User login
Substance abuse boosts COVID hospitalization, death risk, even after vaccination
Individuals with substance use disorders (SUDs) have a twofold increased risk for COVID-related hospitalization and death even after vaccination, new research shows.
Investigators analyzed data on over 10,000 vaccinated individuals with various SUDs and almost 600,000 vaccinated individuals without an SUD. They found about twice as many individuals with an SUD had a breakthrough COVID-19 infection as their counterparts without an SUD, at 7% versus 3.6%, respectively.
In addition, the risks for hospitalizations and death resulting from breakthrough infection were also higher among people with SUD compared to those without.
“It is crucial that clinicians continue to prioritize vaccination among people with SUDs, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19,” co-investigator Nora Volkow, MD, director of the National Institute on Drug Abuse, told this news organization.
“In addition, clinicians should screen their patients for SUDs in order to best understand their risks and care needs [since] many physicians don’t screen or inquire about SUD, which is a tremendous missed opportunity and one that is likely to jeopardize their ability to effectively care for their patients,” she said.
The study was published online October 5 in World Psychiatry.
Worrisome phase
SUDs are “often associated with multiple comorbid conditions that are known risk factors for severe outcome of COVID-19 infection,” the investigators note.
Research published early in the pandemic showed patients with SUDs, including alcohol, cannabis, cocaine, opioid, and tobacco use disorders, were “at increased risk for COVID-19 infection and associated severe outcomes, especially among African Americans,” they add.
To date, no research has focused on the potential risk for COVID in individuals with SUDs following vaccination. In addition, although vaccines are “very effective,” breakthrough infections have been recorded, “highlighting the need to identify populations that might be most vulnerable, as we have entered a worrisome new phase of the pandemic,” the authors write.
to estimate the risk for breakthrough COVID-19 among vaccinated patients with SUD (n = 30,183; mean age 59.3, 51.4% male, 63.2% White, 26.2% African American), compared with vaccinated individuals without SUDs (n = 549,189; mean age 54.7, 43.2% male, 63.4% White, 14.3% African American) between December 2020 and August 2021.
They also conducted statistical analyses to examine how the rate of breakthrough cases changed over that timeframe.
The cohorts were matched by demographics, adverse socioeconomic determinants of health, lifetime medical and psychiatric comorbidities, and vaccine type.
Among vaccinated SUD patients, three-quarters received the Pfizer-BioNTech vaccine, one-fifth received the Moderna vaccine, and 3.3% received the Johnson & Johnson vaccine.
In contrast, among the vaccinated non-SUD population, almost all (88.2%) received the Pfizer-BioNTech vaccine, 10% received Moderna, and only 1.2% received the Johnson & Johnson vaccine.
Underlying drivers
The prevalence of adverse socioeconomic determinants of health was higher in vaccinated individuals with SUDs compared to those without (7.9% vs. 1.2%, respectively). Moreover, vaccinated patients with SUD had a higher lifetime prevalence of all comorbidities as well as transplants (all Ps < .001).
The risk for breakthrough infection was significantly higher in vaccinated individuals with SUDs compared to those without (all Ps < .001).
After controlling for adverse socioeconomic determinants of health and comorbid medical conditions, the risk for breakthrough infection “no longer differed in SUD compared to non-SUD cohorts, except for patients with cannabis use disorder, who remained at significantly increased risk,” the authors report.
In both populations, the rate of breakthrough infections “steadily increased” between January and August 2021.
The risk for hospitalization and death was higher among those with breakthrough infections, compared with those in the matched cohort without breakthrough infections, but the risk for hospitalization and death were higher in the SUD compared with the non-SUD population.
In the SUD patients, after matching an array of demographic, socioeconomic, and medical factors as well as vaccine type, only cannabis use disorder was associated with a higher risk in African Americans, compared with matched Caucasians (HR = 1.63; 95% confidence interval, 1.06-2.51).
“When we adjusted the data to account for comorbidities and for socioeconomic background, we no longer saw a difference between those with substance use disorders and those without – the only exception to this was for people with cannabis use disorder,” said Dr. Volkow.
“This suggests that these factors, which are often associated with substance use disorders, are likely the underlying drivers for the increased risk,” she continued.
She added that it is important for other studies to investigate why individuals with cannabis use disorder had a higher risk for breakthrough infections.
Good news, bad news
Commenting for this news organization, Anna Lembke, MD, professor of psychiatry and behavioral sciences, Stanford (Calif.) University, said the study is important and contains good news and bad news.
The good news, she said, “is that, after controlling for comorbidities and socioeconomic variables, patients with SUDs are no more likely than patients without SUDs to get COVID after getting vaccinated, and the bad news is that if vaccinated patients with SUDs do get COVID, they’re more likely to end up hospitalized or die from it,” said Dr. Lembke, who was not involved with the study.
“The take-home message for clinicians is that if your vaccinated patient with an SUD gets COVID, be on the alert for a more complicated medical outcome and a higher risk of death,” warned Dr. Lembke.
This study was supported by the U.S. National Institute on Drug Abuse, the U.S. National Institute of Aging, and the Clinical and Translational Science Collaborative (CTSC) of Cleveland. No disclosures were listed on the original study. Dr. Lembke has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with substance use disorders (SUDs) have a twofold increased risk for COVID-related hospitalization and death even after vaccination, new research shows.
Investigators analyzed data on over 10,000 vaccinated individuals with various SUDs and almost 600,000 vaccinated individuals without an SUD. They found about twice as many individuals with an SUD had a breakthrough COVID-19 infection as their counterparts without an SUD, at 7% versus 3.6%, respectively.
In addition, the risks for hospitalizations and death resulting from breakthrough infection were also higher among people with SUD compared to those without.
“It is crucial that clinicians continue to prioritize vaccination among people with SUDs, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19,” co-investigator Nora Volkow, MD, director of the National Institute on Drug Abuse, told this news organization.
“In addition, clinicians should screen their patients for SUDs in order to best understand their risks and care needs [since] many physicians don’t screen or inquire about SUD, which is a tremendous missed opportunity and one that is likely to jeopardize their ability to effectively care for their patients,” she said.
The study was published online October 5 in World Psychiatry.
Worrisome phase
SUDs are “often associated with multiple comorbid conditions that are known risk factors for severe outcome of COVID-19 infection,” the investigators note.
Research published early in the pandemic showed patients with SUDs, including alcohol, cannabis, cocaine, opioid, and tobacco use disorders, were “at increased risk for COVID-19 infection and associated severe outcomes, especially among African Americans,” they add.
To date, no research has focused on the potential risk for COVID in individuals with SUDs following vaccination. In addition, although vaccines are “very effective,” breakthrough infections have been recorded, “highlighting the need to identify populations that might be most vulnerable, as we have entered a worrisome new phase of the pandemic,” the authors write.
to estimate the risk for breakthrough COVID-19 among vaccinated patients with SUD (n = 30,183; mean age 59.3, 51.4% male, 63.2% White, 26.2% African American), compared with vaccinated individuals without SUDs (n = 549,189; mean age 54.7, 43.2% male, 63.4% White, 14.3% African American) between December 2020 and August 2021.
They also conducted statistical analyses to examine how the rate of breakthrough cases changed over that timeframe.
The cohorts were matched by demographics, adverse socioeconomic determinants of health, lifetime medical and psychiatric comorbidities, and vaccine type.
Among vaccinated SUD patients, three-quarters received the Pfizer-BioNTech vaccine, one-fifth received the Moderna vaccine, and 3.3% received the Johnson & Johnson vaccine.
In contrast, among the vaccinated non-SUD population, almost all (88.2%) received the Pfizer-BioNTech vaccine, 10% received Moderna, and only 1.2% received the Johnson & Johnson vaccine.
Underlying drivers
The prevalence of adverse socioeconomic determinants of health was higher in vaccinated individuals with SUDs compared to those without (7.9% vs. 1.2%, respectively). Moreover, vaccinated patients with SUD had a higher lifetime prevalence of all comorbidities as well as transplants (all Ps < .001).
The risk for breakthrough infection was significantly higher in vaccinated individuals with SUDs compared to those without (all Ps < .001).
After controlling for adverse socioeconomic determinants of health and comorbid medical conditions, the risk for breakthrough infection “no longer differed in SUD compared to non-SUD cohorts, except for patients with cannabis use disorder, who remained at significantly increased risk,” the authors report.
In both populations, the rate of breakthrough infections “steadily increased” between January and August 2021.
The risk for hospitalization and death was higher among those with breakthrough infections, compared with those in the matched cohort without breakthrough infections, but the risk for hospitalization and death were higher in the SUD compared with the non-SUD population.
In the SUD patients, after matching an array of demographic, socioeconomic, and medical factors as well as vaccine type, only cannabis use disorder was associated with a higher risk in African Americans, compared with matched Caucasians (HR = 1.63; 95% confidence interval, 1.06-2.51).
“When we adjusted the data to account for comorbidities and for socioeconomic background, we no longer saw a difference between those with substance use disorders and those without – the only exception to this was for people with cannabis use disorder,” said Dr. Volkow.
“This suggests that these factors, which are often associated with substance use disorders, are likely the underlying drivers for the increased risk,” she continued.
She added that it is important for other studies to investigate why individuals with cannabis use disorder had a higher risk for breakthrough infections.
Good news, bad news
Commenting for this news organization, Anna Lembke, MD, professor of psychiatry and behavioral sciences, Stanford (Calif.) University, said the study is important and contains good news and bad news.
The good news, she said, “is that, after controlling for comorbidities and socioeconomic variables, patients with SUDs are no more likely than patients without SUDs to get COVID after getting vaccinated, and the bad news is that if vaccinated patients with SUDs do get COVID, they’re more likely to end up hospitalized or die from it,” said Dr. Lembke, who was not involved with the study.
“The take-home message for clinicians is that if your vaccinated patient with an SUD gets COVID, be on the alert for a more complicated medical outcome and a higher risk of death,” warned Dr. Lembke.
This study was supported by the U.S. National Institute on Drug Abuse, the U.S. National Institute of Aging, and the Clinical and Translational Science Collaborative (CTSC) of Cleveland. No disclosures were listed on the original study. Dr. Lembke has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with substance use disorders (SUDs) have a twofold increased risk for COVID-related hospitalization and death even after vaccination, new research shows.
Investigators analyzed data on over 10,000 vaccinated individuals with various SUDs and almost 600,000 vaccinated individuals without an SUD. They found about twice as many individuals with an SUD had a breakthrough COVID-19 infection as their counterparts without an SUD, at 7% versus 3.6%, respectively.
In addition, the risks for hospitalizations and death resulting from breakthrough infection were also higher among people with SUD compared to those without.
“It is crucial that clinicians continue to prioritize vaccination among people with SUDs, while also acknowledging that even after vaccination, this group is at an increased risk and should continue to take protective measures against COVID-19,” co-investigator Nora Volkow, MD, director of the National Institute on Drug Abuse, told this news organization.
“In addition, clinicians should screen their patients for SUDs in order to best understand their risks and care needs [since] many physicians don’t screen or inquire about SUD, which is a tremendous missed opportunity and one that is likely to jeopardize their ability to effectively care for their patients,” she said.
The study was published online October 5 in World Psychiatry.
Worrisome phase
SUDs are “often associated with multiple comorbid conditions that are known risk factors for severe outcome of COVID-19 infection,” the investigators note.
Research published early in the pandemic showed patients with SUDs, including alcohol, cannabis, cocaine, opioid, and tobacco use disorders, were “at increased risk for COVID-19 infection and associated severe outcomes, especially among African Americans,” they add.
To date, no research has focused on the potential risk for COVID in individuals with SUDs following vaccination. In addition, although vaccines are “very effective,” breakthrough infections have been recorded, “highlighting the need to identify populations that might be most vulnerable, as we have entered a worrisome new phase of the pandemic,” the authors write.
to estimate the risk for breakthrough COVID-19 among vaccinated patients with SUD (n = 30,183; mean age 59.3, 51.4% male, 63.2% White, 26.2% African American), compared with vaccinated individuals without SUDs (n = 549,189; mean age 54.7, 43.2% male, 63.4% White, 14.3% African American) between December 2020 and August 2021.
They also conducted statistical analyses to examine how the rate of breakthrough cases changed over that timeframe.
The cohorts were matched by demographics, adverse socioeconomic determinants of health, lifetime medical and psychiatric comorbidities, and vaccine type.
Among vaccinated SUD patients, three-quarters received the Pfizer-BioNTech vaccine, one-fifth received the Moderna vaccine, and 3.3% received the Johnson & Johnson vaccine.
In contrast, among the vaccinated non-SUD population, almost all (88.2%) received the Pfizer-BioNTech vaccine, 10% received Moderna, and only 1.2% received the Johnson & Johnson vaccine.
Underlying drivers
The prevalence of adverse socioeconomic determinants of health was higher in vaccinated individuals with SUDs compared to those without (7.9% vs. 1.2%, respectively). Moreover, vaccinated patients with SUD had a higher lifetime prevalence of all comorbidities as well as transplants (all Ps < .001).
The risk for breakthrough infection was significantly higher in vaccinated individuals with SUDs compared to those without (all Ps < .001).
After controlling for adverse socioeconomic determinants of health and comorbid medical conditions, the risk for breakthrough infection “no longer differed in SUD compared to non-SUD cohorts, except for patients with cannabis use disorder, who remained at significantly increased risk,” the authors report.
In both populations, the rate of breakthrough infections “steadily increased” between January and August 2021.
The risk for hospitalization and death was higher among those with breakthrough infections, compared with those in the matched cohort without breakthrough infections, but the risk for hospitalization and death were higher in the SUD compared with the non-SUD population.
In the SUD patients, after matching an array of demographic, socioeconomic, and medical factors as well as vaccine type, only cannabis use disorder was associated with a higher risk in African Americans, compared with matched Caucasians (HR = 1.63; 95% confidence interval, 1.06-2.51).
“When we adjusted the data to account for comorbidities and for socioeconomic background, we no longer saw a difference between those with substance use disorders and those without – the only exception to this was for people with cannabis use disorder,” said Dr. Volkow.
“This suggests that these factors, which are often associated with substance use disorders, are likely the underlying drivers for the increased risk,” she continued.
She added that it is important for other studies to investigate why individuals with cannabis use disorder had a higher risk for breakthrough infections.
Good news, bad news
Commenting for this news organization, Anna Lembke, MD, professor of psychiatry and behavioral sciences, Stanford (Calif.) University, said the study is important and contains good news and bad news.
The good news, she said, “is that, after controlling for comorbidities and socioeconomic variables, patients with SUDs are no more likely than patients without SUDs to get COVID after getting vaccinated, and the bad news is that if vaccinated patients with SUDs do get COVID, they’re more likely to end up hospitalized or die from it,” said Dr. Lembke, who was not involved with the study.
“The take-home message for clinicians is that if your vaccinated patient with an SUD gets COVID, be on the alert for a more complicated medical outcome and a higher risk of death,” warned Dr. Lembke.
