User login
FDA Approves First Engineered Cell Therapy for a Solid Tumor
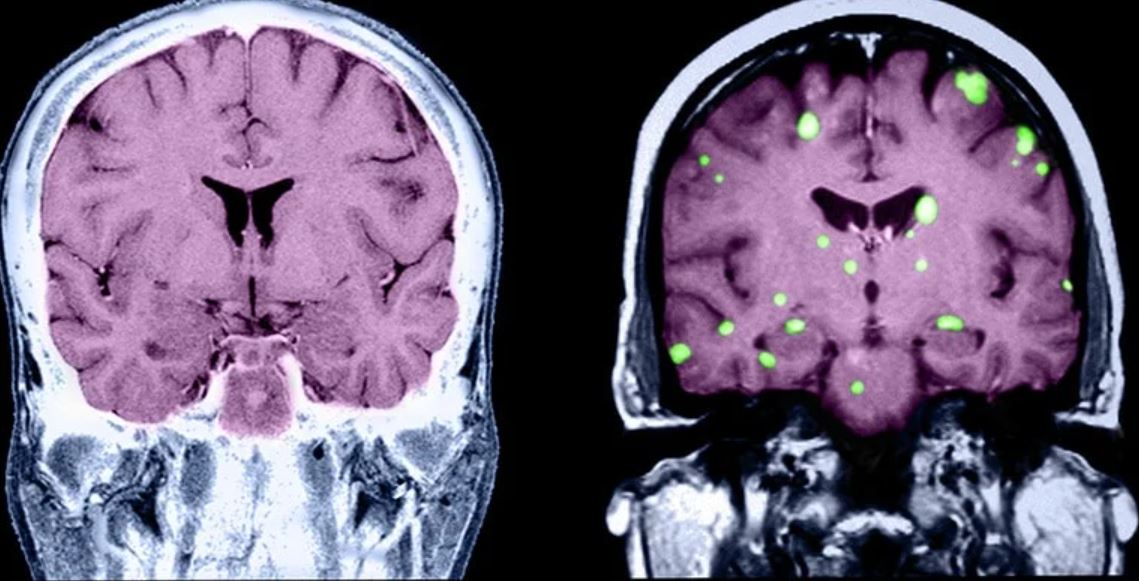
Afami-cel — the first engineered cell therapy for a solid tumor — is indicated specifically for adults with unresectable or metastatic synovial sarcoma who have received prior chemotherapy, are positive for several human leukocyte antigens (HLAs), and whose tumors express melanoma-associated antigen A4, as determined by FDA-authorized companion diagnostic devices.
The single-dose treatment targets solid tumors expressing melanoma-associated antigen A4, a protein highly expressed in synovial sarcoma.
Synovial sarcoma is a rare form of cancer, which affects about 1000 people in the US each year. Malignant cells develop and form a tumor in soft tissues, often in the extremities.
“Adults with metastatic synovial sarcoma, a life-threatening form of cancer, often face limited treatment options in addition to the risk of cancer spread or recurrence,” Nicole Verdun, MD, director of the Office of Therapeutic Products in the FDA’s Center for Biologics Evaluation and Research, said in the agency press release announcing the approval. “Today’s approval represents a significant milestone in the development of an innovative, safe and effective therapy for patients with this rare but potentially fatal disease.”
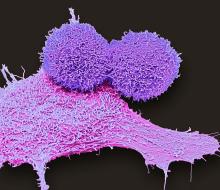
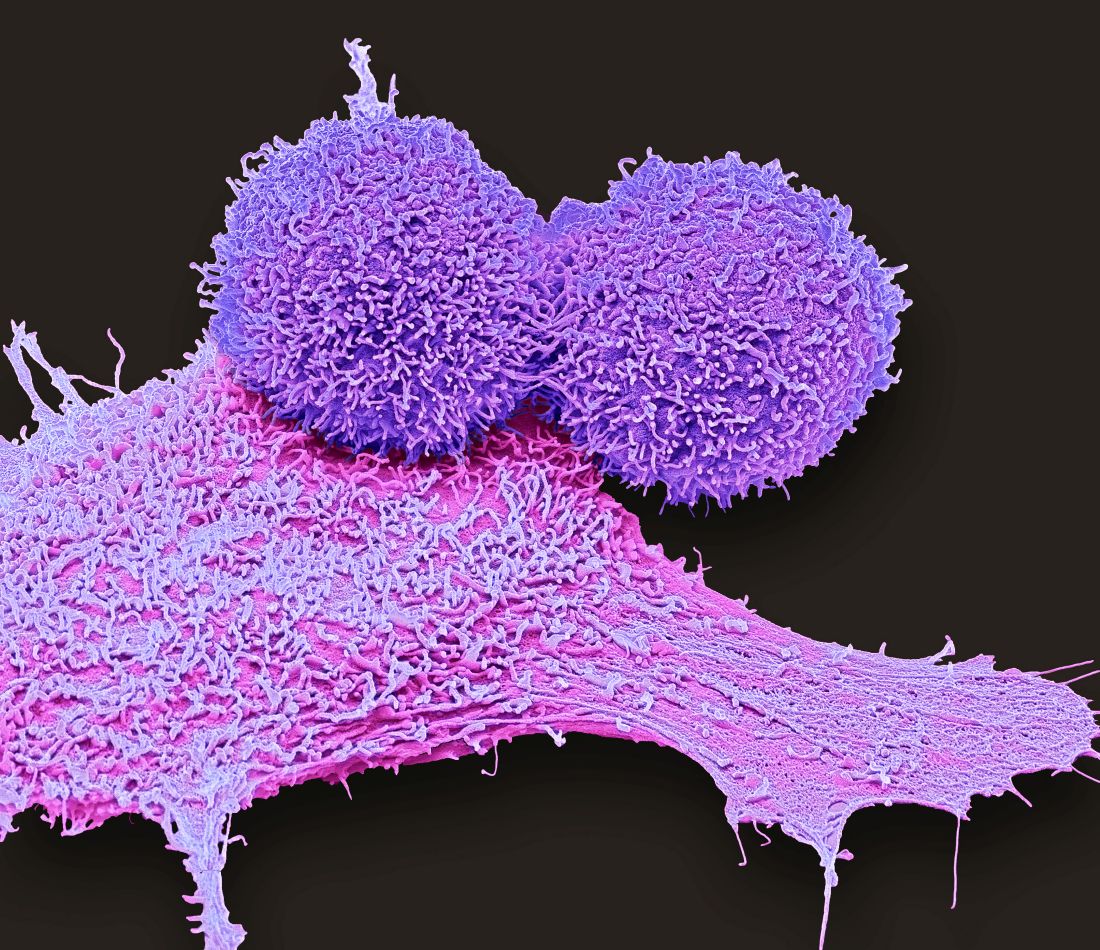
T-cell receptor therapy, like chimeric antigen receptor (CAR) T-cell (CAR-T) therapy, involves altering patient T cells to fight cancer. While CAR-T therapy inserts an artificial receptor to target a specific surface protein on cancer cells, the T-cell receptor therapy modifies existing receptors to recognize an array of antigens on the surface of cancer cells — a promising strategy for targeting solid tumors.
The accelerated approval of afami-cel was based on the phase 2 SPEARHEAD-1 trial in 44 patients with synovial sarcoma who received a single infusion of the therapy. The trial had enrolled 52 patients, but 8 did not receive afami-cel, including 3 who died and 1 who withdrew.
According to the FDA announcement, the overall response rate was 43.2%, with a median time to response of 4.9 weeks. The median duration of response was 6 months (95% CI, 4.6 months to not reached). Among patients who responded, 39% had a duration of response of 12 months or longer.
“These results suggest that a one-time treatment with afami-cel has the potential to extend life while allowing responders to go off chemotherapy,” said lead investigator Sandra D’Angelo, MD, a sarcoma specialist at Memorial Sloan Kettering Cancer Center in New York City, in a company press release.
The prescribing information includes a boxed warning for serious or fatal cytokine release syndrome.
The most common nonlaboratory adverse reactions, occurring in at least 20% of patients, included cytokine release syndrome, nausea, vomiting, fatigue, infections, pyrexia, constipation, dyspnea, tachycardia, hypotension, diarrhea, and edema. The most common grade 3 or 4 laboratory abnormalities, occurring in at least 20% of patients, included decreased lymphocyte count, neutrophil count, white cell blood count, red blood cell, and platelet count.
The recommended dose is between 2.68x109 to 10x109 MAGE-A4 T-cell receptor–positive T-cells. The FDA notice specifies not using a leukodepleting filter or prophylactic systemic corticosteroids.
The list price for the one-time therapy is $727,000, according to Fierce Pharma.
A version of this article first appeared on Medscape.com.
Afami-cel — the first engineered cell therapy for a solid tumor — is indicated specifically for adults with unresectable or metastatic synovial sarcoma who have received prior chemotherapy, are positive for several human leukocyte antigens (HLAs), and whose tumors express melanoma-associated antigen A4, as determined by FDA-authorized companion diagnostic devices.
The single-dose treatment targets solid tumors expressing melanoma-associated antigen A4, a protein highly expressed in synovial sarcoma.
Synovial sarcoma is a rare form of cancer, which affects about 1000 people in the US each year. Malignant cells develop and form a tumor in soft tissues, often in the extremities.
“Adults with metastatic synovial sarcoma, a life-threatening form of cancer, often face limited treatment options in addition to the risk of cancer spread or recurrence,” Nicole Verdun, MD, director of the Office of Therapeutic Products in the FDA’s Center for Biologics Evaluation and Research, said in the agency press release announcing the approval. “Today’s approval represents a significant milestone in the development of an innovative, safe and effective therapy for patients with this rare but potentially fatal disease.”
T-cell receptor therapy, like chimeric antigen receptor (CAR) T-cell (CAR-T) therapy, involves altering patient T cells to fight cancer. While CAR-T therapy inserts an artificial receptor to target a specific surface protein on cancer cells, the T-cell receptor therapy modifies existing receptors to recognize an array of antigens on the surface of cancer cells — a promising strategy for targeting solid tumors.
The accelerated approval of afami-cel was based on the phase 2 SPEARHEAD-1 trial in 44 patients with synovial sarcoma who received a single infusion of the therapy. The trial had enrolled 52 patients, but 8 did not receive afami-cel, including 3 who died and 1 who withdrew.
According to the FDA announcement, the overall response rate was 43.2%, with a median time to response of 4.9 weeks. The median duration of response was 6 months (95% CI, 4.6 months to not reached). Among patients who responded, 39% had a duration of response of 12 months or longer.
“These results suggest that a one-time treatment with afami-cel has the potential to extend life while allowing responders to go off chemotherapy,” said lead investigator Sandra D’Angelo, MD, a sarcoma specialist at Memorial Sloan Kettering Cancer Center in New York City, in a company press release.
The prescribing information includes a boxed warning for serious or fatal cytokine release syndrome.
The most common nonlaboratory adverse reactions, occurring in at least 20% of patients, included cytokine release syndrome, nausea, vomiting, fatigue, infections, pyrexia, constipation, dyspnea, tachycardia, hypotension, diarrhea, and edema. The most common grade 3 or 4 laboratory abnormalities, occurring in at least 20% of patients, included decreased lymphocyte count, neutrophil count, white cell blood count, red blood cell, and platelet count.
The recommended dose is between 2.68x109 to 10x109 MAGE-A4 T-cell receptor–positive T-cells. The FDA notice specifies not using a leukodepleting filter or prophylactic systemic corticosteroids.
The list price for the one-time therapy is $727,000, according to Fierce Pharma.
A version of this article first appeared on Medscape.com.
Afami-cel — the first engineered cell therapy for a solid tumor — is indicated specifically for adults with unresectable or metastatic synovial sarcoma who have received prior chemotherapy, are positive for several human leukocyte antigens (HLAs), and whose tumors express melanoma-associated antigen A4, as determined by FDA-authorized companion diagnostic devices.
The single-dose treatment targets solid tumors expressing melanoma-associated antigen A4, a protein highly expressed in synovial sarcoma.
Synovial sarcoma is a rare form of cancer, which affects about 1000 people in the US each year. Malignant cells develop and form a tumor in soft tissues, often in the extremities.
“Adults with metastatic synovial sarcoma, a life-threatening form of cancer, often face limited treatment options in addition to the risk of cancer spread or recurrence,” Nicole Verdun, MD, director of the Office of Therapeutic Products in the FDA’s Center for Biologics Evaluation and Research, said in the agency press release announcing the approval. “Today’s approval represents a significant milestone in the development of an innovative, safe and effective therapy for patients with this rare but potentially fatal disease.”
T-cell receptor therapy, like chimeric antigen receptor (CAR) T-cell (CAR-T) therapy, involves altering patient T cells to fight cancer. While CAR-T therapy inserts an artificial receptor to target a specific surface protein on cancer cells, the T-cell receptor therapy modifies existing receptors to recognize an array of antigens on the surface of cancer cells — a promising strategy for targeting solid tumors.
The accelerated approval of afami-cel was based on the phase 2 SPEARHEAD-1 trial in 44 patients with synovial sarcoma who received a single infusion of the therapy. The trial had enrolled 52 patients, but 8 did not receive afami-cel, including 3 who died and 1 who withdrew.
According to the FDA announcement, the overall response rate was 43.2%, with a median time to response of 4.9 weeks. The median duration of response was 6 months (95% CI, 4.6 months to not reached). Among patients who responded, 39% had a duration of response of 12 months or longer.
“These results suggest that a one-time treatment with afami-cel has the potential to extend life while allowing responders to go off chemotherapy,” said lead investigator Sandra D’Angelo, MD, a sarcoma specialist at Memorial Sloan Kettering Cancer Center in New York City, in a company press release.
The prescribing information includes a boxed warning for serious or fatal cytokine release syndrome.
The most common nonlaboratory adverse reactions, occurring in at least 20% of patients, included cytokine release syndrome, nausea, vomiting, fatigue, infections, pyrexia, constipation, dyspnea, tachycardia, hypotension, diarrhea, and edema. The most common grade 3 or 4 laboratory abnormalities, occurring in at least 20% of patients, included decreased lymphocyte count, neutrophil count, white cell blood count, red blood cell, and platelet count.
The recommended dose is between 2.68x109 to 10x109 MAGE-A4 T-cell receptor–positive T-cells. The FDA notice specifies not using a leukodepleting filter or prophylactic systemic corticosteroids.
The list price for the one-time therapy is $727,000, according to Fierce Pharma.
A version of this article first appeared on Medscape.com.
The ‘psychological warfare’ of prior authorization
Shikha Jain, MD, felt the urgency of the moment.
It was 10:00 AM. A young patient had stepped into her Chicago cancer clinic. His face was red, and he was struggling to breathe.
The man had primary mediastinal B-cell lymphoma, a rare, aggressive form of non-Hodgkin lymphoma. Many cases involve large, fast‐growing masses that expand into the lungs and compress respiratory pathways, sometimes leaving patients breathless.
Dr. Jain rushed to his side and walked him from the clinic to an ICU bed at the hospital nearby.
“He was so sick,” recalled Dr. Jain, currently a tenured associate professor of medicine in the division of hematology and oncology at the University of Illinois Cancer Center, Chicago. “He needed chemotherapy immediately.”
The standard chemotherapy regimen at the time – R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) – required prior authorization.
Dr. Jain’s patient did not have days to wait, so Dr. Jain requested an expedited approval. The insurance company responded quickly, denying the request for treatment.
That evening, after hours on the phone trying to reverse the denial, Dr. Jain was able to arrange a peer-to-peer conversation with the insurer. She explained her patient’s pressing need for chemotherapy: He would die if he continued to wait.
But Dr. Jain’s argument did not move the reviewer. At that point, she had reached her limit.
“I asked for the gentleman’s full name. I told him he would be responsible for this 30-year-old man’s death, and my next call would be to CNN,” Dr. Jain told this news organization. “And that is how I got my patient’s chemotherapy approved.”
Her patient received the regimen that evening. He later went into remission.
This incident occurred almost a decade ago, but it has stayed with Dr. Jain. She knows that her persistence in that moment meant the difference between her patient’s life and death.
There was the denial for standard-of-care staging and surveillance imaging – dotatate PET/CT – for her patient with neuroendocrine cancer. “The specific insurance company simply doesn’t approve this imaging, despite being around for years,” she said.
There was the patient with metastatic colon cancer who needed third-line therapy. His insurer took more than a month to reverse its denial for a recently approved drug, and in that time, the man’s disease progressed. “He eventually succumbed to the cancer after receiving the drug, but it’s unclear if his life was cut short by the delay in care,” Dr. Jain said.
And there is the maze of insurance company phone calls and transfers. On one call, Dr. Jain recalled being transferred six times before being connected to the right department to discuss approving standard-of-care chemotherapy for a patient. After being denied approval, Dr. Jain was put on hold to speak with a manager, and the call was abruptly disconnected.
“I have wasted so many hours on prior authorization and have seen months and months of patient care delays,” Dr. Jain said. “It’s easy to see why people just give up.”
For Dr. Jain, prior authorization has begun to “feel like psychological warfare,” she said. “To have everything questioned by people who don’t understand the basics of oncology is demoralizing.”
The growing administrative – and emotional – burden of prior authorization is contributing to physician burnout.
According to Medscape’s ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023, more than half of oncologists reported feeling burned out this year – the highest percentage in 5 years. When asked what factors led to burnout, most doctors surveyed pointed to an overabundance of bureaucratic tasks, and specifically, “insurance companies telling me how to practice medicine and controlling what the patients can and can’t do.”
“Burnout is a real problem in medicine,” said Kelly Anderson, PhD, MPP, assistant professor in the department of clinical pharmacy, University of Colorado at Denver, Aurora. “While there are many factors that contribute to burnout, prior authorization is certainly one.”
In a 2022 survey from the American Medical Association, 88% of respondents reported that the burden associated with prior authorization requirements was “high or extremely high.”
Although insurers argue that prior authorization cuts down on unnecessary and expensive care, physicians in the AMA survey reported that this practice often leads to greater overall use of health care resources, including more emergency department and office visits.
“Insurers are confident that prior authorization is saving money overall, but there’s also no clear evidence of that,” Dr. Anderson noted. “Prior authorization may reduce spending without harming patients in some instances, but in others, it’s adding administrative burden, costs, and may be causing harm to patients.”
A version of this article originally appeared on Medscape.com.
Shikha Jain, MD, felt the urgency of the moment.
It was 10:00 AM. A young patient had stepped into her Chicago cancer clinic. His face was red, and he was struggling to breathe.
The man had primary mediastinal B-cell lymphoma, a rare, aggressive form of non-Hodgkin lymphoma. Many cases involve large, fast‐growing masses that expand into the lungs and compress respiratory pathways, sometimes leaving patients breathless.
Dr. Jain rushed to his side and walked him from the clinic to an ICU bed at the hospital nearby.
“He was so sick,” recalled Dr. Jain, currently a tenured associate professor of medicine in the division of hematology and oncology at the University of Illinois Cancer Center, Chicago. “He needed chemotherapy immediately.”
The standard chemotherapy regimen at the time – R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) – required prior authorization.
Dr. Jain’s patient did not have days to wait, so Dr. Jain requested an expedited approval. The insurance company responded quickly, denying the request for treatment.
That evening, after hours on the phone trying to reverse the denial, Dr. Jain was able to arrange a peer-to-peer conversation with the insurer. She explained her patient’s pressing need for chemotherapy: He would die if he continued to wait.
But Dr. Jain’s argument did not move the reviewer. At that point, she had reached her limit.
“I asked for the gentleman’s full name. I told him he would be responsible for this 30-year-old man’s death, and my next call would be to CNN,” Dr. Jain told this news organization. “And that is how I got my patient’s chemotherapy approved.”
Her patient received the regimen that evening. He later went into remission.
This incident occurred almost a decade ago, but it has stayed with Dr. Jain. She knows that her persistence in that moment meant the difference between her patient’s life and death.
There was the denial for standard-of-care staging and surveillance imaging – dotatate PET/CT – for her patient with neuroendocrine cancer. “The specific insurance company simply doesn’t approve this imaging, despite being around for years,” she said.
There was the patient with metastatic colon cancer who needed third-line therapy. His insurer took more than a month to reverse its denial for a recently approved drug, and in that time, the man’s disease progressed. “He eventually succumbed to the cancer after receiving the drug, but it’s unclear if his life was cut short by the delay in care,” Dr. Jain said.
And there is the maze of insurance company phone calls and transfers. On one call, Dr. Jain recalled being transferred six times before being connected to the right department to discuss approving standard-of-care chemotherapy for a patient. After being denied approval, Dr. Jain was put on hold to speak with a manager, and the call was abruptly disconnected.
“I have wasted so many hours on prior authorization and have seen months and months of patient care delays,” Dr. Jain said. “It’s easy to see why people just give up.”
For Dr. Jain, prior authorization has begun to “feel like psychological warfare,” she said. “To have everything questioned by people who don’t understand the basics of oncology is demoralizing.”
The growing administrative – and emotional – burden of prior authorization is contributing to physician burnout.
According to Medscape’s ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023, more than half of oncologists reported feeling burned out this year – the highest percentage in 5 years. When asked what factors led to burnout, most doctors surveyed pointed to an overabundance of bureaucratic tasks, and specifically, “insurance companies telling me how to practice medicine and controlling what the patients can and can’t do.”
“Burnout is a real problem in medicine,” said Kelly Anderson, PhD, MPP, assistant professor in the department of clinical pharmacy, University of Colorado at Denver, Aurora. “While there are many factors that contribute to burnout, prior authorization is certainly one.”
In a 2022 survey from the American Medical Association, 88% of respondents reported that the burden associated with prior authorization requirements was “high or extremely high.”
Although insurers argue that prior authorization cuts down on unnecessary and expensive care, physicians in the AMA survey reported that this practice often leads to greater overall use of health care resources, including more emergency department and office visits.
“Insurers are confident that prior authorization is saving money overall, but there’s also no clear evidence of that,” Dr. Anderson noted. “Prior authorization may reduce spending without harming patients in some instances, but in others, it’s adding administrative burden, costs, and may be causing harm to patients.”
A version of this article originally appeared on Medscape.com.
Shikha Jain, MD, felt the urgency of the moment.
It was 10:00 AM. A young patient had stepped into her Chicago cancer clinic. His face was red, and he was struggling to breathe.
The man had primary mediastinal B-cell lymphoma, a rare, aggressive form of non-Hodgkin lymphoma. Many cases involve large, fast‐growing masses that expand into the lungs and compress respiratory pathways, sometimes leaving patients breathless.
Dr. Jain rushed to his side and walked him from the clinic to an ICU bed at the hospital nearby.
“He was so sick,” recalled Dr. Jain, currently a tenured associate professor of medicine in the division of hematology and oncology at the University of Illinois Cancer Center, Chicago. “He needed chemotherapy immediately.”
The standard chemotherapy regimen at the time – R-CHOP (rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone) – required prior authorization.
Dr. Jain’s patient did not have days to wait, so Dr. Jain requested an expedited approval. The insurance company responded quickly, denying the request for treatment.
That evening, after hours on the phone trying to reverse the denial, Dr. Jain was able to arrange a peer-to-peer conversation with the insurer. She explained her patient’s pressing need for chemotherapy: He would die if he continued to wait.
But Dr. Jain’s argument did not move the reviewer. At that point, she had reached her limit.
“I asked for the gentleman’s full name. I told him he would be responsible for this 30-year-old man’s death, and my next call would be to CNN,” Dr. Jain told this news organization. “And that is how I got my patient’s chemotherapy approved.”
Her patient received the regimen that evening. He later went into remission.
This incident occurred almost a decade ago, but it has stayed with Dr. Jain. She knows that her persistence in that moment meant the difference between her patient’s life and death.
There was the denial for standard-of-care staging and surveillance imaging – dotatate PET/CT – for her patient with neuroendocrine cancer. “The specific insurance company simply doesn’t approve this imaging, despite being around for years,” she said.
There was the patient with metastatic colon cancer who needed third-line therapy. His insurer took more than a month to reverse its denial for a recently approved drug, and in that time, the man’s disease progressed. “He eventually succumbed to the cancer after receiving the drug, but it’s unclear if his life was cut short by the delay in care,” Dr. Jain said.
And there is the maze of insurance company phone calls and transfers. On one call, Dr. Jain recalled being transferred six times before being connected to the right department to discuss approving standard-of-care chemotherapy for a patient. After being denied approval, Dr. Jain was put on hold to speak with a manager, and the call was abruptly disconnected.
“I have wasted so many hours on prior authorization and have seen months and months of patient care delays,” Dr. Jain said. “It’s easy to see why people just give up.”
For Dr. Jain, prior authorization has begun to “feel like psychological warfare,” she said. “To have everything questioned by people who don’t understand the basics of oncology is demoralizing.”
The growing administrative – and emotional – burden of prior authorization is contributing to physician burnout.
According to Medscape’s ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023, more than half of oncologists reported feeling burned out this year – the highest percentage in 5 years. When asked what factors led to burnout, most doctors surveyed pointed to an overabundance of bureaucratic tasks, and specifically, “insurance companies telling me how to practice medicine and controlling what the patients can and can’t do.”
“Burnout is a real problem in medicine,” said Kelly Anderson, PhD, MPP, assistant professor in the department of clinical pharmacy, University of Colorado at Denver, Aurora. “While there are many factors that contribute to burnout, prior authorization is certainly one.”
In a 2022 survey from the American Medical Association, 88% of respondents reported that the burden associated with prior authorization requirements was “high or extremely high.”
Although insurers argue that prior authorization cuts down on unnecessary and expensive care, physicians in the AMA survey reported that this practice often leads to greater overall use of health care resources, including more emergency department and office visits.
“Insurers are confident that prior authorization is saving money overall, but there’s also no clear evidence of that,” Dr. Anderson noted. “Prior authorization may reduce spending without harming patients in some instances, but in others, it’s adding administrative burden, costs, and may be causing harm to patients.”
A version of this article originally appeared on Medscape.com.
Prior authorization has radiation oncologist deferring to business manager
“What am I allowed to do?” radiation oncologist Vivek Kavadi, MD, asked the business manager at Texas Oncology in Sugar Land, Tex.
Dr. Kavadi wanted to give his patient with early-stage breast cancer a standard radiation treatment – hypofractionated 3D conformal radiation therapy – following her lumpectomy.
But his hands were tied.
Dr. Kavadi had submitted a prior authorization request, but the patient’s health insurance was dragging its feet. And without prior authorization, Dr. Kavadi couldn’t schedule his patient’s first treatment.
“I chose the most cost-effective, standard treatment, but nothing could begin without the insurance company’s permission,” he said.
One of the most challenging aspects of the delay was explaining to his patient why he couldn’t schedule her treatment. “We would love to start, but your insurance company has not given us approval. The best I can do is give you a tentative appointment,” he recalled telling her.
After a few days with no word, calls to the insurance company began. “My patient called, I called, my office called,” Dr. Kavadi said. “It was a week or more of aggravation, stress, and time wasted for my patient and my team.”
This type of delay has become increasingly common in radiation oncology. One recent analysis estimated that 97% of radiation oncology services now require prior authorization under Medicare Advantage. And another analysis found that almost all radiation oncologists said prior authorization delays life-saving care for their patients.
Terrence Cunningham, director of administrative simplification policy for the American Hospital Association, told this news organization last year that “prior authorization used to be applied only to new, costly, or high-risk services,” but now “many insurers require authorizations for even routine care, which is inappropriate.”
The growth of prior authorization requirements has forced many doctors, nurses, and pharmacists to dedicate part of their workday to handling requests and appealing denials and has forced many practices to hire staff exclusively for prior authorizations.
This additional work is costly.
