User login
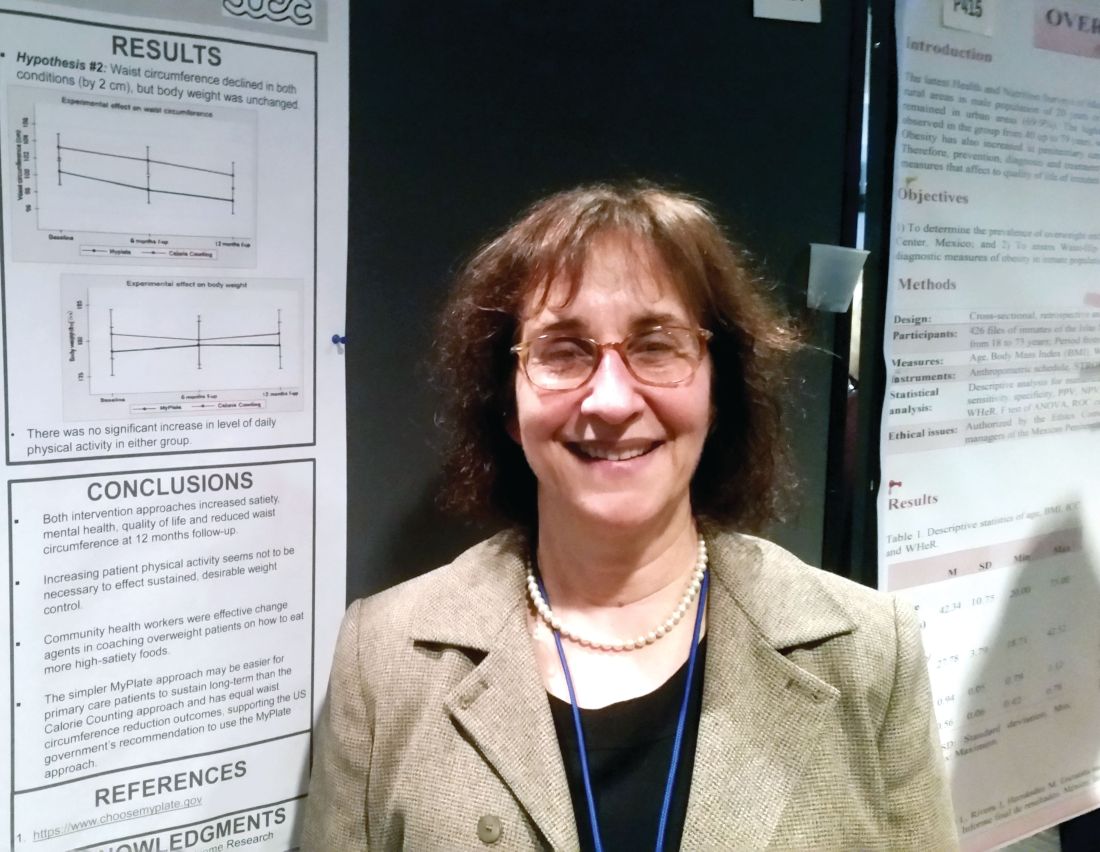
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
MONTREAL – The high-satiety MyPlate approach to weight loss reduced waist circumference, improved mental health and quality of life, and increased satiety 12 months into a study that found the strategy as effective as a conventional calorie-counting approach.
After 12 months, waist circumference had decreased by about 2 cm in study participants, regardless of whether they used the MyPlate approach or counted calories. Body weight was unchanged after a year in both groups.
“The simpler MyPlate approach may be easier for primary care patients to sustain long-term than the calorie-counting approach and has equal waist circumference reduction outcomes, supporting the U.S. government’s recommendation to use the MyPlate approach,” wrote Lillian Gelberg, MD, and her collaborators.
MyPlate recommends eating more fruits and vegetables, making half of grain choices whole grain, replacing sugary drinks with water, limiting sodium intake.
Over the study period, neither group significantly increased their physical activity. “Increasing patient physical activity seems not to be necessary to effect sustained, desirable weight control,” the researchers wrote.
The comparative effectiveness study compared the two weight loss approaches in 261 primarily Hispanic patients at two federally qualified health center clinics.
The primary outcome in the patient-centered study was perceived satiety; secondary outcomes included waist circumference, weight, mental health, quality of life, intake of sugary drinks, water intake, and exercise.
Participants received 11 health coaching sessions from bilingual community health workers, dubbed “promotoras,” over a 6 month period. “Community health workers were effective change agents in coaching overweight patients on how to eat more high-satiety foods,” Dr. Gelberg and her colleagues noted in a poster presentation at the annual meeting of the North American Primary Care Research Group.
Two of the sessions were hour-long home-based sessions; the MyPlate group also received two hour-long cooking demonstrations. Both groups received two hour-long group education sessions, as well as a total of seven 20-minute telephone coaching sessions.
Most participants (56%) were in five sessions during the study period, with a quarter completing 10 of the 11 sessions. At 12 months, 80% of study members were still being followed.
Overall, 95% of the participants were female, and about half (n = 126) did not have a high school diploma or equivalent.
A total of 86% were Hispanic, and Spanish was the preferred language for about three quarters of all participants. Most patients (82%) were born outside the United States.
The mean age at enrollment was 41 years. Mean body mass index was 30 to less than 35 kg/m2 for about half (46%) of the patients; 5% had a BMI of 40 kg/m2 or more.
In an interview, Dr. Gelberg, professor of family medicine and public health and management at the University of California, Los Angeles, said that the investigators had hypothesized that the MyPlate approach would be easier for patients to follow, because it’s easier to understand and less cumbersome in terms of record keeping. The investigators did not think that one approach would result in greater reductions in body weight or waist circumference, a finding borne out by the data presented.
Both groups reduced their intake of sugary drinks and increased the amount of water they drank, but the differences were not statistically significant.
The study was funded by the Patient-Centered Outcome Research Institute. Dr. Gelberg reported no relevant disclosures.
SOURCE: Gelberg L, abstract P414.
This article was updated on 2/13/18
REPORTING FROM NAPCRG 2017
Key clinical point:
Major finding: At 12 months, both approaches reduced waist circumference by 2 cm but didn’t result in weight loss.
Data source: Prospective randomized comparative effectiveness trial of 261 patients.
Disclosures: Dr. Gelberg reported no conflicts of interest. The study was funded by the Patient-Centered Comparative Effectiveness Institute.
Source: Gelberg L, abstract P414.