This study was supported by the U.S. National Institute on Drug Abuse, the U.S. National Institute of Aging, and the Clinical and Translational Science Collaborative (CTSC) of Cleveland. No disclosures were listed on the original study. Dr. Lembke has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Gut health ‘vitally important’ for mental health
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Disturbances in gut microbiota are associated with depletion of anti-inflammatory bacteria and proliferation of proinflammatory bacteria, a pattern tied to several major psychiatric disorders including depression, bipolar disorder (BD), schizophrenia, and anxiety, new research shows.
A meta-analysis of 59 studies, encompassing roughly 2,600 patients with psychiatric conditions, showed a decrease in microbial richness in patients with psychiatric conditions versus controls.
In addition, those with depression, anxiety, BD, and psychosis had a similar set of abnormalities in the microbiota, particularly lower levels of Faecalibacterium and Coprococcus – two types of bacteria that have an anti-inflammatory effect in gut – and higher levels of Eggerthella, a bacterium with proinflammatory effects.
“The wealth of evidence we have summarized clearly demonstrates that the gut microbiota is vitally important to the wider mental health of individuals,” lead author Viktoriya Nikolova, MRes, Centre for Affective Disorders, King’s College London, said in an interview.
“While it is still too early to recommend specific interventions, it’s clear that clinicians need to place a greater awareness of gut health when considering the treatment of certain psychiatric disorders,” she said.
The study was published online Sept. 15, 2021, in JAMA Psychiatry.
Reliable biomarkers
“Evidence of gut microbiota perturbations has accumulated for multiple psychiatric disorders, with microbiota signatures proposed as potential biomarkers,” the authors wrote.
However, “while there is a wealth of evidence to suggest that abnormalities within the composition of the gut microbiota are connected to a number of psychiatric disorders, there haven’t been any attempts to evaluate the specificity of this evidence – that is, if these changes are unique to specific disorders or shared across many,” Ms. Nikolova said.
Previous research in individual disorders has identified “patterns that may be promising biomarker targets,” with the potential to “improve diagnostic accuracy, guide treatment, and assist the monitoring of treatment response,” the authors noted.
“We wanted to see if we could reliably establish biomarkers for individual conditions in an effort to further our understanding of the relationship between mental illness and gut microbiota,” said Ms. Nikolova.
The researchers wanted to “evaluate the specificity and reproducibility of gut microbiota alterations and delineate those with potential to become biomarkers.”
They identified 59 studies (64 case-control comparisons; n = 2,643 patients, 2,336 controls). Most (54.2%) were conducted in East Asia, followed by Westernized populations (40.7%) and Africa (1.7%).
These studies evaluated diversity or abundance of gut microbes in adult populations encompassing an array of psychiatric disorders: major depressive disorder (MDD), BD, psychosis and schizophrenia, eating disorders (anorexia nervosa and bulimia nervosa), anxiety, obsessive-compulsive disorder (OCD), PTSD, and ADHD.
Although studies were similar in exclusion criteria, few attempted to minimize dietary changes or control dietary intake. In addition, use of psychiatric medication also “varied substantially.”
The researchers conducted several analyses, with primary outcomes consisting of “community-level measures of gut microbiota composition (alpha and beta diversity) as well as taxonomic findings at the phylum, family, and genus levels (relative abundance).”
Alpha diversity provides a “summary of the microbial community in individual samples,” which “can be compared across groups to evaluate the role of a particular factor (in this case psychiatric diagnosis) on the richness (number of species) and evenness (how well each species is represented) in the sample.”
Beta diversity, on the other hand, “measures interindividual (between samples) diversity that assesses similarity of communities, compared with the other samples analyzed.”
Control samples consisted of participants without the relevant condition.
Biological overlap?
The alpha-diversity meta-analysis encompassed 34 studies (n = 1,519 patients, 1,429 controls). The researchers found significant decreases in microbial richness in patients, compared with controls (observed species standardized mean difference, −0.26; 95% CI, −0.47 to −0.06; Chao1 SMD, −0.5; 95% CI, −0.79 to −0.21). On the other hand, when they examined each diagnosis separately, they found consistent decreases only in bipolar disorder. There was a small, nonsignificant decrease in phylogenetic diversity between groups.
MDD, psychosis, and schizophrenia were the only conditions in which differences in beta diversity were consistently observed.
“These findings suggest there is reliable evidence for differences in the shared phylogenetic structure in MDD and psychosis and schizophrenia compared with controls,” the authors write.
However, “method of measurement and method of patient classification (symptom vs. diagnosis based) may affect findings,” they added.
When they focused on relative abundance, they found “little evidence” of disorder specificity, but rather a “transdiagnostic pattern of microbiota signatures.”
In particular, depleted levels of Faecalibacterium and Coprococcus and enriched levels of Eggerthella were “consistently shared” between MDD, BD, psychosis and schizophrenia, and anxiety, “suggesting these disorders are characterized by a reduction of anti-inflammatory butyrate-producing bacteria, while proinflammatory genera are enriched.”
“The finding that these perturbations do not appear to be disorder-specific suggests that the microbiota is affected in a similar manner by conditions such as depression, anxiety, bipolar disorder, and psychosis,” said Ms. Nikolova.
“We have seen similar findings from previous meta-analyses of inflammatory marker studies and genetic studies, for example, suggesting that there is a biological overlap between these conditions, which we have now also seen in the microbiota.”
The authors highlighted potential confounders, including study region and medication use.
Conditions such as MDD, psychosis, and schizophrenia were “largely investigated in the East,” while anorexia nervosa and OCD were primarily investigated in the West.
Moreover, comparing results from medication-free studies with those in which 80% or more of patients were taking psychiatric medication showed increases in bacterial families Lactobacillaceae, Klebsiella, Streptococcus, and Megasphaera only in medicated groups, and decreases in Dialister.
In light of these confounders, the findings should be considered “preliminary,” the investigators noted.
Greater standardization needed
Commenting on the study, Emeran Mayer, MD, director of the Oppenheimer Center for Neurobiology of Stress and Resilience at the University of California, Los Angeles, said it is “intriguing to speculate that low-grade immune activation due to reduced production of butyrate may be such a generalized factor affecting microbial composition shared similarly in several brain disorders. However, such a mechanism has not been confirmed in mechanistic studies to date.”
In addition, the study “lumps together a large number of studies and heterogeneous patient populations, with and without centrally acting medication, without adequate dietary history, studied in different ethnic populations, studied with highly variable collection and analysis methods, including highly variable sample and study sizes for different diseases, and using only measures of microbial composition but not function,” cautioned Dr. Mayer, who was not involved in the research.
Future studies “with much greater standardization of subject populations and clinical and biological analyses techniques should be performed to reevaluate the results of the current study and confirm or reject the main hypotheses,” asserted Dr. Mayer, who is also the founding director of the UCLA Brain Gut Microbiome Center.
Ms. Nikolova is funded by a Medical Research Council PhD Studentship. Other sources of funding include the National Institute for Health Research Biomedical Research Centre at South London and Maudsley National Health Service Foundation Trust and King’s College London. Ms. Nikolova has disclosed no relevant financial relationships. Dr. Mayer is a scientific advisory board member of Danone, Axial Therapeutics, Viome, Amare, Mahana Therapeutics, Pendulum, Bloom Biosciences, and APC Microbiome Ireland.
A version of this article first appeared on Medscape.com .
Antipsychotics tied to increased breast cancer risk
Use of antipsychotics that increase prolactin levels is significantly associated with an increased risk for breast cancer in women with schizophrenia, new research suggests. However, at least one expert says that, at this point, clinical implications are premature.
Investigators compared data from Finnish nationwide registers on more than 30,000 women diagnosed with schizophrenia. Of those patients, 1,069 were diagnosed with breast cancer. Results showed that long-term exposure to prolactin-increasing antipsychotics was associated with a 56% increased risk of developing breast cancer in comparison with exposure of short duration. No significant association was found with cumulative exposure to prolactin-sparing antipsychotics.
“In case of planning for long-term antipsychotic [therapy], prefer non–prolactin-raising antipsychotics in females and inform patients about a potential risk to allow for informed shared decision-making,” study coauthor Christoph U. Correll, MD, professor of psychiatry and molecular medicine at Hofstra University, Hempstead, N.Y., told this news organization.
“ he said.
The study was published online Aug. 30, 2021, in The Lancet.
A ‘relevant contribution’
Breast cancer is 25% more prevalent among women with schizophrenia than among women in the general population. Antipsychotics have long been suspected as a potential culprit, but research results have been inconsistent, said Dr. Correll.
In addition, high concentrations of prolactin are associated with a higher risk of developing breast cancer, but most previous research did not distinguish between antipsychotics that increased prolactin levels those that did not.
Dr. Correll and colleagues “wanted to add to this literature by utilizing a generalizable nationwide sample with a sufficient large number of patients and sufficiently long follow-up to address the clinically very relevant question whether antipsychotic use could increase the risk of breast cancer.”
They also believed that grouping antipsychotics into prolactin-raising and non–prolactin-raising agents would be “a relevant contribution.”
The researchers drew on data from several large Finnish databases to conduct a nested case-control study of 30,785 women aged at least16 years who were diagnosed with schizophrenia between 1972 and 2014.
Of these patients, 1,069 received an initial diagnosis of invasive breast cancer (after being diagnosed with schizophrenia) between 2000 and 2017. These case patients were compared to 5,339 matched control patients. The mean age of the case patients and the control patients was 62 years. The mean time since initial diagnosis of schizophrenia was 24 years.
Antipsychotic use was divided into three periods: less than 1 year, 1-4 years, and ≥5 years. Antipsychotics were further divided into prolactin-increasing or prolactin-sparing drugs (for example, clozapine, quetiapine, or aripiprazole). Breast cancer was divided into either lobular or ductal adenocarcinoma.
In their statistical analyses, the researchers adjusted for an array of covariates, including previous diagnoses of other medical conditions, drugs that may modify the risk for breast cancer (for example, beta-blockers, calcium channel blockers, spironolactone, loop diuretics, and statins), substance misuse, suicide attempt, parity, and use of hormone replacement therapy (HRT).
‘Clinically meaningful’ risk
Ductal adenocarcinoma was more common than lobular adenocarcinoma (73% vs. 20% among case patients). A higher proportion of case patients used cardiovascular medications and HRT, compared with control patients.
A higher proportion of case patients had used prolactin-increasing antipsychotics for at least 5 years, compared with control patients (71.4% vs. 64.3%; adjusted odds ratio, 1.56; 95% CI, 1.27-1.92; P < .0001) in comparison with minimal exposure (<1 year) to prolactin-increasing antipsychotics.
On the other hand, a similar proportion of case patients and control patients used prolactin-sparing antipsychotics for at least 5 years (8.3 vs. 8.2%; aOR, 1.19; 95% CI, 0.90-1.58); the OR of 1.19 was not deemed significant.
Although exposure of ≥5 years to prolactin-increasing antipsychotics was associated with an increased risk for both types of adenocarcinoma, the risk was higher for lobular than for ductal disease (aOR, 2.36; 95% CI, 1.46-3.82 vs. aOR, 1.42; 95% CI, 1.12-1.80).
“Conservatively, if we subtract the 19% nonsignificantly increased odds with prolactin-sparing antipsychotics from the 56% significantly increased odds with prolactin-increasing antipsychotics, we obtain a 37% relative increase in odds,” the authors noted.
“Using a lifetime incidence of breast cancer in women in the general population of about 12%, with a somewhat higher lifetime incidence in patients with schizophrenia than the general population, this difference between prolactin-increasing versus prolactin-sparing antipsychotics in breast cancer risk upon exposure of 5 or more years would correspond to about a 4% (37% x 12%) increase in absolute breast cancer odds with prolactin-increasing antipsychotic treatment” – a difference the authors call “clinically meaningful.”
Correll noted that although the study was conducted in a Finnish population, the findings are generalizable to other populations.
Clinical implications premature?
Commenting on the study, Anton Pottegård, MScPharm, PhD, DMSc, professor of pharmacoepidemiology, department of public health, University of Southern Denmark, Odense, expressed concern that “this new study is fairly aggressive in its recommendation [that] we need to pay attention to hyperprolactinemia, as this seems to cause breast cancer.”
Dr. Pottegård, who is also the head of research, Hospital Pharmacy Funen, Odense University Hospital, who was not involved with the study, said he does not “think that the full body of the literature supports such a direct conclusion and/or direct inference to clinical practice.”
Although “this is an important study to further this work, I do not think we are at a place (yet) where it should lead to different action from clinicians,” Dr. Pottegård cautioned.
Also commenting on the study, Mary Seeman, MDCM, DSc, professor emeritus of neurosciences and clinical translation, department of psychiatry, University of Toronto, called the question of whether prolactin-increasing antipsychotics increase breast cancer risk “very complicated because the incidence of breast cancer ... is higher in women with schizophrenia than in other women.”
Dr. Seeman, who was not involved with the study, pointed to other reasons for the increased risk, including higher rates of obesity, substance abuse, cigarette smoking, stress, and sedentary behavior, all of which raise prolactin levels. Additionally, “protective factors such as pregnancies and breastfeeding are less frequent in women with schizophrenia than in their peers.” Women with schizophrenia also “tend not to do breast screening, see their doctors less often, follow doctors’ orders less rigorously, and obtain treatment less often.”
The take-home message “is to prescribe prolactin-sparing medication to women if at all possible – but until we know more, that is good advice, although not always possible because the illness for which the antipsychotics are prescribed may not respond to those particular medications,” Dr. Seeman said.
The study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital. Funding was also provided to individual researchers by the Academy of Finland, the Finnish Medical Foundation, and the Emil Aaltonen foundation. Dr. Correll has been a consultant or advisor to or has received honoraria from numerous companies. He has provided expert testimony for Janssen and Otsuka; received royalties from UpToDate and is a stock option holder of LB Pharma; served on a data safety monitoring board for Lundbeck, Rovi, Supernus, and Teva; and received grant support from Janssen and Takeda. Dr. Pottegård and Dr. Seeman disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of antipsychotics that increase prolactin levels is significantly associated with an increased risk for breast cancer in women with schizophrenia, new research suggests. However, at least one expert says that, at this point, clinical implications are premature.
Investigators compared data from Finnish nationwide registers on more than 30,000 women diagnosed with schizophrenia. Of those patients, 1,069 were diagnosed with breast cancer. Results showed that long-term exposure to prolactin-increasing antipsychotics was associated with a 56% increased risk of developing breast cancer in comparison with exposure of short duration. No significant association was found with cumulative exposure to prolactin-sparing antipsychotics.
“In case of planning for long-term antipsychotic [therapy], prefer non–prolactin-raising antipsychotics in females and inform patients about a potential risk to allow for informed shared decision-making,” study coauthor Christoph U. Correll, MD, professor of psychiatry and molecular medicine at Hofstra University, Hempstead, N.Y., told this news organization.
“ he said.
The study was published online Aug. 30, 2021, in The Lancet.
A ‘relevant contribution’
Breast cancer is 25% more prevalent among women with schizophrenia than among women in the general population. Antipsychotics have long been suspected as a potential culprit, but research results have been inconsistent, said Dr. Correll.