One recent study found that the radiation oncology department of Vanderbilt University, Nashville, Tenn., spent nearly $500,000 annually in employee time to obtain prior authorization for radiation therapy treatments. Extrapolated nationally, the researchers estimated that physicians’ annual compensation for prior authorization duties came to an estimated $46 million. Overall, 86% of these costs were for treatments that were ultimately approved, the majority on initial request and some on appeal.
Dr. Kavadi has five full-time employees dedicated to managing prior authorization requests and challenges.
And after a week of delays and hours on the phone with the insurer, his patient’s radiation treatment was ultimately approved.
Dr. Kavadi wondered why something so simple needed to be so onerous.
Stretching out an approval for a standard radiation treatment “feels like a means of intentionally delaying care,” Dr. Kavadi said. “This is an example of a process that has run so far amok. It’s just a burden across the board.”
And even with his 30 years of experience, “I still have to ask my business supervisor what I am allowed to do,” he said. “I can’t just proceed with what’s best for my patient, what the patient has consented to, and what also happens to be the least expensive option.”
A version of this article first appeared on Medscape.com.
“What am I allowed to do?” radiation oncologist Vivek Kavadi, MD, asked the business manager at Texas Oncology in Sugar Land, Tex.
Dr. Kavadi wanted to give his patient with early-stage breast cancer a standard radiation treatment – hypofractionated 3D conformal radiation therapy – following her lumpectomy.
But his hands were tied.
Dr. Kavadi had submitted a prior authorization request, but the patient’s health insurance was dragging its feet. And without prior authorization, Dr. Kavadi couldn’t schedule his patient’s first treatment.
“I chose the most cost-effective, standard treatment, but nothing could begin without the insurance company’s permission,” he said.
One of the most challenging aspects of the delay was explaining to his patient why he couldn’t schedule her treatment. “We would love to start, but your insurance company has not given us approval. The best I can do is give you a tentative appointment,” he recalled telling her.
After a few days with no word, calls to the insurance company began. “My patient called, I called, my office called,” Dr. Kavadi said. “It was a week or more of aggravation, stress, and time wasted for my patient and my team.”
This type of delay has become increasingly common in radiation oncology. One recent analysis estimated that 97% of radiation oncology services now require prior authorization under Medicare Advantage. And another analysis found that almost all radiation oncologists said prior authorization delays life-saving care for their patients.
Terrence Cunningham, director of administrative simplification policy for the American Hospital Association, told this news organization last year that “prior authorization used to be applied only to new, costly, or high-risk services,” but now “many insurers require authorizations for even routine care, which is inappropriate.”
The growth of prior authorization requirements has forced many doctors, nurses, and pharmacists to dedicate part of their workday to handling requests and appealing denials and has forced many practices to hire staff exclusively for prior authorizations.
This additional work is costly.
One recent study found that the radiation oncology department of Vanderbilt University, Nashville, Tenn., spent nearly $500,000 annually in employee time to obtain prior authorization for radiation therapy treatments. Extrapolated nationally, the researchers estimated that physicians’ annual compensation for prior authorization duties came to an estimated $46 million. Overall, 86% of these costs were for treatments that were ultimately approved, the majority on initial request and some on appeal.
Dr. Kavadi has five full-time employees dedicated to managing prior authorization requests and challenges.
And after a week of delays and hours on the phone with the insurer, his patient’s radiation treatment was ultimately approved.
Dr. Kavadi wondered why something so simple needed to be so onerous.
Stretching out an approval for a standard radiation treatment “feels like a means of intentionally delaying care,” Dr. Kavadi said. “This is an example of a process that has run so far amok. It’s just a burden across the board.”
And even with his 30 years of experience, “I still have to ask my business supervisor what I am allowed to do,” he said. “I can’t just proceed with what’s best for my patient, what the patient has consented to, and what also happens to be the least expensive option.”
A version of this article first appeared on Medscape.com.
“What am I allowed to do?” radiation oncologist Vivek Kavadi, MD, asked the business manager at Texas Oncology in Sugar Land, Tex.
Dr. Kavadi wanted to give his patient with early-stage breast cancer a standard radiation treatment – hypofractionated 3D conformal radiation therapy – following her lumpectomy.
But his hands were tied.
Dr. Kavadi had submitted a prior authorization request, but the patient’s health insurance was dragging its feet. And without prior authorization, Dr. Kavadi couldn’t schedule his patient’s first treatment.
“I chose the most cost-effective, standard treatment, but nothing could begin without the insurance company’s permission,” he said.
One of the most challenging aspects of the delay was explaining to his patient why he couldn’t schedule her treatment. “We would love to start, but your insurance company has not given us approval. The best I can do is give you a tentative appointment,” he recalled telling her.
After a few days with no word, calls to the insurance company began. “My patient called, I called, my office called,” Dr. Kavadi said. “It was a week or more of aggravation, stress, and time wasted for my patient and my team.”
This type of delay has become increasingly common in radiation oncology. One recent analysis estimated that 97% of radiation oncology services now require prior authorization under Medicare Advantage. And another analysis found that almost all radiation oncologists said prior authorization delays life-saving care for their patients.
Terrence Cunningham, director of administrative simplification policy for the American Hospital Association, told this news organization last year that “prior authorization used to be applied only to new, costly, or high-risk services,” but now “many insurers require authorizations for even routine care, which is inappropriate.”
The growth of prior authorization requirements has forced many doctors, nurses, and pharmacists to dedicate part of their workday to handling requests and appealing denials and has forced many practices to hire staff exclusively for prior authorizations.
This additional work is costly.
One recent study found that the radiation oncology department of Vanderbilt University, Nashville, Tenn., spent nearly $500,000 annually in employee time to obtain prior authorization for radiation therapy treatments. Extrapolated nationally, the researchers estimated that physicians’ annual compensation for prior authorization duties came to an estimated $46 million. Overall, 86% of these costs were for treatments that were ultimately approved, the majority on initial request and some on appeal.
Dr. Kavadi has five full-time employees dedicated to managing prior authorization requests and challenges.
And after a week of delays and hours on the phone with the insurer, his patient’s radiation treatment was ultimately approved.
Dr. Kavadi wondered why something so simple needed to be so onerous.
Stretching out an approval for a standard radiation treatment “feels like a means of intentionally delaying care,” Dr. Kavadi said. “This is an example of a process that has run so far amok. It’s just a burden across the board.”
And even with his 30 years of experience, “I still have to ask my business supervisor what I am allowed to do,” he said. “I can’t just proceed with what’s best for my patient, what the patient has consented to, and what also happens to be the least expensive option.”
A version of this article first appeared on Medscape.com.
After cancer, abortion experience highlights post-Roe reality
The drive from Texas to the clinic in Albuquerque, N.M., took 10 hours. It was mid-April of this year. There wasn’t much to see along the mostly barren stretch, and there wasn’t much for Kailee DeSpain to do aside from think about where she was going and why.
Her husband was driving. She sensed his nervous glances toward the passenger seat where she sat struggling to quiet her thoughts.
No, she wasn’t having any pain, she told him. No, she wasn’t feeling like she did the last time or the two times before that.
This pregnancy was different. It was the first in which she feared for her own life. Her fetus – Finley – had triploidy, a rare chromosomal abnormality. Because of the condition, which affects 1%-3% of pregnancies, his heart, brain, and kidneys were not developing properly.
At 19 weeks, Finley was already struggling to draw breath from lungs squeezed inside an overcrowded chest cavity. Ms. DeSpain wanted nothing more than to carry Finley to term, hold him, meet him even for a moment before saying goodbye.
But his condition meant he would likely suffocate in utero well before that. And Ms. DeSpain knew that carrying him longer would likely raise her risk of bleeding and of her blood pressure increasing to dangerous highs.
“This could kill you,” her husband told her. “Do you realize you could die bringing a baby into this world who is not going to live? I don’t want to lose you.’”
Unlike her other pregnancies, the timing of this one and the decision she faced to end it put her health in even greater danger.
Imminent danger
On Sept. 1, 2021, a bill went into effect in Texas that banned abortions from as early as 6 weeks’ gestation. Texas Senate Bill 8 (SB8) became one of the most restrictive abortion laws in the country. It prohibited abortions whenever a fetal heartbeat, defined by lawmakers, could be detected on an ultrasound, often before many women knew they were pregnant.
The Texas abortion law was hardly the last word on the topic. Ms. DeSpain didn’t know it on her drive to New Mexico in April, but the U.S. Supreme Court was weeks away from overturning the landmark Roe v. Wade decision.
On June 24, the Supreme Court delivered its 6-3 ruling overturning Roe v. Wade, the 1973 case that granted women the right to abortion.
This decision set in motion “trigger laws” in some states – laws that essentially fully banned abortions. Those states included Ms. DeSpain’s home state of Texas, where abortion is now a felony except when the life of the mother is in peril.
However, legal definitions of what qualifies as “life-threatening” remain murky.
The law is unclear, says Lisa Harris, MD, PhD, professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “What does the risk of death have to be, and how imminent must it be?” she asked in a recent editorial in the New England Journal of Medicine. Is 25% enough? 50%? Or does a woman have to be moments from dying?
“This whole thing makes me so angry,” says Shikha Jain, MD, a medical oncologist at University of Illinois Health, Chicago. “A patient may not be experiencing an emergency right now, but if we don’t take care of the situation, it may become an emergency in 2 hours or 2 days.”
Even before the Roe v. Wade decision, pregnancy had been a high-stakes endeavor for many women. In 2019, more than 750 women died from pregnancy-related events in the United States. In 2020, that number rose to 850. Each year dozens more suffer pregnancy-related events that require lifesaving interventions.
Now, in a post-Roe world, the number of maternal deaths will likely climb as more abortion bans take effect and fewer women have access to lifesaving care, experts say. A 2021 study that compared 2017 maternal mortality rates in states with different levels of abortion restrictions found that the rate of maternal mortality was almost two times higher in states that restricted abortion access compared with those that protected it – 28.5 per 100,000 women vs. 15.7.
Some women living in states with abortion bans won’t have the resources to cross state lines for care.
“This is just going to widen the health care disparities that are already so prevalent in this country,” Dr. Jain says.
Navigating a crossroads
Ms. DeSpain’s medical history reads like a checklist of pregnancy-related perils: chronic high blood pressure, persistent clotting problems, and a high risk of hemorrhage. She was also diagnosed with cervical cancer in 2020, which left her body more fragile.
Cardiovascular conditions, including hypertension and hemorrhage, are the leading causes of maternal mortality, responsible for more than one-third of pregnancy-related deaths. Preeclampsia, characterized by high blood pressure, accounts for more than 7% of maternal deaths in the United States. Although less common, genetic disorders, such as spinal muscular atrophy and triploidy, or cancer during pregnancy can put a mother and fetus at risk.
Cancer – which affects about 1 in 1,000 pregnant women and results in termination in as many as 28% of cases – brings sharp focus to the new dangers and complex decision-making patients and their doctors face as abortion bans take hold.
Before the Supreme Court decision, a pregnant woman with cancer was already facing great uncertainty. The decision to treat cancer during pregnancy involves “weighing the risk of exposing the fetus to medication vs. the risk to the mother’s untreated illness if you don’t expose the fetus to medication,” Elyce Cardonick, MD, an obstetrician at Cooper University Health Care, Camden, N.J., who specializes in high-risk pregnancies, told the National Cancer Institute.
Oncologists generally agree that it’s safe for pregnant women to receive chemotherapy during the second and third trimesters. But for women with aggressive cancers that are diagnosed in the first trimester, chemotherapy is dangerous. For women who need immunotherapy, the risks of treatment remain unclear.
In these cases, Alice S. Mims, MD, must broach the possibility of terminating the pregnancy.
“Cancer is a very urgent condition,” says Dr. Mims, a hematology specialist at the Ohio State University Comprehensive Cancer Center, Columbus, who sees patients who are pregnant. “These women may have other children at home, and they want to do their best to fight the disease so they can be around for their family long term.”
Now the changing legal landscape on abortion will put hundreds more pregnant women with cancer in danger. In a recent viewpoint article published in JAMA Oncology, Jordyn Silverstein and Katherine Van Loon, MD, MPH, estimate that during the next year, up to 420 pregnant women living in states with restricted abortion access will face threats to their cancer care and potentially their life.
“The repercussions of overturning Roe v. Wade – and the failure of the Supreme Court to provide any guidance on exceptions related to the life and health of the mother – are potentially catastrophic for a subset of women who face a life-threating diagnosis of [pregnancy-associated cancer],” they write.
The choice Ms. DeSpain faced after her cervical cancer diagnosis was different. She was not pregnant at the time, but she was at a crossroads.
Although it was caught early, the cancer was aggressive. Her oncologist recommended that she undergo a hysterectomy – the surgery that would give her the best chance for a cancer-free future. It would also mean she could no longer become pregnant.
With a less invasive procedure, on the other hand, she could still carry a child, but she would face a much greater chance that the cancer would come back.
At 27, Ms. DeSpain was not ready to close the pregnancy door. She opted for a surgery in which part of her cervix was removed, allowing her to try for another baby.
But she faced a ticking clock in the event her cancer returned.
If you want to have a baby, “try soon,” her doctor warned.
A dead end
After her cancer surgery and a third miscarriage, Ms. DeSpain and her husband were surprised and excited when in late 2021 she again became pregnant.
The first trimester seemed blissfully uneventful. As the weeks passed, Finley’s heart started to beat.
But the 16-week ultrasound signaled a turning point. The sonographer was too quiet.
“This is really bad, isn’t it?” Ms. DeSpain asked her sonographer.
The doctors told her he wouldn’t survive. Finley had no heart chambers. His heart couldn’t pump blood properly. He was missing one kidney, and his brain was split in the back. With almost no amniotic fluid, her doctor said he would likely die in utero, crushed to death without support from the protective liquid.
She fought for him anyway. She sought specialty care, followed bed rest orders, and traveled 3 hours to Houston to enroll in a clinical trial.
But every road was a dead end.
Ultimately, testing revealed Finley had triploidy, and all lines led to one point.
“There were too many things wrong, too much wrong for them to fix,” says Ms. DeSpain, recalling the news from her doctor in Houston. “I was in shock. My husband was just sitting with his hands flat on the table, staring at nothing, shaking a little bit.”
However, Finley still had a heartbeat, making an abortion after 6 weeks a felony in Texas. Even a compassionate induction was now out of the question unless her death was imminent.
Ms. DeSpain called the abortion clinic in Albuquerque and made an appointment. She would have to wait 2 weeks because of an influx of pregnant patients coming from Texas.
She welcomed the wait … just in case she changed her mind.
“At that point I wanted to carry him as far as I could,” she says.
For those 2 weeks, Ms. DeSpain remained on bed rest. She cried all day every day. She worried that Finley was experiencing pain.
Through this process, her doctor’s support helped keep her grounded.
“She cried with us in her office and said, ‘I wish that you didn’t have to go, but I think you’re doing the right thing, doing what keeps you safest,’ “ Ms. DeSpain recalls.
Ms. DeSpain declined to share the name of her doctor out of fear that even expressing compassion for a patient’s safety could put the physician in legal jeopardy and provoke harassment.
That fear is warranted. Some doctors will be forced to choose between doing what is legal – even though the law is vague – and doing what is right for patients, says law professor Jamie Abrams, who was recently diagnosed with breast cancer.
To live in a world where there’s talk of criminalizing doctors for taking care of their patients, where there’s “this national movement to position some women to be shunned and exiled for seeking care that’s right for them, their health, and might save their life is staggering and beyond comprehension,” says Ms. Abrams, professor of law at the American University Washington College of Law.
Ms. Abrams, who was diagnosed with hormone receptor–positive invasive breast cancer the same day she read the leaked Supreme Court draft on the decision to end of Roe v. Wade, said that “overnight, I became a person who would need an abortion if I became pregnant, because my treatment would compromise a healthy birth or delay necessary cancer care.” Ms. Abrams was also told she could no longer use hormonal contraception.
Dr. Harris’s advice to clinicians is to try to do what they feel is best for patients, including referring them to centers that have legal resources and protections regarding abortions.
Dr. Mims agrees and recommends that doctors reach out to those with more resources and legal backing for support. “I would advise doctors in [states with restrictive laws] to familiarize themselves with available resources and organizations taking action to deal with questionable cases,” Dr. Mims says.
‘Baby killers work here’
Following her 10-hour drive to Albuquerque, Ms. DeSpain encountered lines of protesters at the clinic. They were holding signs that said, “Abortion is murder,” and “Baby killers work here.”
“Please don’t kill your baby – we have resources for you,” a woman screeched through a megaphone as Ms. DeSpain, nearly 20 weeks’ pregnant, stepped out of the car to enter the clinic.
“I remember turning around, looking at her and making eye contact, and yelling back, ‘My baby has triploidy – he is dying! He is going to suffocate if I carry him full term. You don’t know what you’re talking about!’ “
A nurse held her hand during the procedure.
“He said, ‘You’re doing great, you’re okay,’ “ she recalls. She knew there was a chance that Finley’s face would be crushed by contractions during labor because of the lack of amniotic fluid, but she hoped not. Ms. DeSpain longed for a photo.
There was no photo to take home the next day, but Ms. DeSpain did receive Finley’s footprints, and his heartbeat – as captured by the specialty team in Houston – lives on in a stuffed giraffe.
His ashes arrived a few weeks later.
By then, the Supreme Court draft had been leaked. Ms. DeSpain knew her predicament in Texas would soon affect women across the United States and make any future pregnancy attempt for her even more risky.
The weeks and months that followed were a blur of grief, anger, and medical testing.
But she received some good news. A second triploidy pregnancy was extremely unlikely.
Several weeks later, Ms. DeSpain got more good news.
“I had a follow-up cancer appointment, and everything was completely clear,” she says.
She remains hopeful that she will be able to give birth, but her doctor cautioned that it’s no longer safe to become pregnant in Texas.
“I need you to understand that if you get pregnant and you have complications, we can’t intervene unless the baby doesn’t have a heartbeat, even if it would save your life,” Ms. DeSpain recalls her doctor saying.
If Texas remains a dangerous place to be pregnant, Ms. DeSpain and her husband will have to move.
For now, Ms. DeSpain wants people to know her story and to continue to fight for her right to govern her body.
In a public post to Facebook, she laid bare her pregnancy journey.
“No one should have to share a story like mine to justify abortion,” she wrote. “My choice is not yours to judge, and my rights are not yours to gleefully take away.”
Ms. Abrams, Ms. DeSpain, Dr. Harris, Dr. Jain, and Dr. Mims have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The drive from Texas to the clinic in Albuquerque, N.M., took 10 hours. It was mid-April of this year. There wasn’t much to see along the mostly barren stretch, and there wasn’t much for Kailee DeSpain to do aside from think about where she was going and why.
Her husband was driving. She sensed his nervous glances toward the passenger seat where she sat struggling to quiet her thoughts.
No, she wasn’t having any pain, she told him. No, she wasn’t feeling like she did the last time or the two times before that.
This pregnancy was different. It was the first in which she feared for her own life. Her fetus – Finley – had triploidy, a rare chromosomal abnormality. Because of the condition, which affects 1%-3% of pregnancies, his heart, brain, and kidneys were not developing properly.
At 19 weeks, Finley was already struggling to draw breath from lungs squeezed inside an overcrowded chest cavity. Ms. DeSpain wanted nothing more than to carry Finley to term, hold him, meet him even for a moment before saying goodbye.
But his condition meant he would likely suffocate in utero well before that. And Ms. DeSpain knew that carrying him longer would likely raise her risk of bleeding and of her blood pressure increasing to dangerous highs.
“This could kill you,” her husband told her. “Do you realize you could die bringing a baby into this world who is not going to live? I don’t want to lose you.’”
Unlike her other pregnancies, the timing of this one and the decision she faced to end it put her health in even greater danger.
Imminent danger
On Sept. 1, 2021, a bill went into effect in Texas that banned abortions from as early as 6 weeks’ gestation. Texas Senate Bill 8 (SB8) became one of the most restrictive abortion laws in the country. It prohibited abortions whenever a fetal heartbeat, defined by lawmakers, could be detected on an ultrasound, often before many women knew they were pregnant.
The Texas abortion law was hardly the last word on the topic. Ms. DeSpain didn’t know it on her drive to New Mexico in April, but the U.S. Supreme Court was weeks away from overturning the landmark Roe v. Wade decision.
On June 24, the Supreme Court delivered its 6-3 ruling overturning Roe v. Wade, the 1973 case that granted women the right to abortion.
This decision set in motion “trigger laws” in some states – laws that essentially fully banned abortions. Those states included Ms. DeSpain’s home state of Texas, where abortion is now a felony except when the life of the mother is in peril.
However, legal definitions of what qualifies as “life-threatening” remain murky.
The law is unclear, says Lisa Harris, MD, PhD, professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “What does the risk of death have to be, and how imminent must it be?” she asked in a recent editorial in the New England Journal of Medicine. Is 25% enough? 50%? Or does a woman have to be moments from dying?
“This whole thing makes me so angry,” says Shikha Jain, MD, a medical oncologist at University of Illinois Health, Chicago. “A patient may not be experiencing an emergency right now, but if we don’t take care of the situation, it may become an emergency in 2 hours or 2 days.”
Even before the Roe v. Wade decision, pregnancy had been a high-stakes endeavor for many women. In 2019, more than 750 women died from pregnancy-related events in the United States. In 2020, that number rose to 850. Each year dozens more suffer pregnancy-related events that require lifesaving interventions.
Now, in a post-Roe world, the number of maternal deaths will likely climb as more abortion bans take effect and fewer women have access to lifesaving care, experts say. A 2021 study that compared 2017 maternal mortality rates in states with different levels of abortion restrictions found that the rate of maternal mortality was almost two times higher in states that restricted abortion access compared with those that protected it – 28.5 per 100,000 women vs. 15.7.
Some women living in states with abortion bans won’t have the resources to cross state lines for care.
“This is just going to widen the health care disparities that are already so prevalent in this country,” Dr. Jain says.
Navigating a crossroads
Ms. DeSpain’s medical history reads like a checklist of pregnancy-related perils: chronic high blood pressure, persistent clotting problems, and a high risk of hemorrhage. She was also diagnosed with cervical cancer in 2020, which left her body more fragile.
Cardiovascular conditions, including hypertension and hemorrhage, are the leading causes of maternal mortality, responsible for more than one-third of pregnancy-related deaths. Preeclampsia, characterized by high blood pressure, accounts for more than 7% of maternal deaths in the United States. Although less common, genetic disorders, such as spinal muscular atrophy and triploidy, or cancer during pregnancy can put a mother and fetus at risk.
Cancer – which affects about 1 in 1,000 pregnant women and results in termination in as many as 28% of cases – brings sharp focus to the new dangers and complex decision-making patients and their doctors face as abortion bans take hold.
Before the Supreme Court decision, a pregnant woman with cancer was already facing great uncertainty. The decision to treat cancer during pregnancy involves “weighing the risk of exposing the fetus to medication vs. the risk to the mother’s untreated illness if you don’t expose the fetus to medication,” Elyce Cardonick, MD, an obstetrician at Cooper University Health Care, Camden, N.J., who specializes in high-risk pregnancies, told the National Cancer Institute.
Oncologists generally agree that it’s safe for pregnant women to receive chemotherapy during the second and third trimesters. But for women with aggressive cancers that are diagnosed in the first trimester, chemotherapy is dangerous. For women who need immunotherapy, the risks of treatment remain unclear.
In these cases, Alice S. Mims, MD, must broach the possibility of terminating the pregnancy.
“Cancer is a very urgent condition,” says Dr. Mims, a hematology specialist at the Ohio State University Comprehensive Cancer Center, Columbus, who sees patients who are pregnant. “These women may have other children at home, and they want to do their best to fight the disease so they can be around for their family long term.”
Now the changing legal landscape on abortion will put hundreds more pregnant women with cancer in danger. In a recent viewpoint article published in JAMA Oncology, Jordyn Silverstein and Katherine Van Loon, MD, MPH, estimate that during the next year, up to 420 pregnant women living in states with restricted abortion access will face threats to their cancer care and potentially their life.
“The repercussions of overturning Roe v. Wade – and the failure of the Supreme Court to provide any guidance on exceptions related to the life and health of the mother – are potentially catastrophic for a subset of women who face a life-threating diagnosis of [pregnancy-associated cancer],” they write.
The choice Ms. DeSpain faced after her cervical cancer diagnosis was different. She was not pregnant at the time, but she was at a crossroads.
Although it was caught early, the cancer was aggressive. Her oncologist recommended that she undergo a hysterectomy – the surgery that would give her the best chance for a cancer-free future. It would also mean she could no longer become pregnant.
With a less invasive procedure, on the other hand, she could still carry a child, but she would face a much greater chance that the cancer would come back.
At 27, Ms. DeSpain was not ready to close the pregnancy door. She opted for a surgery in which part of her cervix was removed, allowing her to try for another baby.
But she faced a ticking clock in the event her cancer returned.
If you want to have a baby, “try soon,” her doctor warned.
A dead end
After her cancer surgery and a third miscarriage, Ms. DeSpain and her husband were surprised and excited when in late 2021 she again became pregnant.
The first trimester seemed blissfully uneventful. As the weeks passed, Finley’s heart started to beat.
But the 16-week ultrasound signaled a turning point. The sonographer was too quiet.
“This is really bad, isn’t it?” Ms. DeSpain asked her sonographer.
The doctors told her he wouldn’t survive. Finley had no heart chambers. His heart couldn’t pump blood properly. He was missing one kidney, and his brain was split in the back. With almost no amniotic fluid, her doctor said he would likely die in utero, crushed to death without support from the protective liquid.
She fought for him anyway. She sought specialty care, followed bed rest orders, and traveled 3 hours to Houston to enroll in a clinical trial.
But every road was a dead end.
Ultimately, testing revealed Finley had triploidy, and all lines led to one point.
“There were too many things wrong, too much wrong for them to fix,” says Ms. DeSpain, recalling the news from her doctor in Houston. “I was in shock. My husband was just sitting with his hands flat on the table, staring at nothing, shaking a little bit.”
However, Finley still had a heartbeat, making an abortion after 6 weeks a felony in Texas. Even a compassionate induction was now out of the question unless her death was imminent.
Ms. DeSpain called the abortion clinic in Albuquerque and made an appointment. She would have to wait 2 weeks because of an influx of pregnant patients coming from Texas.
She welcomed the wait … just in case she changed her mind.
“At that point I wanted to carry him as far as I could,” she says.
For those 2 weeks, Ms. DeSpain remained on bed rest. She cried all day every day. She worried that Finley was experiencing pain.
Through this process, her doctor’s support helped keep her grounded.
“She cried with us in her office and said, ‘I wish that you didn’t have to go, but I think you’re doing the right thing, doing what keeps you safest,’ “ Ms. DeSpain recalls.
Ms. DeSpain declined to share the name of her doctor out of fear that even expressing compassion for a patient’s safety could put the physician in legal jeopardy and provoke harassment.
That fear is warranted. Some doctors will be forced to choose between doing what is legal – even though the law is vague – and doing what is right for patients, says law professor Jamie Abrams, who was recently diagnosed with breast cancer.
To live in a world where there’s talk of criminalizing doctors for taking care of their patients, where there’s “this national movement to position some women to be shunned and exiled for seeking care that’s right for them, their health, and might save their life is staggering and beyond comprehension,” says Ms. Abrams, professor of law at the American University Washington College of Law.
Ms. Abrams, who was diagnosed with hormone receptor–positive invasive breast cancer the same day she read the leaked Supreme Court draft on the decision to end of Roe v. Wade, said that “overnight, I became a person who would need an abortion if I became pregnant, because my treatment would compromise a healthy birth or delay necessary cancer care.” Ms. Abrams was also told she could no longer use hormonal contraception.
