User login
Can Telehealth Improve Access to Amyloid-Targeting Therapies for Veterans Living With Alzheimer Disease?
Can Telehealth Improve Access to Amyloid-Targeting Therapies for Veterans Living With Alzheimer Disease?
The Veterans Health Administration (VHA) is the largest US integrated health care system, providing health care to > 9 million veterans annually. Dementia affects > 7.2 million Americans, and an estimated 450,000 veterans live with Alzheimer disease (AD).1,2 Compared with the general population, veterans have a higher burden of chronic medical conditions and are disproportionately affected by AD due to exposure to military-related risk factors (eg, traumatic brain injury and posttraumatic stress disorder) and the high prevalence of nonmilitary risk factors, such as cardiovascular disease. The VHA is a pioneer in dementia care, having established a Dementia System of Care to provide primary and specialty care to veterans with dementia. The VHA also is leading the way in implementing the Institute for Healthcare Improvement Age-Friendly Health Systems (AFHS) framework for providing goal-concordant care in > 100 VHA medical centers. The VHA aims to be the largest AFHS in the country.
AD profoundly affects individuals and their families. The progressive nature of the most common form of dementia diminishes the quality of life for patients as well as their care partners in an ongoing fashion, often leading to emotional, physical, and financial strain. Costs for health and long-term care for people living with AD and other dementias were projected at $360 billion in 2024, largely due to the need for nursing home care.1 Although several oral medications are available, their capacity to effectively mitigate the negative effects of AD is limited. Cholinesterase inhibitors and memantine may offer temporary symptomatic relief, but they do not alter disease progression.3 The use of these agents is relatively low, with about one-third of patients diagnosed with AD receiving these medications.4
Amyloid-Targeting Therapies
Recent advancements in biologics, particularly amyloid-targeting therapies, such as lecanemab and donanemab, offer new hope for managing AD. Older adults treated with these medications show less decline on measures of cognition and function than those receiving a placebo at 18 months.5,6 However, accessing and using these medications is challenging.
Use of amyloid-targeting therapies poses challenges. The medications are expensive, potentially placing a financial burden on patients, families, and health care systems.7 Determining initial eligibility for treatment requires a battery of cognitive assessments, laboratory tests, advanced radiologic studies (eg, magnetic resonance imaging [MRI] of the brain and amyloid positron emission tomography [PET] scans), and possible cerebrospinal fluid (CSF) testing. Frequent ongoing assessments are necessary to monitor safety and efficacy. These treatments carry substantial risks, particularly amyloid-related imaging abnormalities (ARIA) such as cerebral edema, microhemorrhages, and superficial siderosis. Therefore, follow-up assessments typically occur around months 2, 3, 4, and 7, depending on which medication is selected. Finally, at present, both agents must be intravenous (IV)-administered in a monitored clinical setting, which requires additional coordination, transportation, and cost.
Ongoing evaluations and in-person administration particularly affect patients and care partners with limitations regarding transportation, time off work, and navigating complex health care systems.8 VHA clinicians at sites that have implemented or are interested in implementing amyloid-targeting therapy programs endorse similar challenges when implementing these therapies in their US Department of Veterans Affairs (VA) medical centers (VAMCs).9
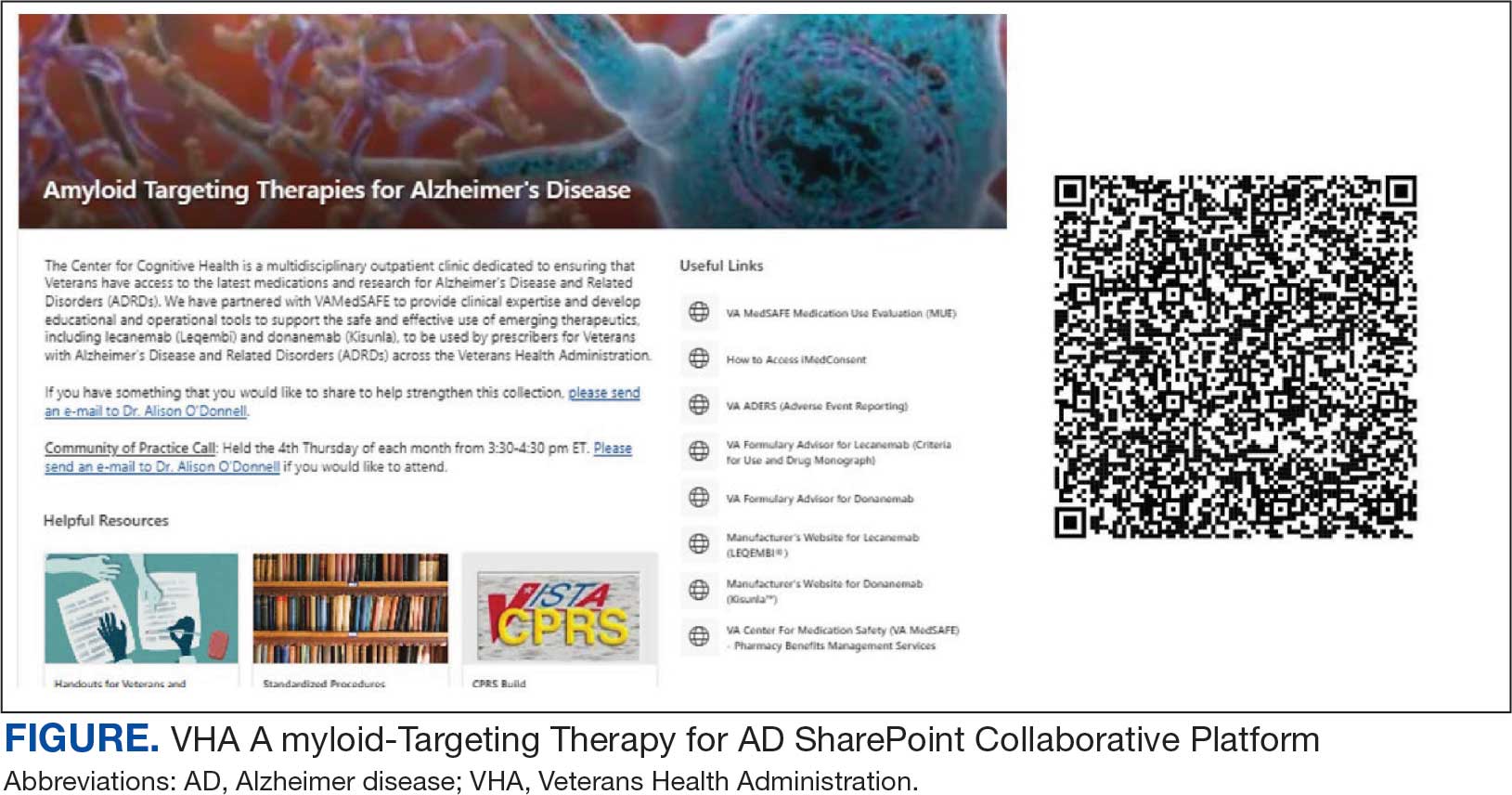
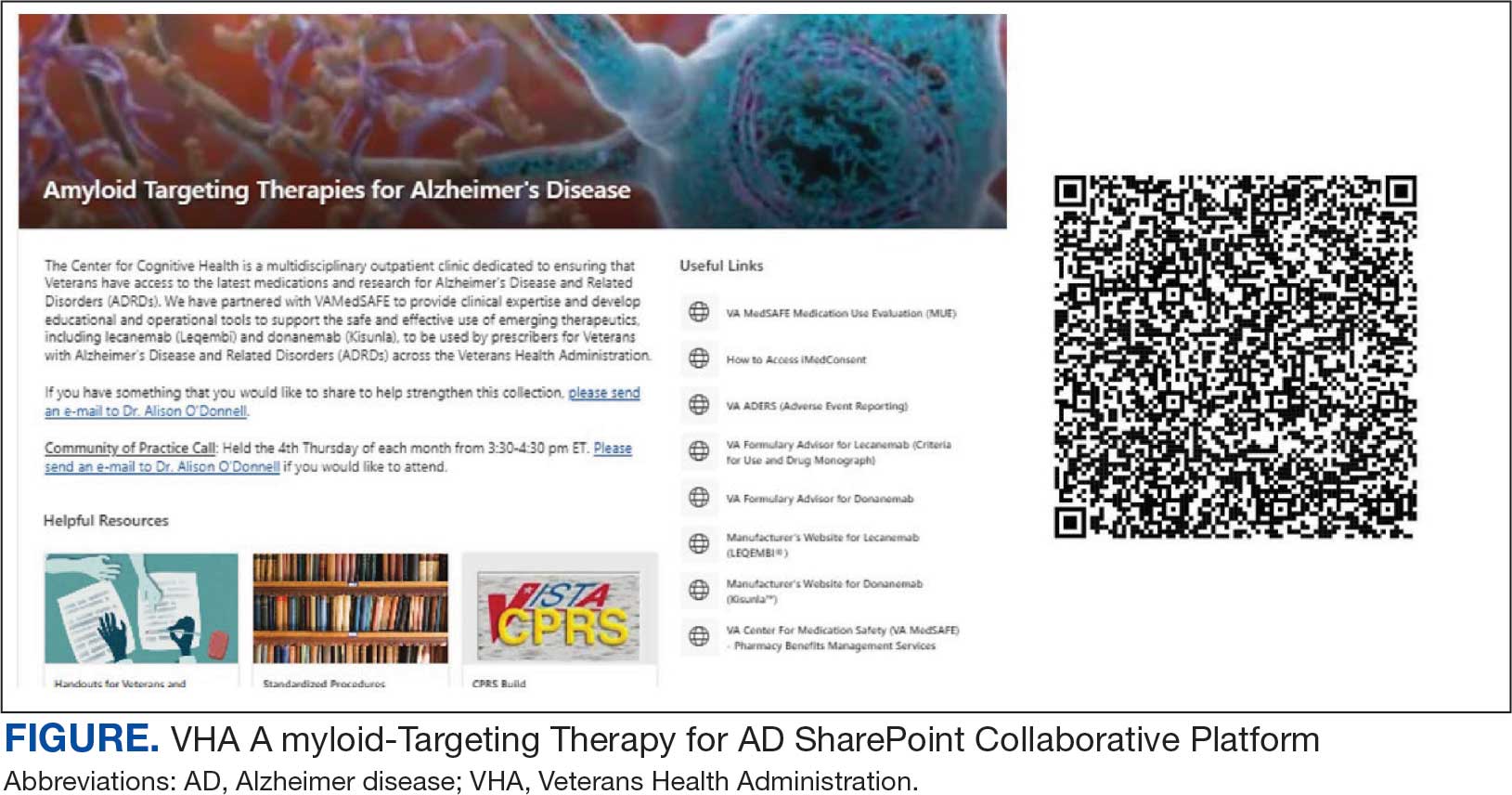
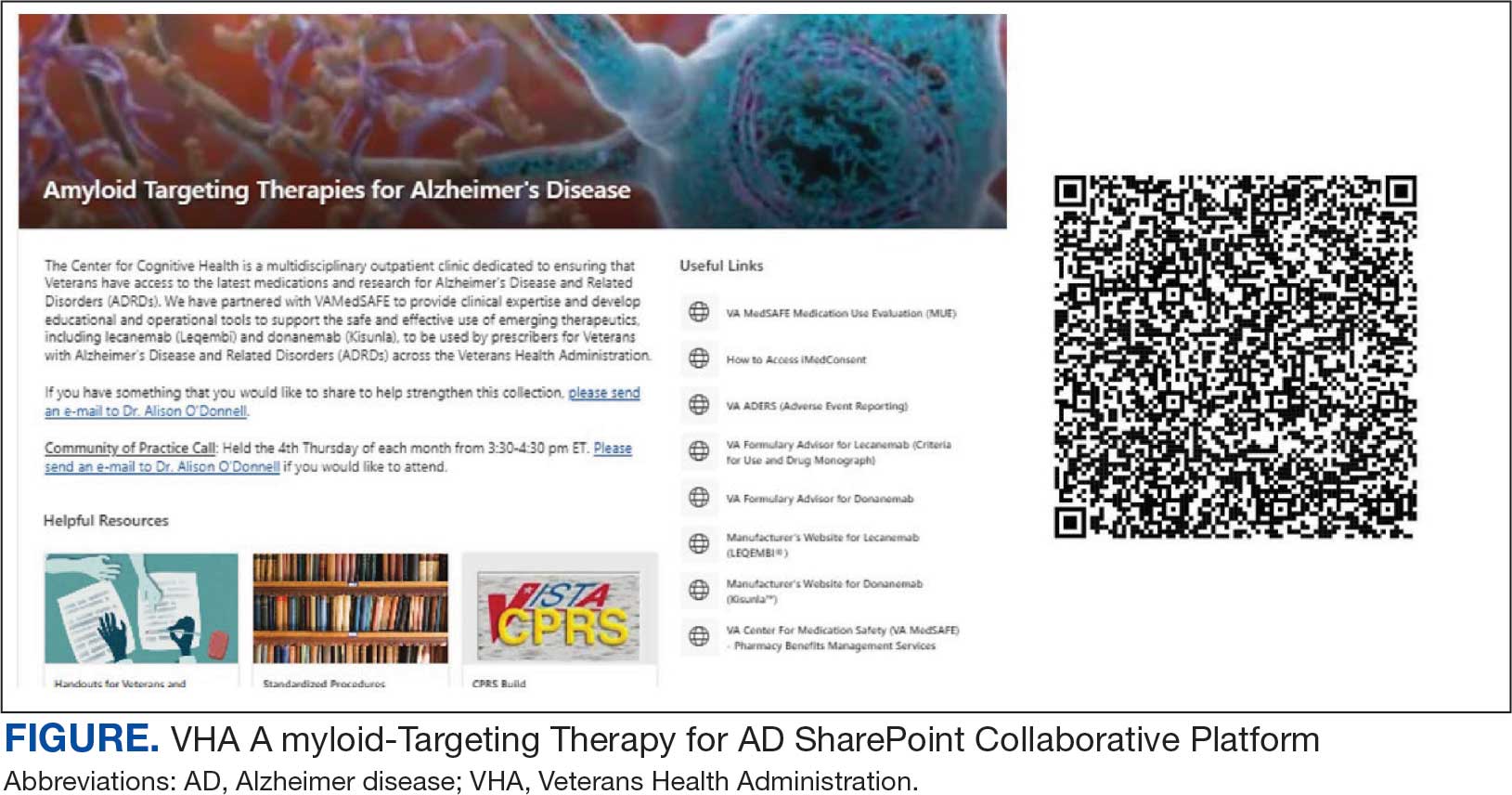
The VHA was one of the first health care systems to use amyloid-targeting therapies, covering the cost of lecanemab and donanemab, in addition to costs associated with concomitant evaluation and testing. However, given the safety concerns with this novel class of medications, the VHA National Formulary Committee developed criteria for use and recommended the VA Center for Medication Safety (VAMedSAFE) conduct a mandatory real-time medication use evaluation (MUE). VAMedSAFE developed the MUE to monitor the safe and appropriate use of amyloid-targeting therapy for AD. Two authors (AJO, SMH) partnered with VAMedSAFE through the VA Pittsburgh Healthcare System Technology Enhancing Cognition and Health–Geriatric Research, Education, and Clinical Center (TECH-GRECC) to provide clinical expertise, substantive feedback for the development of the MUE, and guidance for VHA sites starting amyloid targeting-therapy programs. We started a VHA Amyloid-Targeting Therapy for AD SharePoint collaborative platform and VHA AD Therapeutics Community of Practice (CoP) for shared learning (Figure). The private SharePoint platform houses an array of implementation materials for VAMCs starting programs: key documents and links; educational materials; sample guidelines; note templates; and electronic health record screenshots. The CoP allows VHAs to share best practices and discuss challenges.
Even with these advantages, we found that ensuring the safe and appropriate use of amyloid-targeting therapies did not overcome the barriers associated with their complexity. This was especially true for veterans living in rural areas. Only 4 VAMCs had administered amyloid-targeting therapies in the first year they were available. Preliminary data demonstrated that 27 (84%) of 32 veterans who initiated lecanemab in the VHA between October 2023 and September 2024 resided in urban areas.10 To address the underutilization of amyloid-targeting therapy, we propose leveraging the strengths of VHA telehealth to facilitate expansion of access to these medications for veterans with early AD. Telehealth may substantially increase access to evaluation for veterans with early dementia and, when medically appropriate, to receive amyloid-targeting therapies by reducing transportation needs and mitigating costs while ensuring appropriate monitoring through ongoing clinical assessments.
Using Telehealth
The VHA is a pioneer in telehealth, with programs dating back to 2003.11 Between October 1, 2018, and September 30, 2019, the VHA served > 900,000 veterans through the provision of > 2.6 million episodes of care via telehealth.12 The COVID-19 pandemic further cemented the role of telemedicine as an essential component of health care. Telehealth has demonstrated success in the assessment and management of individuals living with dementia. At the VHA, the GRECC-Connect Project is a partnership between 9 urban GRECC sites that seek to provide consultative geriatric and dementia care to rural veterans through telehealth.13 Additional evidence supports the potential to leverage telehealth to effectively communicate results of amyloid PET scans.14
This approach is not without limitations such as the digital divide, or the gap that separates technology-enabled individuals and those unprepared to adopt technology due to limited digital literacy levels or access to needed hardware, software, and connectivity. The VHA has taken steps to address these digital divide barriers by broadly providing tools—such as tablets and broadband connectivity—to veterans. Specifically, the VHA has instituted digital divide consults to determine whether telehealth could be a potential solution for appropriate veterans and to provide an iPad (if eligible) to connect with VA clinicians. Complementary to the digital divide consult, a VHA-specific telehealth preparedness assessment tool is under development and being tested by 2 authors (JF, SMH). This telehealth preparedness assessment tool is designed to aid in the seamless integration of telehealth services with the support of tailored education materials specific to gaps in digital literacy that a veteran might experience.
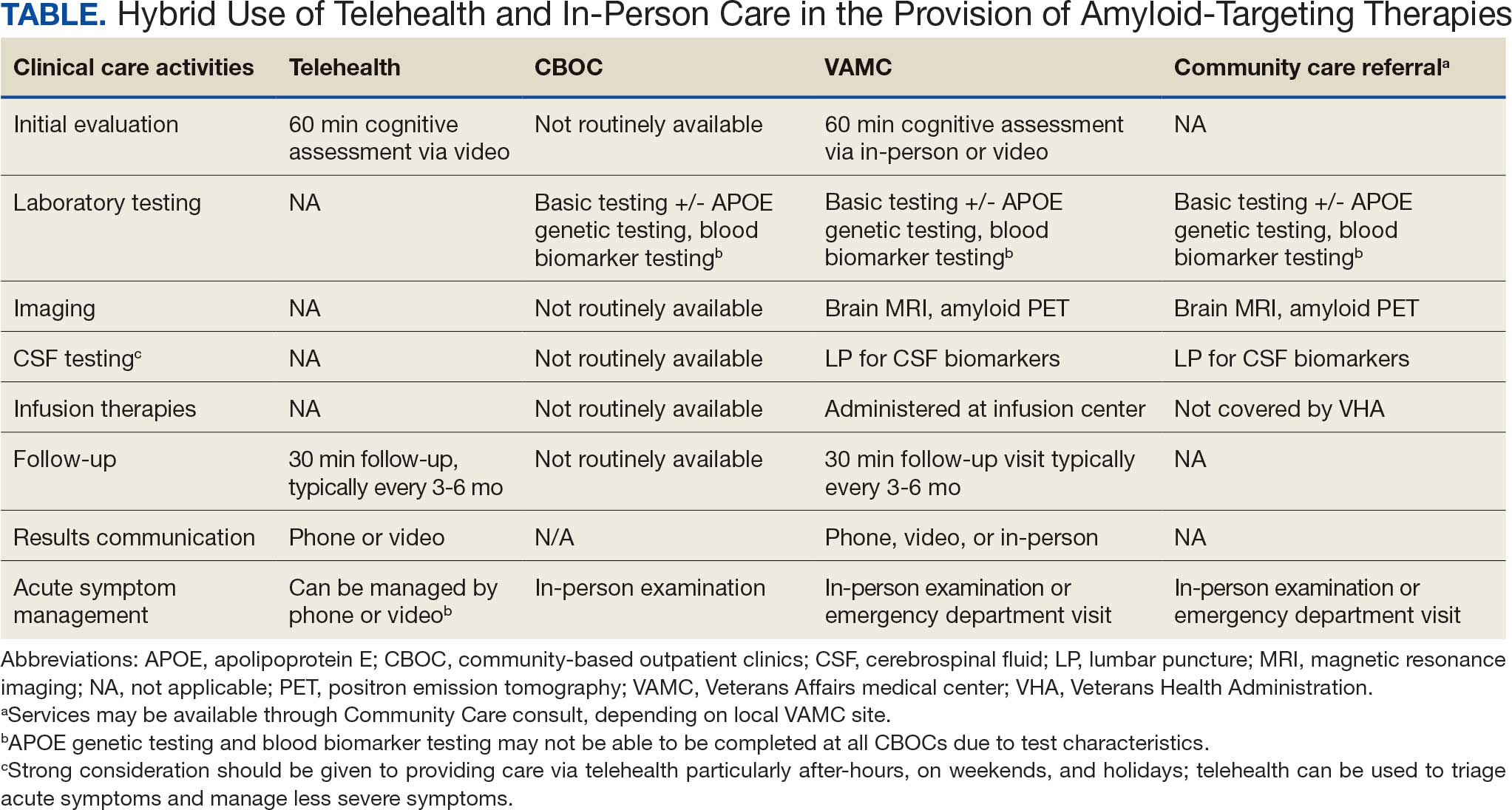
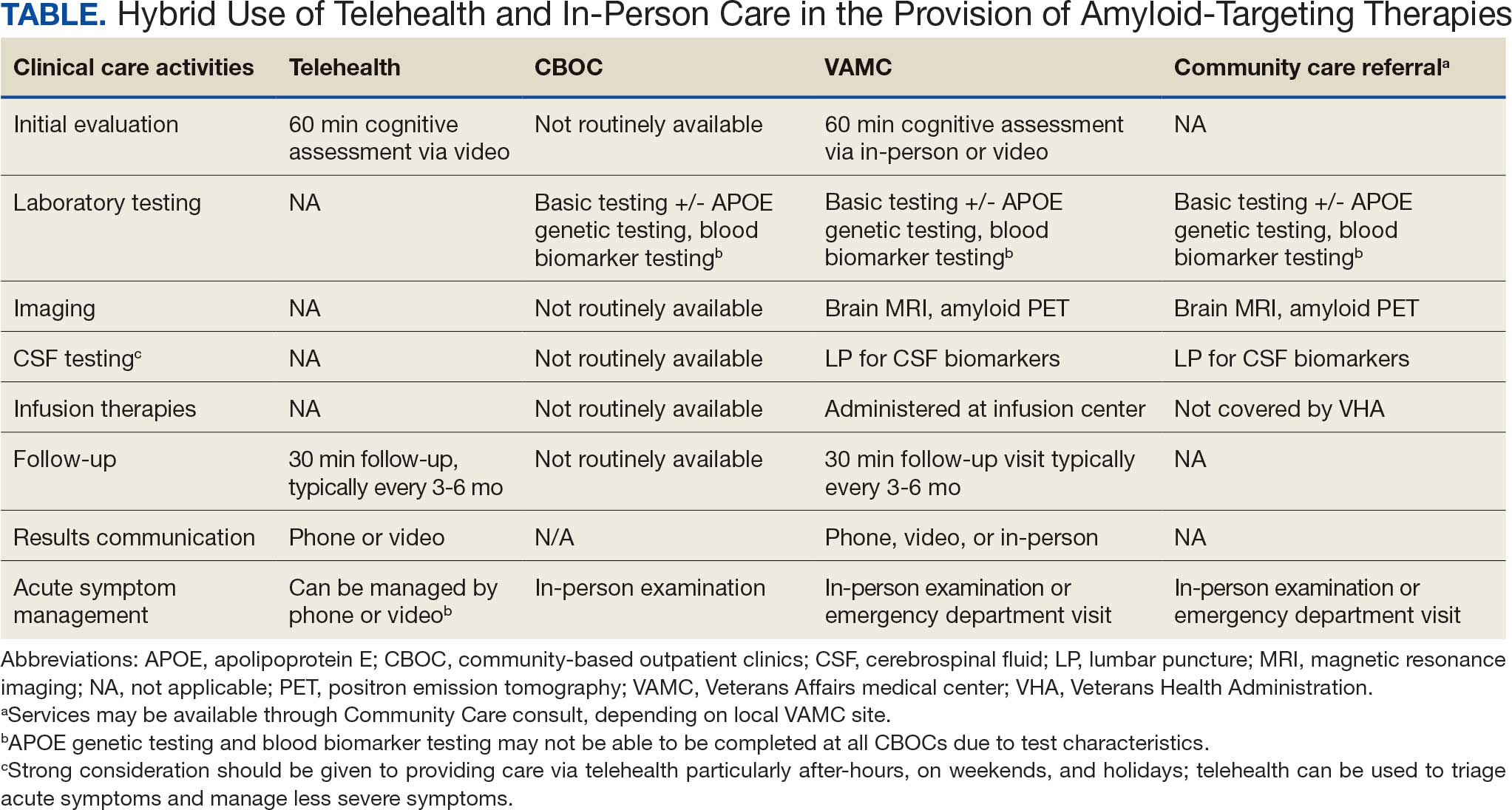
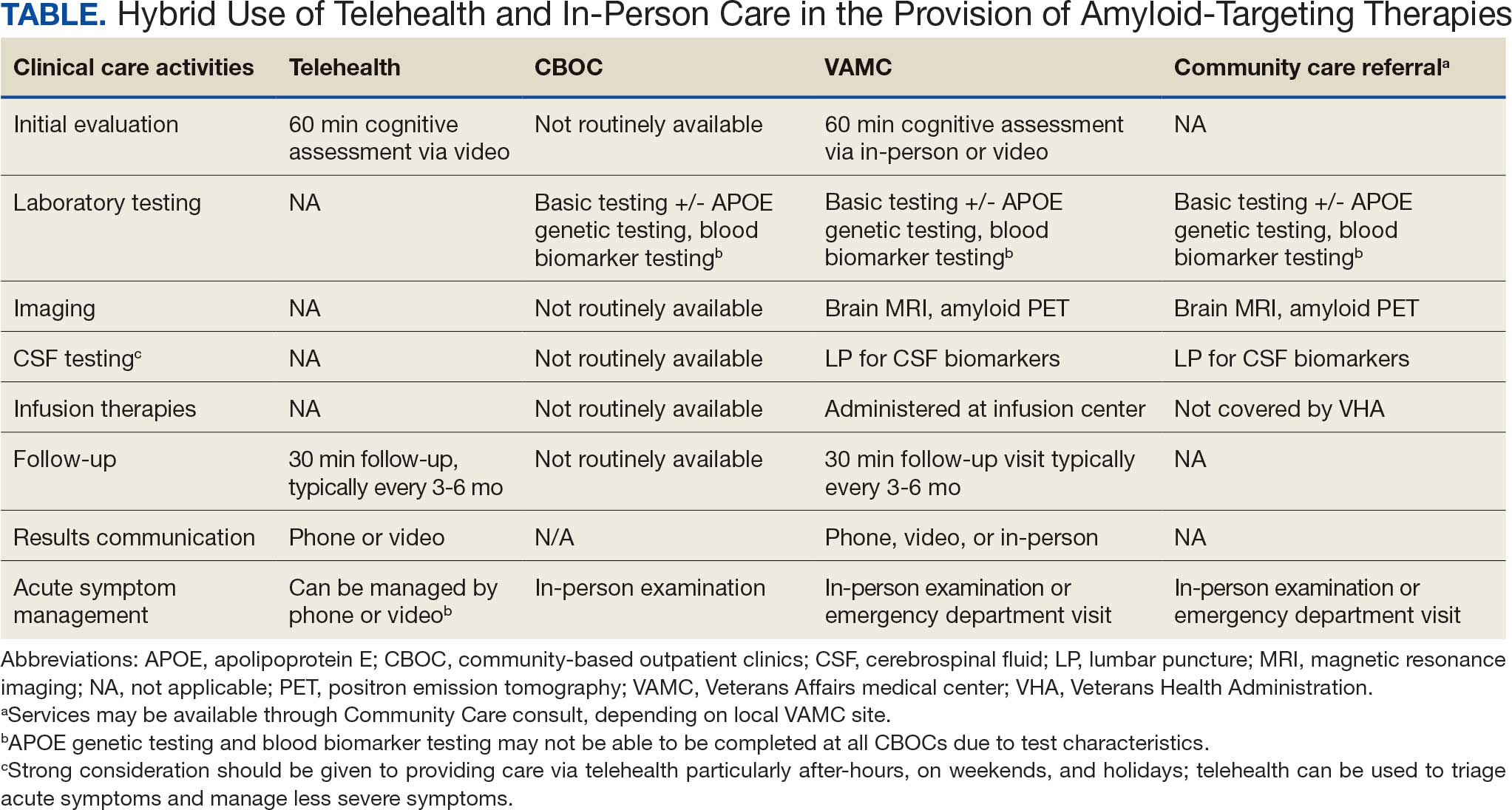
Building on these initiatives, there is an opportunity to expand access to amyloid-targeting therapies, regardless of distance to large VAMCs, by leveraging telehealth as an alternative method of connecting patients with specialty care. Specifically, a hybrid approach could be used to accomplish the myriad initial and follow-up tasks involved in the provision of amyloid-targeting therapies (Table). Not all VHA facilities possess the specialty expertise to prescribe these medications, and local clinicians may not have sufficient knowledge and clinical support to prescribe and monitor these therapies.
