User login
Vaccine update: The latest from ACIP
The 2013 immunization schedules have been published by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP).1,2 Perhaps the most noticeable change is a single schedule for infants, children, and adolescents, instead of the previous 2 schedules (for those ages 0-6 years, and for those ages 7-18 years). Other major new recommendations include the following:
- tetanus-diphtheria-pertussis (Tdap) vaccine for individuals ≥65 years of age
- Tdap for pregnant women during every pregnancy
- meningococcal conjugate vaccine for high-risk infants and children
- pneumococcal conjugate vaccine for high-risk adults.
There are also minor changes in recommendations for the use of measles, mumps, and rubella (MMR) vaccine among those with human immunodeficiency virus (HIV) infection. The new immunization schedules can be found on the CDC’s immunization Web site, at http://www.cdc.gov/vaccines/schedules/index.html.
Previous Practice Alerts have reported on recommendation changes made throughout 2012, including removal of egg allergy as a contraindication for influenza vaccine for those who experience only hives after eating eggs,3 the addition of a simplified algorithm for deciding whether children younger than 9 years need one or 2 doses of influenza vaccine,3 and the addition of human papillomavirus vaccine as a routine recommendation for males ages 11 to 21 years.4
Tdap: Some recommendations are off label
Given the continuing elevated rates of pertussis in the United States and our understanding about the duration of protection and safety of the Tdap vaccine, ACIP has made new recommendations for the use of Tdap, including some off-label uses. Two Tdap products are available: Boostrix, approved for individuals ≥10 years, and Adacel, approved for individuals 11 to 64 years (TABLE 1).5 ACIP states that those ≥65 years may be vaccinated with Tdap, and that an opportunity for vaccination should not be missed; Adacel can be substituted if it is the only product available. To control the spread of pertussis to the most vulnerable, it is especially important to immunize grandparents, childcare providers, and those who are around infants.
TABLE 1
Available tetanus-diphtheria-pertussis vaccines5
| Trade name | Manufacturer | FDA-approved age for use* (y) | Pertussis antigens (mcg) | Diphtheria toxoid (Lf) | Tetanus toxoid (Lf) | |||
|---|---|---|---|---|---|---|---|---|
| PT | FHA | PRN | FIM | |||||
| Boostrix | GlaxoSmithKline Biologicals | ≥10 | 8 | 8 | 2.5 | — | 2.5 | 5 |
| Adacel | Sanofi Pasteur | 11-64 | 2.5 | 5 | 3 | 5† | 2 | 5 |
| FDA, Food and Drug Administration; FHA, filamentous hemagglutinin; FIM, fimbriae; Lf, limit of flocculation units; PRN, pertactin; PT, pertussis toxin. *Indicated as a single dose. †Types 2 and 3. | ||||||||
Wound management. If a tetanus booster is indicated for wound management in an individual ≥19 years who has never received Tdap, this product is preferred to Td.5 There is now no suggested minimum time interval for administering Tdap after Td. Currently only one dose of Tdap is recommended for adults (except for pregnant women, as described in the next section). But this may change as time passes and we learn more about the duration of protection from the acellular pertussis antigen in the vaccine.
Pregnancy. ACIP first recommended the use of Tdap during pregnancy in October 2011, in an attempt to provide protection for newborns through the transfer of maternal antibodies to the fetus.6 Recent evidence indicates that the duration of protective antibody levels wanes between pregnancies and may not be high enough to protect a newborn in subsequent pregnancies.7 ACIP voted in October 2012 to recommend Tdap for pregnant women during each pregnancy, at the gestational age of 27 through 36 weeks. If a mother does not receive Tdap during pregnancy and has never received it, she should be vaccinated soon after delivery.
The safety data for serial vaccination with Tdap in pregnant women is sparse, and ACIP considered this concern. In the opinion of ACIP, the potential benefits to the newborn, coupled with the high rate of pertussis, outweigh this concern, and efforts will be made to monitor for safety issues. If the rate of pertussis declines, ACIP will likely revisit this recommendation.
Meningococcal vaccine: No routine immunization for infants
A previous Practice Alert described 3 new products to protect infants and children against meningococcal disease, and identified issues that make recommendations about their use difficult at a time when rates of meningococcal disease in this age group are very low.8 At its October 2012 meeting, ACIP considered one of these products, HibMenCY (MenHibrix), which contains antigens against meningococcal serogroups C and Y and Haemophilus influenzae B (Hib).
ACIP voted not to recommend routine immunization against meningococcal disease in infants. However, HibMenCY was recommended for high-risk infants, and it was noted that it can be used as an Hib vaccine. The details of the recommendation appear in “When should you use HibMenCY in infants?”.9 The current recommendation also includes vaccinating high-risk infants ages 9 through 23 months with 2 doses of MenACWY-D (Menactra) with at least 8 weeks between doses. Only one of these products should be used, and ACIP does not cite a preference between them.
Vaccinate infants at increased risk for meningococcal disease with 4 doses of HibMenCY at 2, 4, 6, and 12-15 months. Candidates for vaccination are infants with recognized persistent complement pathway deficiencies and infants who have anatomic or functional asplenia (including sickle cell disease).
HibMenCY can also be used for infants ages 2-18 months in communities with serogroup C and Y meningococcal disease outbreaks for which vaccination is recommended.
ACIP does not recommend routine meningococcal vaccination for infants.
HibMenCY is safe and immunogenic and may be administered to infants to complete the routine Hib vaccination series. If HibMenCY is used to achieve protection against serogroups C and Y, HibMenCY should be used for all 4 doses of Hib vaccine.
Pneumococcal conjugate vaccine recommended for high-risk adults
There are now 2 products that provide protection for adults against pneumococcal disease: a 23-valent polysaccharide product (PPSV23) and a 13-valent conjugate product (PCV13). PPSV23 is recommended for all adults ≥65 years and for those <65 who are at high risk for pneumococcal disease or complications from pneumococcal disease. While PCV13 is approved by the FDA for all adults ≥50 years, ACIP recommends it only for those at higher risk for pneumococcal disease.10
ACIP also recommends that those at risk should receive both PCV13 and PPSV23. Give PCV13 first, followed by PPSV23 2 months later.10 However, if PPSV23 is given first, administer PCV13 12 months later. To complicate matters, for some risk categories it is recommended that patients receive a second dose of PPSV23 5 years after the first one. No more than 2 doses of PPSV23 should be given prior to age 65. This complicated set of recommendations is summarized in TABLE 2.10
TABLE 2
Indications for using pneumococcal vaccines in adults ≥19 years*10
| Risk group | Underlying medical conditions | PCV13 | PPSV23 | |
|---|---|---|---|---|
| Recommended | Recommended | Revaccination 5 years after first dose | ||
| Immunocompetent individuals | Chronic heart disease† | √ | ||
| Chronic lung disease‡ | √ | |||
| Diabetes mellitus | √ | |||
| Cerebrospinal fluid leak | √ | √ | ||
| Cochlear implant | √ | √ | ||
| Alcoholism | √ | |||
| Chronic liver disease, cirrhosis | √ | |||
| Cigarette smoking | √ | |||
| Individuals with functional or anatomic asplenia | Sickle cell disease/other hemoglobinopathy | √ | √ | √ |
| Congenital or acquired asplenia | √ | √ | √ | |
| Immunocompromised individuals | Congenital or acquired immunodeficiency§ | √ | √ | √ |
| Human immunodeficiency virus infection | √ | √ | √ | |
| Chronic renal failure | √ | √ | √ | |
| Nephrotic syndrome | √ | √ | √ | |
| Leukemia | √ | √ | √ | |
| Lymphoma | √ | √ | √ | |
| Hodgkin disease | √ | √ | √ | |
| Generalized malignancy | √ | √ | √ | |
| Iatrogenic immunosuppression|| | √ | √ | √ | |
| Solid organ transplant | √ | √ | √ | |
| Multiple myeloma | √ | √ | √ | |
| PCV13, 13-valent pneumococcal conjugate vaccine; PPSV23, 23-valent pneumococcal polysaccharide vaccine. *All adults ≥65 years should receive a dose of PPSV23, regardless of previous history of vaccination with pneumococcal vaccine. †Including congestive heart failure and cardiomyopathies; excluding hypertension. ‡Including chronic obstructive pulmonary disease, emphysema, and asthma. §Including B- (humoral) or T-lymphocyte deficiency, complement deficiencies (particularly C1, C2, C3, and C4 deficiencies), and phagocytic disorders (excluding chronic granulomatous disease). ||Diseases requiring treatment with immunosuppressive drugs, including long-term systemic corticosteroids and radiation therapy. | ||||
MMR for those with HIV and use of IG for measles prevention
The last set of significant changes to the schedules are updated recommendations for the use of MMR vaccine in those who have HIV infection, and the use of immune globulin to prevent measles in those previously unvaccinated who are exposed to the disease. Details of these recommendations can be found at http://www.cdc.gov/vaccines/recs/provisional/downloads/mmr-Oct-2012.pdf.
1. CDC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedules for persons aged 0 through 18 years—United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:2-8.
2. CDC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for adults aged 19 years and older—United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:9-19.
3. Campos-Outcalt D. Battling influenza: changes for the 2012-2013 season. J Fam Pract. 2012;61:606-609.
4. Campos-Outcalt D. HPV is now routinely recommended for males. J Fam Pract. 2012;61:38-40.
5. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2012;61:468-470.
6. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1424-1426.
7. Liang JL. Review of evidence considered for pregnancy Tdap recommendation. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 24, 2012; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2012/02-pertussis-Liang.pdf. Accessed December 15, 2012.
8. Campos-Outcalt D. Meningococcal vaccine for infants? J Fam Pract. 2012;61:482-484.
9. Cohn A. Considerations for use of meningococcal conjugate vaccines in infants. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 24, 2012; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2012/04-MCV-Cohn.pdf. Accessed February 8, 2013.
10. CDC. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816-819.
The 2013 immunization schedules have been published by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP).1,2 Perhaps the most noticeable change is a single schedule for infants, children, and adolescents, instead of the previous 2 schedules (for those ages 0-6 years, and for those ages 7-18 years). Other major new recommendations include the following:
- tetanus-diphtheria-pertussis (Tdap) vaccine for individuals ≥65 years of age
- Tdap for pregnant women during every pregnancy
- meningococcal conjugate vaccine for high-risk infants and children
- pneumococcal conjugate vaccine for high-risk adults.
There are also minor changes in recommendations for the use of measles, mumps, and rubella (MMR) vaccine among those with human immunodeficiency virus (HIV) infection. The new immunization schedules can be found on the CDC’s immunization Web site, at http://www.cdc.gov/vaccines/schedules/index.html.
Previous Practice Alerts have reported on recommendation changes made throughout 2012, including removal of egg allergy as a contraindication for influenza vaccine for those who experience only hives after eating eggs,3 the addition of a simplified algorithm for deciding whether children younger than 9 years need one or 2 doses of influenza vaccine,3 and the addition of human papillomavirus vaccine as a routine recommendation for males ages 11 to 21 years.4
Tdap: Some recommendations are off label
Given the continuing elevated rates of pertussis in the United States and our understanding about the duration of protection and safety of the Tdap vaccine, ACIP has made new recommendations for the use of Tdap, including some off-label uses. Two Tdap products are available: Boostrix, approved for individuals ≥10 years, and Adacel, approved for individuals 11 to 64 years (TABLE 1).5 ACIP states that those ≥65 years may be vaccinated with Tdap, and that an opportunity for vaccination should not be missed; Adacel can be substituted if it is the only product available. To control the spread of pertussis to the most vulnerable, it is especially important to immunize grandparents, childcare providers, and those who are around infants.
TABLE 1
Available tetanus-diphtheria-pertussis vaccines5
| Trade name | Manufacturer | FDA-approved age for use* (y) | Pertussis antigens (mcg) | Diphtheria toxoid (Lf) | Tetanus toxoid (Lf) | |||
|---|---|---|---|---|---|---|---|---|
| PT | FHA | PRN | FIM | |||||
| Boostrix | GlaxoSmithKline Biologicals | ≥10 | 8 | 8 | 2.5 | — | 2.5 | 5 |
| Adacel | Sanofi Pasteur | 11-64 | 2.5 | 5 | 3 | 5† | 2 | 5 |
| FDA, Food and Drug Administration; FHA, filamentous hemagglutinin; FIM, fimbriae; Lf, limit of flocculation units; PRN, pertactin; PT, pertussis toxin. *Indicated as a single dose. †Types 2 and 3. | ||||||||
Wound management. If a tetanus booster is indicated for wound management in an individual ≥19 years who has never received Tdap, this product is preferred to Td.5 There is now no suggested minimum time interval for administering Tdap after Td. Currently only one dose of Tdap is recommended for adults (except for pregnant women, as described in the next section). But this may change as time passes and we learn more about the duration of protection from the acellular pertussis antigen in the vaccine.
Pregnancy. ACIP first recommended the use of Tdap during pregnancy in October 2011, in an attempt to provide protection for newborns through the transfer of maternal antibodies to the fetus.6 Recent evidence indicates that the duration of protective antibody levels wanes between pregnancies and may not be high enough to protect a newborn in subsequent pregnancies.7 ACIP voted in October 2012 to recommend Tdap for pregnant women during each pregnancy, at the gestational age of 27 through 36 weeks. If a mother does not receive Tdap during pregnancy and has never received it, she should be vaccinated soon after delivery.
The safety data for serial vaccination with Tdap in pregnant women is sparse, and ACIP considered this concern. In the opinion of ACIP, the potential benefits to the newborn, coupled with the high rate of pertussis, outweigh this concern, and efforts will be made to monitor for safety issues. If the rate of pertussis declines, ACIP will likely revisit this recommendation.
Meningococcal vaccine: No routine immunization for infants
A previous Practice Alert described 3 new products to protect infants and children against meningococcal disease, and identified issues that make recommendations about their use difficult at a time when rates of meningococcal disease in this age group are very low.8 At its October 2012 meeting, ACIP considered one of these products, HibMenCY (MenHibrix), which contains antigens against meningococcal serogroups C and Y and Haemophilus influenzae B (Hib).
ACIP voted not to recommend routine immunization against meningococcal disease in infants. However, HibMenCY was recommended for high-risk infants, and it was noted that it can be used as an Hib vaccine. The details of the recommendation appear in “When should you use HibMenCY in infants?”.9 The current recommendation also includes vaccinating high-risk infants ages 9 through 23 months with 2 doses of MenACWY-D (Menactra) with at least 8 weeks between doses. Only one of these products should be used, and ACIP does not cite a preference between them.
Vaccinate infants at increased risk for meningococcal disease with 4 doses of HibMenCY at 2, 4, 6, and 12-15 months. Candidates for vaccination are infants with recognized persistent complement pathway deficiencies and infants who have anatomic or functional asplenia (including sickle cell disease).
HibMenCY can also be used for infants ages 2-18 months in communities with serogroup C and Y meningococcal disease outbreaks for which vaccination is recommended.
ACIP does not recommend routine meningococcal vaccination for infants.
HibMenCY is safe and immunogenic and may be administered to infants to complete the routine Hib vaccination series. If HibMenCY is used to achieve protection against serogroups C and Y, HibMenCY should be used for all 4 doses of Hib vaccine.
Pneumococcal conjugate vaccine recommended for high-risk adults
There are now 2 products that provide protection for adults against pneumococcal disease: a 23-valent polysaccharide product (PPSV23) and a 13-valent conjugate product (PCV13). PPSV23 is recommended for all adults ≥65 years and for those <65 who are at high risk for pneumococcal disease or complications from pneumococcal disease. While PCV13 is approved by the FDA for all adults ≥50 years, ACIP recommends it only for those at higher risk for pneumococcal disease.10
ACIP also recommends that those at risk should receive both PCV13 and PPSV23. Give PCV13 first, followed by PPSV23 2 months later.10 However, if PPSV23 is given first, administer PCV13 12 months later. To complicate matters, for some risk categories it is recommended that patients receive a second dose of PPSV23 5 years after the first one. No more than 2 doses of PPSV23 should be given prior to age 65. This complicated set of recommendations is summarized in TABLE 2.10
TABLE 2
Indications for using pneumococcal vaccines in adults ≥19 years*10
| Risk group | Underlying medical conditions | PCV13 | PPSV23 | |
|---|---|---|---|---|
| Recommended | Recommended | Revaccination 5 years after first dose | ||
| Immunocompetent individuals | Chronic heart disease† | √ | ||
| Chronic lung disease‡ | √ | |||
| Diabetes mellitus | √ | |||
| Cerebrospinal fluid leak | √ | √ | ||
| Cochlear implant | √ | √ | ||
| Alcoholism | √ | |||
| Chronic liver disease, cirrhosis | √ | |||
| Cigarette smoking | √ | |||
| Individuals with functional or anatomic asplenia | Sickle cell disease/other hemoglobinopathy | √ | √ | √ |
| Congenital or acquired asplenia | √ | √ | √ | |
| Immunocompromised individuals | Congenital or acquired immunodeficiency§ | √ | √ | √ |
| Human immunodeficiency virus infection | √ | √ | √ | |
| Chronic renal failure | √ | √ | √ | |
| Nephrotic syndrome | √ | √ | √ | |
| Leukemia | √ | √ | √ | |
| Lymphoma | √ | √ | √ | |
| Hodgkin disease | √ | √ | √ | |
| Generalized malignancy | √ | √ | √ | |
| Iatrogenic immunosuppression|| | √ | √ | √ | |
| Solid organ transplant | √ | √ | √ | |
| Multiple myeloma | √ | √ | √ | |
| PCV13, 13-valent pneumococcal conjugate vaccine; PPSV23, 23-valent pneumococcal polysaccharide vaccine. *All adults ≥65 years should receive a dose of PPSV23, regardless of previous history of vaccination with pneumococcal vaccine. †Including congestive heart failure and cardiomyopathies; excluding hypertension. ‡Including chronic obstructive pulmonary disease, emphysema, and asthma. §Including B- (humoral) or T-lymphocyte deficiency, complement deficiencies (particularly C1, C2, C3, and C4 deficiencies), and phagocytic disorders (excluding chronic granulomatous disease). ||Diseases requiring treatment with immunosuppressive drugs, including long-term systemic corticosteroids and radiation therapy. | ||||
MMR for those with HIV and use of IG for measles prevention
The last set of significant changes to the schedules are updated recommendations for the use of MMR vaccine in those who have HIV infection, and the use of immune globulin to prevent measles in those previously unvaccinated who are exposed to the disease. Details of these recommendations can be found at http://www.cdc.gov/vaccines/recs/provisional/downloads/mmr-Oct-2012.pdf.
The 2013 immunization schedules have been published by the Centers for Disease Control and Prevention (CDC)’s Advisory Committee on Immunization Practices (ACIP).1,2 Perhaps the most noticeable change is a single schedule for infants, children, and adolescents, instead of the previous 2 schedules (for those ages 0-6 years, and for those ages 7-18 years). Other major new recommendations include the following:
- tetanus-diphtheria-pertussis (Tdap) vaccine for individuals ≥65 years of age
- Tdap for pregnant women during every pregnancy
- meningococcal conjugate vaccine for high-risk infants and children
- pneumococcal conjugate vaccine for high-risk adults.
There are also minor changes in recommendations for the use of measles, mumps, and rubella (MMR) vaccine among those with human immunodeficiency virus (HIV) infection. The new immunization schedules can be found on the CDC’s immunization Web site, at http://www.cdc.gov/vaccines/schedules/index.html.
Previous Practice Alerts have reported on recommendation changes made throughout 2012, including removal of egg allergy as a contraindication for influenza vaccine for those who experience only hives after eating eggs,3 the addition of a simplified algorithm for deciding whether children younger than 9 years need one or 2 doses of influenza vaccine,3 and the addition of human papillomavirus vaccine as a routine recommendation for males ages 11 to 21 years.4
Tdap: Some recommendations are off label
Given the continuing elevated rates of pertussis in the United States and our understanding about the duration of protection and safety of the Tdap vaccine, ACIP has made new recommendations for the use of Tdap, including some off-label uses. Two Tdap products are available: Boostrix, approved for individuals ≥10 years, and Adacel, approved for individuals 11 to 64 years (TABLE 1).5 ACIP states that those ≥65 years may be vaccinated with Tdap, and that an opportunity for vaccination should not be missed; Adacel can be substituted if it is the only product available. To control the spread of pertussis to the most vulnerable, it is especially important to immunize grandparents, childcare providers, and those who are around infants.
TABLE 1
Available tetanus-diphtheria-pertussis vaccines5
| Trade name | Manufacturer | FDA-approved age for use* (y) | Pertussis antigens (mcg) | Diphtheria toxoid (Lf) | Tetanus toxoid (Lf) | |||
|---|---|---|---|---|---|---|---|---|
| PT | FHA | PRN | FIM | |||||
| Boostrix | GlaxoSmithKline Biologicals | ≥10 | 8 | 8 | 2.5 | — | 2.5 | 5 |
| Adacel | Sanofi Pasteur | 11-64 | 2.5 | 5 | 3 | 5† | 2 | 5 |
| FDA, Food and Drug Administration; FHA, filamentous hemagglutinin; FIM, fimbriae; Lf, limit of flocculation units; PRN, pertactin; PT, pertussis toxin. *Indicated as a single dose. †Types 2 and 3. | ||||||||
Wound management. If a tetanus booster is indicated for wound management in an individual ≥19 years who has never received Tdap, this product is preferred to Td.5 There is now no suggested minimum time interval for administering Tdap after Td. Currently only one dose of Tdap is recommended for adults (except for pregnant women, as described in the next section). But this may change as time passes and we learn more about the duration of protection from the acellular pertussis antigen in the vaccine.
Pregnancy. ACIP first recommended the use of Tdap during pregnancy in October 2011, in an attempt to provide protection for newborns through the transfer of maternal antibodies to the fetus.6 Recent evidence indicates that the duration of protective antibody levels wanes between pregnancies and may not be high enough to protect a newborn in subsequent pregnancies.7 ACIP voted in October 2012 to recommend Tdap for pregnant women during each pregnancy, at the gestational age of 27 through 36 weeks. If a mother does not receive Tdap during pregnancy and has never received it, she should be vaccinated soon after delivery.
The safety data for serial vaccination with Tdap in pregnant women is sparse, and ACIP considered this concern. In the opinion of ACIP, the potential benefits to the newborn, coupled with the high rate of pertussis, outweigh this concern, and efforts will be made to monitor for safety issues. If the rate of pertussis declines, ACIP will likely revisit this recommendation.
Meningococcal vaccine: No routine immunization for infants
A previous Practice Alert described 3 new products to protect infants and children against meningococcal disease, and identified issues that make recommendations about their use difficult at a time when rates of meningococcal disease in this age group are very low.8 At its October 2012 meeting, ACIP considered one of these products, HibMenCY (MenHibrix), which contains antigens against meningococcal serogroups C and Y and Haemophilus influenzae B (Hib).
ACIP voted not to recommend routine immunization against meningococcal disease in infants. However, HibMenCY was recommended for high-risk infants, and it was noted that it can be used as an Hib vaccine. The details of the recommendation appear in “When should you use HibMenCY in infants?”.9 The current recommendation also includes vaccinating high-risk infants ages 9 through 23 months with 2 doses of MenACWY-D (Menactra) with at least 8 weeks between doses. Only one of these products should be used, and ACIP does not cite a preference between them.
Vaccinate infants at increased risk for meningococcal disease with 4 doses of HibMenCY at 2, 4, 6, and 12-15 months. Candidates for vaccination are infants with recognized persistent complement pathway deficiencies and infants who have anatomic or functional asplenia (including sickle cell disease).
HibMenCY can also be used for infants ages 2-18 months in communities with serogroup C and Y meningococcal disease outbreaks for which vaccination is recommended.
ACIP does not recommend routine meningococcal vaccination for infants.
HibMenCY is safe and immunogenic and may be administered to infants to complete the routine Hib vaccination series. If HibMenCY is used to achieve protection against serogroups C and Y, HibMenCY should be used for all 4 doses of Hib vaccine.
Pneumococcal conjugate vaccine recommended for high-risk adults
There are now 2 products that provide protection for adults against pneumococcal disease: a 23-valent polysaccharide product (PPSV23) and a 13-valent conjugate product (PCV13). PPSV23 is recommended for all adults ≥65 years and for those <65 who are at high risk for pneumococcal disease or complications from pneumococcal disease. While PCV13 is approved by the FDA for all adults ≥50 years, ACIP recommends it only for those at higher risk for pneumococcal disease.10
ACIP also recommends that those at risk should receive both PCV13 and PPSV23. Give PCV13 first, followed by PPSV23 2 months later.10 However, if PPSV23 is given first, administer PCV13 12 months later. To complicate matters, for some risk categories it is recommended that patients receive a second dose of PPSV23 5 years after the first one. No more than 2 doses of PPSV23 should be given prior to age 65. This complicated set of recommendations is summarized in TABLE 2.10
TABLE 2
Indications for using pneumococcal vaccines in adults ≥19 years*10
| Risk group | Underlying medical conditions | PCV13 | PPSV23 | |
|---|---|---|---|---|
| Recommended | Recommended | Revaccination 5 years after first dose | ||
| Immunocompetent individuals | Chronic heart disease† | √ | ||
| Chronic lung disease‡ | √ | |||
| Diabetes mellitus | √ | |||
| Cerebrospinal fluid leak | √ | √ | ||
| Cochlear implant | √ | √ | ||
| Alcoholism | √ | |||
| Chronic liver disease, cirrhosis | √ | |||
| Cigarette smoking | √ | |||
| Individuals with functional or anatomic asplenia | Sickle cell disease/other hemoglobinopathy | √ | √ | √ |
| Congenital or acquired asplenia | √ | √ | √ | |
| Immunocompromised individuals | Congenital or acquired immunodeficiency§ | √ | √ | √ |
| Human immunodeficiency virus infection | √ | √ | √ | |
| Chronic renal failure | √ | √ | √ | |
| Nephrotic syndrome | √ | √ | √ | |
| Leukemia | √ | √ | √ | |
| Lymphoma | √ | √ | √ | |
| Hodgkin disease | √ | √ | √ | |
| Generalized malignancy | √ | √ | √ | |
| Iatrogenic immunosuppression|| | √ | √ | √ | |
| Solid organ transplant | √ | √ | √ | |
| Multiple myeloma | √ | √ | √ | |
| PCV13, 13-valent pneumococcal conjugate vaccine; PPSV23, 23-valent pneumococcal polysaccharide vaccine. *All adults ≥65 years should receive a dose of PPSV23, regardless of previous history of vaccination with pneumococcal vaccine. †Including congestive heart failure and cardiomyopathies; excluding hypertension. ‡Including chronic obstructive pulmonary disease, emphysema, and asthma. §Including B- (humoral) or T-lymphocyte deficiency, complement deficiencies (particularly C1, C2, C3, and C4 deficiencies), and phagocytic disorders (excluding chronic granulomatous disease). ||Diseases requiring treatment with immunosuppressive drugs, including long-term systemic corticosteroids and radiation therapy. | ||||
MMR for those with HIV and use of IG for measles prevention
The last set of significant changes to the schedules are updated recommendations for the use of MMR vaccine in those who have HIV infection, and the use of immune globulin to prevent measles in those previously unvaccinated who are exposed to the disease. Details of these recommendations can be found at http://www.cdc.gov/vaccines/recs/provisional/downloads/mmr-Oct-2012.pdf.
