User login
Bariatric surgery tied to less pregnancy weight gain
TOPLINE:
Pregnancy weight gain is lower in women with a history of gastric bypass or sleeve gastrectomy than in those without such a history, especially when the interval between surgery and conception is shorter, new data suggest.
METHODOLOGY:
- Using Swedish national registers, researchers investigated the association of pregnancy weight gain with history in 12,776 pregnancies — 6388 in women with a history of bariatric surgery and 6388 in women without such a history.
- Pregnancies were propensity score matched to patients’ early-pregnancy body mass index (BMI), prepregnancy diabetes, , smoking status, education, height, country of birth, and delivery year.
- Post-gastric bypass pregnancies were matched to post-sleeve gastrectomy pregnancies using the same matching strategy.
- Time from surgery to conception was also assessed.
TAKEAWAY:
- Across all early-pregnancy BMI strata, women with a history of bariatric surgery had lower pregnancy weight gain than matched controls.
- The magnitude of difference was largest for women with normal weight or overweight early-pregnancy BMI status (adjusted mean difference in z score, −0.33), which then decreased stepwise within the subclasses (−0.21, −0.16, and −0.08 for obesity classes I, II, and III, respectively).
- Pregnancy weight gain did not differ by surgery type, but lower pregnancy weight gain was associated with a shorter surgery-to-conception interval (particularly within 1 year) or lower surgery-to-conception weight loss.
IN PRACTICE:
“The highest proportion of weight gain below the recommendations was found among women with a normal weight status. Hence, clinical attention to women with history of bariatric surgery and a normal weight status in early pregnancy might be warranted,” the authors advised.
SOURCE:
The study, with the first author Huiling Xu, MD, MSc, Karolinska Institutet, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
Despite rigorous matching, residual confounding was possible. The sample size was limited for some subgroups, possibly affecting statistical power. Although the study provides an overview of pregnancy outcomes within surgery-to-conception interval and pregnancy weight gain z scores, a more in-depth investigation is needed to understand the associations among bariatric surgery, pregnancy weight gain, and pregnancy outcomes.
DISCLOSURES:
Research for this study was supported by the Swedish Research Council for Health, Working Life and Welfare, and the Swedish Research Council. The authors have no relevant disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Pregnancy weight gain is lower in women with a history of gastric bypass or sleeve gastrectomy than in those without such a history, especially when the interval between surgery and conception is shorter, new data suggest.
METHODOLOGY:
- Using Swedish national registers, researchers investigated the association of pregnancy weight gain with history in 12,776 pregnancies — 6388 in women with a history of bariatric surgery and 6388 in women without such a history.
- Pregnancies were propensity score matched to patients’ early-pregnancy body mass index (BMI), prepregnancy diabetes, , smoking status, education, height, country of birth, and delivery year.
- Post-gastric bypass pregnancies were matched to post-sleeve gastrectomy pregnancies using the same matching strategy.
- Time from surgery to conception was also assessed.
TAKEAWAY:
- Across all early-pregnancy BMI strata, women with a history of bariatric surgery had lower pregnancy weight gain than matched controls.
- The magnitude of difference was largest for women with normal weight or overweight early-pregnancy BMI status (adjusted mean difference in z score, −0.33), which then decreased stepwise within the subclasses (−0.21, −0.16, and −0.08 for obesity classes I, II, and III, respectively).
- Pregnancy weight gain did not differ by surgery type, but lower pregnancy weight gain was associated with a shorter surgery-to-conception interval (particularly within 1 year) or lower surgery-to-conception weight loss.
IN PRACTICE:
“The highest proportion of weight gain below the recommendations was found among women with a normal weight status. Hence, clinical attention to women with history of bariatric surgery and a normal weight status in early pregnancy might be warranted,” the authors advised.
SOURCE:
The study, with the first author Huiling Xu, MD, MSc, Karolinska Institutet, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
Despite rigorous matching, residual confounding was possible. The sample size was limited for some subgroups, possibly affecting statistical power. Although the study provides an overview of pregnancy outcomes within surgery-to-conception interval and pregnancy weight gain z scores, a more in-depth investigation is needed to understand the associations among bariatric surgery, pregnancy weight gain, and pregnancy outcomes.
DISCLOSURES:
Research for this study was supported by the Swedish Research Council for Health, Working Life and Welfare, and the Swedish Research Council. The authors have no relevant disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Pregnancy weight gain is lower in women with a history of gastric bypass or sleeve gastrectomy than in those without such a history, especially when the interval between surgery and conception is shorter, new data suggest.
METHODOLOGY:
- Using Swedish national registers, researchers investigated the association of pregnancy weight gain with history in 12,776 pregnancies — 6388 in women with a history of bariatric surgery and 6388 in women without such a history.
- Pregnancies were propensity score matched to patients’ early-pregnancy body mass index (BMI), prepregnancy diabetes, , smoking status, education, height, country of birth, and delivery year.
- Post-gastric bypass pregnancies were matched to post-sleeve gastrectomy pregnancies using the same matching strategy.
- Time from surgery to conception was also assessed.
TAKEAWAY:
- Across all early-pregnancy BMI strata, women with a history of bariatric surgery had lower pregnancy weight gain than matched controls.
- The magnitude of difference was largest for women with normal weight or overweight early-pregnancy BMI status (adjusted mean difference in z score, −0.33), which then decreased stepwise within the subclasses (−0.21, −0.16, and −0.08 for obesity classes I, II, and III, respectively).
- Pregnancy weight gain did not differ by surgery type, but lower pregnancy weight gain was associated with a shorter surgery-to-conception interval (particularly within 1 year) or lower surgery-to-conception weight loss.
IN PRACTICE:
“The highest proportion of weight gain below the recommendations was found among women with a normal weight status. Hence, clinical attention to women with history of bariatric surgery and a normal weight status in early pregnancy might be warranted,” the authors advised.
SOURCE:
The study, with the first author Huiling Xu, MD, MSc, Karolinska Institutet, Stockholm, Sweden, was published online in JAMA Network Open.
LIMITATIONS:
Despite rigorous matching, residual confounding was possible. The sample size was limited for some subgroups, possibly affecting statistical power. Although the study provides an overview of pregnancy outcomes within surgery-to-conception interval and pregnancy weight gain z scores, a more in-depth investigation is needed to understand the associations among bariatric surgery, pregnancy weight gain, and pregnancy outcomes.
DISCLOSURES:
Research for this study was supported by the Swedish Research Council for Health, Working Life and Welfare, and the Swedish Research Council. The authors have no relevant disclosures.
A version of this article appeared on Medscape.com.
Less is more for axillary surgery in early breast cancer
SAN ANTONIO — than do those who have more extensive surgery, according to findings from a large meta-analysis.
Less extensive surgery also reduced patients’ risk for lymphedema, according to research (abstract GS02-05) presented at the San Antonio Breast Cancer Symposium.
These results, which included data from more than 20,000 women, may “reassure” patients and clinicians that more extensive axillary lymph node dissection “does not improve outcomes in many women with early-stage breast cancer,” said Andrea V. Barrio, MD, a breast surgeon at Memorial Sloan Kettering Cancer Center, New York City, who was not involved in the study.
Gurdeep S. Mannu, DPhil, of the University of Oxford, United Kingdom, who presented the findings at SABCS, explained that the optimal surgical management of the axilla remains uncertain in this patient population.
To better understand the long-term risks and benefits of more vs less aggressive axillary surgery in early breast cancer, Dr. Mannu and colleagues performed a meta-analysis of 29 randomized trials conducted over six decades, which included data on 20,285 women. The trials compared more vs less extensive axillary surgery as well as axillary surgery vs axillary radiotherapy.
In trials comparing more vs less extensive axillary surgery, researchers found that 83% of locoregional recurrences occurred in the breast or in multiple sites/unspecified locations, and the remaining 17% occurred in isolated axilla or other local recurrences, such as in the supraclavicular fossa or internal mammary chain.
Those with recurrences in the breast or multiple sites/unspecified locations did not benefit from more extensive surgery, demonstrating similar recurrence rates (RR) (RR for breast, 1.13; 95% CI, 0.92-1.40; RR for other, 0.89; 95% CI, 0.67-1.18).
The group with recurrences in isolated axilla or other local recurrences tended to do better with more extensive surgery (RR, 0.43 and 0.41, respectively).
Overall though, after a median follow-up of 10 years, differences in locoregional recurrence rates at any site did not differ among patients who had more vs less extensive axillary surgery (RR, 0.91; P = .22). This finding held even when restricting the analysis to women with node-positive disease/unknown nodal status (RR, 1.00; P = .98) and for node-negative women (RR, 0.88; P = .15).
Dr. Mannu and colleagues observed similar findings for distant recurrence, breast cancer mortality, and death from any cause.
“But where there was quite a striking difference was in morbidity,” said Dr. Mannu.
To examine rates of lymphedema — the surgical complication that has been “one of the main motivations” for the deescalation trials of the past few decades — the researchers focused on more recent trials, which “are most relevant to women treated today,” Dr. Mannu explained.
These showed that more extensive axillary surgery was associated with almost 2.5-times the rate of lymphedema compared with less extensive treatment (odds ratio [OR], 2.43).
Finally, the team compared axillary dissection with axillary radiotherapy across five trials and found no significant differences in the treatment approaches in terms of locoregional occurrence, distant recurrence, breast cancer mortality, and death from any cause.
However, once again, a notable difference in rates of lymphedema occurred, with axillary dissection associated with higher rates compared with radiotherapy (OR, 1.79).
This is “probably the largest meta-analysis comparing more vs less axillary surgery,” Dr. Barrio said in an interview.
“When we have one or two positive sentinel nodes, anywhere from 30%-50% of women will have additional positive lymph nodes that we’re not removing” with less extensive surgery, she explained. This study shows that, even then, this “doesn’t seem to impact on survival.”
This is “likely related to better medical treatment and radiation techniques that can treat that disease just as well as big surgery, but with less lymphedema,” she added.
Nevertheless, Dr. Barrio believes that there are “situations where we still feel that axillary lymph node dissection is important: in women with advanced cancer, like inflammatory breast cancer, and in women who’ve received chemotherapy upfront, then had surgery, and still have positive nodes after the chemo.”
The study was funded by Cancer Research UK, British Heart Foundation, Medical Research Council.
No relevant financial relationships have been declared.
A version of this article appeared on Medscape.com.
SAN ANTONIO — than do those who have more extensive surgery, according to findings from a large meta-analysis.
Less extensive surgery also reduced patients’ risk for lymphedema, according to research (abstract GS02-05) presented at the San Antonio Breast Cancer Symposium.
These results, which included data from more than 20,000 women, may “reassure” patients and clinicians that more extensive axillary lymph node dissection “does not improve outcomes in many women with early-stage breast cancer,” said Andrea V. Barrio, MD, a breast surgeon at Memorial Sloan Kettering Cancer Center, New York City, who was not involved in the study.
Gurdeep S. Mannu, DPhil, of the University of Oxford, United Kingdom, who presented the findings at SABCS, explained that the optimal surgical management of the axilla remains uncertain in this patient population.
To better understand the long-term risks and benefits of more vs less aggressive axillary surgery in early breast cancer, Dr. Mannu and colleagues performed a meta-analysis of 29 randomized trials conducted over six decades, which included data on 20,285 women. The trials compared more vs less extensive axillary surgery as well as axillary surgery vs axillary radiotherapy.
In trials comparing more vs less extensive axillary surgery, researchers found that 83% of locoregional recurrences occurred in the breast or in multiple sites/unspecified locations, and the remaining 17% occurred in isolated axilla or other local recurrences, such as in the supraclavicular fossa or internal mammary chain.
Those with recurrences in the breast or multiple sites/unspecified locations did not benefit from more extensive surgery, demonstrating similar recurrence rates (RR) (RR for breast, 1.13; 95% CI, 0.92-1.40; RR for other, 0.89; 95% CI, 0.67-1.18).
The group with recurrences in isolated axilla or other local recurrences tended to do better with more extensive surgery (RR, 0.43 and 0.41, respectively).
Overall though, after a median follow-up of 10 years, differences in locoregional recurrence rates at any site did not differ among patients who had more vs less extensive axillary surgery (RR, 0.91; P = .22). This finding held even when restricting the analysis to women with node-positive disease/unknown nodal status (RR, 1.00; P = .98) and for node-negative women (RR, 0.88; P = .15).
Dr. Mannu and colleagues observed similar findings for distant recurrence, breast cancer mortality, and death from any cause.
“But where there was quite a striking difference was in morbidity,” said Dr. Mannu.
To examine rates of lymphedema — the surgical complication that has been “one of the main motivations” for the deescalation trials of the past few decades — the researchers focused on more recent trials, which “are most relevant to women treated today,” Dr. Mannu explained.
These showed that more extensive axillary surgery was associated with almost 2.5-times the rate of lymphedema compared with less extensive treatment (odds ratio [OR], 2.43).
Finally, the team compared axillary dissection with axillary radiotherapy across five trials and found no significant differences in the treatment approaches in terms of locoregional occurrence, distant recurrence, breast cancer mortality, and death from any cause.
However, once again, a notable difference in rates of lymphedema occurred, with axillary dissection associated with higher rates compared with radiotherapy (OR, 1.79).
This is “probably the largest meta-analysis comparing more vs less axillary surgery,” Dr. Barrio said in an interview.
“When we have one or two positive sentinel nodes, anywhere from 30%-50% of women will have additional positive lymph nodes that we’re not removing” with less extensive surgery, she explained. This study shows that, even then, this “doesn’t seem to impact on survival.”
This is “likely related to better medical treatment and radiation techniques that can treat that disease just as well as big surgery, but with less lymphedema,” she added.
Nevertheless, Dr. Barrio believes that there are “situations where we still feel that axillary lymph node dissection is important: in women with advanced cancer, like inflammatory breast cancer, and in women who’ve received chemotherapy upfront, then had surgery, and still have positive nodes after the chemo.”
The study was funded by Cancer Research UK, British Heart Foundation, Medical Research Council.
No relevant financial relationships have been declared.
A version of this article appeared on Medscape.com.
SAN ANTONIO — than do those who have more extensive surgery, according to findings from a large meta-analysis.
Less extensive surgery also reduced patients’ risk for lymphedema, according to research (abstract GS02-05) presented at the San Antonio Breast Cancer Symposium.
These results, which included data from more than 20,000 women, may “reassure” patients and clinicians that more extensive axillary lymph node dissection “does not improve outcomes in many women with early-stage breast cancer,” said Andrea V. Barrio, MD, a breast surgeon at Memorial Sloan Kettering Cancer Center, New York City, who was not involved in the study.
Gurdeep S. Mannu, DPhil, of the University of Oxford, United Kingdom, who presented the findings at SABCS, explained that the optimal surgical management of the axilla remains uncertain in this patient population.
To better understand the long-term risks and benefits of more vs less aggressive axillary surgery in early breast cancer, Dr. Mannu and colleagues performed a meta-analysis of 29 randomized trials conducted over six decades, which included data on 20,285 women. The trials compared more vs less extensive axillary surgery as well as axillary surgery vs axillary radiotherapy.
