User login
Beware the hidden allergens in nutritional supplements
, Alison Ehrlich, MD, said at the annual meeting of the American Contact Dermatitis Society.
Allergens may be hidden in a range of supplement products, from colorings in vitamin C powders to some vitamins used in hair products and other products.
“In general, our patients do not tell us what supplements they are taking,” said Dr. Ehrlich, a dermatologist who practices in Washington, D.C. Antiaging, sleep, and weight loss/weight control supplements are among the most popular, she said.
Surveys have shown that many patients do not discuss supplement use with their health care providers, in part because they believe their providers would disapprove of supplement use, and patients are not educated about supplements, she said. “This is definitely an area that we should try to learn more about,” she added.
Current regulations regarding dietary supplements stem from the Dietary Supplement Health and Education Act of 1994, which defined dietary supplements as distinct from meals but regulated them as a category of food, not as medications. Dietary supplements can be vitamins, minerals, herbs, and extracts, Dr. Ehrlich said.
“There is not a lot of safety wrapped around how supplements come onto the market,” she explained. “It is not the manufacturer’s responsibility to test these products and make sure they are safe. When they get pulled off the market, it is because safety reports are getting back to the FDA.”
Consequently, a detailed history of supplement use is important, as it may reveal possible allergens as the cause of previously unidentified reactions, she said.
Dr. Ehrlich shared a case involving a patient who claimed to have had a reaction to a “Prevage-like” product that was labeled as a crepe repair cream. Listed among the product’s ingredients was idebenone, a synthetic version of the popular antioxidant known as Coenzyme Q.
Be wary of vitamins
Another potential source of allergy is vitamin C supplements, which became especially popular during the pandemic as people sought additional immune system support, Dr. Ehrlich noted. “What kind of vitamin C product our patients are taking is important,” she said. For example, some vitamin C powders contain coloring agents, such as carmine. Some also contain gelatin, which may cause an allergic reaction in individuals with alpha-gal syndrome, she added.
In general, water-soluble vitamins such as vitamins B1 to B9, B12, and C are more likely to cause an immediate reaction, Dr. Ehrlich said. Fat-soluble vitamins, such as vitamins A, D, E, and K, are more likely to cause a delayed reaction of allergic contact dermatitis.
Dr. Ehrlich described some unusual reactions to vitamins that have been reported, including a systemic allergy associated with vitamin B1 (thiamine), burning mouth syndrome associated with vitamin B3 (nicotinate), contact urticaria associated with vitamin B5 (panthenol), systemic allergy and generalized ACD associated with vitamin E (tocopherol), and erythema multiforme–like ACD associated with vitamin K1.
Notably, vitamin B5 has been associated with ACD as an ingredient in hair products, moisturizers, and wound care products, as well as B-complex vitamins and fortified foods, Dr. Ehrlich said.
Herbs and spices can act as allergens as well. Turmeric is a spice that has become a popular supplement ingredient, she said. Turmeric and curcumin (found in turmeric) can be used as a dye for its yellow color as well as a flavoring but has been associated with allergic reactions. Another popular herbal supplement, ginkgo biloba, has been marketed as a product that improves memory and cognition. It is available in pill form and in herbal teas.
“It’s really important to think about what herbal products our patients are taking, and not just in pill form,” Dr. Ehrlich said. “We need to expand our thoughts on what the herbs are in.”
Consider food additives as allergens
Food additives, in the form of colorants, preservatives, or flavoring agents, can cause allergic reactions, Dr. Ehrlich noted.
The question of whether food-additive contact sensitivity has a role in the occurrence of atopic dermatitis (AD) in children remains unclear, she said. However, a study published in 2020 found that 62% of children with AD had positive patch test reactions to at least one food-additive allergen, compared with 20% of children without AD. The additives responsible for the most reactions were azorubine (24.4%); formic acid (15.6%); and carmine, cochineal red, and amaranth (13.3% for each).
Common colorant culprits in allergic reactions include carmine, annatto, tartrazine, and spices (such as paprika and saffron), Dr. Ehrlich said. Carmine is used in meat to prevent photo-oxidation and to preserve a red color, and it has other uses as well, she said. Carmine has been associated with ACD, AD flares, and immediate hypersensitivity. Annatto is used in foods, including processed foods, butter, and cheese, to provide a yellow color. It is also found in some lipsticks and has been associated with urticaria and angioedema, she noted.
Food preservatives that have been associated with allergic reactions include butylated hydroxyanisole and sulfites, Dr. Ehrlich said. Sulfites are used to prevent food from turning brown, and it may be present in dried fruit, fruit juice, molasses, pickled foods, vinegar, and wine.
Reports of ACD in response to sodium metabisulfite have been increasing, she noted. Other sulfite reactions may occur with exposure to other products, such as cosmetics, body washes, and swimming pool water, she said.
Awareness of allergens in supplements is important “because the number of our patients taking supplements for different reasons is increasing” and allergens in supplements could account for flares, Dr. Ehrlich said. Clinicians should encourage patients to tell them what supplements they use. Clinicians should review the ingredients in these supplements with their patients to identify potential allergens that may be causing reactions, she advised.
Dr. Ehrlich has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, Alison Ehrlich, MD, said at the annual meeting of the American Contact Dermatitis Society.
Allergens may be hidden in a range of supplement products, from colorings in vitamin C powders to some vitamins used in hair products and other products.
“In general, our patients do not tell us what supplements they are taking,” said Dr. Ehrlich, a dermatologist who practices in Washington, D.C. Antiaging, sleep, and weight loss/weight control supplements are among the most popular, she said.
Surveys have shown that many patients do not discuss supplement use with their health care providers, in part because they believe their providers would disapprove of supplement use, and patients are not educated about supplements, she said. “This is definitely an area that we should try to learn more about,” she added.
Current regulations regarding dietary supplements stem from the Dietary Supplement Health and Education Act of 1994, which defined dietary supplements as distinct from meals but regulated them as a category of food, not as medications. Dietary supplements can be vitamins, minerals, herbs, and extracts, Dr. Ehrlich said.
“There is not a lot of safety wrapped around how supplements come onto the market,” she explained. “It is not the manufacturer’s responsibility to test these products and make sure they are safe. When they get pulled off the market, it is because safety reports are getting back to the FDA.”
Consequently, a detailed history of supplement use is important, as it may reveal possible allergens as the cause of previously unidentified reactions, she said.
Dr. Ehrlich shared a case involving a patient who claimed to have had a reaction to a “Prevage-like” product that was labeled as a crepe repair cream. Listed among the product’s ingredients was idebenone, a synthetic version of the popular antioxidant known as Coenzyme Q.
Be wary of vitamins
Another potential source of allergy is vitamin C supplements, which became especially popular during the pandemic as people sought additional immune system support, Dr. Ehrlich noted. “What kind of vitamin C product our patients are taking is important,” she said. For example, some vitamin C powders contain coloring agents, such as carmine. Some also contain gelatin, which may cause an allergic reaction in individuals with alpha-gal syndrome, she added.
In general, water-soluble vitamins such as vitamins B1 to B9, B12, and C are more likely to cause an immediate reaction, Dr. Ehrlich said. Fat-soluble vitamins, such as vitamins A, D, E, and K, are more likely to cause a delayed reaction of allergic contact dermatitis.
Dr. Ehrlich described some unusual reactions to vitamins that have been reported, including a systemic allergy associated with vitamin B1 (thiamine), burning mouth syndrome associated with vitamin B3 (nicotinate), contact urticaria associated with vitamin B5 (panthenol), systemic allergy and generalized ACD associated with vitamin E (tocopherol), and erythema multiforme–like ACD associated with vitamin K1.
Notably, vitamin B5 has been associated with ACD as an ingredient in hair products, moisturizers, and wound care products, as well as B-complex vitamins and fortified foods, Dr. Ehrlich said.
Herbs and spices can act as allergens as well. Turmeric is a spice that has become a popular supplement ingredient, she said. Turmeric and curcumin (found in turmeric) can be used as a dye for its yellow color as well as a flavoring but has been associated with allergic reactions. Another popular herbal supplement, ginkgo biloba, has been marketed as a product that improves memory and cognition. It is available in pill form and in herbal teas.
“It’s really important to think about what herbal products our patients are taking, and not just in pill form,” Dr. Ehrlich said. “We need to expand our thoughts on what the herbs are in.”
Consider food additives as allergens
Food additives, in the form of colorants, preservatives, or flavoring agents, can cause allergic reactions, Dr. Ehrlich noted.
The question of whether food-additive contact sensitivity has a role in the occurrence of atopic dermatitis (AD) in children remains unclear, she said. However, a study published in 2020 found that 62% of children with AD had positive patch test reactions to at least one food-additive allergen, compared with 20% of children without AD. The additives responsible for the most reactions were azorubine (24.4%); formic acid (15.6%); and carmine, cochineal red, and amaranth (13.3% for each).
Common colorant culprits in allergic reactions include carmine, annatto, tartrazine, and spices (such as paprika and saffron), Dr. Ehrlich said. Carmine is used in meat to prevent photo-oxidation and to preserve a red color, and it has other uses as well, she said. Carmine has been associated with ACD, AD flares, and immediate hypersensitivity. Annatto is used in foods, including processed foods, butter, and cheese, to provide a yellow color. It is also found in some lipsticks and has been associated with urticaria and angioedema, she noted.
Food preservatives that have been associated with allergic reactions include butylated hydroxyanisole and sulfites, Dr. Ehrlich said. Sulfites are used to prevent food from turning brown, and it may be present in dried fruit, fruit juice, molasses, pickled foods, vinegar, and wine.
Reports of ACD in response to sodium metabisulfite have been increasing, she noted. Other sulfite reactions may occur with exposure to other products, such as cosmetics, body washes, and swimming pool water, she said.
Awareness of allergens in supplements is important “because the number of our patients taking supplements for different reasons is increasing” and allergens in supplements could account for flares, Dr. Ehrlich said. Clinicians should encourage patients to tell them what supplements they use. Clinicians should review the ingredients in these supplements with their patients to identify potential allergens that may be causing reactions, she advised.
Dr. Ehrlich has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, Alison Ehrlich, MD, said at the annual meeting of the American Contact Dermatitis Society.
Allergens may be hidden in a range of supplement products, from colorings in vitamin C powders to some vitamins used in hair products and other products.
“In general, our patients do not tell us what supplements they are taking,” said Dr. Ehrlich, a dermatologist who practices in Washington, D.C. Antiaging, sleep, and weight loss/weight control supplements are among the most popular, she said.
Surveys have shown that many patients do not discuss supplement use with their health care providers, in part because they believe their providers would disapprove of supplement use, and patients are not educated about supplements, she said. “This is definitely an area that we should try to learn more about,” she added.
Current regulations regarding dietary supplements stem from the Dietary Supplement Health and Education Act of 1994, which defined dietary supplements as distinct from meals but regulated them as a category of food, not as medications. Dietary supplements can be vitamins, minerals, herbs, and extracts, Dr. Ehrlich said.
“There is not a lot of safety wrapped around how supplements come onto the market,” she explained. “It is not the manufacturer’s responsibility to test these products and make sure they are safe. When they get pulled off the market, it is because safety reports are getting back to the FDA.”
Consequently, a detailed history of supplement use is important, as it may reveal possible allergens as the cause of previously unidentified reactions, she said.
Dr. Ehrlich shared a case involving a patient who claimed to have had a reaction to a “Prevage-like” product that was labeled as a crepe repair cream. Listed among the product’s ingredients was idebenone, a synthetic version of the popular antioxidant known as Coenzyme Q.
Be wary of vitamins
Another potential source of allergy is vitamin C supplements, which became especially popular during the pandemic as people sought additional immune system support, Dr. Ehrlich noted. “What kind of vitamin C product our patients are taking is important,” she said. For example, some vitamin C powders contain coloring agents, such as carmine. Some also contain gelatin, which may cause an allergic reaction in individuals with alpha-gal syndrome, she added.
In general, water-soluble vitamins such as vitamins B1 to B9, B12, and C are more likely to cause an immediate reaction, Dr. Ehrlich said. Fat-soluble vitamins, such as vitamins A, D, E, and K, are more likely to cause a delayed reaction of allergic contact dermatitis.
Dr. Ehrlich described some unusual reactions to vitamins that have been reported, including a systemic allergy associated with vitamin B1 (thiamine), burning mouth syndrome associated with vitamin B3 (nicotinate), contact urticaria associated with vitamin B5 (panthenol), systemic allergy and generalized ACD associated with vitamin E (tocopherol), and erythema multiforme–like ACD associated with vitamin K1.
Notably, vitamin B5 has been associated with ACD as an ingredient in hair products, moisturizers, and wound care products, as well as B-complex vitamins and fortified foods, Dr. Ehrlich said.
Herbs and spices can act as allergens as well. Turmeric is a spice that has become a popular supplement ingredient, she said. Turmeric and curcumin (found in turmeric) can be used as a dye for its yellow color as well as a flavoring but has been associated with allergic reactions. Another popular herbal supplement, ginkgo biloba, has been marketed as a product that improves memory and cognition. It is available in pill form and in herbal teas.
“It’s really important to think about what herbal products our patients are taking, and not just in pill form,” Dr. Ehrlich said. “We need to expand our thoughts on what the herbs are in.”
Consider food additives as allergens
Food additives, in the form of colorants, preservatives, or flavoring agents, can cause allergic reactions, Dr. Ehrlich noted.
The question of whether food-additive contact sensitivity has a role in the occurrence of atopic dermatitis (AD) in children remains unclear, she said. However, a study published in 2020 found that 62% of children with AD had positive patch test reactions to at least one food-additive allergen, compared with 20% of children without AD. The additives responsible for the most reactions were azorubine (24.4%); formic acid (15.6%); and carmine, cochineal red, and amaranth (13.3% for each).
Common colorant culprits in allergic reactions include carmine, annatto, tartrazine, and spices (such as paprika and saffron), Dr. Ehrlich said. Carmine is used in meat to prevent photo-oxidation and to preserve a red color, and it has other uses as well, she said. Carmine has been associated with ACD, AD flares, and immediate hypersensitivity. Annatto is used in foods, including processed foods, butter, and cheese, to provide a yellow color. It is also found in some lipsticks and has been associated with urticaria and angioedema, she noted.
Food preservatives that have been associated with allergic reactions include butylated hydroxyanisole and sulfites, Dr. Ehrlich said. Sulfites are used to prevent food from turning brown, and it may be present in dried fruit, fruit juice, molasses, pickled foods, vinegar, and wine.