1. CDC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedules for persons aged 0 through 18 years—United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:2-8.
2. CDC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for adults aged 19 years and older—United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:9-19.
3. Campos-Outcalt D. Battling influenza: changes for the 2012-2013 season. J Fam Pract. 2012;61:606-609.
4. Campos-Outcalt D. HPV is now routinely recommended for males. J Fam Pract. 2012;61:38-40.
5. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2012;61:468-470.
6. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1424-1426.
7. Liang JL. Review of evidence considered for pregnancy Tdap recommendation. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 24, 2012; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2012/02-pertussis-Liang.pdf. Accessed December 15, 2012.
8. Campos-Outcalt D. Meningococcal vaccine for infants? J Fam Pract. 2012;61:482-484.
9. Cohn A. Considerations for use of meningococcal conjugate vaccines in infants. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 24, 2012; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2012/04-MCV-Cohn.pdf. Accessed February 8, 2013.
10. CDC. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816-819.
1. CDC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedules for persons aged 0 through 18 years—United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:2-8.
2. CDC. Advisory Committee on Immunization Practices (ACIP) recommended immunization schedule for adults aged 19 years and older—United States, 2013. MMWR Morb Mortal Wkly Rep. 2013;62:9-19.
3. Campos-Outcalt D. Battling influenza: changes for the 2012-2013 season. J Fam Pract. 2012;61:606-609.
4. Campos-Outcalt D. HPV is now routinely recommended for males. J Fam Pract. 2012;61:38-40.
5. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) vaccine in adults aged 65 years and older—Advisory Committee on Immunization Practices (ACIP), 2012. MMWR Morb Mortal Wkly Rep. 2012;61:468-470.
6. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1424-1426.
7. Liang JL. Review of evidence considered for pregnancy Tdap recommendation. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 24, 2012; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2012/02-pertussis-Liang.pdf. Accessed December 15, 2012.
8. Campos-Outcalt D. Meningococcal vaccine for infants? J Fam Pract. 2012;61:482-484.
9. Cohn A. Considerations for use of meningococcal conjugate vaccines in infants. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); October 24, 2012; Atlanta, Ga. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-oct-2012/04-MCV-Cohn.pdf. Accessed February 8, 2013.
10. CDC. Use of 13-valent pneumococcal conjugate vaccine and 23-valent pneumococcal polysaccharide vaccine for adults with immunocompromising conditions: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2012;61:816-819.
Hepatitis C: New CDC screening recommendations
The Centers for Disease Control and Prevention (CDC) recently released new recommendations for screening for hepatitis C virus (HCV) infection that include a one-time screening for everyone in the United States born between 1945 and 1965, regardless of risk.1 These new recommendations are an enhancement of, but not a replacement for, the recommendations for HCV screening made in 1998, which called for screening those at high risk.2
HCV causes considerable morbidity and mortality in this country. Approximately 17,000 new infections occurred in 2010.1 Between 2.7 and 3.9 million Americans (1%-1.5% of the population) are living with chronic HCV infection, and many do not know they are infected.1 This lack of awareness appears to be due to a failure of both health care providers to offer testing to those at known risk and patients to either acknowledge or recall past high-risk behaviors.
Those at highest risk for HCV infection are current or past users of illegal injected drugs and recipients of a blood transfusion before 1992 (when HCV screening of the blood supply was instituted). Other risk factors are listed in TABLE 1.1 Many of those with HCV infection do not report injection drug use or having received a transfusion prior to 1992, and they are not detected by current risk-based testing.
TABLE 1
Risk factors for HCV infection1
| Most common risks |
|
| Less common risks |
|
| HCV, hepatitis C virus |
Approximately three-fourths of those who acquire HCV are unable to clear the virus and become chronically infected.1 Twenty percent of these individuals will develop cirrhosis and 5% will die from an HCV-related liver disease, such as decompensated cirrhosis or hepatocellular carcinoma (HCC).3
New treatments. In 2011, 2 protease inhibitor drugs, telaprevir and boceprevir, were approved for the treatment of HCV geno-type 1. These are the first generation of a class of drugs called direct-acting antiviral agents (DAAs). When a DAA is added to the standard therapy of ribavirin and pegylated interferon, the rate of viral clearance increases (from 44% to 75% for telaprevir and from 38% to 63% for boceprevir).1 However, the adverse reactions caused by these new drugs can lead to a 34% rise in the rate at which patients stop treatment.1 Twenty potential new HCV antivirals are in clinical trials, and it is expected that treatment recommendations will change rapidly as some of these are approved.
Does treatment improve long-term outcomes?
Clinical guidelines recommend antiviral treatment for anyone with HCV infection and biopsy evidence of bridging fibrosis, septal fibrosis, or cirrhosis.4
A look at Tx and all-cause mortality. Studies looking at patient-oriented outcomes such as all-cause mortality and incidence of HCC have been conducted with pegylated interferon and ribavirin, without the newer DAAs. The most commonly cited study assessed all-cause mortality in a large sample of veterans with multiple comorbidities.
Those who achieved a sustained virological response after treatment exhibited a reduction in all-cause mortality >50% compared with nonresponders. This endpoint included substantially lower rates of liver-related deaths and cirrhosis complicated by ascites, variceal bleeding, or encephalopathy.5 However, in such a nonrandom clinical trial, an improved outcome for responders could be due to their relatively good health, with fewer comorbid conditions, and other undetected biases. While this study attempted to control for such biases, it didn’t provide evidence that treating infection detected by screening a low-risk population would improve intermediate or long-term outcomes.
Observational studies look at carcinoma incidence. Twelve observational studies have addressed treatment effects on HCC incidence. They showed a 75% reduction in HCC rates in those who achieved viral clearance compared with those who did not.1 Again, these studies did not compare treated and untreated patients in a controlled clinical trial; they looked only at treated individuals and compared the outcomes of responders and nonresponders.
HCV transmission research is lacking. The CDC found no studies in its evidence review that addressed the issue of HCV transmission. Nevertheless, the new recommendations state that HCV transmission was a critical factor in determining the strength of the recommendation for age cohort screening. It is expected that those who have a sustained viral response will be less likely to transmit the virus to others.
Why the 1945-1965 birth cohort?
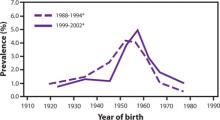
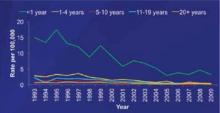
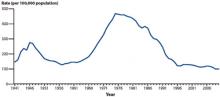
The prevalence of HCV infection in those born between 1945 and 1965 is 3.25%, and three-fourths of all those with HCV infection in the United States are in this cohort. The FIGURE depicts the large difference in prevalence between this age group and others. Within 3 cohorts defined by date of birth (1945-1965, 1950-1970, and 1945-1970), the prevalence of HCV infection is twice as high in men than in women, and in black non-Hispanics than in white non-Hispanics and Mexican Americans. However, extending the birth cohort to those born through 1970 yields only a marginal difference in prevalence figures. The CDC justifies restricting the new universal screening recommendation to the 1945-1965 age group mainly on the results of focus groups in which the public identified this cohort as “baby boomers” who would likely adopt the recommendation.
FIGURE
Prevalence of hepatitis C virus antibody by year of birth1
*National Health and Nutrition Examination Survey, United States, 1988–1994 and 1999–2002.
Two-step screening process
Screen individuals using a test for antibodies to HCV (anti-HCV). If the anti-HCV test result is positive, order a test for HCV nucleic acid that gives either a quantitative measure of viral load or a qualitative assessment of presence or absence of virus. If the confirmatory nucleic acid test result is negative, the individual does not have chronic HCV infection and is among the approximately 25% who clear the virus on their own. They do not need further testing or treatment.
What to tell infected patients
If the confirmatory test result is positive, presume the patient has HCV infection and offer the advice contained in TABLE 2.1 Patients should undergo further assessment for possible chronic liver disease and, with the counsel of their physician, decide whether to initiate treatment. They should also take measures to protect the liver from further damage, such as reducing alcohol consumption, avoiding medication and herbal products that can damage the liver, maintaining an optimal weight, and receiving vaccines against hepatitis A and B, if still susceptible to these viruses. Finally, encourage patients to take steps to avoid transmission of HCV to others.
TABLE 2
Advice for your patients with HCV infection1
Consult a health care provider (either a primary care physician or specialist [eg, in hepatology, gastroenterology, or infectious disease]) for:
|
Protect the liver from further harm by:
|
Maintain optimal weight by:
|
Minimize the risk of infecting others by:
|
| BMI, body mass index; HCV, hepatitis C virus; HIV, human immunodeficiency virus. |
The decision on whether to begin treatment immediately is complicated by the large number of new antivirals in development, which will be available in the near future and may be more effective with fewer adverse effects.
Lingering controversies
Given the lack of evidence of improved outcomes with HCV screening in the general population, it will be interesting to see how widely accepted the new CDC recommendations will be. The US Preventive Services Task Force is in the process of revising its HCV screening recommendations. Given the Task Force’s evidence-based methodology and the lack of evidence on the benefits and harms of screening those with no reported risks, there may be some differences with the new CDC recommendations.
If the CDC’s assumption proves correct—ie, that the benefits of treating high-risk populations will also occur with treating detected infection in the general population—and if the age cohort screening recommendation is fully implemented, 47,000 cases of HCC and 15,000 liver transplants will be prevented.1
1. CDC. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Morb Mortal Wkly Rep. 2012;61:1-18.Available at: http://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf. Accessed October 5, 2012.
2. CDC. Recommendations for prevention and control of hepatitis C virus infection and HCV-related chronic disease. MMWR Morb Mortal Wkly Rep. 1998;47(RR-19):1-54.
3. Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17-35.
4. Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-1374.
5. Backus LI, Boothroyd DB, Phillips BR, et al. A sustained virological response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.
The Centers for Disease Control and Prevention (CDC) recently released new recommendations for screening for hepatitis C virus (HCV) infection that include a one-time screening for everyone in the United States born between 1945 and 1965, regardless of risk.1 These new recommendations are an enhancement of, but not a replacement for, the recommendations for HCV screening made in 1998, which called for screening those at high risk.2
HCV causes considerable morbidity and mortality in this country. Approximately 17,000 new infections occurred in 2010.1 Between 2.7 and 3.9 million Americans (1%-1.5% of the population) are living with chronic HCV infection, and many do not know they are infected.1 This lack of awareness appears to be due to a failure of both health care providers to offer testing to those at known risk and patients to either acknowledge or recall past high-risk behaviors.
Those at highest risk for HCV infection are current or past users of illegal injected drugs and recipients of a blood transfusion before 1992 (when HCV screening of the blood supply was instituted). Other risk factors are listed in TABLE 1.1 Many of those with HCV infection do not report injection drug use or having received a transfusion prior to 1992, and they are not detected by current risk-based testing.
TABLE 1
Risk factors for HCV infection1
| Most common risks |
|
| Less common risks |
|
| HCV, hepatitis C virus |
Approximately three-fourths of those who acquire HCV are unable to clear the virus and become chronically infected.1 Twenty percent of these individuals will develop cirrhosis and 5% will die from an HCV-related liver disease, such as decompensated cirrhosis or hepatocellular carcinoma (HCC).3
New treatments. In 2011, 2 protease inhibitor drugs, telaprevir and boceprevir, were approved for the treatment of HCV geno-type 1. These are the first generation of a class of drugs called direct-acting antiviral agents (DAAs). When a DAA is added to the standard therapy of ribavirin and pegylated interferon, the rate of viral clearance increases (from 44% to 75% for telaprevir and from 38% to 63% for boceprevir).1 However, the adverse reactions caused by these new drugs can lead to a 34% rise in the rate at which patients stop treatment.1 Twenty potential new HCV antivirals are in clinical trials, and it is expected that treatment recommendations will change rapidly as some of these are approved.
Does treatment improve long-term outcomes?
Clinical guidelines recommend antiviral treatment for anyone with HCV infection and biopsy evidence of bridging fibrosis, septal fibrosis, or cirrhosis.4
A look at Tx and all-cause mortality. Studies looking at patient-oriented outcomes such as all-cause mortality and incidence of HCC have been conducted with pegylated interferon and ribavirin, without the newer DAAs. The most commonly cited study assessed all-cause mortality in a large sample of veterans with multiple comorbidities.
Those who achieved a sustained virological response after treatment exhibited a reduction in all-cause mortality >50% compared with nonresponders. This endpoint included substantially lower rates of liver-related deaths and cirrhosis complicated by ascites, variceal bleeding, or encephalopathy.5 However, in such a nonrandom clinical trial, an improved outcome for responders could be due to their relatively good health, with fewer comorbid conditions, and other undetected biases. While this study attempted to control for such biases, it didn’t provide evidence that treating infection detected by screening a low-risk population would improve intermediate or long-term outcomes.
Observational studies look at carcinoma incidence. Twelve observational studies have addressed treatment effects on HCC incidence. They showed a 75% reduction in HCC rates in those who achieved viral clearance compared with those who did not.1 Again, these studies did not compare treated and untreated patients in a controlled clinical trial; they looked only at treated individuals and compared the outcomes of responders and nonresponders.
HCV transmission research is lacking. The CDC found no studies in its evidence review that addressed the issue of HCV transmission. Nevertheless, the new recommendations state that HCV transmission was a critical factor in determining the strength of the recommendation for age cohort screening. It is expected that those who have a sustained viral response will be less likely to transmit the virus to others.
Why the 1945-1965 birth cohort?
The prevalence of HCV infection in those born between 1945 and 1965 is 3.25%, and three-fourths of all those with HCV infection in the United States are in this cohort. The FIGURE depicts the large difference in prevalence between this age group and others. Within 3 cohorts defined by date of birth (1945-1965, 1950-1970, and 1945-1970), the prevalence of HCV infection is twice as high in men than in women, and in black non-Hispanics than in white non-Hispanics and Mexican Americans. However, extending the birth cohort to those born through 1970 yields only a marginal difference in prevalence figures. The CDC justifies restricting the new universal screening recommendation to the 1945-1965 age group mainly on the results of focus groups in which the public identified this cohort as “baby boomers” who would likely adopt the recommendation.
FIGURE
Prevalence of hepatitis C virus antibody by year of birth1
*National Health and Nutrition Examination Survey, United States, 1988–1994 and 1999–2002.
Two-step screening process
Screen individuals using a test for antibodies to HCV (anti-HCV). If the anti-HCV test result is positive, order a test for HCV nucleic acid that gives either a quantitative measure of viral load or a qualitative assessment of presence or absence of virus. If the confirmatory nucleic acid test result is negative, the individual does not have chronic HCV infection and is among the approximately 25% who clear the virus on their own. They do not need further testing or treatment.
What to tell infected patients
If the confirmatory test result is positive, presume the patient has HCV infection and offer the advice contained in TABLE 2.1 Patients should undergo further assessment for possible chronic liver disease and, with the counsel of their physician, decide whether to initiate treatment. They should also take measures to protect the liver from further damage, such as reducing alcohol consumption, avoiding medication and herbal products that can damage the liver, maintaining an optimal weight, and receiving vaccines against hepatitis A and B, if still susceptible to these viruses. Finally, encourage patients to take steps to avoid transmission of HCV to others.
TABLE 2
Advice for your patients with HCV infection1
Consult a health care provider (either a primary care physician or specialist [eg, in hepatology, gastroenterology, or infectious disease]) for:
|
Protect the liver from further harm by:
|
Maintain optimal weight by:
|
Minimize the risk of infecting others by:
|
| BMI, body mass index; HCV, hepatitis C virus; HIV, human immunodeficiency virus. |
The decision on whether to begin treatment immediately is complicated by the large number of new antivirals in development, which will be available in the near future and may be more effective with fewer adverse effects.
Lingering controversies
Given the lack of evidence of improved outcomes with HCV screening in the general population, it will be interesting to see how widely accepted the new CDC recommendations will be. The US Preventive Services Task Force is in the process of revising its HCV screening recommendations. Given the Task Force’s evidence-based methodology and the lack of evidence on the benefits and harms of screening those with no reported risks, there may be some differences with the new CDC recommendations.
If the CDC’s assumption proves correct—ie, that the benefits of treating high-risk populations will also occur with treating detected infection in the general population—and if the age cohort screening recommendation is fully implemented, 47,000 cases of HCC and 15,000 liver transplants will be prevented.1
The Centers for Disease Control and Prevention (CDC) recently released new recommendations for screening for hepatitis C virus (HCV) infection that include a one-time screening for everyone in the United States born between 1945 and 1965, regardless of risk.1 These new recommendations are an enhancement of, but not a replacement for, the recommendations for HCV screening made in 1998, which called for screening those at high risk.2
HCV causes considerable morbidity and mortality in this country. Approximately 17,000 new infections occurred in 2010.1 Between 2.7 and 3.9 million Americans (1%-1.5% of the population) are living with chronic HCV infection, and many do not know they are infected.1 This lack of awareness appears to be due to a failure of both health care providers to offer testing to those at known risk and patients to either acknowledge or recall past high-risk behaviors.
Those at highest risk for HCV infection are current or past users of illegal injected drugs and recipients of a blood transfusion before 1992 (when HCV screening of the blood supply was instituted). Other risk factors are listed in TABLE 1.1 Many of those with HCV infection do not report injection drug use or having received a transfusion prior to 1992, and they are not detected by current risk-based testing.
TABLE 1
Risk factors for HCV infection1
| Most common risks |
|
| Less common risks |
|
| HCV, hepatitis C virus |
Approximately three-fourths of those who acquire HCV are unable to clear the virus and become chronically infected.1 Twenty percent of these individuals will develop cirrhosis and 5% will die from an HCV-related liver disease, such as decompensated cirrhosis or hepatocellular carcinoma (HCC).3
New treatments. In 2011, 2 protease inhibitor drugs, telaprevir and boceprevir, were approved for the treatment of HCV geno-type 1. These are the first generation of a class of drugs called direct-acting antiviral agents (DAAs). When a DAA is added to the standard therapy of ribavirin and pegylated interferon, the rate of viral clearance increases (from 44% to 75% for telaprevir and from 38% to 63% for boceprevir).1 However, the adverse reactions caused by these new drugs can lead to a 34% rise in the rate at which patients stop treatment.1 Twenty potential new HCV antivirals are in clinical trials, and it is expected that treatment recommendations will change rapidly as some of these are approved.
Does treatment improve long-term outcomes?
Clinical guidelines recommend antiviral treatment for anyone with HCV infection and biopsy evidence of bridging fibrosis, septal fibrosis, or cirrhosis.4
A look at Tx and all-cause mortality. Studies looking at patient-oriented outcomes such as all-cause mortality and incidence of HCC have been conducted with pegylated interferon and ribavirin, without the newer DAAs. The most commonly cited study assessed all-cause mortality in a large sample of veterans with multiple comorbidities.
Those who achieved a sustained virological response after treatment exhibited a reduction in all-cause mortality >50% compared with nonresponders. This endpoint included substantially lower rates of liver-related deaths and cirrhosis complicated by ascites, variceal bleeding, or encephalopathy.5 However, in such a nonrandom clinical trial, an improved outcome for responders could be due to their relatively good health, with fewer comorbid conditions, and other undetected biases. While this study attempted to control for such biases, it didn’t provide evidence that treating infection detected by screening a low-risk population would improve intermediate or long-term outcomes.
Observational studies look at carcinoma incidence. Twelve observational studies have addressed treatment effects on HCC incidence. They showed a 75% reduction in HCC rates in those who achieved viral clearance compared with those who did not.1 Again, these studies did not compare treated and untreated patients in a controlled clinical trial; they looked only at treated individuals and compared the outcomes of responders and nonresponders.
HCV transmission research is lacking. The CDC found no studies in its evidence review that addressed the issue of HCV transmission. Nevertheless, the new recommendations state that HCV transmission was a critical factor in determining the strength of the recommendation for age cohort screening. It is expected that those who have a sustained viral response will be less likely to transmit the virus to others.
Why the 1945-1965 birth cohort?
The prevalence of HCV infection in those born between 1945 and 1965 is 3.25%, and three-fourths of all those with HCV infection in the United States are in this cohort. The FIGURE depicts the large difference in prevalence between this age group and others. Within 3 cohorts defined by date of birth (1945-1965, 1950-1970, and 1945-1970), the prevalence of HCV infection is twice as high in men than in women, and in black non-Hispanics than in white non-Hispanics and Mexican Americans. However, extending the birth cohort to those born through 1970 yields only a marginal difference in prevalence figures. The CDC justifies restricting the new universal screening recommendation to the 1945-1965 age group mainly on the results of focus groups in which the public identified this cohort as “baby boomers” who would likely adopt the recommendation.
FIGURE
Prevalence of hepatitis C virus antibody by year of birth1
*National Health and Nutrition Examination Survey, United States, 1988–1994 and 1999–2002.
Two-step screening process
Screen individuals using a test for antibodies to HCV (anti-HCV). If the anti-HCV test result is positive, order a test for HCV nucleic acid that gives either a quantitative measure of viral load or a qualitative assessment of presence or absence of virus. If the confirmatory nucleic acid test result is negative, the individual does not have chronic HCV infection and is among the approximately 25% who clear the virus on their own. They do not need further testing or treatment.
What to tell infected patients
If the confirmatory test result is positive, presume the patient has HCV infection and offer the advice contained in TABLE 2.1 Patients should undergo further assessment for possible chronic liver disease and, with the counsel of their physician, decide whether to initiate treatment. They should also take measures to protect the liver from further damage, such as reducing alcohol consumption, avoiding medication and herbal products that can damage the liver, maintaining an optimal weight, and receiving vaccines against hepatitis A and B, if still susceptible to these viruses. Finally, encourage patients to take steps to avoid transmission of HCV to others.
TABLE 2
Advice for your patients with HCV infection1
Consult a health care provider (either a primary care physician or specialist [eg, in hepatology, gastroenterology, or infectious disease]) for:
|
Protect the liver from further harm by:
|
Maintain optimal weight by:
|
Minimize the risk of infecting others by:
|
| BMI, body mass index; HCV, hepatitis C virus; HIV, human immunodeficiency virus. |
The decision on whether to begin treatment immediately is complicated by the large number of new antivirals in development, which will be available in the near future and may be more effective with fewer adverse effects.
Lingering controversies
Given the lack of evidence of improved outcomes with HCV screening in the general population, it will be interesting to see how widely accepted the new CDC recommendations will be. The US Preventive Services Task Force is in the process of revising its HCV screening recommendations. Given the Task Force’s evidence-based methodology and the lack of evidence on the benefits and harms of screening those with no reported risks, there may be some differences with the new CDC recommendations.
If the CDC’s assumption proves correct—ie, that the benefits of treating high-risk populations will also occur with treating detected infection in the general population—and if the age cohort screening recommendation is fully implemented, 47,000 cases of HCC and 15,000 liver transplants will be prevented.1
1. CDC. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Morb Mortal Wkly Rep. 2012;61:1-18.Available at: http://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf. Accessed October 5, 2012.
2. CDC. Recommendations for prevention and control of hepatitis C virus infection and HCV-related chronic disease. MMWR Morb Mortal Wkly Rep. 1998;47(RR-19):1-54.
3. Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17-35.
4. Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-1374.
5. Backus LI, Boothroyd DB, Phillips BR, et al. A sustained virological response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.
1. CDC. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945-1965. MMWR Morb Mortal Wkly Rep. 2012;61:1-18.Available at: http://www.cdc.gov/mmwr/pdf/rr/rr6104.pdf. Accessed October 5, 2012.
2. CDC. Recommendations for prevention and control of hepatitis C virus infection and HCV-related chronic disease. MMWR Morb Mortal Wkly Rep. 1998;47(RR-19):1-54.
3. Alter HJ, Seeff LB. Recovery, persistence, and sequelae in hepatitis C virus infection: a perspective on long-term outcome. Semin Liver Dis. 2000;20:17-35.
4. Ghany MG, Strader DB, Thomas DL, et al. Diagnosis, management, and treatment of hepatitis C: an update. Hepatology. 2009;49:1335-1374.
5. Backus LI, Boothroyd DB, Phillips BR, et al. A sustained virological response reduces risk of all-cause mortality in patients with hepatitis C. Clin Gastroenterol Hepatol. 2011;9:509-516.
Battling influenza: Changes for the 2012-2013 season
By all measures, last year’s flu season was a mild one that peaked in early March. The number of cases reported, the total number of pneumonia/influenza deaths, and the number of pediatric deaths were all comparatively low.1 The main circulating strains were the same as the previous 2 years, leaving much of the population protected by immunity gained from natural infections. And there was a good match between the vaccine and the circulating strains, leading to higher vaccine effectiveness.
So what’s new—and what remains the same—for the 2012-2013 season? Annual flu vaccination continues to be recommended for everyone ≥6 months of age, starting as soon as the vaccine is available and continuing through the influenza season. This season’s vaccine contains 2 new strains in addition to the A/California/7/2009 (H1N1) strain that has been in the vaccine the past 2 seasons and was used for a monovalent vaccine in 2009. The new strains are A/Victoria/361/2011 (H3N2) and B/Wisconsin/1/2010.2
Each year, influenza experts decide which strains to include in the vaccine based on the ones currently circulating and the ones expected to circulate into the next season. The degree to which vaccine strains match circulating strains will determine the effectiveness of the vaccine.
A variety of products
The number of influenza vaccine products has increased, and they differ in the ages for which they are approved.2 All trivalent inactivated vaccine (TIV) products are given intramuscularly, with the exception of a relatively new product, Fluzone Intradermal (Sanofi Pasteur). There is also FluMist (MedImmune), a live-attenuated influenza vaccine (LAIV), administered as a nasal spray. And, for adults ≥65 years, the product Fluzone High-Dose contains 4 times the antigen content of other vaccines for this age group. The Centers for Disease Control and Prevention (CDC) does not express a preference for any one of the TIV products over the others.