In trials comparing more vs less extensive axillary surgery, researchers found that 83% of locoregional recurrences occurred in the breast or in multiple sites/unspecified locations, and the remaining 17% occurred in isolated axilla or other local recurrences, such as in the supraclavicular fossa or internal mammary chain.
Those with recurrences in the breast or multiple sites/unspecified locations did not benefit from more extensive surgery, demonstrating similar recurrence rates (RR) (RR for breast, 1.13; 95% CI, 0.92-1.40; RR for other, 0.89; 95% CI, 0.67-1.18).
The group with recurrences in isolated axilla or other local recurrences tended to do better with more extensive surgery (RR, 0.43 and 0.41, respectively).
Overall though, after a median follow-up of 10 years, differences in locoregional recurrence rates at any site did not differ among patients who had more vs less extensive axillary surgery (RR, 0.91; P = .22). This finding held even when restricting the analysis to women with node-positive disease/unknown nodal status (RR, 1.00; P = .98) and for node-negative women (RR, 0.88; P = .15).
Dr. Mannu and colleagues observed similar findings for distant recurrence, breast cancer mortality, and death from any cause.
“But where there was quite a striking difference was in morbidity,” said Dr. Mannu.
To examine rates of lymphedema — the surgical complication that has been “one of the main motivations” for the deescalation trials of the past few decades — the researchers focused on more recent trials, which “are most relevant to women treated today,” Dr. Mannu explained.
These showed that more extensive axillary surgery was associated with almost 2.5-times the rate of lymphedema compared with less extensive treatment (odds ratio [OR], 2.43).
Finally, the team compared axillary dissection with axillary radiotherapy across five trials and found no significant differences in the treatment approaches in terms of locoregional occurrence, distant recurrence, breast cancer mortality, and death from any cause.
However, once again, a notable difference in rates of lymphedema occurred, with axillary dissection associated with higher rates compared with radiotherapy (OR, 1.79).
This is “probably the largest meta-analysis comparing more vs less axillary surgery,” Dr. Barrio said in an interview.
“When we have one or two positive sentinel nodes, anywhere from 30%-50% of women will have additional positive lymph nodes that we’re not removing” with less extensive surgery, she explained. This study shows that, even then, this “doesn’t seem to impact on survival.”
This is “likely related to better medical treatment and radiation techniques that can treat that disease just as well as big surgery, but with less lymphedema,” she added.
Nevertheless, Dr. Barrio believes that there are “situations where we still feel that axillary lymph node dissection is important: in women with advanced cancer, like inflammatory breast cancer, and in women who’ve received chemotherapy upfront, then had surgery, and still have positive nodes after the chemo.”
The study was funded by Cancer Research UK, British Heart Foundation, Medical Research Council.
No relevant financial relationships have been declared.
A version of this article appeared on Medscape.com.
FROM SABCS 2023
Hemorrhage-control device holds up in real-world review
Morbidity and mortality related to postpartum hemorrhage (PPH) are often preventable if caught early, but the persistent rise in PPH-associated morbidity illustrates the need for new and innovative treatments, wrote Dena Goffman, MD, of New York-Presbyterian/Columbia University Irving Medical Center, New York, and colleagues.
The device, known as the Jada System, was cleared by the Food and Drug Administration for management of abnormal postpartum uterine bleeding or postpartum hemorrhage (PPH) in August 2020 and showed safety and effectiveness in a registrational study of 106 patients, the researchers said.
In a postmarket registry medical record review known as RUBY (Treating Abnormal Postpartum Uterine Bleeding or Postpartum Hemorrhage with the Jada System), the researchers examined data collected from Oct. 8, 2020, to March 31, 2022, at 16 centers in the United States. The findings were published in Obstetrics & Gynecology.
The study population included all individuals treated with an intrauterine vacuum-induced hemorrhage control device; of these, 530 were vaginal births and 270 were cesarean births. A total of 94.3% had uterine atony, alone or in conjunction with other causes of bleeding. The median maternal age was 30.3 years; approximately 60% and 53% of patients in the vaginal and cesarean groups were White, and approximately 43% and 49% of patients in the two groups, respectively, were nulliparous.
The median blood loss at the time of device insertion was 1,250 mL in vaginal births and 1,980 mL in cesarean births, and the median time from delivery of the placenta to device insertion was 31 minutes and 108 minutes in the two groups, respectively.
The primary endpoint was treatment success, defined as control of bleeding after device insertion, with no escalation of treatment or recurrence of bleeding after the initial bleeding control and device removal.
Treatment success was achieved in 92.5% of vaginal births and 83.7% of cesarean births, and in 95.8% and 88.2%, respectively, among patients with isolated uterine atony. The median insertion time was 3.1 hours for vaginal births and 4.6 hours for cesarean births.
The safety profile was similar to that in the registrational trial and adverse effects were those expected in patients with PPH, the researchers noted.
A total of 14 SAEs were reported in 13 patients with vaginal births, and 22 SAEs were reported in 21 patients with cesarean births. Of these, three were identified as possibly related to the device or procedure (two cases of endometritis in the vaginal birth group and one case of hemorrhagic shock in the cesarean group); no uterine perforations of deaths were reported during the study.
The study was limited by several factors including the use of data mainly from academic centers, which could limit generalizability, and by the use of a mix of estimated and quantitative reporting of blood loss, the researchers noted. Other limitations include the inability to make direct comparisons to other treatments for PPH.
However, the results confirm the safety and efficacy of the device in a real-world setting and support its use as an important new tool in the management of PPH and reducing maternal morbidity and mortality, they concluded.
Two companies were involved in the study; Alydia Health contributed to the concept, design, and analysis, and Organon contributed to data analysis and reviewed the manuscript.
Dr. Goffman disclosed research support from Organon and Alydia Health, as well as serving as a speaker for Haymarket and PRIME PPH education and for Laborie, participation in the Cooper Surgical Obstetrical Safety Council, and serving as an editor for UpToDate. Several coauthors disclosed relationships with multiple companies including Organon and Alydia Health.
Morbidity and mortality related to postpartum hemorrhage (PPH) are often preventable if caught early, but the persistent rise in PPH-associated morbidity illustrates the need for new and innovative treatments, wrote Dena Goffman, MD, of New York-Presbyterian/Columbia University Irving Medical Center, New York, and colleagues.
The device, known as the Jada System, was cleared by the Food and Drug Administration for management of abnormal postpartum uterine bleeding or postpartum hemorrhage (PPH) in August 2020 and showed safety and effectiveness in a registrational study of 106 patients, the researchers said.
In a postmarket registry medical record review known as RUBY (Treating Abnormal Postpartum Uterine Bleeding or Postpartum Hemorrhage with the Jada System), the researchers examined data collected from Oct. 8, 2020, to March 31, 2022, at 16 centers in the United States. The findings were published in Obstetrics & Gynecology.
The study population included all individuals treated with an intrauterine vacuum-induced hemorrhage control device; of these, 530 were vaginal births and 270 were cesarean births. A total of 94.3% had uterine atony, alone or in conjunction with other causes of bleeding. The median maternal age was 30.3 years; approximately 60% and 53% of patients in the vaginal and cesarean groups were White, and approximately 43% and 49% of patients in the two groups, respectively, were nulliparous.
The median blood loss at the time of device insertion was 1,250 mL in vaginal births and 1,980 mL in cesarean births, and the median time from delivery of the placenta to device insertion was 31 minutes and 108 minutes in the two groups, respectively.
The primary endpoint was treatment success, defined as control of bleeding after device insertion, with no escalation of treatment or recurrence of bleeding after the initial bleeding control and device removal.
Treatment success was achieved in 92.5% of vaginal births and 83.7% of cesarean births, and in 95.8% and 88.2%, respectively, among patients with isolated uterine atony. The median insertion time was 3.1 hours for vaginal births and 4.6 hours for cesarean births.
The safety profile was similar to that in the registrational trial and adverse effects were those expected in patients with PPH, the researchers noted.
A total of 14 SAEs were reported in 13 patients with vaginal births, and 22 SAEs were reported in 21 patients with cesarean births. Of these, three were identified as possibly related to the device or procedure (two cases of endometritis in the vaginal birth group and one case of hemorrhagic shock in the cesarean group); no uterine perforations of deaths were reported during the study.
The study was limited by several factors including the use of data mainly from academic centers, which could limit generalizability, and by the use of a mix of estimated and quantitative reporting of blood loss, the researchers noted. Other limitations include the inability to make direct comparisons to other treatments for PPH.
However, the results confirm the safety and efficacy of the device in a real-world setting and support its use as an important new tool in the management of PPH and reducing maternal morbidity and mortality, they concluded.
Two companies were involved in the study; Alydia Health contributed to the concept, design, and analysis, and Organon contributed to data analysis and reviewed the manuscript.
Dr. Goffman disclosed research support from Organon and Alydia Health, as well as serving as a speaker for Haymarket and PRIME PPH education and for Laborie, participation in the Cooper Surgical Obstetrical Safety Council, and serving as an editor for UpToDate. Several coauthors disclosed relationships with multiple companies including Organon and Alydia Health.
Morbidity and mortality related to postpartum hemorrhage (PPH) are often preventable if caught early, but the persistent rise in PPH-associated morbidity illustrates the need for new and innovative treatments, wrote Dena Goffman, MD, of New York-Presbyterian/Columbia University Irving Medical Center, New York, and colleagues.
The device, known as the Jada System, was cleared by the Food and Drug Administration for management of abnormal postpartum uterine bleeding or postpartum hemorrhage (PPH) in August 2020 and showed safety and effectiveness in a registrational study of 106 patients, the researchers said.
In a postmarket registry medical record review known as RUBY (Treating Abnormal Postpartum Uterine Bleeding or Postpartum Hemorrhage with the Jada System), the researchers examined data collected from Oct. 8, 2020, to March 31, 2022, at 16 centers in the United States. The findings were published in Obstetrics & Gynecology.
The study population included all individuals treated with an intrauterine vacuum-induced hemorrhage control device; of these, 530 were vaginal births and 270 were cesarean births. A total of 94.3% had uterine atony, alone or in conjunction with other causes of bleeding. The median maternal age was 30.3 years; approximately 60% and 53% of patients in the vaginal and cesarean groups were White, and approximately 43% and 49% of patients in the two groups, respectively, were nulliparous.
The median blood loss at the time of device insertion was 1,250 mL in vaginal births and 1,980 mL in cesarean births, and the median time from delivery of the placenta to device insertion was 31 minutes and 108 minutes in the two groups, respectively.
The primary endpoint was treatment success, defined as control of bleeding after device insertion, with no escalation of treatment or recurrence of bleeding after the initial bleeding control and device removal.
Treatment success was achieved in 92.5% of vaginal births and 83.7% of cesarean births, and in 95.8% and 88.2%, respectively, among patients with isolated uterine atony. The median insertion time was 3.1 hours for vaginal births and 4.6 hours for cesarean births.
The safety profile was similar to that in the registrational trial and adverse effects were those expected in patients with PPH, the researchers noted.
A total of 14 SAEs were reported in 13 patients with vaginal births, and 22 SAEs were reported in 21 patients with cesarean births. Of these, three were identified as possibly related to the device or procedure (two cases of endometritis in the vaginal birth group and one case of hemorrhagic shock in the cesarean group); no uterine perforations of deaths were reported during the study.
The study was limited by several factors including the use of data mainly from academic centers, which could limit generalizability, and by the use of a mix of estimated and quantitative reporting of blood loss, the researchers noted. Other limitations include the inability to make direct comparisons to other treatments for PPH.
However, the results confirm the safety and efficacy of the device in a real-world setting and support its use as an important new tool in the management of PPH and reducing maternal morbidity and mortality, they concluded.
Two companies were involved in the study; Alydia Health contributed to the concept, design, and analysis, and Organon contributed to data analysis and reviewed the manuscript.
Dr. Goffman disclosed research support from Organon and Alydia Health, as well as serving as a speaker for Haymarket and PRIME PPH education and for Laborie, participation in the Cooper Surgical Obstetrical Safety Council, and serving as an editor for UpToDate. Several coauthors disclosed relationships with multiple companies including Organon and Alydia Health.
FROM OBSTETRICS & GYNECOLOGY
Alternative antirejection regimen is efficacious in pediatric heart transplant
Study challenges everolimus boxed warning
according to the first phase 3 trial to compare antirejection strategies in the pediatric setting.
Even though MMF and tacrolimus have never been evaluated for pediatric cardiac transplant in a controlled trial, this combination is widely considered a standard based on adult data, said Christopher Almond, MD, a professor of pediatric cardiology at Stanford (Calif.) Medicine.
Everolimus has not been widely used in an antirejection regimen in children following heart transplant in part because of a boxed warning. The warning was added to labeling when this agent was associated with increased infection and increased mortality in adults if given within 3 months of transplant.
In this non-inferiority trial, called TEAMMATE, patients were randomized to the MMF-based or everolimus-based regimen 6 months after transplant.
Everolimus- vs. MMF-based antirejection
The study enrolled 210 children and adolescents 21 years of age or younger. The control arm treatment consisted of MMF (660 mg/m2 every 12 hours) plus standard dose of tacrolimus (initially 7-10 ng/mL followed at 6 months by 5-8 ng/mL).
In the experimental arm, patients received everolimus (3-8 ng/mL) plus a low dose of tacrolimus (initially 3-5 ng/mL followed at 6 months by 2.5-4.5 ng/mL).
The primary endpoint was score on the major adverse transplant event (MATE-6) tool. Based on gradations of severity, this assigns values for cardiac allograft vasculopathy (CAV), chronic kidney disease (CKD), acute cellular rejection (ACR), antibody-mediated rejection, infection, and posttransplant lymphoproliferative disorder (PTLD).
Thirty months after randomization, the MATE-6 scores were 1.96 in the everolimus group and 2.18 in the MMF group, which conferred the everolimus-based regimen with a numerical but not a significant advantage over the MMF-based regimen. For the goal of noninferiority, the everolimus regimen “met the prespecified safety criterion for success,” Dr. Almond said.
Numerical advantage for everolimus on efficacy
The primary efficacy endpoint was the MATE-3 score, which is limited to CAV, CKD, and ACR. Again, the mean score on this metric (0.93 vs. 1.25) was lower on the everolimus-based regimen but not significantly different.
Looking at specific events in the MATE-6 score, the everolimus-based regimen was associated with lower numerical rates of CAV and CKD, but a higher rate of PTLD, Dr. Almond reported.
On the MATE-3 efficacy analysis, the everolimus-based regimen was again associated with lower numerical rates of CAV and CKD but higher rates of ACR.
In terms of adverse events, including those involving the gastrointestinal tract, blood cells, proteinuria, and interstitial lung disease, most did not differ markedly even if many were numerically more common in the MMF-based arm. The exception was aphthous stomatitis, which was more common on everolimus (32% vs. 7%; P < .001). There were more discontinuations for an adverse event in the MMF arm (21% vs. 12%; P < .001).