Reports of ACD in response to sodium metabisulfite have been increasing, she noted. Other sulfite reactions may occur with exposure to other products, such as cosmetics, body washes, and swimming pool water, she said.
Awareness of allergens in supplements is important “because the number of our patients taking supplements for different reasons is increasing” and allergens in supplements could account for flares, Dr. Ehrlich said. Clinicians should encourage patients to tell them what supplements they use. Clinicians should review the ingredients in these supplements with their patients to identify potential allergens that may be causing reactions, she advised.
Dr. Ehrlich has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACDS 2023
FMT in a pill: FDA approves second product to prevent C. diff recurrence
The recent approval of the first oral fecal-derived microbiota therapy to prevent the recurrence of Clostridioides difficile (C. diff) infection in patients was welcome news for physicians who’ve struggled under the weight of having too few treatment options for the prevention of C. diff recurrence.
The product, developed by Massachusetts-based Seres Therepeutics and marketed as Vowst, was approved by the U.S. Food and Drug Administration on April 26. It is approved for use in adults who have already been treated with antibiotics for a recurrent infection with C. diff bacteria.
and is designed to be delivered in four capsules taken daily for 3 days.
Gastroenterologist Phillip I. Tarr, MD, division chief of gastroenterology at Washington University, St. Louis, and chair of the American Gastroenterological Association Center for Gut Microbiome Research and Education, said that prevention of recurrent C. diff infection “remains challenging,” and that Vowst “provides the first FDA-approved, orally administered microbiome therapeutic with which to achieve this goal. This advance also makes us optimistic we might soon be able to prevent other disorders by managing gut microbial communities.”
Vowst is the second therapy derived from human stool to be approved for the indication in less than 6 months. In December, the FDA approved Rebyota (Ferring), a rectally delivered treatment that also uses microbes from donor feces. Both products were given priority review, orphan drug, and breakthrough therapy designations by the agency.
C. diff infection can be aggravated by an alteration of normal gut flora associated with antibiotics treatment, leading to cycles of repeated infections. Infection can produce diarrhea, abdominal pain, fever, and severe morbidity. In the United States, an estimated 15,000 to 30,000 deaths per year are linked to C. diff. Risk factors for recurrent infection include being 65 or older, hospitalization, being in a nursing home, a weakened immune system, and previous infection with C. diff.
Therapies transplanting fecal microbiota from donors have been used since the 1950s as treatments for recurrent C. diff infection, and in the past decade, as stool banks recruiting screened donors have made fecal microbiota transplants, or FMT, standard of care. However, only in recent years have fecal-derived therapies become subject to standardized safety and efficacy testing.
Both the current FDA-approved products, Rebyota and Vowst, were shown in randomized controlled trials to reduce recurrence of C. diff infection, compared with placebo. In a phase 3 clinical trial of Rebyota (n = 262) in antibiotic-treated patients, one rectally administered dose reduced recurrence of C. diff infection by 70.6% at 8 weeks, compared with 57.5% for placebo. A phase 3 study of Vowst (n = 281) showed recurrence in treated subjects to be 12.4% at 8 weeks, compared with nearly 40% of those receiving placebo (relative risk, 0.32; 95% confidence interval, 0.18-0.58; P less than .001).
Despite screening protocols that have become increasingly homogenized and rigorous, FMT is associated with the risk of introducing pathogens. Vowst is manufactured with purified bacterial spores derived from donor feces, not whole stool. Nonetheless, FDA noted in its statement that Vowst could still potentially introduce infectious agents or allergens.
Antibiotics are still first-line treatment
In an interview, Jessica Allegretti, MD, MPH, AGAF, medical director of the Crohn’s and Colitis Center at Brigham & Women’s Hospital, Boston, said that having two FDA-approved therapies with different means of administration “is great for the field and great for patients. These are both meant to be used after a course of antibiotics, so antibiotics are still the mainstay of treatment for C. diff and recurrent C. diff, but we now have more options to prevent recurrence.”
The convenience of an oral therapy that can be taken at home is “very attractive,” Dr. Allegretti added, noting that there will also be patients “who either don’t want to or can’t take capsules, for whom a rectal administration [in a health care setting] may be preferred.”
Dr. Allegretti, who has used FMT to treat recurrent C. difficile for more than a decade, said that she expected traditional FMT using screened donor stool to remain available even as the new products are adopted by clinicians. FMT centers like OpenBiome “will continue to provide access for patients who either don’t have the ability to get the FDA-approved products because of insurance coverage, or for financial reasons, or maybe neither of the new products is appropriate for them,” she said. “I do think there will always be a need for the traditional option. The more options that we have available the better.”
TD Cowen analyst Joseph Thome told Reuters that the drug could be priced close to $20,000 per course, expecting peak sales of $750 million in the U.S. in 2033.
Dr. Allegretti disclosed consulting work for Seres Therapeutics, Ferring, and other manufacturers. She is a member of OpenBiome’s clinical advisory board.
The recent approval of the first oral fecal-derived microbiota therapy to prevent the recurrence of Clostridioides difficile (C. diff) infection in patients was welcome news for physicians who’ve struggled under the weight of having too few treatment options for the prevention of C. diff recurrence.
The product, developed by Massachusetts-based Seres Therepeutics and marketed as Vowst, was approved by the U.S. Food and Drug Administration on April 26. It is approved for use in adults who have already been treated with antibiotics for a recurrent infection with C. diff bacteria.
and is designed to be delivered in four capsules taken daily for 3 days.
Gastroenterologist Phillip I. Tarr, MD, division chief of gastroenterology at Washington University, St. Louis, and chair of the American Gastroenterological Association Center for Gut Microbiome Research and Education, said that prevention of recurrent C. diff infection “remains challenging,” and that Vowst “provides the first FDA-approved, orally administered microbiome therapeutic with which to achieve this goal. This advance also makes us optimistic we might soon be able to prevent other disorders by managing gut microbial communities.”
Vowst is the second therapy derived from human stool to be approved for the indication in less than 6 months. In December, the FDA approved Rebyota (Ferring), a rectally delivered treatment that also uses microbes from donor feces. Both products were given priority review, orphan drug, and breakthrough therapy designations by the agency.
C. diff infection can be aggravated by an alteration of normal gut flora associated with antibiotics treatment, leading to cycles of repeated infections. Infection can produce diarrhea, abdominal pain, fever, and severe morbidity. In the United States, an estimated 15,000 to 30,000 deaths per year are linked to C. diff. Risk factors for recurrent infection include being 65 or older, hospitalization, being in a nursing home, a weakened immune system, and previous infection with C. diff.
Therapies transplanting fecal microbiota from donors have been used since the 1950s as treatments for recurrent C. diff infection, and in the past decade, as stool banks recruiting screened donors have made fecal microbiota transplants, or FMT, standard of care. However, only in recent years have fecal-derived therapies become subject to standardized safety and efficacy testing.
Both the current FDA-approved products, Rebyota and Vowst, were shown in randomized controlled trials to reduce recurrence of C. diff infection, compared with placebo. In a phase 3 clinical trial of Rebyota (n = 262) in antibiotic-treated patients, one rectally administered dose reduced recurrence of C. diff infection by 70.6% at 8 weeks, compared with 57.5% for placebo. A phase 3 study of Vowst (n = 281) showed recurrence in treated subjects to be 12.4% at 8 weeks, compared with nearly 40% of those receiving placebo (relative risk, 0.32; 95% confidence interval, 0.18-0.58; P less than .001).
Despite screening protocols that have become increasingly homogenized and rigorous, FMT is associated with the risk of introducing pathogens. Vowst is manufactured with purified bacterial spores derived from donor feces, not whole stool. Nonetheless, FDA noted in its statement that Vowst could still potentially introduce infectious agents or allergens.
Antibiotics are still first-line treatment
In an interview, Jessica Allegretti, MD, MPH, AGAF, medical director of the Crohn’s and Colitis Center at Brigham & Women’s Hospital, Boston, said that having two FDA-approved therapies with different means of administration “is great for the field and great for patients. These are both meant to be used after a course of antibiotics, so antibiotics are still the mainstay of treatment for C. diff and recurrent C. diff, but we now have more options to prevent recurrence.”
The convenience of an oral therapy that can be taken at home is “very attractive,” Dr. Allegretti added, noting that there will also be patients “who either don’t want to or can’t take capsules, for whom a rectal administration [in a health care setting] may be preferred.”
Dr. Allegretti, who has used FMT to treat recurrent C. difficile for more than a decade, said that she expected traditional FMT using screened donor stool to remain available even as the new products are adopted by clinicians. FMT centers like OpenBiome “will continue to provide access for patients who either don’t have the ability to get the FDA-approved products because of insurance coverage, or for financial reasons, or maybe neither of the new products is appropriate for them,” she said. “I do think there will always be a need for the traditional option. The more options that we have available the better.”
TD Cowen analyst Joseph Thome told Reuters that the drug could be priced close to $20,000 per course, expecting peak sales of $750 million in the U.S. in 2033.
Dr. Allegretti disclosed consulting work for Seres Therapeutics, Ferring, and other manufacturers. She is a member of OpenBiome’s clinical advisory board.
The recent approval of the first oral fecal-derived microbiota therapy to prevent the recurrence of Clostridioides difficile (C. diff) infection in patients was welcome news for physicians who’ve struggled under the weight of having too few treatment options for the prevention of C. diff recurrence.
The product, developed by Massachusetts-based Seres Therepeutics and marketed as Vowst, was approved by the U.S. Food and Drug Administration on April 26. It is approved for use in adults who have already been treated with antibiotics for a recurrent infection with C. diff bacteria.
and is designed to be delivered in four capsules taken daily for 3 days.
Gastroenterologist Phillip I. Tarr, MD, division chief of gastroenterology at Washington University, St. Louis, and chair of the American Gastroenterological Association Center for Gut Microbiome Research and Education, said that prevention of recurrent C. diff infection “remains challenging,” and that Vowst “provides the first FDA-approved, orally administered microbiome therapeutic with which to achieve this goal. This advance also makes us optimistic we might soon be able to prevent other disorders by managing gut microbial communities.”
Vowst is the second therapy derived from human stool to be approved for the indication in less than 6 months. In December, the FDA approved Rebyota (Ferring), a rectally delivered treatment that also uses microbes from donor feces. Both products were given priority review, orphan drug, and breakthrough therapy designations by the agency.
C. diff infection can be aggravated by an alteration of normal gut flora associated with antibiotics treatment, leading to cycles of repeated infections. Infection can produce diarrhea, abdominal pain, fever, and severe morbidity. In the United States, an estimated 15,000 to 30,000 deaths per year are linked to C. diff. Risk factors for recurrent infection include being 65 or older, hospitalization, being in a nursing home, a weakened immune system, and previous infection with C. diff.
Therapies transplanting fecal microbiota from donors have been used since the 1950s as treatments for recurrent C. diff infection, and in the past decade, as stool banks recruiting screened donors have made fecal microbiota transplants, or FMT, standard of care. However, only in recent years have fecal-derived therapies become subject to standardized safety and efficacy testing.
Both the current FDA-approved products, Rebyota and Vowst, were shown in randomized controlled trials to reduce recurrence of C. diff infection, compared with placebo. In a phase 3 clinical trial of Rebyota (n = 262) in antibiotic-treated patients, one rectally administered dose reduced recurrence of C. diff infection by 70.6% at 8 weeks, compared with 57.5% for placebo. A phase 3 study of Vowst (n = 281) showed recurrence in treated subjects to be 12.4% at 8 weeks, compared with nearly 40% of those receiving placebo (relative risk, 0.32; 95% confidence interval, 0.18-0.58; P less than .001).
Despite screening protocols that have become increasingly homogenized and rigorous, FMT is associated with the risk of introducing pathogens. Vowst is manufactured with purified bacterial spores derived from donor feces, not whole stool. Nonetheless, FDA noted in its statement that Vowst could still potentially introduce infectious agents or allergens.
Antibiotics are still first-line treatment
In an interview, Jessica Allegretti, MD, MPH, AGAF, medical director of the Crohn’s and Colitis Center at Brigham & Women’s Hospital, Boston, said that having two FDA-approved therapies with different means of administration “is great for the field and great for patients. These are both meant to be used after a course of antibiotics, so antibiotics are still the mainstay of treatment for C. diff and recurrent C. diff, but we now have more options to prevent recurrence.”
The convenience of an oral therapy that can be taken at home is “very attractive,” Dr. Allegretti added, noting that there will also be patients “who either don’t want to or can’t take capsules, for whom a rectal administration [in a health care setting] may be preferred.”
Dr. Allegretti, who has used FMT to treat recurrent C. difficile for more than a decade, said that she expected traditional FMT using screened donor stool to remain available even as the new products are adopted by clinicians. FMT centers like OpenBiome “will continue to provide access for patients who either don’t have the ability to get the FDA-approved products because of insurance coverage, or for financial reasons, or maybe neither of the new products is appropriate for them,” she said. “I do think there will always be a need for the traditional option. The more options that we have available the better.”
TD Cowen analyst Joseph Thome told Reuters that the drug could be priced close to $20,000 per course, expecting peak sales of $750 million in the U.S. in 2033.
Dr. Allegretti disclosed consulting work for Seres Therapeutics, Ferring, and other manufacturers. She is a member of OpenBiome’s clinical advisory board.
What are the main reasons patients sue dermatologists?
PHOENIX – , and the defendants were more likely to be male.
Those are among key findings from a study that aimed to determine the reasons patients pursue litigation against dermatologists.
“The number of lawsuits against physicians continues to climb annually,” Young Lim, MD, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the results were presented during an abstract session. “Depending on the study, anywhere between 75 to 99 percent of physicians will face a lawsuit by age 65. A clear understanding of prior litigations will help mitigate similar errors in future practice and promote safer, higher quality care.”
Dr. Lim, a dermatology resident at Massachusetts General Hospital and Harvard Medical School, Boston, along with Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at MGH, and H. Ray Jalian, MD, a cosmetic dermatologist who practices in Los Angeles, used two large national database repositories, WestlawNext and LexisNexis, to retrospectively analyze legal documents following a query using “dermatology” and “dermatologist” as search terms to capture all variety of litigations. They excluded cases in which litigation did not involve patient care as well as those in which the dermatologist was the plaintiff and those in which the dermatologist was involved as a third party.
The final analysis consisted of 54 claims, comprising 43 state and 11 federal cases. Of the 54 cases, 35 involved a male defendant, 12 involved a female defendant, and 7 cases either did not specify the gender of the defendant or involved multiple defendants. Of the 35 cases involving a male defendant, 23 (66%) were brought by female plaintiffs.