A new algorithm for children <9 years
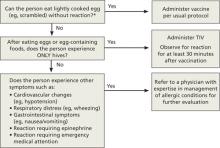
To mount an adequate immune response in children <9 years, 2 doses of vaccine are needed in the first year of receiving vaccine. The time between doses should be at least 4 weeks; longer intervals do not appear to matter. This leads to a complex algorithm when taking into consideration vaccines given in past years. To simplify the issue, the CDC has approved an algorithm for this season that involves only 2 questions (FIGURE 1).
However, strict adherence to this algorithm will result in some children receiving 2 doses when one would suffice. If a child has received at least 2 doses of seasonal influenza vaccine in any prior season, and at least one dose of A/California/7/2009 (H1N1), then just a single dose of vaccine is needed this year. The A/California antigen could have been in the monovalent product in 2009 or the regular trivalent products in the past 2 seasons. If any doubt or confusion exists, administer 2 doses, 4 weeks apart. There is no harm in receiving 2 doses if only one is needed.
FIGURE 1
The CDC’s new dosing algorithm for children 6 months–8 years receiving influenza vaccine in the 2012-2013 flu season2
*Doses should be administered at least 4 weeks apart.
†For simplicity, this algorithm takes into consideration only doses of seasonal influenza vaccine received since July 1, 2010. However, if a child 6 months through 8 years of age is known to have received at least 2 seasonal influenza vaccines during any prior season, and at least one dose of a 2009 (H1N1)-containing vaccine-—ie, either 2010-2011 or 2011-2012 seasonal vaccine or the monovalent 2009 (H1N1) vaccine—then the child needs only one dose for 2012-2013.
Egg allergy precautions
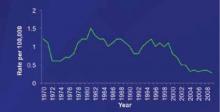
While all influenza vaccines are manufactured by injecting virus into chicken eggs, the amount of egg protein in the vaccine is extremely low. Those who react to egg products only with hives can receive TIV (not LAIV) under the care of a clinician who is familiar with egg allergy manifestations. (Patients should be observed for 30 minutes after vaccine administration.) Those who have more severe reactions to eggs (FIGURE 2) require assessment by a physician with allergy expertise before receiving an influenza vaccine. All facilities that administer vaccines should be equipped to respond to anaphylaxis, and all providers who administer vaccines should be adequately trained in anaphylaxis management. The CDC made these recommendations last year, and there was no increase in egg allergy adverse events following vaccination reported during the 2011-2012 flu season.3
FIGURE 2
ACIP 2012-2013 recommendations regarding influenza vaccination for those with egg allergy2
TIV, trivalent inactivated vaccine.
*Individuals with egg allergy may tolerate egg in baked products (eg, bread, cake). Tolerance to egg-containing foods does not exclude the possibility of egg allergy.
Febrile seizures and vaccine safety
Last flu season, vaccine safety surveillance detected an increased risk for febrile seizures among children 6 months to 4 years during the 24 hours after receiving TIV, when it was given at the same time as 13-valent pneumococcal conjugate vaccine (PCV13).3 This increased risk was <1 per 1000 children vaccinated, and the Advisory Committee on Immunization Practices (ACIP) did not consider it significant enough to warrant any changes in TIV or PCV13 recommendations.
No other safety concerns arose for influenza vaccines last year. The vaccine safety monitoring system looks specifically at Guillain-Barré syndrome (GBS), and it detected no increased risk for GBS related to influenza vaccine.3
Newer quadrivalent vaccines
Historically, influenza vaccines have contained 3 antigens: 2 type A and 1 type B. A newly approved quadrivalent LAIV (FluMist Quadrivalent, MedImmune) contains 2 antigenically different B strains. The inclusion of 2 B strains is expected to increase the likelihood of the vaccine matching the circulating B influenza strains and thereby increase vaccine effectiveness. This new product will probably not be available this coming flu season, but will be marketed for 2013-2014. Other, inactivated, quadrivalent vaccines are also in development and should be available in future flu seasons.
Improving influenza vaccine coverage
In 2011, only 36.3% of people ≥6 months of age had received influenza vaccination by the first week in November (36.7% of children 6 months to 17 years and 36.2% of adults ≥18 years).4 The Community Preventive Services Task Force (a nonfederal group whose members are appointed by the director of the CDC) recommends a number of evidence-based interventions to increase vaccine rates, including patient reminder and recall systems, provider quality assessment and feedback, and standing orders.5 Increased coverage is important if we are to lower the annual morbidity and mortality associated with influenza.
The role of antivirals
All influenza A and B strains currently circulating have low or zero rates of resistance to the neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza). The circulating A strains continue to have high levels of resistance to the adamantanes (amantadine and rimantadine). Therefore, use only the neuraminidase inhibitors to treat influenza, and for pre- and post exposure chemoprevention.1
Those who should receive treatment include anyone with suspected or confirmed influenza who is hospitalized or who meets specific criteria (TABLE). Details regarding influenza antivirals, doses, and duration of treatment—as well as indications for chemoprevention—are on the CDC influenza Web site (http://www.cdc.gov/flu/professionals/antivirals/antiviral-use-influenza.htm#indications).
Table
Indications for treatment of influenza with antivirals
|
| BMI, body mass index; HIV, human immunodeficiency virus. Source: CDC. Antiviral agents for the treatment and chemoprophylaxis of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60:1-24. |
1. Finelli L. Influenza surveillance season summary. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); June 20, 2012; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-jun-2012/02-influenza-finelli.pdf. Accessed July 15, 2012.
2. CDC. Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2012;61:613–618.
3. Shimabukuro T. Update on influenza vaccine safety monitoring. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); June 20, 2012; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-jun-2012/03-influenza-Shimabukuro.pdf. Accessed July 15, 2012.
4. CDC. National mid-season flu vaccination coverage. Available at: http://www.cdc.gov/flu/professionals/vaccination/national-flu-survey.htm. Accessed July 15, 2012.
5. Community Preventive Services Task Force. Vaccines to prevent diseases: universally recommended vaccines. Available at: http://www.thecommunityguide.org/vaccines/universally/index.html. Accessed July 15, 2012.
By all measures, last year’s flu season was a mild one that peaked in early March. The number of cases reported, the total number of pneumonia/influenza deaths, and the number of pediatric deaths were all comparatively low.1 The main circulating strains were the same as the previous 2 years, leaving much of the population protected by immunity gained from natural infections. And there was a good match between the vaccine and the circulating strains, leading to higher vaccine effectiveness.
So what’s new—and what remains the same—for the 2012-2013 season? Annual flu vaccination continues to be recommended for everyone ≥6 months of age, starting as soon as the vaccine is available and continuing through the influenza season. This season’s vaccine contains 2 new strains in addition to the A/California/7/2009 (H1N1) strain that has been in the vaccine the past 2 seasons and was used for a monovalent vaccine in 2009. The new strains are A/Victoria/361/2011 (H3N2) and B/Wisconsin/1/2010.2
Each year, influenza experts decide which strains to include in the vaccine based on the ones currently circulating and the ones expected to circulate into the next season. The degree to which vaccine strains match circulating strains will determine the effectiveness of the vaccine.
A variety of products
The number of influenza vaccine products has increased, and they differ in the ages for which they are approved.2 All trivalent inactivated vaccine (TIV) products are given intramuscularly, with the exception of a relatively new product, Fluzone Intradermal (Sanofi Pasteur). There is also FluMist (MedImmune), a live-attenuated influenza vaccine (LAIV), administered as a nasal spray. And, for adults ≥65 years, the product Fluzone High-Dose contains 4 times the antigen content of other vaccines for this age group. The Centers for Disease Control and Prevention (CDC) does not express a preference for any one of the TIV products over the others.
A new algorithm for children <9 years
To mount an adequate immune response in children <9 years, 2 doses of vaccine are needed in the first year of receiving vaccine. The time between doses should be at least 4 weeks; longer intervals do not appear to matter. This leads to a complex algorithm when taking into consideration vaccines given in past years. To simplify the issue, the CDC has approved an algorithm for this season that involves only 2 questions (FIGURE 1).
However, strict adherence to this algorithm will result in some children receiving 2 doses when one would suffice. If a child has received at least 2 doses of seasonal influenza vaccine in any prior season, and at least one dose of A/California/7/2009 (H1N1), then just a single dose of vaccine is needed this year. The A/California antigen could have been in the monovalent product in 2009 or the regular trivalent products in the past 2 seasons. If any doubt or confusion exists, administer 2 doses, 4 weeks apart. There is no harm in receiving 2 doses if only one is needed.
FIGURE 1
The CDC’s new dosing algorithm for children 6 months–8 years receiving influenza vaccine in the 2012-2013 flu season2
*Doses should be administered at least 4 weeks apart.
†For simplicity, this algorithm takes into consideration only doses of seasonal influenza vaccine received since July 1, 2010. However, if a child 6 months through 8 years of age is known to have received at least 2 seasonal influenza vaccines during any prior season, and at least one dose of a 2009 (H1N1)-containing vaccine-—ie, either 2010-2011 or 2011-2012 seasonal vaccine or the monovalent 2009 (H1N1) vaccine—then the child needs only one dose for 2012-2013.
Egg allergy precautions
While all influenza vaccines are manufactured by injecting virus into chicken eggs, the amount of egg protein in the vaccine is extremely low. Those who react to egg products only with hives can receive TIV (not LAIV) under the care of a clinician who is familiar with egg allergy manifestations. (Patients should be observed for 30 minutes after vaccine administration.) Those who have more severe reactions to eggs (FIGURE 2) require assessment by a physician with allergy expertise before receiving an influenza vaccine. All facilities that administer vaccines should be equipped to respond to anaphylaxis, and all providers who administer vaccines should be adequately trained in anaphylaxis management. The CDC made these recommendations last year, and there was no increase in egg allergy adverse events following vaccination reported during the 2011-2012 flu season.3
FIGURE 2
ACIP 2012-2013 recommendations regarding influenza vaccination for those with egg allergy2
TIV, trivalent inactivated vaccine.
*Individuals with egg allergy may tolerate egg in baked products (eg, bread, cake). Tolerance to egg-containing foods does not exclude the possibility of egg allergy.
Febrile seizures and vaccine safety
Last flu season, vaccine safety surveillance detected an increased risk for febrile seizures among children 6 months to 4 years during the 24 hours after receiving TIV, when it was given at the same time as 13-valent pneumococcal conjugate vaccine (PCV13).3 This increased risk was <1 per 1000 children vaccinated, and the Advisory Committee on Immunization Practices (ACIP) did not consider it significant enough to warrant any changes in TIV or PCV13 recommendations.
No other safety concerns arose for influenza vaccines last year. The vaccine safety monitoring system looks specifically at Guillain-Barré syndrome (GBS), and it detected no increased risk for GBS related to influenza vaccine.3
Newer quadrivalent vaccines
Historically, influenza vaccines have contained 3 antigens: 2 type A and 1 type B. A newly approved quadrivalent LAIV (FluMist Quadrivalent, MedImmune) contains 2 antigenically different B strains. The inclusion of 2 B strains is expected to increase the likelihood of the vaccine matching the circulating B influenza strains and thereby increase vaccine effectiveness. This new product will probably not be available this coming flu season, but will be marketed for 2013-2014. Other, inactivated, quadrivalent vaccines are also in development and should be available in future flu seasons.
Improving influenza vaccine coverage
In 2011, only 36.3% of people ≥6 months of age had received influenza vaccination by the first week in November (36.7% of children 6 months to 17 years and 36.2% of adults ≥18 years).4 The Community Preventive Services Task Force (a nonfederal group whose members are appointed by the director of the CDC) recommends a number of evidence-based interventions to increase vaccine rates, including patient reminder and recall systems, provider quality assessment and feedback, and standing orders.5 Increased coverage is important if we are to lower the annual morbidity and mortality associated with influenza.
The role of antivirals
All influenza A and B strains currently circulating have low or zero rates of resistance to the neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza). The circulating A strains continue to have high levels of resistance to the adamantanes (amantadine and rimantadine). Therefore, use only the neuraminidase inhibitors to treat influenza, and for pre- and post exposure chemoprevention.1
Those who should receive treatment include anyone with suspected or confirmed influenza who is hospitalized or who meets specific criteria (TABLE). Details regarding influenza antivirals, doses, and duration of treatment—as well as indications for chemoprevention—are on the CDC influenza Web site (http://www.cdc.gov/flu/professionals/antivirals/antiviral-use-influenza.htm#indications).
Table
Indications for treatment of influenza with antivirals
|
| BMI, body mass index; HIV, human immunodeficiency virus. Source: CDC. Antiviral agents for the treatment and chemoprophylaxis of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60:1-24. |
By all measures, last year’s flu season was a mild one that peaked in early March. The number of cases reported, the total number of pneumonia/influenza deaths, and the number of pediatric deaths were all comparatively low.1 The main circulating strains were the same as the previous 2 years, leaving much of the population protected by immunity gained from natural infections. And there was a good match between the vaccine and the circulating strains, leading to higher vaccine effectiveness.
So what’s new—and what remains the same—for the 2012-2013 season? Annual flu vaccination continues to be recommended for everyone ≥6 months of age, starting as soon as the vaccine is available and continuing through the influenza season. This season’s vaccine contains 2 new strains in addition to the A/California/7/2009 (H1N1) strain that has been in the vaccine the past 2 seasons and was used for a monovalent vaccine in 2009. The new strains are A/Victoria/361/2011 (H3N2) and B/Wisconsin/1/2010.2
Each year, influenza experts decide which strains to include in the vaccine based on the ones currently circulating and the ones expected to circulate into the next season. The degree to which vaccine strains match circulating strains will determine the effectiveness of the vaccine.
A variety of products
The number of influenza vaccine products has increased, and they differ in the ages for which they are approved.2 All trivalent inactivated vaccine (TIV) products are given intramuscularly, with the exception of a relatively new product, Fluzone Intradermal (Sanofi Pasteur). There is also FluMist (MedImmune), a live-attenuated influenza vaccine (LAIV), administered as a nasal spray. And, for adults ≥65 years, the product Fluzone High-Dose contains 4 times the antigen content of other vaccines for this age group. The Centers for Disease Control and Prevention (CDC) does not express a preference for any one of the TIV products over the others.
A new algorithm for children <9 years
To mount an adequate immune response in children <9 years, 2 doses of vaccine are needed in the first year of receiving vaccine. The time between doses should be at least 4 weeks; longer intervals do not appear to matter. This leads to a complex algorithm when taking into consideration vaccines given in past years. To simplify the issue, the CDC has approved an algorithm for this season that involves only 2 questions (FIGURE 1).
However, strict adherence to this algorithm will result in some children receiving 2 doses when one would suffice. If a child has received at least 2 doses of seasonal influenza vaccine in any prior season, and at least one dose of A/California/7/2009 (H1N1), then just a single dose of vaccine is needed this year. The A/California antigen could have been in the monovalent product in 2009 or the regular trivalent products in the past 2 seasons. If any doubt or confusion exists, administer 2 doses, 4 weeks apart. There is no harm in receiving 2 doses if only one is needed.
FIGURE 1
The CDC’s new dosing algorithm for children 6 months–8 years receiving influenza vaccine in the 2012-2013 flu season2
*Doses should be administered at least 4 weeks apart.
†For simplicity, this algorithm takes into consideration only doses of seasonal influenza vaccine received since July 1, 2010. However, if a child 6 months through 8 years of age is known to have received at least 2 seasonal influenza vaccines during any prior season, and at least one dose of a 2009 (H1N1)-containing vaccine-—ie, either 2010-2011 or 2011-2012 seasonal vaccine or the monovalent 2009 (H1N1) vaccine—then the child needs only one dose for 2012-2013.
Egg allergy precautions
While all influenza vaccines are manufactured by injecting virus into chicken eggs, the amount of egg protein in the vaccine is extremely low. Those who react to egg products only with hives can receive TIV (not LAIV) under the care of a clinician who is familiar with egg allergy manifestations. (Patients should be observed for 30 minutes after vaccine administration.) Those who have more severe reactions to eggs (FIGURE 2) require assessment by a physician with allergy expertise before receiving an influenza vaccine. All facilities that administer vaccines should be equipped to respond to anaphylaxis, and all providers who administer vaccines should be adequately trained in anaphylaxis management. The CDC made these recommendations last year, and there was no increase in egg allergy adverse events following vaccination reported during the 2011-2012 flu season.3
FIGURE 2
ACIP 2012-2013 recommendations regarding influenza vaccination for those with egg allergy2
TIV, trivalent inactivated vaccine.
*Individuals with egg allergy may tolerate egg in baked products (eg, bread, cake). Tolerance to egg-containing foods does not exclude the possibility of egg allergy.
Febrile seizures and vaccine safety
Last flu season, vaccine safety surveillance detected an increased risk for febrile seizures among children 6 months to 4 years during the 24 hours after receiving TIV, when it was given at the same time as 13-valent pneumococcal conjugate vaccine (PCV13).3 This increased risk was <1 per 1000 children vaccinated, and the Advisory Committee on Immunization Practices (ACIP) did not consider it significant enough to warrant any changes in TIV or PCV13 recommendations.
No other safety concerns arose for influenza vaccines last year. The vaccine safety monitoring system looks specifically at Guillain-Barré syndrome (GBS), and it detected no increased risk for GBS related to influenza vaccine.3
Newer quadrivalent vaccines
Historically, influenza vaccines have contained 3 antigens: 2 type A and 1 type B. A newly approved quadrivalent LAIV (FluMist Quadrivalent, MedImmune) contains 2 antigenically different B strains. The inclusion of 2 B strains is expected to increase the likelihood of the vaccine matching the circulating B influenza strains and thereby increase vaccine effectiveness. This new product will probably not be available this coming flu season, but will be marketed for 2013-2014. Other, inactivated, quadrivalent vaccines are also in development and should be available in future flu seasons.
Improving influenza vaccine coverage
In 2011, only 36.3% of people ≥6 months of age had received influenza vaccination by the first week in November (36.7% of children 6 months to 17 years and 36.2% of adults ≥18 years).4 The Community Preventive Services Task Force (a nonfederal group whose members are appointed by the director of the CDC) recommends a number of evidence-based interventions to increase vaccine rates, including patient reminder and recall systems, provider quality assessment and feedback, and standing orders.5 Increased coverage is important if we are to lower the annual morbidity and mortality associated with influenza.
The role of antivirals
All influenza A and B strains currently circulating have low or zero rates of resistance to the neuraminidase inhibitors, oseltamivir (Tamiflu) and zanamivir (Relenza). The circulating A strains continue to have high levels of resistance to the adamantanes (amantadine and rimantadine). Therefore, use only the neuraminidase inhibitors to treat influenza, and for pre- and post exposure chemoprevention.1
Those who should receive treatment include anyone with suspected or confirmed influenza who is hospitalized or who meets specific criteria (TABLE). Details regarding influenza antivirals, doses, and duration of treatment—as well as indications for chemoprevention—are on the CDC influenza Web site (http://www.cdc.gov/flu/professionals/antivirals/antiviral-use-influenza.htm#indications).
Table
Indications for treatment of influenza with antivirals
|
| BMI, body mass index; HIV, human immunodeficiency virus. Source: CDC. Antiviral agents for the treatment and chemoprophylaxis of influenza: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60:1-24. |
1. Finelli L. Influenza surveillance season summary. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); June 20, 2012; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-jun-2012/02-influenza-finelli.pdf. Accessed July 15, 2012.
2. CDC. Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2012;61:613–618.
3. Shimabukuro T. Update on influenza vaccine safety monitoring. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); June 20, 2012; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-jun-2012/03-influenza-Shimabukuro.pdf. Accessed July 15, 2012.
4. CDC. National mid-season flu vaccination coverage. Available at: http://www.cdc.gov/flu/professionals/vaccination/national-flu-survey.htm. Accessed July 15, 2012.
5. Community Preventive Services Task Force. Vaccines to prevent diseases: universally recommended vaccines. Available at: http://www.thecommunityguide.org/vaccines/universally/index.html. Accessed July 15, 2012.
1. Finelli L. Influenza surveillance season summary. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); June 20, 2012; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-jun-2012/02-influenza-finelli.pdf. Accessed July 15, 2012.
2. CDC. Prevention and control of influenza with vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP)—United States, 2012-13 influenza season. MMWR Morb Mortal Wkly Rep. 2012;61:613–618.
3. Shimabukuro T. Update on influenza vaccine safety monitoring. Presented at: meeting of the Advisory Committee on Immunization Practices (ACIP); June 20, 2012; Atlanta, GA. Available at: http://www.cdc.gov/vaccines/acip/meetings/downloads/slides-jun-2012/03-influenza-Shimabukuro.pdf. Accessed July 15, 2012.
4. CDC. National mid-season flu vaccination coverage. Available at: http://www.cdc.gov/flu/professionals/vaccination/national-flu-survey.htm. Accessed July 15, 2012.
5. Community Preventive Services Task Force. Vaccines to prevent diseases: universally recommended vaccines. Available at: http://www.thecommunityguide.org/vaccines/universally/index.html. Accessed July 15, 2012.
Meningococcal vaccine for infants?
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
Meningococcal vaccine for infants?
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
The Advisory Committee on Immunization Practices (ACIP) is evaluating whether to recommend the use of meningococcal vaccines for infants and children <2 years.1 The decision may be made within the next 4 to 8 months. In its deliberation, ACIP must consider several issues, which I review here.
Current and impending vaccine options. Two quadrivalent meningococcal conjugate vaccines (MCV4) are licensed by the US Food and Drug Administration (FDA) for use in the United States: Men ACWY-CRM (Menveo, Novartis) and Men ACWY-D (Menactra, Sanofi Pasteur).2 Both vaccines protect against 4 meningococcal serogroups (A, C, Y, and W-135) and are approved for use among those ages 2 to 55 years. In addition, Menactra was recently licensed as a 2-dose series for children ages 9 to 23 months. ACIP recommends routine use of MCV4 for adolescents ages 11 to 18 years, with a preference for the first dose at ages 11 to 12 years; and for all individuals between the ages of 2 and 55 years who are at increased risk for meningococcal disease ( TABLE ).
Complicating matters is the pending availability of more formulations. In addition to the 2-dose Menactra option for children 9 to 23 months, Novartis has an application before the FDA for a 4-dose schedule with Menveo, given at ages 2, 4, 6, and 12 months. GlaxoSmithKline has just received approval from the FDA for MenHibrix, a combination vaccine that contains antigens against Haemophilus influenzae type b (Hib) and 2 meningococcal serogroups, C and Y, licensed as a 4-dose series given at ages 2, 4, 6, and 12 months.
These vaccines have proven to be immunogenic in infants without diminishing the effectiveness of other, co-administered vaccines in normal infant populations. They also appear to be safe, although the studies to date have not been sufficiently large to detect uncommon adverse events.3-7
Table
Patients at high risk for meningococcal disease
|
| Source: CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76. |
Meningococcal disease incidence and prevalence are declining
One major consideration for ACIP is the changing epidemiology of meningococcal disease and the low prevalence of disease in all age groups, including infants. The incidence of meningococcal disease has declined in the United States since 1980, with a marked and sustained decline since 2000 ( FIGURE 1 ).8 This decline has occurred in all age groups including infants, who have the highest rate of infection ( FIGURE 2 ).8 This decline in incidence occurred for all serogroups, including serogroup B.8
Serogroup B. Among children <5 years, including infants, half of meningococcal disease is caused by serogroup B,8 and these infections would not be prevented by any of the currently licensed vaccines or by those under review. Furthermore, half of all infections occur before age 9 months8 —an age range for which Menactra in not approved.
Serogroup C and Y. One-third of infections with serogroups C and Y occur before the age of 6 months8 and would not be prevented by any of the new products. Also of note: From 2007 to 2009, the mean number of cases of serotype A or C infection occurring each year in children <5 years was 77.8
The impact on children vs adults. Meningococcal disease in children is generally less severe than that occurring in older age groups. Overall case fatality in children is 6%; 10% in those with serogroup B and 1% in those with serogroup Y.8 The disease in children does result in significant sequelae, however, with 10% suffering hearing loss and 1% to 2% requiring amputation. From 2007 to 2009, there were 4 to 8 deaths per year among children under age 5, and 8 to 12 children per year experienced serious sequelae.8
FIGURE 1
The incidence of meningococcal disease has declined steadily since 20008
1970-1996 National Notifiable Diseases Surveillance System data. 1997-2009 Active Bacterial Core surveillance data estimated to the US population.
FIGURE 2
Meningococcal disease has declined among infants and other age groups8
Active Bacterial Core surveillance cases from 1993-2009 estimated to the US population with 18% correction for underreporting.
ACIP’s dilemma
The low morbidity and mortality associated with meningococcal disease is one issue to consider when deciding whether to recommend new vaccines as part of the routine infant and child immunization schedule. The vaccine schedule is already crowded and complex, and parents increasingly are questioning the need for additional antigens.
In addition, the cost of vaccines for children has escalated over the past decade due mainly to the new, more expensive formulations.
The reason for a declining incidence of meningococcal disease is not fully known. It may be partly explained by increasing rates of vaccination among adolescents. However, the overall low rate of disease in the population makes assessing herd immunity difficult.
If ACIP decides to recommend vaccinating infants against meningococcal disease, it is unclear how long immunity will last, potentially necessitating a booster dose before the currently recommended adolescent dose.
Finally, in children at high risk, it is not fully known how meningococcal vaccines will affect the immune response to pneumococcal conjugate vaccine. This is an important consideration because the incidence of pneumococcal disease among these children is much higher than that of meningococcal disease.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
1. CDC. Report from the Advisory Committee on Immunization Practices (ACIP): decision not to recommend routine vaccination of all children aged 2-10 years with quadrivalent meningococcal conjugate vaccine (MCV4). MMWR Morb Mortal Wkly Rep. 2008;57:462-465.
2. CDC. Licensure of a meningococcal conjugate vaccine for children aged 2 through 10 years and updated booster dose guidance for adolescents and other persons at increased risk for meningococcal disease—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1018-1019.
3. Marshall GS, Marchant CD, Blatter M, et al. Immune response and one-year antibody persistence after a fourth dose of a novel Haemophilus influenzae type B and Neisseria meningitides serogroups C and T-tetanus toxoid conjugate vaccine (HibMenCY) at 12 to 15 months of age. Pediatr Infect Dis J. 2010;29:469-471.
4. Nolan T, Richmond P, Marshall H, et al. Immunogenicity and safety of an investigational combined Haemophilus influenzae type B-Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine. Pediatr Infect Dis J. 2011;30:190-196.
5. Bryant KA, Marshall GS, Marchant CD, et al. Immunogenicity and safety of H influenzae type b-N meningitides C/Y conjugate vaccine in infants. Pediatrics. 2011;127:e1375-e1385.
6. Marshall GS, Marchant CD, Blatter M, et al. Co-administration of a novel Haemophilus influenzae type b and Neisseria meningitides serogroups C and Y-tetanus toxoid conjugate vaccine does not interfere with the immune response to antigens contained in infant vaccines routinely used in the United States. Hum Vaccin. 2011;7:258-264.