The first step is identifying local and regional subject matter experts, followed by the development and expansion of these networks. The National TeleNeurology Program is a good example of a national telehealth program that leverages technology to bring specialty services to rural areas with limited access to care. Although amyloid-targeting therapies often require more complex logistics, such as laboratory tests and imaging, these initial hurdles can be overcome through localized services and collaboration between VAMCs.
While treatment and imaging will most likely need to occur at a VAMC, most basic laboratory studies can be performed at community-based outpatient clinics (CBOCs). Some CBOCs may not be able to process more specialized laboratory tests such as apolipoprotein E genetic testing. Samples for these tests can be collected and processed at VAMCs, which usually have contracts with outside laboratories capable of performing these studies. Most, although not all, VAMCs offer advanced imaging, including MRI of the brain and amyloid PETs. VAMCs without those modalities may need to coordinate with other regional VAMCs. Additionally, a pilot program is already underway whereby VAMCs without the ability to quantify the amount of amyloid on PETs are able to leverage technology and collaborations with other VAMCs to obtain these data.
Once the initial phases of evaluation and care are completed, telemedicine can be leveraged for follow-up and ongoing management. Interdisciplinary teams can help facilitate care related to amyloid-targeting therapies, including the close monitoring of veterans for development of ARIA.15 To achieve this monitoring, specialty clinic teams prescribing amyloid-targeting therapies, which may be geographically distant, need to coordinate with local primary care clinical teams and emergency clinicians. All of these health care team members, along with neurologists and neurosurgeons, should be involved in the development and implementation of protocols in the event that patients present to their local primary or specialty care clinics or emergency department with ARIA symptoms.
If amyloid-targeting therapies are to be provided along with other emerging treatments for rural veterans, telehealth must be part of the solution. There is a pressing need to explore innovative evaluation and delivery models for these therapies, particularly as we expect additional diagnostics and therapeutics to be available in the future. With the advent of commercially available blood tests (ie, blood biomarkers) for AD, there is hope for a transition away from PETs and CSF testing given their cost, limited access, and invasiveness for diagnosis and monitoring of AD. These advances will increase the utility of telehealth to help rural veterans access amyloid-targeting therapies.
Additionally, administering the drug at home or at local clinics, supported by a dedicated health care team or home health agency, could further improve accessibility. Telehealth can be leveraged in this scenario, allowing specialty clinics and specialists to connect with patients and clinicians based out of local clinics or even home health agencies. In this scenario, specialists can provide hands-on care guidance and oversight even though they may be geographically distant from care recipients. Transitioning from IV administration to subcutaneous formulations would further enhance convenience and reduce barriers; these formulations may be available soon.16 Addressing logistical challenges to care and access through technology-based solutions will require coordinated efforts and continued VHA investment.
Conclusions
The VHA has a large population of veterans with dementia, and the costs to care for these veterans will only increase. While the current benefits of amyloid-targeting therapies are modest, now is the time to establish care processes that will support future innovations in amyloid-targeting therapies and other treatments and diagnostics. We are developing better ways to detect AD using clinical decision support tools, improving care pathways and the management of AD, and leveraging telehealth to improve access. The VA is conducting research to investigate whether a cognitive screening and laboratory evaluation that includes a telehealth preparedness assessment will be feasible and effective for improving the detection of AD and access to treatment, and we plan to publish the results.
The lessons learned can be extended to non-VHA care settings to help achieve potential benefits for other patients with early AD. Emerging therapies have the potential to improve the quality of life for both patients and care partners, adding life to years and not just years to life. Policymakers and payors must prioritize research funding to evaluate the safety and efficacy of these approaches to the delivery of health services, ensuring that emerging therapies are accessible for all individuals affected by AD.
- Alzheimer’s Association. 2025 Alzheimer’s disease facts and figures. Alzheimers Dement. 2025;21(4):e70235. doi:10.1002/alz.70235
- US Department of Veterans Affairs. Statistical Projections of Alzheimer’s Dementia for VA Patients, VA Enrollees, and US Veterans. December 18, 2020. Accessed November 2, 2025. https://www.va.gov/GERIATRICS/docs/VHA_ALZHEIMERS_DEMENTIA_Statistical_Projections_FY21_and_FY33_sgc121820.pdf
- Casey DA, Antimisiaris D, O’Brien J. Drugs for Alzheimer’s disease: are they effective? P T. 2010;35(4):208-211.
- Barthold D, Joyce G, Ferido P, et al. Pharmaceutical treatment for Alzheimer’s disease and related dementias: utilization and disparities. J Alzheimers Dis. 2020;76(2):579-589. doi:10.3233/JAD-200133
- Sims JR, Zimmer JA, Evans CD, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330(6):512-527. doi:10.1001/jama.2023.13239
- van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
- Tanne JH. Lecanemab: US Veterans Health Administration will cover cost of new Alzheimer’s drug. BMJ. 2023;380:p628. doi:10.1136/bmj.p628
- Nadeau SE. Lecanemab questions. Neurology. 2024;102(7):e209320. doi:10.1212/WNL.0000000000209320 9. O’Donnell AJ, Fortunato AT, Spitznogle BL, et al. Implementation of lecanemab for Alzheimer’s disease: facilitators and barriers. Presented at: American Geriatrics Society 2025 Annual Scientific Meeting, Chicago. May 2025.
- O’Donnell AJ, Zhao X, Parr A, et al. Use of lecanemab for Alzheimer’s disease within the Veteran’s Health Foundation: early findings. Abstract presented at: Alzheimer’s Association International Conference 2025; July 27, 2025; Toronto, Canada.
- O’Donnell AJ, Zhao X, Parr A, et al. Use of lecanemab for Alzheimer’s disease within the Veteran’s Health Foundation: early findings. Abstract presented at: Alzheimer’s Association International Conference 2025; July 27, 2025; Toronto, Canada.
- Hopp F, Whitten P, Subramanian U, et al. Perspectives from the Veterans Health Administration about opportunities and barriers in telemedicine. J Telemed Telecare. 2006;12(8):404-409. doi:10.1258/135763306779378717
- VA reports significant increase in veteran use of telehealth services. News release. US Department of Veterans Affairs. November 22, 2019. Accessed November 19, 2025. https://news.va.gov/press-room/va-reports-significant-increase-in-veteran-use-of-telehealth-services/
- Powers BB, Homer MC, Morone N, et al. Creation of an interprofessional teledementia clinic for rural veterans: preliminary data. J Am Geriatr Soc. 2017;65(5):1092-1099. doi:10.1111/jgs.14839
- Erickson CM, Chin NA, Rosario HL, et al. Feasibility of virtual Alzheimer’s biomarker disclosure: findings from an observational cohort. Alzheimers Dement (N Y). 2023;9(3):e12413. doi:10.1002/trc2.12413
- Turk KW, Knobel MD, Nothern A, et al. An interprofessional team for disease-modifying therapy in Alzheimer disease implementation. Neurol Clin Pract. 2024;14(6):e200346. doi:10.1212/CPJ.0000000000200346
- FDA accepts LEQEMBI® (lecanemab-irmb) biologics license application for subcutaneous maintenance dosing for the treatment of early Alzheimer’s disease. News release. Elsai US. January 13, 2025. Accessed November 2, 2025. https://media-us.eisai.com/2025-01-13-FDA-Accepts-LEQEMBI-R-lecanemab-irmb-Biologics-License-Application-for-Subcutaneous-Maintenance-Dosing-for-the-Treatment-of-Early-Alzheimers-Disease
The Veterans Health Administration (VHA) is the largest US integrated health care system, providing health care to > 9 million veterans annually. Dementia affects > 7.2 million Americans, and an estimated 450,000 veterans live with Alzheimer disease (AD).1,2 Compared with the general population, veterans have a higher burden of chronic medical conditions and are disproportionately affected by AD due to exposure to military-related risk factors (eg, traumatic brain injury and posttraumatic stress disorder) and the high prevalence of nonmilitary risk factors, such as cardiovascular disease. The VHA is a pioneer in dementia care, having established a Dementia System of Care to provide primary and specialty care to veterans with dementia. The VHA also is leading the way in implementing the Institute for Healthcare Improvement Age-Friendly Health Systems (AFHS) framework for providing goal-concordant care in > 100 VHA medical centers. The VHA aims to be the largest AFHS in the country.
AD profoundly affects individuals and their families. The progressive nature of the most common form of dementia diminishes the quality of life for patients as well as their care partners in an ongoing fashion, often leading to emotional, physical, and financial strain. Costs for health and long-term care for people living with AD and other dementias were projected at $360 billion in 2024, largely due to the need for nursing home care.1 Although several oral medications are available, their capacity to effectively mitigate the negative effects of AD is limited. Cholinesterase inhibitors and memantine may offer temporary symptomatic relief, but they do not alter disease progression.3 The use of these agents is relatively low, with about one-third of patients diagnosed with AD receiving these medications.4
Amyloid-Targeting Therapies
Recent advancements in biologics, particularly amyloid-targeting therapies, such as lecanemab and donanemab, offer new hope for managing AD. Older adults treated with these medications show less decline on measures of cognition and function than those receiving a placebo at 18 months.5,6 However, accessing and using these medications is challenging.
Use of amyloid-targeting therapies poses challenges. The medications are expensive, potentially placing a financial burden on patients, families, and health care systems.7 Determining initial eligibility for treatment requires a battery of cognitive assessments, laboratory tests, advanced radiologic studies (eg, magnetic resonance imaging [MRI] of the brain and amyloid positron emission tomography [PET] scans), and possible cerebrospinal fluid (CSF) testing. Frequent ongoing assessments are necessary to monitor safety and efficacy. These treatments carry substantial risks, particularly amyloid-related imaging abnormalities (ARIA) such as cerebral edema, microhemorrhages, and superficial siderosis. Therefore, follow-up assessments typically occur around months 2, 3, 4, and 7, depending on which medication is selected. Finally, at present, both agents must be intravenous (IV)-administered in a monitored clinical setting, which requires additional coordination, transportation, and cost.
Ongoing evaluations and in-person administration particularly affect patients and care partners with limitations regarding transportation, time off work, and navigating complex health care systems.8 VHA clinicians at sites that have implemented or are interested in implementing amyloid-targeting therapy programs endorse similar challenges when implementing these therapies in their US Department of Veterans Affairs (VA) medical centers (VAMCs).9
The VHA was one of the first health care systems to use amyloid-targeting therapies, covering the cost of lecanemab and donanemab, in addition to costs associated with concomitant evaluation and testing. However, given the safety concerns with this novel class of medications, the VHA National Formulary Committee developed criteria for use and recommended the VA Center for Medication Safety (VAMedSAFE) conduct a mandatory real-time medication use evaluation (MUE). VAMedSAFE developed the MUE to monitor the safe and appropriate use of amyloid-targeting therapy for AD. Two authors (AJO, SMH) partnered with VAMedSAFE through the VA Pittsburgh Healthcare System Technology Enhancing Cognition and Health–Geriatric Research, Education, and Clinical Center (TECH-GRECC) to provide clinical expertise, substantive feedback for the development of the MUE, and guidance for VHA sites starting amyloid targeting-therapy programs. We started a VHA Amyloid-Targeting Therapy for AD SharePoint collaborative platform and VHA AD Therapeutics Community of Practice (CoP) for shared learning (Figure). The private SharePoint platform houses an array of implementation materials for VAMCs starting programs: key documents and links; educational materials; sample guidelines; note templates; and electronic health record screenshots. The CoP allows VHAs to share best practices and discuss challenges.
Even with these advantages, we found that ensuring the safe and appropriate use of amyloid-targeting therapies did not overcome the barriers associated with their complexity. This was especially true for veterans living in rural areas. Only 4 VAMCs had administered amyloid-targeting therapies in the first year they were available. Preliminary data demonstrated that 27 (84%) of 32 veterans who initiated lecanemab in the VHA between October 2023 and September 2024 resided in urban areas.10 To address the underutilization of amyloid-targeting therapy, we propose leveraging the strengths of VHA telehealth to facilitate expansion of access to these medications for veterans with early AD. Telehealth may substantially increase access to evaluation for veterans with early dementia and, when medically appropriate, to receive amyloid-targeting therapies by reducing transportation needs and mitigating costs while ensuring appropriate monitoring through ongoing clinical assessments.
Using Telehealth
The VHA is a pioneer in telehealth, with programs dating back to 2003.11 Between October 1, 2018, and September 30, 2019, the VHA served > 900,000 veterans through the provision of > 2.6 million episodes of care via telehealth.12 The COVID-19 pandemic further cemented the role of telemedicine as an essential component of health care. Telehealth has demonstrated success in the assessment and management of individuals living with dementia. At the VHA, the GRECC-Connect Project is a partnership between 9 urban GRECC sites that seek to provide consultative geriatric and dementia care to rural veterans through telehealth.13 Additional evidence supports the potential to leverage telehealth to effectively communicate results of amyloid PET scans.14
This approach is not without limitations such as the digital divide, or the gap that separates technology-enabled individuals and those unprepared to adopt technology due to limited digital literacy levels or access to needed hardware, software, and connectivity. The VHA has taken steps to address these digital divide barriers by broadly providing tools—such as tablets and broadband connectivity—to veterans. Specifically, the VHA has instituted digital divide consults to determine whether telehealth could be a potential solution for appropriate veterans and to provide an iPad (if eligible) to connect with VA clinicians. Complementary to the digital divide consult, a VHA-specific telehealth preparedness assessment tool is under development and being tested by 2 authors (JF, SMH). This telehealth preparedness assessment tool is designed to aid in the seamless integration of telehealth services with the support of tailored education materials specific to gaps in digital literacy that a veteran might experience.
Building on these initiatives, there is an opportunity to expand access to amyloid-targeting therapies, regardless of distance to large VAMCs, by leveraging telehealth as an alternative method of connecting patients with specialty care. Specifically, a hybrid approach could be used to accomplish the myriad initial and follow-up tasks involved in the provision of amyloid-targeting therapies (Table). Not all VHA facilities possess the specialty expertise to prescribe these medications, and local clinicians may not have sufficient knowledge and clinical support to prescribe and monitor these therapies.
The first step is identifying local and regional subject matter experts, followed by the development and expansion of these networks. The National TeleNeurology Program is a good example of a national telehealth program that leverages technology to bring specialty services to rural areas with limited access to care. Although amyloid-targeting therapies often require more complex logistics, such as laboratory tests and imaging, these initial hurdles can be overcome through localized services and collaboration between VAMCs.
While treatment and imaging will most likely need to occur at a VAMC, most basic laboratory studies can be performed at community-based outpatient clinics (CBOCs). Some CBOCs may not be able to process more specialized laboratory tests such as apolipoprotein E genetic testing. Samples for these tests can be collected and processed at VAMCs, which usually have contracts with outside laboratories capable of performing these studies. Most, although not all, VAMCs offer advanced imaging, including MRI of the brain and amyloid PETs. VAMCs without those modalities may need to coordinate with other regional VAMCs. Additionally, a pilot program is already underway whereby VAMCs without the ability to quantify the amount of amyloid on PETs are able to leverage technology and collaborations with other VAMCs to obtain these data.
Once the initial phases of evaluation and care are completed, telemedicine can be leveraged for follow-up and ongoing management. Interdisciplinary teams can help facilitate care related to amyloid-targeting therapies, including the close monitoring of veterans for development of ARIA.15 To achieve this monitoring, specialty clinic teams prescribing amyloid-targeting therapies, which may be geographically distant, need to coordinate with local primary care clinical teams and emergency clinicians. All of these health care team members, along with neurologists and neurosurgeons, should be involved in the development and implementation of protocols in the event that patients present to their local primary or specialty care clinics or emergency department with ARIA symptoms.
If amyloid-targeting therapies are to be provided along with other emerging treatments for rural veterans, telehealth must be part of the solution. There is a pressing need to explore innovative evaluation and delivery models for these therapies, particularly as we expect additional diagnostics and therapeutics to be available in the future. With the advent of commercially available blood tests (ie, blood biomarkers) for AD, there is hope for a transition away from PETs and CSF testing given their cost, limited access, and invasiveness for diagnosis and monitoring of AD. These advances will increase the utility of telehealth to help rural veterans access amyloid-targeting therapies.
Additionally, administering the drug at home or at local clinics, supported by a dedicated health care team or home health agency, could further improve accessibility. Telehealth can be leveraged in this scenario, allowing specialty clinics and specialists to connect with patients and clinicians based out of local clinics or even home health agencies. In this scenario, specialists can provide hands-on care guidance and oversight even though they may be geographically distant from care recipients. Transitioning from IV administration to subcutaneous formulations would further enhance convenience and reduce barriers; these formulations may be available soon.16 Addressing logistical challenges to care and access through technology-based solutions will require coordinated efforts and continued VHA investment.
Conclusions
The VHA has a large population of veterans with dementia, and the costs to care for these veterans will only increase. While the current benefits of amyloid-targeting therapies are modest, now is the time to establish care processes that will support future innovations in amyloid-targeting therapies and other treatments and diagnostics. We are developing better ways to detect AD using clinical decision support tools, improving care pathways and the management of AD, and leveraging telehealth to improve access. The VA is conducting research to investigate whether a cognitive screening and laboratory evaluation that includes a telehealth preparedness assessment will be feasible and effective for improving the detection of AD and access to treatment, and we plan to publish the results.
The lessons learned can be extended to non-VHA care settings to help achieve potential benefits for other patients with early AD. Emerging therapies have the potential to improve the quality of life for both patients and care partners, adding life to years and not just years to life. Policymakers and payors must prioritize research funding to evaluate the safety and efficacy of these approaches to the delivery of health services, ensuring that emerging therapies are accessible for all individuals affected by AD.
The Veterans Health Administration (VHA) is the largest US integrated health care system, providing health care to > 9 million veterans annually. Dementia affects > 7.2 million Americans, and an estimated 450,000 veterans live with Alzheimer disease (AD).1,2 Compared with the general population, veterans have a higher burden of chronic medical conditions and are disproportionately affected by AD due to exposure to military-related risk factors (eg, traumatic brain injury and posttraumatic stress disorder) and the high prevalence of nonmilitary risk factors, such as cardiovascular disease. The VHA is a pioneer in dementia care, having established a Dementia System of Care to provide primary and specialty care to veterans with dementia. The VHA also is leading the way in implementing the Institute for Healthcare Improvement Age-Friendly Health Systems (AFHS) framework for providing goal-concordant care in > 100 VHA medical centers. The VHA aims to be the largest AFHS in the country.
AD profoundly affects individuals and their families. The progressive nature of the most common form of dementia diminishes the quality of life for patients as well as their care partners in an ongoing fashion, often leading to emotional, physical, and financial strain. Costs for health and long-term care for people living with AD and other dementias were projected at $360 billion in 2024, largely due to the need for nursing home care.1 Although several oral medications are available, their capacity to effectively mitigate the negative effects of AD is limited. Cholinesterase inhibitors and memantine may offer temporary symptomatic relief, but they do not alter disease progression.3 The use of these agents is relatively low, with about one-third of patients diagnosed with AD receiving these medications.4
Amyloid-Targeting Therapies
Recent advancements in biologics, particularly amyloid-targeting therapies, such as lecanemab and donanemab, offer new hope for managing AD. Older adults treated with these medications show less decline on measures of cognition and function than those receiving a placebo at 18 months.5,6 However, accessing and using these medications is challenging.
Use of amyloid-targeting therapies poses challenges. The medications are expensive, potentially placing a financial burden on patients, families, and health care systems.7 Determining initial eligibility for treatment requires a battery of cognitive assessments, laboratory tests, advanced radiologic studies (eg, magnetic resonance imaging [MRI] of the brain and amyloid positron emission tomography [PET] scans), and possible cerebrospinal fluid (CSF) testing. Frequent ongoing assessments are necessary to monitor safety and efficacy. These treatments carry substantial risks, particularly amyloid-related imaging abnormalities (ARIA) such as cerebral edema, microhemorrhages, and superficial siderosis. Therefore, follow-up assessments typically occur around months 2, 3, 4, and 7, depending on which medication is selected. Finally, at present, both agents must be intravenous (IV)-administered in a monitored clinical setting, which requires additional coordination, transportation, and cost.