Most cases (49, or 91%) involved a defendant dermatologist in private practice while the remaining 5 involved a defendant dermatologist in an academic setting.
The most common reason for litigation was accidental injury (27 cases, or 50%), followed by incorrect or delayed diagnoses (22 cases, or 41%). Five cases resulted from the dermatologist failing to communicate important information, such as postop care instructions or obtaining informed consent.
Of all 54 cases 30 (56%) were dismissed prior to trial, while 24 (44%) resulted in a judgment for the plaintiff. According to Dr. Lim, payout information was available for only five cases, and ranged from $15,000 (injury from laser) to $1,950,000 (delayed diagnosis of malignant melanoma).
“While lawsuits from patients against dermatologists largely involve injury from elective procedures, clinicians should practice caution regarding missed or delayed diagnoses when practicing medical dermatology,” the authors concluded in their abstract. “Ensuring that critical information is shared with patients and obtaining proper written consent will also safeguard against easily-avoidable litigations.”
Christopher B. Zachary, MBBS, professor and chair emeritus of the department of dermatology at the University of California, Irvine, who was asked to comment on the study, said that the findings are a reminder that lack of attention to the most simply performed aspects of care can be the reasons patients will seek medical malpractice redress.
“Consent requires careful and thoughtful explanation of a planned procedure, which should then be recorded in the chart to avoid future confusion,” Dr. Zachary told this news organization. “A patient’s signature on a consent form obtained by a staff member is clearly inadequate if not accompanied by a clear and understandable preoperative discussion. Words, images, video are all elements that aid patients’ comprehension of a planned procedure. And postoperative instructions given to the patients while on the laser table are commonly forgotten by the patient and must be accompanied by written advice summary. Patients will frequently misremember instructions and can be overwhelmed by medical jargon.”
Neither the researchers nor Dr. Zachary reported having relevant financial disclosures.
PHOENIX – , and the defendants were more likely to be male.
Those are among key findings from a study that aimed to determine the reasons patients pursue litigation against dermatologists.
“The number of lawsuits against physicians continues to climb annually,” Young Lim, MD, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the results were presented during an abstract session. “Depending on the study, anywhere between 75 to 99 percent of physicians will face a lawsuit by age 65. A clear understanding of prior litigations will help mitigate similar errors in future practice and promote safer, higher quality care.”
Dr. Lim, a dermatology resident at Massachusetts General Hospital and Harvard Medical School, Boston, along with Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at MGH, and H. Ray Jalian, MD, a cosmetic dermatologist who practices in Los Angeles, used two large national database repositories, WestlawNext and LexisNexis, to retrospectively analyze legal documents following a query using “dermatology” and “dermatologist” as search terms to capture all variety of litigations. They excluded cases in which litigation did not involve patient care as well as those in which the dermatologist was the plaintiff and those in which the dermatologist was involved as a third party.
The final analysis consisted of 54 claims, comprising 43 state and 11 federal cases. Of the 54 cases, 35 involved a male defendant, 12 involved a female defendant, and 7 cases either did not specify the gender of the defendant or involved multiple defendants. Of the 35 cases involving a male defendant, 23 (66%) were brought by female plaintiffs.
Most cases (49, or 91%) involved a defendant dermatologist in private practice while the remaining 5 involved a defendant dermatologist in an academic setting.
The most common reason for litigation was accidental injury (27 cases, or 50%), followed by incorrect or delayed diagnoses (22 cases, or 41%). Five cases resulted from the dermatologist failing to communicate important information, such as postop care instructions or obtaining informed consent.
Of all 54 cases 30 (56%) were dismissed prior to trial, while 24 (44%) resulted in a judgment for the plaintiff. According to Dr. Lim, payout information was available for only five cases, and ranged from $15,000 (injury from laser) to $1,950,000 (delayed diagnosis of malignant melanoma).
“While lawsuits from patients against dermatologists largely involve injury from elective procedures, clinicians should practice caution regarding missed or delayed diagnoses when practicing medical dermatology,” the authors concluded in their abstract. “Ensuring that critical information is shared with patients and obtaining proper written consent will also safeguard against easily-avoidable litigations.”
Christopher B. Zachary, MBBS, professor and chair emeritus of the department of dermatology at the University of California, Irvine, who was asked to comment on the study, said that the findings are a reminder that lack of attention to the most simply performed aspects of care can be the reasons patients will seek medical malpractice redress.
“Consent requires careful and thoughtful explanation of a planned procedure, which should then be recorded in the chart to avoid future confusion,” Dr. Zachary told this news organization. “A patient’s signature on a consent form obtained by a staff member is clearly inadequate if not accompanied by a clear and understandable preoperative discussion. Words, images, video are all elements that aid patients’ comprehension of a planned procedure. And postoperative instructions given to the patients while on the laser table are commonly forgotten by the patient and must be accompanied by written advice summary. Patients will frequently misremember instructions and can be overwhelmed by medical jargon.”
Neither the researchers nor Dr. Zachary reported having relevant financial disclosures.
PHOENIX – , and the defendants were more likely to be male.
Those are among key findings from a study that aimed to determine the reasons patients pursue litigation against dermatologists.
“The number of lawsuits against physicians continues to climb annually,” Young Lim, MD, PhD, said at the annual conference of the American Society for Laser Medicine and Surgery, where the results were presented during an abstract session. “Depending on the study, anywhere between 75 to 99 percent of physicians will face a lawsuit by age 65. A clear understanding of prior litigations will help mitigate similar errors in future practice and promote safer, higher quality care.”
Dr. Lim, a dermatology resident at Massachusetts General Hospital and Harvard Medical School, Boston, along with Mathew M. Avram, MD, JD, director of laser, cosmetics, and dermatologic surgery at MGH, and H. Ray Jalian, MD, a cosmetic dermatologist who practices in Los Angeles, used two large national database repositories, WestlawNext and LexisNexis, to retrospectively analyze legal documents following a query using “dermatology” and “dermatologist” as search terms to capture all variety of litigations. They excluded cases in which litigation did not involve patient care as well as those in which the dermatologist was the plaintiff and those in which the dermatologist was involved as a third party.
The final analysis consisted of 54 claims, comprising 43 state and 11 federal cases. Of the 54 cases, 35 involved a male defendant, 12 involved a female defendant, and 7 cases either did not specify the gender of the defendant or involved multiple defendants. Of the 35 cases involving a male defendant, 23 (66%) were brought by female plaintiffs.
Most cases (49, or 91%) involved a defendant dermatologist in private practice while the remaining 5 involved a defendant dermatologist in an academic setting.
The most common reason for litigation was accidental injury (27 cases, or 50%), followed by incorrect or delayed diagnoses (22 cases, or 41%). Five cases resulted from the dermatologist failing to communicate important information, such as postop care instructions or obtaining informed consent.
Of all 54 cases 30 (56%) were dismissed prior to trial, while 24 (44%) resulted in a judgment for the plaintiff. According to Dr. Lim, payout information was available for only five cases, and ranged from $15,000 (injury from laser) to $1,950,000 (delayed diagnosis of malignant melanoma).
“While lawsuits from patients against dermatologists largely involve injury from elective procedures, clinicians should practice caution regarding missed or delayed diagnoses when practicing medical dermatology,” the authors concluded in their abstract. “Ensuring that critical information is shared with patients and obtaining proper written consent will also safeguard against easily-avoidable litigations.”
Christopher B. Zachary, MBBS, professor and chair emeritus of the department of dermatology at the University of California, Irvine, who was asked to comment on the study, said that the findings are a reminder that lack of attention to the most simply performed aspects of care can be the reasons patients will seek medical malpractice redress.
“Consent requires careful and thoughtful explanation of a planned procedure, which should then be recorded in the chart to avoid future confusion,” Dr. Zachary told this news organization. “A patient’s signature on a consent form obtained by a staff member is clearly inadequate if not accompanied by a clear and understandable preoperative discussion. Words, images, video are all elements that aid patients’ comprehension of a planned procedure. And postoperative instructions given to the patients while on the laser table are commonly forgotten by the patient and must be accompanied by written advice summary. Patients will frequently misremember instructions and can be overwhelmed by medical jargon.”
Neither the researchers nor Dr. Zachary reported having relevant financial disclosures.
AT ASLMS 2023
NPF provides guidance for virtual psoriasis visits
.
The success of telemedicine in managing chronic inflammatory skin conditions including psoriasis during the COVID-19 pandemic “highlighted that teledermatology can be used beyond the context of a global health crisis to provide continuity of care and improve access to health care more broadly,” the task force wrote in a paper published online in JAAD International.
Co–senior author George Han, MD, PhD, said in an interview that the impetus for the guidelines came from NPF patient advocates, who realized that the organization needed something to take to payers and governmental agencies to advocate for better access to dermatologic care. He is associate professor of dermatology and director of teledermatology at the Hofstra/Northwell department of dermatology, Hyde Park, New York.
“We realized that, in many places around the country, people don’t have access to dermatology.” In upstate New York, said Dr. Han, his anecdotal research has revealed wait times of 6 months or more.
As a guiding principle, the authors pronounce teledermatology “a reasonable alternative for providing long-term management of patients with psoriasis.” Research shows that nearly all dermatologists used teledermatology during the pandemic, the authors noted, and that well-run programs improve Psoriasis Area and Severity Index (PASI) scores and other measures on par with in-person care. Telemedicine may be especially useful for initial visits, they added, particularly when distance, patient incapacity, and circumstances prevent face-to-face evaluation.
Additional position statements emphasize that teledermatology should support rather than supplant in-person visits, and that this balance may be particularly important in cases involving psoriatic arthritis (PsA). “Even though we can’t do a physical exam and palpate some of those joints in person,” said Dr. Han, “tools have been developed that, through a series of questions the patient can answer, can guide you towards whether there is a high index of suspicion for psoriatic arthritis.” Such patients require in-person evaluation with urgency, he said, because delays in PsA diagnosis and treatment can lead to irreversible joint damage and significant functional impairment.
Another motivation for producing the guidelines, said Dr. Han, was that, even when underserved patients get a dermatology appointment, some providers may not have all the latest tools or medicines available for treating psoriasis. In such cases, telemedicine may allow dermatologists specializing in psoriasis care to extend their reach in comanaging patients with primary care physicians and community dermatologists.
Before the appointment, guidelines suggest determining what form of teledermatology will best suit each patient. Authors recommended gauging patients’ savviness with computers and cameras, and counseling patients regarding available virtual evaluation tools – such as live video visits, store-and-forward photo strategies, and assessment-tool training videos.
A subsequent guideline underscores the importance of continuously improving technology to support expeditious image capture and workflows that emulate in-person practice. Dr. Han explained, “we wanted to make sure that on the back end there’s adequate support such that – if through teledermatology, we determine that the patient should get, say, a systemic treatment – the patient is able to get the appropriate lab tests, get the medicine, and know how to inject it.”
Regarding reimbursement, Dr. Han said that policies varied prepandemic, but many commercial insurers covered telemedicine at a rate 20% lower than the in-person rate. During the pandemic, he said, insurers shifted to provide the higher rate for telemedicine, consistent with policies adopted by the Centers for Medicare & Medicaid Services.
“There are differences in coverage and reimbursement from plan to plan,” Dr. Han added. “And even within the same plan, there are carve-outs so that some plans don’t allow certain services. The big picture is that for the most part these services are covered at a level comparable to an in-person visit at present.”
With the Department of Health & Human Services’ public health emergency declaration expiring in May, he said, physicians have worried that some of the allowances made by CMS – such as lifting requirements that Medicare patients in rural areas be seen at care sites – will expire. “It seems that some of those limitations have been addressed, and those allowances are going to be extended until Congress is able to pass something that gives us durable access to telemedicine care. We think that based on the current environment telemedicine is here to stay.”
The study was funded by the NPF. Dr. Han has been an investigator, adviser, speaker, or researcher for AbbVie, Amgen, Apogee Therapeutics, Arcutis, Athenex, Bausch Health, Beiersdorf, Boehringer Ingelheim, Bond Avillion, Bristol Myers Squibb, Celgene, CeraVe, Dermavant, DermTech, Eli Lilly, EPI Health, Janssen Pharmaceuticals, LEO Pharma, L’Oreal, MC2 Therapeutics, Novartis, Ortho Dermatologics, PellePharm, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, SUN Pharmaceuticals, and UCB.
.
The success of telemedicine in managing chronic inflammatory skin conditions including psoriasis during the COVID-19 pandemic “highlighted that teledermatology can be used beyond the context of a global health crisis to provide continuity of care and improve access to health care more broadly,” the task force wrote in a paper published online in JAAD International.
Co–senior author George Han, MD, PhD, said in an interview that the impetus for the guidelines came from NPF patient advocates, who realized that the organization needed something to take to payers and governmental agencies to advocate for better access to dermatologic care. He is associate professor of dermatology and director of teledermatology at the Hofstra/Northwell department of dermatology, Hyde Park, New York.
“We realized that, in many places around the country, people don’t have access to dermatology.” In upstate New York, said Dr. Han, his anecdotal research has revealed wait times of 6 months or more.
As a guiding principle, the authors pronounce teledermatology “a reasonable alternative for providing long-term management of patients with psoriasis.” Research shows that nearly all dermatologists used teledermatology during the pandemic, the authors noted, and that well-run programs improve Psoriasis Area and Severity Index (PASI) scores and other measures on par with in-person care. Telemedicine may be especially useful for initial visits, they added, particularly when distance, patient incapacity, and circumstances prevent face-to-face evaluation.
Additional position statements emphasize that teledermatology should support rather than supplant in-person visits, and that this balance may be particularly important in cases involving psoriatic arthritis (PsA). “Even though we can’t do a physical exam and palpate some of those joints in person,” said Dr. Han, “tools have been developed that, through a series of questions the patient can answer, can guide you towards whether there is a high index of suspicion for psoriatic arthritis.” Such patients require in-person evaluation with urgency, he said, because delays in PsA diagnosis and treatment can lead to irreversible joint damage and significant functional impairment.
Another motivation for producing the guidelines, said Dr. Han, was that, even when underserved patients get a dermatology appointment, some providers may not have all the latest tools or medicines available for treating psoriasis. In such cases, telemedicine may allow dermatologists specializing in psoriasis care to extend their reach in comanaging patients with primary care physicians and community dermatologists.
