User login
Brain imaging gives new insight into hoarding disorder
In a neuroimaging study, investigators led by Taro Mizobe, department of neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, compared brain scans of individuals with and without HD.
Results showed that compared with healthy family members, participants with HD had anatomically widespread abnormalities in WM tracts.
In particular, a broad range of alterations were found in frontal WM related to HD symptom severity, as well as cortical regions involved in cognitive dysfunction.
“The finding of a characteristic association between alterations in the prefrontal WM tract, which connects cortical regions involved in cognitive function and the severity of hoarding symptoms, could provide new insights into the neurobiological basis of HD,” the researchers write.
The findings were published online Jan. 18 in the Journal of Psychiatric Research.
Limited information to date
“Although there are no clear neurobiological models of HD, several neuroimaging studies have found specific differences in specific brain regions” between patients with and without HD, the investigators write.
Structural MRI studies and voxel-based morphometry have shown larger volumes of gray matter in several regions of the brain in patients with HD. However, there have been no reports on alterations in the WM tracts – and studies of patients with obsessive-compulsive disorder and hoarding symptoms have yielded only “limited information” regarding WM tracts, the researchers note.
Diffusion tensor imaging (DTI) studies have yielded “inconsistent” findings, “therefore little is known about the microstructure of WM in the brains of patients with HD,” they add.
The current study was designed “to investigate microstructural alterations in the WM tracts of individuals with HD” by using tract-based spatial statistics – a model typically used for whole-brain, voxel-wise analysis of DTI measures.
DTI neuroimaging can assess the microstructure of WM. In the current study, the investigators focused on the three measures yielded by DTI: fractional anisotropy (FA), which is an index of overall WM integrity; axial diffusivity (AD); and radial diffusivity (RD).
Participants underwent MRI and DTI scans. Brain images of 25 individuals with hoarding disorder (mean age, 43 years; 64% women; 96% right-handed) were compared with those of 36 healthy controls matched for age, sex, and handedness.
Participants with HD had higher scores on the Hamilton Rating Scales for depression and anxiety than those without HD (P < .001 for both).
Of the patients with HD, 10 were taking psychiatric medications such as antidepressants, tranquilizers, or nonstimulant agents for attention-deficit/hyperactivity disorder.
Most (n = 18) were concurrently diagnosed with other psychiatric conditions, including ADHD, anxiety disorder, major depressive disorder, posttraumatic stress disorder, or obsessive-compulsive disorder.
The researchers also conducted a post hoc analysis of regions of interest “to detect correlations with clinical features.”
Microstructural alterations
Compared with healthy controls, patients with hoarding disorder showed decreased FA and increased RD in anatomically widespread WM tracts.
Decreased FA areas included the left superior longitudinal fasciculus (SLF), left uncinate fasciculus, left inferior fronto-occipital fasciculus (IFOF), left anterior thalamic radiation (ATR), left corticospinal tract, and left anterior limb of the internal capsule (ALIC).
Increased RD areas included the bilateral SLF, right IFOF, bilateral anterior and superior corona radiata, left posterior corona radiata, right ATR, left posterior thalamic radiation, right external capsule, and right ALIC.
Post hoc analyses of “regions of interest,” revealed “significant negative correlation” between the severity of hoarding symptoms and FA, particularly in the left anterior limb of the internal capsule, and a positive correlation between HD symptom severity and radial diffusivity in the right anterior thalamic radiation.
Those with HD also showed “a broad range of alterations” in the frontal WM tracts, including the frontothalamic circuit, frontoparietal network, and frontolimbic pathway.
“We found anatomically widespread decreases in FA and increases in WD in many major WM tracts and correlations between the severity of hoarding symptoms and DTI parameters (FA and RD) in the left ALIC and right ATR, which is part of the frontothalamic circuit,” the investigators write.
These findings “suggest that patients with HD have microstructural alterations in the prefrontal WM tracts,” they add.
First study
The researchers say that, to their knowledge, this is the first study to find major abnormalities in WM tracts within the brain and correlations between DTI indexes and clinical features in patients with HD.
The frontothalamic circuit is “thought to play an important role in executive functions, including working memory, attention, reward processing, and decision-making,” the investigators write.
Previous research implied that frontothalamic circuit–related cognitive functions are “impaired in patients with HD” and suggested that these impairments “underlie hoarding symptoms such as acquiring, saving, and cluttering relevant to HD.”
The decreased FA in the left SLF “reflects alterations in WM in the frontoparietal network in these patients and may be associated with cognitive impairments, such as task switching and inhibition, as shown in previous studies,” the researchers write.
Additionally, changes in FA and RD often “indicate myelin pathology,” which suggest that HD pathophysiology “may include abnormalities of myelination.”
However, the investigators cite several study limitations, including the “relatively small” sample size, which kept the DTI analysis from being “robust.” Moreover, many patients with HD had comorbid psychiatric disorders, which have also been associated with microstructural abnormalities in WM, the researchers note.
Novel approach
Commenting for this news organization, Michael Stevens, PhD, director, CNDLAB, Olin Neuropsychiatry Research Center, and adjunct professor of psychiatry at Yale University School of Medicine, New Haven, Conn., said the study “provides useful new clues for understanding HD neurobiology” because of its novel approach in assessing microstructural properties of major WM tracts.
The study’s “main contribution is to identify specific WM pathways between brain regions as worth looking at closely in the future. Some of these regions already have been implicated by brain function neuroimaging as abnormal in patients who compulsively hoard,” said Dr. Stevens, who was not involved in the research.
He noted that, when WM pathway integrity is affected, “it is thought to have an impact on how well information is communicated” between the brain regions.
“So once these specific findings are replicated in a separate study, they hopefully can guide researchers to ask new questions to learn exactly how these WM tracts might contribute to hoarding behavior,” Dr. Stevens said.
The study had no specific funding. The investigators and Dr. Stevens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a neuroimaging study, investigators led by Taro Mizobe, department of neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, compared brain scans of individuals with and without HD.
Results showed that compared with healthy family members, participants with HD had anatomically widespread abnormalities in WM tracts.
In particular, a broad range of alterations were found in frontal WM related to HD symptom severity, as well as cortical regions involved in cognitive dysfunction.
“The finding of a characteristic association between alterations in the prefrontal WM tract, which connects cortical regions involved in cognitive function and the severity of hoarding symptoms, could provide new insights into the neurobiological basis of HD,” the researchers write.
The findings were published online Jan. 18 in the Journal of Psychiatric Research.
Limited information to date
“Although there are no clear neurobiological models of HD, several neuroimaging studies have found specific differences in specific brain regions” between patients with and without HD, the investigators write.
Structural MRI studies and voxel-based morphometry have shown larger volumes of gray matter in several regions of the brain in patients with HD. However, there have been no reports on alterations in the WM tracts – and studies of patients with obsessive-compulsive disorder and hoarding symptoms have yielded only “limited information” regarding WM tracts, the researchers note.
Diffusion tensor imaging (DTI) studies have yielded “inconsistent” findings, “therefore little is known about the microstructure of WM in the brains of patients with HD,” they add.
The current study was designed “to investigate microstructural alterations in the WM tracts of individuals with HD” by using tract-based spatial statistics – a model typically used for whole-brain, voxel-wise analysis of DTI measures.
DTI neuroimaging can assess the microstructure of WM. In the current study, the investigators focused on the three measures yielded by DTI: fractional anisotropy (FA), which is an index of overall WM integrity; axial diffusivity (AD); and radial diffusivity (RD).
Participants underwent MRI and DTI scans. Brain images of 25 individuals with hoarding disorder (mean age, 43 years; 64% women; 96% right-handed) were compared with those of 36 healthy controls matched for age, sex, and handedness.
Participants with HD had higher scores on the Hamilton Rating Scales for depression and anxiety than those without HD (P < .001 for both).
Of the patients with HD, 10 were taking psychiatric medications such as antidepressants, tranquilizers, or nonstimulant agents for attention-deficit/hyperactivity disorder.
Most (n = 18) were concurrently diagnosed with other psychiatric conditions, including ADHD, anxiety disorder, major depressive disorder, posttraumatic stress disorder, or obsessive-compulsive disorder.
The researchers also conducted a post hoc analysis of regions of interest “to detect correlations with clinical features.”
Microstructural alterations
Compared with healthy controls, patients with hoarding disorder showed decreased FA and increased RD in anatomically widespread WM tracts.
Decreased FA areas included the left superior longitudinal fasciculus (SLF), left uncinate fasciculus, left inferior fronto-occipital fasciculus (IFOF), left anterior thalamic radiation (ATR), left corticospinal tract, and left anterior limb of the internal capsule (ALIC).
Increased RD areas included the bilateral SLF, right IFOF, bilateral anterior and superior corona radiata, left posterior corona radiata, right ATR, left posterior thalamic radiation, right external capsule, and right ALIC.
Post hoc analyses of “regions of interest,” revealed “significant negative correlation” between the severity of hoarding symptoms and FA, particularly in the left anterior limb of the internal capsule, and a positive correlation between HD symptom severity and radial diffusivity in the right anterior thalamic radiation.
Those with HD also showed “a broad range of alterations” in the frontal WM tracts, including the frontothalamic circuit, frontoparietal network, and frontolimbic pathway.
“We found anatomically widespread decreases in FA and increases in WD in many major WM tracts and correlations between the severity of hoarding symptoms and DTI parameters (FA and RD) in the left ALIC and right ATR, which is part of the frontothalamic circuit,” the investigators write.
These findings “suggest that patients with HD have microstructural alterations in the prefrontal WM tracts,” they add.
First study
The researchers say that, to their knowledge, this is the first study to find major abnormalities in WM tracts within the brain and correlations between DTI indexes and clinical features in patients with HD.
The frontothalamic circuit is “thought to play an important role in executive functions, including working memory, attention, reward processing, and decision-making,” the investigators write.
Previous research implied that frontothalamic circuit–related cognitive functions are “impaired in patients with HD” and suggested that these impairments “underlie hoarding symptoms such as acquiring, saving, and cluttering relevant to HD.”
The decreased FA in the left SLF “reflects alterations in WM in the frontoparietal network in these patients and may be associated with cognitive impairments, such as task switching and inhibition, as shown in previous studies,” the researchers write.
Additionally, changes in FA and RD often “indicate myelin pathology,” which suggest that HD pathophysiology “may include abnormalities of myelination.”
However, the investigators cite several study limitations, including the “relatively small” sample size, which kept the DTI analysis from being “robust.” Moreover, many patients with HD had comorbid psychiatric disorders, which have also been associated with microstructural abnormalities in WM, the researchers note.
Novel approach
Commenting for this news organization, Michael Stevens, PhD, director, CNDLAB, Olin Neuropsychiatry Research Center, and adjunct professor of psychiatry at Yale University School of Medicine, New Haven, Conn., said the study “provides useful new clues for understanding HD neurobiology” because of its novel approach in assessing microstructural properties of major WM tracts.
The study’s “main contribution is to identify specific WM pathways between brain regions as worth looking at closely in the future. Some of these regions already have been implicated by brain function neuroimaging as abnormal in patients who compulsively hoard,” said Dr. Stevens, who was not involved in the research.
He noted that, when WM pathway integrity is affected, “it is thought to have an impact on how well information is communicated” between the brain regions.
“So once these specific findings are replicated in a separate study, they hopefully can guide researchers to ask new questions to learn exactly how these WM tracts might contribute to hoarding behavior,” Dr. Stevens said.
The study had no specific funding. The investigators and Dr. Stevens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a neuroimaging study, investigators led by Taro Mizobe, department of neuropsychiatry, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, compared brain scans of individuals with and without HD.
Results showed that compared with healthy family members, participants with HD had anatomically widespread abnormalities in WM tracts.
In particular, a broad range of alterations were found in frontal WM related to HD symptom severity, as well as cortical regions involved in cognitive dysfunction.
“The finding of a characteristic association between alterations in the prefrontal WM tract, which connects cortical regions involved in cognitive function and the severity of hoarding symptoms, could provide new insights into the neurobiological basis of HD,” the researchers write.
The findings were published online Jan. 18 in the Journal of Psychiatric Research.
Limited information to date
“Although there are no clear neurobiological models of HD, several neuroimaging studies have found specific differences in specific brain regions” between patients with and without HD, the investigators write.
Structural MRI studies and voxel-based morphometry have shown larger volumes of gray matter in several regions of the brain in patients with HD. However, there have been no reports on alterations in the WM tracts – and studies of patients with obsessive-compulsive disorder and hoarding symptoms have yielded only “limited information” regarding WM tracts, the researchers note.
Diffusion tensor imaging (DTI) studies have yielded “inconsistent” findings, “therefore little is known about the microstructure of WM in the brains of patients with HD,” they add.
The current study was designed “to investigate microstructural alterations in the WM tracts of individuals with HD” by using tract-based spatial statistics – a model typically used for whole-brain, voxel-wise analysis of DTI measures.
DTI neuroimaging can assess the microstructure of WM. In the current study, the investigators focused on the three measures yielded by DTI: fractional anisotropy (FA), which is an index of overall WM integrity; axial diffusivity (AD); and radial diffusivity (RD).
Participants underwent MRI and DTI scans. Brain images of 25 individuals with hoarding disorder (mean age, 43 years; 64% women; 96% right-handed) were compared with those of 36 healthy controls matched for age, sex, and handedness.
Participants with HD had higher scores on the Hamilton Rating Scales for depression and anxiety than those without HD (P < .001 for both).
Of the patients with HD, 10 were taking psychiatric medications such as antidepressants, tranquilizers, or nonstimulant agents for attention-deficit/hyperactivity disorder.
Most (n = 18) were concurrently diagnosed with other psychiatric conditions, including ADHD, anxiety disorder, major depressive disorder, posttraumatic stress disorder, or obsessive-compulsive disorder.
The researchers also conducted a post hoc analysis of regions of interest “to detect correlations with clinical features.”
Microstructural alterations
Compared with healthy controls, patients with hoarding disorder showed decreased FA and increased RD in anatomically widespread WM tracts.
Decreased FA areas included the left superior longitudinal fasciculus (SLF), left uncinate fasciculus, left inferior fronto-occipital fasciculus (IFOF), left anterior thalamic radiation (ATR), left corticospinal tract, and left anterior limb of the internal capsule (ALIC).
Increased RD areas included the bilateral SLF, right IFOF, bilateral anterior and superior corona radiata, left posterior corona radiata, right ATR, left posterior thalamic radiation, right external capsule, and right ALIC.
Post hoc analyses of “regions of interest,” revealed “significant negative correlation” between the severity of hoarding symptoms and FA, particularly in the left anterior limb of the internal capsule, and a positive correlation between HD symptom severity and radial diffusivity in the right anterior thalamic radiation.
Those with HD also showed “a broad range of alterations” in the frontal WM tracts, including the frontothalamic circuit, frontoparietal network, and frontolimbic pathway.
“We found anatomically widespread decreases in FA and increases in WD in many major WM tracts and correlations between the severity of hoarding symptoms and DTI parameters (FA and RD) in the left ALIC and right ATR, which is part of the frontothalamic circuit,” the investigators write.
These findings “suggest that patients with HD have microstructural alterations in the prefrontal WM tracts,” they add.
First study
The researchers say that, to their knowledge, this is the first study to find major abnormalities in WM tracts within the brain and correlations between DTI indexes and clinical features in patients with HD.
The frontothalamic circuit is “thought to play an important role in executive functions, including working memory, attention, reward processing, and decision-making,” the investigators write.
Previous research implied that frontothalamic circuit–related cognitive functions are “impaired in patients with HD” and suggested that these impairments “underlie hoarding symptoms such as acquiring, saving, and cluttering relevant to HD.”
The decreased FA in the left SLF “reflects alterations in WM in the frontoparietal network in these patients and may be associated with cognitive impairments, such as task switching and inhibition, as shown in previous studies,” the researchers write.
Additionally, changes in FA and RD often “indicate myelin pathology,” which suggest that HD pathophysiology “may include abnormalities of myelination.”
However, the investigators cite several study limitations, including the “relatively small” sample size, which kept the DTI analysis from being “robust.” Moreover, many patients with HD had comorbid psychiatric disorders, which have also been associated with microstructural abnormalities in WM, the researchers note.
Novel approach
Commenting for this news organization, Michael Stevens, PhD, director, CNDLAB, Olin Neuropsychiatry Research Center, and adjunct professor of psychiatry at Yale University School of Medicine, New Haven, Conn., said the study “provides useful new clues for understanding HD neurobiology” because of its novel approach in assessing microstructural properties of major WM tracts.
The study’s “main contribution is to identify specific WM pathways between brain regions as worth looking at closely in the future. Some of these regions already have been implicated by brain function neuroimaging as abnormal in patients who compulsively hoard,” said Dr. Stevens, who was not involved in the research.
He noted that, when WM pathway integrity is affected, “it is thought to have an impact on how well information is communicated” between the brain regions.
“So once these specific findings are replicated in a separate study, they hopefully can guide researchers to ask new questions to learn exactly how these WM tracts might contribute to hoarding behavior,” Dr. Stevens said.
The study had no specific funding. The investigators and Dr. Stevens have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intranasal oxytocin shows early promise for cocaine dependence
Intranasal oxytocin (INOT) is showing early promise as a treatment for cocaine dependence, new research suggests.
Results of a small 6-week randomized, placebo-controlled trial in patients with cocaine use disorder showed a high level of abstinence in those who received INOT beginning 2 weeks after treatment initiation.
“In this population of cocaine-dependent individuals in a community clinic setting, , compared to placebo,” lead author Wilfrid Noel Raby, PhD, MD, a Teaneck, N.J.–based psychiatrist, said in an interview.
On the other hand, “the findings were paradoxical because there was a greater dropout rate in the intranasal oxytocin group after week 1, suggesting that oxytocin might have a biphasic effect, which should be addressed in future studies,” added Dr. Raby, who was an adjunct clinical professor of psychiatry, division on substance abuse, Montefiore Medical Center, Albert Einstein College of Medicine, New York, when the trial was conducted.
The study was published in the March issue of Drug and Alcohol Dependence Reports.
‘Crying need’
“Focus on stress reactivity in addiction and on the loss of social norms among drug users has generated interest in oxytocin, due to its purported role in these traits and regulation of stress,” the authors wrote.
Oxytocin is a neuropeptide that regulates autonomic functions. Previous research in cannabis users suggests it may have a role in treating addiction by reportedly reducing cravings. In addition, earlier research also suggests it cuts stress reactivity and state anger in cocaine users.
A previous trial of INOT showed it decreased cocaine craving, and additional research has revealed recurrent cocaine use results in lower endogenous oxytocin levels and depleted oxytocin in the hypothalamus and amygdala.
“The bias of my work is to look for simple, nonaddictive medicinal approaches that can be used in the community settings, because that’s where the greatest crying need lies and where most problems from drug addiction occur,” said Dr. Raby.
“There has been long-standing interest in how the brain adaptive systems, or so-called ‘stress systems,’ adjust in the face of drug dependence in general, and the main focus of the study has been to understand this response and use the insight from these adaptations to develop medicinal treatments for drug abuse, particularly cocaine dependence,” he added.
To investigate the potential for INOT to promote abstinence from cocaine, the researchers randomized 26 patients with cocaine use disorder (73% male, mean [SD] age, 50.2 [5.4] years). Most participants had been using cocaine on a regular basis for about 25 years, and baseline average days of cocaine use was 11.1 (5.7) during the 30 days prior to study entry.
At a baseline, the researchers collected participants’ medical history and conducted a physical examination, urine toxicology, electrocardiogram, comprehensive metabolic panel, and complete blood count. They used the MINI International Neuropsychiatric Interview to confirm the diagnosis of cocaine dependence.
The study began with a 7-day inpatient abstinence induction stage, after which participants were randomized to receive either INOT 24 IU or intranasal placebo (n = 15 and n = 11, respectively).
Patients attended the clinic three times per week. At each visit, they completed the cocaine craving scale, the Perceived Stress Scale, and the Clinician Global Inventory (all self-reports), as well as the Time Line Follow Back (TLFB) to document cocaine use.
Participants were trained to self-administer an intranasal solution at home, with compliance monitored in two ways – staff observed self-administration of the randomized medication at the time of clinic visits and weighed the “at home bottle.”
