User login
Can case management cut hypertension’s consequences?
MONTREAL – who received phone calls, care coordination, and coaching from a nurse case manager, according to a retrospective population-based cohort study of almost 85,000 patients with hypertension.
The reduction yielded a hazard ratio for all-cause mortality of 0.504, with a number needed to treat (NNT) of 25 (P less than .05).
Service utilization also decreased for those participating in the intervention, compared with those receiving usual care: Hospitalizations fell by 7 per 100 patient-years, with greater reductions seen in emergency department, specialist, and primary care utilization (P less than .05 for all).
At the time the study was conceived, the Hong Kong Hospital Authority cared for about 200,000 hypertensive patients, of whom more than 40% hadn’t achieved the target blood pressure of less than 140/90 mm Hg, said Dr. Yu.
Dr. Yu of the department of family medicine and primary care at the University of Hong Kong said there are challenges in bringing more hypertension patients into good blood pressure control in Hong Kong. These include the “idiosyncratic practice” of some frontline physicians, who also often have limited time for patient consultations and only limited access to the services of allied health professionals to help them in their work. Patient adherence, she said, is also an issue.
To tackle these persistent high rates of patients whose blood pressures remained too high, Dr. Yu and her colleagues at the Hospital Authority launched the Risk Assessment and Management Program – Hypertension (RAMP-HT) in 2011. The program, she said, is an “evidence-based, structured, protocol-driven, multidisciplinary program” that includes risk assessment and screening for complications, and uses a risk-guided management approach.
Patients in RAMP-HT received interventions according to a matrix for risk management of patients with hypertension. Patients with a blood pressure between 140/90 and 160/100 mm Hg who were assessed as being low and medium risk according to the Joint British Societies guidelines for cardiovascular risk continued to receive management from their primary care physician. High-risk patients with blood pressure in this range also received a statin if their low-density lipoprotein cholesterol level was suboptimal.
Patients whose blood pressure was at least 160/100 mm Hg were followed by a RAMP-HT nurse. For those with this degree of blood pressure elevation who were already on at least three antihypertensive medications, specialty appointments were also arranged.
Other targeted interventions were also available to participants, including the services of dietitians and physical therapists for those with a body mass index (BMI) of at least 27.5 kg/m2; smoking cessation and mental health services were also available, as appropriate.
After 3 years, those participating in the RAMP-HT program (n = 79,116) were compared with those in the usual care group (n = 43,901). In both arms, adult patients with complete data and without preexisting cardiovascular disease, diabetes, or end-stage renal disease were included. In each group, about 58% of participants were female, and the mean age was about 65 years.
Primary outcome measures included the incidence of cardiovascular disease, an outcome that included coronary heart disease, heart failure, and stroke; end-stage renal disease; and all-cause mortality. The significant reductions in these measures for the RAMP-HT group remained after multivariable analysis accounted for sex, age, smoking status, renal function, lipid values, BMI, comorbidities, and antihypertensive and lipid-lowering medication use.
The reduced care utilization seen among RAMP-HT participants also persisted after multivariable analysis for these potential confounders.
Dr. Yu said the systematic, protocol-driven program was a primary strength of RAMP-HT. The key to the program was use of nurses to provide patient education and physicians and allied health resources only as needed, she said; the program reinforced the importance of self-management and adherence because patients heard a unified message from many different health care professionals.
However, lifestyle factors such as diet and exercise weren’t tracked, and the retrospective study design introduced the potential for some bias, she said. In ongoing work, the long-term efficacy and cost-effectiveness of the RAMP-HT program are being tracked.
Dr. Yu reported that the study was funded by the Hong Kong Health and Medical Research Fund. She reported no relevant conflicts of interest.
SOURCE: Yu, Esther et al. NAPCRG 2017, Abstract HY33.
MONTREAL – who received phone calls, care coordination, and coaching from a nurse case manager, according to a retrospective population-based cohort study of almost 85,000 patients with hypertension.
The reduction yielded a hazard ratio for all-cause mortality of 0.504, with a number needed to treat (NNT) of 25 (P less than .05).
Service utilization also decreased for those participating in the intervention, compared with those receiving usual care: Hospitalizations fell by 7 per 100 patient-years, with greater reductions seen in emergency department, specialist, and primary care utilization (P less than .05 for all).
At the time the study was conceived, the Hong Kong Hospital Authority cared for about 200,000 hypertensive patients, of whom more than 40% hadn’t achieved the target blood pressure of less than 140/90 mm Hg, said Dr. Yu.
Dr. Yu of the department of family medicine and primary care at the University of Hong Kong said there are challenges in bringing more hypertension patients into good blood pressure control in Hong Kong. These include the “idiosyncratic practice” of some frontline physicians, who also often have limited time for patient consultations and only limited access to the services of allied health professionals to help them in their work. Patient adherence, she said, is also an issue.
To tackle these persistent high rates of patients whose blood pressures remained too high, Dr. Yu and her colleagues at the Hospital Authority launched the Risk Assessment and Management Program – Hypertension (RAMP-HT) in 2011. The program, she said, is an “evidence-based, structured, protocol-driven, multidisciplinary program” that includes risk assessment and screening for complications, and uses a risk-guided management approach.
Patients in RAMP-HT received interventions according to a matrix for risk management of patients with hypertension. Patients with a blood pressure between 140/90 and 160/100 mm Hg who were assessed as being low and medium risk according to the Joint British Societies guidelines for cardiovascular risk continued to receive management from their primary care physician. High-risk patients with blood pressure in this range also received a statin if their low-density lipoprotein cholesterol level was suboptimal.
Patients whose blood pressure was at least 160/100 mm Hg were followed by a RAMP-HT nurse. For those with this degree of blood pressure elevation who were already on at least three antihypertensive medications, specialty appointments were also arranged.
Other targeted interventions were also available to participants, including the services of dietitians and physical therapists for those with a body mass index (BMI) of at least 27.5 kg/m2; smoking cessation and mental health services were also available, as appropriate.
After 3 years, those participating in the RAMP-HT program (n = 79,116) were compared with those in the usual care group (n = 43,901). In both arms, adult patients with complete data and without preexisting cardiovascular disease, diabetes, or end-stage renal disease were included. In each group, about 58% of participants were female, and the mean age was about 65 years.
Primary outcome measures included the incidence of cardiovascular disease, an outcome that included coronary heart disease, heart failure, and stroke; end-stage renal disease; and all-cause mortality. The significant reductions in these measures for the RAMP-HT group remained after multivariable analysis accounted for sex, age, smoking status, renal function, lipid values, BMI, comorbidities, and antihypertensive and lipid-lowering medication use.
The reduced care utilization seen among RAMP-HT participants also persisted after multivariable analysis for these potential confounders.
Dr. Yu said the systematic, protocol-driven program was a primary strength of RAMP-HT. The key to the program was use of nurses to provide patient education and physicians and allied health resources only as needed, she said; the program reinforced the importance of self-management and adherence because patients heard a unified message from many different health care professionals.
However, lifestyle factors such as diet and exercise weren’t tracked, and the retrospective study design introduced the potential for some bias, she said. In ongoing work, the long-term efficacy and cost-effectiveness of the RAMP-HT program are being tracked.
Dr. Yu reported that the study was funded by the Hong Kong Health and Medical Research Fund. She reported no relevant conflicts of interest.
SOURCE: Yu, Esther et al. NAPCRG 2017, Abstract HY33.
MONTREAL – who received phone calls, care coordination, and coaching from a nurse case manager, according to a retrospective population-based cohort study of almost 85,000 patients with hypertension.
The reduction yielded a hazard ratio for all-cause mortality of 0.504, with a number needed to treat (NNT) of 25 (P less than .05).
Service utilization also decreased for those participating in the intervention, compared with those receiving usual care: Hospitalizations fell by 7 per 100 patient-years, with greater reductions seen in emergency department, specialist, and primary care utilization (P less than .05 for all).
At the time the study was conceived, the Hong Kong Hospital Authority cared for about 200,000 hypertensive patients, of whom more than 40% hadn’t achieved the target blood pressure of less than 140/90 mm Hg, said Dr. Yu.
Dr. Yu of the department of family medicine and primary care at the University of Hong Kong said there are challenges in bringing more hypertension patients into good blood pressure control in Hong Kong. These include the “idiosyncratic practice” of some frontline physicians, who also often have limited time for patient consultations and only limited access to the services of allied health professionals to help them in their work. Patient adherence, she said, is also an issue.
To tackle these persistent high rates of patients whose blood pressures remained too high, Dr. Yu and her colleagues at the Hospital Authority launched the Risk Assessment and Management Program – Hypertension (RAMP-HT) in 2011. The program, she said, is an “evidence-based, structured, protocol-driven, multidisciplinary program” that includes risk assessment and screening for complications, and uses a risk-guided management approach.
Patients in RAMP-HT received interventions according to a matrix for risk management of patients with hypertension. Patients with a blood pressure between 140/90 and 160/100 mm Hg who were assessed as being low and medium risk according to the Joint British Societies guidelines for cardiovascular risk continued to receive management from their primary care physician. High-risk patients with blood pressure in this range also received a statin if their low-density lipoprotein cholesterol level was suboptimal.
Patients whose blood pressure was at least 160/100 mm Hg were followed by a RAMP-HT nurse. For those with this degree of blood pressure elevation who were already on at least three antihypertensive medications, specialty appointments were also arranged.
Other targeted interventions were also available to participants, including the services of dietitians and physical therapists for those with a body mass index (BMI) of at least 27.5 kg/m2; smoking cessation and mental health services were also available, as appropriate.
After 3 years, those participating in the RAMP-HT program (n = 79,116) were compared with those in the usual care group (n = 43,901). In both arms, adult patients with complete data and without preexisting cardiovascular disease, diabetes, or end-stage renal disease were included. In each group, about 58% of participants were female, and the mean age was about 65 years.
Primary outcome measures included the incidence of cardiovascular disease, an outcome that included coronary heart disease, heart failure, and stroke; end-stage renal disease; and all-cause mortality. The significant reductions in these measures for the RAMP-HT group remained after multivariable analysis accounted for sex, age, smoking status, renal function, lipid values, BMI, comorbidities, and antihypertensive and lipid-lowering medication use.
The reduced care utilization seen among RAMP-HT participants also persisted after multivariable analysis for these potential confounders.
Dr. Yu said the systematic, protocol-driven program was a primary strength of RAMP-HT. The key to the program was use of nurses to provide patient education and physicians and allied health resources only as needed, she said; the program reinforced the importance of self-management and adherence because patients heard a unified message from many different health care professionals.