In addition, high concentrations of prolactin are associated with a higher risk of developing breast cancer, but most previous research did not distinguish between antipsychotics that increased prolactin levels those that did not.
Dr. Correll and colleagues “wanted to add to this literature by utilizing a generalizable nationwide sample with a sufficient large number of patients and sufficiently long follow-up to address the clinically very relevant question whether antipsychotic use could increase the risk of breast cancer.”
They also believed that grouping antipsychotics into prolactin-raising and non–prolactin-raising agents would be “a relevant contribution.”
The researchers drew on data from several large Finnish databases to conduct a nested case-control study of 30,785 women aged at least16 years who were diagnosed with schizophrenia between 1972 and 2014.
Of these patients, 1,069 received an initial diagnosis of invasive breast cancer (after being diagnosed with schizophrenia) between 2000 and 2017. These case patients were compared to 5,339 matched control patients. The mean age of the case patients and the control patients was 62 years. The mean time since initial diagnosis of schizophrenia was 24 years.
Antipsychotic use was divided into three periods: less than 1 year, 1-4 years, and ≥5 years. Antipsychotics were further divided into prolactin-increasing or prolactin-sparing drugs (for example, clozapine, quetiapine, or aripiprazole). Breast cancer was divided into either lobular or ductal adenocarcinoma.
In their statistical analyses, the researchers adjusted for an array of covariates, including previous diagnoses of other medical conditions, drugs that may modify the risk for breast cancer (for example, beta-blockers, calcium channel blockers, spironolactone, loop diuretics, and statins), substance misuse, suicide attempt, parity, and use of hormone replacement therapy (HRT).
‘Clinically meaningful’ risk
Ductal adenocarcinoma was more common than lobular adenocarcinoma (73% vs. 20% among case patients). A higher proportion of case patients used cardiovascular medications and HRT, compared with control patients.
A higher proportion of case patients had used prolactin-increasing antipsychotics for at least 5 years, compared with control patients (71.4% vs. 64.3%; adjusted odds ratio, 1.56; 95% CI, 1.27-1.92; P < .0001) in comparison with minimal exposure (<1 year) to prolactin-increasing antipsychotics.
On the other hand, a similar proportion of case patients and control patients used prolactin-sparing antipsychotics for at least 5 years (8.3 vs. 8.2%; aOR, 1.19; 95% CI, 0.90-1.58); the OR of 1.19 was not deemed significant.
Although exposure of ≥5 years to prolactin-increasing antipsychotics was associated with an increased risk for both types of adenocarcinoma, the risk was higher for lobular than for ductal disease (aOR, 2.36; 95% CI, 1.46-3.82 vs. aOR, 1.42; 95% CI, 1.12-1.80).
“Conservatively, if we subtract the 19% nonsignificantly increased odds with prolactin-sparing antipsychotics from the 56% significantly increased odds with prolactin-increasing antipsychotics, we obtain a 37% relative increase in odds,” the authors noted.
“Using a lifetime incidence of breast cancer in women in the general population of about 12%, with a somewhat higher lifetime incidence in patients with schizophrenia than the general population, this difference between prolactin-increasing versus prolactin-sparing antipsychotics in breast cancer risk upon exposure of 5 or more years would correspond to about a 4% (37% x 12%) increase in absolute breast cancer odds with prolactin-increasing antipsychotic treatment” – a difference the authors call “clinically meaningful.”
Correll noted that although the study was conducted in a Finnish population, the findings are generalizable to other populations.
Clinical implications premature?
Commenting on the study, Anton Pottegård, MScPharm, PhD, DMSc, professor of pharmacoepidemiology, department of public health, University of Southern Denmark, Odense, expressed concern that “this new study is fairly aggressive in its recommendation [that] we need to pay attention to hyperprolactinemia, as this seems to cause breast cancer.”
Dr. Pottegård, who is also the head of research, Hospital Pharmacy Funen, Odense University Hospital, who was not involved with the study, said he does not “think that the full body of the literature supports such a direct conclusion and/or direct inference to clinical practice.”
Although “this is an important study to further this work, I do not think we are at a place (yet) where it should lead to different action from clinicians,” Dr. Pottegård cautioned.
Also commenting on the study, Mary Seeman, MDCM, DSc, professor emeritus of neurosciences and clinical translation, department of psychiatry, University of Toronto, called the question of whether prolactin-increasing antipsychotics increase breast cancer risk “very complicated because the incidence of breast cancer ... is higher in women with schizophrenia than in other women.”
Dr. Seeman, who was not involved with the study, pointed to other reasons for the increased risk, including higher rates of obesity, substance abuse, cigarette smoking, stress, and sedentary behavior, all of which raise prolactin levels. Additionally, “protective factors such as pregnancies and breastfeeding are less frequent in women with schizophrenia than in their peers.” Women with schizophrenia also “tend not to do breast screening, see their doctors less often, follow doctors’ orders less rigorously, and obtain treatment less often.”
The take-home message “is to prescribe prolactin-sparing medication to women if at all possible – but until we know more, that is good advice, although not always possible because the illness for which the antipsychotics are prescribed may not respond to those particular medications,” Dr. Seeman said.
The study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital. Funding was also provided to individual researchers by the Academy of Finland, the Finnish Medical Foundation, and the Emil Aaltonen foundation. Dr. Correll has been a consultant or advisor to or has received honoraria from numerous companies. He has provided expert testimony for Janssen and Otsuka; received royalties from UpToDate and is a stock option holder of LB Pharma; served on a data safety monitoring board for Lundbeck, Rovi, Supernus, and Teva; and received grant support from Janssen and Takeda. Dr. Pottegård and Dr. Seeman disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Use of antipsychotics that increase prolactin levels is significantly associated with an increased risk for breast cancer in women with schizophrenia, new research suggests. However, at least one expert says that, at this point, clinical implications are premature.
Investigators compared data from Finnish nationwide registers on more than 30,000 women diagnosed with schizophrenia. Of those patients, 1,069 were diagnosed with breast cancer. Results showed that long-term exposure to prolactin-increasing antipsychotics was associated with a 56% increased risk of developing breast cancer in comparison with exposure of short duration. No significant association was found with cumulative exposure to prolactin-sparing antipsychotics.
“In case of planning for long-term antipsychotic [therapy], prefer non–prolactin-raising antipsychotics in females and inform patients about a potential risk to allow for informed shared decision-making,” study coauthor Christoph U. Correll, MD, professor of psychiatry and molecular medicine at Hofstra University, Hempstead, N.Y., told this news organization.
“ he said.
The study was published online Aug. 30, 2021, in The Lancet.
A ‘relevant contribution’
Breast cancer is 25% more prevalent among women with schizophrenia than among women in the general population. Antipsychotics have long been suspected as a potential culprit, but research results have been inconsistent, said Dr. Correll.
In addition, high concentrations of prolactin are associated with a higher risk of developing breast cancer, but most previous research did not distinguish between antipsychotics that increased prolactin levels those that did not.
Dr. Correll and colleagues “wanted to add to this literature by utilizing a generalizable nationwide sample with a sufficient large number of patients and sufficiently long follow-up to address the clinically very relevant question whether antipsychotic use could increase the risk of breast cancer.”
They also believed that grouping antipsychotics into prolactin-raising and non–prolactin-raising agents would be “a relevant contribution.”
The researchers drew on data from several large Finnish databases to conduct a nested case-control study of 30,785 women aged at least16 years who were diagnosed with schizophrenia between 1972 and 2014.
Of these patients, 1,069 received an initial diagnosis of invasive breast cancer (after being diagnosed with schizophrenia) between 2000 and 2017. These case patients were compared to 5,339 matched control patients. The mean age of the case patients and the control patients was 62 years. The mean time since initial diagnosis of schizophrenia was 24 years.
Antipsychotic use was divided into three periods: less than 1 year, 1-4 years, and ≥5 years. Antipsychotics were further divided into prolactin-increasing or prolactin-sparing drugs (for example, clozapine, quetiapine, or aripiprazole). Breast cancer was divided into either lobular or ductal adenocarcinoma.
In their statistical analyses, the researchers adjusted for an array of covariates, including previous diagnoses of other medical conditions, drugs that may modify the risk for breast cancer (for example, beta-blockers, calcium channel blockers, spironolactone, loop diuretics, and statins), substance misuse, suicide attempt, parity, and use of hormone replacement therapy (HRT).
‘Clinically meaningful’ risk
Ductal adenocarcinoma was more common than lobular adenocarcinoma (73% vs. 20% among case patients). A higher proportion of case patients used cardiovascular medications and HRT, compared with control patients.
A higher proportion of case patients had used prolactin-increasing antipsychotics for at least 5 years, compared with control patients (71.4% vs. 64.3%; adjusted odds ratio, 1.56; 95% CI, 1.27-1.92; P < .0001) in comparison with minimal exposure (<1 year) to prolactin-increasing antipsychotics.
On the other hand, a similar proportion of case patients and control patients used prolactin-sparing antipsychotics for at least 5 years (8.3 vs. 8.2%; aOR, 1.19; 95% CI, 0.90-1.58); the OR of 1.19 was not deemed significant.
Although exposure of ≥5 years to prolactin-increasing antipsychotics was associated with an increased risk for both types of adenocarcinoma, the risk was higher for lobular than for ductal disease (aOR, 2.36; 95% CI, 1.46-3.82 vs. aOR, 1.42; 95% CI, 1.12-1.80).
“Conservatively, if we subtract the 19% nonsignificantly increased odds with prolactin-sparing antipsychotics from the 56% significantly increased odds with prolactin-increasing antipsychotics, we obtain a 37% relative increase in odds,” the authors noted.
“Using a lifetime incidence of breast cancer in women in the general population of about 12%, with a somewhat higher lifetime incidence in patients with schizophrenia than the general population, this difference between prolactin-increasing versus prolactin-sparing antipsychotics in breast cancer risk upon exposure of 5 or more years would correspond to about a 4% (37% x 12%) increase in absolute breast cancer odds with prolactin-increasing antipsychotic treatment” – a difference the authors call “clinically meaningful.”
Correll noted that although the study was conducted in a Finnish population, the findings are generalizable to other populations.
Clinical implications premature?
Commenting on the study, Anton Pottegård, MScPharm, PhD, DMSc, professor of pharmacoepidemiology, department of public health, University of Southern Denmark, Odense, expressed concern that “this new study is fairly aggressive in its recommendation [that] we need to pay attention to hyperprolactinemia, as this seems to cause breast cancer.”
Dr. Pottegård, who is also the head of research, Hospital Pharmacy Funen, Odense University Hospital, who was not involved with the study, said he does not “think that the full body of the literature supports such a direct conclusion and/or direct inference to clinical practice.”
Although “this is an important study to further this work, I do not think we are at a place (yet) where it should lead to different action from clinicians,” Dr. Pottegård cautioned.
Also commenting on the study, Mary Seeman, MDCM, DSc, professor emeritus of neurosciences and clinical translation, department of psychiatry, University of Toronto, called the question of whether prolactin-increasing antipsychotics increase breast cancer risk “very complicated because the incidence of breast cancer ... is higher in women with schizophrenia than in other women.”
Dr. Seeman, who was not involved with the study, pointed to other reasons for the increased risk, including higher rates of obesity, substance abuse, cigarette smoking, stress, and sedentary behavior, all of which raise prolactin levels. Additionally, “protective factors such as pregnancies and breastfeeding are less frequent in women with schizophrenia than in their peers.” Women with schizophrenia also “tend not to do breast screening, see their doctors less often, follow doctors’ orders less rigorously, and obtain treatment less often.”
The take-home message “is to prescribe prolactin-sparing medication to women if at all possible – but until we know more, that is good advice, although not always possible because the illness for which the antipsychotics are prescribed may not respond to those particular medications,” Dr. Seeman said.
The study was funded by the Finnish Ministry of Social Affairs and Health through the developmental fund for Niuvanniemi Hospital. Funding was also provided to individual researchers by the Academy of Finland, the Finnish Medical Foundation, and the Emil Aaltonen foundation. Dr. Correll has been a consultant or advisor to or has received honoraria from numerous companies. He has provided expert testimony for Janssen and Otsuka; received royalties from UpToDate and is a stock option holder of LB Pharma; served on a data safety monitoring board for Lundbeck, Rovi, Supernus, and Teva; and received grant support from Janssen and Takeda. Dr. Pottegård and Dr. Seeman disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CBT via telehealth or in-person: Which is best for insomnia?
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
Telehealth can be effective for delivering cognitive-behavioral therapy for insomnia (CBT-I) – and is not inferior to in-person treatment, new research suggests.
Results from a study of 60 adults with insomnia disorder showed no significant between-group difference at 3-month follow-up between those assigned to receive in-person CBT-I and those assigned to telehealth CBT-I in regard to change in score on the Insomnia Severity Index (ISI).
In addition, both groups showed significant change compared with a wait-list group, indicating that telehealth was not inferior to the in-person mode of delivery, the investigators note.
“The take-home message is that patients with insomnia can be treated with cognitive-behavioral treatment for insomnia by video telehealth without sacrificing clinical gains,” study investigator Philip Gehrman, PhD, department of psychiatry, University of Pennsylvania, Philadelphia, told this news organization.
“This fits with the broader telehealth literature that has shown that other forms of therapy can be delivered this way without losing efficacy, so it is likely that telehealth is a viable option for therapy in general,” he said.
The findings were published online August 24 in The Journal of Clinical Psychiatry.
Telehealth ‘explosion’
Although CBT-I is the recommended intervention for insomnia, “widespread implementation of CBT-I is limited by the lack of clinicians who are trained in this treatment,” the investigators note. There is a “need for strategies to increase access, particularly for patients in areas with few health care providers.”
Telehealth is a promising technology for providing treatment, without the necessity of having the patient and the practitioner in the same place. There has been an “explosion” in its use because of restrictions necessitated by the COVID-19 pandemic. However, the “rapid deployment of telehealth interventions did not allow time to assess this approach in a controlled manner,” so it is possible that this type of communication might reduce treatment efficacy, the investigators note.
Previous research suggests that telehealth psychotherapeutic treatments in general are not inferior to in-person treatments. One study showed that CBT-I delivered via telehealth was noninferior to in-person delivery. However, that study did not include a control group.
“I have been doing telehealth clinical work for about 10 years – so way before the pandemic pushed everything virtual,” Dr. Gehrman said. “But when I would talk about my telehealth work to other providers, I would frequently get asked whether the advantages of telehealth (greater access to care, reduced travel costs) came at a price of lower efficacy.”
Dr. Gehrman said he suspected that telehealth treatment was just as effective and wanted to formally test this impression to see whether he was correct.
The investigators randomly assigned 60 adults (mean age, 32.72 years; mean ISI score, 17.0; 65% women) with insomnia disorder to in-person CBT-I (n = 20), telehealth-delivered CBT-I (n = 21), or to a wait-list control group (n = 19). For the study, insomnia disorder was determined on the basis of DSM-5 criteria.
Most participants had completed college or postgraduate school (43% and 37%, respectively) and did not have many comorbidities.