Dr. Harris’s advice to clinicians is to try to do what they feel is best for patients, including referring them to centers that have legal resources and protections regarding abortions.
Dr. Mims agrees and recommends that doctors reach out to those with more resources and legal backing for support. “I would advise doctors in [states with restrictive laws] to familiarize themselves with available resources and organizations taking action to deal with questionable cases,” Dr. Mims says.
‘Baby killers work here’
Following her 10-hour drive to Albuquerque, Ms. DeSpain encountered lines of protesters at the clinic. They were holding signs that said, “Abortion is murder,” and “Baby killers work here.”
“Please don’t kill your baby – we have resources for you,” a woman screeched through a megaphone as Ms. DeSpain, nearly 20 weeks’ pregnant, stepped out of the car to enter the clinic.
“I remember turning around, looking at her and making eye contact, and yelling back, ‘My baby has triploidy – he is dying! He is going to suffocate if I carry him full term. You don’t know what you’re talking about!’ “
A nurse held her hand during the procedure.
“He said, ‘You’re doing great, you’re okay,’ “ she recalls. She knew there was a chance that Finley’s face would be crushed by contractions during labor because of the lack of amniotic fluid, but she hoped not. Ms. DeSpain longed for a photo.
There was no photo to take home the next day, but Ms. DeSpain did receive Finley’s footprints, and his heartbeat – as captured by the specialty team in Houston – lives on in a stuffed giraffe.
His ashes arrived a few weeks later.
By then, the Supreme Court draft had been leaked. Ms. DeSpain knew her predicament in Texas would soon affect women across the United States and make any future pregnancy attempt for her even more risky.
The weeks and months that followed were a blur of grief, anger, and medical testing.
But she received some good news. A second triploidy pregnancy was extremely unlikely.
Several weeks later, Ms. DeSpain got more good news.
“I had a follow-up cancer appointment, and everything was completely clear,” she says.
She remains hopeful that she will be able to give birth, but her doctor cautioned that it’s no longer safe to become pregnant in Texas.
“I need you to understand that if you get pregnant and you have complications, we can’t intervene unless the baby doesn’t have a heartbeat, even if it would save your life,” Ms. DeSpain recalls her doctor saying.
If Texas remains a dangerous place to be pregnant, Ms. DeSpain and her husband will have to move.
For now, Ms. DeSpain wants people to know her story and to continue to fight for her right to govern her body.
In a public post to Facebook, she laid bare her pregnancy journey.
“No one should have to share a story like mine to justify abortion,” she wrote. “My choice is not yours to judge, and my rights are not yours to gleefully take away.”
Ms. Abrams, Ms. DeSpain, Dr. Harris, Dr. Jain, and Dr. Mims have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The drive from Texas to the clinic in Albuquerque, N.M., took 10 hours. It was mid-April of this year. There wasn’t much to see along the mostly barren stretch, and there wasn’t much for Kailee DeSpain to do aside from think about where she was going and why.
Her husband was driving. She sensed his nervous glances toward the passenger seat where she sat struggling to quiet her thoughts.
No, she wasn’t having any pain, she told him. No, she wasn’t feeling like she did the last time or the two times before that.
This pregnancy was different. It was the first in which she feared for her own life. Her fetus – Finley – had triploidy, a rare chromosomal abnormality. Because of the condition, which affects 1%-3% of pregnancies, his heart, brain, and kidneys were not developing properly.
At 19 weeks, Finley was already struggling to draw breath from lungs squeezed inside an overcrowded chest cavity. Ms. DeSpain wanted nothing more than to carry Finley to term, hold him, meet him even for a moment before saying goodbye.
But his condition meant he would likely suffocate in utero well before that. And Ms. DeSpain knew that carrying him longer would likely raise her risk of bleeding and of her blood pressure increasing to dangerous highs.
“This could kill you,” her husband told her. “Do you realize you could die bringing a baby into this world who is not going to live? I don’t want to lose you.’”
Unlike her other pregnancies, the timing of this one and the decision she faced to end it put her health in even greater danger.
Imminent danger
On Sept. 1, 2021, a bill went into effect in Texas that banned abortions from as early as 6 weeks’ gestation. Texas Senate Bill 8 (SB8) became one of the most restrictive abortion laws in the country. It prohibited abortions whenever a fetal heartbeat, defined by lawmakers, could be detected on an ultrasound, often before many women knew they were pregnant.
The Texas abortion law was hardly the last word on the topic. Ms. DeSpain didn’t know it on her drive to New Mexico in April, but the U.S. Supreme Court was weeks away from overturning the landmark Roe v. Wade decision.
On June 24, the Supreme Court delivered its 6-3 ruling overturning Roe v. Wade, the 1973 case that granted women the right to abortion.
This decision set in motion “trigger laws” in some states – laws that essentially fully banned abortions. Those states included Ms. DeSpain’s home state of Texas, where abortion is now a felony except when the life of the mother is in peril.
However, legal definitions of what qualifies as “life-threatening” remain murky.
The law is unclear, says Lisa Harris, MD, PhD, professor in the department of obstetrics and gynecology at the University of Michigan, Ann Arbor. “What does the risk of death have to be, and how imminent must it be?” she asked in a recent editorial in the New England Journal of Medicine. Is 25% enough? 50%? Or does a woman have to be moments from dying?
“This whole thing makes me so angry,” says Shikha Jain, MD, a medical oncologist at University of Illinois Health, Chicago. “A patient may not be experiencing an emergency right now, but if we don’t take care of the situation, it may become an emergency in 2 hours or 2 days.”
Even before the Roe v. Wade decision, pregnancy had been a high-stakes endeavor for many women. In 2019, more than 750 women died from pregnancy-related events in the United States. In 2020, that number rose to 850. Each year dozens more suffer pregnancy-related events that require lifesaving interventions.
Now, in a post-Roe world, the number of maternal deaths will likely climb as more abortion bans take effect and fewer women have access to lifesaving care, experts say. A 2021 study that compared 2017 maternal mortality rates in states with different levels of abortion restrictions found that the rate of maternal mortality was almost two times higher in states that restricted abortion access compared with those that protected it – 28.5 per 100,000 women vs. 15.7.
Some women living in states with abortion bans won’t have the resources to cross state lines for care.
“This is just going to widen the health care disparities that are already so prevalent in this country,” Dr. Jain says.
Navigating a crossroads
Ms. DeSpain’s medical history reads like a checklist of pregnancy-related perils: chronic high blood pressure, persistent clotting problems, and a high risk of hemorrhage. She was also diagnosed with cervical cancer in 2020, which left her body more fragile.
Cardiovascular conditions, including hypertension and hemorrhage, are the leading causes of maternal mortality, responsible for more than one-third of pregnancy-related deaths. Preeclampsia, characterized by high blood pressure, accounts for more than 7% of maternal deaths in the United States. Although less common, genetic disorders, such as spinal muscular atrophy and triploidy, or cancer during pregnancy can put a mother and fetus at risk.
Cancer – which affects about 1 in 1,000 pregnant women and results in termination in as many as 28% of cases – brings sharp focus to the new dangers and complex decision-making patients and their doctors face as abortion bans take hold.
Before the Supreme Court decision, a pregnant woman with cancer was already facing great uncertainty. The decision to treat cancer during pregnancy involves “weighing the risk of exposing the fetus to medication vs. the risk to the mother’s untreated illness if you don’t expose the fetus to medication,” Elyce Cardonick, MD, an obstetrician at Cooper University Health Care, Camden, N.J., who specializes in high-risk pregnancies, told the National Cancer Institute.
Oncologists generally agree that it’s safe for pregnant women to receive chemotherapy during the second and third trimesters. But for women with aggressive cancers that are diagnosed in the first trimester, chemotherapy is dangerous. For women who need immunotherapy, the risks of treatment remain unclear.
In these cases, Alice S. Mims, MD, must broach the possibility of terminating the pregnancy.
“Cancer is a very urgent condition,” says Dr. Mims, a hematology specialist at the Ohio State University Comprehensive Cancer Center, Columbus, who sees patients who are pregnant. “These women may have other children at home, and they want to do their best to fight the disease so they can be around for their family long term.”
Now the changing legal landscape on abortion will put hundreds more pregnant women with cancer in danger. In a recent viewpoint article published in JAMA Oncology, Jordyn Silverstein and Katherine Van Loon, MD, MPH, estimate that during the next year, up to 420 pregnant women living in states with restricted abortion access will face threats to their cancer care and potentially their life.
“The repercussions of overturning Roe v. Wade – and the failure of the Supreme Court to provide any guidance on exceptions related to the life and health of the mother – are potentially catastrophic for a subset of women who face a life-threating diagnosis of [pregnancy-associated cancer],” they write.
The choice Ms. DeSpain faced after her cervical cancer diagnosis was different. She was not pregnant at the time, but she was at a crossroads.
Although it was caught early, the cancer was aggressive. Her oncologist recommended that she undergo a hysterectomy – the surgery that would give her the best chance for a cancer-free future. It would also mean she could no longer become pregnant.
With a less invasive procedure, on the other hand, she could still carry a child, but she would face a much greater chance that the cancer would come back.
At 27, Ms. DeSpain was not ready to close the pregnancy door. She opted for a surgery in which part of her cervix was removed, allowing her to try for another baby.
But she faced a ticking clock in the event her cancer returned.
If you want to have a baby, “try soon,” her doctor warned.
A dead end
After her cancer surgery and a third miscarriage, Ms. DeSpain and her husband were surprised and excited when in late 2021 she again became pregnant.
The first trimester seemed blissfully uneventful. As the weeks passed, Finley’s heart started to beat.
But the 16-week ultrasound signaled a turning point. The sonographer was too quiet.
“This is really bad, isn’t it?” Ms. DeSpain asked her sonographer.
The doctors told her he wouldn’t survive. Finley had no heart chambers. His heart couldn’t pump blood properly. He was missing one kidney, and his brain was split in the back. With almost no amniotic fluid, her doctor said he would likely die in utero, crushed to death without support from the protective liquid.
She fought for him anyway. She sought specialty care, followed bed rest orders, and traveled 3 hours to Houston to enroll in a clinical trial.
But every road was a dead end.
Ultimately, testing revealed Finley had triploidy, and all lines led to one point.
“There were too many things wrong, too much wrong for them to fix,” says Ms. DeSpain, recalling the news from her doctor in Houston. “I was in shock. My husband was just sitting with his hands flat on the table, staring at nothing, shaking a little bit.”
However, Finley still had a heartbeat, making an abortion after 6 weeks a felony in Texas. Even a compassionate induction was now out of the question unless her death was imminent.
Ms. DeSpain called the abortion clinic in Albuquerque and made an appointment. She would have to wait 2 weeks because of an influx of pregnant patients coming from Texas.
She welcomed the wait … just in case she changed her mind.
“At that point I wanted to carry him as far as I could,” she says.
For those 2 weeks, Ms. DeSpain remained on bed rest. She cried all day every day. She worried that Finley was experiencing pain.
Through this process, her doctor’s support helped keep her grounded.
“She cried with us in her office and said, ‘I wish that you didn’t have to go, but I think you’re doing the right thing, doing what keeps you safest,’ “ Ms. DeSpain recalls.
Ms. DeSpain declined to share the name of her doctor out of fear that even expressing compassion for a patient’s safety could put the physician in legal jeopardy and provoke harassment.
That fear is warranted. Some doctors will be forced to choose between doing what is legal – even though the law is vague – and doing what is right for patients, says law professor Jamie Abrams, who was recently diagnosed with breast cancer.
To live in a world where there’s talk of criminalizing doctors for taking care of their patients, where there’s “this national movement to position some women to be shunned and exiled for seeking care that’s right for them, their health, and might save their life is staggering and beyond comprehension,” says Ms. Abrams, professor of law at the American University Washington College of Law.
Ms. Abrams, who was diagnosed with hormone receptor–positive invasive breast cancer the same day she read the leaked Supreme Court draft on the decision to end of Roe v. Wade, said that “overnight, I became a person who would need an abortion if I became pregnant, because my treatment would compromise a healthy birth or delay necessary cancer care.” Ms. Abrams was also told she could no longer use hormonal contraception.
Dr. Harris’s advice to clinicians is to try to do what they feel is best for patients, including referring them to centers that have legal resources and protections regarding abortions.
Dr. Mims agrees and recommends that doctors reach out to those with more resources and legal backing for support. “I would advise doctors in [states with restrictive laws] to familiarize themselves with available resources and organizations taking action to deal with questionable cases,” Dr. Mims says.
‘Baby killers work here’
Following her 10-hour drive to Albuquerque, Ms. DeSpain encountered lines of protesters at the clinic. They were holding signs that said, “Abortion is murder,” and “Baby killers work here.”
“Please don’t kill your baby – we have resources for you,” a woman screeched through a megaphone as Ms. DeSpain, nearly 20 weeks’ pregnant, stepped out of the car to enter the clinic.
“I remember turning around, looking at her and making eye contact, and yelling back, ‘My baby has triploidy – he is dying! He is going to suffocate if I carry him full term. You don’t know what you’re talking about!’ “
A nurse held her hand during the procedure.
“He said, ‘You’re doing great, you’re okay,’ “ she recalls. She knew there was a chance that Finley’s face would be crushed by contractions during labor because of the lack of amniotic fluid, but she hoped not. Ms. DeSpain longed for a photo.
There was no photo to take home the next day, but Ms. DeSpain did receive Finley’s footprints, and his heartbeat – as captured by the specialty team in Houston – lives on in a stuffed giraffe.
His ashes arrived a few weeks later.
By then, the Supreme Court draft had been leaked. Ms. DeSpain knew her predicament in Texas would soon affect women across the United States and make any future pregnancy attempt for her even more risky.
The weeks and months that followed were a blur of grief, anger, and medical testing.
But she received some good news. A second triploidy pregnancy was extremely unlikely.
Several weeks later, Ms. DeSpain got more good news.
“I had a follow-up cancer appointment, and everything was completely clear,” she says.
She remains hopeful that she will be able to give birth, but her doctor cautioned that it’s no longer safe to become pregnant in Texas.
“I need you to understand that if you get pregnant and you have complications, we can’t intervene unless the baby doesn’t have a heartbeat, even if it would save your life,” Ms. DeSpain recalls her doctor saying.
If Texas remains a dangerous place to be pregnant, Ms. DeSpain and her husband will have to move.
For now, Ms. DeSpain wants people to know her story and to continue to fight for her right to govern her body.
In a public post to Facebook, she laid bare her pregnancy journey.
“No one should have to share a story like mine to justify abortion,” she wrote. “My choice is not yours to judge, and my rights are not yours to gleefully take away.”
Ms. Abrams, Ms. DeSpain, Dr. Harris, Dr. Jain, and Dr. Mims have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
$3 billion in cancer drug waste: Can it be salvaged?
Three billion dollars: It’s enough to finance the annual out-of-pocket costs for 1 in 7 patients with cancer. It would cover almost half of the National Cancer Institute’s annual budget. And it could fund President Biden’s entire Cancer Moonshot program, with more than a billion to spare.
It’s also how much the United States spends on unused cancer drugs each year, some experts estimate.
Drug companies typically sell infused drugs in one or two single-dose vial sizes, but patients don’t come in such neat packages. A patient may need 300 mg of a drug that is only sold as 200 mg vials, which means half of a vial will go to waste.
Although most oncology drugs don’t incur substantial waste, even small volumes can translate to millions of dollars a year.
But can this money be saved or reallocated, if only we delivered drugs more efficiently?
Some experts don’t believe that’s possible.
“Attempts to recoup money for discarded drugs wouldn’t happen in a vacuum,” said Robin Yabroff, PhD, MBA, an epidemiologist and scientific vice president of Health Services Research at the American Cancer Society, who was part of a committee commissioned to evaluate the costs associated with discarded drugs.
The potential catch of any widespread effort to seek repayment or reduce the amount of discarded drugs, Dr. Yabroff and colleagues note, is that manufacturers would “simply increase the price of the vial.”
In other words, attempting to fix one problem may lead to another — essentially a whack-a-mole of cancer costs, which are projected to balloon to $246 billion by 2030.
What this means is without sweeping policies to rein in cancer care costs, oncologists can only do so much. And every little bit counts.
“We are left chipping away at this monster of cancer care costs,” said Adam Binder, MD, a medical oncologist at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Millions spent on “reasonable amount” of waste
Michal Sarfaty, MD, was excited when enfortumab vedotin came on the market to treat advanced urothelial cancer in late 2019.
The cost of the drug, however, tempered her enthusiasm.
Enfortumab vedotin is a “great drug,” said Dr. Sarfaty, an oncologist at the Sheba Medical Center, Ramat Gan, Israel. But it can cost upwards of $500,000 a year for an average-weight man.
Given the expense, Dr. Sarfaty wanted to understand how much of the drug gets thrown away. During a fellowship at Memorial Sloan Kettering (MSK) Cancer Center in New York, Dr. Sarfaty explored the amount of unused enfortumab vedotin among the 64 patients who received the drug in 2020. She, along with a team at MSK, calculated the price tag of that waste and extrapolated those estimates for patients across the country.
Although waste occurred in almost half of administered doses (367 of 793), only a small volume got discarded — 2.9% per dose, on average.
Multiplying unused milligrams by the cost per milligram, Dr. Sarfaty and colleagues estimated that, for each patient, $3,127 of the drug got discarded. When calculated over the year, the cost came to just over $200,000 at MSK, and nearly $15 million when projected across the approved patient population in the United States.
“Ultimately, we did not see a lot of waste with this specific drug,” Dr. Sarfaty said. “Under 2.9% is considered a reasonable amount, below the 3% threshold Peter Bach, MD, and colleagues recommend. But even with this small amount of waste, the cost per patient and to the system remains notable.”
The problem with recouping drug waste
Estimates from the Centers for Medicare & Medicaid Services (CMS), which tracks costs associated with discarded weight-based drugs covered under Medicare Part B, support the notion that small quantities of discarded drugs can still translate to big bucks.
Since 2017, CMS has required healthcare providers to report the volume of drugs discarded from a single-dose vial using a code, known as the JW modifier. The JW modifier means that providers can be reimbursed for the entire vial amount, not just the quantity the patient used.
In 2019, claims data from Medicare Part B showed that 1.85% of discarded rituximab came to $33.3 million. For infliximab, the 1.55% of discarded liquid translated to $15 million, and just 0.36% of discarded pembrolizumab reached $10 million.
However, experts question whether the JW modifier accurately reflects the quantity of drugs discarded.
According to the 2021 report from the National Academies of Sciences, Engineering, and Medicine (NASEM), most physicians don’t use the JW modifier. Among Medicare claims, 16.2% included the JW modifier in 2017 and 16.9% did in 2018.
The rate was significantly lower for private insurance. Of more than 4 million private insurance claims on 77 drugs made in 2017 and 2018, only 3.6% included the JW modifier; 15 of these drugs had no JW claims.
“Although we found that most physicians don’t use the JW modifier, even those who do, don’t use it consistently, even for the same patient,” said Dr. Yabroff, a co-author on the report.
Going a step further, Dr. Yabroff and colleagues argue that even if everyone used the JW modifier as intended, manufacturers would probably increase the price of drugs to compensate for any loss, potentially eliminating savings for payers.
That’s because, in the United States, manufacturers typically base drug prices on a patient and payers’ “willingness to pay for better health,” not on the volume of liquid used. Take a patient who pays $2,000 to receive the dose they need. If that dose is 600 mg but requires using two vials of 400 mg, then “to the patient, the 600-mg dose is worth $2,000, and the remainder has no value whatsoever,” the NASEM authors argue.
The authors parallel this scenario to purchasing a designer coat or dress. If that item requires alterations that remove a section of material, “the customer does not typically get a rebate because all the fabric was not needed,” the NASEM team writes.
But there’s a flaw in this rationale, argues Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel. A person’s willingness to pay for better health assumes that the price of a drug is based on proper market forces, where a drug’s cost and its effectiveness are in harmony.
“The problem is we’re operating in a broken market where the prices of oncology drugs have no real bearing on their efficacy,” said Dr. Goldstein.
And, as Dr. Bach noted in a 2021 Health Affairs piece, willingness to pay also requires that consumers know what they’re paying and allows them to walk away from an excessively high price.
But neither is a reality.
For one, Dr. Bach explains, companies may lowball the monthly price of a drug. In 2020, GlaxoSmithKline (GSK) announced that its new drug Blenrep would carry a list price of $8,277 per vial, or about $23,900 per month for an average 79 kg (175 lb) patient. That price accounts for two vials of the drug. But, according to Dr. Bach, “what GSK left out is that 44% of U.S. adults weigh more than 80 kg, and above that weight, three vials are needed per dose.” That would raise the average monthly cost to $30,479.
Perhaps more importantly, consumers can’t easily walk away.
“Medicare can’t negotiate prices and is forced to pay what a drug company says,” Dr. Goldstein said. “This is very different to when I buy a coat. If the price is too high, I can walk away.”
Fixed dosing: A solution or a new problem?
Efforts to reduce the financial impact of discarded cancer drugs can blow back on physicians, patients, and payers in other unanticipated ways. Take fixed dosing. Although chemotherapy dosing remains weight-based, many targeted therapies — such as nivolumab and pembrolizumab — recently transitioned to a fixed dosing regimen.
Administering a fixed, instead of weight-based, dose eliminates waste but can create new problems.
“Patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” said Dr. Goldstein. In a 2017 analysis, Dr. Goldstein and colleagues compared dosing strategies in patients with metastatic non–small cell lung cancer who received pembrolizumab. The team found that the total annual cost of weight-based dosing was $2.6 billion, whereas the cost of the fixed dosing strategy was $3.44 billion — 24% more. In other words, personalized weight-based dosing would save more than $825 million dollars in the United States each year.
A 2020 analysis based in France found a similar cost increase of 26% for fixed dosing of pembrolizumab as well as nivolumab.
“I’ve argued we should go back to weight-based dosing,” Dr. Goldstein said. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
Does dose rounding work?
Rose DiMarco, PharmD, BCPS, BCOP, keeps a tight watch on patients being treated at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Dr. DiMarco educates patients about their treatment plan, reviews their lab results, and monitors them for side effects and drug interactions.
She also thinks a lot about costs.
“We spend about $100,000 a day on oncology drugs, and we want to make sure we’re not being wasteful,” Dr. DiMarco said in an interview.
One major initiative to curb waste and reduce costs at Jefferson has centered on dose rounding, which calculates whether a specific dose can be altered slightly to conserve vials and prevent waste. According to the Hematology/Oncology Pharmacy Association, a patient can receive up to 10% more or less of a weight-based dose without impacting treatment efficacy.
If, for instance, a patient requires 380 mg, but two vials come to 400 mg, rounding up that dose by approximately 5% means eliminating 20 mg that would go unused. But if that patient requires 420 mg, rounding down about 5% means substantial savings from not opening a new vial.
At Jefferson, Dr. DiMarco and her pharmacy colleagues map out dose ranges for all patients. Anyone who falls inside the 10% may be eligible for dose rounding. Anyone who doesn’t will receive the usual dose.
Although it is a challenge to implement, dose rounding has become standard of care at many cancer centers across the United States and is linked to substantial savings.
A 2018 analysis projected annual savings of $865,000 associated with rounding down eight monoclonal antibodies for patients with metastatic disease at a community cancer center. A more recent analysis from the Mayo Clinic found that dose rounding saved a total of 9,814 drug vials — 4485 of which were cancer drugs and 5329 of which were biologics — and resulted in $7.3 million in savings over 6 months in 2019 — $1.56 million from oncology agents and $5.7 from biologics.
And in a small 2019 analysis, researchers at Jefferson showed dose rounding of one monoclonal antibody saved approximately $30,000 in just 3 months, Dr. DiMarco noted.
“Not only does this process reduce costs and waste, but it also standardizes the preparation of hazardous medications, which can help prevent medication errors,” Dr. DiMarco said.
Nibbling around the edges
Despite estimates that scale into the billions of dollars, “drug wastage is just a small part of overall cancer costs,” Dr. Sarfaty said.
Fumiko Chino, MD, a radiation oncologist at MSK, agrees. “When we talk about affordability and cost, we can nibble around the edges of what’s really important,” Dr. Chino said. “Discarded drugs may cost a lot when you consider them in aggregate, but they are not as important as negotiated drug prices, which could substantially reduce overall costs.”
And until drug prices are addressed on a broader policy level, the cost of cancer care likely won’t improve in a meaningful way.
“But for the patient sitting in front of me, my focus will always be to provide the best care possible,” Dr. Binder said.
A version of this article first appeared on Medscape.com.
Three billion dollars: It’s enough to finance the annual out-of-pocket costs for 1 in 7 patients with cancer. It would cover almost half of the National Cancer Institute’s annual budget. And it could fund President Biden’s entire Cancer Moonshot program, with more than a billion to spare.
It’s also how much the United States spends on unused cancer drugs each year, some experts estimate.
Drug companies typically sell infused drugs in one or two single-dose vial sizes, but patients don’t come in such neat packages. A patient may need 300 mg of a drug that is only sold as 200 mg vials, which means half of a vial will go to waste.
Although most oncology drugs don’t incur substantial waste, even small volumes can translate to millions of dollars a year.
But can this money be saved or reallocated, if only we delivered drugs more efficiently?
Some experts don’t believe that’s possible.
“Attempts to recoup money for discarded drugs wouldn’t happen in a vacuum,” said Robin Yabroff, PhD, MBA, an epidemiologist and scientific vice president of Health Services Research at the American Cancer Society, who was part of a committee commissioned to evaluate the costs associated with discarded drugs.
The potential catch of any widespread effort to seek repayment or reduce the amount of discarded drugs, Dr. Yabroff and colleagues note, is that manufacturers would “simply increase the price of the vial.”
In other words, attempting to fix one problem may lead to another — essentially a whack-a-mole of cancer costs, which are projected to balloon to $246 billion by 2030.
What this means is without sweeping policies to rein in cancer care costs, oncologists can only do so much. And every little bit counts.
“We are left chipping away at this monster of cancer care costs,” said Adam Binder, MD, a medical oncologist at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Millions spent on “reasonable amount” of waste
Michal Sarfaty, MD, was excited when enfortumab vedotin came on the market to treat advanced urothelial cancer in late 2019.
The cost of the drug, however, tempered her enthusiasm.
Enfortumab vedotin is a “great drug,” said Dr. Sarfaty, an oncologist at the Sheba Medical Center, Ramat Gan, Israel. But it can cost upwards of $500,000 a year for an average-weight man.
Given the expense, Dr. Sarfaty wanted to understand how much of the drug gets thrown away. During a fellowship at Memorial Sloan Kettering (MSK) Cancer Center in New York, Dr. Sarfaty explored the amount of unused enfortumab vedotin among the 64 patients who received the drug in 2020. She, along with a team at MSK, calculated the price tag of that waste and extrapolated those estimates for patients across the country.
Although waste occurred in almost half of administered doses (367 of 793), only a small volume got discarded — 2.9% per dose, on average.
Multiplying unused milligrams by the cost per milligram, Dr. Sarfaty and colleagues estimated that, for each patient, $3,127 of the drug got discarded. When calculated over the year, the cost came to just over $200,000 at MSK, and nearly $15 million when projected across the approved patient population in the United States.
“Ultimately, we did not see a lot of waste with this specific drug,” Dr. Sarfaty said. “Under 2.9% is considered a reasonable amount, below the 3% threshold Peter Bach, MD, and colleagues recommend. But even with this small amount of waste, the cost per patient and to the system remains notable.”
