User login
Myth of the Month: Is Contrast-Induced Acute Kidney Injury Real?
A 59-year-old man presents with abdominal pain. He has a history of small bowel obstruction and diverticulitis. His medical history includes chronic kidney disease (CKD; baseline creatinine, 1.8 mg/dL), hypertension, type 2 diabetes, and depression. He had a colectomy 6 years ago for colon cancer.
He takes the following medications: Semaglutide (1 mg weekly), amlodipine (5 mg once daily), and escitalopram (10 mg once daily). On physical exam his blood pressure is 130/80 mm Hg, his pulse is 90, and his temperature is 37.2 degrees C. He has normal bowel sounds but guarding in the right lower quadrant.
His hemoglobin is 14 g/dL, his blood sodium is 136 mEq/L, his blood potassium is 4.0 mmol/L, his BUN is 26 mg/dL, and his creatinine is 1.9 mg/dL. His kidney, ureter, bladder x-ray is unremarkable.
What imaging would you recommend?
A) CT without contrast
B) CT with contrast
C) MRI
D) Abdominal ultrasound
This patient has several potential causes for his abdominal pain that imaging may clarify. I think a contrast CT scan would be the most likely to provide helpful information. It is likely that if it were ordered, there may be hesitation by the radiologist to perform the scan with contrast because of the patient’s CKD.
Concern for contrast-induced kidney injury has limited diagnostic testing for many years. How strong is the evidence for contrast-induced kidney injury, and should we avoid testing that requires contrast in patients with CKD? McDonald and colleagues performed a meta-analysis with 13 studies meeting inclusion criteria, involving 25,950 patients.1 They found no increased risk of acute kidney injury (AKI) in patients who received contrast medium compared with those who did not receive contrast; relative risk of AKI for those receiving contrast was 0.79 (confidence interval: 0.62-1.02). Importantly, there was no difference in AKI in patients with diabetes or CKD.
Ehmann et al. looked at renal outcomes in patients who received IV contrast when they presented to an emergency department with AKI.2 They found that in patients with AKI, receiving contrast was not associated with persistent AKI at hospital discharge. Hinson and colleagues looked at patients arriving at the emergency department and needing imaging.3 They did a retrospective, cohort analysis of 17,934 patients who had CT with contrast, CT with no contrast, or no CT. Contrast administration was not associated with increased incidence of AKI (odds ratio, 0.96, CI: 0.85-1.08).
Aycock et al. did a meta-analysis of AKI after CT scanning, including 28 studies involving 107,335 patients.4 They found that compared with noncontrast CT, CT scanning with contrast was not associated with AKI (OR, 0.94, CI: 0.83-1.07). Elias and Aronson looked at the risk of AKI after contrast in patients receiving CT scans compared with those who received ventilation/perfusion scans to evaluate for pulmonary embolism.5 There were 44 AKI events (4.5%) in patients exposed to contrast media and 33 events (3.4%) in patients not exposed to contrast media (risk difference: 1.1%, 95% CI: -0.6% to 2.9%; OR, 1.39, CI: 0.86-2.26; P = .18).
Despite multiple studies showing no increased risk, there is still a concern that contrast can cause AKI.6 Animal models have shown iodinated contrast can have a deleterious effect on mitochondria and membrane function.6 Criticisms of the retrospective nature of many of the studies I have shared, and the lack of randomized, controlled trials are that there may be bias in these studies, as the highest-risk patients are the ones most likely not to receive contrast. In a joint guideline from the American College of Radiology and the National Kidney Foundation, this statement was made: “The risk of acute kidney injury developing in patients with reduced kidney function following exposure to intravenous iodinated contrast media has been overstated.”7 Their recommendation was to give contrast if needed in patients with glomerular filtration rates (GFRs) greater than 30.
Myth: Contrast-induced renal injury is a concern.
Clinical impact: For CT scanning, it is OK to give contrast when needed. A conservative cutoff for contrast use would be a GFR less than 30.
Dr. Paauw is professor of medicine in the Division of General Internal Medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. McDonald JS et al. Radiology. 2013:267:119-128.
2. Ehmann MR et al. Intensive Care Med. 2023:49(2):205-215.
3. Hinson JS et al. Ann Emerg Med. 2017;69(5):577-586.
4. Aycock RD et al. Ann Emerg Med. 2018 Jan;71(1):44-53.
5. Elias A, Aronson D. Thromb Haemost. 2021 Jun;121(6):800-807.
6. Weisbord SD, du Cheryon D. Intensive Care Med. 2018;44(1):107-109.
7. Davenport MS et al. Radiology. 2020;294(3):660-668.
A 59-year-old man presents with abdominal pain. He has a history of small bowel obstruction and diverticulitis. His medical history includes chronic kidney disease (CKD; baseline creatinine, 1.8 mg/dL), hypertension, type 2 diabetes, and depression. He had a colectomy 6 years ago for colon cancer.
He takes the following medications: Semaglutide (1 mg weekly), amlodipine (5 mg once daily), and escitalopram (10 mg once daily). On physical exam his blood pressure is 130/80 mm Hg, his pulse is 90, and his temperature is 37.2 degrees C. He has normal bowel sounds but guarding in the right lower quadrant.
His hemoglobin is 14 g/dL, his blood sodium is 136 mEq/L, his blood potassium is 4.0 mmol/L, his BUN is 26 mg/dL, and his creatinine is 1.9 mg/dL. His kidney, ureter, bladder x-ray is unremarkable.
What imaging would you recommend?
A) CT without contrast
B) CT with contrast
C) MRI
D) Abdominal ultrasound
This patient has several potential causes for his abdominal pain that imaging may clarify. I think a contrast CT scan would be the most likely to provide helpful information. It is likely that if it were ordered, there may be hesitation by the radiologist to perform the scan with contrast because of the patient’s CKD.
Concern for contrast-induced kidney injury has limited diagnostic testing for many years. How strong is the evidence for contrast-induced kidney injury, and should we avoid testing that requires contrast in patients with CKD? McDonald and colleagues performed a meta-analysis with 13 studies meeting inclusion criteria, involving 25,950 patients.1 They found no increased risk of acute kidney injury (AKI) in patients who received contrast medium compared with those who did not receive contrast; relative risk of AKI for those receiving contrast was 0.79 (confidence interval: 0.62-1.02). Importantly, there was no difference in AKI in patients with diabetes or CKD.
Ehmann et al. looked at renal outcomes in patients who received IV contrast when they presented to an emergency department with AKI.2 They found that in patients with AKI, receiving contrast was not associated with persistent AKI at hospital discharge. Hinson and colleagues looked at patients arriving at the emergency department and needing imaging.3 They did a retrospective, cohort analysis of 17,934 patients who had CT with contrast, CT with no contrast, or no CT. Contrast administration was not associated with increased incidence of AKI (odds ratio, 0.96, CI: 0.85-1.08).
Aycock et al. did a meta-analysis of AKI after CT scanning, including 28 studies involving 107,335 patients.4 They found that compared with noncontrast CT, CT scanning with contrast was not associated with AKI (OR, 0.94, CI: 0.83-1.07). Elias and Aronson looked at the risk of AKI after contrast in patients receiving CT scans compared with those who received ventilation/perfusion scans to evaluate for pulmonary embolism.5 There were 44 AKI events (4.5%) in patients exposed to contrast media and 33 events (3.4%) in patients not exposed to contrast media (risk difference: 1.1%, 95% CI: -0.6% to 2.9%; OR, 1.39, CI: 0.86-2.26; P = .18).
Despite multiple studies showing no increased risk, there is still a concern that contrast can cause AKI.6 Animal models have shown iodinated contrast can have a deleterious effect on mitochondria and membrane function.6 Criticisms of the retrospective nature of many of the studies I have shared, and the lack of randomized, controlled trials are that there may be bias in these studies, as the highest-risk patients are the ones most likely not to receive contrast. In a joint guideline from the American College of Radiology and the National Kidney Foundation, this statement was made: “The risk of acute kidney injury developing in patients with reduced kidney function following exposure to intravenous iodinated contrast media has been overstated.”7 Their recommendation was to give contrast if needed in patients with glomerular filtration rates (GFRs) greater than 30.
Myth: Contrast-induced renal injury is a concern.
Clinical impact: For CT scanning, it is OK to give contrast when needed. A conservative cutoff for contrast use would be a GFR less than 30.
Dr. Paauw is professor of medicine in the Division of General Internal Medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. McDonald JS et al. Radiology. 2013:267:119-128.
2. Ehmann MR et al. Intensive Care Med. 2023:49(2):205-215.
3. Hinson JS et al. Ann Emerg Med. 2017;69(5):577-586.
4. Aycock RD et al. Ann Emerg Med. 2018 Jan;71(1):44-53.
5. Elias A, Aronson D. Thromb Haemost. 2021 Jun;121(6):800-807.
6. Weisbord SD, du Cheryon D. Intensive Care Med. 2018;44(1):107-109.
7. Davenport MS et al. Radiology. 2020;294(3):660-668.
A 59-year-old man presents with abdominal pain. He has a history of small bowel obstruction and diverticulitis. His medical history includes chronic kidney disease (CKD; baseline creatinine, 1.8 mg/dL), hypertension, type 2 diabetes, and depression. He had a colectomy 6 years ago for colon cancer.
He takes the following medications: Semaglutide (1 mg weekly), amlodipine (5 mg once daily), and escitalopram (10 mg once daily). On physical exam his blood pressure is 130/80 mm Hg, his pulse is 90, and his temperature is 37.2 degrees C. He has normal bowel sounds but guarding in the right lower quadrant.
His hemoglobin is 14 g/dL, his blood sodium is 136 mEq/L, his blood potassium is 4.0 mmol/L, his BUN is 26 mg/dL, and his creatinine is 1.9 mg/dL. His kidney, ureter, bladder x-ray is unremarkable.
What imaging would you recommend?
A) CT without contrast
B) CT with contrast
C) MRI
D) Abdominal ultrasound
This patient has several potential causes for his abdominal pain that imaging may clarify. I think a contrast CT scan would be the most likely to provide helpful information. It is likely that if it were ordered, there may be hesitation by the radiologist to perform the scan with contrast because of the patient’s CKD.
Concern for contrast-induced kidney injury has limited diagnostic testing for many years. How strong is the evidence for contrast-induced kidney injury, and should we avoid testing that requires contrast in patients with CKD? McDonald and colleagues performed a meta-analysis with 13 studies meeting inclusion criteria, involving 25,950 patients.1 They found no increased risk of acute kidney injury (AKI) in patients who received contrast medium compared with those who did not receive contrast; relative risk of AKI for those receiving contrast was 0.79 (confidence interval: 0.62-1.02). Importantly, there was no difference in AKI in patients with diabetes or CKD.
Ehmann et al. looked at renal outcomes in patients who received IV contrast when they presented to an emergency department with AKI.2 They found that in patients with AKI, receiving contrast was not associated with persistent AKI at hospital discharge. Hinson and colleagues looked at patients arriving at the emergency department and needing imaging.3 They did a retrospective, cohort analysis of 17,934 patients who had CT with contrast, CT with no contrast, or no CT. Contrast administration was not associated with increased incidence of AKI (odds ratio, 0.96, CI: 0.85-1.08).
Aycock et al. did a meta-analysis of AKI after CT scanning, including 28 studies involving 107,335 patients.4 They found that compared with noncontrast CT, CT scanning with contrast was not associated with AKI (OR, 0.94, CI: 0.83-1.07). Elias and Aronson looked at the risk of AKI after contrast in patients receiving CT scans compared with those who received ventilation/perfusion scans to evaluate for pulmonary embolism.5 There were 44 AKI events (4.5%) in patients exposed to contrast media and 33 events (3.4%) in patients not exposed to contrast media (risk difference: 1.1%, 95% CI: -0.6% to 2.9%; OR, 1.39, CI: 0.86-2.26; P = .18).
Despite multiple studies showing no increased risk, there is still a concern that contrast can cause AKI.6 Animal models have shown iodinated contrast can have a deleterious effect on mitochondria and membrane function.6 Criticisms of the retrospective nature of many of the studies I have shared, and the lack of randomized, controlled trials are that there may be bias in these studies, as the highest-risk patients are the ones most likely not to receive contrast. In a joint guideline from the American College of Radiology and the National Kidney Foundation, this statement was made: “The risk of acute kidney injury developing in patients with reduced kidney function following exposure to intravenous iodinated contrast media has been overstated.”7 Their recommendation was to give contrast if needed in patients with glomerular filtration rates (GFRs) greater than 30.
Myth: Contrast-induced renal injury is a concern.
Clinical impact: For CT scanning, it is OK to give contrast when needed. A conservative cutoff for contrast use would be a GFR less than 30.
Dr. Paauw is professor of medicine in the Division of General Internal Medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at dpaauw@uw.edu.
References
1. McDonald JS et al. Radiology. 2013:267:119-128.
2. Ehmann MR et al. Intensive Care Med. 2023:49(2):205-215.
3. Hinson JS et al. Ann Emerg Med. 2017;69(5):577-586.
4. Aycock RD et al. Ann Emerg Med. 2018 Jan;71(1):44-53.
5. Elias A, Aronson D. Thromb Haemost. 2021 Jun;121(6):800-807.
6. Weisbord SD, du Cheryon D. Intensive Care Med. 2018;44(1):107-109.
7. Davenport MS et al. Radiology. 2020;294(3):660-668.
Office Procedure Found to Get Stone Fragments Rolling
An experimental handheld ultrasonic device used in an office setting was shown to guide residual kidney stone fragments out of the body and markedly reduce the risk for relapse, researchers reported (Abstract MP29-10) at the 2024 annual meeting of the American Urological Association AUA in San Antonio, Texas.
Mathew Sorensen, MD, MS, an associate professor of urology at the University of Washington, Seattle, and director of the Comprehensive Metabolic Stone Clinic at the Puget Sound VA, said that the risk for relapse of kidney stones was 70% lower in the treatment group than in the control group.
“This is an ultrasound-based propulsion procedure that is not like anything else that has ever existed. There’s nothing else that’s like it,” Dr. Sorensen said. “Essentially, in a session in the office with no anesthesia, we can use ultrasound energy to focus on those fragments and try to push them out of the unfavorable areas of the kidney.”
Roughly 20%-30% of patients who undergo surgery to remove kidney stones have residual fragments that can ultimately cause pain and send them to the emergency department or into hospital admission for treatment.
In the new study, 82 patients with stone fragments ≤ 5 mm were randomly assigned to receive the ultrasound treatment — which Dr. Sorensen and his colleagues developed over the past decade — or no procedure.
During a median follow-up of 2.6 years, 20% of patients in the treatment group experienced relapse of stones compared with 50% of patients in the control group.
Relapse was measured as the future occurrence of urgent medical visits for stone-related symptoms, surgeries, or growth of the residual fragments as measured on annual CT.
Dr. Sorensen and his colleagues found asymptomatic passage of fragments was twelvefold higher in the treatment group in the first 3 weeks (60% vs 5%). Asymptomatic passage was similar in both groups after 3 weeks.
Dr. Sorensen said that mild discomfort after the procedure was common, occurring in 38% of patients who underwent the treatment, but that it was short-lived and resolved without intervention; 8% of the treatment group and 7% of the control group had blood in the urine.
The propulsion device is available at two test sites in the University of Washington system; the manufacturer, SonoMotion Inc, a spinoff from the institution, is seeking US Food and Drug Administration approval for the technology, Dr. Sorensen said.
David Schulsinger, MD, an associate professor in the Department of Urology at Stony Brook University Hospital, Stony Brook, New York, said that patients with stone fragments currently have two options: follow-up surgery or active surveillance.
“With this new device, we actually have the potential for doing one other thing, and that is treating these patients noninvasively and without anesthesia,” Dr. Schulsinger said. “Once it’s ready for prime time, I think [ultrasonic propulsion] will be very well accepted among urologists to manage patients with asymptomatic residual stones.”
Dr. Sorensen is an advisor and equity holder in SonoMotion Inc. Dr. Schulsinger reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
An experimental handheld ultrasonic device used in an office setting was shown to guide residual kidney stone fragments out of the body and markedly reduce the risk for relapse, researchers reported (Abstract MP29-10) at the 2024 annual meeting of the American Urological Association AUA in San Antonio, Texas.
Mathew Sorensen, MD, MS, an associate professor of urology at the University of Washington, Seattle, and director of the Comprehensive Metabolic Stone Clinic at the Puget Sound VA, said that the risk for relapse of kidney stones was 70% lower in the treatment group than in the control group.
“This is an ultrasound-based propulsion procedure that is not like anything else that has ever existed. There’s nothing else that’s like it,” Dr. Sorensen said. “Essentially, in a session in the office with no anesthesia, we can use ultrasound energy to focus on those fragments and try to push them out of the unfavorable areas of the kidney.”
Roughly 20%-30% of patients who undergo surgery to remove kidney stones have residual fragments that can ultimately cause pain and send them to the emergency department or into hospital admission for treatment.
In the new study, 82 patients with stone fragments ≤ 5 mm were randomly assigned to receive the ultrasound treatment — which Dr. Sorensen and his colleagues developed over the past decade — or no procedure.
During a median follow-up of 2.6 years, 20% of patients in the treatment group experienced relapse of stones compared with 50% of patients in the control group.
Relapse was measured as the future occurrence of urgent medical visits for stone-related symptoms, surgeries, or growth of the residual fragments as measured on annual CT.
Dr. Sorensen and his colleagues found asymptomatic passage of fragments was twelvefold higher in the treatment group in the first 3 weeks (60% vs 5%). Asymptomatic passage was similar in both groups after 3 weeks.
Dr. Sorensen said that mild discomfort after the procedure was common, occurring in 38% of patients who underwent the treatment, but that it was short-lived and resolved without intervention; 8% of the treatment group and 7% of the control group had blood in the urine.
The propulsion device is available at two test sites in the University of Washington system; the manufacturer, SonoMotion Inc, a spinoff from the institution, is seeking US Food and Drug Administration approval for the technology, Dr. Sorensen said.
David Schulsinger, MD, an associate professor in the Department of Urology at Stony Brook University Hospital, Stony Brook, New York, said that patients with stone fragments currently have two options: follow-up surgery or active surveillance.
“With this new device, we actually have the potential for doing one other thing, and that is treating these patients noninvasively and without anesthesia,” Dr. Schulsinger said. “Once it’s ready for prime time, I think [ultrasonic propulsion] will be very well accepted among urologists to manage patients with asymptomatic residual stones.”
Dr. Sorensen is an advisor and equity holder in SonoMotion Inc. Dr. Schulsinger reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
An experimental handheld ultrasonic device used in an office setting was shown to guide residual kidney stone fragments out of the body and markedly reduce the risk for relapse, researchers reported (Abstract MP29-10) at the 2024 annual meeting of the American Urological Association AUA in San Antonio, Texas.
Mathew Sorensen, MD, MS, an associate professor of urology at the University of Washington, Seattle, and director of the Comprehensive Metabolic Stone Clinic at the Puget Sound VA, said that the risk for relapse of kidney stones was 70% lower in the treatment group than in the control group.
“This is an ultrasound-based propulsion procedure that is not like anything else that has ever existed. There’s nothing else that’s like it,” Dr. Sorensen said. “Essentially, in a session in the office with no anesthesia, we can use ultrasound energy to focus on those fragments and try to push them out of the unfavorable areas of the kidney.”
Roughly 20%-30% of patients who undergo surgery to remove kidney stones have residual fragments that can ultimately cause pain and send them to the emergency department or into hospital admission for treatment.