Cocaine use was determined via urine toxicology and TLFB self-report.
Threshold period
INOT did not induce ≥ 3 weeks of continuous abstinence. However, beginning with week 3, the odds of weekly abstinence increased dramatically in the INOT group, from 4.61 (95% confidence interval,1.05, 20.3) to 15.0 (1.18, 190.2) by week 6 (t = 2.12, P = .037).
The overall medication group by time interaction across all 6 weeks was not significant (F1,69 = 1.73, P = .19); but when the interaction was removed, the difference between the overall effect of medication (INOT vs. placebo) over all 6 weeks “reached trend-level significance” (F1,70) = 3.42, P = .07).
The subjective rating outcomes (cravings, perceived stress, cocaine dependence, and depression) “did not show a significant medication group by time interaction effect,” the authors reported, although stress-induced cravings did tend toward a significant difference between the groups.
Half of the patients did not complete the full 6 weeks. Of those who discontinued, 85% came from the INOT group and 15% from the placebo group. Of the 11 who dropped out from the treatment group, seven were abstinent at the time of discontinuation for ≥ 1 week.
There were no significant differences in rates of reported side effects between the two groups.
“This study highlights some promise that perhaps there is a threshold period of time you need to cross, after which time oxytocin could really be really helpful as acute or maintenance medication,” said Dr. Raby. The short study duration might have been a disadvantage. “We might have seen better results if the study had been 8 or 12 weeks in duration.”
Using motivational approaches during the early phase – e.g., psychotherapy or a voucher system – might increase adherence, and then “after this initial lag, we might see a more therapeutic effect,” he suggested.
Dr. Raby noted that his group studied stress hormone secretions in the cocaine-dependent study participants during the 7-day induction period and that the findings, when published, could shed light on this latency period. “Cocaine dependence creates adaptations in the stress system,” he said.
‘Nice first step’
Commenting on the study, Jane Joseph, PhD, professor in the department of neurosciences and director of the neuroimaging division at Medical University of South Carolina, Charleston, said it is “nice to see a clinical trial using oxytocin in cocaine dependence [because] preclinical research has shown fairly convincing effects of oxytocin in reducing craving or stress in the context of cocaine seeking, but findings are rather mixed in human studies.”
Dr. Joseph, who was not involved with the study, said her group’s research showed oxytocin to be the most helpful for men with cocaine use disorder who reported childhood trauma, while for women, oxytocin “seemed to worsen their reactivity to cocaine cues.”
She said the current study is a “nice first step” and suggested that future research should include larger sample sizes to “address some of the individual variability in the response to oxytocin by examining sex differences or trauma history.”
The study was supported by an award from the National Institute of Drug Abuse. Dr. Raby and coauthors and Dr. Joseph have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intranasal oxytocin (INOT) is showing early promise as a treatment for cocaine dependence, new research suggests.
Results of a small 6-week randomized, placebo-controlled trial in patients with cocaine use disorder showed a high level of abstinence in those who received INOT beginning 2 weeks after treatment initiation.
“In this population of cocaine-dependent individuals in a community clinic setting, , compared to placebo,” lead author Wilfrid Noel Raby, PhD, MD, a Teaneck, N.J.–based psychiatrist, said in an interview.
On the other hand, “the findings were paradoxical because there was a greater dropout rate in the intranasal oxytocin group after week 1, suggesting that oxytocin might have a biphasic effect, which should be addressed in future studies,” added Dr. Raby, who was an adjunct clinical professor of psychiatry, division on substance abuse, Montefiore Medical Center, Albert Einstein College of Medicine, New York, when the trial was conducted.
The study was published in the March issue of Drug and Alcohol Dependence Reports.
‘Crying need’
“Focus on stress reactivity in addiction and on the loss of social norms among drug users has generated interest in oxytocin, due to its purported role in these traits and regulation of stress,” the authors wrote.
Oxytocin is a neuropeptide that regulates autonomic functions. Previous research in cannabis users suggests it may have a role in treating addiction by reportedly reducing cravings. In addition, earlier research also suggests it cuts stress reactivity and state anger in cocaine users.
A previous trial of INOT showed it decreased cocaine craving, and additional research has revealed recurrent cocaine use results in lower endogenous oxytocin levels and depleted oxytocin in the hypothalamus and amygdala.
“The bias of my work is to look for simple, nonaddictive medicinal approaches that can be used in the community settings, because that’s where the greatest crying need lies and where most problems from drug addiction occur,” said Dr. Raby.
“There has been long-standing interest in how the brain adaptive systems, or so-called ‘stress systems,’ adjust in the face of drug dependence in general, and the main focus of the study has been to understand this response and use the insight from these adaptations to develop medicinal treatments for drug abuse, particularly cocaine dependence,” he added.
To investigate the potential for INOT to promote abstinence from cocaine, the researchers randomized 26 patients with cocaine use disorder (73% male, mean [SD] age, 50.2 [5.4] years). Most participants had been using cocaine on a regular basis for about 25 years, and baseline average days of cocaine use was 11.1 (5.7) during the 30 days prior to study entry.
At a baseline, the researchers collected participants’ medical history and conducted a physical examination, urine toxicology, electrocardiogram, comprehensive metabolic panel, and complete blood count. They used the MINI International Neuropsychiatric Interview to confirm the diagnosis of cocaine dependence.
The study began with a 7-day inpatient abstinence induction stage, after which participants were randomized to receive either INOT 24 IU or intranasal placebo (n = 15 and n = 11, respectively).
Patients attended the clinic three times per week. At each visit, they completed the cocaine craving scale, the Perceived Stress Scale, and the Clinician Global Inventory (all self-reports), as well as the Time Line Follow Back (TLFB) to document cocaine use.
Participants were trained to self-administer an intranasal solution at home, with compliance monitored in two ways – staff observed self-administration of the randomized medication at the time of clinic visits and weighed the “at home bottle.”
Cocaine use was determined via urine toxicology and TLFB self-report.
Threshold period
INOT did not induce ≥ 3 weeks of continuous abstinence. However, beginning with week 3, the odds of weekly abstinence increased dramatically in the INOT group, from 4.61 (95% confidence interval,1.05, 20.3) to 15.0 (1.18, 190.2) by week 6 (t = 2.12, P = .037).
The overall medication group by time interaction across all 6 weeks was not significant (F1,69 = 1.73, P = .19); but when the interaction was removed, the difference between the overall effect of medication (INOT vs. placebo) over all 6 weeks “reached trend-level significance” (F1,70) = 3.42, P = .07).
The subjective rating outcomes (cravings, perceived stress, cocaine dependence, and depression) “did not show a significant medication group by time interaction effect,” the authors reported, although stress-induced cravings did tend toward a significant difference between the groups.
Half of the patients did not complete the full 6 weeks. Of those who discontinued, 85% came from the INOT group and 15% from the placebo group. Of the 11 who dropped out from the treatment group, seven were abstinent at the time of discontinuation for ≥ 1 week.
There were no significant differences in rates of reported side effects between the two groups.
“This study highlights some promise that perhaps there is a threshold period of time you need to cross, after which time oxytocin could really be really helpful as acute or maintenance medication,” said Dr. Raby. The short study duration might have been a disadvantage. “We might have seen better results if the study had been 8 or 12 weeks in duration.”
Using motivational approaches during the early phase – e.g., psychotherapy or a voucher system – might increase adherence, and then “after this initial lag, we might see a more therapeutic effect,” he suggested.
Dr. Raby noted that his group studied stress hormone secretions in the cocaine-dependent study participants during the 7-day induction period and that the findings, when published, could shed light on this latency period. “Cocaine dependence creates adaptations in the stress system,” he said.
‘Nice first step’
Commenting on the study, Jane Joseph, PhD, professor in the department of neurosciences and director of the neuroimaging division at Medical University of South Carolina, Charleston, said it is “nice to see a clinical trial using oxytocin in cocaine dependence [because] preclinical research has shown fairly convincing effects of oxytocin in reducing craving or stress in the context of cocaine seeking, but findings are rather mixed in human studies.”
Dr. Joseph, who was not involved with the study, said her group’s research showed oxytocin to be the most helpful for men with cocaine use disorder who reported childhood trauma, while for women, oxytocin “seemed to worsen their reactivity to cocaine cues.”
She said the current study is a “nice first step” and suggested that future research should include larger sample sizes to “address some of the individual variability in the response to oxytocin by examining sex differences or trauma history.”
The study was supported by an award from the National Institute of Drug Abuse. Dr. Raby and coauthors and Dr. Joseph have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Intranasal oxytocin (INOT) is showing early promise as a treatment for cocaine dependence, new research suggests.
Results of a small 6-week randomized, placebo-controlled trial in patients with cocaine use disorder showed a high level of abstinence in those who received INOT beginning 2 weeks after treatment initiation.
“In this population of cocaine-dependent individuals in a community clinic setting, , compared to placebo,” lead author Wilfrid Noel Raby, PhD, MD, a Teaneck, N.J.–based psychiatrist, said in an interview.
On the other hand, “the findings were paradoxical because there was a greater dropout rate in the intranasal oxytocin group after week 1, suggesting that oxytocin might have a biphasic effect, which should be addressed in future studies,” added Dr. Raby, who was an adjunct clinical professor of psychiatry, division on substance abuse, Montefiore Medical Center, Albert Einstein College of Medicine, New York, when the trial was conducted.
The study was published in the March issue of Drug and Alcohol Dependence Reports.
‘Crying need’
“Focus on stress reactivity in addiction and on the loss of social norms among drug users has generated interest in oxytocin, due to its purported role in these traits and regulation of stress,” the authors wrote.
Oxytocin is a neuropeptide that regulates autonomic functions. Previous research in cannabis users suggests it may have a role in treating addiction by reportedly reducing cravings. In addition, earlier research also suggests it cuts stress reactivity and state anger in cocaine users.
A previous trial of INOT showed it decreased cocaine craving, and additional research has revealed recurrent cocaine use results in lower endogenous oxytocin levels and depleted oxytocin in the hypothalamus and amygdala.
“The bias of my work is to look for simple, nonaddictive medicinal approaches that can be used in the community settings, because that’s where the greatest crying need lies and where most problems from drug addiction occur,” said Dr. Raby.
“There has been long-standing interest in how the brain adaptive systems, or so-called ‘stress systems,’ adjust in the face of drug dependence in general, and the main focus of the study has been to understand this response and use the insight from these adaptations to develop medicinal treatments for drug abuse, particularly cocaine dependence,” he added.
To investigate the potential for INOT to promote abstinence from cocaine, the researchers randomized 26 patients with cocaine use disorder (73% male, mean [SD] age, 50.2 [5.4] years). Most participants had been using cocaine on a regular basis for about 25 years, and baseline average days of cocaine use was 11.1 (5.7) during the 30 days prior to study entry.
At a baseline, the researchers collected participants’ medical history and conducted a physical examination, urine toxicology, electrocardiogram, comprehensive metabolic panel, and complete blood count. They used the MINI International Neuropsychiatric Interview to confirm the diagnosis of cocaine dependence.
The study began with a 7-day inpatient abstinence induction stage, after which participants were randomized to receive either INOT 24 IU or intranasal placebo (n = 15 and n = 11, respectively).
Patients attended the clinic three times per week. At each visit, they completed the cocaine craving scale, the Perceived Stress Scale, and the Clinician Global Inventory (all self-reports), as well as the Time Line Follow Back (TLFB) to document cocaine use.
Participants were trained to self-administer an intranasal solution at home, with compliance monitored in two ways – staff observed self-administration of the randomized medication at the time of clinic visits and weighed the “at home bottle.”
Cocaine use was determined via urine toxicology and TLFB self-report.
Threshold period
INOT did not induce ≥ 3 weeks of continuous abstinence. However, beginning with week 3, the odds of weekly abstinence increased dramatically in the INOT group, from 4.61 (95% confidence interval,1.05, 20.3) to 15.0 (1.18, 190.2) by week 6 (t = 2.12, P = .037).
The overall medication group by time interaction across all 6 weeks was not significant (F1,69 = 1.73, P = .19); but when the interaction was removed, the difference between the overall effect of medication (INOT vs. placebo) over all 6 weeks “reached trend-level significance” (F1,70) = 3.42, P = .07).
The subjective rating outcomes (cravings, perceived stress, cocaine dependence, and depression) “did not show a significant medication group by time interaction effect,” the authors reported, although stress-induced cravings did tend toward a significant difference between the groups.
Half of the patients did not complete the full 6 weeks. Of those who discontinued, 85% came from the INOT group and 15% from the placebo group. Of the 11 who dropped out from the treatment group, seven were abstinent at the time of discontinuation for ≥ 1 week.
There were no significant differences in rates of reported side effects between the two groups.
“This study highlights some promise that perhaps there is a threshold period of time you need to cross, after which time oxytocin could really be really helpful as acute or maintenance medication,” said Dr. Raby. The short study duration might have been a disadvantage. “We might have seen better results if the study had been 8 or 12 weeks in duration.”
Using motivational approaches during the early phase – e.g., psychotherapy or a voucher system – might increase adherence, and then “after this initial lag, we might see a more therapeutic effect,” he suggested.
Dr. Raby noted that his group studied stress hormone secretions in the cocaine-dependent study participants during the 7-day induction period and that the findings, when published, could shed light on this latency period. “Cocaine dependence creates adaptations in the stress system,” he said.
‘Nice first step’
Commenting on the study, Jane Joseph, PhD, professor in the department of neurosciences and director of the neuroimaging division at Medical University of South Carolina, Charleston, said it is “nice to see a clinical trial using oxytocin in cocaine dependence [because] preclinical research has shown fairly convincing effects of oxytocin in reducing craving or stress in the context of cocaine seeking, but findings are rather mixed in human studies.”
Dr. Joseph, who was not involved with the study, said her group’s research showed oxytocin to be the most helpful for men with cocaine use disorder who reported childhood trauma, while for women, oxytocin “seemed to worsen their reactivity to cocaine cues.”
She said the current study is a “nice first step” and suggested that future research should include larger sample sizes to “address some of the individual variability in the response to oxytocin by examining sex differences or trauma history.”
The study was supported by an award from the National Institute of Drug Abuse. Dr. Raby and coauthors and Dr. Joseph have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DRUG AND ALCOHOL DEPENDENCE REPORTS
Dramatic increase in driving high after cannabis legislation
Since Canada legalized marijuana in 2018, there has been a dramatic increase in the number of individuals driving while high, new research shows.
Investigators studied over 4,000 drivers treated after a motor vehicle collision in British Columbia trauma centers and found that, before cannabis was legalized, a THC level greater than 0 ng/mL in the blood was present in roughly 10% of drivers. After the drug was legalized this percentage increased to 18%. The percentages of injured drivers with at least 2 ng/mL, the Canadian legal limit, and at least 5 ng/mL more than doubled.
“It’s concerning that we’re seeing such a dramatic increase,” study investigator Jeffrey Brubacher, MD, associate professor, department of emergency medicine, University of British Columbia, Vancouver, said in a press release.
“There are serious risks associated with driving after cannabis use and our findings suggest more [work] is needed to deter this dangerous behavior in light of legalization,” he said.
The study was published online Jan. 12 in the New England Journal of Medicine.
Impact of legalization?
The investigators note that the Canadian government introduced a law aiming to prevent cannabis-impaired driving by establishing penalties and criminal charges for drivers found with a whole-blood THC level of 2 ng/mL, with more severe penalties for those with a THC level of greater than 5 ng/mL or greater than 2.5 ng/mL combined with a blood alcohol level of .05%.
Cannabis use is “associated with cognitive deficits and psychomotor impairment, and there is evidence that it increases the risk of motor vehicle crashes, especially at higher THC levels,” they noted.
“I’m an emergency physician at Vancouver General Hospital’s trauma center. We’ve been measuring drug levels in injured drivers since 2013 here in British Columbia and, in particular, we’ve been measuring THC levels,” Dr. Brubacher said in an interview. “We thought it would be interesting and important to see what would happen after legalization.”
The investigators studied 4,339 drivers – 3,550 whose accident took place before legalization of cannabis, and 789 after legalization – who had been moderately injured in a motor vehicle collision and presented to four British Columbia trauma centers between January 2013 and March 2020.
said Dr. Brubacher. Drivers included in the study had excess blood remaining after the clinical testing had been completed, which was then used for drug analysis.
Insufficient laws
After legalization there was an increased prevalence of drivers with a THC level greater than 0 ng/mL, a TCH level of at least 2 ng/mL, and a THC level of at least 5 ng/mL.
The largest increases in a THC level of at least 2 ng/mL were in drivers 50 years of age or older and among male drivers (adjusted prevalence ratio, 5.18; 95% confidence interval, 2.49-10.78 and aPR, 2.44; 95% CI, 1.60-3.74, respectively).
“There were no significant changes in the prevalence of drivers testing positive for alcohol,” the authors reported.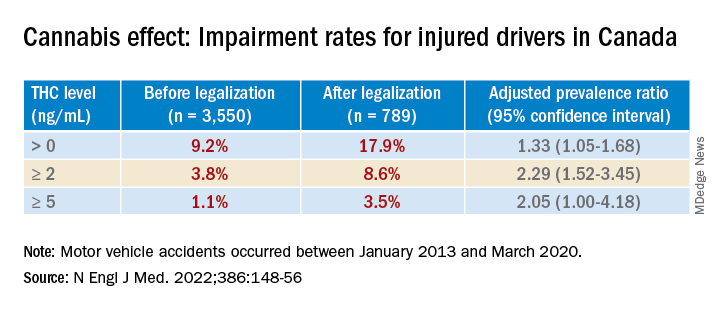
Dr. Brubacher said the evidence suggests these new laws “are not enough to stop everyone from driving after using cannabis.”
The findings have implications for clinicians and patients and for policymakers, he said. “My moderately conservative recommendations are that, if you are going to smoke cannabis, wait at least 4 hours after smoking before you drive. Edibles last longer, and patients should wait least 8 hours after ingesting [edibles] before driving. And of course, if you continue to feel the effects of the THC, you should avoid driving altogether until the time has elapsed and you no longer feel any effects.”
Dr. Brubacher hopes policy makers will use the study’s findings to “design public information campaigns and enforcement measures that encourage drivers, especially older drivers, to separate cannabis use from driving.”
Additionally, “policy makers shouldn’t lose sight of drinking and driving because that’s an even bigger problem than the risk of driving under the influence of cannabis.”
Focus on older adults
In a comment, Anees Bahji, MD, an International Collaborative Addiction Medicine research fellow at the British Columbia Centre on Substance Use, called the study “interesting and relevant.”
He raised several questions regarding the “correlation between the level of a substance in a person’s system and the degree of impairment.” For example, “does the same level of THC in the blood affect us all the same way? And to what extent do the levels detected at the time of the analysis correlate with the level in the person’s system at the time of driving?”
An additional consideration “is for individuals with cannabis use disorder and for those who have developed tolerance to the psychoactive effects of THC: Does it affect their driving skills in the same way as someone who is cannabis naive?” asked Dr. Bahji, a clinical assistant professor at the University of Calgary (Alta.) who was not involved with the study.
Also commenting, Eric Sevigny, PhD, associate professor of criminal justice and criminology at Georgia State University, Atlanta, described it as a “well-designed study that adds yet another data point for considering appropriate road safety policy responses alongside ongoing cannabis liberalization.”
However, the findings “cannot say much about whether cannabis legalization leads to an increase in cannabis-impaired driving, because current research finds little correlation between biological THC concentrations and driving performance,” said Dr. Sevigny, who was not involved with the study.
The finding of “higher THC prevalence among older adults is also relevant for road safety, as this population has a number of concomitant risk factors, such as cognitive decline and prescription drug use,” Dr. Sevigny added.
The study was supported by the Canadian Institutes of Health Research. Dr. Brubacher and Dr. Sevigny disclosed no relevant financial relationships. Dr. Bahji reported receiving research funding from the Canadian Institutes of Health Research, the Calgary Health Trust, the American Psychiatric Association, NIDA, and the University of Calgary.
A version of this article first appeared on Medscape.com.
Since Canada legalized marijuana in 2018, there has been a dramatic increase in the number of individuals driving while high, new research shows.