However, lifestyle factors such as diet and exercise weren’t tracked, and the retrospective study design introduced the potential for some bias, she said. In ongoing work, the long-term efficacy and cost-effectiveness of the RAMP-HT program are being tracked.
Dr. Yu reported that the study was funded by the Hong Kong Health and Medical Research Fund. She reported no relevant conflicts of interest.
SOURCE: Yu, Esther et al. NAPCRG 2017, Abstract HY33.
REPORTING FROM NAPCRG 2017
Key clinical point:
Major finding: The hazard ratio for all-cause mortality was 0.504 for patients in the intervention arm.
Study details: A retrospective population-based cohort study of almost 85,000 Hong Kong patients with hypertension.
Disclosures: The study was funded by the Hong Kong Health and Medical Research Fund. Dr. Yu reported no relevant financial disclosures.
Source: Yu E et al. NAPCRG 2017, Abstract HY33.
Earlier treatment but shorter survival: The rurality paradox in cancer
MONTREAL – Does rurality matter in cancer treatment? According to lessons from a Scottish study, the answer may be yes, but in unexpected ways.
Patients who lived further away from a cancer treatment center were more likely to be treated within the 62 days postreferral window that the Scottish government has set as a target. Compared with those living within 15 minutes of a cancer center, the adjusted odds ratio for patients living at least an hour away to receive timely treatment was 1.42 (95% confidence interval, 1.25-1.61). For those living on remote islands, the aOR was 1.32 (95% CI, 1.09-1.59).
Dr. Murchie, speaking at the annual meeting of the North American Primary Care Research Group, shared results of an updated study that looked at the cancer population in Northeast Scotland to see how living farther from a cancer center might be associated with time to diagnosis and treatment of cancer and with 1-year survival rates.
A “seminal” work that set the background for this study, said Dr. Murchie, was the 2002 publication tracking the relationship between rural residence status and cancer survival (Br J Cancer. 2002;87[6]:585-90). Findings from that study showed that as the distance from the patient’s residence to a cancer center increased, so did the risk that the cancer wasn’t diagnosed before death. Survival, especially for prostate and lung cancer, was found to decrease with increasing distance, said Dr. Murchie.
“This study has been widely replicated in the global literature, but the mechanisms have never been satisfactorily explained,” he said.
For the present study, the primary outcome measure was whether patients achieved treatment within 62 days of referral, the target set by the Scottish government, said Dr. Murchie.
Secondary outcomes included secondary care delay – whether treatment was begun within 31 days of diagnosis – and survival at 1 year after presentation or referral by a general practitioner.
A total of 12,339 patients were included; 74% were older than 60 years. Patients were relatively affluent, with 59% in the two least-deprived quintiles according to Scottish government classification. Dr. Murchie said that this is in keeping with the geographic-socioeconomic status distribution in Scotland. Females made up 56% of the population, and 35% were classified as rural dwelling.
Nearly a third of patients (n = 3,722; 30.6%) had breast cancer. Colorectal cancer was the next most common diagnosis (n = 2,775; 22.5%), followed by prostate cancer, lung cancer, upper gastrointestinal cancer, melanoma, and cervical cancer. Most patients (n = 8,537; 62%) had a Charlson Comorbidity Index score of 0.
Dr. Murchie used the Northeast and Aberdeen Scottish Cancer and Residence Cohort (NASCAR) data gathered during 2007-2014; the cohort’s data came from a variety of sources, including the region’s cancer care pathway database. National cancer registries, morbidity records, and other nationally maintained demographic databases were also used for the NASCAR dataset.
Those building the NASCAR cohort were able to link all of the data from disparate datasets and still keep investigators blinded to patient identity via a “safe harvest” technique that created pseudonyms to harmonize the datasets.
Using patient postal codes, a geographical information systems approach was used to determine traveling time to a cancer center. Travel time, Dr. Murchie pointed out, is a better measure than straight-line distance of true accessibility for rural-dwelling patients.
In discussion, Dr. Murchie said that the correlation between longer distance and shorter time to treatment held even when he and his colleagues controlled for “the most obvious explanation – that disease was more advanced on diagnosis among remoter people.” But, he said, “This does not translate into better survival. Why?”
Hypotheses, said Dr. Murchie, include the many small and large barriers to care that rural-dwelling individuals face. They must find a way to their GP, or place a phone call, and that physician must weigh the risk of a serious complication against the burden to the patient – and that patient’s family – of travel from a remote location to a cancer center.
Dr. Murchie encouraged international collaboration and replication of his work so that cancer researchers and primary care practitioners can reach a better understanding of the unique challenges in treating rural cancer patients.
Dr. Murchie reported that he had no relevant disclosures.
SOURCE: Murchie P. NAPCRG 2017 Abstract CR15.
MONTREAL – Does rurality matter in cancer treatment? According to lessons from a Scottish study, the answer may be yes, but in unexpected ways.
Patients who lived further away from a cancer treatment center were more likely to be treated within the 62 days postreferral window that the Scottish government has set as a target. Compared with those living within 15 minutes of a cancer center, the adjusted odds ratio for patients living at least an hour away to receive timely treatment was 1.42 (95% confidence interval, 1.25-1.61). For those living on remote islands, the aOR was 1.32 (95% CI, 1.09-1.59).
Dr. Murchie, speaking at the annual meeting of the North American Primary Care Research Group, shared results of an updated study that looked at the cancer population in Northeast Scotland to see how living farther from a cancer center might be associated with time to diagnosis and treatment of cancer and with 1-year survival rates.
A “seminal” work that set the background for this study, said Dr. Murchie, was the 2002 publication tracking the relationship between rural residence status and cancer survival (Br J Cancer. 2002;87[6]:585-90). Findings from that study showed that as the distance from the patient’s residence to a cancer center increased, so did the risk that the cancer wasn’t diagnosed before death. Survival, especially for prostate and lung cancer, was found to decrease with increasing distance, said Dr. Murchie.
“This study has been widely replicated in the global literature, but the mechanisms have never been satisfactorily explained,” he said.
For the present study, the primary outcome measure was whether patients achieved treatment within 62 days of referral, the target set by the Scottish government, said Dr. Murchie.
Secondary outcomes included secondary care delay – whether treatment was begun within 31 days of diagnosis – and survival at 1 year after presentation or referral by a general practitioner.
A total of 12,339 patients were included; 74% were older than 60 years. Patients were relatively affluent, with 59% in the two least-deprived quintiles according to Scottish government classification. Dr. Murchie said that this is in keeping with the geographic-socioeconomic status distribution in Scotland. Females made up 56% of the population, and 35% were classified as rural dwelling.
Nearly a third of patients (n = 3,722; 30.6%) had breast cancer. Colorectal cancer was the next most common diagnosis (n = 2,775; 22.5%), followed by prostate cancer, lung cancer, upper gastrointestinal cancer, melanoma, and cervical cancer. Most patients (n = 8,537; 62%) had a Charlson Comorbidity Index score of 0.
Dr. Murchie used the Northeast and Aberdeen Scottish Cancer and Residence Cohort (NASCAR) data gathered during 2007-2014; the cohort’s data came from a variety of sources, including the region’s cancer care pathway database. National cancer registries, morbidity records, and other nationally maintained demographic databases were also used for the NASCAR dataset.
Those building the NASCAR cohort were able to link all of the data from disparate datasets and still keep investigators blinded to patient identity via a “safe harvest” technique that created pseudonyms to harmonize the datasets.
Using patient postal codes, a geographical information systems approach was used to determine traveling time to a cancer center. Travel time, Dr. Murchie pointed out, is a better measure than straight-line distance of true accessibility for rural-dwelling patients.
In discussion, Dr. Murchie said that the correlation between longer distance and shorter time to treatment held even when he and his colleagues controlled for “the most obvious explanation – that disease was more advanced on diagnosis among remoter people.” But, he said, “This does not translate into better survival. Why?”
Hypotheses, said Dr. Murchie, include the many small and large barriers to care that rural-dwelling individuals face. They must find a way to their GP, or place a phone call, and that physician must weigh the risk of a serious complication against the burden to the patient – and that patient’s family – of travel from a remote location to a cancer center.
Dr. Murchie encouraged international collaboration and replication of his work so that cancer researchers and primary care practitioners can reach a better understanding of the unique challenges in treating rural cancer patients.
Dr. Murchie reported that he had no relevant disclosures.
SOURCE: Murchie P. NAPCRG 2017 Abstract CR15.
MONTREAL – Does rurality matter in cancer treatment? According to lessons from a Scottish study, the answer may be yes, but in unexpected ways.
Patients who lived further away from a cancer treatment center were more likely to be treated within the 62 days postreferral window that the Scottish government has set as a target. Compared with those living within 15 minutes of a cancer center, the adjusted odds ratio for patients living at least an hour away to receive timely treatment was 1.42 (95% confidence interval, 1.25-1.61). For those living on remote islands, the aOR was 1.32 (95% CI, 1.09-1.59).
Dr. Murchie, speaking at the annual meeting of the North American Primary Care Research Group, shared results of an updated study that looked at the cancer population in Northeast Scotland to see how living farther from a cancer center might be associated with time to diagnosis and treatment of cancer and with 1-year survival rates.
A “seminal” work that set the background for this study, said Dr. Murchie, was the 2002 publication tracking the relationship between rural residence status and cancer survival (Br J Cancer. 2002;87[6]:585-90). Findings from that study showed that as the distance from the patient’s residence to a cancer center increased, so did the risk that the cancer wasn’t diagnosed before death. Survival, especially for prostate and lung cancer, was found to decrease with increasing distance, said Dr. Murchie.
“This study has been widely replicated in the global literature, but the mechanisms have never been satisfactorily explained,” he said.
For the present study, the primary outcome measure was whether patients achieved treatment within 62 days of referral, the target set by the Scottish government, said Dr. Murchie.
Secondary outcomes included secondary care delay – whether treatment was begun within 31 days of diagnosis – and survival at 1 year after presentation or referral by a general practitioner.
A total of 12,339 patients were included; 74% were older than 60 years. Patients were relatively affluent, with 59% in the two least-deprived quintiles according to Scottish government classification. Dr. Murchie said that this is in keeping with the geographic-socioeconomic status distribution in Scotland. Females made up 56% of the population, and 35% were classified as rural dwelling.
Nearly a third of patients (n = 3,722; 30.6%) had breast cancer. Colorectal cancer was the next most common diagnosis (n = 2,775; 22.5%), followed by prostate cancer, lung cancer, upper gastrointestinal cancer, melanoma, and cervical cancer. Most patients (n = 8,537; 62%) had a Charlson Comorbidity Index score of 0.