In the new study, 82 patients with stone fragments ≤ 5 mm were randomly assigned to receive the ultrasound treatment — which Dr. Sorensen and his colleagues developed over the past decade — or no procedure.
During a median follow-up of 2.6 years, 20% of patients in the treatment group experienced relapse of stones compared with 50% of patients in the control group.
Relapse was measured as the future occurrence of urgent medical visits for stone-related symptoms, surgeries, or growth of the residual fragments as measured on annual CT.
Dr. Sorensen and his colleagues found asymptomatic passage of fragments was twelvefold higher in the treatment group in the first 3 weeks (60% vs 5%). Asymptomatic passage was similar in both groups after 3 weeks.
Dr. Sorensen said that mild discomfort after the procedure was common, occurring in 38% of patients who underwent the treatment, but that it was short-lived and resolved without intervention; 8% of the treatment group and 7% of the control group had blood in the urine.
The propulsion device is available at two test sites in the University of Washington system; the manufacturer, SonoMotion Inc, a spinoff from the institution, is seeking US Food and Drug Administration approval for the technology, Dr. Sorensen said.
David Schulsinger, MD, an associate professor in the Department of Urology at Stony Brook University Hospital, Stony Brook, New York, said that patients with stone fragments currently have two options: follow-up surgery or active surveillance.
“With this new device, we actually have the potential for doing one other thing, and that is treating these patients noninvasively and without anesthesia,” Dr. Schulsinger said. “Once it’s ready for prime time, I think [ultrasonic propulsion] will be very well accepted among urologists to manage patients with asymptomatic residual stones.”
Dr. Sorensen is an advisor and equity holder in SonoMotion Inc. Dr. Schulsinger reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM AUA 2024
Vast Majority of Adults At Risk for Cardiovascular-Kidney-Metabolic Syndrome
TOPLINE:
Nearly 90% of adults were at risk of developing cardiovascular-kidney-metabolic (CKM) syndrome between 2011 and 2020, according to new research published in JAMA.
METHODOLOGY:
- In 2023, the American Heart Association defined to acknowledge how heart and kidney diseases, diabetes, and obesity interact and are increasingly co-occurring conditions.
- Researchers used data from the National Health and Nutrition Examination Survey between 2011 and 2020.
- More than 10,000 adults over age 20 years were included; all of them received a physical and fasting laboratory measurements and self-reported their cardiovascular disease (CVD) status.
- Researchers created categories for risk, ranging from 0 (no risk factors) to 4, using factors such as kidney disease, obesity, and hypertension.
TAKEAWAY:
- (having metabolic risk factors like hypertension or moderate- to high-risk chronic kidney disease).
- 14.6% met the criteria for advanced stage 3 (very high-risk chronic kidney disease or a high risk for 10-year CVD) and stage 4 CKM syndrome (established CVD) combined.
- Men, adults over age 65 years, and Black individuals were at a greater risk for advanced stages of the CKM syndrome.
- Almost half of people met the criteria for stage 2 (having metabolic risk factors like hypertension or moderate- to high-risk chronic kidney disease).
- 14.6% met the criteria for advanced stage 3 (very high-risk chronic kidney disease or a high risk for 10-year CVD) and stage 4 CKM syndrome (established CVD) combined.
- Men, adults over age 65 years, and Black individuals were at a greater risk for advanced stages of the CKM syndrome.
IN PRACTICE:
“Equitable health care approaches prioritizing CKM health are urgently needed,” the study authors wrote.
SOURCE:
The study was led by Muthiah Vaduganathan, MD, MPH, cardiologist and researcher at Brigham and Women’s Hospital, Harvard Medical School, Boston.
LIMITATIONS:
Established CVD statuses were self-reported. Some data that would indicate advanced CKM stages were not available (eg, cardiac biomarkers, echocardiography, and coronary angiography), which may have led to an underestimation of rates.
DISCLOSURES:
One author received grants from Bristol Myers Squibb–Pfizer outside the submitted work. Dr. Vaduganathan received grants from and was an adviser and committee trial member for various pharmaceutical companies outside the submitted work. The authors reported no other disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Nearly 90% of adults were at risk of developing cardiovascular-kidney-metabolic (CKM) syndrome between 2011 and 2020, according to new research published in JAMA.
METHODOLOGY:
- In 2023, the American Heart Association defined to acknowledge how heart and kidney diseases, diabetes, and obesity interact and are increasingly co-occurring conditions.
- Researchers used data from the National Health and Nutrition Examination Survey between 2011 and 2020.
- More than 10,000 adults over age 20 years were included; all of them received a physical and fasting laboratory measurements and self-reported their cardiovascular disease (CVD) status.
- Researchers created categories for risk, ranging from 0 (no risk factors) to 4, using factors such as kidney disease, obesity, and hypertension.
TAKEAWAY:
- (having metabolic risk factors like hypertension or moderate- to high-risk chronic kidney disease).
- 14.6% met the criteria for advanced stage 3 (very high-risk chronic kidney disease or a high risk for 10-year CVD) and stage 4 CKM syndrome (established CVD) combined.
- Men, adults over age 65 years, and Black individuals were at a greater risk for advanced stages of the CKM syndrome.
- Almost half of people met the criteria for stage 2 (having metabolic risk factors like hypertension or moderate- to high-risk chronic kidney disease).
- 14.6% met the criteria for advanced stage 3 (very high-risk chronic kidney disease or a high risk for 10-year CVD) and stage 4 CKM syndrome (established CVD) combined.
- Men, adults over age 65 years, and Black individuals were at a greater risk for advanced stages of the CKM syndrome.
IN PRACTICE:
“Equitable health care approaches prioritizing CKM health are urgently needed,” the study authors wrote.
SOURCE:
The study was led by Muthiah Vaduganathan, MD, MPH, cardiologist and researcher at Brigham and Women’s Hospital, Harvard Medical School, Boston.
LIMITATIONS:
Established CVD statuses were self-reported. Some data that would indicate advanced CKM stages were not available (eg, cardiac biomarkers, echocardiography, and coronary angiography), which may have led to an underestimation of rates.
DISCLOSURES:
One author received grants from Bristol Myers Squibb–Pfizer outside the submitted work. Dr. Vaduganathan received grants from and was an adviser and committee trial member for various pharmaceutical companies outside the submitted work. The authors reported no other disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Nearly 90% of adults were at risk of developing cardiovascular-kidney-metabolic (CKM) syndrome between 2011 and 2020, according to new research published in JAMA.
METHODOLOGY:
- In 2023, the American Heart Association defined to acknowledge how heart and kidney diseases, diabetes, and obesity interact and are increasingly co-occurring conditions.
- Researchers used data from the National Health and Nutrition Examination Survey between 2011 and 2020.
- More than 10,000 adults over age 20 years were included; all of them received a physical and fasting laboratory measurements and self-reported their cardiovascular disease (CVD) status.
- Researchers created categories for risk, ranging from 0 (no risk factors) to 4, using factors such as kidney disease, obesity, and hypertension.
TAKEAWAY:
- (having metabolic risk factors like hypertension or moderate- to high-risk chronic kidney disease).
- 14.6% met the criteria for advanced stage 3 (very high-risk chronic kidney disease or a high risk for 10-year CVD) and stage 4 CKM syndrome (established CVD) combined.
- Men, adults over age 65 years, and Black individuals were at a greater risk for advanced stages of the CKM syndrome.
- Almost half of people met the criteria for stage 2 (having metabolic risk factors like hypertension or moderate- to high-risk chronic kidney disease).
- 14.6% met the criteria for advanced stage 3 (very high-risk chronic kidney disease or a high risk for 10-year CVD) and stage 4 CKM syndrome (established CVD) combined.
- Men, adults over age 65 years, and Black individuals were at a greater risk for advanced stages of the CKM syndrome.
IN PRACTICE:
“Equitable health care approaches prioritizing CKM health are urgently needed,” the study authors wrote.
SOURCE:
The study was led by Muthiah Vaduganathan, MD, MPH, cardiologist and researcher at Brigham and Women’s Hospital, Harvard Medical School, Boston.
LIMITATIONS:
Established CVD statuses were self-reported. Some data that would indicate advanced CKM stages were not available (eg, cardiac biomarkers, echocardiography, and coronary angiography), which may have led to an underestimation of rates.
DISCLOSURES:
One author received grants from Bristol Myers Squibb–Pfizer outside the submitted work. Dr. Vaduganathan received grants from and was an adviser and committee trial member for various pharmaceutical companies outside the submitted work. The authors reported no other disclosures.
A version of this article appeared on Medscape.com.
What Underlies Sex Differences in CKD Cardiovascular Risk?
Older men with chronic kidney disease (CKD) show higher resting muscle sympathetic nerve activity, but not vascular stiffness, compared with older women, offering clues to the underlying reasons why men with CKD have a higher cardiovascular risk than do women with the disease.
“Although it is well established that sympathetic nerve system activity is chronically elevated in patients with impaired kidney function, we show for the first time that males with CKD have higher resting muscle sympathetic nerve activity compared with females with CKD,” report the authors on research published in the American Journal of Physiology-Renal Physiology.
“For clinicians, the key takeaway is the importance of recognizing sex-specific differences in sympathetic activity and vascular function when assessing cardiovascular risk in CKD patients,” first author Matias G. Zanuzzi, MD, of the Division of Renal Medicine, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, told this news organization.
In the general population, cardiovascular risk is lower in younger women vs men, but their risks converge in older age as women develop similar levels of sympathetic overactivity, vascular stiffness, and cardiovascular risk.
However, an exception to that pattern is seen in the CKD population, where men continue to have a higher cardiovascular mortality risk vs women even in older age.
Studies evaluating the reasons for that have been conflicting, with some reporting a tendency of higher muscle sympathetic nerve activity in older women compared with men and others suggest the opposite finding — lower activity vs men.
To further investigate, Dr. Zanuzzi and colleagues enrolled 129 participants, including 96 men and 33 women with stage III or IV CKD.
The mean age of the study participants was 64 years for men and65 years for women. Most had obesity, and importantly, more than 80% of participants in each group was Black. There were no significant differences between the groups in terms of body mass index or comorbidities, including smoking, diabetes, or hypertension.
At two separate study visits, vascular stiffness was assessed with carotid-femoral pulse wave velocity measurement, and resting muscle sympathetic nerve activity was measured using microneurography.
The results showed that men with CKD had significantly higher resting muscle sympathetic nerve activity compared with women with CKD (68 vs 55 bursts per 100 heartbeats; P = .005), whereas no differences in vascular stiffness were observed between the genders (P = .248).
“The findings suggest that the higher cardiovascular disease risk observed in older males with CKD may be influenced by elevated sympathetic activity,” Dr. Zanuzzi explained.
“However, the lack of significant differences in vascular stiffness between genders implies that additional factors beyond vascular remodeling may contribute to the observed sex-specific differences in cardiovascular risk,” he said.
Of note, resting vascular stiffness was not associated with muscular sympathetic nerve activity in either men or women, which was surprising to the authors, Dr. Zanuzzi noted.
“This underscores the multifactorial nature of vascular pathophysiology in CKD and underscores the need for further research to unravel the underlying mechanisms.”
In other findings, although prior studies have shown a positive correlation between age and resting muscle sympathetic nerve activity in White, healthy women and men without obesity,, no similar relationship was observed in men or women with CKD.
“These findings suggest that the protective effect of younger age on sympathetic function may not be present in the setting of decreased kidney function in both males and females,” the authors note.
In addition, whereas previous research has shown a clear association between sympathetic overactivity and a wide variety of measures of obesity, in the current study, that association was only observed in men with CKD.
Important limitations of the study include the cross-sectional design and that the population was predominantly Black, Dr. Zanuzzi noted.
“Generalizability to other demographic groups may be limited, and future longitudinal studies are needed to validate these findings and explore potential causal relationships,” he said.
The findings underscore “the need for novel therapeutic approaches targeting sympathetic overactivity and vascular stiffness in CKD patients, especially considering the observed sex-specific differences,” Dr. Zanuzzi added.
“Potential interventions may include pharmacological agents that modulate sympathetic tone or vascular remodeling pathways,” he said.
“Lifestyle modifications focusing on stress reduction and cardiovascular health promotion could also play a crucial role in mitigating cardiovascular risk.”
Dr. Zanuzzi concluded that “tailoring treatment strategies to address these differences may lead to more personalized and effective management approaches, ultimately improving clinical outcomes in this high-risk population.”
The authors had no disclosures to report.
A version of this article first appeared on Medscape.com.
Older men with chronic kidney disease (CKD) show higher resting muscle sympathetic nerve activity, but not vascular stiffness, compared with older women, offering clues to the underlying reasons why men with CKD have a higher cardiovascular risk than do women with the disease.
“Although it is well established that sympathetic nerve system activity is chronically elevated in patients with impaired kidney function, we show for the first time that males with CKD have higher resting muscle sympathetic nerve activity compared with females with CKD,” report the authors on research published in the American Journal of Physiology-Renal Physiology.
“For clinicians, the key takeaway is the importance of recognizing sex-specific differences in sympathetic activity and vascular function when assessing cardiovascular risk in CKD patients,” first author Matias G. Zanuzzi, MD, of the Division of Renal Medicine, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, told this news organization.
In the general population, cardiovascular risk is lower in younger women vs men, but their risks converge in older age as women develop similar levels of sympathetic overactivity, vascular stiffness, and cardiovascular risk.
However, an exception to that pattern is seen in the CKD population, where men continue to have a higher cardiovascular mortality risk vs women even in older age.
Studies evaluating the reasons for that have been conflicting, with some reporting a tendency of higher muscle sympathetic nerve activity in older women compared with men and others suggest the opposite finding — lower activity vs men.
To further investigate, Dr. Zanuzzi and colleagues enrolled 129 participants, including 96 men and 33 women with stage III or IV CKD.
The mean age of the study participants was 64 years for men and65 years for women. Most had obesity, and importantly, more than 80% of participants in each group was Black. There were no significant differences between the groups in terms of body mass index or comorbidities, including smoking, diabetes, or hypertension.
At two separate study visits, vascular stiffness was assessed with carotid-femoral pulse wave velocity measurement, and resting muscle sympathetic nerve activity was measured using microneurography.
The results showed that men with CKD had significantly higher resting muscle sympathetic nerve activity compared with women with CKD (68 vs 55 bursts per 100 heartbeats; P = .005), whereas no differences in vascular stiffness were observed between the genders (P = .248).
“The findings suggest that the higher cardiovascular disease risk observed in older males with CKD may be influenced by elevated sympathetic activity,” Dr. Zanuzzi explained.
“However, the lack of significant differences in vascular stiffness between genders implies that additional factors beyond vascular remodeling may contribute to the observed sex-specific differences in cardiovascular risk,” he said.
Of note, resting vascular stiffness was not associated with muscular sympathetic nerve activity in either men or women, which was surprising to the authors, Dr. Zanuzzi noted.
“This underscores the multifactorial nature of vascular pathophysiology in CKD and underscores the need for further research to unravel the underlying mechanisms.”
In other findings, although prior studies have shown a positive correlation between age and resting muscle sympathetic nerve activity in White, healthy women and men without obesity,, no similar relationship was observed in men or women with CKD.
“These findings suggest that the protective effect of younger age on sympathetic function may not be present in the setting of decreased kidney function in both males and females,” the authors note.
In addition, whereas previous research has shown a clear association between sympathetic overactivity and a wide variety of measures of obesity, in the current study, that association was only observed in men with CKD.
Important limitations of the study include the cross-sectional design and that the population was predominantly Black, Dr. Zanuzzi noted.
“Generalizability to other demographic groups may be limited, and future longitudinal studies are needed to validate these findings and explore potential causal relationships,” he said.
The findings underscore “the need for novel therapeutic approaches targeting sympathetic overactivity and vascular stiffness in CKD patients, especially considering the observed sex-specific differences,” Dr. Zanuzzi added.
“Potential interventions may include pharmacological agents that modulate sympathetic tone or vascular remodeling pathways,” he said.
“Lifestyle modifications focusing on stress reduction and cardiovascular health promotion could also play a crucial role in mitigating cardiovascular risk.”
Dr. Zanuzzi concluded that “tailoring treatment strategies to address these differences may lead to more personalized and effective management approaches, ultimately improving clinical outcomes in this high-risk population.”
The authors had no disclosures to report.
A version of this article first appeared on Medscape.com.
Older men with chronic kidney disease (CKD) show higher resting muscle sympathetic nerve activity, but not vascular stiffness, compared with older women, offering clues to the underlying reasons why men with CKD have a higher cardiovascular risk than do women with the disease.
“Although it is well established that sympathetic nerve system activity is chronically elevated in patients with impaired kidney function, we show for the first time that males with CKD have higher resting muscle sympathetic nerve activity compared with females with CKD,” report the authors on research published in the American Journal of Physiology-Renal Physiology.
“For clinicians, the key takeaway is the importance of recognizing sex-specific differences in sympathetic activity and vascular function when assessing cardiovascular risk in CKD patients,” first author Matias G. Zanuzzi, MD, of the Division of Renal Medicine, Department of Medicine, Emory University School of Medicine, Atlanta, Georgia, told this news organization.
In the general population, cardiovascular risk is lower in younger women vs men, but their risks converge in older age as women develop similar levels of sympathetic overactivity, vascular stiffness, and cardiovascular risk.
However, an exception to that pattern is seen in the CKD population, where men continue to have a higher cardiovascular mortality risk vs women even in older age.
Studies evaluating the reasons for that have been conflicting, with some reporting a tendency of higher muscle sympathetic nerve activity in older women compared with men and others suggest the opposite finding — lower activity vs men.
To further investigate, Dr. Zanuzzi and colleagues enrolled 129 participants, including 96 men and 33 women with stage III or IV CKD.
The mean age of the study participants was 64 years for men and65 years for women. Most had obesity, and importantly, more than 80% of participants in each group was Black. There were no significant differences between the groups in terms of body mass index or comorbidities, including smoking, diabetes, or hypertension.
At two separate study visits, vascular stiffness was assessed with carotid-femoral pulse wave velocity measurement, and resting muscle sympathetic nerve activity was measured using microneurography.
The results showed that men with CKD had significantly higher resting muscle sympathetic nerve activity compared with women with CKD (68 vs 55 bursts per 100 heartbeats; P = .005), whereas no differences in vascular stiffness were observed between the genders (P = .248).
“The findings suggest that the higher cardiovascular disease risk observed in older males with CKD may be influenced by elevated sympathetic activity,” Dr. Zanuzzi explained.
“However, the lack of significant differences in vascular stiffness between genders implies that additional factors beyond vascular remodeling may contribute to the observed sex-specific differences in cardiovascular risk,” he said.
Of note, resting vascular stiffness was not associated with muscular sympathetic nerve activity in either men or women, which was surprising to the authors, Dr. Zanuzzi noted.
“This underscores the multifactorial nature of vascular pathophysiology in CKD and underscores the need for further research to unravel the underlying mechanisms.”
In other findings, although prior studies have shown a positive correlation between age and resting muscle sympathetic nerve activity in White, healthy women and men without obesity,, no similar relationship was observed in men or women with CKD.
“These findings suggest that the protective effect of younger age on sympathetic function may not be present in the setting of decreased kidney function in both males and females,” the authors note.
In addition, whereas previous research has shown a clear association between sympathetic overactivity and a wide variety of measures of obesity, in the current study, that association was only observed in men with CKD.
Important limitations of the study include the cross-sectional design and that the population was predominantly Black, Dr. Zanuzzi noted.
“Generalizability to other demographic groups may be limited, and future longitudinal studies are needed to validate these findings and explore potential causal relationships,” he said.