Other differences included a lower proportion of patients in the everolimus arm with anti-HLA antibodies (17% vs. 30%; P < .05). Total cholesterol levels at the end of the study were lower but not significantly different in the MMF group, while the higher median glomerular filtration rate was higher on everolimus, and this did reach statistical significance (P < .05).
Infection rates overall were similar, but cytomegalovirus (CMV) infection was more common on the MMF-based regimen. The 30% lower rate of CMV infection in the everolimus proved to be potentially clinically meaningful when it was considered in the context of MATE-3. When these two endpoints were combined (MATE-3 and CMV infection as a prespecified secondary endpoint, the difference was statistically significant (P = .03) in favor of the everolimus-based regimen,
Study supports safety of everolimus regimen
The take-home message is that the everolimus-based regimen, which “is safe in children and young adults when initiated at 6 months after transplant,” can be considered as an alternative to MFF, Dr. Almond concluded.
However, one of the coauthors of the study, Joseph Rossano, MD, chief of the division of cardiology, Children’s Hospital of Philadelphia, suggested a stronger message.
“These data provide compelling reasons to consider initiation of the combination of everolimus and tacrolimus at 6 months post transplant in pediatric heart transplant recipients,” Dr. Rossano said.
Even though the everolimus-based regimen met the terms of noninferiority overall, patients who received this combination rather than the MMF-based regimen “were less likely to have the combined endpoints of vasculopathy, CKD, rejection and CMV infection. Additionally, they were less likely to make donor specific antibodies,” he said.
He also said that this study challenges the current boxed warning for everolimus. He pointed out that the warning, based on early use of everolimus in adults, does not appear to be an issue for children treated at 6 months.
Early mortality based on infection “was not observed in our study,” he said.
The AHA-invited discussant, Antonio G. Cabrera, MD, division chief of pediatric cardiology, University of Utah, Salt Lake City, drew the same conclusions. Based on the study, the everolimus-based regimen can only be described as noninferior to the MMF-based regimen, but Dr. Cabrera listed the same relative advantages as Dr. Rossano, including better kidney function.
Overall, either regimen might be more appealing based on several variables, but Dr. Cabrera said these data suggest everolimus-based treatment “should be considered” as one of two evidence-based options,
Dr. Almond reported no potential financial conflicts of interest. Dr. Rossano reports financial relationships with Abiomed, Bayer, Cytokinetics, Merck, and Myokardia. Dr. Cabrera reported no potential financial conflicts of interest.
Study challenges everolimus boxed warning
Study challenges everolimus boxed warning
according to the first phase 3 trial to compare antirejection strategies in the pediatric setting.
Even though MMF and tacrolimus have never been evaluated for pediatric cardiac transplant in a controlled trial, this combination is widely considered a standard based on adult data, said Christopher Almond, MD, a professor of pediatric cardiology at Stanford (Calif.) Medicine.
Everolimus has not been widely used in an antirejection regimen in children following heart transplant in part because of a boxed warning. The warning was added to labeling when this agent was associated with increased infection and increased mortality in adults if given within 3 months of transplant.
In this non-inferiority trial, called TEAMMATE, patients were randomized to the MMF-based or everolimus-based regimen 6 months after transplant.
Everolimus- vs. MMF-based antirejection
The study enrolled 210 children and adolescents 21 years of age or younger. The control arm treatment consisted of MMF (660 mg/m2 every 12 hours) plus standard dose of tacrolimus (initially 7-10 ng/mL followed at 6 months by 5-8 ng/mL).
In the experimental arm, patients received everolimus (3-8 ng/mL) plus a low dose of tacrolimus (initially 3-5 ng/mL followed at 6 months by 2.5-4.5 ng/mL).
The primary endpoint was score on the major adverse transplant event (MATE-6) tool. Based on gradations of severity, this assigns values for cardiac allograft vasculopathy (CAV), chronic kidney disease (CKD), acute cellular rejection (ACR), antibody-mediated rejection, infection, and posttransplant lymphoproliferative disorder (PTLD).
Thirty months after randomization, the MATE-6 scores were 1.96 in the everolimus group and 2.18 in the MMF group, which conferred the everolimus-based regimen with a numerical but not a significant advantage over the MMF-based regimen. For the goal of noninferiority, the everolimus regimen “met the prespecified safety criterion for success,” Dr. Almond said.
Numerical advantage for everolimus on efficacy
The primary efficacy endpoint was the MATE-3 score, which is limited to CAV, CKD, and ACR. Again, the mean score on this metric (0.93 vs. 1.25) was lower on the everolimus-based regimen but not significantly different.
Looking at specific events in the MATE-6 score, the everolimus-based regimen was associated with lower numerical rates of CAV and CKD, but a higher rate of PTLD, Dr. Almond reported.
On the MATE-3 efficacy analysis, the everolimus-based regimen was again associated with lower numerical rates of CAV and CKD but higher rates of ACR.
In terms of adverse events, including those involving the gastrointestinal tract, blood cells, proteinuria, and interstitial lung disease, most did not differ markedly even if many were numerically more common in the MMF-based arm. The exception was aphthous stomatitis, which was more common on everolimus (32% vs. 7%; P < .001). There were more discontinuations for an adverse event in the MMF arm (21% vs. 12%; P < .001).
Other differences included a lower proportion of patients in the everolimus arm with anti-HLA antibodies (17% vs. 30%; P < .05). Total cholesterol levels at the end of the study were lower but not significantly different in the MMF group, while the higher median glomerular filtration rate was higher on everolimus, and this did reach statistical significance (P < .05).
Infection rates overall were similar, but cytomegalovirus (CMV) infection was more common on the MMF-based regimen. The 30% lower rate of CMV infection in the everolimus proved to be potentially clinically meaningful when it was considered in the context of MATE-3. When these two endpoints were combined (MATE-3 and CMV infection as a prespecified secondary endpoint, the difference was statistically significant (P = .03) in favor of the everolimus-based regimen,
Study supports safety of everolimus regimen
The take-home message is that the everolimus-based regimen, which “is safe in children and young adults when initiated at 6 months after transplant,” can be considered as an alternative to MFF, Dr. Almond concluded.
However, one of the coauthors of the study, Joseph Rossano, MD, chief of the division of cardiology, Children’s Hospital of Philadelphia, suggested a stronger message.
“These data provide compelling reasons to consider initiation of the combination of everolimus and tacrolimus at 6 months post transplant in pediatric heart transplant recipients,” Dr. Rossano said.
Even though the everolimus-based regimen met the terms of noninferiority overall, patients who received this combination rather than the MMF-based regimen “were less likely to have the combined endpoints of vasculopathy, CKD, rejection and CMV infection. Additionally, they were less likely to make donor specific antibodies,” he said.
He also said that this study challenges the current boxed warning for everolimus. He pointed out that the warning, based on early use of everolimus in adults, does not appear to be an issue for children treated at 6 months.
Early mortality based on infection “was not observed in our study,” he said.
The AHA-invited discussant, Antonio G. Cabrera, MD, division chief of pediatric cardiology, University of Utah, Salt Lake City, drew the same conclusions. Based on the study, the everolimus-based regimen can only be described as noninferior to the MMF-based regimen, but Dr. Cabrera listed the same relative advantages as Dr. Rossano, including better kidney function.
Overall, either regimen might be more appealing based on several variables, but Dr. Cabrera said these data suggest everolimus-based treatment “should be considered” as one of two evidence-based options,
Dr. Almond reported no potential financial conflicts of interest. Dr. Rossano reports financial relationships with Abiomed, Bayer, Cytokinetics, Merck, and Myokardia. Dr. Cabrera reported no potential financial conflicts of interest.
according to the first phase 3 trial to compare antirejection strategies in the pediatric setting.
Even though MMF and tacrolimus have never been evaluated for pediatric cardiac transplant in a controlled trial, this combination is widely considered a standard based on adult data, said Christopher Almond, MD, a professor of pediatric cardiology at Stanford (Calif.) Medicine.
Everolimus has not been widely used in an antirejection regimen in children following heart transplant in part because of a boxed warning. The warning was added to labeling when this agent was associated with increased infection and increased mortality in adults if given within 3 months of transplant.
In this non-inferiority trial, called TEAMMATE, patients were randomized to the MMF-based or everolimus-based regimen 6 months after transplant.
Everolimus- vs. MMF-based antirejection
The study enrolled 210 children and adolescents 21 years of age or younger. The control arm treatment consisted of MMF (660 mg/m2 every 12 hours) plus standard dose of tacrolimus (initially 7-10 ng/mL followed at 6 months by 5-8 ng/mL).
In the experimental arm, patients received everolimus (3-8 ng/mL) plus a low dose of tacrolimus (initially 3-5 ng/mL followed at 6 months by 2.5-4.5 ng/mL).
The primary endpoint was score on the major adverse transplant event (MATE-6) tool. Based on gradations of severity, this assigns values for cardiac allograft vasculopathy (CAV), chronic kidney disease (CKD), acute cellular rejection (ACR), antibody-mediated rejection, infection, and posttransplant lymphoproliferative disorder (PTLD).
Thirty months after randomization, the MATE-6 scores were 1.96 in the everolimus group and 2.18 in the MMF group, which conferred the everolimus-based regimen with a numerical but not a significant advantage over the MMF-based regimen. For the goal of noninferiority, the everolimus regimen “met the prespecified safety criterion for success,” Dr. Almond said.
Numerical advantage for everolimus on efficacy
The primary efficacy endpoint was the MATE-3 score, which is limited to CAV, CKD, and ACR. Again, the mean score on this metric (0.93 vs. 1.25) was lower on the everolimus-based regimen but not significantly different.
Looking at specific events in the MATE-6 score, the everolimus-based regimen was associated with lower numerical rates of CAV and CKD, but a higher rate of PTLD, Dr. Almond reported.
On the MATE-3 efficacy analysis, the everolimus-based regimen was again associated with lower numerical rates of CAV and CKD but higher rates of ACR.
In terms of adverse events, including those involving the gastrointestinal tract, blood cells, proteinuria, and interstitial lung disease, most did not differ markedly even if many were numerically more common in the MMF-based arm. The exception was aphthous stomatitis, which was more common on everolimus (32% vs. 7%; P < .001). There were more discontinuations for an adverse event in the MMF arm (21% vs. 12%; P < .001).
Other differences included a lower proportion of patients in the everolimus arm with anti-HLA antibodies (17% vs. 30%; P < .05). Total cholesterol levels at the end of the study were lower but not significantly different in the MMF group, while the higher median glomerular filtration rate was higher on everolimus, and this did reach statistical significance (P < .05).
Infection rates overall were similar, but cytomegalovirus (CMV) infection was more common on the MMF-based regimen. The 30% lower rate of CMV infection in the everolimus proved to be potentially clinically meaningful when it was considered in the context of MATE-3. When these two endpoints were combined (MATE-3 and CMV infection as a prespecified secondary endpoint, the difference was statistically significant (P = .03) in favor of the everolimus-based regimen,
Study supports safety of everolimus regimen
The take-home message is that the everolimus-based regimen, which “is safe in children and young adults when initiated at 6 months after transplant,” can be considered as an alternative to MFF, Dr. Almond concluded.
However, one of the coauthors of the study, Joseph Rossano, MD, chief of the division of cardiology, Children’s Hospital of Philadelphia, suggested a stronger message.
“These data provide compelling reasons to consider initiation of the combination of everolimus and tacrolimus at 6 months post transplant in pediatric heart transplant recipients,” Dr. Rossano said.
Even though the everolimus-based regimen met the terms of noninferiority overall, patients who received this combination rather than the MMF-based regimen “were less likely to have the combined endpoints of vasculopathy, CKD, rejection and CMV infection. Additionally, they were less likely to make donor specific antibodies,” he said.
He also said that this study challenges the current boxed warning for everolimus. He pointed out that the warning, based on early use of everolimus in adults, does not appear to be an issue for children treated at 6 months.
Early mortality based on infection “was not observed in our study,” he said.
The AHA-invited discussant, Antonio G. Cabrera, MD, division chief of pediatric cardiology, University of Utah, Salt Lake City, drew the same conclusions. Based on the study, the everolimus-based regimen can only be described as noninferior to the MMF-based regimen, but Dr. Cabrera listed the same relative advantages as Dr. Rossano, including better kidney function.
Overall, either regimen might be more appealing based on several variables, but Dr. Cabrera said these data suggest everolimus-based treatment “should be considered” as one of two evidence-based options,
Dr. Almond reported no potential financial conflicts of interest. Dr. Rossano reports financial relationships with Abiomed, Bayer, Cytokinetics, Merck, and Myokardia. Dr. Cabrera reported no potential financial conflicts of interest.
FROM AHA 2023
Algorithm cuts time to incision in urgent cesarean deliveries
No specific recommended decision-to-incision time exists for cases of unscheduled, nonemergent cesarean deliveries, although a target of 30 minutes is recommended for emergent deliveries, Lina T. Bernal, MD, of Boston University and colleagues wrote.
The researchers developed a quality improvement project in which a multidisciplinary team defined which unscheduled cesarean deliveries should qualify as urgent, and identified a goal of 40 minutes or less for decision-to-incision time in these cases.
“We defined urgent, unscheduled cesarean delivery as cesarean delivery in patients with the following diagnoses: active phase arrest at 6 cm or greater, category II fetal heart rate tracing during labor requiring delivery per the Shields algorithm, but not meeting emergent category III criteria, any unscheduled cesarean delivery complicated by chorioamnionitis, and failed trial of labor after cesarean,” they wrote.
In a study published in Obstetrics & Gynecology, the researchers compared times from decision to incision before and after the implementation of a multidisciplinary algorithm. The study included 199 urgent, unscheduled deliveries in a single center between May 2019 and November 2019, and implementation period with 283 deliveries from December 2019 to September 2020, and a postimplementation period with 160 deliveries between October 2020 and May 2021.
The primary outcome was the mean time from decision to incision; secondary outcomes were neonatal status based on 5-minute Apgar score and quantitative blood loss during delivery.
Overall, the mean decision-to-incision time improved from 88 minutes during the preimplementation period to 50 minutes in the postimplementation period.
For Black non-Hispanic patients, the mean decision-to-incision time improved from 98 minutes during the preimplementation period to 50 minutes in the postimplementation period. Similarly, mean times among Hispanic patients decreased from 84 minutes to 49 minutes during the pre- and postimplementation periods, respectively.
No significant improvement in decision-to-incision time was noted among patients in other racial and ethnic groups.
In cases of cesarean delivery for fetal indications, 5-minute Apgar scores were significantly higher in the postimplementation period compared with the preimplementation period (8.5 vs. 8.8, P < .01).
No significant associations appeared between maternal quantitative blood loss and the implementation of the algorithm across treatment periods.
Over the course of the study, adjustments to the algorithm included clarification of the criteria, streamlined communication, and expanded use of resources. “There are no prior studies regarding the effects of creation of an urgent category on decision-to-incision time or maternal or neonatal outcomes,” the researchers wrote. “As a result of improved outcomes and appreciation of a standardized approach, the urgent cesarean delivery designation has been incorporated into the labor unit work flow.”