Dr. Murchie used the Northeast and Aberdeen Scottish Cancer and Residence Cohort (NASCAR) data gathered during 2007-2014; the cohort’s data came from a variety of sources, including the region’s cancer care pathway database. National cancer registries, morbidity records, and other nationally maintained demographic databases were also used for the NASCAR dataset.
Those building the NASCAR cohort were able to link all of the data from disparate datasets and still keep investigators blinded to patient identity via a “safe harvest” technique that created pseudonyms to harmonize the datasets.
Using patient postal codes, a geographical information systems approach was used to determine traveling time to a cancer center. Travel time, Dr. Murchie pointed out, is a better measure than straight-line distance of true accessibility for rural-dwelling patients.
In discussion, Dr. Murchie said that the correlation between longer distance and shorter time to treatment held even when he and his colleagues controlled for “the most obvious explanation – that disease was more advanced on diagnosis among remoter people.” But, he said, “This does not translate into better survival. Why?”
Hypotheses, said Dr. Murchie, include the many small and large barriers to care that rural-dwelling individuals face. They must find a way to their GP, or place a phone call, and that physician must weigh the risk of a serious complication against the burden to the patient – and that patient’s family – of travel from a remote location to a cancer center.
Dr. Murchie encouraged international collaboration and replication of his work so that cancer researchers and primary care practitioners can reach a better understanding of the unique challenges in treating rural cancer patients.
Dr. Murchie reported that he had no relevant disclosures.
SOURCE: Murchie P. NAPCRG 2017 Abstract CR15.
REPORTING FROM NAPCRG 2017
Key clinical point: Rural Scottish cancer patients were treated earlier but had shorter survival.
Major finding: Rural patients had an odds ratio of 1.42 for prompt treatment after a cancer diagnosis.
Study details: Study of 12,339 rural and urban patients with cancer living in Scotland.
Disclosures: Dr. Murchie reported no conflicts of interest.
Source: Murchie P. NAPCRG 2017 Abstract CR15.
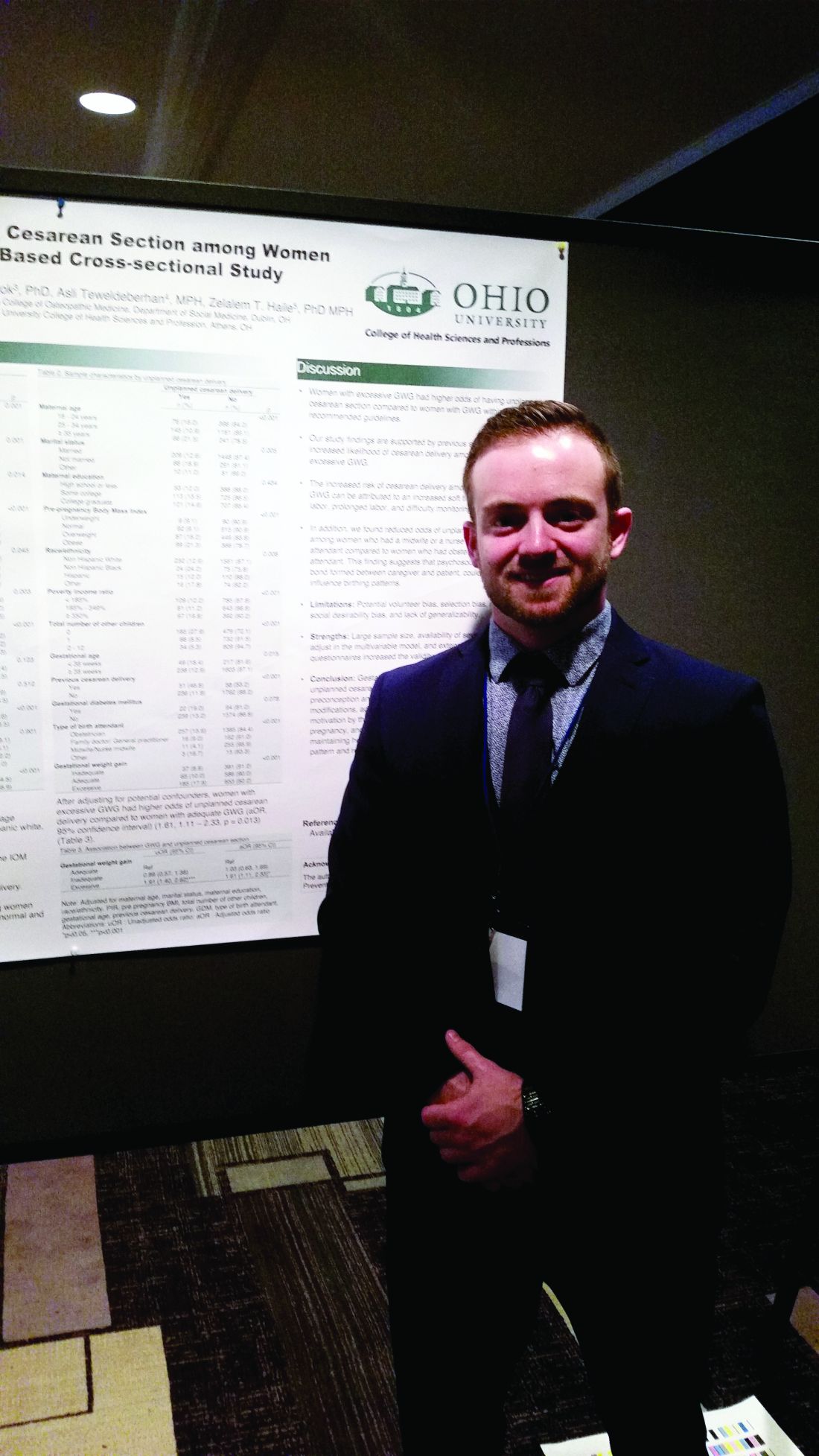
Unplanned cesareans more common with excess gestational weight gain
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
MONTREAL – The risk for unplanned cesarean delivery is increased when maternal gestational weight gain exceeds the recommended amount – as it does in almost half of pregnancies in the United States.
In a new analysis of data from the Infant Feeding Practices Study II (IFPS II), women with excessive gestational weight gain (GWG) were found to have an adjusted odds ratio of 1.61 for unplanned cesarean delivery, compared with women with adequate GWG (95% confidence interval, 1.11-2.33; P = .013).
Maternal obesity is known to be a risk factor for cesarean delivery, at least in part because excess adipose tissue may interfere with the normal ability of the cervix to thin and dilate with contractions, said Mr. Francescon, a medical student at Ohio University Heritage College of Osteopathic Medicine, Athens. Labor can be prolonged, and it’s often difficult to monitor fetal activity with external activity, he said.
To see whether unplanned cesarean deliveries were associated with excess GWG, Mr. Francescon and his collaborators included data from 2,107 of the 3,033 respondents to the IFPS II, excluding those with missing data and those with planned cesarean deliveries.
Weight gain was grouped into three categories – adequate, inadequate, and excessive – according to guidelines set by the Institute of Medicine. The odds of an unplanned cesarean delivery were adjusted by using multivariable analysis that took into account ethnicity, education, poverty status, parity, and previous obstetric history. The statistical analysis also accounted for the presence of gestational diabetes and the type of birth attendant.
A total of 1,038 women (49.3%) had excessive GWG according to the IOM guidelines, and 287 women (13.6%) overall had an unplanned cesarean delivery. After adjusting for the potentially confounding variables, only excessive weight gain was significantly associated with the risk for unplanned cesarean delivery; those with inadequate weight gain had an odds ratio of 1.03 (95% CI, 0.63-1.69; not significant).
, but rather were attended by a nonobstetrician physician or a midwife, said Mr. Francescon. After excluding patients who planned to have cesarean deliveries, 257 of 1,385 (15.6%) of patients seeing obstetricians had unplanned cesarean deliveries; this figure was 9% for nonobstetrician physicians and 4.1% for midwives/nurse midwives.
“This finding suggests that psychosocial factors, such as the bond formed between caregiver and patient, could also potentially influence birthing patterns,” wrote Mr. Francescon and his collaborators.
“Our study findings are supported by previous studies that found increased likelihood of cesarean delivery among women with excessive GWG,” said the investigators.
The study had a large sample size, used well-tested survey instruments, and could include many variables in statistical analysis, all strengths, wrote Mr. Francescon and his coauthors. However, there remained the potential for volunteer bias and recall bias. In addition, weight gain carries social stigma, which could have influence the self-reported results.
“Gestational weight gain is a modifiable risk factor for unplanned cesarean delivery,” Mr. Francescon said. He and his collaborators propose that a comprehensive plan of dietary and lifestyle modifications beginning pre-conception, together with enhanced patient and provider awareness of the risk of unplanned cesarean deliveries with excess gestational weight gain, could help reduce the number of unplanned cesarean deliveries.
The data for the study were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
SOURCE: Francescon J. NAPCRG 2017 Abstract P495.
REPORTING FROM NAPCRG 2017
Key clinical point: The risk for an unplanned cesarean delivery rose with excess gestational weight gain.
Major finding: The adjusted odds ratio for unplanned cesarean was 1.61 for those with excess GWG (P = .013).
Study details: Retrospective analysis of 2,107 responses to the Infant Feeding Practices Study II (IFPSII).
Disclosures: Study data were provided by the Centers for Disease Control and Prevention. Mr. Francescon reported no conflicts of interest.
Source: Francescon J. NAPCRG 2017 Abstract P495.
Length of stay shorter with admission to family medicine, not hospitalist, service
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
MONTREAL – When a family medicine teaching service provided hospital care for local patients, length of stay was almost a third shorter than when care was provided by the hospitalist internal medicine service at a large tertiary care hospital.
What made the difference in length of stay? “,” said Gregory Garrison, MD, of the department of family medicine at the Mayo Clinic, Rochester, Minn. He noted that readmission rates weren’t higher for the patients cared for by the family medicine inpatient service.
The primary outcome measures were length of stay and readmission or death within 30 days of discharge, Dr. Garrison said at the annual meeting of the North American Primary Care Research Group.
A total of 3,125 admissions were seen for 2,138 unique patients. Most admissions (2,651; 84.8%) were for the family medicine service. Demographic characteristics and readmission rates were similar between admissions to the two services, but “hospitalist internal medicine patients were perhaps slightly sicker,” said Dr. Garrison. The mean Charlson comorbidity score was 4 for the family medicine admissions and 5.6 for the hospitalist internal medicine admissions (P less than .001). Also, the patients admitted to the hospitalist service were slightly more likely to have had a previous hospital admission within the prior 12 months.