The findings underscore “the need for novel therapeutic approaches targeting sympathetic overactivity and vascular stiffness in CKD patients, especially considering the observed sex-specific differences,” Dr. Zanuzzi added.
“Potential interventions may include pharmacological agents that modulate sympathetic tone or vascular remodeling pathways,” he said.
“Lifestyle modifications focusing on stress reduction and cardiovascular health promotion could also play a crucial role in mitigating cardiovascular risk.”
Dr. Zanuzzi concluded that “tailoring treatment strategies to address these differences may lead to more personalized and effective management approaches, ultimately improving clinical outcomes in this high-risk population.”
The authors had no disclosures to report.
A version of this article first appeared on Medscape.com.
Barcelona’s Best: Vasculitis Treatment Studies on Stopping Steroids, Abatacept, Plasma Exchange, Vaccination
Some of the best clinical trials of patients with antineutrophil cytoplasmic antibody–associated vasculitis (AAV) that were presented at the 21st International Vasculitis Workshop in Barcelona, Spain, included studies addressing relapse after stopping steroids, preventing relapse with abatacept, improving kidney function with plasma exchange, and vaccinating rituximab-treated patients.
Stopping Steroids After Remission in GPA
In the randomized, open-label TAPIR (The Assessment of Prednisone In Remission Trial) study of 159 adults with GPA in remission who had tapered to a prednisone dose of 5 mg/day, those who remained at that dosage had a significantly lower rate of relapse after 6 months than those who tapered to 0 mg/day (4.2% vs 15.5%; P = .227), according to results reported at the meeting.
However, use of a higher dose of prednisone for disease relapse by 6 months was similar for patients who used rituximab at baseline (8.8% with 0 mg/day vs 6.1% with 5 mg/day; P = .667), and the difference in this primary outcome was more pronounced among patients who did not take rituximab at baseline (20.0% with 0 mg/day vs 2.6% with 5 mg/day; P = .023).
A higher percentage of patients taking prednisone 0 mg/day had disease relapses that were considered minor (14.1% and 4.2%; P = .0391). Major relapses occurred in none of the patients taking 5 mg/day and in 1.4% receiving 0 mg/day. About 90% of patients in either treatment arm completed the trial.
The study, funded by the National Institute of Arthritis and Musculoskelatal and Skin Diseases and the National Heart Lung and Blood Institute, was unique in that half of patients randomized in the study were enrolled at community clinics and half were enrolled at Vasculitis Clinical Research Consortium clinical centers.
Abatacept Falls Short for Preventing Relapse in GPA
Adding abatacept to glucocorticoids failed to reduce risk of relapse, worsening disease, or failure to reach remission in adults with relapsing, nonsevere GPA, based on data from a randomized trial of 65 individuals.
In the 20-site, randomized, double-blind ABROGATE (Abatacept for the Treatment of Relapsing, Non-Severe, Granulomatosis With Polyangiitis) study, 34 patients received 125 mg subcutaneous abatacept once a week or a placebo in addition to 30 mg/day of prednisone that was tapered and discontinued after 12 weeks. Patients who were receiving methotrexate, azathioprine, mycophenolate, or leflunomide at baseline continued the medication at a stable dose.
The primary outcome of disease worsening or relapse occurred in 62% of the abatacept group and 68% of the placebo group, and no significant difference in treatment failure rate appeared between the groups. In addition, key secondary endpoints of time to full remission, duration of glucocorticoid-free remission, relapse severity, prevention of damage, and patient-reported quality of life outcomes were not significantly different between the groups.
A total of 112 adverse events occurred, with similar type and severity between the groups, including incidence of infections.
The findings were limited by the relatively small sample size, but the results suggest a need for further research to determine mechanisms of disease and explore additional novel treatments for this rare patient population, the researchers wrote in their abstract.
The study was funded by the National Institutes of Health and Bristol-Myers Squibb.
Plasma Exchange Improves Kidney Function in AAV
Use of therapeutic plasma exchange (PLEX) as an adjunct treatment improved early kidney function in adults with AAV and glomerulonephritis but did not extend beyond 8 weeks, and recovery of kidney function was no different between patients receiving a regular glucocorticoid regimen versus a reduced course, based on a post-hoc analysis of 691 individuals in the international randomized controlled trial called PEXIVAS.
The primary outcomes of change in kidney function based on estimated glomerular filtration rate (eGFR) from baseline over 1 year and the percentage of patients with improvement in eGFR of at least 15 mL/min/1.73 m2 at weeks 12, 26, and 52.
The rate of improved eGFR was significantly greater in the PLEX group, compared with controls, at 2, 4, and 8 weeks. At 4 weeks, significantly more patients in the PLEX group had an increase in eGFR by at least 15 mL/min/1.73 m2, compared with the control group (relative risk [RR], 1.41; P = .008). In addition, improved kidney function within 4 weeks was significantly associated with lower risk of kidney failure within 1 year, regardless of treatment group.
The original PEXIVAS trial was supported by various government institutes and agencies from multiple countries.
Reinforced Vaccine Strategy with Rituximab Improved Antibody Response in AAV
A vaccine strategy consisting of a double dose of 13-valent antipneumococcal conjugate vaccine (PCV13) at day 0 and day 7 followed by a single dose of 23-valent unconjugated pneumococcal polysaccharide vaccine (PPV23) at 5 months significantly improved antibody responses against Streptococcus pneumoniae in patients with AAV, compared with standard treatment, based on data from 95 individuals in the multicenter, open-label study called PNEUMOVAS.
Adults with newly diagnosed AAV were randomly assigned to one of three treatment arms: a standard regimen of one dose of PCV13 at day 0 and one dose of PPV23 at month 5 (arm 1); a double dose of PCV13 at day 0 and day 7 with a dose of PPV23 at month 5 (arm 2); or four doses of PCV13 at day 0 and one dose of PPV23 at month 5 (arm 3). These patients received PCV13 within 2 days before or after their first infusion of rituximab.
The primary endpoint was positive antibody response against 12 pneumococcal subtypes common to the PCV13 and PCV23 vaccines at 6 months. At 6 months, the immune response to 0-3, 4-6, 7-9, or 10-12 serotypes was 83.3%, 13.3%, 3.3%, and 0%, respectively, in arm 1; 56.3%, 28.1%, 15.6%, and 0% in arm 2; and 60.6%, 33.3%, 6.1%, and 0% in arm 3.
No severe adverse events related to vaccination were observed in any of the groups; a total of eight AAV flares occurred in six patients (one in arm 1, two in arm 2, and three in arm 3). Local and systemic reactions occurred more frequently with the reinforced dose regimens, but these were mostly grade 1 or 2 local reactions.
The study was supported by the French Ministry of Health.
Some of the best clinical trials of patients with antineutrophil cytoplasmic antibody–associated vasculitis (AAV) that were presented at the 21st International Vasculitis Workshop in Barcelona, Spain, included studies addressing relapse after stopping steroids, preventing relapse with abatacept, improving kidney function with plasma exchange, and vaccinating rituximab-treated patients.
Stopping Steroids After Remission in GPA
In the randomized, open-label TAPIR (The Assessment of Prednisone In Remission Trial) study of 159 adults with GPA in remission who had tapered to a prednisone dose of 5 mg/day, those who remained at that dosage had a significantly lower rate of relapse after 6 months than those who tapered to 0 mg/day (4.2% vs 15.5%; P = .227), according to results reported at the meeting.
However, use of a higher dose of prednisone for disease relapse by 6 months was similar for patients who used rituximab at baseline (8.8% with 0 mg/day vs 6.1% with 5 mg/day; P = .667), and the difference in this primary outcome was more pronounced among patients who did not take rituximab at baseline (20.0% with 0 mg/day vs 2.6% with 5 mg/day; P = .023).
A higher percentage of patients taking prednisone 0 mg/day had disease relapses that were considered minor (14.1% and 4.2%; P = .0391). Major relapses occurred in none of the patients taking 5 mg/day and in 1.4% receiving 0 mg/day. About 90% of patients in either treatment arm completed the trial.
The study, funded by the National Institute of Arthritis and Musculoskelatal and Skin Diseases and the National Heart Lung and Blood Institute, was unique in that half of patients randomized in the study were enrolled at community clinics and half were enrolled at Vasculitis Clinical Research Consortium clinical centers.
Abatacept Falls Short for Preventing Relapse in GPA
Adding abatacept to glucocorticoids failed to reduce risk of relapse, worsening disease, or failure to reach remission in adults with relapsing, nonsevere GPA, based on data from a randomized trial of 65 individuals.
In the 20-site, randomized, double-blind ABROGATE (Abatacept for the Treatment of Relapsing, Non-Severe, Granulomatosis With Polyangiitis) study, 34 patients received 125 mg subcutaneous abatacept once a week or a placebo in addition to 30 mg/day of prednisone that was tapered and discontinued after 12 weeks. Patients who were receiving methotrexate, azathioprine, mycophenolate, or leflunomide at baseline continued the medication at a stable dose.
The primary outcome of disease worsening or relapse occurred in 62% of the abatacept group and 68% of the placebo group, and no significant difference in treatment failure rate appeared between the groups. In addition, key secondary endpoints of time to full remission, duration of glucocorticoid-free remission, relapse severity, prevention of damage, and patient-reported quality of life outcomes were not significantly different between the groups.
A total of 112 adverse events occurred, with similar type and severity between the groups, including incidence of infections.
The findings were limited by the relatively small sample size, but the results suggest a need for further research to determine mechanisms of disease and explore additional novel treatments for this rare patient population, the researchers wrote in their abstract.
The study was funded by the National Institutes of Health and Bristol-Myers Squibb.
Plasma Exchange Improves Kidney Function in AAV
Use of therapeutic plasma exchange (PLEX) as an adjunct treatment improved early kidney function in adults with AAV and glomerulonephritis but did not extend beyond 8 weeks, and recovery of kidney function was no different between patients receiving a regular glucocorticoid regimen versus a reduced course, based on a post-hoc analysis of 691 individuals in the international randomized controlled trial called PEXIVAS.
The primary outcomes of change in kidney function based on estimated glomerular filtration rate (eGFR) from baseline over 1 year and the percentage of patients with improvement in eGFR of at least 15 mL/min/1.73 m2 at weeks 12, 26, and 52.
The rate of improved eGFR was significantly greater in the PLEX group, compared with controls, at 2, 4, and 8 weeks. At 4 weeks, significantly more patients in the PLEX group had an increase in eGFR by at least 15 mL/min/1.73 m2, compared with the control group (relative risk [RR], 1.41; P = .008). In addition, improved kidney function within 4 weeks was significantly associated with lower risk of kidney failure within 1 year, regardless of treatment group.
The original PEXIVAS trial was supported by various government institutes and agencies from multiple countries.
Reinforced Vaccine Strategy with Rituximab Improved Antibody Response in AAV
A vaccine strategy consisting of a double dose of 13-valent antipneumococcal conjugate vaccine (PCV13) at day 0 and day 7 followed by a single dose of 23-valent unconjugated pneumococcal polysaccharide vaccine (PPV23) at 5 months significantly improved antibody responses against Streptococcus pneumoniae in patients with AAV, compared with standard treatment, based on data from 95 individuals in the multicenter, open-label study called PNEUMOVAS.
Adults with newly diagnosed AAV were randomly assigned to one of three treatment arms: a standard regimen of one dose of PCV13 at day 0 and one dose of PPV23 at month 5 (arm 1); a double dose of PCV13 at day 0 and day 7 with a dose of PPV23 at month 5 (arm 2); or four doses of PCV13 at day 0 and one dose of PPV23 at month 5 (arm 3). These patients received PCV13 within 2 days before or after their first infusion of rituximab.
The primary endpoint was positive antibody response against 12 pneumococcal subtypes common to the PCV13 and PCV23 vaccines at 6 months. At 6 months, the immune response to 0-3, 4-6, 7-9, or 10-12 serotypes was 83.3%, 13.3%, 3.3%, and 0%, respectively, in arm 1; 56.3%, 28.1%, 15.6%, and 0% in arm 2; and 60.6%, 33.3%, 6.1%, and 0% in arm 3.
No severe adverse events related to vaccination were observed in any of the groups; a total of eight AAV flares occurred in six patients (one in arm 1, two in arm 2, and three in arm 3). Local and systemic reactions occurred more frequently with the reinforced dose regimens, but these were mostly grade 1 or 2 local reactions.
The study was supported by the French Ministry of Health.
Some of the best clinical trials of patients with antineutrophil cytoplasmic antibody–associated vasculitis (AAV) that were presented at the 21st International Vasculitis Workshop in Barcelona, Spain, included studies addressing relapse after stopping steroids, preventing relapse with abatacept, improving kidney function with plasma exchange, and vaccinating rituximab-treated patients.
Stopping Steroids After Remission in GPA
In the randomized, open-label TAPIR (The Assessment of Prednisone In Remission Trial) study of 159 adults with GPA in remission who had tapered to a prednisone dose of 5 mg/day, those who remained at that dosage had a significantly lower rate of relapse after 6 months than those who tapered to 0 mg/day (4.2% vs 15.5%; P = .227), according to results reported at the meeting.
However, use of a higher dose of prednisone for disease relapse by 6 months was similar for patients who used rituximab at baseline (8.8% with 0 mg/day vs 6.1% with 5 mg/day; P = .667), and the difference in this primary outcome was more pronounced among patients who did not take rituximab at baseline (20.0% with 0 mg/day vs 2.6% with 5 mg/day; P = .023).
A higher percentage of patients taking prednisone 0 mg/day had disease relapses that were considered minor (14.1% and 4.2%; P = .0391). Major relapses occurred in none of the patients taking 5 mg/day and in 1.4% receiving 0 mg/day. About 90% of patients in either treatment arm completed the trial.
The study, funded by the National Institute of Arthritis and Musculoskelatal and Skin Diseases and the National Heart Lung and Blood Institute, was unique in that half of patients randomized in the study were enrolled at community clinics and half were enrolled at Vasculitis Clinical Research Consortium clinical centers.
Abatacept Falls Short for Preventing Relapse in GPA
Adding abatacept to glucocorticoids failed to reduce risk of relapse, worsening disease, or failure to reach remission in adults with relapsing, nonsevere GPA, based on data from a randomized trial of 65 individuals.
In the 20-site, randomized, double-blind ABROGATE (Abatacept for the Treatment of Relapsing, Non-Severe, Granulomatosis With Polyangiitis) study, 34 patients received 125 mg subcutaneous abatacept once a week or a placebo in addition to 30 mg/day of prednisone that was tapered and discontinued after 12 weeks. Patients who were receiving methotrexate, azathioprine, mycophenolate, or leflunomide at baseline continued the medication at a stable dose.
The primary outcome of disease worsening or relapse occurred in 62% of the abatacept group and 68% of the placebo group, and no significant difference in treatment failure rate appeared between the groups. In addition, key secondary endpoints of time to full remission, duration of glucocorticoid-free remission, relapse severity, prevention of damage, and patient-reported quality of life outcomes were not significantly different between the groups.
A total of 112 adverse events occurred, with similar type and severity between the groups, including incidence of infections.
The findings were limited by the relatively small sample size, but the results suggest a need for further research to determine mechanisms of disease and explore additional novel treatments for this rare patient population, the researchers wrote in their abstract.
The study was funded by the National Institutes of Health and Bristol-Myers Squibb.
Plasma Exchange Improves Kidney Function in AAV
Use of therapeutic plasma exchange (PLEX) as an adjunct treatment improved early kidney function in adults with AAV and glomerulonephritis but did not extend beyond 8 weeks, and recovery of kidney function was no different between patients receiving a regular glucocorticoid regimen versus a reduced course, based on a post-hoc analysis of 691 individuals in the international randomized controlled trial called PEXIVAS.
The primary outcomes of change in kidney function based on estimated glomerular filtration rate (eGFR) from baseline over 1 year and the percentage of patients with improvement in eGFR of at least 15 mL/min/1.73 m2 at weeks 12, 26, and 52.
The rate of improved eGFR was significantly greater in the PLEX group, compared with controls, at 2, 4, and 8 weeks. At 4 weeks, significantly more patients in the PLEX group had an increase in eGFR by at least 15 mL/min/1.73 m2, compared with the control group (relative risk [RR], 1.41; P = .008). In addition, improved kidney function within 4 weeks was significantly associated with lower risk of kidney failure within 1 year, regardless of treatment group.
The original PEXIVAS trial was supported by various government institutes and agencies from multiple countries.
Reinforced Vaccine Strategy with Rituximab Improved Antibody Response in AAV
A vaccine strategy consisting of a double dose of 13-valent antipneumococcal conjugate vaccine (PCV13) at day 0 and day 7 followed by a single dose of 23-valent unconjugated pneumococcal polysaccharide vaccine (PPV23) at 5 months significantly improved antibody responses against Streptococcus pneumoniae in patients with AAV, compared with standard treatment, based on data from 95 individuals in the multicenter, open-label study called PNEUMOVAS.
Adults with newly diagnosed AAV were randomly assigned to one of three treatment arms: a standard regimen of one dose of PCV13 at day 0 and one dose of PPV23 at month 5 (arm 1); a double dose of PCV13 at day 0 and day 7 with a dose of PPV23 at month 5 (arm 2); or four doses of PCV13 at day 0 and one dose of PPV23 at month 5 (arm 3). These patients received PCV13 within 2 days before or after their first infusion of rituximab.
The primary endpoint was positive antibody response against 12 pneumococcal subtypes common to the PCV13 and PCV23 vaccines at 6 months. At 6 months, the immune response to 0-3, 4-6, 7-9, or 10-12 serotypes was 83.3%, 13.3%, 3.3%, and 0%, respectively, in arm 1; 56.3%, 28.1%, 15.6%, and 0% in arm 2; and 60.6%, 33.3%, 6.1%, and 0% in arm 3.
No severe adverse events related to vaccination were observed in any of the groups; a total of eight AAV flares occurred in six patients (one in arm 1, two in arm 2, and three in arm 3). Local and systemic reactions occurred more frequently with the reinforced dose regimens, but these were mostly grade 1 or 2 local reactions.
The study was supported by the French Ministry of Health.
Metabolite in Red Meat Increases Kidney Disease Risk
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
TOPLINE:
Trimethylamine N-oxide (TMAO) is a gut microbiota-derived metabolite generated by metabolism of dietary L-carnitine, primarily from red meat, and choline, from a variety of animal source foods. TMAO has been shown to cause kidney injury and tubulointerstitial fibrosis in experimental models.
In this study, TMAO was independently associated with higher risks for incident chronic kidney disease (CKD) and faster kidney function decline in humans.
METHODOLOGY:
- Study population was 10,564 participants from two community-based, prospective cohorts without baseline CKD (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2).
- Incident CKD was defined as eGFR decline ≥ 30% from baseline, resulting in eGFR < 60 mL/min/1.73 m2.
TAKEAWAY:
- During a median 9.4 years, 979 incident CKD events occurred.
- Correlation between baseline TMAO and total meat intake was small but statistically significant (P = .08).
- After adjustments for sociodemographic, lifestyle, diet, and cardiovascular risk factors, higher plasma TMAO was associated with more than doubled CKD incidence (hazard ratio, 2.24 for top vs bottom quintile).
- Higher TMAO levels were also associated with greater annual eGFR decline (top vs bottom quintile eGFR change = −0.43 mL/min/1.73 m2 per year.
- Compared with other major CKD risk factors, the association for the top vs bottom TMAO quintile (−0.43 mL/min/1.73 m2 per year) was similar to that seen per 10 years of older age (−0.43) and presence of diabetes (−0.51), and larger than that seen comparing Black vs non-Black race (−0.28) and per 10 mm Hg systolic blood pressure (−0.16).
