day said.
“One question they don’t directly ask is, is this association maybe due to some differences in stress? And the answer from the paper is probably not, because it looks like when we control for these things, we don’t see big differences incident risk factors between race,” he added.
The findings also point to the need for clinicians, especially primary care physicians, to screen patients for stress during routine examinations.
“Every visit is an opportunity to screen for risk factors that are going to set people up for future brain health,” Dr. Day said. “In addition to screening for all of these other risk factors for brain health, maybe it’s worth including some more global assessment of stress in a standard screener.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institutes of Health, and the National Institute on Aging. Dr. Kulshreshtha and Dr. Day report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new study shows.
Individuals with elevated stress levels also had higher rates of diabetes, hypertension, and other cardiovascular disease (CVD) risk factors. But even after controlling for those risk factors, stress remained an independent predictor of cognitive decline.
The national cohort study showed that the association between stress and cognition was similar between Black and White individuals and that those with controlled stress were less likely to have cognitive impairment than those with uncontrolled or new stress.
“We have known for a while that excess levels of stress can be harmful for the human body and the heart, but we are now adding more evidence that excess levels of stress can be harmful for cognition,” said lead investigator Ambar Kulshreshtha, MD, PhD, associate professor of family and preventive medicine and epidemiology at Emory University, Atlanta. “We were able to see that regardless of race or gender, stress is bad.”
The findings were published online in JAMA Network Open.
Independent risk factor
For the study, investigators analyzed data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a national population-based cohort of Black and White participants aged 45 years or older, sampled from the U.S. population.
Participants completed a questionnaire designed to evaluate stress levels when they were enrolled in the study between 2003 and 2007 and again about 11 years after enrollment.
Of the 24,448 participants (41.6% Black) in the study, 22.9% reported elevated stress levels.
Those with high stress were more likely to be younger, female, Black, smokers, and have a higher body mass index and less likely to have a college degree and to be physically active. They also had a lower family income and were more likely to have cardiovascular disease risk factors, such as hypertension, diabetes, and dyslipidemia.
Participants with elevated levels of perceived stress were 37% more likely to have poor cognition after adjustment for sociodemographic variables, cardiovascular risk factors, and depression (adjusted odds ratio, 1.37; 95% confidence interval, 1.22-1.53).
There was no significant difference between Black and White participants.
Damaging consequences
Researchers also found a dose-response relationship, with the greatest cognitive decline found in people who reported high stress at both time points and those who had new stress at follow up (aOR, 1.16; 95% CI, 0.92-1.45), compared with those with resolved stress (aOR, 1.03; 95% CI, 0.81-1.32) or no stress (aOR, 0.81; 95% CI, 0.68-0.97).
A change in perceived stress by 1 unit was associated with 4% increased risk of cognitive impairment after adjusting for sociodemographic variables, CVD risk factors, lifestyle factors, and depressive symptoms (aOR, 1.04; 95% CI, 1.02-1.06).
Although the study didn’t reveal the mechanisms that might link stress and cognition, it does point to stress as a potentially modifiable risk factor for cognitive decline, Dr. Kulshreshtha said.
“One in three of my patients have had to deal with extra levels of stress and anxiety over the past few years,” said Dr. Kulshreshtha. “We as clinicians are aware that stress can have damaging consequences to the heart and other organs, and when we see patients who have these complaints, especially elderly patients, we should spend some time asking people about their stress and how they are managing it.”
Additional screening
Gregory Day, MD, a neurologist at the Mayo Clinic, Jacksonville, Fla., said that the findings help fill a void in the research about stress and cognition.
“It’s a potentially important association that’s easy for us to miss in clinical practice,” said Dr. Day, who was not a part of the study. “It’s one of those things that we can all recognize impacts health, but we have very few large, well thought out studies that give us the data we need to inform its place in clinical decision-making.”
In addition to its large sample size, the overrepresentation of diverse populations is a strength of the study and a contribution to the field, Dr. Day said.
“One question they don’t directly ask is, is this association maybe due to some differences in stress? And the answer from the paper is probably not, because it looks like when we control for these things, we don’t see big differences incident risk factors between race,” he added.
The findings also point to the need for clinicians, especially primary care physicians, to screen patients for stress during routine examinations.