The findings were limited by several factors including the retrospective design, use of data from a single medical center, and the inability to address confounding variables such as age, parity, body mass index, time of delivery, and staffing, the researchers noted. Other limitations include a lack of data on measures of maternal morbidity beyond quantitative blood loss and other neonatal morbidities, and lack of data on patient satisfaction.
However, the results support the use of a standard algorithm to successfully reduce decision-to-incision time in urgent and unscheduled cesarean deliveries, and next steps for further improvement of care should identify which patients are most likely to benefit from a more rapid delivery, the researchers concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
No specific recommended decision-to-incision time exists for cases of unscheduled, nonemergent cesarean deliveries, although a target of 30 minutes is recommended for emergent deliveries, Lina T. Bernal, MD, of Boston University and colleagues wrote.
The researchers developed a quality improvement project in which a multidisciplinary team defined which unscheduled cesarean deliveries should qualify as urgent, and identified a goal of 40 minutes or less for decision-to-incision time in these cases.
“We defined urgent, unscheduled cesarean delivery as cesarean delivery in patients with the following diagnoses: active phase arrest at 6 cm or greater, category II fetal heart rate tracing during labor requiring delivery per the Shields algorithm, but not meeting emergent category III criteria, any unscheduled cesarean delivery complicated by chorioamnionitis, and failed trial of labor after cesarean,” they wrote.
In a study published in Obstetrics & Gynecology, the researchers compared times from decision to incision before and after the implementation of a multidisciplinary algorithm. The study included 199 urgent, unscheduled deliveries in a single center between May 2019 and November 2019, and implementation period with 283 deliveries from December 2019 to September 2020, and a postimplementation period with 160 deliveries between October 2020 and May 2021.
The primary outcome was the mean time from decision to incision; secondary outcomes were neonatal status based on 5-minute Apgar score and quantitative blood loss during delivery.
Overall, the mean decision-to-incision time improved from 88 minutes during the preimplementation period to 50 minutes in the postimplementation period.
For Black non-Hispanic patients, the mean decision-to-incision time improved from 98 minutes during the preimplementation period to 50 minutes in the postimplementation period. Similarly, mean times among Hispanic patients decreased from 84 minutes to 49 minutes during the pre- and postimplementation periods, respectively.
No significant improvement in decision-to-incision time was noted among patients in other racial and ethnic groups.
In cases of cesarean delivery for fetal indications, 5-minute Apgar scores were significantly higher in the postimplementation period compared with the preimplementation period (8.5 vs. 8.8, P < .01).
No significant associations appeared between maternal quantitative blood loss and the implementation of the algorithm across treatment periods.
Over the course of the study, adjustments to the algorithm included clarification of the criteria, streamlined communication, and expanded use of resources. “There are no prior studies regarding the effects of creation of an urgent category on decision-to-incision time or maternal or neonatal outcomes,” the researchers wrote. “As a result of improved outcomes and appreciation of a standardized approach, the urgent cesarean delivery designation has been incorporated into the labor unit work flow.”
The findings were limited by several factors including the retrospective design, use of data from a single medical center, and the inability to address confounding variables such as age, parity, body mass index, time of delivery, and staffing, the researchers noted. Other limitations include a lack of data on measures of maternal morbidity beyond quantitative blood loss and other neonatal morbidities, and lack of data on patient satisfaction.
However, the results support the use of a standard algorithm to successfully reduce decision-to-incision time in urgent and unscheduled cesarean deliveries, and next steps for further improvement of care should identify which patients are most likely to benefit from a more rapid delivery, the researchers concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
No specific recommended decision-to-incision time exists for cases of unscheduled, nonemergent cesarean deliveries, although a target of 30 minutes is recommended for emergent deliveries, Lina T. Bernal, MD, of Boston University and colleagues wrote.
The researchers developed a quality improvement project in which a multidisciplinary team defined which unscheduled cesarean deliveries should qualify as urgent, and identified a goal of 40 minutes or less for decision-to-incision time in these cases.
“We defined urgent, unscheduled cesarean delivery as cesarean delivery in patients with the following diagnoses: active phase arrest at 6 cm or greater, category II fetal heart rate tracing during labor requiring delivery per the Shields algorithm, but not meeting emergent category III criteria, any unscheduled cesarean delivery complicated by chorioamnionitis, and failed trial of labor after cesarean,” they wrote.
In a study published in Obstetrics & Gynecology, the researchers compared times from decision to incision before and after the implementation of a multidisciplinary algorithm. The study included 199 urgent, unscheduled deliveries in a single center between May 2019 and November 2019, and implementation period with 283 deliveries from December 2019 to September 2020, and a postimplementation period with 160 deliveries between October 2020 and May 2021.
The primary outcome was the mean time from decision to incision; secondary outcomes were neonatal status based on 5-minute Apgar score and quantitative blood loss during delivery.
Overall, the mean decision-to-incision time improved from 88 minutes during the preimplementation period to 50 minutes in the postimplementation period.
For Black non-Hispanic patients, the mean decision-to-incision time improved from 98 minutes during the preimplementation period to 50 minutes in the postimplementation period. Similarly, mean times among Hispanic patients decreased from 84 minutes to 49 minutes during the pre- and postimplementation periods, respectively.
No significant improvement in decision-to-incision time was noted among patients in other racial and ethnic groups.
In cases of cesarean delivery for fetal indications, 5-minute Apgar scores were significantly higher in the postimplementation period compared with the preimplementation period (8.5 vs. 8.8, P < .01).
No significant associations appeared between maternal quantitative blood loss and the implementation of the algorithm across treatment periods.
Over the course of the study, adjustments to the algorithm included clarification of the criteria, streamlined communication, and expanded use of resources. “There are no prior studies regarding the effects of creation of an urgent category on decision-to-incision time or maternal or neonatal outcomes,” the researchers wrote. “As a result of improved outcomes and appreciation of a standardized approach, the urgent cesarean delivery designation has been incorporated into the labor unit work flow.”
The findings were limited by several factors including the retrospective design, use of data from a single medical center, and the inability to address confounding variables such as age, parity, body mass index, time of delivery, and staffing, the researchers noted. Other limitations include a lack of data on measures of maternal morbidity beyond quantitative blood loss and other neonatal morbidities, and lack of data on patient satisfaction.
However, the results support the use of a standard algorithm to successfully reduce decision-to-incision time in urgent and unscheduled cesarean deliveries, and next steps for further improvement of care should identify which patients are most likely to benefit from a more rapid delivery, the researchers concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM OBSTETRICS & GYNECOLOGY
Product Update
REVIEW
By James Greenberg, MD
Chief of Gynecology
Associate Professor, Harvard Medical School
Boston, Massachusetts
Guardenia: A “really great solution” for contained tissue extraction
The Guardenia Contained Extraction System, developed by Advanced Surgical Concepts (Wicklow, Ireland), offers a comprehensive approach to contained tissue extraction.
Background. Contained tissue extraction has been an integral part of laparoscopic procedures from at least the late 1980s and early 1990s. Bags of one sort or another are routinely used to remove from the abdomen all sorts of human tissues, including but not limited to ovaries, ectopic pregnancies, gallbladders, kidneys, spleens, and the list goes on. However, after the April 17, 2014, FDA Safety Communication discouraging the use of power morcellators with myomectomy or hysterectomy, the need for more robust contained tissue extraction systems has been ongoing, and there has yet to be a really good solution despite some innovative attempts.
Design/Functionality. Advanced Surgical Concepts’ Guardenia System is the latest attempt to provide a “really great solution” for surgeons to address my 3 “musts” for any system to gain traction in this niche.
- Must #1. An easy method for getting the device into the abdomen.
- Must #2. An easy method for getting the tissue into the bag.
- Must #3. An easy method for getting the tissue out of the body while still containing the cells within the system.
In my opinion based on my usage, Guardenia does a pretty good job addressing all my “musts.”
The Guardenia System is a sterile, single-use device with 3 main components—an introducer with a plunger that will fit through any standard 12-mm trocar, a polyurethane film bag supported by a nitinol ring, and an opening ring with expandable semi-rigid polyethylene “Guard Petals.” When I used it in the operating room to manually morcellate a 10-cm myoma through the umbilicus, I thought it was pretty spot on. Getting the bag into the abdomen is 100% intuitive but even has a nifty up-arrow built onto the tip to make sure the bag is opened in the proper direction. The bag material and the nitinol ring, in combination with the 17.5-cm opening ring, make the process of getting the specimen into the bag and exteriorized easier than any other system I have ever used. And, the opening ring with the Guard Petals yields a very large retraction area for the incision size while providing excellent protection to the surrounding tissues. Overall, Guardenia worked better than anything else I have previously used.
Innovation. Guardenia does not really introduce any fundamentally novel ideas, but it does combine a lot of standard technologies into a product whose sum is much larger than its parts. I would like to see it combined with an occlusive top piece to allow the retractor to be used for single-port laparoscopy as well, but that would just be the cherry on top.
Summary. I have been working on inventing a really good contained tissue extraction system for a long time, and I am a bit chagrined to see someone else outsmart me (low bar), but Advanced Surgical Concepts did, and I really like Guardenia. For pathology that is appropriate for contained morcellation, this device is definitely worth a try, and I suspect many surgeons will switch to it from whatever they are currently using.
FOR MORE INFORMATION, VISIT https://advancedsurgical.ie/guardenia-contained-extraction-system/
The views of the author are personal opinions and do not necessarily represent the views of
REVIEW
By James Greenberg, MD
Chief of Gynecology
Associate Professor, Harvard Medical School
Boston, Massachusetts
Guardenia: A “really great solution” for contained tissue extraction
The Guardenia Contained Extraction System, developed by Advanced Surgical Concepts (Wicklow, Ireland), offers a comprehensive approach to contained tissue extraction.
Background. Contained tissue extraction has been an integral part of laparoscopic procedures from at least the late 1980s and early 1990s. Bags of one sort or another are routinely used to remove from the abdomen all sorts of human tissues, including but not limited to ovaries, ectopic pregnancies, gallbladders, kidneys, spleens, and the list goes on. However, after the April 17, 2014, FDA Safety Communication discouraging the use of power morcellators with myomectomy or hysterectomy, the need for more robust contained tissue extraction systems has been ongoing, and there has yet to be a really good solution despite some innovative attempts.
Design/Functionality. Advanced Surgical Concepts’ Guardenia System is the latest attempt to provide a “really great solution” for surgeons to address my 3 “musts” for any system to gain traction in this niche.
- Must #1. An easy method for getting the device into the abdomen.
- Must #2. An easy method for getting the tissue into the bag.
- Must #3. An easy method for getting the tissue out of the body while still containing the cells within the system.
In my opinion based on my usage, Guardenia does a pretty good job addressing all my “musts.”
The Guardenia System is a sterile, single-use device with 3 main components—an introducer with a plunger that will fit through any standard 12-mm trocar, a polyurethane film bag supported by a nitinol ring, and an opening ring with expandable semi-rigid polyethylene “Guard Petals.” When I used it in the operating room to manually morcellate a 10-cm myoma through the umbilicus, I thought it was pretty spot on. Getting the bag into the abdomen is 100% intuitive but even has a nifty up-arrow built onto the tip to make sure the bag is opened in the proper direction. The bag material and the nitinol ring, in combination with the 17.5-cm opening ring, make the process of getting the specimen into the bag and exteriorized easier than any other system I have ever used. And, the opening ring with the Guard Petals yields a very large retraction area for the incision size while providing excellent protection to the surrounding tissues. Overall, Guardenia worked better than anything else I have previously used.
Innovation. Guardenia does not really introduce any fundamentally novel ideas, but it does combine a lot of standard technologies into a product whose sum is much larger than its parts. I would like to see it combined with an occlusive top piece to allow the retractor to be used for single-port laparoscopy as well, but that would just be the cherry on top.
Summary. I have been working on inventing a really good contained tissue extraction system for a long time, and I am a bit chagrined to see someone else outsmart me (low bar), but Advanced Surgical Concepts did, and I really like Guardenia. For pathology that is appropriate for contained morcellation, this device is definitely worth a try, and I suspect many surgeons will switch to it from whatever they are currently using.
FOR MORE INFORMATION, VISIT https://advancedsurgical.ie/guardenia-contained-extraction-system/
The views of the author are personal opinions and do not necessarily represent the views of
REVIEW
By James Greenberg, MD
Chief of Gynecology
Associate Professor, Harvard Medical School
Boston, Massachusetts
Guardenia: A “really great solution” for contained tissue extraction
The Guardenia Contained Extraction System, developed by Advanced Surgical Concepts (Wicklow, Ireland), offers a comprehensive approach to contained tissue extraction.
Background. Contained tissue extraction has been an integral part of laparoscopic procedures from at least the late 1980s and early 1990s. Bags of one sort or another are routinely used to remove from the abdomen all sorts of human tissues, including but not limited to ovaries, ectopic pregnancies, gallbladders, kidneys, spleens, and the list goes on. However, after the April 17, 2014, FDA Safety Communication discouraging the use of power morcellators with myomectomy or hysterectomy, the need for more robust contained tissue extraction systems has been ongoing, and there has yet to be a really good solution despite some innovative attempts.
Design/Functionality. Advanced Surgical Concepts’ Guardenia System is the latest attempt to provide a “really great solution” for surgeons to address my 3 “musts” for any system to gain traction in this niche.
- Must #1. An easy method for getting the device into the abdomen.
- Must #2. An easy method for getting the tissue into the bag.
- Must #3. An easy method for getting the tissue out of the body while still containing the cells within the system.
In my opinion based on my usage, Guardenia does a pretty good job addressing all my “musts.”
The Guardenia System is a sterile, single-use device with 3 main components—an introducer with a plunger that will fit through any standard 12-mm trocar, a polyurethane film bag supported by a nitinol ring, and an opening ring with expandable semi-rigid polyethylene “Guard Petals.” When I used it in the operating room to manually morcellate a 10-cm myoma through the umbilicus, I thought it was pretty spot on. Getting the bag into the abdomen is 100% intuitive but even has a nifty up-arrow built onto the tip to make sure the bag is opened in the proper direction. The bag material and the nitinol ring, in combination with the 17.5-cm opening ring, make the process of getting the specimen into the bag and exteriorized easier than any other system I have ever used. And, the opening ring with the Guard Petals yields a very large retraction area for the incision size while providing excellent protection to the surrounding tissues. Overall, Guardenia worked better than anything else I have previously used.
Innovation. Guardenia does not really introduce any fundamentally novel ideas, but it does combine a lot of standard technologies into a product whose sum is much larger than its parts. I would like to see it combined with an occlusive top piece to allow the retractor to be used for single-port laparoscopy as well, but that would just be the cherry on top.
Summary. I have been working on inventing a really good contained tissue extraction system for a long time, and I am a bit chagrined to see someone else outsmart me (low bar), but Advanced Surgical Concepts did, and I really like Guardenia. For pathology that is appropriate for contained morcellation, this device is definitely worth a try, and I suspect many surgeons will switch to it from whatever they are currently using.