IN PRACTICE:
“TMAO levels are highly modifiable by both lifestyle-like diet and pharmacologic interventions. Besides using novel drugs to lower TMAO in patients, using dietary interventions to lower TMAO in the general population could be a cost-efficient and low-risk preventive strategy for chronic kidney disease development. ... These findings support future studies to investigate whether lifestyle and pharmacologic interventions to lower TMAO may prevent CKD development and progression.”
SOURCE:
The study was conducted by Meng Wang, PhD, of Tufts University, Boston, and colleagues and published online in the Journal of the American Society of Nephrology.
LIMITATIONS:
Observational design, can’t exclude residual confounding.
Inter-assay variability.
Use of International Classification of Diseases codes for hospitalization-based CKD, subject to reporting errors.
DISCLOSURES:
The study was supported by grants from the National Institutes of Health and an American Heart Association Postdoctoral Fellowship. Dr. Wang had no disclosures but several coauthors have patents on various diagnostics and/or industry disclosures.
A version of this article appeared on Medscape.com.
Immunoglobulin A Nephropathy: 5 Things to Know
Immunoglobulin A (IgA) nephropathy, also known as Berger disease, is a kidney disorder characterized by the deposition of IgA in the glomeruli, leading to inflammation and potential damage. It is the most common primary glomerulonephritis worldwide. Here are five things to know about IgA nephropathy.
1. Disease-modifying therapies for IgA nephropathy have become available only recently.
The past few years have brought development of the first disease-modifying therapies to reduce proteinuria for adults with primary IgA nephropathy who are at risk for rapid disease progression. In 2021, the US Food and Drug Administration (FDA) approved a targeted-release formulation of the corticosteroid budesonide for these patients. This formulation delivers the drug to the distal ileum, targeting Peyer patches — the site of IgA production — while minimizing the adverse effects associated with systemic corticosteroid therapy.
The FDA most recently approved sparsentan, a nonimmunosuppressive therapy that combines an endothelin type A receptor antagonist with an angiotensin II type 1 receptor antagonist, for the same indication in 2023.
In addition, several studies have reported benefits with the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors in the treatment of patients with IgA nephropathy at high risk for progression, although this use is still investigational.
2. The most common sign in patients with IgA nephropathy is blood in the urine.
The most common clinical manifestation of IgA nephropathy is microscopic or gross hematuria. Hematuria is often recurrent and may follow upper respiratory tract or other infections. The presence of blood in the urine may be episodic and can vary in severity.
Proteinuria is another key feature of IgA nephropathy. It may range from mild to moderate and, in some cases, can even progress to nephrotic-range proteinuria. The level of proteinuria is an important indicator of disease severity and prognosis. Persistent and significant proteinuria may be associated with an increased risk for progression to chronic kidney disease.
3. Five histologic features are widely used to predict clinical outcomes.
The Oxford classification of IgA nephropathy, or MEST score, published in 2009, comprises four histologic features that are independent predictors of clinical outcome: mesangial and endocapillary hypercellularity, segmental glomerulosclerosis, and interstitial fibrosis/tubular atrophy. In 2017, the IgA Nephropathy Classification Working Group added glomerular crescent formation to the Oxford classification, to form the MEST-C score.
If any of these features are seen, the prognosis can generally be assumed to be poor. Proteinuria, hypertension, elevated creatinine, and a decreased estimated glomerular filtration rate are some of the other factors that can contribute to poor clinical outcomes in patients with IgA nephropathy.
4. IgA nephropathy can eventually progress to end-stage kidney disease.
Progressive kidney dysfunction can occur in some individuals with IgA nephropathy. This may manifest as a gradual decline in glomerular filtration rate, leading to chronic kidney disease over time. In addition, up to 20% of patients progress to end-stage kidney disease within 10 years. The risk for renal impairment varies among individuals, and certain clinical and histologic features may influence the prognosis.
Hypertension is a common complication of IgA nephropathy. The mechanisms underlying hypertension in IgA nephropathy are complex and may involve alterations in the renin-angiotensin-aldosterone system and salt-water balance. Controlling blood pressure is important in managing IgA nephropathy to help slow the progression of kidney damage.
5. Definitive diagnosis requires a renal biopsy.
There are currently no validated diagnostic serum or urine biomarkers for IgA nephropathy, which, according to KDIGO (Kidney Disease: Improving Global Outcomes), requires a renal biopsy to make a definitive diagnosis. The characteristic finding is the deposition of IgA in the glomeruli, typically in the mesangial area. The biopsy can also provide information about the degree of inflammation, scarring, and other histologic features that help guide treatment decisions and predict outcomes.
Dr. Alper, associate professor, department of medicine, section of nephrology, Tulane University School of Medicine, New Orleans, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Immunoglobulin A (IgA) nephropathy, also known as Berger disease, is a kidney disorder characterized by the deposition of IgA in the glomeruli, leading to inflammation and potential damage. It is the most common primary glomerulonephritis worldwide. Here are five things to know about IgA nephropathy.
1. Disease-modifying therapies for IgA nephropathy have become available only recently.
The past few years have brought development of the first disease-modifying therapies to reduce proteinuria for adults with primary IgA nephropathy who are at risk for rapid disease progression. In 2021, the US Food and Drug Administration (FDA) approved a targeted-release formulation of the corticosteroid budesonide for these patients. This formulation delivers the drug to the distal ileum, targeting Peyer patches — the site of IgA production — while minimizing the adverse effects associated with systemic corticosteroid therapy.
The FDA most recently approved sparsentan, a nonimmunosuppressive therapy that combines an endothelin type A receptor antagonist with an angiotensin II type 1 receptor antagonist, for the same indication in 2023.
In addition, several studies have reported benefits with the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors in the treatment of patients with IgA nephropathy at high risk for progression, although this use is still investigational.
2. The most common sign in patients with IgA nephropathy is blood in the urine.
The most common clinical manifestation of IgA nephropathy is microscopic or gross hematuria. Hematuria is often recurrent and may follow upper respiratory tract or other infections. The presence of blood in the urine may be episodic and can vary in severity.
Proteinuria is another key feature of IgA nephropathy. It may range from mild to moderate and, in some cases, can even progress to nephrotic-range proteinuria. The level of proteinuria is an important indicator of disease severity and prognosis. Persistent and significant proteinuria may be associated with an increased risk for progression to chronic kidney disease.
3. Five histologic features are widely used to predict clinical outcomes.
The Oxford classification of IgA nephropathy, or MEST score, published in 2009, comprises four histologic features that are independent predictors of clinical outcome: mesangial and endocapillary hypercellularity, segmental glomerulosclerosis, and interstitial fibrosis/tubular atrophy. In 2017, the IgA Nephropathy Classification Working Group added glomerular crescent formation to the Oxford classification, to form the MEST-C score.
If any of these features are seen, the prognosis can generally be assumed to be poor. Proteinuria, hypertension, elevated creatinine, and a decreased estimated glomerular filtration rate are some of the other factors that can contribute to poor clinical outcomes in patients with IgA nephropathy.
4. IgA nephropathy can eventually progress to end-stage kidney disease.
Progressive kidney dysfunction can occur in some individuals with IgA nephropathy. This may manifest as a gradual decline in glomerular filtration rate, leading to chronic kidney disease over time. In addition, up to 20% of patients progress to end-stage kidney disease within 10 years. The risk for renal impairment varies among individuals, and certain clinical and histologic features may influence the prognosis.
Hypertension is a common complication of IgA nephropathy. The mechanisms underlying hypertension in IgA nephropathy are complex and may involve alterations in the renin-angiotensin-aldosterone system and salt-water balance. Controlling blood pressure is important in managing IgA nephropathy to help slow the progression of kidney damage.
5. Definitive diagnosis requires a renal biopsy.
There are currently no validated diagnostic serum or urine biomarkers for IgA nephropathy, which, according to KDIGO (Kidney Disease: Improving Global Outcomes), requires a renal biopsy to make a definitive diagnosis. The characteristic finding is the deposition of IgA in the glomeruli, typically in the mesangial area. The biopsy can also provide information about the degree of inflammation, scarring, and other histologic features that help guide treatment decisions and predict outcomes.
Dr. Alper, associate professor, department of medicine, section of nephrology, Tulane University School of Medicine, New Orleans, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Immunoglobulin A (IgA) nephropathy, also known as Berger disease, is a kidney disorder characterized by the deposition of IgA in the glomeruli, leading to inflammation and potential damage. It is the most common primary glomerulonephritis worldwide. Here are five things to know about IgA nephropathy.
1. Disease-modifying therapies for IgA nephropathy have become available only recently.
The past few years have brought development of the first disease-modifying therapies to reduce proteinuria for adults with primary IgA nephropathy who are at risk for rapid disease progression. In 2021, the US Food and Drug Administration (FDA) approved a targeted-release formulation of the corticosteroid budesonide for these patients. This formulation delivers the drug to the distal ileum, targeting Peyer patches — the site of IgA production — while minimizing the adverse effects associated with systemic corticosteroid therapy.
The FDA most recently approved sparsentan, a nonimmunosuppressive therapy that combines an endothelin type A receptor antagonist with an angiotensin II type 1 receptor antagonist, for the same indication in 2023.
In addition, several studies have reported benefits with the use of sodium-glucose cotransporter 2 (SGLT2) inhibitors in the treatment of patients with IgA nephropathy at high risk for progression, although this use is still investigational.
2. The most common sign in patients with IgA nephropathy is blood in the urine.
The most common clinical manifestation of IgA nephropathy is microscopic or gross hematuria. Hematuria is often recurrent and may follow upper respiratory tract or other infections. The presence of blood in the urine may be episodic and can vary in severity.
Proteinuria is another key feature of IgA nephropathy. It may range from mild to moderate and, in some cases, can even progress to nephrotic-range proteinuria. The level of proteinuria is an important indicator of disease severity and prognosis. Persistent and significant proteinuria may be associated with an increased risk for progression to chronic kidney disease.
3. Five histologic features are widely used to predict clinical outcomes.
The Oxford classification of IgA nephropathy, or MEST score, published in 2009, comprises four histologic features that are independent predictors of clinical outcome: mesangial and endocapillary hypercellularity, segmental glomerulosclerosis, and interstitial fibrosis/tubular atrophy. In 2017, the IgA Nephropathy Classification Working Group added glomerular crescent formation to the Oxford classification, to form the MEST-C score.
If any of these features are seen, the prognosis can generally be assumed to be poor. Proteinuria, hypertension, elevated creatinine, and a decreased estimated glomerular filtration rate are some of the other factors that can contribute to poor clinical outcomes in patients with IgA nephropathy.
4. IgA nephropathy can eventually progress to end-stage kidney disease.
Progressive kidney dysfunction can occur in some individuals with IgA nephropathy. This may manifest as a gradual decline in glomerular filtration rate, leading to chronic kidney disease over time. In addition, up to 20% of patients progress to end-stage kidney disease within 10 years. The risk for renal impairment varies among individuals, and certain clinical and histologic features may influence the prognosis.
Hypertension is a common complication of IgA nephropathy. The mechanisms underlying hypertension in IgA nephropathy are complex and may involve alterations in the renin-angiotensin-aldosterone system and salt-water balance. Controlling blood pressure is important in managing IgA nephropathy to help slow the progression of kidney damage.
5. Definitive diagnosis requires a renal biopsy.
There are currently no validated diagnostic serum or urine biomarkers for IgA nephropathy, which, according to KDIGO (Kidney Disease: Improving Global Outcomes), requires a renal biopsy to make a definitive diagnosis. The characteristic finding is the deposition of IgA in the glomeruli, typically in the mesangial area. The biopsy can also provide information about the degree of inflammation, scarring, and other histologic features that help guide treatment decisions and predict outcomes.
Dr. Alper, associate professor, department of medicine, section of nephrology, Tulane University School of Medicine, New Orleans, has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Hair-Straightening Products Entail Acute Kidney Failure Risk
The observation was made by a team of French researchers who tested the suspected straightening product on animals. The product is believed to be the cause of several episodes of renal damage in a young woman.
“The results on mice are striking,” said study author Emmanuel Letavernier, MD, a nephrologist at Tenon Hospital in Paris. “They develop extremely severe acute kidney failure within 24 hours of applying the straightening cream. Samples show the presence of calcium oxalate crystals in all renal tubules.”
Given the potential nephrotoxicity of glyoxylic acid through topical application, products containing this compound should be avoided and ideally withdrawn from the market, the researchers suggested in a letter published in The New England Journal of Medicine. The appropriate departments of the French Agency for Food, Environmental, and Occupational Health and Safety have been alerted, Dr. Letavernier added.
Replacing Formaldehyde
Glyoxylic acid has recently been introduced into certain cosmetic products (such as shampoo, styling lotion, and straightening products), often as a replacement for formaldehyde, which is irritating and possibly carcinogenic. Glyoxylic acid is praised for its smoothing qualities. However, it is recommended to avoid contact with the scalp.
Cases of renal complications could be underdiagnosed, according to the researchers, who are preparing a nationwide survey. Renal failure can be silent. Among the signs that should raise concern are “scalp irritation accompanied by nausea or vomiting after a hair salon visit,” said Dr. Letavernier.
Similar cases have already been reported in the literature. An Israeli team recently described 26 patients treated for acute renal injuries after hair straightening in hair salons. Biopsies revealed calcium oxalate crystals in the kidneys.
The Israeli researchers suspected an effect of glycolic acid, another substance found in many cosmetic products, including straightening products. However, they could not provide evidence.
Glycolic Acid Safe?
By conducting a second animal study, which should be published soon, Dr. Letavernier and his team were able to rule out this hypothesis. “Glycolic acid does not pose a problem. Unlike glyoxylic acid, the application of glycolic acid on the skin of mice does not induce the formation of oxalate crystals in the kidneys, nor acute kidney failure.”
The French clinical case reported in the correspondence concerns a 26-year-old woman with no prior health history who had three episodes of acute renal damage 1 year apart. It turned out that each episode occurred shortly after hair straightening at a hair salon in Marseille.
The patient reported feeling a burning sensation during the hair treatment. Scalp irritations appeared. She then experienced vomiting, diarrhea, fever, and back pain. Analyses revealed high levels of plasma creatinine during each episode, indicating renal failure.
A CT scan showed no signs of urinary tract obstruction. However, the patient had a small kidney stone. Further analysis revealed the presence of blood and leukocytes in the urine. But there was no proteinuria or urinary infection.
Chronic Renal Failure
After each episode, renal function rapidly improved. “The repetition of episodes of acute renal failure is, however, a major risk factor for developing chronic renal failure in the long term,” said Dr. Letavernier.
The cream used in the hair salon to straighten hair was retrieved by the researchers. It contained a significant amount of glyoxylic acid but no glycolic acid.
To explore its potential nephrotoxic effect, they conducted a study on 10 mice. The animals were divided into two groups to test on one side topical application of the product and a gel without active product (control group) on the other.
Mice exposed to the product had oxalate crystals in their urine, unlike mice in the control group. A scan confirmed calcium oxalate deposits in the kidneys. Plasma creatinine levels increased significantly after exposure to glyoxylic acid.
“After passing through the epidermis, glyoxylic acid is rapidly converted in the blood to glyoxylate. In the liver and probably in other organs, glyoxylate is metabolized to become oxalate, which upon contact with calcium in the urine forms calcium oxalate crystals,” explained the specialist.
Excess calcium oxalate crystals causing renal failure are observed in rare conditions such as primary hyperoxaluria, a genetic disease affecting liver metabolism, or enteric hyperoxaluria, which is linked to increased intestinal permeability to oxalate: an anion naturally found in certain plants.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The observation was made by a team of French researchers who tested the suspected straightening product on animals. The product is believed to be the cause of several episodes of renal damage in a young woman.
“The results on mice are striking,” said study author Emmanuel Letavernier, MD, a nephrologist at Tenon Hospital in Paris. “They develop extremely severe acute kidney failure within 24 hours of applying the straightening cream. Samples show the presence of calcium oxalate crystals in all renal tubules.”
Given the potential nephrotoxicity of glyoxylic acid through topical application, products containing this compound should be avoided and ideally withdrawn from the market, the researchers suggested in a letter published in The New England Journal of Medicine. The appropriate departments of the French Agency for Food, Environmental, and Occupational Health and Safety have been alerted, Dr. Letavernier added.
Replacing Formaldehyde
Glyoxylic acid has recently been introduced into certain cosmetic products (such as shampoo, styling lotion, and straightening products), often as a replacement for formaldehyde, which is irritating and possibly carcinogenic. Glyoxylic acid is praised for its smoothing qualities. However, it is recommended to avoid contact with the scalp.
Cases of renal complications could be underdiagnosed, according to the researchers, who are preparing a nationwide survey. Renal failure can be silent. Among the signs that should raise concern are “scalp irritation accompanied by nausea or vomiting after a hair salon visit,” said Dr. Letavernier.
Similar cases have already been reported in the literature. An Israeli team recently described 26 patients treated for acute renal injuries after hair straightening in hair salons. Biopsies revealed calcium oxalate crystals in the kidneys.
The Israeli researchers suspected an effect of glycolic acid, another substance found in many cosmetic products, including straightening products. However, they could not provide evidence.
Glycolic Acid Safe?
By conducting a second animal study, which should be published soon, Dr. Letavernier and his team were able to rule out this hypothesis. “Glycolic acid does not pose a problem. Unlike glyoxylic acid, the application of glycolic acid on the skin of mice does not induce the formation of oxalate crystals in the kidneys, nor acute kidney failure.”
The French clinical case reported in the correspondence concerns a 26-year-old woman with no prior health history who had three episodes of acute renal damage 1 year apart. It turned out that each episode occurred shortly after hair straightening at a hair salon in Marseille.
The patient reported feeling a burning sensation during the hair treatment. Scalp irritations appeared. She then experienced vomiting, diarrhea, fever, and back pain. Analyses revealed high levels of plasma creatinine during each episode, indicating renal failure.
A CT scan showed no signs of urinary tract obstruction. However, the patient had a small kidney stone. Further analysis revealed the presence of blood and leukocytes in the urine. But there was no proteinuria or urinary infection.
Chronic Renal Failure
After each episode, renal function rapidly improved. “The repetition of episodes of acute renal failure is, however, a major risk factor for developing chronic renal failure in the long term,” said Dr. Letavernier.
The cream used in the hair salon to straighten hair was retrieved by the researchers. It contained a significant amount of glyoxylic acid but no glycolic acid.
To explore its potential nephrotoxic effect, they conducted a study on 10 mice. The animals were divided into two groups to test on one side topical application of the product and a gel without active product (control group) on the other.
Mice exposed to the product had oxalate crystals in their urine, unlike mice in the control group. A scan confirmed calcium oxalate deposits in the kidneys. Plasma creatinine levels increased significantly after exposure to glyoxylic acid.
“After passing through the epidermis, glyoxylic acid is rapidly converted in the blood to glyoxylate. In the liver and probably in other organs, glyoxylate is metabolized to become oxalate, which upon contact with calcium in the urine forms calcium oxalate crystals,” explained the specialist.
Excess calcium oxalate crystals causing renal failure are observed in rare conditions such as primary hyperoxaluria, a genetic disease affecting liver metabolism, or enteric hyperoxaluria, which is linked to increased intestinal permeability to oxalate: an anion naturally found in certain plants.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
The observation was made by a team of French researchers who tested the suspected straightening product on animals. The product is believed to be the cause of several episodes of renal damage in a young woman.