Ongoing evaluations and in-person administration particularly affect patients and care partners with limitations regarding transportation, time off work, and navigating complex health care systems.8 VHA clinicians at sites that have implemented or are interested in implementing amyloid-targeting therapy programs endorse similar challenges when implementing these therapies in their US Department of Veterans Affairs (VA) medical centers (VAMCs).9
The VHA was one of the first health care systems to use amyloid-targeting therapies, covering the cost of lecanemab and donanemab, in addition to costs associated with concomitant evaluation and testing. However, given the safety concerns with this novel class of medications, the VHA National Formulary Committee developed criteria for use and recommended the VA Center for Medication Safety (VAMedSAFE) conduct a mandatory real-time medication use evaluation (MUE). VAMedSAFE developed the MUE to monitor the safe and appropriate use of amyloid-targeting therapy for AD. Two authors (AJO, SMH) partnered with VAMedSAFE through the VA Pittsburgh Healthcare System Technology Enhancing Cognition and Health–Geriatric Research, Education, and Clinical Center (TECH-GRECC) to provide clinical expertise, substantive feedback for the development of the MUE, and guidance for VHA sites starting amyloid targeting-therapy programs. We started a VHA Amyloid-Targeting Therapy for AD SharePoint collaborative platform and VHA AD Therapeutics Community of Practice (CoP) for shared learning (Figure). The private SharePoint platform houses an array of implementation materials for VAMCs starting programs: key documents and links; educational materials; sample guidelines; note templates; and electronic health record screenshots. The CoP allows VHAs to share best practices and discuss challenges.
Even with these advantages, we found that ensuring the safe and appropriate use of amyloid-targeting therapies did not overcome the barriers associated with their complexity. This was especially true for veterans living in rural areas. Only 4 VAMCs had administered amyloid-targeting therapies in the first year they were available. Preliminary data demonstrated that 27 (84%) of 32 veterans who initiated lecanemab in the VHA between October 2023 and September 2024 resided in urban areas.10 To address the underutilization of amyloid-targeting therapy, we propose leveraging the strengths of VHA telehealth to facilitate expansion of access to these medications for veterans with early AD. Telehealth may substantially increase access to evaluation for veterans with early dementia and, when medically appropriate, to receive amyloid-targeting therapies by reducing transportation needs and mitigating costs while ensuring appropriate monitoring through ongoing clinical assessments.
Using Telehealth
The VHA is a pioneer in telehealth, with programs dating back to 2003.11 Between October 1, 2018, and September 30, 2019, the VHA served > 900,000 veterans through the provision of > 2.6 million episodes of care via telehealth.12 The COVID-19 pandemic further cemented the role of telemedicine as an essential component of health care. Telehealth has demonstrated success in the assessment and management of individuals living with dementia. At the VHA, the GRECC-Connect Project is a partnership between 9 urban GRECC sites that seek to provide consultative geriatric and dementia care to rural veterans through telehealth.13 Additional evidence supports the potential to leverage telehealth to effectively communicate results of amyloid PET scans.14
This approach is not without limitations such as the digital divide, or the gap that separates technology-enabled individuals and those unprepared to adopt technology due to limited digital literacy levels or access to needed hardware, software, and connectivity. The VHA has taken steps to address these digital divide barriers by broadly providing tools—such as tablets and broadband connectivity—to veterans. Specifically, the VHA has instituted digital divide consults to determine whether telehealth could be a potential solution for appropriate veterans and to provide an iPad (if eligible) to connect with VA clinicians. Complementary to the digital divide consult, a VHA-specific telehealth preparedness assessment tool is under development and being tested by 2 authors (JF, SMH). This telehealth preparedness assessment tool is designed to aid in the seamless integration of telehealth services with the support of tailored education materials specific to gaps in digital literacy that a veteran might experience.
Building on these initiatives, there is an opportunity to expand access to amyloid-targeting therapies, regardless of distance to large VAMCs, by leveraging telehealth as an alternative method of connecting patients with specialty care. Specifically, a hybrid approach could be used to accomplish the myriad initial and follow-up tasks involved in the provision of amyloid-targeting therapies (Table). Not all VHA facilities possess the specialty expertise to prescribe these medications, and local clinicians may not have sufficient knowledge and clinical support to prescribe and monitor these therapies.
The first step is identifying local and regional subject matter experts, followed by the development and expansion of these networks. The National TeleNeurology Program is a good example of a national telehealth program that leverages technology to bring specialty services to rural areas with limited access to care. Although amyloid-targeting therapies often require more complex logistics, such as laboratory tests and imaging, these initial hurdles can be overcome through localized services and collaboration between VAMCs.
While treatment and imaging will most likely need to occur at a VAMC, most basic laboratory studies can be performed at community-based outpatient clinics (CBOCs). Some CBOCs may not be able to process more specialized laboratory tests such as apolipoprotein E genetic testing. Samples for these tests can be collected and processed at VAMCs, which usually have contracts with outside laboratories capable of performing these studies. Most, although not all, VAMCs offer advanced imaging, including MRI of the brain and amyloid PETs. VAMCs without those modalities may need to coordinate with other regional VAMCs. Additionally, a pilot program is already underway whereby VAMCs without the ability to quantify the amount of amyloid on PETs are able to leverage technology and collaborations with other VAMCs to obtain these data.
Once the initial phases of evaluation and care are completed, telemedicine can be leveraged for follow-up and ongoing management. Interdisciplinary teams can help facilitate care related to amyloid-targeting therapies, including the close monitoring of veterans for development of ARIA.15 To achieve this monitoring, specialty clinic teams prescribing amyloid-targeting therapies, which may be geographically distant, need to coordinate with local primary care clinical teams and emergency clinicians. All of these health care team members, along with neurologists and neurosurgeons, should be involved in the development and implementation of protocols in the event that patients present to their local primary or specialty care clinics or emergency department with ARIA symptoms.
If amyloid-targeting therapies are to be provided along with other emerging treatments for rural veterans, telehealth must be part of the solution. There is a pressing need to explore innovative evaluation and delivery models for these therapies, particularly as we expect additional diagnostics and therapeutics to be available in the future. With the advent of commercially available blood tests (ie, blood biomarkers) for AD, there is hope for a transition away from PETs and CSF testing given their cost, limited access, and invasiveness for diagnosis and monitoring of AD. These advances will increase the utility of telehealth to help rural veterans access amyloid-targeting therapies.
Additionally, administering the drug at home or at local clinics, supported by a dedicated health care team or home health agency, could further improve accessibility. Telehealth can be leveraged in this scenario, allowing specialty clinics and specialists to connect with patients and clinicians based out of local clinics or even home health agencies. In this scenario, specialists can provide hands-on care guidance and oversight even though they may be geographically distant from care recipients. Transitioning from IV administration to subcutaneous formulations would further enhance convenience and reduce barriers; these formulations may be available soon.16 Addressing logistical challenges to care and access through technology-based solutions will require coordinated efforts and continued VHA investment.
Conclusions
The VHA has a large population of veterans with dementia, and the costs to care for these veterans will only increase. While the current benefits of amyloid-targeting therapies are modest, now is the time to establish care processes that will support future innovations in amyloid-targeting therapies and other treatments and diagnostics. We are developing better ways to detect AD using clinical decision support tools, improving care pathways and the management of AD, and leveraging telehealth to improve access. The VA is conducting research to investigate whether a cognitive screening and laboratory evaluation that includes a telehealth preparedness assessment will be feasible and effective for improving the detection of AD and access to treatment, and we plan to publish the results.
The lessons learned can be extended to non-VHA care settings to help achieve potential benefits for other patients with early AD. Emerging therapies have the potential to improve the quality of life for both patients and care partners, adding life to years and not just years to life. Policymakers and payors must prioritize research funding to evaluate the safety and efficacy of these approaches to the delivery of health services, ensuring that emerging therapies are accessible for all individuals affected by AD.
- Alzheimer’s Association. 2025 Alzheimer’s disease facts and figures. Alzheimers Dement. 2025;21(4):e70235. doi:10.1002/alz.70235
- US Department of Veterans Affairs. Statistical Projections of Alzheimer’s Dementia for VA Patients, VA Enrollees, and US Veterans. December 18, 2020. Accessed November 2, 2025. https://www.va.gov/GERIATRICS/docs/VHA_ALZHEIMERS_DEMENTIA_Statistical_Projections_FY21_and_FY33_sgc121820.pdf
- Casey DA, Antimisiaris D, O’Brien J. Drugs for Alzheimer’s disease: are they effective? P T. 2010;35(4):208-211.
- Barthold D, Joyce G, Ferido P, et al. Pharmaceutical treatment for Alzheimer’s disease and related dementias: utilization and disparities. J Alzheimers Dis. 2020;76(2):579-589. doi:10.3233/JAD-200133
- Sims JR, Zimmer JA, Evans CD, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330(6):512-527. doi:10.1001/jama.2023.13239
- van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
- Tanne JH. Lecanemab: US Veterans Health Administration will cover cost of new Alzheimer’s drug. BMJ. 2023;380:p628. doi:10.1136/bmj.p628
- Nadeau SE. Lecanemab questions. Neurology. 2024;102(7):e209320. doi:10.1212/WNL.0000000000209320 9. O’Donnell AJ, Fortunato AT, Spitznogle BL, et al. Implementation of lecanemab for Alzheimer’s disease: facilitators and barriers. Presented at: American Geriatrics Society 2025 Annual Scientific Meeting, Chicago. May 2025.
- O’Donnell AJ, Zhao X, Parr A, et al. Use of lecanemab for Alzheimer’s disease within the Veteran’s Health Foundation: early findings. Abstract presented at: Alzheimer’s Association International Conference 2025; July 27, 2025; Toronto, Canada.
- O’Donnell AJ, Zhao X, Parr A, et al. Use of lecanemab for Alzheimer’s disease within the Veteran’s Health Foundation: early findings. Abstract presented at: Alzheimer’s Association International Conference 2025; July 27, 2025; Toronto, Canada.
- Hopp F, Whitten P, Subramanian U, et al. Perspectives from the Veterans Health Administration about opportunities and barriers in telemedicine. J Telemed Telecare. 2006;12(8):404-409. doi:10.1258/135763306779378717
- VA reports significant increase in veteran use of telehealth services. News release. US Department of Veterans Affairs. November 22, 2019. Accessed November 19, 2025. https://news.va.gov/press-room/va-reports-significant-increase-in-veteran-use-of-telehealth-services/
- Powers BB, Homer MC, Morone N, et al. Creation of an interprofessional teledementia clinic for rural veterans: preliminary data. J Am Geriatr Soc. 2017;65(5):1092-1099. doi:10.1111/jgs.14839
- Erickson CM, Chin NA, Rosario HL, et al. Feasibility of virtual Alzheimer’s biomarker disclosure: findings from an observational cohort. Alzheimers Dement (N Y). 2023;9(3):e12413. doi:10.1002/trc2.12413
- Turk KW, Knobel MD, Nothern A, et al. An interprofessional team for disease-modifying therapy in Alzheimer disease implementation. Neurol Clin Pract. 2024;14(6):e200346. doi:10.1212/CPJ.0000000000200346
- FDA accepts LEQEMBI® (lecanemab-irmb) biologics license application for subcutaneous maintenance dosing for the treatment of early Alzheimer’s disease. News release. Elsai US. January 13, 2025. Accessed November 2, 2025. https://media-us.eisai.com/2025-01-13-FDA-Accepts-LEQEMBI-R-lecanemab-irmb-Biologics-License-Application-for-Subcutaneous-Maintenance-Dosing-for-the-Treatment-of-Early-Alzheimers-Disease
- Alzheimer’s Association. 2025 Alzheimer’s disease facts and figures. Alzheimers Dement. 2025;21(4):e70235. doi:10.1002/alz.70235
- US Department of Veterans Affairs. Statistical Projections of Alzheimer’s Dementia for VA Patients, VA Enrollees, and US Veterans. December 18, 2020. Accessed November 2, 2025. https://www.va.gov/GERIATRICS/docs/VHA_ALZHEIMERS_DEMENTIA_Statistical_Projections_FY21_and_FY33_sgc121820.pdf
- Casey DA, Antimisiaris D, O’Brien J. Drugs for Alzheimer’s disease: are they effective? P T. 2010;35(4):208-211.
- Barthold D, Joyce G, Ferido P, et al. Pharmaceutical treatment for Alzheimer’s disease and related dementias: utilization and disparities. J Alzheimers Dis. 2020;76(2):579-589. doi:10.3233/JAD-200133
- Sims JR, Zimmer JA, Evans CD, et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA. 2023;330(6):512-527. doi:10.1001/jama.2023.13239
- van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in early Alzheimer’s disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
- Tanne JH. Lecanemab: US Veterans Health Administration will cover cost of new Alzheimer’s drug. BMJ. 2023;380:p628. doi:10.1136/bmj.p628
- Nadeau SE. Lecanemab questions. Neurology. 2024;102(7):e209320. doi:10.1212/WNL.0000000000209320 9. O’Donnell AJ, Fortunato AT, Spitznogle BL, et al. Implementation of lecanemab for Alzheimer’s disease: facilitators and barriers. Presented at: American Geriatrics Society 2025 Annual Scientific Meeting, Chicago. May 2025.
- O’Donnell AJ, Zhao X, Parr A, et al. Use of lecanemab for Alzheimer’s disease within the Veteran’s Health Foundation: early findings. Abstract presented at: Alzheimer’s Association International Conference 2025; July 27, 2025; Toronto, Canada.
- O’Donnell AJ, Zhao X, Parr A, et al. Use of lecanemab for Alzheimer’s disease within the Veteran’s Health Foundation: early findings. Abstract presented at: Alzheimer’s Association International Conference 2025; July 27, 2025; Toronto, Canada.
- Hopp F, Whitten P, Subramanian U, et al. Perspectives from the Veterans Health Administration about opportunities and barriers in telemedicine. J Telemed Telecare. 2006;12(8):404-409. doi:10.1258/135763306779378717
- VA reports significant increase in veteran use of telehealth services. News release. US Department of Veterans Affairs. November 22, 2019. Accessed November 19, 2025. https://news.va.gov/press-room/va-reports-significant-increase-in-veteran-use-of-telehealth-services/
- Powers BB, Homer MC, Morone N, et al. Creation of an interprofessional teledementia clinic for rural veterans: preliminary data. J Am Geriatr Soc. 2017;65(5):1092-1099. doi:10.1111/jgs.14839
- Erickson CM, Chin NA, Rosario HL, et al. Feasibility of virtual Alzheimer’s biomarker disclosure: findings from an observational cohort. Alzheimers Dement (N Y). 2023;9(3):e12413. doi:10.1002/trc2.12413
- Turk KW, Knobel MD, Nothern A, et al. An interprofessional team for disease-modifying therapy in Alzheimer disease implementation. Neurol Clin Pract. 2024;14(6):e200346. doi:10.1212/CPJ.0000000000200346
- FDA accepts LEQEMBI® (lecanemab-irmb) biologics license application for subcutaneous maintenance dosing for the treatment of early Alzheimer’s disease. News release. Elsai US. January 13, 2025. Accessed November 2, 2025. https://media-us.eisai.com/2025-01-13-FDA-Accepts-LEQEMBI-R-lecanemab-irmb-Biologics-License-Application-for-Subcutaneous-Maintenance-Dosing-for-the-Treatment-of-Early-Alzheimers-Disease
Can Telehealth Improve Access to Amyloid-Targeting Therapies for Veterans Living With Alzheimer Disease?
Can Telehealth Improve Access to Amyloid-Targeting Therapies for Veterans Living With Alzheimer Disease?
Pharmacist-Driven Deprescribing to Reduce Anticholinergic Burden in Veterans With Dementia
Pharmacist-Driven Deprescribing to Reduce Anticholinergic Burden in Veterans With Dementia
Anticholinergic medications block the activity of the neurotransmitter acetylcholine by binding to either muscarinic or nicotinic receptors in both the peripheral and central nervous system. Anticholinergic medications typically refer to antimuscarinic medications and have been prescribed to treat a variety of conditions common in older adults, including overactive bladder, allergies, muscle spasms, and sleep disorders.1,2 Since muscarinic receptors are present throughout the body, anticholinergic medications are associated with many adverse effects (AEs), including constipation, urinary retention, xerostomia, and delirium. Older adults are more sensitive to these AEs due to physiological changes associated with aging.1
The American Geriatric Society Beers Criteria for Potentially Inappropriate Medications Use in Older Adults identifies drugs with strong anticholinergic properties. The Beers Criteria strongly recommends avoiding these medications in patients with dementia or cognitive impairment due to the risk of central nervous system AEs. In the updated 2023 Beers Criteria, the rationale was expanded to recognize the risks of the cumulative anticholinergic burden associated with concurrent anticholinergic use.3,4
Given the prevalent use of anticholinergic medications in older adults, there has been significant research demonstrating their AEs, specifically delirium and cognitive impairment in geriatric patients. A systematic review of 14 articles conducted in 7 different countries of patients with median age of 76.4 to 86.1 years reviewed clinical outcomes of anticholinergic use in patients with dementia. Five studies found anticholinergics were associated with increased all-cause mortality in patients with dementia, and 3 studies found anticholinergics were associated with longer hospital stays. Other studies found that anticholinergics were associated with delirium and reduced health-related quality of life.5
About 35% of veterans with dementia have been prescribed a medication regimen with a high anticholinergic burden.6 In 2018, the US Department of Veterans Affairs (VA) Pharmacy Benfits Management Center for Medical Safety completed a centrally aggregated medication use evaluation (CAMUE) to assess the appropriateness of anticholinergic medication use in patients with dementia. The retrospective chart review included 1094 veterans from 19 sites. Overall, about 15% of the veterans experienced new falls, delirium, or worsening dementia within 30 days of starting an anticholinergic medication. Furthermore, < 40% had documentation of a nonanticholinergic alternative medication trial, and < 20% had documented nonpharmacologic therapy. The documentation of risk-benefit assessment acknowledging the risks of anticholinergic medication use in veterans with dementia occurred only about 13% of the time. The CAMUE concluded that the risks of initiating an anticholinergic medication in veterans with dementia are likely underdocumented and possibly under considered by prescribers.7
Developed within the Veterans Health Administration (VHA), VIONE (Vital, Important, Optional, Not Indicated, Every medication has an indication) is a medication management methodology that aims to reduce polypharmacy and improve patient safety consistent with high-reliability organizations. Since it launched in 2016, VIONE has gradually been implemented at many VHA facilities. The VIONE deprescribing dashboard had not been used at the VA Louisville Healthcare System prior to this quality improvement project.
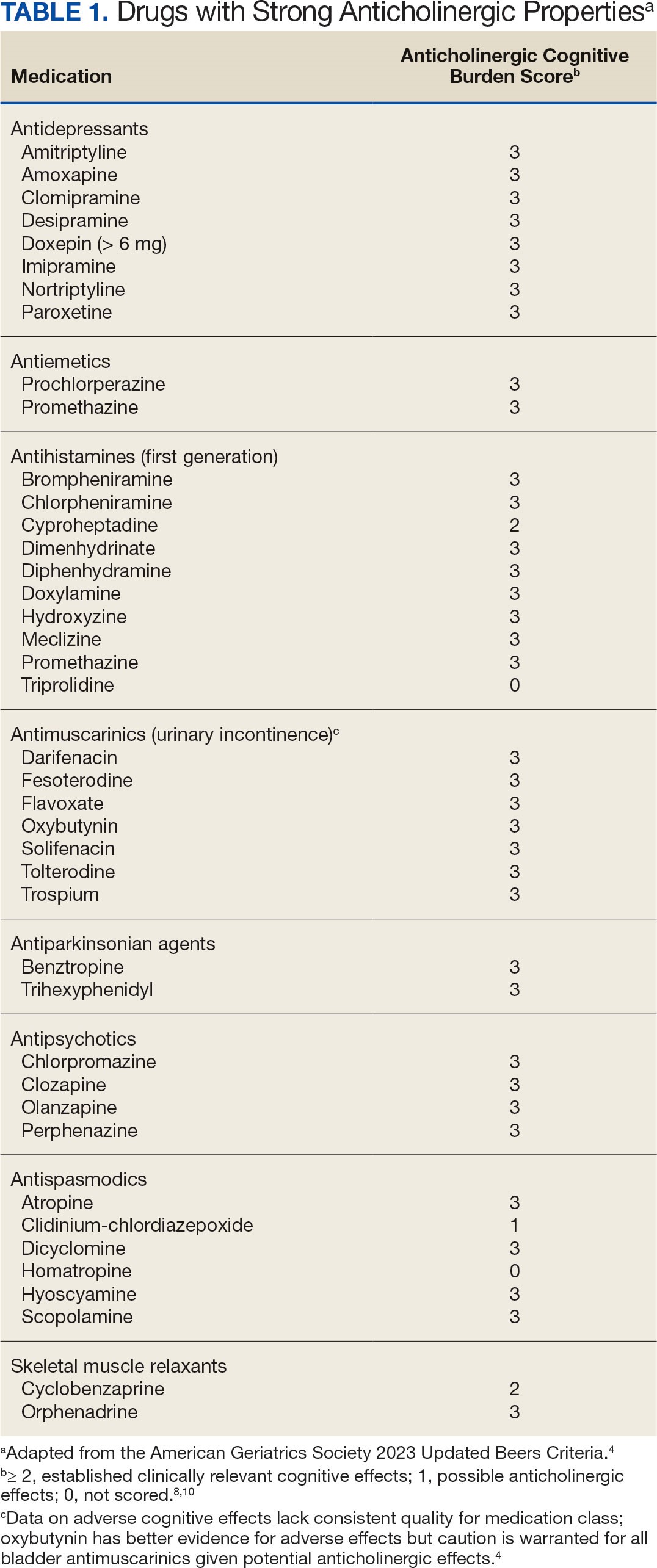
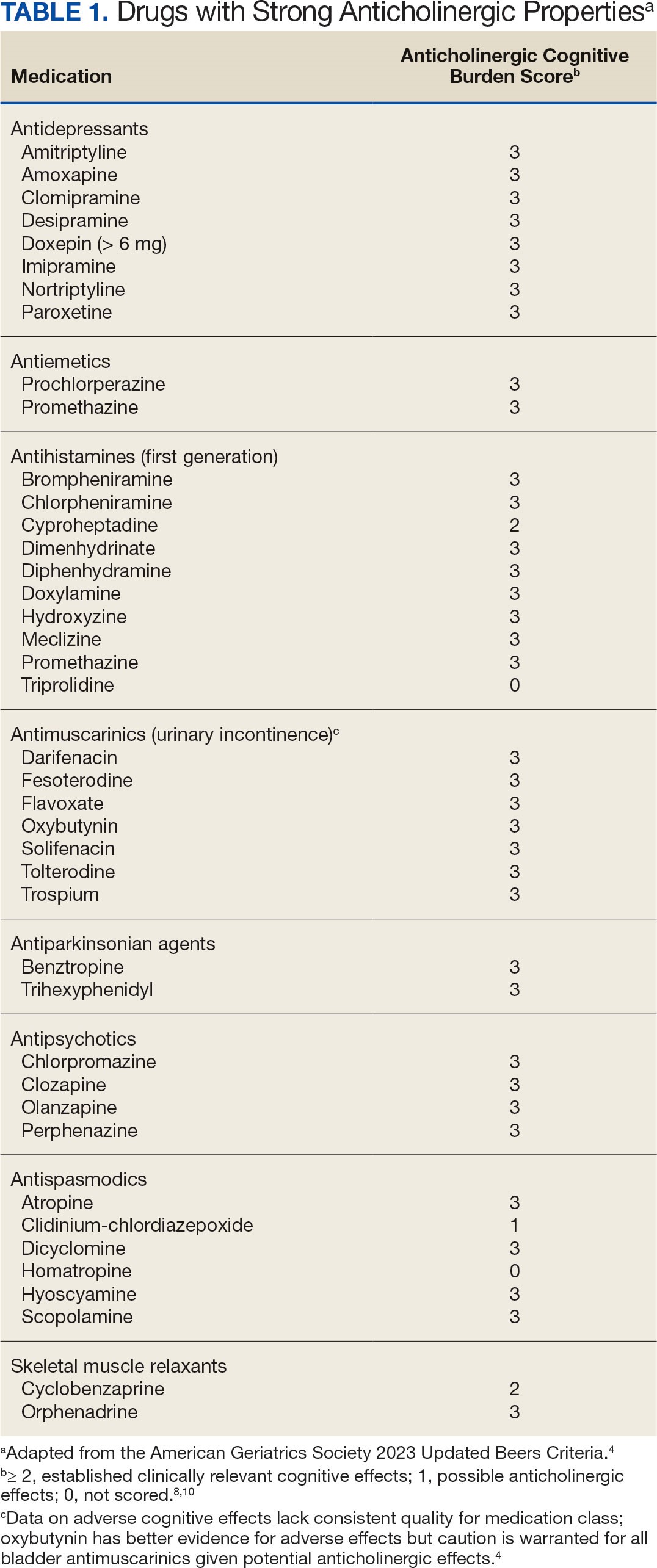
This dashboard uses the Beers Criteria to identify potentially inappropriate anticholinergic medications. It uses the Anticholinergic Cognitive Burden (ACB) scale to calculate the cumulative anticholinergic risk for each patient. Medications with an ACB score of 2 or 3 have clinically relevant cognitive effects such as delirium and dementia (Table 1). For each point increase in total ACB score, a decline in mini-mental state examination score of 0.33 points over 2 years has been shown. Each point increase has also been correlated with a 26% increase in risk of death.8-10
Methods
The purpose of this quality improvement project was to determine the impact of pharmacist-driven deprescribing on the anticholinergic burden in veterans with dementia at VA Louisville Healthcare System. Data were obtained through the Computerized Patient Record System (CPRS) and VIONE deprescribing dashboard and entered in a secure Microsoft Excel spreadsheet. Pharmacist deprescribing steps were entered as CPRS progress notes. A deprescribing note template was created, and 11 templates with indication-specific recommendations were created for each anticholinergic indication identified (contact authors for deprescribing note template examples). Usage of anticholinergic medications was reexamined 3 months after the deprescribing note was entered.