Investigators studied over 4,000 drivers treated after a motor vehicle collision in British Columbia trauma centers and found that, before cannabis was legalized, a THC level greater than 0 ng/mL in the blood was present in roughly 10% of drivers. After the drug was legalized this percentage increased to 18%. The percentages of injured drivers with at least 2 ng/mL, the Canadian legal limit, and at least 5 ng/mL more than doubled.
“It’s concerning that we’re seeing such a dramatic increase,” study investigator Jeffrey Brubacher, MD, associate professor, department of emergency medicine, University of British Columbia, Vancouver, said in a press release.
“There are serious risks associated with driving after cannabis use and our findings suggest more [work] is needed to deter this dangerous behavior in light of legalization,” he said.
The study was published online Jan. 12 in the New England Journal of Medicine.
Impact of legalization?
The investigators note that the Canadian government introduced a law aiming to prevent cannabis-impaired driving by establishing penalties and criminal charges for drivers found with a whole-blood THC level of 2 ng/mL, with more severe penalties for those with a THC level of greater than 5 ng/mL or greater than 2.5 ng/mL combined with a blood alcohol level of .05%.
Cannabis use is “associated with cognitive deficits and psychomotor impairment, and there is evidence that it increases the risk of motor vehicle crashes, especially at higher THC levels,” they noted.
“I’m an emergency physician at Vancouver General Hospital’s trauma center. We’ve been measuring drug levels in injured drivers since 2013 here in British Columbia and, in particular, we’ve been measuring THC levels,” Dr. Brubacher said in an interview. “We thought it would be interesting and important to see what would happen after legalization.”
The investigators studied 4,339 drivers – 3,550 whose accident took place before legalization of cannabis, and 789 after legalization – who had been moderately injured in a motor vehicle collision and presented to four British Columbia trauma centers between January 2013 and March 2020.
said Dr. Brubacher. Drivers included in the study had excess blood remaining after the clinical testing had been completed, which was then used for drug analysis.
Insufficient laws
After legalization there was an increased prevalence of drivers with a THC level greater than 0 ng/mL, a TCH level of at least 2 ng/mL, and a THC level of at least 5 ng/mL.
The largest increases in a THC level of at least 2 ng/mL were in drivers 50 years of age or older and among male drivers (adjusted prevalence ratio, 5.18; 95% confidence interval, 2.49-10.78 and aPR, 2.44; 95% CI, 1.60-3.74, respectively).
“There were no significant changes in the prevalence of drivers testing positive for alcohol,” the authors reported.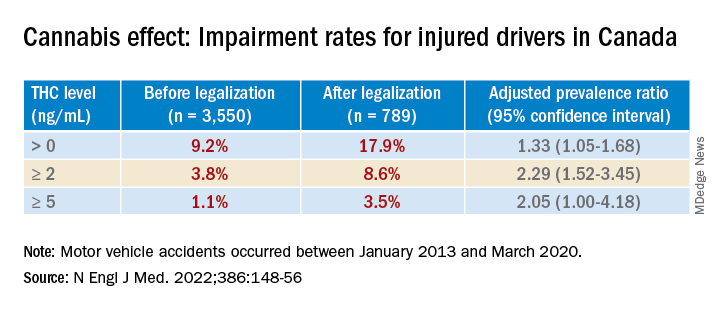
Dr. Brubacher said the evidence suggests these new laws “are not enough to stop everyone from driving after using cannabis.”
The findings have implications for clinicians and patients and for policymakers, he said. “My moderately conservative recommendations are that, if you are going to smoke cannabis, wait at least 4 hours after smoking before you drive. Edibles last longer, and patients should wait least 8 hours after ingesting [edibles] before driving. And of course, if you continue to feel the effects of the THC, you should avoid driving altogether until the time has elapsed and you no longer feel any effects.”
Dr. Brubacher hopes policy makers will use the study’s findings to “design public information campaigns and enforcement measures that encourage drivers, especially older drivers, to separate cannabis use from driving.”
Additionally, “policy makers shouldn’t lose sight of drinking and driving because that’s an even bigger problem than the risk of driving under the influence of cannabis.”
Focus on older adults
In a comment, Anees Bahji, MD, an International Collaborative Addiction Medicine research fellow at the British Columbia Centre on Substance Use, called the study “interesting and relevant.”
He raised several questions regarding the “correlation between the level of a substance in a person’s system and the degree of impairment.” For example, “does the same level of THC in the blood affect us all the same way? And to what extent do the levels detected at the time of the analysis correlate with the level in the person’s system at the time of driving?”
An additional consideration “is for individuals with cannabis use disorder and for those who have developed tolerance to the psychoactive effects of THC: Does it affect their driving skills in the same way as someone who is cannabis naive?” asked Dr. Bahji, a clinical assistant professor at the University of Calgary (Alta.) who was not involved with the study.
Also commenting, Eric Sevigny, PhD, associate professor of criminal justice and criminology at Georgia State University, Atlanta, described it as a “well-designed study that adds yet another data point for considering appropriate road safety policy responses alongside ongoing cannabis liberalization.”
However, the findings “cannot say much about whether cannabis legalization leads to an increase in cannabis-impaired driving, because current research finds little correlation between biological THC concentrations and driving performance,” said Dr. Sevigny, who was not involved with the study.
The finding of “higher THC prevalence among older adults is also relevant for road safety, as this population has a number of concomitant risk factors, such as cognitive decline and prescription drug use,” Dr. Sevigny added.
The study was supported by the Canadian Institutes of Health Research. Dr. Brubacher and Dr. Sevigny disclosed no relevant financial relationships. Dr. Bahji reported receiving research funding from the Canadian Institutes of Health Research, the Calgary Health Trust, the American Psychiatric Association, NIDA, and the University of Calgary.
A version of this article first appeared on Medscape.com.
Since Canada legalized marijuana in 2018, there has been a dramatic increase in the number of individuals driving while high, new research shows.
Investigators studied over 4,000 drivers treated after a motor vehicle collision in British Columbia trauma centers and found that, before cannabis was legalized, a THC level greater than 0 ng/mL in the blood was present in roughly 10% of drivers. After the drug was legalized this percentage increased to 18%. The percentages of injured drivers with at least 2 ng/mL, the Canadian legal limit, and at least 5 ng/mL more than doubled.
“It’s concerning that we’re seeing such a dramatic increase,” study investigator Jeffrey Brubacher, MD, associate professor, department of emergency medicine, University of British Columbia, Vancouver, said in a press release.
“There are serious risks associated with driving after cannabis use and our findings suggest more [work] is needed to deter this dangerous behavior in light of legalization,” he said.
The study was published online Jan. 12 in the New England Journal of Medicine.
Impact of legalization?
The investigators note that the Canadian government introduced a law aiming to prevent cannabis-impaired driving by establishing penalties and criminal charges for drivers found with a whole-blood THC level of 2 ng/mL, with more severe penalties for those with a THC level of greater than 5 ng/mL or greater than 2.5 ng/mL combined with a blood alcohol level of .05%.
Cannabis use is “associated with cognitive deficits and psychomotor impairment, and there is evidence that it increases the risk of motor vehicle crashes, especially at higher THC levels,” they noted.
“I’m an emergency physician at Vancouver General Hospital’s trauma center. We’ve been measuring drug levels in injured drivers since 2013 here in British Columbia and, in particular, we’ve been measuring THC levels,” Dr. Brubacher said in an interview. “We thought it would be interesting and important to see what would happen after legalization.”
The investigators studied 4,339 drivers – 3,550 whose accident took place before legalization of cannabis, and 789 after legalization – who had been moderately injured in a motor vehicle collision and presented to four British Columbia trauma centers between January 2013 and March 2020.
said Dr. Brubacher. Drivers included in the study had excess blood remaining after the clinical testing had been completed, which was then used for drug analysis.
Insufficient laws
After legalization there was an increased prevalence of drivers with a THC level greater than 0 ng/mL, a TCH level of at least 2 ng/mL, and a THC level of at least 5 ng/mL.
The largest increases in a THC level of at least 2 ng/mL were in drivers 50 years of age or older and among male drivers (adjusted prevalence ratio, 5.18; 95% confidence interval, 2.49-10.78 and aPR, 2.44; 95% CI, 1.60-3.74, respectively).
“There were no significant changes in the prevalence of drivers testing positive for alcohol,” the authors reported.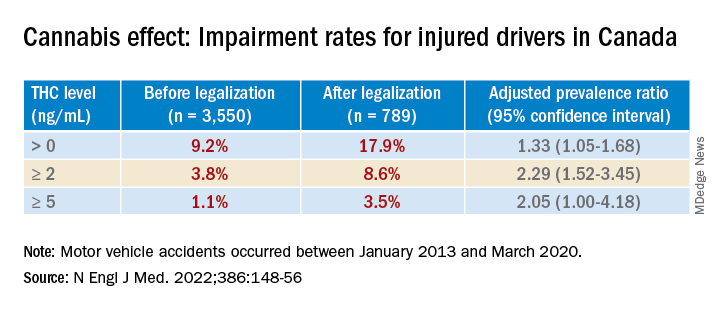
Dr. Brubacher said the evidence suggests these new laws “are not enough to stop everyone from driving after using cannabis.”
The findings have implications for clinicians and patients and for policymakers, he said. “My moderately conservative recommendations are that, if you are going to smoke cannabis, wait at least 4 hours after smoking before you drive. Edibles last longer, and patients should wait least 8 hours after ingesting [edibles] before driving. And of course, if you continue to feel the effects of the THC, you should avoid driving altogether until the time has elapsed and you no longer feel any effects.”
Dr. Brubacher hopes policy makers will use the study’s findings to “design public information campaigns and enforcement measures that encourage drivers, especially older drivers, to separate cannabis use from driving.”
Additionally, “policy makers shouldn’t lose sight of drinking and driving because that’s an even bigger problem than the risk of driving under the influence of cannabis.”
Focus on older adults
In a comment, Anees Bahji, MD, an International Collaborative Addiction Medicine research fellow at the British Columbia Centre on Substance Use, called the study “interesting and relevant.”
He raised several questions regarding the “correlation between the level of a substance in a person’s system and the degree of impairment.” For example, “does the same level of THC in the blood affect us all the same way? And to what extent do the levels detected at the time of the analysis correlate with the level in the person’s system at the time of driving?”
An additional consideration “is for individuals with cannabis use disorder and for those who have developed tolerance to the psychoactive effects of THC: Does it affect their driving skills in the same way as someone who is cannabis naive?” asked Dr. Bahji, a clinical assistant professor at the University of Calgary (Alta.) who was not involved with the study.
Also commenting, Eric Sevigny, PhD, associate professor of criminal justice and criminology at Georgia State University, Atlanta, described it as a “well-designed study that adds yet another data point for considering appropriate road safety policy responses alongside ongoing cannabis liberalization.”
However, the findings “cannot say much about whether cannabis legalization leads to an increase in cannabis-impaired driving, because current research finds little correlation between biological THC concentrations and driving performance,” said Dr. Sevigny, who was not involved with the study.
The finding of “higher THC prevalence among older adults is also relevant for road safety, as this population has a number of concomitant risk factors, such as cognitive decline and prescription drug use,” Dr. Sevigny added.
The study was supported by the Canadian Institutes of Health Research. Dr. Brubacher and Dr. Sevigny disclosed no relevant financial relationships. Dr. Bahji reported receiving research funding from the Canadian Institutes of Health Research, the Calgary Health Trust, the American Psychiatric Association, NIDA, and the University of Calgary.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Antidepressants: Is less more?
When it comes to antidepressant prescribing, less may be more, new research suggests.
A new review suggests antidepressants are overprescribed and that the efficacy of these agents is questionable, leading researchers to recommend that, when physicians prescribe these medications, it should be for shorter periods.
“Antidepressants have never been shown to have a clinically significant difference from placebo in the treatment of depression,” study co\investigator Mark Horowitz, GDPsych, PhD, division of psychiatry, University College London, said in an interview.
He added antidepressants “exert profound adverse effects on the body and brain” and can be difficult to stop because of physical dependence that occurs when the brain adapts to them.
“The best way to take people off these drugs is to do so gradually enough that the unpleasant effects are minimized and in a way that means the reductions in dose get smaller and smaller as the total dose gets lower,” Dr. Horowitz said.
However, at least one expert urged caution in interpreting the review’s findings.
“The reality is that millions of people do benefit from these medications, and this review minimizes those benefits,” Philip Muskin, MD, chief of consultation-liaison for psychiatry and professor of psychiatry, Columbia University Medical Center and New York–Presbyterian Hospital, said when approached for comment.
The findings were published online Dec. 20, 2021, in the Drug and Therapeutics Bulletin.
Personal experience
Prescribing of newer-generation antidepressants, such as SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs), is increasing, with an estimated one in six adults in the United Kingdom receiving at least one prescription in 2019-2020, the investigators noted.
Dr. Horowitz noted a personal motivation for conducting the review. “As well as being an academic psychiatrist, I’m also a patient who has been prescribed antidepressants since age 21, when my mood was poor, due to life circumstances.”
The antidepressant “didn’t have particularly helpful effects,” but Dr. Horowitz continued taking it for 18 years. “I was told it was helpful and internalized that message. I came to understand that much of the information around antidepressants came from the drug companies that manufactured them or from academics paid by these companies.”
Dr. Horowitz is currently discontinuing his medication – a tapering process now in its third year. He said he has come to realize, in retrospect, that symptoms not initially attributed to the drug, such as fatigue, impaired concentration, and impaired memory, have improved since reducing the medication.
“That experience sensitized me to look for these symptoms in my patients and I see them; but most of my patients were told by their doctors that the cause of those problems was the depression or anxiety itself and not the drug,” he said.
Dr. Horowitz collaborated with Michael Wilcock, DTB, Pharmacy, Royal Cornwall Hospitals, NHS Trust, Truro, England, in conducting the review “to provide an independent assessment of benefits and harms of antidepressants.”
“Much of the evidence of the efficacy of antidepressants comes from randomized placebo-controlled trials,” Dr. Horowitz said. Several meta-analyses of these studies showed a difference of about two points between the agent and the placebo on the Hamilton Depression Rating Scale (HAM-D).
“Although this might be statistically significant, it does not meet the threshold for a clinical significance – those aren’t the same thing,” Dr. Horowitz said. Some analyses suggest that a “minimally clinically important difference” on the HAM-D would range from 3 to 6 points.
The findings in adolescents and children are “even less convincing,” the investigators noted, citing a Cochrane review.
“This is especially concerning because the number of children and adolescents being treated with antidepressants is rapidly increasing,” Dr. Horowitz said.
Additionally, the short duration of most trials, typically 6-12 weeks, is “largely uninformative for the clinical treatment of depression.”
Relapse or withdrawal?
The researchers reviewed the adverse effects of long-term antidepressant use, including daytime sleepiness, dry mouth, profuse sweating, weight gain, sexual dysfunction, restlessness, and feeling “foggy or detached.”
“Antidepressants have toxic effects on the brain and cause brain damage when they artificially increase serotonin and modify brain chemistry, which is why people become sick for years after stopping,” Dr. Horowitz said. “When the drug is reduced or stopped, the brain has difficulty dealing with the sudden drop in neurotransmitters, and withdrawal symptoms result, similar to stopping caffeine, nicotine, or opioids.”
He added it is not necessarily the original condition of depression or anxiety that is recurring but rather withdrawal, which can last for months or even years after medication discontinuation.
“Unfortunately, doctors have been taught that there are minimal withdrawal symptoms, euphemized as ‘discontinuation symptoms,’ and so when patients have reported withdrawal symptoms, they have been told it is a return of their underlying condition,” Dr. Horowitz said.
“This has led to many patients being incorrectly told that they need to get back on their antidepressants,” he added.
He likened this approach to “telling people that the need to continue smoking because when they stop, they get more anxiety.” Rather, the “correct response would be that they simply need to taper off the antidepressant more carefully,” he said.
Helpful in the short term
Patients should be informed prior to initiation of antidepressant treatment about the risk of withdrawal effects if they stop the drug, the investigators advise. They reference the Royal College of Psychiatrists’ updated guidance, which recommends slow tapering over a period long enough to mitigate withdrawal symptoms to “tolerable levels.”
The guidance suggests that patients start with a small “test reduction.” Withdrawal symptoms should be monitored for the following 2-4 weeks, using a symptom checklist such as the Discontinuation Emergent Signs and Symptoms Scale, with subsequent reductions based on the tolerability of the process.
Gradual dose reductions and very small final doses may necessitate the use of formulations of medication other than those commonly available in tablet forms, the researchers noted. During the tapering process, patients may benefit from increased psychosocial support.
Dr. Horowitz noted that antidepressants can be helpful on a short-term basis, and likened their use to the use of a cast to stabilize a broken arm.
“It’s useful for a short period. But if you leave someone in a plastic cast permanently, their arm will shrivel and you will disable them. These drugs should be prescribed minimally, and for the shortest possible period of time,” he said.
Dr. Horowitz recommended the recent draft National Institute for Health and Care Excellence depression guidance that recommends multiple other options beyond antidepressants, including cognitive-behavioral therapy, problem solving, counseling, and exercise.
Lack of balance
Dr. Muskin commented that the review is helpful in guiding clinicians on how to approach tapering of antidepressants and making patients aware of discontinuation symptoms.
However, “a lot of people will read this who need treatment, but they won’t get treated because they’ll take away the message that ‘drugs don’t work,’ ” he said.
“As it is, there is already stigma and prejudice toward psychiatric illness and using medications for treatment,” said Dr. Muskin, who was not involved with the research.
The current review “isn’t balanced, in terms of the efficacy of these drugs – both for the spectrum of depressive disorders and for panic or anxiety disorder. And there is nowhere that the authors say these drugs help people,” he added.
Moreover, the investigators’ assertion that long-term use of antidepressants causes harm is incorrect, he said.
“Yes, there are ongoing side effects that impose a burden, but that’s not the same as harm. And while the side effects are sometimes burdensome, ongoing depression is also terribly burdensome,” Dr. Muskin concluded.
Dr. Horowitz, Dr. Wilcock, and Dr. Muskin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When it comes to antidepressant prescribing, less may be more, new research suggests.
A new review suggests antidepressants are overprescribed and that the efficacy of these agents is questionable, leading researchers to recommend that, when physicians prescribe these medications, it should be for shorter periods.
“Antidepressants have never been shown to have a clinically significant difference from placebo in the treatment of depression,” study co\investigator Mark Horowitz, GDPsych, PhD, division of psychiatry, University College London, said in an interview.
He added antidepressants “exert profound adverse effects on the body and brain” and can be difficult to stop because of physical dependence that occurs when the brain adapts to them.
“The best way to take people off these drugs is to do so gradually enough that the unpleasant effects are minimized and in a way that means the reductions in dose get smaller and smaller as the total dose gets lower,” Dr. Horowitz said.
However, at least one expert urged caution in interpreting the review’s findings.
“The reality is that millions of people do benefit from these medications, and this review minimizes those benefits,” Philip Muskin, MD, chief of consultation-liaison for psychiatry and professor of psychiatry, Columbia University Medical Center and New York–Presbyterian Hospital, said when approached for comment.
The findings were published online Dec. 20, 2021, in the Drug and Therapeutics Bulletin.
Personal experience
Prescribing of newer-generation antidepressants, such as SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs), is increasing, with an estimated one in six adults in the United Kingdom receiving at least one prescription in 2019-2020, the investigators noted.
Dr. Horowitz noted a personal motivation for conducting the review. “As well as being an academic psychiatrist, I’m also a patient who has been prescribed antidepressants since age 21, when my mood was poor, due to life circumstances.”
The antidepressant “didn’t have particularly helpful effects,” but Dr. Horowitz continued taking it for 18 years. “I was told it was helpful and internalized that message. I came to understand that much of the information around antidepressants came from the drug companies that manufactured them or from academics paid by these companies.”
Dr. Horowitz is currently discontinuing his medication – a tapering process now in its third year. He said he has come to realize, in retrospect, that symptoms not initially attributed to the drug, such as fatigue, impaired concentration, and impaired memory, have improved since reducing the medication.
“That experience sensitized me to look for these symptoms in my patients and I see them; but most of my patients were told by their doctors that the cause of those problems was the depression or anxiety itself and not the drug,” he said.