The problem with recouping drug waste
Estimates from the Centers for Medicare & Medicaid Services (CMS), which tracks costs associated with discarded weight-based drugs covered under Medicare Part B, support the notion that small quantities of discarded drugs can still translate to big bucks.
Since 2017, CMS has required healthcare providers to report the volume of drugs discarded from a single-dose vial using a code, known as the JW modifier. The JW modifier means that providers can be reimbursed for the entire vial amount, not just the quantity the patient used.
In 2019, claims data from Medicare Part B showed that 1.85% of discarded rituximab came to $33.3 million. For infliximab, the 1.55% of discarded liquid translated to $15 million, and just 0.36% of discarded pembrolizumab reached $10 million.
However, experts question whether the JW modifier accurately reflects the quantity of drugs discarded.
According to the 2021 report from the National Academies of Sciences, Engineering, and Medicine (NASEM), most physicians don’t use the JW modifier. Among Medicare claims, 16.2% included the JW modifier in 2017 and 16.9% did in 2018.
The rate was significantly lower for private insurance. Of more than 4 million private insurance claims on 77 drugs made in 2017 and 2018, only 3.6% included the JW modifier; 15 of these drugs had no JW claims.
“Although we found that most physicians don’t use the JW modifier, even those who do, don’t use it consistently, even for the same patient,” said Dr. Yabroff, a co-author on the report.
Going a step further, Dr. Yabroff and colleagues argue that even if everyone used the JW modifier as intended, manufacturers would probably increase the price of drugs to compensate for any loss, potentially eliminating savings for payers.
That’s because, in the United States, manufacturers typically base drug prices on a patient and payers’ “willingness to pay for better health,” not on the volume of liquid used. Take a patient who pays $2,000 to receive the dose they need. If that dose is 600 mg but requires using two vials of 400 mg, then “to the patient, the 600-mg dose is worth $2,000, and the remainder has no value whatsoever,” the NASEM authors argue.
The authors parallel this scenario to purchasing a designer coat or dress. If that item requires alterations that remove a section of material, “the customer does not typically get a rebate because all the fabric was not needed,” the NASEM team writes.
But there’s a flaw in this rationale, argues Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel. A person’s willingness to pay for better health assumes that the price of a drug is based on proper market forces, where a drug’s cost and its effectiveness are in harmony.
“The problem is we’re operating in a broken market where the prices of oncology drugs have no real bearing on their efficacy,” said Dr. Goldstein.
And, as Dr. Bach noted in a 2021 Health Affairs piece, willingness to pay also requires that consumers know what they’re paying and allows them to walk away from an excessively high price.
But neither is a reality.
For one, Dr. Bach explains, companies may lowball the monthly price of a drug. In 2020, GlaxoSmithKline (GSK) announced that its new drug Blenrep would carry a list price of $8,277 per vial, or about $23,900 per month for an average 79 kg (175 lb) patient. That price accounts for two vials of the drug. But, according to Dr. Bach, “what GSK left out is that 44% of U.S. adults weigh more than 80 kg, and above that weight, three vials are needed per dose.” That would raise the average monthly cost to $30,479.
Perhaps more importantly, consumers can’t easily walk away.
“Medicare can’t negotiate prices and is forced to pay what a drug company says,” Dr. Goldstein said. “This is very different to when I buy a coat. If the price is too high, I can walk away.”
Fixed dosing: A solution or a new problem?
Efforts to reduce the financial impact of discarded cancer drugs can blow back on physicians, patients, and payers in other unanticipated ways. Take fixed dosing. Although chemotherapy dosing remains weight-based, many targeted therapies — such as nivolumab and pembrolizumab — recently transitioned to a fixed dosing regimen.
Administering a fixed, instead of weight-based, dose eliminates waste but can create new problems.
“Patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” said Dr. Goldstein. In a 2017 analysis, Dr. Goldstein and colleagues compared dosing strategies in patients with metastatic non–small cell lung cancer who received pembrolizumab. The team found that the total annual cost of weight-based dosing was $2.6 billion, whereas the cost of the fixed dosing strategy was $3.44 billion — 24% more. In other words, personalized weight-based dosing would save more than $825 million dollars in the United States each year.
A 2020 analysis based in France found a similar cost increase of 26% for fixed dosing of pembrolizumab as well as nivolumab.
“I’ve argued we should go back to weight-based dosing,” Dr. Goldstein said. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
Does dose rounding work?
Rose DiMarco, PharmD, BCPS, BCOP, keeps a tight watch on patients being treated at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Dr. DiMarco educates patients about their treatment plan, reviews their lab results, and monitors them for side effects and drug interactions.
She also thinks a lot about costs.
“We spend about $100,000 a day on oncology drugs, and we want to make sure we’re not being wasteful,” Dr. DiMarco said in an interview.
One major initiative to curb waste and reduce costs at Jefferson has centered on dose rounding, which calculates whether a specific dose can be altered slightly to conserve vials and prevent waste. According to the Hematology/Oncology Pharmacy Association, a patient can receive up to 10% more or less of a weight-based dose without impacting treatment efficacy.
If, for instance, a patient requires 380 mg, but two vials come to 400 mg, rounding up that dose by approximately 5% means eliminating 20 mg that would go unused. But if that patient requires 420 mg, rounding down about 5% means substantial savings from not opening a new vial.
At Jefferson, Dr. DiMarco and her pharmacy colleagues map out dose ranges for all patients. Anyone who falls inside the 10% may be eligible for dose rounding. Anyone who doesn’t will receive the usual dose.
Although it is a challenge to implement, dose rounding has become standard of care at many cancer centers across the United States and is linked to substantial savings.
A 2018 analysis projected annual savings of $865,000 associated with rounding down eight monoclonal antibodies for patients with metastatic disease at a community cancer center. A more recent analysis from the Mayo Clinic found that dose rounding saved a total of 9,814 drug vials — 4485 of which were cancer drugs and 5329 of which were biologics — and resulted in $7.3 million in savings over 6 months in 2019 — $1.56 million from oncology agents and $5.7 from biologics.
And in a small 2019 analysis, researchers at Jefferson showed dose rounding of one monoclonal antibody saved approximately $30,000 in just 3 months, Dr. DiMarco noted.
“Not only does this process reduce costs and waste, but it also standardizes the preparation of hazardous medications, which can help prevent medication errors,” Dr. DiMarco said.
Nibbling around the edges
Despite estimates that scale into the billions of dollars, “drug wastage is just a small part of overall cancer costs,” Dr. Sarfaty said.
Fumiko Chino, MD, a radiation oncologist at MSK, agrees. “When we talk about affordability and cost, we can nibble around the edges of what’s really important,” Dr. Chino said. “Discarded drugs may cost a lot when you consider them in aggregate, but they are not as important as negotiated drug prices, which could substantially reduce overall costs.”
And until drug prices are addressed on a broader policy level, the cost of cancer care likely won’t improve in a meaningful way.
“But for the patient sitting in front of me, my focus will always be to provide the best care possible,” Dr. Binder said.
A version of this article first appeared on Medscape.com.
Three billion dollars: It’s enough to finance the annual out-of-pocket costs for 1 in 7 patients with cancer. It would cover almost half of the National Cancer Institute’s annual budget. And it could fund President Biden’s entire Cancer Moonshot program, with more than a billion to spare.
It’s also how much the United States spends on unused cancer drugs each year, some experts estimate.
Drug companies typically sell infused drugs in one or two single-dose vial sizes, but patients don’t come in such neat packages. A patient may need 300 mg of a drug that is only sold as 200 mg vials, which means half of a vial will go to waste.
Although most oncology drugs don’t incur substantial waste, even small volumes can translate to millions of dollars a year.
But can this money be saved or reallocated, if only we delivered drugs more efficiently?
Some experts don’t believe that’s possible.
“Attempts to recoup money for discarded drugs wouldn’t happen in a vacuum,” said Robin Yabroff, PhD, MBA, an epidemiologist and scientific vice president of Health Services Research at the American Cancer Society, who was part of a committee commissioned to evaluate the costs associated with discarded drugs.
The potential catch of any widespread effort to seek repayment or reduce the amount of discarded drugs, Dr. Yabroff and colleagues note, is that manufacturers would “simply increase the price of the vial.”
In other words, attempting to fix one problem may lead to another — essentially a whack-a-mole of cancer costs, which are projected to balloon to $246 billion by 2030.
What this means is without sweeping policies to rein in cancer care costs, oncologists can only do so much. And every little bit counts.
“We are left chipping away at this monster of cancer care costs,” said Adam Binder, MD, a medical oncologist at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Millions spent on “reasonable amount” of waste
Michal Sarfaty, MD, was excited when enfortumab vedotin came on the market to treat advanced urothelial cancer in late 2019.
The cost of the drug, however, tempered her enthusiasm.
Enfortumab vedotin is a “great drug,” said Dr. Sarfaty, an oncologist at the Sheba Medical Center, Ramat Gan, Israel. But it can cost upwards of $500,000 a year for an average-weight man.
Given the expense, Dr. Sarfaty wanted to understand how much of the drug gets thrown away. During a fellowship at Memorial Sloan Kettering (MSK) Cancer Center in New York, Dr. Sarfaty explored the amount of unused enfortumab vedotin among the 64 patients who received the drug in 2020. She, along with a team at MSK, calculated the price tag of that waste and extrapolated those estimates for patients across the country.
Although waste occurred in almost half of administered doses (367 of 793), only a small volume got discarded — 2.9% per dose, on average.
Multiplying unused milligrams by the cost per milligram, Dr. Sarfaty and colleagues estimated that, for each patient, $3,127 of the drug got discarded. When calculated over the year, the cost came to just over $200,000 at MSK, and nearly $15 million when projected across the approved patient population in the United States.
“Ultimately, we did not see a lot of waste with this specific drug,” Dr. Sarfaty said. “Under 2.9% is considered a reasonable amount, below the 3% threshold Peter Bach, MD, and colleagues recommend. But even with this small amount of waste, the cost per patient and to the system remains notable.”
The problem with recouping drug waste
Estimates from the Centers for Medicare & Medicaid Services (CMS), which tracks costs associated with discarded weight-based drugs covered under Medicare Part B, support the notion that small quantities of discarded drugs can still translate to big bucks.
Since 2017, CMS has required healthcare providers to report the volume of drugs discarded from a single-dose vial using a code, known as the JW modifier. The JW modifier means that providers can be reimbursed for the entire vial amount, not just the quantity the patient used.
In 2019, claims data from Medicare Part B showed that 1.85% of discarded rituximab came to $33.3 million. For infliximab, the 1.55% of discarded liquid translated to $15 million, and just 0.36% of discarded pembrolizumab reached $10 million.
However, experts question whether the JW modifier accurately reflects the quantity of drugs discarded.
According to the 2021 report from the National Academies of Sciences, Engineering, and Medicine (NASEM), most physicians don’t use the JW modifier. Among Medicare claims, 16.2% included the JW modifier in 2017 and 16.9% did in 2018.
The rate was significantly lower for private insurance. Of more than 4 million private insurance claims on 77 drugs made in 2017 and 2018, only 3.6% included the JW modifier; 15 of these drugs had no JW claims.
“Although we found that most physicians don’t use the JW modifier, even those who do, don’t use it consistently, even for the same patient,” said Dr. Yabroff, a co-author on the report.
Going a step further, Dr. Yabroff and colleagues argue that even if everyone used the JW modifier as intended, manufacturers would probably increase the price of drugs to compensate for any loss, potentially eliminating savings for payers.
That’s because, in the United States, manufacturers typically base drug prices on a patient and payers’ “willingness to pay for better health,” not on the volume of liquid used. Take a patient who pays $2,000 to receive the dose they need. If that dose is 600 mg but requires using two vials of 400 mg, then “to the patient, the 600-mg dose is worth $2,000, and the remainder has no value whatsoever,” the NASEM authors argue.
The authors parallel this scenario to purchasing a designer coat or dress. If that item requires alterations that remove a section of material, “the customer does not typically get a rebate because all the fabric was not needed,” the NASEM team writes.
But there’s a flaw in this rationale, argues Daniel Goldstein, MD, a medical oncologist at the Rabin Medical Center, Petah Tikva, Israel. A person’s willingness to pay for better health assumes that the price of a drug is based on proper market forces, where a drug’s cost and its effectiveness are in harmony.
“The problem is we’re operating in a broken market where the prices of oncology drugs have no real bearing on their efficacy,” said Dr. Goldstein.
And, as Dr. Bach noted in a 2021 Health Affairs piece, willingness to pay also requires that consumers know what they’re paying and allows them to walk away from an excessively high price.
But neither is a reality.
For one, Dr. Bach explains, companies may lowball the monthly price of a drug. In 2020, GlaxoSmithKline (GSK) announced that its new drug Blenrep would carry a list price of $8,277 per vial, or about $23,900 per month for an average 79 kg (175 lb) patient. That price accounts for two vials of the drug. But, according to Dr. Bach, “what GSK left out is that 44% of U.S. adults weigh more than 80 kg, and above that weight, three vials are needed per dose.” That would raise the average monthly cost to $30,479.
Perhaps more importantly, consumers can’t easily walk away.
“Medicare can’t negotiate prices and is forced to pay what a drug company says,” Dr. Goldstein said. “This is very different to when I buy a coat. If the price is too high, I can walk away.”
Fixed dosing: A solution or a new problem?
Efforts to reduce the financial impact of discarded cancer drugs can blow back on physicians, patients, and payers in other unanticipated ways. Take fixed dosing. Although chemotherapy dosing remains weight-based, many targeted therapies — such as nivolumab and pembrolizumab — recently transitioned to a fixed dosing regimen.
Administering a fixed, instead of weight-based, dose eliminates waste but can create new problems.
“Patients with cancer not only tend to get too high a dose of the drug, but costs go up significantly,” said Dr. Goldstein. In a 2017 analysis, Dr. Goldstein and colleagues compared dosing strategies in patients with metastatic non–small cell lung cancer who received pembrolizumab. The team found that the total annual cost of weight-based dosing was $2.6 billion, whereas the cost of the fixed dosing strategy was $3.44 billion — 24% more. In other words, personalized weight-based dosing would save more than $825 million dollars in the United States each year.
A 2020 analysis based in France found a similar cost increase of 26% for fixed dosing of pembrolizumab as well as nivolumab.
“I’ve argued we should go back to weight-based dosing,” Dr. Goldstein said. “Why should we give a higher dose with the same efficacy when that dose will cost significantly more and has the potential to increase adverse events?”
Does dose rounding work?
Rose DiMarco, PharmD, BCPS, BCOP, keeps a tight watch on patients being treated at the Sidney Kimmel Cancer Center at Jefferson Health in Philadelphia.
Dr. DiMarco educates patients about their treatment plan, reviews their lab results, and monitors them for side effects and drug interactions.
She also thinks a lot about costs.
“We spend about $100,000 a day on oncology drugs, and we want to make sure we’re not being wasteful,” Dr. DiMarco said in an interview.
One major initiative to curb waste and reduce costs at Jefferson has centered on dose rounding, which calculates whether a specific dose can be altered slightly to conserve vials and prevent waste. According to the Hematology/Oncology Pharmacy Association, a patient can receive up to 10% more or less of a weight-based dose without impacting treatment efficacy.
If, for instance, a patient requires 380 mg, but two vials come to 400 mg, rounding up that dose by approximately 5% means eliminating 20 mg that would go unused. But if that patient requires 420 mg, rounding down about 5% means substantial savings from not opening a new vial.
At Jefferson, Dr. DiMarco and her pharmacy colleagues map out dose ranges for all patients. Anyone who falls inside the 10% may be eligible for dose rounding. Anyone who doesn’t will receive the usual dose.
Although it is a challenge to implement, dose rounding has become standard of care at many cancer centers across the United States and is linked to substantial savings.
A 2018 analysis projected annual savings of $865,000 associated with rounding down eight monoclonal antibodies for patients with metastatic disease at a community cancer center. A more recent analysis from the Mayo Clinic found that dose rounding saved a total of 9,814 drug vials — 4485 of which were cancer drugs and 5329 of which were biologics — and resulted in $7.3 million in savings over 6 months in 2019 — $1.56 million from oncology agents and $5.7 from biologics.
And in a small 2019 analysis, researchers at Jefferson showed dose rounding of one monoclonal antibody saved approximately $30,000 in just 3 months, Dr. DiMarco noted.
“Not only does this process reduce costs and waste, but it also standardizes the preparation of hazardous medications, which can help prevent medication errors,” Dr. DiMarco said.
Nibbling around the edges
Despite estimates that scale into the billions of dollars, “drug wastage is just a small part of overall cancer costs,” Dr. Sarfaty said.
Fumiko Chino, MD, a radiation oncologist at MSK, agrees. “When we talk about affordability and cost, we can nibble around the edges of what’s really important,” Dr. Chino said. “Discarded drugs may cost a lot when you consider them in aggregate, but they are not as important as negotiated drug prices, which could substantially reduce overall costs.”
And until drug prices are addressed on a broader policy level, the cost of cancer care likely won’t improve in a meaningful way.
“But for the patient sitting in front of me, my focus will always be to provide the best care possible,” Dr. Binder said.
A version of this article first appeared on Medscape.com.
Can cancer patients get approved COVID therapies?
In mid-November, Kevin Billingsley, MD, MBA, chief medical officer at Yale Cancer Center, New Haven, Conn., was keeping a close eye on the new COVID variant sweeping across South Africa. Six weeks later, the Omicron variant had become the dominant strain in the U.S. – and the Yale health system was no exception.
“As we entered January, we had a breathtaking rate of infection in our hospital,” said Dr. Billingsley, who also leads clinical care at the Smilow Cancer Hospital. “Some of the newly authorized COVID agents were available but not widely enough to make a clinically meaningful impact to protect all high-risk individuals during this surge.”
That left the team at Yale with difficult decisions about who would receive these treatments and who wouldn’t.
The health system convened a COVID-19 immunocompromised working group to identify which patients should get priority access to one of the promising drugs authorized to treat the infection – the monoclonal antibody sotrovimab and antiviral pills Paxlovid and molnupiravir – or the sole available option to prevent it, Evusheld.
“Although clinically sound, none of these decisions have been easy,” Dr. Billingsley told this news organization. “We have done a lot of case-by-case reviewing and a lot of handwringing. Omicron has been a wild ride for us all, and we have been doing the best we can with limited resources.”
‘We’re seeing incredible variability’
The team at Yale is not alone. The restricted supply of COVID-19 treatments has led many oncologists and other experts across the U.S. to create carefully curated lists of their most vulnerable patients.
In late December, the National Institutes of Health published broad criteria to help clinicians prioritize patients most likely to benefit from these therapies. A handful of state health departments, including those in Michigan and Minnesota, established their own standards. Patients with cancer – specifically those with hematologic malignancies and receiving oncology therapies that compromise the immune system – appeared at the top of everyone’s list.
But ultimately individual decisions about who receives these drugs and how they’re allocated fell to institutions.
“Overall, what we’re seeing is incredible variability across the country, because there’s no uniform agreement on what comprises best practices on allocating scarce resources,” said Matthew Wynia, MD, MPH, professor of medicine and director of the Center for Bioethics and Humanities at the University of Colorado, Aurora. “There are so many people at the top of most lists, and the drugs are in such short supply, that there’s no guarantee even those in the top tier will get it.”
This news organization spoke to experts across the country about their experiences accessing these treatments during the Omicron surge and their strategies prioritizing patients with cancer.
Dealing with limited supply
Overall, the limited supply of COVID-19 drugs means not every patient who’s eligible to receive a treatment will get one.
A snapshot of the past 2 weeks, for instance, shows that the count of new infections hit almost 4.3 million, while distribution of the two antiviral pills Paxlovid and molnupiravir and the monoclonal antibody sotrovimab reached just over 600,000 courses.
Since receiving emergency use authorization in early December, almost 500,000 courses of the pre-exposure prophylactic agent Evusheld – which offers about 6 months of protection for immunocompromised individuals – have been distributed; however, about 7 million adults in the U.S. could potentially benefit from it.
In addition, the distribution of drugs is uneven. The federal government manages the overall distribution to states, but states then decide how to divvy up these allocations to hospitals, pharmacies, and medical centers. In Ohio, for instance, the antivirals go to providers who already receive monoclonal antibodies, while in Tennessee, the supply of antiviral agents only goes to Walmart pharmacies.
This strategy, Dr. Wynia explained, can leave clinicians at the mercy of where and how much states decide to allocate to each location. “I’ve heard of some hospitals and health systems in Colorado that aren’t using all they’ve got, but most don’t have nearly enough,” Dr. Wynia said. However, he noted, “some of that is inevitable. We will never get a perfect distribution of these drugs when there is such variable need and demand.”
And, according to Nicolette Louissaint, PhD, MBA, senior vice president of policy and strategic planning at the Healthcare Distribution Alliance in Arlington, Virginia, “we can take some comfort that the federal government is actively looking at cases from week to week and working with state and local health departments to see who needs these products, which means the process is constantly being reviewed and adjusted.”
Plus, not every positive COVID-19 case, even among immunocompromised individuals, necessarily warrants treatment. “If, for instance, an individual with cancer has a mild case of COVID-19, their provider may not deem it necessary for them to receive treatment,” Dr. Louissaint noted.
Still, given the limited and unpredictable supply, “we have had to be thoughtful about who gets these drugs,” said Derek Raghavan, MD, PhD, president of the Levine Cancer Institute, part of the 40-hospital Atrium Health system in Charlotte, North Carolina.
Dr. Raghavan said the highest priority goes to patients with hematologic malignancies, those receiving or coming off chemotherapy or experiencing myelosuppression and immune paresis, as well as those who have undergone organ transplants. Age and other comorbidities, such as diabetes or obesity, play into the lineup as well.
To further hone their priority list, the Levine Cancer Institute has implemented a cancer-centered Hospital at Home initiative. The program includes 40 oncology nurse navigators who routinely screen and score all cancer patients who test positive for COVID-19 by their symptoms and risk factors. For a time-sensitive treatment like Paxlovid, this close monitoring allows patients with COVID to access the pills within 5 days of symptom onset.
Ultimately, “the decision regarding who gets these drugs is [made] by a team to overcome any risk of personal bias, and some of it just comes down to the interface between clinical judgment and available data,” Dr. Raghavan told this news organization. “Although we’d like to have more COVID drugs available and fewer patients with COVID, we have been able to get adequate supplies for our most at-risk patients.”
Like Dr. Raghavan, Karen Bloch, MD, MPH, the medical director for the COVID Infusion Clinic at Vanderbilt University Medical Center (VUMC), said the clinic has had to be highly selective about which patients would benefit most from the COVID monoclonal antibodies. For patients with cancer, her team prioritizes individuals who would be least able to develop antibodies through vaccination or natural infection – which includes patients with B cell malignancies, acute myeloid leukemia, or multiple myeloma receiving active treatment, as well as those who recently received an allogeneic or autologous stem cell transplant.
“Since our criteria for treatment with therapies such as sotrovimab and Evusheld are pretty stringent, we have had sufficient supply to treat those who meet our internal ‘category 1’ predetermined criteria,” said Dr. Bloch, professor of medicine and associate division director for clinical affairs at VUMC, Nashville. “More recently, as the supply chain has begun to open up, we’ve been able to loosen our criteria for sotrovimab, though not for Evusheld yet.”
The Yale team described a similar evolution. “Initially, only a small subset of oncology patients could get these drugs,” said Osama (Sam) Abdelghany, PharmD, MHA, associate director of Oncology Pharmacy Services at Smilow Cancer Hospital. But as the caseload has diminished, Dr. Abdelghany noted, “we have been able to reach many more patients with COVID-19.”
An equitable system?
Dr. Wynia, who has written many reports on crisis standards of care, has spent thousands of hours delving into the ethics of allocating scarce resources during a disaster.
A core problem arises when there are too many people who need a scarce resource and no way of differentiating among them.
In response to the limited supply of COVID-19 treatments, some institutions, such as the University of Pittsburgh Medical Center and Massachusetts General Hospital, have created a lottery system. Others, such as Johns Hopkins Medicine, have opted for first come, first served. Each strategy comes with caveats.
“First come, first served prioritization may be quicker, but it gives more well-resourced people an advantage and lends itself to people abusing the system or exacerbating existing disparities,” Dr. Wynia said.
While a lottery system may be more equitable, this strategy often comes at the price of efficiency. “The practicality of doing a lottery when you have to make a decision about whether or not to treat the patient sitting in front of you comes with its own challenges,” Dr. Wynia said.
At the University of Colorado, he explained, the health center constantly scans medical records for patients who have been diagnosed with COVID and fall into a high-risk group. That way clinicians can call or email those most likely to benefit from these drugs.
“It ends up being a bit of a first come, first served strategy,” Dr. Wynia said. “But we also do not have a huge supply coming in each week, so reaching out to the most eligible people when we have the drugs in hand means more privileged patients are less likely to game the system.”
To manage the supply of Evusheld, Timothy Kubal, MD, MBA, and colleagues also reach out to patients most likely to benefit – specifically, those who can’t mount an adequate antibody response after vaccination.
“We screen all of our patients who have been receiving anti-CD20 agents and other chemotherapy agents known to suppress antibody response,” Dr. Kubal, a medical oncologist/hematologist at the Moffitt Institute in Tampa, Florida, said in an interview. “We then test those patients for antibodies and deliver Evusheld if they have no evidence of antibodies.”
Fortunately, in the coming months, distribution of these drugs should improve significantly. Pfizer says it expects to deliver 10 million courses of Paxlovid by the end of June, and another 10 million by the end of September. More than 1 million courses of sotrovimab should be distributed by GlaxoSmithKline through the end of March. And, recently, the Biden administration announced it purchased 1.2 million courses of Evusheld from AstraZeneca.
“Every few weeks, because the COVID picture changes, the demand changes,” said Dr. Louissaint. “With vaccination rates going up and cases going down, fewer patients will need these products.”
Still, the constant barrage of supply shortages over the past 2 years – from COVID tests, ventilators, and personal protective equipment early on to COVID vaccines a year later and more recently health care staff and COVID tests once again – has taken its toll.
“We have faced supply challenge after challenge and have had to be creative in each situation,” said Lisa Barbarotta, MSN, APRN, program director of Oncology Education and Clinical Practice at Smilow Cancer Hospital. “Nothing has been easy about this.”
And, Dr. Bloch cautioned, even with broader access to COVID-19 drugs on the horizon, there is still no substitute for vaccination. “Getting vaccinated is the best and first line of defense for most people,” she said.
A version of this article first appeared on Medscape.com.
In mid-November, Kevin Billingsley, MD, MBA, chief medical officer at Yale Cancer Center, New Haven, Conn., was keeping a close eye on the new COVID variant sweeping across South Africa. Six weeks later, the Omicron variant had become the dominant strain in the U.S. – and the Yale health system was no exception.
“As we entered January, we had a breathtaking rate of infection in our hospital,” said Dr. Billingsley, who also leads clinical care at the Smilow Cancer Hospital. “Some of the newly authorized COVID agents were available but not widely enough to make a clinically meaningful impact to protect all high-risk individuals during this surge.”
That left the team at Yale with difficult decisions about who would receive these treatments and who wouldn’t.
The health system convened a COVID-19 immunocompromised working group to identify which patients should get priority access to one of the promising drugs authorized to treat the infection – the monoclonal antibody sotrovimab and antiviral pills Paxlovid and molnupiravir – or the sole available option to prevent it, Evusheld.
“Although clinically sound, none of these decisions have been easy,” Dr. Billingsley told this news organization. “We have done a lot of case-by-case reviewing and a lot of handwringing. Omicron has been a wild ride for us all, and we have been doing the best we can with limited resources.”