“The results on mice are striking,” said study author Emmanuel Letavernier, MD, a nephrologist at Tenon Hospital in Paris. “They develop extremely severe acute kidney failure within 24 hours of applying the straightening cream. Samples show the presence of calcium oxalate crystals in all renal tubules.”
Given the potential nephrotoxicity of glyoxylic acid through topical application, products containing this compound should be avoided and ideally withdrawn from the market, the researchers suggested in a letter published in The New England Journal of Medicine. The appropriate departments of the French Agency for Food, Environmental, and Occupational Health and Safety have been alerted, Dr. Letavernier added.
Replacing Formaldehyde
Glyoxylic acid has recently been introduced into certain cosmetic products (such as shampoo, styling lotion, and straightening products), often as a replacement for formaldehyde, which is irritating and possibly carcinogenic. Glyoxylic acid is praised for its smoothing qualities. However, it is recommended to avoid contact with the scalp.
Cases of renal complications could be underdiagnosed, according to the researchers, who are preparing a nationwide survey. Renal failure can be silent. Among the signs that should raise concern are “scalp irritation accompanied by nausea or vomiting after a hair salon visit,” said Dr. Letavernier.
Similar cases have already been reported in the literature. An Israeli team recently described 26 patients treated for acute renal injuries after hair straightening in hair salons. Biopsies revealed calcium oxalate crystals in the kidneys.
The Israeli researchers suspected an effect of glycolic acid, another substance found in many cosmetic products, including straightening products. However, they could not provide evidence.
Glycolic Acid Safe?
By conducting a second animal study, which should be published soon, Dr. Letavernier and his team were able to rule out this hypothesis. “Glycolic acid does not pose a problem. Unlike glyoxylic acid, the application of glycolic acid on the skin of mice does not induce the formation of oxalate crystals in the kidneys, nor acute kidney failure.”
The French clinical case reported in the correspondence concerns a 26-year-old woman with no prior health history who had three episodes of acute renal damage 1 year apart. It turned out that each episode occurred shortly after hair straightening at a hair salon in Marseille.
The patient reported feeling a burning sensation during the hair treatment. Scalp irritations appeared. She then experienced vomiting, diarrhea, fever, and back pain. Analyses revealed high levels of plasma creatinine during each episode, indicating renal failure.
A CT scan showed no signs of urinary tract obstruction. However, the patient had a small kidney stone. Further analysis revealed the presence of blood and leukocytes in the urine. But there was no proteinuria or urinary infection.
Chronic Renal Failure
After each episode, renal function rapidly improved. “The repetition of episodes of acute renal failure is, however, a major risk factor for developing chronic renal failure in the long term,” said Dr. Letavernier.
The cream used in the hair salon to straighten hair was retrieved by the researchers. It contained a significant amount of glyoxylic acid but no glycolic acid.
To explore its potential nephrotoxic effect, they conducted a study on 10 mice. The animals were divided into two groups to test on one side topical application of the product and a gel without active product (control group) on the other.
Mice exposed to the product had oxalate crystals in their urine, unlike mice in the control group. A scan confirmed calcium oxalate deposits in the kidneys. Plasma creatinine levels increased significantly after exposure to glyoxylic acid.
“After passing through the epidermis, glyoxylic acid is rapidly converted in the blood to glyoxylate. In the liver and probably in other organs, glyoxylate is metabolized to become oxalate, which upon contact with calcium in the urine forms calcium oxalate crystals,” explained the specialist.
Excess calcium oxalate crystals causing renal failure are observed in rare conditions such as primary hyperoxaluria, a genetic disease affecting liver metabolism, or enteric hyperoxaluria, which is linked to increased intestinal permeability to oxalate: an anion naturally found in certain plants.
This story was translated from the Medscape French edition using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication. A version of this article appeared on Medscape.com.
COVID-19 Is a Very Weird Virus
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
In the early days of the pandemic, before we really understood what COVID was, two specialties in the hospital had a foreboding sense that something was very strange about this virus. The first was the pulmonologists, who noticed the striking levels of hypoxemia — low oxygen in the blood — and the rapidity with which patients who had previously been stable would crash in the intensive care unit.
The second, and I mark myself among this group, were the nephrologists. The dialysis machines stopped working right. I remember rounding on patients in the hospital who were on dialysis for kidney failure in the setting of severe COVID infection and seeing clots forming on the dialysis filters. Some patients could barely get in a full treatment because the filters would clog so quickly.
We knew it was worse than flu because of the mortality rates, but these oddities made us realize that it was different too — not just a particularly nasty respiratory virus but one that had effects on the body that we hadn’t really seen before.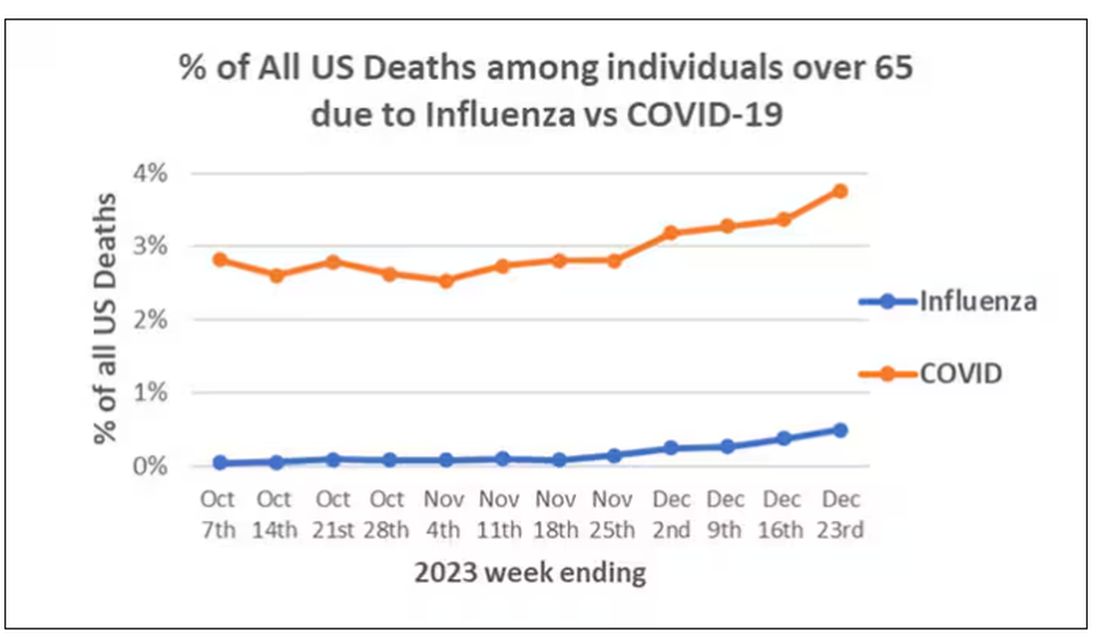
That’s why I’ve always been interested in studies that compare what happens to patients after COVID infection vs what happens to patients after other respiratory infections. This week, we’ll look at an intriguing study that suggests that COVID may lead to autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis.
The study appears in the Annals of Internal Medicine and is made possible by the universal electronic health record systems of South Korea and Japan, who collaborated to create a truly staggering cohort of more than 20 million individuals living in those countries from 2020 to 2021.
The exposure of interest? COVID infection, experienced by just under 5% of that cohort over the study period. (Remember, there was a time when COVID infections were relatively controlled, particularly in some countries.)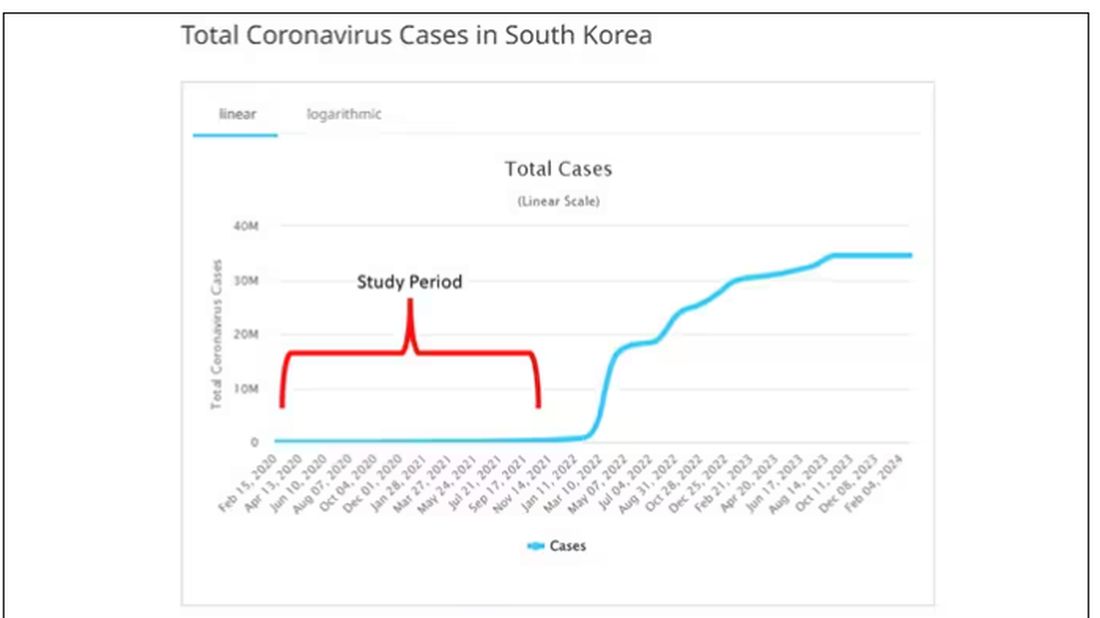
The researchers wanted to compare the risk for autoimmune disease among COVID-infected individuals against two control groups. The first control group was the general population. This is interesting but a difficult analysis, because people who become infected with COVID might be very different from the general population. The second control group was people infected with influenza. I like this a lot better; the risk factors for COVID and influenza are quite similar, and the fact that this group was diagnosed with flu means at least that they are getting medical care and are sort of “in the system,” so to speak.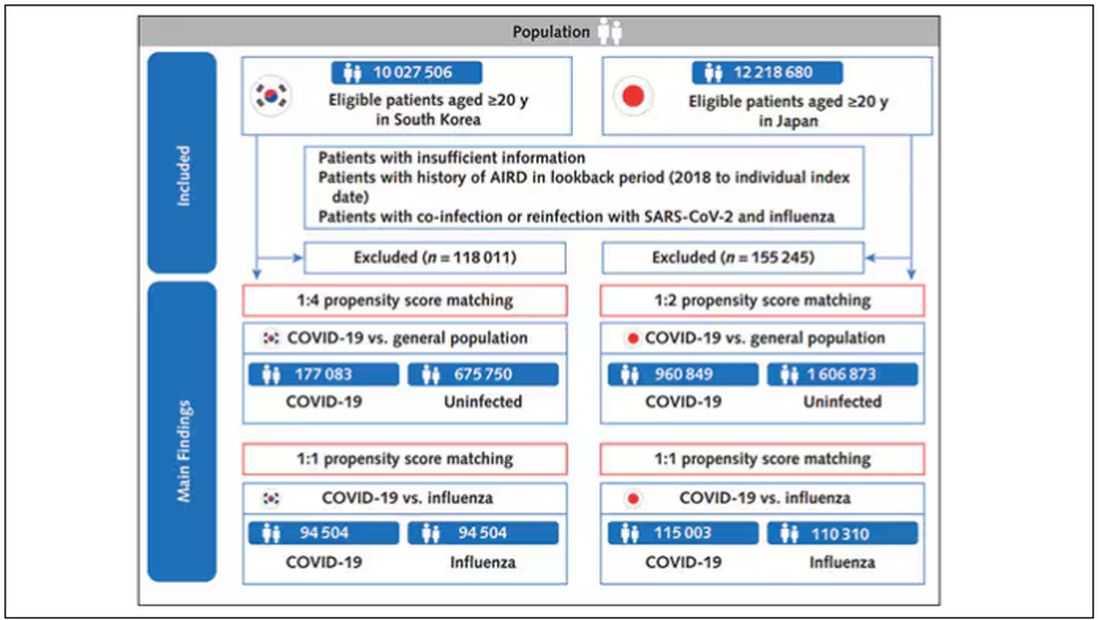
But it’s not enough to simply identify these folks and see who ends up with more autoimmune disease. The authors used propensity score matching to pair individuals infected with COVID with individuals from the control groups who were very similar to them. I’ve talked about this strategy before, but the basic idea is that you build a model predicting the likelihood of infection with COVID, based on a slew of factors — and the slew these authors used is pretty big, as shown below — and then stick people with similar risk for COVID together, with one member of the pair having had COVID and the other having eluded it (at least for the study period).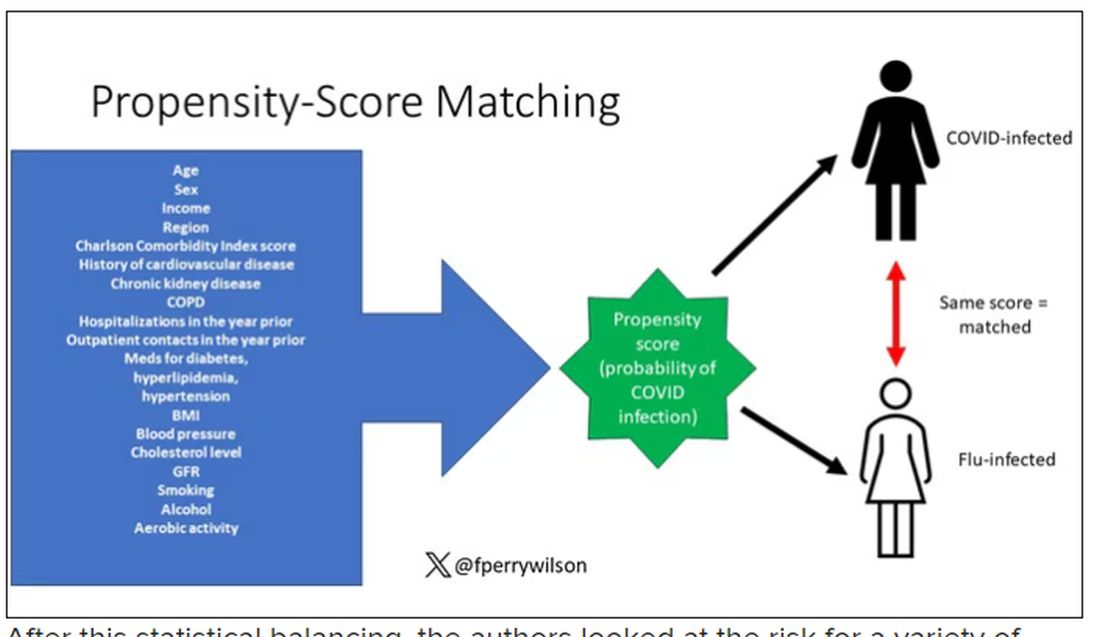
After this statistical balancing, the authors looked at the risk for a variety of autoimmune diseases.
Compared with those infected with flu, those infected with COVID were more likely to be diagnosed with any autoimmune condition, connective tissue disease, and, in Japan at least, inflammatory arthritis.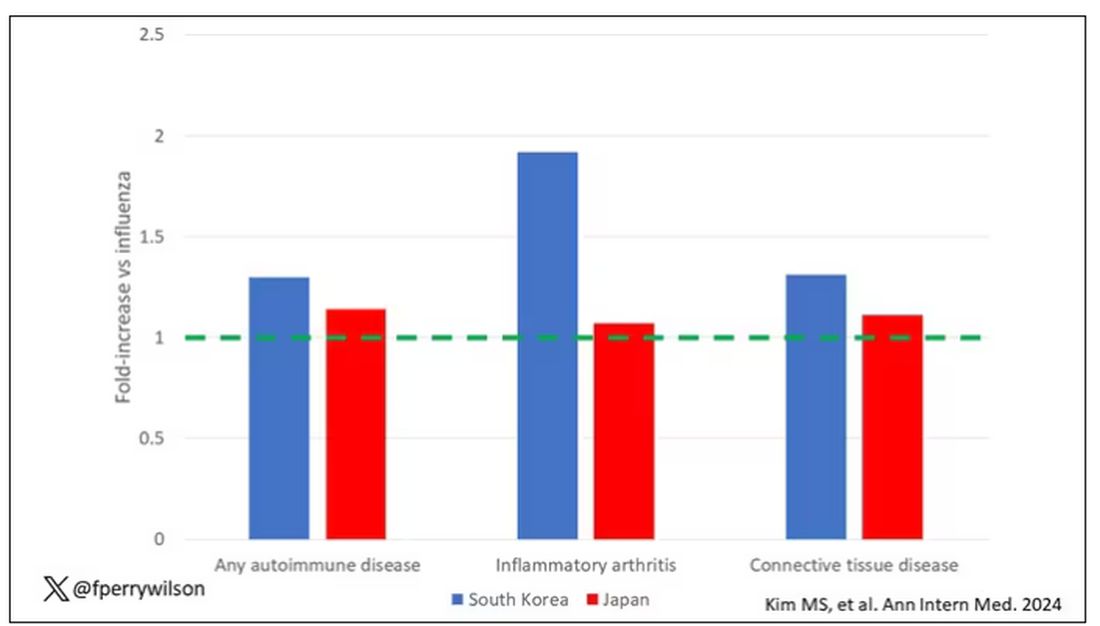
The authors acknowledge that being diagnosed with a disease might not be the same as actually having the disease, so in another analysis they looked only at people who received treatment for the autoimmune conditions, and the signals were even stronger in that group.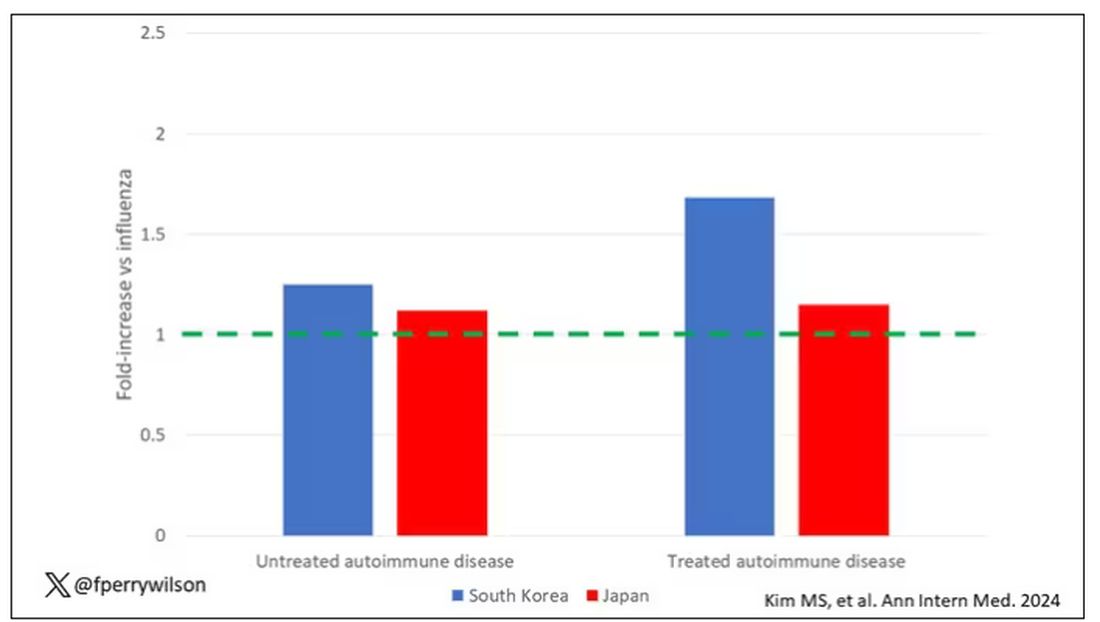
This risk seemed to be highest in the 6 months following the COVID infection, which makes sense biologically if we think that the infection is somehow screwing up the immune system.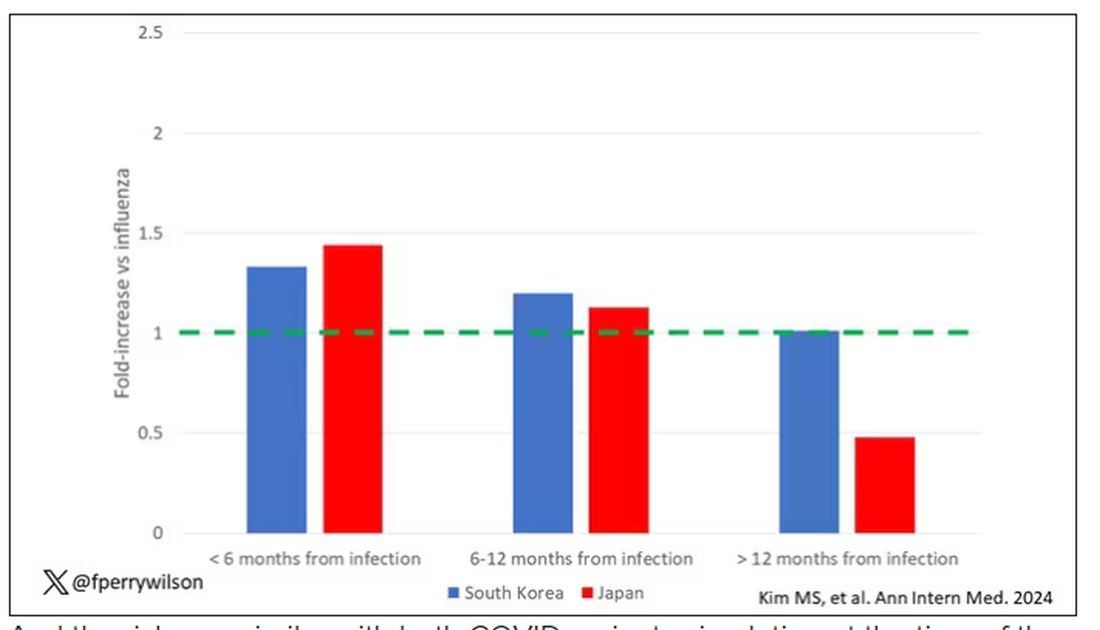
And the risk was similar with both COVID variants circulating at the time of the study.