Examining the unadjusted data, Dr. Garrison and his colleagues found that the family medicine patients had a shorter length of stay, with a mean 2.5 days and a median 1.8 days, compared with the mean 3.8 days and median 2.7 days spent in hospital for the hospitalist internal medicine patients.
The difference remained significant after multivariable analysis to control for several potentially confounding factors, including patient demographics, prior health care utilization, disposition, readmissions, and Charlson comorbidity score.
The adjusted figures showed that length of stay was 31.8% longer for admissions to the hospitalist internal medicine service than for the family medicine service.
In discussion, Dr. Garrison said that he and his colleagues believe that the physicians, social workers, and clinical assistants who make up the family medicine service really understand the “outpatient resources that can be marshaled to help local patients with the transition from hospital to home.”
In practical terms, this can mean that a social worker knows which skilled nursing facilities are likely to accept a Friday admission, or that a physician understands community resources that can help an elderly patient return to her home with a little extra support, he said.
Another practicality, is that “the lack of a census cap on the family medicine inpatient service may incentivize rapid turnover,” he added.
Dr. Garrison reported no outside sources of funding and no conflicts of interest.
SOURCE: Garrison G et al. NAPCRG 2017 Abstract AE32
REPORTING FROM NAPCRG 2017
Key clinical point: Patients’ length of stay was shorter when they were cared for by family medicine doctors and not hospitalists.
Major finding: After multivariable analysis, the adjusted length of stay was 31.8% longer for patients on the hospitalist service than on the family medicine inpatient service.
Study details: A retrospective review of records from 3,125 admissions of 2,138 patients.
Disclosures: Dr. Garrison reported no conflicts of interest and no outside sources of funding.
Source: Garrison G et al. NAPCRG 2017 Abstract AE32.
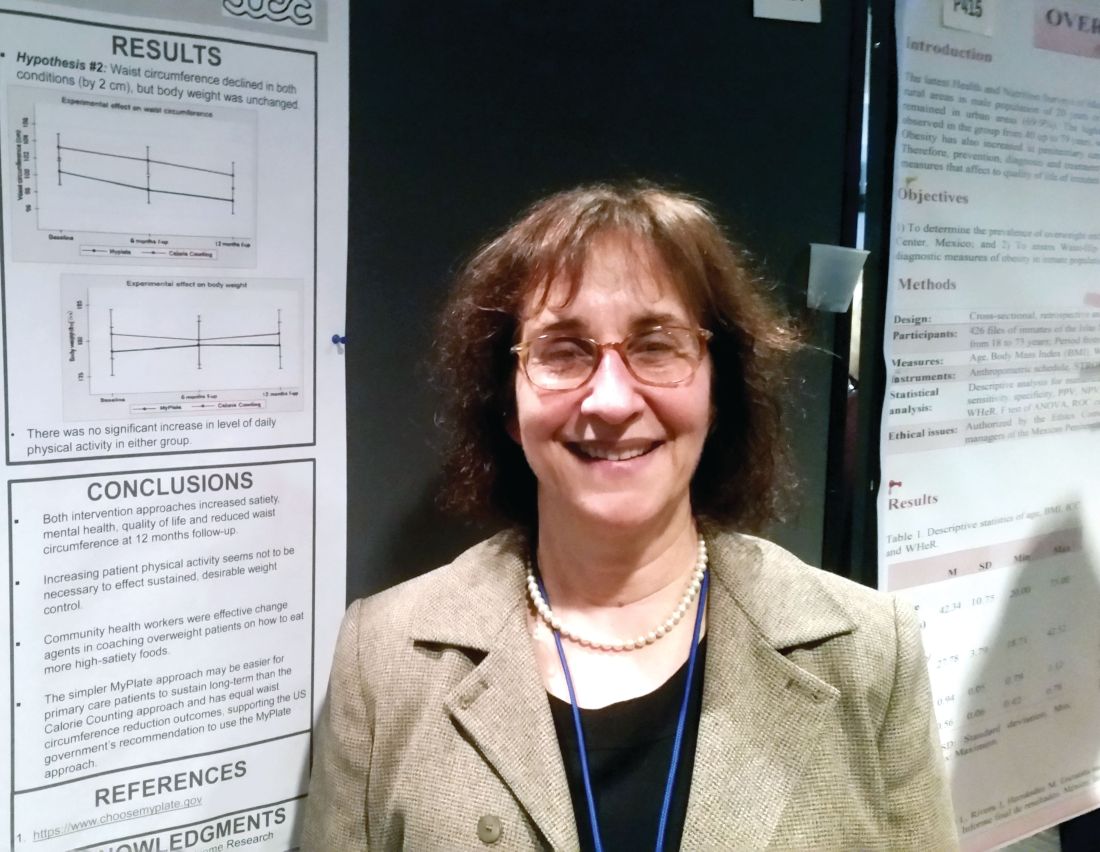
MyPlate as effective as calorie counting after 12 months
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
REPORTING FROM NAPCRG 2017
Key clinical point:
Major finding: At 12 months, both approaches reduced waist circumference by 2 cm but didn’t result in weight loss.
Data source: Prospective randomized comparative effectiveness trial of 261 patients.
Disclosures: Dr. Gelberg reported no conflicts of interest. The study was funded by the Patient-Centered Comparative Effectiveness Institute.
Source: Gelberg L, abstract P414.
E-health app helps weight loss, QOL for African American breast cancer survivors
MONTREAL – African American breast cancer survivors who participated in fitness tracking and an online support program saw small but significant reductions in weight and improvement in quality of life, according to a new study.
Further, patients who reported a low baseline quality of life (QOL) achieved as much or more weight loss as did those whose QOL was initially high, said Jeanne Ferrante, MD, MPH, professor of family medicine and community health at Robert Wood Johnson Medical School, New Brunswick, N.J.
Overall, but not cancer-related, QOL improved during the 6 months of the study as well.
“Low quality of life at baseline was not a barrier to weight loss, and there’s the potential for weight loss to improve quality of life” in this group of cancer survivors, Dr. Ferrante said at the annual meeting of the North American Primary Care Research Group.
Although weight loss is known to improve functional status and QOL, few studies have examined these issues in African American breast cancer survivors, who may have more comorbidities and a greater risk for obesity compared with the general population, said Dr. Ferrante.
Dr. Ferrante and her coinvestigators hypothesized that QOL would be a predictor of weight loss, and that weight loss, in turn, would have a positive impact on QOL. They conducted a secondary data analysis of a trial of participants using a physical activity monitor alone (in this study, a Fitbit), compared with using the wrist-worn activity monitor together with an Internet program, SparkPeople, designed to provide information and support for increased activity and weight loss.
Eligible participants (n = 61) were African American women who had completed treatment for early stage (0-III) breast cancer, were aged 21-75 (mean 62) years, and had a body mass index of at least 25 kg/m2 (mean, 37; range 26-52). They had to be English speaking, and have Internet and smartphone access. Half the number of participants were retired, half were college graduates, and about a third were married.
One-third of the women reported that they had five or more chronic conditions at enrollment. The mean waist circumference at baseline was 45 inches, and the mean weight was 216 pounds. Patients who had bariatric surgery, had recently lost at least 5% of their body weight, or had limitations to exercise participation or other serious medical or psychiatric conditions were excluded.
To assess QOL, the investigators used the Quality of Life in Adult Cancer Survivors (Q-LACS) scale, which measures both generic and cancer-specific quality of life.
The women in the study also reported how many days out of the past 30 days their mental and their physical health was “not good.”
At baseline, the mean QOL was 108, generic quality of life was 70, and cancer-specific quality of life was 39; lower numbers are better on the scale. Patients reported that their mental health had not been good for 9 of the past 30 days, on average, and that their physical health had not been good for a mean of 6 of the past 30 days.
After 6 months (but not at 3 months), the mean improvement for overall QOL on the Q-LACS scale was –7 (P = .054). Generic QOL improved significantly at both 3 and 6 months (P = .051 and P = .017, respectively), but cancer-specific QOL did not change significantly.
The women saw no significant change over the 6 months in the number of “not good” mental and physical health days.
Waist circumference reduction was about a half inch at 3 months (–0.45 inches, not significant), with a drop at 6 months of 0.91 inches from baseline that met criteria for statistical significance. (P = .013).
The study’s limitations included its small sample size and relatively short duration, said Dr. Ferrante; however, the study continued for 12 months and those data are being analyzed now. Some bias may have been introduced by the need for Internet connection and a smartphone as well, she said.
The investigators are now piloting use of a premium version of the SparkPeople app that offers more customization and interaction with participants.
Dr. Ferrante reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – African American breast cancer survivors who participated in fitness tracking and an online support program saw small but significant reductions in weight and improvement in quality of life, according to a new study.
Further, patients who reported a low baseline quality of life (QOL) achieved as much or more weight loss as did those whose QOL was initially high, said Jeanne Ferrante, MD, MPH, professor of family medicine and community health at Robert Wood Johnson Medical School, New Brunswick, N.J.
Overall, but not cancer-related, QOL improved during the 6 months of the study as well.
“Low quality of life at baseline was not a barrier to weight loss, and there’s the potential for weight loss to improve quality of life” in this group of cancer survivors, Dr. Ferrante said at the annual meeting of the North American Primary Care Research Group.
Although weight loss is known to improve functional status and QOL, few studies have examined these issues in African American breast cancer survivors, who may have more comorbidities and a greater risk for obesity compared with the general population, said Dr. Ferrante.
Dr. Ferrante and her coinvestigators hypothesized that QOL would be a predictor of weight loss, and that weight loss, in turn, would have a positive impact on QOL. They conducted a secondary data analysis of a trial of participants using a physical activity monitor alone (in this study, a Fitbit), compared with using the wrist-worn activity monitor together with an Internet program, SparkPeople, designed to provide information and support for increased activity and weight loss.
Eligible participants (n = 61) were African American women who had completed treatment for early stage (0-III) breast cancer, were aged 21-75 (mean 62) years, and had a body mass index of at least 25 kg/m2 (mean, 37; range 26-52). They had to be English speaking, and have Internet and smartphone access. Half the number of participants were retired, half were college graduates, and about a third were married.
One-third of the women reported that they had five or more chronic conditions at enrollment. The mean waist circumference at baseline was 45 inches, and the mean weight was 216 pounds. Patients who had bariatric surgery, had recently lost at least 5% of their body weight, or had limitations to exercise participation or other serious medical or psychiatric conditions were excluded.
To assess QOL, the investigators used the Quality of Life in Adult Cancer Survivors (Q-LACS) scale, which measures both generic and cancer-specific quality of life.
The women in the study also reported how many days out of the past 30 days their mental and their physical health was “not good.”