7. Perrett KP, Snape MD, Ford KJ, et al. Immunogenicity and immune memory of a nonadjuvanted quadrivalent meningococcal glycoconjugate vaccine in infants. Pediatr Infect Dis J. 2009;28:186-193.
8. MacNeil J. Epidemiology of meningococcal diseases in infants and young children. Paper presented at: Meeting of the Advisory Committee on Immunization Practices; October 25, 2011; Atlanta, GA.
The latest recommendations from the USPSTF
Recently, the US Preventive Services Task Force (USPSTF) finalized 7 recommendations on 5 topics and posted draft recommendations on an additional 10 topics. It also implemented new procedures that include posting draft recommendations for public comment (see “A new review process for the USPSTF”). This article reviews the USPSTF activity in 2011, as well as cervical cancer screening recommendations issued earlier this year.
In response to the adverse publicity from the 2009 mammogram recommendations and the increased scrutiny brought on by the affordable care act—which mandates that A and B recommendations from the US Preventive Services Task force are covered preventive services provided at no charge to the patient—the USPSTF developed and implemented a new review procedure. This is intended to increase stakeholder involvement at all steps in the process.
Last year, the USPSTF completed its rollout of this new online review process. The USPSTF now posts all draft recommendations and the evidence report supporting them on its Web site for public comment. final recommendations are posted months later after consideration of the public input. The final recommendations for the 10 topics with draft recommendations posted in 2011 are expected to be released this year.
Potential for confusion. The new process may cause confusion for family physicians. Draft recommendations will receive press coverage and may differ from the final recommendations, as happened with cervical cancer screening recommendations. Physicians will need to familiarize themselves with the process and look for final recommendations on the USPSTF Web site at http://www.uspreventiveservicestaskforce.org/recommendations.htm.
2012 recommendations
Screening for cervical cancer
The USPSTF released its new recommendations on screening for cervical cancer in March (TABLE 1).1 The final document varied from the 2011 draft recommendations in 2 areas: the roles of human papillomavirus (HPV) testing and sexual history.
- The draft issued an I statement (insufficient evidence) for the role of HPV testing. Subsequently, based on stakeholder and public comment (as well as a review of 2 large recently published studies), the USPSTF gave an A recommendation to the use of HPV testing in conjunction with cervical cytology as an option for women ages 30 years and older who want to increase the interval between screening to 5 years.2,3
- The draft stated that the age at which screening should be initiated depends on a patient’s sexual history. The final recommendations state that screening should not begin until age 21, regardless of sexual history.
TABLE 1
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
These new recommendations balance the proven benefits of cervical cytology with the harms from overscreening and are now essentially the same as those of other organizations, including the American Cancer Society, the American Society for Colposcopy and Cervical Pathology, and the American Society for Clinical Pathology. They differ in minor ways from those of the American Congress of Obstetricians and Gynecologists, and the American Academy of Family Physicians is assessing whether to endorse them.
Importantly, the new recommendations identify individuals for whom cervical cytology should be avoided—women younger than age 21, most women older than age 65, and those who have had a hysterectomy with removal of the cervix. A decision to stop screening after the 65th birthday depends on whether the patient has had adequate screening yielding normal findings: This is defined by the USPSTF as 3 consecutive negative cytology results (or 2 consecutive negative co-test results with cytology and HIV testing) within 10 years of the proposed time of cessation, with the most recent test having been performed within 5 years. Avoiding cytology testing after hysterectomy is contingent on the procedure having been performed for an indication other than a high-grade precancerous lesion or cervical cancer. In addition, the recommendations advise against HPV testing in women younger than age 30, as it offers little advantage and leads to much overdiagnosis.
Liquid vs conventional cytology. As a minor point, the USPSTF says the evidence clearly shows that liquid cytology offers no advantage over conventional cytology. But it recognizes that the screening method used is often not determined by the physician.
Recommendations finalized in 2011
TABLE 2 summarizes recommendations completed by the USPSTF last year.
Neonatal gonococcal eye infection prevention
The recommendation to use topical medication (erythromycin ointment) to prevent neonatal gonococcal eye infection is an update and reaffirmation of a previous recommendation. Blindness due to this disease has become rare in the United States because of the routine use of a neonatal topical antibiotic, and there is good evidence that it causes no significant harm. Its use continues to be recommended for all newborns.4
TABLE 2
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
Vision screening for children
Vision screening for preschool children can detect visual acuity problems such as amblyopia and refractive errors. A variety of screening tests are available, including visual acuity, stereoacuity, cover-uncover, Hirschberg light reflex, and auto-refractor tests (automated optical instruments that detect refractive errors). The most benefit is obtained by discovering and correcting amblyopia.
There is no evidence that detecting problems before age 3 years leads to better outcomes than detection between 3 and 5 years of age. Testing is more difficult in younger children and can yield inconclusive or false-positive results more frequently. This led the USPSTF to reaffirm vision testing once for children ages 3 to 5 years, and to state that the evidence is insufficient to make a recommendation for younger children.5
Screening for osteoporosis
The recommendations indicate that all women ages 65 and older should undergo screening, although the optimal frequency of screening is not known. The clinical discussion accompanying the recommendation indicates there is reason to believe that screening men may reduce morbidity and mortality, but that sufficient evidence for or against this is lacking.6
Screening can be done with dual-energy x-ray absorptiometry (DEXA) of the hip and lumbar spine, or quantitative ultrasonography of the calcaneus. DEXA is most commonly used, and is the basis for most treatment recommendations.
The recommendation to screen some women younger than 65 years, based on risk, is somewhat complex. The USPSTF recommends screening younger women if their 10-year risk of fracture is comparable to that of a 65-year-old white woman with no additional risk factors (a risk of 9.3% over 10 years). To calculate that risk, the USPSTF recommends using the FRAX (Fracture Risk Assessment) tool developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom, which is available free to clinicians and the public (www.shef.ac.uk/FRAX/).
Screening for testicular cancer
The recommendation against screening for testicular cancer may surprise many physicians, even though it is a reaffirmation of a previous recommendation. Testicular cancer is uncommon (5 cases per 100,000 males per year) and treatment is successful in a large proportion of patients, regardless of the stage at which it is discovered. Patients or their partners discover these tumors in time for a cure and there is no evidence physician exams improve outcomes. Physician discovery of incidental and inconsequential findings such as spermatoceles and varicoceles can lead to unnecessary testing and follow-up.7
Screening for bladder cancer
The USPSTF issued an I statement for bladder cancer screening because there is little evidence regarding the diagnostic accuracy of available tests (urinalysis for microscopic hematuria, urine cytology, or tests for urine biomarkers) in detecting bladder cancer in asymptomatic patients. In addition, there is no evidence regarding the potential benefits of detecting asymptomatic bladder cancer.8
Current draft recommendations
The USPSTF posts recommendations on its Web site for public comment for 30 days. To see current draft recommendations, go to http://www.uspreventiveservicestaskforce.org/tfcomment.htm.
1. USPSTF. Screening for cervical cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. Accessed March 10, 2012.
2. Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13:78-88.
3. Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663-672.
4. USPSTF. Ocular prophylaxis for gonococcal ophthalmia neonatorum. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgononew.htm. Accessed March 10, 2012.
5. USPSTF. Screening for vision impairment in children ages 1 to 5 years. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsvsch.htm. Accessed March 10, 2012.
6. USPSTF. Screening for osteoporosis. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed March 10, 2012.
7. USPSTF. Screening for testicular cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm. Accessed March 10, 2012.
8. USPSTF. Screening for bladder cancer in adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm. Accessed March 10, 2012.
Recently, the US Preventive Services Task Force (USPSTF) finalized 7 recommendations on 5 topics and posted draft recommendations on an additional 10 topics. It also implemented new procedures that include posting draft recommendations for public comment (see “A new review process for the USPSTF”). This article reviews the USPSTF activity in 2011, as well as cervical cancer screening recommendations issued earlier this year.
In response to the adverse publicity from the 2009 mammogram recommendations and the increased scrutiny brought on by the affordable care act—which mandates that A and B recommendations from the US Preventive Services Task force are covered preventive services provided at no charge to the patient—the USPSTF developed and implemented a new review procedure. This is intended to increase stakeholder involvement at all steps in the process.
Last year, the USPSTF completed its rollout of this new online review process. The USPSTF now posts all draft recommendations and the evidence report supporting them on its Web site for public comment. final recommendations are posted months later after consideration of the public input. The final recommendations for the 10 topics with draft recommendations posted in 2011 are expected to be released this year.
Potential for confusion. The new process may cause confusion for family physicians. Draft recommendations will receive press coverage and may differ from the final recommendations, as happened with cervical cancer screening recommendations. Physicians will need to familiarize themselves with the process and look for final recommendations on the USPSTF Web site at http://www.uspreventiveservicestaskforce.org/recommendations.htm.
2012 recommendations
Screening for cervical cancer
The USPSTF released its new recommendations on screening for cervical cancer in March (TABLE 1).1 The final document varied from the 2011 draft recommendations in 2 areas: the roles of human papillomavirus (HPV) testing and sexual history.
- The draft issued an I statement (insufficient evidence) for the role of HPV testing. Subsequently, based on stakeholder and public comment (as well as a review of 2 large recently published studies), the USPSTF gave an A recommendation to the use of HPV testing in conjunction with cervical cytology as an option for women ages 30 years and older who want to increase the interval between screening to 5 years.2,3
- The draft stated that the age at which screening should be initiated depends on a patient’s sexual history. The final recommendations state that screening should not begin until age 21, regardless of sexual history.
TABLE 1
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
These new recommendations balance the proven benefits of cervical cytology with the harms from overscreening and are now essentially the same as those of other organizations, including the American Cancer Society, the American Society for Colposcopy and Cervical Pathology, and the American Society for Clinical Pathology. They differ in minor ways from those of the American Congress of Obstetricians and Gynecologists, and the American Academy of Family Physicians is assessing whether to endorse them.
Importantly, the new recommendations identify individuals for whom cervical cytology should be avoided—women younger than age 21, most women older than age 65, and those who have had a hysterectomy with removal of the cervix. A decision to stop screening after the 65th birthday depends on whether the patient has had adequate screening yielding normal findings: This is defined by the USPSTF as 3 consecutive negative cytology results (or 2 consecutive negative co-test results with cytology and HIV testing) within 10 years of the proposed time of cessation, with the most recent test having been performed within 5 years. Avoiding cytology testing after hysterectomy is contingent on the procedure having been performed for an indication other than a high-grade precancerous lesion or cervical cancer. In addition, the recommendations advise against HPV testing in women younger than age 30, as it offers little advantage and leads to much overdiagnosis.
Liquid vs conventional cytology. As a minor point, the USPSTF says the evidence clearly shows that liquid cytology offers no advantage over conventional cytology. But it recognizes that the screening method used is often not determined by the physician.
Recommendations finalized in 2011
TABLE 2 summarizes recommendations completed by the USPSTF last year.
Neonatal gonococcal eye infection prevention
The recommendation to use topical medication (erythromycin ointment) to prevent neonatal gonococcal eye infection is an update and reaffirmation of a previous recommendation. Blindness due to this disease has become rare in the United States because of the routine use of a neonatal topical antibiotic, and there is good evidence that it causes no significant harm. Its use continues to be recommended for all newborns.4
TABLE 2
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
Vision screening for children
Vision screening for preschool children can detect visual acuity problems such as amblyopia and refractive errors. A variety of screening tests are available, including visual acuity, stereoacuity, cover-uncover, Hirschberg light reflex, and auto-refractor tests (automated optical instruments that detect refractive errors). The most benefit is obtained by discovering and correcting amblyopia.
There is no evidence that detecting problems before age 3 years leads to better outcomes than detection between 3 and 5 years of age. Testing is more difficult in younger children and can yield inconclusive or false-positive results more frequently. This led the USPSTF to reaffirm vision testing once for children ages 3 to 5 years, and to state that the evidence is insufficient to make a recommendation for younger children.5
Screening for osteoporosis
The recommendations indicate that all women ages 65 and older should undergo screening, although the optimal frequency of screening is not known. The clinical discussion accompanying the recommendation indicates there is reason to believe that screening men may reduce morbidity and mortality, but that sufficient evidence for or against this is lacking.6
Screening can be done with dual-energy x-ray absorptiometry (DEXA) of the hip and lumbar spine, or quantitative ultrasonography of the calcaneus. DEXA is most commonly used, and is the basis for most treatment recommendations.
The recommendation to screen some women younger than 65 years, based on risk, is somewhat complex. The USPSTF recommends screening younger women if their 10-year risk of fracture is comparable to that of a 65-year-old white woman with no additional risk factors (a risk of 9.3% over 10 years). To calculate that risk, the USPSTF recommends using the FRAX (Fracture Risk Assessment) tool developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom, which is available free to clinicians and the public (www.shef.ac.uk/FRAX/).
Screening for testicular cancer
The recommendation against screening for testicular cancer may surprise many physicians, even though it is a reaffirmation of a previous recommendation. Testicular cancer is uncommon (5 cases per 100,000 males per year) and treatment is successful in a large proportion of patients, regardless of the stage at which it is discovered. Patients or their partners discover these tumors in time for a cure and there is no evidence physician exams improve outcomes. Physician discovery of incidental and inconsequential findings such as spermatoceles and varicoceles can lead to unnecessary testing and follow-up.7
Screening for bladder cancer
The USPSTF issued an I statement for bladder cancer screening because there is little evidence regarding the diagnostic accuracy of available tests (urinalysis for microscopic hematuria, urine cytology, or tests for urine biomarkers) in detecting bladder cancer in asymptomatic patients. In addition, there is no evidence regarding the potential benefits of detecting asymptomatic bladder cancer.8
Current draft recommendations
The USPSTF posts recommendations on its Web site for public comment for 30 days. To see current draft recommendations, go to http://www.uspreventiveservicestaskforce.org/tfcomment.htm.
Recently, the US Preventive Services Task Force (USPSTF) finalized 7 recommendations on 5 topics and posted draft recommendations on an additional 10 topics. It also implemented new procedures that include posting draft recommendations for public comment (see “A new review process for the USPSTF”). This article reviews the USPSTF activity in 2011, as well as cervical cancer screening recommendations issued earlier this year.
In response to the adverse publicity from the 2009 mammogram recommendations and the increased scrutiny brought on by the affordable care act—which mandates that A and B recommendations from the US Preventive Services Task force are covered preventive services provided at no charge to the patient—the USPSTF developed and implemented a new review procedure. This is intended to increase stakeholder involvement at all steps in the process.
Last year, the USPSTF completed its rollout of this new online review process. The USPSTF now posts all draft recommendations and the evidence report supporting them on its Web site for public comment. final recommendations are posted months later after consideration of the public input. The final recommendations for the 10 topics with draft recommendations posted in 2011 are expected to be released this year.
Potential for confusion. The new process may cause confusion for family physicians. Draft recommendations will receive press coverage and may differ from the final recommendations, as happened with cervical cancer screening recommendations. Physicians will need to familiarize themselves with the process and look for final recommendations on the USPSTF Web site at http://www.uspreventiveservicestaskforce.org/recommendations.htm.
2012 recommendations
Screening for cervical cancer
The USPSTF released its new recommendations on screening for cervical cancer in March (TABLE 1).1 The final document varied from the 2011 draft recommendations in 2 areas: the roles of human papillomavirus (HPV) testing and sexual history.
- The draft issued an I statement (insufficient evidence) for the role of HPV testing. Subsequently, based on stakeholder and public comment (as well as a review of 2 large recently published studies), the USPSTF gave an A recommendation to the use of HPV testing in conjunction with cervical cytology as an option for women ages 30 years and older who want to increase the interval between screening to 5 years.2,3
- The draft stated that the age at which screening should be initiated depends on a patient’s sexual history. The final recommendations state that screening should not begin until age 21, regardless of sexual history.
TABLE 1
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
These new recommendations balance the proven benefits of cervical cytology with the harms from overscreening and are now essentially the same as those of other organizations, including the American Cancer Society, the American Society for Colposcopy and Cervical Pathology, and the American Society for Clinical Pathology. They differ in minor ways from those of the American Congress of Obstetricians and Gynecologists, and the American Academy of Family Physicians is assessing whether to endorse them.
Importantly, the new recommendations identify individuals for whom cervical cytology should be avoided—women younger than age 21, most women older than age 65, and those who have had a hysterectomy with removal of the cervix. A decision to stop screening after the 65th birthday depends on whether the patient has had adequate screening yielding normal findings: This is defined by the USPSTF as 3 consecutive negative cytology results (or 2 consecutive negative co-test results with cytology and HIV testing) within 10 years of the proposed time of cessation, with the most recent test having been performed within 5 years. Avoiding cytology testing after hysterectomy is contingent on the procedure having been performed for an indication other than a high-grade precancerous lesion or cervical cancer. In addition, the recommendations advise against HPV testing in women younger than age 30, as it offers little advantage and leads to much overdiagnosis.
Liquid vs conventional cytology. As a minor point, the USPSTF says the evidence clearly shows that liquid cytology offers no advantage over conventional cytology. But it recognizes that the screening method used is often not determined by the physician.
Recommendations finalized in 2011
TABLE 2 summarizes recommendations completed by the USPSTF last year.
Neonatal gonococcal eye infection prevention
The recommendation to use topical medication (erythromycin ointment) to prevent neonatal gonococcal eye infection is an update and reaffirmation of a previous recommendation. Blindness due to this disease has become rare in the United States because of the routine use of a neonatal topical antibiotic, and there is good evidence that it causes no significant harm. Its use continues to be recommended for all newborns.4
TABLE 2
*For more on the USPSTF's grade definitions, see http://www.uspreventiveservicestaskforce.org/uspstf/grades.htm.
Vision screening for children
Vision screening for preschool children can detect visual acuity problems such as amblyopia and refractive errors. A variety of screening tests are available, including visual acuity, stereoacuity, cover-uncover, Hirschberg light reflex, and auto-refractor tests (automated optical instruments that detect refractive errors). The most benefit is obtained by discovering and correcting amblyopia.
There is no evidence that detecting problems before age 3 years leads to better outcomes than detection between 3 and 5 years of age. Testing is more difficult in younger children and can yield inconclusive or false-positive results more frequently. This led the USPSTF to reaffirm vision testing once for children ages 3 to 5 years, and to state that the evidence is insufficient to make a recommendation for younger children.5
Screening for osteoporosis
The recommendations indicate that all women ages 65 and older should undergo screening, although the optimal frequency of screening is not known. The clinical discussion accompanying the recommendation indicates there is reason to believe that screening men may reduce morbidity and mortality, but that sufficient evidence for or against this is lacking.6
Screening can be done with dual-energy x-ray absorptiometry (DEXA) of the hip and lumbar spine, or quantitative ultrasonography of the calcaneus. DEXA is most commonly used, and is the basis for most treatment recommendations.
The recommendation to screen some women younger than 65 years, based on risk, is somewhat complex. The USPSTF recommends screening younger women if their 10-year risk of fracture is comparable to that of a 65-year-old white woman with no additional risk factors (a risk of 9.3% over 10 years). To calculate that risk, the USPSTF recommends using the FRAX (Fracture Risk Assessment) tool developed by the World Health Organization Collaborating Centre for Metabolic Bone Diseases, Sheffield, United Kingdom, which is available free to clinicians and the public (www.shef.ac.uk/FRAX/).
Screening for testicular cancer
The recommendation against screening for testicular cancer may surprise many physicians, even though it is a reaffirmation of a previous recommendation. Testicular cancer is uncommon (5 cases per 100,000 males per year) and treatment is successful in a large proportion of patients, regardless of the stage at which it is discovered. Patients or their partners discover these tumors in time for a cure and there is no evidence physician exams improve outcomes. Physician discovery of incidental and inconsequential findings such as spermatoceles and varicoceles can lead to unnecessary testing and follow-up.7
Screening for bladder cancer
The USPSTF issued an I statement for bladder cancer screening because there is little evidence regarding the diagnostic accuracy of available tests (urinalysis for microscopic hematuria, urine cytology, or tests for urine biomarkers) in detecting bladder cancer in asymptomatic patients. In addition, there is no evidence regarding the potential benefits of detecting asymptomatic bladder cancer.8
Current draft recommendations
The USPSTF posts recommendations on its Web site for public comment for 30 days. To see current draft recommendations, go to http://www.uspreventiveservicestaskforce.org/tfcomment.htm.
1. USPSTF. Screening for cervical cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. Accessed March 10, 2012.
2. Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13:78-88.
3. Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663-672.
4. USPSTF. Ocular prophylaxis for gonococcal ophthalmia neonatorum. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgononew.htm. Accessed March 10, 2012.
5. USPSTF. Screening for vision impairment in children ages 1 to 5 years. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsvsch.htm. Accessed March 10, 2012.
6. USPSTF. Screening for osteoporosis. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed March 10, 2012.
7. USPSTF. Screening for testicular cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm. Accessed March 10, 2012.
8. USPSTF. Screening for bladder cancer in adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm. Accessed March 10, 2012.
1. USPSTF. Screening for cervical cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspscerv.htm. Accessed March 10, 2012.
2. Rijkaart DC, Berkhof J, Rozendaal L, et al. Human papillomavirus testing for the detection of high-grade cervical intraepithelial neoplasia and cancer: final results of the POBASCAM randomised controlled trial. Lancet Oncol. 2012;13:78-88.
3. Katki HA, Kinney WK, Fetterman B, et al. Cervical cancer risk for women undergoing concurrent testing for human papillomavirus and cervical cytology: a population-based study in routine clinical practice. Lancet Oncol. 2011;12:663-672.
4. USPSTF. Ocular prophylaxis for gonococcal ophthalmia neonatorum. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgononew.htm. Accessed March 10, 2012.
5. USPSTF. Screening for vision impairment in children ages 1 to 5 years. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsvsch.htm. Accessed March 10, 2012.
6. USPSTF. Screening for osteoporosis. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsoste.htm. Accessed March 10, 2012.
7. USPSTF. Screening for testicular cancer. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspstest.htm. Accessed March 10, 2012.
8. USPSTF. Screening for bladder cancer in adults. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsblad.htm. Accessed March 10, 2012.
ACIP immunization update
In February, the Centers for Disease Control and Prevention (CDC) published the 2012 immunization schedules for infants and children, adolescents, and adults.1,2 The schedules, which are available at http://www.cdc.gov/vaccines/recs/schedules/default.htm, are updated annually and incorporate additions and changes recommended by the Advisory Committee on Immunization Practices (ACIP) over the past year. While there were no major advances in new vaccines in 2011, there were a number of new indications for existing ones.
Human papillomavirus vaccine for males
Quadrivalent vaccine against human papillomavirus is now recommended for routine use for males ages 11 to 12 years to prevent genital warts and anal intraepithelial neoplasia.3,4 Catch-up vaccination is also recommended for males ages 13 to 21 who have not received it. In addition, routine use is recommended for males ages 22 to 26 years who have sex with men or are HIV positive or immuno-compromised.
Tetanus toxoid, reduced strength diphtheria toxoid, and acellular pertussis (Tdap)
Indications for the routine use of Tdap were expanded to include children ages 7 to 10 years, pregnant women, and adults age 65 and older who have contact with infants.5,6 Children ages 7 to 10 years who have not had the full series of DTaP should receive Td/Tdap according to the catch-up schedule,1 with one of the doses being Tdap. Adults older than 65 who have never received Tdap and who have close contact with infants should receive one dose. No minimum interval is required between receipt of the Td and Tdap vaccines. Other older adults who ask for Tdap vaccination should receive it. Use of Tdap in those ages 7 to 10 years or 65 and older is off label.5
Pregnant women who have not received Tdap should receive 1 dose after week 20 of pregnancy, although receiving it earlier is not contraindicated if tetanus toxoid is needed for tetanus prevention following a wound.6
Hepatitis B virus (HBV) vaccine
Added to the list of high-risk adults who should receive HBV vaccine routinely are those ages 19 through 59 years with diabetes.7 Vaccinate as soon as possible after the diabetes diagnosis is confirmed. The decision as to whether to vaccinate patients ≥60 years with diabetes should be based on the likelihood that they will become infected. Considerations include the risks associated with an increased need for help with blood-glucose monitoring in long-term care facilities, the likelihood that the patient will experience chronic sequelae if infected, and the likelihood that the patient will mount a proper immune response to the vaccine.7 (The more frail patients are, the less likely they are to achieve adequate immunity.7)
Meningococcal conjugate vaccine, quadrivalent (MCV4)
An MCV4 vaccine (Menactra) has now been licensed for use in children as young as 9 months.8 At this time, however, neither Menactra nor its competitor, Menveo (licensed for use in those 2 years and older), is recommended for routine administration until the age of 11 to 12 years. Infants and children ages 9 through 23 months with complement deficiencies, or who will be traveling to countries with endemic high levels of meningococcus, should be vaccinated with 2 doses of Menactra 3 months apart, and with a booster dose after 3 years if risk persists. The recommendations regarding the use of MCV4 in those ≤2 years with high-risk conditions are listed in TABLE 1.
In February 2012, the CDC announced results of the 2010 National Health Interview Survey. Increases in immunization coverage occurred only with Tdap vaccination for individuals 19 to 64 years of age (from 6.6% to 8.2%), herpes zoster vaccination among those ≥60 years (from 10% to 14.4%), and ≥1 dose of HPV vaccination for women 19 to 26 years (from 17.1% to 20.7%). Rates of immunization were unchanged for other vaccines. The CDC said a substantial improvement in coverage is needed to reduce vaccine-preventable diseases among adults.
Source: CDC. Adult vaccination coverage—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:66-72.
Another change regarding the use of MCV4 is a recommended booster dose for those age 16 and older who were first vaccinated at age 11 or 12 years.9 For those vaccinated at ages 13 to 15, a booster should be received at ages 16 to 18. No booster is needed if the first MCV4 dose is received at or after age 16. Recommendations for MCV4 use and booster doses for those 2 years and older are listed in TABLE 2.