The only factor that reduced the risk? You guessed it: vaccination. This is a particularly interesting finding because the exposure cohort was defined by having been infected with COVID. Therefore, the mechanism of protection is not prevention of infection; it’s something else. Perhaps vaccination helps to get the immune system in a state to respond to COVID infection more… appropriately?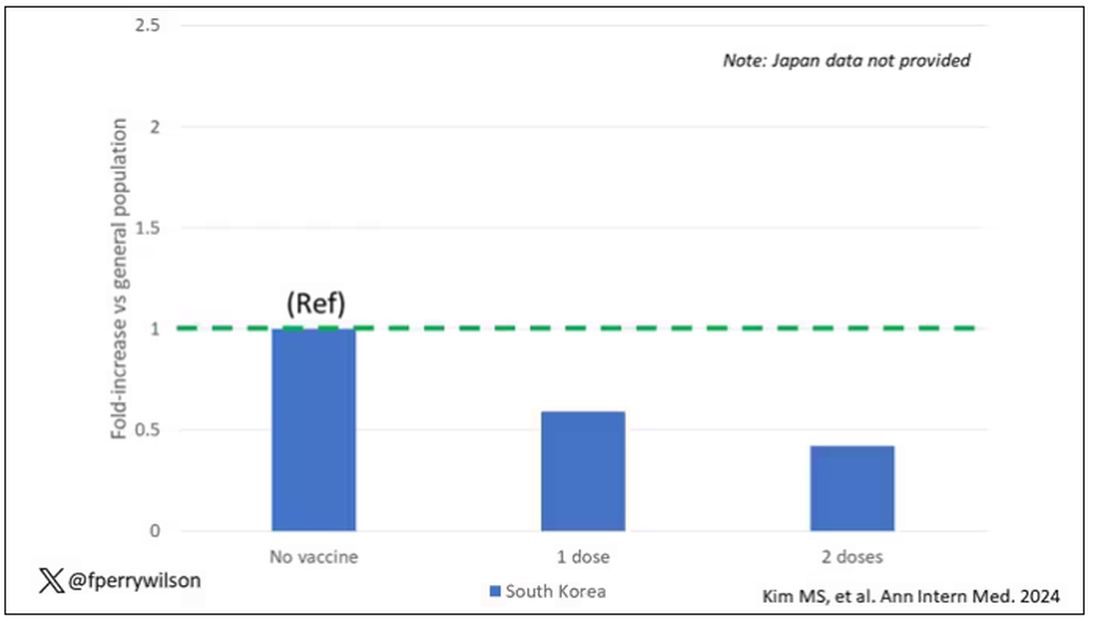
Yes, this study is observational. We can’t draw causal conclusions here. But it does reinforce my long-held belief that COVID is a weird virus, one with effects that are different from the respiratory viruses we are used to. I can’t say for certain whether COVID causes immune system dysfunction that puts someone at risk for autoimmunity — not from this study. But I can say it wouldn’t surprise me.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
In the early days of the pandemic, before we really understood what COVID was, two specialties in the hospital had a foreboding sense that something was very strange about this virus. The first was the pulmonologists, who noticed the striking levels of hypoxemia — low oxygen in the blood — and the rapidity with which patients who had previously been stable would crash in the intensive care unit.
The second, and I mark myself among this group, were the nephrologists. The dialysis machines stopped working right. I remember rounding on patients in the hospital who were on dialysis for kidney failure in the setting of severe COVID infection and seeing clots forming on the dialysis filters. Some patients could barely get in a full treatment because the filters would clog so quickly.
We knew it was worse than flu because of the mortality rates, but these oddities made us realize that it was different too — not just a particularly nasty respiratory virus but one that had effects on the body that we hadn’t really seen before.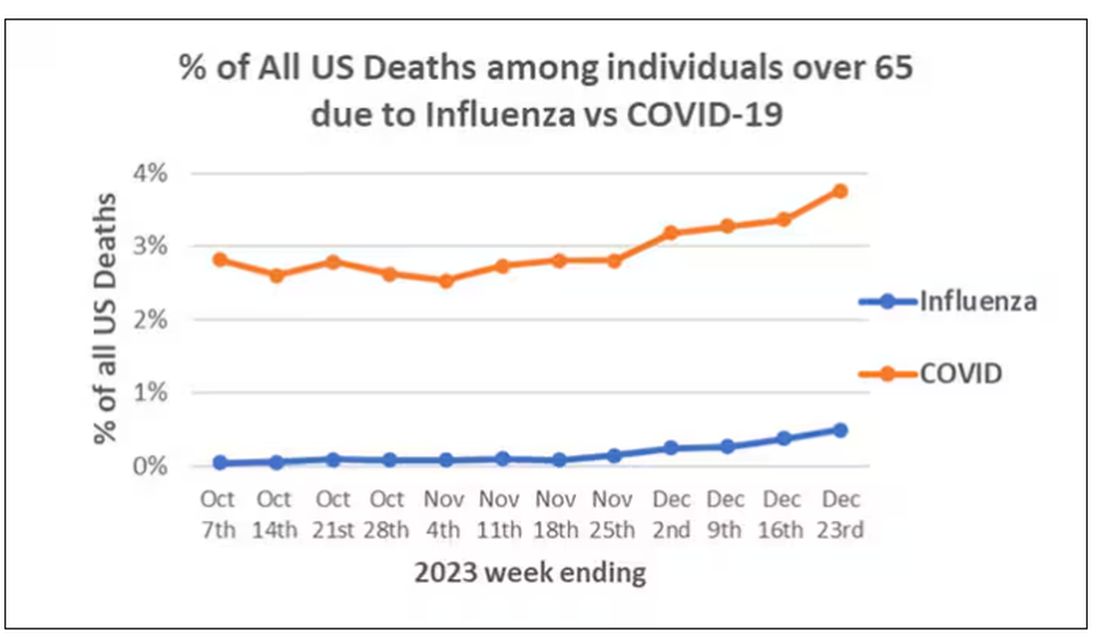
That’s why I’ve always been interested in studies that compare what happens to patients after COVID infection vs what happens to patients after other respiratory infections. This week, we’ll look at an intriguing study that suggests that COVID may lead to autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis.
The study appears in the Annals of Internal Medicine and is made possible by the universal electronic health record systems of South Korea and Japan, who collaborated to create a truly staggering cohort of more than 20 million individuals living in those countries from 2020 to 2021.
The exposure of interest? COVID infection, experienced by just under 5% of that cohort over the study period. (Remember, there was a time when COVID infections were relatively controlled, particularly in some countries.)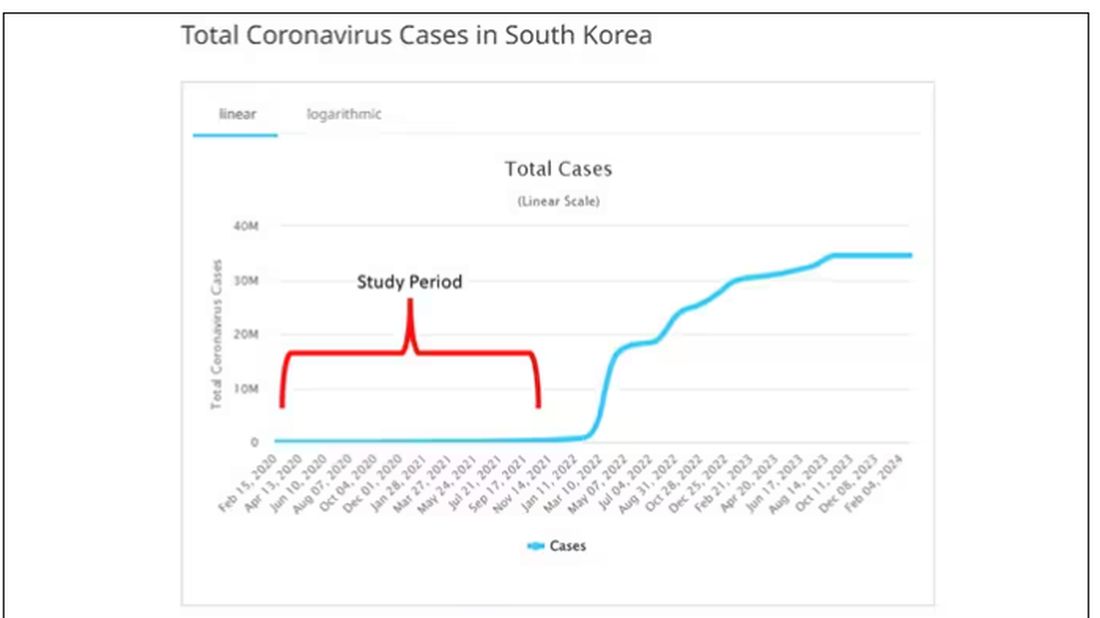
The researchers wanted to compare the risk for autoimmune disease among COVID-infected individuals against two control groups. The first control group was the general population. This is interesting but a difficult analysis, because people who become infected with COVID might be very different from the general population. The second control group was people infected with influenza. I like this a lot better; the risk factors for COVID and influenza are quite similar, and the fact that this group was diagnosed with flu means at least that they are getting medical care and are sort of “in the system,” so to speak.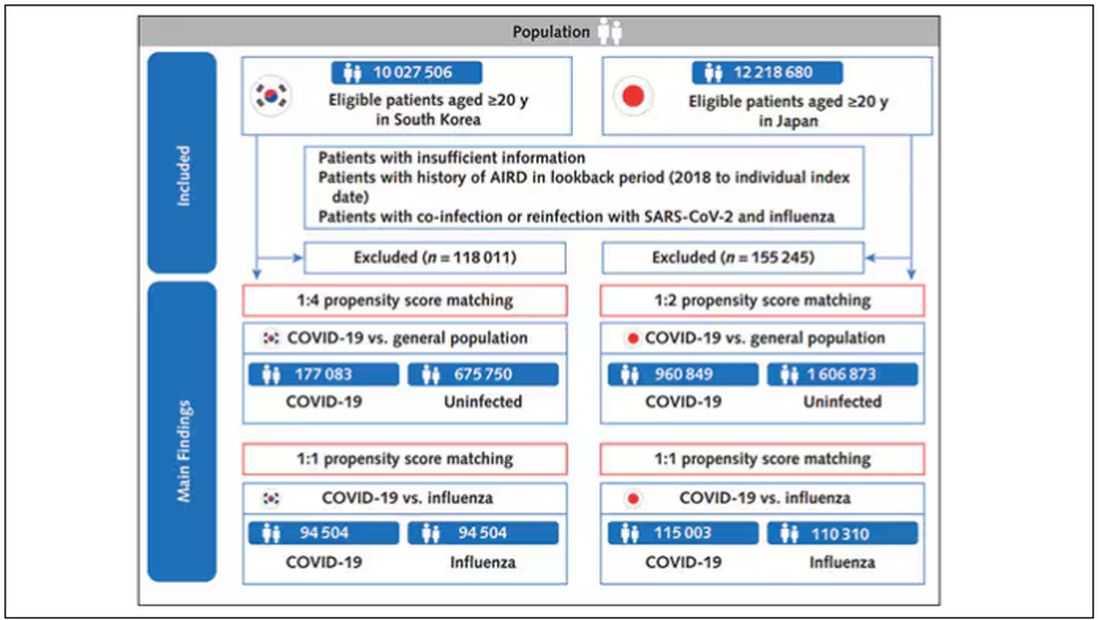
But it’s not enough to simply identify these folks and see who ends up with more autoimmune disease. The authors used propensity score matching to pair individuals infected with COVID with individuals from the control groups who were very similar to them. I’ve talked about this strategy before, but the basic idea is that you build a model predicting the likelihood of infection with COVID, based on a slew of factors — and the slew these authors used is pretty big, as shown below — and then stick people with similar risk for COVID together, with one member of the pair having had COVID and the other having eluded it (at least for the study period).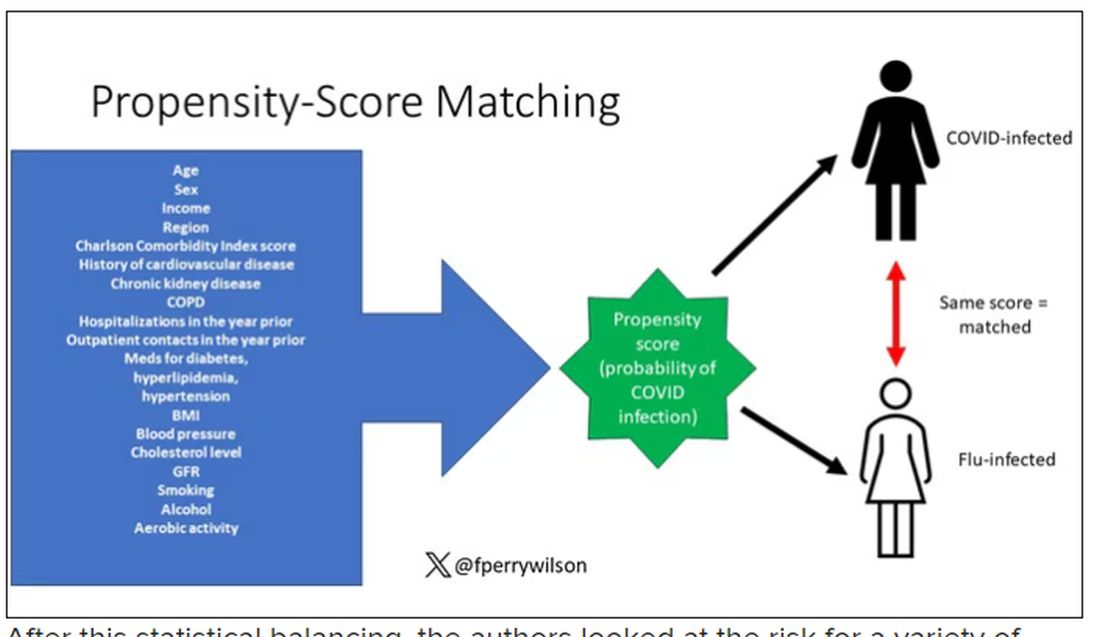
After this statistical balancing, the authors looked at the risk for a variety of autoimmune diseases.