At baseline, the mean QOL was 108, generic quality of life was 70, and cancer-specific quality of life was 39; lower numbers are better on the scale. Patients reported that their mental health had not been good for 9 of the past 30 days, on average, and that their physical health had not been good for a mean of 6 of the past 30 days.
After 6 months (but not at 3 months), the mean improvement for overall QOL on the Q-LACS scale was –7 (P = .054). Generic QOL improved significantly at both 3 and 6 months (P = .051 and P = .017, respectively), but cancer-specific QOL did not change significantly.
The women saw no significant change over the 6 months in the number of “not good” mental and physical health days.
Waist circumference reduction was about a half inch at 3 months (–0.45 inches, not significant), with a drop at 6 months of 0.91 inches from baseline that met criteria for statistical significance. (P = .013).
The study’s limitations included its small sample size and relatively short duration, said Dr. Ferrante; however, the study continued for 12 months and those data are being analyzed now. Some bias may have been introduced by the need for Internet connection and a smartphone as well, she said.
The investigators are now piloting use of a premium version of the SparkPeople app that offers more customization and interaction with participants.
Dr. Ferrante reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – African American breast cancer survivors who participated in fitness tracking and an online support program saw small but significant reductions in weight and improvement in quality of life, according to a new study.
Further, patients who reported a low baseline quality of life (QOL) achieved as much or more weight loss as did those whose QOL was initially high, said Jeanne Ferrante, MD, MPH, professor of family medicine and community health at Robert Wood Johnson Medical School, New Brunswick, N.J.
Overall, but not cancer-related, QOL improved during the 6 months of the study as well.
“Low quality of life at baseline was not a barrier to weight loss, and there’s the potential for weight loss to improve quality of life” in this group of cancer survivors, Dr. Ferrante said at the annual meeting of the North American Primary Care Research Group.
Although weight loss is known to improve functional status and QOL, few studies have examined these issues in African American breast cancer survivors, who may have more comorbidities and a greater risk for obesity compared with the general population, said Dr. Ferrante.
Dr. Ferrante and her coinvestigators hypothesized that QOL would be a predictor of weight loss, and that weight loss, in turn, would have a positive impact on QOL. They conducted a secondary data analysis of a trial of participants using a physical activity monitor alone (in this study, a Fitbit), compared with using the wrist-worn activity monitor together with an Internet program, SparkPeople, designed to provide information and support for increased activity and weight loss.
Eligible participants (n = 61) were African American women who had completed treatment for early stage (0-III) breast cancer, were aged 21-75 (mean 62) years, and had a body mass index of at least 25 kg/m2 (mean, 37; range 26-52). They had to be English speaking, and have Internet and smartphone access. Half the number of participants were retired, half were college graduates, and about a third were married.
One-third of the women reported that they had five or more chronic conditions at enrollment. The mean waist circumference at baseline was 45 inches, and the mean weight was 216 pounds. Patients who had bariatric surgery, had recently lost at least 5% of their body weight, or had limitations to exercise participation or other serious medical or psychiatric conditions were excluded.
To assess QOL, the investigators used the Quality of Life in Adult Cancer Survivors (Q-LACS) scale, which measures both generic and cancer-specific quality of life.
The women in the study also reported how many days out of the past 30 days their mental and their physical health was “not good.”
At baseline, the mean QOL was 108, generic quality of life was 70, and cancer-specific quality of life was 39; lower numbers are better on the scale. Patients reported that their mental health had not been good for 9 of the past 30 days, on average, and that their physical health had not been good for a mean of 6 of the past 30 days.
After 6 months (but not at 3 months), the mean improvement for overall QOL on the Q-LACS scale was –7 (P = .054). Generic QOL improved significantly at both 3 and 6 months (P = .051 and P = .017, respectively), but cancer-specific QOL did not change significantly.
The women saw no significant change over the 6 months in the number of “not good” mental and physical health days.
Waist circumference reduction was about a half inch at 3 months (–0.45 inches, not significant), with a drop at 6 months of 0.91 inches from baseline that met criteria for statistical significance. (P = .013).
The study’s limitations included its small sample size and relatively short duration, said Dr. Ferrante; however, the study continued for 12 months and those data are being analyzed now. Some bias may have been introduced by the need for Internet connection and a smartphone as well, she said.
The investigators are now piloting use of a premium version of the SparkPeople app that offers more customization and interaction with participants.
Dr. Ferrante reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT NAPCRG 2017
Key clinical point:
Major finding: Participants lost a mean 4.79 pounds from baseline (mean 2.14%, P less than .001).
Data source: Subanalysis from study of 61 African American survivors of early stage breast cancer, with BMI of 25 or higher.
Disclosures: Dr. Ferrante reported no conflicts of interest.
E-visits less likely to generate antibiotic prescriptions for common ailments
MONTREAL – When the same patient was assessed in person and via an electronic visit (e-visit) for several common complaints, a prescription for antibiotics was more likely to be generated from the face-to-face encounter.
In a recent study, if antibiotics were prescribed in one setting, but not the other, the office visit rather than the e-visit was where the antibiotic prescription was written in 73% of cases. Visits for sinus problems and vaginal symptoms made up over 80% of these cases of nonconcordant prescribing.
The study compared the diagnosis and treatment of five common acute conditions in an outpatient and e-visit setting, examining the concordance of both diagnosis and treatment between the two settings for complaints of vaginal irritation or discharge, urinary symptoms, sinus problems, rash, and diarrhea.
Outcomes tracked included concordance between the office visits and mock e-visits for the diagnosis, whether antibiotics were prescribed, and the general choice of antibiotics. Determinations about concordance were made by a third provider who was not involved with either the in-person visit or the mock e-visit, said Dr. Player, of the department of family medicine at the Medical University of South Carolina, Charleston.
Nonconcordance in treatment could occur either because an antibiotic was prescribed in one setting, but not the other, or because the broad choice of antibiotic class differed between the two settings.
Adult patients who came to the outpatient clinic and agreed to be enrolled in the study also completed the e-visit questionnaires appropriate to their condition before they saw the provider in an office visit. Thus, mock e-visits were created that mirrored the office visit with the e-visit format used in practice.
At a later point in time, the blinded e-visit questionnaires were given to e-visit providers who treated the patients as they would if the questionnaires had been generated in an actual e-visit.
The study generated a total of 142 office visits with accompanying mock e-visits, but 29 were excluded for lack of completeness or inappropriateness for e-visit care. In all, 113 paired visits were evaluated. All but seven patients (94%) were female; slightly more than half (53%) of patients were aged 45 years or older.
About one-third of visits (34%; n = 38) were for vaginal discharge or irritation. Sinus problems were reported by 36 patients (32%). Twenty-five patients (22%) reported urinary problems, while eight patients (7%) reported diarrhea. Six patients (5%) complained of a rash.
In total, 78 visit pairs (69%) were assessed as being concordant. Of the 35 nonconcordant visits, over half (54%) were for sinus problems, 40% were for vaginal discharge or irritation, and 6% were for rash. None of the visits involving urinary problems or diarrhea were assessed as nonconcordant.
Examining the data another way, Dr. Player and his coinvestigators also looked at how many visits involved antibiotic prescribing, and how many of those visits were assessed as nonconcordant. Of the 96 patients (85%) who were prescribed antibiotics, 37 had office and mock e-visits that were assessed as discordant in antibiotic prescribing.
Of these visit pairs, about half (51%) were for sinus problems, and a third (32%) were for vaginal complaints. Urinary complaints made up 11% of the nonconcordant visit pairs where antibiotics were prescribed, and rashes made up the remaining 5%.
Diagnostic concordance was seen in about two-thirds of rash (67%) and vaginal discharge (63%) visit pairs. Concordance of diagnosis for sinus problems occurred in fewer than half (47%) of visit pairs.
Dr. Player said that the investigators excluded visits involving urinary or vaginal complaints that did not have an accompanying urinalysis or vaginal wet mount. This decision was made because the standard of care for both office visits and e-visits requires these laboratory tests for diagnosis, he said.
The study design came with some limitations, said Dr. Player. “Patients self-select for e-visits, and the patients in this study might be different from those in true e-visit encounters,” he said. Also, the diagnosis and treatment of sinus problems, rash, and diarrhea relied on clinical judgment alone in each visit setting. Still, he said, the study supports what many clinicians report anecdotally: Patients want to leave the office knowing that the clinician has “done something” for them, and often, that means walking out with a prescription in hand.
Dr. Player reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – When the same patient was assessed in person and via an electronic visit (e-visit) for several common complaints, a prescription for antibiotics was more likely to be generated from the face-to-face encounter.
In a recent study, if antibiotics were prescribed in one setting, but not the other, the office visit rather than the e-visit was where the antibiotic prescription was written in 73% of cases. Visits for sinus problems and vaginal symptoms made up over 80% of these cases of nonconcordant prescribing.
The study compared the diagnosis and treatment of five common acute conditions in an outpatient and e-visit setting, examining the concordance of both diagnosis and treatment between the two settings for complaints of vaginal irritation or discharge, urinary symptoms, sinus problems, rash, and diarrhea.
Outcomes tracked included concordance between the office visits and mock e-visits for the diagnosis, whether antibiotics were prescribed, and the general choice of antibiotics. Determinations about concordance were made by a third provider who was not involved with either the in-person visit or the mock e-visit, said Dr. Player, of the department of family medicine at the Medical University of South Carolina, Charleston.
Nonconcordance in treatment could occur either because an antibiotic was prescribed in one setting, but not the other, or because the broad choice of antibiotic class differed between the two settings.
Adult patients who came to the outpatient clinic and agreed to be enrolled in the study also completed the e-visit questionnaires appropriate to their condition before they saw the provider in an office visit. Thus, mock e-visits were created that mirrored the office visit with the e-visit format used in practice.
At a later point in time, the blinded e-visit questionnaires were given to e-visit providers who treated the patients as they would if the questionnaires had been generated in an actual e-visit.
The study generated a total of 142 office visits with accompanying mock e-visits, but 29 were excluded for lack of completeness or inappropriateness for e-visit care. In all, 113 paired visits were evaluated. All but seven patients (94%) were female; slightly more than half (53%) of patients were aged 45 years or older.
About one-third of visits (34%; n = 38) were for vaginal discharge or irritation. Sinus problems were reported by 36 patients (32%). Twenty-five patients (22%) reported urinary problems, while eight patients (7%) reported diarrhea. Six patients (5%) complained of a rash.
In total, 78 visit pairs (69%) were assessed as being concordant. Of the 35 nonconcordant visits, over half (54%) were for sinus problems, 40% were for vaginal discharge or irritation, and 6% were for rash. None of the visits involving urinary problems or diarrhea were assessed as nonconcordant.