Dr. Horowitz collaborated with Michael Wilcock, DTB, Pharmacy, Royal Cornwall Hospitals, NHS Trust, Truro, England, in conducting the review “to provide an independent assessment of benefits and harms of antidepressants.”
“Much of the evidence of the efficacy of antidepressants comes from randomized placebo-controlled trials,” Dr. Horowitz said. Several meta-analyses of these studies showed a difference of about two points between the agent and the placebo on the Hamilton Depression Rating Scale (HAM-D).
“Although this might be statistically significant, it does not meet the threshold for a clinical significance – those aren’t the same thing,” Dr. Horowitz said. Some analyses suggest that a “minimally clinically important difference” on the HAM-D would range from 3 to 6 points.
The findings in adolescents and children are “even less convincing,” the investigators noted, citing a Cochrane review.
“This is especially concerning because the number of children and adolescents being treated with antidepressants is rapidly increasing,” Dr. Horowitz said.
Additionally, the short duration of most trials, typically 6-12 weeks, is “largely uninformative for the clinical treatment of depression.”
Relapse or withdrawal?
The researchers reviewed the adverse effects of long-term antidepressant use, including daytime sleepiness, dry mouth, profuse sweating, weight gain, sexual dysfunction, restlessness, and feeling “foggy or detached.”
“Antidepressants have toxic effects on the brain and cause brain damage when they artificially increase serotonin and modify brain chemistry, which is why people become sick for years after stopping,” Dr. Horowitz said. “When the drug is reduced or stopped, the brain has difficulty dealing with the sudden drop in neurotransmitters, and withdrawal symptoms result, similar to stopping caffeine, nicotine, or opioids.”
He added it is not necessarily the original condition of depression or anxiety that is recurring but rather withdrawal, which can last for months or even years after medication discontinuation.
“Unfortunately, doctors have been taught that there are minimal withdrawal symptoms, euphemized as ‘discontinuation symptoms,’ and so when patients have reported withdrawal symptoms, they have been told it is a return of their underlying condition,” Dr. Horowitz said.
“This has led to many patients being incorrectly told that they need to get back on their antidepressants,” he added.
He likened this approach to “telling people that the need to continue smoking because when they stop, they get more anxiety.” Rather, the “correct response would be that they simply need to taper off the antidepressant more carefully,” he said.
Helpful in the short term
Patients should be informed prior to initiation of antidepressant treatment about the risk of withdrawal effects if they stop the drug, the investigators advise. They reference the Royal College of Psychiatrists’ updated guidance, which recommends slow tapering over a period long enough to mitigate withdrawal symptoms to “tolerable levels.”
The guidance suggests that patients start with a small “test reduction.” Withdrawal symptoms should be monitored for the following 2-4 weeks, using a symptom checklist such as the Discontinuation Emergent Signs and Symptoms Scale, with subsequent reductions based on the tolerability of the process.
Gradual dose reductions and very small final doses may necessitate the use of formulations of medication other than those commonly available in tablet forms, the researchers noted. During the tapering process, patients may benefit from increased psychosocial support.
Dr. Horowitz noted that antidepressants can be helpful on a short-term basis, and likened their use to the use of a cast to stabilize a broken arm.
“It’s useful for a short period. But if you leave someone in a plastic cast permanently, their arm will shrivel and you will disable them. These drugs should be prescribed minimally, and for the shortest possible period of time,” he said.
Dr. Horowitz recommended the recent draft National Institute for Health and Care Excellence depression guidance that recommends multiple other options beyond antidepressants, including cognitive-behavioral therapy, problem solving, counseling, and exercise.
Lack of balance
Dr. Muskin commented that the review is helpful in guiding clinicians on how to approach tapering of antidepressants and making patients aware of discontinuation symptoms.
However, “a lot of people will read this who need treatment, but they won’t get treated because they’ll take away the message that ‘drugs don’t work,’ ” he said.
“As it is, there is already stigma and prejudice toward psychiatric illness and using medications for treatment,” said Dr. Muskin, who was not involved with the research.
The current review “isn’t balanced, in terms of the efficacy of these drugs – both for the spectrum of depressive disorders and for panic or anxiety disorder. And there is nowhere that the authors say these drugs help people,” he added.
Moreover, the investigators’ assertion that long-term use of antidepressants causes harm is incorrect, he said.
“Yes, there are ongoing side effects that impose a burden, but that’s not the same as harm. And while the side effects are sometimes burdensome, ongoing depression is also terribly burdensome,” Dr. Muskin concluded.
Dr. Horowitz, Dr. Wilcock, and Dr. Muskin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When it comes to antidepressant prescribing, less may be more, new research suggests.
A new review suggests antidepressants are overprescribed and that the efficacy of these agents is questionable, leading researchers to recommend that, when physicians prescribe these medications, it should be for shorter periods.
“Antidepressants have never been shown to have a clinically significant difference from placebo in the treatment of depression,” study co\investigator Mark Horowitz, GDPsych, PhD, division of psychiatry, University College London, said in an interview.
He added antidepressants “exert profound adverse effects on the body and brain” and can be difficult to stop because of physical dependence that occurs when the brain adapts to them.
“The best way to take people off these drugs is to do so gradually enough that the unpleasant effects are minimized and in a way that means the reductions in dose get smaller and smaller as the total dose gets lower,” Dr. Horowitz said.
However, at least one expert urged caution in interpreting the review’s findings.
“The reality is that millions of people do benefit from these medications, and this review minimizes those benefits,” Philip Muskin, MD, chief of consultation-liaison for psychiatry and professor of psychiatry, Columbia University Medical Center and New York–Presbyterian Hospital, said when approached for comment.
The findings were published online Dec. 20, 2021, in the Drug and Therapeutics Bulletin.
Personal experience
Prescribing of newer-generation antidepressants, such as SSRIs and serotonin and norepinephrine reuptake inhibitors (SNRIs), is increasing, with an estimated one in six adults in the United Kingdom receiving at least one prescription in 2019-2020, the investigators noted.
Dr. Horowitz noted a personal motivation for conducting the review. “As well as being an academic psychiatrist, I’m also a patient who has been prescribed antidepressants since age 21, when my mood was poor, due to life circumstances.”
The antidepressant “didn’t have particularly helpful effects,” but Dr. Horowitz continued taking it for 18 years. “I was told it was helpful and internalized that message. I came to understand that much of the information around antidepressants came from the drug companies that manufactured them or from academics paid by these companies.”
Dr. Horowitz is currently discontinuing his medication – a tapering process now in its third year. He said he has come to realize, in retrospect, that symptoms not initially attributed to the drug, such as fatigue, impaired concentration, and impaired memory, have improved since reducing the medication.
“That experience sensitized me to look for these symptoms in my patients and I see them; but most of my patients were told by their doctors that the cause of those problems was the depression or anxiety itself and not the drug,” he said.
Dr. Horowitz collaborated with Michael Wilcock, DTB, Pharmacy, Royal Cornwall Hospitals, NHS Trust, Truro, England, in conducting the review “to provide an independent assessment of benefits and harms of antidepressants.”
“Much of the evidence of the efficacy of antidepressants comes from randomized placebo-controlled trials,” Dr. Horowitz said. Several meta-analyses of these studies showed a difference of about two points between the agent and the placebo on the Hamilton Depression Rating Scale (HAM-D).
“Although this might be statistically significant, it does not meet the threshold for a clinical significance – those aren’t the same thing,” Dr. Horowitz said. Some analyses suggest that a “minimally clinically important difference” on the HAM-D would range from 3 to 6 points.
The findings in adolescents and children are “even less convincing,” the investigators noted, citing a Cochrane review.
“This is especially concerning because the number of children and adolescents being treated with antidepressants is rapidly increasing,” Dr. Horowitz said.
Additionally, the short duration of most trials, typically 6-12 weeks, is “largely uninformative for the clinical treatment of depression.”
Relapse or withdrawal?
The researchers reviewed the adverse effects of long-term antidepressant use, including daytime sleepiness, dry mouth, profuse sweating, weight gain, sexual dysfunction, restlessness, and feeling “foggy or detached.”
“Antidepressants have toxic effects on the brain and cause brain damage when they artificially increase serotonin and modify brain chemistry, which is why people become sick for years after stopping,” Dr. Horowitz said. “When the drug is reduced or stopped, the brain has difficulty dealing with the sudden drop in neurotransmitters, and withdrawal symptoms result, similar to stopping caffeine, nicotine, or opioids.”
He added it is not necessarily the original condition of depression or anxiety that is recurring but rather withdrawal, which can last for months or even years after medication discontinuation.
“Unfortunately, doctors have been taught that there are minimal withdrawal symptoms, euphemized as ‘discontinuation symptoms,’ and so when patients have reported withdrawal symptoms, they have been told it is a return of their underlying condition,” Dr. Horowitz said.
“This has led to many patients being incorrectly told that they need to get back on their antidepressants,” he added.
He likened this approach to “telling people that the need to continue smoking because when they stop, they get more anxiety.” Rather, the “correct response would be that they simply need to taper off the antidepressant more carefully,” he said.
Helpful in the short term
Patients should be informed prior to initiation of antidepressant treatment about the risk of withdrawal effects if they stop the drug, the investigators advise. They reference the Royal College of Psychiatrists’ updated guidance, which recommends slow tapering over a period long enough to mitigate withdrawal symptoms to “tolerable levels.”
The guidance suggests that patients start with a small “test reduction.” Withdrawal symptoms should be monitored for the following 2-4 weeks, using a symptom checklist such as the Discontinuation Emergent Signs and Symptoms Scale, with subsequent reductions based on the tolerability of the process.
Gradual dose reductions and very small final doses may necessitate the use of formulations of medication other than those commonly available in tablet forms, the researchers noted. During the tapering process, patients may benefit from increased psychosocial support.
Dr. Horowitz noted that antidepressants can be helpful on a short-term basis, and likened their use to the use of a cast to stabilize a broken arm.
“It’s useful for a short period. But if you leave someone in a plastic cast permanently, their arm will shrivel and you will disable them. These drugs should be prescribed minimally, and for the shortest possible period of time,” he said.
Dr. Horowitz recommended the recent draft National Institute for Health and Care Excellence depression guidance that recommends multiple other options beyond antidepressants, including cognitive-behavioral therapy, problem solving, counseling, and exercise.
Lack of balance
Dr. Muskin commented that the review is helpful in guiding clinicians on how to approach tapering of antidepressants and making patients aware of discontinuation symptoms.
However, “a lot of people will read this who need treatment, but they won’t get treated because they’ll take away the message that ‘drugs don’t work,’ ” he said.
“As it is, there is already stigma and prejudice toward psychiatric illness and using medications for treatment,” said Dr. Muskin, who was not involved with the research.
The current review “isn’t balanced, in terms of the efficacy of these drugs – both for the spectrum of depressive disorders and for panic or anxiety disorder. And there is nowhere that the authors say these drugs help people,” he added.
Moreover, the investigators’ assertion that long-term use of antidepressants causes harm is incorrect, he said.
“Yes, there are ongoing side effects that impose a burden, but that’s not the same as harm. And while the side effects are sometimes burdensome, ongoing depression is also terribly burdensome,” Dr. Muskin concluded.
Dr. Horowitz, Dr. Wilcock, and Dr. Muskin have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE DRUG AND THERAPEUTICS BULLETIN
Ginger for migraine: A new review
in patients who do not want to use or don’t have access to prescription medications, new data suggest.
Conducted by investigators at the National Institute of Mental Health and Neurosciences, Bangalore, India, the review showed ginger root can relieve migraine-related pain, nausea, and vomiting. However, the evidence does not support ginger’s use as a first-line therapy for acute migraine or for migraine prevention.
Study author Chittaranjan Andrade, MD, professor of clinical psychopharmacology and neurotoxicology at the institute, said in an interview that the evidence base is still “too small” to support formal clinical recommendations. However, he added, ginger can be considered as a viable “home-remedy option” for acute migraine.
The review was published online Dec. 2 in The Journal of Clinical Psychiatry.
Potential uses
Used for centuries in traditional medicine, much of the preclinical and clinical research has examined the potential of raw ginger, ginger extracts, and ginger constituents to prevent and treat a wide range of medical conditions. These include nausea and vomiting associated with pregnancy, chemotherapy, postoperative states, motion sickness, and other diseases and disorders, said Dr. Andrade.
Ginger has “long been recommended as an effective home remedy for the acute treatment of migraine, relieving both headache and the associated nausea,” Dr. Andrade noted.
One recommended recipe is stirring half a teaspoon of ground ginger into a glass of water and drinking the “ginger juice,” while another is to drink hot tea made from a teaspoon of freshly ground ginger.
“Patients with a number of common ailments, including migraine, are sometimes caught without medicines; or they may have poor access to medicines,” Dr. Andrade said. “I came across a reference to the use of ginger for migraine in a book on home remedies and I thought that if the research literature supports the use of ginger for migraine episodes, such patients could benefit.”
Large treatment gap
The review and meta-analysis included three randomized controlled trials with 227 patients looking at ginger versus placebo for the treatment.
One of the studies investigated the therapeutic efficacy of a specific proprietary formulation of ginger, combined with feverfew, while two trials were independent of industry.
Of these two, one examined the benefit of add-on dry ginger extract (400 mg; 5% active gingerols) in 50 patients who were also taking ketoprofen to treat migraine episodes, while the other examined the 3-month efficacy of daily dry ginger extract for migraine prophylaxis in 107 patients.
The two studies that examined the therapeutic efficacy of ginger versus placebo showed ginger reduced mean pain scores at 2 hours (mean difference, –1.27 [95% confidence interval, –1.46 to 1,07]) and also increased the proportion of patients who were pain free at 2 hours (RR, 1.79 [1.04 to 3.09]). In addition, compared to placebo, ginger halved the risk of migraine-related nausea and vomiting in all of the studies and was not associated with an increased risk of adverse events.
One RCT investigated prophylactic efficacy and found it to be more effective than placebo in bringing a ≥ 50% reduction in the frequency of monthly migraine episodes (in 42% versus 39% of patients, respectively), but the difference was not deemed statistically significant. In addition, there were no significant differences between the groups in days of pain, severe pain, days requiring use of analgesics, number of migraine episodes, and maximum duration of migraine episodes.
Dr. Andrade noted that ginger has many chemical constituents, including phenolic compounds, terpenes, polysaccharides, lipids, and organic acids of which 6-shogaol, 6-gingerol, and 10-dehydrogingerdione “may be important.”
It also has antioxidant and anti-inflammatory effects, lowering prostaglandins, and reducing several serum lipid and glycemic measures. Additionally, it has “putative” vasculoprotective effects, he added.
“Ginger has a large number of chemical constituents and we do not know which of these, separately or in combination, will help relieve migraine,” he said. “We won’t know the answer unless clinical trials are conducted with the individual constituents rather than with ginger extract.” He compared this to the study of omega-3 fatty acids rather than fish and nuts for various neuropsychiatric or cardiovascular indications.
Nevertheless, given the high global prevalence of migraine and the “large treatment gap [of migraine] in primary care,” it could be common for many affected patients to experience episodes of migraine headache “without recourse to recommended pharmacologic relief,” he noted. “In such cases, the availability of a simple home remedy, such as ginger, could be helpful.”
‘Good additional tool’
Commenting on the study for this news organization, Jessica Ailani, MD, director, MedStar Georgetown Headache Center and professor of clinical neurology, MedStar Georgetown University Hospital, Washington, said that for “people with migraine who are seeking treatment with minimal side effects that they can obtain without counsel of a health care provider, ginger is a good additional tool to have.”
Dr. Ailani, vice cochair of strategic planning in the MedStar department of neurology, who was not involved with the study, said that clinicians can “consider suggesting ginger to patients with migraine that have associated nausea who are interested in nonpharmacologic ways to treat symptoms.”
Since there are “many other effective ways to treat migraine,” she advises “conversing with the patient about speed of onset of efficacy, along with tolerability, and return of migraine symptoms as important factors to evaluate when choosing and staying with a treatment.”
Also commenting on the study for this news organization, Nada Hindiyeh, MD, clinical associate professor, department of neurology, Stanford (Calif.) University, called it a “nice summary of the objective research available for the use of ginger in acute and preventive treatment of migraine.”
Although there is insufficient literature evaluating ginger alone in migraine treatment, so “no definitive conclusions can be drawn,” since it appears to be safe and “somewhat helpful for migraine-associated nausea and vomiting and possibly in frequency of migraine reduction, it remains a considerable alternative for those seeking nonprescription options,” said Dr. Hindiyeh, who was not involved with the study.
Dr. Andrade publishes an e-newsletter supported by Sun Pharmaceuticals, with payments made to charities. He has received payments for developing educational materials for scientific initiatives and programs. Dr. Ailani reports honoraria for independent consulting from various pharmaceutical companies and clinical trial grants to her institution from the American Migraine Foundation, Allergan, Biohaven, Eli Lilly, Satsuma, and Zosano. Dr. Hindiyeh discloses no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in patients who do not want to use or don’t have access to prescription medications, new data suggest.
Conducted by investigators at the National Institute of Mental Health and Neurosciences, Bangalore, India, the review showed ginger root can relieve migraine-related pain, nausea, and vomiting. However, the evidence does not support ginger’s use as a first-line therapy for acute migraine or for migraine prevention.
Study author Chittaranjan Andrade, MD, professor of clinical psychopharmacology and neurotoxicology at the institute, said in an interview that the evidence base is still “too small” to support formal clinical recommendations. However, he added, ginger can be considered as a viable “home-remedy option” for acute migraine.
The review was published online Dec. 2 in The Journal of Clinical Psychiatry.
Potential uses
Used for centuries in traditional medicine, much of the preclinical and clinical research has examined the potential of raw ginger, ginger extracts, and ginger constituents to prevent and treat a wide range of medical conditions. These include nausea and vomiting associated with pregnancy, chemotherapy, postoperative states, motion sickness, and other diseases and disorders, said Dr. Andrade.
Ginger has “long been recommended as an effective home remedy for the acute treatment of migraine, relieving both headache and the associated nausea,” Dr. Andrade noted.
One recommended recipe is stirring half a teaspoon of ground ginger into a glass of water and drinking the “ginger juice,” while another is to drink hot tea made from a teaspoon of freshly ground ginger.
“Patients with a number of common ailments, including migraine, are sometimes caught without medicines; or they may have poor access to medicines,” Dr. Andrade said. “I came across a reference to the use of ginger for migraine in a book on home remedies and I thought that if the research literature supports the use of ginger for migraine episodes, such patients could benefit.”
Large treatment gap
The review and meta-analysis included three randomized controlled trials with 227 patients looking at ginger versus placebo for the treatment.
One of the studies investigated the therapeutic efficacy of a specific proprietary formulation of ginger, combined with feverfew, while two trials were independent of industry.
Of these two, one examined the benefit of add-on dry ginger extract (400 mg; 5% active gingerols) in 50 patients who were also taking ketoprofen to treat migraine episodes, while the other examined the 3-month efficacy of daily dry ginger extract for migraine prophylaxis in 107 patients.
The two studies that examined the therapeutic efficacy of ginger versus placebo showed ginger reduced mean pain scores at 2 hours (mean difference, –1.27 [95% confidence interval, –1.46 to 1,07]) and also increased the proportion of patients who were pain free at 2 hours (RR, 1.79 [1.04 to 3.09]). In addition, compared to placebo, ginger halved the risk of migraine-related nausea and vomiting in all of the studies and was not associated with an increased risk of adverse events.
One RCT investigated prophylactic efficacy and found it to be more effective than placebo in bringing a ≥ 50% reduction in the frequency of monthly migraine episodes (in 42% versus 39% of patients, respectively), but the difference was not deemed statistically significant. In addition, there were no significant differences between the groups in days of pain, severe pain, days requiring use of analgesics, number of migraine episodes, and maximum duration of migraine episodes.
Dr. Andrade noted that ginger has many chemical constituents, including phenolic compounds, terpenes, polysaccharides, lipids, and organic acids of which 6-shogaol, 6-gingerol, and 10-dehydrogingerdione “may be important.”
It also has antioxidant and anti-inflammatory effects, lowering prostaglandins, and reducing several serum lipid and glycemic measures. Additionally, it has “putative” vasculoprotective effects, he added.