Compared with those infected with flu, those infected with COVID were more likely to be diagnosed with any autoimmune condition, connective tissue disease, and, in Japan at least, inflammatory arthritis.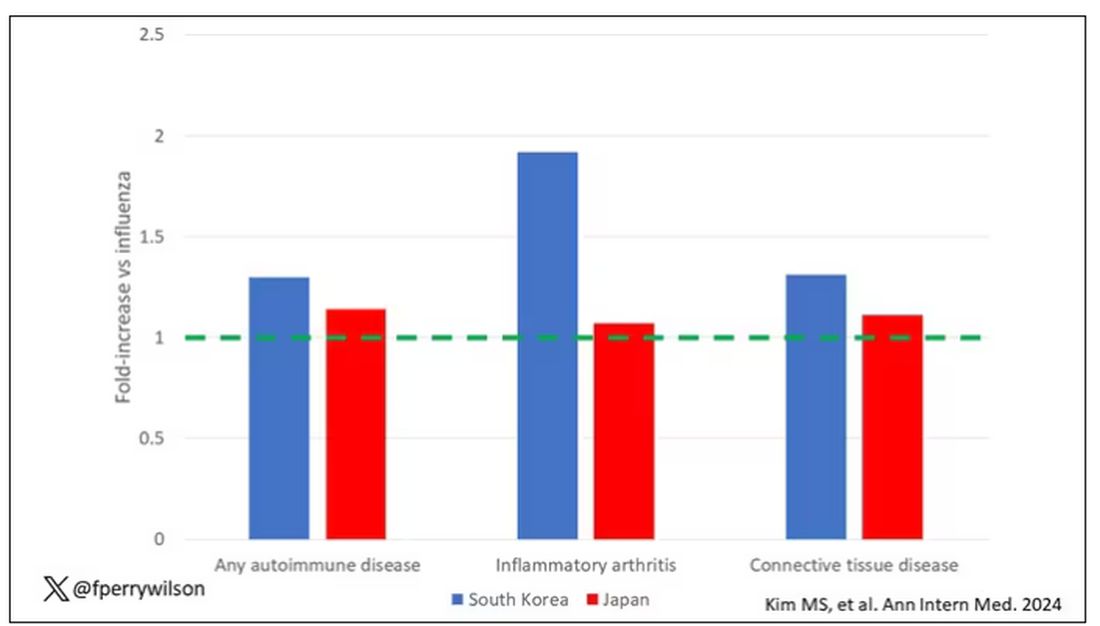
The authors acknowledge that being diagnosed with a disease might not be the same as actually having the disease, so in another analysis they looked only at people who received treatment for the autoimmune conditions, and the signals were even stronger in that group.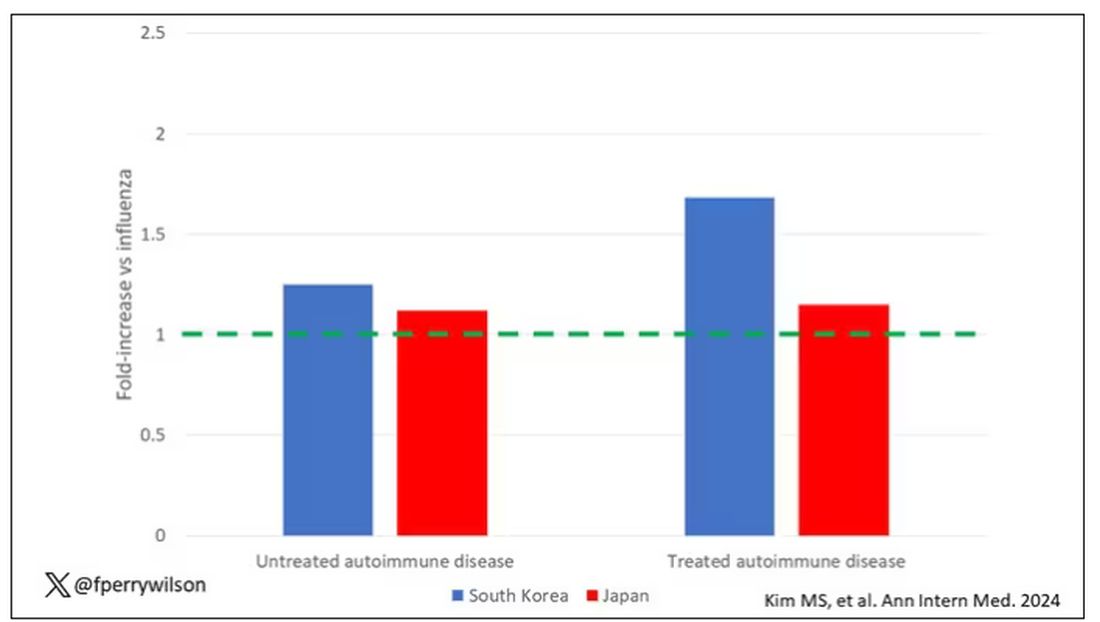
This risk seemed to be highest in the 6 months following the COVID infection, which makes sense biologically if we think that the infection is somehow screwing up the immune system.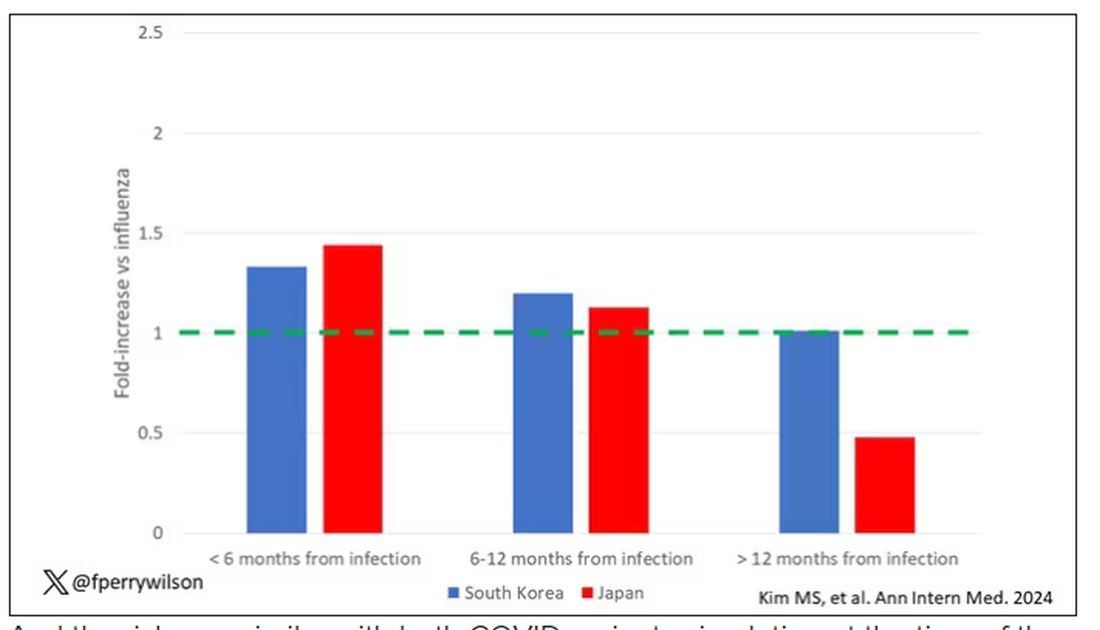
And the risk was similar with both COVID variants circulating at the time of the study.
The only factor that reduced the risk? You guessed it: vaccination. This is a particularly interesting finding because the exposure cohort was defined by having been infected with COVID. Therefore, the mechanism of protection is not prevention of infection; it’s something else. Perhaps vaccination helps to get the immune system in a state to respond to COVID infection more… appropriately?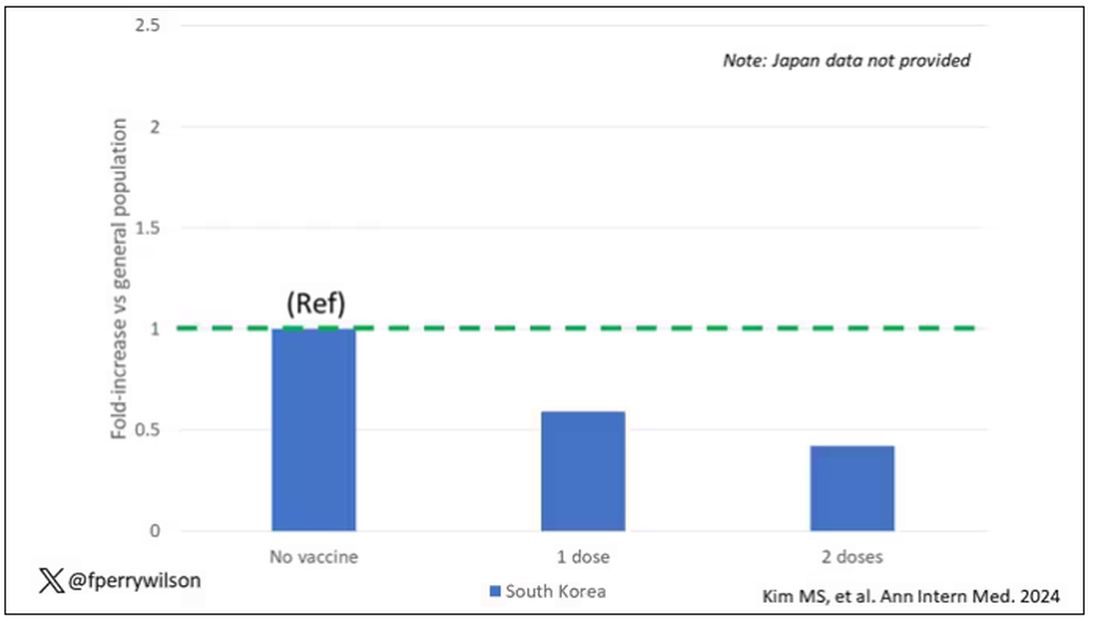
Yes, this study is observational. We can’t draw causal conclusions here. But it does reinforce my long-held belief that COVID is a weird virus, one with effects that are different from the respiratory viruses we are used to. I can’t say for certain whether COVID causes immune system dysfunction that puts someone at risk for autoimmunity — not from this study. But I can say it wouldn’t surprise me.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
This transcript has been edited for clarity.
Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
In the early days of the pandemic, before we really understood what COVID was, two specialties in the hospital had a foreboding sense that something was very strange about this virus. The first was the pulmonologists, who noticed the striking levels of hypoxemia — low oxygen in the blood — and the rapidity with which patients who had previously been stable would crash in the intensive care unit.
The second, and I mark myself among this group, were the nephrologists. The dialysis machines stopped working right. I remember rounding on patients in the hospital who were on dialysis for kidney failure in the setting of severe COVID infection and seeing clots forming on the dialysis filters. Some patients could barely get in a full treatment because the filters would clog so quickly.
We knew it was worse than flu because of the mortality rates, but these oddities made us realize that it was different too — not just a particularly nasty respiratory virus but one that had effects on the body that we hadn’t really seen before.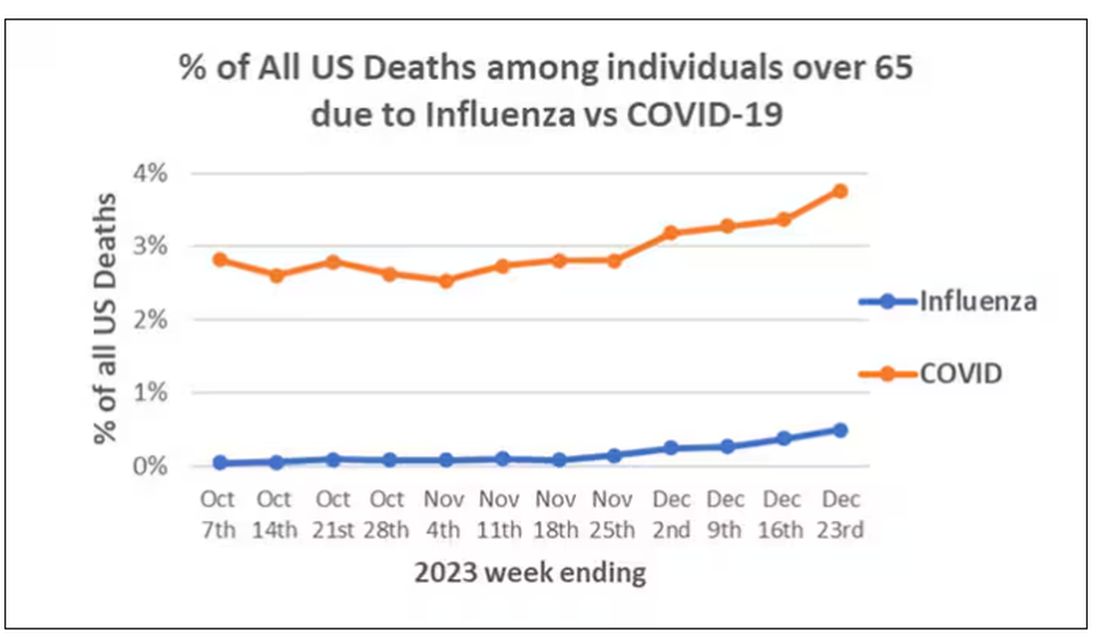
That’s why I’ve always been interested in studies that compare what happens to patients after COVID infection vs what happens to patients after other respiratory infections. This week, we’ll look at an intriguing study that suggests that COVID may lead to autoimmune diseases like rheumatoid arthritis, lupus, and vasculitis.
The study appears in the Annals of Internal Medicine and is made possible by the universal electronic health record systems of South Korea and Japan, who collaborated to create a truly staggering cohort of more than 20 million individuals living in those countries from 2020 to 2021.
The exposure of interest? COVID infection, experienced by just under 5% of that cohort over the study period. (Remember, there was a time when COVID infections were relatively controlled, particularly in some countries.)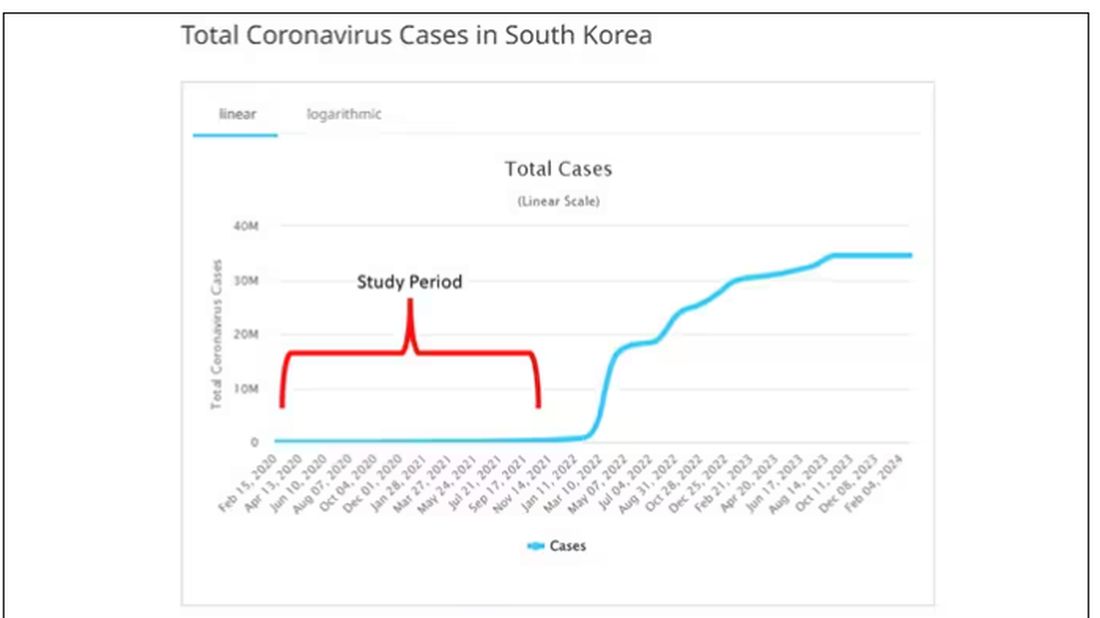
The researchers wanted to compare the risk for autoimmune disease among COVID-infected individuals against two control groups. The first control group was the general population. This is interesting but a difficult analysis, because people who become infected with COVID might be very different from the general population. The second control group was people infected with influenza. I like this a lot better; the risk factors for COVID and influenza are quite similar, and the fact that this group was diagnosed with flu means at least that they are getting medical care and are sort of “in the system,” so to speak.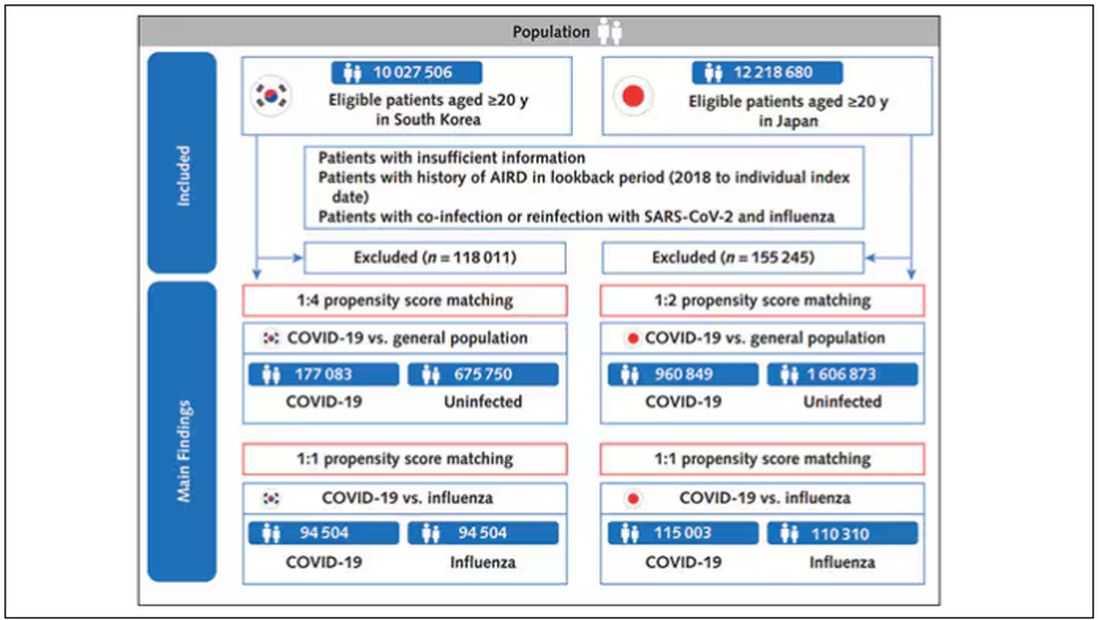
But it’s not enough to simply identify these folks and see who ends up with more autoimmune disease. The authors used propensity score matching to pair individuals infected with COVID with individuals from the control groups who were very similar to them. I’ve talked about this strategy before, but the basic idea is that you build a model predicting the likelihood of infection with COVID, based on a slew of factors — and the slew these authors used is pretty big, as shown below — and then stick people with similar risk for COVID together, with one member of the pair having had COVID and the other having eluded it (at least for the study period).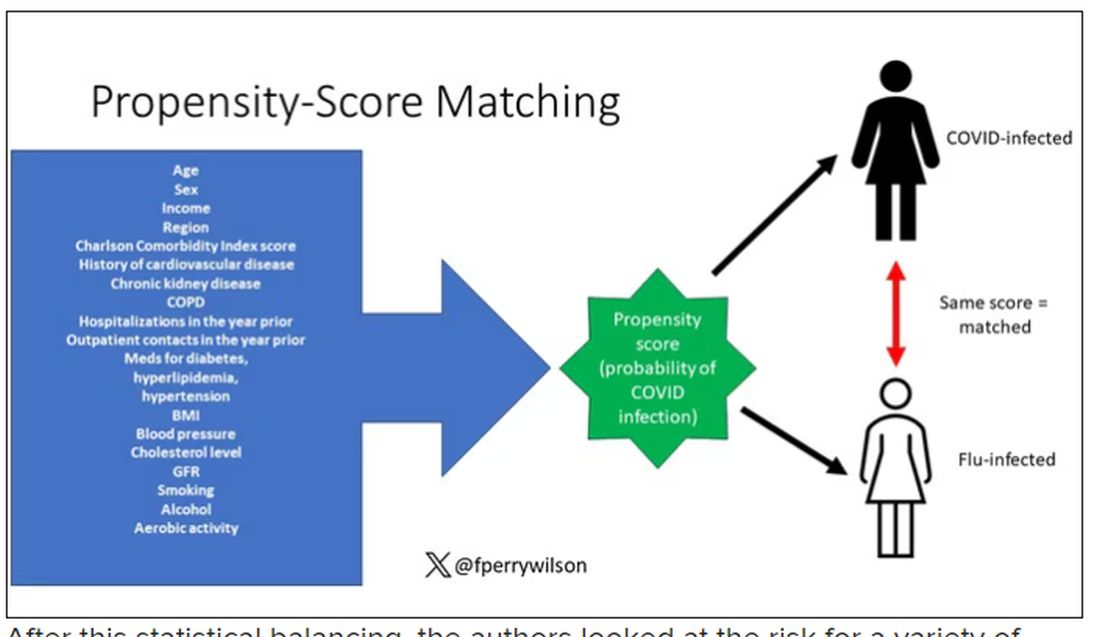
After this statistical balancing, the authors looked at the risk for a variety of autoimmune diseases.