The primary outcome was change on the ISI. Other assessments included measures of depression, anxiety, work and social adjustment, fatigue, and medical outcomes. Participants also completed a home unattended sleep study using a portable monitor to screen participants for obstructive sleep apnea.
Both types of CBT-I were delivered over 6 to 8 weekly sessions, with 2-week and 3-month post-treatment follow-ups.
An a priori margin of -3.0 points was used in the noninferiority analysis, and all analyses were conducted using mixed-effects models, the authors explain.
Necessary evil?
In the primary noninferiority analyses, the mean change in ISI score from baseline to 3-month follow-up was -7.8 points for in-person CBT-I, -7.5 points for telehealth, and -1.6 for wait list.
The difference between the CBT-I groups was not statistically significant (t 28 = -0.98, P = .33).
“The lower confidence limit of this between-group difference in the mean ISI changes was greater than the a priori margin of -3.0 points, indicating that telehealth treatment was not inferior to in-person treatment,” the investigators write.
Although there were significant improvements on most secondary outcome measures related to mood/anxiety and daytime functioning, the investigators found no group differences.
The findings suggest that the benefits of telehealth, including increased access and reduced travel time, “do not come with a cost of reduced efficacy,” the researchers write.
However, the results “underscore that the use of telehealth during the pandemic is not a ‘necessary evil,’ but rather a means of providing high quality care while reducing risks of exposure,” they write.
Benefits, fidelity maintained
Commenting on the study, J. Todd Arnedt, PhD, professor of psychiatry and neurology and co-director of the Sleep and Circadian Research Laboratory, Michigan Medicine, University of Michigan, Ann Arbor, said it is “one of the first studies to clearly demonstrate that the benefits and fidelity of CBT for insomnia, which is most commonly delivered in-person, can be maintained with telehealth delivery.”
Dr. Arnedt is also director of the Behavioral Sleep Medicine Program and was not involved in the study. He said the findings “support the use of this modality by providers to expand access to this highly effective but underutilized insomnia treatment.”
Additionally, telehealth delivery of CBT-I “offers a safe and effective alternative to in-person care for improving insomnia and associated daytime consequences and has the potential to reduce health care disparities by increasing availability to underserved communities,” Dr. Arnedt said.
However, the investigators point out that the utility of this approach for underserved communities needs further investigation. A study limitation was that the participants were “generally healthy and well educated.”
In addition, further research is needed to see whether the findings can be generalized to individuals who have “more complicated health or socioeconomic difficulties,” they write.
The study was funded by a grant from the American Sleep Medicine Foundation and the Doris Duke Charitable Foundation Clinical Scientist Development Award. Dr. Gehrman has received research funding from Merck, is a consultant to WW, and serves on the scientific advisory board of Eight Sleep. The other authors’ disclosures are listed in the original article. Dr. Arnedt reports no relevant financial relationships but notes that he was the principal investigator of a similar study run in parallel to this one that was also funded by the American Academy of Sleep Medicine Foundation at the same time.
A version of this article first appeared on Medscape.com.
The trauma and healing of 9/11 echo in COVID-19
The scope and magnitude of the Sept. 11, 2001, attacks on the World Trade Center and the Pentagon were unprecedented in U.S. history. It was arguably the most serious trauma to beset Americans on U.S. soil. The 20th anniversary of 9/11 will take place during another crisis, not only in American history but also in world history – the COVID-19 pandemic.

“As different as these two events are, there are obvious points of comparison,” Jonathan DePierro, PhD, assistant professor of psychiatry, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Both were unprecedented life-threatening situations, presenting threats to individuals’ lives and profoundly traumatizing not only society as a whole but also first responders.”
Dr. DePierro, who is also the clinical director of the Center for Stress, Resilience, and Personal Growth at Mount Sinai, thinks there are many lessons to be learned from the mental health response to 9/11 that can inform our understanding of and response to the mental health needs of today’s first responders in the COVID-19 crisis, particularly health care professionals.
“Every one of our hospitals became a ‘ground zero’ early during the pandemic, and we see the numbers rising again and hospitals again overwhelmed, so he said.
Placing trauma within a new framework
According to Priscilla Dass-Brailsford, EdD, MPH, professor of psychology, department of psychiatry, Georgetown University, Washington, Sept. 11, 2001, “placed trauma within a new framework.”
“Prior to 9/11, crisis protocols and how to manage stress in the aftermath of violent events were uncommon,” Dr. Dass-Brailsford, a clinical psychologist with expertise in trauma who also chairs a clinical psychology program for the Chicago School of Professional Psychology, said in an interview.
As a first responder, she was involved in early interventions for survivors of 9/11. On Sept. 11, 2001, she had just resigned her position as coordinator of the community crisis response team – the first of its kind in the United States – through the Victims of Violence Program in Cambridge, in Cambridge, Mass.
The program responded to communities in which there were high rates of drive-by shootings and similar acts of violence. Because of her crisis experience, Dr. Dass-Brailsford was asked to conduct debriefings in Boston in the area where the 9/11 terrorists had stayed prior to boarding the planes that were used in the terrorist attacks. She subsequently went to New York City to conduct similar psychological debriefings with affected communities.
“What we’ve learned is that we had no crisis protocol on how to manage the stress in the aftermath of such a violent event, no standard operating procedures. There were very few people trained in crisis and trauma response at that time. Partially spurred by 9/11, trauma training programs became more prolific,” she said. Dr. Dass-Brailsford developed a trauma certification program at Lesley University in Cambridge, Mass., where she began to teach after 9/11. “I saw the importance of having clinicians trained to respond in a crisis, because responding to a crisis is very different from conducting regular mental health interventions.”
Short- and long-term interventions
Dr. DePierro said that Mount Sinai has a 20-year history of responding to the physical and mental health needs of 9/11 responders.
“We saw a number of first responders experiencing clinical depression, anxiety, a lot of worry, symptoms of posttraumatic stress disorder, and an increase in alcohol and/or substance use,” he recounted. In some, these responses were immediate; in others, the onset of symptoms was more gradual. Some responders had acute reactions that lasted for several months to a year, whereas for others, the reactions were prolonged, and they remained “chronically distressed long after the immediate exposure to the event,” he said.
Recent studies have shown that, during the COVID-19 pandemic, health care professionals and many essential workers have experienced similar symptoms, Dr. DePierro noted.
Mental health care professionals who provided interventions for workers involved in recovery and cleanup at the World Trade Center have highlighted the need for long-term monitoring of people on the front lines during the COVID-19 pandemic – especially health care workers, other essential personnel (for example, delivery, postal, and grocery store workers) and surviving family members. “Health monitoring and treatment efforts for 9/11 survivors and responders were put into place soon after the attacks and continue to this day,” using funding provided through the James Zadroga Act, Dr. DePierro said.
“Without similarly unified health registry and treatment services, many individuals – especially from underserved groups – will likely experience chronic mental health consequences and will be unable to access high-quality health care services,” he stated.
‘Psychological first aid’
“Although many people who go through a crisis – whether as a result of terrorism, such as 9/11, or a medical crisis, such as the current pandemic, or a natural disaster, such as Hurricane Katrina – experience PTSD, it’s important to note that not everyone who goes through a crisis and is traumatized will go on to develop PTSD,” Dr. Dass-Brailsford emphasized.
“To me, 9/11 placed psychological first aid on the map. Even if you are not a clinician, you can be trained to provide psychological first aid by becoming familiar with people’s reactions to trauma and how you can support them through it,” she continued.
For example, if a coworker is agitated or “seems to be having a meltdown, you can be there by offering support and getting them the appropriate help.” Research has suggested that having social support before and after a traumatic event can be helpful in determining vulnerability to the development of PTSD and in modulating the impact of the trauma.
Psychological first aid is helpful as an interim measure. “If you see a coworker holding their head in their hands all day and staring at the screen, identifying whether the person might be having a dissociative episode is critical. Providing some support is important, but if more intensive professional support is needed, determining that and making a referral becomes key,” Dr. Dass-Brailsford stated.
Dr. DePierro added: “One of the most important messages that I want health care workers to know from my years of working with 9/11 survivors is that feeling distressed after a traumatic event is very common, but with effective care, one doesn’t necessarily need to be in treatment for years.”
Danielle Ofri, MD, PhD, clinical professor, department of medicine, New York University, agreed. “It is important to continue keeping tabs on each other and remaining sensitive to the collateral struggles of our colleagues. Some have children who are struggling in school, others have parents who have lost a job. Continuing to check in on others and offer support is critical going forward,” she said in an interview.
Cohesiveness and volunteerism
One of the most powerful antidotes to long-term traumatization is a sense of community cohesiveness. This was the case following 9/11, and it is the case during the COVID-19 pandemic, according to Dr. Ofri, an internist at Bellevue Hospital in New York.
“There was an enormous mobilization. Bellevue is a city hospital with a level 1 trauma center, and we expected to be swamped, so the whole hospital shifted into gear,” said Dr. Ofri. “What would have been terrifying seemed tolerable because we felt that we were in it together. We discharged the inpatients to make beds available. Within hours, we had converted clinics into emergency departments and ICUs. We worked seamlessly, and the crisis brought us together ... but then, of course, no patients showed up.”
She described her relationship with her colleagues as “feeling almost like a family, especially during the pandemic, when so many others were in lockdown and feeling isolated and useless.”
She and her colleagues saw each other daily. Although the content of their tasks and responsibilities changed and people were redeployed to other areas, “our workday didn’t really change. It would have been overwhelming if we hadn’t had our daily meetings to regroup and assess where we were. Each day, everything we had learned or implemented the day before – treatment protocols, testing protocols, our understanding of how the virus was communicated – would change and need to be reevaluated. Those morning meetings were critical to staying centered. It felt as though we were building a plane and flying it at the same time, which felt both scary and heady. Luckily, it took place within the fraternity of a committed and caring group.”
Dr. Ofri recounted that, after 9/11, as well as during the pandemic, “professionals kept jumping in from the sidelines to volunteer. Within hours of the collapse of the towers, the ED had filled with staff. People came out of retirement and out from vacation and out of the woodwork. It was very heartening.”
Even more inspiring, “all the departmental barriers seemed to break down. People were willing to step out of their ordinary roles and check their egos at the door. Seasoned physicians were willing to function as medical interns.”
This generosity of time and spirit “helped keep us going,” she said.
Dr. DePierro agreed. “One of the things I’ve seen on medical floors is that COVID actually brought some units together, increasing their cohesion and mutual support and increasing the bonds between people.” These intensified bonds “increased the resilience of everyone involved.”
Commitment to the community
Dr. Ofri recalls families gathering at the hospital after 9/11, watching posters of missing people going up all over the hospital as well as on mailboxes and lampposts. Because the center for missing people was located right next door to Bellevue, there were long lines of families coming in to register. The chief medical office was there, and a huge tent was built to accommodate the families. The tent took up the entire block. “We felt a lot of ownership, because families were coming here,” she said.
The street remained closed even as the days, weeks, and years stretched on, and the tent remained. It was used as a reflection area for families. During the pandemic, that area was used for refrigerated trucks that served as temporary morgues.
“Both logistically and emotionally, we had a feeling during the pandemic of, ‘We’ve been here before, we’ll do it again and be there for the community,’ ” Dr. Ofri said.
She noted that the sense of commitment to the community carried her and fellow clinicians through the toughest parts of 9/11 and of the COVID-19 pandemic.
“People look to the medical system as a lodestar. ‘Where’s my family member? What should I do? Should I be tested? Vaccinated?’ We were there to be a steady presence for the community physically, psychologically, emotionally, and medically, which helped center us as well,” Dr. Ofri said. “If we didn’t have that, we might have all given in to existential panic.”
She added: “Although we had to work twice as hard, often amid great personal risk, we had the good fortune of having a sense of purpose, something to contribute, plus the community of colleagues we cared about and trusted with our lives.”
Crisis and personal growth
Dr. DePierro said that participants who went through 9/11 have been coming to Mount Sinai’s World Trade Center Health Program for care for nearly two decades. “Many are doing quite well, despite the emotional trauma and the dust and toxin exposure, which has given us a window into what makes people resilient.”
Social and community support are key factors in resilience. Another is recognizing opportunities for personal or professional growth during the crisis, according to Dr. DePierro.
During the pandemic, hospital staff were redeployed to departments where they didn’t typically work. They worked with new colleagues and used skills in patient care that they hadn’t needed for years or even decades. “Although this was stressful and distressing, quite a number said they came through with more medical knowledge than before and that they had forged relationships in the trenches that have been lasting and have become important to them,” he reported.
He noted that, during both crises, for first responders and health care practitioners, religious or spiritual faith was a source of resilience. “During the peak of the pandemic, chaplains provided an exorbitant amount of staff support as clinicians turned to the chaplain to help make sense of what they were going through and connect to something greater than themselves.” Similarly, during 9/11, police and fire department chaplains “played a huge role in supporting the first responders,” Dr. DePierro said.
He said that Mount Sinai holds resilience workshops “where we focus on these topics and teach health care workers how to build resilience in their lives, heal day-to-day stressors, and even grow from the experience.”
Dr. Ofri, who is the founder and editor-in-chief of the Bellevue Literary Review, added that the arts played an important role in bolstering resilience and providing a creative outlet for clinicians after 9/11 and again during the pandemic.
The publication is celebrating its twentieth anniversary – its first issue went to press in September 2001. The cover contained an acknowledgment of 9/11.
Dr. Ofri said that a gala event had been planned for Oct. 7, 2001, to celebrate the inaugural issue of the publication. She assumed no one would show up, given that the United States had invaded Afghanistan only hours earlier. To her surprise, over a hundred people attended, “which made me realize the role of the arts during trauma. People were seeking to come together and hear poetry, fiction, and creative nonfiction.”
Dr. Ofri has been “impressed by the amount of incredible creative writing of all sorts that has been submitted [to the publication] during the pandemic, an unexpected flowering of the arts.”
Unique challenges, unique opportunities
All three experts pointed to several noteworthy differences between the experiences of first responders following 9/11 and those of today’s health care professionals during the pandemic.
“What happened on Sept. 11 was one discrete event, and although it obviously led to years of recovering body parts and cleaning up Ground Zero, and on a national level it led to a war, it nevertheless was a single event,” Dr. DePierro observed. By contrast, the COVID-19 pandemic is ongoing, and for health care practitioners, “it’s by no means over. Again and again, they are being thrown back into battle, dealing with fatigue, weariness, and loss of life.”
Moreover, “it is my understanding that immediately following 9/11, there was a general coming together in our country, but it’s obvious that today, there’s a great deal of fractiousness, contention, disagreement, and disunity in our country when it comes to COVID-19,” Dr. DePierro continued.
“This takes a great toll, particularly on health care workers who are dealing with COVID-19 on a daily basis and experience a disconnect between what they see on their floors and ICUs of the hospital, experiencing loss of life they’ve likely never encountered in their careers, and what people are saying when they downplay the seriousness of COVID-19,” he said.
Dr. Ofri agreed. “The fragmentation of our country and the failure of leadership at the highest level to provide even the basics, such as PPE [personal protective equipment] for health care professionals, left us baffled, profoundly hurt, and angry.”