“Ginger has a large number of chemical constituents and we do not know which of these, separately or in combination, will help relieve migraine,” he said. “We won’t know the answer unless clinical trials are conducted with the individual constituents rather than with ginger extract.” He compared this to the study of omega-3 fatty acids rather than fish and nuts for various neuropsychiatric or cardiovascular indications.
Nevertheless, given the high global prevalence of migraine and the “large treatment gap [of migraine] in primary care,” it could be common for many affected patients to experience episodes of migraine headache “without recourse to recommended pharmacologic relief,” he noted. “In such cases, the availability of a simple home remedy, such as ginger, could be helpful.”
‘Good additional tool’
Commenting on the study for this news organization, Jessica Ailani, MD, director, MedStar Georgetown Headache Center and professor of clinical neurology, MedStar Georgetown University Hospital, Washington, said that for “people with migraine who are seeking treatment with minimal side effects that they can obtain without counsel of a health care provider, ginger is a good additional tool to have.”
Dr. Ailani, vice cochair of strategic planning in the MedStar department of neurology, who was not involved with the study, said that clinicians can “consider suggesting ginger to patients with migraine that have associated nausea who are interested in nonpharmacologic ways to treat symptoms.”
Since there are “many other effective ways to treat migraine,” she advises “conversing with the patient about speed of onset of efficacy, along with tolerability, and return of migraine symptoms as important factors to evaluate when choosing and staying with a treatment.”
Also commenting on the study for this news organization, Nada Hindiyeh, MD, clinical associate professor, department of neurology, Stanford (Calif.) University, called it a “nice summary of the objective research available for the use of ginger in acute and preventive treatment of migraine.”
Although there is insufficient literature evaluating ginger alone in migraine treatment, so “no definitive conclusions can be drawn,” since it appears to be safe and “somewhat helpful for migraine-associated nausea and vomiting and possibly in frequency of migraine reduction, it remains a considerable alternative for those seeking nonprescription options,” said Dr. Hindiyeh, who was not involved with the study.
Dr. Andrade publishes an e-newsletter supported by Sun Pharmaceuticals, with payments made to charities. He has received payments for developing educational materials for scientific initiatives and programs. Dr. Ailani reports honoraria for independent consulting from various pharmaceutical companies and clinical trial grants to her institution from the American Migraine Foundation, Allergan, Biohaven, Eli Lilly, Satsuma, and Zosano. Dr. Hindiyeh discloses no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in patients who do not want to use or don’t have access to prescription medications, new data suggest.
Conducted by investigators at the National Institute of Mental Health and Neurosciences, Bangalore, India, the review showed ginger root can relieve migraine-related pain, nausea, and vomiting. However, the evidence does not support ginger’s use as a first-line therapy for acute migraine or for migraine prevention.
Study author Chittaranjan Andrade, MD, professor of clinical psychopharmacology and neurotoxicology at the institute, said in an interview that the evidence base is still “too small” to support formal clinical recommendations. However, he added, ginger can be considered as a viable “home-remedy option” for acute migraine.
The review was published online Dec. 2 in The Journal of Clinical Psychiatry.
Potential uses
Used for centuries in traditional medicine, much of the preclinical and clinical research has examined the potential of raw ginger, ginger extracts, and ginger constituents to prevent and treat a wide range of medical conditions. These include nausea and vomiting associated with pregnancy, chemotherapy, postoperative states, motion sickness, and other diseases and disorders, said Dr. Andrade.
Ginger has “long been recommended as an effective home remedy for the acute treatment of migraine, relieving both headache and the associated nausea,” Dr. Andrade noted.
One recommended recipe is stirring half a teaspoon of ground ginger into a glass of water and drinking the “ginger juice,” while another is to drink hot tea made from a teaspoon of freshly ground ginger.
“Patients with a number of common ailments, including migraine, are sometimes caught without medicines; or they may have poor access to medicines,” Dr. Andrade said. “I came across a reference to the use of ginger for migraine in a book on home remedies and I thought that if the research literature supports the use of ginger for migraine episodes, such patients could benefit.”
Large treatment gap
The review and meta-analysis included three randomized controlled trials with 227 patients looking at ginger versus placebo for the treatment.
One of the studies investigated the therapeutic efficacy of a specific proprietary formulation of ginger, combined with feverfew, while two trials were independent of industry.
Of these two, one examined the benefit of add-on dry ginger extract (400 mg; 5% active gingerols) in 50 patients who were also taking ketoprofen to treat migraine episodes, while the other examined the 3-month efficacy of daily dry ginger extract for migraine prophylaxis in 107 patients.
The two studies that examined the therapeutic efficacy of ginger versus placebo showed ginger reduced mean pain scores at 2 hours (mean difference, –1.27 [95% confidence interval, –1.46 to 1,07]) and also increased the proportion of patients who were pain free at 2 hours (RR, 1.79 [1.04 to 3.09]). In addition, compared to placebo, ginger halved the risk of migraine-related nausea and vomiting in all of the studies and was not associated with an increased risk of adverse events.
One RCT investigated prophylactic efficacy and found it to be more effective than placebo in bringing a ≥ 50% reduction in the frequency of monthly migraine episodes (in 42% versus 39% of patients, respectively), but the difference was not deemed statistically significant. In addition, there were no significant differences between the groups in days of pain, severe pain, days requiring use of analgesics, number of migraine episodes, and maximum duration of migraine episodes.
Dr. Andrade noted that ginger has many chemical constituents, including phenolic compounds, terpenes, polysaccharides, lipids, and organic acids of which 6-shogaol, 6-gingerol, and 10-dehydrogingerdione “may be important.”
It also has antioxidant and anti-inflammatory effects, lowering prostaglandins, and reducing several serum lipid and glycemic measures. Additionally, it has “putative” vasculoprotective effects, he added.
“Ginger has a large number of chemical constituents and we do not know which of these, separately or in combination, will help relieve migraine,” he said. “We won’t know the answer unless clinical trials are conducted with the individual constituents rather than with ginger extract.” He compared this to the study of omega-3 fatty acids rather than fish and nuts for various neuropsychiatric or cardiovascular indications.
Nevertheless, given the high global prevalence of migraine and the “large treatment gap [of migraine] in primary care,” it could be common for many affected patients to experience episodes of migraine headache “without recourse to recommended pharmacologic relief,” he noted. “In such cases, the availability of a simple home remedy, such as ginger, could be helpful.”
‘Good additional tool’
Commenting on the study for this news organization, Jessica Ailani, MD, director, MedStar Georgetown Headache Center and professor of clinical neurology, MedStar Georgetown University Hospital, Washington, said that for “people with migraine who are seeking treatment with minimal side effects that they can obtain without counsel of a health care provider, ginger is a good additional tool to have.”
Dr. Ailani, vice cochair of strategic planning in the MedStar department of neurology, who was not involved with the study, said that clinicians can “consider suggesting ginger to patients with migraine that have associated nausea who are interested in nonpharmacologic ways to treat symptoms.”
Since there are “many other effective ways to treat migraine,” she advises “conversing with the patient about speed of onset of efficacy, along with tolerability, and return of migraine symptoms as important factors to evaluate when choosing and staying with a treatment.”
Also commenting on the study for this news organization, Nada Hindiyeh, MD, clinical associate professor, department of neurology, Stanford (Calif.) University, called it a “nice summary of the objective research available for the use of ginger in acute and preventive treatment of migraine.”
Although there is insufficient literature evaluating ginger alone in migraine treatment, so “no definitive conclusions can be drawn,” since it appears to be safe and “somewhat helpful for migraine-associated nausea and vomiting and possibly in frequency of migraine reduction, it remains a considerable alternative for those seeking nonprescription options,” said Dr. Hindiyeh, who was not involved with the study.
Dr. Andrade publishes an e-newsletter supported by Sun Pharmaceuticals, with payments made to charities. He has received payments for developing educational materials for scientific initiatives and programs. Dr. Ailani reports honoraria for independent consulting from various pharmaceutical companies and clinical trial grants to her institution from the American Migraine Foundation, Allergan, Biohaven, Eli Lilly, Satsuma, and Zosano. Dr. Hindiyeh discloses no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL PSYCHIATRY
Hypertension may double the risk of late-onset epilepsy
new research suggests.
After excluding individuals with normal blood pressure who were taking antihypertensive medication, investigators found hypertension was linked to an almost 2.5-fold higher risk of epilepsy.
“Our findings further expand upon our knowledge of the negative effects hypertension has on brain health and, regarding epilepsy, that effect may be starting even in midlife,” said co–lead author Maria Stefanidou, MD, MSc, of Boston University.
“Practicing clinicians should be vigilant to diagnose hypertension, discuss with patients all potential long-term brain health outcomes, and need for treatment. Furthermore, in those presenting with new-onset epilepsy later in life, screening for potentially undiagnosed hypertension should be included in the initial workup,” she said.
The study was published online Nov. 17, 2021, in Epilepsia.
Unknown etiology
“New-onset epilepsy risk increases with increasing age over the age of 65 and can affect 15-20 per 1,000 older individuals. Although the most common causes for seizures in this age group are prior history of stroke and presence of dementia, for about 30%-40% of patients, the etiology of seizures remains unknown,” Dr. Stefanidou said.
“We wanted to study if modifiable vascular risk factors that are known to contribute both to vascular brain aging and to neurodegeneration may directly predict the development of epilepsy, even in the absence of clinical stroke or dementia,” she added.
To investigate, the researchers turned to data from participants in the Offspring Cohort of the Framingham Health Study (FHS). The original FHS was an ongoing longitudinal community-based study that first began in 1948. Offspring of the original cohort and their spouses (n = 5,124) were enrolled in the Offspring Cohort in 1971, with surveillance of these second-generation participants based on exam visits occurring every 4 years.
The study included participants who had attended exam 5 (1991-1995), were age 45 years or older, had available vascular risk factor (VRF) data, and available follow-up data on epilepsy status (n = 2,986; mean age, 58 years; 48% male).
The investigators conducted two statistical analyses. In the primary model, they adjusted for age and gender, while in a secondary model they also adjusted for prevalent and interim stroke. They also conducted an analysis that excluded participants treated with antihypertensive medication and had normal blood pressure.
Plausible mechanisms
During a mean follow-up of 19.2 years, 55 incident epilepsy cases were identified. The mean age of these patients was 73.8 years.
In the primary model, hypertension was associated with an almost twofold higher risk of developing epilepsy (hazard ratio, 1.97; 95% confidence interval, 1.13-3.45; P = .017).
Interestingly, the Framingham Stroke Risk Profile – a calculation based on an array of factors, including age/sex, systolic blood pressure, antihypertensive therapy, diabetes, history of cardiovascular disease, atrial fibrillation, and cigarette smoking – was not associated with incident epilepsy, and there was no other significant associated between any of the other VRFs when looked at independently.
When the researchers adjusted for prevalent and interim stroke, they continued to find an almost twofold higher risk of developing epilepsy (HR 1.93; 95% CI, 1.10-3.37; P = .022). An analysis that adjusted for competing risk of death obtained similar findings (HR, 1.98; 95% CI, 1.03-3.81; P = .042).
The model that excluded patients receiving antihypertensive treatment, whose blood pressure readings were normal (n = 2,162; 50 incident epilepsy cases) showed an even stronger association (HR, 2.44; 95% CI, 1.36-4.35; P = .003).
“Our results are based on an epidemiological, observational study, therefore our findings point to an association between hypertension and new-onset epilepsy later in life,” said Dr. Stefanidou.
She noted that because it was an observational study, “a cause-effect relationship cannot be established based on these results, but there is growing evidence from our, as well as other, similar cohorts that hypertension, a modifiable vascular risk factor, may indeed be an independent predictor of late-onset epilepsy.”
There are “plausible mechanisms” that support both a direct, and indirect, role of hypertension – for example, through accumulation of small vessel disease in the brain – but further research will be necessary to elucidate the exact mechanisms involved in the process,” she added.
‘Welcome addition’
In a joint comment, Hedley C.A. Emsley, PhD, professor of clinical neuroscience, Lancaster (England) University, and Jasmine Wall, MBBChir, academic clinical fellow in neurology, Lancaster University, described the study as a “welcome addition to this field,” noting that the Framingham Heart Study “lends itself well to an embedded observational study of this nature of late-onset epilepsy.”
Dr. Emsley and Dr. Wall, who were not involved in the research, said that the “apparent magnitude of increased late-onset epilepsy risk association with hypertension in the Stefanidou et al study is quite striking,” even allowing for the “relatively small sample size,” since their analysis and findings appear to “withstand exclusion of individuals who became normotensive on antihypertensive treatment.”
They noted that in recent years there has been a growing body of evidence highlighting the importance of hypertension in late-onset epilepsy epileptogenesis with subclinical cerebrovascular diseases, including “otherwise occult cerebral small vessel disease believed to be a frequent cause.”
The mechanisms “remain unclear,” but they could potentially include diffuse cerebral microangiopathy, structural and physiological changes, and/or blood-brain barrier dysfunction and leakage, they suggested.
“Although there is no current consensus over an age threshold that defines ‘late onset,’ we would argue that age thresholds used in such studies of late-onset epilepsy should be lower, to avoid missing younger adults at risk through vascular mechanisms,” Dr. Emsley and Dr. Wall added.
The study authors suggest that “potential pathophysiologic mechanisms can further be explored in future experimental studies and clinical trials.”
This study was funded by grants from the National Institutes of Health and Finding a Cure for Epilepsy/Seizures. Dr. Stefanidou disclosed relevant financial relationships. Dr. Emsley and Dr. Wall disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
After excluding individuals with normal blood pressure who were taking antihypertensive medication, investigators found hypertension was linked to an almost 2.5-fold higher risk of epilepsy.
“Our findings further expand upon our knowledge of the negative effects hypertension has on brain health and, regarding epilepsy, that effect may be starting even in midlife,” said co–lead author Maria Stefanidou, MD, MSc, of Boston University.
“Practicing clinicians should be vigilant to diagnose hypertension, discuss with patients all potential long-term brain health outcomes, and need for treatment. Furthermore, in those presenting with new-onset epilepsy later in life, screening for potentially undiagnosed hypertension should be included in the initial workup,” she said.
The study was published online Nov. 17, 2021, in Epilepsia.
Unknown etiology
“New-onset epilepsy risk increases with increasing age over the age of 65 and can affect 15-20 per 1,000 older individuals. Although the most common causes for seizures in this age group are prior history of stroke and presence of dementia, for about 30%-40% of patients, the etiology of seizures remains unknown,” Dr. Stefanidou said.
“We wanted to study if modifiable vascular risk factors that are known to contribute both to vascular brain aging and to neurodegeneration may directly predict the development of epilepsy, even in the absence of clinical stroke or dementia,” she added.
To investigate, the researchers turned to data from participants in the Offspring Cohort of the Framingham Health Study (FHS). The original FHS was an ongoing longitudinal community-based study that first began in 1948. Offspring of the original cohort and their spouses (n = 5,124) were enrolled in the Offspring Cohort in 1971, with surveillance of these second-generation participants based on exam visits occurring every 4 years.
The study included participants who had attended exam 5 (1991-1995), were age 45 years or older, had available vascular risk factor (VRF) data, and available follow-up data on epilepsy status (n = 2,986; mean age, 58 years; 48% male).
The investigators conducted two statistical analyses. In the primary model, they adjusted for age and gender, while in a secondary model they also adjusted for prevalent and interim stroke. They also conducted an analysis that excluded participants treated with antihypertensive medication and had normal blood pressure.
Plausible mechanisms
During a mean follow-up of 19.2 years, 55 incident epilepsy cases were identified. The mean age of these patients was 73.8 years.
In the primary model, hypertension was associated with an almost twofold higher risk of developing epilepsy (hazard ratio, 1.97; 95% confidence interval, 1.13-3.45; P = .017).
Interestingly, the Framingham Stroke Risk Profile – a calculation based on an array of factors, including age/sex, systolic blood pressure, antihypertensive therapy, diabetes, history of cardiovascular disease, atrial fibrillation, and cigarette smoking – was not associated with incident epilepsy, and there was no other significant associated between any of the other VRFs when looked at independently.
When the researchers adjusted for prevalent and interim stroke, they continued to find an almost twofold higher risk of developing epilepsy (HR 1.93; 95% CI, 1.10-3.37; P = .022). An analysis that adjusted for competing risk of death obtained similar findings (HR, 1.98; 95% CI, 1.03-3.81; P = .042).
The model that excluded patients receiving antihypertensive treatment, whose blood pressure readings were normal (n = 2,162; 50 incident epilepsy cases) showed an even stronger association (HR, 2.44; 95% CI, 1.36-4.35; P = .003).
“Our results are based on an epidemiological, observational study, therefore our findings point to an association between hypertension and new-onset epilepsy later in life,” said Dr. Stefanidou.
She noted that because it was an observational study, “a cause-effect relationship cannot be established based on these results, but there is growing evidence from our, as well as other, similar cohorts that hypertension, a modifiable vascular risk factor, may indeed be an independent predictor of late-onset epilepsy.”
There are “plausible mechanisms” that support both a direct, and indirect, role of hypertension – for example, through accumulation of small vessel disease in the brain – but further research will be necessary to elucidate the exact mechanisms involved in the process,” she added.
‘Welcome addition’
In a joint comment, Hedley C.A. Emsley, PhD, professor of clinical neuroscience, Lancaster (England) University, and Jasmine Wall, MBBChir, academic clinical fellow in neurology, Lancaster University, described the study as a “welcome addition to this field,” noting that the Framingham Heart Study “lends itself well to an embedded observational study of this nature of late-onset epilepsy.”
Dr. Emsley and Dr. Wall, who were not involved in the research, said that the “apparent magnitude of increased late-onset epilepsy risk association with hypertension in the Stefanidou et al study is quite striking,” even allowing for the “relatively small sample size,” since their analysis and findings appear to “withstand exclusion of individuals who became normotensive on antihypertensive treatment.”
They noted that in recent years there has been a growing body of evidence highlighting the importance of hypertension in late-onset epilepsy epileptogenesis with subclinical cerebrovascular diseases, including “otherwise occult cerebral small vessel disease believed to be a frequent cause.”
The mechanisms “remain unclear,” but they could potentially include diffuse cerebral microangiopathy, structural and physiological changes, and/or blood-brain barrier dysfunction and leakage, they suggested.
“Although there is no current consensus over an age threshold that defines ‘late onset,’ we would argue that age thresholds used in such studies of late-onset epilepsy should be lower, to avoid missing younger adults at risk through vascular mechanisms,” Dr. Emsley and Dr. Wall added.
The study authors suggest that “potential pathophysiologic mechanisms can further be explored in future experimental studies and clinical trials.”
This study was funded by grants from the National Institutes of Health and Finding a Cure for Epilepsy/Seizures. Dr. Stefanidou disclosed relevant financial relationships. Dr. Emsley and Dr. Wall disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
After excluding individuals with normal blood pressure who were taking antihypertensive medication, investigators found hypertension was linked to an almost 2.5-fold higher risk of epilepsy.
“Our findings further expand upon our knowledge of the negative effects hypertension has on brain health and, regarding epilepsy, that effect may be starting even in midlife,” said co–lead author Maria Stefanidou, MD, MSc, of Boston University.
“Practicing clinicians should be vigilant to diagnose hypertension, discuss with patients all potential long-term brain health outcomes, and need for treatment. Furthermore, in those presenting with new-onset epilepsy later in life, screening for potentially undiagnosed hypertension should be included in the initial workup,” she said.
The study was published online Nov. 17, 2021, in Epilepsia.
Unknown etiology
“New-onset epilepsy risk increases with increasing age over the age of 65 and can affect 15-20 per 1,000 older individuals. Although the most common causes for seizures in this age group are prior history of stroke and presence of dementia, for about 30%-40% of patients, the etiology of seizures remains unknown,” Dr. Stefanidou said.
“We wanted to study if modifiable vascular risk factors that are known to contribute both to vascular brain aging and to neurodegeneration may directly predict the development of epilepsy, even in the absence of clinical stroke or dementia,” she added.