‘We’re seeing incredible variability’
The team at Yale is not alone. The restricted supply of COVID-19 treatments has led many oncologists and other experts across the U.S. to create carefully curated lists of their most vulnerable patients.
In late December, the National Institutes of Health published broad criteria to help clinicians prioritize patients most likely to benefit from these therapies. A handful of state health departments, including those in Michigan and Minnesota, established their own standards. Patients with cancer – specifically those with hematologic malignancies and receiving oncology therapies that compromise the immune system – appeared at the top of everyone’s list.
But ultimately individual decisions about who receives these drugs and how they’re allocated fell to institutions.
“Overall, what we’re seeing is incredible variability across the country, because there’s no uniform agreement on what comprises best practices on allocating scarce resources,” said Matthew Wynia, MD, MPH, professor of medicine and director of the Center for Bioethics and Humanities at the University of Colorado, Aurora. “There are so many people at the top of most lists, and the drugs are in such short supply, that there’s no guarantee even those in the top tier will get it.”
This news organization spoke to experts across the country about their experiences accessing these treatments during the Omicron surge and their strategies prioritizing patients with cancer.
Dealing with limited supply
Overall, the limited supply of COVID-19 drugs means not every patient who’s eligible to receive a treatment will get one.
A snapshot of the past 2 weeks, for instance, shows that the count of new infections hit almost 4.3 million, while distribution of the two antiviral pills Paxlovid and molnupiravir and the monoclonal antibody sotrovimab reached just over 600,000 courses.
Since receiving emergency use authorization in early December, almost 500,000 courses of the pre-exposure prophylactic agent Evusheld – which offers about 6 months of protection for immunocompromised individuals – have been distributed; however, about 7 million adults in the U.S. could potentially benefit from it.
In addition, the distribution of drugs is uneven. The federal government manages the overall distribution to states, but states then decide how to divvy up these allocations to hospitals, pharmacies, and medical centers. In Ohio, for instance, the antivirals go to providers who already receive monoclonal antibodies, while in Tennessee, the supply of antiviral agents only goes to Walmart pharmacies.
This strategy, Dr. Wynia explained, can leave clinicians at the mercy of where and how much states decide to allocate to each location. “I’ve heard of some hospitals and health systems in Colorado that aren’t using all they’ve got, but most don’t have nearly enough,” Dr. Wynia said. However, he noted, “some of that is inevitable. We will never get a perfect distribution of these drugs when there is such variable need and demand.”
And, according to Nicolette Louissaint, PhD, MBA, senior vice president of policy and strategic planning at the Healthcare Distribution Alliance in Arlington, Virginia, “we can take some comfort that the federal government is actively looking at cases from week to week and working with state and local health departments to see who needs these products, which means the process is constantly being reviewed and adjusted.”
Plus, not every positive COVID-19 case, even among immunocompromised individuals, necessarily warrants treatment. “If, for instance, an individual with cancer has a mild case of COVID-19, their provider may not deem it necessary for them to receive treatment,” Dr. Louissaint noted.
Still, given the limited and unpredictable supply, “we have had to be thoughtful about who gets these drugs,” said Derek Raghavan, MD, PhD, president of the Levine Cancer Institute, part of the 40-hospital Atrium Health system in Charlotte, North Carolina.
Dr. Raghavan said the highest priority goes to patients with hematologic malignancies, those receiving or coming off chemotherapy or experiencing myelosuppression and immune paresis, as well as those who have undergone organ transplants. Age and other comorbidities, such as diabetes or obesity, play into the lineup as well.
To further hone their priority list, the Levine Cancer Institute has implemented a cancer-centered Hospital at Home initiative. The program includes 40 oncology nurse navigators who routinely screen and score all cancer patients who test positive for COVID-19 by their symptoms and risk factors. For a time-sensitive treatment like Paxlovid, this close monitoring allows patients with COVID to access the pills within 5 days of symptom onset.
Ultimately, “the decision regarding who gets these drugs is [made] by a team to overcome any risk of personal bias, and some of it just comes down to the interface between clinical judgment and available data,” Dr. Raghavan told this news organization. “Although we’d like to have more COVID drugs available and fewer patients with COVID, we have been able to get adequate supplies for our most at-risk patients.”
Like Dr. Raghavan, Karen Bloch, MD, MPH, the medical director for the COVID Infusion Clinic at Vanderbilt University Medical Center (VUMC), said the clinic has had to be highly selective about which patients would benefit most from the COVID monoclonal antibodies. For patients with cancer, her team prioritizes individuals who would be least able to develop antibodies through vaccination or natural infection – which includes patients with B cell malignancies, acute myeloid leukemia, or multiple myeloma receiving active treatment, as well as those who recently received an allogeneic or autologous stem cell transplant.
“Since our criteria for treatment with therapies such as sotrovimab and Evusheld are pretty stringent, we have had sufficient supply to treat those who meet our internal ‘category 1’ predetermined criteria,” said Dr. Bloch, professor of medicine and associate division director for clinical affairs at VUMC, Nashville. “More recently, as the supply chain has begun to open up, we’ve been able to loosen our criteria for sotrovimab, though not for Evusheld yet.”
The Yale team described a similar evolution. “Initially, only a small subset of oncology patients could get these drugs,” said Osama (Sam) Abdelghany, PharmD, MHA, associate director of Oncology Pharmacy Services at Smilow Cancer Hospital. But as the caseload has diminished, Dr. Abdelghany noted, “we have been able to reach many more patients with COVID-19.”
An equitable system?
Dr. Wynia, who has written many reports on crisis standards of care, has spent thousands of hours delving into the ethics of allocating scarce resources during a disaster.
A core problem arises when there are too many people who need a scarce resource and no way of differentiating among them.
In response to the limited supply of COVID-19 treatments, some institutions, such as the University of Pittsburgh Medical Center and Massachusetts General Hospital, have created a lottery system. Others, such as Johns Hopkins Medicine, have opted for first come, first served. Each strategy comes with caveats.
“First come, first served prioritization may be quicker, but it gives more well-resourced people an advantage and lends itself to people abusing the system or exacerbating existing disparities,” Dr. Wynia said.
While a lottery system may be more equitable, this strategy often comes at the price of efficiency. “The practicality of doing a lottery when you have to make a decision about whether or not to treat the patient sitting in front of you comes with its own challenges,” Dr. Wynia said.
At the University of Colorado, he explained, the health center constantly scans medical records for patients who have been diagnosed with COVID and fall into a high-risk group. That way clinicians can call or email those most likely to benefit from these drugs.
“It ends up being a bit of a first come, first served strategy,” Dr. Wynia said. “But we also do not have a huge supply coming in each week, so reaching out to the most eligible people when we have the drugs in hand means more privileged patients are less likely to game the system.”
To manage the supply of Evusheld, Timothy Kubal, MD, MBA, and colleagues also reach out to patients most likely to benefit – specifically, those who can’t mount an adequate antibody response after vaccination.
“We screen all of our patients who have been receiving anti-CD20 agents and other chemotherapy agents known to suppress antibody response,” Dr. Kubal, a medical oncologist/hematologist at the Moffitt Institute in Tampa, Florida, said in an interview. “We then test those patients for antibodies and deliver Evusheld if they have no evidence of antibodies.”
Fortunately, in the coming months, distribution of these drugs should improve significantly. Pfizer says it expects to deliver 10 million courses of Paxlovid by the end of June, and another 10 million by the end of September. More than 1 million courses of sotrovimab should be distributed by GlaxoSmithKline through the end of March. And, recently, the Biden administration announced it purchased 1.2 million courses of Evusheld from AstraZeneca.
“Every few weeks, because the COVID picture changes, the demand changes,” said Dr. Louissaint. “With vaccination rates going up and cases going down, fewer patients will need these products.”
Still, the constant barrage of supply shortages over the past 2 years – from COVID tests, ventilators, and personal protective equipment early on to COVID vaccines a year later and more recently health care staff and COVID tests once again – has taken its toll.
“We have faced supply challenge after challenge and have had to be creative in each situation,” said Lisa Barbarotta, MSN, APRN, program director of Oncology Education and Clinical Practice at Smilow Cancer Hospital. “Nothing has been easy about this.”
And, Dr. Bloch cautioned, even with broader access to COVID-19 drugs on the horizon, there is still no substitute for vaccination. “Getting vaccinated is the best and first line of defense for most people,” she said.
A version of this article first appeared on Medscape.com.
In mid-November, Kevin Billingsley, MD, MBA, chief medical officer at Yale Cancer Center, New Haven, Conn., was keeping a close eye on the new COVID variant sweeping across South Africa. Six weeks later, the Omicron variant had become the dominant strain in the U.S. – and the Yale health system was no exception.
“As we entered January, we had a breathtaking rate of infection in our hospital,” said Dr. Billingsley, who also leads clinical care at the Smilow Cancer Hospital. “Some of the newly authorized COVID agents were available but not widely enough to make a clinically meaningful impact to protect all high-risk individuals during this surge.”
That left the team at Yale with difficult decisions about who would receive these treatments and who wouldn’t.
The health system convened a COVID-19 immunocompromised working group to identify which patients should get priority access to one of the promising drugs authorized to treat the infection – the monoclonal antibody sotrovimab and antiviral pills Paxlovid and molnupiravir – or the sole available option to prevent it, Evusheld.
“Although clinically sound, none of these decisions have been easy,” Dr. Billingsley told this news organization. “We have done a lot of case-by-case reviewing and a lot of handwringing. Omicron has been a wild ride for us all, and we have been doing the best we can with limited resources.”
‘We’re seeing incredible variability’
The team at Yale is not alone. The restricted supply of COVID-19 treatments has led many oncologists and other experts across the U.S. to create carefully curated lists of their most vulnerable patients.
In late December, the National Institutes of Health published broad criteria to help clinicians prioritize patients most likely to benefit from these therapies. A handful of state health departments, including those in Michigan and Minnesota, established their own standards. Patients with cancer – specifically those with hematologic malignancies and receiving oncology therapies that compromise the immune system – appeared at the top of everyone’s list.
But ultimately individual decisions about who receives these drugs and how they’re allocated fell to institutions.
“Overall, what we’re seeing is incredible variability across the country, because there’s no uniform agreement on what comprises best practices on allocating scarce resources,” said Matthew Wynia, MD, MPH, professor of medicine and director of the Center for Bioethics and Humanities at the University of Colorado, Aurora. “There are so many people at the top of most lists, and the drugs are in such short supply, that there’s no guarantee even those in the top tier will get it.”
This news organization spoke to experts across the country about their experiences accessing these treatments during the Omicron surge and their strategies prioritizing patients with cancer.
Dealing with limited supply
Overall, the limited supply of COVID-19 drugs means not every patient who’s eligible to receive a treatment will get one.
A snapshot of the past 2 weeks, for instance, shows that the count of new infections hit almost 4.3 million, while distribution of the two antiviral pills Paxlovid and molnupiravir and the monoclonal antibody sotrovimab reached just over 600,000 courses.
Since receiving emergency use authorization in early December, almost 500,000 courses of the pre-exposure prophylactic agent Evusheld – which offers about 6 months of protection for immunocompromised individuals – have been distributed; however, about 7 million adults in the U.S. could potentially benefit from it.
In addition, the distribution of drugs is uneven. The federal government manages the overall distribution to states, but states then decide how to divvy up these allocations to hospitals, pharmacies, and medical centers. In Ohio, for instance, the antivirals go to providers who already receive monoclonal antibodies, while in Tennessee, the supply of antiviral agents only goes to Walmart pharmacies.
This strategy, Dr. Wynia explained, can leave clinicians at the mercy of where and how much states decide to allocate to each location. “I’ve heard of some hospitals and health systems in Colorado that aren’t using all they’ve got, but most don’t have nearly enough,” Dr. Wynia said. However, he noted, “some of that is inevitable. We will never get a perfect distribution of these drugs when there is such variable need and demand.”
And, according to Nicolette Louissaint, PhD, MBA, senior vice president of policy and strategic planning at the Healthcare Distribution Alliance in Arlington, Virginia, “we can take some comfort that the federal government is actively looking at cases from week to week and working with state and local health departments to see who needs these products, which means the process is constantly being reviewed and adjusted.”
Plus, not every positive COVID-19 case, even among immunocompromised individuals, necessarily warrants treatment. “If, for instance, an individual with cancer has a mild case of COVID-19, their provider may not deem it necessary for them to receive treatment,” Dr. Louissaint noted.
Still, given the limited and unpredictable supply, “we have had to be thoughtful about who gets these drugs,” said Derek Raghavan, MD, PhD, president of the Levine Cancer Institute, part of the 40-hospital Atrium Health system in Charlotte, North Carolina.
Dr. Raghavan said the highest priority goes to patients with hematologic malignancies, those receiving or coming off chemotherapy or experiencing myelosuppression and immune paresis, as well as those who have undergone organ transplants. Age and other comorbidities, such as diabetes or obesity, play into the lineup as well.
To further hone their priority list, the Levine Cancer Institute has implemented a cancer-centered Hospital at Home initiative. The program includes 40 oncology nurse navigators who routinely screen and score all cancer patients who test positive for COVID-19 by their symptoms and risk factors. For a time-sensitive treatment like Paxlovid, this close monitoring allows patients with COVID to access the pills within 5 days of symptom onset.
Ultimately, “the decision regarding who gets these drugs is [made] by a team to overcome any risk of personal bias, and some of it just comes down to the interface between clinical judgment and available data,” Dr. Raghavan told this news organization. “Although we’d like to have more COVID drugs available and fewer patients with COVID, we have been able to get adequate supplies for our most at-risk patients.”
Like Dr. Raghavan, Karen Bloch, MD, MPH, the medical director for the COVID Infusion Clinic at Vanderbilt University Medical Center (VUMC), said the clinic has had to be highly selective about which patients would benefit most from the COVID monoclonal antibodies. For patients with cancer, her team prioritizes individuals who would be least able to develop antibodies through vaccination or natural infection – which includes patients with B cell malignancies, acute myeloid leukemia, or multiple myeloma receiving active treatment, as well as those who recently received an allogeneic or autologous stem cell transplant.
“Since our criteria for treatment with therapies such as sotrovimab and Evusheld are pretty stringent, we have had sufficient supply to treat those who meet our internal ‘category 1’ predetermined criteria,” said Dr. Bloch, professor of medicine and associate division director for clinical affairs at VUMC, Nashville. “More recently, as the supply chain has begun to open up, we’ve been able to loosen our criteria for sotrovimab, though not for Evusheld yet.”
The Yale team described a similar evolution. “Initially, only a small subset of oncology patients could get these drugs,” said Osama (Sam) Abdelghany, PharmD, MHA, associate director of Oncology Pharmacy Services at Smilow Cancer Hospital. But as the caseload has diminished, Dr. Abdelghany noted, “we have been able to reach many more patients with COVID-19.”
An equitable system?
Dr. Wynia, who has written many reports on crisis standards of care, has spent thousands of hours delving into the ethics of allocating scarce resources during a disaster.
A core problem arises when there are too many people who need a scarce resource and no way of differentiating among them.
In response to the limited supply of COVID-19 treatments, some institutions, such as the University of Pittsburgh Medical Center and Massachusetts General Hospital, have created a lottery system. Others, such as Johns Hopkins Medicine, have opted for first come, first served. Each strategy comes with caveats.
“First come, first served prioritization may be quicker, but it gives more well-resourced people an advantage and lends itself to people abusing the system or exacerbating existing disparities,” Dr. Wynia said.
While a lottery system may be more equitable, this strategy often comes at the price of efficiency. “The practicality of doing a lottery when you have to make a decision about whether or not to treat the patient sitting in front of you comes with its own challenges,” Dr. Wynia said.
At the University of Colorado, he explained, the health center constantly scans medical records for patients who have been diagnosed with COVID and fall into a high-risk group. That way clinicians can call or email those most likely to benefit from these drugs.
“It ends up being a bit of a first come, first served strategy,” Dr. Wynia said. “But we also do not have a huge supply coming in each week, so reaching out to the most eligible people when we have the drugs in hand means more privileged patients are less likely to game the system.”
To manage the supply of Evusheld, Timothy Kubal, MD, MBA, and colleagues also reach out to patients most likely to benefit – specifically, those who can’t mount an adequate antibody response after vaccination.
“We screen all of our patients who have been receiving anti-CD20 agents and other chemotherapy agents known to suppress antibody response,” Dr. Kubal, a medical oncologist/hematologist at the Moffitt Institute in Tampa, Florida, said in an interview. “We then test those patients for antibodies and deliver Evusheld if they have no evidence of antibodies.”
Fortunately, in the coming months, distribution of these drugs should improve significantly. Pfizer says it expects to deliver 10 million courses of Paxlovid by the end of June, and another 10 million by the end of September. More than 1 million courses of sotrovimab should be distributed by GlaxoSmithKline through the end of March. And, recently, the Biden administration announced it purchased 1.2 million courses of Evusheld from AstraZeneca.
“Every few weeks, because the COVID picture changes, the demand changes,” said Dr. Louissaint. “With vaccination rates going up and cases going down, fewer patients will need these products.”
Still, the constant barrage of supply shortages over the past 2 years – from COVID tests, ventilators, and personal protective equipment early on to COVID vaccines a year later and more recently health care staff and COVID tests once again – has taken its toll.
“We have faced supply challenge after challenge and have had to be creative in each situation,” said Lisa Barbarotta, MSN, APRN, program director of Oncology Education and Clinical Practice at Smilow Cancer Hospital. “Nothing has been easy about this.”
And, Dr. Bloch cautioned, even with broader access to COVID-19 drugs on the horizon, there is still no substitute for vaccination. “Getting vaccinated is the best and first line of defense for most people,” she said.
A version of this article first appeared on Medscape.com.
The evolving HER2+ metastatic breast cancer landscape: Novel agents and promising combination therapies
Recent therapeutic advances in HER2-positive metastatic breast cancer (MBC) have begun to reshape the treatment landscape for patients. Since late 2019, the U.S. Food and Drug Administration (FDA) has approved a handful of novel agents for HER2-positive MBC — most notably, the antibody-drug conjugate (ADC) trastuzumab deruxtecan in December 2019 and the tyrosine kinase inhibitors (TKIs) tucatinib and neratinib in 2020. According to the National Cancer Institute›s Surveillance, Epidemiology, and End Results (SEER) program, the 5-year survival rate for patients with advanced disease was already on the rise between 2004 and 2018, and
“I’ve been involved in the HER2 space for a long time and have watched the field evolve,” said Adam Brufsky, MD, PhD, associate chief in the division of hematology/oncology and co-director of the Comprehensive Breast Cancer Center at the University of Pittsburgh School of Medicine. “The fact that we’re now talking about fourth- and fifth-line therapies for HER2-positive MBC represents a major advance in the management of these patients.”
Oncologists are still building on this progress, focusing on designing more targeted therapies as well as studying different combinations of available agents. The main goal of treatment, experts say, is to prolong patients’ systemic response and prevent recurrences, especially in the brain. This news organization spoke to Dr. Brufksy and others about promising agents and therapeutic strategies on the horizon to treat HER2-positive MBC.
Inside emerging ADCs
Because many patients develop resistance to trastuzumab emtansine (T-DM1) — the first FDA-approved ADC in breast cancer — researchers have focused on developing the next generation of ADCs with more potent payloads, different linkers, and distinct mechanisms of action, according to Sayeh Lavasani, MD, MS, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
The second-generation ADC trastuzumab deruxtecan showed “really dramatic” results in HER2-positive MBC, demonstrating progression-free survival of 16 months, remarked Kevin Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University. “These outcomes further changed how we treat patients with metastatic disease and prompted considerable excitement over the potential to develop novel ADCs to treat HER2-positive MBC.”
Most recently, two investigational ADCs — trastuzumab duocarmazine (SYD985) and ARX788 — have stood out. The FDA granted fast-track designations to trastuzumab duocarmazine in January 2018 and ARX788 in January 2021. Trastuzumab duocarmazine, the furthest along the pipeline, has shown promising results so far. In June 2021, Netherlands-based biopharmaceutical company Byondis reported preliminary phase 3 data from the TULIP trial. The open-label, randomized phase 3 study enrolled 436 patients with HER2-positive locally advanced or metastatic disease that had progressed on previous anti-HER2 regimens. The company shared early results that trastuzumab duocarmazine achieved its progression-free survival primary endpoint, marking a significant improvement over physician’s choice of chemotherapy, and promised more detailed results to come later this year.
Although only in early-phase trials, ARX788 has also shown robust anti-HER2 activity as well as low toxicity in HER2-positive tumors, according to recent data. The findings from two phase 1 studies, presented at the June 2021 virtual American Society for Clinical Oncology meeting (abstract 1038), revealed an overall response rate of 74% in the breast cancer cohort, but the investigators acknowledged it was too early to report median progression-free survival outcomes. Preclinical data also showed activity in HER2-low and T-DM1–resistant tumors.
Despite the encouraging initial findings, Dr. Kalinsky remains cautiously optimistic about long-term outcomes for both ADCs. “These data are hot off the press, but it’s too soon to know how these two ADCs and others in the pipeline will measure up to approved therapies,” he commented. As experts learn more about the efficacy of these novel ADCs, Dr. Brufsky would also like to better understand resistance mechanisms and how to integrate these agents into current treatment strategies. “The cellular biology of HER2-positive MBC is complicated, and many factors in these tumor cells affect where ADCs are released, how resistance develops, and whether or not resistance to one ADC applies to others,” Dr. Brufsky remarked. “As we gather more data, we’ll understand resistance mechanisms better and begin to figure out where to go with treatment sequencing.”
TKIs and beyond
In addition to ADCs, TKIs continue to make their mark in the targeted HER2 therapeutic space. The approvals of tucatinib and neratinib last year represented an important advance in treating HER2-positive MBC, particularly for patients with brain metastases. The HER2CLIMB trial, for instance, found that tucatinib combined with trastuzumab and capecitabine had a 4.5-month overall survival advantage compared with placebo (21.9 vs 17.4) and a median progression-free survival advantage of 5.4 months in patients with active brain metastases (9.5 vs 4.1) and 8.3 months in patients with stable metastases (13.9 vs 5.6).
Given this progress, experts are looking to add new TKIs to the armamentarium. In particular, pyrotinib — already approved in China for treating HER2-positive MBC — has demonstrated significantly longer progression-free survival compared with a standard TKI, lapatinib. The phase 3 PHOEBE trial results, published in The Lancet in early 2021, found a median progression-free survival of 12.5 months in patients randomly assigned to receive pyrotinib plus capecitabine compared with 6.8 months in those receiving lapatinib plus capecitabine. The investigators also reported “manageable toxicity”; diarrhea was the most common grade 3 adverse event, occurring in 31% of the pyrotinib group vs. 8% of the lapatinib group, and overall serious adverse events occurred in 10% of patients receiving pyrotinib vs. 8% of those receiving lapatinib.
More recent data on pyrotinib come from the phase 2 PERMEATE trial, which focused on the safety and efficacy of the agent in patients with advanced disease and brain metastases. The investigators, who presented their findings at the 2021 virtual ASCO meeting (abstract 1037), reported that radiation therapy–naive patients receiving pyrotinib plus capecitabine had an overall response rate of 74.6% in the central nervous system. Patients experiencing progression after whole-brain or stereotactic radiation therapy, however, had a comparatively lower overall response rate of 42.1%.
Similarly, median progression-free survival was much higher in the radiation therapy–naive patients (12.1 vs 5.6 months in the radiation therapy cohort). Similar to the PHOEBE trial, the most common grade 3 adverse event was diarrhea (23.1%), followed by decreased neutrophil and white blood cell counts (12.8% for both), anemia (9%), and hand-foot syndrome (7.7%). The main question for Dr. Kalinsky is how well pyrotinib will ultimately stack up to tucatinib and neratinib. “Pyrotinib — like neratinib — was shown to be superior to lapatinib plus capecitabine , but its role may be limited by its gastrointestinal toxicity,” he said. In addition to research focused on expanding the selection of novel ADCs and TKIs, researchers are also exploring new combinations of approved treatments and whether these combinations can be used earlier in treatment sequencing.
Take the CompassHER2 trials. The ongoing phase 3 trial in patients with high-risk HER2-positive breast cancer and residual disease will explore whether tucatinib plus T-DM1 compared with T-DM1 alone improves overall survival and recurrence-free survival and prevents brain metastases. Another possibility currently under investigation is pairing tucatinib and trastuzumab deruxtecan, instead of T-DM1. “Overall, it’s exciting that we are increasing the number of therapeutic options and combinations,” commented Debu Tripathy, MD, professor and chairman in the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston. “Having more choices allows us to tailor therapies to manage resistance and prolong patients’ responses.”
Curbing brain metastasis, according to Dr. Brufksy, is particularly important, and experts need to explore the extent to which ADCs can penetrate the blood-brain barrier. Already, a subgroup analysis of the DESTINY-Breast01 trial found that trastuzumab deruxtecan appeared to be active in patients with brain metastases. Investigators reported an overall response rate of 58.3% and a median progression-free survival of 18.1 months — results in line with those in the general study cohort — but the study population did not include patients with untreated or progressive brain metastases. A phase 2 study currently under way will examine whether patients with HER2-positive and HER2-low breast cancer who have untreated or progressive brain metastases respond to trastuzumab deruxtecan as well. Ultimately, Dr. Brufksy hopes the recent successes with preventing brain metastases in pediatric acute lymphoblastic leukemia (ALL) foreshadow what›s to come in HER2-positive MBC.
“When we figured out how to treat brain metastases prophylactically in childhood ALL, we saw a huge improvement in the cure rate, which is ultimately my vision for HER2-positive disease,” Dr. Brufsky remarked. “Are there cures for HER2-positive MBC on the horizon? We don’t know yet, but the field has really exploded in recent years.”
A version of this article first appeared on Medscape.com.
Recent therapeutic advances in HER2-positive metastatic breast cancer (MBC) have begun to reshape the treatment landscape for patients. Since late 2019, the U.S. Food and Drug Administration (FDA) has approved a handful of novel agents for HER2-positive MBC — most notably, the antibody-drug conjugate (ADC) trastuzumab deruxtecan in December 2019 and the tyrosine kinase inhibitors (TKIs) tucatinib and neratinib in 2020. According to the National Cancer Institute›s Surveillance, Epidemiology, and End Results (SEER) program, the 5-year survival rate for patients with advanced disease was already on the rise between 2004 and 2018, and
“I’ve been involved in the HER2 space for a long time and have watched the field evolve,” said Adam Brufsky, MD, PhD, associate chief in the division of hematology/oncology and co-director of the Comprehensive Breast Cancer Center at the University of Pittsburgh School of Medicine. “The fact that we’re now talking about fourth- and fifth-line therapies for HER2-positive MBC represents a major advance in the management of these patients.”
Oncologists are still building on this progress, focusing on designing more targeted therapies as well as studying different combinations of available agents. The main goal of treatment, experts say, is to prolong patients’ systemic response and prevent recurrences, especially in the brain. This news organization spoke to Dr. Brufksy and others about promising agents and therapeutic strategies on the horizon to treat HER2-positive MBC.
Inside emerging ADCs
Because many patients develop resistance to trastuzumab emtansine (T-DM1) — the first FDA-approved ADC in breast cancer — researchers have focused on developing the next generation of ADCs with more potent payloads, different linkers, and distinct mechanisms of action, according to Sayeh Lavasani, MD, MS, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
The second-generation ADC trastuzumab deruxtecan showed “really dramatic” results in HER2-positive MBC, demonstrating progression-free survival of 16 months, remarked Kevin Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University. “These outcomes further changed how we treat patients with metastatic disease and prompted considerable excitement over the potential to develop novel ADCs to treat HER2-positive MBC.”