FOR MORE INFORMATION, VISIT https://advancedsurgical.ie/guardenia-contained-extraction-system/
The views of the author are personal opinions and do not necessarily represent the views of
Surgery approach may improve survival in advanced ovarian cancer
TOPLINE:
Neoadjuvant chemotherapy followed by interval cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) significantly improves progression-free survival (PFS) and overall survival, compared with interval cytoreductive surgery alone, in patients with advanced ovarian cancer, new research shows.
METHODOLOGY:
- Several randomized controlled trials have shown survival benefits with HIPEC followed by interval cytoreductive surgery in advanced ovarian cancer. Despite the data, the use of HIPEC in clinical practice remains limited.
- Potential downsides of HIPEC include longer operative time and treatment-related complications.
- This prospective, multicenter, comparative effectiveness study evaluated the safety and effectiveness of interval cytoreductive surgery with HIPEC versus the surgery alone.
- The study, conducted at seven Korean Gynecologic Oncology Group institutions, included 196 patients (mean age, 58 years) with stage III or IV ovarian cancer who had received at least three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery with HIPEC (n = 109) or without HIPEC (n = 87).
- The researchers reported progression-free survival as well as overall survival and treatment-related toxic effects.
TAKEAWAY:
- During a median follow-up of 28.2 months, 128 patients (65%) had a recurrence and 30 died (15.3%) – 8.3% in the HIPEC group and 24.1% in the non-HIPEC group.
- Compared with no HIPEC, interval cytoreductive surgery with HIPEC led to a significant improvement in median PFS (22.9 months vs. 14.2 months; P = .005) and median overall survival (not reached vs. 53 months; P = .002).
- The frequency of grade 3 or 4 postoperative complications was similar in both groups: 2.8% with HIPEC versus 3.4% without HIPEC.
- Among patients with recurrence, the frequency of peritoneal recurrence was significantly lower among those who received HIPEC (32.8% vs. 64.1% without HIPEC; P = .001).
IN PRACTICE:
“We observed a significantly superior survival benefit associated with [interval cytoreductive surgery] with HIPEC, without higher rates of postoperative complications,” the authors concluded, adding that “the survival benefit remained consistent, irrespective of maintenance therapy.”
SOURCE:
The study, led by Jung-Yun Lee, MD, PhD, Yonsei University College of Medicine, Seoul, Korea, was published online in JAMA Surgery.
LIMITATIONS:
The patients were not randomly assigned and the decision to give HIPEC was at the clinician’s discretion, introducing the possibility of selection and treatment bias. The different types of drugs used in HIPEC could result in bias in data interpretation.
DISCLOSURES:
The authors reported no conflicts of interest. The study had no specific funding.
A version of this article first appeared on Medscape.com.
TOPLINE:
Neoadjuvant chemotherapy followed by interval cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) significantly improves progression-free survival (PFS) and overall survival, compared with interval cytoreductive surgery alone, in patients with advanced ovarian cancer, new research shows.
METHODOLOGY:
- Several randomized controlled trials have shown survival benefits with HIPEC followed by interval cytoreductive surgery in advanced ovarian cancer. Despite the data, the use of HIPEC in clinical practice remains limited.
- Potential downsides of HIPEC include longer operative time and treatment-related complications.
- This prospective, multicenter, comparative effectiveness study evaluated the safety and effectiveness of interval cytoreductive surgery with HIPEC versus the surgery alone.
- The study, conducted at seven Korean Gynecologic Oncology Group institutions, included 196 patients (mean age, 58 years) with stage III or IV ovarian cancer who had received at least three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery with HIPEC (n = 109) or without HIPEC (n = 87).
- The researchers reported progression-free survival as well as overall survival and treatment-related toxic effects.
TAKEAWAY:
- During a median follow-up of 28.2 months, 128 patients (65%) had a recurrence and 30 died (15.3%) – 8.3% in the HIPEC group and 24.1% in the non-HIPEC group.
- Compared with no HIPEC, interval cytoreductive surgery with HIPEC led to a significant improvement in median PFS (22.9 months vs. 14.2 months; P = .005) and median overall survival (not reached vs. 53 months; P = .002).
- The frequency of grade 3 or 4 postoperative complications was similar in both groups: 2.8% with HIPEC versus 3.4% without HIPEC.
- Among patients with recurrence, the frequency of peritoneal recurrence was significantly lower among those who received HIPEC (32.8% vs. 64.1% without HIPEC; P = .001).
IN PRACTICE:
“We observed a significantly superior survival benefit associated with [interval cytoreductive surgery] with HIPEC, without higher rates of postoperative complications,” the authors concluded, adding that “the survival benefit remained consistent, irrespective of maintenance therapy.”
SOURCE:
The study, led by Jung-Yun Lee, MD, PhD, Yonsei University College of Medicine, Seoul, Korea, was published online in JAMA Surgery.
LIMITATIONS:
The patients were not randomly assigned and the decision to give HIPEC was at the clinician’s discretion, introducing the possibility of selection and treatment bias. The different types of drugs used in HIPEC could result in bias in data interpretation.
DISCLOSURES:
The authors reported no conflicts of interest. The study had no specific funding.
A version of this article first appeared on Medscape.com.
TOPLINE:
Neoadjuvant chemotherapy followed by interval cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC) significantly improves progression-free survival (PFS) and overall survival, compared with interval cytoreductive surgery alone, in patients with advanced ovarian cancer, new research shows.
METHODOLOGY:
- Several randomized controlled trials have shown survival benefits with HIPEC followed by interval cytoreductive surgery in advanced ovarian cancer. Despite the data, the use of HIPEC in clinical practice remains limited.
- Potential downsides of HIPEC include longer operative time and treatment-related complications.
- This prospective, multicenter, comparative effectiveness study evaluated the safety and effectiveness of interval cytoreductive surgery with HIPEC versus the surgery alone.
- The study, conducted at seven Korean Gynecologic Oncology Group institutions, included 196 patients (mean age, 58 years) with stage III or IV ovarian cancer who had received at least three cycles of neoadjuvant chemotherapy followed by interval cytoreductive surgery with HIPEC (n = 109) or without HIPEC (n = 87).
- The researchers reported progression-free survival as well as overall survival and treatment-related toxic effects.
TAKEAWAY:
- During a median follow-up of 28.2 months, 128 patients (65%) had a recurrence and 30 died (15.3%) – 8.3% in the HIPEC group and 24.1% in the non-HIPEC group.
- Compared with no HIPEC, interval cytoreductive surgery with HIPEC led to a significant improvement in median PFS (22.9 months vs. 14.2 months; P = .005) and median overall survival (not reached vs. 53 months; P = .002).
- The frequency of grade 3 or 4 postoperative complications was similar in both groups: 2.8% with HIPEC versus 3.4% without HIPEC.
- Among patients with recurrence, the frequency of peritoneal recurrence was significantly lower among those who received HIPEC (32.8% vs. 64.1% without HIPEC; P = .001).
IN PRACTICE:
“We observed a significantly superior survival benefit associated with [interval cytoreductive surgery] with HIPEC, without higher rates of postoperative complications,” the authors concluded, adding that “the survival benefit remained consistent, irrespective of maintenance therapy.”
SOURCE:
The study, led by Jung-Yun Lee, MD, PhD, Yonsei University College of Medicine, Seoul, Korea, was published online in JAMA Surgery.
LIMITATIONS:
The patients were not randomly assigned and the decision to give HIPEC was at the clinician’s discretion, introducing the possibility of selection and treatment bias. The different types of drugs used in HIPEC could result in bias in data interpretation.
DISCLOSURES:
The authors reported no conflicts of interest. The study had no specific funding.
A version of this article first appeared on Medscape.com.
FROM JAMA SURGERY
Minimally invasive surfactant shows some benefit in infants’ first 2 years
Results of the OPTIMIST follow-up study were published online in JAMA.
Researchers, led by Peter A. Dargaville, MD, department of paediatrics, Royal Hobart (Australia) Hospital, found that MIST, which involves administering surfactant via a thin catheter, compared with sham treatment, did not reduce the incidence of death or neurodevelopmental disability (NDD) by 2 years of age.
However, infants who received MIST had lower rates of poor respiratory outcomes during those first 2 years of life.
Study spanned 11 countries
The study was conducted in 33 tertiary neonatal intensive care units (NICUs) in 11 countries, including Australia, Canada, Israel, New Zealand, Qatar, Singapore, Slovenia, the Netherlands, Turkey, the United Kingdom, and the United States.
It included 486 infants 25-28 weeks old supported with CPAP; 453 had follow-up data available and data on the key secondary outcome were available for 434 infants.
The sham treatment consisted of only transient repositioning without airway instruments. Treating clinicians, outcome assessors, and parents were blinded to group status.
No significant difference in deaths, NDD
Death or NDD occurred in 36.3% of the patients in the MIST group and 36.1% in the control group (risk difference, 0%; 95% confidence interval, −7.6% to 7.7%; relative risk, 1.0; 95% confidence interval, 0.81-1.24).
Secondary respiratory outcomes were better in the MIST group:
- Hospitalization with respiratory illness occurred in 25.1% in the MIST group versus 38.2% in the control group (RR, 0.66; 95% CI, 0.54-0.81).
- Parent-reported wheezing or breathing difficulty occurred in 40.6% in the MIST group versus 53.6% in controls (RR, 0.76; 95% CI, 0.63-0.90).
- Asthma diagnosed by a physician was reported in 4.4% and 11.9% of MIST and control-group infants, respectively.
- Reported use of inhaled relievers (beta2 agonists) was 23.9% in the MIST group versus 38.7% in controls.
The previous study of early outcomes of deaths or bronchopulmonary dysplasia (BPD; chronic lung injury in preterm infants) was published by the same group of researchers in 2021.
Important benefit for respiratory health
Suhas G. Kallapur, MD, chief of the divisions of neonatology and developmental biology at University of California, Los Angeles, who was not part of either study, said: “This is one of the largest studies to date examining whether the MIST procedure for surfactant is beneficial in preterm babies born at 25-28 weeks’ gestation.”
Overall, when considering the 2021 and 2023 studies together, it appears that the MIST therapy has important benefits for respiratory health during a NICU stay and in early infancy, even though the primary outcome of death or NDD was not different between the treatment and control groups, Dr. Kallapur said.
“The slight (nonsignificant) increase in deaths in the MIST group was confined to the more immature babies – 25-26 weeks’ gestation at birth,” he pointed out. “In the bigger and more mature babies – 27-28 week gestation infants – the benefits of MIST therapy occurred without any increase in mortality, suggesting that this group of babies may be the group that stands to benefit most from this therapy.”
Dr. Kallapur said new data in the developmental origins of health and disease “now show that the trajectory of respiratory health in infancy is an important determinant of respiratory health into adulthood and older age.”
Therefore, the finding of benefit to respiratory health is particularly important, he said.
He noted that MIST or similar therapy is already in use in many NICUs throughout the world and that those already using it will likely feel vindicated by this study.
“Neonatologists who were on the sidelines will likely see these results – especially childhood respiratory outcomes – as a reason to initiate this procedure in all but the most immature preterm infants,” Dr. Kallapur says.
Dr. Dargaville reports personal fees from AbbVie and Chiesi Farmaceutici and provision of surfactant at reduced cost and support for conference travel from Chiesi Farmaceutici during the conduct of the study; in addition, Dr. Dargaville has been issued a patent for a catheter design. One coauthor reports grants from Chiesi Farmaceutici during the conduct of the study. Another coauthor reports serving as chief investigator for OPTI-SURF, an observational study on United Kingdom neonatal surfactant use in respiratory distress syndrome funded by Chiesi UK outside the submitted work. A third coauthor reports personal fees from Chiesi Farmaceutici outside the submitted work. This study was funded by grants from the Royal Hobart Hospital Research Foundation and the Australian National Health and Medical Research Council. Exogenous surfactant was provided at reduced cost by Chiesi Farmaceutici. Dr. Kallapur has no relevant financial relationships.
Results of the OPTIMIST follow-up study were published online in JAMA.
Researchers, led by Peter A. Dargaville, MD, department of paediatrics, Royal Hobart (Australia) Hospital, found that MIST, which involves administering surfactant via a thin catheter, compared with sham treatment, did not reduce the incidence of death or neurodevelopmental disability (NDD) by 2 years of age.
However, infants who received MIST had lower rates of poor respiratory outcomes during those first 2 years of life.
Study spanned 11 countries
The study was conducted in 33 tertiary neonatal intensive care units (NICUs) in 11 countries, including Australia, Canada, Israel, New Zealand, Qatar, Singapore, Slovenia, the Netherlands, Turkey, the United Kingdom, and the United States.
It included 486 infants 25-28 weeks old supported with CPAP; 453 had follow-up data available and data on the key secondary outcome were available for 434 infants.
The sham treatment consisted of only transient repositioning without airway instruments. Treating clinicians, outcome assessors, and parents were blinded to group status.
No significant difference in deaths, NDD
Death or NDD occurred in 36.3% of the patients in the MIST group and 36.1% in the control group (risk difference, 0%; 95% confidence interval, −7.6% to 7.7%; relative risk, 1.0; 95% confidence interval, 0.81-1.24).
Secondary respiratory outcomes were better in the MIST group:
- Hospitalization with respiratory illness occurred in 25.1% in the MIST group versus 38.2% in the control group (RR, 0.66; 95% CI, 0.54-0.81).
- Parent-reported wheezing or breathing difficulty occurred in 40.6% in the MIST group versus 53.6% in controls (RR, 0.76; 95% CI, 0.63-0.90).
- Asthma diagnosed by a physician was reported in 4.4% and 11.9% of MIST and control-group infants, respectively.
- Reported use of inhaled relievers (beta2 agonists) was 23.9% in the MIST group versus 38.7% in controls.
The previous study of early outcomes of deaths or bronchopulmonary dysplasia (BPD; chronic lung injury in preterm infants) was published by the same group of researchers in 2021.
Important benefit for respiratory health
Suhas G. Kallapur, MD, chief of the divisions of neonatology and developmental biology at University of California, Los Angeles, who was not part of either study, said: “This is one of the largest studies to date examining whether the MIST procedure for surfactant is beneficial in preterm babies born at 25-28 weeks’ gestation.”
Overall, when considering the 2021 and 2023 studies together, it appears that the MIST therapy has important benefits for respiratory health during a NICU stay and in early infancy, even though the primary outcome of death or NDD was not different between the treatment and control groups, Dr. Kallapur said.
“The slight (nonsignificant) increase in deaths in the MIST group was confined to the more immature babies – 25-26 weeks’ gestation at birth,” he pointed out. “In the bigger and more mature babies – 27-28 week gestation infants – the benefits of MIST therapy occurred without any increase in mortality, suggesting that this group of babies may be the group that stands to benefit most from this therapy.”
Dr. Kallapur said new data in the developmental origins of health and disease “now show that the trajectory of respiratory health in infancy is an important determinant of respiratory health into adulthood and older age.”
Therefore, the finding of benefit to respiratory health is particularly important, he said.
He noted that MIST or similar therapy is already in use in many NICUs throughout the world and that those already using it will likely feel vindicated by this study.