A positive difference between the COVID-19 pandemic and the aftermath of 9/11 is the development of sophisticated technology that allows interventions for traumatized individuals – both health care professionals and the general public – through telehealth, Dr. DePierro pointed out.
“I would say that these resources and technologies are a silver lining and should continue to be expanded on,” he said. “Now, busy health care workers can access all manner of supportive services, including teletherapy, right from home or between shifts.”
Another “silver lining” is that the pandemic has shone a spotlight on an issue that predated the pandemic – the mental health of health care professionals. Opening a discussion about this has reduced stigma and hopefully has paved the way for improved treatments and for providing resources.
Dr. Dass-Brailsford added that “it is important, going forward, for all of us to be trauma informed, to know how trauma and trauma-related stress unfolds in both other people and yourself, and to know what coping skills can be used to avoid crises from developing – a task that extends across all types of disasters.”
A version of this article first appeared on Medscape.com.
The scope and magnitude of the Sept. 11, 2001, attacks on the World Trade Center and the Pentagon were unprecedented in U.S. history. It was arguably the most serious trauma to beset Americans on U.S. soil. The 20th anniversary of 9/11 will take place during another crisis, not only in American history but also in world history – the COVID-19 pandemic.

“As different as these two events are, there are obvious points of comparison,” Jonathan DePierro, PhD, assistant professor of psychiatry, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Both were unprecedented life-threatening situations, presenting threats to individuals’ lives and profoundly traumatizing not only society as a whole but also first responders.”
Dr. DePierro, who is also the clinical director of the Center for Stress, Resilience, and Personal Growth at Mount Sinai, thinks there are many lessons to be learned from the mental health response to 9/11 that can inform our understanding of and response to the mental health needs of today’s first responders in the COVID-19 crisis, particularly health care professionals.
“Every one of our hospitals became a ‘ground zero’ early during the pandemic, and we see the numbers rising again and hospitals again overwhelmed, so he said.
Placing trauma within a new framework
According to Priscilla Dass-Brailsford, EdD, MPH, professor of psychology, department of psychiatry, Georgetown University, Washington, Sept. 11, 2001, “placed trauma within a new framework.”
“Prior to 9/11, crisis protocols and how to manage stress in the aftermath of violent events were uncommon,” Dr. Dass-Brailsford, a clinical psychologist with expertise in trauma who also chairs a clinical psychology program for the Chicago School of Professional Psychology, said in an interview.
As a first responder, she was involved in early interventions for survivors of 9/11. On Sept. 11, 2001, she had just resigned her position as coordinator of the community crisis response team – the first of its kind in the United States – through the Victims of Violence Program in Cambridge, in Cambridge, Mass.
The program responded to communities in which there were high rates of drive-by shootings and similar acts of violence. Because of her crisis experience, Dr. Dass-Brailsford was asked to conduct debriefings in Boston in the area where the 9/11 terrorists had stayed prior to boarding the planes that were used in the terrorist attacks. She subsequently went to New York City to conduct similar psychological debriefings with affected communities.
“What we’ve learned is that we had no crisis protocol on how to manage the stress in the aftermath of such a violent event, no standard operating procedures. There were very few people trained in crisis and trauma response at that time. Partially spurred by 9/11, trauma training programs became more prolific,” she said. Dr. Dass-Brailsford developed a trauma certification program at Lesley University in Cambridge, Mass., where she began to teach after 9/11. “I saw the importance of having clinicians trained to respond in a crisis, because responding to a crisis is very different from conducting regular mental health interventions.”
Short- and long-term interventions
Dr. DePierro said that Mount Sinai has a 20-year history of responding to the physical and mental health needs of 9/11 responders.
“We saw a number of first responders experiencing clinical depression, anxiety, a lot of worry, symptoms of posttraumatic stress disorder, and an increase in alcohol and/or substance use,” he recounted. In some, these responses were immediate; in others, the onset of symptoms was more gradual. Some responders had acute reactions that lasted for several months to a year, whereas for others, the reactions were prolonged, and they remained “chronically distressed long after the immediate exposure to the event,” he said.
Recent studies have shown that, during the COVID-19 pandemic, health care professionals and many essential workers have experienced similar symptoms, Dr. DePierro noted.
Mental health care professionals who provided interventions for workers involved in recovery and cleanup at the World Trade Center have highlighted the need for long-term monitoring of people on the front lines during the COVID-19 pandemic – especially health care workers, other essential personnel (for example, delivery, postal, and grocery store workers) and surviving family members. “Health monitoring and treatment efforts for 9/11 survivors and responders were put into place soon after the attacks and continue to this day,” using funding provided through the James Zadroga Act, Dr. DePierro said.
“Without similarly unified health registry and treatment services, many individuals – especially from underserved groups – will likely experience chronic mental health consequences and will be unable to access high-quality health care services,” he stated.
‘Psychological first aid’
“Although many people who go through a crisis – whether as a result of terrorism, such as 9/11, or a medical crisis, such as the current pandemic, or a natural disaster, such as Hurricane Katrina – experience PTSD, it’s important to note that not everyone who goes through a crisis and is traumatized will go on to develop PTSD,” Dr. Dass-Brailsford emphasized.
“To me, 9/11 placed psychological first aid on the map. Even if you are not a clinician, you can be trained to provide psychological first aid by becoming familiar with people’s reactions to trauma and how you can support them through it,” she continued.
For example, if a coworker is agitated or “seems to be having a meltdown, you can be there by offering support and getting them the appropriate help.” Research has suggested that having social support before and after a traumatic event can be helpful in determining vulnerability to the development of PTSD and in modulating the impact of the trauma.
Psychological first aid is helpful as an interim measure. “If you see a coworker holding their head in their hands all day and staring at the screen, identifying whether the person might be having a dissociative episode is critical. Providing some support is important, but if more intensive professional support is needed, determining that and making a referral becomes key,” Dr. Dass-Brailsford stated.
Dr. DePierro added: “One of the most important messages that I want health care workers to know from my years of working with 9/11 survivors is that feeling distressed after a traumatic event is very common, but with effective care, one doesn’t necessarily need to be in treatment for years.”
Danielle Ofri, MD, PhD, clinical professor, department of medicine, New York University, agreed. “It is important to continue keeping tabs on each other and remaining sensitive to the collateral struggles of our colleagues. Some have children who are struggling in school, others have parents who have lost a job. Continuing to check in on others and offer support is critical going forward,” she said in an interview.
Cohesiveness and volunteerism
One of the most powerful antidotes to long-term traumatization is a sense of community cohesiveness. This was the case following 9/11, and it is the case during the COVID-19 pandemic, according to Dr. Ofri, an internist at Bellevue Hospital in New York.
“There was an enormous mobilization. Bellevue is a city hospital with a level 1 trauma center, and we expected to be swamped, so the whole hospital shifted into gear,” said Dr. Ofri. “What would have been terrifying seemed tolerable because we felt that we were in it together. We discharged the inpatients to make beds available. Within hours, we had converted clinics into emergency departments and ICUs. We worked seamlessly, and the crisis brought us together ... but then, of course, no patients showed up.”
She described her relationship with her colleagues as “feeling almost like a family, especially during the pandemic, when so many others were in lockdown and feeling isolated and useless.”
She and her colleagues saw each other daily. Although the content of their tasks and responsibilities changed and people were redeployed to other areas, “our workday didn’t really change. It would have been overwhelming if we hadn’t had our daily meetings to regroup and assess where we were. Each day, everything we had learned or implemented the day before – treatment protocols, testing protocols, our understanding of how the virus was communicated – would change and need to be reevaluated. Those morning meetings were critical to staying centered. It felt as though we were building a plane and flying it at the same time, which felt both scary and heady. Luckily, it took place within the fraternity of a committed and caring group.”
Dr. Ofri recounted that, after 9/11, as well as during the pandemic, “professionals kept jumping in from the sidelines to volunteer. Within hours of the collapse of the towers, the ED had filled with staff. People came out of retirement and out from vacation and out of the woodwork. It was very heartening.”
Even more inspiring, “all the departmental barriers seemed to break down. People were willing to step out of their ordinary roles and check their egos at the door. Seasoned physicians were willing to function as medical interns.”
This generosity of time and spirit “helped keep us going,” she said.
Dr. DePierro agreed. “One of the things I’ve seen on medical floors is that COVID actually brought some units together, increasing their cohesion and mutual support and increasing the bonds between people.” These intensified bonds “increased the resilience of everyone involved.”
Commitment to the community
Dr. Ofri recalls families gathering at the hospital after 9/11, watching posters of missing people going up all over the hospital as well as on mailboxes and lampposts. Because the center for missing people was located right next door to Bellevue, there were long lines of families coming in to register. The chief medical office was there, and a huge tent was built to accommodate the families. The tent took up the entire block. “We felt a lot of ownership, because families were coming here,” she said.
The street remained closed even as the days, weeks, and years stretched on, and the tent remained. It was used as a reflection area for families. During the pandemic, that area was used for refrigerated trucks that served as temporary morgues.
“Both logistically and emotionally, we had a feeling during the pandemic of, ‘We’ve been here before, we’ll do it again and be there for the community,’ ” Dr. Ofri said.
She noted that the sense of commitment to the community carried her and fellow clinicians through the toughest parts of 9/11 and of the COVID-19 pandemic.
“People look to the medical system as a lodestar. ‘Where’s my family member? What should I do? Should I be tested? Vaccinated?’ We were there to be a steady presence for the community physically, psychologically, emotionally, and medically, which helped center us as well,” Dr. Ofri said. “If we didn’t have that, we might have all given in to existential panic.”
She added: “Although we had to work twice as hard, often amid great personal risk, we had the good fortune of having a sense of purpose, something to contribute, plus the community of colleagues we cared about and trusted with our lives.”
Crisis and personal growth
Dr. DePierro said that participants who went through 9/11 have been coming to Mount Sinai’s World Trade Center Health Program for care for nearly two decades. “Many are doing quite well, despite the emotional trauma and the dust and toxin exposure, which has given us a window into what makes people resilient.”
Social and community support are key factors in resilience. Another is recognizing opportunities for personal or professional growth during the crisis, according to Dr. DePierro.
During the pandemic, hospital staff were redeployed to departments where they didn’t typically work. They worked with new colleagues and used skills in patient care that they hadn’t needed for years or even decades. “Although this was stressful and distressing, quite a number said they came through with more medical knowledge than before and that they had forged relationships in the trenches that have been lasting and have become important to them,” he reported.
He noted that, during both crises, for first responders and health care practitioners, religious or spiritual faith was a source of resilience. “During the peak of the pandemic, chaplains provided an exorbitant amount of staff support as clinicians turned to the chaplain to help make sense of what they were going through and connect to something greater than themselves.” Similarly, during 9/11, police and fire department chaplains “played a huge role in supporting the first responders,” Dr. DePierro said.
He said that Mount Sinai holds resilience workshops “where we focus on these topics and teach health care workers how to build resilience in their lives, heal day-to-day stressors, and even grow from the experience.”
Dr. Ofri, who is the founder and editor-in-chief of the Bellevue Literary Review, added that the arts played an important role in bolstering resilience and providing a creative outlet for clinicians after 9/11 and again during the pandemic.
The publication is celebrating its twentieth anniversary – its first issue went to press in September 2001. The cover contained an acknowledgment of 9/11.
Dr. Ofri said that a gala event had been planned for Oct. 7, 2001, to celebrate the inaugural issue of the publication. She assumed no one would show up, given that the United States had invaded Afghanistan only hours earlier. To her surprise, over a hundred people attended, “which made me realize the role of the arts during trauma. People were seeking to come together and hear poetry, fiction, and creative nonfiction.”
Dr. Ofri has been “impressed by the amount of incredible creative writing of all sorts that has been submitted [to the publication] during the pandemic, an unexpected flowering of the arts.”
Unique challenges, unique opportunities
All three experts pointed to several noteworthy differences between the experiences of first responders following 9/11 and those of today’s health care professionals during the pandemic.
“What happened on Sept. 11 was one discrete event, and although it obviously led to years of recovering body parts and cleaning up Ground Zero, and on a national level it led to a war, it nevertheless was a single event,” Dr. DePierro observed. By contrast, the COVID-19 pandemic is ongoing, and for health care practitioners, “it’s by no means over. Again and again, they are being thrown back into battle, dealing with fatigue, weariness, and loss of life.”
Moreover, “it is my understanding that immediately following 9/11, there was a general coming together in our country, but it’s obvious that today, there’s a great deal of fractiousness, contention, disagreement, and disunity in our country when it comes to COVID-19,” Dr. DePierro continued.
“This takes a great toll, particularly on health care workers who are dealing with COVID-19 on a daily basis and experience a disconnect between what they see on their floors and ICUs of the hospital, experiencing loss of life they’ve likely never encountered in their careers, and what people are saying when they downplay the seriousness of COVID-19,” he said.
Dr. Ofri agreed. “The fragmentation of our country and the failure of leadership at the highest level to provide even the basics, such as PPE [personal protective equipment] for health care professionals, left us baffled, profoundly hurt, and angry.”
A positive difference between the COVID-19 pandemic and the aftermath of 9/11 is the development of sophisticated technology that allows interventions for traumatized individuals – both health care professionals and the general public – through telehealth, Dr. DePierro pointed out.
“I would say that these resources and technologies are a silver lining and should continue to be expanded on,” he said. “Now, busy health care workers can access all manner of supportive services, including teletherapy, right from home or between shifts.”
Another “silver lining” is that the pandemic has shone a spotlight on an issue that predated the pandemic – the mental health of health care professionals. Opening a discussion about this has reduced stigma and hopefully has paved the way for improved treatments and for providing resources.
Dr. Dass-Brailsford added that “it is important, going forward, for all of us to be trauma informed, to know how trauma and trauma-related stress unfolds in both other people and yourself, and to know what coping skills can be used to avoid crises from developing – a task that extends across all types of disasters.”
A version of this article first appeared on Medscape.com.
The scope and magnitude of the Sept. 11, 2001, attacks on the World Trade Center and the Pentagon were unprecedented in U.S. history. It was arguably the most serious trauma to beset Americans on U.S. soil. The 20th anniversary of 9/11 will take place during another crisis, not only in American history but also in world history – the COVID-19 pandemic.

“As different as these two events are, there are obvious points of comparison,” Jonathan DePierro, PhD, assistant professor of psychiatry, Icahn School of Medicine at Mount Sinai, New York, said in an interview. “Both were unprecedented life-threatening situations, presenting threats to individuals’ lives and profoundly traumatizing not only society as a whole but also first responders.”
Dr. DePierro, who is also the clinical director of the Center for Stress, Resilience, and Personal Growth at Mount Sinai, thinks there are many lessons to be learned from the mental health response to 9/11 that can inform our understanding of and response to the mental health needs of today’s first responders in the COVID-19 crisis, particularly health care professionals.
“Every one of our hospitals became a ‘ground zero’ early during the pandemic, and we see the numbers rising again and hospitals again overwhelmed, so he said.