Compared with those infected with flu, those infected with COVID were more likely to be diagnosed with any autoimmune condition, connective tissue disease, and, in Japan at least, inflammatory arthritis.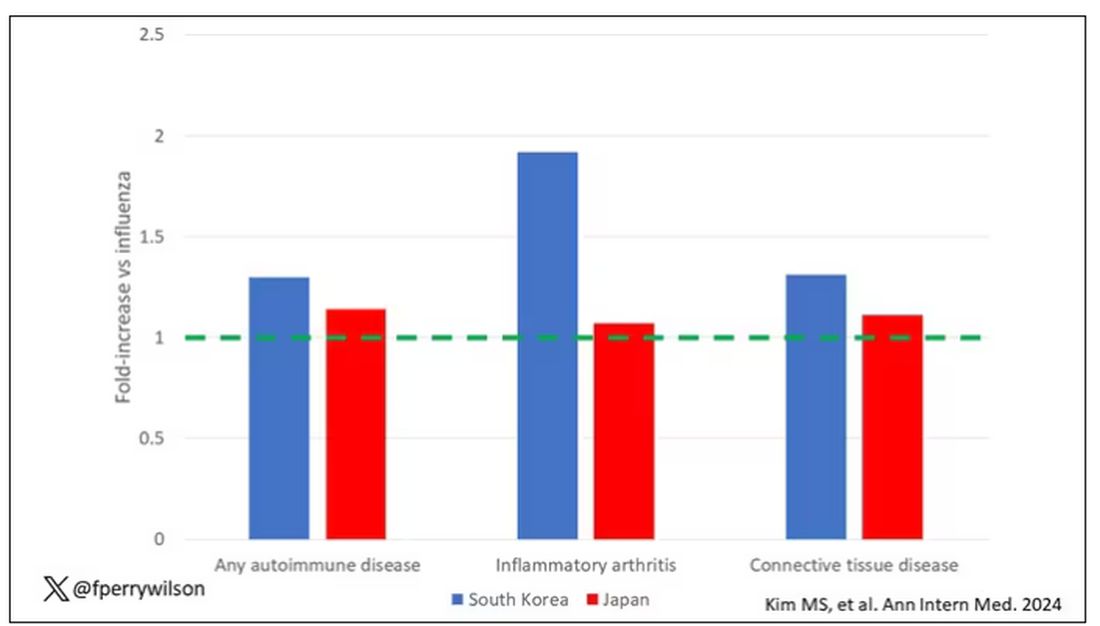
The authors acknowledge that being diagnosed with a disease might not be the same as actually having the disease, so in another analysis they looked only at people who received treatment for the autoimmune conditions, and the signals were even stronger in that group.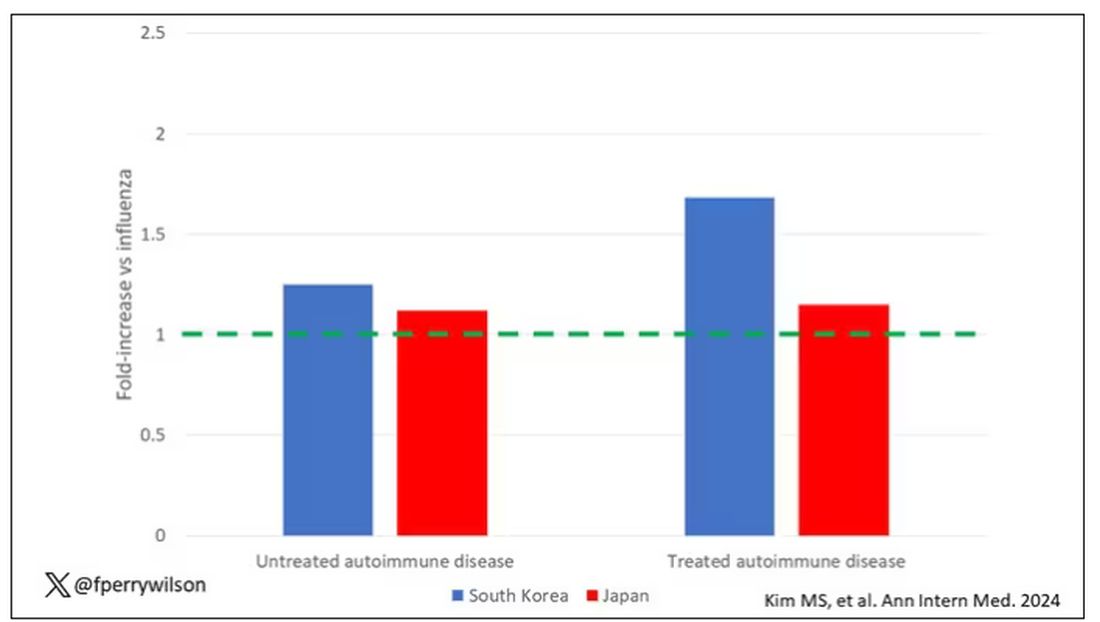
This risk seemed to be highest in the 6 months following the COVID infection, which makes sense biologically if we think that the infection is somehow screwing up the immune system.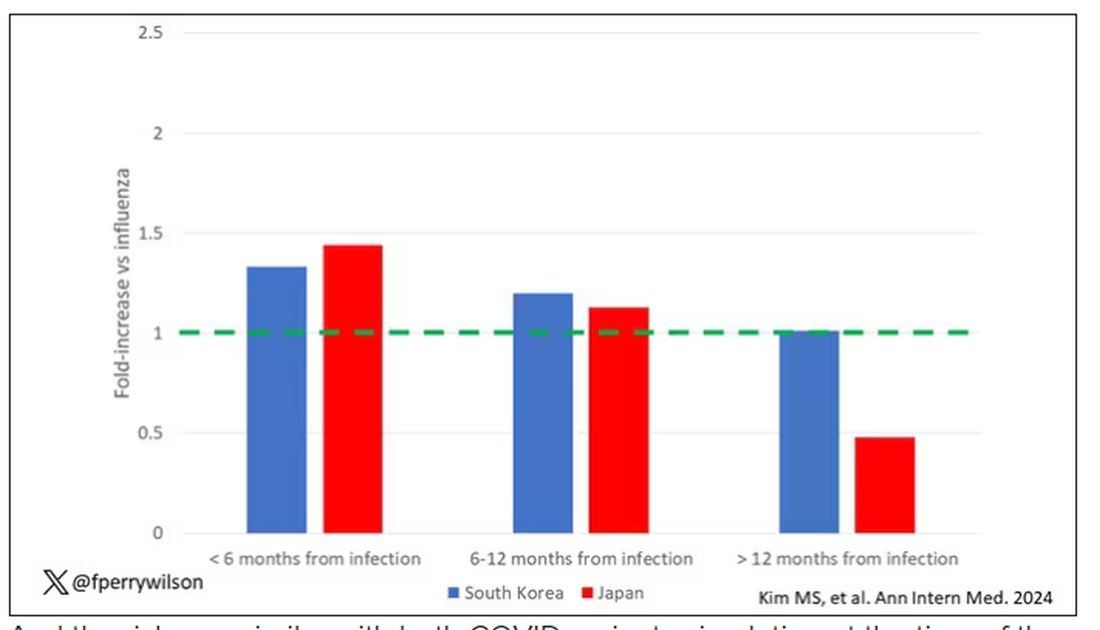
And the risk was similar with both COVID variants circulating at the time of the study.
The only factor that reduced the risk? You guessed it: vaccination. This is a particularly interesting finding because the exposure cohort was defined by having been infected with COVID. Therefore, the mechanism of protection is not prevention of infection; it’s something else. Perhaps vaccination helps to get the immune system in a state to respond to COVID infection more… appropriately?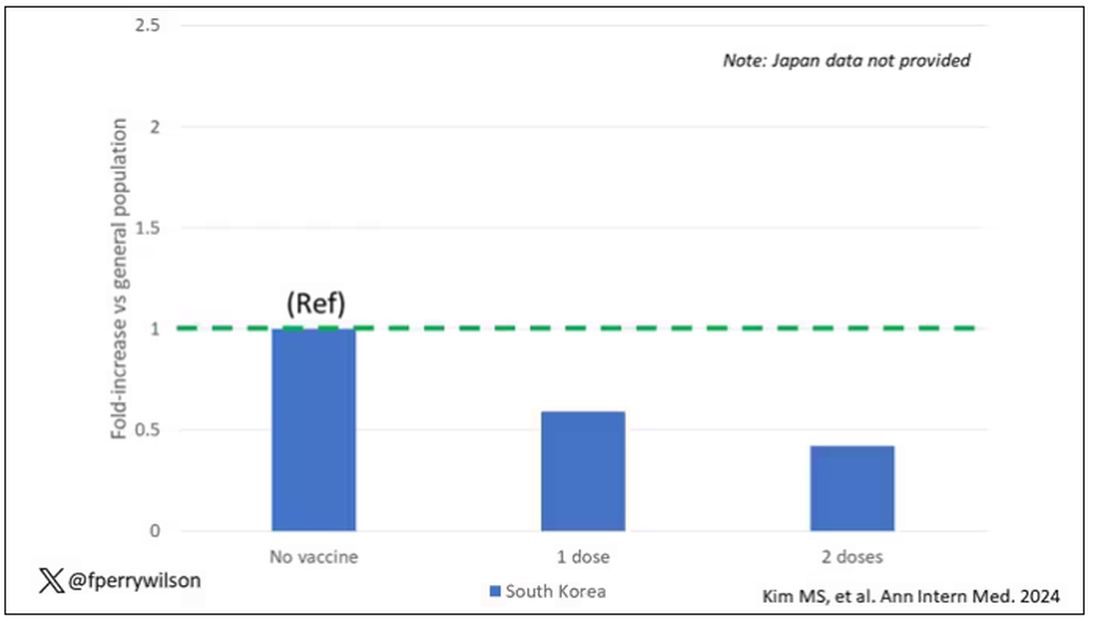
Yes, this study is observational. We can’t draw causal conclusions here. But it does reinforce my long-held belief that COVID is a weird virus, one with effects that are different from the respiratory viruses we are used to. I can’t say for certain whether COVID causes immune system dysfunction that puts someone at risk for autoimmunity — not from this study. But I can say it wouldn’t surprise me.
Dr. F. Perry Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Conn. He has disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Effect of Metformin Across Renal Function States in Diabetes
TOPLINE:
Metformin cuts the risk for diabetic nephropathy (DN) and major kidney and cardiovascular events in patients with newly diagnosed type 2 diabetes (T2D) across various renal function states.
METHODOLOGY:
Metformin is a first-line treatment in US and South Korean T2D management guidelines, except for patients with advanced chronic kidney disease (CKD) (stage, ≥ 4; estimated glomerular filtration rate [eGFR], < 30).
The study used data from the databases of three tertiary hospitals in South Korea to assess the effect of metformin on long-term renal and cardiovascular outcomes across various renal function states in patients with newly diagnosed T2D.
Four groups of treatment-control comparative cohorts were identified at each hospital: Patients who had not yet developed DN at T2D diagnosis (mean age in treatment and control cohorts, 61-65 years) and those with reduced renal function (CKD stages 3A, 3B, and 4).
Patients who continuously received metformin after T2D diagnosis and beyond the observation period were 1:1 propensity score matched with controls who were prescribed oral hypoglycemic agents other than metformin.
Primary outcomes were net major adverse cardiovascular events including strokes (MACEs) or in-hospital death and a composite of major adverse kidney events (MAKEs) or in-hospital death.
TAKEAWAY:
Among patients without DN at T2D diagnosis, the continuous use of metformin vs other oral hypoglycemic agents was associated with a lower risk for:
Overt DN (incidence rate ratio [IRR], 0.82; 95% CI, 0.71-0.95),
MACEs (IRR, 0.76; 95% CI, 0.64-0.92), and
MAKEs (IRR, 0.45; 95% CI, 0.33-0.62).
Compared with non-metformin or discontinued metformin use, the continuous use of metformin was associated with a lower risk for MACE across CKD stages 3A (IRR, 0.70; 95% CI, 0.57-0.87), 3B (IRR, 0.83; 95% CI, 0.74-0.93), and 4 (IRR, 0.71; 95% CI, 0.60-0.85).
Similarly, the risk for MAKE was lower among continuous metformin users than in nonusers or discontinuous metformin users across CKD stage 3A (IRR, 0.39; 95% CI, 0.35-0.43), 3B (IRR, 0.44; 95% CI, 0.40-0.48), and 4 (IRR, 0.45; 95% CI, 0.39-0.51).
IN PRACTICE:
“The significance of the current study is highlighted by its integration of real-world clinical data, which encompasses patients diagnosed with CDK4 [eGRF, 15-29 mL/min/1.73 m2], a group currently considered contraindicated,” the authors wrote.
SOURCE:
The study, led by Yongjin Yi, MD, PhD, Department of Internal Medicine, Dankook University College of Medicine, Cheonan-si, Republic of Korea, was published in Scientific Reports.
LIMITATIONS:
There may be a possibility of selection bias because of the retrospective and observational nature of this study. Despite achieving a 1:1 propensity score matching to address the confounding factors, some variables, such as serum albumin and A1c levels, remained unbalanced after matching. The paper did not include observation length or patient numbers, but in response to an email query from Medscape, Yi notes that in one hospital, the mean duration of observation for the control and treatment groups was about 6.5 years, and the total number in the treatment groups across data from three hospitals was 11,675, with the same number of matched controls.
DISCLOSURES:
This study was supported by a Young Investigator Research Grant from the Korean Society of Nephrology, a grant from the Seoul National University Bundang Hospital Research Fund, and the Bio&Medical Technology Development Program of the National Research Foundation funded by the Korean government. The authors disclosed no competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
Metformin cuts the risk for diabetic nephropathy (DN) and major kidney and cardiovascular events in patients with newly diagnosed type 2 diabetes (T2D) across various renal function states.
METHODOLOGY:
Metformin is a first-line treatment in US and South Korean T2D management guidelines, except for patients with advanced chronic kidney disease (CKD) (stage, ≥ 4; estimated glomerular filtration rate [eGFR], < 30).
The study used data from the databases of three tertiary hospitals in South Korea to assess the effect of metformin on long-term renal and cardiovascular outcomes across various renal function states in patients with newly diagnosed T2D.
Four groups of treatment-control comparative cohorts were identified at each hospital: Patients who had not yet developed DN at T2D diagnosis (mean age in treatment and control cohorts, 61-65 years) and those with reduced renal function (CKD stages 3A, 3B, and 4).
Patients who continuously received metformin after T2D diagnosis and beyond the observation period were 1:1 propensity score matched with controls who were prescribed oral hypoglycemic agents other than metformin.
Primary outcomes were net major adverse cardiovascular events including strokes (MACEs) or in-hospital death and a composite of major adverse kidney events (MAKEs) or in-hospital death.
TAKEAWAY:
Among patients without DN at T2D diagnosis, the continuous use of metformin vs other oral hypoglycemic agents was associated with a lower risk for:
Overt DN (incidence rate ratio [IRR], 0.82; 95% CI, 0.71-0.95),
MACEs (IRR, 0.76; 95% CI, 0.64-0.92), and
MAKEs (IRR, 0.45; 95% CI, 0.33-0.62).
Compared with non-metformin or discontinued metformin use, the continuous use of metformin was associated with a lower risk for MACE across CKD stages 3A (IRR, 0.70; 95% CI, 0.57-0.87), 3B (IRR, 0.83; 95% CI, 0.74-0.93), and 4 (IRR, 0.71; 95% CI, 0.60-0.85).
Similarly, the risk for MAKE was lower among continuous metformin users than in nonusers or discontinuous metformin users across CKD stage 3A (IRR, 0.39; 95% CI, 0.35-0.43), 3B (IRR, 0.44; 95% CI, 0.40-0.48), and 4 (IRR, 0.45; 95% CI, 0.39-0.51).
IN PRACTICE:
“The significance of the current study is highlighted by its integration of real-world clinical data, which encompasses patients diagnosed with CDK4 [eGRF, 15-29 mL/min/1.73 m2], a group currently considered contraindicated,” the authors wrote.
SOURCE:
The study, led by Yongjin Yi, MD, PhD, Department of Internal Medicine, Dankook University College of Medicine, Cheonan-si, Republic of Korea, was published in Scientific Reports.
LIMITATIONS:
There may be a possibility of selection bias because of the retrospective and observational nature of this study. Despite achieving a 1:1 propensity score matching to address the confounding factors, some variables, such as serum albumin and A1c levels, remained unbalanced after matching. The paper did not include observation length or patient numbers, but in response to an email query from Medscape, Yi notes that in one hospital, the mean duration of observation for the control and treatment groups was about 6.5 years, and the total number in the treatment groups across data from three hospitals was 11,675, with the same number of matched controls.
DISCLOSURES:
This study was supported by a Young Investigator Research Grant from the Korean Society of Nephrology, a grant from the Seoul National University Bundang Hospital Research Fund, and the Bio&Medical Technology Development Program of the National Research Foundation funded by the Korean government. The authors disclosed no competing interests.
A version of this article appeared on Medscape.com.
TOPLINE:
Metformin cuts the risk for diabetic nephropathy (DN) and major kidney and cardiovascular events in patients with newly diagnosed type 2 diabetes (T2D) across various renal function states.
METHODOLOGY:
Metformin is a first-line treatment in US and South Korean T2D management guidelines, except for patients with advanced chronic kidney disease (CKD) (stage, ≥ 4; estimated glomerular filtration rate [eGFR], < 30).
The study used data from the databases of three tertiary hospitals in South Korea to assess the effect of metformin on long-term renal and cardiovascular outcomes across various renal function states in patients with newly diagnosed T2D.
Four groups of treatment-control comparative cohorts were identified at each hospital: Patients who had not yet developed DN at T2D diagnosis (mean age in treatment and control cohorts, 61-65 years) and those with reduced renal function (CKD stages 3A, 3B, and 4).
Patients who continuously received metformin after T2D diagnosis and beyond the observation period were 1:1 propensity score matched with controls who were prescribed oral hypoglycemic agents other than metformin.
Primary outcomes were net major adverse cardiovascular events including strokes (MACEs) or in-hospital death and a composite of major adverse kidney events (MAKEs) or in-hospital death.
TAKEAWAY:
Among patients without DN at T2D diagnosis, the continuous use of metformin vs other oral hypoglycemic agents was associated with a lower risk for:
Overt DN (incidence rate ratio [IRR], 0.82; 95% CI, 0.71-0.95),
MACEs (IRR, 0.76; 95% CI, 0.64-0.92), and
MAKEs (IRR, 0.45; 95% CI, 0.33-0.62).
Compared with non-metformin or discontinued metformin use, the continuous use of metformin was associated with a lower risk for MACE across CKD stages 3A (IRR, 0.70; 95% CI, 0.57-0.87), 3B (IRR, 0.83; 95% CI, 0.74-0.93), and 4 (IRR, 0.71; 95% CI, 0.60-0.85).
Similarly, the risk for MAKE was lower among continuous metformin users than in nonusers or discontinuous metformin users across CKD stage 3A (IRR, 0.39; 95% CI, 0.35-0.43), 3B (IRR, 0.44; 95% CI, 0.40-0.48), and 4 (IRR, 0.45; 95% CI, 0.39-0.51).
IN PRACTICE:
“The significance of the current study is highlighted by its integration of real-world clinical data, which encompasses patients diagnosed with CDK4 [eGRF, 15-29 mL/min/1.73 m2], a group currently considered contraindicated,” the authors wrote.
SOURCE:
The study, led by Yongjin Yi, MD, PhD, Department of Internal Medicine, Dankook University College of Medicine, Cheonan-si, Republic of Korea, was published in Scientific Reports.
LIMITATIONS:
There may be a possibility of selection bias because of the retrospective and observational nature of this study. Despite achieving a 1:1 propensity score matching to address the confounding factors, some variables, such as serum albumin and A1c levels, remained unbalanced after matching. The paper did not include observation length or patient numbers, but in response to an email query from Medscape, Yi notes that in one hospital, the mean duration of observation for the control and treatment groups was about 6.5 years, and the total number in the treatment groups across data from three hospitals was 11,675, with the same number of matched controls.
DISCLOSURES:
This study was supported by a Young Investigator Research Grant from the Korean Society of Nephrology, a grant from the Seoul National University Bundang Hospital Research Fund, and the Bio&Medical Technology Development Program of the National Research Foundation funded by the Korean government. The authors disclosed no competing interests.
A version of this article appeared on Medscape.com.