Examining the data another way, Dr. Player and his coinvestigators also looked at how many visits involved antibiotic prescribing, and how many of those visits were assessed as nonconcordant. Of the 96 patients (85%) who were prescribed antibiotics, 37 had office and mock e-visits that were assessed as discordant in antibiotic prescribing.
Of these visit pairs, about half (51%) were for sinus problems, and a third (32%) were for vaginal complaints. Urinary complaints made up 11% of the nonconcordant visit pairs where antibiotics were prescribed, and rashes made up the remaining 5%.
Diagnostic concordance was seen in about two-thirds of rash (67%) and vaginal discharge (63%) visit pairs. Concordance of diagnosis for sinus problems occurred in fewer than half (47%) of visit pairs.
Dr. Player said that the investigators excluded visits involving urinary or vaginal complaints that did not have an accompanying urinalysis or vaginal wet mount. This decision was made because the standard of care for both office visits and e-visits requires these laboratory tests for diagnosis, he said.
The study design came with some limitations, said Dr. Player. “Patients self-select for e-visits, and the patients in this study might be different from those in true e-visit encounters,” he said. Also, the diagnosis and treatment of sinus problems, rash, and diarrhea relied on clinical judgment alone in each visit setting. Still, he said, the study supports what many clinicians report anecdotally: Patients want to leave the office knowing that the clinician has “done something” for them, and often, that means walking out with a prescription in hand.
Dr. Player reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – When the same patient was assessed in person and via an electronic visit (e-visit) for several common complaints, a prescription for antibiotics was more likely to be generated from the face-to-face encounter.
In a recent study, if antibiotics were prescribed in one setting, but not the other, the office visit rather than the e-visit was where the antibiotic prescription was written in 73% of cases. Visits for sinus problems and vaginal symptoms made up over 80% of these cases of nonconcordant prescribing.
The study compared the diagnosis and treatment of five common acute conditions in an outpatient and e-visit setting, examining the concordance of both diagnosis and treatment between the two settings for complaints of vaginal irritation or discharge, urinary symptoms, sinus problems, rash, and diarrhea.
Outcomes tracked included concordance between the office visits and mock e-visits for the diagnosis, whether antibiotics were prescribed, and the general choice of antibiotics. Determinations about concordance were made by a third provider who was not involved with either the in-person visit or the mock e-visit, said Dr. Player, of the department of family medicine at the Medical University of South Carolina, Charleston.
Nonconcordance in treatment could occur either because an antibiotic was prescribed in one setting, but not the other, or because the broad choice of antibiotic class differed between the two settings.
Adult patients who came to the outpatient clinic and agreed to be enrolled in the study also completed the e-visit questionnaires appropriate to their condition before they saw the provider in an office visit. Thus, mock e-visits were created that mirrored the office visit with the e-visit format used in practice.
At a later point in time, the blinded e-visit questionnaires were given to e-visit providers who treated the patients as they would if the questionnaires had been generated in an actual e-visit.
The study generated a total of 142 office visits with accompanying mock e-visits, but 29 were excluded for lack of completeness or inappropriateness for e-visit care. In all, 113 paired visits were evaluated. All but seven patients (94%) were female; slightly more than half (53%) of patients were aged 45 years or older.
About one-third of visits (34%; n = 38) were for vaginal discharge or irritation. Sinus problems were reported by 36 patients (32%). Twenty-five patients (22%) reported urinary problems, while eight patients (7%) reported diarrhea. Six patients (5%) complained of a rash.
In total, 78 visit pairs (69%) were assessed as being concordant. Of the 35 nonconcordant visits, over half (54%) were for sinus problems, 40% were for vaginal discharge or irritation, and 6% were for rash. None of the visits involving urinary problems or diarrhea were assessed as nonconcordant.
Examining the data another way, Dr. Player and his coinvestigators also looked at how many visits involved antibiotic prescribing, and how many of those visits were assessed as nonconcordant. Of the 96 patients (85%) who were prescribed antibiotics, 37 had office and mock e-visits that were assessed as discordant in antibiotic prescribing.
Of these visit pairs, about half (51%) were for sinus problems, and a third (32%) were for vaginal complaints. Urinary complaints made up 11% of the nonconcordant visit pairs where antibiotics were prescribed, and rashes made up the remaining 5%.
Diagnostic concordance was seen in about two-thirds of rash (67%) and vaginal discharge (63%) visit pairs. Concordance of diagnosis for sinus problems occurred in fewer than half (47%) of visit pairs.
Dr. Player said that the investigators excluded visits involving urinary or vaginal complaints that did not have an accompanying urinalysis or vaginal wet mount. This decision was made because the standard of care for both office visits and e-visits requires these laboratory tests for diagnosis, he said.
The study design came with some limitations, said Dr. Player. “Patients self-select for e-visits, and the patients in this study might be different from those in true e-visit encounters,” he said. Also, the diagnosis and treatment of sinus problems, rash, and diarrhea relied on clinical judgment alone in each visit setting. Still, he said, the study supports what many clinicians report anecdotally: Patients want to leave the office knowing that the clinician has “done something” for them, and often, that means walking out with a prescription in hand.
Dr. Player reported no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT NAPCRG 2017
Key clinical point:
Major finding: Antibiotics were given in the office but not the e-visit in 73% of cases.
Data source: Prospective study of 113 office visits that were paired with independently assessed e-visits for the same patient and complaint.
Disclosures: Dr. Player reported no conflicts of interest.
Female family physicians come up short in burnout gender divide
MONTREAL – Female family physicians report more burnout and fewer self-care activities than their male colleagues, according to the results of a survey that found a significant gender divide in physician wellness.
Female respondents to the Texas-wide electronic survey of practicing physicians and residents reported more emotional exhaustion (P = .004) and higher levels of work stress (P = .009) than their male colleagues. Additionally, they reported sleeping less (P = .009), exercising less (P = .001), and eating healthy food less often (P = .005).
In an interview, Dr. Holder said she and her colleagues sent electronic surveys to family physicians, using the Residency Research Network of Texas champion at each of 11 family medicine residency sites. The champion helped with administration to residents, and also engaged community-based physicians in their region to complete the survey.
A total of 324 physicians completed the survey; 54% were female. The female respondents were younger (P = .001) and less likely to be married (P = .019) than the male physicians who responded.
A high level of emotional exhaustion, as assessed by responses on the Maslach Burnout Inventory, was reported by more than a third of physician respondents. Male respondents, however, were more likely to endorse factors protective against burnout, including feeling a higher level of personal accomplishment (P = .004) and having more resilience (P = .002). They also were more likely to participate in activities outside of work (P = .007).
Dr. Holder said she was surprised by the pervasively higher rates of burnout and lower levels of self-care the survey revealed among family physicians in Texas. She would have been less surprised to see the association in female physicians with children, but, she said, unpublished data didn’t bear that association out.
“Creating wellness programs during residency that are aimed at teaching physicians to incorporate self-care into their routines, especially females, may lead to decreased rates of burnout later in physicians’ careers,” said Dr. Holder.
In a discussion during the poster session, Dr. Holder, who is the associate program director for the Baylor Family Medicine residency program in Garland, Tex., said that she herself tries to make room for exercise in a busy schedule and eats so healthily that her residents tease her about it. It’s important to provide positive role modeling for residents, both male and female alike, during their training years, she said.
Dr. Holder reported no relevant financial conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – Female family physicians report more burnout and fewer self-care activities than their male colleagues, according to the results of a survey that found a significant gender divide in physician wellness.
Female respondents to the Texas-wide electronic survey of practicing physicians and residents reported more emotional exhaustion (P = .004) and higher levels of work stress (P = .009) than their male colleagues. Additionally, they reported sleeping less (P = .009), exercising less (P = .001), and eating healthy food less often (P = .005).
In an interview, Dr. Holder said she and her colleagues sent electronic surveys to family physicians, using the Residency Research Network of Texas champion at each of 11 family medicine residency sites. The champion helped with administration to residents, and also engaged community-based physicians in their region to complete the survey.
A total of 324 physicians completed the survey; 54% were female. The female respondents were younger (P = .001) and less likely to be married (P = .019) than the male physicians who responded.
A high level of emotional exhaustion, as assessed by responses on the Maslach Burnout Inventory, was reported by more than a third of physician respondents. Male respondents, however, were more likely to endorse factors protective against burnout, including feeling a higher level of personal accomplishment (P = .004) and having more resilience (P = .002). They also were more likely to participate in activities outside of work (P = .007).
Dr. Holder said she was surprised by the pervasively higher rates of burnout and lower levels of self-care the survey revealed among family physicians in Texas. She would have been less surprised to see the association in female physicians with children, but, she said, unpublished data didn’t bear that association out.
“Creating wellness programs during residency that are aimed at teaching physicians to incorporate self-care into their routines, especially females, may lead to decreased rates of burnout later in physicians’ careers,” said Dr. Holder.
In a discussion during the poster session, Dr. Holder, who is the associate program director for the Baylor Family Medicine residency program in Garland, Tex., said that she herself tries to make room for exercise in a busy schedule and eats so healthily that her residents tease her about it. It’s important to provide positive role modeling for residents, both male and female alike, during their training years, she said.
Dr. Holder reported no relevant financial conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – Female family physicians report more burnout and fewer self-care activities than their male colleagues, according to the results of a survey that found a significant gender divide in physician wellness.
Female respondents to the Texas-wide electronic survey of practicing physicians and residents reported more emotional exhaustion (P = .004) and higher levels of work stress (P = .009) than their male colleagues. Additionally, they reported sleeping less (P = .009), exercising less (P = .001), and eating healthy food less often (P = .005).
In an interview, Dr. Holder said she and her colleagues sent electronic surveys to family physicians, using the Residency Research Network of Texas champion at each of 11 family medicine residency sites. The champion helped with administration to residents, and also engaged community-based physicians in their region to complete the survey.
A total of 324 physicians completed the survey; 54% were female. The female respondents were younger (P = .001) and less likely to be married (P = .019) than the male physicians who responded.
A high level of emotional exhaustion, as assessed by responses on the Maslach Burnout Inventory, was reported by more than a third of physician respondents. Male respondents, however, were more likely to endorse factors protective against burnout, including feeling a higher level of personal accomplishment (P = .004) and having more resilience (P = .002). They also were more likely to participate in activities outside of work (P = .007).
Dr. Holder said she was surprised by the pervasively higher rates of burnout and lower levels of self-care the survey revealed among family physicians in Texas. She would have been less surprised to see the association in female physicians with children, but, she said, unpublished data didn’t bear that association out.