TABLE 1
Recommended Menactra schedule for young children at high risk for invasive meningococcal disease8
| Risk group | Primary vaccination series | Booster dose, if child remains at increased risk |
|---|---|---|
| Children ages 9-23 months at high risk for invasive meningococcal disease,* except those with functional or anatomic asplenia | 2 doses, 3 months apart Catch-up dose at earliest opportunity if dose 2 is not given on schedule | Initial booster 3 years after completing primary series At 5-year intervals after initial booster |
| Children with functional or anatomic asplenia at high risk for invasive meningococcal disease | 2 doses, 2 months apart, starting at age 2 years and ≥4 weeks after completing the PCV13 vaccine series | |
| PCV, pneumococcal conjugate vaccine. *Children who have persistent complement component deficiencies (eg, C5–C9, properdin, factor H, or factor D); those traveling to (or residents of) countries where meningococcal disease is hyperendemic or epidemic; or those who are in a defined risk group during a community or institutional meningococcal outbreak. | ||
TABLE 2
Recommended schedule for meningococcal conjugate vaccine in those ≥2 years, according to risk9
| Risk group | Primary vaccination series | Booster dose |
|---|---|---|
| Individuals ages 11-18 years | 1 dose, preferably at 11 or 12 years | At age 16 years, if primary dose given at age 11 or 12 years Age 16-18 years, if primary dose given at age 13-15 years No booster needed if primary dose given on or after age 16 years |
| Individuals ages 11-18 years infected with HIV | 2 doses, 2 months apart | |
| Individuals ages 2-55 years with persistent complement component deficiency (eg, C5–C9, properdin, or factor D) or functional or anatomical asplenia | 2 doses, 2 months apart | Every 5 years At the earliest opportunity if only 1 primary dose; every 5 years thereafter |
| Individuals ages 2-55 years with prolonged increased risk for exposure, such as microbiologists routinely working with Neisseria meningitides, and travelers to, or residents of, countries where meningococcal disease is hyperendemic or epidemic | 1 dose | After 3 years, if primary dose given at age 2-6 years After 5 years, if primary dose given at ≥7 years and the individual remains at risk Every 5 years thereafter, as long as the risk persists |
| HIV, human immunodeficiency virus. | ||
Herpes zoster vaccine
The herpes zoster vaccine was initially licensed for those 60 years and older. Last year the FDA approved lowering the age to 50 years and older. At this time, however, the ACIP continues to recommend that the vaccine be used routinely starting at age 60 years. The age was not lowered because of a concern about vaccine supply and the uncertainty about the possible need for a booster dose if administered at age 50.10
Influenza vaccine
As described in a previous Practice Alert,11 a history of egg allergy is no longer a strict contraindication for receipt of the influenza vaccine. The other major adjustment is a simplified recommendation on how to determine the required number of doses for a child younger than 9 years. If the child received 1 or both doses of the 2010-2011 vaccine, give just a single dose of the 2011-2012 vaccine. If the history is uncertain, give 2 doses of the new vaccine at least 4 weeks apart.12
1. CDC. Recommended immunization schedules for persons aged 0 through 18 years—United States, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(5):1-4.
2. CDC. Recommended adult immunization schedule—United States, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(4):1-7.
3. Campos-Outcalt D. Human papilloma virus: Vaccine is now routinely indicated for males. J Fam Pract. 2012;61:38-40.
4. CDC. Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1705-1708.
5. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:13-15.
6. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1424-1426.
7. CDC. Use of hepatitis B vaccination for adults with diabetes mellitus: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60:1709-1711.
8. CDC. Recommendation of the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MenACWY-D) among children aged 9 through 23 months at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep. 2011;60:1391-1392.
9. CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76.
10. CDC. Update on herpes zoster vaccine: licensure for persons aged 50 through 59 years. MMWR Morb Mortal Wkly Rep. 2011;60:1528-
11. Campos-Outcalt D. Ready for flu season? The 2011-2012 ACIP recommendations. J Fam Pract. 2011;60:543-544.
12. CDC. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1128-1132.
In February, the Centers for Disease Control and Prevention (CDC) published the 2012 immunization schedules for infants and children, adolescents, and adults.1,2 The schedules, which are available at http://www.cdc.gov/vaccines/recs/schedules/default.htm, are updated annually and incorporate additions and changes recommended by the Advisory Committee on Immunization Practices (ACIP) over the past year. While there were no major advances in new vaccines in 2011, there were a number of new indications for existing ones.
Human papillomavirus vaccine for males
Quadrivalent vaccine against human papillomavirus is now recommended for routine use for males ages 11 to 12 years to prevent genital warts and anal intraepithelial neoplasia.3,4 Catch-up vaccination is also recommended for males ages 13 to 21 who have not received it. In addition, routine use is recommended for males ages 22 to 26 years who have sex with men or are HIV positive or immuno-compromised.
Tetanus toxoid, reduced strength diphtheria toxoid, and acellular pertussis (Tdap)
Indications for the routine use of Tdap were expanded to include children ages 7 to 10 years, pregnant women, and adults age 65 and older who have contact with infants.5,6 Children ages 7 to 10 years who have not had the full series of DTaP should receive Td/Tdap according to the catch-up schedule,1 with one of the doses being Tdap. Adults older than 65 who have never received Tdap and who have close contact with infants should receive one dose. No minimum interval is required between receipt of the Td and Tdap vaccines. Other older adults who ask for Tdap vaccination should receive it. Use of Tdap in those ages 7 to 10 years or 65 and older is off label.5
Pregnant women who have not received Tdap should receive 1 dose after week 20 of pregnancy, although receiving it earlier is not contraindicated if tetanus toxoid is needed for tetanus prevention following a wound.6
Hepatitis B virus (HBV) vaccine
Added to the list of high-risk adults who should receive HBV vaccine routinely are those ages 19 through 59 years with diabetes.7 Vaccinate as soon as possible after the diabetes diagnosis is confirmed. The decision as to whether to vaccinate patients ≥60 years with diabetes should be based on the likelihood that they will become infected. Considerations include the risks associated with an increased need for help with blood-glucose monitoring in long-term care facilities, the likelihood that the patient will experience chronic sequelae if infected, and the likelihood that the patient will mount a proper immune response to the vaccine.7 (The more frail patients are, the less likely they are to achieve adequate immunity.7)
Meningococcal conjugate vaccine, quadrivalent (MCV4)
An MCV4 vaccine (Menactra) has now been licensed for use in children as young as 9 months.8 At this time, however, neither Menactra nor its competitor, Menveo (licensed for use in those 2 years and older), is recommended for routine administration until the age of 11 to 12 years. Infants and children ages 9 through 23 months with complement deficiencies, or who will be traveling to countries with endemic high levels of meningococcus, should be vaccinated with 2 doses of Menactra 3 months apart, and with a booster dose after 3 years if risk persists. The recommendations regarding the use of MCV4 in those ≤2 years with high-risk conditions are listed in TABLE 1.
In February 2012, the CDC announced results of the 2010 National Health Interview Survey. Increases in immunization coverage occurred only with Tdap vaccination for individuals 19 to 64 years of age (from 6.6% to 8.2%), herpes zoster vaccination among those ≥60 years (from 10% to 14.4%), and ≥1 dose of HPV vaccination for women 19 to 26 years (from 17.1% to 20.7%). Rates of immunization were unchanged for other vaccines. The CDC said a substantial improvement in coverage is needed to reduce vaccine-preventable diseases among adults.
Source: CDC. Adult vaccination coverage—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:66-72.
Another change regarding the use of MCV4 is a recommended booster dose for those age 16 and older who were first vaccinated at age 11 or 12 years.9 For those vaccinated at ages 13 to 15, a booster should be received at ages 16 to 18. No booster is needed if the first MCV4 dose is received at or after age 16. Recommendations for MCV4 use and booster doses for those 2 years and older are listed in TABLE 2.
TABLE 1
Recommended Menactra schedule for young children at high risk for invasive meningococcal disease8
| Risk group | Primary vaccination series | Booster dose, if child remains at increased risk |
|---|---|---|
| Children ages 9-23 months at high risk for invasive meningococcal disease,* except those with functional or anatomic asplenia | 2 doses, 3 months apart Catch-up dose at earliest opportunity if dose 2 is not given on schedule | Initial booster 3 years after completing primary series At 5-year intervals after initial booster |
| Children with functional or anatomic asplenia at high risk for invasive meningococcal disease | 2 doses, 2 months apart, starting at age 2 years and ≥4 weeks after completing the PCV13 vaccine series | |
| PCV, pneumococcal conjugate vaccine. *Children who have persistent complement component deficiencies (eg, C5–C9, properdin, factor H, or factor D); those traveling to (or residents of) countries where meningococcal disease is hyperendemic or epidemic; or those who are in a defined risk group during a community or institutional meningococcal outbreak. | ||
TABLE 2
Recommended schedule for meningococcal conjugate vaccine in those ≥2 years, according to risk9
| Risk group | Primary vaccination series | Booster dose |
|---|---|---|
| Individuals ages 11-18 years | 1 dose, preferably at 11 or 12 years | At age 16 years, if primary dose given at age 11 or 12 years Age 16-18 years, if primary dose given at age 13-15 years No booster needed if primary dose given on or after age 16 years |
| Individuals ages 11-18 years infected with HIV | 2 doses, 2 months apart | |
| Individuals ages 2-55 years with persistent complement component deficiency (eg, C5–C9, properdin, or factor D) or functional or anatomical asplenia | 2 doses, 2 months apart | Every 5 years At the earliest opportunity if only 1 primary dose; every 5 years thereafter |
| Individuals ages 2-55 years with prolonged increased risk for exposure, such as microbiologists routinely working with Neisseria meningitides, and travelers to, or residents of, countries where meningococcal disease is hyperendemic or epidemic | 1 dose | After 3 years, if primary dose given at age 2-6 years After 5 years, if primary dose given at ≥7 years and the individual remains at risk Every 5 years thereafter, as long as the risk persists |
| HIV, human immunodeficiency virus. | ||
Herpes zoster vaccine
The herpes zoster vaccine was initially licensed for those 60 years and older. Last year the FDA approved lowering the age to 50 years and older. At this time, however, the ACIP continues to recommend that the vaccine be used routinely starting at age 60 years. The age was not lowered because of a concern about vaccine supply and the uncertainty about the possible need for a booster dose if administered at age 50.10
Influenza vaccine
As described in a previous Practice Alert,11 a history of egg allergy is no longer a strict contraindication for receipt of the influenza vaccine. The other major adjustment is a simplified recommendation on how to determine the required number of doses for a child younger than 9 years. If the child received 1 or both doses of the 2010-2011 vaccine, give just a single dose of the 2011-2012 vaccine. If the history is uncertain, give 2 doses of the new vaccine at least 4 weeks apart.12
In February, the Centers for Disease Control and Prevention (CDC) published the 2012 immunization schedules for infants and children, adolescents, and adults.1,2 The schedules, which are available at http://www.cdc.gov/vaccines/recs/schedules/default.htm, are updated annually and incorporate additions and changes recommended by the Advisory Committee on Immunization Practices (ACIP) over the past year. While there were no major advances in new vaccines in 2011, there were a number of new indications for existing ones.
Human papillomavirus vaccine for males
Quadrivalent vaccine against human papillomavirus is now recommended for routine use for males ages 11 to 12 years to prevent genital warts and anal intraepithelial neoplasia.3,4 Catch-up vaccination is also recommended for males ages 13 to 21 who have not received it. In addition, routine use is recommended for males ages 22 to 26 years who have sex with men or are HIV positive or immuno-compromised.
Tetanus toxoid, reduced strength diphtheria toxoid, and acellular pertussis (Tdap)
Indications for the routine use of Tdap were expanded to include children ages 7 to 10 years, pregnant women, and adults age 65 and older who have contact with infants.5,6 Children ages 7 to 10 years who have not had the full series of DTaP should receive Td/Tdap according to the catch-up schedule,1 with one of the doses being Tdap. Adults older than 65 who have never received Tdap and who have close contact with infants should receive one dose. No minimum interval is required between receipt of the Td and Tdap vaccines. Other older adults who ask for Tdap vaccination should receive it. Use of Tdap in those ages 7 to 10 years or 65 and older is off label.5
Pregnant women who have not received Tdap should receive 1 dose after week 20 of pregnancy, although receiving it earlier is not contraindicated if tetanus toxoid is needed for tetanus prevention following a wound.6
Hepatitis B virus (HBV) vaccine
Added to the list of high-risk adults who should receive HBV vaccine routinely are those ages 19 through 59 years with diabetes.7 Vaccinate as soon as possible after the diabetes diagnosis is confirmed. The decision as to whether to vaccinate patients ≥60 years with diabetes should be based on the likelihood that they will become infected. Considerations include the risks associated with an increased need for help with blood-glucose monitoring in long-term care facilities, the likelihood that the patient will experience chronic sequelae if infected, and the likelihood that the patient will mount a proper immune response to the vaccine.7 (The more frail patients are, the less likely they are to achieve adequate immunity.7)
Meningococcal conjugate vaccine, quadrivalent (MCV4)
An MCV4 vaccine (Menactra) has now been licensed for use in children as young as 9 months.8 At this time, however, neither Menactra nor its competitor, Menveo (licensed for use in those 2 years and older), is recommended for routine administration until the age of 11 to 12 years. Infants and children ages 9 through 23 months with complement deficiencies, or who will be traveling to countries with endemic high levels of meningococcus, should be vaccinated with 2 doses of Menactra 3 months apart, and with a booster dose after 3 years if risk persists. The recommendations regarding the use of MCV4 in those ≤2 years with high-risk conditions are listed in TABLE 1.
In February 2012, the CDC announced results of the 2010 National Health Interview Survey. Increases in immunization coverage occurred only with Tdap vaccination for individuals 19 to 64 years of age (from 6.6% to 8.2%), herpes zoster vaccination among those ≥60 years (from 10% to 14.4%), and ≥1 dose of HPV vaccination for women 19 to 26 years (from 17.1% to 20.7%). Rates of immunization were unchanged for other vaccines. The CDC said a substantial improvement in coverage is needed to reduce vaccine-preventable diseases among adults.
Source: CDC. Adult vaccination coverage—United States, 2010. MMWR Morb Mortal Wkly Rep. 2012;61:66-72.
Another change regarding the use of MCV4 is a recommended booster dose for those age 16 and older who were first vaccinated at age 11 or 12 years.9 For those vaccinated at ages 13 to 15, a booster should be received at ages 16 to 18. No booster is needed if the first MCV4 dose is received at or after age 16. Recommendations for MCV4 use and booster doses for those 2 years and older are listed in TABLE 2.
TABLE 1
Recommended Menactra schedule for young children at high risk for invasive meningococcal disease8
| Risk group | Primary vaccination series | Booster dose, if child remains at increased risk |
|---|---|---|
| Children ages 9-23 months at high risk for invasive meningococcal disease,* except those with functional or anatomic asplenia | 2 doses, 3 months apart Catch-up dose at earliest opportunity if dose 2 is not given on schedule | Initial booster 3 years after completing primary series At 5-year intervals after initial booster |
| Children with functional or anatomic asplenia at high risk for invasive meningococcal disease | 2 doses, 2 months apart, starting at age 2 years and ≥4 weeks after completing the PCV13 vaccine series | |
| PCV, pneumococcal conjugate vaccine. *Children who have persistent complement component deficiencies (eg, C5–C9, properdin, factor H, or factor D); those traveling to (or residents of) countries where meningococcal disease is hyperendemic or epidemic; or those who are in a defined risk group during a community or institutional meningococcal outbreak. | ||
TABLE 2
Recommended schedule for meningococcal conjugate vaccine in those ≥2 years, according to risk9
| Risk group | Primary vaccination series | Booster dose |
|---|---|---|
| Individuals ages 11-18 years | 1 dose, preferably at 11 or 12 years | At age 16 years, if primary dose given at age 11 or 12 years Age 16-18 years, if primary dose given at age 13-15 years No booster needed if primary dose given on or after age 16 years |
| Individuals ages 11-18 years infected with HIV | 2 doses, 2 months apart | |
| Individuals ages 2-55 years with persistent complement component deficiency (eg, C5–C9, properdin, or factor D) or functional or anatomical asplenia | 2 doses, 2 months apart | Every 5 years At the earliest opportunity if only 1 primary dose; every 5 years thereafter |
| Individuals ages 2-55 years with prolonged increased risk for exposure, such as microbiologists routinely working with Neisseria meningitides, and travelers to, or residents of, countries where meningococcal disease is hyperendemic or epidemic | 1 dose | After 3 years, if primary dose given at age 2-6 years After 5 years, if primary dose given at ≥7 years and the individual remains at risk Every 5 years thereafter, as long as the risk persists |
| HIV, human immunodeficiency virus. | ||
Herpes zoster vaccine
The herpes zoster vaccine was initially licensed for those 60 years and older. Last year the FDA approved lowering the age to 50 years and older. At this time, however, the ACIP continues to recommend that the vaccine be used routinely starting at age 60 years. The age was not lowered because of a concern about vaccine supply and the uncertainty about the possible need for a booster dose if administered at age 50.10
Influenza vaccine
As described in a previous Practice Alert,11 a history of egg allergy is no longer a strict contraindication for receipt of the influenza vaccine. The other major adjustment is a simplified recommendation on how to determine the required number of doses for a child younger than 9 years. If the child received 1 or both doses of the 2010-2011 vaccine, give just a single dose of the 2011-2012 vaccine. If the history is uncertain, give 2 doses of the new vaccine at least 4 weeks apart.12
1. CDC. Recommended immunization schedules for persons aged 0 through 18 years—United States, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(5):1-4.
2. CDC. Recommended adult immunization schedule—United States, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(4):1-7.
3. Campos-Outcalt D. Human papilloma virus: Vaccine is now routinely indicated for males. J Fam Pract. 2012;61:38-40.
4. CDC. Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1705-1708.
5. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:13-15.
6. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1424-1426.
7. CDC. Use of hepatitis B vaccination for adults with diabetes mellitus: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60:1709-1711.
8. CDC. Recommendation of the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MenACWY-D) among children aged 9 through 23 months at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep. 2011;60:1391-1392.
9. CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76.
10. CDC. Update on herpes zoster vaccine: licensure for persons aged 50 through 59 years. MMWR Morb Mortal Wkly Rep. 2011;60:1528-
11. Campos-Outcalt D. Ready for flu season? The 2011-2012 ACIP recommendations. J Fam Pract. 2011;60:543-544.
12. CDC. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1128-1132.
1. CDC. Recommended immunization schedules for persons aged 0 through 18 years—United States, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(5):1-4.
2. CDC. Recommended adult immunization schedule—United States, 2012. MMWR Morb Mortal Wkly Rep. 2012;61(4):1-7.
3. Campos-Outcalt D. Human papilloma virus: Vaccine is now routinely indicated for males. J Fam Pract. 2012;61:38-40.
4. CDC. Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1705-1708.
5. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis (Tdap) vaccine from the Advisory Committee on Immunization Practices, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:13-15.
6. CDC. Updated recommendations for use of tetanus toxoid, reduced diphtheria toxoid and acellular pertussis vaccine (Tdap) in pregnant women and persons who have or anticipate having close contact with an infant aged <12 months—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1424-1426.
7. CDC. Use of hepatitis B vaccination for adults with diabetes mellitus: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2011;60:1709-1711.
8. CDC. Recommendation of the Advisory Committee on Immunization Practices (ACIP) for use of quadrivalent meningococcal conjugate vaccine (MenACWY-D) among children aged 9 through 23 months at increased risk for invasive meningococcal disease. MMWR Morb Mortal Wkly Rep. 2011;60:1391-1392.
9. CDC. Updated recommendations for use of meningococcal conjugate vaccines—Advisory Committee on Immunization Practices (ACIP), 2010. MMWR Morb Mortal Wkly Rep. 2011;60:72-76.
10. CDC. Update on herpes zoster vaccine: licensure for persons aged 50 through 59 years. MMWR Morb Mortal Wkly Rep. 2011;60:1528-
11. Campos-Outcalt D. Ready for flu season? The 2011-2012 ACIP recommendations. J Fam Pract. 2011;60:543-544.
12. CDC. Prevention and control of influenza with vaccines: recommendations of the advisory committee on immunization practices (ACIP), 2011. MMWR Morb Mortal Wkly Rep. 2011;60:1128-1132.
HPV vaccine is now routinely indicated for males
At its October 2011 meeting, the Advisory Committee on Immunization Practices (ACIP) recommended to the CDC that quadrivalent human papilloma virus vaccine (HPV4, Gardasil) be routinely given to all males ages 11 to 21 and to men ages 22 to 26 who have sex with men or who are HIV positive, if they have not been previously vaccinated. This replaces a 2009 recommendation that stated HPV4 vaccine could be used in males to prevent genital warts, but stopped short of advocating routine use for all males.1
There were 3 reasons the previous recommendation did not include HPV4 for routine vaccination of males:
- The vaccine had been shown to be effective only for prevention of genital warts.
- The cost effectiveness of the vaccine for use in boys was poor and, in modeling, it yielded less benefit as more females were vaccinated.
- It was thought that a more effective approach to preventing HPV disease would be to emphasize high rates of vaccination of females.
The new recommendation takes into account recent evidence demonstrating that the vaccine prevents anal intraepithelial neoplasia (AIN) in males, in addition to genital warts. Moreover, vaccination rates in females remain low, which makes vaccinating males more cost effective and additionally protective for females.
Female vaccination rates lower than expected
Despite its effectiveness and safety record, HPV vaccination has had a slow rate of acceptance among females ages 13 to 17 years. Coverage for this group documented in the last national vaccine survey was 48.7% for one dose and 32% for the recommended 3 doses.2
The vaccine is effective in preventing cervical intraepithelial neoplasia (TABLE 1),3 condyloma, and vaginal intraepithelial neoplasia in women ~15 to 26 years of age. Large studies of vaccine safety have documented no serious adverse reactions, other than syncope, which could occur as frequently as 17.9/10,000 females and 12.5/10,000 males.4 Another study that involved post-licensure safety data from >600,000 HPV4 doses found no increased risk for a variety of outcomes, including Guillain-Barré syndrome, stroke, venous thromboembolism, appendicitis, seizures, syncope, allergic reactions, and anaphylaxis.5,6
TABLE 1
HPV vaccine efficacy against HPV type-related CIN2+ in females ages ~15 to 26 years3
| Vaccine/HPV type | Vaccine | Placebo | Efficacy | |||
|---|---|---|---|---|---|---|
| N | CIN cases | N | CIN cases | % | CI* | |
| Bivalent HPV 16/18 HPV 16 HPV 18 | 7344 6303 6794 | 4 2 2 | 7312 6165 6746 | 56 46 15 | 93 96 87 | 80-98 83-100 40-99 |
| Quadrivalent HPV 16/18 HPV 16 HPV 18 | 7738 6647 7382 | 2 2 0 | 7714 6455 7316 | 100 81 29 | 98 98 100 | 93-100 91-100 87-100 |
| CI, confidence interval; CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus. *Confidence interval for bivalent results was 96.1%, and for quadrivalent results was 95%. | ||||||
HPV-associated disease in males
HPV causes anal, penile, and oropharyngeal cancers in males, with about 7500 cancers occurring each year in the United States.3 In addition, about 1% of sexually active males in America have genital warts at any one time.7 HPV types 6 and 11 cause about 90% of cases.1
The HPV4 vaccine—when all 3 doses are given—is 89.3% effective in preventing genital warts related to HPV types 6 and 11. Even a single dose is 68.1% effective (95% CI, 48.8–80.7).1 New evidence shows that HPV4 prevents AIN, which can lead to anal cancer.8 Effectiveness in preventing AIN 2/3 is 74.9% (95% CI, 8.8–95.4) in those completing 3 doses before onset of infection with one of the HPV types contained in vaccine. Notably, these results were obtained in a subgroup analysis of men who have sex with men. And although the reduction in AIN is expected to lower the incidence of anal cancer, ongoing studies require time to confirm this. If such a reduction is confirmed (and vaccination is started at age 12 in the general male population), the number-needed-to-vaccinate to prevent one case of genital warts would be 18, and to prevent one case of anal cancer, 1581.6
No studies have evaluated efficacy of HPV4 in preventing penile or oropharyngeal cancers.
Men who have sex with men at high risk
Men who have sex with men have higher rates of AIN, anal cancers, and genital warts than the general male population.3 Those who are additionally HIV positive have higher rates of genital warts, which are also more difficult to treat.3 AIN is also more common in HIV-infected males.3 The HPV4 vaccine is immunogenic in those who are HIV infected, although the resulting antibody titers are lower than in other populations.
A look at the 2 HPV vaccines
Two HPV vaccines are available (TABLE 2).3 HPV4 vaccine protects against HPV 6, 11, 16, and 18. Bivalent (HPV2, Cervarix) vaccine contains antigens from HPV 16 and 18. Both vaccines are approved for use in females for the prevention of cervical cancer; HPV4 is preferred if protection against genital warts is also desired. Only HPV4 has been licensed for use in males.
TABLE 2
A look at the human papillomavirus vaccines3
| Quadrivalent (Gardasil) | Bivalent (Cervarix) | |
|---|---|---|
| Manufacturer/VLP types | Merck/6, 11, 16, 18 | GlaxoSmithKline/16, 18 |
| Date of US licensure | 2006, females 2009, males | 2009, females |
| Dose of protein | 20/40/40/20 μg | 20/20 μg |
| Producer cells | Saccharomyces cerevisiae (yeast) | Baculovirus-infected Trichoplusia ni (insect cell line) |
| Adjuvant | AAHS: 225 μg amorphous aluminum hydroxyphosphate sulfate | AS04: 500 μg aluminum hydroxide; 50 μg 3-O-desacyl-4’-monophosphoryl lipid A |
| Schedule (IM) | 3-dose series | 3-dose series |
| VLP, virus-like particle; IM, intramuscular. | ||
HPV vaccine is effective, but costly
A major consideration with HPV vaccines is their cost. With 3 doses required and each dose costing about $130,9 cost effectiveness is poor when preventing uncommon diseases such as cervical and anal cancer, and a relatively benign disease such as genital warts. Male vaccination at age 12 years, when added to a female vaccination program, costs about $20,000 to $40,000 per quality-adjusted life year (QALY) if all potential HPV morbidity is included, not just that which has been proven to be prevented by the vaccine (assuming oral and penile cancer will also be prevented). Counting only HPV disease demonstrated to be prevented by the vaccine, the result is $75,000 to $250,000+ per QALY.6 Vaccinating males older than 21 years results in a cost per QALY 2 to 4 times that of vaccinating males younger than 18 years.10
A final decision. After considering these factors, ACIP approved a set of recommendations at its October 2011 meeting that will become official once they are published in the Morbidity and Mortality Weekly Report. (See “ACIP recommendations for HPV vaccine use in males”.)
- Routinely vaccinate males ages 11 to 12 years with 3 doses of HPV4. The vaccination series can be started at 9 years of age. (A recommendation)
- Vaccinate males, ages 13 to 21 years, who have not been vaccinated previously or who have not completed the 3-dose series. (A recommendation)
- Consider vaccinating males ages 22 to 26 years. (B recommendation)
- Vaccinate men ages 22 to 26 years of age who have sex with men and those in this age group who are HIV positive, if they have not been previously vaccinated. (A recommendation)
Levels of recommendation
A: Applies to all individuals in an age- or risk factor-based group.
B: Defers to clinician judgment in determining benefit for individuals.