Before the appointment, guidelines suggest determining what form of teledermatology will best suit each patient. Authors recommended gauging patients’ savviness with computers and cameras, and counseling patients regarding available virtual evaluation tools – such as live video visits, store-and-forward photo strategies, and assessment-tool training videos.
A subsequent guideline underscores the importance of continuously improving technology to support expeditious image capture and workflows that emulate in-person practice. Dr. Han explained, “we wanted to make sure that on the back end there’s adequate support such that – if through teledermatology, we determine that the patient should get, say, a systemic treatment – the patient is able to get the appropriate lab tests, get the medicine, and know how to inject it.”
Regarding reimbursement, Dr. Han said that policies varied prepandemic, but many commercial insurers covered telemedicine at a rate 20% lower than the in-person rate. During the pandemic, he said, insurers shifted to provide the higher rate for telemedicine, consistent with policies adopted by the Centers for Medicare & Medicaid Services.
“There are differences in coverage and reimbursement from plan to plan,” Dr. Han added. “And even within the same plan, there are carve-outs so that some plans don’t allow certain services. The big picture is that for the most part these services are covered at a level comparable to an in-person visit at present.”
With the Department of Health & Human Services’ public health emergency declaration expiring in May, he said, physicians have worried that some of the allowances made by CMS – such as lifting requirements that Medicare patients in rural areas be seen at care sites – will expire. “It seems that some of those limitations have been addressed, and those allowances are going to be extended until Congress is able to pass something that gives us durable access to telemedicine care. We think that based on the current environment telemedicine is here to stay.”
The study was funded by the NPF. Dr. Han has been an investigator, adviser, speaker, or researcher for AbbVie, Amgen, Apogee Therapeutics, Arcutis, Athenex, Bausch Health, Beiersdorf, Boehringer Ingelheim, Bond Avillion, Bristol Myers Squibb, Celgene, CeraVe, Dermavant, DermTech, Eli Lilly, EPI Health, Janssen Pharmaceuticals, LEO Pharma, L’Oreal, MC2 Therapeutics, Novartis, Ortho Dermatologics, PellePharm, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, SUN Pharmaceuticals, and UCB.
.
The success of telemedicine in managing chronic inflammatory skin conditions including psoriasis during the COVID-19 pandemic “highlighted that teledermatology can be used beyond the context of a global health crisis to provide continuity of care and improve access to health care more broadly,” the task force wrote in a paper published online in JAAD International.
Co–senior author George Han, MD, PhD, said in an interview that the impetus for the guidelines came from NPF patient advocates, who realized that the organization needed something to take to payers and governmental agencies to advocate for better access to dermatologic care. He is associate professor of dermatology and director of teledermatology at the Hofstra/Northwell department of dermatology, Hyde Park, New York.
“We realized that, in many places around the country, people don’t have access to dermatology.” In upstate New York, said Dr. Han, his anecdotal research has revealed wait times of 6 months or more.
As a guiding principle, the authors pronounce teledermatology “a reasonable alternative for providing long-term management of patients with psoriasis.” Research shows that nearly all dermatologists used teledermatology during the pandemic, the authors noted, and that well-run programs improve Psoriasis Area and Severity Index (PASI) scores and other measures on par with in-person care. Telemedicine may be especially useful for initial visits, they added, particularly when distance, patient incapacity, and circumstances prevent face-to-face evaluation.
Additional position statements emphasize that teledermatology should support rather than supplant in-person visits, and that this balance may be particularly important in cases involving psoriatic arthritis (PsA). “Even though we can’t do a physical exam and palpate some of those joints in person,” said Dr. Han, “tools have been developed that, through a series of questions the patient can answer, can guide you towards whether there is a high index of suspicion for psoriatic arthritis.” Such patients require in-person evaluation with urgency, he said, because delays in PsA diagnosis and treatment can lead to irreversible joint damage and significant functional impairment.
Another motivation for producing the guidelines, said Dr. Han, was that, even when underserved patients get a dermatology appointment, some providers may not have all the latest tools or medicines available for treating psoriasis. In such cases, telemedicine may allow dermatologists specializing in psoriasis care to extend their reach in comanaging patients with primary care physicians and community dermatologists.
Before the appointment, guidelines suggest determining what form of teledermatology will best suit each patient. Authors recommended gauging patients’ savviness with computers and cameras, and counseling patients regarding available virtual evaluation tools – such as live video visits, store-and-forward photo strategies, and assessment-tool training videos.
A subsequent guideline underscores the importance of continuously improving technology to support expeditious image capture and workflows that emulate in-person practice. Dr. Han explained, “we wanted to make sure that on the back end there’s adequate support such that – if through teledermatology, we determine that the patient should get, say, a systemic treatment – the patient is able to get the appropriate lab tests, get the medicine, and know how to inject it.”
Regarding reimbursement, Dr. Han said that policies varied prepandemic, but many commercial insurers covered telemedicine at a rate 20% lower than the in-person rate. During the pandemic, he said, insurers shifted to provide the higher rate for telemedicine, consistent with policies adopted by the Centers for Medicare & Medicaid Services.
“There are differences in coverage and reimbursement from plan to plan,” Dr. Han added. “And even within the same plan, there are carve-outs so that some plans don’t allow certain services. The big picture is that for the most part these services are covered at a level comparable to an in-person visit at present.”
With the Department of Health & Human Services’ public health emergency declaration expiring in May, he said, physicians have worried that some of the allowances made by CMS – such as lifting requirements that Medicare patients in rural areas be seen at care sites – will expire. “It seems that some of those limitations have been addressed, and those allowances are going to be extended until Congress is able to pass something that gives us durable access to telemedicine care. We think that based on the current environment telemedicine is here to stay.”
The study was funded by the NPF. Dr. Han has been an investigator, adviser, speaker, or researcher for AbbVie, Amgen, Apogee Therapeutics, Arcutis, Athenex, Bausch Health, Beiersdorf, Boehringer Ingelheim, Bond Avillion, Bristol Myers Squibb, Celgene, CeraVe, Dermavant, DermTech, Eli Lilly, EPI Health, Janssen Pharmaceuticals, LEO Pharma, L’Oreal, MC2 Therapeutics, Novartis, Ortho Dermatologics, PellePharm, Pfizer, Regeneron Pharmaceuticals, Sanofi Genzyme, SUN Pharmaceuticals, and UCB.
FROM JAAD INTERNATIONAL
FDA clears first patch to treat axillary hyperhidrosis
The Food and Drug Administration on April 13 cleared the first patch to reduce excessive underarm sweating for adults with primary axillary hyperhidrosis.
The single-use, disposable, prescription-only patch will be marketed as Brella. It consists of a sodium sheet with an adhesive overlay. A health care provider applies it to the patient’s underarm for up to 3 minutes and then repeats the process on the other underarm.
The developer, Candesant Biomedical, says the patch uses the company’s patented targeted alkali thermolysis (TAT) technology, which was built on the principle that heat is generated when sodium reacts with water in sweat. “The thermal energy created by the sodium sheet is precisely localized, microtargeting sweat glands to significantly reduce sweat production,” according to the company’s press release announcing the FDA decision.
FDA clearance was based on data from the pivotal randomized, double-blind, multicenter SAHARA study, which indicated that the product is effective and well tolerated.
Patients experienced a reduction in sweat that was maintained for 3 months or longer, according to trial results.
The SAHARA trial results were reported in a late-breaking abstract at the annual meeting of the American Academy of Dermatology in March.
The trial enrolled 110 individuals with Hyperhidrosis Disease Severity Scale (HDSS) scores of 3 or 4 (indicating frequent sweating or sweating that always interferes with daily activities). Trial participants were randomly assigned to receive either an active TAT or a sham patch, which was applied for up to 3 minutes.
At the meeting, lead investigator David M. Pariser, MD, a dermatologist practicing in Norfolk, Va., reported that at 4 weeks, 63.6% of patients in the active patch group achieved an HDSS score of 1 or 2, compared with 44.2% of those in the sham treatment group (P = .0332). Also, 43.2% of those in the active-patch group achieved an improvement of 2 points or greater on the HDSS, as compared with 16.3% of those in the sham treatment group (P = .0107) .
In addition, 9.1% of those in the active-patch group achieved a 3-point improvement on the HDSS, compared with none in the sham group. “That’s an amazing improvement; you’re basically going from moderate or severe to none,” Dr. Pariser said at the meeting.
As for adverse events (AEs), 13 patients in the active-patch group experienced AEs at the treatment site. Six patients experienced erythema; four experienced erosion; two experienced burning, itching, or stinging; and one had underarm odor.
“The two procedure-related AEs in the TAT-treated group were compensatory sweating and irritant contact dermatitis due to the adhesive,” Dr. Pariser said. He noted that most AEs resolved in fewer than 2 weeks, and all AEs were mild to moderate.
According to the International Hyperhidrosis Society, about 1.3 million people in the United States have axillary hyperhidrosis, and about a third report that sweating is barely tolerable and frequently interferes with daily activities or is intolerable and always interferes with daily activities.
The patch will be available within months in select U.S. markets beginning in late summer. The company says the markets will be listed on its website.
A company representative told this news organization that because it is an in-office procedure, pricing will vary, depending on the practice. “With that said, Candesant expects doctors will charge about the same for one session of the Brella SweatControl Patch as they would for a high-end, in-office facial or chemical peel,” the representative said.
Dr. Pariser is a consultant or investigator for Bickel Biotechnology, Biofrontera AG, Bristol-Myers Squibb, the Celgene Corporation, Novartis Pharmaceuticals, Pfizer, Regeneron, and Sanofi.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration on April 13 cleared the first patch to reduce excessive underarm sweating for adults with primary axillary hyperhidrosis.
The single-use, disposable, prescription-only patch will be marketed as Brella. It consists of a sodium sheet with an adhesive overlay. A health care provider applies it to the patient’s underarm for up to 3 minutes and then repeats the process on the other underarm.
The developer, Candesant Biomedical, says the patch uses the company’s patented targeted alkali thermolysis (TAT) technology, which was built on the principle that heat is generated when sodium reacts with water in sweat. “The thermal energy created by the sodium sheet is precisely localized, microtargeting sweat glands to significantly reduce sweat production,” according to the company’s press release announcing the FDA decision.
FDA clearance was based on data from the pivotal randomized, double-blind, multicenter SAHARA study, which indicated that the product is effective and well tolerated.
Patients experienced a reduction in sweat that was maintained for 3 months or longer, according to trial results.
The SAHARA trial results were reported in a late-breaking abstract at the annual meeting of the American Academy of Dermatology in March.
The trial enrolled 110 individuals with Hyperhidrosis Disease Severity Scale (HDSS) scores of 3 or 4 (indicating frequent sweating or sweating that always interferes with daily activities). Trial participants were randomly assigned to receive either an active TAT or a sham patch, which was applied for up to 3 minutes.
At the meeting, lead investigator David M. Pariser, MD, a dermatologist practicing in Norfolk, Va., reported that at 4 weeks, 63.6% of patients in the active patch group achieved an HDSS score of 1 or 2, compared with 44.2% of those in the sham treatment group (P = .0332). Also, 43.2% of those in the active-patch group achieved an improvement of 2 points or greater on the HDSS, as compared with 16.3% of those in the sham treatment group (P = .0107) .
In addition, 9.1% of those in the active-patch group achieved a 3-point improvement on the HDSS, compared with none in the sham group. “That’s an amazing improvement; you’re basically going from moderate or severe to none,” Dr. Pariser said at the meeting.
As for adverse events (AEs), 13 patients in the active-patch group experienced AEs at the treatment site. Six patients experienced erythema; four experienced erosion; two experienced burning, itching, or stinging; and one had underarm odor.
“The two procedure-related AEs in the TAT-treated group were compensatory sweating and irritant contact dermatitis due to the adhesive,” Dr. Pariser said. He noted that most AEs resolved in fewer than 2 weeks, and all AEs were mild to moderate.
According to the International Hyperhidrosis Society, about 1.3 million people in the United States have axillary hyperhidrosis, and about a third report that sweating is barely tolerable and frequently interferes with daily activities or is intolerable and always interferes with daily activities.
The patch will be available within months in select U.S. markets beginning in late summer. The company says the markets will be listed on its website.
A company representative told this news organization that because it is an in-office procedure, pricing will vary, depending on the practice. “With that said, Candesant expects doctors will charge about the same for one session of the Brella SweatControl Patch as they would for a high-end, in-office facial or chemical peel,” the representative said.
Dr. Pariser is a consultant or investigator for Bickel Biotechnology, Biofrontera AG, Bristol-Myers Squibb, the Celgene Corporation, Novartis Pharmaceuticals, Pfizer, Regeneron, and Sanofi.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration on April 13 cleared the first patch to reduce excessive underarm sweating for adults with primary axillary hyperhidrosis.
The single-use, disposable, prescription-only patch will be marketed as Brella. It consists of a sodium sheet with an adhesive overlay. A health care provider applies it to the patient’s underarm for up to 3 minutes and then repeats the process on the other underarm.
The developer, Candesant Biomedical, says the patch uses the company’s patented targeted alkali thermolysis (TAT) technology, which was built on the principle that heat is generated when sodium reacts with water in sweat. “The thermal energy created by the sodium sheet is precisely localized, microtargeting sweat glands to significantly reduce sweat production,” according to the company’s press release announcing the FDA decision.
FDA clearance was based on data from the pivotal randomized, double-blind, multicenter SAHARA study, which indicated that the product is effective and well tolerated.
Patients experienced a reduction in sweat that was maintained for 3 months or longer, according to trial results.
The SAHARA trial results were reported in a late-breaking abstract at the annual meeting of the American Academy of Dermatology in March.
The trial enrolled 110 individuals with Hyperhidrosis Disease Severity Scale (HDSS) scores of 3 or 4 (indicating frequent sweating or sweating that always interferes with daily activities). Trial participants were randomly assigned to receive either an active TAT or a sham patch, which was applied for up to 3 minutes.
At the meeting, lead investigator David M. Pariser, MD, a dermatologist practicing in Norfolk, Va., reported that at 4 weeks, 63.6% of patients in the active patch group achieved an HDSS score of 1 or 2, compared with 44.2% of those in the sham treatment group (P = .0332). Also, 43.2% of those in the active-patch group achieved an improvement of 2 points or greater on the HDSS, as compared with 16.3% of those in the sham treatment group (P = .0107) .
In addition, 9.1% of those in the active-patch group achieved a 3-point improvement on the HDSS, compared with none in the sham group. “That’s an amazing improvement; you’re basically going from moderate or severe to none,” Dr. Pariser said at the meeting.