“Neonatologists who were on the sidelines will likely see these results – especially childhood respiratory outcomes – as a reason to initiate this procedure in all but the most immature preterm infants,” Dr. Kallapur says.
Dr. Dargaville reports personal fees from AbbVie and Chiesi Farmaceutici and provision of surfactant at reduced cost and support for conference travel from Chiesi Farmaceutici during the conduct of the study; in addition, Dr. Dargaville has been issued a patent for a catheter design. One coauthor reports grants from Chiesi Farmaceutici during the conduct of the study. Another coauthor reports serving as chief investigator for OPTI-SURF, an observational study on United Kingdom neonatal surfactant use in respiratory distress syndrome funded by Chiesi UK outside the submitted work. A third coauthor reports personal fees from Chiesi Farmaceutici outside the submitted work. This study was funded by grants from the Royal Hobart Hospital Research Foundation and the Australian National Health and Medical Research Council. Exogenous surfactant was provided at reduced cost by Chiesi Farmaceutici. Dr. Kallapur has no relevant financial relationships.
Results of the OPTIMIST follow-up study were published online in JAMA.
Researchers, led by Peter A. Dargaville, MD, department of paediatrics, Royal Hobart (Australia) Hospital, found that MIST, which involves administering surfactant via a thin catheter, compared with sham treatment, did not reduce the incidence of death or neurodevelopmental disability (NDD) by 2 years of age.
However, infants who received MIST had lower rates of poor respiratory outcomes during those first 2 years of life.
Study spanned 11 countries
The study was conducted in 33 tertiary neonatal intensive care units (NICUs) in 11 countries, including Australia, Canada, Israel, New Zealand, Qatar, Singapore, Slovenia, the Netherlands, Turkey, the United Kingdom, and the United States.
It included 486 infants 25-28 weeks old supported with CPAP; 453 had follow-up data available and data on the key secondary outcome were available for 434 infants.
The sham treatment consisted of only transient repositioning without airway instruments. Treating clinicians, outcome assessors, and parents were blinded to group status.
No significant difference in deaths, NDD
Death or NDD occurred in 36.3% of the patients in the MIST group and 36.1% in the control group (risk difference, 0%; 95% confidence interval, −7.6% to 7.7%; relative risk, 1.0; 95% confidence interval, 0.81-1.24).
Secondary respiratory outcomes were better in the MIST group:
- Hospitalization with respiratory illness occurred in 25.1% in the MIST group versus 38.2% in the control group (RR, 0.66; 95% CI, 0.54-0.81).
- Parent-reported wheezing or breathing difficulty occurred in 40.6% in the MIST group versus 53.6% in controls (RR, 0.76; 95% CI, 0.63-0.90).
- Asthma diagnosed by a physician was reported in 4.4% and 11.9% of MIST and control-group infants, respectively.
- Reported use of inhaled relievers (beta2 agonists) was 23.9% in the MIST group versus 38.7% in controls.
The previous study of early outcomes of deaths or bronchopulmonary dysplasia (BPD; chronic lung injury in preterm infants) was published by the same group of researchers in 2021.
Important benefit for respiratory health
Suhas G. Kallapur, MD, chief of the divisions of neonatology and developmental biology at University of California, Los Angeles, who was not part of either study, said: “This is one of the largest studies to date examining whether the MIST procedure for surfactant is beneficial in preterm babies born at 25-28 weeks’ gestation.”
Overall, when considering the 2021 and 2023 studies together, it appears that the MIST therapy has important benefits for respiratory health during a NICU stay and in early infancy, even though the primary outcome of death or NDD was not different between the treatment and control groups, Dr. Kallapur said.
“The slight (nonsignificant) increase in deaths in the MIST group was confined to the more immature babies – 25-26 weeks’ gestation at birth,” he pointed out. “In the bigger and more mature babies – 27-28 week gestation infants – the benefits of MIST therapy occurred without any increase in mortality, suggesting that this group of babies may be the group that stands to benefit most from this therapy.”
Dr. Kallapur said new data in the developmental origins of health and disease “now show that the trajectory of respiratory health in infancy is an important determinant of respiratory health into adulthood and older age.”
Therefore, the finding of benefit to respiratory health is particularly important, he said.
He noted that MIST or similar therapy is already in use in many NICUs throughout the world and that those already using it will likely feel vindicated by this study.
“Neonatologists who were on the sidelines will likely see these results – especially childhood respiratory outcomes – as a reason to initiate this procedure in all but the most immature preterm infants,” Dr. Kallapur says.
Dr. Dargaville reports personal fees from AbbVie and Chiesi Farmaceutici and provision of surfactant at reduced cost and support for conference travel from Chiesi Farmaceutici during the conduct of the study; in addition, Dr. Dargaville has been issued a patent for a catheter design. One coauthor reports grants from Chiesi Farmaceutici during the conduct of the study. Another coauthor reports serving as chief investigator for OPTI-SURF, an observational study on United Kingdom neonatal surfactant use in respiratory distress syndrome funded by Chiesi UK outside the submitted work. A third coauthor reports personal fees from Chiesi Farmaceutici outside the submitted work. This study was funded by grants from the Royal Hobart Hospital Research Foundation and the Australian National Health and Medical Research Council. Exogenous surfactant was provided at reduced cost by Chiesi Farmaceutici. Dr. Kallapur has no relevant financial relationships.
FROM JAMA
‘Decapitated’ boy saved by surgery team
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: I am joined today by Dr. Ohad Einav. He’s a staff surgeon in orthopedics at Hadassah Medical Center in Jerusalem. He’s with me to talk about an absolutely incredible surgical case, something that is terrifying to most non–orthopedic surgeons and I imagine is fairly scary for spine surgeons like him as well. But what we don’t have is information about how this works from a medical perspective. So, first of all, Dr. Einav, thank you for taking time to speak with me today.
Ohad Einav, MD: Thank you for having me.
Dr. Wilson: Can you tell us about Suleiman Hassan and what happened to him before he came into your care?
Dr. Einav: Hassan is a 12-year-old child who was riding his bicycle on the West Bank, about 40 minutes from here. Unfortunately, he was involved in a motor vehicle accident and he suffered injuries to his abdomen and cervical spine. He was transported to our service by helicopter from the scene of the accident.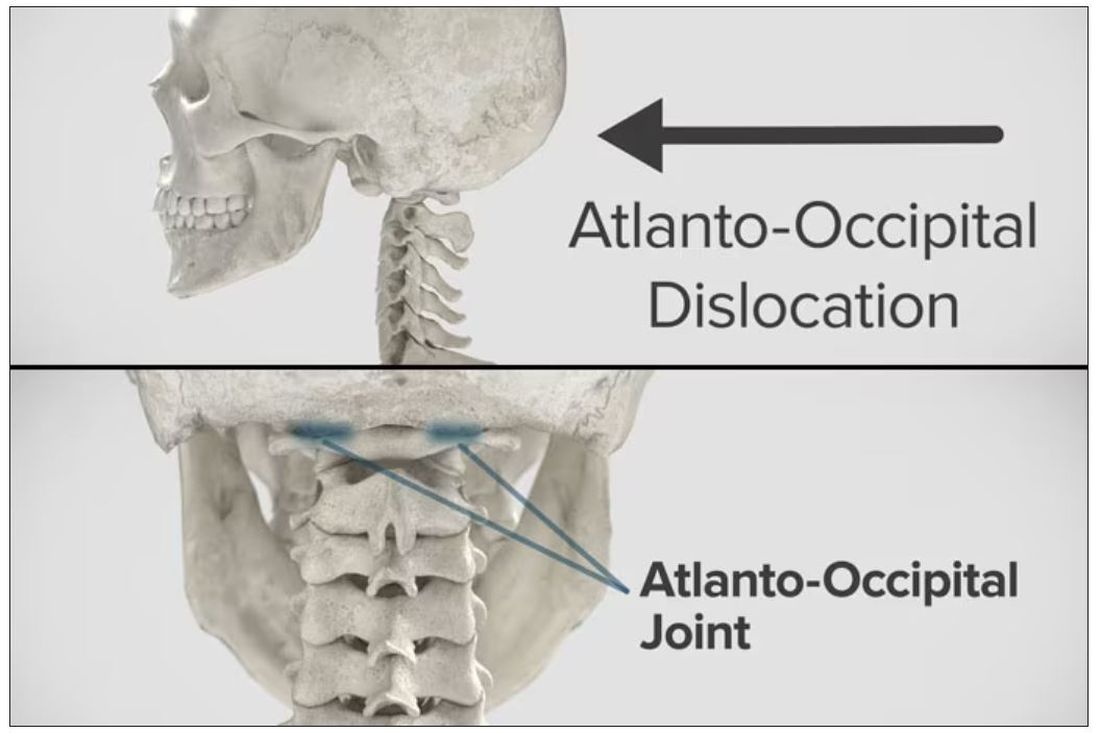
Dr. Wilson: “Injury to the cervical spine” might be something of an understatement. He had what’s called atlanto-occipital dislocation, colloquially often referred to as internal decapitation. Can you tell us what that means? It sounds terrifying.
Dr. Einav: It’s an injury to the ligaments between the occiput and the upper cervical spine, with or without bony fracture. The atlanto-occipital joint is formed by the superior articular facet of the atlas and the occipital condyle, stabilized by an articular capsule between the head and neck, and is supported by various ligaments around it that stabilize the joint and allow joint movements, including flexion, extension, and some rotation in the lower levels.
Dr. Wilson: This joint has several degrees of freedom, which means it needs a lot of support. With this type of injury, where essentially you have severing of the ligaments, is it usually survivable? How dangerous is this?
Dr. Einav: The mortality rate is 50%-60%, depending on the primary impact, the injury, transportation later on, and then the surgery and surgical management.
Dr. Wilson: Tell us a bit about this patient’s status when he came to your medical center. I assume he was in bad shape.
Dr. Einav: Hassan arrived at our medical center with a Glasgow Coma Scale score of 15. He was fully conscious. He was hemodynamically stable except for a bad laceration on his abdomen. He had a Philadelphia collar around his neck. He was transported by chopper because the paramedics suspected that he had a cervical spine injury and decided to bring him to a Level 1 trauma center.
He was monitored and we treated him according to the ATLS [advanced trauma life support] protocol. He didn’t have any gross sensory deficits, but he was a little confused about the whole situation and the accident. Therefore, we could do a general examination but we couldn’t rely on that regarding any sensory deficit that he may or may not have. We decided as a team that it would be better to slow down and control the situation. We decided not to operate on him immediately. We basically stabilized him and made sure that he didn’t have any traumatic internal organ damage. Later on we took him to the OR and performed surgery.
Dr. Wilson: It’s amazing that he had intact motor function, considering the extent of his injury. The spinal cord was spared somewhat during the injury. There must have been a moment when you realized that this kid, who was conscious and could move all four extremities, had a very severe neck injury. Was that due to a CT scan or physical exam? And what was your feeling when you saw that he had atlanto-occipital dislocation?
Dr. Einav: As a surgeon, you have a gut feeling in regard to the general examination of the patient. But I never rely on gut feelings. On the CT, I understood exactly what he had, what we needed to do, and the time frame.
Dr. Wilson: You’ve done these types of surgeries before, right? Obviously, no one has done a lot of them because this isn’t very common. But you knew what to do. Did you have a plan? Where does your experience come into play in a situation like this?
Dr. Einav: I graduated from the spine program of Toronto University, where I did a fellowship in trauma of the spine and complex spine surgery. I had very good teachers, and during my fellowship I treated a few cases in older patients that were similar but not the same. Therefore, I knew exactly what needed to be done.
Dr. Wilson: For those of us who aren’t surgeons, take us into the OR with you. This is obviously an incredibly delicate procedure. You are high up in the spinal cord at the base of the brain. The slightest mistake could have devastating consequences. What are the key elements of this procedure? What can go wrong here? What is the number-one thing you have to look out for when you’re trying to fix an internal decapitation?
Dr. Einav: The key element in surgeries of the cervical spine – trauma and complex spine surgery – is planning. I never go to the OR without knowing what I’m going to do. I have a few plans – plan A, plan B, plan C – in case something fails. So, I definitely know what the next step will be. I always think about the surgery a few hours before, if I have time to prepare.
The second thing that is very important is teamwork. The team needs to be coordinated. Everybody needs to know what their job is. With these types of injuries, it’s not the time for rookies. If you are new, please stand back and let the more experienced people do that job. I’m talking about surgeons, nurses, anesthesiologists – everyone.
Another important thing in planning is choosing the right hardware. For example, in this case we had a problem because most of the hardware is designed for adults, and we had to improvise because there isn’t a lot of hardware on the market for the pediatric population. The adult plates and screws are too big, so we had to improvise.
Dr. Wilson: Tell us more about that. How do you improvise spinal hardware for a 12-year-old?
Dr. Einav: In this case, I chose to use hardware from one of the companies that works with us.
You can see in this model the area of the injury, and the area that we worked on. To perform the surgery, I had to use some plates and rods from a different company. This company’s (NuVasive) hardware has a small attachment to the skull, which was helpful for affixing the skull to the cervical spine, instead of using a big plate that would sit at the base of the skull and would not be very good for him. Most of the hardware is made for adults and not for kids.
Dr. Wilson: Will that hardware preserve the motor function of his neck? Will he be able to turn his head and extend and flex it?
Dr. Einav: The injury leads to instability and destruction of both articulations between the head and neck. Therefore, those articulations won’t be able to function the same way in the future. There is a decrease of something like 50% of the flexion and extension of Hassan’s cervical spine. Therefore, I decided that in this case there would be no chance of saving Hassan’s motor function unless we performed a fusion between the head and the neck, and therefore I decided that this would be the best procedure with the best survival rate. So, in the future, he will have some diminished flexion, extension, and rotation of his head.
Dr. Wilson: How long did his surgery take?
Dr. Einav: To be honest, I don’t remember. But I can tell you that it took us time. It was very challenging to coordinate with everyone. The most problematic part of the surgery to perform is what we call “flip-over.”
The anesthesiologist intubated the patient when he was supine, and later on, we flipped him prone to operate on the spine. This maneuver can actually lead to injury by itself, and injury at this level is fatal. So, we took our time and got Hassan into the OR. The anesthesiologist did a great job with the GlideScope – inserting the endotracheal tube. Later on, we neuromonitored him. Basically, we connected Hassan’s peripheral nerves to a computer and monitored his motor function. Gently we flipped him over, and after that we saw a little change in his motor function, so we had to modify his position so we could preserve his motor function. We then started the procedure, which took a few hours. I don’t know exactly how many.
Dr. Wilson: That just speaks to how delicate this is for everything from the intubation, where typically you’re manipulating the head, to the repositioning. Clearly this requires a lot of teamwork.
What happened after the operation? How is he doing?
Dr. Einav: After the operation, Hassan had a great recovery. He’s doing well. He doesn’t have any motor or sensory deficits. He’s able to ambulate without any aid. He had no signs of infection, which can happen after a car accident, neither from his abdominal wound nor from the occipital cervical surgery. He feels well. We saw him in the clinic. We removed his collar. We monitored him at the clinic. He looked amazing.