Source: ACIP meeting; October 25, 2011; Atlanta, Ga.
1. CDC. FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59:630-632.
2. CDC. National and state vaccination coverage among adolescents aged 13 through 17 years—United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1117-1123.
3. Markowitz L. HPV vaccine for males: background and review of data. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/downloads/mtg-slides-oct11/04-HPV-Markowitz.pdf. Accessed December 2, 2011.
4. Gee J. Safety of quadrivalent human papilloma virus (HPV4) vaccine. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/downloads/ mtg-slides-oct11/02-HPV-Gee.pdf. Accessed December 2, 2011.
5. Gee J, Naleway A, Shui I, et al. Monitoring the safety of quadrivalent human papillomavirus vaccine: findings from the Vaccine Safety Datalink. Vaccine. 2011;29:8279-8284.
6. Dunne EF. HPV vaccine considerations for males. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc. gov/vaccines/recs/acip/downloads/mtg-slides-oct11/05-HPVDunne.pdf. Accessed December 2, 2011.
7. CDC. HPV and men—fact sheet. http://www.cdc.gov/std/hpv/std/hpv/stdfact-hpv-and-men.htm. Accessed December 19, 2011.
8. Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365:1576-1585.
9. CDC. Sexually transmitted diseases (STDs): HPV vaccine information for young women—fact sheet. http://www.cdc.gov/std/hpv/stdfact-hpv-vaccine-young-women.htm. Accessed December 2, 2011.
10. Chesson HW. HPV vaccine cost-effectiveness: updates and review. Presented at: ACIP meeting; June 22, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/down-loads/mtg-slides-jun11/07-5-hpv-cost-effect.pdf. Accessed December 2, 2011.
At its October 2011 meeting, the Advisory Committee on Immunization Practices (ACIP) recommended to the CDC that quadrivalent human papilloma virus vaccine (HPV4, Gardasil) be routinely given to all males ages 11 to 21 and to men ages 22 to 26 who have sex with men or who are HIV positive, if they have not been previously vaccinated. This replaces a 2009 recommendation that stated HPV4 vaccine could be used in males to prevent genital warts, but stopped short of advocating routine use for all males.1
There were 3 reasons the previous recommendation did not include HPV4 for routine vaccination of males:
- The vaccine had been shown to be effective only for prevention of genital warts.
- The cost effectiveness of the vaccine for use in boys was poor and, in modeling, it yielded less benefit as more females were vaccinated.
- It was thought that a more effective approach to preventing HPV disease would be to emphasize high rates of vaccination of females.
The new recommendation takes into account recent evidence demonstrating that the vaccine prevents anal intraepithelial neoplasia (AIN) in males, in addition to genital warts. Moreover, vaccination rates in females remain low, which makes vaccinating males more cost effective and additionally protective for females.
Female vaccination rates lower than expected
Despite its effectiveness and safety record, HPV vaccination has had a slow rate of acceptance among females ages 13 to 17 years. Coverage for this group documented in the last national vaccine survey was 48.7% for one dose and 32% for the recommended 3 doses.2
The vaccine is effective in preventing cervical intraepithelial neoplasia (TABLE 1),3 condyloma, and vaginal intraepithelial neoplasia in women ~15 to 26 years of age. Large studies of vaccine safety have documented no serious adverse reactions, other than syncope, which could occur as frequently as 17.9/10,000 females and 12.5/10,000 males.4 Another study that involved post-licensure safety data from >600,000 HPV4 doses found no increased risk for a variety of outcomes, including Guillain-Barré syndrome, stroke, venous thromboembolism, appendicitis, seizures, syncope, allergic reactions, and anaphylaxis.5,6
TABLE 1
HPV vaccine efficacy against HPV type-related CIN2+ in females ages ~15 to 26 years3
| Vaccine/HPV type | Vaccine | Placebo | Efficacy | |||
|---|---|---|---|---|---|---|
| N | CIN cases | N | CIN cases | % | CI* | |
| Bivalent HPV 16/18 HPV 16 HPV 18 | 7344 6303 6794 | 4 2 2 | 7312 6165 6746 | 56 46 15 | 93 96 87 | 80-98 83-100 40-99 |
| Quadrivalent HPV 16/18 HPV 16 HPV 18 | 7738 6647 7382 | 2 2 0 | 7714 6455 7316 | 100 81 29 | 98 98 100 | 93-100 91-100 87-100 |
| CI, confidence interval; CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus. *Confidence interval for bivalent results was 96.1%, and for quadrivalent results was 95%. | ||||||
HPV-associated disease in males
HPV causes anal, penile, and oropharyngeal cancers in males, with about 7500 cancers occurring each year in the United States.3 In addition, about 1% of sexually active males in America have genital warts at any one time.7 HPV types 6 and 11 cause about 90% of cases.1
The HPV4 vaccine—when all 3 doses are given—is 89.3% effective in preventing genital warts related to HPV types 6 and 11. Even a single dose is 68.1% effective (95% CI, 48.8–80.7).1 New evidence shows that HPV4 prevents AIN, which can lead to anal cancer.8 Effectiveness in preventing AIN 2/3 is 74.9% (95% CI, 8.8–95.4) in those completing 3 doses before onset of infection with one of the HPV types contained in vaccine. Notably, these results were obtained in a subgroup analysis of men who have sex with men. And although the reduction in AIN is expected to lower the incidence of anal cancer, ongoing studies require time to confirm this. If such a reduction is confirmed (and vaccination is started at age 12 in the general male population), the number-needed-to-vaccinate to prevent one case of genital warts would be 18, and to prevent one case of anal cancer, 1581.6
No studies have evaluated efficacy of HPV4 in preventing penile or oropharyngeal cancers.
Men who have sex with men at high risk
Men who have sex with men have higher rates of AIN, anal cancers, and genital warts than the general male population.3 Those who are additionally HIV positive have higher rates of genital warts, which are also more difficult to treat.3 AIN is also more common in HIV-infected males.3 The HPV4 vaccine is immunogenic in those who are HIV infected, although the resulting antibody titers are lower than in other populations.
A look at the 2 HPV vaccines
Two HPV vaccines are available (TABLE 2).3 HPV4 vaccine protects against HPV 6, 11, 16, and 18. Bivalent (HPV2, Cervarix) vaccine contains antigens from HPV 16 and 18. Both vaccines are approved for use in females for the prevention of cervical cancer; HPV4 is preferred if protection against genital warts is also desired. Only HPV4 has been licensed for use in males.
TABLE 2
A look at the human papillomavirus vaccines3
| Quadrivalent (Gardasil) | Bivalent (Cervarix) | |
|---|---|---|
| Manufacturer/VLP types | Merck/6, 11, 16, 18 | GlaxoSmithKline/16, 18 |
| Date of US licensure | 2006, females 2009, males | 2009, females |
| Dose of protein | 20/40/40/20 μg | 20/20 μg |
| Producer cells | Saccharomyces cerevisiae (yeast) | Baculovirus-infected Trichoplusia ni (insect cell line) |
| Adjuvant | AAHS: 225 μg amorphous aluminum hydroxyphosphate sulfate | AS04: 500 μg aluminum hydroxide; 50 μg 3-O-desacyl-4’-monophosphoryl lipid A |
| Schedule (IM) | 3-dose series | 3-dose series |
| VLP, virus-like particle; IM, intramuscular. | ||
HPV vaccine is effective, but costly
A major consideration with HPV vaccines is their cost. With 3 doses required and each dose costing about $130,9 cost effectiveness is poor when preventing uncommon diseases such as cervical and anal cancer, and a relatively benign disease such as genital warts. Male vaccination at age 12 years, when added to a female vaccination program, costs about $20,000 to $40,000 per quality-adjusted life year (QALY) if all potential HPV morbidity is included, not just that which has been proven to be prevented by the vaccine (assuming oral and penile cancer will also be prevented). Counting only HPV disease demonstrated to be prevented by the vaccine, the result is $75,000 to $250,000+ per QALY.6 Vaccinating males older than 21 years results in a cost per QALY 2 to 4 times that of vaccinating males younger than 18 years.10
A final decision. After considering these factors, ACIP approved a set of recommendations at its October 2011 meeting that will become official once they are published in the Morbidity and Mortality Weekly Report. (See “ACIP recommendations for HPV vaccine use in males”.)
- Routinely vaccinate males ages 11 to 12 years with 3 doses of HPV4. The vaccination series can be started at 9 years of age. (A recommendation)
- Vaccinate males, ages 13 to 21 years, who have not been vaccinated previously or who have not completed the 3-dose series. (A recommendation)
- Consider vaccinating males ages 22 to 26 years. (B recommendation)
- Vaccinate men ages 22 to 26 years of age who have sex with men and those in this age group who are HIV positive, if they have not been previously vaccinated. (A recommendation)
Levels of recommendation
A: Applies to all individuals in an age- or risk factor-based group.
B: Defers to clinician judgment in determining benefit for individuals.
Source: ACIP meeting; October 25, 2011; Atlanta, Ga.
At its October 2011 meeting, the Advisory Committee on Immunization Practices (ACIP) recommended to the CDC that quadrivalent human papilloma virus vaccine (HPV4, Gardasil) be routinely given to all males ages 11 to 21 and to men ages 22 to 26 who have sex with men or who are HIV positive, if they have not been previously vaccinated. This replaces a 2009 recommendation that stated HPV4 vaccine could be used in males to prevent genital warts, but stopped short of advocating routine use for all males.1
There were 3 reasons the previous recommendation did not include HPV4 for routine vaccination of males:
- The vaccine had been shown to be effective only for prevention of genital warts.
- The cost effectiveness of the vaccine for use in boys was poor and, in modeling, it yielded less benefit as more females were vaccinated.
- It was thought that a more effective approach to preventing HPV disease would be to emphasize high rates of vaccination of females.
The new recommendation takes into account recent evidence demonstrating that the vaccine prevents anal intraepithelial neoplasia (AIN) in males, in addition to genital warts. Moreover, vaccination rates in females remain low, which makes vaccinating males more cost effective and additionally protective for females.
Female vaccination rates lower than expected
Despite its effectiveness and safety record, HPV vaccination has had a slow rate of acceptance among females ages 13 to 17 years. Coverage for this group documented in the last national vaccine survey was 48.7% for one dose and 32% for the recommended 3 doses.2
The vaccine is effective in preventing cervical intraepithelial neoplasia (TABLE 1),3 condyloma, and vaginal intraepithelial neoplasia in women ~15 to 26 years of age. Large studies of vaccine safety have documented no serious adverse reactions, other than syncope, which could occur as frequently as 17.9/10,000 females and 12.5/10,000 males.4 Another study that involved post-licensure safety data from >600,000 HPV4 doses found no increased risk for a variety of outcomes, including Guillain-Barré syndrome, stroke, venous thromboembolism, appendicitis, seizures, syncope, allergic reactions, and anaphylaxis.5,6
TABLE 1
HPV vaccine efficacy against HPV type-related CIN2+ in females ages ~15 to 26 years3
| Vaccine/HPV type | Vaccine | Placebo | Efficacy | |||
|---|---|---|---|---|---|---|
| N | CIN cases | N | CIN cases | % | CI* | |
| Bivalent HPV 16/18 HPV 16 HPV 18 | 7344 6303 6794 | 4 2 2 | 7312 6165 6746 | 56 46 15 | 93 96 87 | 80-98 83-100 40-99 |
| Quadrivalent HPV 16/18 HPV 16 HPV 18 | 7738 6647 7382 | 2 2 0 | 7714 6455 7316 | 100 81 29 | 98 98 100 | 93-100 91-100 87-100 |
| CI, confidence interval; CIN, cervical intraepithelial neoplasia; HPV, human papillomavirus. *Confidence interval for bivalent results was 96.1%, and for quadrivalent results was 95%. | ||||||
HPV-associated disease in males
HPV causes anal, penile, and oropharyngeal cancers in males, with about 7500 cancers occurring each year in the United States.3 In addition, about 1% of sexually active males in America have genital warts at any one time.7 HPV types 6 and 11 cause about 90% of cases.1
The HPV4 vaccine—when all 3 doses are given—is 89.3% effective in preventing genital warts related to HPV types 6 and 11. Even a single dose is 68.1% effective (95% CI, 48.8–80.7).1 New evidence shows that HPV4 prevents AIN, which can lead to anal cancer.8 Effectiveness in preventing AIN 2/3 is 74.9% (95% CI, 8.8–95.4) in those completing 3 doses before onset of infection with one of the HPV types contained in vaccine. Notably, these results were obtained in a subgroup analysis of men who have sex with men. And although the reduction in AIN is expected to lower the incidence of anal cancer, ongoing studies require time to confirm this. If such a reduction is confirmed (and vaccination is started at age 12 in the general male population), the number-needed-to-vaccinate to prevent one case of genital warts would be 18, and to prevent one case of anal cancer, 1581.6
No studies have evaluated efficacy of HPV4 in preventing penile or oropharyngeal cancers.
Men who have sex with men at high risk
Men who have sex with men have higher rates of AIN, anal cancers, and genital warts than the general male population.3 Those who are additionally HIV positive have higher rates of genital warts, which are also more difficult to treat.3 AIN is also more common in HIV-infected males.3 The HPV4 vaccine is immunogenic in those who are HIV infected, although the resulting antibody titers are lower than in other populations.
A look at the 2 HPV vaccines
Two HPV vaccines are available (TABLE 2).3 HPV4 vaccine protects against HPV 6, 11, 16, and 18. Bivalent (HPV2, Cervarix) vaccine contains antigens from HPV 16 and 18. Both vaccines are approved for use in females for the prevention of cervical cancer; HPV4 is preferred if protection against genital warts is also desired. Only HPV4 has been licensed for use in males.
TABLE 2
A look at the human papillomavirus vaccines3
| Quadrivalent (Gardasil) | Bivalent (Cervarix) | |
|---|---|---|
| Manufacturer/VLP types | Merck/6, 11, 16, 18 | GlaxoSmithKline/16, 18 |
| Date of US licensure | 2006, females 2009, males | 2009, females |
| Dose of protein | 20/40/40/20 μg | 20/20 μg |
| Producer cells | Saccharomyces cerevisiae (yeast) | Baculovirus-infected Trichoplusia ni (insect cell line) |
| Adjuvant | AAHS: 225 μg amorphous aluminum hydroxyphosphate sulfate | AS04: 500 μg aluminum hydroxide; 50 μg 3-O-desacyl-4’-monophosphoryl lipid A |
| Schedule (IM) | 3-dose series | 3-dose series |
| VLP, virus-like particle; IM, intramuscular. | ||
HPV vaccine is effective, but costly
A major consideration with HPV vaccines is their cost. With 3 doses required and each dose costing about $130,9 cost effectiveness is poor when preventing uncommon diseases such as cervical and anal cancer, and a relatively benign disease such as genital warts. Male vaccination at age 12 years, when added to a female vaccination program, costs about $20,000 to $40,000 per quality-adjusted life year (QALY) if all potential HPV morbidity is included, not just that which has been proven to be prevented by the vaccine (assuming oral and penile cancer will also be prevented). Counting only HPV disease demonstrated to be prevented by the vaccine, the result is $75,000 to $250,000+ per QALY.6 Vaccinating males older than 21 years results in a cost per QALY 2 to 4 times that of vaccinating males younger than 18 years.10
A final decision. After considering these factors, ACIP approved a set of recommendations at its October 2011 meeting that will become official once they are published in the Morbidity and Mortality Weekly Report. (See “ACIP recommendations for HPV vaccine use in males”.)
- Routinely vaccinate males ages 11 to 12 years with 3 doses of HPV4. The vaccination series can be started at 9 years of age. (A recommendation)
- Vaccinate males, ages 13 to 21 years, who have not been vaccinated previously or who have not completed the 3-dose series. (A recommendation)
- Consider vaccinating males ages 22 to 26 years. (B recommendation)
- Vaccinate men ages 22 to 26 years of age who have sex with men and those in this age group who are HIV positive, if they have not been previously vaccinated. (A recommendation)
Levels of recommendation
A: Applies to all individuals in an age- or risk factor-based group.
B: Defers to clinician judgment in determining benefit for individuals.
Source: ACIP meeting; October 25, 2011; Atlanta, Ga.
1. CDC. FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59:630-632.
2. CDC. National and state vaccination coverage among adolescents aged 13 through 17 years—United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1117-1123.
3. Markowitz L. HPV vaccine for males: background and review of data. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/downloads/mtg-slides-oct11/04-HPV-Markowitz.pdf. Accessed December 2, 2011.
4. Gee J. Safety of quadrivalent human papilloma virus (HPV4) vaccine. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/downloads/ mtg-slides-oct11/02-HPV-Gee.pdf. Accessed December 2, 2011.
5. Gee J, Naleway A, Shui I, et al. Monitoring the safety of quadrivalent human papillomavirus vaccine: findings from the Vaccine Safety Datalink. Vaccine. 2011;29:8279-8284.
6. Dunne EF. HPV vaccine considerations for males. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc. gov/vaccines/recs/acip/downloads/mtg-slides-oct11/05-HPVDunne.pdf. Accessed December 2, 2011.
7. CDC. HPV and men—fact sheet. http://www.cdc.gov/std/hpv/std/hpv/stdfact-hpv-and-men.htm. Accessed December 19, 2011.
8. Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365:1576-1585.
9. CDC. Sexually transmitted diseases (STDs): HPV vaccine information for young women—fact sheet. http://www.cdc.gov/std/hpv/stdfact-hpv-vaccine-young-women.htm. Accessed December 2, 2011.
10. Chesson HW. HPV vaccine cost-effectiveness: updates and review. Presented at: ACIP meeting; June 22, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/down-loads/mtg-slides-jun11/07-5-hpv-cost-effect.pdf. Accessed December 2, 2011.
1. CDC. FDA licensure of quadrivalent human papillomavirus vaccine (HPV4, Gardasil) for use in males and guidance from the Advisory Committee on Immunization Practices (ACIP). MMWR Morb Mortal Wkly Rep. 2010;59:630-632.
2. CDC. National and state vaccination coverage among adolescents aged 13 through 17 years—United States, 2010. MMWR Morb Mortal Wkly Rep. 2011;60:1117-1123.
3. Markowitz L. HPV vaccine for males: background and review of data. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/downloads/mtg-slides-oct11/04-HPV-Markowitz.pdf. Accessed December 2, 2011.
4. Gee J. Safety of quadrivalent human papilloma virus (HPV4) vaccine. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/downloads/ mtg-slides-oct11/02-HPV-Gee.pdf. Accessed December 2, 2011.
5. Gee J, Naleway A, Shui I, et al. Monitoring the safety of quadrivalent human papillomavirus vaccine: findings from the Vaccine Safety Datalink. Vaccine. 2011;29:8279-8284.
6. Dunne EF. HPV vaccine considerations for males. Presented at: ACIP meeting; October 25, 2011; Atlanta, GA. http://www.cdc. gov/vaccines/recs/acip/downloads/mtg-slides-oct11/05-HPVDunne.pdf. Accessed December 2, 2011.
7. CDC. HPV and men—fact sheet. http://www.cdc.gov/std/hpv/std/hpv/stdfact-hpv-and-men.htm. Accessed December 19, 2011.
8. Palefsky JM, Giuliano AR, Goldstone S, et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011;365:1576-1585.
9. CDC. Sexually transmitted diseases (STDs): HPV vaccine information for young women—fact sheet. http://www.cdc.gov/std/hpv/stdfact-hpv-vaccine-young-women.htm. Accessed December 2, 2011.
10. Chesson HW. HPV vaccine cost-effectiveness: updates and review. Presented at: ACIP meeting; June 22, 2011; Atlanta, GA. http://www.cdc.gov/vaccines/recs/acip/down-loads/mtg-slides-jun11/07-5-hpv-cost-effect.pdf. Accessed December 2, 2011.
CDC update on gonorrhea: Expand treatment to limit resistance
Public health efforts have decreased the incidence of gonorrhea over the past several decades, but this progress is threatened by emergent bacteria resistance to the few remaining antibiotics available to treat it.
Gonococcal resistance to penicillin and tetracycline began in the 1970s and was widespread by the 1980s. Resistance to fluoroquinolones developed during the last decade and led the Centers for Disease Control and Prevention (CDC) in 2007 to stop recommending this class of antibiotics for treatment of gonorrhea.1 (See “The decline of gonorrhea: A success story now threatened by antibiotic resistance”.)
Given the speed with which gonococci developed resistance to fluoroquinolones, the CDC sees as inevitable the eventual development of resistance to cephalosporins—the currently favored agents for gonorrhea.2 This is the main reason behind the new recommendations for treating all cases of gonorrhea with both a cephalosporin and azithromycin, whether or not co-infection with Chlamydia trachomatis is documented or suspected.3
The reported rate of gonorrhea rose steadily from the early 1960s until the mid-1970s, when it was close to 500 cases per 100,000. With implementation of the national gonorrhea control program, the annual rate began to fall, and by the mid-1990s it had declined by 74%. Between 1996 and 2006, the rate remained at about 115 cases per 100,000. Between 2006 and 2009, it decreased to the lowest rate since national reporting began, but increased 2.8% between 2009 and 2010 (FIGURE 1).
The highest rates of gonorrhea are in the South (FIGURE 2) and in women ages 15 to 24 and men ages 20 to 24 (FIGURE 3). Rates are highest among blacks (432.5 cases per 100,000), followed by American Indians/Alaska natives (105.7) and Hispanics (49.9). Between 2009 and 2010, gonorrhea rates increased among American Indians/Alaska natives (21.5%), Asians/Pacific Islanders (13.1%), Hispanics (11.9%), whites (9.0%), and blacks (0.3%).
Recent trends in Gonococcus susceptibility to cephalosporins have the CDC concerned. While cephalosporin resistance remains rare, the proportion of Gonococcus isolates that have shown elevated minimum inhibitory concentrations to cephalosporins has increased.
Gonorrhea control depends in part on appropriate screening of individuals at risk (TABLE). Risk factors for gonorrhea include a history of previous gonorrhea infection, other sexually transmitted infections, new or multiple sexual partners, inconsistent condom use, sex work, and drug use. Risk factors for pregnant women are the same as for nonpregnant women. Prevalence of gonorrhea infection varies widely among communities and patient populations.
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 1
A decline in gonorrhea that began in the mid-1970s*
*The initiation of a national gonorrhea control program reaped immediate benefits that have continued through the present.
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates, United States, 1941-2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 2
Gonorrhea prevalence, 2010
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates by state, United States and outlying areas, 2010. Available at: http://www.cdc.gov/std/10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 3
Gonorrhea prevalence by age and sex, 2010
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates by age and sex, United States, 2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
Augment therapy, follow up thoroughly
Family physicians can assist with public health efforts to control gonorrhea and delay the development of cephalosporin resistance by screening for and detecting the infection, diagnosing those with symptoms, and treating according to newer recommendations. It’s also essential to report cases to local public health departments, assist with finding and treating sexual contacts of infected individuals, and immediately report suspected treatment failures.
A 2-drug regimen is imperative. The latest recommendation for treating gonorrhea is ceftriaxone 250 mg IM in a single dose and azithromycin 1 g orally in a single dose. Until 2010, the dose of ceftriaxone had been 125 mg. This dual drug regimen is recommended for several reasons: As with using multiple drugs to treat tuberculosis, it is hoped dual drug therapy will slow development of resistance to both cephalosporins and azithromycin; co-infection with C trachomatis remains a significant problem; and the combination may be more effective against pharyngeal gonorrhea, which is hard to detect.
Alternative regimens. Cefixime 400 mg orally as a single dose is an option in lieu of ceftriaxone, but is not preferred because of the higher number of reported failures of treatment with oral cephalosporins and less efficacy against pharyngeal disease.3 Other injectable cephalosporins are also an option, but less is known about their effectiveness in treating pharyngeal infection. Injectable options include ceftizoxime 500 mg IM, cefoxitin 2 g IM with probenecid 1 g orally, and cefotaxime 500 mg IM.
Regardless of the cephalosporin chosen, always administer azithromycin. If necessary, an alternative to azithromycin is doxycycline 100 mg orally twice a day. But doxycycline is not preferred because it has a multiple daily dosing requirement and higher levels of gonococcal resistance than is seen with azithromycin.
Necessary follow-up. Although routine testing for cure is not advocated for those treated with a recommended antibiotic regimen, a gonococcal culture and testing for antibiotic susceptibility should be done for any patient whose symptoms persist after treatment. Rapid tests using nucleic acid amplification are unsuitable for testing antibiotic susceptibility. The CDC does recommend retesting patients 3 months after treatment is completed because of a high prevalence of reinfection.3 If cephalosporin resistance becomes prevalent, routine tests of cure might become a recommended standard.
Report all patients with gonorrhea to the local public health department so that sexual contacts within the past 60 days can be notified, tested, and treated presumptively with the dual drug regimen. Recommend simultaneous treatment for all current sex partners, and discourage sexual intercourse until symptoms have resolved. Promptly report any patient with suspected treatment failure to the local health department, and consult the local or state health department for recommendations on subsequent treatment regimens.
The US Preventive Services Task Force (USPSTF) recommends routine screening for asymptomatic infection in women at risk, as per the details in the TABLE.4 While the USPSTF found insufficient evidence to recommend screening of high-risk men, physicians might still consider screening men who have sex with multiple male partners.
TABLE
USPSTF recommendations on screening for gonorrhea4
|
|
|
|
| USPSTF, US Preventive Services Task Force. *For more on the USPSTF’s grade definitions, see: http://www.uspreventiveservicestaskforce.org/uspstf/gradespre.htm#brec. |
Doing our best in the face of uncertainty
Although evidence is lacking that dual drug therapy will delay the progression of resistance, the strategy makes empirical sense. If gonorrhea develops resistance to cephalosporins, it will seriously challenge public health efforts to control this infection. Family physicians have an important role in controlling this sexually transmitted infection and helping to prevent drug resistance.
1. Centers for Disease Control and Prevention. Update to CDC’s sexually transmitted disease treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007;56:332-336.
2. Centers for Disease Control and Prevention. Cephalosporin susceptibility among Neisseria gonorrhoeae isolates—United States 2000-2010. MMWR Morb Mortal Wkly Rep. 2011;60:873-877.
3. Workowski KA, Berman S. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
4. US Preventive Services Task Force. Screening for gonorrhea. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgono.htm. Accessed September 26, 2011.
Public health efforts have decreased the incidence of gonorrhea over the past several decades, but this progress is threatened by emergent bacteria resistance to the few remaining antibiotics available to treat it.
Gonococcal resistance to penicillin and tetracycline began in the 1970s and was widespread by the 1980s. Resistance to fluoroquinolones developed during the last decade and led the Centers for Disease Control and Prevention (CDC) in 2007 to stop recommending this class of antibiotics for treatment of gonorrhea.1 (See “The decline of gonorrhea: A success story now threatened by antibiotic resistance”.)