As for adverse events (AEs), 13 patients in the active-patch group experienced AEs at the treatment site. Six patients experienced erythema; four experienced erosion; two experienced burning, itching, or stinging; and one had underarm odor.
“The two procedure-related AEs in the TAT-treated group were compensatory sweating and irritant contact dermatitis due to the adhesive,” Dr. Pariser said. He noted that most AEs resolved in fewer than 2 weeks, and all AEs were mild to moderate.
According to the International Hyperhidrosis Society, about 1.3 million people in the United States have axillary hyperhidrosis, and about a third report that sweating is barely tolerable and frequently interferes with daily activities or is intolerable and always interferes with daily activities.
The patch will be available within months in select U.S. markets beginning in late summer. The company says the markets will be listed on its website.
A company representative told this news organization that because it is an in-office procedure, pricing will vary, depending on the practice. “With that said, Candesant expects doctors will charge about the same for one session of the Brella SweatControl Patch as they would for a high-end, in-office facial or chemical peel,” the representative said.
Dr. Pariser is a consultant or investigator for Bickel Biotechnology, Biofrontera AG, Bristol-Myers Squibb, the Celgene Corporation, Novartis Pharmaceuticals, Pfizer, Regeneron, and Sanofi.
A version of this article originally appeared on Medscape.com.
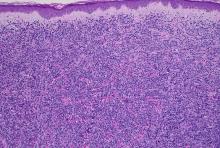
A 50-year-old White male presented with a 4- to 5-year history of progressively growing violaceous lesions on his left lower extremity
with scarce T-cells, classically presenting as rapidly progressive, plum-colored lesions on the lower extremities.1,2 CBCLs, with PCDLBCL-LT accounting for 4%, make up the minority of cutaneous lymphomas in the Western world.1-3 The leg type variant, typically demonstrating a female predominance and median age of onset in the 70s, is clinically aggressive and associated with a poorer prognosis, increased recurrence rate, and 40%-60% 5-year survival rate.1-5
Histologically, this variant demonstrates a diffuse sheet-like growth of enlarged atypical B-cells distinctively separated from the epidermis by a prominent grenz zone. Classic PCDLBCL-LT immunophenotype includes B-cell markers CD20 and IgM; triple expressor phenotype indicating c-MYC, BCL-2, and BCL-6 positivity; as well as CD10 negativity, lack of BCL-2 rearrangement, and presence of a positive MYD-88 molecular result.
Other characteristic histopathological findings include positivity for post-germinal markers IRF4/MUM-1 and FOXP-1, positivity for additional B-cell markers, including CD79 and PAX5, and negativity of t(14;18) (q32;21).1,3-5
This case is of significant interest as it falls within the approximately 10% of PCDLBCL-LT cases demonstrating weak to negative MUM-1 staining, in addition to its presentation in a younger male individual.
While MUM-1 positivity is common in this subtype, its presence, or lack thereof, should not be looked at in isolation when evaluating diagnostic criteria, nor has it been shown to have a statistically significant effect on survival rate – in contrast to factors like lesion location on the leg versus non-leg lesions, multiple lesions at diagnosis, and dissemination to other sites.2,6
PCDLBCL-LT can uncommonly present in non-leg locations and only 10% depict associated B-symptoms, such as fatigue, night sweats, weight loss, or lymphadenopathy.2,6 First-line treatment is with the R-CHOP chemotherapy regimen – consisting of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone – although radiotherapy is sometimes considered in patients with a single small lesion.1,2
Because of possible cutaneous involvement beyond the legs, common lack of systemic symptoms, and variable immunophenotypes, this case of MUM-1 negative PCDLBCL-LT highlights the importance of a clinicopathological approach to differentiate the subtypes of CBCLs, allowing for proper and individualized stratification of risk, prognosis, and treatment.
This case was submitted and written by Marlee Hill, BS, Michael Franzetti, MD, Jeffrey McBride, MD, and Allison Hood, MD, of the University of Oklahoma, Oklahoma City. They also provided the photos. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Willemze R et al. Blood. 2019;133(16):1703-14.
2. Willemze R et al. Blood. 2005;105(10):3768-85.
3. Sukswai N et al. Pathology. 2020;52(1):53-67.
4. Hristov AC. Arch Pathol Lab Med. 2012;136(8):876-81.
5. Sokol L et al. Cancer Control. 2012;19(3):236-44.
6. Grange F et al. Arch Dermatol. 2007;143(9):1144-50.
with scarce T-cells, classically presenting as rapidly progressive, plum-colored lesions on the lower extremities.1,2 CBCLs, with PCDLBCL-LT accounting for 4%, make up the minority of cutaneous lymphomas in the Western world.1-3 The leg type variant, typically demonstrating a female predominance and median age of onset in the 70s, is clinically aggressive and associated with a poorer prognosis, increased recurrence rate, and 40%-60% 5-year survival rate.1-5
Histologically, this variant demonstrates a diffuse sheet-like growth of enlarged atypical B-cells distinctively separated from the epidermis by a prominent grenz zone. Classic PCDLBCL-LT immunophenotype includes B-cell markers CD20 and IgM; triple expressor phenotype indicating c-MYC, BCL-2, and BCL-6 positivity; as well as CD10 negativity, lack of BCL-2 rearrangement, and presence of a positive MYD-88 molecular result.
Other characteristic histopathological findings include positivity for post-germinal markers IRF4/MUM-1 and FOXP-1, positivity for additional B-cell markers, including CD79 and PAX5, and negativity of t(14;18) (q32;21).1,3-5
This case is of significant interest as it falls within the approximately 10% of PCDLBCL-LT cases demonstrating weak to negative MUM-1 staining, in addition to its presentation in a younger male individual.
While MUM-1 positivity is common in this subtype, its presence, or lack thereof, should not be looked at in isolation when evaluating diagnostic criteria, nor has it been shown to have a statistically significant effect on survival rate – in contrast to factors like lesion location on the leg versus non-leg lesions, multiple lesions at diagnosis, and dissemination to other sites.2,6
PCDLBCL-LT can uncommonly present in non-leg locations and only 10% depict associated B-symptoms, such as fatigue, night sweats, weight loss, or lymphadenopathy.2,6 First-line treatment is with the R-CHOP chemotherapy regimen – consisting of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone – although radiotherapy is sometimes considered in patients with a single small lesion.1,2
Because of possible cutaneous involvement beyond the legs, common lack of systemic symptoms, and variable immunophenotypes, this case of MUM-1 negative PCDLBCL-LT highlights the importance of a clinicopathological approach to differentiate the subtypes of CBCLs, allowing for proper and individualized stratification of risk, prognosis, and treatment.
This case was submitted and written by Marlee Hill, BS, Michael Franzetti, MD, Jeffrey McBride, MD, and Allison Hood, MD, of the University of Oklahoma, Oklahoma City. They also provided the photos. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Willemze R et al. Blood. 2019;133(16):1703-14.
2. Willemze R et al. Blood. 2005;105(10):3768-85.
3. Sukswai N et al. Pathology. 2020;52(1):53-67.
4. Hristov AC. Arch Pathol Lab Med. 2012;136(8):876-81.
5. Sokol L et al. Cancer Control. 2012;19(3):236-44.
6. Grange F et al. Arch Dermatol. 2007;143(9):1144-50.
with scarce T-cells, classically presenting as rapidly progressive, plum-colored lesions on the lower extremities.1,2 CBCLs, with PCDLBCL-LT accounting for 4%, make up the minority of cutaneous lymphomas in the Western world.1-3 The leg type variant, typically demonstrating a female predominance and median age of onset in the 70s, is clinically aggressive and associated with a poorer prognosis, increased recurrence rate, and 40%-60% 5-year survival rate.1-5
Histologically, this variant demonstrates a diffuse sheet-like growth of enlarged atypical B-cells distinctively separated from the epidermis by a prominent grenz zone. Classic PCDLBCL-LT immunophenotype includes B-cell markers CD20 and IgM; triple expressor phenotype indicating c-MYC, BCL-2, and BCL-6 positivity; as well as CD10 negativity, lack of BCL-2 rearrangement, and presence of a positive MYD-88 molecular result.
Other characteristic histopathological findings include positivity for post-germinal markers IRF4/MUM-1 and FOXP-1, positivity for additional B-cell markers, including CD79 and PAX5, and negativity of t(14;18) (q32;21).1,3-5
This case is of significant interest as it falls within the approximately 10% of PCDLBCL-LT cases demonstrating weak to negative MUM-1 staining, in addition to its presentation in a younger male individual.
While MUM-1 positivity is common in this subtype, its presence, or lack thereof, should not be looked at in isolation when evaluating diagnostic criteria, nor has it been shown to have a statistically significant effect on survival rate – in contrast to factors like lesion location on the leg versus non-leg lesions, multiple lesions at diagnosis, and dissemination to other sites.2,6
PCDLBCL-LT can uncommonly present in non-leg locations and only 10% depict associated B-symptoms, such as fatigue, night sweats, weight loss, or lymphadenopathy.2,6 First-line treatment is with the R-CHOP chemotherapy regimen – consisting of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone – although radiotherapy is sometimes considered in patients with a single small lesion.1,2
Because of possible cutaneous involvement beyond the legs, common lack of systemic symptoms, and variable immunophenotypes, this case of MUM-1 negative PCDLBCL-LT highlights the importance of a clinicopathological approach to differentiate the subtypes of CBCLs, allowing for proper and individualized stratification of risk, prognosis, and treatment.
This case was submitted and written by Marlee Hill, BS, Michael Franzetti, MD, Jeffrey McBride, MD, and Allison Hood, MD, of the University of Oklahoma, Oklahoma City. They also provided the photos. Donna Bilu Martin, MD, edited the column.
Dr. Bilu Martin is a board-certified dermatologist in private practice at Premier Dermatology, MD, in Aventura, Fla. More diagnostic cases are available at mdedge.com/dermatology. To submit a case for possible publication, send an email to dermnews@mdedge.com.
References
1. Willemze R et al. Blood. 2019;133(16):1703-14.
2. Willemze R et al. Blood. 2005;105(10):3768-85.
3. Sukswai N et al. Pathology. 2020;52(1):53-67.
4. Hristov AC. Arch Pathol Lab Med. 2012;136(8):876-81.
5. Sokol L et al. Cancer Control. 2012;19(3):236-44.
6. Grange F et al. Arch Dermatol. 2007;143(9):1144-50.
There was no cervical, axillary, or inguinal lymphadenopathy.
What are the clinical implications of recent skin dysbiosis discoveries?
NEW ORLEANS – .
“There’s still a lot for us to learn,” Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said at the annual meeting of the American Academy of Dermatology. “Multiple factors contribute to the variability in the skin microbiota, including age, sex, environment, immune system, host genotype, lifestyle, and pathobiology. The question becomes, when do these factors or impacts on the microbiota become clinically significant?”
According to Dr. Friedman, there are 10 times more bacteria cells than human cells in the human body, “but it’s not a fight to the finish; it’s not us versus them,” he said. “Together, we are a super organism.” There are also more than 500 species of bacteria on human skin excluding viruses and fungi, and each person carries up to 5 pounds of bacteria, which is akin to finding a new organ in the body.
“What’s so unique is that we each have our own bacterial fingerprint,” he said. “Whoever is sitting next to you? Their microbiota makeup is different than yours.”
Beyond genetics and environment, activities that can contribute to alterations in skin flora or skin dysbiosis include topical application of steroids, antibiotics, retinoids, harsh soaps, chemical and physical exfoliants, and resurfacing techniques. “With anything we apply or do to the skin, we are literally changing the home of many microorganisms, for good or bad,” he said.
In the realm of atopic dermatitis (AD), Staphylococcus aureus has been implicated as an offender in the pathophysiology of the disease. “It’s not about one single species of Staphylococcus, though,” said Dr. Friedman, who also is director of translational research at George Washington University. “We’re finding out that, depending on the severity of disease, Staph. epidermis may be part of the problem as opposed to it just being about Staph. aureus. Furthermore, and more importantly, these changes in the microbiota, specifically a decrease in microbial diversity, has been shown to precede a disease flare, highlighting the central role of maintaining microbial diversity and by definition, supporting the living barrier in our management of AD.”
With this in mind, researchers in one study used high-throughput sequencing to evaluate the microbial communities associated with affected and unaffected skin of 49 patients with AD before and after emollient treatment. Following 84 days of emollient application, clinical symptoms of AD improved in 72% of the study population and Stenotrophomonas species were significantly more abundant among responders.
Prebiotics, probiotics
“Our treatments certainly can positively impact the microbiota, as we have seen even recently with some of our new targeted therapies, but we can also directly provide support,” he continued. Prebiotics, which he defined as supplements or foods that contain a nondigestible ingredient that selectively stimulates the growth and/or activity of indigenous bacteria, can be found in many over-the-counter moisturizers.
For example, colloidal oatmeal has been found to support the growth of S. epidermidis and enhance the production of lactic acid. “We really don’t know much about what these induced changes mean from a clinical perspective; that has yet to be elucidated,” Dr. Friedman said.
In light of the recent attention to the early application of moisturizers in infants at high risk of developing AD in an effort to prevent or limit AD, “maybe part of this has to do with applying something that’s nurturing an evolving microbiota,” Dr. Friedman noted. “It’s something to think about.”
Yet another area of study involves the use of probiotics, which Dr. Friedman defined as supplements or foods that contain viable microorganisms that alter the microflora of the host. In a first-of-its-kind trial, researchers evaluated the safety and efficacy of self-administered topical Roseomonas mucosa in 10 adults and 5 children with AD. No adverse events or treatment complications were observed, and the topical R. mucosa was associated with significant decreases in measures of disease severity, topical steroid requirement, and S. aureus burden
In a more recent randomized trial of 11 patients with AD, Richard L. Gallo, MD, PhD, chair of dermatology, University of California, San Diego, and colleagues found that application of a personalized topical cream formulated from coagulase-negative Staphylococcus with antimicrobial activity against S. aureus reduced colonization of S. aureus and improved disease severity.
And in another randomized, controlled trial, Italian researchers enrolled 80 adults with mild to severe AD to receive a placebo or a supplement that was a mixture of lactobacilli for 56 days. They found that adults in the treatment arm showed an improvement in skin smoothness, skin moisturization, self-perception, and a decrease in the SCORing Atopic Dermatitis (SCORAD) index as well as in levels of inflammatory markers associated with AD.