Dr. Wilson: That’s incredible. Are there long-term risks for him that you need to be looking out for?
Dr. Einav: Yes, and that’s the reason that we are monitoring him post surgery. While he was in the hospital, we monitored his motor and sensory functions, as well as his wound healing. Later on, in the clinic, for a few weeks after surgery we monitored for any failure of the hardware and bone graft. We check for healing of the bone graft and bone substitutes we put in to heal those bones.
Dr. Wilson: He will grow, right? He’s only 12, so he still has some years of growth in him. Is he going to need more surgery or any kind of hardware upgrade?
Dr. Einav: I hope not. In my surgeries, I never rely on the hardware for long durations. If I decide to do, for example, fusion, I rely on the hardware for a certain amount of time. And then I plan that the biology will do the work. If I plan for fusion, I put bone grafts in the preferred area for a fusion. Then if the hardware fails, I wouldn’t need to take out the hardware, and there would be no change in the condition of the patient.
Dr. Wilson: What an incredible story. It’s clear that you and your team kept your cool despite a very high-acuity situation with a ton of risk. What a tremendous outcome that this boy is not only alive but fully functional. So, congratulations to you and your team. That was very strong work.
Dr. Einav: Thank you very much. I would like to thank our team. We have to remember that the surgeon is not standing alone in the war. Hassan’s story is a success story of a very big group of people from various backgrounds and religions. They work day and night to help people and save lives. To the paramedics, the physiologists, the traumatologists, the pediatricians, the nurses, the physiotherapists, and obviously the surgeons, a big thank you. His story is our success story.
Dr. Wilson: It’s inspiring to see so many people come together to do what we all are here for, which is to fight against suffering, disease, and death. Thank you for keeping up that fight. And thank you for joining me here.
Dr. Einav: Thank you very much.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: I am joined today by Dr. Ohad Einav. He’s a staff surgeon in orthopedics at Hadassah Medical Center in Jerusalem. He’s with me to talk about an absolutely incredible surgical case, something that is terrifying to most non–orthopedic surgeons and I imagine is fairly scary for spine surgeons like him as well. But what we don’t have is information about how this works from a medical perspective. So, first of all, Dr. Einav, thank you for taking time to speak with me today.
Ohad Einav, MD: Thank you for having me.
Dr. Wilson: Can you tell us about Suleiman Hassan and what happened to him before he came into your care?
Dr. Einav: Hassan is a 12-year-old child who was riding his bicycle on the West Bank, about 40 minutes from here. Unfortunately, he was involved in a motor vehicle accident and he suffered injuries to his abdomen and cervical spine. He was transported to our service by helicopter from the scene of the accident.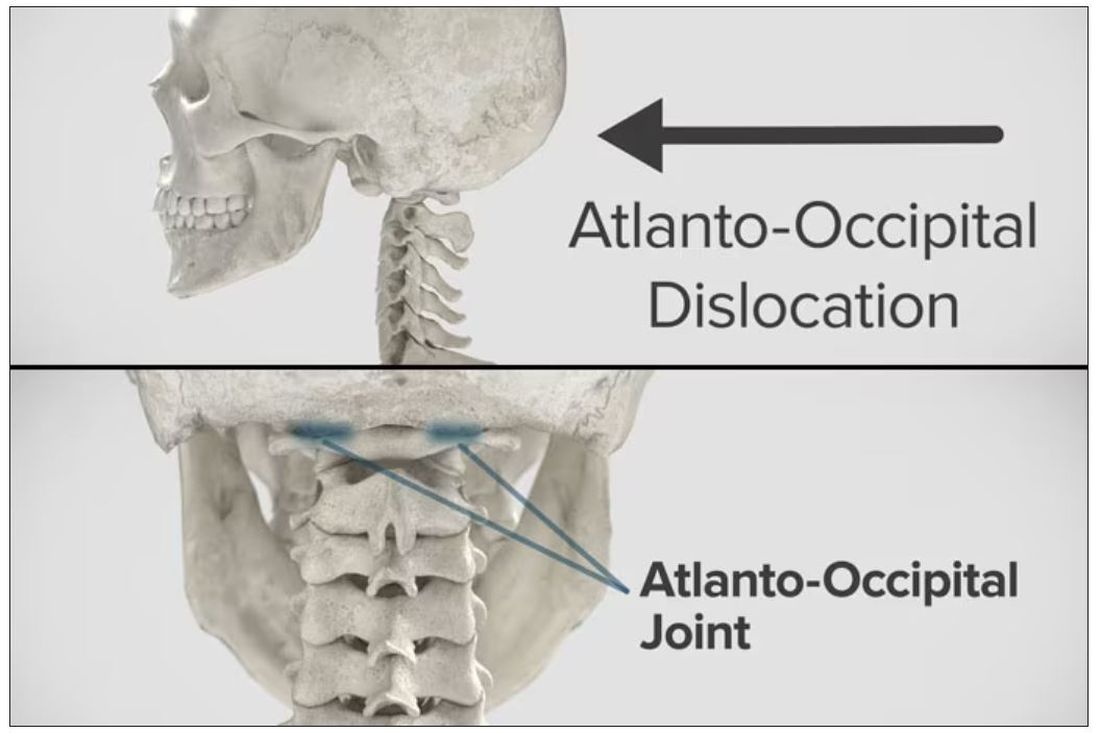
Dr. Wilson: “Injury to the cervical spine” might be something of an understatement. He had what’s called atlanto-occipital dislocation, colloquially often referred to as internal decapitation. Can you tell us what that means? It sounds terrifying.
Dr. Einav: It’s an injury to the ligaments between the occiput and the upper cervical spine, with or without bony fracture. The atlanto-occipital joint is formed by the superior articular facet of the atlas and the occipital condyle, stabilized by an articular capsule between the head and neck, and is supported by various ligaments around it that stabilize the joint and allow joint movements, including flexion, extension, and some rotation in the lower levels.
Dr. Wilson: This joint has several degrees of freedom, which means it needs a lot of support. With this type of injury, where essentially you have severing of the ligaments, is it usually survivable? How dangerous is this?
Dr. Einav: The mortality rate is 50%-60%, depending on the primary impact, the injury, transportation later on, and then the surgery and surgical management.
Dr. Wilson: Tell us a bit about this patient’s status when he came to your medical center. I assume he was in bad shape.
Dr. Einav: Hassan arrived at our medical center with a Glasgow Coma Scale score of 15. He was fully conscious. He was hemodynamically stable except for a bad laceration on his abdomen. He had a Philadelphia collar around his neck. He was transported by chopper because the paramedics suspected that he had a cervical spine injury and decided to bring him to a Level 1 trauma center.
He was monitored and we treated him according to the ATLS [advanced trauma life support] protocol. He didn’t have any gross sensory deficits, but he was a little confused about the whole situation and the accident. Therefore, we could do a general examination but we couldn’t rely on that regarding any sensory deficit that he may or may not have. We decided as a team that it would be better to slow down and control the situation. We decided not to operate on him immediately. We basically stabilized him and made sure that he didn’t have any traumatic internal organ damage. Later on we took him to the OR and performed surgery.
Dr. Wilson: It’s amazing that he had intact motor function, considering the extent of his injury. The spinal cord was spared somewhat during the injury. There must have been a moment when you realized that this kid, who was conscious and could move all four extremities, had a very severe neck injury. Was that due to a CT scan or physical exam? And what was your feeling when you saw that he had atlanto-occipital dislocation?
Dr. Einav: As a surgeon, you have a gut feeling in regard to the general examination of the patient. But I never rely on gut feelings. On the CT, I understood exactly what he had, what we needed to do, and the time frame.
Dr. Wilson: You’ve done these types of surgeries before, right? Obviously, no one has done a lot of them because this isn’t very common. But you knew what to do. Did you have a plan? Where does your experience come into play in a situation like this?
Dr. Einav: I graduated from the spine program of Toronto University, where I did a fellowship in trauma of the spine and complex spine surgery. I had very good teachers, and during my fellowship I treated a few cases in older patients that were similar but not the same. Therefore, I knew exactly what needed to be done.
Dr. Wilson: For those of us who aren’t surgeons, take us into the OR with you. This is obviously an incredibly delicate procedure. You are high up in the spinal cord at the base of the brain. The slightest mistake could have devastating consequences. What are the key elements of this procedure? What can go wrong here? What is the number-one thing you have to look out for when you’re trying to fix an internal decapitation?
Dr. Einav: The key element in surgeries of the cervical spine – trauma and complex spine surgery – is planning. I never go to the OR without knowing what I’m going to do. I have a few plans – plan A, plan B, plan C – in case something fails. So, I definitely know what the next step will be. I always think about the surgery a few hours before, if I have time to prepare.
The second thing that is very important is teamwork. The team needs to be coordinated. Everybody needs to know what their job is. With these types of injuries, it’s not the time for rookies. If you are new, please stand back and let the more experienced people do that job. I’m talking about surgeons, nurses, anesthesiologists – everyone.
Another important thing in planning is choosing the right hardware. For example, in this case we had a problem because most of the hardware is designed for adults, and we had to improvise because there isn’t a lot of hardware on the market for the pediatric population. The adult plates and screws are too big, so we had to improvise.
Dr. Wilson: Tell us more about that. How do you improvise spinal hardware for a 12-year-old?
Dr. Einav: In this case, I chose to use hardware from one of the companies that works with us.
You can see in this model the area of the injury, and the area that we worked on. To perform the surgery, I had to use some plates and rods from a different company. This company’s (NuVasive) hardware has a small attachment to the skull, which was helpful for affixing the skull to the cervical spine, instead of using a big plate that would sit at the base of the skull and would not be very good for him. Most of the hardware is made for adults and not for kids.
Dr. Wilson: Will that hardware preserve the motor function of his neck? Will he be able to turn his head and extend and flex it?
Dr. Einav: The injury leads to instability and destruction of both articulations between the head and neck. Therefore, those articulations won’t be able to function the same way in the future. There is a decrease of something like 50% of the flexion and extension of Hassan’s cervical spine. Therefore, I decided that in this case there would be no chance of saving Hassan’s motor function unless we performed a fusion between the head and the neck, and therefore I decided that this would be the best procedure with the best survival rate. So, in the future, he will have some diminished flexion, extension, and rotation of his head.
Dr. Wilson: How long did his surgery take?
Dr. Einav: To be honest, I don’t remember. But I can tell you that it took us time. It was very challenging to coordinate with everyone. The most problematic part of the surgery to perform is what we call “flip-over.”
The anesthesiologist intubated the patient when he was supine, and later on, we flipped him prone to operate on the spine. This maneuver can actually lead to injury by itself, and injury at this level is fatal. So, we took our time and got Hassan into the OR. The anesthesiologist did a great job with the GlideScope – inserting the endotracheal tube. Later on, we neuromonitored him. Basically, we connected Hassan’s peripheral nerves to a computer and monitored his motor function. Gently we flipped him over, and after that we saw a little change in his motor function, so we had to modify his position so we could preserve his motor function. We then started the procedure, which took a few hours. I don’t know exactly how many.
Dr. Wilson: That just speaks to how delicate this is for everything from the intubation, where typically you’re manipulating the head, to the repositioning. Clearly this requires a lot of teamwork.
What happened after the operation? How is he doing?
Dr. Einav: After the operation, Hassan had a great recovery. He’s doing well. He doesn’t have any motor or sensory deficits. He’s able to ambulate without any aid. He had no signs of infection, which can happen after a car accident, neither from his abdominal wound nor from the occipital cervical surgery. He feels well. We saw him in the clinic. We removed his collar. We monitored him at the clinic. He looked amazing.
Dr. Wilson: That’s incredible. Are there long-term risks for him that you need to be looking out for?
Dr. Einav: Yes, and that’s the reason that we are monitoring him post surgery. While he was in the hospital, we monitored his motor and sensory functions, as well as his wound healing. Later on, in the clinic, for a few weeks after surgery we monitored for any failure of the hardware and bone graft. We check for healing of the bone graft and bone substitutes we put in to heal those bones.
Dr. Wilson: He will grow, right? He’s only 12, so he still has some years of growth in him. Is he going to need more surgery or any kind of hardware upgrade?
Dr. Einav: I hope not. In my surgeries, I never rely on the hardware for long durations. If I decide to do, for example, fusion, I rely on the hardware for a certain amount of time. And then I plan that the biology will do the work. If I plan for fusion, I put bone grafts in the preferred area for a fusion. Then if the hardware fails, I wouldn’t need to take out the hardware, and there would be no change in the condition of the patient.
Dr. Wilson: What an incredible story. It’s clear that you and your team kept your cool despite a very high-acuity situation with a ton of risk. What a tremendous outcome that this boy is not only alive but fully functional. So, congratulations to you and your team. That was very strong work.
Dr. Einav: Thank you very much. I would like to thank our team. We have to remember that the surgeon is not standing alone in the war. Hassan’s story is a success story of a very big group of people from various backgrounds and religions. They work day and night to help people and save lives. To the paramedics, the physiologists, the traumatologists, the pediatricians, the nurses, the physiotherapists, and obviously the surgeons, a big thank you. His story is our success story.
Dr. Wilson: It’s inspiring to see so many people come together to do what we all are here for, which is to fight against suffering, disease, and death. Thank you for keeping up that fight. And thank you for joining me here.
Dr. Einav: Thank you very much.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
F. Perry Wilson, MD, MSCE: I am joined today by Dr. Ohad Einav. He’s a staff surgeon in orthopedics at Hadassah Medical Center in Jerusalem. He’s with me to talk about an absolutely incredible surgical case, something that is terrifying to most non–orthopedic surgeons and I imagine is fairly scary for spine surgeons like him as well. But what we don’t have is information about how this works from a medical perspective. So, first of all, Dr. Einav, thank you for taking time to speak with me today.
Ohad Einav, MD: Thank you for having me.
Dr. Wilson: Can you tell us about Suleiman Hassan and what happened to him before he came into your care?