Given the speed with which gonococci developed resistance to fluoroquinolones, the CDC sees as inevitable the eventual development of resistance to cephalosporins—the currently favored agents for gonorrhea.2 This is the main reason behind the new recommendations for treating all cases of gonorrhea with both a cephalosporin and azithromycin, whether or not co-infection with Chlamydia trachomatis is documented or suspected.3
The reported rate of gonorrhea rose steadily from the early 1960s until the mid-1970s, when it was close to 500 cases per 100,000. With implementation of the national gonorrhea control program, the annual rate began to fall, and by the mid-1990s it had declined by 74%. Between 1996 and 2006, the rate remained at about 115 cases per 100,000. Between 2006 and 2009, it decreased to the lowest rate since national reporting began, but increased 2.8% between 2009 and 2010 (FIGURE 1).
The highest rates of gonorrhea are in the South (FIGURE 2) and in women ages 15 to 24 and men ages 20 to 24 (FIGURE 3). Rates are highest among blacks (432.5 cases per 100,000), followed by American Indians/Alaska natives (105.7) and Hispanics (49.9). Between 2009 and 2010, gonorrhea rates increased among American Indians/Alaska natives (21.5%), Asians/Pacific Islanders (13.1%), Hispanics (11.9%), whites (9.0%), and blacks (0.3%).
Recent trends in Gonococcus susceptibility to cephalosporins have the CDC concerned. While cephalosporin resistance remains rare, the proportion of Gonococcus isolates that have shown elevated minimum inhibitory concentrations to cephalosporins has increased.
Gonorrhea control depends in part on appropriate screening of individuals at risk (TABLE). Risk factors for gonorrhea include a history of previous gonorrhea infection, other sexually transmitted infections, new or multiple sexual partners, inconsistent condom use, sex work, and drug use. Risk factors for pregnant women are the same as for nonpregnant women. Prevalence of gonorrhea infection varies widely among communities and patient populations.
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 1
A decline in gonorrhea that began in the mid-1970s*
*The initiation of a national gonorrhea control program reaped immediate benefits that have continued through the present.
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates, United States, 1941-2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 2
Gonorrhea prevalence, 2010
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates by state, United States and outlying areas, 2010. Available at: http://www.cdc.gov/std/10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 3
Gonorrhea prevalence by age and sex, 2010
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates by age and sex, United States, 2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
Augment therapy, follow up thoroughly
Family physicians can assist with public health efforts to control gonorrhea and delay the development of cephalosporin resistance by screening for and detecting the infection, diagnosing those with symptoms, and treating according to newer recommendations. It’s also essential to report cases to local public health departments, assist with finding and treating sexual contacts of infected individuals, and immediately report suspected treatment failures.
A 2-drug regimen is imperative. The latest recommendation for treating gonorrhea is ceftriaxone 250 mg IM in a single dose and azithromycin 1 g orally in a single dose. Until 2010, the dose of ceftriaxone had been 125 mg. This dual drug regimen is recommended for several reasons: As with using multiple drugs to treat tuberculosis, it is hoped dual drug therapy will slow development of resistance to both cephalosporins and azithromycin; co-infection with C trachomatis remains a significant problem; and the combination may be more effective against pharyngeal gonorrhea, which is hard to detect.
Alternative regimens. Cefixime 400 mg orally as a single dose is an option in lieu of ceftriaxone, but is not preferred because of the higher number of reported failures of treatment with oral cephalosporins and less efficacy against pharyngeal disease.3 Other injectable cephalosporins are also an option, but less is known about their effectiveness in treating pharyngeal infection. Injectable options include ceftizoxime 500 mg IM, cefoxitin 2 g IM with probenecid 1 g orally, and cefotaxime 500 mg IM.
Regardless of the cephalosporin chosen, always administer azithromycin. If necessary, an alternative to azithromycin is doxycycline 100 mg orally twice a day. But doxycycline is not preferred because it has a multiple daily dosing requirement and higher levels of gonococcal resistance than is seen with azithromycin.
Necessary follow-up. Although routine testing for cure is not advocated for those treated with a recommended antibiotic regimen, a gonococcal culture and testing for antibiotic susceptibility should be done for any patient whose symptoms persist after treatment. Rapid tests using nucleic acid amplification are unsuitable for testing antibiotic susceptibility. The CDC does recommend retesting patients 3 months after treatment is completed because of a high prevalence of reinfection.3 If cephalosporin resistance becomes prevalent, routine tests of cure might become a recommended standard.
Report all patients with gonorrhea to the local public health department so that sexual contacts within the past 60 days can be notified, tested, and treated presumptively with the dual drug regimen. Recommend simultaneous treatment for all current sex partners, and discourage sexual intercourse until symptoms have resolved. Promptly report any patient with suspected treatment failure to the local health department, and consult the local or state health department for recommendations on subsequent treatment regimens.
The US Preventive Services Task Force (USPSTF) recommends routine screening for asymptomatic infection in women at risk, as per the details in the TABLE.4 While the USPSTF found insufficient evidence to recommend screening of high-risk men, physicians might still consider screening men who have sex with multiple male partners.
TABLE
USPSTF recommendations on screening for gonorrhea4
|
|
|
|
| USPSTF, US Preventive Services Task Force. *For more on the USPSTF’s grade definitions, see: http://www.uspreventiveservicestaskforce.org/uspstf/gradespre.htm#brec. |
Doing our best in the face of uncertainty
Although evidence is lacking that dual drug therapy will delay the progression of resistance, the strategy makes empirical sense. If gonorrhea develops resistance to cephalosporins, it will seriously challenge public health efforts to control this infection. Family physicians have an important role in controlling this sexually transmitted infection and helping to prevent drug resistance.
Public health efforts have decreased the incidence of gonorrhea over the past several decades, but this progress is threatened by emergent bacteria resistance to the few remaining antibiotics available to treat it.
Gonococcal resistance to penicillin and tetracycline began in the 1970s and was widespread by the 1980s. Resistance to fluoroquinolones developed during the last decade and led the Centers for Disease Control and Prevention (CDC) in 2007 to stop recommending this class of antibiotics for treatment of gonorrhea.1 (See “The decline of gonorrhea: A success story now threatened by antibiotic resistance”.)
Given the speed with which gonococci developed resistance to fluoroquinolones, the CDC sees as inevitable the eventual development of resistance to cephalosporins—the currently favored agents for gonorrhea.2 This is the main reason behind the new recommendations for treating all cases of gonorrhea with both a cephalosporin and azithromycin, whether or not co-infection with Chlamydia trachomatis is documented or suspected.3
The reported rate of gonorrhea rose steadily from the early 1960s until the mid-1970s, when it was close to 500 cases per 100,000. With implementation of the national gonorrhea control program, the annual rate began to fall, and by the mid-1990s it had declined by 74%. Between 1996 and 2006, the rate remained at about 115 cases per 100,000. Between 2006 and 2009, it decreased to the lowest rate since national reporting began, but increased 2.8% between 2009 and 2010 (FIGURE 1).
The highest rates of gonorrhea are in the South (FIGURE 2) and in women ages 15 to 24 and men ages 20 to 24 (FIGURE 3). Rates are highest among blacks (432.5 cases per 100,000), followed by American Indians/Alaska natives (105.7) and Hispanics (49.9). Between 2009 and 2010, gonorrhea rates increased among American Indians/Alaska natives (21.5%), Asians/Pacific Islanders (13.1%), Hispanics (11.9%), whites (9.0%), and blacks (0.3%).
Recent trends in Gonococcus susceptibility to cephalosporins have the CDC concerned. While cephalosporin resistance remains rare, the proportion of Gonococcus isolates that have shown elevated minimum inhibitory concentrations to cephalosporins has increased.
Gonorrhea control depends in part on appropriate screening of individuals at risk (TABLE). Risk factors for gonorrhea include a history of previous gonorrhea infection, other sexually transmitted infections, new or multiple sexual partners, inconsistent condom use, sex work, and drug use. Risk factors for pregnant women are the same as for nonpregnant women. Prevalence of gonorrhea infection varies widely among communities and patient populations.
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 1
A decline in gonorrhea that began in the mid-1970s*
*The initiation of a national gonorrhea control program reaped immediate benefits that have continued through the present.
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates, United States, 1941-2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 2
Gonorrhea prevalence, 2010
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates by state, United States and outlying areas, 2010. Available at: http://www.cdc.gov/std/10/surv2010.pdf. Accessed November 17, 2011.
FIGURE 3
Gonorrhea prevalence by age and sex, 2010
Source: Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2010. Gonorrhea—rates by age and sex, United States, 2010. Available at: http://www.cdc.gov/std/stats10/surv2010.pdf. Accessed November 17, 2011.
Augment therapy, follow up thoroughly
Family physicians can assist with public health efforts to control gonorrhea and delay the development of cephalosporin resistance by screening for and detecting the infection, diagnosing those with symptoms, and treating according to newer recommendations. It’s also essential to report cases to local public health departments, assist with finding and treating sexual contacts of infected individuals, and immediately report suspected treatment failures.
A 2-drug regimen is imperative. The latest recommendation for treating gonorrhea is ceftriaxone 250 mg IM in a single dose and azithromycin 1 g orally in a single dose. Until 2010, the dose of ceftriaxone had been 125 mg. This dual drug regimen is recommended for several reasons: As with using multiple drugs to treat tuberculosis, it is hoped dual drug therapy will slow development of resistance to both cephalosporins and azithromycin; co-infection with C trachomatis remains a significant problem; and the combination may be more effective against pharyngeal gonorrhea, which is hard to detect.
Alternative regimens. Cefixime 400 mg orally as a single dose is an option in lieu of ceftriaxone, but is not preferred because of the higher number of reported failures of treatment with oral cephalosporins and less efficacy against pharyngeal disease.3 Other injectable cephalosporins are also an option, but less is known about their effectiveness in treating pharyngeal infection. Injectable options include ceftizoxime 500 mg IM, cefoxitin 2 g IM with probenecid 1 g orally, and cefotaxime 500 mg IM.
Regardless of the cephalosporin chosen, always administer azithromycin. If necessary, an alternative to azithromycin is doxycycline 100 mg orally twice a day. But doxycycline is not preferred because it has a multiple daily dosing requirement and higher levels of gonococcal resistance than is seen with azithromycin.
Necessary follow-up. Although routine testing for cure is not advocated for those treated with a recommended antibiotic regimen, a gonococcal culture and testing for antibiotic susceptibility should be done for any patient whose symptoms persist after treatment. Rapid tests using nucleic acid amplification are unsuitable for testing antibiotic susceptibility. The CDC does recommend retesting patients 3 months after treatment is completed because of a high prevalence of reinfection.3 If cephalosporin resistance becomes prevalent, routine tests of cure might become a recommended standard.
Report all patients with gonorrhea to the local public health department so that sexual contacts within the past 60 days can be notified, tested, and treated presumptively with the dual drug regimen. Recommend simultaneous treatment for all current sex partners, and discourage sexual intercourse until symptoms have resolved. Promptly report any patient with suspected treatment failure to the local health department, and consult the local or state health department for recommendations on subsequent treatment regimens.
The US Preventive Services Task Force (USPSTF) recommends routine screening for asymptomatic infection in women at risk, as per the details in the TABLE.4 While the USPSTF found insufficient evidence to recommend screening of high-risk men, physicians might still consider screening men who have sex with multiple male partners.
TABLE
USPSTF recommendations on screening for gonorrhea4
|
|
|
|
| USPSTF, US Preventive Services Task Force. *For more on the USPSTF’s grade definitions, see: http://www.uspreventiveservicestaskforce.org/uspstf/gradespre.htm#brec. |
Doing our best in the face of uncertainty
Although evidence is lacking that dual drug therapy will delay the progression of resistance, the strategy makes empirical sense. If gonorrhea develops resistance to cephalosporins, it will seriously challenge public health efforts to control this infection. Family physicians have an important role in controlling this sexually transmitted infection and helping to prevent drug resistance.
1. Centers for Disease Control and Prevention. Update to CDC’s sexually transmitted disease treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007;56:332-336.
2. Centers for Disease Control and Prevention. Cephalosporin susceptibility among Neisseria gonorrhoeae isolates—United States 2000-2010. MMWR Morb Mortal Wkly Rep. 2011;60:873-877.
3. Workowski KA, Berman S. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
4. US Preventive Services Task Force. Screening for gonorrhea. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgono.htm. Accessed September 26, 2011.
1. Centers for Disease Control and Prevention. Update to CDC’s sexually transmitted disease treatment guidelines, 2006: fluoroquinolones no longer recommended for treatment of gonococcal infections. MMWR Morb Mortal Wkly Rep. 2007;56:332-336.
2. Centers for Disease Control and Prevention. Cephalosporin susceptibility among Neisseria gonorrhoeae isolates—United States 2000-2010. MMWR Morb Mortal Wkly Rep. 2011;60:873-877.
3. Workowski KA, Berman S. Centers for Disease Control and Prevention (CDC). Sexually transmitted diseases treatment guidelines, 2010. MMWR Recomm Rep. 2010;59(RR-12):1-110.
4. US Preventive Services Task Force. Screening for gonorrhea. Available at: http://www.uspreventiveservicestaskforce.org/uspstf/uspsgono.htm. Accessed September 26, 2011.
CVD prevention in women: A practice update
Nearly 3 out of 4 (71.9%) US women (and 72.6% of men) ages 60 to 79 years have cardiovascular disease (CVD)—the leading cause of death despite marked improvement in mortality rates in the last 4 decades. In that same age group, the prevalence of cerebral vascular disease is 8.2% in women and 7.2% in men.1
The age-adjusted death rate for all adults is 135.1 in 100,000 for coronary heart disease (CHD) and 44.1 in 100,000 for cerebral vascular disease. In 2007, CVD caused 34.5% of deaths in women and 32.7% of deaths in men.1
Evidence that CVD frequently manifests differently in women than in men led the American Heart Association (AHA) to issue recommendations for the prevention of CVD in women in 1999, and to follow with guidelines in 2004 and an update in 2007.2-4 However, the recommended interventions were, with a few exceptions, the same as the recommendations for men. But that’s changed.
The latest update of the guidelines, published earlier this year, focuses more on sex-based differences, with the addition of pregnancy complications as a major risk factor, for example. (See “AHA’s 2011 CVD guideline update: What’s new?”.) Highlights of the guidelines,5 including the recommended interventions for all women (TABLE 1) and a comparison of its recommendations with those of the US Preventive Services Task Force (USPSTF)6 (TABLE 2)—are detailed here.
The updated guidelines for prevention of CVD in women give more weight to conditions that increase risk for heart disease and stroke primarily or exclusively in women, including gestational diabetes and other complications of pregnancy, lupus, and rheumatoid arthritis. Some of the changes include:
- adding a history of preeclampsia, gestational diabetes, and pregnancy-induced hypertension as criteria for the "at risk" classification
- revising the criterion for "high risk" classification based on risk calculation to ≥10% 10-year predicted risk of CVD (it was previously ≥20%)
- addressing the challenges of diversity, including recommendations that providers develop cultural competence and become aware of, and take steps to reduce, CVD health disparities
- redefining the lowest risk category as "ideal cardiovascular health," for women who have ideal blood pressure, cholesterol, and fasting glucose levels, and adhere to optimal lifestyle/behavioral recommendations.
The AHA indicates that it has changed from evidence-based to effectiveness-based guidelines;5 however, the practical implications within the guidelines themselves are unclear.
TABLE 1
AHA recommends these interventions for all women5
| Avoid smoking (incorporates smoking prevention and cessation advice and assistance, including nicotine replacement, pharmacotherapy, and formal smoking cessation programs) and environmental tobacco smoke |
| Exercise (≥150 minutes of moderate exercise or ≥75 minutes of vigorous exercise per week, with additional benefit gained by more time and higher-level exercise) |
| Consume a healthy diet, rich in fruits and vegetables; whole-grain, high-fiber foods; and fish (at least twice a week); limit intake of saturated fat, cholesterol, alcohol, sodium, and sugar and avoid trans-fatty acids |
| Control your weight (maintain a BMI of <25 kg/m2) |
| Keep blood pressure <120/mm Hg through diet, exercise, and weight control; take medication for BP ≥140/90 mm Hg (or ≥130/80 mm Hg for women with diabetes or chronic kidney disease) |
| Maintain healthy lipid levels (LDL-C <100 mg/dL, HDL-C >50 mg/dL, triglycerides <150 mg/dL, and non-HDL-C [total cholesterol minus HDL] <130 mg/dL) through lifestyle and diet; consider medication for hyperlipidemia based on CVD risk and lipid levels |
| BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; HDL, high-density lipoprotein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol. |
TABLE 2
CVD prevention in women: Comparing AHA1and USPSTF recommendations5,6
| AHA | USPSTF | |
|---|---|---|
| Screening for CVD risks | ||
| Hypertension | Implied, but no specific recommendation | Recommends screening for high BP in women ≥18 y |
| Lipid disorders | Implied, but no specific recommendation | Recommends screening women ≥20 y for lipid disorders if they are at increased risk for CHD (evidence is stronger for women ≥45 y) No recommendation for or against routine screening for lipid disorders in women who are not at increased risk for CHD |
| Obesity | Implied, but no specific recommendation | Recommends screening all adult patients for obesity |
| Diabetes | Implied, but no specific recommendation | Recommends screening for asymptomatic adults with sustained BP (treated or untreated) >135/80 mm Hg Insufficient evidence to assess the balance of benefits and harms of screening asymptomatic adults with BP ≤135/80 mm Hg |
| Tobacco use | Implied, but no specific recommendation | Recommends asking all adults about tobacco use and providing tobacco cessation interventions for those who use tobacco products |
| Nontraditional risk factors | The role that novel CVD risk biomarkers (hs-CRP and advanced lipid testing) and imaging technologies (coronary calcium scoring assessment) is not yet well defined | Insufficient evidence to assess the balance of benefits and harms of using nontraditional risk factors* to screen asymptomatic women with no history of CHD |
| Screening for CVD | ||
| Carotid artery stenosis | Not addressed, but implies it might be useful for classification | Recommends against screening for asymptomatic carotid artery stenosis in the general adult population |
| Peripheral artery disease | Not addressed, but implies it might be useful for classification | Recommends against routine screening for peripheral arterial disease |
| CHD or prediction of CHD | Not addressed, but implies it might be useful for classification | Recommends against routine screening with resting EKG, ETT, or EBCT scanning for coronary calcium for the presence of severe carotid artery stenosis or the prediction of CHD events in adults at low risk for CHD events Insufficient evidence to recommend for or against routine screening with EKG, ETT, or EBCT scanning for coronary calcium for the presence of severe carotid artery stenosis or the prediction of CHD events in adults at increased risk for CHD events |
| Behavioral counseling to reduce risk | ||
| To promote physical activity | Sets physical activity targets but does not address how to achieve them | Insufficient evidence to recommend for or against behavioral counseling in primary care settings to promote physical activity |
| To promote weight loss | Sets ideal weight targets but does not address how to achieve them | Recommends intensive counseling and behavioral interventions+ to promote sustained weight loss for obese adults Insufficient evidence to recommend for or against the use of moderate (monthly) or low-intensity (less than once a month) counseling together with behavioral interventions to promote sustained weight loss in obese adults Insufficient evidence to recommend for or against the use of counseling of any intensity and behavioral interventions to promote sustained weight loss in overweight adults |
| Tobacco use | Recommends smoking prevention and cessation advice and assistance, including nicotine replacement, pharmacotherapy, and formal smoking cessation programs | Recommends tobacco cessation interventions for those who use tobacco products |
| Risk reduction interventions | ||
| Aspirin | Recommends the use of aspirin in women with CHD unless it is contraindicated Says use of aspirin is reasonable in women with diabetes, unless it is contraindicated If aspirin is indicated but not tolerated, clopidogrel should be substituted. Aspirin may be reasonable for women <65 years for stroke prevention, but is not recommended for MI prevention. Aspirin can be useful for women >65 years if BP is controlled; benefit for stroke and MI prevention is likely to outweigh risk of GI bleeding and hemorrhagic stroke | Recommends the use of aspirin for women ages 55 to 79 years when the potential benefit of a reduction in ischemic stroke outweighs the potential harm of an increased risk of GI hemorrhage Insufficient evidence to assess aspirin for cardiovascular disease prevention in women ≥80 years Recommends against the use of aspirin for stroke prevention in women ≤55 years |
| Beta-carotene | Should not be used for prevention of CVD | Recommends against the use of beta-carotene supplements, either alone or in combination, for the prevention of cancer or cardiovascular disease |
| Antioxidants and vitamins | Vitamins E, C, B6, B12, and folic acid should not be used for CVD prevention. | Insufficient evidence to recommend for or against the use of supplements of vitamins A, C, or E; multivitamins with folic acid; or antioxidant combinations for the prevention of cancer or cardiovascular disease |
| Hormonal therapy | Hormone therapy and selective estrogen-receptor modulators should not be used for CVD prevention. | Recommends against the routine use of combined estrogen and progestin for the prevention of chronic conditions in postmenopausal women Recommends against the routine use of unopposed estrogen for the prevention of chronic conditions in postmenopausal women who have had a hysterectomy |
| †;Defined by the USPSTF as >1 individual or group session per month for ≥3 months. *Nontraditional risk factors included in this recommendation are high-sensitivity C-reactive protein, ankle-brachial index, leukocyte count, fasting blood glucose level, periodontal disease, carotid intima-media thickness, coronary artery calcification score on electron-beam computed tomography, homocysteine level, and lipoprotein(a) level. AHA, American Heart Association; BP, blood pressure; CHD, coronary heart disease; CVD, cardiovascular disease; EBCT, electron-beam computed tomography; EKG, electrocardiography; ETT, exercise treadmill test; GI, gastrointestinal; hs-CRP, high-sensitivity C-reactive protein; MI, myocardial infarction; USPSTF, US Preventive Services Task Force. | ||
The AHA’s assessment of risk
The new guideline update recommends assessing each woman’s CVD risk and placing her into one of 3 risk groups—high risk, at risk, and ideal cardiovascular health (TABLE 3)—then using an algorithm to determine which preventive interventions to recommend based on her risk level.
This classification approach is challenging, for several reasons. It lumps women with markedly different risk profiles into the “at risk” group, a category that will likely apply to a high proportion of women. It also appears to encourage the use of diagnostic tests for subclinical vascular disease, for which there is no evidence of effectiveness. In addition, some of the terms used in the at-risk criteria, such as ”physical inactivity” and “poor diet,” are vague.
TABLE 3
Cardiovascular disease: How the AHA classifies women’s risk5
High risk ≥1 of the following: Documented CVD Diabetes Chronic or end-stage renal disease 10-year predicted risk of CVD ≥10%* |
At risk ≥1 of the following major risk factors: Smoking Hypertension (BP ≥120/80 mm Hg, or treated hypertension) Hyperlipidemia (total cholesterol ≥200 mg/dL, HDL cholesterol <50 mg/dL, or treated dyslipidemia) Obesity Poor diet Physical inactivity Premature CVD in a first-degree relative (<55 years for men and <65 for women) Metabolic syndrome Subclinical atherosclerosis Poor exercise tolerance on a treadmill test Systemic autoimmune disease A history of preeclampsia, gestational diabetes, or PIH |
Ideal cardiovascular health All of the following: Total cholesterol <200 mg/dL, untreated BP <120/80 mm Hg, untreated Fasting blood glucose <100 mg/dL, untreated BMI <25 mm/kg2 Nonsmoking Healthy diet (rich in fruits and vegetables; whole-grain, high-fiber foods; and fish, especially oily fish such as salmon and mackerel, at least twice a week; with limited intake of saturated fat, cholesterol, alcohol, sodium, and sugar; and avoidance of trans-fatty acids) Physical activity (≥150 minutes per week at moderate intensity or ≥75 minutes per week at vigorous intensity) |
| *Calculation tools can be found at http://hp2010.nhlbihin.net/atpiii/calculator.asp (for CHD) and at http://www.westernstroke.org/PersonalStrokeRisk1.xls (for stroke). AHA, American Heart Association; BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; HDL, high-density lipoprotein, PIH, pregnancy-induced hypertension. |
Some recommendations apply to all women, regardless of risk
The AHA recommendations for all women (TABLE 1) include smoking prevention or cessation, maintenance of optimal weight, regular physical activity, and a diet aimed at preventing CVD. The guidelines also emphasize that major CVD risks should be controlled, with either lifestyle and diet modifications (preferably) or pharmacotherapy. The aggressiveness of control targets depends on the level of risk and the presence of other risk factors.
The guidelines recommend against some interventions that are often used for CVD prevention, based on a high level of evidence that they are ineffective. These include estrogen or selective estrogen receptor modulators, antioxidant vitamins (vitamins E and C, and beta-carotene), folic acid with or without vitamins B6 and B12, and aspirin (for CHD prevention) for healthy women <65 years old.
The AHA does not take a position for or against several diagnostic and risk classification tools because of a lack of evidence of usefulness. These include CVD risk biomarkers such as high sensitivity C-reactive protein and imaging technologies such as coronary calcium scoring assessment.
AHA and USPSTF diverge, but not by much
Screening for conditions that increase CVD risk is not explicitly addressed in the AHA guidelines. Screening is implied by the proposed classification scheme, which includes the presence or absence of smoking, obesity, diabetes, hypertension, and dyslipidemia, but there is no guidance on when to start or stop screening for these conditions. The AHA and the USPSTF diverge on screening women for dyslipidemia, with the USPSTF recommending screening for lipid disorders only in women at increased risk for CHD.
The recommendations for optimal weight and activity levels in the AHA guidelines do not include advice on how to achieve them, nor do they call for an assessment of the effectiveness of behavioral counseling in the clinical setting. Because the USPSTF includes an assessment of, and recommendations for, asymptomatic patients in primary care settings, its recommendations do not address women with conditions such as established CVD, heart failure, or atrial fibrillation—which the AHA guidelines do.
Overall, the AHA and USPSTF agree more than they disagree, and each covers some areas that the other does not (TABLE 2). Family physicians can use the information provided by both entities to ensure that their female patients receive high-quality preventive care that will minimize their risk for CVD.
1. American Heart Association. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18-e209.
2. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. Circulation. 1999;99:2480-2484.
3. Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
4. Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481-1501.
5. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243-1262.
6. United States Preventive Services Task Force. USPSTF A-Z guide. Available at: www.uspreventiveservicestaskforce.org/uspstopics.htm. Accessed June 7, 2011.