Eligible patients identified in the VIONE deprescribing dashboard had an outpatient order for a medication with strong anticholinergic properties as identified using the Beers Criteria and were aged ≥ 65 years. Patients also had to be diagnosed with dementia or cognitive impairment. Patients were excluded if they were receiving hospice care or if the anticholinergic medication was from a non-VA prescriber or filled at a non-VA pharmacy. The VIONE deprescribing dashboard also excluded skeletal muscle relaxants if the patient had a spinal cord-related visit in the previous 2 years, first-generation antihistamines if the patient had a vertigo diagnosis, hydroxyzine if the indication was for anxiety, trospium if the indication was for overactive bladder, and antipsychotics if the patient had been diagnosed with schizophrenia or bipolar disorder. The following were included in the deprescribing recommendations if the dashboard identified the patient due to receiving a second strongly anticholinergic medication: first generation antihistamines if the patient was diagnosed with vertigo and hydroxyzine if the indication is for anxiety.
Each eligible patient received a focused medication review by a pharmacist via electronic chart review and a templated CPRS progress note with patient-specific recommendations. The prescriber and the patient’s primary care practitioner were recommended to perform a patient-specific risk-benefit assessment, deprescribe potentially inappropriate anticholinergic medications, and consider nonanticholinergic alternatives (both pharmacologic and nonpharmacologic). Data collected included baseline age, sex, prespecified comorbidities (type of dementia, cognitive impairment, delirium, benign prostatic hyperplasia/lower urinary tract symptoms), duration of prescribed anticholinergic medication, indication and deprescribing rate for each anticholinergic agent, and concurrent dementia medications (acetylcholinesterase inhibitors, memantine, or both).
The primary outcome was the number of patients that had = 1 medication with strong anticholinergic properties deprescribed. Deprescribing was defined as medication discontinuation or reduction of total daily dose. Secondary outcomes were the mean change in ACB scale, the number of patients with dose tapering, documented patient-specific risk-benefit assessment, and initiated nonanticholinergic alternative per pharmacist recommendation.
Results
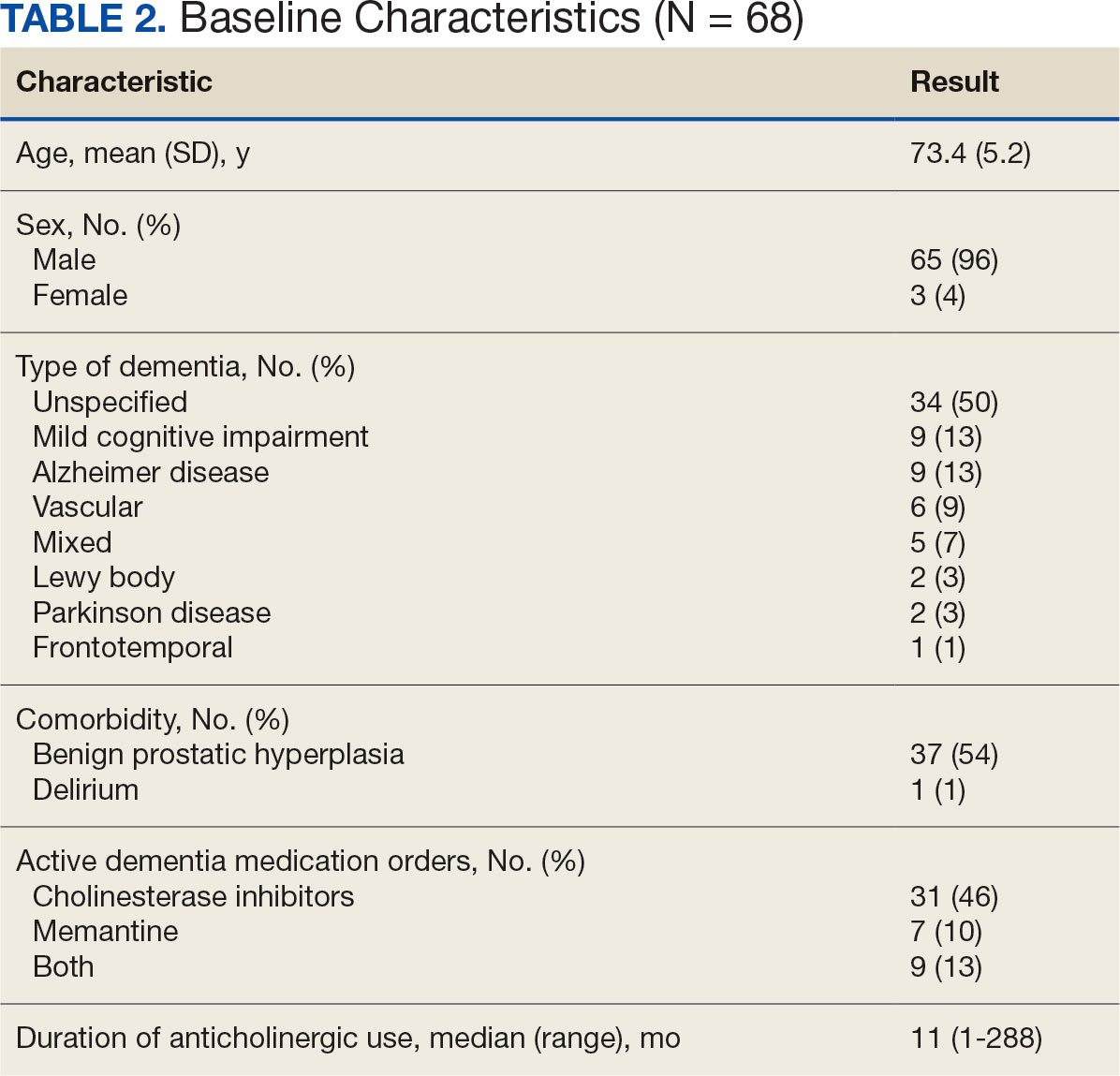
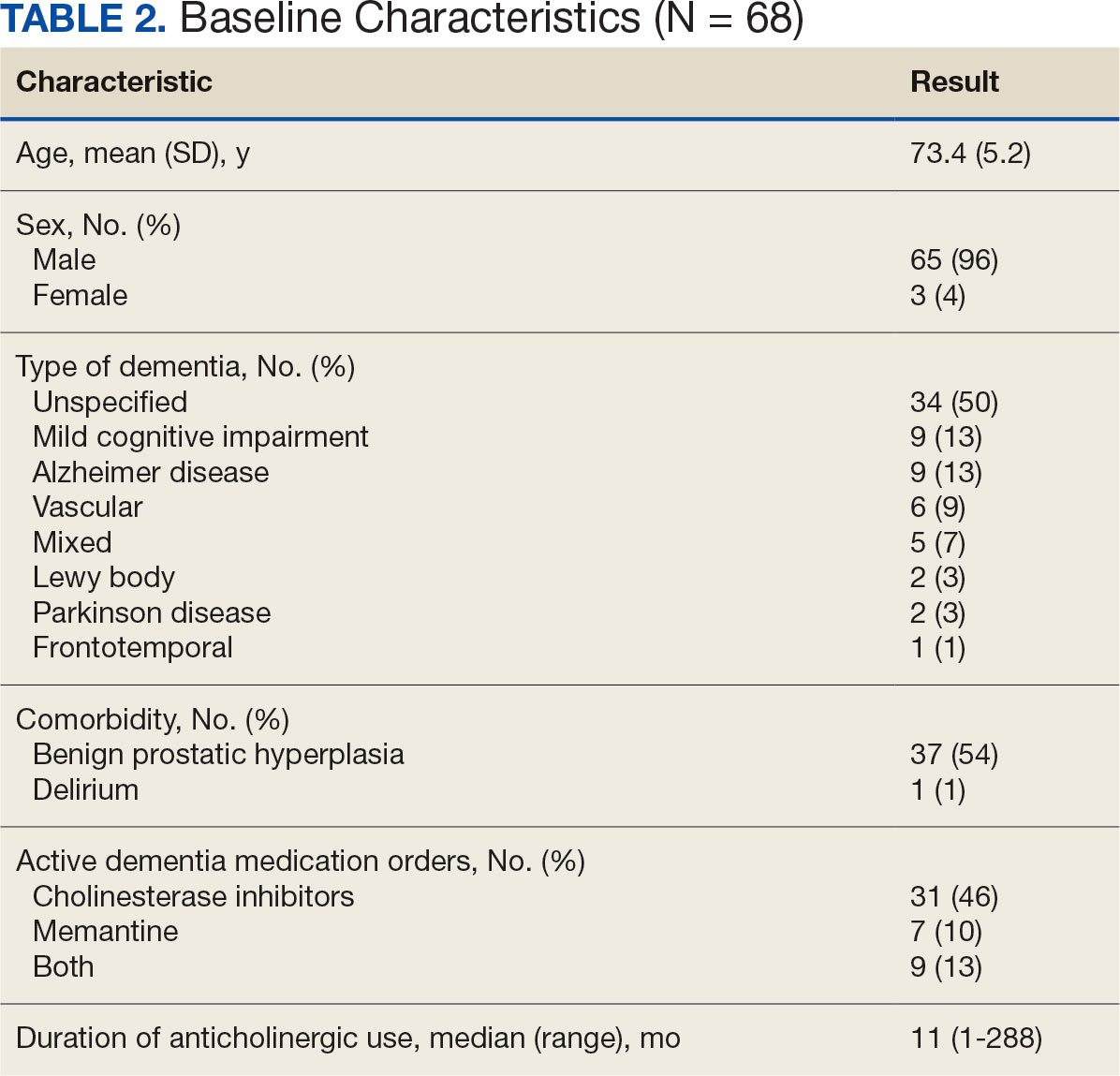
The VIONE deprescribing dashboard identified 121 patients; 45 were excluded for non-VA prescriber or pharmacy, and 8 patients were excluded for other reasons. Sixty-eight patients were included in the deprescribing initiative. The mean age was 73.4 years (range, 67-93), 65 (96%) were male, and 34 (50%) had unspecified dementia (Table 2). Thirty-one patients (46%) had concurrent cholinesterase inhibitor prescriptions for dementia. The median duration of use of a strong anticholinergic medication was 11 months.
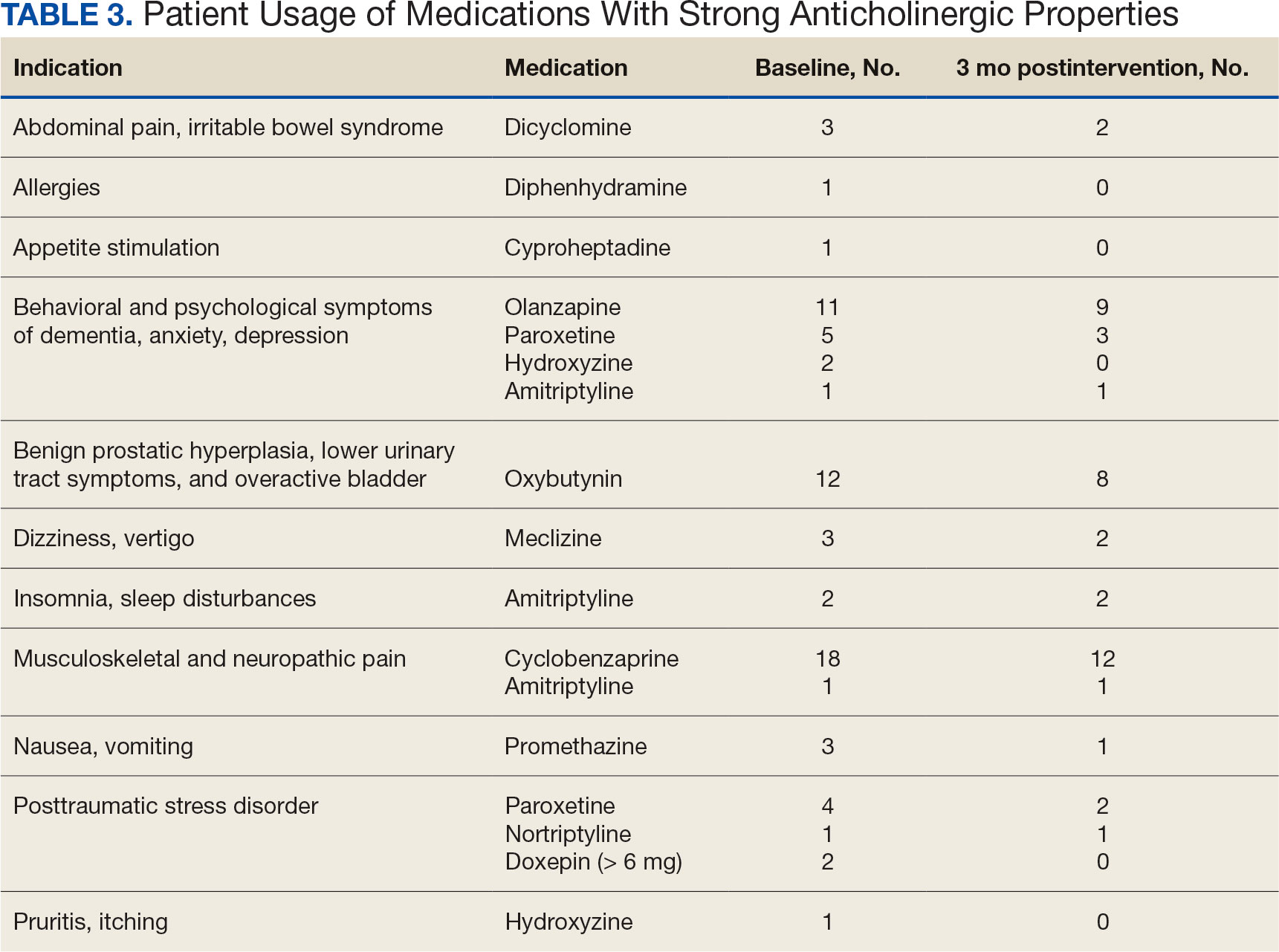
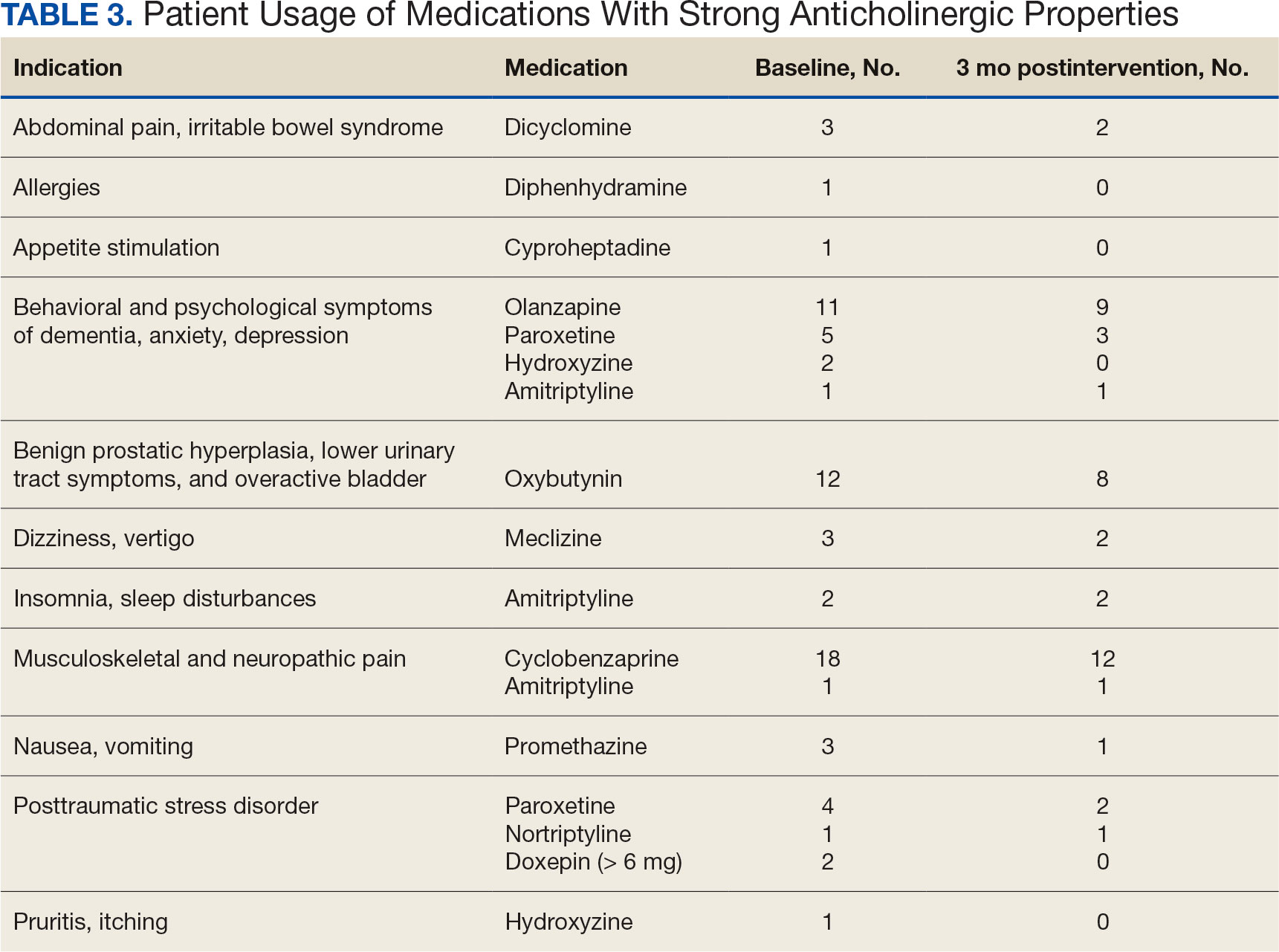
Twenty-nine patients (43%) had ≥ 1 medication with strong anticholinergic properties deprescribed. Anticholinergic medication was discontinued for 26 patients, and the dose was decreased for 3 patients. ACB score fell by a mean of 1.1 per patient. There was an increase in the documented risk-benefit assessment for anticholinergic medications from a baseline of 4 (6%) to 19 (28%) 3 months after the deprescribing note. Cyclobenzaprine, paroxetine, and oxybutynin were deprescribed the most, and amitriptyline had the lowest rate of deprescribing (Table 3). Thirty patients (44%) had a pharmacologic, nonanticholinergic alternative initiated per pharmacist recommendation, and 6 patients (9%) had a nonpharmacologic alternative initiated per pharmacist recommendation.
Discussion
This quality improvement project suggests that with the use of population health management tools such as the VIONE deprescribing dashboard, pharmacists can help identify and deprescribe strong anticholinergic medications in patients with cognitive impairment or dementia. Pharmacists can also aid in deprescribing through evidence-based recommendations to guide risk-benefit discussion and consider safer, nonanticholinergic alternatives. The authors were able to help reduce anticholinergic cognitive burden in 43% of patients in this sample. The mean 1.1 ACB score reduction was considered clinically significant based on prior studies that found that each 1-point increase in ACB score correlated with declined cognition and increased mortality.8,10 The VIONE deprescribing dashboard provided real-time patient data and helped target patients at the highest risk of anticholinergic AEs. The creation of the note templates based on the indication helped streamline recommendations. Typically, the prescriber addressed the recommendations at a routine follow-up appointment. The deprescribing method used in this project was time-efficient and could be easily replicated once the CPRS note templates were created. Future deprescribing projects could consider more direct pharmacist intervention and medication management.
Limitations
There was no direct assessment of clinical outcomes such as change in cognition using cognitive function tests. However, multiple studies have demonstrated AEs associated with strong anticholinergic medication use and additive anticholinergic burden in patients with dementia or cognitive impairment.1,5 Also, the 3-month follow-up period was relatively short. The pharmacist’s deprescribing recommendations may have been accepted after 3 months, or patients could have restarted their anticholinergic medications. Longer follow-up time could provide more robust results and conclusions. Thirdly, there was no formal definition of what constituted a risk-benefit assessment of anticholinergic medications. The risk-benefit assessment was determined at the discretion of the authors, which was subjective and allowed for bias. Finally, 6 patients died during the 3-month follow-up. The data for these patients were included in the baseline characteristics but not in the study outcomes. If these patients had been excluded from the results, a higher percentage of patients (47%) would have had ≥ 1 anticholinergic medication deprescribed.
Conclusions
In collaboration with the interdisciplinary team, pharmacist recommendations resulted in deprescribing of anticholinergic medications in veterans with dementia or cognitive impairment. The VIONE deprescribing dashboard, an easily accessible population health management tool, can identify patients prescribed potentially inappropriate medications and help target patients at the highest risk of anticholinergic AEs. To prevent worsening cognitive impairment, delirium, falls, and other AEs, this deprescribing initiative can be replicated at other VHA facilities. Future projects could have a longer follow-up period, incorporate more direct pharmacist intervention, and assess clinical outcomes of deprescribing.
- Gray SL, Hanlon JT. Anticholinergic medication use and dementia: latest evidence and clinical implications. Ther Adv Drug Saf. 2016;7(5):217-224. doi:10.1177/2042098616658399
- Kersten H, Wyller TB. Anticholinergic drug burden in older people’s brain - how well is it measured? Basic Clin Pharmacol Toxicol. 2014;114(2):151-159. doi:10.1111/bcpt.12140
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
- By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults J Am Geriatr Soc. 2023;71(7):2052-2081. doi:10.1111/jgs.18372
- Wang K, Alan J, Page AT, Dimopoulos E, Etherton-Beer C. Anticholinergics and clinical outcomes amongst people with pre-existing dementia: a systematic review. Maturitas. 2021;151:1-14. doi:10.1016/j.maturitas.2021.06.004
- Thorpe JM, Thorpe CT, Gellad WF, et al. Dual health care system use and high-risk prescribing in patients with dementia: a national cohort study. Ann Intern Med. 2017;166(3):157-163. doi:10.7326/M16-0551
- McCarren M, Burk M, Carico R, Glassman P, Good CB, Cunningham F. Design of a centrally aggregated medication use evaluation (CAMUE): anticholinergics in dementia. Presented at: 2019 HSR&D/QUERI National Conference; October 29-31, 2019; Washington, DC. https://www.hsrd.research.va.gov/meetings/2019/abstract-display.cfm?AbsNum=4027
- Boustani, M, Campbell, N, Munger S, et al. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4(3):311-320. doi:10.2217/1745509.x
- Constantino-Corpuz JK, Alonso MTD. Assessment of a medication deprescribing tool on polypharmacy and cost avoidance. Fed Pract. 2021;38(7):332-336. doi:10.12788/fp.0146
- Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59(8):1477-1483. doi:10.1111/j.1532-5415.2011.03491.x
Anticholinergic medications block the activity of the neurotransmitter acetylcholine by binding to either muscarinic or nicotinic receptors in both the peripheral and central nervous system. Anticholinergic medications typically refer to antimuscarinic medications and have been prescribed to treat a variety of conditions common in older adults, including overactive bladder, allergies, muscle spasms, and sleep disorders.1,2 Since muscarinic receptors are present throughout the body, anticholinergic medications are associated with many adverse effects (AEs), including constipation, urinary retention, xerostomia, and delirium. Older adults are more sensitive to these AEs due to physiological changes associated with aging.1
The American Geriatric Society Beers Criteria for Potentially Inappropriate Medications Use in Older Adults identifies drugs with strong anticholinergic properties. The Beers Criteria strongly recommends avoiding these medications in patients with dementia or cognitive impairment due to the risk of central nervous system AEs. In the updated 2023 Beers Criteria, the rationale was expanded to recognize the risks of the cumulative anticholinergic burden associated with concurrent anticholinergic use.3,4
Given the prevalent use of anticholinergic medications in older adults, there has been significant research demonstrating their AEs, specifically delirium and cognitive impairment in geriatric patients. A systematic review of 14 articles conducted in 7 different countries of patients with median age of 76.4 to 86.1 years reviewed clinical outcomes of anticholinergic use in patients with dementia. Five studies found anticholinergics were associated with increased all-cause mortality in patients with dementia, and 3 studies found anticholinergics were associated with longer hospital stays. Other studies found that anticholinergics were associated with delirium and reduced health-related quality of life.5
About 35% of veterans with dementia have been prescribed a medication regimen with a high anticholinergic burden.6 In 2018, the US Department of Veterans Affairs (VA) Pharmacy Benfits Management Center for Medical Safety completed a centrally aggregated medication use evaluation (CAMUE) to assess the appropriateness of anticholinergic medication use in patients with dementia. The retrospective chart review included 1094 veterans from 19 sites. Overall, about 15% of the veterans experienced new falls, delirium, or worsening dementia within 30 days of starting an anticholinergic medication. Furthermore, < 40% had documentation of a nonanticholinergic alternative medication trial, and < 20% had documented nonpharmacologic therapy. The documentation of risk-benefit assessment acknowledging the risks of anticholinergic medication use in veterans with dementia occurred only about 13% of the time. The CAMUE concluded that the risks of initiating an anticholinergic medication in veterans with dementia are likely underdocumented and possibly under considered by prescribers.7
Developed within the Veterans Health Administration (VHA), VIONE (Vital, Important, Optional, Not Indicated, Every medication has an indication) is a medication management methodology that aims to reduce polypharmacy and improve patient safety consistent with high-reliability organizations. Since it launched in 2016, VIONE has gradually been implemented at many VHA facilities. The VIONE deprescribing dashboard had not been used at the VA Louisville Healthcare System prior to this quality improvement project.