Placing trauma within a new framework
According to Priscilla Dass-Brailsford, EdD, MPH, professor of psychology, department of psychiatry, Georgetown University, Washington, Sept. 11, 2001, “placed trauma within a new framework.”
“Prior to 9/11, crisis protocols and how to manage stress in the aftermath of violent events were uncommon,” Dr. Dass-Brailsford, a clinical psychologist with expertise in trauma who also chairs a clinical psychology program for the Chicago School of Professional Psychology, said in an interview.
As a first responder, she was involved in early interventions for survivors of 9/11. On Sept. 11, 2001, she had just resigned her position as coordinator of the community crisis response team – the first of its kind in the United States – through the Victims of Violence Program in Cambridge, in Cambridge, Mass.
The program responded to communities in which there were high rates of drive-by shootings and similar acts of violence. Because of her crisis experience, Dr. Dass-Brailsford was asked to conduct debriefings in Boston in the area where the 9/11 terrorists had stayed prior to boarding the planes that were used in the terrorist attacks. She subsequently went to New York City to conduct similar psychological debriefings with affected communities.
“What we’ve learned is that we had no crisis protocol on how to manage the stress in the aftermath of such a violent event, no standard operating procedures. There were very few people trained in crisis and trauma response at that time. Partially spurred by 9/11, trauma training programs became more prolific,” she said. Dr. Dass-Brailsford developed a trauma certification program at Lesley University in Cambridge, Mass., where she began to teach after 9/11. “I saw the importance of having clinicians trained to respond in a crisis, because responding to a crisis is very different from conducting regular mental health interventions.”
Short- and long-term interventions
Dr. DePierro said that Mount Sinai has a 20-year history of responding to the physical and mental health needs of 9/11 responders.
“We saw a number of first responders experiencing clinical depression, anxiety, a lot of worry, symptoms of posttraumatic stress disorder, and an increase in alcohol and/or substance use,” he recounted. In some, these responses were immediate; in others, the onset of symptoms was more gradual. Some responders had acute reactions that lasted for several months to a year, whereas for others, the reactions were prolonged, and they remained “chronically distressed long after the immediate exposure to the event,” he said.
Recent studies have shown that, during the COVID-19 pandemic, health care professionals and many essential workers have experienced similar symptoms, Dr. DePierro noted.
Mental health care professionals who provided interventions for workers involved in recovery and cleanup at the World Trade Center have highlighted the need for long-term monitoring of people on the front lines during the COVID-19 pandemic – especially health care workers, other essential personnel (for example, delivery, postal, and grocery store workers) and surviving family members. “Health monitoring and treatment efforts for 9/11 survivors and responders were put into place soon after the attacks and continue to this day,” using funding provided through the James Zadroga Act, Dr. DePierro said.
“Without similarly unified health registry and treatment services, many individuals – especially from underserved groups – will likely experience chronic mental health consequences and will be unable to access high-quality health care services,” he stated.
‘Psychological first aid’
“Although many people who go through a crisis – whether as a result of terrorism, such as 9/11, or a medical crisis, such as the current pandemic, or a natural disaster, such as Hurricane Katrina – experience PTSD, it’s important to note that not everyone who goes through a crisis and is traumatized will go on to develop PTSD,” Dr. Dass-Brailsford emphasized.
“To me, 9/11 placed psychological first aid on the map. Even if you are not a clinician, you can be trained to provide psychological first aid by becoming familiar with people’s reactions to trauma and how you can support them through it,” she continued.
For example, if a coworker is agitated or “seems to be having a meltdown, you can be there by offering support and getting them the appropriate help.” Research has suggested that having social support before and after a traumatic event can be helpful in determining vulnerability to the development of PTSD and in modulating the impact of the trauma.
Psychological first aid is helpful as an interim measure. “If you see a coworker holding their head in their hands all day and staring at the screen, identifying whether the person might be having a dissociative episode is critical. Providing some support is important, but if more intensive professional support is needed, determining that and making a referral becomes key,” Dr. Dass-Brailsford stated.
Dr. DePierro added: “One of the most important messages that I want health care workers to know from my years of working with 9/11 survivors is that feeling distressed after a traumatic event is very common, but with effective care, one doesn’t necessarily need to be in treatment for years.”
Danielle Ofri, MD, PhD, clinical professor, department of medicine, New York University, agreed. “It is important to continue keeping tabs on each other and remaining sensitive to the collateral struggles of our colleagues. Some have children who are struggling in school, others have parents who have lost a job. Continuing to check in on others and offer support is critical going forward,” she said in an interview.
Cohesiveness and volunteerism
One of the most powerful antidotes to long-term traumatization is a sense of community cohesiveness. This was the case following 9/11, and it is the case during the COVID-19 pandemic, according to Dr. Ofri, an internist at Bellevue Hospital in New York.
“There was an enormous mobilization. Bellevue is a city hospital with a level 1 trauma center, and we expected to be swamped, so the whole hospital shifted into gear,” said Dr. Ofri. “What would have been terrifying seemed tolerable because we felt that we were in it together. We discharged the inpatients to make beds available. Within hours, we had converted clinics into emergency departments and ICUs. We worked seamlessly, and the crisis brought us together ... but then, of course, no patients showed up.”
She described her relationship with her colleagues as “feeling almost like a family, especially during the pandemic, when so many others were in lockdown and feeling isolated and useless.”
She and her colleagues saw each other daily. Although the content of their tasks and responsibilities changed and people were redeployed to other areas, “our workday didn’t really change. It would have been overwhelming if we hadn’t had our daily meetings to regroup and assess where we were. Each day, everything we had learned or implemented the day before – treatment protocols, testing protocols, our understanding of how the virus was communicated – would change and need to be reevaluated. Those morning meetings were critical to staying centered. It felt as though we were building a plane and flying it at the same time, which felt both scary and heady. Luckily, it took place within the fraternity of a committed and caring group.”
Dr. Ofri recounted that, after 9/11, as well as during the pandemic, “professionals kept jumping in from the sidelines to volunteer. Within hours of the collapse of the towers, the ED had filled with staff. People came out of retirement and out from vacation and out of the woodwork. It was very heartening.”
Even more inspiring, “all the departmental barriers seemed to break down. People were willing to step out of their ordinary roles and check their egos at the door. Seasoned physicians were willing to function as medical interns.”
This generosity of time and spirit “helped keep us going,” she said.
Dr. DePierro agreed. “One of the things I’ve seen on medical floors is that COVID actually brought some units together, increasing their cohesion and mutual support and increasing the bonds between people.” These intensified bonds “increased the resilience of everyone involved.”
Commitment to the community
Dr. Ofri recalls families gathering at the hospital after 9/11, watching posters of missing people going up all over the hospital as well as on mailboxes and lampposts. Because the center for missing people was located right next door to Bellevue, there were long lines of families coming in to register. The chief medical office was there, and a huge tent was built to accommodate the families. The tent took up the entire block. “We felt a lot of ownership, because families were coming here,” she said.
The street remained closed even as the days, weeks, and years stretched on, and the tent remained. It was used as a reflection area for families. During the pandemic, that area was used for refrigerated trucks that served as temporary morgues.
“Both logistically and emotionally, we had a feeling during the pandemic of, ‘We’ve been here before, we’ll do it again and be there for the community,’ ” Dr. Ofri said.
She noted that the sense of commitment to the community carried her and fellow clinicians through the toughest parts of 9/11 and of the COVID-19 pandemic.
“People look to the medical system as a lodestar. ‘Where’s my family member? What should I do? Should I be tested? Vaccinated?’ We were there to be a steady presence for the community physically, psychologically, emotionally, and medically, which helped center us as well,” Dr. Ofri said. “If we didn’t have that, we might have all given in to existential panic.”
She added: “Although we had to work twice as hard, often amid great personal risk, we had the good fortune of having a sense of purpose, something to contribute, plus the community of colleagues we cared about and trusted with our lives.”
Crisis and personal growth
Dr. DePierro said that participants who went through 9/11 have been coming to Mount Sinai’s World Trade Center Health Program for care for nearly two decades. “Many are doing quite well, despite the emotional trauma and the dust and toxin exposure, which has given us a window into what makes people resilient.”
Social and community support are key factors in resilience. Another is recognizing opportunities for personal or professional growth during the crisis, according to Dr. DePierro.
During the pandemic, hospital staff were redeployed to departments where they didn’t typically work. They worked with new colleagues and used skills in patient care that they hadn’t needed for years or even decades. “Although this was stressful and distressing, quite a number said they came through with more medical knowledge than before and that they had forged relationships in the trenches that have been lasting and have become important to them,” he reported.
He noted that, during both crises, for first responders and health care practitioners, religious or spiritual faith was a source of resilience. “During the peak of the pandemic, chaplains provided an exorbitant amount of staff support as clinicians turned to the chaplain to help make sense of what they were going through and connect to something greater than themselves.” Similarly, during 9/11, police and fire department chaplains “played a huge role in supporting the first responders,” Dr. DePierro said.
He said that Mount Sinai holds resilience workshops “where we focus on these topics and teach health care workers how to build resilience in their lives, heal day-to-day stressors, and even grow from the experience.”
Dr. Ofri, who is the founder and editor-in-chief of the Bellevue Literary Review, added that the arts played an important role in bolstering resilience and providing a creative outlet for clinicians after 9/11 and again during the pandemic.
The publication is celebrating its twentieth anniversary – its first issue went to press in September 2001. The cover contained an acknowledgment of 9/11.
Dr. Ofri said that a gala event had been planned for Oct. 7, 2001, to celebrate the inaugural issue of the publication. She assumed no one would show up, given that the United States had invaded Afghanistan only hours earlier. To her surprise, over a hundred people attended, “which made me realize the role of the arts during trauma. People were seeking to come together and hear poetry, fiction, and creative nonfiction.”
Dr. Ofri has been “impressed by the amount of incredible creative writing of all sorts that has been submitted [to the publication] during the pandemic, an unexpected flowering of the arts.”
Unique challenges, unique opportunities
All three experts pointed to several noteworthy differences between the experiences of first responders following 9/11 and those of today’s health care professionals during the pandemic.
“What happened on Sept. 11 was one discrete event, and although it obviously led to years of recovering body parts and cleaning up Ground Zero, and on a national level it led to a war, it nevertheless was a single event,” Dr. DePierro observed. By contrast, the COVID-19 pandemic is ongoing, and for health care practitioners, “it’s by no means over. Again and again, they are being thrown back into battle, dealing with fatigue, weariness, and loss of life.”
Moreover, “it is my understanding that immediately following 9/11, there was a general coming together in our country, but it’s obvious that today, there’s a great deal of fractiousness, contention, disagreement, and disunity in our country when it comes to COVID-19,” Dr. DePierro continued.
“This takes a great toll, particularly on health care workers who are dealing with COVID-19 on a daily basis and experience a disconnect between what they see on their floors and ICUs of the hospital, experiencing loss of life they’ve likely never encountered in their careers, and what people are saying when they downplay the seriousness of COVID-19,” he said.
Dr. Ofri agreed. “The fragmentation of our country and the failure of leadership at the highest level to provide even the basics, such as PPE [personal protective equipment] for health care professionals, left us baffled, profoundly hurt, and angry.”
A positive difference between the COVID-19 pandemic and the aftermath of 9/11 is the development of sophisticated technology that allows interventions for traumatized individuals – both health care professionals and the general public – through telehealth, Dr. DePierro pointed out.
“I would say that these resources and technologies are a silver lining and should continue to be expanded on,” he said. “Now, busy health care workers can access all manner of supportive services, including teletherapy, right from home or between shifts.”
Another “silver lining” is that the pandemic has shone a spotlight on an issue that predated the pandemic – the mental health of health care professionals. Opening a discussion about this has reduced stigma and hopefully has paved the way for improved treatments and for providing resources.
Dr. Dass-Brailsford added that “it is important, going forward, for all of us to be trauma informed, to know how trauma and trauma-related stress unfolds in both other people and yourself, and to know what coping skills can be used to avoid crises from developing – a task that extends across all types of disasters.”
A version of this article first appeared on Medscape.com.
Early data for experimental THC drug ‘promising’ for Tourette’s
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Oral delta-9-tetrahydracannabinol (delta-9-THC) and palmitoylethanolamide (PEA), in a proprietary combination known as THX-110, is promising for reducing tic symptoms in adults with Tourette syndrome (TS), new research suggests.
In a small phase 2 trial, investigators administered THX-110 to 16 adults with treatment-resistant TS for 12 weeks. Results showed a reduction of more than 20% in tic symptoms after the first week of treatment compared with baseline.
“We conducted an uncontrolled study in adults with severe TS and found that their tics improved over time while they took THX-110,” lead author Michael Bloch, MD, associate professor and co-director of the Tic and OCD Program at the Child Study Center, Yale University, New Haven, Conn., told this news organization.
Dr. Bloch added that the next step in this line of research will be to conduct a placebo-controlled trial of the compound in order to assess whether tic improvement observed over time in this study “was due to the effects of the medication and not related to the natural waxing-and-waning course of tic symptoms or treatment expectancy.”
The findings were published online August 2 in the Journal of Neuropsychiatry and Clinical Neurosciences.
‘Entourage effect’
“Several lines of evidence from clinical observation and even randomized controlled trials” suggest that cannabis (cannabis sativa) and delta-9-THC may be effective in treatment of tic disorders, Dr. Bloch said.
“Cannabinoid receptors are present in the motor regions important for tics, and thus, there is a potential mechanism of action to lead to improvement of tics,” he added.
However, “the major limitations of both cannabis and dronabinol [a synthetic form of delta-9-THC] use are the adverse psychoactive effects they induce in higher doses,” he said.
Dr. Bloch noted that PEA is a lipid messenger “known to mimic several endocannabinoid-driven activities.”
For this reason, combining delta-9-THC with PEA is hypothesized to reduce the dose of delta-9-THC needed to improve tics and also potentially lessen its side effects.
This initial open-label trial examined safety and tolerability of THX-110, as well as its effect on tic symptoms in adults with TS. The researchers hoped to “use the entourage effect to deliver the therapeutic benefits of delta-9-THC in reducing tics with decrease psychoactive effects by combining with PEA.”
The “entourage effect” refers to “endocannabinoid regulation by which multiple endogenous cannabinoid chemical species display a cooperative effect in eliciting a cellular response,” they write.
The investigators conducted a 12-week uncontrolled trial of THX-110, used at its maximum daily dose of delta-9-THC (10 mg) and a constant 800-mg dose of PEA in 16 adults with TS (mean age, 35 years; mean TS illness duration, 26.6 years).
Participants had a mean baseline Yale Global Tic Severity Scale (YGTSS) score of 38.1 and a mean worst-ever total tic score of 45.4.
All participants were experiencing persistent tics, despite having tried an array of previous evidence-based treatments for TS, including antipsychotics, alpha-2 agonists, VMAT2 inhibitors, benzodiazepines, and topiramate (Topamax).
Significant improvement
Results showed significant improvement in tic symptoms with TXH-110 treatment over time (general linear model time factor: F = 3.06, df = 7.91, P = .006).
At first assessment point, mean YGTSS improvement was 3.5 (95% confidence interval, 0.1-6.9; P = .047). The improvement not only remained significant but continued to increase throughout the 12-week trial period.