Dr. Friedman also discussed postbiotics, nonviable bacterial products or metabolic byproducts from probiotic microorganisms that have biologic activity in the host. In one trial, French researchers enrolled 75 people with AD who ranged in age from 6 to 70 years to receive a cream containing a 5% lysate of the nonpathogenic bacteria Vitreoscilla filiformis, or a vehicle cream for 30 days. They found that compared with the vehicle, V. filiformis lysate significantly decreased SCORAD levels and pruritus; active cream was shown to significantly decrease loss of sleep from day 0 to day 29.
Dr. Friedman characterized these novel approaches to AD as “an exciting area, one we need to pay attention to. But what I really want to know is, aside from these purposefully made and marketed products that have pre- and postprobiotics, is there a difference with some of the products we use already? My assumption is that there is, but we need to see that data.”
Dr. Friedman disclosed that he is a consultant and/or advisory board member for Medscape/SanovaWorks, Oakstone Institute, L’Oréal, La Roche Posay, Galderma, Aveeno, Ortho Dermatologic, Microcures, Pfizer, Novartis, Lilly, Hoth Therapeutics, Zylo Therapeutics, BMS, Vial, Janssen, Novocure, Dermavant, Regeneron/Sanofi, and Incyte. He has also received grants from Pfizer, the Dermatology Foundation, Lilly, Janssen, Incyte, and Galderma.
NEW ORLEANS – .
“There’s still a lot for us to learn,” Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said at the annual meeting of the American Academy of Dermatology. “Multiple factors contribute to the variability in the skin microbiota, including age, sex, environment, immune system, host genotype, lifestyle, and pathobiology. The question becomes, when do these factors or impacts on the microbiota become clinically significant?”
According to Dr. Friedman, there are 10 times more bacteria cells than human cells in the human body, “but it’s not a fight to the finish; it’s not us versus them,” he said. “Together, we are a super organism.” There are also more than 500 species of bacteria on human skin excluding viruses and fungi, and each person carries up to 5 pounds of bacteria, which is akin to finding a new organ in the body.
“What’s so unique is that we each have our own bacterial fingerprint,” he said. “Whoever is sitting next to you? Their microbiota makeup is different than yours.”
Beyond genetics and environment, activities that can contribute to alterations in skin flora or skin dysbiosis include topical application of steroids, antibiotics, retinoids, harsh soaps, chemical and physical exfoliants, and resurfacing techniques. “With anything we apply or do to the skin, we are literally changing the home of many microorganisms, for good or bad,” he said.
In the realm of atopic dermatitis (AD), Staphylococcus aureus has been implicated as an offender in the pathophysiology of the disease. “It’s not about one single species of Staphylococcus, though,” said Dr. Friedman, who also is director of translational research at George Washington University. “We’re finding out that, depending on the severity of disease, Staph. epidermis may be part of the problem as opposed to it just being about Staph. aureus. Furthermore, and more importantly, these changes in the microbiota, specifically a decrease in microbial diversity, has been shown to precede a disease flare, highlighting the central role of maintaining microbial diversity and by definition, supporting the living barrier in our management of AD.”
With this in mind, researchers in one study used high-throughput sequencing to evaluate the microbial communities associated with affected and unaffected skin of 49 patients with AD before and after emollient treatment. Following 84 days of emollient application, clinical symptoms of AD improved in 72% of the study population and Stenotrophomonas species were significantly more abundant among responders.
Prebiotics, probiotics
“Our treatments certainly can positively impact the microbiota, as we have seen even recently with some of our new targeted therapies, but we can also directly provide support,” he continued. Prebiotics, which he defined as supplements or foods that contain a nondigestible ingredient that selectively stimulates the growth and/or activity of indigenous bacteria, can be found in many over-the-counter moisturizers.
For example, colloidal oatmeal has been found to support the growth of S. epidermidis and enhance the production of lactic acid. “We really don’t know much about what these induced changes mean from a clinical perspective; that has yet to be elucidated,” Dr. Friedman said.
In light of the recent attention to the early application of moisturizers in infants at high risk of developing AD in an effort to prevent or limit AD, “maybe part of this has to do with applying something that’s nurturing an evolving microbiota,” Dr. Friedman noted. “It’s something to think about.”
Yet another area of study involves the use of probiotics, which Dr. Friedman defined as supplements or foods that contain viable microorganisms that alter the microflora of the host. In a first-of-its-kind trial, researchers evaluated the safety and efficacy of self-administered topical Roseomonas mucosa in 10 adults and 5 children with AD. No adverse events or treatment complications were observed, and the topical R. mucosa was associated with significant decreases in measures of disease severity, topical steroid requirement, and S. aureus burden
In a more recent randomized trial of 11 patients with AD, Richard L. Gallo, MD, PhD, chair of dermatology, University of California, San Diego, and colleagues found that application of a personalized topical cream formulated from coagulase-negative Staphylococcus with antimicrobial activity against S. aureus reduced colonization of S. aureus and improved disease severity.
And in another randomized, controlled trial, Italian researchers enrolled 80 adults with mild to severe AD to receive a placebo or a supplement that was a mixture of lactobacilli for 56 days. They found that adults in the treatment arm showed an improvement in skin smoothness, skin moisturization, self-perception, and a decrease in the SCORing Atopic Dermatitis (SCORAD) index as well as in levels of inflammatory markers associated with AD.
Dr. Friedman also discussed postbiotics, nonviable bacterial products or metabolic byproducts from probiotic microorganisms that have biologic activity in the host. In one trial, French researchers enrolled 75 people with AD who ranged in age from 6 to 70 years to receive a cream containing a 5% lysate of the nonpathogenic bacteria Vitreoscilla filiformis, or a vehicle cream for 30 days. They found that compared with the vehicle, V. filiformis lysate significantly decreased SCORAD levels and pruritus; active cream was shown to significantly decrease loss of sleep from day 0 to day 29.
Dr. Friedman characterized these novel approaches to AD as “an exciting area, one we need to pay attention to. But what I really want to know is, aside from these purposefully made and marketed products that have pre- and postprobiotics, is there a difference with some of the products we use already? My assumption is that there is, but we need to see that data.”
Dr. Friedman disclosed that he is a consultant and/or advisory board member for Medscape/SanovaWorks, Oakstone Institute, L’Oréal, La Roche Posay, Galderma, Aveeno, Ortho Dermatologic, Microcures, Pfizer, Novartis, Lilly, Hoth Therapeutics, Zylo Therapeutics, BMS, Vial, Janssen, Novocure, Dermavant, Regeneron/Sanofi, and Incyte. He has also received grants from Pfizer, the Dermatology Foundation, Lilly, Janssen, Incyte, and Galderma.
NEW ORLEANS – .
“There’s still a lot for us to learn,” Adam Friedman, MD, professor and chair of dermatology at George Washington University, Washington, said at the annual meeting of the American Academy of Dermatology. “Multiple factors contribute to the variability in the skin microbiota, including age, sex, environment, immune system, host genotype, lifestyle, and pathobiology. The question becomes, when do these factors or impacts on the microbiota become clinically significant?”
According to Dr. Friedman, there are 10 times more bacteria cells than human cells in the human body, “but it’s not a fight to the finish; it’s not us versus them,” he said. “Together, we are a super organism.” There are also more than 500 species of bacteria on human skin excluding viruses and fungi, and each person carries up to 5 pounds of bacteria, which is akin to finding a new organ in the body.
“What’s so unique is that we each have our own bacterial fingerprint,” he said. “Whoever is sitting next to you? Their microbiota makeup is different than yours.”
Beyond genetics and environment, activities that can contribute to alterations in skin flora or skin dysbiosis include topical application of steroids, antibiotics, retinoids, harsh soaps, chemical and physical exfoliants, and resurfacing techniques. “With anything we apply or do to the skin, we are literally changing the home of many microorganisms, for good or bad,” he said.
In the realm of atopic dermatitis (AD), Staphylococcus aureus has been implicated as an offender in the pathophysiology of the disease. “It’s not about one single species of Staphylococcus, though,” said Dr. Friedman, who also is director of translational research at George Washington University. “We’re finding out that, depending on the severity of disease, Staph. epidermis may be part of the problem as opposed to it just being about Staph. aureus. Furthermore, and more importantly, these changes in the microbiota, specifically a decrease in microbial diversity, has been shown to precede a disease flare, highlighting the central role of maintaining microbial diversity and by definition, supporting the living barrier in our management of AD.”
With this in mind, researchers in one study used high-throughput sequencing to evaluate the microbial communities associated with affected and unaffected skin of 49 patients with AD before and after emollient treatment. Following 84 days of emollient application, clinical symptoms of AD improved in 72% of the study population and Stenotrophomonas species were significantly more abundant among responders.
Prebiotics, probiotics
“Our treatments certainly can positively impact the microbiota, as we have seen even recently with some of our new targeted therapies, but we can also directly provide support,” he continued. Prebiotics, which he defined as supplements or foods that contain a nondigestible ingredient that selectively stimulates the growth and/or activity of indigenous bacteria, can be found in many over-the-counter moisturizers.
For example, colloidal oatmeal has been found to support the growth of S. epidermidis and enhance the production of lactic acid. “We really don’t know much about what these induced changes mean from a clinical perspective; that has yet to be elucidated,” Dr. Friedman said.
In light of the recent attention to the early application of moisturizers in infants at high risk of developing AD in an effort to prevent or limit AD, “maybe part of this has to do with applying something that’s nurturing an evolving microbiota,” Dr. Friedman noted. “It’s something to think about.”
Yet another area of study involves the use of probiotics, which Dr. Friedman defined as supplements or foods that contain viable microorganisms that alter the microflora of the host. In a first-of-its-kind trial, researchers evaluated the safety and efficacy of self-administered topical Roseomonas mucosa in 10 adults and 5 children with AD. No adverse events or treatment complications were observed, and the topical R. mucosa was associated with significant decreases in measures of disease severity, topical steroid requirement, and S. aureus burden
In a more recent randomized trial of 11 patients with AD, Richard L. Gallo, MD, PhD, chair of dermatology, University of California, San Diego, and colleagues found that application of a personalized topical cream formulated from coagulase-negative Staphylococcus with antimicrobial activity against S. aureus reduced colonization of S. aureus and improved disease severity.
And in another randomized, controlled trial, Italian researchers enrolled 80 adults with mild to severe AD to receive a placebo or a supplement that was a mixture of lactobacilli for 56 days. They found that adults in the treatment arm showed an improvement in skin smoothness, skin moisturization, self-perception, and a decrease in the SCORing Atopic Dermatitis (SCORAD) index as well as in levels of inflammatory markers associated with AD.
Dr. Friedman also discussed postbiotics, nonviable bacterial products or metabolic byproducts from probiotic microorganisms that have biologic activity in the host. In one trial, French researchers enrolled 75 people with AD who ranged in age from 6 to 70 years to receive a cream containing a 5% lysate of the nonpathogenic bacteria Vitreoscilla filiformis, or a vehicle cream for 30 days. They found that compared with the vehicle, V. filiformis lysate significantly decreased SCORAD levels and pruritus; active cream was shown to significantly decrease loss of sleep from day 0 to day 29.
Dr. Friedman characterized these novel approaches to AD as “an exciting area, one we need to pay attention to. But what I really want to know is, aside from these purposefully made and marketed products that have pre- and postprobiotics, is there a difference with some of the products we use already? My assumption is that there is, but we need to see that data.”
Dr. Friedman disclosed that he is a consultant and/or advisory board member for Medscape/SanovaWorks, Oakstone Institute, L’Oréal, La Roche Posay, Galderma, Aveeno, Ortho Dermatologic, Microcures, Pfizer, Novartis, Lilly, Hoth Therapeutics, Zylo Therapeutics, BMS, Vial, Janssen, Novocure, Dermavant, Regeneron/Sanofi, and Incyte. He has also received grants from Pfizer, the Dermatology Foundation, Lilly, Janssen, Incyte, and Galderma.
AT AAD 2023
Anifrolumab shows promise in refractory discoid lupus erythematosus
a small retrospective study reports.
DLE, the most common form of chronic cutaneous lupus erythematosus, can permanently scar and disfigure patients, and traditional treatments such as antimalarials, steroid-sparing immunosuppressive agents, thalidomide, retinoids, and lenalidomide don’t consistently improve refractory DLE, the authors noted.
“All patients demonstrated significant improvement in symptomatology and disease activity within 2 months of initiating anifrolumab,” lead study author Katharina Shaw, MD, of the department of dermatology of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, and colleagues wrote in a research letter published in JAMA Dermatology. “These early results highlight the potential for anifrolumab to be a viable therapeutic option for patients with DLE, particularly those with severe or recalcitrant disease.”
The Food and Drug Administration approved anifrolumab (Saphnelo), a human monoclonal antibody targeting type 1 interferon receptor subunit 1, in 2021 for adults with moderate to severe systemic lupus erythematosus, but it has not been approved for the treatment of DLE.
Dr. Shaw and colleagues queried the medical records from Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, to find all cases of DLE based on biopsy, expert opinion, or both from January 2000 to October 2022.
The researchers identified eight female patients who had received anifrolumab for at least 8 weeks. The women were aged between 19 and 75 years (median, 42.5 years), and all had DLE recalcitrant to standard therapies and had been treated with hydroxychloroquine and between 1 and 10 other drugs, most commonly methotrexate and mycophenolate mofetil (MMF).
The authors looked for improvements in patient-reported symptoms and Cutaneous Lupus Erythematosus Disease Area and Severity Index scores, including CLASI A (activity) score 0-70, and CLASI-D (damage) score 0-56.
All patients showed significantly improved symptoms and disease activity within 2 months of their first infusion of the treatment. The mean decrease and mean percentage decrease in CLASI-A scores were 17.1 and 65.1%, respectively. The mean decrease and mean percentage decrease in CLASI-D scores were 0.5 and 2.9%, respectively.
The rapid clinical improvements with anifrolumab, compared with improvements with traditional medications, were striking, the authors wrote. “Given the risk for permanent scarring, dyspigmentation, and alopecia with poorly controlled DLE, the importance of rapidly mitigating disease activity cannot be overemphasized.”
They acknowledged that the results are limited by the study’s small sample size and retrospective design, and they recommend larger related prospective studies.
Asked to comment on the results, Kaveh Ardalan, MD, MS, assistant professor of pediatrics in the division of pediatric rheumatology at Duke University, Durham, N.C., said that finding new DLE therapeutics is important because of the huge impact of uncontrolled DLE on patients’ quality of life, body image, and social roles.
Dr. Ardalan noted that he sees DLE in his pediatric patients, “either as an isolated finding or in the context of systemic lupus erythematosus. Anifrolumab is not approved by the FDA to treat DLE or children.