“Every visit is an opportunity to screen for risk factors that are going to set people up for future brain health,” Dr. Day said. “In addition to screening for all of these other risk factors for brain health, maybe it’s worth including some more global assessment of stress in a standard screener.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institutes of Health, and the National Institute on Aging. Dr. Kulshreshtha and Dr. Day report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, a new study shows.
Individuals with elevated stress levels also had higher rates of diabetes, hypertension, and other cardiovascular disease (CVD) risk factors. But even after controlling for those risk factors, stress remained an independent predictor of cognitive decline.
The national cohort study showed that the association between stress and cognition was similar between Black and White individuals and that those with controlled stress were less likely to have cognitive impairment than those with uncontrolled or new stress.
“We have known for a while that excess levels of stress can be harmful for the human body and the heart, but we are now adding more evidence that excess levels of stress can be harmful for cognition,” said lead investigator Ambar Kulshreshtha, MD, PhD, associate professor of family and preventive medicine and epidemiology at Emory University, Atlanta. “We were able to see that regardless of race or gender, stress is bad.”
The findings were published online in JAMA Network Open.
Independent risk factor
For the study, investigators analyzed data from the Reasons for Geographic and Racial Differences in Stroke (REGARDS) study, a national population-based cohort of Black and White participants aged 45 years or older, sampled from the U.S. population.
Participants completed a questionnaire designed to evaluate stress levels when they were enrolled in the study between 2003 and 2007 and again about 11 years after enrollment.
Of the 24,448 participants (41.6% Black) in the study, 22.9% reported elevated stress levels.
Those with high stress were more likely to be younger, female, Black, smokers, and have a higher body mass index and less likely to have a college degree and to be physically active. They also had a lower family income and were more likely to have cardiovascular disease risk factors, such as hypertension, diabetes, and dyslipidemia.
Participants with elevated levels of perceived stress were 37% more likely to have poor cognition after adjustment for sociodemographic variables, cardiovascular risk factors, and depression (adjusted odds ratio, 1.37; 95% confidence interval, 1.22-1.53).
There was no significant difference between Black and White participants.
Damaging consequences
Researchers also found a dose-response relationship, with the greatest cognitive decline found in people who reported high stress at both time points and those who had new stress at follow up (aOR, 1.16; 95% CI, 0.92-1.45), compared with those with resolved stress (aOR, 1.03; 95% CI, 0.81-1.32) or no stress (aOR, 0.81; 95% CI, 0.68-0.97).
A change in perceived stress by 1 unit was associated with 4% increased risk of cognitive impairment after adjusting for sociodemographic variables, CVD risk factors, lifestyle factors, and depressive symptoms (aOR, 1.04; 95% CI, 1.02-1.06).
Although the study didn’t reveal the mechanisms that might link stress and cognition, it does point to stress as a potentially modifiable risk factor for cognitive decline, Dr. Kulshreshtha said.
“One in three of my patients have had to deal with extra levels of stress and anxiety over the past few years,” said Dr. Kulshreshtha. “We as clinicians are aware that stress can have damaging consequences to the heart and other organs, and when we see patients who have these complaints, especially elderly patients, we should spend some time asking people about their stress and how they are managing it.”
Additional screening
Gregory Day, MD, a neurologist at the Mayo Clinic, Jacksonville, Fla., said that the findings help fill a void in the research about stress and cognition.
“It’s a potentially important association that’s easy for us to miss in clinical practice,” said Dr. Day, who was not a part of the study. “It’s one of those things that we can all recognize impacts health, but we have very few large, well thought out studies that give us the data we need to inform its place in clinical decision-making.”
In addition to its large sample size, the overrepresentation of diverse populations is a strength of the study and a contribution to the field, Dr. Day said.
“One question they don’t directly ask is, is this association maybe due to some differences in stress? And the answer from the paper is probably not, because it looks like when we control for these things, we don’t see big differences incident risk factors between race,” he added.
The findings also point to the need for clinicians, especially primary care physicians, to screen patients for stress during routine examinations.
“Every visit is an opportunity to screen for risk factors that are going to set people up for future brain health,” Dr. Day said. “In addition to screening for all of these other risk factors for brain health, maybe it’s worth including some more global assessment of stress in a standard screener.”
The study was funded by the National Institute of Neurological Disorders and Stroke, the National Institutes of Health, and the National Institute on Aging. Dr. Kulshreshtha and Dr. Day report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From JAMA Network Open