To investigate, the researchers turned to data from participants in the Offspring Cohort of the Framingham Health Study (FHS). The original FHS was an ongoing longitudinal community-based study that first began in 1948. Offspring of the original cohort and their spouses (n = 5,124) were enrolled in the Offspring Cohort in 1971, with surveillance of these second-generation participants based on exam visits occurring every 4 years.
The study included participants who had attended exam 5 (1991-1995), were age 45 years or older, had available vascular risk factor (VRF) data, and available follow-up data on epilepsy status (n = 2,986; mean age, 58 years; 48% male).
The investigators conducted two statistical analyses. In the primary model, they adjusted for age and gender, while in a secondary model they also adjusted for prevalent and interim stroke. They also conducted an analysis that excluded participants treated with antihypertensive medication and had normal blood pressure.
Plausible mechanisms
During a mean follow-up of 19.2 years, 55 incident epilepsy cases were identified. The mean age of these patients was 73.8 years.
In the primary model, hypertension was associated with an almost twofold higher risk of developing epilepsy (hazard ratio, 1.97; 95% confidence interval, 1.13-3.45; P = .017).
Interestingly, the Framingham Stroke Risk Profile – a calculation based on an array of factors, including age/sex, systolic blood pressure, antihypertensive therapy, diabetes, history of cardiovascular disease, atrial fibrillation, and cigarette smoking – was not associated with incident epilepsy, and there was no other significant associated between any of the other VRFs when looked at independently.
When the researchers adjusted for prevalent and interim stroke, they continued to find an almost twofold higher risk of developing epilepsy (HR 1.93; 95% CI, 1.10-3.37; P = .022). An analysis that adjusted for competing risk of death obtained similar findings (HR, 1.98; 95% CI, 1.03-3.81; P = .042).
The model that excluded patients receiving antihypertensive treatment, whose blood pressure readings were normal (n = 2,162; 50 incident epilepsy cases) showed an even stronger association (HR, 2.44; 95% CI, 1.36-4.35; P = .003).
“Our results are based on an epidemiological, observational study, therefore our findings point to an association between hypertension and new-onset epilepsy later in life,” said Dr. Stefanidou.
She noted that because it was an observational study, “a cause-effect relationship cannot be established based on these results, but there is growing evidence from our, as well as other, similar cohorts that hypertension, a modifiable vascular risk factor, may indeed be an independent predictor of late-onset epilepsy.”
There are “plausible mechanisms” that support both a direct, and indirect, role of hypertension – for example, through accumulation of small vessel disease in the brain – but further research will be necessary to elucidate the exact mechanisms involved in the process,” she added.
‘Welcome addition’
In a joint comment, Hedley C.A. Emsley, PhD, professor of clinical neuroscience, Lancaster (England) University, and Jasmine Wall, MBBChir, academic clinical fellow in neurology, Lancaster University, described the study as a “welcome addition to this field,” noting that the Framingham Heart Study “lends itself well to an embedded observational study of this nature of late-onset epilepsy.”
Dr. Emsley and Dr. Wall, who were not involved in the research, said that the “apparent magnitude of increased late-onset epilepsy risk association with hypertension in the Stefanidou et al study is quite striking,” even allowing for the “relatively small sample size,” since their analysis and findings appear to “withstand exclusion of individuals who became normotensive on antihypertensive treatment.”
They noted that in recent years there has been a growing body of evidence highlighting the importance of hypertension in late-onset epilepsy epileptogenesis with subclinical cerebrovascular diseases, including “otherwise occult cerebral small vessel disease believed to be a frequent cause.”
The mechanisms “remain unclear,” but they could potentially include diffuse cerebral microangiopathy, structural and physiological changes, and/or blood-brain barrier dysfunction and leakage, they suggested.
“Although there is no current consensus over an age threshold that defines ‘late onset,’ we would argue that age thresholds used in such studies of late-onset epilepsy should be lower, to avoid missing younger adults at risk through vascular mechanisms,” Dr. Emsley and Dr. Wall added.
The study authors suggest that “potential pathophysiologic mechanisms can further be explored in future experimental studies and clinical trials.”
This study was funded by grants from the National Institutes of Health and Finding a Cure for Epilepsy/Seizures. Dr. Stefanidou disclosed relevant financial relationships. Dr. Emsley and Dr. Wall disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM EPILEPSIA
Telehealth safe, effective for a challenging psychiatric disorder
Telehealth is safe and effective for the treatment of borderline personality disorder (BPD) and may even have an edge over in-person treatment, new research suggests.
Investigators compared BPD outcomes with therapy delivered in person and via telemedicine and found comparable reductions in depression, anxiety, and anger symptoms as well as improved overall well-being and mental health.
The results also suggest a telehealth advantage with significantly better patient attendance vs. patients treated in-person.
“We found a large effect size of treatment in both groups, as well as comparable levels of satisfaction with treatment, symptom reduction, and improved functioning, coping ability, positive mental health, and general well-being,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., said in an interview.
The study was published online Nov. 8 in the Journal of Personality Disorders.
‘No other option’
Most previous research investigating telehealth has occurred in outpatient, individual treatment settings and has not examined telehealth-delivered group therapy or partial hospitalization, the authors noted.
“Until the pandemic, we were delivering care in person, but when the pandemic began, because of public safety recommendations, we knew that we could no longer continue doing so,” said Dr. Zimmerman, director of the outpatient division at the partial hospital program (PHP), Rhode Island Hospital.
“In switching to a telehealth platform, we were concerned about patient safety and acceptability of delivering care in that manner, especially with patients with BPD, which is associated with impulsive behavior, self-harm, and suicidal behavior, among other problems,” he said. However “we had no other option” than to utilize a telehealth delivery mode, since the alternative was to shut down the program.
The investigators were “interested in whether or not virtual treatment in an acute intensive setting, such as a PHP, would be as safe, acceptable, and effective as in-person treatment.”
The study was part of the ongoing work of the Rhode Island Methods to Improve Diagnostic Assessment and Services.
Additional safety measures
Treatment, consisting of an Acceptance and Commitment Therapy (ACT) treatment model – including intake assessments, individual therapy, psychiatric visits, and group therapy – was delivered by a multidisciplinary team via Zoom.
Dr. Zimmerman noted that the team implemented additional safety precautions, including having patients check in at the beginning of each day to indicate their location, not seeing patients who were out of state, and making sure all patients had a contact person.
In addition, beyond the therapist leading the group, another therapist was always available, overseeing groups and meeting one-on-one (virtually) with participants if they had been triggered by the group process and were highly distressed.
Patients were asked to complete a number of questionnaires, including the Clinically Useful Patient Satisfaction Scale (CUPSS) at the end of their intake session. The primary outcome measure was the Remission from Depression Questionnaire (RDQ-M).
The study was conducted between May 1 and Dec. 15 of 2020 and included 64 patients with BPD who were treated for the first time in the Rhode Island Hospital PHP. They were compared to 117 patients who participated in the in-person program during the same months in 2019.
Participant characteristics were similar – for example, three-quarters of the participants in both groups were female, and the mean age was 34 years.
‘Sea change’
Most patients in the telehealth and in-person groups reported being “very” or “extremely” satisfied with the initial evaluation (90% vs. 85.3%, c2 = 0.74) and were hopeful that they would get better (85.8% vs. 82.1%, c2 = 0.45).
(c2 = 4.62), and “under both telehealth and in-person treatment conditions, the patients significantly improved from admission to discharge on each of the RDQ-M subscales, with large effect sizes found for most of the subscales,” the authors reported.
There were significant differences between the groups in the average number of days of attendance and number of days missed.
A nonsignificantly higher proportion of patients completed the telehealth program, vs. the in-person program (68.8% vs. 59%, c2 = 1.69).
In both programs, transfer to inpatient care and dissatisfaction-related withdrawal from the program were low (both < 2%). Notably, no patients attempted or completed suicide during treatment.
Virtual treatment is more convenient than in-person treatment, Dr. Zimmerman noted. “Some patients – generally those with medical or transportation issues – told us they otherwise would not have been able to participate [in the program] if treatment had been in person.”
He added, “My prediction is that 5 years from now, two-thirds to three-quarters of outpatient visits will be virtual because that is what the patients prefer – and although there will certainly be individuals who prefer in-person care, I think we’ve witnessed a sea change in how behavioral health care will be delivered.”
‘Game changer’
In an interview, Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and a senior fellow at the Personality Disorders Institute, Weill Cornell Medical College, New York, said the study has “a lot of valuable detail about how to set up a virtual PHP, which could guide any group wanting to try this.”
Dr. Carsky, who was not involved with the study, called it “a very important contribution to the research literature on efficacious treatment of BPD,” although it is not a randomized controlled trial.
“Adding more individual attention to the virtual group (e.g., having a co-host in the groups) seems as though it may be an important factor in dealing with the limitations of virtual treatment,” she noted.
However, she continued, “a limitation is that outcome assessment relied on self-administered questionnaires and did not include clinician rating scales, so the response may have been subject to the effects of social desirability bias.”
Donald W. Black, MD, associate chief of staff for mental health at the Iowa City Veterans Administration Hospital, said in an interview that the pandemic has been a “game changer, as we have had to quickly adapt mental health programs to a virtual format.
“For the most part, they have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,” said Dr. Black, who was not associated with the research.
No study funding was listed. The study authors, Dr. Carsky, and Dr. Black have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Telehealth is safe and effective for the treatment of borderline personality disorder (BPD) and may even have an edge over in-person treatment, new research suggests.
Investigators compared BPD outcomes with therapy delivered in person and via telemedicine and found comparable reductions in depression, anxiety, and anger symptoms as well as improved overall well-being and mental health.
The results also suggest a telehealth advantage with significantly better patient attendance vs. patients treated in-person.
“We found a large effect size of treatment in both groups, as well as comparable levels of satisfaction with treatment, symptom reduction, and improved functioning, coping ability, positive mental health, and general well-being,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., said in an interview.
The study was published online Nov. 8 in the Journal of Personality Disorders.
‘No other option’
Most previous research investigating telehealth has occurred in outpatient, individual treatment settings and has not examined telehealth-delivered group therapy or partial hospitalization, the authors noted.
“Until the pandemic, we were delivering care in person, but when the pandemic began, because of public safety recommendations, we knew that we could no longer continue doing so,” said Dr. Zimmerman, director of the outpatient division at the partial hospital program (PHP), Rhode Island Hospital.
“In switching to a telehealth platform, we were concerned about patient safety and acceptability of delivering care in that manner, especially with patients with BPD, which is associated with impulsive behavior, self-harm, and suicidal behavior, among other problems,” he said. However “we had no other option” than to utilize a telehealth delivery mode, since the alternative was to shut down the program.
The investigators were “interested in whether or not virtual treatment in an acute intensive setting, such as a PHP, would be as safe, acceptable, and effective as in-person treatment.”
The study was part of the ongoing work of the Rhode Island Methods to Improve Diagnostic Assessment and Services.
Additional safety measures
Treatment, consisting of an Acceptance and Commitment Therapy (ACT) treatment model – including intake assessments, individual therapy, psychiatric visits, and group therapy – was delivered by a multidisciplinary team via Zoom.
Dr. Zimmerman noted that the team implemented additional safety precautions, including having patients check in at the beginning of each day to indicate their location, not seeing patients who were out of state, and making sure all patients had a contact person.
In addition, beyond the therapist leading the group, another therapist was always available, overseeing groups and meeting one-on-one (virtually) with participants if they had been triggered by the group process and were highly distressed.
Patients were asked to complete a number of questionnaires, including the Clinically Useful Patient Satisfaction Scale (CUPSS) at the end of their intake session. The primary outcome measure was the Remission from Depression Questionnaire (RDQ-M).
The study was conducted between May 1 and Dec. 15 of 2020 and included 64 patients with BPD who were treated for the first time in the Rhode Island Hospital PHP. They were compared to 117 patients who participated in the in-person program during the same months in 2019.
Participant characteristics were similar – for example, three-quarters of the participants in both groups were female, and the mean age was 34 years.
‘Sea change’
Most patients in the telehealth and in-person groups reported being “very” or “extremely” satisfied with the initial evaluation (90% vs. 85.3%, c2 = 0.74) and were hopeful that they would get better (85.8% vs. 82.1%, c2 = 0.45).
(c2 = 4.62), and “under both telehealth and in-person treatment conditions, the patients significantly improved from admission to discharge on each of the RDQ-M subscales, with large effect sizes found for most of the subscales,” the authors reported.
There were significant differences between the groups in the average number of days of attendance and number of days missed.
A nonsignificantly higher proportion of patients completed the telehealth program, vs. the in-person program (68.8% vs. 59%, c2 = 1.69).
In both programs, transfer to inpatient care and dissatisfaction-related withdrawal from the program were low (both < 2%). Notably, no patients attempted or completed suicide during treatment.
Virtual treatment is more convenient than in-person treatment, Dr. Zimmerman noted. “Some patients – generally those with medical or transportation issues – told us they otherwise would not have been able to participate [in the program] if treatment had been in person.”
He added, “My prediction is that 5 years from now, two-thirds to three-quarters of outpatient visits will be virtual because that is what the patients prefer – and although there will certainly be individuals who prefer in-person care, I think we’ve witnessed a sea change in how behavioral health care will be delivered.”
‘Game changer’
In an interview, Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and a senior fellow at the Personality Disorders Institute, Weill Cornell Medical College, New York, said the study has “a lot of valuable detail about how to set up a virtual PHP, which could guide any group wanting to try this.”
Dr. Carsky, who was not involved with the study, called it “a very important contribution to the research literature on efficacious treatment of BPD,” although it is not a randomized controlled trial.
“Adding more individual attention to the virtual group (e.g., having a co-host in the groups) seems as though it may be an important factor in dealing with the limitations of virtual treatment,” she noted.
However, she continued, “a limitation is that outcome assessment relied on self-administered questionnaires and did not include clinician rating scales, so the response may have been subject to the effects of social desirability bias.”
Donald W. Black, MD, associate chief of staff for mental health at the Iowa City Veterans Administration Hospital, said in an interview that the pandemic has been a “game changer, as we have had to quickly adapt mental health programs to a virtual format.
“For the most part, they have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,” said Dr. Black, who was not associated with the research.
No study funding was listed. The study authors, Dr. Carsky, and Dr. Black have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Telehealth is safe and effective for the treatment of borderline personality disorder (BPD) and may even have an edge over in-person treatment, new research suggests.
Investigators compared BPD outcomes with therapy delivered in person and via telemedicine and found comparable reductions in depression, anxiety, and anger symptoms as well as improved overall well-being and mental health.
The results also suggest a telehealth advantage with significantly better patient attendance vs. patients treated in-person.
“We found a large effect size of treatment in both groups, as well as comparable levels of satisfaction with treatment, symptom reduction, and improved functioning, coping ability, positive mental health, and general well-being,” study investigator Mark Zimmerman, MD, professor of psychiatry and human behavior, Brown University, Providence, R.I., said in an interview.
The study was published online Nov. 8 in the Journal of Personality Disorders.
‘No other option’
Most previous research investigating telehealth has occurred in outpatient, individual treatment settings and has not examined telehealth-delivered group therapy or partial hospitalization, the authors noted.
“Until the pandemic, we were delivering care in person, but when the pandemic began, because of public safety recommendations, we knew that we could no longer continue doing so,” said Dr. Zimmerman, director of the outpatient division at the partial hospital program (PHP), Rhode Island Hospital.
“In switching to a telehealth platform, we were concerned about patient safety and acceptability of delivering care in that manner, especially with patients with BPD, which is associated with impulsive behavior, self-harm, and suicidal behavior, among other problems,” he said. However “we had no other option” than to utilize a telehealth delivery mode, since the alternative was to shut down the program.
The investigators were “interested in whether or not virtual treatment in an acute intensive setting, such as a PHP, would be as safe, acceptable, and effective as in-person treatment.”
The study was part of the ongoing work of the Rhode Island Methods to Improve Diagnostic Assessment and Services.
Additional safety measures
Treatment, consisting of an Acceptance and Commitment Therapy (ACT) treatment model – including intake assessments, individual therapy, psychiatric visits, and group therapy – was delivered by a multidisciplinary team via Zoom.
Dr. Zimmerman noted that the team implemented additional safety precautions, including having patients check in at the beginning of each day to indicate their location, not seeing patients who were out of state, and making sure all patients had a contact person.
In addition, beyond the therapist leading the group, another therapist was always available, overseeing groups and meeting one-on-one (virtually) with participants if they had been triggered by the group process and were highly distressed.
Patients were asked to complete a number of questionnaires, including the Clinically Useful Patient Satisfaction Scale (CUPSS) at the end of their intake session. The primary outcome measure was the Remission from Depression Questionnaire (RDQ-M).
The study was conducted between May 1 and Dec. 15 of 2020 and included 64 patients with BPD who were treated for the first time in the Rhode Island Hospital PHP. They were compared to 117 patients who participated in the in-person program during the same months in 2019.
Participant characteristics were similar – for example, three-quarters of the participants in both groups were female, and the mean age was 34 years.
‘Sea change’
Most patients in the telehealth and in-person groups reported being “very” or “extremely” satisfied with the initial evaluation (90% vs. 85.3%, c2 = 0.74) and were hopeful that they would get better (85.8% vs. 82.1%, c2 = 0.45).
(c2 = 4.62), and “under both telehealth and in-person treatment conditions, the patients significantly improved from admission to discharge on each of the RDQ-M subscales, with large effect sizes found for most of the subscales,” the authors reported.
There were significant differences between the groups in the average number of days of attendance and number of days missed.
A nonsignificantly higher proportion of patients completed the telehealth program, vs. the in-person program (68.8% vs. 59%, c2 = 1.69).
In both programs, transfer to inpatient care and dissatisfaction-related withdrawal from the program were low (both < 2%). Notably, no patients attempted or completed suicide during treatment.
Virtual treatment is more convenient than in-person treatment, Dr. Zimmerman noted. “Some patients – generally those with medical or transportation issues – told us they otherwise would not have been able to participate [in the program] if treatment had been in person.”
He added, “My prediction is that 5 years from now, two-thirds to three-quarters of outpatient visits will be virtual because that is what the patients prefer – and although there will certainly be individuals who prefer in-person care, I think we’ve witnessed a sea change in how behavioral health care will be delivered.”
‘Game changer’
In an interview, Monica Carsky, PhD, clinical assistant professor of psychology in psychiatry and a senior fellow at the Personality Disorders Institute, Weill Cornell Medical College, New York, said the study has “a lot of valuable detail about how to set up a virtual PHP, which could guide any group wanting to try this.”
Dr. Carsky, who was not involved with the study, called it “a very important contribution to the research literature on efficacious treatment of BPD,” although it is not a randomized controlled trial.
“Adding more individual attention to the virtual group (e.g., having a co-host in the groups) seems as though it may be an important factor in dealing with the limitations of virtual treatment,” she noted.
However, she continued, “a limitation is that outcome assessment relied on self-administered questionnaires and did not include clinician rating scales, so the response may have been subject to the effects of social desirability bias.”
Donald W. Black, MD, associate chief of staff for mental health at the Iowa City Veterans Administration Hospital, said in an interview that the pandemic has been a “game changer, as we have had to quickly adapt mental health programs to a virtual format.
“For the most part, they have been remarkably successful for a variety of conditions, and Zimmerman and colleagues now show this for BPD families,” said Dr. Black, who was not associated with the research.
No study funding was listed. The study authors, Dr. Carsky, and Dr. Black have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF PERSONALITY DISORDERS
Alopecia tied to a threefold increased risk for dementia
Alopecia areata (AA) has been linked to a significantly increased risk for dementia, new research shows.
After controlling for an array of potential confounders, investigators found a threefold higher risk of developing any form of dementia and a fourfold higher risk of developing Alzheimer’s disease (AD) in those with AA versus the controls.
“AA shares a similar inflammatory signature with dementia and has great psychological impacts that lead to poor social engagement,” lead author Cheng-Yuan Li, MD, MSc, of the department of dermatology, Taipei (Taiwan) Veterans General Hospital.
“Poor social engagement and shared inflammatory cytokines might both be important links between AA and dementia,” said Dr. Li, who is also affiliated with the School of Medicine and the Institute of Brain Science at National Yang Ming Chiao Tung University, Taipei.
The study was published online Oct. 26, 2021, in the Journal of Clinical Psychiatry (doi: 10.4088/JCP.21m13931).