This dashboard uses the Beers Criteria to identify potentially inappropriate anticholinergic medications. It uses the Anticholinergic Cognitive Burden (ACB) scale to calculate the cumulative anticholinergic risk for each patient. Medications with an ACB score of 2 or 3 have clinically relevant cognitive effects such as delirium and dementia (Table 1). For each point increase in total ACB score, a decline in mini-mental state examination score of 0.33 points over 2 years has been shown. Each point increase has also been correlated with a 26% increase in risk of death.8-10
Methods
The purpose of this quality improvement project was to determine the impact of pharmacist-driven deprescribing on the anticholinergic burden in veterans with dementia at VA Louisville Healthcare System. Data were obtained through the Computerized Patient Record System (CPRS) and VIONE deprescribing dashboard and entered in a secure Microsoft Excel spreadsheet. Pharmacist deprescribing steps were entered as CPRS progress notes. A deprescribing note template was created, and 11 templates with indication-specific recommendations were created for each anticholinergic indication identified (contact authors for deprescribing note template examples). Usage of anticholinergic medications was reexamined 3 months after the deprescribing note was entered.
Eligible patients identified in the VIONE deprescribing dashboard had an outpatient order for a medication with strong anticholinergic properties as identified using the Beers Criteria and were aged ≥ 65 years. Patients also had to be diagnosed with dementia or cognitive impairment. Patients were excluded if they were receiving hospice care or if the anticholinergic medication was from a non-VA prescriber or filled at a non-VA pharmacy. The VIONE deprescribing dashboard also excluded skeletal muscle relaxants if the patient had a spinal cord-related visit in the previous 2 years, first-generation antihistamines if the patient had a vertigo diagnosis, hydroxyzine if the indication was for anxiety, trospium if the indication was for overactive bladder, and antipsychotics if the patient had been diagnosed with schizophrenia or bipolar disorder. The following were included in the deprescribing recommendations if the dashboard identified the patient due to receiving a second strongly anticholinergic medication: first generation antihistamines if the patient was diagnosed with vertigo and hydroxyzine if the indication is for anxiety.
Each eligible patient received a focused medication review by a pharmacist via electronic chart review and a templated CPRS progress note with patient-specific recommendations. The prescriber and the patient’s primary care practitioner were recommended to perform a patient-specific risk-benefit assessment, deprescribe potentially inappropriate anticholinergic medications, and consider nonanticholinergic alternatives (both pharmacologic and nonpharmacologic). Data collected included baseline age, sex, prespecified comorbidities (type of dementia, cognitive impairment, delirium, benign prostatic hyperplasia/lower urinary tract symptoms), duration of prescribed anticholinergic medication, indication and deprescribing rate for each anticholinergic agent, and concurrent dementia medications (acetylcholinesterase inhibitors, memantine, or both).
The primary outcome was the number of patients that had = 1 medication with strong anticholinergic properties deprescribed. Deprescribing was defined as medication discontinuation or reduction of total daily dose. Secondary outcomes were the mean change in ACB scale, the number of patients with dose tapering, documented patient-specific risk-benefit assessment, and initiated nonanticholinergic alternative per pharmacist recommendation.
Results
The VIONE deprescribing dashboard identified 121 patients; 45 were excluded for non-VA prescriber or pharmacy, and 8 patients were excluded for other reasons. Sixty-eight patients were included in the deprescribing initiative. The mean age was 73.4 years (range, 67-93), 65 (96%) were male, and 34 (50%) had unspecified dementia (Table 2). Thirty-one patients (46%) had concurrent cholinesterase inhibitor prescriptions for dementia. The median duration of use of a strong anticholinergic medication was 11 months.
Twenty-nine patients (43%) had ≥ 1 medication with strong anticholinergic properties deprescribed. Anticholinergic medication was discontinued for 26 patients, and the dose was decreased for 3 patients. ACB score fell by a mean of 1.1 per patient. There was an increase in the documented risk-benefit assessment for anticholinergic medications from a baseline of 4 (6%) to 19 (28%) 3 months after the deprescribing note. Cyclobenzaprine, paroxetine, and oxybutynin were deprescribed the most, and amitriptyline had the lowest rate of deprescribing (Table 3). Thirty patients (44%) had a pharmacologic, nonanticholinergic alternative initiated per pharmacist recommendation, and 6 patients (9%) had a nonpharmacologic alternative initiated per pharmacist recommendation.
Discussion
This quality improvement project suggests that with the use of population health management tools such as the VIONE deprescribing dashboard, pharmacists can help identify and deprescribe strong anticholinergic medications in patients with cognitive impairment or dementia. Pharmacists can also aid in deprescribing through evidence-based recommendations to guide risk-benefit discussion and consider safer, nonanticholinergic alternatives. The authors were able to help reduce anticholinergic cognitive burden in 43% of patients in this sample. The mean 1.1 ACB score reduction was considered clinically significant based on prior studies that found that each 1-point increase in ACB score correlated with declined cognition and increased mortality.8,10 The VIONE deprescribing dashboard provided real-time patient data and helped target patients at the highest risk of anticholinergic AEs. The creation of the note templates based on the indication helped streamline recommendations. Typically, the prescriber addressed the recommendations at a routine follow-up appointment. The deprescribing method used in this project was time-efficient and could be easily replicated once the CPRS note templates were created. Future deprescribing projects could consider more direct pharmacist intervention and medication management.
Limitations
There was no direct assessment of clinical outcomes such as change in cognition using cognitive function tests. However, multiple studies have demonstrated AEs associated with strong anticholinergic medication use and additive anticholinergic burden in patients with dementia or cognitive impairment.1,5 Also, the 3-month follow-up period was relatively short. The pharmacist’s deprescribing recommendations may have been accepted after 3 months, or patients could have restarted their anticholinergic medications. Longer follow-up time could provide more robust results and conclusions. Thirdly, there was no formal definition of what constituted a risk-benefit assessment of anticholinergic medications. The risk-benefit assessment was determined at the discretion of the authors, which was subjective and allowed for bias. Finally, 6 patients died during the 3-month follow-up. The data for these patients were included in the baseline characteristics but not in the study outcomes. If these patients had been excluded from the results, a higher percentage of patients (47%) would have had ≥ 1 anticholinergic medication deprescribed.
Conclusions
In collaboration with the interdisciplinary team, pharmacist recommendations resulted in deprescribing of anticholinergic medications in veterans with dementia or cognitive impairment. The VIONE deprescribing dashboard, an easily accessible population health management tool, can identify patients prescribed potentially inappropriate medications and help target patients at the highest risk of anticholinergic AEs. To prevent worsening cognitive impairment, delirium, falls, and other AEs, this deprescribing initiative can be replicated at other VHA facilities. Future projects could have a longer follow-up period, incorporate more direct pharmacist intervention, and assess clinical outcomes of deprescribing.
Anticholinergic medications block the activity of the neurotransmitter acetylcholine by binding to either muscarinic or nicotinic receptors in both the peripheral and central nervous system. Anticholinergic medications typically refer to antimuscarinic medications and have been prescribed to treat a variety of conditions common in older adults, including overactive bladder, allergies, muscle spasms, and sleep disorders.1,2 Since muscarinic receptors are present throughout the body, anticholinergic medications are associated with many adverse effects (AEs), including constipation, urinary retention, xerostomia, and delirium. Older adults are more sensitive to these AEs due to physiological changes associated with aging.1
The American Geriatric Society Beers Criteria for Potentially Inappropriate Medications Use in Older Adults identifies drugs with strong anticholinergic properties. The Beers Criteria strongly recommends avoiding these medications in patients with dementia or cognitive impairment due to the risk of central nervous system AEs. In the updated 2023 Beers Criteria, the rationale was expanded to recognize the risks of the cumulative anticholinergic burden associated with concurrent anticholinergic use.3,4
Given the prevalent use of anticholinergic medications in older adults, there has been significant research demonstrating their AEs, specifically delirium and cognitive impairment in geriatric patients. A systematic review of 14 articles conducted in 7 different countries of patients with median age of 76.4 to 86.1 years reviewed clinical outcomes of anticholinergic use in patients with dementia. Five studies found anticholinergics were associated with increased all-cause mortality in patients with dementia, and 3 studies found anticholinergics were associated with longer hospital stays. Other studies found that anticholinergics were associated with delirium and reduced health-related quality of life.5
About 35% of veterans with dementia have been prescribed a medication regimen with a high anticholinergic burden.6 In 2018, the US Department of Veterans Affairs (VA) Pharmacy Benfits Management Center for Medical Safety completed a centrally aggregated medication use evaluation (CAMUE) to assess the appropriateness of anticholinergic medication use in patients with dementia. The retrospective chart review included 1094 veterans from 19 sites. Overall, about 15% of the veterans experienced new falls, delirium, or worsening dementia within 30 days of starting an anticholinergic medication. Furthermore, < 40% had documentation of a nonanticholinergic alternative medication trial, and < 20% had documented nonpharmacologic therapy. The documentation of risk-benefit assessment acknowledging the risks of anticholinergic medication use in veterans with dementia occurred only about 13% of the time. The CAMUE concluded that the risks of initiating an anticholinergic medication in veterans with dementia are likely underdocumented and possibly under considered by prescribers.7
Developed within the Veterans Health Administration (VHA), VIONE (Vital, Important, Optional, Not Indicated, Every medication has an indication) is a medication management methodology that aims to reduce polypharmacy and improve patient safety consistent with high-reliability organizations. Since it launched in 2016, VIONE has gradually been implemented at many VHA facilities. The VIONE deprescribing dashboard had not been used at the VA Louisville Healthcare System prior to this quality improvement project.
This dashboard uses the Beers Criteria to identify potentially inappropriate anticholinergic medications. It uses the Anticholinergic Cognitive Burden (ACB) scale to calculate the cumulative anticholinergic risk for each patient. Medications with an ACB score of 2 or 3 have clinically relevant cognitive effects such as delirium and dementia (Table 1). For each point increase in total ACB score, a decline in mini-mental state examination score of 0.33 points over 2 years has been shown. Each point increase has also been correlated with a 26% increase in risk of death.8-10
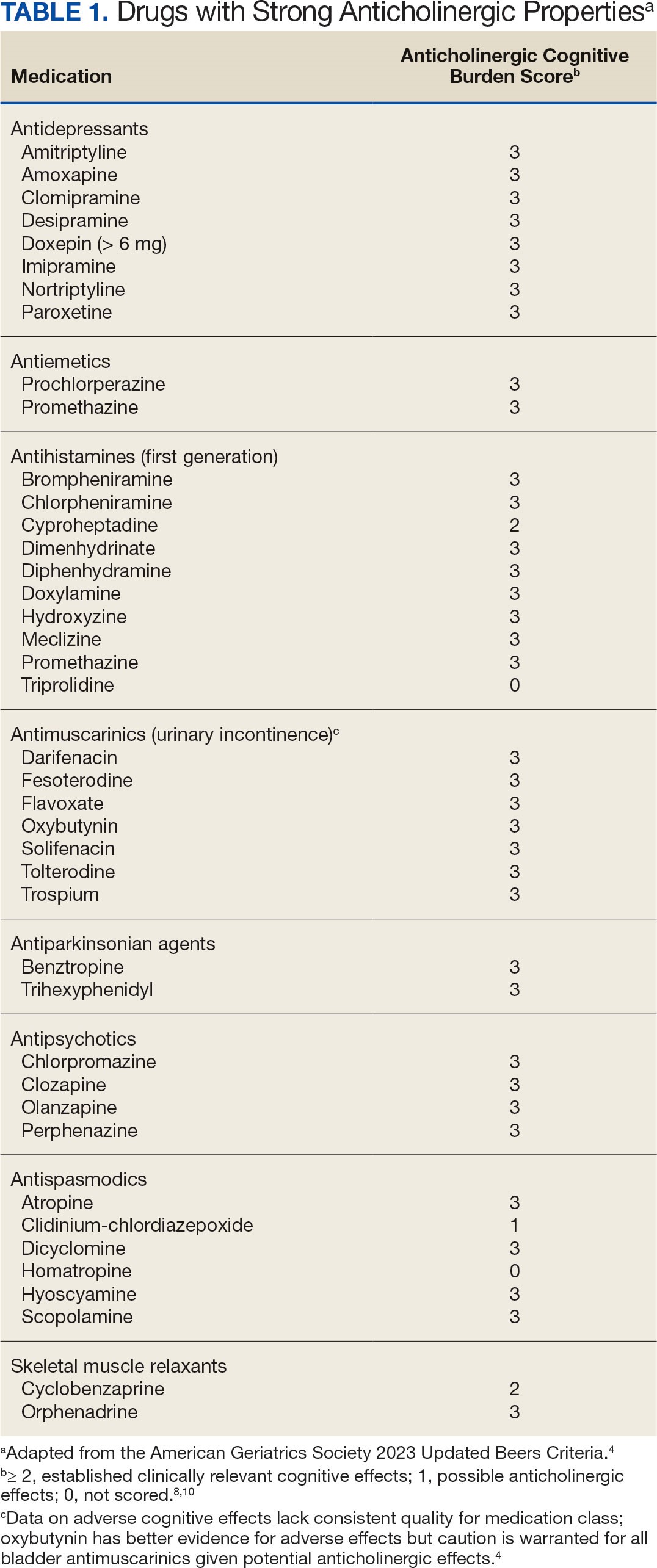
Methods
The purpose of this quality improvement project was to determine the impact of pharmacist-driven deprescribing on the anticholinergic burden in veterans with dementia at VA Louisville Healthcare System. Data were obtained through the Computerized Patient Record System (CPRS) and VIONE deprescribing dashboard and entered in a secure Microsoft Excel spreadsheet. Pharmacist deprescribing steps were entered as CPRS progress notes. A deprescribing note template was created, and 11 templates with indication-specific recommendations were created for each anticholinergic indication identified (contact authors for deprescribing note template examples). Usage of anticholinergic medications was reexamined 3 months after the deprescribing note was entered.
Eligible patients identified in the VIONE deprescribing dashboard had an outpatient order for a medication with strong anticholinergic properties as identified using the Beers Criteria and were aged ≥ 65 years. Patients also had to be diagnosed with dementia or cognitive impairment. Patients were excluded if they were receiving hospice care or if the anticholinergic medication was from a non-VA prescriber or filled at a non-VA pharmacy. The VIONE deprescribing dashboard also excluded skeletal muscle relaxants if the patient had a spinal cord-related visit in the previous 2 years, first-generation antihistamines if the patient had a vertigo diagnosis, hydroxyzine if the indication was for anxiety, trospium if the indication was for overactive bladder, and antipsychotics if the patient had been diagnosed with schizophrenia or bipolar disorder. The following were included in the deprescribing recommendations if the dashboard identified the patient due to receiving a second strongly anticholinergic medication: first generation antihistamines if the patient was diagnosed with vertigo and hydroxyzine if the indication is for anxiety.
Each eligible patient received a focused medication review by a pharmacist via electronic chart review and a templated CPRS progress note with patient-specific recommendations. The prescriber and the patient’s primary care practitioner were recommended to perform a patient-specific risk-benefit assessment, deprescribe potentially inappropriate anticholinergic medications, and consider nonanticholinergic alternatives (both pharmacologic and nonpharmacologic). Data collected included baseline age, sex, prespecified comorbidities (type of dementia, cognitive impairment, delirium, benign prostatic hyperplasia/lower urinary tract symptoms), duration of prescribed anticholinergic medication, indication and deprescribing rate for each anticholinergic agent, and concurrent dementia medications (acetylcholinesterase inhibitors, memantine, or both).
The primary outcome was the number of patients that had = 1 medication with strong anticholinergic properties deprescribed. Deprescribing was defined as medication discontinuation or reduction of total daily dose. Secondary outcomes were the mean change in ACB scale, the number of patients with dose tapering, documented patient-specific risk-benefit assessment, and initiated nonanticholinergic alternative per pharmacist recommendation.
Results
The VIONE deprescribing dashboard identified 121 patients; 45 were excluded for non-VA prescriber or pharmacy, and 8 patients were excluded for other reasons. Sixty-eight patients were included in the deprescribing initiative. The mean age was 73.4 years (range, 67-93), 65 (96%) were male, and 34 (50%) had unspecified dementia (Table 2). Thirty-one patients (46%) had concurrent cholinesterase inhibitor prescriptions for dementia. The median duration of use of a strong anticholinergic medication was 11 months.
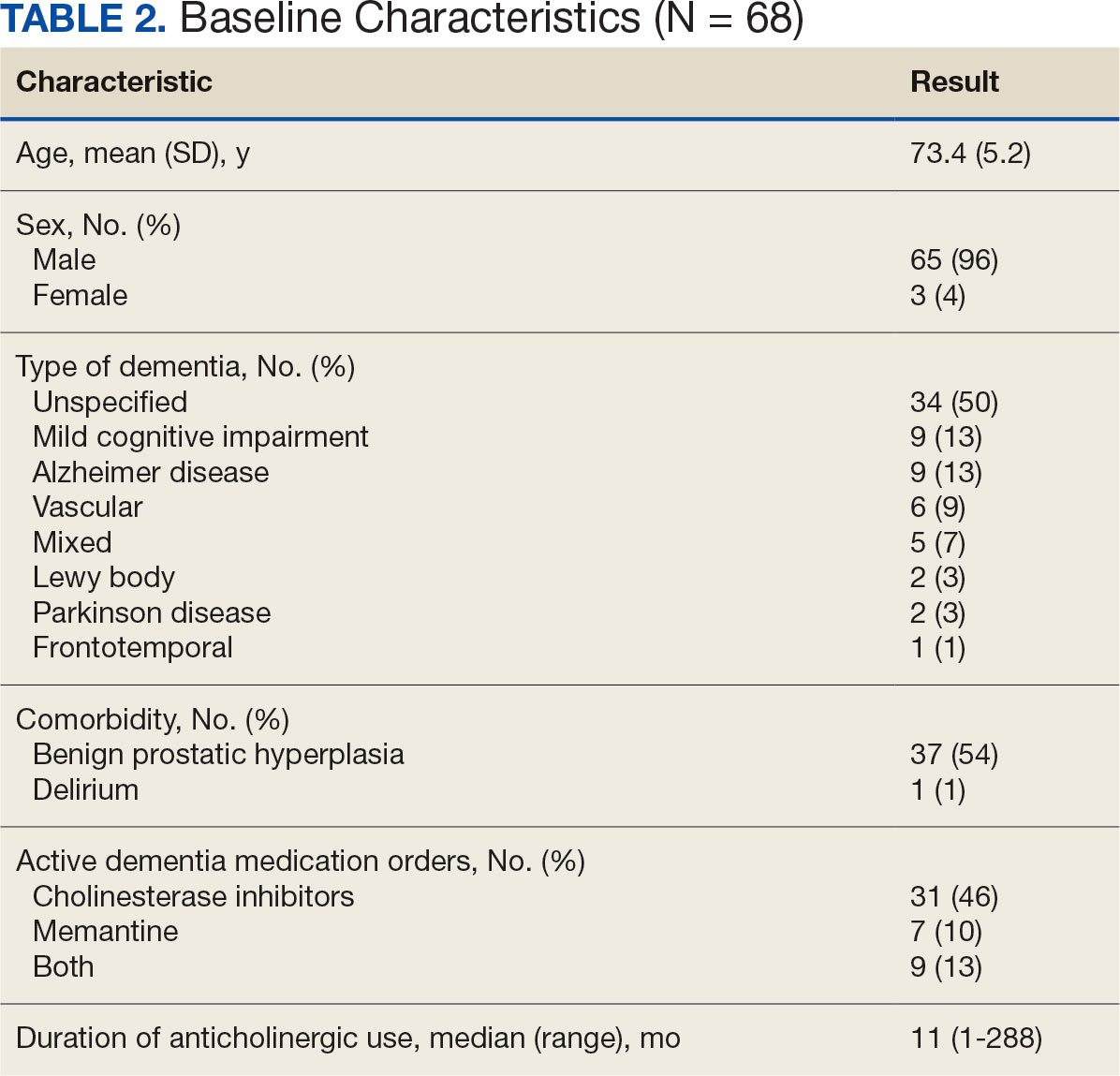
Twenty-nine patients (43%) had ≥ 1 medication with strong anticholinergic properties deprescribed. Anticholinergic medication was discontinued for 26 patients, and the dose was decreased for 3 patients. ACB score fell by a mean of 1.1 per patient. There was an increase in the documented risk-benefit assessment for anticholinergic medications from a baseline of 4 (6%) to 19 (28%) 3 months after the deprescribing note. Cyclobenzaprine, paroxetine, and oxybutynin were deprescribed the most, and amitriptyline had the lowest rate of deprescribing (Table 3). Thirty patients (44%) had a pharmacologic, nonanticholinergic alternative initiated per pharmacist recommendation, and 6 patients (9%) had a nonpharmacologic alternative initiated per pharmacist recommendation.
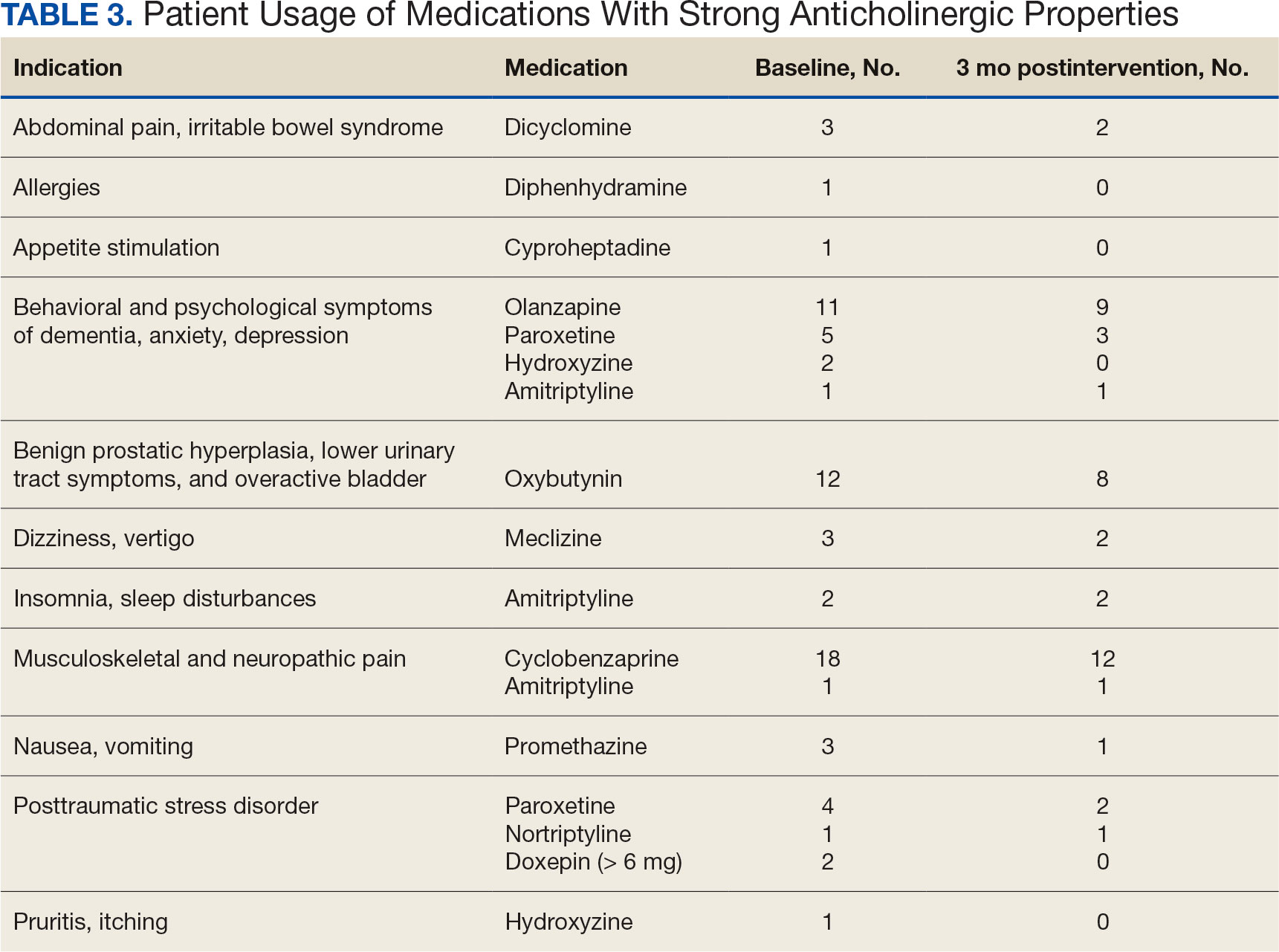
Discussion
This quality improvement project suggests that with the use of population health management tools such as the VIONE deprescribing dashboard, pharmacists can help identify and deprescribe strong anticholinergic medications in patients with cognitive impairment or dementia. Pharmacists can also aid in deprescribing through evidence-based recommendations to guide risk-benefit discussion and consider safer, nonanticholinergic alternatives. The authors were able to help reduce anticholinergic cognitive burden in 43% of patients in this sample. The mean 1.1 ACB score reduction was considered clinically significant based on prior studies that found that each 1-point increase in ACB score correlated with declined cognition and increased mortality.8,10 The VIONE deprescribing dashboard provided real-time patient data and helped target patients at the highest risk of anticholinergic AEs. The creation of the note templates based on the indication helped streamline recommendations. Typically, the prescriber addressed the recommendations at a routine follow-up appointment. The deprescribing method used in this project was time-efficient and could be easily replicated once the CPRS note templates were created. Future deprescribing projects could consider more direct pharmacist intervention and medication management.