Most recently, two investigational ADCs — trastuzumab duocarmazine (SYD985) and ARX788 — have stood out. The FDA granted fast-track designations to trastuzumab duocarmazine in January 2018 and ARX788 in January 2021. Trastuzumab duocarmazine, the furthest along the pipeline, has shown promising results so far. In June 2021, Netherlands-based biopharmaceutical company Byondis reported preliminary phase 3 data from the TULIP trial. The open-label, randomized phase 3 study enrolled 436 patients with HER2-positive locally advanced or metastatic disease that had progressed on previous anti-HER2 regimens. The company shared early results that trastuzumab duocarmazine achieved its progression-free survival primary endpoint, marking a significant improvement over physician’s choice of chemotherapy, and promised more detailed results to come later this year.
Although only in early-phase trials, ARX788 has also shown robust anti-HER2 activity as well as low toxicity in HER2-positive tumors, according to recent data. The findings from two phase 1 studies, presented at the June 2021 virtual American Society for Clinical Oncology meeting (abstract 1038), revealed an overall response rate of 74% in the breast cancer cohort, but the investigators acknowledged it was too early to report median progression-free survival outcomes. Preclinical data also showed activity in HER2-low and T-DM1–resistant tumors.
Despite the encouraging initial findings, Dr. Kalinsky remains cautiously optimistic about long-term outcomes for both ADCs. “These data are hot off the press, but it’s too soon to know how these two ADCs and others in the pipeline will measure up to approved therapies,” he commented. As experts learn more about the efficacy of these novel ADCs, Dr. Brufsky would also like to better understand resistance mechanisms and how to integrate these agents into current treatment strategies. “The cellular biology of HER2-positive MBC is complicated, and many factors in these tumor cells affect where ADCs are released, how resistance develops, and whether or not resistance to one ADC applies to others,” Dr. Brufsky remarked. “As we gather more data, we’ll understand resistance mechanisms better and begin to figure out where to go with treatment sequencing.”
TKIs and beyond
In addition to ADCs, TKIs continue to make their mark in the targeted HER2 therapeutic space. The approvals of tucatinib and neratinib last year represented an important advance in treating HER2-positive MBC, particularly for patients with brain metastases. The HER2CLIMB trial, for instance, found that tucatinib combined with trastuzumab and capecitabine had a 4.5-month overall survival advantage compared with placebo (21.9 vs 17.4) and a median progression-free survival advantage of 5.4 months in patients with active brain metastases (9.5 vs 4.1) and 8.3 months in patients with stable metastases (13.9 vs 5.6).
Given this progress, experts are looking to add new TKIs to the armamentarium. In particular, pyrotinib — already approved in China for treating HER2-positive MBC — has demonstrated significantly longer progression-free survival compared with a standard TKI, lapatinib. The phase 3 PHOEBE trial results, published in The Lancet in early 2021, found a median progression-free survival of 12.5 months in patients randomly assigned to receive pyrotinib plus capecitabine compared with 6.8 months in those receiving lapatinib plus capecitabine. The investigators also reported “manageable toxicity”; diarrhea was the most common grade 3 adverse event, occurring in 31% of the pyrotinib group vs. 8% of the lapatinib group, and overall serious adverse events occurred in 10% of patients receiving pyrotinib vs. 8% of those receiving lapatinib.
More recent data on pyrotinib come from the phase 2 PERMEATE trial, which focused on the safety and efficacy of the agent in patients with advanced disease and brain metastases. The investigators, who presented their findings at the 2021 virtual ASCO meeting (abstract 1037), reported that radiation therapy–naive patients receiving pyrotinib plus capecitabine had an overall response rate of 74.6% in the central nervous system. Patients experiencing progression after whole-brain or stereotactic radiation therapy, however, had a comparatively lower overall response rate of 42.1%.
Similarly, median progression-free survival was much higher in the radiation therapy–naive patients (12.1 vs 5.6 months in the radiation therapy cohort). Similar to the PHOEBE trial, the most common grade 3 adverse event was diarrhea (23.1%), followed by decreased neutrophil and white blood cell counts (12.8% for both), anemia (9%), and hand-foot syndrome (7.7%). The main question for Dr. Kalinsky is how well pyrotinib will ultimately stack up to tucatinib and neratinib. “Pyrotinib — like neratinib — was shown to be superior to lapatinib plus capecitabine , but its role may be limited by its gastrointestinal toxicity,” he said. In addition to research focused on expanding the selection of novel ADCs and TKIs, researchers are also exploring new combinations of approved treatments and whether these combinations can be used earlier in treatment sequencing.
Take the CompassHER2 trials. The ongoing phase 3 trial in patients with high-risk HER2-positive breast cancer and residual disease will explore whether tucatinib plus T-DM1 compared with T-DM1 alone improves overall survival and recurrence-free survival and prevents brain metastases. Another possibility currently under investigation is pairing tucatinib and trastuzumab deruxtecan, instead of T-DM1. “Overall, it’s exciting that we are increasing the number of therapeutic options and combinations,” commented Debu Tripathy, MD, professor and chairman in the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston. “Having more choices allows us to tailor therapies to manage resistance and prolong patients’ responses.”
Curbing brain metastasis, according to Dr. Brufksy, is particularly important, and experts need to explore the extent to which ADCs can penetrate the blood-brain barrier. Already, a subgroup analysis of the DESTINY-Breast01 trial found that trastuzumab deruxtecan appeared to be active in patients with brain metastases. Investigators reported an overall response rate of 58.3% and a median progression-free survival of 18.1 months — results in line with those in the general study cohort — but the study population did not include patients with untreated or progressive brain metastases. A phase 2 study currently under way will examine whether patients with HER2-positive and HER2-low breast cancer who have untreated or progressive brain metastases respond to trastuzumab deruxtecan as well. Ultimately, Dr. Brufksy hopes the recent successes with preventing brain metastases in pediatric acute lymphoblastic leukemia (ALL) foreshadow what›s to come in HER2-positive MBC.
“When we figured out how to treat brain metastases prophylactically in childhood ALL, we saw a huge improvement in the cure rate, which is ultimately my vision for HER2-positive disease,” Dr. Brufsky remarked. “Are there cures for HER2-positive MBC on the horizon? We don’t know yet, but the field has really exploded in recent years.”
A version of this article first appeared on Medscape.com.
Recent therapeutic advances in HER2-positive metastatic breast cancer (MBC) have begun to reshape the treatment landscape for patients. Since late 2019, the U.S. Food and Drug Administration (FDA) has approved a handful of novel agents for HER2-positive MBC — most notably, the antibody-drug conjugate (ADC) trastuzumab deruxtecan in December 2019 and the tyrosine kinase inhibitors (TKIs) tucatinib and neratinib in 2020. According to the National Cancer Institute›s Surveillance, Epidemiology, and End Results (SEER) program, the 5-year survival rate for patients with advanced disease was already on the rise between 2004 and 2018, and
“I’ve been involved in the HER2 space for a long time and have watched the field evolve,” said Adam Brufsky, MD, PhD, associate chief in the division of hematology/oncology and co-director of the Comprehensive Breast Cancer Center at the University of Pittsburgh School of Medicine. “The fact that we’re now talking about fourth- and fifth-line therapies for HER2-positive MBC represents a major advance in the management of these patients.”
Oncologists are still building on this progress, focusing on designing more targeted therapies as well as studying different combinations of available agents. The main goal of treatment, experts say, is to prolong patients’ systemic response and prevent recurrences, especially in the brain. This news organization spoke to Dr. Brufksy and others about promising agents and therapeutic strategies on the horizon to treat HER2-positive MBC.
Inside emerging ADCs
Because many patients develop resistance to trastuzumab emtansine (T-DM1) — the first FDA-approved ADC in breast cancer — researchers have focused on developing the next generation of ADCs with more potent payloads, different linkers, and distinct mechanisms of action, according to Sayeh Lavasani, MD, MS, a medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County.
The second-generation ADC trastuzumab deruxtecan showed “really dramatic” results in HER2-positive MBC, demonstrating progression-free survival of 16 months, remarked Kevin Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University. “These outcomes further changed how we treat patients with metastatic disease and prompted considerable excitement over the potential to develop novel ADCs to treat HER2-positive MBC.”
Most recently, two investigational ADCs — trastuzumab duocarmazine (SYD985) and ARX788 — have stood out. The FDA granted fast-track designations to trastuzumab duocarmazine in January 2018 and ARX788 in January 2021. Trastuzumab duocarmazine, the furthest along the pipeline, has shown promising results so far. In June 2021, Netherlands-based biopharmaceutical company Byondis reported preliminary phase 3 data from the TULIP trial. The open-label, randomized phase 3 study enrolled 436 patients with HER2-positive locally advanced or metastatic disease that had progressed on previous anti-HER2 regimens. The company shared early results that trastuzumab duocarmazine achieved its progression-free survival primary endpoint, marking a significant improvement over physician’s choice of chemotherapy, and promised more detailed results to come later this year.
Although only in early-phase trials, ARX788 has also shown robust anti-HER2 activity as well as low toxicity in HER2-positive tumors, according to recent data. The findings from two phase 1 studies, presented at the June 2021 virtual American Society for Clinical Oncology meeting (abstract 1038), revealed an overall response rate of 74% in the breast cancer cohort, but the investigators acknowledged it was too early to report median progression-free survival outcomes. Preclinical data also showed activity in HER2-low and T-DM1–resistant tumors.
Despite the encouraging initial findings, Dr. Kalinsky remains cautiously optimistic about long-term outcomes for both ADCs. “These data are hot off the press, but it’s too soon to know how these two ADCs and others in the pipeline will measure up to approved therapies,” he commented. As experts learn more about the efficacy of these novel ADCs, Dr. Brufsky would also like to better understand resistance mechanisms and how to integrate these agents into current treatment strategies. “The cellular biology of HER2-positive MBC is complicated, and many factors in these tumor cells affect where ADCs are released, how resistance develops, and whether or not resistance to one ADC applies to others,” Dr. Brufsky remarked. “As we gather more data, we’ll understand resistance mechanisms better and begin to figure out where to go with treatment sequencing.”
TKIs and beyond
In addition to ADCs, TKIs continue to make their mark in the targeted HER2 therapeutic space. The approvals of tucatinib and neratinib last year represented an important advance in treating HER2-positive MBC, particularly for patients with brain metastases. The HER2CLIMB trial, for instance, found that tucatinib combined with trastuzumab and capecitabine had a 4.5-month overall survival advantage compared with placebo (21.9 vs 17.4) and a median progression-free survival advantage of 5.4 months in patients with active brain metastases (9.5 vs 4.1) and 8.3 months in patients with stable metastases (13.9 vs 5.6).
Given this progress, experts are looking to add new TKIs to the armamentarium. In particular, pyrotinib — already approved in China for treating HER2-positive MBC — has demonstrated significantly longer progression-free survival compared with a standard TKI, lapatinib. The phase 3 PHOEBE trial results, published in The Lancet in early 2021, found a median progression-free survival of 12.5 months in patients randomly assigned to receive pyrotinib plus capecitabine compared with 6.8 months in those receiving lapatinib plus capecitabine. The investigators also reported “manageable toxicity”; diarrhea was the most common grade 3 adverse event, occurring in 31% of the pyrotinib group vs. 8% of the lapatinib group, and overall serious adverse events occurred in 10% of patients receiving pyrotinib vs. 8% of those receiving lapatinib.
More recent data on pyrotinib come from the phase 2 PERMEATE trial, which focused on the safety and efficacy of the agent in patients with advanced disease and brain metastases. The investigators, who presented their findings at the 2021 virtual ASCO meeting (abstract 1037), reported that radiation therapy–naive patients receiving pyrotinib plus capecitabine had an overall response rate of 74.6% in the central nervous system. Patients experiencing progression after whole-brain or stereotactic radiation therapy, however, had a comparatively lower overall response rate of 42.1%.
Similarly, median progression-free survival was much higher in the radiation therapy–naive patients (12.1 vs 5.6 months in the radiation therapy cohort). Similar to the PHOEBE trial, the most common grade 3 adverse event was diarrhea (23.1%), followed by decreased neutrophil and white blood cell counts (12.8% for both), anemia (9%), and hand-foot syndrome (7.7%). The main question for Dr. Kalinsky is how well pyrotinib will ultimately stack up to tucatinib and neratinib. “Pyrotinib — like neratinib — was shown to be superior to lapatinib plus capecitabine , but its role may be limited by its gastrointestinal toxicity,” he said. In addition to research focused on expanding the selection of novel ADCs and TKIs, researchers are also exploring new combinations of approved treatments and whether these combinations can be used earlier in treatment sequencing.
Take the CompassHER2 trials. The ongoing phase 3 trial in patients with high-risk HER2-positive breast cancer and residual disease will explore whether tucatinib plus T-DM1 compared with T-DM1 alone improves overall survival and recurrence-free survival and prevents brain metastases. Another possibility currently under investigation is pairing tucatinib and trastuzumab deruxtecan, instead of T-DM1. “Overall, it’s exciting that we are increasing the number of therapeutic options and combinations,” commented Debu Tripathy, MD, professor and chairman in the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston. “Having more choices allows us to tailor therapies to manage resistance and prolong patients’ responses.”
Curbing brain metastasis, according to Dr. Brufksy, is particularly important, and experts need to explore the extent to which ADCs can penetrate the blood-brain barrier. Already, a subgroup analysis of the DESTINY-Breast01 trial found that trastuzumab deruxtecan appeared to be active in patients with brain metastases. Investigators reported an overall response rate of 58.3% and a median progression-free survival of 18.1 months — results in line with those in the general study cohort — but the study population did not include patients with untreated or progressive brain metastases. A phase 2 study currently under way will examine whether patients with HER2-positive and HER2-low breast cancer who have untreated or progressive brain metastases respond to trastuzumab deruxtecan as well. Ultimately, Dr. Brufksy hopes the recent successes with preventing brain metastases in pediatric acute lymphoblastic leukemia (ALL) foreshadow what›s to come in HER2-positive MBC.
“When we figured out how to treat brain metastases prophylactically in childhood ALL, we saw a huge improvement in the cure rate, which is ultimately my vision for HER2-positive disease,” Dr. Brufsky remarked. “Are there cures for HER2-positive MBC on the horizon? We don’t know yet, but the field has really exploded in recent years.”
A version of this article first appeared on Medscape.com.
Liquid biopsy in metastatic breast cancer management: Where does it stand in clinical practice?
Tissue biopsy remains the gold standard for characterizing tumor biology and guiding therapeutic decisions, but liquid biopsies — blood analyses that allow oncologists to detect circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) in the blood — are increasingly demonstrating their value. Last year, the U.S. Food and Drug Administration (FDA) approved two liquid biopsy tests, Guardant360 CDx and FoundationOne Liquid CDx, that can identify more than 300 cancer-related genes in the blood. In 2019, the FDA also approved the first companion diagnostic test, therascreen, to pinpoint PIK3CA gene mutations in patients’ ctDNA and determine whether patients should receive the PI3K inhibitor alpelisib along with fulvestrant.
Here’s an overview of how liquid biopsy is being used in monitoring MBC progression and treatment — and what some oncologists think of it.
What we do and don’t know
“Identifying a patient’s targetable mutations, most notably PIK3CA mutations, is currently the main use of liquid biopsy,” said Pedram Razavi, MD, PhD, a medical oncologist who leads the liquid biopsy program for breast cancer at Memorial Sloan Kettering (MSK) Cancer Center in New York City. “Patients who come to MSK are offered a tumor and liquid biopsy at the time of metastatic diagnosis as part of the standard of care.”
Liquid and tissue biopsy analyses can provide a more complete picture of a patient’s condition. Whereas tissue biopsy allows oncologists to target a more saturated sample of the cancer ecosystem and a wider array of biomarkers, liquid biopsy offers important advantages as well, including a less invasive way to sequence a sample, monitor patients’ treatment response, or track tumor evolution. Liquid biopsy also provides a bigger picture view of tumor heterogeneity by pooling information from many tumor locations as opposed to one.
But, cautioned Yuan Yuan, MD, PhD, liquid biopsy technology is not always sensitive enough to detect CTCs, ctDNA, or all relevant mutations. “When you collect a small tube of blood, you’re essentially trying to catch a small fish in a big sea and wading through a lot of background noise,” said Dr. Yuan, medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County. “The results may be hard to interpret or come back inconclusive.”
And although emerging data suggest that liquid biopsy provides important insights about tumor dynamics — including mapping disease progression, predicting survival, and even detecting signs of cancer recurrence before metastasis develops — the tool has limited utility in clinical practice outside of identifying sensitivity to various therapies or drugs.
“Right now, a lot of research is being done to understand how to use CTC and ctDNA in particular as a means of surveillance in breast cancer, but we’re still in the beginning stages of applying that outside of clinical trials,” said Joseph A. Sparano, MD, deputy director of the Tisch Cancer Institute and chief of the division of hematology and medical oncology, Icahn School of Medicine at Mount Sinai, New York City.
Personalizing treatment
The companion diagnostic test therascreen marked the beginning stages of using liquid biopsy to match treatments to genetic abnormalities in MBC. The SOLAR-1 phase 3 trial, which led to the approval of alpelisib and therascreen, found that the PI3K inhibitor plus fulvestrant almost doubled progression-free survival (PFS) (11 months vs 5.7 months in placebo-fulvestrant group) in patients with PIK3CA-mutated, HR-positive, HER2-negative advanced breast cancer.
More recent studies have shown that liquid biopsy tests can also identify ESR1 mutations and predict responses to inhibitors that target AKT1 and HER2. Investigators presenting at the 2021 American Society of Clinical Oncology meeting reported that next-generation sequencing of ctDNA in patients with HR-positive MBC, HER-positive MBC, or triple-negative breast cancer detected ESR1 mutations in 14% of patients (71 of 501). Moreover, ESR1 mutations were found only in HR-positive patients who had already received endocrine therapy. (The study also examined PIK3CA mutations, which occurred in about one third of patients). A more in-depth look revealed that ESR1 mutations were strongly associated with liver and bone metastases and that mutations along specific codons negatively affected overall survival (OS) and PFS: codons 537 and 538 for OS and codons 380 and 536 for PFS.
According to Debasish Tripathy, MD, professor and chairman of the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston, in addition to tumor sequencing, “liquid biopsy has become a great research tool to track patients in real time and predict, for instance, who will respond to a treatment and identify emerging resistance.”
In terms of predicting responses to treatment, the plasmaMATCH trial assessed ctDNA in 1,034 patients with advanced breast cancer for mutations in ESR1, HER2, and AKT1 using digital droplet polymerase chain reaction (PCR) and Guardant360. Results showed that 357 (34.5%) of these patients had potentially targetable aberrations, including 222 patients with ESR1 mutations, 36 patients with HER2 mutations, and 30 patients with AKT1 mutations.
Agreement between digital droplet PCR and Guardant360 testing was 96%-99%, and liquid biopsy showed 93% sensitivity compared with tumor samples. The investigators also used liquid biopsy findings to match patients’ mutations to targeted treatments: fulvestrant for those with ESR1 mutations, neratinib for HER2 (ERBB2) mutations, and the selective AKT inhibitor capivasertib for estrogen receptor–positive tumors with AKT1 mutations.
Overall, the investigators concluded that ctDNA testing offers “accurate tumor genotyping” in line with tissue-based testing and is ready for routine clinical practice to identify common as well as rare genetic alterations, such as HER2 and AKT1 mutations, that affect only about 5% of patients with advanced disease.
Predicting survival and recurrence
A particularly promising area for liquid biopsy is its usefulness in helping to predict survival outcomes and monitor patients for early signs of recurrence before metastasis occurs. But the data to support this are still in their infancy.
A highly cited study, published over 15 years ago in the New England Journal of Medicine, found that patients with MBC who had five or more CTCs per 7.5 mL of whole blood before receiving first-line therapy exhibited significantly shorter median PFS (2.7 vs 7.0 months) and OS (10 vs > 18 months) compared with patients with fewer than five CTCs. Subsequent analyses performed more than a decade later, including a meta-analysis published last year, helped validate these early findings that levels of CTCs detected in the blood independently and strongly predicted PFS and OS in patients with MBC.
In addition, ctDNA can provide important information about patients’ survival odds. In a retrospective study published last year, investigators tracked changes in ctDNA in 291 plasma samples from 84 patients with locally advanced breast cancer who participated in the I-SPY trial. Patients who remained ctDNA-positive after 3 weeks of neoadjuvant chemotherapy were significantly more likely to have residual disease after completing their treatment compared with patients who cleared ctDNA at that early stage (83% for those with nonpathologic complete response vs 52%). Notably, the presence of ctDNA between therapy initiation and completion was associated with a significantly greater risk for metastatic recurrence, whereas clearance of ctDNA after neoadjuvant therapy was linked to improved survival.
“The study is important because it highlights how tracking circulating ctDNA status in neoadjuvant-treated breast cancer can expose a patient’s risk for distant metastasis,” said Dr. Yuan. But, she added, “I think the biggest attraction of liquid biopsy will be the ability to detect molecular disease even before imaging can, and identify who has a high risk for recurrence.”
Dr. Razavi agreed that the potential to prevent metastasis by finding minimal residual disease (MRD) is the most exciting area of liquid biopsy research. “If we can find tumor DNA early before tumors have a chance to establish themselves, we could potentially change the trajectory of the disease for patients,” he said.
Several studies suggest that monitoring patients’ ctDNA levels after neoadjuvant treatment and surgery may help predict their risk for relapse and progression to metastatic disease. A 2015 analysis, which followed 20 patients with breast cancer after surgery, found that ctDNA monitoring accurately differentiated those who ultimately developed metastatic disease from those who didn’t (sensitivity, 93%; specificity, 100%) and detected metastatic disease 11 months earlier, on average, than imaging did. Another 2015 study found that the presence of ctDNA in plasma after neoadjuvant chemotherapy and surgery predicted metastatic relapse a median of almost 8 months before clinical detection. Other recent data show the power of ultrasensitive blood tests to detect MRD and potentially find metastatic disease early.
Although an increasing number of studies show that ctDNA and CTCs are prognostic for breast cancer recurrence, a major question remains: For patients with ctDNA or CTCs but no overt disease after imaging, will initiating therapy prevent or delay the development of metastatic disease?
“We still have to do those clinical trials to determine whether detecting MRD and treating patients early actually positively affects their survival and quality of life,” Dr. Razavi said.
Tissue biopsy remains the gold standard for characterizing tumor biology and guiding therapeutic decisions, but liquid biopsies — blood analyses that allow oncologists to detect circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) in the blood — are increasingly demonstrating their value. Last year, the U.S. Food and Drug Administration (FDA) approved two liquid biopsy tests, Guardant360 CDx and FoundationOne Liquid CDx, that can identify more than 300 cancer-related genes in the blood. In 2019, the FDA also approved the first companion diagnostic test, therascreen, to pinpoint PIK3CA gene mutations in patients’ ctDNA and determine whether patients should receive the PI3K inhibitor alpelisib along with fulvestrant.
Here’s an overview of how liquid biopsy is being used in monitoring MBC progression and treatment — and what some oncologists think of it.
What we do and don’t know
“Identifying a patient’s targetable mutations, most notably PIK3CA mutations, is currently the main use of liquid biopsy,” said Pedram Razavi, MD, PhD, a medical oncologist who leads the liquid biopsy program for breast cancer at Memorial Sloan Kettering (MSK) Cancer Center in New York City. “Patients who come to MSK are offered a tumor and liquid biopsy at the time of metastatic diagnosis as part of the standard of care.”
Liquid and tissue biopsy analyses can provide a more complete picture of a patient’s condition. Whereas tissue biopsy allows oncologists to target a more saturated sample of the cancer ecosystem and a wider array of biomarkers, liquid biopsy offers important advantages as well, including a less invasive way to sequence a sample, monitor patients’ treatment response, or track tumor evolution. Liquid biopsy also provides a bigger picture view of tumor heterogeneity by pooling information from many tumor locations as opposed to one.
But, cautioned Yuan Yuan, MD, PhD, liquid biopsy technology is not always sensitive enough to detect CTCs, ctDNA, or all relevant mutations. “When you collect a small tube of blood, you’re essentially trying to catch a small fish in a big sea and wading through a lot of background noise,” said Dr. Yuan, medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County. “The results may be hard to interpret or come back inconclusive.”
And although emerging data suggest that liquid biopsy provides important insights about tumor dynamics — including mapping disease progression, predicting survival, and even detecting signs of cancer recurrence before metastasis develops — the tool has limited utility in clinical practice outside of identifying sensitivity to various therapies or drugs.
“Right now, a lot of research is being done to understand how to use CTC and ctDNA in particular as a means of surveillance in breast cancer, but we’re still in the beginning stages of applying that outside of clinical trials,” said Joseph A. Sparano, MD, deputy director of the Tisch Cancer Institute and chief of the division of hematology and medical oncology, Icahn School of Medicine at Mount Sinai, New York City.
Personalizing treatment
The companion diagnostic test therascreen marked the beginning stages of using liquid biopsy to match treatments to genetic abnormalities in MBC. The SOLAR-1 phase 3 trial, which led to the approval of alpelisib and therascreen, found that the PI3K inhibitor plus fulvestrant almost doubled progression-free survival (PFS) (11 months vs 5.7 months in placebo-fulvestrant group) in patients with PIK3CA-mutated, HR-positive, HER2-negative advanced breast cancer.
More recent studies have shown that liquid biopsy tests can also identify ESR1 mutations and predict responses to inhibitors that target AKT1 and HER2. Investigators presenting at the 2021 American Society of Clinical Oncology meeting reported that next-generation sequencing of ctDNA in patients with HR-positive MBC, HER-positive MBC, or triple-negative breast cancer detected ESR1 mutations in 14% of patients (71 of 501). Moreover, ESR1 mutations were found only in HR-positive patients who had already received endocrine therapy. (The study also examined PIK3CA mutations, which occurred in about one third of patients). A more in-depth look revealed that ESR1 mutations were strongly associated with liver and bone metastases and that mutations along specific codons negatively affected overall survival (OS) and PFS: codons 537 and 538 for OS and codons 380 and 536 for PFS.
According to Debasish Tripathy, MD, professor and chairman of the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston, in addition to tumor sequencing, “liquid biopsy has become a great research tool to track patients in real time and predict, for instance, who will respond to a treatment and identify emerging resistance.”
In terms of predicting responses to treatment, the plasmaMATCH trial assessed ctDNA in 1,034 patients with advanced breast cancer for mutations in ESR1, HER2, and AKT1 using digital droplet polymerase chain reaction (PCR) and Guardant360. Results showed that 357 (34.5%) of these patients had potentially targetable aberrations, including 222 patients with ESR1 mutations, 36 patients with HER2 mutations, and 30 patients with AKT1 mutations.
Agreement between digital droplet PCR and Guardant360 testing was 96%-99%, and liquid biopsy showed 93% sensitivity compared with tumor samples. The investigators also used liquid biopsy findings to match patients’ mutations to targeted treatments: fulvestrant for those with ESR1 mutations, neratinib for HER2 (ERBB2) mutations, and the selective AKT inhibitor capivasertib for estrogen receptor–positive tumors with AKT1 mutations.
Overall, the investigators concluded that ctDNA testing offers “accurate tumor genotyping” in line with tissue-based testing and is ready for routine clinical practice to identify common as well as rare genetic alterations, such as HER2 and AKT1 mutations, that affect only about 5% of patients with advanced disease.
Predicting survival and recurrence
A particularly promising area for liquid biopsy is its usefulness in helping to predict survival outcomes and monitor patients for early signs of recurrence before metastasis occurs. But the data to support this are still in their infancy.