Nearly 3 out of 4 (71.9%) US women (and 72.6% of men) ages 60 to 79 years have cardiovascular disease (CVD)—the leading cause of death despite marked improvement in mortality rates in the last 4 decades. In that same age group, the prevalence of cerebral vascular disease is 8.2% in women and 7.2% in men.1
The age-adjusted death rate for all adults is 135.1 in 100,000 for coronary heart disease (CHD) and 44.1 in 100,000 for cerebral vascular disease. In 2007, CVD caused 34.5% of deaths in women and 32.7% of deaths in men.1
Evidence that CVD frequently manifests differently in women than in men led the American Heart Association (AHA) to issue recommendations for the prevention of CVD in women in 1999, and to follow with guidelines in 2004 and an update in 2007.2-4 However, the recommended interventions were, with a few exceptions, the same as the recommendations for men. But that’s changed.
The latest update of the guidelines, published earlier this year, focuses more on sex-based differences, with the addition of pregnancy complications as a major risk factor, for example. (See “AHA’s 2011 CVD guideline update: What’s new?”.) Highlights of the guidelines,5 including the recommended interventions for all women (TABLE 1) and a comparison of its recommendations with those of the US Preventive Services Task Force (USPSTF)6 (TABLE 2)—are detailed here.
The updated guidelines for prevention of CVD in women give more weight to conditions that increase risk for heart disease and stroke primarily or exclusively in women, including gestational diabetes and other complications of pregnancy, lupus, and rheumatoid arthritis. Some of the changes include:
- adding a history of preeclampsia, gestational diabetes, and pregnancy-induced hypertension as criteria for the "at risk" classification
- revising the criterion for "high risk" classification based on risk calculation to ≥10% 10-year predicted risk of CVD (it was previously ≥20%)
- addressing the challenges of diversity, including recommendations that providers develop cultural competence and become aware of, and take steps to reduce, CVD health disparities
- redefining the lowest risk category as "ideal cardiovascular health," for women who have ideal blood pressure, cholesterol, and fasting glucose levels, and adhere to optimal lifestyle/behavioral recommendations.
The AHA indicates that it has changed from evidence-based to effectiveness-based guidelines;5 however, the practical implications within the guidelines themselves are unclear.
TABLE 1
AHA recommends these interventions for all women5
| Avoid smoking (incorporates smoking prevention and cessation advice and assistance, including nicotine replacement, pharmacotherapy, and formal smoking cessation programs) and environmental tobacco smoke |
| Exercise (≥150 minutes of moderate exercise or ≥75 minutes of vigorous exercise per week, with additional benefit gained by more time and higher-level exercise) |
| Consume a healthy diet, rich in fruits and vegetables; whole-grain, high-fiber foods; and fish (at least twice a week); limit intake of saturated fat, cholesterol, alcohol, sodium, and sugar and avoid trans-fatty acids |
| Control your weight (maintain a BMI of <25 kg/m2) |
| Keep blood pressure <120/mm Hg through diet, exercise, and weight control; take medication for BP ≥140/90 mm Hg (or ≥130/80 mm Hg for women with diabetes or chronic kidney disease) |
| Maintain healthy lipid levels (LDL-C <100 mg/dL, HDL-C >50 mg/dL, triglycerides <150 mg/dL, and non-HDL-C [total cholesterol minus HDL] <130 mg/dL) through lifestyle and diet; consider medication for hyperlipidemia based on CVD risk and lipid levels |
| BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; HDL, high-density lipoprotein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol. |
TABLE 2
CVD prevention in women: Comparing AHA1and USPSTF recommendations5,6
| AHA | USPSTF | |
|---|---|---|
| Screening for CVD risks | ||
| Hypertension | Implied, but no specific recommendation | Recommends screening for high BP in women ≥18 y |
| Lipid disorders | Implied, but no specific recommendation | Recommends screening women ≥20 y for lipid disorders if they are at increased risk for CHD (evidence is stronger for women ≥45 y) No recommendation for or against routine screening for lipid disorders in women who are not at increased risk for CHD |
| Obesity | Implied, but no specific recommendation | Recommends screening all adult patients for obesity |
| Diabetes | Implied, but no specific recommendation | Recommends screening for asymptomatic adults with sustained BP (treated or untreated) >135/80 mm Hg Insufficient evidence to assess the balance of benefits and harms of screening asymptomatic adults with BP ≤135/80 mm Hg |
| Tobacco use | Implied, but no specific recommendation | Recommends asking all adults about tobacco use and providing tobacco cessation interventions for those who use tobacco products |
| Nontraditional risk factors | The role that novel CVD risk biomarkers (hs-CRP and advanced lipid testing) and imaging technologies (coronary calcium scoring assessment) is not yet well defined | Insufficient evidence to assess the balance of benefits and harms of using nontraditional risk factors* to screen asymptomatic women with no history of CHD |
| Screening for CVD | ||
| Carotid artery stenosis | Not addressed, but implies it might be useful for classification | Recommends against screening for asymptomatic carotid artery stenosis in the general adult population |
| Peripheral artery disease | Not addressed, but implies it might be useful for classification | Recommends against routine screening for peripheral arterial disease |
| CHD or prediction of CHD | Not addressed, but implies it might be useful for classification | Recommends against routine screening with resting EKG, ETT, or EBCT scanning for coronary calcium for the presence of severe carotid artery stenosis or the prediction of CHD events in adults at low risk for CHD events Insufficient evidence to recommend for or against routine screening with EKG, ETT, or EBCT scanning for coronary calcium for the presence of severe carotid artery stenosis or the prediction of CHD events in adults at increased risk for CHD events |
| Behavioral counseling to reduce risk | ||
| To promote physical activity | Sets physical activity targets but does not address how to achieve them | Insufficient evidence to recommend for or against behavioral counseling in primary care settings to promote physical activity |
| To promote weight loss | Sets ideal weight targets but does not address how to achieve them | Recommends intensive counseling and behavioral interventions+ to promote sustained weight loss for obese adults Insufficient evidence to recommend for or against the use of moderate (monthly) or low-intensity (less than once a month) counseling together with behavioral interventions to promote sustained weight loss in obese adults Insufficient evidence to recommend for or against the use of counseling of any intensity and behavioral interventions to promote sustained weight loss in overweight adults |
| Tobacco use | Recommends smoking prevention and cessation advice and assistance, including nicotine replacement, pharmacotherapy, and formal smoking cessation programs | Recommends tobacco cessation interventions for those who use tobacco products |
| Risk reduction interventions | ||
| Aspirin | Recommends the use of aspirin in women with CHD unless it is contraindicated Says use of aspirin is reasonable in women with diabetes, unless it is contraindicated If aspirin is indicated but not tolerated, clopidogrel should be substituted. Aspirin may be reasonable for women <65 years for stroke prevention, but is not recommended for MI prevention. Aspirin can be useful for women >65 years if BP is controlled; benefit for stroke and MI prevention is likely to outweigh risk of GI bleeding and hemorrhagic stroke | Recommends the use of aspirin for women ages 55 to 79 years when the potential benefit of a reduction in ischemic stroke outweighs the potential harm of an increased risk of GI hemorrhage Insufficient evidence to assess aspirin for cardiovascular disease prevention in women ≥80 years Recommends against the use of aspirin for stroke prevention in women ≤55 years |
| Beta-carotene | Should not be used for prevention of CVD | Recommends against the use of beta-carotene supplements, either alone or in combination, for the prevention of cancer or cardiovascular disease |
| Antioxidants and vitamins | Vitamins E, C, B6, B12, and folic acid should not be used for CVD prevention. | Insufficient evidence to recommend for or against the use of supplements of vitamins A, C, or E; multivitamins with folic acid; or antioxidant combinations for the prevention of cancer or cardiovascular disease |
| Hormonal therapy | Hormone therapy and selective estrogen-receptor modulators should not be used for CVD prevention. | Recommends against the routine use of combined estrogen and progestin for the prevention of chronic conditions in postmenopausal women Recommends against the routine use of unopposed estrogen for the prevention of chronic conditions in postmenopausal women who have had a hysterectomy |
| †;Defined by the USPSTF as >1 individual or group session per month for ≥3 months. *Nontraditional risk factors included in this recommendation are high-sensitivity C-reactive protein, ankle-brachial index, leukocyte count, fasting blood glucose level, periodontal disease, carotid intima-media thickness, coronary artery calcification score on electron-beam computed tomography, homocysteine level, and lipoprotein(a) level. AHA, American Heart Association; BP, blood pressure; CHD, coronary heart disease; CVD, cardiovascular disease; EBCT, electron-beam computed tomography; EKG, electrocardiography; ETT, exercise treadmill test; GI, gastrointestinal; hs-CRP, high-sensitivity C-reactive protein; MI, myocardial infarction; USPSTF, US Preventive Services Task Force. | ||
The AHA’s assessment of risk
The new guideline update recommends assessing each woman’s CVD risk and placing her into one of 3 risk groups—high risk, at risk, and ideal cardiovascular health (TABLE 3)—then using an algorithm to determine which preventive interventions to recommend based on her risk level.
This classification approach is challenging, for several reasons. It lumps women with markedly different risk profiles into the “at risk” group, a category that will likely apply to a high proportion of women. It also appears to encourage the use of diagnostic tests for subclinical vascular disease, for which there is no evidence of effectiveness. In addition, some of the terms used in the at-risk criteria, such as ”physical inactivity” and “poor diet,” are vague.
TABLE 3
Cardiovascular disease: How the AHA classifies women’s risk5
High risk ≥1 of the following: Documented CVD Diabetes Chronic or end-stage renal disease 10-year predicted risk of CVD ≥10%* |
At risk ≥1 of the following major risk factors: Smoking Hypertension (BP ≥120/80 mm Hg, or treated hypertension) Hyperlipidemia (total cholesterol ≥200 mg/dL, HDL cholesterol <50 mg/dL, or treated dyslipidemia) Obesity Poor diet Physical inactivity Premature CVD in a first-degree relative (<55 years for men and <65 for women) Metabolic syndrome Subclinical atherosclerosis Poor exercise tolerance on a treadmill test Systemic autoimmune disease A history of preeclampsia, gestational diabetes, or PIH |
Ideal cardiovascular health All of the following: Total cholesterol <200 mg/dL, untreated BP <120/80 mm Hg, untreated Fasting blood glucose <100 mg/dL, untreated BMI <25 mm/kg2 Nonsmoking Healthy diet (rich in fruits and vegetables; whole-grain, high-fiber foods; and fish, especially oily fish such as salmon and mackerel, at least twice a week; with limited intake of saturated fat, cholesterol, alcohol, sodium, and sugar; and avoidance of trans-fatty acids) Physical activity (≥150 minutes per week at moderate intensity or ≥75 minutes per week at vigorous intensity) |
| *Calculation tools can be found at http://hp2010.nhlbihin.net/atpiii/calculator.asp (for CHD) and at http://www.westernstroke.org/PersonalStrokeRisk1.xls (for stroke). AHA, American Heart Association; BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; HDL, high-density lipoprotein, PIH, pregnancy-induced hypertension. |
Some recommendations apply to all women, regardless of risk
The AHA recommendations for all women (TABLE 1) include smoking prevention or cessation, maintenance of optimal weight, regular physical activity, and a diet aimed at preventing CVD. The guidelines also emphasize that major CVD risks should be controlled, with either lifestyle and diet modifications (preferably) or pharmacotherapy. The aggressiveness of control targets depends on the level of risk and the presence of other risk factors.
The guidelines recommend against some interventions that are often used for CVD prevention, based on a high level of evidence that they are ineffective. These include estrogen or selective estrogen receptor modulators, antioxidant vitamins (vitamins E and C, and beta-carotene), folic acid with or without vitamins B6 and B12, and aspirin (for CHD prevention) for healthy women <65 years old.
The AHA does not take a position for or against several diagnostic and risk classification tools because of a lack of evidence of usefulness. These include CVD risk biomarkers such as high sensitivity C-reactive protein and imaging technologies such as coronary calcium scoring assessment.
AHA and USPSTF diverge, but not by much
Screening for conditions that increase CVD risk is not explicitly addressed in the AHA guidelines. Screening is implied by the proposed classification scheme, which includes the presence or absence of smoking, obesity, diabetes, hypertension, and dyslipidemia, but there is no guidance on when to start or stop screening for these conditions. The AHA and the USPSTF diverge on screening women for dyslipidemia, with the USPSTF recommending screening for lipid disorders only in women at increased risk for CHD.
The recommendations for optimal weight and activity levels in the AHA guidelines do not include advice on how to achieve them, nor do they call for an assessment of the effectiveness of behavioral counseling in the clinical setting. Because the USPSTF includes an assessment of, and recommendations for, asymptomatic patients in primary care settings, its recommendations do not address women with conditions such as established CVD, heart failure, or atrial fibrillation—which the AHA guidelines do.
Overall, the AHA and USPSTF agree more than they disagree, and each covers some areas that the other does not (TABLE 2). Family physicians can use the information provided by both entities to ensure that their female patients receive high-quality preventive care that will minimize their risk for CVD.
Nearly 3 out of 4 (71.9%) US women (and 72.6% of men) ages 60 to 79 years have cardiovascular disease (CVD)—the leading cause of death despite marked improvement in mortality rates in the last 4 decades. In that same age group, the prevalence of cerebral vascular disease is 8.2% in women and 7.2% in men.1
The age-adjusted death rate for all adults is 135.1 in 100,000 for coronary heart disease (CHD) and 44.1 in 100,000 for cerebral vascular disease. In 2007, CVD caused 34.5% of deaths in women and 32.7% of deaths in men.1
Evidence that CVD frequently manifests differently in women than in men led the American Heart Association (AHA) to issue recommendations for the prevention of CVD in women in 1999, and to follow with guidelines in 2004 and an update in 2007.2-4 However, the recommended interventions were, with a few exceptions, the same as the recommendations for men. But that’s changed.
The latest update of the guidelines, published earlier this year, focuses more on sex-based differences, with the addition of pregnancy complications as a major risk factor, for example. (See “AHA’s 2011 CVD guideline update: What’s new?”.) Highlights of the guidelines,5 including the recommended interventions for all women (TABLE 1) and a comparison of its recommendations with those of the US Preventive Services Task Force (USPSTF)6 (TABLE 2)—are detailed here.
The updated guidelines for prevention of CVD in women give more weight to conditions that increase risk for heart disease and stroke primarily or exclusively in women, including gestational diabetes and other complications of pregnancy, lupus, and rheumatoid arthritis. Some of the changes include:
- adding a history of preeclampsia, gestational diabetes, and pregnancy-induced hypertension as criteria for the "at risk" classification
- revising the criterion for "high risk" classification based on risk calculation to ≥10% 10-year predicted risk of CVD (it was previously ≥20%)
- addressing the challenges of diversity, including recommendations that providers develop cultural competence and become aware of, and take steps to reduce, CVD health disparities
- redefining the lowest risk category as "ideal cardiovascular health," for women who have ideal blood pressure, cholesterol, and fasting glucose levels, and adhere to optimal lifestyle/behavioral recommendations.
The AHA indicates that it has changed from evidence-based to effectiveness-based guidelines;5 however, the practical implications within the guidelines themselves are unclear.
TABLE 1
AHA recommends these interventions for all women5
| Avoid smoking (incorporates smoking prevention and cessation advice and assistance, including nicotine replacement, pharmacotherapy, and formal smoking cessation programs) and environmental tobacco smoke |
| Exercise (≥150 minutes of moderate exercise or ≥75 minutes of vigorous exercise per week, with additional benefit gained by more time and higher-level exercise) |
| Consume a healthy diet, rich in fruits and vegetables; whole-grain, high-fiber foods; and fish (at least twice a week); limit intake of saturated fat, cholesterol, alcohol, sodium, and sugar and avoid trans-fatty acids |
| Control your weight (maintain a BMI of <25 kg/m2) |
| Keep blood pressure <120/mm Hg through diet, exercise, and weight control; take medication for BP ≥140/90 mm Hg (or ≥130/80 mm Hg for women with diabetes or chronic kidney disease) |
| Maintain healthy lipid levels (LDL-C <100 mg/dL, HDL-C >50 mg/dL, triglycerides <150 mg/dL, and non-HDL-C [total cholesterol minus HDL] <130 mg/dL) through lifestyle and diet; consider medication for hyperlipidemia based on CVD risk and lipid levels |
| BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; HDL, high-density lipoprotein; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol. |
TABLE 2
CVD prevention in women: Comparing AHA1and USPSTF recommendations5,6
| AHA | USPSTF | |
|---|---|---|
| Screening for CVD risks | ||
| Hypertension | Implied, but no specific recommendation | Recommends screening for high BP in women ≥18 y |
| Lipid disorders | Implied, but no specific recommendation | Recommends screening women ≥20 y for lipid disorders if they are at increased risk for CHD (evidence is stronger for women ≥45 y) No recommendation for or against routine screening for lipid disorders in women who are not at increased risk for CHD |
| Obesity | Implied, but no specific recommendation | Recommends screening all adult patients for obesity |
| Diabetes | Implied, but no specific recommendation | Recommends screening for asymptomatic adults with sustained BP (treated or untreated) >135/80 mm Hg Insufficient evidence to assess the balance of benefits and harms of screening asymptomatic adults with BP ≤135/80 mm Hg |
| Tobacco use | Implied, but no specific recommendation | Recommends asking all adults about tobacco use and providing tobacco cessation interventions for those who use tobacco products |
| Nontraditional risk factors | The role that novel CVD risk biomarkers (hs-CRP and advanced lipid testing) and imaging technologies (coronary calcium scoring assessment) is not yet well defined | Insufficient evidence to assess the balance of benefits and harms of using nontraditional risk factors* to screen asymptomatic women with no history of CHD |
| Screening for CVD | ||
| Carotid artery stenosis | Not addressed, but implies it might be useful for classification | Recommends against screening for asymptomatic carotid artery stenosis in the general adult population |
| Peripheral artery disease | Not addressed, but implies it might be useful for classification | Recommends against routine screening for peripheral arterial disease |
| CHD or prediction of CHD | Not addressed, but implies it might be useful for classification | Recommends against routine screening with resting EKG, ETT, or EBCT scanning for coronary calcium for the presence of severe carotid artery stenosis or the prediction of CHD events in adults at low risk for CHD events Insufficient evidence to recommend for or against routine screening with EKG, ETT, or EBCT scanning for coronary calcium for the presence of severe carotid artery stenosis or the prediction of CHD events in adults at increased risk for CHD events |
| Behavioral counseling to reduce risk | ||
| To promote physical activity | Sets physical activity targets but does not address how to achieve them | Insufficient evidence to recommend for or against behavioral counseling in primary care settings to promote physical activity |
| To promote weight loss | Sets ideal weight targets but does not address how to achieve them | Recommends intensive counseling and behavioral interventions+ to promote sustained weight loss for obese adults Insufficient evidence to recommend for or against the use of moderate (monthly) or low-intensity (less than once a month) counseling together with behavioral interventions to promote sustained weight loss in obese adults Insufficient evidence to recommend for or against the use of counseling of any intensity and behavioral interventions to promote sustained weight loss in overweight adults |
| Tobacco use | Recommends smoking prevention and cessation advice and assistance, including nicotine replacement, pharmacotherapy, and formal smoking cessation programs | Recommends tobacco cessation interventions for those who use tobacco products |
| Risk reduction interventions | ||
| Aspirin | Recommends the use of aspirin in women with CHD unless it is contraindicated Says use of aspirin is reasonable in women with diabetes, unless it is contraindicated If aspirin is indicated but not tolerated, clopidogrel should be substituted. Aspirin may be reasonable for women <65 years for stroke prevention, but is not recommended for MI prevention. Aspirin can be useful for women >65 years if BP is controlled; benefit for stroke and MI prevention is likely to outweigh risk of GI bleeding and hemorrhagic stroke | Recommends the use of aspirin for women ages 55 to 79 years when the potential benefit of a reduction in ischemic stroke outweighs the potential harm of an increased risk of GI hemorrhage Insufficient evidence to assess aspirin for cardiovascular disease prevention in women ≥80 years Recommends against the use of aspirin for stroke prevention in women ≤55 years |
| Beta-carotene | Should not be used for prevention of CVD | Recommends against the use of beta-carotene supplements, either alone or in combination, for the prevention of cancer or cardiovascular disease |
| Antioxidants and vitamins | Vitamins E, C, B6, B12, and folic acid should not be used for CVD prevention. | Insufficient evidence to recommend for or against the use of supplements of vitamins A, C, or E; multivitamins with folic acid; or antioxidant combinations for the prevention of cancer or cardiovascular disease |
| Hormonal therapy | Hormone therapy and selective estrogen-receptor modulators should not be used for CVD prevention. | Recommends against the routine use of combined estrogen and progestin for the prevention of chronic conditions in postmenopausal women Recommends against the routine use of unopposed estrogen for the prevention of chronic conditions in postmenopausal women who have had a hysterectomy |
| †;Defined by the USPSTF as >1 individual or group session per month for ≥3 months. *Nontraditional risk factors included in this recommendation are high-sensitivity C-reactive protein, ankle-brachial index, leukocyte count, fasting blood glucose level, periodontal disease, carotid intima-media thickness, coronary artery calcification score on electron-beam computed tomography, homocysteine level, and lipoprotein(a) level. AHA, American Heart Association; BP, blood pressure; CHD, coronary heart disease; CVD, cardiovascular disease; EBCT, electron-beam computed tomography; EKG, electrocardiography; ETT, exercise treadmill test; GI, gastrointestinal; hs-CRP, high-sensitivity C-reactive protein; MI, myocardial infarction; USPSTF, US Preventive Services Task Force. | ||
The AHA’s assessment of risk
The new guideline update recommends assessing each woman’s CVD risk and placing her into one of 3 risk groups—high risk, at risk, and ideal cardiovascular health (TABLE 3)—then using an algorithm to determine which preventive interventions to recommend based on her risk level.
This classification approach is challenging, for several reasons. It lumps women with markedly different risk profiles into the “at risk” group, a category that will likely apply to a high proportion of women. It also appears to encourage the use of diagnostic tests for subclinical vascular disease, for which there is no evidence of effectiveness. In addition, some of the terms used in the at-risk criteria, such as ”physical inactivity” and “poor diet,” are vague.
TABLE 3
Cardiovascular disease: How the AHA classifies women’s risk5
High risk ≥1 of the following: Documented CVD Diabetes Chronic or end-stage renal disease 10-year predicted risk of CVD ≥10%* |
At risk ≥1 of the following major risk factors: Smoking Hypertension (BP ≥120/80 mm Hg, or treated hypertension) Hyperlipidemia (total cholesterol ≥200 mg/dL, HDL cholesterol <50 mg/dL, or treated dyslipidemia) Obesity Poor diet Physical inactivity Premature CVD in a first-degree relative (<55 years for men and <65 for women) Metabolic syndrome Subclinical atherosclerosis Poor exercise tolerance on a treadmill test Systemic autoimmune disease A history of preeclampsia, gestational diabetes, or PIH |
Ideal cardiovascular health All of the following: Total cholesterol <200 mg/dL, untreated BP <120/80 mm Hg, untreated Fasting blood glucose <100 mg/dL, untreated BMI <25 mm/kg2 Nonsmoking Healthy diet (rich in fruits and vegetables; whole-grain, high-fiber foods; and fish, especially oily fish such as salmon and mackerel, at least twice a week; with limited intake of saturated fat, cholesterol, alcohol, sodium, and sugar; and avoidance of trans-fatty acids) Physical activity (≥150 minutes per week at moderate intensity or ≥75 minutes per week at vigorous intensity) |
| *Calculation tools can be found at http://hp2010.nhlbihin.net/atpiii/calculator.asp (for CHD) and at http://www.westernstroke.org/PersonalStrokeRisk1.xls (for stroke). AHA, American Heart Association; BMI, body mass index; BP, blood pressure; CVD, cardiovascular disease; HDL, high-density lipoprotein, PIH, pregnancy-induced hypertension. |
Some recommendations apply to all women, regardless of risk
The AHA recommendations for all women (TABLE 1) include smoking prevention or cessation, maintenance of optimal weight, regular physical activity, and a diet aimed at preventing CVD. The guidelines also emphasize that major CVD risks should be controlled, with either lifestyle and diet modifications (preferably) or pharmacotherapy. The aggressiveness of control targets depends on the level of risk and the presence of other risk factors.
The guidelines recommend against some interventions that are often used for CVD prevention, based on a high level of evidence that they are ineffective. These include estrogen or selective estrogen receptor modulators, antioxidant vitamins (vitamins E and C, and beta-carotene), folic acid with or without vitamins B6 and B12, and aspirin (for CHD prevention) for healthy women <65 years old.
The AHA does not take a position for or against several diagnostic and risk classification tools because of a lack of evidence of usefulness. These include CVD risk biomarkers such as high sensitivity C-reactive protein and imaging technologies such as coronary calcium scoring assessment.
AHA and USPSTF diverge, but not by much
Screening for conditions that increase CVD risk is not explicitly addressed in the AHA guidelines. Screening is implied by the proposed classification scheme, which includes the presence or absence of smoking, obesity, diabetes, hypertension, and dyslipidemia, but there is no guidance on when to start or stop screening for these conditions. The AHA and the USPSTF diverge on screening women for dyslipidemia, with the USPSTF recommending screening for lipid disorders only in women at increased risk for CHD.
The recommendations for optimal weight and activity levels in the AHA guidelines do not include advice on how to achieve them, nor do they call for an assessment of the effectiveness of behavioral counseling in the clinical setting. Because the USPSTF includes an assessment of, and recommendations for, asymptomatic patients in primary care settings, its recommendations do not address women with conditions such as established CVD, heart failure, or atrial fibrillation—which the AHA guidelines do.
Overall, the AHA and USPSTF agree more than they disagree, and each covers some areas that the other does not (TABLE 2). Family physicians can use the information provided by both entities to ensure that their female patients receive high-quality preventive care that will minimize their risk for CVD.
1. American Heart Association. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18-e209.
2. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. Circulation. 1999;99:2480-2484.
3. Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
4. Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481-1501.
5. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243-1262.
6. United States Preventive Services Task Force. USPSTF A-Z guide. Available at: www.uspreventiveservicestaskforce.org/uspstopics.htm. Accessed June 7, 2011.
1. American Heart Association. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18-e209.
2. Mosca L, Grundy SM, Judelson D, et al. Guide to preventive cardiology for women. AHA/ACC scientific statement, consensus panel statement. Circulation. 1999;99:2480-2484.
3. Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. Circulation. 2004;109:672-693.
4. Mosca L, Banka CL, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation. 2007;115:1481-1501.
5. Mosca L, Benjamin EJ, Berra K, et al. Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: a guideline from the American Heart Association. Circulation. 2011;123:1243-1262.
6. United States Preventive Services Task Force. USPSTF A-Z guide. Available at: www.uspreventiveservicestaskforce.org/uspstopics.htm. Accessed June 7, 2011.