Limitations
There was no direct assessment of clinical outcomes such as change in cognition using cognitive function tests. However, multiple studies have demonstrated AEs associated with strong anticholinergic medication use and additive anticholinergic burden in patients with dementia or cognitive impairment.1,5 Also, the 3-month follow-up period was relatively short. The pharmacist’s deprescribing recommendations may have been accepted after 3 months, or patients could have restarted their anticholinergic medications. Longer follow-up time could provide more robust results and conclusions. Thirdly, there was no formal definition of what constituted a risk-benefit assessment of anticholinergic medications. The risk-benefit assessment was determined at the discretion of the authors, which was subjective and allowed for bias. Finally, 6 patients died during the 3-month follow-up. The data for these patients were included in the baseline characteristics but not in the study outcomes. If these patients had been excluded from the results, a higher percentage of patients (47%) would have had ≥ 1 anticholinergic medication deprescribed.
Conclusions
In collaboration with the interdisciplinary team, pharmacist recommendations resulted in deprescribing of anticholinergic medications in veterans with dementia or cognitive impairment. The VIONE deprescribing dashboard, an easily accessible population health management tool, can identify patients prescribed potentially inappropriate medications and help target patients at the highest risk of anticholinergic AEs. To prevent worsening cognitive impairment, delirium, falls, and other AEs, this deprescribing initiative can be replicated at other VHA facilities. Future projects could have a longer follow-up period, incorporate more direct pharmacist intervention, and assess clinical outcomes of deprescribing.
- Gray SL, Hanlon JT. Anticholinergic medication use and dementia: latest evidence and clinical implications. Ther Adv Drug Saf. 2016;7(5):217-224. doi:10.1177/2042098616658399
- Kersten H, Wyller TB. Anticholinergic drug burden in older people’s brain - how well is it measured? Basic Clin Pharmacol Toxicol. 2014;114(2):151-159. doi:10.1111/bcpt.12140
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
- By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults J Am Geriatr Soc. 2023;71(7):2052-2081. doi:10.1111/jgs.18372
- Wang K, Alan J, Page AT, Dimopoulos E, Etherton-Beer C. Anticholinergics and clinical outcomes amongst people with pre-existing dementia: a systematic review. Maturitas. 2021;151:1-14. doi:10.1016/j.maturitas.2021.06.004
- Thorpe JM, Thorpe CT, Gellad WF, et al. Dual health care system use and high-risk prescribing in patients with dementia: a national cohort study. Ann Intern Med. 2017;166(3):157-163. doi:10.7326/M16-0551
- McCarren M, Burk M, Carico R, Glassman P, Good CB, Cunningham F. Design of a centrally aggregated medication use evaluation (CAMUE): anticholinergics in dementia. Presented at: 2019 HSR&D/QUERI National Conference; October 29-31, 2019; Washington, DC. https://www.hsrd.research.va.gov/meetings/2019/abstract-display.cfm?AbsNum=4027
- Boustani, M, Campbell, N, Munger S, et al. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4(3):311-320. doi:10.2217/1745509.x
- Constantino-Corpuz JK, Alonso MTD. Assessment of a medication deprescribing tool on polypharmacy and cost avoidance. Fed Pract. 2021;38(7):332-336. doi:10.12788/fp.0146
- Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59(8):1477-1483. doi:10.1111/j.1532-5415.2011.03491.x
- Gray SL, Hanlon JT. Anticholinergic medication use and dementia: latest evidence and clinical implications. Ther Adv Drug Saf. 2016;7(5):217-224. doi:10.1177/2042098616658399
- Kersten H, Wyller TB. Anticholinergic drug burden in older people’s brain - how well is it measured? Basic Clin Pharmacol Toxicol. 2014;114(2):151-159. doi:10.1111/bcpt.12140
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 updated AGS beers criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019;67(4):674-694. doi:10.1111/jgs.15767
- By the 2023 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2023 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults J Am Geriatr Soc. 2023;71(7):2052-2081. doi:10.1111/jgs.18372
- Wang K, Alan J, Page AT, Dimopoulos E, Etherton-Beer C. Anticholinergics and clinical outcomes amongst people with pre-existing dementia: a systematic review. Maturitas. 2021;151:1-14. doi:10.1016/j.maturitas.2021.06.004
- Thorpe JM, Thorpe CT, Gellad WF, et al. Dual health care system use and high-risk prescribing in patients with dementia: a national cohort study. Ann Intern Med. 2017;166(3):157-163. doi:10.7326/M16-0551
- McCarren M, Burk M, Carico R, Glassman P, Good CB, Cunningham F. Design of a centrally aggregated medication use evaluation (CAMUE): anticholinergics in dementia. Presented at: 2019 HSR&D/QUERI National Conference; October 29-31, 2019; Washington, DC. https://www.hsrd.research.va.gov/meetings/2019/abstract-display.cfm?AbsNum=4027
- Boustani, M, Campbell, N, Munger S, et al. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4(3):311-320. doi:10.2217/1745509.x
- Constantino-Corpuz JK, Alonso MTD. Assessment of a medication deprescribing tool on polypharmacy and cost avoidance. Fed Pract. 2021;38(7):332-336. doi:10.12788/fp.0146
- Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59(8):1477-1483. doi:10.1111/j.1532-5415.2011.03491.x
Pharmacist-Driven Deprescribing to Reduce Anticholinergic Burden in Veterans With Dementia
Pharmacist-Driven Deprescribing to Reduce Anticholinergic Burden in Veterans With Dementia
Antidepressants and Dementia Risk: New Data
TOPLINE:
Taking antidepressants in midlife was not associated with an increased risk of subsequent Alzheimer’s disease (AD) or AD-related dementias (ADRD), data from a large prospective study of US veterans show.
METHODOLOGY:
- Investigators analyzed data from 35,200 US veterans aged ≥ 55 years diagnosed with major depressive disorder from January 1, 2000, to June 1, 2022, and followed them for ≤ 20 years to track subsequent AD/ADRD diagnoses.
- Health information was pulled from electronic health records of the Veterans Health Administration (VHA) Corporate Data Warehouse, and veterans had to be at the VHA for ≥ 1 year before diagnosis.
- Participants were considered to be exposed to an antidepressant when a prescription lasted ≥ 3 months.
TAKEAWAY:
- A total of 32,500 individuals were diagnosed with MDD. The mean age was 65 years, and 91% were men. 17,000 patients received antidepressants for a median duration of 4 years. Median follow-up time was 3.2 years.
- There was no significant association between antidepressant exposure and the risk for AD/ADRD (events = 1056; hazard ratio, 0.93; 95% CI, 0.80-1.08) vs no exposure.
- In a subgroup analysis, investigators found no significant link between different classes of antidepressants and dementia risk. These included selective serotonin reuptake inhibitors, norepinephrine and dopamine reuptake inhibitors, and serotonin-norepinephrine reuptake inhibitors.
- Investigators emphasized the need for further research, particularly in populations with a larger representation of female patients.
IN PRACTICE:
“A possibility for the conflicting results in retrospective studies is that the heightened risk identified in participants on antidepressants may be attributed to depression itself, rather than the result of a potential pharmacological action. So, this and other clinical confounding factors need to be taken into account,” the investigators noted.
SOURCE:
The study was led by Jaime Ramos-Cejudo, PhD, VA Boston Healthcare System, Boston. It was published online May 8 in Alzheimer’s & Dementia.
LIMITATIONS:
The cohort’s relatively young age limited the number of dementia cases captured. Data from supplemental insurance, including Medicare, were not included, potentially limiting outcome capture.
DISCLOSURES:
The study was supported by the National Institutes of Health and the National Alzheimer’s Coordinating Center. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
Taking antidepressants in midlife was not associated with an increased risk of subsequent Alzheimer’s disease (AD) or AD-related dementias (ADRD), data from a large prospective study of US veterans show.
METHODOLOGY:
- Investigators analyzed data from 35,200 US veterans aged ≥ 55 years diagnosed with major depressive disorder from January 1, 2000, to June 1, 2022, and followed them for ≤ 20 years to track subsequent AD/ADRD diagnoses.
- Health information was pulled from electronic health records of the Veterans Health Administration (VHA) Corporate Data Warehouse, and veterans had to be at the VHA for ≥ 1 year before diagnosis.
- Participants were considered to be exposed to an antidepressant when a prescription lasted ≥ 3 months.
TAKEAWAY:
- A total of 32,500 individuals were diagnosed with MDD. The mean age was 65 years, and 91% were men. 17,000 patients received antidepressants for a median duration of 4 years. Median follow-up time was 3.2 years.
- There was no significant association between antidepressant exposure and the risk for AD/ADRD (events = 1056; hazard ratio, 0.93; 95% CI, 0.80-1.08) vs no exposure.
- In a subgroup analysis, investigators found no significant link between different classes of antidepressants and dementia risk. These included selective serotonin reuptake inhibitors, norepinephrine and dopamine reuptake inhibitors, and serotonin-norepinephrine reuptake inhibitors.
- Investigators emphasized the need for further research, particularly in populations with a larger representation of female patients.
IN PRACTICE:
“A possibility for the conflicting results in retrospective studies is that the heightened risk identified in participants on antidepressants may be attributed to depression itself, rather than the result of a potential pharmacological action. So, this and other clinical confounding factors need to be taken into account,” the investigators noted.
SOURCE:
The study was led by Jaime Ramos-Cejudo, PhD, VA Boston Healthcare System, Boston. It was published online May 8 in Alzheimer’s & Dementia.
LIMITATIONS:
The cohort’s relatively young age limited the number of dementia cases captured. Data from supplemental insurance, including Medicare, were not included, potentially limiting outcome capture.
DISCLOSURES:
The study was supported by the National Institutes of Health and the National Alzheimer’s Coordinating Center. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
TOPLINE:
Taking antidepressants in midlife was not associated with an increased risk of subsequent Alzheimer’s disease (AD) or AD-related dementias (ADRD), data from a large prospective study of US veterans show.
METHODOLOGY:
- Investigators analyzed data from 35,200 US veterans aged ≥ 55 years diagnosed with major depressive disorder from January 1, 2000, to June 1, 2022, and followed them for ≤ 20 years to track subsequent AD/ADRD diagnoses.
- Health information was pulled from electronic health records of the Veterans Health Administration (VHA) Corporate Data Warehouse, and veterans had to be at the VHA for ≥ 1 year before diagnosis.
- Participants were considered to be exposed to an antidepressant when a prescription lasted ≥ 3 months.
TAKEAWAY:
- A total of 32,500 individuals were diagnosed with MDD. The mean age was 65 years, and 91% were men. 17,000 patients received antidepressants for a median duration of 4 years. Median follow-up time was 3.2 years.
- There was no significant association between antidepressant exposure and the risk for AD/ADRD (events = 1056; hazard ratio, 0.93; 95% CI, 0.80-1.08) vs no exposure.
- In a subgroup analysis, investigators found no significant link between different classes of antidepressants and dementia risk. These included selective serotonin reuptake inhibitors, norepinephrine and dopamine reuptake inhibitors, and serotonin-norepinephrine reuptake inhibitors.
- Investigators emphasized the need for further research, particularly in populations with a larger representation of female patients.
IN PRACTICE:
“A possibility for the conflicting results in retrospective studies is that the heightened risk identified in participants on antidepressants may be attributed to depression itself, rather than the result of a potential pharmacological action. So, this and other clinical confounding factors need to be taken into account,” the investigators noted.
SOURCE:
The study was led by Jaime Ramos-Cejudo, PhD, VA Boston Healthcare System, Boston. It was published online May 8 in Alzheimer’s & Dementia.
LIMITATIONS:
The cohort’s relatively young age limited the number of dementia cases captured. Data from supplemental insurance, including Medicare, were not included, potentially limiting outcome capture.
DISCLOSURES:
The study was supported by the National Institutes of Health and the National Alzheimer’s Coordinating Center. The authors declared no conflicts of interest.
This article was created using several editorial tools, including AI, as part of the process. Human editors reviewed this content before publication.
A version of this article appeared on Medscape.com.
U.S. dementia rate drops as education, women’s employment rises
new research shows. New data from the Health and Retirement Study, a nationally representative survey, show that the prevalence of dementia among individuals aged 65 and older dropped from 12.2% in 2000 to 8.5% in 2016 – a 30.1% decrease. In men, the prevalence of dementia fell from 10.2% to 7.0%, while for women, it declined from 13.6% to 9.7%, researchers reported. Their finding were published online in PNAS.
The study also revealed that the proportion of college-educated men in the sample increased from 21.5% in 2000 to 33.7% in 2016, while the proportion of college-educated women increased from 12.3% in 2000 to 23% in 2016.
The findings also show a decline in the dementia prevalence in non-Hispanic Black men, which dropped from 17.2% to 9.9%, a decrease of 42.6%. In non-Hispanic White men, dementia declined 9.3% to 6.6%, or 29.0%.
The investigators also found a substantial increase in the level of education between 2000 and 2016. In addition, they found that, among 74- to 84-year-old women in 2000, 29.5% had worked for more than 30 years during their lifetime versus 59.0% in 2016.
The investigators speculated that the decline in dementia prevalence reflects larger socioeconomic changes in the United States as well as prevention strategies to reduce cardiovascular disease.
A person born around 1920, for example, would have had greater exposure to the Great Depression, while someone born in 1936 would have benefited more from the changes in living standards in the years following World War II, they noted.
“There’s a need for more research on the effect of employment on cognitive reserve. It’s plausible that working is good for your mental cognitive abilities,” said study investigator Péter Hudomiet, PhD, from the RAND Corporation, adding that there may also be benefits that extend beyond working years. It’s possible that women’s greater participation in the workforce gives them more chances to establish relationships that in some cases last well into retirement and provide essential social connection. It’s well known that social isolation has a negative impact on cognition.
“It’s plausible that working is good for your mental cognitive abilities,” he added.
The investigators noted that it is beyond the scope of their study to draw definitive conclusions about the causes of the decline, but they observed that positive trends in employment and standard of living make sense. “They would suggest that as schooling levels continue to rise in the U.S. population in younger generations, the prevalence of dementia would continue to decrease.
The investigators report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows. New data from the Health and Retirement Study, a nationally representative survey, show that the prevalence of dementia among individuals aged 65 and older dropped from 12.2% in 2000 to 8.5% in 2016 – a 30.1% decrease. In men, the prevalence of dementia fell from 10.2% to 7.0%, while for women, it declined from 13.6% to 9.7%, researchers reported. Their finding were published online in PNAS.
The study also revealed that the proportion of college-educated men in the sample increased from 21.5% in 2000 to 33.7% in 2016, while the proportion of college-educated women increased from 12.3% in 2000 to 23% in 2016.
The findings also show a decline in the dementia prevalence in non-Hispanic Black men, which dropped from 17.2% to 9.9%, a decrease of 42.6%. In non-Hispanic White men, dementia declined 9.3% to 6.6%, or 29.0%.
The investigators also found a substantial increase in the level of education between 2000 and 2016. In addition, they found that, among 74- to 84-year-old women in 2000, 29.5% had worked for more than 30 years during their lifetime versus 59.0% in 2016.
The investigators speculated that the decline in dementia prevalence reflects larger socioeconomic changes in the United States as well as prevention strategies to reduce cardiovascular disease.
A person born around 1920, for example, would have had greater exposure to the Great Depression, while someone born in 1936 would have benefited more from the changes in living standards in the years following World War II, they noted.
“There’s a need for more research on the effect of employment on cognitive reserve. It’s plausible that working is good for your mental cognitive abilities,” said study investigator Péter Hudomiet, PhD, from the RAND Corporation, adding that there may also be benefits that extend beyond working years. It’s possible that women’s greater participation in the workforce gives them more chances to establish relationships that in some cases last well into retirement and provide essential social connection. It’s well known that social isolation has a negative impact on cognition.
“It’s plausible that working is good for your mental cognitive abilities,” he added.
The investigators noted that it is beyond the scope of their study to draw definitive conclusions about the causes of the decline, but they observed that positive trends in employment and standard of living make sense. “They would suggest that as schooling levels continue to rise in the U.S. population in younger generations, the prevalence of dementia would continue to decrease.
The investigators report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows. New data from the Health and Retirement Study, a nationally representative survey, show that the prevalence of dementia among individuals aged 65 and older dropped from 12.2% in 2000 to 8.5% in 2016 – a 30.1% decrease. In men, the prevalence of dementia fell from 10.2% to 7.0%, while for women, it declined from 13.6% to 9.7%, researchers reported. Their finding were published online in PNAS.
The study also revealed that the proportion of college-educated men in the sample increased from 21.5% in 2000 to 33.7% in 2016, while the proportion of college-educated women increased from 12.3% in 2000 to 23% in 2016.
The findings also show a decline in the dementia prevalence in non-Hispanic Black men, which dropped from 17.2% to 9.9%, a decrease of 42.6%. In non-Hispanic White men, dementia declined 9.3% to 6.6%, or 29.0%.
The investigators also found a substantial increase in the level of education between 2000 and 2016. In addition, they found that, among 74- to 84-year-old women in 2000, 29.5% had worked for more than 30 years during their lifetime versus 59.0% in 2016.
The investigators speculated that the decline in dementia prevalence reflects larger socioeconomic changes in the United States as well as prevention strategies to reduce cardiovascular disease.
A person born around 1920, for example, would have had greater exposure to the Great Depression, while someone born in 1936 would have benefited more from the changes in living standards in the years following World War II, they noted.
“There’s a need for more research on the effect of employment on cognitive reserve. It’s plausible that working is good for your mental cognitive abilities,” said study investigator Péter Hudomiet, PhD, from the RAND Corporation, adding that there may also be benefits that extend beyond working years. It’s possible that women’s greater participation in the workforce gives them more chances to establish relationships that in some cases last well into retirement and provide essential social connection. It’s well known that social isolation has a negative impact on cognition.
“It’s plausible that working is good for your mental cognitive abilities,” he added.
The investigators noted that it is beyond the scope of their study to draw definitive conclusions about the causes of the decline, but they observed that positive trends in employment and standard of living make sense. “They would suggest that as schooling levels continue to rise in the U.S. population in younger generations, the prevalence of dementia would continue to decrease.
The investigators report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
From PNAS
Mental illness tied to increased dementia risk
Results of a large, longitudinal, population-based study show that individuals hospitalized for a mental health disorder had a fourfold increased relative risk (RR) for developing dementia, compared with those who were not hospitalized with a mental illness.
In addition, those with dementia plus a mental disorder developed dementia almost 6 years earlier than those without a mental illness.
The findings were consistent among men and women, in patients with early- and late-onset dementia, in those with Alzheimer’s and non-Alzheimer’s dementia, and across all mental health disorders – and remained so after accounting for pre-existing physical illness and socioeconomic factors.
“Dementia is not typically treated until later in life, but our study suggests that we need to be thinking about dementia prevention much earlier in the life course,” study investigator Leah Richmond-Rakerd, PhD, assistant professor, department of psychology, University of Michigan, said in an interview.
“Supporting young people’s mental health could be a window of opportunity to help reduce the burden of dementia in older adults,” she said.
The findings were published online Feb. 16.
Underappreciated risk factor
“Recognition of the outsized influence of dementia on later-life functioning has fueled research into modifiable risk factors and prevention targets,” the investigators write.
Previous research suggests mental disorders may “comprise an underappreciated category of modifiable risk factors.” However, those studies focused primarily on midlife and older individuals, not on capturing mental disorders during young adulthood, which is the time of “peak prevalence,” they add. In addition, most studies have not explored the full range of mental disorders.
Dr. Richmond-Rakerd noted that it is well known that mental health disorders peak in adolescence and young adulthood – and are treatable.
“If the same people who have mental disorders when they are young tend to develop dementia when they are older, that would mean that preventing mental health problems in younger people might reduce or delay the burden of dementia in older people,” she said.
The investigators assessed records from the New Zealand Integrated Data Infrastructure, which is a de-identified register that includes the entire New Zealand population. They also examined information about hospitalizations and diagnoses from records kept by the New Zealand Ministry of Health.
The researchers followed 1,711,386 individuals born between 1928 and 1967 (50.6% men, aged 21 to 60 years at baseline) for 30 years. The population was subdivided into age groups based on birth years: 1928-1937 (14.8%), 1938-1947 (20.85%), 1948-1957 (29.35%), and 1958-1967 (35.1%).
Earlier onset
During the study period, 3.8% of individuals were identified as having a mental disorder, and 2% were identified as having dementia. Similar percentages of men and women had a mental disorder, and similar percentages had dementia.
Dementia was “over-represented” among participants with versus without a mental disorder (6.1% vs. 1.8%). This finding held across all age groups.
Those diagnosed with a mental disorder were also more likely to develop dementia, compared with their peers without a mental disorder (RR, 3.51; 95% confidence interval, 3.39-3.64), which is a larger association than that between physical diseases and dementia (RR, 1.19; 95% CI, 1.16-1.21).
These associations were present in both sexes and in all age groups, although the associations were stronger in more recently born cohorts.
A sixfold higher risk for dementia remained even after adjusting for pre-existing physical illnesses (HR, 6.49; 95% CI, 6.25-6.73); and the elevated risk was evident across different lengths of follow-up from the index mental disorder.
When the researchers focused specifically on individuals diagnosed with dementia, they found that those diagnosed with a mental disorder developed dementia a mean of 5.60 years earlier than those without a mental disorder diagnosis – an association observed across both sexes and all age groups.
“Individuals diagnosed with psychotic, substance use, mood, neurotic, and all other mental disorders and who engaged in self-harm were all more likely than those without a mental disorder to be diagnosed with subsequent dementia, even after accounting for their physical disease histories,” the investigators write.
Although there was a link between mental disorders in both Alzheimer’s and non-Alzheimer’s dementias, the association was larger in non-Alzheimer’s.
The researchers note that the study has several limitations, including the fact that it was conducted in New Zealand and therefore the results may not be generalizable to other regions. In addition, inpatient hospital records do not capture less severe mental disorder cases treated in the outpatient setting.
Dr. Richmond-Rakerd suggested several potential mechanisms that could account for the link between mental illness and dementia, including poor lifestyle choices and metabolic side effects associated with some psychiatric medications.
“There could also be shared risk factors for both mental disorders and dementia, such as shared genetics, or individuals may experience a lifelong brain vulnerability that shows up as mental health problems earlier in life and shows up as dementia later in life,” she said.
An important risk factor
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness, said a major strength of the study was its longitudinal scope and large population size.
He described the study as allowing clinicians to “watch the movie,” as opposed to looking at a “snapshot” of data.
“Although you can learn things from snapshots, a large, comprehensive public health system looking at 30 years of claims – something not possible in the U.S. because of our more fragmented health care system – offers more insight,” said Dr. Duckworth, who was not involved with the research.
The investigators are “painting a picture of a correlation of risk, and to me, that’s the beginning of further inquiry,” he added. “Would preventive efforts targeting dementia, such as exercise and socialization, be helpful? It’s a great study that raises these interesting questions.”
Also commenting in an interview, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, said the study “adds a wealth of data to our understanding” of mental disorders as a dementia risk factor.
However, the study was observational, so “the findings cannot imply causation, [and just] because someone has depression, that does not mean they will go on to develop Alzheimer’s,” said Dr. Sexton, who also was not involved with the research.
Still, “these data support the idea that taking care of one’s mental health is incredibly important for overall wellbeing. For providers, it’s important to have mental health evaluation be a part of your patient’s regular checkups,” she added.
Dr. Richmond-Rakerd noted that even if mental health conditions are not a causal risk factor for dementia, “the presence of a mental health problem is still an important indicator of risk. Mental health providers may wish to target other risk factors for dementia that are more common in individuals with mental health conditions, such as social disconnection.”
The study was funded by grants from the National Institute on Aging, the U.K. Medical Research Council, the National Institute of Child Health and Development through the Duke Population Research Center, and the National Institute on Aging through the Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease and Related Dementias. Dr. Richmond-Rakerd reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Sexton and Dr. Duckworth report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large, longitudinal, population-based study show that individuals hospitalized for a mental health disorder had a fourfold increased relative risk (RR) for developing dementia, compared with those who were not hospitalized with a mental illness.
In addition, those with dementia plus a mental disorder developed dementia almost 6 years earlier than those without a mental illness.
The findings were consistent among men and women, in patients with early- and late-onset dementia, in those with Alzheimer’s and non-Alzheimer’s dementia, and across all mental health disorders – and remained so after accounting for pre-existing physical illness and socioeconomic factors.