A highly cited study, published over 15 years ago in the New England Journal of Medicine, found that patients with MBC who had five or more CTCs per 7.5 mL of whole blood before receiving first-line therapy exhibited significantly shorter median PFS (2.7 vs 7.0 months) and OS (10 vs > 18 months) compared with patients with fewer than five CTCs. Subsequent analyses performed more than a decade later, including a meta-analysis published last year, helped validate these early findings that levels of CTCs detected in the blood independently and strongly predicted PFS and OS in patients with MBC.
In addition, ctDNA can provide important information about patients’ survival odds. In a retrospective study published last year, investigators tracked changes in ctDNA in 291 plasma samples from 84 patients with locally advanced breast cancer who participated in the I-SPY trial. Patients who remained ctDNA-positive after 3 weeks of neoadjuvant chemotherapy were significantly more likely to have residual disease after completing their treatment compared with patients who cleared ctDNA at that early stage (83% for those with nonpathologic complete response vs 52%). Notably, the presence of ctDNA between therapy initiation and completion was associated with a significantly greater risk for metastatic recurrence, whereas clearance of ctDNA after neoadjuvant therapy was linked to improved survival.
“The study is important because it highlights how tracking circulating ctDNA status in neoadjuvant-treated breast cancer can expose a patient’s risk for distant metastasis,” said Dr. Yuan. But, she added, “I think the biggest attraction of liquid biopsy will be the ability to detect molecular disease even before imaging can, and identify who has a high risk for recurrence.”
Dr. Razavi agreed that the potential to prevent metastasis by finding minimal residual disease (MRD) is the most exciting area of liquid biopsy research. “If we can find tumor DNA early before tumors have a chance to establish themselves, we could potentially change the trajectory of the disease for patients,” he said.
Several studies suggest that monitoring patients’ ctDNA levels after neoadjuvant treatment and surgery may help predict their risk for relapse and progression to metastatic disease. A 2015 analysis, which followed 20 patients with breast cancer after surgery, found that ctDNA monitoring accurately differentiated those who ultimately developed metastatic disease from those who didn’t (sensitivity, 93%; specificity, 100%) and detected metastatic disease 11 months earlier, on average, than imaging did. Another 2015 study found that the presence of ctDNA in plasma after neoadjuvant chemotherapy and surgery predicted metastatic relapse a median of almost 8 months before clinical detection. Other recent data show the power of ultrasensitive blood tests to detect MRD and potentially find metastatic disease early.
Although an increasing number of studies show that ctDNA and CTCs are prognostic for breast cancer recurrence, a major question remains: For patients with ctDNA or CTCs but no overt disease after imaging, will initiating therapy prevent or delay the development of metastatic disease?
“We still have to do those clinical trials to determine whether detecting MRD and treating patients early actually positively affects their survival and quality of life,” Dr. Razavi said.
Tissue biopsy remains the gold standard for characterizing tumor biology and guiding therapeutic decisions, but liquid biopsies — blood analyses that allow oncologists to detect circulating tumor cells (CTCs) and circulating tumor DNA (ctDNA) in the blood — are increasingly demonstrating their value. Last year, the U.S. Food and Drug Administration (FDA) approved two liquid biopsy tests, Guardant360 CDx and FoundationOne Liquid CDx, that can identify more than 300 cancer-related genes in the blood. In 2019, the FDA also approved the first companion diagnostic test, therascreen, to pinpoint PIK3CA gene mutations in patients’ ctDNA and determine whether patients should receive the PI3K inhibitor alpelisib along with fulvestrant.
Here’s an overview of how liquid biopsy is being used in monitoring MBC progression and treatment — and what some oncologists think of it.
What we do and don’t know
“Identifying a patient’s targetable mutations, most notably PIK3CA mutations, is currently the main use of liquid biopsy,” said Pedram Razavi, MD, PhD, a medical oncologist who leads the liquid biopsy program for breast cancer at Memorial Sloan Kettering (MSK) Cancer Center in New York City. “Patients who come to MSK are offered a tumor and liquid biopsy at the time of metastatic diagnosis as part of the standard of care.”
Liquid and tissue biopsy analyses can provide a more complete picture of a patient’s condition. Whereas tissue biopsy allows oncologists to target a more saturated sample of the cancer ecosystem and a wider array of biomarkers, liquid biopsy offers important advantages as well, including a less invasive way to sequence a sample, monitor patients’ treatment response, or track tumor evolution. Liquid biopsy also provides a bigger picture view of tumor heterogeneity by pooling information from many tumor locations as opposed to one.
But, cautioned Yuan Yuan, MD, PhD, liquid biopsy technology is not always sensitive enough to detect CTCs, ctDNA, or all relevant mutations. “When you collect a small tube of blood, you’re essentially trying to catch a small fish in a big sea and wading through a lot of background noise,” said Dr. Yuan, medical oncologist at City of Hope, a comprehensive cancer center in Los Angeles County. “The results may be hard to interpret or come back inconclusive.”
And although emerging data suggest that liquid biopsy provides important insights about tumor dynamics — including mapping disease progression, predicting survival, and even detecting signs of cancer recurrence before metastasis develops — the tool has limited utility in clinical practice outside of identifying sensitivity to various therapies or drugs.
“Right now, a lot of research is being done to understand how to use CTC and ctDNA in particular as a means of surveillance in breast cancer, but we’re still in the beginning stages of applying that outside of clinical trials,” said Joseph A. Sparano, MD, deputy director of the Tisch Cancer Institute and chief of the division of hematology and medical oncology, Icahn School of Medicine at Mount Sinai, New York City.
Personalizing treatment
The companion diagnostic test therascreen marked the beginning stages of using liquid biopsy to match treatments to genetic abnormalities in MBC. The SOLAR-1 phase 3 trial, which led to the approval of alpelisib and therascreen, found that the PI3K inhibitor plus fulvestrant almost doubled progression-free survival (PFS) (11 months vs 5.7 months in placebo-fulvestrant group) in patients with PIK3CA-mutated, HR-positive, HER2-negative advanced breast cancer.
More recent studies have shown that liquid biopsy tests can also identify ESR1 mutations and predict responses to inhibitors that target AKT1 and HER2. Investigators presenting at the 2021 American Society of Clinical Oncology meeting reported that next-generation sequencing of ctDNA in patients with HR-positive MBC, HER-positive MBC, or triple-negative breast cancer detected ESR1 mutations in 14% of patients (71 of 501). Moreover, ESR1 mutations were found only in HR-positive patients who had already received endocrine therapy. (The study also examined PIK3CA mutations, which occurred in about one third of patients). A more in-depth look revealed that ESR1 mutations were strongly associated with liver and bone metastases and that mutations along specific codons negatively affected overall survival (OS) and PFS: codons 537 and 538 for OS and codons 380 and 536 for PFS.
According to Debasish Tripathy, MD, professor and chairman of the department of breast medical oncology at the University of Texas MD Anderson Cancer Center in Houston, in addition to tumor sequencing, “liquid biopsy has become a great research tool to track patients in real time and predict, for instance, who will respond to a treatment and identify emerging resistance.”
In terms of predicting responses to treatment, the plasmaMATCH trial assessed ctDNA in 1,034 patients with advanced breast cancer for mutations in ESR1, HER2, and AKT1 using digital droplet polymerase chain reaction (PCR) and Guardant360. Results showed that 357 (34.5%) of these patients had potentially targetable aberrations, including 222 patients with ESR1 mutations, 36 patients with HER2 mutations, and 30 patients with AKT1 mutations.
Agreement between digital droplet PCR and Guardant360 testing was 96%-99%, and liquid biopsy showed 93% sensitivity compared with tumor samples. The investigators also used liquid biopsy findings to match patients’ mutations to targeted treatments: fulvestrant for those with ESR1 mutations, neratinib for HER2 (ERBB2) mutations, and the selective AKT inhibitor capivasertib for estrogen receptor–positive tumors with AKT1 mutations.
Overall, the investigators concluded that ctDNA testing offers “accurate tumor genotyping” in line with tissue-based testing and is ready for routine clinical practice to identify common as well as rare genetic alterations, such as HER2 and AKT1 mutations, that affect only about 5% of patients with advanced disease.
Predicting survival and recurrence
A particularly promising area for liquid biopsy is its usefulness in helping to predict survival outcomes and monitor patients for early signs of recurrence before metastasis occurs. But the data to support this are still in their infancy.
A highly cited study, published over 15 years ago in the New England Journal of Medicine, found that patients with MBC who had five or more CTCs per 7.5 mL of whole blood before receiving first-line therapy exhibited significantly shorter median PFS (2.7 vs 7.0 months) and OS (10 vs > 18 months) compared with patients with fewer than five CTCs. Subsequent analyses performed more than a decade later, including a meta-analysis published last year, helped validate these early findings that levels of CTCs detected in the blood independently and strongly predicted PFS and OS in patients with MBC.
In addition, ctDNA can provide important information about patients’ survival odds. In a retrospective study published last year, investigators tracked changes in ctDNA in 291 plasma samples from 84 patients with locally advanced breast cancer who participated in the I-SPY trial. Patients who remained ctDNA-positive after 3 weeks of neoadjuvant chemotherapy were significantly more likely to have residual disease after completing their treatment compared with patients who cleared ctDNA at that early stage (83% for those with nonpathologic complete response vs 52%). Notably, the presence of ctDNA between therapy initiation and completion was associated with a significantly greater risk for metastatic recurrence, whereas clearance of ctDNA after neoadjuvant therapy was linked to improved survival.
“The study is important because it highlights how tracking circulating ctDNA status in neoadjuvant-treated breast cancer can expose a patient’s risk for distant metastasis,” said Dr. Yuan. But, she added, “I think the biggest attraction of liquid biopsy will be the ability to detect molecular disease even before imaging can, and identify who has a high risk for recurrence.”
Dr. Razavi agreed that the potential to prevent metastasis by finding minimal residual disease (MRD) is the most exciting area of liquid biopsy research. “If we can find tumor DNA early before tumors have a chance to establish themselves, we could potentially change the trajectory of the disease for patients,” he said.
Several studies suggest that monitoring patients’ ctDNA levels after neoadjuvant treatment and surgery may help predict their risk for relapse and progression to metastatic disease. A 2015 analysis, which followed 20 patients with breast cancer after surgery, found that ctDNA monitoring accurately differentiated those who ultimately developed metastatic disease from those who didn’t (sensitivity, 93%; specificity, 100%) and detected metastatic disease 11 months earlier, on average, than imaging did. Another 2015 study found that the presence of ctDNA in plasma after neoadjuvant chemotherapy and surgery predicted metastatic relapse a median of almost 8 months before clinical detection. Other recent data show the power of ultrasensitive blood tests to detect MRD and potentially find metastatic disease early.
Although an increasing number of studies show that ctDNA and CTCs are prognostic for breast cancer recurrence, a major question remains: For patients with ctDNA or CTCs but no overt disease after imaging, will initiating therapy prevent or delay the development of metastatic disease?
“We still have to do those clinical trials to determine whether detecting MRD and treating patients early actually positively affects their survival and quality of life,” Dr. Razavi said.
Biomarker testing in metastatic breast cancer management: ‘Essential’
Identifying biomarkers in metastatic breast cancer (MBC) has become an integral part of choosing treatments and understanding disease progression. The American Society of Clinical Oncology Clinical Practice Guideline, published in 2015, recommends an initial biopsy to confirm estrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2) status as well as repeat biopsies to watch for receptor status changes over time.
“Decisions concerning the initiation of systemic therapy or selection of systemic therapy for metastatic breast cancer should be guided by ER, PR, and HER2 status in conjunction with clinical evaluation, judgment, and the patient’s goals for care,” according to the guideline authors.This news organization reached out to Kelly McCann, MD, PhD, a hematologist and oncologist in the department of medicine at the David Geffen School of Medicine, University of California, Los Angeles, to explore the role biomarker testing plays in managing MBC.
Question: How important is biomarker testing in guiding MBC treatments? Is there a standard or recommended process?
Dr. McCann: Biomarker testing is essential to breast cancer treatment and the development of targeted therapies. Oncologists typically identify a tumor’s canonical biomarkers — ER, PR, and HER2 — using immunohistochemistry or fluorescence in situ hybridization (FISH) testing and then try to match the tumor biology to drugs that target that subtype.
For tumors that lack canonical biomarkers — for example, triple-negative breast cancer (TNBC) — I send the tumor tissue for next-generation sequencing at the time of metastatic diagnosis to identify a wider range of potential targets or oncogenic drivers, such as somatic or germline mutations in homologous recombination repair genes ( BRCA1, BRCA2, and PALB2 ) or mutations in the PI3K/AKT/mTOR pathway.
In our attempts to define tumor biology and design a treatment strategy, two additional issues quickly arise. First, tumors are heterogeneous from the start. Second, tumors evolve.
Let’s start with how we define or subtype a tumor. Would you walk us through this process?
Defining a breast tumor can be tricky because these cancers often don’t fit neatly into predefined categories. Let’s take the estrogen receptor. In clinical trials, we need to define the cutoff for what constitutes ER-positive MBC or TNBC. Some trials define ER-positive as 1% or greater, others define it as 10% or greater.
But is a PR- and HER2-negative tumor with 1% or even 5% ER expression really ER-positive in the biological or prognostic sense? Probably not. A tumor with less than 10% ER expression, for instance, will actually behave like a triple-negative tumor. Instead of choosing a regimen targeting the ER-positive cells, I’ll lean more toward cytotoxic chemotherapy, the standard treatment for TNBC.
Tumors may have multiple drivers as well. What are some aberrations in addition to the main subtypes?
Tumors also often harbor more than one targetable driver. For instance, PIK3CA gene mutations are present in about 40% of hormone receptor–positive, HER2-negative tumors. Activating mutations in ESR1 develop in anywhere from 10% to 50% of MBCs as a resistance mechanism to estrogen deprivation therapy, conferring estrogen independence to the cells. Activating mutations in ERBB2, which essentially turns HER2 into an active receptor, are found in 2%-4% of breast cancers, including ER-positive, HER2-mutant breast cancers, and are enriched in lobular breast cancers, which are typically ER positive, HER2 negative.
What about tumor evolution, given the growing body of evidence that biomarker status in MBC can change over time?
Patients with MBC often have several active areas of cancer, and these areas will evolve differently. During each line of treatment, some metastases will develop resistance and others won’t. For instance, if my patient’s liver metastases start to grow, I will change therapy immediately. If, however, a single bone metastasis begins to grow and the liver metastases have responded well, I might consider local therapy — such as radiation — to target that bone metastasis, though this particular approach hasn’t been formally studied.
Ultimately, we can expect tumors to change over time as they become more biologically aggressive or resistant to current therapy. The most common biomarker change is probably loss of ER or PR expression, but the frequency of ER, PR, or HER2 biomarker changes is still not well understood.
Resistance mutations can also happen. When, for instance, activating mutations in ESR1 occur, the estrogen receptor becomes independent of estrogen and tumors then develop resistance to endocrine therapies. We see a similar problem arise in metastatic prostate cancer. With chronic testosterone deprivation, eventually the androgen receptor evolves to become independent of testosterone in a stage known as castrate-resistant prostate cancer.
Which biomarkers or combinations of biomarkers can be paired with an approved treatment?
We have a range of treatments targeting ER-positive and HER2-positive MBC in particular. For tumors harboring additional targetable mutations, preliminary data suggest that HER2-targeted tyrosine kinase inhibitors (TKIs), such as tucatinib and neratinib, are effective against activating mutations in ERBB2.
The PI3K inhibitor alpelisib in combination with fulvestrant has been approved for patients with ER-positive, HER2-negative MBC and mutations in PIK3CA. The mTOR inhibitor everolimus plus exemestane is an option for patients with ER-positive, HER2-negative. And for those with activating mutations in ESR1, I switch patients to a selective estrogen receptor degrader, such as fulvestrant.
PARP inhibitors, including olaparib or talazoparib, target metastatic HR-positive disease or TNBC with deleterious germline BRCA1 or BRCA2 mutations. Sacituzumab govitecan has been approved for treating metastatic TNBC and targets the cell surface protein TROP2, expressed in almost 90% of TNBC tumors.
What targets, on the other hand, are less informative for treatment choice?
When we order next-generation sequencing, we also will get a list of possible targets for which there are currently no therapeutic options, but there may be in the future. I find this knowledge is helpful. For example, an activating mutation in KRAS tells me that the cancer has a very strong oncogenic driver that I won›t be able to target. I know that activating KRAS mutations in lung cancer and colon cancer portend a poorer prognosis, which helps me to prepare the patient and family.
Atezolizumab in combination with paclitaxel has been FDA-approved for PD-L1 TNBC in the first-line setting, though data show that immune checkpoint inhibitors may be effective even without PD-L1 expression. Although cell surface protein TROP2 has emerged as a target in recent years, its expression is so common in TNBC that confirmatory testing for TROP2 expression is not required to prescribe sacituzumab govitecan.
What factors do you weigh when selecting among the large number of tests available for tumor testing?
We have many biomarker tests available, but the National Comprehensive Cancer Network does not have guidelines for tumor genetics testing in breast cancer. That means insurance does not have to cover the cost, and many companies don’t. Ultimately, though, drug companies and some testing companies have an incentive to cover the cost themselves because a companion diagnostic might be linked to their drug — therascreen PIK3CA RGQ PCR kit for alpelisib, for instance.
I tend not to use a companion diagnostic test because I want more information with a wider panel. The tumor tests I often use are FoundationOne CDx, Caris Molecular Intelligence, and Tempus. I use Tempus because their financial aid is very generous and almost all of my patients qualify to be tested for less than $100. For germline genetic testing, Invitae, Myriad, and Color are also options. Invitae and Color are about $250 out of pocket without insurance. Many academic centers have their own gene panels as well.
How far have we come in identifying biomarkers in MBC?
Targeted treatment for breast cancer has advanced significantly since doing my PhD research in cancer biology about 15 years ago. Of course, targeted therapies for ER-positive and HER2-amplified cancers were available at that point, but many more have been developed. The most significant advance has been the development of efficient and affordable genome sequencing, which has led to these large panels and identification of therapeutic targets. We’ve also expanded our knowledge of genetic predispositions for breast cancer beyond BRCA1 and BRCA2, which not only allows us to preemptively advise patients and their families about cancer risks and recommendations for cancer screening, but also to select a therapy to target a cancer’s DNA repair deficits.
I feel that we are in an exciting discovery phase in oncology. We currently rely on biomarkers to manage MBC and will continue to refine our strategies and develop more effective drug therapies as we identify more oncogenic drivers, tumor-specific proteins, and cancer cell vulnerabilities.
Identifying biomarkers in metastatic breast cancer (MBC) has become an integral part of choosing treatments and understanding disease progression. The American Society of Clinical Oncology Clinical Practice Guideline, published in 2015, recommends an initial biopsy to confirm estrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2) status as well as repeat biopsies to watch for receptor status changes over time.
“Decisions concerning the initiation of systemic therapy or selection of systemic therapy for metastatic breast cancer should be guided by ER, PR, and HER2 status in conjunction with clinical evaluation, judgment, and the patient’s goals for care,” according to the guideline authors.This news organization reached out to Kelly McCann, MD, PhD, a hematologist and oncologist in the department of medicine at the David Geffen School of Medicine, University of California, Los Angeles, to explore the role biomarker testing plays in managing MBC.
Question: How important is biomarker testing in guiding MBC treatments? Is there a standard or recommended process?
Dr. McCann: Biomarker testing is essential to breast cancer treatment and the development of targeted therapies. Oncologists typically identify a tumor’s canonical biomarkers — ER, PR, and HER2 — using immunohistochemistry or fluorescence in situ hybridization (FISH) testing and then try to match the tumor biology to drugs that target that subtype.
For tumors that lack canonical biomarkers — for example, triple-negative breast cancer (TNBC) — I send the tumor tissue for next-generation sequencing at the time of metastatic diagnosis to identify a wider range of potential targets or oncogenic drivers, such as somatic or germline mutations in homologous recombination repair genes ( BRCA1, BRCA2, and PALB2 ) or mutations in the PI3K/AKT/mTOR pathway.
In our attempts to define tumor biology and design a treatment strategy, two additional issues quickly arise. First, tumors are heterogeneous from the start. Second, tumors evolve.
Let’s start with how we define or subtype a tumor. Would you walk us through this process?
Defining a breast tumor can be tricky because these cancers often don’t fit neatly into predefined categories. Let’s take the estrogen receptor. In clinical trials, we need to define the cutoff for what constitutes ER-positive MBC or TNBC. Some trials define ER-positive as 1% or greater, others define it as 10% or greater.
But is a PR- and HER2-negative tumor with 1% or even 5% ER expression really ER-positive in the biological or prognostic sense? Probably not. A tumor with less than 10% ER expression, for instance, will actually behave like a triple-negative tumor. Instead of choosing a regimen targeting the ER-positive cells, I’ll lean more toward cytotoxic chemotherapy, the standard treatment for TNBC.
Tumors may have multiple drivers as well. What are some aberrations in addition to the main subtypes?
Tumors also often harbor more than one targetable driver. For instance, PIK3CA gene mutations are present in about 40% of hormone receptor–positive, HER2-negative tumors. Activating mutations in ESR1 develop in anywhere from 10% to 50% of MBCs as a resistance mechanism to estrogen deprivation therapy, conferring estrogen independence to the cells. Activating mutations in ERBB2, which essentially turns HER2 into an active receptor, are found in 2%-4% of breast cancers, including ER-positive, HER2-mutant breast cancers, and are enriched in lobular breast cancers, which are typically ER positive, HER2 negative.
What about tumor evolution, given the growing body of evidence that biomarker status in MBC can change over time?
Patients with MBC often have several active areas of cancer, and these areas will evolve differently. During each line of treatment, some metastases will develop resistance and others won’t. For instance, if my patient’s liver metastases start to grow, I will change therapy immediately. If, however, a single bone metastasis begins to grow and the liver metastases have responded well, I might consider local therapy — such as radiation — to target that bone metastasis, though this particular approach hasn’t been formally studied.
Ultimately, we can expect tumors to change over time as they become more biologically aggressive or resistant to current therapy. The most common biomarker change is probably loss of ER or PR expression, but the frequency of ER, PR, or HER2 biomarker changes is still not well understood.
Resistance mutations can also happen. When, for instance, activating mutations in ESR1 occur, the estrogen receptor becomes independent of estrogen and tumors then develop resistance to endocrine therapies. We see a similar problem arise in metastatic prostate cancer. With chronic testosterone deprivation, eventually the androgen receptor evolves to become independent of testosterone in a stage known as castrate-resistant prostate cancer.
Which biomarkers or combinations of biomarkers can be paired with an approved treatment?
We have a range of treatments targeting ER-positive and HER2-positive MBC in particular. For tumors harboring additional targetable mutations, preliminary data suggest that HER2-targeted tyrosine kinase inhibitors (TKIs), such as tucatinib and neratinib, are effective against activating mutations in ERBB2.
The PI3K inhibitor alpelisib in combination with fulvestrant has been approved for patients with ER-positive, HER2-negative MBC and mutations in PIK3CA. The mTOR inhibitor everolimus plus exemestane is an option for patients with ER-positive, HER2-negative. And for those with activating mutations in ESR1, I switch patients to a selective estrogen receptor degrader, such as fulvestrant.
PARP inhibitors, including olaparib or talazoparib, target metastatic HR-positive disease or TNBC with deleterious germline BRCA1 or BRCA2 mutations. Sacituzumab govitecan has been approved for treating metastatic TNBC and targets the cell surface protein TROP2, expressed in almost 90% of TNBC tumors.
What targets, on the other hand, are less informative for treatment choice?
When we order next-generation sequencing, we also will get a list of possible targets for which there are currently no therapeutic options, but there may be in the future. I find this knowledge is helpful. For example, an activating mutation in KRAS tells me that the cancer has a very strong oncogenic driver that I won›t be able to target. I know that activating KRAS mutations in lung cancer and colon cancer portend a poorer prognosis, which helps me to prepare the patient and family.
Atezolizumab in combination with paclitaxel has been FDA-approved for PD-L1 TNBC in the first-line setting, though data show that immune checkpoint inhibitors may be effective even without PD-L1 expression. Although cell surface protein TROP2 has emerged as a target in recent years, its expression is so common in TNBC that confirmatory testing for TROP2 expression is not required to prescribe sacituzumab govitecan.
What factors do you weigh when selecting among the large number of tests available for tumor testing?
We have many biomarker tests available, but the National Comprehensive Cancer Network does not have guidelines for tumor genetics testing in breast cancer. That means insurance does not have to cover the cost, and many companies don’t. Ultimately, though, drug companies and some testing companies have an incentive to cover the cost themselves because a companion diagnostic might be linked to their drug — therascreen PIK3CA RGQ PCR kit for alpelisib, for instance.
I tend not to use a companion diagnostic test because I want more information with a wider panel. The tumor tests I often use are FoundationOne CDx, Caris Molecular Intelligence, and Tempus. I use Tempus because their financial aid is very generous and almost all of my patients qualify to be tested for less than $100. For germline genetic testing, Invitae, Myriad, and Color are also options. Invitae and Color are about $250 out of pocket without insurance. Many academic centers have their own gene panels as well.
How far have we come in identifying biomarkers in MBC?
Targeted treatment for breast cancer has advanced significantly since doing my PhD research in cancer biology about 15 years ago. Of course, targeted therapies for ER-positive and HER2-amplified cancers were available at that point, but many more have been developed. The most significant advance has been the development of efficient and affordable genome sequencing, which has led to these large panels and identification of therapeutic targets. We’ve also expanded our knowledge of genetic predispositions for breast cancer beyond BRCA1 and BRCA2, which not only allows us to preemptively advise patients and their families about cancer risks and recommendations for cancer screening, but also to select a therapy to target a cancer’s DNA repair deficits.
I feel that we are in an exciting discovery phase in oncology. We currently rely on biomarkers to manage MBC and will continue to refine our strategies and develop more effective drug therapies as we identify more oncogenic drivers, tumor-specific proteins, and cancer cell vulnerabilities.
Identifying biomarkers in metastatic breast cancer (MBC) has become an integral part of choosing treatments and understanding disease progression. The American Society of Clinical Oncology Clinical Practice Guideline, published in 2015, recommends an initial biopsy to confirm estrogen receptor (ER), progesterone receptor (PR), or human epidermal growth factor receptor 2 (HER2) status as well as repeat biopsies to watch for receptor status changes over time.
“Decisions concerning the initiation of systemic therapy or selection of systemic therapy for metastatic breast cancer should be guided by ER, PR, and HER2 status in conjunction with clinical evaluation, judgment, and the patient’s goals for care,” according to the guideline authors.This news organization reached out to Kelly McCann, MD, PhD, a hematologist and oncologist in the department of medicine at the David Geffen School of Medicine, University of California, Los Angeles, to explore the role biomarker testing plays in managing MBC.
Question: How important is biomarker testing in guiding MBC treatments? Is there a standard or recommended process?
Dr. McCann: Biomarker testing is essential to breast cancer treatment and the development of targeted therapies. Oncologists typically identify a tumor’s canonical biomarkers — ER, PR, and HER2 — using immunohistochemistry or fluorescence in situ hybridization (FISH) testing and then try to match the tumor biology to drugs that target that subtype.
For tumors that lack canonical biomarkers — for example, triple-negative breast cancer (TNBC) — I send the tumor tissue for next-generation sequencing at the time of metastatic diagnosis to identify a wider range of potential targets or oncogenic drivers, such as somatic or germline mutations in homologous recombination repair genes ( BRCA1, BRCA2, and PALB2 ) or mutations in the PI3K/AKT/mTOR pathway.