“Randomized controlled trials, including the TULIP-1 and TULIP-2 studies of anifrolumab in systemic lupus, have indicated that lupus skin manifestations can improve in patients who receive anifrolumab,” said Dr. Ardalan, who was not involved in the study. “And we know that type I interferons are major drivers of cutaneous disease activity in patients with lupus, so targeting that mechanism with anifrolumab makes biological sense.”
The authors’ use of the validated CLASI classification system to quantify disease activity and damage over time, and their determination of the length of time for the drug to take effect are strengths of the study, he added.
Funding information was not provided. Two authors reported financial relationships with Pfizer, which does not manufacture anifrolumab. Dr. Ardalan reported no conflicts of interest with the study.
a small retrospective study reports.
DLE, the most common form of chronic cutaneous lupus erythematosus, can permanently scar and disfigure patients, and traditional treatments such as antimalarials, steroid-sparing immunosuppressive agents, thalidomide, retinoids, and lenalidomide don’t consistently improve refractory DLE, the authors noted.
“All patients demonstrated significant improvement in symptomatology and disease activity within 2 months of initiating anifrolumab,” lead study author Katharina Shaw, MD, of the department of dermatology of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, and colleagues wrote in a research letter published in JAMA Dermatology. “These early results highlight the potential for anifrolumab to be a viable therapeutic option for patients with DLE, particularly those with severe or recalcitrant disease.”
The Food and Drug Administration approved anifrolumab (Saphnelo), a human monoclonal antibody targeting type 1 interferon receptor subunit 1, in 2021 for adults with moderate to severe systemic lupus erythematosus, but it has not been approved for the treatment of DLE.
Dr. Shaw and colleagues queried the medical records from Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, to find all cases of DLE based on biopsy, expert opinion, or both from January 2000 to October 2022.
The researchers identified eight female patients who had received anifrolumab for at least 8 weeks. The women were aged between 19 and 75 years (median, 42.5 years), and all had DLE recalcitrant to standard therapies and had been treated with hydroxychloroquine and between 1 and 10 other drugs, most commonly methotrexate and mycophenolate mofetil (MMF).
The authors looked for improvements in patient-reported symptoms and Cutaneous Lupus Erythematosus Disease Area and Severity Index scores, including CLASI A (activity) score 0-70, and CLASI-D (damage) score 0-56.
All patients showed significantly improved symptoms and disease activity within 2 months of their first infusion of the treatment. The mean decrease and mean percentage decrease in CLASI-A scores were 17.1 and 65.1%, respectively. The mean decrease and mean percentage decrease in CLASI-D scores were 0.5 and 2.9%, respectively.
The rapid clinical improvements with anifrolumab, compared with improvements with traditional medications, were striking, the authors wrote. “Given the risk for permanent scarring, dyspigmentation, and alopecia with poorly controlled DLE, the importance of rapidly mitigating disease activity cannot be overemphasized.”
They acknowledged that the results are limited by the study’s small sample size and retrospective design, and they recommend larger related prospective studies.
Asked to comment on the results, Kaveh Ardalan, MD, MS, assistant professor of pediatrics in the division of pediatric rheumatology at Duke University, Durham, N.C., said that finding new DLE therapeutics is important because of the huge impact of uncontrolled DLE on patients’ quality of life, body image, and social roles.
Dr. Ardalan noted that he sees DLE in his pediatric patients, “either as an isolated finding or in the context of systemic lupus erythematosus. Anifrolumab is not approved by the FDA to treat DLE or children.
“Randomized controlled trials, including the TULIP-1 and TULIP-2 studies of anifrolumab in systemic lupus, have indicated that lupus skin manifestations can improve in patients who receive anifrolumab,” said Dr. Ardalan, who was not involved in the study. “And we know that type I interferons are major drivers of cutaneous disease activity in patients with lupus, so targeting that mechanism with anifrolumab makes biological sense.”
The authors’ use of the validated CLASI classification system to quantify disease activity and damage over time, and their determination of the length of time for the drug to take effect are strengths of the study, he added.
Funding information was not provided. Two authors reported financial relationships with Pfizer, which does not manufacture anifrolumab. Dr. Ardalan reported no conflicts of interest with the study.
a small retrospective study reports.
DLE, the most common form of chronic cutaneous lupus erythematosus, can permanently scar and disfigure patients, and traditional treatments such as antimalarials, steroid-sparing immunosuppressive agents, thalidomide, retinoids, and lenalidomide don’t consistently improve refractory DLE, the authors noted.
“All patients demonstrated significant improvement in symptomatology and disease activity within 2 months of initiating anifrolumab,” lead study author Katharina Shaw, MD, of the department of dermatology of Brigham and Women’s Hospital and Harvard Medical School, both in Boston, and colleagues wrote in a research letter published in JAMA Dermatology. “These early results highlight the potential for anifrolumab to be a viable therapeutic option for patients with DLE, particularly those with severe or recalcitrant disease.”
The Food and Drug Administration approved anifrolumab (Saphnelo), a human monoclonal antibody targeting type 1 interferon receptor subunit 1, in 2021 for adults with moderate to severe systemic lupus erythematosus, but it has not been approved for the treatment of DLE.
Dr. Shaw and colleagues queried the medical records from Brigham and Women’s Hospital and Massachusetts General Hospital, Boston, to find all cases of DLE based on biopsy, expert opinion, or both from January 2000 to October 2022.
The researchers identified eight female patients who had received anifrolumab for at least 8 weeks. The women were aged between 19 and 75 years (median, 42.5 years), and all had DLE recalcitrant to standard therapies and had been treated with hydroxychloroquine and between 1 and 10 other drugs, most commonly methotrexate and mycophenolate mofetil (MMF).
The authors looked for improvements in patient-reported symptoms and Cutaneous Lupus Erythematosus Disease Area and Severity Index scores, including CLASI A (activity) score 0-70, and CLASI-D (damage) score 0-56.
All patients showed significantly improved symptoms and disease activity within 2 months of their first infusion of the treatment. The mean decrease and mean percentage decrease in CLASI-A scores were 17.1 and 65.1%, respectively. The mean decrease and mean percentage decrease in CLASI-D scores were 0.5 and 2.9%, respectively.
The rapid clinical improvements with anifrolumab, compared with improvements with traditional medications, were striking, the authors wrote. “Given the risk for permanent scarring, dyspigmentation, and alopecia with poorly controlled DLE, the importance of rapidly mitigating disease activity cannot be overemphasized.”
They acknowledged that the results are limited by the study’s small sample size and retrospective design, and they recommend larger related prospective studies.
Asked to comment on the results, Kaveh Ardalan, MD, MS, assistant professor of pediatrics in the division of pediatric rheumatology at Duke University, Durham, N.C., said that finding new DLE therapeutics is important because of the huge impact of uncontrolled DLE on patients’ quality of life, body image, and social roles.
Dr. Ardalan noted that he sees DLE in his pediatric patients, “either as an isolated finding or in the context of systemic lupus erythematosus. Anifrolumab is not approved by the FDA to treat DLE or children.
“Randomized controlled trials, including the TULIP-1 and TULIP-2 studies of anifrolumab in systemic lupus, have indicated that lupus skin manifestations can improve in patients who receive anifrolumab,” said Dr. Ardalan, who was not involved in the study. “And we know that type I interferons are major drivers of cutaneous disease activity in patients with lupus, so targeting that mechanism with anifrolumab makes biological sense.”
The authors’ use of the validated CLASI classification system to quantify disease activity and damage over time, and their determination of the length of time for the drug to take effect are strengths of the study, he added.
Funding information was not provided. Two authors reported financial relationships with Pfizer, which does not manufacture anifrolumab. Dr. Ardalan reported no conflicts of interest with the study.
FROM JAMA DERMATOLOGY
FDA approves new Merkel cell carcinoma treatment
the agency announced.
This marks the first regulatory approval for the PD-1 inhibitor. The FDA granted accelerated approval for the drug on the basis of tumor response rate and duration of response from the POD1UM-201 trial. Drugmaker Incyte said that “continued approval of Zynyz for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.”
MCC is a rare and aggressive skin cancer with a high rate of metastatic disease and an estimated 5-year overall survival of just 14% among those who present with metastatic disease. Incidence is rapidly increasing in the United States, particularly among adults older than 65 years, Incyte noted.
“More than a third of patients with MCC present with regional or distant metastases, which are associated with high rates of mortality,” principal author Shailender Bhatia, MD, of the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, said in a news release. “The approval of Zynyz offers health care providers another first-line treatment option against MCC that can result in durable responses in patients with metastatic disease.”
POD1UM-201 was an open-label, single-arm, phase 2 study that evaluated the agent in 65 systemic treatment–naive adults with metastatic or recurrent locally advanced MCC.
Overall, 52% of patients had an objective response rate. A complete response was observed in 12 patients (18%), and a partial response was observed in 22 patients (34%).
Duration of response ranged from 1.1 to 24.9 months; 76% of responders experienced responses of 6 months or longer, and 62% experienced responses of 12 months or longer.
Study participants received a 500-mg dose of retifanlimab every 4 weeks for up to 24 weeks or until disease progression or unacceptable toxicity. Serious adverse events occurred in 22% of patients and most often included fatigue, arrhythmia, and pneumonitis; 11% of patients discontinued treatment because of serious adverse events.
Retifanlimab may cause a severe or life-threatening immune response during treatment or after discontinuation. Patients should be advised to immediately report any new or worsening signs or symptoms to their health care provider. Side effects can also be reported to the FDA.
A version of this article first appeared on Medscape.com.
the agency announced.
This marks the first regulatory approval for the PD-1 inhibitor. The FDA granted accelerated approval for the drug on the basis of tumor response rate and duration of response from the POD1UM-201 trial. Drugmaker Incyte said that “continued approval of Zynyz for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.”
MCC is a rare and aggressive skin cancer with a high rate of metastatic disease and an estimated 5-year overall survival of just 14% among those who present with metastatic disease. Incidence is rapidly increasing in the United States, particularly among adults older than 65 years, Incyte noted.
“More than a third of patients with MCC present with regional or distant metastases, which are associated with high rates of mortality,” principal author Shailender Bhatia, MD, of the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, said in a news release. “The approval of Zynyz offers health care providers another first-line treatment option against MCC that can result in durable responses in patients with metastatic disease.”
POD1UM-201 was an open-label, single-arm, phase 2 study that evaluated the agent in 65 systemic treatment–naive adults with metastatic or recurrent locally advanced MCC.
Overall, 52% of patients had an objective response rate. A complete response was observed in 12 patients (18%), and a partial response was observed in 22 patients (34%).
Duration of response ranged from 1.1 to 24.9 months; 76% of responders experienced responses of 6 months or longer, and 62% experienced responses of 12 months or longer.
Study participants received a 500-mg dose of retifanlimab every 4 weeks for up to 24 weeks or until disease progression or unacceptable toxicity. Serious adverse events occurred in 22% of patients and most often included fatigue, arrhythmia, and pneumonitis; 11% of patients discontinued treatment because of serious adverse events.
Retifanlimab may cause a severe or life-threatening immune response during treatment or after discontinuation. Patients should be advised to immediately report any new or worsening signs or symptoms to their health care provider. Side effects can also be reported to the FDA.
A version of this article first appeared on Medscape.com.
the agency announced.
This marks the first regulatory approval for the PD-1 inhibitor. The FDA granted accelerated approval for the drug on the basis of tumor response rate and duration of response from the POD1UM-201 trial. Drugmaker Incyte said that “continued approval of Zynyz for this indication may be contingent upon verification and description of clinical benefit in confirmatory trials.”
MCC is a rare and aggressive skin cancer with a high rate of metastatic disease and an estimated 5-year overall survival of just 14% among those who present with metastatic disease. Incidence is rapidly increasing in the United States, particularly among adults older than 65 years, Incyte noted.
“More than a third of patients with MCC present with regional or distant metastases, which are associated with high rates of mortality,” principal author Shailender Bhatia, MD, of the University of Washington and Fred Hutchinson Cancer Center, both in Seattle, said in a news release. “The approval of Zynyz offers health care providers another first-line treatment option against MCC that can result in durable responses in patients with metastatic disease.”
POD1UM-201 was an open-label, single-arm, phase 2 study that evaluated the agent in 65 systemic treatment–naive adults with metastatic or recurrent locally advanced MCC.
Overall, 52% of patients had an objective response rate. A complete response was observed in 12 patients (18%), and a partial response was observed in 22 patients (34%).
Duration of response ranged from 1.1 to 24.9 months; 76% of responders experienced responses of 6 months or longer, and 62% experienced responses of 12 months or longer.
Study participants received a 500-mg dose of retifanlimab every 4 weeks for up to 24 weeks or until disease progression or unacceptable toxicity. Serious adverse events occurred in 22% of patients and most often included fatigue, arrhythmia, and pneumonitis; 11% of patients discontinued treatment because of serious adverse events.
Retifanlimab may cause a severe or life-threatening immune response during treatment or after discontinuation. Patients should be advised to immediately report any new or worsening signs or symptoms to their health care provider. Side effects can also be reported to the FDA.
A version of this article first appeared on Medscape.com.
Phase 3 prurigo nodularis trial shows positive results for nemolizumab
NEW ORLEANS – demonstrated.
Nemolizumab is a first-in-class investigational monoclonal antibody directed against the interleukin-31 receptor alpha that blocks signaling from IL-31. “From prior studies we know that it modulates pruritus, but also alters keratinocyte differentiation, inflammation, and fibrosis,” one of the investigators, Shawn G. Kwatra, MD, of the department of dermatology, Johns Hopkins University, Baltimore, said during a late-breaking research session at the annual meeting of the American Academy of Dermatology.
OLYMPIA 2 was a phase 3, multicenter, double-blind study in adults with PN presenting with 20 or more nodules, and Investigator’s Global Assessment (IGA) score of 3 or more, and the Peak Pruritus Numerical Rating Scale (PP-NRS) score of 7 or more. Exclusion criteria included chronic pruritus resulting from an active condition other than PN, such as neuropathic and psychogenic pruritus and active atopic dermatitis. In addition, the use of topical steroids, considered a rescue therapy, was not allowed in the trial, Dr. Kwatra said.
After an initial screening period, 274 patients at 73 sites in nine countries were randomized 2:1 either to the nemolizumab monotherapy or placebo. Following an initial 60-mg subcutaneous dose, patients received 30 mg or 60 mg (depending on their baseline weight) every 4 weeks for 16 weeks. The primary endpoint was the proportion of patients with a 4-point or greater improvement in the PP-NRS from baseline at week 16 and the proportion of patients with IGA success at week 16.