“Creating wellness programs during residency that are aimed at teaching physicians to incorporate self-care into their routines, especially females, may lead to decreased rates of burnout later in physicians’ careers,” said Dr. Holder.
In a discussion during the poster session, Dr. Holder, who is the associate program director for the Baylor Family Medicine residency program in Garland, Tex., said that she herself tries to make room for exercise in a busy schedule and eats so healthily that her residents tease her about it. It’s important to provide positive role modeling for residents, both male and female alike, during their training years, she said.
Dr. Holder reported no relevant financial conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT NAPCRG 2017
Key clinical point:
Major finding: Female family physicians are more likely to experience emotional exhaustion than their male counterparts (P = .009).
Data source: A survey of 324 family physicians in Texas.
Disclosures: Dr. Holder reported no relevant financial conflicts of interest.
Can increased scope of practice protect against family physician burnout?
MONTREAL – Have restrictions on scope of practice contributed to primary care physician burnout?
Perhaps they have, according to a recent survey that saw less burnout among recently graduated family physicians who retained inpatient or obstetrics work.
Of the 1,167 family practice physicians surveyed, 42% reported that they felt burned out once per week or more, said Amanda Weidner, MPH, of the University of Washington Family Medicine Residency Network in Seattle. However, some physicians were significantly less likely to experience burnout: those whose practice included adult inpatient medicine (P less than .0001), those currently delivering babies (P = .0007), and those who routinely saw their patients at the hospital or in patients’ homes (P = .0016 and P = .02, respectively).
Surveys of family practice physicians have reported varying levels of burnout, ranging from as low as 24% to as high as 65%. “Either way, we can probably agree that even one quarter of physicians saying they’re burned out is too many,” said Ms. Weidner during a presentation at the annual meeting of the National Association of Primary Care Research Groups.
Ms. Weidner and her colleagues polled young family practice physicians about their feelings of burnout and about their practice scope. She said she and her colleagues wondered about the association between those factors because the scope of primary care practice has been narrowing while primary care physicians have been reporting increasing levels of burnout – and at a higher rate than many other specialties.
Their survey, mailed in 2016, was sent to American Board of Family Medicine (ABFM) diplomates who were 2013 graduates of family practice residencies. Overall, 67% responded to the survey. Ms. Weidner and her colleagues used responses from the 78% of respondents who reported providing outpatient continuity care, rather than those who were hospitalists or who practiced in noncontinuity care areas, such as urgent care or emergency medicine.
Participants were asked to indicate how often they felt burned out in their work, with seven choices that ranged from “every day” to “never.” This single question from the Maslach Burnout Inventory, said Ms. Weidner, has been shown to correlate well with the emotional exhaustion domain of the inventory: Any response indicating feeling burned out at least once a week correlates with burnout.
In addition to asking physicians about the scope of their practice and their practice setting, the investigators assessed their work effort by asking about the number of patient encounters per day and whether respondents had after-hours calls and saw patients on weekends and evenings.
Respondents were, on average, about 36 years old, 58.6% were female, and 84.7% held an MD (rather than a DO). Two-thirds were graduates of U.S. medical schools.
Maintaining a broad scope of practice for family physicians can help fulfill the “triple aims” (enhancing patient experience, improving population health, and reducing costs) – now sometimes characterized as the “quadruple aims”with the addition of preventing burnout – of health system performance, said Ms. Weidner. In addition to proven cost reduction, she said, maintaining a broad scope of practice in family practice can enhance the patient experience and improve population health. If increased scope of practice also is associated with improved physician satisfaction, then it will also contribute to the fourth aim, she said.
Questioners in the audience asked Ms. Weidner and her collaborators to dive a little deeper into the data. One audience member remarked that she sees colleagues scheduling themselves for inpatient coverage or an afternoon of endometrial biopsies and other procedures as a strategy to avoid clinic time. She asked whether it’s the practice variety or the reduced number of clinic hours per week that’s driving the lower burnout rates.
Ms. Weidner acknowledged the possibility that working in other practice settings might reduce workload in terms of paperwork and patient communication. However, she pointed out that the number of hours worked per week was not associated with burnout; additionally, she said, both physicians who reported burnout and those who did not saw about the same number of patients per day.
Another audience member wondered whether some of the burnout – and practice restriction – is related to the fact that fewer physicians own their own practices. Maybe, he said, “There’s less of an obligation to be there to take people through all phases of life.”
Some practice restriction may be self-imposed, as may be the case when physicians don’t want the call obligations associated with obstetrics, but some of it is imposed by the system as an attempt to increase clinic throughput, Ms. Weidner said. “This is something for health systems to pay attention to. It’s less of an individual issue and more of a health system issue.”
Ms. Weidner reported that her work was supported by an ABFM Foundation grant while she was a visiting ABFM scholar.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – Have restrictions on scope of practice contributed to primary care physician burnout?
Perhaps they have, according to a recent survey that saw less burnout among recently graduated family physicians who retained inpatient or obstetrics work.
Of the 1,167 family practice physicians surveyed, 42% reported that they felt burned out once per week or more, said Amanda Weidner, MPH, of the University of Washington Family Medicine Residency Network in Seattle. However, some physicians were significantly less likely to experience burnout: those whose practice included adult inpatient medicine (P less than .0001), those currently delivering babies (P = .0007), and those who routinely saw their patients at the hospital or in patients’ homes (P = .0016 and P = .02, respectively).
Surveys of family practice physicians have reported varying levels of burnout, ranging from as low as 24% to as high as 65%. “Either way, we can probably agree that even one quarter of physicians saying they’re burned out is too many,” said Ms. Weidner during a presentation at the annual meeting of the National Association of Primary Care Research Groups.
Ms. Weidner and her colleagues polled young family practice physicians about their feelings of burnout and about their practice scope. She said she and her colleagues wondered about the association between those factors because the scope of primary care practice has been narrowing while primary care physicians have been reporting increasing levels of burnout – and at a higher rate than many other specialties.
Their survey, mailed in 2016, was sent to American Board of Family Medicine (ABFM) diplomates who were 2013 graduates of family practice residencies. Overall, 67% responded to the survey. Ms. Weidner and her colleagues used responses from the 78% of respondents who reported providing outpatient continuity care, rather than those who were hospitalists or who practiced in noncontinuity care areas, such as urgent care or emergency medicine.
Participants were asked to indicate how often they felt burned out in their work, with seven choices that ranged from “every day” to “never.” This single question from the Maslach Burnout Inventory, said Ms. Weidner, has been shown to correlate well with the emotional exhaustion domain of the inventory: Any response indicating feeling burned out at least once a week correlates with burnout.
In addition to asking physicians about the scope of their practice and their practice setting, the investigators assessed their work effort by asking about the number of patient encounters per day and whether respondents had after-hours calls and saw patients on weekends and evenings.
Respondents were, on average, about 36 years old, 58.6% were female, and 84.7% held an MD (rather than a DO). Two-thirds were graduates of U.S. medical schools.
Maintaining a broad scope of practice for family physicians can help fulfill the “triple aims” (enhancing patient experience, improving population health, and reducing costs) – now sometimes characterized as the “quadruple aims”with the addition of preventing burnout – of health system performance, said Ms. Weidner. In addition to proven cost reduction, she said, maintaining a broad scope of practice in family practice can enhance the patient experience and improve population health. If increased scope of practice also is associated with improved physician satisfaction, then it will also contribute to the fourth aim, she said.
Questioners in the audience asked Ms. Weidner and her collaborators to dive a little deeper into the data. One audience member remarked that she sees colleagues scheduling themselves for inpatient coverage or an afternoon of endometrial biopsies and other procedures as a strategy to avoid clinic time. She asked whether it’s the practice variety or the reduced number of clinic hours per week that’s driving the lower burnout rates.
Ms. Weidner acknowledged the possibility that working in other practice settings might reduce workload in terms of paperwork and patient communication. However, she pointed out that the number of hours worked per week was not associated with burnout; additionally, she said, both physicians who reported burnout and those who did not saw about the same number of patients per day.
Another audience member wondered whether some of the burnout – and practice restriction – is related to the fact that fewer physicians own their own practices. Maybe, he said, “There’s less of an obligation to be there to take people through all phases of life.”
Some practice restriction may be self-imposed, as may be the case when physicians don’t want the call obligations associated with obstetrics, but some of it is imposed by the system as an attempt to increase clinic throughput, Ms. Weidner said. “This is something for health systems to pay attention to. It’s less of an individual issue and more of a health system issue.”
Ms. Weidner reported that her work was supported by an ABFM Foundation grant while she was a visiting ABFM scholar.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – Have restrictions on scope of practice contributed to primary care physician burnout?
Perhaps they have, according to a recent survey that saw less burnout among recently graduated family physicians who retained inpatient or obstetrics work.
Of the 1,167 family practice physicians surveyed, 42% reported that they felt burned out once per week or more, said Amanda Weidner, MPH, of the University of Washington Family Medicine Residency Network in Seattle. However, some physicians were significantly less likely to experience burnout: those whose practice included adult inpatient medicine (P less than .0001), those currently delivering babies (P = .0007), and those who routinely saw their patients at the hospital or in patients’ homes (P = .0016 and P = .02, respectively).
Surveys of family practice physicians have reported varying levels of burnout, ranging from as low as 24% to as high as 65%. “Either way, we can probably agree that even one quarter of physicians saying they’re burned out is too many,” said Ms. Weidner during a presentation at the annual meeting of the National Association of Primary Care Research Groups.
Ms. Weidner and her colleagues polled young family practice physicians about their feelings of burnout and about their practice scope. She said she and her colleagues wondered about the association between those factors because the scope of primary care practice has been narrowing while primary care physicians have been reporting increasing levels of burnout – and at a higher rate than many other specialties.
Their survey, mailed in 2016, was sent to American Board of Family Medicine (ABFM) diplomates who were 2013 graduates of family practice residencies. Overall, 67% responded to the survey. Ms. Weidner and her colleagues used responses from the 78% of respondents who reported providing outpatient continuity care, rather than those who were hospitalists or who practiced in noncontinuity care areas, such as urgent care or emergency medicine.
Participants were asked to indicate how often they felt burned out in their work, with seven choices that ranged from “every day” to “never.” This single question from the Maslach Burnout Inventory, said Ms. Weidner, has been shown to correlate well with the emotional exhaustion domain of the inventory: Any response indicating feeling burned out at least once a week correlates with burnout.
In addition to asking physicians about the scope of their practice and their practice setting, the investigators assessed their work effort by asking about the number of patient encounters per day and whether respondents had after-hours calls and saw patients on weekends and evenings.