“Dementia is not typically treated until later in life, but our study suggests that we need to be thinking about dementia prevention much earlier in the life course,” study investigator Leah Richmond-Rakerd, PhD, assistant professor, department of psychology, University of Michigan, said in an interview.
“Supporting young people’s mental health could be a window of opportunity to help reduce the burden of dementia in older adults,” she said.
The findings were published online Feb. 16.
Underappreciated risk factor
“Recognition of the outsized influence of dementia on later-life functioning has fueled research into modifiable risk factors and prevention targets,” the investigators write.
Previous research suggests mental disorders may “comprise an underappreciated category of modifiable risk factors.” However, those studies focused primarily on midlife and older individuals, not on capturing mental disorders during young adulthood, which is the time of “peak prevalence,” they add. In addition, most studies have not explored the full range of mental disorders.
Dr. Richmond-Rakerd noted that it is well known that mental health disorders peak in adolescence and young adulthood – and are treatable.
“If the same people who have mental disorders when they are young tend to develop dementia when they are older, that would mean that preventing mental health problems in younger people might reduce or delay the burden of dementia in older people,” she said.
The investigators assessed records from the New Zealand Integrated Data Infrastructure, which is a de-identified register that includes the entire New Zealand population. They also examined information about hospitalizations and diagnoses from records kept by the New Zealand Ministry of Health.
The researchers followed 1,711,386 individuals born between 1928 and 1967 (50.6% men, aged 21 to 60 years at baseline) for 30 years. The population was subdivided into age groups based on birth years: 1928-1937 (14.8%), 1938-1947 (20.85%), 1948-1957 (29.35%), and 1958-1967 (35.1%).
Earlier onset
During the study period, 3.8% of individuals were identified as having a mental disorder, and 2% were identified as having dementia. Similar percentages of men and women had a mental disorder, and similar percentages had dementia.
Dementia was “over-represented” among participants with versus without a mental disorder (6.1% vs. 1.8%). This finding held across all age groups.
Those diagnosed with a mental disorder were also more likely to develop dementia, compared with their peers without a mental disorder (RR, 3.51; 95% confidence interval, 3.39-3.64), which is a larger association than that between physical diseases and dementia (RR, 1.19; 95% CI, 1.16-1.21).
These associations were present in both sexes and in all age groups, although the associations were stronger in more recently born cohorts.
A sixfold higher risk for dementia remained even after adjusting for pre-existing physical illnesses (HR, 6.49; 95% CI, 6.25-6.73); and the elevated risk was evident across different lengths of follow-up from the index mental disorder.
When the researchers focused specifically on individuals diagnosed with dementia, they found that those diagnosed with a mental disorder developed dementia a mean of 5.60 years earlier than those without a mental disorder diagnosis – an association observed across both sexes and all age groups.
“Individuals diagnosed with psychotic, substance use, mood, neurotic, and all other mental disorders and who engaged in self-harm were all more likely than those without a mental disorder to be diagnosed with subsequent dementia, even after accounting for their physical disease histories,” the investigators write.
Although there was a link between mental disorders in both Alzheimer’s and non-Alzheimer’s dementias, the association was larger in non-Alzheimer’s.
The researchers note that the study has several limitations, including the fact that it was conducted in New Zealand and therefore the results may not be generalizable to other regions. In addition, inpatient hospital records do not capture less severe mental disorder cases treated in the outpatient setting.
Dr. Richmond-Rakerd suggested several potential mechanisms that could account for the link between mental illness and dementia, including poor lifestyle choices and metabolic side effects associated with some psychiatric medications.
“There could also be shared risk factors for both mental disorders and dementia, such as shared genetics, or individuals may experience a lifelong brain vulnerability that shows up as mental health problems earlier in life and shows up as dementia later in life,” she said.
An important risk factor
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness, said a major strength of the study was its longitudinal scope and large population size.
He described the study as allowing clinicians to “watch the movie,” as opposed to looking at a “snapshot” of data.
“Although you can learn things from snapshots, a large, comprehensive public health system looking at 30 years of claims – something not possible in the U.S. because of our more fragmented health care system – offers more insight,” said Dr. Duckworth, who was not involved with the research.
The investigators are “painting a picture of a correlation of risk, and to me, that’s the beginning of further inquiry,” he added. “Would preventive efforts targeting dementia, such as exercise and socialization, be helpful? It’s a great study that raises these interesting questions.”
Also commenting in an interview, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, said the study “adds a wealth of data to our understanding” of mental disorders as a dementia risk factor.
However, the study was observational, so “the findings cannot imply causation, [and just] because someone has depression, that does not mean they will go on to develop Alzheimer’s,” said Dr. Sexton, who also was not involved with the research.
Still, “these data support the idea that taking care of one’s mental health is incredibly important for overall wellbeing. For providers, it’s important to have mental health evaluation be a part of your patient’s regular checkups,” she added.
Dr. Richmond-Rakerd noted that even if mental health conditions are not a causal risk factor for dementia, “the presence of a mental health problem is still an important indicator of risk. Mental health providers may wish to target other risk factors for dementia that are more common in individuals with mental health conditions, such as social disconnection.”
The study was funded by grants from the National Institute on Aging, the U.K. Medical Research Council, the National Institute of Child Health and Development through the Duke Population Research Center, and the National Institute on Aging through the Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease and Related Dementias. Dr. Richmond-Rakerd reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Sexton and Dr. Duckworth report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Results of a large, longitudinal, population-based study show that individuals hospitalized for a mental health disorder had a fourfold increased relative risk (RR) for developing dementia, compared with those who were not hospitalized with a mental illness.
In addition, those with dementia plus a mental disorder developed dementia almost 6 years earlier than those without a mental illness.
The findings were consistent among men and women, in patients with early- and late-onset dementia, in those with Alzheimer’s and non-Alzheimer’s dementia, and across all mental health disorders – and remained so after accounting for pre-existing physical illness and socioeconomic factors.
“Dementia is not typically treated until later in life, but our study suggests that we need to be thinking about dementia prevention much earlier in the life course,” study investigator Leah Richmond-Rakerd, PhD, assistant professor, department of psychology, University of Michigan, said in an interview.
“Supporting young people’s mental health could be a window of opportunity to help reduce the burden of dementia in older adults,” she said.
The findings were published online Feb. 16.
Underappreciated risk factor
“Recognition of the outsized influence of dementia on later-life functioning has fueled research into modifiable risk factors and prevention targets,” the investigators write.
Previous research suggests mental disorders may “comprise an underappreciated category of modifiable risk factors.” However, those studies focused primarily on midlife and older individuals, not on capturing mental disorders during young adulthood, which is the time of “peak prevalence,” they add. In addition, most studies have not explored the full range of mental disorders.
Dr. Richmond-Rakerd noted that it is well known that mental health disorders peak in adolescence and young adulthood – and are treatable.
“If the same people who have mental disorders when they are young tend to develop dementia when they are older, that would mean that preventing mental health problems in younger people might reduce or delay the burden of dementia in older people,” she said.
The investigators assessed records from the New Zealand Integrated Data Infrastructure, which is a de-identified register that includes the entire New Zealand population. They also examined information about hospitalizations and diagnoses from records kept by the New Zealand Ministry of Health.
The researchers followed 1,711,386 individuals born between 1928 and 1967 (50.6% men, aged 21 to 60 years at baseline) for 30 years. The population was subdivided into age groups based on birth years: 1928-1937 (14.8%), 1938-1947 (20.85%), 1948-1957 (29.35%), and 1958-1967 (35.1%).
Earlier onset
During the study period, 3.8% of individuals were identified as having a mental disorder, and 2% were identified as having dementia. Similar percentages of men and women had a mental disorder, and similar percentages had dementia.
Dementia was “over-represented” among participants with versus without a mental disorder (6.1% vs. 1.8%). This finding held across all age groups.
Those diagnosed with a mental disorder were also more likely to develop dementia, compared with their peers without a mental disorder (RR, 3.51; 95% confidence interval, 3.39-3.64), which is a larger association than that between physical diseases and dementia (RR, 1.19; 95% CI, 1.16-1.21).
These associations were present in both sexes and in all age groups, although the associations were stronger in more recently born cohorts.
A sixfold higher risk for dementia remained even after adjusting for pre-existing physical illnesses (HR, 6.49; 95% CI, 6.25-6.73); and the elevated risk was evident across different lengths of follow-up from the index mental disorder.
When the researchers focused specifically on individuals diagnosed with dementia, they found that those diagnosed with a mental disorder developed dementia a mean of 5.60 years earlier than those without a mental disorder diagnosis – an association observed across both sexes and all age groups.
“Individuals diagnosed with psychotic, substance use, mood, neurotic, and all other mental disorders and who engaged in self-harm were all more likely than those without a mental disorder to be diagnosed with subsequent dementia, even after accounting for their physical disease histories,” the investigators write.
Although there was a link between mental disorders in both Alzheimer’s and non-Alzheimer’s dementias, the association was larger in non-Alzheimer’s.
The researchers note that the study has several limitations, including the fact that it was conducted in New Zealand and therefore the results may not be generalizable to other regions. In addition, inpatient hospital records do not capture less severe mental disorder cases treated in the outpatient setting.
Dr. Richmond-Rakerd suggested several potential mechanisms that could account for the link between mental illness and dementia, including poor lifestyle choices and metabolic side effects associated with some psychiatric medications.
“There could also be shared risk factors for both mental disorders and dementia, such as shared genetics, or individuals may experience a lifelong brain vulnerability that shows up as mental health problems earlier in life and shows up as dementia later in life,” she said.
An important risk factor
Commenting for this article, Ken Duckworth, MD, chief medical officer of the National Alliance on Mental Illness, said a major strength of the study was its longitudinal scope and large population size.
He described the study as allowing clinicians to “watch the movie,” as opposed to looking at a “snapshot” of data.
“Although you can learn things from snapshots, a large, comprehensive public health system looking at 30 years of claims – something not possible in the U.S. because of our more fragmented health care system – offers more insight,” said Dr. Duckworth, who was not involved with the research.
The investigators are “painting a picture of a correlation of risk, and to me, that’s the beginning of further inquiry,” he added. “Would preventive efforts targeting dementia, such as exercise and socialization, be helpful? It’s a great study that raises these interesting questions.”
Also commenting in an interview, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, said the study “adds a wealth of data to our understanding” of mental disorders as a dementia risk factor.
However, the study was observational, so “the findings cannot imply causation, [and just] because someone has depression, that does not mean they will go on to develop Alzheimer’s,” said Dr. Sexton, who also was not involved with the research.
Still, “these data support the idea that taking care of one’s mental health is incredibly important for overall wellbeing. For providers, it’s important to have mental health evaluation be a part of your patient’s regular checkups,” she added.
Dr. Richmond-Rakerd noted that even if mental health conditions are not a causal risk factor for dementia, “the presence of a mental health problem is still an important indicator of risk. Mental health providers may wish to target other risk factors for dementia that are more common in individuals with mental health conditions, such as social disconnection.”
The study was funded by grants from the National Institute on Aging, the U.K. Medical Research Council, the National Institute of Child Health and Development through the Duke Population Research Center, and the National Institute on Aging through the Center for Advancing Sociodemographic and Economic Study of Alzheimer’s Disease and Related Dementias. Dr. Richmond-Rakerd reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Sexton and Dr. Duckworth report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Short sleep predicts incident dementia and all-cause mortality
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).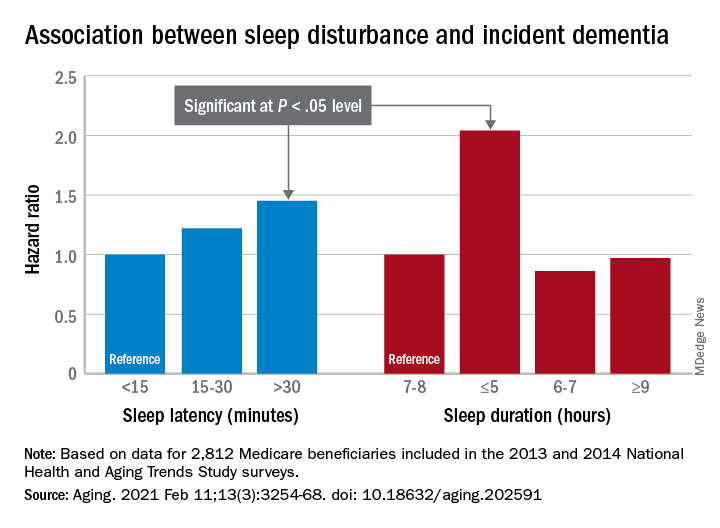
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
More evidence has emerged linking sleep deficiency, dementia, and mortality.
“Sleep disturbance and insufficiency have been shown to be associated with both the development and progression of Alzheimer’s disease and with all-cause mortality,” wrote Rebecca S. Robbins, PhD, of Brigham and Women’s Hospital, Boston, and colleagues. However, research on this topic has yielded conflicting results, and “few studies have included a comprehensive set of sleep characteristics in a single examination of incident dementia and all-cause mortality.”
In a study published in Aging, the researchers identified 2,812 adults aged 65 years and older from the National Health and Aging Trends Study (NHATS), a nationally representative longitudinal study of Medicare beneficiaries aged 65 years and older in the United States.
Participants completed surveys about sleep disturbance and duration in 2013 (1,575 individuals) and in 2014 (1,237 individuals), and the researchers examined the relationship between sleep disturbance and deficiency and incident dementia and all-cause mortality over the next 5 years. The average age of the study participants was 76.9 years, 60% were women, and 72% were White.
Overall, approximately 60% of the participants reported never or rarely having problems with alertness, approximately half said that they rarely or never napped, and more than half said they fell asleep in 15 minutes or less. Approximately 70% rated their sleep quality as good or very good, and more than 90% said they rarely or never snored.
The researchers examined the relationships between sleep characteristics and the development of incident dementia over 5 years. In a fully adjusted Cox multivariate analysis, individuals who slept 5 hours or less per night had approximately twice the risk for incident dementia as those who slept longer (hazard ratio, 2.04); risk of dementia also was higher among those who took 30 minutes or longer to fall asleep (HR, 1.45).
In addition, the risk of all-cause mortality was significantly higher among individuals who reported difficulty maintaining alertness some days or most days/every day (HR, 1.49 and HR, 1.65, respectively), routinely napping some days or most days/every day (HR, 1.38 and HR, 1.73, respectively), poor or very poor sleep quality (HR, 1.75), and sleeping 5 hours or less each night (HR, 2.38).
The study findings were limited by several factors including a population representing only one-quarter of the NHATS cohort, which prevented nationally representative estimates, the availability of only 2 years of sleep data, and small sample size for certain response categories, the researchers noted.
However, “our study offers a contribution to the literature on sleep among aging populations in its assessment of incident dementia and all-cause mortality and a range of sleep characteristics among older adults,” they said. In particular, “short sleep duration was a strong predictor of both incident dementia and all-cause mortality, suggesting this may be a sleep characteristic that is important – over and above the other predictors – of adverse outcomes among older adults,” and future areas for research include the development of novel behavioral interventions to improve sleep in this population.
The study was supported in part by the National Institute for Occupational Safety and Health; the National Heart, Lung, and Blood Institute; the National Institute on Aging; and the Brigham Research Institute Fund to Sustain Research Excellence. Lead author Dr. Robbins disclosed fees from Denihan Hospitality, Rituals Cosmetics, Dagmejan, Asystem, and SleepCycle. Several coauthors disclosed relationships with multiple pharmaceutical companies, and support from various philanthropic organizations.
FROM AGING
Mortality burden of dementia may be greater than estimated
This burden may be greatest among non-Hispanic black older adults, compared with Hispanic and non-Hispanic whites. This burden also is significantly greater among people with less than a high school education, compared with those with a college education.
The study results underscore the importance of broadening access to population-based interventions that focus on dementia prevention and care, the investigators wrote. “Future research could examine the extent to which deaths attributable to dementia and underestimation of dementia as an underlying cause of death on death certificates might have changed over time,” wrote Andrew C. Stokes, PhD, assistant professor of global health at the Boston University School of Public Health, and colleagues.
The study was published online Aug. 24 in JAMA Neurology.
In 2019, approximately 5.6 million adults in the United States who were aged 65 years or older had Alzheimer’s disease, vascular dementia, or mixed-cause dementia. A further 18.8% of Americans in this age group had cognitive impairment without dementia (CIND). About one third of patients with CIND may develop Alzheimer’s disease or related dementias (ADRD) within 5 years.
Research suggests that medical examiners significantly underreport ADRD on death certificates. One community-based study, for example, found that only 25% of deaths in patients with dementia had Alzheimer’s disease listed on the death certificates. Other research found that deaths in patients with dementia were often coded using more proximate causes, such as cardiovascular disease, sepsis, and pneumonia.
Health and retirement study
Dr. Stokes and colleagues examined data from the Health and Retirement Study (HRS) to evaluate the association of dementia and CIND with all-cause mortality. The HRS is a longitudinal cohort study of adults older than 50 years who live in the community. Its sample is nationally representative. The HRS investigators also initiated the Aging, Demographics, and Memory study to develop a procedure for assessing cognitive status in the HRS sample.
In their study, Dr. Stokes and colleagues included adults who had been sampled in the 2000 wave of HRS. They focused on participants between ages 70 and 99 years at baseline, and their final sample included 7,342 older adults. To identify dementia status, the researchers used the Langa–Weir score cutoff, which is based on tests of immediate and delayed recall of 10 words, a serial 7-second task, and a backward counting task. They also classified dementia status using the Herzog–Wallace, Wu, Hurd, and modified Hurd algorithms.
At baseline, the researchers measured age, sex, race or ethnicity, educational attainment, smoking status, self-reported disease diagnoses, and U.S. Census division as covariates. The National Center for Health Statistics linked HRS data with National Death Index records. These linked records include underlying cause of death and any mention of a condition or cause of death on the death certificate. The researchers compared the percentage of deaths attributable to ADRD according to a population attributable fraction estimate with the proportion of dementia-related deaths according to underlying causes and with any mention of dementia on death certificates.
The sample of 7,342 older adults included 4,348 (60.3%) women. Data for 1,030 (13.4%) people were reported by proxy. At baseline, most participants (64.0%) were between ages 70 and 79 years, 31% were between ages 80 and 89, and 5% were between ages 90 and 99 years. The prevalence of dementia in the complete sample was 14.3%, and the prevalence of CIND was 24.7%. The prevalence of dementia (22.4%) and CIND (29.3%) was higher among decedents than among the full population.
The hazard ratio (HR) for mortality was 2.53 among participants with dementia and 1.53 among patients with CIND. Although 13.6% of deaths were attributable to dementia, the proportion of deaths assigned to dementia as an underlying cause on death certificates was 5.0%. This discrepancy suggests that dementia is underreported by more than a factor of 2.7.
The mortality burden of dementia was 24.7% in non-Hispanic black older adults, 20.7% in Hispanic white participants, and 12.2% in non-Hispanic white participants. In addition, the mortality burden of dementia was significantly greater among participants with less than a high school education (16.2%) than among participants with a college education (9.8%).
The degree to which the underlying cause of death underestimated the mortality burden of dementia varied by sociodemographic characteristics, health status, and geography. The burden was underestimated by a factor of 7.1 among non-Hispanic black participants, a factor of 4.1 among Hispanic participants, and a factor of 2.3 among non-Hispanic white participants. The burden was underestimated by a factor of 3.5 in men and a factor of 2.4 in women. In addition, the burden was underestimated by a factor of 3.0 among participants with less than a high school education, by a factor of 2.3 among participants with a high school education, by a factor of 1.9 in participants with some college, and by a factor of 2.5 among participants with a college or higher education.
One of the study’s strengths was its population attributable fraction analysis, which reduced the risk of overestimating the mortality burden of dementia, Dr. Stokes and colleagues wrote. Examining CIND is valuable because of its high prevalence and consequent influence on outcomes in the population, even though CIND is associated with a lower mortality risk, they added. Nevertheless, the investigators were unable to assess mortality for dementia subtypes, and the classifications of dementia status and CIND may be subject to measurement error.
Underestimation is systematic
“This study is eye-opening in that it highlights the systematic underestimation of deaths attributable to dementia,” said Costantino Iadecola, MD, Anne Parrish Titzell professor of neurology and director and chair of the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine in New York. The study’s main strength is that it is nationally representative, but the data must be confirmed in a larger population, he added.
The results will clarify the effect of dementia on mortality for neurologists, and geriatricians should be made aware of them, said Dr. Iadecola. “These data should be valuable to rationalize public health efforts and related funding decisions concerning research and community support.”
Further research could determine the mortality of dementia subgroups, “especially dementias linked to vascular factors in which prevention may be effective,” said Dr. Iadecola. “In the older population, vascular factors may play a more preeminent role, and it may help focus preventive approaches.”
The study was supported by a grant from the National Institute on Aging. Dr. Stokes received grants from Ethicon that were unrelated to this study. Dr. Iadecola serves on the scientific advisory board of Broadview Venture.
SOURCE: Stokes AC et al. JAMA Neurol. 2020 Aug 24. doi: 10.1001/jamaneurol.2020.2831.
This burden may be greatest among non-Hispanic black older adults, compared with Hispanic and non-Hispanic whites. This burden also is significantly greater among people with less than a high school education, compared with those with a college education.
The study results underscore the importance of broadening access to population-based interventions that focus on dementia prevention and care, the investigators wrote. “Future research could examine the extent to which deaths attributable to dementia and underestimation of dementia as an underlying cause of death on death certificates might have changed over time,” wrote Andrew C. Stokes, PhD, assistant professor of global health at the Boston University School of Public Health, and colleagues.
The study was published online Aug. 24 in JAMA Neurology.
In 2019, approximately 5.6 million adults in the United States who were aged 65 years or older had Alzheimer’s disease, vascular dementia, or mixed-cause dementia. A further 18.8% of Americans in this age group had cognitive impairment without dementia (CIND). About one third of patients with CIND may develop Alzheimer’s disease or related dementias (ADRD) within 5 years.
Research suggests that medical examiners significantly underreport ADRD on death certificates. One community-based study, for example, found that only 25% of deaths in patients with dementia had Alzheimer’s disease listed on the death certificates. Other research found that deaths in patients with dementia were often coded using more proximate causes, such as cardiovascular disease, sepsis, and pneumonia.
Health and retirement study
Dr. Stokes and colleagues examined data from the Health and Retirement Study (HRS) to evaluate the association of dementia and CIND with all-cause mortality. The HRS is a longitudinal cohort study of adults older than 50 years who live in the community. Its sample is nationally representative. The HRS investigators also initiated the Aging, Demographics, and Memory study to develop a procedure for assessing cognitive status in the HRS sample.
In their study, Dr. Stokes and colleagues included adults who had been sampled in the 2000 wave of HRS. They focused on participants between ages 70 and 99 years at baseline, and their final sample included 7,342 older adults. To identify dementia status, the researchers used the Langa–Weir score cutoff, which is based on tests of immediate and delayed recall of 10 words, a serial 7-second task, and a backward counting task. They also classified dementia status using the Herzog–Wallace, Wu, Hurd, and modified Hurd algorithms.
At baseline, the researchers measured age, sex, race or ethnicity, educational attainment, smoking status, self-reported disease diagnoses, and U.S. Census division as covariates. The National Center for Health Statistics linked HRS data with National Death Index records. These linked records include underlying cause of death and any mention of a condition or cause of death on the death certificate. The researchers compared the percentage of deaths attributable to ADRD according to a population attributable fraction estimate with the proportion of dementia-related deaths according to underlying causes and with any mention of dementia on death certificates.
The sample of 7,342 older adults included 4,348 (60.3%) women. Data for 1,030 (13.4%) people were reported by proxy. At baseline, most participants (64.0%) were between ages 70 and 79 years, 31% were between ages 80 and 89, and 5% were between ages 90 and 99 years. The prevalence of dementia in the complete sample was 14.3%, and the prevalence of CIND was 24.7%. The prevalence of dementia (22.4%) and CIND (29.3%) was higher among decedents than among the full population.
The hazard ratio (HR) for mortality was 2.53 among participants with dementia and 1.53 among patients with CIND. Although 13.6% of deaths were attributable to dementia, the proportion of deaths assigned to dementia as an underlying cause on death certificates was 5.0%. This discrepancy suggests that dementia is underreported by more than a factor of 2.7.
The mortality burden of dementia was 24.7% in non-Hispanic black older adults, 20.7% in Hispanic white participants, and 12.2% in non-Hispanic white participants. In addition, the mortality burden of dementia was significantly greater among participants with less than a high school education (16.2%) than among participants with a college education (9.8%).
The degree to which the underlying cause of death underestimated the mortality burden of dementia varied by sociodemographic characteristics, health status, and geography. The burden was underestimated by a factor of 7.1 among non-Hispanic black participants, a factor of 4.1 among Hispanic participants, and a factor of 2.3 among non-Hispanic white participants. The burden was underestimated by a factor of 3.5 in men and a factor of 2.4 in women. In addition, the burden was underestimated by a factor of 3.0 among participants with less than a high school education, by a factor of 2.3 among participants with a high school education, by a factor of 1.9 in participants with some college, and by a factor of 2.5 among participants with a college or higher education.