In our attempts to define tumor biology and design a treatment strategy, two additional issues quickly arise. First, tumors are heterogeneous from the start. Second, tumors evolve.
Let’s start with how we define or subtype a tumor. Would you walk us through this process?
Defining a breast tumor can be tricky because these cancers often don’t fit neatly into predefined categories. Let’s take the estrogen receptor. In clinical trials, we need to define the cutoff for what constitutes ER-positive MBC or TNBC. Some trials define ER-positive as 1% or greater, others define it as 10% or greater.
But is a PR- and HER2-negative tumor with 1% or even 5% ER expression really ER-positive in the biological or prognostic sense? Probably not. A tumor with less than 10% ER expression, for instance, will actually behave like a triple-negative tumor. Instead of choosing a regimen targeting the ER-positive cells, I’ll lean more toward cytotoxic chemotherapy, the standard treatment for TNBC.
Tumors may have multiple drivers as well. What are some aberrations in addition to the main subtypes?
Tumors also often harbor more than one targetable driver. For instance, PIK3CA gene mutations are present in about 40% of hormone receptor–positive, HER2-negative tumors. Activating mutations in ESR1 develop in anywhere from 10% to 50% of MBCs as a resistance mechanism to estrogen deprivation therapy, conferring estrogen independence to the cells. Activating mutations in ERBB2, which essentially turns HER2 into an active receptor, are found in 2%-4% of breast cancers, including ER-positive, HER2-mutant breast cancers, and are enriched in lobular breast cancers, which are typically ER positive, HER2 negative.
What about tumor evolution, given the growing body of evidence that biomarker status in MBC can change over time?
Patients with MBC often have several active areas of cancer, and these areas will evolve differently. During each line of treatment, some metastases will develop resistance and others won’t. For instance, if my patient’s liver metastases start to grow, I will change therapy immediately. If, however, a single bone metastasis begins to grow and the liver metastases have responded well, I might consider local therapy — such as radiation — to target that bone metastasis, though this particular approach hasn’t been formally studied.
Ultimately, we can expect tumors to change over time as they become more biologically aggressive or resistant to current therapy. The most common biomarker change is probably loss of ER or PR expression, but the frequency of ER, PR, or HER2 biomarker changes is still not well understood.
Resistance mutations can also happen. When, for instance, activating mutations in ESR1 occur, the estrogen receptor becomes independent of estrogen and tumors then develop resistance to endocrine therapies. We see a similar problem arise in metastatic prostate cancer. With chronic testosterone deprivation, eventually the androgen receptor evolves to become independent of testosterone in a stage known as castrate-resistant prostate cancer.
Which biomarkers or combinations of biomarkers can be paired with an approved treatment?
We have a range of treatments targeting ER-positive and HER2-positive MBC in particular. For tumors harboring additional targetable mutations, preliminary data suggest that HER2-targeted tyrosine kinase inhibitors (TKIs), such as tucatinib and neratinib, are effective against activating mutations in ERBB2.
The PI3K inhibitor alpelisib in combination with fulvestrant has been approved for patients with ER-positive, HER2-negative MBC and mutations in PIK3CA. The mTOR inhibitor everolimus plus exemestane is an option for patients with ER-positive, HER2-negative. And for those with activating mutations in ESR1, I switch patients to a selective estrogen receptor degrader, such as fulvestrant.
PARP inhibitors, including olaparib or talazoparib, target metastatic HR-positive disease or TNBC with deleterious germline BRCA1 or BRCA2 mutations. Sacituzumab govitecan has been approved for treating metastatic TNBC and targets the cell surface protein TROP2, expressed in almost 90% of TNBC tumors.
What targets, on the other hand, are less informative for treatment choice?
When we order next-generation sequencing, we also will get a list of possible targets for which there are currently no therapeutic options, but there may be in the future. I find this knowledge is helpful. For example, an activating mutation in KRAS tells me that the cancer has a very strong oncogenic driver that I won›t be able to target. I know that activating KRAS mutations in lung cancer and colon cancer portend a poorer prognosis, which helps me to prepare the patient and family.
Atezolizumab in combination with paclitaxel has been FDA-approved for PD-L1 TNBC in the first-line setting, though data show that immune checkpoint inhibitors may be effective even without PD-L1 expression. Although cell surface protein TROP2 has emerged as a target in recent years, its expression is so common in TNBC that confirmatory testing for TROP2 expression is not required to prescribe sacituzumab govitecan.
What factors do you weigh when selecting among the large number of tests available for tumor testing?
We have many biomarker tests available, but the National Comprehensive Cancer Network does not have guidelines for tumor genetics testing in breast cancer. That means insurance does not have to cover the cost, and many companies don’t. Ultimately, though, drug companies and some testing companies have an incentive to cover the cost themselves because a companion diagnostic might be linked to their drug — therascreen PIK3CA RGQ PCR kit for alpelisib, for instance.
I tend not to use a companion diagnostic test because I want more information with a wider panel. The tumor tests I often use are FoundationOne CDx, Caris Molecular Intelligence, and Tempus. I use Tempus because their financial aid is very generous and almost all of my patients qualify to be tested for less than $100. For germline genetic testing, Invitae, Myriad, and Color are also options. Invitae and Color are about $250 out of pocket without insurance. Many academic centers have their own gene panels as well.
How far have we come in identifying biomarkers in MBC?
Targeted treatment for breast cancer has advanced significantly since doing my PhD research in cancer biology about 15 years ago. Of course, targeted therapies for ER-positive and HER2-amplified cancers were available at that point, but many more have been developed. The most significant advance has been the development of efficient and affordable genome sequencing, which has led to these large panels and identification of therapeutic targets. We’ve also expanded our knowledge of genetic predispositions for breast cancer beyond BRCA1 and BRCA2, which not only allows us to preemptively advise patients and their families about cancer risks and recommendations for cancer screening, but also to select a therapy to target a cancer’s DNA repair deficits.
I feel that we are in an exciting discovery phase in oncology. We currently rely on biomarkers to manage MBC and will continue to refine our strategies and develop more effective drug therapies as we identify more oncogenic drivers, tumor-specific proteins, and cancer cell vulnerabilities.
Key strategies for managing breast cancer brain metastases
Brain metastases remain a frequent and often fatal consequence of metastatic breast cancer (MBC). MBC carries a median survival of about 3 years, but that rate drops significantly when cancer cells move to the brain. A recent analysis estimates median survival in patients with brain metastases ranges from 6 months in triple-negative breast cancer (TNBC) to 21 months in human epidermal growth factor receptor 2 (HER2)–positive disease.
This news organization spoke to Kevin M. Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University, about the risk for brain metastases in patients with MBC, strategies for screening and treatment, and the work being done to achieve a better understanding of the disease.
Question: Before we dig into strategies to manage MBC brain metastasis, let’s talk about the risks. When and how often do brain metastases present in patients with MBC? What factors increase the likelihood of developing brain metastasis?
Dr. Kalinsky: The biggest risk factor for MBC spreading to the central nervous system (CNS), which includes the brain and spine, is breast cancer subtype. For patients with metastatic TNBC, the risk for brain metastasis can be more than 50%. For patients with HER2-positive disease, the risk may be slightly lower, with estimates in the range of 25%-50%, whereas the likelihood of brain metastasis in patients with hormone receptor–positive MBC is significantly lower at close to 14%. In addition, patients with metastatic TNBC may have brain metastases a little earlier in their disease progression compared with patients with HER2-positive or estrogen receptor–positive breast cancers, where brain metastases generally develop a little later in the disease course.
At what point is it recommended to screen patients with MBC for brain metastasis?
Current guidelines suggest that we scan for brain metastasis in the presence of new neurologic symptoms, such as headache, dizziness, or weakness in the arms or legs. MRI, in particular, is useful for evaluating brain metastasis, especially for smaller lesions, but lesions are sometimes detected through CT imaging of the head, too.
That’s where the guidelines are now. But as our systemic agents improve, there’s always the possibility these recommendations will be revisited and potentially include imaging as screening tools in asymptomatic patients, as well.
How do you assess which patients with MBC should receive local therapy?
Increasingly, because our systemic therapies in breast cancer are getting better in terms of crossing the blood-brain barrier, we think about local therapy on a case-by-case basis. We think about it with the question of whether we delay surgery or radiation — whole brain radiation, in particular — given concerns surrounding the side effects of these modalities, namely cognitive dysfunction for radiation and increased risk of bleeding and infection for surgery.
Giving a patient-directed local therapy, such as Gamma Knife radiosurgery or whole-brain radiotherapy, ultimately depends on the burden of brain metastasis, the status of systemic disease outside of the brain, and the number and size of the lesions seen on imaging. If, for instance, a patient has a large lesion that will immediately impact their neurologic status, we may opt to resect the lesion. If there are innumerable lesions, some of which are large, we may do whole-brain radiotherapy. If, however, a patient has systemic disease that is largely under control but is experiencing local progression in the brain, we may use local radiotherapy while continuing systemic therapy.
What about systemic therapies that cross the blood-brain barrier? What’s available now and how do you choose among the options?The subtype of breast cancer informs treatment with systemic therapies. For instance, patients with HER2-positive disease may receive oral tyrosine kinase inhibitors, such as tucatinib, neratinib, and lapatinib, which have strong CNS penetration. For patients with estrogen receptor–positive, HER2-negative MBC, estrogen therapies including aromatase inhibitors, as well as targeted therapies such as the mTOR inhibitor everolimus, have good CNS penetration. For patients with metastatic TNBC, we have chemotherapies that cross the blood-brain barrier, such as capecitabine and platinum-based chemotherapy.
Evidence suggests that tumors in the brain may harbor different genetic abnormalities from tumors in the breast. How do you consider the potential genetic heterogeneity in CNS tumors vs. the primary breast tumor?When a patient’s disease has spread to the brain, we may preferentially use agents we know cross the blood-brain barrier, so we can obtain systemic control both intracranially and extracranially. If we have already resected or biopsied cancerous brain tissue, it’s good to check the tumor’s estrogen receptor, progesterone receptor, and HER2 status and do next-generation sequencing to see if the tumor has any other targetable mutations, such as PIK3CA mutations.
But when a patient has multiple lesions, we don’t go in and biopsy all of them to check for heterogeneity. We have to make decisions based on samples we have. In cases where we start systemic therapy and notice one lesion is not responding to these agents while others are, the nonresponsive lesion may be an outlier in terms of its biologic characteristics. It may be worth targeting that lesion for biopsy and further sequencing to determine the next best systemic approach.
How do quality of life considerations factor into the management of patients with MBC brain metastases?
We use a multidisciplinary approach when treating patients. This means patient care involves a team of experts, which can include medical oncologists, radiation oncologists, and neuro-oncologists who help determine a treatment plan that takes factors such as survival and quality of life into account.
This is why, for example, we try to delay whole brain radiotherapy when we can. The HER2CLIMB study, which led to the approval of tucatinib as a treatment option for patients with HER2-positive MBC, showed us that patients with treated or untreated brain metastases receiving systemic therapy before local therapy could benefit from the combination of tucatinib, trastuzumab, and capecitabine. These patients exhibited a median progression-free survival of 7.6 months compared with 5.4 months in the placebo group.
HER2CLIMB has been practice changing because it showed us that tucatinib has good CNS activity in patients with brain metastases. The HER2CLIMB findings raise an important question: As our systemic therapies improve, how aggressive do we need to be with local therapy? Can we push off modalities like whole-brain radiotherapy, which are associated with toxicity?
This study also highlights how important it is for patients with metastatic disease to seek clinical trials. Although some trials exclude patients with brain metastases and others may have criteria that require the stability of brain metastasis for a certain amount of time, the knowledge gained can be invaluable.
Where are some of the main gaps in our understanding of brain metastases in patients with MBC?
One issue is our understanding of tropism to the brain. In other words, why does MBC spread to the brain? Once we understand this key piece, we can work on developing more effective therapies and therapeutic combinations to block brain metastasis.
For hormone receptor–positive disease, in particular, a central question is whether the current antiestrogen therapies — such as selective estrogen receptor degraders like fulvestrant, as well as targeted AKT inhibitors — have the potential to affect brain tumor activity. The same holds true for TNBC, where antibody drug conjugates and immunotherapies are being evaluated for treatment of brain tumors. For patients with HER2-positive MBC that has spread to the brain, understanding the continued role for tyrosine kinase inhibitors, such as tucatinib and neratinib, as well as whether antibody drug conjugates, including trastuzumab deruxtecan and trastuzumab emtansine, have CNS activity are important areas to explore further.
The CompassHER2 trial, going on now, is randomizing patients with residual HER2-positive disease after neoadjuvant chemotherapy and HER2-targeted therapy to receive trastuzumab emtansine with or without tucatinib. One of the core questions of this study is whether trastuzumab emtansine/tucatinib lowers the rate of brain metastasis and the incidence of systemic metastasis.
Another area in MBC that requires greater scrutiny is patients who develop leptomeningeal disease, which is when cancer cells spread to the cerebrospinal fluid. These patients have a particularly poor prognosis, and it would be helpful to evaluate the efficacy of existing therapies, but these patients are often excluded from clinical trials.
Overall, the ultimate goal in these endeavors is to decrease the rate of metastasis to the brain and improve survival and quality of life in patients with MBC who do experience brain metastases.
A version of this article first appeared on Medscape.com.
Brain metastases remain a frequent and often fatal consequence of metastatic breast cancer (MBC). MBC carries a median survival of about 3 years, but that rate drops significantly when cancer cells move to the brain. A recent analysis estimates median survival in patients with brain metastases ranges from 6 months in triple-negative breast cancer (TNBC) to 21 months in human epidermal growth factor receptor 2 (HER2)–positive disease.
This news organization spoke to Kevin M. Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University, about the risk for brain metastases in patients with MBC, strategies for screening and treatment, and the work being done to achieve a better understanding of the disease.
Question: Before we dig into strategies to manage MBC brain metastasis, let’s talk about the risks. When and how often do brain metastases present in patients with MBC? What factors increase the likelihood of developing brain metastasis?
Dr. Kalinsky: The biggest risk factor for MBC spreading to the central nervous system (CNS), which includes the brain and spine, is breast cancer subtype. For patients with metastatic TNBC, the risk for brain metastasis can be more than 50%. For patients with HER2-positive disease, the risk may be slightly lower, with estimates in the range of 25%-50%, whereas the likelihood of brain metastasis in patients with hormone receptor–positive MBC is significantly lower at close to 14%. In addition, patients with metastatic TNBC may have brain metastases a little earlier in their disease progression compared with patients with HER2-positive or estrogen receptor–positive breast cancers, where brain metastases generally develop a little later in the disease course.
At what point is it recommended to screen patients with MBC for brain metastasis?
Current guidelines suggest that we scan for brain metastasis in the presence of new neurologic symptoms, such as headache, dizziness, or weakness in the arms or legs. MRI, in particular, is useful for evaluating brain metastasis, especially for smaller lesions, but lesions are sometimes detected through CT imaging of the head, too.
That’s where the guidelines are now. But as our systemic agents improve, there’s always the possibility these recommendations will be revisited and potentially include imaging as screening tools in asymptomatic patients, as well.
How do you assess which patients with MBC should receive local therapy?
Increasingly, because our systemic therapies in breast cancer are getting better in terms of crossing the blood-brain barrier, we think about local therapy on a case-by-case basis. We think about it with the question of whether we delay surgery or radiation — whole brain radiation, in particular — given concerns surrounding the side effects of these modalities, namely cognitive dysfunction for radiation and increased risk of bleeding and infection for surgery.
Giving a patient-directed local therapy, such as Gamma Knife radiosurgery or whole-brain radiotherapy, ultimately depends on the burden of brain metastasis, the status of systemic disease outside of the brain, and the number and size of the lesions seen on imaging. If, for instance, a patient has a large lesion that will immediately impact their neurologic status, we may opt to resect the lesion. If there are innumerable lesions, some of which are large, we may do whole-brain radiotherapy. If, however, a patient has systemic disease that is largely under control but is experiencing local progression in the brain, we may use local radiotherapy while continuing systemic therapy.
What about systemic therapies that cross the blood-brain barrier? What’s available now and how do you choose among the options?The subtype of breast cancer informs treatment with systemic therapies. For instance, patients with HER2-positive disease may receive oral tyrosine kinase inhibitors, such as tucatinib, neratinib, and lapatinib, which have strong CNS penetration. For patients with estrogen receptor–positive, HER2-negative MBC, estrogen therapies including aromatase inhibitors, as well as targeted therapies such as the mTOR inhibitor everolimus, have good CNS penetration. For patients with metastatic TNBC, we have chemotherapies that cross the blood-brain barrier, such as capecitabine and platinum-based chemotherapy.
Evidence suggests that tumors in the brain may harbor different genetic abnormalities from tumors in the breast. How do you consider the potential genetic heterogeneity in CNS tumors vs. the primary breast tumor?When a patient’s disease has spread to the brain, we may preferentially use agents we know cross the blood-brain barrier, so we can obtain systemic control both intracranially and extracranially. If we have already resected or biopsied cancerous brain tissue, it’s good to check the tumor’s estrogen receptor, progesterone receptor, and HER2 status and do next-generation sequencing to see if the tumor has any other targetable mutations, such as PIK3CA mutations.
But when a patient has multiple lesions, we don’t go in and biopsy all of them to check for heterogeneity. We have to make decisions based on samples we have. In cases where we start systemic therapy and notice one lesion is not responding to these agents while others are, the nonresponsive lesion may be an outlier in terms of its biologic characteristics. It may be worth targeting that lesion for biopsy and further sequencing to determine the next best systemic approach.
How do quality of life considerations factor into the management of patients with MBC brain metastases?
We use a multidisciplinary approach when treating patients. This means patient care involves a team of experts, which can include medical oncologists, radiation oncologists, and neuro-oncologists who help determine a treatment plan that takes factors such as survival and quality of life into account.
This is why, for example, we try to delay whole brain radiotherapy when we can. The HER2CLIMB study, which led to the approval of tucatinib as a treatment option for patients with HER2-positive MBC, showed us that patients with treated or untreated brain metastases receiving systemic therapy before local therapy could benefit from the combination of tucatinib, trastuzumab, and capecitabine. These patients exhibited a median progression-free survival of 7.6 months compared with 5.4 months in the placebo group.
HER2CLIMB has been practice changing because it showed us that tucatinib has good CNS activity in patients with brain metastases. The HER2CLIMB findings raise an important question: As our systemic therapies improve, how aggressive do we need to be with local therapy? Can we push off modalities like whole-brain radiotherapy, which are associated with toxicity?
This study also highlights how important it is for patients with metastatic disease to seek clinical trials. Although some trials exclude patients with brain metastases and others may have criteria that require the stability of brain metastasis for a certain amount of time, the knowledge gained can be invaluable.
Where are some of the main gaps in our understanding of brain metastases in patients with MBC?
One issue is our understanding of tropism to the brain. In other words, why does MBC spread to the brain? Once we understand this key piece, we can work on developing more effective therapies and therapeutic combinations to block brain metastasis.
For hormone receptor–positive disease, in particular, a central question is whether the current antiestrogen therapies — such as selective estrogen receptor degraders like fulvestrant, as well as targeted AKT inhibitors — have the potential to affect brain tumor activity. The same holds true for TNBC, where antibody drug conjugates and immunotherapies are being evaluated for treatment of brain tumors. For patients with HER2-positive MBC that has spread to the brain, understanding the continued role for tyrosine kinase inhibitors, such as tucatinib and neratinib, as well as whether antibody drug conjugates, including trastuzumab deruxtecan and trastuzumab emtansine, have CNS activity are important areas to explore further.
The CompassHER2 trial, going on now, is randomizing patients with residual HER2-positive disease after neoadjuvant chemotherapy and HER2-targeted therapy to receive trastuzumab emtansine with or without tucatinib. One of the core questions of this study is whether trastuzumab emtansine/tucatinib lowers the rate of brain metastasis and the incidence of systemic metastasis.
Another area in MBC that requires greater scrutiny is patients who develop leptomeningeal disease, which is when cancer cells spread to the cerebrospinal fluid. These patients have a particularly poor prognosis, and it would be helpful to evaluate the efficacy of existing therapies, but these patients are often excluded from clinical trials.
Overall, the ultimate goal in these endeavors is to decrease the rate of metastasis to the brain and improve survival and quality of life in patients with MBC who do experience brain metastases.
A version of this article first appeared on Medscape.com.
Brain metastases remain a frequent and often fatal consequence of metastatic breast cancer (MBC). MBC carries a median survival of about 3 years, but that rate drops significantly when cancer cells move to the brain. A recent analysis estimates median survival in patients with brain metastases ranges from 6 months in triple-negative breast cancer (TNBC) to 21 months in human epidermal growth factor receptor 2 (HER2)–positive disease.
This news organization spoke to Kevin M. Kalinsky, MD, acting associate professor in the department of hematology and medical oncology at Emory University School of Medicine in Atlanta and director of the Glenn Family Breast Center at the Winship Cancer Institute of Emory University, about the risk for brain metastases in patients with MBC, strategies for screening and treatment, and the work being done to achieve a better understanding of the disease.
Question: Before we dig into strategies to manage MBC brain metastasis, let’s talk about the risks. When and how often do brain metastases present in patients with MBC? What factors increase the likelihood of developing brain metastasis?
Dr. Kalinsky: The biggest risk factor for MBC spreading to the central nervous system (CNS), which includes the brain and spine, is breast cancer subtype. For patients with metastatic TNBC, the risk for brain metastasis can be more than 50%. For patients with HER2-positive disease, the risk may be slightly lower, with estimates in the range of 25%-50%, whereas the likelihood of brain metastasis in patients with hormone receptor–positive MBC is significantly lower at close to 14%. In addition, patients with metastatic TNBC may have brain metastases a little earlier in their disease progression compared with patients with HER2-positive or estrogen receptor–positive breast cancers, where brain metastases generally develop a little later in the disease course.
At what point is it recommended to screen patients with MBC for brain metastasis?
Current guidelines suggest that we scan for brain metastasis in the presence of new neurologic symptoms, such as headache, dizziness, or weakness in the arms or legs. MRI, in particular, is useful for evaluating brain metastasis, especially for smaller lesions, but lesions are sometimes detected through CT imaging of the head, too.
That’s where the guidelines are now. But as our systemic agents improve, there’s always the possibility these recommendations will be revisited and potentially include imaging as screening tools in asymptomatic patients, as well.
How do you assess which patients with MBC should receive local therapy?
Increasingly, because our systemic therapies in breast cancer are getting better in terms of crossing the blood-brain barrier, we think about local therapy on a case-by-case basis. We think about it with the question of whether we delay surgery or radiation — whole brain radiation, in particular — given concerns surrounding the side effects of these modalities, namely cognitive dysfunction for radiation and increased risk of bleeding and infection for surgery.
Giving a patient-directed local therapy, such as Gamma Knife radiosurgery or whole-brain radiotherapy, ultimately depends on the burden of brain metastasis, the status of systemic disease outside of the brain, and the number and size of the lesions seen on imaging. If, for instance, a patient has a large lesion that will immediately impact their neurologic status, we may opt to resect the lesion. If there are innumerable lesions, some of which are large, we may do whole-brain radiotherapy. If, however, a patient has systemic disease that is largely under control but is experiencing local progression in the brain, we may use local radiotherapy while continuing systemic therapy.
What about systemic therapies that cross the blood-brain barrier? What’s available now and how do you choose among the options?The subtype of breast cancer informs treatment with systemic therapies. For instance, patients with HER2-positive disease may receive oral tyrosine kinase inhibitors, such as tucatinib, neratinib, and lapatinib, which have strong CNS penetration. For patients with estrogen receptor–positive, HER2-negative MBC, estrogen therapies including aromatase inhibitors, as well as targeted therapies such as the mTOR inhibitor everolimus, have good CNS penetration. For patients with metastatic TNBC, we have chemotherapies that cross the blood-brain barrier, such as capecitabine and platinum-based chemotherapy.
Evidence suggests that tumors in the brain may harbor different genetic abnormalities from tumors in the breast. How do you consider the potential genetic heterogeneity in CNS tumors vs. the primary breast tumor?When a patient’s disease has spread to the brain, we may preferentially use agents we know cross the blood-brain barrier, so we can obtain systemic control both intracranially and extracranially. If we have already resected or biopsied cancerous brain tissue, it’s good to check the tumor’s estrogen receptor, progesterone receptor, and HER2 status and do next-generation sequencing to see if the tumor has any other targetable mutations, such as PIK3CA mutations.
But when a patient has multiple lesions, we don’t go in and biopsy all of them to check for heterogeneity. We have to make decisions based on samples we have. In cases where we start systemic therapy and notice one lesion is not responding to these agents while others are, the nonresponsive lesion may be an outlier in terms of its biologic characteristics. It may be worth targeting that lesion for biopsy and further sequencing to determine the next best systemic approach.
How do quality of life considerations factor into the management of patients with MBC brain metastases?
We use a multidisciplinary approach when treating patients. This means patient care involves a team of experts, which can include medical oncologists, radiation oncologists, and neuro-oncologists who help determine a treatment plan that takes factors such as survival and quality of life into account.
This is why, for example, we try to delay whole brain radiotherapy when we can. The HER2CLIMB study, which led to the approval of tucatinib as a treatment option for patients with HER2-positive MBC, showed us that patients with treated or untreated brain metastases receiving systemic therapy before local therapy could benefit from the combination of tucatinib, trastuzumab, and capecitabine. These patients exhibited a median progression-free survival of 7.6 months compared with 5.4 months in the placebo group.
HER2CLIMB has been practice changing because it showed us that tucatinib has good CNS activity in patients with brain metastases. The HER2CLIMB findings raise an important question: As our systemic therapies improve, how aggressive do we need to be with local therapy? Can we push off modalities like whole-brain radiotherapy, which are associated with toxicity?
This study also highlights how important it is for patients with metastatic disease to seek clinical trials. Although some trials exclude patients with brain metastases and others may have criteria that require the stability of brain metastasis for a certain amount of time, the knowledge gained can be invaluable.
Where are some of the main gaps in our understanding of brain metastases in patients with MBC?
One issue is our understanding of tropism to the brain. In other words, why does MBC spread to the brain? Once we understand this key piece, we can work on developing more effective therapies and therapeutic combinations to block brain metastasis.
For hormone receptor–positive disease, in particular, a central question is whether the current antiestrogen therapies — such as selective estrogen receptor degraders like fulvestrant, as well as targeted AKT inhibitors — have the potential to affect brain tumor activity. The same holds true for TNBC, where antibody drug conjugates and immunotherapies are being evaluated for treatment of brain tumors. For patients with HER2-positive MBC that has spread to the brain, understanding the continued role for tyrosine kinase inhibitors, such as tucatinib and neratinib, as well as whether antibody drug conjugates, including trastuzumab deruxtecan and trastuzumab emtansine, have CNS activity are important areas to explore further.
The CompassHER2 trial, going on now, is randomizing patients with residual HER2-positive disease after neoadjuvant chemotherapy and HER2-targeted therapy to receive trastuzumab emtansine with or without tucatinib. One of the core questions of this study is whether trastuzumab emtansine/tucatinib lowers the rate of brain metastasis and the incidence of systemic metastasis.
Another area in MBC that requires greater scrutiny is patients who develop leptomeningeal disease, which is when cancer cells spread to the cerebrospinal fluid. These patients have a particularly poor prognosis, and it would be helpful to evaluate the efficacy of existing therapies, but these patients are often excluded from clinical trials.
Overall, the ultimate goal in these endeavors is to decrease the rate of metastasis to the brain and improve survival and quality of life in patients with MBC who do experience brain metastases.
A version of this article first appeared on Medscape.com.