Respondents were, on average, about 36 years old, 58.6% were female, and 84.7% held an MD (rather than a DO). Two-thirds were graduates of U.S. medical schools.
Maintaining a broad scope of practice for family physicians can help fulfill the “triple aims” (enhancing patient experience, improving population health, and reducing costs) – now sometimes characterized as the “quadruple aims”with the addition of preventing burnout – of health system performance, said Ms. Weidner. In addition to proven cost reduction, she said, maintaining a broad scope of practice in family practice can enhance the patient experience and improve population health. If increased scope of practice also is associated with improved physician satisfaction, then it will also contribute to the fourth aim, she said.
Questioners in the audience asked Ms. Weidner and her collaborators to dive a little deeper into the data. One audience member remarked that she sees colleagues scheduling themselves for inpatient coverage or an afternoon of endometrial biopsies and other procedures as a strategy to avoid clinic time. She asked whether it’s the practice variety or the reduced number of clinic hours per week that’s driving the lower burnout rates.
Ms. Weidner acknowledged the possibility that working in other practice settings might reduce workload in terms of paperwork and patient communication. However, she pointed out that the number of hours worked per week was not associated with burnout; additionally, she said, both physicians who reported burnout and those who did not saw about the same number of patients per day.
Another audience member wondered whether some of the burnout – and practice restriction – is related to the fact that fewer physicians own their own practices. Maybe, he said, “There’s less of an obligation to be there to take people through all phases of life.”
Some practice restriction may be self-imposed, as may be the case when physicians don’t want the call obligations associated with obstetrics, but some of it is imposed by the system as an attempt to increase clinic throughput, Ms. Weidner said. “This is something for health systems to pay attention to. It’s less of an individual issue and more of a health system issue.”
Ms. Weidner reported that her work was supported by an ABFM Foundation grant while she was a visiting ABFM scholar.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT NAPCRG 2017
Key clinical point:
Major finding: Doing inpatient work and delivering babies was associated with less burnout for recent graduates (P less than .0001 and P = .007).
Data source: A 2016 survey of American Board of Family Medicine (ABFM) diplomates who were 2013 graduates of residency programs; 1,167 physicians’ practices met inclusion criteria.
Disclosures: Ms. Weidner reported that her work was supported by an ABFM Foundation grant while she was a visiting ABFM scholar.
Interprofessional communication demystified with hands-on EHR training
MONTREAL – A hands-on training program designed to improve communication between physicians and allied health professionals, such as physical therapists, produced gains in comfort and confidence to medical students who completed the training.
After completing the training, which involved both a didactic and a hands-on component, 92.58% of third-year medical students agreed or strongly agreed that they had the skills needed for effective interprofessional communication in the EHR, up from 43.86% before the training.
The idea for the training began when Zaiba Jetpuri, DO, and her physician colleagues at the University of Texas Southwestern Medical Center, Dallas, noticed that medical students and residents often were unsure how best to communicate with nurses, pharmacists, physical therapists, and other members of the healthcare team via the EHR.
Knowing who has what role in an interdisciplinary setting is far from obvious, and knowing how to strike the right tone in EHR communications was a challenge for trainees, Dr. Jetpuri said in an interview during her poster presentation at annual meeting of the North American Primary Care Research Groups.
To address such uncertainties, which can impact both quality and continuity of care, Dr. Jetpuri and her colleagues devised an intervention aimed at third-year medical students who were doing family medicine clerkships. The intervention has been given to about 360 students thus far.
The intervention consisted of two components. The first, a didactic module, delivered information about the importance of professionalism and teamwork and also defined interprofessional roles.
The second phase of the training had students using the “sandbox” of Epic, UT Southwestern’s EHR, to practice responding to hypothetical messages from a patient, a nurse, a pharmacist, and a physical therapist. One message would arrive in the medical student’s EHR inbox each week, and the student would have the week to craft a response.
Dr. Jetpuri said that she and her colleagues worked hard to make the scenarios as realistic as possible: The lengthy patient email included several questions about the safety of taking supplements or herbal remedies. They also tried to make sure that the nuts and bolts of interprofessional communication were covered so that, for example, medical students would end a module knowing what should be included when writing orders for physical therapy and how to place the order correctly.
The responses then went through peer evaluation according to a rubric constructed by the investigators. The training and evaluation were designed to make sure that students acquired a better understanding of the mechanics of EHR interprofessional communication and of the soft skills needed for collegial and professional communication.
Dr. Jetpuri said that she and her colleagues would like to extend this realistic educational tool through the clerkship year for better continuity. They also are working on some technical aspects of the EHR to make communication easier for medical students. Furthermore, they are in the process of validating the peer evaluation process by having instructors use the rubric to duplicate the students’ evaluation. She said, though, that both trainees and faculty see the value in early, realistic experience using the electronic record in a multidisciplinary team.
“Simulated EHR experiences are an important tool to utilize in a medical school curriculum to better train and prepare our students for the postgraduate stage,” wrote Dr. Jetpuri and her colleagues.
Dr. Jetpuri reported that she has no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – A hands-on training program designed to improve communication between physicians and allied health professionals, such as physical therapists, produced gains in comfort and confidence to medical students who completed the training.
After completing the training, which involved both a didactic and a hands-on component, 92.58% of third-year medical students agreed or strongly agreed that they had the skills needed for effective interprofessional communication in the EHR, up from 43.86% before the training.
The idea for the training began when Zaiba Jetpuri, DO, and her physician colleagues at the University of Texas Southwestern Medical Center, Dallas, noticed that medical students and residents often were unsure how best to communicate with nurses, pharmacists, physical therapists, and other members of the healthcare team via the EHR.
Knowing who has what role in an interdisciplinary setting is far from obvious, and knowing how to strike the right tone in EHR communications was a challenge for trainees, Dr. Jetpuri said in an interview during her poster presentation at annual meeting of the North American Primary Care Research Groups.
To address such uncertainties, which can impact both quality and continuity of care, Dr. Jetpuri and her colleagues devised an intervention aimed at third-year medical students who were doing family medicine clerkships. The intervention has been given to about 360 students thus far.
The intervention consisted of two components. The first, a didactic module, delivered information about the importance of professionalism and teamwork and also defined interprofessional roles.
The second phase of the training had students using the “sandbox” of Epic, UT Southwestern’s EHR, to practice responding to hypothetical messages from a patient, a nurse, a pharmacist, and a physical therapist. One message would arrive in the medical student’s EHR inbox each week, and the student would have the week to craft a response.
Dr. Jetpuri said that she and her colleagues worked hard to make the scenarios as realistic as possible: The lengthy patient email included several questions about the safety of taking supplements or herbal remedies. They also tried to make sure that the nuts and bolts of interprofessional communication were covered so that, for example, medical students would end a module knowing what should be included when writing orders for physical therapy and how to place the order correctly.
The responses then went through peer evaluation according to a rubric constructed by the investigators. The training and evaluation were designed to make sure that students acquired a better understanding of the mechanics of EHR interprofessional communication and of the soft skills needed for collegial and professional communication.
Dr. Jetpuri said that she and her colleagues would like to extend this realistic educational tool through the clerkship year for better continuity. They also are working on some technical aspects of the EHR to make communication easier for medical students. Furthermore, they are in the process of validating the peer evaluation process by having instructors use the rubric to duplicate the students’ evaluation. She said, though, that both trainees and faculty see the value in early, realistic experience using the electronic record in a multidisciplinary team.
“Simulated EHR experiences are an important tool to utilize in a medical school curriculum to better train and prepare our students for the postgraduate stage,” wrote Dr. Jetpuri and her colleagues.
Dr. Jetpuri reported that she has no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
MONTREAL – A hands-on training program designed to improve communication between physicians and allied health professionals, such as physical therapists, produced gains in comfort and confidence to medical students who completed the training.
After completing the training, which involved both a didactic and a hands-on component, 92.58% of third-year medical students agreed or strongly agreed that they had the skills needed for effective interprofessional communication in the EHR, up from 43.86% before the training.
The idea for the training began when Zaiba Jetpuri, DO, and her physician colleagues at the University of Texas Southwestern Medical Center, Dallas, noticed that medical students and residents often were unsure how best to communicate with nurses, pharmacists, physical therapists, and other members of the healthcare team via the EHR.
Knowing who has what role in an interdisciplinary setting is far from obvious, and knowing how to strike the right tone in EHR communications was a challenge for trainees, Dr. Jetpuri said in an interview during her poster presentation at annual meeting of the North American Primary Care Research Groups.
To address such uncertainties, which can impact both quality and continuity of care, Dr. Jetpuri and her colleagues devised an intervention aimed at third-year medical students who were doing family medicine clerkships. The intervention has been given to about 360 students thus far.
The intervention consisted of two components. The first, a didactic module, delivered information about the importance of professionalism and teamwork and also defined interprofessional roles.
The second phase of the training had students using the “sandbox” of Epic, UT Southwestern’s EHR, to practice responding to hypothetical messages from a patient, a nurse, a pharmacist, and a physical therapist. One message would arrive in the medical student’s EHR inbox each week, and the student would have the week to craft a response.
Dr. Jetpuri said that she and her colleagues worked hard to make the scenarios as realistic as possible: The lengthy patient email included several questions about the safety of taking supplements or herbal remedies. They also tried to make sure that the nuts and bolts of interprofessional communication were covered so that, for example, medical students would end a module knowing what should be included when writing orders for physical therapy and how to place the order correctly.
The responses then went through peer evaluation according to a rubric constructed by the investigators. The training and evaluation were designed to make sure that students acquired a better understanding of the mechanics of EHR interprofessional communication and of the soft skills needed for collegial and professional communication.
Dr. Jetpuri said that she and her colleagues would like to extend this realistic educational tool through the clerkship year for better continuity. They also are working on some technical aspects of the EHR to make communication easier for medical students. Furthermore, they are in the process of validating the peer evaluation process by having instructors use the rubric to duplicate the students’ evaluation. She said, though, that both trainees and faculty see the value in early, realistic experience using the electronic record in a multidisciplinary team.
“Simulated EHR experiences are an important tool to utilize in a medical school curriculum to better train and prepare our students for the postgraduate stage,” wrote Dr. Jetpuri and her colleagues.
Dr. Jetpuri reported that she has no conflicts of interest.
koakes@frontlinemedcom.com
On Twitter @karioakes
AT NAPCRG 2017
Key clinical point:
Major finding: After the training, 93% of students felt they had the skills needed for effective interprofessional communication via the EHR.
Data source: Summary data from pilot involving about 360 third-year medical students completing family medicine clerkships.
Disclosures: Dr. Jetpuri reported no outside sources of funding and had no relevant disclosures.