At 12 weeks, the maximal improvement in tic symptoms was observed, with a mean YGTSS improvement at endpoint of 7.6 (95% CI, 2.5-12.8; P = .007).
Four patients experienced a greater than 35% improvement in tic symptoms during the trial, whereas 6 experienced a 25% or greater improvement. The mean improvement in tic symptoms over the course of the trial was 20.6%.
There was also a significant improvement between baseline and endpoint on other measures of tic symptoms – but not on premonitory urges.
The patients experienced “modest” but not significant improvement in comorbid symptoms, including attentional, anxiety, depressive, and obsessive-compulsive symptoms.
Adverse events
All participants experienced some mild side effects for “a couple hours” after taking the medication, particularly during the course of dose escalation and maintenance. However, these were not serious enough to warrant stopping the medication.
These effects typically included fatigue/drowsiness, feeling “high,” dry mouth, dizziness/lightheadedness, and difficulty concentrating.
Side effects of moderate or greater severity necessitating changes in medication dosing were “less common,” the investigators report. No participants experienced significant laboratory abnormalities.
One patient discontinued the trial early because he felt that the study medication was not helpful, and a second discontinued because of drowsiness and fatigue related to the study medication.
Twelve participants elected to continue treatment with THX-110 during an open extension phase and 7 of these completed the additional 24 weeks.
“THX-110 treatment led to an average improvement in tic symptoms of roughly 20%, or a 7-point decrease in the YGTSS total tic score. This improvement translates to a large effect size (d = 0.92) of improvement over time,” the investigators write.
More data needed
Commenting on the findings, Yolanda Holler-Managan, MD, assistant professor of pediatrics (neurology), Northwestern University, Chicago, cautioned that this was not a randomized, double-blind, parallel-group placebo-controlled study.
Instead, it was a clinical study to prove safety, tolerability, and dosing of the combination medication in adult patients with TS and “does not provide as much weight, since we do not have many studies on the efficacy of cannabinoids,” said Dr. Holler-Managan, who was not involved with the research.
She noted that the American Academy of Neurology’s 2019 practice guideline recommendations for treatment of tics in individuals with TS and tic disorders reported “limited evidence” that delta-9-THC is “possibly more likely than placebo to reduce tic severity in adults with TS, therefore we need more data.”
The current investigators agree. “Although these initial data are promising, future randomized double-blind placebo-controlled trials are necessary to demonstrate efficacy of TXH-110 treatment,” they write.
They add that the psychoactive properties of cannabis-derived compounds make it challenging to design a properly blinded trial.
“Incorporation of physiologic biomarkers and objective measures of symptoms (e.g., videotaped tic counts by blinded raters) may be particularly important when examining these medications with psychoactive properties that may be prone to reporting bias,” the authors write.
The study was supported by an investigator-initiated grant to Dr. Bloch from Therapix Biosciences. The state of Connecticut also provided resource support via the Abraham Ribicoff Research Facilities at the Connecticut Mental Health Center. Dr. Bloch serves on the scientific advisory boards of Therapix Biosciences, and he receives research support from Biohaven Pharmaceuticals, Janssen Pharmaceuticals, NARSAD, Neurocrine Biosciences, NIH, and the Patterson Foundation. The other investigators and Dr. Holler-Managan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Low depression scores may miss seniors with suicidal intent
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
‘Reassuring’ findings for second-generation antipsychotics during pregnancy
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Second-generation antipsychotics (SGAs) taken by pregnant women are linked to a low rate of adverse effects in their children, new research suggests.
Data from a large registry study of almost 2,000 women showed that 2.5% of the live births in a group that had been exposed to antipsychotics had confirmed major malformations compared with 2% of the live births in a non-exposed group. This translated into an estimated odds ratio of 1.5 for major malformations.
“The 2.5% absolute risk for major malformations is consistent with the estimates of the Centers for Disease Control and Prevention’s national baseline rate of major malformations in the general population,” lead author Adele Viguera, MD, MPH, director of research for women’s mental health, Cleveland Clinic Neurological Institute, told this news organization.
“Our results are reassuring and suggest that second-generation antipsychotics, as a class, do not substantially increase the risk of major malformations,” Dr. Viguera said.
The findings were published online August 3 in the Journal of Clinical Psychiatry.
Safety data scarce
Despite the increasing use of SGAs to treat a “spectrum of psychiatric disorders,” relatively little data are available on the reproductive safety of these agents, Dr. Viguera said.
The National Pregnancy Registry for Atypical Antipsychotics (NPRAA) was established in 2008 to determine risk for major malformation among infants exposed to these medications during the first trimester, relative to a comparison group of unexposed infants of mothers with histories of psychiatric morbidity.
The NPRAA follows pregnant women (aged 18 to 45 years) with psychiatric illness who are exposed or unexposed to SGAs during pregnancy. Participants are recruited through nationwide provider referral, self-referral, and advertisement through the Massachusetts General Hospital Center for Women’s Mental Health website.
Specific data collected are shown in the following table.
Since publication of the first results in 2015, the sample size for the trial has increased – and the absolute and relative risk for major malformations observed in the study population are “more precise,” the investigators note. The current study presented updated previous findings.
Demographic differences
Of the 1,906 women who enrolled as of April 2020, 1,311 (mean age, 32.6 years; 81.3% White) completed the study and were eligible for inclusion in the analysis.
Although the groups had a virtually identical mean age, fewer women in the exposure group were married compared with those in the non-exposure group (77% vs. 90%, respectively) and fewer had a college education (71.2% vs. 87.8%). There was also a higher percentage of first-trimester cigarette smokers in the exposure group (18.4% vs. 5.1%).
On the other hand, more women in the non-exposure group used alcohol than in the exposure group (28.6% vs. 21.4%, respectively).
The most frequent psychiatric disorder in the exposure group was bipolar disorder (63.9%), followed by major depression (12.9%), anxiety (5.8%), and schizophrenia (4.5%). Only 11.4% of women in the non-exposure group were diagnosed with bipolar disorder, whereas 34.1% were diagnosed with major depression, 31.3% with anxiety, and none with schizophrenia.
Notably, a large percentage of women in both groups had a history of postpartum depression and/or psychosis (41.4% and 35.5%, respectively).
The most frequently used SGAs in the exposure group were quetiapine (Seroquel), aripiprazole (Abilify), and lurasidone (Latuda).
Participants in the exposure group had a higher age at initial onset of primary psychiatric diagnosis and a lower proportion of lifetime illness compared with those in the non-exposure group.
Major clinical implication?
Among 640 live births in the exposure group, which included 17 twin pregnancies and 1 triplet pregnancy, 2.5% reported major malformations. Among 704 live births in the control group, which included 14 twin pregnancies, 1.99% reported major malformations.
The estimated OR for major malformations comparing exposed and unexposed infants was 1.48 (95% confidence interval, 0.625-3.517).
The authors note that their findings were consistent with one of the largest studies to date, which included a nationwide sample of more than 1 million women. Its results showed that, among infants exposed to SGAs versus those who were not exposed, the estimated risk ratio after adjusting for psychiatric conditions was 1.05 (95% CI, 0.96-1.16).
Additionally, “a hallmark of a teratogen is that it tends to cause a specific type or pattern of malformations, and we found no preponderance of one single type of major malformation or specific pattern of malformations among the exposed and unexposed groups,” Dr. Viguera said
“A major clinical implication of these findings is that for women with major mood and/or psychotic disorders, treatment with an atypical antipsychotic during pregnancy may be the most prudent clinical decision, much as continued treatment is recommended for pregnant women with other serious and chronic medical conditions, such as epilepsy,” she added.
The concept of ‘satisficing’
Commenting on the study, Vivien Burt, MD, PhD, founder and director/consultant of the Women’s Life Center at the Resnick University of California, Los Angeles (UCLA) Neuropsychiatric Hospital, called the findings “reassuring.”
The results “support the conclusion that in pregnant women with serious psychiatric illnesses, the use of SGAs is often a better option than avoiding these medications and exposing both the women and their offspring to the adverse consequences of maternal mental illness,” she said.
An accompanying editorial co-authored by Dr. Burt and colleague Sonya Rasminsky, MD, introduced the concept of “satisficing” – a term coined by Herbert Simon, a behavioral economist and Nobel Laureate. “Satisficing” is a “decision-making strategy that aims for a satisfactory (‘good enough’) outcome rather than a perfect one.”
The concept applies to decision-making beyond the field of economics “and is critical to how physicians help patients make decisions when they are faced with multiple treatment options,” said Dr. Burt, a professor emeritus of psychiatry at UCLA.
“The goal of ‘satisficing’ is to plan for the most satisfactory outcome, knowing that there are always unknowns, so in an uncertain world, clinicians should carefully help their patients make decisions that will allow them to achieve an outcome they can best live with,” she noted.
The investigators note that their findings may not be generalizable to the larger population of women taking SGAs, given that their participants were “overwhelmingly White, married, and well-educated women.”
They add that enrollment into the NPRAA registry is ongoing and larger sample sizes will “further narrow the confidence interval around the risk estimates and allow for adjustment of likely sources of confounding.”
The NPRAA is supported by Alkermes, Johnson & Johnson/Janssen Pharmaceuticals, Otsuka America Pharmaceutical, Sunovion Pharmaceuticals, SAGE Therapeutics, Teva Pharmaceuticals, and Aurobindo Pharma. Past sponsors of the NPRAA are listed in the original paper. Dr. Viguera receives research support from the NPRAA, Alkermes Biopharmaceuticals, Aurobindo Pharma, Janssen Pharmaceuticals, Otsuka Pharmaceutical, Sunovion Pharmaceuticals, Teva Pharmaceuticals, and SAGE Therapeutics and receives adviser/consulting fees from Up-to-Date. Dr. Burt has been a consultant/speaker for Sage Therapeutics. Dr. Rasminsky has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Short-term approach is best for seizure prevention after intracerebral hemorrhage
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
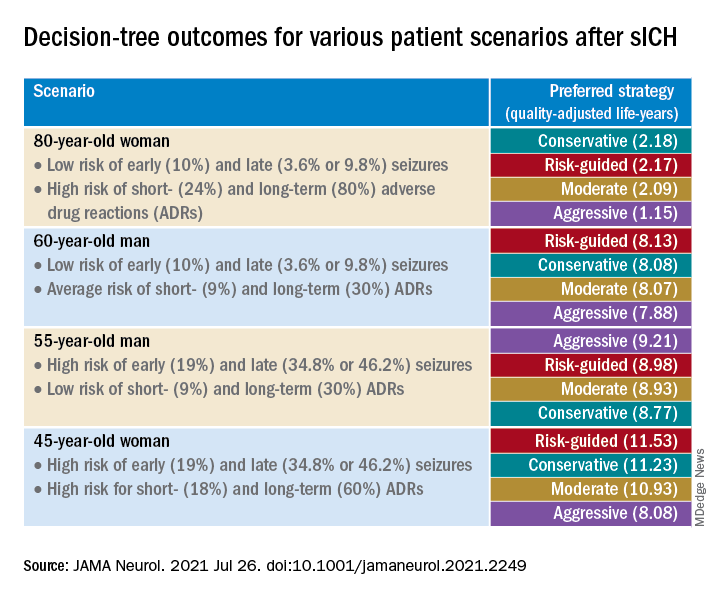
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
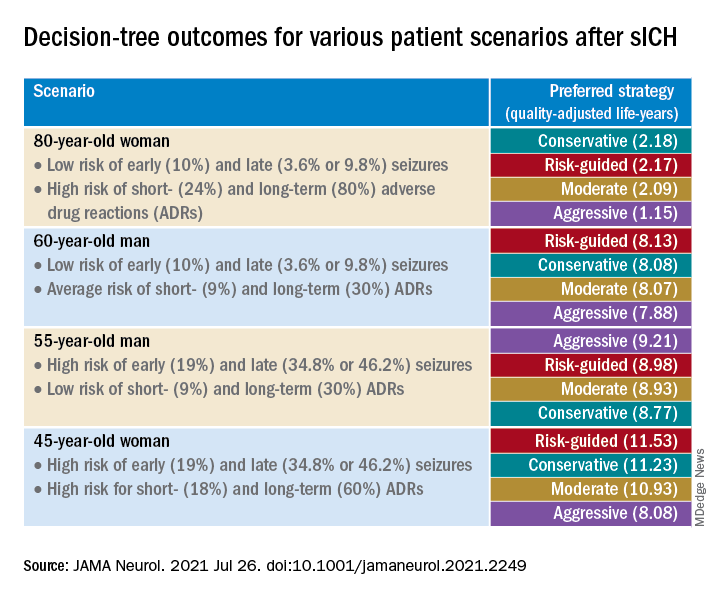
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
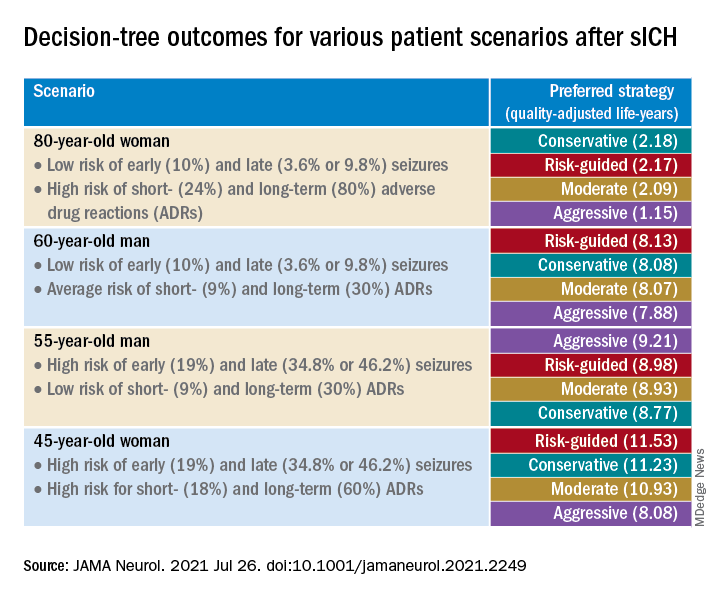
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
Even 10 minutes of daily exercise beneficial after ICD implantation
Small increases in daily physical activity are associated with a boost in 1-year survival in patients with heart failure and coronary disease who received an implantable cardioverter defibrillator (ICD), new research suggests.
“Our study looked at how much exercise was necessary for a better outcome in patients with prior ICD implantation and, for every 10 minutes of exercise, we saw a 1% reduction in the likelihood of death or hospitalization, which is a pretty profound impact on outcome for just a small amount of additional physical activity per day,” lead author Brett Atwater, MD, told this news organization.
“These improvements were achieved outside of a formal cardiac rehabilitation program, suggesting that the benefits of increased physical activity obtained in cardiac rehabilitation programs may also be achievable at home,” he said.
Cardiac rehabilitation (CR) programs have been shown to improve short- and long-term outcomes in patients with heart failure (HF) but continue to be underutilized, especially by women, the elderly, and minorities. Home-based CR could help overcome this limitation but the science behind it is relatively new, noted Dr. Atwater, director of electrophysiology and electrophysiology research, Inova Heart and Vascular Institute, Fairfax, Va.