Significant psychological impact
Patients with AA often experience anxiety and depression, possibly caused by the negative emotional and psychological impact of the hair loss and partial or even complete baldness associated with the disease, the authors noted.
However, AA is also associated with an array of other atopic and autoimmune diseases, including psoriasis and systemic lupus erythematosus (SLE).
Epidemiologic research has suggested a link between dementia and autoimmune diseases such as psoriasis and SLE, with some evidence suggesting that autoimmune and inflammatory mechanisms may “play a role” in the development of AD.
Dementia in general and AD in particular, “have been shown to include an inflammatory component” that may share some of the same mediators seen in AA (eg, IL-1 beta, IL-6, and tumor necrosis factor–alpha).
Moreover, “the great negative psychosocial impact of AA might result in poor social engagement, a typical risk factor for dementia,” said Dr. Li. The investigators sought to investigate whether patients with AA actually do have a higher dementia risk than individuals without AA.
The researchers used data from the Taiwan National Health Insurance Research Database, comparing 2,534 patients with AA against 25,340 controls matched for age, sex, residence, income, dementia-related comorbidities, systemic steroid use, and annual outpatient visits. Participants were enrolled between 1998 and 2011 and followed to the end of 2013.
The mean age of the cohort was 53.9 years, and a little over half (57.6%) were female. The most common comorbidity was hypertension (32.3%), followed by dyslipidemia (27%) and diabetes (15.4%).
Dual intervention
After adjusting for potential confounders, those with AA were more likely to develop dementia, AD, and unspecified dementia, compared with controls. They also had a numerically higher risk for vascular dementia, compared with controls, but it was not statistically significant.
When participants were stratified by age, investigators found a significant association between AA and higher risk for any dementia as well as unspecified dementia in individuals of all ages and an increased risk for AD in patients with dementia age at onset of 65 years and older.
The mean age of dementia diagnosis was considerably younger in patients with AA versus controls (73.4 vs. 78.9 years, P = .002). The risk for any dementia and unspecified dementia was higher in patients of both sexes, but the risk for AD was higher only in male patients.
Sensitivity analyses that excluded the first year or first 3 years of observation yielded similar and consistent findings.
“Intervention targeting poor social engagement and inflammatory cytokines may be beneficial to AA-associated dementia,” said Dr. Li.
“Physicians should be more aware of this possible association, help reduce disease discrimination among the public, and encourage more social engagement for AA patients,” he said.
“Further studies are needed to elucidate the underlying pathophysiology between AA and dementia risk,” he added.
No cause and effect
Commenting on the study, Heather M. Snyder, PhD, vice president of medical and scientific affairs, Alzheimer’s Association, said, “We continue to learn about and better understand factors that may increase or decrease a person’s risk of dementia.”
“While we know the immune system plays a role in Alzheimer’s and other dementia, we are still investigating links between, and impact of, autoimmune diseases – like alopecia areata, rheumatoid arthritis, and others – on our overall health and our brains, [which] may eventually give us important information on risk reduction strategies as well,” said Dr. Snyder, who was not involved in the research.
She cautioned that although the study did show a correlation between AA and dementia risk, this does not equate to a demonstration of cause and effect.
At present, “the message for clinicians is that when a patient comes to your office with complaints about their memory, they should, No. 1, be taken seriously; and, No. 2, receive a thorough evaluation that takes into account the many factors that may lead to cognitive decline,” Dr. Snyder said.
The study was supported by a grant from Taipei Veterans General Hospital and the Ministry of Science and Technology, Taiwan. Dr. Li, coauthors, and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alopecia areata (AA) has been linked to a significantly increased risk for dementia, new research shows.
After controlling for an array of potential confounders, investigators found a threefold higher risk of developing any form of dementia and a fourfold higher risk of developing Alzheimer’s disease (AD) in those with AA versus the controls.
“AA shares a similar inflammatory signature with dementia and has great psychological impacts that lead to poor social engagement,” lead author Cheng-Yuan Li, MD, MSc, of the department of dermatology, Taipei (Taiwan) Veterans General Hospital.
“Poor social engagement and shared inflammatory cytokines might both be important links between AA and dementia,” said Dr. Li, who is also affiliated with the School of Medicine and the Institute of Brain Science at National Yang Ming Chiao Tung University, Taipei.
The study was published online Oct. 26, 2021, in the Journal of Clinical Psychiatry (doi: 10.4088/JCP.21m13931).
Significant psychological impact
Patients with AA often experience anxiety and depression, possibly caused by the negative emotional and psychological impact of the hair loss and partial or even complete baldness associated with the disease, the authors noted.
However, AA is also associated with an array of other atopic and autoimmune diseases, including psoriasis and systemic lupus erythematosus (SLE).
Epidemiologic research has suggested a link between dementia and autoimmune diseases such as psoriasis and SLE, with some evidence suggesting that autoimmune and inflammatory mechanisms may “play a role” in the development of AD.
Dementia in general and AD in particular, “have been shown to include an inflammatory component” that may share some of the same mediators seen in AA (eg, IL-1 beta, IL-6, and tumor necrosis factor–alpha).
Moreover, “the great negative psychosocial impact of AA might result in poor social engagement, a typical risk factor for dementia,” said Dr. Li. The investigators sought to investigate whether patients with AA actually do have a higher dementia risk than individuals without AA.
The researchers used data from the Taiwan National Health Insurance Research Database, comparing 2,534 patients with AA against 25,340 controls matched for age, sex, residence, income, dementia-related comorbidities, systemic steroid use, and annual outpatient visits. Participants were enrolled between 1998 and 2011 and followed to the end of 2013.
The mean age of the cohort was 53.9 years, and a little over half (57.6%) were female. The most common comorbidity was hypertension (32.3%), followed by dyslipidemia (27%) and diabetes (15.4%).
Dual intervention
After adjusting for potential confounders, those with AA were more likely to develop dementia, AD, and unspecified dementia, compared with controls. They also had a numerically higher risk for vascular dementia, compared with controls, but it was not statistically significant.
When participants were stratified by age, investigators found a significant association between AA and higher risk for any dementia as well as unspecified dementia in individuals of all ages and an increased risk for AD in patients with dementia age at onset of 65 years and older.
The mean age of dementia diagnosis was considerably younger in patients with AA versus controls (73.4 vs. 78.9 years, P = .002). The risk for any dementia and unspecified dementia was higher in patients of both sexes, but the risk for AD was higher only in male patients.
Sensitivity analyses that excluded the first year or first 3 years of observation yielded similar and consistent findings.
“Intervention targeting poor social engagement and inflammatory cytokines may be beneficial to AA-associated dementia,” said Dr. Li.
“Physicians should be more aware of this possible association, help reduce disease discrimination among the public, and encourage more social engagement for AA patients,” he said.
“Further studies are needed to elucidate the underlying pathophysiology between AA and dementia risk,” he added.
No cause and effect
Commenting on the study, Heather M. Snyder, PhD, vice president of medical and scientific affairs, Alzheimer’s Association, said, “We continue to learn about and better understand factors that may increase or decrease a person’s risk of dementia.”
“While we know the immune system plays a role in Alzheimer’s and other dementia, we are still investigating links between, and impact of, autoimmune diseases – like alopecia areata, rheumatoid arthritis, and others – on our overall health and our brains, [which] may eventually give us important information on risk reduction strategies as well,” said Dr. Snyder, who was not involved in the research.
She cautioned that although the study did show a correlation between AA and dementia risk, this does not equate to a demonstration of cause and effect.
At present, “the message for clinicians is that when a patient comes to your office with complaints about their memory, they should, No. 1, be taken seriously; and, No. 2, receive a thorough evaluation that takes into account the many factors that may lead to cognitive decline,” Dr. Snyder said.
The study was supported by a grant from Taipei Veterans General Hospital and the Ministry of Science and Technology, Taiwan. Dr. Li, coauthors, and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Alopecia areata (AA) has been linked to a significantly increased risk for dementia, new research shows.
After controlling for an array of potential confounders, investigators found a threefold higher risk of developing any form of dementia and a fourfold higher risk of developing Alzheimer’s disease (AD) in those with AA versus the controls.
“AA shares a similar inflammatory signature with dementia and has great psychological impacts that lead to poor social engagement,” lead author Cheng-Yuan Li, MD, MSc, of the department of dermatology, Taipei (Taiwan) Veterans General Hospital.
“Poor social engagement and shared inflammatory cytokines might both be important links between AA and dementia,” said Dr. Li, who is also affiliated with the School of Medicine and the Institute of Brain Science at National Yang Ming Chiao Tung University, Taipei.
The study was published online Oct. 26, 2021, in the Journal of Clinical Psychiatry (doi: 10.4088/JCP.21m13931).
Significant psychological impact
Patients with AA often experience anxiety and depression, possibly caused by the negative emotional and psychological impact of the hair loss and partial or even complete baldness associated with the disease, the authors noted.
However, AA is also associated with an array of other atopic and autoimmune diseases, including psoriasis and systemic lupus erythematosus (SLE).
Epidemiologic research has suggested a link between dementia and autoimmune diseases such as psoriasis and SLE, with some evidence suggesting that autoimmune and inflammatory mechanisms may “play a role” in the development of AD.
Dementia in general and AD in particular, “have been shown to include an inflammatory component” that may share some of the same mediators seen in AA (eg, IL-1 beta, IL-6, and tumor necrosis factor–alpha).
Moreover, “the great negative psychosocial impact of AA might result in poor social engagement, a typical risk factor for dementia,” said Dr. Li. The investigators sought to investigate whether patients with AA actually do have a higher dementia risk than individuals without AA.
The researchers used data from the Taiwan National Health Insurance Research Database, comparing 2,534 patients with AA against 25,340 controls matched for age, sex, residence, income, dementia-related comorbidities, systemic steroid use, and annual outpatient visits. Participants were enrolled between 1998 and 2011 and followed to the end of 2013.
The mean age of the cohort was 53.9 years, and a little over half (57.6%) were female. The most common comorbidity was hypertension (32.3%), followed by dyslipidemia (27%) and diabetes (15.4%).
Dual intervention
After adjusting for potential confounders, those with AA were more likely to develop dementia, AD, and unspecified dementia, compared with controls. They also had a numerically higher risk for vascular dementia, compared with controls, but it was not statistically significant.
When participants were stratified by age, investigators found a significant association between AA and higher risk for any dementia as well as unspecified dementia in individuals of all ages and an increased risk for AD in patients with dementia age at onset of 65 years and older.
The mean age of dementia diagnosis was considerably younger in patients with AA versus controls (73.4 vs. 78.9 years, P = .002). The risk for any dementia and unspecified dementia was higher in patients of both sexes, but the risk for AD was higher only in male patients.
Sensitivity analyses that excluded the first year or first 3 years of observation yielded similar and consistent findings.
“Intervention targeting poor social engagement and inflammatory cytokines may be beneficial to AA-associated dementia,” said Dr. Li.
“Physicians should be more aware of this possible association, help reduce disease discrimination among the public, and encourage more social engagement for AA patients,” he said.
“Further studies are needed to elucidate the underlying pathophysiology between AA and dementia risk,” he added.
No cause and effect
Commenting on the study, Heather M. Snyder, PhD, vice president of medical and scientific affairs, Alzheimer’s Association, said, “We continue to learn about and better understand factors that may increase or decrease a person’s risk of dementia.”
“While we know the immune system plays a role in Alzheimer’s and other dementia, we are still investigating links between, and impact of, autoimmune diseases – like alopecia areata, rheumatoid arthritis, and others – on our overall health and our brains, [which] may eventually give us important information on risk reduction strategies as well,” said Dr. Snyder, who was not involved in the research.
She cautioned that although the study did show a correlation between AA and dementia risk, this does not equate to a demonstration of cause and effect.
At present, “the message for clinicians is that when a patient comes to your office with complaints about their memory, they should, No. 1, be taken seriously; and, No. 2, receive a thorough evaluation that takes into account the many factors that may lead to cognitive decline,” Dr. Snyder said.
The study was supported by a grant from Taipei Veterans General Hospital and the Ministry of Science and Technology, Taiwan. Dr. Li, coauthors, and Dr. Snyder disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Social determinants of health may drive CVD risk in Black Americans
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).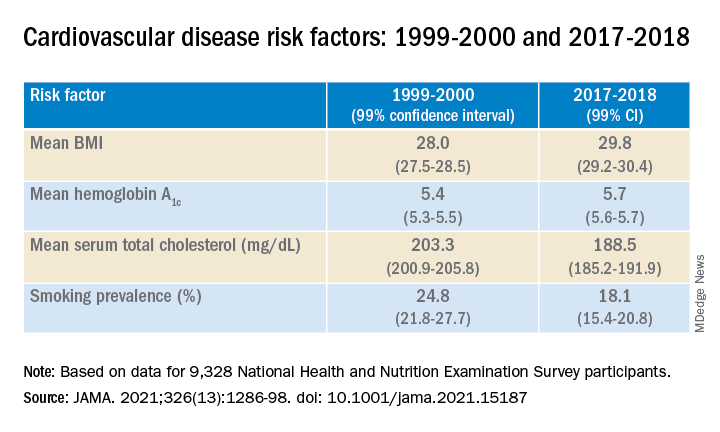
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).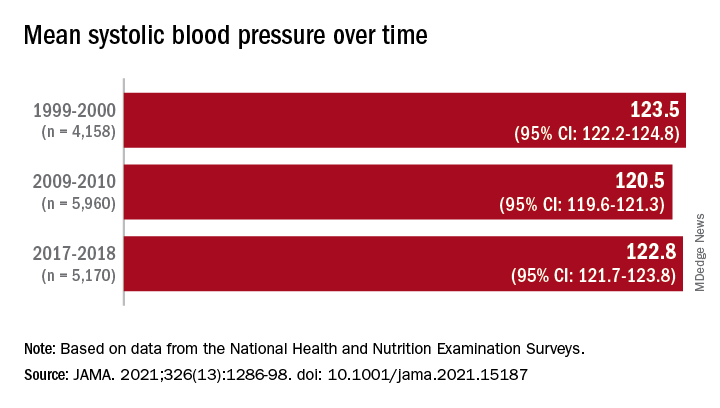
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).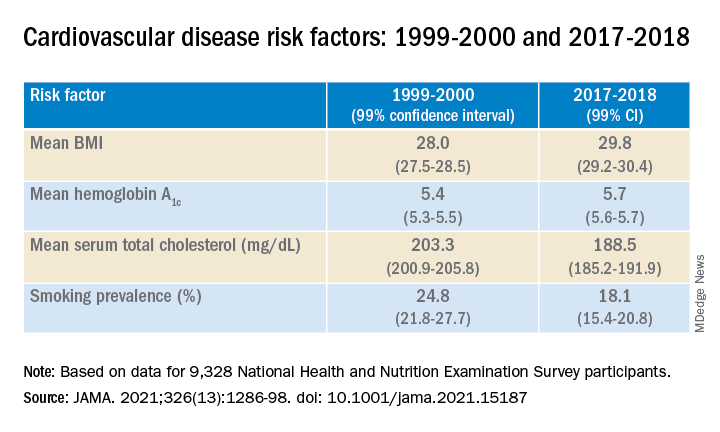
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).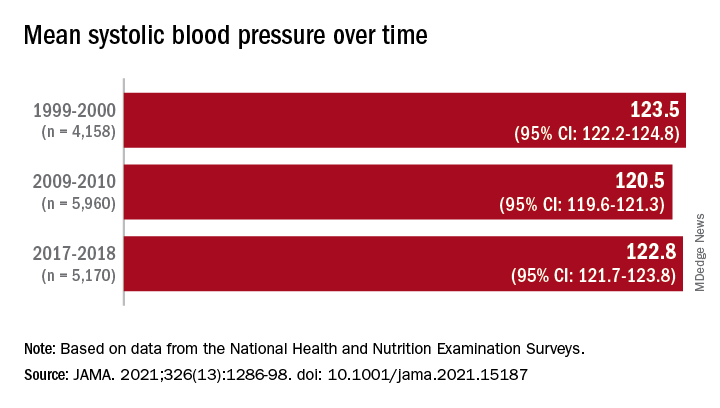
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Investigators analyzed 20 years of data on over 50,500 U.S. adults drawn from the National Health and Nutrition Examination Surveys (NHANES) and found that, in the overall population, body mass index and hemoglobin A1c were significantly increased between 1999 and 2018, while serum total cholesterol and cigarette smoking were significantly decreased. Mean systolic blood pressure decreased between 1999 and 2010, but then increased after 2010.
The mean age- and sex-adjusted estimated 10-year risk for atherosclerotic cardiovascular disease (ASCVD) was consistently higher in Black participants vs. White participants, but the difference was attenuated after further adjusting for education, income, home ownership, employment, health insurance, and access to health care.
“These findings are helpful to guide the development of national public health policies for targeted interventions aimed at eliminating health disparities,” Jiang He, MD, PhD, Joseph S. Copes Chair and professor of epidemiology, Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
“Interventions on social determinants of cardiovascular health should be tested in rigorous designed intervention trials,” said Dr. He, director of the Tulane University Translational Science Institute.
The study was published online Oct. 5 in JAMA.
‘Flattened’ CVD mortality?
Recent data show that the CVD mortality rate flattened, while the total number of cardiovascular deaths increased in the U.S. general population from 2010 to 2018, “but the reasons for this deceleration in the decline of CVD mortality are not entirely understood,” Dr. He said.
Moreover, “racial and ethnic differences in CVD mortality persist in the U.S. general population [but] the secular trends of cardiovascular risk factors among U.S. subpopulations with various racial and ethnic backgrounds and socioeconomic status are [also] not well understood,” he added. The effects of social determinants of health, such as education, income, home ownership, employment, health insurance, and access to health care on racial/ethnic differences in CVD risk, “are not well documented.”
To investigate these questions, the researchers drew on data from NHANES, a series of cross-sectional surveys in nationally representative samples of the U.S. population aged 20 years and older. The surveys are conducted in 2-year cycles and include data from 10 cycles conducted from 1999-2000 to 2017-2018 (n = 50,571, mean age 49.0-51.8 years; 48.2%-51.3% female).
Every 2 years, participants provided sociodemographic information, including age, race/ethnicity, sex, education, income, employment, housing, health insurance, and access to health care, as well as medical history and medication use. They underwent a physical examination that included weight and height, blood pressure, lipid levels, plasma glucose, and hemoglobin A1c.
Social determinants of health
Between 1999-2000 and 2017-2018, age- and sex-adjusted mean BMI and hemoglobin A1c increased, while mean serum total cholesterol and prevalence of smoking decreased (all P < .001).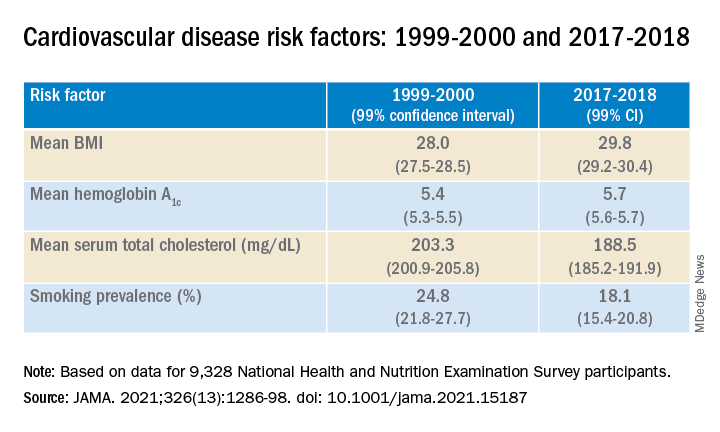
Age- and sex-adjusted 10-year atherosclerotic cardiovascular disease (ASCVD) risk decreased from 7.6% (6.9%-8.2%) in 1999-2000 to 6.5% (6.1%-6.8%) in 2011-2012, with no significant changes thereafter.