Selected key secondary endpoints included the proportion of patients with a 4 point or greater improvement from baseline in the PP-NRS at week 4, the Sleep Disturbance Numerical Rating Scale at week 4, and the SD-NRS at week 16. Safety endpoints included the incidence and severity of all adverse events.
Of the 274 patients randomized, 183 received nemolizumab and 91 received placebo. A total of 174 patients in the nemolizumab group completed the study, compared with 88 in the placebo group. The mean age of study participants was 53 years, 61% were women, 79% were White, 14% were Asian, and the rest were from other racial groups. More than half (57%) had IGA category 3 disease (moderate) and the remainder had IGA category 4 disease (severe); 63% had 20-100 lesions, and the remainder had more than 100. About one-third of study enrollees (32%) had a history of atopy.
Primary, secondary endpoint results
Dr. Kwatra reported that 56.3% of the patients in the nemolizumab group achieved a 4-point or greater improvement in the PP-NRS at week 16, compared with 20.9% of those in the placebo group (P < .0001), while 37.7% of those in the nemolizumab group achieved IGA success at week 16, compared with 11% of those in the placebo group (P < .0001).
As for secondary endpoints, 41% of patients in the nemolizumab group achieved a 4-point or greater improvement in PP-NRS at week 4, compared with 7.7% of those in the placebo group (P < .0001); and 37.2% of patients in the nemolizumab group achieved a 4-point or greater improvement in SD-NRS at week 4, compared with 9.9% of those in the placebo group (P < .0001). Almost 52% of patients in the nemolizumab group achieved a 4-point or greater improvement in SD-NRS at week 16, compared with 20.9% of those in the placebo group (P < .0001); and 9.8% of those in the nemolizumab group achieved IGA success at week 4, compared with 1.1% of those in the placebo group (P < .0074).
Adverse events
Treatment-emergent adverse events occurred in 61.2% of subjects in the nemolizumab group, compared with 52.7% of those in the placebo group. “There were no imbalances overall, [including] no injection-related reactions in either group,” Dr. Kwatra said. There was one case of newly diagnosed asthma in the placebo arm, and none in the treatment arm.
The researchers observed a slightly increased onset of atopic dermatitis in the treatment arm, compared with the placebo arm (5.5% vs. 0%). “Seven out of those 10 patients actually had a history of atopic dermatitis or high IgE [levels] and they were mostly managed with topical steroids without study drug discontinuation,” Dr. Kwatra added. Neurodermatitis, or worsening of PN, occurred in 3.8% of patients in the nemolizumab group, compared with 11% of those in the placebo group.
“The results of this study extend the efficacy and safety findings from the phase 2 study of nemolizumab in patients with PN,” Dr. Kwatra concluded. “I think they also help to usher in a new era of PN [treatment] in prime time.”
Kenneth B. Gordon, MD, who chairs the department of dermatology at the Medical College of Wisconsin, Milwaukee, and was asked to comment on the study, was impressed with nemolizumab’s propensity for blocking IL-31. “To be able to treat PN effectively by simply blocking the itch and not having a significant inflammatory function is really interesting,” he said in an interview at the meeting. If approved, nemolizumab “gives us another treatment option for a disease that is really debilitating. It’s very promising and we hope [the drug] will be available to us in the near future.”
Nemolizumab is being developed by Galderma. According to a press release from the company, nemolizumab was granted Breakthrough Therapy designation by the Food and Drug Administration in December 2019 for the treatment of pruritus associated with PN, a status that was reconfirmed in February 2023.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Galderma, AbbVie, Amgen, Arcutis, ASLAN Pharmaceuticals, Cara Therapeutics, Castle Biosciences, Celldex, Incyte, Johnson and Johnson, Leo Pharma, Novartis, Pfizer, Regeneron, and Sanofi. Dr. Gordon disclosed that he is a consultant to, an investigator for, and/or a member of the advisory board for several pharmaceutical companies, but not Galderma.
NEW ORLEANS – demonstrated.
Nemolizumab is a first-in-class investigational monoclonal antibody directed against the interleukin-31 receptor alpha that blocks signaling from IL-31. “From prior studies we know that it modulates pruritus, but also alters keratinocyte differentiation, inflammation, and fibrosis,” one of the investigators, Shawn G. Kwatra, MD, of the department of dermatology, Johns Hopkins University, Baltimore, said during a late-breaking research session at the annual meeting of the American Academy of Dermatology.
OLYMPIA 2 was a phase 3, multicenter, double-blind study in adults with PN presenting with 20 or more nodules, and Investigator’s Global Assessment (IGA) score of 3 or more, and the Peak Pruritus Numerical Rating Scale (PP-NRS) score of 7 or more. Exclusion criteria included chronic pruritus resulting from an active condition other than PN, such as neuropathic and psychogenic pruritus and active atopic dermatitis. In addition, the use of topical steroids, considered a rescue therapy, was not allowed in the trial, Dr. Kwatra said.
After an initial screening period, 274 patients at 73 sites in nine countries were randomized 2:1 either to the nemolizumab monotherapy or placebo. Following an initial 60-mg subcutaneous dose, patients received 30 mg or 60 mg (depending on their baseline weight) every 4 weeks for 16 weeks. The primary endpoint was the proportion of patients with a 4-point or greater improvement in the PP-NRS from baseline at week 16 and the proportion of patients with IGA success at week 16.
Selected key secondary endpoints included the proportion of patients with a 4 point or greater improvement from baseline in the PP-NRS at week 4, the Sleep Disturbance Numerical Rating Scale at week 4, and the SD-NRS at week 16. Safety endpoints included the incidence and severity of all adverse events.
Of the 274 patients randomized, 183 received nemolizumab and 91 received placebo. A total of 174 patients in the nemolizumab group completed the study, compared with 88 in the placebo group. The mean age of study participants was 53 years, 61% were women, 79% were White, 14% were Asian, and the rest were from other racial groups. More than half (57%) had IGA category 3 disease (moderate) and the remainder had IGA category 4 disease (severe); 63% had 20-100 lesions, and the remainder had more than 100. About one-third of study enrollees (32%) had a history of atopy.
Primary, secondary endpoint results
Dr. Kwatra reported that 56.3% of the patients in the nemolizumab group achieved a 4-point or greater improvement in the PP-NRS at week 16, compared with 20.9% of those in the placebo group (P < .0001), while 37.7% of those in the nemolizumab group achieved IGA success at week 16, compared with 11% of those in the placebo group (P < .0001).
As for secondary endpoints, 41% of patients in the nemolizumab group achieved a 4-point or greater improvement in PP-NRS at week 4, compared with 7.7% of those in the placebo group (P < .0001); and 37.2% of patients in the nemolizumab group achieved a 4-point or greater improvement in SD-NRS at week 4, compared with 9.9% of those in the placebo group (P < .0001). Almost 52% of patients in the nemolizumab group achieved a 4-point or greater improvement in SD-NRS at week 16, compared with 20.9% of those in the placebo group (P < .0001); and 9.8% of those in the nemolizumab group achieved IGA success at week 4, compared with 1.1% of those in the placebo group (P < .0074).
Adverse events
Treatment-emergent adverse events occurred in 61.2% of subjects in the nemolizumab group, compared with 52.7% of those in the placebo group. “There were no imbalances overall, [including] no injection-related reactions in either group,” Dr. Kwatra said. There was one case of newly diagnosed asthma in the placebo arm, and none in the treatment arm.
The researchers observed a slightly increased onset of atopic dermatitis in the treatment arm, compared with the placebo arm (5.5% vs. 0%). “Seven out of those 10 patients actually had a history of atopic dermatitis or high IgE [levels] and they were mostly managed with topical steroids without study drug discontinuation,” Dr. Kwatra added. Neurodermatitis, or worsening of PN, occurred in 3.8% of patients in the nemolizumab group, compared with 11% of those in the placebo group.
“The results of this study extend the efficacy and safety findings from the phase 2 study of nemolizumab in patients with PN,” Dr. Kwatra concluded. “I think they also help to usher in a new era of PN [treatment] in prime time.”
Kenneth B. Gordon, MD, who chairs the department of dermatology at the Medical College of Wisconsin, Milwaukee, and was asked to comment on the study, was impressed with nemolizumab’s propensity for blocking IL-31. “To be able to treat PN effectively by simply blocking the itch and not having a significant inflammatory function is really interesting,” he said in an interview at the meeting. If approved, nemolizumab “gives us another treatment option for a disease that is really debilitating. It’s very promising and we hope [the drug] will be available to us in the near future.”
Nemolizumab is being developed by Galderma. According to a press release from the company, nemolizumab was granted Breakthrough Therapy designation by the Food and Drug Administration in December 2019 for the treatment of pruritus associated with PN, a status that was reconfirmed in February 2023.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Galderma, AbbVie, Amgen, Arcutis, ASLAN Pharmaceuticals, Cara Therapeutics, Castle Biosciences, Celldex, Incyte, Johnson and Johnson, Leo Pharma, Novartis, Pfizer, Regeneron, and Sanofi. Dr. Gordon disclosed that he is a consultant to, an investigator for, and/or a member of the advisory board for several pharmaceutical companies, but not Galderma.
NEW ORLEANS – demonstrated.
Nemolizumab is a first-in-class investigational monoclonal antibody directed against the interleukin-31 receptor alpha that blocks signaling from IL-31. “From prior studies we know that it modulates pruritus, but also alters keratinocyte differentiation, inflammation, and fibrosis,” one of the investigators, Shawn G. Kwatra, MD, of the department of dermatology, Johns Hopkins University, Baltimore, said during a late-breaking research session at the annual meeting of the American Academy of Dermatology.
OLYMPIA 2 was a phase 3, multicenter, double-blind study in adults with PN presenting with 20 or more nodules, and Investigator’s Global Assessment (IGA) score of 3 or more, and the Peak Pruritus Numerical Rating Scale (PP-NRS) score of 7 or more. Exclusion criteria included chronic pruritus resulting from an active condition other than PN, such as neuropathic and psychogenic pruritus and active atopic dermatitis. In addition, the use of topical steroids, considered a rescue therapy, was not allowed in the trial, Dr. Kwatra said.
After an initial screening period, 274 patients at 73 sites in nine countries were randomized 2:1 either to the nemolizumab monotherapy or placebo. Following an initial 60-mg subcutaneous dose, patients received 30 mg or 60 mg (depending on their baseline weight) every 4 weeks for 16 weeks. The primary endpoint was the proportion of patients with a 4-point or greater improvement in the PP-NRS from baseline at week 16 and the proportion of patients with IGA success at week 16.
Selected key secondary endpoints included the proportion of patients with a 4 point or greater improvement from baseline in the PP-NRS at week 4, the Sleep Disturbance Numerical Rating Scale at week 4, and the SD-NRS at week 16. Safety endpoints included the incidence and severity of all adverse events.
Of the 274 patients randomized, 183 received nemolizumab and 91 received placebo. A total of 174 patients in the nemolizumab group completed the study, compared with 88 in the placebo group. The mean age of study participants was 53 years, 61% were women, 79% were White, 14% were Asian, and the rest were from other racial groups. More than half (57%) had IGA category 3 disease (moderate) and the remainder had IGA category 4 disease (severe); 63% had 20-100 lesions, and the remainder had more than 100. About one-third of study enrollees (32%) had a history of atopy.
Primary, secondary endpoint results
Dr. Kwatra reported that 56.3% of the patients in the nemolizumab group achieved a 4-point or greater improvement in the PP-NRS at week 16, compared with 20.9% of those in the placebo group (P < .0001), while 37.7% of those in the nemolizumab group achieved IGA success at week 16, compared with 11% of those in the placebo group (P < .0001).
As for secondary endpoints, 41% of patients in the nemolizumab group achieved a 4-point or greater improvement in PP-NRS at week 4, compared with 7.7% of those in the placebo group (P < .0001); and 37.2% of patients in the nemolizumab group achieved a 4-point or greater improvement in SD-NRS at week 4, compared with 9.9% of those in the placebo group (P < .0001). Almost 52% of patients in the nemolizumab group achieved a 4-point or greater improvement in SD-NRS at week 16, compared with 20.9% of those in the placebo group (P < .0001); and 9.8% of those in the nemolizumab group achieved IGA success at week 4, compared with 1.1% of those in the placebo group (P < .0074).
Adverse events
Treatment-emergent adverse events occurred in 61.2% of subjects in the nemolizumab group, compared with 52.7% of those in the placebo group. “There were no imbalances overall, [including] no injection-related reactions in either group,” Dr. Kwatra said. There was one case of newly diagnosed asthma in the placebo arm, and none in the treatment arm.
The researchers observed a slightly increased onset of atopic dermatitis in the treatment arm, compared with the placebo arm (5.5% vs. 0%). “Seven out of those 10 patients actually had a history of atopic dermatitis or high IgE [levels] and they were mostly managed with topical steroids without study drug discontinuation,” Dr. Kwatra added. Neurodermatitis, or worsening of PN, occurred in 3.8% of patients in the nemolizumab group, compared with 11% of those in the placebo group.
“The results of this study extend the efficacy and safety findings from the phase 2 study of nemolizumab in patients with PN,” Dr. Kwatra concluded. “I think they also help to usher in a new era of PN [treatment] in prime time.”
Kenneth B. Gordon, MD, who chairs the department of dermatology at the Medical College of Wisconsin, Milwaukee, and was asked to comment on the study, was impressed with nemolizumab’s propensity for blocking IL-31. “To be able to treat PN effectively by simply blocking the itch and not having a significant inflammatory function is really interesting,” he said in an interview at the meeting. If approved, nemolizumab “gives us another treatment option for a disease that is really debilitating. It’s very promising and we hope [the drug] will be available to us in the near future.”
Nemolizumab is being developed by Galderma. According to a press release from the company, nemolizumab was granted Breakthrough Therapy designation by the Food and Drug Administration in December 2019 for the treatment of pruritus associated with PN, a status that was reconfirmed in February 2023.
Dr. Kwatra disclosed that he is an advisory board member/consultant for Galderma, AbbVie, Amgen, Arcutis, ASLAN Pharmaceuticals, Cara Therapeutics, Castle Biosciences, Celldex, Incyte, Johnson and Johnson, Leo Pharma, Novartis, Pfizer, Regeneron, and Sanofi. Dr. Gordon disclosed that he is a consultant to, an investigator for, and/or a member of the advisory board for several pharmaceutical companies, but not Galderma.
AT AAD 2023