As reported in Circulation Cardiovascular Quality and Outcomes, the study involved 41,731 Medicare beneficiaries (mean age, 73.5 years) who received an ICD from 2014 to 2016.
ICD heart rate and activity sensor measurements were used to establish a personalized physical activity (PA) threshold for each patient in the first 3 weeks after ICD implantation. Thereafter, the ICD logged PA when the personalized PA threshold was exceeded. The mean baseline PA level was 128.9 minutes/day.
At 3 years’ follow-up, one-quarter of the patients had died and half had been hospitalized for HF. Of the total population, only 3.2% participated in CR.
Compared with nonparticipants, CR participants were more likely to be White (91.0% versus 87.3%), male (75.5% versus 72.2%), and to have diabetes (48.8% versus 44.1%), ischemic heart disease (91.4% versus 82.1%), or congestive heart failure (90.4% versus 83.4%).
CR participants attended a median of 24 sessions, during which time daily PA increased by a mean of 9.7 minutes per day. During the same time, PA decreased by a mean of 1.0 minute per day in non-CR participants (P < .001).
PA levels remained “relatively constant” for the first 36 months of follow-up among CR participants before showing a steep decline, whereas levels gradually declined throughout follow-up among nonparticipants, with a median annual change of –4.5 min/day.
In adjusted analysis, every 10 minutes of increased daily PA was associated with a 1.1% reduced risk for death (hazard ratio, 0.989; 95% confidence interval, 0.979-0.996) and a 1% reduced risk for HF hospitalization (HR, 0.99; 95% CI, 0.986-0.995) at 1-year follow-up (P < .001).
After propensity score was used to match CR participants with nonparticipants by demographic characteristics, comorbidities, and baseline PA level, CR participants had a significantly lower risk for death at 1 year (HR, 0.76; 95% CI, 0.69-0.85). This difference in risk remained at 2- and 3-year follow-ups.
However, when the researchers further adjusted for change in PA during CR or the same time period after device implantation, no differences in mortality were found between CR participants and nonparticipants at 1 year (HR, 1.00; 95% CI, 0.82-1.21) or at 2 or 3 years.
The risk for HF hospitalization did not differ between the two groups in either propensity score model.
Unlike wearable devices, implanted devices “don’t give that type of feedback to patients regarding PA levels – only to providers – and it will be interesting to discover whether providing feedback to patients can motivate them to do more physical activity,” Dr. Atwater commented.
The team is currently enrolling patients in a follow-up trial, in which patients will be given feedback from their ICD “to move these data from an interesting observation to something that can drive outcomes,” he said.
Commenting for this news organization, Melissa Tracy, MD, Rush University Medical Center, Chicago, said the study reiterates the “profound” underutilization of CR.
“Only about 3% of patients who should have qualified for cardiac rehabilitation actually attended, which is startling considering that it has class 1A level of evidence supporting its use,” she said.
Dr. Tracy, who is also a member of the American College of Cardiology’s Prevention of Cardiovascular Disease Section Leadership Council, described the study as “another notch in the belt of positive outcomes supporting the need for cardiac rehabilitation” and emphasizing the importance of a home-based alternative.
“One of the reasons women, minorities, and older patients don’t go to cardiac rehabilitation is they have to get there, rely on someone to drive them, or they have other responsibilities – especially women, who are often primary caretakers of others,” she said. “For women and men, the pressure to get back to work and support their families means they don’t have the luxury to go to cardiac rehabilitation.”
Dr. Tracy noted that home-based CR is covered by CMS until the end of 2021. “An important take-home is for providers and patients to understand that they do have a home-based option,” she stated.
Limitations of the study are that only 24% of patients were women, only 6% were Black, and the results might not be generalizable to patients younger than 65 years, note Dr. Atwater and colleagues. Also, previous implantation might have protected the cohort from experiencing arrhythmic death, and it remains unclear if similar results would be obtained in patients without a previous ICD.
This research was funded through the unrestricted Abbott Medical-Duke Health Strategic Alliance Research Grant. Dr. Atwater receives significant research support from Boston Scientific and Abbott Medical, and modest honoraria from Abbott Medical, Medtronic, and Biotronik. Coauthor disclosures are listed in the paper. Dr. Tracy has created cardiac prevention programs with Virtual Health Partners (VHP) and owns the intellectual property and consults with VHP but receives no monetary compensation.
A version of this article first appeared on Medscape.com.
Small increases in daily physical activity are associated with a boost in 1-year survival in patients with heart failure and coronary disease who received an implantable cardioverter defibrillator (ICD), new research suggests.
“Our study looked at how much exercise was necessary for a better outcome in patients with prior ICD implantation and, for every 10 minutes of exercise, we saw a 1% reduction in the likelihood of death or hospitalization, which is a pretty profound impact on outcome for just a small amount of additional physical activity per day,” lead author Brett Atwater, MD, told this news organization.
“These improvements were achieved outside of a formal cardiac rehabilitation program, suggesting that the benefits of increased physical activity obtained in cardiac rehabilitation programs may also be achievable at home,” he said.
Cardiac rehabilitation (CR) programs have been shown to improve short- and long-term outcomes in patients with heart failure (HF) but continue to be underutilized, especially by women, the elderly, and minorities. Home-based CR could help overcome this limitation but the science behind it is relatively new, noted Dr. Atwater, director of electrophysiology and electrophysiology research, Inova Heart and Vascular Institute, Fairfax, Va.
As reported in Circulation Cardiovascular Quality and Outcomes, the study involved 41,731 Medicare beneficiaries (mean age, 73.5 years) who received an ICD from 2014 to 2016.
ICD heart rate and activity sensor measurements were used to establish a personalized physical activity (PA) threshold for each patient in the first 3 weeks after ICD implantation. Thereafter, the ICD logged PA when the personalized PA threshold was exceeded. The mean baseline PA level was 128.9 minutes/day.
At 3 years’ follow-up, one-quarter of the patients had died and half had been hospitalized for HF. Of the total population, only 3.2% participated in CR.
Compared with nonparticipants, CR participants were more likely to be White (91.0% versus 87.3%), male (75.5% versus 72.2%), and to have diabetes (48.8% versus 44.1%), ischemic heart disease (91.4% versus 82.1%), or congestive heart failure (90.4% versus 83.4%).
CR participants attended a median of 24 sessions, during which time daily PA increased by a mean of 9.7 minutes per day. During the same time, PA decreased by a mean of 1.0 minute per day in non-CR participants (P < .001).
PA levels remained “relatively constant” for the first 36 months of follow-up among CR participants before showing a steep decline, whereas levels gradually declined throughout follow-up among nonparticipants, with a median annual change of –4.5 min/day.
In adjusted analysis, every 10 minutes of increased daily PA was associated with a 1.1% reduced risk for death (hazard ratio, 0.989; 95% confidence interval, 0.979-0.996) and a 1% reduced risk for HF hospitalization (HR, 0.99; 95% CI, 0.986-0.995) at 1-year follow-up (P < .001).
After propensity score was used to match CR participants with nonparticipants by demographic characteristics, comorbidities, and baseline PA level, CR participants had a significantly lower risk for death at 1 year (HR, 0.76; 95% CI, 0.69-0.85). This difference in risk remained at 2- and 3-year follow-ups.
However, when the researchers further adjusted for change in PA during CR or the same time period after device implantation, no differences in mortality were found between CR participants and nonparticipants at 1 year (HR, 1.00; 95% CI, 0.82-1.21) or at 2 or 3 years.
The risk for HF hospitalization did not differ between the two groups in either propensity score model.
Unlike wearable devices, implanted devices “don’t give that type of feedback to patients regarding PA levels – only to providers – and it will be interesting to discover whether providing feedback to patients can motivate them to do more physical activity,” Dr. Atwater commented.
The team is currently enrolling patients in a follow-up trial, in which patients will be given feedback from their ICD “to move these data from an interesting observation to something that can drive outcomes,” he said.
Commenting for this news organization, Melissa Tracy, MD, Rush University Medical Center, Chicago, said the study reiterates the “profound” underutilization of CR.
“Only about 3% of patients who should have qualified for cardiac rehabilitation actually attended, which is startling considering that it has class 1A level of evidence supporting its use,” she said.
Dr. Tracy, who is also a member of the American College of Cardiology’s Prevention of Cardiovascular Disease Section Leadership Council, described the study as “another notch in the belt of positive outcomes supporting the need for cardiac rehabilitation” and emphasizing the importance of a home-based alternative.
“One of the reasons women, minorities, and older patients don’t go to cardiac rehabilitation is they have to get there, rely on someone to drive them, or they have other responsibilities – especially women, who are often primary caretakers of others,” she said. “For women and men, the pressure to get back to work and support their families means they don’t have the luxury to go to cardiac rehabilitation.”
Dr. Tracy noted that home-based CR is covered by CMS until the end of 2021. “An important take-home is for providers and patients to understand that they do have a home-based option,” she stated.
Limitations of the study are that only 24% of patients were women, only 6% were Black, and the results might not be generalizable to patients younger than 65 years, note Dr. Atwater and colleagues. Also, previous implantation might have protected the cohort from experiencing arrhythmic death, and it remains unclear if similar results would be obtained in patients without a previous ICD.
This research was funded through the unrestricted Abbott Medical-Duke Health Strategic Alliance Research Grant. Dr. Atwater receives significant research support from Boston Scientific and Abbott Medical, and modest honoraria from Abbott Medical, Medtronic, and Biotronik. Coauthor disclosures are listed in the paper. Dr. Tracy has created cardiac prevention programs with Virtual Health Partners (VHP) and owns the intellectual property and consults with VHP but receives no monetary compensation.
A version of this article first appeared on Medscape.com.
Small increases in daily physical activity are associated with a boost in 1-year survival in patients with heart failure and coronary disease who received an implantable cardioverter defibrillator (ICD), new research suggests.
“Our study looked at how much exercise was necessary for a better outcome in patients with prior ICD implantation and, for every 10 minutes of exercise, we saw a 1% reduction in the likelihood of death or hospitalization, which is a pretty profound impact on outcome for just a small amount of additional physical activity per day,” lead author Brett Atwater, MD, told this news organization.
“These improvements were achieved outside of a formal cardiac rehabilitation program, suggesting that the benefits of increased physical activity obtained in cardiac rehabilitation programs may also be achievable at home,” he said.
Cardiac rehabilitation (CR) programs have been shown to improve short- and long-term outcomes in patients with heart failure (HF) but continue to be underutilized, especially by women, the elderly, and minorities. Home-based CR could help overcome this limitation but the science behind it is relatively new, noted Dr. Atwater, director of electrophysiology and electrophysiology research, Inova Heart and Vascular Institute, Fairfax, Va.
As reported in Circulation Cardiovascular Quality and Outcomes, the study involved 41,731 Medicare beneficiaries (mean age, 73.5 years) who received an ICD from 2014 to 2016.
ICD heart rate and activity sensor measurements were used to establish a personalized physical activity (PA) threshold for each patient in the first 3 weeks after ICD implantation. Thereafter, the ICD logged PA when the personalized PA threshold was exceeded. The mean baseline PA level was 128.9 minutes/day.
At 3 years’ follow-up, one-quarter of the patients had died and half had been hospitalized for HF. Of the total population, only 3.2% participated in CR.
Compared with nonparticipants, CR participants were more likely to be White (91.0% versus 87.3%), male (75.5% versus 72.2%), and to have diabetes (48.8% versus 44.1%), ischemic heart disease (91.4% versus 82.1%), or congestive heart failure (90.4% versus 83.4%).
CR participants attended a median of 24 sessions, during which time daily PA increased by a mean of 9.7 minutes per day. During the same time, PA decreased by a mean of 1.0 minute per day in non-CR participants (P < .001).
PA levels remained “relatively constant” for the first 36 months of follow-up among CR participants before showing a steep decline, whereas levels gradually declined throughout follow-up among nonparticipants, with a median annual change of –4.5 min/day.
In adjusted analysis, every 10 minutes of increased daily PA was associated with a 1.1% reduced risk for death (hazard ratio, 0.989; 95% confidence interval, 0.979-0.996) and a 1% reduced risk for HF hospitalization (HR, 0.99; 95% CI, 0.986-0.995) at 1-year follow-up (P < .001).
After propensity score was used to match CR participants with nonparticipants by demographic characteristics, comorbidities, and baseline PA level, CR participants had a significantly lower risk for death at 1 year (HR, 0.76; 95% CI, 0.69-0.85). This difference in risk remained at 2- and 3-year follow-ups.
However, when the researchers further adjusted for change in PA during CR or the same time period after device implantation, no differences in mortality were found between CR participants and nonparticipants at 1 year (HR, 1.00; 95% CI, 0.82-1.21) or at 2 or 3 years.
The risk for HF hospitalization did not differ between the two groups in either propensity score model.
Unlike wearable devices, implanted devices “don’t give that type of feedback to patients regarding PA levels – only to providers – and it will be interesting to discover whether providing feedback to patients can motivate them to do more physical activity,” Dr. Atwater commented.
The team is currently enrolling patients in a follow-up trial, in which patients will be given feedback from their ICD “to move these data from an interesting observation to something that can drive outcomes,” he said.
Commenting for this news organization, Melissa Tracy, MD, Rush University Medical Center, Chicago, said the study reiterates the “profound” underutilization of CR.
“Only about 3% of patients who should have qualified for cardiac rehabilitation actually attended, which is startling considering that it has class 1A level of evidence supporting its use,” she said.
Dr. Tracy, who is also a member of the American College of Cardiology’s Prevention of Cardiovascular Disease Section Leadership Council, described the study as “another notch in the belt of positive outcomes supporting the need for cardiac rehabilitation” and emphasizing the importance of a home-based alternative.
“One of the reasons women, minorities, and older patients don’t go to cardiac rehabilitation is they have to get there, rely on someone to drive them, or they have other responsibilities – especially women, who are often primary caretakers of others,” she said. “For women and men, the pressure to get back to work and support their families means they don’t have the luxury to go to cardiac rehabilitation.”
Dr. Tracy noted that home-based CR is covered by CMS until the end of 2021. “An important take-home is for providers and patients to understand that they do have a home-based option,” she stated.
Limitations of the study are that only 24% of patients were women, only 6% were Black, and the results might not be generalizable to patients younger than 65 years, note Dr. Atwater and colleagues. Also, previous implantation might have protected the cohort from experiencing arrhythmic death, and it remains unclear if similar results would be obtained in patients without a previous ICD.
This research was funded through the unrestricted Abbott Medical-Duke Health Strategic Alliance Research Grant. Dr. Atwater receives significant research support from Boston Scientific and Abbott Medical, and modest honoraria from Abbott Medical, Medtronic, and Biotronik. Coauthor disclosures are listed in the paper. Dr. Tracy has created cardiac prevention programs with Virtual Health Partners (VHP) and owns the intellectual property and consults with VHP but receives no monetary compensation.
A version of this article first appeared on Medscape.com.