Dr. Einav: Hassan is a 12-year-old child who was riding his bicycle on the West Bank, about 40 minutes from here. Unfortunately, he was involved in a motor vehicle accident and he suffered injuries to his abdomen and cervical spine. He was transported to our service by helicopter from the scene of the accident.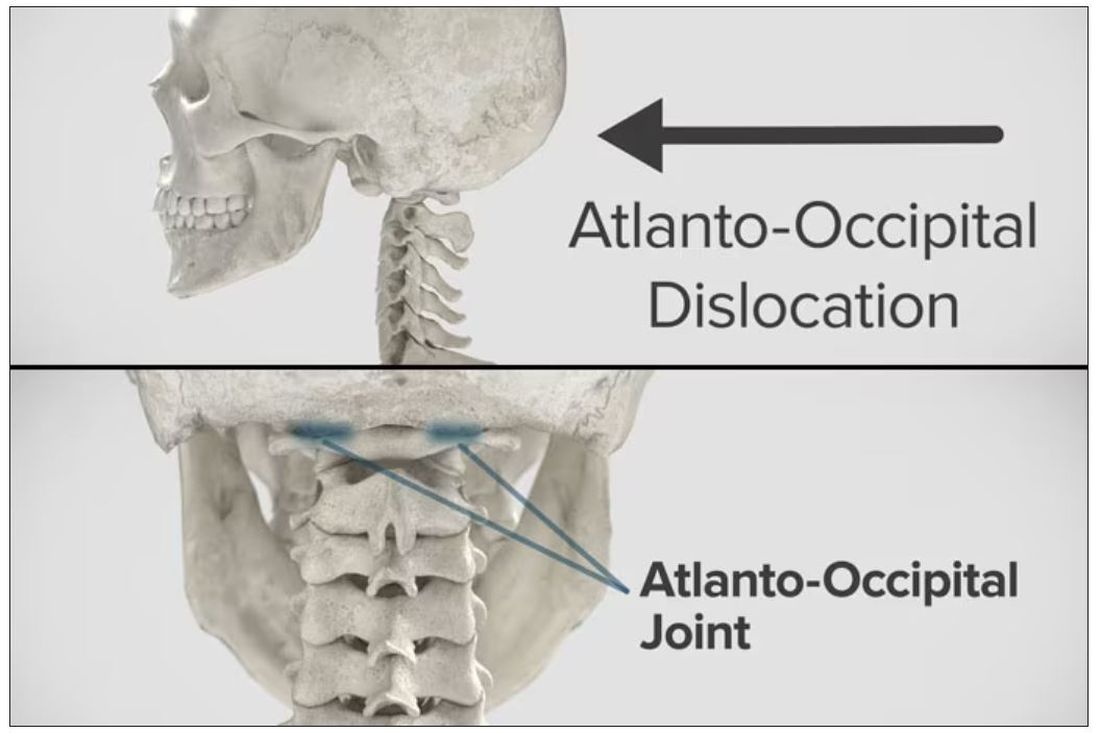
Dr. Wilson: “Injury to the cervical spine” might be something of an understatement. He had what’s called atlanto-occipital dislocation, colloquially often referred to as internal decapitation. Can you tell us what that means? It sounds terrifying.
Dr. Einav: It’s an injury to the ligaments between the occiput and the upper cervical spine, with or without bony fracture. The atlanto-occipital joint is formed by the superior articular facet of the atlas and the occipital condyle, stabilized by an articular capsule between the head and neck, and is supported by various ligaments around it that stabilize the joint and allow joint movements, including flexion, extension, and some rotation in the lower levels.
Dr. Wilson: This joint has several degrees of freedom, which means it needs a lot of support. With this type of injury, where essentially you have severing of the ligaments, is it usually survivable? How dangerous is this?
Dr. Einav: The mortality rate is 50%-60%, depending on the primary impact, the injury, transportation later on, and then the surgery and surgical management.
Dr. Wilson: Tell us a bit about this patient’s status when he came to your medical center. I assume he was in bad shape.
Dr. Einav: Hassan arrived at our medical center with a Glasgow Coma Scale score of 15. He was fully conscious. He was hemodynamically stable except for a bad laceration on his abdomen. He had a Philadelphia collar around his neck. He was transported by chopper because the paramedics suspected that he had a cervical spine injury and decided to bring him to a Level 1 trauma center.
He was monitored and we treated him according to the ATLS [advanced trauma life support] protocol. He didn’t have any gross sensory deficits, but he was a little confused about the whole situation and the accident. Therefore, we could do a general examination but we couldn’t rely on that regarding any sensory deficit that he may or may not have. We decided as a team that it would be better to slow down and control the situation. We decided not to operate on him immediately. We basically stabilized him and made sure that he didn’t have any traumatic internal organ damage. Later on we took him to the OR and performed surgery.
Dr. Wilson: It’s amazing that he had intact motor function, considering the extent of his injury. The spinal cord was spared somewhat during the injury. There must have been a moment when you realized that this kid, who was conscious and could move all four extremities, had a very severe neck injury. Was that due to a CT scan or physical exam? And what was your feeling when you saw that he had atlanto-occipital dislocation?
Dr. Einav: As a surgeon, you have a gut feeling in regard to the general examination of the patient. But I never rely on gut feelings. On the CT, I understood exactly what he had, what we needed to do, and the time frame.
Dr. Wilson: You’ve done these types of surgeries before, right? Obviously, no one has done a lot of them because this isn’t very common. But you knew what to do. Did you have a plan? Where does your experience come into play in a situation like this?
Dr. Einav: I graduated from the spine program of Toronto University, where I did a fellowship in trauma of the spine and complex spine surgery. I had very good teachers, and during my fellowship I treated a few cases in older patients that were similar but not the same. Therefore, I knew exactly what needed to be done.
Dr. Wilson: For those of us who aren’t surgeons, take us into the OR with you. This is obviously an incredibly delicate procedure. You are high up in the spinal cord at the base of the brain. The slightest mistake could have devastating consequences. What are the key elements of this procedure? What can go wrong here? What is the number-one thing you have to look out for when you’re trying to fix an internal decapitation?
Dr. Einav: The key element in surgeries of the cervical spine – trauma and complex spine surgery – is planning. I never go to the OR without knowing what I’m going to do. I have a few plans – plan A, plan B, plan C – in case something fails. So, I definitely know what the next step will be. I always think about the surgery a few hours before, if I have time to prepare.
The second thing that is very important is teamwork. The team needs to be coordinated. Everybody needs to know what their job is. With these types of injuries, it’s not the time for rookies. If you are new, please stand back and let the more experienced people do that job. I’m talking about surgeons, nurses, anesthesiologists – everyone.
Another important thing in planning is choosing the right hardware. For example, in this case we had a problem because most of the hardware is designed for adults, and we had to improvise because there isn’t a lot of hardware on the market for the pediatric population. The adult plates and screws are too big, so we had to improvise.
Dr. Wilson: Tell us more about that. How do you improvise spinal hardware for a 12-year-old?
Dr. Einav: In this case, I chose to use hardware from one of the companies that works with us.
You can see in this model the area of the injury, and the area that we worked on. To perform the surgery, I had to use some plates and rods from a different company. This company’s (NuVasive) hardware has a small attachment to the skull, which was helpful for affixing the skull to the cervical spine, instead of using a big plate that would sit at the base of the skull and would not be very good for him. Most of the hardware is made for adults and not for kids.
Dr. Wilson: Will that hardware preserve the motor function of his neck? Will he be able to turn his head and extend and flex it?
Dr. Einav: The injury leads to instability and destruction of both articulations between the head and neck. Therefore, those articulations won’t be able to function the same way in the future. There is a decrease of something like 50% of the flexion and extension of Hassan’s cervical spine. Therefore, I decided that in this case there would be no chance of saving Hassan’s motor function unless we performed a fusion between the head and the neck, and therefore I decided that this would be the best procedure with the best survival rate. So, in the future, he will have some diminished flexion, extension, and rotation of his head.
Dr. Wilson: How long did his surgery take?
Dr. Einav: To be honest, I don’t remember. But I can tell you that it took us time. It was very challenging to coordinate with everyone. The most problematic part of the surgery to perform is what we call “flip-over.”
The anesthesiologist intubated the patient when he was supine, and later on, we flipped him prone to operate on the spine. This maneuver can actually lead to injury by itself, and injury at this level is fatal. So, we took our time and got Hassan into the OR. The anesthesiologist did a great job with the GlideScope – inserting the endotracheal tube. Later on, we neuromonitored him. Basically, we connected Hassan’s peripheral nerves to a computer and monitored his motor function. Gently we flipped him over, and after that we saw a little change in his motor function, so we had to modify his position so we could preserve his motor function. We then started the procedure, which took a few hours. I don’t know exactly how many.
Dr. Wilson: That just speaks to how delicate this is for everything from the intubation, where typically you’re manipulating the head, to the repositioning. Clearly this requires a lot of teamwork.
What happened after the operation? How is he doing?
Dr. Einav: After the operation, Hassan had a great recovery. He’s doing well. He doesn’t have any motor or sensory deficits. He’s able to ambulate without any aid. He had no signs of infection, which can happen after a car accident, neither from his abdominal wound nor from the occipital cervical surgery. He feels well. We saw him in the clinic. We removed his collar. We monitored him at the clinic. He looked amazing.
Dr. Wilson: That’s incredible. Are there long-term risks for him that you need to be looking out for?
Dr. Einav: Yes, and that’s the reason that we are monitoring him post surgery. While he was in the hospital, we monitored his motor and sensory functions, as well as his wound healing. Later on, in the clinic, for a few weeks after surgery we monitored for any failure of the hardware and bone graft. We check for healing of the bone graft and bone substitutes we put in to heal those bones.
Dr. Wilson: He will grow, right? He’s only 12, so he still has some years of growth in him. Is he going to need more surgery or any kind of hardware upgrade?
Dr. Einav: I hope not. In my surgeries, I never rely on the hardware for long durations. If I decide to do, for example, fusion, I rely on the hardware for a certain amount of time. And then I plan that the biology will do the work. If I plan for fusion, I put bone grafts in the preferred area for a fusion. Then if the hardware fails, I wouldn’t need to take out the hardware, and there would be no change in the condition of the patient.
Dr. Wilson: What an incredible story. It’s clear that you and your team kept your cool despite a very high-acuity situation with a ton of risk. What a tremendous outcome that this boy is not only alive but fully functional. So, congratulations to you and your team. That was very strong work.
Dr. Einav: Thank you very much. I would like to thank our team. We have to remember that the surgeon is not standing alone in the war. Hassan’s story is a success story of a very big group of people from various backgrounds and religions. They work day and night to help people and save lives. To the paramedics, the physiologists, the traumatologists, the pediatricians, the nurses, the physiotherapists, and obviously the surgeons, a big thank you. His story is our success story.
Dr. Wilson: It’s inspiring to see so many people come together to do what we all are here for, which is to fight against suffering, disease, and death. Thank you for keeping up that fight. And thank you for joining me here.
Dr. Einav: Thank you very much.
A version of this article first appeared on Medscape.com.
Five ways to avert a malpractice lawsuit with better EHR techniques
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.
Although most physicians have gotten used to working with EHRs, despite their irritations, the use of EHRs has contributed to a growing number of malpractice lawsuits. Defense attorneys say that
According to a study in the Journal of Patient Safety, more than 30% of all EHR-related malpractice cases are associated with medication errors; 28% with diagnosis; and 31% with a complication of treatment, such as entering wrong information, entering information in the wrong place, and overlooking EHR flags and warnings for interactions or contraindications.
The study gave these examples of EHR-related errors that led to patient harm and ultimately to malpractice lawsuits:
- A discharge order omitted a patient’s medication that prevented strokes; the patient had a stroke days later.
- An electronic order for morphine failed to state the upper dose limit; the patient died.
- A physician meant to click on “discontinue” for an anticoagulant but mistakenly clicked on “continue” for home use.
Catching potential issues such as drug interactions or critical medical history that should inform treatment is more important than ever. “We know from safety engineering principles that just relying on vigilance is not a long-term safety strategy,” says Aaron Zach Hettinger, MD, chief research information officer at MedStar Health Research Institute, Washington, D.C. “So, it’s critical that we design these safe systems and leverage the data that’s in them.”
Here are five smart EHR practices to help protect your patients’ health and your own liability.
1. Double-check dropdown boxes
When it comes to user error, it’s easy to click the wrong choice from a drop-down menu. Better to take the time to explain your answer in a box, even if it takes a few more minutes. Or if you are choosing from a menu, proofread any information it auto-fills in the chart.
Dr. Hettinger says you can strike a balance between these templated approaches to diagnosis and long-term care by working with third-party systems and your organization or vendor IT department to help with follow-up questions to keep populated data in check.
“Make sure you have a back-end system that can help monitor that structured data,” says Dr. Hettinger. Structured data are the patient’s demographic information, like name, address, age, height, weight, vital signs, and data elements like diagnosis, medications, and lab results. “Wherever you can leverage the underlying tools that are part of the electronic health record to make sure that we’re constantly checking the right results, that helps reduce the workload so that clinicians can focus on taking care of the patients and doing the right thing and not be as focused on entering data into the system.”
2. Supplement EHR notes with direct communication
The failure to diagnose cancer because one physician doesn’t know what another physician saw in an imaging report is one of the most common claims in the cases he tries, says Aaron Boeder, a plaintiff’s medical negligence lawyer in Chicago.
Physicians often assume that if they put a note in the electronic chart, others will look for it, but Mr. Boeder says it’s far more prudent to communicate directly.
“Let’s say a radiologist interprets a scan and sees what might be cancer,” he says. “If the ordering doctor is an orthopedist who’s ordered a CT scan for DVT, there’s going to be a report for that scan. It’s going to get auto-populated back into that physician’s note,” says Mr. Boeder.
The physician may or may not look at it, but it will be in their note, and they’re supposed to follow up on it because they ordered the scan. “But they may not follow up on it, and they may not get a call from the radiologist,” he says.
“Next thing you know, 2 or 3 years later, that patient is diagnosed with very advanced cancer.”
3. Tailor auto-fill information to your common practices
Suppose, as a physician, you find that you need to change a default setting time and time again. Dr. Hettinger says it’s worth your time to take an extra couple of minutes to work with your vendor or your health system to try and make changes to auto-population settings that align with your practices.
“Let’s say a default dose of 20 milligrams of a medication is what automatically pops up, but in reality, your practice is to use a smaller dose because it’s safer, even though they’re all within the acceptable realm of what you would order,” he says. “Rather than have the default to the higher dose, see if you can change the default to a lower dose. And that way, you don’t have to catch yourself every time.”
If your auto-fills are amounts that constantly need changing, an interruption could easily knock you off course before you make that correction.
“If there are ways to have the system defaults be safer or more in line with your clinical practice, and especially across a group, then you’re designing a safer system and not relying on vigilance or memory prone to interruptions,” says Dr. Hettinger.
4. Curb the copy and paste
It’s tempting to copy a note from a previous patient visit and make only minimal changes as needed, but you risk including outdated information if you do. Even if you’re repeating questions asked by the intake nurse, it is safer to not to rely on that information, says Beth Kanik, a defense medical malpractice attorney in Atlanta.
“If it later goes into litigation, the argument then becomes that it looks like you didn’t do your job,” says Ms. Kanik. “Instead, try to ask questions in a way that would elicit responses that may be a little different than what the nurse got, so that it’s clear you asked the questions and didn’t just simply rely upon someone else’s information.”
5. Separate typing from listening
While EHR may be an excellent tool for data collection and safety checking, it’s not a stand-in for doctor-patient interaction. As technology practices push medicine toward more and more efficiency, Mr. Boeder says it’s most often listening over all else that makes the difference in the quality of care. And good listening requires full attention.
“A real concern for physicians is the number of visits they’re expected to accomplish in a set amount of time,” says Mr. Boeder. “Often this translates into a doctor talking to a patient while typing notes or while reading a note from the last time the patient was in.”
Taking the time to pause after entering data and briefly reviewing your understanding of what your patient has told you can be invaluable and may save you – and your patient – problems later.
“In so many cases, it comes down to people not being heard,” says Mr. Boeder. “So listen to what your patients are saying.”
A version of this article first appeared on Medscape.com.