One of the study’s strengths was its population attributable fraction analysis, which reduced the risk of overestimating the mortality burden of dementia, Dr. Stokes and colleagues wrote. Examining CIND is valuable because of its high prevalence and consequent influence on outcomes in the population, even though CIND is associated with a lower mortality risk, they added. Nevertheless, the investigators were unable to assess mortality for dementia subtypes, and the classifications of dementia status and CIND may be subject to measurement error.
Underestimation is systematic
“This study is eye-opening in that it highlights the systematic underestimation of deaths attributable to dementia,” said Costantino Iadecola, MD, Anne Parrish Titzell professor of neurology and director and chair of the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine in New York. The study’s main strength is that it is nationally representative, but the data must be confirmed in a larger population, he added.
The results will clarify the effect of dementia on mortality for neurologists, and geriatricians should be made aware of them, said Dr. Iadecola. “These data should be valuable to rationalize public health efforts and related funding decisions concerning research and community support.”
Further research could determine the mortality of dementia subgroups, “especially dementias linked to vascular factors in which prevention may be effective,” said Dr. Iadecola. “In the older population, vascular factors may play a more preeminent role, and it may help focus preventive approaches.”
The study was supported by a grant from the National Institute on Aging. Dr. Stokes received grants from Ethicon that were unrelated to this study. Dr. Iadecola serves on the scientific advisory board of Broadview Venture.
SOURCE: Stokes AC et al. JAMA Neurol. 2020 Aug 24. doi: 10.1001/jamaneurol.2020.2831.
This burden may be greatest among non-Hispanic black older adults, compared with Hispanic and non-Hispanic whites. This burden also is significantly greater among people with less than a high school education, compared with those with a college education.
The study results underscore the importance of broadening access to population-based interventions that focus on dementia prevention and care, the investigators wrote. “Future research could examine the extent to which deaths attributable to dementia and underestimation of dementia as an underlying cause of death on death certificates might have changed over time,” wrote Andrew C. Stokes, PhD, assistant professor of global health at the Boston University School of Public Health, and colleagues.
The study was published online Aug. 24 in JAMA Neurology.
In 2019, approximately 5.6 million adults in the United States who were aged 65 years or older had Alzheimer’s disease, vascular dementia, or mixed-cause dementia. A further 18.8% of Americans in this age group had cognitive impairment without dementia (CIND). About one third of patients with CIND may develop Alzheimer’s disease or related dementias (ADRD) within 5 years.
Research suggests that medical examiners significantly underreport ADRD on death certificates. One community-based study, for example, found that only 25% of deaths in patients with dementia had Alzheimer’s disease listed on the death certificates. Other research found that deaths in patients with dementia were often coded using more proximate causes, such as cardiovascular disease, sepsis, and pneumonia.
Health and retirement study
Dr. Stokes and colleagues examined data from the Health and Retirement Study (HRS) to evaluate the association of dementia and CIND with all-cause mortality. The HRS is a longitudinal cohort study of adults older than 50 years who live in the community. Its sample is nationally representative. The HRS investigators also initiated the Aging, Demographics, and Memory study to develop a procedure for assessing cognitive status in the HRS sample.
In their study, Dr. Stokes and colleagues included adults who had been sampled in the 2000 wave of HRS. They focused on participants between ages 70 and 99 years at baseline, and their final sample included 7,342 older adults. To identify dementia status, the researchers used the Langa–Weir score cutoff, which is based on tests of immediate and delayed recall of 10 words, a serial 7-second task, and a backward counting task. They also classified dementia status using the Herzog–Wallace, Wu, Hurd, and modified Hurd algorithms.
At baseline, the researchers measured age, sex, race or ethnicity, educational attainment, smoking status, self-reported disease diagnoses, and U.S. Census division as covariates. The National Center for Health Statistics linked HRS data with National Death Index records. These linked records include underlying cause of death and any mention of a condition or cause of death on the death certificate. The researchers compared the percentage of deaths attributable to ADRD according to a population attributable fraction estimate with the proportion of dementia-related deaths according to underlying causes and with any mention of dementia on death certificates.
The sample of 7,342 older adults included 4,348 (60.3%) women. Data for 1,030 (13.4%) people were reported by proxy. At baseline, most participants (64.0%) were between ages 70 and 79 years, 31% were between ages 80 and 89, and 5% were between ages 90 and 99 years. The prevalence of dementia in the complete sample was 14.3%, and the prevalence of CIND was 24.7%. The prevalence of dementia (22.4%) and CIND (29.3%) was higher among decedents than among the full population.
The hazard ratio (HR) for mortality was 2.53 among participants with dementia and 1.53 among patients with CIND. Although 13.6% of deaths were attributable to dementia, the proportion of deaths assigned to dementia as an underlying cause on death certificates was 5.0%. This discrepancy suggests that dementia is underreported by more than a factor of 2.7.
The mortality burden of dementia was 24.7% in non-Hispanic black older adults, 20.7% in Hispanic white participants, and 12.2% in non-Hispanic white participants. In addition, the mortality burden of dementia was significantly greater among participants with less than a high school education (16.2%) than among participants with a college education (9.8%).
The degree to which the underlying cause of death underestimated the mortality burden of dementia varied by sociodemographic characteristics, health status, and geography. The burden was underestimated by a factor of 7.1 among non-Hispanic black participants, a factor of 4.1 among Hispanic participants, and a factor of 2.3 among non-Hispanic white participants. The burden was underestimated by a factor of 3.5 in men and a factor of 2.4 in women. In addition, the burden was underestimated by a factor of 3.0 among participants with less than a high school education, by a factor of 2.3 among participants with a high school education, by a factor of 1.9 in participants with some college, and by a factor of 2.5 among participants with a college or higher education.
One of the study’s strengths was its population attributable fraction analysis, which reduced the risk of overestimating the mortality burden of dementia, Dr. Stokes and colleagues wrote. Examining CIND is valuable because of its high prevalence and consequent influence on outcomes in the population, even though CIND is associated with a lower mortality risk, they added. Nevertheless, the investigators were unable to assess mortality for dementia subtypes, and the classifications of dementia status and CIND may be subject to measurement error.
Underestimation is systematic
“This study is eye-opening in that it highlights the systematic underestimation of deaths attributable to dementia,” said Costantino Iadecola, MD, Anne Parrish Titzell professor of neurology and director and chair of the Feil Family Brain and Mind Research Institute at Weill Cornell Medicine in New York. The study’s main strength is that it is nationally representative, but the data must be confirmed in a larger population, he added.
The results will clarify the effect of dementia on mortality for neurologists, and geriatricians should be made aware of them, said Dr. Iadecola. “These data should be valuable to rationalize public health efforts and related funding decisions concerning research and community support.”
Further research could determine the mortality of dementia subgroups, “especially dementias linked to vascular factors in which prevention may be effective,” said Dr. Iadecola. “In the older population, vascular factors may play a more preeminent role, and it may help focus preventive approaches.”
The study was supported by a grant from the National Institute on Aging. Dr. Stokes received grants from Ethicon that were unrelated to this study. Dr. Iadecola serves on the scientific advisory board of Broadview Venture.
SOURCE: Stokes AC et al. JAMA Neurol. 2020 Aug 24. doi: 10.1001/jamaneurol.2020.2831.
FROM JAMA NEUROLOGY
Repetitive hits to the head tied to depression, poor cognition in later life
A history of repetitive hits to the head (RHI), even without noticeable symptoms, is linked to a significantly increased risk of depression and poorer cognition later in life, new research shows.
“We found that a history of exposure to [repetitive hits to the head] from contact sports, military service, or physical abuse, as well as a history of TBI (traumatic brain injury), corresponded to more symptoms of later life depression and worse cognitive function,” lead author Michael Alosco, PhD, associate professor of neurology and codirector of the Boston University Alzheimer’s Disease Center Clinical Core, told Medscape Medical News.
He added that the findings underscore the importance of assessing repetitive head impacts (RHI).
The study was published online June 26 in Neurology.
Largest study to date
It is well known that sustaining a TBI is associated with worse later life cognition or mood problems, said Alosco. However, in the current research the investigators hypothesized that RHI may be a key driver of some of these outcomes, Alosco said.
Previous studies have been small or have only examined male former football players.
“What’s unique about our study is that we focused on a history of RHIs, and it is the largest study of its kind, incorporating over 30,000 males and females with different types of exposure to these RHIs.”
The researchers used data from the Brain Health Registry, an internet-based registry that longitudinally monitors cognition and functioning of participants (age 40 years and older).
Participants completed the Ohio State University TBI Identification Method (OSU TBI-ID) and answered a yes/no question: “Have you ever had a period of time in which you experienced multiple, repeated impacts to your head (eg, history of abuse, contact sports, military duty)?”
Participants also completed the Geriatric Depression Scale (GDS-15), the CogState Battery (CBB), and the Lumos Labs NeuroCognitive Performance Tests (NCPT). Demographic information included age, sex, race/ethnicity, and level of education.
Negative synergistic effect
Of the total sample (N = 13,323, mean age 62 years, 72.5% female, 88.6% White) 725 participants (5%) reported exposure to RHI, with contact sports as the most common cause, followed by physical abuse and then military duty; about 55% (7277 participants) reported TBI.
The researchers noted that 44.4% of those exposed to RHI and 70.3% of those who reported TBI were female. However, those with a history of contact sports were predominantly male and those reporting a history of abuse were predominantly women.
Among study participants who completed the GDS-15, 16.4% reported symptoms of depression, similar to rates reported among community-dwelling older adults.
Compared to the unexposed group, participants who reported TBI with loss of consciousness (LOC) and participants who reported TBI without LOC both had higher scores on the GDS-15 (beta = 0.75 [95% CI, 0.59-0.91] and beta = 0.43 [95% CI, 0.31-0.54], respectively).
A history of RHI was associated with an even higher depression score (beta = 1.24 [95% CI, 0.36-2.12).
Depression increased in tandem with increased exposure, with the lowest GDS-15 scores found in the unexposed group and subsequent increases in scores as exposure to RHI was introduced and TBI severity increased. The GDS scores were highest in those who had RHI plus TBI with LOC.
Participants with a history of RHI and/or TBI also had worse scores on tests of memory, learning, processing speed, and reaction time, compared with unexposed participants.
In particular, TBI with LOC had the most neuropsychological associations.
TBI without LOC had a negative effect on CogState tests measuring Identification and processing speed (beta = 0.004 [95% CI, 0-0.01] and beta = 0.004 [95% CI, 0.0002-0.01], respectively), whereas RHI predicted a worse processing speed score (beta = .02 [95% CI, 0.01-0.05]).
The presence of both RHI and TBI (with or without LOC) had a “synergistic negative effect” on neuropsychological performance, with a “consistent statistically significant finding” for worse neuropsychological test performance for those who had RHI and TBI with LOC, compared with those who had not sustained RHI.
Alosco said the findings highlight the need for clinicians to educate and inform parents/guardians of kids playing (or considering playing) contact sports about the research and potential risks associated with these activities.
If we want to prevent long-term problems, one way is not to expose [people] to these hits. Everyone takes risks in life with everything, but the more we can understand and mitigate the risks, the better,” Alosco said.
“A significant contribution”
Commenting on the findings for Medscape Medical News, Temitayo Oyegbile-Chidi, MD, PhD, a pediatric neurologist with Health Peak Inc, McLean, Virginia, and a member of the American Academy of Neurology, said the study “makes a significant contribution to the literature, as neurologists who specialized in TBI have long yearned to understand the long-term effects of repeated head impact on the brain and cognition.”
Clinicians should “inquire about a history of prior head impacts on all our patients, regardless of age, especially if they are experiencing or showing signs of unexpected cognitive dysfunction or mental health concerns,” said Oyegbile-Chidi, who was not involved with the study.
For those who have sustained single or repeated head impacts with or without associated LOC in the past, “it is important … to keep in mind that depression and cognitive dysfunction may persist or present even many years after the impact was sustained,” she added.
The study was supported by a grant from the National Institutes of Health. Alosco has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Oyegbile-Chidi has disclosed no relevant financial relationships.
A history of repetitive hits to the head (RHI), even without noticeable symptoms, is linked to a significantly increased risk of depression and poorer cognition later in life, new research shows.
“We found that a history of exposure to [repetitive hits to the head] from contact sports, military service, or physical abuse, as well as a history of TBI (traumatic brain injury), corresponded to more symptoms of later life depression and worse cognitive function,” lead author Michael Alosco, PhD, associate professor of neurology and codirector of the Boston University Alzheimer’s Disease Center Clinical Core, told Medscape Medical News.
He added that the findings underscore the importance of assessing repetitive head impacts (RHI).
The study was published online June 26 in Neurology.
Largest study to date
It is well known that sustaining a TBI is associated with worse later life cognition or mood problems, said Alosco. However, in the current research the investigators hypothesized that RHI may be a key driver of some of these outcomes, Alosco said.
Previous studies have been small or have only examined male former football players.
“What’s unique about our study is that we focused on a history of RHIs, and it is the largest study of its kind, incorporating over 30,000 males and females with different types of exposure to these RHIs.”
The researchers used data from the Brain Health Registry, an internet-based registry that longitudinally monitors cognition and functioning of participants (age 40 years and older).
Participants completed the Ohio State University TBI Identification Method (OSU TBI-ID) and answered a yes/no question: “Have you ever had a period of time in which you experienced multiple, repeated impacts to your head (eg, history of abuse, contact sports, military duty)?”
Participants also completed the Geriatric Depression Scale (GDS-15), the CogState Battery (CBB), and the Lumos Labs NeuroCognitive Performance Tests (NCPT). Demographic information included age, sex, race/ethnicity, and level of education.
Negative synergistic effect
Of the total sample (N = 13,323, mean age 62 years, 72.5% female, 88.6% White) 725 participants (5%) reported exposure to RHI, with contact sports as the most common cause, followed by physical abuse and then military duty; about 55% (7277 participants) reported TBI.
The researchers noted that 44.4% of those exposed to RHI and 70.3% of those who reported TBI were female. However, those with a history of contact sports were predominantly male and those reporting a history of abuse were predominantly women.
Among study participants who completed the GDS-15, 16.4% reported symptoms of depression, similar to rates reported among community-dwelling older adults.
Compared to the unexposed group, participants who reported TBI with loss of consciousness (LOC) and participants who reported TBI without LOC both had higher scores on the GDS-15 (beta = 0.75 [95% CI, 0.59-0.91] and beta = 0.43 [95% CI, 0.31-0.54], respectively).
A history of RHI was associated with an even higher depression score (beta = 1.24 [95% CI, 0.36-2.12).
Depression increased in tandem with increased exposure, with the lowest GDS-15 scores found in the unexposed group and subsequent increases in scores as exposure to RHI was introduced and TBI severity increased. The GDS scores were highest in those who had RHI plus TBI with LOC.
Participants with a history of RHI and/or TBI also had worse scores on tests of memory, learning, processing speed, and reaction time, compared with unexposed participants.
In particular, TBI with LOC had the most neuropsychological associations.
TBI without LOC had a negative effect on CogState tests measuring Identification and processing speed (beta = 0.004 [95% CI, 0-0.01] and beta = 0.004 [95% CI, 0.0002-0.01], respectively), whereas RHI predicted a worse processing speed score (beta = .02 [95% CI, 0.01-0.05]).
The presence of both RHI and TBI (with or without LOC) had a “synergistic negative effect” on neuropsychological performance, with a “consistent statistically significant finding” for worse neuropsychological test performance for those who had RHI and TBI with LOC, compared with those who had not sustained RHI.
Alosco said the findings highlight the need for clinicians to educate and inform parents/guardians of kids playing (or considering playing) contact sports about the research and potential risks associated with these activities.
If we want to prevent long-term problems, one way is not to expose [people] to these hits. Everyone takes risks in life with everything, but the more we can understand and mitigate the risks, the better,” Alosco said.
“A significant contribution”
Commenting on the findings for Medscape Medical News, Temitayo Oyegbile-Chidi, MD, PhD, a pediatric neurologist with Health Peak Inc, McLean, Virginia, and a member of the American Academy of Neurology, said the study “makes a significant contribution to the literature, as neurologists who specialized in TBI have long yearned to understand the long-term effects of repeated head impact on the brain and cognition.”
Clinicians should “inquire about a history of prior head impacts on all our patients, regardless of age, especially if they are experiencing or showing signs of unexpected cognitive dysfunction or mental health concerns,” said Oyegbile-Chidi, who was not involved with the study.
For those who have sustained single or repeated head impacts with or without associated LOC in the past, “it is important … to keep in mind that depression and cognitive dysfunction may persist or present even many years after the impact was sustained,” she added.
The study was supported by a grant from the National Institutes of Health. Alosco has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Oyegbile-Chidi has disclosed no relevant financial relationships.
A history of repetitive hits to the head (RHI), even without noticeable symptoms, is linked to a significantly increased risk of depression and poorer cognition later in life, new research shows.
“We found that a history of exposure to [repetitive hits to the head] from contact sports, military service, or physical abuse, as well as a history of TBI (traumatic brain injury), corresponded to more symptoms of later life depression and worse cognitive function,” lead author Michael Alosco, PhD, associate professor of neurology and codirector of the Boston University Alzheimer’s Disease Center Clinical Core, told Medscape Medical News.
He added that the findings underscore the importance of assessing repetitive head impacts (RHI).
The study was published online June 26 in Neurology.
Largest study to date
It is well known that sustaining a TBI is associated with worse later life cognition or mood problems, said Alosco. However, in the current research the investigators hypothesized that RHI may be a key driver of some of these outcomes, Alosco said.
Previous studies have been small or have only examined male former football players.
“What’s unique about our study is that we focused on a history of RHIs, and it is the largest study of its kind, incorporating over 30,000 males and females with different types of exposure to these RHIs.”
The researchers used data from the Brain Health Registry, an internet-based registry that longitudinally monitors cognition and functioning of participants (age 40 years and older).
Participants completed the Ohio State University TBI Identification Method (OSU TBI-ID) and answered a yes/no question: “Have you ever had a period of time in which you experienced multiple, repeated impacts to your head (eg, history of abuse, contact sports, military duty)?”
Participants also completed the Geriatric Depression Scale (GDS-15), the CogState Battery (CBB), and the Lumos Labs NeuroCognitive Performance Tests (NCPT). Demographic information included age, sex, race/ethnicity, and level of education.
Negative synergistic effect
Of the total sample (N = 13,323, mean age 62 years, 72.5% female, 88.6% White) 725 participants (5%) reported exposure to RHI, with contact sports as the most common cause, followed by physical abuse and then military duty; about 55% (7277 participants) reported TBI.
The researchers noted that 44.4% of those exposed to RHI and 70.3% of those who reported TBI were female. However, those with a history of contact sports were predominantly male and those reporting a history of abuse were predominantly women.
Among study participants who completed the GDS-15, 16.4% reported symptoms of depression, similar to rates reported among community-dwelling older adults.
Compared to the unexposed group, participants who reported TBI with loss of consciousness (LOC) and participants who reported TBI without LOC both had higher scores on the GDS-15 (beta = 0.75 [95% CI, 0.59-0.91] and beta = 0.43 [95% CI, 0.31-0.54], respectively).
A history of RHI was associated with an even higher depression score (beta = 1.24 [95% CI, 0.36-2.12).
Depression increased in tandem with increased exposure, with the lowest GDS-15 scores found in the unexposed group and subsequent increases in scores as exposure to RHI was introduced and TBI severity increased. The GDS scores were highest in those who had RHI plus TBI with LOC.
Participants with a history of RHI and/or TBI also had worse scores on tests of memory, learning, processing speed, and reaction time, compared with unexposed participants.
In particular, TBI with LOC had the most neuropsychological associations.
TBI without LOC had a negative effect on CogState tests measuring Identification and processing speed (beta = 0.004 [95% CI, 0-0.01] and beta = 0.004 [95% CI, 0.0002-0.01], respectively), whereas RHI predicted a worse processing speed score (beta = .02 [95% CI, 0.01-0.05]).
The presence of both RHI and TBI (with or without LOC) had a “synergistic negative effect” on neuropsychological performance, with a “consistent statistically significant finding” for worse neuropsychological test performance for those who had RHI and TBI with LOC, compared with those who had not sustained RHI.
Alosco said the findings highlight the need for clinicians to educate and inform parents/guardians of kids playing (or considering playing) contact sports about the research and potential risks associated with these activities.
If we want to prevent long-term problems, one way is not to expose [people] to these hits. Everyone takes risks in life with everything, but the more we can understand and mitigate the risks, the better,” Alosco said.
“A significant contribution”
Commenting on the findings for Medscape Medical News, Temitayo Oyegbile-Chidi, MD, PhD, a pediatric neurologist with Health Peak Inc, McLean, Virginia, and a member of the American Academy of Neurology, said the study “makes a significant contribution to the literature, as neurologists who specialized in TBI have long yearned to understand the long-term effects of repeated head impact on the brain and cognition.”
Clinicians should “inquire about a history of prior head impacts on all our patients, regardless of age, especially if they are experiencing or showing signs of unexpected cognitive dysfunction or mental health concerns,” said Oyegbile-Chidi, who was not involved with the study.
For those who have sustained single or repeated head impacts with or without associated LOC in the past, “it is important … to keep in mind that depression and cognitive dysfunction may persist or present even many years after the impact was sustained,” she added.
The study was supported by a grant from the National Institutes of Health. Alosco has disclosed no relevant financial relationships. The other authors’ disclosures are listed on the original paper. Oyegbile-Chidi has disclosed no relevant financial relationships.
Daily Recap 6/17
Here are the stories our MDedge editors across specialties think you need to know about today:
Comorbidities increase COVID-19 deaths by factor of 12
COVID-19 patients with an underlying condition are 6 times as likely to be hospitalized and 12 times as likely to die, compared with those who have no such condition, according to the CDC.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females.
The pandemic “continues to affect all populations and result in severe outcomes including death,” noted the CDC, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.” Read more.
Preventive services coalition recommends routine anxiety screening for women
Women and girls aged 13 years and older with no current diagnosis of anxiety should be screened routinely for anxiety, according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.” Read more.
High-fat, high-sugar diet may promote adult acne
A diet higher in fat, sugar, and milk was associated with having acne in a cross-sectional study of approximately 24,000 adults in France.
Although acne patients may believe that eating certain foods exacerbates acne, data on the effects of nutrition on acne, including associations between acne and a high-glycemic diet, are limited and have produced conflicting results, noted investigators.
“The results of our study appear to support the hypothesis that the Western diet (rich in animal products and fatty and sugary foods) is associated with the presence of acne in adulthood,” the researchers concluded.
Population study supports migraine-dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that migraine with aura and frequent hospital contacts significantly increased dementia risk after age 60 years, according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Sabrina Islamoska said.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Comorbidities increase COVID-19 deaths by factor of 12
COVID-19 patients with an underlying condition are 6 times as likely to be hospitalized and 12 times as likely to die, compared with those who have no such condition, according to the CDC.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females.
The pandemic “continues to affect all populations and result in severe outcomes including death,” noted the CDC, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.” Read more.
Preventive services coalition recommends routine anxiety screening for women
Women and girls aged 13 years and older with no current diagnosis of anxiety should be screened routinely for anxiety, according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.” Read more.
High-fat, high-sugar diet may promote adult acne
A diet higher in fat, sugar, and milk was associated with having acne in a cross-sectional study of approximately 24,000 adults in France.
Although acne patients may believe that eating certain foods exacerbates acne, data on the effects of nutrition on acne, including associations between acne and a high-glycemic diet, are limited and have produced conflicting results, noted investigators.
“The results of our study appear to support the hypothesis that the Western diet (rich in animal products and fatty and sugary foods) is associated with the presence of acne in adulthood,” the researchers concluded.
Population study supports migraine-dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that migraine with aura and frequent hospital contacts significantly increased dementia risk after age 60 years, according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Sabrina Islamoska said.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Comorbidities increase COVID-19 deaths by factor of 12
COVID-19 patients with an underlying condition are 6 times as likely to be hospitalized and 12 times as likely to die, compared with those who have no such condition, according to the CDC.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females.
The pandemic “continues to affect all populations and result in severe outcomes including death,” noted the CDC, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.” Read more.
Preventive services coalition recommends routine anxiety screening for women
Women and girls aged 13 years and older with no current diagnosis of anxiety should be screened routinely for anxiety, according to a new recommendation from the Women’s Preventive Services Initiative.
The lifetime prevalence of anxiety disorders in women in the United States is 40%, approximately twice that of men, and anxiety can be a manifestation of underlying issues including posttraumatic stress, sexual harassment, and assault.
“The WPSI based its rationale for anxiety screening on several considerations,” the researchers noted. “Anxiety disorders are the most prevalent mental health disorders in women, and the problems created by untreated anxiety can impair function in all areas of a woman’s life.” Read more.
High-fat, high-sugar diet may promote adult acne
A diet higher in fat, sugar, and milk was associated with having acne in a cross-sectional study of approximately 24,000 adults in France.
Although acne patients may believe that eating certain foods exacerbates acne, data on the effects of nutrition on acne, including associations between acne and a high-glycemic diet, are limited and have produced conflicting results, noted investigators.
“The results of our study appear to support the hypothesis that the Western diet (rich in animal products and fatty and sugary foods) is associated with the presence of acne in adulthood,” the researchers concluded.
Population study supports migraine-dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that migraine with aura and frequent hospital contacts significantly increased dementia risk after age 60 years, according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Sabrina Islamoska said.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.