When the researchers looked at specific racial and ethnic groups, they found that age- and sex-adjusted BMI, systolic BP, and hemoglobin A1c were “consistently higher” in non-Hispanic Black participants compared with non-Hispanic White participants, but total cholesterol was lower (all P < .001).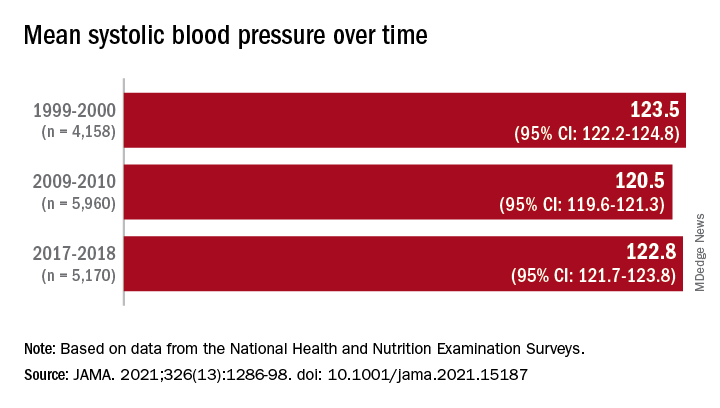
Participants with at least a college education or high family income had “consistently lower levels” of cardiovascular risk factors. And although the mean age- and sex-adjusted 10-year risk for ASCVD was significantly higher in non-Hispanic Black vs. non-Hispanic White participants (difference, 1.4% [1.0%-1.7%] in 1999-2008 and 2.0% [1.7%-2.4%] in 2009-2018), the difference was attenuated (by –0.3% in 1999-2008 and 0.7% in 2009-2018) after the researchers further adjusted for education, income, home ownership, employment, health insurance, and access to health care.
The differences in cardiovascular risk factors between Black and White participants “may have been moderated by social determinants of health,” the authors noted.
Provide appropriate education
Commenting on the study in an interview, Mary Ann McLaughlin, MD, MPH, associate professor of medicine, cardiology, Icahn School of Medicine at Mount Sinai, New York, pointed out that two important cardiovascular risk factors associated with being overweight – hypertension and diabetes – remained higher in the Black population compared with the White population in this analysis.
“Physicians and health care systems should provide appropriate education and resources regarding risk factor modification regarding diet, exercise, and blood pressure control,” advised Dr. McLaughlin, who was not involved with the study.
“Importantly, smoking rates and cholesterol levels are lower in the Black population, compared to the White population, when adjusted for many important socioeconomic factors,” she pointed out.
Dr. McLaughlin added that other “important social determinants of health, such as neighborhood and access to healthy food, were not measured and should be addressed by physicians when optimizing cardiovascular risk.”
The research reported in this publication was supported by the National Heart, Lung, and Blood Institute and by the National Institute of General Medical Sciences. One of the researchers, Joshua D. Bundy, PhD, was supported by a grant from the National Institutes of Health/Eunice Kennedy Shriver National Institute of Child Health and Human Development. Dr. He and the other coauthors and Dr. McLaughlin reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
What if your patient refuses to disrobe?
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.
Sterling Ransone Jr., MD, a family physician in Deltaville, Va., knocked on the exam room door and entered to find the patient, a 28-year-old woman, seated on the examination table. She was complaining about a fever, sore throat, and congestion.
Dr. Ransone asked if it was okay for him to lift her shirt and listen to her heart. She shook her head slightly. He decided to listen without removing the clothing, but when he put one hand on her shoulder and the stethoscope on her back, she flinched.
Instead of proceeding with the examination, Dr. Ransone, who is president-elect of the American Academy of Family Physicians, asked the patient whether everything was okay. It turned out that she had been the victim of a sexual assault and did not want a male to remove any clothing or touch her chest or back. Fortunately, Dr. Ransone’s practice had a female partner, who came in and listened to the patient’s chest.
“I’m glad I asked the patient what was going on for her because otherwise, I wouldn’t have known what she was going through,” Dr. Ransone said. “The patient felt respected and safe, and the therapeutic relationship was enhanced instead of compromised.”
Patient dignity is one of Dr. Ransone’s most important professional values. He recounts that during rounds in medical school, the attending and several interns and students crowded into the semiprivate room of an elderly woman who was lying in bed. The attending pulled off the bed covers, leaving the patient exposed while he discussed her case.
“I was mortified for her, and I learned a lot from watching this unfold, just seeing this woman lying naked in front all of these strangers and God,” said Dr. Ransone, physician practice director at Riverside Fishing Bay Family Practice, Deltaville, and assistant clinical professor of family medicine and population health at Virginia Commonwealth University, in Richmond. “I’ve been in practice for 25 years, and making sure the patient feels comfortable and respected is one of my priorities that dates back to that very first encounter.”
Trauma-informed care
Trauma is a common reason why patients feel reluctant to remove their clothing, according to Lauren Radziejewski, DNP, ANP-BC, clinical program manager, Mount Sinai Center for Transgender Medicine and Surgery, New York.
“We teach and endorse trauma-informed care for any type of procedure that is potentially triggering, and I would certainly put any type of care where people have to take off their clothes as potentially triggering,” she said.
Trauma can be caused by many factors. “Traumas of a sexual nature – having been subjected to sexual violence, for example – are the most obvious that come to mind, but any trauma that involves violation and disempowerment, even a nonsexual one, can make people more reluctant to be in a sensitive situation that can be perceived as invasive or disempowering,” Dr. Radziejewski said.
Talk before you touch
There are other reasons, often multiple intersecting reasons, why patients are reluctant to disrobe, according to Alicia Arbaje, MD, MPH, PhD, associate professor of medicine and director of transitional care research at the Center for Transformative Geriatrics Research, division of geriatric medicine and gerontology, Johns Hopkins University, Baltimore. These include culture and religion, generational sensitivities, and body discomfort associated with transitional times in life (e.g., teen or menopausal years).
Some general approaches apply, regardless of the reason for the patient’s discomfort. Others are specific to the patient’s particular problem or concern, Dr. Arbaje said.
“So much of medicine in this day and age is to quickly get down to business, hurry, and move on to the next patient,” said Dr. Arbaje, who also serves as chair of the American Geriatric Society’s Public Education Committee. “But establishing a little bit of a relationship is crucial before beginning the physical exam with any patient, especially with seniors or other patients who might have particular discomforts.”
She advises practitioners to “spend time talking before touching.” In other words, “Find a way to create some kind of meeting, even very briefly, and establish rapport before the patient changes into a gown and before you touch the patient to examine him or her.”
She acknowledged this might be difficult to do in certain clinical settings, but “to whatever extent you can, try to build this extra time and extra step into your workflow.”
She suggested that physicians first meet with the patient in the office or examining room to hear about his or her concerns. If a gown is necessary, the patient can change into one after the physician leaves the room. This builds trust and rapport.
Choice of language is important, especially when talking with older individuals. “Address the patient by their title until you are told not to – Ms. or Mrs. Smith, or Mr. Jones – or ask, ‘How would you like to be addressed?’ And don’t use terms of endearment, like ‘dear’ or ‘sweetie,’ or the plural, such as ‘How are we feeling today?’ “ These are “infantilizing and patronizing” and can impact the patient’s level of comfort with the entire appointment, including undressing and being examined.
Regarding transgender people, “many have experienced sexual violence and inappropriate touching, but even those fortunate enough to have escaped that type of common problem typically have still undergone traumatic experiences just by being transgender, having been socialized incorrectly, misunderstood, or having the ‘wrong’ genitalia,” said Dr. Radziejewski.
Particularly when dealing with a transgender patient, “you have to assume that there may be a history of trauma. Be sensitive to the patient’s discomforts about disrobing, recognize the examination itself as a potential trigger, and take appropriate measures to mitigate the trauma.”
To do this, Dr. Radziejewski gives her patients a “menu of options,” because “when people are navigating the world after trauma, including marginalized identity, they often have a complete loss of control, so the key is to give them as much control as possible every step of the way.”
For example, Dr. Radziejewski might tell a transgender masculine patient, “I’m looking through your chart and see no documented Pap test.” She acknowledges that after explaining why the test is recommended, the patient might be uncomfortable with it. She then makes a series of suggestions that range from being completely noninvasive to more invasive.
“You can say you don’t want it at all, or you can take a swab that I will give you and do it in the bathroom yourself. If you’re more comfortable with a man performing it, I can arrange that, or if you’re more comfortable with someone other than myself – your regular provider – I can arrange that, too.” By the end of the interaction, most patients are comfortable with Dr. Radziejewski performing the exam.
Regarding invasive exams, she recommends setting up an appointment specifically dedicated to that exam, rather than trying to cram a sensitive process into the time allotted for a patent visit, when other topics are also being discussed. “This also reinforces a sense of control,” she said.
This approach is relevant not only for transgender patients but also for any patient who has experienced trauma or some type of shame associated with the body, she said.
Dr. Ransone asks transgender patients what pronoun they would like him to use when he addresses them.
Prior to the examination, talking about what will be done and why further enhances trust, comfort, and rapport.
Who should be present?
Dr. Arbaje suggested that the pre-examination conversation should include a discussion of who the patient would like to have present during the exam. This is particularly relevant with a geriatric patient who might have been brought in by a family member or caregiver.
Similarly, adolescents may not feel comfortable with a parent being present for an examination. To protect the teen’s privacy, Dr. Ransone asks parents to step out. “There are also subjects that adolescents won’t bring up if their parents are there,” he said.
A question that is relevant in many clinical settings is whether the presence of a chaperone enhances or detracts from the patient’s comfort. Although the use of chaperones is recommended by many societies, it is a judgment call whether a chaperone should be present during all examinations – unless the state in which one practices requires it. Seven states mandate the presence of a chaperone during an intimate exam: Alabama, Delaware, Georgia, Montana, New Jersey, Ohio, and Tennessee.
Dr. Ransone utilizes a medical scribe to take notes on patient visits. The nurse or medical assistant who escorts the patient into the exam room informs the patient that a scribe will be in the room but that the patient should feel free to say whether he or she wants to talk about something privately, in which case the scribe will leave.
Dr. Ransone’s scribe is female and serves as the chaperone during an intimate exam of a female patient. “I have assumed, and my established patients know, that there will be a chaperone present, but my patients also know they can ask for the chaperone to step out,” he said. “When that happens, I document the discussion in the patient’s chart for my own legal protection.”
He recommended that practices consider posting signage or including information about chaperones in the practice’s informational brochures regarding policies and procedures.
Armin Brott, MBA, senior editor of Talking About Men’s Health , said that having a chaperone in the room when a female practitioner is examining a male patient – even if the chaperone is male – would be “extremely uncomfortable, weird, and even voyeuristic for the male patient.”
He noted that typically, male physicians use a chaperone when examining a female patient “for their own legal self-protection and maybe to make the female patient more comfortable, but female physicians are typically less concerned about potentially being accused of violating a male patient and typically do not have chaperones.”
Men face unique challenges
Men have “unique needs and challenges” when it comes to healthcare, said Mr. Brott, an advisory board member of the Men’s Health Network.
Mr. Brott cited research showing that men do not seek healthcare as frequently as women do. “So it’s already hard to get men in the door of a doctor, no matter what the provider’s gender is,” he said. Notably, men are even less likely to seek medical care when the clinician is female, owing to discomfort at having to undergo an intimate exam.
“I think that many men have issues about sexuality and of becoming aroused during an exam if it’s a female practitioner doing the exam,” said Mr. Brott. “I’m sure this is something physicians and nurses are accustomed to, but for the patient, it’s extremely embarrassing. The man may worry that he’ll be perceived as making unwanted sexual overtures to the practitioner.”
The way to mitigate these concerns is through communication, according to Mr. Brott. He recalled his own experience during a catherization conducted by a female practitioner he had never met. “She came in and started dealing with me as if I wasn’t even a person. She didn’t say much. It would have helped if she had created some type of human connection and talked to me – something like, ‘I’ve done this a thousand times and here’s what you’ll be feeling,’ or, “Would you like me to describe what I’m doing, or just do it as quickly as possible?’ ”
On another occasion, Mr. Brott underwent a procedure that was performed by two female practitioners, who were more communicative and even brought some light humor to the encounter, “which set me at ease,” he said.
If a man does become aroused, reassurance would be helpful, Mr. Brott said. “You can say something like, ‘Don’t worry, it’s perfectly natural, it happens all the time. Let’s finish up, and I’ll be out of your way as soon as I can.’ ”
Explain at every step of the way
All the experts emphasize the critical importance of continuing to offer explanations throughout the exam, even if the exam has been discussed beforehand.
“During the exam, it’s key to explain what you’re doing each step of the way – especially with seniors, but with other patients too,” said Arbaje. “For example, ‘I’d like you to remove your arms from your shirt so I can examine the joint better.’ Often there’s apprehension about what you’re going to do next. You can also ask, ‘Is there anything I should know before I examine this part of you? How are you doing?’ “ She advised asking the patient for “ongoing feedback. ‘Is this okay? Is this too rough?’ “
This is especially important when conducting a pelvic exam or palpating the patient’s abdomen, which is a more personal area than, say, the knee. Only the body part that is being examined should be uncovered, and it should be re-covered after the exam of that body part is complete and a different body part is to then be examined.
Asking for feedback is especially important, because many older patients have been acculturated not to question physicians and other medical authorities and may suffer a sense of humiliation silently.
Dr. Arbaje noted that feedback can be nonverbal: “For example, wincing or flinching are signs of discomfort you should ask the patient about or empathetically acknowledge.”
Rapport building doesn’t end after the examination
Dr. Arbaje advises physicians to “spend a little more time with the patient after the examination and not just walk out the door, leaving the person as they are, half undressed or in a gown.”
In the case of an older person, this might involve helping patients get their shoes and socks on or helping them get off the table. “Spend some time closing the encounter, not just doing what you need to do and then leaving or leaving it for someone else or family to do, which can be very dehumanizing,” she said. Even a few minutes of human contact beyond the examination can enhance rapport and help the patient feel respected and more comfortable.
Setting the stage: Create a conducive office environment
Setting patients at ease begins well before the patient enters the examination room, experts say. The overall atmosphere of the practice – the professionalism, courtesy, and friendliness of the staff – contributes to a sense of safety that will set the stage for the patient to feel more comfortable disrobing, if necessary, and being examined.
Mr. Brott pointed out that most medical offices tend to be more “female-friendly” in decor, utilizing pastel colors and flower motifs, for example, and displaying women’s magazines in the waiting room. Gender-neutral decor and different types of reading materials might set men at ease. Receptionists and medical staff are often female, and it is helpful for practices to employ male staff to bring the patient into the examination room or check vital signs. “This would go a long way toward making a man feel welcome and comfortable, even if the physician is female,” he said.
Dr. Radziejewski agreed: “If possible, having male and female support staff available will set patients of any gender at their ease.”
The setup of the examination room may contribute to a patient’s level of comfort. In Dr. Ransone’s examination room, the patient faces the door when on the table, and the door is locked during the exam so that no one can enter.
“I think that if patients are facing away from the door, they may feel claustrophobic or trapped, and I don’t want to position myself between the patient and an exit,” Dr. Ransone said. “My exam room happens to have no windows, but I’ve seen situations where the patient is lying on the table, exposed in front of the window, which can feel vulnerable, even if the office is on a high floor and no one can see into the window.”
Dr. Ransone positions the scribe or chaperone to the side, where the patient can see them, but not directly in front, where the examination might be visible to them. “I think it would be more uncomfortable and anxiety provoking knowing that someone is standing behind me and I can’t see them,” he said.
Choosing the best gown ... when necessary
Is it necessary for patients to disrobe and put on a gown — especially in light of the fact that research suggests that wearing a gown can induce psychological distress?
Danielle Ofri, MD, PhD, clinical professor, department of medicine, NYU Grossman School of Medicine, New York, said that in her practice, patients wear street clothes unless the patient is to undergo a full physical exam.
Even an abdominal exam can be conducted by loosening and slightly lowering the pants. Dr. Ofri stresses that patients should retain full control over how much to expose: “The patient should always take the lead in adjusting or opening clothing for a focused physical exam. And, of course, we always need to ask permission before starting any part of the exam.”
A gown is more conducive for certain exams, such as pelvic or breast exams. Dr. Ransone said that cloth gowns are preferable to paper gowns, which can tear more easily and so lead to unnecessary exposure. Gowns that hang open at the back should be avoided. If that’s the only type available, a second gown can be provided so as to cover the backside.
This is especially important if the examination involves walking across the room – for example, to evaluate gait – or standing on the scale. Alternatively, the patient can be given a sheet to drape over the gown, which can be moved around during the examination.
Dr. Ransome’s own practice uses gowns that fully wrap around the person. “I’ve seen too many people in gowns that are too small, so I make sure the patient has an appropriately sized gown. The extra material also leaves room for draping, while exposing only the part of the body that’s necessary,” he said.
Numerous types of modest gowns are now available, including kimono-type gowns with ties and snaps that allow partial exposure. All the experts encouraged utilizing these or similar types of gowns if possible.
Cultural and religious considerations
It is important for clinicians to be sensitive to cultural and religious factors that might affect patients’ attitudes toward attire and opposite-sex practitioners, said Dr. Ofri, an internist at Bellevue Hospital, New York.
For example, in Islamic and ultra-Orthodox Jewish traditions, certain parts of the body may not be exposed in the presence of a man who is unrelated by blood or marriage. Studies have shown that Hispanic and Asian women have avoided mammography because of embarrassment.
Dr. Arbaje described a 90-year-old patient whose physician ordered a pelvic ultrasound. The ultrasound department conducted the test transvaginally. “The patient, a widow, came from a Catholic background and regarded this as tantamount to ‘cheating’ on her deceased husband, and she felt violated and ashamed,” Dr. Arbaje said.
Dr. Ofri, who is the author of Medicine in Translation: Journeys With My Patients, said that she has Muslim and Orthodox Jewish male patients who allow her to examine their knees but won’t shake her hand because of the prohibition against touching an unrelated woman. Muslim female patients are willing to unsnap their veils because Dr. Ofri is female, but they would be uncomfortable with a male practitioner.
Whenever possible, gender-concordant care should be provided. If that is not possible, patients should be offered the option of not undergoing the examination, unless it’s an emergent situation, Dr. Ofri said. It may be necessary to reschedule the appointment to a time when a same-sex practitioner is available or to refer the patient to another practitioner.
Keeping cultural and religious considerations in mind is important, but there are variations in any given culture or religion. Practitioners should take cues directly from the patient, the experts advise.
Meeting the needs of cognitively impaired patients
Patients who are cognitively impaired have particular needs, Dr. Arbaje says. Many such patients are seniors with dementia, although developmental disabilities, neurodegenerative diseases, and other problems that affect cognition can occur among patients of any age and stage of life.
“People with dementia don’t necessarily understand what you’re doing and why you’re touching them. Even people with advanced dementia often retain a sense of modesty and may feel humiliated by an examination,” Dr. Arbaje said.
Dr. Arbaje encourages offering clear explanations of what is being done. The language one uses should be respectful and nonpatronizing, even if the patient does not understand what is being said. However, the bulk of one’s communication should be nonverbal. “Convey gentleness, safety, and reassurance through your tone and touch,” Dr. Arbaje said.
For cognitively impaired patient, it is helpful for a trusted family member or caregiver to be present during the examination, rather than a stranger. Depending on the degree of impairment, it might also be helpful for them to have a familiar object, perhaps a blanket; the odor and texture can convey familiarity and reassurance.
Nonclinical touch can also be reassuring. “We’re often scared of touching a patient because we don’t want to be considered inappropriate, but people who have dementia in later life are often understimulated, in terms of loving and caring touch,” she said. “For people in that situation, touch is typically of a practical or clinical nature – like bathing the person or taking their blood pressure. Providing reassuring touch or having someone else present to do so can help ease the patient’s fear and can be very healing.”
Making your patient’s eyes light up
“I can’t even count how many times I’ve had patients thank me for just explaining things clearly and giving them the right to opt out of wearing a gown or having an examination or procedure,” Dr. Radziejewski said.
“Obviously, I express recommendations, strong recommendations, but people like to know this is a place where they’ll be acknowledged for who they are, where they can feel safe and their dignity will be preserved. That should be the environment for any patient, whatever their culture, religion, age, background, or sexual identity. Offering that type of venue makes their eyes light up and makes all the difference in adherence to my recommendations and feeling empowered to truly care for their health,” she said.
A version of this article first appeared on Medscape.com.








